- Case report
- Open access
- Published: 11 September 2017

A case of a four-year-old child adopted at eight months with unusual mood patterns and significant polypharmacy
- Magdalena Romanowicz ORCID: orcid.org/0000-0002-4916-0625 1 ,
- Alastair J. McKean 1 &
- Jennifer Vande Voort 1
BMC Psychiatry volume 17 , Article number: 330 ( 2017 ) Cite this article
42k Accesses
2 Citations
1 Altmetric
Metrics details
Long-term effects of neglect in early life are still widely unknown. Diversity of outcomes can be explained by differences in genetic risk, epigenetics, prenatal factors, exposure to stress and/or substances, and parent-child interactions. Very common sub-threshold presentations of children with history of early trauma are challenging not only to diagnose but also in treatment.
Case presentation
A Caucasian 4-year-old, adopted at 8 months, male patient with early history of neglect presented to pediatrician with symptoms of behavioral dyscontrol, emotional dysregulation, anxiety, hyperactivity and inattention, obsessions with food, and attachment issues. He was subsequently seen by two different child psychiatrists. Pharmacotherapy treatment attempted included guanfacine, fluoxetine and amphetamine salts as well as quetiapine, aripiprazole and thioridazine without much improvement. Risperidone initiated by primary care seemed to help with his symptoms of dyscontrol initially but later the dose had to be escalated to 6 mg total for the same result. After an episode of significant aggression, the patient was admitted to inpatient child psychiatric unit for stabilization and taper of the medicine.
Conclusions
The case illustrates difficulties in management of children with early history of neglect. A particular danger in this patient population is polypharmacy, which is often used to manage transdiagnostic symptoms that significantly impacts functioning with long term consequences.
Peer Review reports
There is a paucity of studies that address long-term effects of deprivation, trauma and neglect in early life, with what little data is available coming from institutionalized children [ 1 ]. Rutter [ 2 ], who studied formerly-institutionalized Romanian children adopted into UK families, found that this group exhibited prominent attachment disturbances, attention-deficit/hyperactivity disorder (ADHD), quasi-autistic features and cognitive delays. Interestingly, no other increases in psychopathology were noted [ 2 ].
Even more challenging to properly diagnose and treat are so called sub-threshold presentations of children with histories of early trauma [ 3 ]. Pincus, McQueen, & Elinson [ 4 ] described a group of children who presented with a combination of co-morbid symptoms of various diagnoses such as conduct disorder, ADHD, post-traumatic stress disorder (PTSD), depression and anxiety. As per Shankman et al. [ 5 ], these patients may escalate to fulfill the criteria for these disorders. The lack of proper diagnosis imposes significant challenges in terms of management [ 3 ].
J is a 4-year-old adopted Caucasian male who at the age of 2 years and 4 months was brought by his adoptive mother to primary care with symptoms of behavioral dyscontrol, emotional dysregulation, anxiety, hyperactivity and inattention, obsessions with food, and attachment issues. J was given diagnoses of reactive attachment disorder (RAD) and ADHD. No medications were recommended at that time and a referral was made for behavioral therapy.
She subsequently took him to two different child psychiatrists who diagnosed disruptive mood dysregulation disorder (DMDD), PTSD, anxiety and a mood disorder. To help with mood and inattention symptoms, guanfacine, fluoxetine, methylphenidate and amphetamine salts were all prescribed without significant improvement. Later quetiapine, aripiprazole and thioridazine were tried consecutively without behavioral improvement (please see Table 1 for details).
No significant drug/substance interactions were noted (Table 1 ). There were no concerns regarding adherence and serum drug concentrations were not ordered. On review of patient’s history of medication trials guanfacine and methylphenidate seemed to have no effect on J’s hyperactive and impulsive behavior as well as his lack of focus. Amphetamine salts that were initiated during hospitalization were stopped by the patient’s mother due to significant increase in aggressive behaviors and irritability. Aripiprazole was tried for a brief period of time and seemed to have no effect. Quetiapine was initially helpful at 150 mg (50 mg three times a day), unfortunately its effects wore off quickly and increase in dose to 300 mg (100 mg three times a day) did not seem to make a difference. Fluoxetine that was tried for anxiety did not seem to improve the behaviors and was stopped after less than a month on mother’s request.
J’s condition continued to deteriorate and his primary care provider started risperidone. While initially helpful, escalating doses were required until he was on 6 mg daily. In spite of this treatment, J attempted to stab a girl at preschool with scissors necessitating emergent evaluation, whereupon he was admitted to inpatient care for safety and observation. Risperidone was discontinued and J was referred to outpatient psychiatry for continuing medical monitoring and therapy.
Little is known about J’s early history. There is suspicion that his mother was neglectful with feeding and frequently left him crying, unattended or with strangers. He was taken away from his mother’s care at 7 months due to neglect and placed with his aunt. After 1 month, his aunt declined to collect him from daycare, deciding she was unable to manage him. The owner of the daycare called Child Services and offered to care for J, eventually becoming his present adoptive parent.
J was a very needy baby who would wake screaming and was hard to console. More recently he wakes in the mornings anxious and agitated. He is often indiscriminate and inappropriate interpersonally, unable to play with other children. When in significant distress he regresses, and behaves as a cat, meowing and scratching the floor. Though J bonded with his adoptive mother well and was able to express affection towards her, his affection is frequently indiscriminate and he rarely shows any signs of separation anxiety.
At the age of 2 years and 8 months there was a suspicion for speech delay and J was evaluated by a speech pathologist who concluded that J was exhibiting speech and language skills that were solidly in the average range for age, with developmental speech errors that should be monitored over time. They did not think that issues with communication contributed significantly to his behavioral difficulties. Assessment of intellectual functioning was performed at the age of 2 years and 5 months by a special education teacher. Based on Bailey Infant and Toddler Development Scale, fine and gross motor, cognitive and social communication were all within normal range.
J’s adoptive mother and in-home therapist expressed significant concerns in regards to his appetite. She reports that J’s biological father would come and visit him infrequently, but always with food and sweets. J often eats to the point of throwing up and there have been occasions where he has eaten his own vomit and dog feces. Mother noticed there is an association between his mood and eating behaviors. J’s episodes of insatiable and indiscriminate hunger frequently co-occur with increased energy, diminished need for sleep, and increased speech. This typically lasts a few days to a week and is followed by a period of reduced appetite, low energy, hypersomnia, tearfulness, sadness, rocking behavior and slurred speech. Those episodes last for one to 3 days. Additionally, there are times when his symptomatology seems to be more manageable with fewer outbursts and less difficulty regarding food behaviors.
J’s family history is poorly understood, with his biological mother having a personality disorder and ADHD, and a biological father with substance abuse. Both maternally and paternally there is concern for bipolar disorder.
J has a clear history of disrupted attachment. He is somewhat indiscriminate in his relationship to strangers and struggles with impulsivity, aggression, sleep and feeding issues. In addition to early life neglect and possible trauma, J has a strong family history of psychiatric illness. His mood, anxiety and sleep issues might suggest underlying PTSD. His prominent hyperactivity could be due to trauma or related to ADHD. With his history of neglect, indiscrimination towards strangers, mood liability, attention difficulties, and heightened emotional state, the possibility of Disinhibited Social Engagement Disorder (DSED) is likely. J’s prominent mood lability, irritability and family history of bipolar disorder, are concerning for what future mood diagnosis this portends.
As evidenced above, J presents as a diagnostic conundrum suffering from a combination of transdiagnostic symptoms that broadly impact his functioning. Unfortunately, although various diagnoses such as ADHD, PTSD, Depression, DMDD or DSED may be entertained, the patient does not fall neatly into any of the categories.
This is a case report that describes a diagnostic conundrum in a young boy with prominent early life deprivation who presented with multidimensional symptoms managed with polypharmacy.
A sub-threshold presentation in this patient partially explains difficulties with diagnosis. There is no doubt that negative effects of early childhood deprivation had significant impact on developmental outcomes in this patient, but the mechanisms that could explain the associations are still widely unknown. Significant family history of mental illness also predisposes him to early challenges. The clinical picture is further complicated by the potential dynamic factors that could explain some of the patient’s behaviors. Careful examination of J’s early life history would suggest such a pattern of being able to engage with his biological caregivers, being given food, being tended to; followed by periods of neglect where he would withdraw, regress and engage in rocking as a self-soothing behavior. His adoptive mother observed that visitations with his biological father were accompanied by being given a lot of food. It is also possible that when he was under the care of his biological mother, he was either attended to with access to food or neglected, left hungry and screaming for hours.
The current healthcare model, being centered on obtaining accurate diagnosis, poses difficulties for treatment in these patients. Given the complicated transdiagnostic symptomatology, clear guidelines surrounding treatment are unavailable. To date, there have been no psychopharmacological intervention trials for attachment issues. In patients with disordered attachment, pharmacologic treatment is typically focused on co-morbid disorders, even with sub-threshold presentations, with the goal of symptom reduction [ 6 ]. A study by dosReis [ 7 ] found that psychotropic usage in community foster care patients ranged from 14% to 30%, going to 67% in therapeutic foster care and as high as 77% in group homes. Another study by Breland-Noble [ 8 ] showed that many children receive more than one psychotropic medication, with 22% using two medications from the same class.
It is important to note that our patient received four different neuroleptic medications (quetiapine, aripiprazole, risperidone and thioridazine) for disruptive behaviors and impulsivity at a very young age. Olfson et al. [ 9 ] noted that between 1999 and 2007 there has been a significant increase in the use of neuroleptics for very young children who present with difficult behaviors. A preliminary study by Ercan et al. [ 10 ] showed promising results with the use of risperidone in preschool children with behavioral dyscontrol. Review by Memarzia et al. [ 11 ] suggested that risperidone decreased behavioral problems and improved cognitive-motor functions in preschoolers. The study also raised concerns in regards to side effects from neuroleptic medications in such a vulnerable patient population. Younger children seemed to be much more susceptible to side effects in comparison to older children and adults with weight gain being the most common. Weight gain associated with risperidone was most pronounced in pre-adolescents (Safer) [ 12 ]. Quetiapine and aripiprazole were also associated with higher rates of weight gain (Correll et al.) [ 13 ].
Pharmacokinetics of medications is difficult to assess in very young children with ongoing development of the liver and the kidneys. It has been observed that psychotropic medications in children have shorter half-lives (Kearns et al.) [ 14 ], which would require use of higher doses for body weight in comparison to adults for same plasma level. Unfortunately, that in turn significantly increases the likelihood and severity of potential side effects.
There is also a question on effects of early exposure to antipsychotics on neurodevelopment. In particular in the first 3 years of life there are many changes in developing brains, such as increase in synaptic density, pruning and increase in neuronal myelination to list just a few [ 11 ]. Unfortunately at this point in time there is a significant paucity of data that would allow drawing any conclusions.
Our case report presents a preschool patient with history of adoption, early life abuse and neglect who exhibited significant behavioral challenges and was treated with various psychotropic medications with limited results. It is important to emphasize that subthreshold presentation and poor diagnostic clarity leads to dangerous and excessive medication regimens that, as evidenced above is fairly common in this patient population.
Neglect and/or abuse experienced early in life is a risk factor for mental health problems even after adoption. Differences in genetic risk, epigenetics, prenatal factors (e.g., malnutrition or poor nutrition), exposure to stress and/or substances, and parent-child interactions may explain the diversity of outcomes among these individuals, both in terms of mood and behavioral patterns [ 15 , 16 , 17 ]. Considering that these children often present with significant functional impairment and a wide variety of symptoms, further studies are needed regarding diagnosis and treatment.
Abbreviations
Attention-Deficit/Hyperactivity Disorder
Disruptive Mood Dysregulation Disorder
Disinhibited Social Engagement Disorder
Post-Traumatic Stress Disorder
Reactive Attachment disorder
Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349. https://doi.org/10.1371/journal.pmed.1001349 . Epub 2012 Nov 27
Article PubMed PubMed Central Google Scholar
Kreppner JM, O'Connor TG, Rutter M, English and Romanian Adoptees Study Team. Can inattention/overactivity be an institutional deprivation syndrome? J Abnorm Child Psychol. 2001;29(6):513–28. PMID: 11761285
Article CAS PubMed Google Scholar
Dejong M. Some reflections on the use of psychiatric diagnosis in the looked after or “in care” child population. Clin Child Psychol Psychiatry. 2010;15(4):589–99. https://doi.org/10.1177/1359104510377705 .
Article PubMed Google Scholar
Pincus HA, McQueen LE, Elinson L. Subthreshold mental disorders: Nosological and research recommendations. In: Phillips KA, First MB, Pincus HA, editors. Advancing DSM: dilemmas in psychiatric diagnosis. Washington, DC: American Psychiatric Association; 2003. p. 129–44.
Google Scholar
Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR, Altman SE. Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. J Child Psychol Psychiatry. 2009;50:1485–94.
AACAP. Practice parameter for the assessment and treatment of children and adolescents with reactive attachment disorder of infancy and early childhood. J Am Acad Child Adolesc Psychiatry. 2005;44:1206–18.
Article Google Scholar
dosReis S, Zito JM, Safer DJ, Soeken KL. Mental health services for youths in foster care and disabled youths. Am J Public Health. 2001;91(7):1094–9.
Article CAS PubMed PubMed Central Google Scholar
Breland-Noble AM, Elbogen EB, Farmer EMZ, Wagner HR, Burns BJ. Use of psychotropic medications by youths in therapeutic foster care and group homes. Psychiatr Serv. 2004;55(6):706–8.
Olfson M, Crystal S, Huang C. Trends in antipsychotic drug use by very young, privately insured children. J Am Acad Child Adolesc Psychiatry. 2010;49:13–23.
PubMed Google Scholar
Ercan ES, Basay BK, Basay O. Risperidone in the treatment of conduct disorder in preschool children without intellectual disability. Child Adolesc Psychiatry Ment Health. 2011;5:10.
Memarzia J, Tracy D, Giaroli G. The use of antipsychotics in preschoolers: a veto or a sensible last option? J Psychopharmacol. 2014;28(4):303–19.
Safer DJ. A comparison of risperidone-induced weight gain across the age span. J Clin Psychopharmacol. 2004;24:429–36.
Correll CU, Manu P, Olshanskiy V. Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA. 2009;302:1765–73.
Kearns GL, Abdel-Rahman SM, Alander SW. Developmental pharmacology – drug disposition, action, and therapy in infants and children. N Engl J Med. 2003;349:1157–67.
Monk C, Spicer J, Champagne FA. Linking prenatal maternal adversity to developmental outcomes in infants: the role of epigenetic pathways. Dev Psychopathol. 2012;24(4):1361–76. https://doi.org/10.1017/S0954579412000764 . Review. PMID: 23062303
Cecil CA, Viding E, Fearon P, Glaser D, McCrory EJ. Disentangling the mental health impact of childhood abuse and neglect. Child Abuse Negl. 2016;63:106–19. https://doi.org/10.1016/j.chiabu.2016.11.024 . [Epub ahead of print] PMID: 27914236
Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89(5):892–909. https://doi.org/10.1016/j.neuron.2016.01.019 . Review. PMID: 26938439
Download references
Acknowledgements
We are also grateful to patient’s legal guardian for their support in writing this manuscript.
Availability of data and materials
Not applicable.
Author information
Authors and affiliations.
Mayo Clinic, Department of Psychiatry and Psychology, 200 1st SW, Rochester, MN, 55901, USA
Magdalena Romanowicz, Alastair J. McKean & Jennifer Vande Voort
You can also search for this author in PubMed Google Scholar
Contributions
MR, AJM, JVV conceptualized and followed up the patient. MR, AJM, JVV did literature survey and wrote the report and took part in the scientific discussion and in finalizing the manuscript. All the authors read and approved the final document.
Corresponding author
Correspondence to Magdalena Romanowicz .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Written consent was obtained from the patient’s legal guardian for publication of the patient’s details.
Competing interests
The author(s) declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Romanowicz, M., McKean, A.J. & Vande Voort, J. A case of a four-year-old child adopted at eight months with unusual mood patterns and significant polypharmacy. BMC Psychiatry 17 , 330 (2017). https://doi.org/10.1186/s12888-017-1492-y
Download citation
Received : 20 December 2016
Accepted : 01 September 2017
Published : 11 September 2017
DOI : https://doi.org/10.1186/s12888-017-1492-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Polypharmacy
- Disinhibited social engagement disorder
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
- Theresa Cerulli, MD
- Tina Matthews-Hayes, DNP, FNP, PMHNP
Custom Around the Practice Video Series
Experts in psychiatry review the case of a 27-year-old woman who presents for evaluation of a complex depressive disorder.

EP: 1 . Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
Ep: 2 . clinical significance of bipolar disorder, ep: 3 . clinical impressions from patient case #1, ep: 4 . diagnosis of bipolar disorder, ep: 5 . treatment options for bipolar disorder, ep: 6 . patient case #2: 47-year-old man with treatment resistant depression (trd), ep: 7 . patient case #2 continued: novel second-generation antipsychotics, ep: 8 . role of telemedicine in bipolar disorder.
Michael E. Thase, MD : Hello and welcome to this Psychiatric Times™ Around the Practice , “Identification and Management of Bipolar Disorder. ”I’m Michael Thase, professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Joining me today are: Dr Gustavo Alva, the medical director of ATP Clinical Research in Costa Mesa, California; Dr Theresa Cerulli, the medical director of Cerulli and Associates in North Andover, Massachusetts; and Dr Tina Matthew-Hayes, a dual-certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.
Today we are going to highlight challenges with identifying bipolar disorder, discuss strategies for optimizing treatment, comment on telehealth utilization, and walk through 2 interesting patient cases. We’ll also involve our audience by using several polling questions, and these results will be shared after the program.
Without further ado, welcome and let’s begin. Here’s our first polling question. What percentage of your patients with bipolar disorder have 1 or more co-occurring psychiatric condition? a. 10%, b. 10%-30%, c. 30%-50%, d. 50%-70%, or e. more than 70%.
Now, here’s our second polling question. What percentage of your referred patients with bipolar disorder were initially misdiagnosed? Would you say a. less than 10%, b. 10%-30%, c. 30%-50%, d. more than 50%, up to 70%, or e. greater than 70%.
We’re going to go ahead to patient case No. 1. This is a 27-year-old woman who’s presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode. It began back in the fall, and she described the episode as occurring right “out of the blue.” Further discussion revealed, however, that she had talked with several confidantes about her problems and that she realized she had been disappointed and frustrated for being passed over unfairly for a promotion at work. She had also been saddened by the unusually early death of her favorite aunt.
Now, our patient has a past history of ADHD [attention-deficit/hyperactivity disorder], which was recognized when she was in middle school and for which she took methylphenidate for adolescence and much of her young adult life. As she was wrapping up with college, she decided that this medication sometimes disrupted her sleep and gave her an irritable edge, and decided that she might be better off not taking it. Her medical history was unremarkable. She is taking escitalopram at the time of our initial evaluation, and the dose was just reduced by her PCP [primary care physician]from 20 mg to 10 mg because she subjectively thought the medicine might actually be making her worse.
On the day of her first visit, we get a PHQ-9 [9-item Patient Health Questionnaire]. The score is 16, which is in the moderate depression range. She filled out the MDQ [Mood Disorder Questionnaire] and scored a whopping 10, which is not the highest possible score but it is higher than 95% of people who take this inventory.
At the time of our interview, our patient tells us that her No. 1 symptom is her low mood and her ease to tears. In fact, she was tearful during the interview. She also reports that her normal trouble concentrating, attributable to the ADHD, is actually substantially worse. Additionally, in contrast to her usual diet, she has a tendency to overeat and may have gained as much as 5 kg over the last 4 months. She reports an irregular sleep cycle and tends to have periods of hypersomnolence, especially on the weekends, and then days on end where she might sleep only 4 hours a night despite feeling tired.
Upon examination, her mood is positively reactive, and by that I mean she can lift her spirits in conversation, show some preserved sense of humor, and does not appear as severely depressed as she subjectively describes. Furthermore, she would say that in contrast to other times in her life when she’s been depressed, that she’s actually had no loss of libido, and in fact her libido might even be somewhat increased. Over the last month or so, she’s had several uncharacteristic casual hook-ups.
So the differential diagnosis for this patient included major depressive disorder, recurrent unipolar with mixed features, versus bipolar II disorder, with an antecedent history of ADHD. I think the high MDQ score and recurrent threshold level of mixed symptoms within a diagnosable depressive episode certainly increase the chances that this patient’s illness should be thought of on the bipolar spectrum. Of course, this formulation is strengthened by the fact that she has an early age of onset of recurrent depression, that her current episode, despite having mixed features, has reverse vegetative features as well. We also have the observation that antidepressant therapy has seemed to make her condition worse, not better.
Transcript Edited for Clarity
Dr. Thase is a professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Dr. Alva is the medical director of ATP Clinical Research in Costa Mesa, California.
Dr. Cerulli is the medical director of Cerulli and Associates in Andover, Massachusetts.
Dr. Tina Matthew-Hayes is a dual certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.

The Week in Review: April 1-5

Blue Light, Depression, and Bipolar Disorder

An Update on Bipolar I Disorder

Four Myths About Lamotrigine

Recap: Mood Disorders 2024
Evidence-Based Novel Therapies for Bipolar Depression: Top 5 Takeaways
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
DSM-5 Clinical Cases
- Rachel A. Davis , M.D.
Search for more papers by this author
DSM-5 Clinical Cases makes the rather overwhelming DSM-5 much more accessible to mental health clinicians by using clinical examples—the way many clinicians learn best—to illustrate the changes in diagnostic criteria from DSM-IV-TR to DSM-5. More than 100 authors contributed to the 103 case vignettes and discussions in this book. Each case is concise but not oversimplified. The cases range from straightforward and typical to complicated and unusual, providing a nice repertoire of clinical material. The cases are realistic in that many portray scenarios that are complicated by confounding factors or in which not all information needed to make a diagnosis is available. The authors are candid in their discussions of difficulties arriving at the correct diagnoses, and they acknowledge the limitations of DSM-5 when appropriate.
The book is conveniently organized in a manner similar to DSM-5. The 19 chapters in DSM-5 Clinical Cases correspond to the first 19 chapters in section 2 of DSM-5. As in DSM-5, DSM-5 Clinical Cases begins with diagnoses that tend to manifest earlier in life and advances to diagnoses that usually occur later in life. Each chapter begins with a discussion of changes from DSM-IV. These changes are further explored in the cases that follow.
Each case vignette is titled with the presenting problem. The cases are formatted similarly throughout and include history of present illness, collateral information, past psychiatric history, social history, examination, any laboratory findings, any neurocognitive testing, and family history. This is followed by the diagnosis or diagnoses and the case discussion. In the discussions, the authors highlight the key symptoms relevant to DSM-5 criteria. They explore the differential diagnosis and explain their rational for arriving at their selected diagnoses versus others they considered as well. In addition, they discuss complicating factors that make the diagnoses less clear and often mention what additional information they would like to have. Each case is followed by a list of suggested readings.
As an example, case 6.1 is titled Depression. This case describes a 52-year-old man, “Mr. King,” presenting with the chief complaint of depressive symptoms for years, with minimal response to medication trials. The case goes on to describe that Mr. King had many anxieties with related compulsions. For example, he worried about contracting diseases such as HIV and would wash his hands repeatedly with bleach. He was able to function at work as a janitor by using gloves but otherwise lived a mostly isolative life. Examination was positive for a strong odor of bleach, an anxious, constricted affect, and insight that his fears and behaviors were “kinda crazy.” No laboratory findings or neurocognitive testing is mentioned.
The diagnoses given for this case are “OCD, with good or fair insight,” and “major depressive disorder.” The discussants acknowledge that evaluation for OCD can be difficult because most patients are not so forthcoming with their symptoms. DSM-5 definitions of obsessions and compulsions are reviewed, and the changes to the description of obsessions are highlighted: the term urge is used instead of impulse so as to minimize confusion with impulse-control disorders; the term unwanted instead of inappropriate is used; and obsessions are noted to generally (rather than always) cause marked anxiety or distress to reflect the research that not all obsessions result in marked anxiety or distress. The authors review the remaining DSM-5 criteria, that OCD symptoms must cause distress or impairment and must not be attributable to a substance use disorder, a medical condition, or another mental disorder. They discuss the two specifiers: degree of insight and current or past history of a tic disorder. They briefly explore the differential diagnosis, noting the importance of considering anxiety disorders and distinguishing the obsessions of OCD from the ruminations of major depressive disorder. They also point out the importance of looking for comorbid diagnoses, for example, body dysmorphic disorder and hoarding disorder.
This brief case, presented and discussed in less than three pages, leaves the reader with an overall understanding of the diagnostic criteria for OCD, as well as a good sense of the changes in DSM-5.
DSM-5 Clinical Cases is easy to read, interesting, and clinically relevant. It will improve the reader’s ability to apply the DSM-5 diagnostic classification system to real-life practice and highlights many nuances to DSM-5 that one might otherwise miss. This book will serve as a valuable supplementary manual for clinicians across many different stages and settings of practice. It may well be a more practical and efficient way to learn the DSM changes than the DSM-5 itself.
The author reports no financial relationships with commercial interests.
- Cited by None

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.13(1); 2021 Jan

Illness Anxiety Disorder: A Case Report and Brief Review of the Literature
Eduardo d espiridion.
1 Psychiatry, Drexel University College of Medicine, Philadelphia, USA
2 Psychiatry, West Virginia School of Osteopathic Medicine, Lewisburg, USA
3 Psychiatry, West Virginia University School of Medicine, Martinsburg, USA
4 Psychiatry, Philadelphia College of Osteopathic Medicine, Philadelphia, USA
5 Psychiatry, Reading Hospital Tower Health, West Reading, USA
6 Medicine, Drexel University College of Medicine, Philadelphia, USA
Adeolu O Oladunjoye
7 Critical Care Medicine, Boston Children's Hospital, Boston, USA
Illness anxiety disorder (IAD) is defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V) as the preoccupation with having or acquiring a serious illness, in the absence of somatic symptoms (or, if present, symptoms that are only mild in severity). Patients with IAD experience persistent anxiety or fear of having or acquiring a serious illness, which adversely affects their daily life. They remain unsatisfied with their physician’s reassurances to the contrary, mainly because their distress is created by the anxiety of the meaning, significance, and cause of the complaints and not necessarily due to the physical presentations. IAD remains a huge burden on both the health facility and for the managing healthcare provider. In this report, we present the case of a patient with IAD, which has been managed for the past five years with recurrent visits to the physician with no resolution of signs and symptoms. Despite extensive medical workup over this period, which repeatedly showed normal test results, the patient continued to have anxiety over his ill health and complained of recurrent mild somatic symptoms. After his most recent appointment, he got very upset and booked a flight to his home country to have a second opinion to validate his illness. Physicians are encouraged to build a therapeutic alliance with patients with IAD, rather than ordering expensive or unnecessary diagnostic tests or treatment.
Introduction
Illness anxiety disorder (IAD), previously known as hypochondriasis, is defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V) as the preoccupation with having or acquiring a serious illness, in the absence of somatic symptoms (or, if present, symptoms that are only mild in severity) [ 1 - 2 ]. Patients with IAD experience a high level of anxiety about their health and they are easily alarmed by their health status [ 1 ]. They experience persistent anxiety or fear of having or acquiring a serious illness, adversely affecting their daily life [ 2 - 3 ]. They remain unsatisfied with their physician’s reassurances, mainly because their distress arises from the anxiety of the meaning, significance, and cause of the complaints and not necessarily from the physical presentation. These individuals engage in excessive health-related behaviors (e.g., repeated checks on the body for signs of illness) or exhibit maladaptive avoidance (e.g., avoiding doctor appointments and hospitals) [ 1 ]. The diagnosis requires the existence of the preoccupation for at least six months, but specific illnesses may change over that period of time [ 1 ]. The illness is not better explained by other mental disorders. There are two types of IAD: care-seeking type and care-avoidant type [ 1 - 2 ]. The care-seeking type involves those who frequently utilize the healthcare system and medical resources, including physician visits and undergoing multiple tests and procedures [ 2 , 4 ]. The care-avoidant type, on the other hand, refers to patients with severe anxiety who hold the belief that their physician visit or laboratory test will reveal life-threatening illnesses such as cancer [ 2 , 4 ]. In this report, we present a patient with IAD whose disease course has been characterized by recurrent visits to the physician in the past five years with no resolution of signs and symptoms.
Case presentation
History of the presenting complaint
The patient was a 34-year-old male immigrant to the US from Asia who was admitted to the medical floor of a community hospital for the management of his medical problems. He had experienced a recurrent history of anxiety and mild somatic symptoms for the past five years. He reported sleeping difficulties, panic attacks, ruminative worries, muscle tension, body weakness, and chest discomfort. The patient had a prior psychiatric history and hospitalization for anxiety and depression. He had been admitted for anxiety and depression in a free-standing health facility five years ago and had been treated with medications. He had been prescribed sertraline and quetiapine but had self-discontinued because of tolerability issues. He had continued to be anxious with mild somatic symptoms. The patient denied any manic or psychotic symptoms or any neurological symptoms. The patient also denied any suicidal or homicidal ideations. He had no history of substance use or alcohol intake. He had a family history of anxiety disorder, described as an obsessive-compulsive disorder in his mother. In 2019, he had consulted a physician who had performed an extensive medical workup. All test results were unremarkable; he was reassured and his symptoms improved. During the two to three weeks prior to the current presentation, his anxiety and somatic symptoms had recurred and had subsequently worsened. He was then admitted for further investigation.
Examination
The mental status examination revealed a young man who was neat and well-groomed. He was cooperative, calm, and made appropriate eye contact. His speech was normal. He described his mood as anxious and his affect was constricted. His thought process was normal and linear. There was no suicidal or homicidal ideation. No delusions or hallucinations were reported. He was awake, alert, and oriented to time, place, people, and events. His judgment and insight were fair.
Investigation
He underwent a 12-lead electrocardiogram, which showed a ventricular rate of 80 beats/minute (reference range: 60-100 beats/minute), atrial rate of 80 beats/minute (reference range: 60-100 beats/minute), PR interval of 148 milliseconds (reference range: 120-200 milliseconds), QRS duration of 94 milliseconds (reference range: 80-100 milliseconds), QT interval of 350 milliseconds (reference range: 360-430 milliseconds), and QTC calculation (Bazett) of 403 milliseconds (reference range: ≤440 milliseconds) with normal sinus rhythm.
Other medical workups done revealed thyroid-stimulating hormone of 2.398 uIU/mL (reference range: 0.35-5.5 uIU/mL), hemoglobin A1c of 5.6% (reference range: <5.7%), and urinalysis showing no ketones or proteins. Lipid profile showed cholesterol of 182 milligrams per deciliter (reference range: <200 milligrams per deciliter), high-density lipoprotein of 39 milligrams per deciliter (reference range: <40 milligrams per deciliter), low-density lipoproteins of 103.8 milligrams per deciliter (reference range: <100 milligrams per deciliter), and a slightly elevated triglyceride of 196 milligrams per deciliter (reference range: <150 milligrams per deciliter). His basic metabolic panel was as follows: sodium of 140 millimoles per liter (reference range: 136-145 millimoles per liter), potassium of 4.1 millimoles per liter (reference range: 3.6-5.2 millimoles per liter), chloride of 104 millimoles per liter (reference range: 98-106 millimoles per liter), glucose of 93 milligrams per deciliter (reference range: 70-100 milligrams per deciliter), calcium of 9.3 milligrams per deciliter (reference range: 8.5-10.5 milligrams per deciliter), phosphorus of 4.0 milligrams per deciliter (reference range: 3.4-4.5 milligrams per deciliter), blood urea nitrogen of 9 milligrams per deciliter (reference range: 7-20 milligrams per deciliter), and creatinine of 1.0 milligrams per deciliter (reference range: 0.84-1.21 milligrams per deciliter). His complete blood count revealed a hematocrit of 48.9% (reference range: 38.3-48.6%), mean corpuscular volume of 84.7 femtoliters (reference range: 80-96 femtoliters), and red cell distribution width of 12.5% (reference range: 11.8-14.5%). All of these results were unremarkable. Also, an MRI of the brain without contrast was unremarkable. His vitamin B12 was unremarkable as well: 337 picograms per milliliter (reference range: 160-950 picograms per milliliter).
Both the hospitalist and cardiologist cleared him for any medical issues. Despite this reassurance, he got very upset and booked a flight to his home country to have a second opinion to validate his illness.
The cause of IAD is largely unknown. However, several risk factors have been implicated in the development of IAD. These include an underlying anxiety disorder, excess amount of time spent reviewing health-related materials (e.g., on the internet), history of previous serious childhood illness or illness of the patient's caregiver, family history of anxiety, and discussions and experience that involve labeling normal body sensations as pathological [ 2 , 3 - 5 ]. Our patient did not present with any of these risk factors; however, he had a history of anxiety and depression. These patients usually present with comorbidities such as anxiety and depression and need to be treated for these conditions [ 6 ]. What is not known is whether psychiatric history was a trigger to IAD, or if these psychiatric conditions coexisted in our patient from the onset. This patient had discontinued treatment for his anxiety and depression, which may have also triggered IAD in him.
IAD is a diagnosis of exclusion. It is important that a comprehensive examination and testing be conducted to exclude any organic disease before establishing a diagnosis of IAD [ 2 , 4 ]. Patients with IAD typically utilize several medical facilities. They are seen by multiple physicians with repeated negative tests each time they visit a health facility [ 1 ]. Frequently, the physician will carry out unnecessary and costly tests without achieving satisfying results; though the patient is deemed healthy, the anxiety persists [ 7 ]. Therefore, patients continue to visit multiple physicians due to their frustration with repeatedly normal or negative test results and unsuccessful physician reassurance. In the case of our patient, after several visits with physicians in the US, he got upset with his management and decided to travel to see another physician in his home country for a second opinion.
Patients with IAD are more often found in primary care centers than in mental health clinics, resulting in a delay in treatment and subsequent worsening of their psychiatric condition [ 7 , 8 ]. The primary care provider (PCP) is typically trained to identify physical symptoms that are not found in patients with IAD. This results in excessive use of scarce medical resources, worsening the depletion of the health resources apart from wasting the physician’s time and efforts [ 9 ]. It is not known how much money has been spent on this patient in total, but it is expected to run into several thousands of US dollars. It was estimated that 10-20% of the US medical budget is spent on patients with some form of somatization or IADs [ 10 ].
The most important aspect in the management of IAD is for the physician to establish a longitudinal trust relationship with the patient [ 11 ]. Communication should focus on empathy, open dialog, coordination of testing, and consistent delivery of messages [ 3 ]. The physician should first acknowledge their fears and concerns with the patient. Patients need to be reassured that although there is no specific treatment for the unexplained symptoms, the symptom is not fatal or catastrophic and that the physician will continue to work with patients on their path back to health and well-being. Holder-Perkins et al. have proposed that the physician should focus on psychosocial problems instead of the somatic concerns of the patient [ 8 ]. Patients can have regular follow-up visits with their PCP and psychiatrist to address new complaints, triggers, or stressors [ 4 ]. This will ultimately reduce unnecessary visits to the emergency department or other physicians.
Psychotherapy is the first-line treatment for IAD and has been shown to reduce symptoms associated with the condition [ 2 ]. This includes cognitive-behavioral therapy, which focuses on eradicating dysfunctional maladaptive cognitive beliefs by means of behavioral modification strategies [ 2 , 4 ]. Other therapy options include mindfulness-based cognitive therapy, group-therapies, attention training, and acceptance and commitment therapy [ 2 , 7 ]. Psychotropic medications have also been helpful in treating marked comorbidity of anxiety and depressive symptoms in patients with IAD [ 8 ]. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) have been proven to be effective in patients with IAD [ 2 ]. However, the challenges of prescribing these drugs include the patient’s misinterpretation of this as an attempt to dismiss their unexplained symptoms, as well as the side effects of these medications. Patients should be reassured about using medications and given very detailed information about the management plan during scheduled visits.
Conclusions
Physicians are encouraged to build a therapeutic alliance with patients with IAD as they work with them on their path back to health. This is essential to reduce the tremendous burden on the healthcare system caused by the wastage of physician resources and ordering of expensive or unnecessary investigations while caring for patients with IAD.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study

- Neuroscience
The Neuroscience of Behavior: Five Famous Cases
Five patients who shaped our understanding of behavior and the brain..
Posted January 16, 2020 | Reviewed by Lybi Ma
“Considering everything, it seems we are dealing here with a special illness… There are certainly more psychiatric illnesses than are listed in our textbooks.” —Alois Alzheimer (In: Benjamin, 2018)
Once thought to be the product of demonic possession, immorality, or imbalanced humors, we now know that psychiatric symptoms are often caused by changes in the brain. Read on to learn about the people who helped us understand the brain as the driving force behind our behaviors.
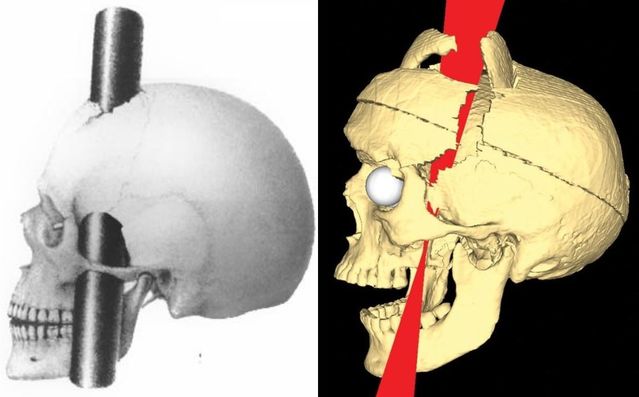
Phineas Gage
In 1848, John Harlow first described the case of a 25-year-old railroad foreman named Phineas Gage. Gage was a "temperate" man: hardworking, polite, and well-liked by all those around him. One day, Gage was struck through the skull by an iron rod launched in an accidental explosion. The rod traveled through the prefrontal cortex of his brain. Remarkably, he survived with no deficits in his motor function or memory . However, his family and friends noticed major changes in his personality . He became impatient, unreliable, vulgar, and was even described as developing the "animal passions of a strong man." This was the first glimpse into the important role of the prefrontal cortex in personality and social behavior (David, 2009; Thiebaut de Schotten, 2015; Benjamin, 2018).
Louis Victor Leborgne
Pierre Broca first published the case of 50-year-old Louis Victor Leborgne in 1861. Despite normal intelligence , Leborgne inexplicably lost the ability to speak. His nickname was Tan, after this became the only word he ever uttered. He was otherwise unaffected and seemed to follow directions and understand others without difficulty. After he died, Broca examined his brain, finding an abnormal area of brain tissue only in the left anterior frontal lobe. This suggested that the left and right sides of the brain were not always symmetric in their functions, as previously thought. Broca later went on to describe several other similar cases, cementing the role of the left anterior frontal lobe (now called Broca’s area) as a crucial region for producing (but not understanding) language (Dronkers, 2007; David, 2009; Thiebaut de Schotten, 2015).
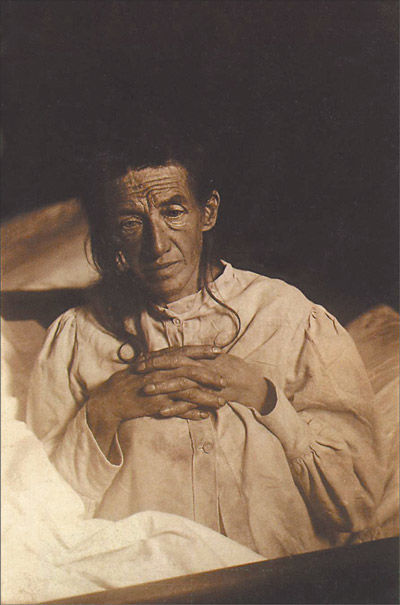
Auguste Deter
Psychiatrist and neuropathologist Aloysius Alzheimer described the case of Auguste Deter, a 56-year-old woman who passed away in 1906 after she developed strange behaviors, hallucinations, and memory loss. When Alzheimer looked at her brain under the microscope, he described amyloid plaques and neurofibrillary tangles that we now know are a hallmark of the disease that bears his name. This significant discovery was the first time that a biological molecule such as a protein was linked to a psychiatric illness (Shorter, 1997; David, 2009; Kalia & Costa e Silva, 2015).
In 1933, Spafford Ackerly described the case of "JP” who, beginning at a very young age, would do crude things like defecate on others' belongings, expose himself, and masturbate in front of other children at school. These behaviors worsened as he aged, leading to his arrest as a teenager . He was examined by Ackerly who found that the boy had a large cyst, likely present from birth, that caused severe damage to his prefrontal cortices. Like the case of Phineas Gage, JP helped us understand the crucial role that the prefrontal cortex plays in judgment, decision-making , social behaviors, and personality (Benjamin, 2018).
HM (Henry Gustav Molaison)
William Scoville first described the case of HM, a 29-year-old man whom he had treated two years earlier with an experimental surgery to remove his medial temporal lobes (including the hippocampus and amygdala on both sides). The hope was that the surgery would control his severe epilepsy, and it did seem to help. But with that improvement came a very unexpected side effect: HM completely lost the ability to form certain kinds of new memories. While he was still able to form new implicit or procedural memories (like tying shoes or playing the piano), he was no longer able to form new semantic or declarative memories (like someone’s name or major life events). This taught us that memories were localized to a specific brain region, not distributed throughout the whole brain as previously thought (David, 2009; Thiebaut de Schotten, 2015; Benjamin, 2018).
Facebook /LinkedIn image: Gorodenkoff/Shutterstock
Benjamin, S., MacGillivray, L., Schildkrout, B., Cohen-Oram, A., Lauterbach, M.D., & Levin, L.L. (2018). Six landmark case reports essential for neuropsychiatric literacy. J Neuropsychiatry Clin Neurosci, 30 , 279-290.
Shorter, E., (1997). A history of psychiatry: From the era of the asylum to the age of Prozac. New York: John Wiley & Sons, Inc.
Thiebaut de Schotten, M., Dell'Acqua, F., Ratiu, P. Leslie, A., Howells, H., Cabanis, E., Iba-Zizen, M.T., Plaisant, O., Simmons, A, Dronkers, N.F., Corkin, S., & Catani, M. (2015). From Phineas Gage and Monsieur Leborgne to H.M.: Revisiting disconnection syndromes. Cerebral Cortex, 25 , 4812-4827.
David, A.S., Fleminger, S., Kopelman, M.D., Lovestone, S., & Mellers, J. (2009). Lishman's organic psychiatry: A textbook of neuropsychiatry. Hoboken, NJ: Wiley-Blackwell.
Kalia, M., & Costa e Silva, J. (2015). Biomarkers of psychiatric diseases: Current status and future prospects. Metabolism, 64, S11-S15.
Dronkers, N.F., Plaisant, O., Iba-Zizen, M.T., & Cabanis, E.A. (2007). Paul Broca's historic cases: High resolution MR Imaging of the brains of Leborgne and Lelong. Brain , 130, 1432–1441.
Scoville, W.B., & Milner, B. (1957). Loss of recent memory after bilateral hippocampal lesions. J. Neurol. Neurosurg. Psychiat., 20, 11-21.

Melissa Shepard, MD , is an assistant professor of psychiatry at the Johns Hopkins School of Medicine.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
143 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health
At Tracking Happiness, we’re dedicated to helping others around the world overcome struggles of mental health.
In 2022, we published a survey of 5,521 respondents and found:
- 88% of our respondents experienced mental health issues in the past year.
- 25% of people don’t feel comfortable sharing their struggles with anyone, not even their closest friends.
In order to break the stigma that surrounds mental health struggles, we’re looking to share your stories.
Overcoming struggles
They say that everyone you meet is engaged in a great struggle. No matter how well someone manages to hide it, there’s always something to overcome, a struggle to deal with, an obstacle to climb.
And when someone is engaged in a struggle, that person is looking for others to join him. Because we, as human beings, don’t thrive when we feel alone in facing a struggle.
Let’s throw rocks together
Overcoming your struggles is like defeating an angry giant. You try to throw rocks at it, but how much damage is one little rock gonna do?
Tracking Happiness can become your partner in facing this giant. We are on a mission to share all your stories of overcoming mental health struggles. By doing so, we want to help inspire you to overcome the things that you’re struggling with, while also breaking the stigma of mental health.
Which explains the phrase: “Let’s throw rocks together”.
Let’s throw rocks together, and become better at overcoming our struggles collectively. If you’re interested in becoming a part of this and sharing your story, click this link!
Case studies
April 11, 2024
How a Mindset Change Helped Me Break Free From Childhood Trauma and Toxicity
“My mother said she wanted to end it in bloodshed and she waited for him to come home from his late-night meeting. She thought better of it when he was late arriving home. She was overwhelmed with thoughts of her in prison and me in foster care. To say that she made the right decision in achieving the goal of a good life is an answer I struggled to answer for many years.”
Struggled with: Abuse Anxiety Childhood CPTSD Depression
Helped by: Mindfulness Reinventing yourself Self-improvement Therapy
April 9, 2024
Healing From Postpartum Depression With Therapy, Friends & Exercise
“I wasn’t sure how to feel better for a while. People talk about ‘getting help’ but that’s a blanket term and unfortunately it’s not a band-aid you can just put on and suddenly be yourself again. It takes time to find the right therapist, medication if that’s what you decide to do, to find a new rhythm with family, and in my case, I really needed friends locally.”
Struggled with: Postpartum depression
Helped by: Exercise Social support Therapy
April 4, 2024
My Journey from Loneliness and Isolation to Creating an Online Haven for Seniors
“When one is home alone, all day, with nothing to do, nobody to speak with, stuck with their thoughts both good and bad, it’s easy to slip back into a depressive state. Feeling unneeded, unwanted, no happiness, no joy, no reason to get out of bed – just suffering with “the blahs”.”
Struggled with: Depression Loneliness
Helped by: Self-improvement Social support
April 2, 2024
Surviving a Workplace Shooting and Navigating PTSD, Insomnia With Marathons and Prayers
“My symptoms began immediately following a workplace shooting on Saturday, November 28, 2015, and were exasperated due to the activity of the company, the criminals, and the cops. The company treated me as if I were a criminal, the criminals attempted to kill me three additional times, and the cops (Houston Police Department Organized Crime Unit) treated me as if I was a thorn in their flesh.”
Struggled with: Depression Insomnia PTSD Stress
Helped by: Exercise Religion Treatment Volunteering
March 28, 2024

How The Support of Others Helped Me Heal After a Mental Breakdown
“I do not recommend having a breakdown when trying to raise boys. I would cry, eat all the time, and feel like my brain was full of fuzz. I could barely function. There was that day when I got home from taking the kids to school, and thought to myself that if there was a gun in the house, someone else would have had to pick them up from school that day.”
Struggled with: Depression Divorce Stress
Helped by: Journaling Social support Therapy
March 26, 2024
Journaling and Therapy Helped Me After Surviving a Car Accident and a Late Pregnancy Loss
“I vividly remember one day a few months after getting hit by the car when I wondered if my life would ever feel peaceful, pain-free, or joyful again. I was simply getting in and out of the passenger seat of a vehicle, my whole body gripped with pain and stiffness when I experienced a flash of fear that my health would never improve.”
Struggled with: Chronic pain Depression Grief PTSD
Helped by: Journaling Therapy
March 21, 2024
From the C-Suites to the Streets and Back – Overcoming Addiction, Anxiety, Depression and PTSD
“Over the past decade, I have struggled with substance abuse immensely leading to anxiety, depression, and PTSD. After losing thirteen corporate jobs and ending up homeless, beaten up, and absolutely broken on the streets I have finally come to terms with my situation and am finding a path towards long-term sobriety and happiness.”
Struggled with: Addiction Anxiety Depression PTSD
Helped by: Mindfulness Rehab Religion Self-improvement Social support
March 19, 2024
My Journey to Self-Compassion Amidst Depression, Anxiety and Suicidal Thoughts
“This suicidal edge coupled with stress, anxiety, and loneliness made me stop working as a human being. In just two months I had spiraled down into the darkest hole which has ever existed for me. There didn’t exist Marina anymore, merely a depressive and neurotic copy of her, who was unable to laugh and sleep.”
Struggled with: Anxiety Depression Panic attacks Stress Suicidal
Helped by: Self-acceptance Self-improvement Therapy
March 14, 2024
How EMDR Therapy Helped Me Navigate Childhood Trauma and Rediscover Myself
“As my anxiety levels grew, I turned to alcohol and then combined that with Vicodin to fend off the bad feelings. I would drink to the point of blacking out on a regular basis, sometimes never knowing how I got home.”
Struggled with: Abuse Addiction Bullying Childhood CPTSD
Helped by: Reinventing yourself Therapy
March 12, 2024
How Self-Care and My Infrared Sauna Blanket Help Me Navigate CPTSD and Fascia Pain
“I’m sure that other people around me knew that I was struggling, but I only shared this with a couple of people. People in my immediate physical ecosphere didn’t offer up any kind of empathy either. In fact, the exact opposite. Which I think made the condition even worse.”
Struggled with: Chronic pain CPTSD
Helped by: Journaling Meditation Self-Care
Module 12: Personality Disorders
Case studies: personality disorders, learning objectives.
- Identify personality disorders in case studies
Case Study: Latasha
Latasha was a 20-year-old college student who lived in the dorms on campus. Classmates described Latasha as absent-minded and geeky because she didn’t interact with others and rarely, if ever, engaged with classmates or professors in class. She usually raced back to her dorm as soon as classes were over. Latasha primarily stayed in her room, did not appear to have any friends, and had no interest in the events happening on campus. Latasha even asked for special permission to stay on campus when most students went home for Thanksgiving break.
Now let’s examine some fictional case studies.
Case Study: The Mad Hatter
The Mad Hatter, from Alice in Wonderland , appears to be living in a forest that is part of Alice’s dream. He appears to be in his mid-thirties, is Caucasian, and dresses vibrantly. The Mad Hatter climbs on a table, walks across it, and breaks plates and teacups along the way. He is rather protective of Alice; when the guards of the Queen of Hearts come, he hides Alice in a tea kettle. Upon making sure that Alice is safe, Mad Hatter puts her on his hat, after he had shrunk her, and takes her for a walk. While walking, he starts to talk about the Jabberwocky and becomes enraged when Alice tells him that she will not slay the Jabberwocky. Talking to Alice about why she needs to slay the Jabberwocky, the Mad Hatter becomes emotional and tells Alice that she has changed.
The Mad Hatter continues to go to lengths to protect Alice; he throws his hat with her on it across the field, so the Queen of Heart’s guards do not capture her. He lies to the Queen and indicates he has not seen Alice, although she is clearly sitting next to the Queen. He decides to charm the Queen, by telling her that he wants to make her a hat for her rather large head. Once the White Queen regained her land again, the Mad Hatter is happy.
Case Study: The Grinch

The Grinch, who is a bitter and cave-dwelling creature, lives on the snowy Mount Crumpits, a high mountain north of Whoville. His age is undisclosed, but he looks to be in his 40s and does not have a job. He normally spends a lot of his time alone in his cave. He is often depressed and spends his time avoiding and hating the people of Whoville and their celebration of Christmas. He disregards the feelings of the people, knowingly steals and destroys their property, and finds pleasure in doing so. We do not know his family history, as he was abandoned as a child, but he was taken in by two ladies who raised him with a love for Christmas. He is green and fuzzy, so he stands out among the Whos, and he was often ridiculed for his looks in school. He does not maintain any social relationships with his friends and family. The only social companion the Grinch has is his dog, Max. The Grinch had no goal in his life except to stop Christmas from happening. There is no history of drug or alcohol use.
- Modification, adaptation, and original content. Authored by : Julie Manley for Lumen Learning. Provided by : Lumen Learning. License : CC BY: Attribution
- Case Studies: The Grinch. Authored by : Dr. Caleb Lack and students at the University of Central Oklahoma and Arkansas Tech University. Located at : https://courses.lumenlearning.com/abnormalpsychology/chapter/antisocial-personality-disorder/ . License : CC BY-NC-SA: Attribution-NonCommercial-ShareAlike
- The Mad Hatter. Authored by : Loren Javier. Located at : https://www.flickr.com/photos/lorenjavier/4031000212/ . License : CC BY-ND: Attribution-NoDerivatives
- The Grinch. Located at : https://pixy.org/1066311/ . License : CC0: No Rights Reserved

- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is a Case Study?
Weighing the pros and cons of this method of research
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
Verywell / Colleen Tighe
- Pros and Cons
What Types of Case Studies Are Out There?
Where do you find data for a case study, how do i write a psychology case study.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The point of a case study is to learn as much as possible about an individual or group so that the information can be generalized to many others. Unfortunately, case studies tend to be highly subjective, and it is sometimes difficult to generalize results to a larger population.
While case studies focus on a single individual or group, they follow a format similar to other types of psychology writing. If you are writing a case study, we got you—here are some rules of APA format to reference.
At a Glance
A case study, or an in-depth study of a person, group, or event, can be a useful research tool when used wisely. In many cases, case studies are best used in situations where it would be difficult or impossible for you to conduct an experiment. They are helpful for looking at unique situations and allow researchers to gather a lot of˜ information about a specific individual or group of people. However, it's important to be cautious of any bias we draw from them as they are highly subjective.
What Are the Benefits and Limitations of Case Studies?
A case study can have its strengths and weaknesses. Researchers must consider these pros and cons before deciding if this type of study is appropriate for their needs.
One of the greatest advantages of a case study is that it allows researchers to investigate things that are often difficult or impossible to replicate in a lab. Some other benefits of a case study:
- Allows researchers to capture information on the 'how,' 'what,' and 'why,' of something that's implemented
- Gives researchers the chance to collect information on why one strategy might be chosen over another
- Permits researchers to develop hypotheses that can be explored in experimental research
On the other hand, a case study can have some drawbacks:
- It cannot necessarily be generalized to the larger population
- Cannot demonstrate cause and effect
- It may not be scientifically rigorous
- It can lead to bias
Researchers may choose to perform a case study if they want to explore a unique or recently discovered phenomenon. Through their insights, researchers develop additional ideas and study questions that might be explored in future studies.
It's important to remember that the insights from case studies cannot be used to determine cause-and-effect relationships between variables. However, case studies may be used to develop hypotheses that can then be addressed in experimental research.
Case Study Examples
There have been a number of notable case studies in the history of psychology. Much of Freud's work and theories were developed through individual case studies. Some great examples of case studies in psychology include:
- Anna O : Anna O. was a pseudonym of a woman named Bertha Pappenheim, a patient of a physician named Josef Breuer. While she was never a patient of Freud's, Freud and Breuer discussed her case extensively. The woman was experiencing symptoms of a condition that was then known as hysteria and found that talking about her problems helped relieve her symptoms. Her case played an important part in the development of talk therapy as an approach to mental health treatment.
- Phineas Gage : Phineas Gage was a railroad employee who experienced a terrible accident in which an explosion sent a metal rod through his skull, damaging important portions of his brain. Gage recovered from his accident but was left with serious changes in both personality and behavior.
- Genie : Genie was a young girl subjected to horrific abuse and isolation. The case study of Genie allowed researchers to study whether language learning was possible, even after missing critical periods for language development. Her case also served as an example of how scientific research may interfere with treatment and lead to further abuse of vulnerable individuals.
Such cases demonstrate how case research can be used to study things that researchers could not replicate in experimental settings. In Genie's case, her horrific abuse denied her the opportunity to learn a language at critical points in her development.
This is clearly not something researchers could ethically replicate, but conducting a case study on Genie allowed researchers to study phenomena that are otherwise impossible to reproduce.
There are a few different types of case studies that psychologists and other researchers might use:
- Collective case studies : These involve studying a group of individuals. Researchers might study a group of people in a certain setting or look at an entire community. For example, psychologists might explore how access to resources in a community has affected the collective mental well-being of those who live there.
- Descriptive case studies : These involve starting with a descriptive theory. The subjects are then observed, and the information gathered is compared to the pre-existing theory.
- Explanatory case studies : These are often used to do causal investigations. In other words, researchers are interested in looking at factors that may have caused certain things to occur.
- Exploratory case studies : These are sometimes used as a prelude to further, more in-depth research. This allows researchers to gather more information before developing their research questions and hypotheses .
- Instrumental case studies : These occur when the individual or group allows researchers to understand more than what is initially obvious to observers.
- Intrinsic case studies : This type of case study is when the researcher has a personal interest in the case. Jean Piaget's observations of his own children are good examples of how an intrinsic case study can contribute to the development of a psychological theory.
The three main case study types often used are intrinsic, instrumental, and collective. Intrinsic case studies are useful for learning about unique cases. Instrumental case studies help look at an individual to learn more about a broader issue. A collective case study can be useful for looking at several cases simultaneously.
The type of case study that psychology researchers use depends on the unique characteristics of the situation and the case itself.
There are a number of different sources and methods that researchers can use to gather information about an individual or group. Six major sources that have been identified by researchers are:
- Archival records : Census records, survey records, and name lists are examples of archival records.
- Direct observation : This strategy involves observing the subject, often in a natural setting . While an individual observer is sometimes used, it is more common to utilize a group of observers.
- Documents : Letters, newspaper articles, administrative records, etc., are the types of documents often used as sources.
- Interviews : Interviews are one of the most important methods for gathering information in case studies. An interview can involve structured survey questions or more open-ended questions.
- Participant observation : When the researcher serves as a participant in events and observes the actions and outcomes, it is called participant observation.
- Physical artifacts : Tools, objects, instruments, and other artifacts are often observed during a direct observation of the subject.
If you have been directed to write a case study for a psychology course, be sure to check with your instructor for any specific guidelines you need to follow. If you are writing your case study for a professional publication, check with the publisher for their specific guidelines for submitting a case study.
Here is a general outline of what should be included in a case study.
Section 1: A Case History
This section will have the following structure and content:
Background information : The first section of your paper will present your client's background. Include factors such as age, gender, work, health status, family mental health history, family and social relationships, drug and alcohol history, life difficulties, goals, and coping skills and weaknesses.
Description of the presenting problem : In the next section of your case study, you will describe the problem or symptoms that the client presented with.
Describe any physical, emotional, or sensory symptoms reported by the client. Thoughts, feelings, and perceptions related to the symptoms should also be noted. Any screening or diagnostic assessments that are used should also be described in detail and all scores reported.
Your diagnosis : Provide your diagnosis and give the appropriate Diagnostic and Statistical Manual code. Explain how you reached your diagnosis, how the client's symptoms fit the diagnostic criteria for the disorder(s), or any possible difficulties in reaching a diagnosis.
Section 2: Treatment Plan
This portion of the paper will address the chosen treatment for the condition. This might also include the theoretical basis for the chosen treatment or any other evidence that might exist to support why this approach was chosen.
- Cognitive behavioral approach : Explain how a cognitive behavioral therapist would approach treatment. Offer background information on cognitive behavioral therapy and describe the treatment sessions, client response, and outcome of this type of treatment. Make note of any difficulties or successes encountered by your client during treatment.
- Humanistic approach : Describe a humanistic approach that could be used to treat your client, such as client-centered therapy . Provide information on the type of treatment you chose, the client's reaction to the treatment, and the end result of this approach. Explain why the treatment was successful or unsuccessful.
- Psychoanalytic approach : Describe how a psychoanalytic therapist would view the client's problem. Provide some background on the psychoanalytic approach and cite relevant references. Explain how psychoanalytic therapy would be used to treat the client, how the client would respond to therapy, and the effectiveness of this treatment approach.
- Pharmacological approach : If treatment primarily involves the use of medications, explain which medications were used and why. Provide background on the effectiveness of these medications and how monotherapy may compare with an approach that combines medications with therapy or other treatments.
This section of a case study should also include information about the treatment goals, process, and outcomes.
When you are writing a case study, you should also include a section where you discuss the case study itself, including the strengths and limitiations of the study. You should note how the findings of your case study might support previous research.
In your discussion section, you should also describe some of the implications of your case study. What ideas or findings might require further exploration? How might researchers go about exploring some of these questions in additional studies?
Need More Tips?
Here are a few additional pointers to keep in mind when formatting your case study:
- Never refer to the subject of your case study as "the client." Instead, use their name or a pseudonym.
- Read examples of case studies to gain an idea about the style and format.
- Remember to use APA format when citing references .
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011;11:100.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011 Jun 27;11:100. doi:10.1186/1471-2288-11-100
Gagnon, Yves-Chantal. The Case Study as Research Method: A Practical Handbook . Canada, Chicago Review Press Incorporated DBA Independent Pub Group, 2010.
Yin, Robert K. Case Study Research and Applications: Design and Methods . United States, SAGE Publications, 2017.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
Bipolar I disorder and anxiety disorder with spontaneous ejaculations
- Open access
- Published: 10 April 2024
- Volume 4 , article number 37 , ( 2024 )
Cite this article
You have full access to this open access article
- Deeksha Chakrabarty 1 ,
- Irina Tardif 1 &
- Rachel Carpenter 1
Anxiety and ejaculation share similar sympathetic neuronal pathways and hence they may coincide. In this case report, we describe a 30-year-old male with ongoing perceptual disturbances and spontaneous ejaculations that occur without sexual arousal. The patient ultimately benefited from pharmacological therapy with risperidone.
Avoid common mistakes on your manuscript.
1 Introduction
The autonomic nervous system, consisting of the sympathetic and parasympathetic pathways, plays an important part in the symptomatology of both anxiety and ejaculation. Anxiety leads to an increase in sympathetic activity, leading to an increase in norepinephric and dopaminergic neurotransmitters [ 1 ]. Additionally, the sympathetic neuronal pathways in the pelvis plexus are primarily responsible for the physiology of ejaculation, primarily through the release of norepinephrine. Hence, the two processes could occur concurrently [ 3 ]. Even though there is a well-known association between anxiety and sexual arousal, the literature only finds two case reports documenting the association between anxiety and spontaneous ejaculations [ 5 , 6 ]. The following is a case report of a patient experiencing spontaneous ejaculations in the setting of acute psychosis, managed successfully by pharmacological therapy.
2 Case presentation
A 30 year old African-American male with no documented past psychiatric history was brought to the emergency room by his grandmother for bizarre and erratic behavior developing over the past 1–2 years. According to his grandmother, he had been exhibiting paranoid ideation, had recently lost his job and had been severing close relationships. Patient’s grandmother also stated that she and other members of his family had observed the patient responding to internal stimuli. Upon evaluation in the emergency department, he denied all symptoms reported by his family; however, he exhibited flight of ideas, rapid pressured speech, hyper-religiosity and paranoid delusions with religious undertones. He was deemed a danger to himself and/or to others and hence was placed on involuntary psychiatric hold and was admitted to the inpatient psychiatric department. In the inpatient unit, the patient underwent further evaluation with differential diagnoses including bipolar disorder with psychotic features, schizophrenia and schizoaffective spectrum disorders. He was initially managed with oral risperidone 0.5 mg twice daily, with an alternative of intramuscular olanzapine 2.5 mg twice daily if he refused oral medication. His regimen also included oral lorazepam 2 mg and oral haloperidol as needed for agitation and anxiety. He tolerated these medications well and did not report any adverse effects.
Upon further evaluation in the inpatient unit, the patient was hyperverbal with tangential thought process and demonstrated a preoccupation with losing body fluids due to routine blood draw performed on the previous day. He also reported having frequent spontaneous ejaculations in the setting of anxiety and loud noises for the past 6 years. He stated that the emissions were not preceded by penile erection or stimulation, and they were not associated with sexual arousal. The patient stated that these episodes distressed him; however, he denied any associated pleasure or guilt in relation to them. Physical and neurological examination findings were unremarkable.
In response to these complaints and continued symptoms of mania and psychosis, risperidone was increased to 2 mg orally twice daily with nightly quetiapine 200 mg per oral to augment, as patient continued to struggle with sleep. Once improvement and tolerability were established orally, he was subsequently transitioned to the long-acting injectable formulation of paliperidone palmitate to ensure medication adherence as well as decrease rehospitalization.
The patient reported two events of spontaneous ejaculations occurring during his admission prior to increase in dosage of risperidone and initiation of quetiapine. With this change in his medication regimen, he reported improvement in his manic symptomatology as well as cessation in spontaneous ejaculations until discharge. Total length of stay was 10 days. The frequency of spontaneous ejaculations was reduced to a mean of once every week as reported by the patient during follow-up phone call 2 weeks after discharge.
3 Discussion
Ejaculation is a physiologic process that is regulated by the autonomic nervous system. Sympathetic neuronal pathways of the pelvic plexus that primarily secrete norepinephrine are the neuronal basis for ejaculation [ 2 ]. The role of serotonin in this phenomenon of ejaculation has been well-documented. 5HT receptor agonism has been found to have an overall inhibitory effect on ejaculation; 5HT1A receptors have a cumulative facilitatory effect, whereas 5HT1B and 5HT2C receptors have an inhibitory effect on the process [ 3 ]. Penile erection, on the other hand, is primarily mediated by the parasympathetic nervous system through the sacral reflex arc [ 2 ]. Anxiety decreases parasympathetic activity, thereby inhibiting penile erection while simultaneously increasing sympathetic activity, which could trigger ejaculation. An increase in sympathetic activity is associated with an increase in noradrenergic and dopaminergic activity and a decrease in serotonergic activity. Therefore, the neuronal pathways between anxiety and ejaculations are linked and are not necessarily associated with penile erection and/or sexual arousal.
The patient, whose history is previously described, was diagnosed with bipolar I disorder with psychotic features and anxiety disorder, unspecified, associated with spontaneous ejaculation. Antipsychotics have documented side effects of sexual dysfunction, predominantly due to their strong dopaminergic effect and increase in prolactin levels. Risperidone is a second-generation atypical antipsychotic that exhibits its effect by blocking dopamine and serotonin receptors [ 4 ]. Hence, it was an appropriate choice, with its dual neurotransmitter effect, to successfully manage both the symptoms of psychosis/mania and spontaneous ejaculations simultaneously.
Upon review of literature, the authors found two previously documented case reports of individuals with anxiety disorder presenting with spontaneous ejaculations. Freeman SA [ 5 ] describes the case of a 42-year-old male with panic attacks associated with spontaneous ejaculation who was successfully treated with citalopram and clonazepam. Senormanci et al. [ 6 ] present the case of a 20-year-old male with panic disorder with spontaneous ejaculations which was pharmacologically managed by sertraline and alprazolam. Both case reports hypothesize similar mechanisms for simultaneous presentation of anxiety and spontaneous ejaculations. They further express that it is unclear whether the spontaneous ejaculations resolved upon resolution of anxiety or if it was due to the effect of the SSRI on serotonergic receptors. By the resolution of spontaneous ejaculations by use of risperidone, we hypothesize that spontaneous ejaculations can effectively be controlled by blockade of serotonergic receptors and suppression of dopaminergic activity at the mesolimbic dopaminergic circuit.
Assessment of the presented case in the light of the scarce literature indicates that spontaneous ejaculations without sexual stimulus can gradually subside with introduction of D2 and serotonin antagonists such as risperidone or paliperidone. Our patient had spontaneous ejaculations for about 6 years without sexual desires in the context of anxiety promoting situations during these ejaculations until he was admitted to inpatient psychiatric unit where he received appropriate treatment with antipsychotic drugs for diagnosed bipolar 1 disorder. Therefore, spontaneous ejaculation occurring in situations without apparent or direct sexual precipitation should be questioned in patients with psychiatric problems concurrent with anxiety symptoms. Consciously patients may feel embarrassed or fear humiliation and never disclose this information to anyone including family members as in this case or even a treating provider. Consequently, the role of inpatient psychiatric stabilization with initiation of antipsychotic drugs in decreasing the frequency of spontaneous ejaculation in the presented case is also thought to have occurred via control of psychiatric symptoms and its adverse effects on ejaculation.
Since this patient was seen only on the acute inpatient unit without long term outpatient follow up after discharge, historical data was challenging to validate as extended observation could not be obtained. Nevertheless, the lack of research on the interaction between psychopharmacological agents and spontaneous ejaculation constitutes a limitation for analyzing the presented case where our conclusions were based on treatment response to clinical observations.
Data availability
The author confirms that all data generated or analysed during this study are included in this published article.
Hoehn-Saric R, McLeod DR. The peripheral sympathetic nervous system. Its role in normal and pathologic anxiety. Psychiatr Clin North Am. 1988;11(2):375–86.
Article PubMed Google Scholar
Alwaal A, Breyer BN, Lue TF. Normal male sexual function: emphasis on orgasm and ejaculation. Fertil Steril. 2015;104(5):1051–60.
Article PubMed PubMed Central Google Scholar
Giuliano F, Clément P. Physiology of ejaculation: emphasis on serotonergic control. Eur Urol. 2005;48(3):408–17.
McNeil SE, Gibbons JR, Cogburn M. Risperidone. In: McNeil SE, editor. StatPearls. Treasure Island: StatPearls Publishing; 2022.
Google Scholar
Freeman SA. Panic attacks with spontaneous ejaculation successfully treated with citalopram and clonazepam. J Clin Psychopharmacol. 2004;24(4):463–4.
Senormanci G, Kilic OH, Senormanci O. A case of spontaneous ejaculation associated with panic disorder which was treated with sertraline and alprazolam. Psychiatry Behav Sci. 2017;7(3):173.
Download references
Author information
Authors and affiliations.
Department of Psychiatry, UF Health, Jacksonville, FL, USA
Deeksha Chakrabarty, Irina Tardif & Rachel Carpenter
You can also search for this author in PubMed Google Scholar
Contributions
DC wrote the manuscript text. IT and RC modified the manuscript text. All authors reviewed the manuscript.
Corresponding author
Correspondence to Deeksha Chakrabarty .
Ethics declarations
Ethics approval and consent to participate.
This case report was approved as nonhuman and exempt research under 45 CFR 46.101(b) in compliance with the federal Office of Human Research Protections guidance. Approval was granted by the University of Florida (Date 8/26/23/No. NH00020132).
Informed consent
The participant has consented to the submission of the case report to the journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Chakrabarty, D., Tardif, I. & Carpenter, R. Bipolar I disorder and anxiety disorder with spontaneous ejaculations. Discov Psychol 4 , 37 (2024). https://doi.org/10.1007/s44202-024-00136-3
Download citation
Received : 08 August 2023
Accepted : 28 February 2024
Published : 10 April 2024
DOI : https://doi.org/10.1007/s44202-024-00136-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Spontaneous ejaculations
- Bipolar disorder
- Find a journal
- Publish with us
- Track your research
ORIGINAL RESEARCH article
This article is part of the research topic.
Eating Behavior and Chronic Diseases: Research Evidence from Population Studies
Comparison of Dutch healthy eating and healthy eating indexes and anthropometry in patients with major depression with health subjects: a case-control study Provisionally Accepted

- 1 Science and Research Branch, Islamic Azad University, Iran
The final, formatted version of the article will be published soon.
Background: Diseases and disorders related to mental health are spreading like other chronic diseases all around the world. Considering the role of food in the prevention and treatment of these disorders, including major depression, investigating the relationship between different food patterns and this disorder is of particular importance. The aim of this study was to compare Dutch healthy eating and healthy eating indexes and anthropometry in patients with major depression with healthy individuals.Methods: In this case-control study, the final analysis was performed on 67 men and 111 women with an age range of 20-30 years. Height (cm), weight (kg), food frequency questionnaire (FFQ), physical activity (MET-min/week), demographic and PHQ-9 questionnaires were taken from all participants. In the following, all the food ingredients and their components were extracted and used to calculate HEI-2015 and DHD. Statistical analysis was performed using SPSS software with independent t-test, logistic regression and chi-square.Results: It was found that people with major depression in this study were mostly women and occupied. The average HEI-2015 in healthy people and those with major depression was 58 and 54.3, respectively. Also, the average DHD in these people was 60.5 and 55, respectively. HEI-2015 and DHD had a significant negative correlation with depression score (r= -0.16, p-value= 0.03) (r= -0.19, p-value= 0.01). Also, in the logistic regression model, before and even after adjusting confounders, HEI-2015 and DHD had a reduced odds ratio in people suffering from major depression. The two groups did not differ significantly in terms of the average factors of height, weight and body mass index (BMI).Conclusion: It seems that HEI2015 and DHD have a significant relationship in reducing major depression. However, due to the small number of studies in this regard, especially in the field of DHD, the need for more studies seems necessary.
Keywords: major depression, Dutch Healthy Diet index, Healthy Eating Index 2015, PHQ9, HEI
Received: 14 Jan 2024; Accepted: 08 Apr 2024.
Copyright: © 2024 Tohidi-Nafe, Movahedi and Djazayery. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Mrs. Melika Tohidi-Nafe, Science and Research Branch, Islamic Azad University, Tehran, Iran
People also looked at

COMMENTS
Sara, a 35-year-old married female. Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks. Bleiberg, K.L., & Markowitz, J.C. (2008).
The case illustrates difficulties in management of children with early history of neglect. ... Pincus HA, McQueen LE, Elinson L. Subthreshold mental disorders: Nosological and research recommendations. ... Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. J Child ...
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
Psychotic-like experiences are highly prevalent in the general population, with figures of 20% or above being reported in some studies. 1 Major self-mutilation (or NSSI) is a rare but potentially catastrophic complication of severe mental illness. Most people who inflict NSSI have a psychotic disorder, usually a schizophrenia spectrum psychosis.
Case Study Details. Mike is a 20 year-old who reports to you that he feels depressed and is experiencing a significant amount of stress about school, noting that he'll "probably flunk out.". He spends much of his day in his dorm room playing video games and has a hard time identifying what, if anything, is enjoyable in a typical day.
This case study deals with Sara, a 37-year-old social phobic woman who suffered from a primary fear of blushing as well as comorbid disorders, including obsessive-compulsive disorder, generalized anxiety disorder and spider phobia. The client was treated in an intensive, one-week group cognitive-behavioral therapy program in an educational university clinic in Aarhus, Denmark.
DSM-5 Clinical Cases makes the rather overwhelming DSM-5 much more accessible to mental health clinicians by using clinical examples—the way many clinicians learn best—to illustrate the changes in diagnostic criteria from DSM-IV-TR to DSM-5. More than 100 authors contributed to the 103 case vignettes and discussions in this book. Each case is concise but not oversimplified.
Illness anxiety disorder (IAD) is defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V) as the preoccupation with having or acquiring a serious illness, in the absence of somatic symptoms (or, if present, symptoms that are only mild in severity). Patients with IAD experience persistent anxiety or fear of ...
Paranoid personality disorder (PPD) is a severe condition, lacking specialized and empirically supported treatment. To provide the clinician with insights into how to treat this condition, we present a case study of a 61‐year‐old man with severe PPD who presented with ideas of persecution, emotionally charged hostility, and comorbid antisocial personality disorder.
An anxiety disorder case study. March 2020; Authors: Steliana Rizeanu. Hyperion University, Bucharest, Romania ... Pathological gambling is a psychological disorder that usually begins as an ...
Finding order within the disorder: a case study exploring the meaningfulness of delusions - Volume 46 Issue 2. ... When do beliefs become a symptom of mental disorder? Focusing on the psychological and sociological features (such as distress, harm and dysfunction) associated with certain unusual convictions might be a better way forward for ...
Case Study of Client Diagnosed with Major Depressive Disorder 2005 Dr. Janet Cahill Applied Psychology Program The purpose of this study was to determine the best practice for a client diagnosed with major depressive disorder whom was referred for treatment at a community mental health facility.
Like the case of Phineas Gage, JP helped us understand the crucial role that the prefrontal cortex plays in judgment, decision-making, social behaviors, and personality (Benjamin, 2018). HM (Henry ...
Case Study: Ashlynn. Ashlynn is a 21-year-old college student and political science major who has struggled with depression on and off since beginning college. She was picked up by campus police after being caught vandalizing a man's apartment and was recommended to a psychiatrist after exhibiting erratic behavior.
In 2022, we published a survey of 5,521 respondents and found: 88% of our respondents experienced mental health issues in the past year. 25% of people don't feel comfortable sharing their struggles with anyone, not even their closest friends. In order to break the stigma that surrounds mental health struggles, we're looking to share your ...
Case Study: The Grinch. The Grinch, who is a bitter and cave-dwelling creature, lives on the snowy Mount Crumpits, a high mountain north of Whoville. His age is undisclosed, but he looks to be in his 40s and does not have a job. He normally spends a lot of his time alone in his cave. He is often depressed and spends his time avoiding and hating ...
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
Persistent depressive disorder, anorexia and obsessive-compulsive disorder are each psychopathologic entities with suicidal risk. When they appear together it is a must that a multidisciplinary ...
Case study The International Journal of Indian Psychology ISSN 2348-5396 (Online) | ISSN: 2349-3429 (Print) ... interpersonal and social problems while treating individuals with mood disorders. The empirical evidence identifies the implication of CBT for clinical social workers, provided have proper training and appropriate clinical supervision ...
current issue. current issue; browse recently published; browse full issue index; learning/cme
Check your understanding of psychological disorders by reading the information on the following cases, and stating the most appropriate diagnosis for each person. Explain the rationale for each of your diagnoses. Some of these cases may not have disorders. In that case, indicate that the person does not have a mood disorder, and indicate why this
Autism Spectrum Disorder (ASD) is widely regarded as the most severe childhood behavioral disorder. However, society's lack of awareness regarding neurodevelopmental disorders, like autism, has led to a limited understanding of their profound impact on children and their families.
Generalized anxiety disorders (GAD) is a chronic anxiety disorder characterized by autonomic excitability and hypervigilance. However, there was currently a lack of a quantitative synthesis of this time-varying science, as well as a measure of researchers' networks and scientific productivity. Searching from the Web of Science Core Collection, PubMed, and Scopus on January 31st, 2024. The ...
Markers of metabolic syndrome were associated with an increased risk for the three common mental health disorders up to 20 years later, results of a large longitudinal study showed.
The study is the first and largest to use an entire country's data to confirm genetic transmission of TRD across families and an association with other major psychiatric disorders, said senior ...
Anxiety and ejaculation share similar sympathetic neuronal pathways and hence they may coincide. In this case report, we describe a 30-year-old male with ongoing perceptual disturbances and spontaneous ejaculations that occur without sexual arousal. The patient ultimately benefited from pharmacological therapy with risperidone.
The aim of the presented study is to make an attempt at capturing the specificity of psychosocial and temporal functioning and their possible changes in men serving prison sentences. ... Based on in-depth analysis of two case studies, exemplary directions for social rehabilitation and psychological support for prisoners, which consider their ...
Background: Diseases and disorders related to mental health are spreading like other chronic diseases all around the world. Considering the role of food in the prevention and treatment of these disorders, including major depression, investigating the relationship between different food patterns and this disorder is of particular importance. The aim of this study was to compare Dutch healthy ...