

Why climate change is still the greatest threat to human health
Polluted air and steadily rising temperatures are linked to health effects ranging from increased heart attacks and strokes to the spread of infectious diseases and psychological trauma.
People around the world are witnessing firsthand how climate change can wreak havoc on the planet. Steadily rising average temperatures fuel increasingly intense wildfires, hurricanes, and other disasters that are now impossible to ignore. And while the world has been plunged into a deadly pandemic, scientists are sounding the alarm once more that climate change is still the greatest threat to human health in recorded history .
As recently as August—when wildfires raged in the United States, Europe, and Siberia—World Health Organization Director-General Tedros Adhanom Ghebreyesus said in a statement that “the risks posed by climate change could dwarf those of any single disease.”
On September 5, more than 200 medical journals released an unprecedented joint editorial that urged world leaders to act. “The science is unequivocal,” they write. “A global increase of 1.5°C above the pre-industrial average and the continued loss of biodiversity risk catastrophic harm to health that will be impossible to reverse.”
Despite the acute dangers posed by COVID-19, the authors of the joint op-ed write that world governments “cannot wait for the pandemic to pass to rapidly reduce emissions.” Instead, they argue, everyone must treat climate change with the same urgency as they have COVID-19.
Here’s a look at the ways that climate change can affect your health—including some less obvious but still insidious effects—and why scientists say it’s not too late to avert catastrophe.
Air pollution
Climate change is caused by an increase of carbon dioxide and other greenhouse gases in Earth’s atmosphere, mostly from fossil fuel emissions. But burning fossil fuels can also have direct consequences for human health. That’s because the polluted air contains small particles that can induce stroke and heart attacks by penetrating the lungs and heart and even traveling into the bloodstream. Those particles might harm the organs directly or provoke an inflammatory response from the immune system as it tries to fight them off. Estimates suggest that air pollution causes anywhere between 3.6 million and nine million premature deaths a year.
“The numbers do vary,” says Andy Haines , professor of environmental change and public health at the London School of Hygiene and Tropical Medicine and author of the recently published book Planetary Health . “But they all agree that it’s a big public health burden.”

People over the age of 65 are most susceptible to the harmful effects of air pollution, but many others are at risk too, says Kari Nadeau , director of the Sean N. Parker Center for Allergy and Asthma Research at Stanford University. People who smoke or vape are at increased risk, as are children with asthma.
Air pollution also has consequences for those with allergies. Carbon dioxide increases the acidity of the air, which then pulls more pollen out from plants. For some people, this might just mean that they face annoyingly long bouts of seasonal allergies. But for others, it could be life-threatening.
“For people who already have respiratory disease, boy is that a problem,” Nadeau says. When pollen gets into the respiratory pathway, the body creates mucus to get rid of it, which can then fill up and suffocate the lungs.
Even healthy people can have similar outcomes if pollen levels are especially intense. In 2016, in the Australian state of Victoria, a severe thunderstorm combined with high levels of pollen to induce what The Lancet has described as “the world’s largest and most catastrophic epidemic of thunderstorm asthma.” So many residents suffered asthma attacks that emergency rooms were overwhelmed—and at least 10 people died as a result.
Climate change is also causing wildfires to get worse, and wildfire smoke is especially toxic. As one recent study showed, fires can account for 25 percent of dangerous air pollution in the U.S. Nadeau explains that the smoke contains particles of everything that the fire has consumed along its path—from rubber tires to harmful chemicals. These particles are tiny and can penetrate even deeper into a person’s lungs and organs. ( Here’s how breathing wildfire smoke affects the body .)
Extreme heat
Heat waves are deadly, but researchers at first didn’t see direct links between climate change and the harmful impacts of heat waves and other extreme weather events. Haines says the evidence base has been growing. “We have now got a number of studies which has shown that we can with high confidence attribute health outcomes to climate change,” he says.

Most recently, Haines points to a study published earlier this year in Nature Climate Change that attributes more than a third of heat-related deaths to climate change. As National Geographic reported at the time , the study found that the human toll was even higher in some countries with less access to air conditioning or other factors that render people more vulnerable to heat. ( How climate change is making heat waves even deadlier .)
That’s because the human body was not designed to cope with temperatures above 98.6°F, Nadeau says. Heat can break down muscles. The body does have some ways to deal with the heat—such as sweating. “But when it’s hot outside all the time, you cannot cope with that, and your heart muscles and cells start to literally die and degrade,” she says.
If you’re exposed to extreme heat for too long and are unable to adequately release that heat, the stress can cause a cascade of problems throughout the body. The heart has to work harder to pump blood to the rest of the organs, while sweat leeches the body of necessary minerals such as sodium and potassium. The combination can result in heart attacks and strokes .
Dehydration from heat exposure can also cause serious damage to the kidneys, which rely on water to function properly. For people whose kidneys are already beginning to fail—particularly older adults—Nadeau says that extreme heat can be a death sentence. “This is happening more and more,” she says.
Studies have also drawn links between higher temperatures and preterm birth and other pregnancy complications. It’s unclear why, but Haines says that one hypothesis is that extreme heat reduces blood flow to the fetus.
Food insecurity
One of the less direct—but no less harmful—ways that climate change can affect health is by disrupting the world’s supply of food.
You May Also Like

This brain-eating amoeba is on the rise

2024 hurricane season forecasted to be record-breaking year

‘Corn sweat’—and other weird weather phenomena—explained
Climate change both reduces the amount of food that’s available and makes it less nutritious. According to an Intergovernmental Panel on Climate Change (IPCC) special report , crop yields have already begun to decline as a result of rising temperatures, changing precipitation patterns, and extreme weather events. Meanwhile, studies have shown that increased carbon dioxide in the atmosphere can leech plants of zinc, iron, and protein—nutrients that humans need to survive.

Malnutrition is linked to a variety of illnesses, including heart disease, cancer, and diabetes. It can also increase the risk of stunting, or impaired growth , in children, which can harm cognitive function.
Climate change also imperils what we eat from the sea. Rising ocean temperatures have led many fish species to migrate toward Earth’s poles in search of cooler waters. Haines says that the resulting decline of fish stocks in subtropic regions “has big implications for nutrition,” because many of those coastal communities depend on fish for a substantial amount of the protein in their diets.
This effect is likely to be particularly harmful for Indigenous communities, says Tiff-Annie Kenny, a professor in the faculty of medicine at Laval University in Quebec who studies climate change and food security in the Canadian Arctic. It’s much more difficult for these communities to find alternative sources of protein, she says, either because it’s not there or because it’s too expensive. “So what are people going to eat instead?” she asks.
Infectious diseases
As the planet gets hotter, the geographic region where ticks and mosquitoes like to live is getting wider. These animals are well-known vectors of diseases such as the Zika virus, dengue fever, and malaria. As they cross the tropics of Cancer and Capricorn, Nadeau says, mosquitoes and ticks bring more opportunities for these diseases to infect greater swaths of the world.
“It used to be that they stayed in those little sectors near the Equator, but now unfortunately because of the warming of northern Europe and Canada, you can find Zika in places you wouldn’t have expected,” Nadeau says.
In addition, climate conditions such as temperature and humidity can impact the life cycle of mosquitoes. Haines says there’s particularly good evidence showing that, in some regions, climate change has altered these conditions in ways that increase the risk of mosquitos transmitting dengue .
There are also several ways in which climate change is increasing the risk of diseases that can be transmitted through water, such as cholera, typhoid fever, and parasites. Sometimes that’s fairly direct, such as when people interact with dirty floodwaters. But Haines says that drought can have indirect impacts when people, say, can’t wash their hands or are forced to drink from dodgier sources of freshwater.
Mental health
A common result of any climate-linked disaster is the toll on mental health. The distress caused by drastic environmental change is so significant that it has been given its own name— solastalgia .

Nadeau says that the effects on mental health have been apparent in her studies of emergency room visits arising from wildfires in the western U.S. People lose their homes, their jobs, and sometimes their loved ones, and that takes an immediate toll. “What’s the fastest acute issue that develops? It’s psychological,” she says. Extreme weather events such as wildfires and hurricanes cause so much stress and anxiety that they can lead to post-traumatic stress disorder and even suicide in the long run.
Another common factor is that climate change causes disproportionate harm to the world’s most vulnerable people. On September 2, the Environmental Protection Agency (EPA) released an analysis showing that racial and ethnic minority communities are particularly at risk . According to the report, if temperatures rise by 2°C (3.6°F), Black people are 40 percent more likely to live in areas with the highest projected increases in related deaths. Another 34 percent are more likely to live in areas with a rise in childhood asthma.
Further, the effects of climate change don’t occur in isolation. At any given time, a community might face air pollution, food insecurity, disease, and extreme heat all at once. Kenny says that’s particularly devastating in communities where the prevalence of food insecurity and poverty are already high. This situation hasn’t been adequately studied, she says, because “it’s difficult to capture these shocks that climate can bring.”
Why there’s reason for hope
In recent years, scientists and environmental activists have begun to push for more research into the myriad health effects of climate change. “One of the striking things is there’s been a real dearth of funding for climate change and health,” Haines says. “For that reason, some of the evidence we have is still fragmentary.”
Still, hope is not lost. In the Paris Agreement, countries around the world have pledged to limit global warming to below 2°C (3.6°F)—and preferably to 1.5°C (2.7°F)—by cutting their emissions. “When you reduce those emissions, you benefit health as well as the planet,” Haines says.
Meanwhile, scientists and environmental activists have put forward solutions that can help people adapt to the health effects of climate change. These include early heat warnings and dedicated cooling centers, more resilient supply chains, and freeing healthcare facilities from dependence on the electric grid.
Nadeau argues that the COVID-19 pandemic also presents an opportunity for world leaders to think bigger and more strategically. For example, the pandemic has laid bare problems with efficiency and equity that have many countries restructuring their healthcare facilities. In the process, she says, they can look for new ways to reduce waste and emissions, such as getting more hospitals using renewable energy.
“This is in our hands to do,” Nadeau says. “If we don’t do anything, that would be cataclysmic.”
Related Topics
- AIR POLLUTION
- WATER QUALITY
- NATURAL DISASTERS
- PUBLIC HEALTH
- CLIMATE CHANGE

What we're learning from lung cancer patients who never smoked

The U.S. plans to limit PFAS in drinking water. What does that really mean?

Extreme heat is the future. Here are 10 practical ways to manage it.

Here’s what extreme heat does to the body

Some antibiotics are no longer as effective. That's as concerning as it sounds.
- Environment
- Paid Content
History & Culture
- History & Culture
- Destination Guide
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 11, Issue 6
- Health effects of climate change: an overview of systematic reviews
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-4548-2229 Rhea J Rocque 1 ,
- Caroline Beaudoin 2 ,
- http://orcid.org/0000-0002-4716-6505 Ruth Ndjaboue 2 , 3 ,
- Laura Cameron 1 ,
- Louann Poirier-Bergeron 2 ,
- Rose-Alice Poulin-Rheault 2 ,
- Catherine Fallon 2 , 4 ,
- http://orcid.org/0000-0002-4114-8971 Andrea C Tricco 5 , 6 ,
- http://orcid.org/0000-0003-4192-0682 Holly O Witteman 2 , 3
- 1 Prairie Climate Centre , The University of Winnipeg , Winnipeg , Manitoba , Canada
- 2 Faculty of Medicine , Université Laval , Quebec , QC , Canada
- 3 VITAM Research Centre for Sustainable Health , Quebec , QC , Canada
- 4 CHUQ Research Centre , Quebec , QC , Canada
- 5 Li Ka Shing Knowledge Institute , Toronto , Ontario , Canada
- 6 Dalla Lana School of Public Health , University of Toronto , Toronto , Ontario , Canada
- Correspondence to Dr Rhea J Rocque; rhea.rocque{at}gmail.com
Objectives We aimed to develop a systematic synthesis of systematic reviews of health impacts of climate change, by synthesising studies’ characteristics, climate impacts, health outcomes and key findings.
Design We conducted an overview of systematic reviews of health impacts of climate change. We registered our review in PROSPERO (CRD42019145972). No ethical approval was required since we used secondary data. Additional data are not available.
Data sources On 22 June 2019, we searched Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, Cochrane and Web of Science.
Eligibility criteria We included systematic reviews that explored at least one health impact of climate change.
Data extraction and synthesis We organised systematic reviews according to their key characteristics, including geographical regions, year of publication and authors’ affiliations. We mapped the climate effects and health outcomes being studied and synthesised major findings. We used a modified version of A MeaSurement Tool to Assess systematic Reviews-2 (AMSTAR-2) to assess the quality of studies.
Results We included 94 systematic reviews. Most were published after 2015 and approximately one-fifth contained meta-analyses. Reviews synthesised evidence about five categories of climate impacts; the two most common were meteorological and extreme weather events. Reviews covered 10 health outcome categories; the 3 most common were (1) infectious diseases, (2) mortality and (3) respiratory, cardiovascular or neurological outcomes. Most reviews suggested a deleterious impact of climate change on multiple adverse health outcomes, although the majority also called for more research.
Conclusions Most systematic reviews suggest that climate change is associated with worse human health. This study provides a comprehensive higher order summary of research on health impacts of climate change. Study limitations include possible missed relevant reviews, no meta-meta-analyses, and no assessment of overlap. Future research could explore the potential explanations between these associations to propose adaptation and mitigation strategies and could include broader sociopsychological health impacts of climate change.
- public health
- social medicine
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. All data relevant to the study are included in the article or uploaded as supplementary information. Additional data are not available.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-046333
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
A strength of this study is that it provides the first broad overview of previous systematic reviews exploring the health impacts of climate change. By targeting systematic reviews, we achieve a higher order summary of findings than what would have been possible by consulting individual original studies.
By synthesising findings across all included studies and according to the combination of climate impact and health outcome, we offer a clear, detailed and unique summary of the current state of evidence and knowledge gaps about how climate change may influence human health.
A limitation of this study is that we were unable to access some full texts and therefore some studies were excluded, even though we deemed them potentially relevant after title and abstract inspection.
Another limitation is that we could not conduct meta-meta-analyses of findings across reviews, due to the heterogeneity of the included systematic reviews and the relatively small proportion of studies reporting meta-analytic findings.
Finally, the date of the systematic search is a limitation, as we conducted the search in June 2019.
Introduction
The environmental consequences of climate change such as sea-level rise, increasing temperatures, more extreme weather events, increased droughts, flooding and wildfires are impacting human health and lives. 1 2 Previous studies and reviews have documented the multiple health impacts of climate change, including an increase in infectious diseases, respiratory disorders, heat-related morbidity and mortality, undernutrition due to food insecurity, and adverse health outcomes ensuing from increased sociopolitical tension and conflicts. 2–5 Indeed, the most recent Lancet Countdown report, 2 which investigates 43 indicators of the relationship between climate change and human health, arrived at their most worrisome findings since the beginning of their on-going annual work. This report underlines that the health impacts of climate change continue to worsen and are being felt on every continent, although they are having a disproportionate and unequal impact on populations. 2 Authors caution that these health impacts will continue to worsen unless we see an immediate international response to limiting climate change.
To guide future research and action to mitigate and adapt to the health impacts of climate change and its environmental consequences, we need a complete and thorough overview of the research already conducted regarding the health impacts of climate change. Although the number of original studies researching the health impacts of climate change has greatly increased in the recent decade, 2 these do not allow for an in-depth overview of the current literature on the topic. Systematic reviews, on the other hand, allow a higher order overview of the literature. Although previous systematic reviews have been conducted on the health impacts of climate change, these tend to focus on specific climate effects (eg, impact of wildfires on health), 6 7 health impacts (eg, occupational health outcomes), 8 9 countries, 10–12 or are no longer up to date, 13 14 thus limiting our global understanding of what is currently known about the multiple health impacts of climate change across the world.
In this study, we aimed to develop such a complete overview by synthesising systematic reviews of health impacts of climate change. This higher order overview of the literature will allow us to better prepare for the worsening health impacts of climate change, by identifying and describing the diversity and range of health impacts studied, as well as by identifying gaps in previous research. Our research objectives were to synthesise studies’ characteristics such as geographical regions, years of publication, and authors’ affiliations, to map the climate impacts, health outcomes, and combinations of these that have been studied, and to synthesise key findings.
We applied the Cochrane method for overviews of reviews. 15 This method is designed to systematically map the themes of studies on a topic and synthesise findings to achieve a broader overview of the available literature on the topic.
Research questions
Our research questions were the following: (1) What is known about the relationship between climate change and health, as shown in previous systematic reviews? (2) What are the characteristics of these studies? We registered our plan (CRD42019145972 16 ) in PROSPERO, an international prospective register of systematic reviews and followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 17 to report our findings, as a reporting guideline for overviews is still in development. 18
Search strategy and selection criteria
To identify relevant studies, we used a systematic search strategy. There were two inclusion criteria. We included studies in this review if they (1) were systematic reviews of original research and (2) reported at least one health impact as it related (directly or indirectly) to climate change.
We defined a systematic review, based on Cochrane’s definition, as a review of the literature in which one ‘attempts to identify, appraise and synthesize all the empirical evidence that meets pre-specified eligibility criteria to answer a specific research question [by] us[ing] explicit, systematic methods that are selected with a view aimed at minimizing bias, to produce more reliable findings to inform decision making’. 19 We included systematic reviews of original research, with or without meta-analyses. We excluded narrative reviews, non-systematic literature reviews and systematic reviews of materials that were not original research (eg, systematic reviews of guidelines.)
We based our definition of health impacts on the WHO’s definition of health as, ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. 20 Therefore, health impacts included, among others, morbidity, mortality, new conditions, worsening/improving conditions, injuries and psychological well-being. Included studies could refer to climate change or global warming directly or indirectly, for instance, by synthesising the direct or indirect health effects of temperature rises or of natural conditions/disasters made more likely by climate change (eg, floods, wildfires, temperature variability, droughts.) Although climate change and global warming are not equivalent terms, in an effort to avoid missing relevant literature, we included studies using either term. We included systematic reviews whose main focus was not the health impacts of climate change, providing they reported at least one result regarding health effects related to climate change (or consequences of climate change.) We excluded studies if they did not report at least one health effect of climate change. For instance, we excluded studies which reported on existing measures of health impacts of climate change (and not the health impact itself) and studies which reported on certain health impacts without a mention of climate change, global warming or environmental consequences made more likely by climate change.
On 22 June 2019, we retrieved systematic reviews regarding the health effects of climate change by searching from inception the electronic databases Medline, CINAHL, Embase, Cochrane, Web of Science using a structured search (see online supplemental appendix 1 for final search strategy developed by a librarian.) We did not apply language restrictions. After removing duplicates, we imported references into Covidence. 21
Supplemental material
Screening process and data extraction.
To select studies, two trained analysts first screened independently titles and abstracts to eliminate articles that did not meet our inclusion criteria. Next, the two analysts independently screened the full text of each article. A senior analyst resolved any conflict or disagreement.
Next, we decided on key information that needed to be extracted from studies. We extracted the first author’s name, year of publication, number of studies included, time frame (in years) of the studies included in the article, first author’s institution’s country affiliation, whether the systematic review included a meta-analysis, geographical focus, population focus, the climate impact(s) and the health outcome(s) as well as the main findings and limitations of each systematic review.
Two or more trained analysts (RR, CB, RN, LC, LPB, RAPR) independently extracted data, using Covidence and spreadsheet software (Google Sheets). An additional trained analyst from the group or senior research team member resolved disagreements between individual judgments.
Coding and data mapping
To summarise findings from previous reviews, we first mapped articles according to climate impacts and health outcomes. To develop the categories of climate impacts and health outcomes, two researchers (RR and LC) consulted the titles and abstracts of each article. We started by identifying categories directly based on our data and finalised our categories by consulting previous conceptual frameworks of climate impacts and health outcomes. 1 22 23 The same two researchers independently coded each article according to their climate impact and health outcome. We then compared coding and resolved disagreements through discussion.
Next, using spreadsheet software, we created a matrix to map articles according to their combination of climate impacts and health outcomes. Each health outcome occupied one row, whereas climate impacts each occupied one column. We placed each article in the matrix according to the combination(s) of their climate impact(s) and health outcome(s). For instance, if we coded an article as ‘extreme weather’ for climate and ‘mental health’ for health impact, we noted the reference of this article in the cell at the intersection of these two codes. We calculated frequencies for each cell to identify frequent combinations and gaps in literature. Because one study could investigate more than one climate impact and health outcome, the frequency counts for each category could exceed the number of studies included in this review.
Finally, we re-read the Results and Discussion sections of each article to summarise findings of the studies. We first wrote an individual summary for each study, then we collated the summaries of all studies exploring the same combination of categories to develop an overall summary of findings for each combination of categories.
Quality assessment
We used a modified version of AMSTAR-2 to assess the quality of the included systematic reviews ( online supplemental appendix 2 ). The purpose of this assessment was to evaluate the quality of the included studies as a whole to get a sense of the overall quality of evidence in this field. Therefore, individual quality scores were not compiled for each article, but scores were aggregated according to items. Since AMSTAR-2 was developed for syntheses of systematic reviews of randomised controlled trials, working with a team member with expertise in knowledge synthesis (AT), we adapted it to suit a research context that is not amenable to randomised controlled trials. For instance, we changed assessing and accounting for risk of bias in studies’ included randomised controlled trials to assessing and accounting for limitations in studies’ included articles. Complete modifications are presented in online supplemental appendix 2 .
Patient and public involvement
Patients and members of the public were not involved in this study.
Articles identified
As shown in the PRISMA diagram in figure 1 , from an initial set of 2619 references, we retained 94 for inclusion. More precisely, following screening of titles and abstracts, 146 studies remained for full-text inspection. During full-text inspection, we excluded 52 studies, as they did not report a direct health effect of climate change (n=17), did not relate to climate change (n=15), were not systematic reviews (n=10), or we could not retrieve the full text (n=10).
- Download figure
- Open in new tab
- Download powerpoint
The flow chart for included articles in this review.
Study descriptions
A detailed table of all articles and their characteristics can be found in online supplemental appendix 3 . Publication years ranged from 2007 to 2019 (year of data extraction), with the great majority of included articles (n=69; 73%) published since 2015 ( figure 2 ). A median of 30 studies had been included in the systematic reviews (mean=60; SD=49; range 7–722). Approximately one-fifth of the systematic reviews included meta-analyses of their included studies (n=18; 19%). The majority of included systematic reviews’ first authors had affiliations in high-income countries, with the largest representations by continent in Europe (n=30) and Australia (n=24) ( figure 3 ). Countries of origin by continents include (from highest to lowest frequency, then by alphabetical order): Europe (30); UK (9), Germany (6), Italy (4), Sweden (4), Denmark (2), France (2), Georgia (1), Greece (1) and Finland (1); Australia (24); Asia (21); China (11), Iran (4), India (1), Jordan (1), Korea (1), Nepal (1), Philippines (1), Taiwan (1); North America (16); USA (15), Canada (1); Africa (2); Ethiopia (1), Ghana (1), and South America (1); Brazil (1).
Number of included systematic reviews by year of publication.
Number of publications according to geographical affiliation of the first author.
Regarding the geographical focus of systematic reviews, most of the included studies (n=68; 72%) had a global focus or no specified geographical limitations and therefore included studies published anywhere in the world. The remaining systematic reviews either targeted certain countries (n=12) (1 for each Australia, Germany, Iran, India, Ethiopia, Malaysia, Nepal, New Zealand and 2 reviews focused on China and the USA), continents (n=5) (3 focused on Europe and 2 on Asia), or regions according to geographical location (n=6) (1 focused on Sub-Saharan Africa, 1 on Eastern Mediterranean countries, 1 on Tropical countries, and 3 focused on the Arctic), or according to the country’s level of income (n=3) (2 on low to middle income countries, 1 on high income countries).
Regarding specific populations of interest, most of the systematic reviews did not define a specific population of interest (n=69; 73%). For the studies that specified a population of interest (n=25; 26.6%), the most frequent populations were children (n=7) and workers (n=6), followed by vulnerable or susceptible populations more generally (n=4), the elderly (n=3), pregnant people (n=2), people with disabilities or chronic illnesses (n=2) and rural populations (n=1).
We assessed studies for quality according to our revised AMSTAR-2. Complete scores for each article and each item are available in online supplemental appendix 4 . Out of 94 systematic reviews, the most commonly fully satisfied criterion was #1 (Population, Intervention, Comparator, Outcome (PICO) components) with 81/94 (86%) of included systematic reviews fully satisfying this criterion. The next most commonly satisfied criteria were #16 (potential sources of conflict of interest reported) (78/94=83% fully), #13 (account for limitations in individual studies) (70/94=75% fully and 2/94=2% partially), #7 (explain both inclusion and exclusion criteria) (64/94=68% fully and 19/94=20% partially), #8 (description of included studies in adequate detail) (36/94=38% fully and 41/94=44% partially), and #4 (use of a comprehensive literature search strategy) (0/94=0% fully and 80/94=85% partially). For criteria #11, #12, and #15, which only applied to reviews including meta-analyses, 17/18 (94%) fully satisfied criterion #11 (use of an appropriate methods for statistical combination of results), 12/18 (67%) fully satisfied criterion #12 (assessment of the potential impact of Risk of Bias (RoB) in individual studies) (1/18=6% partially), and 11/18 (61%) fully satisfied criterion #15 (an adequate investigation of publication bias, small study bias).
Climate impacts and health outcomes
Regarding climate impacts, we identified 5 mutually exclusive categories, with 13 publications targeting more than one category of climate impacts: (1) meteorological (n=71 papers) (eg, temperature, heat waves, humidity, precipitation, sunlight, wind, air pressure), (2) extreme weather (n=24) (eg, water-related, floods, cyclones, hurricanes, drought), (3) air quality (n=7) (eg, air pollution and wildfire smoke exposure), (4) general (n=5), and (5) other (n=3). Although heat waves could be considered an extreme weather event, papers investigating heat waves’ impact on health were classified in the meteorological impact category, since some of these studies treated them with high temperature. ‘General’ climate impacts included articles that did not specify climate change impacts but stated general climate change as their focus. ‘Other’ climate impacts included studies investigating other effects indirectly related to climate change (eg, impact of environmental contaminants) or general environmental risk factors (eg, environmental hazards, sanitation and access to clean water.)
We identified 10 categories to describe the health outcomes studied by the systematic reviews, and 29 publications targeted more than one category of health outcomes: (1) infectious diseases (n=41 papers) (vector borne, food borne and water borne), (2) mortality (n=32), (3) respiratory, cardiovascular and neurological (n=23), (4) healthcare systems (n=16), 5) mental health (n=13), (6) pregnancy and birth (n=11), 7) nutritional (n=9), (8) skin diseases and allergies (n=8), (9) occupational health and injuries (n=6) and (10) other health outcomes (n=17) (eg, sleep, arthritis, disability-adjusted life years, non-occupational injuries, etc)
Figure 4 depicts the combinations of climate impact and health outcome for each study, with online supplemental appendix 5 offering further details. The five most common combinations are studies investigating the (1) meteorological impacts on infectious diseases (n=35), (2) mortality (n=24) and (3) respiratory, cardiovascular and neurological outcomes (n=17), (4) extreme weather events’ impacts on infectious diseases (n=14), and (5) meteorological impacts on health systems (n=11).
Summary of the combination of climate impact and health outcome (frequencies). The total frequency for one category of health outcome could exceed the number of publications included in this health outcome, since one publication could explore the health impact according to more than one climate factor (eg, one publication could explore both the impact of extreme weather events and temperature on mental health).
For studies investigating meteorological impacts on health, the three most common health outcomes studied were impacts on (1) infectious diseases (n=35), (2) mortality (n=24) and (3) respiratory, cardiovascular and neurological outcomes (n=17). Extreme weather event studies most commonly reported health outcomes related to (1) infectious diseases (n=14), (2) mental health outcomes (n=9) and (3) nutritional outcomes (n=6) and other health outcomes (eg, injuries, sleep) (n=6). Studies focused on the impact of air quality were less frequent and explored mostly health outcomes linked to (1) respiratory, cardiovascular and neurological outcomes (n=6), (2) mortality (n=5) and (3) pregnancy and birth outcomes (n=3).
Summary of findings
Most reviews suggest a deleterious impact of climate change on multiple adverse health outcomes, with some associations being explored and/or supported with consistent findings more often than others. Some reviews also report conflicting findings or an absence of association between the climate impact and health outcome studied (see table 1 for a detailed summary of findings according to health outcomes).
- View inline
Summary of findings from systematic reviews according to health outcome and climate impact
Notable findings of health outcomes according to climate impact include the following. For meteorological factors (n=71), temperature and humidity are the variables most often studied and report the most consistent associations with infectious diseases and respiratory, cardiovascular, and neurological outcomes. Temperature is also consistently associated with mortality and healthcare service use. Some associations are less frequently studied, but remain consistent, including the association between some meteorological factors (eg, temperature and heat) and some adverse mental health outcomes (eg, hospital admissions for mental health reasons, suicide, exacerbation of previous mental health conditions), and the association between heat and adverse occupational outcomes and some adverse birth outcomes. Temperature is also associated with adverse nutritional outcomes (likely via crop production and food insecurity) and temperature and humidity are associated with some skin diseases and allergies. Some health outcomes are less frequently studied, but studies suggest an association between temperature and diabetes, impaired sleep, cataracts, heat stress, heat exhaustion and renal diseases.
Extreme weather events (n=24) are consistently associated with mortality, some mental health outcomes (eg, distress, anxiety, depression) and adverse nutritional outcomes (likely via crop production and food insecurity). Some associations are explored less frequently, but these studies suggest an association between drought and respiratory and cardiovascular outcomes (likely via air quality), between extreme weather events and an increased use of healthcare services and some adverse birth outcomes (likely due to indirect causes, such as experiencing stress). Some health outcomes are less frequently studied, but studies suggest an association between extreme weather events and injuries, impaired sleep, oesophageal cancer and exacerbation of chronic illnesses. There are limited and conflicting findings for the association between extreme weather events and infectious diseases, as well as for certain mental health outcomes (eg, suicide and substance abuse). At times, different types of extreme weather events (eg, drought vs flood) led to conflicting findings for some health outcomes (eg, mental health outcomes, infectious diseases), but for other health outcomes, the association was consistent independently of the extreme weather event studied (eg, mortality, healthcare service use and nutritional outcomes).
The impact of air quality on health (n=7) was less frequently studied, but the few studies exploring this association report consistent findings regarding an association with respiratory-specific mortality, adverse respiratory outcomes and an increase in healthcare service use. There is limited evidence regarding the association between air quality and cardiovascular outcomes, limited and inconsistent evidence between wildfire smoke exposure and adverse birth outcomes, and no association is found between exposure to wildfire smoke and increase in use of health services for mental health reasons. Only one review explored the impact of wildfire smoke exposure on ophthalmic outcomes, and it suggests that it may be associated with eye irritation and cataracts.
Reviews which stated climate change as their general focus and did not specify the climate impact(s) under study were less frequent (n=5), but they suggest an association between climate change and pollen allergies in Europe, increased use of healthcare services, obesity, skin diseases and allergies and an association with disability-adjusted life years. Reviews investigating the impact of other climate-related factors (n=3) show inconsistent findings concerning the association between environmental pollutant and adverse birth outcomes, and two reviews suggest an association between environmental risk factors and pollutants and childhood stunting and occupational diseases.
Most reviews concluded by calling for more research, noting the limitations observed among the studies included in their reviews, as well as limitations in their reviews themselves. These limitations included, among others, some systematic reviews having a small number of publications, 24 25 language restrictions such as including only papers in English, 26 27 arriving at conflicting evidence, 28 difficulty concluding a strong association due to the heterogeneity in methods and measurements or the limited equipment and access to quality data in certain contexts, 24 29–31 and most studies included were conducted in high-income countries. 32 33
Previous authors also discussed the important challenge related to exploring the relationship between climate change and health. Not only is it difficult to explore the potential causal relationship between climate change and health, mostly due to methodological challenges, but there are also a wide variety of complex causal factors that may interact to determine health outcomes. Therefore, the possible causal mechanisms underlying these associations were at times still unknown or uncertain and the impacts of some climate factors were different according to geographical location and specificities of the context. Nonetheless, some reviews offered potential explanations for the climate-health association, with the climate factor at times, having a direct impact on health (eg, flooding causing injuries, heat causing dehydration) and in other cases, having an indirect impact (eg, flooding causing stress which in turn may cause adverse birth outcomes, heat causing difficulty concentrating leading to occupational injuries.)
Principal results
In this overview of systematic reviews, we aimed to develop a synthesis of systematic reviews of health impacts of climate change by mapping the characteristics and findings of studies exploring the relationship between climate change and health. We identified four key findings.
First, meteorological impacts, mostly related to temperature and humidity, were the most common impacts studied by included publications, which aligns with findings from a previous scoping review on the health impacts of climate change in the Philippines. 10 Indeed, meteorological factors’ impact on all health outcomes identified in this review are explored, although some health outcomes are more rarely explored (eg, mental health and nutritional outcomes). Although this may not be surprising given that a key implication of climate change is the long-term meteorological impact of temperature rise, this finding suggests we also need to undertake research focused on other climate impacts on health, including potential direct and indirect effects of temperature rise, such as the impact of droughts and wildfire smoke. This will allow us to better prepare for the health crises that arise from these ever-increasing climate-related impacts. For instance, the impacts of extreme weather events and air quality on certain health outcomes are not explored (eg, skin diseases and allergies, occupational health) or only rarely explored (eg, pregnancy outcomes).
Second, systematic reviews primarily focus on physical health outcomes, such as infectious diseases, mortality, and respiratory, cardiovascular and neurological outcomes, which also aligns with the country-specific previous scoping review. 10 Regarding mortality, we support Campbell and colleagues’ 34 suggestion that we should expand our focus to include other types of health outcomes. This will provide better support for mitigation policies and allow us to adapt to the full range of threats of climate change.
Moreover, it is unclear whether the distribution of frequencies of health outcomes reflects the actual burden of health impacts of climate change. The most commonly studied health outcomes do not necessarily reflect the definition of health presented by the WHO as, ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. 20 This suggests that future studies should investigate in greater depth the impacts of climate change on mental and broader social well-being. Indeed, some reviews suggested that climate change impacts psychological and social well-being, via broader consequences, such as political instability, health system capacity, migration, and crime, 3 4 35 36 thus illustrating how our personal health is determined not only by biological and environmental factors but also by social and health systems. The importance of expanding our scope of health in this field is also recognised in the most recent Lancet report, which states that future reports will include a new mental health indicator. 2
Interestingly, the reviews that explored the mental health impacts of climate change were focused mostly on the direct and immediate impacts of experiencing extreme weather events. However, psychologists are also warning about the long-term indirect mental health impacts of climate change, which are becoming more prevalent for children and adults alike (eg, eco-anxiety, climate depression). 37 38 Even people who do not experience direct climate impacts, such as extreme weather events, report experiencing distressing emotions when thinking of the destruction of our environment or when worrying about one’s uncertain future and the lack of actions being taken. To foster emotional resilience in the face of climate change, these mental health impacts of climate change need to be further explored. Humanity’s ability to adapt to and mitigate climate change ultimately depends on our emotional capacity to face this threat.
Third, there is a notable geographical difference in the country affiliations of first authors, with three quarters of systematic reviews having been led by first authors affiliated to institutions in Europe, Australia, or North America, which aligns with the findings of the most recent Lancet report. 2 While perhaps unsurprising given the inequalities in research funding and institutions concentrated in Western countries, this is of critical importance given the significant health impacts that are currently faced (and will remain) in other parts of the world. Research funding organisations should seek to provide more resources to authors in low-income to middle-income countries to ensure their expertise and perspectives are better represented in the literature.
Fourth, overall, most reviews suggest an association between climate change and the deterioration of health in various ways, illustrating the interdependence of our health and well-being with the well-being of our environment. This interdependence may be direct (eg, heat’s impact on dehydration and exhaustion) or indirect (eg, via behaviour change due to heat.) The most frequently explored and consistently supported associations include an association between temperature and humidity with infectious diseases, mortality and adverse respiratory, cardiovascular and neurological outcomes. Other less frequently studied but consistent associations include associations between climate impacts and increased use of healthcare services, some adverse mental health outcomes, adverse nutritional outcomes and adverse occupational health outcomes. These associations support key findings of the most recent Lancet report, in which authors report, among others, increasing heat exposure being associated with increasing morbidities and mortality, climate change leading to food insecurity and undernutrition, and to an increase in infectious disease transmission. 2
That said, a number of reviews included in this study reported limited, conflicting and/or an absence of evidence regarding the association between the climate impact and health outcome. For instance, there was conflicting or limited evidence concerning the association between extreme weather events and infectious diseases, cardiorespiratory outcomes and some mental health outcomes and the association between air quality and cardiovascular-specific mortality and adverse birth outcomes. These conflicting and limited findings highlight the need for further research. These associations are complex and there exist important methodological challenges inherent to exploring the causal relationship between climate change and health outcomes. This relationship may at times be indirect and likely determined by multiple interacting factors.
The climate-health link has been the target of more research in recent years and it is also receiving increasing attention from the public and in both public health and climate communication literature. 2 39–41 However, the health framing of climate change information is still underused in climate communications, and researchers suggest we should be doing more to make the link between human health and climate change more explicit to increase engagement with the climate crisis. 2 41–43 The health framing of climate communication also has implications for healthcare professionals 44 and policy-makers, as these actors could play a key part in climate communication, adaptation and mitigation. 41 42 45 These key stakeholders’ perspectives on the climate-health link, as well as their perceived role in climate adaptation and mitigation could be explored, 46 since research suggests that health professionals are important voices in climate communications 44 and especially since, ultimately, these adverse health outcomes will engender pressure on and cost to our health systems and health workers.
Strengths and limitations
To the best of our knowledge, the current study provides the first broad overview of previous systematic reviews exploring the health impacts of climate change. Our review has three main strengths. First, by targeting systematic reviews, we achieve a higher order summary of findings than what would have been possible by consulting individual original studies. Second, by synthesising findings across all included studies and according to the combination of climate impact and health outcome, we offer a clear, detailed and unique summary of the current state of evidence and knowledge gaps about how climate change may influence human health. This summary may be of use to researchers, policy-makers and communities. Third, we included studies published in all languages about any climate impact and any health outcome. In doing so, we provide a comprehensive and robust overview.
Our work has four main limitations. First, we were unable to access some full texts and therefore some studies were excluded, even though we deemed them potentially relevant after title and abstract inspection. Other potentially relevant systematic reviews may be missing due to unseen flaws in our systematic search. Second, due to the heterogeneity of the included systematic reviews and the relatively small proportion of studies reporting meta-analytic findings, we could not conduct meta-meta-analyses of findings across reviews. Future research is needed to quantify the climate and health links described in this review, as well as to investigate the causal relationship and other interacting factors. Third, due to limited resources, we did not assess overlap between the included reviews concerning the studies they included. Frequencies and findings should be interpreted with potential overlap in mind. Fourth, we conducted the systematic search of the literature in June 2019, and it is therefore likely that some recent systematic reviews are not included in this study.
Conclusions
Overall, most systematic reviews of the health impacts of climate change suggest an association between climate change and the deterioration of health in multiple ways, generally in the direction that climate change is associated with adverse human health outcomes. This is worrisome since these outcomes are predicted to rise in the near future, due to the rise in temperature and increase in climate-change-related events such as extreme weather events and worsened air quality. Most studies included in this review focused on meteorological impacts of climate change on adverse physical health outcomes. Future studies could fill knowledge gaps by exploring other climate-related impacts and broader psychosocial health outcomes. Moreover, studies on health impacts of climate change have mostly been conducted by first authors affiliated with institutions in high-income countries. This inequity needs to be addressed, considering that the impacts of climate change are and will continue to predominantly impact lower income countries. Finally, although most reviews also recommend more research to better understand and quantify these associations, to adapt to and mitigate climate change’s impacts on health, it will also be important to unpack the ‘what, how, and where’ of these effects. Health effects of climate change are unlikely to be distributed equally or randomly through populations. It will be important to mitigate the changing climate’s potential to exacerbate health inequities.
Ethics statements
Patient consent for publication.
Not required.
Acknowledgments
The authors gratefully acknowledge the contributions of Selma Chipenda Dansokho, as research associate, and Thierry Provencher, as research assistant, to this project, and of Frederic Bergeron, for assistance with search strategy, screening and selection of articles for the systematic review.
- Portier C ,
- Arnell N , et al
- Hsiang SM ,
- Frumkin H ,
- Holloway T , et al
- Alderman K ,
- Turner LR ,
- Coates SJ ,
- Davis MDP ,
- Andersen LK
- Jin H , et al
- Azizi M , et al
- Dorotan MM ,
- Sigua JA , et al
- Mcintyre M , et al
- Liu J , et al
- Herlihy N ,
- Bar-Hen A ,
- Verner G , et al
- Hosking J ,
- Campbell-Lendrum D
- Pollock M ,
- Fernandes RM ,
- Witteman HO ,
- Dansokho SC ,
- McKenzie J ,
- Pieper D , et al
- ↵ About Cochrane reviews . Available: https://www.cochranelibrary.com/about/about-cochrane-reviews [Accessed 14 Sept 2020 ].
- World Health Organization
- ↵ Covidence systematic review software . Available: www.covidence.org
- Schlosberg D , et al
- Amegah AK ,
- Jaakkola JJK
- Zheng S , et al
- Leyva EWA ,
- Davidson PM
- Phalkey RK ,
- Aranda-Jan C ,
- Marx S , et al
- Porpora MG ,
- Piacenti I ,
- Scaramuzzino S , et al
- Morton LC ,
- Zhu R , et al
- Rutherford S , et al
- Klinger C ,
- Xu D , et al
- Campbell S ,
- Remenyi TA ,
- White CJ , et al
- Palmer J , et al
- Benevolenza MA ,
- Davenport L
- Maibach EW ,
- Baldwin P , et al
- Schütte S ,
- Nisbet MC ,
- Maibach EW , et al
- Costello A ,
- Montgomery H ,
- Hess J , et al
- Berhane K ,
- Bernhardt V ,
- Finkelmeier F ,
- Verhoff MA , et al
- de Sousa TCM ,
- Amancio F ,
- Hacon SdeS , et al
- Bai Z , et al
- Roda Gracia J ,
- Schumann B ,
- Hedlund C ,
- Blomstedt Y ,
- Aghamohammadi N , et al
- Khader YS ,
- Abdelrahman M ,
- Abdo N , et al
- Matysiak A ,
- Mackenzie JS , et al
- Nichols A ,
- Maynard V ,
- Goodman B , et al
- Tong S , et al
- Swynghedauw B
- Emelyanova A ,
- Oksanen A , et al
- Su H , et al
- Mengersen K ,
- Dale P , et al
- Veenema TG ,
- Thornton CP ,
- Lavin RP , et al
- Gatton ML ,
- Ghazani M ,
- FitzGerald G ,
- Hu W , et al
- Lu Y , et al
- Fearnley E ,
- Woster AP ,
- Goldstein RS , et al
- Philipsborn R ,
- Brosi BJ , et al
- Semenza JC ,
- Rechenburg A , et al
- Stensgaard A-S ,
- Vounatsou P ,
- Sengupta ME , et al
- Shipp-Hilts A ,
- Eidson M , et al
- Thomas DR ,
- Salmon RL , et al
- Prudhomme C , et al
- Wildenhain J ,
- Vandenbergh A , et al
- Barnett AG ,
- Wang X , et al
- Ghanizadeh G ,
- Heidari M ,
- Lawton EM ,
- Liang R , et al
- Moghadamnia MT ,
- Ardalan A ,
- Mesdaghinia A , et al
- Parthasarathy R ,
- Krishnan A , et al
- Sanderson M ,
- Arbuthnott K ,
- Kovats S , et al
- Schubert AJ ,
- Jehn M , et al
- Sheffield PE ,
- Guo Y , et al
- Daniels A , et al
- Madaniyazi L ,
- Yu W , et al
- Pereira G ,
- Uhl SA , et al
- Johnston FH , et al
- Youssouf H ,
- Liousse C ,
- Roblou L , et al
- Agnew M , et al
- Zhang Y , et al
- Crooks JL ,
- Davies JM , et al
- Sawatzky A ,
- Cunsolo A ,
- Jones-Bitton A , et al
- Duan J , et al
- Kunzweiler K ,
- Garthus-Niegel S
- Fernandez A ,
- Jones M , et al
- Saha S , et al
- Carolan-Olah M ,
- Frankowska D
- McCormick S
- Poursafa P ,
- Kelishadi R
- Vilcins D ,
- Huang K-C ,
- Yang T-Y , et al
- Augustin J ,
- Franzke N ,
- Augustin M , et al
- Binazzi A ,
- Bonafede M , et al
- Bonafede M ,
- Marinaccio A ,
- Asta F , et al
- Flouris AD ,
- Ioannou LG , et al
- Kjellstrom T ,
- Baldasseroni A
- Varghese BM ,
- Bi P , et al
- Wimalawansa SA ,
- Wimalawansa SJ
- Ahn HS , et al
- Otte im Kampe E ,
- Rifkin DI ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
- Data supplement 4
- Data supplement 5
Twitter @RutNdjab, @ATricco, @hwitteman
Contributors RN, CF, ACT, HOW contributed to the design of the study. CB, RN, LPB, RAPR and HOW contributed to the systematic search of the literature and selection of studies. RR, HOW, LC conducted data analysis and interpretation. RR and HOW drafted the first version of the article with early revision by CB, LC and RN. All authors critically revised the article and approved the final version for submission for publication. RR and HOW had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Funding This study was funded by the Canadian Institutes of Health Research (CIHR) FDN-148426. The CIHR had no role in determining the study design, the plans for data collection or analysis, the decision to publish, nor the preparation of this manuscript. ACT is funded by a Tier 2 Canada Research Chair in Knowledge Synthesis. HOW is funded by a Tier 2 Canada Research Chair in Human-Centred Digital Health.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Newsroom Post
Climate change: a threat to human wellbeing and health of the planet. taking action now can secure our future.
BERLIN, Feb 28 – Human-induced climate change is causing dangerous and widespread disruption in nature and affecting the lives of billions of people around the world, despite efforts to reduce the risks. People and ecosystems least able to cope are being hardest hit, said scientists in the latest Intergovernmental Panel on Climate Change (IPCC) report, released today.
“This report is a dire warning about the consequences of inaction,” said Hoesung Lee, Chair of the IPCC. “It shows that climate change is a grave and mounting threat to our wellbeing and a healthy planet. Our actions today will shape how people adapt and nature responds to increasing climate risks.”
The world faces unavoidable multiple climate hazards over the next two decades with global warming of 1.5°C (2.7°F). Even temporarily exceeding this warming level will result in additional severe impacts, some of which will be irreversible. Risks for society will increase, including to infrastructure and low-lying coastal settlements.
The Summary for Policymakers of the IPCC Working Group II report, Climate Change 2022: Impacts, Adaptation and Vulnerability was approved on Sunday, February 27 2022, by 195 member governments of the IPCC, through a virtual approval session that was held over two weeks starting on February 14.
Urgent action required to deal with increasing risks
Increased heatwaves, droughts and floods are already exceeding plants’ and animals’ tolerance thresholds, driving mass mortalities in species such as trees and corals. These weather extremes are occurring simultaneously, causing cascading impacts that are increasingly difficult to manage. They have exposed millions of people to acute food and water insecurity, especially in Africa, Asia, Central and South America, on Small Islands and in the Arctic.
To avoid mounting loss of life, biodiversity and infrastructure, ambitious, accelerated action is required to adapt to climate change, at the same time as making rapid, deep cuts in greenhouse gas emissions. So far, progress on adaptation is uneven and there are increasing gaps between action taken and what is needed to deal with the increasing risks, the new report finds. These gaps are largest among lower-income populations.
The Working Group II report is the second instalment of the IPCC’s Sixth Assessment Report (AR6), which will be completed this year.
“This report recognizes the interdependence of climate, biodiversity and people and integrates natural, social and economic sciences more strongly than earlier IPCC assessments,” said Hoesung Lee. “It emphasizes the urgency of immediate and more ambitious action to address climate risks. Half measures are no longer an option.”
Safeguarding and strengthening nature is key to securing a liveable future
There are options to adapt to a changing climate. This report provides new insights into nature’s potential not only to reduce climate risks but also to improve people’s lives.
“Healthy ecosystems are more resilient to climate change and provide life-critical services such as food and clean water”, said IPCC Working Group II Co-Chair Hans-Otto Pörtner. “By restoring degraded ecosystems and effectively and equitably conserving 30 to 50 per cent of Earth’s land, freshwater and ocean habitats, society can benefit from nature’s capacity to absorb and store carbon, and we can accelerate progress towards sustainable development, but adequate finance and political support are essential.”
Scientists point out that climate change interacts with global trends such as unsustainable use of natural resources, growing urbanization, social inequalities, losses and damages from extreme events and a pandemic, jeopardizing future development.
“Our assessment clearly shows that tackling all these different challenges involves everyone – governments, the private sector, civil society – working together to prioritize risk reduction, as well as equity and justice, in decision-making and investment,” said IPCC Working Group II Co-Chair Debra Roberts.
“In this way, different interests, values and world views can be reconciled. By bringing together scientific and technological know-how as well as Indigenous and local knowledge, solutions will be more effective. Failure to achieve climate resilient and sustainable development will result in a sub-optimal future for people and nature.”
Cities: Hotspots of impacts and risks, but also a crucial part of the solution
This report provides a detailed assessment of climate change impacts, risks and adaptation in cities, where more than half the world’s population lives. People’s health, lives and livelihoods, as well as property and critical infrastructure, including energy and transportation systems, are being increasingly adversely affected by hazards from heatwaves, storms, drought and flooding as well as slow-onset changes, including sea level rise.
“Together, growing urbanization and climate change create complex risks, especially for those cities that already experience poorly planned urban growth, high levels of poverty and unemployment, and a lack of basic services,” Debra Roberts said.
“But cities also provide opportunities for climate action – green buildings, reliable supplies of clean water and renewable energy, and sustainable transport systems that connect urban and rural areas can all lead to a more inclusive, fairer society.”
There is increasing evidence of adaptation that has caused unintended consequences, for example destroying nature, putting peoples’ lives at risk or increasing greenhouse gas emissions. This can be avoided by involving everyone in planning, attention to equity and justice, and drawing on Indigenous and local knowledge.
A narrowing window for action
Climate change is a global challenge that requires local solutions and that’s why the Working Group II contribution to the IPCC’s Sixth Assessment Report (AR6) provides extensive regional information to enable Climate Resilient Development.
The report clearly states Climate Resilient Development is already challenging at current warming levels. It will become more limited if global warming exceeds 1.5°C (2.7°F). In some regions it will be impossible if global warming exceeds 2°C (3.6°F). This key finding underlines the urgency for climate action, focusing on equity and justice. Adequate funding, technology transfer, political commitment and partnership lead to more effective climate change adaptation and emissions reductions.
“The scientific evidence is unequivocal: climate change is a threat to human wellbeing and the health of the planet. Any further delay in concerted global action will miss a brief and rapidly closing window to secure a liveable future,” said Hans-Otto Pörtner.
For more information, please contact:
IPCC Press Office, Email: [email protected] IPCC Working Group II: Sina Löschke, Komila Nabiyeva: [email protected]
Notes for Editors
Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change
The Working Group II report examines the impacts of climate change on nature and people around the globe. It explores future impacts at different levels of warming and the resulting risks and offers options to strengthen nature’s and society’s resilience to ongoing climate change, to fight hunger, poverty, and inequality and keep Earth a place worth living on – for current as well as for future generations.
Working Group II introduces several new components in its latest report: One is a special section on climate change impacts, risks and options to act for cities and settlements by the sea, tropical forests, mountains, biodiversity hotspots, dryland and deserts, the Mediterranean as well as the polar regions. Another is an atlas that will present data and findings on observed and projected climate change impacts and risks from global to regional scales, thus offering even more insights for decision makers.
The Summary for Policymakers of the Working Group II contribution to the Sixth Assessment Report (AR6) as well as additional materials and information are available at https://www.ipcc.ch/report/ar6/wg2/
Note : Originally scheduled for release in September 2021, the report was delayed for several months by the COVID-19 pandemic, as work in the scientific community including the IPCC shifted online. This is the second time that the IPCC has conducted a virtual approval session for one of its reports.
AR6 Working Group II in numbers
270 authors from 67 countries
- 47 – coordinating authors
- 184 – lead authors
- 39 – review editors
- 675 – contributing authors
Over 34,000 cited references
A total of 62,418 expert and government review comments
(First Order Draft 16,348; Second Order Draft 40,293; Final Government Distribution: 5,777)
More information about the Sixth Assessment Report can be found here .
Additional media resources
Assets available after the embargo is lifted on Media Essentials website .
Press conference recording, collection of sound bites from WGII authors, link to presentation slides, B-roll of approval session, link to launch Trello board including press release and video trailer in UN languages, a social media pack.
The website includes outreach materials such as videos about the IPCC and video recordings from outreach events conducted as webinars or live-streamed events.
Most videos published by the IPCC can be found on our YouTube channel. Credit for artwork
About the IPCC
The Intergovernmental Panel on Climate Change (IPCC) is the UN body for assessing the science related to climate change. It was established by the United Nations Environment Programme (UNEP) and the World Meteorological Organization (WMO) in 1988 to provide political leaders with periodic scientific assessments concerning climate change, its implications and risks, as well as to put forward adaptation and mitigation strategies. In the same year the UN General Assembly endorsed the action by the WMO and UNEP in jointly establishing the IPCC. It has 195 member states.
Thousands of people from all over the world contribute to the work of the IPCC. For the assessment reports, IPCC scientists volunteer their time to assess the thousands of scientific papers published each year to provide a comprehensive summary of what is known about the drivers of climate change, its impacts and future risks, and how adaptation and mitigation can reduce those risks.
The IPCC has three working groups: Working Group I , dealing with the physical science basis of climate change; Working Group II , dealing with impacts, adaptation and vulnerability; and Working Group III , dealing with the mitigation of climate change. It also has a Task Force on National Greenhouse Gas Inventories that develops methodologies for measuring emissions and removals. As part of the IPCC, a Task Group on Data Support for Climate Change Assessments (TG-Data) provides guidance to the Data Distribution Centre (DDC) on curation, traceability, stability, availability and transparency of data and scenarios related to the reports of the IPCC.
IPCC assessments provide governments, at all levels, with scientific information that they can use to develop climate policies. IPCC assessments are a key input into the international negotiations to tackle climate change. IPCC reports are drafted and reviewed in several stages, thus guaranteeing objectivity and transparency. An IPCC assessment report consists of the contributions of the three working groups and a Synthesis Report. The Synthesis Report integrates the findings of the three working group reports and of any special reports prepared in that assessment cycle.
About the Sixth Assessment Cycle
At its 41st Session in February 2015, the IPCC decided to produce a Sixth Assessment Report (AR6). At its 42nd Session in October 2015 it elected a new Bureau that would oversee the work on this report and the Special Reports to be produced in the assessment cycle.
Global Warming of 1.5°C , an IPCC special report on the impacts of global warming of 1.5 degrees Celsius above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty was launched in October 2018.
Climate Change and Land , an IPCC special report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems was launched in August 2019, and the Special Report on the Ocean and Cryosphere in a Changing Climate was released in September 2019.
In May 2019 the IPCC released the 2019 Refinement to the 2006 IPCC Guidelines for National Greenhouse Gas Inventories , an update to the methodology used by governments to estimate their greenhouse gas emissions and removals.
In August 2021 the IPCC released the Working Group I contribution to the AR6, Climate Change 2021, the Physical Science Basis
The Working Group III contribution to the AR6 is scheduled for early April 2022.
The Synthesis Report of the Sixth Assessment Report will be completed in the second half of 2022.
For more information go to www.ipcc.ch
Related Content
Remarks by the ipcc chair during the press conference to present the working group ii contribution to the sixth assessment report.
Monday, 28 February 2022 Distinguished representatives of the media, WMO Secretary-General Petteri, UNEP Executive Director Andersen, We have just heard …
February 2022
Fifty-fifth session of the ipcc (ipcc-55) and twelfth session of working group ii (wgii-12), february 14, 2022, working group report, ar6 climate change 2022: impacts, adaptation and vulnerability.
- Ways to Give
- Contact an Expert
- Explore WRI Perspectives
Filter Your Site Experience by Topic
Applying the filters below will filter all articles, data, insights and projects by the topic area you select.
- All Topics Remove filter
- Climate filter site by Climate
- Cities filter site by Cities
- Energy filter site by Energy
- Food filter site by Food
- Forests filter site by Forests
- Freshwater filter site by Freshwater
- Ocean filter site by Ocean
- Business filter site by Business
- Economics filter site by Economics
- Finance filter site by Finance
- Equity & Governance filter site by Equity & Governance
Search WRI.org
Not sure where to find something? Search all of the site's content.

How Climate Change Affects Health and How Countries Can Respond
- Climate Resilience
- adaptation finance
- climate change
- climatewatch-pinned
Since early 2020, the world’s attention has been on the global coronavirus pandemic. The pandemic continues to put massive stress on existing health systems, exposing their fault lines. As nations think about how to make health systems more resilient to current and future threats, one threat must not be overlooked: climate change is also impacting human health and straining heavily burdened health services everywhere.
Health-related risks linked to climate change range widely, from increased likelihood of transmitting vector-borne diseases to decreased access to services as a result of natural disasters. For example, air pollution — the sources of which are often the same as those that drive climate change — kills 4.2 million people every year and makes countless more sick and debilitated. Ground-level ozone, a key component of air pollution, is even more harmful to human health when temperatures are higher. Climate change events like hurricanes and floods can also destroy or limit access to health infrastructure and services.
Human health is a priority in 59% of countries’ national climate adaptation commitments under the Paris Agreement and close to half of countries acknowledge the negative health effects of climate change. However, countries struggle to understand specific climate risks to health, as well as how to identify and fund comprehensive health adaptation actions. Only 0.5% of multilateral climate finance targets health projects. Domestic funding for this issue is also minimal or nonexistent.
This is unacceptable considering the need for resilient and stable health systems.
A new paper by WRI showcases how countries can integrate health-related risks from climate change into their national climate and health strategies and put them into action. Doing so is essential, not only in preventing the worst impacts of climate change, but in keeping people healthy and nations prosperous.
How Does Climate Change Affect Human Health?
There are many ways health risks link to climate change, which often intersect with one another. Common risks include:
1. Increased risk of vector- and water-borne diseases.
Climate change is redistributing and increasing the optimal habitats for mosquitoes and other pathogens that carry disease. In some cases, these pathogens are bringing infectious diseases into communities that had not encountered them before. For example, warmer temperatures expand mosquito breeding ranges, causing malaria to shift upslope into new villages.
One study projects that, because of climate change, up to an additional 51.3 million people will be at risk from exposure to malaria in Western Africa by 2050. These shifts can heighten suffering, increase countries’ burdens of disease and cause epidemics. The World Health Organization (WHO) estimates that one-sixth of illness and disability suffered globally is due to vector-borne diseases, which are predicted to spread due to climate change.
Climate effects related to changing rainfall patterns, water quality and water scarcity can also trigger or worsen diseases within a country. For example, Ghana is now facing a higher prevalence of cholera, diarrhea, malaria and meningitis because flooding contaminates and exacerbates sanitation problems and water quality. Cholera outbreaks in Ghana have a high fatality rate and are particularly frequent during the rainy seasons and in coastal regions.
2. Increased risks to lives and livelihoods.
Similarly, higher temperatures and extreme events — such as intense rainfall, stronger cyclones and increased risk of landslides — can cause physical injuries, water contamination , decreased labor productivity and mental stress such as anxiety, depression and post-traumatic stress disorders. Hot weather and more intense heat waves reduce people’s ability to work and stay healthy; an environment that is too hot and humid makes it impossible for the human body to sweat and can lead to overheating and death.
Changes in the rainy seasons and other, slower-onset climate change risks like salt intrusion from rising sea levels can also negatively impact crop yields and food quality over time. This can lead to greater food insecurity and undernutrition. Bangladesh has the largest delta of any country in the world, and increasing salinity has already negatively affected its crop, fish and livestock production.
Even in places where agriculture yields may be boosted due to climate change, evidence has emerged that such increases can come at the expense of nutrition. These food security threats, in turn, affect people’s every day health, especially when it comes to child growth and development .
Environmental degradation and natural resources instability and competition exacerbated by climate impacts can also contribute to forced migration and social conflict . This can expose people to physical and mental health stressors, exacerbate existing health issues, lead to poorer living conditions and reduce access to affordable medical care.
3. Greater risk of social inequities.
The effects of climate change are especially felt by the most vulnerable , including people living in poverty, those who are marginalized or socially excluded, women, children, the elderly and those who are already ill or living with a disability. Without adequate support and funding, vulnerable groups will continue to suffer the most from the impacts of climate change on health.
The rising frequency, intensity and duration of extreme weather events will disproportionately impact the physical and economic capacities of people and households already struggling with weakened health and chronic disease. Due to their already debilitated or weakened immune systems, people with cardiovascular diseases, respiratory diseases and other pre-existing health conditions are at higher risk of injury or sickness from natural disasters and other climate-related risks.
The elderly and people who perform heavy physical labor, including agricultural laborers, are especially at risk from the effects of increasing heat and heat wave events, which stress the heart (possibly leading to cardiac arrest) and can cause severe dehydration, which damages other vital organs like the kidneys.
When combined with poorer nutrition and water stress, the result is often worse existing health problems, which can further entrench generational poverty and systemic vulnerabilities . This, in turn, contributes to heightened mortality and morbidity at a wider scale, increasing countries’ disease burdens.

What Are the Challenges to Integrating Climate Adaptation into Health Plans?
Several technical and financial challenges remain when it comes to incorporating climate-sensitive risks into health systems. Many countries and groups lack a strong understanding of the links between climate change and health. This is made more complicated when considering that cause-and-effect is difficult, and at times impossible, to prove.
While environmental health and public health officers can see the connections, policymakers may not understand them without proper training. These knowledge gaps can lead to inconsistent policies and a lack of adaptation activities in health budgets.
Many countries also have inadequate finance to implement adaptation and health activities.
As our case study illustrates, in Ghana, for instance, policymakers have limited human resources and skills available to identify and develop appropriate adaptation measures to reduce climate-sensitive health risks. As a result, it is difficult to persuade Parliament to dedicate an adequate budget for such activities. Frequent changes in administration can also make it difficult to ensure consistent allocation of public resources for adaptation in the health sector.
Despite being a priority in national policies and international commitments, technical and financial support requests to the NDC Partnership and multilateral climate funds like the Green Climate Fund often vastly underrepresent health-specific activities.
In a global review of more than 100 countries, the UN found that only one in five countries is spending enough to implement climate-related health commitments. This gap will be further exacerbated by 2030, when the direct damage costs to health are expected to be between $2 billion to $4 billion per year — even without considering indirect effects.
How Can Governments Adapt to Protect Human Health from the Effects of Climate Change?
While it can be difficult to identify, understand and reduce climate-sensitive health risks, a lack of information should not prevent action or delay no-regrets adaptation measures to strengthen health care systems. No-regrets measures include actions that protect communities whether climate impacts materialize as severely as expected or not, such as building robust food and medical supply chains, retrofitting technology and equipment, increasing training of medical staff and establishing protections against interrupted health services.
Governments can establish policy frameworks and collaboration mechanisms to provide needed guidance and support for no-regrets adaptation measures. Champions of climate and health issues inside and outside of the health sector can rally critical supporters and resources to influence policies and drive action.
Fiji, one of the most climate-vulnerable countries in the world, provides an excellent example of how to advance solutions. The nation developed and implemented its national Climate Change and Health Strategic Action Plan and integrated it into various policies and plans. The adaptation and health activities in Fiji’s plan are expected to increase the nation’s ability to provide and use reliable information on climate-sensitive health risks through an early warning system; improve capacity within health sector institutions to respond to these risks; and allow the nation to pilot disease prevention measures in higher-risk areas.
Fiji also set up a Climate Change and Health Unit within its Ministry of Health and allocated domestic funding to advance climate-health activities, like early warning systems, and build the capacity of health institutions to respond to climate threats. Health and climate change also remain on the political agenda thanks to the continuous efforts of and leadership from its Permanent Secretaries of the Ministry of Health, who encourage collaboration with other ministries.

Protecting the Health of Current and Future Generations
The links between climate change and health continue to grow in clarity and evidence. Policymakers can seize on the political momentum created by the global pandemic to strengthen their countries’ abilities to respond to a range of shocks and stressors — including the linked challenges of infectious disease and climate change. Strengthening the overall capacities and resources of health systems will increase adaptive capacity to deal with climate impacts, ensuring that current and future generations remain healthy.
Relevant Work
What happens when extreme heat and air pollution collide, key investments can build resilience to pandemics and climate change, global emissions and local deforestation are combining to create dangerous levels of heat stress in the tropics, 6 big findings from the ipcc 2022 report on climate impacts, adaptation and vulnerability, how you can help.
WRI relies on the generosity of donors like you to turn research into action. You can support our work by making a gift today or exploring other ways to give.
Stay Informed
World Resources Institute 10 G Street NE Suite 800 Washington DC 20002 +1 (202) 729-7600
© 2024 World Resources Institute
Envision a world where everyone can enjoy clean air, walkable cities, vibrant landscapes, nutritious food and affordable energy.
- Research article
- Open access
- Published: 01 June 2010
Reframing climate change as a public health issue: an exploratory study of public reactions
- Edward W Maibach 1 ,
- Matthew Nisbet 1 , 2 ,
- Paula Baldwin 1 ,
- Karen Akerlof 1 &
- Guoqing Diao 3
BMC Public Health volume 10 , Article number: 299 ( 2010 ) Cite this article
56k Accesses
267 Citations
210 Altmetric
Metrics details
Climate change is taking a toll on human health, and some leaders in the public health community have urged their colleagues to give voice to its health implications. Previous research has shown that Americans are only dimly aware of the health implications of climate change, yet the literature on issue framing suggests that providing a novel frame - such as human health - may be potentially useful in enhancing public engagement. We conducted an exploratory study in the United States of people's reactions to a public health-framed short essay on climate change.
U.S. adult respondents (n = 70), stratified by six previously identified audience segments, read the essay and were asked to highlight in green or pink any portions of the essay they found "especially clear and helpful" or alternatively "especially confusing or unhelpful." Two dependent measures were created: a composite sentence-specific score based on reactions to all 18 sentences in the essay; and respondents' general reactions to the essay that were coded for valence (positive, neutral, or negative). We tested the hypothesis that five of the six audience segments would respond positively to the essay on both dependent measures.
There was clear evidence that two of the five segments responded positively to the public health essay, and mixed evidence that two other responded positively. There was limited evidence that the fifth segment responded positively. Post-hoc analysis showed that five of the six segments responded more positively to information about the health benefits associated with mitigation-related policy actions than to information about the health risks of climate change.
Conclusions
Presentations about climate change that encourage people to consider its human health relevance appear likely to provide many Americans with a useful and engaging new frame of reference. Information about the potential health benefits of specific mitigation-related policy actions appears to be particularly compelling. We believe that the public health community has an important perspective to share about climate change, a perspective that makes the problem more personally relevant, significant, and understandable to members of the public.
Peer Review reports
Climate change is already taking a toll on human health in the United States [ 1 ] and other nations worldwide [ 2 ]. Unless greenhouse gas emissions worldwide are sharply curtailed - and significant actions taken to help communities adapt to changes in their climate that are unavoidable - the human toll of climate change is likely to become dramatically worse over the next several decades and beyond [ 3 ]. Globally, the human health impacts of climate change will continue to differentially affect the world's poorest nations, where populations endemically suffer myriad health burdens associated with extreme poverty that are being exacerbated by the changing climate. As stated in a recent British Medical Journal editorial, failure of the world's nations to successfully curtail emissions will likely lead to a "global health catastrophe" [ 4 ]. In developed countries such as the United States, the segments of the population most at risk are the poor, the very young, the elderly, those already in poor health, the disabled, individuals living alone, those with inadequate housing or basic services, and/or individuals who lack access to affordable health care or who live in areas with weak public health systems. These population segments disproportionately include racial, ethnic, and indigenous minorities [ 5 ].
While legislation to reduce U.S. greenhouse gas (GHG) emissions has stalled in Congress, in December 2009 the Environmental Protection Agency (EPA) moved toward regulating carbon dioxide and five other of the gases under the Clean Air Act, citing its authority to protect public health and welfare from the impacts of global warming [ 5 ]. The agency found that global warming poses public health risks - including increased morbidity and mortality - due to declining air quality, rising temperatures, increased frequency of extreme weather events, and higher incidences of food- and water-borne pathogens and allergens.
This finding comes as a relatively small group of public health professionals are working rapidly to better comprehend and quantify the nature and magnitude of these threats to human health and wellbeing [ 6 ]. This new but rapidly advancing public health focus has received minimal news media attention, even at internationally leading news organizations such as the New York Times [unpublished data]. It is not surprising therefore that the public also has yet to fully comprehend the public health implications of climate change. Recent surveys of Americans [ 7 ], Canadians [ 8 ], and Maltese [ 9 ] demonstrate that the human health consequences of climate change are seriously underestimated and/or poorly understood, if grasped at all. About half of American survey respondents, for example, selected "don't know" (rather than "none," "hundreds," "thousands," or "millions") when asked the estimated number of current and future (i.e. 50 years hence) injuries and illnesses, and death due to climate change. An earlier survey of Americans [ 10 ] demonstrated that most people see climate change as a geographically and temporally distant threat to the non-human environment. Notably, not a single survey respondent freely associated climate change as representing a threat to people. Similarly, few Canadians, without prompting, can name any specific human health threat linked to climate change impacts in their country [ 8 ].
Cognitive research over the past several decades has shown that how people "frame" an issue - i.e., how they mentally organize and discuss with others the issue's central ideas - greatly influences how they understand the nature of the problem, who or what they see as being responsible for the problem, and what they feel should be done to address the problem [ 11 , 12 ]. The polling data cited above [ 7 – 9 ] suggests that the dominant mental frame used by most members of the public to organize their conceptions about climate change is that of "climate change as an environmental problem." However, when climate change is framed as an environmental problem, this interpretation likely distances many people from the issue and contributes to a lack of serious and sustained public engagement necessary to develop solutions. This focus is also susceptible to a dominant counter frame that the best solution is to continue to grow the economy - paying for adaptive measures in the future when, theoretically, society will be wealthier and better able to afford them - rather than focus on the root causes of the environmental problem [ 13 ]. This economic frame likely leaves the public ambivalent about policy action and works to the advantage of industries that are reluctant to reduce their carbon intensity. Indeed, it is precisely the lack of a countervailing populist movement on climate change that has made policy solutions so difficult to enact [ 13 , 14 ].
Significant efforts have been made over the past several years by public health organizations to raise awareness of the public health implications of climate change and prepare the public health workforce to respond, although as noted above, it is not clear the extent to which public health professionals, journalists, or most importantly, the public and policy makers have taken notice. In the United States, National Public Health Week 2008 was themed "Climate Change: Our Health in the Balance," the Centers for Disease Control and Prevention created a Climate Change and Public Health program, and several professional associations assessed the public health system's readiness to respond to the emerging threat [ 15 – 17 ]. Globally, World Health Day 2008 was themed "Protecting Health from Climate Change," and the World Health Organization has developed a climate change and health work plan, the first objective of which is "raising awareness of the effects of climate change on health, in order to prompt action for public health measures" [ 18 ]. Several prominent medical journals have released special issues on climate change and health [ 19 – 21 ], and these and other medical journals [ 4 ] have issued strongly worded editorials urging health professionals to give voice to the health implications of climate change.
An important assumption in these calls to action is that there may be considerable value in introducing a public health frame into the ongoing public - and policy - dialogue about climate change. While there is indeed solid theoretical basis for this assumption, to the best of our knowledge there is not yet empirical evidence to support the validity of the assumption [ 22 ].
The purpose of this study therefore was to explore how American adults respond to an essay about climate change framed as a public health issue. Our hypothesis was that a public health-framed explanation of climate change would be perceived as useful and personally relevant by readers, with the exception of members of one small segment of Americans who dismiss the notion that human-induced climate change is happening. We used two dependent measures in this hypothesis: a composite score based on respondent reactions to each sentence in the essay, and the overall valence of respondents' general comments made after reading the essay.
Our study builds on previous research that identified six distinct segments of Americans, termed Global Warming's Six Americas [ 7 ]. These six segments of Americans - the Alarmed (18% of the adult population), the Concerned (33%), the Cautious (19%), the Disengaged (12%), the Doubtful (11%), and the Dismissive (7%) - fall along a continuum from those who are engaged on the issue and looking for ways to take appropriate actions (the Alarmed) to those who actively deny its reality and are looking for ways to oppose societal action (the Dismissive; see Figure 1 ). The four segments in the middle of the continuum are likely to benefit most from a reframing of climate change as a human health problem because, to a greater or lesser degree, they are not yet sure that they fully understand the issue and are still, if motivated to do so, relatively open to learning about new perspectives.
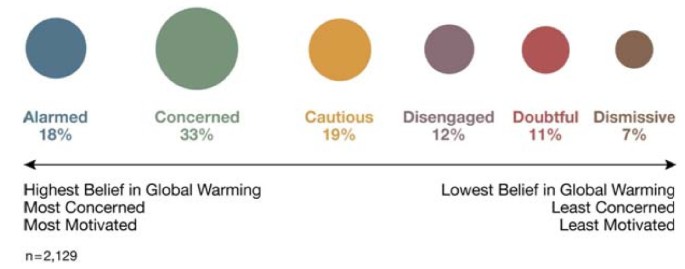
Global Warming's Six Americas . A nationally representative sample of American adults classified into six unique audience segments based on their climate change-related beliefs, behaviors and policy preferences.
Between May and August 2009, 74 adults were recruited to participate in semi-structured in-depth elicitation interviews that lasted an average of 43 minutes (ranging from 16 to 124 minutes) and included the presentation of a public health framed essay on climate change. The recruitment process was designed to yield completed interviews with a demographically and geographically diverse group of at least 10 people from each of the previously identified "Six Americas" [ 7 ]. Four respondents were dropped from this study due to incomplete data, leaving a sample size of 70. Audience segment status (i.e., which one of the "Six Americas" a person belonged) was assessed with a previously developed 15-item screening questionnaire that identifies segment status with 80% accuracy [unpublished data].
To achieve demographic diversity in the sample, we recruited an approximately balanced number of men and women, and an approximately balanced number of younger (18 to 30), middle-aged (31 to 50), and older (51 and older) adults (see Table 1 ). We did not set recruitment quotas for racial/ethnic groups, but did make an effort to recruit a mix of people from various racial/ethnic backgrounds.
To achieve geographic diversity, we recruited participants in one of two ways. The majority of participants (n = 56) were recruited - and then interviewed - face-to-face in one of two locations: out-of-town visitors were interviewed at a central location on the National Mall in Washington, DC (a national park situated between the U.S. Capitol, the Smithsonian Museum buildings, and the Lincoln Memorial); and shoppers were interviewed at an "outlet" mall (i.e., discount branded merchandise shopping mall) adjacent to an interstate freeway in Hagerstown, MD. The outlet mall is more than an hour driving distance outside of Washington, DC and attracts shoppers from Maryland, Pennsylvania, and West Virginia, as well as visitors from further away who are driving the interstate freeway. The remaining study participants were recruited via email from among participants to a nationally representative survey that we conducted in Fall 2008 [ 7 ]. They were interviewed subsequently by telephone, after being mailed a copy of the test "public health essay" - described below - in a sealed envelope marked "do not open until asked to do so by the interviewer." As an incentive to participate, all respondents were given a $50 gift card upon completion of their interview. George Mason University Human Subjects Review Board provided approval for the study protocol (reference #6161); all potential respondents received written consent information prior to participation.
The 70 study participants resided in 29 states. Using U.S. Census Bureau classifications, 14% (n = 10) were from the Northeast region, 21% (n = 15) were from the Midwest, 40% (n = 28) from the South, and 23% (n = 16) were from the West; state and region were unknown for one participant. In 2006, the geographic distribution of the overall U.S. population was 18%, 22%, 36% and 23% in the Northeast, Midwest, South and West, respectively [ 23 ].
Data Collection and Coding
The majority of the interview was devoted to open-ended questions intended to establish the respondent's emotions, attitudes, beliefs, knowledge and behavior relative to global warming's causes and consequences. For example, respective open-ended questions asked alternatively if, how, and for whom global warming was a problem; how global warming is caused; if and how global warming can be stopped or limited; and what, if anything, an individual could do to help limit global warming. Toward the end of the interview, respondents were asked to read "a brief essay about global warming" (see Appendix 1), which was designed to frame climate change as a human health issue. Respondents were also given a green and a pink highlighting pen and asked to "use the green highlighter pen to mark any portions of the essay that you feel are especially clear or helpful, and use the pink highlighter pen to mark any portions of the essay that are particularly confusing or unhelpful."
As shown in Appendix 1, the one page essay was organized into four sections: an opening paragraph that introduced the public health frame (5 total sentences); a paragraph that emphasized how human health will be harmed if action is not taken to stop, limit, and/or protect against global warming (i.e., a description of the threat; 7 sentences); a paragraph that discussed several mitigation-focused policy actions and their human health-related benefits if adopted (4 sentences); and a brief concluding paragraph intended to reinforce the public health frame (2 sentences).
When respondents finished the reading, they were asked to describe in an open-ended format their "general reaction to this essay." (Note: This question was inadvertently not asked of one respondent, therefore the sample size for analysis of this data is 69.) For each portion of the essay they marked in green, they were subsequently asked: "What about each of these sentences was especially clear or helpful to you?" For each portion of the essay they marked in pink, they were also asked: "What about each of these sentences was especially confusing or unhelpful to you?"
To evaluate the respondent's general reactions to the essay we reviewed their individual statements (n = 193), defined as discrete thoughts or concepts. Based on this review, we iteratively developed eight thematic categories that captured the range of statements made by respondents. Table 2 defines and describe these themes.
Two graduate student coders were then trained to code each statement into one of the thematic categories. The coders were also instructed to assess the overall valence of each respondent's statements - the first of our dependent measures - rating them as: -1 (entirely negative comments); 0 (mixed, including both positive and negative comments); or 1 (entirely positive comments). Following standard content analysis procedures, we tested inter-coder agreement on approximately 50 statements, making sure that a full range of possible types of coding decisions were required of the coders. To assess reliability, we used Krippendorff's alpha [ 24 , 25 ], a conservative measure that corrects for chance agreement among coders; a K-alpha of .70 or higher is considered sufficient and .80 or higher is considered excellent. For 7 of the 8 thematic categories, we achieved a reliability of .80 or higher; "Lack of Evidence or Stylistically Confusing" was the exception, with an inter-coder reliability of .70. After establishing reliability, the two coders then went on to categorize the rest of the remaining statements from the sample of respondents.
To code the respondent's sentence-specific reactions made with the highlighting pens, sentences marked with only green on at least one word were scored +1 (i.e. indicating "especially clear or useful"), sentences marked with only pink on at least one word were scored -1 (i.e. indicating "especially confusing or unhelpful), and sentences with either no highlighting, or both green and pink, were scored 0. Composite scores were created for each of the four sections of the essay - the opening, the threat section, the benefit section, and the conclusion - by summing the sentence-specific scores in the section and dividing by the number of sentences. A composite score for the entire essay - the second of the dependent measures in our hypothesis - was created by summing the sentence scores across each segment and dividing by the number of respondents per segment. Population estimates, which can be taken solely as preliminary indicators given the non-probabilistic nature of our sampling, were estimated by weighting the mean values for each of the six segments according to its prevalence in the U.S. population (see Figure 1 ).
Data Analysis
To test the between-segment differences in our dependent measures - overall reactions to the essay (i.e., valence) and composite sentence-specific reactions to the entire essay - we used the nonparametric Kruskal-Wallis test (see Figures 2 , 3 ). To test if the median response to the essay on each dependent measure was greater than zero (i.e., a positive reaction) for our full sample, we used the Wilcoxon signed rank test. Lastly, for both dependent measures, we used the Wilcoxon signed rank test to test our hypothesis that five of the six segments (the Dismissive being the one exception) would respond positively to the essay; the null hypothesis was that the median score for each of the five segments did not differ from zero. The Wilcoxon signed rank test is appropriate for small sample sizes and non-normal distributions, both of which are the case for at least some segments in our data.
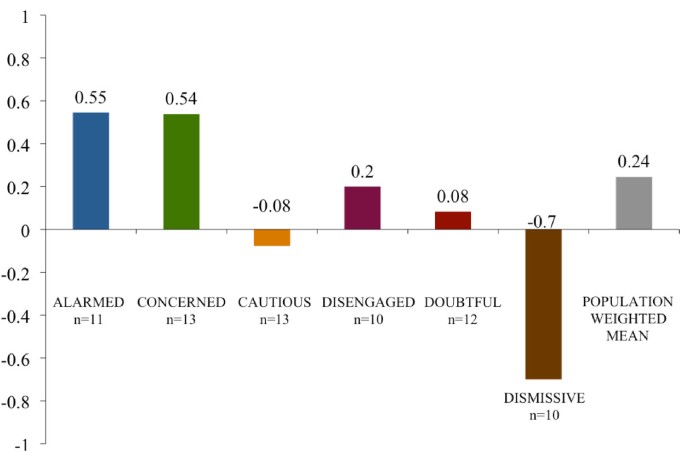
Average valence of respondents' general essay comments . The mean valence of respondent comments when asked their general reactions to the public health essay by audience segment and by a national population estimate. Note: 1 = (entirely positive comments); 0 = (mixed, including both positive and negative comments); and -1 = (entirely negative comments).
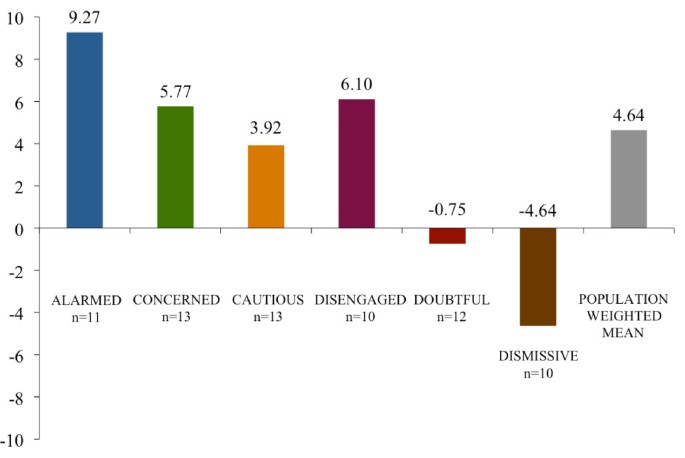
Composite essay scores by segment . Scores reflect respondent average values by segment for the difference between the number of times each of 18 sentences were marked "especially clear or helpful" and "especially confusing or unhelpful" with a full range of possible values between 18 and -18. The scores are adjusted for unequal numbers of respondents within each segment by re-weighting values to represent n = 10.
Post-hoc - after examining the visualized data (see Figures 4 , 5 and 6 ) - we decided to test for two possible main effects in the data. To examine the possibility that the essay's later focus on the public health benefits of mitigation-related policy actions was seen by respondents as clearer and more useful than the essay's earlier focus on public health-related threats, we calculated the difference between the re-scaled (by a factor of 10) average response to both the benefit and the threat sections and then used the Wilcoxon signed rank test to test, by segment, whether the median of these differences was greater than zero. We then evaluated the overall main effect of the essay - across all segments - using the weighted t-test on the differences with weights corresponding to the frequencies of the segments in the population.
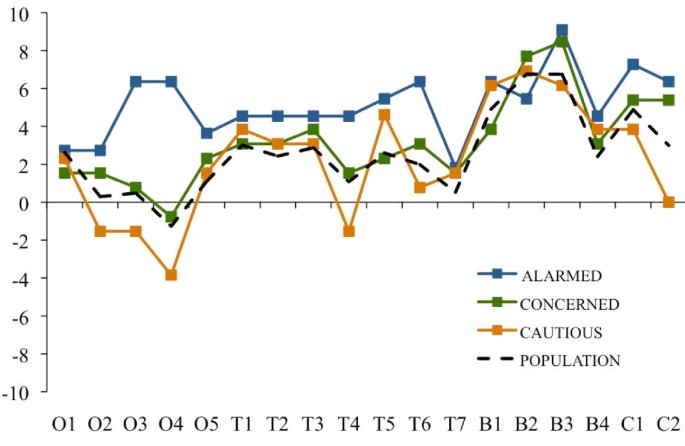
Essay evaluations by sentence: Alarmed, Concerned and Cautious segments . Sentence-specific evaluations of the public health essay by respondents in the Alarmed, Concerned and Cautious segments and by a national population estimate. Note: Scores reflect the difference between the number of times a sentence was marked as "especially clear or helpful" and the number of times it was marked as "especially confusing or unhelpful," adjusting for unequal numbers of respondents within each segment by re-weighting values to represent n = 10. Sentence abbreviations correspond to O = opening section (5 sentences); T = climate change health threat related section (7 sentences); B = mitigation-related policy actions and their health benefits (4 sentences); and C = concluding section (2 sentences). The national population estimate was created by weighting the values for each of the six segments according to their relative proportion of American adults.
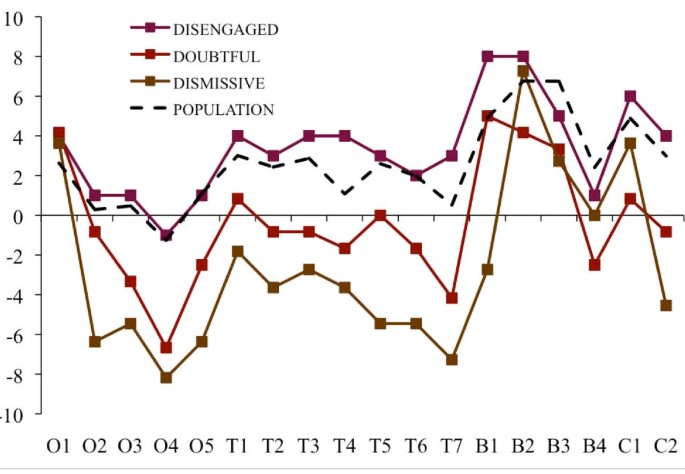
Essay evaluations by sentence: Disengaged, Doubtful and Dismissive segments . Sentence-specific evaluations of the public health essay by respondents in the Disengaged, Doubtful and Dismissive segments and by a national population estimate. Note: Scores reflect the difference between the number of times within a sentence was marked as "especially clear or helpful" and the number of times it was marked as "especially confusing or unhelpful," adjusting for unequal numbers of respondents within each segment by re-weighting values to represent n = 10. Sentence abbreviations correspond to O = opening section (5 sentences); T = climate change health threat related section (7 sentences); B = mitigation-related policy actions and their health benefits (4 sentences); and C = concluding section (2 sentences). The national population estimate was created by weighting the values for each of the six segments according to their relative proportion of American adults.
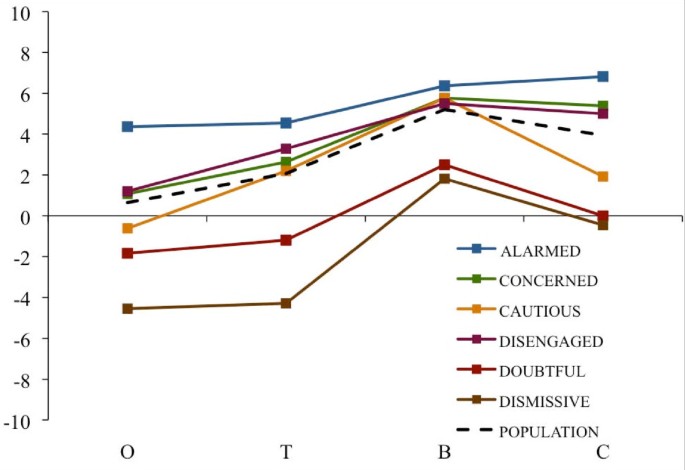
Essay evaluations by section (opening, threat, benefits, closing) . Average section-specific evaluations of the public health essay by respondents in each of the six audience segments and by a national population estimate. Note: Scores reflect the difference between the number of sentences within each section marked by a respondent as "especially clear or helpful" and those marked as "especially confusing or unhelpful" with those values averaged across the number of sentences per section and rescaled by a factor of 10. Section abbreviations correspond to O = opening section (5 sentences); T = climate change health threat related section (7 sentences); B = mitigation-related policy actions and their health benefits (4 sentences); and C = concluding section (2 sentences). The national population estimate was created by weighting the mean values for each of the six segments according to their relative proportion of American adults.
Lastly, to examine for the possibility that the concluding framing section of the essay was perceived by respondents as clearer and more useful than the opening framing section, we calculated the difference between the re-scaled average response to both the opening and the concluding sections and then used the Wilcoxon signed rank test to test, by segment, whether the median of these differences was greater than zero. We then evaluated the overall main effect - across all segments - using the weighted t-test on the differences with weights corresponding to the frequencies of the segments in the population.
Overall Sample Response and Between-Group Differences
The results of non-parametric Kruskal-Wallis tests indicate that there are significant between-group differences for both dependent measures: valence ( p = .001)and the composite sentence-specific score ( p < .0001). For the overall sample, the Wilcoxon signed rank tests indicated a positive response on the sentence-specific composite score ( p < .001) but not on the valence score ( p = .12). The average valence scores - on a scale of 1 to -1 - spanned from .55 (Alarmed) to -.7 (Dismissive) (see Figure 2 ). The average sentence-specific composite scores - on a scale of 18 to -18 - ranged from 9.27 (Alarmed) to -4.64 (Dismissive) (see Figure 3 ).
Hypothesis Test
The Wilcoxon signed rank tests indicated only partial support for our hypothesis. Using valence as the dependent measure, the null hypothesis can be rejected only for the Alarmed ( p = .04) and Concerned ( p = .02) segments, but not for the Cautious ( p = .50), Disengaged ( p = .36) or Doubtful segments ( p = .50). Using the composite sentence-specific score as the dependent measure, the null hypothesis can be rejected for the Alarmed ( p = .001), Concerned ( p < .01) and Cautious ( p = .01) segments, and marginally rejected for the Disengaged segment ( p = .06), but not for the Doubtful segment ( p = .61) segment.
In sum, there was clear evidence that the Alarmed and Concerned segments responded positively to the public health essay, and mixed evidence that the Cautious and Disengaged responded positively. There was no evidence that the Doubtful responded positively. It is worthy of note, however, that all six segments agreed with the essay's opening frame device (O1) that "good health is a great blessing," suggesting that human health and wellbeing is a widely shared value.
Table 3 summarizes the thematic content of the statements made by respondents when they were asked to discuss their general reactions to the public health essay. Across segments, not surprisingly, a substantial proportion of comments focused on the presentation of evidence or the stylistic tone of the essay. For the Alarmed and Concerned segments, roughly a third of their statements reflected personal agreement with the essay. In contrast, among the Dismissive, roughly a third of their statements characterized the essay as biased or alarmist. Relative to other possible reactions, substantial proportions of the statements made by the Concerned (18%), Cautious (19%), Disengaged (13%); and Doubtful (16%) indicated that the essay was informative and/or thought provoking.
Benefit versus Threat Statements
The Wilcoxon signed rank tests used to compare segments on the perceived clarity and helpfulness of the threat statements in the first part of the essay against the health benefits of mitigation-related policy actions in the second part of the essay showed a significant main effect ( p ≤ .05) for all segments except the Alarmed ( p = .17). The Dismissive segment showed the largest difference between the sections of the essay (6.10), followed by the Doubtful (3.69), the Cautious (3.57), the Concerned (3.13), and the Disengaged (2.12). Using a weighted t-test, the estimated gain from the Threat to Benefits sections across all segments was 3.17 ( p < .0001), with a 95% confidence interval of 1.85 to 4.49. In short, the health benefits associated with mitigation-related policy actions were seen as clearer and more useful than the preceding threat statements in the essay.
Also worthy of note, as Figures 4 and 5 indicate, is that all six segments reacted positively to the following statements focusing on specific mitigation-related policy actions that lead to human health benefits:
"Taking actions to limit global warming - by making our energy sources cleaner and our cars and appliances more efficient, by making our cities and towns friendlier to trains, buses, and bikers and walkers, and by improving the quality and safety of our food - will improve the health of almost every American."
"Cleaner energy sources and more efficient use of energy will lead to healthier air for children and adults to breathe."
"Improving the design of our cities and towns in ways that make it easier to get around on foot, by bike and on mass transit will reduce the number of cars and help people become more physically active, lose weight."
Conversely, respondents in all segments responded less positively to the statement:
"Increasing our consumption of fruits and vegetables, and reducing our intake of meat - especially beef - will help people maintain a healthy weight, will help prevent heart disease and cancer, and will play an important role in limiting global warming."
Opening versus Concluding Framing Statements
The Wilcoxon signed rank test used to compare segments on their reactions to the opening versus concluding framing statements for each segment showed a significant or marginally significant main effect in the Alarmed ( p = .07), Concerned ( p < .01), Cautious ( p = .05), Disengaged ( p = .03) and Dismissive ( p < .01) segments; the trend was not significant in the Doubtful ( p = .14) segment. The largest differences were seen in the Concerned segment (4.31), followed by the Dismissive (4.09), Disengaged (3.8), Cautious (2.54) and the Alarmed segment (2.45). Again using a weighted t-test, the estimated increase from the Opening to Concluding sections across all segments was 3.30 ( p < .0001), with a 95% confidence interval of 2.14 to 4.47.
On the whole, people who read our public health-framed essay about climate change reacted positively to the information. People in the Alarmed and the Concerned segments demonstrated consistent positive response to the information, while people in the Cautious, Disengaged, and Doubtful segments were less consistent. Although we did not treat it as a dependent measure per se, many of the respondents in all five segments made open-ended comments about the essay that demonstrated a positive engagement with the material. For example, nearly half (44%) of the comments made by the Disengaged segment indicated that the essay reflected their personal point of view, was informative or thought-provoking, or offered valuable prescriptive information on how to take action relative to the climate problem. Similarly, 39% of the comments made by respondents in the Doubtful segment reflected one of these three themes. Moreover, the ascending sentence-specific evaluations between the opening and concluding sections of the essay, for the sample overall and for all of the segments (excluding the Dismissive), suggest that the value of the public health frame may not be immediate, but rather may manifest more fully after people have had time to consider the evidence, especially when this evidence is presented with specific mitigation-related policy actions that are likely to have human health benefits.
One of the most intriguing findings in the study - albeit not definitive due to the order effect of the information in the essay - is the robustness of the response across all six segments to information about the health benefits of taking action to address global warming.
Overall, we interpret these collective findings as providing partial support for our hypothesis that information about climate change framed in ways that encourage people to consider its human health context provides many Americans with a useful and engaging new frame of reference and that this new interpretation may broaden the personal significance and relevance of the issue. Our methods were exploratory, however, and additional research on this question is needed. To that end, we are further analyzing the data already collected to determine more systematically which specific ideas are most and also least resonant with members of each segment. We are also planning an experimental test of climate education material framed in various ways, including a public health frame. Additional research is needed to determine if these findings generalize across nations and other populations.
In the U.S., these findings are especially relevant given the "issue fatigue" that appears to be developing with regard to climate change among at least certain segments of the American public [ 26 ]. Recent public opinion polls in the U.S. have shown a marked decline in the proportion of adults who are worried about global warming, and even relative to the proportion who are convinced that global warming is happening [ 27 – 29 ]. The public health voice may offer an important hedge against such issue fatigue.
Suggesting a novel frame for climate change - i.e., a frame that people had not previously considered - is potentially useful when it helps people understand the issue more clearly by providing additional personal and societal relevance [ 30 , 31 ]. Re-defining climate change in public health terms should help people make connections to already familiar problems such as asthma, allergies, and infectious diseases experienced in their communities, while shifting the visualization of the issue away from remote Arctic regions, and distant peoples and animals. In the process, giving climate change a public health focus suggests that there is a need to both mitigate (i.e. reduce greenhouse gas emissions) and adapt to the problem (i.e. protect communities and people from current and future health related impacts). The frame also presents the opportunity to involve additional trusted communication partners on the issue, notably public health experts and local community leaders [ 13 ].
In conclusion, we believe that the public health community has an important perspective to share about climate change, a perspective that potentially offers the public a more salient way to comprehend an issue that has proven deeply difficult for many people to fully comprehend. Moreover, the public health perspective offers a vision of a better, healthier future - not just a vision of environmental disaster averted, and it focuses on a range of possible policy actions that offer local as well as global benefits. Many leading experts in climate change communication, including the present authors, have suggested that a positive vision for the future and a localization of the issue is precisely what has been missing from the public dialogue on climate change thus far [ 13 , 22 , 32 ].
Not all aspects of the public health implications, however, may be engaging. Certain key recommendations, such as eating less meat, tended to elicit counter-arguments among people in many of the segments in our research. Our research provides clues about specific public health messages that might not be helpful, and suggests the need in future research to look carefully for examples or associations that trigger counter-arguments and negative reactions.
There is an urgent need for the public health community to successfully educate the public and policy makers about the serious human health implications of climate change, and to engage those publics in appropriate preventive and adaptive responses. As a point of strategy, however, our findings may suggest that continuing to communicate about the problem of climate change is not likely to generate wider public engagement. Instead public health voices may be wise to focus their communication on the solutions and the many co-benefits that matter most to people.
Global Warming is a Threat to Peoples' Health & Wellbeing
Most people agree with the sentiment that "good health is a great blessing." Although not yet widely known, global warming poses a very real threat to the health and wellbeing of Americans and other people around the world. Experts at the World Health Organization say that global warming is already leading to an increase in the rate of some diseases and is causing many deaths. If our government and other governments around the world do not soon take steps to limit global warming, a growing number of people in the United States will likely be harmed and killed. Conversely, if our government does take steps to limit global warming, our health and wellbeing will likely improve in a number of important ways.
Our health will suffer if we don't take action
Global warming can harm people both directly and indirectly. Directly, global warming causes more extreme weather patterns including more frequent heat waves, more violent storms, and rising sea-levels - all of which can lead to people being harmed or killed. Indirectly, global warming harms the quality of our water, air and food, and our ecosystems, all of which can lead to increasing rates of disease and death. If we do not act now to limit global warming, experts at the U.S. Centers for Disease Control and Prevention say that global warming will harm people in every region of the United States. As a result of the poor air quality caused by global warming, children will become more likely to develop asthma, and the asthma they suffer from will be more severe; adults who have heart and lung diseases will become more likely to be hospitalized or die from their illness. An increasing number of extreme heat waves, floods, storms, fires and droughts caused by the changes in our climate will lead to more people being injured or killed. New infectious diseases (such as West Nile Virus) and old infectious diseases that we had previously eradicated from the United States (such as malaria and Dengue Fever) are likely to become an increasing problem for us as our climate warms.
Our health will benefit if we do take action
According to a recent study published in the medical journal Lancet, taking actions to limit global warming - by making our energy sources cleaner and our cars and appliances more efficient, by making our cities and towns friendlier to trains, buses, and bikers and walkers, and by improving the quality and safety of our food - will improve the health of almost every American. Cleaner energy sources and more efficient use of energy will lead to healthier air for children and adults to breathe. Improving the design of our cities and towns in ways that make it easier and safer to get around on foot, by bike and on mass transit will reduce the number of cars on our roads and will help people become more physically active and lose weight. Increasing our consumption of fruits and vegetables, and reducing our intake of meat - especially beef - will help people maintain a healthy weight, will help prevent heart disease and cancer, and will play an important role in limiting global warming.
Peoples' health is dependent on the health of the environment in which we live. Global warming offers America an opportunity to make choices that are healthier for us, and for our climate.
Karl TR, Melillo JM, Peterson TC, (Eds): Global climate change impacts in the United States. 2009, Cambridge University Press
Google Scholar
IPCC: Climate change 2007: impacts, adaptation and vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Edited by: Parry ML, Canziani OF, Palutikof JP, van der Linden PJ, Hanson CE. 2007, Cambridge University Press
Frumkin H, McMichael AJ: Climate change and public health: thinking, acting and communicating. American Journal of Preventive Medicine. 2008, 35 (5): 403-410. 10.1016/j.amepre.2008.08.019.
Article PubMed Google Scholar
Jay M, Marmot MG: Health and climate change: will a global commitment be made at the UN climate change conference in December?. BMJ. 2009, 339: 645-646. 10.1136/bmj.b3669.
Article Google Scholar
Environmental Protection Agency: Endangerment and cause or contribute findings for greenhouse gases under Section 202(a) of the Clean Air Act. Federal Register. 2009, 74 (239): 66495-66546. [ http://www.epa.gov/climatechange/endangerment/downloads/Federal_Register-EPA-HQ-OAR-2009-0171-Dec.15-09.pdf ]
McMichael AJ, Woodruff RE, Hales S: Climate change and human health: present and future risks. Lancet. 2006, 367: 859-69. 10.1016/S0140-6736(06)68079-3.
Maibach EW, Roser-Renouf C, Leiserowitz A: Global warming's Six Americas 2009: an audience segmentation analysis. 2009, [ http://climatechange.gmu.edu ]
Berry P, Clarke K, Pajot M, Hutton D, Verret M: The role of risk perception and health communication in adapting to the health impacts of climate change in Canada. Natural Resources Canada. 2009, Ottawa, Canada
DeBono R: Maltese public perceptions on climate change and health. MPH thesis. 2009, University of Malta, Faculty of Medicine and Surgery
Leiserowitz A: American risk perceptions: is climate change dangerous?. Risk Anal. 2005, 25: 1433-42. 10.1111/j.1540-6261.2005.00690.x.
Gamson WA, Croteau D, Hoynes W, Sasson T: Media images and the social construction of reality. Annual Review of Sociology. 1992, 18: 373-93. 10.1146/annurev.so.18.080192.002105.
Price V, Nir L, Capella JN: Framing public discussion of gay civil unions. Public Opinion Quarterly. 2005, 69 (2): 179-212. 10.1093/poq/nfi014.
Nisbet MC: Communicating climate change: why frames matter to public engagement. Environment. 2009, 51 (2): 514-518.
Ockwell D, Whitmarsh L, O'Neill S: Reorienting climate change communication for effective mitigation: forcing people to be green or fostering grass roots engagement?. Science Communication. 2009, 30 (3): 305-327. 10.1177/1075547008328969.
Balbus J, Ebi K, Finzer L, Malina C, Chadwick A, McBride D, Chuk M, Maibach E: Are we ready?: preparing for the public health challenges of climate change. Environmental Defense Fund. 2008
Maibach EW, Chadwick A, McBride D, Chuk M, Ebi K, Balbus J: Climate change and local public health in the United States: Preparedness, programs and perceptions of local public health department directors. PLoS ONE. 2008, 3 (7): 10.1371/journal.pone.0002838.
Association of State and Territorial Health Officials: Climate change: a serious threat to public health. 2009, [ http://www.astho.org/Search.aspx?s=climate%20change ]
World Health Organization: WHO workplan on climate change and health. 2009, [ http://www.who.int/globalchange/wha_plans_objectives/en/index1.html ]
The Lancet. 2007, 370 (9591):
The Lancet. 2009, 374 (9707):
Frumkin H, McMichael AJ, Hess JJ, (Eds): Climate change and the health of the public. American Journal of Preventive Medicine. 2008, 35 (5):
Maibach EW, Roser-Renouf C, Leiserowitz A: Communication and marketing as climate change-intervention assets: A public health perspective. American Journal of Preventive Medicine. 2008, 35 (5): 488-500. 10.1016/j.amepre.2008.08.016.
U. S. Census Bureau: Census Bureau Regions and Divisions with State FIPS Codes. Retrieved April 21, 2010, [ http://www.census.gov/geo/www/us_regdiv.pdf ]
Hayes AF, Krippendorff K: Answering the call for a standard reliability measure for coding data. Communication Methods and Measures. 2007, 1: 77-89.
Krippendorff K: Content Analysis: An Introduction to Its Methodology. 1980, Newbury Park, CA: Sage
Kerr RA: Amid worrisome signs of warming, 'climate fatigue' sets in. Science. 2009, 326: 926-928. 10.1126/science.326.5955.926.
Article CAS PubMed Google Scholar
ABC News/Washington Post: Conservatives, Republicans move away from belief that the Earth is warming. [ http://abcnews.go.com/images/PollingUnit/1096a7GlobalWarming.pdf ]
Pew Research Center for the People & the Press: Fewer Americans see solid evidence of global warming. [ http://people-press.org/report/556/global-warming ]
Gallup: Increased number think global warming is "exaggerated.". [ http://www.gallup.com/poll/116590/Increased-Number-Think-Global-Warming-Exaggerated.aspx ]
Price V, Tewksbury D: News values and public opinion: a theoretical account of media priming and framing. Progress in the Communication Sciences. Edited by: Barnett GA, Boster FJ. 1997, New York: Ablex, 13: 173-212.
Scheufele DA, Tewksbury D: Framing, agenda setting and priming: the evolution of three media effects models. Journal of Communication. 2007, 57 (1): 9-20.
Moser SC, Dilling L: Creating a Climate for Change: Communicating Climate Change and Facilitating Social Change. 2007, Cambridge, UK: Cambridge University Press
Book Google Scholar
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/10/299/prepub
Download references
Acknowledgements
This research was supported by a Robert Wood Johnson Foundation Health Policy Investigator Award.
Author information
Authors and affiliations.
Center for Climate Change Communication, Department of Communication, George Mason University, Fairfax, VA, USA
Edward W Maibach, Matthew Nisbet, Paula Baldwin & Karen Akerlof
School of Communication, American University, Washington, DC, USA
Matthew Nisbet
Department of Statistics, George Mason University, Fairfax, VA, USA
Guoqing Diao
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Edward W Maibach .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
EWM and MN developed the research question, participated in all aspects of the research, and wrote the first draft of the paper. PB coded and conducted preliminary data analysis. KA managed the data collection, conducted data analysis and prepared all figures and tables. GD conducted the final data analysis. All authors contributed to the final draft of the paper.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.

Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, authors’ original file for figure 6, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Maibach, E.W., Nisbet, M., Baldwin, P. et al. Reframing climate change as a public health issue: an exploratory study of public reactions. BMC Public Health 10 , 299 (2010). https://doi.org/10.1186/1471-2458-10-299
Download citation
Received : 04 January 2010
Accepted : 01 June 2010
Published : 01 June 2010
DOI : https://doi.org/10.1186/1471-2458-10-299
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Climate Change
- Global Warming
- West Nile Virus
- Dependent Measure
- Public Engagement
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.11(6); 2021

Original research
Health effects of climate change: an overview of systematic reviews, rhea j rocque.
1 Prairie Climate Centre, The University of Winnipeg, Winnipeg, Manitoba, Canada
Caroline Beaudoin
2 Faculty of Medicine, Université Laval, Quebec, QC, Canada
Ruth Ndjaboue
3 VITAM Research Centre for Sustainable Health, Quebec, QC, Canada
Laura Cameron
Louann poirier-bergeron, rose-alice poulin-rheault, catherine fallon.
4 CHUQ Research Centre, Quebec, QC, Canada
Andrea C Tricco
5 Li Ka Shing Knowledge Institute, Toronto, Ontario, Canada
6 Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada
Holly O Witteman
Associated data.
bmjopen-2020-046333supp001.pdf
bmjopen-2020-046333supp002.pdf
bmjopen-2020-046333supp003.pdf
bmjopen-2020-046333supp004.pdf
bmjopen-2020-046333supp005.pdf
Data sharing not applicable as no datasets generated and/or analysed for this study. All data relevant to the study are included in the article or uploaded as supplementary information. Additional data are not available.
We aimed to develop a systematic synthesis of systematic reviews of health impacts of climate change, by synthesising studies’ characteristics, climate impacts, health outcomes and key findings.
We conducted an overview of systematic reviews of health impacts of climate change. We registered our review in PROSPERO (CRD42019145972). No ethical approval was required since we used secondary data. Additional data are not available.
Data sources
On 22 June 2019, we searched Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, Cochrane and Web of Science.
Eligibility criteria
We included systematic reviews that explored at least one health impact of climate change.
Data extraction and synthesis
We organised systematic reviews according to their key characteristics, including geographical regions, year of publication and authors’ affiliations. We mapped the climate effects and health outcomes being studied and synthesised major findings. We used a modified version of A MeaSurement Tool to Assess systematic Reviews-2 (AMSTAR-2) to assess the quality of studies.
We included 94 systematic reviews. Most were published after 2015 and approximately one-fifth contained meta-analyses. Reviews synthesised evidence about five categories of climate impacts; the two most common were meteorological and extreme weather events. Reviews covered 10 health outcome categories; the 3 most common were (1) infectious diseases, (2) mortality and (3) respiratory, cardiovascular or neurological outcomes. Most reviews suggested a deleterious impact of climate change on multiple adverse health outcomes, although the majority also called for more research.
Conclusions
Most systematic reviews suggest that climate change is associated with worse human health. This study provides a comprehensive higher order summary of research on health impacts of climate change. Study limitations include possible missed relevant reviews, no meta-meta-analyses, and no assessment of overlap. Future research could explore the potential explanations between these associations to propose adaptation and mitigation strategies and could include broader sociopsychological health impacts of climate change.
Strengths and limitations of this study
- A strength of this study is that it provides the first broad overview of previous systematic reviews exploring the health impacts of climate change. By targeting systematic reviews, we achieve a higher order summary of findings than what would have been possible by consulting individual original studies.
- By synthesising findings across all included studies and according to the combination of climate impact and health outcome, we offer a clear, detailed and unique summary of the current state of evidence and knowledge gaps about how climate change may influence human health.
- A limitation of this study is that we were unable to access some full texts and therefore some studies were excluded, even though we deemed them potentially relevant after title and abstract inspection.
- Another limitation is that we could not conduct meta-meta-analyses of findings across reviews, due to the heterogeneity of the included systematic reviews and the relatively small proportion of studies reporting meta-analytic findings.
- Finally, the date of the systematic search is a limitation, as we conducted the search in June 2019.
Introduction
The environmental consequences of climate change such as sea-level rise, increasing temperatures, more extreme weather events, increased droughts, flooding and wildfires are impacting human health and lives. 1 2 Previous studies and reviews have documented the multiple health impacts of climate change, including an increase in infectious diseases, respiratory disorders, heat-related morbidity and mortality, undernutrition due to food insecurity, and adverse health outcomes ensuing from increased sociopolitical tension and conflicts. 2–5 Indeed, the most recent Lancet Countdown report, 2 which investigates 43 indicators of the relationship between climate change and human health, arrived at their most worrisome findings since the beginning of their on-going annual work. This report underlines that the health impacts of climate change continue to worsen and are being felt on every continent, although they are having a disproportionate and unequal impact on populations. 2 Authors caution that these health impacts will continue to worsen unless we see an immediate international response to limiting climate change.
To guide future research and action to mitigate and adapt to the health impacts of climate change and its environmental consequences, we need a complete and thorough overview of the research already conducted regarding the health impacts of climate change. Although the number of original studies researching the health impacts of climate change has greatly increased in the recent decade, 2 these do not allow for an in-depth overview of the current literature on the topic. Systematic reviews, on the other hand, allow a higher order overview of the literature. Although previous systematic reviews have been conducted on the health impacts of climate change, these tend to focus on specific climate effects (eg, impact of wildfires on health), 6 7 health impacts (eg, occupational health outcomes), 8 9 countries, 10–12 or are no longer up to date, 13 14 thus limiting our global understanding of what is currently known about the multiple health impacts of climate change across the world.
In this study, we aimed to develop such a complete overview by synthesising systematic reviews of health impacts of climate change. This higher order overview of the literature will allow us to better prepare for the worsening health impacts of climate change, by identifying and describing the diversity and range of health impacts studied, as well as by identifying gaps in previous research. Our research objectives were to synthesise studies’ characteristics such as geographical regions, years of publication, and authors’ affiliations, to map the climate impacts, health outcomes, and combinations of these that have been studied, and to synthesise key findings.
We applied the Cochrane method for overviews of reviews. 15 This method is designed to systematically map the themes of studies on a topic and synthesise findings to achieve a broader overview of the available literature on the topic.
Research questions
Our research questions were the following: (1) What is known about the relationship between climate change and health, as shown in previous systematic reviews? (2) What are the characteristics of these studies? We registered our plan (CRD42019145972 16 ) in PROSPERO, an international prospective register of systematic reviews and followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 17 to report our findings, as a reporting guideline for overviews is still in development. 18
Search strategy and selection criteria
To identify relevant studies, we used a systematic search strategy. There were two inclusion criteria. We included studies in this review if they (1) were systematic reviews of original research and (2) reported at least one health impact as it related (directly or indirectly) to climate change.
We defined a systematic review, based on Cochrane’s definition, as a review of the literature in which one ‘attempts to identify, appraise and synthesize all the empirical evidence that meets pre-specified eligibility criteria to answer a specific research question [by] us[ing] explicit, systematic methods that are selected with a view aimed at minimizing bias, to produce more reliable findings to inform decision making’. 19 We included systematic reviews of original research, with or without meta-analyses. We excluded narrative reviews, non-systematic literature reviews and systematic reviews of materials that were not original research (eg, systematic reviews of guidelines.)
We based our definition of health impacts on the WHO’s definition of health as, ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. 20 Therefore, health impacts included, among others, morbidity, mortality, new conditions, worsening/improving conditions, injuries and psychological well-being. Included studies could refer to climate change or global warming directly or indirectly, for instance, by synthesising the direct or indirect health effects of temperature rises or of natural conditions/disasters made more likely by climate change (eg, floods, wildfires, temperature variability, droughts.) Although climate change and global warming are not equivalent terms, in an effort to avoid missing relevant literature, we included studies using either term. We included systematic reviews whose main focus was not the health impacts of climate change, providing they reported at least one result regarding health effects related to climate change (or consequences of climate change.) We excluded studies if they did not report at least one health effect of climate change. For instance, we excluded studies which reported on existing measures of health impacts of climate change (and not the health impact itself) and studies which reported on certain health impacts without a mention of climate change, global warming or environmental consequences made more likely by climate change.
On 22 June 2019, we retrieved systematic reviews regarding the health effects of climate change by searching from inception the electronic databases Medline, CINAHL, Embase, Cochrane, Web of Science using a structured search (see online supplemental appendix 1 for final search strategy developed by a librarian.) We did not apply language restrictions. After removing duplicates, we imported references into Covidence. 21
Supplementary data
Screening process and data extraction.
To select studies, two trained analysts first screened independently titles and abstracts to eliminate articles that did not meet our inclusion criteria. Next, the two analysts independently screened the full text of each article. A senior analyst resolved any conflict or disagreement.
Next, we decided on key information that needed to be extracted from studies. We extracted the first author’s name, year of publication, number of studies included, time frame (in years) of the studies included in the article, first author’s institution’s country affiliation, whether the systematic review included a meta-analysis, geographical focus, population focus, the climate impact(s) and the health outcome(s) as well as the main findings and limitations of each systematic review.
Two or more trained analysts (RR, CB, RN, LC, LPB, RAPR) independently extracted data, using Covidence and spreadsheet software (Google Sheets). An additional trained analyst from the group or senior research team member resolved disagreements between individual judgments.
Coding and data mapping
To summarise findings from previous reviews, we first mapped articles according to climate impacts and health outcomes. To develop the categories of climate impacts and health outcomes, two researchers (RR and LC) consulted the titles and abstracts of each article. We started by identifying categories directly based on our data and finalised our categories by consulting previous conceptual frameworks of climate impacts and health outcomes. 1 22 23 The same two researchers independently coded each article according to their climate impact and health outcome. We then compared coding and resolved disagreements through discussion.
Next, using spreadsheet software, we created a matrix to map articles according to their combination of climate impacts and health outcomes. Each health outcome occupied one row, whereas climate impacts each occupied one column. We placed each article in the matrix according to the combination(s) of their climate impact(s) and health outcome(s). For instance, if we coded an article as ‘extreme weather’ for climate and ‘mental health’ for health impact, we noted the reference of this article in the cell at the intersection of these two codes. We calculated frequencies for each cell to identify frequent combinations and gaps in literature. Because one study could investigate more than one climate impact and health outcome, the frequency counts for each category could exceed the number of studies included in this review.
Finally, we re-read the Results and Discussion sections of each article to summarise findings of the studies. We first wrote an individual summary for each study, then we collated the summaries of all studies exploring the same combination of categories to develop an overall summary of findings for each combination of categories.
Quality assessment
We used a modified version of AMSTAR-2 to assess the quality of the included systematic reviews ( online supplemental appendix 2 ). The purpose of this assessment was to evaluate the quality of the included studies as a whole to get a sense of the overall quality of evidence in this field. Therefore, individual quality scores were not compiled for each article, but scores were aggregated according to items. Since AMSTAR-2 was developed for syntheses of systematic reviews of randomised controlled trials, working with a team member with expertise in knowledge synthesis (AT), we adapted it to suit a research context that is not amenable to randomised controlled trials. For instance, we changed assessing and accounting for risk of bias in studies’ included randomised controlled trials to assessing and accounting for limitations in studies’ included articles. Complete modifications are presented in online supplemental appendix 2 .
Patient and public involvement
Patients and members of the public were not involved in this study.
Articles identified
As shown in the PRISMA diagram in figure 1 , from an initial set of 2619 references, we retained 94 for inclusion. More precisely, following screening of titles and abstracts, 146 studies remained for full-text inspection. During full-text inspection, we excluded 52 studies, as they did not report a direct health effect of climate change (n=17), did not relate to climate change (n=15), were not systematic reviews (n=10), or we could not retrieve the full text (n=10).

The flow chart for included articles in this review.
Study descriptions
A detailed table of all articles and their characteristics can be found in online supplemental appendix 3 . Publication years ranged from 2007 to 2019 (year of data extraction), with the great majority of included articles (n=69; 73%) published since 2015 ( figure 2 ). A median of 30 studies had been included in the systematic reviews (mean=60; SD=49; range 7–722). Approximately one-fifth of the systematic reviews included meta-analyses of their included studies (n=18; 19%). The majority of included systematic reviews’ first authors had affiliations in high-income countries, with the largest representations by continent in Europe (n=30) and Australia (n=24) ( figure 3 ). Countries of origin by continents include (from highest to lowest frequency, then by alphabetical order): Europe (30); UK (9), Germany (6), Italy (4), Sweden (4), Denmark (2), France (2), Georgia (1), Greece (1) and Finland (1); Australia (24); Asia (21); China (11), Iran (4), India (1), Jordan (1), Korea (1), Nepal (1), Philippines (1), Taiwan (1); North America (16); USA (15), Canada (1); Africa (2); Ethiopia (1), Ghana (1), and South America (1); Brazil (1).

Number of included systematic reviews by year of publication.

Number of publications according to geographical affiliation of the first author.
Regarding the geographical focus of systematic reviews, most of the included studies (n=68; 72%) had a global focus or no specified geographical limitations and therefore included studies published anywhere in the world. The remaining systematic reviews either targeted certain countries (n=12) (1 for each Australia, Germany, Iran, India, Ethiopia, Malaysia, Nepal, New Zealand and 2 reviews focused on China and the USA), continents (n=5) (3 focused on Europe and 2 on Asia), or regions according to geographical location (n=6) (1 focused on Sub-Saharan Africa, 1 on Eastern Mediterranean countries, 1 on Tropical countries, and 3 focused on the Arctic), or according to the country’s level of income (n=3) (2 on low to middle income countries, 1 on high income countries).
Regarding specific populations of interest, most of the systematic reviews did not define a specific population of interest (n=69; 73%). For the studies that specified a population of interest (n=25; 26.6%), the most frequent populations were children (n=7) and workers (n=6), followed by vulnerable or susceptible populations more generally (n=4), the elderly (n=3), pregnant people (n=2), people with disabilities or chronic illnesses (n=2) and rural populations (n=1).
We assessed studies for quality according to our revised AMSTAR-2. Complete scores for each article and each item are available in online supplemental appendix 4 . Out of 94 systematic reviews, the most commonly fully satisfied criterion was #1 (Population, Intervention, Comparator, Outcome (PICO) components) with 81/94 (86%) of included systematic reviews fully satisfying this criterion. The next most commonly satisfied criteria were #16 (potential sources of conflict of interest reported) (78/94=83% fully), #13 (account for limitations in individual studies) (70/94=75% fully and 2/94=2% partially), #7 (explain both inclusion and exclusion criteria) (64/94=68% fully and 19/94=20% partially), #8 (description of included studies in adequate detail) (36/94=38% fully and 41/94=44% partially), and #4 (use of a comprehensive literature search strategy) (0/94=0% fully and 80/94=85% partially). For criteria #11, #12, and #15, which only applied to reviews including meta-analyses, 17/18 (94%) fully satisfied criterion #11 (use of an appropriate methods for statistical combination of results), 12/18 (67%) fully satisfied criterion #12 (assessment of the potential impact of Risk of Bias (RoB) in individual studies) (1/18=6% partially), and 11/18 (61%) fully satisfied criterion #15 (an adequate investigation of publication bias, small study bias).
Climate impacts and health outcomes
Regarding climate impacts, we identified 5 mutually exclusive categories, with 13 publications targeting more than one category of climate impacts: (1) meteorological (n=71 papers) (eg, temperature, heat waves, humidity, precipitation, sunlight, wind, air pressure), (2) extreme weather (n=24) (eg, water-related, floods, cyclones, hurricanes, drought), (3) air quality (n=7) (eg, air pollution and wildfire smoke exposure), (4) general (n=5), and (5) other (n=3). Although heat waves could be considered an extreme weather event, papers investigating heat waves’ impact on health were classified in the meteorological impact category, since some of these studies treated them with high temperature. ‘General’ climate impacts included articles that did not specify climate change impacts but stated general climate change as their focus. ‘Other’ climate impacts included studies investigating other effects indirectly related to climate change (eg, impact of environmental contaminants) or general environmental risk factors (eg, environmental hazards, sanitation and access to clean water.)
We identified 10 categories to describe the health outcomes studied by the systematic reviews, and 29 publications targeted more than one category of health outcomes: (1) infectious diseases (n=41 papers) (vector borne, food borne and water borne), (2) mortality (n=32), (3) respiratory, cardiovascular and neurological (n=23), (4) healthcare systems (n=16), 5) mental health (n=13), (6) pregnancy and birth (n=11), 7) nutritional (n=9), (8) skin diseases and allergies (n=8), (9) occupational health and injuries (n=6) and (10) other health outcomes (n=17) (eg, sleep, arthritis, disability-adjusted life years, non-occupational injuries, etc)
Figure 4 depicts the combinations of climate impact and health outcome for each study, with online supplemental appendix 5 offering further details. The five most common combinations are studies investigating the (1) meteorological impacts on infectious diseases (n=35), (2) mortality (n=24) and (3) respiratory, cardiovascular and neurological outcomes (n=17), (4) extreme weather events’ impacts on infectious diseases (n=14), and (5) meteorological impacts on health systems (n=11).

Summary of the combination of climate impact and health outcome (frequencies). The total frequency for one category of health outcome could exceed the number of publications included in this health outcome, since one publication could explore the health impact according to more than one climate factor (eg, one publication could explore both the impact of extreme weather events and temperature on mental health).
For studies investigating meteorological impacts on health, the three most common health outcomes studied were impacts on (1) infectious diseases (n=35), (2) mortality (n=24) and (3) respiratory, cardiovascular and neurological outcomes (n=17). Extreme weather event studies most commonly reported health outcomes related to (1) infectious diseases (n=14), (2) mental health outcomes (n=9) and (3) nutritional outcomes (n=6) and other health outcomes (eg, injuries, sleep) (n=6). Studies focused on the impact of air quality were less frequent and explored mostly health outcomes linked to (1) respiratory, cardiovascular and neurological outcomes (n=6), (2) mortality (n=5) and (3) pregnancy and birth outcomes (n=3).
Summary of findings
Most reviews suggest a deleterious impact of climate change on multiple adverse health outcomes, with some associations being explored and/or supported with consistent findings more often than others. Some reviews also report conflicting findings or an absence of association between the climate impact and health outcome studied (see table 1 for a detailed summary of findings according to health outcomes).
Summary of findings from systematic reviews according to health outcome and climate impact
| Climate impact | n | Summary of findings |
| ) | ||
| ) | ||
| Meteorological | 22 | Systematic reviews suggest that meteorological factors, such as temperature, precipitation, humidity, and wind, are associated with diverse vector-borne infectious diseases, including malaria and dengue. This association was mostly proportional (eg, higher temperature and increased rainfall associated with vector-borne diseases), although findings were at times conflicting, with some suggesting an inversely proportional association (eg, decreased rainfall) or no association at all (eg, with the human puumala hantavirus Infection.) Geographical location, seasonality and potential interaction with other climate-related factors may partly explain these inconsistencies. Temperature, humidity and rainfall were the most common and important meteorological factors reported by reviews and factors such as wind, air pressure and sunshine were reported less often. |
| Extreme weather | 7 | There are limited and conflicting findings concerning the association of extreme weather events with vector-borne diseases. Some reviews suggest water-related extreme events and flooding are associated with an increased risk of vector-borne diseases, while drought is associated with a reduction of dengue incidence. Other reviews focused specifically on Puerto Rico and Australia did not find an association between hurricanes and/or floods and mosquito-borne disease transmission. |
| ) | ||
| Meteorological | 14 | Reviews suggest that meteorological factors, such as temperature, precipitation and humidity, are associated with diverse food-borne and water-borne infectious diseases, in particular, cholera, schistosomiasis, salmonella and gastroenteritis. Overall, higher temperatures and humidity, along with lower precipitation was associated with these infectious diseases. Directionality and strength of the association seemed to vary according to disease and pathogens, seasons and geographical region. |
| Extreme weather | 10 | Reviews suggest a proportional association between extreme water-related events, such as flooding and heavy rainfall, and food-borne and water-borne diseases, including diarrhoea, food contamination, cholera. Drought may also be proportionally associated with food-borne and water-borne disease, but these associations are less consistent than those with water-related extreme events. |
| ) | ||
| Meteorological | 8 | Reviews suggest an association of most meteorological factors, such as temperature and humidity, with various other infectious diseases, including meningitis, Ebola, influenza, and paediatric infectious diseases such as hand-foot-and-mouth disease. This association was mostly proportional for meteorological factors such as temperature, diurnal temperature range and humidity, although some meteorological factors, such as air pressure and lower temperatures were inversely proportional to these diseases. Some conflicting evidence is reported concerning the association with some meteorological factors, such as sunshine with hand-foot-and-mouth disease, and humidity and paediatric infectious diseases. No association was found between some meteorological factors, such as precipitation, wind speed and sunshine with hand-foot-and-mouth disease. |
| ) | ||
| Meteorological | 24 | Reviews suggest that temperature (high, low, or diurnal range) was consistently associated with all-cause and cause-specific mortality. A strong association was reported between heat (including heat waves) and mortality (all-cause), heat related, stroke related, cardiovascular related, and respiratory related, especially in rural, very young children and ageing populations. Mortality seems to be the most frequent health outcome studied in association with heatwaves. Inconsistent results are found concerning the association between heat and childhood mortality. Due to limited evidence, this association was weaker in some geographical regions. Also, heat wave intensity (compared with duration) was more strongly associated with heat-related mortality. Finally, although less studied, low temperature was also associated with mortality, specifically respiratory, stroke and cardiovascular mortality. |
| Extreme weather | 5 | Reviews suggest an association between extreme weather events such as floods, droughts, cyclones and other water-related events, with direct (eg, drowning) and indirect long-term mortality (eg, due to malnutrition, environmental toxin exposure, armed conflict, etc). |
| Air quality | 5 | Reviews suggest an association between exposure to air pollution or wildfire smoke and air pollution related-mortality, such as respiratory-specific mortality. There is currently limited evidence, but reviews suggest a potential association between wildfire smoke exposure and cardiovascular-specific mortality. |
| ) | ||
| General | 1 | A review suggests a proportional association between climate change, in general, and ragweed pollen allergies in Europe. |
| Meteorological | 17 | Reviews suggest an association between meteorological factors, such as temperature and humidity, and cardiovascular, respiratory and neurological outcomes. Exposure to high temperatures and extreme heat are associated to cardiovascular and respiratory diseases, stroke, long-term neurological outcomes (due to heat strokes), myocardial infarction, and childhood asthma and paediatric respiratory diseases. A review also suggests a beneficial association between heat and the shortening of a respiratory virus season. Exposure to low temperature (cold), temperature drop, or diurnal temperature range was associated with cardiovascular and respiratory diseases, stroke, and myocardial infarctions. Humidity (most often high humidity, but also lower humidity) and low temperatures were also associated with respiratory diseases in children, including childhood asthma. |
| Extreme weather | 1 | A previous review suggests an association between drought and respiratory and cardiovascular outcomes, most likely due to droughts leading to increased dust in the air. |
| Air quality | 6 | Reviews suggest a proportional association between exposure to air pollution or wildfire smoke exposure and respiratory outcomes, including asthma, chronic obstructive pulmonary disease, coughing, wheezing and overall lung function. Although there is currently limited evidence, reviews also suggest a potential association between air pollution or wildfire smoke exposure and cardiovascular outcomes. |
| ) | ||
| General | 1 | A previous review suggests that climate change in general puts a strain on public health resources, via population health issues and shows that using an integrated surveillance system may guide future adaptation to climate change. |
| Meteorological | 11 | Previous reviews suggest an association between temperature change extreme heat, aridity and cold temperatures and an increase in use of healthcare services (mostly linked to heat-related health impacts), such as an increase in emergency department visits, hospital admissions and use of ambulances. |
| Extreme weather | 2 | Reviews suggest that extreme weather events and flooding may be associated with an increase in use of healthcare services (eg, increased hospitalisations) and a compromised quality of care as extreme weather events may lead to power outages. |
| Air quality | 2 | Reviews suggest an association between wildfire smoke exposure and an increase in use of healthcare services, such as an increase in emergency department visits. |
| ) | ||
| Meteorological | 3 | Reviews suggest an association of most meteorological factors such as temperature increase, aridity, heat and heat waves with mental health outcomes, including hospital admissions for mental health reasons, suicide, and exacerbation of pre-existing mental health conditions, difficulty sleeping and fatigue. No association was found between sunlight duration and suicide incidence. |
| Extreme weather | 9 | Most reviews reported a proportional association of extreme weather events, flooding and drought with diverse mental health issues, including, psychological distress, post-traumatic stress disorder, anxiety, depression, psychotropic medication use, alcohol consumption. There was conflicting evidence regarding the association of floods with suicide, tobacco, alcohol and substance abuse. No association was found between drought and suicide. |
| Air quality | 1 | A previous review suggests no association between wildfire smoke exposure and mental health, as measured by physician visits and hospitalizations for mental health reasons during wildfires. |
| ) | ||
| Meteorological | 5 | Reviews suggest that adverse birth outcomes may be higher among people exposed to meteorological factors such as high temperature, heat, sunlight intensity, cold and humidity. These outcomes include low birth weight, preterm birth, eclampsia and preeclampsia, hypertension and length of pregnancy. The association between heat and adverse birth outcomes seems to have stronger support than the association with cold temperatures. |
| Extreme Weather | 2 | Reviews suggest a potential association of extreme weather events and flooding with adverse birth outcomes, such as low birth weight, preterm birth and preeclampsia. It is suggested that extreme weather events may indirectly affect birth outcomes via the pregnant person’s well-being (eg, stress and worry during pregnancy.) |
| Air quality | 3 | There is limited and inconsistent evidence concerning the association between wildfire smoke exposure and adverse birth outcomes, but reviews suggest a potential proportional association between wildfire smoke exposure and lower birth weight. |
| Other | 1 | The association between environmental pollutants and adverse birth outcomes (ie, preterm birth) remains unclear due to conflicting evidence. |
| ) | ||
| General | 1 | A review suggests an association between climate change and obesity. |
| Meteorological | 4 | Reviews suggest an association between meteorological factors, such as changes in temperature, heat and precipitation, with diverse nutritional outcomes, including undernutrition, malnutrition and child stunting. This association may be explained by the impact of meteorological factors, such as temperature increase and precipitation decrease, on crop production and food insecurity. |
| Extreme Weather | 6 | Reviews suggest an association between extreme weather events, such as flooding and droughts, and diverse nutritional outcomes, including malnutrition and undernutrition in children and adults via, among others, crops production and food insecurity (eg, low food aid following flooding. |
| Other | 1 | A review suggests a potential association between certain environmental risk factors (eg, sanitation, cooking fuels and food-borne mycotoxins), and childhood stunting, which could be aggravated by climate change. |
| ) | ||
| General | 1 | A review suggests a potential proportional association between climate change, in general, and skin and soft-tissue infections (eg, fatal vibrio vulnificus necrotising). |
| Meteorological | 7 | Reviews suggest an association of meteorological factors, such as ultraviolet light exposure, temperature and humidity, with diverse skin diseases and allergies, including skin cancer, sunburn, acute urticaria, eczema and paediatric skin irritabilities. Higher temperature and ultraviolet light exposure is proportionally associated with sunburn and skin cancer, while low humidity and low temperatures were associated with eczema and skin irritabilities in children. |
| ) | ||
| Meteorological | 6 | Reviews suggest that heat is associated with adverse occupational health outcomes, including injuries (eg, slips, trips, falls, wounds, lacerations and amputations), heat strain, dehydration and kidney diseases. This association was found in many occupational settings, including agriculture, construction, transport and fishing, and seems to affect both outdoor and indoor workers. This association may be explained by a combination of direct (eg, dehydration) and indirect factors (eg, impaired cognitive and physical performance.) |
| Other | 1 | A review suggests a potential association between environmental pollution (eg, heavy metals, fertilisers, etc) and occupational diseases, such as chronic kidney disease. This association is suggested to be affected by increasing temperatures. |
| ) | ||
| General | 1 | A review suggests a potential association between climate change in general and disability-adjusted life years, which is an indicator that quantifies ‘the burden of disease attributable to climate change’. Authors suggest that the cost of disability-adjusted life years could be high, especially in low-income to middle-income countries. |
| Meteorological | 10 | Reviews suggests an association between increasing temperatures and temperature changes, and other various health outcomes, including acute gouty arthritis, unintentional injuries, diabetes, genitourinary diseases, impaired sleep time and quality, cataracts (indirectly associated via people spending more time outside and therefore increased exposure to ultraviolet light), heat stress, heat exhaustion and kidney failure, and renal diseases, fever and electrolyte imbalance in children. |
| Extreme weather | 6 | Reviews suggests an association between extreme weather events, such as flooding, cyclones, hurricanes and drought, and other various health outcomes including injuries (eg, debris, diving in water that is shallower than expected), impaired sleep, oesophageal cancer (likely linked to high salinity of water due to droughts), and exacerbation of chronic illnesses. |
| Air quality | 1 | There is limited evidence, but a systematic review suggests a potential association between wildfire smoke exposure and ophthalmic outcomes, such as eye irritation and cataracts. |
Reviews that covered multiple climate impacts are listed in each relevant category.
Notable findings of health outcomes according to climate impact include the following. For meteorological factors (n=71), temperature and humidity are the variables most often studied and report the most consistent associations with infectious diseases and respiratory, cardiovascular, and neurological outcomes. Temperature is also consistently associated with mortality and healthcare service use. Some associations are less frequently studied, but remain consistent, including the association between some meteorological factors (eg, temperature and heat) and some adverse mental health outcomes (eg, hospital admissions for mental health reasons, suicide, exacerbation of previous mental health conditions), and the association between heat and adverse occupational outcomes and some adverse birth outcomes. Temperature is also associated with adverse nutritional outcomes (likely via crop production and food insecurity) and temperature and humidity are associated with some skin diseases and allergies. Some health outcomes are less frequently studied, but studies suggest an association between temperature and diabetes, impaired sleep, cataracts, heat stress, heat exhaustion and renal diseases.
Extreme weather events (n=24) are consistently associated with mortality, some mental health outcomes (eg, distress, anxiety, depression) and adverse nutritional outcomes (likely via crop production and food insecurity). Some associations are explored less frequently, but these studies suggest an association between drought and respiratory and cardiovascular outcomes (likely via air quality), between extreme weather events and an increased use of healthcare services and some adverse birth outcomes (likely due to indirect causes, such as experiencing stress). Some health outcomes are less frequently studied, but studies suggest an association between extreme weather events and injuries, impaired sleep, oesophageal cancer and exacerbation of chronic illnesses. There are limited and conflicting findings for the association between extreme weather events and infectious diseases, as well as for certain mental health outcomes (eg, suicide and substance abuse). At times, different types of extreme weather events (eg, drought vs flood) led to conflicting findings for some health outcomes (eg, mental health outcomes, infectious diseases), but for other health outcomes, the association was consistent independently of the extreme weather event studied (eg, mortality, healthcare service use and nutritional outcomes).
The impact of air quality on health (n=7) was less frequently studied, but the few studies exploring this association report consistent findings regarding an association with respiratory-specific mortality, adverse respiratory outcomes and an increase in healthcare service use. There is limited evidence regarding the association between air quality and cardiovascular outcomes, limited and inconsistent evidence between wildfire smoke exposure and adverse birth outcomes, and no association is found between exposure to wildfire smoke and increase in use of health services for mental health reasons. Only one review explored the impact of wildfire smoke exposure on ophthalmic outcomes, and it suggests that it may be associated with eye irritation and cataracts.
Reviews which stated climate change as their general focus and did not specify the climate impact(s) under study were less frequent (n=5), but they suggest an association between climate change and pollen allergies in Europe, increased use of healthcare services, obesity, skin diseases and allergies and an association with disability-adjusted life years. Reviews investigating the impact of other climate-related factors (n=3) show inconsistent findings concerning the association between environmental pollutant and adverse birth outcomes, and two reviews suggest an association between environmental risk factors and pollutants and childhood stunting and occupational diseases.
Most reviews concluded by calling for more research, noting the limitations observed among the studies included in their reviews, as well as limitations in their reviews themselves. These limitations included, among others, some systematic reviews having a small number of publications, 24 25 language restrictions such as including only papers in English, 26 27 arriving at conflicting evidence, 28 difficulty concluding a strong association due to the heterogeneity in methods and measurements or the limited equipment and access to quality data in certain contexts, 24 29–31 and most studies included were conducted in high-income countries. 32 33
Previous authors also discussed the important challenge related to exploring the relationship between climate change and health. Not only is it difficult to explore the potential causal relationship between climate change and health, mostly due to methodological challenges, but there are also a wide variety of complex causal factors that may interact to determine health outcomes. Therefore, the possible causal mechanisms underlying these associations were at times still unknown or uncertain and the impacts of some climate factors were different according to geographical location and specificities of the context. Nonetheless, some reviews offered potential explanations for the climate-health association, with the climate factor at times, having a direct impact on health (eg, flooding causing injuries, heat causing dehydration) and in other cases, having an indirect impact (eg, flooding causing stress which in turn may cause adverse birth outcomes, heat causing difficulty concentrating leading to occupational injuries.)
Principal results
In this overview of systematic reviews, we aimed to develop a synthesis of systematic reviews of health impacts of climate change by mapping the characteristics and findings of studies exploring the relationship between climate change and health. We identified four key findings.
First, meteorological impacts, mostly related to temperature and humidity, were the most common impacts studied by included publications, which aligns with findings from a previous scoping review on the health impacts of climate change in the Philippines. 10 Indeed, meteorological factors’ impact on all health outcomes identified in this review are explored, although some health outcomes are more rarely explored (eg, mental health and nutritional outcomes). Although this may not be surprising given that a key implication of climate change is the long-term meteorological impact of temperature rise, this finding suggests we also need to undertake research focused on other climate impacts on health, including potential direct and indirect effects of temperature rise, such as the impact of droughts and wildfire smoke. This will allow us to better prepare for the health crises that arise from these ever-increasing climate-related impacts. For instance, the impacts of extreme weather events and air quality on certain health outcomes are not explored (eg, skin diseases and allergies, occupational health) or only rarely explored (eg, pregnancy outcomes).
Second, systematic reviews primarily focus on physical health outcomes, such as infectious diseases, mortality, and respiratory, cardiovascular and neurological outcomes, which also aligns with the country-specific previous scoping review. 10 Regarding mortality, we support Campbell and colleagues’ 34 suggestion that we should expand our focus to include other types of health outcomes. This will provide better support for mitigation policies and allow us to adapt to the full range of threats of climate change.
Moreover, it is unclear whether the distribution of frequencies of health outcomes reflects the actual burden of health impacts of climate change. The most commonly studied health outcomes do not necessarily reflect the definition of health presented by the WHO as, ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. 20 This suggests that future studies should investigate in greater depth the impacts of climate change on mental and broader social well-being. Indeed, some reviews suggested that climate change impacts psychological and social well-being, via broader consequences, such as political instability, health system capacity, migration, and crime, 3 4 35 36 thus illustrating how our personal health is determined not only by biological and environmental factors but also by social and health systems. The importance of expanding our scope of health in this field is also recognised in the most recent Lancet report, which states that future reports will include a new mental health indicator. 2
Interestingly, the reviews that explored the mental health impacts of climate change were focused mostly on the direct and immediate impacts of experiencing extreme weather events. However, psychologists are also warning about the long-term indirect mental health impacts of climate change, which are becoming more prevalent for children and adults alike (eg, eco-anxiety, climate depression). 37 38 Even people who do not experience direct climate impacts, such as extreme weather events, report experiencing distressing emotions when thinking of the destruction of our environment or when worrying about one’s uncertain future and the lack of actions being taken. To foster emotional resilience in the face of climate change, these mental health impacts of climate change need to be further explored. Humanity’s ability to adapt to and mitigate climate change ultimately depends on our emotional capacity to face this threat.
Third, there is a notable geographical difference in the country affiliations of first authors, with three quarters of systematic reviews having been led by first authors affiliated to institutions in Europe, Australia, or North America, which aligns with the findings of the most recent Lancet report. 2 While perhaps unsurprising given the inequalities in research funding and institutions concentrated in Western countries, this is of critical importance given the significant health impacts that are currently faced (and will remain) in other parts of the world. Research funding organisations should seek to provide more resources to authors in low-income to middle-income countries to ensure their expertise and perspectives are better represented in the literature.
Fourth, overall, most reviews suggest an association between climate change and the deterioration of health in various ways, illustrating the interdependence of our health and well-being with the well-being of our environment. This interdependence may be direct (eg, heat’s impact on dehydration and exhaustion) or indirect (eg, via behaviour change due to heat.) The most frequently explored and consistently supported associations include an association between temperature and humidity with infectious diseases, mortality and adverse respiratory, cardiovascular and neurological outcomes. Other less frequently studied but consistent associations include associations between climate impacts and increased use of healthcare services, some adverse mental health outcomes, adverse nutritional outcomes and adverse occupational health outcomes. These associations support key findings of the most recent Lancet report, in which authors report, among others, increasing heat exposure being associated with increasing morbidities and mortality, climate change leading to food insecurity and undernutrition, and to an increase in infectious disease transmission. 2
That said, a number of reviews included in this study reported limited, conflicting and/or an absence of evidence regarding the association between the climate impact and health outcome. For instance, there was conflicting or limited evidence concerning the association between extreme weather events and infectious diseases, cardiorespiratory outcomes and some mental health outcomes and the association between air quality and cardiovascular-specific mortality and adverse birth outcomes. These conflicting and limited findings highlight the need for further research. These associations are complex and there exist important methodological challenges inherent to exploring the causal relationship between climate change and health outcomes. This relationship may at times be indirect and likely determined by multiple interacting factors.
The climate-health link has been the target of more research in recent years and it is also receiving increasing attention from the public and in both public health and climate communication literature. 2 39–41 However, the health framing of climate change information is still underused in climate communications, and researchers suggest we should be doing more to make the link between human health and climate change more explicit to increase engagement with the climate crisis. 2 41–43 The health framing of climate communication also has implications for healthcare professionals 44 and policy-makers, as these actors could play a key part in climate communication, adaptation and mitigation. 41 42 45 These key stakeholders’ perspectives on the climate-health link, as well as their perceived role in climate adaptation and mitigation could be explored, 46 since research suggests that health professionals are important voices in climate communications 44 and especially since, ultimately, these adverse health outcomes will engender pressure on and cost to our health systems and health workers.
Strengths and limitations
To the best of our knowledge, the current study provides the first broad overview of previous systematic reviews exploring the health impacts of climate change. Our review has three main strengths. First, by targeting systematic reviews, we achieve a higher order summary of findings than what would have been possible by consulting individual original studies. Second, by synthesising findings across all included studies and according to the combination of climate impact and health outcome, we offer a clear, detailed and unique summary of the current state of evidence and knowledge gaps about how climate change may influence human health. This summary may be of use to researchers, policy-makers and communities. Third, we included studies published in all languages about any climate impact and any health outcome. In doing so, we provide a comprehensive and robust overview.
Our work has four main limitations. First, we were unable to access some full texts and therefore some studies were excluded, even though we deemed them potentially relevant after title and abstract inspection. Other potentially relevant systematic reviews may be missing due to unseen flaws in our systematic search. Second, due to the heterogeneity of the included systematic reviews and the relatively small proportion of studies reporting meta-analytic findings, we could not conduct meta-meta-analyses of findings across reviews. Future research is needed to quantify the climate and health links described in this review, as well as to investigate the causal relationship and other interacting factors. Third, due to limited resources, we did not assess overlap between the included reviews concerning the studies they included. Frequencies and findings should be interpreted with potential overlap in mind. Fourth, we conducted the systematic search of the literature in June 2019, and it is therefore likely that some recent systematic reviews are not included in this study.
Overall, most systematic reviews of the health impacts of climate change suggest an association between climate change and the deterioration of health in multiple ways, generally in the direction that climate change is associated with adverse human health outcomes. This is worrisome since these outcomes are predicted to rise in the near future, due to the rise in temperature and increase in climate-change-related events such as extreme weather events and worsened air quality. Most studies included in this review focused on meteorological impacts of climate change on adverse physical health outcomes. Future studies could fill knowledge gaps by exploring other climate-related impacts and broader psychosocial health outcomes. Moreover, studies on health impacts of climate change have mostly been conducted by first authors affiliated with institutions in high-income countries. This inequity needs to be addressed, considering that the impacts of climate change are and will continue to predominantly impact lower income countries. Finally, although most reviews also recommend more research to better understand and quantify these associations, to adapt to and mitigate climate change’s impacts on health, it will also be important to unpack the ‘what, how, and where’ of these effects. Health effects of climate change are unlikely to be distributed equally or randomly through populations. It will be important to mitigate the changing climate’s potential to exacerbate health inequities.
Supplementary Material
Acknowledgments.
The authors gratefully acknowledge the contributions of Selma Chipenda Dansokho, as research associate, and Thierry Provencher, as research assistant, to this project, and of Frederic Bergeron, for assistance with search strategy, screening and selection of articles for the systematic review.
Twitter: @RutNdjab, @ATricco, @hwitteman
Contributors: RN, CF, ACT, HOW contributed to the design of the study. CB, RN, LPB, RAPR and HOW contributed to the systematic search of the literature and selection of studies. RR, HOW, LC conducted data analysis and interpretation. RR and HOW drafted the first version of the article with early revision by CB, LC and RN. All authors critically revised the article and approved the final version for submission for publication. RR and HOW had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Funding: This study was funded by the Canadian Institutes of Health Research (CIHR) FDN-148426. The CIHR had no role in determining the study design, the plans for data collection or analysis, the decision to publish, nor the preparation of this manuscript. ACT is funded by a Tier 2 Canada Research Chair in Knowledge Synthesis. HOW is funded by a Tier 2 Canada Research Chair in Human-Centred Digital Health.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Ethics statements, patient consent for publication.
Not required.
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
Heat and health
- Heat is an important environmental and occupational health hazard. Heat stress is the leading cause of weather-related deaths and can exacerbate underlying illnesses including cardiovascular disease, diabetes, mental health, asthma, and can increase the risk of accidents and transmission of some infectious diseases. Heatstroke is a medical emergency with a high-case fatality rate.
- The number of people exposed to extreme heat is growing exponentially due to climate change in all world regions. Heat-related mortality for people over 65 years of age increased by approximately 85% between 2000–2004 and 2017–2021 (1) .
- Between 2000–2019 studies show approximately 489 000 heat-related deaths occur each year, with 45% of these in Asia and 36% in Europe (2) . In Europe alone in the summer of 2022, an estimated 61 672 heat-related excess deaths occurred (3) . High intensity heatwave events can bring high acute mortality; in 2003, 70 000 people in Europe died as a result of the June–August event. In 2010, 56 000 excess deaths occurred during a 44–day heatwave in the Russian Federation.
- Vulnerability to heat is shaped by both physiological factors, such as age and health status, and exposure factors such as occupation and socio-economic conditions.
- The negative health impacts of heat are predictable and largely preventable with specific public health and multi-sectoral policies and interventions. WHO has issued guidance for public health institutions to identify and manage extreme heat risks. Action on climate change combined with comprehensive preparedness and risk management can save lives now and in the future.
A heatwave is a period where local excess heat accumulates over a sequence of unusually hot days and nights. Heatwaves and prolonged excess heat conditions are increasing in frequency, duration, intensity and magnitude due to climate change. Even low and moderate intensity heat waves can impact the health and well-being of vulnerable populations.
The frequency and intensity of extreme heat and heat waves will continue to rise in the 21st century because of climate change. Extended periods of high day and nighttime temperature conditions create cumulative stress on the human body, increasing the risk of illness and death from heat exposure. Heatwaves can acutely impact large populations for short periods of time, often trigger public health emergencies, and result in excess mortality and cascading socioeconomic impacts (for example, lost work capacity and labour productivity). They can also cause loss of health service delivery capacity, when power shortages accompany heatwaves and disrupt health facilities, transport and water infrastructure.
Population ageing and the growing prevalence of non-communicable diseases (respiratory and cardiovascular diseases, diabetes, dementia, renal disease and musculoskeletal disease) means that populations are becoming more susceptible to negative heat impacts. Cities are not being designed to minimize the accumulation and generation of urban heat, with a loss of greenspace and inappropriate housing materials (for example, metal roofs) that amplify human exposure to excess heat.
Awareness among health workers and the public remains insufficient of the health risks posed by heat. Health professionals should adjust their guidance, planning and interventions to account for increasing heat exposures, as well as to manage acute increases in admissions associated with heatwaves. Practical, feasible and often low-cost interventions at the individual, community, organizational, governmental and societal levels can save lives.
Who is affected?
Many populations in tropical and subtropical climates are chronically exposed to high temperatures. In mid to high latitudes, population exposure excess heat is seasonal.
Individual vulnerability to heat for physiological or clinical factors in adults is well described (4) . Heat can affect health through a variety of direct and indirect mechanisms. There is limited research on the impact of chronic (sustained) exposure to high temperatures and humidity.
Outdoor and manual workers, athletes and civil protection employees are exposed to excess heat because of their work and susceptible to exertional heat stress.
Urban and rural poor are often disproportionately exposed to overheating due to low quality housing and lack of access to cooling. Due to building materials, informal settlements are often hotter than other urban areas in some cities. Gender can play an important role in determining heat exposure, for example where women are primarily responsible for cooking indoors during hot weather.
Infographic: Main heat vulnerability factors
How does heat impact health?
The amount of heat stored in the human body is determined by a combination of (a) an inability to eliminate internally generated heat from metabolic processes due to environmental heat stress (for example, high temperature, high humidity, low wind, high thermal radiation), (b) clothing creating a barrier to heat loss, (c) external heat gain from the environment.
The body’s inability to regulate internal temperature and eliminate heat gain in such conditions increases the risk of heat exhaustion and heatstroke. The strain put on the body as it tries to cool itself also stresses the heart and kidneys. As a result, heat extremes can worsen health risks from chronic conditions (cardiovascular, mental, respiratory and diabetes related conditions) and cause acute kidney injury.
Deaths and hospitalizations triggered by extreme hot weather occur rapidly (same day and following days), which means interventions also need to be rapid when a heat alert is issued.
Heat can also disrupt and compromise essential health services, such as the loss of power supply and transport. Heat will reduce working productivity and increases the risk of accidents. It is difficult to complete work or learning in very hot weather and heatwaves may lead schools and other institutions to close. Heatwaves can also be associated with hazardous air pollution events.
The scale and nature of the health impacts of heat depend on the timing, intensity and duration of a heat event, and the level of acclimatization and adaptability of the local population, infrastructure and institutions to the prevailing climate.
Infographic: Scale and nature of the health impacts of heat
What actions should the public take?
Stay out of the heat.
- Avoid going outside and doing strenuous activity during the hottest time of day.
- Stay in the shade. Remember that perceived temperatures in the sun can be 10–15 ˚C higher.
- Spend 2–3 hours during the day in a cool place.
- Be aware of the risk of drowning. Never swim alone.
- Stay informed about official heat warnings.
Keep your home cool
- Use the night air to cool down your home by opening windows after dark when the outdoor temperature is lower than the indoor temperature.
- During the day when outdoor temperatures are higher than indoors, close windows and cover them with blinds or shutters to block direct sunlight. Turn off as many electrical devices as possible.
- Use electric fans only when temperatures are below 40 ˚C / 104 ˚F. In temperatures above 40 ˚C / 104 ˚F, fans will heat the body.
- If using air conditioning, set the thermostat to 27 ˚C / 81 ˚F and turn on an electric fan – this will make the room feel 4 ˚C cooler . It can also save up to 70% on your electricity bill for cooling.
- Remember that it may be cooler outdoors in the shade.
Keep your body cool and hydrated
- Use light and loose-fitting clothing and bed linens.
- Take cool showers or baths.
- Wet your skin using a damp cloth, spray, or wet light clothing.
- Drink water regularly (1 cup of water per hour and at least 2–3 litres per day).
- Regularly check in with vulnerable people in your circle – especially people over 65 years old and those with heart, lung or kidney conditions, a disability, and living alone.
Protect infants and children
- Never leave children or animals in parked vehicles for any amount of time, as temperatures can quickly become dangerously high.
- Avoid direct exposure to the sun during peak hours, seeking shade or staying indoors instead. Shade can reduce how hot you feel by more than 10 °C.
- Never cover an infant stroller / pram with dry fabric – this makes it hotter inside the carriage. Instead, use a wet, thin cloth and re-wet as necessary to lower the temperature. Combine with a portable fan for even greater cooling.
- Dress children in lightweight, loose-fitting clothing that covers their skin, and use wide-brimmed hats, sunglasses and sunscreen to protect them from the sun’s rays.
- Follow the guidance on keeping your home cool to maintain a safe indoor temperature.
Download: Signs of heat stroke
WHO response
Mitigating climate change by reducing greenhouse gas emissions is imperative and urgent to limit the magnitude of human costs from extreme heat. WHO is addressing climate change through the Alliance for Transformational Change in Climate and Health (ATACH) , as well as country support of technical and policy resources to help the health sector and communities adapt to the risks of climate change.
WHO works with the health sector to strengthen governance, preparedness and response to acute impacts of heatwaves by developing heat action plans, heat early warning systems and advisories, and emergency response plans that map the risks, vulnerable populations, available capacities and resources. These plans protect high risk populations such as those in health facilities, nursing homes and schools which do not have access to cooling.
WHO co-sponsors the Global Heat Health Information Network to accelerate sharing and learning about the risks and solutions to address extreme heat. WHO partners closely with the World Meteorological Organization on the development of Heat Health Warning Systems.
- Lancet Countdown: Heat-related Mortality. 2023. https://www.lancetcountdown.org/data-platform/health-hazards-exposures-and-impacts/1-1-health-and-heat/1-1-5-heat-and-sentiment
- Zhao et al, 2021 Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study https://pubmed.ncbi.nlm.nih.gov/34245712/
- Heat-related mortality in Europe during the summer of 2022 https://www.nature.com/articles/s41591-023-02419-z
- Hot weather and heat extremes: health risks. The Lancet. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01208-3/fulltext
- Signs of heat stroke
- WHO's work on heatwaves
- Global Heat Health Information Network
- WHO's work on climate change
- World Meteorological Organization: Heatwave
- Preparing for warm and dry summers
- Evidence for effective protection
- #KeepCool videos

The lifelong impacts of climate change on people and what we can do about them
Germán caruso, inés de marcos.

In our last post , we explored the crucial role of investing in human capital—our health, knowledge, and skills—in addressing the climate crisis.
Today, we examine how climate change affects us from birth to old age, profoundly shaping our lives and communities. Imagine a baby enduring a heat wave or a child missing school due to flooding. These events can have lifelong consequences, affecting health, education, income, and overall well-being.
At the World Bank’s Human Capital Project, our team is dedicated to understanding these challenges and identifying innovative solutions to protect people at every stage of life.

Source: Climate and Development Brief: Delivering for People and the Planet . Washington, D.C.: World Bank Group, 2022.
How does climate change affect us throughout the life cycle?
Climate change has lasting impacts on health outcomes, starting as early as in utero. It increases mortality rates and causes permanent cognitive and educational setbacks among infants and young children. Higher temperatures and changing weather patterns are projected to result in over 21 million additional deaths linked to five major health-related issues by 2050 , with infants being the most affected. A key factor in this is the increased prevalence of vector-borne diseases and reduced access to clean water. For instance, flooding in Bangladesh has been linked to higher rates of stunting in children due to increased water-borne diseases. Working in extreme heat doubles the risks associated with pregnancy. Extreme weather events also hinder pregnant women from accessing medical care, leading to higher rates of newborn deaths and low birth weights.
Climate shocks disrupt education for school-age children and potentially cost them opportunities over their lifetime. Events like flooding or cyclones prevent children from attending school and limit their access to healthcare. In Mozambique , for example, flooding destroyed over 500 schools in one year, drastically affecting children's education.
A new report on education and climate highlights that these disruptions are more widespread than previously thought. Since 2022, a staggering 400 million students globally have experienced school closures due to extreme weather events. The impacts are most severe in low- and middle-income countries, where education systems are already vulnerable to climate shocks. These short-term events can have longer-term impacts. Many kids do not return to school after the shock subsides. A striking graph illustrates how flooding in Latin America can significantly reduce education, especially for children who are not yet in school during the flood.

Source: Caruso, G. D. (2017) . The legacy of natural disasters: The intergenerational impact of 100 years of disasters in Latin America
Climate change reduces productivity and earnings for working-age adults. Over the last 60 years, rising temperatures lengthened the transition season for malaria , increasing by 32% in the Americas and 14% in highlands Africa. This surge in disease, especially among vulnerable workers, leads to higher absenteeism and decreased productivity. As working-age adults work less and are not as productive, they earn less income and face increased poverty. This graph clearly illustrates how extreme heat reduces productivity, with earnings lost to heat as a share of GDP across different regions and industrial sectors. Agricultural workers in poorer regions, like Africa and South-East Asia, are the most affected.

Source: The 2023 report of the Lancet Countdown
Climate change poses significant health risks for older adults. Heat waves are particularly dangerous for older adults. In Latin America , comparing the 95th and 75th percentiles of daily mean apparent temperature—what the temperature feels like to the human body—reveals an increase in mortality for those over 65. The elderly have higher rates of preexisting health conditions and mobility challenges, making it difficult to evacuate during disasters and recover afterward. Poor health also heightens the risks of illness from worsening air quality. In South Korea , outdoor air pollution has been shown to decrease cognitive function, especially among elderly women in urban areas.
Investing in human capital across all ages to address climate change impacts
Combatting climate change and building resilience across all life stages is crucial. The World Bank’s Human Capital Project works to generate evidence and knowledge to help identify country-specific needs and inform investments. This involves systematically assessing climate-related vulnerabilities in developing countries, focusing on impacts on lives, livelihoods, and economies, and identifying ‘best buys’ for climate and human capital investments. Here are some examples of World Bank programs addressing risks for specific age groups:
- Early childhood: Cash and in-kind transfers are vital for protecting human capital from the impacts of climate shocks, such as food insecurity and lost income. The Mauritania Social Safety Net System is a lifeline to many, providing regular cash transfers to over 90,000 households and maintaining a social registry with information on 300,000 potentially vulnerable households. When the 2022 lean season hit, the government quickly reached an additional 70,000 food-insecure households. These transfers ensure families can provide adequate nutrition and healthcare, directly supporting the healthy development of young children.
- School-age children: Integrating climate resilience into school infrastructure and curricula can also protect education outcomes. Nigeria’s Adolescent Girls Initiative for Learning and Empowerment invests in constructing climate-resilient, energy-efficient, and eco-friendly schools. These schools feature adaptations like rainwater harvesting structures to combat both immediate climate shocks such as floods and long-term trends related to water availability. Additionally, the program offers digital literacy and remote learning, ensuring education continues even during climate disruptions.
- Working-age adults: In response to climate change impacts on the agricultural system, the government of Lesotho , in collaboration with the World Bank, has developed initiatives to build a more resilient agricultural sector, ensuring that working-age adults can maintain stable incomes and contribute to the country's food security and economic growth.
- The elderly: As climate-related health risks rise, it’s crucial to protect the most vulnerable populations, including the elderly. A new Climate and Health Program aims to improve healthcare infrastructure and services, ensuring elderly individuals receive the care they need during climate-induced health crises.
This is the second blog in series that showcases recent World Bank research to explore how human capital is critical for climate resilience, adaptation, and action. Check out the first blog here .
We are especially grateful to Gabriel Demombynes, Dani Clark, Jing Guo, Christina Nelson, and Sarah Eleuterio Comer for their insightful feedback and valuable comments on this blog.
To receive weekly articles, sign-up here
Get updates from Protect and Invest in People
Thank you for choosing to be part of the Protect and Invest in People community!
Your subscription is now active. The latest blog posts and blog-related announcements will be delivered directly to your email inbox. You may unsubscribe at any time.

Senior Economist, Human Capital Project, World Bank

Consultant, Human Capital Project, World Bank
Join the Conversation
- Share on mail
- comments added

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
JavaScript appears to be disabled on this computer. Please click here to see any active alerts .
Climate Change and Human Health
On this page:
How Climate Change Affects Human Health
Related resources.
Climate change poses many threats to the health and well-being of all Americans. Climate change affects the food we eat, the air we breathe, the water we drink, and the places that provide us with shelter. Climate change can also impact people’s health and well-being by altering the frequency or intensity of extreme weather events and spread of certain pests and diseases.

Climate change affects people’s health in two main ways:
- By changing the seriousness or frequency of health problems that people already face.
- By creating new or unanticipated health problems in people or places where they have not been before.
The health effects of climate change include respiratory and heart diseases, pest-related diseases like Lyme disease and West Nile Virus , water- and food-related illnesses, and injuries and deaths. Climate change has also been linked to increases in violent crime and overall poor mental health.
Who’s Most at Risk?

Certain groups are at more risk than others due to both climate and non-climate factors.
- What Can We Do?

There are many things we can do to protect people’s health from the impacts of climate change.
How is EPA helping?

EPA is supporting communities by helping them deliver critical resources even as the climate changes.
People can face multiple climate change effects at the same time, at different stages of their life, or over the course of their lifetime. A person’s vulnerability to climate change impacts depends on three key factors:
- Exposure. People will encounter climate hazards differently. Exposure will depend on where and how long people spend time and what they do. For example, people who spend a lot of time outdoors may be more exposed to extreme heat .
- Sensitivity. Some people are more sensitive than others to climate hazards due to factors like age and health condition . For example, children and adults with asthma are particularly sensitive to air pollutants and wildfire smoke.
- Adaptive capacity. People can adjust to, take advantage of, or respond to climate change hazards. A person’s ability to adapt may depend upon their income, age, living situation, access to health care, and many other factors.
Learn more about the connections between climate change and health .
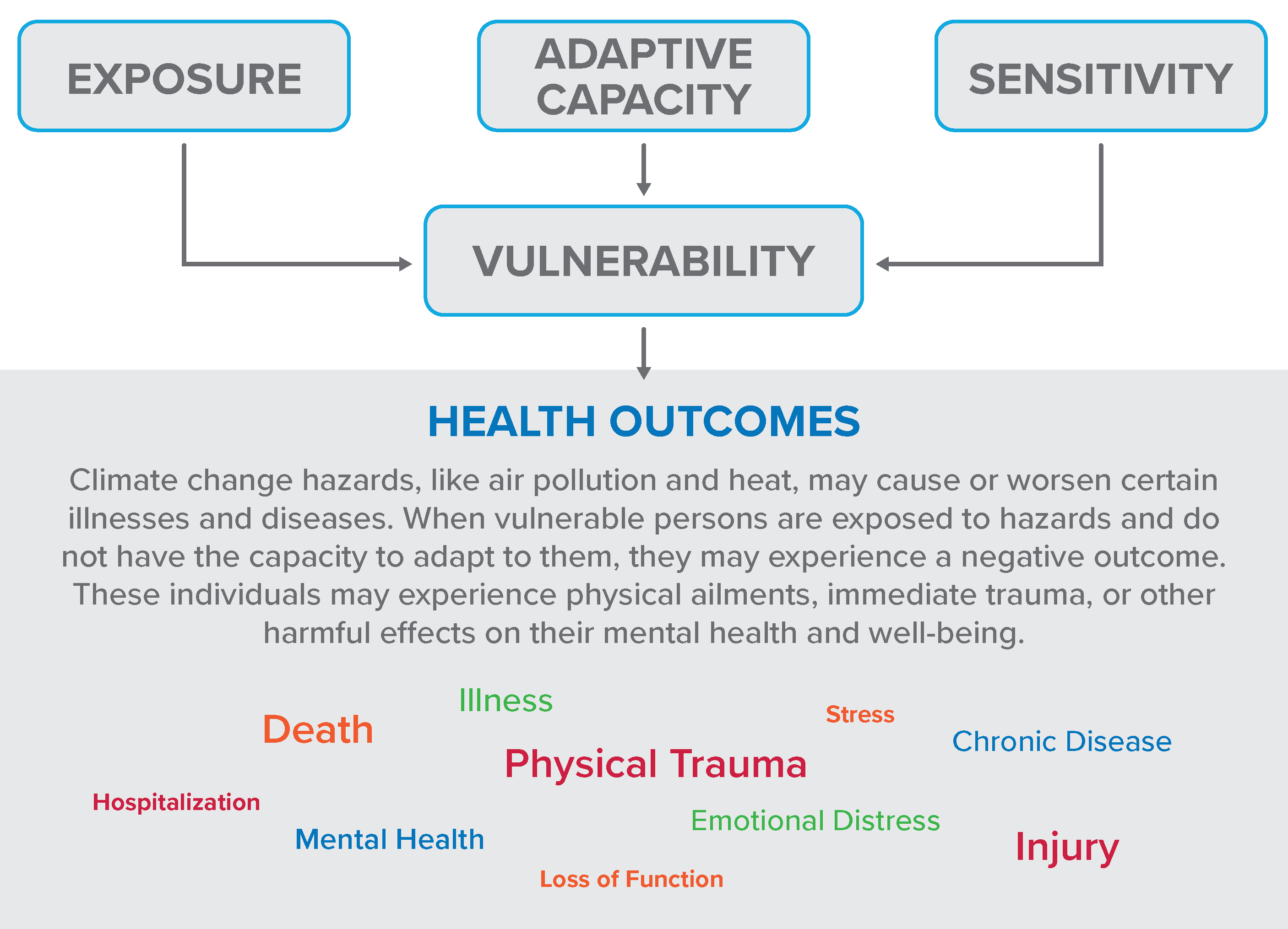
- Understanding the Connections Between Climate Change and Human Health
- Climate Change Indicators: Health and Society
- National Climate Assessment
- National Climate Assessment, Chapter 15: Human Health
- The Impacts of Climate Change on Human Health in the United States
- Centers for Disease Control and Prevention: Climate and Health Program
- Climate Change Impacts Home
- Impacts by Sector
- Socially Vulnerable People
- Indigenous Populations
- Older Adults
- People with Chronic Medical Conditions
- People with Disabilities
- Pregnant, Breastfeeding, and Postpartum Women
- State and Regional Impacts
- Climate Equity
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Climate change and human health
Affiliation.
- 1 Global Climate Change, Division of Environmental Hazards and Health Effects, National Center for Environmental Health, CDC, 4770 Buford Highway, NE, MS F-57, Atlanta, Georgia 30341, USA. [email protected]
- PMID: 19768168
- PMCID: PMC2744549
Climate change science points to an increase in sea surface temperature, increases in the severity of extreme weather events, declining air quality, and destabilizing natural systems due to increases in greenhouse gas emissions. The direct and indirect health results of such a global imbalance include excessive heat-related illnesses, vector- and waterborne diseases, increased exposure to environmental toxins, exacerbation of cardiovascular and respiratory diseases due to declining air quality, and mental health stress among others. Vulnerability to these health effects will increase as elderly and urban populations increase and are less able to adapt to climate change. In addition, the level of vulnerability to certain health impacts will vary by location. As a result, strategies to address climate change must include health as a strategic component on a regional level. The co-benefits of improving health while addressing climate change will improve public health infrastructure today, while mitigating the negative consequences of a changing climate for future generations.
PubMed Disclaimer
Conflict of interest statement
Potential Conflicts of Interest: None disclosed
Similar articles
- When it rains, it pours: future climate extremes and health. Patz JA, Grabow ML, Limaye VS. Patz JA, et al. Ann Glob Health. 2014 Jul-Aug;80(4):332-44. doi: 10.1016/j.aogh.2014.09.007. Epub 2014 Nov 25. Ann Glob Health. 2014. PMID: 25459335 Free PMC article. Review.
- Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Bezirtzoglou C, Dekas K, Charvalos E. Bezirtzoglou C, et al. Anaerobe. 2011 Dec;17(6):337-40. doi: 10.1016/j.anaerobe.2011.05.016. Epub 2011 Jun 2. Anaerobe. 2011. PMID: 21664978
- Climate Change, Human Rights, and Social Justice. Levy BS, Patz JA. Levy BS, et al. Ann Glob Health. 2015 May-Jun;81(3):310-22. doi: 10.1016/j.aogh.2015.08.008. Ann Glob Health. 2015. PMID: 26615065 Review.
- Climate change and health: impacts, vulnerability, adaptation and mitigation. Kjellstrom T, Weaver HJ. Kjellstrom T, et al. N S W Public Health Bull. 2009 Jan-Feb;20(1-2):5-9. doi: 10.1071/nb08053. N S W Public Health Bull. 2009. PMID: 19261209 Review.
- US local action on heat and health: are we prepared for climate change? O'Neill MS, Jackman DK, Wyman M, Manarolla X, Gronlund CJ, Brown DG, Brines SJ, Schwartz J, Diez-Roux AV. O'Neill MS, et al. Int J Public Health. 2010 Apr;55(2):105-12. doi: 10.1007/s00038-009-0071-5. Epub 2009 Sep 23. Int J Public Health. 2010. PMID: 19774340
- Redefining exposure science to advance research supporting cumulative impacts, environmental justice, and decision-making. Tulve NS, Guiseppi-Elie A, Geller AM, Ward-Caviness CK, Paul SJ, Lavoie ET, Rivers L, Frey HC. Tulve NS, et al. J Expo Sci Environ Epidemiol. 2023 Nov;33(6):843-845. doi: 10.1038/s41370-023-00610-5. Epub 2023 Nov 9. J Expo Sci Environ Epidemiol. 2023. PMID: 37945924 Free PMC article. No abstract available.
- Mapping Heat Vulnerability of a Community Mental Health Center Population. Dumont CR, Mathis WS. Dumont CR, et al. Community Ment Health J. 2023 Oct;59(7):1330-1340. doi: 10.1007/s10597-023-01119-9. Epub 2023 Apr 4. Community Ment Health J. 2023. PMID: 37014585
- Spatial and temporal patterns of agrometeorological indicators in maize producing provinces of South Africa. Simanjuntak C, Gaiser T, Ahrends HE, Srivastava AK. Simanjuntak C, et al. Sci Rep. 2022 Jul 15;12(1):12072. doi: 10.1038/s41598-022-15847-7. Sci Rep. 2022. PMID: 35840590 Free PMC article.
- Modeling heat stress changes based on wet-bulb globe temperature in respect to global warming. Nassiri P, Monazzam MR, Golbabaei F, Farhang Dehghan S, Shamsipour A, Ghanadzadeh MJ, Asghari M. Nassiri P, et al. J Environ Health Sci Eng. 2020 May 4;18(2):441-450. doi: 10.1007/s40201-020-00472-1. eCollection 2020 Dec. J Environ Health Sci Eng. 2020. PMID: 33312573 Free PMC article.
- Fundamental Concepts of Human Thermoregulation and Adaptation to Heat: A Review in the Context of Global Warming. Lim CL. Lim CL. Int J Environ Res Public Health. 2020 Oct 24;17(21):7795. doi: 10.3390/ijerph17217795. Int J Environ Res Public Health. 2020. PMID: 33114437 Free PMC article. Review.
- Solomon S, Qin D, Manning M, et al., editors. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK, and New York: Cambridge University Press; 2007. Climate Change 2007: The Physical Science Basis. (Accessed at http://www.ipcc.ch/ipccreports/ar4-wgl.htm .)
- United Nations. World Urbanization Prospects: the 2005 revision. In: Department of Economic and Social Affairs, Population Division: Working Paper ESA/P/WP/2000 2006.
- Luber G, McGeehin M. Climate change and extreme heat events. American Journal of Preventive Medicine. 2008;35:429–35. - PubMed
- U.S. Environmental Protection Agency. Heat Island Effect. U.S. Environmental Protection Agency. 2005. (Accessed at http://www.epa.gov/heatisland/index.htm .)
- Vose RS, Karl TR, Easterling DR, Williams CN, Menne MJ. Impact of land-use change on climate. Nature. 2004;427:213–4. - PubMed
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- PubMed Central
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 17 September 2024
Countering the impact of the climate crisis on health will require data
Nature Medicine volume 30 , page 2379 ( 2024 ) Cite this article
Metrics details
As drastically rising global temperatures threaten the health and wellbeing of populations, solutions that drive policy action must be based on scientific evidence of which strategies work in different scenarios.
The year of 2023 was the hottest on record. In July 2024, the world experienced the two hottest record-breaking days consecutively. Despite broad agreement that human-induced climate change is driving the rise in global temperatures, exacerbating the duration of heatwaves and increasing the frequency of natural disasters such as wildfires and tropical cyclones, the world remains unprepared, and 2.4 billion people from the most vulnerable regions and communities are at high risk from the deadly impacts of extreme heat.
Climate advocates have made progress to get policymakers to acknowledge some of the health impacts of climate change. During the 77th World Health Assembly, held from 27 May to 1 June 2024, World Health Organization Member States agreed on a climate change resolution committed to prioritizing health considerations in climate policy frameworks. But the translation from promise to action remains severely limited. Only 23% of the countries that signed the Paris Agreement on Climate Change assess the impact of climate policies on health and wellbeing, and less than 10% quantify the health co-benefits of climate mitigation plans. Health-specific climate action remains underfunded, with 2% of funding allocated to climate adaptation projects that directly aim to improve health. The Green Climate Fund, established as part of the UN Framework Convention on Climate Change to finance climate adaptation and resilience measures in low- and middle-income countries, allocates only 15% of the US $1.15 billion to implementing measures that specifically address health 1 , despite the fact that all of the countries probably need at least $11 billion per year to adequately address the health impacts of climate change.
Scientific research provides essential data for decision-makers to invest in and prioritize climate policies aimed at delivering effective, actionable and affordable measures that protect the health of communities. However, the current research landscape on climate and health is misaligned with those needs. There is substantial research on the health and mortality impacts of climate change, particularly from modeling and projections. But evidence is lacking on the feasibility, effectiveness and economic costs of climate adaptation and mitigation measures that protect health, or the positive and negative health consequences of current climate policies. Furthermore, climate research output is predominantly from high-income countries and China 2 . There is disproportionately limited research output from Latin America, sub-Saharan Africa and small island states that are experiencing the worst impact of climate change already, and there is a dire need to implement evidence-based measures to address the challenges that these regions face.
Climate and health research is also siloed within disciplines and academic circles, with fragmented engagement across sectors or partnerships between researchers and local policymakers, community, youth and indigenous groups. The consequences of this lack of multi-sector partnerships in supporting implementation are evident. For instance, the Great Green Wall project, an ambitious multinational reforestation initiative that aims to restore 250 million hectares of degraded land in the Sahara, is collapsing in part because of the lack of political engagement, resources and sustainable financing infrastructures in place for the initiative to succeed. Engaging with policymakers and communities most at risk in climate and health research would ensure that proposed intervention measures are supported by evidence showing that they are feasible, acceptable and sustainably integrated into communities, health systems and policies. Funding support for research investigating these climate measures is also crucial. The Wellcome Trust recently invested £17.5 million in the health co-benefits of community-based adaptation projects in vulnerable regions. This decision is an important first step that we hope other research funders will follow in investing in such initiatives.
Encouragingly, evidence that climate adaptation and mitigation interventions provide health returns is beginning to accumulate. Changes in housing designs to reduce indoor temperatures in rural settlements in the Gambia have been shown to decrease the risk of malaria 3 . Climate-friendly urban planning initiatives, including urban cable-cars in Bogota, Colombia, as sustainable transport systems, and green city projects that involve expanding tree canopies in Philadelphia, USA, are delivering benefits of improved health and wellbeing 4 . China’s Air Pollution Prevention and Control Action Plan, a national policy initiative established in 2013 to improve air quality and monitoring, resulted in substantial reductions in mortality attributed to air pollution within 5 years of its implementation 5 .
Climate and health research must now cross disciplines and involve policymakers and local communities to ensure that scientific evidence is incorporated into policies that directly impact health. We at Nature Medicine encourage submissions of research on the testing and implementation of climate adaptation and mitigation measures that provide benefits to health. Focusing on research into the health benefits of implementing such intervention measures will close evidence gaps that are preventing the development of effective health policies, and will inspire similar communities and regions to adopt workable solutions at scale.
Romanello, M. et al. Lancet 400 , 1619–1654 (2022).
Article PubMed Google Scholar
Berrang-Ford, L. et al. Lancet Planet. Health 5 , e514–e525 (2021).
Article PubMed PubMed Central Google Scholar
Jatta, E. et al. Lancet Planet. Health 2 , e498–e508 (2018).
Kondo, M. C. et al. Lancet Planet. Health 4 , e149–e157 (2020).
Huang, J., Pan, X., Guo, X. & Li, G. Lancet Planet. Health 2 , e313–e323 (2018).
Download references
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Countering the impact of the climate crisis on health will require data. Nat Med 30 , 2379 (2024). https://doi.org/10.1038/s41591-024-03276-0
Download citation
Published : 17 September 2024
Issue Date : September 2024
DOI : https://doi.org/10.1038/s41591-024-03276-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Essay: To fix climate anxiety (and also climate change), we first have to fix individualism
- Copy Link URL Copied!
How do you cope? I feel the sorrow, the quiet plea for guidance every time someone asks me this question. As an environmental reporter dedicated to helping people make sense of climate change, I know I should have answers. But the truth is, it took me until now to face my own grief.
My heart keeps breaking whenever I meet yet another child struggling with asthma amid orange, smoke-filled skies. I, too, am reeling from the whiplash of extreme drought and extreme rain , and I’m still haunted by the thought of a mother having to call each of her daughters to say goodbye as the homes around her cave to fire.
Each year, as I reflect on my own reporting on the floods that keep getting worse and the toxic pollution building up in all forms of life , I find myself questioning whether I could ever justify bringing my own children into this world. I agonize over the amount of plastic we can’t avoid using and mourn the monarch butterflies that have vanished. With each new heat record shattered, and each new report declaring a code red for humanity , I can’t help but feel like we’re just counting down the days to our own extinction.
In the face of sea level rise, can we reimagine California’s vanishing coastline?
“Climate anxiety” is the term we now use to describe these feelings, but I must confess, I was perplexed when I first heard these words a few years ago. Anger, frustration, helplessness, exhaustion — these are the emotions I come across more often when getting to know the communities bracing for, or recovering from, the devastation of what they’ve long considered home.
Then a college student asked me about climate anxiety. It came up again on social media, and again in personal essays and polls. This paralyzing dread was suddenly the talk of the town — but it has also, very noticeably, remained absent in some circles.
All this has led me to wonder: What, exactly, is climate anxiety? And how should we cope? At first blush, this anxiety seems rooted in a fear that we’ll never go back to normal, that the future we were once promised is now gone. But who this “normal” is even for (and what we’re actually afraid of losing) speaks to a much more complicated question:
Is this anxiety pointing to a deeper responsibility that we all must face — and ultimately, is this anxiety something we can transcend?
For Jade Sasser, whose research on climate emotions has been grounded by her own experiences as a Black woman, these questions sharpened into focus during a research-methods seminar that she was teaching early last year at UC Riverside.
The class — all female, many from low-income immigrant communities — had been a fairly quiet group all quarter, so Sasser was surprised when the room completely erupted after she broached what she thought would be an academic, somewhat dispassionate discussion about climate change and the future.
Every student was suddenly talking, even yelling, over one another. Thought after thought tumbled out as they shared that not only does the future feel bleak when it comes to the job market, the housing crisis and whether their generation will ever be able to “settle down with kids” — but all this is many times worse when you’re not white, not documented and not born into a college-educated family.
How can they feel hopeful about the future, they asked, when, on top of everything already stacked against them, they also have to worry about wildfires, extreme heat and air pollution getting out of control?
‘It’s almost shameful to want to have children’
‘Climate Anxiety and the Kid Question’ asks: With American society feeling more socially and politically polarized than ever, is it right to bring another person into the world?
“It was literally a collective meltdown unlike anything I had ever experienced,” said Sasser, whose podcast and book, “ Climate Anxiety and the Kid Question, ” were largely inspired by her students that day. “I understood in that moment that you cannot assume someone does not also experience anxiety simply because their way of talking about it may not be the same as yours.”
It doesn’t help, she added, that many people don’t realize what they’re feeling is climate anxiety because the way we talk about it tends to center the experiences of white and more privileged people — people who have been insulated from oppression and have rarely (until now) had to worry about the safety of their own future.
“For a lot of people, climate anxiety looks a certain way: It looks very scared, it looks very sad, and it looks like a person who is ready, willing and able to talk about it,” Sasser said. “But for those who are experiencing many compounding forms of vulnerability at the same time, you can’t just pick out one part of it and say, ‘Oh, this is what’s causing me to feel this way.’”
A brave first step is to acknowledge privilege — and to support, and perhaps even learn, from those who have had to be resilient long before climate change became so overwhelming.
“For me, this work is a matter of survival,” said Kevin J. Patel, who grew up in South L.A. and has been fighting for climate justice since he was 11. He was contemplative, nodding, when I shared what I learned from Sasser, and he gently added that one privilege many communities don’t have is the ability to turn it off. Not everyone can go on a vacation or take a day to recharge, he said. Even having the time to talk about your sadness can be a luxury.
Feeling climate anxiety? These books offer glimmers of hope — and much-needed wisdom
Patel learned at a young age that not all communities get the same level of care. Growing up with hazy air, in a neighborhood hemmed in by the 10 and 110 freeways, Patel almost collapsed one day in front of his sixth-grade class when his heart suddenly started pounding at more than 300 beats per minute.
His parents, farmers from Gujarat, India, rushed Patel to the emergency room and held his hand while everyone around him thought he was dying. After months of hospital visits and procedures, doctors determined that he had developed a severe heart condition in large part due to the smog.

‘For me, this work is a matter of survival.’
— Kevin J. Patel
As he learned to live with an irregular heartbeat, he found joy in his family’s tiny garden and marveled at all the ladybugs that gathered on the tulsi, a special type of basil. He taught his classmates that food came from the ground, not the grocery store, and together, they went on to form an environmental club.
Today, Patel speaks with the hardened wisdom of someone who has experienced much more than the typical 23-year-old. He’s constantly doing something — whether it’s supporting a neighbor, getting water bottle refill stations installed at his school, or turning the idea of a Los Angeles County Youth Climate Commission into reality. For years, he has guided other marginalized youth through OneUpAction , a grassroots environmental group that he built from the ground up.
Even if he doesn’t call it anxiety, he admits he sometimes has trouble focusing, and there’s a tenseness in his body that can be hard to shake off. But he’s usually able to turn it around by talking to his friends or elders, or by reciting his favorite proverb:
They tried to bury us, but they didn’t know we were seeds.
“It’s not about what I need, it’s about what my community needs,” he said. “There is joy in caring for one another. There is joy in coming together to fight for a future that we believe in.”
When talking about climate anxiety, it’s important to differentiate whether you’re assessing these emotions as a mental health condition, or as a cultural phenomenon.
Let’s start with mental health: Polls show climate anxiety is on the rise and that people all around the world are losing sleep over climate change. Organizations like the Climate-Aware Therapist Directory and the American Psychiatric Assn. have put together an increasing number of guides and resources to help more people understand how climate change has affected our emotional well-being.
Poll shows Californians’ climate anxiety is on the rise
Just knowing that climate change is getting worse can trigger serious psychological responses. And the shock and trauma are all the more great if you’ve already had to live through the kinds of disasters that keep the rest of us up at night.
It’s also important to note that social media has magnified our sense of doom. What you see on social media tends to be a particularly intense and cherry-picked version of reality, but studies show that’s exactly how the vast majority of young people are getting their information about climate change: online rather than in school.
But you can’t treat climate anxiety like other forms of anxiety, and here’s where the cultural politics come in: The only way to make climate anxiety go away is to make climate change go away, and given the fraught and deeply systemic underpinnings of climate change, we must also consider this context when it comes to our climate emotions. How we feel is just as much a product of the narratives that have shaped the way we perceive and respond to the world.
“Climate anxiety can’t be limited to just a clinical setting — we have to take it out of the therapy room and look at it through a lens of privilege, and power, and the economic, historical and social structures that are at the root of the problem,” said Sarah Jaquette Ray, whose book “ A Field Guide to Climate Anxiety ” is a call to arms to think more expansively about our despair. “Treating a person’s climate anxiety without challenging these systems only addresses the symptoms, not the causes... and if white or more privileged emotions get the most airtime, and if we don’t see how climate is intersecting with all these other problems, that can result in a greater silencing of the people most impacted.”

Ray, an environmental humanist who chairs the environmental studies program at Cal Poly Humboldt, also emphasized that our distress can actually be a catalyst for much-needed change. These emotions are meant to shake us out of complacency, to sound the alarm to the very real crisis before us. But if we don’t openly talk about climate anxiety as something that is not only normal but also expected, we run the risk of further individualizing the problem. We already have a tendency to shut down and feel alone in our sorrows, which traps us into thinking only about ourselves.
“One huge reason why climate anxiety feels so awful is this feeling of not being able to do anything about it,” Ray said. “But if you actually saw yourself as part of a collective, as interconnected with all these other movements doing meaningful things, you wouldn’t be feeling this despair and loneliness.”
The trick to fixing climate anxiety is to fix individualism, she said. Start small, tap into what you’re already good at, join something bigger than yourself.
And by fixing individualism, as many young activists like Patel have already figured out, we just might have a better shot at fixing climate change.
Let us consider, for a moment, how the words that we use can also limit the way we think about our vulnerability and despair.
Something as simple as the “climate” in “climate anxiety” and how we define “environment” can unintentionally reinforce who we center in the conversation.
“In Nigeria, what we call our environment — it’s not just trees and mountains — it’s also about our food, our jobs, the biodiversity that gives us the life support that we need to thrive every day. That’s what we call our environment; it’s about our people,” said Jennifer Uchendu, who founded SustyVibes , a youth-led sustainability group based in her home country, as well as the Eco-Anxiety in Africa Project , which seeks to validate the emotions and experiences of communities often overlooked in climate conversations. “So if people are being oppressed by the system, it is still linked to our idea of the environment.”
Many of Uchendu’s elders have expressed a lifetime of feeling frustrated and powerless, for example, but she said they didn’t immediately connect these feelings to climate change because “climate anxiety” sounded to them like a new and elite phenomenon.
Editorial: California can make climate polluters pay for the mess they have made of Earth
We hear so often today that climate change is the existential crisis of our time, but that dismisses the trauma and violence to all the people who have been fighting to survive for centuries. Colonization, greed and exploitation are inseparable from climate change, Uchendu said, but we miss these connections when we consider our emotions only through a Western lens.
For Jessa Calderon, a Chumash and Tongva songwriter, these disconnects are ever-present in the concrete-hardened rivers snaking through Los Angeles, and the sour taste of industrialization often singeing the air. In her darkest moments, her heart hurts wondering if her son, Honor, will grow up to know clean water.
Her voice cracked as she recalled a brown bear that had been struck dead on the freeway near the Cajon Pass. As she watched strangers gawk at the limp body and share videos online, she wished she had been able to put the bear to rest and sing him into the spirit world.
“If we don’t see them as our people, then we have no hope for ourselves as a people, because we’re showing that we care about nothing more than ourselves,” she said. “And if we care about nothing more than ourselves, then we’re going to continue to devastate each other and the land.”
It is not too late to turn your climate anxiety into climate empathy. Acknowledging the emotional toll on people beyond yourself can be an opportunity to listen and support one another. Embracing our feelings — and then finding others who also want to turn their fear into action — can be the missing spark to much-needed social and environmental healing.
There is also wisdom to be learned in the songs and traditions of past movements, when people banded together — for civil rights, for women’s suffrage — and found ways to keep hope alive against all odds. And the more we look to the young people still caring for their elders in Nigeria, and to our Indigenous neighbors who continue to sing and love and tend to every living being, the better we might also comprehend the resilience required of all of us in the warming years ahead.
Opinion: Here are the places that could become too hot for humans due to climate change
So how should we cope? For Patel, living with his irregular but unwavering heartbeat, he finds strength in the words of adrienne maree brown, who famously wrote in “ Emergent Strategy ” that in the same way our lives are shaped today by our ancestors, we ourselves are future ancestors. Calderon, who similarly taught her son to leave this Earth better with every passing generation, confided to me that on the days when the sorrow feels too great, she sneaks off to plant native manzanita seeds in neighborhoods stripped of plants and trees.
As I’m reminded of all the love we can still sow for the future, I think of Phoenix Armenta, a longtime climate justice organizer in Oakland who has inspired numerous people, including myself, to take heart in all the times we actually got it right. (Remember acid rain? It was a huge problem, but collective action inspired multiple countries to join forces in the 1980s, and we did what needed to be done.)
“Imagine what kind of world you actually want to live in and start working to make that happen,” said Armenta, who recently made the switch to government planning to help more communities find their voice and determine their own visions for the future.
To grieve the world as we know it is to miss out on opportunities to transform our world for the better. To believe we have nothing left to hope for is a self-fulfilling void. We must find the courage to care, to change, to reimagine the systems that got us into such a devastating crisis in the first place — and we must allow ourselves to dream.
“But it can’t just be my dream, or your dream. It has to be our collective dream,” Armenta said. “I’ve known for a very long time that I can’t save the world, but we can save the world together.”
More to Read
Demanding to be heard
Sept. 15, 2024

What will happen if someone you love has asthma and can’t breathe?

Sometimes we have to escalate to be heard when we’re demanding a livable future

Rosanna Xia is an environment reporter for the Los Angeles Times, where she specializes in stories about the coast and ocean. She was a Pulitzer Prize finalist in 2020 for explanatory reporting, and her award-winning book, “ California Against the Sea ,” has been praised as a poetic and mind-expanding exploration of what we stand to lose in the face of rising water.
More From the Los Angeles Times

Climate & Environment
A decade after signing of California groundwater law, major challenges remain
Sept. 17, 2024

Google to invest in satellites and AI to better detect wildfires

California extreme weather shift: From record heat to cold, rain, even snow
Sept. 16, 2024

An oasis where kids learn to be climate literate amid trees, flower beds and herbs

- Focus Areas
- Engage With Us
- Global Health Hub

IMAGES
VIDEO
COMMENTS
Air pollution is detrimental to human health. Malnutrition is linked to a variety of illnesses, including heart disease, cancer, and diabetes. It can also increase the risk of stunting, or ...
These changes pose fundamental threats to human well-being and health. 4,7 For example, a positive relationship has been observed between regional trends in climate (rising temperatures and ...
Research on climate change and human health is a rapidly growing field, with the number of articles published each year surging more than sixfold over the past decade 43. Despite the increase in ...
Climate change induces both immediate mental health issues, like anxiety and post-traumatic stress, and long-term disorders due to factors like displacement and disrupted social cohesion. Recent research attributes 37% of heat-related deaths to human-induced climate change. Heat-related deaths among those over 65 have risen by 70% in two decades.
The environmental consequences of climate change such as sea-level rise, increasing temperatures, more extreme weather events, increased droughts, flooding and wildfires are impacting human health and lives.1 2 Previous studies and reviews have documented the multiple health impacts of climate change, including an increase in infectious ...
Ebi KL, Vanos J, Baldwin JW, et al. Extreme weather and climate change: population health and health system implications. Annu Rev Public Health 2021;42:293-315. Crossref
These include the inaugural Declaration on Climate and Health at COP28, the publication of the report Quantifying the Impact of Climate Change on Human Health 1 by the World Economic Forum, and a ...
Metrics. Climate change is a health emergency, impacting multiple facets of human well-being via direct and indirect pathways. Nature Climate Change asked experts from different health fields to ...
curbing climate change. Inaction on climate change would result in far reaching and devastating health consequences, particularly for the poor; on the other hand, a strong and equitably distributed cap on greenhouse gas emissions (GHG) would bring major and lasting global health improvements and reduce the global disease burden by more than 25%.
Climate change impacts human health in both direct and indirect ways 1 , 2 . Extreme heat waves, rising sea level, changes in precipitation resulting in flooding and droughts, and intense hurricanes can directly cause injury, illness, and even death 3 . The effects of climate change can also indirectly affect health through alterations to the ...
For the assessment reports, IPCC scientists volunteer their time to assess the thousands of scientific papers published each year to provide a comprehensive summary of what is known about the drivers of climate change, its impacts and future risks, and how adaptation and mitigation can reduce those risks.
Chapter 1. Global climate change and health: an old story writ large 1 Introduction 1 Recognising the complexity of systems upon which life depends: an ecological perspective 3 Climate change: overview of recent scientific assessments 5 Climate and human health: an ancient struggle 8 Potential health impacts of climate change 10
One study projects that, because of climate change, up to an additional 51.3 million people will be at risk from exposure to malaria in Western Africa by 2050. These shifts can heighten suffering, increase countries' burdens of disease and cause epidemics. The World Health Organization (WHO) estimates that one-sixth of illness and disability ...
Background In the past decades, climate change has been impacting human lives and health via extreme weather and climate events and alterations in labour capacity, food security, and the prevalence and geographical distribution of infectious diseases across the globe. Climate change and health indicators (CCHIs) are workable tools designed to capture the complex set of interdependent ...
Climate change is taking a toll on human health, and some leaders in the public health community have urged their colleagues to give voice to its health implications. Previous research has shown that Americans are only dimly aware of the health implications of climate change, yet the literature on issue framing suggests that providing a novel frame - such as human health - may be potentially ...
Climate change is profoundly impacting human health, with direct and indirect effects on physical, mental and social health. In light of the growing recognition of the climate change-health ...
Some efects of climate change are less direct and involve shifts in our environment that, in turn, can afect human health. For example, changes in temperatures and rainfall can afect the lifecycles of insects that transmit Lyme disease and West Nile virus, leading to new or varied outbreaks. Rising sea levels can worsen the fooding from ...
Introduction. The environmental consequences of climate change such as sea-level rise, increasing temperatures, more extreme weather events, increased droughts, flooding and wildfires are impacting human health and lives. 1 2 Previous studies and reviews have documented the multiple health impacts of climate change, including an increase in infectious diseases, respiratory disorders, heat ...
Mitigating climate change by reducing greenhouse gas emissions is imperative and urgent to limit the magnitude of human costs from extreme heat. WHO is addressing climate change through the Alliance for Transformational Change in Climate and Health (ATACH) , as well as country support of technical and policy resources to help the health sector ...
Source: The 2023 report of the Lancet Countdown Climate change poses significant health risks for older adults. Heat waves are particularly dangerous for older adults. In Latin America, comparing the 95th and 75th percentiles of daily mean apparent temperature—what the temperature feels like to the human body—reveals an increase in mortality for those over 65.
Climate change affects people's health in two main ways: By changing the seriousness or frequency of health problems that people already face. By creating new or unanticipated health problems in people or places where they have not been before. The health effects of climate change include respiratory and heart diseases, pest-related diseases ...
The Journal of Climate Change and Health is a worldwide scientific peer reviewed gold open access medical journal that seeks to publish high quality scientific works related to acute and chronic climate related disasters, migration, changing patterns of disease and the impacts of climate change on individuals and health systems.. The journal seeks to publish articles related to best practices ...
Health Promotion. Hot Temperature / adverse effects. Humans. Public Health. Stress, Physiological. Weather. Climate change science points to an increase in sea surface temperature, increases in the severity of extreme weather events, declining air quality, and destabilizing natural systems due to increases in greenhouse gas emissions.
As the world's climate negotiators convene for COP27, a key theme to be addressed is the impact of climate change on human health and evidence-based solutions and adaptation actions. Please submit your paper by April 28, 2023 to be considered for inclusion in this collection. Apr 28 2023. Submit to PLOS Climate or. " Vitor Monthay " by ...
The year of 2023 was the hottest on record. In July 2024, the world experienced the two hottest record-breaking days consecutively. Despite broad agreement that human-induced climate change is ...
Then a college student asked me about climate anxiety. It came up again on social media, and again in personal essays and polls. This paralyzing dread was suddenly the talk of the town — but it ...
© 2024 by the President and Fellows of Harvard College. Privacy Accesibility Accesibility