An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BJPsych Bull
- v.44(5); 2020 Oct


Homelessness, housing instability and mental health: making the connections
Deborah k. padgett.
1 New York University
Associated Data
For supplementary material accompanying this paper visit https://doi.org/10.1192/bjb.2020.49.
Research on the bi-directional relationship between mental health and homelessness is reviewed and extended to consider a broader global perspective, highlighting structural factors that contribute to housing instability and its mental ill health sequelae. Local, national and international initiatives to address housing and mental health include Housing First in Western countries and promising local programmes in India and Africa. Ways that psychiatrists and physicians can be agents of changes range from brief screening for housing stability to structural competence training. Narrow medico-scientific framing of these issues risks losing sight of the foundational importance of housing to mental health and well-being.
Mental illness and homelessness
The bi-directional relationship between mental ill health and homelessness has been the subject of countless reports and a few misperceptions. Foremost among the latter is the popular notion that mental illness accounts for much of the homelessness visible in American cities. To be sure, the failure of deinstitutionalisation, where psychiatric hospitals were emptied, beginning in the 1960s, led to far too many psychiatric patients being consigned to group homes, shelters and the streets. 1 However, epidemiological studies have consistently found that only about 25–30% of homeless persons have a severe mental illness such as schizophrenia. 2
At the same time, the deleterious effects of homelessness on mental health have been established by research going back decades. Early epidemiological studies, comparing homeless persons with their domiciled counterparts, found that depression and suicidal thoughts were far more prevalent, along with symptoms of trauma and substance misuse. 2 , 3 A recent meta-analysis found that more than half of homeless and marginally housed individuals had traumatic brain injuries – a rate far exceeding that of the general population. 4 Qualitative interviews with street homeless persons bring to life the daily struggles and emotional toll of exposure not only to the elements but to scorn and harassment from passers-by and the police. 5
In the USA, healthcare professionals were among the first responders to the homelessness ‘epidemic’ of the 1980s. The Robert Wood Johnson Foundation Health Care for the Homeless initiative funded 19 health clinics around the nation, beginning in 1985. Individual physicians, including Jim Withers in Pittsburgh and Jim O'Connell in Boston, made it their mission to go out on the streets rather than participating in the ‘institutional circuit’ 6 that led so many homeless men and women to cycle in and out of emergency departments, hospitals and jails. Health problems such as skin ulcerations, respiratory problems, and injuries were the visible indicia of what foretold a shortened lifespan. 7 Less visible but no less dire are the emotional sequelae of being unhoused – children are especially susceptible to the psychological effects of homelessness and housing instability. 8 The gap between mental health needs and service availability for the homeless population is vast.
The bigger picture: global housing instability and structural factors
Literal homelessness – sleeping rough in places unfit for human habitation – can be seen as the tip of an iceberg of housing insecurity affecting millions of people around the world. 9 As with attempts to count the number of homeless people and the definitional difficulties attending such counts, 10 providing an estimate of the number of housing-unstable persons globally is definitionally and logistically challenging. In terms of slum dwellers (a prevalent form of housing instability), Habitat for Humanity cites estimates ranging from 900 000 to 1.6 billion. 11 The Dharavi slum in Mumbai has one million residents squeezed into two square kilometres, one of the densest human settlements in the world. 11 Substandard housing affects the well-being of inhabitants – crowding, poor sanitation and infestations bring their own risks to health and mental health. 12
Severe housing shortages in low-income countries contrast with the greater availability of housing in higher-income countries. And yet the visibility and persistence of homelessness in wealthier nations attests to the effects of growing income inequities in the midst of plenty. In the USA, attempts to address homelessness must take several structural barriers into account. First, housing is fundamentally viewed as a commodity and is bound up with economic gains in the forms of tax benefits for homeowners and builders, equity or wealth accumulation from owning property, and developers’ profits from housing market speculation. 13 The worst ‘slumlords’ (landlords who own and rent decrepit properties to poor families) reap greater levels of profit than their counterparts who build for affluent buyers or renters. 14 Second, exclusionary zoning ordinances ensure protection of single-family properties, thus reducing housing availability for renters and preventing multi-family dwellings. 15 Finally, access to housing is not a purely economic proposition. The effects of centuries of de facto and de jure racial exclusion continue to uniquely harm African Americans in denying them access to housing and associated wealth accumulation, thus contributing to their disproportionate representation among homeless persons in the USA. 15
The ultimate causes of homelessness are upstream, i.e. a profound lack of affordable housing due in large part to neo-liberal government austerity policies that prevent or limit public funding for housing, gentrification that displaces working and poor families, and growing income disparities that make paying the rent beyond the means of millions of households. Currently, more than half of US households must devote over 50% of their income to paying for housing, an unprecedented level of rent burden. 14 Farmer refers to this phenomenon as ‘structural violence’: the combined and cumulative effects of entrenched socioeconomic inequities that give rise to varied forms of social suffering. 16 Social suffering does not easily align with existing psychiatric nomenclatures and diagnostic algorithms, but its influence on health through chronic stress and allostatic overload weakens immune systems and erodes emotional well-being. 17
International and national initiatives
Interestingly, since its 1948 declaration of a right to housing, 18 the United Nations (UN) has generally steered clear of re-enunciating such a right until the Sustainable Development Goals (SDGs) were announced in 2015. Subsumed within SDG #11, labelled ‘sustainable cities and communities’, is Target 11.1 of ‘safe and affordable housing for all by 2030’. 19 The UN Special Rapporteur on the right to adequate housing, Leilani Farha, recently submitted a set of guidelines for achieving this goal. 20
In the global south, access to mental healthcare for the most vulnerable is extremely limited despite legislative initiatives to expand such care 21 , 22 and reduce human rights abuses against psychiatric patients. 23 The Global Mental Health Movement (GMHM), which began with a series of articles in the Lancet in 2007 asserting ‘no health without mental health’, 24 came together to address a crisis that results in a ‘monumental loss in human capabilities and avoidable suffering’. 21 The Lancet Commission on Global Mental Health and Sustainable Development, part of the GMHM, has strategically partnered with the UN's SDGs to ensure that mental health and substance misuse are integral to the SDGs moving forward. 21 And there are signs of progress – most originating in the work of citizen advocates and patients working through non-profit rather than formal government channels. In Chennai, India, a visionary non-profit known as The Banyan has pioneered a culturally and socially innovative approach, ‘Home Again’, to help homeless persons with severe mental illness recover their lives and live independently or return to their family homes. 25 In West Africa, advocates for AIDS and leprosy patients have turned their talents and expertise to developing programmes for persons with mental illness that are inclusive, rehabilitative and rights based. 23 Zimbabwe's ‘Friendship Bench’ programme, which situates attention to mental health within ongoing community activities, has been replicated worldwide. 26 Although the African approaches are not targeted at homeless persons, they have been heralded as low-barrier and inclusive – and by their location are likely to assist persons with housing insecurity problems among others. 21 The recent Lancet Commission report on global mental health 21 included mention of homelessness as both a cause and consequence of poor mental health.
The advent of Housing First has been a rare success story at the programmatic and systems levels in the US, Canada and Western Europe. 27 Begun in New York City as a small but determined counterpoint to ‘treatment first’ approaches making access to housing contingent on adherence, Housing First has achieved an impressive evidence base and extensive adaptations to new populations such as homeless youth, families and opioid users. 27 By reversing the usual care continuum of first requiring medication adherence, abstinence and proof of ‘housing worthiness’, Housing First is the prime exemplar of an evidence-based, cost-saving enactment of the right to housing. Importantly, it is not ‘housing only’, i.e. support services including mental healthcare are essential to its success. 28 Early reliance on assertive community treatment in Housing First support services was eventually expanded to include less-intensive case management supports for clients whose mental health recovery had proceeded further. 27
Another evidence-based programme known as critical time intervention (CTI) has proven effective in preventing homelessness pending discharge from institutional care. 29 Using time-sensitive intensive supports before and after discharge, CTI connects the patient or client with housing and support services to ease return to the community and avert falling into homelessness. 29 Like Housing First, CTI has focused on persons with mental disorders but has since been adapted for other at-risk groups, such as clients leaving substance misuse treatment settings or prisons.
In the USA, there are a few signs that housing as a social determinant of health is receiving greater recognition. The Obama-era Affordable Care Act offered states the opportunity to expand Medicaid eligibility to millions of low-income households, including coverage for mental healthcare. 30 Although federal rules prohibit use of Medicaid funds to pay for housing (with the exception of nursing homes), some states have creatively used Medicaid funds for all housing-related services short of rent, including move-in costs and follow-up supports. 30 Unfortunately, capital funding for building and developing new housing units remains woefully inadequate, and it is too often left up to the private sector to act on a profit motive incentivised by government subsidies and tax incentives. 15 Given the current national political situation in the US, positive change at the federal level is unlikely, but states and cities continue to independently seek ways to move from shelters to housing. 30
The healthcare landscape in the UK offers opportunities for service integration under coordinated national healthcare, and the link between housing and health is evident in recent cooperation between the National Housing Federation and the Mental Health Foundation in providing supported accommodation for persons with mental disorders. 31 In Western Europe, the establishment of FEANTSA (European Federation of National Organizations Working with the Homeless; www.feantsa.org ) in 1989 with support from the European Commission has brought together representatives from 30 nations for programmatic and research initiatives (many using Housing First). Consideration of mental problems as cause and consequence of homelessness is a key component of FEANTSA's work, with psychiatrists actively involved in research at several sites, e.g. France's multi-city randomised trial of Housing First. 32
Psychiatrists and physicians as agents of change
In what ways can healthcare providers help? For housing-related risk assessment, family or general care physicians may make use of brief screening items inquiring about recent moves, evictions and rent arrears 33 as a means of ascertaining a patient's housing instability. Regrettably, there are limited programmes available to which to refer patients with ‘positive’ screens, but raising awareness and knowing a patient's life challenges can only improve care. Calls for medical training to include ‘structural competency’ 34 point to the broader importance of practitioners becoming versed in patients’ life circumstances linked to poverty to contextualise their health problems. According to Metzl and Hansen, 34 structural competency is the practitioners’ trained ability to recognise that patients’ problems defined clinically as symptoms, attitudes or disease also represent the downstream implications of upstream decisions about housing affordability, healthcare availability, food delivery systems and other infrastructure supports.
Some physicians have called for the right to prescribe housing as a means of solving this underlying problem, with the added advantage of reducing medical costs. 35 Prescribing housing as a form of ‘preventive neuroscience’ has received support from the O'Neill Institute as a cost-saving humane investment in children's brain development. 36 Such attention to social and environmental determinants of health is hardly misplaced, as they account for 90% of health status, with only 10% attributable to medical care. 30
Homeless men and women have few encounters with physicians, much less psychiatrists and other formal mental healthcare providers. Those with diagnoses of severe mental illnesses might have an assigned psychiatrist to prescribe anti-psychotic medications, but these are brief encounters at best. Even in wealthier nations, psychiatrists working in the public sector are relatively fewer in number, overworked, underpaid and rarely able to address the hidden crisis of mental ill health wrought by homelessness and housing instability. In low-income nations, the service gap is even wider. 22
A recent US report on the alarming lack of access to mental healthcare even for the well insured points to a broad-based crisis in mental health services. 37 Ignoring laws ensuring parity, insurers provide much lower coverage for mental health treatment than would be tolerated for cardiac or cancer care, and out-of-pocket costs can run as high as $400 per private psychiatrist visit. 37 The prospects for a homeless man or woman who is feeling anxious, depressed or suicidal are indeed dismal. Although many homeless and other low-income individuals in the US are enrolled in Medicaid, an acute scarcity of psychiatrists who accept Medicaid patients renders such coverage virtually unattainable in many parts of the US. 37
A caveat about the medico-scientific approach moving forward
Attempts to incorporate social determinants thinking into public policy discourse on the mental health benefits of stable housing still have some way to go in jurisdictions where the medico-scientific approach holds sway. As a case in point, witness the recent report by the prestigious US National Academy of Science, Engineering and Medicine (NASEM) on the health benefits of permanent supportive housing (PSH), a major source of housing and supports for formerly homeless persons with severe mental illness. 38 Acknowledging that research on the topic was severely limited owing to the recency of PSH and its many poorly defined iterations, the NASEM report nevertheless concluded that the health benefits of such housing were minimal, with the possible exception of persons with HIV/AIDS having improved outcomes. 38 The report argued for the need to identify ‘housing-sensitive’ health conditions to point future researchers in the right direction. 38
Such delimiting of what is important to ‘housing-sensitive’ medical conditions exemplifies the narrowness of the medico-scientific model set against a social determinants model combined with human rights. In response to such reductionism, the British Psychological Society recently proposed the Power Threat Meaning Framework as an alternative to the medicalisation of mental illness, 39 proposing that greater attention be given to the implications of power and inequality.
Homelessness represents an existential crisis that threatens mind and body alike. The concept of ontological security, having its modern origins in the writings of sociologist Anthony Giddens, offers phenomenological insights into the benefits of stable housing that domiciled persons easily take for granted. As noted by this author, 40 going from the streets to a home enhances one's ontological security, as such a transition affords a sense of safety, constancy in everyday life, privacy, and a secure platform for identity development. 40 As with Maslow's hierarchy, 41 fundamental human needs must be met in order to satisfy higher-order needs such as belonging and self-actualisation.
Despite a plethora of research linking mental and physical health to housing stability, the salience of structural barriers is too often submerged in ‘blaming the victim’ for her or his plight. Physicians and healthcare providers receive little training in social determinants and often view them as off-limits or distracting from attention to signs and symptoms. Yet psychiatrists and other mental health professionals can become agents of change by paying greater attention to the social determinants of mental health and seeking structural competence in their practice. It is difficult to overestimate the benefits of having a stable, safe home as fundamental to mental health and well-being.
About the author
Deborah K. Padgett , PhD, MPH, is a Professor at the Silver School of Social Work at New York University (NYU). She is also an Affiliated Professor with NYU's Department of Anthropology and College of Global Public Health.
Declaration of interest
Supplementary material.
Loading metrics
Open Access
Peer-reviewed
Research Article
The prevalence of mental disorders among homeless people in high-income countries: An updated systematic review and meta-regression analysis
Contributed equally to this work with: Stefan Gutwinski, Stefanie Schreiter
Roles Conceptualization, Data curation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing
Affiliation Department of Psychiatry and Psychotherapy, Charité–Universitätsmedizin Berlin, Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany
Roles Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing
Affiliations Department of Psychiatry and Psychotherapy, Charité–Universitätsmedizin Berlin, Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany, Biomedical Innovation Academy, Berlin Institute of Health, Berlin, Germany
Roles Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing
Roles Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Psychiatry, University of Oxford, Oxford, United Kingdom
- Stefan Gutwinski,
- Stefanie Schreiter,
- Karl Deutscher,
- Seena Fazel

- Published: August 23, 2021
- https://doi.org/10.1371/journal.pmed.1003750
- Peer Review
- Reader Comments
Homelessness continues to be a pressing public health concern in many countries, and mental disorders in homeless persons contribute to their high rates of morbidity and mortality. Many primary studies have estimated prevalence rates for mental disorders in homeless individuals. We conducted a systematic review and meta-analysis of studies on the prevalence of any mental disorder and major psychiatric diagnoses in clearly defined homeless populations in any high-income country.
Methods and findings
We systematically searched for observational studies that estimated prevalence rates of mental disorders in samples of homeless individuals, using Medline, Embase, PsycInfo, and Google Scholar. We updated a previous systematic review and meta-analysis conducted in 2007, and searched until 1 April 2021. Studies were included if they sampled exclusively homeless persons, diagnosed mental disorders by standardized criteria using validated methods, provided point or up to 12-month prevalence rates, and were conducted in high-income countries. We identified 39 publications with a total of 8,049 participants. Study quality was assessed using the JBI critical appraisal tool for prevalence studies and a risk of bias tool. Random effects meta-analyses of prevalence rates were conducted, and heterogeneity was assessed by meta-regression analyses. The mean prevalence of any current mental disorder was estimated at 76.2% (95% CI 64.0% to 86.6%). The most common diagnostic categories were alcohol use disorders, at 36.7% (95% CI 27.7% to 46.2%), and drug use disorders, at 21.7% (95% CI 13.1% to 31.7%), followed by schizophrenia spectrum disorders (12.4% [95% CI 9.5% to 15.7%]) and major depression (12.6% [95% CI 8.0% to 18.2%]). We found substantial heterogeneity in prevalence rates between studies, which was partially explained by sampling method, study location, and the sex distribution of participants. Limitations included lack of information on certain subpopulations (e.g., women and immigrants) and unmet healthcare needs.
Conclusions
Public health and policy interventions to improve the health of homeless persons should consider the pattern and extent of psychiatric morbidity. Our findings suggest that the burden of psychiatric morbidity in homeless persons is substantial, and should lead to regular reviews of how healthcare services assess, treat, and follow up homeless people. The high burden of substance use disorders and schizophrenia spectrum disorders need particular attention in service development. This systematic review and meta-analysis has been registered with PROSPERO (CRD42018085216).
Trial registration
PROSPERO CRD42018085216 .
Author summary
Why was this study done.
- Homelessness continues to affect a large number of people in high-income countries and is associated with an increased risk of mental disorders.
- To guide service development, further research, and public policy, reliable estimates on the prevalence of mental disorders among homeless individuals are needed.
- Many primary investigations into rates of mental disorders have been published since a previous comprehensive quantitative synthesis in 2008.
What did the researchers do and find?
- We performed a systematic database search, extracted data from primary reports, and assessed their risk of bias, resulting in a sample of 39 studies including information from over 8,000 homeless individuals in 11 countries.
- We conducted random effects meta-analyses of 7 common diagnostic categories. Prevalence estimates were all increased in homeless individuals compared with those in the general population. Alcohol use disorders had the highest absolute rate, at 37%, with substantially elevated proportional excesses compared to the general population for schizophrenia spectrum disorders and drug use disorders as well.
- There was substantial between-study variation in prevalence estimates, and meta-regression analyses found that sampling method, participant sex distribution, and study country explained some of the heterogeneity.
What do these findings mean?
- The high burden of substance use disorders and severe mental illness in homeless people represents a unique challenge to public health and policy.
- Future research should prioritize quantification of unmet healthcare needs, and how they can be identified and effectively treated. Research on subgroups, including younger people and immigrant populations, is a priority for prevalence work.
Citation: Gutwinski S, Schreiter S, Deutscher K, Fazel S (2021) The prevalence of mental disorders among homeless people in high-income countries: An updated systematic review and meta-regression analysis. PLoS Med 18(8): e1003750. https://doi.org/10.1371/journal.pmed.1003750
Academic Editor: Vikram Patel, Harvard Medical School, UNITED STATES
Received: February 2, 2021; Accepted: August 2, 2021; Published: August 23, 2021
Copyright: © 2021 Gutwinski et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The Wellcome Trust ( https://wellcome.org ) granted the submission fee for this review to SF (grant number 202836/Z/16/Z). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: CI, confidence interval; DSM, Diagnostic and Statistical Manual of Mental Disorders; PI, prediction interval
Introduction
Homelessness is recognized by the United Nations Economic and Social Council as an issue of global importance [ 1 ]. In high-income countries, around 2 million people have been homeless over the past decade [ 2 ]. In the US, the lifetime prevalence of homelessness is estimated at 4.2% [ 3 ], with around 550,000 individuals lacking fixed, regular, and adequate residence on any given night [ 4 ]. Patterns over time have differed by country, although homelessness has increased in many high-income countries in recent years, including in the US and UK since 2017 [ 2 ].
There has been an increasing recognition of the public health importance of homeless persons, with many studies reporting high rates of acute hospitalization, chronic diseases, and mortality [ 5 – 13 ]. Comorbidities increase these risks, particularly mental disorder comorbidities. For example, in a Danish population study, comorbidity of psychiatric disorders increased mortality rates by 70% [ 14 ]. Furthermore, mental illness among homeless individuals has been associated with elevated rates of criminal behavior and victimization [ 15 , 16 ], prolonged courses of homelessness [ 17 , 18 ], and perceived discrimination [ 19 ]. Mental disorders among homeless individuals are mostly treatable and represent an important opportunity to address health inequalities.
Information on the overall extent and pattern of mental disorders among homeless people is necessary to inform resource allocation and service development, and to allow researchers, clinicians, and policymakers to consider evidence gaps. The large number of primary studies, of varying quality and samples, means that systematic reviews are required to clarify and synthesize the evidence, underscore main findings, and consider implications. According to a recent umbrella review, there have been at least 7 systematic reviews with quantitative data synthesis in the past 2 decades [ 20 ]; however, most of them focused on individual diagnostic categories [ 21 – 24 ], examined specific age bands [ 24 , 25 ], or were limited to a single country [ 26 ]. The last meta-analysis to our knowledge that provided a comprehensive account of the prevalence of major mental disorders in homeless adults in high-income countries completed its search in 2007 [ 27 ], and since then, a considerable number of primary studies have been published [ 28 , 29 ]. Thus, we conducted an updated systematic review and meta-analysis on the prevalence of mental disorders among homeless people in high-income countries, and added the diagnostic categories of any mental disorder and bipolar disorder.
Search strategy
We searched for studies that determined prevalence rates for at least 1 of the following disorders among homeless persons: (1) schizophrenia spectrum disorders, (2) major depressive disorder, (3) bipolar disorder, (4) alcohol use disorders, (5) drug use disorders, (6) personality disorders, and (7) any current mental disorder (Axis I disorders in the Diagnostic and Statistical Manual of Mental Disorders [DSM] multiaxial system [ 30 ]).
We have updated an earlier review [ 27 ] that was based on a search for articles published up until December 2007, so we targeted new primary studies published between 1 January 2008 and 1 April 2021. We searched Embase via OvidSP, Medline via OvidSP and via PubMed, and PsycInfo via EBSCOhost. Additionally, we searched Google Scholar using a search query and screened all literature citing the previous review. Finally, we screened reference lists of relevant publications. Each search employed a specific combination of search terms designed to fit the databases’ respective syntaxes and thesaurus systems ( S1 Table ). Articles written in languages other than English or German were translated by professional translators. The protocol for this systematic review and meta-analysis has been published (PROSPERO CRD42018085216). We followed Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines for extracting and assessing data [ 31 ]. This systematic review adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (see S2 Table ) [ 32 ].
Eligibility criteria and study selection
Inclusion criteria were as follows: (1) homelessness status of study participants was validated by an operationalized definition or a sampling method that specifically targeted homeless population; (2) standardized criteria for the psychiatric disorders specified above, based on the International Classification of Diseases (ICD) or DSM, were applied; (3) psychiatric diagnoses were made by clinical examination or interviews using validated semi-structured diagnostic instruments; (4) for any psychiatric disorders except for personality disorders (where lifetime rates were used), prevalence rates were reported within 12 months; and (5) study location was a high-income country according to the classification of the World Bank [ 33 ].
Surveys that reported a response rate of less than 50% or exclusively sampled from selected subpopulations (such as elderly homeless, homeless youth, or homeless single parents) were excluded.
In order to assess all results from the bibliographic search process, researchers SS, SG, and KD each carried out a multilevel screening process independently from one another. Any differences between results were resolved by consensus between all the authors.
Data collection and quality assessment
Information from included surveys was extracted on study location, year of diagnostic assessment, operational definition of homelessness status, sampling method, diagnostic procedures, diagnostic criteria, professional qualification of interviewers, response rate, dropout rate, number of participants by sex, sample mean age, current accommodation of participants, sample mean duration of homelessness, and number of participants diagnosed with schizophrenia spectrum disorders, major depressive disorder, bipolar disorder, alcohol- and drug-related disorders, personality disorders, and any primary diagnosis of a mental disorder apart from personality and developmental disorders (i.e., Axis I disorders in DSM). If data regarding any of these categories were unclear in the published study, we corresponded with the primary study authors.
Each included publication was rated on methodological quality by 2 sets of criteria specifically designed to assess prevalence studies: the JBI critical appraisal tool for prevalence studies [ 34 ] and a risk of bias tool [ 35 ]. This process was carried out by SS, SG, and KD independently, and any differences were resolved by discussion.
Statistical analysis
Random effects meta-analyses and meta-regression analyses were performed on each diagnostic category independently—prevalence data for alcohol misuse/abuse and alcohol dependence were both entered into the single category of alcohol use disorders, in accordance with current diagnostic approaches. All analyses were done in R, version 4.0.4 [ 36 ]. The package “metafor,” version 2.4–0, was utilized for meta-analysis and meta-regression analysis, supplemented by “glmulti,” version 1.0.8, for multivariable model selection and “mice”, version 3.13.0, for multivariate imputation [ 37 – 39 ].
Prevalence estimates were transformed on the double arcsine function in order to avoid variance instability and confidence intervals (CIs) exceeding the interval (0 ≤ x ≤ 1) in which prevalence proportions can be meaningfully defined [ 40 ]. We calculated random effects models, which we deemed appropriate considering sampling differences. The Paule–Mandel estimator was chosen to measure between-study variance due to its reliability for different types of models [ 41 ]. A Q- test for heterogeneity was conducted. To quantify measures of between-study heterogeneity, we report the test statistic Q E and corresponding p- value as well as the I 2 statistic. Additionally, we calculated 95% prediction intervals (PIs) for all meta-analytical models [ 42 ]. Because the “metafor::predict.rma” function unrealistically assumed that the model variance τ 2 was a known value [ 43 ], we instead implemented a method proposed by Higgins and colleagues that accounts for τ 2 being an estimate with limited precision ([ 44 ], expression 12).
Additional meta-analyses were carried out in each diagnostic category for low-risk-of-bias studies, assigned during quality assessment [ 35 ]. Subgroup analyses comparing low-risk-of-bias and moderate-risk-of-bias studies were performed through a Q- test. In cases of significant between-subgroup difference, a meta-regression model with risk of bias assessment as a single independent variable was computed to estimate the proportion of variance explained by disparities in methodological quality.
For each diagnostic category, meta-regression analyses were performed to investigate potential sources of heterogeneity. Continuous independent variables for single factor meta-regression were number of participants, sex distribution (female/all), and final year of diagnostic assessments. Categorial independent factors were diagnostic method (structured/semi-structured interview versus non-structured clinical evaluation), sampling method (randomized versus non-randomized sampling methods), and study location (US, UK, or Germany). The 3 study locations were prespecified as predictor variables due to a preponderance of primary studies in each of these countries.
Multivariable meta-regression models were also calculated. The respective independent variables were chosen through automated, information-criterion-based model selection with generalized linear models [ 38 ]. For models with 20 or more included studies, the Akaike information criterion (AIC) was used; for models with fewer than 20 included studies, we utilized the corrected version for small sample sizes (AIC C ) to avoid over-fitting.
The proportion of variance of prevalence estimates explained by any meta-regression model was estimated by the R 2 statistic [ 45 ].
We assumed that missingness was at random [ 46 ], so missing values in independent variables (that were missing despite requests for additional information to primary study authors) were replaced through multiple imputation by chained equations [ 47 ]. For models including incomplete predictor variables, results of meta-regression on imputed data are presented as the primary analysis; meta-regression results on only complete cases are provided as sensitivity analyses [ 48 ].
Description of included studies
The systematic literature search returned 5,886 distinct records, of which 144 full texts were assessed (see S3 Table for reasons for exclusion). We identified a total of 39 studies comprising data on 8,049 homeless individuals [ 28 , 29 , 49 – 85 ] (see Fig 1 for flow chart of screening process). This included 10 additional studies for this update [ 28 , 29 , 53 – 55 , 57 , 59 , 62 , 75 , 76 ], and 2 previous investigations were further clarified [ 81 , 83 ].
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1003750.g001
Out of the 39 included studies, 27 publications reported age (mean of 41.1 years) [ 28 , 49 – 57 , 59 , 64 , 65 , 67 , 70 – 73 , 75 , 76 , 78 – 82 , 84 , 85 ], and the proportion of women was 22.3% (based on 38 studies) [ 28 , 29 , 49 – 65 , 67 – 85 ]. Eleven studies [ 52 , 56 , 68 , 71 – 74 , 80 , 82 , 83 , 85 ] investigated male-only samples, and 5 studies [ 59 , 65 , 78 , 81 , 84 ] solely women. Of the 39 studies, 27 were from 3 countries: 11 from the US ( n = 2,694 participants) [ 57 , 59 , 60 , 64 , 69 , 75 , 77 , 79 , 83 – 85 ], 7 from the UK ( n = 1,390 participants) [ 49 , 61 , 66 , 67 , 70 , 78 , 82 ], and 9 from Germany ( n = 936 participants) [ 28 , 50 , 51 , 56 , 65 , 71 – 73 , 80 , 81 ]. Six studies were from other European countries ( n = 2,301 participants) [ 29 , 52 , 55 , 58 , 62 , 76 ], 1 study was from Canada ( n = 60 participants) [ 69 ], 2 were from Japan ( n = 194 participants) [ 53 , 54 ], and 2 were from Australia ( n = 667 participants) [ 63 , 74 ]. Fourteen studies reported a response rate of 85% or above [ 49 , 60 , 65 , 66 , 69 – 73 , 78 , 81 , 82 , 84 , 85 ], 20 studies reported a response rate below 85% [ 28 , 29 , 50 – 52 , 54 – 56 , 58 , 59 , 61 – 64 , 68 , 74 , 76 , 79 , 80 , 83 ], and 5 did not report participation rate [ 53 , 57 , 67 , 75 , 77 ]. In 13 studies, participants were accommodated in shelters, hostels, or residential care when assessed [ 28 , 49 , 63 , 66 , 70 , 72 , 74 , 76 – 78 , 81 – 83 ] while in 3 they were rough sleeping [ 54 , 62 , 67 ]; 22 studies had mixed samples regarding accommodation or provided incomplete information [ 29 , 50 – 53 , 55 – 61 , 64 , 65 , 68 , 69 , 71 , 73 , 75 , 79 , 80 , 84 , 85 ]. S4 Table provides further information on methodological and sample characteristics. For quality ratings, see S5 and S6 Tables. S7 Table provides all extracted data that meta-analyses and meta-regression analyses were based on.
Any current mental disorders
There were 8 surveys reporting on homeless people having at least 1 diagnosis of a current mental disorder [ 28 , 51 , 54 , 62 , 71 – 73 , 81 ], with a random effects pooled prevalence estimated at 76.2% (95% CI 64.0% to 86.6%) ( Fig 2 ). Individual study prevalence rates ranged from 56.3% to 93.3%, with substantial heterogeneity ( I 2 = 88% [95% CI 72% to 97%]). The 95% PI was 40% to 99%. Univariable meta-regression analysis revealed that studies with randomized sampling procedures reported significantly higher prevalence estimates than ones with other sampling procedures, accounting for a large proportion of heterogeneity ( R 2 = 59%) (see S8 Table ). Sampling procedure was chosen as the only predictor variable by multivariable model selection (see Table 1 ).
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval.
https://doi.org/10.1371/journal.pmed.1003750.g002
https://doi.org/10.1371/journal.pmed.1003750.t001
In a subgroup analysis of 4 low-risk-of-bias studies [ 62 , 71 , 73 , 81 ], the random effects prevalence was 75.3% (95% CI 50.2% to 93.6%; I 2 = 81% [95% CI 32% to 99%]). There was no significant difference between quality subgroups ( Q = 0.03, p = 0.87).
Schizophrenia spectrum disorders
There were 35 surveys reporting on any schizophrenia spectrum disorder [ 28 , 29 , 49 , 51 – 58 , 60 – 74 , 76 – 78 , 80 – 85 ], and the random effects prevalence was 12.4% (95% CI 9.5% to 15.7%) ( Fig 3 ), with substantial heterogeneity ( I 2 = 93% [95% CI 89% to 96%]; 95% PI 0% to 34%). Primary investigation estimates ranged between 2.0% and 42.2%. No single model coefficient in univariable meta-regression was statistically significant. A multivariable model with sample size, proportion of female participants, and study location in Germany accounted for a small share of the heterogeneity ( R 2 = 16%). The latter model indicated that studies with smaller samples had significantly higher prevalence rates, but only when based on imputed values (see Table 1 ).
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval; RE, random effects.
https://doi.org/10.1371/journal.pmed.1003750.g003
A subgroup analysis of 17 low-risk-of-bias studies [ 29 , 49 , 52 , 55 , 58 , 60 , 62 , 65 , 67 , 69 , 71 , 73 , 78 , 80 , 81 , 84 , 85 ] revealed a random effects pooled prevalence of 10.5% (95% CI 6.2% to 15.7%; I 2 = 94% [95% CI 88% to 98%]). The subgroup difference between low-risk-of-bias and moderate-risk-of-bias studies was non-significant, with the low-risk group resulting in a marginally lower weighted mean ( Q = 1.59, p = 0.21).
Major depression
We identified 18 studies reporting prevalence estimates on major depressive disorder [ 28 , 49 , 52 , 55 , 57 – 60 , 62 , 63 , 65 , 67 , 71 , 77 , 80 , 81 , 84 , 85 ], with a random effects pooled prevalence of 12.6% (95% CI 7.9% to 18.2%) ( Fig 4 ). Individual study estimates ranged between 0% and 40.6% and showed substantial heterogeneity ( I 2 = 95% [95% CI 90% to 98%]; 95% PI 0% to 40%). Univariable meta-regression analysis produced no significant models (see S8 Table ). For multivariable regression, independent variable sampling procedure and proportion of female participants were selected; the model indicated that studies with randomized sampling reported significantly higher prevalence rates (see Table 1 ).
https://doi.org/10.1371/journal.pmed.1003750.g004
In a subgroup analysis of 13 low-risk-of-bias studies [ 49 , 52 , 55 , 58 , 60 , 62 , 65 , 67 , 71 , 80 , 81 , 84 , 85 ], the random effects pooled prevalence was 13.0% (95% CI 6.7% to 20.9%; I 2 = 96% [95% CI 90% to 99%]). There were no significant differences in between risk of bias subgroups ( Q = 0.09, p = 0.76).
Bipolar disorder
Fourteen surveys with prevalence estimates on bipolar disorder were identified [ 28 , 49 , 55 , 57 – 59 , 62 , 63 , 65 , 67 , 71 , 77 , 84 , 85 ]. Three studies reported on solely type I bipolar disorder [ 49 , 57 , 85 ], 4 examined all bipolar disorder subtypes [ 28 , 59 , 65 , 71 ], and 7 did not specify [ 55 , 58 , 62 , 63 , 67 , 77 , 84 ]. The random effects pooled prevalence was 4.1% (95% CI 2.0% to 6.7%) ( Fig 5 ), with substantial heterogeneity ( I 2 = 89% [95% CI 77% to 96%]; 95% PI 0% to 16%). Individual estimates ranged from 1.0% to 13.5%. Univariable regression models indicated that studies with higher proportions of female participants reported significantly higher rates of bipolar disorder (see S8 Table ). In the multivariable model, prevalence estimates from studies with randomized sampling were significantly lower than those from studies with other sampling methods (see Table 1 ).
https://doi.org/10.1371/journal.pmed.1003750.g005
A subgroup analysis of 9 low-risk-of-bias surveys [ 49 , 55 , 58 , 62 , 65 , 67 , 71 , 84 , 85 ] resulted in a random effects pooled prevalence of 2.6% (95% CI 1.0% to 4.9%), with moderate heterogeneity ( I 2 = 78% [95% CI 29% to 96%]). The difference between low-risk-of-bias and moderate-risk-of-bias studies was non-significant ( Q = 2.29, p = 0.13).
Findings for any affective disorder (which included depression and bipolar disorder) are reported in S1 Text and S6 Table .
Alcohol use disorders
Estimates on alcohol use disorders could be extracted from 29 surveys [ 28 , 29 , 51 – 66 , 68 , 71 – 73 , 76 , 77 , 79 – 81 , 84 , 85 ]. The random effects pooled prevalence was 36.7% (95% CI 27.7% to 46.2%) ( Fig 6 ), with individual study estimates ranging from 5.5% to 71.7%, and with substantial between-study heterogeneity ( I 2 = 98% [95% CI 97% to 99%]; 95% PI 2% to 85%). Univariable meta-regression models indicated that studies with smaller samples and studies from Germany (compared to other locations) reported significantly higher rates of alcohol use disorders (see S8 Table ). In multivariable analysis, the best selected model included only study location as a predictor variable, with higher prevalences reported in Germany and North America (see Table 1 ).
https://doi.org/10.1371/journal.pmed.1003750.g006
In a subgroup analysis of 14 low-risk-of-bias studies [ 29 , 52 , 55 , 58 , 60 , 62 , 65 , 71 , 73 , 79 – 81 , 84 , 85 ], the random effects pooled prevalence was 36.9% (95% CI 21.1% to 54.3%; I 2 = 99% [95% CI 98% to 100%]). There was no significant difference between risk of bias subgroups ( Q < 0.01, p = 0.96).
Drug use disorders
We identified 23 surveys reporting prevalence estimates on drug use disorders [ 28 , 29 , 52 , 53 , 55 – 65 , 71 , 73 , 76 , 79 , 80 , 82 , 84 , 85 ] ( Fig 7 ). A random effects pooled prevalence of 21.7% (95% CI 13.1% to 31.7%) was found, with very high heterogeneity ( I 2 = 99% [95% CI 98% to 99%]; 95% PI 0% to 74%); individual estimates ranged between 0% and 72.1%. According to univariable meta-regression, studies with randomized sampling (as opposed to other sampling methods) estimated significantly lower prevalence rates (see S8 Table ). The selected multivariable model showed that studies from the UK reported lower prevalence rates. These results were confirmed by a secondary complete case analysis.
Analytic weights are from random effects meta-analysis. Grey boxes represent study estimates; their size is proportional to the respective analytical weight. Lines through the boxes represent the 95% CIs around the study estimates. The blue diamond represents the mean estimate and its 95% CI. The vertical red dashed line indicates the mean estimate. CI, confidence interval; PI, prediction interval; RE: random effects.
https://doi.org/10.1371/journal.pmed.1003750.g007
A subgroup analysis of 13 low-risk-of-bias studies [ 29 , 52 , 55 , 58 , 60 , 62 , 65 , 71 , 73 , 79 , 80 , 84 , 85 ] resulted in a random effects pooled prevalence of 18.1% (95% CI 10.5% to 27.2%), with substantial heterogeneity ( I 2 = 97% [95% CI 94% to 99%]). The difference between subgroups was not significant ( Q = 0.65, p = 0.42).
Personality disorders
Fourteen studies reported prevalence estimates on lifetime personality disorders [ 28 , 51 – 53 , 62 , 64 , 67 , 75 – 77 , 80 , 82 , 84 , 85 ], with a random effects pooled prevalence of 25.4% (95% CI 10.9% to 43.6%) ( Fig 8 ). Individual estimates ranged between 0% and 98.3%, resulting in substantial heterogeneity ( I 2 = 99% [95% CI 97% to 99%]; 95% PI 0% to 91%). Univariable regression models did not yield significant results (see S8 Table ), and neither did the selected multivariable model (see Table 1 ).
https://doi.org/10.1371/journal.pmed.1003750.g008
In a subgroup analysis of 6 low-risk-of-bias studies [ 52 , 62 , 67 , 80 , 84 , 85 ], the random effects pooled prevalence was 21.0% (95% CI 4.7% to 44.5%), with substantial heterogeneity ( I 2 = 97% [95% CI 92% to 100%]). The difference between subgroups was not significant ( Q = 0.32, p = 0.57).
This systematic review and meta-analysis of the prevalence of mental illness among homeless people in high-income countries included 39 studies comprising a total of 8,049 participants. We investigated 7 common psychiatric diagnoses, and examined possible explanations for the between-study heterogeneity. We report 3 main findings.
With a pooled prevalence of around 37%, alcohol-related disorders were the most prevalent diagnostic category. This prevalence estimate is around 10-fold greater than general population estimates: An EU study reported a 12-month prevalence of 3.4% in the general population [ 86 ]. Correspondingly, drug-related disorders were the second most common current mental disorder, with a pooled prevalence of 22% (which can be compared with the 12-month prevalence in the US general population of 2.5% [ 87 ]). We found substantial variation between the individual studies contributing to these estimates, with individual study estimates ranging from 5.5% to 71.7% for alcohol-related disorders; this variation was partially accounted for by study location. Particularly, German-based samples typically had higher prevalence rates of alcohol use disorders than those from other nations. This might highlight geographical differences regarding the affordability and availability of substances, including a comparatively low alcohol tax in Germany [ 88 ]. Irrespective of this moderating factor, the strong association between homelessness and substance abuse reflects a bidirectional relationship: Alcohol and drug use represent possible coping strategies in marginalized housing situations. At the same time, substance abuse and other psychiatric disorders precede the onset of homelessness in many people, with alcohol use disorders in particular emerging at an earlier point in life compared to age-matched non-homeless comparisons [ 89 ], suggesting that substance use might contribute to the deterioration of an individual’s housing situation. Such deterioration is consistent with the links between substance use disorders and excess mortality in homeless people [ 11 ], homelessness chronicity, psychosocial problems [ 90 ], and poorer long-term housing stability [ 91 ].
A second main finding was that some study characteristics consistently explained the variations in prevalence. In 5 diagnostic groups, methods were important, specifically the number of included participants and the sampling procedure. Unexpectedly, the latter had differential effects by diagnostic group. In bipolar disorder and drug use disorders, randomization was associated with lower prevalence estimates, whereas for any current mental disorder and major depression, it was associated with higher estimates. These findings underline the importance of standardized methodological procedures for homelessness research. We recommend that new research studies should base their inclusion criteria on a standardized definition of homelessness based on ETHOS criteria [ 92 ] and use randomized sampling, standardized diagnostic instruments, and trained interviewers with clinical backgrounds (including nurses, psychologists, and medical doctors).
Our third main finding was high prevalence rates for treatable mental illnesses, with 1 in 8 homeless individuals having either major depression (12.6%) or schizophrenia spectrum disorders (12.4%). This represents a high rate of schizophrenia spectrum disorders among homeless people, and a very large excess compared to the 12-month prevalence in the general population, which for schizophrenia is estimated around 0.7% in high-income countries [ 86 ]. For major depression, the difference from the general population is not marked, as the 12-month prevalence in the US general population is estimated at 10% [ 93 ], although comparisons would need to account for the differences in age and sex structure between the samples contributing to this review and the general population. Depression remains important because it is modifiable, and because of its effects on adverse outcomes. In addition, a recent cohort study based in Vancouver, Canada, found that substance use disorders were associated with worsening of psychosis in homeless people, underscoring the links between these mental disorders, and the importance of treatment in mitigating their effects directly and indirectly [ 13 ]. This study also found elevated risks of mortality in those with psychosis and alcohol use disorders [ 13 ].
Overall, our findings underscore the importance of mental health problems among homeless individuals. This review is complemented by other research on the often precarious financial and housing situation of psychiatric patients, for whom high rates of homelessness, indebtedness, and lack of bank account ownership have been reported [ 94 – 97 ]. Being homeless and having mental disorders are therefore closely interrelated. Fragmented and siloed services will therefore be typically unable to address these linked psychosocial and health problems. The mental disorders reported in this study are typically associated with unmet needs in the homeless population [ 51 , 98 – 100 ], which further indicates the need for integrated approaches. Many different initiatives to address these needs have been researched over the last decade, among them Housing First, Intensive Case Management, Assertive Community Treatment, and Critical Time Intervention. Randomized controlled studies using these approaches have generally resulted in positive effects on housing stability, but only moderate or no effects on most indicators of mental health in comparison to usual care, including for substance use [ 101 – 104 ]. Therefore, further improvements in management and treatment are necessary that focus on these common mental disorders.
The COVID-19 pandemic has put homeless people at particular risk of infection and further marginalization [ 105 ]. But it has shown what is possible—government agencies and charity organizations managed to quickly provide accommodation to a large number of rough-sleeping homeless people in some European regions [ 106 , 107 ].
Some limitations to this review need to be considered. We searched a limited number of databases, so it is possible that we missed certain primary reports, although this possibility was minimized by searching through reference lists and Google Scholar citations. Furthermore, despite the high rate of multimorbidity in homeless populations [ 108 , 109 ], included studies lacked information on comorbidity. With most of the primary studies reporting prevalence rates of more than 1 of the investigated diagnostic categories, effects from the same sample were in many cases entered into multiple meta-analytical models. This may have led to measurement error and overestimation if diagnostic criteria overlap, but without diagnostic validity studies specific to homeless persons, this remains uncertain. We limited the number of demographic variables that we conducted heterogeneity analyses on, because of variations in measurement and reporting detail. Future work, including individual participant meta-analysis, could standardize information on age, socioeconomic background, and ethnicity, for example.
The present review focuses on high-income countries because sample and diagnostic heterogeneity would presumably increase if a wider range of countries was included. It is important to note, however, that homeless populations in low- and middle-income countries need investigation, and may have higher rates of trauma-related symptoms [ 110 , 111 ]. The prevalence of the mental disorders reported in the current review does not consider unmet healthcare needs or treatment provision, which are additional elements to consider in developing services. Finally, several subpopulations were underrepresented: migrants and refugees (individuals who did not speak the local language were excluded from some study samples), the “hidden homeless” population (e.g., “couch-surfers”) [ 112 ] (sampling procedures were often not able to identify this group), and, importantly, homeless women. Twenty-two percent of participants in the included studies were female, lower than most estimates of the proportion of women among homeless populations, which range between 25% and 40% [ 4 , 113 ].
In summary, we found high prevalence of mental disorders among homeless people in high-income countries, with around three-quarters having any mental disorder and a third having alcohol use disorders. Future research should focus on integrated service models addressing the identified needs of substance use disorders, schizophrenia spectrum disorders, and depression in homeless individuals as a priority. In addition, new work could consider focusing on underrepresented subpopulations like homeless women and migrants. Furthermore, longitudinal studies could examine mechanisms linking homelessness and mental disorders in order to develop more effective preventive measures.
Supporting information
S1 table. database search strings..
https://doi.org/10.1371/journal.pmed.1003750.s001
S2 Table. PRISMA 2009 checklist.
https://doi.org/10.1371/journal.pmed.1003750.s002
S3 Table. Studies excluded at full-text screening, with reasons.
https://doi.org/10.1371/journal.pmed.1003750.s003
S4 Table. Study characteristics.
https://doi.org/10.1371/journal.pmed.1003750.s004
S5 Table. JBI checklist for prevalence studies.
https://doi.org/10.1371/journal.pmed.1003750.s005
S6 Table. Risk of bias tool.
https://doi.org/10.1371/journal.pmed.1003750.s006
S7 Table. Data basis for meta-analyses and meta-regression analyses.
https://doi.org/10.1371/journal.pmed.1003750.s007
S8 Table. Univariable regression models.
https://doi.org/10.1371/journal.pmed.1003750.s008
S9 Table. Results of single factor meta-regression models for affective disorders (pooled).
https://doi.org/10.1371/journal.pmed.1003750.s009
S10 Table. Results of multiple factor meta-regression for affective disorders (pooled).
https://doi.org/10.1371/journal.pmed.1003750.s010
S1 Text. Affective disorders.
Results of meta-analysis and meta-regression analysis.
https://doi.org/10.1371/journal.pmed.1003750.s011
Acknowledgments
We are grateful to authors of included and non-included publications who provided additional details about their studies: C. Adams, H.-J. Salize, A. Greifenhagen, C. Vazquez, U. Beijer, C. Siegel, and G. Gilchrist. We are also grateful to the professional translator N. Spennemann for assistance with Japanese studies.
- 1. United Nations Commission for Social Development. Affordable housing and social protection systems for all to address homelessness. Report of the Secretary-General. E/CN.5/2020/3. New York: United Nations Commission for Social Development; 2019 Nov 27 [cited 2020 May 10]. Available from: https://undocs.org/en/E/CN.5/2020/3 .
- 2. Directorate of Employment, Labour and Social Affairs. HC3.1 Homeless population. Paris: Organisation for Economic Co-operation and Development; 2020 [cited 2020 May 3]. Available from: https://www.oecd.org/els/family/HC3-1-Homeless-population.pdf .
- View Article
- PubMed/NCBI
- Google Scholar
- 4. Henry M, Mahathey A, Morrill T, Robinson A, Shivji A, Watt R. The 2018 Annual Homeless Assessment Report (AHAR) to Congress. Part 1: point-in-time estimates of homelessness. Washington (DC): US Department of Housing and Urban Development; 2018 Dec [cited 2020 May 10]. Available from: https://www.huduser.gov/portal/sites/default/files/pdf/2018-AHAR-Part-1.pdf .
- 28. Bäuml J, Brönner M, Baur B, Pitschel-Walz GG, Jahn T, Bäuml J. Die SEEWOLF-Studie: seelische Erkrankungsrate in den Einrichtungen der Wohnungslosenhilfe im Großraum München. Archiv für Wissenschaft und Praxis der sozialen Arbeit. Freiburg im Breisgau: Lambertus-Verlag; 2017.
- 33. World Bank. World Bank country and lending groups. Washington (DC): World Bank; 2020 [cited 2020 Sep 11]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups .
- 34. JBI. Critical appraisal tools. Adelaide: University of Adelaide; 2021 [cited 2021 Aug 12]. Available from: https://jbi.global/critical-appraisal-tools .
- 43. Viechtbauer W. Package ‘metafor.’ Version 2.4–0. Comprehensive R Archive Network; 2020 [cited 2021 Apr 21]. Available from: https://cran.r-project.org/web/packages/metafor/metafor.pdf .
- 106. Ministry of Housing, Communities & Local Government, Jenrick R. 6,000 new supported homes as part of landmark commitment to end rough sleeping. London: Ministry of Housing, Communities & Local Government; 2020 May 24 [cited 2021 Jan 1]. Available from: https://www.gov.uk/government/news/6-000-new-supported-homes-as-part-of-landmark-commitment-to-end-rough-sleeping .
- 107. Deutsche Welle. Berlin opens first hostel for the homeless amid coronavirus pandemic. Deutsche Welle. 2020 Mar 31 [cited 2021 Jan 2]. Available from: https://www.dw.com/en/berlin-opens-first-hostel-for-the-homeless-amid-coronavirus-pandemic/a-52972263 .
- 113. Neupert P. Statistikbericht 2017. Berlin: Bundesarbeitsgemeinschaft Wohnungslosenhilfe. 2018 [cited 2020 Jul 18]. Available from: https://www.bagw.de/fileadmin/bagw/media/Doc/STA/STA_Statistikbericht_2017.pdf .

The Complex Link Between Homelessness and Mental Health
Many americans are at heightened risk of homelessness due to the pandemic..
Posted May 21, 2021 | Reviewed by Hara Estroff Marano
- An estimated 20 to 25 percent of the U.S. homeless population suffers from severe mental illness, compared to 6 percent of the general public.
- The combination of mental illness, substance abuse, and poor physical health makes it difficult to maintain employment and residential stability.
- Better mental health services would combat not only mental illness but homelessness as well.
This post was written by Lenni Marcus, Cameron Johnson, and Danna Ramirez.
For many Americans, the prospect of losing their homes and falling into uncertain housing situations became excruciatingly prescient during the economic downturn caused by the impact of the coronavirus outbreak. A 2019 study suggested that even at that time, 40 percent of Americans were already one missed paycheck away from poverty.
And though governmental policies have temporarily slowed or halted evictions in many places, many individuals and families are still at risk of homelessness, or have already fallen through the cracks. Few are on a path to financial recovery and the profound aftershocks of this crisis will be felt far beyond the upcoming months and may impact families and their mental health for years to come.

Many homeless people share similar experiences, but a substantial subgroup of the homeless population struggle with severe mental illness as well. Yet the resilience of this group is often understated. Some just need help accessing resources, including mental health services, to reach a stable housing and financial situation. To understand how to better provide resources to break the cycle of homelessness, it is important to understand the many factors that may contribute to their impoverished state.
Homelessness and Mental Health
The idea that mental illness alone causes homelessness is naive and inaccurate, for two major reasons. First, the overwhelming majority of those living with mental illness are not homeless (and studies have failed to demonstrate a causal relationship between the two).
These types of distortions can have dangerous implications, wrongly focusing the attention on the individual rather than on the institutions that perpetuate housing insecurity. As a result, the illusory division between the “mentally ill homeless” and the “non-mentally ill homeless” casts the former as more deserving of intervention and services and the latter as seemingly “unworthy” or “undeserving” of support.
Though there is no causal relationship between mental illness and homelessness, those who suffer from housing insecurity are struggling significantly, both psychologically and emotionally. The constellation of economics, subsistence living, family breakdown, psychological deprivation, and impoverished self-esteem all contribute to the downward cycle of poverty.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), in 2010, 26.2 percent of all sheltered persons who were homeless had a severe mental illness, and 34.7 percent of all sheltered adults who were homeless had chronic substance use issues. Of those who experience chronic/long-term homelessness, approximately 30 percent have mental health conditions and 50 percent have co-occurring substance use problems. Also, they typically endure traumatic experiences that could potentially lead to mental health struggles, and certain environmental factors may increase the likelihood that they encounter future traumas.
Over 92 percent of mothers who are homeless have experienced severe physical and/or sexual abuse during their lifetime, and about two-thirds of homeless mothers have histories of domestic violence . Mothers who are homeless have three times the rate of PTSD and twice the rate of drug and alcohol dependence of their low-income housed counterparts. Left untreated, these stressors can further damage their mental health, potentially triggering maladaptive coping and putting them at risk for future traumatic events.
Breaking the Cycle of Homelessness
Homelessness is a social problem with complex and multifactorial origins. It underlies economic , social , and biographical risk factors such as poverty, lack of affordable housing, community and family breakdown, childhood adversity, neglect, and lack of social support, to name a few. These factors contribute to the onset, duration, frequency, and type of homelessness amongst individuals of all ages.
About 3 percent of Americans experience at least one episode of homelessness throughout their lives. Many enter an unbreakable cycle of homeless living due to the lack of access to adequate resources.
There are many components involved in the healthy exit of homelessness, with two of the most important being housing and social support . Meaningful and sustainable employment is fundamental to creating and maintaining housing stability. At the same time, individuals experiencing homelessness face many barriers to finding and maintaining employment . Most organizations that provide brief employment interventions assist individuals with only their most immediate employment needs (e.g., resume preparing); frequently these have little or no beneficial effects.

More intensive interventions that include an educational and/or training component are effective for those who participate regularly. Connecting people experiencing homelessness with job training and placement programs provides them with the necessary tools for long-term stability and success.
Access to housing and effective employment programs alone do not address other issues, such as loneliness , social exclusion, or any psychological problems that might have emerged. Promoting social connections as part of the transition out of homelessness plays a major role in improving outcomes.
Social support is a multidimensional concept that is measured by the size of a social network , received social support, and perceived social support. Received and perceived social support can each consist of different components: emotional support (the expression of positive affect and empathetic understanding), financial support (the provision of financial advice or aid), and instrumental support (tangible, material, or behavioral assistance). Therefore, programs providing training in job and life skills should also address how to navigate through social networking and how to maintain healthy social relations.
Breaking the cycle of homelessness requires institutions and policymakers to focus their efforts on multifaceted programs that are as complex as the social problem itself.
About the Authors
Lenni Marcus is a former social worker at the Compass program for young adults at The Menninger Clinic.
Cameron Johnson is a research assistant at The Menninger Clinic . Cameron collects and manages treatment outcomes survey data, which Menninger uses to help track the symptoms of patients.
Danna Ramirez is the Clinical Research Informatics Engineer at The Menninger Clinic . Her research interests include the neurobiology of psychiatric disorders, especially personality disorders and mood disorders

Mind Matters is a collaborative blog written by Menninger staff and an occasional invited guest to increase awareness about mental health. Launched in 2019, Mind Matters is curated and edited by an expert clinical team, which is led by Robyn Dotson Martin, LPC-S. Martin serves as an Outpatient Assessment team leader and staff therapist.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 05 April 2024
Addressing health needs in people with mental illness experiencing homelessness
- Nick Kerman ORCID: orcid.org/0000-0001-5219-0449 1 &
- Vicky Stergiopoulos ORCID: orcid.org/0000-0003-3941-9434 1 , 2
Nature Mental Health volume 2 , pages 354–366 ( 2024 ) Cite this article
881 Accesses
12 Altmetric
Metrics details
- Social sciences
Homelessness among people with mental illness is a prevalent and persisting problem. This Review examines the intersection between mental illness and homelessness in high-income countries, including prevalence rates and changes over time, the harmful effects of homelessness, and evidence-based health and housing interventions for homeless people with mental illness. Special populations and their support needs are also highlighted. Throughout this Review, policy and service implementation failures that have precipitated and perpetuated homelessness among people with mental illness are discussed, and policy and practice priorities critical to reducing homelessness and improving health outcomes in this population are proposed.
You have full access to this article via your institution.
Similar content being viewed by others

Determinants of behaviour and their efficacy as targets of behavioural change interventions

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

Psilocybin microdosers demonstrate greater observed improvements in mood and mental health at one month relative to non-microdosing controls
Homelessness is an extreme form of material deprivation that occurs when people do not have permanent, safe and adequate accommodations. Although there is no consensus on the types of living situation that constitute homelessness, definitions often include temporarily residing in emergency accommodations (such as shelters), living on the streets, in cars or in buildings not intended for human habitation or staying temporarily with family and friends (that is, hidden homelessness) 1 , 2 . People experiencing homelessness are also overrepresented in hospitals and jails, making these institutions central to some experiences of homelessness 3 , 4 .
Homelessness in its various forms is an enduring social problem that is widespread in high-income countries. An estimated 2.1 million people experience homelessness every year across 36 member countries of the Organisation for Economic Co-operation and Development (OECD) 5 . As shown in Table 1 , homelessness estimates and trends vary considerably among high-income countries. However, comparisons between countries are challenging due to different methodological approaches and definitions of homelessness. Still, there are evident prevalence trends in some countries. In the USA, there was a very slight, gradual decline in daily homelessness rates from 647,258 in 2007 to 582,462 in 2022, before increasing to 653,104 in 2023, as measured by annual point-in-time counts 6 . Similarly, homelessness has stagnated or increased in many European countries during the past decade, with the notable exception of Finland, which has observed sizable decreases in the number of people experiencing homelessness over the past decade 7 , 8 . Other high-income countries have failed to monitor homelessness rates at the population level, or have done so very narrowly, yielding a lack of clarity about the extent of the problem and the effectiveness of the investments made to address it.
Homelessness is fundamentally a housing problem, with the limited availability of affordable housing being a foremost contributor to homelessness in communities 9 . However, other key structural- and individual-level factors can also affect rates of homelessness. For example, both unemployment and the quality of the social safety net, such as income support programs, have been tied to homelessness rates 10 , 11 , 12 . In addition, poor health, early childhood adversity and trauma, and involvement in the criminal justice system are associated with increased risk of homelessness 12 . Thus, populations experiencing marginalization, such as people with mental illness, that are disproportionately affected by these structural- and individual-level factors are at higher risk of homelessness. It is estimated that 76.2% of people experiencing homelessness have a current mental disorder 13 .
Given the persistence of homelessness in many jurisdictions and the prevalence of mental illness among people experiencing homelessness, this Review will discuss the intersection of mental illness and homelessness, and identify urgent priorities for action in high-income countries.
Mental illness and homelessness: emergence of an intractable problem
The intersection between mental illness and homelessness in many high-income countries is often described as having its modern origins in deinstitutionalization. Beginning in the 1960s, many psychiatric hospitals were closed in response to growing concerns about the poor quality of care in those facilities, emerging evidence on recovery in mental illness and advancements in psychotropic medications. The scale of the psychiatric hospital closures during deinstitutionalization transformed mental health systems. Of the 559,000 state psychiatric hospital beds that existed in the USA in 1955, over 400,000 had been closed by the early 1980s 14 . Similar reductions in psychiatric inpatient beds occurred in Canada (a 70.6% decline from 1965 to 1981) 15 and in the UK (a 60.0% decrease from 1954 to 1990) 16 . As a result, many long-stay hospital patients with serious mental illness were discharged to community settings. This transformational shift corresponded with rising rates of homelessness among people with mental illness during these decades. This led to assumptions that an insufficient supply of appropriate housing and mental health support alternatives had resulted in increased rates of homelessness for this population 17 . Recent research has questioned the extent to which there was a causal relationship between deinstitutionalization and homelessness rates among people with mental illness, with evidence that this may have been confounded by other societal changes that occurred during subsequent decades 18 . Nevertheless, deinstitutionalization precipitated the transformation of mental health systems, marked by the limited availability of community services and funding in some regions—ill-enduring effects with which community mental health systems continue to grapple and that disproportionally affect people with mental illness who experience homelessness 16 , 17 .
Over the past half-century, other macro-level social policies, societal factors and systemic issues have been identified as yielding multiple pathways into homelessness for people with mental illness. This includes high rates of unemployment and precarious employment among people with mental illness, coupled with insufficient minimum wages and income support rates, as well as shortages in affordable and supportive housing, that make it challenging to find and keep housing 19 , 20 , 21 . Criminal record histories and substance use yield additional challenges to obtaining housing and employment 22 , 23 , 24 . At the systems level, fragmentation within and between health and social services can undermine efforts by homeless people with mental illness to achieve positive housing outcomes 25 . Furthermore, childhood family instability and lower educational attainment have been identified as early-life experiences that may affect homelessness risk and trajectories among people with mental illness 22 , 24 . Thus, the evolution of mental health service systems and inadequate social policies, potentially exacerbated by other forms of social exclusion, have contributed to homelessness among people with mental illness becoming an intractable problem.
Prevalence of mental illness among homeless populations
Similar to research on the rates of homelessness, studies examining the prevalence of mental illness, including substance use disorders, among homeless populations use different methodologies and samples. In addition, there has been a limited number of longitudinal studies on prevalence rates from the past decade. As a result, to understand emergent trends in prevalence, particularly with regard to problematic drug use among people experiencing homelessness, it is necessary to integrate research that examines epidemiology, treatment seeking and mortality rates. In this Review, comparisons of estimates are made only when there is sufficient methodological consistency between studies.
The rates of mental illness among people experiencing homelessness in high-income countries are high. As shown in Table 2 , a recent meta-analysis of 39 publications from 1979 to 2019 indicated that between 64.0 and 86.6% of people experiencing homelessness have at least one diagnosable current mental disorder (defined as any Axis I disorder in the multiaxial system previously used by the Diagnostic and Statistical Manual of Mental Disorders ) 13 . Of the non-substance use disorder diagnostic categories examined in the meta-analysis, personality disorders were identified as the most prevalent (10.9–43.6%), followed by major depression (7.9–18.2%), schizophrenia spectrum disorders (9.5–15.7%) and bipolar disorders (2.0–6.7%). Compared to an earlier meta-analysis that comprised studies up to 2005, these prevalence rate estimates have been mostly stable 26 . Although post-traumatic stress disorder (PTSD) was not examined in the aforementioned studies, its prevalence among people experiencing homelessness has been investigated in another recent meta-analysis. Findings showed that between 22.0 and 33.6% of people experiencing homelessness met the diagnostic criteria for PTSD, with significant heterogeneity in prevalence rates across high-income countries 27 . Similarly, a synthesis on intellectual disability among people experiencing homelessness found that prevalence estimates ranged from 12.0 to 38.9%, as determined via intellectual functioning assessments using intelligence quotient (IQ) estimates (IQ < 70 or IQ ≤ 70) 28 . However, there was considerable variation between and within samples, and adaptive functioning was not assessed, which may overestimate the prevalence of intellectual disability among homeless populations 28 . More broadly, meta-analyses have demonstrated high rates of ‘cognitive impairment’ within the population, with a pooled estimate of approximately 25% (ref. 29 ).
The prevalence of mental illness and addictions among homeless populations has changed over time. Early research involving three studies conducted in ten-year intervals using the same methods showed that the lifetime prevalence of non-substance use DSM Axis I disorders increased significantly for both men and women from 1980 to 2000 30 . Major depression was the foremost contributor to the sharp increase in prevalence over the two decades, with rates of bipolar disorder and panic disorder also increasing to a lesser extent. By contrast, the prevalence of schizophrenia changed minimally. A more recent repeated longitudinal survey conducted every three years from 2000 to 2018 in the US state of Minnesota found increased rates of self-reported depression (from 24.3 to 44.3%), PTSD (from 13.1 to 35.6%), bipolar disorder (from 12.3 to 23.9%) and schizophrenia (from 6.4 to 10.9%) across the study period 31 . The prevalence rates in this study exceed the aforementioned meta-analysis estimates probably due to the use of unstandardized self-report tools, necessitating the need for interpretational caution. However, trend patterns over time may reflect changes in the types of disorder among people experiencing homelessness in the post-deinstitutionalization era. The rise was gradual for all disorders, with the exception of schizophrenia, which plateaued from 2006 onward. Thus, major mood disorders and the effects of trauma may be growing issues within homeless populations.
Substance use disorders are among the most prevalent mental disorders among homelessness populations. In the meta-analysis by Gutwinski and colleagues, prevalence estimates for alcohol use disorder and drug use disorder (excluding tobacco use disorder) ranged from 27.7 to 46.2% and from 13.1 to 31.7%, respectively 13 . However, tobacco is the most commonly used drug. A systematic review of smoking prevalence among adults experiencing homelessness ranged from 57.3 to 81.7% (ref. 32 ). Other types of drug commonly used by people experiencing homelessness include opioids, methamphetamine and cocaine. Drug use patterns and disorder rates have changed over time, and these trends are probably shaped by evolving supplies of street drugs and laws about the legality of the substances. With regard to opioids, a large cohort study of people experiencing homelessness in the US city of Boston found a more than 1,400% increase in the synthetic opioid mortality rate from 2013 to 2018 33 . The same study also demonstrated that polysubstance overdose deaths involving opioids had surpassed opioid-only deaths, attributable to increases in concurrent use of opioids with cocaine, benzodiazepine and alcohol over the study period. Other research has demonstrated an increase in concurrent methamphetamine and opioid use in recent years. In a national retrospective US study of people accessing substance use treatment from 2013 to 2017, the rate of concurrent methamphetamine use among people with opioid use disorder also experiencing homelessness increased from 13.8 to 25.0% (ref. 34 ). Earlier research also supports changing rates of methamphetamine and amphetamine use. A serial cross-sectional study of homeless and marginally housed people in the US city of San Francisco found that methamphetamine use within the past 30 days had nearly quadrupled among those under 35 years of age from 1996 (8.8%) to 2003 (33.0%) 35 . As for cocaine use disorder, according to a recent systematic review, lifetime prevalence among homeless populations increased from a median estimate of 16% among studies published in the 1980s to 37% among studies from 1990 to 2012 36 . Gambling disorder has also been found to be many times higher among people experiencing homelessness than in the general population, with past-year prevalence estimates ranging from 9.0 to 25.7% (ref. 37 ).
Premature mortality among homeless people with mental illness
Mortality rates among people experiencing homelessness are many times higher than in the general population—a finding that has been replicated in multiple high-income countries 38 , 39 . Unsheltered homelessness further exacerbates this mortality disparity 40 . Life-expectancy estimates differ between studies, as well as by age and gender, but people experiencing homelessness generally live 16–28 fewer years than same-aged peers in the general population 41 . The noted variations in mortality rates and life expectancies between high-income countries may be attributable to differences in health systems, including universal coverage and social issues (for example, violence and homicide rates) 42 .
The effects of mental illness on mortality rates among people experiencing homelessness have been insufficiently studied. A ten-year follow-up study found that homeless men with schizophrenia in Australia had a non-significantly lower standardized mortality ratio than those without schizophrenia, but were more likely to die by suicide at a significantly younger age 43 . In a smaller five-year follow-up study of homeless men in Sweden, there were no deaths among men with schizophrenia, whereas many of those who died had substance use problems 44 . Similarly, a national study conducted in Denmark found that schizophrenia spectrum disorders were a non-significant predictor of mortality among women experiencing sheltered homelessness, whereas men with schizophrenia spectrum disorders had a lower probability of dying than men without contact with the mental health system 45 . Earlier research has also found mental illness to be a non-significant predictor of mortality among people experiencing homelessness, with one study from 1999 reporting that men with mental illness had a lower likelihood of mortality over a seven-year period than men without mental illness 38 . As for suicide as a cause of death among homeless people with mental illness, high attempt rates have been found in additional research 46 .
Although the relationship between mental illness, homelessness and mortality requires further investigation, the effects of substance use disorders on mortality among people experiencing homelessness are more evident and alarming. Homeless people with substance use disorders are at increased risk of mortality 45 . However, this association was not replicated in a recent study of predictors of mortality among older adults experiencing homelessness 47 , suggesting that the risk may be greater among younger cohorts. The relationship between substance use disorders and mortality risk is probably partially attributable to drug overdose being one of the leading causes of death among people experiencing homelessness 48 . Moreover, overdose as a cause of death among homeless populations is worsening. In a Boston cohort study from 2003 to 2018, the drug overdose mortality rate increased 9.35% annually 48 . Accordingly, the overdose crisis is a grievous and worsening threat facing homeless populations in high-income countries.
Few studies have examined the role of physical health conditions on mortality among homeless people with mental illness. However, physical health problems are prevalent among this population. The risk of cardiovascular disease, a leading cause of death among homeless populations, has been found to be more than two times higher among homeless people with mental illness than the reference normal risk 49 . Rates of chronic diseases are also high, with hypertension, migraine, arthritis and asthma being among the most common, as are blood-borne pathogens, such as HIV and viral hepatitis 50 , 51 . The disease burden of these conditions among homeless people with mental illness is critical for interventions to consider and warrants further investigation.
Living at the margins
Homelessness can be experienced transitionally, episodically or chronically. Studies from North America have demonstrated that most people have brief episodes of homelessness that are a few in number (that is, transitional homelessness) 52 , 53 . Fewer people have repeated episodes of homelessness over a short period of time or longer shelter stays that last years (that is, episodic and chronic homelessness, respectively). Research on the relationship between mental illness and type of homelessness experienced has produced varying findings. In a study of shelter-use patterns in two US cities, people with mental illness were more likely to experience episodic or chronic homelessness and less likely to be transitionally homeless 53 . By contrast, a similar study in Denmark found high rates of mental illness across each type of homelessness, but this was marginally lower among the chronically homeless group 10 . Similar results emerged in recent Canadian research, with lower mental health functioning being associated with trajectories of higher housing stability 54 . The differing findings suggest that the broader social policy and system contexts may affect how people with mental illness experience homelessness and its associated harms.
In all of its forms, homelessness is a period of instability and social exclusion that can precipitate and exacerbate mental illness, yielding a bidirectional relationship between the two experiences 55 . There are several factors that impel deteriorations in mental health. First, people experiencing homelessness have ‘competing priorities’ among multiple unmet needs 56 . This can lead to needs that are less immediate than shelter, food and safety to go unaddressed, such as healthcare. One US study found than approximately 20% of people experiencing homelessness reported a past-year unmet need for mental health services 57 . Poor care quality, inadequate continuity, and stigma and discrimination are additional barriers to addressing mental health and addiction needs 58 , 59 , 60 . These impediments contribute to an overreliance on acute care services, such as emergency departments, that have limited effectiveness in addressing long-term health needs 60 , 61 .
Exposure to trauma, violence and victimization is another factor that can negatively affect mental health. Although such experiences are prevalent before people become unhoused, homelessness yields a heightened risk of victimization 22 , 62 . Estimates of recent violent victimization among homeless adults with serious mental illness found prevalence rates of 45.0 and 76.7% for the past month and two months, respectively 63 . Other forms of trauma, including pedestrian-strike, self-injurious and burn injuries, are also more common among homeless populations than those with housing 64 , 65 . Traumatic events during homelessness can be among the most debilitating problems experienced by people with mental illness and complicate their mental health recovery trajectories 66 .
Enforcement responses to homelessness by police, bylaw authorities, courts and other legal institutions can cause additional harms. Interactions between people experiencing homelessness and the police are common. In a study of over 500 homeless adults with mental illness in Toronto, Canada, 55.8% had interactions with the police in the past year 67 . Some interactions were deemed unnecessary, as shown by 12.6% receiving charges for acts of living, such as substance use in public, indecent acts, fouling in a street or solicitation. Similar results were found in a US study, with people experiencing homelessness reporting that policing aimed at restricting the overnight use of public spaces was more harassing than helpful 68 . Concerns about police contact can also lead people experiencing homelessness to seek more isolated and unsafe sleeping locations where the risk of violent victimization is greater 69 . Furthermore, displacement practices, such as ‘sweeps’ and ‘cleanups,’ have been used in some cities to remove people experiencing unsheltered homelessness from public spaces. This approach not only fails to address the basic needs of people who are displaced but may also undermine safety and increase drug-related morbidity and mortality. In a simulation study, continual displacement of people experiencing unsheltered homelessness who inject drugs contributed to an additional 15.6–24.4% of deaths over a ten-year period 70 .
Coping with the adversities of homelessness and mental illness takes different forms. Street-based survival strategies, such as intentional avoidance, hypervigilance and the establishment of outward appearances of strength, are a common adaptation to living in hostile and stressful environments 71 , 72 . Substance use is another frequently used coping strategy, yet it is one that carries heightened risk due to unregulated street-drug supplies, barriers to substance use treatment and limited access to places to safely use drugs. The role of social support in the context of homelessness is complex and varied. Although other individuals experiencing homelessness can be a source of community and belonging, there is the risk of victimization and the adoption of unhealthy behaviors, which is heightened among people with mental illness, especially women 63 , 73 , 74 . Trusted and compassionate service providers offer another valuable source of support 75 , although negative experiences using health, social and community services due to stigma and discrimination can be a barrier to the development of positive working relationships and a reason for service avoidance 76 . Overall, the coping mechanisms used by people experiencing homelessness are focused on immediate survival and may conflict with longer-term goals.
Interventions for improving housing and health outcomes
A range of interventions have been developed over the past four decades to address the housing and health needs of homeless people with mental illness. Several interventions, including Housing First, Assertive Community Treatment (ACT), Intensive Case Management (ICM) and Critical Time Intervention (CTI), have been extensively studied and are recognized as effective with this population. Common across all of these interventions is the provision of community-based types of support, on either an ongoing or a time-limited basis. These interventions can be differentiated from each other by their intensity of support, with ACT being most appropriate for those who have higher, ongoing needs, ICM being suitable for individuals with moderate, ongoing needs and CTI being used for those in need of time-limited support during service transitions. Housing First is unique from these other three interventions as it includes access to permanent housing in addition to different types of community support. These four interventions are described in more detail below, followed by promising practices that require further study.
Housing First is widely regarded as a best practice intervention for people experiencing chronic homelessness and mental illness. The intervention involves the provision of permanent housing in the form of a rental subsidy or an affordable housing unit, with accompanying community-based support such as ACT or ICM. Key tenets that guide the intervention include: no requirements for sobriety or medication adherence, the separation of housing and supports, service user choice and use of a harm-reduction and mental health recovery orientation. The robust evidence base for Housing First includes rigorous randomized trials from Canada and France, which demonstrate that the intervention is highly effective in improving housing stability 77 , 78 , 79 . Studies have increasingly involved longer follow-up periods, demonstrating that most people continue to experience housing stability after six years 79 . Multiple systematic reviews have also concluded that Housing First is effective in reducing emergency department visits and hospital admissions 80 , 81 . These service use reductions contribute to Housing First being a cost-effective intervention, especially for people with high support needs 82 . As for health and social outcomes, intervention effects have been less impactful 80 . However, greater program fidelity is linked to more positive outcomes, including adaptive functioning, underscoring the importance of adherence to the Housing First model 83 . Ongoing experiences of poverty among Housing First service users and the need for chronic health problems to be treated over a longer duration have been discussed as potential contributory factors to the limited improvements in health and social outcomes, despite favorable service experiences 84 . It would be prudent for future research to consider the effects of long-standing interpersonal and structural trauma among people living in Housing First programs, as well as the needs of those that may not be able to live independently in the community. Greater integration of intensive treatment for trauma may reduce behaviors that could cause housing loss.
In addition to its role in Housing First, ACT is a standalone evidence-based intervention used with homeless adults that experience serious mental illness. ACT, using multidisciplinary teams with small caseloads that offer intensive contact and 24-hour coverage, has been found to yield greater reductions in homelessness and improvements in psychiatric symptom severity compared with standard case management in randomized controlled trials 85 , 86 . Unsurprisingly, the effects of ACT alone on housing outcomes are smaller than those found in Housing First 87 . ACT is similarly associated with reductions in hospitalization and emergency department visits in randomized controlled trials, although the findings are not unequivocal 86 . The effects of the intervention on quality of life and income are more limited, with no known studies examining employment outcomes 86 . Fewer studies have examined service users’ care experiences with ACT, although there is evidence of higher satisfaction with this model than standard care 88 .
ICM is another standalone community mental health intervention that is commonly used with homeless people who experience mental illness. ICM involves the provision of community-based supports via a case manager who has small caseloads to facilitate weekly contact and coordinate care with other service providers. On its own, ICM yields small reductions in the number of days spent homeless compared with usual care 86 . These effects are smaller than those found in ACT, with a recent meta-analysis suggesting that a team-based support approach may yield better housing outcomes than the individualized approach of ICM 87 . Improvements in quality of life, substance use and access to income supports have been found with ICM, whereas the intervention’s effects on mental health, hospitalization and employment outcomes are more limited 86 .
CTI is a time-limited case management intervention to reduce the risk of homelessness and enhance the continuity of care during service transitions (for example, following hospital discharge or entry into housing programs from homelessness). As with ICM, CTI workers are responsible for service provision and coordination. Randomized trials have found that CTI cam improve housing and service use outcomes among homeless people with serious mental illness during transition periods 86 , 89 . One non-randomized pre–post cohort study also found improvements in mental health symptoms and substance use problems, as well as reductions in the number of days spent in institutions 90 . No changes in income were found among CTI recipients in a single randomized trial 89 .
A recent trend in intervention research with homeless people that experience mental illness has been the adaptation of Housing First and case management-type interventions to include new supports and implementation contexts. For example, supported employment has been integrated into Housing First, which increased the likelihood of service users obtaining competitive employment 91 . Multidisciplinary adaptations of CTI have been used successfully with homeless people who have unmet mental health needs following hospital discharge 92 . Moreover, financial incentives have been used to promote service engagement in a variety of settings, with promising but mixed effects 93 . Thus, there is a current and ongoing research focus on how to augment evidence-based interventions to more effectively improve service engagement, health and housing outcomes among homeless people with mental illness.
In addition to the evidenced-based interventions described above, there are promising approaches that warrant further research. Peer-navigation interventions involve support delivered by people with lived experience to address unmet health needs and improve access to services. Although such services exist in many forms, research on peer navigation targeted to individuals at the intersection of homelessness and mental illness is more limited. One randomized trial of peer navigation with Black homeless adults who experience serious mental illness found that the intervention had small to moderate effects on health status, mental health recovery and quality of life 94 . A harm-reduction-based peer-navigation intervention for homeless people with problematic substance use was also found to be acceptable and yielded promising findings in a feasibility study 95 . The use of peer navigation could be leveraged in future work with other groups experiencing multiple disadvantage, such as homeless migrants with mental illness who face additional barriers to accessing health and social services.
Income support interventions are another promising approach, albeit one with considerable variability in intervention components and practices. One approach is the use of larger cash transfers to overcome the financial barriers to exiting homelessness 77 . A recent randomized controlled trial in Canada examined the effects of a single unconditional cash transfer of CAD$7,500 (ranging from approximately US$5,652–5,788 at the time of distribution) on adults experiencing homelessness with non-severe mental health and addiction symptoms 96 . Findings showed that the intervention significantly reduced the number of days spent homeless and did not change spending on substances over the one-year study period, suggesting that the cash transfer may hasten exits from homelessness 96 . Although this approach has yet to be tested with homeless people who experience mental illness, it has the potential to address a key problem faced by this population: income support rates being insufficient to access affordable housing. Accordingly, income support interventions and other basic income schemes warrant further investigation.
Experiences and support needs of special populations
There are many groups, including women, youth, older adults, people of diverse sexual orientations and gender identities (LGBT+), people with substance use disorders, people with intellectual disabilities and racialized individuals and migrants, who have unique needs and support considerations as well as some shared vulnerabilities (see Table 3 ). Most notable are the relationship conflicts and terminations that become a pathway into homelessness, as well as high rates of trauma and victimization risk once homeless. Ongoing discrimination in the context of homelessness is another critical issue for some groups, such as LGBT+ community members and racialized and migrant groups. These homelessness pathways and experiences highlight the importance of creating service settings that are perceived as safe by these groups and involve the provision of holistic, person-centered and trauma-informed supports. Furthermore, they underscore the need for transformative social change to prevent homelessness caused by housing exclusion and structural racism.
Evidence gaps
In light of the evidence presented in this narrative review, several key avenues for future research are proposed, which include changes in psychiatric epidemiology among homelessness populations, stigma-reduction strategies in mainstream health and social services, approaches to enhancing service engagement and the standardized measurement of homelessness, as detailed below.
The transformation of community mental health systems following deinstitutionalization led to multi-decades growth in research on the intersection of homelessness and mental illness. However, the structural and systemic factors that determine homelessness and its sequelae have continued to evolve, and knowledge development has not kept pace. Evidence on changes over time in the prevalence rates of mental illness among homeless populations remains limited. In addition, there is continued ambiguity with regard to the effects of mental illness on premature mortality in the context of homelessness. As people with mental illness are at higher risk of cardiovascular and metabolic diseases than those without mental illness 97 , it is also critical to understand how homelessness may exacerbate associated health disparities and the extent to which service innovations effectively address them. With the advancement of research using administrative health data repositories and public health surveillance data, there are likely to be opportunities to sustainably address this evidence gap to enable health and social service systems to respond to changes at the population level in a more timely manner.
Another key evidence gap centers on approaches for improving the quality of care for people experiencing homelessness in mainstream health services. Experiences of stigma and discrimination by health professionals are commonly reported among homeless people with mental illness 71 , 76 . Although specialized health services for homeless and unstably housed populations have been developed to create more accessible and welcoming programs, the marginalization and stigmatization of homeless populations persists in mainstream health services. Moreover, specialized services are less likely to be available in smaller cities and rural communities, and most do not provide continuous care once housed. Accordingly, there is a need to develop and evaluate stigma-reduction approaches for facilitating humanizing healthcare experiences among homeless people with mental illness in mainstream settings.
The delivery of health services to homeless people with mental illness is fraught with challenges. Although some systemic and structural barriers require innovation at the policy level, other problems, including service engagement, can be potentially addressed via improvements to service delivery approaches, including among specialized services for this population. Key factors that shape service engagement among homeless people with mental illness include self-perceived need, support availability and relational factors 75 , 76 . Given this, simply expanding mental health services without attending to care philosophy and recovery orientation may not precipitate increased service engagement among those in need. Thus, further research is warranted on person-centered practices for enhancing health service engagement among homeless people with mental illness. Peer-led interventions and the integration of people with lived experience in outreach engagement teams could be beneficial for strengthening working relationships between service users and providers. Advancing the evidence base on intervention considerations for special populations, such as those outlined in Table 3 , will also be beneficial for adapting service approaches to improve engagement and outcomes.
Lastly, long-standing variations in the definitions and measurement of homelessness have hindered comparisons in prevalence rates between regions and countries, and deeper understandings of experiences within homeless populations. On the latter, for example, as unsheltered homelessness is associated with greater health harms than sheltered homelessness, aggregating these forms of homelessness may obscure differences between them. Thus, there is a critical need for future research to consistently define and measure homelessness. Leveraging existing typologies of homelessness 1 , 2 will yield stronger methodological parallels between studies. With more homelessness research using administrative health datasets, integrating typologies of homelessness into these data-collection systems will enable more nuanced examinations of differences within homeless populations in future research. Use of the Residential Time-Line Follow-Back inventory, a self-report housing history measure with strong psychometric properties, is also recommended for measuring housing outcomes, especially in clinical trials and longitudinal research with people experiencing homelessness 98 .
Practice and policy priorities
Effectively addressing the intractable problem of homelessness and mental illness requires investments that are comprehensive, multifaceted and evidence-based. Accordingly, we propose three practice and policy priorities that are critical for improving the health and wellness of homeless people with mental illness: (1) scale up ‘what works’, (2) strengthen upstream prevention and (3) establish needed downstream prevention supports (Fig. 1 ).
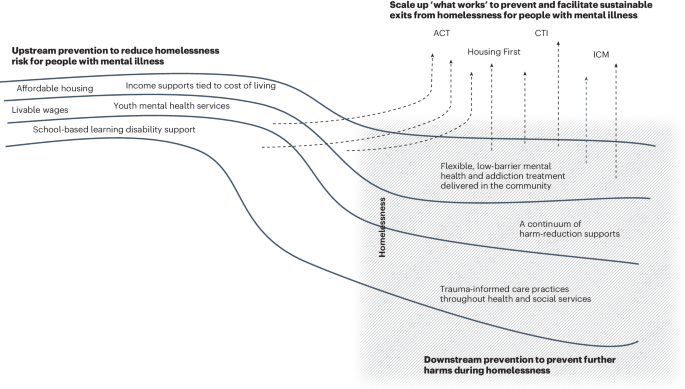
Improving the health and wellness of homeless people with mental illness requires more upstream prevention to reduce homelessness risk. Without this, people with mental illness are at greater risk of becoming homeless (as shown by the grey shaded box). Scaling up evidence-based interventions, such as Housing First, Assertive Community Treatment (ACT), Intensive Case Management (ICM), and Critical Time Intervention (CTI), is also key to preventing and facilitating exits from homelessness (as shown by the arrows that circumvent or direct away from homelessness). Downstream prevention are support services and orientations needed for preventing additional harms among people who are currently experiencing homelessness.
Scale up ‘what works’
Interventions such as Housing First, ACT, ICM and CTI are effective for improving housing and other outcomes among homeless people with mental illness. These interventions have been rigorously and extensively studied, demonstrating their generalizability to various homeless populations and service delivery contexts. Thus, there is a need to meaningfully scale up these evidence-based practices to meet the level of community need. The success of scale-up efforts is dependent on ensuring that services are sufficiently resourced to provide high-quality care with strong fidelity to program models. Too often, housing-focused interventions are implemented in real-world settings with a fraction of the resources used in research trials. Intermediary and purveyor organizations, which support the implementation and sustainability of evidence-based practices, can be leveraged to ensure that community mental health agencies have the tools to deliver high-quality services 99 . Although scaling up what works will require sizable resource investments, the achievement of cost offsets and superior outcomes would constitute fiscally smart spending.
Strengthen upstream prevention
Childhood adversity, pre-existing poverty, lower educational achievement and other forms of social exclusion are prevalent among homeless people with mental illness 22 , 66 , making upstream prevention a critical policy and intervention target. Investments to strengthen social safety nets, including more affordable housing, livable wages and income supports tied to the cost of living, will create a strong foundation for homelessness prevention among people with mental illness. Such upstream prevention efforts would align highly with an enhanced prioritization to scale up evidence-based interventions, such as Housing First, as demonstrated in Finland. Beginning in 2008, Finland undertook a highly successful national program to end chronic homelessness using a Housing First approach 100 . A key component of the program’s effectiveness was an emphasis on homelessness prevention through the development of social housing, which was targeted to young people 100 , 101 . Thus, Finland’s national program represents a concurrent investment in what works and upstream prevention, and holds great promise.
As the onset of many mental illnesses occurs by early adulthood, early intervention during childhood is another important upstream approach for preventing trajectories into homelessness. Reducing waiting lists for youth mental health and addiction treatment, and ensuring that these programs are integrated into community settings that serve at-risk groups are key to facilitating timely access to needed services. The detection of learning disabilities during childhood is another key preventive practice, given the overrepresentation of people with learning disabilities among homeless people with mental illness and their association with lower education attainment and poorer health outcomes 102 .
Establish needed downstream prevention supports
It is anticipated that prioritizing the other two policy and practice domains will reduce the need for downstream prevention supports, which should nonetheless remain a focus of intervention development and implementation. It is important to acknowledge and address the dire circumstances in which homeless people with mental illness are currently living and dying. Overdose fatalities and barriers to accessing mental health and addiction services are key problems that are currently faced by homeless populations and direct service providers 33 , 59 , 103 . Accordingly, there is an urgent need to increase the supply of person-centered, flexible, low-barrier mental health and addiction services, as well as harm-reduction supports for this population. Embedding trauma-informed practices throughout health and social services is instrumental for promoting service engagement and preventing further traumatization among this vulnerable population 104 .
Comprehensive policy and practice initiatives are needed to address the prevalent and persisting problem of homelessness among people with mental illness. Centering this work on upstream prevention and the scaling up of evidence-based practices, with concurrent, wraparound investments in accessible health and social services for homeless people with mental illness, will be best positioned to achieve sustainable, positive outcomes.
Gaetz, S. et al. Canadian Definition of Homelessness (Canadian Observatory on Homelessness Press, 2012).
FEANTSA. ETHOS – European Typology on Homelessness and Housing Exclusion ; https://www.feantsa.org/en/toolkit/2005/04/01/ethos-typology-on-homelessness-and-housing-exclusion (2017).
Greenberg, G. A. & Rosenheck, R. A. Jail incarceration, homelessness, and mental health: a national study. Psychiatr. Serv. 59 , 170–177 (2008).
Article PubMed Google Scholar
Lin, W. C., Bharel, M., Zhang, J., O’Connell, E. & Clark, R. E. Frequent emergency department visits and hospitalizations among homeless people with Medicaid: implications for Medicaid expansion. Am. J. Public Health 105 , S716–S722 (2015).
Article PubMed PubMed Central Google Scholar
HC3.1. Homeless population. OECD Affordable Housing Database https://www.oecd.org/els/family/HC3-1-Homeless-population.pdf (2021).
de Souza, T. et al. The 2023 Annual Homelessness Assessment Report (AHAR) to Congress. Part 1: Point-in-Time Estimates of Homelessness (US Department of Housing and Urban Development, 2023).
Fondation Abbé Pierre and FEANTSA. Fifth Overview of Housing Exclusion in Europe ; https://www.feantsa.org/en/news/2020/07/23/fifth-overview-of-housing-exclusion-in-europe-2020 (2020).
The Housing Finance and Development Centre of Finland. Homelessness in Finland 2022; https://www.ara.fi/en-US/Materials/Homelessness_reports/Homelessness_in_Finland_2022(65349) (2023).
Hanratty, M. Do local economic conditions affect homelessness? Impact of area housing market factors, unemployment, and poverty on community homeless rates. Hous. Policy Debate 27 , 640–655 (2017).
Article Google Scholar
Benjaminsen, L. & Andrade, S. B. Testing a typology of homelessness across welfare regimes: shelter use in Denmark and the USA. Hous. Stud. 30 , 858–876 (2015).
Giano, Z. et al. Forty years of research on predictors of homelessness. Community Ment. Health J. 56 , 692–709 (2020).
Nilsson, S. F., Nordentoft, M. & Hjorthøj, C. Individual-level predictors for becoming homeless and exiting homelessness: a systematic review and meta-analysis. J. Urban Health 96 , 741–750 (2019).
Gutwinski, S., Schreiter, S., Deutscher, K. & Fazel, S. The prevalence of mental disorders among homeless people in high-income countries: an updated systematic review and meta-regression analysis. PLoS Med. 18 , e1003750 (2021).
Lamb, H. R. Deinstitutionalization and the homeless mentally ill. Hosp. Community Psychiatry 35 , 899–907 (1984).
PubMed Google Scholar
Sealy, P. & Whitehead, P. C. Forty years of deinstitutionalization of psychiatric services in Canada: an empirical assessment. Can. J. Psychiatry 49 , 249–257 (2004).
Craig, T. & Timms, P. W. Out of the wards and onto the streets? Deinstitutionalization and homelessness in Britain. J. Ment. Health 1 , 265–275 (1992).
Sylvestre, J., Nelson, G. & Aubry, T. (eds) Housing, Citizenship, and Communities for People with Serious Mental Illness: Theory, Research, Practice, and Policy Perspectives (Oxford Univ. Press, 2017).
Winkler, P. et al. Deinstitutionalised patients, homelessness and imprisonment: systematic review. Br. J. Psychiatry 208 , 421–428 (2016).
Forchuk, C. et al. Housing, income support and mental health: points of disconnection. Health Res. Policy Sys. 5 , 14 (2007).
Padgett, D. K. Homelessness, housing instability and mental health: making the connections. BJPsych Bull. 44 , 197–201 (2020).
Piat, M. et al. Pathways into homelessness: understanding how both individual and structural factors contribute to and sustain homelessness in Canada. Urban Stud. 52 , 2366–2382 (2015).
Fitzpatrick, S., Bramley, G. & Johnsen, S. Pathways into multiple exclusion homelessness in seven UK cities. Urban Stud. 50 , 148–168 (2013).
Poremski, D., Whitley, R. & Latimer, E. Barriers to obtaining employment for people with severe mental illness experiencing homelessness. J. Ment. Health 23 , 181–185 (2014).
Sullivan, G., Burnam, A. & Koegel, P. Pathways to homelessness among the mentally ill. Soc. Psychiatry Psychiatr. Epidemiol. 35 , 444–450 (2000).
Rosenheck, R. et al. Service system integration, access to services, and housing outcomes in a program for homeless persons with severe mental illness. Am. J. Public Health 88 , 1610–1615 (1998).
Fazel, S., Khosla, V., Doll, H. & Geddes, J. The prevalence of mental disorders among the homeless in Western countries: systematic review and meta-regression analysis. PLoS Med. 5 , e225 (2008).
Ayano, G., Solomon, M., Tsegay, L., Yohannes, K. & Abraha, M. A systematic review and meta-analysis of the prevalence of post-traumatic stress disorder among homeless people. Psychiatr. Q. 91 , 949–963 (2020).
Durbin, A. et al. Intellectual disability and homelessness: a synthesis of the literature and discussion of how supportive housing can support wellness for people with intellectual disability. Curr. Dev. Disord. Rep. 5 , 125–131 (2018).
Depp, C. A., Vella, L., Orff, H. J. & Twamley, E. W. A quantitative review of cognitive functioning in homeless adults. J. Nerv. Ment. Dis. 203 , 126–131 (2015).
North, C. S., Eyrich, K. M., Pollio, D. E. & Spitznagel, E. L. Are rates of psychiatric disorders in the homeless population changing? Am. J. Public Health 94 , 103–108 (2004).
Vickery, K. D. et al. Trends in trimorbidity among adults experiencing homelessness in Minnesota, 2000–2018. Med. Care 59 , S220–S227 (2021).
Soar, K., Dawkins, L., Robson, D. & Cox, S. Smoking amongst adults experiencing homelessness: a systematic review of prevalence rates, interventions and the barriers and facilitators to quitting and staying quit. J. Smok. Cessat. 15 , 94–108 (2020).
Fine, D. R. et al. Drug overdose mortality among people experiencing homelessness, 2003 to 2018. JAMA Netw. Open 5 , e2142676 (2022).
Han, B. H., Doran, K. M. & Krawczyk, N. National trends in substance use treatment admissions for opioid use disorder among adults experiencing homelessness. J. Subst. Abuse Treat. 132 , 108504 (2022).
Das-Douglas, M., Colfax, G., Moss, A. R., Bangsberg, D. R. & Hahn, J. A. Tripling of methamphetamine/amphetamine use among homeless and marginally housed persons, 1996–2003. J. Urban Health 85 , 239–249 (2008).
Perez, G. R., Ustyol, A., Mills, K. J., Raitt, J. M. & North, C. S. The prevalence of cocaine use in homeless populations: a systematic review. Curr. Treat. Options Psychiatry 9 , 246–279 (2022).
Deutscher, K. et al. The prevalence of problem gambling and gambling disorder among homeless people: a systematic review and meta-analysis. J. Gambl. Stud. 39 , 467–482 (2023).
Barrow, S. M., Herman, D. B., Córdova, P. & Struening, E. L. Mortality among homeless shelter residents in New York City. Am. J. Public Health 89 , 529–534 (1999).
Seastres, R. J. et al. Long‐term effects of homelessness on mortality: a 15‐year Australian cohort study. Aust. N. Z. J. Public Health 44 , 476–481 (2020).
Roncarati, J. S. et al. Mortality among unsheltered homeless adults in Boston, Massachusetts, 2000–2009. JAMA Intern. Med. 178 , 1242–1248 (2018).
Romaszko, J., Cymes, I., Dragańska, E., Kuchta, R. & Glińska-Lewczuk, K. Mortality among the homeless: causes and meteorological relationships. PLoS ONE 12 , e0189938 (2017).
Liu, M. & Hwang, S. W. Health care for homeless people. Nat. Rev. Dis. Primers 7 , 5 (2021).
Babidge, N. C., Buhrich, N. & Butler, T. Mortality among homeless people with schizophrenia in Sydney, Australia: a 10-year follow-up. Acta Psychiatr. Scand. 103 , 105–110 (2001).
Beijer, U., Andréasson, A., Agren, G. & Fugelstad, A. Mortality, mental disorders and addiction: a 5-year follow-up of 82 homeless men in Stockholm. Nord. J. Psychiatry 61 , 363–368 (2007).
Nielsen, S. F., Hjorthøj, C. R., Erlangsen, A. & Nordentoft, M. Psychiatric disorders and mortality among people in homeless shelters in Denmark: a nationwide register-based cohort study. Lancet 377 , 2205–2214 (2011).
Prigerson, H. G., Desai, R. A., Liu-Mares, W. & Rosenheck, R. A. Suicidal ideation and suicide attempts in homeless mentally ill persons: age-specific risks of substance abuse. Soc. Psychiatry Psychiatr. Epidemiol. 38 , 213–219 (2003).
Brown, R. T. et al. Factors associated with mortality among homeless older adults in California: the HOPE HOME study. JAMA Intern. Med. 182 , 1052–1060 (2022).
Dickins, K. A. et al. Mortality trends among adults experiencing homelessness in Boston, Massachusetts from 2003 to 2018. JAMA Intern. Med. 183 , 488–490 (2023).
Gozdzik, A., Salehi, R., O’Campo, P., Stergiopoulos, V. & Hwang, S. W. Cardiovascular risk factors and 30-year cardiovascular risk in homeless adults with mental illness. BMC Public Health 15 , 165 (2015).
Mejia-Lancheros, C. et al. Dental problems and chronic diseases in mentally ill homeless adults: a cross-sectional study. BMC Public Health 20 , 419 (2020).
Klinkenberg, W. D. et al. Prevalence of human immunodeficiency virus, hepatitis B, and hepatitis C among homeless persons with co-occurring severe mental illness and substance use disorders. Compr. Psychiatry 44 , 293–302 (2003).
Aubry, T., Farrell, S., Hwang, S. W. & Calhoun, M. Identifying the patterns of emergency shelter stays of single individuals in Canadian cities of different sizes. Hous. Stud. 28 , 910–927 (2013).
Kuhn, R. & Culhane, D. P. Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: results from the analysis of administrative data. Am. J. Community Psychol. 26 , 207–232 (1998).
Aubry, T. et al. Housing trajectories, risk factors, and resources among individuals who are homeless or precariously housed. Ann. Am. Acad. Pol. Soc. Sci. 693 , 102–122 (2021).
Nilsson, S. F. et al. The bidirectional association between psychiatric disorders and sheltered homelessness. Psychol. Med. 8 , 1–11 (2023).
Google Scholar
Gelberg, L., Gallagher, T. C., Andersen, R. M. & Koegel, P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am. J. Public Health 87 , 217–220 (1997).
Baggett, T. P., O’Connell, J. J., Singer, D. E. & Rigotti, N. A. The unmet health care needs of homeless adults: a national study. Am. J. Public Health 100 , 1326–1333 (2010).
Kerman, N. & Sylvestre, J. Surviving versus living life: capabilities and service user among adults with mental health problems and histories of homelessness. Health Soc. Care Community 28 , 414–422 (2021).
Lamanna, D. et al. Promoting continuity of care for homeless adults with unmet health needs: the role of brief interventions. Health Soc. Care Community 26 , 56–64 (2018).
Skosireva, A. et al. Different faces of discrimination: perceived discrimination among homeless adults with mental illness in healthcare settings. BMC Health Serv. Res. 14 , 376 (2014).
Folsom, D. P. et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public health mental system. Am. J. Psychiatry 162 , 370–376 (2005).
Ellsworth, J. T. Street crime victimization among homeless adults: a review of the literature. Vict. Offender. 14 , 96–118 (2019).
Roy, L., Crocker, A. G., Nicholls, T. L., Latimer, E. A. & Ayllon, A. R. Criminal behavior and victimization among homeless individuals with severe mental illness: a systematic review. Psychiatr. Serv. 65 , 739–750 (2014).
Silver, C. M. et al. Injury patterns and hospital admission after trauma among people experiencing homelessness. JAMA Netw. Open 6 , e2320862 (2023).
Vrouwe, S. Q. et al. The homelessness crisis and burn injuries: a cohort study. J. Burn Care Res. 41 , 820–827 (2020).
Padgett, D. K., Tiderington, E., Smith, B. T., Derejko, K.-S. & Henwood, B. F. Complex recovery: understanding the lives of formerly homeless adults with complex needs. J. Soc. Distress Homeless. 25 , 60–70 (2016).
Kouyoumdjian, F. G. et al. Interactions between police and persons who experience homelessness and mental illness in Toronto, Canada: findings from a prospective study. Can. J. Psychiatry 64 , 718–725 (2019).
PubMed PubMed Central Google Scholar
Robinson, T. No right to rest: police enforcement patterns and quality of life consequences of the criminalization of homelessness. Urban Aff. Rev. 55 , 41–73 (2019).
Westbrook, M. & Robinson, T. Unhealthy by design: health & safety consequences of the criminalization of homelessness. J. Soc. Distress Homeless. 30 , 107–115 (2021).
Barocas, J. A. et al. Population-level health effects of involuntary displacement of people experiencing unsheltered homelessness who inject drugs in US cities. JAMA 329 , 1478–1486 (2023).
Karadzhov, D., Yuan, Y. & Bond, L. Coping amidst an assemblage of disadvantage: a qualitative metasynthesis of first-person accounts of managing severe mental illness while homeless. J. Psychiatr. Ment. Health Nurs. 27 , 4–24 (2020).
Paul, S., Corneau, S., Boozary, T. & Stergiopoulos, V. Coping and resilience among ethnoracial individuals experiencing homelessness and mental illness. Int. J. Soc. Psychiatry 64 , 189–197 (2018).
Duke, A. & Searby, A. Mental ill health in homeless women: a review. Issues Ment. Health Nurs. 40 , 605–612 (2019).
Phipps, M., Dalton, L., Maxwell, H. & Cleary, M. Women and homelessness, a complex multidimensional issue: findings from a scoping review. J. Soc. Distress Homeless. 28 , 1–13 (2019).
Cummings, C., Lei, Q., Hochberg, L., Hones, V. & Brown, M. Social support and networks among people experiencing chronic homelessness: a systematic review. Am. J. Orthopsychiatry 92 , 349–363 (2022).
Kerman, N., Gran-Ruaz, S., Lawrence, M. & Sylvestre, J. Perceptions of service use among currently and formerly homeless adults with mental health problems. Community Ment. Health J. 55 , 777–783 (2019).
Aubry, T. et al. Effectiveness of permanent supportive housing and income assistance interventions for homeless individuals in high-income countries: a systematic review. Lancet Public Health 5 , e342–e360 (2020).
Loubière, S. et al. Housing First for homeless people with severe mental illness: extended 4-year follow-up and analysis of recovery and housing stability from the randomized Un Chez Soi d’Abord trial. Epidemiol. Psychiatr. Sci. 31 , e14 (2022).
Stergiopoulos, V. et al. Long-term effects of rent supplements and mental health support services on housing and health outcomes of homeless adults with mental illness: extension study of the At Home/Chez Soi randomised controlled trial. Lancet Psychiatry 6 , 915–925 (2019).
Baxter, A. J., Tweed, E. J., Katikireddi, S. V. & Thomson, H. Effects of Housing First approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. J. Epidemiol. Community Health 73 , 379–387 (2019).
Peng, Y. et al. Permanent supportive housing with Housing First to reduce homelessness and promote health among homeless populations with disability: a community guide systematic review. J. Public Health Manag. Pract. 26 , 404–411 (2020).
Latimer, E. A. et al. Cost-effectiveness of Housing First with Assertive Community Treatment: results from the Canadian At Home/Chez Soi trial. Psychiatr. Serv. 71 , 1020–1030 (2020).
Goering, P. et al. Further validation of the Pathways Housing First fidelity scale. Psychiatr. Serv. 67 , 111–114 (2016).
Nelson, G. et al. Life changes among homeless persons with mental illness: a longitudinal study of Housing First and usual treatment. Psychiatr. Serv. 66 , 592–597 (2015).
Coldwell, C. M. & Bender, W. S. The effectiveness of Assertive Community Treatment for homeless populations with severe mental illness: a meta-analysis. Am. J. Psychiatry 164 , 393–399 (2007).
Ponka, D. et al. The effectiveness of case management interventions for the homeless, vulnerably housed and persons with lived experience: a systematic review. PLoS ONE 15 , e0230896 (2020).
Weightman, A. L. et al. Exploring the effect of case management in homelessness per components: a systematic review of effectiveness and implementation, with meta-analysis and thematic synthesis. Campbell Syst. Rev. 19 , e1329 (2023).
Morse, G. A. et al. Treating homeless clients with severe mental illness and substance use disorders: costs and outcomes. Community Ment. Health J. 42 , 377–404 (2006).
Jones, K. et al. Cost-effectiveness of Critical Time Intervention to reduce homelessness among persons with mental illness. Psychiatr. Serv. 54 , 884–890 (2003).
Kasprow, W. J. & Rosenheck, R. A. Outcomes of Critical Time Intervention case management of homeless veterans after psychiatric hospitalization. Psychiatr. Serv. 58 , 929–935 (2007).
Poremski, D., Rabouin, D. & Latimer, E. A randomised controlled trial of evidence based supported employment for people who have recently been homeless and have a mental illness. Adm. Policy Ment. Health 44 , 217–224 (2017).
Stergiopoulos, V. et al. Bridging hospital and community care for homeless adults with mental health needs: outcomes of a brief interdisciplinary intervention. Can. J. Psychiatry 63 , 774–784 (2018).
Hollenberg, E. et al. Using financial incentives to improve health service engagement and outcomes of adults experiencing homelessness: a scoping review of the literature. Health Soc. Care Community 30 , e3406–e3434 (2022).
Corrigan, P. et al. Using peer navigators to address the integrated health care needs of homeless African Americans with serious mental illness. Psychiatr. Serv. 68 , 264–270 (2017).
Parkes, T. et al. A peer-delivered intervention to reduce harm and improve the well-being of homeless people with problem substance use: the SHARPS feasibility mixed-methods study. Health Technol. Assess. 26 , 1–128 (2022).
Dwyer, R., Palepu, A., Williams, C., Daly-Grafstein, D. & Zhao, J. Unconditional cash transfers reduce homelessness. Proc. Natl Acad. Sci. USA 120 , e2222103120 (2023).
Firth, J. et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry 6 , 675–712 (2019).
Tsemberis, S., McHugo, G., Williams, V., Hanrahan, P. & Stefancic, A. Measuring homelessness and residential stability: the residential time-line follow-back inventory. J. Community Psychol. 35 , 29–42 (2007).
Dixon, L. B. & Patel, S. R. The application of implementation science to community mental health. World Psychiatry 19 , 173–174 (2020).
Kaakinen, J. & Turunen, S. Finnish but not yet finished – successes and challenges of Housing First in Finland. Eur. J. Homeless. 15 , 81–84 (2021).
Pleace, N., Baptista, I. & Knutagård, M. Housing First in Europe: An Overview of Implementation, Strategy and Fidelity (Housing First Europe Hub, 2019).
Patterson, M. L., Moniruzzaman, A., Frankish, C. J. & Somers, J. M. Missed opportunities: childhood learning disabilities as early indicators of risk among homeless adults with mental illness in Vancouver, British Columbia. BMJ Open 2 , e001586 (2012).
Kerman, N., Ecker, J., Tiderington, E., Gaetz, S. & Kidd, S. A. Workplace trauma and chronic stressor exposure among direct service providers working with people experiencing homelessness. J. Ment. Health 32 , 424–433 (2023).
Barry, A. R. et al. Trauma-informed interactions within a trauma-informed homeless service provider: staff and client perspectives. J. Community Psychol. 52 , 415–434 (2024).
Australian Bureau of Statistics. Estimating Homelessness: Census ; https://www.abs.gov.au/statistics/people/housing/estimating-homelessness-census/latest-release (2023).
Fondation Abbé Pierre and FEANTSA. Eighth Overview of Housing Exclusion in Europe ; https://www.feantsa.org/en/event/2023/09/05/?bcParent=27 (2023).
Gaetz, S., Gulliver, T. & Richter, T. The State of Homelessness in Canada: 2014 (The Homeless Hub Press, 2014).
Government of Canada. Everyone Counts 2020–2022: Preliminary Highlights report ; https://www.infrastructure.gc.ca/homelessness-sans-abri/reports-rapports/pit-counts-dp-2020-2022-highlights-eng.html (2023).
Amore, K., Viggers, H. & Howden-Chapman, P. H. Severe Housing Deprivation in Aotearoa New Zealand, 2018: June 2021 Update (Te Tūāpapa Kura Kāinga – Ministry of Housing and Urban Development, 2021).
Halseth, L., Larsson, T. & Urstad, H. in Homeless in Europe: National Strategies for Fighting Homelessness 20–26 (FEANTSA, 2022).
Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R. & Walters, E. E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62 , 617–627 (2005).
Kessler, R. C. et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R). Biol. Psychiatry 58 , 668–676 (2005).
The Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Lenzenweger, M. F., Lane, M. C., Loranger, A. W. & Kessler, R. C. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 62 , 553–564 (2007).
Grant, B. F. et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA Psychiatry 73 , 39–47 (2016).
Andermann, A. et al. Evidence-informed interventions and best practices for supporting women experiencing or at risk of homelessness: a scoping review with gender and equity analysis. Health Promot. Chronic Dis. Prev. Can. 41 , 1–13 (2021).
Milaney, K., Williams, N., Lockerbie, S. L., Dutton, D. J. & Hyshka, E. Recognizing and responding to women experiencing homelessness with gendered and trauma-informed care. BMC Public Health 20 , 397 (2020).
Schwan, K. et al. The State of Women’s Housing Need & Homelessness in Canada: A Literature Review (Canadian Observatory on Homelessness Press, 2020).
Speirs, V., Johnson, M. & Jirojwong, S. A systematic review of interventions for homeless women. J. Clin. Nurs. 22 , 1080–1093 (2013).
Davies, B. R. & Allen, N. B. Trauma and homelessness in youth: psychopathology and intervention. Clin. Psychol. Rev. 54 , 17–28 (2017).
Edidin, J. P., Ganim, Z., Hunter, S. J. & Karnik, N. S. The mental and physical health of homeless youth: a literature review. Child Psychiatry Hum. Dev. 43 , 354–375 (2012).
Winiarski, D. A., Glover, A. C., Bounds, D. T. & Karnik, N. S. Addressing intersecting social and mental health needs among transition-age homeless youths: a review of the literature. Psychiatr. Serv. 72 , 317–324 (2021).
Kozloff, N. et al. The unique needs of homeless youths with mental illness: baseline findings from a Housing First trial. Psychiatr. Serv. 67 , 1083–1090 (2016).
Kidd, S. A. et al. The second national Canadian homeless youth survey: mental health and addiction findings. Can. J. Psychiatry 66 , 897–905 (2021).
Brown, R. T., Thomas, M. L., Cutler, D. F. & Hinderlie, M. Meeting the housing and care needs of older homeless adults: a permanent supportive housing program targeting homeless elders. Seniors Hous. Care J. 21 , 126–135 (2013).
Grenier, A. et al. A literature review of homelessness and aging: suggestions for a policy and practice-relevant research agenda. Can. J. Aging 35 , 28–41 (2016).
Stergiopoulos, V. & Herrmann, N. Old and homeless: a review and survey of older adults who use shelters in an urban setting. Can. J. Psychiatry 48 , 374–380 (2003).
Canham, S. L., Custodio, K., Mauboules, C., Good, C. & Bosma, H. Health and psychosocial needs of older adults who are experiencing homelessness following hospital discharge. Gerontologist 60 , 715–724 (2020).
Humphries, J. & Canham, S. L. Conceptualizing the shelter and housing needs and solutions of older people experiencing homelessness. Hous. Stud. 36 , 157–179 (2021).
Canham, S., Humphries, J., Moore, P., Burns, V. & Mahmood, A. Shelter/housing options, supports and interventions for older people experiencing homelessness. Ageing Soc. 42 , 2615–2641 (2022).
Johnson, G. & Chamberlain, C. Homelessness and substance abuse: which comes first? Aust. Soc. Work 61 , 342–356 (2006).
Schütz, C. G. Homelessness and addiction: causes, consequences and interventions. Curr. Treat. Options Psychiatry 3 , 303–313 (2016).
Schütz, C. et al. Living with dual diagnosis and homelessness: marginalized within a marginalized group. J. Dual Diagn. 15 , 88–94 (2019).
Bauer, L. K., Brody, J. K., León, C. & Baggett, T. P. Characteristics of homeless adults who died of drug overdoses: a retrospective record review. J. Health Care Poor Underserved 27 , 846–859 (2016).
Riggs, K. R. et al. Prevalence of and risk factors associated with nonfatal overdose among veterans who have experienced homelessness. JAMA Netw. Open 3 , e201190 (2020).
Miler, J. A. et al. What treatment and services are effective for people who are homeless and use drugs? A systematic ‘review of reviews’. PLoS ONE 16 , e0254729 (2021).
Brown, M. & McCann, E. Homelessness and people with intellectual disabilities: a systematic review of the international research evidence. J. Appl. Res. Intellect. Disabil. 34 , 390–401 (2021).
Lougheed, D. C. & Farrell, S. The challenge of a ‘triple diagnosis’: identifying and serving homeless Canadian adults with a dual diagnosis. J. Policy Pract. Intellect. Disabil. 10 , 230–235 (2013).
Abramovich, A. Preventing, reducing and ending LGBTQ2S youth homelessness: the need for targeted strategies. Soc. Incl. 4 , 86–96 (2016).
Ecker, J., Aubry, T. & Sylvestre, J. A review of the literature on LGBTQ adults who experience homelessness. J. Homosex. 66 , 297–323 (2019).
Spicer, S. S. Healthcare needs of the transgender homeless population. J. Gay Lesbian Ment. Health 14 , 320–339 (2010).
Abramovich, I. A. No safe place to go – LGBTQ youth homelessness in Canada: reviewing the literature. Can. J. Fam. Youth 4 , 29–51 (2012).
Maccio, E. M. & Ferguson, K. M. Services to LGBTQ runaway and homeless youth: gaps and recommendations. Child. Youth Serv. Rev. 63 , 47–57 (2016).
Fowle, M. Z. Racialized homelessness: a review of historical and contemporary causes of racial disparities in homelessness. Hous. Policy Debate 32 , 940–967 (2022).
Jones, M. M. Does race matter in addressing homelessness? A review of the literature. World Med. Health Policy 8 , 139–156 (2016).
Kaur, H. et al. Understanding the health and housing experiences of refugees and other migrant populations experiencing homelessness or vulnerable housing: a systematic review using GRADE-CERQual. CMAJ Open 9 , e681–e692 (2021).
Olivet, J. et al. Racial inequity and homelessness: findings from the SPARC study. Ann. Am. Acad. Pol. Soc. Sci. 693 , 82–100 (2021).
Paul, D. W. et al. Racial discrimination in the life course of older adults experiencing homelessness: results from the HOPE HOME study. J. Soc. Distress Homeless. 29 , 184–193 (2020).
Zerger, S. et al. Differential experiences of discrimination among ethnoracially diverse persons experiencing mental illness and homelessness. BMC Psychiatry 14 , 353 (2014).
Download references
Acknowledgements
We thank A. Sosnowski for assistance with the literature search, as well as A. Abramovich, S. Canham, A. Durbin, J. Ecker, S. Kidd, N. Kozloff and P. O’Campo for their feedback on the special populations section of this article. This work was funded by the Canadian Institutes of Health Research (CIHR Foundation Grant Number 143259). The funder did not have any involvement in the preparation of this article.
Author information
Authors and affiliations.
Centre for Addiction and Mental Health, Toronto, Ontario, Canada
Nick Kerman & Vicky Stergiopoulos
Department of Psychiatry, University of Toronto, Toronto, Ontario, Canada
Vicky Stergiopoulos
You can also search for this author in PubMed Google Scholar
Contributions
Both authors collaboratively conceptualized this Review. N.K. drafted the Review, with input and critical review by V.S. Both authors read and approved the final paper.
Corresponding author
Correspondence to Vicky Stergiopoulos .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Mental Health thanks Jed Boardman, Seena Fazel and Debbie Robson for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Kerman, N., Stergiopoulos, V. Addressing health needs in people with mental illness experiencing homelessness. Nat. Mental Health 2 , 354–366 (2024). https://doi.org/10.1038/s44220-024-00218-0
Download citation
Received : 14 March 2023
Accepted : 21 February 2024
Published : 05 April 2024
Issue Date : April 2024
DOI : https://doi.org/10.1038/s44220-024-00218-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Reimagining Institutionalization and a Continuum of Care for People Experiencing Homelessness and Mental Illness
- 1 Department of Psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts
- 2 Boston Health Care for the Homeless Program, Boston, Massachusetts
- 3 Harvard Medical School, Boston, Massachusetts
- Editorial Involuntary Displacements Margot Kushel, MD JAMA
- Original Investigation Health Effects of Involuntary Displacement of Homeless Individuals Who Inject Drugs Joshua A. Barocas, MD; Samantha K. Nall, MPH; Sarah Axelrath, MD; Courtney Pladsen, DNP; Alaina Boyer, BS; Alex H. Kral, PhD; Ashley A. Meehan, MPH; Alexandra Savinkina, MSPH; David Peery, JD; Michael Bien, MPH; Christine Agnew-Brune, PhD; Jesse Goldshear, MPH; Joey Chiang, MD; Benjamin P. Linas, MD; Gregg Gonsalves, PhD; Ricky N. Bluthenthal, PhD; Emily Mosites, PhD; NHBS Study Group; Pascale Wortley; Jeff Todd; David Melton; Colin Flynn; Danielle German; Monina Klevens; Rose Doherty; Conall O'Cleirigh; Antonio Jimenez; Thomas Clyde; Jonathon Poe; Margaret Vaaler; Jie Deng; Alia Al-Tayyib; Danielle Shodell; Emily Higgins; Vivian Griffin; Corrine Sanger; Salma Khuwaja; Zaida Lopez; Paige Padgett; Ekow Kwa Sey; Yingbo Ma; Hugo Santacruz; Meredith Brantley; Christopher Mathews; Jack Marr; Emma Spencer; Willie Nixon; David Forrest; Bridget Anderson; Ashley Tate; Meaghan Abrego; William T. Robinson; Narquis Barak; Jeremy M. Beckford; Sarah Braunstein; Alexis Rivera; Sidney Carrillo; Abdel R. Ibrahim; Afework Wogayehu; Luis Moraga; Kathleen A. Brady; Jennifer Shinefeld; Chrysanthus Nnumolu; Timothy W. Menza; E. Roberto Orellana; Amisha Bhattari; Anna Flynn; Onika Chambers; Marisa Ramos; Will McFarland; Jessica Lin; Desmond Miller; Sandra Miranda De Leon; Yadira Rolon-Colon; Maria P. Martinez; Tom Jaenicke; Saral Glick; Jennifer Kienzle; Brandie Smith; Toyah Reid; Jenevieve Opoku; Irene Kuo; Monica Adams; Amy Baugher; Dita Broz; Janet Burnett; Susan Chambers; Johanna Chapin-Bardales; Paul Denning; Teresa Finlayson; Senad Handanagic; Terence Hickey; Dafna Kanny; Kathryn Lee; Rashunda Lewis; Elana Morris; Evelyn Olansky; Taylor Robbins; Catlainn Sionean; Amanda Smith; Anna Teplinskaya; Kindsay Trujillo; Cyprian Wejnert; Ari Whiteman; Mingjing Xia JAMA
- Research Letter Recuperation Units and Hospitalization Rates Among People Experiencing Homelessness With COVID-19 Joshua A. Barocas, MD; Mam Jarra Gai, MPH; Laura F. White, PhD; Deanna Faretra, RN, BSN; Kerry Sachs, MBA; Miriam Komaromy, MD JAMA Network Open
Current rates of suffering, abuse, neglect, and incarceration of those experiencing homelessness and mental illness represent an unacceptable humanitarian crisis. Political will to invest in solutions appears to be growing. New York City Mayor Eric Adams recently announced a plan to lower the threshold for involuntary commitment of people with mental illness living on the street. Portland Mayor Ted Wheeler declared similar intentions. In California, the newly enacted CARE (Community Assistance, Recovery, and Empowerment) Act intends to leverage courts to bring people with severe mental illness and substance use disorders into a system of care. Most recently, New York Governor Kathy Hochul pledged more than $1 billion for a comprehensive plan integrating hospitalization and community-based care. Although each proposal has prompted debate on ethical and practical grounds, this momentum provides an urgent opportunity to implement community-based care options, reimagine institutionalization, and finally build a functional continuum of care for those experiencing homelessness and mental illness.
- Editorial Involuntary Displacements JAMA
Read More About
Koh KA , Gorman BL. Reimagining Institutionalization and a Continuum of Care for People Experiencing Homelessness and Mental Illness. JAMA. 2023;329(17):1449–1450. doi:10.1001/jama.2023.6132
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

The Never-Ending Loop: Homelessness, Psychiatric Disorder, and Mortality
- Jack Tsai, PhD
Mental health conditions are highly prevalent in homeless populations. Further research and advocacy are needed to address the obstacles that homeless individuals encounter in accessing mental health care.

Table 1 and 2. Solutions to addressing barriers to mental health care in homeless populations
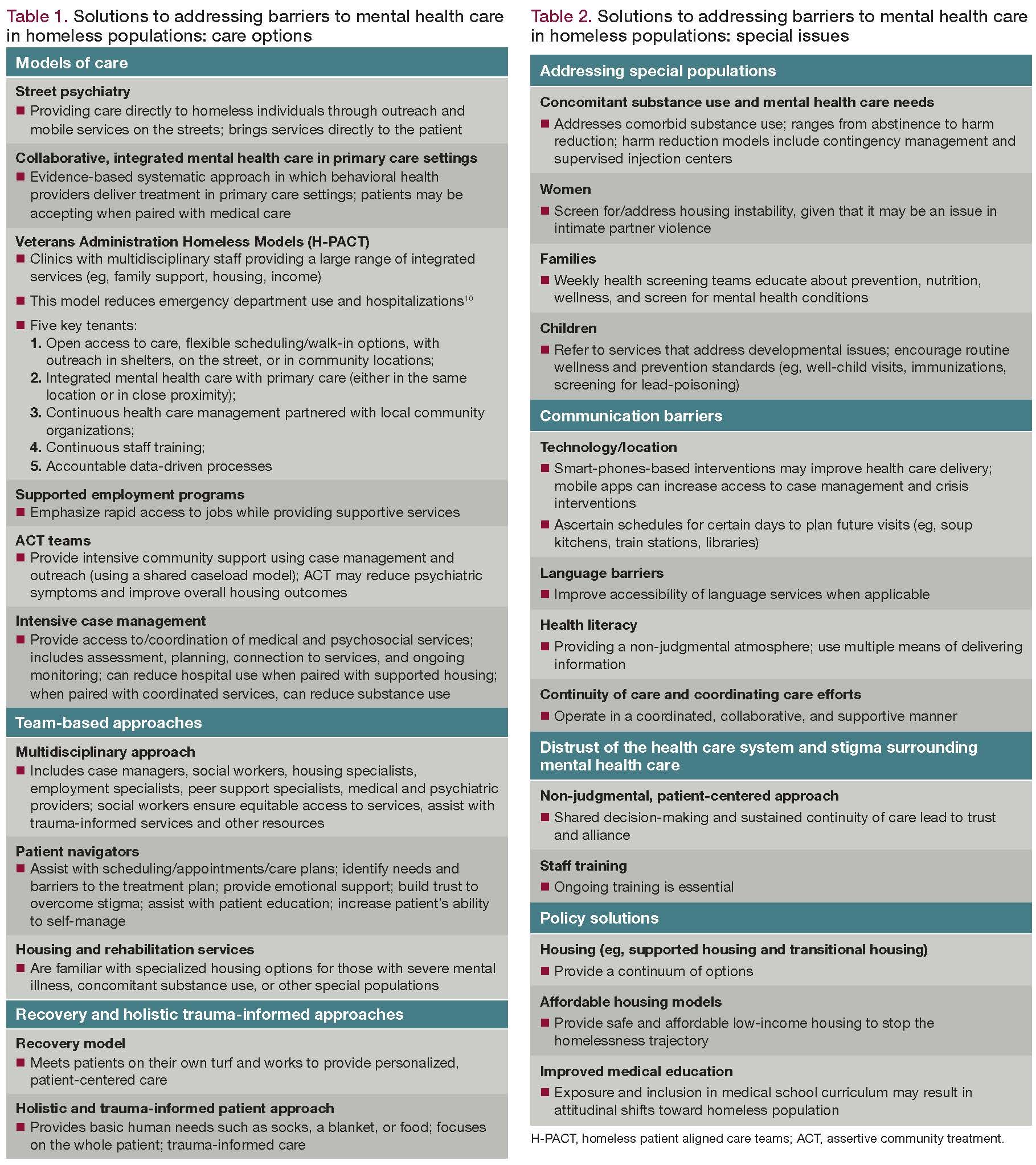
With a lifetime and 1-year prevalence of homelessness in the US population found to be 4.2% and 1.5%, respectively, and the total number of people who experience some form of homelessness over the course of a year is estimated to be 2.5 to 3.5 million individuals, homelessness is a serious problem. Mental illness, in addition to adverse childhood experiences and substance use, are risk factors for homelessness. Although estimates of the prevalence of mental illness vary, studies looking at mental illness in the homeless population have generally found a high prevalence of mental disorders. The most common disorders may be alcohol and drug dependence ( Figure ). 1
There is clearly a link between psychiatric disorders and homelessness; disentangling the nature of this relationship is complicated. Regardless of mental health status, people who are homeless generally have a history marked by poverty and social disadvantage, including considerable poverty in childhood and lower levels of education, and they are likely to belong to an ethnic minority. 2 Mental illness had preceded homelessness in about two-thirds of the cases.
Homelessness in turn has been associated with poorer mental health outcomes and may trigger or exacerbate certain types of disorders. For example, findings indicate that homelessness is related to higher levels of psychiatric distress and lower perceived levels of recovery from serious mental illness. 3
Impact of homelessness on premature morbidity
Homelessness is associated with substantially increased morbidity and mortality from many causes including infectious diseases, cardiovascular disease, cancer, unintentional injury, suicide, homicide, and substance use. The unsheltered homeless have an even greater burden, with higher mortality than sheltered homeless. Among a large group of homeless adults in Boston, disparities in deaths attributed to tobacco, alcohol, and drug use accounted for almost 60% of the mortality gap between homeless adults and the general population. 4
In accordance with findings in the general population, there also is a strong association between psychiatric disorders and suicide in homeless populations. The prevalence of suicidal ideation and suicide attempts is extremely high in mentally ill homeless persons. In a large sample of homeless adults with serious mental illness, almost 8% reported a suicide attempt within the previous 30 days. 5 The highest rates of suicidal ideation and suicide attempts were in the group aged 30 to 39 years, in contrast to the general population with peaks of suicidality in young adults and the elderly.
Challenges in accessing psychiatric care
General guidelines were created for primary care physicians working with the homeless in the US in 2004, and in 2018 the Street Medicine Institute began publishing international clinical guidelines targeting the primary care needs of specifically street-dwelling homeless individuals. 6,7 Unfortunately, similar guidelines for psychiatrists working with the street-homeless population are still lacking.
When thinking about challenges to accessing care, it is critical to understand the heterogeneous nature of homelessness. The structures of support and oppression for each individual may vary significantly based on the surrounding community and resources.
Fundamental basic needs. A qualitative study highlighted the basic human needs that often take priority over seeking psychiatric care. 8 Access to adequate nutrition, water, shelter, and protection from the elements are the reality homeless individuals encounter daily, and these issues take priority over psychiatric needs, which are often not addressed until a crisis occurs.
The effects of illness. Having mental health care needs itself may be a barrier to accessing psychiatric care. Motivation to make and attend appointments may be low if an individual is suffering from depression, amotivation, anhedonia, anxiety, paranoia, hypervigilance, history of trauma, substance use, or negative past experiences with the health care system related to mental illness. Moreover, homeless people may have experienced greater trauma, have traumatic brain injuries, and cognitive impairment-all of which may affect interactions with the health care system and health literacy.
Similarly, comorbid medical illness may be a barrier, as these needs may take priority over psychiatric care. Many homeless people have medical issues such as diabetes, hypertension, tuberculosis, and ischemic heart disease. These needs often necessitate resources such as intensive case management and assertive outreach to maintain treatment.
Transportation. Homeless individuals often lack adequate transportation; consequently they are unable to do the necessary tasks involved in care-getting laboratory work completed, picking up medications, and getting to mental health appointments. Public transportation may not always be a solution, as it often requires multiple transfers, can be unreliable and, in some areas, may be limited or may not exist. Most significantly, homeless individuals may lack the resources to pay for fares.
Cost of care. For persons who are homeless, small expenses can be a significant barrier to accessing mental health care. Moreover, they may not be cognizant of resources available to them through Medicaid or the Affordable Care Act.
Communication. Although some homeless adults and youth have access to cell phones, there is higher turnover of both phones and phone numbers, which can pose a barrier to consistent communication. Keeping a cell phone charged is a challenge for those without reliable access to electricity. Similarly, with lower internet use, homeless people are likely to have less access to important information, including care and resources. Language barriers may also affect access to care, particularly in limited resource settings.
Stigma and vulnerability. Stigma and discrimination continue against homeless individuals who also have mental health conditions. Setting health care goals may feel unattainable when pressing issues like basic survival are more salient. Homeless people with mental illness are also highly vulnerable to violence, with a reported lifetime incidence of 74% to 87% of violence being perpetrated against them. 9 Psychiatric care may include prescribed psychotropics that affect alertness and pose a danger for someone who is at increased risk for victimization and violence. Furthermore, those who have a history with the legal system, reintegrating into society, parole, or strained finances may further impact their ability to acquire care.
Briefly, solutions to the problem of homelessness include finding and implementing innovative models of care such as street psychiatry, integrated primary care, and mental health care models; Veterans Administration Homeless Models (Homeless Patient Aligned Care Teams H-PACT); and utilizing allies in the housing and rehabilitation services domains to find specialized housing opportunities. Taking a team-based approach is essential, as the mental health care needs of homeless people are often complex and include many aspects of the social determinants of health. Multidisciplinary teams often include case managers, social workers, housing specialists, and vocational specialists. Medical students can also play an integral part in providing mental health care for homeless persons. (For a full and detailed list of potential solutions, please see Table 1 and Table 2 .)
Recovery models and holistic, patient-centered, trauma-informed care are important as perceived discrimination, stigma, and distrust may be present. Communication barriers must also be addressed. This includes the advance development of plans regarding communications and finding creative ways to address potential barriers. Solutions should be tailored to fit the individual needs of the patient, including special needs that may occur around patients with dual diagnoses, women, families, and children. Although beyond the scope of this article, effective public policy can play a role in reducing homelessness.
Mental health conditions are highly prevalent in homeless populations. Although homeless individuals have higher mortality related to many causes, access to care is poorer than that for the general population. Further research and advocacy are needed to address the obstacles that homeless individuals encounter in accessing mental health care.
Disclosures:
Dr Balasuriya is a Medical Resident and Dr Buelt is an Instructor, Department of Psychiatry, Yale University School of Medicine, New Haven, CT; Dr Tsai is Campus Dean and Professor, School of Public Health, University of Texas Health Science Center, Houston, TX. The authors report no conflicts of interest concerning the subject matter of this article.
References:
1. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med . 2008;5:e225.
2. Sullivan G, Burnam A, Koegel P. Pathways to homelessness among the mentally ill. Soc Psychiatry Psychiatr Epidemiol . 2000;35:444-450.
3. Castellow J KB, Townley G. Previous homelessness as a risk factor for recovery from serious mental illness. Community Ment Health J . 2015;51:674-684.
4. Baggett TP, Chang Y, Singer DE, et al. Tobacco-, alcohol-, and drug-attributable deaths and their contribution to mortality disparities in a cohort of homeless adults in Boston. Am J Public Health . 2015;105:1189-1197.
5. Prigerson HG, Desai RA, Liu-Mares W, Rosenheck RA. Suicidal ideation and suicide attempts in homeless mentally ill persons: age-specific risks of substance abuse. Soc Psychiatry Psychiatr Epidemiol . 2003;38:213-219.
6. Bonin E, Hoeft J, Brehove T, et al. General Recommendations for the Care of Homeless Patients. Adapting Your Practice . 2010.
7. Board of Directors, Street Medicine Institute. Street Medicine Clinical Guidelines, 2018.
8. Paudyal V, MacLure K, Buchanan C, et al. “When you are homeless, you are not thinking about your medication, but your food, shelter or heat for the night”: behavioural determinants of homeless patients’ adherence to prescribed medicines. Public Health . 2017;148:1-8.
9. Roy L, Crocker AG, Nicholls TL, et al. Criminal behavior and victimization among homeless individuals with severe mental illness: a systematic review. Psychiatr Serv . 2014;65:739-750.
10. O’Toole TP, Johnson EE, Aiello R, et al. Tailoring care to vulnerable populations by incorporating social determinants of health: the Veterans Health Administration’s “Homeless Patient Aligned Care Team” program. Prev Chronic Dis . 2016;13:E44.
Tips for Managing Multiple Medication Use

Polypharmacy in Older Adults

Correlates of Antipsychotic Polypharmacy in Taiwanese Patients With Schizophrenia

Polypharmacy in Traumatic Brain Injury

Connections Between Food Additives and Psychiatric Disorders

Unraveling Minds: The Impact of Global Climate Change on Mental Health
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


Homelessness, housing instability and mental health: making the connections
Affiliation.
- 1 New York University.
- PMID: 32538335
- PMCID: PMC7525583
- DOI: 10.1192/bjb.2020.49
Research on the bi-directional relationship between mental health and homelessness is reviewed and extended to consider a broader global perspective, highlighting structural factors that contribute to housing instability and its mental ill health sequelae. Local, national and international initiatives to address housing and mental health include Housing First in Western countries and promising local programmes in India and Africa. Ways that psychiatrists and physicians can be agents of changes range from brief screening for housing stability to structural competence training. Narrow medico-scientific framing of these issues risks losing sight of the foundational importance of housing to mental health and well-being.
Keywords: Homelessness; housing instability; human rights; mental health; structural competence.
- Research article
- Open access
- Published: 12 July 2022
Homelessness and health-related outcomes: an umbrella review of observational studies and randomized controlled trials
- Michele Fornaro 1 ,
- Elena Dragioti ORCID: orcid.org/0000-0001-9019-4125 2 ,
- Michele De Prisco 1 ,
- Martina Billeci 1 ,
- Anna Maria Mondin 1 ,
- Raffaella Calati 3 , 4 ,
- Lee Smith 5 ,
- Simon Hatcher 6 , 7 , 8 ,
- Mark Kaluzienski 6 , 7 ,
- Jess G. Fiedorowicz 6 , 7 , 8 ,
- Marco Solmi 6 , 7 , 8 , 9 , 10 ,
- Andrea de Bartolomeis 1 , 11 &
- André F. Carvalho 12
BMC Medicine volume 20 , Article number: 224 ( 2022 ) Cite this article
8620 Accesses
10 Citations
5 Altmetric
Metrics details
Homelessness has been associated with multiple detrimental health outcomes across observational studies. However, relatively few randomized controlled trials (RCTs) have been conducted on people who experience homelessness (PEH). Thus, this umbrella review ranked the credibility of evidence derived from systematic reviews (SRs) and meta-analyses (MAs) of observational studies investigating the associations between homelessness and any health outcome as well as RCTs targeting health needs in this population.
Several databases were systematically searched from inception through April 28, 2021. Any SR and/or MA reporting quantitative data and providing a control group were eligible for inclusion. The credibility of the evidence derived from observational studies was appraised by considering the significance level of the association and the largest study, the degree of heterogeneity, the presence of small-study effects as well as excess significance bias. The credibility of evidence was then ranked in five classes. For SRs and/or MAs of RCTs, we considered the level of significance and whether the prediction interval crossed the null. The AMSTAR-2 and AMSTAR-plus instruments were adopted to further assess the methodological quality of SRs and/or MAs. The Newcastle-Ottawa Scale (NOS) was employed to further appraise the methodological quality of prospective cohort studies only; a sensitivity analysis limited to higher quality studies was conducted.
Out of 1549 references, 8 MAs and 2 SRs were included. Among those considering observational studies, 23 unique associations were appraised. Twelve of them were statistically significant at the p ≤0.005 level. Included cases had worst health-related outcomes than controls, but only two associations reached a priori-defined criteria for convincing (class I) evidence namely hospitalization due to any cause among PEH diagnosed with HIV infection, and the occurrence of falls within the past year among PEH. According to the AMSTAR-2 instrument, the methodological quality of all included SRs and/or MAs was “critically low.” Interventional studies were scant.
While homelessness has been repeatedly associated with detrimental health outcomes, only two associations met the criteria for convincing evidence. Furthermore, few RCTs were appraised by SRs and/or MAs. Our umbrella review also highlights the need to standardize definitions of homelessness to be incorporated by forthcoming studies to improve the external validity of the findings in this vulnerable population.
Peer Review reports
Homelessness is an important social, public health, and human rights issue worldwide. The prevalence of homelessness varies among diverse countries and cultures around the world. Lifetime prevalence estimates from representative samples are 4.2% in the USA [ 1 ] to 4.9% in Europe [ 2 ]. However, high-quality data on the prevalence of homelessness in low- and middle-income countries (LMICs) is scant.
The operational definitions for homelessness likewise vary across different literature sources and settings [ 3 ] although a commonly accepted and implemented definition of homelessness globally comes from the European Typology of Homeless and Housing Exclusion study [ 4 ].
People experiencing homelessness (PEH) may face social and economic challenges that may lead to poor health, such as poverty, poor nutrition, and social exclusion. People who lack stable and appropriate housing appear to be at relatively high risk for a broad range of acute and chronic illnesses, especially infectious diseases, heart diseases, substance use disorders, and severe mental disorders [ 5 ]. However, it is unclear whether homelessness causes these disorders or otherwise these illnesses per se contribute to homelessness. Finally, evidence indicates that PEH has a lower probability of receiving proper care for their health conditions compared to the general population [ 6 ].
Data about differences in the prevalence of multiple health conditions between PEH and the general population is substantially unreliable, as exemplified by current knowledge about mental health [ 7 ] and infectious diseases among PEH [ 8 ]. Cohort and case-control studies have reported various health outcomes associated with homelessness, and several health outcomes have been the subject of a multitude of systematic reviews (SRs) and meta-analyses (MAs). While informative, this latter knowledge synthesis is usually restricted to a single outcome, and some of their results may be affected by biases, which are often poorly appraised [ 9 ]. Furthermore, randomized controlled trials (RCTs) targeting health-related outcomes in homeless populations are few, thus providing limited evidence to inform health policies [ 10 ]. Specifically, significant associations claimed by the original observational studies, or their pooled synthesis may be susceptible to biases such as excess significance [ 11 ], publication bias, reporting bias, and residual confounding, leading to misleading or inflated estimates of these associations [ 12 ].
Umbrella reviews (URs)—a systematic collection and appraisal of SRs and MAs performed on a specific topic [ 13 ]—can disentangle the aforementioned biases through appraising the quality and comprehensiveness of the data, and hence, assess which associations derived from observational studies are supported by the most credible evidence. Likewise, URs can provide a methodological appraisal of RCTs targeting a specific population or condition. Thus, in the current report, we aimed to conduct an umbrella review of the evidence from observational studies and RCTs considering multiple health outcomes involving PEH. In particular, we aimed at (i) assessing the reported association measures between homelessness and any health outcome and (ii) appraising the interventions targeting any health outcome among PEH.
Search strategy
We performed an umbrella review that included observational or RCTs that investigated the association between homelessness and any health outcome. The PubMed/MEDLINE, EMBASE, and SCOPUS databases were systematically searched from inception up to April 28, 2021. The following string was adopted for PubMed: (((“homeless persons”[MeSH Terms]) OR (“homeless youth”[MeSH Terms])) OR (“vulnerable populations”[MeSH Terms]) OR (homeless*[Title/Abstract])) AND (((((“meta analysis as topic”[MeSH Terms]) OR (“systematic reviews as topic”[MeSH Terms])) OR (“meta analysis”[Title/Abstract])) OR (“systematic review”[Title/Abstract]))). Please see Additional file 1 : material 1. The definition of homelessness and related phenomena were independently recorded by two investigators.
Eligibility criteria
For the synthesis of evidence from SRs and MAs of observational studies, we included those studies reporting any health outcome among PEH compared to the general population or otherwise provided controls (i.e., people who are not experiencing homelessness, PEH without a particular exposure). We excluded those SRs or MAs of observational studies that only provided prevalence estimates of a given health condition in PEH without providing a measure of association. Specifically, those studies reporting interventions just targeting housing, but not the related health status, were likewise excluded. The SRs and MAs of RCTs suitable for inclusion were those documenting interventions targeting any health outcome among PEH; controls were PEH exposed to a health-targeting intervention different from the health-outcome intervention delivered to PEH cases. Eligible quantitative SRs and MAs of observational studies had to include at least 3 studies; eligible SRs and MAs of intervention studies had to include at least 5 studies. The rationale for this inclusion criterion is explained in detail elsewhere [ 14 ]. In the case of multiple MAs reporting on the same topic (i.e., overlapping with the same type of intervention or exposure), we considered only the one that included the largest number of studies as it is a standard procedure in previously conducted umbrella reviews [ 15 , 16 ]. In cases there were two or more MAs pooling the same number of studies, we retained the most recent one. Qualitative reports were excluded. There were no language restrictions for the inclusion of studies for this umbrella review.
The protocol for this study was registered in PROSPERO with the following numbers: CRD42021252185, for the protocol investigating observational studies, and CRD42021252191 for the protocol that assessed evidence from intervention studies, respectively. Complete versions of each protocol are fully available online at https://osf.io/am67d/ and https://osf.io/58mhu/ .
Data extraction
Three investigators (MDP, MB, MF) independently searched title/abstracts of retrieved references for eligibility, and when a consensus could not be achieved, additional authors with considerable expertise in umbrella reviews (AFC, MS, LS) and the study of homelessness (LS, JGF, SH, MK) were consulted. The same procedure was followed at the full-text level. The reference lists of included studies were also searched for the identification of additional eligible references. Among other variables, we recorded the following: publication year, considered health outcome, study design, number of the included studies, total sample size, homelessness definition, and disclosure of sponsorship. For each primary study included in the SRs or MAs, we additionally recorded the first author, year of publication, study design (i.e., cohort, case-control, cross-sectional, RCT), setting of the study (i.e., inpatients, outpatients, population-based), number of subjects included in the study (total sample, cases, and controls), sex, ethnicity, both adjusted and unadjusted effect sizes (ES), and 95% confidence interval (CI). Intervention and mean duration of RCT studies were likewise extracted.
Data analysis and assessment of the credibility of evidence
We re-analyzed each eligible MA using the extracted individual study estimates to compute the summary effect estimates and the exact p-value under the random-effects model with DerSimonian and Laird method if included studies were equal or more than 10, and Hartung, Knapp, Sidik, and Jonkman (HKSJ) if less than 10 [ 17 , 18 ]. Cochran’s Q test and the I 2 statistics were computed for the evaluation of heterogeneity across studies ( I 2 >50% indicated high heterogeneity) [ 19 , 20 ]. To further account for heterogeneity between studies, we computed 95% prediction intervals for the summary random-effect estimates [ 21 ]. We evaluated the presence of small-study effects (i.e., large studies fetching significantly more conservative results than smaller studies) by adopting the Egger’s regression asymmetry test ( p ≤0.10) [ 22 ]. For statistically significant MAs, we assessed the presence of excess significance bias by evaluating whether the number of observed studies with nominally statistically significant results was different from the expected number of studies with statistically significant results [ 23 ]. The expected number of statistically significant studies in each association was calculated from the sum of the statistical power estimates for each component study using an algorithm from a non-central t distribution [ 24 , 25 , 26 ]. The power estimates of each component study depended on the plausible effect size of the tested association, which was assumed to be the effect size of the largest study in each MA [ 27 ]. The presence of excess significance bias for individual MAs was considered at p ≤0.10. The credibility of the evidence of each association provided by MAs of observational studies was assessed using the criteria previously applied in various medical fields [ 26 , 28 , 29 ], waiving the “number of cases” criterion since some health outcomes of PEH represent infrequent events. Briefly, the associations that presented nominally significant random-effect summary estimates were considered as “convincing” (Class I), “highly suggestive” (Class II), “suggestive” (Class III), “weak evidence” (Class IV), or “non-significant” (NS). Please, see the credibility box in Additional file 1 : Table S1. For MAs of intervention studies, we assessed the significance of the pooled effect size as P <0.005, P =0.005–0.005, and P ≥0.05 [ 30 ], the 95% prediction interval (excluding the null or not), the significance of the effect size of the largest study, and the presence of large heterogeneity (i.e., I 2 >50%) [ 31 ]. In addition, the methodological quality of those SRs and/or MAs was further appraised with the Assessment of Multiple Systematic Reviews Plus (AMSTAR-Plus) instrument [ 32 ]. All statistical tests were two-tailed. The data abstraction was performed using pre-defined Microsoft Excel® forms, while the statistical computations were carried out by an expert senior author (ED) using the STATA/SE, version 17.0 (StataCorp LLC) software. For each eligible quantitative report, two investigators (MDP and MB) independently rated the methodological quality using the AMSTAR-2 (Assessment of multiple SRs) tool [ 33 ] for quantitative SRs or MAs of observational studies. The prospective cohort studies included in the quantitative SRs or MAs of observational studies were rated for quality using the Newcastle-Ottawa scale (NOS) [ 34 ]. Finally, we adopted the following thresholds for the NOS scores: “good quality” (3-4 stars in the “selection domain” AND 1-2 stars in the “comparability” domain AND 2-3 stars in the “outcome” domain), “fair quality” (2 stars in the “selection domain” AND 1-2 stars in the “comparability” domain AND 2-3 stars in the “outcome” domain), and “poor quality” (0-1 stars in the “selection domain” OR 0 stars in the “comparability” domain OR 0-1 star in the “outcome” domain) [ 35 ].
The search returned 1549 potentially eligible records, of which 11 records were manually retrieved. Upon title and abstract screening, 189 records were further assessed at the full-text level, of which 179 were excluded with reasons as detailed in Additional file 1 : Table S2 [ 7 , 8 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 , 193 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 ]. Nine SRs or MAs of observational studies [ 211 , 212 , 213 , 214 , 215 , 216 , 217 , 218 , 219 ] were included, which yielded 23 comparisons. One MA of interventional studies [ 220 ] fetched two comparisons. Figure 1 provides a flowchart for study selection.
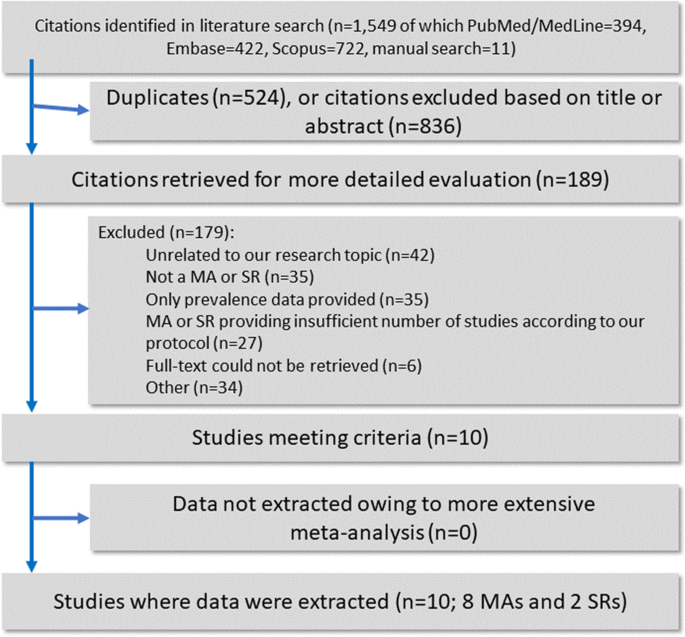
Flowchart of the literature search and evaluation process returning 10 systematic reviews and meta-analyses
Given the scant evidence for intervention studies, we decided to combine the reporting of both registration protocols into a single publication.
Descriptive characteristics of the 10 included eligible SRs and MAs of observational and intervention studies are outlined in Table 1 . The observational studies had the following control groups: PEH without SUD [ 211 ], PEH who did not inject drugs [ 212 ], people not experiencing homelessness [ 213 , 214 , 215 , 218 , 219 ], or the general population [ 216 , 217 ]. Although substantially overlapping, we nonetheless recorded “people not experiencing homelessness” and “general population” controls, as documented by the original study at review. The included MA of RCTs controlled for various treatment exposures [ 220 ].
Description and summary of associations
Observational studies.
Nine eligible SRs and/or MAs of observational studies assessed 23 associations, evaluated by 122 individual studies from 73 original reports, estimating adverse health outcomes associated with homelessness. Six (26.1%) associations concerned various causes of mortality among PEH, five (21.7%) associations regarded health outcomes related to HIV infection, and four (17.4%) associations inquired about premature geriatric syndromes (e.g., falls, functional limitations). Please refer to Fig. 2 for additional details. Twelve out of 23 (52.2%) associations were nominally statistically significant at a p ≤0.005 level based on the random-effects model, and 7 (30.4%) reached p ≤1×10 −6 . Fifteen associations (65.2%) had large heterogeneity, and the 95% prediction interval excluded the null value for only five associations (21.7%). In twenty associations (86.9%), the effect of the largest study was statistically significant at p ≤0.05. A small-study effect was detected in one association (4.3%), and excess significance bias occurred in one out of ten studies suitable for such estimation (10%). Please refer to Table 2 for details.
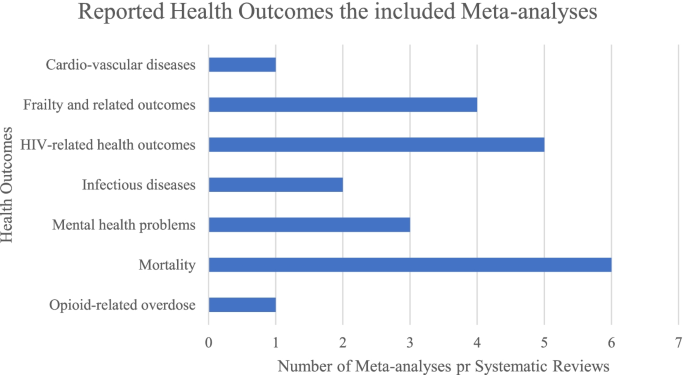
Number of systematic reviews or meta-analyses of observational studies reporting health outcomes among PEH by category of health outcome
Intervention studies
One eligible MA of intervention studies documented two therapeutic interventions, evaluated by 10 unique RCTs from 10 original reports, estimating interventions associated with mental health status among PEH [ 220 ]. One association concerned the psychological interventions among PEH diagnosed with depression, while the remaining one dealt with psychological interventions for anxiety. None of the assessed associations reached a statistically significant value at p ≤0.005 based on the random-effects model [ 30 ]. The degree of heterogeneity of the documented associations was quantified in I 2 =42.5% for depression and 39.9% for anxiety. The 95% prediction intervals crossed the null for the outcomes of both interventions. Neither of the largest studies of the two associations was statistically significant at p ≤0.05. Please refer to Table 3 for details.
Grading of systematic reviews and meta-analyses of observational studies
Concerning the SRs and/or MAs of observational studies, none of them concurrently reached a “convincing evidence” threshold, according to the adapted credibility box, and a “high quality” score based on the AMSTAR-2 tool. According to the latter, every SR and/or MA included in the present study was rated as having “critically low” methodological quality. Please refer to Additional file 1 : Table S3 [ 211 , 212 , 213 , 214 , 215 , 216 , 217 , 218 , 219 ].
Convincing evidence
Among the 23 associations, two (8.7%) were supported by “convincing evidence”: hospitalization due to any cause among PEH diagnosed with HIV infection and the occurrence of falls within the past year among PEH. Both health outcomes were more common among PEH compared to non-homeless controls.
Highly suggestive evidence
Five (21.7%) associations were rated “highly suggestive evidence”: (1) mortality due to any cause; (2) mortality due to external causes (i.e., intentional injury, unintentional injury, poisoning) among PEH compared to the general population; (3) HCV-infection among PEH using injection drugs compared to those who did not; (4) the presence of limitations in activities of daily living (ADL, e.g., dressing, eating, toileting); and (5) instrumental activities of daily living (IADL, e.g., using telephone, using transportations, taking medications) among PEH compared to non-homeless controls. These above-mentioned health outcomes were more common among PEH compared to their respective controls. Mortality due to any cause and mortality due to external causes had high standardized mortality ratios=6.22 (95% C.I.=4.2–9.2), and SMR=15.75 (95% C.I.=10.58–23.44), respectively.
Suggestive, weak, and no evidence
Five (21.7%) associations were rated “suggestive evidence,” four (17.4%) were “weak evidence,” while “no significant evidence” was found in seven (30.5%) associations.
Grading of systematic reviews and meta-analyses of intervention studies
Concerning intervention studies, the sole MA retrieved obtained a score of “10” at the AMSTAR-plus. Please refer to Table 3 for details.
Sensitivity analysis
A sensitivity analysis limited to high-quality prospective cohort studies included eleven (47.8%) associations, rated according to the NOS. Upon sensitivity analysis, two associations worsen, and one association improved in terms of credibility evidence. Hospitalization due to any cause among PEH with HIV infection shifted from “convincing evidence” to “highly suggestive evidence”, non-adherence to antiretroviral therapy (ART) among PEH with HIV infection shifted from “suggestive evidence” to “weak evidence”, and mortality due to any cause among PEH with SUD up-graded from “no significant evidence” to “highly suggestive evidence”. Please refer to Additional file 1 : Table S4 [ 211 , 214 , 217 , 219 ].
Statement of principal findings
We found convincing evidence that all-cause hospitalization in people with HIV infection and the occurrence of falls within the past year were more common among PEH compared to comparison populations. We also found highly suggestive evidence that mortality due to any cause; mortality due to external causes; hepatitis C infection among PEH using injection drugs; limitations in activities of daily living; and limitations in instrumental activities of daily living were significantly more common in PEH compared to their comparison populations. Mortality due to any cause and mortality due to external causes had high standardized mortality ratios such that PEH had a mortality rate six times their comparison groups and they were about 15 times more likely to die from either accidents or intentional self-harm.
Strengths and limitations
To our knowledge, this study is the first umbrella review that systematically inquired about any health-related outcomes and interventions among PEH, grading the evidence by using previously adopted and widely accepted criteria of credibility [ 14 , 16 , 29 , 31 , 221 ]. All SRs/or MAs of observational studies were graded as having “critically low” methodological quality according to the AMSTAR-2 instrument. Among the associations rated with “highly suggestive evidence”, two were not deemed as “convincing” due to high heterogeneity. Overall, 65.2% of the associations covered by the present umbrella review were hampered by high heterogeneity, which held upon controlling for high-quality prospective studies (seven out of eleven associations—63.6%—had an I 2 >50%).
The differences in definitions of “homelessness” and thus categories of homelessness (for example individuals without permanent housing who may live on the streets; stay in a shelter, mission, single room occupancy facilities, abandoned building or vehicle; or in any other unstable or non-permanent situation) adopted by the authors of the included SRs or MAs could likewise account for the high rates of heterogeneity. Half of the appraised studies lacked a “homelessness” definition, and the remaining half provided a broad definition, as detailed in Table 1 . The timeframe for the homelessness definition, or its related labels, varied across the individual studies included by the appraised SRs or MAs, often merging people who were currently homeless with people who were experiencing this condition within varying timeframes (i.e., 30-day, 6-month, or 12-month intervals, as usually documented by the authors of the original studies). Future research should, therefore, rely on consistent operational definitions, or otherwise stratify their results accordingly, especially considering that substantial variability of the adopted definitions exists across different world regions [ 222 ].
The limitations of this review include the exclusion of RCTs on the impact of housing interventions (Housing First) on PEH. However, such interventions were not deemed eligible for inclusion according to our a priori criteria since we focused on those interventions directly targeting health outcomes in PEH rather than on interventions aimed at reducing the burden of homelessness. Sensitivity analyses were restricted to high-quality prospective studies. Because of the lack of relevant SRs or MAs, we could not appraise otherwise relevant associations between homelessness and health outcomes such as alcohol-related issues, cancer, or infectious diseases other than HIV or HCV. Mental illness-related issues were only accounted for by three comparisons focusing on children experiencing homelessness [ 223 ].
Comparison with previous studies
Considering the two associations reaching “convincing evidence” before sensitivity analysis, the documented hospitalization trend due to any cause in people with HIV is consistent with a recent retrospective cohort study [ 224 ]. A significant increase in “falls during the previous year” may be the result of high rates of concurrent geriatric syndromes, alcohol use disorders, and drug abuse as described elsewhere [ 225 ].
Hence, upstream (e.g., poverty, poor nutrition, barriers to healthcare, and HIV treatment) and downstream factors (i.e., comorbidities and multimorbidity) significantly affect PEH [ 5 ], jeopardize their healthcare, and inflate their hospitalization rates compared to the general population [ 222 ].
Although we were unable to include any SR and MA reporting on the relationship between the COVID-19 pandemic and homelessness, PEH could be at higher risk also at developing hospitalization or fatalities due to COVID-19 according to recent evidence [ 226 ] although this finding deserves replication, providing evidence for the need of well-designed interventions targeting this vulnerable population.
Conclusions and implications for further research
This review adds weight to arguments about why reducing homelessness should be a priority beyond human rights justification. The evidence that experiencing homelessness leads to worse health outcomes is only a secondary consideration for providing affordable housing albeit an important one. Housing reduces hospitalization rates according to RCTs involving PEH with chronic illnesses [ 227 , 228 ]. This study demonstrates that a readily treatable illness such as HIV is not adequately managed in PEH resulting in significant downstream healthcare costs in addition to preventable patient suffering. A recent SR identified that housing PEH (in the short term) improves some aspects of health in this population with HIV, anxiety, and depression [ 229 ].
However, focusing just on providing housing for this population does not mean that an individual’s health needs are automatically solved. We know from Housing First studies that just providing housing does not result in improvements in mental health or addictions after a year, especially in people who have experienced significant trauma [ 55 ]. This umbrella review suggests that the health effects of homelessness are serious, longstanding, and involve all parts of the health system. Finally, while psychological interventions are expected to be more effective than TAU in reducing the burden of the associated health condition among clinical and non-clinical populations [ 230 ], the herein reviewed MA focusing on PEH on the matter [ 220 ] failed to reach a statistically significant threshold according to our conservative p value set at p =.005, though it could not be excluded the condition of homelessness itself could attenuate the effects of such psychological interventions.
What is needed now are studies that look at better coordination of care for this population that may involve hospitals and community partners as well as programs to address health issues in people recently housed after experiencing homelessness. In addition, it should be reiterated that there is an urgent need for international standardization of housing status to improve research rigor that could improve the external generalizability of this field and hence direct policy. Furthermore, more studies should be conducted in low- and middle-income countries as the vast majority of studies to date on this topic have been performed in developed nations. Such bias related to the geographical region may depend on a variety of issues, including, but not necessarily limited to, public health policies as well as the limited funding in LMICs. Lastly, more SRs and MAs with enhanced methodological quality are an unmet need in this field.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and are available online at https://osf.io/am67d/ and https://osf.io/58mhu/ .
The additional file includes the following: material 1 – [search strings]; table S 1 - [criteria for the evaluation of the credibility of the evidence of observational studies]; table S 2 – [excluded studies with reasons]; table S 3 – [quality rating of the included SRs or MAs of observational studies, according to the AMSTAR-2]; table S 4 – [sensitivity analysis].
Abbreviations
Activities of daily living
Assessment of Multiple Systematic Reviews 2
Assessment of Multiple Systematic Reviews Plus
Antiretroviral therapy
Confidence interval
Coronavirus disease 2019
Effect size
Hepatitis C virus
Human immunodeficiency virus
Instrumental activities of daily living
Low- and middle-income countries
Meta-analysis
Newcastle-Ottawa Scale
People experiencing homelessness
Randomized controlled trial
Standardized mortality ratio
Systematic review
Substance use disorder
Tsai J. Lifetime and 1-year prevalence of homelessness in the US population: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Public Health. 2018;40(1):65–74.
Article Google Scholar
Taylor O, Loubiere S, Tinland A, Vargas-Moniz M, Spinnewijn F, Manning R, et al. Lifetime, 5-year and past-year prevalence of homelessness in Europe: a cross-national survey in eight European nations. BMJ Open. 2019;9(11):e033237.
Article PubMed PubMed Central Google Scholar
Bensken WP. How do we define homelessness in large health care data? Identifying variation in composition and comorbidities. Health Serv Outcomes Res Methodol. 2021;21(1):145–66.
EUROPEAN TYPOLOGY OF HOMELESSNESS AND HOUSING EXCLUSION (ETHOS) [ https://www.feantsa.org/download/ethos2484215748748239888.pdf ]
Liu M, Hwang SW. Health care for homeless people. Nat Rev Dis Prim. 2021;7(1):1–2.
Google Scholar
Gilmer C, Buccieri K. Homeless patients associate clinician bias with suboptimal care for mental illness, addictions, and chronic pain. J Prim Care Commun Health. 2020;11:2150132720910289.
Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225.
Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859–70.
Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2(8):e124.
Ojo-Fati O, Joseph AM, Ig-Izevbekhai J, Thomas JL, Everson-Rose SA, Pratt R, et al. Practical issues regarding implementing a randomized clinical trial in a homeless population: strategies and lessons learned. Trials. 2017;18(1):1–10.
Ioannidis JP, Munafo MR, Fusar-Poli P, Nosek BA, David SP. Publication and other reporting biases in cognitive sciences: detection, prevalence, and prevention. Trends Cognit Sci. 2014;18(5):235–41.
Ioannidis JP. Why most discovered true associations are inflated. Epidemiology. 2008;19(5):640–8. https://doi.org/10.1097/EDE.0b013e31818131e7 .
Ioannidis JP. Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Cmaj. 2009;181(8):488–93.
Dragioti E, Evangelou E, Larsson B, Gerdle B. Effectiveness of multidisciplinary programmes for clinical pain conditions: An umbrella review. J Rehabil Med. 2018;50(9):779–91.
Article PubMed Google Scholar
Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JP. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ. 2015;350:g7607.
Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JP. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ. 2014;348:g2035. https://doi.org/10.1136/bmj.g2035 .
DerSimonian R, Laird N. Meta-analysis in clinical trials. Contr Clin Trials. 1986;7(3):177–88.
Article CAS Google Scholar
IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14(1):1–12.
Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101–29.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. https://doi.org/10.1136/bmj.d549 .
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. https://doi.org/10.1136/bmj.d4002 .
Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4(3):245–53.
Tsilidis KK, Papatheodorou SI, Evangelou E, Ioannidis JP. Evaluation of excess statistical significance in meta-analyses of 98 biomarker associations with cancer risk. J Natl Cancer Inst. 2012;104(24):1867–78.
Article CAS PubMed Google Scholar
Tsilidis KK, Panagiotou OA, Sena ES, Aretouli E, Evangelou E, Howells DW. Salman RA-S, Macleod MR, Ioannidis JP: Evaluation of excess significance bias in animal studies of neurological diseases. PLoS Biol. 2013;11(7):e1001609.
Article CAS PubMed PubMed Central Google Scholar
Dragioti E, Karathanos V, Gerdle B, Evangelou E. Does psychotherapy work? An umbrella review of meta-analyses of randomized controlled trials. Acta Psychiatrica Scandinavica. 2017;136(3):236–46.
Ioannidis JP. Clarifications on the application and interpretation of the test for excess significance and its extensions. J Math Psychol. 2013;57(5):184–7.
Bellou V, Belbasis L, Tzoulaki I, Evangelou E, Ioannidis JP. Environmental risk factors and Parkinson's disease: an umbrella review of meta-analyses. Parkinson Relat Disord. 2016;23:1–9.
Bortolato B, Köhler CA, Evangelou E, León-Caballero J, Solmi M, Stubbs B, et al. Systematic assessment of environmental risk factors for bipolar disorder: an umbrella review of systematic reviews and meta-analyses. Bipolar Disord. 2017;19(2):84–96.
Koletsi D, Solmi M, Pandis N, Fleming PS, Correll CU, Ioannidis JP. Most recommended medical interventions reach P < 0.005 for their primary outcomes in meta-analyses. Int J Epidemiol. 2020;49(3):885–93.
Li X, Meng X, Timofeeva M, Tzoulaki I, Tsilidis KK, Ioannidis JP, et al. Serum uric acid levels and multiple health outcomes: umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. BMJ. 2017;357:j2376.
Correll CU, Rubio JM, Inczedy-Farkas G, Birnbaum ML, Kane JM, Leucht S. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatr. 2017;74(7):675–84.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford: 2000.
Sharmin S, Kypri K, Khanam M, Wadolowski M, Bruno R, Mattick RP. Parental supply of alcohol in childhood and risky drinking in adolescence: systematic review and meta-analysis. Int J Environ Res Public Health. 2017;14(3):287.
Article PubMed Central Google Scholar
Ontario HQ. Interventions to Improve Access to Primary Care for People Who Are Homeless: A Systematic Review. Ont Health Technol Assess Ser. 2016;16(9):1–50.
Abad N, Baack B, O'Leary A, Lyles C. A review of HIV/STD behavioral prevention interventions for female sex workers in the United States. Sexual Transmit Dis. 2014;41:S114.
Adams-Guppy JR, Guppy A. A systematic review of interventions for homeless alcohol-abusing adults. Drugs. 2016;23(1):15–30.
Alividza V, Mariano V, Ahmad R, Charani E, Rawson TM, Holmes AH, et al. Investigating the impact of poverty on colonization and infection with drug-resistant organisms in humans: a systematic review. Infect Dis Poverty. 2018;7(1):76.
Altena AM, Brilleslijper-Kater SN, Wolf JL. Effective interventions for homeless youth: a systematic review. Am J Prev Med. 2010;38(6):637–45.
Altena AM, Brilleslijper-Kater SN, Wolf JLM. Effective Interventions for Homeless Youth. A Systematic Review. Am J Prevent Med. 2010;38(6):637–45.
Andrade FMR, Figueiredo AS, Capelas ML, Charepe Z, Deodato S. Experiences of homeless families in parenthood: a systematic review and synthesis of qualitative evidence. Int J Environ Res Public Health. 2020;17(8):2712. https://doi.org/10.3390/ijerph17082712 .
Aubry T, Bloch G, Brcic V, Saad A, Magwood O, Abdalla T, et al. Effectiveness of permanent supportive housing and income assistance interventions for homeless individuals in high-income countries: a systematic review. Lancet Public Health. 2020;5(6):e342–60.
Auerswald C, Woan J, Lin J. The health status of street children in low-and middle-income countries: A systematic review. Turk Pediatri Arsivi. 2013;48:75.
Ayano G, Shumet S, Tesfaw G, et al. A systematic review and meta-analysis of the prevalence of bipolar disorder among homeless people. BMC Public Health. 2020;20:731. https://doi.org/10.1186/s12889-020-08819-x .
Ayano G, Belete A, Duko B, Tsegay L, Dachew BA. Systematic review and meta-analysis of the prevalence of depressive symptoms, dysthymia and major depressive disorders among homeless people. BMJ Open. 2021;11(2):e040061.
Ayano G, Shumet S, Tesfaw G, Tsegay L. A systematic review and meta-analysis of the prevalence of bipolar disorder among homeless people. BMC Public Health. 2020;20(1):731.
Ayano G, Solomon M, Tsegay L, Yohannes K, Abraha M. A Systematic Review and Meta-Analysis of the Prevalence of Post-Traumatic Stress Disorder among Homeless People. Psychiatr Q. 2020;91(4):949–63.
Ayano G, Tesfaw G, Shumet S. The prevalence of schizophrenia and other psychotic disorders among homeless people: a systematic review and meta-analysis. BMC Psychiatry. 2019;19(1):370.
Ayano G, Tsegay L, Abraha M, Yohannes K. Suicidal Ideation and Attempt among Homeless People: a Systematic Review and Meta-Analysis. Psychiatr Q. 2019;90(4):829–42.
Bahji A, Bajaj N. Opioids on trial: a systematic review of interventions for the treatment and prevention of opioid overdose. Can J Addict. 2018;9(1):26–33.
Banks S, McHugo GJ, Williams V, Drake RE, Shinn M. A prospective meta-analytic approach in a multisite study of homelessness prevention. New Direct Eval. 2002;2002(94):45–60.
Barajas-Nava L. Oral substitution treatment of injecting opioid users for prevention of HIV infection. J Assoc Nurs AIDS Care. 2017;28(5):832–3.
Batra K, Pharr J, Olawepo JO, Cruz P. Understanding the multidimensional trajectory of psychosocial maternal risk factors causing preterm birth: A systematic review. Asian J Psychiatr. 2020;54:102436.
Baxter AJ, Tweed EJ, Katikireddi SV, Thomson H. Effects of Housing First approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. J Epidemiol Community Health. 2019;73(5):379–87.
Bazzi AR, Drainoni ML, Biancarelli DL, Hartman JJ, Mimiaga MJ, Mayer KH, et al. Systematic review of HIV treatment adherence research among people who inject drugs in the United States and Canada: evidence to inform pre-exposure prophylaxis (PrEP) adherence interventions. BMC Public Health. 2019;19(1):31.
Bazzi AR, Drainoni ML, Biancarelli DL, Hartman JJ, Mimiaga MJ, Mayer KH, et al. Systematic review of HIV treatment adherence research among people who inject drugs in the United States and Canada: Evidence to inform pre-exposure prophylaxis (PrEP) adherence interventions 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Public Health. 2019;19(1):1.
Behzadifar M, Gorji HA, Rezapour A, Bragazzi NL. Prevalence of hepatitis C virus among street children in Iran. Infect Dis Poverty. 2018;7(1):88.
Benston EA. Housing Programs for Homeless Individuals With Mental Illness: Effects on Housing and Mental Health Outcomes. Psychiatr Serv. 2015;66(8):806–16.
Bernstein RS, Meurer LN, Plumb EJ, Jackson JL. Diabetes and hypertension prevalence in homeless adults in the United States: a systematic review and meta-analysis. Am J Public Health. 2015;105(2):e46–60.
Blanquet M, Legrand A, Pélissier A, Mourgues C. Socio-economics status and metabolic syndrome: A meta-analysis. Diab Metab Syndr. 2019;13(3):1805–12.
Bonner A, Luscombe C. Suicide and homelessness. J Public Mental Health. 2009;8(3):7–19.
Borkhoff CM, Wieland ML, Myasoedova E, Ahmad Z, Welch V, Hawker GA, et al. Reaching those most in need: a scoping review of interventions to improve health care quality for disadvantaged populations with osteoarthritis. Arthritis Care Res (Hoboken). 2011;63(1):39–52.
Brownfield NR, Thielking M, Bates G, Morrison F. Does poverty impact student academic outcomes and wellbeing in australian universities? A systematic review. J Soc Inclusion. 2020;11(2):4–19.
Bryant J, Bonevski B, Paul C, McElduff P, Attia J. A systematic review and meta-analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction. 2011;106(9):1568–85.
Burra TA, Stergiopoulos V, Rourke SB. A systematic review of cognitive deficits in homeless adults: implications for service delivery. Can J Psychiatr. 2009;54(2):123–33.
Byrne T, Montgomery AE, Dichter ME. Homelessness among female veterans: a systematic review of the literature. Women Health. 2013;53(6):572–96.
Campos-Matos I, Russo G, Perelman J. Connecting the dots on health inequalities - A systematic review on the social determinants of health in Portugal. Int J Equity Health. 2016;15(1):26.
Carver H, Ring N, Miler J, Parkes T. What constitutes effective problematic substance use treatment from the perspective of people who are homeless? A systematic review and meta-ethnography. Harm Reduct J. 2020;17(1):10.
Cassone A. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Pathog Glob Health. 2012;106(7):377.
Chandler CE, Austin AE, Shanahan ME. Association of Housing Stress With Child Maltreatment: A Systematic Review. Trauma Violence Abuse. 2020;23:639–59.
Chant C, Smith O, Wang A, Burns K, Dos Santos CC, Friedrich JO, et al. Critical illness in homeless persons: A systematic review of the literature. Intens Care Med. 2013;39:S512.
Chant C, Smith O, Wang A, Hwang S, Friedrich JO, Burns KEA, et al. Homelessness and critical care: a systematic review of the literature. Intensive Care Med. 2014;40(1):123–5. https://doi.org/10.1007/s00134-013-3124-4 .
Chant C, Wang A, Burns KE, dos Santos CC, Hwang SW, Friedrich JO, et al. Critical illness in homeless persons is poorly studied: a systematic review of the literature. Intensive Care Med. 2014;40(1):123–5.
Charron CB, Hayes T, Pakhale S. A systematic review of interventions for smoking tobacco in low socio-economic populations. Am J Respir Crit Care Med. 2018;197. https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2018.197.1_MeetingAbstracts.A6253 .
Clark NC, Lintzeris N, Gijsbers A, Whelan G, Dunlop A, Ritter A, et al. LAAM maintenance vs methadone maintenance for heroin dependence. Cochrane Database Syst Rev. 2002;2:CD002210.
Coldwell CM, Bender WS. The effectiveness of assertive community treatment for homeless populations with severe mental illness: a meta-analysis. Am J Psychiatry. 2007;164(3):393–9.
Conn VS, Ruppar TM. Medication adherence outcomes of 771 intervention trials: Systematic review and meta-analysis. Prev Med. 2017;99:269–76.
Constance J, Lusher JM. Diabetes management interventions for homeless adults: a systematic review. Int J Public Health. 2020;65(9):1773–83.
Coren E, Hossain R, Pardo JP, Veras MM, Chakraborty K, Harris H, et al. Interventions for promoting reintegration and reducing harmful behaviour and lifestyles in street-connected children and young people. Evid Based Child Health. 2013;8(4):1140–272.
Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, et al. Global Morbidity and Mortality of Leptospirosis: A Systematic Review. PLoS Negl Trop Dis. 2015;9(9):e0003898.
Coufopoulos A, McDowell G, Roe B, Maden M. Interventions to improve nutrition and nutrition related health amongst homeless mothers and their children: a systematic review. Proceed Nutr Soc. 2012;71(OCE2):E161. https://doi.org/10.1017/S0029665112002182 .
Cumber SN, Tsoka-Gwegweni JM. The Health Profile of Street Children in Africa: A Literature Review. J Public Health Afr. 2015;6(2):566.
PubMed PubMed Central Google Scholar
Curtis J. Impact of x-ray screening programmes for active tuberculosis in homeless populations: a systematic review of original studies. J Public Health (Oxf). 2016;38(1):106–14.
da Silva TFC, Lovisi GM, Verdolin LD, Cavalcanti MT. Adherence to drug treatment among schizophrenic spectrum patients: A systematic review of the literature. Jornal Brasileiro de Psiquiatria. 2012;61(4):242–51.
Dalton-Locke C, Marston L, McPherson P, Killaspy H. The Effectiveness of Mental Health Rehabilitation Services: A Systematic Review and Narrative Synthesis. Front Psychiatry. 2020;11:607933.
de Vet R, van Luijtelaar MJ, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JR. Effectiveness of case management for homeless persons: a systematic review. Am J Public Health. 2013;103(10):e13–26.
De Vet R, Van Luijtelaar MJA, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JRLM. Effectiveness of case management for homeless persons: A systematic review. Am J Public Health. 2013;103(10):e13–26.
Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–207.
Doran KM, Ragins KT, Gross CP, Zerger S. Medical respite programs for homeless patients: a systematic review. J Health Care Poor Underserved. 2013;24(2):499–524.
Dorney-Smith S, Thomson E, Hewett N, Burridge S, Khan Z. Homeless medical respite service provision in the UK. House Care Support. 2019;22(1):40–53.
Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62(5):1353–63.
El Baba R, Colucci E. Post-traumatic stress disorders, depression, and anxiety in unaccompanied refugee minors exposed to war-related trauma: a systematic review. Int J Cult Mental Health. 2018;11(2):194–207.
Embleton L, Mwangi A, Vreeman R, Ayuku D, Braitstein P. The epidemiology of substance use among street children in resource-constrained settings: a systematic review and meta-analysis. Addiction. 2013;108(10):1722–33.
Ennis N, Roy S, Topolovec-Vranic J. Memory impairment among people who are homeless: a systematic review. Memory. 2015;23(5):695–713.
Fitzpatrick-Lewis D, Ganann R, Krishnaratne S, Ciliska D, Kouyoumdjian F, Hwang SW. Effectiveness of interventions to improve the health and housing status of homeless people: a rapid systematic review. BMC Public Health. 2011;11:638.
Flach Y, Razza TS. Suicidality in homeless children and adolescent: a systematic review. Aggress Violent Behav. 2022;64:101575.
Folsom D, Jeste DV. Schizophrenia in homeless persons: a systematic review of the literature. Acta Psychiatr Scand. 2002;105(6):404–13.
Formosa EA, Kishimoto V, Orchanian-Cheff A, Hayman K. Emergency department interventions for homelessness: a systematic review. Cjem. 2021;23(1):111–22.
Formosa EA, Kishimoto V, Orchanian-Cheff A, Hayman KG. 302 Emergency Department Interventions for Homelessness: A Systematic Review. Ann Emerg Med. 2019;74(4):S119.
Fry CE, Langley K, Shelton KH. A systematic review of cognitive functioning among young people who have experienced homelessness, foster care, or poverty. Child Neuropsychol. 2017;23(8):907–34.
Gentry S, Forouhi NG, Notley C. Are Electronic Cigarettes an Effective Aid to Smoking Cessation or Reduction Among Vulnerable Groups? A Systematic Review of Quantitative and Qualitative Evidence. Nicotine Tob Res. 2019;21(5):602–16.
Getty CA, Morande A, Lynskey M, Weaver T, Metrebian N. Mobile telephone-delivered contingency management interventions promoting behaviour change in individuals with substance use disorders: a meta-analysis. Addiction. 2019;114(11):1915–25.
Gulati G, Keating N, O'Neill A, Delaunois I, Meagher D, Dunne CP. The prevalence of major mental illness, substance misuse and homelessness in Irish prisoners: systematic review and meta-analyses. Ir J Psychol Med. 2019;36(1):35–45.
Hamilton K, Tolfree R, Mytton J. A systematic review of active case-finding strategies for tuberculosis in homeless populations. Int J Tuberc Lung Dis. 2018;22(10):1135–44.
Hamilton K, Tolfree R, Mytton J. Impact and implementation of active case finding for tuberculosis in homeless populations: a systematic review. Lancet. 2019;394:S48.
Hanlon P, Yeoman L, Gibson L, Esiovwa R, Williamson AE, Mair FS, et al. A systematic review of interventions by healthcare professionals to improve management of non-communicable diseases and communicable diseases requiring long-term care in adults who are homeless. BMJ Open. 2018;8(4):e020161.
Heerde JA, Hemphill SA. A systematic review of associations between perpetration of physically violent behaviors and property offenses, victimization and use of substances among homeless youth. Children Youth Serv Rev. 2014;44:265–77.
Heerde JA, Hemphill SA. Is Substance Use Associated with Perpetration and Victimization of Physically Violent Behavior and Property Offences Among Homeless Youth? A Systematic Review of International Studies. Child Youth Care Forum. 2015;44(2):277–307.
Heerde JA, Hemphill SA. The role of risk and protective factors in the modification of risk for sexual victimization, sexual risk behaviors, and survival sex among homeless youth: A meta-analysis. J Investig Psychol Offend Profil. 2017;14(2):150–74.
Heerde JA, Hemphill SA. Associations between individual-level characteristics and exposure to physically violent behavior among young people experiencing homelessness: A meta-analysis. Aggress Violent Behav. 2019;47:46–57.
Heerde JA, Scholes-Balog KE, Hemphill SA. Associations between youth homelessness, sexual offenses, sexual victimization, and sexual risk behaviors: a systematic literature review. Arch Sex Behav. 2015;44(1):181–212.
Herrman H. Mental disorders among homeless people in western countries. PLoS Med. 2008;5(12):e237.
Heuvelings CC, de Vries SG, Greve PF, Visser BJ, Bélard S, Janssen S, et al. Effectiveness of interventions for diagnosis and treatment of tuberculosis in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. Lancet Infect Dis. 2017;17(5):e144–58.
Heuvelings CC, Greve PF, de Vries SG, Visser BJ, Bélard S, Janssen S, et al. Effectiveness of service models and organisational structures supporting tuberculosis identification and management in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. BMJ Open. 2018;8(9):e019642.
Hino P, Yamamoto TT, Bastos SH, Beraldo AA, Figueiredo T, Bertolozzi MR. Tuberculosis in the street population: a systematic review. Rev Esc Enferm USP. 2021;55:e03688.
Hino P, Yamamoto TT, Bastos SH, Beraldo AA, Figueiredo TMRM, Bertolozzi MR. Tuberculosis in the street population: a systematic review. Revista da Escola de Enfermagem da U S P. 2021;55:e03688.
Hodgson KJ, Shelton KH, van den Bree MB, Los FJ. Psychopathology in young people experiencing homelessness: a systematic review. Am J Public Health. 2013;103(6):e24–37.
Hodgson KJ, Shelton KH, Van Den Bree MBM, Los FJ. Psychopathology in young people experiencing homelessness: A systematic review. Am J Public Health. 2013;103(6):e24–37.
Hoell A, Franz M, Salize HJ. Healthcare for homeless people with mental illness-A review of results of current interventions. Psychiatrie. 2017;14(2):75–85.
Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal Self-Directed Violence Among Homeless US Veterans: A Systematic Review. Suicide Life Threat Behav. 2018;48(4):481–98.
Hossain MM, Purohit N, Sultana A, Ma P, McKyer ELJ, Ahmed HU. Prevalence of mental disorders in South Asia: An umbrella review of systematic reviews and meta-analyses. Asian J Psychiatr. 2020;51:102041.
Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: a systematic review. Am J Prev Med. 2005;29(4):311–9.
Ijaz S, Jackson J, Thorley H, Porter K, Fleming C, Richards A, et al. Nutritional deficiencies in homeless persons with problematic drinking: a systematic review. Int J Equity Health. 2017;16(1):71.
Ijaz S, Thorley H, Porter K, Fleming C, Jones T, Kesten J, et al. Interventions for preventing or treating malnutrition in homeless problem-drinkers: a systematic review. Int J Equity Health. 2018;17(1):8.
Karki P, Shrestha R, Huedo-Medina TB, Copenhaver M. The impact of methadone maintenance treatment on HIV risk behaviors among high-risk injection drug users: a systematic review. Evid Based Med Public Health. 2016;2:e1229.
Kenworthy J, Ayyub R, Rtveladze K, Wright D, Xia A, Fordham R. A systematic literature review of the societal costs and consequences of heroin addiction. Value Health. 2017;20(9):A497.
Klop HT, de Veer AJE, van Dongen SI, Francke AL, Rietjens JAC, Onwuteaka-Philipsen BD. Palliative care for homeless people: a systematic review of the concerns, care needs and preferences, and the barriers and facilitators for providing palliative care. BMC Palliat Care. 2018;17(1):67.
Krahn J, Caine V, Chaw-Kant J, Singh AE. Housing interventions for homeless, pregnant/parenting women with addictions: a systematic review. J Soc Distress Homeless. 2018;27(1):75–88.
Kyle T, Dunn JR. Effects of housing circumstances on health, quality of life and healthcare use for people with severe mental illness: a review. Health Soc Care Community. 2008;16(1):1–15.
Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007;11(6 Suppl):85–100.
Leibler JH, Zakhour CM, Gadhoke P, Gaeta JM. Zoonotic and Vector-Borne Infections Among Urban Homeless and Marginalized People in the United States and Europe, 1990-2014. Vector Borne Zoonotic Dis. 2016;16(7):435–44.
Lowrie R, Stock K, Lucey S, Knapp M, Williamson A, Montgomery M, et al. Pharmacist led homeless outreach engagement and non-medical independent prescribing (Rx) (PHOENIx) intervention for people experiencing homelessness: a non- randomised feasibility study. Int J Equity Health. 2021;20(1):19.
Luong CT, Rew L, Banner M. Suicidality in Young Men Who Have Sex with Men: A Systematic Review of the Literature. Issues Ment Health Nurs. 2018;39(1):37–45.
Ly A, Latimer E. Housing First Impact on Costs and Associated Cost Offsets: A Review of the Literature. Can J Psychiatry. 2015;60(11):475–87.
Ly TDA, Castaneda S, Hoang VT, Dao TL, Gautret P. Vaccine-preventable diseases other than tuberculosis, and homelessness: A scoping review of the published literature, 1980 to 2020. Vaccine. 2021;39(8):1205–24.
Maglione MA, Raaen L, Chen C, Azhar G, Shahidinia N, Shen M, et al. Effects of medication assisted treatment (MAT) for opioid use disorder on functional outcomes: a systematic review. J Subst Abuse Treatment. 2018;89:28–51.
Magwood O, Salvalaggio G, Beder M, Kendall C, Kpade V, Daghmach W, et al. The effectiveness of substance use interventions for homeless and vulnerably housed persons: A systematic review of systematic reviews on supervised consumption facilities, managed alcohol programs, and pharmacological agents for opioid use disorder. PLoS One. 2020;15(1):e0227298.
Martinez O, Wu E, Sandfort T, Dodge B, Carballo-Dieguez A, Pinto R, et al. Evaluating the Impact of Immigration Policies on Health Status Among Undocumented Immigrants: A Systematic Review. J Immigrant Minor Health. 2015;17(3):947–70.
Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009;3:CD002209.
Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;2:CD002207.
McInnes DK, Li AE, Hogan TP. Opportunities for engaging low-income, vulnerable populations in health care: a systematic review of homeless persons' access to and use of information technologies. Am J Public Health. 2013;103(Suppl 2):e11–24.
McPherson P, Krotofil J, Killaspy H. Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry. 2018;18(1):128.
Mendes KT, Ronzani TM, de Paiva FS. Homeless population, vulnerabilities and drugs: a systematic review. Psicol Soc. 2019;31:e169056. https://doi.org/10.1590/1807-0310/2019v31169056 .
Moe J, Kirkland SW, Rawe E, Ospina MB, Vandermeer B, Campbell S, et al. Effectiveness of Interventions to Decrease Emergency Department Visits by Adult Frequent Users: A Systematic Review. Acad Emerg Med. 2017;24(1):40–52.
Momsen AM, Rasmussen JO, Nielsen CV, Iversen MD, Lund H. Multidisciplinary team care in rehabilitation: An overview of reviews. J Rehabil Med. 2012;44(11):901–12.
Moniruzzaman A, Kazanjian A, Wong H, Chowdhury MM, Elwood RK, Fitzgerald JM. A systematic review on risk factors of mortality among Tb patients. Am J Respir Crit Care Med. 2010;181. https://doi.org/10.1164/ajrccm-conference.2010.181.1_MeetingAbstracts.A5460 .
Morton MH, Kugley S, Epstein R, Farrell A. Interventions for youth homelessness: A systematic review of effectiveness studies. Child Youth Serv Rev. 2020;116:105096.
Murray RL, Bauld L, Hackshaw LE, McNeill A. Improving access to smoking cessation services for disadvantaged groups: a systematic review. J Public Health (Oxf). 2009;31(2):258–77.
Muzzey FK, Fortenberry JD, Maas MK, Holtrop K, McCauley H. 169. Sexual and Gender Minority Homeless Youth and Their Sexual Relationships: A Systematic Review of Recent Literature. J Adolesc Health. 2020;66(2):S86.
Nevard I, Green C, Bell V, Gellatly J, Brooks H, Bee P. Conceptualising the social networks of vulnerable children and young people: a systematic review and narrative synthesis. Soc Psychiatry Psychiatr Epidemiol. 2021;56(2):169–82.
Nilsson S, Nordentoft M, Hjorthoj C. Psychiatric predictors for becoming homeless and exiting homelessness: A systematic review and meta-analysis. Schizophrenia Bull. 2020;46:S278.
Noh D. Psychological Interventions for Runaway and Homeless Youth. J Nurs Scholar. 2018;50(5):465–72.
Omerov P, Craftman Å, Mattsson E, Klarare A. Homeless persons' experiences of health- and social care: A systematic integrative review. Health Soc Care Community. 2020;28(1):1–11.
Paisi M, March-McDonald J, Burns L, Snelgrove-Clarke E, Withers L, Shawe J. Perceived barriers and facilitators to accessing and utilising sexual and reproductive healthcare for people who experience homelessness: a systematic review. BMJ Sex Reprod Health. 2020;47:211–20.
Paisi MD, March-Mcdonald J, Burns L, Snelgrove-Clarke E, Withers L, Shawe J. Perceived barriers and facilitators to accessing and utilising sexual and reproductive healthcare for people who experience homelessness: A systematic review. BMJ Sex Reprod Health. 2020;47:211–20.
Paquette K, Cheng MP, Kadatz MJ, Cook VJ, Chen W, Johnston JC. Chest radiography for active tuberculosis case finding in the homeless: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2014;18(10):1231–6.
Parks RW, Stevens RJ, Spence SA. A systematic review of cognition in homeless children and adolescents. J R Soc Med. 2007;100(1):46–50.
Parriott A, Malekinejad M, Miller AP, Marks SM, Horvath H, Kahn JG. Care Cascade for targeted tuberculosis testing and linkage to Care in Homeless Populations in the United States: a meta-analysis. BMC Public Health. 2018;18(1):485.
Peng Y, Hahn RA, Finnie RKC, Cobb J, Williams SP, Fielding JE, et al. Permanent Supportive Housing With Housing First to Reduce Homelessness and Promote Health Among Homeless Populations With Disability: A Community Guide Systematic Review. J Public Health Manag Pract. 2020;26(5):404–11.
Polcin DL. Co-occurring substance abuse and mental health problems among homeless persons: Suggestions for research and practice. J Soc Distress Homeless. 2016;26(1):1–10.
Polillo A, Gran-Ruaz S, Sylvestre J, Kerman N. The use of eHealth interventions among persons experiencing homelessness: A systematic review. Digit Health. 2021;7:2055207620987066.
Ponka D, Agbata E, Kendall C, Stergiopoulos V, Mendonca O, Magwood O, et al. The effectiveness of case management interventions for the homeless, vulnerably housed and persons with lived experience: A systematic review. PLoS One. 2020;15(4):e0230896.
Rajendran M, Zaki RA, Aghamohammadi N. Contributing risk factors towards the prevalence of multidrug-resistant tuberculosis in Malaysia: A systematic review. Tuberculosis (Edinb). 2020;122:101925.
Rezaei O, Ghiasvand H, Higgs P, Noroozi A, Noroozi M, Rezaei F, et al. Factors associated with injecting-related risk behaviors among people who inject drugs: a systematic review and meta-analysis study. J Addict Dis. 2020;38(4):420–37.
Richter D, Hoffmann H. Independent housing and support for people with severe mental illness: systematic review. Acta Psychiatr Scand. 2017;136(3):269–79.
Riquelme-Miralles D, Palazón-Bru A, Sepehri A, Gil-Guillén VF. A systematic review of non-pharmacological interventions to improve therapeutic adherence in tuberculosis. Heart Lung. 2019;48(5):452–61.
Roy L. Criminal behavior and victimization among homeless individuals with severe mental illness: A systematic review (Psychiatric Services (2014)). Psychiatr Serv. 2014;65(7):896.
Roy L, Crocker AG, Nicholls TL, Latimer EA, Ayllon AR. Criminal behavior and victimization among homeless individuals with severe mental illness: a systematic review. Psychiatr Serv. 2014;65(6):739–50.
Sandgren A, Vonk Noordegraaf-Schouten M, van Kessel F, Stuurman A, Oordt-Speets A, van der Werf MJ. Initiation and completion rates for latent tuberculosis infection treatment: a systematic review. BMC Infect Dis. 2016;16:204.
Article PubMed PubMed Central CAS Google Scholar
Saulle R, Vecchi S, Gowing L. Supervised dosing with a long-acting opioid medication in the management of opioid dependence. Cochrane Database Syst Rev. 2017;4:CD011983.
PubMed Google Scholar
Sayal AP, Slomovic J, Bhambra NS, Popovic MM, Lichter M. Visual impairment and the prevalence of ocular pathology in homeless children and adults globally: a systematic review. Can J Ophthalmol. 2020;56:158–65.
Scappaticci ALSS, Blay SL. Homeless adolescent mothers: A systematic review of the literature. Revista de Psiquiatria do Rio Grande do Sul. 2010;32(1):3–15.
Schneider JA, Skaathun B, Michaels S, Young L, Green K, Morgan E, et al. Drivers of HIV treatment success among a population-based sample of younger black MSM. Top Antiviral Med. 2015;23:494–5.
Schreiter S, Bermpohl F, Krausz M, Leucht S, Rössler W, Schouler-Ocak M, et al. The Prevalence of Mental Illness in Homeless People in Germany. Dtsch Arztebl Int. 2017;114(40):665–72.
Schreiter S, Bermpohl F, Krausz M, Leucht S, Rössler W, Schouler-Ocak M, et al. The prevalence of mental illness in homeless people in Germany - A systematic review and meta-analysis. Deutsches Arzteblatt Int. 2017;114(40):665–72.
Schumacher JE, Milby JB, Wallace D, Meehan DC, Kertesz S, Vuchinich R, et al. Meta-analysis of day treatment and contingency-management dismantling research: Birmingham Homeless Cocaine Studies (1990-2006). J Consult Clin Psychol. 2007;75(5):823–8.
Shortt SE, Hwang S, Stuart H, Bedore M, Zurba N, Darling M. Delivering primary care to homeless persons: a policy analysis approach to evaluating the options. Healthc Policy. 2008;4(1):108–22.
CAS PubMed PubMed Central Google Scholar
Silva EN, da Silva Pereira ACE, de Araújo WN, Elias FTS. A systematic review of economic evaluations of interventions to tackle tuberculosis in homeless people. Revista Panamericana de Salud Publica/Pan Am J Public Health. 2018;42:e40.
Silva EN, Pereira A, de Araújo WN, Elias FTS. A systematic review of economic evaluations of interventions to tackle tuberculosis in homeless people. Rev Panam Salud Publica. 2018;42:e40.
Simmonds M, Simmonds K, Weleff J. Prevalence and problems of pain in the homeless: A systematic review. J Pain. 2016;17(4):S12–3.
Simoens S, Matheson C, Bond C, Inkster K, Ludbrook A. The effectiveness of community maintenance with methadone or buprenorphine for treating opiate dependence. Br J Gen Pract. 2005;55(511):139–46.
Soar K, Dawkins L, Robson D, Cox S. Smoking amongst adults experiencing homelessness: A systematic review of prevalence rates, interventions and the barriers and facilitators to quitting and staying quit. J Smok Cessation. 2020;15:94–108.
Speirs V, Johnson M, Jirojwong S. A systematic review of interventions for homeless women. J Clin Nurs. 2013;22(7-8):1080–93.
Spence S, Stevens R, Parks R. Cognitive dysfunction in homeless adults: a systematic review. J R Soc Med. 2004;97(8):375–9.
Strang J, Groshkova T, Uchtenhagen A, Van Den Brink W, Haasen C, Schechter MT, et al. Heroin on trial: systematic review and meta-analysis of randomised trials of diamorphine-prescribing as treatment for refractory heroin addiction. Br J Psychiatr. 2015;207(1):5–14.
Stubbs JL, Thornton AE, Sevick JM, Silverberg ND, Barr AM, Honer WG, et al. Traumatic brain injury in homeless and marginally housed individuals: a systematic review and meta-analysis. Lancet Public Health. 2020;5(1):e19–32.
Sudarsanam TD, Tharyan P. Rifampicin compared to isoniazid for preventing active TB in HIV-negative people at risk of developing active TB: Implications for public health. Clin Epidemiol Global Health. 2014;2(1):28–36.
Sumalinog R, Harrington K, Dosani N, Hwang SW. Advance care planning, palliative care, and end-of-life care interventions for homeless people: A systematic review. Palliat Med. 2017;31(2):109–19.
Sundin EC. Homelessness and experiences of psychological trauma in the western world: A research review and a qualitative study. Eur Psychiatry. 2011;26:1811.
Tankimovich M. Barriers to and interventions for improved tuberculosis detection and treatment among homeless and immigrant populations: a literature review. J Community Health Nurs. 2013;30(2):83–95.
Thomas CP, Fullerton CA, Kim M, Montejano L, Lyman DR, Dougherty RH, et al. Medication-assisted treatment with buprenorphine: assessing the evidence. Psychiatric Serv. 2014;65(2):158–70.
Thomas Y, Gray M, McGinty S. A systematic review of occupational therapy interventions with homeless people. Occup Ther Health Care. 2011;25(1):38–53.
Thorley H, Porter K, Fleming C, Jones T, Kesten J, Marques E, et al. Interventions for preventing or treating malnutrition in problem drinkers who are homeless or vulnerably housed: protocol for a systematic review. Syst Rev. 2015;4:131.
To MJ, Brothers TD, Van Zoost C. Foot Conditions among Homeless Persons: A Systematic Review. PLoS One. 2016;11(12):e0167463.
Topolovec-Vranic J, Ennis N, Colantonio A, Cusimano MD, Hwang SW, Kontos P, et al. Traumatic brain injury among people who are homeless: a systematic review. BMC Public Health. 2012;12:1059.
Tsai J, Rosenheck RA. Risk factors for homelessness among US veterans. Epidemiol Rev. 2015;37:177–95.
Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414.
Vijayaraghavan M, Elser H, Frazer K, Lindson N, Apollonio D. Interventions to reduce tobacco use in people experiencing homelessness. Cochrane Database Syst Rev. 2020;12:CD013413.
Wang JZ, Mott S, Magwood O, Mathew C, McLellan A, Kpade V, et al. The impact of interventions for youth experiencing homelessness on housing, mental health, substance use, and family cohesion: a systematic review. BMC Public Health. 2019;19(1):1528.
Weber JJ. A systematic review of nurse-led interventions with populations experiencing homelessness. Public Health Nurs. 2019;36(1):96–106.
White BM, Newman SD. Access to primary care services among the homeless: a synthesis of the literature using the equity of access to medical care framework. J Prim Care Community Health. 2015;6(2):77–87.
Whitney B, Kruszka B, Lorvick J, Lucas GM, Wechsberg W, Kuo I, et al. Association between housing stability and new HIV diagnosis in seek and test studies. Topics Antiviral Med. 2017;25(1):362s–3s.
Wilson MG, Aidala A, Gogolishvili D, Shubert V, Rueda S, Bozack A, et al. Housing status and the health of people living with HIV/AIDS: A systematic review. Can J Infect Dis Med Microbiol. 2012;23:40A–1A.
Woan J, Lin J, Auerswald C. The health status of street children and youth in low- and middle-income countries: a systematic review of the literature. J Adolesc Health. 2013;53(3):314–321.e312.
Wright N, Walker J. Homelessness and drug use - A narrative systematic review of interventions to promote sexual health. AIDS Care Psycholog Socio Med Aspects AIDS/HIV. 2006;18(5):467–78.
Wright NM, Walker J. Homelessness and drug use - a narrative systematic review of interventions to promote sexual health. AIDS Care. 2006;18(5):467–78.
Xiang J, Kaminga AC, Wu XY, Lai Z, Yang J, Lian Y, et al. Lifetime prevalence of suicidal attempt among homeless individuals in North America: a meta-analysis. J Affect Disord. 2021;287:341–9.
Yadee J, Bangpan M, Thavorn K, Welch V, Tugwell P, Chaiyakunapruk N. Assessing evidence of interventions addressing inequity among migrant populations: A two-stage systematic review. Int J Equity Health. 2019;18(1):64.
Zlotnick C, Tam T, Zerger S. Common needs but divergent interventions for U.S. homeless and foster care children: results from a systematic review. Health Soc Care Community. 2012;20(5):449–76.
Tweed EJ, Thomson RM, Lewer D, Sumpter C, Kirolos A, Southworth PM, et al. Health of people experiencing co-occurring homelessness, imprisonment, substance use, sex work and/or severe mental illness in high-income countries: a systematic review and meta-analysis. J Epidemiol Community Health. 2021;75:1010–8.
Arum C, Fraser H, Artenie AA, Bivegete S, Trickey A, Alary M, et al. Homelessness, unstable housing, and risk of HIV and hepatitis C virus acquisition among people who inject drugs: a systematic review and meta-analysis. Lancet Public Health. 2021;6:e309–23.
Suh K, Beck J, Katzman W, Allen DD. Homelessness and rates of physical dysfunctions characteristic of premature geriatric syndromes: systematic review and meta-analysis. Physiother Theory Pract. 2020;38:1–10.
Al-Shakarchi NJ, Evans H, Luchenski SA, Story A, Banerjee A. Cardiovascular disease in homeless versus housed individuals: a systematic review of observational and interventional studies. Heart. 2020;106(19):1483–8.
van Draanen J, Tsang C, Mitra S, Karamouzian M, Richardson L. Socioeconomic marginalization and opioid-related overdose: A systematic review. Drug Alcohol Depend. 2020;214:108127.
Lin D, Zhang CY, He ZK, Zhao XD. How does hard-to-reach status affect antiretroviral therapy adherence in the HIV-infected population? Results from a meta-analysis of observational studies. BMC Public Health. 2019;19(1):789.
Aldridge RW, Story A, Hwang SW, Nordentoft M, Luchenski SA, Hartwell G, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. 2018;391(10117):241–50.
Bassuk EL, Richard MK, Tsertsvadze A. The prevalence of mental illness in homeless children: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2015;54(2):86–96.e82.
Aidala AA, Wilson MG, Shubert V, Gogolishvili D, Globerman J, Rueda S, et al. Housing Status, Medical Care, and Health Outcomes Among People Living With HIV/AIDS: A Systematic Review. Am J Public Health. 2016;106(1):e1–e23.
Hyun M, Bae SH, Noh D. Systematic review and meta-analyses of randomized control trials of the effectiveness of psychosocial interventions for homeless adults. J Adv Nurs. 2020;76(3):773–86.
Dragioti E, Solmi M, Favaro A, Fusar-Poli P, Dazzan P, Thompson T, et al. Association of antidepressant use with adverse health outcomes: a systematic umbrella review. JAMA Psychiatry. 2019;76(12):1241–55.
Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–40.
Smartt C, Prince M, Frissa S, Eaton J, Fekadu A, Hanlon C. Homelessness and severe mental illness in low-and middle-income countries: scoping review. BJPsych Open. 2019;5(4):e57.
Clemenzi-Allen A, Neuhaus J, Geng E, Sachdev D, Buchbinder S, Havlir D, et al. Housing instability results in increased acute care utilization in an urban HIV clinic cohort. In: Open forum infectious diseases: Oxford University Press US; 2019. p. ofz148.
Brown RT, Kiely DK, Bharel M, Mitchell SL. Factors associated with geriatric syndromes in older homeless adults. J Health Care Poor Underserved. 2013;24:456–68.
Culhane D, Treglia D, Steif K, Kuhn R, Byrne T. Estimated emergency and observational/quarantine capacity need for the US homeless population related to COVID-19 exposure by county; projected hospitalizations, intensive care units and mortality. 2020. https://endhomelessness.org/wp-content/uploads/2020/03/COVID-paper_clean-636pm.pdf .
Buchanan D, Kee R, Sadowski LS, Garcia D. The health impact of supportive housing for HIV-positive homeless patients: a randomized controlled trial. Am J Public Health. 2009;99(S3):S675–80.
Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. Jama. 2009;301(17):1771–8.
Onapa H, Sharpley CF, Bitsika V, McMillan ME, MacLure K, Smith L, et al. The physical and mental health effects of housing homeless people: A systematic review. Health Soc Care Community. 2021;30:448–68.
van Agteren J, Iasiello M, Lo L, Bartholomaeus J, Kopsaftis Z, Carey M, et al. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat Human Behav. 2021;5(5):631–52.
Download references
Acknowledgments
Open access funding provided by Linköping University. This study received no funding.
Author information
Authors and affiliations.
Section of Psychiatry, Department of Neuroscience, Reproductive Science, and Odontostomatology, Federico Ii University of Naples, Naples, Italy
Michele Fornaro, Michele De Prisco, Martina Billeci, Anna Maria Mondin & Andrea de Bartolomeis
Pain and Rehabilitation Centre, and Department of Medical and Health Sciences, Linköping University, SE-581 85, Linköping, Sweden
Elena Dragioti
Department of Psychology, University of Milan-Bicocca, Piazza dell’Ateneo Nuovo, 1, 20126, Milan, Italy
Raffaella Calati
Department of Adult Psychiatry, Nimes University Hospital, 4 Rue du Professeur Robert Debré, 30029, Nimes, France
Cambridge Centre for Health, Performance and Wellbeing, Anglia Ruskin University, Cambridge, UK
Department of Psychiatry, University of Ottawa, Ottawa, ON, Canada
Simon Hatcher, Mark Kaluzienski, Jess G. Fiedorowicz & Marco Solmi
Department of Mental Health, The Ottawa Hospital, Ottawa, ON, Canada
Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, ON, Canada
Simon Hatcher, Jess G. Fiedorowicz & Marco Solmi
Early Psychosis: Interventions and Clinical-Detection (EPIC) Lab, Department of Psychosis Studies, Institute of Psychiatry, Psychology, London, UK
Marco Solmi
Faculty of Environmental and Life Sciences, Center for Innovation in Mental Health, School of Psychology, University of Southampton, Southampton, UK
UNESCO staff, Chair - “Education for Health and Sustainable Development”, University of Naples, Federico II Naples, Naples, Italy
Andrea de Bartolomeis
IMPACT, The Institute for Mental and Physical Health and Clinical Translation, School of Medicine, Barwon Health, Deakin University, Geelong, Australia
André F. Carvalho
You can also search for this author in PubMed Google Scholar
Contributions
MF and AFC conceived the study together with MS. MS and AFC provided input over the study process. MDP, MB, and AM extracted the data, assisting in manuscript drafting under MF guidance. ED performed the analyses. AdB, LS, RC, SH, JGF, ED, and MK provided expert input over the review process and final drafting. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Elena Dragioti .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: material 1..
adopted search strings. Table S1. criteria for the evaluation of the credibility of the evidence of observational studies. Please note that criterion n.1 (sample size of cases) was purposely waived as outlined in the main-text, methods section. Table S2. List of the 179 excluded records, with the reason(s). Note: duplicate records may appear multiple times for consistency issues. Table S3. Included SRs or MAs of observational studies; quality rating according to the AMSTAR-2. Table S4. Sensitivity analysis of evidence from SRs or MAs of observational studies for the association between homelessness and any health outcome.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fornaro, M., Dragioti, E., De Prisco, M. et al. Homelessness and health-related outcomes: an umbrella review of observational studies and randomized controlled trials. BMC Med 20 , 224 (2022). https://doi.org/10.1186/s12916-022-02423-z
Download citation
Received : 19 January 2022
Accepted : 30 May 2022
Published : 12 July 2022
DOI : https://doi.org/10.1186/s12916-022-02423-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health outcomes
- Severe mental illness
- Umbrella review
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Media Center
- Events & Webinars
- Healthy Minds TV
- Email Signup
- Get Involved
- Anxiety Disorders
- Attention-Deficit Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder (ASD)
- Bipolar Disorder
- Borderline Personality Disorder (BPD)
- Eating Disorders
- Mental Illness (General)
- Inaccessible
- Obsessive-Compulsive Disorder (OCD)
- Post-Traumatic Stress Disorder (PTSD)
- Schizophrenia
- Suicide Prevention
- Other Brain-Related Illnesses
- Basic Research
- New Technologies
- Early Intervention/ Diagnostic Tools
- Next Generation Therapies
- Donate Today
- Make a Memorial/Tribute Gift
- Create an Event/Memorial Page
- Find an Event/Memorial Page
- Make a Stock/Securities Gift/IRA Charitable Rollover Gift
- Donate Cryptocurrency
- Other Giving Opportunities
- Monthly Giving
- Planned Giving
- Research Partners
- Donor Advised Funds
- Workplace Giving
- Team Up for Research!
- Sponsorship Opportunities
Homelessness and Mental Illness: A Challenge to Our Society

What is the prevalence of mental illness among people experiencing homelessness in the U.S.?
According to a 2015 assessment by the U.S. Department of Housing and Urban Development, 564,708 people were homeless on a given night in the United States. At a minimum, 140,000 or 25 percent of these people were seriously mentally ill, and 250,000 or 45 percent had any mental illness. By comparison, a 2016 study found that 4.2 percent of U.S. adults have been diagnosed with a serious mental illness.
What are the most common types of mental illness among people experiencing homelessness?
Affective disorders such as depression and bipolar disorder, schizophrenia, anxiety disorders and substance abuse disorders are among the most common types of mental illness in the homeless population.
How are homelessness and mental illness connected?
Most researchers agree that the connection between homelessness and mental illness is a complicated, two-way relationship. An individual’s mental illness may lead to cognitive and behavioral problems that make it difficult to earn a stable income or to carry out daily activities in ways that encourage stable housing. Several studies have shown, however, that individuals with mental illnesses often find themselves homeless primarily as the result of poverty and a lack of low-income housing. The combination of mental illness and homelessness also can lead to other factors such as increased levels of alcohol and drug abuse and violent victimization that reinforce the connection between health and homelessness.
Can homelessness exacerbate an existing mental illness?
Studies do show that homelessness can be a traumatic event that influences a person’s symptoms of mental illness. Having ever been homeless and the time spent homeless can be related to higher levels of psychiatric distress, higher levels of alcohol use and lower levels of perceived recovery in people with previous mental illness.
How do homelessness and mental illness influence a person's interactions with police and the justice system?
In general, homelessness among people with mental illness can lead to more encounters with police and the courts. For instance, rates of contact with the criminal justice system and victimization among homeless adults with severe symptoms such as psychosis, are higher than among housed adults with severe mental illness. Homeless adults with mental illness who experienced abuse or neglect in childhood are more likely to be arrested for a crime or be the victim of crime.
How does homelessness affect mental illness within families?
One of the biggest impacts of homelessness on mental illness comes through its effect on the mothers of families. For instance, mothers who experience postpartum depression during the first year after birth are at higher risk for homelessness or factors leading to homelessness such as evictions or frequent moves in the two to three years after the postpartum year. One of the largest studies of children and homelessness (17,000 children in Denmark) found a higher incidence of psychiatric disorders, including substance abuse, among adolescents with a mother or both parents with a history of homelessness.
What kinds of interventions help people with mental illness experiencing homelessness?
Programs that provide long-term (a year or longer) stable housing for people with mental illnesses can help to improve mental health outcomes, including reducing the number of visits to inpatient psychiatric hospitals. A 2015 study concluded that services that deliver cognitive and social skill training, particularly in developing and maintaining relationships, would be useful in helping people with mental illnesses and homelessness regain housing.
— Written By Peter Tarr, Ph.D.
Click here to read the Brain & Behavior Magazine's September 2018 issue
1. U.S. Department of Housing and Urban Development, 2015 Annual Homelessness Assessment Report: Part 1: Point-in-Time Estimates of Homelessness in the U.S. https://www.hudexchange.info/resources/documents/2015-AHAR-Part-1.pdf . 2. Substance Abuse and Mental Health Services Administration, Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.htm . 3. S. Fazel et al. The prevalence of mental disorders among the homeless in western countries: Systematic review and meta-regression analysis. PLoS Medicine, Volume 5, Pages e225, December 2008. 4. National Coalition for the Homeless, “Mental Illness and Homelessness,” http://www.nationalhomeless.org/factsheets/Mental_Illness.pdf . 5. A. Mathieu. The medicalization of homelessness and the theater of repression. Medical Anthropology Quarterly, Volume 7, Pages 170-184, June 1993. 6. M Shinn and C Gillespie. The roles of housing and poverty in the origins of homelessness. American Behavioral Scientist, Volume 34, Pages 505-521, 1994. 7. AM Fox et al. Untangling the relationship between mental health and homelessness among a sample of arrestees. Crime and Delinquency, Volume 62, Pages 592-613, November 2013. 8. J Castellow et al. Previous homelessness as a risk factor for recovery from serious mental illnesses. Community Mental Health Journal, Volume 51, Pages 674-684, 2015. 9. L Roy et al. Criminal behavior and victimization among homeless individuals with severe mental illness: A systematic review. Psychiatric Services, Volume 65, Pages 739-750, June 2014. 10. H Edalati et al. Adverse childhood experiences and the risk of criminal justice involvement and victimization among homeless adults with mental illness. Psychiatric Services, Volume 68, Pages 1288-1295, September 2017. 11. M Curtis et al. Maternal depression as a risk factor for family homelessness. American Journal of Public Health, Volume 104, Pages 1664- 1670, September 2014. 12. SF Nilsson et al. Risk of psychosis in offspring of parents with a history of homelessness during childhood and adolescence: A nationwide, registerbased, cohort study. Schizophrenia Bulletin, Volume 44, Pages S111, April 2018. 13. N Kerman et al. The effects of housing stability on service use among homeless adults with mental illness in a randomized controlled trial of Housing First. BMC Health Services Research, Volume 18, Pages 190-197, 2018. 14. S Gabrielian et al. Factors affecting exits from homelessness among persons with serious mental illness and substance use disorders. The Journal of Clinical Psychiatry, Volume 76, Pages e469-e476, 2015.
TOP VIEWED POSTS
Reasons to Feel Empowered About Depression Prevention
Meet Our 2016 NARSAD Distinguished Investigators
Solving Treatment-Resistant Depression
The Disease of Addiction: What Goes Wrong When Drugs Enter the Brain
What Do We Know About Depression in Preschoolers?
Donations are welcome
100% of every dollar donated for research is invested in our research grants. Our operating expenses are covered by separate foundation grants.
The Brain & Behavior Research Foundation is a 501(c)(3) nonprofit organization, our Tax ID # is 31-1020010.

Exploring the Link Between Housing Stability and Mental Health
- Share this page on Facebook facebook
- Share this page on Twitter twitter
- Share this page on LinkedIn linkedin
- Health & Wellness
By Mia Chapman
Millions of people in the United States living with mental health challenges face barriers to finding and maintaining stable housing. Mental health encompasses emotional, psychological, and social well-being, and mental health illnesses are some of the most common health conditions across the country. There are myriad causes of mental health illnesses and challenges, however, there is evidence that the accessibility of stable and affordable housing can improve mental health. As much as the benefits of stable housing can help uplift mental health, the repercussions of a lack of stable and affordable housing can exacerbate mental health challenges. This is a trend identified among both renters and homeowners, with similar mental health repercussions reported on those experiencing mortgage strain .
Repercussions of Unstable Housing on Mental Health
A recent study reported that individuals with mental health challenges are at-risk of experiencing exacerbated mental health symptoms as a result of housing instability. With the growing housing affordability crisis, individuals and families experiencing high cost burdens are numerous. Those experiencing long-term housing affordability stress report significant negative effects on mental health related to social, emotional, and mental functioning.
The eviction process has also been found to have serious mental health repercussions on renters. In the two years following an eviction , people were more likely to visit the emergency room or require hospitalization for a mental health condition (compared to those who had not experienced an eviction). Eviction is more common among low-income tenants and disproportionately affects renters who are black, indigenous, and people of color (BIPOC).
Reducing cost burdens and long-term affordability stress can help alleviate less-severe mental health challenges. Those experiencing serious mental illnesses may find it significantly more difficult to access stable housing; the number of Fair Housing complaints related to mental illness and disability has in recent years. Furthermore, many people with serious mental illnesses rely on Social Security Insurance (SSI) and Social Security Disability Insurance (SSDI) payments , making many housing options unaffordable. Individuals experiencing chronic unsheltered homelessness also experience daily struggles and face emotional tolls of exposure to the elements, difficulty meeting basic needs, and a lack of economic opportunity.

While mental illness does not cause homelessness, the experience of homelessness exacerbates mental health conditions and symptoms of mental illness. Source: National Library of Medicine
Policies and Programs to Support Mental Health Through Housing
There is an array of federal policies and housing programs that aim to support mental health through the provision of housing or related funding and services. The American Rescue Plan Act (ARPA) of 2021 and the Emergency Rental Assistance (ERA) program have helped provide rental assistance to state and local program grantees to support those in need. State and local governments have used State and Local Fiscal Recovery Funds (SLFRF) provided through ARPA to distribute additional rent, mortgage, or utility assistance to more than 700,000 households and provided eviction prevention services to more than 100,000 households in 2021.
In 2021, the U.S. Department of Housing and Urban Development (HUD), in collaboration with the Department of Health and Human Services (DHHS), established the Housing and Services Resource Center . The center strives to provide federal resources to individuals seeking housing and social services support, including behavioral health, personal care, transportation, and community living options. As a response to the growing mental health crisis, HUD is also training housing counselors, housing-based services coordinators, and Fair Housing grantee staff in basic mental health skills.
The Substance Abuse and Mental Health Services Administration (SAMHSA) has funding available for homelessness services through the Projects for Assistance in Transition from Homelessness (PATH) program. Source: SAMSHA

The PATH program is intended to fund services for people with serious mental illnesses experiencing homelessness and is part of the first major federal legislative response to homelessness. PATH grants are distributed annually at the state level, where each state or territory solicits proposals and awards funds to local public or nonprofit organizations, which are known as PATH providers. The PATH program has reached over 100,000 individuals and enrolled nearly 60,000 PATH-eligible clients in a variety of services .
How Are Cities Supporting Mental Health Through Housing?
Cities are developing programs to provide mental health services alongside providing housing, in addition to leveraging federal policies and funding to provide services to the local community. Mental health services and policies can often be most impactful at the local community level, making city initiatives vital in the provision of mental health services.
- Boise, ID – The New Path Community Housing project was developed in collaboration with the City of Boise, Ada County, and the HUD Supportive Housing Program. New Path strives to address homelessness through the provision of permanent supportive housing and has been one of Boise’s biggest accomplishments in its efforts to address homelessness since 2009. New Path is a 40-unit apartment building for those who have experienced chronic homelessness and their partners. Most New Path residents have chronic or debilitating health conditions such as mental health challenges or brain disorders, long-term substance use disorders, or trauma. To adequately support residents, these residents receive daily or weekly support from onsite staff, such as case management, physical and mental health care, substance abuse counseling, life skills training, and peer support groups.
- Seattle, WA – Plymouth on First Hill is a permanent supportive housing development in Seattle that provides 77 units of housing to individuals experiencing chronic homelessness. The project was designed specifically for residents with physical and mental illnesses, even winning an award for housing accessibility. Many of the units are fully compliant with the Americans with Disabilities Act (ADA) standards, and the rest comply with universal design principles, making all units easily accessible for those living with mental health challenges, substance use disorders, and physical disabilities.
- Santa Monica, CA – The City of Santa Monica has partnered with the Los Angeles County Department of Mental Health to equip first responders with behavioral health teams to more appropriately provide mental health services to those experiencing homelessness. The pilot program provides a therapeutic transport team to assist first responders in Santa Monica and is part of the city’s holistic approach to addressing homelessness. By scaling solutions, such as immediate mental health support services, the city hopes to holistically address homelessness and work towards securing stable housing for all residents.
About the Authors
You may also like:.

Healthy Housing Innovation Cohort Info Session

Advancing Inclusive Mental Health Policies in the Workplace & Addressing the Behavioral Health Workforce Shortage

- Community & Economic Development
Using National Opioid Settlement Funds: Local Strategies and Solutions

- Legal Advocacy
Recent Litigation Activity That Local Governments Should Know About
- McKaia Dykema
- Carolyn Berndt
- Stephanie Martinez-Ruckman
What We’ve Learned from Two Years of the 988 Suicide & Crisis Lifeline

Launching NLC’s National Opioid Settlement Dashboard: Focusing on Solutions

- Sarah Minster

Mental health and homelessness: get to know the facts
Although we don't have a vaccine for mental health or substance use disorders, we do have practical and effective solutions. They are the effective and evidence-based practices we know work — access to treatment, harm reduction services, mental health support, peer support groups, and perhaps most importantly, educating our community to reduce stigma and promote compassion. Andrew Bove, Preble Street Vice President of Social Work
Access to healthcare, especially mental health care and substance use treatment, is difficult for many people in our community, especially people who are unhoused. Living in high-stress situations on the streets or in crowded shelters with limited access to treatment makes people experiencing homelessness particularly vulnerable to chronic mental health issues and co-occurring substance use disorders.
Across all of our programs, Preble Street serves some of the most vulnerable Mainers, people with complex mental and behavioral health needs. People who have experienced chronic homelessness and who have a mental health and/or substance abuse disorder require trauma-informed care and treatment as they work towards their goals. But, this treatment is often difficult to access because of the many barriers to access and an overall dysfunctional mental healthcare system.
M ental health and homelessness are inter connected , and t his May, during Mental Health Awareness Month, take a few minutes to learn more about the relationship between mental health and homelessness and what Maine can do to impact the mental health care crisis it is experiencing.
While people experiencing homelessness report higher rates of serious mental illness (e.g. schizophrenia, bipolar disorder, etc.) than the general public, the number of people who report a serious mental illness is still part of the overall number of people experiencing homelessness.
Full 2023 Maine PIT count.
People lose housing for many reasons – economic reasons, death of a family member, domestic violence, end of relationship, etc. – and research shows that increases in homelessness are not strongly connected with the number of individuals who have mental illnesses or substance abuse disorders. In fact, mental or behavioral health disorders and substance abuse are many times outcomes of experiencing homelessness. The stress and trauma of homelessness makes it a known risk factor for creating the conditions for mental illness and substance abuse disorders (3), and people who experience chronic homelessness have a far higher risk of mental illness, disability, or a substance abuse disorder.
On a single night in the U.S. in January 2023...
Click here for the full 2023 US PIT count.
*Chronic homelessness describes someone who has experienced homelessness for at least a year — or repeatedly — while struggling with a disabling condition, like a serious mental illness, substance use disorder, or physical disability.
The best predictor we have for homelessness is a lack of affordable housing in an area (4). High rent prices and low vacancy rates are shown to increase homelessness, while mental illness and substance abuse do not have a demonstrated connection to increases in homelessness rates (5). Survey data from the last 10 years also supports this. When asked, people say economic reasons are the cause for losing their housing – job loss, eviction, rent increase, money challenges, etc. – not mental illness (6-7).
What are the solutions?
For there to be any real “solution” to homelessness, we must focus on prevention and fixing the broken systems of care that exist in our society. Social and economic factors, like adverse childhood experiences, lacking mental health services, racial inequities, economic inequality, the rise of housing costs, etc., all contribute to rising rates of homelessness, especially among people with mental illness, and must be addressed with joint policy and advocacy efforts.
Maine’s critically important low-barrier shelters recently received three years of $2.5M in annual funding — a total of $7.5M — in the 2024 supplemental budget signed by Governor Janet Mills. These shelters fill a critical gap in meeting the needs of people with complex medical needs, histories of trauma, and untreated substance use and mental health disorders.
There is no one-size-fits-all housing solution for people experiencing homelessness, but Site-based Housing First, which prioritizes access to permanent, long-term housing, has proven effective for people with complex needs who have experienced chronic homelessness. Preble Street’s three Site-based Housing-First programs, Logan Place , Florence House , and Huston Commons all demonstrate the effectiveness of this model in stably housing people with complex needs.
When people are provided a safe, healing environment, support from a compassionate and professional social worker, and low-barrier access to mental health treatment hope and opportunity arise. To save more lives, Maine — and the rest of the U.S. — must continue to invest in a trauma-informed, dignified shelter system and Site-based Housing First alongside large-scale changes in how we care for people suffering from mental illness.
1. U.S. Department of Housing and Urban Development (2023). Part 1 – Point in Time Estimates of Homelessness. Abt Associates.
2. MaineHousing (2023). 2023 Point in Time Count. Maine State Housing Authority.
3. Goodman, Lisa A, Leonard Saxe, and Mary Harvey (1991). Homelessness as psychological trauma. American Psychologist , 46(11): 1219–1225. Corcoran, C., Walker, E., Huot, R., Mittal, V., Tessner, K., Kestler, L., & Malaspina, D. (2003). The stress cascade and schizophrenia: Etiology and onset. Schizophrenia Bulletin , 29(4): 671–692. Castellow, Jennifer, Bret Kloos, and Greg Townley (2015). Previous homelessness as a risk factor for recovery from serious mental illnesses. Community Mental Health Journal , 51: 674-684.
4. Shinn, Marybeth, Jim Baumohl, and Kim Hopper (2001). The prevention of homelessness revisited. Analyses of Social Issues and Public Policy , 1.1: 95-127. Shinn, Marybeth (2009). Ending Homelessness for Families: The Evidence for Affordable Housing. Washington, DC: National Alliance to End Homelessness and Enterprise Community Partners. Colburn, G., & Aldern, C. P. Homelessness is a housing problem: How structural factors explain US patterns. Univ of California Press, 2022. National Coalition for the Homeless (June 2007). Why Are People Homeless ? National Coalition for the Homeless.
5. All Home & Applied Survey Research (2019). Count Us In: Seattle/King County Point-In-Time Count of Persons Experiencing Homelessness.
6. Snow, David A. and Rachel E. Goldberg (June 2017). Homelessness In Orange County: The Costs to Our Community.
7. Applied Survey Research (2022). 2022 Alameda County Homeless Count And Survey Comprehensive Report.

Landlords are a part of the solution
To address homelessness and housing insecurity in Maine, the help and support of landlords is critical. Preble Street works closely with landlords to identify and maintain stable housing for clients. Their partnership is crucial to successfully housing people, who are transitioning from shelter or the street. Veteran’s Housing Services (VHS), in particular, frequently works alongside landlords

Although we don’t have a vaccine for mental health or substance use disorders, we do have practical and effective solutions. They are the effective and evidence-based practices we know work — access to treatment, harm reduction services, mental health support, peer support groups, and perhaps most importantly, educating our community to reduce stigma and promote

Understanding low barrier shelters
What does a low-barrier shelter look like? At a time when unsheltered homelessness is increasing exponentially in our community and the shortage of low-barrier shelter beds has created a state-wide homelessness crisis, Elena’s Way and Florence House are a model for how we can take care of the most vulnerable people in our community. The

Celebrating advocacy wins
Low-barrier shelters receive funding for the next three years… On April 22, 2024, Governor Janet Mills signed the supplemental budget into law, which includes three years of $2.5M in annual funding — a total of $7.5M — to directly support emergency low-barrier shelters. This funding will be incredibly impactful for Maine’s five privately operated, low-barrier

19 years of Site-based Housing First at Logan Place
“For me, eventually, is a key word. It’s my first apartment in 14 years,” shares Kabir. Kabir is the newest resident of Logan Place, Maine’s first Site-based Housing First building, which opened 19 years ago this month. Logan Place has 30 efficiency apartments, with 24-hour on-site support for adults who have experienced chronic homelessness. Kabir
The Importance of Low-Barrier Shelters in Our Community
What does a low-barrier shelter look like? At a time when unsheltered homelessness is increasing exponentially in our community and the shortage of low-barrier shelter beds has created a state-wide crisis, Elena’s Way and Florence House are a model for how we can take care of the most vulnerable people in our community. The staff
SIGN UP FOR E-NEWS & ADVOCACY ALERTS
The mission of Preble Street is to provide accessible barrier-free services to empower people experiencing problems with homelessness, housing, hunger, and poverty, and to advocate for solutions to these problems.
You Can Help

Copyright © 2020 • Preble Street • All Rights Reserved • View Privacy Policy
More older Californians are falling into homelessness. A new study examines why

- Show more sharing options
- Copy Link URL Copied!
Good morning. It’s Tuesday, May 28 . Here’s what you need to know to start your day.
A new study examines homelessness among older Californians
- A tree-killing beetle is decimating Southern California’s oaks
- 24 superb things to do around L.A. to kick off the summer of 2024
- And here’s today’s e-newspaper
You're reading the Essential California newsletter
Our reporters guide you through our biggest news, features and recommendations every morning
You may occasionally receive promotional content from the Los Angeles Times.
If you’ve been following the news in recent decades, it’s no surprise that the Golden State is the U.S. capital for homelessness . And among the Californians experiencing homelessness, the group rising the fastest by proportion is older adults — defined as anyone 50 and older.
A major study on homelessness in California, released last year by UC San Francisco’s Benioff Homelessness and Housing Initiative (BHHI), includes two notable findings: 48% of all unhoused single adults in the state are 50 or older and 41% of unhoused older adults became homeless for the first time after age 50.
Now a follow-up study from BHHI researchers dives further into that alarming trend, which they note is expected to continue as “the proportion of people age 65 and older experiencing homelessness in the United States [is] expected to triple between 2017 and 2030.”
The new report, titled “ Toward Dignity: Understanding Older Adult Homelessness ,” explores how older adults lost housing, what their lives have been like since, and the barriers they face to get back into housing. The authors also include policy recommendations to address the crisis.
“We are failing our older adults by allowing them to spend their last years on our streets and in our shelters,” Margot Kushel, director of BHHI and the study’s lead author, said in a news release. “The dramatic rise in homelessness among older adults has severe consequences for the health and safety of those who experience it, and for our society at large. Now is the time for investments in real solutions to prevent and end homelessness among this vulnerable population.”
The study builds off what BHHI called the largest representative study of homelessness in decades, which traced the “causes and consequences” of homelessness in the state and challenged myths about unhoused people. Researchers surveyed nearly 3,200 people experiencing homelessness across eight California counties in the state and conducted in-depth interviews with 365 of those participants.
One common misconception you might have heard: Unhoused people are moving to California in droves.
According to the study, 91% of older homeless adults in the state lost their last stable housing in California, and more than 75% were last housed in the same county where they were currently experiencing homelessness.
“Older homeless adults’ lives have been marked by deep poverty and trauma,” the authors wrote. More than two-thirds of those surveyed reported experiencing physical violence and 19% reported experiencing sexual violence — many before age 18.
“People who experience homelessness have higher rates of mental health conditions and substance use than the general population,” the authors wrote, adding that many of those struggles existed before those individuals lost housing.
More than 80% of unhoused older adults said they’d experienced at least one significant mental health symptom at some point in their lifetime. The most common symptoms were related to anxiety and depression.
Researchers included a quote from one unhoused 57-year-old woman, who shared:
“I’ve felt like walking in front of the train every day for the last three years since I lost my house… It’s the first time I’ve ever contemplated suicide ever in my life. I’m always upbeat and I’m such a positive person until I got out here…Everything is so hard, just my age and just physically… I hurt all the time and I’m in pain and everything is just a struggle, just to do laundry, just to, you know, food. The younger crowd seems to do better, but I’m older and it’s hard. It’s just hard…”
Here are a few more key findings from the report:
- According to the report: “Being single is a risk factor for homelessness.” Of the older adults surveyed, 52% were single and never married; 17% reported being married or partnered. More than a quarter were divorced or separated, and 4% were widowed.
- “More than 80% of older adults entered homelessness from housing: 46% from non-leaseholding arrangements and 35% from leaseholding arrangements. The other 19% entered homelessness from institutions, which included time in jail, prison or healthcare settings.
- Poor health is a common reality among older adults experiencing homelessness. More than two-thirds reported having at least one significant chronic health condition. About a quarter of those surveyed said they’d experienced a time when they couldn’t get healthcare or obtain medication they needed.
- While people of color are overrepresented overall within the state’s unhoused population, older Black adults are particularly overrepresented. The report notes that 31% of older adults experiencing homelessness identified as Black, compared with 6% of all Californians age 50 or older. Older adults who identified as Native American or Indigenous and multiracial were also overrepresented, the survey found.
- The majority of older adults surveyed expressed optimism that “well-timed financial support would have staved off homelessness,” the authors wrote. Many believed that a modest monthly subsidy ($300 to $500), a one-time payment ($5,000 to $10,000) or something akin to a housing voucher would have allowed them to stay in their homes.
The study’s authors recommended policies meant to “reduce and end homelessness among older adults.” Those include increasing the state’s dismal stock of affordable housing and removing barriers that older adults have in navigating complex programs and processes.
The authors also called on policymakers to strengthen eviction protections and do more to prevent older adults who exit jails and prisons from ending up on the streets, noting that many in that population are entering homelessness “directly from institutional settings.”
Other recommendations included increasing incomes for older adults in extreme poverty, expanding outreach to older adults experiencing homelessness and prioritizing racial equity within the systems that respond to homelessness.
As we covered in this newsletter last month, those systems are struggling, and lasting solutions are difficult to achieve . And even though the state has poured billions of dollars into programs meant to reverse our nation-leading homelessness, we have little to show for it — and don’t really know how well all that money is being spent .
Today’s top stories
COVID in California
- COVID is rising in California . Here’s how to protect yourself from FLiRT subvariants.
- Early signs of rising COVID in California as new FLiRT subvariants dominate.
Remembering Bill Walton
- Bill Walton, UCLA legend, NBA star and Pac-12 advocate, dies at age 71 .
- Appreciation: Bill Walton’s kindness and wonderful wackiness made us the grateful ones.
- ‘General Hospital’ actor Johnny Wactor’s slaying during L.A. theft sparks shock, anger, mourning.
- A 14-year-old girl out walking on the holiday weekend in Newport Beach is fatally struck by a car .
More big stories
- UCLA and UC Davis brace for strike as union alleges free speech violations in pro-Palestinian protests.
- Hollywood crews in ‘crisis’ : ‘Everyone’s just in panic mode’ as jobs decline.
- A tree-killing beetle is on a death march through Southern California’s oaks. Can it be stopped?
- Ocean technology hub AltaSea blooms on the San Pedro waterfront .
- Mike Tyson is ‘doing great’ after a medical emergency on a flight to L.A.
Get unlimited access to the Los Angeles Times. Subscribe here .
Commentary and opinions
- Doyle McManus: Trump fans say he speaks his mind. But on some subjects, he’s as slippery as an eel .
- George Skelton: Unaffordable homeowner’s insurance is leaving Californians exposed to the elements.
- Anita Chabria: What I got wrong in the ‘bad built’ blowup .
- Editorial: Metro’s ‘surge’ of police isn’t the long-term solution L.A. needs for safer buses and trains.
- LZ Granderson: LeBron James is the aging icon we all need .
- Jenn Harris: At my favorite new restaurant, the room is red and the chef is a doctor .
- Jonah Goldberg: What’s convincing voters that the economy is worse than it ever was?
- Mark Z. Barabak: Will abortion rights boost Biden and fellow Democrats? Arizona offers a test case.
Today’s great reads
City National is Hollywood’s ‘Bank to the Stars.’ Now a lawsuit says it aided a Ponzi scheme . City National Bank has been sued for nearly $800 million for allegedly bankrolling a Hollywood Ponzi scheme, the latest in a series of controversies involving one of L.A.’s best-known banks.
Other great reads
- How the small screen breathes new life into classic film noir .
- Artists priced out of Los Angeles head to this creative hub in the high desert .
How can we make this newsletter more useful? Send comments to [email protected] .
For your downtime
- 🏖️ 24 superb things to do around L.A. to kick off the summer of 2024.
- 🥾For your L.A. bucket list: An epic city hike that has it all .
- ⛰️ The 101 best West Coast experiences .
- 📺 Ricky Martin is livin’ the good life back in front of the camera in ‘Palm Royale’ on Apple TV+.
- 🍪 Here are 9 of our favorite cookie recipes for baking right now .
- ✏️ Get our free daily crossword puzzle, sudoku, word search and arcade games .
And finally ... a great photo
Show us your favorite place in California! We’re running low on submissions. Send us photos that scream California and we may feature them in an edition of Essential California.

Today’s great photo is from Times photographer Genaro Molina at Dillon Beach, one of the few communities that will be allowed to grow its short-term rental market under a new Marin County ordinance.
Have a great day, from the Essential California team
Ryan Fonseca, reporter Kevinisha Walker, multiplatform editor and Saturday reporter
Check our top stories , topics and the latest articles on latimes.com .
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.

Ryan Fonseca writes the Los Angeles Times’ Essential California newsletter. A lifelong SoCal native, he has worked in a diverse mix of newsrooms across L.A. County, including radio, documentary, print and television outlets. Most recently, he was an associate editor for LAist.com and KPCC-FM (89.3) public radio, covering transportation and mobility. He returns to The Times after previously working as an assistant web editor for Times Community News, where he helped manage the websites and social media presence of the Burbank Leader, Glendale News-Press and La Cañada Valley Sun. Fonseca studied journalism at Cal State Northridge, where he now teaches the next generation of journalists to develop their voice and digital skills.
More From the Los Angeles Times
Was my favorite teacher gay? Maybe a belly dancer could find out

Climate & Environment
As Los Angeles plans to take less water, environmentalists celebrate a win for Mono Lake

For some incarcerated women, getting ahold of menstrual products is a nightmare

Extreme heat forecast for Western U.S. may kick off sweltering summer. Here’s the outlook
Night Owls Could Be Upping Their Mental Health Risks

FRIDAY, May 31, 2024 (HealthDay News) -- People who regularly stay up until the wee hours of the morning could be harming their mental health, a new study finds.
Regardless of whether people were morning larks or a night owls, they tended to have higher rates of mental and behavioral disorders if they stayed up late, researchers found.
The mental health risk associated with staying up late cropped up regardless of a person’s preferred sleep timing, also known as their chronotype.
“We found that alignment with your chronotype is not crucial here, and that really it’s being up late that is not good for your mental health,” said senior researcher Jamie Zeitzer , a professor of psychiatry and behavioral sciences at Stanford Medicine, in California. “The big unknown is why.”
U.S. Cities With the Most Homelessness

These findings run counter to previous studies which found that people who stick to their chronotype tend to be healthier, Zeitzer added.
For the study, researchers tracked nearly 74,000 middle-aged and older people in the United Kingdom.
More than 19,000 said they were morning types, while about 6,800 identified as evening types. The rest fell somewhere in the middle.
The participants were asked to wear an activity monitor to track their sleep over seven days. Their preferred sleep timing was then compared to both their actual sleep and their mental health, which was determined through their health records.
Analysis showed that night owls who stayed up late, in alignment with their preferred sleep timing, had higher rates of mental health disorders like depression and anxiety.
Night owls being true to their nature were 20% to 40% more likely to be diagnosed with a mental health problem, compared to evening types who nonetheless slept like a morning person or an average person.
“The worst-case scenario is definitely the late-night people staying up late,” Zeitzer said.
Morning larks who rose with the sun tended to have the best mental health of all, researchers found. But if they had to stay up late, their mental health suffered as well, although not as much as night owls’.
Zeitzer suspects these differences come down to the poor decisions people make in the early hours of the morning.
Suicide, violent crime, drinking, substance use and overeating are all more common at night, Zeitzer noted.
One theory called the “mind after midnight” hypothesis holds that body and brain changes late at night can make people more impulsive, negative and apt to take risks, the researchers said.
That might explain why morning people have an advantage even if they stay up late, Zeitzer said.
“If I had to hazard a guess, morning people who are up late are quite cognizant of the fact that their brain isn’t working quite right, so they may put off making bad decisions,” Zeitzer said in a Stanford news release. “Meanwhile, the evening person who is up late thinks, ‘I’m feeling great. This is a great decision I’m making at 3 o’clock in the morning.’”
The increased risk also might vary depending on where you are in the world.
For example, the United States and the United Kingdom tend to close down at night, with few people up and active.
On the other hand, nights are more gregarious in Mediterranean cultures, and it might be okay or even good for mental health to stay up late in those locales, researchers said.
“Maybe there are fewer social constraints late at night because you have fewer people around who are awake,” Zeitzer said.
The new study was published recently in the journal Psychiatry Research .
Zeitzer advises night owls to get to sleep before 1 a.m., but he admits that is easier said than done. Sleep patterns are stubbornly persistent.
His team plans to examine whether changing particular late-night behaviors, rather than sleep timing, could improve mental health.
“If you like being up late and just do what people normally do at 10 p.m., but you do it at 2 or 3 a.m. -- maybe that’s not a problem,” he said.
More information
The Sleep Foundation has more about chronotypes .
SOURCE: Stanford Medicine, news release, May 19, 2024
Copyright © 2024 HealthDay . All rights reserved.
Join the Conversation
Tags: psychology , depression
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

NYC’s Verdict on Trump: Not One of Us
Lincoln Mitchell June 1, 2024

Will Trump’s Guilty Verdict Help Biden?
Susan Milligan May 31, 2024

Texas Court Punts Abortion Ban Challenge
Aneeta Mathur-Ashton May 31, 2024

Key Reactions to Trump’s Guilty Verdict
Lauren Camera and Laura Mannweiler May 31, 2024

5 Key Questions About Trump Verdict
Cecelia Smith-Schoenwalder May 31, 2024

His Own Worst Enemy?
Lauren Camera May 31, 2024


IMAGES
COMMENTS
Abstract. Research on the bi-directional relationship between mental health and homelessness is reviewed and extended to consider a broader global perspective, highlighting structural factors that contribute to housing instability and its mental ill health sequelae. Local, national and international initiatives to address housing and mental ...
Furthermore, mental illness among homeless individuals has been associated with elevated rates of criminal behavior and victimization [15,16], prolonged courses of homelessness [17,18], and perceived discrimination . Mental disorders among homeless individuals are mostly treatable and represent an important opportunity to address health ...
People experiencing homelessness have elevated rates of mental health conditions and substance use disorders. 20 The California study cited above found that 82 percent of homeless adults in ...
Homelessness is a major public health problem that has received considerable attention from clinicians, researchers, administrators, and policymakers in recent years. In 2016, 550,000 individuals were homeless in the United States (U.S. Department of Housing and Urban Development, 2016) with 4.2% of individuals in the United States experiencing homelessness for over 1 month sometime in their ...
An estimated 20 to 25 percent of the U.S. homeless population suffers from severe mental illness, compared to 6 percent of the general public. The combination of mental illness, substance abuse ...
Earlier research has also found mental illness to be a non-significant predictor of mortality among people experiencing homelessness, with one study from 1999 reporting that men with mental ...
Homelessness creates a significant social and economic burden in the society. Homelessness and mental illness are two interconnected social issues that poses challenges to individuals and communities across the globe. This systematic review aims to synthesize the existing literature on interventions for the homeless persons with mental illness.
As mental health providers, we have an opportunity and responsibility to understand the relationship between homelessness and mental illness, address risk factors for homelessness, and provide evidence-based interventions for our patients experiencing homelessness and mental illness. ... Sustaining Housing First After a Successful Research ...
Of more than 580 000 individuals in the US who experience homelessness on a single night, estimates suggest that more than half have a mental illness or substance use disorder and at least 1 in 5 have severe mental illness. 1-3 Limited mental health care for this population forces individuals into emergency departments, where they are ...
Homelessness itself is a highly risky condition contributing to mental illness, and its association with poverty and poor resources available for living in adequate housing adds to the problem (Geoffrey et al., 2010).It is inevitable that those who are living on the streets or in housing shelters and are also additionally vulnerable due to their mental illness will become victims of violence ...
Unsheltered homelessness is rising, particularly in the Western U.S. •. We reviewed studies that compared health outcomes by shelter status. •. Unsheltered populations have higher rates of physical and mental illness and substance use. •. Unsheltered populations use health care less and often lack health insurance. •.
Homelessness is a traumatic event for individuals and families who experience it. It can lead to disruption in relationships, health, work, and education. According to the U.S. Department of Housing and Urban Development's (HUD's) Annual Point in Time Count, nearly 570,000 people had no place to sleep on January 23, 2020 .
Further research and advocacy are needed to address the obstacles that homeless individuals encounter in accessing mental health care. Disclosures: Dr Balasuriya is a Medical Resident and Dr Buelt is an Instructor, Department of Psychiatry, Yale University School of Medicine, New Haven, CT; Dr Tsai is Campus Dean and Professor, School of Public ...
Abstract. Research on the bi-directional relationship between mental health and homelessness is reviewed and extended to consider a broader global perspective, highlighting structural factors that contribute to housing instability and its mental ill health sequelae. Local, national and international initiatives to address housing and mental ...
Homelessness has been associated with multiple detrimental health outcomes across observational studies. However, relatively few randomized controlled trials (RCTs) have been conducted on people who experience homelessness (PEH). Thus, this umbrella review ranked the credibility of evidence derived from systematic reviews (SRs) and meta-analyses (MAs) of observational studies investigating the ...
The co-occurring problems of homelessness and mental illness is addressed through Participatory Action Research. A group of five people who have experienced homelessness and mental illness collaborated with the principal researcher through interviews and a working group in order to generate responses to the challenges they encounter.
According to a 2015 assessment by the U.S. Department of Housing and Urban Development, 564,708 people were homeless on a given night in the United States. At a minimum, 140,000 or 25 percent of these people were seriously mentally ill, and 250,000 or 45 percent had any mental illness.
The PATH program is intended to fund services for people with serious mental illnesses experiencing homelessness and is part of the first major federal legislative response to homelessness. PATH grants are distributed annually at the state level, where each state or territory solicits proposals and awards funds to local public or nonprofit ...
ma, mental health and substance use problems, and involvement with the criminal legal system. Those who were first homeless in late life were less likely to have experienced mental health problems, substance use problems, and incarceration than those with early life homelessness who remained homeless in late life. FIGURE 7 Older Adult Regular ...
There are many misconceptions about the relationship between homelessness and mental illness. People can lose housing for many reasons - economic reasons, death of a family member, domestic violence, end of relationship, etc. - and research shows that increases in homelessness are not strongly connected with the number of individuals who have mental illnesses or substance abuse disorders.
Julie Nordgaard a Mental Health Center Amager, Copenhagen University Hospital - Mental ... knowledge of these issues remains scarce. The purpose of this study was to explore substance use in homeless patients with mental disorders and their subjective perspectives on their substance use. ... Due to the nature of the research, due to ethical ...
A new study examines homelessness among older Californians. If you've been following the news in recent decades, it's no surprise that the Golden State is the U.S. capital for homelessness.And ...
Night owls being true to their nature were 20% to 40% more likely to be diagnosed with a mental health problem, compared to evening types who nonetheless slept like a morning person or an average ...
Projects for Assistance in Transition from Homelessness (PATH) Military Cultural Competence Training Behavioral Health Services for LGBTQI Community Support Program ... Shapiro Administration Highlights Mental Health and Substance Use Disorder Resources for Older Pennsylvanians, Governor's Proposed Investments in Behavioral Health Funding.