Hand Hygiene and Handwashing

Learn about hand hygiene and handwashing and its importance in providing nursing care.

Table of Contents
Types of hand hygiene, indicators of hand hygiene, supplies needed, antiseptic handrub, antiseptic handwash.
- Surgical Antisepsis
Practice Quiz: Hand Hygiene and Handwashing
Handwashing is the act of cleaning one’s hands with the use of any liquid with or without soap for the purpose of removing dirt or microorganisms. It is the most effective measure in reducing the risk of transmitting infectious diseases.
It cannot be said too often that hand washing is the most important and most basic technique in preventing and controlling infections. It is the single most effective infection control measure.
Handwashing is under the umbrella of hand hygiene . Hand hygiene is defined by the World Health Organization as a general term that applies to handwashing, antiseptic handwash, antiseptic hand rub or surgical hand antisepsis.
To understand this study guide better, familiarize yourself with the terms used:
- Hand Hygiene. It is a general term that applies to handwashing, antiseptic handwash, antiseptic hand rub, or surgical hand antisepsis
- Hand Washing. It is defined as the washing of hands with plain (i.e., non-antimicrobial) soap and water.
- Antiseptic Handwash. A term that applies to handwashing with an antimicrobial soap and water.
- Surgical Hand Antisepsis. Commonly called as a surgical hand scrub. This is to remove as many microorganisms from the hands as possible before the sterile procedure.
Principles and concepts surrounding hand hygiene:
- You must use running water in a sink that drains out instead of using a basin.
- You may use soap – antibacterial soap if necessary.
- You must rub your hands against each other for at least 30 seconds to facilitate removal of microorganisms.
- Long nails and jewelry trap germs. It is best to keep fingernails short. If you wear a ring, it is better not to remove the ring before hand washing so that it can be washed too.
- It is always better to use disposable paper towels than to use cloth towel when drying hands to ensure that you can only use those once.
- The faucet is always considered dirty and it is recommended to turn it off using a paper towel in the absence of the ideal sensor or foot pedal.
- Dispensers of soap should be used until completely empty. Once emptied, it should be washed before refilled.
The purposes of hand hygiene are:
- Hand washing can prevent infection
- Avoid pathogenic microorganisms and to avoid transmitting them
The following are the types of hand hygiene:
- Routine handwash. Use of water and non-antimicrobial soap for the purpose of removing soil and transient microorganisms.
- Antiseptic handwash. Use of water and antimicrobial soap (e.g., chlorhexidine, iodine and iodophors, chloroxylenol [PCMX], triclosan) for the purpose of removing or destroying transient microorganisms and reduce resident flora.
- Antiseptic handrub. Use of alcohol-based handrub.
- Surgical antisepsis. Use of water and antimicrobial soap (e.g., chlorhexidine, iodine and iodophors, chloroxylenol [PCMX], triclosan) for the purpose of removing or destroying transient microorganisms and reduce resident flora. Recommended duration is 2-6 minutes.
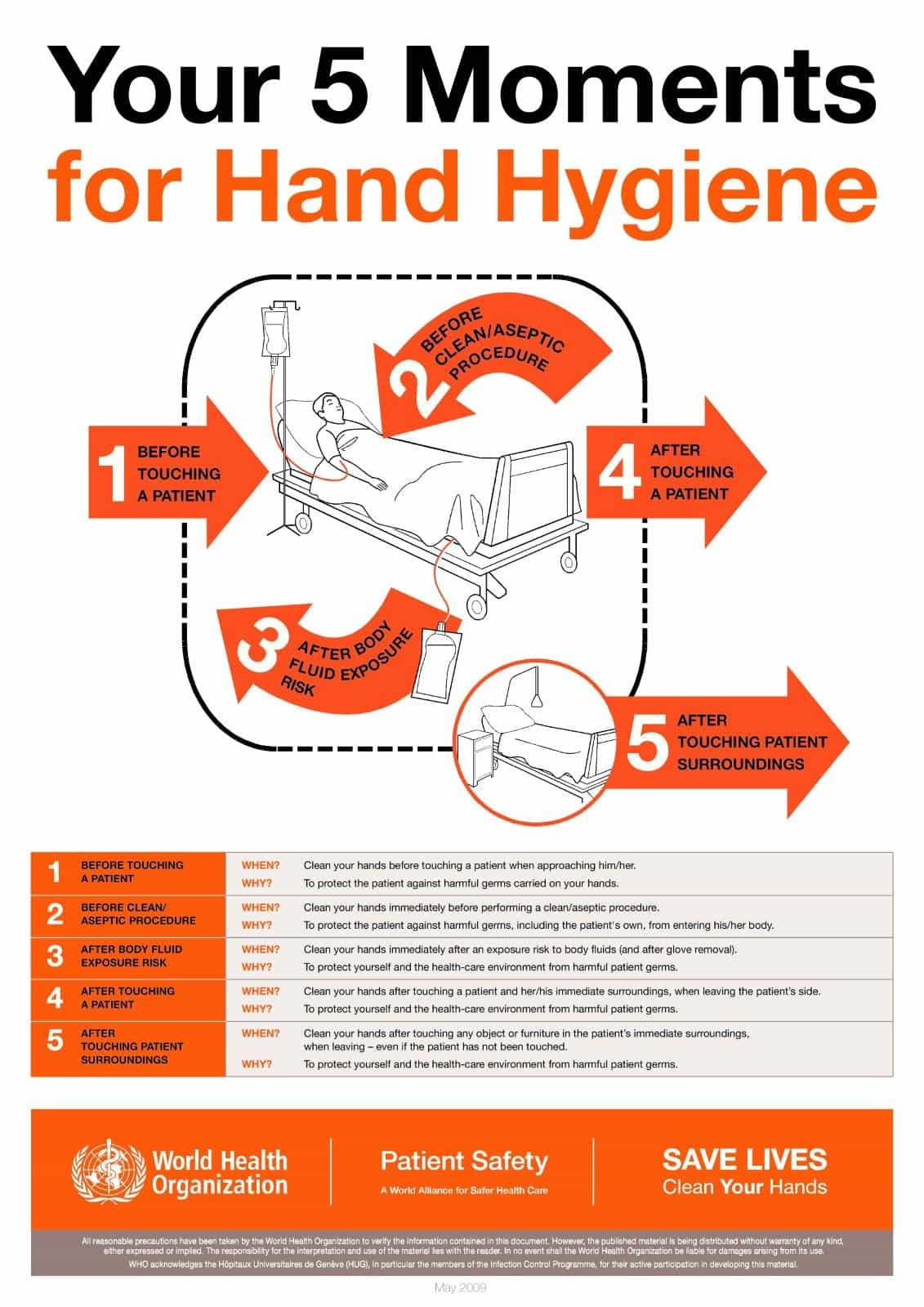
According to the World Health Organization (WHO), there are Five Moments for Hand Hygiene:
- Before Patient Contact.
- Before and Antiseptic Task.
- After Body Fluid Exposure Risk.
- After Patient Contact.
- After Contact with Patient Surroundings.
The following materials or equipment are needed to perform hand washing:
- Soap or detergent
- Warm running water
- Paper towels
- Optional: Antiseptic cleaner, fingernail brush, plastic cuticle stick
Below are the step-by-step guide for different hand hygiene methods:
The use of alcohol-based handrub.
1. Ensure jewellery has been removed
2. Apply quantity of alcohol-based hand hygiene product as per manufacturer’s recommendations into cupped hand.
3. Rub hands palm to palm
4. Right palm over left dorsum with interlaced fingers and vice versa.
5. Palm to palm with fingers interlaced
6. Backs of fingers to opposing palms with fingers interlaced
7. Rotational rubbing of left thumb clasped in right palm and vice versa
8. Rotational rubbing, backwards and forwards with clasped fingers of right hand in left palm and vice versa
9. Rubbing hands together until hands are dry before continuing with patient care, do not rub off excess product
Also known as clean technique, includes procedures used to reduce the number of organisms on hands.
1. Gather the necessary supplies. Stand in front of the sink.
2. Wet the hands and wrist area. Keep hands lower than elbows to allow water to flow towards the fingertips.
3. Cover all areas of hands with soap.
4. With firm rubbing and circular motions, wash the palms and backs of the hands, each finger, the knuckles, wrists, and forearms. Continue this friction motion for 30 seconds.
5. Rinse thoroughly with water flowing towards the fingertips.
6. Pat hands dry, beginning with the fingers and moving upward towards forearms, with a paper towel and discard immediately.
7. In the absence of sensors or foot pedal, use another clean paper towel to turn off the faucet.
Surgical Antisepsis
Also known as sterile technique, prevents contamination of an open wound, serves to isolate the operative area from the unsterile environment, and maintains a sterile field for surgery .
1. Remove all pieces of jewelry.
2. Wet hands using sterile water with water closest to your body temperature.
3. Wash hands using antimicrobial soap and/or povidone-iodine.
4. Clean subungual areas with a nail file.
5. Scrub each side of each finger, between the fingers, and the backs and fronts of the hands for at least 4 minutes.
6. Proceed to scrub the hands, keeping the hand higher than the arm at all times to prevent bacteria-laden soap and water from contaminating the hands.
7. Rinse hands and arms by passing them through the flowing water in one direction only, from fingertips to elbow.
8. Proceed to the operating room holding hands above elbows.
9. Dry hands and arms using sterile towel observing aseptic technique.
1. What is the act of cleaning one’s hands with the use of any liquid with or without soap for the purpose of removing dirt or microorganisms?
A. Aseptic Technique B. Handwashing C. Medical Asepsis D. Surgical Asepsis
2. What is known as clean technique which includes procedures used to reduce the number of organisms on hands?
3. What is known as sterile technique, prevents contamination of an open wound, serves to isolate the operative area from the unsterile environment, and maintains a sterile field for surgery?
4. What are we trying to reduce or eliminate when we are doing handwashing?
A. Viruses B. Bacteria C. Fungi D. All of the above
5. The clinical instructor asks her students the rationale for handwashing. The students are correct if they answered that handwashing is expected to remove:
A. transient flora from the skin. B. resident flora from the skin. C. all microorganisms from the skin. D. media for bacterial growth.
Answers and Rationale
1. Answer: B. Handwashing
2. Answer: C. Medical Asepsis.
Medical asepsis or clean technique includes procedures used to reduce the number of organisms on hands.
3. Answer: D. Surgical Asepsis
Sterile Technique prevents contamination of an open wound, serves to isolate the operative area from the unsterile environment, and maintains a sterile field for surgery.
4. Answer: D. All of the above.
In handwashing, we are trying to reduce or eliminate microorganisms and these include viruses, bacteria, and fungi.
5. Answer: A. transient flora from the skin.
There are two types of normal flora: transient and resident. Transient flora are normal flora that a person picks up by coming in contact with objects or another person (e.g., when you touch a soiled dressing ). You can remove these with hand washing. Resident flora live deep in skin layers where they live and multiply harmlessly. They are permanent inhabitants of the skin and cannot usually be removed with routine hand washing. Removing all microorganisms from the skin (sterilization) is not possible without damaging the skin tissues. To live and thrive in humans, microbes must be able to use the body’s precise balance of food, moisture, nutrients, electrolytes , pH, temperature, and light. Food, water, and soil that provide these conditions may serve as nonliving reservoirs. Hand washing does little to make the skin uninhabitable for microorganisms, except perhaps briefly when an antiseptic agent is used for cleansing.
2 thoughts on “Hand Hygiene and Handwashing”
There should be some images of handwashing techniques
Could we also get some case scenarios where applicable
Leave a Comment Cancel reply
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Determinants of hand hygiene compliance among nurses in US hospitals: A formative research study
Madeline sands.
1 Department of Infectious Disease, London School of Hygiene and Tropical Medicine, London, United Kingdom
2 University of Arizona College of Medicine, Tucson, Arizona, United States of America
Robert Aunger
Associated data.
All relevant data are within the manuscript and its Supporting Information files.
Hand hygiene is the simplest and most effective measure for preventing healthcare-associated infections. Despite the simplicity of this procedure and advances made in infection control, hospital health care workers’ compliance to hand hygiene recommendations is generally low. Nurses have the most frequent patient care interactions, and thus more opportunities to practice hand hygiene. As such, it is important to identify and understand determinants of nurses’ reported compliance. Formative research was undertaken to assess the potential impact of several unexamined factors that could influence HH among nurses: professional role and status, social affiliation, social norms, and physical modifications to the work environment (as well as institutional factors like safety climate). A survey questionnaire was developed primarily to inform the creation of a behaviour change intervention. The survey looked at how these factors influence HH among nurses and sought to identify barriers and levers to reported hand hygiene. It was administered to a survey panel of acute care nurses, working in US hospitals, with a year or more of experience. Multivariate regression modelling suggested that reported hand hygiene compliance was most likely to be a function of a hospital management’s communication openness, perceived performance by peers, increased interactions with patients and other staff members, and the reduction in stress, busyness, and cognitive load associated with role performance. A powerful, effective intervention on HH among nurses therefore could be directed at improving communication openness, consider the impact of perceived performance by peers, increase interactions with patients and staff, and determine how to reduce the stress and cognitive load associated with role performance.
Introduction
Hand hygiene (HH) is the simplest and most effective measure for preventing healthcare-associated infections (HAIs).[ 1 ] Despite the simplicity of this procedure and advances made in infection control, hospital health care workers’ compliance to HH recommendations is generally low.[ 2 ] Nurses have the most frequent patient care interactions, and thus more opportunities to practice HH.[ 3 ] As such, it is important to identify and understand determinants of nurses’ reported compliance.
Hand hygiene is a complex behaviour with a myriad of motivators and barriers.[ 1 , 4 ] While the basic behavioural aspects surrounding HH practices in hospital settings have been widely researched, there remain gaps in the literature regarding effective psychological promotion of hand hygiene compliance (HHC).[ 4 ] Psychological frameworks have been shown to lead to behaviour change in a wide variety of contexts, especially in the behaviour of healthcare workers (HCWs).[ 5 ] Therefore, focusing on determinants of behaviour change and employing psychological behaviour change models can better inform HH improvement strategies.
Behaviour Centred Design (BCD) is a general approach to behaviour change that offers both a Theory of Change for behaviours in addition to a practical process for designing and evaluating interventions.[ 6 ] The BCD’s Theory of Change incorporates concepts such as reinforcement learning theory,[ 7 ] the evolution of behavioural control,[ 8 ] the evolved structure of human motivation,[ 9 ] and behaviour settings theory.[ 10 , 6 ] The behaviour settings theory explains the relationship between individuals and the environment—both physical and social.[ 10 ] Behaviour is a function of the setting within which it takes place. As such, behaviour settings are situations where people have learned what to expect from the environment and from other people’s behaviours. Each setting has a purpose, a designated place, a set of objects, and a prescribed set of behaviours. Therefore, each person entering a setting expects others, who are also participants, to perform their designated roles.
BCD is associated with a checklist of factors that determine human behaviour, which can be used to direct empirical investigations prior to the design of public health interventions. This checklist includes environmental determinants such as the props and infrastructure that support performance of the behaviour, as well as the psychological characteristics and personal traits required.
The aim of this study is to use the BCD approach to identify determinants that impact the HHC of nurses in intensive and acute care hospital units. A combination of literature review and formative research are used to identify prospective strategies for a behaviour change intervention. Recognizing what motivates and hinders a nurse from practicing HH should aid in the development of successful strategies seeking to improve nurses’ HHC.
Given the complexity of institutional settings for behaviour change, our data gathering strategy focussed on potentially important factors that have not yet been found to be significant. The literature search began with a background search to develop an understanding for the breadth of the body of literature. The iterative search process became more refined and developed as the review progressed. Once the volume and general scope of the HH field had been determined, parameters were set and search strings were developed [ S1 File ]. Search strings were developed for concepts encompassing behaviour change, hand hygiene compliance, healthcare workers, healthcare-associated infections, hand hygiene, and interventions. Medline, Web of Science, CINAHL, and Google Scholar databases were electronically searched selecting only for papers written in English. A total of 187 publications were identified this way; after filtering for papers published from January 2002- January 2015, there were 89 papers left to be reviewed. Additional papers and grey literature were identified by searching the references lists of the retrieved papers. We used the WHO’s tables of factors (WHO Table I.2.1) as well as hand hygiene improvement interventions (WHO Table I.2.2) as a framework.[ 1 ]
Categorizing and identifying modifiable factors using BCD
The BCD Checklist itemises all the types of behavioural determinants identified by the BCD approach. Placing the factors from the literature known to influence HHC ( Table 1 ) into the BCD Checklist enables us to see what categories of factors have potential for deeper investigation and could serve as the foundation for further research into HHC (see Table 2 ). This analysis shows that only a few of these categories have been investigated by intervention-based studies in the literature, and it is apparent that whole categories of factors have not yet been examined by the public health community. Types of potential factors that have been completely ignored thus far are listed without entries in Table 1 . It should be noted that even some categories with entries below have not been fully investigated; additional factors could be identified and explored. If we restrict our attention to categories—either with or without entries—which can be readily changed by the types of mechanisms that are both acceptable and within the budget of an average hospital administration, we arrive at the following list of five categories: (1) motivational psychology , (2) reactive psychology (i.e. habit formation), (3) modification of the relevant behaviour setting stage , (4) role change , and ( 5) social norm manipulation . These categories will be the focus of this formative research.
Importance of this formative research
Formative research is a critical step in the development of health behaviour change interventions.[ 6 , 11 ] The purpose of formative research is to assess individuals’ beliefs, perceptions, behaviours, and the structure of the environment itself that may help or hinder program effectiveness. Typically, such research involves significant fieldwork in the relevant context. In the case of this study, the ability of the research team to obtain a comprehensive view of the factors associated with HHC was limited by the logistics of access to hospitals. It was neither possible to take nurses from the floor during their shift nor to engage in substantial observation of their practices without introducing bias into the data collection. Further, there is considerable variation and organization-specific intricacies when it comes to the institutional contexts of HHC, which needs to be understood and considered when creating interventions intended to be widely used. Thus, the decision was made to administer a survey to a large number of nurses with a range variety of experiences across the United States, gaining in breadth what was lacking in terms of depth in the investigation. This survey sought to assess the behavioural change potential of the factors identified by the analysis above.
Ethics approval was attained from the London School of Hygiene and Tropical Medicine’s Observational and Interventions Research Ethics Committee (reference number is 14411).
Sampling procedure
An anonymous internet-based cross-sectional survey was administered between November to December 2015 by a global online sampling and digital data collection company called Dynata—formerly known as Research Now—to a survey panel of acute care nurses, working in various types of hospitals that are geographically distributed across the US, with at least a year or more of experience. There were 19,969 hospital nurses available to take the survey. With a confidence interval of 95% and a margin of error 5%, we calculated that we need a minimum of 377 completed surveys. Dynata screened and recruited participants, and it used an incentive scale based on set time increments. Incentive options allowed panellists to redeem from a range of gift cards, charitable contributions, and other products or services upon completing the survey.
Survey design
The survey concentrates on the five unexamined but modifiable factors that are potential determinants of HHC: (1) motivation, (2) habit, (3) roles, (4) behaviour setting stage, and (5) norms. The survey questions, which draw upon various concepts and measurement tools from fields such as sociology and psychology, are designed to measure the degree to which these factors influence reported HHC [ S2 File ]. In doing so, a novel questionnaire was developed using techniques—such as vignettes and the self-reported habit index (SRHI)[ 12 ]—that have not been commonly or consistently used in HH questionnaires before. The movement of the respondent through the survey is depicted in Fig 1 . The explanation of the theoretical underpinnings of the survey with their respective survey questions follow.

To make a more succinct and pertinent list of risk factors for this research project, we first determined which factors have already been found to have a significant impact on HH behaviour from a literature search and review.
The role of the nurses was explored through professional identity. Identities are the traits and characteristics, social relations, roles, and social group memberships that define an individual.[ 13 ] A professional identity is the sense of self that is associated with the enactment of a professional role.[ 14 , 15 ] This identity gives members of a profession a definition of self-in-role and the goals, values, norms, and interaction patterns that are associated with their job.[ 16 ] This definition of identity is critical to how professionals interpret and behave in various work situations, with identity being both a product of situations and a determinant of behaviour within situations.[ 13 , 17 ] Identity is (a) predicted to influence what individuals are motivated to do, (b) encompasses how individuals think and makes sense of themselves and others, (c) the actions the individuals take, and (d) the individuals’ feelings and abilities to control or regulate themselves.[ 18 , 19 ]
By learning what qualities, skills, and traits nurses value, the perceived responsibilities of the professional role can be modified to include the responsibility of practicing HH. There is potential for hand hygiene to be integrated into the qualities that nurses perceive to be what a “good” or “ideal” nurse possesses. Respondents are therefore asked to choose five qualities or traits they wish they had exhibited more of during their most recent shift. The following qualities and traits were identified from the literature:[ 20 – 27 ]
Respondents were then asked to choose five statements they would least like to hear said about them as a nurse. The statements address undesirable qualities and traits or unfavourable working conditions identified in the literature.[ 20 – 27 ]
A social norm is a rule of behaviour that individuals conform to conditionally based on the beliefs that (a) most people in their relevant network conform to this behaviour (this is referred to as an empirical expectation ), (b) they themselves believe that they should perform the behaviour ( normative personal belief ), and (c) that most people in their relevant network believe they ought to conform to this behaviour as deviations from the norm could result in potential punishment (referred to as a normative expectation ).[ 28 ] Social norms direct human action, however, norms are situationally contingent, meaning that a norm’s salience and one’s compliance to this norm are conditional upon the situation.[ 29 ] To understand and predict behaviour, it is important to know which social norms individuals find salient in particular contexts—that is, which norms are likely to be dependent on particular settings.[ 30 , 31 ]
The normative system of nursing with respect to HH behaviour can be measured through learning about (a) individual’s preferences for ‘proper’ HH action, (b) expectations of others’ HH behaviour, and (c) beliefs about the expectations others have of them in this regard. We sought to identify nurses’ social norms regarding hand hygiene and whether the social norms have a causal influence on behaviour. Bicchieri (2014) devised a series of questions that diagnose, explain, and predict collective patterns of behaviour, which were adapted for the research purposes here.[ 28 ] This involves ascertaining several aspects of a normative system, including empirical expectations, normative beliefs, and normative expectations. To test empirical expectations, respondents were asked about their own beliefs regarding the prevalence of HH behaviour among their peers; respondents were asked to disclose how many nurses out of a group of ten would always practice HH at the various indications.
To test normative personal beliefs, respondents were also asked if they think they should practice HH at six various moments: (1) before entering a patient’s room, (2) when exiting a patient’s room, (3) after taking a patient’s vitals, (4) after cleaning a patient’s wound, (5) before charting in the nurse station, and (6) after talking with fellow nurses in the break room. Responses along a Likert scale from Never to Always were offered. To test normative expectations, respondents were asked if they believed that other nurses thought that they should use hand sanitizer or soap at the same moments provided above. Once again, the same Likert scale offered five response options.
Habits are defined as psychological tendencies to respond automatically to environmental stimuli, acquired through repeated practice in particular contexts.[ 32 , 33 ] Habitual actions are triggered in response to contextual cues associated with their performance: for example, automatically putting on a seatbelt (action) after getting into the car (contextual cue) or washing hands (action) after using the toilet (contextual cue).[ 34 ] Habit strength is a continuum. Habits that are considered to be of weak or moderate strength are performed with less frequency than strong habits.[ 35 ]
Participants were asked about the strength of their HH habits using the Self-Report Habit Index (SRHI) developed by Vernplanken et al. (1994).[ 36 ] The SRHI is a tool used either as a dependent variable, or to determine or monitor habit strength without measuring behavioural frequency. It discriminates between behaviours varying in frequency and between daily vs. weekly habits. The index is based on features of habit: a history of repetition, automaticity, and expressing one’s identity. Respondents answer the degree to which they felt the statement affected them using a 5-point Likert scale (from Strongly Disagree to Strongly Agree). There is evidence that the SRHI can solicit accurate answers comparable to real behaviours.[ 37 ] The index in this case is phrased to ask respondents about practicing HH before entering and after exiting a patient’s room.
Motives are evolved psychological mechanisms that help individuals choose the appropriate goal-directed behavioural strategy in response to a situation.[ 38 ] An appropriate strategy would most likely lead to a satisfactory outcome in terms of the benefits accruing from that interaction with the environment.[ 9 ] A satisfactory outcome involves an experience that is rewarding—be it a sensory pleasure, a metabolic benefit for the body, or a change to one’s place in the social world.
This research sought to identify what motivates people to practice HH. Thus, the objective of the motive questions was to determine if a person of higher status—such as a nurse manager or direct supervisor—or someone who is dependent on the nurse—such as patient—is a likely motivator of HH. The BCD’s motive mapping technique is used.[ 6 ] Motive mapping attempts to reduce psychological ‘distance’ by simulating the behavioural context using a narrative, and attempts to minimize the participant’s reflection by focusing directly on the rewards from performance.
Participants responded to three scenarios asking about how feedback is likely to influence their own HH behaviour. In each of the scenarios, participants were told that they had taken a patient’s vitals and immediately practiced HH upon exiting the room. At the end of each scenario, positive feedback regarding the practicing of HH was shared with the nurse by the nurse manger, a fellow nurse, and the patient. Respondents answered to what degree they feel this feedback makes them more likely to use hand sanitizer in the future as compared to normal usage. A five-point Likert scale measured responses.
Situational constraints: Vignettes
Participants were asked to judge their likely compliance to HH in varying situations known as vignettes. Vignettes are closer to real-life judgment-making situations than relatively abstract questions that are typical of most surveys. Respondents were asked to reflect on whether they would practice HH in the following situations: (1) exiting a patient’s room after taking the patient’s vitals, (2) entering a patient’s room before taking vitals, (3) exiting a patient’s room after cleaning and bandaging the patient’s diabetic foot wound, and (4) entering a patient’s room before cleaning and bandaging the patient’s foot wound. These situations were altered slightly for each follow-up question by introducing either a facilitator or a barrier to practicing HH, such as:
- Large patient load, which measures busyness
- Already wearing gloves, which measures the nurse’s inclination to practice HH when wearing protective equipment
- Being observed by the infection prevention manager, which measures higher status social influence
- Being observed by a fellow nurse, which measures peer influence
- Trying to practice hand hygiene but the dispenser is empty, which measures perception of ease
- An interruption during patient care requiring the immediate assistance of the nurse, which measures interruption
- An emergency requiring CPR, which measures reaction to emergency
Through vignettes, we sought to determine the extent to which these factors impact HH behaviour. Responses were presented on a five-point Likert scale based on the likelihoods of behavioural response.
Institutional factors: Safety culture and familiarity with hand hygiene
Nurse behaviour takes place within the context of hospital life. Hospitals can be considered institutions, which have an impact on the settings that occur within them. Therefore, this research sought to assess the culture of safety within the respondents’ institutions. It has been widely accepted that the safety culture of one’s hospital affects HHC rates.[ 1 , 39 – 41 ] To measure the safety culture of the hospitals where the respondents work, the research team selected and modified questions from the hospital survey on patient safety culture developed by the US Agency for Healthcare Research and Quality.[ 42 ] Questions were grouped according to the safety culture dimensions they are intended to measure. Groups included: rating overall perceptions of safety, frequency of event reporting, supervisor/manager expectations and actions, teamwork within units, closeness, communication openness, feedback and communication about error, non-punitive response to error, staffing, and hospital management support. Five point Likert scales asking for agreement/disagreement and frequency were used.
Participants were also asked about their engagement and participation in past HH training and interventions, both as nursing students and as practicing professionals. In addition, participants were asked about their hospital’s own HH programs. Questions were all phrased so that a yes/no response was appropriate.
Modification to physical setting
Finally, the research aimed to investigate various ways to disrupt a behaviour setting, specifically by identifying how the stage and arrangement of props of the setting surrounding the act of HH serve as constraints or opportunities to practicing HH. Respondents are presented with two photos—one of a hallway in a non-descript hospital and one of a patient’s room—and then asked how both the hallway and the room could be altered to better facilitate HH. These questions allowed for open-ended responses.
Formatting the survey
The survey was a self-administered online task. Each question was presented on its own webpage. Respondents were first asked a series of screener questions to determine if they were eligible: they had to be an acute care nurse, working in a US hospital, with a year or more of experience.
Those who are eligible were then presented with a series of photos related to the modification of the physical setting. These questions were asked first because the research team wanted responses that were not influenced by other questions in the survey. In addition, the photos served to ground the respondents in the survey by providing visual context. The vignettes immediately followed; the research team reasoned that the vignettes would likely solicit the most accurate responses about HH performance. As such, the vignettes were placed early in the survey so that the respondents were not biased or primed by subsequent specific queries. The professional identity questions were asked next as these questions tapped into values. Questions about norms followed and were followed by questions on habit and motivation. The final questions focused on the safety culture of the hospital as well as the respondents’ history with HH interventions and programs. A diagram of the survey questions and flow are provided in Fig 2 .

The survey is broken into sections; the movement of the respondent through the survey is depicted in this figure.
Analysis of the survey
Descriptive statistics were first used to characterize the sample. Univariate analyses were therefore first conducted to determine which variables were associated with reported levels of HHC. Next, a multivariate regression of the variable of interest—reported HH on exiting a patient room after taking vitals—was conducted on demographic, role, safety culture, and norm variables. This variable of interest was chosen as it was asked in the form of a vignette, which is closer to real-life judgment-making situations and thus provided a better sense of compliance than asking respondents directly about their HHC. In addition, this specific vignette question was used as nurses are more likely to practice HH upon exiting a room, but less likely to practice HH after conducting a low-risk procedure. As an ordinary least squares regression of outcome on predictors was inappropriate for a model with this number of predictors but only 500 observations, we performed a bidirectional stepwise procedure to build the model, using the Akaike Information Criterion (AIC) as the model-building criterion for adding or removing variables; any variable that, when removed, changed the model AIC by ≤ 1 was discarded by the procedure.
Study population
A total of 540 surveys were completed. Table 2 summarizes selected characteristics of the participants. The median age was 49 (range: 24–70). In a typical workday, more than two-thirds of the respondents (68%) reported spending 80% or more of their time performing direct patient care. Familiarity with HH practices was indicated by 459 (85%) of respondents, who reported that HH was emphasized during professional training to be a nurse. Furthermore, the clear majority of respondents (456, or 84%) had participated in a hospital-led hand hygiene initiative before.
Summary variables were standardized before analysis. Variables included habit , safety culture , norms , motivation , role , hand hygiene familiarity , and demographics . Means were taken across Likert scale questions per the prescribed groupings. Sums were calculated across yes/no variables and demographic variables were encoded with a binary number system.
Univariate analysis
The results for each of the five main potential determinants of HHC have been provided in their respective tables and figures enumerated below. Major findings have been summarized for norms , habit , and motives .
The results for every question in this section of the survey are included in Table 3 . The most salient findings were that nurses were more likely to practice HH upon exiting a patient’s room than entering, and that when the procedure was perceived as being high-risk—such as cleaning and bandaging a wound—there was an increased likelihood of practicing HH. Most notably, 90.7% (n = 490) of nurse respondents reported being likely to practice HH upon exiting a patient’s room after cleaning and bandaging the diabetic foot wound.
The results for empirical expectations, normative personal beliefs, and normative expectations have been presented in Table 4 . Regarding empirical expectations , respondents felt that most nurses practiced hand hygiene before entering a patient’s room, when exiting a patient’s room, after taking a patient’s vitals, and after cleaning a patient’s wound. Concerning normative personal beliefs , for each moment apart from charting, most respondents claimed that HH should always be practiced. Of the 540 respondents, 81.7% (n = 441) of respondents said it should always be practiced before entering a patient’s room, 90.4% (n = 488) when exiting a patient’s room, 75.6% (n = 408) after taking patient’s vitals, and 98.7% (n = 533) after cleaning a patient’s wound. With normative expectations , over 50% of respondents claimed that most other nurses always think that one should practice hand hygiene before entering a patient’s room, when exiting a patient’s room, after taking a patient’s vitals, and after cleaning a patient’s wound. [Figs H and I in the S1 Fig display the results.]
Respondents answered the SRHI about practicing HH before entering a patient’s room and after exiting a patient’s room. Responses were made on five point Likert scales anchored by the terms strongly agree-strongly disagree and were coded such that high values indicated strong habits (1 = strongly disagreeing and 5 = strongly agreeing). The means of the questions were calculated, and these in turn became the habit strength scores. Regarding HH upon entering a room, 59.1% (n = 319) of respondents had a score of 4.5 or over ( Fig 3 ). In the case of exiting, 68.0% (n = 367) of respondents had a habit strength score of 4.5 and over ( Fig 4 ).

Upon receiving feedback from nurse managers and fellow nurses, 50.7% (n = 274) of participants and 55.4% (n = 299) said that there would be no difference in future HH action, respectively. Regarding receiving feedback from patients, 59.3% (n = 320) respondents said that feedback would positively impact their HH behaviour in the future. Results are summarized in Table 5 .
Safety culture
The results for each question in this section of the survey are included in Table 6 .
Multivariate regression
Presented in Table 7 are the results from the bidirectional stepwise procedure to analyse the relationships between various predictors and the outcome: reported HH on exiting a patient room after taking vitals. Included in the table are only the variables which met the selection criteria. Values are provided for the regression Estimate, as well as its Standard Error, T-value, and Pr(>|t|) coefficients. Coefficients were assigned to each predictor; the sign on the coefficient (positive or negative) provides the direction of the effect of the predictor on the outcome variable.
The reported higher likelihood of practicing HH upon performing a high-risk procedure as compared to a low-risk procedure aligns with the literature which shows that HHC is greater when involving higher-risk tasks.[ 2 , 43 , 44 ] In addition, nurses reported being more likely to practice HH upon exiting a patient’s room than entering, which is interpreted as nurses practicing HH as a form of self-protection.[ 44 ]
Nurses work in close relationships with patients who are vulnerable and largely dependent on the nurse for care.[ 45 ] Nurses work with one another and on inter-professional healthcare teams to deliver care and provide support. Fagermoen’s (1997) proposed theoretical model for professional identity of nurses maintains that nurses’ perceptions of the ‘professional self’ focuses on both other-oriented and self-oriented values .[ 45 ] Other-oriented values encompass the nurse’s actions on behalf of the patient’s well-being and the interactions with patients in providing care. Self-oriented work values include work performance and collaboration with other professionals. While self-oriented work values directly impact the self, these values also affect the care delivered. For instance, better stress management can lead to a nurse feeling more confident, capable, and in control, which can then lead to better care delivered.
When asked which values the participants wish they had exhibited more of during their last shift, the traits most widely selected were those of self-oriented values such as stress management, patience, good communication, and physical and mental endurance. These in turn impact other-oriented values to a degree since work performance directly influences the kind of care delivered. Other-oriented values are the foundation of nursing care and an integral part of the nurses’ relationships with patients. Areas of improvement could be seen in how nurses engage in the work-setting and the actualization of the other-oriented values . When asked what the nurses would least like to hear said about them, the top responses were about the inadequacy in the delivery of care. This again demonstrates how integral other-oriented values are to the discipline of nursing.
There is agreement amongst participants as to when to practice HH—upon entering and exiting a patients’ room and after performing a procedure such as vitals or cleaning a wound. It is apparent that participants believed these to be norms, and believed others to hold the same norms in addition to conforming to such norms. This suggests that HH indications are well understood and agreed upon by nurses.
Habit is the cognitive mechanism by which actions occur reflexively and in a fixed sequence.[ 46 ] Habit scores were quite high, which is not unexpected for a behaviour that is practiced many times a day. This suggests that the SRHI may not be useful in measuring behaviour that is already being practiced intensively.
Over half of participants indicated that receiving feedback from a patient or a colleague would likely lead to an increase in future HH action. There is evidence that HH behaviour of HCWs is positively influenced by the presence and proximity of peers.[ 47 , 48 ] Regarding patients, patient involvement in supporting their own safety has been widely discussed. [ 49 – 51 ]. Patient involvement in HH—such as praising HCWs for practicing HH or reminding HCWs to wash their hands—and its impact on HH behaviour has not been extensively studied [ 51 ], but our results show that it would be acceptable to HCWs for patients to recognize nurses for practicing HH.
The variable of interest was the reported HHC upon exiting a patient’s room after taking their vitals. This question had the most variance in responses. The regression analysis shows that reported HHC is a function of specific variables at all possible levels: the hospital, unit, and individual. At the hospital level, increased openness of communication —which was asked about in the safety culture portion of the survey—led to a higher reporting of HHC. There is evidence that features of a hospital’s safety climate are related to how well standard precautions and safety practices, such as HH, are adhered to.[ 52 – 54 ] Communication openness is a component of a hospital’s patient safety culture and is defined as the extent to which the staff freely speak up if they see something that may negatively affect a patient and/or question those with more authority.[ 40 , 55 ] A core tenet behind communication openness is that all have a responsibility to speak out when certain actions, objects, or processes pose danger to the safety of the patient and others, and those who speak out should be able to do so without fear of being reprimanded. It could be surmised that those who are comfortable enough to speak out about threats to patient safety would also act on their own accord to protect patient safety by practicing HH at the proper indications.
At the unit level, the type of hospital unit played a role in the HHC reported—overall, participants who work in an emergency department reported lower HHC rates. This could be attributed to the fact that nurses must respond to various unpredictable situations that could be life-threatening to the patient, and the patient’s need for immediate attention and care is put first before practicing HH. Practicing HH in an emergency could be perceived as dilatory. This could also be because the emergency department is an environment with a high density of invasive procedures that require glove usage, and there is evidence that glove usage is inversely correlated with adequate HH. [ 1 , 56 , 57 ]
An interesting finding was that nurses who indicated having a higher proportion of shift time allocated to interaction with patients and with fellow healthcare professionals reported higher HHC. More time spent with a patient could lead to more opportunities to practice HH and thus more events completed. However, this challenges the notion that the higher the demand for hygiene (the more opportunities to practice it), the lower the adherence rates. Nevertheless, the more time spent with other HCWs could result in a nurse feeling the ‘watching eyes’ effect thus leading to increased HHC. More time with the patient could also result in the nurse bonding with the patient and is thus more cognisant of practicing HH to ensure the patient’s safety.
At the individual level, one’s personal ability to manage subjectively important aspects of the professional role—such as stress management, communication skills, and being confident in one’s self as a nurse—leads to increased reporting of HHC. All the individual-level variables in the analysis could be defined as other-oriented to a degree as presumably successful stress management can lead to providing better care. The significant individual variables show other-oriented values involving care and communication as being of highest professional importance to nurses, and this orientation fosters better HH.
It has been noted in the literature that poor working conditions, increased levels of stress, and insufficient communication have a direct negative impact on the quality of nursing and have severe consequences for patients.[ 58 – 61 ] In addition, low HHC can result from fatigue or burnout. As a nurses’ shift progresses, HHC declines towards the end of the shift.[ 62 ] Continuous long shifts can lead to nurse burnout which in turn has been associated with increased HAI levels.[ 63 ] Thus, nurses who feel in control, confident in their abilities, supported, and have lower stress levels can better focus on and execute safety procedures such as HH.
Limitations
Surveys administered to HCWs are relatively inexpensive and allow for HCWs to focus and reflect on their own practices. However, self-report of infection prevention can be flawed, especially as reported HH practices and actual HH practice can differ significantly.[ 54 , 64 , 65 ] In using vignettes, we may have reduced socially desirable responses by allowing participants to report their HH practice and the practices of others through the vignette character(s) and situations.[ 65 , 66 ] This may have reduced the potential for disparity between reported and actual behaviour. Additionally, generalizability of the findings may be limited by certain characteristics of the sample, achieved through online data recruitment. This limitation was addressed by administering the survey online, which allowed for us to collect responses from a wide variety of participants located in different regions and hospitals of the United States with varying degrees of experience and specialisation.
Formative research was undertaken to assess the potential impact of several unexamined factors that could influence HH among nurses: professional role and status , social affiliation , social norms , and physical modifications to the work environment , as well as institutional factors (like safety climate). A survey questionnaire looked at how these factors influence nurses’ reported HHC and also sought to identify barriers and levers to HH. Multivariate regression modelling suggested that HHC was most likely to be a function of a hospital management’s ‘openness’, perceived performance by peers, increased interactions with patients and other staff members, and the reduction in stress, busyness, and cognitive load associated with role performance. Thus, a powerful and effective intervention focusing on nurses’ HHC should address improving communication openness, consider the impact of perceived performance by peers, increase interactions with patients and staff, and determine how to reduce the stress and cognitive load associated with role performance. Use of Behaviour Centred Design increased the informativeness of the survey tool, and could be used more widely in formative research studies.
Supporting information
Concepts and their corresponding search strings.
Acknowledgments
We are grateful to Rahul Singh for guiding the preliminary analysis of formative research results and for writing the code in R-studio for the multivariate analysis.
Abbreviations
Funding statement.
MHS and RA received financial compensation as affiliates of the London School of Hygiene and Tropical Medicine, which served as a paid consultant to GOJO Industries, Inc. for the creation and evaluation of the intervention. The funders had no role in study design, data analysis, decision to publish, or preparation of the manuscript.
Data Availability
Healthcare Providers
New Training and Education Resources available . Hand Hygiene in Healthcare Settings Video Series link: Education Courses | Hand Hygiene | CDC

Clean Hands Count for Healthcare Providers
Protect yourself and your patients from potentially deadly germs by cleaning your hands. Be sure you clean your hands the right way at the right times.
Introduction to Hand Hygiene
Hand Hygiene means cleaning your hands by using either handwashing (washing hands with soap and water), antiseptic hand wash, antiseptic hand rub (i.e. alcohol-based hand sanitizer including foam or gel), or surgical hand antisepsis
Cleaning your hands reduces:
- The spread of potentially deadly germs to patients
- The risk of healthcare provider colonization or infection caused by germs acquired from the patient
- Alcohol-based hand sanitizers are the most effective products for reducing the number of germs on the hands of healthcare providers.
- Alcohol-based hand sanitizers are the preferred method for cleaning your hands in most clinical situations.
- Wash your hands with soap and water whenever they are visibly dirty, before eating, and after using the restroom.
During Routine Patient Care:
Use an Alcohol-Based Hand Sanitizer
Wash with Soap and Water
- Immediately before touching a patient
- When hands are visibly soiled
- Before performing an aseptic task (e.g., placing an indwelling device) or handling invasive medical devices
- After caring for a person with known or suspected infectious diarrhea
- Before moving from work on a soiled body site to a clean body site on the same patient
- After known or suspected exposure to spores (e.g. B. anthracis, C difficile outbreaks)
- After touching a patient or the patient’s immediate environment
- After contact with blood, body fluids or contaminated surfaces
- Immediately after glove removal
When and How to Perform Hand Hygiene
The safety of refilling or “topping off” containers of ABHS has not been well studied. ABHS is an FDA regulated over-the counter drug and should be stored and dispensed in a manner that ensures safety and effectiveness. Potential safety risks that may be associated with refilling or “topping off” containers of ABHS include inadvertent contamination, reduced effectiveness from the evaporation of alcohol, and irritant effects from mixing formulations. Therefore, refilling or “topping off” ABHS dispensers should only be considered in accordance with manufacturer’s guidance and FDA regulations. Refilling or “topping off” containers of liquid soap has been associated with outbreaks of pathogenic bacteria. The 2002 Guidelines for Hand Hygiene in Healthcare Settings recommends that soap should not be added to partially empty soap dispensers.
Multiple opportunities for hand hygiene may occur during a single care episode. Following are the clinical indications for hand hygiene:
When using alcohol-based hand sanitizer:
- Put product on hands and rub hands together
- Cover all surfaces until hands feel dry
- This should take around 20 seconds
- When cleaning your hands with soap and water, wet your hands first with water, apply the amount of product recommended by the manufacturer to your hands, and rub your hands together vigorously for at least 15 seconds, covering all surfaces of the hands and fingers.
- Rinse your hands with water and use disposable towels to dry. Use towel to turn off the faucet.
- Avoid using hot water, to prevent drying of skin.
- Other entities have recommended that cleaning your hands with soap and water should take around 20 seconds.
- Either time is acceptable. The focus should be on cleaning your hands at the right times.
- Wear gloves, according to Standard Precautions, when it can be reasonably anticipated that contact with blood or other potentially infectious materials, mucous membranes, non-intact skin, potentially contaminated skin or contaminated equipment could occur.
- If your task requires gloves, perform hand hygiene prior to donning gloves, before touching the patient or the patient environment.
- Perform hand hygiene immediately after removing gloves.
- gloves become damaged,
- gloves become visibly soiled with blood or body fluids following a task,
- moving from work on a soiled body site to a clean body site on the same patient or if another clinical indication for hand hygiene occurs.
- Never wear the same pair of gloves in the care of more than one patient.
- Carefully remove gloves to prevent hand contamination.

Hand Hygiene for Surgery
- Remove rings, watches, and bracelets before beginning the surgical hand scrub
- Remove debris from underneath fingernails using a nail cleaner under running water
- Performing surgical hand antisepsis using either an antimicrobial soap or an alcohol-based hand sanitizer with persistent activity is recommended before donning sterile gloves when performing surgical procedures
- When performing surgical hand antisepsis using an antimicrobial soap, scrub hands and forearms for the length of time recommended by the manufacturer, usually 2–6 minutes.
- Long scrub times (e.g., 10 minutes) are not necessary
- When using an alcohol-based surgical hand-scrub product with persistent activity, follow the manufacturer’s instructions
- Before applying the alcohol solution, prewash hands and forearms with a non-antimicrobial soap and dry hands and forearms completely
- After application of the alcohol-based product as recommended, allow hands and forearms to dry thoroughly before donning sterile gloves
- Double gloving is advised during invasive procedures, such as surgery, that pose an increased risk of blood exposure
- Bacteria on the hands of surgeons can cause wound infections if introduced into the operative field during surgery
- Rapid multiplication of bacteria occurs under surgical gloves if hands are washed with a non-antimicrobial soap
- Bacterial growth is slowed after preoperative scrubbing with an antiseptic agent
- Reducing resident skin flora on the hands of the surgical team for the duration of a procedure reduces the risk of bacteria being released into the surgical field if gloves become punctured or torn during surgery
Skin and Nail Care
- Lotions and creams can prevent and decrease skin dryness that happens from cleaning your hands
- Use only hand lotions approved by your healthcare facility because they won’t interfere with hand sanitizing products
- Germs can live under artificial fingernails both before and after using an alcohol-based hand sanitizer and handwashing
- It is recommended that healthcare providers do not wear artificial fingernails or extensions when having direct contact with patients at high risk (e.g., those in intensive-care units or operating rooms)
- Keep natural nail tips less than ¼ inch long
- Some studies have shown that skin underneath rings contains more germs than comparable areas of skin on fingers without rings
- Further studies are needed to determine if wearing rings results in an increased spread of potentially deadly germs
- Guideline for Hand Hygiene in Healthcare Settings; 17-18 [PDF – 495 KB] .
- Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings .
- Guideline for Prevention of Surgical Site Infection; pp. 258 and 267 .
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

Nursing: Handwashing
- Reference Resources
- Books & Ebooks
- Articles & Databases
- Web Resources
- Evidence Based Practice
- Research Checklist
- Streaming Videos
- Reserve Materials
- Handwashing
- Book-A-Librarian This link opens in a new window
- Anatomy & Physiology
Infection Control Basics
There are 2 tiers of recommended precautions to prevent the spread of infections in healthcare settings: Standard Precautions and Transmission-Based Precautions. Standard Precautions are used for all patient care. They’re based on a risk assessment and make use of common sense practices and personal protective equipment use that protect healthcare providers from infection and prevent the spread of infection from patient to patient.
- Hand hygiene .
- Use of personal protective equipment (e.g., gloves , gowns, masks)
- Safe injection practices .
- Safe handling of potentially contaminated equipment or surfaces in the patient environment, and.
- Respiratory hygiene / cough etiquette. Source: Guideline for Isolation Precautions and Infection Prevention and you
Introduction
This is a gathering of resources that are relevant to washing one's hands. Hygiene and cleanliness are one of the most important duties that a person in the health care field can perform. Proper hand washing ensures that germs and the spread of disease is kept to a minimum.
- Hand Healthy Guidelines Hand washing, also referred to as hand hygiene, is one of the best ways to avoid getting sick and spreading infections to others, in the home, at work, at school, when traveling, or in a healthcare setting. The attention to prevention of spreading the COVID-19 pandemic has helped propel this “simple” measure into the spotlight as a new habit to stay healthy and prevent the spread of infections like flu, colds or intestinal illnesses. Hand washing requires only soap and water or an alcohol-based hand sanitizer.
CDC Basic Handwashing Video
Wash your hands: the right way, when should you wash your hands.
- Before, during, and after preparing food
- Before eating food
- Before and after caring for someone who is sick
- Before and after treating a cut or wound
- After using the toilet
- After changing diapers or cleaning up a child who has used the toilet
- After blowing your nose, coughing, or sneezing
- After touching an animal or animal waste
- After touching garbage
- CDC Handwashing: Clean Hands Saves Lives Scientists estimate that people are not washing their hands often or well enough and may transmit up to 80% of all infections by their hands. From doorknobs to animals to food, harmful germs can live on almost everything. Handwashing may be your single most important act to help stop the spread of infection and stay healthy.
CDC Handwashing Hygiene
- Guideline for Hand Hygiene in Health-Care Settings
The link is for the CDC Webasite on Hand Hygiene in Healthcare setting. Taken from the page description, "Hand Hygiene in Healthcare Settings provides healthcare workers and patients with a variety of resources including guidelines for providers, patient empowerment materials, the latest technological advances in hand hygiene adherence measurement, frequently asked questions, and links to promotional and educational tools published by the WHO, universities, and health departments."
CDC Guidelines
"The Guideline for Hand Hygiene in Health-Care Settings provides health-care workers (HCWs) with a review of data regarding handwashing and hand antisepsis in health-care settings."
- Guidelines for Hand Hygiene in Healthcare Settings Published 2002 CDC Healthcare Handwash Guidelines
Resources for Correct Handwashing Procedures
- Five Key Moments for Hand Hygiene 1. Before touching a patient 2. Before clean/aseptic procedures 3. After body fluid exposure risks 4. After touching a patient 5. After touching patient surroundings
Clean Hands Save Lives - PDF Poster
- PDF Poster Shows Dirty Hands 29" x 19" high quality poster for placing throughout your facility. Shows bugs that can lead to infection and may be found on unclean healthcare worker's hands.
WHO Guidelines on Hand Hygiene in Health Care
- << Previous: Reserve Materials
- Next: Book-A-Librarian >>
- Last Updated: Mar 6, 2024 1:23 PM
- URL: https://libguides.bristolcc.edu/Nursing

Assignment: Hand Hygiene Evidence Based Practice
- Uncategorized
Assignment: Hand Hygiene Evidence-Based Practice
Hand hygiene compliance.
Nurses as important part of the healthcare system and care provision should support interventions that improve patient safety and quality care outcomes. Hand hygiene plays a major role in reducing and eliminating the spread of germs and infections from healthcare providers to patients. Good hand hygiene is considered an effective way to prevent infections among all stakeholders, especially from providers to patients (Martos-Cabrera et al., 2019). Infectious diseases and hospital acquired infections (HAIs) are critical risks to young, the elderly, and those with preexisting conditions as well as individuals with a compromised immune system. Hand hygiene compliance among nurses is an effective way to reduce and prevent infections and promote patient safety as well as quality outcomes.
Comparison of the Pro and Con Sides of Hand Hygiene
Hand hygiene as an essential aspect of patient safety is essential with existing studies demonstrating its efficacy and effectiveness in reducing and preventing the spread and transmission of infections among patients and even providers. According to a systematic review on hand hygiene of nurses and patient safety, Malliarou (2018) asserts that nurses should wash their hands not only to prevent their contact with germs and infections that could lead to sickness but to protect their patients from getting healthcare associated infections (HAIs). The study notes that noncompliance to hand hygiene is a primary cause of nosocomial infections in healthcare settings. Good hand hygiene plays a significant part in reducing and eliminating the spread of germs and infections among patients. As such, there are several benefits to hand hygiene practices by healthcare providers as opposed to possible negative effects.
A core con revealed from existing evidence is that a significant number of healthcare providers clean their hands less than half of the times that they should. As such, limited compliance to hand hygiene measures means that these providers contribute to the spread of healthcare associated infections which impact one in every 31 hospital patients on any day. The Centers for Disease Control and Prevention (CDC) is categorical that every patient is at risk of acquiring an infection as they get treated for different diagnoses. The prevention of germs spread is essential and does not constitute any adverse effects on facilities, patients, and providers.
Impact of the Issue on Delivery of Health and Nursing Profession
Sufficient research evidence shows that hand hygiene measures affect the overall delivery of health and the nursing profession. In their systematic review of literature on hand hygiene knowledge and compliance among nursing students, Labrague et al. (2020) assert that there is low-to-moderate awareness and compliance among this group. The study shows the impact of enhancing knowledge among nursing students so that they comply with hand hygiene measures as demonstrated by higher rates among their medical counterparts.
Again, the study by Hillier (2020) emphasizes the effective use of hand hygiene practices to prevent and control infections. The study asserts that decontamination using hand hygiene is one of the most critical and effective ways for nurses and other healthcare providers to minimize and prevent the occurrence of HAIs and cross-infections among patients. The article demonstrates correct procedures that providers can use to attain effective hand hygiene. The article is categorical that nurses should be up-to-date with the evidence-based guidelines on hand hygiene like the use of hand sanitizers and hand washing approaches. The use of alcohol-based hand gels and the soap and water are considered in different measures as effective to attaining compliance on hand hygiene. The author shows that the emergence of the COVID-19 pandemic raised the need for optimal hand hygiene practices to reduce cross-contamination and spread of the infectious disease.
The study by Sandbol et al. (2022) compared the levels of hand hygiene compliance among healthcare worker before and during the COVID-19 pandemic. The study argues that unlike other findings that demonstrate a rise in hand hygiene compliance levels before the pandemic, it did not find any significant difference between the rates before and during the pandemic. This implies that nurses and other healthcare providers should increase their compliance to hand hygiene measures not just at times of pandemics and serious infections but all the times. Hand hygiene is essential because it reduce the rate of infections.
Personal Statement on Hand Hygiene Compliance
It is evident that hand hygiene compliance is essential for nurses and other healthcare professionals like physicians. Therefore, nurses should embrace evidence-based hand hygiene practices like the use of alcohol-based sanitizers and soap and water. Cleaning hands by rubbing alcohol-based formulation is an effective hand sanitizing technique if the hand are not visibly soiled (Martos-Cabrera et al., 2019). This approach is faster and better tolerated compared to washing hand with soap and water. However, handwashing using soap and water remains the most effective and affordable intervention despite its unpopularity among healthcare workers.
Hand hygiene measures are essential for healthcare providers, especially nurses and physicians to reduce susceptibility to infections. Compliance to hand hygiene is an effective way to enhance patient safety and improve overall care provision among nurses. As demonstrated since Nightingale’s time, hand hygiene is a core part of the nursing profession as nurses create an environment free from infections and aimed at promoting recovery from illnesses. The implication is that providers cannot attain better care delivery without following hand hygiene protocols.
Centers for Disease Control and Prevention (CDC) (2020). Clean Hands Count for Safe
Healthcare. https://www.cdc.gov/patientsafety/features/clean-hands-count.html
Hillier, M. D. (2020). Using effective hand hygiene practice to prevent and control infection.
Nursing Standard, 35(5), 45-50. DOI: 10.7748/ns. 2020.e11552
Labrague, L. J., McEnroe‐Petitte, D. M., Van de Mortel, T., & Nasirudeen, A. M. A. (2018). A
systematic review on hand hygiene knowledge and compliance in student nurses. International nursing review, 65(3), 336-348. DOI: 10.1111/inr.12410
Martos-Cabrera, M. B., Mota-Romero, E., Martos-García, R., Gómez-Urquiza, J. L., Suleiman-
Martos, N., Albendín-García, L., & Cañadas-De la Fuente, G. A. (2019). Hand hygiene teaching strategies among nursing staff: a systematic review. International journal of environmental research and public health, 16(17), 3039. DOI: 10.3390/ijerph16173039
Malliarou, M. (2018). Hand Hygiene of Nurses and Patient Safety. International Journal of
Nursing & Clinical Practices, 4(217). https://doi.org/10.15344/2394-4978/2017/217
Sandbøl, S. G., Glassou, E. N., Ellermann-Eriksen, S., & Haagerup, A. (2022). Hand hygiene
compliance among healthcare workers before and during the COVID-19 pandemic. American Journal of Infection Control, 50(7), 719-723. DOI: 10.1016/j.ajic.2022.03.014.
Question Description
I don’t know how to handle this Health & Medical question and need guidance.
PICOT: “Does compliance with hand washing measures (I) for direct care staff in a hospital setting (P), as compared to non-compliance with hand washing measures (C), help improve patient safety by decreasing healthcare associated infections (O) during hospitalization (T)?”
Write a 500-750 word paper (excluding the title and reference pages) for your proposed evidence-based practice project solution. Consider the following criteria:
(a) Describe the proposed solution (or intervention) for the problem and how it is (are) consistent with current evidence. Make extensive use of references and evidence to support your solution or intervention. (b) Consider whether the intervention is realistic in your setting, too expensive, or there is a lack of appropriate training to deliver the intervention. If the intervention is unrealistic, you may need to revise your PICOT before proceeding. Organization Culture: Describe how the proposed solution is consistent with the culture and resources of the organization or community. Expected Outcomes: Describe the project’s expected outcomes. The results should follow from the PICOT. Method for Achieving Results: Create a plan for achieving the desired results. List any specific barriers that must be assessed and removed. Make a note of any assumptions or limitations that must be addressed. Impact of Outcomes: Describe how the outcomes will affect one or more of the following indicators: quality care improvement, patient-centered quality care, process efficiency, environmental changes, and/or professional expertise. Prepare this assignment in accordance with the APA guidelines found in the Student Success Center’s APA Style Guide. There is no need for an abstract.
rubric print format.xlsx\sreferences.docx
You should proofread your paper. However, do not rely solely on your computer’s spell-checker and grammar-checker; failure to do so indicates a lack of effort on your part, and your grade will suffer as a result. Papers with a high number of misspelled words and grammatical errors will be penalized. Before submitting your paper, go over it in silence and then aloud, and make any necessary changes. It is often beneficial to have a friend proofread your paper for obvious errors. Uncorrected mistakes are preferable to handwritten corrections.
Click here to ORDER an A++ paper from our MASTERS and DOCTORATE WRITERS: Assignment: Hand Hygiene Evidence Based Practice
Use a standard 10 to 12 point typeface (10 to 12 characters per inch). Smaller or compressed type, as well as papers with narrow margins or single spacing, are difficult to read. It is preferable to allow your essay to exceed the recommended number of pages rather than attempting to compress it into fewer pages.
Large type, large margins, large indentations, triple-spacing, increased leading (space between lines), increased kerning (space between letters), and other such attempts at “padding” to increase the length of a paper are also unacceptable, waste trees, and will not fool your professor.
The paper must be neatly formatted, double-spaced, and have a one-inch margin on all four sides of each page. When submitting hard copies, use white paper and print with dark ink. It will be difficult to follow your argument if it is difficult to read your essay.
ADDITIONAL INSTRUCTIONS FOR THE CLASS
Discussion Questions (DQ)
Initial responses to the DQ should address all components of the questions asked, include a minimum of one scholarly source, and be at least 250 words. Successful responses are substantive (i.e., add something new to the discussion, engage others in the discussion, well-developed idea) and include at least one scholarly source. One or two sentence responses, simple statements of agreement or “good post,” and responses that are off-topic will not count as substantive. Substantive responses should be at least 150 words. I encourage you to incorporate the readings from the week (as applicable) into your responses. Weekly Participation
Your initial responses to the mandatory DQ do not count toward participation and are graded separately. In addition to the DQ responses, you must post at least one reply to peers (or me) on three separate days, for a total of three replies. Participation posts do not require a scholarly source/citation (unless you cite someone else’s work). Part of your weekly participation includes viewing the weekly announcement and attesting to watching it in the comments. These announcements are made to ensure you understand everything that is due during the week. APA Format and Writing Quality
Familiarize yourself with APA format and practice using it correctly. It is used for most writing assignments for your degree. Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for APA paper templates, citation examples, tips, etc. Points will be deducted for poor use of APA format or absence of APA format (if required). Cite all sources of information! When in doubt, cite the source. Paraphrasing also requires a citation. I highly recommend using the APA Publication Manual, 6th edition. Use of Direct Quotes
I discourage overutilization of direct quotes in DQs and assignments at the Masters’ level and deduct points accordingly. As Masters’ level students, it is important that you be able to critically analyze and interpret information from journal articles and other resources. Simply restating someone else’s words does not demonstrate an understanding of the content or critical analysis of the content. It is best to paraphrase content and cite your source. LopesWrite Policy
For assignments that need to be submitted to LopesWrite, please be sure you have received your report and Similarity Index (SI) percentage BEFORE you do a “final submit” to me. Once you have received your report, please review it. This report will show you grammatical, punctuation, and spelling errors that can easily be fixed. Take the extra few minutes to review instead of getting counted off for these mistakes. Review your similarities. Did you forget to cite something? Did you not paraphrase well enough? Is your paper made up of someone else’s thoughts more than your own? Visit the Writing Center in the Student Success Center, under the Resources tab in LoudCloud for tips on improving your paper and SI score. Late Policy
The university’s policy on late assignments is 10% penalty PER DAY LATE. This also applies to late DQ replies. Please communicate with me if you anticipate having to submit an assignment late. I am happy to be flexible, with advance notice. We may be able to work out an extension based on extenuating circumstances. If you do not communicate with me before submitting an assignment late, the GCU late policy will be in effect. I do not accept assignments that are two or more weeks late unless we have worked out an extension. As per policy, no assignments are accepted after the last day of class. Any assignment submitted after midnight on the last day of class will not be accepted for grading. Communication
Communication is so very important. There are multiple ways to communicate with me: Questions to Instructor Forum: This is a great place to ask course content or assignment questions. If you have a question, there is a good chance one of your peers does as well. This is a public forum for the class. Individual Forum: This is a private forum to ask me questions or send me messages. This will be checked at least once every 24 hours.
- Click here - to use the wp menu builder

- Privacy Policy
- Refund Policy
- Terms Of Service
- Nursing notes PDF
- Nursing Foundations
- Medical Surgical Nursing
- Maternal Nursing
- Pediatric Nursing
- Behavioural sciences
- BSC NURSING
- GNM NURSING
- MSC NURSING
- PC BSC NURSING
- HPSSB AND HPSSC
- Nursing Assignment
Purpose of Hand Washing in Nursing
Purpose of Hand Washing in Nursing-What is Hand Washing,Hand Hygiene Guidelines,Nurse’s Role In Hand washing,Purpose of Hand Washing in Nursing,Why is handwashing so important in nursing?
Table of Contents
What is Hand Washing?
In order to rid the skin of dirt, germs, and other dangerous microorganisms, handwashing is the process of washing one’s hands with water, soap, or a hand sanitizer. Handwashing is a quick and easy technique to stop the transmission of infectious diseases including COVID-19, the flu, and the common cold.
Nurse’s Role In Hand washing
Infections and diseases can be transmitted rapidly through poor hand hygiene, and nurses are particularly susceptible because of their exposure to sick patients. Not only can they themselves be susceptible to illness, they could also be transmitters when they touch affected patients or objects and then happen to pass on infections and viruses to other patients, visitors, or other staff members. This is why the management and minimization of healthcare-associated infections are incredibly important. It is also vital to minimize the risk of dreaded antibacterial resistance and ‘super bugs’ that defy treatment.
Hand washing is an essential practice in nursing that aims to prevent the spread of infection and disease among patients, healthcare workers, and the community. The purpose of hand washing in nursing is to:
Reduce the risk of infections
Hands are a primary vehicle for the transmission of infections. Healthcare workers come into contact with various types of bacteria, viruses, and other microorganisms that can be easily transmitted to patients. Hand washing helps to reduce the spread of infections, including healthcare-associated infections (HAIs), by removing harmful microorganisms from the hands.
Protect vulnerable patients
Patients who are already sick or immunocompromised are particularly vulnerable to infections. Healthcare workers must take every precaution to prevent the transmission of infections from one patient to another. Hand washing is an effective way to prevent the spread of infections and protect vulnerable patients.
Prevent cross-contamination
Cross-contamination occurs when microorganisms are transferred from one surface or person to another. Hand washing helps to prevent cross-contamination by removing microorganisms from the hands of healthcare workers.
Ensure the safety of healthcare workers
Healthcare workers are also at risk of contracting infections from patients. Hand washing is a simple and effective way to protect healthcare workers from exposure to harmful microorganisms.
Proper technique for hand washing
Proper hand washing technique is essential to remove harmful microorganisms from your hands effectively. Here are the general steps for proper hand washing in a healthcare setting:
- Wet your hands with clean, running water, and apply soap. Avoid using hot water, as it can be damaging to your skin and does not kill germs better than warm water.
- Lather your hands with soap, making sure to get the soap on all surfaces of your hands, including between your fingers, the backs of your hands, and under your nails.
- Scrub your hands for at least 20 seconds. You can time yourself by singing “Happy Birthday” twice or another song that lasts around 20 seconds.
- Rinse your hands thoroughly under clean, running water to remove all soap and lather.
- Dry your hands using a clean towel or air dryer. If possible, use a single-use towel or a paper towel to avoid the risk of contamination.
- Turn off the faucet using the towel or your elbow to avoid recontaminating your hands.
Hand Hygiene Guidelines
Hand hygiene guidelines are recommendations for proper hand hygiene practices to prevent the spread of infection. The guidelines are typically issued by healthcare organizations such as the World Health Organization ( WHO ) and the Centers for Disease Control and Prevention (CDC). Here are some general hand hygiene guidelines:
- Wash your hands with soap and water for at least 20 seconds, or use an alcohol-based hand sanitizer with at least 60% alcohol if soap and water are not available.
- Wash your hands before and after caring for a patient, before and after eating, after using the restroom, and after touching anything that could be contaminated.
- Use gloves when in contact with bodily fluids or contaminated surfaces, but remember that gloves are not a substitute for hand hygiene. You should always wash your hands before and after wearing gloves.
- Cover your nose and mouth with a tissue or your sleeve when coughing or sneezing, and dispose of tissues in a trash can.
- Avoid touching your face, especially your eyes, nose, and mouth, as this can transfer germs to your body.
- Regularly clean and disinfect frequently touched surfaces such as doorknobs, light switches, and countertops.
- Monitor and maintain hand hygiene compliance rates in healthcare settings through regular training, observation, and feedback.
Some questions about the Purpose of Hand Washing in Nursing
Why is handwashing so important in nursing?
In order to stop the spread of infections in medical facilities, handwashing is essential in nursing. Patients with compromised immune systems who are more prone to infections are frequently in the company of nurses. Nurses can lessen the possibility of passing harmful microorganisms to their patients by regularly and properly washing their hands.
When should nurses wash their hands?
Every time a nurse interacts with a patient, as well as before and after any activity that might involve contact with potentially infectious materials, like handling contaminated equipment or undergoing invasive procedures, they should wash their hands.
What is the proper way to wash your hands?
You should wet your hands with clean running water, put soap on them, lather them for at least 20 seconds, rinse them thoroughly, and then dry them with a clean towel or an air dryer. It’s crucial to wash the hands thoroughly, including the backs, the spaces in between the fingers, and the areas under the nails.
What type of soap should nurses use for handwashing?
For handwashing, nurses should use an antimicrobial soap or an alcohol-based hand rub. For the soap to be effective against the majority of pathogens, it must be FDA-approved and contain at least 60% alcohol or another antimicrobial substance.
How can nurses encourage patients to practice good hand hygiene?
Nurses can encourage patients to practice good hand hygiene by setting an example and washing hands frequently. They can also educate patients about the importance of hand washing and provide them with resources, such as posters and brochures, to promote hand hygiene. Additionally, nurses can make hand sanitizer and hand washing equipment easily accessible to patients.
Hope you Like this Article Purpose of Hand Washing in Nursing.
Please note that this article is for informational purposes only and should not substitute professional medical advice.
Leave a Reply Cancel reply
Recent articles, navigating the currents: conflict resolution in nursing, health assessment in nursing importance, purpose, and process, use and care of microscopes, causes of terminal illness symptoms diagnosis and coping strategies, six aims of quality of care, continuous bladder irrigation: a comprehensive guide, download nursing notes pdf, staff nurse syllabus and exam pattern question bank -1, medical surgical nursing notes, anatomy and physiology of female reproductive system, mental health nursing process recording, mental health nursing history collection, human anatomy introduction nursing pdf, aiims recruitment question with answers, hpssb & hpssc staff nurse recuirment exam study material - ii, more like this, five legal requirements for nursing documentation, the crucial role of research in nursing care, 5 essential principles of bedmaking, the vital role of public health nurses in our communities, mental health nursing diagnosis care plan pdf, child pediatric health nursing notes -bsc nursing, mid-wifery pdf notes for nursing students, national health programmes in india pdf, reproductive system nursing notes pdf, primary health care nursing notes pdf, psychology note nursing pdf, nursingenotes.com.
- STUDY NOTES
- SUBJECT NOTES
A Digital Platform For Nursing Study Materials
Latest Articles
Cultural competence in healthcare, the advantages of electronic health records, most popular.
© Nursingenotes.com | All rights reserved |

IMAGES
VIDEO
COMMENTS
4. Clean subungual areas with a nail file. 5. Scrub each side of each finger, between the fingers, and the backs and fronts of the hands for at least 4 minutes. 6. Proceed to scrub the hands, keeping the hand higher than the arm at all times to prevent bacteria-laden soap and water from contaminating the hands. 7.
Hand hygiene is a critical practice for healthcare personnel to prevent infections and protect patients. This pdf document provides an overview of the core concepts, evidence, and recommendations for hand hygiene in healthcare settings. Learn how to perform, monitor, and improve hand hygiene practices with this resource from CDC.
2.2. Study Selection, Data Collection, Critical Review, and Level of Evidence. The inclusion criteria were clinical trials; analyzing handwashing techniques and the effectiveness of different methods used by nurses or nursing students; being published in English or Spanish during the period January 2008 to July 2018; and being related to the subject of the present study.
with hand hygiene practices. Nursing Standard . 29, 35, 40-46. doi: 10.7748/ns. 29.35.40.e9929 ... Hand hygiene audit data and a cross-sectional survey were used to measure the impact of the ...
Decontamination using hand hygiene remains one of the most important and effective methods for reducing healthcare-associated infections and cross-infection between patients. In 1860, Florence Nightingale wrote that nurses should wash their hands frequently throughout the day, demonstrating an early awareness of the effectiveness of this simple ...
Hand hygiene basics. Hand hygiene includes washing your hands with soap and water, using an antiseptic hand wash or rub, and surgical hand antisepsis. Hand washing with soap and water entails lathering your hands and vigorously rubbing them together, followed by rinsing with warm (not hot) water.
Despite many efforts, health care-associated infections (HAI) continue to be a threat to hospital patients. Whereas various factors account for HAIs,1 contact transmission is a key pathway.2 Thus, hand hygiene (HH) with soap and water or alcohol-based handrub (ABHR) is regarded as among the most important interventions to prevent HAI.3 As far as 150 years ago, Ignaz Semmelweis described a ...
Dinah Gould. Hand hygiene is the cornerstone of infection prevention but is poorly undertaken and under-appreciated by medical, nursing, and other health care students. This systematic review aimed to identify and describe strategies used to teach the theory and practice of hand hygiene, determine impact on knowledge and practice, and identify ...
10 steps to effective hand washing. Wet hands and forearms. Soap up rubbing palm to palm. Rub with fingers interlaced. Massage between fingers, right palm over back of left hand, left palm over back of right hand Scrub with fingers locked including finger tips. Rub rotationally with thumbs locked Rinse thoroughly.
Introduction. Hand hygiene (HH) is the simplest and most effective measure for preventing healthcare-associated infections (HAIs).[] Despite the simplicity of this procedure and advances made in infection control, hospital health care workers' compliance to HH recommendations is generally low.[] Nurses have the most frequent patient care interactions, and thus more opportunities to practice ...
When assisting with client care, consistent, proper, and meticulous hand hygiene is the single easiest and most effective practice to reduce the risk of transmission of infection to and from the client. Hand hygiene mainly includes handwashing with soap and water and using an alcohol -based hand rub. Now, depending on your facility's policy ...
The CDC Guideline for Hand Hygiene in Healthcare Settings [PDF - 1.3 MB] recommends: . When cleaning your hands with soap and water, wet your hands first with water, apply the amount of product recommended by the manufacturer to your hands, and rub your hands together vigorously for at least 15 seconds, covering all surfaces of the hands and fingers.
A 2020-2021 study published by the U.S. Department of Agriculture discovered that 95 percent of people don't wash their hands properly. This is a pretty shocking discovery that should give everyone pause, especially those who care for sick patients on a regular basis like nurses.. Keep in mind, though, that there are a lot of opinions out there about the "right" way to wash your hands.
This is a reflective essay based on personal experience of hand washing and hand hygiene practices in clinical practice. It focuses on the most recent policy and guidelines from the National Health Service (NHS) England and NHS Improvement which will be discussed in more detail below. Reflective practice is commonly used by nurses and other ...
Recommended publications. PDF | On Dec 3, 2013, Michael Bunyan published A lesson plan for practicing nurses to promote effective hand hygiene | Find, read and cite all the research you need on ...
Methods. A multi-disciplinary team was formed comprising infection control physicians and nurses and the nursing education team. It established an approach to promote better hand hygiene practice among nursing students as well as to drive an innovative learning experience based on previous positive results with medical students [].A hand hygiene auditor training programme was incorporated into ...
The link is for the CDC Webasite on Hand Hygiene in Healthcare setting. Taken from the page description, "Hand Hygiene in Healthcare Settings provides healthcare workers and patients with a variety of resources including guidelines for providers, patient empowerment materials, the latest technological advances in hand hygiene adherence measurement, frequently asked questions, and links to ...
Utilising Evidence Based Care. This essay endeavours to investigate hand hygiene, and feel I need to gain more knowledge in this field by utilising the available evidence effectively. I also intend to discuss nurse held traditions, customs and rituals. The common method of handwasing is usually with unmedicated soaps, whist an anti-bacterial ...
Therefore, nurses should embrace evidence-based hand hygiene practices like the use of alcohol-based sanitizers and soap and water. Cleaning hands by rubbing alcohol-based formulation is an effective hand sanitizing technique if the hand are not visibly soiled (Martos-Cabrera et al., 2019). This approach is faster and better tolerated compared ...
Nurse's Role In Hand washing. Purpose of Hand Washing in Nursing. Reduce the risk of infections. Protect vulnerable patients. Prevent cross-contamination. Ensure the safety of healthcare workers. Proper technique for hand washing. Hand Hygiene Guidelines.
Assignment on Hand washing | Nursing students #bscnursing #nursing #video.
Hand washing Hand washing. Purpose: Effective hand hygiene to reduce the incidence of healthcare-associated infectionsPolicy: All members of the healthcare team will comply with current CDC hand hygiene guidelines. Procedure Indications for HandwashingIndications for Handwashing Wash hands when hands are visibly dirty. Wash hands using antimicrobial soap and water before eating and after using ...