May 10, 2021

The Forgotten History of the World's First Trans Clinic
The Institute for Sexual Research in Berlin would be a century old if it hadn’t fallen victim to Nazi ideology
By Brandy Schillace
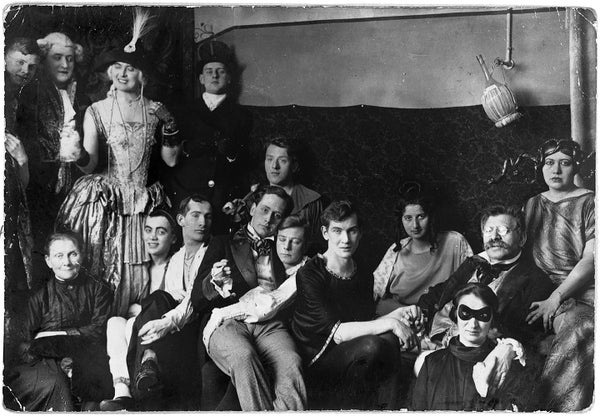
Costume party at the Institute for Sexual Research in Berlin, date and photographer unknown. Magnus Hirschfeld ( in glasses ) holds hands with his partner, Karl Giese ( center ).
Magnus-Hirschfeld-Gesellschaft e.V., Berlin
Late one night on the cusp of the 20th century, Magnus Hirschfeld, a young doctor, found a soldier on the doorstep of his practice in Germany. Distraught and agitated, the man had come to confess himself an Urning —a word used to refer to homosexual men. It explained the cover of darkness; to speak of such things was dangerous business. The infamous “Paragraph 175” in the German criminal code made homosexuality illegal; a man so accused could be stripped of his ranks and titles and thrown in jail.
Hirschfeld understood the soldier’s plight—he was himself both homosexual and Jewish—and did his best to comfort his patient. But the soldier had already made up his mind. It was the eve of his wedding, an event he could not face . Shortly after, he shot himself.
The soldier bequeathed his private papers to Hirschfeld, along with a letter: “The thought that you could contribute to [a future] when the German fatherland will think of us in more just terms,” he wrote, “sweetens the hour of death.” Hirschfeld would be forever haunted by this needless loss; the soldier had called himself a “curse,” fit only to die, because the expectations of heterosexual norms, reinforced by marriage and law, made no room for his kind. These heartbreaking stories, Hirschfeld wrote in The Sexual History of the World War , “bring before us the whole tragedy [in Germany]; what fatherland did they have, and for what freedom were they fighting?” In the aftermath of this lonely death, Hirschfeld left his medical practice and began a crusade for justice that would alter the course of queer history.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Hirschfeld sought to specialize in sexual health, an area of growing interest. Many of his predecessors and colleagues believed that homosexuality was pathological, using new theories from psychology to suggest it was a sign of mental ill health. Hirschfeld, in contrast, argued that a person may be born with characteristics that did not fit into heterosexual or binary categories and supported the idea that a “third sex” (or Geschlecht ) existed naturally. Hirschfeld proposed the term “sexual intermediaries” for nonconforming individuals. Included under this umbrella were what he considered “situational” and “constitutional” homosexuals—a recognition that there is often a spectrum of bisexual practice—as well as what he termed “transvestites.” This group included those who wished to wear the clothes of the opposite sex and those who “from the point of view of their character” should be considered as the opposite sex. One soldier with whom Hirschfeld had worked described wearing women’s clothing as the chance “to be a human being at least for a moment.” He likewise recognized that these people could be either homosexual or heterosexual, something that is frequently misunderstood about transgender people today.
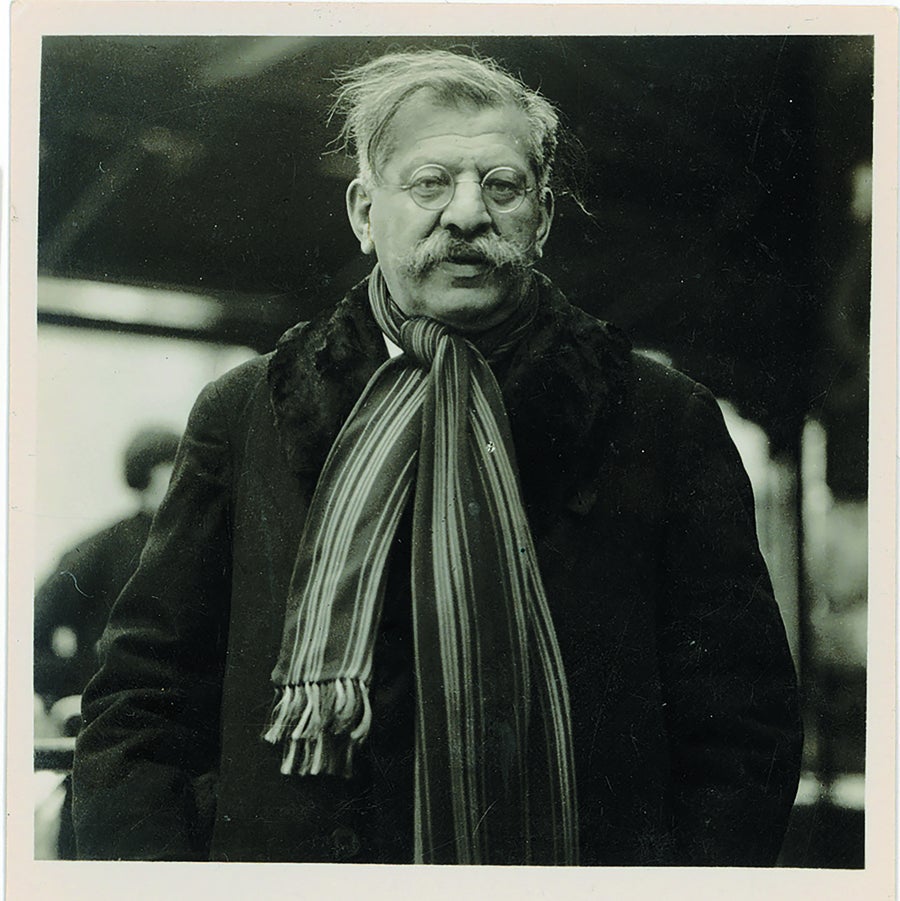
Magnus Hirschfeld, director of the Institute for Sexual Research, in an undated portrait. Credit: Magnus-Hirschfeld-Gesellschaft e.V., Berlin
Perhaps even more surprising was Hirschfeld’s inclusion of those with no fixed gender, akin to today’s concept of gender-fluid or nonbinary identity (he counted French novelist George Sand among them). Most important for Hirschfeld, these people were acting “in accordance with their nature,” not against it.
If this seems like extremely forward thinking for the time, it was. It was possibly even more forward than our own thinking, 100 years later. Current anti-trans sentiments center on the idea that being transgender is both new and unnatural. In the wake of a U.K. court decision in 2020 limiting trans rights, an editorial in the Economist argued that other countries should follow suit , and an editorial in the Observer praised the court for resisting a “disturbing trend” of children receiving gender-affirming health care as part of a transition.
Related: The Disturbing History of Research into Transgender Identity
But history bears witness to the plurality of gender and sexuality. Hirschfeld considered Socrates, Michelangelo and Shakespeare to be sexual intermediaries; he considered himself and his partner Karl Giese to be the same. Hirschfeld’s own predecessor in sexology, Richard von Krafft-Ebing, had claimed in the 19th century that homosexuality was natural sexual variation and congenital.
Hirschfeld’s study of sexual intermediaries was no trend or fad; instead it was a recognition that people may be born with a nature contrary to their assigned gender. And in cases where the desire to live as the opposite sex was strong, he thought science ought to provide a means of transition. He purchased a Berlin villa in early 1919 and opened the Institut für Sexualwissenschaft (the Institute for Sexual Research) on July 6. By 1930 it would perform the first modern gender-affirmation surgeries in the world.
A Place of Safety
A corner building with wings to either side, the institute was an architectural gem that blurred the line between professional and intimate living spaces. A journalist reported it could not be a scientific institute, because it was furnished, plush and “full of life everywhere.” Its stated purpose was to be a place of “research, teaching, healing, and refuge” that could “free the individual from physical ailments, psychological afflictions, and social deprivation.” Hirschfeld’s institute would also be a place of education. While in medical school, he had experienced the trauma of watching as a gay man was paraded naked before the class, to be verbally abused as a degenerate.
Hirschfeld would instead provide sex education and health clinics, advice on contraception, and research on gender and sexuality, both anthropological and psychological. He worked tirelessly to try to overturn Paragraph 175. Unable to do so, he got legally accepted “transvestite” identity cards for his patients, intended to prevent them from being arrested for openly dressing and living as the opposite sex. The grounds also included room for offices given over to feminist activists, as well as a printing house for sex reform journals meant to dispel myths about sexuality. “Love,” Hirschfeld said, “is as varied as people are.”
The institute would ultimately house an immense library on sexuality, gathered over many years and including rare books and diagrams and protocols for male-to-female (MTF) surgical transition. In addition to psychiatrists for therapy, he had hired Ludwig Levy-Lenz, a gynecologist. Together, with surgeon Erwin Gohrbandt, they performed male-to-female surgery called Genitalumwandlung —literally, “transformation of genitals.” This occurred in stages: castration, penectomy and vaginoplasty. (The institute treated only trans women at this time; female-to-male phalloplasty would not be practiced until the late 1940s.) Patients would also be prescribed hormone therapy, allowing them to grow natural breasts and softer features.
Their groundbreaking studies, meticulously documented, drew international attention. Legal rights and recognition did not immediately follow, however. After surgery, some trans women had difficulty getting work to support themselves, and as a result, five were employed at the institute itself. In this way, Hirschfeld sought to provide a safe space for those whose altered bodies differed from the gender they were assigned at birth—including, at times, protection from the law.

1926 portrait of Lili Elbe, one of Hirschfeld's patients. Elbe's story inspired the 2015 film The Danish Girl . Credit: https://wellcomeimages.org/indexplus/image/L0031864.html (CC BY 4.0)
Lives Worth Living
That such an institute existed as early as 1919, recognizing the plurality of gender identity and offering support, comes as a surprise to many. It should have been the bedrock on which to build a bolder future. But as the institute celebrated its first decade, the Nazi party was already on the rise. By 1932 it was the largest political party in Germany, growing its numbers through a nationalism that targeted the immigrant, the disabled and the “genetically unfit.” Weakened by economic crisis and without a majority, the Weimar Republic collapsed.
Adolf Hitler was named chancellor on January 30, 1933, and enacted policies to rid Germany of Lebensunwertes Leben , or “lives unworthy of living.” What began as a sterilization program ultimately led to the extermination of millions of Jews, Roma, Soviet and Polish citizens—and homosexuals and transgender people.
When the Nazis came for the institute on May 6, 1933, Hirschfeld was out of the country. Giese fled with what little he could. Troops swarmed the building, carrying off a bronze bust of Hirschfeld and all his precious books, which they piled in the street. Soon a towerlike bonfire engulfed more than 20,000 books, some of them rare copies that had helped provide a historiography for nonconforming people.
The carnage flickered over German newsreels. It was among the first and largest of the Nazi book burnings. Nazi youth, students and soldiers participated in the destruction, while voiceovers of the footage declared that the German state had committed “the intellectual garbage of the past” to the flames. The collection was irreplaceable.
Levy-Lenz, who like Hirschfeld was Jewish, fled Germany. But in a dark twist, his collaborator Gohrbandt, with whom he had performed supportive operations, joined the Luftwaffe as chief medical adviser and later contributed to grim experiments in the Dachau concentration camp. Hirschfeld’s likeness would be reproduced on Nazi propaganda as the worst kind of offender (both Jewish and homosexual) to the perfect heteronormative Aryan race.
In the immediate aftermath of the Nazi raid, Giese joined Hirschfeld and his protégé Li Shiu Tong, a medical student, in Paris. The three would continue living together as partners and colleagues with hopes of rebuilding the institute, until the growing threat of Nazi occupation in Paris required them to flee to Nice. Hirschfeld died of a sudden stroke in 1935 while still on the run. Giese died by suicide in 1938. Tong abandoned his hopes of opening an institute in Hong Kong for a life of obscurity abroad.
Over time their stories have resurfaced in popular culture. In 2015, for instance, the institute was a major plot point in the second season of the television show Transparent , and one of Hirschfeld’s patients, Lili Elbe, was the protagonist of the film The Danish Girl . Notably, the doctor’s name never appears in the novel that inspired the movie, and despite these few exceptions the history of Hirschfeld’s clinic has been effectively erased. So effectively, in fact, that although the Nazi newsreels still exist, and the pictures of the burning library are often reproduced, few know they feature the world’s first trans clinic. Even that iconic image has been decontextualized, a nameless tragedy.
The Nazi ideal had been based on white, cishet (that is, cisgender and heterosexual) masculinity masquerading as genetic superiority. Any who strayed were considered as depraved, immoral, and worthy of total eradication. What began as a project of “protecting” German youth and raising healthy families had become, under Hitler, a mechanism for genocide.

One of the first and largest Nazi book burnings destroyed the library at the Institute for Sexual Research. Credit: Ullstein Bild and Getty Images
A Note for the Future
The future doesn’t always guarantee progress, even as time moves forward, and the story of the Institute for Sexual Research sounds a warning for our present moment. Current legislation and indeed calls even to separate trans children from supportive parents bear a striking resemblance to those terrible campaigns against so-labeled aberrant lives.
Studies have shown that supportive hormone therapy, accessed at an early age, lowers rates of suicide among trans youth. But there are those who reject the evidence that trans identity is something you can be “born with.” Evolutionary biologist Richard Dawkins was recently stripped of his “humanist of the year” award for comments comparing trans people to Rachel Dolezal , a civil rights activist who posed as a Black woman, as though gender transition were a kind of duplicity. His comments come on the heels of legislation in Florida aiming to ban trans athletes from participating in sports and an Arkansas bill denying trans children and teens supportive care.
Looking back on the story of Hirschfeld’s institute—his protocols not only for surgery but for a trans-supportive community of care, for mental and physical healing, and for social change—it’s hard not to imagine a history that might have been. What future might have been built from a platform where “sexual intermediaries” were indeed thought of in “more just terms”? Still, these pioneers and their heroic sacrifices help to deepen a sense of pride—and of legacy—for LGBTQ+ communities worldwide. As we confront oppressive legislation today, may we find hope in the history of the institute and a cautionary tale in the Nazis who were bent on erasing it.
Brandy Schillace is editor in chief of BMJ's Medical Humanities journal and author of the recently released book Mr. Humble and Doctor Butcher , a biography of Robert White, who aimed to transplant the human soul.
November 16, 2016
A History of Transgender Health Care
As the stigma of being transgender begins to ease, medicine is starting to catch up
By Farah Naz Khan
This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
An estimated 1.4 million Americans, close to 0.6 percent of the population of the United States, identify as transgender. And, today, the topic of transgender health care is more widely discussed than ever before. Despite this, lost in the shuffle between conversations about equal access to bathrooms and popular culture icons is the history of a piece of modern medicine that should no longer remain so elusive. To be willing to embrace the future of this pivotal area of healthcare, it is imperative to understand the piecemeal roots and evolution of transgender medicine.
Magnus Hirschfeld, a German physician who could easily be considered the father of transgender health care, coined the term “ transvestite ” in 1918 at his Institute for Sexual Science in Berlin. Defining transvestism as the desire to express one’s gender in opposition to their defined sex, Hirschfeld and his colleagues used this now antiquated label as a gateway to the provision of sex changing therapies and as a means to protect his patients. Going against the grain, Hirschfeld was one of the first to offer his patients the means to achieve sex change, either through hormone therapy, sex change operations, or both.
In a time when his contemporaries aimed to “cure” transgender patients of their alleged mental affliction, Hirschfeld’s Adaptation Theory supported those who wanted to live according to the gender they felt most aligned with, as opposed to the gender that their sex obligated them to abide by. Much of the history of the institute’s early works were destroyed in the wake of the Nazi book burnings in 1933, but as far as history can prove, Hirschfeld’s institute was the first to offer gender reassignment surgery.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
In 1922, Hirschfeld performed castration on Dora Richter , one of the institute’s employees who later went on to complete her sex reassignment in 1931 with further surgeries at the institute. The institute's most famous patient was arguably Danish painter Lili Elbe (born Einar Wegener) whose life story has been fictionalized in the popular film The Danish Girl . Starting in 1930, Elbe had five surgeries performed as part of her male-to-female transition. Unfortunately, Elbe died from infection-related complications of her final surgery in 1931.
World War II and Nazi Germany forced Hirschfeld into exile and this along with the destruction of his Berlin institute, minimal further advancements were made by his group at that time. Pioneering influences in America began emerging in the 1940s, including Dr. Alfred Kinsey , the biologist who founded the Institute for Sex Research at Indiana University in 1947 (now known as the Kinsey Institute). Kinsey was one of the first to use the term transsexual in his gender studies, and he helped introduce America to a concept that for some reason still seems foreign to many today despite its obvious place in history for years.
The first American to undergo a sex change operation was Christine Jorgensen, who brought significant attention to the transgender revolution in America when her story hit New York Times headlines in 1952. Jorgensen’s willingness to publicly tell her story helped bring a face to the growing transgender revolution in the states, but at the time the lack of quality transgender healthcare in the U.S. meant that Jorgensen had to travel to Denmark to get the treatment she needed.
Following Jorgensen's successful treatment in Denmark by Dr. Christian Hamburger , many other transgender Americans wrote to Hamburger for similar treatment. Hamburger referred these individuals to endocrinologist Henry Benjamin, who had offices in both New York City and San Francisco. Benjamin had been studying transgender issues since at least the 1950s , but it was his 1966 book The Transsexual Phenomenon that left the most indelible impact on American transgender healthcare.
Having spent time with Hirschfeld and his Berlin institute, Benjamin supported the same principles, that those who feel their sex to be discordant from their gender deserve treatment in the form of hormonal therapy and reassignment surgeries and not psychotherapy for a “cure.” In covering such a highly stigmatized health care issue at the time of its publication, The Transsexual Phenomenon laid the foundation for modern transgender healthcare.
Over a decade later, a 1979 study out of Johns Hopkins called sex reassignment surgeries into question by suggesting that psychosocial outcomes in transgender patients who underwent reassignment surgery were not better than those who went without surgery. Despite criticism and a nod to flaws in its methodology, the study led to the closure of the Johns Hopkins Gender Identity Clinic and an end to the sex reassignment surgeries offered there.
In an attempt to standardize care in response to this study’s accusations, the Henry Benjamin International Gender Dysphoria Association, now better known as the World Professional Association for Transgender Health (WPATH), created the first version of Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. Now in its seventh iteration, the WPATH Standards of Care provide guidance on everything from hormone therapy to surgical interventions and everything in between.
Despite all of the apparent advancements in transgender health care noted above, the 1980 addition of “ gender identity disorder ” to the American Psychiatric Association’s (APA) third Diagnostic and Statistical Manual (DSM-3) seemed like a giant leap backwards, but this controversial move actually helped transgender individuals gain access to an often impenetrable healthcare system. Slowly, but surely, strides were made towards removing the notion of “ disorder ” in the context of gender identity, and with the release of the DSM-5 in 2013, gender identity disorder was replaced with the diagnosis “gender dysphoria.”
Destigmatization of this diagnosis was a major milestone for transgender individuals in America, and further strides were achieved when a government appeals board in 2014 ruled that Medicare must cover surgery for gender transitions, overturning a policy that had been in place since the 1980s. Given that the surgeries are no longer experimental in nature and that the updated WPATH standards of care reference many studies which have proven the beneficial effects of sex reassignment therapy for transgender individuals, this ruling was a long time coming.
Gone are the days of rudimentary surgeries and experimental therapies, because we now know what works. And in an effort to make treatment of transgender patients even easier and more accessible for providers everywhere, in 2009, the Endocrine Society put together brief clinical practice guidelines . These guidelines cover diagnosis, treatment, and preventive care needs for transgender patients, while also drawing attention to the potential risks associated with gender transition therapies.
Modern transgender healthcare encompasses all of the above, along with a shift in focus on patient care. Our transgender patients are like all of our other patients, and their gender identity is just one facet of their overall identity. Multidisciplinary clinics that focus on key issues for transgender patients are important, because they can provide access to subspecialists who can focus on hormone therapy, fertility questions, mental health, etc—but equally important is the understanding that transgender patients need to be able to see a primary care physician for their common cold without fear of stigma due to their gender identity. We can only hope that these widespread stigmas and hesitancies will dissipate with time, because as history has clearly proven, where there is a will, there most certainly is a way.
Advertisement
Stages of Gender Reassignment
- Share Content on Facebook
- Share Content on LinkedIn
- Share Content on Flipboard
- Share Content on Reddit
- Share Content via Email

The idea of getting stuck in the wrong body sounds like the premise for a movie in "Freaky Friday," a mother and a daughter swap bodies, and in "Big" and "13 Going on 30," teenagers experience life in an adult's body. These movies derive their humor from the ways in which the person's attitude and thoughts don't match their appearance. A teenager trapped in her mother's body, for example, revels in breaking curfew and playing air guitar, while a teenager trapped in an adult's body is astounded by the trappings of wealth that come with a full-time job. We laugh because the dialogue and actions are so contrary to what we'd expect from someone who is a mother, or from someone who is an employed adult.
But for some people, living as an incongruous gender is anything but a joke. A transgender person is someone who has a different gender identity than their birth sex would indicate. We interchange the words sex, sexuality and gender all the time, but they don't actually refer to the same thing. Sex refers to the parts we were born with; boys, we assume, have a penis, while girls come equipped with a vagina. Sexuality generally refers to sexual orientation , or who we're attracted to in a sexual and/or romantic sense. Gender expression refers to the behavior used to communicate gender in a given culture. Little girls in the U.S., for example, would be expected express their feminine gender by playing with dolls and wearing dresses, and little boys would be assumed to express their masculinity with penchants for roughhousing and monster trucks. Another term is g ender identity, the private sense or feeling of being either a man or woman, some combination of both or neither [source: American Psychological Association ].
Sometimes, a young boy may want to wear dresses and have tea parties, yet it's nothing more than a phase that eventually subsides. Other times, however, there is a longing to identify with another gender or no gender at all that becomes so intense that the person experiencing it can't function anymore. Transgender is an umbrella term for people who identify outside of the gender they were assigned at birth and for some gender reassignment surgeries are crucial to leading a healthy, happy life.
Gender Dysphoria: Diagnosis and Psychotherapy
Real-life experience, hormone replacement therapy, surgical options: transgender women, surgical options: transgender men, gender reassignment: regrets.

Transgender people may begin identifying with a different gender, rather than the one assigned at birth, in early childhood, which means they can't remember a time they didn't feel shame or distress about their bodies. For other people, that dissatisfaction with their biological sex begins later, perhaps around puberty or early adulthood, though it can occur later in life as well.
It's estimated that about 0.3 percent of the U.S. population self-identify as transgender, but not all who are transgender will choose to undergo a gender transition [source: Gates ]. Some may choose to affirm their new gender through physically transforming their bodies from the top down, while others may prefer to make only certain cosmetic changes, such as surgeries to soften facial features or hair removal procedures, for example.
Not all who identify with a gender different than their birth sex suffer from gender dysphoria or go on to seek surgery. Transgender people who do want gender reassignment surgery, however, must follow the standards of care for gender affirmation as defined by the World Professional Association for Transgender Health (WPATH).
In 1980, when gender identity disorder (GID) was first recognized, it was considered a psychiatric disorder. In 2013, though, GID was, in part, reconsidered as biological in nature, and renamed gender dysphoria . It was reclassified as a medical condition in the American Psychological Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-V), a common language and standards protocol manual for the classification of mental disorders. With this classification, transgender people must be diagnosed prior to any treatment [source: International Foundation for Gender Education ].
Gender dysphoria is diagnosed when a person has a persistent desire to become a different gender. The desire may manifest itself as disgust for one's reproductive organs, hatred for the clothing and other outward signs of one's given gender, and/or a desire to act and be recognized as another gender. This desire must be continuously present for six months in order to be recognized as a disorder [source: WPATH].
In addition to receiving the diagnosis from a mental health professional, a person seeking reassignment must also take part in psychotherapy. The point of therapy isn't to ignite a change, begin a conversion or otherwise convince a transgender person that it's wrong to want to be of a different gender (or of no specific gender at all) . Rather, counseling is required to ensure that the person is realistic about the process of gender affirmation and understands the ramifications of not only going through with social and legal changes but with permanent options such as surgery. And because feeling incongruous with your body can be traumatizing and frustrating, the mental health professional will also work to identify any underlying issues such as anxiety, depression, substance abuse or borderline personality disorder.
The mental health professional can also help to guide the person seeking gender reassignment through the next step of the process: real-life experience.

WPATH requires transgender people desiring gender reassignment surgery to live full-time as the gender that they wish to be before pursuing any permanent options as part of their gender transition. This period is a known as real-life experience (RLE) .
It's during the RLE that the transgender person often chooses a new name appropriate for the desired gender, and begins the legal name-change process. That new name often comes with a set of newly appropriate pronouns, too; for example, when Chastity Bono, biologically born as Sonny and Cher's daughter in 1969, began her transition in 2008 she renamed herself as Chaz and instructed people to use "he" rather than "she" [source: Donaldson James ].
In addition to a new name and pronouns, during this time gender-affirming men and women are expected to also adopt the clothing of their desired gender while maintaining their employment, attending school or volunteering in the community. Trans women might begin undergoing cosmetic procedures to rid themselves of body hair; trans men might take voice coaching in attempt to speak in a lower pitch. The goal of real-life experience is to expose social issues that might arise if the individual were to continue gender reassignment. How, for example, will a boss react if a male employee comes to work as a female? What about family? Or your significant other? Sometimes, during RLE people realize that living as the other gender doesn't bring the happiness they thought it would, and they may not continue to transition. Other times, a social transition is enough, and gender reassignment surgery isn't pursued. And sometimes, this test run is the confirmation people need to pursue physical changes in order to fully become another gender.
In addition to the year-long real-life experience requirement before surgical options may be pursued, WPATH recommends hormonal therapy as a critical component to transitioning before surgery. Candidates for hormone therapy may choose to complete a year-long RLE and counseling or complete six months of a RLE or three-months of a RLE/three months of psychotherapy before moving ahead with hormone therapy.
Upon successfully completing a RLE by demonstrating stable mental health and a healthy lifestyle, the transitioning individual becomes eligible for genital reconstructive surgery — but it can't begin until a mental health professional submits a letter (or letters) of recommendation indicating that the individual is ready to move forward [source: WPATH].

Hormone replacement therapy (HRT) , also called cross-sex hormones, is a way for transgender individuals to feel and look more like the gender they identify with, and so it's a major step in gender reassignment. In order to be eligible for hormone therapy, participants must be at least 18 years old (though sometimes, younger adolescents are allowed to take hormone blockers to prohibit their naturally occurring puberty) and demonstrate to a mental health professional that they have realistic expectations of what the hormones will and won't do to their bodies. A letter from that mental health professional is required, per the standards of care established by WPATH.
Hormone therapy is used to balance a person's gender identity with their body's endocrine system. Male-to-female candidates begin by taking testosterone-blocking agents (or anti-androgens ) along with female hormones such as estrogen and progesterone . This combination of hormones is designed to lead to breast growth, softer skin, less body hair and fewer erections. These hormones also change the body by redistributing body fat to areas where women tend to carry extra weight (such as around the hips) and by decreasing upper body strength. Female-to-male candidates begin taking testosterone , which will deepen the voice and may cause some hair loss or baldness. Testosterone will also cause the clitoris to enlarge and the person's sex drive to increase. Breasts may slightly shrink, while upper body strength will increase [source: WPATH].
It usually takes two continuous years of treatment to see the full results of hormone therapy. If a person were to stop taking the hormones, then some of these changes would reverse themselves. Hormone therapy is not without side effects — both men and women may experience an increased risk for cardiovascular disease, and they are also at risk for fertility problems. Some transgender people may choose to bank sperm or eggs if they wish to have children in the future.
Sometimes hormonal therapy is enough to make a person feel he or she belongs to the desired gender, so treatment stops here. Others may pursue surgical means as part of gender reassignment.

Surgical options are usually considered after at least two years of hormonal therapy, and require two letters of approval by therapists or physicians. These surgeries may or may not be covered by health insurance in the U.S. — often only those that are considered medically necessary to treat gender dysphoria are covered, and they can be expensive. Gender reassignment costs vary based on each person's needs and desires; expenses often range between $7,000 and $50,000 (in 2014), although costs may be much greater depending upon the type (gender reconstructive surgeries versus cosmetic procedures) and number of surgeries as well as where in the world they are performed [source: AP ].
Gender affirmation is done with an interdisciplinary team, which includes mental health professionals, endocrinologists, gynecologists, urologists and reconstructive cosmetic surgeons.
One of the first surgeries male-to-female candidates pursue is breast augmentation, if HRT doesn't enlarge their breasts to their satisfaction. Though breast augmentations are a common procedure for cisgender women (those who identify with the gender they were assigned at birth), care must be taken when operating on a biologically male body, as there are structural differences, like body size, that may affect the outcome.
The surgical options to change male genitalia include orchiectomy (removal of the testicles), penile inversion vaginoplasty (creation of a vagina from the penis), clitoroplasty (creation of a clitoris from the glans of the penis) and labiaplasty (creation of labia from the skin of the scrotum) [source: Nguyen ]. The new vagina, clitoris and labia are typically constructed from the existing penile tissue. Essentially, after the testicles and the inner tissue of the penis is removed and the urethra is shortened, the skin of the penis is turned inside out and fashioned into the external labia and the internal vagina. A clitoris is created from excess erectile tissue, while the glans ends up at the opposite end of the vagina; these two sensitive areas usually mean that orgasm is possible once gender reassignment is complete. Male-to-female gender reconstructive surgery typically takes about four or five hours [source: University of Michigan ]. The major complication from this surgery is collapse of the new vaginal cavity, so after surgery, patients may have to use dilating devices.
Trans women may also choose to undergo cosmetic surgeries to further enhance their femininity. Procedures commonly included with feminization are: blepharoplasty (eyelid surgery); cheek augmentation; chin augmentation; facelift; forehead and brow lift with brow bone reduction and hair line advance; liposuction; rhinoplasty; chondrolargynoplasty or tracheal shave (to reduce the appearance of the Adam's apple); and upper lip shortening [source: The Philadelphia Center for Transgender Surgery]. Trans women may pursue these surgeries with any cosmetic plastic surgeon, but as with breast augmentation, a doctor experienced with this unique situation is preferred. One last surgical option is voice modification surgery , which changes the pitch of the voice (alternatively, there is speech therapy and voice training, as well as training DVDs and audio recordings that promise the same thing).

Female-to-male surgeries are pursued less often than male-to-female surgeries, mostly because when compared to male-to-female surgeries, trans men have limited options; and, historically, successful surgical outcomes haven't been considered on par with those of trans women. Still, more than 80 percent of surgically trans men report having sexual intercourse with orgasm [source: Harrison ].
As with male-to-female transition, female-to-male candidates may begin with breast surgery, although for trans men this comes in the form of a mastectomy. This may be the only surgery that trans men undergo in their reassignment, if only because the genital surgeries available are still far from perfect. Forty percent of trans men who undergo genital reconstructive surgeries experience complications including problems with urinary function, infection and fistulas [sources: Harrison , WPATH].
Female-to-male genital reconstructive surgeries include hysterectomy (removal of the uterus) and salpingo-oophorectomy (removal of the fallopian tubes and ovaries). Patients may then elect to have a metoidioplasty , which is a surgical enlargement of the clitoris so that it can serve as a sort of penis, or, more commonly, a phalloplasty . A phalloplasty includes the creation of a neo-phallus, clitoral transposition, glansplasty and scrotoplasty with prosthetic testicles inserted to complete the appearance.
There are three types of penile implants, also called penile prostheses: The most popular is a three-piece inflatable implant, used in about 75 percent of patients. There are also two-piece inflatable penile implants, used only 15 percent of the time; and non-inflatable (including semi-rigid) implants, which are used in fewer than 10 percent of surgeries. Inflatable implants are expected to last about five to 10 years, while semi-rigid options typically have a lifespan of about 20 years (and fewer complications than inflatable types) [source: Crane ].
As with trans women, trans men may elect for cosmetic surgery that will make them appear more masculine, though the options are slightly more limited; liposuction to reduce fat in areas in which cisgender women i tend to carry it is one of the most commonly performed cosmetic procedures.

As surgical techniques improve, complication rates have fallen too. For instance, long-term complication risks for male-to-female reconstructive surgeries have fallen below 1 percent. Despite any complications, though, the overwhelming majority of people who've undergone surgical reconstruction report they're satisfied with the results [source: Jarolím ]. Other researchers have noted that people who complete their transition process show a marked improvement in mental health and a substantial decrease in substance abuse and depression. Compare these results to 2010 survey findings that revealed that 41 percent of transgender people in the U.S. attempted suicide, and you'll see that finally feeling comfortable in one's own skin can be an immensely positive experience [source: Moskowitz ].
It's difficult, though, to paint a complete picture of what life is like after people transition to a new gender, as many people move to a new place for a fresh start after their transition is complete. For that reason, many researchers, doctors and therapists have lost track of former patients. For some people, that fresh start is essential to living their new lives to the fullest, while others have found that staying in the same job, the same marriage or the same city is just as rewarding and fulfilling and vital to their sense of acceptance.
In many ways, the process of gender affirmation is ongoing. Even after the surgeries and therapies are complete, people will still have to deal with these discrimination issues. Transgender people are often at high risk for hate crimes. Regular follow-ups will be necessary to maintain both physical and mental health, and many people continue to struggle with self-acceptance and self-esteem after struggling with themselves for so long. Still, as more people learn about gender reassignment, it seems possible that that these issues of stigma and discrimination won't be so prevalent.
As many as 91 percent Americans are familiar with the term "transgender" and 76 percent can correctly define it; 89 percent agree that transgender people deserve the same rights, privileges and protections as those who are cisgender [source: Public Religion Research Institute ]. But that's not to say that everything becomes completely easy once a person transitions to his or her desired gender.
Depending upon where you live, non-discrimination laws may or may not cover transgender individuals, so it's completely possible to be fired from one's job or lose one's home due to gender expression. Some people have lost custody of their children after divorces and have been unable to get courts to recognize their parental rights. Historically, some marriages were challenged — consider, for example, what happens when a man who is married to a woman decides to become a woman; after the surgery, if the two people decide to remain married, it now appears to be a same-sex marriage, which is now legalized in the U.S. Some organizations and governments refuse to recognize a person's new gender unless genital reconstructive surgery has been performed, despite the fact that some people only pursue hormone therapy or breast surgery [sources: U.S. Office of Personnel Management , Glicksman ].
Lots More Information
Author's note: stages of gender reassignment.
It's interesting how our terminology changes throughout the years, isn't it? (And in some cases for the better.) What we used to call a sex change operation is now gender realignment surgery. Transsexual is now largely replaced with transgender. And with good reason, I think. Knowing that sex, sexuality and gender aren't interchangeable terms, updating "sex change" to "gender reassignment" or "gender affirmation" and "transsexual" to "transgender" moves the focus away from what sounds like something to do with sexual orientation to one that is a more accurate designation.
Related Articles
- How Gender Identity Disorder Works
- Is gender just a matter of choice?
- What is transgender voice therapy?
- How fluid is gender?
- Why do girls wear pink and boys wear blue?
More Great Links
- DSM-5: Gender Dysphoria
- National Center for Transgender Equality
- The Williams Institute
- American Medical Student Association (AMSA). "Transgender Health Resources." 2014. (April 20, 2015) http://www.amsa.org/AMSA/Homepage/About/Committees/GenderandSexuality/TransgenderHealthCare.aspx
- American Psychological Association (APA). "Definition of Terms: Sex, Gender, Gender Identity, Sexual Orientation." 2011. (July 1, 2015) http://www.apa.org/pi/lgbt/resources/sexuality-definitions.pdf
- AP. "Medicare ban on sex reassignment surgery lifted." May 30, 2014. (April 20, 2015) http://www.usatoday.com/story/news/nation/2014/05/30/medicare-sex-reassignment/9789675/
- Belkin, Lisa. "Smoother Transitions." The New York Times. Sept. 4, 2008. (Aug. 1, 2011) http://www.nytimes.com/2008/09/04/fashion/04WORK.html
- Crane, Curtis. "The Total Guide to Penile Implants For Transsexual Men." Transhealth. May 2, 2014. (April 20, 2015) http://www.trans-health.com/2013/penile-implants-guide/
- Donaldson James, Susan. "Trans Chaz Bono Eyes Risky Surgery to Construct Penis." ABC News. Jan. 6, 2012. (April 20, 2015) http://abcnews.go.com/Health/transgender-chaz-bono-seeks-penis-genital-surgery-risky/story?id=15299871Gates, Gary J. "How many people are lesbian, gay, bisexual, and transgender?" April 2011. (July 29, 2015) http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf
- Glicksman, Eve. "Transgender today." Monitor on Psychology. Vol. 44, no. 4. Page 36. April 2013. (April 20, 2015) http://www.apa.org/monitor/2013/04/transgender.aspx
- Harrison, Laird. "Sex-Change Operations Mostly Successful." Medscape Medical News. May 20, 2013. (April 20, 2015) http://www.medscape.com/viewarticle/804432
- HealthResearchFunding.org (HRF). "14 Unique Gender Identity Disorder Statistics." July 28, 2014. (April 20, 2015) http://healthresearchfunding.org/gender-identity-disorder-statistics/
- International Foundation for Gender Education. "APA DSM-5 Sexual and Gender Identity Disorders: 302.85 Gender Identity Disorder in Adolescents or Adults." (April 20, 2015) http://www.ifge.org/302.85_Gender_Identity_Disorder_in_Adolescents_or_Adults
- Moskowitz, Clara. "High Suicide Risk, Prejudice Plague Transgender People." LiveScience. Nov. 18, 2010. (April 20, 2015) http://www.livescience.com/11208-high-suicide-risk-prejudice-plague-transgender-people.html
- Nguyen, Tuan A. "Male-To-Female Procedures." Lake Oswego Plastic Surgery. 2013. (April 20, 2015) http://www.lakeoswegoplasticsurgery.com/grs/grs_procedures_mtf.html
- Public Religion Research Institute. "Survey: Strong Majorities of Americans Favor Rights and Legal Protections for Transgender People." Nov. 3, 2011. (April 20, 2015) http://publicreligion.org/research/2011/11/american-attitudes-towards-transgender-people/#.VSmlgfnF9bw
- Steinmetz, Katy. "Board Rules That Medicare Can Cover Gender Reassignment Surgery." Time. (April 20, 2015) http://time.com/2800307/medicare-gender-reassignment/
- The Philadelphia Center for Transgender Surgery. "Phalloplasty: Frequently Asked Questions." (April 20, 2015) http://www.thetransgendercenter.com/index.php/surgical-procedures/phalloplasty-faqs.html
- U.S. Office of Personnel Management. "Guidance Regarding the Employment of Transgender Individuals in the Federal Workplace." 2015. (April 20, 2015) http://www.opm.gov/diversity/Transgender/Guidance.asp
- University of California, San Francisco - Department of Family and Community Medicine, Center of Excellence for Transgender Health. "Primary Care Protocol for Transgender Patient Care." April 2011. (April 20, 2015) http://transhealth.ucsf.edu/trans?page=protocol-hormones
- University of Miami - Miller School of Medicine, Department of Surgery, Plastic, Aesthetic and Reconstructive Surgery. "Transgender Reassignment." 2015. (April 20, 2015) http://surgery.med.miami.edu/plastic-and-reconstructive/transgender-reassignment-surgery
- University of Michigan Health System. "Gender Affirming Surgery." (April 20, 2015) http://www.uofmhealth.org/medical-services/gender-affirming-surgery
- World Professional Association for Transgender Health (WPATH). "Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People." Version 7. 2012. (April 20, 2015) http://www.wpath.org/uploaded_files/140/files/Standards%20of%20Care,%20V7%20Full%20Book.pdf
- World Professional Association for Transgender Health (WPATH). "WPATH Clarification on Medical Necessity of Treatment, Sex Reassignment, and Insurance Coverage for Transgender and Transsexual People Worldwide." 2015. (April 20, 2015) http://www.wpath.org/site_page.cfm?pk_association_webpage_menu=1352&pk_association_webpage=3947
Please copy/paste the following text to properly cite this HowStuffWorks.com article:

- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Gender Confirmation Surgery (GCS)
What is Gender Confirmation Surgery?
- Transfeminine Tr
Transmasculine Transition
- Traveling Abroad
Choosing a Surgeon
Gender confirmation surgery (GCS), known clinically as genitoplasty, are procedures that surgically confirm a person's gender by altering the genitalia and other physical features to align with their desired physical characteristics. Gender confirmation surgeries are also called gender affirmation procedures. These are both respectful terms.
Gender dysphoria , an experience of misalignment between gender and sex, is becoming more widely diagnosed. People diagnosed with gender dysphoria are often referred to as "transgender," though one does not necessarily need to experience gender dysphoria to be a member of the transgender community. It is important to note there is controversy around the gender dysphoria diagnosis. Many disapprove of it, noting that the diagnosis suggests that being transgender is an illness.
Ellen Lindner / Verywell
Transfeminine Transition
Transfeminine is a term inclusive of trans women and non-binary trans people assigned male at birth.
Gender confirmation procedures that a transfeminine person may undergo include:
- Penectomy is the surgical removal of external male genitalia.
- Orchiectomy is the surgical removal of the testes.
- Vaginoplasty is the surgical creation of a vagina.
- Feminizing genitoplasty creates internal female genitalia.
- Breast implants create breasts.
- Gluteoplasty increases buttock volume.
- Chondrolaryngoplasty is a procedure on the throat that can minimize the appearance of Adam's apple .
Feminizing hormones are commonly used for at least 12 months prior to breast augmentation to maximize breast growth and achieve a better surgical outcome. They are also often used for approximately 12 months prior to feminizing genital surgeries.
Facial feminization surgery (FFS) is often done to soften the lines of the face. FFS can include softening the brow line, rhinoplasty (nose job), smoothing the jaw and forehead, and altering the cheekbones. Each person is unique and the procedures that are done are based on the individual's need and budget,
Transmasculine is a term inclusive of trans men and non-binary trans people assigned female at birth.
Gender confirmation procedures that a transmasculine person may undergo include:
- Masculinizing genitoplasty is the surgical creation of external genitalia. This procedure uses the tissue of the labia to create a penis.
- Phalloplasty is the surgical construction of a penis using a skin graft from the forearm, thigh, or upper back.
- Metoidioplasty is the creation of a penis from the hormonally enlarged clitoris.
- Scrotoplasty is the creation of a scrotum.
Procedures that change the genitalia are performed with other procedures, which may be extensive.
The change to a masculine appearance may also include hormone therapy with testosterone, a mastectomy (surgical removal of the breasts), hysterectomy (surgical removal of the uterus), and perhaps additional cosmetic procedures intended to masculinize the appearance.
Paying For Gender Confirmation Surgery
Medicare and some health insurance providers in the United States may cover a portion of the cost of gender confirmation surgery.
It is unlawful to discriminate or withhold healthcare based on sex or gender. However, many plans do have exclusions.
For most transgender individuals, the burden of financing the procedure(s) is the main difficulty in obtaining treatment. The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed.
A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019.
Traveling Abroad for GCS
Some patients seek gender confirmation surgery overseas, as the procedures can be less expensive in some other countries. It is important to remember that traveling to a foreign country for surgery, also known as surgery tourism, can be very risky.
Regardless of where the surgery will be performed, it is essential that your surgeon is skilled in the procedure being performed and that your surgery will be performed in a reputable facility that offers high-quality care.
When choosing a surgeon , it is important to do your research, whether the surgery is performed in the U.S. or elsewhere. Talk to people who have already had the procedure and ask about their experience and their surgeon.
Before and after photos don't tell the whole story, and can easily be altered, so consider asking for a patient reference with whom you can speak.
It is important to remember that surgeons have specialties and to stick with your surgeon's specialty. For example, you may choose to have one surgeon perform a genitoplasty, but another to perform facial surgeries. This may result in more expenses, but it can result in a better outcome.
A Word From Verywell
Gender confirmation surgery is very complex, and the procedures that one person needs to achieve their desired result can be very different from what another person wants.
Each individual's goals for their appearance will be different. For example, one individual may feel strongly that breast implants are essential to having a desirable and feminine appearance, while a different person may not feel that breast size is a concern. A personalized approach is essential to satisfaction because personal appearance is so highly individualized.
Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review . Transgend Health . 2018;3(1):159-169. doi:10.1089/trgh.2018.0014
Morrison SD, Vyas KS, Motakef S, et al. Facial Feminization: Systematic Review of the Literature . Plast Reconstr Surg. 2016;137(6):1759-70. doi:10.1097/PRS.0000000000002171
Hadj-moussa M, Agarwal S, Ohl DA, Kuzon WM. Masculinizing Genital Gender Confirmation Surgery . Sex Med Rev . 2019;7(1):141-155. doi:10.1016/j.sxmr.2018.06.004
Dowshen NL, Christensen J, Gruschow SM. Health Insurance Coverage of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information . Transgend Health . 2019;4(1):131-135. doi:10.1089/trgh.2018.0055
American Society of Plastic Surgeons. Rhinoplasty nose surgery .
Rights Group: More U.S. Companies Covering Cost of Gender Reassignment Surgery. CNS News. http://cnsnews.com/news/article/rights-group-more-us-companies-covering-cost-gender-reassignment-surgery
The Sex Change Capital of the US. CBS News. http://www.cbsnews.com/2100-3445_162-4423154.html
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.
This is the beneficial effect of sex-reassignment surgery early on in a transition

Surgery "is often the last and the most considered step in the treatment process for gender dysphoria". Image: REUTERS/Gleb Garanich
.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Reuters Staff

.chakra .wef-9dduvl{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-9dduvl{font-size:1.125rem;}} Explore and monitor how .chakra .wef-15eoq1r{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;color:#F7DB5E;}@media screen and (min-width:56.5rem){.chakra .wef-15eoq1r{font-size:1.125rem;}} SDG 10: Reduced Inequalities is affecting economies, industries and global issues

.chakra .wef-1nk5u5d{margin-top:16px;margin-bottom:16px;line-height:1.388;color:#2846F8;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-1nk5u5d{font-size:1.125rem;}} Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:, sdg 10: reduced inequalities.
When transgender people undergo sex-reassignment surgery, the beneficial effect on their mental health is still evident - and increasing - years later, a Swedish study suggests.
Overall, people in the study with gender incongruence - that is, their biological gender doesn’t match the gender with which they identify - were six times more likely than people in the general population to visit a doctor for mood and anxiety disorders. They were also three times more likely to be prescribed antidepressants, and six times more likely to be hospitalized after a suicide attempt, researchers found.
But among trans people who had undergone gender-affirming surgery, the longer ago their surgery, the less likely they were to suffer anxiety, depression or suicidal behavior during the study period, researchers reported in The American Journal of Psychiatry.
Surgery to modify a person’s sex characteristics “is often the last and the most considered step in the treatment process for gender dysphoria,” according to the World Professional Association for Transgender Health.
Many transsexual, transgender, and gender-nonconforming individuals "find comfort with their gender identity, role, and expression without surgery," but for others, "surgery is essential and medically necessary to alleviate their gender dysphoria," according to the organization. (bit.ly/2WEn9Lg)
Have you read?
This is the state of lgbti rights around the world in 2018.
While the new study confirms that transgender individuals are more likely to use mental health treatments, it also shows that gender-affirming therapy might reduce this risk, coauthor Richard Branstrom of the Karolinska Institutet in Stockholm told Reuters Health by email.
Branstrom and colleague John Pachankis of the Yale School of Public Health in New Haven, Connecticut found that as of 2015, 2,679 people in Sweden had a diagnosis of gender incongruence, out of the total population of 9.7 million.
That year, 9.3% of people with gender incongruence visited a doctor for mood disorders, 7.4% saw a doctor for anxiety disorders, and 29% were on antidepressants. In the general population, those percentages were 1%, 0.6% and 9.4%, respectively.
Just over 70% of people with gender incongruence were receiving feminizing or masculinizing hormones to modify outward sexual features such as breasts, body fat distribution, and facial hair, and 48% had undergone gender-affirming surgery. Nearly all of those who had surgery also received hormone therapy.
The benefit of hormone treatment did not increase with time. But “increased time since last gender-affirming surgery was associated with fewer mental health treatments,” the authors report.
In fact, they note, “The likelihood of being treated for a mood or anxiety disorder was reduced by 8% for each year since the last gender-affirming surgery,” for up to 10 years.
Transgender individuals’ use of mental health care still exceeded that of the general Swedish population, which the research team suggests is due at least partly to stigma, economic inequality and victimization.
“We need greater visibility and knowledge about challenges people are confronted with while breaking gender and identity norms,” Branstrom said.
Dr. Joshua Safer, executive director at Mount Sinai Center for Transgender Medicine and Surgery in New York City, told Reuters Health by email, “If anything, the study likely under-reports mental health benefits of medical and surgical care for transgender individuals.”
Safer, who was not involved in the study, said the fact that mental health continued to improve for years after surgery “suggests (surgery provides) extended and ongoing benefit to patients living according to gender identity.”
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
The agenda .chakra .wef-n7bacu{margin-top:16px;margin-bottom:16px;line-height:1.388;font-weight:400;} weekly.
A weekly update of the most important issues driving the global agenda
.chakra .wef-1dtnjt5{display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;} More on Wellbeing and Mental Health .chakra .wef-17xejub{-webkit-flex:1;-ms-flex:1;flex:1;justify-self:stretch;-webkit-align-self:stretch;-ms-flex-item-align:stretch;align-self:stretch;} .chakra .wef-nr1rr4{display:-webkit-inline-box;display:-webkit-inline-flex;display:-ms-inline-flexbox;display:inline-flex;white-space:normal;vertical-align:middle;text-transform:uppercase;font-size:0.75rem;border-radius:0.25rem;font-weight:700;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;line-height:1.2;-webkit-letter-spacing:1.25px;-moz-letter-spacing:1.25px;-ms-letter-spacing:1.25px;letter-spacing:1.25px;background:none;padding:0px;color:#B3B3B3;-webkit-box-decoration-break:clone;box-decoration-break:clone;-webkit-box-decoration-break:clone;}@media screen and (min-width:37.5rem){.chakra .wef-nr1rr4{font-size:0.875rem;}}@media screen and (min-width:56.5rem){.chakra .wef-nr1rr4{font-size:1rem;}} See all

Olena Zelenska: War is harming global mental health — even for people living in safety
Olena Zelenska
May 31, 2024

Improving workplace productivity requires a holistic approach to employee health and well-being
Susan Garfield, Ruma Bhargava and Eric Kostegan
May 30, 2024

Why movement is the best prescription for a healthy workforce
Emma Mason Zwiebler
May 28, 2024

The fascinating link between biodiversity and mental wellbeing
Andrea Mechelli
May 15, 2024

How philanthropy is empowering India's mental health sector
Kiran Mazumdar-Shaw
May 2, 2024

From 'Quit-Tok' to proximity bias, here are 11 buzzwords from the world of hybrid work
Kate Whiting
April 17, 2024
When Transgender Kids Transition, Medical Risks are Both Known and Unknown

The last couple of years have seen burgeoning awareness in society of what it means to be transgender as an adult. But now doctors, like those at Ann and Robert H. Lurie Children’s Hospital of Chicago, are helping children who identify as transgender negotiate their journey into adulthood.
For earlier generations of transgender people, the only way to transition physically was through surgery or taking hormones as adults. However, new medical options are allowing transgender children to start the process of transitioning at younger ages.
But doctors tread carefully, navigating medical interventions that carry risks that are both known and unknown.
PUTTING A PAUSE ON PUBERTY
When someone makes the decision to transition, part of that process can be social — choosing a new name, changing pronouns, wearing different clothes — and part of it can be medical.
One of the more recent medical developments is the use of puberty blockers to treat children who are transgender or gender non-conforming. The medications, which suppress the body’s production of estrogen or testosterone, essentially pause the changes that would occur during puberty.
“That’s really what these pubertal blockers do,” Dr. Rob Garofalo told FRONTLINE. Garofalo is the director of the Lurie Children’s Hospital’s Gender and Sex Development Program. “They allow these families the opportunity to hit a pause button, to prevent natal puberty … until we know that that’s either the right or the wrong direction for their particular child.”
Doctors who use puberty blockers say they allow children who experience gender dysphoria — the feeling that they’re in the wrong body — the time and space to explore and settle on their gender identity. What makes treatment tricky is that there is no test that can tell whether a child experiencing distress about their gender will grow up to be transgender. The handful of studies that do exist suggest that gender dysphoria persists in a minority of children, but they involved very few children and were done mostly abroad.
Puberty blockers have been tested and used for children who start puberty very young — if their bodies start to change before the age of eight or nine. Dr. Courtney Finlayson, a pediatric endocrinologist at Lurie Children’s Hospital, said, “We have a lot of experience in pediatric endocrinology using pubertal blockers. And from all the evidence we have they are generally a very safe medication.”
But their use in treating transgender children is a relatively new practice, first prescribed in the United States by the Gender Management Service at Boston Children’s Hospital in 2007, and recommended in the Endocrine Society’s guidelines for the treatment of transgender people in 2009.
Doctors say the benefit of using puberty blockers is that they block hormone-induced biological changes, such as vocal chord changes, the development of breast tissue or changes in facial structure, that are irreversible and can be especially distressing to children who are gender-non conforming or transgender.
“One of the challenges that’s been faced in the past is that treatment of the transgender population really didn’t start until they were either at least older adolescents or adults,” said Finlayson. “And by that time they’ve had all of the pubertal and physical changes that go along with their … natal sex.”
With the use of puberty blockers, “we’re really starting to some extent from a little bit more of a blank slate,” Finlayson explained. “We don’t have to be erasing or trying to get rid of all these other changes that occurred that they don’t want.”
However, the use of puberty blockers to treat transgender children is what’s considered an “off label” use of the medication — something that hasn’t been approved by the Food and Drug Administration. And doctors say their biggest concern is about how long children stay on the medication, because there isn’t enough research into the effects of stalling puberty at the age when children normally go through it.
The Endocrine Society’s guidelines suggest starting puberty blockers for transgender children when they hit a stage of development known as Tanner stage 2 — usually around 10 or 11 years old for a girl and 11 or 12 years old for a boy. The same guidelines suggest giving cross sex hormones — estrogen for transgender girls and testosterone for transgender boys — at age 16. However, doctors caution that estrogen and testosterone, the hormones that are blocked by these medications, also play a role in a child’s neurological development and bone growth.
“We do know that there is some decrease in bone density during treatment with pubertal suppression,” Finlayson said, adding that initial studies have shown that starting estrogen and testosterone can help regain the bone density. What Finlayson said there isn’t enough research on is whether someone who was on puberty blockers will regain all their bone strength, or if they might be at risk for osteoporosis in the future.
Another area where doctors say there isn’t enough research is the impact that suppressing puberty has on brain development.
“The bottom line is we don’t really know how sex hormones impact any adolescent’s brain development,” Dr. Lisa Simons, a pediatrician at Lurie Children’s, told FRONTLINE. “We know that there’s a lot of brain development between childhood and adulthood, but it’s not clear what’s behind that.” What’s lacking, she said, are specific studies that look at the neurocognitive effects of puberty blockers.
“I wouldn’t use [puberty blockers] if I didn’t think that they were safe, or that the benefits didn’t outweigh the potential risks,” Finlayson said. “But we always have this conversation with families before we start.”
STARTING HORMONES
The stakes are higher for children who want to continue physically transitioning by taking the hormones of their desired gender. Doctors grapple with when to start cross-sex hormones, and they say it really depends on the child’s readiness and stability in their gender identity.
While the Endocrine Society’s guidelines suggest 16, more and more children are starting hormones at 13 or 14 once their doctors, therapists and families have agreed that they are mentally and emotionally prepared. The shift is because of the concerns over the impact that delaying puberty for too long can have on development, physically, emotionally and socially.
The physical changes that hormones bring about are irreversible, making the decision more weighty than taking puberty blockers. Some of the known side effects of hormones include things that might sound familiar: acne and changes in mood. Patients are also warned that they may be at higher risk for heart disease or diabetes later in life. The risk of blood clots increases for those who start estrogen. And the risk for cancer is an unknown, but it is included in the warnings doctors give their patients.
Another potential dilemma facing transgender children, their families and their doctors is this: Taking cross hormones can reduce fertility. And there isn’t enough research to find out of it is reversible or not. So when children make the decision to start taking hormones, they have to consider whether they ever want to have biological children.
“I think it’s really important to talk to these children and families about fertility,” Finlayson says. “I do worry that at that stage in life many of them may not be able to realize how important that would be to them someday.”
It’s an ethical question that each family has to deal with in their own way, because if a child goes from taking puberty blockers to taking hormones, they may no longer have viable eggs or sperm at the age when they decide they would like to have children. They do have the option to start their puberty and delay their treatment in order to store eggs or sperm, but some of them may not want to.
While transgender adults have taken hormones sometimes for years, the generation growing up now is among the first to start taking hormones so young. Since most people who start hormones take them for life, doctors say there also isn’t enough research into the long-term impact of taking estrogen or testosterone for what could end up being 50 to 70 years.
“There are so many unanswered questions around the long-term consequences, and whether your health risk profile really becomes that of a male or female,” Garofalo says. “If we start testosterone today, will you have the cardiac risk profile of a male or female as you grow older? Will you develop breast cancer because we’re administering estrogen?
“I think those are the unanswered questions that really trouble me, and can only be answered with long-term follow-up studies.”
THE COST OF TRANSITIONING
Most of these treatments are still very expensive and often out of reach for people without the help of insurance. The cost of puberty blockers is approximately $1,200 per month for injections and can range from $4,500 to $18,000 for an implant. The least expensive form of estrogen, a pill, can cost anywhere between $4 to $30 a month, according to Simons, while testosterone can be anywhere between $20 to $200 a vial.
“What we’re seeing in the clinic is that whether or not specific insurance plans cover medication or not is completely arbitrary,” Simons said. “It really can’t be predicted very easily.”
“We almost always just expect a denial,” she said.
“Though it is not the only treatment, doctor-supervised medical transition is critically important to aid people in the treatment of gender dysphoria,” Vincent Paolo Villano, the director of communications at the National Center for Transgender Equality, told FRONTLINE. “Access to medical transition is often unobtainable due to cost and insurance discrimination.”
“Transgender people experience twice the rate of unemployment as non-transgender people, which means they often lack insurance to gain access to health care, period,” Villano said. “And even for trans people with insurance, health plans often outright ban coverage of transition-related care, forcing transgender people to pay outrageous out-of-pocket expenses for medically-necessary procedures that are covered without question for non-transgender people.”
But the trend might be changing, with some insurance companies starting to cover the cost of transitioning. The team at Lurie Children’s Hospital says it has seen several cases in recent months that did not require appeals, or covered the medication after the first appeal.
Ultimately, the doctors working in clinics like the one at Lurie Children’s hope to spare transgender children some of the anguish and societal isolation that earlier generations of transgender people went through. But they too would like the answers to the unknown consequences of these medications.
“The stakes are super high, and we don’t have all the answers,” Garofalo says. “Hopefully, there’s going to be more research and some of those unanswered questions, hopefully, will begin to be answered.”

Priyanka Boghani , Digital Editor , FRONTLINE
More stories.

A Historic Criminal Conviction and Trump’s Ex-‘Fixer’

FRONTLINE’s Reporting on the Israeli-Palestinian conflict

Families of Uvalde Shooting Victims Sue Texas DPS Officers for Waiting To Confront Gunman

Where Does School Segregation Stand, 70 Years After Brown v. Board of Education?
Documenting police use of force, get our newsletter, follow frontline, frontline newsletter, we answer to no one but you.
You'll receive access to exclusive information and early alerts about our documentaries and investigations.
I'm already subscribed
The FRONTLINE Dispatch
Don't miss an episode. sign-up for the frontline dispatch newsletter., sign-up for the unresolved newsletter..
Transgender Health Program
Gender-affirming surgery.
OHSU surgeons are leaders in gender-diverse care. We provide specialized services tailored to the needs and goals of each patient. We offer:
- Specialists who do hundreds of surgeries a year.
- Plastic surgeons, urologists and other specialists who are leading experts in bottom surgery, top surgery and other gender-affirming options.
- Vocal surgery with a highly trained ear, nose and throat doctor.
- Peer volunteers who can provide support during visits.
- Welcoming care for every patient, every gender and every journey.
Our surgical services
We offer many gender-affirming surgery options for transgender and nonbinary patients, including options within the following types. We also welcome you to request a procedure that isn’t listed on our pages.
Top surgery:
- Gender-affirming mastectomy
- Gender-affirming breast augmentation
Bottom surgery:
- Phalloplasty and metoidioplasty , including vagina-preserving options
- Vaginoplasty and vulvoplasty , including penile-preserving options
Hysterectomy
Nullification surgery, oophorectomy, orchiectomy.
Bottom surgery options also include:
- Scrotectomy
- Scrotoplasty
- Urethroplasty
- Vaginectomy
Additional gender-affirming options:
- Adam’s apple surgery
Vocal surgery
Face and body surgery, preparing for surgery.
Please see our patient guide page to learn about:
- Steps to surgery
- WPATH standards of care
- The letter of support needed for some surgeries
For patients
Request services.
Please fill out an online form:
- I am seeking services for myself.
- I am seeking services for someone else.
Other questions and concerns
Contact us at:
- 503-494-7970
- [email protected]
Refer a patient
- Please complete our Request for Transgender Health Services referral form and fax with relevant medical records to 503-346-6854 .
- Learn more on our For Health Care Professionals page.
At OHSU, our gynecologic surgeon, Dr. Lishiana Shaffer, specializes in hysterectomies (uterus and cervix removal; often combined with oophorectomy, or ovary removal) for gender-diverse patients. She does more than 150 a year.
We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Some patients choose hysterectomy to:
- More closely align their bodies with their gender identity.
- With ovary removal, to remove a main source of the hormone estrogen.
- To end pain caused by testosterone therapy that shrinks the uterus.
- To end the need for some gynecologic exams, such Pap smears.
Preparation: We usually recommend a year of hormone therapy first, to shrink the uterus. We don’t require a year of social transition.
How hysterectomy is done
Most often, we use a minimally invasive laparoscope and small incisions in the belly. We usually recommend removing fallopian tubes as well, to greatly reduce the risk of ovarian cancer.
Most patients spend one night in the hospital. Recovery typically takes about two weeks. You’re encouraged to walk during that time but to avoid heavy lifting or strenuous exercise.
Considerations and risks
Hysterectomy is usually safe, and we have a low rate of complications. Risks can include blood clots, infection and scar tissue. Because of a possible link between hysterectomy and higher risk of cardiovascular disease, your doctors may recommend regular tests.
Removing the uterus also ends the ability to carry a child. OHSU fertility experts offer options such as egg freezing before treatment, and connecting patients with a surrogacy service.
OHSU offers nullification surgery to create a gender-neutral look in the groin area.
Nullification surgery may include:
- Removing the penis (penectomy)
- Removing the testicles (orchiectomy)
- Reducing or removing the scrotum (scrotectomy)
- Shortening the urethra
- Removing the uterus (hysterectomy)
- Removing the vagina (vaginectomy)
The procedure takes several hours. Patients can expect to spend one to two nights in the hospital. Recovery typically takes six to eight weeks. Patients are asked to limit walking and to stick to light to moderate activity for four weeks. They should wait three months before bicycling or strenuous activity.
Nullification surgery cannot be reversed. Risks can include:
- Changes in sensation
- Dissatisfaction with the final look
- Healing problems
Removing the penis and testicles or the uterus also affects the ability to conceive a child. OHSU fertility experts offer options such as freezing eggs and connecting patients with a surrogacy service.
Having a gynecologic surgeon remove one or both ovaries is often done at the same time as a hysterectomy. We do nearly all these surgeries with a minimally invasive laparoscope and small incisions in the belly.
Most patients spend one night in the hospital and return to their regular routine in about two weeks.
The ovaries produce estrogen, which helps prevent bone loss and the thickening of arteries. After removal, a patient should be monitored long-term for the risk of osteoporosis and cardiovascular disease.
We encourage patients to keep at least one ovary to preserve fertility without egg freezing. This also preserves some hormone production, which can avoid early menopause.
At OHSU, expert urologists do orchiectomies (testicle removal). Patients may choose this option:
- To remove the body’s source of testosterone
- As part of a vaginoplasty or vulvoplasty (surgeries that create a vagina and/or vulva)
- To relieve dysphoria (some patients choose only this surgery)
Removing the testicles usually means a patient can stop taking a testosterone blocker. Patients may also be able to lower estrogen therapy.
How orchiectomy is done
The surgeon makes an incision in the scrotum. The testicles and the spermatic cord, which supplies blood, are removed. Scrotal skin is removed only if the patient specifically requests it. The skin is used if the patient plans a vaginoplasty or vulvoplasty.
You will probably go home the same day. Patients can typically resume normal activities in a week or two.
Reducing testosterone production may increase the risk of bone loss and cardiovascular disease, so we recommend regular tests. Without prior fertility treatment, orchiectomy also ends the ability to produce children. Serious risks are uncommon but include bleeding, infection, nerve damage and scarring.
Adam’s apple reduction (laryngochrondoplasty)
Dr. Joshua Schindler, an ear, nose and throat doctor who does Adam’s apple and vocal surgeries, completed his training at Johns Hopkins University.
Laryngochrondoplasty is also known as Adam’s apple reduction or a tracheal shave (though the trachea, or windpipe, is not affected).
A surgeon removes thyroid cartilage at the front of the throat to give your neck a smoother appearance. This procedure can often be combined with facial surgery.
Thin incision: At OHSU, this procedure can be done by an ear, nose and throat doctor (otolaryngologist) with detailed knowledge of the neck’s anatomy. The surgeon uses a thin incision, tucked into a neck line or fold. It can also be done by one of our plastic surgeons, typically with other facial surgery.
In an office or an operating room: Our team can do a laryngochrondoplasty in either setting, which may limit a patient’s out-of-pocket expenses.
OHSU also offers Adams’ apple enhancement surgery.
Many patients find that hormone therapy and speech therapy help them achieve a voice that reflects their identity. For others, vocal surgery can be added to raise the voice’s pitch.
Voice therapy: Patients have voice and communication therapy before we consider vocal surgery. Your surgeon and your speech therapist will assess your voice with tests such as videostroboscopy (allowing us to see how your vocal cords work) and acoustic voice analysis.
Effective surgery: We use a surgery called a Wendler glottoplasty. It’s done through the mouth under general anesthesia. The surgeon creates a small controlled scar between the two vocal cords, shortening them to increase tension and raise pitch. Unlike techniques that can lose effectiveness over time, this surgery offers permanent results.
Hormone therapy can bring out desired traits, but it can’t change the underlying structure or remove hair follicles. Our highly trained surgeons and other specialists offer options. Patients usually go home the same day or spend one night in a private room.
Face options:
- Browlift (done with the forehead)
- Cheek augmentation
- Chin surgery (genioplasty), including reductive, implants or bone-cut options
- Eyelid surgery
- Face-lift, neck lift
- Forehead lengthening
- Forehead reduction, including Type 3 sinus setback and orbital remodeling
- Hairline advancement (done with the forehead)
- Jawline contouring
- Lip lift and/or augmentation
- Lipofilling (transferring fat using liposuction and filling)
- Nose job (rhinoplasty)
Body options:
Hormone treatment may not result in fat distribution consistent with your gender. We offer liposuction and fat grafting to reshape areas of the body.
The Ethical Intricacies of Transgender Surgery

Illustration by Taimi Xu
Article by Leyla Giordano
Over the past decade, the transgender population has increased in visibility dramatically in the United States. The medical field has made progress when it comes to access to gender-affirming surgery; however, the progress has not rid society of discrimination and bias towards the transgender population, and access to care is still limited. Thus, it is essential to train medical professionals to care for this vulnerable population with compassion and knowledge. During the summer of 2018, I interned at the Gender Reassignment Department of Mount Sinai Hospital, where Dr. Jess Ting pioneered New York City’s first surgical program dedicated to transgender surgery. I learned that he transforms bodies every day in his operating room and cares for his patients with empathy, but he also struggles with feelings of helplessness when his patients share their devastating stories and disappointment when his surgeries are unable to live up to their expectations.
The American Psychiatric Association defines transgender as “a person whose sex assigned at birth (i.e. the sex assigned at birth, usually based on external genitalia) does not align with their gender identity (i.e., one’s psychological sense of their gender).” 1 Further, a subset of transgender individuals will experience gender dysphoria, defined by the American Psychiatric Association as “psychological distress that results from an incongruence between one’s sex assigned at birth and one’s gender identity.” 1 Thus, the dysphoria refers to the psychological distress that can often result from being transgender. In response to gender dysphoria, one may seek affirmations in several areas, including but not limited to social, legal, medical, or surgical. Medical and surgical affirmations are two ways in which one’s true identity can be revealed externally to society. Gender affirming surgery includes vaginoplasty, facial feminization surgery, breast augmentation, masculine chest reconstruction, and others. 3 Surgeries like these can help reduce an individual’s gender dysphoria so that their physical body matches their gender identity.
Overall, transgender surgery improves lives because it gives trans individuals a body in which they feel more like themselves. However, the transgender population faces significant disparities in social determinants of health. These detrimental determinants limit Dr. Ting’s ability to heal this vulnerable population, frustrating him as he is ultimately unable to fix the discriminatory social context they encounter outside of the hospital. This paper will first discuss what it means to be transgender and how Dr. Ting’s work improves their life experiences. It will then move into the broader traumas that transgender individuals face. Finally, this paper will discuss the limitations and frustrations of Dr. Ting’s practice and how they have affected his approach.
Being transgender in our society and life-changing surgery
Since the 1900s, historians, activists, anthropologists, and many others have engaged in the debate between sex and gender. The social presentation and embodiment of one’s gender can differ from the anatomy or chromosomes with which one is born. Until recently, people have assumed that females act feminine because they have a uterus, not because they identify as a “female.” Society has assigned certain characteristics to what it means to be a girl, such as wanting to wear lipstick and play with Barbies. In the 1960s, a white and Western feminist theory emerged that posits that sex refers to the natural anatomical features, whereas gender refers to the culturally constructed norms that have been built based on one’s sex. 2 This theory persisted into the 1990s, when Judith Butler argued that, in addition to gender, sex is also a social construct. She posited that if gender and sex are both social constructs, then these two terms are essentially the same. 2
For decades, long-standing ideologies have informed beliefs that the trans identity is unacceptable since it runs contrary to the societally constructed connection between sex and gender. However, individuals like Dr. Jess Ting are contributing to the current shift in that dialogue surrounding the acceptance of trans identities. The Gender Reassignment Department that Dr. Jess Ting helped create at Mount Sinai Hospital gives transgender individuals the medical care that they need, changing the discourse around the transgender identity from taboo to celebrated. For example, in an interview I conducted with Dr. Ting, he recounted a memory about his oldest patient, who has stayed with him for five years. She was 77 years old and had been married to a man for many years. She told Dr. Ting that “this [surgery] is something I want to do for myself. I’ve wanted it since I was five years old, and I have never been able to get it.” As soon as Dr. Ting began to sign her up for surgery, she began to cry. She said, “I thought you were going to tell me that I was too old for surgery.” This story has stuck with Dr. Ting ever since because, as he says, “it’s powerful to give someone something that they have wanted for their whole life.” This patient had previously not gone to a doctor for the surgery out of fear that she herself and her identity would never be accepted. She also never had access to surgery because until 2016, no surgical programs existed in the state of New York. However, at the age of 77, the discussion around the transgender population has become significantly more welcoming and access to these operations increased such that Dr. Ting’s patient was able to finally get the gender-affirming surgery for herself.
A significant number of Dr. Ting’s operations are facial feminization surgeries. Facial feminization surgery, which includes shaving the male protruding forehead and brow ridge and softening the nose and jaw, are sought out by transgender individuals who identify as women and hope to have society externally view them as women. It is difficult to masculinize a face, but facial feminization surgery is extremely effective in giving a patient the stereotypical female features, such as a less-protruding forehead. Society consistently puts pressure on each gender to embody certain characteristics, as Eric Plemons points out in The Look of a Woman : “Yes, [the operating room] was the precise location in which patients’ longed-for physical transformations took place. But it was also a place whose material dynamics pushed and pulled at conceptual frameworks of embodiment and selfhood that lay at the heart of trans-body projects.” 3 Dr. Ting revealed to me that the most common reaction he gets from his patients post-surgery is, “I just feel like me now,” as the material change in their appearance is an important part of what finally allows them to externally embody their ideal selves. Thus, the operating room becomes a place where the physical transformation makes it possible for a transgender individual to finally fit their own vision of themselves.
In a visual society such as ours, one’s facial features become the most salient factor in society’s recognition of one’s sex. As Plemons mentions, “Facial feminization surgery is guided by hope for future phenomenological integration and social recognition the creation of a body that (re)presents the self.” 3 Transgender individuals are unable to embody their ideal selves when they remain in the body they were given at birth. However, through facial feminization surgery, a transgender female can be outwardly recognized as a woman, making gendered embodiment a social phenomenon. As Rosalind expresses in Plemons’ article, “‘I’ve spent twenty-five years of my life thinking about not looking like I do now. I want that to go away. Constant thinking about that ruins the mind. After this I’ll be able to think of other things, everyday things.’” 3 Rosalind’s inability to embody her ideal self consumes her, as she is told every day by society that her gender identity is based off her recognizable characteristics like her Adam’s apple and her “Neanderthal brow.” 3 Facial feminization surgery is, thus, a popular way to experience the world in a body that is outwardly recognizable and accepted as female.
The stereotypical facial features of a woman are what have been defined as “normal” to society. These features include a softer brow ridge and forehead, eyebrows with a slight arch, fuller lips, no facial hair, and a smaller nose. Society defines these characteristics as female, and it also defines a binary of female and male as the only acceptable genders. According to Abramowitz’s three definitions of “normal,”—socially accepted or morally condoned, statistically most common, and frequently occurring in everyday life—each society determines that a specific anomaly is not “normal.” 4 Using these definitions, society sees transgender individuals as not “normal.” However, this is not how society should see the transgender population. This isolation is the exact disposition that leads to transphobia and a lack of transgender-specialized healthcare in the United States. Transgender individuals have reported that the most significant barrier to health care is the lack of physicians who are culturally competent and knowledgeable on the population. 5 Dr. Ting echoed this shortage when he discussed his introduction into the field: “When we started our program in 2016, there was no place in New York City to access transgender surgery.” Despite the discrimination they face, transgender individuals are normal and should be considered normal by society; they are simply human beings who do not feel comfortable in their own bodies. Through his work at Mount Sinai Hospital, Dr. Ting became a pioneer in this field of medicine, making the transition to an embodiment of transgender individuals’ ideal selves possible.
The broader traumas
Trans individuals’ health outcomes are negatively impacted through several factors, such as intense stigma, increased harassment, and restricted access to employment, healthcare, and insurance. The detrimental effect that these factors cause can extend as far as suicide. Dr. Ting revealed, “The thing that was most impactful for me was when we first started seeing patients. One of the patients that I had interviewed and was going to schedule for surgery killed themselves. And up until that moment, I did not understand what the trans experience meant. That’s how I came to understand why these surgeries can be lifesaving.” Despite the beneficial impact of transgender surgery, it cannot rid the United States of its unequal structural and social determinants of health. Transgender individuals often have restricted access to employment, healthcare, and housing compared to cisgender individuals. 6 Dr. Ting mentioned in our interview, “So many of my patients are sex workers, are undomiciled, and are living in shelters. This made me realize that I was judgmental. There’s not much that separates us from people who live on the streets or who are sex workers. When you have no other options, that is your only way of surviving.” The lack of these fundamental resources can lead to increased stress and poor physical and mental health, such as depression, suicidality, and chronic illnesses. 6
The othering of the transgender population leads to an intense and detrimental stigma surrounding the trans identity. Transgender individuals experience structural stigma (societal norms), interpersonal stigma (verbal harassment, physical violence, sexual assault), and individual stigma (the feelings these individuals hold about themselves that may shape future behavior such as the anticipation of discrimination). Structural stigma originates from the socially constructed gender binary, and therefore marginalizes those that are considered “abnormal.” This stigma may “therefore operate as a form of symbolic violence in which structures, such as communities, institutions, or governments, […] restrict and forcibly reshape transgender individuals in ways that ultimately serve to maintain the power and privilege of the cisgender majority.” 6 For example, a lack of insurance within the transgender population may lead trans individuals to pay out of pocket for procedures, which therefore makes it more likely that they feel they have no option other than to use cheaper street hormones acquired through friends or online. 6 Secondly, interpersonal stigma refers to the increased levels of physical and sexual harassment:“It is theorized that gender nonconformity causes perpetrators of violence to become anxious and angry, ultimately enacting violence against transgender people as a means of rejecting and diminishing that which they fear.” 6 Further, a national survey showed that, out of 402 transgender individuals, 47% had been assaulted and 14% of the 47% had been raped or survived attempted rape. 7 Thus, transgender individuals experience disproportionate abuse in their lifetimes, whether that be in the form of hate crimes, sexual assault, or verbal abuse. Finally, individual stigma refers to transgender individuals’ negative image of themselves. This stigma makes them anxious to seek out healthcare and destroys their ability to deal with external stressors, leading to an increase in preventable deaths such as suicide.
Another crucial example of negative health outcomes among the transgender population is the increased rate of HIV. According to the Journal of Virus Eradication , “transgender women have a pooled HIV prevalence of 19.1%, […] For transgender women sex workers, HIV prevalence is even greater, estimated at 27.3%.” 8 Researchers believe that the increased risk is multifactorial and may be “due to differing psychosocial risk factors, poorer access to transgender-specific healthcare, a higher likelihood of using exogenous hormones or fillers without direct medical supervision, interactions between hormonal therapy and antiretroviral therapy, and direct effects of hormonal therapy on HIV acquisition and immune control.” 8 The fear of the medical setting that is present in the transgender population could lead to decrease testing for sexually transmitted infections, and therefore higher rates of HIV. Additionally, the stigma that surrounds the trans population leads to an alarming amount of trans individuals going into sex work due to the absence of other employment opportunities, which could also lead to increased levels of HIV.
The aforementioned factors contribute to a symbolic violence in which transgender individuals internalize the social asymmetries they experience. 9 This internalization can lead to a reactive personality and may even culminate in a personality disorder such as borderline personality disorder, since transgender individuals become used to the abuse and thus have learned to fight for themselves. As Dr. Ting reflected, “When anything goes wrong, [my patients’] reactions can be overwhelming and out of proportion to what you would expect. They blow up at me all the time. […] Trans people have a lived experience where […] they are subjected to abuse, and they are ignored. When you live like that, you build up your fences and you learn that you have to fight and scream for just regular occurrences.” Every day, Dr. Ting sees first-hand the internalization of the stigma that the transgender population faces. Trans individuals begin to view themselves and their self-worth through how they are negatively treated, prompting the development of a personality that is programmed to protect oneself against the world.
Limitations of Dr. Ting’s practice and their effects
The discrimination and abuse that Dr. Ting’s patients experience often exceed the medical realm, so an approach that focuses on narrative medicine and listening to his patients’ personal stories is important. 10 In “Narrative Medicine: Attention, Representation, Affiliation,” Rita Charon moves past the narrow focus on her patients’ physical bodies and approaches her patients with a dedication to their stories. 11 As Charon writes about a patient, “It was not just a matter of my having to know which section of his brain infarcted in his stroke but also what his stroke made of him, what it did to him, how he fought back from it, […] whether he will be the person he once was. It mattered to him and to our future clinical relationship that I know these things, that I have heard his fears and rage and grieving.” 11 Similarly, Dr. Ting is committed to listening to his patients’ personal stories about their experiences as transgender individuals. In our interview, he emphasized how important it was to him to listen to his patients and their concerns, as his patients often lack a support system. In this way, similarly to Dr. Charon, Dr. Ting acts as an empathic witness for his suffering patients. 10
However, physicians can only open themselves up to others’ suffering to a certain extent, and this balance has been difficult for Dr. Ting. When his patients come to his office, they have looked forward to their gender-affirming surgery for years, putting immense pressure on the outcome. This pressure can also lead to a dependency on the physician after a successful surgery for further help; however, Dr. Ting can only accept so much responsibility. During our interview, Dr. Ting reflected on a close relationship he built with one of his patients that caused him a large amount of grief: “One of my patients killed himself. He didn’t have a very smooth postoperative course. During Thanksgiving, he was texting me and meeting with a urologist. The urologist didn’t like the way that this patient was speaking to him. He can be a little rough, and the urologist [denied him care]. He then texted me saying, ‘What am I going to do now?’ I remember that I was out of town, and I responded ‘Don’t worry, we’ll find you someone else. It’s going to be okay.’ And he texted a few more times on Thursday or Friday, and then over the weekend, I noticed that I hadn’t heard from him in a while. I texted him on Monday to ask how he was doing, and I never heard back. A few days later, I found out that he had killed himself on the Monday after Thanksgiving.” With this news, Dr. Ting blamed himself, thinking that it was the complications from his surgery that made his patient commit suicide.
Physicians around the country experience burnout from job demands such as an overwhelming workload and emotional demands. Research on the mental health of psychologists and other physicians shows that these occupations aim to help people in need, leading to a high level of responsibility and increased emotional and interpersonal stressors for the physicians themselves. 12 Dr. Ting could not help but assign blame to himself for his patient’s suicide. In the process of doing so, the high level of compassion and empathy required of him negatively affected Dr. Ting. For psychologists, emotional exhaustion is the most commonly reported cause of burnout. 12 Although Dr. Ting is not a psychologist, his patients often depend on him for matters that extend past his office due to their lack of a support system. Dr. Ting provides life-changing surgeries to a very vulnerable population and deeply cares about his patients, and that type of work requires high levels of involvement, which can lead to burnout. As a consequence of burnout, research has shown that physicians then “seek an escape or distance themselves from their work both emotionally and cognitively, and [the burnout] is thought to lead on to feelings of cynicism.” 12 Dr. Ting felt himself burning out from the emotional burden he experienced while forming close relationships with his patients, and it forced him to place distance between him and his patients.
Thus, especially after his patient’s suicide, Dr. Ting decided to set a boundary between him and his patients by strictly keeping his relationships to his office. It was necessary for Dr. Ting to adopt a medical gaze to take care of himself. 13 In the process, he lamented the loss of the personal relationships he had built:
In the beginning, I would find myself getting very close to patients, sharing lots of details of their lives. In a way, that was really gratifying and rewarding for them to share emotionally fraught things. That’s why you become a healer. You want to heal people, and part of that is the positive feedback you get back from patients. Over time, I found that 99% of patients would be great, but the one complication would take so much out of me mentally. I could feel myself burning out a lot, so now, I am much more careful with patients in terms of creating boundaries. I don’t get as close to patients, which is sad, but it is necessary to protect myself. When I go see patients after surgery, and they tell me that I changed their lives, [saying] “How can I ever thank you?”, I feel like I have become a little numb to that, and I put up the boundaries where I’m afraid to let myself get close with patients.
Dr. Ting struggles between his commitment to his patients on a personal level and protecting himself from extreme responsibility for his patients’ distress. This complicated experience unfortunately limits the extent of his care. Despite the loss of many relationships that he values and his commitment to his patients past their physical bodies, Dr. Ting finds himself having to take a step back to separate himself from the burden of his patients’ trauma.
Overall, Dr. Ting changes his patients’ lives by giving them a body they can finally love and claim as their own. However, this responsibility brings a lot of pressure, as Dr. Ting expressed in our interview: “There is this tendency to idealize what’s going to happen or to feel like this surgery will cure everything – it will cure ‘all my ails.’ It doesn’t do that, it doesn’t cure all the ails of society – it makes your body align better with your internal identity, but you still have to go out into the world, and the world is not a better place.” Dr. Ting’s contributions to the transgender community supersede all expectations and grant so many the bodies and comfort they so desperately need, but he himself cannot change the society that transgender individuals enter back into when they leave the hospital. Despite the intense grief that Dr. Ting conveyed when he talked about the suicide of a patient and close friend, he ended our interview by relaying an encouraging conversation he had with his late patient’s partner: “She told me that the patient loved the body that I made for him, even with the complications. She told me that if he hadn’t had that surgery earlier, he would’ve died even sooner. He would not have even lived this long. For me, that lifted a heavy burden. I realized that maybe it wasn’t my fault, and that I did help him.” It’s clear that to Dr. Ting, the complicated moral experience that he faces within and beyond his office is worth it when he can aid individuals that are so desperately in need of his care.
- “What is Gender Dysphoria?” American Psychiatric Association . https://www.psychiatry.org/patients-families/gender-dysphoria/what-is-gender-dysphoria
- Mason, Katherine. “Embodiment.” (Brown University, February 14, 2022).
- Plemons, Eric. “The Operating Room | The Look of a Woman: Facial Feminization Surgery and the Aims of Trans- Medicine | Books Gateway | Duke University Press,” Chapter 5.
- Mason, Katherine. “The Normal and the Abnormal.” (Brown University, February 7, 2022).
- Safer, Joshua D., Eli Coleman, Jamie Feldman, Robert Garofalo, Wylie Hembree, Asa Radix, and Jae Sevelius. “Barriers to health care for transgender individuals.” Current opinion in endocrinology, diabetes, and obesity 23, no. 2 (2016): 168-171. 10.1097/MED.0000000000000227
- White Hughto, Jaclyn M., Sari L. Reisner, and John E. Pachankis. “Transgender Stigma and Health: A Critical Review of Stigma Determinants, Mechanisms, and Interventions.” Social Science & Medicine 147 (December 1, 2015): 222–31. https://doi.org/10.1016/j.socscimed.2015.11.010 .
- Mizock, Lauren, and Thomas K. Lewis. “Trauma in Transgender Populations: Risk, Resilience, and Clinical Care.” Journal of Emotional Abuse 8, no. 3 (August 26, 2008): 335–54. https://doi.org/10.1080/10926790802262523 .
- Wansom, Tanyaporn, Thomas E. Guadamuz, and Sandhya Vasan. “Transgender Populations and HIV: Unique Risks, Challenges and Opportunities.” Journal of Virus Eradication 2, no. 2 (April 1, 2016): 87–93. https://doi.org/10.1016/S2055-6640(20)30475-1 .
- Mason, Katherine. “Narrative, Stories, and Healing.” (Brown University, February 23, 2022).
- Charon, Rita. “Narrative Medicine: Attention, Representation, Affiliation.” Narrative 13, no. 3 (2005): 261-270. https://library.brown.edu/reserves/pdffiles/55716_rita_charon.pdf .
- McCormack, Hannah M., Tadhg E. MacIntyre, Deirdre O’Shea, Matthew P. Herring, and Mark J. Campbell. “The prevalence and cause (s) of burnout among applied psychologists: A systematic review.” Frontiers in psychology (2018): 1897. https://doi.org/10.3389/fpsyg.2018.01897
- Mason, Katherine. “(Bio)medical Training and Professions.” (Brown University, March 7, 2022).
- Media & Government
- News and Views
The history of gender reassignment surgeries in the UK
For Pride Month, we are recognising the plastic surgeons who pioneered gender reassignment surgeries (GRS) in the UK. Gender reassignment surgery, also known as gender confirmation surgery or gender affirmation surgery, is a sub-speciality within plastic surgery, developed based on reconstructive procedures used in trauma and in congenital malformations. The specific procedures used for GRS have only been practised in the last 100 years.
Over the last decade, there has been an increase in society acknowledgement and acceptance of gender diverse persons. This catalysed an increase in referrals to gender identity clinics and an increase in the number of gender affirmation surgeries. GRS help by bringing fulfilment to many people who experience gender dysphoria. Gender dysphoria - a distress caused by the incongruence of a person's gender identity and their biological sex, drives the person to seek medical or surgical intervention to align some or all of their physical appearance with their gender identity. Patients with gender dysphoria experience higher rates of psychiatric disorders such as depression and anxiety. Gender-affirming medical intervention tends to resolve the psychiatric disorders that are a direct consequence of gender dysphoria.
Norman Haire (1892-1952) was a medical practitioner and a Sexologist. In his book, The Encyclopaedia of Sexual Knowledge (1933), he describes the first successful GRS. His patient, Dora Richter underwent 3 procedures reassigning from male to female between 1922-1931. The procedures included a vaginoplasty (surgical procedure where a vagina is created).
In the UK, gender reassignment surgeries were pioneered by Sir Harold Gillies. Harold Gillies is most famous for the development of a new method of facial reconstructive surgery, in 1917. During the Second World War, he organized plastic surgery units in various parts of Britain and inspired colleagues to do the same, training many doctors in this field. During the war, Gillies performed genital reconstruction surgeries for wounded soldiers.
British physician Laurence Michael Dillon (born Laura Maude Dillon) felt that they were not truly a woman. Gillies performed the first phalloplasty (surgery performed to construct the penis) on Dillon in 1946. In transitioning from female to male, Dillon underwent a total of 13 operations, over a period of 4 years.
Roberta Cowell (born Robert Marshall Cowell) is the first known Brit to undergo male to female GRS. After meeting Dillon and becoming close, Dillon operated illegally on Cowell. The operation helped her obtain documents confirming that she was intersex and have her birth gender formally re-registered as female. The operation that helped her transition was forbidden as it was considered “disfiguring” of a man who was otherwise qualified to serve in the military. Consequently, Gillies, assisted by American surgeon Ralph Millard performed a vaginoplasty on Roberta in 1951. The technique pioneered by Harold Gillies remained the standard for 40 years.
Gillies requested no publicity for his gender affirmation work. In response to the objections received from his peers, he replied that he was satisfied by the patient's written sentiments: “To Sir Harold Gillies, I owe my life and my happiness”. “If it gives real happiness,” Gillies wrote of his procedures, “that is the most that any surgeon or medicine can give.” These words highlight the importance of plastic surgery in the mental wellbeing of transgender patients.
The BAPRAS Collection and Archive has an extraordinary assembly of fascinating archive and historical surgical instruments dating from 1900. Visit https://www.bapras.org.uk/professionals/About/bapras-archive or email [email protected] for more information.
Please refer to our Privacy policy for important information on the use of cookies. By continuing to use this website, you agree to this.
Sorry, your browser isn't supported
Please click here to find out about upgrading.
You can also view the BAPRAS website on your tablet or mobile.
Putting numbers on the rise in children seeking gender care
By ROBIN RESPAUT and CHAD TERHUNE
Filed Oct. 6, 2022, 11 a.m. GMT

Thousands of children in the United States now openly identify as a gender different from the one they were assigned at birth, their numbers surging amid growing recognition of transgender identity and rights even as they face persistent prejudice and discrimination.
As the number of transgender children has grown, so has their access to gender-affirming care, much of it provided at scores of clinics at major hospitals.
Reliable counts of adolescents receiving gender-affirming treatment have long been guesswork – until now. Reuters worked with health technology company Komodo Health Inc to identify how many youths have sought and received care. The data show that more and more families across the country are grappling with profound questions about what type of care to pursue for their children, placing them at the center of a vitriolic national political debate over what it means to protect youth who identify as transgender.
Diagnoses of youths with gender dysphoria surge
In 2021, about 42,000 children and teens across the United States received a diagnosis of gender dysphoria, nearly triple the number in 2017, according to data Komodo compiled for Reuters. Gender dysphoria is defined as the distress caused by a discrepancy between a person’s gender identity and the one assigned to them at birth.
Overall, the analysis found that at least 121,882 children ages 6 to 17 were diagnosed with gender dysphoria from 2017 through 2021. Reuters found similar trends when it requested state-level data on diagnoses among children covered by Medicaid, the public insurance program for lower-income families.
Gender-affirming care for youths takes several forms, from social recognition of a preferred name and pronouns to medical interventions such as hormone therapy and, sometimes, surgery. A small but increasing number of U.S. children diagnosed with gender dysphoria are choosing medical interventions to express their identity and help alleviate their distress.
These medical treatments don’t begin until the onset of puberty, typically around age 10 or 11.
For children at this age and stage of development, puberty-blocking medications are an option. These drugs, known as GnRH agonists, suppress the release of the sex hormones testosterone and estrogen. The U.S. Food and Drug Administration has approved the drugs to treat prostate cancer, endometriosis and central precocious puberty, but not gender dysphoria. Their off-label use in gender-affirming care, while legal, lacks the support of clinical trials to establish their safety for such treatment.
Over the last five years, there were at least 4,780 adolescents who started on puberty blockers and had a prior gender dysphoria diagnosis.
This tally and others in the Komodo analysis are likely an undercount because they didn’t include treatment that wasn’t covered by insurance and were limited to pediatric patients with a gender dysphoria diagnosis. Practitioners may not log this diagnosis when prescribing treatment.
By suppressing sex hormones, puberty-blocking medications stop the onset of secondary sex characteristics, such as breast development and menstruation in adolescents assigned female at birth. For those assigned male at birth, the drugs inhibit development of a deeper voice and an Adam’s apple and growth of facial and body hair. They also limit growth of genitalia.
Without puberty blockers, such physical changes can cause severe distress in many transgender children. If an adolescent stops the medication, puberty resumes.
The medications are administered as injections, typically every few months, or through an implant under the skin of the upper arm.
After suppressing puberty, a child may pursue hormone treatments to initiate a puberty that aligns with their gender identity. Those for whom the opportunity to block puberty has already passed or who declined the option may also pursue hormone therapy.
At least 14,726 minors started hormone treatment with a prior gender dysphoria diagnosis from 2017 through 2021, according to the Komodo analysis.
Hormones – testosterone for adolescents assigned female at birth and estrogen for those assigned male – promote development of secondary sex characteristics. Adolescents assigned female at birth who take testosterone may notice that fat is redistributed from the hips and thighs to the abdomen. Arms and legs may appear more muscular. The brow and jawline may become more pronounced. Body hair may coarsen and thicken. Teens assigned male at birth who take estrogen may notice the hair on their body softens and thins. Fat may be redistributed from the abdomen to the buttocks and thighs. Their testicles may shrink and sex drive diminish. Some changes from hormone treatment are permanent.
Hormones are taken in a variety of ways: injections, pills, patches and gels. Some minors will continue to take hormones for many years well into adulthood, or they may stop if they achieve the physical traits they want.
Hormone treatment may leave an adolescent infertile, especially if the child also took puberty blockers at an early age. That and other potential side effects are not well-studied, experts say.
The ultimate step in gender-affirming medical treatment is surgery, which is uncommon in patients under age 18. Some children’s hospitals and gender clinics don’t offer surgery to minors, requiring that they be adults before deciding on procedures that are irreversible and carry a heightened risk of complications.
The Komodo analysis of insurance claims found 56 genital surgeries among patients ages 13 to 17 with a prior gender dysphoria diagnosis from 2019 to 2021. Among teens, “top surgery” to remove breasts is more common. In the three years ending in 2021, at least 776 mastectomies were performed in the United States on patients ages 13 to 17 with a gender dysphoria diagnosis, according to Komodo’s data analysis of insurance claims. This tally does not include procedures that were paid for out of pocket.
A note on the data
Komodo’s analysis draws on full or partial health insurance claims for about 330 million U.S. patients over the five years from 2017 to 2021, including patients covered by private health plans and public insurance like Medicaid. The data include roughly 40 million patients annually, ages 6 through 17, and comprise health insurance claims that document diagnoses and procedures administered by U.S. clinicians and facilities.
To determine the number of new patients who initiated puberty blockers or hormones, or who received an initial dysphoria diagnosis, Komodo looked back at least one year prior in each patient’s record. For the surgery data, Komodo counted multiple procedures on a single day as one procedure.
For the analysis of pediatric patients initiating puberty blockers or hormones, Komodo searched for patients with a prior gender dysphoria diagnosis. Patients with a diagnosis of central precocious puberty were removed. A total of 17,683 patients, ages 6 through 17, with a prior gender dysphoria diagnosis initiated either puberty blockers or hormones or both during the five-year period. Of these, 4,780 patients had initiated puberty blockers and 14,726 patients had initiated hormone treatment.
Youth in Transition
By Robin Respaut and Chad Terhune
Photo editing: Corrine Perkins
Art direction: John Emerson
Edited by Michele Gershberg and John Blanton
- Follow Reuters Investigates
Other Reuters investigations

The Gender Reassignment Controversy
When people opt for surgery, are they satisfied with the outcome.
Posted March 16, 2018 | Reviewed by Ekua Hagan
In an age of increasing gender fluidity, it is surprising that so many find it difficult to accept the gender of their birth and take the drastic step of changing it through surgery. What are their motives? Are they satisfied with the outcome?
Gender may be the most important dimension of human variation, whether that is either desirable, or inevitable. In every society, male and female children are raised differently and acquire different expectations, and aspirations, for their work lives, emotional experiences, and leisure pursuits.
These differences may be shaped by how children are raised but gender reassignment, even early in life, is difficult, and problematic. Reassignment in adulthood is even more difficult.
Such efforts are of interest not just for medical reasons but also for the light they shed on gender differences.
The first effort at reassignment, by John Money, involved David Reimer whose penis was accidentally damaged at eight months due to a botched circumcision.
The Money Perspective
Money believed that while children are mostly born with unambiguous genitalia, their gender identity is neutral. He felt that which gender a child identifies with is determined primarily by how parents treat it and that parental views are shaped by the appearance of the genitals.
Accordingly, Money advised the parents to have the child surgically altered to resemble a female and raise it as “Brenda.” For many years, Money claimed that the reassignment had been a complete success. Such was his influence as a well-known Johns Hopkins gender researcher that his views came to be widely accepted by scholars and the general public.
Unfortunately for Brenda, the outcome was far from happy. When he was 14, Reimer began the process of reassignment to being a male. As an adult, he married a woman but depression and drug abuse ensued, culminating in suicide at the age of 38 (1).
Money's ideas about gender identity were forcefully challenged by Paul McHugh (2), a leading psychiatrist at the same institution as Money. The brunt of this challenge came from an analysis of gender reassignment cases in terms of both motivation and outcomes.
Adult Reassignment Surgery Motivation
Why do people (predominantly men) seek surgical reassignment (as a woman)? In a controversial take, McHugh argued that there are two main motives.
In one category fall homosexual men who are morally uncomfortable about their orientation and see reassignment as a way of solving the problem. If they are actually women, sexual interactions with men get redefined as heterosexual.
McHugh argued that many of the others seeking reassignment are cross-dressers. These are heterosexual men who derive sexual pleasure from wearing women's clothing. According to McHugh, surgery is the logical extreme of identifying with a female identity through cross-dressing.
If his thesis is correct, McHugh denies that reassignment surgery is ever either medically necessary or ethically defensible. He feels that the surgeon is merely cooperating with delusional thinking. It is analogous to providing liposuction treatment for an anorexic who is extremely slender but believes themselves to be overweight.
To bolster his case, McHugh looked at the clinical outcomes for gender reassignment surgeries.
Adult Reassignment Results
Anecdotally, the first hurdle for reassignment is how the result is perceived by others. This problem is familiar to anyone who looked at Dustin Hoffman's depiction of a woman ( Tootsie ). Diligent as the actor was in his preparation, his character looked masculine.
For male-to-female transsexuals, the toughest audience to convince is women. As McHugh reported, one of his female colleagues said: “Gals know gals, and that's a guy.”
According to McHugh, although transsexuals did not regret their surgery, there were little or no psychological benefits:
“They had much the same problems with relationships, work, and emotions, as before. The hope that they would emerge now from their emotional difficulties to flourish psychologically had not been fulfilled (2)”.

Thanks to McHugh's influence, gender reassignment surgeries were halted at Johns Hopkins. The surgeries were resumed, however, and are now carried out in many hospitals here and around the world.
What changed? One likely influence was the rise of the gay rights movement that now includes transgender people under its umbrella and has made many political strides in work and family.
McHugh's views are associated with the religious right-wing that has lost ground in this area.
Transgender surgery is now covered by medical insurance reflecting more positive views of the psychological benefits.
Aspirational Surgery
Why do people who are born as males want to be women? Why do females want to be men? There seems to be no easy biological explanation for the transgender phenomenon (2).
Transgender people commonly report a lifelong sense that they feel different from their biological category and express satisfaction after surgery (now called gender affirmation) that permits them to be who they really are.
The motivation for surgical change is thus aspirational rather than medical, as is true of most cosmetic surgery also. Following surgery, patients report lower gender dysphoria and improved sexual relationships (3).
All surgeries have potential costs, however. According to a Swedish study of 324 patients (3, 41 percent of whom were born female) surgery was associated with “considerably higher risks for mortality, suicidal behavior, and psychiatric morbidity than the general population.”
1 Blumberg, M. S. (2005). Basic instinct: The genesis of behavior. New York: Thunder's Mouth Press.
2 McHugh, P. R. (1995). Witches, multiple personalities, and other psychiatric artifacts. Nature Medicine, 1, 110-114.
3 Dhejne, S., Lichtenstein, P., Boman, M., et al. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study of Sweden . Plos One.

Nigel Barber, Ph.D., is an evolutionary psychologist as well as the author of Why Parents Matter and The Science of Romance , among other books.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

Quality of life improves early after gender reassignment surgery in transgender women
Affiliations.
- 1 Clinic for Reconstructive Plastic Surgery, Karolinska University Hospital, 171 76 Stockholm, Sweden.
- 2 Dept. of Molecular Medicine and Surgery, Karolinska Institute, 171 77 Stockholm, Sweden.
- 3 Stockholm Craniofacial Center, Clinic for Reconstructive Plastic Surgery, A2:04, Karolinska University Hospital, 171 76 Stockholm, Sweden.
- PMID: 28603386
- PMCID: PMC5440516
- DOI: 10.1007/s00238-016-1252-0
Background: Few studies have examined the long-term quality of life (QoL) of individuals with gender dysphoria, or how it is affected by treatment. Our aim was to examine the QoL of transgender women undergoing gender reassignment surgery (GRS).
Methods: We performed a prospective cohort study on 190 patients undergoing male-to-female GRS at Karolinska University Hospital between 2003 and 2015. We used the Swedish version of the Short Form-36 Health Survey (SF-36), which measures QoL across eight domains. The questionnaire was distributed to patients pre-operatively, as well as 1, 3, and 5 years post-operatively. The results were compared between the different measure points, as well as between the study group and the general population.
Results: On most dimensions of the SF-36 questionnaire, transgender women reported a lower QoL than the general population. The scores of SF-36 showed a non-significant trend to be lower 5 years post-GRS compared to pre-operatively, a decline consistent with that of the general population. Self-perceived health compared to 1 year previously rose in the first post-operative year, after which it declined.
Conclusions: To our knowledge, this is the largest prospective study to follow a group of transgender patients with regards to QoL over continuous temporal measure points. Our results show that transgender women generally have a lower QoL compared to the general population. GRS leads to an improvement in general well-being as a trend but over the long-term, QoL decreases slightly in line with that of the comparison group. Level of evidence: Level III, therapeutic study.
Keywords: Gender dysphoria; Gender reassignment surgery; Quality of life; SF-36.
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Starting Point: the World Professional Association of Transgender Health Standards of Care
Initial ethics discussions, is there a sound medical rationale for the treatment or surgery to be provided through the center is such treatment or surgery consistent with the practice of evidence-based medicine, is establishment of the center consistent with the hospital’s mission, does the establishment of the center, and the delivery of its services, demonstrate respect for human dignity and worth, does the establishment of the center, and delivery of its services, demonstrate respect for patient autonomy, if the procedures performed by the center elicit some public criticism on the basis of religious or moral views, how should the hospital respond, how will the center show respect for, and accommodate, religious or moral objections by staff to participating in the procedures offered by the center, how should the center allocate resources in the event that the need for services exceeds capacity, the dilemma of patient age, conclusions, acknowledgments, ethical issues considered when establishing a pediatrics gender surgery center.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Elizabeth R. Boskey , Judith A. Johnson , Charlotte Harrison , Jonathan M. Marron , Leah Abecassis , Allison Scobie-Carroll , Julian Willard , David A. Diamond , Amir H. Taghinia , Oren Ganor; Ethical Issues Considered When Establishing a Pediatrics Gender Surgery Center. Pediatrics June 2019; 143 (6): e20183053. 10.1542/peds.2018-3053
Download citation file:
- Ris (Zotero)
- Reference Manager
As part of establishing a gender surgery center at a pediatric academic hospital, we undertook a process of identifying key ethical, legal, and contextual issues through collaboration among clinical providers, review by hospital leadership, discussions with key staff and hospital support services, consultation with the hospital’s ethics committee, outreach to other institutions providing transgender health care, and meetings with hospital legal counsel. This process allowed the center to identify key issues, formulate approaches to resolving those issues, and develop policies and procedures addressing stakeholder concerns. Key issues identified during the process included the appropriateness of providing gender-affirming surgeries to adolescents and adults, given the hospital’s mission and emphasis on pediatric services; the need for education on the clinical basis for offered procedures; methods for obtaining adequate informed consent and assent; the lower and upper acceptable age limits for various procedures; the role of psychological assessments in determining surgical eligibility; the need for coordinated, multidisciplinary patient care; and the importance of addressing historical access inequities affecting transgender patients. The process also facilitated the development of policies addressing the identified issues, articulation of a guiding mission statement, institution of ongoing educational opportunities for hospital staff, beginning outreach to the community, and guidance as to future avenues of research and policy development. Given the sensitive nature of the center’s services and the significant clinical, ethical, and legal issues involved, we recommend such a process when a establishing a program for gender surgery in a pediatric institution.
As part of the development of the Center for Gender Surgery at Boston Children’s Hospital (BCH), the surgical team decided to initiate a process of ethical and legal consultation. As the first gender surgical center to be housed in a pediatric facility in the United States, it was expected that there would be ethical and legal concerns that were unique to the setting, in addition to the broader concerns around gender surgery raised by other authors. 1 , 2 In the fall of 2017, these concerns were raised over a series of discussions with the hospital’s administration, ethics committee, legal team, community members, and other stakeholders, and several concerns were identified that might be relevant to both this center and other centers working with younger transgender patients.
The World Professional Association of Transgender Health (WPATH) has laid out standards of care (SOC) 3 for the treatment of gender-nonconforming people. Although these SOC are in the process of being reviewed and revised, 4 and are not without controversy, 2 , 5 , – 8 the center team decided to use them as a starting point for policy development. As a starting point, the center decided to follow recommendations in the SOC that state that patients are not eligible for genital surgery until they have reached the age of majority and have lived for at least a year in their affirmed gender. Twelve months of hormone therapy is also required, unless hormone therapy is not clinically indicated. 3 With respect to chest surgeries, the SOC state that “Chest surgery in [female-to-male] patients could be conducted earlier, preferably after ample time of living in the desired gender role and after one year of testosterone treatment. 3 ” Other requirements for chest surgery in both men and women are persistent, well-documented gender dysphoria; capacity to make an informed decision; and evidence that any significant medical and mental health conditions are well controlled. (Note, the requirements for living in the affirmed gender do not require living in a binary gender.) Another important aspect of the SOC guidelines is the requirement for screening by a behavioral health professional, which is designed to provide the surgeon with relevant information about the patient’s gender identity and overall mental health. That screening is provided to the surgeon in the form of a letter, required for most insurance authorizations, that establishes the patient's suitability for gender affirming surgery. This requirement is somewhat controversial and has occasionally been referred to as “gatekeeping.”
Despite their awareness of this controversy, the center staff believed it was appropriate for the care paradigm to include a surgery-specific behavioral health assessment. The implemented protocol covers general readiness for surgery, case management issues that may occur around the time of surgery, assessment of whether the patient’s expectations for surgery are realistic, awareness of postsurgical care requirements and likelihood of compliance, gender history, and fertility assessment.
The center staff consists of a multidisciplinary team of surgeons (2 plastic surgeons, 1 urologist), midlevel providers, nurses, a social worker and researcher, an administrator, and a designated research specialist. The idea for the center originated with the 3 surgeons, who serve as codirectors. After a year of planning and seeking out professional development options in transgender care, the codirectors brought the social worker and researcher onto the team because of her extensive experience working with the gender-diverse patient population. Together, those 4 team members drafted an evidence-based proposal for how the center would be structured and how care would be delivered. They also prepared a presentation in which they highlighted the needs of young people for gender-affirming surgery, key criteria and conceptual underpinnings for offering the surgery (including the SOC), and specific surgical solutions. This material was then presented to the hospital ethics committee for discussion. The ethics committee includes members from a range of medical and surgical services, nursing, patient care services, social services, pastoral care, and other clinical services as well as community representatives and ex-officio participants from administration and legal counsel. 9
The ethics committee meeting lasted ∼2 hours, and there was a vigorous discussion of concerns across a broad range of domains. A smaller team of ethics committee members and ethics staff then distilled the discussion points into an outline of ethical issues and general recommendations for approaches the center might follow in determining how to address them. This document was brought back to center staff and used to inform policy development and help formulate the center’s mission and values statements ( Fig 1 ). As additional issues, particularly those around the intersection of hospital policy, state law, and fertility preservation, arose for center staff, less-formal discussions were held with ethics and/or legal teams to explore relevant factors to be considered by the center in developing its policies.

Mission statement and values.
Key questions that arose from the ethics discussions are addressed below.
Gender dysphoria is defined in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition as the distress that occurs when there is a marked incongruence between the gender a person was assigned at birth and the gender that they experience or express. 10 The experience of gender dysphoria, and/or identifying as transgender, has been associated with a number of serious physical and mental health disparities, including elevated risks of depression, anxiety, suicidality, substance abuse, and HIV. 11 , – 15 Some of these disparities can be reduced with access to transgender-affirming health care and gender affirmation procedures. 11 , 16
The center planned to offer gender affirmation chest reconstruction, phalloplasty, and metoidioplasty for transmasculine individuals (those assigned female at birth with a more male gender identity) and breast augmentation and vaginoplasty for transfeminine individuals (those assigned male at birth with a more female gender identity). Although the quality of the evidence base is low and relies mostly on short-term follow-up, the limited existing reports suggest that these treatments can be an effective way to improve gender congruence and body satisfaction for transgender individuals who are interested in such surgeries, and they have also been shown to improve depression, anxiety, and overall quality of life. 17 , – 24 Reports of regret do occur, but they are rare, affecting <1% of patients in 1 large study. 25 This rate is substantially lower than for breast reconstruction after mastectomy, a contextually similar surgical procedure (reconstructive but optional, often involving body image and sexuality) for which decision regret has been studied. 26 , 27 On the basis of research in the field, the clinicians were able to present solid evidence that the treatments to be provided at the center were medically sound and necessary to improve the health and well-being of the patients to whom they would be provided, including reduction or alleviation of symptoms of gender dysphoria.
Genital affirmation surgeries, such as vaginoplasty and phalloplasty, are generally offered to adult patients rather than pediatric patients. Therefore, one of the questions that received substantial discussion at the ethics meeting was whether and how these surgeries fit into the mission of a pediatric hospital, including its primary commitment to the health and well-being of pediatric patients. The hospital’s patient care policy defines pediatric patients as those who are under the age of 21.
The conclusion that the program was consistent with the hospital’s mission was based on several factors. First, the hospital’s mission statement addresses the importance of serving unmet need. Because of this mission, the hospital had previously established that it is appropriate to follow pediatric conditions into adulthood when other specialty care for these conditions is not available. In fact, a number of hospital departments, including surgical specialties, already provided care for patients into or through adulthood, and the hospital also had standard criteria for patients being treated through age 35. Because gender dysphoria is often a condition that originates in childhood, it meets the basis of that criteria to the extent that equivalent care is not available. 28 , 29 Evidence was presented that there was currently a significant unmet need for gender affirmation procedures in New England. Although several surgeons offered chest surgeries in the Boston area, there was limited access to care for adolescents. There was one other surgical team in the area offering genital affirmation surgeries for transgender women, but genital affirmation surgeries for transgender men were completely unavailable in the area before the opening of the center. As such, one of the motivations for forming the center was the community reaching out to local hospitals looking for providers to address this gap in care. While it might, on the surface, make more sense to offer genital surgeries for transgender men at an adult hospital, at the time the center was formed, there were no surgeons in local adult facilities interested in providing that care. In contrast, the center surgeons had both appropriate expertise and interest in addressing the unmet need.
In addition to the unmet need in the area as a whole, clinical leaders at BCH also recognized an unmet need affecting current patients and appealed to the hospital for support. The hospital houses the Gender Management Service 30 , 31 (GeMS), a leader in medical gender affirmation for transgender youth that was founded in 2007 and currently works with hundreds of patients a year. However, when GeMS patients were ready to surgically transition, their care had to be referred outside of the hospital system. There was agreement by center staff and hospital leaders that a dedicated gender surgery center would best serve the hospital’s mission by providing comprehensive care options and continuity of care for those transgender adolescents and young adults who had been treated in GeMS and were interested in surgical affirmation. Although the 2 programs run entirely separately, the location of the center in a pediatric hospital, with access to the expertise of GeMS providers, meant that it was also well placed to address the particular psychological and medical challenges experienced by transgender youth, including an elevated risk of bullying, violence, and other forms of school-based harrassment. 32 , – 34
The hospital’s mission also includes research and education. Given its academic nature, and the presence of the GeMS program, the center is well situated to contribute to research in the field of transgender care (especially continuity of care from prepuberty to adult transitioning). The center can also support the hospital’s commitment to education, as is more fully described below.
Respect for human dignity and worth, including support for individual self-determination, are fundamental elements of medical ethics. 35 The hospital has a stated commitment to serving a diverse population, representing many nationalities, cultures, faiths, and value systems as well as those with diverse gender identities and sexual preferences. The ethics discussion process addressed this question by examining research in which it was shown that identifying with a gender that is inconsistent with one’s physical characteristics can lead to psychosocial difficulties and a decreased sense of self-worth. 36 , – 41 Although not all transgender individuals want surgery, treatment to help reduce the dissonance between physical body and gender identity has the potential to restore individuals’ sense of dignity and worth. In support of this goal, the ethics team recommended that the center provide services designed to meet patients’ psychosocial, emotional, and spiritual needs. This recommendation was addressed by the integration of a social worker with transgender health experience and training in the core team, who would explore patients’ motivations for surgery as part of the assessment ( Fig 2 ), and by the availability of transgender-affirming chaplaincy staff within the hospital. Center staff also determined that discussions of any surgical procedure should be instituted by the patient rather than offered by the team, to avoid giving the impression that providers felt any particular surgery was a necessary component of transition. The ethics team also recommended that center staff identify avenues for increasing understanding of the population served by the center, both within and outside the walls of BCH; fostering sensitivity and support throughout the center and the hospital for this population; and including input of this community into the development and operations of the center. In agreement with this goal, center staff have sought out opportunities to train providers and community members both inside and outside of the hospital 42 and continue to seek out opportunities to provide professional and community education whenever possible. This includes participation in the Care for Patients with Diverse Sexual Orientations and Gender Identities elective at Harvard Medical School and offering medical students opportunities to engage in additional research and practice with this population. The center has also sought input from community members and actively recruited transgender staff.

Patient care flow sheet. MD, medical doctor; NP, nurse practitioner; PA, physician’s assistant; SW, social worker.
Respect for patient autonomy is the ethical principle that generated the most controversy when developing the center’s policies and practices for patient care. Questions of respect for patient autonomy are at the core of much of the debate around the current WPATH SOC and screening guidelines, specifically care structures that require behavioral health professionals to provide approval to access care rather than prioritizing access through a process of informed consent, a model that is being adopted more and more often for hormone treatment. 6 This is true not just in the adult setting, but in the pediatric setting, as well. Although the GeMS model requires extensive psychological screening, 30 other models are also in place for pediatric hormone access, 43 , 44 and the center sees patients who have taken various routes to medical transition.
Debate on this topic is not restricted to medical transition care. There is also substantial disagreement among providers and others as to whether the current guidelines requiring one or more mental health assessments for patients to move forward with gender affirmation surgeries are critical to providing quality care, are problematic gatekeeping, or are something in between. 45 , – 51 Because a clear answer to the appropriateness of these guidelines is not supported in the current evidence base, the center decided that the most-appropriate way to address the controversy would be to follow the SOC while researching the burdens and benefits of the behavioral health requirements, particularly with respect to providing services to adolescents. To date, the center has enrolled over 70 patients into a longitudinal study in which researchers are assessing quality of life, mental health, and issues and costs of health care access in the context of gender-affirming surgery.
A related issue was whether minors were able to provide informed assent to the kinds of procedures being offered. Addressing this issue is a required component of the outside letters of support needed to access surgery. In addition, it has been previously established that minors legally and ethically can provide informed consent, without parent permission, for many medical therapies related to sexual and mental health. 52
Another issue raised around informed consent was specific to the pediatric population, namely the role of parents and guardians in providing informed consent (sometimes referred to as informed permission), because minors generally can provide assent but not consent for care. 52 There was substantial discussion among the ethics team, hospital counsel, and center providers as to whether the consent of both parents must be required for minor patients to undergo gender-affirming surgery. Although consent from both parents, alongside assent from the minor, is the standard for care in the hospital’s GeMS program, many transgender youth have complicated family situations. 32 , 53 , – 57 This may make acquiring 2-parent consent to perform surgery on an adolescent unfeasible or impossible, particularly when 1 parent is no longer involved in the minor’s life. Eventually, the center decided on a policy incorporating the standard of 2-parent consent but with the intention to develop formal procedures allowing for appeal in cases in which such a requirement appears to interfere unduly with the informed choices of minors and raises the possibility of significant harm.
Although for some people the requirements for parental consent and behavioral health assessment raised questions about the autonomy of adolescent patients, for others it was reassuring. There is substantial debate around adolescents’ capacity for decision-making and ability to conceptualize long-term outcomes. 58 , – 60 The involvement of both parents and multiple behavioral health providers in the process of determining eligibility for surgery, as well as the patients’ discussion with the interdisciplinary team of the benefits and risks (including possible regrets), serves as a check on the possibility of impulsivity and reduces the likelihood that age-related cognitive factors would lead to decision regret.
As such, the role of parents is not simply to provide informed consent. They are also important sources of insight and support throughout the gender affirmation process. Parental concerns can give important insights into adolescent maturity, gender stability, mental health, and well-being and provide a window into additional areas that the behavioral health provider might need to explore before surgical approval. Because of this, parent and guardian education is an important part of the consult process for minors seeking surgery, as is assessment of those adults’ interest in and willingness to support the patient through surgery. Situations in which parents disagree with each other are particularly challenging and addressed on a case-by-case basis.
Members of the ethics committee brought up a concern that some members of the public may have moral or religious objections to transgender surgery. Objections had been raised when the GeMS program was first started, including some death threats to staff, and it was thought that it would be important to prepare for any similar backlash in response to the start of the center. The possibility of moral or religious objections to surgery was not seen as a barrier to providing these services, and the ethics team recommended that appropriate hospital staff, including public relations staff, familiarize themselves with the nature of possible objections to the establishment of the center and with the underlying medical and ethical reasons for establishing the center to be able to engage in informed communication with the public. To accomplish this goal, center staff worked with marketing and communications staff at the hospital to develop evidenced-based messaging and responses to expected objections and to increase staff confidence with transgender issues. Center staff have also offered, and continue to provide in an ongoing manner, training to health care and support professionals throughout the hospital on both how to support patients and the importance of gender-affirming care for individual well-being.
The hospital has some existing policies related to religious and moral objections by staff. The personnel policy on “Requests to be excused from Patient Care Responsibilities,” for example, states that the hospital “will consider a request by a staff member not to participate in aspects of a patient’s care or treatment when such care or treatment conflicts with a staff member’s bona fide ethical or religious beliefs.” However, the policy is also clear that such a request cannot be accommodated if it will negatively affect care for the patient.
All participants involved in the discussions recognized the importance of education in addressing staff moral and religious concerns. To help accomplish this goal, center staff involved in education attempt to provide a safe space for questioning and discussion of care practices. 42 In addition, center staff are currently in the process of deploying a validated survey 61 to examine provider attitudes about and self-assessed competence in lesbian, gay, bisexual, and transgender health care across the hospital. It is suggested in the preliminary results that provider attitudes are primarily positive, although there were some responses expressing moral concerns about working with lesbian, gay, bisexual, and transgender patients and families. Results also suggest that providers were consistently less comfortable, and felt less competent, about working with transgender patients and families than lesbian, gay, and bisexual patients and families. 62 This is being addressed through offering increased opportunities for professional education on gender surgery and gender-affirming care throughout the hospital. Center staff offered more than 20 trainings to BCH staff between December 2017 and December 2018, and trainings continue to be requested across a variety of units and departments.
There is a documented unmet need for gender-affirming services, including surgical procedures. 32 , 63 , – 66 This was clearly visible in the fact that, within a few months of Boston Medical Center starting to offer insurance-covered vaginoplasty, their waitlist quickly grew to over 200 patients. 67 Because of the possibility of waitlists for the center’s services, the ethics team recommended that the center have a clear and consistent method of prioritizing patients for care. The center decided to take a first-come, first-served approach to initial consultation with patients. However, the center recognized there would be a need to undertake further exploration of methods for allocating resources in the event that limits were reached. From the beginning, center staff anticipated that hair removal would likely provide the primary scheduling barrier for patients seeking genital affirmation, and that has proven to be the case. (Hair removal is a requirement for genital surgery because of concerns about the presence of hair in the neourethra or neovagina.) Chest surgery scheduling is more straightforward and primarily limited by the availability of operating room time. While continuing to use the first come, first served principle, the center is working on ways to shorten waiting times whenever feasible.
After the initial ethical discussions were conducted, there remained several questions that the center wished to explore further. One such question was determining an appropriate age range for patients to be able to access each type of gender-affirming surgical procedure. Because the hospital is a pediatric institution, with policies about the age ranges for which it is appropriate to provide care, this discussion needed to address both the lower and upper bounds of care.
The WPATH SOC state that genital surgery should not be done until the age of majority in any given country (18 in the United States), but that it may be reasonable for chest surgeries to be done earlier. 3 Unfortunately, there is extremely limited published research on the impact of chest surgeries on the pediatric and young adult population. In what research there is, it is suggested that chest surgery can make it easier for young transmasculine individuals to participate more fully in society, including making it easier to exercise and maintain their health. 68 This research is supported by the clinical experience of center staff. Breast augmentation also has the potential to allow young transfeminine individuals to present more effectively as feminine, although fewer transfeminine than transmasculine individuals are interested in chest surgery. 32
After weighing the guidelines and feedback from stakeholders, the center decided to deviate from the SOC and set 15 as a minimum age for undergoing a chest reconstruction or breast augmentation, with surgery at age 15 only being appropriate for those individuals who have had a strong and consistent gender identity and, in rare cases, those who are significantly limited in life activities by the presence of their breasts. Because the risk of desistence of a transgender identity declines sharply after puberty, 22 , 69 the center thought that this allowed for a reasonable balance of recognizing the possible risk of a premature decision with respecting patients’ current needs and preferences.
Determining the minimum age for genital surgeries was somewhat more complicated. Although all center staff felt comfortable with requiring phalloplasty candidates to wait until the age of majority for surgery, the same was not true for vaginoplasty candidates. Transgender women who have not undergone vaginoplasty may face a number of challenges related to the existential threat that is sometimes perceived to accrue through the presence of male genitalia in a women’s-only space. 42 This concern may be particularly salient for young transgender women who are going off to college and who want to live, and be treated, like any other young women on campus. As a result, a number of American surgeons perform vaginoplasty procedures in patients under the age of 18 to allow young women to begin their adult lives feeling safe and affirmed in their gender. 5 Although mental health outcomes associated with vaginoplasty have generally been shown to be quite positive, to date there have been few published studies specifically exploring the psychosocial outcomes of vaginoplasty in minors. 70 , 71 Two studies following the same small population of girls who underwent vaginoplasty during adolescence did report improved psychological functioning and decreased gender dysphoria at 1 and 5 years follow-up. 72 , 73
However, performing vaginoplasty in patients under the age of 18 raises several particular concerns. 1 These include the ability of the patient to adequately provide assent 52 and a detailed assessment of whether the young woman will be capable of the extensive postsurgical care required by the procedure. 72 , 74 It is also critical to explicitly address the fact that the procedure will render the patient permanently sterile and attempt to determine whether the patient is capable of making an informed decision to permanently impact their fertility. Although fertility assessment is, in theory, a standard part of assessment earlier in the transition process, the center team felt it was critical to include such an assessment as part of the initial social work consult with every potential patient, regardless of age. This fertility assessment includes questions about whether the patient wants to have biological children, any history of gamete preservation, and appropriate referrals as necessary. The center team has found that doing such an assessment is critical because a sizeable minority of patients do not have a clear understanding of the fertility impacts of gender transition at the time of the initial consult.
The center staff eventually came to the conclusion that it is appropriate to offer vaginoplasties to certain individuals before the age of majority so that they can safely embark on their adult lives. However, to address legal concerns related to performing vaginoplasties in Massachusetts minors, it was necessary to institute a policy requiring such patients to either have undergone fertility preservation or to seek out a court order granting permission for surgery. To date, the only family to which this option has been offered has decided to pursue the court order.
Building a gender surgery center in a pediatric setting requires institutions to address unique ethical and legal challenges. It is important for providers and administrators to have a clear understanding of the local legal environment and relevant ethical principles. Plans for navigation of ethical challenges should be discussed early in the process, and institutions should plan to respond to ethical and moral considerations brought up by staff, patients, and the public at large. Ongoing ethical and legal consultation, as well as a broad range of staff, patient, and public educational opportunities, are likely to be needed. Such processes are necessary to provide optimal care for members of the transgender community in an ethically responsible fashion.
Dr Boskey copresented to the ethics committee, provided topic-specific documentation to the committee for review, drafted the manuscript, and oversaw all revisions; Ms Johnson led the drafting of the ethics committee response to the initial committee consultation, which was used in the drafting of the manuscript, and contributed significantly to revisions; Dr Harrison, Dr Marron, Ms Abecassis, Ms Scobie-Carroll, and Dr Willard contributed to the ethics committee consultation and contributed significantly to revisions; and Drs Diamond, Taghinia, and Ganor initiated the ethics consultation process, copresented to the ethics committee, worked on all consultations, and contributed significantly to revisions; and all authors approved the final manuscript as submitted.
FUNDING: No external funding.
The authors thank the members of Boston Children’s Hospital Ethics Advisory Committee for thoughtful comments and insights during their meeting to discuss this topic.
Boston Children’s Hospital
Gender Management Service
standards of care
World Professional Association of Transgender Health
Competing Interests
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Breaking News
RELIST WATCH
Restrictions on gender-affirming medical care – and assault weapons.

The Relist Watch column examines cert petitions that the Supreme Court has “relisted” for its upcoming conference. A short explanation of relists is available here .
After going two conferences without any new relists, the Supreme Court ended the relist drought this week with a vengeance. We have 12 new relists, several of which are potential blockbusters if the court grants review.
Gender-affirming care
Three of the cases involve constitutional challenges brought against state prohibitions on providing gender-affirming care to minors: United States v. Skrmetti , L. W. v. Skrmetti , and Jane Doe 1 v. Kentucky ex rel. Cameron . Last year, Tennessee and Kentucky were among a group of more than 20 states that enacted laws that prohibit giving transgender youths under the age of 18 medical treatment to align their appearance with their gender identity.
Tennessee’s law forbids medical treatments that are intended to allow a minor “to identify with, or live as, a purported identity inconsistent with the minor’s sex” or to treat “purported discomfort or distress from a discordance between the minor’s sex and asserted identity.” Kentucky’s law prohibits medical treatments “for the purpose of attempting to alter the appearance of, or to validate a minor’s perception of, [a] minor’s sex.” Both provisions outlaw a range of treatments, including gender-reassignment surgery. But the challenges before the court specifically concern two nonsurgical treatments: the administration of puberty blockers to stop physical changes brought on by puberty; and hormone therapy, which seeks to produce physiological changes to conform physical appearance with gender identity.
Transgender youths and their parents in both states quickly brought constitutional challenges in federal court, seeking to enjoin the laws before they went into effect. The challengers first argue that the restrictions discriminate on the basis of sex and therefore violate the 14th Amendment’s equal protection clause. They contend that the laws allow the use of puberty blockers and hormone therapy to conform a minor’s appearance to their birth sex, while barring transgender minors from using the same treatments. Second, the challengers argue that the prohibitions violate the 14th Amendment’s due process clause by infringing upon parents’ rights to make medical decisions for their children. The Biden administration intervened on the challengers’ side in the Tennessee case.
Federal district courts in both states granted the challengers’ requests to block the laws from going into effect. Kentucky and Tennessee then asked the U.S. Court of Appeals for the 6th Circuit to lift those orders while they appealed. The court of appeals refused, instead expediting argument. By a split vote, the 6th Circuit then reversed the lower courts’ rulings , concluding that the states were likely to win their appeals. The court thus allowed the laws go into effect.
The Biden administration, together with the Tennessee and Kentucky families, seek reversal of the 6th Circuit’s ruling. All three challengers maintain that the laws violate the equal protection clause, arguing that under Bostock v. Clayton County (in which the Supreme Court held that firing transgender employees on the basis of their gender identity violates federal employment discrimination laws) drawing distinctions on the basis of gender identity constitute prohibited action on the basis of sex. The private challengers also argue that the laws violate the due process clause because the Supreme Court has repeatedly struck down state restrictions on parents’ ability to raise their children as they see fit.
Just last month, the Supreme Court granted Idaho’s request for a partial stay of a lower-court injunction, thus permitting the state’s ban on gender-affirming care to go into effect until the court rules on any cert petition – although the injunction still remained in force as to the plaintiffs in that case, thus permitting the plaintiffs there to receive treatment.
There are some differences in the case – in the Idaho case, the district court’s decision to grant relief beyond the plaintiffs – a so-called “universal injunction” – was more prominent. But the grant of a stay suggests that a majority of the court believes the issue is certworthy and that the state is likely to succeed. A grant in this case would make next term very interesting indeed.
Assault weapons
In early 2023, Illinois adopted the Protect Illinois Communities Act, which prohibits the possession of assault weapons and high-capacity magazines. The state law’s definition of “assault weapon” essentially followed the federal-law definition. The act prohibits possession of certain semiautomatic pistols and rifles. A semiautomatic rifle falls under the law’s proscriptions if it has a detachable magazine and one or more of the following features: a pistol grip or thumbhole stock; any feature capable of functioning as a protruding grip for the non-trigger hand; a folding, telescoping, thumbhole, or detachable stock or a stock that otherwise enhances the concealability of the weapon; a flash suppressor; a grenade launcher; or a barrel shroud. The definition also includes a semiautomatic rifle with a fixed magazine capacity of more than 10 rounds (except those that accept only .22 caliber rimfire ammunition). Finally, there is a lengthy list of particular models that fall within the scope of the statute, notably all “AK” weapons (modeled after the Russian AK-47) and all “AR” weapons (those modeled after the AR-15). People who owned such weapons before the effective date of the law are permitted to retain them, subject to some geographic restrictions on use; otherwise, possession is a crime. Several Illinois municipalities adopted similar legislation.
Gun owners, dealers, and interest groups brought a number of lawsuits arguing that the law violated their rights under the Second Amendment to keep and bear arms and sought to block the state from enforcing the law. Roughly speaking, plaintiffs in northern Illinois, which is more urban, lost; plaintiffs in southern Illinois, which is more rural, were successful, and a judge there held that the statute was unconstitutional in all its applications and barred the state from enforcing it.
In a consolidated appeal, a divided panel of the U.S. Court of Appeals for the 7th Circuit affirmed the denial of relief for the northern cases and reversed the grant of relief for the southern ones. The panel said that, “[u]sing the tools of history and tradition to which the Supreme Court directed us in [ District of Columbia v. ] Heller and [ New York State Rifle & Pistol Ass’n v. ] Bruen ,” which instructed courts to look for analogous laws in history when considering the constitutionality of restrictions on the personal right to bear arms, “the state and the affected subdivisions have a strong likelihood of success in the pending litigation.” The 7th Circuit reasoned that “these assault weapons and high-capacity magazines are much more like machineguns and military-grade weaponry” that are not protected by the Second Amendment “than they are like the many different types of firearms that are used for individual self-defense,” and thus they can be regulated or banned.
Six petitions have been filed seeking review of that determination: Harrel v. Raoul , Herrera v. Raoul , Barnett v. Raoul , National Association for Gun Rights v. City of Naperville, Illinois , Langley v. Kelly , and Gun Owners of America, Inc. v. Raoul . Given the ubiquity of AR- and AK-type firearms, this case will likely be a blockbuster if granted.
Environmental law
The Clean Water Act of 1972 regulates the discharge of pollutants into regulated waters. The city and county of San Francisco received a permit from the EPA under the law’s National Pollutant Discharge Elimination System that allowed San Francisco to discharge from its wastewater treatment facility into the Pacific Ocean. San Francisco challenged the terms of its permit, arguing that the permit contained terms so vague that it failed to tell the city how much it needed to limit or treat its discharges to comply with the act, while simultaneously exposing it to liability for violating the permit provisions. After exhausting administrative remedies, San Francisco petitioned the U.S. Court of Appeals for the 9th Circuit for review.
A divided panel of the 9th Circuit denied San Francisco’s petition , concluding that the provisions are not unduly vague and are “consistent with the CWA and its implementing regulations.” In dissent, Judge Daniel Collins concluded that those provisions were “inconsistent with the text of the CWA.” He argued that the permit violated the CWA by making the permittee responsible for maintaining water quality standards without specifying what limitations on discharges would satisfy its responsibility.
San Francisco now seeks review , arguing that the 9th Circuit’s decision conflicts with decisions of the U.S. Court of Appeals for the 2nd Circuit and the Supreme Court itself. The government denies that there’s any such split.
Yes, that Michael Avenatti
Michael Avenatti enjoyed his 15 minutes of fame representing porn star Stormy Daniels in her suit against then-President Donald Trump. Afterwards, while representing youth basketball coach Gary Franklin in sponsorship negotiations with sports clothing company Nike, Avenatti threatened to disclose certain documents (that his client had not authorized him to disclose) unless Nike paid him and a colleague more than $10 million to do an “internal investigation” into sports corruption. Based on the conduct, Avenatti was convicted in federal court of extortion and fraud for depriving his client of his “honest services,” prohibited by 18 U.S.C. § 1346. The U.S. Court of Appeals for the 2nd Circuit affirmed his conviction.
In his petition in Avenatti v. United States , Avenatti raises two claims . First, he argues that 18 U.S.C. § 1346 is void “both on its face and” as applied to him because, as Justice Neil Gorsuch said in his concurring opinion in last year’s Percoco v. United States , “[t]o this day, no one knows what ‘honest-services fraud’ encompasses.” Avenatti claims that he did not defraud his client – he “at worst … abus[ed] his fiduciary duty as Franklin’s attorney by leveraging Franklin’s claims to pursue compensation for himself.” Second, he argues that most courts besides the 2nd Circuit have held that civil litigation conduct — and in particular, an attorney’s settlement demand — cannot support federal criminal extortion liability. Avenetti argues that under the 2nd Circuit’s rule, what would normally be handled by bar discipline is converted into a 20-year felony. The government responds that Avenatti raised neither claim before the court of appeals and that they are therefore procedurally defaulted; and even if they weren’t, those claims are meritless.
The Surpeme Court has long been skeptical of the honest-services fraud statute and the risks of overcriminalizing sharp business dealings, so one or more of the justices is surely taking a close look at this case.
Last up is a capital case, Medrano v. Texas . Rodolfo Medrano was a member of a south Texas gang charged with capital murder for the shooting deaths of six rival gang members during a robbery. When Medrano was arrested, he invoked his Miranda rights and told police he wanted to speak to an attorney. Police then spoke to Medrano’s wife and told her (falsely) that he was not believed to be involved and would be released if he spoke to police. She persuaded Medrano to talk, and he confessed to providing the guns. Medrano protested that he only provided guns for a robbery and was not present and did not expect the shootings to occur, but the jury found him criminally responsible. That testimony was then introduced against him at trial, and he was convicted of murder and sentenced to death. His conviction and sentence were affirmed on appeal, and his first petition for state post-conviction relief was denied.
Medrano then filed a second petition for state post-conviction relief, alleging that his Miranda rights were violated because police responded to his invocation of his right to silence by persuading his wife to talk to him. He also argued that expert testimony introduced against him violated his due process rights. The Texas Court of Criminal Appeals concluded that Medrano’s application failed to satisfy a state rule of criminal procedure governing successive petitions, and therefore dismissed his application as an “abuse of the writ” of habeas corpus.
In his petition , Medrano renews his argument that law enforcement officers violated his Miranda rights by using his wife to circumvent his invocation of his right to silence. He also argues that the rule invoked by the Texas Court of Criminal Appeals was not actually an “adequate and independent state ground” precluding review of his petition on the merits. He explains that the rule itself permitted a subsequent petition if the defendant could make a showing that but for a violation of the Constitution, no rational juror could have found him guilty. That condition is satisfied here, Medrano says, because the principal evidence introduced against him was the confession he says was improperly procured. In a supplemental brief , Medrano says that his second question is related to an issue the court will be considering next term in Glossip v. Oklahoma , so at minimum, the court should hold his petition for resolution of that case.
We’ll know more soon. Until next time!
New Relists
L.W. v. Skrmetti , 23-466 Issues : (1) Whether Tennessee’s Senate Bill 1 , which categorically bans gender-affirming healthcare for transgender adolescents, triggers heightened scrutiny and likely violates the 14th Amendment’s equal protection clause; and (2) whether Senate Bill 1 likely violates the fundamental right of parents to make decisions concerning the medical care of their children guaranteed by the 14th Amendment’s due process clause. (rescheduled before the Mar. 15, Mar. 22, Mar. 28, Apr. 12, Apr. 19, Apr. 26 and May 9 conferences; relisted after the May 16 conference)
United States v. Skrmetti , 23-477 Issue : Whether Tennessee Senate Bill 1 , which prohibits all medical treatments intended to allow “a minor to identify with, or live as, a purported identity inconsistent with the minor’s sex” or to treat “purported discomfort or distress from a discordance between the minor’s sex and asserted identity,” violates the equal protection clause of the 14th Amendment. (rescheduled before the Mar. 15, Mar. 22, Mar. 28, Apr. 12, Apr. 19, Apr. 26 and May 9 conferences; relisted after the May 16 conference)
Jane Doe 1 v. Kentucky ex rel. Coleman, Attorney General , 23-492 Issues : (1) Whether, under the 14th Amendment’s due process clause, Kentucky Revised Statutes Section 311.372(2) , which bans medical treatments “for the purpose of attempting to alter the appearance of, or to validate a minor’s perception of, the minor’s sex, if that appearance or perception is inconsistent with the minor’s sex,” should be subjected to heightened scrutiny because it burdens parents’ right to direct the medical treatment of their children; (2) whether, under the 14th Amendment’s equal protection clause, § 311.372(2) should be subjected to heightened scrutiny because it classifies on the basis of sex and transgender status; and (3) whether petitioners are likely to show that § 311.372(2) does not satisfy heightened scrutiny. (rescheduled before the Mar. 15, Mar. 22, Mar. 28, Apr. 12, Apr. 19, Apr. 26 and May 9 conferences; relisted after the May 16 conference)
City and County of San Francisco v. Environmental Protection Agency , 23-753 Issue : Whether the Clean Water Act allows the Environmental Protection Agency (or an authorized state) to impose generic prohibitions in National Pollutant Discharge Elimination System permits that subject permit-holders to enforcement for violating water quality standards without identifying specific limits to which their discharges must conform. (relisted after the May 16 conference)
Harrel v. Raoul , 23-877 Issues : (1) Whether the Constitution allows the government to prohibit law-abiding, responsible citizens from protecting themselves, their families, and their homes with semiautomatic firearms that are in common use for lawful purposes; (2) whether the Constitution allows the government to prohibit law-abiding, responsible citizens from protecting themselves, their families, and their homes with ammunition magazines that are in common use for lawful purposes; and (3) whether enforcement of Illinois’s semiautomatic firearm and ammunition magazine bans should be enjoined. (relisted after the May 16 conference)
Herrera v. Raoul , 23-878 Issues : (1) Whether semiautomatic rifles and standard handgun and rifle magazines do not count as “Arms” within the ordinary meaning of the Second Amendment’s plain text; and (2) whether there is a broad historical tradition of states banning protected arms and standard magazines from law-abiding citizens’ homes. (relisted after the May 16 conference)
Barnett v. Raoul , 23-879 Issue : Whether Illinois’ sweeping ban on common and long-lawful arms violates the Second Amendment. (relisted after the May 16 conference)
National Association for Gun Rights v. City of Naperville, Illinois , 23-880 Issues : (1) Whether the state of Illinois’ ban of certain handguns is constitutional in light of the holding in District of Columbia v. Heller that handgun bans are categorically unconstitutional; (2) whether the “in common use” test announced in Heller is hopelessly circular and therefore unworkable; and (3) whether the government can ban the sale, purchase, and possession of certain semi-automatic firearms and firearm magazines that are possessed by millions of law-abiding Americans for lawful purposes when there is no analogous Founding-era regulation. (relisted after the May 16 conference)
Langley v. Kelly , 23-944 Issues : (1) Whether the state of Illinois’ absolute ban of certain commonly owned semi-automatic handguns is constitutional in light of the holding in District of Columbia v. Heller that handgun bans are categorially unconstitutional; (2) whether the state of Illinois’ absolute ban of all commonly owned semi-automatic handgun magazines over 15 rounds is constitutional in light of the holding in Heller that handgun bans are categorially unconstitutional; and (3) whether the government can ban the sale, purchase, possession, and carriage of certain commonly owned semi-automatic rifles, pistols, shotguns, and standard-capacity firearm magazines, tens of millions of which are possessed by law-abiding Americans for lawful purposes, when there is no analogous historical ban as required by Heller and New York State Rifle & Pistol Ass’n, Inc. v. Bruen . (relisted after the May 16 conference)
Gun Owners of America, Inc. v. Raoul , 23-1010 Issue : Whether Illinois’ categorical ban on millions of the most commonly owned firearms and ammunition magazines in the nation, including the AR-15 rifle, violates the Second Amendment. (relisted after the May 16 conference)
Medrano v. Texas , 23-5597 Issues : (1) Whether under all the circumstances, including an officer’s knowing and deliberate deployment of Petitioner’s wife to elicit statements from Petitioner while he was in custody, the falsity of the information the officer gave her to convey to the petitioner, the strength of the incentive he proffered to induce the Petitioner to speak, and the fact that similar tactics were deliberately employed to obtain confessions Petitioner’s codefendants, introduction of the resulting statement Petitioner’s Fifth and Fourteenth Amendment rights under Miranda v. Arizona, 384 U.S. 436 (1966); (2) Whether the Texas Court of Criminal Appeals’ determination that the Petitioner’s subsequent petition failed to satisfy the requirements of Article 11.071, § 5(a)(2) was an adequate and independent state ground precluding merits review of his claim where that provision authorizes a subsequent petition when “by a preponderance of the evidence, but for a violation of the United States Constitution no rational juror could have found the applicant guilty beyond a reasonable doubt” and the confession whose constitutionality Petitioner is challenging was the only significant evidence linking him to the capital murder with which he was charged. (relisted after the May 16 conference)
Avenatti v. United States , 23-6753 Issues : (1) whether 18 U.S.C. § 1346, making it a crime to engage in “honest services fraud,” is void for vagueness; (2); whether civil litigation conduct – in particular, an attorney’s settlement demand – can support federal criminal extortion liability. (relisted after the May 16 conference)
Returning Relists
Hamm v. Smith , 23-167 Issues : (1) Whether Hall v. Florida and Moore v. Texas mandate that courts deem the standard of “significantly subaverage intellectual functioning” for determining intellectual disability in Atkins v. Virginia satisfied when an offender’s lowest IQ score, decreased by one standard error of measurement, is 70 or below; and (2) whether the court should overrule Hall and Moore , or at least clarify that they permit courts to consider multiple IQ scores and the probability that an offender’s IQ does not fall at the bottom of the lowest IQ score’s error range. (relisted after the Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22, Mar. 28, Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Cunningham v. Florida , 23-5171 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Nov. 17, Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Guzman v. Florida , 23-5173 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Crane v. Florida , 23-5455 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Arellano-Ramirez v. Florida , 23-5567 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Jackson v. Florida , 23-5570 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Sposato v. Florida , 23-5575 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Morton v. Florida , 23-5579 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to trial by a 12-person jury when the defendant is charged with a felony (rescheduled before the Dec. 1, Dec. 8, Jan. 5, Jan. 12, Jan. 19, Feb. 16, Feb. 23, Mar. 1, Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Aiken v. Florida , 23-5794 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (rescheduled before the Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Enrriquez v. Florida , 23-5965 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (rescheduled before the Mar. 15, Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Bartee v. Florida , 23-6143 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Manning v. Florida , 23-6049 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (rescheduled before the Mar. 22 and Mar 28 conferences; relisted after the Apr. 12, Apr. 19, Apr. 26, May 9 and May 16 conferences)
Tillman v. Florida , 23-6304 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (relisted after the Apr. 19, Apr. 26, May 9 and May 16 conferences)
Sanon v. Florida , 23-6289 Issue: Whether the Sixth and Fourteenth Amendments guarantee the right to a trial by a 12-person jury when the defendant is charged with a felony. (relisted after the Apr. 19, Apr. 26, May 9 and May 16 conferences)
Posted in Cases in the Pipeline
Cases: L. W. v. Skrmetti , Medrano v. Texas , United States v. Skrmetti , Avenatti v. United States , Jane Doe 1 v. Kentucky ex rel. Coleman, Attorney General , City and County of San Francisco v. Environmental Protection Agency , Harrel v. Raoul , Herrera v. Raoul , Barnett v. Raoul , National Association for Gun Rights v. City of Naperville, Illinois , Langley v. Kelly , Hamm v. Smith , Gun Owners of America, Inc. v. Raoul
Recommended Citation: John Elwood, Restrictions on gender-affirming medical care – and assault weapons , SCOTUSblog (May. 24, 2024, 10:49 AM), https://www.scotusblog.com/2024/05/restrictions-on-gender-affirming-medical-care-and-assault-weapons/
Privacy Overview
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.82(4); November, 2015
Transsexual attractions and sexual reassignment surgery: Risks and potential risks
Transsexual issues and sexual reassignment surgery (SRS) are receiving a great deal of attention and support in the media, schools, and government. Given the early age at which youth seek treatment for transsexual attractions (TSA) and gender dysphoria and given the serious risks associated with such treatment, it is essential that family and youth be advised about these risks and alternative treatment options. Physicians and mental-health professionals have a professional responsibility to know and communicate the serious risks, in particular risk of suicide, that are associated with SRS; the spontaneous resolution of TSA in youth; the psychological conflicts that have been identified in such patients and in their parents; the successful treatment of conflicts associated TSA and the regrets of those who have been through SRS. SRS and gender theory are also viewed from the faith perspective of Pope Francis and Pope Emeritus Benedict XVI.
Lay summary : Transsexuals and sex-change operations are receiving a great deal of attention. Young people may seek treatment for transsexual attractions at an early age even though these attractions may go away on their own. Psychological conflicts have been identified in these patients and their parents and may be successfully treated. There are serious risks associated with sex change. They include the risk of depressive illness and suicide. Physicians and mental-health professionals should know these risks and the regrets of those who have been through sex-change operations. These patients and their families also should be informed of other treatment options.
Transsexual issues and sexual reassignment surgery are receiving a great deal of attention and support in the media, schools, government and in health professionals today.
Dr. Paul McHugh, former chairperson of the Department of Psychiatry at Johns Hopkins Hospital, has written that,
The idea that one's sex is fluid and a matter open to choice runs unquestioned through our culture and is reflected everywhere in the media, the theater, the classroom, and in many medical clinics. It has taken on cult-like features: its own special lingo, Internet chat rooms providing slick answers to new recruits, and clubs for easy access to dresses and styles supporting the sex change. It is doing much damage to families, adolescents, and children and should be confronted as an opinion without biological foundation wherever it emerges. ( McHugh 2015 )
Transsexual issues are creating a new controversy in our elementary and high schools today as a result of youth and their parents asserting a right to identify the sex of their child without regard to the biological and genetic realities. The parents and child may insist that the child's name be changed to one of the opposite sex and that the child be allowed to wear clothing of the opposite sex and use opposite-sex bathrooms.
These families are often preparing their children for sexual reassignment surgery (SRS) without being given the knowledge of the serious, documented risks associated with such surgery or other treatment options for gender dysphoria, referred to in the past as gender identity disorder (GID). Endocrinologists who are giving hormones to these youth, mental-health professionals who are affirming SRS surgery, and surgeons have a professional responsibility to understand these grave risks; and these patients also should be apprised of these risks.
An early study of these risks included one hundred patients seeking SRS, sixty-six of whom had surgery and 34 of whom did not ( Meyer and Reter 1979 ). The operated-upon groups were followed from the time of surgery, the unoperated-upon group from the time of initial interview at the Gender Identity Clinic at Johns Hopkins. Of those operated on, twenty-one had a trial period (taking hormones and working in the opposite-gender role) while the other thirteen had been well-established in the cross-gender role at the time of surgery but did not have a formal trial period. Follow-up was successful in fifty-two patients, of whom fifty consented to have their data published. Follow-up interviews covered three main areas: adaptation; family relationships and adaptational patterns at major life intervals; and fantasy, dreams, and sexual activity. 73–80 percent of the patients were male. Average follow-up for operated-upon patients was sixty-two months and twenty-five months for the unoperated-upon group.
Residential instability was similar in the groups (average of twenty months between moves in the operated-upon group pre-surgery, eighteen months post-surgery, and twelve months pre-contact and ten months post-contact in the unoperated-upon group). Job levels indicated a slight upward trend in both groups. Changes in psychiatric contacts were also similar in the two groups.
A third group was found that went elsewhere for surgery when this was not performed at Hopkins. Adjustment scores were improved in the surgery and unoperated-upon group to a similar extent, with no significant difference between the groups, but the group that sought surgery elsewhere did less well (although there was no statistical significance to the difference).
As stated by the authors, “At the most simple level, these data suggest that significant change in adjustment scores may be achieved either through surgery or through the passage of time in association with some contact and acceptance into an organized evaluation program” ( Meyer and Reter 1979 ). The conclusion was that SRS was not successful in treating this condition and led to the discontinuation of SRS at Johns Hopkins.
In spite of these early findings, and lack of contravening evidence that SRS conveyed any benefits compared with any unoperated-upon control groups, the practice of SRS has continued and has been extended into younger age groups. In a 2015, Boston study of 180 transsexual youth who had undergone SRS (106 female-to-male; 74 male-to-female), these youth had a twofold to threefold increased risk of psychiatric disorders, including depression, anxiety disorder, suicidal ideation, suicide attempt, self-harm without lethal intent, and both inpatient and outpatient mental health treatment compared to a control group of youth ( Reisner et al. 2015 ).
(An important research study would be that of determining how many of these youth, and their parents or guardians, were informed about the psychiatric risks associated with the surgery which is described in the mental health literature and which should be known by the treating health professionals. Since the mean age at which youth presented for consideration for SRS surgery in the Boston study was age 9, providing this information in a way that the children would understand would be challenging but nonetheless could be done in regard to discussing suicide risks and successful alternative treatments for gender dysphoria. The primary childhood psychological conflicts that interfere with the appreciation of the goodness of a child's masculinity or femininity should be given.)
The largest study to date of the long-term psychological state of post-SRS persons was an analysis of over three hundred people who had undergone SRS in Sweden over the past thirty years. This 2011 study demonstrated that persons after sex reassignment, have considerably higher risks for mortality, suicidal behavior, and psychiatric morbidity than the general population ( Dhejne et al. 2011 ).
In 2014, Dr. Paul McHugh wrote in The Wall Street Journal about this research, “Most shockingly, their suicide mortality rose almost 20-fold above the comparable non-transgender population. This disturbing result has as yet no explanation but probably reflects the growing sense of isolation reported by the aging transgendered after surgery. The high suicide rate certainly challenges the surgery prescription” ( McHugh 2014 ).
In the same article, Dr. McHugh has also described his study of people with gender confusion over the past forty years, twenty-six of which he spent as the psychiatrist in chief of Johns Hopkins Hospital. He wrote, “In fact, gender dysphoria—the official psychiatric term for feeling oneself to be of the opposite sex—belongs in the family of similarly disordered assumptions about the body, such as anorexia nervosa and body dysmorphic disorder. Its treatment should not be directed at the body as with surgery and hormones any more than one treats obesity-fearing anorexic patients with liposuction.” He went on, “The treatment should strive to correct the false, problematic nature of the assumption and to resolve the psychological conflicts provoking it. With youngsters, this is best done in family therapy” ( McHugh 2014 ).
Important medical and psychological issues need to be considered before the educational, medical, political, and judicial systems rush headlong into a process of affirming in youth and in their parents a fixed, false belief that a person can be a sex that is not consistent with their biological and genetic identity and that such individuals have the right to transsexual surgery. Fixed, false beliefs are identified in the mental-health field as manifestations of a serious thinking disorder, specifically a delusion. Health professionals should not be supporting this delusional belief in these youth and their parents.
An understanding of what motivates youth to identify with the opposite sex is essential as well as the reasons why parents would encourage or support transsexual attraction. Dale O'Leary, the author of the important book The Gender Agenda , has co-authored an important 2015 research paper, “Understanding and Responding to the Transgender Movement” ( O'Leary and Sprigg 2015 ). Parents, youth and adults with TSA and health professionals would benefit from reviewing this important research paper.
GID/Gender Dysphoria: The Most Common Precursor to Transsexual Conflicts
Many youths who identify as persons of the opposite sex meet the earlier DSM criteria for GID. GID is a childhood psychiatric disorder (DSM IV TR) in which there is a strong and persistent cross-gender identification with at least four of the following preferences:
- • repeated stated desire to be of the opposite sex,
- • in boys, a preference for cross-dressing or simulating female attire and, in girls, wearing stereotypical masculine clothing and a rejection of feminine clothing such as skirts,
- • a strong and persistent preference for cross-sex role in play,
- • a strong preference for playmates of the opposite sex, and
- • an intense desire to participate in games and pastimes typical of the opposite sex.
The DSM 5 has replaced the diagnosis GID with a new diagnosis, gender dysphoria. It also describes the symptoms that arise from the failure to identify with one's biological sex.
Children who seek SRS should be evaluated for psychological conflicts but regularly are not. A Dutch researcher and clinician, who specializes in treating such youth, Dr. Peggy T. Cohen-Kettenis has written in this regard:
The percentage of children coming to our clinic with GID as adolescents wanting sex reassignment is much higher than the reported percentages in the literature … We believe (psychological) treatment should be available for all children with GID, regardless of their eventual sexual orientation. ( Cohen-Kettenis 2001 )
A Study of Youth from a Gender Identity Center
A 2013 study from a gender identity service in Toronto, that consisted of a sample of 577 children (ages 3–12) and 253 adolescents (ages 13–20), reported a number of findings and comments. These included:
- • A sharp increase in adolescent referrals starting with the 2004–2007 cohort and this increased even more so in the last cohort, 2008–2011.
- • For the first six cohorts (1976–1999), the percentage of boys always exceeded 75 percent, with the sex ratio ranging from a low of 4.61:1 (1988–1991) to a high of 12:1 of boys to girls (1992–1995), but for the last three cohorts (2000–2011) hovered around 75 percent, with the sex ratio ranging from 2.77:1 (2000–2003) to 3.41:1 (2008–2011) of boys to girls.
- • The adolescent sex ratios were closer to parity. Of note, there were two cohorts (1988–1991 and 2008–2011) in which the number of girls exceeded the number of boys.
- • The adolescent cases increased even more from the 2004 to 2007 cohort; and in the 2008 to 2011 cohort, the number of adolescent cases exceeded the number of child cases for the first time since the inception of their clinic in the mid-1970s.
- • For the adolescents, data on sexual orientation were available for 248 patients. The percentage of girls classified as homosexual was greater than the percentage of boys classified as homosexual (76.0% vs. 56.7%).
For the children, 66.4 percent were in two-parent families at the time of assessment compared with 45.8 percent of the adolescents ( Wood et al. 2013 ). Another parameter that struck them as clinically important was that a number of youth commented that, in some ways, it was easier to be transsexual than to be gay or lesbian.
Along similar lines, they have also wondered whether, in some ways, identifying as transsexual has come to occupy a more valued social status than identifying as gay or lesbian in some youth subcultures. Perhaps this social force explains, at least partially, the particularly dramatic increase in female adolescent cases in the 2008–2011 cohort.
Another factor that impressed them in accounting for the increase in adolescent referrals pertained to youth with gender identify disorder who also had an autism spectrum disorder which has been reported by others ( de Varies et al. 2010 ). A center in the Netherlands reported the co-occurrence of GID and autism spectrum disorders (ASD) in a study of children and adolescents (115 boys and 89 girls, mean age 10.8). The incidence of ASD was 7.8 percent. The authors recommended acquiring a greater awareness “of co-occurring ASD and GID and the challenges it generates in clinical management.”
Family Conflicts in Youth with Gender Identity Confusion/Gender Dysphoria
Drs. Zucker and Bradley in Toronto have been recognized as leaders in the study of GID. They have identified a number of conflicts in the families of children with GID that included:
A composite measure of maternal psychopathology correlated quite strongly with Child Behavior Checklist indices of behavior problems in boys with GID.
The rate of maternal psychopathology is high by any standard and includes depression and bipolar disorder.
The boy, who is highly sensitive to maternal signals, perceives the mother's feelings of depression and anger. Because of his own insecurity, he is all the more threatened by his mother's anger or hostility, which he perceives as directed at him. His worry about the loss of his mother intensifies his conflict over his own anger, resulting in high levels of arousal or anxiety. The father's own difficulty with affect regulation and inner sense of inadequacy usually produces withdrawal rather than approach.
The parents have difficulty resolving the conflicts they experience in their own marital relations, and fail to provide support to each other. This produces an intensified sense of conflict and hostility.
In this situation, the boy becomes increasingly unsure about his own self-value because of the mother's withdrawal or anger and the father's failure to intercede. This anxiety and insecurity intensify, as does his anger.
These men (fathers) are often easily threatened and feel inadequate themselves. These qualities appear to make it very difficult for them to connect with sons who display non-masculine behavior.” Withdrawing from their feminine sons, “they often deal with their conflicts by overwork or distancing themselves from their families. The fathers’ difficulty expressing feelings, and their inner sense of inadequacy are the roots of this emotional withdrawal.
Fathers demonstrate depression and substance abuse disorder.
Parental psychopathology among the parents of children with GID deserves thoughtful consideration. ( Zucker et al. 2003 )
Also, Dr. Bradley has described additional maternal conflicts in these youth,
boys with GID appear to believe that they will be more valued by their families or that they will get in less trouble as girls than as boys. These beliefs are related to parents’ experiences within their families of origin especially tendencies on the part of mothers to be frightened by male aggression or to be in need of nurturing, which they perceive as a female characteristic. ( Bradley 2003 , 201–202)
Zucker et al. (2012 ) also found that GID youth had high rates of general behavior problems and poor peer relations.
It should be noted that these observations are not derived from controlled studies. As such, there is no comparison to the prevalence of such conflicts among control groups. Thus the specificity of these conflicts (or their prevalence in children with gender dysphoria) is not clear. There is no conclusive evidence of the role of such conflicts in the development of gender dysphoria or whether treatment aimed at correcting these leads to improvement. However, the comments of Zucker and Bradley do seem relevant to understanding the development of GID.
Additional conflicts that we have seen in engaging in the family therapy recommended by Dr. Paul McHugh include:
In females’ relationships with their fathers, observed conflicts may include:
- 1. Excessive fear of the father's anger or his controlling behaviors, leading to a fear of being hurt due to being a woman, coupled with a belief that being a male would help them feel stronger and safer;
- 2. Severe mistrust of the father because of his insensitive and angry treatment of the mother, because of his harming the family by abandonment or because of his emotional, personality, or behavioral conflicts;
- 3. The father's failure to affirm his daughter's feminine goodness and gifts, to critique and protect her from gender theory errors, and to communicate that fulfillment and happiness can be found in being a psychologically healthy female.
In males’ relationships with their mothers, observed conflicts may include:
- 1. The mother's mistrust of and anxiety with males as a result of growing up with a harsh, angry, distant, or addicted father (the child's grandfather);
- 2. Her desire that her son had been a daughter, leading to initiating or supporting cross dressing and cross-sexual identification;
- 3. A boy's fears that he does not please his mother as a male, together with his unconscious belief that he might receive more love and acceptance from his mother if he identified with femininity;
- 4. A mother's failure to support and encourage her son to have same-sex friendships;
- 5. A failure to critique and protect him from gender theory errors;
- 6. A failure to communicate that fulfillment and happiness can be found in being a psychologically healthy male.
In males’ relationships with their fathers, observed conflicts may include:
- 1. Failure to develop a secure father–son relationship because of a father's emotionally distant behaviors or severe male insecurity;
- 2. A father's excessive anger or rejecting behaviors that undermine a son's ability to model after his father or that create a negative view of masculinity;
- 3. A father's failure to support a son's strong creative and artistic gifts;
- 4. A failure to protect the son from abusive behaviors by siblings or by same-sex peers that contribute to a son's failure to identify with the goodness of masculinity;
- 5. A failure to support same-sex friendships in childhood and adolescence;
- 6. A failure to critique and protect youth from gender theory errors;
- 7. A failure to communicate that fulfillment and happiness can be found in being a psychologically healthy male.
In females’ relationships with their mothers, observed conflicts may include:
- 1. An emotionally distant, angry, selfish, depressed, or critical mother who failed to bond closely with her daughter for any number of reasons, including unresolved anger with the maternal grandmother that was misdirected at the daughter;
- 2. The failure to affirm the daughter's goodness and female gifts;
- 3. A failure to support and encourage same sex friendships;
- 4. A failure to critique and protect her daughter from gender theory errors;
- 5. A failure to communicate that fulfillment and happiness can be found in being a psychologically healthy female.
Other factors and conflicts observed in males may include:
- 1. A keen appreciation and love for beauty that is often associated more with femininity than masculinity and a desire to be what one loves;
- 2. A poor body image and the belief that one would be more attractive if he were of the opposite sex;
- 3. Severe childhood rejection by same-sex peers, creating a sense of not fitting in with them, which results in intense fears of rejection and an unconscious belief that one would feel safer if he were of the opposite sex;
- 4. Repeated failures in relationships with women, associated with a severe loss of self-esteem;
- 5. A sense of pleasure in rejecting the values and moral code of his parents;
- 6. The belief that his sex is not a gift, but a constraint that must be overcome;
- 7. Pressure from a significant other to cross dress, take hormones, and move toward SRS;
- 8. Severe narcissism and acceptance of gender theory with a delusional belief that he can create himself as he wants.
Other factors and conflicts observed in females may include:
- 1. The absence of close female friendships and a sense of not fitting in, along with a belief that she would be less lonely and happier if she were a male;
- 2. In strong, young females, a love for what is perceived as male strength and preferential treatment for males, together with the desire to become what she loves;
- 3. Poor body image and a belief that she would be more attractive if she were of the opposite sex;
- 4. In very athletic and strong young females an intense bonding and identification with young males through athletic activities;
- 5. A sense of failure as a female and a delusional belief that she would feel more confident and happy being a member of the opposite sex;
- 6. Repeated failures in relationships with males with severe loss of self-esteem;
- 8. A sense of pleasure in rejecting the values and moral code of her parents;
- 9. The view that her sex is not a gift but as a constraint that must be overcome;
- 10. Acceptance of gender theory, along with a delusional belief that she can create herself as she wants.
The exposure of youth to gender theory in college can result in their embrace of postmodern philosophies focused on freedom as an end in and of itself. Such ideas come from various sources, including the writings of Friedrich Nietzsche and Jean-Paul Sartre. If freedom (some would call it license) is the greatest good in the world, then why should anyone be constrained by biology? One's sex as male and female is seen not as a gift but as a constraint that must be overcome. So if technology can alter one's body, then so be it.
PC Medicine
Some medical centers fail to or refuse to diagnose the psychological difficulties youth have in accepting and appreciating their biological sex. They neglect to provide proper counseling about treatment and the risks of sexual-reassignment surgery. Instead, they support the beliefs of the youths and their parents and initiate hormone treatments in preparation for eventual body-mutilating surgery.
A pediatric specialist at Boston has a program for boys who feel like girls and girls who want to be boys. He offers his patients—some as young as seven years old—counseling about the “naturalness” of their feelings and hormones to delay the onset of puberty. These drugs stop the natural process of sexual development that would make it more surgically difficult to have a sex alteration later in life.
This physician alleges that those whom he labels as transsexual children are deeply troubled by a lack of understanding of their feelings and have a high level of suicide attempts. While this physician is accurate in his interpretation of the literature—that children with GID and transsexual ideation are deeply troubled—his claims of a high level of suicide attempts in children with GID is not substantially supported by the medical literature. In fact, the literature demonstrates a shocking increase in suicide and in psychiatric illness after sexual reassignment surgery ( Dhejne et al. 2011 ).
In his 2014 Wall Street Journal article, Dr. McHugh wrote that “misguided doctors at medical centers including Boston's Children's Hospital have begun trying to treat” transgenderism in youths “even though the drugs stunt the children's growth and risk causing sterility.” He recommends “a better way to help these children: with devoted parenting” ( McHugh 2014 ).
The Treatment of Youth with Transsexual Confusion
According to Drs. Zucker and Bradley:
The fantasy solution provides relief but at a cost. They are unhappy children who are using their cross-gender behaviors to deal with their distress.
Treatment goal is to develop same-sex skills and friendships.
In general, we concur with those who believe that the earlier treatment begins, the better … It has been our experience that a sizable number of children and their families can achieve a great deal of change.
In these cases, the gender identity disorder resolves fully, and nothing in the children's behavior or fantasy suggest that gender identity issues remain problematic … All things considered, however, we take the position that in such cases clinicians should be optimistic, not nihilistic, about the possibility of helping the children to become more secure in their gender identity. ( Zucker and Bradley 1995 , 281–282)
Zucker and Bradley have been providing sensitive treatment to children with the precursor of transsexual conflicts. They have written that the goal of treatment is to develop skills associated with children of their own biological sex and friendships with such children. We have found a similar treatment approach to be beneficial in treating such children ( Fitzgibbons 2015 ). While data from controlled clinical studies are not available to measure the effectiveness of these therapies, it seems reasonable to follow the recommendations of those with extensive clinical experience until such time as controlled trials are performed.
Also, Dr. McHugh has written that transsexual attractions are often fluid and can change. “When children who reported transsexual feelings were tracked without medical or surgical treatment at both Vanderbilt University and London's Portman Clinic, 70 to 80 percent of them spontaneously lost those feelings” ( McHugh 2014 ). Dr. McHugh has described also his research experiences at Johns Hopkins:
As for the adults who came to us claiming to have discovered their true sexual identity and to have heard about sex-change operations, we psychiatrists have been distracted from studying the causes and natures of their mental misdirections by preparing them for surgery and for a life in the other sex. We have wasted scientific and technical resources and damaged our professional credibility by collaborating with madness rather than trying to study, cure, and ultimately prevent it.
One might expect that those who claim that sexual identity has no biological or physical basis would bring forth more evidence to persuade others. But as I've learned, there is a prejudice in favor of the idea that nature is totally malleable.
A practice that appears to give people what they want turns out to be difficult to combat with ordinary professional experience and wisdom. Even controlled trials or careful follow-up studies to ensure that the practice itself is not damaging are often resisted and the results rejected. ( McHugh 2004 )
Sexual Reassignment Surgery
SRS violates basic medical and ethical principles and is therefore not ethically or medically appropriate.
- 1 SRS mutilates a healthy, non-diseased body. To perform surgery on a healthy body involves unnecessary risks; therefore, SRS violates the principle primum non nocere , “first, do no harm.”
- 2 Candidates for SRS may believe that they are trapped in the bodies of the wrong sex and therefore desire or, more accurately, demand SRS; however, this belief is generated by a disordered perception of self. Such a fixed, irrational belief is appropriately described as a delusion.
- 3 SRS, therefore, is a “category mistake”—it offers a surgical solution for psychological problems, such as a failure to accept the goodness of one's masculinity or femininity, lack of secure attachment relationships in childhood with same-sex peers or a parent, self-rejection, untreated GID, addiction to masturbation and fantasy, poor body image, excessive anger and rebelliousness, and severe psychopathology in a parent.
- 4 SRS does not accomplish what it claims to accomplish. It does not change a person's sex; therefore, it provides no true benefit.
- 5 SRS is a “permanent,” effectively unchangeable, and often unsatisfying surgical attempt to change what may be only a temporary (i.e., psychotherapeutically changeable) psychological/psychiatric condition. ( Fitzgibbons, Sutton, and O'Leary 2009 )
Regrets over SRS
Dr. Renee Richards, a former professional tennis player, has written that her transition failed to meet even her own expectations. She wrote,
I wish that there could have been an alternative way, but there wasn't in 1975. If there was a drug that I could have taken that would have reduced the pressure, I would have been better off staying the way I was—a totally intact person. I know deep down that I'm a second-class woman. I get a lot of inquiries from would-be transsexuals, but I don't want anyone to hold me out as an example to follow. Today there are better choices, including medication, for dealing with the compulsion to cross-dress and the depression that comes from gender confusion. As far as being fulfilled as a woman, I'm not as fulfilled as I dreamed of being. I get a lot of letters from people who are considering having this operation … and I discourage them all. ( Richards 1999 )
Walt Heyer, who went through SRS, also exposes the origins of the practice and its often tragic results in his article ( Heyer 2015 ).
Youth, their parents, and adults who are considering SRS should be informed by their doctors and psychologists about the serious regrets many people have who underwent SRS. This information should also be communicated in schools where SRS is being taught as a healthy step to seeking greater happiness and fulfillment in life.
Parental Responses to Youth with Transsexual Attractions
As the protectors of their children, the first step parents can take is to understand possible reasons why their child is identifying with the opposite sex and has difficulty in embracing the goodness of his masculinity or her femininity. Then parents should learn about the serious health risks associated with SRS. Next, it is essential to do what most health professionals, educators, and the media fail to do, warn their children of the serious psychiatric dangers associated with SRS, especially the risk of suicide.
Many parents report the benefits of limiting time on the Internet for their children with this conflict. They believe that communication with those who are supporting and encouraging SRS reinforces the false belief that their thinking can determine their sex, that they have no emotional conflicts, and that SRS is a path they should pursue.
The leading experts in GID, Zucker and Bradley, have written, “parental ambivalence is, in most cases part of the problem.” Parents, particularly mothers, who might rationalize that it is “cute” to have a boy wear female clothing, often ignore or excuse obvious appearances of effeminacy in males. These psychologists encourage early intervention to prevent the suffering of isolation, unhappiness, and low self-esteem in children who fail to appreciate their goodness as boys or girls.
Children are born with a drive to seek love and acceptance from each parent, as well as siblings and peers. If this need is met, children develop a positive identification with their masculinity or femininity. When this developmental task is successfully completed, the child is free to choose gender-atypical activities. Boys and girls with gender-identity problems are not freely experimenting with gender-atypical activities. They are constrained by deep insecurities and fears and are reacting against the reality of their own sexual identity, often as a result of failing to experience secure attachment relationships with the parents, siblings, or same-sex peers.
Mistakes parents make with children who have transsexual attractions (TSA) may include:
- • failing to identify a child's weakness in embracing the goodness of his masculinity or her femininity;
- • allowing a child unsupervised time on the Internet, especially in the evenings, during which the delusional belief that one can change one's sex can be communicated and affirmed;
- • failing to help understand the causes of their conflicts;
- • failing to warn about the severe dangers of SRS;
- • enabling the delusional thinking that one can change one's sex;
- • depending too much on acceptance by a child;
- • allowing a child to see a health professional who fails to provide adequate information and who fails to explore possible psychological origins of the failure to embrace the goodness of masculinity or femininity;
- • failing to get a professional opinion about the origins of transsexual attractions and the serious risks associated with sexual reassignment surgery;
- • supporting the controlling behavior of the child who insists upon being called by a name of the opposite sex at home and at school;
- • enabling communication with peers and others who encourage SRS.
Children can also learn to correct their cognitive distortions in regard to their natural goodness and beauty as a male or female. The responses could include thinking:
“I can grow to appreciate the goodness of my body and masculinity and femininity.”
“I can be thankful for my special masculinity or femininity.”
“I can grow to feel more comfortable and confident in being who I am.”
While there are no controlled clinical data to support specific interventions in treating children with transsexual conflicts, the following recommendations could be helpful if incorporated into a family therapy treatment program. For boys with transsexual conflicts:
- • increasing quality time for bonding with the father;
- • increasing affirmation of the son's masculine gifts by the father;
- • bonding with the son in his artistic or creative activities;
- • participating in and support for the son's creative efforts by the father;
- • encouraging same-sex friendships and diminishing time with opposite-sex friends;
- • slowly diminishing play with opposite-sex toys;
- • encouraging the boy to be thankful for his special male gifts;
- • working at forgiving boys who may have hurt him;
- • communicating with other parents whose children have been treated successfully for GID and who have come to appreciate and to embrace the goodness of their masculinity and femininity;
- • addressing the emotional conflicts in a mother who wants her son to be a girl;
- • in those with faith, encouraging thankfulness for one's special, God-given masculine gifts.
For girls with transsexual conflicts:
- • encouraging the daughter to appreciate the goodness and beauty of her femininity, including her body;
- • encouraging same-sex friendships and activities;
- • increasing the mother–child quality time;
- • praising their daughter's special goodness and gifts;
- • working with the daughter to forgive peers who have hurt her;
- • encouraging pursuit of a balance in athletic activities;
- • addressing conflicts in a parent who may want her to be a boy;
- • in those with faith, encouraging thankfulness for one's special, God-given femininity.
Transsexual Indoctrination in Schools
Some school districts have been attempting to incorporate transsexual education into the required health programs in junior and senior high schools. In the Fairfax County, Virginia, School District, parents’ groups strongly objected to this attempt; and the program was left in the family life section which is not required for students. In an important article, “Gender Free Children: The newest fad in public education,” the British Columbia Teachers Federation handbook on gender education was cited. It stated that “gender is a product of the mind … Being transgender or gender non-conforming is normal and healthy.”
Author Lee Duigon wrote,
Coming soon, to a public school near you: the teaching that “gender is a spectrum,’ and ‘gender identity” a state of mind, a social construct—and it's all part of a top-down campaign to convince your children that they can be “whoever they want to be.” Boys can be girls and girls can be boys. ( Duigon 2011 )
The author noted that the Redwood Heights Elementary School in Oakland, California, has already installed a “gender coach” in the classroom to teach very young children that “you can be a boy or a girl, or both.” The “coach” was provided by an organization called Gender Spectrum (http:// www.genderspectrum.org ) which presumably would not exist if it did not perceive a demand for its services.
In addition, school principals are placing children at risk and are creating confusion in the minds of many children by giving in to the requests of parents to allow young children to change their names to those of the opposite sex, cross dress, and be accepted as being of the sex opposite of their biological sex. These school administrators either do not know or ignore medical and psychological science and research on transsexual issues and SRS. They are participating in a false belief that the children are not of their biological sex. Such a fixed, false belief is identified in the mental health field as a delusion.
Faith and Transsexual Issues
While he has not specifically addressed the issue of transsexualism, Pope Francis has repeatedly criticized gender theory indoctrination of youth. On January 19, 2015, in an in-flight interview returning from Manila, he described the forcing of gender ideology onto students in schools as a form of “ideological colonization” comparable to Hitler youth indoctrination ( Westen 2015 ). Pope Francis commented on April 15, 2015, at his weekly general audience: “if so-called gender theory is not an expression of frustration and resignation, that aims to cancel out sexual difference as it is no longer able to face it. Yes, we run the risk of taking a step backwards. Indeed, the removal of difference is the problem, not the solution” ( White 2015 ). On June 8, 2015, he stated that so-called gender ideology is challenging the complementarity between a man and a woman under the guise of seeking a more just society. He related, “Let me draw your attention to the value and beauty of marriage. The differences between men and women are not of the order of opposition or subordination, but rather communion and generation, always as the image and semblance of God” ( Montagna 2015 ).
Similarly, Pope Benedict XVI strongly criticized gender theory in his Christmas address to the Roman Curia, December 22, 2008. He stated,
She [the Church] has a responsibility towards creation, and must also publicly assert this responsibility. In so doing, she must not only defend earth, water and air as gifts of creation belonging to all. She must also protect man from self-destruction … .
What is often expressed and understood by the term “gender” ultimately ends up being man's attempt at self-emancipation from creation and the Creator. Man wants to be his own master, and alone—always and exclusively—to determine everything that concerns him. Yet in this way he lives in opposition to the truth, in opposition to the Creator Spirit.
Rain forests deserve indeed to be protected, but no less so does man, as a creature having an innate “message” which does not contradict our freedom, but is instead its very premise. ( Benedict XVI 2008 )
Youth have the right to be provided, by physicians, mental health professionals, school nurses, and the media, with accurate information about gender confusion, the serious medical and psychiatric associated with SRS, and the excellent prognosis associated with an alternative proven treatment described in the medical literature.
Parents, family members, educators, politicians, and clergy have a moral responsibility to be familiar with medical science and to provide prudent counsel to youth that will protect and not harm them.
Biographical Note
Richard Fitzgibbons, M.D., has practiced psychiatry for forty years. He trained at the Hospital of the University of Pennsylvania and the Philadelphia Child Guidance Center. He has worked extensively with marital and family conflicts.
- Benedict Pope., XVI 2008. Address “To the members of the Roman Curia for the traditional exchange of Christmas greetings.” December 22. http://w2.vatican.va/content/benedict-xvi/en/speeches/2008/december/documents/hf_ben-xvi_spe_20081222_curia-romana.html .
- Bradley Susan. 2003. Affect regulation and the development of psychopathology . New York: Guilford Press. [ Google Scholar ]
- Cohen-Kettenis Peggy. 2001. Gender identity disorder in the DSM? Journal of the American Academy of Child and Adolescent Psychiatry 40 : 391. [ PubMed ] [ Google Scholar ]
- de Varies Annelou L., Noens Ilse L.J., Cohen-Kettenis Peggy T., van Berckelaer-Onnes Ina A., and Doreleijers Theo A.. 2010. Autism spectrum disorders in gender dysphoric children and adolescents . Journal of Autism and Developmental Disorders 40 : 930–936. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dhejne Cecilia, Lichtenstein Paul, Boman Marcus, Johansson Anna L. V., Långström Niklas, and Landén Mikael. 2011. Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study in Sweden . PLoS ONE 6 : e16885. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Duigon Lee. 2011. Gender free children: The newest fad in public education. ghalcedon. http://chalcedon.edu/research/articles/gender-free-children-the-newest-fad-in-public-education/ .
- Fitzgibbons Richard. 2015. Gender dysphoria, gender identity disorder and informed consent. http://www.childhealing.com/articles/genderidentitydisorder.php .
- Fitzgibbons Richard, Philip M.Sutton, and O'Leary Dale. 2009. The psychopathology of “sex reassignment” surgery: Assessing its medical, psychological, and ethical appropriateness . National Catholic Bioethics Quarterly 9.1 : 109–37. [ Google Scholar ]
- Heyer Walt. 2015. Sex change surgery: What Bruce Jenner, Diane Sawyer and you should know. April 27. http://www.thepublicdiscourse.com/2015/04/14905 .
- McHugh Paul. 2004. Surgical sex . First Things 147 ( November ): 34–38. [ Google Scholar ]
- McHugh Paul. 2014. Transgender surgery isn't the solution. The Wall Street Journal . June 12. http://www.wsj.com/articles/paul-mchugh-transgender-surgery-isnt-the-solution-1402615120 .
- McHugh Paul. 2015. Transgenderism: A pathogenic meme. Public Discourse . June 10. http://www.thepublicdiscourse.com/2015/06/15145 .
- Meyer Jon K., and Reter Donna J.. 1979. Sex reassignment. Follow-up . Archives of General Psychiatry 36 : 1010–5. [ PubMed ] [ Google Scholar ]
- Montagna Diane. 2015. Pope Francis: Gender theory is a threat to society. Aleteia.org . June 9. http://aleteia.org/2015/06/09/pope-francis-gender-theory-is-a-threat-to-society/ .
- O'Leary Dale, and Sprigg Peter. 2015. Understanding and responding to the transgender movement. Family Research Council. http://downloads.frc.org/EF/EF15F45.pdf .
- Reisner Sari, Vetters Ralph, Leclerc M., Zaslow Shayne, Wolfrum Sarah, Shumer Daniel, and Mimiaga Matthew J.. 2015. Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study . Journal of Adolescent Health 56 : 274–79. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Richards Renee. 1999. The Liaison Legacy. Tennis Magazine . March.
- Westen John-Henry. 2015. Pope Francis condemns gender theory a third time: “The family is under attack.” Lifesitenews.com . March 23. https://www.lifesitenews.com/news/pope-francis-condemns-gender-theory-a-third-time-the-family-is-under-attack .
- White Hilary. 2015. Pope Francis blasts “gender theory” again: rejecting sexual difference is “a step backwards.” Lifesitenews.com . April 15. http://www.lifesitenews.com/news/pope-francis-blasts-gender-theory-again-rejecting-sexual-difference-is-a-st .
- Wood Hayley, Sasakia Shoko, Bradleya Susan J., Singha Devita, Fantusa Sophia, Owen-Andersona Allison, Di Giacomoa Alexander, Bainb Jerald, and Zucker Kenneth J.. 2013. Patterns of referral to a gender identity service for children and adolescents (1976–2011) age, sex ratio, and sexual orientation . Journal of Sex & Marital Therapy 39 : 1–6. [ PubMed ] [ Google Scholar ]
- Zucker Kenneth, and Bradley Susan. 1995. Gender identity disorder and psychosexual problems in children and adolescents . New York: Guilford Publications. [ PubMed ] [ Google Scholar ]
- Zucker Kenneth, Bradleya Susan J., Owen-Andersona Allison, Kibblewhitea Sarah J., Wooda Hayley, Singha Devita, and Choia Kathryn. 2012. Demographics, behavior problems, and psychosexual characteristics of adolescents with gender identity disorder or transvestic fetishism . Journal of Sex & Marital Therapy 38 : 151–89. [ PubMed ] [ Google Scholar ]
- Zucker Kenneth, Bradley Susan J., Ben-Dat Dahlia N., Ho Caroline, Johnson Laurel, and Owen Allison. 2003. Psychopathology in the parents of boys with gender identity disorder . Journal of the American Academy of Child and Adolescent Psychiatry 42 : 2–4. [ PubMed ] [ Google Scholar ]
Politics Analysis

Trump Vows to Fight On Despite Conviction
Law News

Soros-Backed DA’s Office Gave Free Consultations to Illegal Aliens Charged With Violent Crimes
Economy Commentary

Biden Turns American Dream of Retirement Into a Nightmare
Society Commentary

The Sick, Sociopathic Symbiosis of the Woke Left and Jihadi Enthusiasts
Security Commentary

Videos Uncover Illegal Immigration Realities the Media Tries to Hide: The BorderLine
Security Analysis

Illegal Immigration Has Created ‘High Threat Level’ for Terrorist Attack in US, Expert Says
Security News

Agents Arrest 10 Members of Infamous Venezuelan Prison Gang at Southern Border
Health Care Commentary

What Are NIH Officials Hiding?: Fauci to Testify on America’s Response to COVID-19
Security Commentary

China’s Land Purchases in US Spark Outcry for Federal Solution

Loose Talk About the End of Everything
Security News

EXCLUSIVE: Fauci ‘Could Be Indicted’ for Destruction of Records, Rand Paul Says
Economy News

Biden’s Regulations Cost American Households Tens of Thousands, Report Says
Security Commentary

5 Americans Remain Hostages in Gaza. Does Biden Have a Plan to Bring Them Home?
Politics News

Political World Erupts After Jury Declares Trump Guilty on All 34 Counts
Law Analysis

Former Prosecutor Weighs in on Jury Deliberations in Trump’s Criminal Case
Law Commentary

Judge’s Problematic Jury Instructions in Trump’s Hush Money Trial
Politics Commentary

EXCLUSIVE: Sen. Rubio’s Killer Video Blow to the Left’s Depressive Values

EXCLUSIVE: Ted Cruz Sets the Record Straight After SPLC Claims He Spread ‘Antisemitic Trope’
Society Analysis

EXCLUSIVE: Federal Farm Credit Agency Plows Ahead With DEI, ‘Queer’ Farming

EXCLUSIVE: DOJ’s Kristen Clarke Testified She Was Never Arrested. Court Records and Text Messages Indicate She Was.
International News

Iran’s Supreme Leader Endorses US Campus Protests as Part of ‘Resistance Front’

Rep. Tlaib Addresses Conference Endorsed by Founding Member of Palestinian Terrorist Group

Yes, Trump Could Be Elected President From Prison

How ‘Faith and Reason Can Win the Culture War’
Society News
Study Finds Gender-Transition Surgeries Drastically Increase Suicide Risk
A new study shows gender-transition surgeries increase the risk of patient suicide, a finding consistent with previous research. Pictured: Adm. Rachel L. Levine, center, assistant secretary for health in the U.S. Department of Health and Human Services, is flanked onstage Oct. 21 by Jesse Ehrenfeld, president of the American Medical Association, and Charlotte Clymer, a transgender activist and military veteran, during PFLAG's national convention in Washington. (Photo: Paul Morigi/Getty Images)

Get your FREE digital copy of The Heritage Foundation’s Founders’ Almanac.
While some in the U.S. health community continue to claim that gender-transition procedures save lives, a new study shows that these surgeries increase the risk of suicide.
A study published last month entitled “Risk of Suicide and Self-Harm Following Gender-Affirmation Surgery” evaluated patient data from nearly 60 U.S. health care organizations, comprising millions of patients.
Over 1,500 patients, called “Cohort A,” were described as “adults aged 18-60 who had gender-affirming surgery and an emergency visit”; nearly 16 million patients, called “Cohort B,” who were a “control group of adults with emergency visits but no gender-affirming surgery.”
Almost 150,000 patients, “Cohort C,” were described as “adults with emergency visits, tubal ligation or vasectomy, but no gender-affirming surgery.” A fourth group, “Cohort D,” was examined to “validate the results from Cohort C.”
Data analyzed covered 20 years, from Feb. 4, 2003, to Feb. 4, 2023. The study concluded: “Individuals who underwent gender-affirming surgery had a 12.12-fold higher suicide attempt risk than those who did not.”
Those who had undergone gender-transition surgeries were nearly five times more likely to attempt suicide than those who had undergone tubal ligations or vasectomies, the study found. It warned: “Gender-affirming surgery is significantly associated with elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support.”
The findings are in line with the conclusions of numerous other studies. For example, research published in the journal BMJ Mental Health earlier this year found that gender-transition procedures such as hormone drugs and surgeries have “not been shown to reduce even suicidal ideation, and suicidal ideation is not equal to actual suicide risk.”
And in Sweden, an extensive 30-year-long study concluded that suicide rates increase after gender-transition surgeries, rising to at least 20 times the suicide rate of the general population.
A report from the U.K. last year found that over a third of children who were prescribed puberty blockers and hormone drugs suffered worsened mental health. And a study from Finland discovered that those who identify as transgender typically manifest “many more common psychiatric needs” than the general population, but that gender-transition procedures don’t alleviate or cure those mental health issues.
Countless other studies have shown that gender-transition procedures are harmful, especially to children. A study published in March suggested that puberty blockers have numerous harmful effects on children, including an increased risk of cancer in boys.
As it turns out, transgenderism activists have been aware of the “debilitating” effects of gender-transition procedures for years. Leaked internal files from the World Professional Association for Transgender Health, or WPATH, demonstrated that members of the organization were acutely aware of the “debilitating” and “potentially fatal” effects of gender-transition procedures, which they also implied they didn’t “fully understand.”
This was further confirmed earlier this year with publication of a series of video presentations from WPATH’s 2022 Global Education Institute .
In those videos, WPATH “experts” discussed how they know little about the long-term effects of hormone drugs, other than the permanent damage done to fertility.
The organization’s experts also discussed how puberty blockers are irreversible and may have devastating impacts on both future fertility and current brain development; how gender-transition procedures don’t alleviate mental health issues and may make them worse; and the dangers associated with surgical interventions, including high complication rates, severe damage to healthy tissue, and potential side effects such as healing delays or necrosis.
Lately, experts outside the U.S. have sounded the alarm over the potential and largely unstudied dangers of gender-transition procedures, especially for children.
Both England and Scotland have halted the prescription of puberty blockers and hormone drugs to minors, with England’s National Health Service warning that “there is not enough evidence of safety and clinical effectiveness” to support their use.
Some leading clinical psychologists publicly apologized for their profession’s role in promoting “gender-affirming care” and called for a thorough review and possible reform of the psychological and psychiatric profession’s standards. And the NHS revised its official constitution to declare sex a “biological” reality, instead of giving preference to “gender identity.”
The U.K. is 1 of 5 European countries that have put the brakes on gender-transition procedures for minors. France, Sweden, Finland, and Norway all also warned that there is insufficient evidence to support puberty blockers, hormone drugs, and surgeries for children; the U.S. has become an “outlier” by continuing to endorse the practice.
Last year, Assistant Health and Human Services Secretary Rachel Levine, a man who identifies as a woman, declared : “We often say that gender-affirming care is health care, gender-affirming care is mental health care, and gender-affirming care is literally suicide prevention care.”
However, when pressed to provide evidence supporting the claim, Levine could produce only a single, two-page PDF document citing one study conducted by an LGBTQ activist group.
Originally published by The Washington Stand
Related posts:
- Will the ‘Invisible Hand’ Finally Stop Doctors From Putting Kids on Experimental Gender Drugs?
- ‘We Will Not Stand By’: Florida Sues Biden Admin to Block New Trans Health Care Rule
- United Kingdom Orders ‘Emergency Ban’ on Puberty Blockers for Minors
South Carolina Gov. McMaster signs bill outlawing transgender care for trans youth
South Carolina Gov. Henry McMaster signed a bill banning certain medical care for transgender youth on Tuesday.
House Bill 4624, called the “Help not Harm” bill by legislators, prohibits anyone under the age of 18 from receiving gender reassignment surgery or any form of puberty-blocking or hormone therapy. The bill became effective immediately.
The bill also makes it a felony to perform gender reassignment surgery on those under the age of 18.
McMaster said a ceremonial bill signing with legislators would take place in the Upstate next week.
Under the new bill, minors can still be prescribed puberty blockers or hormone therapy to treat certain conditions like precocious puberty or endometriosis.
The new law also bans the South Carolina Medicaid program from providing coverage for gender reassignment surgery or hormone therapy to adults and minors.
The bill passed on the last day of the legislative session after the House agreed to accept the Senate’s changes to the law. The Senate's major change was an amendment requiring public school principals and vice principals to report students to parents if their child informed officials that they were identifying as a different gender from their assigned sex or using different pronouns.
More: As SC legislature winds down, bill banning transgender youth medical care returns to House
Opponents of the amendment argued the measure would be a forced outing and worried it could put a child in an uncomfortable or potentially dangerous situation if their parent or guardian were not accepting. Supporters of the amendment said parents have a right to know if their children are identifying as transgender or requesting to change their pronouns.
Dr. Elizabeth Mack, president of the South Carolina chapter of the American Academy of Pediatrics testified against the bill during a Senate medical affairs subcommittee in February, noting there are “less than 2,000 trans kids in the state.”
Still, supporters of the bill pushed for it, saying its intention was to protect children, while others say it does the opposite.
“We stand in grief and solidarity with LGBTQ South Carolinians, who are increasingly under attack by our own government,” Executive Director of ACLU South Carolina Jace Woodrum said in a statement on X, formerly known as Twitter. “We can put to rest the notion that the government cares about limited government and personal freedom. With a stroke of a pen, he (McMaster) has chosen to insert the will of politicians into healthcare decisions, trample on the liberties of trans South Carolinians, and deny the rights of the parents of trans minors.”
South Carolina joins 25 states to outlaw transgender care for minors. It was also one of the only states that did not have a ban on transgender care in the South, with Virginia now being the lone Southern state with access.
Savannah Moss covers politics for the Greenville News. Reach her at [email protected] or follow her on X @Savmoss.

IMAGES
VIDEO
COMMENTS
Together, with surgeon Erwin Gohrbandt, they performed male-to-female surgery called Genitalumwandlung—literally, “transformation of genitals.” This occurred in stages: castration, penectomy ...
Opinion. Late one night on the cusp of the 20th century, Magnus Hirschfeld, a young doctor, found a soldier on the doorstep of his practice in Germany. Distraught and agitated, the man had come to ...
The first physician to perform sex reassignment surgery in the United States was Los Angeles-based urologist Elmer Belt, who quietly performed operations from the early 1950s until 1968. [citation needed] In 1966, Johns Hopkins University opened the first sex reassignment surgery clinic in America. The Hopkins Gender Identity Clinic was made up ...
The early history of sex reassignment surgery in transgender people has been reviewed by various authors. Prevalence. The prevalence of transgender-related surgeries is difficult to measure and likely underestimated. In 2015, the largest survey of transgender people in the United States reported that 25% of respondents reported having undergone ...
Much of the history of the institute's early works were destroyed in the wake of the Nazi book burnings in 1933, ... Hirschfeld's institute was the first to offer gender reassignment surgery. ...
gender-affirming surgery, medical procedure in which the physical sex characteristics of an individual are modified. Gender-affirming surgery typically is undertaken when an individual chooses to align their physical appearance with their gender identity, enabling the individual to achieve a greater sense of self and helping to reduce psychological distress that may be associated with gender ...
Gender dysphoria, earlier known as gender identity disorder, describes a heterogeneous group of individuals having the desire to possess secondary sexual characteristics of the opposite sex and possessing varying degrees of dissatisfaction regarding their anatomical gender . Gender reassignment surgery (GRS) has proven to be a revolutionary ...
Not all who identify with a gender different than their birth sex suffer from gender dysphoria or go on to seek surgery. Transgender people who do want gender reassignment surgery, however, must follow the standards of care for gender affirmation as defined by the World Professional Association for Transgender Health (WPATH).
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
A study has found that trans people who had undergone gender-affirming surgery, the longer ago their surgery, the less likely they were to suffer anxiety, depression or suicidal behavior. ... This is the beneficial effect of sex-reassignment surgery early on in a transition Nov 13, 2019. This article is published in collaboration with Thomson ...
Quality of life improves early after gender reassignment surgery in transgender women. ... (F64.0 in ICD-10) undergoing male-to-female gender reassignment surgery at Karolinska University Hospital between 2003 and 2015. All patients presenting at the clinic were invited to participate. No exclusion criterion was applied.
New medical options are allowing transgender children to start the process of transitioning at younger and younger ages. But doctors tread carefully, lacking research on some of the long-term effects.
She does more than 150 a year. We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Thus, it is essential to train medical professionals to care for this vulnerable population with compassion and knowledge. During the summer of 2018, I interned at the Gender Reassignment Department of Mount Sinai Hospital, where Dr. Jess Ting pioneered New York City's first surgical program dedicated to transgender surgery.
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Gender surgery improves quality of life. Dr. Hess and colleagues surveyed 156 people who had all had gender reassignment surgery 6.61 years prior to the study, on average. The survey included open ...
As sex reassignment surgery often constitutes the final step of sex reassignment measures, hormone therapy as well as accompanying psychotherapy may have had a confounding effect. ... Quality of life improves early after gender reassignment surgery in transgender women. Eur J Plast Surg. 2017; 40:223-226. [PMC free article] [Google Scholar] 24.
The procedures included a vaginoplasty (surgical procedure where a vagina is created). In the UK, gender reassignment surgeries were pioneered by Sir Harold Gillies. Harold Gillies is most famous for the development of a new method of facial reconstructive surgery, in 1917. During the Second World War, he organized plastic surgery units in ...
About 42,000 U.S. children ages 6 to 17 were diagnosed with gender dysphoria in 2021, nearly triple the number in 2017, a unique data analysis for Reuters found.
When he was 14, Reimer began the process of reassignment to being a male. As an adult, he married a woman but depression and drug abuse ensued, culminating in suicide at the age of 38 (1). Money's ...
Background: Few studies have examined the long-term quality of life (QoL) of individuals with gender dysphoria, or how it is affected by treatment. Our aim was to examine the QoL of transgender women undergoing gender reassignment surgery (GRS). Methods: We performed a prospective cohort study on 190 patients undergoing male-to-female GRS at Karolinska University Hospital between 2003 and 2015.
As part of establishing a gender surgery center at a pediatric academic hospital, we undertook a process of identifying key ethical, legal, and contextual issues through collaboration among clinical providers, review by hospital leadership, discussions with key staff and hospital support services, consultation with the hospital's ethics committee, outreach to other institutions providing ...
The prevalence decreased to 4% when they reached 26 years of age: "Gender dissatisfaction, although relatively common during early adolescence, in general decreases with age, and seems to be ...
Both provisions outlaw a range of treatments, including gender-reassignment surgery. But the challenges before the court specifically concern two nonsurgical treatments: the administration of puberty blockers to stop physical changes brought on by puberty; and hormone therapy, which seeks to produce physiological changes to conform physical ...
Abstract. Transsexual issues and sexual reassignment surgery (SRS) are receiving a great deal of attention and support in the media, schools, and government. Given the early age at which youth seek treatment for transsexual attractions (TSA) and gender dysphoria and given the serious risks associated with such treatment, it is essential that ...
Data analyzed covered 20 years, from Feb. 4, 2003, to Feb. 4, 2023. The study concluded: "Individuals who underwent gender-affirming surgery had a 12.12-fold higher suicide attempt risk than ...
The bill also makes it a felony to perform gender reassignment surgery on those under the age of 18. McMaster said a ceremonial bill signing with legislators would take place in the Upstate next week.
Dr. Milton Diamond PhD, Professor Emeritus of Anatomy and Reproductive Biology at the University of Hawaiʻi at Mānoa, John A. Burns School of Medicine, died in Honolulu, Hawai'i, on March 20, 2024 at the age of 90 from cardiac arrest. He was internationally known for investigating the case of David Reimer, which had been claimed to show ...
TAIPEI (Taiwan News) — A Taipei court has ruled in favor of a man seeking to change his legal gender without undergoing gender reassignment surgery, in a first for Taiwan. The Taipei High Administrative Court ruled in favor of transgender man Nemo's right to change his legal gender from female to male on Thursday (May 30), after a nearly two year legal battle.