- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games

Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Delivery, face and brow presentation.
Julija Makajeva ; Mohsina Ashraf .
Affiliations
Last Update: January 9, 2023 .
- Continuing Education Activity
Face and brow presentation is a malpresentation during labor when the presenting part is either the face or, in the case of brow presentation, it is the area between the orbital ridge and the anterior fontanelle. This activity reviews the evaluation and management of these two presentations and explains the role of the interprofessional team in managing delivery safely for both the mother and the baby.
- Describe the mechanism of labor in the face and brow presentation.
- Summarize potential maternal and fetal complications during the face and brow presentations.
- Review different management approaches for the face and brow presentation.
- Outline some interprofessional strategies that will improve patient outcomes in delivery cases with face and brow presentation issues.
- Introduction
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference.
Face presentation – an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3]
In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries. [3]
Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, polyhydramnios. [2] [4] [5]
These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse.
Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. [6] The ultrasound imaging can show a reduced angle between the occiput and the spine or, the chin is separated from the chest. However, ultrasound does not provide much predicting value in the outcome of the labor. [7]
- Anatomy and Physiology
Before discussing the mechanism of labor in the face or brow presentation, it is crucial to highlight some anatomical landmarks and their measurements.
Planes and Diameters of the Pelvis
The three most important planes in the female pelvis are the pelvic inlet, mid pelvis, and pelvic outlet.
Four diameters can describe the pelvic inlet: anteroposterior, transverse, and two obliques. Furthermore, based on the different landmarks on the pelvic inlet, there are three different anteroposterior diameters, named conjugates: true conjugate, obstetrical conjugate, and diagonal conjugate. Only the latter can be measured directly during the obstetric examination. The shortest of these three diameters is obstetrical conjugate, which measures approximately 10.5 cm and is a distance between the sacral promontory and 1 cm below the upper border of the symphysis pubis. This measurement is clinically significant as the fetal head must pass through this diameter during the engagement phase. The transverse diameter measures about 13.5cm and is the widest distance between the innominate line on both sides.
The shortest distance in the mid pelvis is the interspinous diameter and usually is only about 10 cm.
Fetal Skull Diameters
There are six distinguished longitudinal fetal skull diameters:
- Suboccipito-bregmatic: from the center of anterior fontanelle (bregma) to the occipital protuberance, measuring 9.5 cm. This is the presenting diameter in vertex presentation.
- Suboccipito-frontal: from the anterior part of bregma to the occipital protuberance, measuring 10 cm
- Occipito-frontal: from the root of the nose to the most prominent part of the occiput, measuring 11.5cm
- Submento-bregmatic: from the center of the bregma to the angle of the mandible, measuring 9.5 cm. This is the presenting diameter in face presentation where the neck is hyperextended.
- Submento-vertical: from the midpoint between fontanelles and the angle of the mandible, measuring 11.5cm
- Occipito-mental: from the midpoint between fontanelles and the tip of the chin, measuring 13.5 cm. It is the presenting diameter in brow presentation.
Cardinal Movements of Normal Labor
- Neck flexion
- Internal rotation
- Extension (delivers head)
- External rotation (Restitution)
- Expulsion (delivery of anterior and posterior shoulders)
Some of the key movements are not possible in the face or brow presentations.
Based on the information provided above, it is obvious that labor will be arrested in brow presentation unless it spontaneously changes to face or vertex, as the occipito-mental diameter of the fetal head is significantly wider than the smallest diameter of the female pelvis. Face presentation can, however, be delivered vaginally, and further mechanisms of face delivery will be explained in later sections.
- Indications
As mentioned previously, spontaneous vaginal delivery can be successful in face presentation. However, the main indication for vaginal delivery in such circumstances would be a maternal choice. It is crucial to have a thorough conversation with a mother, explaining the risks and benefits of vaginal delivery with face presentation and a cesarean section. Informed consent and creating a rapport with the mother is an essential aspect of safe and successful labor.
- Contraindications
Vaginal delivery of face presentation is contraindicated if the mentum is lying posteriorly or is in a transverse position. In such a scenario, the fetal brow is pressing against the maternal symphysis pubis, and the short fetal neck, which is already maximally extended, cannot span the surface of the maternal sacrum. In this position, the diameter of the head is larger than the maternal pelvis, and it cannot descend through the birth canal. Therefore the cesarean section is recommended as the safest mode of delivery for mentum posterior face presentations.
Attempts to manually convert face presentation to vertex, manual or forceps rotation of the persistent posterior chin to anterior are contraindicated as they can be dangerous.
Persistent brow presentation itself is a contraindication for vaginal delivery unless the fetus is significantly small or the maternal pelvis is large.
Continuous electronic fetal heart rate monitoring is recommended for face and brow presentations, as heart rate abnormalities are common in these scenarios. One study found that only 14% of the cases with face presentation had no abnormal traces on the cardiotocograph. [8] It is advised to use external transducer devices to prevent damage to the eyes. When internal monitoring is inevitable, it is suggested to place monitoring devices on bony parts carefully.
People who are usually involved in the delivery of face/ brow presentation are:
- Experienced midwife, preferably looking after laboring woman 1:1
- Senior obstetrician
- Neonatal team - in case of need for resuscitation
- Anesthetic team - to provide necessary pain control (e.g., epidural)
- Theatre team - in case of failure to progress and an emergency cesarean section will be required.
- Preparation
No specific preparation is required for face or brow presentation. However, it is essential to discuss the labor options with the mother and birthing partner and inform members of the neonatal, anesthetic, and theatre co-ordinating teams.
- Technique or Treatment
Mechanism of Labor in Face Presentation
During contractions, the pressure exerted by the fundus of the uterus on the fetus and pressure of amniotic fluid initiate descent. During this descent, the fetal neck extends instead of flexing. The internal rotation determines the outcome of delivery, if the fetal chin rotates posteriorly, vaginal delivery would not be possible, and cesarean section is permitted. The approach towards mentum-posterior delivery should be individualized, as the cases are rare. Expectant management is acceptable in multiparous women with small fetuses, as a spontaneous mentum-anterior rotation can occur. However, there should be a low threshold for cesarean section in primigravida women or women with large fetuses.
When the fetal chin is rotated towards maternal symphysis pubis as described as mentum-anterior; in these cases further descend through the vaginal canal continues with approximately 73% cases deliver spontaneously. [9] Fetal mentum presses on the maternal symphysis pubis, and the head is delivered by flexion. The occiput is pointing towards the maternal back, and external rotation happens. Shoulders are delivered in the same manner as in vertex delivery.
Mechanism of Labor in Brow Presentation
As this presentation is considered unstable, it is usually converted into a face or an occiput presentation. Due to the cephalic diameter being wider than the maternal pelvis, the fetal head cannot engage; thus, brow delivery cannot take place. Unless the fetus is small or the pelvis is very wide, the prognosis for vaginal delivery is poor. With persistent brow presentation, a cesarean section is required for safe delivery.
- Complications
As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly. [10]
However, there are still some complications associated with the nature of labor in face presentation. Due to the fetal head position, it is more challenging for the head to engage in the birth canal and descend, resulting in prolonged labor.
Prolonged labor itself can provoke foetal distress and arrhythmias. If the labor arrests or signs of fetal distress appear on CTG, the recommended next step in management is an emergency cesarean section, which in itself carries a myriad of operative and post-operative complications.
Finally, due to the nature of the fetal position and prolonged duration of labor in face presentation, neonates develop significant edema of the skull and face. Swelling of the fetal airway may also be present, resulting in respiratory distress after birth and possible intubation.
- Clinical Significance
During vertex presentation, the fetal head flexes, bringing the chin to the chest, forming the smallest possible fetal head diameter, measuring approximately 9.5cm. With face and brow presentation, the neck hyperextends, resulting in greater cephalic diameters. As a result, the fetal head will engage later, and labor will progress more slowly. Failure to progress in labor is also more common in both presentations compared to vertex presentation.
Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis. As a result, descend through the birth canal is impossible. Such presentation is considered undeliverable vaginally and requires an emergency cesarean section.
Manual attempts to change face presentation to vertex, manual or forceps rotation to mentum anterior are considered dangerous and are discouraged.
- Enhancing Healthcare Team Outcomes
A multidisciplinary team of healthcare experts supports the woman and her child during labor and the perinatal period. For a face or brow presentation to be appropriately diagnosed, an experienced midwife and obstetrician must be involved in the vaginal examination and labor monitoring. As fetal anomalies, such as anencephaly or goiter, can contribute to face presentation, sonographers experienced in antenatal scanning should also be involved in the care. It is advised to inform the anesthetic and neonatal teams in advance of the possible need for emergency cesarean section and resuscitation of the neonate. [11] [12]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Julija Makajeva declares no relevant financial relationships with ineligible companies.
Disclosure: Mohsina Ashraf declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Makajeva J, Ashraf M. Delivery, Face and Brow Presentation. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. [Am J Obstet Gynecol MFM. 2020] Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Bellussi F, Livi A, Cataneo I, Salsi G, Lenzi J, Pilu G. Am J Obstet Gynecol MFM. 2020 Nov; 2(4):100217. Epub 2020 Aug 18.
- Review Sonographic evaluation of the fetal head position and attitude during labor. [Am J Obstet Gynecol. 2022] Review Sonographic evaluation of the fetal head position and attitude during labor. Ghi T, Dall'Asta A. Am J Obstet Gynecol. 2022 Jul 6; . Epub 2022 Jul 6.
- Stages of Labor. [StatPearls. 2024] Stages of Labor. Hutchison J, Mahdy H, Hutchison J. StatPearls. 2024 Jan
- Leopold Maneuvers. [StatPearls. 2024] Leopold Maneuvers. Superville SS, Siccardi MA. StatPearls. 2024 Jan
- Review Labor with abnormal presentation and position. [Obstet Gynecol Clin North Am. ...] Review Labor with abnormal presentation and position. Stitely ML, Gherman RB. Obstet Gynecol Clin North Am. 2005 Jun; 32(2):165-79.
Recent Activity
- Delivery, Face and Brow Presentation - StatPearls Delivery, Face and Brow Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
Fetal Positions for Labor and Birth
Knowing your baby's position can you help ease pain and speed up labor
In the last weeks of pregnancy , determining your baby's position can help you manage pain and discomfort. Knowing your baby's position during early labor can help you adjust your own position during labor and possibly even speed up the process.
Right or Left Occiput Anterior
Illustration by JR Bee, Verywell
Looking at where the baby's head is in the birth canal helps determine the fetal position.The front of a baby's head is referred to as the anterior portion and the back is the posterior portion. There are two different positions called occiput anterior (OA) positions that may occur.
The left occiput anterior (LOA) position is the most common in labor. In this position, the baby's head is slightly off-center in the pelvis with the back of the head toward the mother's left thigh.
The right occiput anterior (ROA) presentation is also common in labor. In this position, the back of the baby is slightly off-center in the pelvis with the back of the head toward the mother's right thigh.
In general, OA positions do not lead to problems or additional pain during labor or birth.
Right or Left Occiput Transverse
Illustration by JR Bee, Verywell
When facing out toward the mother's right thigh, the baby is said to be left occiput transverse (LOT). This position is halfway between a posterior and anterior position. If the baby was previously in a posterior position (in either direction), the LOT position indicates positive movement toward an anterior position.
When the baby is facing outward toward the mother's left thigh, the baby is said to be right occiput transverse (ROT). Like the previous presentation, ROT is halfway between a posterior and anterior position. If the baby was previously in a posterior position, ROT is a sign the baby is making a positive move toward an anterior position.
When a baby is in the left occiput transverse position (LOT) or right occiput transverse (ROT) position during labor, it may lead to more pain and a slower progression.
Tips to Reduce Discomfort
There are several labor positions a mother can try to alleviate pain and encourage the baby to continue rotating toward an anterior position, including:
- Pelvic tilts
- Standing and swaying
A doula , labor nurse, midwife , or doctor may have other suggestions for positions.
Right or Left Occiput Posterior
When facing forward, the baby is in the occiput posterior position. If the baby is facing forward and slightly to the left (looking toward the mother's right thigh) it is in the left occiput posterior (LOP) position. This presentation can lead to more back pain (sometimes referred to as " back labor ") and slow progression of labor.
In the right occiput posterior position (ROP), the baby is facing forward and slightly to the right (looking toward the mother's left thigh). This presentation may slow labor and cause more pain.
To help prevent or decrease pain during labor and encourage the baby to move into a better position for delivery, mothers can try a variety of positions, including:
- Hands and knees
- Pelvic rocking
Mothers may try other comfort measures, including:
- Bathtub or shower (water)
- Counter pressure
- Movement (swaying, dancing, sitting on a birth ball )
- Rice socks (heat packs)
How a Doctor Determines Baby's Position
Leopold's maneuvers are a series of hands-on examinations your doctor or midwife will use to help determine your baby's position. During the third trimester , the assessment will be done at most of your prenatal visits. Knowing the baby's position before labor begins can help you prepare for labor and delivery.
Once labor begins, a nurse, doctor, or midwife will be able to get a more accurate sense of your baby's position by performing a vaginal exam. When your cervix is dilated enough, the practitioner will insert their fingers into the vagina and feel for the suture lines of the baby's skull as it moves down in the birth canal. It's important to ensure the baby is head down and moving in the right direction.
Labor and delivery may be more complicated if the baby is not in a head-down position, such as in the case of a breech presentation.
How You Can Determine Baby's Position
While exams by health practitioners are an important part of your care, from the prenatal period through labor and delivery, often the best person to assess a baby's position in the pelvis is you. Mothers should pay close attention to how the baby moves and where different movements are felt.
A technique called belly mapping can help mothers ask questions of themselves to assess their baby's movement and get a sense of the position they are in as labor approaches.
For example, the position of your baby's legs can be determined by asking questions about the location and strength of the kicking you feel. The spots where you feel the strongest kicks are most likely where your baby's feet are.
Other landmarks you can feel for include a large, flat plane, which is most likely your baby's back. Sometimes you can feel the baby arching his or her back.
At the top or bottom of the flat plane, you may feel either a hard, round shape (most likely your baby's head) or a soft curve (most likely to be your baby's bottom).
Guittier M, Othenin-Girard V, de Gasquet B, Irion O, Boulvain M. Maternal positioning to correct occiput posterior fetal position during the first stage of labour: a randomised controlled trial . BJOG: An International Journal of Obstetrics & Gynaecology . 2016;123(13):2199-2207. doi:10.1111/1471-0528.13855
Gizzo S, Di Gangi S, Noventa M, Bacile V, Zambon A, Nardelli G. Women’s Choice of Positions during Labour: Return to the Past or a Modern Way to Give Birth? A Cohort Study in Italy . Biomed Res Int . 2014;2014:1-7. doi:10.1155/2014/638093
Ahmad A, Webb S, Early B, Sitch A, Khan K, MacArthur C. Association between fetal position at onset of labor and mode of delivery: a prospective cohort study . Ultrasound in Obstetrics & Gynecology . 2014;43(2):176-182. doi:10.1002/uog.13189
Nishikawa M, Sakakibara H. Effect of nursing intervention program using abdominal palpation of Leopold’s maneuvers on maternal-fetal attachment . Reprod Health . 2013;10(1). doi:10.1186/1742-4755-10-12
Choi S, Park Y, Lee D, Ko H, Park I, Shin J. Sonographic assessment of fetal occiput position during labor for the prediction of labor dystocia and perinatal outcomes . The Journal of Maternal-Fetal & Neonatal Medicine . 2016;29(24):3988-3992. doi:10.3109/14767058.2016.1152250
Bamberg C, Deprest J, Sindhwani N et al. Evaluating fetal head dimension changes during labor using open magnetic resonance imaging . J Perinat Med . 2017;45(3). doi:10.1515/jpm-2016-0005
Gabbe S, Niebyl J, Simpson J et al. Obstetrics . Philadelphia, Pa.: Elsevier; 2012.
By Robin Elise Weiss, PhD, MPH Robin Elise Weiss, PhD, MPH is a professor, author, childbirth and postpartum educator, certified doula, and lactation counselor.
- Face Presentation
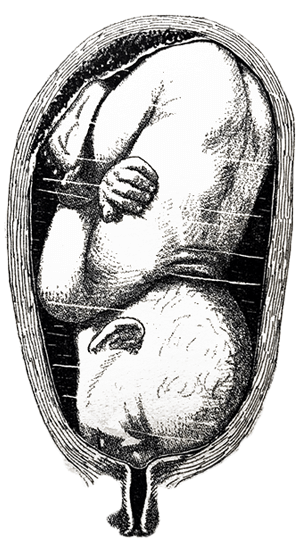
Pictoral Midwifery, Comyns Berkely, 4th Edition. 1941
Face it. We have a lot to learn about fetal positioning. The old paradigm is fetal positions are random. The new paradigm is that babies match the space available.
Face and brow presentations occur when baby’s spine extended until the head is shifted back so baby’s face comes through the pelvis first.
Baby may settle in a face or brow presentation before labor or they may become a face or brow presentation, usually when a posterior baby has it’s chin pushed further up by the pelvic floor during descent.
A baby who is in a face-first or forehead-first position often started as an extended (chin up) occiput posterior or occiput transverse position. Coming down on to the pelvic floor with the forehead leading then “converted” this baby’s head to the face first position.
The baby’s face may be bruised for a couple days after the birth. The brow presentation may cause a redness but only occasionally will cause a bruise.
Mobility of the pelvis and the freedom of maternal movements often help bring the face-first baby down through the pelvis with good strong, uterine surges.
But not always. Sometimes the labor can’t move baby down. Cesareans are more common, but a portion of the higher surgical rate is because time is not given to the mother to begin or continue labor, or to be out of bed for this labor. Monitoring becomes important. Expect a bit of an unusual heart rate to contraction pattern seen in these labors.
- When is Breech an Issue?
- Belly Mapping® Breech
- Flip a Breech
- When Baby Flips Head Down
- Breech & Bicornuate Uterus
- Breech for Providers
- What if My Breech Baby Doesn't Turn?
- Belly Mapping ®️ Method
- After Baby Turns
- Head Down is Not Enough
- Sideways/Transverse
- Asynclitism
- Oblique Lie
- Left Occiput Transverse
- Right Occiput Anterior
- Right Occiput Posterior
- Right Occiput Transverse
- Left Occiput Anterior
- OP Truths & Myths
- Anterior Placenta
- Body Balancing
What makes labor easier for a face-first baby and you?
Balance the body and the baby will thank you by curling into position to aim, not their face, but the crown of their head.
Flexion is physiological. So support physiology and the baby will change their position. We may need a little physics.
In Labor with a Face or Brow Presentation
Back baby up!
Forward-leaning Inversion with a jiggle of the buttocks right through 1-2 contractions often backs baby up so they can tuck their chin. Then they can aim into the pelvis with an easier position.

Shake the Apples in Forward-leaning Inversion with hands
A little effort can make labor a lot easier!
Only after baby’s crown is first, then do Side-lying Release in labor.
Before Labor with a face or brow presentation
Face presentation may reflect a psoas/pelvic floor imbalance with a collapse in the front body.
Free the piriformis, strengthen the buttocks, lengthen the hamstrings, squat for lengthening the pelvic floor, don’t worry about strengthening the pelvic floor right now. Alignment, walking, stabilizing and lengthening will tone the pelvic floor. Use it by breathing with your whole body.
Before labor, it’s safe to do Side-lying Release when baby’s face-first head isn’t in the pelvis yet.
Free the way
The psoas is the upper guide, the pelvic floor is the lower guide. release spasms and lengthen both.
Make room for the baby by releasing muscles that spasm, lengthen ligaments that are shortened, and support the abdominal muscles by attending to the muscles that interact with them, don’t go directly to the front first.

Pin It on Pinterest
Appointments at Mayo Clinic
- Labor and delivery, postpartum care
Stages of labor and birth: Baby, it's time!
Labor is a natural process. Here's what to expect during the three stages of labor and birth — and what you can do to promote comfort.
Labor is a unique experience. Sometimes it's over in a matter of hours. In other cases, labor tests a mother's physical and emotional stamina.
You won't know how labor and childbirth will unfold until it happens. However, you can prepare by understanding the typical sequence of events.
Stage 1: Early labor and active labor
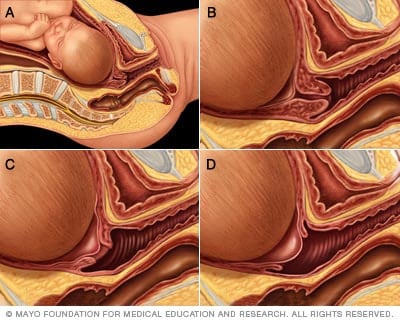
Cervical effacement and dilation
During the first stage of labor, the cervix opens (dilates) and thins out (effaces) to allow the baby to move into the birth canal. In figures A and B, the cervix is tightly closed. In figure C, the cervix is 60% effaced and 1 to 2 cm dilated. In figure D, the cervix is 90% effaced and 4 to 5 cm dilated. The cervix must be 100% effaced and 10 cm dilated before a vaginal delivery.
The first stage of labor and birth occurs when you begin to feel persistent contractions. These contractions become stronger, more regular and more frequent over time. They cause the cervix to open (dilate) and soften as well as shorten and thin (efface) to allow your baby to move into the birth canal.
The first stage is the longest of the three stages. It's actually divided into two phases — early labor and active labor.
Early labor
During early labor, your cervix dilates and effaces. You'll likely feel mild, irregular contractions.
As your cervix begins to open, you might notice a clear pink or slightly bloody discharge from your vagina. This is likely the mucus plug that blocks the cervical opening during pregnancy.
How long it lasts: Early labor is unpredictable. For first-time moms, the average length varies from hours to days. It's often shorter for subsequent deliveries.
What you can do: For many women, early labor isn't particularly uncomfortable, but contractions may be more intense for some. Try to stay relaxed.
To promote comfort during early labor:
- Go for a walk
- Take a shower or bath
- Listen to relaxing music
- Try breathing or relaxation techniques taught in childbirth class
- Change positions
If you're having an uncomplicated pregnancy, you may spend most of your early labor at home until your contractions start to increase in frequency and intensity. Your health care provider will instruct you on when to leave for the hospital or birthing center. If your water breaks or you experience significant vaginal bleeding, call your health care provider right away.
Active labor
During active labor, your cervix will dilate from 6 centimeters (cm) to 10 cm. Your contractions will become stronger, closer together and regular. Your legs might cramp, and you might feel nauseated. You might feel your water break — if it hasn't already — and experience increasing pressure in your back. If you haven't headed to your labor and delivery facility yet, now's the time.
Don't be surprised if your initial excitement wanes as labor progresses and your discomfort intensifies. Ask for pain medication or anesthesia if you want it. Your health care team will partner with you to make the best choice for you and your baby. Remember, you're the only one who can judge your need for pain relief.
How long it lasts: Active labor often lasts 4 to 8 hours or more. On average, your cervix will dilate at approximately 1 cm an hour.
What you can do: Look to your labor partner and health care team for encouragement and support. Try breathing and relaxation techniques to relieve your discomfort. Use what you learned in childbirth class or ask your health care team for suggestions.
Unless you need to be in a specific position to allow for close monitoring of you and your baby, consider these ways to promote comfort during active labor:
- Roll on a large rubber ball (birthing ball)
- Take a warm shower or bath
- Take a walk, stopping to breathe through contractions
- Have a gentle massage between contractions
If you need to have a Cesarean delivery (C-section), having food in your stomach can lead to complications. If your health care provider thinks you might need a C-section, he or she might recommend small amounts of clear liquids, such as water, ice chips, popsicles and juice, instead of solid foods.
The last part of active labor — often referred to as transition — can be particularly intense and painful. Contractions will come close together and can last 60 to 90 seconds. You'll experience pressure in your lower back and rectum. Tell your health care provider if you feel the urge to push.
If you want to push but you're not fully dilated, your health care provider will ask you to hold back. Pushing too soon could make you tired and cause your cervix to swell, which might delay delivery. Pant or blow your way through the contractions. Transition typically lasts 15 to 60 minutes.
Stage 2: The birth of your baby
It's time! You'll deliver your baby during the second stage of labor.
How long it lasts: It can take from a few minutes to a few hours or more to push your baby into the world. It might take longer for first-time moms and women who've had an epidural.
What you can do: Push! Your health care provider will ask you to bear down during each contraction or tell you when to push. Or you might be asked to push when you feel the urge to do so.
When it's time to push, you may experiment with different positions until you find one that feels best. You can push while squatting, sitting, kneeling — even on your hands and knees.
At some point, you might be asked to push more gently — or not at all. Slowing down gives your vaginal tissues time to stretch rather than tear. To stay motivated, you might ask if you could feel the baby's head between your legs or see it in a mirror.
After your baby's head is delivered, the rest of the baby's body will follow shortly. The baby's airway will be cleared if necessary. If you've had an uncomplicated delivery, your health care provider may wait a few seconds to a few minutes before the umbilical cord is cut. Delaying clamping and cutting the umbilical cord after delivery increases the flow of nutrient-rich blood from the cord and the placenta to the baby. This increases the baby's iron stores and reduces the risk of anemia, promoting healthy development and growth.
Stage 3: Delivery of the placenta
After your baby is born, you'll likely feel a great sense of relief. You might hold the baby in your arms or on your abdomen. Cherish the moment. But a lot is still happening. During the third stage of labor, you will deliver the placenta.
How long it lasts: The placenta is typically delivered in 30 minutes, but the process can last as long as an hour.
You'll continue to have mild, less painful contractions that are close together. The contractions help move the placenta into the birth canal. You'll be asked to push gently one more time to deliver the placenta. You might be given medication before or after the placenta is delivered to encourage uterine contractions and minimize bleeding.
Your health care provider will examine the placenta to make sure it's intact. Any remaining fragments must be removed from the uterus to prevent bleeding and infection. If you're interested, ask to see the placenta.
After you deliver the placenta, your uterus will continue to contract to help it return to its normal size.
A member of your health care team may massage your abdomen. This may help the uterus contract to decrease bleeding.
Your health care provider will also determine whether you need repair of any tears of your vaginal region. If you don't have anesthesia, you'll receive an injection of local anesthetic in the area to be stitched.
Savor this special time with your baby. Your preparation, pain and effort have paid off. Revel in the miracle of birth.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Funai EF, et al. Management of normal labor and delivery. https://www.uptodate.com/contents/search. Accessed Oct. 28, 2021.
- Caughey AB, et al. Nonpharmacologic approaches to management of labor pain. https://www.uptodate.com/contents/search. Accessed Oct. 28, 2021.
- Satin AJ. Labor: Diagnosis and management of the latent phase. https://www.uptodate.com/contents/search. Accessed Oct. 28, 2021.
- American College of Obstetricians and Gynecologists. Labor and delivery. In: Your Pregnancy and Childbirth: Month to Month. Kindle edition. 7th ed. American College of Obstetricians and Gynecologists; 2021. Accessed Oct. 28, 2021.
- Landon MB, et al. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. http://www.clinicalkey.com. Accessed Oct. 28, 2021.
- Meek JY, et al. The first feedings. In: The American Academy of Pediatrics New Mother's Guide to Breastfeeding. Kindle edition. 3rd ed. Bantam Books; 2017. Accessed Oct. 28, 2021.
- Cunningham FG, et al. Normal labor. In: Williams Obstetrics. 25th ed. McGraw-Hill; 2018. https://www.accessmedicine.com. Accessed Oct. 28, 2021.
- Wick MJ (expert opinion). Mayo Clinic. Dec. 6, 2021.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Can vaginal tears during childbirth be prevented?
- Fetal presentation before birth
- High-risk pregnancy
- Inducing labor
- Labor pain medications
- Labor positions
- Repeat C-sections
- Signs of labor
- Tailbone pain
- Vaginal tears in childbirth
- Considering VBAC
- The epidural block
- Water breaking
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Stages of labor and birth Baby its time
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Malpresentation
8-minute read
If you feel your waters break and you have been told that your baby is not in a head-first position, seek medical help immediately .
- Malpresentation is when your baby is not facing head-first down the birth canal as birth approaches.
- The most common type of malpresentation is breech — when your baby’s bottom or feet are facing downwards.
- A procedure called external cephalic version can sometimes turn a breech baby into a head-first position at 36 weeks.
- Most babies with malpresentation are born by caesarean, but you may be able to have a vaginal birth if your baby is breech.
- There is a serious risk of cord prolapse if your waters break and your baby is not head-first.
What are presentation and malpresentation?
‘Presentation’ describes how your baby is facing down the birth canal. The ‘presenting part’ is the part of your baby’s body that is against the cervix .
The ideal presentation is head-first, with the crown (top) of the baby’s head against the cervix, with the chin tucked into the baby’s chest. This is called ‘vertex presentation’.
If your baby is in any other position, it’s called ‘malpresentation’. Malpresentation can mean your baby’s face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix.
It’s safest for your baby’s head to come out first. If any other body part goes down the birth canal first, the risks to you and your baby may be higher. Malpresentation increases the chance that you will have a more complex vaginal birth or a caesarean.
If my baby is not head-first, what position could they be in?
Malpresentation is caused by your baby’s position (‘lie’). There are different types of malpresentation.
Breech presentation
This is when your baby is lying with their bottom or feet facing down. Sometimes one foot may enter the birth canal first (called a ‘footling presentation’).
Breech presentation is the most common type of malpresentation.
Face presentation
This is when your baby is head-first but stretching their neck, with their face against the cervix.
Transverse lie
This is when your baby is lying sideways. Their back, shoulders, arms or legs may be the first to enter the birth canal.
Oblique lie
This is when your baby is lying diagonally. No particular part of their body is against the cervix.
Unstable lie
This is when your baby continually changes their position after 36 weeks of pregnancy.
Cord presentation
This is when the umbilical cord is against the cervix, between your baby and the birth canal. It can happen in any situation where your baby’s presenting part is not sitting snugly in your pelvis. It can become an emergency if it leads to cord prolapse (when the cord is born before your baby, potentially reducing placental blood flow to your baby).
What is malposition?
If your baby is lying head-first, the best position for labour is when their face is towards your back.
If your baby is facing the front of your body (posterior position) or facing your side (transverse position) this is called malposition. Transverse position is not the same as transverse lie. A transverse position means your labour may take a bit longer and you might feel more pain in your back. Often your baby will move into a better position before or during labour.
Why might my baby be in the wrong position?
Malpresentation may be caused by:
- a low-lying placenta
- too much or too little amniotic fluid
- many previous pregnancies, making the muscles of the uterus less stable
- carrying twins or more
Often no cause is found.
Is it likely that my baby will be in the wrong position?
Many babies are in a breech position during pregnancy. They usually turn head-first as pregnancy progresses, and more than 9 in 10 babies in Australia have a vertex presentation (ideal presentation, head-first) at birth.
You are more likely to have a malpresentation if:
- this is your first baby
- you are over 40 years old
- you've had a previous breech baby
- you go into labour prematurely
How is malpresentation diagnosed?
Malpresentation is normally diagnosed when your doctor or midwife examines you, from 36 weeks of pregnancy. If it’s not clear, it can be confirmed with an ultrasound.
Can my baby’s position be changed?
If you are 36 weeks pregnant , it may be possible to gently turn your baby into a head-first position. This is done by an obstetrician using a technique called external cephalic version (ECV).
Some people try different postures or acupuncture to correct malpresentation, but there isn’t reliable evidence that either of these work.

Will I need a caesarean if my baby has a malpresentation?
Most babies with a malpresentation close to birth are born by caesarean . You may be able to have a vaginal birth with a breech baby, but you will need to go to a hospital that can offer you and your baby specialised care.
If your baby is breech, an elective (planned) caesarean is safer for your baby than a vaginal birth in the short term. However, in the longer term their health will be similar, on average, regardless of how they were born.
A vaginal birth is safer for you than an elective caesarean. However, about 4 in 10 people planning a vaginal breech birth end up needing an emergency caesarean . If this happens to you, the risk of complications will be higher.
Your doctor can talk to you about your options. Whether it’s safe for you to try a vaginal birth will depend on many factors. These include how big your baby is, the position of your baby, the structure of your pelvis and whether you’ve had a caesarean in the past.
What are the risks if I have my baby when it’s not head-first?
If your waters break when your baby is not head-first, there is a risk of cord prolapse. This is an emergency.
Vaginal breech birth
Risks to your baby can include:
- Erb’s palsy
- fractures, dislocations or other injuries
- bleeding in your baby’s brain
- low Apgar scores
- their head getting stuck – this is an emergency
Risks to you include:
- blood loss or blood clots
- infection in the wound
- problems with the anaesthetic
- damage to other organs nearby, such as your bladder
- a higher chance of problems in future pregnancies
- a longer recovery time than after a vaginal birth
Risks to your baby include:
- trouble with breathing — this is temporary
- getting a small cut during the surgery
Will I have a malpresentation in my future pregnancies?
If you had a malpresentation in one pregnancy, you have a higher chance of it happening again, but it won’t necessarily happen in future pregnancies. If you’re worried, it may help to talk to your doctor or midwife so they can explain what happened.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: July 2022
Related pages
Labour complications.
- Interventions during labour
- Giving birth - stages of labour
Breech pregnancy
Search our site for.
- Caesarean Section
- Foetal Version
Need more information?
Top results
When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

Presentation and position of baby through pregnancy and at birth
Presentation and position refer to where your baby’s head and body is in relation to your birth canal. Learn why it’s important for labour and birth.
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
- Getting pregnant
- Preschooler
- Life as a parent
- Baby essentials
- Find your birth club
- Free antenatal classes
- Meet local parents & parents-to-be
- See all in Community
- Ovulation calculator
- Am I pregnant quiz
- How to get pregnant fast
- Best sex positions
- Signs of pregnancy
- How many days after your period can you get pregnant?
- How age affects fertility
- Very early signs of pregnancy
- What fertile cervical mucus looks like
- Think you're pregnant but the test is negative?
- Faint line on pregnancy test
- See all in Getting pregnant
- Pregnancy week by week
- How big is my baby?
- Due date calculator
- Baby movements week by week
- Symptoms you should never ignore
- Hospital bag checklist
- Signs of labour
- Your baby's position in the womb
- Baby gender predictor
- Vaginal spotting
- Fetal development chart
- See all in Pregnancy
- Baby names finder
- Baby name inspiration
- Popular baby names 2022
- Numerology calculator
- Gender-neutral names
- Old-fashioned names
- See all in Baby names
- Your baby week by week
- Baby milestones by month
- Baby rash types
- Baby poop chart
- Ways to soothe a crying baby
- Safe co-sleeping
- Teething signs
- Growth spurts
- See all in Baby
- Your toddler month by month
- Toddler development milestones
- Dealing with tantrums
- Toddler meals
- Food & fussy eating
- When to start potty training
- Moving from a cot to a bed
- Help your child sleep through
- Games & activities
- Vomiting: what's normal?
- See all in Toddler
- Your child month by month
- Food ideas & nutrition
- How kids learn to share
- Coping with aggression
- Bedtime battles
- Anxiety in children
- Dealing with public tantrums
- Great play ideas
- Is your child ready for school?Top tips for starting school
- See all in Preschooler
- Postnatal symptoms to watch out for
- Stitches after birth
- Postpartum blood clots
- Baby showers
- Sex secrets for parents
- See all in Life as a parent
- Best baby products
- Best formula and bottles for a windy baby
- Best car seats if you need three to fit
- Best nappies
- Best Moses baskets
- Best baby registries
- Best baby sleeping bags
- Best baby humidifier
- Best baby monitors
- Best baby bath seat
- Best baby food
- See all in Baby essentials
- Back pain in pregnancy
- Pelvic girdle pain
- Perineal massage
- Signs you're having a boy
- Signs you're having a girl
- Can you take fish oil while pregnant?
- 18 weeks pregnant bump
- Can you eat salami when pregnant?
- Edwards' syndrome
- Missed miscarriage
- Should I harvest my colostrum?
- Rhesus positive vs. Rhesus negative
- What do contractions feel like?
- Hunger in early pregnancy
- First poop after birth
- When do babies sit up?
- When can babies have salt?
- MMR vaccine rash
- Vaping while breastfeeding
- How to transition from formula to milk
- When do babies start grabbing things?
- Sperm allergy: can sperm cause itching?
- How long after taking folic acid can I get pregnant?
What is brow presentation?

- the size or shape of your pelvis
- because your baby is premature
- an abnormality that prevents your baby from tucking in her chin
- having too much amniotic fluid ( polyhydramnios )
Was this article helpful?
What is a doula and how can she help? (Video)

Parents' tips: nursery lighting

Would you use complementary therapies during labour?
What is asynclitic presentation.

Where to go next

Abnormal Fetal Position and Presentation
Under normal circumstances, a baby is in the vertex (cephalic) position before delivery. In the vertex position, the baby’s head is at the lower part of the abdomen, and the baby is born head-first. However, some babies present differently before delivery. In these cases, abnormal presentations may place the baby at risk of experiencing umbilical cord problems and/or a birth trauma (1). Types of abnormal fetal positions and presentations include the following. We’ll cover each in more detail on this page.
What is the difference between fetal presentation and position?
In the womb, a fetus has both a presentation and a position . Presentation refers to the baby’s body that leads, or is expected to lead, out of the birth canal (9). For example, if a baby’s rear is set to come out of the birth canal first, the baby is said to be in “breech presentation.” Position refers to the direction the baby is facing in relation to the mother’s spine (9). A baby could be lying face-first against a mother’s spine, or face up towards the mother’s belly.
What way should a baby come out during birth?
Vertex presentation is the ‘normal’ way that a baby is positioned for birth and the lowest-risk presentation for vaginal birth (1). In vertex presentation, the baby is positioned head-first with their occiput (the part of the head close to the base of the skull) entering the birth canal first. In this position, the baby’s chin is tucked into their chest and they are facing the mother’s back (occipito-anterior position). Any position other than vertex position is abnormal and can make vaginal delivery much more difficult or sometimes impossible (2). If a baby’s chin isn’t tucked into their chest, they may come out face-first (face presentation), which can cause birth injury (1).
What happens if a baby isn’t in the standard vertex position during birth?
Before delivery, it is critical that the fetus is in the standard vertex presentation and within the normal range for weight and size. This helps ensure the safety of both baby and mother during labor. When the baby’s size or position is abnormal, physician intervention is usually warranted (1). This may mean simple manual procedures to help reposition the baby or, in many cases, a planned C-section delivery . The failure of healthcare professionals to identify and quickly resolve issues related to fetal size, weight, and presentation is medical malpractice . There are numerous complications related to abnormal weight, size, abnormal position, or abnormal presentation.
Compound presentation
In the safest presentation (vertex presentation), the baby is born head first, with the rest of the body following. In a compound presentation, however, there are multiple presenting parts. Most commonly, this means that the baby’s head and an arm come out first at the same time. Sometimes compound presentation can occur with twins where the head of the first twin presents with the extremity of the second twin (3).
Risk factors for compound presentation include (3):
- Prematurity
- Intrauterine growth restriction (IUGR)
- Multiple gestations ( twins , triplets, etc.)
- Polyhydramnios
- A large pelvis
- External cephalic version
- Rupture of membranes at high station
Compound presentations can be detected via ultrasound before the mother’s water breaks. During labor, compound presentation is identified as an irregular finding during a cervical examination (3).
If a mother has polyhydramnios, the risk of compound presentation is higher, as the flow of amniotic fluid when the membranes rupture can sweep extremities into the birth canal, or cause a cord prolapse , which is a medical emergency (3). If compound presentation continues, it is likely to cause dystocia (the baby becoming stuck in the birth canal), which is also a medical emergency (3). Often, the safest way to deliver a baby with compound presentation is C-section, because complications like dystocia and cord prolapse carry risks of severe adverse outcomes, including cerebral palsy , intellectual and developmental disabilities, and hypoxic-ischemic encephalopathy (HIE) (3).
Limb presentation
Limb presentation during childbirth means that the part of the baby’s body that emerges first is a limb – an arm or a leg. Babies with limb presentation cannot be delivered safely via vaginal delivery; they must be delivered quickly by emergency C-section (4). Limb presentation poses a large risk for dystocia (the baby getting stuck on the mother’s pelvis), which is a medical emergency.
Occipitoposterior (OP) position
Approximately 1 out of 19 babies present in a posterior position rather than an anterior position. This is called an occipitoposterior (OP) position or occiput posterior position (3) In OP position, the baby is head-first with the back part of the head turned towards the mother’s back, rotated to the right (right occipitoposterior position, or ROP), or to the left (left occipitoposterior position, or LOP) of the sacroiliac joint. Occipitoposterior position increases the baby’s risk of experiencing prolonged labor , prolapsed umbilical cord , and use of delivery instruments, such as forceps and vacuum extractors (5). These conditions can cause brain bleeds , a lack of oxygen to the brain, and birth asphyxia .
When OP position is present, if a manual rotation cannot be quickly and effectively performed in the face of fetal distress, the baby should be delivered via C-section (5). A C-section can help prevent oxygen deprivation caused by prolonged labor, umbilical cord prolapse, or forceps and vacuum extractor use.
A nurse explains posterior position
Breech presentation
Breech presentation is normal throughout pregnancy. However, by the 37th week, the baby should turn to the cephalic position in time for labor. Breech presentation occurs when a baby’s buttocks or legs are positioned to descend the birth canal first. Breech positions are dangerous because when vaginal delivery is attempted, a baby is at increased risk for prolapsed umbilical cord, traumatic head injury, spinal cord fracture, fatality, and other serious problems with labor (6).
There are 4 types of breech positions:
- Footling breech presentation : In footling position, one or both feet enter the birth canal first, with the buttocks at a higher position than the feet.
- Kneeling breech presentation : This is when the baby has one or both legs extended at the hips and flexed at the knees.
- Frank breech presentation : This is when the baby’s buttocks present first, the legs are flexed at the hip and extended at the knees, and the feet are near the ears.
- Complete breech presentation : In this position, the baby’s hips and knees are flexed so that the baby is sitting cross-legged, with the feet beside the buttocks.
When a baby is in breech position, physicians often try to maneuver the baby into a head-first position. This should only be attempted if fetal heart tracings are normal (the baby is not in distress ) (7). The only type of breech position that may allow for a vaginal delivery is frank breech , and the following conditions must be met:
- The baby’s heart rate is being closely monitored and the baby is not in distress.
- Cephalopelvic disproportion (CPD) is not present; x-rays and ultrasound show that the size of the mother’s pelvis will allow a safe vaginal birth.
- The hospital is equipped for and the physician is skilled in performing an emergency C-section .
If these conditions are not present, vaginal birth should not be attempted. Most experts recommend C-section delivery for all types of breech positions because it is the safest method of delivery and it helps avoid birth injuries (6). Mismanaged breech birth can result in the following conditions:
- Brain bleeds, intracranial hemorrhages
- Spinal cord fractures
- Hypoxic-ischemic encephalopathy (HIE)
- Cerebral palsy
- Intellectual disabilities
- Developmental delays
Face presentation
A face presentation occurs when the face is the presenting part of the baby. In this position, the baby’s neck is deflexed (extended backward) so that the back of the head touches the baby’s back. This prevents head engagement and descent of the baby through the birth canal. In some cases of face presentation, the trauma of a vaginal delivery causes face deformation and fluid build-up (edema) in the face and upper airway, which often means the baby will need a breathing tube placed in the airway to maintain airway patency and assist breathing (1).
Image by healthhand.com
There are three types of face presentation:
- Mentum anterior (MA) : In this position, the chin is facing the front of the mother.
- Mentum posterior (MP) : The chin is facing the mother’s back, pointing down towards her buttocks in mentum posterior position. In this position, the baby’s head, neck, and shoulders enter the pelvis at the same time, and the pelvis is usually not large enough to accommodate this. Also, an open fetal mouth can push against the bone (sacrum) at the upper and back part of the pelvis, which also can prevent descent of the baby through the birth canal.
- Mentum transverse (MT) : The baby’s chin is facing the side of the birth canal in this position.
Trauma is very common during vaginal delivery of a baby in face presentation, so parents must be warned that their baby may be bruised and that a C-section is available to avoid this trauma.
Babies presenting face-first can sometimes be delivered vaginally, as long as the baby is in MA position (1). Safe vaginal delivery of a term-sized infant in persistent MP position is impossible due to the presenting part of the baby compared to the size of the mother’s pelvis (1). Babies in MP position must be delivered by C-section. Babies in MT position must also be delivered by C-section. Some babies in the MP and MT positions will spontaneously convert to the MA position during the course of labor, which makes vaginal delivery a possibility. If the baby is in the MA position and vaginal delivery is able to proceed, engagement of the presenting part of the baby probably will not occur until the face is at a +2 station (1).
The management of face presentation requires close observation of the progress of labor due to the high incidence of CPD with face presentation. In face presentation, the diameter of the presenting part of the head is, on average, 0.7 cm greater than in the normal vertex position (1).
In any face presentation situation, if progress in dilation and descent ceases despite adequate contractions, delivery must occur by C-section. In fact, when face presentation occurs, experts recommend liberal use of C-section (1).
Since there is an increased risk of trauma to the baby when the face presents, the physician should not try to rotate the baby internally. In addition, the physician must not use vacuum extractors or manual extraction (grasping the baby with hands) to extract the baby from the uterine cavity. Outlet forceps should only be used by experienced physicians; these forceps increase the risk of trauma and brain bleeds. In almost all clinical circumstances a cesarean delivery is the safest method of delivery.
Listed below are complications that can occur if face presentation is mismanaged by the medical team:
- Prolonged labor
- Facial trauma
- Facial and upper airway edema (fluid build-up in the face, often caused by trauma)
- Skull molding (abnormal head shape that results from pressure on the baby’s head during childbirth)
- Respiratory distress or difficulty in ventilation (the baby being able to move air in and out of lungs) due to upper airway trauma and edema
- Spinal cord injury
- Abnormal fetal heart rate patterns
- 10-fold increase in fetal compromise
- Brain bleeds
- Intracranial hemorrhages
- Permanent brain damage
Brow presentation
Brow presentation is similar to face presentation, but the baby’s neck is less extended. A fetus in brow presentation has the chin untucked, and the neck is extended slightly backward. As the term “brow presentation” suggests, the brow (forehead) is the part that is situated to go through the pelvis first. Vaginal delivery can be difficult or impossible with brow presentation, because the diameter of the presenting part of the head may be too big to safely fit through the pelvis.
Risk factors and conditions associated with brow presentation
Brow presentation has been linked to several risk factors and co-occurring conditions. These include:
- Multiparity (having previously given birth)
- Premature delivery
- Fetal anomalies such as anencephaly (an absence of major parts of the brain and skull) or anterior neck mass (a growth on the front of the neck)
- Previous c-section delivery
- Polyhydramnios (excessive amniotic fluid: infants swallow amniotic fluid while in utero, but this may be difficult if their neck is extended)
Diagnosis of brow presentation
Brow presentation can often be diagnosed through a vaginal examination during labor. If there are no conclusive signs from the physical examination alone, an ultrasound can also be used. Warning signs of brow presentation may include signs of fetal distress or lack of labor progression.
Management of brow presentation
Infants who assume a brow presentation early in labor may spontaneously move into a more optimal position during the delivery process. Additionally, safe delivery in brow presentation may be possible if the infant is unusually small and/or the mother’s pelvic opening is unusually large. For these reasons, physicians occasionally recommend vaginal delivery of infants in brow presentation.
Doctors attempting vaginal delivery of a baby in brow presentation must be very careful to watch for signs of fetal distress (such as an abnormal heart rate), and to monitor the progression of labor. Prolonged labor can cause extended periods of fetal oxygen deprivation, which can cause birth asphyxia and permanent injury. Signs of fetal distress can indicate that a baby is in danger of sustaining serious brain damage if action is not quickly taken to prevent this. If an infant in brow presentation begins to show signs of distress, or if labor progress stops or slows significantly, physicians should be ready to move on to a cesarean delivery.
Labor induction or augmentation with the drug Pitocin (synthetic oxytocin) is very dangerous in cases of brow presentation. Pitocin can lead to excessive uterine contractions, which can put pressure on the infant’s head and cut off their oxygen supply; this is especially risky when safe fetal descent is already compromised, such as in cases of brow presentation.
Complications of brow presentation
If brow presentation is diagnosed in a timely fashion and is appropriately managed, there are typically no serious negative effects on the mother or baby. However, if medical professionals fail to recognize brow presentation and intervene as necessary, there can be lasting consequences. Infants may suffer oxygen deprivation due to prolonged labor, or traumatic injuries from a difficult delivery. Some of the most severe conditions resulting from mismanaged brow presentation births include:
- Hypoxic-ischemic encephalopathy
- Periventricular leukomalacia
- Seizure disorders
- Developmental disabilities
Shoulder presentation (transverse lie)
Shoulder presentation (transverse lie) is when the arm, shoulder or trunk of the baby enter the birth canal first. When a baby is in a transverse lie position during labor, C-section is almost always used as the delivery method (8). Mothers who have polyhydramnios (too much amniotic fluid), are pregnant with more than one baby, have placenta previa, or have a baby with intrauterine growth restriction (IUGR) are more likely to have a baby in the transverse lie position (8). Once the membranes rupture, there is an increased risk of umbilical cord prolapse in this position; thus, a C-section should ideally be performed before the membranes break (8). Failure to quickly deliver the baby by C-section when transverse lie presentation is present can cause severe birth asphyxia due to cord compression and trauma to the baby. This can cause hypoxic-ischemic encephalopathy (HIE), seizures, permanent brain damage, and cerebral palsy.
Legal help for birth injuries from abnormal position or presentation
The award-winning birth injury attorneys at ABC Law Centers have over 100 years of joint experience handling birth trauma cases related to abnormal position or presentation. If you believe your loved one’s birth injury resulted from an instance of medical malpractice, you may be entitled to compensation from a medical malpractice or personal injury case. During your free legal consultation, our birth injury attorneys will discuss your case with you, determine if negligence caused your loved one’s injuries, identify the negligent party, and discuss your legal options with you.
- Free Case Review
- Available 24/7
- No Fee Unless We Win
Featured Videos
Testimonial from keziah’s family, posterior position, hypoxic-ischemic encephalopathy (hie).
Featured Testimonial
What Our Clients Say…
After the traumatic birth of my son, I was left confused, afraid, and seeking answers. We needed someone we could trust and depend on . ABC Law Centers was just that.
Helpful resources
More about our firm.
- Meet our birth injury attorneys
- Meet our in-house medical staff
- Verdicts and settlements
- Testimonials
- Julien, S., and Galerneau, F. (2017). Face and brow presentations in labor. Retrieved from https://www.uptodate.com/contents/face-and-brow-presentations-in-labor .
- World Health Organization, UNICEF, and United Nations Population Fund. Malpositions and malpresentations. Retrieved from http://hetv.org/resources/reproductive-health/impac/Symptoms/Malpositions__malpresetations_S69_S81.html .
- Barth, W. (2016). Compound fetal presentation. Retrieved from https://www.uptodate.com/contents/compound-fetal-presentation .
- Gabbe, S.G., … Grobman, W.A. (2017). Compound Presentation. Retrieved from https://expertconsult.inkling.com/read/gabbe-obstetrics-normal-problem-pregnancies-7e/chapter-17/compound-presentation .
- Argani, C.H. and Satin, A.J. (2018) Occiput posterior position. Retrieved from https://www.uptodate.com/contents/occiput-posterior-position .
- Hofmeyr, G.J. (2018). Overview of issues related to breech presentation. Retrieved from https://www.uptodate.com/contents/overview-of-issues-related-to-breech-presentation .
- Hofmeyr, G.J. (2017). Delivery of the fetus in breech presentation. Retrieved from https://www.uptodate.com/contents/delivery-of-the-fetus-in-breech-presentation .
- Strauss, R.A. (2017). Transverse fetal lie. Retrieved from https://www.uptodate.com/contents/transverse-fetal-lie .
- Moldenhauer, J.S. (2018). Abnormal Position and Presentation of the Fetus. Retrieved from https://www.merckmanuals.com/home/women-s-health-issues/complications-of-labor-and-delivery/abnormal-position-and-presentation-of-the-fetus .
Over $350 Million Recovered
In Verdicts, Settlements, & Judgements
$4.75 Million
$3.9 Million
$5.85 Million
Awards & Memberships
Emergency Obstetrics and Pediatrics
2-19. limb presentation.
Transport the mother to the hospital immediately if an arm or leg is presented first. Keep the mother in the delivery position (follow local guidelines.) DO NOT attempt to deliver the baby.
CAUTION: DO NOT try to pull on the presenting limb.
DO NOT try to replace the limb into the vagina.
DO NOT place your hand into the vagina unless there is a prolapsed cord.
A Distance Learning Course
Planning for a baby?
- Preconception Health
- Preparing for Pregnancy
- Assisted Pregnancy
- Second Pregnancy
Already Pregnant?
- Pregnancy Week by Week
- Health & Safety
- Live life better
- Preparing for the baby
- Pregnancy Diet & Fitness
Have a Baby?
- Baby Milestones
- Baby Basics
- Mother Care
- Activity & Fun
Have a Toddler?
- Toddler Mile Stones
- Toddler Basics
- Food & Feeding
- Child Safety & Health
- Games & Playtime
- Special Child
Positive Parenting
- Health & Hyginie
- Learning and Development
- Family Basics
Child Safety
- Special child Care
- Planning for Future
- Play, Games, activity & Fun
Life Skills
Premature baby, baby products, health & safety, what is brow presentation what are its complications.
Written by Editorial Team

Editorial Team
With a rich experience in pregnancy and parenting, our team of experts create insightful, well-curated, and easy-to-read content for our to-be-parents and parents at all stages of parenting..
What Is Brow Presentation?
What leads to brow presentation, diagnosis of brow presentation, how to avoid c-section if baby is in brow presentation, what complications can arise due to brow presentation.

- Polyhydramnios : Excess amniotic fluid can make it difficult for the baby’s head to take a flexed position
- Size and shape of the pelvis: Abnormally shaped and sized pelvis can make it difficult for the baby to pick up a vertex presentation. Android pelvis, which has a triangular or heart-shaped inlet with a narrower front part, is usually behind most of the brow presentations. Similarly, contracted pelvis, a pelvis that is abnormally small, can cause brow presentation
- Fetal abnormality: Fetal abnormalities such as hydrocephalus, anencephaly and neck masses accounts for the majority of brow presentations
- Premature birth/low birth weight baby: If the baby is born prematurely or if the baby is having low birth weight , the chances of brow presentation increases
- Big baby : If the baby is larger than normal size, the baby tends to extend its head instead of curling inward
- Multiple pregnancies: Multiple pregnancies also increase the risk of brow presentation
- Multiple nuchal cords: If the umbilical cord wraps around the baby’s neck, obviously, it cannot tuck its chin into the chest. In such cases, the baby tends to be brow or face presentations
- Laxity of the uterus: If the uterine wall loses its firmness, the baby may not able to hold its chin tucked to the chest firmly and the baby tends to be in brow presentation
- Cephalopelvic disproportion (CPD): If the mother’s pelvis and the baby’s head are not proportionate to each other, brow presentation can happen

- Manual rotation: Doctor inserts his hand through the cervix and tries to flex the baby’s head
- The baby’s head should be engaged in the pelvis and should be in a front anterior position
- The pelvis should have sufficient room to permit the ventouse cup to be inserted posteriorly and to reach the occiput
- Ability and experience of the obstetrician
- How favorable is the position of the baby’s head inside the pelvis
- Available space inside the pelvis
- Increased chances of spinal cord injury are associated with brow presentation
- Fetal distress
- Abnormal shape of the baby’s head after delivery
- Prolonged labor
- Increased chances of using forceps which in turn increases the chances of facial trauma
- Obstructed labor
Advantages Of Saffron During Pregnancy
Saffron is the dried stigma of Crocus Sativus flower, i.e. the thread-like part at the centre which contains pollen.

Editorial Team,
With a rich experience in pregnancy and parenting, our team of experts create insightful, well-curated, and easy-to-read content for our to-be-parents and parents at all stages of parenting. Read more.

Responses (0)
Want curated content sharply tailored for your exact stage of parenting, read this next, related articles.

Repeat C-Sections – How Many Can Woman Have Safely

Top 500 Latest Baby Boy Names Starting With Y

Top 500 Baby Boy Names That Start With B

Lamb during Pregnancy – Safety, Benefits & Side Effects

Black Salt During Pregnancy – Is it Safe, Benefits and Side Effects

Top 500 Latest Baby Girl Names Starting With M
Sponsored content
Discover great local businesses around you for your kids..
Get regular updates, great recommendations and other right stuff at the right time.
Premium Access
Join our community of 50K+ Moms and get access to exclusive features & resources in our app.
Pay Rs 25/- and read this article (One time access)

Our site uses cookies to make your experience on this site even better. We hope you think that is sweet.
Create account
Focus your wanderlust. create your account to get curated stories and recommendations., already have an account sign in.
Don't have an account? Sign up forgot password?
Get curated personalized content., articles and resources served personalized as per the stage of your parenting., already have an account login, choose one..

Enter dates

What is ADHD?
Signs and symptoms.
- Managing Symptoms
ADHD in Adults
More information.
ADHD is one of the most common neurodevelopmental disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. Children with ADHD may have trouble paying attention, controlling impulsive behaviors (may act without thinking about what the result will be), or be overly active.
It is normal for children to have trouble focusing and behaving at one time or another. However, children with ADHD do not just grow out of these behaviors. The symptoms continue, can be severe, and can cause difficulty at school, at home, or with friends.
A child with ADHD might:
- daydream a lot
- forget or lose things a lot
- squirm or fidget
- talk too much
- make careless mistakes or take unnecessary risks
- have a hard time resisting temptation
- have trouble taking turns
- have difficulty getting along with others
Learn more about signs and symptoms

Get information and support from the National Resource Center on ADHD
There are three different ways ADHD presents itself, depending on which types of symptoms are strongest in the individual:
- Predominantly Inattentive Presentation: It is hard for the individual to organize or finish a task, to pay attention to details, or to follow instructions or conversations. The person is easily distracted or forgets details of daily routines.
- Predominantly Hyperactive-Impulsive Presentation: The person fidgets and talks a lot. It is hard to sit still for long (e.g., for a meal or while doing homework). Smaller children may run, jump or climb constantly. The individual feels restless and has trouble with impulsivity. Someone who is impulsive may interrupt others a lot, grab things from people, or speak at inappropriate times. It is hard for the person to wait their turn or listen to directions. A person with impulsiveness may have more accidents and injuries than others.
- Combined Presentation: Symptoms of the above two types are equally present in the person.
Because symptoms can change over time, the presentation may change over time as well.
Learn about symptoms of ADHD, how ADHD is diagnosed, and treatment recommendations including behavior therapy, medication, and school support.
Causes of ADHD
Scientists are studying cause(s) and risk factors in an effort to find better ways to manage and reduce the chances of a person having ADHD. The cause(s) and risk factors for ADHD are unknown, but current research shows that genetics plays an important role. Recent studies link genetic factors with ADHD. 1
In addition to genetics, scientists are studying other possible causes and risk factors including:
- Brain injury
- Exposure to environmental risks (e.g., lead) during pregnancy or at a young age
- Alcohol and tobacco use during pregnancy
- Premature delivery
- Low birth weight
Research does not support the popularly held views that ADHD is caused by eating too much sugar, watching too much television, parenting, or social and environmental factors such as poverty or family chaos. Of course, many things, including these, might make symptoms worse, especially in certain people. But the evidence is not strong enough to conclude that they are the main causes of ADHD.

Download and Print this fact sheet [PDF – 473 KB]
Deciding if a child has ADHD is a process with several steps. There is no single test to diagnose ADHD, and many other problems, like anxiety, depression, sleep problems, and certain types of learning disabilities, can have similar symptoms. One step of the process involves having a medical exam, including hearing and vision tests , to rule out other problems with symptoms like ADHD. Diagnosing ADHD usually includes a checklist for rating ADHD symptoms and taking a history of the child from parents, teachers, and sometimes, the child.
Learn more about the criteria for diagnosing ADHD

In most cases, ADHD is best treated with a combination of behavior therapy and medication. For preschool-aged children (4-5 years of age) with ADHD, behavior therapy, particularly training for parents, is recommended as the first line of treatment before medication is tried. What works best can depend on the child and family. Good treatment plans will include close monitoring, follow-ups, and making changes, if needed, along the way.
Learn more about treatments
Managing Symptoms: Staying Healthy
Being healthy is important for all children and can be especially important for children with ADHD. In addition to behavioral therapy and medication, having a healthy lifestyle can make it easier for your child to deal with ADHD symptoms. Here are some healthy behaviors that may help:
- Developing healthy eating habits such as eating plenty of fruits, vegetables, and whole grains and choosing lean protein sources
- Participating in daily physical activity based on age
- Limiting the amount of daily screen time from TVs, computers, phones, and other electronics
- Getting the recommended amount of sleep each night based on age
If you or your doctor has concerns about ADHD, you can take your child to a specialist such as a child psychologist, child psychiatrist, or developmental pediatrician, or you can contact your local early intervention agency (for children under 3) or public school (for children 3 and older).
The Centers for Disease Control and Prevention (CDC) funds the National Resource Center on ADHD , a program of CHADD – Children and Adults with Attention-Deficit/Hyperactivity Disorder. Their website has links to information for people with ADHD and their families. The National Resource Center operates a call center (1-866-200-8098) with trained staff to answer questions about ADHD.
For more information on services for children with special needs, visit the Center for Parent Information and Resources. To find the Parent Center near you, you can visit this website.
ADHD can last into adulthood. Some adults have ADHD but have never been diagnosed. The symptoms can cause difficulty at work, at home, or with relationships. Symptoms may look different at older ages, for example, hyperactivity may appear as extreme restlessness. Symptoms can become more severe when the demands of adulthood increase. For more information about diagnosis and treatment throughout the lifespan, please visit the websites of the National Resource Center on ADHD and the National Institutes of Mental Health .
- National Resource Center on ADHD
- National Institute of Mental Health (NIMH)
- Faraone, S. V., Banaschewski, T., Coghill, D., Zheng, Y., Biederman, J., Bellgrove, M. A., . . . Wang, Y. (2021). The World Federation of ADHD International Consensus Statement: 208 evidence-based conclusions about the disorder. Neuroscience & Biobehavioral Reviews. doi:10.1016/j.neubiorev.2021.01.022
To receive email updates about this topic, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Ask a Pharmacist: The first over-the-counter birth control pill
by CNY Central
Opill is the first and only FDA-approved daily oral contraceptive for over-the-counter use, meaning no prescription is required. It’s 98% effective at preventing pregnancy when taken at the same time every day and starts working within 48 hours of taking the first pill.
The pill is estrogen-free and only contains the hormone progestin, which works to prevent pregnancy by affecting ovulation, thickening cervical mucus and changing the uterine lining.
Opill is not an emergency contraceptive and does not protect from sexually transmitted diseases.
Approximately one in three adult women who have tried to get a prescription or a refill for birth control face roadblocks or are unable to get their next supply in time. Having the over-the-counter option of Opill eliminates many barriers for women who want to protect against unwanted pregnancy.
Opill is available at Kinney Drugs in the family planning section and it can also be delivered through Kinney Drugs’ Instacart service.
If you have any questions about Opill, ask your Kinney pharmacist!
Watch the video above to learn more.
Ask a Pharmacist is sponsored by Kinney Drugs.

IMAGES
VIDEO
COMMENTS
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech ...
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
Presentation refers to the part of the fetus's body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way. Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput ...
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin.
There are several types of breech presentation. Frank breech: The fetal hips are flexed, and the knees extended (pike position). Complete breech: The fetus seems to be sitting with hips and knees flexed. Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Presentation refers to which part of your baby's body is facing towards your birth canal. Position refers to the direction your baby's head or back is facing. Your baby's presentation will be checked at around 36 weeks of pregnancy. Your baby's position is most important during labour and birth.
This presentation can lead to more back pain (sometimes referred to as "back labor") and slow progression of labor. In the right occiput posterior position (ROP), the baby is facing forward and slightly to the right (looking toward the mother's left thigh). This presentation may slow labor and cause more pain. Tips to Reduce Discomfort
Presentation of twins in Der Rosengarten ("The Rose Garden"), a standard medical text for midwives published in 1513. In obstetrics, the presentation of a fetus about to be born specifies which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal. According to the leading part, this is identified as a cephalic, breech, or shoulder presentation.
Vertex Presentation. A vertex presentation is the ideal position for a fetus to be in for a vaginal delivery. It means the fetus is head down, headfirst and facing your spine with its chin tucked to its chest. Vertex presentation describes a fetus being head-first or head down in the birth canal.
This is the most common position for babies in-utero. In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest delivery, as baby's head can easily move down the birth canal and under the pubic bone during childbirth.
In a face presentation, the fetal head and neck are hyperextended, causing the occiput to come in contact with the upper back of the fetus while lying in a longitudinal axis. The presenting portion of the fetus is the fetal face between the orbital ridges and the chin. The fetal chin (mentum) is the point designated for reference during an ...
Face presentation may reflect a psoas/pelvic floor imbalance with a collapse in the front body. Free the piriformis, strengthen the buttocks, lengthen the hamstrings, squat for lengthening the pelvic floor, don't worry about strengthening the pelvic floor right now. Alignment, walking, stabilizing and lengthening will tone the pelvic floor.
presentation. breech birth, in childbirth, position of the fetus in which the buttocks or feet are presented first. About 3 to 4 percent of babies are in a breech presentation at the onset of labour. In nearly all other cases, babies born vaginally are born headfirst, since they are in a head-down position in the mother's uterus.
Presentation, in childbirth, the position of the fetus at the time of delivery. The presenting part is the part of the fetus that can be touched by the obstetrician when he probes with his finger through the opening in the cervix, the outermost portion of the uterus, which projects into the vagina.
Stage 1: Early labor and active labor. Cervical effacement and dilation. The first stage of labor and birth occurs when you begin to feel persistent contractions. These contractions become stronger, more regular and more frequent over time. They cause the cervix to open (dilate) and soften as well as shorten and thin (efface) to allow your baby ...
'Presentation' describes how your baby is facing down the birth canal. The 'presenting part' is the part of your baby's body that is against the cervix. The ideal presentation is head-first, with the crown (top) of the baby's head against the cervix, with the chin tucked into the baby's chest. This is called 'vertex presentation'.
Face Presentation Causes & Risk Factors. These conditions may increase the likelihood of a face presentation birth: A Very Big Baby (Fetal Macrosomia): Larger babies may have trouble fitting into the birth canal in the standard position, leading to alternative presentations. Prematurity: Premature infants are more likely to have non-standard presentations, including face presentation, because ...
Brow presentation is a rare complication, which affects only one in every 500 to one in every 1,400 births. So the chances of it happening are low. If a brow presentation is picked up in early labour, your baby may still flex her head in time for the birth. Alternatively, she may tip her head further back and be born face first.
Vertex presentation is the 'normal' way that a baby is positioned for birth and the lowest-risk presentation for vaginal birth (1). In vertex presentation, the baby is positioned head-first with their occiput (the part of the head close to the base of the skull) entering the birth canal first. In this position, the baby's chin is tucked ...
LIMB PRESENTATION - Emergency Obstetrics and Pediatrics. 2-19. LIMB PRESENTATION. Transport the mother to the hospital immediately if an arm or leg is presented first. Keep the mother in the delivery position (follow local guidelines.) DO NOT attempt to deliver the baby. CAUTION: DO NOT try to pull on the presenting limb.
One such complication that can come at the last minute of any delivery is the presentation of the baby. Normally, babies bow down their chin well tucked into the chest during their journey through the birth canal. This position is called flexed position or vertex presentation. This is the ideal position that makes delivery easier as the baby ...
Types. There are three different ways ADHD presents itself, depending on which types of symptoms are strongest in the individual: Predominantly Inattentive Presentation: It is hard for the individual to organize or finish a task, to pay attention to details, or to follow instructions or conversations. The person is easily distracted or forgets details of daily routines.
Opill is the first and only FDA-approved daily oral contraceptive for over-the-counter use, meaning no prescription is required. It's 98% effective at preventin