Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center


Factors that impact residents' transition and psychological adjustment to long-term aged care: A systematic literature review

Related Papers
Graham Rowles
Naomi Young
Ageing and Society
Pamela Dawson
Western Journal of Nursing Research
Jaclene Zauszniewski
Relocation is a major life event for elders and has been found to adversely affect their adjustment and ability to perform daily activities. Rosenbaum's theory of learned resourcefulness suggests that such adverse effects can be minimized if elders have positive cognitions and are resourceful. A cross-sectional design was used to examine the hypothesized relationships among the study variables in a sample of 104 cognitively unimpaired elders (aged 65+ years) who have relocated to retirement communities in Northeast Ohio. Results indicate that positive cognitions had a direct positive effect on learned resourcefulness and on relocation adjustment. Furthermore, learned resourcefulness had a moderating effect on the relationship between relocation controllability and relocation adjustment when controlling for covariates. It is imperative to generate interventions to enhance positive thinking and learned resourcefulness for elders facing the need to relocate and to create the therap...
Aging & Mental Health
Linda Garcia
David Ekerdt
Open Longevity Science
Loren Lovegreen
Journal of the American Medical Directors Association
Heather Allore , Thomas Gill , Evelyne Gahbauer
Ryan Woolrych
Although moving from institutional to home-like long-term care (LTC) settings can promote and sustain the health and wellbeing of older adults, there has been little research examining how home is perceived by older adults when moving between care settings. A qualitative study was conducted over a two-year period during the relocation of residents and staff from an institutional LTC home to a purpose-built LTC home in Western Canada. The study explored perceptions of home amongst residents, family members and staff. Accordingly, 210 semi-structured interviews were conducted at five time-points with 35 residents, 23 family members and 81 staff. Thematic analyses generated four superordinate themes that are suggestive of how to create and enhance a sense of home in LTC settings: (a) physical environment features; (b) privacy and personalisation; (c) autonomy, choice and flexibility; and (d) connectedness and togetherness. The findings reveal that the physical environment features are ...
Doctoral Dissertation
Heidi H Ewen
The decision to relocate or to age in place can be a difficult one, mitigated by a variety of influencing factors such as finances, physical abilities, as well as social and instrumental support from family and others. This study focuses on the stresses of residential relocation to independent and assisted living facilities among older women living in Lexington, Kentucky. Participation
RELATED PAPERS
Farhat Ben Amor
Rafik Shalaby
Biological & pharmaceutical bulletin
Prof. Raymond R Tjandrawinata, PhD, MS, MBA, FRSC, FRSPH
European Journal of Biochemistry
Véronique BOZON
Seray Doğan
Health and Social Care Chaplaincy
BMC Infectious Diseases
Valdiléa G. Veloso
Revista Brasileira de Fruticultura
Endson Nunes
Sisilia Ratri
Research, Society and Development
Felipe Caldeira
Proceedings of the 3rd International Conference on Economics, Business and Economic Education Science, ICE-BEES 2020, 22-23 July 2020, Semarang, Indonesia
Seng Hansen
THE 8TH INTERNATIONAL SEMINAR ON AEROSPACE SCIENCE AND TECHNOLOGY – ISAST 2020
BIOFIX Scientific Journal
Matheus Gueri
nadiyah elias
cumincades.scix.net
Maria C F Rocha
Ksawery Krenc
Frontiers in Immunology
Simonetta Baraldo
Microscopy and Microanalysis
Zhengran Ji
Journal of the European Ceramic Society
Monica Popa , Maria Zaharescu
Sabuco Revista De Estudios Albacetenses
Fernando Mejia Bautista
Journal of Applied Microbiology
Bjarnheiður K Guðmundsdóttir
乔治布朗学院毕业证办理成绩单 购买加拿大GBC文凭学历证书
Revista de la Sociedad Científica del Paraguay
Bianca Salinas
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Measuring safety in older adult care homes: a scoping review of the international literature.
Rand S, Smith N, Jones K, et al. Measuring safety in older adult care homes: a scoping review of the international literature. BMJ Open. 2021;11(3):e043206. doi: 10.1136/bmjopen-2020-043206.
Care home settings, such as nursing homes or residential care homes, present unique challenges to patient safety. This systematic review identified several gaps in the available safety measures used for quality monitoring and improvement in older adult care homes, including patient experience (e.g., quality of life or other resident-reported indicators of safety), psychological harm related to the care home environment, abusive or neglectful practices, and the absence of processes for integrated learning.
Exploring patient safety outcomes for people with learning disabilities in acute hospital settings: a scoping review. June 30, 2021
Dimensions of safety culture: a systematic review of quantitative, qualitative and mixed methods for assessing safety culture in hospitals. September 1, 2021
Quality standards for safe medication in nursing homes: development through a multistep approach including a Delphi consensus study. October 27, 2021
Recommendations for the safety of hospitalised patients in the context of the COVID-19 pandemic: a scoping review. October 5, 2022
How do patients respond to safety problems in ambulatory care? Results of a retrospective cross-sectional telephone survey. December 1, 2021
Suicide as an incident of severe patient harm: a retrospective cohort study of investigations after suicide in Swedish healthcare in a 13-year perspective. March 31, 2021
Exploring the factors that promote or diminish a psychologically safe environment: a qualitative interview study with critical care staff. September 22, 2021
Incidence, duration and risk factors associated with delayed and missed diagnostic opportunities related to tuberculosis: a population-based longitudinal study. March 24, 2021
'It's all about patient safety': an ethnographic study of how pharmacy staff construct medicines safety in the context of polypharmacy. March 10, 2021
NHS ‘Learning from Deaths’ reports: a qualitative and quantitative document analysis of the first year of a countrywide patient safety programme. July 21, 2021
Instruments for measuring patient safety competencies in nursing: a scoping review. June 15, 2022
Interventions promoting employee "speaking-up" within healthcare workplaces: a systematic narrative review of the international literature. June 2, 2021
Heatwaves, hospitals and health system resilience in England: a qualitative assessment of frontline perspectives from the hot summer of 2019. March 22, 2023
Checklists to reduce diagnostic error: a systematic review of the literature using a human factors framework. June 1, 2022
Patient safety in inpatient mental health settings: a systematic review. February 5, 2020
The effect of providing staff training and enhanced support to care homes on care processes, safety climate and avoidable harms: evaluation of a care home quality improvement programme in England. August 18, 2021
Patients' perceptions of safety in emergency medical services: an interview study. December 2, 2020
Towards safer healthcare: qualitative insights from a process view of organisational learning from failure. August 25, 2021
Safe opioid prescribing: a prognostic machine learning approach to predicting 30-day risk after an opioid dispensation in Alberta, Canada. June 16, 2021
Predictors of response rates of safety culture questionnaires in healthcare: a systematic review and analysis. October 26, 2022
User-testing guidelines to improve the safety of intravenous medicines administration: a randomised in situ simulation study. July 29, 2020
Exploration of prescribing error reporting across primary care: a qualitative study. April 13, 2022
Effects of interorganisational information technology networks on patient safety: a realist synthesis. December 9, 2020
Can SBAR be implemented with high fidelity and does it improve communication between healthcare workers? A systematic review. January 12, 2022
Responses of physicians to an objective safety and quality knowledge test: a cross-sectional study. October 6, 2021
Safe clinical practice for patients hospitalised in mental health wards during a suicidal crisis: qualitative study of patient experiences. December 23, 2020
Patient feedback for safety improvement in primary care: results from a feasibility study. July 29, 2020
Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. August 1, 2012
Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. November 28, 2018
Documenting the indication for antimicrobial prescribing: a scoping review. November 2, 2022
Role of the regulator in enabling a just culture: a qualitative study in mental health and hospital care. August 10, 2022
Evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. January 12, 2022
Unintended consequences: quantifying the benefits, iatrogenic harms and downstream cascade costs of musculoskeletal MRI in UK primary care. August 11, 2021
Eliciting willingness-to-pay to prevent hospital medication administration errors in the UK: a contingent valuation survey. February 16, 2022
Explaining the negative effects of patient participation in patient safety: an exploratory qualitative study in an academic tertiary healthcare centre in the Netherlands. February 1, 2023
For-profit long-term care homes and the risk of COVID-19 outbreaks and resident deaths. August 19, 2020
Assessing quality of older persons' emergency transitions between long-term and acute care settings: a proof-of-concept study. May 18, 2022
Higher incidence of adverse events in isolated patients compared with non-isolated patients: a cohort study. November 18, 2020
Evaluation of effectiveness and safety of pharmacist independent prescribers in care homes: cluster randomised controlled trial. March 1, 2023
Results and lessons from a hospital-wide initiative incentivised by delivery system reform to improve infection prevention and sepsis care. March 17, 2021
Cohort study of diagnostic delay in the clinical pathway of patients with chronic wounds in the primary care setting. December 14, 2022
The role of organizational and professional cultures in medication safety: a scoping review of the literature. January 15, 2020
The standardisation of handoffs in a large academic paediatric emergency department using I-PASS. July 28, 2021
Adverse event reviews in healthcare: what matters to patients and their family? A qualitative study exploring the perspective of patients and family. June 1, 2022
Sustaining improvement of hospital-wide initiative for patient safety and quality: a systematic scoping review. February 1, 2023
Enhancing teamwork communication and patient safety responsiveness in a paediatric intensive care unit using the daily safety huddle tool. March 18, 2020
Associations of workflow disruptions in the operating room with surgical outcomes: a systematic review and narrative synthesis. June 17, 2020
Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. August 8, 2012
Promoting patient and nurse safety: testing a behavioural health intervention in a learning healthcare system: results of the DEMEANOR pragmatic, cluster, cross-over trial. March 2, 2022
Incidence, nature and causes of avoidable significant harm in primary care in England: retrospective case note review. December 16, 2020
Understanding the factors influencing implementation of a new national patient safety policy in England: lessons from 'Learning from Deaths'. May 18, 2022
Creating psychological safety in interprofessional simulation for health professional learners: a scoping review of the barriers and enablers. May 18, 2022
Psychological impact and recovery after involvement in a patient safety incident: a repeated measures analysis. September 21, 2016
Use of FMEA analysis to reduce risk of errors in prescribing and administering drugs in paediatric wards: a quality improvement report. January 16, 2013
A 6-year thematic review of reported incidents associated with cardiopulmonary resuscitation calls in a United Kingdom hospital. April 27, 2022
Medication errors and processes to reduce them in care homes in the United Kingdom: a scoping review. March 23, 2022
A meta-review of methods of measuring and monitoring safety in primary care. September 15, 2021
Changes in weekend and weekday care quality of emergency medical admissions to 20 hospitals in England during implementation of the 7-day services national health policy. November 25, 2020
Prioritising recommendations following analyses of adverse events in healthcare: a systematic review. November 4, 2020
The development of the concept of return-on-investment from large-scale quality improvement programmes in healthcare: an integrative systematic literature review. January 11, 2023
Quality and safety outcomes of a hospital merger following a full integration at a safety net hospital. March 16, 2022
Medication-related interventions to improve medication safety and patient outcomes on transition from adult intensive care settings: a systematic review and meta-analysis. February 2, 2022
The impact of drug error reduction software on preventing harmful adverse drug events in England: a retrospective database study. August 24, 2022
Defining diagnostic error: a scoping review to assess the impact of the National Academies' report Improving Diagnosis in Health Care. May 25, 2022
Experience of hospital-initiated medication changes in older people with multimorbidity: a multicentre mixed-methods study embedded in the OPtimising thERapy to prevent Avoidable hospital admissions in Multimorbid older people (OPERAM) trial. December 7, 2022
Systematic review of the impact of physician implicit racial bias on clinical decision making. May 5, 2017
Surgical safety checklist audits may be misleading! Improving the implementation and adherence of the surgical safety checklist: a quality improvement project. December 22, 2021
The use of anatomical side markers in general radiology: a systematic review of the current literature. August 26, 2020
A realist synthesis of pharmacist-conducted medication reviews in primary care after leaving hospital: what works for whom and why? December 2, 2020
Severe illness getting noticed sooner - SIGNS-for-Kids: developing an illness recognition tool to connect home and hospital. January 15, 2020
Association of current opioid use with serious adverse events among older adult survivors of breast cancer. October 14, 2020
Systematic review and meta-analysis of interventions for operating room to intensive care unit handoffs. March 10, 2021
Ethical issues in patient safety research: a systematic review of the literature. September 9, 2015
Healthcare professionals' perception of safety culture and the Operating Room (OR) Black Box technology before clinical implementation: a cross-sectional survey. March 22, 2023
Optimizing post-acute care patient safety: a scoping review of multifactorial fall prevention interventions for older adults. July 13, 2022
Medication-related interventions delivered both in hospital and following discharge: a systematic review and meta-analysis. August 19, 2020
Assisting beginners in root cause analysis operations: analysis and recommendations regarding the spread of COVID-19 in nursing facilities for the elderly. September 30, 2020
A scoping review of adverse incidents research in aged care homes: learnings, gaps, and challenges. February 8, 2023
Measuring psychological safety and local learning to enable high reliability organisational change. November 9, 2022
Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. August 19, 2020
Assessing the perceived level of institutional support for the second victim after a patient safety event. June 10, 2015
Prospective validation of classification of intraoperative adverse events (ClassIntra): international, multicentre cohort study. October 7, 2020
Early prescribing outcomes after exporting the EQUIPPED medication safety improvement programme. January 19, 2022
Defining and studying errors in surgical care: a systematic review. August 17, 2022
The COVID-19 pandemic: resilient organisational response to a low-chance, high-impact event. July 15, 2020
The scientific literature on Coronaviruses, COVID-19 and its associated safety-related research dimensions: a scientometric analysis and scoping review. July 15, 2020
Misdiagnosis of acute myocardial infarction: a systematic review of the literature. October 6, 2021
Incidence, origins and avoidable harm of missed opportunities in diagnosis: longitudinal patient record review in 21 English general practices. June 30, 2021
The value of learning from near misses to improve patient safety: a scoping review. January 25, 2023
Using social and behavioural science to support COVID-19 pandemic response. June 3, 2020
Prevalence of potentially inappropriate medication use in older adults living in nursing homes: a systematic review. August 17, 2016
Indicators for implementation outcome monitoring of reporting and learning systems in hospitals: an underestimated need for patient safety. May 4, 2022
Interventions targeted at reducing diagnostic error: systematic review. September 8, 2021
A comprehensive quality assurance program for personnel and procedures in radiation oncology: value of voluntary error reporting and checklists. August 7, 2013
Safety implications of remote assessments for suspected COVID-19: qualitative study in UK primary care. March 23, 2022
A scoping review of real-time automated clinical deterioration alerts and evidence of impacts on hospitalised patient outcomes. August 3, 2022
Using participatory design to engage physicians in the development of a provider-level performance dashboard and feedback system. February 2, 2022
Potentially inappropriate prescribing in older people with dementia in care homes: a retrospective analysis. February 15, 2012
Impact of providing patients access to electronic health records on quality and safety of care: a systematic review and meta-analysis. July 8, 2020
What do patients and their carers do to support the safety of cancer treatment and care? A scoping review. December 14, 2022
Systemic failures in nursing home care--a scoping study. February 14, 2024
Patient safety in nursing homes from an ecological perspective: an integrated review. January 17, 2024
Aging stigma and the health of US adults over 65: what do we know? January 10, 2024
The relationship between nursing home staffing and resident safety outcomes: a systematic review of reviews. December 6, 2023
Bringing the equity lens to patient safety event reporting. October 25, 2023
American Geriatrics Society 2023 updated AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. August 16, 2023
Drug-related problems among older people with dementia: a systematic review. July 5, 2023
Factors differentiating nursing homes with strong resident safety climate: a qualitative study of leadership and staff perspectives. February 15, 2023
Nursing home patient safety culture perceptions among licensed practical nurses. February 1, 2023
Interventions to increase patient safety in long-term care facilities-umbrella review. January 25, 2023
Patient safety measurement tools used in nursing homes: a systematic literature review. December 7, 2022
Exploring the intersection of structural racism and ageism in healthcare. December 7, 2022
Patient safety culture in assisted living: staff perceptions and association with state regulations. November 30, 2022
How do hospital inpatients conceptualise patient safety? A qualitative interview study using constructivist grounded theory. October 19, 2022
Factors associated with potentially harmful medication prescribing in nursing homes: a scoping review. September 28, 2022
Impact of medication reviews on potentially inappropriate medications and associated costs among older women in aged care. September 21, 2022
Using health information technology in residential aged care homes: an integrative review to identify service and quality outcomes. August 17, 2022
Iatrogenesis in the context of residential dementia care: a concept analysis. August 3, 2022
Long-term care healthcare-associated infections in 2021: an analysis of 17,971 reports. July 13, 2022
Supplemental Item Set for Nursing Home SOPS: Call for Pilot Participants. July 6, 2022
Standardized assessment of medication reconciliation in post-acute care. April 27, 2022
The National Imperative to Improve Nursing Home Quality: Honoring Our Commitment to Residents, Families, and Staff. April 20, 2022
SOPS Nursing Home Survey: What You Need to Know. May 3, 2022
Qualitative content analysis: a framework for the substantive review of hospital incident reports. March 23, 2022
Implementation of an antibiotic stewardship program in long-term care facilities across the US. March 9, 2022
Sources of medication omissions among hospitalized older adults with polypharmacy. March 9, 2022

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
- Open access
- Published: 08 July 2023
Understanding geriatric models of care for older adults living with HIV: a scoping review and qualitative analysis
- Kristina Marie Kokorelias 1 , 2 , 3 ,
- Anna Grosse 1 , 4 ,
- Alice Zhabokritsky 5 , 6 , 7 &
- Luxey Sirisegaram 1 , 4
BMC Geriatrics volume 23 , Article number: 417 ( 2023 ) Cite this article
1434 Accesses
1 Citations
7 Altmetric
Metrics details
Advances in Human Immunodeficiency Virus (HIV) treatment have reduced mortality rates and consequently increased the number of individuals with HIV living into older age. Despite this, people aged 50 years and older have been left behind in recent HIV treatment and prevention campaigns, and a gold-standard model of care for this population has not yet been defined. Developing evidence-based geriatric HIV models of care can support an accessible, equitable, and sustainable HIV health care system that ensures older adults have access to care that meets their needs now and in the future.
Guided by Arksey & O’Malley (2005)’s methodological framework, a scoping review was conducted to determine the key components of, identify gaps in the literature about, and provide recommendations for future research into geriatric models of care for individuals with HIV. Five databases and the grey literature were systematically searched. The titles, abstracts and full texts of the search results were screened independently in duplicate. Data were analyzed using a qualitative case study and key component analysis approach to identify necessary model components.
5702 studies underwent title and abstract screening, with 154 entering full-text review. 13 peer-reviewed and 0 grey literature sources were included. Most articles were from North America. We identified three primary model of care components that may improve the successful delivery of geriatric care to people living with HIV: Collaboration and Integration; Organization of Geriatric Care; and Support for Holistic Care. Most articles included some aspects of all three components.
To provide effective geriatric care to older persons living with HIV, health services and systems are encouraged to use an evidence-based framework and should consider incorporating the distinct model of care characteristics that we have identified in the literature. However, there is limited data about models in developing countries and long-term care settings, and limited knowledge of the role of family, friends and peers in supporting the geriatric care of individuals living with HIV. Future evaluative research is encouraged to determine the impact of optimal components of geriatric models of care on patient outcomes.
Peer Review reports
Human immunodeficiency virus (HIV) continues to be characterized as one of the most prominent public health threats [ 1 ], although advances in antiretroviral therapy (ART) have reduced mortality rates and transformed HIV into a manageable, chronic disease [ 2 ]. The life expectancy for people living with HIV who have had early and sustained access to ART is now similar to that of HIV-negative populations [ 3 , 4 , 5 ]. Thus, there is now an increase in the number of individuals living with HIV into older age [ 6 ] and the number of older adults (aged ≥ 50 years [ 7 ]) living with HIV is expected to increase even further in the coming years [ 8 ]. The proportion of older adults living with HIV has nearly tripled since 2000 [ 9 ].
Older adults with HIV have an increased risk of dementia, diabetes, frailty, depression, osteoporosis, and some cancers, compared to those who are HIV negative [ 10 , 11 , 12 ]. Comorbidities commonly associated with ageing (e.g., diabetes) have been found to increase the risk of opportunistic infections (e.g., HIV-related concerns) in older adults with HIV [ 13 , 14 , 15 , 16 ]. Moreover, stigma is associated with higher rates of loneliness, social isolation and depression in the HIV population [ 17 ]. Despite their increased risk of poor health and social outcomes, older adults living with HIV face many challenges accessing appropriate health and social care, further exacerbating their poor health outcomes [ 18 ]. The stigma associated with HIV may result in a fear of disclosure that delays treatment [ 19 ], and individuals with HIV can feel discriminated against by healthcare providers, resulting in hesitation about or refusal to seek medical care [ 20 , 21 ]. Older adults also tend to not access social services designed for the HIV-infected population because of their own assumption that these programs are created only for younger individuals [ 22 ]. Consequently, HIV scholars have urged for a health and social care system where knowledge and communication about geriatric HIV care are encouraged amongst advocates who work directly with this population, such as geriatric healthcare workers [ 23 ].
Geriatric specialists have expertise in managing many comorbidities that share associations with both ageing and HIV, despite geriatricians being hesitant to take a prominent role in the care of HIV in older adults [ 24 ] due to a lack of experience and training [ 25 ]. While health policy reports a preference for general practice-based HIV care over specialist care [ 26 , 27 ], general practitioners may have a less nuanced understanding about the holistic care of an older adult with complex comorbidities, geriatric syndromes, and metabolic complications when compared with geriatricians [ 28 ]. The use of the Comprehensive Geriatric Assessment (CGA) has been explored, and may lead to improved health and social outcomes in the older adult-HIV population [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ], and may be used to measure outcomes in clinical trials that aim to improve the delivery of HIV care for the older adult-HIV population [ 36 ]. However, in the absence of specialized geriatric models of HIV care, many older adults with HIV fail to receive a CGA [ 37 , 38 ] and the recommendations from CGAs are rarely implemented due to a lack of feasibility following a geriatric consult for older adults with HIV [ 39 ].
Numerous models of care, defined as “the way health services are delivered” [ 40 ] (pg., 3), have been developed for older adults with HIV. Many involve geriatric specialists in HIV care, with geriatricians taking on various responsibilities ranging from consultation to leadership roles [ 36 , 41 ]. However, the gold-standard model of care for older adults living with HIV have not yet been defined [ 34 , 35 ], and geriatric care is often delivered by non-geriatric specialists [ 16 ]. Instead of examining models of care, recent literature reviews have tended to focus on the prevalence and experiences of older adults in HIV care [7, NaN], or the experiences of geriatricians [ 24 ]. As implementing geriatric models of HIV care into healthcare settings requires unique considerations [ 28 ], an improved understanding of existing models of care may inform best-practices. This approach has been done to inform the design and delivery of other models of healthcare [ 42 , 43 , 44 , 45 ]. Therefore, we conducted a scoping review of the existing evidence about geriatric models of care for older adults within the context of HIV. To our knowledge, this is the first review to systematically identify the core operational components of existing models of care specific to older adults living with HIV.
A scoping review was selected to map the available literature on geriatric models of care for older adults within the context HIV [ 46 ]. The protocol for our scoping review followed the well-established framework outlined by Arksey and O’Malley [ 46 ] and later refined by Levac et al. [ 47 ] and Colquhoun et al. [ 48 ]. The framework was selected as it provides guidance to ensure a rigorous scoping review approach utilizing a comprehensive search strategy [ 46 ]. Our protocol has been published elsewhere (blinded for review #1) but is briefly described within this section of the manuscript. There were no deviations from our protocol. The framework includes five steps: 1) identifying the research questions; 2) identifying relevant literature; 3) study selection; 4) charting the data; 5) collating, summarizing and reporting the results [ 46 ]. The optional sixth step of consulting with key stakeholders was not followed due to financial resource constraints. We briefly summarize each step and report our findings in accordance with The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews (PRISMA-Scr) [ 49 ] (see Supplemental Material A).
Step 1: Identifying the research questions
Our questions were developed to support a knowledge synthesis that could mobilize the current evidence into practice. Our study aimed to answer: What are the key components of the existing models of HIV care for older adults (aged ≥ 50 years [ 7 , 29 ])?
Step 2: Searching for relevant studies
To identify studies, we developed a comprehensive search strategy with an experienced medical information specialist (CDC) who first conducted the search in MEDLINE(R) ALL (in Ovid, including Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily) and then translated it into NLM’s PubMed OVID Embase + Embase Classic, EBSCO’s CINAHL Complete, Clarivate’s Web of Science Core Collection, and Elsevier’s Scopus from the earliest record to 2022 (see Supplemental Material B for the full strategies ) . The search strategy was peer-reviewed according to the peer-review of electronic search strategy guidelines (the PRESS strategy) [ 50 ]. MeSH terms were used. All searches were limited to English language. The final searches were completed on Friday, October 21, 2022. Duplicates were removed using the Bramer method in EndNote [ 51 ]. Covidence was used to manage the review process, including the deduplication of database results [ 52 ].
Gray literature and non-indexed articles were searched for using Google Scholar, Open Grey, open Google searches and relevant websites, including the World Health Organization, UK National Research Register, CADTH’s “Grey Matters”, New York Academy of Medicine's Grey Literature Report, the Canadian Medical Association InfoBase and the National Institute for Heath and Care Excellence – Guidance. Similar search terms used in the scientific search were used. We also consulted with stakeholders of our research (i.e. geriatricians, infectious disease specialists) for any gray literature missed.
Step 3: Selecting studies
Three reviewers (LS, KMK and AG) independently screened article titles and abstracts (level 1-screening) and then full articles (level 2-screening) were screened in duplicate to identify potentially relevant studies. In both levels of screening, any disagreements were resolved through team-based discussion. Articles were included if they described an implemented model or models of care to treat older adults living with HIV exclusively (i.e., not as part of the treatment for multi-morbidity including HIV) and included a registered healthcare provider that specialized in geriatric care (e.g., gerontology social worker, geriatric clinical nurse specialist, geriatrician). Perspective (viewpoint) papers that describe implemented models of HIV care were also included. Book sections, theses, film broadcasts, abstracts without adequate data, and literature reviews were excluded. Articles were also excluded if they: (1) did not propose an original model of HIV care specifically for older adults (i.e., models of care for all adults or models that may include older adults), (2) focused on ethical issues or the theoretical understandings of HIV care or geriatric care, (3) focused on training healthcare providers on how to deliver HIV and/or geriatric care; and (4) described social support, rather than care in a clinical, health-care context. Forward and backward searching were conducted on the final full-text articles to ensure a broad search using EndNote and Citationchaser [ 53 , 54 ].
Step 4: Charting the data
The same three reviewers independently extracted data from the included studies using a data abstraction form that was developed and pilot tested by two researchers (LS and KMK). The data form was tested on five articles for consistency in understanding and ensuring that all relevant data was captured. No changes were made after comparing the pilot test results. The fields for abstraction included author last name, year, study type, setting, geographic location (country), methodology, characteristics of intervention (model of care) and delivery method, participant and provider characteristics, patient inclusion and exclusion criteria, desired outcomes (primary and secondary), results and key conclusions.
Step 5: Collating, summarizing and reporting the results
Data were analyzed using a systematic qualitative case study analytic approach [ 55 ]. First, each author reviewed the abstracted data and independently noted the core operational components (i.e., model structure and process for delivery) described in the models of care. Then the authors came together to list all the identified model components across the included articles, by exploring the similar and different terms to describe the same model components. Each model component was given a label and a definition. These components became the basis of codes that were then appropriately applied by one author (KMK) to each article using NVivo 12 software [ 56 ]. Next the coded data was reviewed by all authors to determine how each model of care described in the articles adhered or did not adhere to each of the particular model components (codes). The authors met weekly to discuss the process of adherence. This discussion process was informed by adherence analyses [ 57 ]. During this process, authors were encouraged to identify any components that were potentially originally overlooked. No additional suggestions were made on key model components. The model components adhered to across the articles and models of care formed the basis of the results.
After a comprehensive list of the identified model components had been determined, two authors (KMK and AG) went through each article and identified them as either adhering or not adhering to each particular characteristic component, as determined by written evidence within the articles. This was done by having the two authors each providing their vote (i.e., adhering or not) and then comparing the two scoring. Any uncertainty in adherence assignment or discrepancies in voting was resolved through discussion amongst all the investigators as done in other reviews with similar methodologies [ 42 ].
Step 6: Consultation
To further contribute to our component adherence, we shared our model components with the senior investigators of our peer-reviewed articles for feedback. We also asked the investigators to assess their level of agreement with our interpretations of their study's component adherence. Lastly, we asked authors to send along any studies that they believed would be relevant to our review. This was done via email by the first (KMK) and senior author (LS) in December 2022. After two months, we only received five replies from 13 potential authors (n = 5/13, 38%) and all five authors agreed with the adherence we provided their article with, suggesting an accurate adherence analysis. No investigators provided us with additional materials or feedback on the model components, rather just commenting on their article specifically.
The databases search yielded a total of 5699 unique citations, from which 151 articles were selected for full text review. Of these 151 articles, 12 peer-reviewed articles were included. An additional peer-reviewed article was obtained from hand searching. No grey literature was included. Thirteen articles were included in the final analysis (see Fig. 1 PRISMA flow chart).
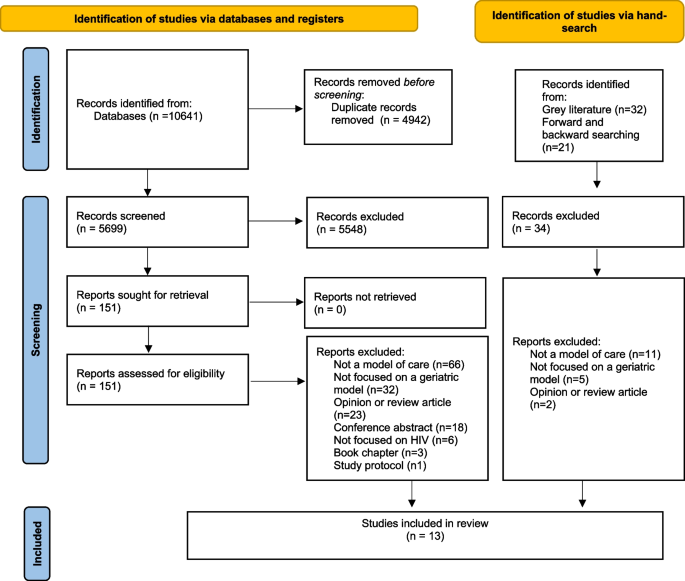
PRISMA flow chat diagram
Most ( n = 10/13, 77%) of the publication activity occurred in the United States (USA) [ 28 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 ]. The remaining three articles ( n = 3/13,23%) were from the United Kingdom (UK)[ 66 , 67 , 68 ]. Over half ( n = 9/13,69%) of the articles were published in the last 5 years (2018–2023) [ 28 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 ]. In published papers, the most common research methods were qualitative. The key description from these studies were abstracted and are summarized in Table 1 .
Patient population
Patients in the included models of care ranged from 48 [ 60 ]–87 years of age [ 67 ]. The number of patients served ranged from 76 [ 39 ] over 4 years to a maximum of 4000 at the time of data collection (period unspecified) [ 66 ]. Of those articles that reported sex ( n = 9/13,69%), the majority described primarily male samples [ 39 , 60 , 61 , 62 , 63 , 64 , 65 , 68 ]. Articles that reported race/ethnicity ( n = 7/13, 54%), described including participants who were mostly White [ 60 , 61 , 67 ] or African American [ 39 , 62 , 63 , 65 , 68 ]. These articles all included White individuals. Of the two ( n = 2/13, 15%) studies that reported the median time since HIV diagnosis [ 39 ], the average was 12.5 [ 63 ]- 21.5 [ 39 ] years. Medicaid was used as the patients’ primary health insurance in the USA [ 39 , 61 , 62 ].
Key operational components of geriatric models of HIV care
The qualitative analysis identified three distinct model of care components, each with one or more sub-components. These components are listed and described in Table 2 . Table 3 also lists the articles adherent to each component. These model components entail: Collaboration and Integration; Organization of Geriatric Care; and Support for Holistic Care. These three components are described and are illustrated in Fig. 2 .
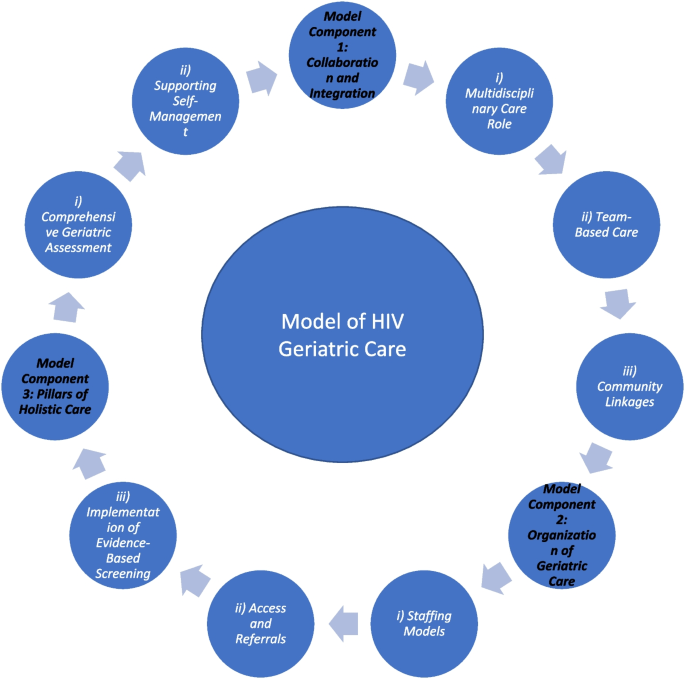
Main Model Components
Model Component 1: Collaboration and integration
Eleven ( n = 11/13, 85%) [ 28 , 39 , 41 , 59 , 60 , 61 , 64 , 65 , 66 , 67 , 68 ] articles described the importance of collaboration and integration for providers caring for older adults with HIV. Models of care frequently incorporated a team of multidisciplinary professionals from the health and social care sectors that were linked in with community supports to improve healthcare delivery for older adults with HIV.
i) Multidisciplinary care roles
Multidisciplinary teams supported the care of older adults living with HIV in all eleven articles that adhered to the Collaboration and Integration model component ( n = 11/13, 85%). These articles described several provider roles, including designated HIV specialists (infectious diseases or internal medicine physicians) [ 39 , 41 , 60 , 61 , 65 , 66 , 67 , 68 ], geriatricians [ 39 , 41 , 60 , 61 , 64 , 65 , 67 , 68 ] and/or dual-trained HIV and geriatric physicians. Other physician roles included psychiatrists [ 39 ], endocrinologists [ 65 ], cardiologists [ 41 , 60 , 61 , 68 ] and medicine fellows [ 64 ]. Numerous nursing roles [ 41 , 59 , 60 , 61 , 64 , 65 ] were involved, such as HIV clinical nurse specialists [ 41 , 66 , 67 ] and nurse practioners [ 41 , 64 , 65 ]. Allied health professionals included dieticians [ 39 , 65 , 66 ]/ nutritionists[ 41 ], social workers[ 39 , 41 , 59 , 61 , 65 , 66 , 68 ], phsysiotherapists [ 41 , 59 , 66 ], occupational therapists [ 41 , 59 , 66 ], speech-language pathologists[ 59 ], counselors/therapists [ 59 ], homecare aides [ 59 ], clinical psychologists [ 65 , 66 ] and specialist pharmacists [ 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 ].
In addition to healthcare providers, several models of care also included research team members (i.e. research coordinators [ 39 ], research assistants [ 39 ], graduate students in gerontology and epidemiology [ 41 ]), medical directors and administrative staff [ 59 , 61 ] (e.g., program coordinator[ 60 ], a gerontologist [i.e., non-clinician] [ 41 ]), chaplains [ 59 ] and volunteers [ 59 ]. Peer navigator roles were also described [ 28 , 41 , 65 , 68 ].
The key responsibilities of these providers differed between models of care and many had overlapping functions. Physicians [ 39 , 41 , 60 , 61 , 64 , 65 , 66 , 67 , 68 ] and nurses [ 41 , 59 , 60 , 61 , 64 , 65 ] were often responsible for overseeing and ensuring appropriate medical care, such as disease and symptom management. Other healthcare professional roles and designated navigation-specific roles [ 28 , 65 , 68 ], provided medication, rehabilitation [ 41 , 59 , 66 ], dietary [ 39 , 59 , 65 , 66 ], or emotional counseling to patients and caregivers [ 59 ]. Geriatricians, in particular, provided evidence-based, best-practice advice that was shared with patients’ primary care providers [ 39 , 41 , 60 , 61 , 64 , 65 , 67 , 68 ]. HIV specialists generally oversaw HIV-related treatments and community services [ 39 , 41 , 60 , 61 , 65 , 66 , 67 , 68 ]. Pharmacists often provided medication instructions and explained care protocols [ 41 , 60 , 65 , 66 , 67 ]. All care providers were described as providing informational and tangible (i.e., hands-on care) support. Administrative and research staff were responsible for documenting relevant information accurately [ 39 , 41 , 59 , 61 ]. Only one article mentioned the role of non-professional caregivers (i.e., spouse, partner, or friend) as part of the care team [ 59 ], in which they were described as providing much of the personal care involved in the home management of HIV [ 59 ].
Administrative team members and researchers support the collection of client information to systematically standardize clinical and research operations [ 39 , 41 , 59 , 60 , 61 ].
ii) Team-Based care
Ten articles ( n = 10/13, 77%) described the team-based delivery of multidisciplinary care, which was facilitated by several different mechanisms. Informational continuity was identified as being vital in ensuring a consistent and coherent approach to the management of older adults’ evolving needs [ 67 ]. A shared electronic health record was found to enable team-based care, including the ability for multiple providers to chat in real-time [ 28 , 41 , 60 , 61 , 68 ]. Moreover, the multidisciplinary team would often meet to discuss each patient’s background, their outcome measures, current clinical problems, and anticipated needs [ 28 ]. Consequently, the team would facilitate the appropriate screenings through access to different providers, services, and resources [ 28 , 39 , 41 , 60 , 61 , 65 , 68 ]. Following a referral and initial clinical visit, the HIV-geriatric specialists would maintain communication with the primary care team [ 28 ], make recommendations based on the identified age-related needs for care [ 28 ], initiate referrals to other specialist care providers and communicate with community stakeholders to meet other needs [ 59 ]. Team-based care allowed for all members of the circle of care to have a comprehensive knowledge of patients’ health and social care needs (e.g., functional, cognitive) [ 28 ]. Results from retrospective medical and pharmacy chart reviews helped inform all team decisions [ 65 ]. When deemed necessary, the team would be able to create a new action plan [ 39 ] and determine follow-up [ 64 ]. Nurses who worked in case manager roles helped to facilitate this care by coordinating a comprehensive, holistic care plan in collaboration with the patient, caregiver(s), physician(s), and other members of the care team [ 59 ]. Team-based models of care were felt to improve the coordination of care [ 41 ].
iii) Community linkages
Nine articles ( n = 9/13, 69%) described how the management of HIV in older adults involved active, collaborative partnerships between multidisciplinary healthcare providers and the various community resources available to individuals living with HIV. Models of care were often delivered in linkage with community resources (e.g., social groups) [ 41 ] and through community partners (e.g., volunteer organizations) [ 41 ]. Social workers often helped to facilitate community linkages [ 59 ], and grant-funding helped to pay for community services [ 65 ]. By working with community partners [ 41 ], models of care were able to deliver both nonclinical care [ 39 ] (e.g., peer support to decrease isolation and depression [ 41 ]), as well as clinical care [ 28 ] (e.g., care facilitated by a community nurse [ 39 ]). Community outreach also helped to foster friendships amongst older adults living with HIV through social and community-building activities including dinners, speeches, dances, and trips [ 59 ]. Local partner agencies assisted with meeting the housing needs for patients with marginal housing [ 61 ], and with the provision of legal services [ 61 ]. Partnering medical HIV-geriatric services with community services was thought to result in improved access to services [ 28 ], reduced social isolation [ 60 ], improved home safety management [ 59 ] and the provision of spiritual care such as priests, rabbis, or pastoral personnel [ 59 ].
Model Component 2: Organization of geriatric care
The specific organizational structure of each model of care varied, particularly as it related to staffing models, processes for access and referrals, and the implementation of evidence-based, best-practice care and follow-up. All articles adhered and contributed to this model component. Models of care were often delivered through clinics that were predominantly hospital-based (i.e., operating within a hospital) [ 39 , 60 , 61 , 65 , 66 , 67 ]. Additionally, geriatric clinics were outpatient clinics housed within existing HIV clinics [ 41 ] or community-based services providing home care [ 59 ]. Some models of care were able to be delivered virtually, either solely via phone [ 62 ] or in addition to in-person delivery [ 65 , 66 ]. Some clinics ran weekly [ 66 ], bi-weekly [ 65 ] or monthly [ 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 ], whereas others were full-time [ 39 , 65 ].
i) Staffing models
Within the identified models of care, various staffing models were described. All articles contributed to this sub-component. The Geriatrician-Referral model included a geriatrician who consulted on patients [ 39 , 41 , 60 , 61 , 64 , 65 ] based on a referral from the primary care team (often an HIV provider [ 41 ]), according to the perceived need (e.g., cognitive concerns). Six articles ( n = 6/13, 46%) adhered to this. The Joint-Clinic model involved a geriatrician and HIV physician who were present in a single, combined clinic [ 41 , 66 , 67 , 68 ]. Four articles ( n = 4/13, 31%) adhered to this model. The HIV-Physician-led model involved staffing clinics with a HIV physician and clinical nurse specialist trained in geriatrics, without geriatrician involvement [ 65 , 66 ]. Two articles ( n = 2/13, 15%) adhered to this model. A further staffing model, the Dual-Trained Provider model, involved a dually-trained HIV and geriatrics provider, as either a physician [ 41 , 68 ] or psychotherapist [ 62 , 63 ]. Four articles ( n = 4/13, 31%) adhered to this model. The Nurse-led model, involved nurse-lead teams of allied health professionals [ 59 ]. Only one article ( n = 1/13, 8%) adhered to this model [ 59 ].
i) Access and referrals
All articles described processes to ensure appropriate access to care, and thus contributed to this sub-component. Referrals and on-call services [ 59 ] were used to facilitate access to care [ 59 ]. In some models of care, older adults were only able to access geriatric services via a referral from their HIV primary care team [ 39 , 41 , 60 , 61 , 67 ], while in other models, referrals were triggered by a combination of age (i.e., 50 years of age or older) and need (e.g., complexity) [ 28 , 66 , 67 , 68 ]. The process of receiving geriatric care often began with an assessment of patients’ needs and functional status (e.g., cognition) [ 39 ] and the collection of demographic information (e.g., age, sex, race/ethnicity, HIV risk factors, marital status, insurance status [ 39 ])[ 28 , 61 , 65 ]. Provider referrals were often documented through tracking scheduled appointments [ 60 , 61 , 68 ], however, limitations of this method included HIV providers not remembering to refer [ 41 ] and patient barriers such as confusion over the need for the referral which may result in skipping geriatric appointments [ 41 ]. One model of care implemented patient reminders to help ensure appointments were attended [ 64 ]. Two articles ( n = 2/13, 15%) relied on referrals through an AIDS service organization [ 62 , 63 ]Moreover, across the models, patients could choose to be referred to one service (e.g. cardiology clinic) or multiple (e.g., geriatrics clinic) [ 60 , 68 ]. Patients could choose to have follow up with the geriatrician[ 28 ] and/or be connected with a primary care provider [ 41 ]. Clinics have developed guidelines and policies to guide the operation of services [ 28 ].
ii) Implementation of evidence-based screening
All articles described the incorporation of gold-standard, evidence-based screening practices into their geriatric care. Mood symptoms were assessed using the Hospital Anxiety and Depression Scale [ 60 , 62 , 63 , 67 ], the Geriatric Depression Scale [ 62 , 63 ], the Older Peoples’ Quality of Life Questionnaire [ 67 ] and/or the Patient Health Questionnaire [ 39 ], while cognition was assessed using tools such as the Montreal Cognitive Assessment [ 60 ]. CGAs were followed up with direct actions such as counseling (e.g., about ageing) [ 28 , 39 , 60 ], assessments of comorbidities, age-appropriate preventative health screening[ 41 , 60 , 61 ], and pharmacist reviews targeting polypharmacy and drug safety [4, NaN]. In addition to the CGA, clinics offered British HIV Association (BHIVA)-recommended screening (i.e., guidelines for the management of HIV), an antiretroviral review, a functional review and full medication review [ 28 , 66 ]. Emotional support was monitored using the ‘Therapy Content Checklist’ [ 62 , 63 ]. The goal of using valid measurements was to promote best practice [ 59 ].
Model Component 3: Support for holistic care
As older persons are more likely to experience cumulative health challenges that affect their quality of life, models of care for people ageing with HIV have incorporated a comprehensive holistic management approach. All included articles adhered and contributed to this model component. Clinics provided care for patients with multimorbidity [ 60 , 61 , 66 , 67 ] and helped them to overcome socioeconomic challenges [ 41 ], substance use disorders [ 60 , 65 ] and social isolation [ 60 , 62 , 63 ] by understanding their backgrounds[ 41 ]. Physical health consultations considered cardiovascular disease, dental health, eye health and bone health[ 28 , 41 , 60 , 61 , 64 , 68 ] to address HIV and metabolic-related complications [ 41 ]. Care plans incorporated medication prescriptions [ 28 , 39 , 60 , 61 , 66 , 67 , 68 ], preventative screening [ 28 , 39 , 60 , 61 , 64 , 65 , 66 , 67 , 68 ], age-related disease processes (e.g., cognitive-testing) [ 28 , 39 , 41 , 59 , 60 , 61 , 64 , 65 , 66 , 67 , 68 ], psychosocial interventions to improve social networks and mental health [ 28 , 39 , 59 , 60 , 62 , 63 , 64 , 65 ], exercise and nutrition regimens [ 39 ] and behavioural health supports (e.g., smoking cessation, therapy) [ 28 , 39 , 59 , 60 , 61 , 62 , 63 , 64 , 67 ] to meet the holistic needs of each patient. Spiritual support delivered through religious leaders, mental health counselors/therapists, and emotional support volunteers was also offered [ 59 , 64 ].
i)Comprehensive geriatric assessment
Most models of care ( n = 8/13,61.5%) involved a CGA [ 28 , 39 , 41 , 60 , 61 , 66 , 68 ] or utilized geriatric screening tools [ 65 ] to guide holistic care plans. Most CGAs were delivered by geriatricians who would write full consultation notes [ 39 , 60 , 61 ], although non-geriatrician health care providers were often trained to administer geriatric screening tests [ 41 , 64 ]. The CGA provided an overview of physical and mental health, as well as social support systems [ 39 ], using validated scales [ 39 ].
ii)Supporting self-management
The models of care in six articles ( n = 6/13, 46%) aimed to support the self-management of older adults living with HIV. The goal of self-management was to enable patients to better manage their health outside of the clinic setting by involving older adults in medical decision-making [ 60 , 68 ] and managing their chronic illnesses [ 59 , 60 , 61 ]. Self-management involved education [ 39 , 59 , 60 , 65 ] and coaching [ 28 ] about health behaviours, guidance for choosing appropriate interventions [ 39 , 59 , 65 ] to improve a patient’s health status [ 28 , 65 ], and increased health care utilization to improve patient involvement in care [ 60 , 65 ]. Some models involved classes where older adults could learn about various health conditions [ 60 , 61 , 62 , 63 ]. Where self-management was not possible due to cognitive or functional impairments, healthcare professionals provided education to individuals’ social support networks such as to encourage their inclusion in care [ 39 , 59 ]. To evaluate self-management, some studies included surveys about knowledge in the evaluations of the clinic models [ 60 , 61 ].
Our scoping review of the literature identified thirteen articles describing geriatric models of care for older adults living with HIV. The identified models came from two countries, the USA and the United Kingdom, and incorporated screening for geriatric syndromes [ 28 , 39 , 41 , 60 , 61 , 65 , 66 , 68 ]. From these articles, we identified three overarching key model components: Collaboration and Integration; Organization of Geriatric Care; and Support for Holistic Care. The models of care were largely delivered by a consulting geriatrician [ 39 , 41 , 60 , 61 , 64 , 65 ] via a referral from an HIV provider [ 41 ], from a joint clinic model involving a geriatrician and HIV physician[ 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 ], or through a dually-trained HIV-geriatrics provider [ 41 , 62 , 63 , 68 ]. However, some models did not involve a geriatrician [59, NaN]. Table 4 summarizes the future recommendations from the included articles.
Our review identified that most models of geriatric-HIV care are delivered by multidisciplinary teams that facilitate integrated health and social care. Multidisciplinary providers who work in team-based care models have been shown to improve clinical outcomes among HIV patients [ 70 , 71 , 72 , 73 ]. This study provided examples of collaborations in which practitioners worked together to meet the diverse needs of patients. Our data expand this finding by suggesting that multidisciplinary care providers help to facilitate referrals to even more providers, particularly those working in community settings, to ensure care continuity and care coordination to meet holistic needs for support. However, it is important for future research to further understand what staffing model of multidisciplinary team care contributes best to the quadruple aim of optimizing health system performance (i.e., improving the individual experience of care; improving the health of populations; reducing the per capita cost of healthcare and creating better provider experiences [ 74 ]) and the limitations of the existing approaches. Moreover, given the shortage of geriatricians [ 45 ] to meet patient needs, it is important to consider the transferability of models that involve a geriatrician [ 39 , 41 , 60 , 61 , 64 , 65 ][ 66 , 67 , 68 ], or dually-trained HIV-geriatrics provider [ 41 , 62 , 63 , 68 ].
The increasing proportion of older adults living with multimorbidity, including HIV, has evoked calls for tailored geriatric services that respond to their evolving needs. Our results suggest that care delivery should address multiple complex and multidimensional aspects of health and wellness, including psychosocial needs such as strategies to reduce social isolation. However, none of the articles discussed the provision of palliative or hospice care. Palliative care has been posited to augment HIV patients’ health and social care outcomes [ 75 ]. Implementation science may help researchers identify how to implement novel palliative care interventions into exiting practices and support uptake and sustainability by considering why, how and in what circumstances barriers and facilitators may be present [ 76 ]. In addition, older adults were described as being decision makers in their care such as being able to choose the follow up services they receive [ 60 , 68 ]. While some programs sought the input of older adults (e.g., through focus groups, none explicitly mentioned partnering with older adults to co-design their models of HIV care. Other HIV interventions have included individuals living with HIV on their steering committees and in development teams, such that care meaningfully reflects their wishes and preferences [ 77 , 78 , 79 ]. These interventions do not include older adults. Future models of care may wish to engage older adults in co-design to conceptualize and brainstorm program delivery [ 80 , 81 ].
Our review identified several areas of research with limited information. Most literature was published in the USA. Only one article mentioned the role of family caregivers in the care of HIV [ 59 ]. However, individuals living with HIV may receive support from non-kin family caregivers, such as friends [ 82 ]. Research is needed to better understand how broader conceptualizations of family can be embedded into the multidisciplinary care teams to help facilitate family-centered care [ 43 , 83 ]. Moreover, none of the articles mentioned care being delivered in the context of nursing or long-term care homes, nor did they mention offered referrals to long-term care facilities or services. Research is needed to determine the optimal approach for delivering geriatric services in long-term care settings to older adults living with HIV. Strategies are also needed to effectively embed HIV care into the already overburdened and under-resourced long-term care sector. While telehealth has proven to be an effective strategy for delivering HIV care [ 84 , 85 ], particularly in rural and remote communities where specialists may not be readily available [ 86 ], additional research is needed to identify the best practices and limitations for delivering geriatric-focused models of care virtually. Lastly, no studies have evaluated how to best incorporate culturally-sensitive geriatric care across racial and ethnic groups [ 87 , 88 ]. Thus, more data are needed to develop culturally-informed models of care to better engage and care for diverse populations of older adults living with HIV, particularly for adults with certain racial and ethnic backgrounds who may face pervasive stigma for accessing HIV care [ 89 , 90 ].
Limitations
As with any review, our findings must be considered within the context of the limitations. Despite our best efforts (i.e., multiple databases, peer-reviewed strategy, screening in duplicate, bibliographic searches, contacting authors of the reviewed articles), we may have inadvertently missed potentially relevant articles. Moreover, we may have missed papers of programs not yet described in the literature, such as those recently funded or piloted. Similarly, we limited the inclusion criteria to studies available in English due to resource constraints (i.e., lack of funding to support translation) and, consequently, may have biased our included studies to those published in English-speaking countries [ 91 ]. However, the intention of scoping reviews is to provide an overview or “map” of the breadth of existing literature, and thus, future exploration is warranted that builds upon our search strategy. Studies focused on individuals with HIV, but did not include description of older adults living with co-morbidities that impair healthcare decision-making, such as dementia, making it difficult to comment about models of care for individuals who require decision-making support. Lastly, stakeholders in implementing, delivering and receiving models of care (e.g., individuals with HIV, policy-makers, healthcare professionals) were not involved in the study design nor analysis.
Conclusions
Our review suggests that novel models of geriatric care for older adults living with HIV should include collaboration and integration, an organization of care that considers appropriate and timely referrals, communication of medical information and the implementation of evidence-based recommendations, as well as a holistic understanding of the dimensions of care, such that they support self-management. This proposed geriatric-based model can provide the framework to inform future implementation science and evaluative research to support further refining and developing this model. However, further research is needed to inform models of geriatric-HIV care in long-term care settings. Given the increasing number of older adults living with HIV, the development of best-practice models of integrated care can hopefully guide healthcare professionals to provide optimal care in the context of the complexities of care for older adults with HIV.
Availability of data and materials
The analysis files and data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Comprehensive Geriatric Assessment
Human Immunodeficiency Virus
Organization WH. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach: World Health Organization 2021.
Gardner EM, McLees MP, Steiner JF, et al. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800.
Article PubMed PubMed Central Google Scholar
Higgins JA, Hoffman S, Dworkin SL. Rethinking gender, heterosexual men, and women’s vulnerability to HIV/AIDS. Am J Public Health. 2010;100(3):435–45.
Marcus JL, Chao CR, Leyden WA, et al. Narrowing the gap in life expectancy between HIV-infected and HIV-uninfected individuals with access to care. Journal of acquired immune deficiency syndromes (1999) 2016;73(1):39.
Nakagawa F, May M, Phillips A. Life expectancy living with HIV: recent estimates and future implications. Curr Opin Infect Dis. 2013;26(1):17–25.
Article PubMed Google Scholar
Guaraldi G, Milic J, Mussini C. Aging with HIV. Curr HIV/AIDS Rep. 2019;16(6):475–81.
Sankar A, Nevedal A, Neufeld S, et al. What do we know about older adults and HIV? A review of social and behavioral literature. AIDS Care. 2011;23(10):1187–207.
Flaer PJ, Benjamin PL, Malow RM, et al. The growing cohort of seniors with HIV/AIDS: changing the scope of Medicare Part D. AIDS Care. 2010;22(7):903–8.
Autenrieth CS, Beck EJ, Stelzle D, et al. Global and regional trends of people living with HIV aged 50 and over: Estimates and projections for 2000–2020. PLoS ONE. 2018;13(11): e0207005.
Yendewa GA, Poveda E, Yendewa SA, et al. HIV/AIDS in Sierra Leone: Characterizing the hidden epidemic. AIDS Reviews 2018;20(2):104–13. doi: https://dx.doi.org/ https://doi.org/10.24875/AIDSRev.M18000022
Desmarais P, Gao AF, Lanctôt K, et al. White matter hyperintensities in autopsy-confirmed frontotemporal lobar degeneration and Alzheimer’s disease. Alzheimer’s research & therapy. 2021;13(1):129. https://doi.org/10.1186/s13195-021-00869-6[publishedOnlineFirst:2021/07/15] .
Article Google Scholar
Buchacz K, Baker RK, Palella FJ Jr, et al. Disparities in prevalence of key chronic diseases by gender and race/ethnicity among antiretroviral-treated HIV-infected adults in the US. Antivir Ther. 2013;18(1):65–75.
Mateen FJ, Mills EJ. Aging and HIV-Related Cognitive Loss. JAMA, J Am Med Assoc. 2012;308(4):349–50. https://doi.org/10.1001/jama.2012.8538 .
Article CAS Google Scholar
Kong AM, Pozen A, Anastos K, et al. Non-HIV Comorbid Conditions and Polypharmacy Among People Living with HIV Age 65 or Older Compared with HIV-Negative Individuals Age 65 or Older in the United States: A Retrospective Claims-Based Analysis. AIDS Patient Care STDS. 2019;33(3):93–103. https://doi.org/10.1089/apc.2018.0190 .
McMillan JM, Gill MJ, Power C, et al. Comorbidities in Older Persons with Controlled HIV Infection: Correlations with Frailty Index Subtypes. AIDS Patient Care STDS. 2020;34(7):284–94. https://doi.org/10.1089/apc.2020.0051 .
Erlandson KM, Karris MY. HIV and aging: reconsidering the approach to management of comorbidities. Infect Dis Clin. 2019;33(3):769–86.
Emlet CA, Brennan DJ, Brennenstuhl S, et al. The impact of HIV-related stigma on older and younger adults living with HIV disease: does age matter? AIDS Care. 2015;27(4):520–8.
Emlet CA. Social, economic, and health disparities among LGBT older adults. Generations. 2016;40(2):16–22.
PubMed PubMed Central Google Scholar
Alexandra Marshall S, Brewington KM, Kathryn Allison M, et al. Measuring HIV-related stigma among healthcare providers: a systematic review. AIDS Care. 2017;29(11):1337–45.
Article CAS PubMed Google Scholar
Hibbert M, Wolton A, Crenna-Jennings W, et al. Experiences of stigma and discrimination in social and healthcare settings among trans people living with HIV in the UK. AIDS Care. 2018;30(7):836–43.
Emlet CA, Brennan DJ, Brennenstuhl S, et al. Protective and risk factors associated with stigma in a population of older adults living with HIV in Ontario. Canada AIDS care. 2013;25(10):1330–9.
Fritsch T. HIV/AIDS and the older adult: An exploratory study of the age-related differences in access to medical and social services. J Appl Gerontol. 2005;24(1):35–54.
Wallach IS, Brotman SH. Gaps in health and social care services to older adults living with HIV: a qualitative study on the perspectives of older adults and service providers. NursCare Open Access J. 2019;6(1):28–33.
Google Scholar
Jones HT, Barber TJ. How do geriatricians feel about managing older people living with HIV? A scoping review European geriatric medicine. 2022;13(4):987–97. https://doi.org/10.1007/s41999-022-00642-4 .
Chambers LA, Wilson MG, Rueda S, et al. Evidence Informing the Intersection of HIV, Aging and Health: A Scoping Review. AIDS Behav. 2014;18(4):661. https://doi.org/10.1007/s10461-013-0627-5 .
Liddy C, Shoemaker ES, Crowe L, et al. How the delivery of HIV care in Canada aligns with the Chronic care model: A qualitative study. PLoS ONE. 2019;14(7):e0220516-e220616. https://doi.org/10.1371/journal.pone.0220516 .
Article CAS PubMed PubMed Central Google Scholar
Mapp F, Hutchinson J, Estcourt C. A systematic review of contemporary models of shared HIV care and HIV in primary care in high-income settings. Int J STD AIDS. 2015;26(14):991–7. https://doi.org/10.1177/0956462415577496 .
Siegler EL, Burchett CO, Glesby MJ. Older people with HIV are an essential part of the continuum of HIV care. Journal of the International AIDS Society 2018;21(10):e25188-n/a. doi: https://doi.org/10.1002/jia2.25188
Sánchez-Conde M, Díaz-Alvarez J, Dronda F, et al. Why are people with HIV considered “older adults” in their fifties? European Geriatric Medicine. 2019;10(2):183–8.
Grov C, Golub SA, Parsons JT, et al. Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS Care. 2010;22(5):630–9.
Greene M, Shi Y, Boscardin J, Sudore R, Gandhi M, Covinsky K. Geriatric conditions and healthcare utilisation in older adults living with HIV. Age and Ageing. 2022 May;51(5):afac093.
Sangarlangkarn A, Appelbaum JS. Comprehensive Geriatric Assessment in Older Persons With HIV. Open forum infectious diseases 2020;7(11):ofaa485-ofaa85. doi: https://doi.org/10.1093/ofid/ofaa485
Yip KF, Wong TH, Alhamid SM, et al. Integrating advance care planning as part of comprehensive geriatric assessment for hospitalised frail elderly patients: findings of a cross-sectional study. Singapore Med J. 2020;61(5):254–9. https://doi.org/10.11622/smedj.2019098 .
Guaraldi G. Rockwood K. Geriatric-HIV medicine is born: Oxford University Press US; 2017. p. 507–9.
Guaraldi G, Palella FJ Jr. Clinical implications of aging with HIV infection: perspectives and the future medical care agenda. AIDS (London, England). 2017;31:S129–35.
Brañas F, Ryan P, Troya J, et al. Geriatric-HIV Medicine: the geriatrician’s role. European geriatric medicine. 2019;10(2):259–65. https://doi.org/10.1007/s41999-018-0144-1 .
Sangarlangkarn A, Apornpong T, Justice AC, et al. Screening tools for targeted comprehensive geriatric assessment in HIV-infected patients 50 years and older. Int J STD AIDS. 2019;30(10):1009–17. https://doi.org/10.1177/0956462419841478 .
Morrow H, Horner M, Thomson-Glover R. 992 RESULTS OF A PILOT HIV/FRAILTY CLINIC - CAN COMPREHENSIVE GERIATRIC ASSESSMENT BENEFIT FRAIL PEOPLE LIVING WITH HIV? Age and ageing 2022;51(Supplement_2) doi: https://doi.org/10.1093/ageing/afac126.043
Bitas C, Jones S, Singh HK, et al. Adherence to Recommendations from Comprehensive Geriatric Assessment of Older Individuals with HIV. Journal of the International Association of Providers of AIDS Care. 2019;18:2325958218821656–56. https://doi.org/10.1177/2325958218821656 .
Innovation AfC. Understanding the Process to Develop a Model of Care: An ACI Framework: Agency for Clinical Innovation Chatswood NSW, 2013.
Davis AJ, Greene M, Siegler E, et al. Strengths and Challenges of Various Models of Geriatric Consultation for Older Adults Living With Human Immunodeficiency Virus. Clin Infect Dis. 2022;74(6):1101–6. https://doi.org/10.1093/cid/ciab682 .
Sinha SK, Bessman ES, Flomenbaum N, et al. A systematic review and qualitative analysis to inform the development of a new emergency department-based geriatric case management model. Ann Emerg Med. 2011;57(6):672–82.
Kokorelias KM, Gignac MA, Naglie G, et al. Towards a universal model of family centered care: a scoping review. BMC Health Serv Res. 2019;19(1):1–11.
Korthuis PT, McCarty D, Weimer M, et al. Primary care–based models for the treatment of opioid use disorder: A scoping review. Ann Intern Med. 2017;166(4):268–78.
Krause KE, Kokorelias KM, Sinha SK. A systematic review and qualitative analysis of geriatric models of care for rural and remote populations. Rural Remote Health. 2022;22(3):7486–586.
PubMed Google Scholar
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):1–9.
Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4.
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
McGowan J, Sampson M, Salzwedel DM, et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
Bramer WM, Giustini D, de Jonge GB, et al. De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association: JMLA. 2016;104(3):240.
Babineau J. Product review: covidence (systematic review software). Journal of the Canadian Health Libraries Association/Journal de l’Association des bibliothèques de la santé du Canada. 2014;35(2):68–71.
Bramer WM, Milic J, Mast F. Reviewing retrieved references for inclusion in systematic reviews using EndNote. Journal of the Medical Library Association: JMLA. 2017;105(1):84.
Haddaway NR, Grainger MJ, Gray CT. Citationchaser: A tool for transparent and efficient forward and backward citation chasing in systematic searching. Research Synthesis Methods 2022
Miles MB, Huberman AM, Saldaña J. Qualitative data analysis: A methods sourcebook: Sage publications 2018.
Beekhuyzen J. Putting the pieces of the puzzle together: Using Nvivo for a literature review. Proceedings of QualIT2007: Qualitative Research, From the Margins to the Mainstream, Wellington, New Zealand, Victoria University of Wellington 2007:18–20.
Bissonnette JM. Adherence: a concept analysis. J Adv Nurs. 2008;63(6):634–43.
Bhatta M, Nandi S, Dutta N, et al. HIV care among elderly population: Systematic review and meta-analysis. AIDS research and human retroviruses 2020;36(ja):475–89. doi: https://doi.org/10.1089/AID.2019.0098
Garvey C. AIDS care for the elderly: A community-based approach. AIDS Patient Care. 1994;8(3):118–20. https://doi.org/10.1089/apc.1994.8.118 .
Greene M, Myers J, Tan JY, et al. The Golden Compass Program: Overview of the Initial Implementation of a Comprehensive Program for Older Adults Living with HIV. Journal of the International Association of Providers of AIDS Care. 2020;19:2325958220935267–67. https://doi.org/10.1177/2325958220935267 .
Greene ML, Tan JY, Weiser SD, et al. Patient and provider perceptions of a comprehensive care program for HIV-positive adults over 50 years of age: The formation of the Golden Compass HIV and aging care program in San Francisco. PLoS ONE. 2018;13(12):e0208486-e208586. https://doi.org/10.1371/journal.pone.0208486 .
Heckman TG, Heckman BD, Anderson T, et al. Common Factors and Depressive Symptom Relief Trajectories in Group Teletherapy for Persons Ageing with HIV: Common Factors and Depression in HIV-infected Older Adults. Clin Psychol Psychother. 2017;24(1):139–48. https://doi.org/10.1002/cpp.1989 .
Heckman TG, Sikkema KJ, Hansen N, et al. A randomized clinical trial of a coping improvement group intervention for HIV-infected older adults. J Behav Med. 2010;34(2):102–11. https://doi.org/10.1007/s10865-010-9292-6 .
Ruiz M, Cefalu C, Ogbuokiri J. A Dedicated Screening Program for Geriatric HIV-Infected Patients Integrating HIV and Geriatric Care. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill : 2002) 2010;9(3):157–61. doi: https://doi.org/10.1177/1545109710367519
Schmalzle SA, Viviano NA, Mohanty K, et al. People aging with HIV - protecting a population vulnerable to effects of COVID-19 and its control measures. AIDS Care. 2022;34(11):1355–63. https://doi.org/10.1080/09540121.2021.2020208 .
Cresswell FV, Levett T. Specialist care of older adults with HIV infection in the UK: a service evaluation. HIV Med. 2017;18(7):519–24. https://doi.org/10.1111/hiv.12481 .
Levett T, Alford K, Roberts J, et al. Evaluation of a combined hiv and geriatrics clinic for older people living with hiv: The silver clinic in brighton, uk. Geriatrics (Basel, Switzerland). 2020;5(4):1–12. https://doi.org/10.3390/geriatrics5040081 .
Tan JY, Greene M, Blat C, et al. Examining the Impact of the Golden Compass Clinical Care Program for Older People with HIV: A Qualitative Study. AIDS Behav. 2022;26(5):1562–71. https://doi.org/10.1007/s10461-021-03509-0 .
Siegler, E. L., Burchett, C. O., & Glesby, M. J. (2018). Older people with HIV are an essential part of the continuum of HIV care. Journal of the International AIDS Society , 21 (10).
Elgalib A, Al-Sawafi H, Kamble B, et al. Multidisciplinary care model for HIV improves treatment outcome: a single-centre experience from the Middle East. AIDS Care. 2018;30(9):1114–9.
Handford CD, Tynan A-M, Agha A, et al. Organization of care for persons with HIV-infection: a systematic review. AIDS Care. 2017;29(7):807–16.
Sherer R, Stieglitz K, Narra J, et al. HIV multidisciplinary teams work: support services improve access to and retention in HIV primary care. AIDS Care. 2002;14(sup1):31–44.
Soto TA, Bell J, Pillen M, et al. Literature on integrated HIV care: a review. AIDS Care. 2004;16(sup1):43–55.
Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. The Annals of Family Medicine. 2014;12(6):573–6.
Simms V, Higginson IJ, Harding R. Integration of palliative care throughout HIV disease. Lancet Infect Dis. 2012;12(7):571–5.
Demiris G, Parker Oliver D, Capurro D, et al. Implementation science: implications for intervention research in hospice and palliative care. Gerontologist. 2014;54(2):163–71.
Mackworth-Young C, Dringus S, Dauya E, et al. Putting youth at the centre: co-design of a community-based intervention to improve HIV outcomes among youth in Zimbabwe. Wellcome open research. 2022;7:53.
Marent B, Henwood F, Darking M, et al. Development of an mHealth platform for HIV care: gathering user perspectives through co-design workshops and interviews. JMIR Mhealth Uhealth. 2018;6(10): e9856.
Lee MJ, Onyango D, Hamza H, et al. Surveying testing preferences in Black, Latin American, and other minorities for the co-design of digital vending machines for HIV self-testing. Int J STD AIDS. 2020;31(2):158–65.
Tong C, Kernoghan A, Lemmon K, et al. Lessons and Reflections From an Extended Co-design Process Developing an mHealth App With and for Older Adults: Multiphase, Mixed Methods Study. JMIR aging. 2022;5(4): e39189.
Long-term co-design guidelines: Empowering older adults as co-designers of social robots. 2021 30th IEEE International Conference on Robot & Human Interactive Communication (RO-MAN); 2021. IEEE.
Prachakul W, Grant JS. Informal caregivers of persons with HIV/AIDS: A review and analysis. J Assoc Nurses AIDS Care. 2003;14(3):55–71.
Nelson MK. Fictive kin, families we choose, and voluntary kin: What does the discourse tell us? J Fam Theory Rev. 2013;5(4):259–81.
Dandachi D, Dang BN, Lucari B, et al. Exploring the attitude of patients with HIV about using telehealth for HIV care. AIDS Patient Care STDS. 2020;34(4):166–72.
Dandachi D, Lee C, Morgan RO, et al. Integration of telehealth services in the healthcare system: with emphasis on the experience of patients living with HIV. J Investig Med. 2019;67(5):815–20.
Ohl M, Dillon D, Moeckli J, et al. Mixed-methods evaluation of a telehealth collaborative care program for persons with HIV infection in a rural setting. J Gen Intern Med. 2013;28(9):1165–73.
Bucharski D, Reutter LI, Ogilvie LD. “You need to know where we’re coming from”: Canadian aboriginal women’s perspectives on culturally appropriate HIV counseling and testing. Health Care Women Int. 2006;27(8):723–47.
Sauceda JA, Brooks RA, Xavier J, et al. From theory to application: a description of transnationalism in culturally-appropriate HIV interventions of outreach, access, and retention among Latino/a populations. J Immigr Minor Health. 2019;21(2):332–45.
Chakrapani V, Gulfam FR, Arumugam V, et al. Intersectional stigma and gender non-affirmation hinder HIV care engagement among transgender women living with HIV in India. AIDS care 2022:1–9.
Ziersch A, Walsh M, Baak M, et al. “It is not an acceptable disease”: A qualitative study of HIV-related stigma and discrimination and impacts on health and wellbeing for people from ethnically diverse backgrounds in Australia. BMC Public Health. 2021;21(1):1–15.
Neimann Rasmussen L, Montgomery P. The prevalence of and factors associated with inclusion of non-English language studies in Campbell systematic reviews: A survey and meta-epidemiological study. Syst Rev. 2018;7(1):129–229. https://doi.org/10.1186/s13643-018-0786-6 .
Download references
Acknowledgements
We would like to thank and acknowledge the contributions of Charmaine De Castro, Information Specialist at the Mount Sinai Hospital– Sinai Health System, for providing guidance on the search strategy development, and conducting the literature search. We would like to thank and acknowledge the contributions of the authors who replied to our emails for contributing to our analysis.
This work was supported by Sinai Health’s Healthy Ageing and Geriatrics Program Research Fund.
Author information
Authors and affiliations.
Division of Geriatric Medicine, Department of Medicine, Sinai Health System and University Health Network, Suite 475 - 600 University Avenue, Toronto, ON, M5G 1X5, Canada
Kristina Marie Kokorelias, Anna Grosse & Luxey Sirisegaram
Department of Occupational Science & Occupational Therapy, Temerty Faculty of Medicine, University of Toronto, 160 - 500 University Ave, Toronto, ON, M5G 1V7, Canada
Kristina Marie Kokorelias
Rehabilitation Sciences Institute, University of Toronto, Toronto, Canada
Division of Geriatric Medicine, Department of Medicine, Medical Sciences Building, University of Toronto, 1 King’s College Cir, Toronto, ON, M5S 1A8, Canada
Anna Grosse & Luxey Sirisegaram
Department of Medicine, Medical Sciences Building, The University of Toronto, King’s College Cir, Toronto, ON, M5S 1A8, Canada
Alice Zhabokritsky
Infectious Diseases, Department of Medicine, University Health Network, 610 University Ave, Toronto, Toronto, ON, M5G 2M9, Canada
CIHR Canadian HIV Trails Network, 570-1081 Burrard Street, Vancouver, BC, V6Z 1Y6, Canada
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the project idea and initiated the project. KMK and LS conceptualized the study design. KMK wrote the first draft of this manuscript and revised the article during the review process. KMK and LS provided guidance to the Information Specialist with respect to the design of the search strategy. All authors finalized the literature search strategy. KMK piloted the search strategy. AG and LS were involved in editing and revising the manuscript. All authors approved the final version of the protocol and are accountable for all aspects of the work.
Corresponding author
Correspondence to Luxey Sirisegaram .
Ethics declarations
Ethics approval and consent to participate.
Not Required.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kokorelias, K.M., Grosse, A., Zhabokritsky, A. et al. Understanding geriatric models of care for older adults living with HIV: a scoping review and qualitative analysis. BMC Geriatr 23 , 417 (2023). https://doi.org/10.1186/s12877-023-04114-7
Download citation
Received : 18 January 2023
Accepted : 16 June 2023
Published : 08 July 2023
DOI : https://doi.org/10.1186/s12877-023-04114-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Models of care
- Older adults
- Qualitative
- Scoping review
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 19 April 2024
Person-centered care assessment tool with a focus on quality healthcare: a systematic review of psychometric properties
- Lluna Maria Bru-Luna 1 ,
- Manuel Martí-Vilar 2 ,
- César Merino-Soto 3 ,
- José Livia-Segovia 4 ,
- Juan Garduño-Espinosa 5 &
- Filiberto Toledano-Toledano 5 , 6 , 7
BMC Psychology volume 12 , Article number: 217 ( 2024 ) Cite this article
372 Accesses
Metrics details
The person-centered care (PCC) approach plays a fundamental role in ensuring quality healthcare. The Person-Centered Care Assessment Tool (P-CAT) is one of the shortest and simplest tools currently available for measuring PCC. The objective of this study was to conduct a systematic review of the evidence in validation studies of the P-CAT, taking the “Standards” as a frame of reference.
First, a systematic literature review was conducted following the PRISMA method. Second, a systematic descriptive literature review of validity tests was conducted following the “Standards” framework. The search strategy and information sources were obtained from the Cochrane, Web of Science (WoS), Scopus and PubMed databases. With regard to the eligibility criteria and selection process, a protocol was registered in PROSPERO (CRD42022335866), and articles had to meet criteria for inclusion in the systematic review.
A total of seven articles were included. Empirical evidence indicates that these validations offer a high number of sources related to test content, internal structure for dimensionality and internal consistency. A moderate number of sources pertain to internal structure in terms of test-retest reliability and the relationship with other variables. There is little evidence of response processes, internal structure in measurement invariance terms, and test consequences.
The various validations of the P-CAT are not framed in a structured, valid, theory-based procedural framework like the “Standards” are. This can affect clinical practice because people’s health may depend on it. The findings of this study show that validation studies continue to focus on the types of validity traditionally studied and overlook interpretation of the scores in terms of their intended use.
Peer Review reports
Person-centered care (PCC)
Quality care for people with chronic diseases, functional limitations, or both has become one of the main objectives of medical and care services. The person-centered care (PCC) approach is an essential element not only in achieving this goal but also in providing high-quality health maintenance and medical care [ 1 , 2 , 3 ]. In addition to guaranteeing human rights, PCC provides numerous benefits to both the recipient and the provider [ 4 , 5 ]. Additionally, PCC includes a set of necessary competencies for healthcare professionals to address ongoing challenges in this area [ 6 ]. PCC includes the following elements [ 7 ]: an individualized, goal-oriented care plan based on individuals’ preferences; an ongoing review of the plan and the individual’s goals; support from an interprofessional team; active coordination among all medical and care providers and support services; ongoing information exchange, education and training for providers; and quality improvement through feedback from the individual and caregivers.
There is currently a growing body of literature on the application of PCC. A good example of this is McCormack’s widely known mid-range theory [ 8 ], an internationally recognized theoretical framework for PCC and how it is operationalized in practice. This framework forms a guide for care practitioners and researchers in hospital settings. This framework is elaborated in PCC and conceived of as “an approach to practice that is established through the formation and fostering of therapeutic relationships between all care providers, service users, and others significant to them, underpinned by values of respect for persons, [the] individual right to self-determination, mutual respect, and understanding” [ 9 ].
Thus, as established by PCC, it is important to emphasize that reference to the person who is the focus of care refers not only to the recipient but also to everyone involved in a care interaction [ 10 , 11 ]. PCC ensures that professionals are trained in relevant skills and methodology since, as discussed above, carers are among the agents who have the greatest impact on the quality of life of the person in need of care [ 12 , 13 , 14 ]. Furthermore, due to the high burden of caregiving, it is essential to account for caregivers’ well-being. In this regard, studies on professional caregivers are beginning to suggest that the provision of PCC can produce multiple benefits for both the care recipient and the caregiver [ 15 ].
Despite a considerable body of literature and the frequent inclusion of the term in health policy and research [ 16 ], PCC involves several complications. There is no standard consensus on the definition of this concept [ 17 ], which includes problematic areas such as efficacy assessment [ 18 , 19 ]. In addition, the difficulty of measuring the subjectivity involved in identifying the dimensions of the CPC and the infrequent use of standardized measures are acute issues [ 20 ]. These limitations and purposes motivated the creation of the Person-Centered Care Assessment Tool (P-CAT; [ 21 ]), which emerged from the need for a brief, economical, easily applied, versatile and comprehensive assessment instrument to provide valid and reliable measures of PCC for research purposes [ 21 ].
Person-centered care assessment tool (P-CAT)
There are several instruments that can measure PCC from different perspectives (i.e., the caregiver or the care recipient) and in different contexts (e.g., hospitals and nursing homes). However, from a practical point of view, the P-CAT is one of the shortest and simplest tools and contains all the essential elements of PCC described in the literature. It was developed in Australia to measure the approach of long-term residential settings to older people with dementia, although it is increasingly used in other healthcare settings, such as oncology units [ 22 ] and psychiatric hospitals [ 23 ].
Due to the brevity and simplicity of its application, the versatility of its use in different medical and care contexts, and its potential emic characteristics (i.e., constructs that can be cross-culturally applicable with reasonable and similar structure and interpretation; [ 24 ]), the P-CAT is one of the most widely used tests by professionals to measure PCC [ 25 , 26 ]. It has expanded to several countries with cultural and linguistic differences. Since its creation, it has been adapted in countries separated by wide cultural and linguistic differences, such as Norway [ 27 ], Sweden [ 28 ], China [ 29 ], South Korea [ 30 ], Spain [ 25 ], and Italy [ 31 ].
The P-CAT comprises 13 items rated on a 5-point ordinal scale (from “strongly disagree” to “strongly agree”), with high scores indicating a high degree of person-centeredness. The scale consists of three dimensions: person-centered care (7 items), organizational support (4 items) and environmental accessibility (2 items). In the original study ( n = 220; [ 21 ]), the internal consistency of the instrument yielded satisfactory values for the total scale ( α = 0.84) and good test-retest reliability ( r =.66) at one-week intervals. A reliability generalization study conducted in 2021 [ 32 ] that estimated the internal consistency of the P-CAT and analyzed possible factors that could affect the it revealed that the mean α value for the 25 meta-analysis samples (some of which were part of the validations included in this study) was 0.81, and the only variable that had a statistically significant relationship with the reliability coefficient was the mean age of the sample. With respect to internal structure validity, three factors (56% of the total variance) were obtained, and content validity was assessed by experts, literature reviews and stakeholders [ 33 ].
Although not explicitly stated, the apparent commonality between validation studies of different versions of the P-CAT may be influenced by an influential decades-old validity framework that differentiates three categories: content validity, construct validity, and criterion validity [ 34 , 35 ]. However, a reformulation of the validity of the P-CAT within a modern framework, which would provide a different definition of validity, has not been performed.
Scale validity
Traditionally, validation is a process focused on the psychometric properties of a measurement instrument [ 36 ]. In the early 20th century, with the frequent use of standardized measurement tests in education and psychology, two definitions emerged: the first defined validity as the degree to which a test measures what it intends to measure, while the second described the validity of an instrument in terms of the correlation it presents with a variable [ 35 ].
However, in the past century, validity theory has evolved, leading to the understanding that validity should be based on specific interpretations for an intended purpose. It should not be limited to empirically obtained psychometric properties but should also be supported by the theory underlying the construct measured. Thus, to speak of classical or modern validity theory suggests an evolution in the classical or modern understanding of the concept of validity. Therefore, a classical approach (called classical test theory, CTT) is specifically differentiated from a modern approach. In general, recent concepts associated with a modern view of validity are based on (a) a unitary conception of validity and (b) validity judgments based on inferences and interpretations of the scores of a measure [ 37 , 38 ]. This conceptual advance in the concept of validity led to the creation of a guiding framework to for obtaining evidence to support the use and interpretation of the scores obtained by a measure [ 39 ].
This purpose is addressed by the Standards for Educational and Psychological Testing (“Standards”), a guide created by the American Educational Research Association (AERA), the American Psychological Association (APA) and the National Council on Measurement in Education (NCME) in 2014 with the aim of providing guidelines to assess the validity of the interpretations of scores of an instrument based on their intended use. Two conceptual aspects stand out in this modern view of validity: first, validity is a unitary concept centered on the construct; second, validity is defined as “the degree to which evidence and theory support the interpretations of test scores for proposed uses of tests” [ 37 ]. Thus, the “Standards” propose several sources that serve as a reference for assessing different aspects of validity. The five sources of valid evidence are as follows [ 37 ]: test content, response processes, internal structure, relations to other variables and consequences of testing. According to AERA et al. [ 37 ], test content validity refers to the relationship of the administration process, subject matter, wording and format of test items to the construct they are intended to measure. It is measured predominantly with qualitative methods but without excluding quantitative approaches. The validity of the responses is based on analysis of the cognitive processes and interpretation of the items by respondents and is measured with qualitative methods. Internal structure validity is based on the interrelationship between the items and the construct and is measured by quantitative methods. Validity in terms of the relationship with other variables is based on comparison between the variable that the instrument intends to measure and other theoretically relevant external variables and is measured by quantitative methods. Finally, validity based on the results of the test analyses consequences, both intended and unintended, that may be due to a source of invalidity. It is measured mainly by qualitative methods.
Thus, although validity plays a fundamental role in providing a strong scientific basis for interpretations of test scores, validation studies in the health field have traditionally focused on content validity, criterion validity and construct validity and have overlooked the interpretation and use of scores [ 34 ].
“Standards” are considered a suitable validity theory-based procedural framework for reviewing the validity of questionnaires due to its ability to analyze sources of validity from both qualitative and quantitative approaches and its evidence-based method [ 35 ]. Nevertheless, due to a lack of knowledge or the lack of a systematic description protocol, very few instruments to date have been reviewed within the framework of the “Standards” [ 39 ].
Current study
Although the P-CAT is one of the most widely used instruments by professionals and has seven validations [ 25 , 27 , 28 , 29 , 30 , 31 , 40 ], no analysis has been conducted of its validity within the framework of the “Standards”. That is, empirical evidence of the validity of the P-CAT has not been obtained in a way that helps to develop a judgment based on a synthesis of the available information.
A review of this type is critical given that some methodological issues seem to have not been resolved in the P-CAT. For example, although the multidimensionality of the P-CAT was identified in the study that introduced it, Bru-Luna et al. [ 32 ] recently stated that in adaptations of the P-CAT [ 25 , 27 , 28 , 29 , 30 , 40 ], the total score is used for interpretation and multidimensionality is disregarded. Thus, the multidimensionality of the original study was apparently not replicated. Bru-Luna et al. [ 32 ] also indicated that the internal structure validity of the P-CAT is usually underreported due to a lack of sufficiently rigorous approaches to establish with certainty how its scores are calculated.
The validity of the P-CAT, specifically its internal structure, appears to be unresolved. Nevertheless, substantive research and professional practice point to this measure as relevant to assessing PCC. This perception is contestable and judgment-based and may not be sufficient to assess the validity of the P-CAT from a cumulative and synthetic angle based on preceding validation studies. An adequate assessment of validity requires a model to conceptualize validity followed by a review of previous studies of the validity of the P-CAT using this model.
Therefore, the main purpose of this study was to conduct a systematic review of the evidence provided by P-CAT validation studies while taking the “Standards” as a framework.
The present study comprises two distinct but interconnected procedures. First, a systematic literature review was conducted following the PRISMA method ( [ 41 ]; Additional file 1; Additional file 2) with the aim of collecting all validations of the P-CAT that have been developed. Second, a systematic description of the validity evidence for each of the P-CAT validations found in the systematic review was developed following the “Standards” framework [ 37 ]. The work of Hawkins et al. [ 39 ], the first study to review validity sources according to the guidelines proposed by the “Standards”, was also used as a reference. Both provided conceptual and pragmatic guidance for organizing and classifying validity evidence for the P-CAT.
The procedure conducted in the systematic review is described below, followed by the procedure for examining the validity studies.
Systematic review
Search strategy and information sources.
Initially, the Cochrane database was searched with the aim of identifying systematic reviews of the P-CAT. When no such reviews were found, subsequent preliminary searches were performed in the Web of Science (WoS), Scopus and PubMed databases. These databases play a fundamental role in recent scientific literature since they are the main sources of published articles that undergo high-quality content and editorial review processes [ 42 ]. The search formula was as follows. The original P-CAT article [ 21 ] was located, after which all articles that cited it through 2021 were identified and analyzed. This approach ensured the inclusion of all validations. No articles were excluded on the basis of language to avoid language bias [ 43 ]. Moreover, to reduce the effects of publication bias, a complementary search in Google Scholar was also performed to allow the inclusion of “gray” literature [ 44 ]. Finally, a manual search was performed through a review of the references of the included articles to identify other articles that met the search criteria but were not present in any of the aforementioned databases.
This process was conducted by one of the authors and corroborated by another using the Covidence tool [ 45 ]. A third author was consulted in case of doubt.
Eligibility criteria and selection process
The protocol was registered in PROSPERO, and the search was conducted according to these criteria. The identification code is CRD42022335866.
The articles had to meet the following criteria for inclusion in the systematic review: (a) a methodological approach to P-CAT validations, (b) an experimental or quasiexperimental studies, (c) studies with any type of sample, and (d) studies in any language. We discarded studies that met at least one of the following exclusion criteria: (a) systematic reviews or bibliometric reviews of the instrument or meta-analyses or (b) studies published after 2021.
Data collection process
After the articles were selected, the most relevant information was extracted from each article. Fundamental data were recorded in an Excel spreadsheet for each of the sections: introduction, methodology, results and discussion. Information was also recorded about the limitations mentioned in each article as well as the practical implications and suggestions for future research.
Given the aim of the study, information was collected about the sources of validity of each study, including test content (judges’ evaluation, literature review and translation), response processes, internal structure (factor analysis, design, estimator, factor extraction method, factors and items, interfactor R, internal replication, effect of the method, and factor loadings), and relationships with other variables (convergent, divergent, concurrent and predictive validity) and consequences of measurement.
Description of the validity study
To assess the validity of the studies, an Excel table was used. Information was recorded for the seven articles included in the systematic review. The data were extracted directly from the texts of the articles and included information about the authors, the year of publication, the country where each P-CAT validation was produced and each of the five standards proposed in the “Standards” [ 37 ].
The validity source related to internal structure was divided into three sections to record information about dimensionality (e.g., factor analysis, design, estimator, factor extraction method, factors and items, interfactor R, internal replication, effect of the method, and factor loadings), reliability expression (i.e., internal consistency and test-retest) and the study of factorial invariance according to the groups into which it was divided (e.g., sex, age, profession) and the level of study (i.e., metric, intercepts). This approach allowed much more information to be obtained than relying solely on source validity based on internal structure. This division was performed by the same researcher who performed the previous processes.
Study selection and study characteristics
The systematic review process was developed according to the PRISMA methodology [ 41 ].
The WoS, Scopus, PubMed and Google Scholar databases were searched on February 12, 2022 and yielded a total of 485 articles. Of these, 111 were found in WoS, 114 in Scopus, 43 in PubMed and 217 in Google Scholar. In the first phase, the title and abstracts of all the articles were read. In this first screening, 457 articles were eliminated because they did not include studies with a methodological approach to P-CAT validation and one article was excluded because it was the original P-CAT article. This resulted in a total of 27 articles, 19 of which were duplicated in different databases and, in the case of Google Scholar, within the same database. This process yielded a total of eight articles that were evaluated for eligibility by a complete reading of the text. In this step, one of the articles was excluded due to a lack of access to the full text of the study [ 31 ] (although the original manuscript was found, it was impossible to access the complete content; in addition, the authors of the manuscript were contacted, but no reply was received). Finally, a manual search was performed by reviewing the references of the seven studies, but none were considered suitable for inclusion. Thus, the review was conducted with a total of seven articles.
Of the seven studies, six were original validations in other languages. These included Norwegian [ 27 ], Swedish [ 28 ], Chinese (which has two validations [ 29 , 40 ]), Spanish [ 25 ], and Korean [ 30 ]. The study by Selan et al. [ 46 ] included a modification of the Swedish version of the P-CAT and explored the psychometric properties of both versions (i.e., the original Swedish version and the modified version).
The item selection and screening process are illustrated in detail in Fig. 1 .
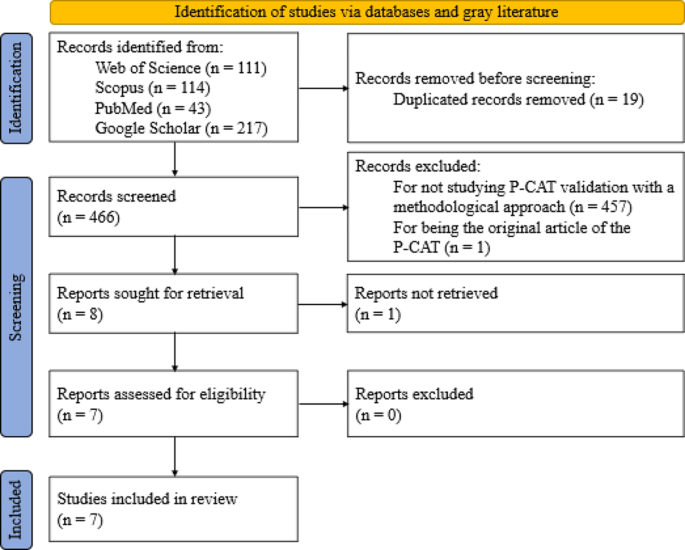
PRISMA 2020 flow diagram for new systematic reviews including database searches
Validity analysis
To provide a clear overview of the validity analyses, Table 1 descriptively shows the percentages of items that provide information about the five standards proposed by the “Standards” guide [ 37 ].
The table shows a high number of validity sources related to test content and internal structure in relation to dimensionality and internal consistency, followed by a moderate number of sources for test-retest and relationship with other variables. A rate of 0% is observed for validity sources related to response processes, invariance and test consequences. Below, different sections related to each of the standards are shown, and the information is presented in more detail.
Evidence based on test content
The first standard, which focused on test content, was met for all items (100%). Translation, which refers to the equivalence of content between the original language and the target language, was met in the six articles that conducted validation in another language and/or culture. These studies reported that the validations were translated by bilingual experts and/or experts in the area of care. In addition, three studies [ 25 , 29 , 40 ] reported that the translation process followed International Test Commission guidelines, such as those of Beaton et al. [ 47 ], Guillemin [ 48 ], Hambleton et al. [ 49 ], and Muñiz et al. [ 50 ]. Evaluation by judges, who referred to the relevance, clarity and importance of the content, was divided into two categories: expert evaluation (a panel of expert judges for each of the areas to consider in the evaluation instrument) and experiential evaluation (potential participants testing the test). The first type of evaluation occurred in three of the articles [ 28 , 29 , 46 ], while the other occurred in two [ 25 , 40 ]. Only one of the items [ 29 ] reported that the scale contained items that reflected the dimension described in the literature. The validity evidence related to the test content presented in each article can be found in Table 2 .
Evidence based on response processes
The second standard, related to the validity of the response process, was obtained according to the “Standards” from the analysis of individual responses: “questioning test takers about their performance strategies or response to particular items (…), maintaining records that monitor the development of a response to a writing task (…), documentation of other aspects of performance, like eye movement or response times…” [ 37 ] (p. 15). According to the analysis of the validity of the response processes, none of the articles complied with this evidence.
Evidence based on internal structure
The third standard, validity related to internal structure, was divided into three sections. First, the dimensionality of each study was examined in terms of factor analysis, design, estimator, factor extraction method, factors and items, interfactor R, internal replication, effect of the method, and factor loadings. Le et al. [ 40 ] conducted an exploratory-confirmatory design while Sjögren et al. [ 28 ] conducted a confirmatory-exploratory design to assess construct validity using confirmatory factor analysis (CFA) and investigated it further using exploratory factor analysis (EFA). The remaining articles employed only a single form of factor analysis: three employed EFA, and two employed CFA. Regarding the next point, only three of the articles reported the factor extraction method used, including Kaiser’s eigenvalue, criterion, scree plot test, parallel analysis and Velicer’s MAP test. Instrument validations yielded a total of two factors in five of the seven articles, while one yielded a single dimension [ 25 ] and the other yielded three dimensions [ 29 ], as in the original instrument. The interfactor R was reported only in the study by Zhong and Lou [ 29 ], whereas in the study by Martínez et al. [ 25 ], it could be easily obtained since it consisted of only one dimension. Internal replication was also calculated in the Spanish validation by randomly splitting the sample into two to test the correlations between factors. The effectiveness of the method was not reported in any of the articles. This information is presented in Table 3 in addition to a summary of the factor loadings.
The second section examined reliability. All the studies presented measures of internal consistency conducted in their entirety with Cronbach’s α coefficient for both the total scale and the subscales. The ω coefficient of McDonald was not used in any case. Four of the seven articles performed a test-retest test. Martínez et al. [ 25 ] conducted a test-retest after a period of seven days, while Le et al. [ 40 ] and Rokstad et al. [ 27 ] performed it between one and two weeks later and Sjögren et al. [ 28 ] allowed approximately two weeks to pass after the initial test.
The third section analyzes the calculation of invariance, which was not reported in any of the studies.
Evidence based on relationships with other variables
In the fourth standard, based on validity according to the relationship with other variables, the articles that reported it used only convergent validity (i.e., it was hypothesized that the variables related to the construct measured by the test—in this case, person-centeredness—were positively or negatively related to another construct). Discriminant validity hypothesizes that the variables related to the PCC construct are not correlated in any way with any other variable studied. No article (0%) measured discriminant evidence, while four (57%) measured convergent evidence [ 25 , 29 , 30 , 46 ]. Convergent validity was obtained through comparisons with instruments such as the Person-Centered Climate Questionnaire–Staff Version (PCQ-S), the Staff-Based Measures of Individualized Care for Institutionalized Persons with Dementia (IC), the Caregiver Psychological Elder Abuse Behavior Scale (CPEAB), the Organizational Climate (CLIOR) and the Maslach Burnout Inventory (MBI). In the case of Selan et al. [ 46 ], convergent validity was assessed on two items considered by the authors as “crude measures of person-centered care (i.e., external constructs) giving an indication of the instruments’ ability to measure PCC” (p. 4). Concurrent validity, which measures the degree to which the results of one test are or are not similar to those of another test conducted at more or less the same time with the same participants, and predictive validity, which allows predictions to be established regarding behavior based on comparison between the values of the instrument and the criterion, were not reported in any of the studies.
Evidence based on the consequences of testing
The fifth and final standard was related to the consequences of the test. It analyzed the consequences, both intended and unintended, of applying the test to a given sample. None of the articles presented explicit or implicit evidence of this.
The last two sources of validity can be seen in Table 4 .
Table 5 shows the results of the set of validity tests for each study according to the described standards.
The main purpose of this article is to analyze the evidence of validity in different validation studies of the P-CAT. To gather all existing validations, a systematic review of all literature citing this instrument was conducted.
The publication of validation studies of the P-CAT has been constant over the years. Since the publication of the original instrument in 2010, seven validations have been published in other languages (taking into account the Italian version by Brugnolli et al. [ 31 ], which could not be included in this study) as well as a modification of one of these versions. The very unequal distribution of validations between languages and countries is striking. A recent systematic review [ 51 ] revealed that in Europe, the countries where the PCC approach is most widely used are the United Kingdom, Sweden, the Netherlands, Northern Ireland, and Norway. It has also been shown that the neighboring countries seem to exert an influence on each other due to proximity [ 52 ] such that they tend to organize healthcare in a similar way, as is the case for Scandinavian countries. This favors the expansion of PCC and explains the numerous validations we found in this geographical area.
Although this approach is conceived as an essential element of healthcare for most governments [ 53 ], PCC varies according to the different definitions and interpretations attributed to it, which can cause confusion in its application (e.g., between Norway and the United Kingdom [ 54 ]). Moreover, facilitators of or barriers to implementation depend on the context and level of development of each country, and financial support remains one of the main factors in this regard [ 53 ]. This fact explains why PCC is not globally widespread among all territories. In countries where access to healthcare for all remains out of reach for economic reasons, the application of this approach takes a back seat, as does the validation of its assessment tools. In contrast, in a large part of Europe or in countries such as China or South Korea that have experienced decades of rapid economic development, patients are willing to be involved in their medical treatment and enjoy more satisfying and efficient medical experiences and environments [ 55 ], which facilitates the expansion of validations of instruments such as the P-CAT.
Regarding validity testing, the guidelines proposed by the “Standards” [ 37 ] were followed. According to the analysis of the different validations of the P-CAT instrument, none of the studies used a structured validity theory-based procedural framework for conducting validation. The most frequently reported validity tests were on the content of the test and two of the sections into which the internal structure was divided (i.e., dimensionality and internal consistency).
In the present article, the most cited source of validity in the studies was the content of the test because most of the articles were validations of the P-CAT in other languages, and the authors reported that the translation procedure was conducted by experts in all cases. In addition, several of the studies employed International Test Commission guidelines, such as those by Beaton et al. [ 47 ], Guillemin [ 48 ], Hambleton et al. [ 49 ], and Muñiz et al. [ 50 ]. Several studies also assessed the relevance, clarity and importance of the content.
The third source of validity, internal structure, was the next most often reported, although it appeared unevenly among the three sections into which this evidence was divided. Dimensionality and internal consistency were reported in all studies, followed by test-retest consistency. In relation to the first section, factor analysis, a total of five EFAs and four CFAs were presented in the validations. Traditionally, EFA has been used in research to assess dimensionality and identify key psychological constructs, although this approach involves a number of inconveniences, such as difficulty testing measurement invariance and incorporating latent factors into subsequent analyses [ 56 ] or the major problem of factor loading matrix rotation [ 57 ]. Studies eventually began to employ CFA, a technique that overcame some of these obstacles [ 56 ] but had other drawbacks; for example, the strict requirement of zero cross-loadings often does not fit the data well, and misspecification of zero loadings tends to produce distorted factors [ 57 ]. Recently, exploratory structural equation modeling (ESEM) has been proposed. This technique is widely recommended both conceptually and empirically to assess the internal structure of psychological tools [ 58 ] since it overcomes the limitations of EFA and CFA in estimating their parameters [ 56 , 57 ].
The next section, reliability, reports the total number of items according to Cronbach’s α reliability coefficient. Reliability is defined as a combination of systematic and random influences that determine the observed scores on a psychological test. Reporting the reliability measure ensures that item-based scores are consistent, that the tool’s responses are replicable and that they are not modified solely by random noise [ 59 , 60 ]. Currently, the most commonly employed reliability coefficient in studies with a multi-item measurement scale (MIMS) is Cronbach’s α [ 60 , 61 ].
Cronbach’s α [ 62 ] is based on numerous strict assumptions (e.g., the test must be unidimensional, factor loadings must be equal for all items and item errors should not covary) to estimate internal consistency. These assumptions are difficult to meet, and their violation may produce small reliability estimates [ 60 ]. One of the alternative measures to α that is increasingly recommended by the scientific literature is McDonald’s ω [ 63 ], a composite reliability measure. This coefficient is recommended for congeneric scales in which tau equivalence is not assumed. It has several advantages. For example, estimates of ω are usually robust when the estimated model contains more factors than the true model, even with small samples, or when skewness in univariate item distributions produces lower biases than those found when using α [ 59 ].
The test-retest method was the next most commonly reported internal structure section in these studies. This type of reliability considers the consistency of the scores of a test between two measurements separated by a period [ 64 ]. It is striking that test-retest consistency does not have a prevalence similar to that of internal consistency since, unlike internal consistency, test-retest consistency can be assessed for practically all types of patient-reported outcomes. It is even considered by some measurement experts to report reliability with greater relevance than internal consistency since it plays a fundamental role in the calculation of parameters for health measures [ 64 ]. However, the literature provides little guidance regarding the assessment of this type of reliability.
The internal structure section that was least frequently reported in the studies in this review was invariance. A lack of invariance refers to a difference between scores on a test that is not explained by group differences in the structure it is intended to measure [ 65 ]. The invariance of the measure should be emphasized as a prerequisite in comparisons between groups since “if scale invariance is not examined, item bias may not be fully recognized and this may lead to a distorted interpretation of the bias in a particular psychological measure” [ 65 ].
Evidence related to other variables was the next most reported source of validity in the studies included in this review. Specifically, the four studies that reported this evidence did so according to convergent validity and cited several instruments. None of the studies included evidence of discriminant validity, although this may be because there are currently several obstacles related to the measurement of this type of validity [ 66 ]. On the one hand, different definitions are used in the applied literature, which makes its evaluation difficult; on the other hand, the literature on discriminant validity focuses on techniques that require the use of multiple measurement methods, which often seem to have been introduced without sufficient evidence or are applied randomly.
Validity related to response processes was not reported by any of the studies. There are several methods to analyze this validity. These methods can be divided into two groups: “those that directly access the psychological processes or cognitive operations (think aloud, focus group, and interviews), compared to those which provide indirect indicators which in turn require additional inference (eye tracking and response times)” [ 38 ]. However, this validity evidence has traditionally been reported less frequently than others in most studies, perhaps because there are fewer clear and accepted practices on how to design or report these studies [ 67 ].
Finally, the consequences of testing were not reported in any of the studies. There is debate regarding this source of validity, with two main opposing streams of thought. On the one hand [ 68 , 69 ]) suggests that consequences that appear after the application of a test should not derive from any source of test invalidity and that “adverse consequences only undermine the validity of an assessment if they can be attributed to a problem of fit between the test and the construct” (p. 6). In contrast, Cronbach [ 69 , 70 ] notes that adverse social consequences that may result from the application of a test may call into question the validity of the test. However, the potential risks that may arise from the application of a test should be minimized in any case, especially in regard to health assessments. To this end, it is essential that this aspect be assessed by instrument developers and that the experiences of respondents be protected through the development of comprehensive and informed practices [ 39 ].
This work is not without limitations. First, not all published validation studies of the P-CAT, such as the Italian version by Brugnolli et al. [ 31 ], were available. These studies could have provided relevant information. Second, many sources of validity could not be analyzed because the studies provided scant or no data, such as response processes [ 25 , 27 , 28 , 29 , 30 , 40 , 46 ], relationships with other variables [ 27 , 28 , 40 ], consequences of testing [ 25 , 27 , 28 , 29 , 30 , 40 , 46 ], or invariance [ 25 , 27 , 28 , 29 , 30 , 40 , 46 ] in the case of internal structure and interfactor R [ 27 , 28 , 30 , 40 , 46 ], internal replication [ 27 , 28 , 29 , 30 , 40 , 46 ] or the effect of the method [ 25 , 27 , 28 , 29 , 30 , 40 , 46 ] in the case of dimensionality. In the future, it is hoped that authors will become aware of the importance of validity, as shown in this article and many others, and provide data on unreported sources so that comprehensive validity studies can be performed.
The present work also has several strengths. The search was extensive, and many studies were obtained using three different databases, including WoS, one of the most widely used and authoritative databases in the world. This database includes a large number and variety of articles and is not fully automated due to its human team [ 71 , 72 , 73 ]. In addition, to prevent publication bias, gray literature search engines such as Google Scholar were used to avoid the exclusion of unpublished research [ 44 ]. Finally, linguistic bias was prevented by not limiting the search to articles published in only one or two languages, thus avoiding the overrepresentation of studies in one language and underrepresentation in others [ 43 ].
Conclusions
Validity is understood as the degree to which tests and theory support the interpretations of instrument scores for their intended use [ 37 ]. From this perspective, the various validations of the P-CAT are not presented in a structured, valid, theory-based procedural framework like the “Standards” are. After integration and analysis of the results, it was observed that these validation reports offer a high number of sources of validity related to test content, internal structure in dimensionality and internal consistency, a moderate number of sources for internal structure in terms of test-retest reliability and the relationship with other variables, and a very low number of sources for response processes, internal structure in terms of invariance, and test consequences.
Validity plays a fundamental role in ensuring a sound scientific basis for test interpretations because it provides evidence of the extent to which the data provided by the test are valid for the intended purpose. This can affect clinical practice as people’s health may depend on it. In this sense, the “Standards” are considered a suitable and valid theory-based procedural framework for studying this modern conception of questionnaire validity, which should be taken into account in future research in this area.
Although the P-CAT is one of the most widely used instruments for assessing PCC, as shown in this study, PCC has rarely been studied. The developers of measurement tests applied to the health care setting, on which the health and quality of life of many people may depend, should use this validity framework to reflect the clear purpose of the measurement. This approach is important because the equity of decision making by healthcare professionals in daily clinical practice may depend on the source of validity. Through a more extensive study of validity that includes the interpretation of scores in terms of their intended use, the applicability of the P-CAT, an instrument that was initially developed for long-term care homes for elderly people, could be expanded to other care settings. However, the findings of this study show that validation studies continue to focus on traditionally studied types of validity and overlook the interpretation of scores in terms of their intended use.
Data availability
All data relevant to the study were included in the article or uploaded as additional files. Additional template data extraction forms are available from the corresponding author upon reasonable request.
Abbreviations
American Educational Research Association
American Psychological Association
Confirmatory factor analysis
Organizational Climate
Caregiver Psychological Elder Abuse Behavior Scale
Exploratory factor analysis
Exploratory structural equation modeling
Staff-based Measures of Individualized Care for Institutionalized Persons with Dementia
Maslach Burnout Inventory
Multi-item measurement scale
Maximum likelihood
National Council on Measurement in Education
Person-Centered Care Assessment Tool
- Person-centered care
Person-Centered Climate Questionnaire–Staff Version
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
International Register of Systematic Review Protocols
Standards for Educational and Psychological Testing
weighted least square mean and variance adjusted
Web of Science
Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy; 2001.
Google Scholar
International Alliance of Patients’ Organizations. What is patient-centred healthcare? A review of definitions and principles. 2nd ed. London, UK: International Alliance of Patients’ Organizations; 2007.
World Health Organization. WHO global strategy on people-centred and integrated health services: interim report. Geneva, Switzerland: World Health Organization; 2015.
Britten N, Ekman I, Naldemirci Ö, Javinger M, Hedman H, Wolf A. Learning from Gothenburg model of person centred healthcare. BMJ. 2020;370:m2738.
Article PubMed Google Scholar
Van Diepen C, Fors A, Ekman I, Hensing G. Association between person-centred care and healthcare providers’ job satisfaction and work-related health: a scoping review. BMJ Open. 2020;10:e042658.
Article PubMed PubMed Central Google Scholar
Ekman N, Taft C, Moons P, Mäkitalo Å, Boström E, Fors A. A state-of-the-art review of direct observation tools for assessing competency in person-centred care. Int J Nurs Stud. 2020;109:103634.
American Geriatrics Society Expert Panel on Person-Centered Care. Person-centered care: a definition and essential elements. J Am Geriatr Soc. 2016;64:15–8.
Article Google Scholar
McCormack B, McCance TV. Development of a framework for person-centred nursing. J Adv Nurs. 2006;56:472–9.
McCormack B, McCance T. Person-centred practice in nursing and health care: theory and practice. Chichester, England: Wiley; 2016.
Nolan MR, Davies S, Brown J, Keady J, Nolan J. Beyond person-centred care: a new vision for gerontological nursing. J Clin Nurs. 2004;13:45–53.
McCormack B, McCance T. Person-centred nursing: theory, models and methods. Oxford, UK: Wiley-Blackwell; 2010.
Book Google Scholar
Abraha I, Rimland JM, Trotta FM, Dell’Aquila G, Cruz-Jentoft A, Petrovic M, et al. Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop series. BMJ Open. 2017;7:e012759.
Anderson K, Blair A. Why we need to care about the care: a longitudinal study linking the quality of residential dementia care to residents’ quality of life. Arch Gerontol Geriatr. 2020;91:104226.
Bauer M, Fetherstonhaugh D, Haesler E, Beattie E, Hill KD, Poulos CJ. The impact of nurse and care staff education on the functional ability and quality of life of people living with dementia in aged care: a systematic review. Nurse Educ Today. 2018;67:27–45.
Smythe A, Jenkins C, Galant-Miecznikowska M, Dyer J, Downs M, Bentham P, et al. A qualitative study exploring nursing home nurses’ experiences of training in person centred dementia care on burnout. Nurse Educ Pract. 2020;44:102745.
McCormack B, Borg M, Cardiff S, Dewing J, Jacobs G, Janes N, et al. Person-centredness– the ‘state’ of the art. Int Pract Dev J. 2015;5:1–15.
Wilberforce M, Challis D, Davies L, Kelly MP, Roberts C, Loynes N. Person-centredness in the care of older adults: a systematic review of questionnaire-based scales and their measurement properties. BMC Geriatr. 2016;16:63.
Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70:351–79.
Sharma T, Bamford M, Dodman D. Person-centred care: an overview of reviews. Contemp Nurse. 2016;51:107–20.
Ahmed S, Djurkovic A, Manalili K, Sahota B, Santana MJ. A qualitative study on measuring patient-centered care: perspectives from clinician-scientists and quality improvement experts. Health Sci Rep. 2019;2:e140.
Edvardsson D, Fetherstonhaugh D, Nay R, Gibson S. Development and initial testing of the person-centered Care Assessment Tool (P-CAT). Int Psychogeriatr. 2010;22:101–8.
Tamagawa R, Groff S, Anderson J, Champ S, Deiure A, Looyis J, et al. Effects of a provincial-wide implementation of screening for distress on healthcare professionals’ confidence and understanding of person-centered care in oncology. J Natl Compr Canc Netw. 2016;14:1259–66.
Degl’ Innocenti A, Wijk H, Kullgren A, Alexiou E. The influence of evidence-based design on staff perceptions of a supportive environment for person-centered care in forensic psychiatry. J Forensic Nurs. 2020;16:E23–30.
Hulin CL. A psychometric theory of evaluations of item and scale translations: fidelity across languages. J Cross Cult Psychol. 1987;18:115–42.
Martínez T, Suárez-Álvarez J, Yanguas J, Muñiz J. Spanish validation of the person-centered Care Assessment Tool (P-CAT). Aging Ment Health. 2016;20:550–8.
Martínez T, Martínez-Loredo V, Cuesta M, Muñiz J. Assessment of person-centered care in gerontology services: a new tool for healthcare professionals. Int J Clin Health Psychol. 2020;20:62–70.
Rokstad AM, Engedal K, Edvardsson D, Selbaek G. Psychometric evaluation of the Norwegian version of the person-centred Care Assessment Tool. Int J Nurs Pract. 2012;18:99–105.
Sjögren K, Lindkvist M, Sandman PO, Zingmark K, Edvardsson D. Psychometric evaluation of the Swedish version of the person-centered Care Assessment Tool (P-CAT). Int Psychogeriatr. 2012;24:406–15.
Zhong XB, Lou VW. Person-centered care in Chinese residential care facilities: a preliminary measure. Aging Ment Health. 2013;17:952–8.
Tak YR, Woo HY, You SY, Kim JH. Validity and reliability of the person-centered Care Assessment Tool in long-term care facilities in Korea. J Korean Acad Nurs. 2015;45:412–9.
Brugnolli A, Debiasi M, Zenere A, Zanolin ME, Baggia M. The person-centered Care Assessment Tool in nursing homes: psychometric evaluation of the Italian version. J Nurs Meas. 2020;28:555–63.
Bru-Luna LM, Martí-Vilar M, Merino-Soto C, Livia J. Reliability generalization study of the person-centered Care Assessment Tool. Front Psychol. 2021;12:712582.
Edvardsson D, Innes A. Measuring person-centered care: a critical comparative review of published tools. Gerontologist. 2010;50:834–46.
Hawkins M, Elsworth GR, Nolte S, Osborne RH. Validity arguments for patient-reported outcomes: justifying the intended interpretation and use of data. J Patient Rep Outcomes. 2021;5:64.
Sireci SG. On the validity of useless tests. Assess Educ Princ Policy Pract. 2016;23:226–35.
Hawkins M, Elsworth GR, Osborne RH. Questionnaire validation practice: a protocol for a systematic descriptive literature review of health literacy assessments. BMJ Open. 2019;9:e030753.
American Educational Research Association, American Psychological Association. National Council on Measurement in Education. Standards for educational and psychological testing. Washington, DC: American Educational Research Association; 2014.
Padilla JL, Benítez I. Validity evidence based on response processes. Psicothema. 2014;26:136–44.
PubMed Google Scholar
Hawkins M, Elsworth GR, Hoban E, Osborne RH. Questionnaire validation practice within a theoretical framework: a systematic descriptive literature review of health literacy assessments. BMJ Open. 2020;10:e035974.
Le C, Ma K, Tang P, Edvardsson D, Behm L, Zhang J, et al. Psychometric evaluation of the Chinese version of the person-centred Care Assessment Tool. BMJ Open. 2020;10:e031580.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2008;22:338–42.
Grégoire G, Derderian F, Le Lorier J. Selecting the language of the publications included in a meta-analysis: is there a tower of Babel bias? J Clin Epidemiol. 1995;48:159–63.
Arias MM. Aspectos metodológicos Del metaanálisis (1). Pediatr Aten Primaria. 2018;20:297–302.
Covidence. Covidence systematic review software. Veritas Health Innovation, Australia. 2014. https://www.covidence.org/ . Accessed 28 Feb 2022.
Selan D, Jakobsson U, Condelius A. The Swedish P-CAT: modification and exploration of psychometric properties of two different versions. Scand J Caring Sci. 2017;31:527–35.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25:3186–91.
Guillemin F. Cross-cultural adaptation and validation of health status measures. Scand J Rheumatol. 1995;24:61–3.
Hambleton R, Merenda P, Spielberger C. Adapting educational and psychological tests for cross-cultural assessment. Mahwah, NJ: Lawrence Erlbaum Associates; 2005.
Muñiz J, Elosua P, Hambleton RK. International test commission guidelines for test translation and adaptation: second edition. Psicothema. 2013;25:151–7.
Rosengren K, Brannefors P, Carlstrom E. Adoption of the concept of person-centred care into discourse in Europe: a systematic literature review. J Health Organ Manag. 2021;35:265–80.
Alharbi T, Olsson LE, Ekman I, Carlström E. The impact of organizational culture on the outcome of hospital care: after the implementation of person-centred care. Scand J Public Health. 2014;42:104–10.
Bensbih S, Souadka A, Diez AG, Bouksour O. Patient centered care: focus on low and middle income countries and proposition of new conceptual model. J Med Surg Res. 2020;7:755–63.
Stranz A, Sörensdotter R. Interpretations of person-centered dementia care: same rhetoric, different practices? A comparative study of nursing homes in England and Sweden. J Aging Stud. 2016;38:70–80.
Zhou LM, Xu RH, Xu YH, Chang JH, Wang D. Inpatients’ perception of patient-centered care in Guangdong province, China: a cross-sectional study. Inquiry. 2021. https://doi.org/10.1177/00469580211059482 .
Marsh HW, Morin AJ, Parker PD, Kaur G. Exploratory structural equation modeling: an integration of the best features of exploratory and confirmatory factor analysis. Annu Rev Clin Psychol. 2014;10:85–110.
Asparouhov T, Muthén B. Exploratory structural equation modeling. Struct Equ Model Multidiscip J. 2009;16:397–438.
Cabedo-Peris J, Martí-Vilar M, Merino-Soto C, Ortiz-Morán M. Basic empathy scale: a systematic review and reliability generalization meta-analysis. Healthc (Basel). 2022;10:29–62.
Flora DB. Your coefficient alpha is probably wrong, but which coefficient omega is right? A tutorial on using R to obtain better reliability estimates. Adv Methods Pract Psychol Sci. 2020;3:484–501.
McNeish D. Thanks coefficient alpha, we’ll take it from here. Psychol Methods. 2018;23:412–33.
Hayes AF, Coutts JJ. Use omega rather than Cronbach’s alpha for estimating reliability. But… Commun Methods Meas. 2020;14:1–24.
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334.
McDonald R. Test theory: a unified approach. Mahwah, NJ: Erlbaum; 1999.
Polit DF. Getting serious about test-retest reliability: a critique of retest research and some recommendations. Qual Life Res. 2014;23:1713–20.
Ceylan D, Çizel B, Karakaş H. Testing destination image scale invariance for intergroup comparison. Tour Anal. 2020;25:239–51.
Rönkkö M, Cho E. An updated guideline for assessing discriminant validity. Organ Res Methods. 2022;25:6–14.
Hubley A, Zumbo B. Response processes in the context of validity: setting the stage. In: Zumbo B, Hubley A, editors. Understanding and investigating response processes in validation research. Cham, Switzerland: Springer; 2017. pp. 1–12.
Messick S. Validity of performance assessments. In: Philips G, editor. Technical issues in large-scale performance assessment. Washington, DC: Department of Education, National Center for Education Statistics; 1996. pp. 1–18.
Moss PA. The role of consequences in validity theory. Educ Meas Issues Pract. 1998;17:6–12.
Cronbach L. Five perspectives on validity argument. In: Wainer H, editor. Test validity. Hillsdale, MI: Erlbaum; 1988. pp. 3–17.
Birkle C, Pendlebury DA, Schnell J, Adams J. Web of Science as a data source for research on scientific and scholarly activity. Quant Sci Stud. 2020;1:363–76.
Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017;6:245.
Web of Science Group. Editorial selection process. Clarivate. 2024. https://clarivate.com/webofsciencegroup/solutions/%20editorial-selection-process/ . Accessed 12 Sept 2022.
Download references

Acknowledgements
The authors thank the casual helpers for their aid in information processing and searching.
This work is one of the results of research project HIM/2015/017/SSA.1207, “Effects of mindfulness training on psychological distress and quality of life of the family caregiver”. Main researcher: Filiberto Toledano-Toledano Ph.D. The present research was funded by federal funds for health research and was approved by the Commissions of Research, Ethics and Biosafety (Comisiones de Investigación, Ética y Bioseguridad), Hospital Infantil de México Federico Gómez, National Institute of Health. The source of federal funds did not control the study design, data collection, analysis, or interpretation, or decisions regarding publication.
Author information
Authors and affiliations.
Departamento de Educación, Facultad de Ciencias Sociales, Universidad Europea de Valencia, 46010, Valencia, Spain
Lluna Maria Bru-Luna
Departamento de Psicología Básica, Universitat de València, Blasco Ibáñez Avenue, 21, 46010, Valencia, Spain
Manuel Martí-Vilar
Departamento de Psicología, Instituto de Investigación de Psicología, Universidad de San Martín de Porres, Tomás Marsano Avenue 242, Lima 34, Perú
César Merino-Soto
Instituto Central de Gestión de la Investigación, Universidad Nacional Federico Villarreal, Carlos Gonzalez Avenue 285, 15088, San Miguel, Perú
José Livia-Segovia
Unidad de Investigación en Medicina Basada en Evidencias, Hospital Infantil de México Federico Gómez Instituto Nacional de Salud, Dr. Márquez 162, 06720, Doctores, Cuauhtémoc, Mexico
Juan Garduño-Espinosa & Filiberto Toledano-Toledano
Unidad de Investigación Multidisciplinaria en Salud, Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra, México-Xochimilco 289, Arenal de Guadalupe, 14389, Tlalpan, Mexico City, Mexico
Filiberto Toledano-Toledano
Dirección de Investigación y Diseminación del Conocimiento, Instituto Nacional de Ciencias e Innovación para la Formación de Comunidad Científica, INDEHUS, Periférico Sur 4860, Arenal de Guadalupe, 14389, Tlalpan, Mexico City, Mexico
You can also search for this author in PubMed Google Scholar
Contributions
L.M.B.L. conceptualized the study, collected the data, performed the formal anal- ysis, wrote the original draft, and reviewed and edited the subsequent drafts. M.M.V. collected the data and reviewed and edited the subsequent drafts. C.M.S. collected the data, performed the formal analysis, wrote the original draft, and reviewed and edited the subsequent drafts. J.L.S. collected the data, wrote the original draft, and reviewed and edited the subsequent drafts. J.G.E. collected the data and reviewed and edited the subsequent drafts. F.T.T. conceptualized the study and reviewed and edited the subsequent drafts. L.M.B.L. conceptualized the study and reviewed and edited the subsequent drafts. M.M.V. conceptualized the study and reviewed and edited the subsequent drafts. C.M.S. reviewed and edited the subsequent drafts. J.G.E. reviewed and edited the subsequent drafts. F.T.T. conceptualized the study; provided resources, software, and supervision; wrote the original draft; and reviewed and edited the subsequent drafts.
Corresponding author
Correspondence to Filiberto Toledano-Toledano .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Commissions of Research, Ethics and Biosafety (Comisiones de Investigación, Ética y Bioseguridad), Hospital Infantil de México Federico Gómez, National Institute of Health. HIM/2015/017/SSA.1207, “Effects of mindfulness training on psychological distress and quality of life of the family caregiver”.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bru-Luna, L.M., Martí-Vilar, M., Merino-Soto, C. et al. Person-centered care assessment tool with a focus on quality healthcare: a systematic review of psychometric properties. BMC Psychol 12 , 217 (2024). https://doi.org/10.1186/s40359-024-01716-7
Download citation
Received : 17 May 2023
Accepted : 07 April 2024
Published : 19 April 2024
DOI : https://doi.org/10.1186/s40359-024-01716-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Person-centered care assessment tool
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Open access
- Published: 24 April 2024
Breast cancer screening motivation and behaviours of women aged over 75 years: a scoping review
- Virginia Dickson-Swift 1 ,
- Joanne Adams 1 ,
- Evelien Spelten 1 ,
- Irene Blackberry 2 ,
- Carlene Wilson 3 , 4 , 5 &
- Eva Yuen 3 , 6 , 7 , 8
BMC Women's Health volume 24 , Article number: 256 ( 2024 ) Cite this article
137 Accesses
Metrics details
This scoping review aimed to identify and present the evidence describing key motivations for breast cancer screening among women aged ≥ 75 years. Few of the internationally available guidelines recommend continued biennial screening for this age group. Some suggest ongoing screening is unnecessary or should be determined on individual health status and life expectancy. Recent research has shown that despite recommendations regarding screening, older women continue to hold positive attitudes to breast screening and participate when the opportunity is available.
All original research articles that address motivation, intention and/or participation in screening for breast cancer among women aged ≥ 75 years were considered for inclusion. These included articles reporting on women who use public and private breast cancer screening services and those who do not use screening services (i.e., non-screeners).
The Joanna Briggs Institute (JBI) methodology for scoping reviews was used to guide this review. A comprehensive search strategy was developed with the assistance of a specialist librarian to access selected databases including: the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Web of Science and PsychInfo. The review was restricted to original research studies published since 2009, available in English and focusing on high-income countries (as defined by the World Bank). Title and abstract screening, followed by an assessment of full-text studies against the inclusion criteria was completed by at least two reviewers. Data relating to key motivations, screening intention and behaviour were extracted, and a thematic analysis of study findings undertaken.
A total of fourteen (14) studies were included in the review. Thematic analysis resulted in identification of three themes from included studies highlighting that decisions about screening were influenced by: knowledge of the benefits and harms of screening and their relationship to age; underlying attitudes to the importance of cancer screening in women's lives; and use of decision aids to improve knowledge and guide decision-making.
The results of this review provide a comprehensive overview of current knowledge regarding the motivations and screening behaviour of older women about breast cancer screening which may inform policy development.
Peer Review reports
Introduction
Breast cancer is now the most commonly diagnosed cancer in the world overtaking lung cancer in 2021 [ 1 ]. Across the globe, breast cancer contributed to 25.8% of the total number of new cases of cancer diagnosed in 2020 [ 2 ] and accounts for a high disease burden for women [ 3 ]. Screening for breast cancer is an effective means of detecting early-stage cancer and has been shown to significantly improve survival rates [ 4 ]. A recent systematic review of international screening guidelines found that most countries recommend that women have biennial mammograms between the ages of 40–70 years [ 5 ] with some recommending that there should be no upper age limit [ 6 , 7 , 8 , 9 , 10 , 11 , 12 ] and others suggesting that benefits of continued screening for women over 75 are not clear [ 13 , 14 , 15 ].
Some guidelines suggest that the decision to end screening should be determined based on the individual health status of the woman, their life expectancy and current health issues [ 5 , 16 , 17 ]. This is because the benefits of mammography screening may be limited after 7 years due to existing comorbidities and limited life expectancy [ 18 , 19 , 20 , 21 ], with some jurisdictions recommending breast cancer screening for women ≥ 75 years only when life expectancy is estimated as at least 7–10 years [ 22 ]. Others have argued that decisions about continuing with screening mammography should depend on individual patient risk and health management preferences [ 23 ]. This decision is likely facilitated by a discussion between a health care provider and patient about the harms and benefits of screening outside the recommended ages [ 24 , 25 ]. While mammography may enable early detection of breast cancer, it is clear that false-positive results and overdiagnosis Footnote 1 may occur. Studies have estimated that up to 25% of breast cancer cases in the general population may be over diagnosed [ 26 , 27 , 28 ].
The risk of being diagnosed with breast cancer increases with age and approximately 80% of new cases of breast cancer in high-income countries are in women over the age of 50 [ 29 ]. The average age of first diagnosis of breast cancer in high income countries is comparable to that of Australian women which is now 61 years [ 2 , 4 , 29 ]. Studies show that women aged ≥ 75 years generally have positive attitudes to mammography screening and report high levels of perceived benefits including early detection of breast cancer and a desire to stay healthy as they age [ 21 , 30 , 31 , 32 ]. Some women aged over 74 participate, or plan to participate, in screening despite recommendations from health professionals and government guidelines advising against it [ 33 ]. Results of a recent review found that knowledge of the recommended guidelines and the potential harms of screening are limited and many older women believed that the benefits of continued screening outweighed the risks [ 30 ].
Very few studies have been undertaken to understand the motivations of women to screen or to establish screening participation rates among women aged ≥ 75 and older. This is surprising given that increasing age is recognised as a key risk factor for the development of breast cancer, and that screening is offered in many locations around the world every two years up until 74 years. The importance of this topic is high given the ambiguity around best practice for participation beyond 74 years. A preliminary search of Open Science Framework, PROSPERO, Cochrane Database of Systematic Reviews and JBI Evidence Synthesis in May 2022 did not locate any reviews on this topic.
This scoping review has allowed for the mapping of a broad range of research to explore the breadth and depth of the literature, summarize the evidence and identify knowledge gaps [ 34 , 35 ]. This information has supported the development of a comprehensive overview of current knowledge of motivations of women to screen and screening participation rates among women outside the targeted age of many international screening programs.
Materials and methods
Research question.
The research question for this scoping review was developed by applying the Population—Concept—Context (PCC) framework [ 36 ]. The current review addresses the research question “What research has been undertaken in high-income countries (context) exploring the key motivations to screen for breast cancer and screening participation (concepts) among women ≥ 75 years of age (population)?
Eligibility criteria
Participants.
Women aged ≥ 75 years were the key population. Specifically, motivations to screen and screening intention and behaviour and the variables that discriminate those who screen from those who do not (non-screeners) were utilised as the key predictors and outcomes respectively.
From a conceptual perspective it was considered that motivation led to behaviour, therefore articles that described motivation and corresponding behaviour were considered. These included articles reporting on women who use public (government funded) and private (fee for service) breast cancer screening services and those who do not use screening services (i.e., non-screeners).
The scope included high-income countries using the World Bank definition [ 37 ]. These countries have broadly similar health systems and opportunities for breast cancer screening in both public and private settings.
Types of sources
All studies reporting original research in peer-reviewed journals from January 2009 were eligible for inclusion, regardless of design. This date was selected due to an evaluation undertaken for BreastScreen Australia recommending expansion of the age group to include 70–74-year-old women [ 38 ]. This date was also indicative of international debate regarding breast cancer screening effectiveness at this time [ 39 , 40 ]. Reviews were also included, regardless of type—scoping, systematic, or narrative. Only sources published in English and available through the University’s extensive research holdings were eligible for inclusion. Ineligible materials were conference abstracts, letters to the editor, editorials, opinion pieces, commentaries, newspaper articles, dissertations and theses.
This scoping review was registered with the Open Science Framework database ( https://osf.io/fd3eh ) and followed Joanna Briggs Institute (JBI) methodology for scoping reviews [ 35 , 36 ]. Although ethics approval is not required for scoping reviews the broader study was approved by the University Ethics Committee (approval number HEC 21249).
Search strategy
A pilot search strategy was developed in consultation with an expert health librarian and tested in MEDLINE (OVID) and conducted on 3 June 2022. Articles from this pilot search were compared with seminal articles previously identified by the members of the team and used to refine the search terms. The search terms were then searched as both keywords and subject headings (e.g., MeSH) in the titles and abstracts and Boolean operators employed. A full MEDLINE search was then carried out by the librarian (see Table 1 ). This search strategy was adapted for use in each of the following databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medical Literature Analysis and Retrieval System Online (MEDLINE), Web of Science and PsychInfo databases. The references of included studies have been hand-searched to identify any additional evidence sources.
Study/source of evidence selection
Following the search, all identified citations were collated and uploaded into EndNote v.X20 (Clarivate Analytics, PA, USA) and duplicates removed. The resulting articles were then imported into Covidence – Cochrane’s systematic review management software [ 41 ]. Duplicates were removed once importation was complete, and title and abstract screening was undertaken against the eligibility criteria. A sample of 25 articles were assessed by all reviewers to ensure reliability in the application of the inclusion and exclusion criteria. Team discussion was used to ensure consistent application. The Covidence software supports blind reviewing with two reviewers required at each screening phase. Potentially relevant sources were retrieved in full text and were assessed against the inclusion criteria by two independent reviewers. Conflicts were flagged within the software which allows the team to discuss those that have disagreements until a consensus was reached. Reasons for exclusion of studies at full text were recorded and reported in the scoping review. The Preferred Reporting Items of Systematic Reviews extension for scoping reviews (PRISMA-ScR) checklist was used to guide the reporting of the review [ 42 ] and all stages were documented using the PRISMA-ScR flow chart [ 42 ].
Data extraction
A data extraction form was created in Covidence and used to extract study characteristics and to confirm the study’s relevance. This included specific details such as article author/s, title, year of publication, country, aim, population, setting, data collection methods and key findings relevant to the review question. The draft extraction form was modified as needed during the data extraction process.
Data analysis and presentation
Extracted data were summarised in tabular format (see Table 2 ). Consistent with the guidelines for the effective reporting of scoping reviews [ 43 ] and the JBI framework [ 35 ] the final stage of the review included thematic analysis of the key findings of the included studies. Study findings were imported into QSR NVivo with coding of each line of text. Descriptive codes reflected key aspects of the included studies related to the motivations and behaviours of women > 75 years about breast cancer screening.
In line with the reporting requirements for scoping reviews the search results for this review are presented in Fig. 1 [ 44 ].
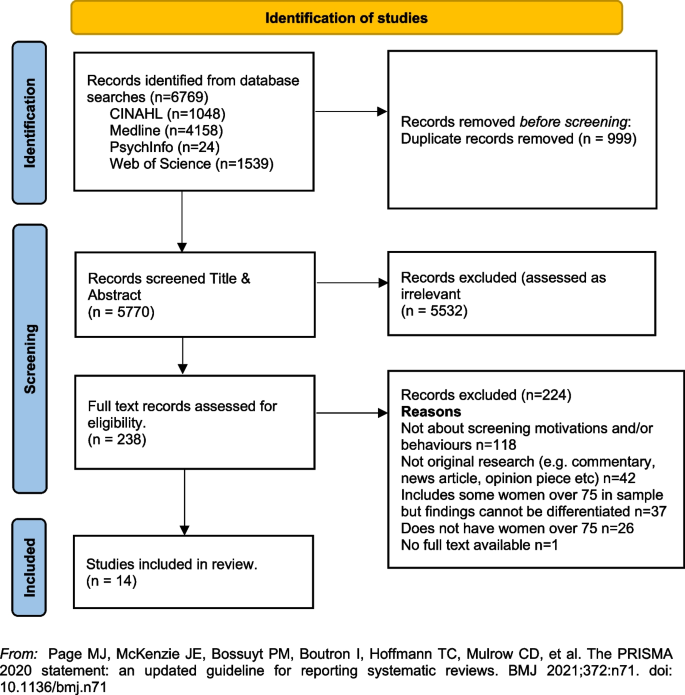
PRISMA Flowchart. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
A total of fourteen [ 14 ] studies were included in the review with studies from the following countries, US n = 12 [ 33 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 ], UK n = 1 [ 23 ] and France n = 1 [ 56 ]. Sample sizes varied, with most containing fewer than 50 women ( n = 8) [ 33 , 45 , 46 , 48 , 51 , 52 , 55 ]. Two had larger samples including a French study with 136 women (a sub-set of a larger sample) [ 56 ], and one mixed method study in the UK with a sample of 26 women undertaking interviews and 479 women completing surveys [ 23 ]. One study did not report exact numbers [ 50 ]. Three studies [ 47 , 53 , 54 ] were undertaken by a group of researchers based in the US utilising the same sample of women, however each of the papers focused on different primary outcomes. The samples in the included studies were recruited from a range of locations including primary medical care clinics, specialist medical clinics, University affiliated medical clinics, community-based health centres and community outreach clinics [ 47 , 53 , 54 ].
Data collection methods varied and included: quantitative ( n = 8), qualitative ( n = 5) and mixed methods ( n = 1). A range of data collection tools and research designs were utilised; pre/post, pilot and cross-sectional surveys, interviews, and secondary analysis of existing data sets. Seven studies focused on the use of a Decision Aids (DAs), either in original or modified form, developed by Schonberg et al. [ 55 ] as a tool to increase knowledge about the harms and benefits of screening for older women [ 45 , 47 , 48 , 49 , 52 , 54 , 55 ]. Three studies focused on intention to screen [ 33 , 53 , 56 ], two on knowledge of, and attitudes to, screening [ 23 , 46 ], one on information needs relating to risks and benefits of screening discontinuation [ 51 ], and one on perceptions about discontinuation of screening and impact of social interactions on screening [ 50 ].
The three themes developed from the analysis of the included studies highlighted that decisions about screening were primarily influenced by: (1) knowledge of the benefits and harms of screening and their relationship to age; (2) underlying attitudes to the importance of cancer screening in women's lives; and (3) exposure to decision aids designed to facilitate informed decision-making. Each of these themes will be presented below drawing on the key findings of the appropriate studies. The full dataset of extracted data can be found in Table 2 .
Knowledge of the benefits and harms of screening ≥ 75 years
The decision to participate in routine mammography is influenced by individual differences in cognition and affect, interpersonal relationships, provider characteristics, and healthcare system variables. Women typically perceive mammograms as a positive, beneficial and routine component of care [ 46 ] and an important aspect of taking care of themselves [ 23 , 46 , 49 ]. One qualitative study undertaken in the US showed that few women had discussed mammography cessation or the potential harms of screening with their health care providers and some women reported they would insist on receiving mammography even without a provider recommendation to continue screening [ 46 ].
Studies suggested that ageing itself, and even poor health, were not seen as reasonable reasons for screening cessation. For many women, guidance from a health care provider was deemed the most important influence on decision-making [ 46 ]. Preferences for communication about risk and benefits were varied with one study reporting women would like to learn more about harms and risks and recommended that this information be communicated via physicians or other healthcare providers, included in brochures/pamphlets, and presented outside of clinical settings (e.g., in community-based seniors groups) [ 51 ]. Others reported that women were sometimes sceptical of expert and government recommendations [ 33 ] although some were happy to participate in discussions with health educators or care providers about breast cancer screening harms and benefits and potential cessation [ 52 ].
Underlying attitudes to the importance of cancer screening at and beyond 75 years
Included studies varied in describing the importance of screening, with some attitudes based on past attendance and some based on future intentions to screen. Three studies reported findings indicating that some women intended to continue screening after 75 years of age [ 23 , 45 , 46 ], with one study in the UK reporting that women supported an extension of the automatic recall indefinitely, regardless of age or health status. In this study, failure to invite older women to screen was interpreted as age discrimination [ 23 ]. The desire to continue screening beyond 75 was also highlighted in a study from France that found that 60% of the women ( n = 136 aged ≥ 75) intended to pursue screening in the future, and 27 women aged ≥ 75, who had never undergone mammography previously (36%), intended to do so in the future [ 56 ]. In this same study, intentions to screen varied significantly [ 56 ]. There were no sociodemographic differences observed between screened and unscreened women with regard to level of education, income, health risk behaviour (smoking, alcohol consumption), knowledge about the importance and the process of screening, or psychological features (fear of the test, fear of the results, fear of the disease, trust in screening impact) [ 56 ]. Further analysis showed that three items were statistically correlated with a higher rate of attendance at screening: (1) screening was initiated by a physician; (2) the women had a consultation with a gynaecologist during the past 12 months; and (3) the women had already undergone at least five screening mammograms. Analysis highlighted that although average income, level of education, psychological features or other types of health risk behaviours did not impact screening intention, having a mammogram previously impacted likelihood of ongoing screening. There was no information provided that explained why women who had not previously undergone screening might do so in the future.
A mixed methods study in the UK reported similar findings [ 23 ]. Utilising interviews ( n = 26) and questionnaires ( n = 479) with women ≥ 70 years (median age 75 years) the overwhelming result (90.1%) was that breast screening should be offered to all women indefinitely regardless of age, health status or fitness [ 23 ], and that many older women were keen to continue screening. Both the interview and survey data confirmed women were uncertain about eligibility for breast screening. The survey data showed that just over half the women (52.9%) were unaware that they could request mammography or knew how to access it. Key reasons for screening discontinuation were not being invited for screening (52.1%) and not knowing about self-referral (35.1%).
Women reported that not being invited to continue screening sent messages that screening was no longer important or required for this age group [ 23 ]. Almost two thirds of the women completing the survey (61.6%) said they would forget to attend screening without an invitation. Other reasons for screening discontinuation included transport difficulties (25%) and not wishing to burden family members (24.7%). By contrast, other studies have reported that women do not endorse discontinuation of screening mammography due to advancing age or poor health, but some may be receptive to reducing screening frequency on recommendation from their health care provider [ 46 , 51 ].
Use of Decision Aids (DAs) to improve knowledge and guide screening decision-making
Many women reported poor knowledge about the harms and benefits of screening with studies identifying an important role for DAs. These aids have been shown to be effective in improving knowledge of the harms and benefits of screening [ 45 , 54 , 55 ] including for women with low educational attainment; as compared to women with high educational attainment [ 47 ]. DAs can increase knowledge about screening [ 47 , 49 ] and may decrease the intention to continue screening after the recommended age [ 45 , 52 , 54 ]. They can be used by primary care providers to support a conversation about breast screening intention and reasons for discontinuing screening. In one pilot study undertaken in the US using a DA, 5 of the 8 women (62.5%) indicated they intended to continue to receive mammography; however, 3 participants planned to get them less often [ 45 ]. When asked whether they thought their physician would want them to get a mammogram, 80% said “yes” on pre-test; this figure decreased to 62.5% after exposure to the DA. This pilot study suggests that the use of a decision-aid may result in fewer women ≥ 75 years old continuing to screen for breast cancer [ 45 ].
Similar findings were evident in two studies drawing on the same data undertaken in the US [ 48 , 53 ]. Using a larger sample ( n = 283), women’s intentions to screen prior to a visit with their primary care provider and then again after exposure to the DA were compared. Results showed that 21.7% of women reduced their intention to be screened, 7.9% increased their intentions to be screened, and 70.4% did not change. Compared to those who had no change or increased their screening intentions, women who had a decrease in screening intention were significantly less likely to receive screening after 18 months. Generally, studies have shown that women aged 75 and older find DAs acceptable and helpful [ 47 , 48 , 49 , 55 ] and using them had the potential to impact on a women’s intention to screen [ 55 ].
Cadet and colleagues [ 49 ] explored the impact of educational attainment on the use of DAs. Results highlight that education moderates the utility of these aids; women with lower educational attainment were less likely to understand all the DA’s content (46.3% vs 67.5%; P < 0.001); had less knowledge of the benefits and harms of mammography (adjusted mean ± standard error knowledge score, 7.1 ± 0.3 vs 8.1 ± 0.3; p < 0.001); and were less likely to have their screening intentions impacted (adjusted percentage, 11.4% vs 19.4%; p = 0.01).
This scoping review summarises current knowledge regarding motivations and screening behaviours of women over 75 years. The findings suggest that awareness of the importance of breast cancer screening among women aged ≥ 75 years is high [ 23 , 46 , 49 ] and that many women wish to continue screening regardless of perceived health status or age. This highlights the importance of focusing on motivation and screening behaviours and the multiple factors that influence ongoing participation in breast screening programs.
The generally high regard attributed to screening among women aged ≥ 75 years presents a complex challenge for health professionals who are focused on potential harm (from available national and international guidelines) in ongoing screening for women beyond age 75 [ 18 , 20 , 57 ]. Included studies highlight that many women relied on the advice of health care providers regarding the benefits and harms when making the decision to continue breast screening [ 46 , 51 , 52 ], however there were some that did not [ 33 ]. Having a previous pattern of screening was noted as being more significant to ongoing intention than any other identified socio-demographic feature [ 56 ]. This is perhaps because women will not readily forgo health care practices that they have always considered important and that retain ongoing importance for the broader population.
For those women who had discontinued screening after the age of 74 it was apparent that the rationale for doing so was not often based on choice or receipt of information, but rather on factors that impact decision-making in relation to screening. These included no longer receiving an invitation to attend, transport difficulties and not wanting to be a burden on relatives or friends [ 23 , 46 , 51 ]. Ongoing receipt of invitations to screen was an important aspect of maintaining a capacity to choose [ 23 ]. This was particularly important for those women who had been regular screeners.
Women over 75 require more information to make decisions regarding screening [ 23 , 52 , 54 , 55 ], however health care providers must also be aware that the element of choice is important for older women. Having a capacity to choose avoids any notion of discrimination based on age, health status, gender or sociodemographic difference and acknowledges the importance of women retaining control over their health [ 23 ]. It was apparent that some women would choose to continue screening at a reduced frequency if this option was available and that women should have access to information facilitating self-referral [ 23 , 45 , 46 , 51 , 56 ].
Decision-making regarding ongoing breast cancer screening has been facilitated via the use of Decision Aids (DAs) within clinical settings [ 54 , 55 ]. While some studies suggest that women will make a decision regardless of health status, the use of DAs has impacted women’s decision to screen. While this may have limited benefit for those of lower educational attainment [ 48 ] they have been effective in improving knowledge relating to harms and benefits of screening particularly where they have been used to support a conversation with women about the value of screening [ 54 , 55 , 56 ].
Women have identified challenges in engaging in conversations with health care providers regarding ongoing screening, because providers frequently draw on projections of life expectancy and over-diagnosis [ 17 , 51 ]. As a result, these conversations about screening after age 75 years often do not occur [ 46 ]. It is likely that health providers may need more support and guidance in leading these conversations. This may be through the use of DAs or standardised checklists. It may be possible to incorporate these within existing health preventive measures for this age group. The potential for advice regarding ongoing breast cancer screening to be available outside of clinical settings may provide important pathways for conversations with women regarding health choices. Provision of information and advice in settings such as community based seniors groups [ 51 ] offers a potential platform to broaden conversations and align sources of information, not only with health professionals but amongst women themselves. This may help to address any misconception regarding eligibility and access to services [ 23 ]. It may also be aligned with other health promotion and lifestyle messages provided to this age group.
Limitations of the review
The searches that formed the basis of this review were carried in June 2022. Although the search was comprehensive, we have only captured those studies that were published in the included databases from 2009. There may have been other studies published outside of these periods. We also limited the search to studies published in English with full-text availability.
The emphasis of a scoping review is on comprehensive coverage and synthesis of the key findings, rather than on a particular standard of evidence and, consequently a quality assessment of the included studies was not undertaken. This has resulted in the inclusion of a wide range of study designs and data collection methods. It is important to note that three studies included in the review drew on the same sample of women (283 over > 75)[ 49 , 53 , 54 ]. The results of this review provide valuable insights into motivations and behaviours for breast cancer screening for older women, however they should be interpreted with caution given the specific methodological and geographical limitations.
Conclusion and recommendations
This scoping review highlighted a range of key motivations and behaviours in relation to breast cancer screening for women ≥ 75 years of age. The results provide some insight into how decisions about screening continuation after 74 are made and how informed decision-making can be supported. Specifically, this review supports the following suggestions for further research and policy direction:
Further research regarding breast cancer screening motivations and behaviours for women over 75 would provide valuable insight for health providers delivering services to women in this age group.
Health providers may benefit from the broader use of decision aids or structured checklists to guide conversations with women over 75 regarding ongoing health promotion/preventive measures.
Providing health-based information in non-clinical settings frequented by women in this age group may provide a broader reach of information and facilitate choices. This may help to reduce any perception of discrimination based on age, health status or socio-demographic factors.
Availability of data and materials
All data generated or analysed during this study is included in this published article (see Table 2 above).
Cancer Australia, in their 2014 position statement, define “overdiagnosis” in the following way. ‘’Overdiagnosis’ from breast screening does not refer to error or misdiagnosis, but rather refers to breast cancer diagnosed by screening that would not otherwise have been diagnosed during a woman’s lifetime. “Overdiagnosis” includes all instances where cancers detected through screening (ductal carcinoma in situ or invasive breast cancer) might never have progressed to become symptomatic during a woman’s life, i.e., cancer that would not have been detected in the absence of screening. It is not possible to precisely predict at diagnosis, to which cancers overdiagnosis would apply.” (accessed 22. nd August 2022; https://www.canceraustralia.gov.au/resources/position-statements/overdiagnosis-mammographic-screening ).
World Health Organization. Breast Cancer Geneva: WHO; 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=Reducing%20global%20breast%20cancer%20mortality,and%20comprehensive%20breast%20cancer%20management .
International Agency for Research on Cancer (IARC). IARC Handbooks on Cancer Screening: Volume 15 Breast Cancer Geneva: IARC; 2016 [Available from: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Handbooks-Of-Cancer-Prevention/Breast-Cancer-Screening-2016 .
Australian Institute of Health and Welfare. Cancer in Australia 2021 [Available from: https://www.canceraustralia.gov.au/cancer-types/breast-cancer/statistics .
Breast Cancer Network Australia. Current breast cancer statistics in Australia 2020 [Available from: https://www.bcna.org.au/media/7111/bcna-2019-current-breast-cancer-statistics-in-australia-11jan2019.pdf .
Ren W, Chen M, Qiao Y, Zhao F. Global guidelines for breast cancer screening: A systematic review. The Breast. 2022;64:85–99.
Article PubMed PubMed Central Google Scholar
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(8):1194–220.
Article CAS PubMed Google Scholar
Hamashima C, Hattori M, Honjo S, Kasahara Y, Katayama T, Nakai M, et al. The Japanese guidelines for breast cancer screening. Jpn J Clin Oncol. 2016;46(5):482–92.
Article PubMed Google Scholar
Bevers TB, Helvie M, Bonaccio E, Calhoun KE, Daly MB, Farrar WB, et al. Breast cancer screening and diagnosis, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Net. 2018;16(11):1362–89.
Article Google Scholar
He J, Chen W, Li N, Shen H, Li J, Wang Y, et al. China guideline for the screening and early detection of female breast cancer (2021, Beijing). Zhonghua Zhong liu za zhi [Chinese Journal of Oncology]. 2021;43(4):357–82.
CAS PubMed Google Scholar
Cancer Australia. Early detection of breast cancer 2021 [cited 2022 25 July]. Available from: https://www.canceraustralia.gov.au/resources/position-statements/early-detection-breast-cancer .
Schünemann HJ, Lerda D, Quinn C, Follmann M, Alonso-Coello P, Rossi PG, et al. Breast Cancer Screening and Diagnosis: A Synopsis of the European Breast Guidelines. Ann Intern Med. 2019;172(1):46–56.
World Health Organization. WHO Position Paper on Mammography Screening Geneva WHO. 2016.
Google Scholar
Lansdorp-Vogelaar I, Gulati R, Mariotto AB. Personalizing age of cancer screening cessation based on comorbid conditions: model estimates of harms and benefits. Ann Intern Med. 2014;161:104.
Lee CS, Moy L, Joe BN, Sickles EA, Niell BL. Screening for Breast Cancer in Women Age 75 Years and Older. Am J Roentgenol. 2017;210(2):256–63.
Broeders M, Moss S, Nystrom L. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J Med Screen. 2012;19(suppl 1):14.
Oeffinger KC, Fontham ETH, Etzioni R, Herzig A, Michaelson JS, Shih YCT, et al. Breast cancer screening for women at average risk: 2015 Guideline update from the American cancer society. JAMA - Journal of the American Medical Association. 2015;314(15):1599–614.
Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA. 2014;311:1336.
Article CAS PubMed PubMed Central Google Scholar
Braithwaite D, Walter LC, Izano M, Kerlikowske K. Benefits and harms of screening mammography by comorbidity and age: a qualitative synthesis of observational studies and decision analyses. J Gen Intern Med. 2016;31:561.
Braithwaite D, Mandelblatt JS, Kerlikowske K. To screen or not to screen older women for breast cancer: a conundrum. Future Oncol. 2013;9(6):763–6.
Demb J, Abraham L, Miglioretti DL, Sprague BL, O’Meara ES, Advani S, et al. Screening Mammography Outcomes: Risk of Breast Cancer and Mortality by Comorbidity Score and Age. Jnci-Journal of the National Cancer Institute. 2020;112(6):599–606.
Demb J, Akinyemiju T, Allen I, Onega T, Hiatt RA, Braithwaite D. Screening mammography use in older women according to health status: a systematic review and meta-analysis. Clin Interv Aging. 2018;13:1987–97.
Qaseem A, Lin JS, Mustafa RA, Horwitch CA, Wilt TJ. Screening for Breast Cancer in Average-Risk Women: A Guidance Statement From the American College of Physicians. Ann Intern Med. 2019;170(8):547–60.
Collins K, Winslow M, Reed MW, Walters SJ, Robinson T, Madan J, et al. The views of older women towards mammographic screening: a qualitative and quantitative study. Br J Cancer. 2010;102(10):1461–7.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605–13.
Hersch J, Jansen J, Barratt A, Irwig L, Houssami N, Howard K, et al. Women’s views on overdiagnosis in breast cancer screening: a qualitative study. BMJ : British Medical Journal. 2013;346:f158.
De Gelder R, Heijnsdijk EAM, Van Ravesteyn NT, Fracheboud J, Draisma G, De Koning HJ. Interpreting overdiagnosis estimates in population-based mammography screening. Epidemiol Rev. 2011;33(1):111–21.
Monticciolo DL, Helvie MA, Edward HR. Current issues in the overdiagnosis and overtreatment of breast cancer. Am J Roentgenol. 2018;210(2):285–91.
Shepardson LB, Dean L. Current controversies in breast cancer screening. Semin Oncol. 2020;47(4):177–81.
National Cancer Control Centre. Cancer incidence in Australia 2022 [Available from: https://ncci.canceraustralia.gov.au/diagnosis/cancer-incidence/cancer-incidence .
Austin JD, Shelton RC, Lee Argov EJ, Tehranifar P. Older Women’s Perspectives Driving Mammography Screening Use and Overuse: a Narrative Review of Mixed-Methods Studies. Current Epidemiology Reports. 2020;7(4):274–89.
Austin JD, Tehranifar P, Rodriguez CB, Brotzman L, Agovino M, Ziazadeh D, et al. A mixed-methods study of multi-level factors influencing mammography overuse among an older ethnically diverse screening population: implications for de-implementation. Implementation Science Communications. 2021;2(1):110.
Demb J, Allen I, Braithwaite D. Utilization of screening mammography in older women according to comorbidity and age: protocol for a systematic review. Syst Rev. 2016;5(1):168.
Housten AJ, Pappadis MR, Krishnan S, Weller SC, Giordano SH, Bevers TB, et al. Resistance to discontinuing breast cancer screening in older women: A qualitative study. Psychooncology. 2018;27(6):1635–41.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil HAE, et al. Chapter 11: Scoping reviews. JBI Manual for Evidence Synthesis 2020 [Available from: https://jbi-global-wiki.refined.site/space/MANUAL .
Peters MD, Godfrey C, McInerney P, Khalil H, Larsen P, Marnie C, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI evidence synthesis. 2022;20(4):953–68.
Fantom NJ, Serajuddin U. The World Bank’s classification of countries by income. World Bank Policy Research Working Paper; 2016.
Book Google Scholar
BreastScreen Australia Evaluation Taskforce. BreastScreen Australia Evaluation. Evaluation final report: Screening Monograph No 1/2009. Canberra; Australia Australian Government Department of Health and Ageing; 2009.
Nelson HD, Cantor A, Humphrey L. Screening for breast cancer: a systematic review to update the 2009 U.S. Preventive Services Task Force recommendation2016.
Woolf SH. The 2009 breast cancer screening recommendations of the US Preventive Services Task Force. JAMA. 2010;303(2):162–3.
Covidence systematic review software. [Internet]. Veritas-Health-Innovation 2020. Available from: https://www.covidence.org/ .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16(1):15.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Beckmeyer A, Smith RM, Miles L, Schonberg MA, Toland AE, Hirsch H. Pilot Evaluation of Patient-centered Survey Tools for Breast Cancer Screening Decision-making in Women 75 and Older. Health Behavior and Policy Review. 2020;7(1):13–8.
Brotzman LE, Shelton RC, Austin JD, Rodriguez CB, Agovino M, Moise N, et al. “It’s something I’ll do until I die”: A qualitative examination into why older women in the U.S. continue screening mammography. Canc Med. 2022;11(20):3854–62.
Article CAS Google Scholar
Cadet T, Pinheiro A, Karamourtopoulos M, Jacobson AR, Aliberti GM, Kistler CE, et al. Effects by educational attainment of a mammography screening patient decision aid for women aged 75 years and older. Cancer. 2021;127(23):4455–63.
Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Gilliam EA, Primeau S, et al. Evaluation of a mammography decision aid for women 75 and older at risk for lower health literacy in a pretest-posttest trial. Patient Educ Couns. 2021;104(9):2344–50.
Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Siska M, Schonberg MA. Modifying a mammography decision aid for older adult women with risk factors for low health literacy. Health Lit Res Prac. 2021;5(2):e78–90.
Gray N, Picone G. Evidence of Large-Scale Social Interactions in Mammography in the United States. Atl Econ J. 2018;46(4):441–57.
Hoover DS, Pappadis MR, Housten AJ, Krishnan S, Weller SC, Giordano SH, et al. Preferences for Communicating about Breast Cancer Screening Among Racially/Ethnically Diverse Older Women. Health Commun. 2019;34(7):702–6.
Salzman B, Bistline A, Cunningham A, Silverio A, Sifri R. Breast Cancer Screening Shared Decision-Making in Older African-American Women. J Natl Med Assoc. 2020;112(5):556–60.
PubMed Google Scholar
Schoenborn NL, Pinheiro A, Kistler CE, Schonberg MA. Association between Breast Cancer Screening Intention and Behavior in the Context of Screening Cessation in Older Women. Med Decis Making. 2021;41(2):240–4.
Schonberg MA, Kistler CE, Pinheiro A, Jacobson AR, Aliberti GM, Karamourtopoulos M, et al. Effect of a Mammography Screening Decision Aid for Women 75 Years and Older: A Cluster Randomized Clinical Trial. JAMA Intern Med. 2020;180(6):831–42.
Schonberg MA, Hamel MB, Davis RB. Development and evaluation of a decision aid on mammography screening for women 75 years and older. JAMA Intern Med. 2014;174:417.
Eisinger F, Viguier J, Blay J-Y, Morère J-F, Coscas Y, Roussel C, et al. Uptake of breast cancer screening in women aged over 75years: a controversy to come? Eur J Cancer Prev. 2011;20(Suppl 1):S13-5.
Schonberg MA, Breslau ES, McCarthy EP. Targeting of Mammography Screening According to Life Expectancy in Women Aged 75 and Older. J Am Geriatr Soc. 2013;61(3):388–95.
Download references
Acknowledgements
We would like to acknowledge Ange Hayden-Johns (expert librarian) who assisted with the development of the search criteria and undertook the relevant searches and Tejashree Kangutkar who assisted with some of the Covidence work.
This work was supported by funding from the Australian Government Department of Health and Aged Care (ID: Health/20–21/E21-10463).
Author information
Authors and affiliations.
Violet Vines Centre for Rural Health Research, La Trobe Rural Health School, La Trobe University, P.O. Box 199, Bendigo, VIC, 3552, Australia
Virginia Dickson-Swift, Joanne Adams & Evelien Spelten
Care Economy Research Institute, La Trobe University, Wodonga, Australia
Irene Blackberry
Olivia Newton-John Cancer Wellness and Research Centre, Austin Health, Melbourne, Australia
Carlene Wilson & Eva Yuen
Melbourne School of Population and Global Health, Melbourne University, Melbourne, Australia
Carlene Wilson
School of Psychology and Public Health, La Trobe University, Bundoora, Australia
Institute for Health Transformation, Deakin University, Burwood, Australia
Centre for Quality and Patient Safety, Monash Health Partnership, Monash Health, Clayton, Australia
You can also search for this author in PubMed Google Scholar
Contributions
VDS conceived and designed the scoping review. VDS & JA developed the search strategy with librarian support, and all authors (VDS, JA, ES, IB, CW, EY) participated in the screening and data extraction stages and assisted with writing the review. All authors provided editorial support and read and approved the final manuscript prior to submission.
Corresponding author
Correspondence to Joanne Adams .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics approval and consent to participate was not required for this study.
Consent for publication
Consent for publication was not required for this study.
Competing interest
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dickson-Swift, V., Adams, J., Spelten, E. et al. Breast cancer screening motivation and behaviours of women aged over 75 years: a scoping review. BMC Women's Health 24 , 256 (2024). https://doi.org/10.1186/s12905-024-03094-z
Download citation
Received : 06 September 2023
Accepted : 15 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12905-024-03094-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Mammography
- Older women
- Scoping review
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Integr Healthc J
- v.4(1); 2022
- PMC10327458

Equity in healthcare access and service coverage for older people: a scoping review of the conceptual literature
Christopher carroll.
1 School of Health and Related Research (ScHARR), The University of Sheffield, Sheffield, UK
Katie Sworn
Andrew booth, aki tsuchiya.
2 Department of Economics, The University of Sheffield, Sheffield, UK
Michelle Maden
3 Institute of Population Health, University of Liverpool, Liverpool, UK
Megumi Rosenberg
4 Centre for Health Development, World Health Organization, Kobe, Hyogo, Japan
Associated Data
ihj-2021-000092supp001.pdf
ihj-2021-000092supp002.pdf
ihj-2021-000092supp003.pdf
There is currently no global review of the conceptual literature on the equity of healthcare coverage (including access) for older people. It is important to understand the factors affecting access to health and social care for this group, so that policy and service actions can be taken to reduce potential inequities.
A scoping review of published and grey literature was conducted with the aim of summarising how health and social care service access and coverage for older people has been conceptualised. PubMed, MEDLINE, PsycINFO, CINAHL, Web of Science, SciELO, LILACS, BIREME and Global Index Medicus were searched. Selection of sources and data charting were conducted independently by two reviewers.
The database searches retrieved 10 517 citations; 32 relevant articles were identified for inclusion from a global evidence base. Data were summarised and a meta-framework and model produced listing concepts specific to equitable health and social care service coverage relating to older people. The meta-framework identified the following relevant factors: acceptability, affordability, appropriateness, availability and resources, awareness, capacity for decision-making, need, personal social and cultural circumstances, physical accessibility.
This scoping review is relevant to the development and specification of policy for older people. It conceptualises those factors, such as acceptability and affordability, that affect an older person’s ability and capacity to access integrated, person-centred health and social care services in a meaningful way. These factors should be taken into account when seeking to determine whether equity in service use or access is being achieved for older people.
Significance of the study
What is already known about this subject.
- Age is a known factor predicting inequity of access to healthcare.
- Multiple factors affecting different groups of people, such as age, income, education, location, are known to be relevant in accessing healthcare.
- Individual factors such as literacy, ethnicity, minority status and location, have been explored in empirical and conceptual studies examining older people’s access of services
What does this study add?
- To our knowledge, this is the first global review of the conceptual literature on equity of health and social care coverage (including access) for older people.
- It conceptualises exactly those factors that might affect equity of access to integrated and person-centred health and social care services for older people, including the availability and affordability of services, and older people’s own capacities, needs and perceptions of what is acceptable.
- It conceptualises the dynamic relationships between the individual older person, available services and social and political infrastructures
How might this impact on clinical practice or future developments?
This review is relevant to the development and specification of policy for older people because:
- It outlines factors that need to be taken into account when seeking to monitor or measure whether equity in service use or access is being achieved for older people in any country or setting, for example, are older people aware of services and their eligibility for certain services; are appropriate services available, do they satisfy their needs in an acceptable manner; can they afford them; can they access them—physically and intellectually (health literacy), etc.
- It highlights how new, more holistic and complex means of collecting data about older people, and their needs, is required if the local nature of inequity is to be understood, so that it can be addressed by policy.
Introduction
A sizeable body of literature addresses equity and health service coverage or access, though there is no universal consensus on definitions of these terms or the optimal perspective to be taken. Authors might variously assume a conceptual or theoretical perspective, might consider specific countries and systems, 1–5 or employ a policy perspective driven by the principle of universal health coverage (UHC). 6–8 Principles such as UHC link ideas of access to the performance of healthcare systems. 9 10 Researchers have also considered this challenge both for whole populations and for particular disadvantaged groups. 11 The literature defining health service access is often limited to using broad terms, such as availability, coverage and provision. 3 In its broadest sense, it might be considered to refer to a person’s ability, capacity or eligibility to use or potentially use a relevant service. Equity in healthcare has been defined as the 'just distribution of healthcare according to need', 8 but different definitions of what is ‘just’ and what constitutes ‘need’ are possible, and ‘distribution’ represents a different concept from access. 12 However, reviews of equity find that the term is often not clearly defined, even in policy documents. Instead it is only implied, using concepts and values such as social justice or inclusion, and typically assessed in simple terms for example, by gender, socioeconomic factors or place of residence. 3 13 Although age is frequently considered among potential predictors of access in quantitative analyses (usually defined in terms of actual service use because this is easier to measure), 13 it is much less common to conceptualise equity in health service use for older people, as a distinct group.
Conceptual content often proves elusive within the literature, especially when factors must be identified from within empirical papers, theoretical discussions or parent theories. 14 Recent reviews of existing frameworks relevant to equity and UHC 3 15 do include a review of the conceptual literature, 16 but we are not aware of any on the combined challenges of equity, UHC and older people. Yet older people represent a particular, potentially disadvantaged group because of their more extensive and complex healthcare needs, and the challenges they are likely to experience accessing relevant services. It is therefore important to understand those factors that affect access to healthcare for this group so that any given national health system can monitor them, and take appropriate action to reduce potential inequities. This scoping review of the conceptual (that is, theory-developing/generating) literature therefore explores the potential factors affecting healthcare access and service coverage for older people. Given the diversity of definitions and conceptualisations, we chose not to limit our conceptualisations to particular definitions of equity, need or access, but rather to include any articles that used these terms and concepts, however, defined.
Research question
What are the potential factors affecting equity in healthcare access and service coverage for older people as conceptualised in the literature?
We conducted a scoping review using the five-stage framework outlined by Arksey and O’Malley 17 : (1) identifying the research question, (2) identifying relevant studies, (3) reviewing and selecting relevant studies for the final review, (4) charting the data or key information from the studies under review and (5) summarising and reporting the results. The protocol is available. 18
Inclusion criteria
To be included in the review, studies were required to satisfy the following criteria ( table 1 ). In minor revisions to the original protocol, to ensure manageable but meaningful quantities of literature for exploring relevant concepts, publications had to focus exclusively on older people, rather than merely including older people alongside other groups and, aligned with an approach proposed elsewhere, 19 20 were restricted to the conceptually richer papers (that developed frameworks, models of theories, with relationships between themes, rather than just a list of themes; in other words that had greater potential to provide ‘in-depth insights into the phenomenon of interest, allowing the researcher to better interpret the meaning and context of findings’. 19
Inclusion and exclusion criteria
Information sources and search strategies
We searched nine databases for relevant published and unpublished literature, without limits of publication type, date or language, from inception to May and June 2020: PubMed, MEDLINE (Ovid), PsycINFO (Ovid), CINAHL (Ovid), Web of Science, SciELO, LILACS, BIREME, Global Index Medicus. Searches combined thesaurus and free-text terms for models/frameworks/theories, older people, equity/disparity and need or coverage/utilisation/access (strategies are available in online supplemental files 1 and 2 ). In July 2020, citation searches (Google Scholar and Social Science Citation Index) and related-studies’ searches (PubMed and CoCites database) were performed on all included studies. Reference checking of all included studies was also conducted and experts in the project team consulted for any additional, relevant papers that might have been missed by the extensive searches. In doing so, we were able to take advantage of the opportunity to collaborate with Japanese researchers conducting a search of Japanese bibliographic databases (Ichushi-web and CiNii Articles) in order to expand coverage of the literature—that is, including a language that is often not included in literature reviews—especially considering the potential knowledge/evidence that could be obtained from/about Japan, the most aged society in the world with one of the highest levels of population health. This comprehensive, multifaceted search was undertaken because identifying conceptual papers using conventional search techniques can often prove challenging.
Supplementary data
Study selection, extraction and appraisal.
Two reviewers (CC and KS) conducted independent study screening of 10% of all titles and abstracts (538/5379) to ensure consistent interpretation and application of the inclusion criteria (data not available). Each reviewer then screened 50% of the remaining titles and abstracts (approximately 2400 each). In case of doubts over inclusion, the article was subsequently considered at full text. Following the search for related studies, text-mining techniques were employed to manage the large numbers and identify the potentially most relevant articles. 21 Full texts of all potential includes from these processes were independently screened by both reviewers (CC and KS). In the event of disagreements, a third project team member was available to make the final decision (AB), but this did not prove necessary.
Data items and data charting process
Two reviewers (KS and CC) developed, piloted (and revised, with the addition of fields such as care setting) a data extraction form based on independent extraction by two reviewers (CC and KS) of the the first three available studies. 22–24 The following data were then extracted from all studies: study first author; publication date; language; country of study; setting (type of health service, for example, home care); population; definitions of the key concepts of equity, need, access and coverage; each theory or framework’s listed domains and definitions, if provided, of factors affecting access to services, and equity of service coverage. All data charting was conducted independently by two reviewers (KS and CC) with inconsistencies resolved by discussion. Consultation with a third reviewer was not necessary (AB). Scoping reviews do not typically undertake quality assessment and this was not required in this instance (there is currently no published tool for appraising conceptual studies). 25 26
Summarising and reporting the results
This process involved identifying and grouping similar concepts from across studies. The factors identified as being important in older people’s equitable access of health and social care in each study were extracted and listed, and their definitions recorded. Using these definitions, similar factors for example, costs of medications and availability of public insurance, were then grouped under higher-order concepts that reflected these factors, for example, affordability. These higher-order concepts were not based on any a priori framework, but were defined based-on the factors they contained. This summary of findings represented a new conceptual meta-framework. The relationships between these higher-order concepts were then explored; this led to the development of an emerging conceptual model. This process, initiated by the lead reviewers (CC and KS), involved consultation and discussion with all authors: reviewers and experts in equity, older people, and healthcare and social care services (AB, AT, MM and MR).
Details of the study selection process are presented in figure 1 . The search of databases retrieved 6636 potentially relevant records. After deduplication, 5073 papers were excluded at title and abstract stage, and a further 281 papers were excluded at the full text stage. The principal reasons for exclusion of these papers were: the focus was not older people alone; the focus was not equity; the outcome was not access, use or need for health services or service coverage, but an individual health outcome; the study was a statistical analysis. Twenty-five studies were identified from the original database searches.

PRISMA flow diagram.
The complementary citation and related-studies searches retrieved an additional four relevant articles. 27–30 One additional article 31 was identified following reference tracking. Finally, a related review of the Japanese literature, applying the same methods and approaches but also including empirical quantitative literature, conducted by colleagues at Osaka University, identified two additional, relevant articles. 32 33 The final number of included studies was 32.
Included studies
Details of the characteristics of each of the 32 included articles are summarised in table 2 . All studies either generated new models from research or developed existing models, frameworks or theories, and used those conceptualisations to organise and interpret findings from primary or secondary research. Eleven articles were reviews or purely conceptual papers; 15 studies were qualitative primary research studies; three studies applied a form of data modelling; two studies used concept mapping, and one study used participatory action research, that is, a type of research that specifically seeks to bring about change through the participation and actions of key stakeholders.
Study characteristics
The largest group of studies by country were conducted in and concerned with populations of older people in the USA (n=14), followed by Australia (n=3) and China (n=3). Two studies were conducted in Japan. 32 33 One study was conducted in, and concerned older people in, each of the following: Canada, Chile, Hong Kong, Poland, Portugal, the Netherlands, Singapore and Sweden. One study was conducted from an international and one study from a European perspective. Thirty studies were published in English, one in Japanese, 33 and one in Spanish. 34 Seventeen studies considered access to or need for all types of healthcare services (n=17); nine focused on various types of long-term care services, including in the home or community (n=9). In addition, two focused on primary care, 23 35 two on dental care 24 29 and one each on mental health services 36 and rehabilitation services. 37
Sixteen studies considered older people generally (aged 50 years or older), while the other 16 studies considered access relating to specific groups of older people, and the implications for equity: racial, ethnic or immigrant minorities (n=7), sexual minorities (n=2), those with particular disabilities or chronic conditions (n=6), and those designated specifically as ‘underserved’ (n=1). Studies most frequently assumed a joint perspective of both demand (patients’ perspective and needs) and supply (service perspective) (n=16), with fewer studies focusing on demand (n=11) or supply (n=5) alone.
It should be noted that the searches captured relevant literature up to 2020; 27 out of 32 articles (84%) were published in 2015 or later, which reflects the growing interest in older populations, and specific groups within those populations. This sample of 32 studies derives from 14 different countries from North and South America, Europe, Asia and Australia, as well as covering multiple healthcare settings experienced by older people, from acute secondary care to long-term care in the community.
Authors typically developed or based their model or conceptual framework on a variety of existing theories, models or frameworks, which differed in terms of their focus (equity, diversity or rights; access, use or provision; ageing or behaviour) and academic origin. The most commonly used, adapted or augmented pre-existing models for organising concepts were the Andersen Behavioural Model of Healthcare Access (n=6) 38 and the Levesque model of healthcare access (n=3). 16 The Andersen model conceptualises access in terms of a population’s characteristics: their predisposing factors (attitudes, beliefs, sociodemographics); need factors (objective and subjective needs) and enabling factors (resources enabling access to and use of healthcare services). 38 The Levesque conceptual framework constructs a path from healthcare needs, through healthcare seeking, to healthcare reaching and utilisation, and ultimately, the health consequences of this use or non-use. 16 The framework captures the dimension of access and then the dimension of the services user’s ability to access as a set of further characteristics. Both are generic population models. Table 3 lists the models or frameworks identified in included articles and provides a basic summary of how access to healthcare and service coverage have been approached conceptually, though few focus on equity. Models were generally concerned with either access or equity or rights. The remaining models drew on broad conceptual frameworks relating to behaviour, care or successful ageing.
List of models in included studies and conceptual focus
Definitions of key terms, or explanations of key terms, where they were provided, are detailed in online supplemental file 3 . For example, a paper might provide definitions of more than one relevant term 27 : equity: ‘access to care … granted primarily according to need and not to other factors such as income or availability of resources’; access: ‘access to care is best evaluated by the actual use of services’; need: ‘A person’s need refers to the severity of illness and is the factor most directly responsible for use’. However, despite a focus on equity of health service coverage or access by older people, or the healthcare needs of older people, few papers explicitly defined all such terms in this way. The majority provided no such detail or only very broad definitions. More typically, the meaning of these terms was assumed implicitly within the papers, that is, the term was used but no definition was given. This observation may reflect their focus on processes that enable/constrain receipt of healthcare rather than on whether patterns of receipt are equitable.
The higher-order concepts identified for our meta-framework were: acceptability, affordability, appropriateness, availability and resources, awareness, capacity to make decisions, need, personal economic, social and cultural circumstances influencing access, and physical accessibility. These concepts emerged from the concepts identified within the data, linked to the findings of each study, and are described below, with reference to some nuances in the data:
- Acceptability—The data highlighted the effect of negative patient perceptions of inclusivity, discrimination, trust, respect and cultural knowledge and awareness among providers. For example, a perception of the lack of engagement from services in a review of health disparities for lesbian, gay and bisexual older people. 39
- Affordability—Patients’ real or perceived ability to pay for care or services. Affordability included individual financial resources in different health contexts 23 40 and the affordability and supports of insurance cover or services.
- Appropriateness—Providers’ engagement with patients to identify appropriate services, and how to supply services that satisfy patients’ needs in an appropriate way. Appropriateness is a characteristic of person-centred care. It is determined by cultural knowledge, racial or other bias or discrimination, attitudes to inclusivity and overall quality of care. Chui et al 41 undertook an analysis of relatives of older people who had died in a care setting to identify the presence of: structural barriers (cultural inclusivity); knowledge barriers (public education and participation) and attitudinal barriers (public education and intercultural exchange); all of which affected the provision of appropriate care services.
- Availability and resources—Providers’ ability to make available timely and adequate services or resources. The data highlighted the impact of availability at multiple levels. For example macrolevel factors: healthcare providers’ availability and capacity 42 ; local or community capacity 43 and service level resources. 32 44 45 This concept included review evidence on the requirement for resources in long-term care in a Japanese context. 32 Indeed, an aspect of ‘availability and resources’ that affects older people differently from younger age groups is that they have a need for services (ie, social care/long term care) that fall outside of the scope of typical ‘healthcare services’. This is a fundamental element of integrated care.
- Awareness—Patients’ awareness of the existence of relevant services and financial support (eg, knowledge of insurance options and eligibility for using these services). 46 Patients should be able to identify that some form of care services exist, can be reached, and can have an impact on the health of the individual. 36 From a service perspective, awareness includes the provision of service information to eligible individuals.
- Capacity to make decisions—Patients’ ability to understand their care needs and the services required (health literacy), and their ability to make decisions and to act. Data showed this could reflect a lack of knowledge for certain topics such as oral health or the capacity to make decisions might be compromised by personal limitations beyond service knowledge, such as limited capacity for lifestyle modification. 40 Providers may have limited ability themselves to understand the education and care needs, and the services required by older people.
- Need—Patients’ real or perceived need for healthcare services based on their age, multimorbidities, chronicity or complexity of care needs, and cultural or family expectations, which might in turn affect candidacy. 47 Issues relating to need might include preventative care such as screening services to enable identification of needs 28 ; and providers’ ability to anticipate and identify patient and population care needs, including through screening and monitoring.
- Personal economic, social and cultural circumstances influencing access—A patient’s personal circumstances or social context that might shape their choice or ability to access services. Data emphasised the diverse characteristics that could affect the service needs of older people, such as age, sex, marital status, education, race/ethnicity, and occupation. 22 Circumstances also included the context of familial support, which can shape elders’ perceptions of healthcare.
- Physical accessibility—Patients’ ability to access services due to requirements relating to mobility and transportation. The proximity of services was important. 24 34 36 40 45 48–50 From a provider perspective, this entails the provision of relevant services that are easily usable, requiring an appropriate transport infrastructure (even in more economically developed settings, such as the USA). 43
The summary of concepts, and the grouping of included studies by common elements, is presented in table 4 . The sources of the individual concepts are listed in the first column, that is, the included studies. Individual concepts identified by, or presented in, included studies are reported in the second column, and then grouped within a higher-order concept in the third column. These higher-order concepts correspond in part to some of the themes of the Levesque model of healthcare access (eg, Acceptability, Affordability), 16 reflecting common terminology, but often masking a different definition of the term. Where study-specific concepts were positioned in relation to the higher-order concepts was determined by how each paper had defined that concept. So, for example, one study defines its concept of ‘approachability’ in terms of ‘awareness of services’, 51 and so this appears under Awareness in our meta-framework, rather than ‘approachability’. Awareness does not appear in the Levesque model. 16
Summary of concepts from included studies
An emerging conceptual model
The relationships between the higher-order concepts are represented by the conceptual model presented in figure 2 . Clear relationships and overlaps can be observed between concepts, for example, the availability and expectation of family support for an older person shapes their need for and relationship with services; the resources available at policy level to provide local services can affect availability and accessibility of such services.

Conceptual model of relationships between summarised higher-order concepts relating to access to health services.
Figure 2 shows an emerging model for further consideration beyond the scope of this review, based on the summary of findings ( table 4 ). Although the summary identified demand and supply requirements or needs for some but not all concepts, this model attempts to locate each concept within personal, service and wider societal spheres: person-centred, integrated care is at the heart of the model. The model maps different levels: from the individual experience; to an individual’s interaction with health and social care services, and then to the broader infrastructure or policy levels at which decisions about service coverage or funding are made. Arrows in the model demonstrate the interlinkage of factors relating to access and the perception of access for the individual, services and wider infrastructure. Evidence suggests service level decisions are ideally shaped through an understanding about the individual, that is, person-centred care. These factors could function as barriers if not considered by services. Affordability of services is determined by a combination of individual means and the cost of the health-related systems in place. Physical accessibility is shaped by the individuals’ personal physical ability in combination with service availability and accessibility.
This review has identified potential factors affecting equity in healthcare access and service coverage for older people as conceptualised in the literature, falling under the concepts of acceptability, affordability, appropriateness, availability and resources, awareness, capacity to make decisions, need, personal economic, social and cultural circumstances influencing access, and physical accessibility. This review also presents a novel conceptual framework and model relating to integrated health and social care access to be developed with specific reference to older people. While multiple access models and frameworks have been developed for populations generally, 16 38 and then adapted to certain populations, such as certain vulnerable groups (excluding older people), 52 this is the first framework to our knowledge to target older people specifically. The Levesque framework often applies different definitions and perspectives, not specific to older people, and the Andersen model of access is high level and discusses factors affecting populations in general terms. 38 Certain factors therefore achieve greater prominence in our framework and model than in these generic access frameworks as a result of the prevalence of multimorbidity, complex care needs and capacity and accessibility concerns among older people as a group—and within groups of older people. This framework is also generated from literature exploring the concept of equity in relation to ageing populations’ access to and use of long-term health and social care services and facilities; other frameworks only consider primary or secondary care.
Results from this scoping review suggest healthcare service access for older people is constructed between individuals and services/infrastructure. It is not simply a case of either the provision of top-down resources or the prominence of personal characteristics at the individual level. 53 The availability, appropriateness and affordability of resources, in combination with service communication and competency, can facilitate or hinder access based on an understanding of personal (such as needs) and interactional factors. While this dynamic is not new, 9 38 the diversity of personal or demographic characteristics or circumstances affecting older people is both unique and substantial. Multimorbidity, that is, the presence of two or more chronic conditions 54 is certainly known to be both more prevalent in elderly populations than other age groups, 54–57 and also to be increasing. 58 The combination of mental and physical comorbidities is also known to reduce the likelihood of accessing relevant healthcare, 57 which therefore has yet further equity implications for this group. Multimorbidity is therefore an element in a number of our factors such as awareness, capacity to make decisions, need, personal economic, social and cultural circumstances influencing access, and physical accessibility. Some factors apply equally to older as to other age groups, such as need and personal economic, social and cultural circumstances, 59 but worldwide the majority of older people are female, which raises particular issues for healthcare seeking and access. 60 Multiple vulnerabilities can arise from the complex interaction between the sociopolitical, economic, structural, cultural and interpersonal circumstances and older people are more exposed to these than other age groups.
What emerges is a lack of a more sophisticated understanding and acknowledgement of the dimensions of difference in older people’s experience of services: frameworks can homogenise older people into one group thereby omitting clear differences in healthcare needs within this group, based on factors such as age, comorbidities, minority status, financial and familial resources. Previous recommendations for monitoring equity of UHC suggest a need to apply metrics to subgroups, based on factors such as residence (urban/rural), gender or economic status, and age. 61 This review suggests that older people also cannot simply be treated as a homogeneous subgroup: intersectionality applies; the equity or inequity of a system is determined by multiple factors and the interactions between them. For example, our framework and model highlights factors such as discrimination, based on minority status and capacity, and need based on individual physical, cultural and financial circumstances. Factors such as these that might apply to one older person, might not apply to another, with different implications for equity of access. The framework and model presents ideas for targeting older people, an approach which is commensurate with the idea of ‘progressive universalism’ 62 and is in line with current policy movements, such as around the creation of a United Nations Convention on the Rights of Older Persons. When seeking to measure equity in UHC, policy-makers need to take into account metrics that consider not just older people as a group, but subgroups of older people based on personal social, cultural and economic circumstances, for example, those with local health and social care services or available means of accessing them, compared with those who lack such means or must travel further (and this might not be a simple rural/urban division). These metrics need to be developed within indicator frameworks—published frameworks guiding what should be measured—at a national level.
Strengths of the review
A major strength of this scoping review is its comprehensive literature search strategy and robust conduct: the study selection, double-checking of all full text inclusions/exclusions, and data extraction and charting by two experienced reviewers. The summary of findings provides a rich analysis of interacting factors within frameworks, rather than a linear list of relevant frameworks or models. Also, this is a review of the global literature, so its findings may have limited generalisability to individual countries.
Limitations of the review
It is possible that some relevant studies were missed, despite the extensive use of complementary search techniques. And the selection of the primary studies based on the potential richness of their conceptualisation might be considered arbitrary. However, the number of studies supporting each concept suggests that a degree of conceptual saturation has been achieved. The addition of yet more studies is unlikely to add much to the overall findings.
This is the first review to the authors’ knowledge to explore the published conceptual literature explicitly on older people, equity and health and social care service coverage, and consider its implications in the current policy context. A key feature of the factors influencing older people’s equitable access to services is the complexity and diversity of the intersection of personal factors surrounding individual identity, healthcare need and socioeconomic circumstances. The access needs of an older person can be highly individual. The United Nations has recently highlighted the specific issues affecting older people with its proposal for a Convention of Human Rights for Older people, and the need for policy that strengthens healthcare and social protection systems, and improves access to care and support, including long-term care. This review’s framework has relevance to the development and specification of policy for older people because it conceptualises exactly those factors that affect equity of access to person-centred, integrated healthcare and social care services for older people.
Acknowledgments
We would like to thank the team at Osaka University, led by Professor Iso Hiroyasu, who have conducted a ‘sister’ scoping review of the Japanese literature, for the identification and summary of two additional, relevant articles included in this review. We would also like to acknowledge the input of Professors Sarah Salway and Peter Bath of the University of Sheffield, and Drs Anjana Bhushan and Manfred Huber of WHO, at the inception of this project. This scoping review was commissioned and funded by the World Health Organization (WHO) through the WHO Centre for Health Development (WHO Kobe Centre), Japan; reference number: K19010. The authors do not have any conflicts of interest. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Contributors: CC, AB, KS, AT and MM acquired financial support; CC, AB, KS, AT, MM and MR conceived and designed the study; AB conducted data management; CC and KS conducted the investigation; CC and KS performed the formal analysis; CC and KS wrote the initial drafts; CC, KS, AB, AT, MM and MR all offered critical commentary of the manuscript.
Funding: This study was funded by WHO Centre for Health Development (WHO Kobe Centre; reference number K19010).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Open material: I cannot see the Open Access statement, but we require a revision:
Replace the current statement with the following statement as indicated in the standing license agreement signed between BMJ and WHO:
This is an open access article distributed under the terms of the Creative Commons Attribution N-Noncommercial IGO License ( https://creativecommons.org/licenses/by/3.0/igo/ ), which permits use, distribution, and reproduction for non-commercial purposes in any medium, provided the original work is properly cited. In any reproduction of this article there should not be any suggestion that WHO or this article endorse any specific organization or products. The use of the WHO logo is not permitted. This notice should be preserved along with the article's original URL.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication.
Not applicable.
A pre-post study of pharmacist-led medication reviews within a hospital-based residential aged care support service
Affiliations.
- 1 Pharmacy Department, Residential Aged Care District Assessment and Referral, Metro North Health, Brisbane, Australia.
- 2 Pharmacy, Gold Coast Health, Gold Coast, Australia.
- 3 Statistics Unit, QIMR Berghofer Medical Research Institute, Brisbane, Australia.
- 4 Prince Charles Hospital Northside Clinical Unit, Faculty of Medicine, University of Queensland, Brisbane, Australia.
- 5 Safe and Effective Medication Research Collaborative, Faculty of Health and Behavioural Science/Faculty of Medicine at the University of Queensland and Metro North Health, Brisbane, Australia.
- 6 Rural Clinical School, Faculty of Medicine, University of Queensland, Australia.
- PMID: 38652509
- DOI: 10.1093/ijpp/riae018
Background: Hospital-based residential aged-care support service teams typically consist of doctors and nurses who provide hospital substitutive care to aged-care residents. There is limited literature evaluating the pharmacist's role in such aged-care support teams.
Objective: To analyse the effect of residential aged-care support service pharmacist-led medication reviews on polypharmacy, drug burden index, potentially inappropriate medications, and potential prescribing omissions for aged-care residents.
Methods: Residents referred to a residential aged-care support service pharmacist for medication review over a 12-month period were included. The pharmacist communicated medication-related problems and recommendations to the resident's general practitioner and residential aged-care support service medical practitioner. Residents' medication histories were obtained at baseline and one-month postintervention. The number of medications and their associated drug burden indices were compared using paired t-tests; potentially inappropriate medications and potential prescribing omissions were compared using Wilcoxon's signed rank test.
Key findings: Of 175 residents (mean age 84 years) referred for pharmacist-led medication review, 146 had postintervention evaluation after one-month (median 29 days). Mean number of medications reduced from 12.47 at baseline to 11.84 postintervention (mean difference (95% CI): 0.63(0.33-0.93), P < .001). Mean drug burden index score reduced from 1.54 at baseline to 1.37 postintervention (mean difference (95% CI): 0.17(0.10-0.24), P < .001). More residents experienced a decrease in inappropriate medications (median (IQR) pre: 2(1-3), post: 1(0-2), P < .001) and prescribing omissions (median (IQR) pre: 0(0-1), post: 0(0-0), P = .003) compared with those that had an increase.
Conclusions: Medication reviews performed by pharmacists embedded in hospital-based residential aged-care support services may improve medication prescribing. Further research into such preventative health service models is required.
Keywords: homes for the aged; medication review; nursing homes; pharmacists.
© The Author(s) 2024. Published by Oxford University Press on behalf of the Royal Pharmaceutical Society.
ORIGINAL RESEARCH article
Clinical analysis and literature review of two paediatric cases of anti-iglon5 antibody-related encephalitis.

- Hunan Children's Hospital, Changsha, China
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
Introduction: Anti-IgLON5 antibody-related encephalitis is a rare autoimmune disorder of the central nervous system, predominantly occurring in middle-aged elderly individuals, with paediatric cases being exceptionally rare. This study aims to enhance the understanding of paediatric anti-IgLON5 antibody-related encephalitis by summarising its clinical and therapeutic characteristics. Method: A retrospective analysis was conducted on two paediatric patients diagnosed with anti-IgLON5 antibody-related encephalitis at Hunan Children's Hospital from August 2022 to November 2023. This involved reviewing their medical records and follow-up data, in addition to a literature review.The study involved two patients, one male and one female, aged between 2.5 and 9.6 years, both presenting with an acute/subacute course of illness. Clinically, both exhibited movement disorders (including dystonia, involuntary movements, and ataxia), cognitive impairments, sleep disturbances, and psychiatric symptoms. Patient 1 experienced epileptic seizures, while Patient 2 exhibited brainstem symptoms and abnormal eye movements. Neither patient showed autonomic dysfunction. Patient 1 had normal cerebrospinal fluid (CSF) and Brain MRI findings, whereas Patient 2 showed moderate leukocytosis and mild protein elevation in the CSF, and Brain MRI revealed symmetrical lesions in the basal ganglia and cerebellum. Oligoclonal bands in the CSF were positive in both cases. Both patients tested negative for HLA-DQB*05:01 and HLA-DRB*10:01. They received both first-line and second-line immunotherapies, with Patient 2 showing a poor response to treatment. Discussion: Paediatric cases of anti-IgLON5 antibody-related encephalitis similarly present sleep disturbances as a core symptom, alongside various forms of movement disorders. Immunotherapy is partially effective. Compared to adult patients, these paediatric cases tend to exhibit more pronounced psychiatric symptoms, a more rapid onset, and more evident inflammatory changes in the CSF. The condition appears to have a limited association with HLA-DQB*05:01 and HLA-DRB*10:01 polymorphisms.
Keywords: Children, anti-IgLON5 antibody, autoimmune encephalitis, Sleep disturbances, Immunotherapy
Received: 20 Feb 2024; Accepted: 22 Apr 2024.
Copyright: © 2024 Feng, Zhou, Kang, Wang, Tang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Zhen Zhou, Hunan Children's Hospital, Changsha, China Miao Wang, Hunan Children's Hospital, Changsha, China Jingwen Tang, Hunan Children's Hospital, Changsha, China Liwen Wu, Hunan Children's Hospital, Changsha, China
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
A comprehensive literature review was undertaken to search and identify the literature (grey and peer reviewed) relating to quality of care and/or person-centered care in aged care. The review identified nine key themes as salient to the quality of care experience, which include treating the older person with respect and dignity; acknowledging ...
A comprehensive literature review was undertaken to search and identify the literature (grey and peer reviewed) relating to quality of care and/or person-centered care in aged care. The review identified nine key themes as salient to the quality of care experience, which include treating the older person with respect and dignity; acknowledging ...
This literature review was designed to support and expand this activity, by providing a foundation for enquiry and analysis, identifying key concepts and definitions, and informing the development of the questions that the empirical study would seek to answer. ... Walker B, Haslett T. System dynamics and action research in aged care. Australian ...
Consumer engagement in aged care Literature review agedcarequality.gov.au 5 Key phrases and terms that have been applied in the review of literature on Google Scholar and Pub Med Central have included: • co-design in aged care • co-design best practice models • person-centred care in aged care • co-production in aged care • consumer ...
1. Introduction. The rapidly aging population combined with the weakening of traditional family aged care support [1,2,3,4] has received much attention in institutional elder care research which is reflected by exponential growth in relevant academic literature in recent years [].Scholars have made fruitful advances in the research theme of institutional elder care.
There is increasing interest in harnessing aged care residents' perspectives to drive quality improvement in aged care homes. We conducted a systematic review of qualitative evidence including literature examining residents' descriptions of "quality of care" in aged care homes, using database searches and screening records according to eligibility criteria.
Therefore, this literature review included 27 relevant publications covering 26 original studies for data extraction and quality appraisal (Figure 1). Open in a separate window. ... To add to what is known about living in a residential aged care facilities, and such associated issues, from the perspectives of those who are currently residents ...
This same review further indicated that management practices influence work satisfaction and the quality of care, and a recent literature review highlighted that care staff skills are an important ...
The rapidly aging population combined with the weakening of traditional family aged care support [1,2,3,4] has received much attention in institutional elder care research which is reflected by exponential growth in relevant academic literature in recent years [].Scholars have made fruitful advances in the research theme of institutional elder care.
Quality indicators for home- and community-based aged care: A critical literature review to inform policy directions Australas J Ageing. 2022 Sep;41(3):383-395. doi: 10.1111/ajag.13103. Epub 2022 Jul 3. Authors Hui Yuan Foong 1 ... (QIs) in home- and community-based aged care. This research aimed to identify and appraise home care QI sets used ...
Results: 47 articles and books were included in the review that introduce solutions and innovative strategies that could be used to improve students' attitudes to learning in aged care and from older people. The literature review was categorized into three main themes, including: barriers to working with older people; the need for pedagogical ...
The first literature review and the Technology Roadmap for Aged Care were developed by a team from the. Flinders University Medical Device Research Institute led by Professor Karen Reynolds, with ...
The review found that staff training, having personnel or champions as facilitators, and the organisational culture were key factors in using VR to decrease loneliness and improve social engagement in aged care settings. 50 In addition, the quality of the VR videos was found to be important in terms of how immersive the experiences are, and ...
Retention of care support workers in residential aged care facilities and home-based, domiciliary aged care is a global challenge, with rapid turnover, low job satisfaction, and poorly defined career pathways. A mixed-methods systematic review of the workforce literature was conducted to understand the factors that attract and retain care staff across the aged care workforce. The search ...
required care services in accordance with their self-determined care plan. Cash-for-Care schemes thereby emphasise budgeting and marketisation of care (the purchase of aged care services in the market place as opposed to the provision of aged care by government agencies) as the key to more choice. In the evaluation literature, consumer choice is
The purpose of this literature review is to identify the factors that influence residents' transition and adjustment Please cite this article in press as: Brownie, S., et al., Factors that impact residents' transition and psychological adjustment to long-term aged care: A systematic literature review. Int. J. Nurs. Stud.
2 The first literature review and the Technology Roadmap for Aged Care were developed by a team from the Flinders University Medical Device Research Institute led by Professor Karen Reynolds, with ...
1. INTRODUCTION. Aged care services were provided to 1.3 million older Australians in 2019-20 at a cost to the government of $21.2 billion. 1 As our population ages, the quality of aged care will play a critical role in determining the health and well‐being of an increasing number of older Australians and their informal carers. However, a series of inquiries, including the Royal Commission ...
1 INTRODUCTION. Aged care services were provided to 1.3 million older Australians in 2019-20 at a cost to the government of $21.2 billion. 1 As our population ages, the quality of aged care will play a critical role in determining the health and well-being of an increasing number of older Australians and their informal carers. However, a series of inquiries, including the Royal Commission ...
Care home settings, such as nursing homes or residential care homes, present unique challenges to patient safety. This systematic review identified several gaps in the available safety measures used for quality monitoring and improvement in older adult care homes, including patient experience (e.g., quality of life or other resident-reported indicators of safety), psychological harm related to ...
A review of available literature relating to undergraduate nursing students' attitudes, perceptions and experiences in the aged care setting, or in the care of older adults. Data sources CINAHL Plus with Full Text was the primary database used.
A scoping review was selected to map the available literature on geriatric models of care for older adults within the context HIV [].The protocol for our scoping review followed the well-established framework outlined by Arksey and O'Malley [] and later refined by Levac et al. [] and Colquhoun et al. [].The framework was selected as it provides guidance to ensure a rigorous scoping review ...
The person-centered care (PCC) approach plays a fundamental role in ensuring quality healthcare. The Person-Centered Care Assessment Tool (P-CAT) is one of the shortest and simplest tools currently available for measuring PCC. The objective of this study was to conduct a systematic review of the evidence in validation studies of the P-CAT, taking the "Standards" as a frame of reference.
A literature review of research evidence on quality of life issues among residential care home elders. ... 'residential care home' or 'aged care home', were combined with 'quality of life' and used to identify relevant studies. The studies were excluded if they: (1) examined a single domain of QoL; (2) included samples of certain ...
This scoping review aimed to identify and present the evidence describing key motivations for breast cancer screening among women aged ≥ 75 years. Few of the internationally available guidelines recommend continued biennial screening for this age group. Some suggest ongoing screening is unnecessary or should be determined on individual health status and life expectancy.
yoga on balance and falls in a residential care setting: a randomised controlled trial. Contemp Nurse 2014;48:5231-55. 27 Hewitt J, Goodall S, Clemson L, et al. Progressive resistance and balance training for falls prevention in long-term residential aged care: a cluster randomized trial of the Sunbeam program. J Am Med Dir Assoc 2018;19:361-9.
New model: Diversity Conceptual Model for aged care with a focus on diversity characteristics that may be creating benefits and disadvantages for a consumer to participate in their healthcare: A novel conceptual model (DEMAND and SUPPLY) McMaughan, 2020 34: Review of the equity literature: English: Australia: All services: Older adults, aged 65 ...
Background: Hospital-based residential aged-care support service teams typically consist of doctors and nurses who provide hospital substitutive care to aged-care residents. There is limited literature evaluating the pharmacist's role in such aged-care support teams. Objective: To analyse the effect of residential aged-care support service pharmacist-led medication reviews on polypharmacy ...
This involved reviewing their medical records and follow-up data, in addition to a literature review.The study involved two patients, one male and one female, aged between 2.5 and 9.6 years, both presenting with an acute/subacute course of illness.
28. Naidu SS, Baran DA, Jentzer JC, et al. SCAI SHOCK stage classification expert consensus update: a review and incorporation of validation studies: this statement was endorsed by the American College of Cardiology (ACC), American College of Emergency Physicians (ACEP), American Heart Association (AHA), European Society of Cardiology (ESC) Association for Acute Cardiovascular Care (ACVC ...