7 Solution-Focused Therapy Techniques and Worksheets (+PDF)

It has analyzed a person’s problems from where they started and how those problems have an effect on that person’s life.
Out of years of observation of family therapy sessions, the theory and applications of solution-focused therapy developed.
Let’s explore the therapy, along with techniques and applications of the approach.
Before you read on, we thought you might like to download our three Positive Psychology Exercises for free . These science-based exercises will explore fundamental aspects of positive psychology including strengths, values, and self-compassion, and will give you the tools to enhance the wellbeing of your clients, students, or employees.

This Article Contains:
5 solution-focused therapy techniques, handy sft worksheets (pdf), solution-focused therapy interventions, 5 sft questions to ask clients, solution-focused brief therapy (sfbt techniques), 4 activities & exercises, best sft books, a take-home message.
Solution-focused therapy is a type of treatment that highlights a client’s ability to solve problems, rather than why or how the problem was created. It was developed over some time after observations of therapists in a mental health facility in Wisconsin by Steve de Shazer and Insoo Kim Berg and their colleagues.
Like positive psychology, Solution Focused Therapy (SFT) practitioners focus on goal-oriented questioning to assist a client in moving into a future-oriented direction.
Solution-focused therapy has been successfully applied to a wide variety of client concerns due to its broad application. It has been utilized in a wide variety of client groups as well. The approach presupposes that clients have some knowledge of what will improve their lives.
The following areas have utilized SFT with varying success:
- relationship difficulties
- drug and alcohol abuse
- eating disorders
- anger management
- communication difficulties
- crisis intervention
- incarceration recidivism reduction
Goal clarification is an important technique in SFT. A therapist will need to guide a client to envision a future without the problem with which they presented. With coaching and positive questioning, this vision becomes much more clarified.
With any presenting client concern, the main technique in SFT is illuminating the exception. The therapist will guide the client to an area of their life where there is an exception to the problem. The exception is where things worked well, despite the problem. Within the exception, an approach for a solution may be forged.
The ‘miracle question’ is another technique frequently used in SFT. It is a powerful tool that helps clients to move into a solution orientation. This question allows clients to begin small steps toward finding solutions to presenting problems (Santa Rita Jr., 1998). It is asked in a specific way and is outlined later in this article.
Experiment invitation is another way that therapists guide clients into solution orientation. By inviting clients to build on what is already working, clients automatically focus on the positive. In positive psychology, we know that this allows the client’s mind to broaden and build from that orientation.
Utilizing what has been working experimentally allows the client to find what does and doesn’t work in solving the issue at hand. During the second half of a consultation with a client, many SFT therapists take a break to reflect on what they’ve learned during the beginning of the session.
Consultation breaks and invitations for more information from clients allow for both the therapist and client to brainstorm on what might have been missed during the initial conversations. After this break, clients are complemented and given a therapeutic message about the presenting issue. The message is typically stated in the positive so that clients leave with a positive orientation toward their goals.
Here are four handy worksheets for use with solution-focused therapy.
- Miracle worksheet
- Exceptions to the Problem Worksheet
- Scaling Questions Worksheet
- SMART+ Goals Worksheet

Download 3 Free Positive Psychology Exercises (PDF)
Enhance wellbeing with these free, science-based exercises that draw on the latest insights from positive psychology.
Download 3 Free Positive Psychology Tools Pack (PDF)
By filling out your name and email address below.
Compliments are frequently used in SFT, to help the client begin to focus on what is working, rather than what is not. Acknowledging that a client has an impact on the movement toward a goal allows hope to become present. Once hope and perspective shift occurs, a client can decide what daily actions they would like to take in attaining a goal.
Higher levels of hope and optimism can predict the following desirable outcomes (Peterson & Seligman, 2004):
- achievement in all sorts of areas
- freedom from anxiety and depression
- improved social relationships
- improved physical well being
Mind mapping is an effective intervention also used to increase hope and optimism. This intervention is often used in life coaching practices. A research study done on solution-focused life coaching (Green, Oades, & Grant, 2006) showed that this type of intervention increases goal striving and hope, in addition to overall well-being.
Though life coaching is not the same as therapy, this study shows the effectiveness of improving positive behavior through solution-focused questioning.
Mind mapping is a visual thinking tool that helps structure information. It helps clients to better analyze, comprehend, and generate new ideas in areas they might not have been automatically self-generated. Having it on paper gives them a reference point for future goal setting as well.
Empathy is vital in the administration of SFBT. A client needs to feel heard and held by the practitioner for any forward movement to occur. Intentionally leaning in to ensure that a client knows that the practitioner is engaged in listening is recommended.
Speaking to strengths and aligning those strengths with goal setting are important interventions in SFT. Recognizing and acknowledging what is already working for the client validates strengths. Self-recognition of these strengths increases self-esteem and in turn, improves forward movement.
The questions asked in Solution-Focused Therapy are positively directed and in a goal-oriented stance. The intention is to allow a perspective shift by guiding clients in the direction of hope and optimism to lead them to a path of positive change. Results and progress come from focusing on the changes that need to be made for goal attainment and increased well being.
1. Miracle Question
Here is a clear example of how to administer the miracle question. It should be delivered deliberately. When done so, it allows the client to imagine the miracle occurring.
“ Now, I want to ask you a strange question. Suppose that while you are sleeping tonight and the entire house is quiet, a miracle happens. The miracle is that the problem which brought you here is solved. However, because you are sleeping, you don’t know that the miracle has happened. So, when you wake up tomorrow morning, what will be different that will tell you that a miracle has happened and the problem which brought you here is solved? ” (de Shazer, 1988)
2. Presupposing change questions
A practitioner of solution-focused therapy asks questions in an approach derived way.
Here are a few examples of presupposing change questions:
“What stopped complete disaster from occurring?” “How did you avoid falling apart.” “What kept you from unraveling?”
3. Exception Questions
Examples of exception questions include:
1. Tell me about times when you don’t get angry. 2. Tell me about times you felt the happiest. 3. When was the last time that you feel you had a better day? 4. Was there ever a time when you felt happy in your relationship? 5. What was it about that day that made it a better day? 6. Can you think of a time when the problem was not present in your life?
4. Scaling Questions
These are questions that allow a client to rate their experience. They also allow for a client to evaluate their motivation to change their experience. Scaling questions allow for a practitioner to add a follow-up question that is in the positive as well.
An example of a scaling question: “On a scale of 1-10, with 10 representing the best it can be and one the worst, where would you say you are today?”
A follow-up question: “ Why a four and not a five?”
Questions like these allow the client to explore the positive, as well as their commitment to the changes that need to occur.
5. Coping Questions
These types of questions open clients up to their resiliency. Clients are experts in their life experience. Helping them see what works, allows them to grow from a place of strength.
“How have you managed so far?” “What have you done to stay afloat?” “What is working?”
3 Scaling questions from Solution Focused Therapy – Uncommon Practitioners
The main idea behind SFBT is that the techniques are positively and solution-focused to allow a brief amount of time for the client to be in therapy. Overall, improving the quality of life for each client, with them at the center and in the driver’s seat of their growth. SFBT typically has an average of 5-8 sessions.
During the sessions, goals are set. Specific experimental actions are explored and deployed into the client’s daily life. By keeping track of what works and where adjustments need to be made, a client is better able to track his or her progress.
A method has developed from the Miracle Question entitled, The Miracle Method . The steps follow below (Miller & Berg, 1996). It was designed for combatting problematic drinking but is useful in all areas of change.
- State your desire for something in your life to be different.
- Envision a miracle happening, and your life IS different.
- Make sure the miracle is important to you.
- Keep the miracle small.
- Define the change with language that is positive, specific, and behavioral.
- State how you will start your journey, rather than how you will end it.
- Be clear about who, where, and when, but not the why.
World’s Largest Positive Psychology Resource
The Positive Psychology Toolkit© is a groundbreaking practitioner resource containing over 500 science-based exercises , activities, interventions, questionnaires, and assessments created by experts using the latest positive psychology research.
Updated monthly. 100% Science-based.
“The best positive psychology resource out there!” — Emiliya Zhivotovskaya , Flourishing Center CEO
A short selection of exercises which can be used
1. Solution-focused art therapy/ letter writing
A powerful in-session task is to request a client to draw or write about one of the following, as part of art therapy :
- a picture of their miracle
- something the client does well
- a day when everything went well. What was different about that day?
- a special person in their life
2. Strengths Finders
Have a client focus on a time when they felt their strongest. Ask them to highlight what strengths were present when things were going well. This can be an illuminating activity that helps clients focus on the strengths they already have inside of them.
A variation of this task is to have a client ask people who are important in their lives to tell them how they view the client’s strengths. Collecting strengths from another’s perspective can be very illuminating and helpful in bringing a client into a strength perspective.
3. Solution Mind Mapping
A creative way to guide a client into a brainstorm of solutions is by mind mapping. Have the miracle at the center of the mind map. From the center, have a client create branches of solutions to make that miracle happen. By exploring solution options, a client will self-generate and be more connected to the outcome.
4. Experiment Journals
Encourage clients to do experiments in real-life settings concerning the presenting problem. Have the client keep track of what works from an approach perspective. Reassure the client that a variety of experiments is a helpful approach.
17 Top-Rated Positive Psychology Exercises for Practitioners
Expand your arsenal and impact with these 17 Positive Psychology Exercises [PDF] , scientifically designed to promote human flourishing, meaning, and wellbeing.
Created by Experts. 100% Science-based.
These books are recommended reads for solution-focused therapy.
1. The Miracle Method: A Radically New Approach to Problem Drinking – Insoo Kim Berg and Scott D. Miller Ph.D.
The Miracle Method by Scott D. Miller and Insoo Kim Berg is a book that has helped many clients overcome problematic drinking since the 1990s.
By utilizing the miracle question in the book, those with problematic drinking behaviors are given the ability to envision a future without the problem.
Concrete, obtainable steps in reaching the envisioned future are laid out in this supportive read.
Available on Amazon .
2. Solution Focused Brief Therapy: 100 Key Points and Techniques – Harvey Ratney, Evan George and Chris Iveson
Solution Focused Brief Therapy: 100 Key Points and Techniques is a well-received book on solution-focused therapy. Authors Ratner, George, and Iveson provide a concisely written and easily understandable guide to the approach.
Its accessibility allows for quick and effective change in people’s lives.
The book covers the approach’s history, philosophical underpinnings, techniques, and applications. It can be utilized in organizations, coaching, leadership, school-based work, and even in families.
The work is useful for any practitioner seeking to learn the approach and bring it into practice.
3. Handbook of Solution-Focused Brief Therapy (Jossey-Bass Psychology) – Scott D. Miller, Mark Hubble and Barry L. Duncan
It includes work from 28 of the lead practitioners in the field and how they have integrated the solution-focused approach with the problem-focused approach.
It utilizes research across treatment modalities to better equip new practitioners with as many tools as possible.
4. More Than Miracles: The State of the Art of Solution -Focused Therapy (Routledge Mental Health Classic Editions) – Steve de Shazer and Yvonne Dolan
It allows the reader to peek into hundreds of hours of observation of psychotherapy.
It highlights what questions work and provides a thoughtful overview of applications to complex problems.
Solution-Focused Therapy is an approach that empowers clients to own their abilities in solving life’s problems. Rather than traditional psychotherapy that focuses on how a problem was derived, SFT allows for a goal-oriented focus to problem-solving. This approach allows for future-oriented, rather than past-oriented discussions to move a client forward toward the resolutions of their present problem.
This approach is used in many different areas, including education, family therapy , and even in office settings. Creating cooperative and collaborative opportunities to problem solve allows mind-broadening capabilities. Illuminating a path of choice is a compelling way to enable people to explore how exactly they want to show up in this world.
Thanks for reading!
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free .
- de Shazer, S. (1988). Clues: Investigating solutions in brief therapy. New York, NY: W.W. Norton and Co. https://www.amazon.com/dp/0393700542/
- Green, L. S., Oades, L. G., & Grant, A. M. (2006). Cognitive-behavioral, solution-focused life coaching: Enhancing goal striving, well-being, and hope. The Journal of Positive Psychology, 1 (3), 142-149. https://doi.org/10.1080/17439760600619849
- Miller, S. D., & Berg, I. K. (1996). The miracle method: A radically new approach to problem drinking. New York, NY: W.W. Norton and Co. https://www.amazon.com/dp/0393315339/
- Peterson, C., & Seligman, M. E. P., (2004). Character strengths and virtues: A handbook and classification (Vol. 1). New York, NY: Oxford University Press. https://www.amazon.com/dp/0195167015/
- Santa Rita Jr, E. (1998). What do you do after asking the miracle question in solution-focused therapy. Family Therapy, 25( 3), 189-195.
Share this article:
Article feedback
What our readers think.
This was so amazing and helpful
excellent article and useful for applications in day today life activities .I will like at use when required and feasible to practice.
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

The Empty Chair Technique: How It Can Help Your Clients
Resolving ‘unfinished business’ is often an essential part of counseling. If left unresolved, it can contribute to depression, anxiety, and mental ill-health while damaging existing [...]

29 Best Group Therapy Activities for Supporting Adults
As humans, we are social creatures with personal histories based on the various groups that make up our lives. Childhood begins with a family of [...]
47 Free Therapy Resources to Help Kick-Start Your New Practice
Setting up a private practice in psychotherapy brings several challenges, including a considerable investment of time and money. You can reduce risks early on by [...]
Read other articles by their category
- Body & Brain (52)
- Coaching & Application (39)
- Compassion (23)
- Counseling (40)
- Emotional Intelligence (22)
- Gratitude (18)
- Grief & Bereavement (18)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (16)
- Mindfulness (40)
- Motivation & Goals (41)
- Optimism & Mindset (29)
- Positive CBT (28)
- Positive Communication (23)
- Positive Education (37)
- Positive Emotions (32)
- Positive Leadership (16)
- Positive Parenting (14)
- Positive Psychology (21)
- Positive Workplace (35)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (39)
- Self Awareness (20)
- Self Esteem (37)
- Strengths & Virtues (29)
- Stress & Burnout Prevention (33)
- Theory & Books (42)
- Therapy Exercises (37)
- Types of Therapy (54)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10464969

Problem-solving interventions and depression among adolescents and young adults: A systematic review of the effectiveness of problem-solving interventions in preventing or treating depression
Kristina Metz
1 Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States of America
2 Centre for Evidence and Implementation, London, United Kingdom
Jade Mitchell
Sangita chakraborty, bryce d. mcleod.
3 Department of Psychology, Virginia Commonwealth University, Richmond, VA, United States of America
Ludvig Bjørndal
Robyn mildon.
4 Centre for Evidence and Implementation, Melbourne, Victoria, Australia
Aron Shlonsky
5 Department of Social Work, Monash University, Melbourne, Victoria, Australia
Associated Data
All relevant methods and data are within the paper and its Supporting Information files.
Problem-solving (PS) has been identified as a therapeutic technique found in multiple evidence-based treatments for depression. To further understand for whom and how this intervention works, we undertook a systematic review of the evidence for PS’s effectiveness in preventing and treating depression among adolescents and young adults. We searched electronic databases ( PsycINFO , Medline , and Cochrane Library ) for studies published between 2000 and 2022. Studies meeting the following criteria were included: (a) the intervention was described by authors as a PS intervention or including PS; (b) the intervention was used to treat or prevent depression; (c) mean or median age between 13–25 years; (d) at least one depression outcome was reported. Risk of bias of included studies was assessed using the Cochrane Risk of Bias 2.0 tool. A narrative synthesis was undertaken given the high level of heterogeneity in study variables. Twenty-five out of 874 studies met inclusion criteria. The interventions studied were heterogeneous in population, intervention, modality, comparison condition, study design, and outcome. Twelve studies focused purely on PS; 13 used PS as part of a more comprehensive intervention. Eleven studies found positive effects in reducing depressive symptoms and two in reducing suicidality. There was little evidence that the intervention impacted PS skills or that PS skills acted as a mediator or moderator of effects on depression. There is mixed evidence about the effectiveness of PS as a prevention and treatment of depression among AYA. Our findings indicate that pure PS interventions to treat clinical depression have the strongest evidence, while pure PS interventions used to prevent or treat sub-clinical depression and PS as part of a more comprehensive intervention show mixed results. Possible explanations for limited effectiveness are discussed, including missing outcome bias, variability in quality, dosage, and fidelity monitoring; small sample sizes and short follow-up periods.
Introduction
Depression among adolescents and young adults (AYA) is a serious, widespread problem. A striking increase in depressive symptoms is seen in early adolescence [ 1 ], with rates of depression being estimated to almost double between the age of 13 (8.4%) and 18 (15.4%) [ 2 ]. Research also suggests that the mean age of onset for depressive disorders is decreasing, and the prevalence is increasing for AYA. Psychosocial interventions, such as cognitive-behavioural therapy (CBT) and interpersonal therapy (IPT), have shown small to moderate effects in preventing and treating depression [ 3 – 6 ]. However, room for improvement remains. Up to half of youth with depression do not receive treatment [ 7 ]. When youth receive treatment, studies indicate that about half of youth will not show measurable symptom reduction across 30 weeks of routine clinical care for depression [ 8 ]. One strategy to improve the accessibility and effectiveness of mental health interventions is to move away from an emphasis on Evidence- Based Treatments (EBTs; e.g., CBT) to a focus on discrete treatment techniques that demonstrate positive effects across multiple studies that meet certain methodological standards (i.e., common elements; 9). Identifying common elements allows for the removal of redundant and less effective treatment content, reducing treatment costs, expanding available service provision and enhancing scability. Furthermore, introducing the most effective elements of treatment early may improve client retention and outcomes [ 9 – 13 ].
A potential common element for depression intervention is problem-solving (PS). PS refers to how an individual identifies and applies solutions to everyday problems. D’Zurilla and colleagues [ 14 – 17 ] conceptualize effective PS skills to include a constructive attitude towards problems (i.e., a positive problem-solving orientation) and the ability to approach problems systematically and rationally (i.e., a rational PS style). Whereas maladaptive patterns, such as negative problem orientation and passively or impulsively addressing problems, are ineffective PS skills that may lead to depressive symptoms [ 14 – 17 ]. Problem Solving Therapy (PST), designed by D’Zurilla and colleagues, is a therapeutic approach developed to decrease mental health problems by improving PS skills [ 18 ]. PST focuses on four core skills to promote adaptive problem solving, including: (1) defining the problem; (2) brainstorming possible solutions; (3) appraising solutions and selecting the best one; and (4) implementing the chosen solution and assessing the outcome [ 14 – 17 ]. PS is also a component in other manualized approaches, such as CBT and Dialectical Behavioural Therapy (DBT), as well as imbedded into other wider generalized mental health programming [ 19 , 20 ]. A meta-analysis of over 30 studies found PST, or PS skills alone, to be as effective as CBT and IPT and more effective than control conditions [ 21 – 23 ]. Thus, justifying its identification as a common element in multiple prevention [ 19 , 24 ] and treatment [ 21 , 25 ] programs for adult depression [ 9 , 26 – 28 ].
PS has been applied to youth and young adults; however, no manuals specific to the AYA population are available. Empirical studies suggest maladaptive PS skills are associated with depressive symptoms in AYA [ 5 , 17 – 23 ]. Furthermore, PS intervention can be brief [ 29 ], delivered by trained or lay counsellors [ 30 , 31 ], and provided in various contexts (e.g., primary care, schools [ 23 ]). Given PS’s versatility and effectiveness, PS could be an ideal common element in treating AYA depression; however, to our knowledge, no reviews or meta-analyses on PS’s effectiveness with AYA specific populations exist. This review aimed to examine the effectiveness of PS as a common element in the prevention and treatment of depression for AYA within real-world settings, as well as to ascertain the variables that may influence and impact PS intervention effects.
Identification and selection of studies
Searches were conducted using PsycInfo , Medline , and Cochrane Library with the following search terms: "problem-solving", “adolescent”, “youth”, and” depression, ” along with filters limiting results to controlled studies looking at effectiveness or exploring mechanisms of effectiveness. Synonyms and derivatives were employed to expand the search. We searched grey literature using Greylit . org and Opengrey . eu , contacted experts in the field and authors of protocols, and searched the reference lists of all included studies. The search was undertaken on 4 th June 2020 and updated on 11 th June 2022.
Studies meeting the following criteria were included: (a) the intervention was described by authors as a PS intervention or including PS; (b) the intervention was used to treat or prevent depression; (c) mean or median age between 13–25 years; and (d) at least one depression outcome was reported. Literature in electronic format published post 2000 was deemed eligible, given the greater relevance of more recent usage of PS in real-world settings. There was no exclusion for gender, ethnicity, or country setting; only English language texts were included. Randomized controlled trials (RCTs), quasi-experimental designs (QEDs), systematic reviews/meta-analyses, pilots, or other studies with clearly defined comparison conditions (no treatment, treatment as usual (TAU), or a comparator treatment) were included. We excluded studies of CBT, IPT, Acceptance and Commitment Therapy (ACT), Dialectical Behaviour Therapy (DBT), and modified forms of these treatments. These treatments include PS and have been shown to demonstrate small to medium effects on depression [ 13 , 14 , 32 ], but the unique contribution of PS cannot be disentangled. The protocol for this review was not registered; however, all data collection forms, extraction, coding and analyses used in the review are available upon inquiry from the first author.
Study selection
All citations were entered into Endnote and uploaded to Covidence for screening and review against the inclusion/exclusion criteria. Reviewers with high inter-rater reliability (98%) independently screened the titles and abstracts. Two reviewers then independently screened full text of articles that met criteria. Duplicates, irrelevant studies, and studies that did not meet the criteria were removed, and the reason for exclusion was recorded (see S1 File for a list of excluded studies). Discrepancies were resolved by discussion with the team leads.
Data extraction
Two reviewers independently extracted data that included: (i) study characteristics (author, publication year, location, design, study aim), (ii) population (age, gender, race/ethnicity, education, family income, depression status), (iii) setting, (iv) intervention description (therapeutic or preventative, whether PS was provided alone or as part of a more comprehensive intervention, duration, delivery mode), (v) treatment outcomes (measures used and reported outcomes for depression, suicidality, and PS), and (vi) fidelity/implementation outcomes. For treatment outcomes, we included the original statistical analyses and/or values needed to calculate an effect size, as reported by the authors. If a variable was not included in the study publication, we extracted the information available and made note of missing data and subsequent limitations to the analyses.
RCTs were assessed for quality (i.e., confidence in the study’s findings) using the Cochrane Risk of Bias 2.0 tool [ 33 ] which includes assessment of the potential risk of bias relating to the process of randomisation; deviations from the intended intervention(s); missing data; outcome measurement and reported results. Risk of bias pertaining to each domain is estimated using an algorithm, grouped as: Low risk; Some concerns; or High risk. Two reviewers independently assessed the quality of included studies, and discrepancies were resolved by consensus.
We planned to conduct one or more meta-analyses if the studies were sufficiently similar. Data were entered into a summary of findings table as a first step in determining the theoretical and practical similarity of the population, intervention, comparison condition, outcome, and study design. If there were sufficiently similar studies, a meta-analysis would be conducted according to guidelines contained in the Cochrane Collaboration Handbook of Systematic Reviews, including tests of heterogeneity and use of random effects models where necessary.
The two searches yielded a total number of 874 records (after the removal of duplicates). After title and abstract screening, 184 full-text papers were considered for inclusion, of which 25 studies met the eligibility criteria and were included in the systematic review ( Fig 1 ). Unfortunately, substantial differences (both theoretical and practical) precluded any relevant meta-analyses, and we were limited to a narrative synthesis.

Risk of bias assessment
Risk of bias assessments were conducted on the 23 RCTs ( Fig 2 ; assessments by study presented in S1 Table ). Risk of bias concerns were moderate, and a fair degree of confidence in the validity of study findings is warranted. Most studies (81%) were assessed as ‘some concerns’ (N = 18), four studies were ‘low risk’, and one ‘high risk’. The most frequent areas of concern were the selection of the reported result (n = 18, mostly due to inadequate reporting of a priori analytic plans); deviations from the intended intervention (N = 17, mostly related to insufficient information about intention-to-treat analyses); and randomisation process (N = 13).

Study designs and characteristics
Study design.
Across the 25 studies, 23 were RCTs; two were QEDs. Nine had TAU or wait-list control (WLC) comparator groups, and 16 used active control groups (e.g., alternative treatment). Eleven studies described fidelity measures. The sample size ranged from 26 to 686 and was under 63 in nine studies.
Selected intervention
Twenty interventions were described across the 25 studies ( Table 1 ). Ten interventions focused purely on PS. Of these 10 interventions: three were adaptations of models proposed by D’Zurilla and Nezu [ 20 , 34 ] and D’Zurilla and Goldfried [ 18 ], two were based on Mynors-Wallis’s [ 35 ] Problem-Solving Therapy (PST) guide, one was a problem-orientation video intervention adapted from D’Zurilla and Nezu [ 34 ], one was an online intervention adapted from Method of Levels therapy, and three did not specify a model. Ten interventions used PS as part of a larger, more comprehensive intervention (e.g., PS as a portion of cognitive therapy). The utilization and dose of PS steps included in these interventions were unclear. Ten interventions were primary prevention interventions–one of these was universal prevention, five were indicated prevention, and four were selective prevention. Ten interventions were secondary prevention interventions. Nine interventions were described as having been developed or adapted for young people.
| 1 | Bird et al., 2018 UK | Selective prevention Problem-related distress | MYLO: Online, individual problem-solving program Self-delivered Duration participants’ choice (minimum 15 minutes) Based on PCT principles | RCT N = 213 | ELIZA text-based programme emulating Rogerian psychotherapy | University students aged 16–70 years Mean age: 22.08 years No inclusion criteria for depression | No significant change in depression on the DASS-21. Main effect of group: ( (1,157) = .16, n.s.). Interaction effect between time and group ( (2,314) = .39, n.s.) No significant change in problem-related distress (study developed rating), time x group interaction: (2,338) = 1.32, = .27 No significant change in participants’ ratings of problem resolution (study-developed rating). Main effect: ( (1,60) = 2.49, n.s.) | Some concerns |
| 2 | Chibanda et al., 2014 Zimbabwe | Secondary prevention Postnatal depression | PST: Group, face-to-face PST intervention Delivered by trainer peer counselors 2, 60-minute sessions per week for 6 weeks Based on Mynors-Wallis (2005) | RCT N = 58 | Amitriptyline (antidepressant) and peer education | Women attending primary care clinics over the age of 18 Mean age: 25 years Met criteria for post-partum depression (DSM-IV) | Significant reduction in postnatal depression (EPDS) post intervention. PST group (M = 8.22, SD = 3.6), pharmacotherapy group (M = 10.7, SD = 2.7), = 0.0097. | Some concerns |
| 3 | Eskin et al., 2008 Turkey | Secondary prevention Depression | PST: Individual, face-to-face PST intervention Delivered by graduate clinical psychology students 6 weekly sessions Based on D’Zurilla and Goldfried (1971) and D’Zurilla and Nezu (1999) | RCT N = 46 | WLC | High school and university students Mean age: 19.1 years Diagnosed with MDD (SCIV) | Significant reduction in depression at the end of treatment on the BDI (ANOVA (1, 42) = 10.3, < 0.01; adjusted effect size 1.6); HDRS ( (1, 42) = 37.7, < 0.0001; adjusted effect size 2.2) and suicide potential (SPS– (1, 42) = 7.3, < 0.05; adjusted effect size 0.21). No significant improvement in problem-solving skills on the PSI. Time x interaction effect: (1, 42) = 2.2, > 0.05. Main effect for time: (1, 42) = 6.4, < .05, with post-treatment scores being lower than pre-treatment. Follow-up PSI scores were significantly lower than pre-treatment (Z = 3.7, < 0.0001) and post-treatment PSI scores (Z = 2.0, 0.05). Significant post-treatment depression recovery, BDI: 77% of PST participants and 15.8% of control participants achieved full or partial recovery, x = 19.3, d.f. = 2, 0.0001; HDRS: 96.3% of PST participants and 21.1% of control participants achieved full or partial recovery, x = 31.1, d.f. = 2, < 0.0001. Follow-up BDI scores were statistically significantly lower than pre-treatment BDI scores (Z = 4.1, < 0.0001), but similar to post-treatment BDI scores (Z = 1.6, > 0.05). Follow-up HDRS scores were statistically significantly lower than pre-treatment HDRS scores (Z = 4.1, < 0.0001), but similar to post-treatment HDRS scores (Z = 0.1, > 0.05). | Some concerns |
| 4 | Fitzpatrick et al., 2005 US | Secondary prevention Suicidal ideation | Problem-orientation intervention: video focusing on PS and coping styles Self-delivered 35-minute video, one session with 2 modules to be completed Based on D’Zurilla and Nezu’s (1999) Problem-Solving Therapy manual | RCT N = 110 | Single session video covering health issues including diet exercise and sleep | University students aged 18–24 years Mean age: 19.02 years With suicidal ideation (≥ 6 BSS or endorsing active ideation) | Both suicidal ideation–BSS (Z = 2.17) and depression -BDI (Z = 2.72) had significant decreases pre- and post-treatment. However, these changes diminished over time. At follow-up, BSS differences were no longer significant and BDI differences were significant but small (ETA ). No significant change in problem-solving skills or orientation SPSI-R. | Some concerns |
| 5 | Gaffney et al., 2014 UK | Selective prevention Problem-related distress | MYLO: Online, individual PS program Self-delivered Duration participants’ choice (average time 19.23 minutes) Based on PCT principles | Pilot RCT N = 48 | ELIZA text-based programme emulating Rogerian psychotherapist | University students aged 18–32 years Mean age: 21.4 years No inclusion criteria for depression | No significant change in depression (DASS-21), time x group interaction: (1.24, 49.57) = .50, = .52 No significant change in problem-solving (study-developed rating), time x group interaction: (1, 40) = 3.62, = .06. No significant change in problem-related distress (study-developed rating), time x group interaction: (2, 80) = 1.00, = .37 | Some concerns |
| 6 | Hoek et al., 2012 Netherlands | Indicated prevention Depression | PST: Individual, online PST intervention Delivered by mental health care professionals 5 weekly sessions | RCT N = 45 | WLC | Recruitment through community and via parents treated for depression and anxiety aged 12–21 years Mean age: 16.07 years Self-report of mild or moderate depression and anxiety. Excluded severe depression (>40 on CES-D). | No significant change in depression (CES-D) after 4 months, group x time interaction: B = 0.54, SE = 1.14, = 0.637. Recovery from clinical depression (CES-D) effects were not significantly different between intervention and waiting list groups.) | Some concerns |
| 7 | Houston et al., 2017 US | Universal prevention Resilience | Resilience and Coping Intervention: Group-based, face-to-face intervention to identify thoughts, feelings and coping strategies using PS techniques. Delivered by trained social workers 3, 45-minute weekly sessions | RCT N = 129 | TAU | University students aged 18–23 years Mean age: Not stated No inclusion criteria for depression | Significant reduction in depression (CES-D): F(1, 117) D = 5.36, p = .02; small effect size: Cohen’s ƒ = 0.05. | Some concerns |
| 8 | Malik et al., 2021 India | Indicated prevention Common adolescent mental health problems | PS intervention: Individual face-to-face Delivered by college graduate counsellors with no formal training in psychological treatments 4–5, 30-minute sessions delivered over 2–3 weeks | RCT N = 251 | PS booklets without counsellor treatment | High school students aged 12–20 years Mean age: 15.61 years Elevated mental health symptoms and distress/functional impairment (≥ 19 for boys and 20 for girls on SDQ Total Difficulties scale, ≥ 2 SDQ Impact Scale, > 1 month on SDQ chronicity index) | Significant reduction in psychosocial problems (YTP) at 12 months: adjusted mean difference = −0.75, 95% CI = [−1.47, −0.03], = 0.04. Significant reduction in mental health symptoms (SDQ Total Difficulties Score) at 12 months: adjusted mean difference = −1.73, 95% CI = [−3.47, 0.02], = 0.05. Significant intervention effect on both SDQ Total Difficulties and YTP scores over 12 months (SDQ Total Difficulties: adjusted mean difference = −1.23, 95% CI = [−2.37, −0.09]; d = 0.21, 95% CI = [0.05, 0.36]; = 0.03; YTP: adjusted mean difference = −0.98; 95% CI = [−1.51, −0.45]; d = 0.34, 95% CI = [0.19, 0.50]; < 0.001. Significant intervention effect on secondary outcomes including internalising symptoms (SDQ internalising symptoms subscale): adjusted mean difference = −0.76, 95% CI = [−1.42, −0.10]; d = 0.22, 95% CI = [0.06, 0.37]; = 0.03; impairment (SDQ impact score): adjusted mean difference = −0.51, 95% CI = [−0.93, −0.09]; d = 0.21, 95% CI = [0.06, 0.36]; = 0.02); and perceived stress (PSS-4): adjusted mean difference = −0.54 95% CI = [−1.00, −0.08]; d = 0.21, 95% CI = [0.06, 0.36]; = 0.02) over 12 months. No significant effect on wellbeing (SWEMWBS): adjusted mean difference = 1.16, 95% CI = [−0.07, 2.38]; d = 0.19, 95% CI = [0.04, 0.34]; = 0.06; externalising symptoms (SDQ externalising symptoms subscale): adjusted mean difference = −0.47, 95% CI = [−1.09, 0.14]; d = 0.14, 95% CI = [0.01, 0.30]; = 0.13; or remission adjusted mean difference = 1.47, 95% CI = [0.73, 2.96]; = 0.28 over 12 months. | Low risk of bias |
| 9 | Michelson et al., 2020 India | Indicated prevention Common adolescent mental health problems | PS intervention: Individual face-to-face Delivered by college graduate counsellors with no formal training in psychological treatments 4–5, 30-minute sessions delivered over 2–3 weeks | RCT N = 251 | PS booklets without counsellor treatment | High school students aged 12–20 years Mean age: 15.61 years Elevated mental health symptoms (≥ 19 for boys and 20 for girls on SDQ Total Difficulties scale, ≥ 2 SDQ Impact Scale, > 1 month on SDQ chronicity index) | Significant reduction in psychosocial problems (YTP) at 6 weeks (adjusted mean difference = –1·01, 95% CI [–1·63, –0·38]; adjusted effect size = 0.36, 95% CI [0·11, 0·61], = 0·0015), and at 12 weeks (adjusted mean difference = –1.03, 95% CI [–1·60, –0·47]; adjusted effect size = 0.35, 95% CI [0.18, 0·54]; = 0·0004). No significant change in mental health symptoms (SDQ Total Difficulties score) at 6 weeks (adjusted mean difference = –0·86, 95% CI [–2·14, 0·41]; adjusted effect size = 0·16, 95% CI [0·09, 0.41]; = 0·18) or 12 weeks (adjusted mean difference = –1.12, 95% CI [–2.33, 0.10]; adjusted effect size = 0.20, 95% CI [0.02, 0.37], = 0.072. No significant change in internalising symptoms (SDQ Internalising symptoms subscale) at 12 weeks (adjusted mean difference = –0.61, 95% CI [–1.32, 0.09]; adjusted effect size = 0.18, 95% CI [0.002, 0.36], = 0.089. | Low risk of bias |
| 10 | Parker et al., 2016 Australia | Indicated prevention Depression | PST: Face-to-face; Not specified whether group or individual Delivered by research psychologists 6 weekly sessions Based on Mynors-Wallis (2005) | RCT N = 176 | Control treatment based on general counselling principles informed by NICE guidelines for mild to moderate depression | Young people recruited from youth mental health services aged 15–25 years Mean age: 17.6 years Elevated symptoms not specific to depression indicating a mild disorder (K10 score ≥ 20) | No significant change in depression on the BDI-II (difference in change between interventions = 0.13, 95% CI [–3.10, 3.36], = 0.935) or on the MADRS (difference in change between interventions = 0.29, 95% CI [–2.66, 3.24], = 0.847. | Some concerns |
| 11 | Tezel & Gözüm, 2006 Turkey | Indicated prevention Postnatal depression | PST: Individual, face-to-face Delivered by nurse researchers 6, 30–50-minute weekly sessions Based on D’Zurilla and Goldfield (1971) | QED N = 62 | Nursing intervention | Mothers vising postnatal care service Mean age: 24.6 years (care group); 25.4 years (training group) At risk of post-partum depression (>11 EPDS) but without major depressive symptoms | Significant reduction pre-test to post-test in depression (BDI) for PST ( = 5.462, < 0.05) and the nursing intervention ( = 10.062, < 0.05). However, the nursing intervention was significantly more effective than PST at reducing depressive symptoms ( = 4.529, < 0.05). | NA |
| 12 | Xavier et al., 2019 Brazil | Secondary prevention Suicidal behaviour | PST: Group, face-to-face Delivered by experienced psychologist 5, 120-minute weekly sessions Based on D’Zurilla and Nezu (2007) and Vazquez et al. 2015) [ ] | RCT N = 100 | TAU | Poorly performing students aged 15–19 years recruited from 3 public schools Mean age: 17.2 years Met criteria for depression (≥ 16 CES-D) and high risk of suicide (score total ≥ 45 or critical item score ≥3 on ISO-30) but not major depression | Significant intervention effect for depression (CES-D) across time points: (3.58, 351.24) = 140.81, < .001, = 0.59). Post-treatment: = 28.00, = 5.60, 95% CI [4.57, -6.60]. 6-month follow-up: = 22.65, = 4.53, 9%% CI [3.72, -3.26]. Significant intervention effect for suicidal orientation (ISO-30): (3.39, 312.51) = 104.75, < .001, = 0.52. Significantly more participants no longer at risk of suicide in the PST group (96%) compared to the control group (0%) at post-test (x (1) = 92.3, 0.001) and at 6-moth follow-up (x (1) = 92.3, <0.001). Post-treatment: t = 30.29, d = 6.05, 95% CI [5.11–6.99]. 6-month follow-up: t = 14.08, d = 2.82, 95% CI [2.21, -3.41]. No significant difference in suicide plans or attempts ( = .495). global problem-solving skills and in functional problem-solving skills (SPSR-I) mediated the relationship between the experimental condition and the pre-/posttreatment change in suicidal orientation, with significant effects of mediation of 20.46, 95% CI [23.32, 57.35] and 13.99, 95% CI [33.18–57.96], respectively. These explained 34.5% and 23.6% of the total effect of the intervention on the change in suicidal orientation. | Low risk of bias |
| | ||||||||
| 13 | Brugha et al., 2000 UK | Indicated prevention Postnatal depression | Preparing for Parenthood: Group, face-to-face cognitive, PS, and social support intervention Delivered by nurses and occupational therapists 6, 120-minute weekly sessions Based on an international, collaborative review of the social support intervention literature (Brugha, 1995). [ ] | RCT N = 292 | TAU | Mothers attending antenatal clinics aged 16–38 years Median age: 19 years Increased risk of post-natal depression (1+ items on modified GHQ) | No significant change in postnatal depression (EPDS: OR = 0.82, 95% CI [0.39, 1.75], = 0.61); GHQ-D: OR = 1.22, 95% CI [0.63, 2.39], = 0.55); SCAN ICD-10: OR = 0.48, 95% CI [0.12, 1.99], = 0.30). Intervention group significantly more likely to adopt an avoidant problem-solving style (OR = 2.23, 95% CI [1.23, 4.06], = .009). No significant group differences in confidence in ability to solve problems (OR = 0.69, 95% CI [0.25, 1.90], = 0.48) or belief in personal control when solving problems (OR = 1.13, 95% CI [0.64, 2.00], = 0.67). | Some concerns |
| 14 | Dietz et al., 2014 US | Secondary prevention Depression | SBFT aimed to treat family dysfunction and teach PS skills to families Delivered by trained therapists Phase 1 involved 12–16 weekly sessions, phase 2 involved 2–4 booster sessions | RCT N = 63 | CBT or NST | Patients recruited from 2 mental health clinics aged 13–18 years Mean age: 15.6 years Met DSM criteria for MDD (≥ 13 BDI) | This report focused on whether the PS components of CBT and SFBT mediated the effectiveness of these interventions for remission of major depressive disorder. PS mediated the association between CBT, but not SFBT, and remission from depression such that there was no significant association between SBFT and remission status (K-SADS-P; Wald = 0.00, = 0.99) and there was a significant association between CBT and remission status (K-SADS-P; Wald = 4.64, = 0.03). CBT (B = 0.41, CI [.29, 1.67], = 2.85, = 0.0006) and SFBT (B = 0.30, CI [0.2, 1.47], = 2.07, = 0.04) were both associated with increased PS (video rating). | Some concerns |
| 15 | Gureje et al., 2019 Nigeria | Secondary prevention Perinatal depression | Individual, face-to-face PS intervention Delivered by primary maternal care providers 8, 30–45-minute initial weekly sessions, followed by 4, 30–45-minute fortnightly sessions, third stage with option of pharmacotherapy/specialist referral for patients with higher EPDS scores Adapted from PST-PC. | RCT N = 686 | Enhanced care as usual including psycho-education and social support | Mothers attending childcare clinics aged 16–45 years Mean age: 24.7 years Met criteria for major depression (≥ 12 EPDS) | Significant reduction in depression symptoms (EPDS) at 6 months: between group adjusted mean difference over four follow-up time points: -0.8, 95% CI [-1.3, 0.2], p = 0.007. No significant difference in remission rate (EPDS): adjusted risk difference = 4%, 95% CI [-4.1%, 12.0%]. Significant increase in remission rate for subgroup of women with more severe baseline depression compared to control (OR = 2.29, 95% CI [1.01, 5.20,] p = 0.047). | Some concerns |
| 16 | Haeffel et al., 2017 US | Selective prevention Depression | Social Problem-Solving Therapy: Group, face-to-face intervention designed to increase social PS and social skills Delivered by trained correctional officers 10, 60-minute sessions Based on the Viewpoints manual (Guerra, Moore, & Slaby, 1995 [ ]; Guerra & Slaby, 1990 [ ]; Guerra & Williams, 2012).[ ] | RCT N = 296 | TAU–psychosocial support | Juvenile detainees in state-run detention centres aged 11–16 years Mean age: 14.97 years No inclusion criteria for depression | No significant change in depression (CDI) compared to control: (1, 139) = 0.02, = 0.89, η . . Significant reduction in depression (CDI) for sub-group with higher intelligence and significant increase in depression for participants with lower intelligence: = -0.34, = -2.26, = 0.03, partial correlation = -.19, change in = .02. Simple slope gradient for those with higher and lower levels of intelligence was significantly different depending on intervention type: = –2.11, = 0.03, partial correlation = –.27; effect size in the medium range. | High risk of bias |
| 17 | Hallford & Mellor, 2016 Australia | Secondary prevention Depression | Cognitive Reminiscence Therapy: Individual, face-to-face cognitive therapy that included brief PST Delivered by registered provisional psychologist 6 weekly sessions Based on the protocol by Watt and Cappeliez (2000) [ ] | RCT N = 26 | Brief evidence-based treatment | Young people recruited from a community youth mental health service aged 12–25 years Mean age: 20.8 years At least moderate depression (score ≥ 7 on DASS-21) | No significant reduction in depression (DASS-21: (1, 24) = 1.9, = 0.146) | Some concerns |
| 18 | Hood et al., 2018 US | Selective prevention Diabetes distress | Penn Resilience Program Type 1 Diabetes: Group, face-to-face resilience enhancing intervention with a focus on diabetes management. Teaches cognitive-behavioural, social, and PS skills. Delivered by masters-level clinicians 9, 90–120 minute bi-weekly sessions Adapted from the University of Pennsylvania Penn Resilience Program (Gillham et al., 2006) | RCT N = 264 | Diabetes educational intervention | Patients from diabetes clinics aged 14–18 years Mean age: 15.74 years No inclusion criteria for depression—excluded with depression diagnosis or treatment | No significant reduction in depression (CDI). Symptoms remined stable over time across groups (slope intercept values > 0.05) and no significant group differences found (treatment-intercept and treatment-slope effect values > 0.05). No significant reduction in PS (SPSR-I) between groups ( >.05). | Some concerns |
| 19 | Kolko et al. (2000) | Secondary prevention Depression | SBFT aimed to treat family dysfunction and teach PS skills to families. Delivered by trained therapists Phase 1 involved 12–16 weekly sessions, phase 2 involved 2–4 booster sessions Based on Functional Family Therapy (Alexander & Parsons, 1982) [ ] and the PS model developed by Robin and Foster (1989) [ ] | RCT N = 107 | CBT or NST | Patients recruited from 2 mental health clinics aged 13–18 years Mean age: 15.6 years Met DSM criteria for MDD (≥ 13 BDI) | No significant reduction in depression post treatment (BDI treatment x time interaction: < .08; DEP-13 treatment x time interaction: < .41) or after 24-months follow-up (BDI: < .62; DEP-13: < .92) | Some concerns |
| 20 | Makover et al., 2019 US | Secondary prevention Depression | High School Transition Program: Group and individual, face-to-face intervention designed to increase social and academic PS skills Delivered by trained mental health counsellors 12, 60 -minute group sessions followed by 4 individual booster sessions Based on CAST (Eggert et al., 2002) [ ] | RCT N = 497 | Interview and clinical follow-up without active therapy | Middle and high school students in 8 and 9 grade Mean age: Not stated Met criteria for depression (score ≥ 15 on MFQ) | No significant reduction in depression (MFQ: (1) = 2.18, = .08) | Some concerns |
| 21 | Miklowitz et al., 2014 US | Secondary prevention Mood episodes (including BP and MDD) | Family-Focused Therapy: Face-to-face family-based sessions including psychoeducation, communication, and PS skills training. Delivered by trained therapists 21, 50-minute weekly/bi-weekly sessions | RCT N = 145 | Pharmacotherapy | Adolescents with a DSM-IV-TR diagnosis of bipolar I or II disorder aged 12–18 years Mean age: 15.6 years Symptoms of at least moderate severity (a score >17 on the K-SADS Mania Rating Scale or a score >16 on the Depression Rating Scale) | No significant group differences in time No significant group differences in time free of mood symptoms (depressive or manic symptoms), or percentage of weeks with mood symptoms or depressive symptoms. Family-focused therapy had a greater increase from year 1 to year 2 than enhanced care in the proportion of weeks without mania/ hypomania symptoms (F = 4.02, df = 1, 87, p = 0.048) Family-focused treatment showed greater improvements in mean Psychiatric Status Rating Scale scores for mania/ hypomania across 3-month intervals than enhanced care (F = 1.98, df = 8, 742, p = 0.046) | Some concerns |
| 22 | Miklowitz et al., 2020 US | Secondary prevention Mood episodes (including BP and MDD) | Family-Focused Therapy: Face-to-face family-based sessions including psychoeducation, communication, and PS skills training Delivered by trained therapists 12, 60-minute weekly/bi-weekly sessions | RCT N = 127 | Enhanced care (EC) including family and individual psychoeducation | High risk youths aged 9–17 years and their parents Mean age: 13.2 years Met DSM-IV/DSM-5 criteria for BD or MDD First or second degree relative with lifetime history of BD-I or BD-II Moderate current mood symptoms (prior week YMRS ≥ 11 or 2-week CDRS-R > 29) | No significant difference in time to recovery. In the Family Focused Therapy (FFT group), 47 of 61 participants (77.0%) recovered in a median of 24 weeks (95% CI, 17–33 weeks) compared with 43 of 66 (65.2%) in the EC group in 23 weeks (95% CI, 17–29 weeks) (log-rank χ2 = 0.01; = .93; unadjusted hazard ratio [HR] for FFT vs EC, 1.02; 95% CI, 0.67–1.54). Among participants who recovered (N = 90) FFT participants experienced longer times with- out a new mood episode than EC participants (unadjusted, treatment of the treated log-rank χ2 = 5.44; = .02; HR, 0.55; 95% CI, 0.48–0.92). The estimated median time from randomization to a new mood episode was 73 weeks (95% CI, 55–82 weeks) in the intent-to- treat sample (n = 127), with a median of 81 weeks (95% CI, 56–123 weeks) for those in the FFT group and 63 weeks (95% CI, 44–78 weeks) for those in the EC group. Patients in the FFT group had longer intervals of wellness before new mood episodes than patients in the EC group (χ2 = 4.44; = .03; HR, 0.59; 95% CI, 0.35–0.97) Significantly longer intervals between recovery and next mood episode (A-LIFE and PSRs: χ2 = 5.44; P = .02; hazard ratio, 0.55; 95% CI, 0.48–0.92;), and from randomisation to the next mood episode (A-LIFE and PSRs: χ2 = 4.44; P = .03; hazard ratio, 0.59; 95% CI, 0.35–0.97). | Low risk of bias |
| 23 | Noh, 2018 South Korea | Selective prevention Build resilience and reduce impact of trauma | Resilience enhancement program: Group, face-to-face intervention designed to increase resilience with a component on PS Delivered by the author and a psychiatric nurse 2, 90-minute sessions per week for 4 weeks | QED N = 32 | TAU by youth shelters | Runaway youths from homeless shelters aged 12–21 years Mean age: 16.69 years No inclusion criteria for depression—excluded young people receiving psychiatric interventions | Significant reduction in depression (BDI-II) at post-test (beta = -5.33, = 0.036) but not at one-month follow-up (beta = -4.48, = 0.120). | NA |
| 24 | Psaros et al. 2022 South Africa | Secondary prevention Depression | PST: Individual, face-to-face PST plus LifeSteps adherence intervention Delivered by a trained lay counsellor 8 weekly sessions Based on PST (Bell & D’Zurilla, 2009; Nezu, Maguth Nezu & D’Zurilla 2013) [ ] | RCT N = 23 | TAU | Pregnant women with HIV aged 18–45 years Median age: 24 years Met criteria for current major depressive episode (data from a structured clinical interview, self-report measure, and team consensus based on clinical impressions) | Significant reduction in depression (BDI-II) at post-test (beta = -5.33, = 0.036) but not at one-month follow-up (beta = -4.48, = 0.120). | Some concerns |
| 25 | Weissberg-Benchell et al., 2020 US | Selective prevention Diabetes distress | Penn Resilience Program Type 1 Diabetes: Group, face-to-face resilience enhancing intervention with a focus on diabetes management. Teaches cognitive-behavioural, social and PS skills. Delivered by masters-level clinicians 9, 90-120-minute bi-weekly sessions Adapted from the University of Pennsylvania Penn Resilience Program (Gillham et al., 2006) [ ] | RCT N = 264 | Diabetes educational intervention | Patients from diabetes clinics aged 14–18 years Mean age: 15.7 years No inclusion criteria for depression—excluded with depression diagnosis or treatment | Stable depressive symptoms (CDI) from 0 to 16 months (slope : = 0.41, = 0.28, .139, β = 0.16; quadratic slope = 0.07, = 0.07, = .269, β = 0.10). Decline in depressive symptoms from 16 to 40 months (slope : -0.17, = 0.07, = .018, β = 0.20). The effect size of change in depressive symptoms from 16 to 40 months was = 0.12. Follow-up assessment of change in depressive symptoms from 16 to 40 months separated by intervention group indicated that there was a significant decline in depressive symptoms for the intervention participants, -0.31, = 0.11, = .005, β = -0.31, but not for control participants, -0.01, = 0.09, = .936, β = -0.01. No significant difference in depressive symptoms at 40 months, = -1.76, = 0.94, = .060, β = -0.13, = 0.23. | Some concerns |
Notes: Psychiatric measures: A-LIFE = Adolescent Longitudinal Interval Follow-up Evaluation; BDI = Beck Depression Inventory; BDI-II = Beck Depression Inventory-II; BSS = Beck Suicide Scale; CDI = Children’s Depression Inventory; CDRS-R = Children’s Depression Rating Scale, Revised; CES-D = Centre for Epidemiological Studies Depression Scale; DASS-21 = Depression Anxiety Stress Scale-21; DEP13 = 13 items from Schedule for Affective Disorders and Schizophrenia for School-Age Children; DSM-IV = Diagnostic and Statistical Manual of Mental Health Disorders, fourth edition; DSM-IV-TR = Diagnostic and Statistical Manual of Mental Health Disorders, fourth edition, text revision; DSM-5 = Diagnostic and Statistical Manual of Mental Health Disorders, fifth edition; EPDS = Edinburgh Postnatal Depression Scale; GHQ = General Health Questionnaire; GHQ-D = General Health Questionnaire Depression Scale; HDRS = Hamilton Depression Rating Scale; ICD-10 = International Classification of Diseases, 10 th revision
ISO-30 = Inventory of Suicide Orientation; K10 = Kessler Psychological Distress Scale; K-SADS = Kiddie Schedule for Affective Disorders and Schizophrenia; MADRS = Montgomery-Åsberg Depression Rating Scale; MFQ = Mood and Feelings Questionnaire; PSRs = Psychiatric Status Ratings; PSS-4 = Perceived Stress Scale-4; SCAN = Schedules for Clinical Assessment in Neuropsychiatry; SCIV = Structured Clinical Interview Clinical Version for DSM-IV Axis 1; SDQ = Strengths and Difficulties Questionnaire; SPS = Suicide Probability Scale; SWEMWBS = Short Warwick–Edinburgh Mental Well-Being Scale; YMRS = Young Mania Rating Scale; YTP = Youth Top Problems
Problem-solving measures: PSI = Problem Solving Inventory; SPSI = Social Problem-Solving Inventory; SPSI-R = Social Problem-Solving Inventory-Revised
Other terms: CAST = Coping and Support Training; CBT = Cognitive Behavioural Therapy; MYLO = Manage Your Life Online; NICE = National Institute of Health and Care Excellence; NST = Nondirective Supportive Therapy; PCT = Perceptual Control Therapy; PS = Problem Solving; PST = Problem-Solving Therapy; PST-PC = Problem-Solving Therapy for Pediatric Care; QED = Quasi-Experimental Design; RCT = Randomized Controlled Trial; SBFT = Systematic-Behavioural Family Therapy; TAU = Treatment As Usual; WLC = Waitlist Control; BP = Bipolar Disorder; MDD = major depressive disorder
Intervention delivery
Of the 20 interventions, eight were delivered individually, eight were group-based, two were family-based, one was mixed, and in one, the format of delivery was unclear. Seventeen were delivered face-to-face and three online. Dosage ranged from a single session to 21, 50-minute sessions (12 weekly sessions, then 6 biweekly sessions); the most common session formar was once weekly for six weeks (N = 5).
Intervention setting and participants
Seventeen studies were conducted in high-income countries (UK, US, Australia, Netherlands, South Korea), four in upper-middle income (Brazil, South Africa, Turkey), and four in low- and middle-income countries (Zimbabwe, Nigeria, India). Four studies included participants younger than 13 and four older than 25. Nine studies were conducted on university or high school student populations and five on pregnant or post-partum mothers. The remaining 11 used populations from mental health clinics, the community, a diabetes clinic, juvenile detention, and a runaway shelter.
Sixteen studies included participants who met the criteria for a depressive, bipolar, or suicidal disorder (two of these excluded severe depression). Nine studies did not use depression symptoms in the inclusion criteria (one of these excluded depression). Several studies excluded other significant mental health conditions.
Outcome measures
Eight interventions targeted depression, four post/perinatal depression, two suicidal ideation, two resilience, one ‘problem-related distress’, one ‘diabetes distress’, one common adolescent mental health problem, and one mood episode. Those targeting post/perinatal depression used the Edinburgh Postnatal Depression Scale as the outcome measure. Of the others, six used the Beck Depression Inventory (I or II), two the Children’s Depression Inventory, three the Depression Anxiety Stress Scale-21, three the Centre for Epidemiologic Studies Depression Scale, one the Short Mood and Feelings Questionnaire, one the Hamilton Depression Rating Scale, one the depression subscale on the Schedule for Affective Disorders and Schizophrenia for School-Age Children, one the Strengths and Difficulties Questionnaire, one the Youth Top Problems Score, one the Adolescent Longitudinal Interval Follow-up Evaluation and Psychiatric Status Ratings, one the Kiddie Schedule for Affective Disorders and Schizophrenia, and one the Mini International Neuropsychiatric Interview.
Only eight studies measured PS skills or orientation outcomes. Three used the Social Problem-Solving Inventory-Revised, one the Problem Solving Inventory, two measured the extent to which the nominated problem had been resolved, one observed PS in video-taped interactions, and one did not specify the measure.
The mixed findings regarding the effectiveness of PS for depression may depend on the type of intervention: primary (universal, selective, or indicated), secondary or tertiary prevention. Universal prevention interventions target the general public or a population not determined by any specific criteria [ 36 ]. Selective prevention interventions target specific populations with an increased risk of developing a disorder. Indicated prevention interventions target high-risk individuals with sub-clinical symptoms of a disorder. Secondary prevention interventions include those that target individuals diagnosed with a disorder. Finally, tertiary prevention interventions refer to follow-up interventions designed to retain treatment effects. Outcomes are therefore grouped by intervention prevention type and outcome. Within these groupings, studies with a lower risk of bias (RCTs) are presented first. According to the World Health Organisation guidelines, interventions were defined as primary, secondary or tertiary prevention [ 36 ].
Universal prevention interventions
One study reported on a universal prevention intervention targeting resilience and coping strategies in US university students. The Resilience and Coping Intervention, which includes PS as a primary component of the intervention, found a significant reduction in depression compared to TAU (RCT, N = 129, moderate risk of bias) [ 37 ].
Selective prevention interventions
Six studies, including five RCTs and one QED, tested PS as a selective prevention intervention. Two studies investigated the impact of the Manage Your Life Online program, which includes PS as a primary component of the intervention, compared with an online programme emulating Rogerian psychotherapy for UK university students (RCT, N = 213, moderate risk of bias [ 38 ]; RCT, N = 48, moderate risk of bias [ 39 ]). Both studies found no differences in depression or problem-related distress between groups.
Similarly, two studies explored the effect of adapting the Penn Resilience Program, which includes PS as a component of a more comprehensive intervention for young people with diabetes in the US (RCT, N = 264, moderate risk of bias) [ 40 , 41 ]. The initial study showed a moderate reduction in diabetes distress but not depression at 4-, 8-, 12- and 16-months follow-up compared to a diabetes education intervention [ 40 ]. The follow-up study found a significant reduction in depressive symptoms compared to the active control from 16- to 40-months; however, this did not reach significance at 40-months [ 41 ].
Another study that was part of wider PS and social skills intervention among juveniles in state-run detention centres in the US found no impacts (RCT, N = 296, high risk of bias) [ 42 ]. A QED ( N = 32) was used to test the effectiveness of a resilience enhancement and prevention intervention for runaway youth in South Korea [ 43 ]. There was a significant decrease in depression for the intervention group compared with the control group at post-test, but the difference was not sustained at one-month follow-up.
Indicated prevention interventions
Six studies, including five RCTs and one QED, tested PS as an indicated prevention intervention. Four of the five RCTs tested PS as a primary component of the intervention. A PS intervention for common adolescent mental health problems in Indian high school students (RCT, N = 251, low risk of bias) led to a significant reduction in psychosocial problems at 6- and 12 weeks; however, it did not have a significant impact on mental health symptoms or internalising symptoms compared to PS booklets without counsellor treatment at 6- and 12-weeks [ 31 ]. A follow-up study showed a significant reduction in overall psychosocial problems and mental health symptoms, including internalizing symptoms, over 12 months [ 44 ]. Still, these effects no longer reached significance in sensitivity analysis adjusting for missing data (RCT, N = 251, low risk of bias). Furthermore, a 2x2 factorial RCT ( N = 176, moderate risk of bias) testing PST among youth mental health service users with a mild mental disorder in Australia found that the intervention was not superior to supportive counselling at 2-weeks post-treatment [ 30 ]. Similarly, an online PS intervention delivered to young people in the Netherlands to prevent depression (RCT, N = 45, moderate risk of bias) found no significant difference between the intervention and WLC in depression level 4-months post-treatment [ 45 ].
One RCT tested PS approaches in a more comprehensive manualized programme for postnatal depression in the UK and found no significant differences in depression scores between intervention and TAU at 3-months post-partum (RCT, N = 292, moderate risk of bias) [ 46 ].
A study in Turkey used a non-equivalent control group design (QED, N = 62) to test a nursing intervention against a PS control intervention [ 47 ]. Both groups showed a reduction in depression, but the nursing care intervention demonstrated a larger decrease post-intervention than the PS control intervention.
Secondary prevention interventions
Twelve studies, all RCTs, tested PS as a secondary prevention intervention. Four of the 12 RCTs tested PS as a primary component of the intervention. An intervention among women in Zimbabwe (RCT, N = 58, moderate risk of bias) found a larger decrease in the Edinburgh Postnatal Depression Scale score for the intervention group compared to control (who received the antidepressant amitriptyline and peer education) at 6-weeks post-treatment [ 48 ]. A problem-orientation intervention covering four PST steps and involving a single session video for US university students (RCT, N = 110, moderate risk of bias), compared with a video covering other health issues, resulted in a moderate reduction in depression post-treatment; however, results were no longer significant at 2-weeks, and 1-month follow up [ 49 ].
Compared to WLC, a study of an intervention for depression and suicidal proneness among high school and university students in Turkey (RCT, N = 46, moderate risk of bias) found large effect sizes on post-treatment depression scores for intervention participants post-treatment compared with WLC. At 12-month follow-up, these improvements were maintained compared to pre-test but not compared to post-treatment scores. Significant post-treatment depression recovery was also found in the PST group [ 12 ]. Compared to TAU, a small but high-quality (low-risk of bias) study focused on preventing suicidal risk among school students in Brazil (RCT, N = 100, low risk of bias) found a significant, moderate reduction in depression symptoms for the treatment group post-intervention that was maintained at 1-, 3- and 6-month follow-up [ 50 ].
Seven of the 12 RCTs tested PS as a part of a more comprehensive intervention. Two interventions targeted mood episodes and were compared to active control. These US studies focused on Family-Focused Therapy as an intervention for mood episodes, which included sessions on PS [ 51 , 52 ]. One of these found that Family-Focused Therapy for AYA with Bipolar Disorder (RCT, N = 145, moderate risk of bias) had no significant impact on mood or depressive symptoms compared to pharmacotherapy. However, Family-Focused Therapy had a greater impact on the proportion of weeks without mania/hypomania and mania/hypomania symptoms than enhanced care [ 53 ]. Alternatively, while the other study (RCT, N = 127, low risk of bias) found no significant impact on time to recovery, Family-Focused Therapy led to significantly longer intervals of wellness before new mood episodes, longer intervals between recovery and the next mood episode, and longer intervals of randomisation to the next mood episode in AYA with either Bipolar Disorder (BD) or Major Depressive Disorder (MDD), compared to family and individual psychoeducation [ 52 ].
Two US studies used a three-arm trial to compare Systemic-behavioural Family Therapy (SBFT) with elements of PS, to CBT and individual Non-directive Supportive therapy (NST) (RCT, N = 107, moderate risk of bias) [ 53 , 54 ]. One study looked at whether the PS elements of CBT and SFBT mediated the effectiveness of these interventions for the remission of MDD. It found that PS mediated the association between CBT, but not SFBT, and remission from depression. There was no significant association between SBFT and remission status, though there was a significant association between CBT and remission status [ 53 ]. The other study found no significant reduction in depression post-treatment or at 24-month follow-up for SBFT [ 54 ].
A PS intervention tested in maternal and child clinics in Nigeria RCT ( N = 686, moderate risk of bias) compared with enhanced TAU involving psychosocial and social support found no significant difference in the proportion of women who recovered from depression at 6-months post-partum [ 55 ]. However, there was a small difference in depression scores in favour of PS averaged across the 3-, 6-, 9-, and 12-month follow-up points. Cognitive Reminiscence Therapy, which involved recollection of past PS experiences and drew on PS techniques used for 12-25-year-olds in community mental health services in Australia (RCT, N = 26, moderate risk of bias), did not reduce depression symptoms compared with a brief evidence-based treatment at 1- or 2-month follow-up [ 56 ]. Additionally, the High School Transition Program in the US (RCT, N = 497, moderate risk of bias) aimed to prevent depression, anxiety, and school problems in youth transitioning to high school [ 57 ]. There was no reduction in the percentage of intervention students with clinical depression compared to the control group. Similarly, a small study focused on reducing depression symptoms, and nonadherence to antiretroviral therapy in pregnant women with HIV in South Africa (RCT, N = 23, some concern) found a significant reduction in depression symptoms compared to TAU, with the results being maintained at the 3-month follow-up [ 58 ].
Reduction in suicidality
Three studies measured a reduction in suicidality. A preventive treatment found a large reduction in suicidal orientation in the PS group compared to control post-treatment. In contrast, suicidal ideation scores were inconsistent at 1-,3- and 6- month follow-up, they maintained an overall lower score [ 50 ]. Furthermore, at post-test, significantly more participants in the PS group were no longer at risk of suicide. No significant differences were found in suicide plans or attempts. In a PST intervention, post-treatment suicide risk scores were lower than pre-treatment for the PST group but unchanged for the control group [ 12 ]. An online treatment found a moderate decline in ideation for the intervention group post-treatment compared to the control but was not sustained at a one-month follow-up [ 49 ].
Mediators and moderators
Eight studies measured PS skills or effectiveness. In two studies, despite the interventions reducing depression, there was no improvement in PS abilities [ 12 , 52 ]. One found that change in global and functional PS skills mediated the relationship between the intervention group and change in suicidal orientation, but this was not assessed for depression [ 50 ]. Three other studies found no change in depression symptoms, PS skills, or problem resolution [ 38 – 40 ]. Finally, CBT and SBFT led to significant increases in PS behaviour, and PS was associated with higher rates of remission across treatments but did not moderate the relationship between SBFT and remission status [ 53 ]. Another study found no changes in confidence in the ability to solve problems or belief in personal control when solving problems. Furthermore, the intervention group was more likely to adopt an avoidant PS style [ 46 ].
A high-intensity intervention for perinatal depression in Nigeria had no treatment effect on depression remission rates for the whole sample. Still, it was significantly effective for participants with more severe depression at baseline [ 55 ]. A PS intervention among juvenile detainees in the US effectively reduced depression for participants with higher levels of fluid intelligence, but symptoms increased for those with lower levels [ 42 ].The authors suggest that individuals with lower levels of fluid intelligence may have been less able to cope with exploring negative emotions and apply the skills learned.
This review has examined the evidence on the effectiveness of PS in the prevention or treatment of depression among 13–25-year-olds. We sought to determine in what way, in which contexts, and for whom PS appears to work in addressing depression. We found 25 studies involving 20 interventions. Results are promising for secondary prevention interventions, or interventions targeting clinical level populations, that utilize PS as the primary intervention [ 12 , 47 – 49 ]. These studies not only found a significant reduction in depression symptoms compared to active [ 48 , 49 ] and non-active [ 12 , 47 ] controls but also found a significant reduction in suicidal orientation and ideation [ 12 , 47 , 49 ]. These findings are consistent with meta-analyses of adult PS interventions [ 21 , 22 , 23 ], highlighting that PS interventions for AYA can be effective in real-world settings.
For other types of interventions (i.e., universal, selective prevention, indicated prevention), results were mixed in reducing depression. The one universal program was found to have a small, significant effect in reducing depression symptoms compared to a non-active control [ 37 ]. Most selective prevention programs were not effective [ 39 , 40 , 56 ], and those that did show small, significant effects had mixed outcomes for follow-up maintenance [ 41 , 42 ]. Most indicated prevention programs were not effective [ 30 , 31 , 45 – 47 ], yet a follow-up study showed a significant reduction in internalizing symptoms at 12-month post-treatment compared to an active control [ 44 ]. Given that these studies targeted sub-clinical populations and many of them had small sample sizes, these mixed findings may be a result of not having sufficient power to detect a meaningful difference.
Our review found limited evidence about PS skills as mediator or moderator of depression. Few studies measured improvements in PS skills; fewer still found interventions to be effective. The absence of evidence for PS abilities as a pathway is puzzling. It may be that specific aspects of PS behaviours and processes, such as problem orientation [ 59 ], are relevant. Alternatively, there may be a mechanism other than PS skills through which PS interventions influence depression.
Studies with PS as part of a wider intervention also showed mixed results, even amongst clinical populations. Although there was no clear rationale for the discrepancies in effectiveness between the studies, it is possible that the wider program dilutes the focus and impact of efficacious therapeutic elements. However, this is difficult to discern given the heterogeneity in the studies and limited information on study treatments and implementation factors. A broad conclusion might be that PS can be delivered most effectively with clinical populations in its purest PS form and may be tailored to a range of different contexts and forms, a range of populations, and to address different types of problems; however, this tailoring may reduce effectiveness.
Although the scale of impact is broadly in line with the small to moderate effectiveness of other treatments for youth depression [ 6 ], our review highlights shortcomings in study design, methods, and reporting that would allow for a better understanding of PS effectiveness and pathways. Studies varied in how well PS was operationalised. Low dosage is consistent with usage described in informal conversations with practitioners but may be insufficient for effectiveness. Fidelity was monitored in only half the studies despite evidence that monitoring implementation improves effectiveness [ 60 ]. There were references to implementation difficulties, including attrition, challenges in operationalizing online interventions, and skills of those delivering. Furthermore, most of the studies had little information about comorbidity and no analysis of whether it influenced outcomes. Therefore, we were unable to fully examine and conceptualize the ways, how and for whom PS works. More information about study populations and intervention implementation is essential to understand the potential of PS for broader dissemination.
Our review had several limitations. We excluded studies that included four treatments known to be effective in treating depression among AYA (e.g., CBT) but where the unique contribution of PS to clinical outcome could not be disentangled. Furthermore, we relied on authors’ reporting to determine if PS was included: details about operationalization of PS were often scant. Little evidence addressing the fit, feasibility, or acceptability of PS interventions was found, reflecting a limited focus on implementation. We included only English-language texts: relevant studies in other languages may exist, though our post-2000 inclusion criteria may limit this potential bias due to improved translation of studies to English over the years. Finally, the heterogeneity of study populations, problem severity, comparison conditions, outcome measures, and study designs, along with a relatively small number of included studies, limits confidence in what we can say about implementation and treatment outcomes.
Overall, our review indicates that PS may have the best results when implemented its purest form as a stand-alone treatment with clinical level AYA populations; tailoring or imbedding PS into wider programming may dilute its effectiveness. Our review also points to a need for continued innovation in treatment to improve the operationalizing and testing of PS, especially when included as a part of a more comprehensive intervention. It also highlights the need for study methods that allow us to understand the specific effects of PS, and that measure the frequency, dosage, and timing of PS to understand what is effective for whom and in what contexts.
Supporting information
Acknowledgments.
All individuals that contributed to this paper are included as authors.
Funding Statement
This work was commissioned by Wellcome Trust and was conducted independently by the evaluators (all named authors). No grant number is available. Wellcome Trust had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. The authors declare no financial or other competing interests, including their relationship and ongoing work with Wellcome Trust. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
Data Availability
- PLoS One. 2023; 18(8): e0285949.
Decision Letter 0
PONE-D-23-00042Problem-solving interventions and depression among adolescents and young adults: A systematic review of the effectiveness of problem-solving interventions in preventing or treating depression among 13-25-year-oldsPLOS ONE
Dear Dr. Metz,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
==============================
Please submit your revised manuscript by Apr 22 2023 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: https://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols . Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols .
We look forward to receiving your revised manuscript.
Kind regards,
Thiago Fernandes, PhD
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
Thank you for stating the following in the Competing Interests/Financial Disclosure * (delete as necessary) section:
"This work was supported by Wellcome Trust and was conducted independently by the evaluators (all named authors). No grant number is available. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
" ext-link-type="uri" xlink:type="simple">https://wellcome.org/"
We note that you received funding from a commercial source: "Wellcome Trust"
Please provide an amended Competing Interests Statement that explicitly states this commercial funder, along with any other relevant declarations relating to employment, consultancy, patents, products in development, marketed products, etc.
Within this Competing Interests Statement, please confirm that this does not alter your adherence to all PLOS ONE policies on sharing data and materials by including the following statement: "This does not alter our adherence to PLOS ONE policies on sharing data and materials.” (as detailed online in our guide for authors http://journals.plos.org/plosone/s/competing-interests ). If there are restrictions on sharing of data and/or materials, please state these. Please note that we cannot proceed with consideration of your article until this information has been declared.
Please include your amended Competing Interests Statement within your cover letter. We will change the online submission form on your behalf.
2. We note that you have indicated that data from this study are available upon request. PLOS only allows data to be available upon request if there are legal or ethical restrictions on sharing data publicly. For more information on unacceptable data access restrictions, please see http://journals.plos.org/plosone/s/data-availability#loc-unacceptable-data-access-restrictions .
In your revised cover letter, please address the following prompts:
a) If there are ethical or legal restrictions on sharing a de-identified data set, please explain them in detail (e.g., data contain potentially sensitive information, data are owned by a third-party organization, etc.) and who has imposed them (e.g., an ethics committee). Please also provide contact information for a data access committee, ethics committee, or other institutional body to which data requests may be sent.
b) If there are no restrictions, please upload the minimal anonymized data set necessary to replicate your study findings as either Supporting Information files or to a stable, public repository and provide us with the relevant URLs, DOIs, or accession numbers. For a list of acceptable repositories, please see http://journals.plos.org/plosone/s/data-availability#loc-recommended-repositories .
We will update your Data Availability statement on your behalf to reflect the information you provide.
Additional Editor Comments:
Please respond each comment AND highlight each of them.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: N/A
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Thank you for providing a very well-written, clear, and detailed manuscript of a very interesting and worthwhile study. It was a pleasure to read and I commend you on your work. I have only a few minor comments which are mostly just points of proofreading:
- Some abbreviations in Table 1 are either not detailed before usage here, or in fact aren't expanded upon at all. Please check and detail abbreviations in your notes section (namely PST, PCT, PST-PC, NST, DSM). I recognise that readers may be familiar with some of these or could hazard a well-educated guess, but for ease of readability and for clarity it would be beneficial to amend this.
- It would be beneficial, if possible from your data, to add more detail about the ages of participant in Table 1, or to provide more details in your results section. You explained that some studies included under 13s and/or over 25s, but it is unclear which studies did so. It would also help the reader to assess the included literature more effectively if the mean/median age of participants (as per your inclusion criteria) was noted in the table.
- Lines 200-202 are unclear and confusing to read
- While I recognise the need for your review, I'm not entirely sold on your research question by your introduction section. Particularly, why you have chosen this specific intervention for this population. It may be beneficial to expand on the final paragraph (lines 83-95).
- It may be beneficial to also add your thoughts on what your results mean for clinical practitioners in your discussion. You provide some good recommendations for research, but general expansion here would be helpful.
These are the only minor edits I see as being required as your paper is strong. The results and conclusion are well written and thorough. Thank you also for providing detailed supplementary materials.
Best of luck with your ongoing work
Reviewer #2: The systematic review summarizes 25 studies concerning the efficacy of problem-solving interventions for preventing or treating depression. The topic is thoroughly examined, and the results provide insight into the development of evidence-based interventions and the enhancement of mental health outcomes for adolescents and young adults.
I have some minor concerns which I will elaborate on below:
1. The use of "13-25 years olds" in the title can be misleading as it implies a full age range rather than the mean or median age.
Introduction:
2. While the introduction is logically structured, it would be beneficial to introduce problem-solving (PS) as a technique for depression treatment early on. PS intervention is a key concept, yet it is not mentioned until the last paragraph.
3. The rationale for focusing on the effect of PS interventions on depression needs further clarification. What makes PS a more relevant technique than other techniques? I agree that maladaptive PS is associated with depressive symptoms (line 84), while the construct of PS as a coping strategy may be different from PS as an intervention technique.
4. The relationship between PS technique and evidence-based treatments is slightly confusing. EBTs such as CBT have shown small to moderate effects in preventing and treating depression (line 66), so emphasis might move to discrete treatment techniques such as PS (line 75). However, PS is usually a component of CBT, a technique used in multiple sessions. What might account for a part of the therapy being more effective than the entire therapy?
5. Line 90 refers to the complex relationship between PS and depression. Although details can be found in the results section, it would be clearer to provide a specific explanation here for “complex.”
Discussion:
6. In line 381, the authors “sought to determine in what way, in which contexts, and for whom PS appears to work in addressing depression.” However, outcomes are not discussed by context or study population. Studies conducted among students could differ from those conducted among peripartum women. Did the comparisons between contexts/populations bring forth any conclusions?
7. Among studies that found a significant reduction in depression, some reported that the effect was not sustained (e.g., line 262, line 268, line 302) while others reported the opposite (e.g., line 311, line 350). Is there a possible explanation for this discrepancy?
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: No
Reviewer #2: Yes: Tianyue Mi
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Author response to Decision Letter 0
24 Apr 2023
See below. Also replicated in the "Response to Reviewers" document.
Thank you to the two reviewers for their thoughtful and comprehensive review of our manuscript. We have carefully considered all the comments and made requested modifications. As a result, we believe that the manuscript is improved.
Reviewer #1: Yes
Reviewer #2: Yes
Reviewer #1: N/A
Response to Reviewer 1 comments:
Reviewer #1: Thank you for providing a very well-written, clear, and detailed manuscript of a very interesting and worthwhile study. It was a pleasure to read and I commend you on your work. I have only a few minor comments which are mostly just points of proofreading:
Thank you for your keen eye and this suggestion. We have updated the manuscript to ensure that all acronyms in the table are in the notes section.
Thank you for this suggestion. We have added this information into the Table 1 under the “study population” information.
Thank you for this feedback. We have adjusted the sentence to hopefully increase comprehension. Please let us know if the sentence (now lines 198-199) is still unclear and/or confusing to read.
Thank you for this feedback. We have re-worked the introduction section to include more information on PS and its potential as an active ingredient for AYA depression treatment. Please see lines 71-94.
Thank you for this feedback. We have summarized the recommendations more clearly at the end of the paper. Please see lines 436-437 for clinical implications.
Thank you so much for the thorough and thoughtful review. We believe your comments aided to the creation of an improved manuscript.
Response to Reviewer 2 comments:
Reviewer #2: The systematic review summarizes 25 studies concerning the efficacy of problem-solving interventions for preventing or treating depression. The topic is thoroughly examined, and the results provide insight into the development of evidence-based interventions and the enhancement of mental health outcomes for adolescents and young adults.
Thank you for this suggestion. We have edited the title to only include the reference to adolescents and young adults to be more fitting.
Thank you for this feedback. We have re-worked the introduction section to have PS introduced earlier in the introduction.
Thank you for this feedback. We have re-worked the introduction section to include more information on background treatments using PS amongst adults and its potential as an active ingredient for AYA depression treatment. Please see lines 71-94.
Thank you for this feedback and question. We have added information to the manuscript that discusses a meta-analysis on PS within adult populations that found Problem Solving Therapy (PST) to be as effective as CBT and IPT, and more effective than WLC. We have additionally added information around the potential benefits of distilling common elements with this AYA population. Please see lines 71-94.
Thank you for this feedback and question. Due to all the additional PS information added to the introduction, we removed this statement and only addressed in the discussion section.
Thank you for this feedback and question. Unfortunately, due to the heterogeneity in the study samples and settings as well as limited implementation factors discussed in the publications, these factors were unable to be explored. I added this limitation to lines 412-423.
Thank you for this question. Unfortunately, the heterogeneity of study populations, problem severity, comparison conditions, outcome measures, and study designs, along with a relatively small number of included studies, limits confidence in what we can say about implementation and treatment outcomes. This includes an explanation for the discrepancies in sustained effects.
6. PLOS authors have the option to publish the peer review history of their article (what does this mean?). If published, this will include your full peer review and any attached files.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy.
Reviewer #1: No
Reviewer #2: Yes: Tianyue Mi
Submitted filename: Response to Reviewers.docx
Decision Letter 1
PONE-D-23-00042R1
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Thiago P. Fernandes, PhD
Additional Editor Comments (optional):
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: All comments have been addressed
Reviewer #2: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: Thank you for returning the manuscript with all comments addressed. I feel this manuscript is now strong and of good quality and details an interesting, well articulated, and important piece of research.
Reviewer #2: (No Response)
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Reviewer #1: Yes: Leah Attwell
Reviewer #2: No
Acceptance letter
11 May 2023
Dear Dr. Metz:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Thiago P. Fernandes
Problem-Solving Theory: The Task-Centred Model
- Living reference work entry
- First Online: 12 April 2022
- Cite this living reference work entry
- Blanca M. Ramos 5 &
- Randall L. Stetson 6
Part of the book series: Social Work ((SOWO))
614 Accesses
This chapter examines the task-centred model to illustrate the application of problem-solving theory for social work intervention. First, it provides a brief description of the problem-solving model. Its historical development and key principles and concepts are presented. Next, the chapter offers a general overview of the crisis intervention model. The task-centred model and crisis intervention share principles and methods drawn from problem-solving theory. The remainder of the chapter focuses on the task-centred model. It reviews its historical background, viability as a framework for social work generalist practice, as well as its applicability with diverse client populations and across cultural settings. The structured steps that guide task-centred implementation throughout the helping process are described. A brief critical review of the model’s strengths and limitations is provided. The chapter concludes with a brief summary and some closing thoughts.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Similar content being viewed by others
Conceptual framework for task shifting and task sharing: an international Delphi study

Action in Counselling: A Contextual Action Theory Perspective
Brieland D (1977) Historical overview. Soc Work 22(5):341–346. http://www.jstor.org.libezproxy2.syr.edu/stable/23712810
Google Scholar
Coady N, Lehmann P (2016) The problem-solving model: a framework for integrating the science and art of practice. In: Lehmann P, Coady N (eds) Theoretical perspectives for direct social work practice: a generalist-eclectic approach, 3rd edn. Springer
Chapter Google Scholar
D’Zurilla TJ, Goldfried MR (1971) Problem solving and behavior modification. J Abnorm Psychol 78(1):107–126. https://doi.org/10.1037/h0031360
Article Google Scholar
Dattilio F (1998) Cognitive behavioral therapy. In: Dattilio M (ed) Case studies in couple and family therapy: systems and cognitive perspectives. Guilford, New York, pp 62–82
Dohert W (1981) Cognitive processes in intimate conflicts: extending attribution theory. Am J Fam Ther 9:3–12
Duckword G (1967) A project in crisis intervention. Soc Casework 48(4):227–231
Fortune AE (2012) Development of the task-centered model. In: Rzepnicki TL, McCracken SG, Briggs HE (eds) From task-centered social work to evidence-based and integrative practice: reflections on history and implementation. Oxford University Press, pp 15–39
Fortune AE, Reid WJ (2011) Task-centered social work. In: Turner F (ed) Social work treatment: interlocking theoretical approaches, 6th edn. Oxford University Press, New York, pp 513–532
Fortune AE, McCallion P, Briar-Lawson K (Eds.) (2010) Social work practice research for the 21st century. New York: Columbia University Press
Fortune AE, Ramos BM, Reid WJ (2022) Task-Centered practice. In: Lisa Rapp-McCall, Kevin Corcoran & Albert R. Roberts, (eds.), Social workers’ desk reference, 4th edn Oxford University Press, New York
Fortune AE, Ramos BM, Reid WJ (2022) Task-Centered Practice. In: Lisa Rapp-McCall, Kevin Corcoran, Albert R Roberts, (Eds.). Social Workers’ Desk Reference, 4th edition. New York: Oxford University Press
Garfield SL (1994) Research on client variables in psychotherapy. In: Bergin A, Garfield S (eds) Handbook of psychotherapy and behavior change, 4th edn. Wiley, New York, pp 190–228
Golan N, Carey H, Hyttinnen E (1969) The emerging role of the social worker in the psychiatric emergency service. Community Ment Health J 5(1):55–61
Gorey KM, Thyer BA, Pawfuck DE (1998) Differential effectiveness of prevalent social work practice models: a meta-analysis. Soc Work 43:269–278
Hollis F (1970) The psychosocial approach to the practice of casework. In: Theories of social casework. University of Chicago Press, pp 33–75
Hoyt MF (2000) Some stories are better than others: doing what works in brief therapy and managed care. Brunner/Mazel, Philadelphia
Hubble M, Duncan B, Miller S (1999) Introduction. In: Hubble M, Duncan B, Miller S (eds) The heart and soul of change: what works in therapy. American Psychological Association, Washington, DC
Huh NS, Koh YS (2010) Task-centered practice in South Korea. In: Fortune AE, McCallion P, Briar-Lawson K (eds) Social work practice research for the 21st century. Columbia University Press, New York, pp 235–239
Jagt N, Jagt L (2010) Task-centered practice in the Netherlands. In: Fortune AE, McCallion P, Briar-Lawson K (eds) Social work practice research for the 21st century. Columbia University Press, New York, pp 208–212
Lo TW (2010) Task-centered practice in Hong Kong. In: Fortune AE, McCallion P, Briar-Lawson K (eds) Social work practice research for the 21st century. Columbia University Press, New York, pp 240–244
Malouff JM, Thorsteinsson EB, Schutte NS (2007) The efficacy of problem-solving therapy in reducing mental and physical health problems: a meta-analysis. Clin Psychol Rev 27(1):46–57
Marsh P (2010) Task-centered practice in Great Britain. In: Fortune AE, McCallion P, Briar-Lawson K (eds) Social work practice research for the 21st century. Columbia University Press, New York, pp 203–2007
Marsh P, Doel M (2005) The task-centred book. Routledge, Abingdon/New York
Book Google Scholar
Miley K, O’Melia M, DuBois (2017) Generalist social work practice: an empowering approach. Allyn & Bacon, Boston
Morris B (1968) Crisis intervention in a public welfare agency. Soc Casework 49(10):612–617
Naleppa M (2010) Task-centered practice in Germany. In: Fortune AE, McCallion P, Briar-Lawson K (eds) Social work practice research for the 21st century. Columbia University Press, New York, pp 213–216
Nezu AM, Nezu CM, D’Zurilla T (2012) Problem-solving therapy: a treatment manual. Springer
Nichols M, Schwartz R (2001) Family therapy. Allyn and Bacon, Needham Heights
Parad HJ (1958) Ego psychology and dynamic casework. Family Association of America, New York
Parad H (1965) Preventive casework: problems and implications. In: Parad H (ed) Crisis intervention: selected readings. Family Service Association of America, New York
Parad H (1966) The use of time-limited crisis interventions in community mental health programming. Soc Serv Rev 40(3):275–282
Parad H, Capland G (1960) A framework for studying families in crisis. Soc Work 5(3):3–15
Parad H, Parad G (1968) A study of crisis oriented planned short-term treatment. Soc Casework 49(6):346–355
Payne M (2014) Modern social work theory, 3rd edn. Palgrave Macmillan, Basingstoke
Perlman HH (1957) Social casework: a problem-solving process. University of Chicago Press, Chicago
Poal P (1990) Introduction to the theory and practice of crisis intervention. Quadernos Psicol 10:121–140
Ramos BM, Garvin C (2003) Task centered treatment with culturally diverse populations. In: Tolson E, Reid W, Garvin C (eds) Generalist practice: a task centered approach, pp. Columbia University Press, New York, pp 441–463
Ramos B, Tolson E (2016) The task-centered model. In: Lehmann P, Coady N (eds) Theoretical perspectives for direct social work practice: a generalist-eclectic approach, 3rd edn. Springer
Regehr C (2017) Crisis theory and social work treatment. In: Turner F (ed) Social work treatment: interlocking theoretical approaches. Oxford University Press
Reid WJ (1992) Task strategies: an empirical approach to social work practice. Columbia University Press, New York
Reid WJ, Epstein L (eds) (1972) Task-centered casework. Columbia University Press, New York
Reid W, Ramos B (2002) Intervención “Centrada en la Tarea”, un Modelo de Práctica de Trabajo Social. Rev Treball Soc 168:6–22
Reid WJ, Shyne AW (1969) Brief and extended casework. Columbia University Press, New York
Roberts A (2005) Bridging the past and present to the future of crisis intervention and case management. In: Roberts A (ed) Crisis intervention handbook: assessment, treatment, and research, 3rd edn. Oxford University Press
Rooney RH (2010) Task-centered practice in the United States. In: Fortune AE, McCallion P, Briar-Lawson K (eds) Social work practice research for the 21st century. Columbia University Press, New York, pp 195–202
Ruben D (1998) Social exchange theory: dynamics of a system governing the dysfunctional family and guide to assessment. J Contemp Psychother 8(3):307–325
Schatz MS, Jenkins LE, Sheafor BW (1990) Milford redefined: a model of initial and advanced generalist social work [Article]. J Soc Work Educ 26(3):217–231. https://doi.org/10.1080/10437797.1990.10672154
Strean HS (1968) Some reactions of case workers to the war on poverty. J Contemp Psychother 1:43–48
Strickler M (1965) Applying crisis theory in a community clinic. Soc Casework 46:150–154
Studt E (1968) Social work theory and implication for the practice of methods. Soc Work Educ Report 16:22–46
Tolson R, Reid W, Garvin C (2003) Generalist practice: a task-centered approach, 2nd edn. Columbia University Press, New York
Trotter C (2010) Task-centred practice in Australia. In Fortune AE, McCallion P, Briar-Lawson K (Eds.), Social work practice research for the 21st century, 235–239. New York: Columbia University Press
Watzlawick P, Bervin J, Jackson D (1967) Pragmatics of human communication. W.W. Norton, New York
Download references
Author information
Authors and affiliations.
State University of New York at Albany, Albany, NY, USA
Blanca M. Ramos
State University of New York at Oswego, Oswego, NY, USA
Randall L. Stetson
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Blanca M. Ramos .
Editor information
Editors and affiliations.
School of Human Services and Social Work, Griffith University, Meadowbrook, QLD, Australia
Dorothee Hölscher
School of Social Sciences, UNSW Sydney, Sydney, NSW, Australia
Richard Hugman
Donna McAuliffe
Rights and permissions
Reprints and permissions
Copyright information
© 2022 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry.
Ramos, B.M., Stetson, R.L. (2022). Problem-Solving Theory: The Task-Centred Model. In: Hölscher, D., Hugman, R., McAuliffe, D. (eds) Social Work Theory and Ethics. Social Work. Springer, Singapore. https://doi.org/10.1007/978-981-16-3059-0_9-1
Download citation
DOI : https://doi.org/10.1007/978-981-16-3059-0_9-1
Received : 24 December 2021
Accepted : 25 January 2022
Published : 12 April 2022
Publisher Name : Springer, Singapore
Print ISBN : 978-981-16-3059-0
Online ISBN : 978-981-16-3059-0
eBook Packages : Social Sciences Reference Module Humanities and Social Sciences Reference Module Business, Economics and Social Sciences
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Problem-solving interventions and depression among adolescents and young adults: A systematic review of the effectiveness of problem-solving interventions in preventing or treating depression
Roles Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States of America
Roles Conceptualization, Writing – original draft
Affiliation Centre for Evidence and Implementation, London, United Kingdom
Roles Data curation
Roles Conceptualization, Writing – review & editing
Affiliation Department of Psychology, Virginia Commonwealth University, Richmond, VA, United States of America
Roles Conceptualization, Methodology
Roles Conceptualization, Project administration, Writing – review & editing
Affiliation Centre for Evidence and Implementation, Melbourne, Victoria, Australia
Roles Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing
Affiliation Department of Social Work, Monash University, Melbourne, Victoria, Australia
- Kristina Metz,
- Jane Lewis,
- Jade Mitchell,
- Sangita Chakraborty,
- Bryce D. McLeod,
- Ludvig Bjørndal,
- Robyn Mildon,
- Aron Shlonsky

- Published: August 29, 2023
- https://doi.org/10.1371/journal.pone.0285949
- Peer Review
- Reader Comments
Problem-solving (PS) has been identified as a therapeutic technique found in multiple evidence-based treatments for depression. To further understand for whom and how this intervention works, we undertook a systematic review of the evidence for PS’s effectiveness in preventing and treating depression among adolescents and young adults. We searched electronic databases ( PsycINFO , Medline , and Cochrane Library ) for studies published between 2000 and 2022. Studies meeting the following criteria were included: (a) the intervention was described by authors as a PS intervention or including PS; (b) the intervention was used to treat or prevent depression; (c) mean or median age between 13–25 years; (d) at least one depression outcome was reported. Risk of bias of included studies was assessed using the Cochrane Risk of Bias 2.0 tool. A narrative synthesis was undertaken given the high level of heterogeneity in study variables. Twenty-five out of 874 studies met inclusion criteria. The interventions studied were heterogeneous in population, intervention, modality, comparison condition, study design, and outcome. Twelve studies focused purely on PS; 13 used PS as part of a more comprehensive intervention. Eleven studies found positive effects in reducing depressive symptoms and two in reducing suicidality. There was little evidence that the intervention impacted PS skills or that PS skills acted as a mediator or moderator of effects on depression. There is mixed evidence about the effectiveness of PS as a prevention and treatment of depression among AYA. Our findings indicate that pure PS interventions to treat clinical depression have the strongest evidence, while pure PS interventions used to prevent or treat sub-clinical depression and PS as part of a more comprehensive intervention show mixed results. Possible explanations for limited effectiveness are discussed, including missing outcome bias, variability in quality, dosage, and fidelity monitoring; small sample sizes and short follow-up periods.
Citation: Metz K, Lewis J, Mitchell J, Chakraborty S, McLeod BD, Bjørndal L, et al. (2023) Problem-solving interventions and depression among adolescents and young adults: A systematic review of the effectiveness of problem-solving interventions in preventing or treating depression. PLoS ONE 18(8): e0285949. https://doi.org/10.1371/journal.pone.0285949
Editor: Thiago P. Fernandes, Federal University of Paraiba, BRAZIL
Received: January 2, 2023; Accepted: May 4, 2023; Published: August 29, 2023
Copyright: © 2023 Metz et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant methods and data are within the paper and its Supporting Information files.
Funding: This work was commissioned by Wellcome Trust and was conducted independently by the evaluators (all named authors). No grant number is available. Wellcome Trust had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. The authors declare no financial or other competing interests, including their relationship and ongoing work with Wellcome Trust. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Depression among adolescents and young adults (AYA) is a serious, widespread problem. A striking increase in depressive symptoms is seen in early adolescence [ 1 ], with rates of depression being estimated to almost double between the age of 13 (8.4%) and 18 (15.4%) [ 2 ]. Research also suggests that the mean age of onset for depressive disorders is decreasing, and the prevalence is increasing for AYA. Psychosocial interventions, such as cognitive-behavioural therapy (CBT) and interpersonal therapy (IPT), have shown small to moderate effects in preventing and treating depression [ 3 – 6 ]. However, room for improvement remains. Up to half of youth with depression do not receive treatment [ 7 ]. When youth receive treatment, studies indicate that about half of youth will not show measurable symptom reduction across 30 weeks of routine clinical care for depression [ 8 ]. One strategy to improve the accessibility and effectiveness of mental health interventions is to move away from an emphasis on Evidence- Based Treatments (EBTs; e.g., CBT) to a focus on discrete treatment techniques that demonstrate positive effects across multiple studies that meet certain methodological standards (i.e., common elements; 9). Identifying common elements allows for the removal of redundant and less effective treatment content, reducing treatment costs, expanding available service provision and enhancing scability. Furthermore, introducing the most effective elements of treatment early may improve client retention and outcomes [ 9 – 13 ].
A potential common element for depression intervention is problem-solving (PS). PS refers to how an individual identifies and applies solutions to everyday problems. D’Zurilla and colleagues [ 14 – 17 ] conceptualize effective PS skills to include a constructive attitude towards problems (i.e., a positive problem-solving orientation) and the ability to approach problems systematically and rationally (i.e., a rational PS style). Whereas maladaptive patterns, such as negative problem orientation and passively or impulsively addressing problems, are ineffective PS skills that may lead to depressive symptoms [ 14 – 17 ]. Problem Solving Therapy (PST), designed by D’Zurilla and colleagues, is a therapeutic approach developed to decrease mental health problems by improving PS skills [ 18 ]. PST focuses on four core skills to promote adaptive problem solving, including: (1) defining the problem; (2) brainstorming possible solutions; (3) appraising solutions and selecting the best one; and (4) implementing the chosen solution and assessing the outcome [ 14 – 17 ]. PS is also a component in other manualized approaches, such as CBT and Dialectical Behavioural Therapy (DBT), as well as imbedded into other wider generalized mental health programming [ 19 , 20 ]. A meta-analysis of over 30 studies found PST, or PS skills alone, to be as effective as CBT and IPT and more effective than control conditions [ 21 – 23 ]. Thus, justifying its identification as a common element in multiple prevention [ 19 , 24 ] and treatment [ 21 , 25 ] programs for adult depression [ 9 , 26 – 28 ].
PS has been applied to youth and young adults; however, no manuals specific to the AYA population are available. Empirical studies suggest maladaptive PS skills are associated with depressive symptoms in AYA [ 5 , 17 – 23 ]. Furthermore, PS intervention can be brief [ 29 ], delivered by trained or lay counsellors [ 30 , 31 ], and provided in various contexts (e.g., primary care, schools [ 23 ]). Given PS’s versatility and effectiveness, PS could be an ideal common element in treating AYA depression; however, to our knowledge, no reviews or meta-analyses on PS’s effectiveness with AYA specific populations exist. This review aimed to examine the effectiveness of PS as a common element in the prevention and treatment of depression for AYA within real-world settings, as well as to ascertain the variables that may influence and impact PS intervention effects.
Identification and selection of studies
Searches were conducted using PsycInfo , Medline , and Cochrane Library with the following search terms: "problem-solving", “adolescent”, “youth”, and” depression, ” along with filters limiting results to controlled studies looking at effectiveness or exploring mechanisms of effectiveness. Synonyms and derivatives were employed to expand the search. We searched grey literature using Greylit . org and Opengrey . eu , contacted experts in the field and authors of protocols, and searched the reference lists of all included studies. The search was undertaken on 4 th June 2020 and updated on 11 th June 2022.
Studies meeting the following criteria were included: (a) the intervention was described by authors as a PS intervention or including PS; (b) the intervention was used to treat or prevent depression; (c) mean or median age between 13–25 years; and (d) at least one depression outcome was reported. Literature in electronic format published post 2000 was deemed eligible, given the greater relevance of more recent usage of PS in real-world settings. There was no exclusion for gender, ethnicity, or country setting; only English language texts were included. Randomized controlled trials (RCTs), quasi-experimental designs (QEDs), systematic reviews/meta-analyses, pilots, or other studies with clearly defined comparison conditions (no treatment, treatment as usual (TAU), or a comparator treatment) were included. We excluded studies of CBT, IPT, Acceptance and Commitment Therapy (ACT), Dialectical Behaviour Therapy (DBT), and modified forms of these treatments. These treatments include PS and have been shown to demonstrate small to medium effects on depression [ 13 , 14 , 32 ], but the unique contribution of PS cannot be disentangled. The protocol for this review was not registered; however, all data collection forms, extraction, coding and analyses used in the review are available upon inquiry from the first author.
Study selection
All citations were entered into Endnote and uploaded to Covidence for screening and review against the inclusion/exclusion criteria. Reviewers with high inter-rater reliability (98%) independently screened the titles and abstracts. Two reviewers then independently screened full text of articles that met criteria. Duplicates, irrelevant studies, and studies that did not meet the criteria were removed, and the reason for exclusion was recorded (see S1 File for a list of excluded studies). Discrepancies were resolved by discussion with the team leads.
Data extraction
Two reviewers independently extracted data that included: (i) study characteristics (author, publication year, location, design, study aim), (ii) population (age, gender, race/ethnicity, education, family income, depression status), (iii) setting, (iv) intervention description (therapeutic or preventative, whether PS was provided alone or as part of a more comprehensive intervention, duration, delivery mode), (v) treatment outcomes (measures used and reported outcomes for depression, suicidality, and PS), and (vi) fidelity/implementation outcomes. For treatment outcomes, we included the original statistical analyses and/or values needed to calculate an effect size, as reported by the authors. If a variable was not included in the study publication, we extracted the information available and made note of missing data and subsequent limitations to the analyses.
RCTs were assessed for quality (i.e., confidence in the study’s findings) using the Cochrane Risk of Bias 2.0 tool [ 33 ] which includes assessment of the potential risk of bias relating to the process of randomisation; deviations from the intended intervention(s); missing data; outcome measurement and reported results. Risk of bias pertaining to each domain is estimated using an algorithm, grouped as: Low risk; Some concerns; or High risk. Two reviewers independently assessed the quality of included studies, and discrepancies were resolved by consensus.
We planned to conduct one or more meta-analyses if the studies were sufficiently similar. Data were entered into a summary of findings table as a first step in determining the theoretical and practical similarity of the population, intervention, comparison condition, outcome, and study design. If there were sufficiently similar studies, a meta-analysis would be conducted according to guidelines contained in the Cochrane Collaboration Handbook of Systematic Reviews, including tests of heterogeneity and use of random effects models where necessary.
The two searches yielded a total number of 874 records (after the removal of duplicates). After title and abstract screening, 184 full-text papers were considered for inclusion, of which 25 studies met the eligibility criteria and were included in the systematic review ( Fig 1 ). Unfortunately, substantial differences (both theoretical and practical) precluded any relevant meta-analyses, and we were limited to a narrative synthesis.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0285949.g001
Risk of bias assessment
Risk of bias assessments were conducted on the 23 RCTs ( Fig 2 ; assessments by study presented in S1 Table ). Risk of bias concerns were moderate, and a fair degree of confidence in the validity of study findings is warranted. Most studies (81%) were assessed as ‘some concerns’ (N = 18), four studies were ‘low risk’, and one ‘high risk’. The most frequent areas of concern were the selection of the reported result (n = 18, mostly due to inadequate reporting of a priori analytic plans); deviations from the intended intervention (N = 17, mostly related to insufficient information about intention-to-treat analyses); and randomisation process (N = 13).
https://doi.org/10.1371/journal.pone.0285949.g002
Study designs and characteristics
Study design..
Across the 25 studies, 23 were RCTs; two were QEDs. Nine had TAU or wait-list control (WLC) comparator groups, and 16 used active control groups (e.g., alternative treatment). Eleven studies described fidelity measures. The sample size ranged from 26 to 686 and was under 63 in nine studies.
Selected intervention.
Twenty interventions were described across the 25 studies ( Table 1 ). Ten interventions focused purely on PS. Of these 10 interventions: three were adaptations of models proposed by D’Zurilla and Nezu [ 20 , 34 ] and D’Zurilla and Goldfried [ 18 ], two were based on Mynors-Wallis’s [ 35 ] Problem-Solving Therapy (PST) guide, one was a problem-orientation video intervention adapted from D’Zurilla and Nezu [ 34 ], one was an online intervention adapted from Method of Levels therapy, and three did not specify a model. Ten interventions used PS as part of a larger, more comprehensive intervention (e.g., PS as a portion of cognitive therapy). The utilization and dose of PS steps included in these interventions were unclear. Ten interventions were primary prevention interventions–one of these was universal prevention, five were indicated prevention, and four were selective prevention. Ten interventions were secondary prevention interventions. Nine interventions were described as having been developed or adapted for young people.
https://doi.org/10.1371/journal.pone.0285949.t001

Intervention delivery.
Of the 20 interventions, eight were delivered individually, eight were group-based, two were family-based, one was mixed, and in one, the format of delivery was unclear. Seventeen were delivered face-to-face and three online. Dosage ranged from a single session to 21, 50-minute sessions (12 weekly sessions, then 6 biweekly sessions); the most common session formar was once weekly for six weeks (N = 5).
Intervention setting and participants.
Seventeen studies were conducted in high-income countries (UK, US, Australia, Netherlands, South Korea), four in upper-middle income (Brazil, South Africa, Turkey), and four in low- and middle-income countries (Zimbabwe, Nigeria, India). Four studies included participants younger than 13 and four older than 25. Nine studies were conducted on university or high school student populations and five on pregnant or post-partum mothers. The remaining 11 used populations from mental health clinics, the community, a diabetes clinic, juvenile detention, and a runaway shelter.
Sixteen studies included participants who met the criteria for a depressive, bipolar, or suicidal disorder (two of these excluded severe depression). Nine studies did not use depression symptoms in the inclusion criteria (one of these excluded depression). Several studies excluded other significant mental health conditions.
Outcome measures.
Eight interventions targeted depression, four post/perinatal depression, two suicidal ideation, two resilience, one ‘problem-related distress’, one ‘diabetes distress’, one common adolescent mental health problem, and one mood episode. Those targeting post/perinatal depression used the Edinburgh Postnatal Depression Scale as the outcome measure. Of the others, six used the Beck Depression Inventory (I or II), two the Children’s Depression Inventory, three the Depression Anxiety Stress Scale-21, three the Centre for Epidemiologic Studies Depression Scale, one the Short Mood and Feelings Questionnaire, one the Hamilton Depression Rating Scale, one the depression subscale on the Schedule for Affective Disorders and Schizophrenia for School-Age Children, one the Strengths and Difficulties Questionnaire, one the Youth Top Problems Score, one the Adolescent Longitudinal Interval Follow-up Evaluation and Psychiatric Status Ratings, one the Kiddie Schedule for Affective Disorders and Schizophrenia, and one the Mini International Neuropsychiatric Interview.
Only eight studies measured PS skills or orientation outcomes. Three used the Social Problem-Solving Inventory-Revised, one the Problem Solving Inventory, two measured the extent to which the nominated problem had been resolved, one observed PS in video-taped interactions, and one did not specify the measure.
The mixed findings regarding the effectiveness of PS for depression may depend on the type of intervention: primary (universal, selective, or indicated), secondary or tertiary prevention. Universal prevention interventions target the general public or a population not determined by any specific criteria [ 36 ]. Selective prevention interventions target specific populations with an increased risk of developing a disorder. Indicated prevention interventions target high-risk individuals with sub-clinical symptoms of a disorder. Secondary prevention interventions include those that target individuals diagnosed with a disorder. Finally, tertiary prevention interventions refer to follow-up interventions designed to retain treatment effects. Outcomes are therefore grouped by intervention prevention type and outcome. Within these groupings, studies with a lower risk of bias (RCTs) are presented first. According to the World Health Organisation guidelines, interventions were defined as primary, secondary or tertiary prevention [ 36 ].
Universal prevention interventions
One study reported on a universal prevention intervention targeting resilience and coping strategies in US university students. The Resilience and Coping Intervention, which includes PS as a primary component of the intervention, found a significant reduction in depression compared to TAU (RCT, N = 129, moderate risk of bias) [ 37 ].
Selective prevention interventions
Six studies, including five RCTs and one QED, tested PS as a selective prevention intervention. Two studies investigated the impact of the Manage Your Life Online program, which includes PS as a primary component of the intervention, compared with an online programme emulating Rogerian psychotherapy for UK university students (RCT, N = 213, moderate risk of bias [ 38 ]; RCT, N = 48, moderate risk of bias [ 39 ]). Both studies found no differences in depression or problem-related distress between groups.
Similarly, two studies explored the effect of adapting the Penn Resilience Program, which includes PS as a component of a more comprehensive intervention for young people with diabetes in the US (RCT, N = 264, moderate risk of bias) [ 40 , 41 ]. The initial study showed a moderate reduction in diabetes distress but not depression at 4-, 8-, 12- and 16-months follow-up compared to a diabetes education intervention [ 40 ]. The follow-up study found a significant reduction in depressive symptoms compared to the active control from 16- to 40-months; however, this did not reach significance at 40-months [ 41 ].
Another study that was part of wider PS and social skills intervention among juveniles in state-run detention centres in the US found no impacts (RCT, N = 296, high risk of bias) [ 42 ]. A QED ( N = 32) was used to test the effectiveness of a resilience enhancement and prevention intervention for runaway youth in South Korea [ 43 ]. There was a significant decrease in depression for the intervention group compared with the control group at post-test, but the difference was not sustained at one-month follow-up.
Indicated prevention interventions
Six studies, including five RCTs and one QED, tested PS as an indicated prevention intervention. Four of the five RCTs tested PS as a primary component of the intervention. A PS intervention for common adolescent mental health problems in Indian high school students (RCT, N = 251, low risk of bias) led to a significant reduction in psychosocial problems at 6- and 12 weeks; however, it did not have a significant impact on mental health symptoms or internalising symptoms compared to PS booklets without counsellor treatment at 6- and 12-weeks [ 31 ]. A follow-up study showed a significant reduction in overall psychosocial problems and mental health symptoms, including internalizing symptoms, over 12 months [ 44 ]. Still, these effects no longer reached significance in sensitivity analysis adjusting for missing data (RCT, N = 251, low risk of bias). Furthermore, a 2x2 factorial RCT ( N = 176, moderate risk of bias) testing PST among youth mental health service users with a mild mental disorder in Australia found that the intervention was not superior to supportive counselling at 2-weeks post-treatment [ 30 ]. Similarly, an online PS intervention delivered to young people in the Netherlands to prevent depression (RCT, N = 45, moderate risk of bias) found no significant difference between the intervention and WLC in depression level 4-months post-treatment [ 45 ].
One RCT tested PS approaches in a more comprehensive manualized programme for postnatal depression in the UK and found no significant differences in depression scores between intervention and TAU at 3-months post-partum (RCT, N = 292, moderate risk of bias) [ 46 ].
A study in Turkey used a non-equivalent control group design (QED, N = 62) to test a nursing intervention against a PS control intervention [ 47 ]. Both groups showed a reduction in depression, but the nursing care intervention demonstrated a larger decrease post-intervention than the PS control intervention.
Secondary prevention interventions
Twelve studies, all RCTs, tested PS as a secondary prevention intervention. Four of the 12 RCTs tested PS as a primary component of the intervention. An intervention among women in Zimbabwe (RCT, N = 58, moderate risk of bias) found a larger decrease in the Edinburgh Postnatal Depression Scale score for the intervention group compared to control (who received the antidepressant amitriptyline and peer education) at 6-weeks post-treatment [ 48 ]. A problem-orientation intervention covering four PST steps and involving a single session video for US university students (RCT, N = 110, moderate risk of bias), compared with a video covering other health issues, resulted in a moderate reduction in depression post-treatment; however, results were no longer significant at 2-weeks, and 1-month follow up [ 49 ].
Compared to WLC, a study of an intervention for depression and suicidal proneness among high school and university students in Turkey (RCT, N = 46, moderate risk of bias) found large effect sizes on post-treatment depression scores for intervention participants post-treatment compared with WLC. At 12-month follow-up, these improvements were maintained compared to pre-test but not compared to post-treatment scores. Significant post-treatment depression recovery was also found in the PST group [ 12 ]. Compared to TAU, a small but high-quality (low-risk of bias) study focused on preventing suicidal risk among school students in Brazil (RCT, N = 100, low risk of bias) found a significant, moderate reduction in depression symptoms for the treatment group post-intervention that was maintained at 1-, 3- and 6-month follow-up [ 50 ].
Seven of the 12 RCTs tested PS as a part of a more comprehensive intervention. Two interventions targeted mood episodes and were compared to active control. These US studies focused on Family-Focused Therapy as an intervention for mood episodes, which included sessions on PS [ 51 , 52 ]. One of these found that Family-Focused Therapy for AYA with Bipolar Disorder (RCT, N = 145, moderate risk of bias) had no significant impact on mood or depressive symptoms compared to pharmacotherapy. However, Family-Focused Therapy had a greater impact on the proportion of weeks without mania/hypomania and mania/hypomania symptoms than enhanced care [ 53 ]. Alternatively, while the other study (RCT, N = 127, low risk of bias) found no significant impact on time to recovery, Family-Focused Therapy led to significantly longer intervals of wellness before new mood episodes, longer intervals between recovery and the next mood episode, and longer intervals of randomisation to the next mood episode in AYA with either Bipolar Disorder (BD) or Major Depressive Disorder (MDD), compared to family and individual psychoeducation [ 52 ].
Two US studies used a three-arm trial to compare Systemic-behavioural Family Therapy (SBFT) with elements of PS, to CBT and individual Non-directive Supportive therapy (NST) (RCT, N = 107, moderate risk of bias) [ 53 , 54 ]. One study looked at whether the PS elements of CBT and SFBT mediated the effectiveness of these interventions for the remission of MDD. It found that PS mediated the association between CBT, but not SFBT, and remission from depression. There was no significant association between SBFT and remission status, though there was a significant association between CBT and remission status [ 53 ]. The other study found no significant reduction in depression post-treatment or at 24-month follow-up for SBFT [ 54 ].
A PS intervention tested in maternal and child clinics in Nigeria RCT ( N = 686, moderate risk of bias) compared with enhanced TAU involving psychosocial and social support found no significant difference in the proportion of women who recovered from depression at 6-months post-partum [ 55 ]. However, there was a small difference in depression scores in favour of PS averaged across the 3-, 6-, 9-, and 12-month follow-up points. Cognitive Reminiscence Therapy, which involved recollection of past PS experiences and drew on PS techniques used for 12-25-year-olds in community mental health services in Australia (RCT, N = 26, moderate risk of bias), did not reduce depression symptoms compared with a brief evidence-based treatment at 1- or 2-month follow-up [ 56 ]. Additionally, the High School Transition Program in the US (RCT, N = 497, moderate risk of bias) aimed to prevent depression, anxiety, and school problems in youth transitioning to high school [ 57 ]. There was no reduction in the percentage of intervention students with clinical depression compared to the control group. Similarly, a small study focused on reducing depression symptoms, and nonadherence to antiretroviral therapy in pregnant women with HIV in South Africa (RCT, N = 23, some concern) found a significant reduction in depression symptoms compared to TAU, with the results being maintained at the 3-month follow-up [ 58 ].
Reduction in suicidality
Three studies measured a reduction in suicidality. A preventive treatment found a large reduction in suicidal orientation in the PS group compared to control post-treatment. In contrast, suicidal ideation scores were inconsistent at 1-,3- and 6- month follow-up, they maintained an overall lower score [ 50 ]. Furthermore, at post-test, significantly more participants in the PS group were no longer at risk of suicide. No significant differences were found in suicide plans or attempts. In a PST intervention, post-treatment suicide risk scores were lower than pre-treatment for the PST group but unchanged for the control group [ 12 ]. An online treatment found a moderate decline in ideation for the intervention group post-treatment compared to the control but was not sustained at a one-month follow-up [ 49 ].
Mediators and moderators
Eight studies measured PS skills or effectiveness. In two studies, despite the interventions reducing depression, there was no improvement in PS abilities [ 12 , 52 ]. One found that change in global and functional PS skills mediated the relationship between the intervention group and change in suicidal orientation, but this was not assessed for depression [ 50 ]. Three other studies found no change in depression symptoms, PS skills, or problem resolution [ 38 – 40 ]. Finally, CBT and SBFT led to significant increases in PS behaviour, and PS was associated with higher rates of remission across treatments but did not moderate the relationship between SBFT and remission status [ 53 ]. Another study found no changes in confidence in the ability to solve problems or belief in personal control when solving problems. Furthermore, the intervention group was more likely to adopt an avoidant PS style [ 46 ].
A high-intensity intervention for perinatal depression in Nigeria had no treatment effect on depression remission rates for the whole sample. Still, it was significantly effective for participants with more severe depression at baseline [ 55 ]. A PS intervention among juvenile detainees in the US effectively reduced depression for participants with higher levels of fluid intelligence, but symptoms increased for those with lower levels [ 42 ].The authors suggest that individuals with lower levels of fluid intelligence may have been less able to cope with exploring negative emotions and apply the skills learned.
This review has examined the evidence on the effectiveness of PS in the prevention or treatment of depression among 13–25-year-olds. We sought to determine in what way, in which contexts, and for whom PS appears to work in addressing depression. We found 25 studies involving 20 interventions. Results are promising for secondary prevention interventions, or interventions targeting clinical level populations, that utilize PS as the primary intervention [ 12 , 47 – 49 ]. These studies not only found a significant reduction in depression symptoms compared to active [ 48 , 49 ] and non-active [ 12 , 47 ] controls but also found a significant reduction in suicidal orientation and ideation [ 12 , 47 , 49 ]. These findings are consistent with meta-analyses of adult PS interventions [ 21 , 22 , 23 ], highlighting that PS interventions for AYA can be effective in real-world settings.
For other types of interventions (i.e., universal, selective prevention, indicated prevention), results were mixed in reducing depression. The one universal program was found to have a small, significant effect in reducing depression symptoms compared to a non-active control [ 37 ]. Most selective prevention programs were not effective [ 39 , 40 , 56 ], and those that did show small, significant effects had mixed outcomes for follow-up maintenance [ 41 , 42 ]. Most indicated prevention programs were not effective [ 30 , 31 , 45 – 47 ], yet a follow-up study showed a significant reduction in internalizing symptoms at 12-month post-treatment compared to an active control [ 44 ]. Given that these studies targeted sub-clinical populations and many of them had small sample sizes, these mixed findings may be a result of not having sufficient power to detect a meaningful difference.
Our review found limited evidence about PS skills as mediator or moderator of depression. Few studies measured improvements in PS skills; fewer still found interventions to be effective. The absence of evidence for PS abilities as a pathway is puzzling. It may be that specific aspects of PS behaviours and processes, such as problem orientation [ 59 ], are relevant. Alternatively, there may be a mechanism other than PS skills through which PS interventions influence depression.
Studies with PS as part of a wider intervention also showed mixed results, even amongst clinical populations. Although there was no clear rationale for the discrepancies in effectiveness between the studies, it is possible that the wider program dilutes the focus and impact of efficacious therapeutic elements. However, this is difficult to discern given the heterogeneity in the studies and limited information on study treatments and implementation factors. A broad conclusion might be that PS can be delivered most effectively with clinical populations in its purest PS form and may be tailored to a range of different contexts and forms, a range of populations, and to address different types of problems; however, this tailoring may reduce effectiveness.
Although the scale of impact is broadly in line with the small to moderate effectiveness of other treatments for youth depression [ 6 ], our review highlights shortcomings in study design, methods, and reporting that would allow for a better understanding of PS effectiveness and pathways. Studies varied in how well PS was operationalised. Low dosage is consistent with usage described in informal conversations with practitioners but may be insufficient for effectiveness. Fidelity was monitored in only half the studies despite evidence that monitoring implementation improves effectiveness [ 60 ]. There were references to implementation difficulties, including attrition, challenges in operationalizing online interventions, and skills of those delivering. Furthermore, most of the studies had little information about comorbidity and no analysis of whether it influenced outcomes. Therefore, we were unable to fully examine and conceptualize the ways, how and for whom PS works. More information about study populations and intervention implementation is essential to understand the potential of PS for broader dissemination.
Our review had several limitations. We excluded studies that included four treatments known to be effective in treating depression among AYA (e.g., CBT) but where the unique contribution of PS to clinical outcome could not be disentangled. Furthermore, we relied on authors’ reporting to determine if PS was included: details about operationalization of PS were often scant. Little evidence addressing the fit, feasibility, or acceptability of PS interventions was found, reflecting a limited focus on implementation. We included only English-language texts: relevant studies in other languages may exist, though our post-2000 inclusion criteria may limit this potential bias due to improved translation of studies to English over the years. Finally, the heterogeneity of study populations, problem severity, comparison conditions, outcome measures, and study designs, along with a relatively small number of included studies, limits confidence in what we can say about implementation and treatment outcomes.
Overall, our review indicates that PS may have the best results when implemented its purest form as a stand-alone treatment with clinical level AYA populations; tailoring or imbedding PS into wider programming may dilute its effectiveness. Our review also points to a need for continued innovation in treatment to improve the operationalizing and testing of PS, especially when included as a part of a more comprehensive intervention. It also highlights the need for study methods that allow us to understand the specific effects of PS, and that measure the frequency, dosage, and timing of PS to understand what is effective for whom and in what contexts.
Supporting information
S1 file. list of excluded studies..
https://doi.org/10.1371/journal.pone.0285949.s001
S2 File. PRISMA checklist.
https://doi.org/10.1371/journal.pone.0285949.s002
S1 Table. Individual risk of bias assessments using cochrane RoB2 tool by domain (1–5) and overall (6).
https://doi.org/10.1371/journal.pone.0285949.s003
Acknowledgments
All individuals that contributed to this paper are included as authors.
- 1. Dietz LJ, Silk J, Amole M. Depressive disorders. In: Ollendick TH, White SW, White BA, editors. The Oxford Handbook of Clinical Child and Adolescent Psychology. Oxford University Press, New York, NY; 2019. p. 280–297.
- View Article
- PubMed/NCBI
- Google Scholar
- 14. Nezu AM, Nezu CM, D’Zurilla T. Problem-solving therapy: A treatment manual. Springer Publishing Company. 2012.
- 15. D’Zurilla TJ, Nezu AM. Problem-solving therapy. In: Handbook of Cognitive-Behavioral Therapies. Third. New York, NY: Guilford Press; 2010. p. 197–225.
- 17. D’Zurilla TJ, Nezu AM, Maydeu-Olivares A. Social Problem Solving: Theory and Assessment. In: Chang EC D’Zurilla TJ, Sanna LJ, editors. Social problem solving: Theory, research, and training: American Psychological Association; 2004. p. 11–27.
- 20. D’Zurilla TJ, Nezu AM. (2007). Problem-solving therapy: A positive approach to clinical intervention (3rd edition) New York: Spring Publishing Company.
- 34. D’Zurilla TJ, Nezu AM. Problem-solving therapy: A social competence approach to clinical intervention. 2nd ed. New York: Springer. 1999.
- 35. Mynors-Wallis LM. Problem-solving treatment for anxiety and depression: A practical guide. Oxford University Press: Oxford. 2005.
- 62. Brugha T. (1995). Social support and psychiatric disorder: Overview of evidence. In Brugha T. (Ed.), Social Support and Psychiatric Disorder : Research Findings and Guidelines for Clinical Practice (Studies in Social and Community Psychiatry, pp. 1–38). Cambridge: Cambridge University Press. https://doi.org/10.1017/CBO9780511526749.002
- 66. Guerra N. G. (1995). Viewpoints : A Guide to Conflict Resolution and Decision Making for Adolescents . Research Press, 2612 North Mattis Avenue, Champaign, IL 61821.
- 67. Guerra N. G., & Williams K. R. (2012). Implementing evidence-based practices for juvenile justice prevention and treatment in communities. In Grigorenko E. L. (Ed.), Handbook of juvenile forensic psychology and psychiatry (pp. 297–308). New York: Springer
- 68. Nezu A. M., Maguth Nezu C., & D’Zurilla T. J. (2013). Problem-solving therapy : A treatment manual . Springer Publishing Co.
- 69. Robin A. L., & Foster S. L. (1989). Negotiating parent-adolescent conflict: A behavioral-family systems approach. New York, NY: Guilford Press.
- 70. VAZQUEZ F. L., OTERO P., BLANCO V., & TORRES A. (2015). Terapia de solucion de problemas para la depresion. Una breve guıa practica en grupo. [Problem-solving therapy for depression: A brife guide for group practice]. Madrid: Alianza Editorial.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is Problem-Solving Therapy?
Verywell / Madelyn Goodnight
Problem-Solving Therapy Techniques
How effective is problem-solving therapy, things to consider, how to get started.
Problem-solving therapy is a brief intervention that provides people with the tools they need to identify and solve problems that arise from big and small life stressors. It aims to improve your overall quality of life and reduce the negative impact of psychological and physical illness.
Problem-solving therapy can be used to treat depression , among other conditions. It can be administered by a doctor or mental health professional and may be combined with other treatment approaches.
At a Glance
Problem-solving therapy is a short-term treatment used to help people who are experiencing depression, stress, PTSD, self-harm, suicidal ideation, and other mental health problems develop the tools they need to deal with challenges. This approach teaches people to identify problems, generate solutions, and implement those solutions. Let's take a closer look at how problem-solving therapy can help people be more resilient and adaptive in the face of stress.
Problem-solving therapy is based on a model that takes into account the importance of real-life problem-solving. In other words, the key to managing the impact of stressful life events is to know how to address issues as they arise. Problem-solving therapy is very practical in its approach and is only concerned with the present, rather than delving into your past.
This form of therapy can take place one-on-one or in a group format and may be offered in person or online via telehealth . Sessions can be anywhere from 30 minutes to two hours long.
Key Components
There are two major components that make up the problem-solving therapy framework:
- Applying a positive problem-solving orientation to your life
- Using problem-solving skills
A positive problem-solving orientation means viewing things in an optimistic light, embracing self-efficacy , and accepting the idea that problems are a normal part of life. Problem-solving skills are behaviors that you can rely on to help you navigate conflict, even during times of stress. This includes skills like:
- Knowing how to identify a problem
- Defining the problem in a helpful way
- Trying to understand the problem more deeply
- Setting goals related to the problem
- Generating alternative, creative solutions to the problem
- Choosing the best course of action
- Implementing the choice you have made
- Evaluating the outcome to determine next steps
Problem-solving therapy is all about training you to become adaptive in your life so that you will start to see problems as challenges to be solved instead of insurmountable obstacles. It also means that you will recognize the action that is required to engage in effective problem-solving techniques.
Planful Problem-Solving
One problem-solving technique, called planful problem-solving, involves following a series of steps to fix issues in a healthy, constructive way:
- Problem definition and formulation : This step involves identifying the real-life problem that needs to be solved and formulating it in a way that allows you to generate potential solutions.
- Generation of alternative solutions : This stage involves coming up with various potential solutions to the problem at hand. The goal in this step is to brainstorm options to creatively address the life stressor in ways that you may not have previously considered.
- Decision-making strategies : This stage involves discussing different strategies for making decisions as well as identifying obstacles that may get in the way of solving the problem at hand.
- Solution implementation and verification : This stage involves implementing a chosen solution and then verifying whether it was effective in addressing the problem.
Other Techniques
Other techniques your therapist may go over include:
- Problem-solving multitasking , which helps you learn to think clearly and solve problems effectively even during times of stress
- Stop, slow down, think, and act (SSTA) , which is meant to encourage you to become more emotionally mindful when faced with conflict
- Healthy thinking and imagery , which teaches you how to embrace more positive self-talk while problem-solving
What Problem-Solving Therapy Can Help With
Problem-solving therapy addresses life stress issues and focuses on helping you find solutions to concrete issues. This approach can be applied to problems associated with various psychological and physiological symptoms.
Mental Health Issues
Problem-solving therapy may help address mental health issues, like:
- Chronic stress due to accumulating minor issues
- Complications associated with traumatic brain injury (TBI)
- Emotional distress
- Post-traumatic stress disorder (PTSD)
- Problems associated with a chronic disease like cancer, heart disease, or diabetes
- Self-harm and feelings of hopelessness
- Substance use
- Suicidal ideation
Specific Life Challenges
This form of therapy is also helpful for dealing with specific life problems, such as:
- Death of a loved one
- Dissatisfaction at work
- Everyday life stressors
- Family problems
- Financial difficulties
- Relationship conflicts
Your doctor or mental healthcare professional will be able to advise whether problem-solving therapy could be helpful for your particular issue. In general, if you are struggling with specific, concrete problems that you are having trouble finding solutions for, problem-solving therapy could be helpful for you.
Benefits of Problem-Solving Therapy
The skills learned in problem-solving therapy can be helpful for managing all areas of your life. These can include:
- Being able to identify which stressors trigger your negative emotions (e.g., sadness, anger)
- Confidence that you can handle problems that you face
- Having a systematic approach on how to deal with life's problems
- Having a toolbox of strategies to solve the issues you face
- Increased confidence to find creative solutions
- Knowing how to identify which barriers will impede your progress
- Knowing how to manage emotions when they arise
- Reduced avoidance and increased action-taking
- The ability to accept life problems that can't be solved
- The ability to make effective decisions
- The development of patience (realizing that not all problems have a "quick fix")
Problem-solving therapy can help people feel more empowered to deal with the problems they face in their lives. Rather than feeling overwhelmed when stressors begin to take a toll, this therapy introduces new coping skills that can boost self-efficacy and resilience .
Other Types of Therapy
Other similar types of therapy include cognitive-behavioral therapy (CBT) and solution-focused brief therapy (SFBT) . While these therapies work to change thinking and behaviors, they work a bit differently. Both CBT and SFBT are less structured than problem-solving therapy and may focus on broader issues. CBT focuses on identifying and changing maladaptive thoughts, and SFBT works to help people look for solutions and build self-efficacy based on strengths.
This form of therapy was initially developed to help people combat stress through effective problem-solving, and it was later adapted to address clinical depression specifically. Today, much of the research on problem-solving therapy deals with its effectiveness in treating depression.
Problem-solving therapy has been shown to help depression in:
- Older adults
- People coping with serious illnesses like cancer
Problem-solving therapy also appears to be effective as a brief treatment for depression, offering benefits in as little as six to eight sessions with a therapist or another healthcare professional. This may make it a good option for someone unable to commit to a lengthier treatment for depression.
Problem-solving therapy is not a good fit for everyone. It may not be effective at addressing issues that don't have clear solutions, like seeking meaning or purpose in life. Problem-solving therapy is also intended to treat specific problems, not general habits or thought patterns .
In general, it's also important to remember that problem-solving therapy is not a primary treatment for mental disorders. If you are living with the symptoms of a serious mental illness such as bipolar disorder or schizophrenia , you may need additional treatment with evidence-based approaches for your particular concern.
Problem-solving therapy is best aimed at someone who has a mental or physical issue that is being treated separately, but who also has life issues that go along with that problem that has yet to be addressed.
For example, it could help if you can't clean your house or pay your bills because of your depression, or if a cancer diagnosis is interfering with your quality of life.
Your doctor may be able to recommend therapists in your area who utilize this approach, or they may offer it themselves as part of their practice. You can also search for a problem-solving therapist with help from the American Psychological Association’s (APA) Society of Clinical Psychology .
If receiving problem-solving therapy from a doctor or mental healthcare professional is not an option for you, you could also consider implementing it as a self-help strategy using a workbook designed to help you learn problem-solving skills on your own.
During your first session, your therapist may spend some time explaining their process and approach. They may ask you to identify the problem you’re currently facing, and they’ll likely discuss your goals for therapy .
Keep In Mind
Problem-solving therapy may be a short-term intervention that's focused on solving a specific issue in your life. If you need further help with something more pervasive, it can also become a longer-term treatment option.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
Shang P, Cao X, You S, Feng X, Li N, Jia Y. Problem-solving therapy for major depressive disorders in older adults: an updated systematic review and meta-analysis of randomized controlled trials . Aging Clin Exp Res . 2021;33(6):1465-1475. doi:10.1007/s40520-020-01672-3
Cuijpers P, Wit L de, Kleiboer A, Karyotaki E, Ebert DD. Problem-solving therapy for adult depression: An updated meta-analysis . Eur Psychiatry . 2018;48(1):27-37. doi:10.1016/j.eurpsy.2017.11.006
Nezu AM, Nezu CM, D'Zurilla TJ. Problem-Solving Therapy: A Treatment Manual . New York; 2013. doi:10.1891/9780826109415.0001
Owens D, Wright-Hughes A, Graham L, et al. Problem-solving therapy rather than treatment as usual for adults after self-harm: a pragmatic, feasibility, randomised controlled trial (the MIDSHIPS trial) . Pilot Feasibility Stud . 2020;6:119. doi:10.1186/s40814-020-00668-0
Sorsdahl K, Stein DJ, Corrigall J, et al. The efficacy of a blended motivational interviewing and problem solving therapy intervention to reduce substance use among patients presenting for emergency services in South Africa: A randomized controlled trial . Subst Abuse Treat Prev Policy . 2015;10(1):46. doi:doi.org/10.1186/s13011-015-0042-1
Margolis SA, Osborne P, Gonzalez JS. Problem solving . In: Gellman MD, ed. Encyclopedia of Behavioral Medicine . Springer International Publishing; 2020:1745-1747. doi:10.1007/978-3-030-39903-0_208
Kirkham JG, Choi N, Seitz DP. Meta-analysis of problem solving therapy for the treatment of major depressive disorder in older adults . Int J Geriatr Psychiatry . 2016;31(5):526-535. doi:10.1002/gps.4358
Garand L, Rinaldo DE, Alberth MM, et al. Effects of problem solving therapy on mental health outcomes in family caregivers of persons with a new diagnosis of mild cognitive impairment or early dementia: A randomized controlled trial . Am J Geriatr Psychiatry . 2014;22(8):771-781. doi:10.1016/j.jagp.2013.07.007
Noyes K, Zapf AL, Depner RM, et al. Problem-solving skills training in adult cancer survivors: Bright IDEAS-AC pilot study . Cancer Treat Res Commun . 2022;31:100552. doi:10.1016/j.ctarc.2022.100552
Albert SM, King J, Anderson S, et al. Depression agency-based collaborative: effect of problem-solving therapy on risk of common mental disorders in older adults with home care needs . The American Journal of Geriatric Psychiatry . 2019;27(6):619-624. doi:10.1016/j.jagp.2019.01.002
By Arlin Cuncic, MA Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.
- Open access
- Published: 24 August 2021
Problem-solving training as an active ingredient of treatment for youth depression: a scoping review and exploratory meta-analysis
- Karolin R. Krause ORCID: orcid.org/0000-0003-3914-7272 1 , 2 ,
- Darren B. Courtney ORCID: orcid.org/0000-0003-1491-0972 1 , 3 ,
- Benjamin W. C. Chan 4 ,
- Sarah Bonato ORCID: orcid.org/0000-0002-5174-0047 1 ,
- Madison Aitken ORCID: orcid.org/0000-0002-4921-5462 1 , 3 ,
- Jacqueline Relihan 1 ,
- Matthew Prebeg 1 ,
- Karleigh Darnay ORCID: orcid.org/0000-0002-0395-8674 1 ,
- Lisa D. Hawke ORCID: orcid.org/0000-0003-1108-9453 1 , 3 ,
- Priya Watson ORCID: orcid.org/0000-0001-9753-6490 1 , 3 &
- Peter Szatmari ORCID: orcid.org/0000-0002-4535-115X 1 , 3 , 5
BMC Psychiatry volume 21 , Article number: 397 ( 2021 ) Cite this article
6809 Accesses
13 Citations
34 Altmetric
Metrics details
Problem-solving training is a common ingredient of evidence-based therapies for youth depression and has shown effectiveness as a versatile stand-alone intervention in adults. This scoping review provided a first overview of the evidence supporting problem solving as a mechanism for treating depression in youth aged 14 to 24 years.
Five bibliographic databases (APA PsycINFO, CINAHL, Embase, MEDLINE, Web of Science) and the grey literature were systematically searched for controlled trials of stand-alone problem-solving therapy; secondary analyses of trial data exploring problem-solving-related concepts as predictors, moderators, or mediators of treatment response within broader therapies; and clinical practice guidelines for youth depression. Following the scoping review, an exploratory meta-analysis examined the overall effectiveness of stand-alone problem-solving therapy.
Inclusion criteria were met by four randomized trials of problem-solving therapy (524 participants); four secondary analyses of problem-solving-related concepts as predictors, moderators, or mediators; and 23 practice guidelines. The only clinical trial rated as having a low risk of bias found problem-solving training helped youth solve personal problems but was not significantly more effective than the control at reducing emotional symptoms. An exploratory meta-analysis showed a small and non-significant effect on self-reported depression or emotional symptoms (Hedges’ g = − 0.34; 95% CI: − 0.92 to 0.23) with high heterogeneity. Removing one study at high risk of bias led to a decrease in effect size and heterogeneity (g = − 0.08; 95% CI: − 0.26 to 0.10). A GRADE appraisal suggested a low overall quality of the evidence. Tentative evidence from secondary analyses suggested problem-solving training might enhance outcomes in cognitive-behavioural therapy and family therapy, but dedicated dismantling studies are needed to corroborate these findings. Clinical practice guidelines did not recommend problem-solving training as a stand-alone treatment for youth depression, but five mentioned it as a treatment ingredient.
Conclusions
On its own, problem-solving training may be beneficial for helping youth solve personal challenges, but it may not measurably reduce depressive symptoms. Youth experiencing elevated depressive symptoms may require more comprehensive psychotherapeutic support alongside problem-solving training. High-quality studies are needed to examine the effectiveness of problem-solving training as a stand-alone approach and as a treatment ingredient.
Peer Review reports
Depressive disorders are a common mental health concern in adolescence [ 1 , 2 , 3 ] and associated with functional impairment [ 4 ] and an increased risk of adverse mental health, physical health, and socio-economic outcomes in adulthood [ 5 , 6 , 7 , 8 ]. Early and effective intervention is needed to reduce the burden arising from early-onset depression. Several psychotherapies have proven modestly effective at reducing youth depression, including cognitive-behavioural therapy (CBT) and interpersonal therapy (IPT) [ 9 , 10 ]. Room for improvement remains; around half of youth do not show measurable symptom reduction after an average of 30 weeks of routine clinical care for depression or anxiety [ 11 ]. One barrier to greater impact is a lack of understanding of which treatment ingredients are most critical [ 12 , 13 ]. Identifying the “active ingredients” that underpin effective approaches, and understanding when and for whom they are most effective is an important avenue for enhancing impact [ 13 ]. Distilling interventions to their most effective ingredients while removing redundant content may also help reduce treatment length and cost, freeing up resources to expand service provision. Given that youth frequently drop out of treatment early [ 14 ], introducing the most effective ingredients at the start may also help improve outcomes.
One common ingredient in the treatment of youth depression is problem-solving (PS) training [ 15 ]. Problem solving in real-life contexts (also called social problem solving) describes “the self-directed process by which individuals attempt to identify [ …] adaptive coping solutions for problems, both acute and chronic, that they encounter in everyday living” (p.8) [ 16 ]. Within a relational/problem-solving model of stress and well-being, mental health difficulties are viewed as the result of maladaptive coping behaviours that cannot adequately safeguard an individual’s well-being against chronic or acute stressors [ 17 ]. According to a conceptual model developed by D’Zurilla and colleagues ([ 16 , 17 , 18 , 19 ]; see Fig. 1 ), effective PS requires a constructive and confident attitude towards problems (i.e., a positive problem orientation ), and the ability to approach problems rationally and systematically (i.e., rational PS style ). Defeatist or catastrophizing attitudes (i.e., a negative problem orientation ), passively waiting for problems to resolve (i.e., avoidant style ), or acting impulsively without thinking through possible consequences and alternative solutions (i.e., impulsive/careless style ) are considered maladaptive [ 16 , 18 , 20 ]. Empirical studies suggest maladaptive PS is associated with depressive symptoms in adolescents and young adults [ 21 , 22 , 23 , 24 , 25 ].
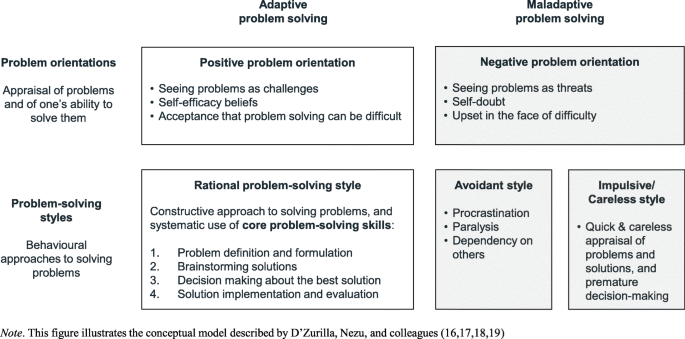
Dimensions of Problem-Solving (PS) Ability
Problem-Solving Therapy (PST) is a therapeutic approach developed by D’Zurilla and Goldfried [ 26 ] in the 1970s, to alleviate mental health difficulties by improving PS ability. Conceptually rooted in Social Learning Theory [ 27 ], PST aims to promote adaptive PS by helping clients foster an optimistic and self-confident attitude towards problems (i.e., a positive problem orientation), and by helping them develop and internalize four core PS skills: (a) defining the problem; (b) brainstorming possible solutions; (c) appraising solutions and selecting the most promising one; (d) implementing the preferred solution and reflecting on the outcome ([ 16 , 17 , 18 , 19 ]; see Fig. 1 ). PST is distinct from Solution-Focused Brief Therapy (SFBT), which has different conceptual roots and emphasizes the construction of solutions over the in-depth formulation of problems [ 28 ].
PS training is also a common ingredient of other psychosocial depression treatments [ 15 , 20 ], such as CBT and Dialectical Behaviour Therapy (DBT) [ 15 , 29 , 30 , 31 , 32 ] that typically focus on strengthening PS skills rather than problem orientation [ 20 ]. In IPT, PS training focuses on helping youth understand and resolve relationship problems [ 29 , 30 , 33 , 34 ]. PS training is also a common component of family therapy [ 35 ], cognitive reminiscence therapy [ 36 ], and adventure therapy [ 37 ]. The extent to which PS training in these contexts follows the conceptual model by D’Zurilla and colleagues varies. Hereafter, we will use the term PST (“Problem-Solving Therapy”) where problem-solving training constitutes a stand-alone intervention; and we will use the term “PS training” where it is mentioned as a part of other therapies or discussed more broadly as an active ingredient of treatment for youth depression.
Meta-analyses considering over 30 randomized control trials (RCTs) of stand-alone PST for adult depression suggest it is as effective as CBT and IPT, and more effective than waitlist or attention controls [ 38 , 39 , 40 ]. PST has been applied with children, adolescents, and young adults [ 41 , 42 , 43 , 44 , 45 , 46 ], but dedicated manuals for different developmental stages are not readily available. In an assessment of fit between evidence-based therapy components and everyday coping skills used by school children, PS skills were the third most frequently endorsed skill set in terms of frequency of habitual use and perceived effectiveness, suggesting these skills are highly transferable and relevant to youth [ 47 ]. PS training can be brief (i.e., involve fewer than 10 sessions) [ 38 ], and has been delivered to youth by trained clinicians [ 45 ], lay counsellors [ 46 ], and via online platforms [ 44 ]. It can also be adapted for primary care [ 40 ]. In light of its versatility and of its effectiveness in adults, PS training is a prime candidate for a treatment ingredient that deserves greater scrutiny in the context of youth depression. However, no systematic evidence synthesis has yet examined its efficacy and effectiveness in this population.
This study had two sequential parts. First, we conducted a mixed-methods scoping review to map the available evidence relating to PS training as an active ingredient for treating youth depression. Youth were defined as aged 14 to 24 years, broadly aligning with United Nations definitions [ 48 ]. In a subsequent step, we conducted an exploratory meta-analysis to examine the overall efficacy of free-standing PST, based on clinical trials identified in the scoping review.
Scoping review
Scoping review methodology was used to provide an initial overview of the available evidence [ 49 ]. The review was pre-registered on the Open Science Framework [ 50 ] and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) extension for Scoping Reviews checklist [ 51 ] (Additional File 1 ). The review was designed to integrate four types of literature: (a) qualitative studies reporting on young people’s experiences with PS training; (b) controlled clinical trials testing the efficacy of stand-alone PST; (c) studies examining PS-related concepts as predictors, moderators, or mediators of treatment response within broader therapeutic interventions (e.g., CBT); and (d) clinical practice guidelines (CPGs) for youth depression. In addition, the search strategy included terms designed to identify relevant conceptual articles that are discussed here as part of the introduction [ 52 ].
Search strategy
Five bibliographic databases (APA PsycINFO, CINAHL, Embase, MEDLINE, Web of Science) and the grey literature were systematically searched for (a) empirical studies published from database inception through June 2020, and (b) CPGs published between 2005 and July 2020. Reference lists of key studies were searched manually, and records citing key studies were searched using Google Scholar’s “search within citing articles” function [ 52 ]. The search strategy was designed in collaboration with a research librarian (SB) and combined topic-specific terms defining the target population (e.g., “depression”; “adolescent?”) and intervention (e.g., “problem-solving”) with methodological search filters combining database-specific subject headings (e.g., “randomized controlled trial”) and recommended search terms. The search for CPGs built upon a previous systematic search [ 53 , 54 ], which was updated and expanded to cover additional languages and databases. A multi-pronged grey literature search retrieved records from common grey literature databases and CPG repositories, websites of relevant associations, charities, and government agencies. The search strategy is provided in Additional File 2 .
Inclusion and exclusion criteria
Empirical studies were included if the mean participant age fell within the eligible range of 14 to 24 years, and at least 50% of participants showed above-threshold depressive or emotional symptoms on a validated screening tool. Controlled clinical trials had to compare the efficacy or effectiveness of PST as a free-standing intervention with a control group or waitlist condition. Secondary analyses were considered for their assessment of PS ability as a predictor, moderator, or mediator of treatment response if they reported on data from controlled clinical trials of broader therapy packages. Records were included as CPGs if labelled as practice guidelines, practice parameters, or consensus or expert committee recommendations, or explicitly aimed to develop original clinical guidance [ 53 , 54 ]; and if focused on indicated psychosocial treatments for youth depression (rather than prevention, screening, or pharmacological treatment). Doctoral dissertations were included. Conference abstracts, non-controlled trials, and prevention studies were excluded. Language of publication was restricted to English, French, German, and Spanish.
All records identified were imported into the EPPI-Reviewer 4.0 review software [ 55 ], and underwent a two-stage screening process (Fig. 2 ). Title and abstract screening was conducted in duplicate for 10% of the identified records, yielding substantial inter-rater agreement ( kappa = .75 and .86, for empirical studies and CPGs, respectively). Of studies retained for full text screening, 20% were screened in duplicate, yielding substantial agreement ( kappa = .68 and .71, for empirical studies and CPGs, respectively). Disagreements were resolved through discussion.
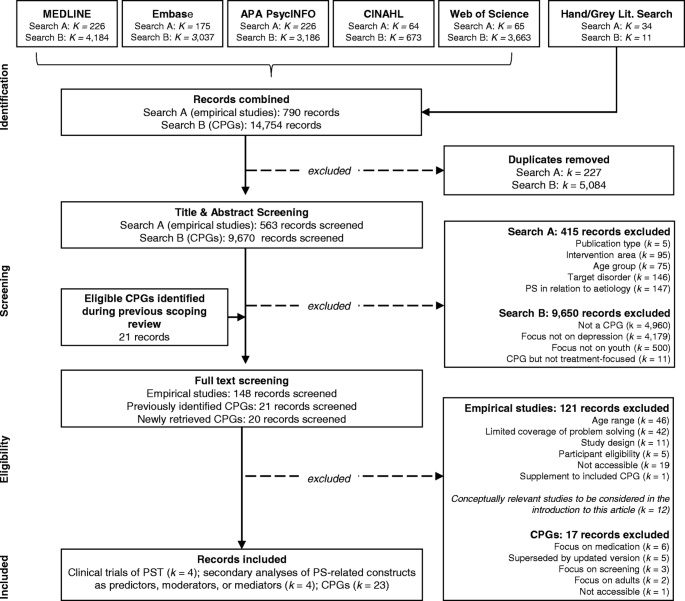
PRISMA Flow Chart of the Study Selection Process
Data extraction and synthesis
Data were extracted using templates tailored to each literature type (e.g., the Cochrane data collection form for RCTs). Information extracted included: citation details; study design; participant characteristics; and relevant qualitative or quantitative results. Additional information extracted from CPGs included the issuing authority, the target population, the treatment settings to which the guideline applied, and any recommendations in relation to PS training. Data from clinical trials and secondary analyses were extracted in duplicate, and any discrepancies were discussed and resolved. Data synthesis followed a five-step process of data reduction, display, comparison, conclusion drawing, and verification [ 56 ]. Scoping review findings were summarized in narrative format. In addition, effect sizes reported in PST trials for depression severity were entered into an exploratory meta-analysis (see below).
The Centre for Addiction and Mental Health (CAMH) implements a Youth Engagement Initiative that brings the voices of youth with lived experience of mental health difficulties into research and service design [ 57 , 58 , 59 ]. Two youth partners were co-investigators in this review and consulted with a panel of twelve CAMH youth advisors to inform the review process and help contextualize findings. Formal approval by a Research Ethics Board (REB) was not required, as youth were research partners rather than participants.
To incorporate a variety of perspectives, the review team convened for an inference workshop where emerging review findings and feedback from youth advisors were discussed and interpreted. The multidisciplinary team involved a methodologist; two child and adolescent psychiatrists with expertise in CBT, DBT, and IPT; a psychologist with expertise in parent-adolescent therapy; a research librarian; a family doctor; a biostatistician; a clinical epidemiologist; two youth research partners; and a youth engagement coordinator.
Exploratory Meta-analysis
Although meta-analyses are not typical components of scoping reviews [ 60 ], an exploratory meta-analysis was conducted following completion of the scoping review and narrative synthesis, to obtain an initial indication of the efficacy of stand-alone PST based on the clinical trials identified in the review. The PICO statement that guided the meta-analysis is shown in Table 1 .
Quality assessment
Risk of bias for included PST trials was appraised using the Cochrane Collaborations Risk of Bias (ROB) 2 tool [ 61 ]. Ratings were performed independently by two reviewers (KRK and MA), and consensus was formed through discussion. In addition, a Grading of Recommendations Assessment, Development, and Evaluation (GRADE) appraisal was conducted (using the GRADEpro software; [ 62 ] to characterize the quality of the overall evidence. The evidence was graded for risk of bias, imprecision, indirectness, inconsistency, and publication bias [ 63 ]. A GRADE of “high quality” indicates a high level of confidence that the true effect lies close to the estimate; “moderate quality” indicates moderate confidence; “low quality” indicates limited confidence; and “very low quality” indicates very little confidence in the estimate. ROB ratings and GRADE appraisal results are provided in Additional File 6 .
Statistical analysis
The meta-analysis was conducted using the meta suite of commands in Stata 16.1. Effect sizes (Hedges’ g) and their confidence intervals were calculated based on the mean difference in depression severity scores between the PST and control conditions at the first post-treatment assessment [ 64 ]. Hedges’ g is calculated by subtracting the post-treatment mean score of the intervention group from the score of the control group, and by dividing the mean difference by the pooled standard deviation. Effect sizes between g = 0.2 and 0.5 indicate a small effect; g = 0.5 to 0.8 indicates a moderate effect; and g ≥ 0.8 indicates a large effect. Effect sizes were adjusted using the Hedges and Olkin small sample correction [ 64 ]. Pooled effect sizes were computed using a random effects model to account for heterogeneity in intervention settings, modes of delivery, and participant age and depression severity. The I 2 statistic was computed as an indicator of effect size heterogeneity. Higgins et al. [ 65 ] suggest that an I 2 below 30% represents low heterogeneity while an I 2 above 75% represents substantial heterogeneity. Investigations of heterogeneity are unlikely to generate valuable insights in small study samples, with at least ten studies recommended for meta-regression [ 65 ]. We conducted limited exploratory subgroup analysis by computing a separate effect size after excluding studies with high risk of bias. We inspected the funnel plot and considered conducting Egger’s test to examine the likelihood and extent of publication bias [ 66 ].
Selection and inclusion of studies
The search for empirical studies identified 563 unique records (Fig. 2 ), of which 148 were screened in full. Inclusion criteria were met by four RCTs of free-standing PST and four secondary analyses of clinical trials investigating PS-related concepts as predictors, mediators, or moderators of treatment response. No eligible qualitative studies that explicitly examined youth experiences of PS training were identified. The search for CPGs identified 9691 unique records, of which 41 were subject to full text screening, and 23 were included in the review. Below we present scoping review findings for all literature types, followed by the results from the meta-analysis for stand-alone PST trials.
Clinical trials of PST
Characteristics of the included PST trials are shown in Table 2 . Studies were published between 2008 and 2020 and included 524 participants (range: 45 to 251), with a mean age of 16.7 years (range: 12–25; 48% female). Participants had a diagnosis of major depressive disorder (MDD; k = 1), elevated anxiety or depressive symptoms ( k = 1), or various mild presenting problems including depression ( k = 2). Treatment covered PS skills but not problem orientation (i.e., youth’s problem appraisals) and was delivered face to face ( k = 3) or online ( k = 1) in five to six sessions. PST was compared with waitlist controls ( k = 2), PS booklets ( k = 1), and supportive counselling ( k = 1). Risk of bias was rated as medium for two [ 44 , 45 ], and high for one study [ 43 ] due to concerns about missing outcome data and the absence of a study protocol.
Eskin and colleagues [ 43 ] randomized 53 Turkish high school and university students with MDD to six sessions of PST or a waitlist. The study reports a significant treatment effect on self-reported depressive symptoms (d = − 1.20; F [1, 42] = 10.3, p < .01.), clinician-reported depressive symptoms (d = − 2.12; F [1, 42] = 37.7, p < .001), and recovery rates, but not on self-reported PS ability (d = − 0.46; F [1, 42] = 2.2, p > .05). Risk of bias was rated as high due to 37% of missing outcome data in the control group and the absence of a published trial protocol.
Michelson and colleagues [ 46 ] compared PST delivered by lay counsellors in combination with booklets, to PS booklets alone in 251 high-school students with mild mental health difficulties (53% emotional problems) in low-income communities in New Delhi, India. At six weeks, the intervention group showed significantly greater progress towards overcoming idiographic priority problems identified at baseline (d = 0.36, p = .002), but no significant difference in self-reported mental health difficulties (d = 0.16, p = .18). Results were similar at 12 weeks, including no significant difference in self-reported emotional symptoms (d = 0.18, p = .089). As there was no long-term follow-up, it is unknown whether reduced personal problems translated into reduced emotional symptoms in the longer term. Perceived stress at six weeks was found to mediate treatment effect on idiographic problems, accounting for 15% of the overall effect at 12 weeks.
Two trials found no significant effect of PST on primary or secondary outcomes: Hoek and colleagues [ 44 ] randomized 45 youth with elevated depression or anxiety symptoms to five sessions of online PST or a waitlist control; Parker and colleagues [ 45 ] randomized 176 youth with mixed presenting problems (54% depression) to either PST with physical activity or PST with psychoeducation, compared with supportive counselling with physical activity or psychoeducation [ 45 ]. Drop-out from PST was high in both studies, ranging from 41.4% [ 45 ] to 72.7% [ 44 ].
PS-related concepts as predictors, moderators, or mediators of treatment response
The review identified four secondary analyses of RCT data that examined PS-related concepts as predictors, moderators, or mediators of treatment response (see Table 3 , below). Studies were published between 2005 and 2014 and included data from 761 participants with MDD diagnoses, and a mean age of 15.2 years (range: 12–18; 61.2% female).
A secondary analysis of data from the Treatment for Adolescents with Depression Study (TADS, n = 439) [ 79 ] explored whether baseline problem orientation and PS styles were significant predictors or moderators of treatment response to Fluoxetine, CBT, or a combination treatment at 12 weeks [ 70 ]. Negative problem orientation and avoidant PS style each predicted less improvement in depression symptom severity ( p = .001 and p = .003, respectively), while positive problem orientation predicted greater improvement ( p = .002). There was no significant moderation effect. Neither rational PS style nor impulsive-careless PS style predicted or moderated change in depressive symptoms.
A secondary analysis of data from the Treatment of Resistant Depression in Adolescents (TORDIA) study [ 80 ] examined the impact of specific CBT components on treatment response at 12 weeks in youth treated with a selective serotonin reuptake inhibitor (SSRI) in combination with CBT ( n = 166) [ 71 ]. Youth who received PS training were 2.3 times ( p = .03) more likely to have a positive treatment response than those not receiving this component. A significant effect was also observed for social skills training (Odds Ratio [OR] = 2.6, p = .04) but not for seven other CBT components. PS and social skills training had the most equal allocation ratios between youth who received them (52 and 54%, respectively) and youth who did not. Balanced allocation provides maximum power for a given sample size [ 81 ]. With allocation ratios between 1:3 and 1:5, analysis of the remaining seven components may have been underpowered. Of further note, CBT components were not randomly assigned but selected based on individual clinical needs. The authors did not correct for multiple comparisons as part of this exploratory analysis.
Dietz and colleagues [ 73 ] explored the impact of social problem solving on treatment outcome based on data from a trial comparing CBT and Systemic Behaviour Family Therapy (SBFT) with elements of PS training on the one hand, with Non-Directive Supportive Therapy on the other hand ( n = 63). Both CBT and SBFT were associated with significant improvements in young people’s interpersonal PS behaviour (measured by coding videotaped interactions between youth and their mothers) over the course of treatment (CBT: b* = 0.41, p = .006; SBFT: b* = 0.30, p = .04), which in turn were associated with higher rates of remission (Wald z = 6.11, p = .01). However, there was no significant indirect effect of treatment condition via youth PS behaviour, and hence, no definitive evidence of a formal mediation effect [ 82 ].
Kaufman and colleagues [ 72 ] examined data from a trial comparing an Adolescent Coping with Depression (CWD-A) group-based intervention with a life-skills control condition in 93 youth with comorbid depression and conduct disorder. The secondary analysis explored whether change in six CBT-specific factors, including the use of PS and conflict resolution skills, mediated the effectiveness of CWD-A. There was no significant improvement in PS ability in CWD-A, compared with the control, and hence no further mediation analysis was conducted.
PS training in clinical practice guidelines
We identified 23 CPGs from twelve countries relevant to youth depression (see Additional File 4 ), issued by governments ( k = 6), specialty societies ( k = 3), health care providers ( k = 4), independent expert groups ( k = 2), and others, or a combination of these. Of these 23 CPGs, 15 mentioned PS training in relation to depression treatment for youth, as a component of CBT ( k = 7), IPT ( k = 4), supportive therapy or counselling ( k = 3), family therapy ( k = 1), DBT ( k = 1), and psychoeducation ( k = 1).
None of the reviewed CPGs recommended free-standing PST as a first-line treatment for youth depression. However, five CPGs mentioned PS training as a treatment ingredient or adjunct component in the context of recommending broader therapeutic approaches. The World Health Organization’s updated Mental Health Gap Action Programme guidelines recommended PS training as an adjunct treatment (e.g., in combination with antidepressant medication) for older adolescents [ 83 ]. A guideline by Orygen (Australia) suggested that for “persistent sub-threshold depressive symptoms (including dysthymia) or mild to moderate depression”, options should include “6–8 sessions of individual guided self-help based on the principles of CBT, including behavioural activation and problem-solving techniques” [ 84 ]. The Chilean Ministry of Health recommended supportive clinical care with adjunctive psychoeducation and PS tools, or supportive counselling for individuals aged 15 and older with mild depression (p. 52) [ 85 ]. The Cincinnati Children’s Hospital Medical Centre recommended four to eight sessions of supportive therapy for mild or uncomplicated depression, highlighting “problem solving coping skills” as one element of supportive therapy (p. 1) [ 86 ]. Fifth, the American Academy of Child and Adolescent Psychiatry’s 2007 practice parameter suggested each phase of treatment for youth depression should include psychoeducation and supportive management, which might include PS training (p. 1510) [ 87 ]. CPGs did not specify whether PS training should incorporate specific modules, or whether the term was used loosely to describe unstructured PS support.
Meta-analysis
Each of the four RCTs of free-standing PST identified by the scoping review contributed one comparison to the exploratory meta-analysis of overall PST efficacy (see Fig. 3 ). Self-rated depression or emotional symptom severity scores were reported by all four studies and constituted the primary outcome for the meta-analysis. We conducted additional exploratory analysis for clinician-rated depression severity as reported in two studies [ 43 , 45 ]. The pooled effect size for self-reported depression severity was g = − 0.34 (95% CI: − 0.92 to 0.23). Heterogeneity was high ( I 2 = 88.37%; p < .001). Due to the small number of studies included, analysis of publication bias via an examination of the funnel plot and tests of funnel plot asymmetry could not be meaningfully conducted [ 88 , 89 ]. The funnel plot is provided in Additional File 5 for reference (Fig. S3).
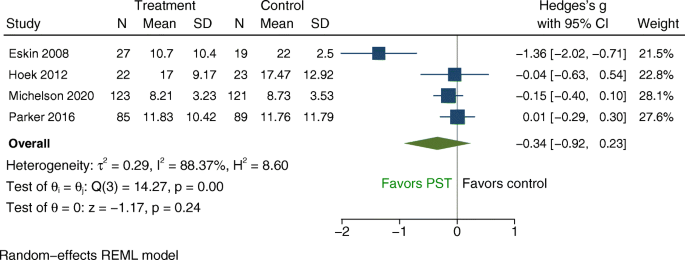
Forest Plot: Random Effects Model with Self-Reported Depression or Emotional Symptoms as Primary Outcome (Continuous)
To achieve the best possible estimate of the true effect size and reduce heterogeneity we computed a second model excluding the one study with high risk of bias (i.e., [ 43 ]). The resulting effect size was g = − 0.08 (95% CI: − 0.26 to 0.10), with no significant heterogeneity ( I 2 = 0.00%; p = 0.72; see Fig. S1 in Additional File 5 ). The pooled effect size for clinician-rated depression severity was g = − 1.39 with a wide confidence interval (95% CI: − 4.03 to 1.42) and very high heterogeneity ( I 2 = 97.41%, p < 0.001; see Fig. S2 in Additional File 5 ).
Overall quality of the evidence
According to the GRADE assessment, the overall quality of the evidence was very low, with concerns related to risk of bias, the inconsistency of results across studies, the indirectness of the evidence with regards to the population of interest (i.e., only one trial focused exclusively on youth with depression), and imprecision in the effect estimate (Table S4 in Additional File 6 ).
This scoping review aimed to provide a first comprehensive overview of the evidence relating to PS training as an active ingredient for treating youth depression. The evidence base relating to the efficacy of PST as a stand-alone intervention was scarce and of low quality. Overall, data from four trials suggested no significant effect on depression symptoms. The scoping review identified some evidence suggesting PS training may enhance treatment response in CBT. However, this conclusion was drawn from secondary analyses where youth were not randomized to treatment with and without PS training, and where primary studies were not powered to test these differences. Disproportionate exposure to comparator CBT components also limits these findings. PST was not recommended as a stand-alone treatment for youth depression in any of the 23 reviewed CPGs; however, one guideline suggested it could be provided alongside other treatments for older adolescents, and four suggested PS training as a component of low-intensity psychosocial interventions for youth with mild to moderate depression.
Given the limited evidence base, only tentative suggestions can be made as to when and for whom PS training is effective. The one PST trial with a low risk of bias enrolled high-school students from low-income communities in New Delhi, and found that PST delivered by lay counselors in combination with PST booklets was more effective at reducing idiographic priority problems than booklets alone, but not at reducing mental health symptoms [ 46 ]. Within a needs-based framework of service delivery (e.g., [ 90 ]), PST may be offered as a low-intensity intervention to youth who experience challenges and struggle with PS—including in low-resource contexts. Future research could explore whether PS training might be particularly helpful for youth facing socioeconomic hardship and related chronic stressors by attenuating potentially harmful impacts on well-being [ 91 ]. If findings are promising, PS training may be considered for targeted prevention (e.g., [ 42 ]). However, at this time there is insufficient evidence to support PS training on its own as an intervention aimed at providing symptom relief for youth experiencing depression.
The PST manual suggests cognitive overload, emotional dysregulation, negative thinking and hopelessness can interfere with PS [ 16 ]. Youth whose depression hinders their ability to engage in PST may require additional support through more comprehensive therapy packages such as CBT or IPT with PS training. In the TORDIA study [ 80 ], where PS training was found to be one of the most effective components, it was generally taught alongside cognitive restructuring, behavioural activation, and emotion regulation, which may have facilitated youths’ ability to absorb PS training [ 71 ]. The focus of these other CBT components on changing negative cognitions and attributions may fulfil a similar function as problem orientation modules in stand-alone PST. Research that is powered to explore such mechanisms is needed. Future research should also apply methodologies designed to identify the most critical elements in a larger treatment package (e.g., dismantling studies; or sequential, multiple assignment, randomized trials) to examine the role of PS training when delivered alongside other components. While one trial focusing on CBT components is currently underway [ 92 ], similar research is needed for other therapies (e.g., IPT, DBT, family therapy).
The included PST trials provided between five and six sessions and covered PS skills but not problem orientation. Meta-analyses of PST for adult depression suggest treatment effectiveness may be enhanced by longer treatment duration (≥ 10 sessions) [ 38 ], and coverage of problem orientation alongside PS skills [ 39 ]. As per the PST treatment manual, strengthening problem orientation fosters motivation and self-efficacy and is an important precondition for enhancing skills [ 93 , 94 ]. In addition, only one youth PST trial assessed PS ability at baseline [ 43 ]. A meta-analysis of PST for adult depression [ 39 ] suggests that studies including such assessments show larger effect sizes, with therapists better able to tailor PST to individual needs. Future research should seek to replicate these findings specifically for youth depression.
Drop out from stand-alone PST was high in two out of four studies, ranging from 41.4% [ 45 ] to 72.7% [ 44 ]. Since its development in the 1970s, PST has undergone several revisions [ 16 , 93 , 95 , 96 , 97 ] but tailoring to youth has been limited. To contextualize the review findings, the review team consulted a panel of twelve youth advisors at the Centre for Addiction and Mental Health (without sharing emerging findings so as not to steer the conversation). Most had participated in PS training as part of other therapies, but none had received formal PST. A key challenge identified by youth advisors was how to provide PS training that is universally applicable and relevant to different youth without being too generic, rigid or schematic; and how to accommodate youth perspectives, complex problems, and individual situations and dispositions. Youth advisors suggested reviewing and reworking PS training with youth in mind, to ensure it is youth-driven, strengths-based, comprehensive, and personalized (see Fig. S4 in Additional File 7 for more detail). Youth advisors emphasized that PS training should identify the root causes underpinning superficial problems and address these through suitable complementary intervention approaches, if needed.
Solution-focused brief therapy (SFBT) has emerged as an antithesis to PST where more emphasis is given to envisaging and constructing solutions rather than analysing problems [ 28 ]. This may be more consistent with youth preferences for strengths-based approaches but may provide insufficiently comprehensive problem appraisals. Future research should compare the effectiveness and acceptability of PST and SFBT and consider possible benefits of combining the advantages of both approaches, to provide support that is strengths-based and targets root problems. More generally, given the effectiveness of PST in adults, future studies could examine whether there are developmental factors that might contribute to reduced effectiveness in youth and should be considered when adapting PST to this age group.
Strengths and limitations
This scoping review applied a broad and systematic approach to study identification and selection. We searched five bibliographic databases, and conducted an extensive grey literature search, considering records published in four languages. Nevertheless, our search may have missed relevant studies published in other languages. We found only a small number of eligible empirical studies, several of which were likely underpowered. As stated above, studies analysing PS-related concepts as predictors, moderators, or mediators of treatment response within broader therapies were heterogenous and limited by design and sample size constraints.
Similarly, there was heterogeneity in recruitment and intervention settings, age groups, and delivery formats across the four RCTs of stand-alone PST, and the overall quality of the evidence was very low. As reflected in our GRADE appraisal, one important limitation was the indirectness of the available evidence: Only one PST trial focused specifically on youth with an MDD diagnosis, while the remaining three included youth with a mix of mental health problems. Although outcomes were reported in terms of depression or emotional symptom severity, this was not based on a subgroup analysis focused specifically on youth with depression. Impact on this group may therefore have been underestimated. In addition, the only PST trial with a low risk of bias did not administer a dedicated depression symptom scale. Instead, our exploratory meta-analysis included scores from the 5-item SDQ emotional problems subscale, which assesses unhappiness, worries, clinginess, fears, and somatic symptoms—and may not have captured nuanced change in depression severity [ 98 , 99 ]. Other concerns that led us to downgrade the quality of the evidence related to considerable risk of bias, with only one out of four studies rated as having a low risk; and imprecision with several studies involving very small samples. Due to the small number of eligible studies, it was not possible to identify the factors driving treatment efficacy via meta-regression. The long-term effectiveness of PS training, or the conditions under which long-term benefits are likely to be realized also could not be examined [ 38 ].
PS training is a core component of several evidence-based therapies for youth depression. However, the evidence base supporting its efficacy as a stand-alone treatment is limited and of low quality. There is tentative evidence suggesting PS-training may drive positive outcomes when provided alongside other treatment components. On its own, PS training may be beneficial for youth who are not acutely distressed or impaired but require support with tackling personal problems. Youth experiencing moderate or severe depressive symptoms may require more comprehensive psychotherapeutic support alongside PS training, as there is currently no robust evidence for the ability of free-standing PST to effectively reduce depression symptoms.
High-quality trials are needed that assess PST efficacy in youth with mild, moderate, and severe depression, in relation to both symptom severity and idiographic treatment goals or priority problems. These studies should examine the influence of treatment length and module content on treatment impact. Dedicated studies are also needed to shed light on the role of PS training as an active ingredient of more comprehensive therapies such as CBT, DBT, IPT, and family therapy. Future studies should include assessments of adverse events and of cost effectiveness. Given high drop-out rates in several youth PST trials, it is important to adapt PS training approaches and therapy manuals as needed, following a youth-engaged research and service development approach [ 57 ], to ensure their relevance and acceptability to this age group.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
Avoidance style
Beck Depression Inventory
Centre for Addiction and Mental Health
Cognitive behavioural therapy
Children’s Depression Rating Scale—Revised
Center for Epidemiologic Studies Depression Scale
Clinical Global Impression Scale—Improvement
Cumulative Index to Nursing and Allied Health Literature
Clinical practice guideline
Adolescent Coping with Depression [intervention name]
Dialectical behaviour therapy
Grading of Recommendations Assessment, Development, and Evaluation
Impulsivity/Carelessness Style
Interpersonal psychotherapy
The Kiddie Schedule for Affective Disorders and Schizophrenia
Lifeskills training
Major depressive disorder
Medical Literature Analysis and Retrieval System Online
Negative problem orientation
Nondirective supportive therapy
Positive problem orientation
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- Problem solving
Problem-solving training
Problem-Solving Therapy
Randomized controlled trial
Research ethics board
Risk of bias
Rational problem-solving style
Systemic Behaviour Family Therapy
Strengths and Difficulties Questionnaire
Solution-Focused Brief Therapy
Social Problem-Solving Inventory Revised
Selective serotonin reuptake inhibitors
Treatment for Adolescents with Depression Study
Treatment of Resistant Depression in Adolescents
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–65. https://doi.org/10.1111/jcpp.12381 .
Article PubMed Google Scholar
Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major Depression in the National Comorbidity Survey–Adolescent Supplement: Prevalence, Correlates, and Treatment. J Am Acad Child Adolesc Psychiatry. 2015;54(1):37–44 e2.
Article Google Scholar
Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377(9783):2093–102. https://doi.org/10.1016/S0140-6736(11)60512-6 .
Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59(3):225–31. https://doi.org/10.1001/archpsyc.59.3.225 .
Jonsson U, Bohman H, von Knorring L, Olsson G, Paaren A, von Knorring A-L. Mental health outcome of long-term and episodic adolescent depression: 15-year follow-up of a community sample. J Affect Disord. 2011;130(3):395–404. https://doi.org/10.1016/j.jad.2010.10.046 .
Article CAS PubMed Google Scholar
Clayborne ZM, Varin M, Colman I. Systematic review and Meta-analysis: adolescent depression and long-term psychosocial outcomes. J Am Acad Child Adolesc Psychiatry. 2019;58(1):72–9. https://doi.org/10.1016/j.jaac.2018.07.896 .
Fletcher JM. Adolescent depression: diagnosis, treatment, and educational attainment. Health Econ. 2008;17(11):1215–35. https://doi.org/10.1002/hec.1319 .
Article PubMed PubMed Central Google Scholar
Fletcher JM. Adolescent depression and adult labor market outcomes. South Econ J. 2013;80(1):26–49. https://doi.org/10.4284/0038-4038-2011.193 .
Zhou X, Hetrick SE, Cuijpers P, Qin B, Barth J, Whittington CJ, et al. Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: a systematic review and network meta-analysis. World Psychiatry. 2015;14(2):207–22. https://doi.org/10.1002/wps.20217 .
Zhou X, Teng T, Zhang Y, Del Giovane C, Furukawa TA, Weisz JR, et al. Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: a systematic review and network meta-analysis. Lancet Psychiatry. 2020;7(7):581–601. https://doi.org/10.1016/S2215-0366(20)30137-1 .
Bear HA, Edbrooke-Childs J, Norton S, Krause KR, Wolpert M. Systematic review and Meta-analysis: outcomes of routine specialist mental health Care for Young People with Depression and/or anxiety. J Am Acad Child Adolesc Psychiatry. 2020;59(7):810–41. https://doi.org/10.1016/j.jaac.2019.12.002 .
Cuijpers P, Stringaris A, Wolpert M. Treatment outcomes for depression: challenges and opportunities. Lancet Psychiatry. 2020;7(11):925–7. https://doi.org/10.1016/S2215-0366(20)30036-5 .
Kazdin AE. Understanding how and why psychotherapy leads to change. Psychother Res. 2009;19(4–5):418–28. https://doi.org/10.1080/10503300802448899 .
de Haan AM, Boon AE, de Jong JTVM, Hoeve M, Vermeiren RRJM. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin Psychol Rev. 2013;33(5):698–711. https://doi.org/10.1016/j.cpr.2013.04.005 .
Chorpita BF, Daleiden EL. Mapping evidence-based treatments for children and adolescents: application of the distillation and matching model to 615 treatments from 322 randomized trials. J Consult Clin Psychol. 2009;77(3):566–79. https://doi.org/10.1037/a0014565 .
Nezu AM, Nezu CM, D’Zurilla TJ. Problem-solving therapy: A treatment manual. Problem-solving therapy: A treatment manual: Springer Publishing Company; 2013. x, 323–x, 323
D’Zurilla TJ, Nezu AM. Problem-solving therapy. In: Handbook of Cognitive-Behavioral Therapies. Third. New York, NY: Guilford Press; 2010. p. 197–225.
Google Scholar
Nezu AM. Problem solving and behavior therapy revisited. Behav Ther. 2004;35(1):1–33. https://doi.org/10.1016/S0005-7894(04)80002-9 .
D’Zurilla TJ, Nezu AM, Maydeu-Olivares A. Social Problem Solving: Theory and Assessment. In: Chang EC, D’Zurilla TJ, Sanna LJ, editors. Social problem solving: Theory, research, and training: American Psychological Association; 2004. p. 11–27.
Ugueto AM, Santucci LC, Krumholz LS, Weisz JR. Problem-Solving Skills Training. In: Sburlati ES, Lyneham HJ, Schniering CA, Rapee RM, editors. Evidence-based CBT for anxiety and depression in children and adolescents: a competencies-based approach. Chichester, UK: John Wiley & Sons; 2014. p. 247–59. https://doi.org/10.1002/9781118500576.ch17 .
Chapter Google Scholar
D’Zurilla TJ, Chang EC, Nottingham EJ IV, Faccini L. Social problem-solving deficits and hopelessness, depression, and suicidal risk in college students and psychiatric inpatients. J Clin Psychol. 1998;54(8):1091–107. https://doi.org/10.1002/(SICI)1097-4679(199812)54:8<1091::AID-JCLP9>3.0.CO;2-J .
Haugh JA. Specificity and social problem-solving: relation to depressive and anxious symptomology. J Soc Clin Psychol. 2006;25(4):392–403. https://doi.org/10.1521/jscp.2006.25.4.392 .
Nezu AM. Cognitive appraisal of problem solving effectiveness: relation to depression and depressive symptoms. J Clin Psychol. 1986;42(1):42–8. https://doi.org/10.1002/1097-4679(198601)42:1<42::AID-JCLP2270420106>3.0.CO;2-2 .
Reinecke MA, Dubois DL, Schultz TM. Social problem solving, mood, and suicidality among inpatient adolescents. Cognit Ther Res. 2001;25(6):743–56. https://doi.org/10.1023/A:1012971423547 .
Siu AMH, Shek DTL. Social problem solving as a predictor of well-being in adolescents and young adults. Soc Indic Res. 2010;95(3):393–406. https://doi.org/10.1007/s11205-009-9527-5 .
D’Zurilla TJ, Goldfried MR. Problem solving and behavior modification. J Abnorm Psychol. 1971;78(1):107–26. https://doi.org/10.1037/h0031360 .
Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977.
Gingerich WJ, Eisengart S. Solution-focused brief therapy: a review of the outcome research. Fam Process. 2000;39(4):477–98. https://doi.org/10.1111/j.1545-5300.2000.39408.x .
Boyd RC, Lewis J, Borreggine K, Benton TD. Adolescent depression: identification and treatment. Curr Treat Options Pediatr. 2018;4(3):350–62. https://doi.org/10.1007/s40746-018-0135-y .
Hamrin V, Pachler MC. Child & adolescent depression: review of the latest evidence-based treatments. J Psychosoc Nurs Ment Health Serv. 2005;43(1):54–63. https://doi.org/10.3928/02793695-20050101-08 .
McCarty CA, Weisz JR. Effects of psychotherapy for depression in children and adolescents: what we can (and can’t) learn from meta-analysis and component profiling. J Am Acad Child Adolesc Psychiatry. 2007;46(7):879–86. https://doi.org/10.1097/chi.0b013e31805467b3 .
Fréchette-Simard C, Plante I, Bluteau J. Strategies included in cognitive behavioral therapy programs to treat internalized disorders: a systematic review. Cogn Behav Ther. 2018;47(4):263–85. https://doi.org/10.1080/16506073.2017.1388275 .
Verdeli H, Mufson L, Lee L, Keith J. Review of evidence-based psychotherapies for pediatric mood and anxiety disorders. Curr Psychiatr Rev. 2006;2(3):395–421. https://doi.org/10.2174/157340006778018102 .
Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 1999;56(6):573–9. https://doi.org/10.1001/archpsyc.56.6.573 .
Diamond G, Siqueland L. Family therapy for the treatment of depressed adolescents. Psychotherapy. 1995;32(1):77–90. https://doi.org/10.1037/0033-3204.32.1.77 .
Hallford DJ, Mellor D. Cognitive-reminiscence therapy and usual care for depression in young adults: study protocol for a randomized controlled trial. Trials. 2013;14(1):1–8.
Richardson ED. Adventure-based therapy and self-efficacy theory: Test of a treatment model for late adolescents with depressive symptomatology. Blacksburg, VA: Virginia Polytechnic Institute and State University; 1998.
Cuijpers P, de Wit L, Kleiboer A, Karyotaki E, Ebert DD. Problem-solving therapy for adult depression: an updated meta-analysis. Eur Psychiatry. 2018;48(1):27–37. https://doi.org/10.1016/j.eurpsy.2017.11.006 .
Bell AC, D’Zurilla TJ. Problem-solving therapy for depression: a meta-analysis. Clin Psychol Rev. 2009;29(4):348–53. https://doi.org/10.1016/j.cpr.2009.02.003 .
Zhang A, Park S, Sullivan JE, Jing S. The effectiveness of problem-solving therapy for primary care patients’ depressive and/or anxiety disorders: a systematic review and meta-analysis. J Am Board Fam Med. 2018;31(1):139–50. https://doi.org/10.3122/jabfm.2018.01.170270 .
Stark KD, Reynolds WM, Kaslow NJ. A comparison of the relative efficacy of self-control therapy and a behavioral problem-solving therapy for depression in children. J Abnorm Child Psychol. 1987;15(1):91–113. https://doi.org/10.1007/BF00916468 .
Spence SH, Sheffield JK, Donovan CL. Preventing adolescent depression: an evaluation of the problem solving for life program. J Consult Clin Psychol. 2003;71(1):3–13. https://doi.org/10.1037/0022-006X.71.1.3 .
Eskin M, Ertekin K, Demir H. Efficacy of a problem-solving therapy for depression and suicide potential in adolescents and young adults. Cognit Ther Res. 2008;32(2):227–45. https://doi.org/10.1007/s10608-007-9172-8 .
Hoek W, Schuurmans J, Koot HM, Cuijpers P. Effects of internet-based guided self-help problem-solving therapy for adolescents with depression and anxiety: a randomized controlled trial. PLoS One. 2012;7(8):1–7.
Parker AG, Hetrick SE, Jorm AF, Mackinnon AJ, McGorry PD, Yung AR, et al. The effectiveness of simple psychological and physical activity interventions for high prevalence mental health problems in young people: a factorial randomised controlled trial. J Affect Disord. 2016;196:200–9. https://doi.org/10.1016/j.jad.2016.02.043 .
Michelson D, Malik K, Parikh R, Weiss HA, Doyle AM, Bhat B, et al. Effectiveness of a brief lay counsellor-delivered, problem-solving intervention for adolescent mental health problems in urban, low-income schools in India: a randomised controlled trial. Lancet Child Adolesc Heal. 2020;4(8):571–82. https://doi.org/10.1016/S2352-4642(20)30173-5 .
Ng MY, Eckshtain D, Weisz JR. Assessing fit between evidence-based psychotherapies for youth depression and real-life coping in early adolescence. J Clin Child Adolesc Psychol. 2016;45(6):732–48. https://doi.org/10.1080/15374416.2015.1041591 .
United Nations. Youth [Internet]. 2020 [cited 2020 Nov 4]. Available from: https://www.un.org/esa/socdev/documents/youth/fact-sheets/youth-definition.pdf .
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1–7.
Krause KR, Courtney DB, Bonato S, Aitken M, Hawke LD, Szatmari P. Problem Solving as an Active Ingredient of Treatment for Youth Depression: A Scoping Review [Protocol] [Internet]. [cited 2021 Jan 13]. Available from: osf.io/ydxge
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850 .
Booth A, Carroll C. Systematic searching for theory to inform systematic reviews: is it feasible? Is it desirable? Health Inf Libr J. 2015;32(3):220–35. https://doi.org/10.1111/hir.12108 .
Courtney DB, Duda S, Szatmari P, Henderson J, Bennett K. Systematic review and quality appraisal of practice guidelines for self-harm in children and adolescents. Suicide Life-Threatening Behav. 2019;49(3):707–23. https://doi.org/10.1111/sltb.12466 .
Bennett K, Duda S, Brouwers M, et al Towards high-quality, useful practice guidelines for child and youth mental health disorders: protocol for a systematic review and consensus exercise BMJ Open. 2018;8:e018053. https://doi.org/10.1136/bmjopen-2017-018053 .
Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4.0: software for research synthesis; 2010.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53. https://doi.org/10.1111/j.1365-2648.2005.03621.x .
Heffernan OS, Herzog TM, Schiralli JE, Hawke LD, Chaim G, Henderson JL. Implementation of a youth-adult partnership model in youth mental health systems research: challenges and successes. Health Expect. 2017;20(6):1183–8. https://doi.org/10.1111/hex.12554 .
Hawke LD, Darnay K, Relihan J, Khaleghi-Moghaddam M, Barbic S, Lachance L, et al. Enhancing researcher capacity to engage youth in research: researchers’ engagement experiences, barriers and capacity development priorities. Health Expect. 2020;23(3):584–92. https://doi.org/10.1111/hex.13032 .
Hawke LD, Relihan J, Miller J, McCann E, Rong J, Darnay K, et al. Engaging youth in research planning, design and execution: practical recommendations for researchers. Health Expect. 2018;21(6):944–9. https://doi.org/10.1111/hex.12795 .
Peters M, Godfrey C, McInerney P, Munn Z, Trico A, Khalil H. Chapter 11: Scoping Reviews. In: JBI Manual for Evidence Synthesis [Internet]. JBI; 2020. Available from: https://wiki.jbi.global/display/MANUAL/Chapter+11%3A+Scoping+reviews . Accessed 20 Dec 2020.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:1–8.
GRADEpro GDT. GRADEpro Guideline Development Tool [Software] [Internet]. McMaster University (developed by Evidence Prime, Inc.); 2020. Available from: gradepro.org . Accessed 20 Dec 2020.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. https://doi.org/10.1136/bmj.39489.470347.AD .
Hedges LV. A random effects model for effect sizes. Psychol Bull. 1983;93(2):388–95. https://doi.org/10.1037/0033-2909.93.2.388 .
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Cochrane Handbook for Systematic Reviews of Interventions: John Wiley & Sons; 2019. https://doi.org/10.1002/9781119536604 .
Book Google Scholar
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629 .
Article CAS PubMed PubMed Central Google Scholar
Beck AT, Steer RA. Internal consistencies of the original and revised beck depression inventory. J Clin Psychol. 1984;40(6):1365–7. https://doi.org/10.1002/1097-4679(198411)40:6<1365::AID-JCLP2270400615>3.0.CO;2-D .
Radloff LS. The CES-D scale. Appl Psychol Meas. 1977;1(3):385–401. https://doi.org/10.1177/014662167700100306 .
Goodman R. Psychometric properties of the strengths and difficulties questionnaire (SDQ). J Am Acad Child Adolesc Psychiatry. 2001;40(11):1337–45. https://doi.org/10.1097/00004583-200111000-00015 .
Becker-Weidman EG, Jacobs RH, Reinecke MA, Silva SG, March JS. Social problem-solving among adolescents treated for depression. Behav Res Ther. 2010;48(1):11–8. https://doi.org/10.1016/j.brat.2009.08.006 .
Kennard BD, Clarke GN, Weersing VR, Asarnow JR, Shamseddeen W, Porta G, et al. Effective components of TORDIA cognitive–behavioral therapy for adolescent depression: preliminary findings. J Consult Clin Psychol. 2009;77(6):1033–41. https://doi.org/10.1037/a0017411 .
Kaufman NK, Rohde P, Seeley JR, Clarke GN, Stice E. Potential mediators of cognitive-behavioral therapy for adolescents with comorbid major depression and conduct disorder. J Consult Clin Psychol. 2005;73(1):38–46. https://doi.org/10.1037/0022-006X.73.1.38 .
Dietz LJ, Marshal MP, Burton CM, Bridge JA, Birmaher B, Kolko D, et al. Social problem solving among depressed adolescents is enhanced by structured psychotherapies. J Consult Clin Psychol. 2014;82(2):202–11. https://doi.org/10.1037/a0035718 .
Beck AT, Steer RA, Brown GK. Beck depression inventory-ii. San Antonio, TX: Psychological Corporation; 1996.
Poznanski E, Mokros H. Children’s depression rating scale–revised (CDRS-R). Los Angeles, CA: Western Psychological Services; 1996.
Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007;4(7):28–37.
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–8. https://doi.org/10.1097/00004583-199707000-00021 .
D’Zurilla TJ, Nezu AM. Maydeu- Olivares a. social problem-solving inventory - revised: technical manual. North Tonawanda, NY: Multi-Health Systems; 2002.
March JS, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, et al. The treatment for adolescents with depression study (TADS). Arch Gen Psychiatry. 2007;64(10):1132–43. https://doi.org/10.1001/archpsyc.64.10.1132 .
Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression. JAMA. 2008;299(8):901–13. https://doi.org/10.1001/jama.299.8.901 .
Brysbaert M. How many participants do we have to include in properly powered experiments? A tutorial of power analysis with some simple guidelines. J Cogn. 2019;2(1):1–38.
MacKinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behav Res. 1995;30(1):41–62. https://doi.org/10.1207/s15327906mbr3001_3 .
World Health Organization. Update of the Mental Health Gap Action Programme (mhGAP) guidelines for mental, neurological and substance use disorders [Internet]. 2015. Available from: https://www.who.int/maternal_child_adolescent/documents/health-promotion-interventions/en/ . Accessed 20 Dec 2020.
Orygen. Treating depression in young people: Guidance, resources and tools for assessment and management [Internet]. Orygen. 2017. Available from: https://www.orygen.org.au/Training/Resources/Depression/Clinical-practice-points/Treating-depression-in-yp . Accessed 20 Dec 2020.
Ministerio de Salud. Guía Clínica Depresión en personas de 15 años y más [Internet]. Santiago, Chile; 2013. Available from: https://www.minsal.cl/portal/url/item/7222754637c08646e04001011f014e64.pdf . Accessed 20 Dec 2020.f
Cincinnati Children's Hospital Medical Center. Best Evidence Statement (BESt): Treatment of Children and Adolescents With Major Depressive Disorder (MDD) During the Acute Phase. Cincinnati: Cincinnati Children's Hospital Medical Center; 2010.
Birmaher B. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503–26. https://doi.org/10.1097/chi.0b013e318145ae1c .
Lau J, Ioannidis JPA, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. Br Med J. 2006;333(7568):597–600. https://doi.org/10.1136/bmj.333.7568.597 .
Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343(7818):1–8.
Wolpert M, Harris R, Hodges S, Fuggle P, James R, Wiener A, et al. THRIVE framework for system change. London: United Kingdom; 2019.
Hostinar CE, Miller GE. Protective factors for youth confronting economic hardship: current challenges and future avenues in resilience research. Am Psychol. 2019;74(6):641–52. https://doi.org/10.1037/amp0000520 .
Van Den Heuvel MWH, Bodden DHM, Moerbeek M, Smit F, Engels RCME. Dismantling the relative effectiveness of core components of cognitive behavioural therapy in preventing depression in adolescents: protocol of a cluster randomized microtrial. BMC Psychiatry. 2019;19(1):1–13.
Nezu AM, Perri MG. Social problem-solving therapy for unipolar depression: an initial dismantling investigation. J Consult Clin Psychol. 1989;57(3):408–13. https://doi.org/10.1037/0022-006X.57.3.408 .
D’Zurilla TJ, Nezu AM. Problem-solving therapy: a positive approach to clinical intervention. 3rd ed. New York, NY: Spring Publishing Company; 2007. 261 p.
Chang EC, D’Zurilla TJ, Sanna LJ. Social problem solving: theory, research, and training: American Psychological Association; 2004. https://doi.org/10.1037/10805-000 .
Nezu AM, Nezu CM, Perri MG. Problem-solving therapy for depression: theory, research, and clinical guidelines. New York, NY: Wiley; 1989.
Nezu AM. A problem-solving formulation of depression: a literature review and proposal of a pluralistic model. Clin Psychol Rev. 1987;7(2):121–44. https://doi.org/10.1016/0272-7358(87)90030-4 .
Goodman R, Meltzer H, Bailey V. The strengths and difficulties questionnaire: a pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry. 1998;7(3):125–30. https://doi.org/10.1007/s007870050057 .
Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiat. 1997;38(5):581–6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x .
Download references
Acknowledgments
We would like to thank the members of the Centre for Addiction and Mental Health (CAMH) youth advisory group for their valuable insights and suggestions. The systematic search for clinical practice guidelines presented in this review was based on a search strategy developed by Dr. Kathryn Bennett. We would like to thank Dr. Bennett for agreeing to the reuse of the strategy as part of this review. We would also like to thank the Cundill Centre for Child and Youth Depression for providing institutional support to this project.
This work was funded by a Wellcome Trust Mental Health Priority Area “Active Ingredients” commission awarded to KRK, DBC and PS, and the Centre for Addiction and Mental Health, Toronto, Canada.
Author information
Authors and affiliations.
Cundill Centre for Child and Youth Depression, Centre for Addiction and Mental Health (CAMH), 80 Workman Way, Toronto, ON, M6J 1H4, Canada
Karolin R. Krause, Darren B. Courtney, Sarah Bonato, Madison Aitken, Jacqueline Relihan, Matthew Prebeg, Karleigh Darnay, Lisa D. Hawke, Priya Watson & Peter Szatmari
Evidence Based Practice Unit, University College London and Anna Freud National Centre for Children and Families, London, UK
Karolin R. Krause
Department of Psychiatry, University of Toronto, Toronto, ON, Canada
Darren B. Courtney, Madison Aitken, Lisa D. Hawke, Priya Watson & Peter Szatmari
Independent Family Doctor, Toronto, ON, Canada
Benjamin W. C. Chan
Hospital for Sick Children, Toronto, ON, Canada
Peter Szatmari
You can also search for this author in PubMed Google Scholar
Contributions
KRK, DBC and PS formulated the research questions and designed the study. SB conducted the systematic search for clinical practice guidelines and the grey literature search, and advised on the search for retrieving empirical studies, which was led by KRK. KRK, DBC and BWCC performed the screening of records for inclusion criteria. Data extraction was performed by KRK and BWCC. The risk of bias assessment for included randomized control trials was conducted by KRK and MA. The youth consultation was led by JR, MP and KD with input from LDH and KRK. Data analysis was led by KRK. All authors contributed to the interpretation of emerging findings through an internal findings workshop and through several rounds of feedback on the draft manuscript, which was drafted by KRK. All authors have reviewed and approved the final manuscript.
Corresponding author
Correspondence to Karolin R. Krause .
Ethics declarations
Ethics approval and consent to participate.
Formal approval by a Research Ethics Board was not required, as youth were consulted as research partners rather than research subjects and provided no individual data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Additional file 2.
Search Strategy.
Additional file 3.
List of Studies Included in the Scoping Review.
Additional file 4.
Characteristics of Included Clinical Practice Guidelines.
Additional file 5.
Additional Data and Outputs from the Meta-Analysis.
Additional file 6.
Risk of Bias Assessment and GRADE Appraisal.
Additional file 7.
Illustration of Insights from the Consultation of Youth Advisors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Krause, K.R., Courtney, D.B., Chan, B.W.C. et al. Problem-solving training as an active ingredient of treatment for youth depression: a scoping review and exploratory meta-analysis. BMC Psychiatry 21 , 397 (2021). https://doi.org/10.1186/s12888-021-03260-9
Download citation
Received : 26 January 2021
Accepted : 28 April 2021
Published : 24 August 2021
DOI : https://doi.org/10.1186/s12888-021-03260-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescence
- Active ingredient
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]
Problem Solving

Download or send
Choose your language, professional version.
A PDF of the resource, theoretical background, suggested therapist questions and prompts.
Premium Feature
Client version.
A PDF of the resource plus client-friendly instructions where appropriate.
Fillable version (PDF)
A fillable version of the resource. This can be edited and saved in Adobe Acrobat, or other PDF editing software.
Editable version (PPT)
An editable Microsoft PowerPoint version of the resource.
Translation Template
Are you a qualified therapist who would like to help with our translation project?
Languages this resource is available in
- Chinese (Simplified)
- Chinese (Traditional)
- English (GB)
- English (US)
- Spanish (International)
Mechanisms associated with this resource
- Skills deficit
Introduction & Theoretical Background
Problem Solving is a helpful intervention whenever clients present with difficulties, dilemmas, and conundrums, or when they experience repetitive thought such as rumination or worry. Effective problem solving is an essential life skill and this Problem Solving worksheet is designed to guide adults through steps which will help them to generate solutions to ‘stuck’ situations in their lives. It follows the qualities of effective problem solving outlined by Nezu, Nezu & D’Zurilla (2013), namely: clearly defining a problem; generation of alternative solutions; deliberative decision making; and the implementation of the chosen solution.
The therapist’s stance during problem solving should be one of collaborative curiosity. It is not for the therapist to pass judgment or to impose their preferred solution. Instead it is the clinician’s role to sit alongside clients and to help them examine the advantages and disadvantages of their options and, if the client is ‘stuck’ in rumination or
Get access to this resource
View all plans and pricing options
Therapist Guidance
- What is the nature of the problem?
- What are my goals?
- What is getting the way of me reaching my goals?
- “Can you think of any ways that you could make this problem not be a problem any more?”
- “What’s keeping this problem as a problem? What could you do
References And Further Reading
- Beck, A.T., Rush, A.J., Shaw, B.F., & Emery, G. (1979). Cognitive therapy of depression . New York: Guilford. Nezu, A. M., Nezu, C. M., D’Zurilla, T. J. (2013). Problem-solving therapy: a treatment manual . New York: Springer.
- For clinicians
- For students
- Resources at your fingertips
- Designed for effectiveness
- Resources by problem
- Translation Project
- Help center
- Try us for free
- Terms & conditions
- Privacy Policy
- Cookies Policy

COMMENTS
excellent work history, many interpersonal and supervisory skills; reliable, productive, responsible. Good problem-solver, good common sense. Had made a reasonable living; always budgeted and saved money. Likeable, a "good family man;" good relationships with children/grandchildren, a cousin, two male friends; made a reasonable living;
Straighten your head forward, pressing your chin to your chest. Feel the tension in your throat and the back of your neck (reader—pause for 3 seconds). Now relax . . . allow your head to return to a comfortable position. Let the relaxation spread over your shoulders (reader—pause for 3 seconds).
We have included three of our favorite books on the subject of Problem-Solving Therapy below. 1. Problem-Solving Therapy: A Treatment Manual - Arthur Nezu, Christine Maguth Nezu, and Thomas D'Zurilla. This is an incredibly valuable book for anyone wishing to understand the principles and practice behind PST.
Mind mapping is an effective intervention also used to increase hope and optimism. This intervention is often used in life coaching practices. A research study done on solution-focused life coaching (Green, Oades, & Grant, 2006) showed that this type of intervention increases goal striving and hope, in addition to overall well-being.
Problem-Solving Therapy (PST) is an evidenced-based intervention to facilitate behavioral changes through a variety of skill training. PST identifies strategies to support people to cope with difficulties in life and take the initiative to solve everyday problems. Using cognitive behavioral theories, effective and successful problem solving
worksheet. Guide your clients and groups through the problem solving process with the help of the Problem Solving Packet. Each page covers one of five problem solving steps with a rationale, tips, and questions. The steps include defining the problem, generating solutions, choosing one solution, implementing the solution, and reviewing the process.
Of these 10 interventions: three were adaptations of models proposed by D'Zurilla and Nezu [20, 34] and D'Zurilla and Goldfried , two were based on Mynors-Wallis's Problem-Solving Therapy (PST) guide, one was a problem-orientation video intervention adapted from D'Zurilla and Nezu , one was an online intervention adapted from Method of ...
The problem-solving intervention has been found to be effective in treating depression in younger adults (Nezu, 1986), older adults (Areán, et al., 1993; Alexopolous, Raue and Areán, in press), and persons with mental retardation (Nezu, Nezu & Areán, 1990). Problem solving training has been found to be an
problems, and instead focuses on clients' strengths and previous successes. There is a focus on working from the client's understandings of her/his concern/situation and what the client might want different. The basic tenets that inform Solution-Focus Brief Therapy are as follows: It is based on solution-building rather than problem-solving.
mann 2016). The systematic application of a generic problem-solving process that can be applied to ameliorate client difficulties and a focus of intervention on problems of living rather than on clients' personality issues are at the root of the generalist perspective. The problem-solving model has also informed the development of some promi-
Problem-Solving Therapy Arthur M. Nezu Christine Maguth Nezu Thomas J. D'Zurilla INTRODUCTION AND HISTORICAL BACKGROUND Problem-solving therapy (PST) is a cognitive-behavioral intervention that focuses on training in the adoption and effective application of adap-tive problem-solving attitudes and skills. The general aim of this positive
Problem-solving (PS) has been identified as a therapeutic technique found in multiple evidence-based treatments for depression. To further understand for whom and how this intervention works, we undertook a systematic review of the evidence for PS's effectiveness in preventing and treating depression among adolescents and young adults. We searched electronic databases (PsycINFO, Medline, and ...
Problem-solving therapy is a brief intervention that provides people with the tools they need to identify and solve problems that arise from big and small life stressors. It aims to improve your overall quality of life and reduce the negative impact of psychological and physical illness. Problem-solving therapy can be used to treat depression ...
Problem-solving training is a common ingredient of evidence-based therapies for youth depression and has shown effectiveness as a versatile stand-alone intervention in adults. This scoping review provided a first overview of the evidence supporting problem solving as a mechanism for treating depression in youth aged 14 to 24 years. Five bibliographic databases (APA PsycINFO, CINAHL, Embase ...
Step 2: Set a realistic, achievable goals within our control. ~ 15 minutes. Step 3: Brainstorm solutions. Step 4: Compare solutions by evaluating the pros and cons. Step 5: Choose the preferred solution. Step 6: Make an action plan to implement the solution. Step 7: Monitor and evaluate the outcome.
Problem Solving is a helpful intervention whenever clients present with difficulties, dilemmas, and conundrums, or when they experience repetitive thought such as rumination or worry. Effective problem solving is an essential life skill and this Problem Solving worksheet is designed to guide adults through steps which will help them to generate ...
Skill-building interventions teach youth skills to manage social interactions and control executive responses such as anger and impulsivity. Skills may be interpersonal skills, problem solving skills, mindfulness strategies for managing emotions, stress, and improving focus, and other similar skills. Our recommendations are specific to the ...
Problem-solving (PS) has been identified as a therapeutic technique found in multiple evidence-based treatments for depression. To further understand for whom and how this intervention works, we ...
general can be improved by about 10% a fter a group problem solving intervention. Furthermore we find differences in improvem ent depending upon the students' level of. logical thinking and ...
Now, as I count from 5 to 1, feel yourself become more alert... 5 bringing your attention to this room... 4 feeling calm and relaxed... 3 start to wiggle your fingers and toes... 2 slowly start to move and stretch your muscles... 1 open your eyes, feeling refreshed and rejuvenated. Used with permission.
al intervention techniques may be used on an emergency basis. hese techniques are to be used only until the person is calm. Such techniques are only used after other methods of intervention (early intervention, non-verbal, and verbal calming techniques) have been considered, and determined to be clinically inappro.
This article provides an overview of a new crisis intervention model, the Integrated Problem-Solving Model (IPSM), and demonstrates its application to a specific crisis, sexual assault.
necessary to ensure the intervention was delivered as intended. If fidelity is good, the team should return to the problem-solving process to determine a more appropriate and effective intervention. Four-step problem solving is cyclical and self-correcting, in that teams return to previous steps of the process until the desired outcomes are ...
Results . This paper outlines a modularised approach to working with people with psychosis and in crisis. It outlines the key values underpinning the protocol, and the key modules of: engagement, assessment and identifying priorities; formulation of the crisis, stabilisation, safety, and problem solving, crisis plans and crisis cards, change strategy work focusing on crisis appraisals, and ...