Information
- Author Services

Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
The cardiac effects of performance-enhancing medications: caffeine vs. anabolic androgenic steroids.

1. Introduction
2. materials and methods, 3.1. caffeine as a performance enhancing agent, 3.1.1. caffeine pharmacology and cardiac physiology, 3.1.2. caffeine and risk of arrhythmia, 3.1.3. caffeine genetics, 3.1.4. caffeine in sudden cardiac death, 3.2. anabolic androgenic steroids as a performance enhancing agent, 3.2.1. aass pharmacology and cardiac physiology, 3.2.2. aass and risk of arrhythmia, 3.2.3. aass genetics, 3.2.4. aass in sudden cardiac death, 4. discussion, clinical pitfalls and future directions, 5. conclusions, author contributions, conflicts of interest.
Click here to enlarge figure
- Pickering, C.; Kiely, J. Are the Current Guidelines on Caffeine Use in Sport Optimal for Everyone? Inter-individual Vari-ation in Caffeine Ergogenicity, and a Move Towards Personalised Sports Nutrition. Sports Med. 2018 , 48 , 7–16. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Berglund, B.; Hemmingsson, P. Effects of Caffeine Ingestion on Exercise Performance at Low and High Altitudes in Cross-Country Skiers. Int. J. Sports Med. 1982 , 3 , 234–236. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Stadheim, H.K.; Nossum, E.M.; Olsen, R.; Spencer, M.; Jensen, J. Caffeine improves performance in double poling during acute exposure to 2,000-m altitude. J. Appl. Physiol. 2015 , 119 , 1501–1509. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Powers, S.K.; Byrd, R.J.; Tulley, R.; Callender, T. Effects of caffeine ingestion on metabolism and performance during graded exercise. Graefe’s Arch. Clin. Exp. Ophthalmol. 1983 , 50 , 301–307. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Grgic, J.; Grgic, I.; Pickering, C.; Schoenfeld, B.J.; Bishop, D.J.; Virgile, A.; Pedisic, Z. Infographic. Wake up and smell the coffee: Caffeine supplementation and exercise performance. Br. J. Sports Med. 2020 , 54 , 304–305. [ Google Scholar ] [ CrossRef ]
- Mullen, C.; Whalley, B.J.; Schifano, F.; Baker, J.S. Anabolic androgenic steroid abuse in the United Kingdom: An update. Br. J. Pharmacol. 2020 , 177 , 2180–2198. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sagoe, D.; Molde, H.; Andreassen, C.S.; Torsheim, T.; Pallesen, S. The global epidemiology of anabolic-androgenic steroid use: A meta-analysis and meta-regression analysis. Ann. Epidemiol. 2014 , 24 , 383–398. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Reyes-Vallejo, L. Current use and abuse of anabolic steroids. Actas Urológicas Españolas (Engl. Ed.) 2020 , 44 , 309–313. [ Google Scholar ] [ CrossRef ]
- Tsatsakis, A.; Docea, A.O.; Calina, D.; Tsarouhas, K.; Zamfira, L.-M.; Mitrut, R.; Sharifi-Rad, J.; Kovatsi, L.; Siokas, V.; Dardiotis, E.; et al. A Mechanistic and Pathophysiological Approach for Stroke Associated with Drugs of Abuse. J. Clin. Med. 2019 , 8 , 1295. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- McCullough, D.; Webb, R.; Enright, K.J.; Lane, K.E.; McVeigh, J.; Stewart, C.E.; Davies, I.G. How the love of muscle can break a heart: Impact of anabolic androgenic steroids on skeletal muscle hypertrophy, metabolic and cardiovascular health. Rev. Endocr. Metab. Disord. 2020 , 1–17. [ Google Scholar ] [ CrossRef ]
- Payne, J.R.; Kotwinski, P.J.; E Montgomery, H. Cardiac effects of anabolic steroids. Heart 2004 , 90 , 473–475. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Southward, K.; Rutherfurd-Markwick, K.J.; Ali, A. The Effect of Acute Caffeine Ingestion on Endurance Performance: A Systematic Review and Meta-Analysis. Sports Med. 2018 , 48 , 1913–1928. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Babu, K.M.; Church, R.J.; Lewander, W. Energy Drinks: The New Eye-Opener For Adolescents. Clin. Pediatr. Emerg. Med. 2008 , 9 , 35–42. [ Google Scholar ] [ CrossRef ]
- Espinola, E.; Dias, R.; Mattei, R.; Carlini, E. Pharmacological activity of Guarana (Paullinia cupana Mart.) in laboratory animals. J. Ethnopharmacol. 1997 , 55 , 223–229. [ Google Scholar ] [ CrossRef ]
- Glatter, K.A.; Myers, R.; Chiamvimonvat, N. Recommendations regarding dietary intake and caffeine and alcohol con-sumption in patients with cardiac arrhythmias: What do you tell your patients to do or not to do? Curr. Treat. Options Cardiovasc. Med. 2012 , 14 , 529–535. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Seifert, S.M.; Schaechter, J.L.; Hershorin, E.R.; Lipshultz, S.E. Health Effects of Energy Drinks on Children, Adolescents, and Young Adults. Pediatrics 2011 , 127 , 511–528. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Spriet, L.L. Exercise and Sport Performance with Low Doses of Caffeine. Sports Med. 2014 , 44 , 175–184. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Del Coso, J.; Muñoz-Fernández, V.E.; Muñoz, G.; Fernández-Elías, V.E.; Ortega, J.F.; Hamouti, N.; Barbero, J.C.; Muñoz-Guerraet, J. Effects of a caffeine containing energy drink on simulated soccer performance. PLoS ONE 2012 , 7 , e31380. [ Google Scholar ] [ CrossRef ]
- Pickering, C.; Grgic, J. Caffeine and Exercise: What Next? Sports Med. 2019 , 49 , 1007–1030. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Trapp, G.S.; Allen, K.; O’Sullivan, T.A.; Robinson, M.; Jacoby, P.; Oddy, W.H. ENERGY DRINK CONSUMPTION IS ASSOCIATED WITH ANXIETY IN AUSTRALIAN YOUNG ADULT MALES. Depress. Anxiety 2013 , 31 , 420–428. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Graham, T.E.; Rush, J.W.E.; Van Soeren, M.H. Caffeine and Exercise: Metabolism and Performance. Can. J. Appl. Physiol. 1994 , 19 , 111–138. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gonzaga, L.A.; Vanderlei, L.C.M.; Gomes, R.L.; Valenti, V.E. Caffeine affects autonomic control of heart rate and blood pressure recovery after aerobic exercise in young adults: A crossover study. Sci. Rep. 2017 , 7 , 14091. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Skinner, T.L.; Desbrow, B.; Arapova, J.; Schaumberg, M.A.; Osborne, J.; Grant, G.D.; Anoopkumar-Dukie, S.; Leveritt, M.D. Women Experience the Same Ergogenic Response to Caffeine as Men. Med. Sci. Sports Exerc. 2019 , 51 , 1195–1202. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Haller, C.A.; Jacob, P.; Benowitz, N.L. Pharmacology of ephedra alkaloids and caffeine after single-dose dietary supplement use*. Clin. Pharmacol. Ther. 2002 , 71 , 421–432. [ Google Scholar ] [ CrossRef ]
- Loftfield, E.; Freedman, N.D.; Graubard, B.I.; Guertin, K.A.; Black, A.; Huang, W.-Y.; Shebl, F.M.; Mayne, S.T.; Sinha, R. Association of Coffee Consumption With Overall and Cause-Specific Mortality in a Large US Prospective Cohort Study. Am. J. Epidemiol. 2015 , 182 , 1010–1022. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Rosenberg, L.; Palmer, J.R.; Kelly, J.P.; Kaufman, D.W.; Shapiro, S. Coffee drinking and nonfatal myocardial infarction in men under 55 years of age. Am. J. Epidemiol. 1988 , 128 , 570–578. [ Google Scholar ] [ CrossRef ]
- Lacroix, A.Z.; Mead, L.A.; Liang, K.-Y.; Thomas, C.B.; Pearson, T.A. Coffee Consumption and the Incidence of Coronary Heart Disease. New Engl. J. Med. 1986 , 315 , 977–982. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Happonen, P.; Voutilainen, S.; Salonen, J.T. Coffee Drinking Is Dose-Dependently Related to the Risk of Acute Coronary Events in Middle-Aged Men. J. Nutr. 2004 , 134 , 2381–2386. [ Google Scholar ] [ CrossRef ]
- Goldfarb, M.; Tellier, C.; Thanassoulis, G. Review of Published Cases of Adverse Cardiovascular Events After Ingestion of Energy Drinks. Am. J. Cardiol. 2014 , 113 , 168–172. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Avcı, S.; Sarıkaya, R.; Büyükcam, F. Death of a young man after overuse of energy drink. Am. J. Emerg. Med. 2013 , 31 , 1624.e3–1624.e4. [ Google Scholar ] [ CrossRef ]
- Frost, L.; Vestergaard, P. Caffeine and risk of atrial fibrillation or flutter: The Danish Diet, Cancer, and Health Study. Am. J. Clin. Nutr. 2005 , 81 , 578–582. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Sanchis-Gomar, F.; Pareja-Galeano, H.; Cervellin, G.; Lippi, G.; Earnest, C.P. Energy Drink Overconsumption in Adolescents: Implications for Arrhythmias and Other Cardiovascular Events. Can. J. Cardiol. 2015 , 31 , 572–575. [ Google Scholar ] [ CrossRef ]
- Zuchinali, P.; Zimerman, A.; Giaretta, V.; Salamoni, J.; Fracasso, B.; Pimentel, M.; Souza, G.C.; Chemello, D.; I Zimerman, L.; E Rohde, L. Short-term Effects of High-Dose Caffeine on Cardiac Arrhythmias in Patients With Heart Failure: A Randomized Clinical Trial. JAMA Intern. Med. 2016 , 176 , 1752–1759. [ Google Scholar ] [ CrossRef ]
- Voskoboinik, A.; Kalman, J.M.; Kistler, P.M. Caffeine and Arrhythmias: Time to Grind the Data. JACC Clin. Electrophysiol. 2018 , 4 , 425–432. [ Google Scholar ] [ CrossRef ]
- Souza, D.B.; Del Coso, J.; Casonatto, J.; Polito, M.D. Acute effects of caffeine-containing energy drinks on physical perfor-mance: A systematic review and meta-analysis. Eur. J. Nutr. 2017 , 56 , 13–27. [ Google Scholar ] [ CrossRef ]
- Fletcher, E.A.; Lacey, C.S.; Aaron, M.; Kolasa, M.; Occiano, A.; Shah, S.A. Randomized Controlled Trial of High-Volume Energy Drink Versus Caffeine Consumption on ECG and Hemodynamic Parameters. J. Am. Hear. Assoc. 2017 , 6 . [ Google Scholar ] [ CrossRef ]
- Cornelis, M.C.; Monda, K.L.; Yu, K.; Paynter, N.; Azzato, E.M.; Bennett, S.N.; Berndt, S.I.; Boerwinkle, E.; Chanock, S.; Chatterjee, N.; et al. Genome-Wide Meta-Analysis Identifies Regions on 7p21 (AHR) and 15q24 (CYP1A2) As Determinants of Habitual Caffeine Consumption. PLoS Genet. 2011 , 7 , e1002033. [ Google Scholar ] [ CrossRef ]
- Sulem, P.; Gudbjartsson, D.F.; Geller, F.; Prokopenko, I.; Feenstra, B.; Aben, K.K.H.; Franke, B.; den Heijer, M.; Kovacs, P.; Stumvoll, M.; et al. Sequence variants at CYP1A1- CYP1A2 and AHR associate with coffee consumption. Hum. Mol. Genet. 2011 , 20 , 2071–2077. [ Google Scholar ] [ CrossRef ]
- Denden, S.; Bouden, B.; Khelil, A.H.; Ben Chibani, J.; Hamdaoui, M. Gender and ethnicity modify the association between the CYP1A2 rs762551 polymorphism and habitual coffee intake: Evidence from a meta-analysis. Genet. Mol. Res. 2016 , 15 . [ Google Scholar ] [ CrossRef ]
- Happonen, P.; Voutilainen, S.; Tuomainen, T.-P.; Salonen, J.T. Catechol-O-Methyltransferase Gene Polymorphism Modifies the Effect of Coffee Intake on Incidence of Acute Coronary Events. PLoS ONE 2006 , 1 , e117. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Enriquez, A.; Frankel, D.S. Arrhythmogenic effects of energy drinks. J. Cardiovasc. Electrophysiol. 2017 , 28 , 711–717. [ Google Scholar ] [ CrossRef ]
- Bird, S.R.; Goebel, C.; Burke, L.M.; Greaves, R.F. Doping in sport and exercise: Anabolic, ergogenic, health and clinical issues. Ann. Clin. Biochem. 2016 , 53 , 196–221. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Torrisi, M.; Pennisi, G.; Russo, I.; Amico, F.; Esposito, M.; Liberto, A.; Cocimano, G.; Salerno, M.; Rosi, G.L.; Di Nunno, N.; et al. Sudden Cardiac Death in Anabolic-Androgenic Steroid Users: A Literature Review. Medicina 2020 , 56 , 587. [ Google Scholar ] [ CrossRef ]
- Marsh, J.D.; Lehmann, M.H.; Ritchie, R.H.; Gwathmey, J.K.; Green, G.E.; Schiebinger, R.J. Androgen receptors mediate hyper-trophy in cardiac myocytes. Circulation 1998 , 98 , 256–261. [ Google Scholar ] [ CrossRef ]
- Perry, J.C.; Schuetz, T.M.; Memon, M.D.; Faiz, S.; Cancarevic, I. Anabolic Steroids and Cardiovascular Outcomes: The Controversy. Cureus 2020 , 12 , e9333. [ Google Scholar ] [ CrossRef ]
- Thiblin, I.; Garmo, H.; Garle, M.; Holmberg, L.; Byberg, L.; Michaëlsson, K.; Gedeborg, R. Anabolic steroids and cardiovascular risk: A national population-based cohort study. Drug Alcohol Depend. 2015 , 152 , 87–92. [ Google Scholar ] [ CrossRef ]
- Montisci, M.; El Mazloum, R.; Cecchetto, G.; Terranova, C.; Ferrara, S.D.; Thiene, G.; Basso, C. Anabolic androgenic steroids abuse and cardiac death in athletes: Morphological and toxicological findings in four fatal cases. Forensic Sci. Int. 2012 , 217 , e13–e18. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Achar, S.; Rostamian, A.; Narayan, S.M. Cardiac and Metabolic Effects of Anabolic-Androgenic Steroid Abuse on Lipids, Blood Pressure, Left Ventricular Dimensions, and Rhythm. Am. J. Cardiol. 2010 , 106 , 893–901. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Sachtleben, T.R.; Berg, K.E.; Elias, B.A.; Cheatham, J.P.; Felix, G.L.; Hofschire, P.J. The effects of anabolic steroids on myocardial structure and cardiovascular fitness. Med. Sci. Sports Exerc. 1993 , 25 , 1240–1245. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- D’Andrea, A.; Caso, P.; Salerno, G.; Scarafile, R.; De Corato, G.; Mita, C.; Di Salvo, G.; Severino, S.; Cuomo, S.; Liccardo, B.; et al. Left ventricular early myocardial dysfunction after chronic misuse of anabolic androgenic steroids: A Doppler myocardial and strain imaging analysis * COMMENTARY. Br. J. Sports Med. 2007 , 41 , 149–155. [ Google Scholar ] [ CrossRef ]
- Baggish, A.L.; Weiner, R.B.; Kanayama, G.; Hudson, J.I.; Picard, M.H.; Hutter, A.M.; Pope, H.G. Long-Term Anabolic-Androgenic Steroid Use Is Associated With Left Ventricular Dysfunction. Circ. Hear. Fail. 2010 , 3 , 472–476. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Riezzo, I.; Di Paolo, M.; Neri, M.; Bello, S.; Cantatore, S.; D’Errico, S.; Dinucci, D.; Parente, R.; Pomara, C.; Rabozzi, R.; et al. Anabolic Steroid - and Exercise - Induced Cardio-Depressant Cytokines and Myocardial β1 Receptor Expression in CD1 Mice. Curr. Pharm. Biotechnol. 2011 , 12 , 275–284. [ Google Scholar ] [ CrossRef ]
- Lieberherr, M.; Grosse, B. Androgens increase intracellular calcium concentration and inositol 1,4,5-trisphosphate and diacylglycerol formation via a pertussis toxin-sensitive G-protein. J. Biol. Chem. 1994 , 269 , 7217–7223. [ Google Scholar ] [ CrossRef ]
- D’Andrea, A.; Radmilovic, J.; Caselli, S.; Carbone, A.; Scarafile, R.; Sperlongano, S.; Tocci, G.; Formisano, T.; Martone, F.; Liccardo, B.; et al. Left atrial myocardial dysfunction after chronic abuse of anabolic andro-genic steroids: A speckle tracking echocardiography analysis. Int. J. Cardiovasc. Imaging. 2018 , 34 , 1549–1559. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hernández-Guerra, A.I.; Tapia, J.; Menéndez-Quintanal, L.M.; Lucena, J.S. Sudden cardiac death in anabolic androgenic ster-oids abuse: Case report and literature review. Forensic Sci. Res. 2019 , 4 , 267–273. [ Google Scholar ]
- Zhu, D.; Hadoke, P.W.; Wu, J.; Vesey, A.T.; Lerman, D.A.; Dweck, M.R.; Newby, D.E.; Smith, L.B.; MacRae, V.E. Ablation of the an-drogen receptor from vascular smooth muscle cells demonstrates a role for testosterone in vascular calcification. Sci. Rep. 2016 , 20 , 24807. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Liu, J.-D.; Wu, Y.-Q. Anabolic-androgenic steroids and cardiovascular risk. Chin. Med J. 2019 , 132 , 2229–2236. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sculthorpe, N.; Grace, F.; Jones, P.; Davies, B. Evidence of altered cardiac electrophysiology following prolonged an-drogenic anabolic steroid use. Cardiovasc. Toxicol. 2010 , 10 , 239–243. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Alizade, E.; Avcı, A.; Fidan, S.; Tabakçı, M.; Bulut, M.; Zehir, R.; Simsek, Z.; Evlice, M.; Arslantaş, U.; Çakır, H.; et al. The effect of chronic anabolic-androgenic steroid use on TpE interval, Tp-E/Qt ratio, and Tp-E/Qtc ratio in male bodybuilders. Ann. Noninvasive Electrocardiol. 2015 , 20 , 592–600. [ Google Scholar ] [ CrossRef ]
- Shirpoor, A.; Heshmatian, B.; Tofighi, A.; Eliasabad, S.N.; Kheradmand, F.; Zerehpoosh, M. Nandrolone administration with or without strenuous exercise increases cardiac fatal genes overexpression, calcium/calmodulin-dependent protein kinaseiiδ, and monoamine oxidase activities and enhances blood pressure in adult wistar rats. Gene 2019 , 697 , 131–137. [ Google Scholar ] [ CrossRef ]
- Pärssinen, M.; Kujala, U.; Vartiainen, E.; Sarna, S.; Seppälä, T. Increased premature mortality of competitive powerlifters suspected to have used anabolic agents. Int. J. Sports. Med. 2000 , 21 , 225–227. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Melchert, R.B.; Welder, A.A. Cardiovascular effects of androgenic-anabolic steroids. Med. Sci. Sports Exerc. 1995 , 27 , 1252–1262. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rothman, R.D.; Weiner, R.B.; Pope, H.G.; Kanayama, G.; Hutter, A.M.; A Fifer, M.; Dec, G.W.; Baggish, A.L. Anabolic androgenic steroid induced myocardial toxicity: An evolving problem in an ageing population. BMJ Case Rep. 2011 , 2011 . [ Google Scholar ] [ CrossRef ]
- Finocchiaro, G.; Papadakis, M.; Robertus, J.L.; Dhutia, H.; Steriotis, A.K.; Tome, M.; Mellor, G.; Merghani, A.; Malhotra, A.; Behr, E.; et al. Etiology of Sudden Death in Sports: Insights From a United Kingdom Regional Registry. J. Am. Coll. Cardiol. 2016 , 67 , 2108–2115. [ Google Scholar ] [ CrossRef ]
- Sheppard, M.N. Aetiology of sudden cardiac death in sport: A histopathologist’s perspective. Br. J. Sports Med. 2012 , 46 , i15–i21. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sessa, F.; Salerno, M.; Di Mizio, G.; Bertozzi, G.; Messina, G.; Tomaiuolo, B.; Pisanelli, D.; Maglietta, F.; Ricci, P.; Pomara, C. Anabolic Androgenic Steroids: Searching New Molecular Biomarkers. Front. Pharmacol. 2018 , 9 , 1321. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Soplinska, A.; Zareba, L.; Wicik, Z.; Eyileten, C.; Jakubik, D.; Siller-Matula, J.M.; De Rosa, S.; Malek, L.A.; Postula, M. MicroRNAs as Biomarkers of Systemic Changes in Response to Endurance Exercise—A Comprehensive Review. Diagnostics 2020 , 10 , 813. [ Google Scholar ] [ CrossRef ]
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Sivalokanathan, S.; Małek, Ł.A.; Malhotra, A. The Cardiac Effects of Performance-Enhancing Medications: Caffeine vs. Anabolic Androgenic Steroids. Diagnostics 2021 , 11 , 324. https://doi.org/10.3390/diagnostics11020324
Sivalokanathan S, Małek ŁA, Malhotra A. The Cardiac Effects of Performance-Enhancing Medications: Caffeine vs. Anabolic Androgenic Steroids. Diagnostics . 2021; 11(2):324. https://doi.org/10.3390/diagnostics11020324
Sivalokanathan, Sanjay, Łukasz A. Małek, and Aneil Malhotra. 2021. "The Cardiac Effects of Performance-Enhancing Medications: Caffeine vs. Anabolic Androgenic Steroids" Diagnostics 11, no. 2: 324. https://doi.org/10.3390/diagnostics11020324
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Open access
- Published: 17 October 2021
Generating evidence on the use of Image and performance enhancing drugs in the UK: results from a scoping review and expert consultation by the Anabolic Steroid UK network
- Jim McVeigh ORCID: orcid.org/0000-0001-5319-6885 1 ,
- Evelyn Hearne 2 ,
- Ian Boardley 3 ,
- Geoff Bates 4 ,
- Vivian Hope 2 ,
- Rob Ralphs 1 &
- Marie Claire Van Hout 5
Harm Reduction Journal volume 18 , Article number: 107 ( 2021 ) Cite this article
6928 Accesses
12 Citations
19 Altmetric
Metrics details
The use of anabolic androgenic steroids (AAS) and associated image and performance enhancing drugs (IPEDs) is now a global phenomenon. There is a need to develop evidence to support the development of interventions to prevent the commencement of use, to minimise the potential harms or to support those in their cessation of use. While the United Kingdom (UK) is no exception to this issue, its public health and legislative response to the phenomenon differs to other countries and requires the examination of research specific to the UK. Therefore, a scoping review has been conducted to examine the recent relevant literature to help inform the development and evaluation of effective interventions to reduce the harmful use of IPEDs.
A comprehensive search strategy was developed for multiple bibliographic databases, supported by and iterative citation searching process and complimented by expert input from the Anabolic Steroid UK Network. Research conducted by or UK academics or within the UK were eligible, if published in the previous five years.
In total 87 eligible outputs were identified, including 26 review articles, 25 qualitative papers and 24 quantitative papers. together with small numbers of clinical studies/case reports (6) and commentaries/correspondence (6). The most common topics of research were public health, treatment and harm reduction (41), followed by studies focusing on epidemiology, sub-groups of people using IPEDs and motivations for use (34). The studies illustrated the diverse populations of people who use a range of enhancement drugs including concomitant psychoactive drug use. A number of papers focused on blood borne viruses and associated issues, while others reported on the uptake of needle and syringe programmes. No effectiveness evaluations related to any aspect of treatment, harm reduction or other intervention were published during study period.
There is a need for the development of effectiveness evaluations of current interventions and any future service provision for people using image and performance enhancing drugs. While there have been no studies of this nature to date, this review illustrates the rich data that has been gathered through diverse methodologies, that will assist in the development of future effectiveness evaluations.
Image and performance and enhancing drugs (IPEDs) include a wide range of drugs across various pharmacological categories. Their common features are the function of their use: the alteration of physical performance, or appearance. IPEDs [ 1 ] form a subset of human enhancement drugs (HEDs) [ 1 , 2 , 3 ], and are predominantly those that promote lean muscle mass (e.g., anabolic androgenic steroids [AAS], human growth hormone [hGH]) but may also include weight loss products such as dinitrophenol or skin tanning injections (e.g., melanotan II). Whilst the use of IPEDs is by no means a new phenomenon, until relatively recently attention has been largely restricted to professional/elite athletes and bodybuilders. However, IPED use has moved beyond the sporting arena and is now commonplace amongst non-elite, recreational trainers within mainstream gymnasia [ 1 , 2 , 3 , 4 , 5 , 6 , 7 ]. This situation is not unique to the United Kingdom (UK) and other high-income countries such as the United States of America (USA), Australia and those within Western Europe. Research has identified widespread use of IPEDs in countries across the globe [ 8 ], including countries in the Middle East [ 9 ] and South America [ 10 , 11 ].
The UK is unique in its response to the use of IPEDs. In the 1990s, on the recommendation of the Advisory Council for the Misuse of Drugs, a decision was made not to criminalise the personal possession of these drugs, but to focus legislation on manufacture, distribution, and possession with intent to supply [ 12 ]. Subsequently, this principle has been maintained, with adjustments to curtail purchasing of AAS from overseas websites but no change to the legality of personal possession of AAS and associated IPEDs [ 13 ]. This approach is supported by a comprehensive network of needle and syringe programmes (NSPs) across the UK. Whilst NSPs were originally established in the 1980s in response to the HIV threat posed to people who injected heroin, people who inject IPEDs now constitute the largest client group for many NSPs in the UK [ 13 , 14 , 15 ]. The specific situation in the UK regarding the legality of AAS possession and the engagement of large numbers of people who use AAS, with a network of NSPs provides a unique backdrop to the development of effective interventions for this population. Therefore, in order to identify relevant evidence to support the development of these effectiveness evaluations it is necessary to identify collate and review the literature that is specific to the UK.
Unlike the evidence that is specific to the AAS environment in the UK, much of our knowledge in relation to the pharmacological effects of IPEDs is generalisable from research around the world and includes an increasing body of evidence highlighting physical and psychological harms stemming from AAS use. While harms to major organs and systems, in particular the heart and cardiovascular, have long been associated with the use of AAS [ 16 ], it is only over the last decade that the significance of long-term, high-dosage AAS has become apparent [ 17 , 18 , 19 ]. Alongside the recognised physical and mental health impacts, new concerning evidence is emerging in relation to long-term use being associated with structural changes to the brain, deviant brain aging, and impaired cognition. Recent studies of AAS use and the brain have also concluded that AAS dependence is associated with thinner cortex in widespread regions, specifically in prefrontal areas involved in inhibitory control and emotional regulation, compared with non-dependent AAS users [ 20 ]. Recently we have also seen greater recognition of prolonged and sometimes irreversible hypogonadism in men after long-term use of AAS [ 21 , 22 ] and how the symptoms of this, including reduced libido [ 23 ], may lead to continuation or resumption of AAS use. There remains significant debate regarding the issue of aggression and violence being associated with AAS use. Recent research has concluded that for some, AAS use may contribute to aggression levels [ 24 ]. Also, while there remains the need to elucidate the mechanisms involved [ 25 ], an association between aggression and AAS dependence has been identified [ 26 ].
While the majority of people who use AAS and associated IPEDs inject at least some of these drugs [ 27 , 28 ],a recent review of blood borne virus (BBV) infection amongst people who use AAS and associated IPEDs highlighted the paucity of relevant robust data globally [ 29 ]. Just nine papers published since 2000 were identified, four from the UK and Australia respectively and one from the USA. Whilst several of these studies were focused on AAS use within populations of gay and bisexual men, the large-scale UK research studies recruited AAS users from NSPs or directly from gyms. The UK study of 2010/11 identified 2% of the 395 participants as HIV positive, similar levels to those seen amongst people who inject psychoactive drugs [ 30 ]. This was supported by further data collection and analyses of surveillance data dating back to 1992, using a sample of 1296 people who had injected IPEDs. Results indicated that HIV had been present within this population for some time and provided an HIV prevalence of 1% for this period [ 31 ]. As yet we do not know the route of transmission of infection and the role that sexual contact and psychoactive drug injection may play. Furthermore, we do not know if this pattern of HIV infection amongst people who inject IPEDs is mirrored in other countries. Injection site infection and injury is a widely recognised issue. Pain and inflammation at injections sites have been identified at significant levels in studies from the UK [ 32 ], USA [ 33 ], Australia [ 34 ] and Holland [ 35 ]. While poor injecting techniques contribute to these localised infections, adulterated and contaminated products, an inevitable by-product of the illicit market is an ongoing issue on a global scale and overseas [ 36 , 37 , 38 , 39 ].
While AAS are the most used IPEDs, polypharmacy is the norm [ 7 , 40 ]. Additional anabolic substances, such as human growth hormone (hGH) and a range of new peptide hormones (e.g., growth hormone-releasing peptide-6) are commonly used. Drugs to prevent or mitigate side-effects (e.g., tamoxifen to counter gynaecomastia), human chorionic gonadotrophin (for the resumption of normal testicular function) and a range of weight loss drugs (e.g., ephedrine, dinitrophenol, clenbuterol) are also part of the established pharmacopeia. Low-cost production and distribution, combined with the increasing sourcing routes via the internet has resulted in substances that were once prohibitively expensive now being commonplace [ 41 ]. Furthermore, the use of other human enhancement drugs including melanotan II and sildenafil combined with psychoactive drugs is prevalent amongst some cohorts who use IPEDs, sometimes with significant potential for harmful interactions with certain drugs (e.g., cocaine) [ 42 ].
People who use AAS and associated IPEDs are by no means a homogenous group. Recent work has highlighted various typologies of user comprised of multiple subgroups with varied characteristics, risk behaviours and levels of engagement with support services [ 43 , 44 , 45 ]. While the focus of much of the research has centred on male use of these substances use, women do use IPEDs and in some cases use AAS, for those women using AAS the potential harms are more significant and sometimes compounded by an added sense of stigma and reluctance to engage with support services or healthcare [ 46 ].
The need for evidence to support our understanding of interventions that can reduce the harmful use of IPEDs is increasingly recognised (e.g. [ 47 , 48 ]). As attention from the research community on IPEDs has amplified substantially in recent decades [ 15 ], the enlarged evidence base may provide valuable insights that will support those working to reduce harm amongst people who use IPEDs and ensure that approaches are based on a thorough understanding of up to date evidence. The review therefore sought to identify and explore evidence that will support the development and evaluation of effective interventions to reduce the harmful use of IPEDs. The underpinning research question developed by the research team was “how has the academic literature base on the use of IPEDs in the UK developed in the past five years and what does it tell us?”. Specifically, we sought to gain insight into the characteristics of studies investigating IPED use including: the methods used, topics of research, the characteristics of study populations, and key themes within study findings and recommendations. We conducted a scoping review of UK literature on the use of IPEDs to map and describe extant UK based literature, and in partial fulfilment of the UK National Institute for Health Research development grant (NIHR 132730), Image and Performance Enhancing Drugs (IPEDs): Assessment of available intelligence and research gaps to inform intervention evaluation’ [ 47 ]. While the international evidence base pertaining to the pharmacological effects of AAS and associated IPEDs is largely applicable to the UK, the specific situation in the UK warranted a review of the UK published literature over the last five years. It is within this environment that we sought to identify the current research landscape to ultimately inform the development of evidence based effective interventions. Therefore, this review looked specifically at the AAS/IPED outputs from UK academics/institutions. These results compliment related NIHR research activity comprising estimations of the size of the population of people who use AAS, the extent and characteristics of service provision for this group and the systems mapping of factors that influence the harmful use of IPEDs.
Methodology
A scoping review design was chosen to map and describe what is known about the current status and focus of research in relation to IPEDs in the UK. Scoping reviews were first proposed by Arksey and O'Malley [ 49 ] and have been further advanced by others over the last decade [ 50 , 51 , 52 ]. More recently, Tricco, Lillie [ 53 ] defined scoping reviews as “a type of knowledge synthesis, follow a systematic approach to map evidence on a topic and identify main concepts, theories, sources, and knowledge gaps” . This independent research methodology addresses broader research questions than systematic reviews can answer [ 49 , 50 , 51 , 52 ]. Scoping reviews are generally conducted to identify knowledge gaps, examine the extent (i.e. size), range (i.e. variety), and nature (i.e. characteristics) of a specific topic, summarise the findings of a heterogeneous body of knowledge, and propose agendas for future policy and research [ 49 , 52 , 54 , 55 ].
Search strategy
Arksey and O'Malley [ 49 ] five-stage iterative scoping review methodology was adhered to, namely: [ 1 ] identifying the essential research question, [ 2 ] identifying relevant studies, [ 3 ] study selection, [ 4 ] charting the data, and [ 5 ] collecting, summarising, and reporting the results. A search was undertaken in January 2021, in Liverpool John Moores University Library catalogues using the following databases: Web of Science; MEDLINE; Science Direct; PsycINFO; SPORTDiscus; CINHAL Plus; PubMed; Google Scholar, and Google. Search terms were compiled and agreed by the research team who had extensive knowledge and experience of public health, addiction, and IPED research (see Table 1 ).
Study selection
The initial search identified 4,882 articles based on the search terms outlined above (see Table 1 ), References were imported to Endnote® citation manager where they were organised. An initial examination of the articles indicated the possibility of many irrelevant articles. Duplicates were removed ( n = 1279) followed by title and abstract screening of the remainder ( n = 3461), where inclusion and exclusion criteria were applied to all citations. Studies included were: all published empirical research including articles in peer-reviewed journals and book chapters; and grey literature such as national policy reports and documents, needs assessments, service evaluations, and locally commissioned research. Date range was restricted to between January 1 st 2016 and December 31 st 2020 to capture current, relevant literature to inform the development and evaluation of effective interventions to reduce harmful IPED use, and studies conducted by UK academics or those with a UK focus due to the unique situation in the UK relating to legislation and NSP provision. Academic theses, animal models, and in-vitro studies were excluded. A total of 77 records were identified at this stage of the search (see Fig. 1 ). Papers were subsequently reviewed and screened to ensure those included met the inclusion criteria and discrepancies resolved [ 54 ]. Manual searching of the reference lists of the 77 records was conducted to identify any relevant literature that was not captured in the initial search. Subsequently, consultation with academics and healthcare professionals with relevant expertise (accessed through the Academic Steroid UK Network) was conducted to ensure all relevant literature was included, as recommended by Daudt, van Mossel [ 54 ]. This was a valuable step in the process as the depth and breadth of knowledge each expert brought strengthened the review and consequently, the richness of the findings. A final number of 87 sources were included in the review (see Fig. 1 ).
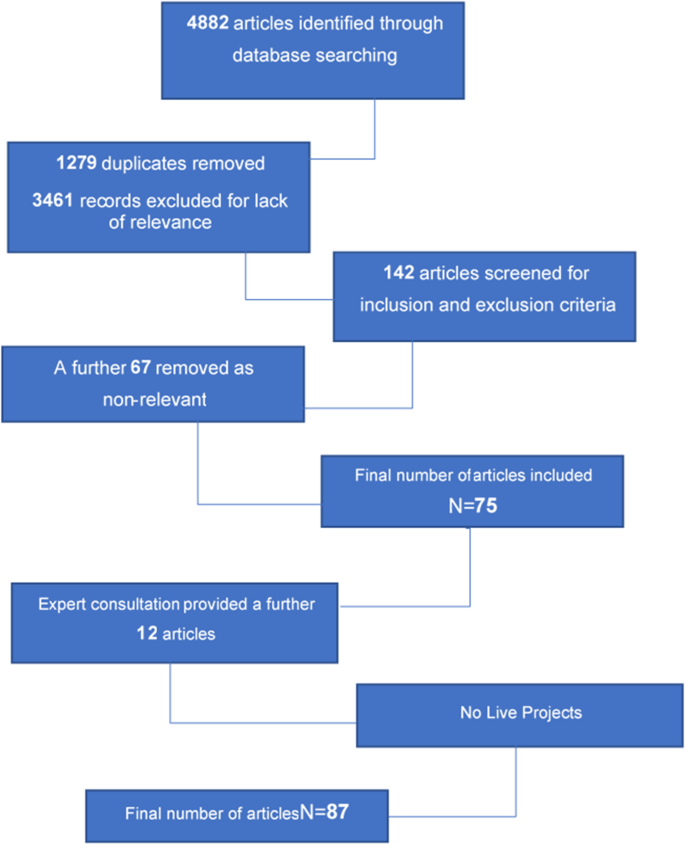
Flow chart of the search strategy used to identify image & performance enhancing drug research outputs 2016–2020
Data extraction and charting
Data were extracted to form a dataset which included all author names and institutions, year of publication, aim and method, population, key findings, implications for policy and practice, and identified research gaps in each source.
Additional file 1 : Table 2 provides a detailed overview of UK academic publications on the use of anabolic androgenic steroids and IPEDs, presenting an overview of this research to illustrate its volume and main characteristics, together with summaries of key findings.
Profile of studies reviewed
The final sample of 87 records present a range of methodologies and foci on AAS and other IPEDs within the UK. The majority of evidence was gleaned from the review of 69 journal articles and supplemented by 12 relevant academic book chapters and six public health reports. There is no discernible trend in the volume, methodologies used or focus of research outputs over the five-year period. Apart from 2019, the number of outputs per year ranged between 12 and 17 publications. The high number of outputs in 2019 [ 29 ] can be explained by the inclusion of 8 chapters from one book on the use of human enhancement drugs [ 1 ]. These records are comprised of a variety of methodologies and approaches including qualitative, quantitative and review. In a small minority of cases several methods were reported within the research output, however in all cases there was a clear predominant method applied. For example, the book chapter ‘The supply of image and performance enhancing drugs (IPED) to local non-elite users in England [ 56 ], forensic analysis of a small number IPEDs was used to support the findings of two qualitative studies and was therefore recorded as a qualitative paper. Figure 2 illustrates these methodologies in an aggregated form. The 26 review articles (including systematic, scoping, and non-specific reviews) account for the largest proportion of outputs(30%), followed by 25 predominantly qualitative (29%), 24 quantitative papers (27%) with 6 (7%) commentary papers and clinical case studies respectively.
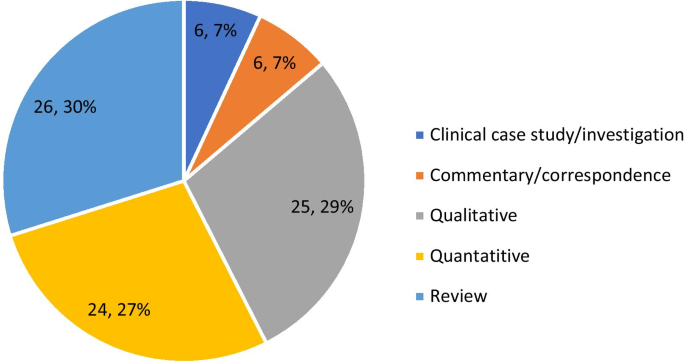
Methodologies of image & performance enhancing drug research outputs 2016–2020
Additional file 1 : Table 2 also includes the main topics of each output. It is important to note that while the category of sport/doping control is included, outputs were excluded if this was the sole area of focus. Outputs may be attributed to two are more categories. Figure 3 summarises these categories within the year of publication. The most common topic of research, included in 41 academic outputs, was public health/care (including harm reduction and treatment). This was consistent across each year apart from 2018 when epidemiology was the major category, this being the second most common topic overall [ 34 ].
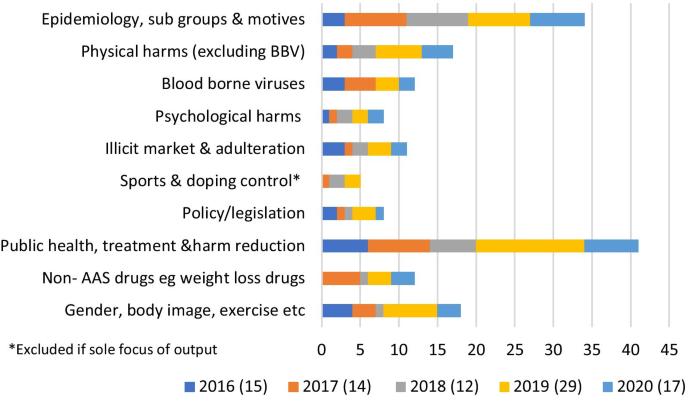
Focus of image & performance enhancing drugs research outputs 2016–2020
Key findings
The UK research from the last 5-years provided a broad spectrum of evidence related to various facets of IPED use, from across the full extent of the UK. An indication of the diversity of drugs used is provided, together with specific implications. The vast majority of the work was in relation to the use of AAS includingone paper looking at the concomitant use of stimulants [ 42 ] Four papers focusing solely on the use of weight loss drugs [ 57 , 58 , 59 , 60 ], two papers examining the use of the skin tanning drug melanotan [ 61 , 62 ], two academic outputs describing the emerging use of the respective peptide hormones metformin and CJC-1295 [ 63 , 64 ], and one article examining the use of synthol (a site enhancement oil) [ 65 ]. One paper focused specifically onthose solely taking oral AAS and associated drugs [ 66 ], two papers examined the relationshipbetween supplements IPED use [ 67 , 68 ], whilethe role of concomitant psychoactive drugs was emphasised as a cause for concern in one paper [ 7 ]. Six outputs provided accounts of the ease of availability and affordability of drugs within a dynamic IPED market [ 56 , 69 , 70 , 71 , 72 , 73 ], with the internet playing an important role with a significant market crossover with other drug using populations [ 74 , 75 , 76 , 77 ].
Research focused on epidemiology, sub-groups, and motives, indicates a complex landscape of diverse sub-populations of IPED users, going beyond the stereotypical young male AAS user. Different populations and practices were identified with specific practices and risks. Significant sub-groups included women using a range of substances [ 78 , 79 , 80 , 81 , 82 ] and older men using AAS [ 28 ]. While research that only focused on elite sport and doping control was excluded, sport clearly plays a significant role in the use of IPEDs [ 83 ] and remains a public policy concern [ 84 ]. IPED use was also associated with specific occupations as diverse as those in the military to those engaged in dance [ 85 , 86 ]. The majority of the literature in this review examined the use of AAS, in particular the use of AAS by men. Only four papers solely focused on the use of IPEDs by women [ 57 , 64 , 78 , 81 ].
This literature also provides an improved understanding of some of the motives for commencement of use or abstinence, in particular those related to self-esteem, body image and masculinity [ 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 ]. The continuation or resumption of AAS use driven by symptoms of hypogonadism [ 97 , 98 , 99 , 100 ] was a significant finding, together with wider issues related to sexual health [ 101 ]. Harms associated with IPED use were commonly described [ 18 , 19 , 102 , 103 ], together with the risk environment [ 6 ] and efforts by individuals to mitigate these adverse consequences [ 104 ].
Common features within studies centred on public health, treatment, and harm reduction included the increasing number of AAS users engaging with NSPs [ 28 , 105 , 106 ] and barriers to service engagement including a lack of confidence in practitioners’ knowledge, perceived stigma. A failure to recognise the beneficial effects of AAS was identified together with an overemphasis of the harms [ 107 , 108 , 109 , 110 ], while the need for non-judgemental specialised services was emphasised [ 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 ]. A greater understanding of the need for a multi-layered approach to preventing both IPED use in general, and harmful use in particular, was emphasised [ 91 , 120 , 121 ]. The need for an understanding of the culture as well as the behaviours of people who use IPEDs was deemed essential, together with an appreciation that IPEDs may have potential benefits to the user [ 58 , 108 , 110 ].
Another recurring theme within this literature was the need for health practitioners to demonstrate both a non-judgemental attitude and have a demonstrable level of knowledge of both IPEDs and how they are used. This was considered a prerequisite if the current barriers to service engagement are to be overcome [ 110 ]. Practitioners must have an appreciation of the complex relationship between AAS use and body image [ 96 ] and an understanding that there is a perceived normalisation of IPED use within some social groups, with concepts around masculinity and muscularity being highly influential on decisions to use IPEDs [ 91 ]. While the majority of the literature referred to practitioners in general, the potential for an increased role for both social workers [ 115 ] and endocrinologists [ 116 ] was highlighted.
Various aspects of a potential continuum of care and support were also discussed. These ranged from prevention activities within a generic health promotion approach, recognising the complex factors that make children, youth and adults vulnerable to IPEDs [ 42 , 120 , 121 ], through to the need for relapse prevention to divert former AAS users from a focus on their body as their major source of self-esteem [ 94 ]. However, the main area of discussion related to existing and potential harm reduction interventions and services [ 7 , 15 , 111 ]. In addition to the expansion of innovative development and activity within NSPs [ 107 , 122 ], other venues and modes of engagement to promote sexual health [ 101 ] and ensure non-stigmatising environments were called for [ 28 , 29 , 123 , 124 ]. There were also calls for the implementation of effective assertive outreach [ 125 ] and the adjustment of health and social care settings to enhance on-site engagement with people who use IPEDs [ 107 ].
As part of service provision there were also calls for comprehensive testing including physiological indicators of harm [ 112 ] together with testing for BBVs [ 126 ] and psychosocial support regarding body image. Such testing for BBVs could draw upon the improved understanding of injecting beliefs and behaviours [ 101 ], including BBV risks [ 25 , 27 , 102 , 103 , 104 , 105 , 106 , 107 ], evident in the review. Information of nutrition and exercise [ 113 ], building self-esteem [ 97 ], psychological services to address dependence and muscle dysmorphia [ 82 , 97 ], and other body image vulnerabilities [ 59 ] were also considered necessary. There were consistent findings regarding the need for practitioners to have an understanding of the diverse populations of people who use IPEDS [ 45 ], the episodic nature of use [ 74 ], polydrug use [ 7 ], those who do not inject [ 66 ] and those using drugs other than AAS [ 58 , 60 , 127 ]. An understanding of the market was considered necessary in order to provide credible health related information on risks of active ingredients and the quality products obtained through the illicit market [ 64 ].
The diversity of UK published research between 2016 and 2020 reflects a growing scientific and academic interest in this phenomenon and underpins the complex issues related to the use of available IPEDs. They also indicate the multidisciplinary response that is required if, as researchers, practitioners, policy makers, and all importantly, people who use these drugs, are going to synergise and work collaboratively to raise awareness increase our understanding and ultimately reduce the harms associated with use. The research findings, together with the stated implications for policymakers, practitioners and the research community illustrate the broad spectrum of opportunities to reduce harm, including prevention, diversion, treatment, cessation support and policies that directly affect the illicit market. However, notable by their absence and as highlighted within many of the publications is the lack of robust effectiveness of evaluations in relation to interventions focused on the use of IPEDs. While the focus of this paper is on recently published UK research, due to the unique position we are in, in relation to legislation and needle and syringe provision, it is worth noting that this dearth of intervention effectiveness evidence is replicated around the globe.
Findings also underscore the need for future efforts to develop and evaluate interventions should see the involvement of people who use IPEDs as an essential component during all stages of the research process. For example, many included records emphasised that interventions should encompass peer support groups and educators [ 113 , 125 ], and a client-centred approach [ 79 , 106 ]. Thus, there was a recurring theme within the UK literature of the recognition of the need to effectively engage with the communities of people who use IPEDs. It is a widely held belief that the required interventions and the research that is needed to test and evaluate them can only be achieved with the participation of those who use IPEDs. This belief is supported not only by the IPED-specific literature reviewed here, but also by the broader literature relevant to the development and evaluation of interventions aimed at enhancing or protecting physical and psychological health. Often referred to as patient and public involvement (PPI), research funders now frequently endorse and sometimes obligate PPI during all stages of health and social care research [ 129 , 130 ]. Incorporating PPI can benefit research by promoting recruitment [ 131 ], which can enhance its validity and reduce costs [ 132 ]. Moreover, the efficacy of PPI is greatest when those with lived experience of the behaviour/condition being studied are represented as research partners, supporting the benefits of harnessing knowledge from such experience-based experts alongside that of scientists and professionals when designing, delivering, and disseminating research [133]. The importance of involving those with lived experience of IPED use in research and in developing and evaluating harm reduction interventions for IPED use is perhaps even more important than in other fields given evidence demonstrating a lack of trust in healthcare professionals when it comes to IPED use [134–136].
The research literature provided a wealth of far-reaching recommendations for future research. It is essential that researchers engage and collaborate with the communities of people who use IPEDs to better understand the patterns of drug-use behaviours, motives and associated risks [ 28 ]. Future research should focus on delivery of holistic healthcare and early intervention for those attending NSPs and outreach services [ 42 ]. However, harm reduction should look beyond NSPs to meet the needs of those who do not inject [ 66 ].
While the evidence base related to harms stemming from AAS use has developed over the last 5 years, there needs to be a continued focus on specific adverse effects for the full range of IPEDs [ 18 , 19 , 65 , 117 , 123 ], so that policy makers have a comprehensive understanding of the drivers and motives for use and cessation, and the associated harms for AAS [ 6 , 79 , 91 , 114 , 117 , 124 ] and other IPEDs [ 15 , 57 , 58 , 59 , 60 , 61 , 64 , 68 , 73 , 104 , 122 , 128 ]. We should also develop the evidence and increase our understanding of the issues associated with the diverse populations that use IPEDs [ 95 , 105 ]. More specifically, research should focus on those people using IPEDs who may be particularly vulnerable [ 76 ], including women [ 78 , 81 ], those in prison [ 117 ], those with specific occupations and those engaging in pertinent activities such as sport [ 67 , 83 , 85 , 86 , 90 , 93 ].
Motives for commencement, continuation, and potential cessation of IPED use should also receive continued research attention [ 92 , 98 , 120 ]. Key examples identified for further attention include body image [ 96 , 97 , 129 ], muscle dysmorphia [ 94 ], muscularity [ 82 ], masculinity [ 87 , 130 ], and hypogonadism [ 99 , 113 , 115 ]. Research findings indicate a combination of routinely available data, survey data and other novel data collection methods should be employed [ 95 ], including online methodologies to gain a better understanding of the prevalence of use and associated behaviours [ 15 , 45 , 64 , 74 , 116 , 127 ]. Research is also needed into the clinical treatment of adverse effects [ 102 ] and how stigma and barriers within generic health services may be effectively addressed [ 112 ]. This is especially pertinent in relation BBV services [ 28 , 31 , 119 , 126 , 131 , 132 ] and sexual health services [ 31 ], including men who have sex with men and women who have sex with women [ 101 ]. We also need to gain a better understanding of the supply and distribution of IPED, the role of the internet, potential for a more regulated market and the harms caused by the illicit market [ 6 , 7 , 15 , 63 , 69 , 73 , 74 , 75 ]. The overarching them in relation to identified research gaps and recommended focus of attention is the evaluation of interventions to identify cost-effective demand reduction and harm reduction solutions [ 104 , 105 , 107 , 111 , 128 ]. Further attention is warranted by policymakers and public health surveillance systems to track and monitor this emerging and increasingly mainstream form of body modification and consumerism of IPED pharmaceuticals.
The UK IPED research community has been highly active over the last five years. This review evidences a wealth of data relating to people who use IPEDs, including their practices and associated harms. However, where interventions are a focus of the research, findings tend to be descriptive and their remains a paucity of effectiveness studies. The literature highlights the need for meaningful involvement of people with lived experience, reinforcing the principles of co-production in the development of future intervention evaluations to reduce the harms associated with this form of substance use.
Van de Ven K, Mulrooney KJ, McVeigh J. Human enhancement drugs. 1st ed. Abigdon: Routledge; 2019.
Book Google Scholar
Evans-Brown M, McVeigh J, Perkins C, Bellis M. Human enhancement drugs: the emerging challenges to public health. Liverpool: North West Public Health Observatory; 2012.
Google Scholar
McVeigh J, Evans-Brown M, Bellis MA. Human enhancement drugs and the pursuit of perfection. Adicciones. 2012;24(3):185–90.
Article PubMed Google Scholar
McVeigh J, Begley E. Anabolic steroids in the UK: an increasing issue for public health. Drugs Educ Prevent Policy. 2017;24(3):278–85.
Article Google Scholar
Coomber R, Pavlidis A, Santos GH, Wilde M, Schmidt W, Redshaw C. The supply of steroids and other performance and image enhancing drugs (PIEDs) in one English city: fakes, counterfeits, supplier trust, common beliefs and access. Perform Enhanc Health. 2014;3(3):135–44.
Hanley Santos G, Coomber R. The risk environment of anabolic-androgenic steroid users in the UK: examining motivations, practices and accounts of use. Int J Drug Policy. 2017;40:35–43.
Salinas M, Floodgate W, Ralphs R. Polydrug use and polydrug markets amongst image and performance enhancing drug users: implications for harm reduction interventions and drug policy. Int J Drug Policy. 2019;67:43–51.
Sagoe D, Pallesen S. Androgen abuse epidemiology. Curr Opin Endocrinol Diabetes Obes. 2018;25(3):185–94.
Article CAS PubMed Google Scholar
Hearne E, Wazaify M, Van Hout MC, Atkinson A, McVeigh J. Anabolic-androgenic steroid use in the Eastern Mediterranean region: a scoping review of extant empirical literature. Int J Mental Health Addict. 2020;19:1162–89.
de Siqueira Nogueira FR, de Freitas BA, de Oliveira CVC, Vieira TI, Beniz Gouveia RL. Anabolic–androgenic steroid use among Brazilian bodybuilders. Subst Use Misuse. 2014;49(9):1138–45.
Abrahin OSC, de Sousa EC, Santos AM. Prevalence of the use of anabolic-androgenic steroids in Brazil: A systematic review. Subst Use Misuse. 2014;49(9):1156–62.
Druglink. ACMD recommends new controls on steroids. Druglink. 1993;September/October 1993.
ACMD. Consideration of the Anabolic Steroids. London (UK); 2010.
Kimergard A, McVeigh J. Variability and dilemmas in harm reduction for anabolic steroid users in the UK: a multi-area interview study. Harm Reduct J. 2014;11(ARTN 19):19.
Article PubMed PubMed Central Google Scholar
McVeigh J, Begley E. Anabolic steroids in the UK: an increasing issue for public health. Drug-Educ Prev Polic. 2017;24(3):278–85.
Hartgens F, Kuipers H, Wijnen JAG, Keizer HA. Body composition, cardiovascular risk factors and liver function in long term androgenic-anabolic steroids using bodybuilders three months after drug withdrawal. Int J Sports Med. 1996;17(6):429–33.
Baggish AL, Weiner RB, Kanayama G, Hudson JI, Lu MT, Hoffmann U, et al. Cardiovascular toxicity of illicit anabolic-androgenic steroid use. Circulation. 2017;135(21):1991–2002.
Article CAS PubMed PubMed Central Google Scholar
Angell PJ, Green DJ, Lord R, Gaze D, Whyte G, George KP. Acute cardiovascular responses to resistance exercise in anabolic steroids users: a preliminary investigation. Sci Sports. 2018;33(6):339–46.
McCullough D, Webb R, Enright KJ, Lane KE, McVeigh J, Stewart CE, et al. How the love of muscle can break a heart: Impact of anabolic androgenic steroids on skeletal muscle hypertrophy, metabolic and cardiovascular health. Rev Endocr Metab Disord. 2020;22(2):389–405.
Article PubMed PubMed Central CAS Google Scholar
Hauger LE, Westlye LT, Fjell AM, Walhovd KB, Bjornebekk A. Structural brain characteristics of anabolic-androgenic steroid dependence in men. Addiction. 2019;114:1405–15.
Kanayama G, Kaufman MJ, Pope HG. Public health impact of androgens. Curr Opin Endocrinol. 2018;25(3):218–23.
Article CAS Google Scholar
Pope HG Jr, Wood RI, Rogol A, Nyberg F, Bowers L, Bhasin S. Adverse health consequences of performance-enhancing drugs: an Endocrine Society scientific statement. Endocr Rev. 2014;35(3):341–75.
Harvey O, Parrish M, van Teijlingen E, Trenoweth S. Libido as a motivator for starting and restarting non-prescribed anabolic androgenic steroid use among men: a mixed-methods study. Drug-Educ Prev Polic. 2021. https://doi.org/10.1080/09687637.2021.1882940 .
Chegeni R, Pallesen S, McVeigh J, Sagoe D. Anabolic-androgenic steroid administration increases self-reported aggression in healthy males: a systematic review and meta-analysis of experimental studies. Psychopharmacology (Berl). 2021. https://doi.org/10.1007/s00213-021-05818-7 .
Pope HG, Jr., Kanayama G, Hudson JI, Kaufman MJ. Review article: anabolic-androgenic steroids, violence, and crime: two cases and literature review. Am J Addict. 2021;30(5):423–32.
Hauger LE, Havnes IA, Jorstad ML, Bjornebekk A. Anabolic androgenic steroids, antisocial personality traits, aggression and violence. Drug Alcohol Depend. 2021;221:108604.
Bonnecaze AK, O’Connor T, Aloi JA. Characteristics and attitudes of men using anabolic androgenic steroids (AAS): a survey of 2385 men. Am J Mens Health. 2020;14(6):1557988320966536.
Begley E, McVeigh J, Hope V, Bates G, Glass R, Campbell J, et al. Image and performance enhancing drugs: 2016 National Survey Results. Liverpool: Liverpool John Moores University; 2017.
Hope V, Iversen J. Infections and risk among people who use image and performance enhancing drugs. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Humam enhancement drugs. Abingdon: Routledge; 2019.
Hope VD, McVeigh J, Marongiu A, Evans-Brown M, Smith J, Kimergard A, et al. Prevalence of, and risk factors for, HIV, hepatitis B and C infections among men who inject image and performance enhancing drugs: a cross-sectional study. BMJ Open. 2013;3(9):e003207.
Hope VD, Harris R, McVeigh J, Cullen KJ, Smith J, Parry JV, et al. Risk of HIV and hepatitis B and C over time among men who inject image and performance enhancing drugs in england and wales: results from cross-sectional prevalence surveys, 1992–2013. J Acquir Immune Defic Syndr. 2016;71(3):331–7.
Hope VD, McVeigh J, Marongiu A, Evans-Brown M, Smith J, Kimergard A, et al. Injection site infections and injuries in men who inject image- and performance-enhancing drugs: prevalence, risks factors, and healthcare seeking. Epidemiol Infect. 2015;143(1):132–40.
Ip EJ, Barnett MJ, Tenerowicz MJ, Perry PJ. The anabolic 500 survey: characteristics of male users versus nonusers of anabolic-androgenic steroids for strength training. Pharmacotherapy. 2011;31(8):757–66.
Larance B, Degenhardt L, Copeland J, Dillon P. Injecting risk behaviour and related harm among men who use performance- and image-enhancing drugs. Drug Alcohol Rev. 2008;27(6):679–86.
Smit DL, Buijs MM, de Hon O, den Heijer M, de Ronde W. Positive and negative side effects of androgen abuse. The HAARLEM study: a one year prospective cohort study in 100 men. Scand J Med Sci Sports. 2020;30(3):531–39.
Fabresse N, Gheddar L, Kintz P, Knapp A, Larabi IA, Alvarez JC. Analysis of pharmaceutical products and dietary supplements seized from the black market among bodybuilders. Forensic Sci Int. 2021;322:110771.
Cho SH, Park HJ, Lee JH, Do JA, Heo S, Jo JH, et al. Determination of anabolic-androgenic steroid adulterants in counterfeit drugs by UHPLC-MS/MS. J Pharm Biomed Anal. 2015;111:138–46.
Evans-Brown M, Kimergard A, McVeigh J. Elephant in the room? The methodological implications for public health research of performance-enhancing drugs derived from the illicit market. Drug Test Anal. 2009;1(7):323–6.
Ribeiro MVD, Boralle N, Felippe LG, Pezza HR, Pezza L. H-1 NMR determination of adulteration of anabolic steroids in seized drugs. Steroids. 2018;138:47–56.
Sagoe D, McVeigh J, Bjornebekk A, Essilfie MS, Andreassen CS, Pallesen S. Polypharmacy among anabolic-androgenic steroid users: a descriptive metasynthesis. Subst Abuse Treat Prev Policy. 2015;10(ARTN 12):12.
Evans-Brown M, McVeigh J. Injecting human growth hormone as a performance-enhancing drug-perspectives from the United Kingdom. J Subst Use. 2009;14(5):267–88.
Zahnow R, McVeigh J, Bates G, Winstock AR. Motives and correlates of anabolic-androgenic steroid use with stimulant polypharmacy. Contemp Drug Probl. 2020;47(2):118–35.
Christiansen AV. Gym culture, identity and performance-enhancing drugs: tracing a typology of steroid use. Oxon: Routledge; 2020.
Christiansen AV, Vinther AS, Liokaftos D. Outline of a typology of men’s use of anabolic androgenic steroids in fitness and strength training environments. Drugs Educ Prevent Policy. 2016;24(3):295–305.
Zahnow R, McVeigh J, Bates G, Hope V, Kean J, Campbell J, et al. Identifying a typology of men who use anabolic androgenic steroids (AAS). Int J Drug Policy. 2018;55:105–12.
Havnes IA, Jorstad ML, Innerdal I, Bjornebekk A. Anabolic-androgenic steroid use among women—A qualitative study on experiences of masculinizing, gonadal and sexual effects. Int J Drug Policy. 2020:102876. https://doi.org/10.1016/j.drugpo.2020.102876 .
McVeigh J. Application Development Award Image and Performance Enhancing Drugs (IPEDs): Assessment of available intelligence and research gaps to inform intervention evaluation: NIHR; 2021 [Available from: https://www.journalslibrary.nihr.ac.uk/programmes/phr/NIHR132730/ #/.
Bates G, Shepherd S, McVeigh J. Harm reduction strategies for androgen users: providing appropriate support and improving engagement with healthcare. Curr Opin Endocrinol Diabetes Obes. 2021. https://doi.org/10.1097/MED.0000000000000676 .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D. An evidence-based approach to scoping reviews. Worldviews Evid Based Nurs. 2016;13(2):118–23.
Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13(1):48.
Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16:15.
Coomber R, Salinas M. The supply of image and performance enhancing drugs (IPED) to local non-elite users in England: Resilient traditional and newly emergent methods. Human enhancement drugs. Abingdon: Routledge; 2019.
Germain DJ, Leavey DC, Van Hout PMC, McVeigh PJ. 2,4 dinitrophenol: It's not just for men. Int J Drug Policy. 2020:102987. https://doi.org/10.1016/j.drugpo.2020.102987 .
McVeigh J, Germain J, Van Hout MC. 2,4-Dinitrophenol, the inferno drug: a netnographic study of user experiences in the quest for leanness. J Subst Use. 2017;22(2):131–8.
Germain J, McLean C, Leavey C. One size does not fit all: Tackling the issue of weight-loss drug use. In: van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Ainsworth NP, Vargo EJ, Petroczi A. Being in control? A thematic content analysis of 14 in-depth interviews with 2,4-dinitrophenol users. Int J Drug Policy. 2018;52:106–14.
Van Hout MC, McVeigh J. The use of sunless synthetic tanning products. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Dreyer BA, Amer T, Fraser M. Melanotan-induced priapism: a hard-earned tan. BMJ Case Rep. 2019;12(2):e227644. https://doi.org/10.1136/bcr-2018-227644
Graham MR, Baker JS, Davies B. Peptide hormones, metformin and new-wave practices and research therapies. In: Hall M, Grogan S, Gough B, editors. Chemically modified bodies. London: Palgrave Macmillan; 2016.
Van Hout MC, Hearne E. Netnography of female use of the synthetic growth hormone CJC-1295: pulses and potions. Subst Use Misuse. 2016;51(1):73–84.
Hall M, Grogan S, Gough B. Bodybuilders’ accounts of synthol use: The construction of lay expertise online. J Health Psychol. 2016;21(9):1939–48.
van de Ven K, Zahnow R, McVeigh J, Winstock A. The modes of administration of anabolic-androgenic steroid (AAS) users: are non-injecting people who use steroids overlooked? Drug Educ Prev Policy. 2019;27(2):131–5.
Boardley ID. Licit forms of performance enhancement and possible links with IPED use: Current knowledge and future directions. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Mooney R, Simonato P, Ruparelia R, Roman-Urrestarazu A, Martinotti G, Corazza O. The use of supplements and performance and image enhancing drugs in fitness settings: A exploratory cross-sectional investigation in the United Kingdom. Hum Psychopharmacol Clin Exp. 2017;32:e2619. https://doi.org/10.1002/hup.2619 .
Turnock LA. Inside a steroid ‘brewing’ and supply operation in South-West England: An ‘ethnographic narrative case study.’ Perform Enhancem Health. 2020;7:3–4.
Hall A, Antonopoulos GA. The (online) supply of illicit lifestyle medicines: a criminological study. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Coomber-Moore J. An exploration of evolving forms of access to performance and image enhancing drugs (PIED), and body image, on Gold Coast, Australia, with particular emphasis on how users reconcile their drift into criminality. Essex: University of Essex; 2017.
Hall A, Koenraadt R, Antonopoulos GA. Illicit pharmaceutical networks in Europe: organising the illicit medicine market in the United Kingdom and the Netherlands. Trends Organ Crime. 2017;20(3–4):296–315.
Hall A, Antonopoulos A. Fake meds online the internet and the transnational market in illicit pharmaceuticals. London: Palgrave Macmillan; 2016.
Tay Wee Teck J, McCann M. Tracking internet interest in anabolic-androgenic steroids using Google Trends. Int J Drug Policy. 2018;51:52–5.
Antonopoulos GA, Hall A. “Gain with no pain’’: anabolic-androgenic steroids trafficking in the UK.” Eur J Criminol. 2016;13(6):696–713.
Chatwin C, Measham F, O’Brien K, Sumnall H. New drugs, new directions? Research priorities for new psychoactive substances and human enhancement drugs. Int J Drug Policy. 2017;40:1–5.
McVeigh J, Salinas M, Ralphs R. A sentinel population: The public health benefits of monitoring enhanced body builders. Int J Drug Policy. 2020:102890. https://doi.org/10.1016/j.drugpo.2020.102890 .
Kotzé J, Richardson A, Antonopoulos GA. Looking ‘acceptably’ feminine: A single case study of a female bodybuilder’s use of steroids. Perform Enhanc Health. 2020;8:2–3.
Richardson A, Dixon K, Kean J. Superheroes—Image and performance enhancing drug (IPED) use within the UK, social media and gym culture. J Forensic Leg Med. 2019;64:28–30.
Richardson A, Antonopoulos GA. Anabolic-androgenic steroids (AAS) users on AAS use: Negative effects, “code of silence”, and implications for forensic and medical professionals. J Forensic Leg Med. 2019;68:101871.
Henning A, Andreasson J. "Yay, Another Lady Starting a Log!": Women's Fitness Doping and the Gendered Space of an Online Doping Forum. Commun Sport. 2019. https://doi.org/10.1177/2167479519896326 .
Harris MA, Dunn M, Alwyn T. Symptoms of muscle dysmorphia between users of anabolic androgenic steroids with varying usage and bodybuilding experience. Eur J Health Psychol. 2019;26(1):21–24.
UKAD. Image and performance enhancing drugs. London: UK Anti-Doping; 2019.
Chester N, McVeigh J. Drug use in society and the impact on the anti-doping movement. In: Mottram DR, Chester N, editors. Drugs in Sport. London: Routledge; 2018.
Whyte I, Pattinson E, Leyland S, Soos I, Ling J. Performance and image enhancing drugs use in active military personnel and veterans: A contemporary review. Transl Sports Med. 2020;4(1):72–87.
Boardley ID, Allen N, Simmons A, Laws H. Nutritional, medicinal, and performance enhancing supplementation in dance. Perform Enhanc Health. 2016;4(1–2):3–11.
Cranswick I, Richardson D, Littlewood M, Tod D. “Oh take some man-up pills”: A life-history study of muscles, masculinity, and the threat of injury. Perform Enhanc Health. 2020;8:2–3.
Kotze J, Antonopoulos GA. Boosting bodily capital: Maintaining masculinity, aesthetic pleasure and instrumental utility through the consumption of steroids. J Consumer Cult. 2019;21(3):683–700.
Corazza O, Simonato P, Demetrovics Z, Mooney R, van de Ven K, Roman-Urrestarazu A, et al. The emergence of Exercise Addiction, Body Dysmorphic Disorder, and other image-related psychopathological correlates in fitness settings: A cross sectional study. PLoS ONE. 2019;14(4):e0213060.
Boardley ID, Smith AL, Mills J, Grix J, Wynne C, Wilkins L. Development of moral disengagement and self-regulatory efficacy assessments relevant to doping in sport and exercise. Psychol Sport Exerc. 2018;36:57–70.
Bates G, Tod D, Leavey C, McVeigh J. An evidence-based socioecological framework to understand men’s use of anabolic androgenic steroids and inform interventions in this area. Drugs Educ Prev Policy. 2018;26(6):484–92.
Harris M, Dunn M, Alwyn T. Intrasexual competition as a potential influence on anabolic-androgenic steroid use initiation. J Health Psychol. 2017;24(9):1210–20.
Boardley ID, Smith AL, Mills JP, Grix J, Wynne C. Empathic and Self-Regulatory Processes Governing Doping Behavior. Front Psychol. 2017;8.
Smith D, Rutty MC, Olrich TW. Muscle dysmorphia and anabolic-androgenic steroid use. In: Hall M, Grogan S, editors. Chemically modified bodies. London: Palgrave Macmillan; 2016.
Joubert HE, Melluish S. Considering anabolic androgenic steroid use in relation to non-substance related diagnostic categories with special emphasis on eating disorders: a systematic review. J Subst Use. 2016;21(2):210–6.
Harris MA, Dunn M, Alwyn T. A qualitative exploration of the motivations underlying anabolic-androgenic steroid use from adolescence into adulthood. Health Psychol Rep. 2016;4(4):315–20.
Greenway CW, Price C. Muscle dysmorphia and self-esteem in former and current users of anabolic-androgenic steroids. Perform Enhanc Health. 2020;7:3–4.
Greenway CW, Price C. A qualitative study of the motivations for anabolic-androgenic steroid use: the role of muscle dysmorphia and self-esteem in long-term users. Perform Enhanc Health. 2018;6(1):12–20.
Coxon J. Hypogonadism persistence after long-term illicit use of anabolic-androgenic steroids. J Sex Med. 2016;13(5):S180-S.
Mossman JA, Pacey AA. The fertility fitness paradox of anabolic-androgenic steroid abuse in men. J Intern Med. 2019;286(2):231–2.
CAS PubMed Google Scholar
Hibbert MP, Brett CE, Porcellato LA, Hope VD. Image and performance enhancing drug use among men who have sex with men and women who have sex with women in the UK. Int J Drug Policy. 2020:102933. https://doi.org/10.1016/j.drugpo.2020.102933 .
Amaral JMX, Padilha MC, Chagas SV, Baker JS, Mullen C, Vieira Neto L, et al. Effective treatment and prevention of attempted suicide, anxiety, and aggressiveness with fluoxetine, despite proven use of androgenic anabolic steroids. Drug Test Anal. 2021;13(1):197–202.
Woodward C, Smith J, Acreman D, Kumar N. Hepatocellular carcinoma in body builders; an emerging rare but serious complication of androgenic anabolic steroid use. Ann Hepatobiliary Pancreat Surg. 2019;23:174–7.
Brennan R, Wells J, Van Hout MC. “Blood letting”-Self-phlebotomy in injecting anabolic-androgenic steroids within performance and image enhancing drug (PIED) culture. Int J Drug Policy. 2018;55:47–50.
Bates G, McVeigh J. Image and performance enhancing drugs 2015 survey results. Liverpool: Centre for Public Health: Liverpool John Moores University; 2016.
Gilmore H, Shannon S, Leavey G, Dempster M, Gallagher S, Breslin G. Help-seeking beliefs among anabolic androgenic steroid users experiencing side effects: an interpretive phenomenological analysis. J Clin Sport Psychol. 2020;14(4):359–75.
Hope V, Leavey G, Morgan G, Acreman D, Turmer D, Smith J. Facilitators and barriers to health care access amongst people using image and performance enhancing drugs in wales: findings & outcomes. Cardiff: Public Health Wales; 2020.
Mulrooney KJ, van de Ven K, McVeigh J, Collins R. Commentary: Steroid Madness- has the dark side of anabolic-androgenic steroids (AAS) been over-stated? Perform Enhanc Health. 2019;6(3–4):98–102.
McVeigh J. Engaging with people who use image and performance enhancing drugs: One size does not fit all. Int J Drug Policy. 2019;71:1–2.
Zahnow R, McVeigh J, Ferris J, Winstock A. Adverse effects, health service engagement, and service satisfaction among anabolic androgenic steroid users. Contemp Drug Probl. 2017;44(1):69–83.
Henning A, Andreasson J. Preventing, producing, or reducing harm? Fitness doping risk and enabling environments. Drugs Educ Prev Policy. 2020:1–10. https://doi.org/10.1080/09687637.2020.1865273 .
Hill SA, Waring WS. Pharmacological effects and safety monitoring of anabolic androgenic steroid use: differing perceptions between users and healthcare professionals. Ther Adv Drug Saf. 2019;10:2042098619855291.
Harvey O, Parrish M, van Teijlingen E, Trenoweth S. Support for non-prescribed anabolic androgenic steroids users: a qualitative exploration of their needs. Drug-Educ Prev Polic. 2020;27(5):377–86.
Harvey O, Parrish M. Social work implications of anabolic-androgenic steroid use, particularly among young people: a literature review. Practice. 2019;32(3):209–28.
Harvey O. ‘Shades of Grey’: the ethics of social work practice in relation to un-prescribed anabolic androgenic steroid use. Practice. 2018;31(4):239–58.
SDF Working Group on IPEDS. Image and Performance Enhancing Drugs (IPEDS) in Scotland. SDF; 2018.
Miller R. Building Bodies: Investigating Image and Performance Enhancing Drugs (IPEDs) Use in Scotland. Edinburgh: Scottish Government; 2017.
Iversen J, Hope VD, McVeigh J. Access to needle and syringe programs by people who inject image and performance enhancing drugs. Int J Drug Policy. 2016;31:199–200.
McVeigh J, Kimergard A, Bates G, Hope VD, Ncube F. Harm reduction interventions should encompass people who inject image and performance enhancing drugs. BMJ. 2016;353:i1889.
Bates G, Backhouse S. Preventing image and performance enhancing drug use: it’s not all chalk and talk. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Bates G, Begley E, Tod D, Jones L, Leavey C, McVeigh J. A systematic review investigating the behaviour change strategies in interventions to prevent misuse of anabolic steroids. J Health Psychol. 2019;24(11):1595–612.
Brennan R, Wells JSG, Van Hout MC. “Beauty through the eye of a needle”—an online study of the practices and beliefs of people who inject performance and image enhancing drugs (PIEDs). In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Mullen C, Whalley BJ, Schifano F, Baker JS. Anabolic androgenic steroid abuse in the United Kingdom: an update. Br J Pharmacol. 2020;177(10):2180–98.
Harvey O, Keen S, Parrish M, van Teijlingen E. Support for people who use Anabolic Androgenic Steroids: A Systematic Scoping Review into what they want and what they access. BMC Public Health. 2019;19(1):1024.
Glass R, Hope VD, Njoroge J, Edmundson C, Smith J, McVeigh J, et al. Secondary distribution of injecting equipment obtained from needle and syringe programmes by people injecting image and performance enhancing drugs: England and Wales, 2012–15. Drug Alcohol Depend. 2019;195:40–4.
Hope VD, McVeigh J, Begley E, Glass R, Edmundson C, Heinsbroek E, et al. Factors associated with hepatitis C and HIV testing uptake among men who inject image and performance enhancing drugs. Drug Alcohol Rev. 2020;40(4):586–96.
Brennan R, Wells JSG, Van Hout MC. The injecting use of image and performance-enhancing drugs (IPED) in the general population: a systematic review. Health Soc Care Community. 2017;25(5):1459–531.
Brennan R, Wells JSG, Van Hout MC. “Raw juicing” – an online study of the home manufacture of anabolic androgenic steroids (AAS) for injection in contemporary performance and image enhancement (PIED) culture. Perform Enhanc Health. 2018;6(1):21–7.
Edwards C, Tod D, Molnar G, Markland D. Predicting muscularity-related behavior, emotions, and cognitions in men: The role of psychological need thwarting, drive for muscularity, and mesomorphic internalization. Body Image. 2016;18:108–12.
Cranswick I. Beyond the muscles: exploring the meaning and role of muscularity in identity. Liverpool: Liverpool John Moores University; 2019.
Hope VD, McVeigh J, Smith J, Glass R, Njoroge J, Tanner C, et al. Low levels of hepatitis C diagnosis and testing uptake among people who inject image and performance enhancing drugs in England and Wales, 2012–15. Drug Alcohol Depend. 2017;179:83–6.
Bates G, Hope V, McVeigh J. HIV among people using anabolic steroids in the United Kingdom: an overview. HIV Nursing: Sharing best practice in HIV care. 2017;17(20-23).
Download references
Acknowledgements
The authors would like to thank the members of both the Study Steering Committee and the Public Expert Advisory Board for their advice and support throughout this project.
The research was funded by the NIHR, grant holder Professor Jim McVeigh under grant number NIHR132730. The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care.
Author information
Authors and affiliations.
Substance Use & Associated Behaviours, Department of Sociology, Manchester Metropolitan University, Manchester, UK
Jim McVeigh & Rob Ralphs
Public Health Institute, Liverpool John Moores University, Liverpool, UK
Evelyn Hearne & Vivian Hope
School of Sport, Exercise and Rehabilitation Sciences, University of Birmingham, Birmingham, UK
Ian Boardley
Institute for Policy Research, University of Bath, Bath, UK
Geoff Bates
Faculty of Health, Public Health Institute, Liverpool John Moores University, Liverpool, UK
Marie Claire Van Hout
You can also search for this author in PubMed Google Scholar
Contributions
All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jim McVeigh .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table 2.
. Charted Records of United Kingdom publications on anabolic androgenic steroids and associated IPED use (2016-2020).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
McVeigh, J., Hearne, E., Boardley, I. et al. Generating evidence on the use of Image and performance enhancing drugs in the UK: results from a scoping review and expert consultation by the Anabolic Steroid UK network. Harm Reduct J 18 , 107 (2021). https://doi.org/10.1186/s12954-021-00550-z
Download citation
Received : 01 July 2021
Accepted : 23 September 2021
Published : 17 October 2021
DOI : https://doi.org/10.1186/s12954-021-00550-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Image and performance enhancement drugs
- United Kingdom
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]

TOBIE SMITH, MD, MPH, Georgetown University Medical Center, Washington, District of Columbia
MATTHEW FEDORUK, PhD, AND AMY EICHNER, PhD, U.S. Anti-Doping Agency, Colorado Springs, Colorado
Am Fam Physician. 2021;103(4):203-204
Author disclosure: No relevant financial affiliations.
Family physicians may be surprised to learn the number of their patients who use performance-enhancing drugs, either deliberately to improve athletic performance or unknowingly through contaminated dietary supplements. Elite athletes account for only a small fraction of the approximately 3 million users of ergogenic drugs in the United States. 1 Sports organizations have broadened their efforts to detect and deter doping (i.e., the use of performance-enhancing drugs in competitive sports) at all levels of competition, resulting in a surprising number of positive doping test results in masters and recreational level athletes. 2 Recreational athletes who have been caught intentionally doping have reported many reasons for doing so, including keeping up with others in their age group in training and competition and for faster recovery from training and competitions so that they can continue to compete at a maximal level. 2 – 4
The prevalence of performance-enhancing drug use among athletes and the general public has led the World Health Organization to recognize the use of these drugs as a public health issue. 3 Over the past decade, the emergence of novel doping agents (particularly drugs aimed at boosting endogenous hormone levels and anabolic agents), increased acceptance of complementary and lifestyle medications, and increased contamination of dietary supplements have contributed to this growing public health concern.
The physical and psychological adverse effects of anabolic androgenic steroids (e.g., kidney and liver damage, acne, gynecomastia, suppression of normal testosterone production, aggression, depression) are well established. What physicians may not recognize are the potential adverse effects of novel, investigational drugs that are being used as doping agents. These include selective androgen receptor modulators (e.g., the investigational drugs ostarine [Enobosarm] and LGD-4033 [Ligandrol]), which have substantial anabolic effects on muscle and bone and significant potential for misuse in sports. These modulators are not approved for human use, and the adverse effects have not been well documented because they are still in clinical trials. Despite their experimental status, selective androgen receptor modulators have been found in dozens of dietary supplements and have caused more than 250 positive doping test results since 2010. 5 – 7 Growth hormone (GH) fragments (e.g., AOD-9604) and GH-releasing peptides, GH secretagogues (e.g., ibutamoren), metabolic modulators (e.g., meldonium), off-market drugs (e.g., sibutramine [Meridia]), and a handful of illegal designer stimulants (e.g., higenamine, 8 methylhexanamine, 9 octodrine 10 ) and other small molecules have also emerged on the doping stage. Consumers can easily buy all of these on the internet.
Even for the astute family physician, it can be difficult to identify patients who are using performance-enhancing drugs. Patients taking dietary supplements may be unintentionally ingesting performance-enhancing drugs because of contamination, and patients commonly do not disclose use of dietary supplements to their physicians. 11 Patients are less likely to disclose supplement use if the physician does not ask about it or if they believe that their physician is not knowledgeable about supplements. 11 Despite anti-doping agencies' warnings to elite athletes about supplement contamination risks, nonelite athletes are rarely educated about these risks.
Patients who are deliberately using performance-enhancing drugs may not disclose use because of shame, legality concerns, or lack of trust. In fact, users of performance-enhancing drugs often are not candid with their physicians about their use of these drugs. In one study, 56% of anabolic steroid users reported that they had never disclosed their use to their physician. 7 The adverse effects of many of the novel performance-enhancing drugs are not well documented or understood and thus may not trigger red flag findings on clinical history and physical examination that would alert a family physician to potential users of these drugs.
Patronage of wellness and antiaging clinics may also put recreational athletes at risk of inadvertent positive doping test results because treatments prescribed at these centers often include hormone replacement. Athletes can apply for a therapeutic use exemption for certain prescribed medications that are prohibited in competition (i.e., beta 2 agonists for asthma, glucocorticoids for inflammatory diseases, hormones for endocrine deficiencies); no exemptions are typically given for medications prescribed solely for symptom relief, antiaging purposes, or other purported health and wellness benefits (i.e., testosterone to treat “low” testosterone levels or nonspecific symptoms).
The family physician is a critical player in addressing the use of performance-enhancing drugs in recreational athletes of all ages. Family physicians should continue to be alert to signs of use of traditional performance-enhancing drugs, such as anabolic-androgenic steroids and stimulants, and also be aware of the emergence and accessibility of novel doping agents. In addition to the potential health risks of the performance-enhancing drug itself, harms of a positive doping test result can include the negative health and social impacts of sanctions prohibiting participation and the potential emotional damage related to being labeled a cheater.
Physicians should be aware of the competition status of athletic patients and consult the appropriate banned substances list (e.g., the World Anti-Doping Agency prohibited list) before prescribing medication and also understand the therapeutic use exemption process ( Table 1 ) . Family physicians should also be aware of the emergence of novel performance-enhancing drugs and their use among the general population; screen patients for use; and be prepared to discuss the safety, effectiveness, legality, and ethics of performance-enhancing drug use. 12
| Global Drug Reference Online | Database for the anti-doping status of medications |
| U.S. Anti-Doping Agency | |
| Therapeutic use exemption: frequently asked questions and application process | |
| Online educational module for health care professionals (CME credits available through Stanford University) | |
| Information on dietary supplements, including a list of dietary supplements at high risk of contamination | |
| Drug reference and email support for anti-doping and medication information | |
| World Anti-Doping Agency | Anti-doping e-learning platform, including a module for health care professionals |
Pope HG, Kanayama G, Athey A, et al. The lifetime prevalence of anabolic-androgenic steroid use and dependence in Americans: current best estimates. Am J Addict. 2014;23(4):371-377.
Henning AD, Dimeo P. The complexities of anti-doping violations: a case study of sanctioned cases in all performance levels of USA cycling. Perform Enhanc Health. 2014;3(3–4):159-166.
Dreier F. Wider testing reveals doping among amateur cyclists, too. July 27, 2012. Accessed November 2, 2020. https://www.nytimes.com/2012/07/28/sports/cycling/doping-in-cycling-reaches-into-amateur-ranks.html
Henning AD, Dimeo P. The new front in the war on doping: amateur athletes. Int J Drug Policy. 2018;51:128-136.
Van Wagoner RM, Eichner A, Bhasin S, et al. Chemical composition and labeling of substances marketed as selective androgen receptor modulators and sold via the internet [published correction appears in JAMA . 2018; 319(7):724]. JAMA. 2017;318(20):2004-2010.
U.S. Anti-Doping Agency. Supplement 411: realize, recognize, reduce. High-risk supplement list; 2019. Accessed April 24, 2020. https://www.supplement411.org
World Anti-Doping Agency. Anti-doping testing figures report. December 20, 2019. Accessed April 24, 2020. https://www.wada-ama.org/en/resources/laboratories/anti-doping-testing-figures-report
Cohen PA, Travis JC, Keizers PHJ, et al. The stimulant higenamine in weight loss and sports supplements. Clin Toxicol (Phila). 2019;57(2):125-130.
Eliason MJ, Eichner A, Cancio A, et al. Case reports: death of active duty soldiers following ingestion of dietary supplements containing 1,3-dimethylamylamine (DMAA). Mil Med. 2012;177(12):1455-1459.
Cohen PA, Travis JC, Keizers PHJ, et al. Four experimental stimulants found in sports and weight loss supplements: 2-amino-6-methylheptane (octodrine), 1,4-dimethylamylamine (1,4-DMAA), 1,3-dimethylamylamine (1,3-DMAA) and 1,3-dimethylbutylamine (1,3-DMBA). Clin Toxicol (Phila). 2018;56(6):421-426.
Guzman JR, Paterniti DA, Liu Y, et al. Factors related to disclosure and nondisclosure of dietary supplements in primary care, integrative medicine, and naturopathic medicine. J Fam Med Dis Prev. 2019;5(4) ):10.23937/2469-5793/1510109.
Jenkinson DM, Harbert AJ. Supplements and sports. Am Fam Physician. 2008;78(9):1039-1046. Accessed November 2, 2020. https://www.aafp.org/afp/2008/1101/p1039.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- About The Journalist’s Resource
- Follow us on Facebook
- Follow us on Twitter
- Criminal Justice
- Environment
- Politics & Government
- Race & Gender
Expert Commentary
Performance-enhancing drugs in athletics: Research roundup
2015 roundup of research on the use of performance-enhancing drugs in athletics and academics as well as their potential health effects.

Republish this article

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License .
by Leighton Walter Kille, The Journalist's Resource June 9, 2015
This <a target="_blank" href="https://journalistsresource.org/health/athletic-academic-performance-enhancing-drugs-research-roundup/">article</a> first appeared on <a target="_blank" href="https://journalistsresource.org">The Journalist's Resource</a> and is republished here under a Creative Commons license.<img src="https://journalistsresource.org/wp-content/uploads/2020/11/cropped-jr-favicon-150x150.png" style="width:1em;height:1em;margin-left:10px;">
Performance-enhancing drugs have a long history in sports, of course, but pharmacological research has led to a surge in the number of substances available, each with its own potential for misuse.
Given the potential financial rewards of athletic success, it’s no surprise that we’ve been witness to a seemingly endless procession of allegations and scandals. Sluggers Barry Bonds (steroids) and Alex Rodriguez (human growth hormone); cyclists Lance Armstrong (EPO), Floyd Landis (testosterone) and Alberto Contador (clenbuterol); runners Tyson Gay (steroids) and Justin Gatlin (testosterone); and golfer Vijay Singh (IGF-1) are only some of the more prominent professionals implicated in such behavior. The complicity of medical professionals and shadowy labs is often involved, and a 2015 report from the International Cycling Union (UCI) found the sport’s own governing body bore significant responsibility.
Not surprisingly, hard numbers on rates of usage are difficult to come by, but anecdotal evidence isn’t lacking and anonymous surveys have provided some insight. Questionable use of medications and supplements have also been reported in the U.S. armed forces , fire and police departments , amateur athletics , and even high schools .
Below is a selection of studies on a range of issues related to performance-enhancing drugs. It has sections on their potential economic impacts, prevalence , health effects and athletes’ attitudes . For additional studies on these topics, you can search PubMed , which is the federal clearinghouse for all medical research. At bottom, we have also included some studies relating to cognitive-enhancing drugs and the related academic dimensions of this issue.
—————————-
“The Economics of Corruption in Sports: The Special Case of Doping” Dimant, Eugen; Deutscher, Christian. Edmond J. Safra Working Papers, No. 55, January 2015.
Abstract: “Corruption in general and doping in particular are ubiquitous in both amateur and professional sports and have taken the character of a systemic threat. In creating unfair advantages, doping distorts the level playing field in sporting competition. With higher stakes involved, such distortions create negative externalities not only on the individual level (lasting health damages, for example) but also frictions on the aggregate level (such as loss of media interest) and erode the principle of sports. In this paper, we provide a comprehensive literature overview of the individual’s incentive to dope, the concomitant detrimental effects and respective countermeasures. In explaining the athlete’s motivation to use performance enhancing drugs, we enrich the discussion by adapting insights from behavioral economics. These insights help to understand such an athlete’s decision beyond a clear-cut rationale but rather as a product of the interaction with the underlying environment. We stress that in order to ensure clean sports and fair competition, more sophisticated measurement methods have to be formulated, and the respective data made publicly available in order to facilitate more extensive studies in the future. So far, the lack of data is alarming, especially in the area of elite sports where the stakes are high and doping has a substantial influence.”
“The Frequency of Doping in Elite Sport: Results of a Replication Study” Pitsch, Werner; Emrich, Eike. International Review for the Sociology of Sport , October 2012, Vol. 47, No. 5, 559-580. doi: 10.1177/1012690211413969.
Abstract: “The difficulty of measuring the prevalence of doping in elite sport is a recurring topic in the scientific literature on doping. The Randomized Response Technique is a method for asking such embarrassing or even threatening questions while allowing the respondents to answer honestly. It was used to measure the prevalence of doping among German squad athletes by Pitsch et al. (2005, 2007). In a replication study with better sampling control, it was possible to replicate the general trend of the data from the 2005 study…. The paper-based survey resulted in a rate of 10.2% ‘honest dopers,’ irrespective of the disciplines, obtained with the question: ‘Have you ever knowingly used illicit drugs or methods in order to enhance your performance?’ By adding the rate of cheaters (24.7%), whose behaviour the researchers know nothing about, one can calculate the interval (10.2%, 34.9%), which should include the true rate of dopers throughout their career among German elite athletes. In contrast, this means that the larger proportion of athletes, namely, 65.2%, represents ‘honest non-dopers.’ In the 2008 season, this figure was 65%.”
“Growth Hormone Doping in Sports: A Critical Review of Use and Detection Strategies” Baumann, Gerhard P. Endocrine Reviews , April 2012, Vol. 33, No. 2 155-186. doi: 10.1210/er.2011-1035.
Abstract: “[Growth hormone] is believed to be widely employed in sports as a performance-enhancing substance. Its use in athletic competition is banned by the World Anti-Doping Agency, and athletes are required to submit to testing for GH exposure…. The scientific evidence for the [performance-enhancing characteristics] of GH is weak, a fact that is not widely appreciated in athletic circles or by the general public. Also insufficiently appreciated is the risk of serious health consequences associated with high-dose, prolonged GH use. This review discusses the GH biology relevant to GH doping; the virtues and limitations of detection tests in blood, urine, and saliva; secretagogue efficacy; IGF-I doping; and information about the effectiveness of GH as a performance-enhancing agent.”
“Supplements in Top-Level Track and Field Athletes” Tscholl, Philippe; Alonso, Juan M.; Dollé, Gabriel; Junge, Astrid; Dvorak, Jiri. American Journal of Sports Medicine , January 2010, Vol. 38, No. 1, 133-140. doi: 10.1177/0363546509344071.
Abstract: “Analysis of 3,887 doping control forms undertaken during 12 International Association of Athletics Federations World Championships and one out-of-competitions season in track and field. Results: There were 6,523 nutritional supplements (1.7 per athlete) and 3,237 medications (0.8 per athlete) reported. Nonsteroidal anti-inflammatory drugs (NSAIDs; 0.27 per athlete, n = 884), respiratory drugs (0.21 per athlete, n = 682), and alternative analgesics (0.13, n = 423) were used most frequently. Medication use increased with age (0.33 to 0.87 per athlete) and decreased with increasing duration of the event (from sprints to endurance events; 1.0 to 0.63 per athlete). African and Asian track and field athletes reported using significantly fewer supplements (0.85 vs. 1.93 per athlete) and medications (0.41 vs. 0.96 per athlete) than athletes from other continents. The final ranking in the championships was unrelated to the quantity of reported medications or supplements taken. Compared with middle-distance and long-distance runners, athletes in power and sprint disciplines reported using more NSAIDs, creatine, and amino acids, and fewer antimicrobial agents. Conclusion: The use of NSAIDs in track and field is less than that reported for team-sport events. However, nutritional supplements are used more than twice as often as they are in soccer and other multisport events; this inadvertently increases the risk of positive results of doping tests.”
“Alcohol, Tobacco, Illicit Drugs and Performance Enhancers: A Comparison of Use by College Student Athletes and Nonathletes” Yusko, David A.; et al. American Journal of Sports Medicine, August 2010. doi: 10.3200/JACH.57.3.281-290.
Abstract: Compares the prevalence and pattern of substance use in undergraduate student athletes and nonathletes from 2005-2006. Data was collected using questionnaires from male (n = 418) and female (n = 475) student athletes and nonathletes from 2005-2006 to assess prevalence, quantity, and frequency of alcohol and drug use, and to determine patterns of student athletes’ alcohol and drug use during their athletic season versus out of season. Male student athletes were found to be at high risk for heavy drinking and performance-enhancing drug use. Considerable in-season versus out-of-season substance use fluctuations were identified in male and female student athletes. Additional, and possibly alternative, factors are involved in a student athlete’s decision-making process regarding drug and alcohol use, which suggests that the development of prevention programs that are specifically designed to meet the unique needs of the college student athlete may be beneficial.”
Health effects
“Performance Enhancing Drug Abuse and Cardiovascular Risk in Athletes” Angell, Peter J.; Chester, Neil; Sculthorpe, Nick; Whyte, Greg; George, Keith; Somauroo, John. British Journal of Sports Medicine , July 2012. doi:10.1136/bjsports-2012-091186.
Abstract: “Despite continuing methodological developments to detect drug use and associated punishments for positive dope tests, there are still many athletes who choose to use performance- and image-enhancing drugs. Of primary concern to this review are the health consequences of drug use by athletes…. We will address current knowledge, controversies and emerging evidence in relation to cardiovascular (CV) health of athletes taking drugs. Further, we delimit our discussion to the CV consequences of anabolic steroids and stimulant (including amphetamines and cocaine) use. These drugs are reported in the majority of adverse findings in athlete drug screenings and thus are more likely to be relevant to the healthcare professionals responsible for the well-being of athletes.”
“Illicit Anabolic-Androgenic Steroid Use” Kanayama, Gen; Hudson, James I.; Pope Jr., Harrison G. Hormones and Behavior , Volume 58, Issue 1, June 2010, Pages 111-121. doi: 10.1016/j.yhbeh.2009.09.006.
Abstract: “The anabolic-androgenic steroids (AAS) are a family of hormones that includes testosterone and its derivatives. These substances have been used by elite athletes since the 1950s, but they did not become widespread drugs of abuse in the general population until the 1980s. Thus, knowledge of the medical and behavioral effects of illicit AAS use is still evolving. Surveys suggest that many millions of boys and men, primarily in Western countries, have abused AAS to enhance athletic performance or personal appearance. AAS use among girls and women is much less common. Taken in supraphysiologic doses, AAS show various long-term adverse medical effects, especially cardiovascular toxicity. Behavioral effects of AAS include hypomanic or manic symptoms, sometimes accompanied by aggression or violence, which usually occur while taking AAS, and depressive symptoms occurring during AAS withdrawal. However, these symptoms are idiosyncratic and afflict only a minority of illicit users; the mechanism of these idiosyncratic responses remains unclear. AAS users may also ingest a range of other illicit drugs, including both “body image” drugs to enhance physical appearance or performance, and classical drugs of abuse. In particular, AAS users appear particularly prone to opioid use. There may well be a biological basis for this association, since both human and animal data suggest that AAS and opioids may share similar brain mechanisms. Finally, AAS may cause a dependence syndrome in a substantial minority of users. AAS dependence may pose a growing public health problem in future years but remains little studied.”
“Adverse Health Effects of Anabolic-Androgenic Steroids” Van Amsterdama, Jan; Opperhuizena, Antoon; Hartgensb, Fred. Regulatory Toxicology and Pharmacology , Volume 57, Issue 1, June 2010, Pages 117-123. doi: 10.1016/j.yrtph.2010.02.001.
Abstract: “Anabolic-androgenic steroids (AAS) are synthetic drugs derived from testosterone. Illegally, these drugs are regularly self-administered by body builders and power lifters to enhance their sportive performance. Adverse side effects of AAS include sexual dysfunction, alterations of the cardiovascular system, psyche and behavior, and liver toxicity. However, severe side effects appear only following prolonged use of AAS at high dose and their occurrence is limited…. The overwhelming stereotype about AAS is that these compounds cause aggressive behavior in males. However, the underlying personality traits of a specific subgroup of the AAS abusers, who show aggression and hostility, may be relevant, as well. Use of AAS in combination with alcohol largely increases the risk of violence and aggression. The dependence liability of AAS is very low, and withdrawal effects are relatively mild. Based on the scores for acute and chronic adverse health effects, the prevalence of use, social harm and criminality, AAS were ranked among 19 illicit drugs as a group of drugs with a relatively low harm.”
“Effects of Growth Hormone Therapy on Exercise Performance in Men” Triay, Jessica M.; Ahmad, Bushra N. Trends in Urology & Men’s Health , July/August 2012, Vol. 3, Issue 4, 23-26. doi: 10.1002/tre.274.
Conclusions: “In the athletic arena, [growth hormone] doping is considered to be widespread and used in combination with other agents, and regimens vary depending on individual preferences and cost implications…. It must be recognised that the effects of GH administration in adults with a normal GH/IGF-1 axis are not comparable to those in GH deficiency and that the complexity of processes influencing GH release and peripheral actions means that overall performance should be considered as opposed to isolated effects. Although studies to date have been small in both subject numbers and treatment times, they have demonstrated measurable changes in GH and IGF-1 levels, as well as possible deleterious effects on exercise performance that should be taken seriously.”
“Performance-Enhancing Drugs on the Web: A Growing Public-Health Issue” Brennan, Brian P.; Kanayama, Gen; Pope Jr., Harrison G. American Journal on Addictions , March-April 2013, Vol. 22, Issue 2, 158-161. doi: 10.1111/j.1521-0391.2013.00311.x.
Abstract: “Today’s Internet provides extensive “underground” guidelines for obtaining and using illicit substances, including especially anabolic-androgenic steroids (AAS) and other appearance- and performance-enhancing drugs (APEDs). We attempted to qualitatively characterize APED-related Internet sites. We used relevant Internet search terms [and] found thousands of sites involving AAS and other APEDs. Most sites presented an unabashedly pro-drug position, often openly questioning the qualifications and motivations of mainstream medical practitioners. Offers of AAS and other APEDs for sale, together with medical advice of varying legitimacy, was widespread across sites. Importantly, many sites provided detailed guidelines for exotic forms of APED use, some likely associated with serious health risks, which are probably unknown to most practicing clinicians.”
“Doping in Sport: A Review of Elite Athletes’ Attitudes, Beliefs and Knowledge” Morente-Sánchez, Jaime; Zabala, Mikel. Sports Medicine , March 2013. doi: 10.1007/s40279-013-0037-x.
Abstract: “Although most athletes acknowledge that doping is cheating, unhealthy and risky because of sanctions, its effectiveness is also widely recognized. There is a general belief about the inefficacy of anti-doping programmes, and athletes criticise the way tests are carried out. Most athletes consider the severity of punishment is appropriate or not severe enough. There are some differences between sports, as team-based sports and sports requiring motor skills could be less influenced by doping practices than individual self-paced sports. However, anti-doping controls are less exhaustive in team sports. The use of banned substance also differs according to the demand of the specific sport. Coaches appear to be the main influence and source of information for athletes, whereas doctors and other specialists do not seem to act as principal advisors. Athletes are becoming increasingly familiar with anti-doping rules, but there is still a lack of knowledge that should be remedied using appropriate educational programmes. There is also a lack of information on dietary supplements and the side effects of [performance-enhancing substances].”
“Age and Gender Specific Variations in Attitudes to Performance Enhancing Drugs and Methods” Singhammer, John. Sport Science Review , December 2012. doi: 10.2478/v10237-012-0017-3.
Abstract: “Using a population-based cross-sectional sample of 1,703 Danish men and women aged 15-60 years, the present study examined age and gender variation in attitudes to performance enhancing drugs and methods…. Overall, participants held negative attitudes to drugs and methods enhancing predominantly cognitive-abilities-enhancing performance drugs and to appearance-modifying methods, but were positive to drugs for restoring physical functioning conditions. However, attitudes varied nonlinearly across age. Lenient attitudes peaked at around age 25 and subsequently decreased. Lenient attitudes to use of drugs against common disorders decreased in a linear fashion. No gender differences were observed and attitude did not vary with level of education, self-reported health or weekly hours of physical activity.”
“Drugs, Sweat and Gears: An Organizational Analysis of Performance Enhancing Drug Use in the 2010 Tour De France” Palmer, Donald; Yenkey, Christopher. University of California, Davis; University of Chicago. March 2013.
Abstract: “This paper seeks a more comprehensive explanation of wrongdoing in organizations by theorizing two under-explored causes: the criticality of a person’s role in their organization’s strategy-based structure, and social ties to known deviants within their organization and industry. We investigate how these factors might have influenced wrongdoing in the context of professional cyclists’ use of banned performance enhancing drugs (PEDs) in advance of the 2010 Tour de France….. We find substantial support for our prediction that actors who are more critical to the organization’s strategy-based structure are more likely to engage in wrongdoing. Further, we find that while undifferentiated social ties to known wrongdoers did not increase the likelihood of wrongdoing, ties to unpunished offenders increased the probability of wrongdoing and ties to severely punished offenders decreased it. These effects were robust to consideration of other known causes of wrongdoing: weak governance regimes and permissive cultural contexts, performance strain, and individual propensities to engage in wrongdoing.”
“Elite Athletes’ Estimates of the Prevalence of Illicit Drug Use: Evidence for the False Consensus Effect” Dunn, Matthew; Thomas, Johanna O.; Swift, Wendy; Burns, Lucinda. Drug and Alcohol Review , January 2012, Vol. 31, Issue 1, 27-32. doi: 10.1111/j.1465-3362.2011.00307.x.
Abstract: “The false consensus effect (FCE) is the tendency for people to assume that others share their attitudes and behaviours to a greater extent than they actually do…. The FCE was investigated among 974 elite Australian athletes who were classified according to their drug use history. Participants tended to report that there was a higher prevalence of drug use among athletes in general compared with athletes in their sport, and these estimates appeared to be influenced by participants’ drug-use history. While overestimation of drug use by participants was not common, this overestimation also appeared to be influenced by athletes’ drug use history.”
“The Role of Sports Physicians in Doping: A Note on Incentives” Korn, Evelyn; Robeck, Volker. Philipps-Universitat, Marburg, March 2013.
Abstract: “How to ban the fraudulent use of performance-enhancing drugs is an issue in all professional — and increasingly in amateur — sports. The main effort in enforcing a ‘clean sport’ has concentrated on proving an abuse of performance-enhancing drugs and on imposing sanctions on teams and athletes. An investigation started by Freiburg university hospital against two of its employees who had been working as physicians for a professional cycling team has drawn attention to another group of actors: physicians. It reveals a multi-layered contractual relations between sports teams, physicians, hospitals, and sports associations that provided string incentives for the two doctors to support the use performance-enhancing drugs. This paper argues that these misled incentives are not singular but a structural part of modern sports caused by cross effects between the labor market for sports medicine specialists (especially if they are researchers) and for professional athletes.”
“Socio-economic Determinants of Adolescent Use of Performance Enhancing Drugs” Humphreys, Brad R.; Ruseski, Jane E. Journal of Socio-Economics , April 2011, Vol. 40, Issue 2, 208-216. doi: 10.1016/j.socec.2011.01.008.
Abstract: “Evidence indicates that adolescents (athletes and non-athletes use performance enhancing drugs. We posit that adolescent athletes have different socio-economic incentives to use steroids than non-athletes. We examine adolescent steroid use using data from the Youth Risk Behavior Surveillance System. Multi-sport upperclassmen and black males have a higher probability of steroid use. Steroid use is associated with motivations to change physical appearance and experimentation with illicit substances. These results suggest there are different socio-economic motivations for adolescent steroid use and that steroid use is an important component of overall adolescent drug use.”
Cognitive-enhancing drugs
“Randomized Response Estimates for the 12-Month Prevalence of Cognitive-Enhancing Drug Use in University Students” Dietz, Pavel; et al. Pharmacotherapy , January 2013, Vol. 33, Issue 1, 44-50. doi: 10.1002/phar.1166.
Results: “An anonymous, specialized questionnaire that used the randomized response technique was distributed to students at the beginning of classes and was collected afterward. From the responses, we calculated the prevalence of students taking drugs only to improve their cognitive performance and not to treat underlying mental disorders such as attention-deficit-hyperactivity disorder, depression, and sleep disorders. The estimated 12-month prevalence of using cognitive-enhancing drugs was 20%. Prevalence varied by sex (male 23.7%, female 17.0%), field of study (highest in students studying sports-related fields, 25.4%), and semester (first semester 24.3%, beyond first semester 16.7%).”
“The Diversion and Misuse of Pharmaceutical Stimulants: What Do We Know and Why Should We Care?” Kaye, Sharlene; Darke, Shane. Addiction , February 2012, Vol. 107, Issue 3, 467-477. doi: 10.1111/j.1360-0443.2011.03720.x.
Results: “The evidence to date suggests that the prevalence of diversion and misuse of pharmaceutical stimulants varies across adolescent and young adult student populations, but is higher than that among the general population, with the highest prevalence found among adults with attention deficit-hyperactive disorder (ADHD) and users of other illicit drugs. Concerns that these practices have become more prevalent as a result of increased prescribing are not supported by large-scale population surveys…. Despite recognition of the abuse liability of these medications, there is a paucity of data on the prevalence, patterns and harms of diversion and misuse among populations where problematic use and abuse may be most likely to occur (e.g. adolescents, young adults, illicit drug users). Comprehensive investigations of diversion and misuse among these populations should be a major research priority, as should the assessment of abuse and dependence criteria among those identified as regular users.”
“Adderall Abuse on College Campuses: A Comprehensive Literature Review” Varga, Matthew D. Journal of Evidence-Based Social Work , 2012, Vol. 9, Issue 3. doi: 10.1080/15433714.2010.525402.
Abstract: “Prescription stimulant abuse has dramatically increased over the past 10 years, but the amount of research regarding college students and illicit prescription stimulant use is still very limited. This has important implications for college mental health professionals and higher education administrators. In this comprehensive literature review the author explores factors contributing to illicit use, self-medication, and recreational use of controlled prescription stimulants; discusses the potential consequences for those students abusing stimulants; and provides recommendations for educating, combating, and assisting students who illicitly use prescription stimulants on college campuses.”
“A Comparison of Attitudes Toward Cognitive Enhancement and Legalized Doping in Sport in a Community Sample of Australian Adults” Partridge, Brad; Lucke, Jayne; Hall, Wayne. AJOB Primary Research , November 2012. doi: 10.1080/21507716.2012.720639.
Abstract: “This article compares public attitudes toward the use of prescription drugs for cognitive enhancement with the use of performance enhancing drugs in sport. We explore attitudes toward the acceptability of both practices; the extent to which familiarity with cognitive enhancement is related to its perceived acceptability; and relationships between the acceptability of cognitive enhancement and legalized doping in sport. Of 1,265 [survey] participants, 7% agreed that cognitive enhancement is acceptable; 2.4% of the total sample said they had taken prescription drugs to enhance their concentration or alertness in the absence of a diagnosed disorder, and a further 8% said they knew someone who had done so. These participants were twice as likely to think cognitive enhancement was acceptable. Only 3.6% of participants agreed that people who play professional sport should be allowed to use performance-enhancing drugs if they wanted to. Participants who found cognitive enhancement acceptable were 9.5 times more likely to agree with legalized doping.”
Keywords: drugs, youth, sports, cheating, higher education, corruption, ADHD, research roundup
About The Author
Leighton Walter Kille
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- New editors
- BMJ Journals
You are here
- Volume 46, Issue Suppl 1
- Performance enhancing drug abuse and cardiovascular risk in athletes: implications for the clinician
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Peter J Angell 1 ,
- Neil Chester 1 ,
- Nick Sculthorpe 2 ,
- Greg Whyte 1 ,
- Keith George 1 ,
- John Somauroo 1 , 3
- 1 Research Institute for Sport and Exercise Sciences, Liverpool John Moores University, Liverpool, UK
- 2 School of Sport and Exercise Science, University of Bedfordshire, Bedford, UK
- 3 Cardiorespiratory and Vascular Department, Countess of Chester NHS Foundation Trust Hospital, Countess of Chester Health Park, Chester, Cheshire, UK
- Correspondence to Dr Peter J Angell, Research Institute for Sport and Exercise Sciences, Liverpool John Moores University, Tom Reilly Building, Byrom Street Campus, Liverpool L3 3AF, UK; P.Angell{at}2004.ljmu.ac.uk
The use of performance-enhancing and social drugs by athletes raises a number of ethical and health concerns. The World Anti-Doping Agency was constituted to address both of these issues as well as publishing a list of, and testing for, banned substances in athletes. Despite continuing methodological developments to detect drug use and associated punishments for positive dope tests, there are still many athletes who choose to use performance and image enhancing drugs. Of primary concern to this review are the health consequences of drug use by athletes. For such a large topic we must put in place delimitations. Specifically, we will address current knowledge, controversies and emerging evidence in relation to cardiovascular (CV) health of athletes taking drugs. Further, we delimit our discussion to the CV consequences of anabolic steroids and stimulant (including amphetamines and cocaine) use. These drugs are reported in the majority of adverse findings in athlete drug screenings and thus are more likely to be relevant to the healthcare professionals responsible for the well-being of athletes. In detailing CV health issues related to anabolic steroid and stimulant abuse by athletes we critique current research evidence, present exemplar case studies and suggest important avenues for on-going research. Specifically we prompt the need for awareness of clinical staff when assessing the potential CV consequences of drug use in athletes.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-commercial License, which permits use, distribution, and reproduction in any medium, provided the original work is properly cited, the use is non commercial and is otherwise in compliance with the license. See: http://creativecommons.org/licenses/by-nc/3.0/ and http://creativecommons.org/licenses/by-nc/3.0/legalcode
https://doi.org/10.1136/bjsports-2012-091186

Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
In a bid to improve performance and/or aid recovery, various pharmaceutical products have been used, both openly (legally) and in a clandestine manner against the rules of governing bodies, by a broad array of athletes. 1 The World Anti-Doping Agency (WADA) strictly regulates the use of pharmaceutical products in competitive sport. WADA produced and regularly updates the World Anti-Doping Code that includes a prohibited drug list. This list dictates what is and is not acceptable, from a doping perspective, within sport ( table 1 ). The list has various subsections with some drugs banned both ‘in’ and ‘out’ of competition, while others are banned ‘in’ competition only (eg, ephedrine and the cannabinoids). The WADA list of prohibited substances is further broken down into several subcategories of specific products, including anabolic agents, peptide hormones and growth factors; β-2 agonists; hormone and metabolic modulators; diuretics and masking agents; stimulants; narcotics; cannabinoids; and glucocortocosteroids ( table 1 ). Despite strict rules and punishments being in place in an attempt to limit doping offences, there continues to be those who choose to try and gain an unfair advantage in sport by taking drugs. 3
- View inline
WADA prohibited substance list (Adapted from WADA 2012 Prohibited List 2 )
As well as the concerns of WADA in defending the spirit of free and fair competition, awareness is also raised when there are known health consequences of drug abuse. The negative health consequences of doping for athletes and the education of support staff are the focus of this narrative review. Clearly, doping and athlete health is a vast area and so two points of delimitation are made up-front. First, we concentrate on cardiovascular (CV) health consequences of drug use. Second, this review focuses on anabolic agents and stimulants. According to WADA's adverse analytical findings report from 2010, anabolic agents accounted for around 60% of adverse findings, with stimulants contributing around 10%. 4 Consequently, the clinical support teams working with athletes must understand the potential CV health consequences when athletes abuse these drugs. Finally, we will discuss the CV effects of cocaine use, as it is one of the most widely used recreational drugs detected in athletes. 4 As well as reflecting on previous data related to the CV health consequences of anabolic steroid, stimulant and cocaine use we have attempted to provide extra context and information in the form of brief case-study exemplars on anabolic steroid and cocaine abuse.
Anabolic agents
There are a number of drugs that are used in an attempt to increase lean muscle mass. Of these, the most well known is the steroid hormone testosterone (T) and the various analogues that are based around testosterone, usually referred to as androgenic anabolic steroids (AS). In addition to AS there are non-steroid agents that are used in an attempt to generate the same anabolic effects. These include the β-2 agonist, clenbuterol (which is additionally used as an anorectic agent to reduce body fat), human growth hormone (HGH) and insulin/insulin-like growth factors. Other growth factors are commonly used in between courses of anabolic agent use and these include human chorionic gonadotropin (HCG) and erythropoietin (EPO) and more recently selective androgen receptor modulators. Whatever the classification, the purpose of anabolic and growth factors is to stimulate skeletal muscle growth and promote rapid recovery following intensive training. From a clinical perspective it is also worth noting that EPO is predominantly used to boost endurance exercise performance and in general has not crossed over to amateur and recreational sports performers. AS, HGH, HCG and insulin/insulin-like growth factors, however, are routinely used by professional, amateur and recreational athletes. 5 Consequently, the likelihood of clinicians coming across users of these particular drugs is much greater.
It is worthy to note that the classification of AS covers a number of structural variants. Classically, AS are classified as water-soluble orally active forms (17-α-alkylated) and lipid-soluble parenteral forms (17-β-esterified). In addition, they are often also classified as either testosterone-based, dihydrotestosterone-based (DHT) or 19-nortestosterone-based (Nandrolone) all of which have differing properties and expected side effects. The situation is further complicated by belief among users, often stemming from anecdotal advice, that some AS are better for predominantly ‘bulking’ (eg. Deca-Durabolin) while others are better suited to losing body fat or ‘cutting’ (eg. Winstrol). Users will often use these different forms of AS in varying quantities. The use of AS is also characterised by periods of use followed by periods of abstinence, or ‘cycles’. This helps to maximise the effects of the drugs while also limiting the negative consequences and allowing the body to normalise following an ‘on’ cycle. Furthermore, users will often supplement their cycles with additional pharmaceutical agents both when bulking (eg, Insulin, human growth hormone) and when losing body fat (clenbuterol, cytomel, 2,4, dinitrophenol). Finally, there are a surprising number of drugs used to attempt to limit side effects of AS use or normalise the hypothalamo-pituitary-gonadal (HPG) axis following an AS cycle. These include estrogen receptor antagonists (tamoxifen), selective estrogen receptor inhibitors (clomifene), aromatase inhibitors (arimidex), 5-α reductase inhibitors (finesteride) and HPG axis stimulators such as HCG.
Evidence of athlete use of AS has been available since the 1950s with AS contributing to c. 60% of adverse findings according to recent WADA reports. 6 In the general population there are data showing an increase in the prevalence of AS use. 7 Despite such widespread use there is still some controversy as to the CV health consequences of taking AS. 8 Large sample epidemiological evidence of the CV health consequences of long-term AS use is lacking, likely because of the reluctance to admit use and/or possession. In addition, evidence for a link between AS use and CV disease outcomes or end-points is mostly limited to case study reports. Published case studies include AS use associated with myocardial infarction, 9 stroke, 10 embolism 11 and other CV health issues ( table 2 ). Although caution should be expressed in implying cause and effect from case studies, 8 they can provide direction for case series and experimental studies as well as informing/educating clinical practitioners.
Cardiovascular events and risk factors from AS use
Significant research attention has focused on the impact of AS use on CV disease risk factors namely blood pressure, lipid profile, left ventricular (LV) mass, cardiac function and arterial function. Elevated systemic arterial blood pressure is associated with an increased CV disease risk. Compared to healthy controls, AS users have increased resting 22 , 26 and exercise 22 systolic blood pressure. Conversely, other studies have not observed increased blood pressure in AS user. 6 , 24 Differences in the training level of the participants along with age could be responsible for the differences seen in these studies.
AS have also been associated with negative alterations in lipid profiles. 27 Changes reported include a decrease in high-density lipoprotein (HDL), 28 an elevation in low-density lipoprotein (LDL) 24 and reduced apolipoprotein levels, 29 possibly through up-regulation of hepatic triglyceride lipase. 30 The changes in lipid profiles indicate an increase in atherosclerotic risk. Increases in homocysteine, a naturally occurring amino-acid thought to have a role in vaso-control, and C-reactive proteins (CRP), an acute-phase protein that rises in response to inflammation, have been implicated as risk factors for CV disease. Grace and Davies 25 demonstrated a significant increase in CRP in AS users. While Zmuda et al 31 observed no significant increases in homocysteine in a group of AS users, Graham et al 32 noted a significant elevation in homocysteine in AS users as well as those who had abstained from AS use for 3 months, indicating a possible effect of AS on vitamin B absorption. Previous studies have also suggested a possible link between AS use and thrombotic risk through alterations in haemoglobin levels. 33
An increase in LV mass is an independent risk factor for CV disease. 34 AS use has been associated with an increase in LV mass, 35 , 36 but there is conflicting data. 27 , 37 , 38 There are some data in AS users that suggest a reduction in systolic cardiac function 38 although this is not a consistent finding between studies. 8 A reduction in diastolic function has been observed more frequently and it has been suggested that a reduction in myocardial relaxation/elastance is associated with AS use. 27 , 37 , 38 AS use has also been associated with reduced endothelial function in conduit arteries. 6 , 24 , 39 Ebenbichler et al 40 and Sader et al 6 noted a reduced flow-mediated dilation in AS users as well as a reduced vasodilator response to glyceryl-trinitrate.
There is a growing evidence base that AS use can have a negative effect on multiple CV disease risk factors. We present a case study exemplar to illustrate the broad effect of AS use on the CV system.
Case study 1
A 25-year-old bodybuilder who was enrolled into a research study gave a detailed history of prolonged AS use. He self-reported no cardiac health problems. The participant was 1.93 m and 127 kg with an LV mass of 218 g on cardiac MRI. While absolute LV mass was high this was normalised when indexed for fat free mass. Left ventricular (LV) ejection fraction was normal (63%), while right ventricular (RV) ejection fraction was slightly reduced at 49%. LV diastolic function, measured using ultrasound echocardiography, was moderately depressed (significant increases in late atrial filling and tissue velocities). Heart rate was 75 beats per min and the ECG was unremarkable. Blood pressure was 131/71 mm/Hg. Total cholesterol was within normal clinical limits (4.6 mmol/l), but high-density lipoproteins were significantly reduced in the participant at 0.46 mmol/l. Low-density lipoproteins were above clinically acceptable levels at 3.77 mmol/l. The participant had an elevated level of alanine transaminase indicative of reduction in liver function. In addition, both testosterone and sex-hormone binding globulin were well below those expected within a male, at 2.13 and 6 nmol/l, respectively. Gamma glutamyltransferase was not assessed. Based on changes to numerous CV risk factors, this athlete was informed of the test outcomes and was directed to seek a general practitioner consultation.
While recent data have started to paint a clearer picture of some of the negative CV consequences of AS use, longitudinal data are still lacking making the long-term chronic effects of AS use difficult to ascertain. 8 There is also uncertainty in relation to the impact of withdrawal of AS use on CV risk factors. Inherently, the study of AS use is complicated by many factors. Specifically, most studies recruit diverse cohorts of self-selected AS users. In these groups there is likely great heterogeneity in total AS dose, poly-drug regimens employed as well the difficulty in verifying the ‘true’ dosages used. 8
There is little direction given to clinicians and health practitioners regarding the identification of clandestine AS use. One of the reasons for athletes engaging in illicit AS use is that there are few ‘tell tale’ signs particularly in those sports where elevated strength and/or fat free mass is relatively commonplace. AS use occurs predominantly but not exclusively in strength and/or power athletes. Of the nine adverse findings for AS by the UK Anti-Doping Agency, three were from professional rugby players. 41 It is worth noting that clinicians are far more likely to encounter recreational athletes using AS, training for predominantly aesthetic purposes. AS users may have rapid increases in lean mass, excessive hypertrophy of the trapezius, the shoulder musculature 42 and a large neck circumference 43 possibly due to higher androgen receptor levels. 41 Other signs of AS use include puffy swelling around the face 42 and acne which occurs in approximately 50% of users (including acne fulminans and acne conglobata). 44 Consequently, clinicians may be suspicious of AS use in muscular individuals with acne (and/or scarring from previous eruptions) extending beyond the face to the back, chest and upper arms. 44 . Another common side effect of AS use is the development of female breast tissue (gynaecomastia) because of the aromotisation of AS to estrogen. The size and rate of development will vary depending on the type and duration of AS exposure with cases ranging from small areas of puffy tissue behind the nipple to easily recognisable breast tissue. It must be stressed however that these are general signs that may indicate AS use, but clinicians should be wary of unfairly targeting individuals who are simply prone to acne, or have a genetic basis for a muscular shoulder girdle.
Stimulants—amphetamines
Stimulants consist of psychoactive drugs, including amphetamines and its derivatives, as well as cocaine, caffeine and nicotine and are used to increase psychological activity, thereby inducing improvements in mental aptitude, physical function or both. Stimulants used for performance enhancement are typically those that affect the central nervous system (CNS); however, concurrent effects on the CV system are common. Amphetamines affect the CNS and autonomic nervous systems causing tachycardia and vasoconstriction as well as having psychological effects, increasing mental alertness and decreased fatigue. Cocaine has similar affects to amphetamines and also exerts its effect through the CNS causing an increase in the release of catecholamines, such as norepinephrine, as well as causing an increase of circulating dopamine. Ephedrine and its isomers are sympathomimetic agonists at both α- and β-adrenergic receptors and also have potent CV effects including increasing heart rate and blood pressure through vasoconstriction. The CV effects of stimulants have been shown to have a detrimental effect on CV health. 45
There have been numerous reported cases of serious adverse CV events, including fatalities, linked with the use of ephedrine's. 46 , 47 The use of ephedrine has also been linked to cardiomyopathy 48 and stroke 49 while pseudoephedrine use has also been linked with stroke 50 and coronary artery spasm with myocardial infarction. 51 Further, there are numerous case reports of significant cardiovascular events following the administration of over-the-counter stimulants. 46 As with AS use, the interpretation of such case reports is difficult, since it may be that serious adverse events are as a consequence of preexisting medical conditions combined with drug use. What case studies do promote is further experimental study. For example, doses equivalent to three to four times greater than the recommended therapeutic dose of pseudoephedrine have raised diastolic blood pressure above 90 mm Hg. 52 These results were in accord with two other studies: Bye et al 53 reported significant increases in heart rate and systolic blood pressure following relatively high doses of pseudoephedrine (120 and 180 mg); Empey et al 54 noted that doses of 120 and 180 mg produced statistically significant increases in both pulse and systolic blood pressure. The clinical relevance of these blood pressure changes is not known.
Reports of the CV effects of sympathomimetics in therapeutic doses have been conflicting. Bye et al 53 observed that a single dose of ephedrine (25 mg) significantly elevated both heart rate and systolic blood pressure while a single therapeutic dose of pseudoephedrine (60 mg) significantly elevated only systolic arterial blood pressure. Bright et al 55 and Empey et al 54 noted little change in CV function following therapeutic doses. Increased blood pressure has been demonstrated in cases whereby ephedrine's have been co-administered with a moderate dose of caffeine. 56 Caffeine is thought to exacerbate the action of ephedrine's since it too may cause vasoconstriction through antagonism of adenosine and release of catecholamines.
All stimulants structurally related to amphetamine can cause catecholamine-mediated cardiotoxicity. Increased catecholamine levels can lead to vasoconstriction, vasospasm, tachycardia and hypertension and it is as a result of these responses that oxygen supply to the heart is compromised and hypertrophy, fibrosis and necrosis can result. 57 Clearly, such conditions develop over time, as a consequence of chronic exposure to amphetamines and the repercussions may include myocardial infarction, aortic dissection and sudden cardiac death. 57
Little has been done by way of measuring both the acute/chronic effects of stimulant use/abuse on a range of CV risk factors. While significant CV events are associated with their use, the effect on long-term atherosclerotic risk even with moderate usage, through negative alterations in known CV risk factors is worthy of further examination. With regard to amphetamines, emphasis has largely focused on the adverse effects relating to the CNS; however, it is clear that their effects can be wide-ranging and no less significant.
Stimulants—cocaine and others
Cocaine is one of the most frequently used recreational drugs worldwide. The prevalence of use in the UK has been steadily increasing over recent years with 6.6% of 16–24 year olds admitting to regular use and figures suggesting over 1 million current cocaine users in the UK. 58 Despite limited use as a performance-enhancing drug, there is still a relatively high level of adverse findings for cocaine use in athletes. According to WADA around 11.3% of adverse findings for stimulants were as a result of cocaine use. 4 Athletes are not immune to the lure of social drugs like cocaine.
The use of cocaine has been associated with acute and chronic cardiovascular disease. 59 , 60 Cocaine inhibits norepinephrine reuptake in the sympathetic system leading to overstimulation 60 and may cause release of catecholamines from central and peripheral stores. 61 Acute coronary syndromes (including myocardial ischemia and infarction) are the commonest cardiac events secondary to cocaine abuse. 60 , 61 This may be due to coronary artery spasm, increase in myocardial oxygen consumption from increases in heart rate and blood pressure, and a prothrombotic state. 62 , 63 Most myocardial infarctions occur in the absence of atherosclerotic coronary disease and are unrelated to the dose and frequency of cocaine use. 64 Cocaine abuse may however also lead to premature coronary disease sometimes with quite rapid onset. 65 Cocaine abuse may also lead to coronary artery aneurysms, aortic dissection, rupture, vasculitis and stroke. 66–68
Arrhythmias are not common with cocaine use, but sinus tachycardia, sinus bradycardia, supraventricular, ventricular arrhythmias and bundle branch blocks have been reported. 59 , 69 , 70 A dilated cardiomyopathy can be caused by cocaine use and a cocaine-induced myocarditis has been reported at postmortem in 20–30% of cases. 71 Myocarditic changes, however, may be fully reversible if identified early and abstention from further cocaine abuse occurs. In the case study detailed the ECG changes with a significant cardiac event are shown in a young professional athlete who has a cocaine abuse history.
Case study 2
We briefly describe the case of a 27-year-old professional skater with a history of cocaine abuse. He developed retrosternal chest pain and ECG changes of inferolateral ST elevation ( figure 1 ) after taking cocaine. His symptoms settled with nitrates and he developed T-wave inversion on his ECG the following day ( figure 2 ) with a rise in Troponin I of 18.5 µg/l. He had normal left ventricular systolic function on echocardiography. On cardiac catheterisation he had a smooth 40% stenosis in the ostial left anterior descending artery with the other coronary branches normal ( figure 3 ). He was initially treated with antiplatelets, heparin and a β-blocker, but as it was felt that he had sustained a myocardial infarction due to coronary artery spasm, the β-blocker was substituted with a calcium channel blocker prior to discharge from hospital. He remained pain-free when further reviewed at 3 months.
- Download figure
- Open in new tab
- Download powerpoint
ECG 1: inferolateral ST elevation with chest pain. This figure is only reproduced in colour in the online version.
ECG 2: Inferior T-wave inversion with lateral biphasic T wave. This figure is only reproduced in colour in the online version.
Coronary angiography: 40% stenosis in ostial left anterior descending artery (arrow) with other coronary branches normal.
While detection of cocaine use, unless openly admitted, can be problematic for the practitioner there are certain psychological and physiological indications that may help inform the healthcare provider. Cocaine use can produce euphoria, decreased appetite and need for sleep, but may also cause anxiety, irritability, paranoia and hallucinations. There may be associated tachycardia, sweating, pupil dilatation and nausea. Withdrawal after chronic use mainly causes psychological symptoms including depression, anxiety and increased sleep.
Other common stimulants used by athletes include caffeine and nicotine (from smoking tobacco, chewing tobacco and smoking cessation products). Both caffeine and nicotine have been shown to have cardiac effects. Caffeine is used by athletes as a stimulant to decrease the feelings of fatigue and elevate heart rate and neural activity. The effect of caffeine will increase myocardial O 2 and has been shown to increase blood pressure as well as raises the level of free-fatty acids in the blood, thereby increasing blood viscosity. If used in moderate doses there are minimal long-term side effects to caffeine use; however, extremely high doses have been associated with cardiac arrhythmias 72 and events in otherwise healthy individuals. 73 , 74 Cigarette smoking has long been known to promote atherosclerosis, with an increased risk of sudden death, 75 myocardial infarction 76 , 77 and stroke. 78 The use of nicotine therapies such as transdermal patches, inhalators and gum as well as the common use of chewing tobacco in some sports has also been associated with an increased cardiovascular event risk. 79 , 80 Again, much of these data have come from case study and anecdotal data, with larger studies not observing a significant increase in risk of cardiovascular events. 81 Like most other stimulants further research is required and given that both caffeine and nicotine are not completely banned admission and monitoring of use may be easier than with other drugs.
This review has attempted to describe available data and exemplar case studies detailing the potential CV health issues surrounding the use of some of the most common drugs detected in doping screens on athletes. Negative CV health effects do occur but more controlled research trials are required alongside longitudinal studies of chronic drug use. Available data demonstrate enough concern in relation to CV health and drug use that healthcare practitioners should be fully educated to help detect signs and symptoms and support athlete treatment and recovery where appropriate.
- Yesalis CE ,
- ↵ WADA . The 2012 prohibited list International Standard . http://wwwwada-amaorg/Documents/World_Anti-Doping_Program/WADP-Prohibited-list/2012/WADA_Prohibited_List_2012_ENpdf (serial on the Internet) , 2012 .
- ↵ <WADA_2010_Laboratory_Statistics_Report.pdf> .
- Graham MR ,
- Griffiths KA ,
- McCredie RJ ,
- McVeigh J ,
- Chester N ,
- Appleby M ,
- Santamarina RD ,
- Besocke AG ,
- Romano LM ,
- Liljeqvist S ,
- Hellden A ,
- Bergman U ,
- Lunghetti S ,
- Fineschi V ,
- Centini F ,
- Watkins S ,
- Ahlgrim C ,
- Frogel JK ,
- Sullivan ML ,
- Martinez CM ,
- Gallagher EJ
- Schofield RS
- Alhadad A ,
- Wysoczanski M ,
- Bergmann SR
- Fernhall B ,
- Thompson PD
- Longson D ,
- Hartgens F ,
- Rietjens G ,
- Keizer HA ,
- Applebaum-Bowden D ,
- Haffner SM ,
- Bausserman LL ,
- Maceroni D ,
- Boobier W ,
- Savage DD ,
- Dannenberg AL ,
- Sachtleben TR ,
- Nguyen LD ,
- D'Andrea A ,
- Salerno G ,
- Baggish AL ,
- Weiner RB ,
- Kanayama G ,
- Kasikcioglu E ,
- Ebenbichler CF ,
- ↵ Anti-Doping U . UK National Anti-Doping Programme Quarterly Report . 2011 .
- Van Marken Lichtenbelt WD ,
- Haller CA ,
- Benowitz NL
- Shekelle PG ,
- Morton SC ,
- Sangster J ,
- Rampling D ,
- Murillo-Bonilla LM ,
- Tilkian AG ,
- Palazzolo M
- Sandage B ,
- McKetin R ,
- Fletcher K ,
- Collinson J
- Schwartz BG ,
- Rezkalla S ,
- Figueredo VM ,
- Lynn Morris D
- Cigarroa RG ,
- Yancy CW Jr . ,
- Heesch CM ,
- Wilhelm CR ,
- Ristich J ,
- Hollander JE ,
- Dressler FA ,
- Malekzadeh S ,
- Salinas CL ,
- Bolger AF ,
- Martinez N ,
- Diez-Tejedor E ,
- Filipenko JD
- Berger AJ ,
- Hallstrom AP ,
- Sugiishi M ,
- Wright RA ,
- Labinjoh C ,
- D'Agostino RB ,
- Kannel WB ,
- Ottervanger JP ,
- Festen JM ,
- de Vries AG ,
- Joseph AM ,
- Norman SM ,
Contributors All authors have contributed substantially to the conception and design of the paper with PJA, JS and KG contributing to data analysis and interpretation. All authors have also contributed significantly to the drafting and revising of the article before approving the final draft.
Competing interests None.
Patient consent Obtained.
Ethics approval Liverpool John Moores University.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Should athletes be...
Should athletes be allowed to use performance enhancing drugs?
- Related content
- Peer review
- Julian Savulescu , Uehiro chair in practical ethics 1 ,
- Leon Creaney , consultant in sport and exercise medicine 2 ,
- Anna Vondy , ST6 emergency medicine 3
- 1 University of Oxford, Oxford, UK
- 2 Trauma and Orthopaedics, University Hospital Birmingham, Birmingham, UK
- 3 Emergency Department, Royal Liverpool University Hospital, Merseyside, UK
- Correspondence to: J Savulescu julian.savulescu{at}philosophy.ox.ac.uk , L Creaney leon.creaney{at}uhb.nhs.uk
Stories about illegal doping in sport are a regular occurrence. Julian Savulescu argues that rather than banning performance enhancing drugs we should regulate their use, but Leon Creaney and Anna Vondy say this would lead to escalating use and call for tougher enforcement
Yes— Julian Savulescu
The zero tolerance ban on doping has failed. The second fastest runner ever, the American Tyson Gay, recently tested positive for a banned substance, along with Jamaican sprinters Asafa Powell and Sherone Simpson. There is evidence of widespread doping across many sports including athletics, tennis, and cycling. 1 Recent evidence from Germany suggests doping is rife in football. 2 Despite apparent advances in the “war on doping,” our success in detecting drug misuse is limited. In 2000, the first tests for erythropoietin were introduced. 3 Yet in 2012, the US Anti-Doping Agency expert Larry Bowers said that a negative test cannot be equated with the absence of doping. 4
According to Hermann and Henneberg, “Using typical values of detectability . . . the probability of detecting a cheater who uses doping methods every week is only 2.9% per test.” 5 It is time for a different approach.
Human nature
It appears we reached the limits of human performance in sprinting about 15 years ago. Starting with Ben Johnson in 1988, only 10 men have ever run under 9.8 sec. Only two (including Usain Bolt) are currently untainted by doping.
To keep improving, to keep beating records, to continue to train at the peak of fitness, to recover from the injury that modern training inevitably inflicts, athletes need enhanced physiology. We have exhausted human potential. But to be human is to be better, and doping is not going to go away.
Regulation could improve safety
The strongest argument against doping is safety. Since there have been no scientific tests of the effects of doping …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £50 / $60/ €56 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Subst Abuse Rehabil
Drug abuse in athletes
Claudia l reardon.
Department of Psychiatry, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA
Shane Creado
Drug abuse occurs in all sports and at most levels of competition. Athletic life may lead to drug abuse for a number of reasons, including for performance enhancement, to self-treat otherwise untreated mental illness, and to deal with stressors, such as pressure to perform, injuries, physical pain, and retirement from sport. This review examines the history of doping in athletes, the effects of different classes of substances used for doping, side effects of doping, the role of anti-doping organizations, and treatment of affected athletes. Doping goes back to ancient times, prior to the development of organized sports. Performance-enhancing drugs have continued to evolve, with “advances” in doping strategies driven by improved drug testing detection methods and advances in scientific research that can lead to the discovery and use of substances that may later be banned. Many sports organizations have come to ban the use of performance-enhancing drugs and have very strict consequences for people caught using them. There is variable evidence for the performance-enhancing effects and side effects of the various substances that are used for doping. Drug abuse in athletes should be addressed with preventive measures, education, motivational interviewing, and, when indicated, pharmacologic interventions.
Introduction
Doping, defined as use of drugs or other substances for performance enhancement, has become an important topic in virtually every sport 1 and has been discovered in athletes of all ages and at every level of competition. 2 – 4 See Table 1 for rates of use of a variety of substances, whether doping agents or recreational substances, among different populations of athletes as reported in various recent research studies. 5 – 10 Of note, self-reports are generally felt likely to yield under-reported figures. 5 Importantly, performance-enhancing drugs (PEDs) are not restricted to illegal drugs or prescription medications, such as anabolic steroids. 11 They include dietary supplements and a variety of compounds that are available at grocery and health food stores and online. 12
Substance use rates among different populations of athletes as reported in various recent research studies
| Substance | Athlete population | Percentage of athletes using substance |
|---|---|---|
| Any substances banned by WADA | Elite athletes across sports (positive drug tests) | 2% over past year |
| Alcohol | College athletes (self report) | 75%–93% for male athletes; 71%–93% for female athletes over past year 85% over past year |
| Anabolic steroids | High school students (self report) | 0.7%–6.6% over past year |
| College athletes (self report) | 0.2%–5% for males depending on sport; 0.0%–1.6% for females depending on sport over past year , | |
| Professional football players (self report) | 9% used at some point in career | |
| Competitive power lifters (self report) | 67% used at some point in career | |
| Cannabis | College athletes (self report) | 28% over past year |
| Opiates | Professional football players (self report) | 52% used at some point in career (71% of those misused at some point in career) |
| Smokeless tobacco | College athletes (self report) | 23% over past year |
| College baseball players (self report) | 40%–50% over past year | |
| Professional baseball players (self report) | 35%–40% over past year | |
| Professional football players (self report) | 20%–30% over past year | |
| Stimulants | College athletes (self report) | 3% over past year |
Abbreviation: WADA, World Anti-Doping Agency.
Drug abuse in the athlete population may involve doping in an effort to gain a competitive advantage. Alternatively, it may involve use of substances such as alcohol or marijuana without the intent of performance enhancement, since athletes may develop substance use disorders just as any nonathlete may.
Athletes may turn to substances to cope with numerous stressors, including pressure to perform, injuries, physical pain, and retirement from a life of sport (which happens much earlier than retirement from most other careers). 13 Additionally, athletes may be significantly less likely to receive treatment for underlying mental illnesses such as depression. 14 Athletes receive comprehensive treatment and rehabilitation for physical injuries, but this may be less often the case for mental illness, because of their sometimes viewing mental illness as a sign of weakness. 14 Untreated mental illness is often associated with substance use, perhaps in an effort to self-treat. Alternatively, substances of abuse may cause mental illness. 15
We will especially focus on doping in this review, which specifically aims to serve as a single paper that provides a broad overview of the history of doping in athletes, the effects of different classes of drugs used for doping, side effects of doping, the role of anti-doping organizations, and the treatment of affected athletes.
Materials and methods
For this review, we identified studies through a MEDLINE search. Search terms included the following, individually and in combination: “doping”, “athletes”, “steroids”, “drug abuse”, “mental illness”, “drug testing”, “anti-doping”, “psychiatry”, “sports”, “depression”, “substance abuse”, “substance dependence”, “addiction”, “history”, “side effects”, “drug testing”, “treatment”, “androgens”, “testosterone”, “growth hormone”, “growth factors”, “stimulants”, “supplements”, “erythropoietin”, “alcohol”, “marijuana”, “narcotics”, “nicotine”, “Beta agonists”, “Beta blockers”, “diuretics”, “masking agents”, “gene doping”, “National Collegiate Athletic Association”, and “World Anti-Doping Agency”. We restricted results to the English language and used no date restrictions. We retrieved all papers discussing drug abuse in athletes. We reviewed the findings of each article, and reviewed the references of each paper for additional papers that had been missed in the initial search and that might include findings relevant to the scope of our review. Ultimately, 67 manuscripts or chapters were felt relevant and representative for inclusion among those referenced in this paper.
History of doping in athletes
The belief that doping is only a recent phenomenon that has arisen solely from increasing financial rewards offered to modern day elite athletes is incorrect. 16 In fact, doping is older than organized sports. Ancient Greek Olympic athletes dating back to the third century BC used various brandy and wine concoctions and ate hallucinogenic mushrooms and sesame seeds to enhance performance. Various plants were used to improve speed and endurance, while others were taken to mask pain, allowing injured athletes to continue competing. 17 – 19 Yet, even in ancient times, doping was considered unethical. In ancient Greece, for example, identified cheaters were sold into slavery. 1
The modern era of doping dates to the early 1900s, with the illegal drugging of racehorses. Its use in the Olympics was first reported in 1904. Up until the 1920s, mixtures of strychnine, heroin, cocaine, and caffeine were not uncommonly used by higher level athletes. 16
By 1930, use of PEDs in the Tour de France was an accepted practice, and when the race changed to national teams that were to be paid by the organizers, the rule book distributed to riders by the organizer reminded them that drugs were not among items with which they would be provided. 20
In the 1950s, the Soviet Olympic team began experimenting with testosterone supplementation to increase strength and power. 16 This was part of a government-sponsored program of performance enhancement by national team trainers and sports medicine doctors without knowledge of the short-term or long-term negative consequences. Additionally, when the Berlin Wall fell, the East German government’s program of giving PEDs to young elite athletes was made public. 1 Many in the sporting world had long questioned the remarkable success of the East German athletes, particularly the females, and their rapid rise to dominance in the Olympics. Young female athletes experienced more performance enhancement than did male athletes. Unfortunately, they also suffered significant and delayed side effects, including reports of early death in three athletes. 19
The specific substances used to illegally enhance performance have continued to evolve. 21 The “advances” in doping strategies have been driven, in part, by improved drug testing detection methods. 21 To avoid detection, various parties have developed ever more complicated doping techniques. 21 Further, new doping strategies may result from advances in scientific research that can lead to the discovery and use of substances that may later be banned. Over the past 150 years, no sport has had more high-profile doping allegations than cycling. 16 However, few sports have been without athletes found to be doping.
Many sports organizations have come to ban the use of PEDs and have very strict rules and consequences for people who are caught using them. The International Association of Athletics Federations was the first international governing body of sport to take the situation seriously. 22 In 1928, they banned participants from doping, 22 but with little in the way of testing available, they had to rely on the word of athletes that they were not doping. It was not until 1966 that the Federation Internationale de Football Association and Union Cycliste Internationale joined the International Association of Athletics Federations in the fight against drugs, closely followed by the International Olympic Committee (IOC) the following year. 23
The first actual drug testing of athletes occurred at the 1966 European Championships, and 2 years later the IOC implemented their first drug tests at both the Summer and Winter Olympics. 24 Anabolic steroids became even more prevalent during the 1970s, and after a method of detection was found, they were added to the IOC’s prohibited substances list in 1976. This resulted in a marked increase in the number of doping-related disqualifications in the late 1970s, 24 notably in strength-related sports, such as throwing events and weightlifting.
While the fight against stimulants and steroids was producing results, 24 the main front in the anti-doping war was rapidly shifting to blood doping. 25 This removal and subsequent reinfusion of an athlete’s blood in order to increase the level of oxygen-carrying hemoglobin has been practiced since the 1970s. 25 The IOC banned blood doping in 1986. 25 Other ways of increasing the level of hemoglobin were being tried, however. One of these was erythropoietin. 25 Erythropoietin was included in the IOC’s list of prohibited substances in 1990, but the fight against erythropoietin was long hampered by the lack of a reliable testing method. An erythropoietin detection test was first implemented at the 2000 Olympic Games. 25
In the 1970s and 1980s, there were suspicions of state-sponsored doping practices in some countries. The former German Democratic Republic substantiated these suspicions. 25 The most prominent doping case of the 1980s concerned Ben Johnson, the 100 meter dash champion who tested positive for the anabolic steroid stanozolol at the 1988 Olympic Games in Seoul. 25 In the 1990s, there was a noticeable correlation between more effective test methods and a drop in top results in some sports. 25
In 1998, police found a large number of prohibited substances, including ampoules of erythropoietin, in a raid during the Tour de France. 25 , 26 The scandal led to a major reappraisal of the role of public authorities in anti-doping affairs. As early as 1963, France had been the first country to enact anti-doping legislation. Other countries followed suit, but international cooperation in anti-doping affairs was long restricted to the Council of Europe. In the 1980s, there was a marked increase in cooperation between international sports authorities and various governmental agencies. Before 1998, debate was still taking place in several discrete forums (IOC, sports federations, individual governments), resulting in differing definitions, policies, and sanctions. Athletes who had received doping sanctions were sometimes taking these sanctions, with their lawyers, to civil courts and sometimes were successful in having the sanctions overturned. The Tour de France scandal highlighted the need for an independent, nonjudicial international agency that would set unified standards for anti-doping work and coordinate the efforts of sports organizations and public authorities. The IOC took the initiative and convened the First World Conference on Doping in Sport in Lausanne in February 1999. Following the proposal of the Conference, the World Anti-Doping Agency (WADA) was established later in 1999.
Performance-enhancing effects of substances used by athletes
There is a research base demonstrating that many doping agents are in fact performance-enhancing. However, some substances (eg, selective androgen receptor modulators, antiestrogens, and aromatase inhibitors), used in an effort to enhance performance, have little data to back up their effectiveness for such a purpose. Note that the studies cited in this paper are chosen as being historically important or representative of the bulk of the research on the topic, and the broad overview provided in this paper does not aim to cite all evidence on the effects of these substances. Additionally, research on this topic is limited by the difficulty in performing ethical studies due to the high doses of doping agents used, potential side effects, and lack of information on actual practice.
Androgens include exogenous testosterone, synthetic androgens (eg, danazol, nandrolone, stanozolol), androgen precursors (eg, androstenedione, dehydroepiandrosterone), selective androgen receptor modulators, and other forms of androgen stimulation. The latter categories of substances have been used by athletes in an attempt to increase endogenous testosterone in a way that may circumvent the ban enforced on natural or synthetic androgens by WADA.
Amounts of testosterone above those normally found in the human body have been shown to increase muscle strength and mass. For example, a representative randomized, double-blind study involved 43 men being randomized to four different groups: testosterone enanthate 600 mg once per week with strength training exercise; placebo with strength training exercise; testosterone enanthate 600 mg once per week with no exercise; and placebo with no exercise. This was a critical study in demonstrating that administration of testosterone increased muscle strength and fat-free mass in all recipients, and even moreso in those who exercised. 27 A second study from the same investigators 5 years later further demonstrated a dose–response relationship between testosterone and strength. 28 Another double-blind trial of exogenous testosterone involved 61 males randomized to five different doses of testosterone enanthate, ranging from 25 mg to 600 mg, along with treatment with a gonadotropin-releasing hormone agonist to suppress endogenous testosterone secretion. That study demonstrated findings similar to the previous one, in showing a dose-dependent increase in leg power and leg press strength, which correlated with serum total testosterone concentrations. 29
Androgen precursors include androstenedione and dehydroepiandrosterone (DHEA). We found no evidence that androstenedione increases muscle strength. 30 DHEA is available as a nutritional supplement that is widely advertised in body building magazines as a substance that will improve strength. However, results from placebo-controlled studies of DHEA in males have been mixed. 30 , 31 One study involved 40 trained males being given DHEA 100 mg per day, androstenedione, or placebo, with no resulting differences in muscle mass or fat-free mass between groups. 30 A second study involved nine males and ten females randomized to receive DHEA 100 mg daily or placebo for 6 months, who were then crossed over to the other group for a further 6 months. The males but not females showed increased knee and lumbar back strength during DHEA treatment. 31
Selective androgen receptor modulators are not approved for use in humans in any country, but athletes are able to obtain these substances on the Internet. 32 No studies were found looking at the effects of selective androgen receptor modulators on muscle strength or mass in humans.
Other forms of androgen stimulation include exogenous human chorionic gonadotropin, antiestrogens such as tamoxifen, clomiphene, and raloxifene, and aromatase inhibitors such as testolactone, letrozole, and anastrozole. These substances may result in increased serum testosterone. 33 However, we found minimal research demonstrating an effect on muscle strength. 34 While androgens of different forms have been shown to improve muscle strength and mass, they have not been shown to improve whole body endurance per se. 35
Growth hormone and growth factors
Growth hormone and growth factors are also banned by WADA. Research shows recombinant human growth hormone to increase muscle mass and decrease adipose tissue. One representative study randomized male recreational athletes to growth hormone 2 mg/day subcutaneously, testosterone 250 mg weekly intramuscularly, a combination of the two treatments, or placebo. 36 Female recreational athletes were randomized to growth hormone 2 mg daily or placebo. In both males and females, growth hormone was associated with significantly decreased fat mass, increased lean body mass, and improved sprint capacity (although with no change in strength, power, or endurance). Sprint capacity improvement was even greater when growth hormone and testosterone were coadministered to males.
Growth factors include insulin-like growth factor and insulin. They are presumed to have similar effects to growth hormone, but have not been studied in athletes. 37 Athletes use these substances because of their apparent anabolic effect on muscle. 37
Stimulants include amphetamine, D-methamphetamine, methylphenidate, ephedrine, pseudoephedrine, caffeine, dimethylamylamine, cocaine, fenfluramine, pemoline, selegiline, sibutramine, strychnine, and modafinil. Research has shown stimulants to improve endurance, increase anaerobic performance, decrease feelings of fatigue, improve reaction time, increase alertness, and cause weight loss. 38 Of note, while WADA bans stimulants as a class, it does allow use of caffeine. Energy beverages now often include a variety of stimulants and other additives including not only caffeine, but also the amino acids taurine and L-carnitine, glucuronolactone, ginkgo biloba, ginseng, and others. 39 Caffeine content can be up to 500 mg per can or bottle. The potential performance benefits of the other ingredients in energy beverages are unclear. For example, taurine may improve exercise capacity by attenuating exercise-induced DNA damage, but the amounts found in popular beverages are probably far below the amounts needed to be of performance-enhancing benefit. 39
Of note, the number of athletes, especially at top levels of competition, reported to be using stimulant medications has markedly increased in recent years. In the USA, the National Collegiate Athletic Association acknowledged that the number of student athletes testing positive for stimulant medications has increased three-fold in recent years. 40 There has also been concern about inappropriate use of stimulants in major league baseball in the USA. According to a report released in January 2009, 106 players representing 8% of major league baseline players obtained therapeutic use exemptions for stimulants in 2008, which was a large increase from 28 players in 2006. 41 Therapeutic use exemptions allow athletes to take otherwise banned and performance-enhancing substances if their physician attests that they should for medical reasons.
Nutritional supplements
Nutritional supplements include vitamins, minerals, herbs, extracts, and metabolites. 39 Importantly, the purity of these substances cannot be guaranteed, such that they may contain banned substances without the athlete or manufacturer being aware. Studies have shown that many nutritional supplements purchased online and in retail stores are contaminated with banned steroids and stimulants. 42 Thus, athletes could end up failing doping tests without intentionally having ingested banned substances. 42 Creatine is not currently on the WADA banned list and is the most popular nutritional supplement for performance enhancement. 3 Studies demonstrate increased maximum power output and lean body mass from creatine. 43 , 44 As such, some allowable nutritional supplements may have ergogenic effects, but may have insufficient evidence supporting their ergogenic properties to rise to the level of being banned.
Methods to increase oxygen transport
Substances athletes use to increase oxygen transport include blood transfusions, erythropoiesis-stimulating agents such as recombinant human erythropoietin and darbepoetin alfa, hypoxia mimetics that stimulate endogenous erythropoietin production such as desferrioxamine and cobalt, and artificial oxygen carriers. Transfusions and erythropoiesis-stimulating agents have been shown to increase aerobic power and physical exercise tolerance. 45 However, the ergogenic effects of the other agents are debatable. 45
Other recreational drugs
Other recreational drugs that may be used in an attempt to enhance performance include alcohol, cannabinoids, narcotics, and nicotine. 13 WADA does not currently ban nicotine but bans cannabinoids and narcotics. Alcohol is banned in six sports during competition only. All of these substances may be used by athletes to reduce anxiety, which may be a form of performance enhancement, but we found little research looking at actual performance enhancement from these agents. Narcotics are used to decrease pain while practicing or playing. Nicotine may enhance weight loss and improve attention. 46
Beta agonists
There is debate as to whether beta-2 adrenergic agonists, for example, albuterol, formoterol, and salmeterol, are ergogenic. 47 There is anecdotal evidence of improvements in swimmers who use these substances prior to racing. 48 Additionally, oral beta agonists may increase skeletal muscle, inhibit breakdown of protein, and decrease body fat. 48 However, there is some evidence suggesting that swimmers may have a relatively high prevalence of airway hyperresponsiveness due to hours spent breathing byproducts of chlorine, such that beta agonists may be needed to restore normal, not enhanced, lung function. 49
Beta blockers
Beta blockers such as propranolol result in a decreased heart rate, reduction in hand tremor, and anxiolysis. These effects may be performance-enhancing in sports in which it is beneficial to have increased steadiness, such as archery, shooting, and billiards. 48
Other prescription drugs
Diuretics and other masking agents may be used as doping agents. 12 Diuretics can result in rapid weight loss such that they may be used for a performance advantage in sports with weight classes, such as wrestling and boxing. 12 Diuretics may also be used to hasten urinary excretion of other PEDs, thereby decreasing the chances that athletes will test positive for other banned substances that they may be using. 12 Masking agents in general conceal prohibited substances in urine or other body samples, and include diuretics, epitestosterone (to normalize urine testosterone to epitestosterone ratios), probenecid, 5-alpha reductase inhibitors, and plasma expanders (eg, glycerol, intravenous administration of albumin, dextra, and mannitol). 50
Glucocorticoids are sometimes used by athletes in an attempt to enhance performance because of their anti-inflammatory and analgesic properties. 12 However, there is minimal research to show any performance benefits of this class of drugs.
Athletes may also use phosphodiesterase-5 inhibitors in an attempt to attain increased oxygenation and exercise capacity, since they have vasodilatory effects. 51 However, again, little research exists to support a performance benefit from these substances.
Psychiatric medications, including antidepressants, anxiolytics, antipsychotics, and anticonvulsants, are generally not on the WADA banned list. 14 Bupropion is an antidepressant that is on the WADA 2014 monitoring list, meaning WADA is monitoring for any concerning trends of inappropriate use. One small study of nine males suggested that bupropion, when used acutely in warm environments, may allow athletes to push themselves to higher body temperature and heart rates without perceiving greater effort. 52 Otherwise, there is very minimal evidence that any of these classes of psychiatric medications enhance performance. 14
Nondrug performance-enhancing measures
Gene doping is a concerning potential method of nondrug performance enhancement and is banned by WADA. The potential to directly affect strength and endurance through gene manipulation has been demonstrated in laboratory mice, but no human athletes thus far have been found to be using this method. 16
Additionally, athletes may legally attempt to improve physical performance in a number of nondrug ways. 53 These have varying degrees of research into their effectiveness and safety, and include hypoxia induction techniques. 53 For example, athletes may train at high altitudes, which can result in erythrocytosis. Some studies suggest that a high–low method of sleeping at high altitude followed by training at low altitude is a better training strategy than training or sleeping at either high or low altitudes alone. 54 Some athletes have tried sleeping at simulated high altitude by using low oxygen tents. Athletes may also make dietary changes to try to increase hemoglobin levels. 55 , 56
Side effects of substances used by athletes
It is presumed that most if not all doping agents have potential short-term and/or long-term side effects. Unfortunately, given the high doses of these agents used by athletes, it is difficult to confirm such effects. It would be unethical to give dosages as high as those used by athletes for performance enhancement effects to participants in research studies. 16 Knowledge about side effects may be gleaned from empirical observation, reports of admitted users, and effects in patients prescribed such agents for medical conditions. Table 2 lists the potential side effects of various forms of doping. 57 – 59
Potential side effects of different substances and methods of doping
| Substance/method | Potential side effects |
|---|---|
| Androgens (eg, testosterone, danazol, nandrolone, stanozolol) | • Reproductive: diminished spermatogenesis and gynecomastia in men, decreased fertility, decreased testicular size, possible benign prostatic hypertrophy or prostate cancer • Cardiovascular: decreased high-density lipoprotein cholesterol, increased low-density lipoprotein cholesterol • Hepatic: hepatotoxicity • Neuropsychiatric: depression, mania, psychosis, aggression • Other: hastened epiphyseal closure in adolescents, acne, hirsutism, temporal hair recession, clitoromegaly, voice deepening, and oligomenorrhea/amenorrhea in women, infections (abscesses at injection sites, septic arthritis, and hepatitis/human immunodeficiency virus from sharing needles), tendon rupture |
| Growth hormone and growth factors (eg, insulin-like growth factor, insulin) | • I nsulin resistance, hyperglycemia, diabetes mellitus, cardiomegaly, hastened epiphyseal closure in adolescents, myopathy, hypertension, edema, carpal tunnel syndrome |
| Stimulants (eg, amphetamine, D-methamphetamine, methylphenidate, ephedrine, pseudoephedrine, caffeine, cocaine) | • Hypertension, tachycardia, myocardial infarction, stroke, heat stroke, weight loss, rhabdomyolysis, headache, nausea, tremor, insomnia, anxiety/panic attacks, agitation, aggression, psychosis |
| Methods to increase oxygen transport (eg, blood transfusions, recombinant human erythropoietin, darbepoetin alfa) | • Myocardial infarction, stroke, deep vein thrombosis/pulmonary embolism, hypertension, antibody-mediated anemia |
| Nutritional supplements (eg, vitamins, minerals, herbs, extracts, metabolites) | • Depends on the components • Creatine: acute interstitial nephritis, more rapid progression of chronic kidney disease , |
| Other recreational drugs | • Alcohol: sedation, decreased concentration and coordination • Cannabinoids: reduced alertness, impaired short-term memory, psychomotor retardation, dysphoria, anxiety, psychosis • Narcotics: physical dependence, nausea/vomiting, constipation, decreased concentration and coordination, fatigue • Nicotine: chronic use associated with cardiovascular disease, chronic obstructive lung disease, and many types of cancer |
| Beta agonists (eg, albuterol, formoterol, salmeterol)) | • Tachycardia, arrhythmias, hypokalemia, hyperglycemia, tremor |
| Beta blockers (eg, propranolol) | • Bradycardia, increased airway resistance, decreased endurance |
| Other prescription drugs | • Diuretics and other masking agents: dizziness, muscle cramps, rash, gout, renal insufficiency, electrolyte imbalances, gynecomastia (spironolactone) • Glucocorticoids: hyperglycemia, fluid retention, depression, mania, psychosis, chronic use may result in reduced muscle mass/weakness, osteoporosis, diabetes mellitus, hypertension, weight gain, central obesity, and cataracts |
| Gene doping | • Unknown |
Note: Copyright © 2013. John Wiley & Sons. Adapted with permission from Baron DA, Reardon CL, Baron SH. Doping in sport. In: Baron DA, Reardon CL, Baron SH, editors. Clinical Sports Psychiatry: An International Perspective . Oxford, UK: Wiley; 2013. 16
Anti-doping organizations, drug testing in athletes, and rules
Drug testing typically occurs only in organized, competitive sports. At the college level, organizations such as the National Collegiate Athletic Association 60 and individual member institutions conduct standard drug testing programs and enforce penalties for positive tests.
Elite athletes competing at international and national levels are subject to standardized anti-doping guidelines under the auspices of WADA and related national organizations. WADA is the international independent agency that publishes the World Anti-Doping Code, which is the document harmonizing anti-doping policies in all sports and all countries. 61 The Code was first adopted in 2003 and became effective in 2004. The Code sets forth specific anti-doping rules and principles that are to be followed by the anti-doping organizations responsible for adopting, implementing, or enforcing anti-doping rules within their authority, including the IOC, International Paralympic Committee, international sport federations (for example, the International Cycling Union), major event organizations, and national anti-doping organizations (for example, the US Anti-Doping Agency).
WADA revises and publishes its list of banned substances approximately annually. It specifies those banned substances and methods that are prohibited at all times (both in-competition and out-of-competition) because of their potential to enhance performance in future competitions or their masking potential, and those substances and methods that are prohibited in-competition only. The list may be expanded by WADA for a particular sport.
WADA has also taken the lead in the development of the athlete biological passport concept. 61 WADA’s athlete biological passport operating guidelines took effect in 2009. The fundamental principle of the athlete biological passport is based on the monitoring of selected parameters over time that indirectly reveal the effect of doping, as opposed to the traditional direct detection of doping by analytical means. This concept gained momentum as a result of questions raised during the 2006 Olympic Winter Games surrounding suspensions of athletes by their federations following health checks that reported high hemoglobin levels. An athlete’s passport purports to establish individual baseline hormone/blood levels, which are monitored over time for significant changes. A positive test result would consist of too dramatic a change from the established individual baseline. This approach is intended to protect athletes from false-positive tests resulting from naturally occurring high levels of endogenous substances, while catching those attempting to cheat by using naturally occurring substances.
In the event that an athlete and his or her medical providers feel it necessary, for documented medical reasons, that he or she continue to take a banned substance, WADA may consider granting a therapeutic use exemption, a concept mentioned earlier. A therapeutic use exemption must be on file before an athlete tests positive for the substance allowed by that therapeutic use exemption.
Treatment of affected athletes, including counseling and psychiatric support
The first level of addressing the problem of drug abuse by athletes is prevention. 13 Drug screening is used in higher-level athletics both to deter athletes from using drugs and to punish and offer opportunities for rehabilitation to those who are found to have done so. Didactic education is another method aimed at prevention. 62 On the one hand, some authors and clinicians feel that among the most effective preventive strategies for drug abuse in sports is frequent, accurate, very closely observed, truly random urine drug testing. 13 , 63 However, some view drug testing as ineffective at preventing use of PEDs. 64 The argument for the latter is that these interventions target doping behavior rather than athlete attitudes. Athletes ultimately focus on their performance, and thus may view doping as rational behavior. 63 Moreover, knowledge of the potentially dangerous consequences from doping imparted via didactic education does not necessarily dissuade athletes. For example, in 1997, Bamberger and Yaeger surveyed 198 Olympic athletes. When asked if they would use PEDs under the hypothetical conditions of knowing they would not be caught and knowing their use would result in victory, 195 of 198 responded “yes”. Moreover, if the caveat was added that they would die within 5 years, 61% of the athletes still said they would use them. 65
There is little research available to guide counseling and psychiatric approaches to treatment of athletes who abuse drugs. 64 However, motivational interviewing approaches have been suggested for athletes with drug abuse or doping problems, since athletes may often present in the precontemplation stage of change. 13 , 64 Important elements of motivational interviewing include: 64
- Clinician empathy
- Developing discrepancies between where the athlete wants to go in life after sport and the impact that continued use of the substance might have on those goals. During this process, the provider helps athletes to clarify conflict among their values, motives, interest, and behaviors.
- Rolling with resistance. When resistance inevitably occurs, providers should avoid arguing with athletes, as that can exacerbate resistance to change. The provider may “agree to disagree” on certain points with some athletes. Providers may propose or “wonder about” certain alternative viewpoints or actions, but they do not impose or insist upon them.
- Encouragement of self-efficacy. Athletes may need to shift their viewpoint from one of being willing to do whatever it takes to win, to acknowledging that they would use PEDs only if ultimately incapable of succeeding without them (with the hope that athletes will never get to that point). If an athlete is physically dependent on a drug, then additional strategies may be needed. These may include pharmacologic interventions such as naltrexone, acamprosate, or disulfiram for alcohol dependence, or buprenorphine for opiate dependence. 13 Additionally, providers should assess for comorbid mental illness, since co-occurrence of physical dependence and mental illness is commonplace. 13 Any underlying mental illness should be treated. 13 A recent review paper on the epidemiology of mental illness in athletes noted that some mental illnesses such as depression are probably as common in athletes as nonathletes. 14 Twelve-step facilitation, cognitive behavioral therapy, and network therapy are also approaches that may be helpful for athletes who are abusing drugs, although studies are preliminary. 10 , 13 , 66
Conclusion and suggestions
Drug abuse in athletes is a significant problem that has many potential underlying causes. The drive to be the best in sport dates to ancient times, as does the use of performance-enhancing substances. With the ever-mounting pressures faced by athletes, it is not surprising that drug abuse by athletes exists across essentially all sports and age groups.
Suggestions for those undertaking research and clinical work with athletes include:
- If providers become aware of an athlete using PEDs, they should educate the athlete about the potential risks of continued use, regardless of any evidence that suggests this may not be influential for all athletes. Providers should encourage discontinuation of the abused substance(s).
- There is great variance in drug testing programs in different sports and at different levels of competition. 13 More high-quality, prospective, randomized trials should be undertaken to determine the deterrent efficacy of various types of PED screening programs, and changes should be made to those types of screening programs found to be ineffective. 8
Common signs and symptoms of substances relatively commonly used by athletes
| Substance | Common signs and symptoms of use |
|---|---|
| Alcohol | Sedation, decreased concentration and coordination, disinhibition, slurred speech, vomiting |
| Anabolic steroids | Acne, rapid muscle gain, irritability, gynecomastia and hair loss in males, deepening of voice and facial hair in females, visible injection sites and cysts |
| Cannabinoids | Bloodshot eyes, increased appetite, slowed responses, cough, lack of motivation, paranoia |
| Opiates | Constricted pupils, sedation, slowed responses, slurred speech, constipation |
| Stimulants | Dilated pupils, anxiety, jitteriness, increased heart rate and blood pressure, loss of appetite, tics |
Note: Copyright © 2013. John Wiley & Sons. Adapted with permission from Morse ED. Substance use in athletes. In: Baron DA, Reardon CL, Baron SH, editors. Clinical Sports Psychiatry: An International Perspective . Oxford, UK: Wiley; 2013. 8 , 13
- The efficacy of education about PED use as a preventative measure needs further study. Early integration of well designed prevention curricula into sports programs may be beneficial. 8 However, as alluded to earlier, at least one preliminary study suggests that educational programs that solely emphasize the negative effects of PEDs may be ineffective for young athletes. 67
- Mental health professionals should be included in the network of team doctors and other health care providers readily available to athletes. Psychiatrists are often helpful in developing strong drug prevention policies that emphasize education and treatment and not just sanctions. 13 Mental health care professionals should have a year-round presence with the athletes and teams with whom they are working so as to build trust. 13
- Screening for and treatment of underlying mental illnesses such as depression that may contribute to self-treatment with drugs by athletes should be increased. The effectiveness of this screening should be studied.
- Athletes who are using drugs are often skeptical of the medical field. This may be partly with good reason, as many health care professionals are unfamiliar with the mentality of athletes or common drug abuse patterns in this population. Accordingly, referral networks or team assistance programs consisting of health care professionals familiar with these issues should be established for athletes and teams. 62 The effectiveness of these models should be studied.
- Research should examine differences in treatment approaches that may be needed for athletes who have been using drugs for a shorter versus longer period of time.
Trainers, coaches, and health care providers should provide evidence-based, safe alternatives to PED use, including optimal nutrition, weight-training strategies, and psychological approaches to improving performance, all of which may help with athletes’ confidence in their natural abilities.
The authors report no conflicts of interest in this work.

IMAGES
COMMENTS
The integrity of sport is predicated on the assumption that all athletes compete on a level playing field. Unfortunately, the use and abuse of performance-enhancing drugs has become ubiquitous, creating complex challenges for the governing bodies of individual ...
Performance-enhancing drug (PED) use by children and teenagers rose sharply in the past decade. One study shows 3.3% of high school students admit anabolic steroid use; another finds 8% of girls and 12% of boys report using products to improve appearance, muscle mass, or strength. Pediatrics clinicians must monitor PED usage trends, screen ...
Despite the high prevalence of performance-enhancing drug (PED) use, media attention has focused almost entirely on PED use by elite athletes to illicitly gain a competitive advantage in sports, and not on the health risks of PEDs. There is a widespread ...
The prevalence of legal performance-enhancing substance use and potential cognitive and or physical doping in German recreational triathletes, assessed via the randomised response technique.
In addition to the injustice of unfair advantage for dishonest athletes, significant potential health risks are associated with performance-enhancing drugs. Performance-enhancing drugs may have an effect on the cardiovascular system by means of directly altering the myocardium, vasculature, and metabolism. However, less frequently considered is ...
Existing data reveals prevalent performance and image-enhancing drug (PIED) use in specific global regions and higher rates among athletes, however, research on performance-enhancement experiences ...
Which drugs and which doses to allow should be determined not by athletes' actual choices but by the hypothetical choices of the reasonable athlete. The resulting sport-specific drug policy would carve a justifiable middle path between complete prohibition and complete permission. KEYWORDS: Performance-enhancing drugs doping fairness coercion ...
Several performance-enhancing or ergogenic drugs have been linked to both significant adverse cardiovascular effects and increased cardiovascular risk. Even with increased scrutiny on the governance of performance-enhancing drugs (PEDs) in professional sport and heightened awareness of the associated cardiovascular risk, there are some who are prepared to risk their use to gain competitive ...
The use of performance-enhancing substances in sports undermines values and risks athletes' health. This study analyzes doping literature, identifying influential documents and research domains. Whil...
The studies illustrated the diverse populations of people who use a range of enhancement drugs including concomitant psychoactive drug use. A number of papers focused on blood borne viruses and associated issues, while others reported on the uptake of needle and syringe programmes.
Research has documented the harms associated with performance and image enhancing drug (PIED) use and lack of disclosure of use to healthcare providers (HCPs). Given that the relationship between HCPs and PIED consumers plays an important role in harm reduction, research is required to understand the barriers and facilitators for consumers to ...
The prevalence of performance-enhancing drug use among athletes and the general public has led the World Health Organization to recognize the use of these drugs as a public health issue. 3 Over ...
Abstract The rules of fair play in sport generally prohibit the use of performance-enhancing drugs (PEDs). The World Anti-Doping Agency (WADA) oversees global antidoping regulations and testing for elite athletes participating in Olympic sports. Efforts to enforce antidoping policies are complicated by the diverse and evolving compounds and strategies employed by athletes to gain a competitive ...
Caffeine use is increasing worldwide. The underlying motivations are mainly concentration and memory enhancement and physical performance improvement. Coffee and caffeine-containing products affect the cardiovascular system, with their positive inotropic and chronotropic effects, and the central nervous system, with their locomotor activity ...
Abstract Doping, or performance enhancing drug use, has long been a social and health problem among athletes. Despite the issues associated with doping and the illegality of using these drugs, little criminological research has examined why athletes engage in this deviant behavior.
In addition to the injustice of unfair advantage for dishonest athletes, significant potential health risks are associated with performance-enhancing drugs. Performance-enhancing drugs may have an effect on the cardiovascular system by means of directly altering the myocardium, vasculature, and metabolism. However, less frequently considered is ...
Background Healthcare professionals (HCPs) provide an important point of contact through which people who use performance and image enhancing drugs (PIEDs) could access reliable information, advice, and interventions on a range of PIEDs, their use and related harms. However, HCPs often report difficulties engaging and building rapport with people who use PIEDs, and research suggests that they ...
2015 roundup of research on the use of performance-enhancing drugs in athletics and academics as well as their potential health effects.
Performance Enhancing Drugs (PED ' s) refers to drugs that have a po-. tential to alter the human body and its b iological functions so as to im-. prove his/her own performan ce. ese drugs do ...
The use of performance-enhancing and social drugs by athletes raises a number of ethical and health concerns. The World Anti-Doping Agency was constituted to address both of these issues as well as publishing a list of, and testing for, banned substances in athletes. Despite continuing methodological developments to detect drug use and associated punishments for positive dope tests, there are ...
Pe rformance enhancing drugs and sports. Dheeraj Kumar Mishra and Dr. Vikram Singh. Abstract. This study aims to analyze the use of PEDs or doping in the world of spo rts. Drugs allow for harder ...
Stories about illegal doping in sport are a regular occurrence. Julian Savulescu argues that rather than banning performance enhancing drugs we should regulate their use, but Leon Creaney and Anna Vondy say this would lead to escalating use and call for tougher enforcement The zero tolerance ban on doping has failed. The second fastest runner ever, the American Tyson Gay, recently tested ...
Doping goes back to ancient times, prior to the development of organized sports. Performance-enhancing drugs have continued to evolve, with "advances" in doping strategies driven by improved drug testing detection methods and advances in scientific research that can lead to the discovery and use of substances that may later be banned.
Another performance-enhancing drug that made the 1996 Summer Olympic Games memorable for the wrong reason was bromantane, a sort of stimulant and masking agent combined. ... According to research ...