- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
- Signs of Burnout
- Stress and Weight Gain
- Stress Reduction Tips
- Self-Care Practices
- Mindful Living

What Is Stress?
Stress is Inevitable - Learn to Maintain Your Emotional and Physical Well-Being
The Inner-Workings of the Stress Response
Ways to cope with stress, final thoughts.
- Next in How Stress Impacts Your Health Guide How to Recognize Burnout Symptoms
Stress can be defined as any type of change that causes physical, emotional, or mental strain. Stress is your body's response to anything that requires attention or action.
Everyone experiences stress to some degree. The way you respond to stress, however, makes a big difference to your overall mental and physical well-being.
Verywell / Brianna Gilmartin
Sometimes, the best way to manage your stress involves changing your situation. At other times, the best strategy involves changing the way you respond to the situation.
Developing a clear understanding of how stress impacts your physical and mental health is important. It's also important to recognize how your mental and physical health affects your stress level.
Watch Now: 5 Ways Stress Can Cause Weight Gain
Clues that indicate you might be stressed.
Stress is not always easy to recognize, but there are some ways to identify some signs that you might be experiencing too much pressure. Sometimes stress can come from an obvious source, but sometimes even small daily stresses from work, school, family, and friends can take a toll on your mind and body.
If you think stress might be affecting you, there are a few things you can watch for:
- Cognitive signs such as difficulty concentrating, worrying, anxiety, and trouble remembering
- Emotional signs such as being angry, irritated, fearful, or moody
- Physical signs such as high blood pressure, headaches , clammy/sweaty hands, muscle tension and neck pain , changes in weight, frequent colds or infections , teeth grinding, digestive problems , and changes in the menstrual cycle and sex drive
- Behavioral signs such as poor self-care, not having time for the things you enjoy, or relying on drugs and alcohol to cope
What Does Stress Feel Like?
Stress can manifest in a variety of ways in your mind and body, and there is no one-size-fits-all answer. It can contribute to feelings of frustration, worry, and burnout. You may feel physically exhausted, worn out, and unable to cope.
Stress vs. Anxiety: What's the Difference?
Stress can sometimes be mistaken for anxiety, and experiencing a great deal of stress can contribute to feelings of anxiety. Stress and anxiety both contribute to nervousness, poor sleep, high blood pressure , muscle tension, and excess worry. Experiencing anxiety can make it more difficult to cope with stress and may contribute to other health issues, including increased depression, susceptibility to illness, and digestive problems.
In most cases, stress is caused by external events, while anxiety is caused by your internal reaction to stress. Stress may go away once the threat or the situation resolves, whereas anxiety may persist even after the original stressor is gone.
The Usual Suspects: Main Causes of Stress
There are many different things in life that can cause stress. Some of the main sources of stress include work, finances, relationships, parenting, and day-to-day inconveniences.
Mental Health in the Workplace Webinar
On May 19, 2022, Verywell Mind hosted a virtual Mental Health in the Workplace webinar, hosted by Amy Morin, LCSW. If you missed it, check out this recap to learn ways to foster supportive work environments and helpful strategies to improve your well-being on the job.
The Four Types of Stress
Not all types of stress are harmful or even negative. Some of the different types of stress that you might experience include:
- Acute stress : Acute stress is a very short-term type of stress that can be upsetting or traumatic ; this is the type of stress that is out of the ordinary, such as a car accident, assault, or natural disaster.
- Chronic stress : Chronic stress is what we most often encounter in day-to-day life and seems never-ending and inescapable, like the stress of a bad marriage or an extremely taxing job.
- Episodic acute stress : Episodic acute stress is acute stress that seems to run rampant and be a way of life, creating a life of ongoing distress; episodic stress can be recurring illness, ongoing domestic violence, child abuse , and living through conflict and war.
- Eustress : Eustress , on the other hand, is fun and exciting. It's known as a positive type of stress that can keep you energized. It's associated with surges of adrenaline, such as when you are skiing or racing to meet a deadline.
Harmful Types of Stress:
The main harmful types of stress are acute stress, chronic stress, and episodic acute stress. Acute stress is usually brief, chronic stress is prolonged, and episodic acute stress is short-term but frequent. Positive stress, known as eustress, can be fun and exciting, but it can also take a toll if you don't keep your life in balance.
Stress can trigger the body’s response to a perceived threat or danger, known as the fight-or-flight response . During this reaction, certain hormones like adrenaline and cortisol are released. This speeds the heart rate, slows digestion, shunts blood flow to major muscle groups, and changes various other autonomic nervous functions, giving the body a burst of energy and strength.
Originally named for its ability to enable us to physically fight or run away when faced with danger, the fight-or-flight response is now activated in situations where neither response is appropriate—like in traffic or during a stressful day at work.
When the perceived threat is gone, systems are designed to return to normal function via the relaxation response . But in cases of chronic stress, the relaxation response doesn't occur often enough, and being in a near-constant state of fight-or-flight can cause damage to the body.
Stress can also lead to some unhealthy habits that have a negative impact on your health. For example, many people cope with stress by eating too much or by smoking. These unhealthy habits damage the body and create bigger problems in the long term.
Brace For Impact: How Stress Affects Your Health
Stress can have several effects on your health and well-being. It can make it more challenging to deal with life's daily hassles, affect your interpersonal relationships, and have detrimental effects on your health. The connection between your mind and body is apparent when you examine stress's impact on your life.
Feeling stressed over a relationship, money, or living situation can create physical health issues. The inverse is also true. Health problems, whether you're dealing with high blood pressure or diabetes , will also affect your stress level and mental health. When your brain experiences high degrees of stress , your body reacts accordingly.
Serious acute stress, like being involved in a natural disaster or getting into a verbal altercation, can trigger heart attacks, arrhythmias, and even sudden death. However, this happens mostly in individuals who already have heart disease.
Stress also takes an emotional toll. While some stress may produce feelings of mild anxiety or frustration, prolonged stress can also lead to burnout , anxiety disorders , and depression.
Chronic stress can have a serious impact on your health as well. If you experience chronic stress, your autonomic nervous system will be overactive, which is likely to damage your body.
Stress-Influenced Conditions
- Chronic Pain
- Inflammatory diseases
- Heart disease
- Hyperthyroidism
- Sexual dysfunction
- Skin problems
- Sleep disorders
- Tooth and gum disease
What Can I Do When I Have Too Much Stress?
There are some treatment options for acute and chronic stress, as well as a variety of stress management strategies you can implement on your own. Stress may be inevitable; however, whenever possible, prevention is the best strategy.
An Old Proverb by Benjamin Franklin
An ounce of prevention is worth a pound of cure
Treatment Options
Stress is not a distinct medical diagnosis and there is no single, specific treatment for it. Treatment for stress focuses on changing the situation, developing stress-coping skills , implementing relaxation techniques, and treating symptoms or conditions that may have been caused by chronic stress.
Some interventions that may be helpful include therapy, medication, and complementary and alternative medicine (CAM).
Psychotherapy
Some forms of therapy that may be particularly helpful in addressing symptoms of stress including cognitive behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) . CBT focuses on helping people identify and change negative thinking patterns, while MBSR utilizes meditation and mindfulness to help reduce stress levels.
Medication may sometimes be prescribed to address some specific symptoms that are related to stress. Such medications may include sleep aids, antacids, antidepressants, and anti-anxiety medications.
Complementary and Alternative Medicine
Some complementary approaches that may also be helpful for reducing stress include acupuncture, aromatherapy, massage, yoga, and meditation .
Although stress is inevitable, it can be manageable. When you understand the toll it takes on you and the steps to combat stress, you can take charge of your health and reduce the impact stress has on your life.
Press Play for Advice On Managing Stress
Hosted by therapist Amy Morin, LCSW, this episode of The Verywell Mind Podcast featuring professor Elissa Epel, shares ways to manage stress. Click below to listen now.
Follow Now : Apple Podcasts / Spotify / Google Podcasts / Amazon Music
Here are a few things to get you started:
- Learn to recognize the signs of burnout. High levels of stress may place you at a high risk of burnout. Burnout can leave you feeling exhausted and apathetic about your job. When you start to feel symptoms of emotional exhaustion, it's a sign that you need to find a way to get a handle on your stress.
- Try to get regular exercise. Physical activity has a big impact on your brain and your body . Whether you enjoy a walk in the park, stretching, pilates, or you want to begin jogging, exercise reduces stress and improves many symptoms associated with mental illness.
- Take care of yourself. Incorporating regular self-care activities into your daily life is essential to stress management. Learn how to take care of your mind, body, and spirit and discover how to equip yourself to live your best life.
- Practice mindfulness in your life. Mindfulness isn't just something you practice for 10 minutes each day. It can also be a way of life. Discover how to live more mindfully throughout your day so you can become more awake and conscious throughout your life.
If you or a loved one are struggling with stress, contact the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-4357 for information on support and treatment facilities in your area.
For more mental health resources, see our National Helpline Database .
Stress is a part of life and comes in all shapes and sizes. There are things we can do to minimize or even prevent much of the stress in our lives. But some stress is unavoidable.
If you find you are overwhelmed by an acute stressor, or the daily grind, there are ways to cope and recover. Whether you try some stress management strategies on your own or seek professional help... it is important to keep stress levels in check to avoid the negative impact on your cognitive, emotional, and physical well being.
National Institute of Mental Health. I'm so stressed out! Fact sheet .
Goldstein DS. Adrenal responses to stress . Cell Mol Neurobiol . 2010;30(8):1433–1440. doi:10.1007/s10571-010-9606-9
Stahl JE, Dossett ML, LaJoie AS, et al. Relaxation response and resiliency training and its effect on healthcare resource utilization . PLoS ONE . 2015;10(10). doi:10.1371/journal.pone.0140212
Chi JS, Kloner RA. Stress and myocardial infarction . Heart . 2003;89(5):475–476. doi:10.1136/heart.89.5.475
Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies . PLoS ONE . 2017;12(10). doi:10.1371%2Fjournal.pone.0185781
Bitonte RA, DeSanto DJ II. Mandatory physical exercise for the prevention of mental illness in medical students . Ment Illn . 2014;6(2):5549. doi:10.4081/mi.2014.5549
Ayala EE, Winseman JS, Johnsen RD, Mason HRC. U.S. medical students who engage in self-care report less stress and higher quality of life . BMC Med Educ . 2018;18(1):189. doi:10.1186/s12909-018-1296-x
Richards KC, Campenni CE, Muse-Burke JL. Self-care and well-being in mental health professionals: The mediating effects of self-awareness and mindfulness . J Ment Health Couns . 2010;32(3):247. doi:10.17744/mehc.32.3.0n31v88304423806.
American Psychological Association. Stress in America 2023 .
Krantz DS, Whittaker KS, Sheps DS. Psychosocial risk factors for coronary heart disease: Pathophysiologic mechanisms . In Heart and Mind: The Practice of Cardiac Psychology (2nd Ed.). American Psychological Association; 2011:91-113. doi:10.1037/13086-004
By Elizabeth Scott, PhD Elizabeth Scott, PhD is an author, workshop leader, educator, and award-winning blogger on stress management, positive psychology, relationships, and emotional wellbeing.
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Questions and answers /
Stress can be defined as a state of worry or mental tension caused by a difficult situation. Stress is a natural human response that prompts us to address challenges and threats in our lives. Everyone experiences stress to some degree. The way we respond to stress, however, makes a big difference to our overall well-being.
Stress affects both the mind and the body. A little bit of stress is good and can help us perform daily activities. Too much stress can cause physical and mental health problems. Learning how to cope with stress can help us feel less overwhelmed and support our mental and physical well-being.
Stress makes it hard for us to relax and can come with a range of emotions, including anxiety and irritability. When stressed, we may find it difficult to concentrate. We may experience headaches or other body pains, an upset stomach or trouble sleeping. We may find we lose our appetite or eat more than usual. Chronic stress can worsen pre-existing health problems and may increase our use of alcohol, tobacco and other substances.
Stressful situations can also cause or exacerbate mental health conditions, most commonly anxiety and depression, which require access to health care. When we suffer from a mental health condition, it may be because our symptoms of stress have become persistent and have started affecting our daily functioning, including at work or school.
No, everyone reacts differently to stressful situations. Coping styles and symptoms of stress vary from person to person.
Yes, it is natural to feel stressed in challenging situations such as job interviews, school exams, unrealistic workloads, an insecure job, or conflict with family, friends or colleagues. For many people stress reduces over time as the situation improves or as they learn to cope emotionally with the situation. Stress tends to be widespread during events such as major economic crises, disease outbreaks, natural disasters, war, and community violence.
Most of us manage stress well and continue to function. If we have difficulties coping with stress, we should seek help from a trusted health-care provider or from another trusted person in our community.
Learn stress management
WHO’s stress management guide – Doing what matters in times of stress – aims to equip people with practical skills to cope with stress. A few minutes each day are enough to practise the guide’s self-help techniques. The guide can be used alone or with its accompanying audio exercises.
Keep a daily routine
Having a daily schedule can help us use our time efficiently and feel more in control. Set time for regular meals, time with family members, exercise, daily chores and other recreational activities.
Get plenty of sleep
Getting enough sleep is important for both body and mind. Sleep repairs, relaxes and rejuvenates our body and can help reverse the effect of stress.
Good sleep habits (also known as sleep hygiene) include:
- Be consistent. Go to bed at the same time each night and get up at the same time each morning, including on the weekends.
- If possible, make your sleeping area quiet, dark, relaxing and at a comfortable temperature.
- Limit your use of electronic devices, such as TVs, computers and smart phones, before sleeping.
- Avoid large meals, caffeine and alcohol before bedtime.
- Get some exercise. Being physically active during the day can help you fall asleep more easily at night.
Connect with others
Keep in touch with family and friends and share your concerns and feelings with people you trust. Connecting with others can lift our mood and help us feel less stressed.
Eat healthy
What we eat and drink can affect our health. Try to eat a balanced diet and to eat at regular intervals. Drink enough fluids. Eat lots of fresh fruits and vegetables if you can.
Exercise regularly
Regular daily exercise can help to reduce stress. This can include walking, as well as more intensive exercise.
Limit time following news
Spending too much time following news on television and social media can increase stress. Limit the time you spend following the news if it increases your stress.
Doing What Matters in Times of Stress: An Illustrated Guide

Stress effects on the body
Stress affects all systems of the body including the musculoskeletal, respiratory, cardiovascular, endocrine, gastrointestinal, nervous, and reproductive systems.

Our bodies are well equipped to handle stress in small doses, but when that stress becomes long-term or chronic, it can have serious effects on your body.
Musculoskeletal system
When the body is stressed, muscles tense up. Muscle tension is almost a reflex reaction to stress—the body’s way of guarding against injury and pain.
With sudden onset stress, the muscles tense up all at once, and then release their tension when the stress passes. Chronic stress causes the muscles in the body to be in a more or less constant state of guardedness. When muscles are taut and tense for long periods of time, this may trigger other reactions of the body and even promote stress-related disorders.
For example, both tension-type headache and migraine headache are associated with chronic muscle tension in the area of the shoulders, neck and head. Musculoskeletal pain in the low back and upper extremities has also been linked to stress, especially job stress.
Millions of individuals suffer from chronic painful conditions secondary to musculoskeletal disorders. Often, but not always, there may be an injury that sets off the chronic painful state. What determines whether or not an injured person goes on to suffer from chronic pain is how they respond to the injury. Individuals who are fearful of pain and re-injury, and who seek only a physical cause and cure for the injury, generally have a worse recovery than individuals who maintain a certain level of moderate, physician-supervised activity. Muscle tension, and eventually, muscle atrophy due to disuse of the body, all promote chronic, stress-related musculoskeletal conditions.
Relaxation techniques and other stress-relieving activities and therapies have been shown to effectively reduce muscle tension, decrease the incidence of certain stress-related disorders, such as headache, and increase a sense of well-being. For those who develop chronic pain conditions, stress-relieving activities have been shown to improve mood and daily function.
Respiratory system
The respiratory system supplies oxygen to cells and removes carbon dioxide waste from the body. Air comes in through the nose and goes through the larynx in the throat, down through the trachea, and into the lungs through the bronchi. The bronchioles then transfer oxygen to red blood cells for circulation.
Stress and strong emotions can present with respiratory symptoms, such as shortness of breath and rapid breathing, as the airway between the nose and the lungs constricts. For people without respiratory disease, this is generally not a problem as the body can manage the additional work to breathe comfortably, but psychological stressors can exacerbate breathing problems for people with pre-existing respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD; includes emphysema and chronic bronchitis).
Some studies show that an acute stress—such as the death of a loved one—can actually trigger asthma attacks. In addition, the rapid breathing—or hyperventilation—caused by stress can bring on a panic attack in someone prone to panic attacks.
Working with a psychologist to develop relaxation, breathing, and other cognitive behavioral strategies can help.
Cardiovascular system
The heart and blood vessels comprise the two elements of the cardiovascular system that work together in providing nourishment and oxygen to the organs of the body. The activity of these two elements is also coordinated in the body’s response to stress. Acute stress—stress that is momentary or short-term such as meeting deadlines, being stuck in traffic or suddenly slamming on the brakes to avoid an accident—causes an increase in heart rate and stronger contractions of the heart muscle, with the stress hormones—adrenaline, noradrenaline, and cortisol—acting as messengers for these effects.
In addition, the blood vessels that direct blood to the large muscles and the heart dilate, thereby increasing the amount of blood pumped to these parts of the body and elevating blood pressure. This is also known as the fight or flight response. Once the acute stress episode has passed, the body returns to its normal state.
Chronic stress, or a constant stress experienced over a prolonged period of time, can contribute to long-term problems for heart and blood vessels. The consistent and ongoing increase in heart rate, and the elevated levels of stress hormones and of blood pressure, can take a toll on the body. This long-term ongoing stress can increase the risk for hypertension, heart attack, or stroke.
Repeated acute stress and persistent chronic stress may also contribute to inflammation in the circulatory system, particularly in the coronary arteries, and this is one pathway that is thought to tie stress to heart attack. It also appears that how a person responds to stress can affect cholesterol levels.
The risk for heart disease associated with stress appears to differ for women, depending on whether the woman is premenopausal or postmenopausal. Levels of estrogen in premenopausal women appears to help blood vessels respond better during stress, thereby helping their bodies to better handle stress and protecting them against heart disease. Postmenopausal women lose this level of protection due to loss of estrogen, therefore putting them at greater risk for the effects of stress on heart disease.
Endocrine system
When someone perceives a situation to be challenging, threatening, or uncontrollable, the brain initiates a cascade of events involving the hypothalamic-pituitary-adrenal (HPA) axis, which is the primary driver of the endocrine stress response. This ultimately results in an increase in the production of steroid hormones called glucocorticoids, which include cortisol, often referred to as the “stress hormone”.
The HPA axis During times of stress, the hypothalamus, a collection of nuclei that connects the brain and the endocrine system, signals the pituitary gland to produce a hormone, which in turn signals the adrenal glands, located above the kidneys, to increase the production of cortisol.
Cortisol increases the level of energy fuel available by mobilizing glucose and fatty acids from the liver. Cortisol is normally produced in varying levels throughout the day, typically increasing in concentration upon awakening and slowly declining throughout the day, providing a daily cycle of energy.
During a stressful event, an increase in cortisol can provide the energy required to deal with prolonged or extreme challenge.
Stress and health Glucocorticoids, including cortisol, are important for regulating the immune system and reducing inflammation. While this is valuable during stressful or threatening situations where injury might result in increased immune system activation, chronic stress can result in impaired communication between the immune system and the HPA axis.
This impaired communication has been linked to the future development of numerous physical and mental health conditions, including chronic fatigue, metabolic disorders (e.g., diabetes, obesity), depression, and immune disorders.
Gastrointestinal system
The gut has hundreds of millions of neurons which can function fairly independently and are in constant communication with the brain—explaining the ability to feel “butterflies” in the stomach. Stress can affect this brain-gut communication, and may trigger pain, bloating, and other gut discomfort to be felt more easily. The gut is also inhabited by millions of bacteria which can influence its health and the brain’s health, which can impact the ability to think and affect emotions.
Stress is associated with changes in gut bacteria which in turn can influence mood. Thus, the gut’s nerves and bacteria strongly influence the brain and vice versa.
Early life stress can change the development of the nervous system as well as how the body reacts to stress. These changes can increase the risk for later gut diseases or dysfunctioning.
Esophagus When stressed, individuals may eat much more or much less than usual. More or different foods, or an increase in the use of alcohol or tobacco, can result in heartburn or acid reflux. Stress or exhaustion can also increase the severity of regularly occurring heartburn pain. A rare case of spasms in the esophagus can be set off by intense stress and can be easily mistaken for a heart attack.
Stress also may make swallowing foods difficult or increase the amount of air that is swallowed, which increases burping, gassiness, and bloating.
Stomach Stress may make pain, bloating, nausea, and other stomach discomfort felt more easily. Vomiting may occur if the stress is severe enough. Furthermore, stress may cause an unnecessary increase or decrease in appetite. Unhealthy diets may in turn deteriorate one’s mood.
Contrary to popular belief, stress does not increase acid production in the stomach, nor causes stomach ulcers. The latter are actually caused by a bacterial infection. When stressed, ulcers may be more bothersome.
Bowel Stress can also make pain, bloating, or discomfort felt more easily in the bowels. It can affect how quickly food moves through the body, which can cause either diarrhea or constipation. Furthermore, stress can induce muscle spasms in the bowel, which can be painful.
Stress can affect digestion and what nutrients the intestines absorb. Gas production related to nutrient absorption may increase.
The intestines have a tight barrier to protect the body from (most) food related bacteria. Stress can make the intestinal barrier weaker and allow gut bacteria to enter the body. Although most of these bacteria are easily taken care of by the immune system and do not make us sick, the constant low need for inflammatory action can lead to chronic mild symptoms.
Stress especially affects people with chronic bowel disorders, such as inflammatory bowel disease or irritable bowel syndrome. This may be due to the gut nerves being more sensitive, changes in gut microbiota, changes in how quickly food moves through the gut, and/or changes in gut immune responses.
Nervous system
The nervous system has several divisions: the central division involving the brain and spinal cord and the peripheral division consisting of the autonomic and somatic nervous systems.
The autonomic nervous system has a direct role in physical response to stress and is divided into the sympathetic nervous system (SNS), and the parasympathetic nervous system (PNS). When the body is stressed, the SNS contributes to what is known as the “fight or flight” response. The body shifts its energy resources toward fighting off a life threat, or fleeing from an enemy.
The SNS signals the adrenal glands to release hormones called adrenalin (epinephrine) and cortisol. These hormones, together with direct actions of autonomic nerves, cause the heart to beat faster, respiration rate to increase, blood vessels in the arms and legs to dilate, digestive process to change and glucose levels (sugar energy) in the bloodstream to increase to deal with the emergency.
The SNS response is fairly sudden in order to prepare the body to respond to an emergency situation or acute stress—short term stressors. Once the crisis is over, the body usually returns to the pre-emergency, unstressed state. This recovery is facilitated by the PNS, which generally has opposing effects to the SNS. But PNS over-activity can also contribute to stress reactions, for example, by promoting bronchoconstriction (e.g., in asthma) or exaggerated vasodilation and compromised blood circulation.
Both the SNS and the PNS have powerful interactions with the immune system, which can also modulate stress reactions. The central nervous system is particularly important in triggering stress responses, as it regulates the autonomic nervous system and plays a central role in interpreting contexts as potentially threatening.
Chronic stress, experiencing stressors over a prolonged period of time, can result in a long-term drain on the body. As the autonomic nervous system continues to trigger physical reactions, it causes a wear-and-tear on the body. It’s not so much what chronic stress does to the nervous system, but what continuous activation of the nervous system does to other bodily systems that become problematic.
Male reproductive system
The male reproductive system is influenced by the nervous system. The parasympathetic part of the nervous system causes relaxation whereas the sympathetic part causes arousal. In the male anatomy, the autonomic nervous system, also known as the fight or flight response, produces testosterone and activates the sympathetic nervous system which creates arousal.
Stress causes the body to release the hormone cortisol, which is produced by the adrenal glands. Cortisol is important to blood pressure regulation and the normal functioning of several body systems including cardiovascular, circulatory, and male reproduction. Excess amounts of cortisol can affect the normal biochemical functioning of the male reproductive system.
Sexual desire Chronic stress, ongoing stress over an extended period of time, can affect testosterone production resulting in a decline in sex drive or libido, and can even cause erectile dysfunction or impotence.
Reproduction Chronic stress can also negatively impact sperm production and maturation, causing difficulties in couples who are trying to conceive. Researchers have found that men who experienced two or more stressful life events in the past year had a lower percentage of sperm motility (ability to swim) and a lower percentage of sperm of normal morphology (size and shape), compared with men who did not experience any stressful life events.
Diseases of the reproductive system When stress affects the immune system, the body can become vulnerable to infection. In the male anatomy, infections to the testes, prostate gland, and urethra, can affect normal male reproductive functioning.
Female reproductive system
Menstruation Stress may affect menstruation among adolescent girls and women in several ways. For example, high levels of stress may be associated with absent or irregular menstrual cycles, more painful periods, and changes in the length of cycles.
Sexual desire Women juggle personal, family, professional, financial, and a broad range of other demands across their life span. Stress, distraction, fatigue, etc., may reduce sexual desire—especially when women are simultaneously caring for young children or other ill family members, coping with chronic medical problems, feeling depressed, experiencing relationship difficulties or abuse, dealing with work problems, etc.
Pregnancy Stress can have significant impact on a woman’s reproductive plans. Stress can negatively impact a woman’s ability to conceive, the health of her pregnancy, and her postpartum adjustment. Depression is the leading complication of pregnancy and postpartum adjustment.
Excess stress increases the likelihood of developing depression and anxiety during this time. Maternal stress can negatively impact fetal and ongoing childhood development and disrupt bonding with the baby in the weeks and months following delivery.
Premenstrual syndrome Stress may make premenstrual symptoms worse or more difficult to cope with and premenses symptoms may be stressful for many women. These symptoms include cramping, fluid retention and bloating, negative mood (feeling irritable and “blue”) and mood swings.
Menopause As menopause approaches, hormone levels fluctuate rapidly. These changes are associated with anxiety, mood swings, and feelings of distress. Thus menopause can be a stressor in and of itself. Some of the physical changes associated with menopause, especially hot flashes, can be difficult to cope with.
Furthermore, emotional distress may cause the physical symptoms to be worse. For example, women who are more anxious may experience an increased number of hot flashes and/or more severe or intense hot flashes.
Diseases of the reproductive system When stress is high, there is increased chance of exacerbation of symptoms of reproductive disease states, such as herpes simplex virus or polycystic ovarian syndrome. The diagnosis and treatment of reproductive cancers can cause significant stress, which warrants additional attention and support.
Stress management
These recent discoveries about the effects of stress on health shouldn’t leave you worrying. We now understand much more about effective strategies for reducing stress responses. Such beneficial strategies include:
- Maintaining a healthy social support network
- Engaging in regular physical exercise
- Getting an adequate amount of sleep each night
These approaches have important benefits for physical and mental health, and form critical building blocks for a healthy lifestyle. If you would like additional support or if you are experiencing extreme or chronic stress, a licensed psychologist can help you identify the challenges and stressors that affect your daily life and find ways to help you best cope for improving your overall physical and mental well-being.
APA gratefully acknowledges the assistance of William Shaw, PhD; Susan Labott-Smith, PhD, ABPP; Matthew M. Burg, PhD; Camelia Hostinar, PhD; Nicholas Alen, BA; Miranda A.L. van Tilburg, PhD; Gary G. Berntson, PhD; Steven M. Tovian, PhD, ABPP, FAClinP, FAClinHP; and Malina Spirito, PsyD, MEd; in developing this article.
Recommended Reading

You may also like

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Publications about Stress

This fact sheet is intended for teens and young adults and presents information about stress, anxiety, and ways to cope when feeling overwhelmed.

This infographic briefly presents information about stress, anxiety, and ways to cope when feeling overwhelmed. It was developed for use on social media to highlight the “I’m So Stressed Out” fact sheet.

This fact sheet presents information about how to assess your mental health and determine if you need help. It provides examples of mild and severe symptoms, as well as self-care activities and options for professional help.

This free, printable coloring and activity book for children ages 8-12 teaches kids about stress and anxiety and offers tips for coping in a healthy way.

The Stress Catcher is a printable, “fortune teller” craft for children that offers coping strategies to help manage stress and other difficult emotions. Instructions on how to create and use the Stress Catcher are provided.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

STRESS AND HEALTH: Psychological, Behavioral, and Biological Determinants
Stressors have a major influence upon mood, our sense of well-being, behavior, and health. Acute stress responses in young, healthy individuals may be adaptive and typically do not impose a health burden. However, if the threat is unremitting, particularly in older or unhealthy individuals, the long-term effects of stressors can damage health. The relationship between psychosocial stressors and disease is affected by the nature, number, and persistence of the stressors as well as by the individual’s biological vulnerability (i.e., genetics, constitutional factors), psychosocial resources, and learned patterns of coping. Psychosocial interventions have proven useful for treating stress-related disorders and may influence the course of chronic diseases.
INTRODUCTION
Claude Bernard (1865/1961) noted that the maintenance of life is critically dependent on keeping our internal milieu constant in the face of a changing environment. Cannon (1929) called this “homeostasis.” Selye (1956) used the term “stress” to represent the effects of anything that seriously threatens homeostasis. The actual or perceived threat to an organism is referred to as the “stressor” and the response to the stressor is called the “stress response.” Although stress responses evolved as adaptive processes, Selye observed that severe, prolonged stress responses might lead to tissue damage and disease.
Based on the appraisal of perceived threat, humans and other animals invoke coping responses ( Lazarus & Folkman 1984 ). Our central nervous system (CNS) tends to produce integrated coping responses rather than single, isolated response changes ( Hilton 1975 ). Thus, when immediate fight-or-flight appears feasible, mammals tend to show increased autonomic and hormonal activities that maximize the possibilities for muscular exertion ( Cannon 1929 , Hess 1957 ). In contrast, during aversive situations in which an active coping response is not available, mammals may engage in a vigilance response that involves sympathetic nervous system (SNS) arousal accompanied by an active inhibition of movement and shunting of blood away from the periphery ( Adams et al. 1968 ). The extent to which various situations elicit different patterns of biologic response is called “situational stereotypy” ( Lacey 1967 ).
Although various situations tend to elicit different patterns of stress responses, there are also individual differences in stress responses to the same situation. This tendency to exhibit a particular pattern of stress responses across a variety of stressors is referred to as “response stereotypy” ( Lacey & Lacey 1958 ). Across a variety of situations, some individuals tend to show stress responses associated with active coping, whereas others tend to show stress responses more associated with aversive vigilance ( Kasprowicz et al. 1990 , Llabre et al. 1998 ).
Although genetic inheritance undoubtedly plays a role in determining individual differences in response stereotypy, neonatal experiences in rats have been shown to produce long-term effects in cognitive-emotional responses ( Levine 1957 ). For example, Meaney et al. (1993) showed that rats raised by nurturing mothers have increased levels of central serotonin activity compared with rats raised by less nurturing mothers. The increased serotonin activity leads to increased expression of a central glucocorticoid receptor gene. This, in turn, leads to higher numbers of glucocorticoid receptors in the limbic system and improved glucocorticoid feedback into the CNS throughout the rat’s life. Interestingly, female rats who receive a high level of nurturing in turn become highly nurturing mothers whose offspring also have high levels of glucocorticoid receptors. This example of behaviorally induced gene expression shows how highly nurtured rats develop into low-anxiety adults, who in turn become nurturing mothers with reduced stress responses.
In contrast to highly nurtured rats, pups separated from their mothers for several hours per day during early life have a highly active hypothalamic-pituitary adrenocortical axis and elevated SNS arousal ( Ladd et al. 2000 ). These deprived rats tend to show larger and more frequent stress responses to the environment than do less deprived animals.
Because evolution has provided mammals with reasonably effective homeostatic mechanisms (e.g., baroreceptor reflex) for dealing with short-term stressors, acute stress responses in young, healthy individuals typically do not impose a health burden. However, if the threat is persistent, particularly in older or unhealthy individuals, the long-term effects of the response to stress may damage health ( Schneiderman 1983 ). Adverse effects of chronic stressors are particularly common in humans, possibly because their high capacity for symbolic thought may elicit persistent stress responses to a broad range of adverse living and working conditions. The relationship between psychosocial stressors and chronic disease is complex. It is affected, for example, by the nature, number, and persistence of the stressors as well as by the individual’s biological vulnerability (i.e., genetics, constitutional factors) and learned patterns of coping. In this review, we focus on some of the psychological, behavioral, and biological effects of specific stressors, the mediating psychophysiological pathways, and the variables known to mediate these relationships. We conclude with a consideration of treatment implications.
PSYCHOLOGICAL ASPECTS OF STRESS
Stressors during childhood and adolescence and their psychological sequelae.
The most widely studied stressors in children and adolescents are exposure to violence, abuse (sexual, physical, emotional, or neglect), and divorce/marital conflict (see Cicchetti 2005 ). McMahon et al. (2003) also provide an excellent review of the psychological consequences of such stressors. Psychological effects of maltreatment/abuse include the dysregulation of affect, provocative behaviors, the avoidance of intimacy, and disturbances in attachment ( Haviland et al. 1995 , Lowenthal 1998 ). Survivors of childhood sexual abuse have higher levels of both general distress and major psychological disturbances including personality disorders ( Polusny & Follett 1995 ). Childhood abuse is also associated with negative views toward learning and poor school performance ( Lowenthal 1998 ). Children of divorced parents have more reported antisocial behavior, anxiety, and depression than their peers ( Short 2002 ). Adult offspring of divorced parents report more current life stress, family conflict, and lack of friend support compared with those whose parents did not divorce ( Short 2002 ). Exposure to nonresponsive environments has also been described as a stressor leading to learned helplessness ( Peterson & Seligman 1984 ).
Studies have also addressed the psychological consequences of exposure to war and terrorism during childhood ( Shaw 2003 ). A majority of children exposed to war experience significant psychological morbidity, including both post-traumatic stress disorder (PTSD) and depressive symptoms. For example, Nader et al. (1993) found that 70% of Kuwaiti children reported mild to severe PTSD symptoms after the Gulf War. Some effects are long lasting: Macksound & Aber (1996) found that 43% of Lebanese children continued to manifest post-traumatic stress symptoms 10 years after exposure to war-related trauma.
Exposure to intense and chronic stressors during the developmental years has long-lasting neurobiological effects and puts one at increased risk for anxiety and mood disorders, aggressive dyscontrol problems, hypo-immune dysfunction, medical morbidity, structural changes in the CNS, and early death ( Shaw 2003 ).
Stressors During Adulthood and Their Psychological Sequelae
Life stress, anxiety, and depression.
It is well known that first depressive episodes often develop following the occurrence of a major negative life event ( Paykel 2001 ). Furthermore, there is evidence that stressful life events are causal for the onset of depression (see Hammen 2005 , Kendler et al. 1999 ). A study of 13,006 patients in Denmark, with first psychiatric admissions diagnosed with depression, found more recent divorces, unemployment, and suicides by relatives compared with age- and gender-matched controls ( Kessing et al. 2003 ). The diagnosis of a major medical illness often has been considered a severe life stressor and often is accompanied by high rates of depression ( Cassem 1995 ). For example, a meta-analysis found that 24% of cancer patients are diagnosed with major depression ( McDaniel et al. 1995 ).
Stressful life events often precede anxiety disorders as well ( Faravelli & Pallanti 1989 , Finlay-Jones & Brown 1981 ). Interestingly, long-term follow-up studies have shown that anxiety occurs more commonly before depression ( Angst &Vollrath 1991 , Breslau et al. 1995 ). In fact, in prospective studies, patients with anxiety are most likely to develop major depression after stressful life events occur ( Brown et al. 1986 ).
DISORDERS RELATED TO TRAUMA
Lifetime exposure to traumatic events in the general population is high, with estimates ranging from 40% to 70% ( Norris 1992 ). Of note, an estimated 13% of adult women in the United States have been exposed to sexual assault ( Kilpatrick et al. 1992 ). The Diagnostic and Statistical Manual (DSM-IV-TR; American Psychiatric Association 2000 ) includes two primary diagnoses related to trauma: Acute Stress Disorder (ASD) and PTSD. Both these disorders have as prominent features a traumatic event involving actual or threatened death or serious injury and symptom clusters including re-experiencing of the traumatic event (e.g., intrusive thoughts), avoidance of reminders/numbing, and hyperarousal (e.g., difficulty falling or staying asleep). The time frame for ASD is shorter (lasting two days to four weeks), with diagnosis limited to within one month of the incident. ASD was introduced in 1994 to describe initial trauma reactions, but it has come under criticism ( Harvey & Bryant 2002 ) for weak empirical and theoretical support. Most people who have symptoms of PTSD shortly after a traumatic event recover and do not develop PTSD. In a comprehensive review, Green (1994) estimates that approximately 25% of those exposed to traumatic events develop PTSD. Surveys of the general population indicate that PTSD affects 1 in 12 adults at some time in their life ( Kessler et al. 1995 ). Trauma and disasters are related not only to PTSD, but also to concurrent depression, other anxiety disorders, cognitive impairment, and substance abuse ( David et al. 1996 , Schnurr et al. 2002 , Shalev 2001 ).
Other consequences of stress that could provide linkages to health have been identified, such as increases in smoking, substance use, accidents, sleep problems, and eating disorders. Populations that live in more stressful environments (communities with higher divorce rates, business failures, natural disasters, etc.) smoke more heavily and experience higher mortality from lung cancer and chronic obstructive pulmonary disorder ( Colby et al. 1994 ). A longitudinal study following seamen in a naval training center found that more cigarette smoking occurred on high-stress days ( Conway et al. 1981 ). Life events stress and chronically stressful conditions have also been linked to higher consumption of alcohol ( Linsky et al. 1985 ). In addition, the possibility that alcohol may be used as self-medication for stress-related disorders such as anxiety has been proposed. For example, a prospective community study of 3021 adolescents and young adults ( Zimmerman et al. 2003 ) found that those with certain anxiety disorders (social phobia and panic attacks) were more likely to develop substance abuse or dependence prospectively over four years of follow-up. Life in stressful environments has also been linked to fatal accidents ( Linsky & Strauss 1986 ) and to the onset of bulimia ( Welch et al. 1997 ). Another variable related to stress that could provide a link to health is the increased sleep problems that have been reported after sychological trauma ( Harvey et al. 2003 ). New onset of sleep problems mediated the relationship between post-traumatic stress symptoms and decreased natural killer (NK) cell cytotoxicity in Hurricane Andrew victims ( Ironson et al. 1997 ).
Variations in Stress Responses
Certain characteristics of a situation are associated with greater stress responses. These include the intensity or severity of the stressor and controllability of the stressor, as well as features that determine the nature of the cognitive responses or appraisals. Life event dimensions of loss, humiliation, and danger are related to the development of major depression and generalized anxiety ( Kendler et al. 2003 ). Factors associated with the development of symptoms of PTSD and mental health disorders include injury, damage to property, loss of resources, bereavement, and perceived life threat ( Freedy et al. 1992 , Ironson et al. 1997 , McNally 2003 ). Recovery from a stressor can also be affected by secondary traumatization ( Pfefferbaum et al. 2003 ). Other studies have found that multiple facets of stress that may work synergistically are more potent than a single facet; for example, in the area of work stress, time pressure in combination with threat ( Stanton et al. 2001 ), or high demand in combination with low control ( Karasek & Theorell 1990 ).
Stress-related outcomes also vary according to personal and environmental factors. Personal risk factors for the development of depression, anxiety, or PTSD after a serious life event, disaster, or trauma include prior psychiatric history, neuroticism, female gender, and other sociodemographic variables ( Green 1996 , McNally 2003 , Patton et al. 2003 ). There is also some evidence that the relationship between personality and environmental adversity may be bidirectional ( Kendler et al. 2003 ). Levels of neuroticism, emotionality, and reactivity correlate with poor interpersonal relationships as well as “event proneness.” Protective factors that have been identified include, but are not limited to, coping, resources (e.g., social support, self-esteem, optimism), and finding meaning. For example, those with social support fare better after a natural disaster ( Madakaisira & O’Brien 1987 ) or after myocardial infarction ( Frasure-Smith et al. 2000 ). Pruessner et al. (1999) found that people with higher self-esteem performed better and had lower cortisol responses to acute stressors (difficult math problems). Attaching meaning to the event is another protective factor against the development of PTSD, even when horrific torture has occurred. Left-wing political activists who were tortured by Turkey’s military regime had lower rates of PTSD than did nonactivists who were arrested and tortured by the police ( Basoğlu et al. 1994 ).
Finally, human beings are resilient and in general are able to cope with adverse situations. A recent illustration is provided by a study of a nationally representative sample of Israelis after 19 months of ongoing exposure to the Palestinian intifada. Despite considerable distress, most Israelis reported adapting to the situation without substantial mental health symptoms or impairment ( Bleich et al. 2003 ).
BIOLOGICAL RESPONSES TO STRESSORS
Acute stress responses.
Following the perception of an acute stressful event, there is a cascade of changes in the nervous, cardiovascular, endocrine, and immune systems. These changes constitute the stress response and are generally adaptive, at least in the short term ( Selye 1956 ). Two features in particular make the stress response adaptive. First, stress hormones are released to make energy stores available for the body’s immediate use. Second, a new pattern of energy distribution emerges. Energy is diverted to the tissues that become more active during stress, primarily the skeletal muscles and the brain. Cells of the immune system are also activated and migrate to “battle stations” ( Dhabar & McEwen 1997 ). Less critical activities are suspended, such as digestion and the production of growth and gonadal hormones. Simply put, during times of acute crisis, eating, growth, and sexual activity may be a detriment to physical integrity and even survival.
Stress hormones are produced by the SNS and hypothalamic-pituitary adrenocortical axis. The SNS stimulates the adrenal medulla to produce catecholamines (e.g., epinephrine). In parallel, the paraventricular nucleus of the hypothalamus produces corticotropin releasing factor, which in turn stimulates the pituitary to produce adrenocorticotropin. Adrenocorticotropin then stimulates the adrenal cortex to secrete cortisol. Together, catecholamines and cortisol increase available sources of energy by promoting lipolysis and the conversion of glycogen into glucose (i.e., blood sugar). Lipolysis is the process of breaking down fats into usable sources of energy (i.e., fatty acids and glycerol; Brindley & Rollan 1989 ).
Energy is then distributed to the organs that need it most by increasing blood pressure levels and contracting certain blood vessels while dilating others. Blood pressure is increased with one of two hemodynamic mechanisms ( Llabre et al.1998 , Schneiderman & McCabe 1989 ). The myocardial mechanism increases blood pressure through enhanced cardiac output; that is, increases in heart rate and stroke volume (i.e., the amount of blood pumped with each heart beat). The vascular mechanism constricts the vasculature, thereby increasing blood pressure much like constricting a hose increases water pressure. Specific stressors tend to elicit either myocardial or vascular responses, providing evidence of situational stereotypy ( Saab et al. 1992 , 1993 ). Laboratory stressors that call for active coping strategies, such as giving a speech or performing mental arithmetic, require the participant to do something and are associated with myocardial responses. In contrast, laboratory stressors that call for more vigilant coping strategies in the absence of movement, such as viewing a distressing video or keeping one’s foot in a bucket of ice water, are associated with vascular responses. From an evolutionary perspective, cardiac responses are believed to facilitate active coping by shunting blood to skeletal muscles, consistent with the fight-or-flight response. In situations where decisive action would not be appropriate, but instead skeletal muscle inhibition and vigilance are called for, a vascular hemodynamic response is adaptive. The vascular response shunts blood away from the periphery to the internal organs, thereby minimizing potential bleeding in the case of physical assault.
Finally, in addition to the increased availability and redistribution of energy, the acute stress response includes activation of the immune system. Cells of the innate immune system (e.g., macrophages and natural killer cells), the first line of defense, depart from lymphatic tissue and spleen and enter the bloodstream, temporarily raising the number of immune cells in circulation (i.e., leukocytosis). From there, the immune cells migrate into tissues that are most likely to suffer damage during physical confrontation (e.g., the skin). Once at “battle stations,” these cells are in position to contain microbes that may enter the body through wounds and thereby facilitate healing ( Dhabar & McEwen 1997 ).
Chronic Stress Responses
The acute stress response can become maladaptive if it is repeatedly or continuously activated ( Selye 1956 ). For example, chronic SNS stimulation of the cardiovascular system due to stress leads to sustained increases in blood pressure and vascular hypertrophy ( Henry et al. 1975 ). That is, the muscles that constrict the vasculature thicken, producing elevated resting blood pressure and response stereotypy, or a tendency to respond to all types of stressors with a vascular response. Chronically elevated blood pressure forces the heart to work harder, which leads to hypertrophy of the left ventricle ( Brownley et al. 2000 ). Over time, the chronically elevated and rapidly shifting levels of blood pressure can lead to damaged arteries and plaque formation.
The elevated basal levels of stress hormones associated with chronic stress also suppress immunity by directly affecting cytokine profiles. Cytokines are communicatory molecules produced primarily by immune cells (see Roitt et al. 1998 ). There are three classes of cytokines. Proinflammatory cytokines mediate acute inflammatory reactions. Th1 cytokines mediate cellular immunity by stimulating natural killer cells and cytotoxic T cells, immune cells that target intracellular pathogens (e.g., viruses). Finally, Th2 cytokines mediate humoral immunity by stimulating B cells to produce antibody, which “tags” extracellular pathogens (e.g., bacteria) for removal. In a meta-analysis of over 30 years of research, Segerstrom & Miller (2004) found that intermediate stressors, such as academic examinations, could promote a Th2 shift (i.e., an increase in Th2 cytokines relative to Th1 cytokines). A Th2 shift has the effect of suppressing cellular immunity in favor of humoral immunity. In response to more chronic stressors (e.g., long-term caregiving for a dementia patient), Segerstrom & Miller found that proinflammatory, Th1, and Th2 cytokines become dysregulated and lead both to suppressed humoral and cellular immunity. Intermediate and chronic stressors are associated with slower wound healing and recovery from surgery, poorer antibody responses to vaccination, and antiviral deficits that are believed to contribute to increased vulnerability to viral infections (e.g., reductions in natural killer cell cytotoxicity; see Kiecolt-Glaser et al. 2002 ).
Chronic stress is particularly problematic for elderly people in light of immunosenescence, the gradual loss of immune function associated with aging. Older adults are less able to produce antibody responses to vaccinations or combat viral infections ( Ferguson et al. 1995 ), and there is also evidence of a Th2 shift ( Glaser et al. 2001 ). Although research has yet to link poor vaccination responses to early mortality, influenza and other infectious illnesses are a major cause of mortality in the elderly, even among those who have received vaccinations (e.g., Voordouw et al. 2003 ).
PSYCHOSOCIAL STRESSORS AND HEALTH
Cardiovascular disease.
Both epidemiological and controlled studies have demonstrated relationships between psychosocial stressors and disease. The underlying mediators, however, are unclear in most cases, although possible mechanisms have been explored in some experimental studies. An occupational gradient in coronary heart disease (CHD) risk has been documented in which men with relatively low socioeconomic status have the poorest health outcomes ( Marmot 2003 ). Much of the risk gradient in CHD can be eliminated, however, by taking into account lack of perceived job control, which is a potent stressor ( Marmot et al. 1997 ). Other factors include risky behaviors such as smoking, alcohol use, and sedentary lifestyle ( Lantz et al. 1998 ), which may be facilitated by stress. Among men ( Schnall et al. 1994 ) and women ( Eaker 1998 ), work stress has been reported to be a predictor of incident CHD and hypertension ( Ironson 1992 ). However, in women with existing CHD, marital stress is a better predictor of poor prognosis than is work stress ( Orth-Gomer et al. 2000 ).
Although the observational studies cited thus far reveal provocative associations between psychosocial stressors and disease, they are limited in what they can tell us about the exact contribution of these stressors or about how stress mediates disease processes. Animal models provide an important tool for helping to understand the specific influences of stressors on disease processes. This is especially true of atherosclerotic CHD, which takes multiple decades to develop in humans and is influenced by a great many constitutional, demographic, and environmental factors. It would also be unethical to induce disease in humans by experimental means.
Perhaps the best-known animal model relating stress to atherosclerosis was developed by Kaplan et al. (1982) . Their study was carried out on male cynomolgus monkeys, who normally live in social groups. The investigators stressed half the animals by reorganizing five-member social groups at one- to three-month intervals on a schedule that ensured that each monkey would be housed with several new animals during each reorganization. The other half of the animals lived in stable social groups. All animals were maintained on a moderately atherogenic diet for 22 months. Animals were also assessed for their social status (i.e., relative dominance) within each group. The major findings were that ( a ) socially dominant animals living in unstable groups had significantly more atherosclerosis than did less dominant animals living in unstable groups; and ( b ) socially dominant male animals living in unstable groups had significantly more atherosclerosis than did socially dominant animals living in stable groups. Other important findings based upon this model have been that heart-rate reactivity to the threat of capture predicts severity of atherosclerosis ( Manuck et al. 1983 ) and that administration of the SNS-blocking agent propranolol decreases the progression of atherosclerosis ( Kaplan et al. 1987 ). In contrast to the findings in males, subordinate premenstrual females develop greater atherosclerosis than do dominant females ( Kaplan et al. 1984 ) because they are relatively estrogen deficient, tending to miss ovulatory cycles ( Adams et al. 1985 ).
Whereas the studies in cynomolgus monkeys indicate that emotionally stressful behavior can accelerate the progression of atherosclerosis, McCabe et al. (2002) have provided evidence that affiliative social behavior can slow the progression of atherosclerosis in the Watanabe heritable hyperlipidemic rabbit. This rabbit model has a genetic defect in lipoprotein clearance such that it exhibits hypercholesterolemia and severe atherosclerosis. The rabbits were assigned to one of three social or behavioral groups: ( a ) an unstable group in which unfamiliar rabbits were paired daily, with the pairing switched each week; ( b ) a stable group, in which littermates were paired daily for the entire study; and ( c ) an individually caged group. The stable group exhibited more affiliative behavior and less agonistic behavior than the unstable group and significantly less atherosclerosis than each of the other two groups. The study emphasizes the importance of behavioral factors in atherogenesis, even in a model of disease with extremely strong genetic determinants.
Upper Respiratory Diseases
The hypothesis that stress predicts susceptibility to the common cold received support from observational studies ( Graham et al. 1986 , Meyer & Haggerty 1962 ). One problem with such studies is that they do not control for exposure. Stressed people, for instance, might seek more outside contact and thus be exposed to more viruses. Therefore, in a more controlled study, people were exposed to a rhinovirus and then quarantined to control for exposure to other viruses ( Cohen et al. 1991 ). Those individuals with the most stressful life events and highest levels of perceived stress and negative affect had the greatest probability of developing cold symptoms. In a subsequent study of volunteers inoculated with a cold virus, it was found that people enduring chronic, stressful life events (i.e., events lasting a month or longer including unemployment, chronic underemployment, or continued interpersonal difficulties) had a high likelihood of catching cold, whereas people subjected to stressful events lasting less than a month did not ( Cohen et al. 1998 ).
Human Immunodeficiency Virus
The impact of life stressors has also been studied within the context of human immunodeficiency virus (HIV) spectrum disease. Leserman et al. (2000) followed men with HIV for up to 7.5 years and found that faster progression to AIDS was associated with higher cumulative stressful life events, use of denial as a coping mechanism, lower satisfaction with social support, and elevated serum cortisol.
Inflammation, the Immune System, and Physical Health
Despite the stress-mediated immunosuppressive effects reviewed above, stress has also been associated with exacerbations of autoimmune disease ( Harbuz et al. 2003 ) and other conditions in which excessive inflammation is a central feature, such as CHD ( Appels et al. 2000 ). Evidence suggests that a chronically activated, dysregulated acute stress response is responsible for these associations. Recall that the acute stress response includes the activation and migration of cells of the innate immune system. This effect is mediated by proinflammatory cytokines. During periods of chronic stress, in the otherwise healthy individual, cortisol eventually suppresses proinflammatory cytokine production. But in individuals with autoimmune disease or CHD, prolonged stress can cause proinflammatory cytokine production to remain chronically activated, leading to an exacerbation of pathophysiology and symptomatology.
Miller et al. (2002) proposed the glucocorticoid-resistance model to account for this deficit in proinflammatory cytokine regulation. They argue that immune cells become “resistant” to the effects of cortisol (i.e., a type of glucocorticoid), primarily through a reduction, or downregulation, in the number of expressed cortisol receptors. With cortisol unable to suppress inflammation, stress continues to promote proinflammatory cytokine production indefinitely. Although there is only preliminary empirical support for this model, it could have implications for diseases of inflammation. For example, in rheumatoid arthritis, excessive inflammation is responsible for joint damage, swelling, pain, and reduced mobility. Stress is associated with more swelling and reduced mobility in rheumatoid arthritis patients ( Affleck et al. 1997 ). Similarly, in multiple sclerosis (MS), an overactive immune system targets and destroys the myelin surrounding nerves, contributing to a host of symptoms that include paralysis and blindness. Again, stress is associated with an exacerbation of disease ( Mohr et al. 2004 ). Even in CHD, inflammation plays a role. The immune system responds to vascular injury just as it would any other wound: Immune cells migrate to and infiltrate the arterial wall, setting off a cascade of biochemical processes that can ultimately lead to a thrombosis (i.e., clot; Ross 1999 ). Elevated levels of inflammatory markers, such as C-reactive protein (CRP), are predictive of heart attacks, even when controlling for other traditional risk factors (e.g., cholesterol, blood pressure, and smoking; Morrow & Ridker 2000 ). Interestingly, a history of major depressive episodes has been associated with elevated levels of CRP in men ( Danner et al. 2003 ).
Inflammation, Cytokine Production, and Mental Health
In addition to its effects on physical health, prolonged proinflammatory cytokine production may also adversely affect mental health in vulnerable individuals. During times of illness (e.g., the flu), proinflammatory cytokines feed back to the CNS and produce symptoms of fatigue, malaise, diminished appetite, and listlessness, which are symptoms usually associated with depression. It was once thought that these symptoms were directly caused by infectious pathogens, but more recently, it has become clear that proinflammatory cytokines are both sufficient and necessary (i.e., even absent infection or fever) to generate sickness behavior ( Dantzer 2001 , Larson & Dunn 2001 ).
Sickness behavior has been suggested to be a highly organized strategy that mammals use to combat infection ( Dantzer 2001 ). Symptoms of illness, as previously thought, are not inconsequential or even maladaptive. On the contrary, sickness behavior is thought to promote resistance and facilitate recovery. For example, an overall decrease in activity allows the sick individual to preserve energy resources that can be redirected toward enhancing immune activity. Similarly, limiting exploration, mating, and foraging further preserves energy resources and reduces the likelihood of risky encounters (e.g., fighting over a mate). Furthermore, decreasing food intake also decreases the level of iron in the blood, thereby decreasing bacterial replication. Thus, for a limited period, sickness behavior may be looked upon as an adaptive response to the stress of illness.
Much like other aspects of the acute stress response, however, sickness behavior can become maladaptive when repeatedly or continuously activated. Many features of the sickness behavior response overlap with major depression. Indeed, compared with healthy controls, elevated rates of depression are reported in patients with inflammatory diseases such as MS ( Mohr et al. 2004 ) or CHD ( Carney et al. 1987 ). Granted, MS patients face a number of stressors and reports of depression are not surprising. However, when compared with individuals facing similar disability who do not have MS (e.g., car accident victims), MS patients still report higher levels of depression ( Ron & Logsdail 1989 ). In both MS ( Fassbender et al. 1998 ) and CHD ( Danner et al. 2003 ), indicators of inflammation have been found to be correlated with depressive symptomatology. Thus, there is evidence to suggest that stress contributes to both physical and mental disease through the mediating effects of proinflammatory cytokines.
HOST VULNERABILITY-STRESSOR INTERACTIONS AND DISEASE
The changes in biological set points that occur across the life span as a function of chronic stressors are referred to as allostasis, and the biological cost of these adjustments is known as allostatic load ( McEwen 1998 ). McEwen has also suggested that cumulative increases in allostatic load are related to chronic illness. These are intriguing hypotheses that emphasize the role that stressors may play in disease. The challenge, however, is to show the exact interactions that occur among stressors, pathogens, host vulnerability (both constitutional and genetic), and such poor health behaviors as smoking, alcohol abuse, and excessive caloric consumption. Evidence of a lifetime trajectory of comorbidities does not necessarily imply that allostatic load is involved since immunosenescence, genetic predisposition, pathogen exposure, and poor health behaviors may act as culprits.
It is not clear, for example, that changes in set point for variables such as blood pressure are related to cumulative stressors per se, at least in healthy young individuals. Thus, for example, British soldiers subjected to battlefield conditions for more than a year in World War II showed chronic elevations in blood pressure, which returned to normal after a couple of months away from the front ( Graham 1945 ). In contrast, individuals with chronic illnesses such as chronic fatigue syndrome may show a high rate of relapse after a relatively acute stressor such as a hurricane ( Lutgendorf et al. 1995 ). Nevertheless, by emphasizing the role that chronic stressors may play in multiple disease outcomes, McEwen has helped to emphasize an important area of study.
TREATMENT FOR STRESS-RELATED DISORDERS
For PTSD, useful treatments include cognitive-behavioral therapy (CBT), along with exposure and the more controversial Eye Movement Desensitization and Reprocessing ( Foa & Meadows 1997 , Ironson et al. 2002 , Shapiro 1995 ). Psychopharmacological approaches have also been suggested ( Berlant 2001 ). In addition, writing about trauma has been helpful both for affective recovery and for potential health benefit ( Pennebaker 1997 ). For outpatients with major depression, Beck’s CBT ( Beck 1976 ) and interpersonal therapy ( Klerman et al. 1984 ) are as effective as psychopharmacotherapy ( Clinical Practice Guidelines 1993 ). However, the presence of sleep problems or hypercortisolemia is associated with poorer response to psychotherapy ( Thase 2000 ). The combination of psychotherapy and pharmacotherapy seems to offer a substantial advantage over psychotherapy alone for the subset of patients who are more severely depressed or have recurrent depression ( Thase et al. 1997 ). For the treatment of anxiety, it depends partly on the specific disorder [e.g., generalized anxiety disorder (GAD), panic disorder, social phobia], although CBT including relaxation training has demonstrated efficacy in several subtypes of anxiety ( Borkovec & Ruscio 2001 ). Antidepressants such as selective serotonin reuptake inhibitors also show efficacy in anxiety ( Ballenger et al. 2001 ), especially when GAD is comorbid with major depression, which is the case in 39% of subjects with current GAD ( Judd et al. 1998 ).
BEHAVIORAL INTERVENTIONS IN CHRONIC DISEASE
Patients dealing with chronic, life-threatening diseases must often confront daily stressors that can threaten to undermine even the most resilient coping strategies and overwhelm the most abundant interpersonal resources. Psychosocial interventions, such as cognitive-behavioral stress management (CBSM), have a positive effect on the quality of life of patients with chronic disease ( Schneiderman et al. 2001 ). Such interventions decrease perceived stress and negative mood (e.g., depression), improve perceived social support, facilitate problem-focused coping, and change cognitive appraisals, as well as decrease SNS arousal and the release of cortisol from the adrenal cortex. Psychosocial interventions also appear to help chronic pain patients reduce their distress and perceived pain as well as increase their physical activity and ability to return to work ( Morley et al. 1999 ). These psychosocial interventions can also decrease patients’ overuse of medications and utilization of the health care system. There is also some evidence that psychosocial interventions may have a favorable influence on disease progression ( Schneiderman et al. 2001 ).
Morbidity, Mortality, and Markers of Disease Progression
Psychosocial intervention trials conducted upon patients following acute myocardial infarction (MI) have reported both positive and null results. Two meta-analyses have reported a reduction in both mortality and morbidity of approximately 20% to 40% ( Dusseldorp et al. 1999 , Linden et al. 1996 ). Most of these studies were carried out in men. The major study reporting positive results was the Recurrent Coronary Prevention Project (RCPP), which employed group-based CBT, and decreased hostility and depressed affect ( Mendes de Leon et al. 1991 ), as well as the composite medical end point of cardiac death and nonfatal MI ( Friedman et al. 1986 ).
In contrast, the major study reporting null results for medical end points was the Enhancing Recovery in Coronary Heart Disease (ENRICHD) clinical trial ( Writing Committee for ENRICHD Investigators 2003 ), which found that the intervention modestly decreased depression and increased perceived social support, but did not affect the composite medical end point of death and nonfatal MI. However, a secondary analysis, which examined the effects of the psychosocial intervention within gender by ethnicity subgroups, found significant decreases approaching 40% in both cardiac death and nonfatal MI for white men but not for other subgroups such as minority women ( Schneiderman et al. 2004 ). Although there were important differences between the RCPP and ENRICHD in terms of the objectives of psychosocial intervention and the duration and timing of treatment, it should also be noted that more than 90% of the patients in the RCPP were white men. Thus, because primarily white men, but not other subgroups, may have benefited from the ENRICHD intervention, future studies need to attend to variables that may have prevented morbidity and mortality benefits among gender and ethnic subgroups other than white men.
Psychosocial intervention trials conducted upon patients with cancer have reported both positive and null results with regard to survival ( Classen 1998 ). A number of factors that generally characterized intervention trials that observed significant positive effects on survival were relatively absent in trials that failed to show improved survival. These included: ( a ) having only patients with the same type and severity of cancer within each group, ( b ) creation of a supportive environment, ( c ) having an educational component, and ( d ) provision of stress-management and coping-skills training. In one study that reported positive results, Fawzy et al. (1993) found that patients with early stage melanoma assigned to a six-week cognitive-behavioral stress management (CBSM) group showed significantly longer survival and longer time to recurrence over a six-year follow-up period compared with those receiving surgery and standard care alone. The intervention also significantly reduced distress, enhanced active coping, and increased NK cell cytotoxicity compared with controls.
Although published studies have not yet shown that psychosocial interventions can decrease disease progression in HIV/AIDS, several studies have significantly influenced factors that have been associated with HIV/AIDS disease progression ( Schneiderman & Antoni 2003 ). These variables associated with disease progression include distress, depressed affect, denial coping, low perceived social support, and elevated serum cortisol ( Ickovics et al. 2001 , Leserman et al. 2000 ). Antoni et al. have used group-based CBSM (i.e., CBT plus relaxation training) to decrease the stress-related effects of HIV+ serostatus notification. Those in the intervention condition showed lower distress, anxiety, and depressed mood than did those in the control condition as well as lower antibody titers of herpesviruses and higher levels of T-helper (CD4) cells, NK cells, and lymphocyte proliferation ( Antoni et al. 1991 , Esterling et al. 1992 ). In subsequent studies conducted upon symptomatic HIV+ men who were not attempting to determine their HIV serostatus, CBSM decreased distress, dysphoria, anxiety, herpesvirus antibody titers, cortisol, and epinephrine ( Antoni et al. 2000a , b ; Lutgendorf et al. 1997 ). Improvement in perceived social support and adaptive coping skills mediated the decreases in distress ( Lutgendorf et al. 1998 ). In summary, it appears that CBSM can positively influence stress-related variables that have been associated with HIV/AIDS progression. Only a randomized clinical trial, however, could document that CBSM can specifically decrease HIV/AIDS disease progression.
Stress is a central concept for understanding both life and evolution. All creatures face threats to homeostasis, which must be met with adaptive responses. Our future as individuals and as a species depends on our ability to adapt to potent stressors. At a societal level, we face a lack of institutional resources (e.g., inadequate health insurance), pestilence (e.g., HIV/AIDS), war, and international terrorism that has reached our shores. At an individual level, we live with the insecurities of our daily existence including job stress, marital stress, and unsafe schools and neighborhoods. These are not an entirely new condition as, in the last century alone, the world suffered from instances of mass starvation, genocide, revolutions, civil wars, major infectious disease epidemics, two world wars, and a pernicious cold war that threatened the world order. Although we have chosen not to focus on these global threats in this paper, they do provide the backdrop for our consideration of the relationship between stress and health.
A widely used definition of stressful situations is one in which the demands of the situation threaten to exceed the resources of the individual ( Lazarus & Folkman 1984 ). It is clear that all of us are exposed to stressful situations at the societal, community, and interpersonal level. How we meet these challenges will tell us about the health of our society and ourselves. Acute stress responses in young, healthy individuals may be adaptive and typically do not impose a health burden. Indeed, individuals who are optimistic and have good coping responses may benefit from such experiences and do well dealing with chronic stressors ( Garmezy 1991 , Glanz & Johnson 1999 ). In contrast, if stressors are too strong and too persistent in individuals who are biologically vulnerable because of age, genetic, or constitutional factors, stressors may lead to disease. This is particularly the case if the person has few psychosocial resources and poor coping skills. In this chapter, we have documented associations between stressors and disease and have described how endocrine-immune interactions appear to mediate the relationship. We have also described how psychosocial stressors influence mental health and how psychosocial treatments may ameliorate both mental and physical disorders. There is much we do not yet know about the relationship between stress and health, but scientific findings being made in the areas of cognitive-emotional psychology, molecular biology, neuroscience, clinical psychology, and medicine will undoubtedly lead to improved health outcomes.
ACKNOWLEDGMENTS
Preparation of this manuscript was supported by NIH grants P01-MH49548, P01- HL04726, T32-HL36588, R01-MH66697, and R01-AT02035. We thank Elizabeth Balbin, Adam Carrico, and Orit Weitzman for library research.
LITERATURE CITED
- Adams DB, Bacelli G, Mancia G, Zanchetti A. Cardiovascular changes during naturally elicited fighting behavior in the cat. Am. J. Physiol. 1968; 216 :1226–1235. [ PubMed ] [ Google Scholar ]
- Adams MR, Kaplan JR, Koritnik DR. Psychosocial influences on ovarian, endocrine and ovulatory function in Macaca fascicularis . Physiol. Behav. 1985; 35 :935–940. [ PubMed ] [ Google Scholar ]
- Affleck G, Urrows S, Tennen H, Higgins P, Pav D, Aloisi R. A dual pathway model of daily stressor effects on rheumatoid arthritis. Ann. Behav. Med. 1997; 19 :161–170. [ PubMed ] [ Google Scholar ]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders IV-TR. 4th ed. Washington, DC: Am. Psychiatr. Assoc.; 2000. [ Google Scholar ]
- Angst J, Vollrath M. The natural history of anxiety disorders. Acta Psychiatr. Scand. 1991; 84 :446–452. [ PubMed ] [ Google Scholar ]
- Antoni MH, Baggett L, Ironson G, LaPerriere A, Klimas N, et al. Cognitive behavioral stress management intervention buffers distress responses and elevates immunologic markers following notification of HIV-1 seropositivity. J. Consult. Clin. Psychol. 1991; 59 :906–915. [ PubMed ] [ Google Scholar ]
- Antoni MH, Cruess DG, Cruess S, Lutgendorf S, Kumar M, et al. Cognitive behavioral stress management intervention effects on anxiety, 24-hour urinary catecholamine output, and T-cytotoxic/suppressor cells over time among symptomatic HIV-infected gay men. J. Consult. Clin. Psychol. 2000a; 68 :31–45. [ PubMed ] [ Google Scholar ]
- Antoni MH, Cruess S, Cruess DG, Kumar M, Lutgendorf S, et al. Cognitive-behavioral stress management reduces distress and 24-hour urinary free cortisol output among symptomatic HIV-infected gay men. Ann. Behav. Med. 2000b; 22 :29–37. [ PubMed ] [ Google Scholar ]
- Appels A, Bar FW, Bar J, Bruggeman C, de Bates M. Inflammation, depressive symptomatology, and coronary artery disease. Psychosom. Med. 2000; 62 :601–605. [ PubMed ] [ Google Scholar ]
- Ballenger JC, Davidson JRT, Lecrubier Y, Nutt DJ, Borkovec TD, et al. Consensus statement on generalized anxiety disorder from the international consensus group on depression and anxiety. J. Clin. Psychiatry. 2001; 62 :53–58. [ PubMed ] [ Google Scholar ]
- Başoğlu M, Parker M, Parker Ö, Özmen E, Marks I, et al. Psychological effects of torture: a comparison of tortured with non-tortured political activists in Turkey. Am. J. Psychiatry. 1994; 151 :76–81. [ PubMed ] [ Google Scholar ]
- Baum A. Stress, intrusive imagery, and chronic distress. Health Psychol. 1990; 9 :653–675. [ PubMed ] [ Google Scholar ]
- Beck AT. Cognitive Therapy and the Emotional Disorders. New York: Int. Univ. Press; 1976. [ Google Scholar ]
- Berlant JL. Topiramate in posttraumatic stress disorder: preliminary clinical observations. J. Clin. Psychiatry. 2001; 62 :60–63. [ PubMed ] [ Google Scholar ]
- Bernard C. An Introduction to the Study of Experimental Medicine. Transl. HC Greene. New York: Collier; 18651961. [ Google Scholar ]
- Bleich A, Gelkopf M, Solomon Z. Exposure to terrorism, stress-related mental health symptoms, and coping behaviors among a nationally representative sample in Israel. JAMA. 2003; 290 :612–620. [ PubMed ] [ Google Scholar ]
- Borkovec TD, Ruscio AM. Psychotherapy for generalized anxiety disorder. J. Clin. Psychiatry. 2001; 61 :37–42. [ PubMed ] [ Google Scholar ]
- Breslau N, Davis GC, Andreski P, Peterson E. Sex differences in depression: a role for preexisting anxiety. Psychiatr. Res. 1995; 58 :1–12. [ PubMed ] [ Google Scholar ]
- Brindley D, Rollan Y. Possible connections between stress, diabetes, obesity, hypertension, and altered lipoprotein metabolism that may result in atherosclerosis. Clin. Sci. 1989; 77 :453–461. [ PubMed ] [ Google Scholar ]
- Brown GW, Bifulco A, Harris T, Bridge L. Life stress, chronic subclinical symptoms and vulnerability to clinical depression. J. Affect. Disord. 1986; 11 :1–19. [ PubMed ] [ Google Scholar ]
- Brownley KA, Hurwitz BE, Schneiderman N. Cardiovascular psychophysiology. In: Cacioppo JT, Tassinary LG, Berntson GG, editors. Handbook of Psychophysiology. 2nd ed. New York: Cambridge Univ.; 2000. pp. 224–264. [ Google Scholar ]
- Cannon WB. Bodily Changes in Pain, Hunger, Fear and Rage. 2nd ed. New York: Appleton; 1929. [ Google Scholar ]
- Carney RM, Rich MW, Tevelde A, Saini J, Clark K, Jaffe AS. Major depressive disorder in coronary artery disease. Am. J. Cardiol. 1987; 60 :1273–1275. [ PubMed ] [ Google Scholar ]
- Cassem EH. Depressive disorders in the medically ill: an overview. Psychosomatics. 1995; 36 :S2–S10. [ PubMed ] [ Google Scholar ]
- Cicchetti D. Child maltreatment. Annu. Rev. Clin. Psychol. 2005; 1 :409–438. [ PubMed ] [ Google Scholar ]
- Classen C, Sephton SE, Diamond S, Spiegel D. Studies of life-extending psychosocial interventions. In: Holland J, editor. Textbook of Psycho-Oncology. New York: Oxford Univ. Press; 1998. pp. 730–742. [ Google Scholar ]
- Clinical Practice Guidelines. No. 5. Depression in Primary Care. Vol. 2: Treatment of Major Depression. Rockville, MD: US Dept. Health Hum. Serv., Agency Health Care Policy Res.; 1993. AHCPR Publ. 93-0551.
- Cohen S, Frank E, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM., Jr Types of stressors that increase susceptibility to the common cold in healthy adults. Health Psychol. 1998; 17 :214–223. [ PubMed ] [ Google Scholar ]
- Cohen S, Tyrrell DA, Smith AP. Psychological stress and susceptibility to the common cold. N. Engl. J. Med. 1991; 325 :606–612. [ PubMed ] [ Google Scholar ]
- Colby JP, Linsky AS, Straus MA. Social stress and state-to-state differences in smoking-related mortality in the United States. Soc. Sci. Med. 1994; 38 :373–381. [ PubMed ] [ Google Scholar ]
- Conway TL, Vickers RR, Ward HW, Rahe RH. Occupational stress and variation in cigarette, coffee and alcohol consumption. J. Health Soc. Behav. 1981; 22 :156–165. [ PubMed ] [ Google Scholar ]
- Danner M, Kasl SV, Abramson JL, Vaccarion V. Association between depression and elevated C-reactive protein. Psychosom. Med. 2003; 65 :347–356. [ PubMed ] [ Google Scholar ]
- Dantzer R. Cytokine-induced sickness behavior: Where do we stand? Brain Behav. Immun. 2001; 15 :7–24. [ PubMed ] [ Google Scholar ]
- David D, Mellman TA, Mendoza LM, Kulick-Bell R, Ironson G, Schneiderman N. Psychiatric morbidity following Hurricane Andrew. Int. Soc. Trauma. Stress Stud. 1996; 9 :607–612. [ PubMed ] [ Google Scholar ]
- Dhabar FS, McEwen BS. Acute stress enhances while chronic stress suppresses cell-mediated immunity in vivo: a potential role for leukocyte trafficking. Brain Behav. Immun. 1997; 11 :286–306. [ PubMed ] [ Google Scholar ]
- Dusseldorp E, van Elderen T, Maes S, Meulman J, Kraaij V. A meta-analysis of psychoeducational programs for coronary heart disease patients. Health Psychol. 1999; 18 :506–519. [ PubMed ] [ Google Scholar ]
- Eaker ED. Psychosocial risk factors for coronary heart disease in women. Cardiovasc. Clin. 1998; 16 :103–111. [ PubMed ] [ Google Scholar ]
- Esterling BA, Antoni MH, Schneiderman N, Carver CS, LaPerriere A, et al. Psychosocial modulation of antibody to Epstein-Barr viral capsid antigen and herpes virus type-6 HIV-1 infected and at-risk gay men. Psychosom. Med. 1992; 54 :354–371. [ PubMed ] [ Google Scholar ]
- Faravelli C, Pallanti S. Recent life events and panic disorder. Am. J. Psychiatry. 1989; 146 :622–626. [ PubMed ] [ Google Scholar ]
- Fassbender K, Schmidt R, Mossner R, Kischka U, Kuhnen J, et al. Mood disorders and dysfunction of the hypothalamic-pituitary-adrenal axis in multiple sclerosis: associations with cerebral inflammation. Arch. Neurol. 1998; 55 :66–72. [ PubMed ] [ Google Scholar ]
- Fawzy FI, Fawzy NW, Hyun CS, Elashoff R, Guthrie D, et al. Malignant melanoma. Effects of an early structured psychiatric intervention, coping and affective state on recurrence and survival 6 years later. Arch. Gen. Psychol. 1993; 50 :681–689. [ PubMed ] [ Google Scholar ]
- Ferguson RG, Wikby A, Maxson P, Olsson J, Johansson B. Immune parameters in a longitudinal study of a very old population of Swedish people: a comparison between survivors and nonsurvivors. J. Gerontol. 1995; 50 :B378–B382. [ PubMed ] [ Google Scholar ]
- Finlay-Jones R, Brown GW. Types of stressful life events and the onset of anxiety and depressive disorders. Psychol. Med. 1981; 11 :803–815. [ PubMed ] [ Google Scholar ]
- Foa EB, Meadows EA. Psychosocial treatments for posttraumatic stress disorder: critical review. Annu. Rev. Psychol. 1997; 48 :449–480. [ PubMed ] [ Google Scholar ]
- Frasure-Smith N, Lespérance F, Gravel G, Masson A, Juneau M, et al. Social support, depression, and mortality during the first year after myocardial infarction. Circulation. 2000; 101 :1919–1924. [ PubMed ] [ Google Scholar ]
- Freedy JR, Shaw DL, Jarrell MP, Masters CR. Towards an understanding of the psychological impact of natural disasters: an application of the conservation of resources stress model. J. Trauma. Stress. 1992; 5 :441–454. [ Google Scholar ]
- Friedman M, Thoresen CE, Gill JJ, Ulmer D, Powell LH, et al. Alteration of type A behavior and its effects on cardiac recurrences in post myocardial patients: summary results of the Recurrent Coronary Prevention Project. Am. Heart J. 1986; 112 :653–665. [ PubMed ] [ Google Scholar ]
- Garmezy N. Resiliency and vulnerability to adverse developmental outcomes associated with poverty. Am. Behav. Sci. 1991; 34 :416–430. [ Google Scholar ]
- Glanz MD, Johnson JL. Resilience and Development: Positive Life Adaptations. New York: Kluwer Acad./Plenum; 1999. [ Google Scholar ]
- Glaser R, MacCallum RC, Laskowski BF, Malarkey WB, Sheridan JF, Kiecolt-Glaser JK. Evidence for a shift in the Th-1 to Th-2 cytokine response associated with chronic stress and aging. J. Gerontol. 2001; 56 :M477–M482. [ PubMed ] [ Google Scholar ]
- Graham JDP. High blood pressure after battle. Lancet. 1945; 248 :239–240. [ Google Scholar ]
- Graham NMH, Douglas RB, Ryan P. Stress and acute respiratory infection. Am. J. Epidemiol. 1986; 124 :389–401. [ PubMed ] [ Google Scholar ]
- Green BL. Psychosocial research in traumatic stress: an update. J. Trauma. Stress. 1994; 7 :341–362. [ PubMed ] [ Google Scholar ]
- Green BL. Traumatic stress and disaster: mental health effects and factors influencing adaptation. In: Mak FL, Nadelson C, editors. International Review of Psychiatry. Washington, DC: Am. Psychiatr. Press; 1996. pp. 177–211. [ Google Scholar ]
- Hammen C. Stress and depression. Annu. Rev. Clin. Psychol. 2005; 1 :293–319. [ PubMed ] [ Google Scholar ]
- Harbuz MS, Chover-Gonzalez AJ, Jessop DS. Hypothalamo-pituitary-adrenal axis and chronic immune activation. Ann. NY Acad. Sci. 2003; 992 :99–106. [ PubMed ] [ Google Scholar ]
- Harvey AG, Bryant RA. Acute stress disorder: a synthesis and critique. Psychol. Bull. 2002; 128 :886–902. [ PubMed ] [ Google Scholar ]
- Harvey AG, Jones C, Schmidt DA. Sleep and posttraumatic stress disorder: a review. Clin. Psychol. Rev. 2003; 23 :377–407. [ PubMed ] [ Google Scholar ]
- Haviland MG, Sonne JL, Woods LR. Beyond posttraumatic stress disorder: object relations and reality testing disturbances in physically and sexually abused adolescents. J. Am. Acad. Child Adolesc. Psychiatry. 1995; 34 :1054–1059. [ PubMed ] [ Google Scholar ]
- Henry JP, Stephens PM, Santisteban GA. A model of psychosocial hypertension showing reversibility and progression of cardiovascular complications. Circ. Res. 1975; 36 :156–164. [ PubMed ] [ Google Scholar ]
- Hess WR. Functional Organization of the Diencephalons. New York: Grune & Stratton; 1957. [ Google Scholar ]
- Hilton SM. Ways of viewing the central nervous control of the circulation—old and new. Brain Res. 1975; 87 :213–228. [ PubMed ] [ Google Scholar ]
- Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schumm P, Boland RJ. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women. JAMA. 2001; 285 :1466–1474. [ PubMed ] [ Google Scholar ]
- Ironson GH. Job stress and health. In: Cranny CJ, Smith PC, Stone EF, editors. Job Satisfaction: How People Feel About Their Jobs and How It Affects Their Performance. New York: Lexington; 1992. pp. 219–239. [ Google Scholar ]
- Ironson GH, Freund B, Strauss JL, Williams J. Comparison of two treatments for traumatic stress: a community-based study of EMDR and prolonged exposure. J. Clin. Psychol. 2002; 58 :113–128. [ PubMed ] [ Google Scholar ]
- Ironson GH, Wynings C, Schneiderman N, Baum A, Rodriguez M, et al. Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosom. Med. 1997; 59 :128–141. [ PubMed ] [ Google Scholar ]
- Judd LL, Kessler RC, Paulus MP, Zeller PV, Whittchen HU, Kunovac JL. Comorbidity as a fundamental feature of generalized anxiety disorders: results from the National Comorbidity Survey (NCS) Acta Psychiatr. Scand. Suppl. 1998; 393 :6–11. [ PubMed ] [ Google Scholar ]
- Kaplan JR, Adams MR, Clarkson TB, Koritnik DR. Psychosocial influences on female “protection” among cynomolgues macaques. Atherosclerosis. 1984; 53 :283–295. [ PubMed ] [ Google Scholar ]
- Kaplan JR, Manuck SB, Adams MR, Weingard KW, Clarkson TB. Inhibition of coronary atherosclerosis by propranolol in behaviorally predisposed monkeys fed an atherogenic diet. Circulation. 1987; 76 :1364–1372. [ PubMed ] [ Google Scholar ]
- Kaplan JR, Manuck SB, Clarkson TB, Lusso FM, Taub DM. Social status, environment and atherosclerosis in cynomolgus monkeys. Arteriosclerosis. 1982; 2 :359–368. [ PubMed ] [ Google Scholar ]
- Karasek RA, Theorell TG. Healthy Work. New York: Basic Books; 1990. [ Google Scholar ]
- Kasprowicz AL, Manuck SB, Malkoff SB, Krantz DS. Individual differences in behaviorally evoked cardiovascular response: temporal stability and hemodynamic patterning. Psychophysiology. 1990; 27 :605–619. [ PubMed ] [ Google Scholar ]
- Kendler KS, Gardner CO, Prescott CA. Personality and the experience of environmental adversity. Psychol. Med. 2003; 33 :1193–1202. [ PubMed ] [ Google Scholar ]
- Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment and danger in the prediction of onsets of major depression and generalized anxiety. Arch. Gen. Psychiatry. 2003; 60 :789–796. [ PubMed ] [ Google Scholar ]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am. J. Psychiatry. 1999; 156 :837–841. [ PubMed ] [ Google Scholar ]
- Kessing LV, Agerbro E, Mortensen PB. Does the impact of major stressful life events on the risk of developing depression change throughout life? Psychol. Med. 2003; 33 :1177–1184. [ PubMed ] [ Google Scholar ]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry. 1995; 52 :1048–1060. [ PubMed ] [ Google Scholar ]
- Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology: psychological influences on immune function and health. J. Consult. Clin. Psychol. 2002; 70 :537–547. [ PubMed ] [ Google Scholar ]
- Kilpatrick DG, Edmunds CN, Seymour AK. Rape in America: A Report to the Nation. Arlington, VA: Natl. Victims Cent.; 1992. [ Google Scholar ]
- Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal Psycho-Therapy of Depression. New York: Basic Books; 1984. [ Google Scholar ]
- Lacey JI. Somatic response patterning and stress: some revisions of activation theory. In: Appleyo MH, Trumble R, editors. Psychological Stress. New York: Appleton-Century-Crofts; 1967. p. 14. [ Google Scholar ]
- Lacey JL, Lacey BC. Verification and extension of the principle of autonomic response stereotyping. Am. J. Psychol. 1958; 71 :50–73. [ PubMed ] [ Google Scholar ]
- Ladd CO, Huot RL, Thrivikraman P, Nemeroff CB, Meaney MJ, Plotsky PM. Long-term behavioral and neuroendocrine adaptations to adverse early experience. Prog. Brain Res. 2000; 122 :79–101. [ PubMed ] [ Google Scholar ]
- Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from nationally representative prospective study of US adults. JAMA. 1998; 279 :1703–1708. [ PubMed ] [ Google Scholar ]
- Larson SJ, Dunn AJ. Behavioral effects of cytokines. Brain Behav. Immun. 2001; 15 :371–387. [ PubMed ] [ Google Scholar ]
- Lazarus RS, Folkman S. Stress, Appraisal and Coping. New York: Springer; 1984. [ Google Scholar ]
- Leserman J, Pettito JM, Golden RN, Gaynes BN, Gu H, Perkins DO. The impact of stressful life events, depression, social support, coping and cortisol on progression to AIDS. Am. J. Psychiatry. 2000; 57 :1221–1228. [ PubMed ] [ Google Scholar ]
- Levine S. Infantile experience and resistance to physiological stress. Science. 1957; 126 :405–406. [ PubMed ] [ Google Scholar ]
- Linden W, Stossel C, Maurice J. Psychosocial interventions for patients with coronary artery disease. Arch. Intern. Med. 1996; 156 :745–752. [ PubMed ] [ Google Scholar ]
- Linsky AS, Strauss M. Social Stress in the United States: Links to Regional Patterns in Crime and Illness. Dover, MA: Auburn House; 1986. [ Google Scholar ]
- Linsky AS, Strauss MA, Colby JP. Stressful events, stressful conditions, and alcohol problems in the United States: a partial test of the Bales theory of alcoholism. J. Stud. Alcohol. 1985; 46 :72–80. [ PubMed ] [ Google Scholar ]
- Llabre MM, Klein BR, Saab PG, McCalla JB, Schneiderman N. Classification of individual differences in cardiovascular responsivity. The contribution of reactor type controlling for race and gender. Int. J. Behav. Med. 1998; 5 :213–229. [ PubMed ] [ Google Scholar ]
- Lowenthal B. The effects of early childhood abuse and the development of resiliency. Early Child Dev. Care. 1998; 142 :43–52. [ Google Scholar ]
- Lutgendorf S, Antoni MH, Ironson G, Fletcher MA, Penedo F, Van Riel F. Physical symptoms of chronic fatigue syndrome are exacerbated by the stress of Hurricane Andrew. Psychiatr. Med. 1995; 57 :310–325. [ PubMed ] [ Google Scholar ]
- Lutgendorf S, Antoni MH, Ironson G, Klimas N, Fletcher MA, Schneiderman N. Cognitive processing style, mood, and immune function following HIV seropositivity notification. Cogn. Ther. Res. 1997; 21 :157–184. [ Google Scholar ]
- Lutgendorf S, Antoni MH, Ironson G, Starr K, Costello N, et al. Changes in cognitive coping skills and social support mediate distress outcomes in symptomatic HIV-seropositive gay men during a cognitive behavioral stress management intervention. Psychosom. Med. 1998; 60 :204–214. [ PubMed ] [ Google Scholar ]
- Macksound M, Aber J. The war experience and psychosocial development of children in Lebanon. Child Dev. 1996; 67 :70–88. [ PubMed ] [ Google Scholar ]
- Madakasira S, O’Brien KF. Acute post-traumatic stress disorder in victims of a natural disaster. J. Nerv. Ment. Dis. 1987; 175 :286–290. [ PubMed ] [ Google Scholar ]
- Manuck SB, Kamarack TW, Kasprowica AS, Waldstein SR. Stability and patterning of behaviorally evoked cardiovascular reactivity. In: Blascovich J, Katkin ES, editors. Cardiovascular Reactivity to Psychological Stress and Disease. Washington, DC: Am. Psychol. Assoc.; 1993. pp. 111–134. [ Google Scholar ]
- Manuck SB, Kaplan JR, Clarkson TB. Behaviorally induced heart rate reactivity and atherosclerosis in cynomolgus monkeys. Psychosom. Med. 1983; 45 :95–108. [ PubMed ] [ Google Scholar ]
- Marmot M. Social resources and health. In: Kessel F, Rosenfield PL, Anderson NB, editors. Expanding the Boundaries of Health and Social Science. New York: Oxford Univ. Press; 2003. pp. 259–285. [ Google Scholar ]
- Marmot MG, Bosma H, Hemingway H, Brunner EJ, Stansfeld S. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997; 350 :235–239. [ PubMed ] [ Google Scholar ]
- McCabe PM, Gonzalez JA, Zaias J, Szeto A, Kumar M, et al. Social environment influences the progression of atherosclerosis in the Watanabe heritable hyperlipidemic rabbit. Circulation. 2002; 105 :354–359. [ PubMed ] [ Google Scholar ]
- McDaniel JS, Musselman DL, Porter MR, Reed DA, Nemeroff CB. Depression in patients with cancer. diagnosis biology and treatment. Arch. Gen. Psychiatry. 1995; 2 :89–99. [ PubMed ] [ Google Scholar ]
- McEwen BS. Protective and damaging effects of stress mediators. N. Engl. J. Med. 1998; 338 :171–179. [ PubMed ] [ Google Scholar ]
- McEwen BS, Steller E. Stress and the individual: mechanisms leading to disease. Arch. Intern. Med. 1993; 153 :2093–2101. [ PubMed ] [ Google Scholar ]
- McMahon SD, Grant KE, Compas BE, Thurm AE, Ey S. Stress and psychopathology in children and adolescents: Is there evidence of specificity? J. Child Psychol. Psychiatry. 2003; 44 :107–133. [ PubMed ] [ Google Scholar ]
- McNally RJ. Psychological mechanisms in acute response to trauma. Biol. Psychiatry. 2003; 53 :779–788. [ PubMed ] [ Google Scholar ]
- Meaney MJ, Bhatnagan S, Dioria J, Larogue S, Francis D, et al. Molecular basis for the development of individual differences in the hypothalamic-pituitary-adrenal stress response. Cell. Mol. Neurobiol. 1993; 13 :321–347. [ PubMed ] [ Google Scholar ]
- Mendes de Leon CF, Powell LH, Kaplan BH. Change in coronary-prone behaviors in the recurrent coronary prevention project. Psychosom. Med. 1991; 53 :407–419. [ PubMed ] [ Google Scholar ]
- Meyer RJ, Haggerty RJ. Streptococcal infection in families. Pediatrics. 1962; 29 :539–549. [ PubMed ] [ Google Scholar ]
- Miller GE, Cohen S, Ritchey AK. Chronic psychological stress and regulation of pro-inflammatory cytokines: a glucocorticoid-resistance model. Health Psychol. 2002; 21 :531–541. [ PubMed ] [ Google Scholar ]
- Mohr DC, Classen C, Barrera M. The relationship between social support, depression and treatment for depression in people with multiple sclerosis. Psychol. Med. 2004; 34 :533–541. [ PubMed ] [ Google Scholar ]
- Mohr DC, Hart SL, Julian L, Cox D, Pelletier D. Association between stressful life events and exacerbation in multiple sclerosis: a meta-analysis. Br. Med. J. 2004; 328 :731. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy and behavior therapy for chronic pain in adults, excluding headache. Pain. 1999; 80 :1–13. [ PubMed ] [ Google Scholar ]
- Morrow DA, Ridker PM. C-reactive protein, inflammation, and coronary disease. Med. Clin. North Am. 2000; 81 :149–161. [ PubMed ] [ Google Scholar ]
- Nader KO, Pynoos RS, Fairbanks LA, al Ajeel M, al-Asfour A. A preliminary study of PTSD and grief among the children of Kuwait following the Gulf crisis. Br. J. Clin. Psychol. 1993; 32 :407–416. [ PubMed ] [ Google Scholar ]
- Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J. Consult. Clin. Psychol. 1992; 60 :409–418. [ PubMed ] [ Google Scholar ]
- O’Donnell ML, Creamer M, Bryant RA, Schnyder U, Shalev A. Posttraumatic disorders following injury: an empirical and methodological review. Clin. Psychol. Rev. 2003; 23 :587–603. [ PubMed ] [ Google Scholar ]
- Orth-Gomér K, Wamala SP, Horsten M, Schenk-Gustafsson K, Schneiderman N, Mittleman MA. Marital stress worsens prognosis in women with coronary heart disease. JAMA. 2000; 284 :3008–3014. [ PubMed ] [ Google Scholar ]
- Patton GC, Coffey C, Posterino M, Carlin JB, Bowes G. Life events and early onset depression: cause or consequence? Psychol. Med. 2003; 33 :1203–1210. [ PubMed ] [ Google Scholar ]
- Paykel ES. Stress and affective disorders in humans. Semin. Clin. Neuropsychiatry. 2001; 6 :4–11. [ PubMed ] [ Google Scholar ]
- Pennebaker JW. Writing about emotional experiences as a therapeutic process. Psychol. Sci. 1997; 8 :162–164. [ Google Scholar ]
- Peterson C, Seligman MEP. Causal explanations as a risk factor for depression: theory and evidence. Psychol. Rev. 1984; 91 :347–374. [ PubMed ] [ Google Scholar ]
- Pfefferbaum B, Sconzo GM, Flynn BW, Kearns LJ, Doughty DE, et al. Case finding and mental health services for children in the aftermath of the Oklahoma City bombing. J. Behav. Health Serv. Res. 2003; 30 :215–227. [ PubMed ] [ Google Scholar ]
- Polusny MA, Follette VM. Long-term correlates of childhood sexual abuse: theory and review of the empirical literature. Appl. Prev. Psychol. 1995; 4 :143–166. [ Google Scholar ]
- Pruessner JC, Hellhammer DH, Kirschbaum C. Low self-esteem, induced failure and the adrenocortical stress response. Personal. Individ. Differ. 1999; 27 :477–489. [ Google Scholar ]
- Roitt I, Brostoff J, Male D. Immunology. 5th ed. London: Mosby Int.; 1998. p. 125. [ Google Scholar ]
- Ron M, Logsdail S. Psychiatric morbidity in multiple sclerosis: a clinical and MRI study. Psychol. Med. 1989; 19 :887–895. [ PubMed ] [ Google Scholar ]
- Ross R. Atherosclerosis—an inflammatory disease. N. Engl. J. Med. 1999; 340 :115–126. [ PubMed ] [ Google Scholar ]
- Saab PG, Llabre MM, Hurwitz BE, Frame CA, Reineke LJ, et al. Myocardial and peripheral vascular responses to behavioral changes and their stability in black and white Americans. Psychophysiology. 1992; 29 :384–397. [ PubMed ] [ Google Scholar ]
- Saab PG, Llabre MM, Hurwitz BE, Schneiderman N, Wohlgemuth W, et al. The cold pressor test: vascular and myocardial response patterns and their stability. Psychophysiology. 1993; 30 :366–373. [ PubMed ] [ Google Scholar ]
- Schnall PL, Landsbergis PA, Baker D. Job strain and cardiovascular disease. Annu. Rev. Public Health. 1994; 15 :381–411. [ PubMed ] [ Google Scholar ]
- Schneiderman N. Pathophysiology in animals. In: Dembroski TM, Schmidt TH, Blümhen G, editors. Biobehavioral Bases of Coronary Heart Disease. Basel: Karger; 1983. pp. 304–364. [ Google Scholar ]
- Schneiderman N, Antoni MH. Learning to cope with HIV/AIDS. In: Kessel F, Rosenfield PL, Anderson NB, editors. Expanding the Boundaries of Health and Social Science. New York: Oxford Univ. Press; 2003. pp. 316–347. [ Google Scholar ]
- Schneiderman N, Antoni MH, Saab PG, Ironson G. Health psychology: psychosocial and biobehavioral aspects of chronic disease management. Annu. Rev. Psychol. 2001; 52 :555–580. [ PubMed ] [ Google Scholar ]
- Schneiderman N, McCabe P. Psychophysiologic strategies in laboratory research. In: Schneiderman N, Weiss SM, Kaufmann PG, editors. Handbook of Research Methods in Cardiovascular Behavioral Medicine. New York: Plenum; 1989. pp. 349–364. [ Google Scholar ]
- Schneiderman N, Saab PG, Catellier DJ, Powell LH, DeBusk RF, et al. Psychosocial treatment within gender by ethnicity subgroups in the enhancing recovery in coronary heart disease (ENRICHD) clinic trial. Psychosom. Med. 2004; 66 :475–483. [ PubMed ] [ Google Scholar ]
- Schnurr PP, Friedman J, Bernardy NC. Research on posttraumatic stress disorder: epidemiology, pathophysiology and assessment. Psychother. Pract. 2002; 58 :877–889. [ PubMed ] [ Google Scholar ]
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analysis of 30 years of inquiry. Psychol. Bull. 2004; 130 :601–630. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Selye H. The Stress of Life. New York: McGraw-Hill; 1956. [ Google Scholar ]
- Shalev AY. What is posttraumatic stress disorder? J. Clin. Psychiatry. 2001; 62 :4–10. [ PubMed ] [ Google Scholar ]
- Shapiro F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols, and Procedures. New York: Guilford; 1995. [ Google Scholar ]
- Shaw JA. Children exposed to war/terrorism. Clin. Child Fam. Psychol. Rev. 2003; 6 :237–246. [ PubMed ] [ Google Scholar ]
- Short JL. The effects of parental divorce during childhood on college students. J. Divorce Remarriage. 2002; 38 :143–156. [ Google Scholar ]
- Stanton JM, Balzer WK, Smith PC, Parra LF, Ironson G. A general measure of work stress: the stress in general scale. Educ. Psychol. Meas. 2001; 61 :866–888. [ Google Scholar ]
- Thase ME. Treatment of severe depression. J. Clin. Psychiatry. 2000; 61 :17–25. [ PubMed ] [ Google Scholar ]
- Thase ME, Greenhouse JB, Frank E. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Arch. Gen. Psychiatry. 1997; 54 :1009–1015. [ PubMed ] [ Google Scholar ]
- Voordouw BC, van der Linden PD, Simonia S, van der Lei J, Sturkenboom MC, Stricker BH. Influenza vaccination in community-dwelling elderly: impact on mortality and influenza-associated morbidity. Arch. Intern. Med. 2003; 163 :1089–1094. [ PubMed ] [ Google Scholar ]
- Welch SL, Doll HA, Fairburn CG. Life events and the onset of bulimia nervosa: a controlled study. Psychol. Med. 1997; 27 :515–522. [ PubMed ] [ Google Scholar ]
- Writing Committee for ENRICHD Investigators. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease patients (ENRICHD) randomized trial. JAMA. 2003; 289 :3106–3116. [ PubMed ] [ Google Scholar ]
- Zimmerman P, Wittchen HU, Hofler M, Pfister H, Kessler RC, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: a 4-year community study of adolescents and young adults. Psychol. Med. 2003; 33 :1211–1222. [ PubMed ] [ Google Scholar ]
- How Brain Rot is silently ruining our lives: A Psychological Perspective
- 5 Hacks to Increase Self-Awareness
- Is Gambling Evil?: Understanding Gambling Disorder and its Causes
- We all need to (and can) get back on our feet after facing an Academic Failure
- Study Reveals Potential Link Between Multiple Sclerosis and Reduced Alzheimer’s Risk

Your cart is empty

7 Ways to Manage Assignment Stress in Students
- by Psychologs Magazine
- April 3, 2024
- 5 minutes read
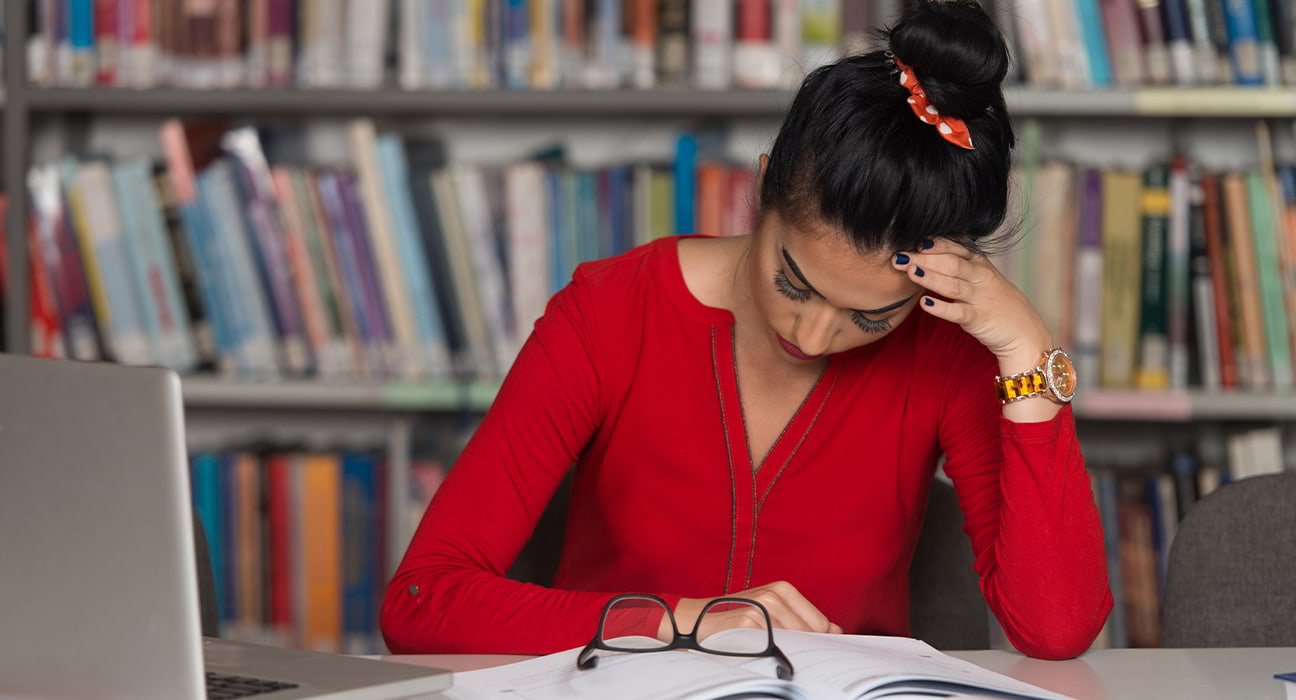
The experience of attending university may be both thrilling and stressful at the same time. Beginning college, tests, homework due dates, living with strangers, and future-focused thoughts can all cause stress. Stress is a normal emotion that is meant to assist you deal with difficult circumstances. It might be beneficial in moderation since it motivates you to put in your best effort and work hard—for example, during exams. However, extreme stress or the belief that you are unable to control your stress can result in mental health issues including anxiety and depression. It might also have an impact on your academic standing. Let’s find some effective strategies to help students manage assignment stress with some practical tips.
Students and Stress
Every student experiences stress at some point, whether it’s from having five assignments due on the same day or what seems like endless back-to-back tests. And you have to be superhuman if you don’t.
The American College Health Association (ACHA) reports that 12.7% of college students report having excessive stress, while 44.9% report having stress levels that are above normal. It’s normal for students to experience periods of extreme stress due to the numerous obligations and demands placed on them by their academic programs. However, you need to identify the source of your stress and learn coping mechanisms when it interferes with your everyday tasks.
Also Read: NMC Sets up National Task Force to Address Mental Health of medical students
Students may experience increased stress, and anxiety as a result of the pressure to serve well academically and complete their assignments. It can be extremely stressful to constantly, worry about turning in homework on time and getting good grades.
Here are the ways by which assignment stress can be reduced in College Students:
Making a study schedule:.
The reason most students fail or are unable to complete the given assignment at the right time is that they don’t have a study schedule that corresponds with their academic schedule. They underestimate the amount of study time required to complete tasks and overestimate the amount of time they have available. Also, they mistakenly believe they have enough time to finish their assignments on time because of their current schedule—or lack thereof. They begin too late, get behind, and ultimately take shortcuts. Reaching parity is nearly unattainable.

Making a study timetable is just meant to help you figure out when you have time to study, which will help you become more efficient at task scheduling. This implies that you must schedule time on your calendar for tasks other than studying. Stress levels rise, grades decline, and important time spent with friends, taking care of oneself, or spending time with family is lost.
Set Priority:
College students who prioritize their responsibilities will be more productive, organized, and less likely to feel overwhelmed. Setting priorities can also assist students in achieving their objectives, lowering stress, and managing their time better. You can know what homework assignments to perform and when to finish them if you prioritize your tasks. Setting priorities for your assignment will also aid you when making templates for your homework schedule and completing assignments before the due date.
Also Read: NIMHANS help tribal department for school students’ well-being and mental health
Time Management and Plan:
Although it requires discipline and experience, effective time management can greatly increase your productivity, lower your stress level, and help you succeed as a college student overall.
To keep your obligations, projects, and assignments organized, make a to-do list or utilize a task management app. Establish due dates for all of your tasks and make a realistic timetable that allows time for studying, going to class, finishing assignments, and taking breaks. Acknowledge that unforeseen circumstances or shifts in priorities can happen, and be ready to modify your goals and timetable as necessary. Be adaptable and modify your time management techniques to take into account new information.
Understanding what is required of you before taking on any projects, assignments, or chores lowers your chance of making mistakes. You can finish a task more quickly and accurately if you ask questions to clarify the topic. For instance, you can ask questions that lead to useful responses if an assignment isn’t giving you a sense of direction. Asking clarifying questions might also help you troubleshoot unclear instructions. This will aid in reducing the Anxiety and also improve the performance.
Maintaining your physical and mental health is essential while stressing over incomplete assignments. Exercise, which might include taking a stroll or any other physical activity, is one powerful self-care tactic. You can also de-stress by indulging in a hot bath or relaxing with calming music. Effective stress management techniques can include writing, mindfulness or meditation, and socializing with loved ones. Make sure you eat healthily, exercise frequently, get adequate sleep, and take breaks to refuel. Maintaining your mental well-being through mindfulness exercises or getting help when required can also keep you concentrated and productive.
Break Large Tasks into Smaller steps

It is beneficial to divide a large work into smaller, more manageable ingredients when faced with it. You can prevent tension and procrastination by doing this. Procrastinators frequently lament how overwhelming and unachievable the task seems when they wait until the last minute. If you are prone to procrastination, creating a prioritized to-do list could be beneficial. Work your way down the list, setting reasonable deadlines for yourself.
Even if something isn’t completed right away, there are situations when writing something down can make you feel better about it. As you complete the tasks at hand, make time for yourself to focus on them in short bursts. Multitasking or task-switching can be stressful in and of itself. The work is less daunting and more manageable when priorities are established and the larger project is divided into smaller tasks.
Also Read: Stress from pre-board exams among students: how to minimize exam stress?
Seek Professional Help
Professionals in mental health can offer evidence-based therapies, like counseling and medication, to assist manage symptoms and enhance general functioning. Higher levels of contentment, happiness, and life quality may result from this. Seek assistance before you feel that you can no longer manage the stress. Take the time to speak with a professional or find out what resources your school provides for mental health issues. A mental health specialist can identify the sources of your stress, create a mental health plan, and plan constructive strategies to manage stress.
At last, the idea behind assigning tasks comes from the way that pupils learn. It facilitates the assessment of students’ subject-matter comprehension by teachers. Assignments broaden their knowledge base and help them acquire a variety of practical abilities. Education experts say that if students acquire and hone these skills, learning a subject is not insurmountable. Moreover, having a hectic amount of assignments can drain your mental well-being. It’s also important to look after you through the ways of stress management.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9169886/
- https://www.healthline.com/nutrition/16-ways-relieve-stress-anxiety
Share This Post:
The role of chatbots in mental health services: how does it impact people, kolam and cognition, leave feedback about this cancel reply.
- Rating 5 4 3 2 1
Related Post

Cultivating a Compassionate Classroom

Behind the Mask: The Impact of Anonymity and

To be a Polyglot: How it affects Cognitive

10 Things You Didn’t Know About Psychology Before

Precognitive Dreams: Glimpses of What’s to Come
Relaxation Techniques for Stress Relief
Quick stress relief.
- How to Stop Worrying and End Anxious Thoughts
Journaling for Mental Health and Wellness
Stress relief guide, social support for stress relief, 12 ways to reduce stress with music, surviving tough times by building resilience.
- Online Therapy: Is it Right for You?
- Mental Health
- Health & Wellness
- Children & Family
- Relationships
Are you or someone you know in crisis?
- Bipolar Disorder
- Eating Disorders
- Grief & Loss
- Personality Disorders
- PTSD & Trauma
- Schizophrenia
- Therapy & Medication
- Exercise & Fitness
- Healthy Eating
- Well-being & Happiness
- Weight Loss
- Work & Career
- Illness & Disability
- Heart Health
- Learning Disabilities
- Family Caregiving
- Teen Issues
- Communication
- Emotional Intelligence
- Love & Friendship
- Domestic Abuse
- Healthy Aging
- Alzheimer’s Disease & Dementia
- End of Life
- Meet Our Team
What is stress management?
- Identify the causes
- Replace unhealthy coping strategies
- Practice the 4 As
Avoid unnecessary stress
Alter the situation, adapt to the stressor.
- Accept the things you can't change
Move more during your day
- Time management
- Reach out and connect
Make time for fun and relaxation
Maintain balance with a healthy lifestyle.
- Reducing stress in the moment
Stress Management Techniques & Strategies to Deal with Stress
While it may seem like there’s nothing you can do about stress in your life, there are healthy steps you can take to destress and regain control.

It may seem like there’s nothing you can do about stress—no way to avoid it and no way to de-stress completely when it hits. The bills won’t stop coming, there will never be more hours in the day, and your work and family responsibilities will always be demanding. But the truth is, you have a lot more control over stress than you may think. In fact, the simple realization that you’re in control of your life is the foundation of stress management.
Managing stress is all about taking charge: of your thoughts, emotions, schedule, environment, and the way you deal with problems. The ultimate goal is a balanced life, with time for work, relationships, relaxation, and fun—plus the ability to hold up under pressure and meet challenges head on.
Stress management involves using various techniques and coping strategies to improve the way you react to stressful things in your life and build resilience . But it’s not one-size-fits-all. That’s why it’s important to experiment and find out what works best for you. Whether you’re looking to reduce your overall stress levels, avoid unnecessary stressors in your life, or deal with stress in the moment, the following stress management techniques and strategies can help.
Why does stress management matter?
If you’re living with high levels of stress, you’re putting your entire well-being at risk. Stress wreaks havoc on your emotional equilibrium, as well as your overall physical and mental health. It narrows your ability to think clearly, function effectively, and enjoy life.
Identify the causes of stress in your life
Stress management starts with identifying the sources of stress in your life. This isn’t as straightforward as it sounds. While it’s easy to identify major stressors such as changing jobs, moving, or going through a divorce, pinpointing the sources of chronic stress can be more complicated.
It’s all too easy to overlook how your own thoughts, feelings, and behaviors contribute to your everyday stress levels. Sure, you may know that you’re constantly worried about work deadlines, but maybe it’s your procrastination, rather than the actual job demands, that is causing the stress.
To identify what’s really stressing you out, look closely at your habits, attitude, and excuses:
- Do you explain away stress as temporary (“I just have a million things going on right now”) even though you can’t remember the last time you took a breather?
- Do you define stress as an integral part of your work or home life (“Things are always crazy around here”) or as a part of your personality (“I have a lot of nervous energy, that’s all”)?
- Do you blame your stress on other people or outside events, or view it as entirely normal and unexceptional?
Until you accept responsibility for the role you play in creating or maintaining it, your stress level will remain outside your control.
Keep a stress journal
A stress journal can help you identify the regular stressors in your life and the way you deal with them. Each time you feel stressed, make a note of it in your journal or use a stress tracker on your phone. As you keep a daily log, you will begin to see patterns and common themes. Write down:
- What caused your stress (make a guess if you’re unsure).
- How you felt, both physically and emotionally.
- How you acted in response.
- What you did to make yourself feel better.
Replace unhealthy coping strategies with healthy ones
Think about the ways you currently manage and cope with stress in your life. Your stress journal can help you identify them. Are your coping strategies healthy or unhealthy? Many of us cope with stress in ways that make us feel better temporarily—but compound the problem in the long run.

Unhealthy ways of dealing with stress
- Using alcohol or drugs to relax .
- Bingeing on junk or comfort food.
- Zoning out for hours on your phone or TV.
- Withdrawing from friends, family, and social activities.
- Sleeping too much.
- Filling up every minute of the day to avoid facing problems.
- Taking out your stress on others
- Procrastinating.
If your methods of coping with stress aren’t contributing to your greater emotional and physical health, it’s time to find healthier ones. No single method works for everyone or in every situation, so experiment with different stress management techniques and strategies. Focus on what makes you feel calm and in control.
Practice the 4 As of stress management
There are many healthy ways to reduce stress or cope with its effects, but they all require change. You can either change the situation or change your reaction. When deciding which option to choose, it’s helpful to think of the four As: avoid , alter , accept , or adapt .
Not all stress can be avoided, and it’s not healthy to avoid a situation that needs to be addressed. But you may be surprised by the number of stressors in your life that you can eliminate.
Learn how to say “no.” Know your limits and stick to them. Whether in your personal or professional life, taking on more than you can handle is a surefire recipe for stress.
Avoid people who stress you out. If someone consistently causes stress in your life, limit the amount of time you spend with that person, or end the relationship.
Take control of your environment. If the evening news makes you anxious, turn off the TV. If traffic makes you tense, take a longer but less-traveled route. If going to the market is an unpleasant chore, do your grocery shopping online.
Avoid hot-button topics . If you get upset over religion or politics, cross them off your conversation list. If you repeatedly argue about the same subject with the same people, stop bringing it up or excuse yourself when it’s the topic of discussion.
Pare down your to-do list. Analyze your schedule, responsibilities, and daily tasks. If you’ve got too much on your plate, distinguish between the “shoulds” and the “musts.” Drop tasks that aren’t truly necessary to the bottom of the list or eliminate them entirely.
If you can’t avoid a stressful situation, try to alter it. Often, this involves changing the way you communicate and operate in your daily life.
Express your feelings instead of bottling them up. If something or someone is bothering you, communicate your concerns in an open and respectful way. If you don’t voice your feelings, resentment will build and the stress will increase.
Be willing to compromise. When you ask someone to change their behavior, be willing to do the same. If you both are willing to bend at least a little, you’ll have a good chance of finding a happy middle ground.
Be more assertive. Don’t take a backseat in your own life. Deal with problems head on, doing your best to anticipate and prevent them. If you’ve got an exam to study for and your chatty roommate just got home, say up front that you only have five minutes to talk.
Find balance. All work and no play is a recipe for burnout. Try to find a balance between work and family life, social activities and solitary pursuits, daily responsibilities and downtime.
If you can’t change the stressor, change yourself. You can adapt to stressful situations and regain your sense of control by changing your expectations and attitude.
Reframe problems. Try to view stressful situations from a more positive perspective. Rather than fuming about a traffic jam, look at it as an opportunity to pause and regroup, listen to your favorite radio station, or enjoy some alone time.
Look at the big picture. Take perspective of the stressful situation. Ask yourself how important it will be in the long run. Will it matter in a month? A year? Is it really worth getting upset over? If the answer is no, focus your time and energy elsewhere.
Adjust your standards. Perfectionism is a major source of avoidable stress. Stop setting yourself up for failure by demanding perfection. Set reasonable standards for yourself and others, and learn to be okay with “good enough.”
Practice gratitude. When stress is getting you down, take a moment to reflect on all the things you appreciate in your life , including your own positive qualities and gifts. This simple strategy can help you keep things in perspective.
Accept the things you can’t change
Some sources of stress are unavoidable. You can’t prevent or change stressors such as the death of a loved one, a serious illness, or a national recession. In such cases, the best way to cope with stress is to accept things as they are. Acceptance may be difficult, but in the long run, it’s easier than railing against a situation you can’t change.
Don’t try to control the uncontrollable. Many things in life are beyond our control, particularly the behavior of other people. Rather than stressing out over them, focus on the things you can control such as the way you choose to react to problems.
Look for the upside. When facing major challenges, try to look at them as opportunities for personal growth. If your own poor choices contributed to a stressful situation, reflect on them and learn from your mistakes.
Learn to forgive. Accept the fact that we live in an imperfect world and that people make mistakes. Let go of anger and resentments. Free yourself from negative energy by forgiving and moving on.
Share your feelings. Expressing what you’re going through can be very cathartic, even if there’s nothing you can do to alter the stressful situation. Talk to a trusted friend or make an appointment with a therapist.
Speak to a Licensed Therapist
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
When you’re stressed, the last thing you probably feel like doing is getting up and exercising. But physical activity is a huge stress reliever—and you don’t have to be an athlete or spend hours in a gym to experience the benefits. Exercise releases endorphins that make you feel good, and it can also serve as a valuable distraction from your daily worries.
While you’ll get the most benefit from regularly exercising for 30 minutes or more, it’s okay to build up your fitness level gradually. Even very small activities can add up over the course of a day. The first step is to get yourself up and moving. Here are some easy ways to incorporate exercise into your daily schedule:
- Put on some music and dance around.
- Take your dog for a walk .
- Walk or cycle to the grocery store.
- Use the stairs at home or work rather than an elevator.
- Park your car in the farthest spot in the lot and walk the rest of the way.
- Pair up with an exercise partner and encourage each other as you work out.
- Play ping-pong or an activity-based video game with your kids.
Using mindful rhythmic exercise to manage stress
While just about any form of physical activity can help burn away tension and stress, rhythmic activities are especially effective. Good choices include walking, running, swimming, dancing, cycling, tai chi, and aerobics. But whatever you choose, make sure it’s something you enjoy so you’re more likely to stick with it.
While you’re exercising, make a conscious effort to pay attention to your body and the physical (and sometimes emotional) sensations you experience as you’re moving. Focus on coordinating your breathing with your movements, for example, or notice how the air or sunlight feels on your skin. Adding this mindfulness element will help you break out of the cycle of negative thoughts that often accompanies overwhelming stress.
Learn to manage your time better
Poor time management can cause a lot of stress. When you’re stretched too thin and running behind, it’s hard to stay calm and focused. Plus, you’ll be tempted to avoid or cut back on all the healthy things you should be doing to keep stress in check, like socializing and getting enough sleep. The good news: there are things you can do to achieve a healthier work-life balance.
Don’t over-commit yourself. Avoid scheduling things back-to-back or trying to fit too much into one day. All too often, we underestimate how long things will take.
Prioritize tasks. Make a list of tasks you have to do, and tackle them in order of importance. Do the high-priority items first. If you have something particularly unpleasant or stressful to do, get it over with early. The rest of your day will be more pleasant as a result.
Break projects into small steps. If a large project seems overwhelming, make a step-by-step plan. Focus on one manageable step at a time, rather than taking on everything at once.
Delegate responsibility. You don’t have to do it all yourself, whether at home, school, or on the job. If other people can take care of the task, why not let them? Let go of the desire to control or oversee every little step. You’ll be letting go of unnecessary stress in the process.
Reach out and connect to people who make you feel good
There is nothing more calming than spending quality time with another human being who makes you feel safe and understood. In fact, face-to-face interaction triggers a cascade of hormones that counteracts the body’s defensive “fight-or-flight” response. It’s nature’s natural stress reliever (as an added bonus, it also helps stave off depression and anxiety). So make it a point to connect regularly—and in person—with family and friends.
[Read: Social Support for Stress Relief]
Keep in mind that the people you talk to don’t have to be able to fix your stress. They simply need to be good listeners. And try not to let worries about looking weak or being a burden keep you from opening up. The people who care about you will be flattered by your trust. It will only strengthen your bond.
Of course, you may not always have someone close by to lean on when you feel overwhelmed by stress, but by building and maintaining a network of close friends you can improve your resiliency to life’s stressors.
Tips for building relationships
- Reach out to a colleague at work.
- Help someone else by volunteering .
- Have lunch or coffee with a friend.
- Ask a loved one to check in with you regularly.
- Call or email an old friend.
- Go for a walk with a workout buddy.
- Schedule a weekly dinner date.
- Meet new people by taking a class or joining a club.
- Confide in a clergy member, teacher, or sports coach.
- Join a support group—either in-person or via on online therapy platform .
Beyond a take-charge approach and a positive attitude, you can reduce stress in your life by carving out “me” time. Don’t get so caught up in the hustle and bustle of life that you forget to take care of your own needs. Nurturing yourself is a necessity, not a luxury. If you regularly make time for fun and relaxation, you’ll be in a better place to handle life’s stressors.
Set aside leisure time. Include rest and relaxation in your daily schedule. Don’t allow other obligations to encroach. This is your time to take a break from all responsibilities and recharge your batteries.
Do something you enjoy every day. Make time for leisure activities that bring you joy, whether it be stargazing, playing the piano, or working on your bike.
Keep your sense of humor. This includes the ability to laugh at yourself. The act of laughing helps your body fight stress in a number of ways.
Take up a relaxation practice. Relaxation techniques such as yoga, meditation, and deep breathing activate the body’s relaxation response , a state of restfulness that is the opposite of the fight or flight or mobilization stress response. As you learn and practice these techniques, your stress levels will decrease and your mind and body will become calm and centered.
In addition to regular exercise, there are other healthy lifestyle choices that can increase your resistance to stress.
Eat a healthy diet . Well-nourished bodies are better prepared to cope with stress, so be mindful of what you eat. Start your day right with breakfast, and keep your energy up and your mind clear with balanced, nutritious meals throughout the day.
Reduce caffeine and sugar. The temporary “highs” caffeine and sugar provide often end with a crash in mood and energy. By reducing the amount of coffee, soft drinks, chocolate, and sugar snacks in your diet , you’ll feel more relaxed and you’ll sleep better.
Avoid alcohol, cigarettes, and drugs. Self-medicating with alcohol or drugs may provide an easy escape from stress, but the relief is only temporary. Don’t avoid or mask the issue at hand; deal with problems head on and with a clear mind.
Get enough sleep. Adequate sleep fuels your mind, as well as your body. Feeling tired will increase your stress because it may cause you to think irrationally.
Tips for reducing stress in the moment
When you’re frazzled by your morning commute, stuck in a stressful meeting at work, or fried from another argument with your spouse, you need a way to manage your stress levels right now . That’s where quick stress relief comes in.
The fastest way to reduce stress is by taking a deep breath and using your senses—what you see, hear, taste, and touch—or through a soothing movement. By viewing a favorite photo, smelling a specific scent, listening to a favorite piece of music, tasting a piece of gum, or hugging a pet, for example, you can quickly relax and focus yourself.
[Read: Quick Stress Relief]
Of course, not everyone responds to each sensory experience in the same way. The key to quick stress relief is to experiment and discover the unique sensory experiences that work best for you.
More Information
- Special Health Report - Special Health Report from Harvard Medical School on Stress. (Harvard Health)
- Tolerating Distress - Workbook and information sheets to help you manage feelings of distress. (Centre for Clinical Interventions)
- How To Relax (Video) - Video to help you ease stress. (Mind)
- Trauma- and Stressor-Related Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders . American Psychiatric Association. Link
- Can, Yekta Said, Heather Iles-Smith, Niaz Chalabianloo, Deniz Ekiz, Javier Fernández-Álvarez, Claudia Repetto, Giuseppe Riva, and Cem Ersoy. “How to Relax in Stressful Situations: A Smart Stress Reduction System.” Healthcare 8, no. 2 (April 16, 2020): 100. Link
- Norelli, Samantha K., Ashley Long, and Jeffrey M. Krepps. “Relaxation Techniques.” In StatPearls . Treasure Island (FL): StatPearls Publishing, 2021. Link
- Toussaint, Loren, Quang Anh Nguyen, Claire Roettger, Kiara Dixon, Martin Offenbächer, Niko Kohls, Jameson Hirsch, and Fuschia Sirois. “Effectiveness of Progressive Muscle Relaxation, Deep Breathing, and Guided Imagery in Promoting Psychological and Physiological States of Relaxation.” Evidence-Based Complementary and Alternative Medicine 2021 (July 3, 2021): e5924040. Link
- Unger, Cynthia A, David Busse, and Ilona S Yim. “The Effect of Guided Relaxation on Cortisol and Affect: Stress Reactivity as a Moderator.” Journal of Health Psychology 22, no. 1 (January 1, 2017): 29–38. Link
- Singh, Karuna. “Nutrient and Stress Management.” Journal of Nutrition & Food Sciences 6, no. 4 (2016). Link
- Katsarou, Alexia L., Marios M. Vryonis, Athanassios D. Protogerou, Evangelos C. Alexopoulos, Apostolos Achimastos, Dimitrios Papadogiannis, George P. Chrousos, and Christina Darviri. “Stress Management and Dietary Counseling in Hypertensive Patients: A Pilot Study of Additional Effect.” Primary Health Care Research & Development 15, no. 1 (January 2014): 38–45. Link
- Errisuriz, Vanessa L., Keryn E. Pasch, and Cheryl L. Perry. “Perceived Stress and Dietary Choices: The Moderating Role of Stress Management.” Eating Behaviors 22 (August 1, 2016): 211–16. Link
- Choi, Dong-Woo, Sung-Youn Chun, Sang Ah Lee, Kyu-Tae Han, and Eun-Cheol Park. “Association between Sleep Duration and Perceived Stress: Salaried Worker in Circumstances of High Workload.” International Journal of Environmental Research and Public Health 15, no. 4 (April 2018): 796. Link
- Blaxton, Jessica M., Cindy S. Bergeman, Brenda R. Whitehead, Marcia E. Braun, and Jessic D. Payne. “Relationships Among Nightly Sleep Quality, Daily Stress, and Daily Affect.” The Journals of Gerontology: Series B 72, no. 3 (May 1, 2017): 363–72. Link
- Saleh, Dalia, Nathalie Camart, Fouad Sbeira, and Lucia Romo. “Can We Learn to Manage Stress? A Randomized Controlled Trial Carried out on University Students.” PLOS ONE 13, no. 9 (September 5, 2018): e0200997. Link
- Loprinzi, Paul D., and Emily Frith. “Protective and Therapeutic Effects of Exercise on Stress-Induced Memory Impairment.” The Journal of Physiological Sciences: JPS 69, no. 1 (January 2019): 1–12. Link
- Salmon, P. “Effects of Physical Exercise on Anxiety, Depression, and Sensitivity to Stress: A Unifying Theory.” Clinical Psychology Review 21, no. 1 (February 2001): 33–61. Link
More in Stress
The power of the relaxation response to reduce stress and boost mood

Using your senses to relieve stress on the spot

How to Stop Worrying
Self-help strategies for anxiety relief

Tips and prompts to journal

Quick tips for when you’re short on time

Using close relationships to manage stress and improve well-being

Fill your life with music that reduces daily stress

Tips for overcoming adversity

Professional therapy, done online
BetterHelp makes starting therapy easy. Take the assessment and get matched with a professional, licensed therapist.
Help us help others
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
mind remake project
A therapy and mental health resource site
75+ Free Mental Health Worksheets & Handouts
75+ free mental health worksheets, handouts, and forms for mental health professionals or self-help.
(Updated 2/13/24) This is a list of nearly 100 mental health worksheets, handouts, forms, and more for substance use, mental health, and wellness.
Please repost and share with anyone who might benefit! New resources are added on a regular basis.
For more free downloads, click here for a list of PDF workbooks, manuals, and self-help guides.
For free mental health worksheets and resources from other sites, check out TherapistAid , GetSelfHelpUK , and Taking the Escalator .
Mental Health Worksheets & Handouts
Group ideas & topics.
A 3-page handout for group facilitators with strategies for managing resistance, disruptive behaviors, and a lack of engagement in group therapy.
A list of topics for substance use groups.
A 2-page handout for clinicians who facilitate group therapy with (adult) clients and their families. The questions were developed for an inpatient SUD setting.
A list of specific topics for substance use groups, such as refusal skills, the difference between a lapse and a relapse, and fun in recovery.
A list of group openers for substance use groups; can also be used in individual counseling sessions.
A list of questions for exploring the following topics: Conversation starters, mental health, addiction, personal development, values, family, relationships, and emotions. These questions can be used in a group setting, individually, or as journal prompts.
Group Activities
A worksheet with prompts for writing a short autobiography to be presented to the group.
Intended audience: Adults
A worksheet for clients to pass around to group members so each person can write a positive affirmation.
Intended audience : Adolescents, Teens, Adults
Good for newly formed groups. Each group member writes down their “first impression” of other group members. The facilitator then reads off the different categories and group members have the opportunity to share their answers.
Intended audience : Adults
An icebreaker activity, good for new groups. Give group members 15-20 minutes to collect signatures. The first person to collect all signatures wins.
Clinical Film Discussion Questions
- Ben Is Back -Discussion Questions
- Girl, Interrupted -Discussion Questions
- Pay It Forward -Discussion Questions
- The Perks of Being a Wallflower -Discussion Questions
- Rachel Getting Married -Discussion Questions
- When a Man Loves a Woman -Discussion Questions
A printable deck of cards with 128 coping skills for managing stress, anxiety, and other difficult emotions. Each card includes one simple coping skill.
Print/cut the cards, fold, and place in a container. Group members take turns drawing the cards and answering the questions.
A printable deck of cards with 40 positive quotes that can be used as affirmations.
A printable card deck with 27 affirmations for healing and empowerment.
These cards can be used in a SUD inpatient or outpatient setting to facilitate group discussions about recovery. Group members take turns drawing a card and answering questions. The facilitator can vary things up by letting group members pick someone else to answer their question once they’ve finished sharing. Alternatively, group members can take turns drawing cards, but all group members are encouraged to share their answers. This activity works best with a working group.
This is a revised version of the Recovery Question Cards.
Rumi Quote Cards
25 cards with Rumi quotes on love, suffering, and healing.
A card deck with 104 cards with thought-provoking questions intended to promote discussion. Topics include goals, values, emotions, relationships, spirituality, and more.
These cards can be used in a group or individual setting. The last page of the PDF includes additional values exercises for journaling, clinical supervision, couples, and groups. Tip: Print the cards on patterned scrapbook paper (blank on one side).
Mental Health Handouts
4 ways to stay calm before a stressful event.
A 1-page handout with simple “in-the-moment” calming strategies for anxiety-provoking events.
A simple 1-page handout that shows the 6 basic emotions.
A comprehensive list of 12-step and other support groups , such as AA, NA, SMART Recovery, Dual Recovery Anonymous, NAMI, etc.
A 1-page DBT-based handout with 25 examples of dialectics (i.e., two things that seem opposite and are at the same time both true).
These journal prompts can also be used in a group setting. The prompts include questions about values, potential, expectations, and more.
Instructions for Living from the Dalai Lama
A 1-page handout with 25 quotes from the Dalai Lama on topics such as kindness and happiness. Can be used in a group setting.
A 1-page handout that debunks five common grief myths and provides the truth about each one.
A 2-page handout with nine creative and soothing outlets for grief , such as music, dance, light therapy, and aromatherapy.
A 2-page handout with journal prompts for recovery, based on material from The Sober Survival Guide (created with the author’s permission).
Kindness To-Do List
A to-do list of kind deeds with blank spaces to write in your own ideas for spreading kindness.
A colorful 3-page handout with ideas for hobbies that fall under the following categories: Animals/nature, arts/crafts, collections, cooking/baking, entertainment, home improvement/DIY, outdoor/adventure, self-improvement, sports, travel, and misc.
A list with links to online grief support groups, forums, and communities.
A 1-page handout on PTG and how it may impact a person’s life, and the factors that contribute to PTG.
A 1-page handout with resources for suicide , including recommended books, apps, crisis lines, and suicide warning signs.
A 2-page handout that describes seven uncommon grief experiences, such as delayed or disenfranchised grief.
A list of 38 unique coping skills for managing difficult emotions.
A 2-page handout that lists values. Can be used as a standalone handout or with the values card deck .
A 2-page handout with two exercise routines, one designed for beginners and the other for more advanced exercisers.
Mental Health Worksheets
A 1-page worksheet for identifying things to be grateful for in different life areas.
A 1-page checklist with 30 ideas for spreading kindness.
A 1-page worksheet for exploring what makes someone a good friend.
Art Activity: H-T-P Test
In the House-Tree-Person Test, the picture of the house is supposed to represent how the individual feels about their family. The tree elicits feelings of strength or weakness. The person represents how the individual feels about themselves. (Source: How Projective Tests Are Used to Measure Personality – Simply Psychology )
Art Activity: Outer & Inner Masks
This art activity can be done in a group setting or individually. Clients design both outer – what the world sees – and inner – the hidden self – masks. The third page has questions for discussion. This activity can be used to target all sorts of issues from body image to values to character defects (in addiction) and more.
Art Activity: Self-Portraits
This worksheet can be used in groups or as a homework assignment. Encourage clients to be creative; instead of just drawing or coloring, they can use magazine cutouts, stickers, photos, etc. Suggested questions for discussion: How did you decide which identities to portray? Which portrait best represents your true self? Which portrait do others see the most? What, if anything, would you like to change about your portraits?
A 2-page worksheet for exploring the consequences of addiction.
Coping with Cravings
A 3-page worksheet with DBT-based skills for coping with cravings.
Coping with Jealousy
A worksheet for understanding jealousy, its impact, whether it’s pathological, and how to manage jealous feelings.
Couples Exercise: Affirmations
A 3-page worksheet for sharing self-affirmations and partner affirmations, including suggested questions for discussion.
Couples Exercise: Our Bucket List
A 3-page worksheet for couples to create a shared list of meaningful “bucket list” items to do together.
Couples Exercise: Our Bucket List (with dates)
A shared bucket list that includes spaces to write in when an item was added to the list and when it was completed.
A 1-page worksheet for affirmations, positive self-talk, and problem-solving strategies for daily challenges.
A basic mood tracker with emoji faces.
A blank schedule with hourly slots starting at 6:00 a.m. and ending at 10:00 p.m. Can be used as part of a relapse prevention, for depression management, or as a planner.
A 3-page worksheet for substance use recovery for planning leisure activities and enhancing wellness/spirituality.
A letter template for individuals entering long-term residential treatment for substance use, to be opened and read at treatment completion.
An 8-page goal-setting worksheet for health/wellness, relationships/social health, emotional wellness, intellectual wellness, education/career, financial health, spirituality, and leisure.
A 3-page worksheet for identifying and managing substance use relapse triggers.
A 1-page worksheet for identifying things that promote addiction and ways to get rid of or avoid these things.
A 3-page goal-setting worksheet for short-term and long-term goals.
A 12-step-based worksheet for identifying and exploring resentments.
A worksheet for creating poetry; print, laminate, and cut out the words.
A 1-page worksheet for examining past substance use relapses and strategies for avoiding future relapses.
A 5-page template for creating a substance use relapse prevention plan.
A 1-page worksheet for exploring ways to resist urges to use in early recovery.
A 1-page checklist with quick tips, self-soothing, and indulgent ideas for self-care.
A 3-page worksheet for developing a colorful self-care “map” to explore patterns and identify new practices.
A 3-page template for creating a self-care “menu.”
A 2-page writing assignment for self-discovery and awareness.
A 2-page worksheet for developing self-esteem.
A 1-page worksheet for exploring motivation for substance use recovery.
A fun worksheet for creating a bucket list of things that are only possible in sobriety.
Stress Management Worksheet
This 6-page worksheet helps with identifying and exploring stressors. From there, the worksheet can be used to build a stress management plan.
7 pages of feelings words.
A 6-page worksheet for describing problem areas, identifying goals, and exploring what has (and has not) been helpful in the past. This worksheet can be used to develop a collaborative treatment plan.
A 2-page worksheet for identifying and exploring wants and needs.
A simple form for tracking daily meals and snacks for one week.
A 2-page worksheet for identifying things that are controllable versus things that can’t be controlled.
A 3-page narrative therapy worksheet for exploring a past substance use relapse.
Laminate and use with fine-tip dry erase markers.
Workbooks & Bonus Materials
100-page printable workbook for working through grief and loss.
A companion workbook meant to be used with the book Staying Sober Without God (created with the author’s permission).
Daily Self-Inventory for Mental Health Professionals
A 10th step-based inventory for self-reflection for counselors and other mental health workers.
Free Coloring Pages for Adults
Links to 15 websites with free printable coloring sheets for adults.
Miscellaneous Printables
A list of 20 openers for individual therapy sessions.
A 2-page form for case conceptualization with sections for demographics, key findings, background info, case formulation, interventions/plans, and requested feedback or suggestions.
A list of interventions (action words) for clinical documentation.
A template for tracking attendance, cases discussed, and any other group topics.
A foldable coloring book with eight different designs.

Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
29 thoughts on “75+ Free Mental Health Worksheets & Handouts”
- Pingback: Sites with Free Therapy Worksheets & Handouts – Mind ReMake Project
- Pingback: Books & Resources for Therapists – Mind ReMake Project
- Pingback: Free Printable PDF Workbooks, Manuals, & Self-Help Guides – Mind ReMake Project
- Pingback: Group Therapy Resource Guide – Mind ReMake Project
Thank you for giving away this valuable information. I am a Adult Mental Health Case Manager and I use things from here in my weekly group meetings!
I do also, but for juveniles. These tools are extremely helpful.
- Pingback: Mental Health Resources Master List – Sandeep's Mind
Thank you so much for providing these free handouts. During these tough times, I find these handouts to be extremely useful. A million thank you’s!
These valuable materials are so much of a blessing, thank you so much for the gracious kindness!!!
I’m a drug and alcohol counselor and I find this site very helpful!
It is great to see that someone else wants to promote better care for clients and therapists alike using comprehensive resources (that are free!). Thank you!!!
I love this site i am a Mental Health Professional and I find these very helpful with my group sessions.
Thank you very much!! I have a son struggling with depression and suicide. This will help very much.
- Pingback: Group Therapy Curriculum Pdf – Explore Recent
- Pingback: Relapse Prevention Worksheets - Worksheets List
This is a wonderful site. I deeply appreciate the effort and time it took to put this together. Thank you very much.
I can’t tell you how fortunate I am to have stumbled onto this. I am a Behavioral Health PSS in a drug and alcohol treatment facility and am looking forward to sharing some of these materials with our clients. I love the group activities and discussion prompts and will be using some in my next group. Fantastic resource! There is something for everyone here! Thank you so much for this. Be well 🙂
Hope you guys add a Domestic Violence section
Thank you for giving us free worksheets. It’s really helpful.
- Pingback: 10 Ways To Kill Time On A Long Flight
- Pingback: Map Your Healing Journey
Thank you!!
- Pingback: 161 Powerful Questions to Explore Values, Ideas, & Beliefs - mind remake project
- Pingback: What is mental health? worksheet - HappierTHERAPY
I am a mental health therapist and I really struggle for group therapy ideas. Thank you for sharing. Your site has been very helpful for me to find new ideas.
- Pingback: 250+ Sites with Free Therapy Worksheets - mind remake project
- Pingback: Boost Your Emotional Wellness: Exercises, Worksheets, And Resources For A Happier Life » LifeWhims
- Pingback: Assignment | Extracting Relevant Resources for Life Coaching and Self Worth Title: "Exploring Resources for Life Coaching and Self Worth: A Comprehensive Review of Workbooks, Assessments, and Questionnaires"
Leave a Reply Cancel reply
Discover more from mind remake project.
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
- Election 2024
- Entertainment
- Newsletters
- Photography
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Delegate Tracker
- AP & Elections
- College football
- Auto Racing
- Movie reviews
- Book reviews
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
How do you deal with stress? In Nigeria, swinging a sledgehammer in a ‘rage room’ helps
Olaribigbe Akeem, wearing protective gear, uses a sledgehammer to break a television set to vent his anger inside the Shadow Rage Room in Lagos, Nigeria, Sunday, July 28, 2024. (AP Photo/Sunday Alamba)
A man laughs after breaking a television set to vent his anger outside the Shadow Rage Room in Lagos, Nigeria, Sunday, July 28, 2024. (AP Photo/Sunday Alamba)
James Babajide Banjoko, the founder of the Shadow Rage Room, speaks during an interview in Lagos, Nigeria, Sunday, July 28, 2024. (AP Photo/Sunday Alamba)
People wearing protective gear use sledgehammers to break a television set to vent their anger outside the Shadow Rage Room in Lagos, Nigeria, Sunday, July 28, 2024. (AP Photo/Sunday Alamba)
Olaribigbe Akeem, reacts after breaking a television set to vent his anger inside the Shadow Rage Room in Lagos, Nigeria, Sunday, July 28, 2024. (AP Photo/Sunday Alamba)
Eka Stephanie Paul, wearing protective gear, uses a bat to break a television set to vent her anger inside the Shadow Rage Room in Lagos, Nigeria, Sunday, July 28, 2024. (AP Photo/Sunday Alamba)
- Copy Link copied
LAGOS, Nigeria (AP) — How do you deal with stress?
In Lagos, Nigeria’s largest city, people are finding their reset button in a “rage room” where they pay to smash electronics and furniture with a sledgehammer as a break from the worst cost-of-living crisis in a generation .
The Shadow Rage Room, apparently the first of its kind in Nigeria, offers “a safe space” for people to let out pent-up emotions, according to Dr. James Babajide Banjoko, the founder and a physician. The idea, he said, came during the COVID-19 pandemic in 2020 after he lost his mother and struggled with work.
For 7,500 naira ($5), customers are left alone with protective gear and a sledgehammer or bat in a room for a 30-minute session with the items that are later recycled.
Times are tough in Nigeria , a country of over 200 million people where growing frustration among youths led to recent mass protests in which several people were killed by security forces . The inflation rate has reached a 28-year-high of 33.4%, while the naira currency has fallen to record lows against the dollar.
Mental health services remain foreign or unaffordable for many in Africa’s most populous country, where 40% of citizens live below $2 per day.
The West African nation has fewer than 400 registered psychologists, according to the Nigerian Association of Clinical Psychologists. That means one psychologist for about every half a million people.
Even when therapy is available, stigma remains a challenge, NACP president Gboyega Emmanuel Abikoye said in an interview.
Rage rooms aren’t necessarily new in other parts of the world. There is no documented evidence of their mental health benefits beyond the momentary relief that comes with venting your feelings, Abikoye said.
Experts in Nigeria instead see a growing need for more long-term emotional support, especially among young people.
In Lagos, an overcrowded city of about 20 million people and a magnet for those seeking better opportunities, such needs are even more pronounced. Daily stressors include traffic jams notorious for trapping drivers and passengers on streets for hours in heat and smog in one of the world’s most polluted cities.
Some Nigerians have turned to social media platforms like Tiktok as a way to cope with stress. Some find support in communities wherever they can, from the church or mosque to the gym.
And now there’s the rage room, which opens on weekends and is usually fully booked up to two weeks ahead, according to Banjoko, the founder.
At the end of one session of smashing, Olaribigbe Akeem, a recent visitor, came out sweating but relieved and visibly happy.
“As an average Nigerian, you get to deal with a lot every day,” Akeem said. “The anger has been piling up (and) instead of venting on somebody, this is the best avenue for me, and I feel a lot renewed.”
Rage room visitors also include couples who want to get something off their chest.
At times, people come in for recreation but find something more.
“My favorite people are those that … just want to try it, and at the end of the day, you see them, they break down, they cry, they become very expressive,” Banjoko said. He said he often refers them to therapy.
Dr. Maymunah Yusuf Kadiri, a Lagos-based psychiatrist, said any benefit from smashing things is usually short-lived and can’t be a replacement for therapy.
There is also the risk of such a practice making someone less likely to use “healthy coping strategies,” she said, and expressed concern that “repeated engagement … might reinforce aggressive tendencies.”
At the rage room, some customers said their problems feel lighter only until they leave and re-enter daily life.
But being vulnerable with yourself while inside, sledgehammer in hand, is still worth it, said Eka Stephanie Paul, an actor and TV host.
“Problem no dey finish anyway,” she said in the pidgin widely spoken across Nigeria, acknowledging that the rage room is hardly a cure. “But right now, I feel very light.”
Asadu reported from Abuja, Nigeria.
For more news on Africa and development: https://apnews.com/hub/africa-pulse
The Associated Press receives financial support for global health and development coverage in Africa from the Bill & Melinda Gates Foundation Trust. The AP is solely responsible for all content. Find AP’s standards for working with philanthropies, a list of supporters and funded coverage areas at AP.org .

Weekend Appointments Available!

Let's work together to improve your mood and daily life!
I offer Mental Health Counseling for:
Major and Seasonal Depressive Disorders
Generalized Anxiety and Frequent Panic Attacks
Post Traumatic Stress Disorder
Military and First Responder Trauma
Religious, Spiritual and Existential Crisis
Grief, Bereavement, and Adjustment Disorders
Chronic Negative Self-Talk and Low Self-Esteem
Distress Associated with Autoimmune Disorders
about Cheryl McGill, LPC
"Sounds great! But, Who are you?"
I'm a Licensed Professional Counselor in the state of Idaho. I utilize Dialectical Behavior Therapy and Cognitive Behavior Therapy to help clients build effective coping strategies for a variety of mental health disorders. I've earned a Master's degree in Clinical Mental Health Counseling with a specialization in working with Military Personnel and Veterans. I have worked professionally in the field of emotional support and life enhancement since 2017.

What Counseling looks like
Initial Intake Session:
We'll discuss the symptoms you're experiencing and how long these have been present
I'll ask you about the ways you've been coping with your presenting symptoms and what's been working and what hasn't
We'll explore your family history of mental health and your personal medical history relating to your symptoms
Together, we will develop a personalized treatment plan based on the severity of your symptoms and your goals for treatment
Ongoing Treatment Sessions:
We'll talk about your experiences since your last session and what your symptoms were like
I'll challenge any ongoing beliefs or thought patterns that interfere with your treatment progress
Together, we will practice and role play coping skills and continue to build on strengths
We'll explore any adjustments to your treatment plan that may be needed based on your progress toward your overall treatment goals
Frequently Asked Questions
What is Depression?
Depression can manifest differently for everyone and isn't always expressed in the same way. Yet, there are symptoms that represent "Depression" such as:
feeling sad, empty, or hopeless for most of the day and nearly everyday
experiencing a significant lack of interest or pleasure in most, or all, activities throughout the day
loss of appetite or overeating
inability to sleep or sleeping too much
moving noticeably slower that usual
excessive fatigue
difficulty concentrating or making decisions
feelings of worthlessness or thoughts of suicide
What is a Panic Attack?
While panic attacks are not a mental health disorder in itself, they often occur as a manifestation of intense emotional response related to other mental health disorders such as anxiety, trauma, stress, depression, and substance use.
Symptoms of panic attack include: pounding heart, sweating, shaking, shortness of breath, sensation of choking, chest pain, nausea, feeling dizzy or light-headed, numbness, chills, heat, feeling detached from reality, a sense of losing control, and fear of dying.
What is Anxiety?
Anxiety is noted as experiencing excessive and uncontrollable worry, apprehension, and fear for more days than not for at least six months. Symptoms include:
feeling restless or on edge
being easily fatigued
mind going blank
feeling irritable or easily agitated
muscle tension difficulty relaxing
difficulty falling asleep or staying asleep
Do you prescribe medications for depression or anxiety?
No. Medications need to be prescribed by your medical provider. I can work collaboratively with your provider to monitor your progress with prescribed medications and identify any potential side effects you may experience.
Do you take insurance?
No. There are several benefits to clients for not accepting insurance. Some benefits include not being limited to the number of sessions you can attend and not having a diagnosis on your medical record. However, I accept HSA cards and can provide a Superbill for clients to submit to their insurance provider for reimbursement of out-of-network treatment. I offer a Military discount for active duty members and Veterans.
Individual Counseling
When symptoms related to mental health are interfering with daily functioning, it's time to identify what's contributing to the problem and develop effective tools to cope. With time, you can learn, practice, and utilize these tools to improve your mood and your daily life.
$135 per Session
12 Most Reliable Mental Health Assessment Tools

Typically, these assessments invite clients to respond to questions about their mental state and subjective experiences.
Psychologists and therapists depend on these tools to make decisions about the best course of treatment for clients seeking support for their mental health. Therefore, it’s worth taking a little time to explore their variations and how to use them most effectively.
In this article, we’ll explore some of the most commonly used and reliable mental health assessments, as well as their applications at different stages of the therapeutic process. We’ll also walk through some ways you can automate and simplify the administration of these assessments.
Before you continue, we thought you might like to download our three Positive Psychology Exercises for free . These science-based exercises explore fundamental aspects of positive psychology, including strengths, values, and self-compassion, and will give you the tools to enhance the wellbeing of your clients, students, or employees.
This Article Contains:
What are psychological assessments 3 examples, how to use therapy assessment tools, 3 reliable psychological tests & assessments, 13 questions and worksheets to assess clients, using online tools for psychology assessments, crafting assessments in quenza: 3 templates, helpful resources from positivepsychology.com, a take-home message.
Whether it’s a pop psychology quiz online or a validated assessment by a therapist, psychological assessments share one thing in common.
They all function as
“a systematic procedure for comparing the behavior of two or more persons.”
Cronbach, 1949, p. 21
In recent years, scientists have begun making distinctions between psychological tests versus assessments .
While tests are typically thought of as pen-and-paper or computer-based tools for considering differences between people, the term ‘assessment’ acknowledges the wide variety of other approaches a psychologist may use to evaluate these differences. Examples of such approaches include interviews , observations, and recording physiological functions (Goldstein, Allen, & DeLuca, 2019).
To begin, here are three examples of mental health tests commonly used among mental health practitioners.
1. Minnesota Multiphasic Personality Inventory (MMPI-2)
First published in 1989, the MMPI-2 is the world’s most widely used psychometric test for measuring mental health ailments that feature as forms of psychopathology (Rogers, Robinson, & Jackson, 2016).
The scale features 567 true–false statements, which assess 10 clinical sub-scales (Butcher, Dahlstrom, Graham, Tellegen, & Kaemmer, 1989):
- Hypochondriasis
- Psychopathic deviate
- Masculinity/Femininity
- Psychasthenia
- Schizophrenia
- Social introversion
In addition to these 10 primary clinical scales, the MMPI-2 also contains three sub-scales to detect lying, defensiveness, and inconsistent responses.
It also features many additional content scales assessing specific cognitions, behaviors, physical experiences, and motivations, such as self-doubt, competitive drive, and gastrointestinal issues.
If you’re interested in administering this assessment yourself, you can order a copy of the test from the Pearson Assessments website.
2. Beck Anxiety Inventory
Another commonly used mental health assessment is the Beck Anxiety Inventory. This inventory is a brief self-report test used to assess the severity of symptoms of anxiety . It includes detailed scoring to help practitioners identify whether clients’ presenting symptoms of anxiety are within a normal range or severe and debilitating.
The scale comprises 21 common symptoms of anxiety. Examples include:
- Hands trembling
- Fear of dying
- Hot/cold sweats
Respondents indicate the frequency with which each symptom has bothered them for the past month on a 4-point scale, where 0 is ‘not at all,’ and 3 is ‘severely – it bothered me a lot.’
You can access a copy of the test for free from the Great Plains Health website .
3. Beck Depression Inventory
Finally, a standard complement to the Beck Anxiety Inventory is the Beck Depression Inventory. Again, this inventory consists of 21 items and contains detailed scoring information to indicate whether symptoms are in a normal range or severe.
Respondents complete each item of the scale by selecting the statement that best reflects their current emotional state. For example, the first item and accompanying scoring are as follows:
- 0 – I do not feel sad.
- 1 – I feel sad.
- 2 – I am sad all the time, and I can’t snap out of it.
- 3 – I am so sad and unhappy that I can’t stand it.
If you’re interested, the Beck Depression Inventory with scoring information is freely available to download.
Beck’s depression inventory – Practical Psychology
Using tests for holistic mental health assessments
Regardless of which test you use, each can form part of a holistic mental assessment for clients that guides the design of subsequent therapeutic interventions.
To illustrate, consider this sample interpretive report following the administration of the MMPI-2 (Pearson Education, 2014).
The assessment results for this example patient, Karen, point toward a likely diagnosis of schizophrenia or major affective disorder as well as potential challenges in the therapeutic process. Namely, several of her responses suggest that she may possess little faith in her ability to improve her mental health and a lack of trust that may impact her relationship with a therapist.
It is subsequently suggested that she may benefit from minimal face-to-face contact and brief, periodic visits with a mental health professional.
Information such as this can form part of a holistic assessment, which monitors Karen’s ongoing engagement with therapeutic interventions (or lack thereof) and determines her likelihood of seeing positive improvements to her mental health.
It might even inform a therapist’s hypothesis that Karen could benefit from therapy of particular duration, such as solution-focused brief therapy , or specific modes of delivery, such as teletherapy or blended modes of treatment.
Next, we’ll consider some of these different delivery modes as well as blended technology’s uses for facilitating ongoing mental health assessment.
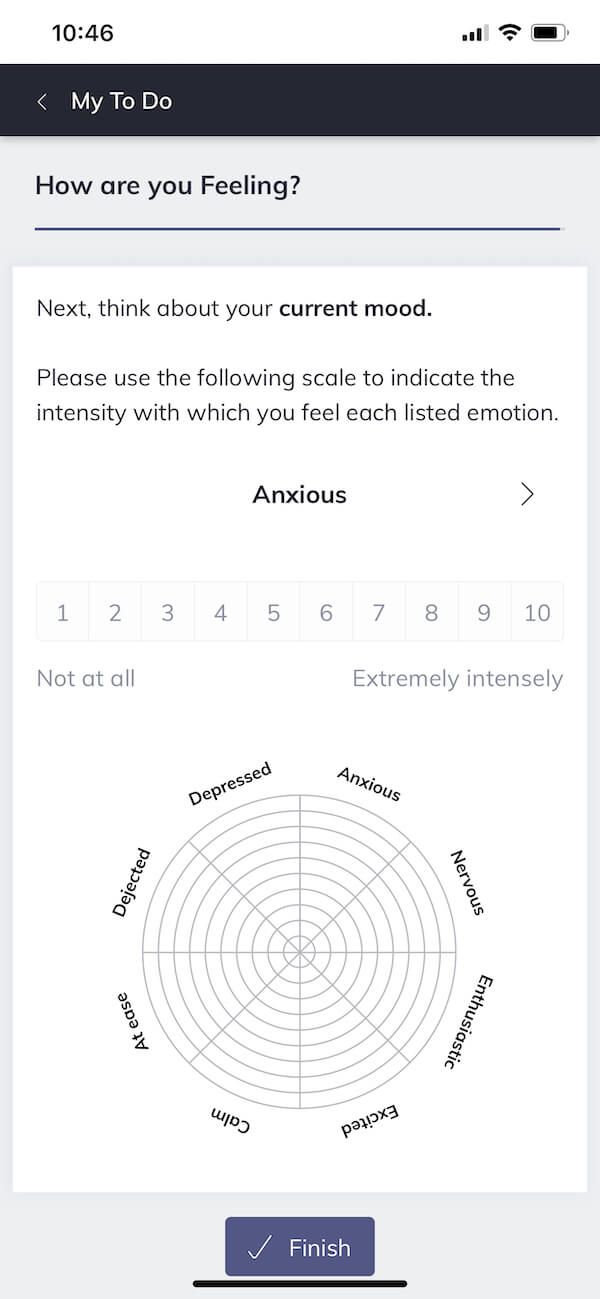
Therapists can use mental health assessments to achieve a range of goals at different stages of the therapeutic process, all of which can be streamlined using online tools.
Throughout this article, we’ll explore the applications of the online psychotherapy tool Quenza (pictured here), which is a powerful platform that helps practitioners automate and scale several aspects of the assessment process.
At the beginning of the therapeutic relationship , practitioners using the platform will send a digital invitation to their clients to sign up for a free account.
Following this initial step, most of the client’s engagement with the platform will occur when prompted via push notifications on their smartphone.
Once a client is registered, Quenza can help the practitioner carry out two key aspects of a mental health assessment. These include pre- and post-treatment assessments and ongoing assessment of intervention efficacy using repeated measurements across time.
Pre-treatment assessments can help practitioners determine which mode of treatment or intervention is most likely to have the greatest benefit based on presenting symptoms.
Likewise, the therapist may administer a post-treatment test to determine how effective an intervention has been at reducing symptoms or increasing signs of psychological flourishing .
Regarding ongoing assessments, it can be helpful to encourage clients to provide regular feedback on aspects of their treatment. Using Quenza, this can be accomplished by assigning brief tests or reflections assessing factors like mood, cognitions, and behaviors, which clients can complete at regular intervals.
For instance, pictured here is a daily emotion reflection, which clients can complete each day on their smartphone to help track changes in their emotions. The practitioner can then review a client’s aggregate responses to these reflections via Quenza’s online dashboard to make inferences about the effectiveness of ongoing interventions.
A key advantage of using an online platform to conduct these one-off and ongoing assessments is that it allows the practitioner to monitor their clients’ progress with interventions between sessions.

Download 3 Free Positive Psychology Exercises (PDF)
Enhance wellbeing with these free, science-based exercises that draw on the latest insights from positive psychology.
Download 3 Free Positive Psychology Tools Pack (PDF)
By filling out your name and email address below.
So far, we’ve looked at the MMPI-2 and the Beck Inventories as examples of reliable and widely used psychological tests for assessing mental health. We’ve also considered how we might administer these tests efficiently as part of a one-off or ongoing assessment.
Let’s now consider three more freely available tests for assessing experiences reflective of one’s mental health.
But before we dive in, a quick note. These assessments are not designed to be self-administered. Rather, they should be administered by licensed practitioners and only within the bounds of your professional expertise.
Dissociation – Brief Dissociative Experiences Scale
Dissociation is a common characteristic of a range of mental health disorders, including post-traumatic stress disorder and bipolar disorder (Hariri et al., 2015). Therefore, when clients show signs of dissociation, it may be wise to administer an assessment.
One widely used test assessing dissociation is the Brief Dissociative Experiences Scale.
This measure consists of eight items assessing the frequency with which a client has experienced various dissociative symptoms over the past seven days.
Example items from the scale are:
- I find myself staring into space and thinking of nothing.
- People, objects, or the world around me seem strange or unreal.
- When I am alone, I talk out loud to myself.
All items are presented on 5-point scales, where 0 is ‘not at all,’ and 4 is ‘more than once a day.’
A full copy of the scale and scoring information can be downloaded from the American Psychiatric Association website .
World’s Largest Positive Psychology Resource
The Positive Psychology Toolkit© is a groundbreaking practitioner resource containing over 500 science-based exercises , activities, interventions, questionnaires, and assessments created by experts using the latest positive psychology research.
Updated monthly. 100% Science-based.
“The best positive psychology resource out there!” — Emiliya Zhivotovskaya , Flourishing Center CEO
Misophonia – Amsterdam Misophonia Scale
Misophonia is defined as
“a relatively unexplored chronic condition in which a person experiences autonomic arousal (analogous to an involuntary ‘fight-or-flight’ response) to certain innocuous or repetitive sounds such as chewing, pen clicking, and lip smacking.”
Edelstein, Brang, Rouw, & Ramachandran, 2013
The experience of misophonia can compel someone to avoid situations that may trigger this autonomic arousal, potentially making it difficult to work and socialize. Misophonic experiences have the potential to negatively impact mental health and quality of life .
One tool for assessing the experience of misophonia is the Amsterdam Misophonia Scale (Schröder, Vulink, & Denys, 2013).
This scale comprises six items assessing different features of misophonic experiences, including their frequency and the extent to which they disrupt a patient’s day-to-day functioning.
- How much of your time is occupied by misophonic sounds?
- How much distress do the misophonic sounds cause you?
- How much effort do you make to resist the (thoughts about the) misophonic sounds?
A free copy of the scale can be obtained from the Misophonia Treatment website .
Intolerance of Uncertainty – Intolerance of Uncertainty Scale Short Form
The inability to tolerate uncertainty can have direct deleterious effects on mental wellbeing (Satici, Saricali, Satici, & Griffiths, in press). Therefore, how a client tolerates uncertainty may sometimes be a relevant focus for assessment.
The Short Form Intolerance of Uncertainty Scale (Carleton, Norton, & Asmundson, 2007) is one of the most commonly used scales for assessing uncertainty intolerance and its effects on mental health.
This scale consists of 12 items asking respondents to indicate the extent to which they agree with a list of statements.
- Unforeseen events upset me greatly.
- I can’t stand being taken by surprise.
- The smallest doubt can stop me from acting.
All items are presented on 5-point scales, where 1 is ‘not at all characteristic of me,’ and 5 is ‘entirely characteristic of me.’

However, there are also questions and exercises that may flag the potential need for these more specific diagnoses. This may require practitioners to ask a series of general therapy questions before diving in for a deeper analysis of specific symptoms.
To help, here are seven useful questions you might ask your clients early in the therapeutic process or session (adapted from Aidala, Havens, Peake, & Keane, 2002).
Note that these questions could invite a combination of open-ended responses and numerical responses on Likert scales.
- How have things been going for you in terms of your mood or feelings?
- Were there any periods when you were very sad or depressed?
- How about any times when you were very nervous, frightened, or worried about things?
- Were there times when you were so active or hyper that you couldn’t slow down?
Depending on when symptoms of ill mental health started presenting (or in cases where an event triggered them), you may find it helpful to anchor the mental health questions in specific timeframes, such as in the following examples:
- During the last month, was there a time when you had little interest or pleasure in doing things? If so, how often did you feel that way?
- Over the last week, how often have you had trouble falling or staying asleep? What about sleeping too much?
- In the last four weeks, have you had an anxiety attack (i.e., sudden feelings of fear or panic)?
In addition to the above questions, here are six worksheets that can support you in exploring your clients’ mental health. Several of these are preloaded activities on Quenza , which you can access and try for yourself via the platform’s no-risk 30-day trial .
1. Moving from Cognitive Fusion to Defusion
Central to the practice of Cognitive-Behavioral Therapy is the understanding that our thoughts have the potential to strengthen or weaken emotional states brought about by events in our environment. Therefore, we can change our emotional experiences by changing our thoughts.
The Cognitive Fusion to Defusion worksheet on Quenza is designed to help your clients take a step back when growing overwhelmed by self-critical thoughts. In particular, the worksheet invites the user to begin noticing their thoughts nonjudgmentally as opposed to getting caught up in them. Consequently, they can reduce their belief that intrusive thoughts are true or must dictate their behaviors.
2. S.O.B.E.R. Stress Interruption Technique
For some clients, difficulties managing stress can exacerbate problems with mental health. For these clients, try inviting them to apply the S.O.B.E.R. Stress Interruption Technique. This exercise and accompanying worksheet are available digitally through Quenza’s Expansion Library.
The acronym S.O.B.E.R. stands for Stop , Observe , Breathe , Expand awareness , and Respond with awareness . To apply the technique during stressful times, clients begin by listening to an eight-minute audio meditation that guides them through the five S.O.B.E.R. steps. The activity then concludes with a reflection, encouraging them to consider other situations in which they may benefit from applying the technique.
3. Brief Needs Check-In
The final worksheet we’ll look at from Quenza is the Brief Needs Check-In .
A core part of caring for our mental health involves recognizing and taking the time to meet our emotional needs. The Brief Needs Check-in is useful for helping clients anchor themselves in the present moment and stop to consider their needs. The activity then guides clients as they plan out how to satisfy any unmet emotional needs in an act of self-care .
4. Preventing Mental Health Relapse
When clients are undertaking therapy for mental health conditions, there are likely to be times when they fall back into old or unhelpful habits .
The Preventing Mental Health Relapse worksheet is designed to help your clients track the symptoms of mental illness, recognize early signs that they may be ‘relapsing’ (e.g., falling into a depressive spell), and plan adaptive strategies to help them cope.
5. Self-Care Checkup
Whether we have a mental illness or not, all of us need to take time out for ourselves to maintain good mental health.
The Self-Care Checkup worksheet lists a wide range of self-care activities and invites your clients to consider which ones they typically engage in. In doing so, the worksheet encourages clients to assess the frequency and quality of their self-care across the emotional, physical, social, professional, and spiritual domains of their life.
6. Understanding Mental Health Stigma
It is not uncommon for therapy clients to experience embarrassment or shame at needing support for their mental health. Likewise, others in their life may hold a stigmatizing view about mental illness or attending therapy.
The Understanding Mental Health Stigma worksheet explores some dangers of mental health stigma and makes recommendations for how we might reduce misunderstanding around mental illness. In particular, this worksheet may serve as a handy communication aid for clients looking to start a constructive conversation about mental health with others in their life.
Let’s now delve into some practical applications of these assessment tools with an example designed in Quenza .
Quenza allows practitioners to draw on a growing library of tests and assessments or design their own.
These can focus on a broad range of themes, including wellbeing, interpersonal functioning, and emotional volatility.
Therapists can then administer these activities to their clients digitally to be completed via their own smartphone or tablet.
For instance, therapists can choose to administer a single test, such as the Beck Depression Inventory (pictured here) or administer a sequence of tests as part of an ongoing assessment. In Quenza, this sequence is referred to as a pathway .
For instance, a therapist might schedule a pathway of mental health activities assessing the intensity of emotions throughout a week. Using Quenza, the therapist can automatically send these according to a pre-programmed schedule and then facilitate a discussion regarding patterns in these responses during their next in-person session with the client.
Additionally, practitioners using Quenza are not limited to designing and administering assessments. Rather, they can create any number of activities, including audio meditations and lessons.
For example, as a part of a mental health intervention , a therapist might record one week’s worth of five-minute meditations and send a push notification to their client each morning, reminding them to meditate.
They might then follow up each meditation with a digital reflection that invites clients to consider their emotional health following the period of meditation.
For an entirely fresh approach, therapists may even wish to design toolkits of activities, meditations, and videos that clients can draw on as needed, rather than according to a schedule. That way, clients will have a bank of custom-made tools in their back pocket to help them cope during times of stress.
These are just a few examples of the different ways you can use this platform to administer your mental health assessments.
Let’s now look at three useful activity templates in Quenza you can use to design a mental health assessment pathway of your own. You’ll find each of these in Quenza’s ever-growing Expansion Library.
Stress Diary Pathway
Among Quenza’s ready-to-use tools is its Stress Diary . This preloaded expansion is a complete pathway that invites your clients to reflect on their experience of stress for seven days.
Each day, your client will receive a push notification reminding them to complete their day’s diary entry. They will be prompted to rate the intensity of their stress reactions, note the day’s most stressful event, reflect on their emotional responses to stress, and consider their chosen coping strategies.
At the end of the week, clients will review their diary entries and analyze them for patterns.
The Stress Diary can serve as a valuable exercise to help clients practice noticing their emotional reactions, which is a behavior that in itself may take practice. Likewise, the diary can serve as a form of ongoing assessment during particularly stressful periods or as a way to capture improvements (e.g., the use of positive coping strategies ) throughout the therapeutic process.
Life Domain Satisfaction Activity
Many clients who seek therapy do so because challenges with their mental health have hampered their ability to function across different domains of life.
Quenza’s Life Domain Satisfaction activity can serve as an enlightening activity to assess these impacts as part of a pre/post-assessment of change. In short, this activity invites clients to rate their satisfaction across 16 domains of life using 10-point rating scales.
Given that all of Quenza’s preloaded activities are fully customizable, practitioners can easily adapt this template to invite open-ended responses exploring the impact that the client’s mental health has had on their satisfaction with each of these domains.
These responses may then serve as useful signposts for whether mental health interventions are enabling clients to achieve their initial aims for seeking therapy and deriving greater satisfaction from life .
Outcome Rating Scale Activity
Finally, Quenza’s Outcome Rating Scale activity is a useful tool for assessing improvements to a client’s mental health. In particular, it quickly assesses four areas of functioning known to change as a result of therapeutic intervention relating to wellbeing and interpersonal functioning using 10-point rating scales.
Again, practitioners may choose to combine this single activity template with a range of other activities in a pathway as part of an ongoing mental health assessment.
For instance, if a client is practicing mindfulness as part of a mental health intervention, the practitioner may alternate sending weekly meditations via Quenza with the Outcome Rating Scale to assess trajectories in mental wellbeing flowing from the intervention.
17 Top-Rated Positive Psychology Exercises for Practitioners
Expand your arsenal and impact with these 17 Positive Psychology Exercises [PDF] , scientifically designed to promote human flourishing, meaning, and wellbeing.
Created by Experts. 100% Science-based.
Looking for more tools to help assess your clients’ mental health and wellbeing? Check out the following free assessment tools from our blog.
- Perfectionist Beliefs ‘Flexibility’ Self-Assessment This short assessment presents a series of questions to help clients identify areas where their thinking is rigid and instances when they might benefit from relaxing perfectionist tendencies.
- Self-Care Check-In This self-assessment uses ratings and reflection questions to help clients determine how they can better meet their self-care needs.
- Thoughts and Feelings: Struggle or Acceptance? This 15-item questionnaire will help you quickly assess the extent to which a client adopts an attitude of acceptance when facing unavoidable discomfort and challenges.
- Codependency Questionnaire This questionnaire , adapted from research, presents 20 statements assessing a client’s tendency to display symptoms of codependency.
If you’re looking for more science-based ways to help others enhance their wellbeing, this signature collection contains 17 validated positive psychology tools for practitioners. Use them to help others flourish and thrive.
It’s clear that assessment tools are critical for mental health professionals to do their work.
Thankfully, researchers and practitioners have designed a vast array of tools and tests to assess everything from the common experience of anxiety to the lesser known disturbances associated with misophonia.
Further, clinicians are becoming increasingly creative in their application of these tools. Rather than the standard pre/post-assessments that once dominated therapeutic practice, modern technologies are making it easier to conduct ongoing assessments involving repeated measurements across time.
If you’re a mental health practitioner, we hope this article has inspired you to consider how you might better use the tools at your disposal to assess your clients’ mental health.
And if it has, let us know what you’re planning to do differently in the comments. We’d love to hear from you.
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free .
- Aidala, A., Havens, J., Peake, M., & Keane, T. (2002). Use of Client Diagnostic Questionnaire (CDQ): Training manual . Retrieved from https://targethiv.org/sites/default/files/file-upload/resources/Client_Diagnostic_Questionnaire.pdf
- Butcher, J. N., Dahlstrom, W. G., Graham, J. R., Tellegen, A., & Kaemmer, B. (1989). Manual for administration and scoring: MMPI-2 . University of Minnesota Press.
- Carleton, R. N., Norton, M. P. J., & Asmundson, G. J. (2007). Fearing the unknown: A short version of the Intolerance of Uncertainty Scale. Journal of Anxiety Disorders , 21 (1), 105–117.
- Cronbach, L. J. (1949). Essentials of psychological testing . Harper.
- Edelstein, M., Brang, D., Rouw, R., & Ramachandran, V. S. (2013). Misophonia: Physiological investigations and case descriptions. Frontiers in Human Neuroscience , 7 , 296.
- Goldstein, G., Allen, D. N., & Deluca, J. (2019). Historical perspective. In G. Goldstein, D. N. Allen, D. N., & J. Deluca (Eds.), Handbook of psychological assessment (4th ed.). Elsevier.
- Hariri, A. G., Gulec, M. Y., Orengul, F. F. C., Sumbul, E. A., Elbay, R. Y., & Gulec, H. (2015). Dissociation in bipolar disorder: Relationships between clinical variables and childhood trauma. Journal of Affective Disorders , 184 , 104–110.
- Park, C. L., Cohen, L. H., & Murch, R. L. (1996). Assessment and prediction of stress‐related growth. Journal of Personality , 64 (1), 71–105.
- Pearson Education. (2014). Case description: Karen Z–Inpatient mental health interpretive report . Retrieved from https://images.pearsonclinical.com/images/Assets/MMPI-2Clinical/MMPI-2_AdultClinical_Inpatient-Mental-Health.pdf
- Prochaska, J. O., Norcross, J. C., & DiClemente, C. C. (1994). Changing for good: The revolutionary program that explains the six stages of change and teaches you how to free yourself from bad habits . Morrow.
- Rogers, R., Robinson, E. V., & Jackson, R. L. (2016). Forensic psychiatry and forensic psychology: Malingering and related response styles. In J. Payne-James & R. W. Byard (Eds.), Encyclopedia of forensic and legal medicine (2nd ed.) (pp. 627–633). Elsevier.
- Satici, B., Saricali, M., Satici, S. A., & Griffiths, M. D. (in press). Intolerance of uncertainty and mental wellbeing: Serial mediation by rumination and fear of COVID-19. International Journal of Mental Health and Addiction .
- Schröder, A., Vulink, N., & Denys, S. (2013). Misophonia: Diagnostic criteria for a new psychiatric disorder. PLoS ONE , 8 (1).
Share this article:
Article feedback
What our readers think.
I am a counselor and missionary in Colombia and with great joy I serve the people of that country who have great difficulties finding mental health and professional counselors. Your resources here are proving very handy for me to use in preparing myself for my next trip. Thank you so very much for making all this available here online.
Clive Wilson
Need a professional mental evaluation with MRI for my son who was born with mental disability.
You can find a directory of licensed therapists here (and note that you can change the country setting in the top-right corner). You’ll also find there are a range of filters to help you drill down to the type of support you need: https://www.psychologytoday.com/us/therapists
I hope this helps.
– Nicole | Community Manager
Thank you for sharing your experience and knowledge with us. Love your resources and they are definitely will be utalised to make a difference in many who are needing care and support in improving their mental health well-being. All the best with your ongoing research. Take care and stay safe.
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

High-Functioning Autism: 23 Strengths-Based Daily Worksheets
Autism diagnoses are rising exponentially. A study by Russell et al. (2022) reported a 787% increase in UK diagnoses between 1998 and 2018. Similarly, 1 [...]

Treating Phobias With Positive Psychology: 15 Approaches
Phobophobia is a fear of phobias. That is just one in our list of 107 phobias. Clearly a person suffering from phobophobia has a lot [...]

How to Fuel Positive Change by Leveraging Episodic Memory
Some researchers believe that our memory didn’t evolve for us to only remember but to imagine all that might be (Young, 2019). Episodic memory is [...]
Read other articles by their category
- Body & Brain (52)
- Coaching & Application (39)
- Compassion (23)
- Counseling (40)
- Emotional Intelligence (21)
- Gratitude (18)
- Grief & Bereavement (18)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (16)
- Mindfulness (40)
- Motivation & Goals (41)
- Optimism & Mindset (29)
- Positive CBT (28)
- Positive Communication (23)
- Positive Education (36)
- Positive Emotions (32)
- Positive Leadership (16)
- Positive Parenting (14)
- Positive Psychology (21)
- Positive Workplace (35)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (38)
- Self Awareness (20)
- Self Esteem (37)
- Strengths & Virtues (29)
- Stress & Burnout Prevention (33)
- Theory & Books (42)
- Therapy Exercises (37)
- Types of Therapy (54)
3 Positive Psychology Tools (PDF)

IMAGES
COMMENTS
This can put you at increased risk for a variety of physical and mental health problems, including anxiety, depression, digestive issues, headaches, muscle tension and pain, heart disease, heart attack, high blood pressure, stroke, sleep problems, weight gain, and memory and concentration impairment. Chronic stress may also cause disease ...
Stress and anxiety both contribute to nervousness, poor sleep, high blood pressure, muscle tension, and excess worry. Experiencing anxiety can make it more difficult to cope with stress and may contribute to other health issues, including increased depression, susceptibility to illness, and digestive problems.
Our 3 Favorite Stress-Management Worksheets. A 2022 report found that in the UK alone, 17 million working days were lost due to stress, depression, and anxiety.. But help is at hand. Multiple, evidence-based stress reduction techniques have been shown to lower stress levels, "resulting in a reduction of disease symptoms, lowering of biological indicators of disease, prevention of disease and ...
1.1 Define stress as a psychophysiological response to the environment. 1.2 Explain sources of stress across the lifespan. 1.3 Explain physiological and psychological consequences of stress for health and wellness. 1.4 Explain physiological, cognitive, and behavioral strategies to deal with stress.
Chronic stress can have negative effects on your body and mind and create a multitude of unpleasant physical and psychological symptoms. For example, it can cause tension, leading to muscle pain ...
Focusing on your breath is a long-held tenet of meditation for stress. Learning to control your breathing can keep you anchored in the present moment. Sometimes, reminding yourself of what's ...
Anxiety is your body's reaction to stress and can occur even if there is no current threat. If that anxiety doesn't go away and begins to interfere with your life, it could affect your health. You could experience problems with sleeping, or with your immune, digestive, cardiovascular, and reproductive systems.
loss of your sense of humor. feelings of overwhelm. depression. loss of interest in life or activities. existing mental health conditions get worse. Physical symptoms of stress may include the ...
Stress can be defined as a state of worry or mental tension caused by a difficult situation. Stress is a natural human response that prompts us to address challenges and threats in our lives. Everyone experiences stress to some degree. The way we respond to stress, however, makes a big difference to our overall well-being.
Stress and health Glucocorticoids, including cortisol, are important for regulating the immune system and reducing inflammation. ... This impaired communication has been linked to the future development of numerous physical and mental health conditions, including chronic fatigue, metabolic disorders (e.g., diabetes, obesity), depression, and ...
This Understanding Mental Health Stigma sheet can be used as an aid to help raise awareness of the stigma that surrounds mental illness, as well as what it looks like. 5. Mental Health Management Bingo. Mental Health Management Bingo is a fun classroom game that can be played with slightly older students.
The Self-Care Vision Board exercise is a positive and practical way for you to personalize the list of items under each dimension (physical, psychological, emotional, spiritual, personal, and professional). It consists of four steps: Brainstorm self-care activities. Collect positive images for the vision board.
This free, printable coloring and activity book for children ages 8-12 teaches kids about stress and anxiety and offers tips for coping in a healthy way. The Stress Catcher is a printable, "fortune teller" craft for children that offers coping strategies to help manage stress and other difficult emotions. Instructions on how to create and ...
Stressors have a major influence upon mood, our sense of well-being, behavior, and health. Acute stress responses in young, healthy individuals may be adaptive and typically do not impose a health burden. However, if the threat is unremitting, particularly in older or unhealthy individuals, the long-term effects of stressors can damage health.
A mental health specialist can identify the sources of your stress, create a mental health plan, and plan constructive strategies to manage stress. At last, the idea behind assigning tasks comes from the way that pupils learn. It facilitates the assessment of students' subject-matter comprehension by teachers. Assignments broaden their ...
The act of laughing helps your body fight stress in a number of ways. Take up a relaxation practice. Relaxation techniques such as yoga, meditation, and deep breathing activate the body's relaxation response, a state of restfulness that is the opposite of the fight or flight or mobilization stress response.
A printable deck of cards with 128 coping skills for managing stress, anxiety, and other difficult emotions. Each card includes one simple coping skill. Print/cut the cards, fold, and place in a container. Group members take turns drawing the cards and answering the questions.
Anxiety in college is very common. According to the American College Health Association Fall 2018 National College Health Assessment, 63% of college students in the US felt overwhelming anxiety in the past year. In the same survey, 23% reported being diagnosed or treated by a mental health professional for anxiety in the past year.
LAGOS, Nigeria (AP) — How do you deal with stress? In Lagos, Nigeria's largest city, people are finding their reset button in a "rage room" where they pay to smash electronics and furniture with a sledgehammer as a break from the worst cost-of-living crisis in a generation.. The Shadow Rage Room, apparently the first of its kind in Nigeria, offers "a safe space" for people to let ...
When symptoms related to mental health are interfering with daily functioning, it's time to identify what's contributing to the problem and develop effective tools to cope. With time, you can learn, practice, and utilize these tools to improve your mood and your daily life. $135 per Session. Mental Health Counseling in Moscow, Idaho.
Search our database of carefully reviewed and verified therapists to find a local therapist, counsellor, psychologist, psychiatrist, or social worker in Moscow. We publish expert-written articles to help you get the most from therapy, better understand each therapy service, and choose the right therapy for your needs.
1. Minnesota Multiphasic Personality Inventory (MMPI-2) First published in 1989, the MMPI-2 is the world's most widely used psychometric test for measuring mental health ailments that feature as forms of psychopathology (Rogers, Robinson, & Jackson, 2016). The scale features 567 true-false statements, which assess 10 clinical sub-scales ...
©2015-2024 Mental Health Center Call us +7 495-108-04-63. Address. Moscow, Palikha str. 13/1, building 2, 2nd floor. Make an appointment ...
Mental health services remain foreign or unaffordable for many in Africa's most populous country, where 40% of citizens live below $2 per day. ... Some Nigerians have turned to social media ...
Mental health refers to emotional, psychological, bio-chemical, and social well-being. It can be found in the name of health ministry departments, or used as a polite euphemism, or even made fun ...