Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.


£42.7 million funding boost for mental health research

Published: 30 May 2023
A new £42.7 million investment into mental health research has been announced by the NIHR and the Office for Life Sciences.
The new Mental Health Mission (MHM) will develop innovative new treatments and technologies. The Mission will work with patients, NHS staff and clinicians and innovators to make the UK a leading location in which to test and trial new products.
Two Co-Chairs have been appointed:
- Kathryn Abel, Professor of Psychological Medicine and Reproductive Psychiatry at the University of Manchester
- Husseini Manji, Visiting Professor at Oxford and Duke Universities.
Together, they will:
- set the overarching strategic direction
- drive forward its delivery
- build strong, collaborative working relationships across the wider clinical and research communities
- represent the Mission nationally and internationally.
The Mental Health Mission will be delivered via the NIHR’s Mental Health Translational Research Collaboration (MH-TRC) .
This is a network of leading investigators who specialise in mental health research. It is led by Professor John Geddes of the University of Oxford, and Professor Rachel Upthegrove of the University of Birmingham.
Professor Lucy Chappell, Chief Executive of the NIHR, said:
“Mental ill health affects many people. This investment in the Mental Health Mission aims to deliver a truly exciting range of innovative therapies and technologies that could greatly improve people's lives.
"For example, the development of wellbeing apps, games and services to diagnose child mental health problems early could provide valuable new methods of treatment.
"And in the true spirit of collaboration, the work has intentionally been spread across the country so that more people are able to participate in world-leading mental health research than ever before.”
Professor Abel and Professor Manji said:
“We are delighted to be working together to make the new Mental Health Mission a truly revolutionary force behind mental health research. We want the Mission to create tangible differences to the lives of patients, both in the UK and internationally. Between us, we bring a wealth of experience in mental health research and innovation, and a commitment to genuine collaboration with patients, industry and healthcare staff.
"Bringing together the public sector, patients and industry as equal partners, the Mission will work with the Office for Life Sciences and the NIHR to support the NHS and NIHR to capitalise on its size and scope, and on the depth of its data resources. Alongside additional investment in mental health research and infrastructure, the Mission will foster a step change in the way we think about mental health, mental illness and its treatment. This will support development of the critically needed treatments across the spectrum of mental illness.
"We want the UK to be the most attractive place to conduct robust, high impact mental health research, ensuring people have access to the best, and newest, treatments. We are confident that the Mission will be unique in its ability to convene and challenge national partners to make this happen.”
Demonstrator sites
Of the total investment, more than £20 million will go towards establishing demonstrator sites in Birmingham and Liverpool (£9.9m and £10.5m over five years respectively).
The new centre in Liverpool will help people look after their mental health by understanding how mental, physical and social conditions interlink.
The site in Birmingham will support research and the development of novel treatments for:
- early intervention in psychosis, depression and children
- young people suffering from mental ill health.
The remainder of the £42.7m fund will go to UK-wide work focussed on conditions such as depression and early psychosis. It also help to build mental health research capacity in the NHS, and embedding research findings into practice.
The establishment of sites in the Midlands and the North further demonstrates the Government’s commitment to Levelling Up. It will ensure communities across the UK get to take part in, and benefit from research.
The Mental Health Mission is one of the healthcare research priorities announced by the government as part of its Life Sciences Vision. It will take a Vaccine Taskforce style approach to tackling some of the biggest public health challenges facing the UK.
Building on the model which led to one of the most successful vaccine roll outs in the world and ensured millions got a Covid-19 jab, the government will continue to:
- harness world-leading research expertise
- remove unnecessary bureaucracy
- strengthen partnerships
- support the new healthcare challenges.
According to NHS England, one in four adults and one in 10 children experience mental illness. Bolstering research in this area could help millions of people across the country. The mission will engage with industry by eliminating barriers to develop and test new products, attracting additional private investment and cementing the UK as a life sciences superpower.
Read more about the Mental Health Translational Research Collaboration.
Latest news
Blood tests for diagnosing dementia a step closer for UK
NIHR launches new funding stream to support global health researchers
UK-US collaboration continues to support the next generation of cancer research leaders
App can help people reduce their alcohol intake
Handing out vapes in A&E helps smokers quit
- 1" class="nav-item" v-on:click="getDoc($event, item['0C13'].replaceAll(/ ]*?>/g, ''))"> Progress report - year 1
- 1" class="nav-item" v-on:click="getDoc($event, item['0C14'].replaceAll(/ ]*?>/g, ''))"> Progress report - year 2
- 1" class="nav-item" v-on:click="getDoc($event, item['0C15'].replaceAll(/ ]*?>/g, ''))"> Progress report - year 3
- 1" class="nav-item" v-on:click="getDoc($event, item['0C16'].replaceAll(/ ]*?>/g, ''))"> Progress report - year 4
- 1" class="nav-item" v-on:click="getDoc($event, item['0C17'].replaceAll(/ ]*?>/g, ''))"> Progress report - final
1" v-html="item['0C7']">
Supervisor(s):
1">Read 's thesis online at
')" v-html="p">
Project abstract
Project aims, progress report - year 1, progress report - year 2, progress report - year 3, progress report - year 4, progress report - final year, mental health research uk, the first uk charity dedicated to raising funds for research into mental illnesses, their causes and cures., since 2008, we have ....
in scholarships
research students
research publications
Mental Health Research UK aims to make a significant improvement to the lives of people with mental illness, by funding research into causes and cures. We know it is often challenging to find resources to support PhD studentships and that is why we focus our funding on these awards, supporting mental health researchers of the future.
Although only registered with the Charity Commission in 2008, Mental Health Research UK has already made {{scholarshipsFundedCount}} research awards; the first being funded jointly with the University of Nottingham.
Select the sub-headings below to learn more ...
What we fund
We fund research into:
- The underlying causes of mental ill health
- Treatments for mental health problems
We do not fund research into autism or dementia. Nor do we fund research that involves laboratory animals.
Mental Health Research UK has one competitive round of PhD Scholarship awards per year, launched in the spring, for submission in May, with decisions made in the autumn to start the following year. The annual timeline is as follows:
- March: Scholarships are advertised via our mailing list and listed on our website.
- Mid-May: Closing date for applications.
- July: The panel meets and shortlists applications. Those not shortlisted are informed at once. References and service user reports are organized.
- September: Deadline for the receipt of references and service user reports.
- Late September: The panel meets and selects applicants to be offered a scholarship.
- October: All applicants are notified of the outcome of their application by the end of the month.
Research topics
Mental Health Research UK makes research awards focusing on research into the causes of, or cures for, mental illnesses.
The specific research topics of interest are selected year-on-year by the Trustees. However, the Schizophrenia Research Fund John Grace QC PhD Scholarship award always focuses on Schizophrenia.
Our awards cover fees and stipend only and are based on the Medical Research Council’s minimum stipend and fees for UK students, currently as follows:
2023/24 stipend: Outside London: £18,662; Inside London: £20,622
2023/24 fees: £4,712
Funding will cease at 4 years or on submission of the PhD thesis, whichever is earlier.
The fourth year is regarded as a ‘writing up’ year and the grant will be the stipend and thesis fee only.
In the event of early submission, a brief application to retain the student for the remainder of the period within the total cost envelope will be considered. College fees will be considered, where advertised by the university as being in addition to the tuition fee.
Mental Health Research UK will consider a small grant towards travel and conference allowances, where the student is presenting, subject to prior approval. No contribution will be made towards Research Training and Support grants.
If your university fees or stipend are different from the above, we will consider these provided you advise us with your application.
MD(Res) awards
Please note that applications are not currently being considered.
The Trustees of Mental Health Research UK have, since 2018, supported the MD(Res) degree at the Institute of Psychiatry, Psychology and Neuroscience (IOPPN) at King's College, London.
Mental Health Research UK wishes to support young psychiatrists with an interest in mental health research by offering scholarships for this programme because we need to encourage more people to develop careers within academic psychiatry. We are keen to provide a supportive community within Mental Health Research UK for all our scholars, which the MD(Res) award holders will join. This will help doctors thrive in their studies and ensure progress is made towards improving the lives of people with mental health problems, through scientific advances.
Dr Gareth Owen, Chair of the MD(Res) committee, IOPPN said:
"Doctors working in mental health sometimes come to research questions later in their careers with the benefit of clinical experience and training. It is hugely important that their experience and research energy is tapped and academic awards make a real difference to enabling such innovation. These awards from MHRUK are an excellent way to bring clinical experience and high quality research supervision together to foster an exciting new cohort of clinical academics in mental health."
Eligibility
Applications for our awards need to come from UK universities. Research supervisors must be based at UK universities.
We accept one application per scholarship award from any one university. A university may apply for more than one scholarship if they wish.
Please note that we do not accept any requests for funding from individuals, including current PhD students.
User and carer involvement
Best practice will be followed to ensure that service users and carers are involved at all stages with the prioritization of research topics and the commissioning of research.
All research project applications will be peer-reviewed by service user reviewers as well as academic reviewers.
NIHR and NHS information
Mental Health Research UK is a National Institute for Health Research (NIHR) non-commercial Partner . This means the studies that we fund may be eligible to access the NIHR Study Support Service which is provided by the NIHR Clinical Research Network. The NIHR Clinical Research Network can now support health and social care research taking place in non-NHS settings, such as studies running in care homes or hospices, or public health research taking place in schools and other community settings. Read the full policy: Eligibility Criteria for NIHR Clinical Research Network Support . In partnership with your local R&D office, we encourage MHRUK award holders to involve your local NIHR Clinical Research Network team in discussions as early as possible when planning your study. This will enable you to fully benefit from the support available through the NIHR Study Support Service.
If your study involves NHS sites in England or Wales you will need to apply for Health Research Authority (HRA) and Health and Care Research Wales (HCRW) Approval .
Open Access publication of research results
Students can download our application form for open access publication of research results here .
PhD Competition {{ ' ' + scholarshipsAvailableYear}}
Mental Health Research UK (incorporating the Schizophrenia Research Fund) is pleased to announce a competition for {{scholarshipsAvailableCount}} PhD Scholarship s beginning September {{scholarshipsAvailableYear}} .
Please note that our PhD scholarship competition is currently closed
We are inviting applications for PhD scholarships under the theme of maternal mental health . We view this topic in its broadest sense inviting proposals that cover all aspects of mental health during pregnancy and in the first year afterwards. We are interested in proposals that aim to understand causes, risk factors, mechanisms, or treatments. MHRUK does not fund health services research.
{{ item['0C0'] + ' ' + item['0C3'] + ': ' + item['0C1']}}
{{item['0C2']}}
We invite applications from UK Universities for these scholarships. The deadline for applications is {{item['0C6']}} .
The full terms and conditions can be found here .
If you have any queries regarding the application process, please read the guidance above and check our FAQs document . If this does not provide the information that you need, please contact [email protected] .
Please note that for each individual scholarship we can accept only one application per university. A university may apply for more than one scholarship if they wish.
Scholarships Awarded
Find out more about the scholarships that we have awarded..
Use the buttons below to filter the list.
1" span v-html="item['0C7']">
Select from the tags below to filter by topic:

Mental Health Research Matters
Funding Opportunities

External – funding opportunities beyond the UKRI Networks
If you’re looking for mental health research funding opportunities, this is a great place to start. See below for a list of funders for mental health research. UKRI – Find the latest funding opportunities from UK Research and Innovation, including mental health. Look out for opportunities from the MRC, and even the EPSRC. NIHR –...

Emerging Minds
In 2021/22, Emerging Minds are focusing particularly on their ‘Big Question Research challenge’ which was identified as a priority in our original consultation workshops with stakeholders.

Violence, Abuse and Mental Health
There are no open funding opportunities for VAMHN network at the moment. Early Career Researcher Bursary Awards The network is delighted to launch another round of the Early Career Researcher (ECR) Training Bursary Scheme, which aims to support junior researchers to attend training courses, research placements at institutions other than their own, and conferences. Applicants...

Closing the Gap
Closing the Gap launched The Impact Accelerator Award, their final funding call, on 27th September 2021.
The aim of the call is to provide support for knowledge mobilisation activities and impact that address the challenge of reducing the health gap for people with experience of severe mental-ill health.

No open funding calls Previous funding calls SMaRteN are pleased to invite proposals for research projects to address student’s key questions about student mental health. Funding is available as part of the UKRI ‘plus’ funding scheme for Mental Health Networks. The deadline for proposals is 17:00 on the 14th of April 2021 This funding call...

MARCH: Social, Cultural and Community Assets for Mental Health
No open funding calls Previous funding calls Second funding round (closed) The MARCH Network’s second round of funding closed on Sunday 31st May 2020. Four projects which answered one of two specific high-priority questions were selected for larger investment of £50K, along with three projects addressing two broader priority questions for innovation grants of £20K,...

eNurture’s final funding round is now closed. eNurture’s third and final funding call is now live. The network is looking to fund research within the following thematic areas: A Focus on Families: The Digital World A Focus on Schools/Peers: The Digital World New Practice Models: Families and Schools Policy, Legal and Regulatory Frameworks Key dates:...

No open funding calls Previous funding calls The TRIUMPH Network plus-funding call for research projects closed in July 2020. They are delighted to announce that grants have been awarded to support the following projects that will start from October 2020. Co-production or adaptation of online interventions for foster care: Promoting the mental health and wellbeing...

Loneliness and Social Isolation Network
No open funding calls Previous funding calls October 2020 – Up to £50K was available from the Loneliness and Social Isolation in Mental Health network as part of their second funding call on interventions. Grants were available for £15K and £50K for small or large projects respectively, provided at 80% of full economic costing. For...
Privacy Overview
Funding opportunity: MRC neurosciences and mental health research grant: Sep 2021
Funding is available from MRC’s Neurosciences and Mental Health Board to support focused research projects on neurosciences and mental health.
We award research grants to UK-based research organisations, and research grants may involve more than one research group or institution.
There is no limit to the funding you can request, but it should be appropriate to the project. Typically awards are up to £1 million. We will usually fund up to 80% of your project’s full economic cost.
Projects can last up to five years and are typically 3-4 years.
Who can apply
Any UK-based researcher with an employment contract at an eligible research organisation can apply. You will need to:
- have at least a graduate degree, although we usually expect most applicants to have a PhD or medical degree
- show that you will direct the project and be actively engaged in the work.
You can include one or more industry partners as project partners in your application. International co-investigators can be included if they provide expertise not available in the UK.
The focus of this funding opportunity is neurosciences and mental health research. There are similar opportunities across other areas of medical research within our remit , including molecular and cellular medicine, infections and immunity, population and systems medicine, and applied global health. There are also other types of awards including programmes, partnerships and new investigator.
You should contact us if you are not sure which opportunity to apply to.
What we're looking for
The MRC’s Neurosciences and Mental Health Board funds research in neurosciences, mental health and disorders of the human nervous system. We aim to transform our understanding of the physiology and behaviour of the human nervous system throughout the life course in health and in illness, as well as how to treat and prevent disorders of the brain.
The research we support includes the interactions between the nervous system and other parts of the body – the brain, mental health and physical health. We are also interested in how episodes throughout life impact on lifelong mental and neurological health.
Research we fund includes, but is not limited to, the following areas:
- neurodegeneration
- clinical neurology and neuroinflammation
- mental health
- addictions and substance misuse
- behavioural and learning disorders including autism
- cognitive and behavioural neuroscience and cognitive systems
- sensory neuroscience including vision and hearing
- neurobiology and neurophysiology
- underpinning support – such as neuroimaging technology, brain banking and neuroinformatics
Find out more about science areas we support and our current board opportunity areas .
We encourage you to contact us first to discuss your application, especially if you believe your research may cross MRC research board or research council interests. If your application fits another research board remit better we may decide to transfer it there to be assessed.
Medical Research Council neurosciences and mental health research grants:
- are suitable for focused short or long-term research projects
- can support method development or development and continuation of research facilities
- may involve more than one research group or institution.
We will fund projects lasting up to five years, although projects typically last 3 to 4 years. If your project will last more than three years, you must justify the reason for this; for example, if you need time for data collection or follow-up.
If your project will last less than two years, it must be for proof of principle or pilot work only. We expect proof of principle proposals to support high-risk or high-reward research by critically testing a key hypothesis or demonstrating feasibility of an approach that could lead to fundamentally new avenues of research.
Contact one of our programme managers for advice if you would like to apply for a short or long-duration project.
You can request funding for costs such as:
- a contribution to the salary of the principal investigator and co-investigators
- support for other posts such as research and technical
- research consumables
- travel costs
- data preservation, data sharing and dissemination costs
- estates/indirect costs.
We won’t fund:
- research involving randomised trials of clinical treatments
- funding to use as a ‘bridge’ between grants
- costs for PhD studentships
- publication costs.
How to apply
Application deadlines for Neurosciences and Mental Health Board funding are usually around January, May and September/October, although sometimes dates can change, so check the Funding finder for details.
You can submit to any of the available deadlines in the year. We do not expect you to submit more than two applications at the same time and encourage you to focus on application quality, not the number you can submit. Read our guidance for applicants for details of our resubmission process .
Applying through Je-S
You must apply through the Joint Electronic Submission system (Je-S) . Please read the Je-S how to apply guidance (PDF, 190KB) for more information. If you need help applying, you can contact Je-S on 01793 444164 or by email [email protected] .
You should give your administrative department at least two weeks’ notice that you intend to apply. You must submit your application before 4pm on the deadline date.
When applying select:
● council: MRC ● document type: standard proposal ● scheme: research grant ● call/type/mode: research boards Sep 2021 submissions
Indicating the proposal is a research grant
Select the ‘grant type’ option from the proposal document menu, within the Je-S proposal form. Within the section, select the radio button adjacent to the ‘research grant’ option and select the ‘save’ button.
Guidance for applicants
Our guidance for applicants will:
- help you check your eligibility
- guide you through preparing a proposal
- show you how to prepare a case for support
- provide details of any ethical and regulatory requirements that may apply.
Industrial partners
If you want to include one or more industry partners as a project partner, you must also:
- complete the project partner section in Je-S
- submit an MRC industrial collaboration agreement (MICA) form and heads of terms
- include ‘MICA’ as a prefix to your project title.
Find out more about MRC industry collaboration agreements .
Longitudinal population studies
If your application is to fund new or existing longitudinal population studies, you must first submit an outline application for joint review by the Longitudinal Population Studies Strategic Advisory Panel and the Research Board. Should a full application be invited, this may be submitted within a 12-month window.
Applications for longitudinal population studies must be for core infrastructure only, applications may include associated research only if it is for proof of principle work.
Applicants must speak to the relevant programme manager at least 6 weeks before the outline submission deadline to confirm the eligibility of their application.
Please email [email protected] for the outline template, timeline for review and next outline submission deadline. Applications for funding for clinical (meaning, patient-specific or disease-focused) cohorts are exempt from this process.
How we will assess your application
When we receive your application, it will be peer-reviewed by independent experts from the UK and overseas.
You can nominate up to three independent reviewers. We will invite only one to assess your application, and may decide not to approach any of your nominated reviewers.
Peer reviewers will assess your application and provide comments. They will also score it using the peer reviewer scoring system against the following criteria:
- importance: how important are the questions, or gaps in knowledge, that are being addressed?
- scientific potential: what are the prospects for good scientific progress?
- resources requested: are the requested funds essential for the work? And do the importance and scientific potential justify funding on the scale requested? Does the proposal represent good value for money?
Read the detailed assessment criteria for each grant type .
We will review these scores and comments at a triage meeting and expect to continue with the highest-quality applications with potential to be funded. If your application passes the triage stage, we will give you the chance to respond to reviewers’ comments.
A board meeting will then discuss your proposal and decide if it is suitable for funding. We make a decision within six months of receiving your application.
Find out more about our peer review process .
Contact details
Visit our science contacts page or contact the programme manager most relevant to your research area for advice on developing your application and which board to apply to:
- head of programme – mental health: Dr Karen Brakspear – [email protected]
- programme manager for cognition and developmental disorders: Dr Charlotte Inchley – [email protected]
- programme manager for neuronal function: Dr Simon Fisher – [email protected]
- programme manager for neurodegeneration: Dr Clara Fons – [email protected]
- programme manager for pain and addiction: Dr Siv Vingill – [email protected]
- programme manager for neurological disorders: Dr Steph Migchelsen – [email protected]
- programme manager for adolescent mental health: Dr Victoria Swann – [email protected]
Other contacts
- for queries about submitting your application using Je-S, email [email protected] or call 01793 444164
- for general enquiries about your application contact [email protected]
For general queries about MRC policy and eligibility or if you are not sure who to contact, get in touch with our research funding policy and delivery team:
- [email protected]
- 01793 416440
Additional info
Supporting documents.
- Je-S how to apply guidance (PDF, 190KB)
This is the website for UKRI: our seven research councils, Research England and Innovate UK. Let us know if you have feedback or would like to help improve our online products and services .
Header menu - Mobile | United Kingdom
Header menu - drawer | united kingdom, investment into mental health research: statistics.
In recent years, there has been an acknowledgement that mental health research is significantly below the equivalent of physical health.
As measured by Years Lived with Disability, mental disorders account for at least 21% of the UK disease burden 1 , although further research suggests this has been underestimated by at least a third. 2 In 2018, only 6.1% of the UK’s health research budget was spent on mental health 3 and funding has remained largely unchanged for a decade. 4
There have been recent boosts to mental health research; for example, the Department of Health and Social Care (DHSC) and the NIHR have announced a new £30 million Mental Health Research Initiative in 2021 5, and in May 2023, a new £42.7 million investment into mental health research has been announced by the NIHR and the Office for Life Sciences. 6
But the Royal College of Psychiatrists have stated that “We urgently need more funding for mental health research. If we’re serious about treating mental and physical health equally, funding for mental health research needs to increase exponentially.” 7
GBD results
Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171-178.
UK Clinical Research Collaboration. UK Health Research Analysis 2018. January 2020.
MQ. UK Mental Health Research Funding 2014–2017. 2017
£30 million investment to rebalance the scale of mental health research
£42.7 million funding boost for mental health services
RCPsych supports Government funding for research into severe mental illness
See all mental health statistics

Was this content useful?
- International edition
- Australia edition
- Europe edition

Mental illness costs England £300bn a year, study shows
Yearly cost to people, business and public sector found to be twice as big as NHS England’s annual budget
Mental illness costs England £300bn a year, equivalent to nearly double its NHS budget, according to research.
Researchers for the Centre for Mental Health thinktank analysed the economic, health and care impact of mental ill health, as well as human costs from reduced quality of life and wellbeing.
The report , commissioned by the NHS Confederation’s mental health network, calculated that in 2022, mental illness cost £130bn in human costs, £110bn in economic costs and £60bn in health and care costs.
The £300bn cost in 2022 equates to nearly double the NHS’s entire £153bn budget in England in the same year and is a “comparable impact, economically, to having a pandemic every year”, the report concludes.
The greatest financial impact, £175bn, falls on people living with mental health difficulties and their families, while the public sector incurs £25bn and business £101bn.
For the first time, the report also assessed some wider financial impacts of mental illness such as presenteeism, staff turnover and lost tax revenues from economic inactivity.
The authors calculate that presenteeism – where someone is less productive at work due to impaired cognitive function and emotional distress caused by their mental ill health – cost £41.8bn, while staff turnover due to mental illness cost £43.1bn and lost tax revenues cost £5.7bn.
The report concludes that even the £300bn is likely to be a significant underestimate. If other impacts of mental ill health were included, such as the £10bn to £16bn cost of physical and mental health comorbidities and the £2.1bn cost of mental ill health in prisons, the total would be even higher.
The figures underline the scale of the mental health crisis. Referrals to NHS mental health services in England rose 44% between 2016-17 and from 4.4m to 6.4m in 2021-22, while the number of people in contact with mental health services rose from 3.6 million to 4.5 million during that same period, the National Audit Office calculated.
According to the Department of Health and Social Care, mental health accounts for just 9% of NHS spending despite taking up 23% of the “burden of disease”.
In 2002 the estimated cost of mental ill health in England was £76.3bn. Further analysis of the figures suggests that even accounting for inflation and stripping out any costs in the 2022 figures not included in the 2002 figure, there has been a 40% increase in the cost of mental illness in England in the past two decades.
Andy Bell, the chief executive of the Centre for Mental Health, said ministers “cannot afford to ignore the devastating impact of mental ill health”, adding: “A pound sign can never fully reflect the suffering caused by mental ill health.
“Rising inequality, austerity and cuts to early support have contributed to a nation with overall poorer mental health, and have led to more people reaching crisis point before they get support.”
The NHS Confederation’s mental health network chief executive, Sean Duggan, reiterated the call for action from ministers, saying: “The false economy of failing to invest in mental health is making the country poorer and causing unspoken anguish to so many people and their loved ones. It is vital that we now invest in effective interventions that bring us closer to a mentally healthier nation for all.”
Wes Streeting, the shadow health secretary, said: “The failure of the Conservatives to support people out of lockdown, in particular young people who have felt the effects worse than most, has stored up huge problems for our society, economy and the public finances.”
Brian Dow, the deputy chief executive of Rethink Mental Illness, called mental ill health rates “one of the greatest challenges of the 21st century”.
The report’s release came as a coalition of leading health organisations signed a joint letter urging Victoria Atkins, the health secretary, to take “urgent steps” to protect the mental health and wellbeing of health and care staff as specialist hubs “continue to close”.
Ringfenced funding for NHS mental health and wellbeing hubs was cut a year ago, the organisations said, and as a result, staff in need of support face a “postcode lottery” of care. Of the original 40 hubs, 18 have closed since March 2023, they said.
A government spokesperson said: “We’ve increased spending on mental health by £4.7bn since 2018/19, to support even more people.
“We are also continuing to roll out mental health support teams in schools and colleges, investing £8m in 24 early support hubs and expanding talking therapies services so people get help early on with their mental health.”
- Mental health

Police in England must keep answering mental health calls, charity urges

20,000 people off work in the UK every month for mental ill health

People in 20s more likely to be out of work because of poor mental health than those in early 40s

Children’s emergency mental health referrals in England soar by 53%

Early release of mental health patients in England presents suicide risk, report finds

UK homeowners with mental health problems ‘spend less on essentials to pay mortgage’

Experts call for fewer antidepressants to be prescribed in UK

Third of UK carers with poor mental health have thoughts of suicide, survey finds
Most viewed.
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Education, training and skills
- Senior mental health lead training grant funding
- Education & Skills Funding Agency
Senior mental health lead training: conditions of grant for the 2024 to 2025 financial year
Updated 2 April 2024
Applies to England

© Crown copyright 2024
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected] .
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at https://www.gov.uk/government/publications/senior-mental-health-lead-training-grant-funding/senior-mental-health-lead-training-conditions-of-grant-for-the-2024-to-2025-financial-year
1. Introduction
The Department for Education ( DfE ) is offering a grant of £1,200 in the 2024 to 2025 financial year for eligible state-funded schools and colleges to train a senior mental health lead.
We encourage eligible settings that want to develop, or introduce, their whole school or college approach to mental health and wellbeing to apply for a grant. You must identify a senior mental health lead who can begin training by 31 March 2025.
The government remains committed to offering senior mental health lead training to all eligible state-funded schools and colleges by 2025.
2. Purpose of the senior mental health lead training grant
We will provide grants to cover, or contribute towards, the cost of DfE quality assured training for a senior member of school or college staff to train as the ‘senior mental health lead’ for that setting. The training will develop the knowledge and skills to implement an effective whole school or college approach to mental health and wellbeing in that setting.
All eligible education settings can benefit from this training, and courses are available to meet a variety of learning needs and preferences of senior leads depending on their level of experience, type of setting or location.
3. Grant allocation and eligibility
Each eligible setting that successfully submits both stages of the application process will receive a fixed grant of £1,200 to train a senior mental health lead who will be expected to implement and sustain an effective whole school or college approach to mental health and wellbeing.
Eligible schools and colleges that claimed a grant in a previous financial year can claim a second £1,200 grant if the senior mental health lead they previously trained left their setting before embedding a whole school or college approach.
4. Eligible settings
All state-funded education settings receiving Education and Skills Funding Agency ( ESFA ) pre-16 revenue, high needs block or 16 to 19 programme funding are eligible for the grant, including:
- mainstream academies and local authority maintained schools
- special academies and local authority maintained special schools (including alternative provision)
- independent special schools whose pupils’ education is funded by their local authority
- further education ( FE ) colleges attended by under-18-year-olds (one claim per campus ID)
- sixth-form colleges
- special post-16 institutions
- non-maintained special schools
- local authorities
- independent training providers
Grant applications can only be submitted by individual settings. Settings within a multi-academy trust must claim individually. Distinct institutions (with a DfE campus ID) within larger FE colleges will each be eligible for a training grant.
Some independent alternative provision settings will be eligible for a grant if the majority of their pupils are funded by the local authority.
4.1 Who is not eligible
Independent institutions (with fee-paying pupils and students) that do not receive the funding types outlined above are not eligible for a grant. Ineligible settings can still access DfE quality assured training courses independently.
This training grant is not available for leaders of early years settings. The department has published a mental health and wellbeing resource article on the Help for early years providers platform on GOV.UK.
If you believe you are eligible, but are experiencing application issues, contact us at [email protected] .
5. Terms on which the grant is allocated to eligible schools and colleges
5.1 before you submit your grant claim.
- have the commitment of your school or college senior leadership team to implement a whole school or college approach to mental health and wellbeing in your setting
- have identified a senior mental health lead, ready to start training by 31 March 2025, and oversee your setting’s whole school or college approach
You should read the accompanying guidance and reflect on the learning outcomes for the training .
When you apply for the grant, you will be asked to declare that these terms are met.
5.2 Permissible spend
The grant must be used to pay for DfE quality assured senior mental health training, to develop the knowledge and skills necessary to implement and sustain an effective whole school or college approach to mental health and wellbeing in a setting. It will be paid as stated in section 14 of the Education Act 2002 .
You can view the full published list of DfE quality assured courses .
Any element of the grant not spent on a DfE quality assured course can then be used:
- for supply cover for the senior mental health lead, should a school or college need to backfill a senior lead while undertaking training
- to fund further training, activity or resources that support the development of a senior mental health lead, and contribute to the implementation of an effective whole school or college approach to mental health and wellbeing in a setting
Further training, activity or resources may include:
- additional courses or coaching that support the further development of the senior mental health lead, enabling them to establish, implement or sustain a whole school or college approach to mental health and wellbeing
- external support to assess your existing school or college approach to promoting and supporting mental health, to identify strengths, weaknesses and areas for improvement
- online resources and toolkits that support the senior lead, or other staff, to embed, sustain or, otherwise, improve the effectiveness of their whole school or college approach to mental health and wellbeing (many resources are available for free)
- other activities by the senior lead within their setting that focus on raising wider awareness and understanding of their whole school or college approach to better promote and support mental health (for example, promotion materials or awareness sessions for education staff)
We do not consider the following expenditure as falling within the scope of further activity:
- employing counsellors or other professional individuals or groups to provide specific social, emotional or mental health interventions for children and young people

5.3 Applying for a grant
You can now apply for a grant if you are able to begin training by 31 March 2025.
Follow these steps to apply:
Complete application form 1 to reserve a grant. This form checks your eligibility. You will be asked to make a series of declarations as described in these conditions of grant.
You will receive confirmation that we have successfully received your application. This will tell you to book a DfE quality assured training course that must start by 31 March 2025. Keep evidence of your booking as you need this when you submit application form 2.
You must submit application form 2 to upload your booking evidence and claim your grant.
The second form asks you to provide evidence you have booked a quality assured course. This can be a scanned copy, screenshot or photograph of your confirmation email or invoice from your training provider. You should ensure that your evidence includes:
- title of the training course
- name of the training provider
If you are applying for a second grant, make sure you ‘tick’ the declaration to confirm your previous senior mental health lead has left. We will not pay your grant if you do not confirm this.
You will have up to 3 weeks to submit the second form. If you do not submit within 3 weeks, we may release your place to applicants on our waiting list.
5.4 When you will be paid
Once you have submitted evidence of your course booking in application form 2, we will review the information provided. We will email you to let you know we have approved your application and confirm when your grant will be paid.
We will make payments on a quarterly basis. When you receive your grant will depend on when you complete the second stage of your application.
Most settings will get their payments on the last working day of:
- September 2024
- December 2024
Academies will get their payments on the first working day of:
- October 2024
- January 2025
Maintained schools and maintained alternative provision settings will receive payment via their local authority. All other settings will receive payment directly. We will make this payment alongside your regular funding and it will appear as a separate line on that remittance.
We will provide local authorities with a breakdown of which schools to pass funding to. Maintained schools and settings should contact their local authority if they have not received their funds.
6. How we will use the data you provide
DfE will collect and use the data submitted through the online forms to compile aggregate statistical information for developing and measuring the impact of the service; and for the purposes of satisfying any legal, accounting or reporting requirements.
When applying for a grant, we will ask you to confirm that you will provide feedback on your training when contacted by DfE .
Your school or college will also be included on a list of published grant claims .
7. Record keeping
You should retain records to show that the grant has been used for the intended purposes for 6 years after the end of the financial year in which the expenditure has taken place.
The books and records of the school or college claiming the grant are open to inspection by the National Audit Office and our representatives.
We may request further information to determine if your school or college has complied with these conditions of grant.
Failure to provide this information may result in the whole or part of the grant paid being recouped.
8. Other terms
You must inform us if your senior mental health lead is unable to complete the training or meet the other terms of this grant.
We reserve the right to withhold payment or seek reimbursement of payments already made if we consider that you have:
- not spent the funding in accordance with this agreement
- breached any other terms of this agreement
- provided false or incorrect statements or information in your funding claim
The school or college will be informed of the above, in writing, along with the sum that immediately becomes payable, by the school or college, back to DfE .
9. Further information
If you have a query about the grant or eligibility criteria which is not covered in these terms and conditions or the guidance below, please contact us using our customer help centre .
Use the links below to find out more about:
- senior mental health lead training
- promoting and supporting mental health and wellbeing in schools and colleges
Is this page useful?
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
Institute of Mental Health Research

The History, Present & Future of LGBTQ+ Mental Health
- Date and time: Wednesday 21 February 2024, 3pm to 4.45pm
- Location: PS/A/202, Lecture Room (Venables Room), Psychology Building, Campus West, University of York ( Map )
- Audience: Open to staff, students, the public
- Admission: Free admission, booking not required
Event details
Three invited speakers will give short talks considering the historical context of LGBTQ+ mental health, the inequalities in mental health faced by these communities today, and how we can improve treatment in the future. This will be followed by a panel discussion drawing on our speakers’ experiences researching the mental health of LGBTQ+ people, working with these groups clinically, and teaching future clinicians to reflect on their practice. These discussions will be relevant to everyone, including LGBTQ+ staff and students and their personal supervisors, as well as those who aim to work clinically, assessing and improving mental health with diverse sexualities and genders.
Dr. Qazi Rahman , Co-director of the LGBT Mental Health Research Group, King's College London
Dr. Ruth Knight , Lecturer, York St Johns
Dr. Miles Rogish , University of York & York House Acquired Brain Injury Service
Note: The University of York is committed to making its events as welcoming and inclusive as possible. Please let us know in advance if you have any accessibility requirements , either by emailing [email protected] or calling 01904 325264: we will make every effort to accommodate your needs.
Venue details
- Wheelchair accessible
Rebecca Jackson

Charity funders of mental health research

Where can I find out about potential charity funding for my study? If you aren’t a well-established researcher, it can be very difficult to know where to start. Even if you are, mental health remains an underfunded area with far fewer charities with either open or themed calls compared to other health conditions. But there are starting points. We worked with Vanessa Pinfold, Chair of the Alliance for Mental Health Funders and Director of the McPin Foundation, on this guide to help mental health researchers navigate a tricky and sparse funding landscape.
The Alliance of Mental Health Research Funders is a consortium of 17 charities with a strong interest in mental health research. The members can broadly be categorised using three groups:
Mental health research funders (sole interest)
Mental Health Research UK (MHRUK) and MQ are both charities whose primary aim is to fund mental health research. They were both set up about 10 years ago. Everything they do is structured around the importance of mental health research and raising funds to invest in new programmes of research.
MHRUK has a PhD scholarship programme with calls for applications once a year – they are often themed calls such as children and young people’s mental health or schizophrenia research. MQ invests every year into new research including an MQ Fellows Award scheme. The MQ Fellows Award supports early career scientists who are asking challenging questions that will contribute to transformative advances in mental health research. The next MQ Fellows Awards round launches in Feb 2022 on the theme of preventing early death. A newer charity in Scotland is called Miricyl with a focus on digital solutions for young people and their family and carers affected by mental illness. There are some charities, often set up in memory of a family member who died that focus on one aspect of mental health research including Orchard OCD that have calls for proposals every two years and The Foundation for Young People’s Mental Health (YPMH) which focuses on supporting the translation of research into innovations in practice and policy. Both work with specific academic teams as well as issuing general research calls. Other research charities with a focus on a particular condition, for example Autistica , which focuses on autism, are health research charities which fund mental health as part of their portfolio.
Mental health research funding is one aspect of their work (and often a very small part).
There are quite a few charities in this group. Some issue commissions to evaluate work being undertaken internally such as Mind , the Samaritans , Mental Health Foundation , and NSPCC as well as research projects on specific topics. They tend to issue a tender specification and have to respond and are scored against set criteria. There are also charities who fund research alongside policy, training and campaigning activities. This can be funding a professorship position such as Charlie Waller Trust , or funding occasional PhD students as in McPin Foundation . The British Association of Counselling and Psychotherapy (BACP) occasionally provides financial support for students undertaking PhD research in counselling and psychotherapy, and offers bursaries and award schemes to help support researchers who are contributing to the evidence-base for the counselling professions. Other institutions such as the Maudsley Charity fund a mix of mental health research and non-research projects. It aims to have national impact but its primary focus is South London.
Mental health research funder allies
There are charities whose work relies on research, who help champion the importance of mental health research and may themselves occasionally fund research activities. From our Alliance this includes the Centre for Mental Health where research is a major part of their own activities, and Bipolar UK .
“There is no equivalent of CRUK or BHF for mental health. I think the bottom line is very few charity mental health funders have open funding calls. But they do have calls from time to time so it’s a good idea to sign up to their newsletters and follow them on twitter”.
Funding calls
Overall, it’s worth making links and keeping an eye on the charity sector as organisations do issue one off calls and new charities set up – such as the Prudence Trust which focuses on young people’s mental health including research for invited applicants. It’s also a good idea to get on the mailing lists so you make sure you hear about the opportunities as soon as they arise.
Mental Health Research UK charity - annual PhD scholarship programme
MQ mental health charity - MQ fellows applications launches in February 2022
Foundation for Young People's Mental Health
Orchard OCD
Mental Health Foundation
Charlie Waller Trust
McPin Foundation
British Association of Counselling and Psychotherapy
Maudsley Charity
Newsletter sign up
By clicking sign up I confirm that I have read and agree with the privacy policy

The use and impact of surveillance-based technology initiatives in inpatient and acute mental health settings: A systematic review
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Jessica L. Griffiths
- For correspondence: [email protected]
- ORCID record for Katherine R. K. Saunders
- ORCID record for Una Foye
- ORCID record for Anna Greenburgh
- ORCID record for Antonio Rojas-Garcia
- ORCID record for Brynmor Lloyd-Evans
- ORCID record for Sonia Johnson
- ORCID record for Alan Simpson
- Info/History
- Supplementary material
- Preview PDF
Background: The use of surveillance technologies is becoming increasingly common in inpatient mental health settings, commonly justified as efforts to improve safety and cost-effectiveness. However, the use of these technologies has been questioned in light of limited research conducted and the sensitivities, ethical concerns and potential harms of surveillance. This systematic review aims to: 1) map how surveillance technologies have been employed in inpatient mental health settings, 2) identify any best practice guidance, 3) explore how they are experienced by patients, staff and carers, and 4) examine evidence regarding their impact. Methods: We searched five academic databases (Embase, MEDLINE, PsycInfo, PubMed and Scopus), one grey literature database (HMIC) and two pre-print servers (medRxiv and PsyArXiv) to identify relevant papers published up to 18/09/2023. We also conducted backwards and forwards citation tracking and contacted experts to identify relevant literature. Quality was assessed using the Mixed Methods Appraisal Tool. Data were synthesised using a narrative approach. Results: A total of 27 studies were identified as meeting the inclusion criteria. Included studies reported on CCTV/video monitoring (n = 13), Vision-Based Patient Monitoring and Management (VBPMM) (n = 6), Body Worn Cameras (BWCs) (n = 4), GPS electronic monitoring (n = 2) and wearable sensors (n = 2). Twelve papers (44.4%) were rated as low quality, five (18.5%) medium quality, and ten (37.0%) high quality. Five studies (18.5%) declared a conflict of interest. We identified minimal best practice guidance. Qualitative findings indicate that patient, staff and carer perceptions and experiences of surveillance technologies are mixed and complex. Quantitative findings regarding the impact of surveillance on outcomes such as self-harm, violence, aggression, care quality and cost-effectiveness were inconsistent or weak. Discussion: There is currently insufficient evidence to suggest that surveillance technologies in inpatient mental health settings are achieving the outcomes they are employed to achieve, such as improving safety and reducing costs. The studies were generally of low methodological quality, lacked lived experience involvement, and a substantial proportion (18.5%) declared conflicts of interest. Further independent coproduced research is needed to more comprehensively evaluate the impact of surveillance technologies in inpatient settings, including harms and benefits. If surveillance technologies are to be implemented, it will be important to engage all key stakeholders in the development of policies, procedures and best practice guidance to regulate their use, with a particular emphasis on prioritising the perspectives of patients.
Competing Interest Statement
AS and UF have undertaken and published research on BWCs. We have received no financial support from BWC or any other surveillance technology companies. All other authors declare no competing interests.
Clinical Protocols
https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=463993
Funding Statement
This study is funded by the National Institute for Health and Care Research (NIHR) Policy Research Programme (grant no. PR-PRU-0916-22003). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. ARG was supported by the Ramon y Cajal programme (RYC2022-038556-I), funded by the Spanish Ministry of Science, Innovation and Universities.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
The template data extraction form is available in Supplementary 1. MMAT quality appraisal ratings for each included study are available in Supplementary 2. All data used is publicly available in the published papers included in this review.
View the discussion thread.
Supplementary Material
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
- Addiction Medicine (316)
- Allergy and Immunology (617)
- Anesthesia (159)
- Cardiovascular Medicine (2276)
- Dentistry and Oral Medicine (279)
- Dermatology (201)
- Emergency Medicine (370)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (798)
- Epidemiology (11573)
- Forensic Medicine (10)
- Gastroenterology (678)
- Genetic and Genomic Medicine (3575)
- Geriatric Medicine (336)
- Health Economics (616)
- Health Informatics (2304)
- Health Policy (913)
- Health Systems and Quality Improvement (863)
- Hematology (335)
- HIV/AIDS (752)
- Infectious Diseases (except HIV/AIDS) (13149)
- Intensive Care and Critical Care Medicine (755)
- Medical Education (359)
- Medical Ethics (100)
- Nephrology (388)
- Neurology (3346)
- Nursing (191)
- Nutrition (506)
- Obstetrics and Gynecology (651)
- Occupational and Environmental Health (645)
- Oncology (1756)
- Ophthalmology (524)
- Orthopedics (209)
- Otolaryngology (284)
- Pain Medicine (223)
- Palliative Medicine (66)
- Pathology (437)
- Pediatrics (1001)
- Pharmacology and Therapeutics (422)
- Primary Care Research (406)
- Psychiatry and Clinical Psychology (3058)
- Public and Global Health (5983)
- Radiology and Imaging (1221)
- Rehabilitation Medicine and Physical Therapy (714)
- Respiratory Medicine (811)
- Rheumatology (367)
- Sexual and Reproductive Health (350)
- Sports Medicine (316)
- Surgery (386)
- Toxicology (50)
- Transplantation (170)
- Urology (142)
- Open access
- Published: 03 April 2024
Women’s experiences of attempted suicide in the perinatal period (ASPEN-study) – a qualitative study
- Kaat De Backer ORCID: orcid.org/0000-0001-5202-2808 1 ,
- Alexandra Pali ORCID: orcid.org/0009-0009-5817-156X 1 , 2 ,
- Fiona L. Challacombe ORCID: orcid.org/0000-0002-3316-8155 3 ,
- Rosanna Hildersley ORCID: orcid.org/0000-0002-1850-6101 3 ,
- Mary Newburn ORCID: orcid.org/0000-0001-9471-0908 4 ,
- Sergio A. Silverio ORCID: orcid.org/0000-0001-7177-3471 5 , 6 ,
- Jane Sandall ORCID: orcid.org/0000-0003-2000-743X 1 ,
- Louise M. Howard ORCID: orcid.org/0000-0001-9942-744X 3 &
- Abigail Easter ORCID: orcid.org/0000-0002-4462-6537 1
BMC Psychiatry volume 24 , Article number: 255 ( 2024 ) Cite this article
122 Accesses
2 Altmetric
Metrics details
Suicide is a leading cause of maternal death during pregnancy and the year after birth (the perinatal period). While maternal suicide is a relatively rare event with a prevalence of 3.84 per 100,000 live births in the UK [ 1 ], the impact of maternal suicide is profound and long-lasting. Many more women will attempt suicide during the perinatal period, with a worldwide estimated prevalence of 680 per 100,000 in pregnancy and 210 per 100,000 in the year after birth [ 2 ]. Qualitative research into perinatal suicide attempts is crucial to understand the experiences, motives and the circumstances surrounding these events, but this has largely been unexplored.
Our study aimed to explore the experiences of women and birthing people who had a perinatal suicide attempt and to understand the context and contributing factors surrounding their perinatal suicide attempt.
Through iterative feedback from a group of women with lived experience of perinatal mental illness and relevant stakeholders, a qualitative study design was developed. We recruited women and birthing people ( N = 11) in the UK who self-reported as having undertaken a suicide attempt. Interviews were conducted virtually, recorded and transcribed. Using NVivo software, a critical realist approach to Thematic Analysis was followed, and themes were developed.
Three key themes were identified that contributed to the perinatal suicide attempt. The first theme ‘Trauma and Adversities’ captures the traumatic events and life adversities with which participants started their pregnancy journeys. The second theme, ‘Disillusionment with Motherhood’ brings together a range of sub-themes highlighting various challenges related to pregnancy, birth and motherhood resulting in a decline in women’s mental health. The third theme, ‘Entrapment and Despair’, presents a range of factors that leads to a significant deterioration of women’s mental health, marked by feelings of failure, hopelessness and losing control.
Conclusions
Feelings of entrapment and despair in women who are struggling with motherhood, alongside a background of traumatic events and life adversities may indicate warning signs of a perinatal suicide. Meaningful enquiry around these factors could lead to timely detection, thus improving care and potentially prevent future maternal suicides.
Peer Review reports
Pregnancy, childbirth, and the postnatal period are a positive and empowering experience for many women and birthing people Footnote 1 . Yet it is widely accepted that the perinatal period is also a time of significant stress, with one in four women experiencing mental health difficulties during this time [ 3 ]. Evidence on the impact of perinatal mental ill-health on the mother [ 4 ], her children [ 5 ], the wider family [ 6 ] and society [ 7 ] has grown in the last decade and worldwide, maternal suicide has been identified as a global public health issue [ 8 ]. In European countries with enhanced surveillance systems for maternal mortality maternal suicide has been identified as one of the leading causes of maternal death [ 9 ]. In the UK, the Confidential Enquiries into Maternal Deaths (MBRRACE-UK) have repeatedly highlighted similar findings, leading to the development and expansion of specialist perinatal mental health services in the UK [ 10 ]. Despite this, there has been no sign of a reduction in suicide rates [ 11 , 12 , 13 , 14 ]. The UK Government has therefore identified pregnant women and new mothers for the first time as a priority group in the recent Suicide Prevention Strategy [ 15 ].
While maternal suicide is a relatively rare event with a prevalence of 3.84 per 100,000 live births (95% CI 2.55–5.55) in the UK [ 1 ], many more women will attempt suicide during pregnancy and the year after birth. Worldwide, the pooled prevalence of perinatal suicide attempts has been estimated to be 680 per 100,000 (95% CI 0.10–4.69%) during pregnancy and 210 per 100,000 (95% CI 0.01–3.21%) during the first-year postpartum [ 2 ]. As well as distressing in their own right, perinatal suicide attempts are known to increase the risk of future fatal acts [ 16 ]. Antenatal [ 17 ] and postnatal suicide attempts [ 18 ] are also associated with increased maternal and neonatal morbidity, adverse birth outcomes, and further suicide attempts.
It is important to note that terminology in suicide research has been a contentious issue and a wide range of definitions have been used in various contexts. The US National Center for Injury and Control issued guidance on uniform definitions in the context of self-directed violence’ [ 19 ], which has informed our study definition of ‘suicide attempt’: “a non-fatal, self-directed, potentially injurious behaviour with intent to die as a result of the behaviour. A suicide attempt might not result in injury”. This definition contains three components worth highlighting, i.e. (1) suicidal ideation, (2) suicidal intent and (3) suicidal behaviour. ‘Suicidal ideation’, also known as ‘suicidality’ (i.e. thoughts of engaging in suicide-related behaviour) [ 19 ] is a known risk factor for suicide [ 20 ] but does not necessarily lead to suicidal behaviours (e.g., behaviour that is self-directed and deliberately results in injury or the potential for injury to oneself, with implicit or explicit evidence of suicidal intent’) [ 19 ]. ‘Suicide attempt’ must also be distinguished from ‘near-fatal deliberate self-harm’, which was defined by Douglas et al (2004) as ‘an act of self-harm using a method that would usually lead to death, or self-injury to a “vital” body area, or self-poisoning that requires admission to an intensive care unit or is judged to be potentially lethal [ 21 ]’. This definition does not contain an element of ‘suicidal intent’, ie. explicit or implicit evidence that at the time of injury the individual intended to kill self or wished to die, and that the individual understood the probable consequences of his or her actions [ 19 ].
To date, perinatal suicide research has predominately been based on case note reviews [ 1 ], retrospective cohort studies [ 22 ], or qualitative studies focussing on suicidal ideation [ 23 ]. Research into suicide attempts in the perinatal period is therefore acutely needed, to gain a better understanding of the circumstances surrounding maternal suicide, the support available to perinatal women and how future deaths can be avoided. To our knowledge, no studies in the UK have used qualitative methods to explore the experiences of women who undertook a suicide attempt in pregnancy or during the postnatal period, yet survived. A better understanding of these events could help refine support and early interventions for women and birthing people at risk.
Aim of the study
The aim of this study was to explore the experiences of women and birthing people who had undertaken one or more suicide attempts during the perinatal period.
Study design
The ASPEN-study (Attempted Suicide during the PEriNatal period) utilised a qualitative design, using semi-structured interviews, to allow for an in-depth understanding of the contextual factors of perinatal suicide attempts, and to demystify the taboos and misunderstanding that are enshrouding this phenomenon [ 24 ]. Qualitative methods are particularly helpful to study sensitive topics [ 25 ] and can facilitate a deeper understanding of suicide attempts, beyond merely explaining [ 26 ]. We adopted a critical realist ontology, meaning participants’ accounts were seen as ‘truths’, even when their reported recall might have been impacted by serious mental illness and/or distress at the time of events [ 27 ]. We also adopted an objectivist epistemological stance meaning our belief system of how we acquire knowledge is one of reality existing and not being constructed, thus enabling an approach to participants’ narratives with no preconceived notions of how the participants may experience the phenomenon of interest [ 28 ]. Drawing on our epistemological and ontological positions, a critical realist approach to Thematic Analysis was best aligned with our philosophical underpinnings. Critical realist TA is an alternative approach to Thematic Analysis, that differs from codebook TA with its positivistic assumptions [ 29 ], or reflexive TA that is grounded in philosophical constructivism [ 30 , 31 ]. Critical realist TA is an explanatory approach that aims to produce causal knowledge through qualitative research on phenomena in the world around us [ 32 , 33 ]. We wanted to go beyond merely ‘exploring’ the phenomenon of perinatal suicide attempt, but aimed to understand what women had experienced during this time, such as any significant life course events they identified as relevant to their perinatal suicide attempt, the specific circumstances in the lead-up to the suicide attempt, their views of motherhood and how this impacted their mental health and any key elements or milestones that made a substantial difference on their journey to recovery. As such, this approach informed our development and structure of the interview schedule and analysis of the data to ensure that this was captured.
Participants and recruitment
The study was advertised through social media and third sector organisations in the field of perinatal mental health and suicide prevention (see Acknowledgements). Interested participants were included if they: (1) were 18 years of age or older; (2) had one or more suicide attempts during the perinatal period (i.e. from pregnancy up to the first year after giving birth), including when the attempt was prevented by self, a loved one or a member of the public; (3) and this happened less than 10 years ago; (4) were residing in the UK; and (5) were not receiving inpatient psychiatric care or experiencing an acute episode of a psychiatric disorder at the time of recruitment. The latter exclusion criterium was adopted in line with our safety protocol, to prevent delays in recovery by addressing such a difficult event outside a therapeutic environment. We used both convenience sampling and purposive sampling techniques: we interviewed anyone who responded to our recruitment materials, met the inclusion criteria and wanted to participate in the study after reading the participant information sheet (convenience sampling). Simultaneously, we also made concerted efforts through intense collaboration with community leaders and third sector organisations to recruit a diverse sample of women and birthing people from different ethnic, cultural, socio-economic and religious backgrounds (purposive sampling). A total of twelve women and birthing people contacted the research team with an interest in the study. Eligibility for the study was explored in a sensitive way, against the overall inclusion criteria and the three components of the study’s definition of ‘suicide attempt’ (suicidal ideation, intent and behaviour). Where in doubt, eligibility was discussed with the wider supervision team. In total, eleven interviews were conducted. A twelfth interested participant did not attend the (online) interview and did not respond to any follow-up emails. Recruitment was finalised when no new themes were being generated from data analysis of the last two interviews [ 34 ]. Participants received reimbursement of £50 for their time to complete the interview and a short demographic survey.
Data collection and analysis
Semi-structured interviews lasted between 38 and 115 min ( MTime = 65 min) and were conducted via video-conference software (Microsoft Teams) by one researcher (KDB) between October 2022 and April 2023. Interviews were audio-recorded, transcribed and de-identified by a professional transcription company. Field notes were taken during the interview. Transcriptions were checked for accuracy by two researchers (KDB, AP). The interview schedule, which was co-designed with a panel of women with lived experience of perinatal mental illness, aimed to explore experiences of mental health difficulties prior to and during the perinatal period, the circumstances in the lead-up to the suicide attempt, and those following the suicide attempt. The interview schedule was used flexibly and did not prevent participants from sharing their story in the order they preferred, but instead, was used as an aid to prompt where required. Interview data was so rich that a secondary analysis focusing on social support prior and after women’s suicide attempts was undertaken, to be published separately.
Thematic Analysis (TA) [ 30 , 31 , 33 ] of the interview data was conducted using NVivo software while adopting a critical realist approach to Thematic Analysis [ 30 , 31 , 33 ]. The process of data analysis is rarely a linear event, and guided by Fryer’s previous work on critical realist TA [ 33 ], our approach to data analysis is presented in Fig. 1 and can best be described as follows:
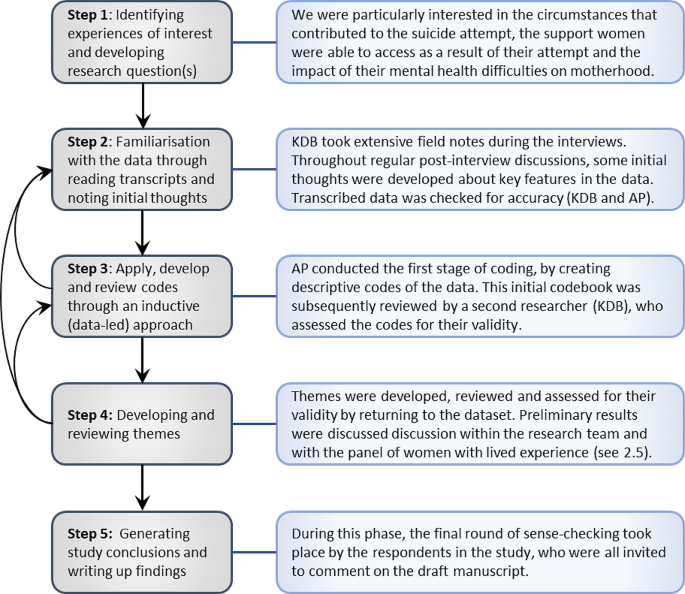
Display of critical realist approach to thematic analysis
Public and patient involvement and engagement (PPIE)
An established advisory panel of women with lived experience of perinatal mental illness was consulted during different phases of the study with additional feedback sought from key stakeholders in the field of perinatal mental illness (see Acknowledgements). The process of PPIE during the study design and data collection phase of this study has been documented elsewhere [ 35 ]. A draft manuscript was shared with research participants to sense-check findings and comment on the manuscript. Participants were also given the opportunity to select a pseudonym of their choice. A total of 8 participants reviewed the draft manuscript and their feedback was incorporated in the final version of this paper.
The study team and reflexivity
The research team are a multidisciplinary team of researchers and clinical academics, with backgrounds in psychology (FLC, AE, RH, SAS, AP), psychiatry (LMH), and midwifery (KDB, JS), and several had clinical experience of supporting women who attempted suicide during the perinatal period (KDB, FLC, LMH). Within the research team, there was a balance between those who were parents and those who did not have children and researchers were at different stages of their life, spanning nearly three generations. The phenomenon of suicidality in the perinatal period was familiar to most of the research team, through extensive clinical experience and/or previous research in the field of perinatal mental health. Our positionality is therefore best described as ‘hybrid’, concordant with our critical realist ontology, as we aimed to align our existing knowledge and understanding (i.e. being embedded in the data) with the uniqueness and unfamiliarity of each individual story that was shared with us as a ‘truth’ (i.e. being an objective onlooker), in order to analyse the data in a coherent and sensitive matter [ 36 ]. Data were collected by one researcher (KDB) who was trained in advanced qualitative research techniques as well as having clinical experience as a perinatal mental health midwife. Analysis was conducted by the same researcher and a MSc Student with a background in clinical psychology (AP). Regular team meetings were held throughout the data collection and analysis phase to discuss and sense-check the developing themes and sub-themes.
Participant safety and researcher wellbeing
The safety and emotional wellbeing of all participants was key throughout the study. Thus, we adopted key elements of trauma-informed care into our study design [ 37 ]. A robust safety protocol, with clear pathways for escalation if required, was developed with the input of the PPIE advisory panel [ 38 ]. The study team undertook bespoke training in trauma-informed interviewing and the interview schedule was developed with this in mind. A safety check prior and after the interview was carried out by the same researcher (KDB), either via email or by phone and all participants were offered a confidential de-brief session with an independent clinical psychologist. The psychological safety of the researchers was also considered [ 25 ] and supported by access to regular reflective supervision sessions provided by a clinical psychologist and regular debrief sessions with supervisors to process any difficult emotions arising from conducting the interviews [ 39 ]. We were acutely aware of the potentially triggering content of the audio files and raised this with the transcription company [ 40 ]. When sending audio recordings for transcription, a summary of triggering content was provided to ensure the transcription would be appropriately allocated.
The majority of our sample ( N = 11) were White British women ( n = 10), with one woman from a mixed ethnic background. Participants were predominantly married ( n = 8) and had higher education qualifications ( n = 7). All but one participant had received a mental health diagnosis by a doctor or other healthcare professional in the past although the demographic survey did not allow to ascertain when this diagnosis had been given. More than half of the participants in our sample were given multiple diagnoses, indicating a high level of complexity in mental health presentation. In most cases, pregnancies had been planned ( n = 9). All but two women were multiparous, with half of the sample having two children ( n = 6), and three participants having three or more children. Two women were first-time mothers at the time of the attempt. Four women undertook their suicide attempt during pregnancy, with a fifth woman being pregnant whilst her older child was still under the age of one. The remaining six women undertook a suicide attempt within the year after giving birth. Four participants had a stay in an inpatient psychiatric Mother and Baby Unit (MBU), and for three of them the admission was preceded by their suicide attempt. For one participant, the admission in the Mother and Baby Unit was subsequently followed by an admission in a general psychiatric hospital, where she undertook the actual suicide attempt. A full table of demographic and clinical information can be found in Table 1 .
Qualitative analysis resulted in the identification of three key themes that played a significant role in the deterioration of women’s mental health during the perinatal period, ultimately culminating into a suicide attempt. Saturation for all themes and sub-themes was achieved after nine interviews when no new themes or subthemes were generated. Data from the remaining two interviews confirmed our analysis and provided additional depth and detail [ 34 ]. The three overarching themes are presented in Fig. 2 : Theme 1 ‘Trauma and Adversities’ , consisting of family history of perinatal mental illness and psycho-social adversities, including grief and trauma; Theme 2 ‘Disillusionment with Motherhood’ , marked by a variety of challenges that arose during pregnancy or the postnatal period; and Theme 3 ‘Entrapment and Despair’ , where multiple stressors piled up with no respite or support available, leading to a severe deterioration of mental ill-health, and ultimately, the suicide attempt.
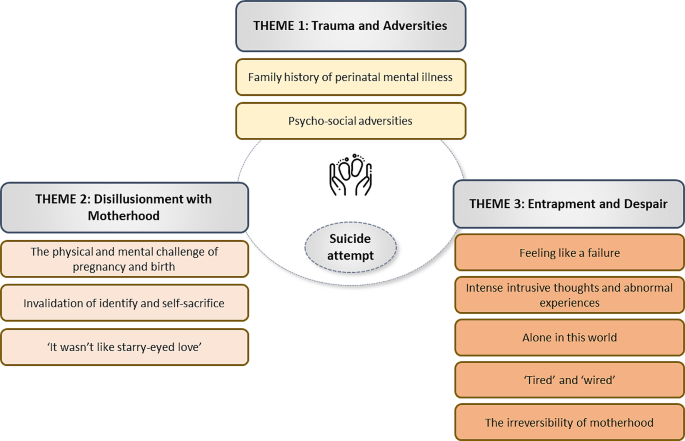
Display of themes and sub-themes
Qualitative data is presented below, with the most representative quotations in text and an additional table of supplementary of quotations included in Supplementary Material 1 .
Theme 1: trauma and adversities
All respondents in our sample started their pregnancy journeys with a range of vulnerabilities, such as previous mental health difficulties, loss, trauma, or social risk factors including domestic abuse and substance misuse. Nevertheless, participants were not always aware of the profound impact these would have on their mental health later in pregnancy and in the postnatal period. Subthemes contributing to this were:
Psycho-social adversities
Many women had experienced mental health difficulties at some point in their life, and most were fully aware of their potentially devastating impact. Some had experienced poor mental health during adolescence and young adulthood and anticipated mental health problems during the perinatal period.
“I’ve had some terrible things happen in my life about failed marriage and fertility problems. Big, big things that I’ve sort of managed with a strength of mine that I perhaps didn’t have in my late teens or early 20s to overcome. So I guess it was always on my radar knowing the stats around you are more likely to have perinatal mental health problems if you’ve had bouts of depression in the past.” – Rosy .
In contrast, others had dealt with traumatic experiences in their life, but could not see how this would be relevant to their mental health during pregnancy and the postnatal period. They started their pregnancy unaware of any potential risks to their mental health.
“I lost my brother when he was 18. […] And I didn’t get a lot of time off work, I was kind of straight back into work. I’m a [professional role in mental health], so I was working in acute psychiatry. Back to work, dealing with other people’s trauma and I don’t think I really dealt with my own particularly well. And it was kind of I think eight months later I had an episode of depression, just very low mood, apathy, poor motivation, poor concentration, was treated briefly with antidepressants and then just kind of did okay after that. So there had been nothing.” – Simone .
Previous trauma was reported by almost all respondents, whether it being through a bereavement, or traumatic life experiences, such as miscarriage and infertility, domestic abuse, fractured relationships, or suicide of a loved one. Two women reported having experienced domestic abuse. One of them reported the abuse, which she described as a ‘punishment’, only started after informing her partner of the pregnancy.
“It was a punishment actually that I dared to be pregnant even though he knew I wasn’t on any contraception or anything. And it really shocked me because he had never ever been like that before.” – Lauren .
For the other respondent, the domestic abuse had been long-lasting and led her to seek coping strategies to deal with the trauma and pain. Being in an abusive relationship created the worst possible start for pregnancy, with no support available.
“Well, it was my first pregnancy. I was 24 so I still hadn’t grown up properly, and I was in a really bad domestic violence relationship so there was a lot going on around that. I was getting no support [for] my pregnancy. I was also using as well which I regret profoundly, but I was drinking, like I drank occasionally because of my mental health, and my mental health was just all over the place; I was really, really unwell.” – Selina .
For some, their previous mental health difficulties were related to an earlier pregnancy or birth experience:
“I had huge amounts of birth trauma from my first, which I had a debrief for from the hospital, which was incredibly unhelpful. And it ended in emergency caesarean [section], after nine days of labour, and being in hospital, as a very naïve 19-year-old, having her first baby; looking back on it, feeling quite coerced by doctors, but not realising at the time that that’s what was happening. And that has impacted me for the rest of my life.” – Sam .
The severity of previous perinatal mental health problems was varied, with one woman having experienced postpartum psychosis after the birth of her first child. Going into the second pregnancy, the risk of relapse was hanging over her like a dark cloud:
“I remember sort of going to the 12-week scan with [second pregnancy] and getting the picture and thinking like shit, it’s really real now and it could all happen again. So I was really scared about that. Because the reccurrence rates are quite high for psychosis, so it’s quite likely that I was going to become unwell. So I was worried, yes, I was really concerned.” – Marie .
This feeling of worry was also reported by women with mild to moderate mental health difficulties and was compounded by a fear of being dismissed and not being able to access support if they would require it.
“I think there was something about the anxiousness of doing it all again, because I think I had some prenatal depression with my first, that wasn’t picked up, and then postnatal anxiety through the roof, that was also never picked up, and was told that was normal.” – Sam .
Family history of perinatal mental illness
Several respondents had a family history of perinatal mental illness and were vigilant that they might experience something similar. To mitigate this risk, they actively sought perinatal mental health support at the earliest opportunity.
“My mum had severe perinatal mental illness, she was hospitalised after my older brother for a year without him […]. At the time they didn’t really have Mother and Baby Units. Then I came [a few] years later and she was hospitalised again but with me for six months, and she passed away […] So my dad said she was saying the same things as each time she’d been sectioned; she would present with very religious ideation and stuff like this, so it was exactly the same stuff, and she died by suicide. So because of that collective history, when we were trying to get pregnant we thought “We need to let someone know we’re trying to get pregnant,” and so I was referred then to a Perinatal Psychiatrist before we got pregnant” - Sarah .
For others, this family history was not something which was spoken about prior to their own experiences of perinatal mental illness. One respondent mentioned she had never been aware of her mother’s history of postnatal depression until she herself started to experience postnatal depression.
“I didn’t know that my mum had postnatal depression. That’s not anything that she’d shared until… I knew that my brother cried a lot and I think he had a cows’ milk protein intolerance, but I didn’t know that my mum…” – Rosy .
Theme 2: disillusionment with motherhood
While previous mental health challenges or trauma were present in the background, all women were profoundly disillusioned with motherhood which contributed to a deterioration in their mental health. This theme of ‘Disillusionment with Motherhood’ captures three sub-themes that reflect a discrepancy between what women thought or hoped motherhood would be like, and the crushing reality they found themselves in. Together, these sub-themes compounded each other and became a catalyst for worsening mental health. The following sub-themes address the various areas of disillusionment that women in our sample reported: in their bodies, in their identity and in the bond with their baby.
The physical and mental struggle of pregnancy and birth
All participants held hopes and expectations of what their pregnancy, birth or the postnatal period would be like. For some first-time mothers, it soon became clear that the societal rosy-hued image of pregnancy was very far removed from their own experience of pregnancy. As they came to grips with how pregnancy was unfolding, the harsh contrast between expectation and reality was so high that many struggled to adjust to this:
“There’s all this thing about pregnancy you’re supposed to be glowing and it’s all marvellous and you’ve got these wonderful hormones, but I was just beached on the sofa feeling hot and sweaty thinking when is this baby going to come out, when’s it going to come out?” – Simone .
For those who had been pregnant before, the reality of another pregnancy, knowing full well what was in store, started to dawn on them:
“I don’t know, it hit me like a ton of bricks. Like oh shit, I’m doing this again. I’m pregnant again.” – Liv .
In addition to these psychological adjustments to reality, respondents mentioned how the physical toll of pregnancy and childbirth played a significant role in the deterioration of their mental health. This close correlation between physical issues and mental health decline was abundantly clear across the sample.
“I was horribly, horribly sick [hyperemesis]; that got worse each pregnancy. I don’t know if that’s normal; I’d heard it is. But horribly sick, which makes you absolutely miserable anyway.” – Sam . “I just sort of couldn’t wait for it [the pregnancy] to end. Yes, I just wanted to give birth. So when they said that they were going to induce me at 40 weeks I thought thank goodness, because my sickness started again quite late on. Again, I don’t know if it was because of the pre-eclampsia. But yes, I was just very ready, very ready to have little one.” – Hannah .
In the most extreme cases, pregnancy was not viewed as something to be enjoyed, but something that left women feeling repulsive.
“So since the pregnancy, just my life fell apart really, I was unemployed, and I just felt the whole way through not just sick and ill, absolutely physically repulsive, like I just felt like an absolute filthy animal. I can’t describe the disgust I felt for myself and the bigger my bump grew, the more disgusting I felt. And I don’t know, it’s just everything was awful, every day was awful.” – Lauren .
For other women physical injuries as a result of childbirth left them unable to function and to enjoy the things they were looking forward to as a new mother.
“I had some tearing and I’d had an episiotomy and they hadn’t healed, so my episiotomy had opened up and there were lots of A&E [Accidents and Emergency] visits and an operation eventually, but I think that really didn’t help my mental health because obviously if you’re in pain all the time then, it just drags you down, doesn’t it? So I wasn’t able to do my normal stuff, I wasn’t able to just carry on with life because I was in pain, I couldn’t sit and I felt like I couldn’t do mummy things.” – Mel .
Apart from the physical repercussions of pregnancy and childbirth, it was the trauma of giving birth and its psychological sequalae which triggered a marked deterioration in the mental health of several women in our sample.
“It was just sort of like you couldn’t expect it to happen, it was like a poor pregnancy and sort of felt like, you know, the birth went wrong as well.” – Hannah . “I had a premature baby. And I went on, I don’t know, like trauma response. Like totally numb. I suppose the adrenalin, the shock, everything…” – Liv .
Invalidation of identity and self-sacrifice
Almost all respondents encountered negative experiences with healthcare professionals at some point during pregnancy or the postnatal period and felt invalidated and dismissed by these. Women reported they were not seen as a person, with a complete identity, but reduced to a vessel for their baby, with little consideration given to their own feelings. This led to a profound loss of identity, exacerbating feelings of being invisible, inadequate and unimportant.
“It was never about me. And I know it’s not all about me, but when I’m wanting to commit suicide, it is very much about me and not one person asked me if I was alright, they were more concerned if the baby was alright, which I was as well, but they just completely bypassed that there was any reason I would do it.“ – Selina .
There seemed to be a lack of professional inquisitiveness to understand why a mother(-to-be) would consider suicide. Instead, all attention was directed towards the well-being of the baby, leading to multiple missed opportunities for timely care and support. In some cases, women reached out but their calls for help were simply ignored while their mood was rapidly deteriorating. These experiences would have devastating consequences on their further help-seeking behaviour.
“What really killed me, what was like the punch in the face that I needed was when I had my midwife appointment at, I don’t know, eight, ten weeks, something like that, and I told her ‘you know what, I’m not feeling right. There’s something bubbling inside me that is not alright, is not correct. I feel more anxious than normal, I can’t sleep, it’s all very weird’. And she just said ‘okay, I’m going to pin that down here to talk about in your next appointment. But we’re not going to do anything right now’. I never saw her again, by the way.” – Liv .
Invalidating encounters like the one described above would have a profound impact on how women viewed healthcare professionals as a source of support and whether they would reach out to them and share the extent of their mental health problems.
“I just felt like nobody was listening at all, just not heard one bit.” – Anna .
For some, the invalidating experience would almost become a motivator to succeed in their suicide plans, as they felt the severity of their mental health problems was brushed under the carpet. One participant sought help after a first suicide attempt through a medication overdose and shared the following:
“So then I think a few more weeks went by and I went back to the doctor’s. I said to the doctor, ’I want to kill myself’. My medication and stuff, I was honest with him, I said the medications and stuff that he was put… I think he tried me on Zopiclone as well with not sleeping and he said, ‘Well if you wanted to kill yourself, you would have done it by now’. I was just… I sort of felt then I’ve got something to prove.” – Hannah .
The loss of identity made respondents feel invisible to healthcare professionals and went hand in hand with exhausting themselves to be the best possible mother for their baby. Women described feelings of total self-sacrifice to meet this perceived standard of ‘the perfect mother’.
“I think I sort of went into supermum mode when I came home, like I had something to prove, and again, it’s that background of failure. I think I’m quite hard on myself anyway and I’m quite… If something goes wrong, I’m probably harder on myself in my head than somebody else would be and I maybe got a bit of a perfectionist trait, so I really didn’t want to rely on anybody, I didn’t ask for help with anything regarding my little boy, and I had a really, really strong bond with him which was really positive, but I think I was sort of going like overkill with not asking for help.” – Hannah .
However, as women started to experience the hard reality of caring for a newborn, they felt unable to meet this impossible standard. The perceived pressure to achieve (unrealistic) goals as well as their feelings of failure to do so started to take a significant strain on their mental health.
“No one had ever told me that before. No one had ever said that you don’t just have to drop everything and run to your child. Because I thought that that was what a secure bond was; and obviously now I’ve learnt about attachment theory and things. I thought that, for her to be securely bonded with me, I had to give every last drop of myself to be her mum.” – Sam .
‘It wasn’t like starry-eyed love’
Closely linked with the previous sub-theme, was the realisation for many women that they did not feel an instant rush of love for their baby. Several women reported feeling unsettled and flawed as a mother when they felt distant and detached from their baby. Women tried their very best to ‘act as a mother’ and do whatever their baby required, but this did not mean they also ‘felt like a mother’.
“So, at the beginning it was very strange. It, because like I said, I was determined to do anything in my power to get that baby out of NICU [Neonatal Intensive Care Unit]. Like whatever it takes, whatever the cost. So it never felt like oh, it’s my baby. I would have jumped in front of a train for him but it was not like a starry-eyed love. And that kept going.” – Liv . “In terms of motherhood, yes, I don’t know whether I just felt I was failing at it or… [pause] I don’t know, I felt very not connected to the baby. I had felt very, very bonded and very connected, and then I wasn’t at all.” – Sarah .
Sadly, for some, this lack of bonding with their baby persisted for a long time, with enduring consequences on their mental health and family happiness, leading to feelings of guilt and shame with which they still are coming to terms with.
“I had no attachment to him probably for about five years, nothing at all, just this ongoing sense of regret and I remember thinking daily I’ve made such a massive mistake in my life and almost this like realisation you are never going to get back what you had before, so just this real hopelessness actually at life.” – Lauren . “I just couldn’t, I couldn’t bond with, I couldn’t. Even still now I love her to pieces but we’re not like mother and daughter, we’re not.” – Anna .
Theme 3: entrapment and despair
In the final phase leading up to the suicide attempt, women experienced an accumulation of stressors, unleashing an overwhelming feeling of hopelessness and entrapment, with seemingly no way out of the situation they found themselves in. The sub-themes identified under this theme of ‘Entrapment and Despair’ left women no breathing space or respite. A perfect storm was brewing, for which women only started to see one way out, and that was by taking their own life.
Feeling like a failure
All respondents expressed a pervasive feeling of utter failure, intersecting their different identifies as a woman, mother and partner. Their perceived inability to meet expectations, whether this related to giving birth, feeding their baby, or functioning as a mother and partner stood in sharp contrast with how they viewed other mothers, who seemed to be effortlessly successful in doing so.
“You sort of just blame yourself. So I can just remember looking at him when he was asleep thinking like, ’Oh you’ve failed, I can’t do this, I’ve already failed at being a mum, but I can’t do this’, and I can just remember just thinking that, looking at him. So I think even though I know it wasn’t my fault, you really felt like a failure and I felt like it was me, like there was something wrong with me, because a lot of women around me, like even family, they never really had experiences like that, they would have like a good pregnancy, like a vaginal birth, a normal birth, so I really felt like I had failed and I really blamed myself for that.” – Hannah .
This feeling of being a total failure created a sense of dread, leaving them fearful every day that their inability and incompetence as a mother would be further exposed.
“I remember seeing the light coming in through the curtains in the morning and just thinking “Oh my god, no, I can’t, I can’t do another day,” like my heart would go, and it was that dread, that whole dread would come over me and I’d think “I can’t do another day today, I just can’t do it. I can’t do it.” It was like a… Yes, it was really hard. I just felt like I don’t know, it felt like I just wasn’t good enough for her, I wasn’t good enough. […] It just felt like I wasn’t good enough to be her mum.” – Mel .
This overwhelming sense of incompetence erased feelings of love, enjoyment or hope and instilled a feeling that their baby and loved ones would be better off without them.
“So it just escalated. This what was going on in my head about, you know, me not being good enough, a failure, just escalated even more, that now I was thinking they are going to take him away, everyone will know how rubbish I am. So it was later that week where I still wasn’t sleeping and I just thought, do you know what, the both of them would be better off without me, because I’ve just failed, I’m just a failure. They will be better off without me.” – Simone . “…That just made me feel so, so low that I think that spiral of internalised feelings and negativity compounded with this sort of isolation and lack of sleep just led me to think they’d be better off without me around, they’d have a parent maybe or a family that would be able to meet their needs.” – Rosy .
Intense intrusive thoughts and abnormal experiences
More than half of the women in our sample reported intrusive ideas or unsettling experiences in the period preceding their suicide attempt. For many, this came as a total surprise as they were unaware this could happen and they felt unable to express the extent of their intrusive thoughts to anyone.
“I remember getting up and going to the bathroom to brush my teeth and then started hearing voices. So this voice, I didn’t recognise it, was just chanting, ‘stinky [name of baby], stinky [name of baby]’, which is my baby’s name and I was like why’s that happening? I don’t understand. Where’s that coming from? And then later that day I remember looking at my husband and thinking you’re the father of this baby, but I’m not its mother. It was a really odd thought, because I was like I know I’ve been pregnant and I know I’ve just been through all that labour, but I look at this baby and it’s not mine, but I know you are the dad. It was really odd.”- Simone . “They [the intrusive thoughts] were really, really scary. And totally uncontrollable as well. They were so vivid and they used to make me feel really upset because they happened quite early on, probably when she was only a few weeks old and I remembering googling them and reading loads of things about it didn’t mean that you were not coping, it didn’t meant that you were going to hurt your baby, it didn’t mean that you were depressed, but I think maybe I should have perhaps seen that as a bit of a sign that I needed to get some help because it was weeks and weeks later that I finally did. But yes, they did upset me and I only told my mum, I didn’t tell anybody else because I just felt as though are people going to think that I’m going to hurt her? Am I going to hurt her if I talk about it more? Yes, they were really scary.” – Rosy .
For some, these ideas were extremely horrific and a symptom of their psychotic illness at the time. Unfortunately, this was left undiagnosed and untreated, leaving them totally desperate and isolated while these unsettling thoughts became their lived reality.
“[…] I started to think ‘oh I’ve committed all these awful crimes in my life’ and I was kind of struggling to process what they were and I was thinking have I killed people and maybe buried them and I don’t know where they are or have I kind of done a big theft or something but not been able to quite work out where I’d stolen the money from. But I was kind of panicking that I’d either buried these bodies or hidden this money and I couldn’t remember where they were, so I was panicking someone else is going to find them and then I’m going to be put in prison. So I had this kind of I want to die because I’m scared I’m going to go to prison because I’ve done all these awful things. And I just felt absolutely desperate.” – Lauren .
Alone in this world
While these distressing experiences of failure and intrusive thoughts invaded women’s mindset, women felt profoundly alone and isolated. Social isolation was reported as a catalyst for their suicide attempt by every woman in the sample. For some, it was a continuation of the situation they had already been in, but during this stage everything felt more desperate, more alone.
“I think by that point I wasn’t talking to anybody at all, not family, certainly not the kids’ dad. The kids’ dad… […] I just totally blocked his number and I wasn’t seeing anybody else. And actually, in some ways, I don’t think anybody wanted to see me because they were just like, “Why have you had another kid?” So the only people that I saw were my own kids, maybe the odd school teacher at pickup but that was it. No one from work. No friends really.” – Lauren .
For others, it was the absence of their partner, who had to return to work after paternity leave, that served as a lever for an acute deterioration of their mental health.
“Everything was fine until about three weeks after the birth and we were back at home, and my husband went back to work; it was him going back to work and I just, yes, fell apart.” – Sarah .
Some respondents had their baby during one of the COVID-19 pandemic lockdowns, when social restrictions meant they were unable to meet with friends or family or seek peer support from other mothers. Instead, they felt cooped up inside their house, alone and isolated, with their suicidal thoughts.
“Completely isolated. Not being able to, like I could have been going to, I don’t know, prenatal yoga. Or breastfeeding groups or toddler groups. Anything else that would take me out of that loop. So I think obviously that made it a lot worse. I don’t think that it would have been… – I don’t know.” – Liv . “So she was three or four months old when Covid hit and it was the whole lockdown and yes, everything just got ten times worse because I couldn’t do anything then; I couldn’t go and talk to my mum, I couldn’t go out, I couldn’t even have doctor’s appointments, I couldn’t have hospital appointments which made me worry even more, and my husband’s a key worker so I was just on my own all the time. Yes, and I think that’s when it got to the point where I just felt like I couldn’t cope anymore.” – Mel .
Several respondents recalled how this feeling of loneliness instilled a determination in them to retreat into isolation further. This meant they no longer wanted to speak to or be around others, even when they had a supportive network in place. An unstoppable cycle of isolation and socially avoidant behaviour was set in motion.
“I just stopped talking to people. That’s when I stopped talking to anybody and I got really ill with my mental health because of it, but I thought “Well, why am I going to talk to people when they don’t listen to me anyway?”- Selina . “I knew exactly what I was doing. I knew how I was going to do it. I just wanted it done. So I thought I have to tell him. I have to tell him. But I couldn’t tell him that I was off to kill myself.” – Simone .
‘Tired’ and ‘wired’
All but two respondents mentioned sleep deprivation as a major contributing factor to the accumulation of despair in the days or weeks before the suicide attempt. The sheer exhaustion they felt prevented them from thinking clearly or having the energy to face their circumstances and get better.
“My little boy slept really well from, gosh, about three weeks, maybe less than that, he would sleep through the night which was really, really lucky, but I couldn’t sleep and I think, yes, the problems of not sleeping had a snowball effect.” – Hannah .
This level of hypervigilance and restlessness was for many women the reason why they were unable to sleep. While women reported to feel exhausted on one hand, they also reported to experience an unhealthy level of drive, anger or arousal, leaving them ‘tired and wired’.
“I stopped sleeping entirely; I was so angry all the time – it’s all the textbook depression symptoms, but I was so angry all the time. I was so tired all the time, but just wired, couldn’t sleep.”- Sam . “I remember thinking I’m just so tired, I just want to go to sleep. I just want to be asleep and not be disturbed. But my mind was just so busy.” – Simone .
Some displayed agitated and manic behaviour to such an extent that they struggled to understand how this went unnoticed.
“I live three miles from the hospital and after they sent me home the next day, I walked back to the hospital with [the] kids and I was mowing the lawn five days after he was born and cleaning the house from top to bottom and driving all over the city after a [caesarean] section and you kind of just think like why did nobody notice? How can you think that that’s normal behaviour? Because I just felt this constant need, like I’ve got to be constantly doing things, constantly cleaning things, constantly walking places or doing things, alongside this absolute anger.” – Lauren .
The irreversibility of motherhood
A majority of respondents described they came to a very agonising realisation that they were unable to get out of being a mother and that they found themselves in an irreversible situation, with no going back. The feeling of being ‘stuck’ was so pervasive, that many expressed they wanted either the pregnancy to end, or to not wake up. The irreversibility of motherhood was surrounded by feelings of deep regret and an admission that this had been their own fault and responsibility.
“I remember actually hoping he would be stillborn towards the end, I think after the bridge. I just really wanted for him to be stillborn because if he was then it would all be over but it wouldn’t be my fault, and then I couldn’t go back. I think there was this constant sense of wanting to go back before any of it had happened and I just have my [older] children and I was working and I was happy and I kept seeking these ways just to go back and there weren’t any and I just got more and more desperate as time went on.” – Lauren .
Many respondents shared their conflicting emotions towards their baby, who they viewed as the cause of their distress on the one hand, and as the reason to stay alive on the other.
“[…] I simply could not do it anymore. Help, or don’t help. Whatever. I’m just not going to be around. And it’s almost like this feeling of, you want someone to take the baby off you, so that the baby’s not around, or that’s how I felt. The baby is your reason to stay alive, but the baby’s also the thing that’s causing you so much anguish. And that conflict is just so hard.” – Sam .
Women were desperate to get a grip on the situation, yet it all felt in vain, with no improvement in sight. An overwhelming feeling of hopelessness took over, leaving women with no light at the end of the tunnel and only one option: taking their own life.
“I don’t know how to explain it. I was feeling like all the things that I had to do were like water in my hands. I could see it. I could feel it. I could hold it. But it was coming through my fingers and I couldn’t do anything about it.” – Liv .
Our study identified three overarching themes, marking different phases during which women’s mental health gradually deteriorated. Whilst not all sub-themes under these themes were necessarily reported by every respondent, they paint a comprehensive picture of the distressing feelings and contributing factors that women experienced in the days and weeks prior to their suicide attempt. Nearly half of our sample undertook a suicide attempt during pregnancy. This is in line with evidence suggesting antepartum suicide attempts are an important complication of pregnancy [ 2 ] and act as a strong predictor for postnatal suicidal behaviour, including completed suicide [ 41 ]. In addition, participants in our sample whose suicide attempt occurred during the postnatal period reported suicidal ideation had started during pregnancy, making the antenatal period a critical period for both antenatal and postnatal suicide prevention.
Our first theme, ‘Trauma and adversities’, captures vulnerabilities prior to conception and during pregnancy and has two key elements: (1) psycho-social adversities, including grief and trauma and (2) having a family history of perinatal mental health difficulties. Women with previous mental health difficulties, in particular those with a history of depression and mood disorders, are known to have an increased risk of fatal and non-fatal perinatal suicide attempts [ 3 , 42 , 43 ]. In addition, previous adverse life events and abuse, especially when these occurred during childhood, [ 44 , 45 ], perinatal bereavement and infertility [ 46 ], comorbid substance use disorders and intimate partner violence [ 47 ], have also been associated with an increased risk of perinatal suicidal thoughts and suicidal behaviour. While the need for trauma-informed maternity services has become a public health priority [ 37 ], it is not always matched by a general awareness of the importance to raise these issues during pregnancy or the postnatal period [ 48 ]. This is reflected in our findings, where several of the respondents had experienced significant trauma and adverse life events prior to becoming pregnant but did not feel this was particularly relevant. Similarly, for some respondents a significant family history of perinatal mental health problems was unbeknown to them until their own mental health deteriorated. In contrast, those respondents who started pregnancy with an alertness of the risk of perinatal mental health problems in light of their own previous mental health difficulties or those of close relatives, reported to have prophylactic support measures in place, for instance by accessing a community perinatal mental health service during pregnancy. While this did not prevent their mental health from deteriorating, it did shorten the referral and escalation times when they reached a point of crisis. Having meaningful conversations about the prevalence of perinatal mental ill-health early on in pregnancy and undertaking a thorough assessment of mental health-related risk factors, such as previous mental health history, domestic abuse, substance misuse, previous trauma, among others, at every contact with maternity services is therefore essential to mitigate these pre-existing vulnerabilities [ 49 ].
In our second theme, ‘Disillusionment with Motherhood’, we identified a range of triggering factors that caused women’s mental health to decline. A first and often overlooked sub-theme that we identified was the impact of a physically and mentally challenging pregnancy and birth and their role in a subsequent mental health deterioration. This was often exacerbated when women received unkind, disrespectful care, which made them feel invisible. Whilst there are no studies to our knowledge that directly associate birth trauma with an increased risk of perinatal suicide, the association between birth trauma and postpartum post-traumatic stress disorder (PTSD) is well established [ 50 , 51 , 52 , 53 ]. Postpartum PTSD in turn is associated with poor coping and stress and highly co-morbid with depression [ 50 ]. Less evidence is available on the association between pregnancy and birth complications and perinatal suicide risk. One study found no association between maternal complications in pregnancy and during birth with hospitalisation for a suicide attempt [ 54 ]. Yet, as illustrated by our study sample, not all suicide attempts will result in an admission to a general hospital for medical treatment. Thus, further evidence is needed to understand the role of physical health complications, both during pregnancy, childbirth and the postnatal period, and their role in mood deterioration.
The subsequent sub-themes of ‘Invalidation of identify and self-sacrifice’ and ‘It wasn’t like starry-eyed love’ are closely intertwined and bring the complexity of women’s conflicting emotions towards motherhood to light [ 55 ]. The desire to be a good mother as a newly found identify often came to the detriment of their own personal self, with many women reporting situations of total self-sacrifice [ 56 ]. These daily struggles, of trying to be the perfect mother on the one hand, while trying to bond with their baby on the other hand, was in many cases fertile soil to start feeling obsolete as a person and feeling disillusioned in motherhood. Our findings build on previous work from Reid et al. (2022), who identified key factors in the context of a perinatal suicide attempt, such as a strained mother-infant bond, lack of social support, loneliness and hopelessness [ 44 ]. This resonates with our sub-themes of “Feeling like a failure”, “Alone in this world” and “Irreversibility of motherhood”. Our final theme “Entrapment and Despair” is in line with Reid et al. (2022)’s final phase, called ‘Darkness Descends’ [ 23 ] and is marked by pervasive feelings of hopelessness and failed motherhood. Under this theme, a turbulent accumulation of negative factors resulting in a fast deterioration of their mental health was reported by all respondents. These feelings of hopelessness and being totally entrapped were so all-encompassing, that participants felt no other way out than by attempting to take their own life. However, in this third stage, women did not just feel disillusioned, they felt totally incompetent as a mother, to a point they believed their baby and family would be better off without them. The finality of motherhood, with no way to turn back time or to escape their fate (‘Irreversibility of Motherhood’), drove them further to despair [ 55 ]. The MBRRACE-UK reports have repeatedly raised such feelings of incompetence as a mother and estrangement of the infant as a ‘red flag’ which should be taken seriously to prevent future maternal deaths by suicide [ 1 , 13 , 57 ].
Another factor we identified in this phase was the occurrence of intrusive thoughts and unsettling (psychotic) experiences, brought together in the subtheme ‘Intense intrusive thoughts and abnormal experiences’. The majority of our respondents reported abnormal experiences that were very unsettling to them. For some, these could be described as intrusive thoughts in the context of Obsessive Compulsive Disorder. Although intrusive thoughts are common among new parents, such experiences are often misunderstood, surrounded by stigma, and sometimes being misdiagnosed or over-normalised and dismissed, preventing timely and effective intervention [ 58 ]. For others in our sample, these experiences may have been delusions or hallucinations as part of a psychotic presentation. For all respondents who had them, the experiences were intense, frightening and difficult to understand at the time. Practitioner knowledge, sensitive risk assessment and careful diagnostic consideration about the nature and type of internal experiences is fundamental to appropriately treat women experiencing these upsetting experiences [ 59 ]. Yet equally important is increased public awareness on the occurrence and impact of such experiences, so women can seek timely support when they experience these frightening thoughts or delusions.
A third common factor we identified was sleep deprivation during pregnancy and the postnatal period and its profound impact on women’s mental health. Sleep disturbance is very common in relation to mental illness, and was highlighted in the most recent MBRRACE-UK report as marked and persistent in those women who died by suicide, even when treated with hypnotic medication [ 1 ]. A recent systematic review by Palagini et al. (2023) showed insomnia and poor sleep quality increased the odds of suicidal risk in pregnant and postpartum women by more than threefold, independently from psychiatric comorbidity [ 60 ]. Especially in a context of onset of psychotic illness, such as bipolar disorder, insomnia often precipitates other psychotic symptoms such as restlessness, irritability and rapid mood changes [ 61 ]. Unfortunately, as sleep loss is generally accepted as a common ‘side effect’ of pregnancy and having a newborn baby, its severity and potential devastating consequences are poorly understood and often minimised. Overall, the theme of ‘Entrapment and Despair’ captures the sheer hopelessness and inability to gain control over a rapidly escalating situation, in line with Klonsky and May’s Three-Step-Theory of suicide [ 62 ]. This theoretical model of suicide considers three steps to suicide. Being in pain and hopelessness leads to suicidal ideation (Step 1), which can be exacerbated by isolation or countered by connectedness (Step 2). The final step is marked by one’s capability of attempting suicide (Step 3). The pervasive feeling of hopelessness and lack of control gradually paved the way for a solid belief it would be better to no longer be here. Participants in our sample shared how they accepted this belief and waited for an opportunity to carry out their suicide plan. This combination of hopelessness and rejection of motherhood, a belief that death would be preferred and an opportunity to act on these thoughts has been previously theorised as a culmination of factors for perinatal suicide [ 23 ]. In line with findings from previous MBRRACE-UK reports, the vast majority of respondents in our sample turned to violent methods for suicide, such as jumping, hanging, suffocation, using sharp objects or stepping in front of traffic, reflecting the high level of distress women found themselves in and the determination with which they wanted to carry out their plan.
Strengths and limitation
Our study is the first to our knowledge to focus on suicide attempts during the perinatal period and offers a rich understanding of women’s experiences surrounding these highly distressing events. A strength of this study is the recruitment of participants across the UK, rather than one geographical area, with diversity in the sample regarding age, parity, psychiatric morbidity, social support, educational attainment and socio-economic status. Significant efforts were made to recruit women from diverse ethnic, cultural, and religious backgrounds, through invitations and meetings with community leaders and designated support groups. Despite our efforts, we did not achieve diversity regarding ethnic and cultural background, one of the limitations of this study. Ethnicity data from the latest MBRRCACE-UK report showed that women who died by suicide were predominately white (86%), with no further ethnicity details on the remaining 14% [ 1 ]. As a result, although this was never our intention, we are aware our study findings are focusing on the experiences of White women in the UK and not transferrable to an ethnically and culturally more diverse sample, or to other countries across the globe. In addition, our sample consisted predominantly of participants with higher educational qualification, in positions of employment. Therefore, our analysis was unable to explore the impact of poverty on women’s suicidality, which is known to be an important driver of poor (perinatal) mental health [ 63 , 64 ]. We are aware a more ethnically, culturally, religiously and socio-economically heterogenous sample is likely to represent a diversity of perspectives, highlighting these issues. Another limitation was the design of the demographic survey, which did not specifically differentiate between mental health diagnosis given during the life course or specifically at the time of the suicide attempt. Suicide research, especially in a perinatal context, is notorious for its recruitment challenges. Saturation for all themes and sub-themes was achieved well within the available sample and is one of the strengths of this study. Another strength of our study is the sensitivity and rigour of patient and public involvement throughout the various phases of the study. This was crucial to do justice to the courage which participants had shown by sharing their stories and to keep respondents safe throughout their research participation.
Implications for clinical practice and care and future research
Our study highlights the importance of routine inquiry of previous mental health difficulties and family history of perinatal mental health problems at the first encounter during pregnancy. Yet, such an assessment needs to be more comprehensive than a tick-box exercise and should be accompanied by a personalised conversation about prevalence of perinatal mental health problems and potential triggers, including trauma and grief. Professionals should be given adequate time during antenatal encounters to explore this in depth and, where required, receive additional training in perinatal mental health to build confidence in doing so. The perinatal period is often described as a ‘window of opportunity’, but this goes both ways: While every encounter creates opportunity for screening, detection and support, it also has the potential for invoking or deepening trauma. Our study revealed the devastating and long-lasting impact of unkind, careless and dismissive remarks by healthcare professionals on women’s mental health, thus instilling a feeling of failure by throw-away comments that would ripple on weeks and months after they were uttered. Perinatal healthcare professionals need to understand the weight of their words, how they can provide hope when women are struggling, but equally how they can push women further into isolation and despair. Culturally aware and trauma-informed clinical practice is essential to achieve this, whilst also recognising the impact of burn-out and carer’s fatigue in an overstretched and under-resourced healthcare service. Healthcare professionals need to be cautious about the difference between normalising and dismissing distressing feelings. In addition, professionals need to fully understand the profound impact of physical, social and psychological risk factors as identified by our study. The physical and mental challenge of pregnancy and childbirth, often in combination with a traumatic birth experience should not be underestimated. An impaired mother-infant dyad, feelings of resentment of motherhood, and the discrepancy between women’s expectations and their lived reality are all key triggers that should be discussed, identified and addressed at the earliest opportunity, in a non-judgemental and sensitive way to avoid further escalation. Women need to be validated and reassured by professionals when disclosing these feelings, and be informed that support is available to help them transition into motherhood. Continuity of care throughout the perinatal period, if done with sensitivity and person-centredness, can foster trusting relationship so women feel safe and supported to disclose distressing feelings. Similarly, insomnia and sleep disturbance, albeit in combination with restlessness and irritability, intrusive thoughts and feelings of lack of control and failure are red flags for severe and rapid mental health deterioration that required prompt and effective action. More than anything, women need to feel safe and listened to, so they can share their feelings with healthcare professionals without fear of judgement, shame and stigma. Our study showed that women will often retreat into silence prior to a suicide attempt and in that moment more than ever rely on attentive, educated and compassionate support networks to avoid a suicide attempt.
Future research into perinatal suicide attempt should focus on developing effective preventative interventions and public health strategies, both in an antenatal and postnatal context, with their distinct healthcare professionals’ involvement and resource challenges. By using implementation science methods, these interventions should be tested and evaluated on their efficacy and effectiveness, in order to reduce future maternal suicides.
This study is the first UK-based qualitative study looking at suicide attempts during the perinatal period. Our findings identified three themes with several contributing factors which led women to undertake a suicide attempt. It is important to understand the impact of previous trauma and life adversity when going through pregnancy and the postnatal period. Feelings of disillusionment with motherhood and feeling entrapped in a hopeless situation were key phases women experienced in the lead-up to their suicide attempt. Our study findings have important implications for clinical practice and healthcare professionals should be aware of warning signs, to improve timely detection and facilitate meaningful inquiry, in order to improve care and prevent future maternal suicide deaths.
Data availability
The datasets generated and analysed during the current study are not publicly available due to the privacy of the participants in the study and the sensitive nature of the data. Further inquiries can be directed to the corresponding author ([email protected]).
We acknowledge not all people who give birth and go through the perinatal period identity as women, female or mothers. While this paper utilises predominantly the terms women and mothers, we aim to include also those who identify as transgender, non-binary or any other gender identity.
Knight M, Bunch K, Patel R, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk J. Saving lives, improving mothers’ Care Core Report - lessons learned to inform maternity care from the UK and Ireland Confidential enquiries into maternal deaths and morbidity 2018-20. In. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2022.
Google Scholar
Rao WW, Yang Y, Ma TJ, Zhang Q, Ungvari GS, Hall BJ, Xiang YT. Worldwide prevalence of suicide attempt in pregnant and postpartum women: a meta-analysis of observational studies. Soc Psychiatry Psychiatr Epidemiol. 2021;56(5):711–20.
Article PubMed Google Scholar
Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. In: World Psychiatry vol. 19; 2020: 313–327.
Gold KJ, Singh V, Marcus SM, Palladino CL. Mental health, substance use and intimate partner problems among pregnant and postpartum suicide victims in the National Violent Death Reporting System. Gen Hosp Psychiatry. 2012;34(2):139–45.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, Pariante CM. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–19.
Letourneau NL, Dennis C-L, Benzies K, Duffett-Leger L, Stewart M, Tryphonopoulos PD, Este D, Watson W. Postpartum Depression is a Family Affair: addressing the impact on mothers, fathers, and children. Issues Ment Health Nurs. 2012;33(7):445–57.
Bauer A, Parsonage M, Knapp M, Iemmi V, Adelaja B. The costs of perinatal mental health problems. Lond School Econ 2014.
Chin K, Wendt A, Bennett IM, Bhat A. Suicide and maternal mortality. Curr Psychiatry Rep. 2022;24(4):239–75.
Article PubMed PubMed Central Google Scholar
Diguisto C, Saucedo M, Kallianidis A, Bloemenkamp K, Bodker B, Buoncristiano M, Donati S, Gissler M, Johansen M, Knight M, et al. Maternal mortality in eight European countries with enhanced surveillance systems: descriptive population based study. BMJ. 2022;379:e070621.
Cantwell R. Perinatal mental health service development across the UK – many achievements, growing challenges. Ir J Psychol Med 2022:1–4.
Knight M, Bunch K, Tuffnell D, Patel R, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ. Saving Lives, Improving Mothers’ Care - Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2017-19. In. Oxford; 2021.
Knight M, Nair M, Tuffnell D, Shakespeare J, Kenyon S, Kurinczuk JJ. Saving Lives, Improving Mothers’ Care Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2013-15 Maternal, Newborn and Infant. Clinical Outcome Review Programme; 2017.
Knight M, Bunch K, Tuffnell D, Jayakody H, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ. Saving Lives, Improving Mothers’ Care Maternal, Newborn and Infant Clinical Outcome Review Programme; 2018.
Knight M, Bunch K, Cairns A, Cantwell R, Cox P, Kenyon S, Kotnis R, Lucas N, Lucas S, Marshall L, et al. Saving Lives, Improving Mothers’ Care Rapid report: Learning from SARS-CoV-2-related and associated maternal deaths in the UK Maternal. Newborn and Infant Clinical Outcome Review Programme; 2020.
Department of Health and Social Care. Suicide prevention in England: 5 year cross-sector strategy. In.; 2023.
Orsolini L, Valchera A, Vecchiotti R, Tomasetti C, Iasevoli F, Fornaro M, De Berardis D, Perna G, Pompili M, Bellantuono C. Suicide during Perinatal Period: epidemiology, risk factors, and clinical correlates. Front Psychiatry. 2016;7:138.
Gandhi SG, Gilbert WM, McElvy SS, El Kady D, Danielson B, Xing G, Smith LH. Maternal and neonatal outcomes after attempted suicide. Obstet Gynecol. 2006;107(5):984–90.
Schiff MA, Grossman DC. Adverse perinatal outcomes and risk for postpartum suicide attempt in Washington state, 1987–2001. Pediatrics. 2006;118(3):e669–675.
Crosby A, Ortega L, Melanson C. Self-directed violence surveillance; uniform definitions and recommended data elements. In.: National Center for Injury Prevention and Control (U.S.). Division of Violence Prevention; 2011.
Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68(3):371–7.
Article CAS PubMed Google Scholar
Douglas J, Cooper J, Amos T, Webb R, Guthrie E, Appleby L. Near-fatal deliberate self-harm: characteristics, prevention and implications for the prevention of suicide. J Affect Disord. 2004;79(1):263–8.
Johannsen BM, Larsen JT, Laursen TM, Ayre K, Howard LM, Meltzer-Brody S, Bech BH, Munk-Olsen T. Self-harm in women with postpartum mental disorders. Psychol Med. 2020;50(9):1563–9.
Reid H, Pratt D, Edge D, Wittkowski A. What makes a perinatal woman suicidal? A grounded theory study. BMC Psychiatry. 2022;22(1):386.
Al-Halabi S, Garcia-Haro J, de la Fe Rodriguez-Munoz M, Fonseca-Pedrero E. Suicidal behavior and the perinatal period: taboo and misunderstanding. Psychol Papers. 2021;42(3):161–9.
Silverio SA, Sheen KS, Bramante A, Knighting K, Koops TU, Montgomery E, November L, Soulsby LK, Stevenson JH, Watkins M, et al. Sensitive, challenging, and difficult topics: experiences and practical considerations for qualitative researchers. Int J Qualitative Methods. 2022;21:16094069221124739.
Article Google Scholar
Hjelmeland H, Knizek BL. Why we need qualitative research in Suicidology. Suicide Life-Threatening Behav. 2010;40(1):74–80.
O’Mahoney J. Critical realism and qualitative research: an introductory overview. In, edn.; 2016.
Williams R. The epistemology of knowledge and the knowledge process cycle: beyond the objectivist vs interpretivist. J Knowl Manage. 2008;12(4):72–85.
Article CAS Google Scholar
Boyatzis RE. Transforming qualitative information: thematic analysis and Code Development. Thousand Oaks, CA: Sage; 1998.
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qualitative Res Sport Exerc Health. 2019;11(4):589–97.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Wiltshire G, Ronkainen N. A realist approach to thematic analysis: making sense of qualitative data through experiential, inferential and dispositional themes. J Crit Realism. 2021;20(2):159–80.
Fryer T. A critical realist approach to thematic analysis: producing causal explanations. J Crit Realism. 2022;21(4):365–84.
Vasileiou K, Barnett J, Thorpe S, Young T. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol. 2018;18(1):148.
De Backer K, Newburn M, Hildersley R, Easter A. Conducting a sensitive research study on perinatal suicide attempts — the power of patient and public involvement and Engagement (PPIE). MIDIRS Midwifery Digest. 2023;33(2):115–8.
Martinez Dy A, Martin L, Marlow S. Developing a critical Realist positional Approach to Intersectionality. J Crit Realism. 2014;13(5):447–66.
Law C, Wolfenden L, Sperlich M, Taylor J. A good practice guide to support implementation of trauma-informed care in the perinatal period. In.; 2021.
Gibson S, Benson O, Brand SL. Talking about suicide: confidentiality and anonymity in qualitative research. Nurs Ethics. 2013;20(1):0969733012452684.
Johnson B, Clarke JM. Collecting Sensitive Data: the impact on researchers. Qual Health Res. 2003;13(3):421–34.
Kiyimba N, O’Reilly M. An exploration of the possibility for secondary traumatic stress among transcriptionists: a grounded theory approach. Qualitative Res Psychol. 2016;13(1):92–108.
Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77–87.
Gressier F, Guillard V, Cazas O, Falissard B, Glangeaud-Freudenthal NMC, Sutter-Dallay A-L. Risk factors for suicide attempt in pregnancy and the post-partum period in women with serious mental illnesses. J Psychiatr Res. 2017;84:284–91.
Taylor CL, Broadbent M, Khondoker M, Stewart RJ, Howard LM. Predictors of severe relapse in pregnant women with psychotic or bipolar disorders. J Psychiatr Res. 2018;104:100–7.
Reid H, Pratt D, Edge D, Wittkowski A. Maternal suicide ideation and Behaviour during pregnancy and the First Postpartum Year: a systematic review of psychological and psychosocial risk factors. Front Psychiatry 2022, 13.
Bright AM, Doody O, Tuohy T. Women with perinatal suicidal ideation-A scoping review of the biopsychosocial risk factors to inform health service provision and research. PLoS ONE. 2022;17(9):e0274862.
Article CAS PubMed PubMed Central Google Scholar
Weng S-C, Chang J-C, Yeh M-K, Wang S-M, Lee C-S, Chen Y-H. Do stillbirth, miscarriage, and termination of pregnancy increase risks of attempted and completed suicide within a year? A population-based nested case–control study. BJOG: Int J Obstet Gynecol. 2018;125(8):983–90.
Forray A, Yonkers KA. The Collision of Mental Health, Substance Use Disorder, and suicide. Obstet Gynecol. 2021;137(6):1083–90.
Cull J, Thomson G, Downe S, Fine M, Topalidou A. Views from women and maternity care professionals on routine discussion of previous trauma in the perinatal period: a qualitative evidence synthesis. PLoS ONE. 2023;18(5):e0284119.
National Institute for Health Care Excellence. Antenatal and postnatal mental health: Antenatal and postnatal mental health: clinical management and service clinical management and service guidance guidance clinical guideline. In.; 2014.
Ayers S, Bond R, Bertullies S, Wijma K. The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychol Med. 2016;46(6):1121–34.
Sheen K, Slade P. The efficacy of ‘debriefing’ after childbirth: is there a case for targeted intervention? J Reproductive Infant Psychol. 2015;33:308–20.
Sheen K, Slade P. Examining the content and moderators of women’s fears for giving birth: a meta-synthesis. J Clin Nurs. 2018;27(13–14):2523–35.
Jomeen J, Martin CR, Jones C, Marshall C, Ayers S, Burt K, Frodsham L, Horsch A, Midwinter D, O’Connell M, et al. Tokophobia and fear of birth: a workshop consensus statement on current issues and recommendations for future research. J Reprod Infant Psychol. 2021;39(1):2–15.
Schiff M, Grossman D. Adverse perinatal outcomes and risk for postpartum suicide attempt in Washington State, 1987–2001. Pediatrics. 2006;118(3):e669–75.
Nicolson P. Loss, happiness and postpartum depression: the ultimate paradox. Can Psychol. 1999;40:162–78.
Staneva AA, Bogossian F, Wittkowski A. The experience of psychological distress, depression, and anxiety during pregnancy: a meta-synthesis of qualitative research. Midwifery. 2015;31(6):563–73.
Knight M, Bunch K, Tuffnell D, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ. Saving Lives, Improving Mothers’ Care Maternal, Newborn and Infant Clinical Outcome Review Programme. In. Oxford; 2020.
Fairbrother N, Woody SR. New mothers’ thoughts of harm related to the newborn. Arch Womens Ment Health. 2008;11(3):221–9.
Challacombe FL, Bavetta M, DeGiorgio S. Intrusive thoughts in perinatal obsessive-compulsive disorder. BMJ. 2019;367:l6574.
Palagini L, Cipriani E, Miniati M, Bramante A, Gemignani A, Geoffroy PA, Riemann D. Insomnia, poor sleep quality and perinatal suicidal risk: a systematic review and meta-analysis. J Sleep Res 2023:e14000.
Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5(2):98–105.
Klonsky ED, May AM, 3ST). The Three-Step Theory (: A New Theory of Suicide Rooted in the Ideation-to-Action Framework. International Journal of Cognitive Therapy 2015, 8(2):114–129.
Mathieu S, Treloar A, Hawgood J, Ross V, Kõlves K. The role of unemployment, Financial Hardship, and economic recession on suicidal behaviors and interventions to mitigate their impact: a review. Front Public Health. 2022;10:907052.
Parra-Saavedra M, Miranda J. Maternal mental health is being affected by poverty and COVID-19. Lancet Global Health. 2021;9(8):e1031–2.
Download references
Acknowledgements
We would like to thank all the women and birthing people who took part in this study, for their time, their bravery and the honesty with which they shared their story. Their commitment to improve care for others who find themselves in a similar position was a privilege to witness. We thank Dr Clare Dolman, the Patient Advisory Group at the Section for Women’s Mental Health at King’s College London, the South London Applied Research Collaboration Maternity and Perinatal Mental Health theme Patient and Public Involvement and Engagement group for their suggestions and feedback throughout the different stages of this study. We also like to thank the third sector partners that were closely involved in the study journey, such as Maternal Mental Health Alliance, Mothers for Mothers, the Institute of Health Visiting, the Motherhood Group, REFORM, National Childbirth Trust (NCT), and Maternity Action.
This work was supported by the National Institute for Health and Care Research (NIHR) South London Applied Research Collaboration (NIHR200152). Patient and public involvement engagement activities undertaken for this study were funded through a King’s Engaged Research Network (KERN) Public Engagement Small Grant Award. Kaat De Backer, Sergio A. Silverio, Professor Jane Sandall and Dr Abigail Easter are supported by the NIHR Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust. Kaat De Backer (King’s College London) is also in receipt of an NIHR Doctoral Research Fellowship (NIHR302565). Sergio A. Silverio (King’s College London) is currently in receipt of a Personal Doctoral Fellowship from the NIHR ARC South London Capacity Building Theme [NIHR-INF-2170]. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
Department of Women & Children’s Health, School of Life Course and Population Sciences, Faculty of Life Sciences & Medicine, King’s College London, 10th Floor North Wing, St. Thomas’ Hospital, Westminster Bridge Road, Lambeth, London, SE1 7EH, UK
Kaat De Backer, Alexandra Pali, Jane Sandall & Abigail Easter
Department of Clinical Psychological Science, Faculty of Psychology and Neuroscience, Maastricht University, Maastricht, The Netherlands
Alexandra Pali
Section of Women’s Mental Health, Institute of Psychiatry, Psychology, and Neuroscience, King’s College London, Denmark Hill, 16 De Crespigny Park, London, SE5 8AF, England
Fiona L. Challacombe, Rosanna Hildersley & Louise M. Howard
Patient and Public Involvement and Engagement Lead for ARC South London, Maternity and Perinatal Mental health theme, Department of Women & Children’s Health, School of Life Sciences and Medicine, King’s College London, 10th Floor North Wing, St. Thomas’ Hospital, Westminster Bridge Road, Lambeth, London, SE1 7EH, UK
Mary Newburn
Department of Women & Children’s Health, School of Life Course & Population Sciences, Faculty of Life Sciences & Medicine, King’s College London, 6th Floor Addison House, Great Maze Pond, Southwark, London, SE1 1UK, UK
Sergio A. Silverio
School of Psychology, Faculty of Health, Liverpool John Moores University, Liverpool, Merseyside, L3 3AF, UK
You can also search for this author in PubMed Google Scholar
Contributions
AE, LMH, JS, RH, KDB conceived the work and designed the study. SAS and MN contributed to the development of the design. MN led the Public and Patient Involvement and Engagement. KDB, AP, AE, FLC contributed to data acquisition. KDB, AP, AE, FLC interpreted the data. KDB drafted the manuscript and incorporated revisions from all other authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Abigail Easter .
Ethics declarations
Ethical approval and consent to participate.
Ethical approvals were sought and granted by the King’s College London Health Faculties Research Ethics Committee, in January 2021 (reference HR-20/21-20092), with a further amendment in June 2022, after further feedback from the advisory panel and stakeholder meeting (reference MOD-21/22-20092). The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Consent for publication
Written informed consent was obtained from all participants in the study. Participants were also invited to proof-read the manuscript to ensure they were satisfied with selection of quotations.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
De Backer, K., Pali, A., Challacombe, F.L. et al. Women’s experiences of attempted suicide in the perinatal period (ASPEN-study) – a qualitative study. BMC Psychiatry 24 , 255 (2024). https://doi.org/10.1186/s12888-024-05686-3
Download citation
Received : 22 December 2023
Accepted : 14 March 2024
Published : 03 April 2024
DOI : https://doi.org/10.1186/s12888-024-05686-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Women’s mental health
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
University of Hertfordshire to support delivery of £1.1 million project to provide digital innovations for vulnerable residents

In a successful joint application with Bedfordshire, Luton and Milton Keynes Integrated Care System’s (BLMK ICS) Digitising Social Care (DiSC) programme and Health Innovation England, a team of researchers from the University of Hertfordshire has secured £1.1m funding from the latest wave of NHS England’s Adult Social Care Technology Fund. This will be used to develop digital innovations that support vulnerable adults including people living with dementia.
Supported by the Applied Research Collaboration East of England and The Office of Health Economics, the research will evaluate the impact of introducing new pain assessment technologies and robotic companions in different adult social care settings. In particular, the innovations aim to support older people, particularly those living with dementia, and their carers.
One such innovation is PainChek, an electronic device that identifies and manages pain for those who are unable to communicate it verbally. It uses artificial intelligence (AI) to spot small changes in facial expressions and voice to quantify a pain score and guide carers to provide the right support. The funding will enable around 1,000 residents in a variety of settings to be assessed by their care provider.
Additionally, as part of the initiative, around 1,300 care home residents will be provided with a robotic companion to provide comfort and decrease loneliness. Robopets are intended to provide a calming influence, give people greater independence and confidence, and to improve mental health and wellbeing.
Dr Jenni Lynch, Reader in Social Care, Technology and Knowledge Mobilisation at the University of Hertfordshire who is leading the implementation arm of the project, said: “We are absolutely delighted with this opportunity. Our researchers have worked extremely hard to secure this funding as we know that around 50% of people living with dementia have undetected and untreated pain, leading to huge amounts of distress. Loneliness and social isolation are also major factors affecting the wellbeing of people living with dementia. With this project we can hopefully shed more light on how advanced digital technologies can be used to tackle issues that really affect people's quality of life.”
It is hoped that both innovations will improve overall wellbeing and quality of life for residents by reducing distress and anxiety, which will also have a positive effect on families and carers.
Through a number of methods and processes, including focus groups and observations, researchers will capture the experiences of service users, carers and key staff. These insights will inform the development of an evidence-based plan for scale and spread across BLMK ICS.
Clare Steward, DiSC Programme Director, said: “We are very aware that depression, loneliness and dementia are real challenges for our ageing population, and are keen to invest in solutions that would help improve the quality of life of our residents and reduce pressure on care services.”
“Co-production and collaboration have always been very important to our team and after looking at a number of potential innovations, we have worked closely with our stakeholders and local care providers to agree which two schemes would most benefit our residents and providers.”
Find out more about the DiSC programme

IMAGES
COMMENTS
A new £42.7 million investment into mental health research has been announced by the NIHR and the Office for Life Sciences. The new Mental Health Mission (MHM) will develop innovative new treatments and technologies. The Mission will work with patients, NHS staff and clinicians and innovators to make the UK a leading location in which to test ...
To fund research that gives hope and improves lives, providing a better future for everyone affected by mental health problems. Our focus To fund talented early-career UK-based mental health research scientists whose work will lead to the prevention, early diagnosis, or treatment of mental ill-health.
Funding. Mental Health Research UK aims to make a significant improvement to the lives of people with mental illness, by funding research into causes and cures. We know it is often challenging to find resources to support PhD studentships and that is why we focus our funding on these awards, supporting mental health researchers of the future.
MQ is the first major charity that funds mental health research. We connect scientists with supporters to understand, treat and prevent mental illness. ... In 2015, MQ compiled a comprehensive data set on mental health-related research grants awarded by major funders in the UK between 2008 and 2013 - the first of its kind. ...
MRC supports world-class mental health research, creating new opportunities to treat and prevent mental health illness, such as anxiety and depression, which are estimated to affect around one in six people at any time in the UK. Budget: MRC has invested more than £140 million over the last five years in research directly addressing mental ...
On 28 November 2022, the government launched the Mental Health Mission ( MHM), with funding to support innovation in mental health research, services, and digital technology. On 25 May 2023, £42. ...
Using grants data retrieved from the Dimensions database, we have calculated funding of mental health research by UK funding bodies from 2014-17 as approximately GBP£125 million per year. This result is comparable to GBP£115 million in the previous MQ analysis covering the period from 2008-13, 6. MQ: Transforming Mental Health ...
Publication date: 15 February 2024. Opening date: 15 February 2024 9:00am UK time. Closing date: 15 May 2024 4:00pm UK time. Start application. Apply for funding to support research projects focused on neurosciences and mental health. You must be a researcher employed by a research organisation eligible to apply for Medical Research Council ...
High-quality data on funding for mental health research are essential to mapping funding levels, identifying gaps in the funding landscape, and tracking the impact of research funding. To date, quantitative analyses of research funding in mental health have been restricted in scope. In this Health Policy paper, we present a comprehensive analysis of grant funding for mental health research as ...
Take the next step. First steps in research. Start publishing. Join a research project. Set up your own research project. Fellowships in mental health research. Do further training. Find a mentor. Patient and public involvement in mental health research.
The Three NIHR Research Schools have announced a further £4.98m of additional funding for phase two of their support programme for mental health research. This funding is available in the form of 3 structured open calls, at the moment, each aimed at people at different stages in their research career. This one is for 8….
Researchers apply for fellowships and research grants to support mental health research studies, and there are lots of different options depending on your career stage and experience. Fellowships support an individual researcher's development, whereas grants support individual studies. The research councils offer largescale funding opportunities.
MQ is the first major charity that funds mental health research. We connect scientists with supporters to understand, treat and prevent mental illness. ... In 2015, MQ compiled a comprehensive data set on mental health-related research grants awarded by major funders in the UK between 2008 and 2013 - the first of its kind. ...
No open funding calls Previous funding calls October 2020 - Up to £50K was available from the Loneliness and Social Isolation in Mental Health network as part of their second funding call on interventions. Grants were available for £15K and £50K for small or large projects respectively, provided at 80% of full economic costing.
Research. We are passionate about the transformative power of mental health research to create change in people's lives, their communities and workplaces regarding services and policy. We aim to contribute to the mental health evidence base by: undertaking original research. synthesising existing knowledge. translating this research to ...
29 September 2021 4:00pm UK time. Funding is available from MRC's Neurosciences and Mental Health Board to support focused research projects on neurosciences and mental health. We award research grants to UK-based research organisations, and research grants may involve more than one research group or institution.
Table 1. Total UK funding for mental health research by year (nominal amounts) What is mental health research? Increases in mental health research funding between 2008 and 2014 have been minimal - whilst the overall grants budget in the UK has grown by 7% during this time.4 Setting the scene: UK mental health research funding 2014-2017
UK Health Research Analysis 2018. January 2020. MQ. UK Mental Health Research Funding 2014-2017. 2017. £30 million investment to rebalance the scale of mental health research. £42.7 million funding boost for mental health services. RCPsych supports Government funding for research into severe mental illness. See all mental health statistics.
This is just over 6% of the population, varying from 16.7% of 11 to 15 year olds and 14.6% of 16 to 19 year olds to 3.2% of 65 to 69 year olds. Access to and contact with mental health services varies across the country. The highest was Hull, where 10.8% of the adult population were in contact with mental health services during 2022/23.
The government is investing £150 million of capital in NHS mental health crisis response and urgent and emergency care services up to April 2025. This includes £7 million for the procurement of ...
Last modified on Wed 27 Mar 2024 03.55 EDT. Mental illness costs England £300bn a year, equivalent to nearly double its NHS budget, according to research. Researchers for the Centre for Mental ...
The Department for Education ( DfE) is offering a grant of £1,200 in the 2024 to 2025 financial year for eligible state-funded schools and colleges to train a senior mental health lead. We ...
The History, Present & Future of LGBTQ+ Mental Health. Panel discussion. Talk. This event has now finished. Date and time: Wednesday 21 February 2024, 3pm to 4.45pm. Location: PS/A/202, Lecture Room (Venables Room), Psychology Building, Campus West, University of York ( Map) Audience:
Mental Health Research UK (MHRUK) and MQ are both charities whose primary aim is to fund mental health research. They were both set up about 10 years ago. Everything they do is structured around the importance of mental health research and raising funds to invest in new programmes of research. MHRUK has a PhD scholarship programme with calls ...
Background: The use of surveillance technologies is becoming increasingly common in inpatient mental health settings, commonly justified as efforts to improve safety and cost-effectiveness. However, the use of these technologies has been questioned in light of limited research conducted and the sensitivities, ethical concerns and potential harms of surveillance. This systematic review aims to ...
Suicide is a leading cause of maternal death during pregnancy and the year after birth (the perinatal period). While maternal suicide is a relatively rare event with a prevalence of 3.84 per 100,000 live births in the UK [1], the impact of maternal suicide is profound and long-lasting. Many more women will attempt suicide during the perinatal period, with a worldwide estimated prevalence of ...
Press Office [email protected] +44 (0)1707 285 770. Herts is supporting the delivery of a £1.1m digital innovations project to provide two social care technologies for people living with dementia, to improve their mental health and wellbeing. Robopets uses AI to respond to voice commands and interact through realistic movement; PainChek uses ...
According to RAF Benevolent Fund research, there was a 93 per cent increase in its family counselling programme between 2020 and last year. The number of RAF children seeking help for mental ...