- Subscribe Today!
- Ophthalmology

Safer eye floater treatments come with a burst of nanobubbles
Between invasive surgery or risky laser therapy, people suffering from severe eye floaters have no great treatment options. now, with the development of a safer and less invasive nanoparticle-based therapy, people with floaters may finally get their vision and quality of life back..

Stephanie joined Drug Discovery News as an Assistant Editor in 2021. She earned her PhD from the University of California Los Angeles in 2019 and has written for Discover Magazine,...
Sometimes they sit just out of sight in the corner of your eye. Other times they waft across your vision, and when you shift your gaze to look at them, they fly out of sight. These pesky obstructions, commonly referred to as floaters, are a visual phenomenon caused by small clumps of collagen in the eye called vitreous opacities.
While floaters are very common, they are typically unobtrusive enough that people ignore them. Sometimes, however, floaters can be so dark and numerous that they obscure large swaths of a person’s vision. These severe floaters impair people’s ability to drive, work, and simply enjoy their lives, often leading to depression (1).

“There are millions of people in the world suffering from floaters,” said Yannis Paulus, a vitreoretinal surgeon and clinician scientist at the University of Michigan. “Currently, they’re stuck with bad options,” he added. The only available treatments have a significant number of risks.
These treatments include vitrectomy, the surgical removal of the clear gel-like vitreous of the eye that contains the collagen clumps, and laser vitreolysis, shining high-energy light pulses directed at the fibers to break them apart. Vitrectomy is more effective than laser vitreolysis, but patients have experienced retinal tears, detached retinas, and vitreous hemorrhage with both treatments.
While investigating how to make vitrectomy and laser vitreolysis safer and more effective, scientists are also developing new nanobubble-based technologies that may prove even safer and less invasive than the current treatments, improving the quality of life for the many people around the world suffering from disruptive floaters.
Clumps of collagen
The most common cause of floaters is simply getting older. In young eyes, collagen fibers bound to hyaluronan molecules hold together the gel-like structure of the vitreous. As people age, the collagen and hyaluronan begin to dissociate, and the gel becomes more liquid-like, causing the collagen fibers in the vitreous to collapse onto each other and form clumps, which are perceived as floaters.
People over 60 years old often begin to see more floaters due to their vitreous pulling away from the back of the eye in a phenomenon called posterior vitreous detachment. But because this de-gelling process happens faster in people with nearsightedness, nearsighted people in their 20s, 30s, and 40s can also experience floaters.

For people who notice a sudden burst of many new floaters, ophthalmologists first check for any signs of retinal detachments or injuries to the eye. But after ruling out an acute cause, doctors usually suggest that people wait a few weeks or months to see if their floaters seem to fade or become less noticeable. Usually, people experience some neuroadaptation, and the brain tunes out the floaters. But if the floaters don’t get better and they continue to detrimentally affect daily life, people return to their doctors seeking help.
“Unfortunately, the most common form of treatment is to dismiss them and ignore them and send the patient home frustrated and unhappy,” said Jerry Sebag, a vitreoretinal surgeon and floaters researcher at the Vitreous Macula Retina (VMR) Institute. “I started to realize that these patients are being dismissed because we had no way of identifying if they really have a problem, or if they're just overreacting to something that we all experience.”
Sebag and his colleagues developed quantitative assessments to measure how floaters affect people’s vision. They demonstrated that they could use quantitative ultrasound to characterize the density of the entire vitreous with floaters showing up as points and lines of increased density (2). Sebag’s team also reported that floaters decreased a person’s contrast sensitivity , meaning that people with floaters were less able to distinguish between differences in shading and patterns (3).
“With a quantitative component, it enables you to classify conditions as mild, moderate, and severe,” said Sebag. “It enabled me to select patients for treatment.”
Surgical incisions clear out floaters
The most effective way to treat floaters is to physically remove them. By performing a surgery called a vitrectomy, surgeons remove the vitreous from the eye and replace it with a clear gel.
While there are risks of retinal tears and detachments during vitrectomy, “you can usually identify those problems during the surgery. If you see a torn retina, you can laser it during the operation,” said Jason Hsu, a vitreoretinal surgeon and researcher at Thomas Jefferson University.
Vitreoretinal surgeons have recently made improvements to vitrectomies to make these retinal tears less likely. For example, they now use smaller gauge instruments to perform the surgery, meaning that they can make smaller incisions. Sebag has adapted his vitrectomy procedure with this modification and improved the method so that it doesn’t induce a posterior vitreous detachment during the surgery. With these safety modifications, Sebag’s team reported in a clinical study of 195 eyes from 145 patients that vitrectomy led to a 94.1% reduction in vitreous echodensity, indicating successful removal of the vitreous opacities that cause the appearance of floaters (4). The patient’s contrast sensitivity also improved to the level of healthy control eyes after surgery. Out of the 195 eyes operated on, there were three retinal tears and three retinal detachments, but these were successfully repaired during the surgery.
While vitrectomy is relatively safe and effective at treating severe floaters, it does lead to an increased risk for developing cataracts (5). Because of this and because other long-term risks of vitrectomy are unknown, Sebag and other vitreoretinal surgeons hesitate to operate on younger patients.
“I just haven't followed people for 30 years, so I can't answer that question,” said Sebag. As an alternative to vitrectomy, some ophthalmologists turned to a risky and somewhat controversial treatment: laser vitreolysis.
An explosion in the eye
Rather than physically removing the vitreous opacities that cause floaters, some ophthalmologists have tried blasting them apart with pulses of a yttrium-aluminum-garnet (YAG) laser.
“It's not like a typical laser beam that we think of like in Star Wars or something where it's burning tissue. The YAG laser is like a little explosion in the eye,” said Hsu. “It’s almost like evaporating some of the tissue with this high concentrated energy.” This process breaks up large aggregates of collagen into smaller pieces, reducing the appearance of floaters.
Ophthalmologists have used YAG lasers for decades to remove cloudy layers of scar tissue that form after cataract surgery and in the treatment of specific kinds of glaucoma, but their use to treat floaters is relatively new and somewhat controversial.
In the only clinical trial so far investigating the effectiveness of YAG laser vitreolysis for floaters, 54% of the patients who received the YAG treatment reported improvement in the appearance of floaters (6). None of the patients in the trial experienced any adverse effects.
There are, however, substantial risks associated with YAG laser treatment. The laser energies needed to blast apart the fibers that cause floaters are double or triple that of the energies used for the other more routine uses of YAG lasers. Even with the higher energy laser pulses, a person may need to sit through multiple sessions of YAG laser treatment to effectively break up a bothersome floater. In some instances, surgeons have focused the laser too close to the front or back of the eye, causing direct damage to the lens or the retina.

Citing these concerns, Inder Paul Singh, an ophthalmologist at the Eye Centers of Racine and Kenosha, explained that newer YAG lasers allow for better illumination of the vitreous, which helps ophthalmologists more easily orient themselves in the eye, decreasing the risks of damaging vital structures.
“Not every floater is a good candidate for YAG laser vitreolysis,” he said, but for example, if “the floater is in the middle of the vitreous where you can correlate signs and symptoms well, this can be a fantastic opportunity to avoid something like a vitrectomy and not to make [the patient] suffer living with it.”
While Singh has had much success treating floaters with YAG vitreolysis in his practice, that has not been the case for many other doctors.
“There is no protocol to guide the use of YAG laser, either in terms of which patients to select or in terms of how to really do the treatment in a reproducible scientific fashion,” Sebag said. He is organizing a study on how to make YAG vitreolysis more reproducible and safer using quantitative ultrasonography, among other methods, to measure outcomes.
Singh agreed that proper training on how to perform YAG vitreolysis is integral to successful floater treatment.
“The laser is not unsafe. It’s we as doctors who can be unsafe,” he said. “It's important for doctors to feel comfortable understanding where they are in the vitreous and learning how to maximize that view.”
He and others are investigating the use of systems to track floaters more accurately in the vitreous and the use of the more efficient femtosecond laser rather than a YAG laser for floater treatment, which would decrease the number of laser sessions needed to destroy floaters.
With the current risks associated with both vitrectomy and laser vitreolysis, researchers are looking for new strategies to treat floaters.
Nanobubbles bust up floaters
Before presenting his research at the Academy of Medicine in Belgium years ago, Stefaan De Smedt, a drug delivery researcher at Ghent University, had never considered nanobubbles as the next frontier in eye floater treatment. He and his team were interested in using vapor nanobubbles, which are produced by shining a laser at nanoparticles, as a method to deliver nucleic acids into cells.
When scientists shine a laser of a certain frequency at nanoparticles that are close together, the nanoparticles absorb the energy from the laser, which heats up the solution surrounding the nanoparticles, causing the liquid to evaporate and create nanobubbles. These nanobubbles expand and then pop tens to hundreds of nanoseconds after they form (7), leading to the creation of a mechanical force that can poke a hole in a cell membrane.
“I was talking to an ophthalmologist, [and] he said maybe it could be useful as well to see whether this kind of nanobubbles could be valuable to destroy aggregates,” De Smedt said.
Intrigued by the possibility, De Smedt and his postdoctoral fellow Félix Sauvage began testing the ability of vapor nanobubbles produced by different kinds of nanoparticles to destroy the collagen aggregates that cause floaters. In a new study published in Nature Nanotechnology , De Smedt and Sauvage, working in collaboration with Sebag, Paulus, and others, reported the success of nanobubbles produced by gold nanoparticles and an ophthalmologic dye to destroy collagen aggregates in vivo for the first time (8).
The researchers demonstrated that both gold nanoparticles coated in hyaluronan and the ophthalmologic dye indocyanine green (ICG) preferentially bound to and destroyed human vitreous opacities that had been isolated from vitrectomy patients in Sebag’s practice. Because the particles specifically bound to the collagen aggregates, the creation of nanobubbles only occurred at the aggregates. This means that even if the laser shines on a place in the eye with no nanoparticles or dye, no nanobubbles will be created to potentially damage other structures in the eye.
“The threshold to generate bubbles is very high,” explained Sauvage. “We have a selective manner to trigger the generation of bubbles.”
Encouraged by how well their technology worked in an ex vivo system, De Smedt’s team searched for the best animal model to test it in vivo . This proved to be somewhat of a challenge, because, as Paulus quipped, “you don't have a mouse telling you that it has floaters in its vision.”
The team finally landed on rabbits with their relatively large eyes, which are closer in size to those of humans, making them ideal models.
De Smedt, Sauvage, and their colleagues injected rabbit eyes with collagen fibers to give the rabbits vitreous opacities, then they either injected the gold nanoparticles or ICG and shined laser pulses into the rabbits’ eyes. They found that they only needed to use an average of five laser pulses to completely remove the collagen aggregates.
“When we saw that data about how effective it was, it was pretty stunning to me,” said Paulus. When the team assessed the safety of their technique, they found that it had no adverse effects on the rabbits’ retinas.
Because the nanoparticles and dye bind directly to the collagen fibers, the researchers could remove the vitreous opacities from locations in the eye that would be impossible using a YAG laser, such as close to the retina. Similarly, the aggregation of the particles allowed the researchers to use a lower energy laser to induce nanobubbles than that required for a YAG laser to break up fibers, vastly improving safety.
This technology also improves on vitrectomy because it does not require a risky surgery, rather simply an injection of nanoparticles or dye into the eye. Eye injections are a common procedure for vitreoretinal surgeons, Paulus added.
“It's taking two things that we do in essence almost independently — these eye injections and the laser — and combining them,” he said.
Moving forward, De Smedt and his team are interested in investigating the pharmacokinetics of their gold nanoparticles and ICG in humans. While both gold nanoparticles and ICG are biocompatible, only ICG is biodegradable, making it the more likely of the two to move forward into future human clinical trials.
“Certainly, there's additional work in terms of clinical trials that we need to do before this is readily available for everyone, but I think it would really be a game changer in terms of the ability to treat these floaters in a manner that's minimally invasive with low risk. And I think it would really transform our care for patients,” said Paulus.
Although De Smedt did not initially set out to develop new treatments for floaters, he now understands what a non-invasive and effective treatment would mean for people suffering from floaters. After his team published their first paper on nanoparticles and floaters (9), he and Sauvage received hundreds of questions from people all over the world asking about the potential of the technology to treat floaters.
“I try to imagine how it feels to open your eyes and to feel always depressed about the fact that you cannot really see,” De Smedt said. “It can contribute to giving vision back to people, which means to give quality of life.”
- Kim, Y-K. et al. Psychological Distress in Patients with Symptomatic Vitreous Floaters. Journal of Ophthalmology 2017 , 3191576 (2017).
- Mamou, J. et al. Ultrasound-Based Quantification of Vitreous Floaters Correlates with Contrast Sensitivity and Quality of Life. Investigative Ophthalmology & Visual Science 56 , 1611-1617 (2015).
- Garcia, G.A. et al. Degradation of Contrast Sensitivity Function Following Posterior Vitreous Detachment. American Journal of Ophthalmology 172 , 7-12 (2016).
- Sebag, J. et al. Long-Term Safety and Efficacy of Limited Vitrectomy for Vision Degrading Vitreopathy Resulting from Vitreous Floaters. Ophthalmology Retina 2 , 881-887 (2018).
- Yee, K.M.P. et al. Incidence of Cataract Surgery after Vitrectomy for Vitreous Opacities. Ophthalmology Retina 1 , 154-157 (2017).
- Shah, C.P. & Heier, J.S. YAG Laser Vitreolysis vs Sham YAG Vitreolysis for Symptomatic Vitreous Floaters: A Randomized Clinical Trial. JAMA Ophthalmol 135 , 918-923 (2017).
- Xiong, R. et al. Comparison of gold nanoparticle mediated photoporation: vapor nanobubbles outperform direct heating for delivering macromolecules in live cells. ACS Nano 8 , 6288-6296 (2014).
- Sauvage, F. et al. Laser-induced nanobubbles safely ablate vitreous opacities in vivo. Nat Nanotechnol (2022).
- Sauvage, F. et al. Photoablation of Human Vitreous Opacities by Light-Induced Vapor Nanobubbles. ACS Nano 13 , 8401-8416 (2019).

Stay connected with all of the latest from Drug Discovery News.

Latest Issue
• Volume 20 • Issue 3 • May 2024
May 2024 Issue
More From Forbes
A clearer future for eye floaters.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Eye floaters
This story is part of a series on the current progression in Regenerative Medicine. This piece is part of a series dedicated to the eye and improvements in restoring vision.
In 1999, I defined regenerative medicine as the collection of interventions that restore tissues and organs damaged by disease, injured by trauma, or worn by time to normal function. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
Have you ever noticed specks or strings drifting across your vision?
If so, you may be one of the estimated 70% of people worldwide who experience eye floaters at some point. While this condition is not typically considered severe, it can still be frustrating and uncomfortable, affecting your vision and quality of life.
Usually, the brain ignores these floaters, and they go unnoticed. However, when they increase in number or become more concentrated in a particular area, they can cause annoyance or discomfort.
There are several treatments available to help ease the symptoms of eye floaters. This article will discuss the different options and advances in artificial intelligence that can educate patients and enhance the management of this common condition.
What are Floaters?
Eye floaters are specks or strands that can appear in the field of vision and move around when the eyes move. These floaters are caused by the shrinking of the vitreous, a gel-like substance that fills the eye. The vitreous becomes more liquid and less gel-like as we age, causing the collagen fibers to clump together and form specks or strands.
Diagram of floaters but Exeter Eye
Best High-Yield Savings Accounts Of 2024
Best 5% interest savings accounts of 2024.
While most floaters are harmless and do not require treatment, some may indicate a severe eye condition, such as retinal detachment or inflammation. Aside from that, eye floaters can be distracting and, at times, concerning significantly when their numbers increase. Some individuals may experience significant interference with their vision, compromising their quality of life and overall well-being.
Treating Eye Floaters
Fortunately, several current treatments address eye floaters, with various approaches depending on the individual's condition and overall severity of symptoms.
Laser Floater Treatment (LFT) is a non-surgical procedure performed in the office that is used as one of the current treatments for eye floaters. LFT uses laser light to dissolve eye floaters, reducing their visibility in the patient's field of vision. It has emerged as a viable alternative for people who are hesitant to undergo surgery, as it poses minimal risk of complications and is a less invasive option than surgical treatments.
Studies have shown that LFT is effective in treating eye floaters. One such investigation , which assessed the safety and effectiveness of YAG laser vitreolysis as a treatment for vitreous floaters, concluded that LFT is a suitable option for patients hesitant to undergo surgery due to its minimal risk of complications. The study also found that LFT shows promising results in improving subjective and objective outcomes for symptomatic floaters. However, given the limited available evidence, further research is needed to determine the exact role of YAG laser vitreolysis in treating vitreous floaters.
Another current treatment option for eye floaters is vitrectomy, a surgical procedure that involves removing the vitreous, the jelly-like substance inside the eye where the floaters are suspended. This approach is relatively uncommon and is typically reserved for extreme cases where the floaters interfere significantly with the individual's vision. Vitrectomy carries some risks, including infection and retinal detachment.
Eye floaters can also be treated through medical management and patient education, especially if an underlying medical condition causes them. For instance, if the floaters result from inflammation or bleeding due to diabetes, controlling or treating the underlying condition can help alleviate the floaters.
The Role of Patient Education in Treating Floaters
Educating patients regarding eye floaters and related disorders is paramount to successful treatment. Patients should understand the condition, including its causes and available treatment options. Additionally, they should be informed about the risk factors, such as age, eye trauma, and specific medical conditions that can lead to eye floaters. By being mindful of these risk factors, patients can take preventative measures to avoid the development of eye floaters.
The study published in Investigative Ophthalmology & Visual Science examined AI chatbots for patient education on retinal floaters. The study assessed multiple AI chatbots and their ability to help provide practical and actionable patient education. It also highlights AI systems' accuracy in answering questions related to floaters from a retinal specialist point of view.
The researchers found that both ChatGPT™ and Google Assistant™ had weak scores, indicating the bots were inadequate in providing in-depth specialist information. Additionally, while AI chatbots can be a helpful tool for patient education, they should not replace the need for a qualified healthcare professional. Patients must be encouraged to seek medical advice and not rely solely on AI chatbots for diagnosis and treatment.
To a Clearer Future
Eye floaters are a common condition that can be uncomfortable and negatively impact one's quality of life significantly as the number of floaters increases. Fortunately, several treatments are available for eye floaters, including Laser Floater Treatment (LFT). Studies show that LFT effectively treats vitreous floaters and has promising results in improving subjective and objective outcomes for symptomatic floaters.
As technology advances and shapes the healthcare industry, the future of eye floater treatment looks promising. Integrating artificial intelligence and human expertise can improve patient care by providing accurate and tailored information and guidance to patients and caregivers, helping them make informed decisions about their health. We can look forward to a future where AI and human expertise work together to provide the best possible patient care.
To learn more about the eye, read more stories at www.williamhaseltine.com
- Editorial Standards
- Reprints & Permissions
15 Oct New study proves effectiveness of a non-surgical, dietary solution for ‘Eye floaters’
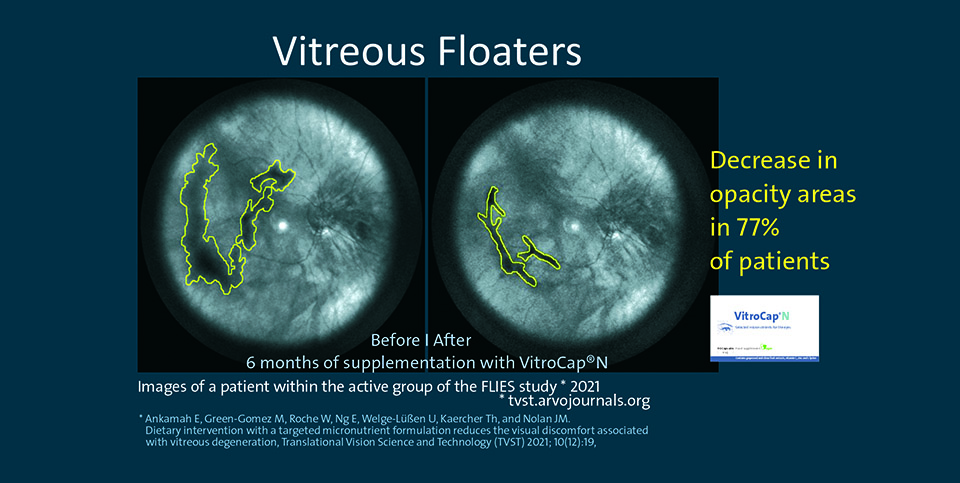
A new study published in the Translational Vision Science and Technology (TVST), an ARVO journal, has revealed that targeted nutrition can significantly reduce ‘eye floaters’ as well as their associated discomforts. This study reports the outcomes of the Floater Intervention Study (FLIES), which was led by the Nutrition Research Centre Ireland (NRCI, Waterford Institute of Technology), in collaboration with local optometrists and the Institute of Eye Surgery at UPMC Whitfield Hospital.
Floaters are spots in your vision like black or grey specks, strings, or cobwebs that drift about when you move your eyes. According to the National Eye Institute, “almost everyone develops floaters as they get older”, but floaters can also occur from a very young age and especially in short-sighted people. Most eye floaters are caused by age-related changes in the vitreous (the jelly part of the eye). Floaters are painless and mostly harmless, but they regularly cause significant visual discomfort and, at times, mental stress for the sufferers. In some cases, floaters may be associated with retinal tears, a potential sight-threatening complication that requires immediate medical attention.
The FLIES trial is the first double-blind, placebo-controlled clinical trial in patients with primary floaters that demonstrated reduction in floater suffering as well as improvements in visual function in the active group compared to placebo, following a 6-month dietary intervention with a formulation consisting of 125mg l-lysine, 40mg vitamin C, 26.3mg Vitis vinifera extract, 5mg zinc, and 100mg Citrus aurantium.
Dr. Emmanuel Ankamah, the main researcher on the FLIES trial, says “I am delighted to see the outcomes of this exciting trial published in TVST, a high impact journal in vision science. Indeed, this trial provides the evidence to support the use of targeted nutritional intervention as a management strategy for vitreous floaters. This gives us more confidence that using antioxidative and antiglycation micronutrients can improve vitreous health.”
According to Professor John Nolan, the Director of the NRCI and Principal Investigator of the FLIES trial, “This study is very interesting, as it is the first of its kind to examine the benefits of nutritional supplementation for patients suffering with vitreous floaters. Notably, a large percentage of patients (77%) on the active supplement demonstrated a reduction in vitreous floaters and associated improvements in vision-related quality of life was seen in 67% of patients. So, while not all participants on the active arm of the trial experienced improvements, this work provides clear evidence that this nutritional intervention is effective for certain patients. We look forward to continuing our studies on this important area of research. While we are hopeful that this research will inform eye-care, and offer an option to eye-care professionals and patients to enhance the health of the vitreous, we strongly advise that patients seek advice from a qualified eye-care professional.”
The FLIES trial was sponsored by Waterford Institute of Technology and ebiga-VISION GmbH through a WIT Co-Fund PhD scholarship (WD_2007_43). To read the newly published study, which is open access and freely available for download, see the manuscript link at Publication https://tvst.arvoj ournals.org/article.aspx?artic leid=2777982
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 26 April 2021
Acute symptomatic vitreous floaters assessed with ultra-wide field scanning laser ophthalmoscopy and spectral domain optical coherence tomography
- Gisung Son 1 , 2 ,
- Joonhong Sohn 1 &
- Mingui Kong 1 , 2
Scientific Reports volume 11 , Article number: 8930 ( 2021 ) Cite this article
3447 Accesses
8 Citations
1 Altmetric
Metrics details
- Diagnostic markers
- Medical research
To describe the eyes with vitreous floaters and to analyze the development of acute symptomatic posterior vitreous detachment (PVD). A retrospective review of medical records was performed on patients with the vitreous floater developed for the first time of their life. Peripapillary vitreous opacity (pVO) was searched in Ultra-wide field (UWF) scanning laser ophthalmoscopy and PVD stage was assessed through spectral-domain optical coherence tomography (SD-OCT). 196 patients (55 males and 141 females), who were 58.4 (± 9.1) years old, visited a retinal clinic 9.4 (± 9.1) days after they experienced vitreous floaters. In 196 eyes, pVO was noticed in 122 eyes (62.2%) at UWF. In 106 eyes where SD-OCT data were available, PVD was noticed in 100 eyes (94.3%). Symptomatic eyes showed more advanced stage of PVD (p < 0.001) than symptom free eyes. Eyes with floaters were more myopic (− 0.7 ± 2.2D vs − 0.5 ± 1.9D, p = 0.02), and had lower intraocular pressure (IOP) (14.7 ± 3.2 mmHg vs 15.2 ± 3.0 mmHg, p = 0.02) than the other symptom free eyes. In patients with first floater symptoms, PVD was in progress in most of the eyes not only the symptomatic eyes but also on the contralateral symptom free eyes. Eyes with vitreous floaters were more myopic and had lower IOP than the opposite symptom free eyes.
Similar content being viewed by others
Investigation of the myopic outcomes of the newer intraocular lens power calculation formulas in Korean patients with long eyes

OCTDL: Optical Coherence Tomography Dataset for Image-Based Deep Learning Methods

Long-term myopia control effect and safety in children wearing DIMS spectacle lenses for 6 years
Introduction.
Vitreous floaters are entoptic images of opacity in vitreous cavity 1 . Substantial portion of patients visit retina clinics complaining symptomatic degenerative floaters. Although floater symptoms often become asymptomatic within a few months from onset, they do cause visual discomfort such as blurred vision, glare and haze in daily living for months or years 2 . Moreover, degenerative vitreous floaters related with posterior vitreous detachment (PVD) could be more clinically significant because they can be followed by pathologic conditions such as vitreous hemorrhage, retinal tear or retinal detachment 3 . Therefore, characterizing the status of PVD could provide important information on eyes with acute vitreous floaters.
Recently, detailed evaluation of vitreoretinal interface has been possible since the introduction of spectral domain optical coherence tomography (SD-OCT) 4 , 5 , 6 , 7 , 8 . And ultra-wide field retinal imaging (UWF) devices allow us to evaluate posterior pole and wide range of the peripheral retina simultaneously 9 . We hypothesized that the SD-OCT and UWF examination will allow us to identify and record PVD status more accurately. Thus, we investigated patients with acute symptomatic vitreous floaters using these two modalities to determine the relationship between floaters and PVD. By comparing eyes with and without floater symptoms, we also intended to find out when floater symptoms occur on the process of PVD.
The mean age was 58.38 (± 9.14) years old in average, consisting of 141 women and 55 men (Table 1 ). The BCVA of 196 eyes was 0.06 (± 0.10) in average, SE was − 0.70 (± 2.09) diopter, and intraocular pressure (IOP) was 15.05 (± 6.20) mmHg. There was no difference between men and women in BCVA (p = 0.64), SE (p = 0.45) and IOP (p = 0.11). In 33 patients (17.3%), vitreous floaters were found in both eyes. Patients visited our retina clinic after an average of 9.41 (± 9.05) days after symptom onset, and 23 patients (11.74%) had ‘flashing light’ symptom before the floater. 24 patients (12.24%) needed laser treatment on peripheral retinal break which was observed in their clinical visit. In 3 eyes (1.53%), glaucoma was diagnosed incidentally and those 3 eyes were excluded from the pRNFL analysis.
Of the 196 eyes with floater, 97 eyes (49.5%) were emmetropic (− 1D < SE < + 1D), 61 eyes (31.1%) were myopic (SE ≤ − 1D) and 38 eyes (19.4%) were hyperopic (SE ≥ + 1D). Myopic eyes tend to present vitreous floater symptoms earlier (r = 0.406, p < 0.001, Fig. 1 ). This was the same for both the male group (r = 0.352, p = 0.008) and the female group (r = 0.463, p < 0.001). In addition, thinner pRNFL was observed in Myopic patients (r = 0.299, p = 0.011), and SE was not significantly related to central macular thickness (CMT) (r = 0.072, p = 0.471).
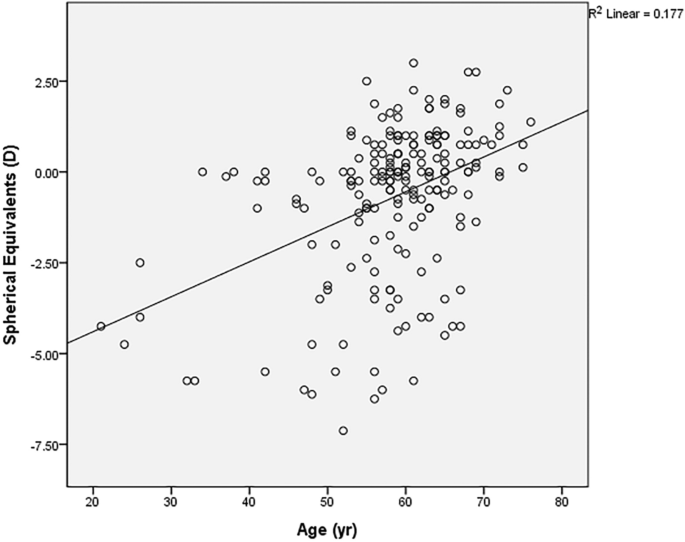
X-axis presents the age when the first vitreous floater symptom occurred, while Y-axis presents the spherical equivalent value in diopters (D). The oblique line of best fit is showing a positive correlation between the spherical equivalent value and age. (r = 0.421, p < 0.001 in the Pearson’s correlation analysis).
Peripapillary vitreous opacity (pVO) was observed in 62.2% (122 out of 196 eyes) in the UWF image. Among 106 symptomatic eyes where SD-OCT data were available, PVD was identified in 94.3% on SD-OCT. PVD was staged based on the morphology of the vitreomacular interphase assessed with SD-OCT, from stage 0 to 4. In 106 symptomatic eyes, 6 eyes were categorized as stage 0, while 8 eyes as stage 1, 6 eyes as stage 2, 5 eyes as stage 3 and 81 eyes as stage 4. Interestingly, almost every eye with the pVO had the evidence of PVD on SD-OCT (98.7%, 75 out of 76 eyes). While, 75.0% (75 eyes out of 100 eyes) of eyes with SD-OCT proven PVD had pVO on UWF images.
We compared the ophthalmologic examination results of the symptomatic study eyes with floaters and the symptom free contralateral eyes without floaters in 163 patients who had symptoms only in the unilateral eye (Table 2 ). The eyes with floaters were more myopic than those without floaters (− 0.7 ± 2.2D vs − 0.5 ± 1.9D, p = 0.02), and had lower intraocular pressure (14.7 ± 3.2 mmHg vs 15.2 ± 3.0 mmHg, p = 0.02). Visual acuity (0.06 ± 0.11 vs 0.04 ± 0.08, p = 0.09), CMT (259.4 ± 20.2 vs 260.0 ± 19.5, p = 0.56) or pRNFL (100.7 ± 11.6 μm vs 100.5 ± 11.4 μm, p = 0.08) did not differ between the two groups. More pVO on UWF (63.2% vs 18.4%, p = 0.04) and more advantaged PVD stage on SD-OCT (p < 0.001) was observed in the eyes with floater symptoms than the symptom free collateral eyes.
We could verify a high degree of agreement on the interpretation of UWF and SD-OCT images between two investigators (GSS, MGK) In UWF image analyses, the judgments were in agreement in 190 eyes (96.9%). Regarding SD-OCT image analyses, the ICC value between the two investigators was 0.977. There were six discordant interpretations on UWF images of myopic eyes with tessellated fundus. And there were three disagreements on SD-OCT images where background reflectivity of vitreous cavity was difficult to be determined as vitreous body or not.
Additional ophthalmological analyses were performed on 33 patients with floater symptoms on both eyes (Supplementary Table 1 ). The comparison was conducted between eyes with earlier floater symptoms versus eyes with more recently occurred floater symptoms. BCVA, SE, IOP, CMT and pRNFL thickness were not different each other (p = 0.48, 0.39, 0.24, 0.65, 0.71 respectively). The prevalence of the pVO on the UWF were not different between 2 groups, (57.6% vs 36.4, p = 0.505) neither so PVD stage (p = 0.90).
This study provides novel information regarding the vitreoretinal interface of patients experiencing their lifetime’s first floater symptom. Meanwhile, through this study, we were able to confirm several facts that have been reported about PVD in previous studies. First, the first vitreous floater in life showed at an average age of 58.4 years, similar to the previous studies 10 , 11 , 12 , 13 . The female predominance of PVD in this study (72% in female) has been also reported several times in previous studies 10 , 13 . In addition, the earlier onset of PVD in the myopic eye in this study has also been reported in several other previous studies 10 , 14 , 15 .
The usefulness of SD-OCT in the diagnosis of PVD was recently presented in a previous prospective study. Moon et al. 16 analyzed 124 eyes with PVD examined using ultrasonography and SD-OCT and showed the usefulness of adding peripapillary OCT scans in the diagnosis of PVD considering lower inter-examiner agreement of ocular ultrasound scanning. Our data could be convincing evidences supporting their hypothesis. Instead of ultrasonography, however, we described the inter-correlation of UWF and SD-OCT assessing eyes with vitreous floaters. We believe that our study could describe more ‘real world’ clinical situation than their data analyzed from prospectively enrolled patients.
Most of the eyes with floaters had PVD in progress, and the proportion was 94.3% as determined by the SD-OCT. Interestingly, PVD was also progressing in most of the asymptomatic eyes. We confirmed the evidence of PVD assessed with SD-OCT in 89.5% of the symptom free contralateral eyes. This inconsistency between presence of PVD on SD-OCT and absence of subjective symptoms could be explained by the PVD stage of the opposite symptom free eye which was earlier than the other symptomatic eye. In other words, the degree of detached membrane might be relatively small to be noticed in earlier PVD stage. Since this study is cross sectional, it was difficult to accurately determine at which point the floater occurred during the PVD process. However, we could confirm that the eyes with floater present more advanced PVD stage on SD-OCT and more eyes with pVO on UWF than the symptom free contralateral eyes.
The fact that the eyes with floaters were more myopic and had lower IOP can be explained in relation to changes in the eyeball as PVD progresses. Myopic eyes have longer axial length, so maybe easily affected by the shrinkage of the vitreous body. We can also infer that a more myopic eye in a single person might expect earlier vitreous floaters than the other eye. Meanwhile, the measurement of low intraocular pressure in PVD eyes can be explained by the fact that stiffer vitreous in eyes without PVD may present a stronger rebound than liquefied vitreous in eyes with PVD during the measurement of IOP.
Peripapillary vitreous opacity presented on UWF could be thought as a convincing evidence of PVD. This can be intuitively understood, because the pVO is likely to be found in UWF after PVD initiation. Weiss ring, which is the representative form of pVO in the advanced stage PVD, is noticed when complete PVD occurs after the detachment of the vitreopapillary adhesion. Also in this study, almost every eyes with visible pVO were proven to have PVD through SD-OCT examination. For a few exceptional cases (2 eyes, 2.67%), pVO could be positioned perpendicular to the front, difficult to be photographed. Considering this, if Weiss ring is observed in UWF, ophthalmologists who are practicing in the environment without SD-OCT equipment could be more confident in the presence of the PVD.
Based on this study results, retinal examinations of both eyes are recommendable on the patients complaining of floaters. This is because described above, PVD was occurring in 89.5% of the contralateral eyes even without subjective floater symptoms. If early-staged PVD findings on SD-OCT are observed in the opposite eye, the patient can be explained in advance that floater symptoms may also occur in the symptom free eyes. In addition, in 6 eyes (1.95%) of the study cohort, a peripheral retinal break requiring laser photocoagulation treatment was found in the opposite eye rather than in the symptomatic eye.
Despite high degree of agreement, discrepancy in the interpretation of UWF and SD-OCT tests between the two investigators should not be ignored. In 6 UWF images, there was a disagreement whether the spots on the photos to be judged by vitreous opacity or peripapillary pigments. The ambiguity got bigger in myopic eyes with tessellated fundus. In 3 SD-OCT images, it was difficult to determine whether PVD stage be categorized into stage 1 or stage 2. Serial checks-up of the test, correlations with the stereoscopic fundus examination findings or performing swept-source OCT covering more extensive retina could be helpful approaches for solving the discrepancy.
Although it is useful to examine UWF and SD-OCT together in patients with vitreous floaters, yet detailed medical history and meticulous retinal observation through a microscope should not be overlooked. This is because floater symptoms are not necessarily caused by PVD. If we listen to the patients carefully through detailed medical history, we can better understand the patients-reporting ‘floaters’ symptoms. Thorough retinal examination should be performed to conclude whether vitreous opacities are related with PVD or not.
We are mindful of the limitations of this study, such as its retrospective and cross-sectional nature performed on single-ethnic population background. In addition, section bias should be mentioned as we analyzed only the patients who visited clinic. In addition, SD-OCT was performed on 106 patients (53%) who were willing to pay for the examination. However, as we know of, this is the first attempt to analyze lifetime’s first vitreous floaters using both of the UWF scanning laser ophthalmoscopy and the SD-OCT images. We believe our study might provide useful information to ophthalmologists regarding vitreous floaters and PVD in real clinical world. Further prospective studies might warrant for more useful information of when and in what percent the vitreous floater symptoms fades away.
We retrospectively analyzed the medical records of patients who visited our retina clinic due to newly developed vitreous floaters within a month from July 2017 to May 2020. All patients received thorough ophthalmological examination including BCVA, manifest refraction, IOP (NT-530P, Nidek, Aichi, Japan), retinal examination after mydriasis, SD-OCT (Version 5.3.2.0; Heidelberg Engineering, Heidelberg, Germany) and UWF (Optomap, Optos PLC, Dunfermline, Fife, Scotland, UK) were performed. We conducted SD-OCT line and raster scan in all eyes centered at the fovea. Automatic real-time (ART) mode was activated when horizontal and vertical line scans were conducted with 25 frames averaged. In the raster scan image, a 30 × 25 degree 2 area was covered with 31 b-scans (consisting of 768 A-scans), which are 9.0 mm in length, and spaced at 240 μm apart. The peripapillary region was scanned using a circular scan 12° in diameter, centered on the optic disc (Fig. 2 ). Every retinal examination was performed on both eyes. All the images information was assessed by saved data on digital files before in-depth analyses.
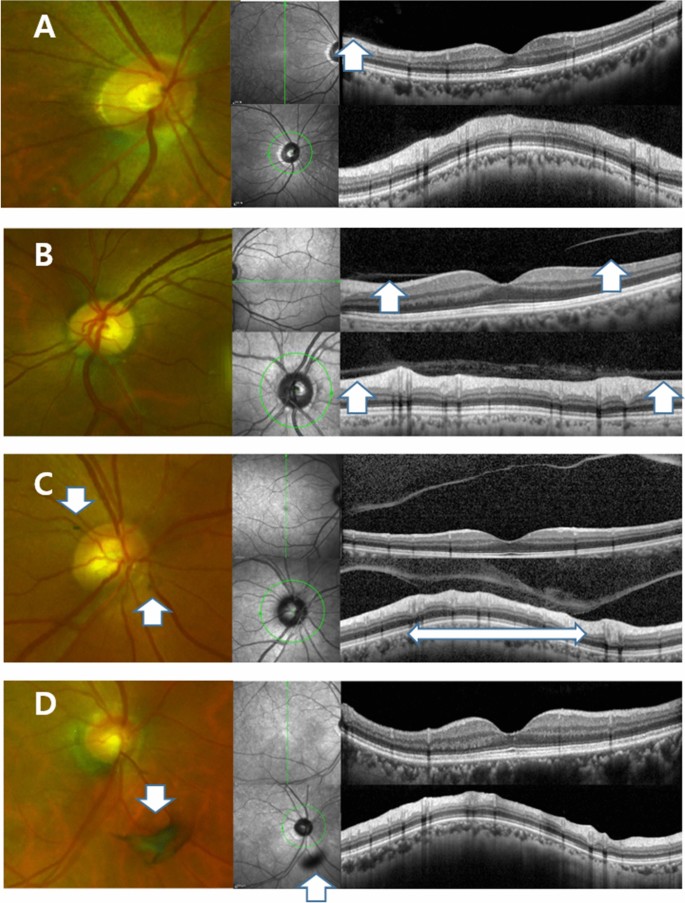
Ultra-wide field scanning laser ophthalmoscopy (UWF) and Spectral Domain Optical Coherence Tomography (SD-OCT) images of patients who experienced floater for the first time in their life. ( A ) PVD stage 1. 59 year-old male. No definite change was noticed around optic disc in UWF. Note subtle change which is presenting the initiation of PVD (Posterior Vitreous Detachment, white arrow). ( B ) PVD stage 2. 60 year-old female. No definite change was noticed around optic disc in UWF. In the macular SD-OCT image, perifoveal posterior vitreous detachment (PVD) is in progress (white arrows) remaining posterior vitreous attached to fovea. In glaucomatous SD-OCT, PVD is in progress in some part of the optic disc margin (arrow), while most of the optic disc remains attached to the vitreous body. ( C ) PVD stage 3. 61 year-old male. Note two pVOs (peripapillary vitreous opacity, white arrows) noticed around the optic disc. In the macular SD-OCT image, PVD occurred throughout the entire macula. In the glaucomatous SD-OCT image, PVD is in progress while about half of the optic disc margin is detached to the vitreous body (a wide bidirectional arrow). ( D ) PVD stage 4. 66 year-old female. Note a dense pVO (white arrow) resembling a Weiss ring. In the macular SD-OCT image, reflectivity of vitreous body is not observed in hollow vitreous cavity. In glaucomatous SD-OCT image, reflectivity of vitreous body is not observed either. A shadow of pVO (arrow) is identified.
Study subjects and vitreous floaters
Eligible subjects were adults older than 20 years old who experienced acute symptom (onset ≤ 1 month) of vitreous floaters for the first time of their life. In patients with floater symptoms in both eyes, eyes with more recently developed floater symptom were selected for the analysis. Exclusion criteria includes history of ocular surgery including cataract operation, history of ocular injections, any retinopathy including diabetic retinopathy or retinal vein occlusion, medial opacity including severe cataract or corneal opacity or eyes with obscure image which were not suitable for proper analyses. Eyes received refractive surgeries were excluded from the refraction analyses.
In this study, vitreous floaters were defined as symptoms of unprecedented amorphous ‘floating’ material. Other confusing symptoms such as fixed spots interrupts visual axis, transient wavy visual disturbance or metamorphopsia were excluded with through history taking. Concurrent subjective symptoms such as headaches, flashes, or ocular pain were asked also.
Analyses of ophthalmologic outcomes
Best-corrected visual acuity was measured with the manifest refraction test and was recorded in logMAR (logarithm of minimal angle of resolution). The spherical equivalent and cylindrical value were expressed in diopter. CMT at the 1-mm center of the fovea was measured using a built-in software (Heidelberg Eye Explorer, version 1.10.2.0, Heidelberg Engineering, Heidelberg, Germany), which recorded the distance between the vitreoretinal surface and the border between the retinal pigment epithelium and the Bruch’s membrane. Peripapillary RNFL (pRNFL) thickness was measured using the identical software.
Analysis of peripapillary vitreous opacity in UWF imaging
The presence of pVO was observed in UWF images taken on the eyes, after pupil dilation. The vitreous opacity found within 3 disc diameters from the center of the disc was included (Fig. 2 ). In cases where it was difficult to judge by pictures alone, the precise fundus examination with indirect ophthalmoscopy was considered together for the determination. The two investigators (GSS, MK) each independently analyzed the image, and for the inconsistencies, the senior investigator (JHS) made a final decision.
Anaylsis of PVD stage in SD-OCT imaging
The staging of PVD was performed base on the previously published paper 17 . In brief, stage 0 = no PVD; stage 1 = PVD at mid-periphery and possible subtle PVD in the posterior retina; stage 2 = PVD, except for persistent adhesion to the papilla and fovea; stage 3 = PVD, except for persistent adhesion to the papilla; and Stage 4 = complete PVD (Fig. 2 ). The two investigators (GSS, MK) analyzed PVD respectively, and the opinions of senior investigator (JHS) were sought for discordant findings.
Statistical analyses
Continuous values were expressed as “average ± standard deviation,” and categorical variables were described as proportions; differences between groups were determined using the Chi-squared test or Fisher’s exact test. Comparison of ophthalmological values between eyes with/without vitreous floaters was performed using the paired t test. Pearson’s correlation analyses were performed among various continuous values. Inter-class correlation (ICC) value was calculated to determine how consistent the two investigators’ interpretations on PVD at SD-OCT images were. All data were inserted into an Excel spreadsheet (Microsoft Corp.) and analyzed using SPSS software (version 23; IBM Corp, New York, NY). A P-value less than 0.05 was considered statistically significant.
Ethics approval and patient consent
This study was approved by the Institutional Review Board (IRB) of Hangil Eye Hospital (IRB number: IRB-20006) and complied with the Declaration of Helsinki in conducting the study. Given the retrospective design of this study and the use of anonymized data, requirements for informed consent were waived by the IRB.
Mossa, F., Delaney, Y. M., Rosen, P. H. & Rahman, R. Floaterectomy: Combined phacoemulsification and deep anterior vitrectomy. J. Cataract Refract. Surg. 28 , 589–592 (2002).
Article Google Scholar
Wagle, A. M., Lim, W.-Y., Yap, T.-P., Neelam, K. & Eong, K.-G.A. Utility values associated with vitreous floaters. Am. J. Ophthalmol. 152 , 60-65.e61 (2011).
Byer, N. E. Natural history of posterior vitreous detachment with early management as the premier line of defense against retinal detachment. Ophthalmology 101 , 1503–1514 (1994).
Article CAS Google Scholar
Sebag, J. Imaging vitreous. Eye 16 , 429–439 (2002).
Hee, M. R. et al. Optical coherence tomography of macular holes. Ophthalmology 102 , 748–756 (1995).
Gallemore, R. P., Jumper, J. M., Jaffe, G., Postel, E. & Toth, C. Diagnosis of vitreoretinal adhesions in macular disease with optical coherence tomography. Retina (Philadelphia, Pa.) 20 , 115–120 (2000).
Mirza, R. G., Johnson, M. W. & Jampol, L. M. Optical coherence tomography use in evaluation of the vitreoretinal interface: A review. Surv. Ophthalmol. 52 , 397–421 (2007).
Koizumi, H. et al. Three-dimensional evaluation of vitreomacular traction and epiretinal membrane using spectral-domain optical coherence tomography. Am. J. Ophthalmol. 145 , 509-517.e501 (2008).
Anderson, L., Friberg, T. & Singh, J. Seminars in ophthalmology 43–47 (Taylor & Francis, 2007).
Google Scholar
Sebag, J. The Vitreous 73–95 (Springer, 1989).
Book Google Scholar
Foos, R. Y. & Wheeler, N. C. Vitreoretinal juncture: Synchysis senilis and posterior vitreous detachment. Ophthalmology 89 , 1502–1512 (1982).
Sebag, J. Ageing of the vitreous. Eye 1 , 254–262 (1987).
Larsson, L. & Österlin, S. Posterior vitreous detachment. Graefes Arch. Clin. Exp. Ophthalmol. 223 , 92–95 (1985).
Linder, B. Acute posterior vitreous detachment and its retinal complications: A clinical biomicroscopic study. Acta Ophthalmol. 87 , S1–S108 (1966).
Yonemoto, J. et al. The age of oneset of posterior vitreous detachment. Graefes Arch. Clin. Exp. Ophthalmol. 232 , 67–70 (1994).
Moon, S. Y., Park, S. P. & Kim, Y.-K. Evaluation of posterior vitreous detachment using ultrasonography and optical coherence tomography. Acta Ophthalmol. https://doi.org/10.1111/aos.14189 (2019).
Article PubMed Google Scholar
Johnson, M. W. Perifoveal vitreous detachment and its macular complications. Trans. Am. Ophthalmol. Soc. 103 , 537 (2005).
PubMed PubMed Central Google Scholar
Download references
Author information
Authors and affiliations.
Department of Retinal Service, Hangil Eye Hospital, Incheon, South Korea
Gisung Son, Joonhong Sohn & Mingui Kong
Department of Ophthalmology, Catholic Kwandong University College of Medicine, Incheon, 22711, South Korea
Gisung Son & Mingui Kong
You can also search for this author in PubMed Google Scholar
Contributions
G.S.: design of the work, the acquisition, analysis, and interpretation of data, drafting the important intellectual content, final approval of the version to be published. J.H.S.: design of the work, final approval of the version to be published. M.K.: design of the work, the acquisition, analysis, and interpretation of data, drafting the important intellectual content, final approval of the version to be published.
Corresponding author
Correspondence to Mingui Kong .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary table 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Son, G., Sohn, J. & Kong, M. Acute symptomatic vitreous floaters assessed with ultra-wide field scanning laser ophthalmoscopy and spectral domain optical coherence tomography. Sci Rep 11 , 8930 (2021). https://doi.org/10.1038/s41598-021-88371-9
Download citation
Received : 30 December 2020
Accepted : 08 April 2021
Published : 26 April 2021
DOI : https://doi.org/10.1038/s41598-021-88371-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Vision degrading myodesopsia assessed with optos ultra-widefield scanning laser ophthalmoscope.
BMC Ophthalmology (2023)
The Efficacy and Safety of YAG Laser Vitreolysis for Symptomatic Vitreous Floaters of Complete PVD or Non-PVD
- Tongtong Li
Ophthalmology and Therapy (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.

- Science and vision
Study proves effectiveness of non-surgical, dietary treatment for vitreous opacities
Advertorial
In a new publication, an international team of researchers confirmed the impact of targeted nutritional intervention via supplementation for patients suffering from vitreous floaters

Advertorial content is paid for and produced by a sponsor, and is reviewed and edited by the OT team before publication.
13 December 2022
The double-blind, placebo-controlled, monocentric Floater Invention Study (FLIES) examined subjects of all ages over a period of six months and was able to demonstrate significant improvements in subjective visual disturbances as well as in the objective parameters ‘vitreous opacity density’ and ‘contrast sensitivity.’ The success rate among the subjects was 77% for the objective improvements (reduction of floater opacity areas) and 67% for the subjective ones (complaint score). The product used in the study in the verum group was VitroCap®N.
Vitreous opacity and the need of the vitreous body for micronutrients
Vitreous opacities, caused by the aggregation of collagen fibres in the vitreous, appear frequently. They are perceived as spots, specks or thread-like structures and arise from shadows, cast on the retina by the clumped collagen fibres interfering with the incident light. They also cause a reduction of visual functions, detectable in the reduced contrast sensitivity. Vitreous opacities are painless and usually harmless but often lead to serious problems in the form of visual disorders and psychological burdens for those affected. After analysing the existing literature on the metabolism and micronutrient supply of the vitreous body, the FLIES researchers at the Nutrition Research Centre Ireland (NRCI), which is renowned for its research on the correlation between nutrition and eye diseases, came to the conclusion that oxidative stress is associated with an undersupply of antioxidants from food (similar to other chronic eye diseases such as AMD and cataracts) and subsequent glycation of collagen fibres (crosslinking via sugar molecules). These two processes may be key mechanisms of vitreous degeneration. Conversely, if the supply of micronutrients found in the vitreous body is optimised, an improvement should potentially be detectable. To test their hypothesis, they chose the scientific gold standard – a prospective, double-blind, randomised supplementation study – and the VitroCap®N capsule as the micronutrient complex to be tested. The study was published online in October 2021 after a peer review in the ARVO journal TVST (Translational Vision Science and Technology) .
Gold standard FLIES study proves subjective and – for the first time – also objective effectiveness of a dietary intervention in vitreous opacity
The FLIES study shows a significant decrease after six months of dietary supplementation with a formulation consisting of 125 mg L-lysine, 40 mg vitamin C, 26.3 mg grape seed extract, 5 mg zinc and 60 mg citrus flavonoids (available as VitroCap®N) in subjective visual symptoms (67%), a significant decrease in vitreous opacity (success rate 76.9%) and a significant improvement in contrast sensitivity compared to placebo. The study included 61 patients with symptomatic, long-standing vitreous opacities. Randomised and blinded, the subjects took one capsule of the micronutrient supplement (verum) or placebo daily for six months. Before and after the supplementation, various visual function tests (visual acuity, contrast vision) as well as imaging and video examinations of the vitreous to quantify the opacities (optical coherence tomography - OCT, Spectralis®, Heidelberg Engineering GmbH) were carried out. These objective and subjective clinical findings confirm the original hypothesis that the optimisation of vitreous supply by supplementation with relevant micronutrients with antioxidant and antiglycating properties are suitable to regulate the mechanisms of vitreous degeneration and thereby reduce the visual complaints associated with vitreous floaters.
More information
- Find out more about Professor John Nolan
- Find out more about Nutrition Research Centre Ireland (NRCI)
- Find out more about the product, or order free sample packs and information material.
VivaQuity Ltd Tel. +353 87 60 90 557 [email protected]
- Ankamah E, Green-Gomez M, Roche W, Ng E, Welge-Lüßen U, Kaercher Th, Barbur J, Nolan JM. Impact of symptomatic vitreous degeneration on photopic and mesopic contrast thresholds, Clinical and Experimental Optometry. 2021, DOI: 10.1080/08164622.2021.1981116
- Mamou J, Wa CA, Yee KMP, et al . Ultrasound-based quantification of vitreous floaters correlates with contrast sensitivity and quality of life. Invest Ophthalmol Vis Sci . 2015;56:1611–1617
- Sebag J, Yee KMP, Wa CA, et al . Vitrectomy for floaters: prospective efficacy analyses and retrospective safety profile. Retina . 2014;34:1062–1068
- Garcia GA, Khoshnevis M, Yee KMP, et al . Degradation of contrast sensitivity function following posterior vitreous detachment. Am J Ophthalmol . 2016;172:7–12
- Garcia GA, Khoshnevis M, Yee KMP, et al . The effects of aging vitreous on contrast sensitivity function. Graefes Arch Clin Exp Ophthalmol . 2018;256:919–925
- Sebag J, Yee KMP, Nguyen JH, et al . Long-term safety and efficacy of limited vitrectomy for vision degrading vitreopathy resulting from vitreous floaters. Ophthalmol Retina . 2018;2:881–887
Do you know someone who might enjoy this article?
Share it here:
Most popular across OT
Eid al-fitr 2024: “a time of sharing and being grateful”, optometry education in scotland and independent prescribing, supporting ip in optometry, “the smiles on their faces have been the motivation” .
Scientists Are Working on a Way to Treat Eye Floaters With Lasers
By michele debczak | jul 24, 2017.

Even people with 20/20 eyesight should be familiar with this scenario: You're enjoying a clear view when a faint doodle shape drifts into your peripheral vision like an organism under a microscope. Floaters affect almost everyone, but there's currently no medically accepted, non-invasive way to treat them. Two doctors with Ophthalmic Consultants of Boston are working to change that. As IFLScience reports, the team believes that lasers may be the solution to bothersome eye squiggles.
As Chirag Shah and Jeffrey Heier write in their study in the journal JAMA Ophthalmology, lasers can be used to safely combat the underlying causes of floaters. Also known as muscae volitantes , Latin for “hovering flies,” the condition comes from physical debris leaking into your eyeball. The front of your eyes is filled with a liquid called vitreous humor, and when drops of that gelatinous substance break off from the whole, the bits cast shadows on your retinas that look like gray blobs. Because floaters literally float inside your eyes, trying to focus on one is almost impossible.
These spots aren't typically a problem for young people, but as you get older your vitreous humor becomes more watery, which increases the chance of it slipping out and clouding your vision. Retinal detachment and retinal tears are also rare but serious causes of symptomatic floaters.
Shah and Heier tested a new method of pinpointing and eliminating floaters with a YAG laser (a type of laser often used in cataract surgery) on 36 patients. An additional 16 test subjects were treated with a sham laser as a placebo. They found that 54 percent of the treated participants saw their floaters decrease over six months, compared to just 9 percent of the control group. So far, the procedure appears be safe and free of side effects, but researchers noted that more follow-up time is needed to determine if those results are long-term.
At the moment, people with symptomatic floaters can choose between surgery or living with the ailment for the rest of their lives. YAG laser treatment may one day offer a safe and easy alternative, but the researchers say they will need to expand the size of future studies before the treatment is ready to go public.
[h/t IFLScience ]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Design of a Functional Eye Dressing for Treatment of the Vitreous Floater
Wen-shuang fan.
1 Department of Ophthalmology, Dalin Tzu Chi General Hospital, 2, Min-Sheng Rd., Dalin Town, Chia-Yi 62247, Taiwan
Shuan-Yu Huang
2 Department of Optometry, Central Taiwan University of Science and Technology, No.666, Buzih Road, Beitun District, Taichung City 406053, Taiwan
Hong-Thai Nguyen
3 Department of Mechanical Engineering, Advanced Institute of Manufacturing with High Tech Innovations (AIM-HI) and Center for Innovative Research on Aging Society (CIRAS), National Chung Cheng University, 168, University Rd., Min Hsiung, Chia Yi 62102, Taiwan
Wen-Tsung Ho
4 Master’s Program in Wellbeing Technology and Biomedical Engineering, Yuanpei University of Medical Technology, No.306, Yuanpei Street, Hsinchu 30015, Taiwan
5 TO2M Corporation, 5F., No. 2, Kedong 3rd Rd., Zhunan Township, Miaoli County 35053, Taiwan
Wen-Hung Chao
Fen-chi lin.
6 Department of Ophthalmology, Kaohsiung Armed Forces General Hospital, 2, Zhongzheng 1st.Rd., Lingya District, Kaohsiung City 80284, Taiwan
Hsiang-Chen Wang
Associated data.
The data presented in this study are available in this article.
With the rapid development of display technology, related diseases of the human eye are also increasing day by day. Eye floaters are one of the diseases that affect humans. Herein, we present a functional ophthalmic dressing that can permeate the skin tissues of the eyes through oxygen and hydrogen to improve the symptoms of floaters. In clinical tests, the symptoms of sensory floaters improved in 28 patients, and the recovery rates of mild, moderate, and severe floaters were about 70%, 66.7%, and 83.3%, respectively.
1. Introduction
In the past, 90% of vitreous floaters were caused by aging [ 1 ]. With the development of 3C (computer, consumer electronics, and communication) products and the increase in myopia, 15% of people aged 20–29 years will develop lymphadenopathy, indicating the gradual acceleration of the eye-aging rate. Lymphadenopathy refers to the presence of floating objects in the eye caused by thickened clumps of vitreous jelly [ 2 , 3 , 4 , 5 , 6 , 7 ]. After the age of 40, the vitreous will become dense and gel-like, in which some denser bundles of collagen fibers form. For people with high myopia, the anterior–posterior diameter of the eye axis is stretched, destroying the dense structure of the vitreous and leading to vitreous degeneration and turbidity. When light is projected to the eyeball, it passes through the interface of the thicker fiber bundle. The vitreous jelly blocks light coming from the front of the eye and casts shadows on the retina. This phenomenon is called degenerative floaters [ 8 , 9 , 10 , 11 , 12 , 13 , 14 ].
Pathological floaters are another type of vitreous floater. Pathological floaters occur when there is a sudden increase in floaters or when the light and shadow of lightning can be observed. Although pathological floaters only account for 5% of floaters, they may seriously harm eyesight. The causes include retinal tears, accompanying retinal detachment, bleeding caused by retinal vein vascular occlusion, diabetic retinopathy, and macular degeneration, which causes blood to flow into the vitreous. At present, the diagnosis of pathological floaters depends on the experience of ophthalmologists. Primary vitreous floaters are mainly produced by the intrinsic structure of the vitreous, and the stacked collagen fiber bundles form visible fibers, which first appear in the central vitreous, where they have a linear structure. With age, they become more and more thick and irregular and are common in young axial myopia. In old age, the glass body liquefies and forms a cavity, and light scattering from the glass cavity wall may cause a floating phenomenon [ 15 , 16 , 17 , 18 , 19 ]. Secondary floaters are exogenous turbidity in the vitreous that is usually composed of protein, amyloids, or cells. However, the most common cause of secondary vitreous floaters is anterior or vitreous hemorrhage, which can cause a sudden onset of floaters and blurred vision [ 20 , 21 ]. Inflammatory diseases (infectious or non-infectious) or malignant tumors (such as lymphoma) can cause an increase in vitreous cells. If the number is large, it may also cause symptomatic vitreous floaters.
The currently available treatments for floaters include vitrectomy and Nd: YAG laser vitrectomy. Many studies have evaluated the success and potential risks of vitrectomy for vitreous floaters [ 22 , 23 , 24 , 25 , 26 , 27 , 28 ]. Although vitrectomy is an effective treatment method, it may affect the lens and accelerate the occurrence or deterioration of postoperative cataracts. On the other hand, Nd: YAG laser vitreous dissolution is used to destroy the vitreous collagen fiber bundles. It only treats the fiber bundles that are relatively far from the retina. However, it only destroys the aggregation and cannot remove the aging cells from the body. It is better for larger aggregations. Nd: YAG laser vitreous dissolution using newer technology has been proven to be safe and effective in treating symptomatic Weiss ring vitreous floaters. The primary outcome measures were the percentage of symptom improvement after treatment and the rate of postoperative complications. In the study, Delaney et al. [ 23 ] reported that the Nd: YAG vitreous improved symptoms in only one-third of patients. Furthermore, clinical improvement was only moderate, subjectively graded to no greater than 50% among 93.3% of patients. Only 38% of the 39 eyes with vitreous floaters showed symptomatic improvement moderately after Nd: YAG laser treatment; not only that, the symptoms could not be improved in terms of complete vision resolution. Moreover, this method of laser therapy also causes complications that are not completely reported. Specifically, complications after surgery can be mentioned as complications of retinal detachment, focal lens opacities, and minor retinal hemorrhages. The exact pathogenesis of this complication is unknown but may involve shock wave generation, vitreous disturbances, or the formation of cellular debris or inclusions. A study by Nguyen et al. [ 25 ] proposed a method to evaluate the recovery of patients with vitreous floaters after treatment with Nd: YAG. Evaluation methods are based on visual function questionnaires, comparative statistical methods are based on quantitative ultrasonography index and contrast sensitivity. There were 38 eyes with vitreous floaters status examined after performing Nd: YAG treatment. Of these, 13 cases showed improvement in symptoms after surgery. However, there were still 25 cases who feel unsatisfied with the results of vision therapy. Another study by Souza et al. [ 26 ] reported no side effects or a recurrence of vitreous floaters. The study used color photo imaging to evaluate YAG laser vitreolysis for symptomatic vitreous floaters. A total of 32 patients were participating in the survey based on the visual function questionnaire. After 6 months of follow-ups, color imaging showed improvement in vitreous opacity over time in 93.7% of study eyes. In trials, symptomatic amorphous posterior clinical vitreous floaters were detected by a novel optical coherence tomography (OCT) [ 27 ] and successfully treated with a YAG laser optimized for vitreous dissolution. A study by Landa et al. [ 27 ] has shown that the spectral domain OCT can assist in the diagnosis of retinal detachment that cannot be excluded only on clinical examination. In general, laser therapy, particularly Nd: YAG, was found to be more effective and safer in the treatment of vitreous floaters. OCT is one method to evaluate the results after treatment is relatively effective. However, the limitation of laser therapy is that it brings many complications and the success rate of vision recovery is not high. The reason may be that this is an invasive method to the vitreous in the retina, causing disturbances in the retinal environment after treatment, and leading to complications. This means that laser treatment is considered when used as a method of vitrectomy.
In this study, we propose a functional dressing for eye floaters as a non-surgical, semi-invasive treatment with no direct impact on vitreous humor. We demonstrate a functional dressing, which has a structure that effectively allows oxygen and hydrogen to penetrate the skin. After the dressing is attached to the skin, it can generate hydrogen and oxygen through moisture. The function of oxygen is to increase blood oxygen, and the function of hydrogen is to fight inflammation and cell apoptosis in the eye and inhibit the production of excessive active oxygen. The dressing uses hydrogen and oxygen to penetrate tissues, and protect wounds from infections, creating a favorable environment for the recovery of lesions around the eye area. We propose a technique to evaluate post-treatment outcomes by analyzing OCT images, providing a more advanced visual assessment than traditional assessment methods through the visual functioning questionnaire system or other measures such as quantitative ultrasonography or contrast sensitivity.
2. Materials and Methods
2.1. oxygen therapy.
The purpose of oxygen therapy is to treat hypoxia and reduce the clinical symptoms caused by hypoxia. Reactive oxygen species (ROS) are small molecules derived from oxygen and are a by-product of biological aerobic metabolism. They can be used as oxidants or are easily converted into oxygen-free radicals, which are one of the most important elements in oxygen therapy. They react with a variety of molecules, including other small organic molecules such as carbohydrates, lipids, proteins, and nucleic acids. However, excessively high levels of ROS can cause damage to the cell and gene structure. Usually, cells pass enzymes (e.g., superoxide dismutase) to reduce the damaging effect of ROS on cells. Oxygen therapy is also used to treat some patients with chronic oxygen deficiency, such as patients with chronic obstructive pulmonary disease or cystic fibrosis. On the other hand, oxygen is needed in every synthetic action of wound repair, including the synthesis of adenosine triphosphate, collagen, protein, and phagocytes, as shown in Figure 1 a. Nitrogen oxides (NOx) enzyme is the main source of ROS. The production of ROS during wound healing is essential for cell-signal transduction, angiogenesis, and wound disinfection. Oxygen generates superoxide anions through the catalysis of NOx to generate hydrogen peroxide and, subsequently, undergoes the action of redox signals until angiogenesis, as shown in Figure 1 b. In addition, as shown in Figure 1 c, hyperbaric oxygen therapy can increase the level of vascular endothelial growth factor in the wound and monoxide and enzymes in the bone, allowing vascular endothelial stem cells to return to the wound. The ischemic site merges into new blood vessels [ 29 ]. After receiving oxygen, nitric oxide (NO) and enzymes will be affected by enzyme catalysis to synthesize NO and help regulate blood vessel tension and angiogenesis, as shown in Figure 1 d. In the human eye, supersaturated oxygen emulsion can also be used for the local treatment of ocular trauma. Oxygen therapy can improve limbal ischemia, accelerate the formation of corneal epithelium, increase corneal transparency, and reduce corneal blood vessel formation [ 30 ].

Oxygen repair cell derivation process. ( a ) Synthesis of adenosine triphosphate (ATP), collagen, protein, phagocytes, and oxygen. ( b ) Enzyme-catalyzed redox repair in the cell. ( c ) Hyperbaric oxygen therapeutic cell repair. ( d ) Synthesis of nitric oxide (NO) angiogenesis. Vascular endothelial growth factor (VEGF).
2.2. Hydrogen Therapy
Hydrogen is one of the most common substances in nature. It can selectively neutralize cytotoxic ROS and reduce inflammation. Hydrogen is used in a variety of medical applications. At present, the concentration of H 2 in the air does not exceed 4%. Low-H 2 concentrations exhibit therapeutic effects on local inflammation of the eyes, ears, nose, and liver, as well as pancreatitis, systemic inflammatory syndrome, sepsis, and neurodegenerative diseases. In 1975, high concentrations of H 2 were found to inhibit tumor growth [ 31 ]. Hydrogen can play a protective role in various ROS-related diseases, including reducing bowel transplant damage in organ transplantation, treating chronic inflammation, and reducing ischemia-reperfusion injury. Hydrogen is also used to treat various ocular diseases, especially in the retina, which is a place where oxygen is highly needed. However, if excessive free radicals accumulate and increase oxidative pressure, they will peroxidize the lipids in the retina, causing retinal hypoxia. Once hypoxia will cause the production of new blood vessels, hydrogen molecules play a very important role at this time. H 2 is a perfect anti-free radical, and it can protect the retina from vascular proliferation. Oxidative stress triggers the development of a variety of human diseases and injuries, including eye diseases. The human body will induce an oxidative stress response due to excessive production of ROS or reduced production of antioxidants. In order to replace these weakened antioxidants, substances with effective antioxidant properties are needed to inhibit oxidative stress and promote healing. Molecular hydrogen (H 2 ) is very suitable for this purpose due to its unique properties. H 2 is the only antioxidant that crosses the blood–brain barrier and the blood–eye barrier. Due to its small molecular weight, it can quickly penetrate tissues and effectively remove active oxygen. H 2 mainly removes hydroxyl free radicals and peroxynitrite. In addition to its antioxidant effect, H 2 also has anti-inflammatory, anti-apoptotic, cell protection, and mitosis effects. Even when used at high concentrations, H 2 still maintains its non-toxic properties. Figure 2 shows the biological effect mechanism of hydrogen. The main molecular target of the biological effect of H 2 is ROS. The effects on chronic inflammation, signal transduction, genes, immunity, and metabolism (mitochondria) are essentially exerted through ROS. Exogenous damage caused by radiation and other factors induces excessive cellular ROS production [ 31 ]. H 2 penetrates the biomembrane and effectively reaches the cell nucleus. H 2 will selectively remove OH and ONOO−, thereby, preventing DNA damage, as shown in Figure 2 a. H 2 reduces the number of apoptotic factors such as caspase-3, caspase-12, caspase-8, and Bax. Some regulatory apoptosis factors such as Bcl-2 and Bcl-xL exhibit an increasing trend, making human cells have anti-apoptotic effects, as shown in Figure 2 b. In addition, H 2 reduces the number of inflammatory cytokines such as interleukin (IL)-1β, IL-6, tumor necrosis factor-α, intercellular adhesion molecule-1, and high mobility group protein-1, leading to anti-inflammatory effects in human cells, as shown in Figure 2 c. H 2 also regulates the signal transduction within and between many pathways, but the exact target and molecular mechanism need to be further studied, as shown in Figure 2 d. In general, H 2 reduces the risk of oxidative stress related to lifestyle and environment by reacting with strong ROS in a cell-free reaction.

Biological effect mechanism of hydrogen. ( a ) H 2 selective removal of -OH and ONOO−. ( b ) H 2 stimulating human apoptosis factor cell regulation. ( c ) H 2 promoting human inflammatory factor cell regulation. ( d ) Unknown molecular mechanism of H 2 regulation.
2.3. Functional Dressing
Oxygen is a vital source of energy necessary for cell repair and renewal. Once in the lungs, oxygen is carried to the cells through the blood in the capillaries. Due to hypoxia, epidermal cells appear inactive and hibernate, leading to the appearance of grayish-yellow and dark black oxidation marks and dryness, roughness, wrinkles, and sagging of the skin. Air pollution, dust, various toxic substances, and computer radiation are the most likely to cause cell hypoxia, which will cause skin cells to repair themselves, store water, and decrease their defenses. With the exception of supplemental oxygen, all other treatments are nearly futile as they only correct the symptoms but do not treat the root cause. Oxygen not only plays an important role in maintaining the health of our skin but also in wound healing and preventing infection. Oxygen can effectively increase the speed of wound healing. In a low-oxygen environment, healing might be delayed. By contrast, healing is accelerated and the risk of infection is greatly reduced in a high-oxygen environment. In addition to wound healing and infection prevention, oxygen can also be in the form of active oxygen, which can effectively reduce the production of melanin and scars and improve skin tone. Figure 3 shows the structure of the functional dressing used in the study. The functional dressing is from TO2M Co. (Miaoli County, Taiwan), model BXX01. This dressing contains sodium peroxide, sodium hydroxide, aluminum powder, and oxalic acid. It generates hydrogen by adding water [ 32 , 33 ]. It can not only protect the wound but also combine oxygen (O 2 ) and hydrogen (H 2 ) to provide an ideal environment for the affected area, block foreign bodies, and reduce the chance of infection.

Structure of the functional dressing. The outer film layer has a structure that allows the penetration of H 2 O easily, the middle layer consists of chemical compounds that generate hydrogen and oxygen, and sequentially escape through the inner film layer.
2.4. Type B Ultrasonic Scanner (Nidek RS-3000)
Type B ultrasonic scanner includes choroidal mode, which provides a comprehensive evaluation for choroid, retina, and glaucoma analysis. The principle of OCT scanning is to use the spectral domain of OCT with a scan range X axis is 3–12 mm, the Y axis is 3–9 mm, and the Z axis is 2.1 mm, using an 880 nm Super-Luminescent Diode light source. Scan speed can achieve up to 85,000 A-scans/s with averaging 120 images. The device can perform retina analysis, glaucoma analysis, angio-scan, or real-time compensation for eye movements which ensures higher image quality and maximum reproducibility. The advanced mode of RS-3000 can be used for measurement with ultra-low sensitivity depending on the pathology to be evaluated. The 9 mm × 9 mm wide-area scan ensures excellent coverage of the entire retinal structure. The unique Eye Tracer technology can use fundus information obtained from high-definition images for precise measurement. The Eye Tracer technology combines positioning, tracking, and automatic shooting functions for convenient and rapid measurement. During the macular line scan, micro-tracking and other involuntary eye movements can be compensated by the “Tracking HD” function. This function ensures that up to 120 macular scan images are aligned to enhance image averaging. Subsequent images are precisely aligned with the baseline data to achieve high reproducibility. The automatic registration function can compensate for the knob in the image acquisition process, thereby, improving the quality of subsequent data. The B-mode ultrasound scanner is an important diagnostic and predictive tool to determine diseases at the back of the eyeball when obvious vitreous opacity is present. There have been many research trials using Scan-B Ultrasound to detect vitreous floaters. Oksala et al. [ 34 ] used ultrasound to detect echoes from vitreous collagens. Mamou et al. [ 35 ] effectuated similar experiments by analyzing the contrast sensitivity obtained from this ultrasound device. Hence, ultrasound is typically used to assess the diagnosis of vitreous floaters.
2.5. Symptoms of Vitreous Floaters
In the imaging of the B-mode ultrasound scanner, vertical and horizontal analysis diagrams inside the vitreous body and OCT assist the doctor to make more accurate judgments and treatments. Patients with mild clinical symptoms will see black lines floating and occasional flashes of tiny spots of light that may not affect vision. Under the analysis of the B-mode ultrasonic scanner, the turbid part of the vitreous is not obvious, but a slight shadow and blackness can still be seen on the vitreous. Patients with moderate clinical symptoms have increased dark shadows and light spots in front of their eyes ( Figure 4 a). In the imaging of the B-mode ultrasound scanner, local shadows begin to appear inside the vitreous, as shown in Figure 4 b. When this symptom persists, the condition is worsening, and the patient must seek a medical facility for treatment. Finally, patients with severe and more significant turbidity have a large number of black shadows in front of their eyes, and their vision may even be reduced by varying degrees. Dust or thick flocculent blocks floating may be present near the vitreous body and the macula. As shown in Figure 4 c, when the vision is severely affected, surgical treatment should be considered. Clinical symptoms and details of pathological signs diagnosed and consulted by doctors represented in OCT images are shown in Table 1 .

Measurement results of B-type ultrasound scanner. ( a – c ) Imaging analysis of mild, moderate, and severe floaters, respectively. The figure on the right is the OCT in the horizontal and vertical directions.
The clinical symptoms and pathological sign details are shown on OCT images for levels of vitreous floater.
| Levels of Floaters | Mild | Moderate | Severe |
|---|---|---|---|
| Number of patients | 10 | 12 | 6 |
| Clinical symptoms | |||
| Pathological signs shown in OCT | Slight shadow and blackness appear on the vitreous | Local shadows appear inside the vitreous | The shadows and blackness appear wider and darker |
3. Results and Discussions
Figure 5 a–c show the measurement results of the ultrasound scan of patient A before and after treatment. In Figure 5 a, before treatment, patient A has a darker shade in the center of the macula in the middle of the vitreous, and many tiny floating objects can be observed in the vitreous. In Figure 5 b, the shadow of the fovea gradually fades after 2 months of treatment, and the floating objects are also reduced and lighter. In Figure 5 c, 4 months after treatment, the shadow of the fovea is lighter, and the floating objects are almost disappeared. Figure 5 d–f show the results of the ultrasound scanner measurement of patient B before and after treatment. In Figure 5 d, the shadow covers almost the entire macula and is even more severe than the symptoms of patient A. The vitreous body is also full of many tiny floating objects. After 2 months of treatment, the shadow of the macula is significantly lighter, the treatment effect has not decreased due to more serious symptoms, and the number of floating objects is reduced (see Figure 5 e). After 4 months of treatment, the macular shadows and floating objects almost completely disappear, as shown in Figure 5 f. The diagnosis of vitreous floaters through ultrasound scanners provides a fairly reliable basis. Type-B ultrasound systems are capable of assessing changes from the wave at interfaces of tissues with different densities, i.e., interfaces between liquid and gel vitreous or echoes from vitreous collagens. This was confirmed in some references that found that vitreous opacity in the vitreous vestibule was most correlated with diminishing contrast. When the amount of echoes from gel-liquid interfaces tend to decrease, it shows that the environment in the retina is gradually returning to equilibrium [ 24 , 34 , 35 ].

Comparative analysis of clinical treatment effects. Results showed improvement of eye floaters symptoms through fading of macular shadows and floating objects compared to baseline disease ( a , d ), after 2 months of treatment ( b , e ), and after 4 months of treatment ( c , f ) of 2 patients A and B.
Recently, due to aging or excessive use of 3C products, glass floaters have continued to increase. When the vitreous body of the eye is chaotic, vitreous floaters cast shadows on the retina, making it seem like something is floating in front of the eyes [ 36 ]. In a previous clinical trial, 10, 12, and 6 subjects had mild, moderate, and severe floaters, respectively. After 2 months of treatment for patients with mild floaters, seven patients almost no longer had symptoms of floaters. However, some patients had bad eye habits. Three patients with mild symptoms had improper eye habits, such as using mobile phones in dark places, staying up late, and overuse of eyes, resulting in symptoms of floaters. After 2 months of treatment for patients with moderate floaters, eight patients had mild symptoms, and the other 4 are due to complications such as recurrent vitreous hemorrhage and corneal edema. As well as poor healing of the corneal epithelium, postoperative intraocular pressure increase, retinal tears, etc., continuous regular follow-up and treatment are required to achieve the therapeutic effect. However, new complications may continue to occur in the acute phase. Thus, 1 week after diagnosis, close follow-up visits are required within 3 months. If patients remain stable, regular visits will be made for 3–6 months. However, patients with severe floaters usually have pathological floaters, which are more likely to occur over 50 years of age. People with high myopia, diabetes, high blood pressure, cataract surgery, eye injury, and eye inflammation. Due to the rupture of blood vessels in the retina, retinal tears or detachment of the retina result in inflammation of the tissues around the vitreous body, causing a large amount of white blood cell suspension to leak out from the vitreous body. Usually, the flying mosquitoes seen by the patient are a thick black shadow, which seriously affects the vision and needs immediate treatment. After 2 months of clinical trial treatment, six patients had moderate symptoms of floaters. Among the six patients with severe floaters, the use of functional dressings can improve the treatment effect due to the relatively large volume of floating objects. Among these patients, five had obvious treatment effects. The floating objects were not only greatly reduced, but the poor vision was also slightly improved. However, floating objects may not be removed by a single treatment. Multiple treatments and continuous follow-ups are required, and the other one is due to the usual and continuous improper use of the eyes, which results in the lack of effectiveness of the treatment. Taken together, when patients see floaters in front of their eyes, they should visit the ophthalmology department for a thorough retinal examination of the fundus. Patients with mild symptoms of floaters may have these symptoms throughout their lives, but they still need to be monitored regularly by an ophthalmologist. After a period of adaptation, floaters usually leave the field of vision and gradually disappear. Patients can also try to move their eyes (looking up and down) to make the fluid in the eyes form fluctuations, which can temporarily make floaters disappear. However, pathological floaters caused by vitreous hemorrhage, peripheral retinal tears, and retinal detachment require more aggressive treatment to avoid further deterioration. The number of patients who recovered positively after 2 months of therapy is shown in Table 2 .
The number of patients participating in clinical trials and the number of patients recovering actively after 2 months of treatment.
| Levels of Floaters | Mild | Moderate | Severe |
|---|---|---|---|
| Number of patients | 10 | 12 | 6 |
| Number of recovery patients | 7 | 8 | 6 |
| Avarage recovery rate | 70.0% | 66.7% | 83.3% |
4. Conclusions
The treatment of vitreous floaters is currently attracting doctors’ and researchers’ attention. There are many advanced solutions to this problem. Our method has shown the patient’s recovery effect in more than 4 months of intensive treatment. Compared with laser therapy, using a functional eye dressing has more potential treatment results and does not cause side effects with the ingredients in the device. Functional eye dressing offers a novel solution for semi-invasive therapy, providing potential therapeutic results and no side effects with ingredients in the device. Our method is portable, compact, and suitable for treatment in the eye and face area. The treatment results achieved for the three grades of vitreous floaters disease were 70%, 66.7%, and 83.3%, respectively. Moreover, the evaluation of treatment results visualized by analyzing through OCT images will bring essential assistance to doctors in the diagnosis and conclusion of treatment regimens. We hope that the use of functional eye dressing will be a new solution in the treatment of vitreous floaters.
Funding Statement
This research was supported by the National Science and Technology Council, China under the grants NSTC111-2221-E-194-007. This work was financially/partially supported by the Advanced Institute of Manufacturing with High-tech Innovations (AIM-HI) and the Center for Innovative Research on Aging Society (CIRAS) from The Featured Areas Research Center Program within the frame-work of the Higher Education Sprout Project by the Ministry of Education (MOE), and Kaohsiung Armed Forces General Hospital research project MAB107-097 in Taiwan.
Author Contributions
Conceptualization, W.-S.F. and S.-Y.H.; methodology, H.-T.N.; software, H.-T.N.; validation, W.-T.H. and H.-C.W.; formal analysis, W.-S.F.; investigation, W.-T.H.; resources, W.-H.C.; data curation, W.-S.F. and S.-Y.H.; writing—Original draft preparation, H.-T.N.; writing—Review and editing, F.-C.L. and H.-C.W.; supervision, H.-C.W.; project administration, H.-C.W. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Dalin Tzu Chi General Hospital (B11001017).
Informed Consent Statement
Written informed consent was waived in this study because of the retrospective anonymized nature of study design.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- 0800 086 1064
- Book a Free Consultation
0% Finance Available – Book FREE Consultation.
Optegra Leads the Way in Successful New Treatment for Floaters
3 June 2021
By Author: Alex J Shortt
Medically reviewed on 17-August-2023
Specialist eye hospital group, Optegra, is leading the way in developing a new method to treat floaters , an eye condition which mainly affects young adults whom to date have been told there is little or no treatment and whose distressing symptoms are frequently dismissed.
Symptoms of floaters include dots, shadows or long strands blocking everyday vision , caused by debris floating in the eye’s vitreous solution and which disturb clear sight at all times, often leading to a huge impact on confidence, attitude and outlook of the sufferer.
Niall Patton, Consultant Surgeon at the Optegra Manchester Eye Hospital , utilises micro-incision sutureless surgery, called vitrectomy (which involves removing the vitreous fluid behind the lens of the eye) for patients with floaters, with remarkable results.
He explains: “Floaters can torment people as these ‘clouds’ in their vision move as their eyes move, so sufferers will constantly have their vision affected. Whilst for many patients, floaters are an everyday part of life and do not bother them, in a significant percentage of individuals, this can lead to substantial detriment to a patient’s quality of life and can even result in depressive symptoms. Sufferers may become withdrawn, or seek psychiatric help. Some individuals can be concerned that they are imagining the symptoms, but they are real.
“The long standing view has been that little can be done for these sufferers, but by applying the very latest modern sutureless techniques to this condition, patients can often have their lives transformed with complete alleviation of their symptoms.
“We have now removed floaters on a number of patients, with excellent results. Because we largely use suture-free surgery, recovery can be very quick, often within a few days/weeks and the patients notice almost immediately that their floaters are gone. What once was a long, difficult and potentially hazardous operation is becoming as reliable and as routine as cataract surgery , usually taking less than an hour to complete. It is fantastic that we can make a dramatic impact on patients’ quality of life.”
Download Information Pack
Learn more about how our latest vision correction techniques could improve your vision and change your life. Or Book Free Consultation .
Read our terms & conditions. Read our privacy policy
Please note – by providing these details, you agree that we can contact you via these methods
Caroline Broadley, 33, from the Wirral, started suffering from floaters when she was seven months pregnant. Describing a big black mark in her eye, constantly whizzing around, Caroline felt that the latter stages of pregnancy and early months with her daughter were spoilt with anxiety and depression.
She says: “This floater was not just affecting my vision, it was affecting my sanity. I felt like I was going mad as my doctor and my local hospital just told me I was hormonal, and I should go away and take some vitamin C!
“I knew it was so much more than that, but people don’t realise how serious floaters can be. I got to the point I was too anxious to leave the house, and would sit in a darkened room hour after hour – as natural daylight made my vision even worse. I just wanted to sleep to escape it.”
After six months, and having been put on anti-depressants, Caroline had the vitrectomy with Mr Patton. She says: “It was amazing. Having become almost agoraphobic for six months, my vision was suddenly crystal clear. I felt as though I got my life back – and could enjoy my daughter, enjoy the sunshine and start living again.”
Floaters are present in the vitreous behind the lens, and move with the eye to disrupt vision. The procedure takes up to one hour, and removes this fluid, taking the floaters with it. Results can be seen within a few days, and full impact within a matter of weeks.
Martin Baldwin, 56, managing director of a mobility aid company in Lancashire, suffered for three years with floaters, and became desperate to find a solution. He explains: “After previous emergency eye surgery for retinal problems, I was left with floaters and told I had to just put up with them. But it felt like a cloud over my central vision, and I would move my eyes around to shift the cloud, but it would pop straight back into the centre of my eye. It’s as though it was on a piece of elastic and would always ping back into place.
“Having always had great vision, it was incredibly frustrating to have this affecting my computer work, my driving, everything I did. I was even contemplating going to America to explore treatment options, when I discovered Niall Patton at Optegra. It was a life changing operation for me – these floaters were driving me mad, I could not escape them, and now thanks to this new procedure I can see as well as I could in my twenties!”
For information on this treatment, please contact us online to arrange a free consultation or call 0800 086 1064.
Notes to editors:
1) Optegra is committed to the world-wide development of eye sciences and championing the latest innovations in vision correction.
Optegra does this by partnering with leading UK universities in the research and development of the next generation of ophthalmic services and technologies.
Optegra operates five private eye hospitals: Surrey Eye Hospital (Guildford), Birmingham Eye Hospital (Aston), Yorkshire Eye Hospital (Apperley Bridge and Laser Eye Centre in Leeds City Centre); Solent Eye Hospital (Whiteley) and Optegra Manchester Eye Hospital, (Didsbury).
All are supported by over 60 consultant level ophthalmic surgeons who provide a wide range of ophthalmic procedures including: Clarivu (refractive lens exchange), laser vision correction, cataract removal, glaucoma, AMD and cosmetic procedures.
2) Floaters are small pieces of debris that ‘float’ in the vitreous humour of the eye. They occur behind the lens (the transparent window through which light enters the eye), and in front of the retina (the light sensitive tissue that lines the back of the eye). Vitreous humour is a clear, jelly-like substance that fills the space in the middle of the eyeball. It is 99% water and 1% substances that help to maintain the shape of the vitreous. Floaters cast shadows on the retina, and it is these shadows which people can see.
3) Niall Patton MB ChB, MD, FRCOphth; Consultant Ophthalmologist, Cataract and Vitreoretinal Surgeon, Optegra Manchester Eye Hospital. Niall graduated in Medicine from the University of Manchester in 1996. He completed his ophthalmic surgical training at the Manchester Royal Eye Hospital and the Princess Alexandra Eye Pavilion, Edinburgh. In addition, he has undertaken four years of specialist Vitreoretinal surgical fellowship training at the Lions Eye Institute, Western Australia, Princess Alexandra Eye Pavilion, Edinburgh, Tennant Eye Institute, Glasgow and Moorfield’s Eye Hospital, London. In addition to his clinical expertise, Niall Patton has completed ophthalmic research in a variety of different ophthalmic fields and has been successful in procuring research grants from the Royal College of Surgeons, Edinburgh. His research culminated in the award of a Doctorate from the University of Manchester in 2006. He has spoken at national and international ophthalmology meetings, including the United States, Australia, and Europe. In addition to 49 peer-reviewed publications in ophthalmic journals, he has also co-authored a chapter of a textbook and has served as a reviewer for major international ophthalmology journals, including Investigative Ophthalmology & Visual Science, Ophthalmology, Archives of Ophthalmology & Journal of Applied Physiology.

Mr Shortt is a leading ophthalmic surgeon and an expert in the fields of cornea, cataract and refractive surgery.
Medically Reviewed Date: 17th August 2023

Download a free infopack
Not ready for a consultation? Learn more about our range of treatments, doctors and hospitals
Free Virtual Consultation
Book your virtual consultation with our top rated eye hospitals
Call us free
We'll answer any questions you may have about treatment.
Private Patients - 0800 086 1064 NHS Patients - 0207 509 4186
Private: Mon-Thu: 8am-7pm, Fri: 8am - 5.30pm NHS: Mon-Fri: 8am - 6pm
Patient Portal
Manage your existing bookings & payments
Request received
Many thanks. We will be in touch shortly.
Research Communities by Springer Nature
Towards a safe treatment of eye floaters by light-induced vapor nanobubbles.
Share this post
Choose a social network to share with, or copy the shortened URL to share elsewhere
Share with...
...or copy the link.
communities.springernature.com
Read the paper
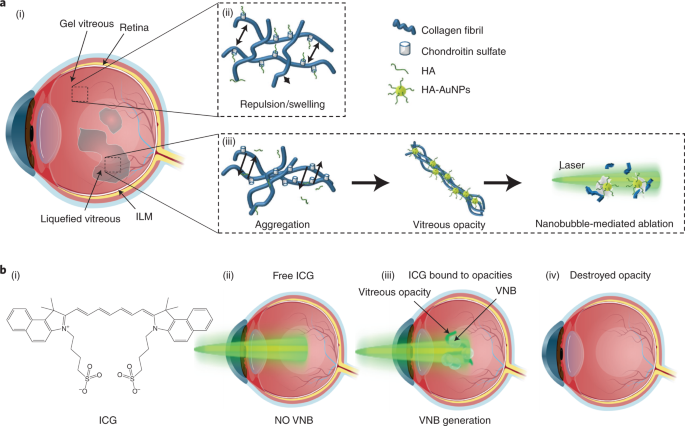
Laser-induced nanobubbles safely ablate vitreous opacities in vivo - Nature Nanotechnology
Vitreous opacities, which are collagen aggregates that form in the eye and cause vision impairment (eye floaters), are currently treated with invasive surgical intervention or high-energy laser photoablation. In this paper, the authors show that exposing gold nanoparticles or indocyanine green to lo…
The vitreous of the eye is a transparent gel mainly composed of water, glycosaminoglycans and a network of collagen fibrils. In healthy eyes, collagen fibrils are spaced apart by hyaluronic acid (HA), an anionic glycosaminoglycan which attracts water and generates a swelling pressure that inflates the gel to maintain its transparency. Vitreous collagen fibrils are heterotypic in composition. They contain collagen type II, V, IX and XI. Type IX collagen has chondroitin sulfate glycosaminoglycan chains which extend away from the fibril surfaces; they space apart the collagen fibrils, thereby preventing the aggregation of collagen fibrils. With aging, myopia or diabetes, there is a progressive ‘liquefaction’ of the vitreous inducing the formation of collagen aggregates that scatter light and can strongly impact vision and quality of life.

Figure 1. Dark-field slit microscopy of dissected human vitreous body reveals aging structure. (A) Homogeneous vitreous of a 33-week old fetus. (B) Fusion of collagen fibrils in the central part of the vitreous (white arrow) of an 59-year-old human. (C) Extensive fibrous liquefaction in the degenerated vitreous of an 88-year-old woman. This degeneration is accelerated in myopia and simultaneously forms vitreous opacities (D) 1 .
In most cases, vitreous opacities are left untreated and patients must cope with at times debilitating symptoms. While vitrectomy (i.e. surgical excision of vitreous) is currently performed to cure eye floaters, it is invasive, costly, and carries risks. Laser treatment has unproven efficacy and remains rather limited because vitreous opacities have to be located sufficiently far from the retina to avoid photomechanical collateral damage. Thus, an approach to increase patient eligibility and reduce laser intensity would meet an unmet medical need.
Exploiting the plasmonic properties of gold nanoparticles, surrounding water evaporates when illuminated with a pulsed-laser, forming ‘vapor nanobubbles’ (VNBs). In 2019, we reported that when nanobubbles collapse, the accompanying mechanical forces destroy vitreous opacities onto which gold nanoparticles are bound. 2 This was achieved with a laser fluence 1000 times lower than currently used clinically. These in vitro and ex vivo studies showed proof of principle requiring corroboration in vivo , but no experimental model existed.
For the first time, we demonstrate safe destruction of vitreous opacities in live rabbits using gold nanoparticles as well as indocyanine green (ICG), a dye which is clinically used in ophthalmology for choroidal angiography 3 and chromodissection. 4 We observed in situ preferential binding to vitreous opacities that were previously obtained from patients during vitrectomy. VNBs were generated in a targeted fashion due to preferential accumulation on the surface of the opacities, thus leaving the surrounding vitreous untouched. In rabbits, it was observed that both gold nanoparticles and ICG were well tolerated and destroyed opacities after few pulses at 1.9 J/cm²; for ICG, at a lower concentration than used during chromodissection. 5

Figure 2 Following (A) gold nanoparticles (10 12 NPs/ml) or (B) ICG injection (0.625 mg/mL), laser irradiation (<7ns; 532 nm (gold) or 800 nm (ICG); 1.9 J/cm²) enabled the ablation of exogenous collagen opacities after few pulses.
Importantly, this occurs at a laser energy which is one thousand times less than the (YAG laser) energies typically employed clinically, making this highly attractive for safe treatments. Taken together, these results suggest that VNBs generated from gold nanoparticles or ocular dyes like ICG hold great promise for safe laser ablation of vitreous opacities, curing vision degrading myodesopsia. 1 With these encouraging results, we aim at expanding nanobubble-mediated ablation more generally to ocular surgery by further increasing safety and precision.
Félix Sauvage
Stefaan C. De Smedt
- Sebag, J. Vitreous and Vision Degrading Myodesopsia. Progress in Retinal and Eye Research 100847 (2020) doi:10.1016/j.preteyeres.2020.100847.
- Sauvage, F. et al. Photoablation of Human Vitreous Opacities by Light-Induced Vapor Nanobubbles. ACS Nano 13 , 8401–8416 (2019).
- Desmettre, T., Devoisselle, J. M. & Mordon, S. Fluorescence Properties and Metabolic Features of Indocyanine Green (ICG) as Related to Angiography. Survey of Ophthalmology 45 , 15–27 (2000).
- Burk, S. E., Da Mata, A. P., Snyder, M. E., Rosa, R. H. & Foster, R. E. Indocyanine green-assisted peeling of the retinal internal limiting membrane. Ophthalmology 107 , 2010–2014 (2000).
- Haritoglou C, Sebag J: Indications and considerations for chromodissection. Retinal Physician 11:34-39, (2014).
Contributors
PharmD, PhD, Ghent University
Contributing authors
J. Sebag, MD, FACS, FRCOphth, FARVO
Professor of Clinical Ophthalmology , UCLA, Founding Director & President, VMR Institute for Vitreous Macula Retina
stefaan de smedt
Prof, Ghent Univ
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
Subscribe to the Topic

Nature Nanotechnology
An interdisciplinary journal that publishes papers of the highest quality and significance in all areas of nanoscience and nanotechnology.
Latest Content
Divergent evolution of the human heart: what we can learn from our evolutionary cousins.

Mycofluidics of clocks in single filaments of Neurospora crassa
Zn2+-mediated catalysis for fast-charging aqueous zn-ion batteries.

Tumor suppressor Par-4 activates autophagy-dependent ferroptosis

Chalcone derivatives with strong nonlinear optical activity
We use cookies to ensure the functionality of our website, to personalize content and advertising, to provide social media features, and to analyze our traffic. If you allow us to do so, we also inform our social media, advertising and analysis partners about your use of our website. You can decide for yourself which categories you want to deny or allow. Please note that based on your settings not all functionalities of the site are available.
Further information can be found in our privacy policy .
Cookie Control
Customise your preferences for any tracking technology
The following allows you to customize your consent preferences for any tracking technology used to help us achieve the features and activities described below. To learn more about how these trackers help us and how they work, refer to the cookie policy. You may review and change your preferences at any time.
These trackers are used for activities that are strictly necessary to operate or deliver the service you requested from us and, therefore, do not require you to consent.
These trackers help us to deliver personalized marketing content and to operate, serve and track ads.
These trackers help us to deliver personalized marketing content to you based on your behaviour and to operate, serve and track social advertising.
These trackers help us to measure traffic and analyze your behaviour with the goal of improving our service.
These trackers help us to provide a personalized user experience by improving the quality of your preference management options, and by enabling the interaction with external networks and platforms.

- For Ophthalmologists
- For Practice Management
- For Clinical Teams
- For Public & Patients
Museum of the Eye
- Latest Issue
- Back Issues (Nov. 2012 to present)
- Archive Highlights (pre Oct. 2012)
- Dr. Richard Mills' Opinions, 2002 to 2016
- Write For Us
- Corporate Webinars
- EyeNet Magazine
- / March 2018
- / To Treat—or Not to Treat—Vitreous Floaters
To Treat—or Not to Treat—Vitreous Floaters
- Mark Complete
Download PDF
Pick virtually any ophthalmologist’s practice and you’ll find patients who complain of vitreous floaters. When, if ever, should these patients receive treatment? Like most of his colleagues, Chirag P. Shah, MD, MPH, with Ophthalmic Consultants of Boston, prefers observation in 99.9% of these cases. “However,” he said, “I do think that paradigm is slowly changing.”
A combination of more sophisticated patient selection and enhanced technology and techniques may be diminishing some concerns about the risks of surgery for vitreous floaters. And although a recent study 1 conducted by Dr. Shah also suggested that YAG vitreolysis may offer benefits for troublesome floaters, it also raises questions about its efficacy and safety, as well as the necessity for multiple costly sessions.
Three vitreoretinal surgeons offer their perspectives on whether, and how, to treat vitreous floaters.
Troublesome Vitreous Floaters
Vitreous floaters may occur following a retinal tear, retinopexy, scleral buckling, or vitreous hemorrhage associated with a tear, said Gaurav K. Shah, MD, with The Retina Institute in St. Louis, Missouri. But most patients who experience vitreous floaters fall into 2 groups: those with a posterior vitreous detachment (PVD) or myopic vitreopathy.
PVD and myopic vitreopathy. People in their 50s, 60s, or 70s may develop a PVD and have more significant floaters, said Dr. Chirag Shah. “Most of the time, patients can cope with them because the brain neuroadapts. But a certain percentage of patients continue to be bothered by the floaters.” People in their 20s and 30s may also develop opacities in their vitreous as a result of myopia, said Jerry Sebag, MD, at VMR Institute for Vitreous Macula Retina in Huntington Beach, California.
Impact of light. “Because the impact is greater in bright light, individuals with floaters—often younger people—typically complain about the inability to work long hours on computers,” said Dr. Sebag. In addition, snow reflections, bright skies, and looking at the ocean may be bothersome. “I’ve had patients tell me they’ve stopped camping, fishing, or skiing because they no longer find these activities pleasurable. Some even tell me they can’t wait to go to sleep at night.”
Why worse for some? Why some people are more afflicted than others is not fully understood, said Dr. Sebag. It may be connected to more than 1 factor, he said, such as biochemistry and the effects of aging, genetics, hormones, and the ability to neuroadapt. “For example, some have a denser posterior vitreous cortex, and these people won’t be able to adapt well to their floaters.”
What is clear, he said, is that many of these patients feel ignored by the medical profession. “What they are complaining about may not fit neatly into our diagnostic boxes, but that doesn’t mean they don’t have a problem.”
Evaluating Vitreous Floaters
Fewer than 5% of Dr. Chirag Shah’s patients complain of floaters. Given that not all floaters are created equally, he said, it’s important to demonstrate a correlation between what the patient is experiencing and what the physician is seeing. “Deciding who to treat ends up being the key to success.”
Basic exams. Why do physicians underestimate serious symptoms of vitreous floaters? “One reason is that we usually check patients’ visual acuity and visual fields,” said Dr. Chirag Shah, “but we don’t check contrast sensitivity, which can be degraded by significant floaters.” Also, floaters may move into the patient’s central vision, affecting their ability to read or drive, but doctors rarely check reading speed.
Dr. Sebag was the first to discover that patients with significant vitreous floaters are bothered with decreased contrast sensitivity function. 2-4 He coined the diagnostic term “vision-degrading vitreopathy” to help distinguish debilitating floaters from those that are relatively benign. “Screening with vitreous-specific questionnaires, structural assessments with ultrasound, and contrast sensitivity functional (CSF) assessments give me the ability to diagnose vision-degrading vitreopathy and make me more comfortable about offering treatment,” he said.
Floaters questionnaire. Dr. Sebag and colleagues devised a screening tool called the Vitreous Floaters Functional Questionnaire (VFFQ) to help evaluate the impact of floaters on patients’ quality of life. “We’ve shown a statistically significant correlation between the VFFQ and the National Eye Institute’s (NEI’s) Visual Function Questionnaire, a gold standard for assessing vision in more general terms,” he said. In addition, there is a high correlation among the results of the VFFQ and CSF and the density of the vitreous body as assessed by ultrasound.
Contrast sensitivity function. A CSF assessment provides a functional evaluation of the impact of vitreous (as well as cornea or lens) opacification on vision, by measuring the ability to distinguish shades of gray, said Dr. Sebag. One of his studies found that patients with bothersome floaters had a 67% reduction in CSF compared with age-matched controls. 2
“These days, I never operate on someone with normal CSF,” said Dr. Sebag. More than 140 patients with abnormal CSF on whom he has performed vitrectomy attained normal CSF within 1 week of surgery. 2-4 Dr. Sebag has followed these patients for an average of nearly 3 years; during this time, their CSF has remained normal.
Quantitative ultrasound (QUS). Dr. Sebag also advocates the use of quantitative ultrasound, which gives an index of the structure of the vitreous body. “The quantitative ultrasound measurements we perform clearly show that the greater the density of the vitreous, the more patients are bothered by their floaters,” he said. He added that QUS is also a useful way to show patients what’s going on inside their eyes and to assess the effectiveness of vitrectomy.
Wide-angle color photography. In his clinical study, Dr. Chirag Shah used wide-angle color photography to visualize floaters. “Oftentimes, patients would look at their color photographs and say, ‘That’s the bug-like floater that keeps going in and out of my vision,’” he said. “If a patient had significant symptoms but the photograph was crystal clear except for a few normal vitreous wisps, that patient may not be easy to satisfy.”
OCT. To assess floaters, Dr. Gaurav Shah takes optical coherence tomography (OCT) infrared video scans. “This allows us to see what the patients are seeing,” he said. “If I do a video scan and don’t see much, the patient’s symptoms are not from the eye, and I won’t treat them with vitrectomy. If patients truly have something, it is a very dramatic demonstration of their symptoms.”
Vitrectomy for Troublesome Floaters
“Vitrectomy is valuable for some patients with floaters, but I tend to reserve it only for those with the most debilitating floaters because of the potential side-effect profile,” said Dr. Chirag Shah. Vitrectomy is invasive, agreed Dr. Gaurav Shah. “But it has evolved and been vindicated by improvements in technology and technique. My patients have been ecstatic with the results, although it’s first critical to determine that they are truly symptomatic and have been given a chance to neuroadapt or to allow the floaters to resolve.”
Exclusion criteria. Dr. Sebag uses the VFFQ, CSF, and QUS to select the best candidates for vitrectomy. “I don’t take surgery lightly,” he said, explaining that he’s performed only about 200 surgical floater cases in over 8 years. “I rarely meet someone and say, ‘Let’s operate.’” In fact, he said the average time between the first onset of symptoms and surgery is more than 30 months.
Dr. Gaurav Shah uses slightly different criteria for excluding patients.“I exclude patients who are phakic, who have 360 degrees of lattice or a lot of peripheral retinal problems, or who have expectations that are way beyond what the surgery can provide.” To help assess expectations, he asks his patients, “If you are driving on a road and the entire windshield is clear except for one little spot, does that bother you?” If the answer is “yes,” he is more concerned about the ability to please the patient with surgery.
Risks of vitrectomy. “With vitrectomy, you are creating 3 holes in the eye,” said Dr. Chirag Shah, “which carries a small risk of infection.” Vitrectomy also accelerates cataract formation, because of increased oxygen concentration in the vitreous cavity following removal of the vitreous. “But for me, retinal detachment is the most concerning risk, with published reports as high as 10.9%,” he said.
Presenting vitrectomy findings from 151 eyes at the 2016 Academy annual meeting, Dr. Sebag reported no cases of endophthalmitis or hypotony; 1 case each of glaucoma, cystoid macular edema, and retinal break; 2 cases of retinal detachments that were surgically corrected; and 6 cases of vitreous hemorrhage, which all cleared spontaneously.
Reducing risks. Dr. Gaurav Shah has found that being discerning in choosing patients has resulted in fewer complications. Operating on 5 to 10 floaters patients last year, he has had no patients experience retinal tears or detachments. The key, he said, is 27-gauge topical vitrectomy, which minimizes complications with blocks and intraoperative issues. Dr. Sebag also credits the development of sutureless, small-gauge vitrectomy in reducing risks, as well as a couple of other techniques.
Reduce risk of endophthalmitis. To this end, Dr. Sebag creates highly beveled incisions and uses nonhollow probes for cannula extraction.
Leave a little vitreous. “I have modified my approach by leaving a few milli-meters of vitreous behind the lens. The antioxidants in the vitreous gel help mitigate cataract formation,” Dr. Sebag said. He and his colleagues compared the incidence of cataract using this modified approach with extensive vitrectomy, which is used at the University of Amsterdam. At 24 months, the incidence of cataract was 35% with the modified approach and 87% with the extensive approach. The time until cataract formation was also 5 months longer with a limited vitrectomy. 5
Two philosophies on surgical PVD. Younger patients have vitreous floaters because of collagen cross-linking in the vitreous body, not because of PVD, said Dr. Sebag. To reduce the risk of tears in these patients, he recommends simply removing the central vitreous and not separating the posterior vitreous from the retina. By contrast, Dr. Gaurav Shah said that he always creates a complete PVD because he’s concerned that contracture of the residual cortical vitreous may cause problems in the future. That has not been the case in Dr. Sebag’s experience of 200 cases, where only 1% experienced retinal detachment.
YAG Laser Vitreolysis for Troublesome Floaters
Before conducting the first randomized clinical trial of YAG vitreolysis for symptomatic Weiss ring floaters, Dr. Chirag Shah wondered whether lasers could provide a niche between performing vitrectomy and doing nothing. “I was very skeptical going into the study, and I’m not currently performing this procedure,” he said, “but the study has shown me that YAG vitreolysis may have some value.”
Laser study results. In the trial, 54% of the laser group reported symptom improvement after 1 treatment. In addition, no differences in adverse events were identified between the laser and sham groups. 1 “We need to do larger studies of longer duration to determine the best candidates and the number of treatments needed, as well as [the treatment’s] true risks and benefits,” said Dr. Chirag Shah.
Although more than half of the patients in Dr. Chirag Shah’s study reported significant or complete resolution of their vitreous floaters, only about one-third of patients in an earlier study by Delaney et al. reported similar results. 6 “We used a higher laser power in our study, which may account for the differences in response,” said Dr. Chirag Shah. “At a lower power, you’re doing more fractionating, but when you turn the power up, you form plasma and can see the tissue vaporize into gas bubbles.”
Dr. Sebag, however, disputes this assertion, saying that YAG laser does not vaporize tissue. “YAG lasers are photodisruptors,” he said. “They take something large and break it into smaller pieces.”
Anomalous? In Dr. Chirag Shah’s trial, 8 patients self-reported zero improvement out of a scale of 100 despite color photography showing significant or complete objective improvement. “Some patients recognized that the floater was virtually gone, but a little speck that was mobile, possibly more than previously, annoyed them to the same degree as their large floater did,” he said.
Exclusion criteria. In Dr. Chirag Shah’s study, the following patients were excluded: those with Snellen best-corrected visual acuity worse than 20/50 in the nonstudy eye; history of retinal tear, retinal detachment, uveitis, diabetic retinopathy, macular edema, retinal vein occlusion, or aphakia in the study eye; and history of glaucoma or high intraocular pressure.
Risks and costs of laser. “To my knowledge, just a handful of doctors are doing YAG vitreolysis, and with variable results,” said Dr. Chirag Shah. With no dedicated insurance code, the procedure is done off-label, he said. In his study, Dr. Chirag Shah only did 1 treatment session because he could not treat patients with 2 sham lasers without unmasking them. “In the real world, patients may require 2 or more laser sessions to vaporize the majority of their floaters.”
With YAG vitreolysis, there is a risk of glaucoma, retinal tear, retinal detachment, cataract if you hit the lens, and retinal damage if you hit the retina, said Dr. Chirag Shah. To minimize risks of lens or retinal damage, he recommends ensuring a safe distance between the focal point of the laser and the retina and crystalline lens. In the study, he required the Weiss ring floater to be 5 mm posterior to the posterior capsule of the crystalline lens and 3 mm anterior of the retina, as measured by B-scan ultrasonography.
Dr. Gaurav Shah has not personally used laser for floaters but is concerned that it may be a time-consuming procedure, and he noted, “Although laser appeared quite safe in this recent laser study, it may have potential drawbacks.”
He added, “It’s important to remember that the vast majority of patients don’t require intervention. However, there are those who are truly symptomatic and might require a procedure—and, even more importantly, [who may benefit from] a conversation that acknowledges their pathology.”
___________________________
1 Shah CP, Heier JS . JAMA Ophthalmol. 2017;135(9):918-923.
2 Sebag J et al. Retina . 2014;34(6):1062-1068.
3 Garcia GA et al. Am J Ophthalmol. 2016;172:7-12.
4 Milston R et al. Surv Ophthalmol. 2016;61(2):211-227.
5 Yee KMP et al. Ophthalmol Retina. 2017;1(2):154-157.
6 Delaney YM et al. Eye (Lond). 2002;16(1):21-26.
___________________________
Dr. Sebag is a vitreo-retinal specialist at the VMRInstitute for Vitreous Macula Retina in Huntington Beach, Calif., and professor of clinical ophthalmology at the Doheny Eye Institute in Los Angeles. Relevant financial disclosures: Abbott Labs: C; Johnson & Johnson: C.
Dr. Chirag Shah is a retina specialist at the Ophthalmic Consultants of Boston; fellowship codirector of the combined Tufts New England Medical Center/Ophthalmic Consultants ofBoston vitreoretinal surgery fellowship; and assistant professor at Tufts University School of Medicine, all in Boston. Relevant financial disclosures: Ellex: L.
Dr. Gaurav Shah is a retina specialist and codirector of the retina fellowship at The Retina Institute in St. Louis, Mo. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
| Abbott Labs: C; Johnson & Johnson: C; Roche Pharmaceuticals: C. Ellex: C; Genentech: S; Johnson & Johnson: S; National Eye Institute: S; Ophthalmic Consultants-Boston: E; Regeneron: S. Allergan: C,S; Bausch + Lomb: L; DORC: C; Regeneron: C,L; Spark: C.
All content on the Academy’s website is protected by copyright law and the Terms of Service . This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
FOLLOW THE ACADEMYMedical Professionals Public & Patients  At a glance: FloatersSmall dark spots or squiggly lines that float across your vision Dilated eye exam None (in most cases), surgery What are floaters?Floaters are small dark shapes that float across your vision. They can look like spots, threads, squiggly lines, or even little cobwebs. Most people have floaters that come and go, and they often don’t need treatment. But sometimes floaters can be a sign of a more serious eye condition. So if you notice new floaters that appear suddenly and don’t go away, it’s important to tell your eye doctor. What are the symptoms of floaters?Floaters move as your eyes move — so when you try to look at them directly, they seem to move away. When your eyes stop moving, floaters keep drifting across your vision. You may notice floaters more when you look at something bright, like white paper or a blue sky. Am I at risk for floaters?Almost everyone develops floaters as they get older, but some people are at higher risk. You’re at higher risk if you:
What causes floaters?Floaters usually happen because of normal changes in your eyes. As you age, tiny strands of your vitreous (the gel-like fluid that fills your eye) stick together and cast shadows on your retina (the light-sensitive layer of tissue at the back of the eye). Those shadows appear as floaters. Sometimes floaters have more serious causes, including:
 When to get help right awaySometimes new floaters can be a sign of a retinal tear or retinal detachment — when the retina gets torn or pulled from its normal position at the back of the eye. Symptoms can include:
Retinal tear or detachment can be a medical emergency . If you have these symptoms, it’s important to go to your eye doctor or the emergency room right away. How will my eye doctor check for floaters?Your eye doctor can check for floaters as part of a dilated eye exam. Your doctor will give you some eye drops to dilate (widen) your pupil and then check your eyes for floaters and other eye problems. This exam is usually painless. The doctor may press on your eyelids to check for retinal tears, which may be uncomfortable for some people. What’s the treatment for floaters?Treatment for floaters depends on the cause. If your floaters are caused by another eye condition, you may need treatment for that condition. If your floaters are caused by aging and they don’t bother you, then you probably won’t need any treatment. If your floaters make it hard to see clearly and interfere with your daily life, your eye doctor might suggest a surgery called a vitrectomy to remove the floaters. Talk with your doctor about the risks and benefits of this surgery. Last updated: November 15, 2023 NEWS AND RESOURCES Yag Laser Vitreolysis ProgramThe YAG Laser Vitreolysis (YLV) program addresses an unmet need – to determine the efficacy of YLV in treating disturbing floaters from vitreous opacities. To  VMRR PROJECTS 2024-26Over the past years, the VMR Research Foundation has been at the forefront of efforts to shed light on vision-degrading myodesopsia (VDM) and elevate its  EYE FLOATERS RESEARCH: UPDATE APRIL 2023Dear Sufferers, Recently Dr. Sebag released a brief interview with some important updates for the VDM PROJECT. The VMR RESEARCH FOUNDATION, along with prominent partners   VMR RESEARCH FOUNDATION | ACHIEVEMENTS 2022Alfredo A. Sadun, MD, PhD, Vice-Chair Ophthalmology, Doheny Eye Institute/UCLAJean-Louis Selam, MD, President, University Clinical Investigators, Irvine, CAHoward Slavin, Esq.Gregory C. Beck, CPAJ. Sebag, MD,  Recent Publication on VDM (Part 1 of 3): Etiology and Diagnosis of Vision Degrading MyodesopsiaAttached please find part 1 of a 3-part series on VDM. As you can see, this work was supported in part by the VMR Research  VDM Project Expense ReportDear supporters, Thanks to your generous contributions to our efforts, the VDM Project is proud to announce a list of projects completed by the VMR  Eye Floaters Research: UPDATE JUNE 2022Dear supporters, To offer full transparency, our webinar with Dr. Sebag (dated June 5th 2022) has been recorded and is available to view. We’ll continue  Eye Floaters Prevalence StudyEye Floater Prevalence Study The VDM Project is currently in the process of commissioning a study on the prevalence of vitreous floaters among adults in the United  Dr. Sebag Live Webinar & Q&A (Jan 2021)Dear supporters, To offer full transparency, our webinar with Dr. Sebag (dated January 17th 2021) has been recorded and is available to view. In this  Research Update: January 2021Dear VDM Project supporters, As 2021 begins, we are continuing our fight to find a safe and effective cure for Vision Degrading Myodesopsia (Eye Floaters). Subscribe to the newsletterStay up to date with latest research, goals and plans. Wee need your support. Together, we must unite for clear vision. © 2020 All Rights Reserved | VMR RESEARCH FOUNDATION | IRS Registration EIN: 61-1888947  By Michelle Stephenson, Contributing Editor Treating Floaters: The Pros, Cons and TechniquesSome retinal surgeons are modifying their stance on treating floaters in certain symptomatic patients.. F loaters are a common complaint of patients of all ages, often caused by myopia in younger patients, and posterior vitreous detachment in older people. Until recently, vitreous floaters weren’t viewed as something to be treated, and patients just had to cope with them as best as they could. Here, retina specialists discuss the sometimes controversial topic of actually treating these annoying, but sometimes debilitating, opacities. Changing Attitudes “Historically, floaters were dismissed by ophthalmologists, and I was one of those doctors for a very long time,” says Jerry Sebag, MD, FACS, senior scientist at the Doheny Eye Institute/UCLA in Pasadena. “This stemmed from a lack of understanding of the origin of patient complaints and a lack of the ability to clinically measure things to characterize the condition as mild, moderate or severe. We didn’t have those tools and were therefore left to determine whether an individual claiming disturbance by floaters was justified or overreacting. About 15 years ago, I started listening to these patients, and I started to believe them.”
“I realized that we need to begin considering floaters a disease in some people,” Dr. Sebag adds. “Many people have floaters that are inconsequential, but there are also many people who are debilitated by the opacities that induce floaters. ‘Floaters’ is a term that’s misused. It’s mistakenly used to refer to structures within the eye, but floaters are not structures. They’re a visual phenomenon that is created by opacities within the vitreous. When you use ultrasound to image the structures within the eye that cause the visual phenomenon of floaters, we use the term ‘echodensity,’ ” he adds. To further clarify things, Dr. Sebag coined the term “vision degrading myodesopsia” to refer to patients who have clinically significant vitreous floaters. 1 “This term doesn’t roll off your tongue easily, but it sure sounds like a disease. And that’s what’s needed to stimulate the paradigm shift in our perception that must occur if we’re going to help those people who are afflicted, in many cases severely,” Dr. Sebag says. In collaboration with acoustic engineers in New York, and with Dr. Alfredo Sadun at the Doheny Eye Institute in Pasadena, Dr. Sebag developed metrics that he now uses on a routine basis to evaluate patients who complain of floaters. The first metric measures the density of vitreous using quantitative ultrasonography. 2 “Ultrasound used to be a mainstay in evaluating the eye, but ever since optical coherence tomography came along, people tend to default to that rather than use ultrasound to image the structures within the eye. OCT is excellent for the retina, but it’s poor to evaluate vitreous, and so ultrasound has filled that void. We worked with acoustic engineers and developed ways to quantify ultrasound imaging to assess the severity of the structural changes within the vitreous body that cause the visual phenomenon of floaters,” he adds. The other useful metric was to measure contrast sensitivity. 3,4 “While this has been available for many years, ophthalmologists tend not to routinely do that test. Instead, we rely on visual acuity as a measure of the person’s ocular health. While that’s useful for evaluating some diseases, it’s not good in evaluating the visual impact of vitreous opacities. Contrast sensitivity, however, is a very useful way to measure the impact of vitreous opacities on vision and to explain why people are so unhappy,” Dr. Sebag describes. According to Jennifer I. Lim, MD, director of the Retina Service at University of Illinois Health, there are two schools of thought on how to surgically treat floaters. First is a core vitrectomy where the vitreous gel and any visible opacities are removed centrally. Second is the complete vitrectomy with creation of a PVD. “I perform complete vitrectomies, and I induce a PVD if there’s not one already,” she says. Dr. Lim mentions that floaters originate in some patients who are very nearsighted or have other vitreous abnormalities, from vitreous degeneration and liquefaction. “In the other group of patients, where the PVD has occurred, the floaters result from collapse of the vitreous gel and opacities within the gel,” she says. “Floaters may result from liberated tissue/blood/pigment as the vitreous separates from the underlying retina and can also result from a retinal tear, or from a retinal detachment if it occurs during the patient’s PVD. Of course, the risks of inducing a retinal tear are higher while you create a PVD surgically especially in highly myopic eyes with thin retinas. However, if you don’t induce a PVD, over the course of time, that patient will eventually develop a PVD, and when he or she does, that patient will develop floaters, in addition to being at risk for a retinal tear or a retinal detachment at that time. Thus, I like to create the PVD in the operating room where it’s very controlled, and then not have to worry about the patient undergoing a PVD in the future and getting floaters back again.” Dr. Sebag has studied this and found that it occurs in only 14.1 percent of individuals who have undergone limited vitrectomy without intraoperative PVD induction. 5 None of those cases developed retinal tears or detachments. Dr. Lim adds that, “Once you navigate the psychosocial and physical exam aspects of it, it’s a reasonable procedure to do. I’m quite pleased that my patients are doing well. This includes both the older patients who have the PVD, as well as the younger ones who just have the liquified vitreous and are very bothered by the floaters. Some of them—who have floaters in both eyes—after they have one eye done, want the other eye done as well because they’re so happy to be free of floaters. I have patients who are several years out from surgery, and they’re quite pleased with their outcome.”
If a patient has a cataract and vitreous floaters, she performs a combined case and has an anterior segment surgeon remove the cataract. Then, she performs the vitrectomy for the floaters. Dr. Sebag’s procedure of choice is a limited vitrectomy. “I leave 3 or 4 mm of gel vitreous behind the lens intact to mitigate against cataract formation, and if the patient doesn’t have a PVD, I don’t induce one surgically, to minimize the risks of retinal tears and detachments but also to limit the increase of intravitreal oxygen levels that occurs following vitrectomy,” he says. “It’s the increase of O 2 in vitreous that causes the changes in the lens that result in cataract formation. So, limited vitrectomy was developed in recognition of the fact that doing vitrectomy for floaters needed to be as safe as possible. To increase the safety profile, I avoided inducing a PVD and hoped that, as a result, the incidence of retinal tears and detachments would be lower. It turns out that this only occurs 1.5 percent of the time, meaning that limited vitrectomy is 98.5-percent safe,” he says. In 2018, he published a study of 195 subjects who were treated with limited vitrectomy. 6 This study had a high success rate as determined by quantitative ultrasonography and by measuring contrast sensitivity. “Concerning the latter,” says Dr. Sebag, “in 139 consecutive cases who preoperatively had an average degradation in contrast sensitivity of 91 percent in comparison to controls, contrast sensitivity was normal in each case within a week of limited vitrectomy, and that was sustained for months and years thereafter. Cataract surgery was required in only 16.9 percent of cases, and retinal detachments only occurred in 1.5 percent of cases.
“Moreover, the patients were extremely happy, and we also documented that quantitative ultrasonography was significantly better in this series of patients,” Dr. Sebag adds. “The complication rates were very acceptable. This study showed that limited vitrectomy was highly effective and safe.” Studies have also shown that, after limited vitrectomy in patients who are unhappy after cataract surgery with multifocal IOL implantation, contrast sensitivity improved, in spite of the multifocal intraocular lens. 7 Dr. Sebag therefore recommends vitreous evaluation in patients who are unhappy with multifocal pseudophakia and that there be consideration of limited vitrectomy for these unhappy patients. He has performed more than 300 limited vitrectomies on all types of patients. “So far, limited vitrectomy has been found to be more cost effective than amblyopia therapy, cataract surgery, and retinal detachment repair,” 8 he says. YAG laser vitreolysis (YLV) is an alternative to vitrectomy, because surgery isn’t for everyone. “In spite of being highly skeptical of YLV in the past, I’ve opened my mind to the possibility that YLV has a role in certain cases,” says Dr. Sebag. “Whereas YLV has been done for years all over the world, it hasn’t been embraced by the vitreoretinal surgery community. It’s being done by general ophthalmologists, and I wonder whether it might be embraced by the vitreoretinal community and perhaps be done with greater precision and efficacy if it could be shown to be effective in a subgroup of individuals.”
He believes that YLV will be somewhat successful, but not in all patients. “The reason is that there’s more than one cause for vision-degrading myodesopsia and vitreous floaters,” he notes. “The leading cause is a PVD, which tends to be the case in older individuals. I think that in those individuals, it will turn out that YAG laser isn’t effective, except for the subset of people who have a disturbing Weiss ring or a particularly prominent central vitreous opacity in whom YLV might be effective, at least subjectively by questionnaire evaluation and perhaps also by contrast sensitivity measurements.” He believes that patients with myopic vitreopathy, which is the second leading cause for vitreous floaters and vision-degrading myodysopsia, 9 may be good candidates for YAG laser treatment. “These people tend to be younger and don’t have a PVD, so those may be the individuals who should be treated with YAG laser. We’re currently conducting a prospective clinical trial of YLV and hope to report the results in the not-too-distant future,” he says. Other technologies are currently being considered for treating vitreous floaters. “Picosecond and femtosecond lasers may prove to be more effective than YAG laser, especially if the treatment can be localized with 3D imaging guidance of the laser energy,” says Dr. Sebag. “That would help YLV, as well, but with more powerful lasers, we will probably be able to ablate the opacities rather than just break them down, which is what’s occurring now with the YAG laser. Pharmacologic vitreolysis may also play an important role in chemically breaking down the aggregates of collagen that are in the vitreous body that cause the shadows that result in the visual phenomenon of floaters and degradation of contrast sensitivity. I’m very excited about the possibility of developing drugs and injecting them into the vitreous body to treat vitreous floaters and vision degrading myodesopsia. “Following the recent anti-VEGF experience,” Dr. Sebag continues, “we’re all comfortable injecting drugs into the vitreous body, so it wouldn’t be that hard to get the community to accept pharmacologic vitreolysis as a treatment paradigm for vision degrading myodesopsia, but we need to develop the right drugs and use them at the right dose, so a lot of work needs to be done in that regard.” Another approach is being developed at the University of Ghent in Belgium using nanoparticles that are specifically designed to adhere to the opacities within the vitreous body that are causing floaters and vision-degrading myodesopsia. 10 “After injecting the nanoparticles, a low-energy laser is used to treat the vitreous body, which doesn’t have to be targeted because the nanoparticles chemically adhere to the opacities and preferentially absorb the laser energy, creating localized nanobubbles that break up the membranes and aggregates of collagen that are causing the floaters and vision degrading myodesopsia,” explains Dr. Sebag. “This has been developed in vitro and has been tested in rabbits in vivo . 10 It’s been shown that the laser energy levels that are required are 1,000 times less than what’s currently being used for YLV. I would like to see it developed further for the treatment of patients with vitreous floaters.” Then, there is an optical approach. “If we understood the optics and physics of how light is interacting with the structures within the vitreous body that are causing floaters and inducing vision-degrading myodesopsia, 11 perhaps that could be corrected with an optical apparatus that counteracts the untoward effects of light scattering, which degrade contrast sensitivity. If we neutralize that, maybe we could decrease the symptoms and lessen the impact by treating optically,” Dr. Sebag says. Dr. Sebag concludes that, “It’s not often that you come across an unmet medical need, where simply opening your mind and heart not only opens new diagnostic and therapeutic avenues, but resonates with patients. They feel ignored, they feel dismissed, they sometimes even feel insulted by the approach that we’ve taken up until now. But, as is always the case with increased knowledge and good science, we become armed with the tools that will help us understand the plight of our patients and enable us to develop better ways to evaluate what’s happening to them, as well as more effective and safer ways to treat them.” Dr. Lim has no financial interests to disclose. Dr. Sebag has IP interests in the patents for quantitative ultrasonography and Nanobubble therapy. 1. Sebag J. Vitreous and vision degrading myodesopsia. Prog Retinal Eye Res 2020;100847. 2. Mamou J, Wa CA, Yee KM, et al. Ultrasound-based quantification of vitreous floaters correlates with contrast sensitivity and quality of life. Invest Ophthalmol Vis Sci 2015;56:1611-1617. 3. Garcia G, Khoshnevis M, Yee KM, Nguyen-Cuu J, Nguyen JH, Sebag J. Degradation of contrast sensitivity following posterior vitreous detachment. Am J Ophthalmol 2016;172:7-12. 4. Garcia G, Khoshnevis M, Nguyen-Cuu J, et al. The effects of aging vitreous on contrast sensitivity function. Graefe’s Arch Clin Exp Ophthalmol 2018;256:919-925. 5. Boneva SK, Nguyen JH, Gui W, et al. Recurrent floaters following limited vitrectomy for vision degrading myodesopsia. Retina 2023;43:1114-1121. 6. Sebag J, Yee KMP, Nguyen JH, Nguyen-Cuu J. Long-term safety and efficacy of limited vitrectomy for vision degrading myodesopsia resulting from vitreous floaters. Ophthalmology Retina 2018;2:881-887. 7. Nguyen JH, Yee KMP, Nguyen-Cuu, et al. Vitrectomy improves contrast sensitivity in multifocal pseudophakia with vision degrading myodesopsia. Am J Ophthalmol 2022;244:196-204. 8. Rostami B, Nguyen-Cuu J, Brown G, et al. Cost-effectiveness of limited vitrectomy for vision degrading myodesopsia. Am J Ophthalmol 2019;204:1-6. 9. Nguyen JH, Nguyen-Cuu J, Mamou J, et al. Vitreous structure and visual function in myopic vitreopathy causing vision degrading myodesopsia. Am J Ophthalmol 2021;224:246-253. 10. Sauvage F, Nguyen VP, Li Y, et al. Laser-induced nanobubbles safely ablate vitreous opacities in vivo. Nature Nanotechnology 2022;17:552-559. 11. Paniagua-Diaz A, Nguyen JH, Artal P, Sebag J. Light scattering by vitreous of humans with Vision Degrading Myodesopsia from floaters. Invest Ophthalmol Vis Sci 2024 (In Press). Related ArticlesDistinguishing infection post-intravitreal injection, updates from the pro study group, study examines features of early glaucoma. 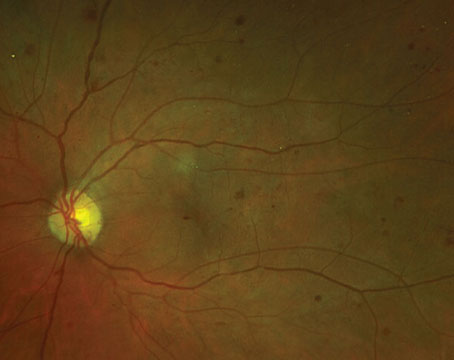 Diabetic Retinopathy: Planning Your TreatmentAddressing the anti-vegf treatment burden, current issue.  Table of ContentsRead digital edition, read pdf edition, subscriptions.
 Copyright © 2024 Jobson Medical Information LLC unless otherwise noted. All rights reserved. Reproduction in whole or in part without permission is prohibited.
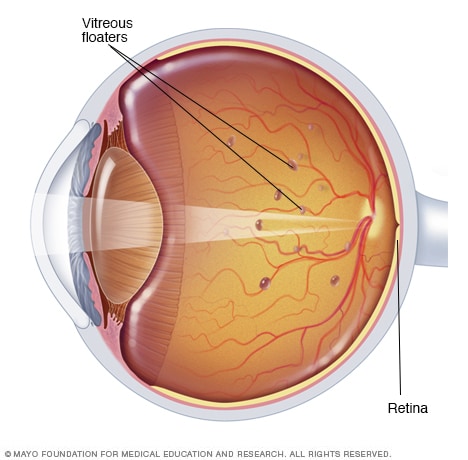 As you age, the vitreous — a jelly-like material inside your eyes — liquifies and contracts. When this happens, microscopic collagen fibers in the vitreous tend to clump together. These scattered pieces cast tiny shadows onto your retina. The shadows you see are called floaters. Eye floaters are spots in your vision. They may look to you like black or gray specks, strings, or cobwebs. They may drift about when you move your eyes. Floaters appear to dart away when you try to look at them directly. Most eye floaters are caused by age-related changes that occur as the jelly-like substance (vitreous) inside your eyes liquifies and contracts. Scattered clumps of collagen fibers form within the vitreous and can cast tiny shadows on your retina. The shadows you see are called floaters. If you notice a sudden increase in eye floaters, contact an eye specialist immediately — especially if you also see light flashes or lose your vision. These can be symptoms of an emergency that requires prompt attention. Products & Services
Symptoms of eye floaters may include:
When to see a doctorContact an eye specialist immediately if you notice:
These painless symptoms could be caused by a retinal tear, with or without a retinal detachment. This is a sight-threatening condition that requires immediate attention.
Jason Howland: Having vision problems? Do you see black or gray specks, strings or cobwebs that drift about when you move your eyes? It could be eye floaters. Amir Khan, M.D., Consultant, Ophthalmology, Mayo Clinic: In the back of our eyes, we have a substance called "the vitreous." When we're young, it's a firm clump of jelly. As we age, this firm clump of jelly can liquefy and break up into smaller pieces. Those smaller pieces are what you may notice as floater. Mr. Howland: Eye floaters are more common as you get older and if you're nearsighted. The biggest concern – they can cause retinal tears. Dr. Khan: If a tear develops in the retina, fluid can get in underneath that tear and just lift the retina off like wallpaper off a wall and that's a retinal detachment. Mr. Howland: And that can cause blindness, which is why it's especially important to have a dilated eye exam within days of noticing new floaters or changes in vision. Most eye floaters don't require treatment, but your eye doctor likely will recommend regular eye exams to ensure the condition doesn't worsen. For the Mayo Clinic Newsnetwork, I'm Jason Howland. There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form. From Mayo Clinic to your inboxSign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required Error Include a valid email address To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Thank you for subscribing!You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Sorry something went wrong with your subscriptionPlease, try again in a couple of minutes 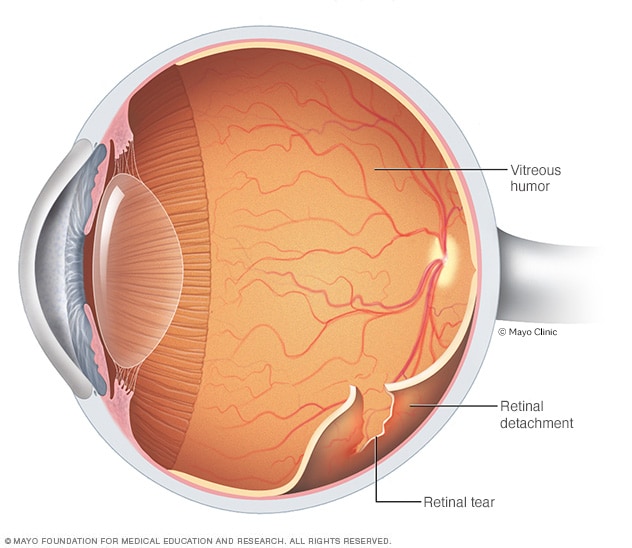 Retinal detachmentRetinal detachment describes an emergency situation in which a thin layer of tissue (the retina) at the back of the eye pulls away from the layer of blood vessels that provides it with oxygen and nutrients. Retinal detachment is often accompanied by flashes and floaters in your vision. Eye floaters may be caused by vitreous changes related to aging or from other diseases or conditions: Age-related eye changes. The vitreous is a jelly-like substance made primarily of water, collagen (a type of protein) and hyaluronan (a type of carbohydrate). The vitreous fills the space in your eye between the lens and retina and helps the eye maintain its round shape. As you age, the vitreous changes. Over time, it liquifies and contracts — a process that causes it to pull away from the eyeball's inside surface. As the vitreous changes, collagen fibers within the vitreous form clumps and strings. These scattered pieces block some of the light passing through the eye. This casts tiny shadows on your retina that are seen as floaters.
Risk factorsFactors that can increase your risk of eye floaters include:
News from Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Mayo Clinic PressCheck out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
We’re transforming healthcareMake a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.  New Research Could Mean Less Invasive Eye Floater Treatment A non-invasive method of treating eye floaters has yet to be devised, forcing patients to either undergo surgery or learn to live with the ailment. However, a pair of doctors at Ophthalmic Consultants of Boston may have discovered a solution involving the use of YAG lasers. These lasers are typically used for surgeries involving cataracts. After testing over thirty patients, over fifty percent of the patients that received treatment saw a decrease in floaters over a six month period compared to the nine percent that received a placebo. The results of the testing have yet to show any side effects and the treatment appears to be safe, but it remains to be seen if any issues will arise in the long term. The future bodes well for using YAG lasers to one day treat floaters in a less invasive way. This information is presented by Retina Macula Specialists of Miami, the largest private retina practice in the city. We are a nationally acclaimed retina practice dedicated to the medical and surgical management of vitreoretinal diseases. Each of our extensively trained doctors are Diplomates of the American Board of Ophthalmology and are highly qualified to treat a wide variety of retinal conditions including but not limited to diabetic retinopathy, retinal detachment, vitreous hemorrhage treatment macular problems, age-related macular degeneration , and CSR. We have three convenient locations in Miami, Coral Gables, and North Miami Beach. For contact information or to request an appointment, please visit https://www.retinamaculamiami.com . Tags: retina macula specialists , vitreous hemorrhage treatment Leave a Reply Cancel replyYour email address will not be published. Required fields are marked * Save my name, email, and website in this browser for the next time I comment. Quick Links
Retinal Diseases
Download Forms
 Our OfficesDesign and Development by AdviceMedia | MedNet Sitemap | Terms of Use Eye Floaters News and ResearchFurther reading.
 FDA approves first targeted RNA-based treatment for rare, fatal genetic diseaseThe U.S. Food and Drug Administration today approved Onpattro (patisiran) infusion for the treatment of peripheral nerve disease (polyneuropathy) caused by hereditary transthyretin-mediated amyloidosis (hATTR) in adult patients.  ThromboGenics receives FDA approval for Jetrea to treat symptomatic vitreomacular adhesionOn Oct. 17, the U.S. Food and Drug Administration approved Jetrea (ocriplasmin), the first drug approved to treat an eye condition called symptomatic vitreomacular adhesion (VMA).
 Revolutionizing Life Science: An Interview with SCIEX on ASMS, the SCIEX 7500+ System, and AI-Driven QuantitationJose Castro-Perez and Chris Lock, SCIEX In our latest interview, News Medical speaks with SCIEX, a global leader in life science analytical technologies, about their exciting announcements at ASMS, the SCIEX 7500+ System, and how they utilize AI quantitation software to streamline solutions.  From Discovery Biology to ELRIG ChairMelanie Leveridge In this interview, we speak with Melanie Leveridge, Vice President of Discovery Biology at AstraZeneca and Chair of the Board for ELRIG UK, to discuss her extensive career in the pharmaceutical industry, her role in fostering scientific innovation, and her vision for ELRIG's future.  Breathing New Life into Diagnostics: Plasmion's SICRIT TechnologyRevolutionizing Non-Invasive Diagnostics with Plasmion’s SICRIT Breath Analysis.  Latest News Your AI Powered Scientific Assistant Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net. A few things you need to know before we start. Please read and accept to continue.
Great. Ask your question. Azthena may occasionally provide inaccurate responses. Read the full terms . While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided. Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles. Please do not ask questions that use sensitive or confidential information. Read the full Terms & Conditions . Provide Feedback
Mayo Clinic Q and A: Most eye floaters caused by age-related changesCynthia Weiss Share this: DEAR MAYO CLINIC: My dad mentioned to me that he has several dark spots and cobweblike strings that interfere with his vision. Is this something to be concerned about? What is needed to fix this condition? ANSWER: Dark spots, such as those you describe, may be eye floaters . These black or gray specks, strings, or cobwebs typically drift about when you move your eyes and appear to dart away when you look at them directly. They may be most noticeable when you look at a plain, bright background, like the blue sky or a white wall. People who need glasses to see distance, called being nearsighted , are more likely to get floaters. They also are more common in adults older than 50, as well as in people who’ve experienced eye trauma or inflammation inside the eye. The presence of a few long-standing floaters usually is not a cause for concern. Most are caused by age-related changes that occur as the jellylike substance inside the eye, called vitreous, becomes more liquid. When this happens, tiny fibers within the vitreous tend to clump and can cast tiny shadows on the retina. 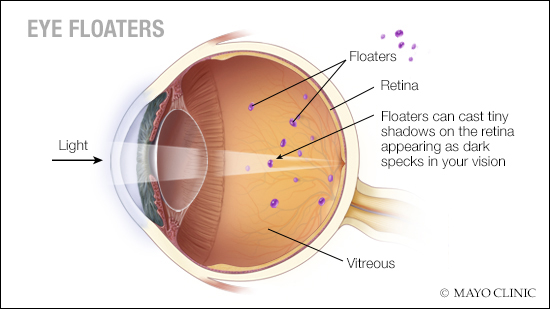 Although usually harmless, not all floaters are nonthreatening clumps of vitreous, so it is a good idea to have any new floaters examined with a dilated eye exam by an optometrist or an ophthalmologist. If he has not already done so, you should suggest to your father that he see a local eye specialist. In the event that your father notices a sudden increase in floaters in one eye, he should seek immediate medical attention. In particular, prompt attention is needed if he sees light flashes or experiences a loss of peripheral vision. These changes may signal the presence of a retinal tear or a retinal detachment. If caught early, a retinal tear may be able to be treated with laser. If the tear has progressed to a retinal detachment , then surgery in the operating room is needed to repair the detachment. If left untreated, full detachment can lead to vision loss in the affected eye. In rare situations an eye care professional may recommend surgical treatment. That can involve surgery to remove the vitreous, which is called a vitrectomy. However, there are risks, including bleeding and retinal tears, and the surgery may not remove all the floaters. Another treatment used infrequently for impaired vision caused by eye floaters is laser therapy. This treatment uses a laser to break up the floaters, making them less noticeable. Laser therapy risks still are not completely known. As with any eye problem, if you are concerned about eye floaters, it is best to discuss your situation with an eye care professional, who will conduct a complete eye exam. By examining the back of the eyes and the vitreous, your eye care professional can determine the cause of the floaters. — Dr. Amir Khan , Ophthalmology, Mayo Clinic, Rochester, Minnesota
Related Articles Malaysia falls to 34th in IMD World Competitiveness Ranking, now below Thailand and Indonesia E-hailing driver charged with outraging modesty of female shopper in Selayang First look at Malaysia’s first Apple Store at The Exchange TRX, four days to its official launch Kajang goldsmith robbery: RM3.2m in losses, seven questioned, say police (VIDEO) MCA chief suggests egg price cut could backfire on government MAHB: KLIA aerotrain project to be completed by January 31, 2025, ahead of schedule China’s Premier Li Qiang arrives in Malaysia for official visit to mark 50 years of diplomatic ties Malaysia ready to roll out dual 5G network, says Fahmi Tesla Cybertruck coming soon to Penang PM Anwar: Implications of MACC oversight by Parliament must be considered Afghanistan: What happens to single moms under Taliban rule? Domestic Trade Ministry to take action against trader for selling cooking gas above controlled price in viral video Cops: Unemployed man caught with nearly 100kg of cannabis in Penang raid Sarawak MP moots training Malaysian teachers in China, Taiwan instead of western countries for cheaper and higher standards Thailand passes landmark bill recognising marriage equalitySeeing worms and webs expert says eye floaters eventually fade but get them checked first. KUALA LUMPUR, June 18 — Tuan Amira Nadhirah Tuan Yunazri started noticing “tiny creatures” floating whenever she moved her head when she was seven years old. At first, she kept rubbing her eyes to remove what she thought was debris but the strange shapes persisted. “Sometimes, I would wonder if I was dizzy or whether I was just imagining the dots, worm-like threads or cobwebs that I saw. “Now, I have got used to living with eye floaters although they can be quite annoying, especially when I am driving or reading,” the 28-year-old lawyer from Johor Baru said. Eye floaters appear when the gel-like vitreous located between the lens and the retina begins to dissolve and becomes watery at the centre as we age. Through a process called posterior vitreous detachment (PVD), the peripheral vitreous gel breaks loose from the retina, leaving behind some undissolved gel particles or floaters. Floaters are common, affecting seven out of 10 people of all ages and is generally more prevalent among individuals over the age of 50. However, Pantai Hospital Ampang ophthalmologist Dr Sunita Padmanabhan noted a higher prevalence of eye floaters among younger people, citing a 2013 study published in the International Journal of Ophthalmology. The study, which surveyed 603 smartphone users, found that 76.3 per cent of respondents under 23 years old and 77.6 per cent of those aged between 24 and 34 years old had eye floaters. “The advent of digital gadgets means we use our vision a lot more now, resulting in more strain on our eyes. “Floaters, however, eventually settle down beneath your field of vision and become less noticeable unless you stare into a bright light or at the sky. “So, it is extremely rare for those with floaters to undergo treatment unless the condition is caused by retinal damage,” Dr Sunita explained. Near-sighted individuals, she said, may notice floaters at an early age because the elongated shape of their eyes increases the likelihood for PVD to happen. Similarly, she said trauma induced to the eyes, such as cataract surgery, can also cause floaters. Although floaters are typically harmless, Dr Sunita cautioned that they could be a warning sign of retinal tear or detachment that could potentially lead to loss of vision. In such cases, she said the retina must be reattached as soon as possible to restore eye function and avoid permanent blindness. “Get your eyes checked immediately if the number of floaters increases suddenly or if you see light flashes (photopsia). Photopsia occurs if your retina is tugged, torn or detached. “Otherwise, floaters are harmless. So, the best advice is to try and ignore them and go about your life as you normally would. “Trust me, you will see them less often. “If in doubt, always consult your ophthalmologist and seek their advice. Prevention is better than cure," she said. You May Also LikeRelated articles.  Pharrell Williams kicks off Paris Fashion Week with Louis Vuitton show at Unesco Sitting watching TV could be particularly harmful to health, study shows A consistent routine is crucial to avoiding children’s bedtime battles, scientists say Consumers welcome egg price cut but want broader reductions in essential food items Premier Li Qiang ready to build stronger China-Malaysia community during visit COVID can seriously damage your vision, even if you didn’t have symptoms, new study says. Experts say to watch for these signs If you’ve had COVID-19, you may want to have your eyes checked. SARS-CoV-2, the coronavirus that causes the disease, can infect the inside of your eyes, according to research published in April in the journal PLOS Pathogens . This holds true even if the virus didn’t enter your body through the surface of your eyes. Pawan Kumar Singh, PhD , an assistant professor of ophthalmology at the University of Missouri School of Medicine , led a team of researchers who found that inhaled viruses can reach highly protected organs such as the eyes, potentially causing long-term damage. SARS-CoV-2 does so by breaching the blood-retinal barrier , layers of cells that shield the retina , the part of your eye that senses light, from microbial pathogens. “Earlier, researchers were primarily focused on the ocular surface exposure of the virus,” Singh said in a news release . “However, our findings reveal that SARS-CoV-2 not only reaches the eye during systemic infection but induces a hyperinflammatory response in the retina and causes cell death in the blood-retinal barrier. The longer viral remnants remain in the eye, the risk of damage to the retina and visual function increases.” Using a humanized mice model, Singh and his team showed that the prolonged presence of SARS-CoV-2 spike proteins can cause problems such as:
“For those who have been diagnosed with COVID-19, we recommend you ask your ophthalmologist to check for signs of pathological changes to the retina,” Singh said. “Even those who were asymptomatic could suffer from damage in the eyes over time because of COVID-19-associated complications.” What are symptoms of retinal disease?The following symptoms may indicate retinal disease, according to the National Eye Institute :
If you don’t have an ophthalmologist, your primary care physician can refer you to one and help determine the best course of treatment. Though the blood-retinal barrier of people with compromised immune systems is known to be susceptible to bacteria and viruses, MU claims Singh’s study is the first to suggest SARS-CoV-2 can infect that of otherwise healthy people. That said, immunocompromised people and those with diabetes or high blood pressure may face more severe COVID-related eye health issues if left untreated. “Now that we know the risk of COVID-19 to the retina, our goal is to better understand the cellular and molecular mechanisms of how this virus breaches the blood-retinal barrier and associated pathological consequences in hopes of informing development of therapies to prevent and treat COVID-19-induced eye complications before a patient’s vision is compromised,” Singh said. For more on COVID-19:
Most Popular Researchers film energy materials as they formEyes glued to a live transmission from inside a reaction vessel. Shooting a movie in the lab requires special equipment. Especially when the actors are molecules -- invisible to the naked eye -- reacting with each other. "Imagine trying to film tiny lava flows during a volcanic eruption. Your smartphone camera wouldn't be up to the job. First, you'd need to develop a special method to make the action you want to capture visible," says Prof. Emiliano Cortés, Professor of Experimental Physics and Energy Conversion at LMU. But the effort is worth it -- particularly when the product of the reaction is a promising energy material: so-called covalent organic frameworks (COFs). Still quite young, this material class has great potential for applications in battery technology and the manufacture of hydrogen. But despite 20 years of intensive research, scientists have been unable to fully elucidate what actually happens during the synthesis of COFs. As such, materials are often developed by trial and error. This has also been the case for COFs where several molecular components have to find the correct place during synthesis. Only then does the desired porous framework form over large areas. "Finding out why synthesis only works under certain conditions and not under others has intrigued me since my master's days. Our approach in this project was to use the tools of physics to support chemists in their work. We wanted to shed more light on the complex synthesis processes and thus optimize them," explains Christoph Gruber, who is researching this topic in Cortés's team as part of his doctoral dissertation. To this end, the two scientists turned to the research group of LMU chemist Prof. Dana Medina, who is specialized in the synthesis of COFs, to establish a collaboration. For the film shoot with the molecular stars, Gruber used a special microscope. With this tool, the team managed to follow the formation mechanism of the COFs at the nano level. The LMU researchers recently published their groundbreaking results in the journal Nature , accompanied by a video showing the processes that occur during synthesis in real time. Their research was made possible by funding from the e-conversion Cluster of Excellence (DFG), the Center for Nanoscience (CeNS), the Bavarian solar technologies program SolTech, and the European Commission (EC). Early order is critical Synthesis of the molecular frameworks demands one thing above all: precise control of the reaction and self-assembly of the molecular building blocks present. "Only when you have this control it is probable to obtain a highly crystalline structure with an extensive order and, ultimately, the desired functionality," says Medina. "However, our knowledge particularly of the early stages of nucleation and growth is full of gaps. And this has thwarted the development of effective synthesis protocols. We therefore were extremely intrigued to visualize the reaction as it unfolds and set the focus on the earliest stages when the mixed molecular components are starting to react." This is precisely where Gruber started with his investigations, choosing what would seem at first glance to be an unconventional method to cast light on the opening scene of COF formation: iSCAT microscopy. The abbreviation stands for interferometric scattering, and biophysicists often use this technology to investigate things like the interaction of proteins. "The measurement principle is based on the fact that even the tiniest of particles, made up of just a few molecules, scatter incident light. If these scattered light waves overlap, we get interference -- just like water waves in a pool. That is to say, we get larger and smaller waves depending on how the waves overlap. We record these light patterns with a high-resolution camera and, with subsequent image processing, we obtain pictures that reveal, for example, nano-scale COF particles," explains Gruber. And here's the kicker: the iSCAT method is suitable for capturing dynamic processes and thus for real-time measurements. This allows the researchers to watch the synthesis live, as it were. Droplets got talent Immediately after the reaction started, the researchers were surprised to observe the presence of tiny structures in the transparent reaction medium. "The images showed us that nanometer-scale droplets can play an essential role in the synthesis. Although they are extremely small, they control the entire kinetics at the beginning of the reaction," says Gruber. "Nothing was known about their existence before now, but for the formation of the COFs we studied, the nano-droplets turned out to be extremely important. If they are absent, the whole reaction happens too quickly and the desired order is lost." Using the iSCAT method, the LMU team managed to record a film showing the formation of the molecular frameworks from the beginning -- with a sensitivity of just a few nanometers. "Existing techniques couldn't capture the start of the reaction, with these nano-scale and millisecond-long processes, in real time," says Cortés. "Through our research, we've now managed to close this gap in our knowledge. At the same time, we're getting a holistic picture of the early stages of the reaction and the progressive formation of the COFs." Energy-efficient synthesis Furthermore, the researchers used the film clip and the resulting analyses to design an energy-efficient synthesis concept. "Building on our results, we discovered how to rationally design the reaction conditions," explains Medina. "By adding normal table salt, for example, we were able to massively reduce the temperature, such that the molecular frameworks form at room temperature as opposed to 120 degrees Celsius." The researchers are convinced their results will transform how we think about the synthesis of the over 300 different COFs and could therefore drive forward advances in industrial COF production. Moreover, the results could have far-reaching effects on the synthesis of other materials and on chemical reactions that have not yet been observed in real time. The LMU researchers are excited about shooting new films with molecules in the starring role.
Story Source: Materials provided by Ludwig-Maximilians-Universität München . Note: Content may be edited for style and length. Journal Reference :
Cite This Page : Explore More
Trending TopicsStrange & offbeat.  Suggested SearchesClimate Change
Humans in Space Earth & ClimateThe solar system, the universe, aeronautics, learning resources, news & events.  NASA, MagniX Altitude Tests Lay Groundwork for Hybrid Electric Planes Perseverance Finds Popcorn on Planet Mars NASA Satellites Find Snow Didn’t Offset Southwest US Groundwater Loss
 NASA Releases Hubble Image Taken in New Pointing Mode Investigating the Origins of the Crab Nebula With NASA’s Webb Lakita Lowe: Leading Space Commercialization Innovations and Fostering STEM Engagement Former Astronaut Russell L. “Rusty” Schweickart NASA’s Repository Supports Research of Commercial Astronaut Health NASA-Led Mission to Map Air Pollution Over Both U.S. Coasts NASA Announces New System to Aid Disaster Response Tropical Solstice Shadows NASA’s LRO Spots China’s Chang’e 6 Spacecraft on Lunar Far Side The Next Full Moon is the Strawberry Moon Hubble Observes a Cosmic Fossil Happy Birthday, Redshift Wrangler! Sols 4216-4218: Another ‘Mammoth’ Plan! Globetrotting NASA Research Model Increases Accuracy ARMD Solicitations Flight Test Sheds New Light on In-Space 3D Printing, Propellant Slosh NASA’s Roman Mission Gets Cosmic ‘Sneak Peek’ From Supercomputers Ed Stone, Former Director of JPL, Voyager Project Scientist, Dies Slow Your Student’s ‘Summer Slide’ and Beat Boredom With NASA STEM 15 Years Ago: Lunar Reconnaissance Orbiter Begins Moon Mapping Mission NASA Interns Blast Off for Their First Week at Goddard NASA Announces Winners of 2024 Student Launch Competition Astronauta de la NASA Frank Rubio Diez maneras en que los estudiantes pueden prepararse para ser astronautas Astronauta de la NASA Marcos BerríosNasa, global astronomers await rare nova explosion.  Beth RidgewayFinding t coronae borealis, a coordinated scientific approach.  Around the world this summer, professional and amateur astronomers alike will be fixed on one small constellation deep in the night sky. But it’s not the seven stars of Corona Borealis, the “Northern Crown,” that have sparked such fascination. It’s a dark spot among them where an impending nova event – so bright it will be visible on Earth with the naked eye – is poised to occur. “It’s a once-in-a-lifetime event that will create a lot of new astronomers out there, giving young people a cosmic event they can observe for themselves, ask their own questions, and collect their own data,” said Dr. Rebekah Hounsell, an assistant research scientist specializing in nova events at NASA’s Goddard Space Flight Center in Greenbelt, Maryland. “It’ll fuel the next generation of scientists.” T Coronae Borealis, dubbed the “Blaze Star” and known to astronomers simply as “T CrB,” is a binary system nestled in the Northern Crown some 3,000 light-years from Earth. The system is comprised of a white dwarf – an Earth-sized remnant of a dead star with a mass comparable to that of our Sun – and an ancient red giant slowly being stripped of hydrogen by the relentless gravitational pull of its hungry neighbor. The hydrogen from the red giant accretes on the surface of the white dwarf, causing a buildup of pressure and heat. Eventually, it triggers a thermonuclear explosion big enough to blast away that accreted material. For T CrB, that event appears to reoccur, on average, every 80 years. Don’t confuse a nova with a supernova, a final, titanic explosion that destroys some dying stars, Hounsell said. In a nova event, the dwarf star remains intact, sending the accumulated material hurtling into space in a blinding flash. The cycle typically repeats itself over time, a process which can carry on for tens or hundreds of thousands of years. “There are a few recurrent novae with very short cycles, but typically, we don’t often see a repeated outburst in a human lifetime, and rarely one so relatively close to our own system,” Hounsell said. “It’s incredibly exciting to have this front-row seat.”  The first recorded sighting of the T CrB nova was more than 800 years ago, in autumn 1217, when a man named Burchard, abbot of Ursberg, Germany, noted his observance of “a faint star that for a time shone with great light.” The T CrB nova was last seen from Earth in 1946. Its behavior over the past decade appears strikingly similar to observed behavior in a similar timeframe leading up to the 1946 eruption. If the pattern continues, some researchers say, the nova event could occur by September 2024. What should stargazers look for? The Northern Crown is a horseshoe-shaped curve of stars west of the Hercules constellation, ideally spotted on clear nights. It can be identified by locating the two brightest stars in the Northern Hemisphere – Arcturus and Vega – and tracking a straight line from one to the other, which will lead skywatchers to Hercules and the Corona Borealis. The outburst will be brief. Once it erupts, it will be visible to the naked eye for a little less than a week – but Hounsell is confident it will be quite a sight to see. To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video Dr. Elizabeth Hays, chief of the Astroparticle Physics Laboratory at NASA Goddard, agreed. She said part of the fun in preparing to observe the event is seeing the enthusiasm among amateur stargazers, whose passion for extreme space phenomena has helped sustain a long and mutually rewarding partnership with NASA. “ Citizen scientists and space enthusiasts are always looking for those strong, bright signals that identify nova events and other phenomena,” Hays said. “Using social media and email, they’ll send out instant alerts, and the flag goes up. We’re counting on that global community interaction again with T CrB.” Hays is the project scientist for NASA’s Fermi Gamma-ray Space Telescope , which has made gamma-ray observations from low Earth orbit since 2008. Fermi is poised to observe T CrB when the nova eruption is detected, along with other space-based missions including NASA’s James Webb Space Telescope , Neil Gehrels Swift Observatory , IXPE ( Imaging X-ray Polarimetry Explorer ), NuSTAR ( Nuclear Spectroscopic Telescope Array ), NICER ( Neutron star Interior Composition Explorer ), and the European Space Agency’s INTEGRAL ( Extreme Universe Surveyor ). Numerous ground-based radio telescopes and optical imagers, including the National Radio Astronomy Observatory’s Very Large Array in New Mexico, also will take part. Collectively, the various telescopes and instruments will capture data across the visible and non-visible light spectrum. “We’ll observe the nova event at its peak and through its decline, as the visible energy of the outburst fades,” Hounsell said. “But it’s equally critical to obtain data during the early rise to eruption – so the data collected by those avid citizen scientists on the lookout now for the nova will contribute dramatically to our findings.” For astrophysics researchers, that promises a rare opportunity to shed new light on the structure and dynamics of recurring stellar explosions like this one. “Typically, nova events are so faint and far away that it’s hard to clearly identify where the erupting energy is concentrated,” Hays said. “This one will be really close, with a lot of eyes on it, studying the various wavelengths and hopefully giving us data to start unlocking the structure and specific processes involved. We can’t wait to get the full picture of what’s going on.” Some of those eyes will be very new. Gamma-ray imagers didn’t exist the last time T CrB erupted in 1946, and IXPE’s polarization capability – which identifies the organization and alignment of electromagnetic waves to determine the structure and internal processes of high-energy phenomena – is also a brand-new tool in X-ray astronomy. Combining their data could offer unprecedented insight into the lifecycles of binary systems and the waning but powerful stellar processes that fuel them. Is there a chance September will come and go without the anticipated nova outburst from T CrB? Experts agree there are no guarantees – but hope abides. “Recurrent novae are unpredictable and contrarian,” said Dr. Koji Mukai, a fellow astrophysics researcher at NASA Goddard. “When you think there can’t possibly be a reason they follow a certain set pattern, they do – and as soon as you start to rely on them repeating the same pattern, they deviate from it completely. We’ll see how T CrB behaves.” Learn more about NASA astrophysics at: https://science.nasa.gov/astrophysics Jonathan Deal Marshall Space Flight Center, Huntsville, Ala. 256-544-0034 [email protected] Related Terms
Explore More The Marshall Star for June 18, 2024 NASA’s Hubble Space Telescope has taken its first new images since changing to an alternate…  About one year ago the Redshift Wrangler project first asked you to help examine “spectra” of distant… Discover More Topics From NASA Solar System 
Construction impacts Walker Engineering entrances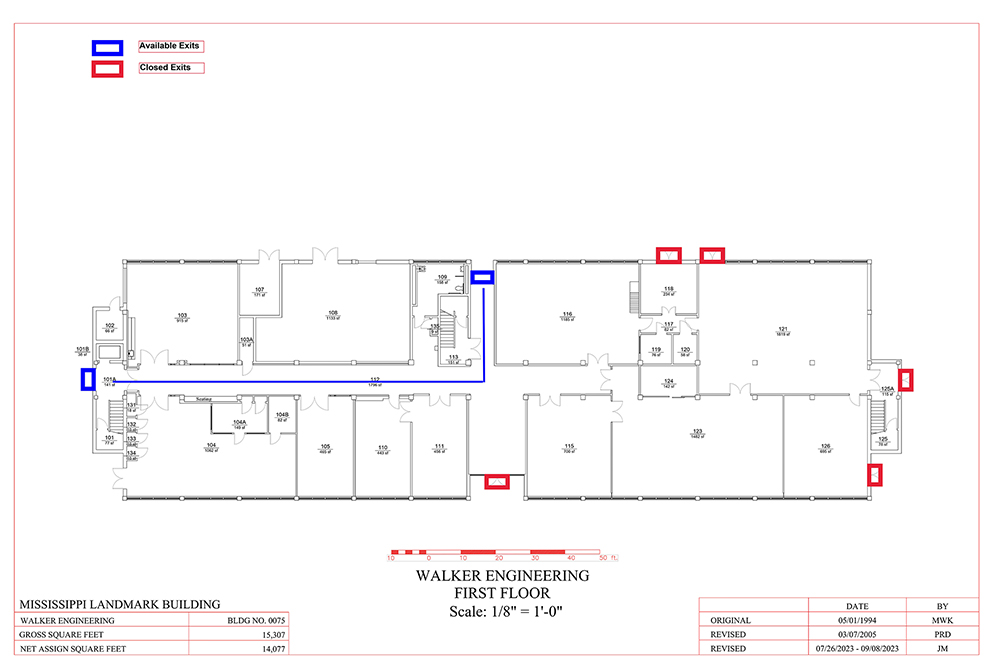 Beginning Wednesday [June 19], access to Walker Engineering will be limited to two entrances due to installation of a new sewer line on the east side of the building. Students, faculty, staff and visitors should use the south and southwest doors highlighted in blue on the map to enter and exit the building. All other entrances will be closed while the project is underway. Work is expected to be completed in mid to late July. Contact the Facilities Management Service Desk at 662-325-2005 with questions. Tuesday, June 18, 2024 - 4:40 pm
You may also be interested in…Booneville high graduates create annual msu scholarship honoring beloved classmate. May 24, 2024 MSU’s Stennis Institute hosting Junior Civics Leadership Academy in JulyJune 12, 2024 MSU's Keith is Iowa State's next provostMay 21, 2024
 |
IMAGES
VIDEO
COMMENTS
Now, with the development of a safer and less invasive nanoparticle-based therapy, people with floaters may finally get their vision and quality of life back. Clumps of collagen float through the vitreous of a patient's eye, causing the appearance of floaters. Credit: Inder Paul Singh. May 01, 2022 | 10 min read. Stephanie DeMarco, PhD.
Laser Floater Treatment (LFT) is a non-surgical procedure performed in the office that is used as one of the current treatments for eye floaters. LFT uses laser light to dissolve eye floaters ...
The severity of floaters and efficacy of treatment options for floaters is evaluated, both in research and ... The most-often used PROM in studies on patients with floaters was the National Eye Institute ... Because of the absence of a reliable and valid PROM with the appropriate content for patients with floaters, the development of a new PROM ...
Vitreous floaters are caused by degenerative or pathologic alterations in the vitreous ultrastructure and perceived as shadows or fly-like obscurations to vision [1,2,3].While patients with ...
A new study published in the Translational Vision Science and Technology (TVST), an ARVO journal, has revealed that targeted nutrition can significantly reduce 'eye floaters' as well as their associated discomforts. This study reports the outcomes of the Floater Intervention Study (FLIES), which was led by the Nutrition Research Centre ...
The primary etiologies of floaters are age, environmental factors (i.e., UV light, blue light), high myopia, and oxidative stress . Additionally, VH-induced ocular floaters are produced from diabetic retinopathy, hypertensive retinopathy, and ocular trauma. In clinics, excessive ocular floaters are too small to be observed by eye doctors.
To describe the eyes with vitreous floaters and to analyze the development of acute symptomatic posterior vitreous detachment (PVD). A retrospective review of medical records was performed on ...
References. Ankamah E, Green-Gomez M, Roche W, Ng E, Welge-Lüßen U, Kaercher Th, Barbur J, Nolan JM. Impact of symptomatic vitreous degeneration on photopic and mesopic contrast thresholds, Clinical and Experimental Optometry. 2021, DOI: 10.1080/08164622.2021.1981116 Mamou J, Wa CA, Yee KMP, et al.Ultrasound-based quantification of vitreous floaters correlates with contrast sensitivity and ...
Shah and Heier tested a new method of pinpointing and eliminating floaters with a YAG laser (a type of laser often used in cataract surgery) on 36 patients. An additional 16 test subjects were ...
The study used color photo imaging to evaluate YAG laser vitreolysis for symptomatic vitreous floaters. A total of 32 patients were participating in the survey based on the visual function questionnaire. After 6 months of follow-ups, color imaging showed improvement in vitreous opacity over time in 93.7% of study eyes.
General practitioners are aware of the visual consequences when both flashes and floaters are present. 23,24 The need to see an ophthalmologist is important because floaters can lead to retinal diseases such as diabetes and retinal detachment. 20,23,24 In contrast, the LLM and virtual assistants do not emphasize the need to see an eye MD.
Medically reviewed on 17-August-2023. Specialist eye hospital group, Optegra, is leading the way in developing a new method to treat floaters, an eye condition which mainly affects young adults whom to date have been told there is little or no treatment and whose distressing symptoms are frequently dismissed.. Symptoms of floaters include dots, shadows or long strands blocking everyday vision ...
While vitrectomy (i.e. surgical excision of vitreous) is currently performed to cure eye floaters, it is invasive, costly, and carries risks. Laser treatment has unproven efficacy and remains rather limited because vitreous opacities have to be located sufficiently far from the retina to avoid photomechanical collateral damage. ... Progress in ...
But most patients who experience vitreous floaters fall into 2 groups: those with a posterior vitreous detachment (PVD) or myopic vitreopathy. PVD and myopic vitreopathy. People in their 50s, 60s, or 70s may develop a PVD and have more significant floaters, said Dr. Chirag Shah. "Most of the time, patients can cope with them because the ...
Most eye floaters don't require treatment. However, any medical condition that is the cause of eye floaters, such as bleeding from diabetes or inflammation, should be treated. Eye floaters can be frustrating and adjusting to them can take time. Once you know the floaters will not cause any more problems, over time you may be able to ignore them ...
A safe and effective cure for eye floaters is our goal - as soon as possible. SUPPORT THE PROJECT ... A new questionnaire created by the VMR Research Foundation specifically measures the negative impact of eye floaters with quantifiable metrics, so we can accurately measure the magnitude of this problem for individuals as well as populations ...
Floaters are small dark shapes that float across your vision. They can look like spots, threads, squiggly lines, or even little cobwebs. Most people have floaters that come and go, and they often don't need treatment. But sometimes floaters can be a sign of a more serious eye condition. So if you notice new floaters that appear suddenly and ...
NEWS AND RESOURCES. NEWS AND RESOURCES. SUPPORT THE PROJECT. News; About Us; Advisory; Research plans; ... EYE FLOATERS RESEARCH: UPDATE APRIL 2023 . ... As 2021 begins, we are continuing our fight to find a safe and effective cure for Vision Degrading Myodesopsia (Eye Floaters). Read More » January 16, 2021 No Comments . Older Post.
Treatment. According to Jennifer I. Lim, MD, director of the Retina Service at University of Illinois Health, there are two schools of thought on how to surgically treat floaters. First is a core vitrectomy where the vitreous gel and any visible opacities are removed centrally. Second is the complete vitrectomy with creation of a PVD.
Many more eye floaters than usual; A sudden onset of new floaters; Flashes of light in the same eye as the floaters; A gray curtain or blurry area that blocks part of your vision; Darkness on a side or sides of your vision (peripheral vision loss) These painless symptoms could be caused by a retinal tear, with or without a retinal detachment.
When the eye's gel-like substance called the vitreous humor breaks off, these drops may cause retina shadows as they float around. Even if you have 20/20 vision, floaters can still happen to you. A non-invasive method of treating eye floaters has yet to be devised, forcing patients to either undergo surgery or learn to live with the ailment.
On Oct. 17, the U.S. Food and Drug Administration approved Jetrea (ocriplasmin), the first drug approved to treat an eye condition called symptomatic vitreomacular adhesion (VMA). 19 Oct 2012
The presence of a few long-standing floaters usually is not a cause for concern. Most are caused by age-related changes that occur as the jellylike substance inside the eye, called vitreous, becomes more liquid. When this happens, tiny fibers within the vitreous tend to clump and can cast tiny shadows on the retina.
The study, which surveyed 603 smartphone users, found that 76.3 per cent of respondents under 23 years old and 77.6 per cent of those aged between 24 and 34 years old had eye floaters. "The advent of digital gadgets means we use our vision a lot more now, resulting in more strain on our eyes.
SARS-CoV-2, the coronavirus that causes COVID-19, can cause ocular infection by breaching the blood-retinal barrier, layers of cells that shield the retina, the part of your eye that senses light ...
Shooting a movie in the lab requires special equipment. Especially when the actors are molecules -- invisible to the naked eye -- reacting with each other. 'Imagine trying to film tiny lava flows ...
Some of those eyes will be very new. Gamma-ray imagers didn't exist the last time T CrB erupted in 1946, and IXPE's polarization capability - which identifies the organization and alignment of electromagnetic waves to determine the structure and internal processes of high-energy phenomena - is also a brand-new tool in X-ray astronomy.
Beginning Wednesday [June 19], access to Walker Engineering will be limited to two entrances due to installation of a new sewer line on the east side of the building. Students, faculty, staff and visitors should use the south and southwest doors highlighted in blue on the map to enter and exit the building.