

ANA Nursing Resources Hub
Search Resources Hub

Critical Thinking in Nursing: Tips to Develop the Skill
4 min read • February, 09 2024
Critical thinking in nursing helps caregivers make decisions that lead to optimal patient care. In school, educators and clinical instructors introduced you to critical-thinking examples in nursing. These educators encouraged using learning tools for assessment, diagnosis, planning, implementation, and evaluation.
Nurturing these invaluable skills continues once you begin practicing. Critical thinking is essential to providing quality patient care and should continue to grow throughout your nursing career until it becomes second nature.
What Is Critical Thinking in Nursing?
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Reflection comes next. Carefully consider whether your actions led to the right solution or if there may have been a better course of action.
Remember, there's no one-size-fits-all treatment method — you must determine what's best for each patient.
How Is Critical Thinking Important for Nurses?
As a patient's primary contact, a nurse is typically the first to notice changes in their status. One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes.
Elements of Critical Thinking in Nursing
To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
- Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing intervention is needed. Keep in mind that there may be multiple options. Use your critical-thinking skills to interpret and understand the importance of test results and the patient’s clinical presentation, including their vital signs. Then prioritize interventions and anticipate potential complications.
- Patient safety. Recognize deviations from the norm and take action to prevent harm to the patient. Suppose you don't think a change in a patient's medication is appropriate for their treatment. Before giving the medication, question the physician's rationale for the modification to avoid a potential error.
- Communication and collaboration. Ask relevant questions and actively listen to others while avoiding judgment. Promoting a collaborative environment may lead to improved patient outcomes and interdisciplinary communication.
- Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues .

How to Develop and Apply Critical-Thinking Skills in Nursing
Critical-thinking skills develop as you gain experience and advance in your career. The ability to predict and respond to nursing challenges increases as you expand your knowledge and encounter real-life patient care scenarios outside of what you learned from a textbook.
Here are five ways to nurture your critical-thinking skills:
- Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice . That knowledge helps you make informed decisions in stressful moments.
- Practice reflection. Allow time each day to reflect on successes and areas for improvement. This self-awareness can help identify your strengths, weaknesses, and personal biases to guide your decision-making.
- Open your mind. Don't assume you're right. Ask for opinions and consider the viewpoints of other nurses, mentors , and interdisciplinary team members.
- Use critical-thinking tools. Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize information, evaluate options, and identify underlying issues.
- Be curious. Challenge assumptions by asking questions to ensure current care methods are valid, relevant, and supported by evidence-based practice .
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart

What is Critical Thinking in Nursing? (Explained W/ Examples)
Last updated on August 23rd, 2023
Critical thinking is a foundational skill applicable across various domains, including education, problem-solving, decision-making, and professional fields such as science, business, healthcare, and more.
It plays a crucial role in promoting logical and rational thinking, fostering informed decision-making, and enabling individuals to navigate complex and rapidly changing environments.
In this article, we will look at what is critical thinking in nursing practice, its importance, and how it enables nurses to excel in their roles while also positively impacting patient outcomes.
What is Critical Thinking?
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
It’s a mental activity that goes beyond simple memorization or acceptance of information at face value.
Critical thinking involves careful, reflective, and logical thinking to understand complex problems, consider various perspectives, and arrive at well-reasoned conclusions or solutions.
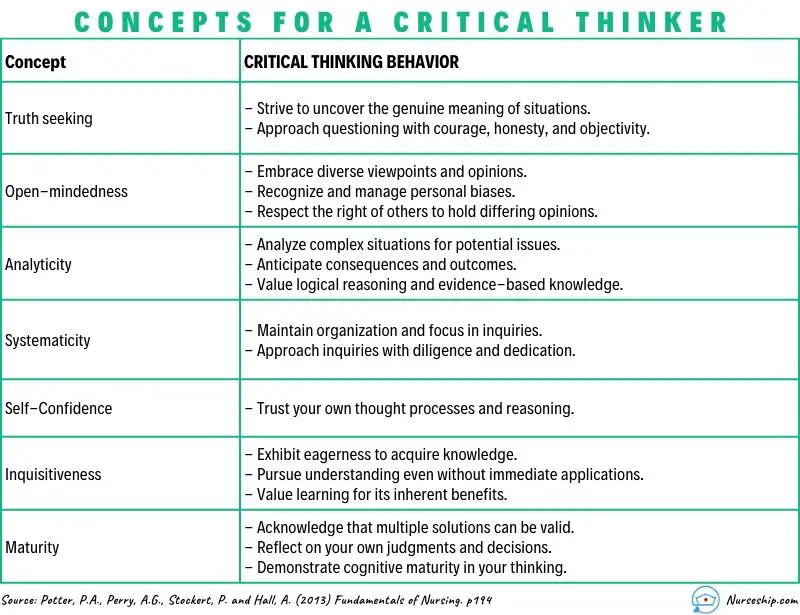
Key aspects of critical thinking include:
- Analysis: Critical thinking begins with the thorough examination of information, ideas, or situations. It involves breaking down complex concepts into smaller parts to better understand their components and relationships.
- Evaluation: Critical thinkers assess the quality and reliability of information or arguments. They weigh evidence, identify strengths and weaknesses, and determine the credibility of sources.
- Synthesis: Critical thinking involves combining different pieces of information or ideas to create a new understanding or perspective. This involves connecting the dots between various sources and integrating them into a coherent whole.
- Inference: Critical thinkers draw logical and well-supported conclusions based on the information and evidence available. They use reasoning to make educated guesses about situations where complete information might be lacking.
- Problem-Solving: Critical thinking is essential in solving complex problems. It allows individuals to identify and define problems, generate potential solutions, evaluate the pros and cons of each solution, and choose the most appropriate course of action.
- Creativity: Critical thinking involves thinking outside the box and considering alternative viewpoints or approaches. It encourages the exploration of new ideas and solutions beyond conventional thinking.
- Reflection: Critical thinkers engage in self-assessment and reflection on their thought processes. They consider their own biases, assumptions, and potential errors in reasoning, aiming to improve their thinking skills over time.
- Open-Mindedness: Critical thinkers approach ideas and information with an open mind, willing to consider different viewpoints and perspectives even if they challenge their own beliefs.
- Effective Communication: Critical thinkers can articulate their thoughts and reasoning clearly and persuasively to others. They can express complex ideas in a coherent and understandable manner.
- Continuous Learning: Critical thinking encourages a commitment to ongoing learning and intellectual growth. It involves seeking out new knowledge, refining thinking skills, and staying receptive to new information.
Definition of Critical Thinking
Critical thinking is an intellectual process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
What is Critical Thinking in Nursing?
Critical thinking in nursing is a vital cognitive skill that involves analyzing, evaluating, and making reasoned decisions about patient care.
It’s an essential aspect of a nurse’s professional practice as it enables them to provide safe and effective care to patients.
Critical thinking involves a careful and deliberate thought process to gather and assess information, consider alternative solutions, and make informed decisions based on evidence and sound judgment.
This skill helps nurses to:
- Assess Information: Critical thinking allows nurses to thoroughly assess patient information, including medical history, symptoms, and test results. By analyzing this data, nurses can identify patterns, discrepancies, and potential issues that may require further investigation.
- Diagnose: Nurses use critical thinking to analyze patient data and collaboratively work with other healthcare professionals to formulate accurate nursing diagnoses. This is crucial for developing appropriate care plans that address the unique needs of each patient.
- Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient’s preferences, medical history, and evidence-based practices.
- Evaluate Outcomes: After implementing interventions, critical thinking enables nurses to evaluate the outcomes of their actions. If the desired outcomes are not achieved, nurses can adapt their approach and make necessary changes to the care plan.
- Prioritize Care: In busy healthcare environments, nurses often face situations where they must prioritize patient care. Critical thinking helps them determine which patients require immediate attention and which interventions are most essential.
- Communicate Effectively: Critical thinking skills allow nurses to communicate clearly and confidently with patients, their families, and other members of the healthcare team. They can explain complex medical information and treatment plans in a way that is easily understood by all parties involved.
- Identify Problems: Nurses use critical thinking to identify potential complications or problems in a patient’s condition. This early recognition can lead to timely interventions and prevent further deterioration.
- Collaborate: Healthcare is a collaborative effort involving various professionals. Critical thinking enables nurses to actively participate in interdisciplinary discussions, share their insights, and contribute to holistic patient care.
- Ethical Decision-Making: Critical thinking helps nurses navigate ethical dilemmas that can arise in patient care. They can analyze different perspectives, consider ethical principles, and make morally sound decisions.
- Continual Learning: Critical thinking encourages nurses to seek out new knowledge, stay up-to-date with the latest research and medical advancements, and incorporate evidence-based practices into their care.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed.
It’s a dynamic process that enhances clinical reasoning , problem-solving, and overall patient outcomes.
What are the Levels of Critical Thinking in Nursing?
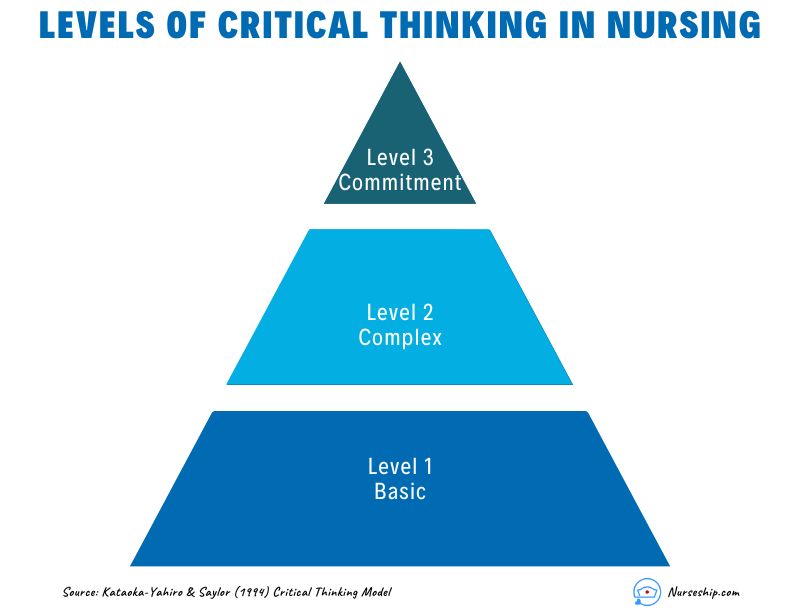
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment.
The Kataoka-Yahiro and Saylor model outlines this progression.
1. Basic Critical Thinking:
At this level, learners trust experts for solutions. Thinking is based on rules and principles. For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted.
2. Complex Critical Thinking:
Learners start to analyze choices independently and think creatively. They recognize conflicting solutions and weigh benefits and risks. Thinking becomes innovative, with a willingness to consider various approaches in complex situations.
3. Commitment:
At this level, individuals anticipate decision points without external help and take responsibility for their choices. They choose actions or beliefs based on available alternatives, considering consequences and accountability.
As nurses gain knowledge and experience, their critical thinking evolves from relying on experts to independent analysis and decision-making, ultimately leading to committed and accountable choices in patient care.
Why Critical Thinking is Important in Nursing?
Critical thinking is important in nursing for several crucial reasons:
Patient Safety:
Nursing decisions directly impact patient well-being. Critical thinking helps nurses identify potential risks, make informed choices, and prevent errors.
Clinical Judgment:
Nursing decisions often involve evaluating information from various sources, such as patient history, lab results, and medical literature.
Critical thinking assists nurses in critically appraising this information, distinguishing credible sources, and making rational judgments that align with evidence-based practices.
Enhances Decision-Making:
In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and weigh different options based on evidence and analysis.
This process empowers them to make informed decisions about patient care, treatment plans, and interventions, ultimately leading to better outcomes.
Promotes Problem-Solving:
Nurses encounter complex patient issues that require effective problem-solving.
Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient.
Drives Creativity:
Nursing care is not always straightforward. Critical thinking encourages nurses to think creatively and explore innovative approaches to challenges, especially when standard protocols might not suffice for unique patient situations.
Fosters Effective Communication:
Communication is central to nursing. Critical thinking enables nurses to clearly express their thoughts, provide logical explanations for their decisions, and engage in meaningful dialogues with patients, families, and other healthcare professionals.
Aids Learning:
Nursing is a field of continuous learning. Critical thinking encourages nurses to engage in ongoing self-directed education, seeking out new knowledge, embracing new techniques, and staying current with the latest research and developments.
Improves Relationships:
Open-mindedness and empathy are essential in nursing relationships.
Critical thinking encourages nurses to consider diverse viewpoints, understand patients’ perspectives, and communicate compassionately, leading to stronger therapeutic relationships.
Empowers Independence:
Nursing often requires autonomous decision-making. Critical thinking empowers nurses to analyze situations independently, make judgments without undue influence, and take responsibility for their actions.
Facilitates Adaptability:
Healthcare environments are ever-changing. Critical thinking equips nurses with the ability to quickly assess new information, adjust care plans, and navigate unexpected situations while maintaining patient safety and well-being.
Strengthens Critical Analysis:
In the era of vast information, nurses must discern reliable data from misinformation.
Critical thinking helps them scrutinize sources, question assumptions, and make well-founded choices based on credible information.
How to Apply Critical Thinking in Nursing? (With Examples)
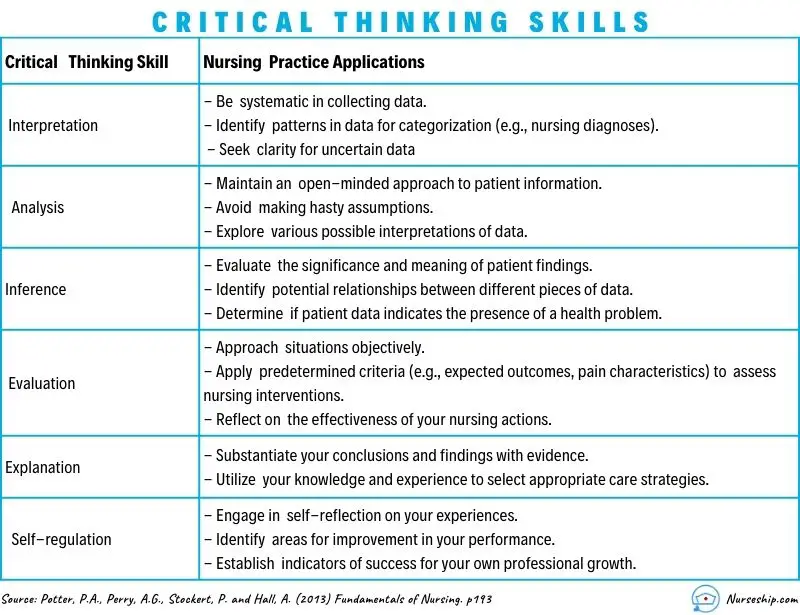
Here are some examples of how nurses can apply critical thinking.
Assess Patient Data:
Critical Thinking Action: Carefully review patient history, symptoms, and test results.
Example: A nurse notices a change in a diabetic patient’s blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions before adjusting the treatment plan.
Diagnose Patient Needs:
Critical Thinking Action: Analyze patient data to identify potential nursing diagnoses.
Example: After reviewing a patient’s lab results, vital signs, and observations, a nurse identifies “ Risk for Impaired Skin Integrity ” due to the patient’s limited mobility.
Plan and Implement Care:
Critical Thinking Action: Develop a care plan based on patient needs and evidence-based practices.
Example: For a patient at risk of falls, the nurse plans interventions such as hourly rounding, non-slip footwear, and bed alarms to ensure patient safety.
Evaluate Interventions:
Critical Thinking Action: Assess the effectiveness of interventions and modify the care plan as needed.
Example: After administering pain medication, the nurse evaluates its impact on the patient’s comfort level and considers adjusting the dosage or trying an alternative pain management approach.
Prioritize Care:
Critical Thinking Action: Determine the order of interventions based on patient acuity and needs.
Example: In a busy emergency department, the nurse triages patients by considering the severity of their conditions, ensuring that critical cases receive immediate attention.
Collaborate with the Healthcare Team:
Critical Thinking Action: Participate in interdisciplinary discussions and share insights.
Example: During rounds, a nurse provides input on a patient’s response to treatment, which prompts the team to adjust the care plan for better outcomes.
Ethical Decision-Making:
Critical Thinking Action: Analyze ethical dilemmas and make morally sound choices.
Example: When a terminally ill patient expresses a desire to stop treatment, the nurse engages in ethical discussions, respecting the patient’s autonomy and ensuring proper end-of-life care.
Patient Education:
Critical Thinking Action: Tailor patient education to individual needs and comprehension levels.
Example: A nurse uses visual aids and simplified language to explain medication administration to a patient with limited literacy skills.
Adapt to Changes:
Critical Thinking Action: Quickly adjust care plans when patient conditions change.
Example: During post-operative recovery, a nurse notices signs of infection and promptly informs the healthcare team to initiate appropriate treatment adjustments.
Critical Analysis of Information:
Critical Thinking Action: Evaluate information sources for reliability and relevance.
Example: When presented with conflicting research studies, a nurse critically examines the methodologies and sample sizes to determine which study is more credible.
Making Sense of Critical Thinking Skills
What is the purpose of critical thinking in nursing.
The purpose of critical thinking in nursing is to enable nurses to effectively analyze, interpret, and evaluate patient information, make informed clinical judgments, develop appropriate care plans, prioritize interventions, and adapt their approaches as needed, thereby ensuring safe, evidence-based, and patient-centered care.
Why critical thinking is important in nursing?
Critical thinking is important in nursing because it promotes safe decision-making, accurate clinical judgment, problem-solving, evidence-based practice, holistic patient care, ethical reasoning, collaboration, and adapting to dynamic healthcare environments.
Critical thinking skill also enhances patient safety, improves outcomes, and supports nurses’ professional growth.
How is critical thinking used in the nursing process?
Critical thinking is integral to the nursing process as it guides nurses through the systematic approach of assessing, diagnosing, planning, implementing, and evaluating patient care. It involves:
- Assessment: Critical thinking enables nurses to gather and interpret patient data accurately, recognizing relevant patterns and cues.
- Diagnosis: Nurses use critical thinking to analyze patient data, identify nursing diagnoses, and differentiate actual issues from potential complications.
- Planning: Critical thinking helps nurses develop tailored care plans, selecting appropriate interventions based on patient needs and evidence.
- Implementation: Nurses make informed decisions during interventions, considering patient responses and adjusting plans as needed.
- Evaluation: Critical thinking supports the assessment of patient outcomes, determining the effectiveness of intervention, and adapting care accordingly.
Throughout the nursing process , critical thinking ensures comprehensive, patient-centered care and fosters continuous improvement in clinical judgment and decision-making.
What is an example of the critical thinking attitude of independent thinking in nursing practice?
An example of the critical thinking attitude of independent thinking in nursing practice could be:
A nurse is caring for a patient with a complex medical history who is experiencing a new set of symptoms. The nurse carefully reviews the patient’s history, recent test results, and medication list.
While discussing the case with the healthcare team, the nurse realizes that the current treatment plan might not be addressing all aspects of the patient’s condition.
Instead of simply following the established protocol, the nurse independently considers alternative approaches based on their assessment.
The nurse proposes a modification to the treatment plan, citing the rationale and evidence supporting the change.
This demonstrates independent thinking by critically evaluating the situation, challenging assumptions, and advocating for a more personalized and effective patient care approach.
How to use Costa’s level of questioning for critical thinking in nursing?
Costa’s levels of questioning can be applied in nursing to facilitate critical thinking and stimulate a deeper understanding of patient situations. The levels of questioning are as follows:
| Level 1: Gathering | 1. What are the common side effects of the prescribed medication? 2. When was the patient’s last bowel movement? 3. Who is the patient’s emergency contact person? 4. Describe the patient’s current level of pain. 5. What information is in the patient’s medical record? |
| 1. What would happen if the patient’s blood pressure falls further? 2. Compare the patient’s oxygen saturation levels before and after administering oxygen. 3. What other nursing interventions could be considered for wound care? 4. Infer the potential reasons behind the patient’s increased heart rate. 5. Analyze the relationship between the patient’s diet and blood glucose levels. | |
| 1. What do you think will be the patient’s response to the new pain management strategy? 2. Could the patient’s current symptoms be indicative of an underlying complication? 3. How would you prioritize care for patients with varying acuity levels in the emergency department? 4. What evidence supports your choice of administering the medication at this time? 5. Create a care plan for a patient with complex needs requiring multiple interventions. |
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
Critical thinking in nursing is the foundation that underpins safe, effective, and patient-centered care.
Critical thinking skills empower nurses to navigate the complexities of their profession while consistently providing high-quality care to diverse patient populations.
Reading Recommendation
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What is Critical Thinking in Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
You are using an outdated browser
Unfortunately Ausmed.com does not support your browser. Please upgrade your browser to continue.
Cultivating Critical Thinking in Healthcare
Published: 06 January 2019

Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).
Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught , assessed and integrated into the design and development of staff and nurse education and training programs (Papp et al. 2014).
So, what exactly is critical thinking and how can healthcare educators cultivate it amongst their staff?
What is Critical Thinking?
In general terms, ‘ critical thinking ’ is often used, and perhaps confused, with problem-solving and clinical decision-making skills .
In practice, however, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions .
Several formal definitions of critical thinking can be found in literature, but in the view of Kahlke and Eva (2018), most of these definitions have limitations. That said, Papp et al. (2014) offer a useful starting point, suggesting that critical thinking is:
‘The ability to apply higher order cognitive skills and the disposition to be deliberate about thinking that leads to action that is logical and appropriate.’
The Foundation for Critical Thinking (2017) expands on this and suggests that:
‘Critical thinking is that mode of thinking, about any subject, content, or problem, in which the thinker improves the quality of his or her thinking by skillfully analysing, assessing, and reconstructing it.’
They go on to suggest that critical thinking is:
- Self-directed
- Self-disciplined
- Self-monitored
- Self-corrective.

Key Qualities and Characteristics of a Critical Thinker
Given that critical thinking is a process that encompasses conceptualisation , application , analysis , synthesis , evaluation and reflection , what qualities should be expected from a critical thinker?
In answering this question, Fortepiani (2018) suggests that critical thinkers should be able to:
- Formulate clear and precise questions
- Gather, assess and interpret relevant information
- Reach relevant well-reasoned conclusions and solutions
- Think open-mindedly, recognising their own assumptions
- Communicate effectively with others on solutions to complex problems.
All of these qualities are important, however, good communication skills are generally considered to be the bedrock of critical thinking. Why? Because they help to create a dialogue that invites questions, reflections and an open-minded approach, as well as generating a positive learning environment needed to support all forms of communication.
Lippincott Solutions (2018) outlines a broad spectrum of characteristics attributed to strong critical thinkers. They include:
- Inquisitiveness with regard to a wide range of issues
- A concern to become and remain well-informed
- Alertness to opportunities to use critical thinking
- Self-confidence in one’s own abilities to reason
- Open mindedness regarding divergent world views
- Flexibility in considering alternatives and opinions
- Understanding the opinions of other people
- Fair-mindedness in appraising reasoning
- Honesty in facing one’s own biases, prejudices, stereotypes or egocentric tendencies
- A willingness to reconsider and revise views where honest reflection suggests that change is warranted.
Papp et al. (2014) also helpfully suggest that the following five milestones can be used as a guide to help develop competency in critical thinking:
Stage 1: Unreflective Thinker
At this stage, the unreflective thinker can’t examine their own actions and cognitive processes and is unaware of different approaches to thinking.
Stage 2: Beginning Critical Thinker
Here, the learner begins to think critically and starts to recognise cognitive differences in other people. However, external motivation is needed to sustain reflection on the learners’ own thought processes.
Stage 3: Practicing Critical Thinker
By now, the learner is familiar with their own thinking processes and makes a conscious effort to practice critical thinking.
Stage 4: Advanced Critical Thinker
As an advanced critical thinker, the learner is able to identify different cognitive processes and consciously uses critical thinking skills.
Stage 5: Accomplished Critical Thinker
At this stage, the skilled critical thinker can take charge of their thinking and habitually monitors, revises and rethinks approaches for continual improvement of their cognitive strategies.
Facilitating Critical Thinking in Healthcare
A common challenge for many educators and facilitators in healthcare is encouraging students to move away from passive learning towards active learning situations that require critical thinking skills.
Just as there are similarities among the definitions of critical thinking across subject areas and levels, there are also several generally recognised hallmarks of teaching for critical thinking . These include:
- Promoting interaction among students as they learn
- Asking open ended questions that do not assume one right answer
- Allowing sufficient time to reflect on the questions asked or problems posed
- Teaching for transfer - helping learners to see how a newly acquired skill can apply to other situations and experiences.
(Lippincott Solutions 2018)
Snyder and Snyder (2008) also make the point that it’s helpful for educators and facilitators to be aware of any initial resistance that learners may have and try to guide them through the process. They should aim to create a learning environment where learners can feel comfortable thinking through an answer rather than simply having an answer given to them.
Examples include using peer coaching techniques , mentoring or preceptorship to engage students in active learning and critical thinking skills, or integrating project-based learning activities that require students to apply their knowledge in a realistic healthcare environment.
Carvalhoa et al. (2017) also advocate problem-based learning as a widely used and successful way of stimulating critical thinking skills in the learner. This view is echoed by Tsui-Mei (2015), who notes that critical thinking, systematic analysis and curiosity significantly improve after practice-based learning .
Integrating Critical Thinking Skills Into Curriculum Design
Most educators agree that critical thinking can’t easily be developed if the program curriculum is not designed to support it. This means that a deep understanding of the nature and value of critical thinking skills needs to be present from the outset of the curriculum design process , and not just bolted on as an afterthought.
In the view of Fortepiani (2018), critical thinking skills can be summarised by the statement that 'thinking is driven by questions', which means that teaching materials need to be designed in such a way as to encourage students to expand their learning by asking questions that generate further questions and stimulate the thinking process. Ideal questions are those that:
- Embrace complexity
- Challenge assumptions and points of view
- Question the source of information
- Explore variable interpretations and potential implications of information.
To put it another way, asking questions with limiting, thought-stopping answers inhibits the development of critical thinking. This means that educators must ideally be critical thinkers themselves .
Drawing these threads together, The Foundation for Critical Thinking (2017) offers us a simple reminder that even though it’s human nature to be ‘thinking’ most of the time, most thoughts, if not guided and structured, tend to be biased, distorted, partial, uninformed or even prejudiced.
They also note that the quality of work depends precisely on the quality of the practitioners’ thought processes. Given that practitioners are being asked to meet the challenge of ever more complex care, the importance of cultivating critical thinking skills, alongside advanced problem-solving skills , seems to be taking on new importance.
Additional Resources
- The Emotionally Intelligent Nurse | Ausmed Article
- Refining Competency-Based Assessment | Ausmed Article
- Socratic Questioning in Healthcare | Ausmed Article
- Carvalhoa, D P S R P et al. 2017, 'Strategies Used for the Promotion of Critical Thinking in Nursing Undergraduate Education: A Systematic Review', Nurse Education Today , vol. 57, pp. 103-10, viewed 7 December 2018, https://www.sciencedirect.com/science/article/abs/pii/S0260691717301715
- Fortepiani, L A 2017, 'Critical Thinking or Traditional Teaching For Health Professionals', PECOP Blog , 16 January, viewed 7 December 2018, https://blog.lifescitrc.org/pecop/2017/01/16/critical-thinking-or-traditional-teaching-for-health-professions/
- Jacob, E, Duffield, C & Jacob, D 2017, 'A Protocol For the Development of a Critical Thinking Assessment Tool for Nurses Using a Delphi Technique', Journal of Advanced Nursing, vol. 73, no. 8, pp. 1982-1988, viewed 7 December 2018, https://onlinelibrary.wiley.com/doi/10.1111/jan.13306
- Kahlke, R & Eva, K 2018, 'Constructing Critical Thinking in Health Professional Education', Perspectives on Medical Education , vol. 7, no. 3, pp. 156-165, viewed 7 December 2018, https://link.springer.com/article/10.1007/s40037-018-0415-z
- Lippincott Solutions 2018, 'Turning New Nurses Into Critical Thinkers', Lippincott Solutions , viewed 10 December 2018, https://www.wolterskluwer.com/en/expert-insights/turning-new-nurses-into-critical-thinkers
- Papp, K K 2014, 'Milestones of Critical Thinking: A Developmental Model for Medicine and Nursing', Academic Medicine , vol. 89, no. 5, pp. 715-720, https://journals.lww.com/academicmedicine/Fulltext/2014/05000/Milestones_of_Critical_Thinking___A_Developmental.14.aspx
- Snyder, L G & Snyder, M J 2008, 'Teaching Critical Thinking and Problem Solving Skills', The Delta Pi Epsilon Journal , vol. L, no. 2, pp. 90-99, viewed 7 December 2018, https://dme.childrenshospital.org/wp-content/uploads/2019/02/Optional-_Teaching-Critical-Thinking-and-Problem-Solving-Skills.pdf
- The Foundation for Critical Thinking 2017, Defining Critical Thinking , The Foundation for Critical Thinking, viewed 7 December 2018, https://www.criticalthinking.org/pages/our-conception-of-critical-thinking/411
- Tsui-Mei, H, Lee-Chun, H & Chen-Ju MSN, K 2015, 'How Mental Health Nurses Improve Their Critical Thinking Through Problem-Based Learning', Journal for Nurses in Professional Development , vol. 31, no. 3, pp. 170-175, viewed 7 December 2018, https://journals.lww.com/jnsdonline/Abstract/2015/05000/How_Mental_Health_Nurses_Improve_Their_Critical.8.aspx
Anne Watkins View profile
Help and feedback, publications.
Ausmed Education is a Trusted Information Partner of Healthdirect Australia. Verify here .
An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Developing critical thinking skills for delivering optimal care
Scott IA, Hubbard RE, Crock C, et al. Developing critical thinking skills for delivering optimal care. Intern Med J. 2021;51(4):488-493. doi: 10.1111/imj.15272
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care – clinical reasoning, evidence-informed decision-making, and systems thinking – and approaches to develop these skills during clinician training.
Medication use and cognitive impairment among residents of aged care facilities. June 23, 2021
COVID-19 pandemic and the tension between the need to act and the need to know. October 14, 2020
Choosing wisely in clinical practice: embracing critical thinking, striving for safer care. April 6, 2022
Scoping review of studies evaluating frailty and its association with medication harm. June 22, 2022
Countering cognitive biases in minimising low value care. June 7, 2017
'More than words' - interpersonal communication, cognitive bias and diagnostic errors. August 11, 2021
A partially structured postoperative handoff protocol improves communication in 2 mixed surgical intensive care units: findings from the Handoffs and Transitions in Critical Care (HATRICC) prospective cohort study. February 6, 2019
Enabling a learning healthcare system with automated computer protocols that produce replicable and personalized clinician actions. August 4, 2021
Analysis of lawsuits related to diagnostic errors from point-of-care ultrasound in internal medicine, paediatrics, family medicine and critical care in the USA. June 24, 2020
Developing and aligning a safety event taxonomy for inpatient psychiatry. July 13, 2022
Changes in unprofessional behaviour, teamwork, and co-operation among hospital staff during the COVID-19 pandemic. September 28, 2022
Pharmacists reducing medication risk in medical outpatient clinics: a retrospective study of 18 clinics. March 8, 2023
Prevalence and causes of diagnostic errors in hospitalized patients under investigation for COVID-19. April 12, 2023
Barriers to accessing nighttime supervisors: a national survey of internal medicine residents. March 17, 2021
Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016 March 3, 2017
Seroprevalence of SARS-CoV-2 among frontline health care personnel in a multistate hospital network--13 academic medical centers, April-June 2020. September 23, 2020
Transforming the medication regimen review process using telemedicine to prevent adverse events. December 16, 2020
The MedSafer study-electronic decision support for deprescribing in hospitalized older adults: a cluster randomized clinical trial. February 2, 2022
Perceived patient safety culture in a critical care transport program. July 31, 2013
Video-based communication assessment of physician error disclosure skills by crowdsourced laypeople and patient advocates who experienced medical harm: reliability assessment with generalizability theory. May 18, 2022
Implementation of the I-PASS handoff program in diverse clinical environments: a multicenter prospective effectiveness implementation study. November 16, 2022
Patient harm from cardiovascular medications. August 25, 2021
Delays in diagnosis, treatment, and surgery: root causes, actions taken, and recommendations for healthcare improvement. June 1, 2022
Influence of opioid prescription policy on overdoses and related adverse effects in a primary care population. May 19, 2021
Evaluation of a second victim peer support program on perceptions of second victim experiences and supportive resources in pediatric clinical specialties using the second victim experience and support tool (SVEST). November 3, 2021
Diagnostic errors in hospitalized adults who died or were transferred to intensive care. January 17, 2024
Estimation of breast cancer overdiagnosis in a U.S. breast screening cohort. March 16, 2022
Multiple meanings of resilience: health professionals' experiences of a dual element training intervention designed to help them prepare for coping with error. March 31, 2021
Care coordination strategies and barriers during medication safety incidents: a qualitative, cognitive task analysis. March 10, 2021
TRIAD IX: can a patient testimonial safely help ensure prehospital appropriate critical versus end-of-life care? September 15, 2021
An act of performance: exploring residents' decision-making processes to seek help. April 14, 2021
Preventing home medication administration errors. March 14, 2022
A randomized trial of a multifactorial strategy to prevent serious fall injuries. July 29, 2020
Clinical predictors for unsafe direct discharge home patients from intensive care units. October 21, 2020
Association between limiting the number of open records in a tele-critical care setting and retract-reorder errors. July 21, 2021
Standardized assessment of medication reconciliation in post-acute care. April 27, 2022
Estimating the economic cost of nurse sensitive adverse events amongst patients in medical and surgical settings. June 16, 2021
Survey of nurses' experiences applying The Joint Commission's medication management titration standards. November 3, 2021
Effectiveness of acute care remote triage systems: a systematic review. February 5, 2020
Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. September 23, 2020
Physician task load and the risk of burnout among US physicians in a national survey. December 2, 2020
Patient and physician perspectives of deprescribing potentially inappropriate medications in older adults with a history of falls: a qualitative study. May 5, 2021
We asked the experts: the WHO Surgical Safety Checklist and the COVID-19 pandemic: recommendations for content and implementation adaptations. March 17, 2021
Association between surgeon technical skills and patient outcomes. September 9, 2020
Influence of psychological safety and organizational support on the impact of humiliation on trainee well-being. June 8, 2022
Developing the Safer Dx Checklist of Ten Safety Recommendations for Health Care Organizations to address diagnostic errors. October 12, 2022
Comparison of health care worker satisfaction before vs after implementation of a communication and optimal resolution program in acute care hospitals. April 5, 2023
Not overstepping professional boundaries: the challenging role of nurses in simulated error disclosures. September 21, 2011
Temporal associations between EHR-derived workload, burnout, and errors: a prospective cohort study. July 20, 2022
Adherence to national guidelines for timeliness of test results communication to patients in the Veterans Affairs health care system. May 4, 2022
Deferral of care for serious non-COVID-19 conditions: a hidden harm of COVID-19. November 18, 2020
An observational study of postoperative handoff standardization failures. June 23, 2021
Content analysis of patient safety incident reports for older adult patient transfers, handovers, and discharges: do they serve organizations, staff, or patients? January 8, 2020
Exploring the impact of employee engagement and patient safety. September 14, 2022
Deprescribing for community-dwelling older adults: a systematic review and meta-analysis. September 16, 2020
The abrupt expansion of ambulatory telemedicine: implications for patient safety. February 9, 2022
Nurse's Achilles Heel: using big data to determine workload factors that impact near misses. April 14, 2021
A diagnostic time-out to improve differential diagnosis in pediatric abdominal pain. July 14, 2021
What safety events are reported for ambulatory care? Analysis of incident reports from a patient safety organization. October 21, 2020
Expert consensus on currently accepted measures of harm. September 9, 2020
The July Effect in podiatric medicine and surgery residency. July 14, 2021
Missed nursing care in the critical care unit, before and during the COVID-19 pandemic: a comparative cross-sectional study. June 22, 2022
The calm before the storm: utilizing in situ simulation to evaluate for preparedness of an alternative care hospital during COVID-19 pandemic. June 2, 2021
The association between nurse staffing and omissions in nursing care: a systematic review. July 11, 2018
Creating a learning health system for improving diagnostic safety: pragmatic insights from US health care organizations. June 22, 2022
Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. June 8, 2016
Impact of the initial response to COVID-19 on long-term care for people with intellectual disability: an interrupted time series analysis of incident reports. October 14, 2020
Pediatric surgical errors: a systematic scoping review. July 20, 2022
Racial bias in pulse oximetry measurement. December 20, 2020
Accuracy of practitioner estimates of probability of diagnosis before and after testing. May 5, 2021
Recommendations for the safe, effective use of adaptive CDS in the US healthcare system: an AMIA position paper. April 21, 2021
Impact of interoperability of smart infusion pumps and an electronic medical record in critical care. September 23, 2020
Decreased incidence of cesarean surgical site infection rate with hospital-wide perioperative bundle. September 29, 2021
Association of diagnostic stewardship for blood cultures in critically ill children with culture rates, antibiotic use, and patient outcomes: results of the Bright STAR Collaborative. May 18, 2022
Second victim experiences of nurses in obstetrics and gynaecology: a Second Victim Experience and Support Tool Survey December 23, 2020
Understanding the second victim experience among multidisciplinary providers in obstetrics and gynecology. May 19, 2021
eSIMPLER: a dynamic, electronic health record-integrated checklist for clinical decision support during PICU daily rounds. June 16, 2021
Treatment patterns and clinical outcomes after the introduction of the Medicare Sepsis Performance Measure (SEP-1). May 5, 2021
Organizational safety climate and job enjoyment in hospital surgical teams with and without crew resource management training, January 26, 2022
Evaluation of effectiveness and safety of pharmacist independent prescribers in care homes: cluster randomised controlled trial. March 1, 2023
The Critical Care Safety Study: the incidence and nature of adverse events and serious medical errors in intensive care. August 24, 2005
Safety II behavior in a pediatric intensive care unit. August 1, 2018
Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. October 21, 2020
The working hours of hospital staff nurses and patient safety. January 9, 2005
Effects of tall man lettering on the visual behaviour of critical care nurses while identifying syringe drug labels: a randomised in situ simulation. April 20, 2022
Family Input for Quality and Safety (FIQS): using mobile technology for in-hospital reporting from families and patients. March 2, 2022
Improving self-reported empathy and communication skills through harm in healthcare response training. January 26, 2022
Bundle interventions including nontechnical skills for surgeons can reduce operative time and improve patient safety. December 9, 2020
COVID-19: an emerging threat to antibiotic stewardship in the emergency department. October 21, 2020
Predicting avoidable hospital events in Maryland. December 1, 2021
Association between in-clinic opioid administration and discharge opioid prescription in urgent care: a retrospective cohort study. February 17, 2021
Why do hospital prescribers continue antibiotics when it is safe to stop? Results of a choice experiment survey. September 2, 2020
Specificity of computerized physician order entry has a significant effect on the efficiency of workflow for critically ill patients. April 21, 2005
COVID-19: patient safety and quality improvement skills to deploy during the surge. June 24, 2020
Patient safety skills in primary care: a national survey of GP educators. February 4, 2015
Implementing human factors in anaesthesia: guidance for clinicians, departments and hospitals: Guidelines from the Difficult Airway Society and the Association of Anaesthetists. March 1, 2023
Can an electronic prescribing system detect doctors who are more likely to make a serious prescribing error? June 8, 2011
Training in safe opioid prescribing and treatment of opioid use disorder in internal medicine residencies: a national survey of program directors. October 12, 2022
Diagnostic discordance, health information exchange, and inter-hospital transfer outcomes: a population study. June 20, 2018
What has been the impact of Covid-19 on safety culture? A case study from a large metropolitan healthcare trust. September 2, 2020
Racial and ethnic harm in patient care is a patient safety issue. May 15, 2024
All in Her Head. The Truth and Lies Early Medicine Taught Us About Women's Bodies and Why It Matters Today. March 20, 2024
The racial disparities in maternal mortality and impact of structural racism and implicit racial bias on pregnant Black women: a review of the literature. December 6, 2023
A scoping review exploring the confidence of healthcare professionals in assessing all skin tones. October 4, 2023
Patient safety in palliative care at the end of life from the perspective of complex thinking. August 16, 2023
Only 1 in 5 people with opioid addiction get the medications to treat it, study finds. August 16, 2023
Factors influencing in-hospital prescribing errors: a systematic review. July 19, 2023
Introducing second-year medical students to diagnostic reasoning concepts and skills via a virtual curriculum. June 28, 2023
Context matters: toward a multilevel perspective on context in clinical reasoning and error. June 21, 2023
The good, the bad, and the ugly: operative staff perspectives of surgeon coping with intraoperative errors. June 14, 2023
Explicitly addressing implicit bias on inpatient rounds: student and faculty reflections. June 7, 2023
The time is now: addressing implicit bias in obstetrics and gynecology education. May 17, 2023
Listen to the whispers before they become screams: addressing Black maternal morbidity and mortality in the United States. May 3, 2023
Annual Perspective
Formalizing the hidden curriculum of performance enhancing errors. March 22, 2023
Implicit racial bias, health care provider attitudes, and perceptions of health care quality among African American college students in Georgia, USA. January 18, 2023
Structural racism and impact on sickle cell disease: sickle cell lives matter. January 11, 2023
The REPAIR Project: a prospectus for change toward racial justice in medical education and health sciences research: REPAIR project steering committee. January 11, 2023
Using the Assessment of Reasoning Tool to facilitate feedback about diagnostic reasoning. January 11, 2023
Exploring the intersection of structural racism and ageism in healthcare. December 7, 2022
Calibrate Dx: A Resource to Improve Diagnostic Decisions. October 19, 2022
Improved Diagnostic Accuracy Through Probability-Based Diagnosis. September 28, 2022
Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. September 21, 2022
A state-of-the-art review of speaking up in healthcare. August 24, 2022
Skin cancer is a risk no matter the skin tone. But it may be overlooked in people with dark skin. August 17, 2022
Oxford Professional Practice: Handbook of Patient Safety. July 27, 2022
Narrowing the mindware gap in medicine. July 20, 2022
From principles to practice: embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. June 15, 2022
A call to action: next steps to advance diagnosis education in the health professions. June 8, 2022
Does a suggested diagnosis in a general practitioners' referral question impact diagnostic reasoning: an experimental study. April 27, 2022

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection

Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Critical Thinking in Critical Care: Five Strategies to Improve Teaching and Learning in the Intensive Care Unit
Affiliations.
- 1 1 Division of Pulmonary, Critical Care and Sleep Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts.
- 2 2 Shapiro Institute for Education and Research at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, Massachusetts; and.
- 3 3 Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda, Massachusetts.
- PMID: 28157389
- PMCID: PMC5461985
- DOI: 10.1513/AnnalsATS.201612-1009AS
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. Without critical thinking, physicians, and particularly residents, are prone to cognitive errors, which can lead to diagnostic errors, especially in a high-stakes environment such as the intensive care unit. Although challenging, critical thinking skills can be taught. At this time, there is a paucity of data to support an educational gold standard for teaching critical thinking, but we believe that five strategies, routed in cognitive theory and our personal teaching experiences, provide an effective framework to teach critical thinking in the intensive care unit. The five strategies are: make the thinking process explicit by helping learners understand that the brain uses two cognitive processes: type 1, an intuitive pattern-recognizing process, and type 2, an analytic process; discuss cognitive biases, such as premature closure, and teach residents to minimize biases by expressing uncertainty and keeping differentials broad; model and teach inductive reasoning by utilizing concept and mechanism maps and explicitly teach how this reasoning differs from the more commonly used hypothetico-deductive reasoning; use questions to stimulate critical thinking: "how" or "why" questions can be used to coach trainees and to uncover their thought processes; and assess and provide feedback on learner's critical thinking. We believe these five strategies provide practical approaches for teaching critical thinking in the intensive care unit.
Keywords: cognitive errors; critical care; critical thinking; medical education.
PubMed Disclaimer
Five strategies to teach critical…
Five strategies to teach critical thinking skills in a critical care environment.
The revised Bloom’s taxonomy. This…
The revised Bloom’s taxonomy. This schematic, first created in 1956, depicts six levels…
Schematic representations of deductive (…
Schematic representations of deductive ( 1 ) and inductive ( 2 ) reasoning…
( A ) A mechanism…
( A ) A mechanism map of a 45-year-old man presenting with cough,…
- Teaching: A Newer Face. Dries DJ. Dries DJ. Air Med J. 2017 Nov-Dec;36(6):282-286. doi: 10.1016/j.amj.2017.09.006. Air Med J. 2017. PMID: 29132587 Review. No abstract available.
Similar articles
- Promoting Critical Thinking in Your Intensive Care Unit Team. Richards JB, Schwartzstein RM. Richards JB, et al. Crit Care Clin. 2022 Jan;38(1):113-127. doi: 10.1016/j.ccc.2021.08.002. Crit Care Clin. 2022. PMID: 34794626 Review.
- Teaching Clinical Reasoning and Critical Thinking: From Cognitive Theory to Practical Application. Richards JB, Hayes MM, Schwartzstein RM. Richards JB, et al. Chest. 2020 Oct;158(4):1617-1628. doi: 10.1016/j.chest.2020.05.525. Epub 2020 May 22. Chest. 2020. PMID: 32450242 Review.
- Reclaiming magical incantation in graduate medical education. Katz JD, George DT. Katz JD, et al. Clin Rheumatol. 2020 Mar;39(3):703-707. doi: 10.1007/s10067-019-04812-x. Epub 2019 Nov 14. Clin Rheumatol. 2020. PMID: 31724095 Review.
- Intensive Care Unit Educators: A Multicenter Evaluation of Behaviors Residents Value in Attending Physicians. Santhosh L, Jain S, Brady A, Sharp M, Carlos WG. Santhosh L, et al. Ann Am Thorac Soc. 2017 Apr;14(4):513-516. doi: 10.1513/AnnalsATS.201612-996BC. Ann Am Thorac Soc. 2017. PMID: 28287827
- Current teaching and evaluation methods in critical care medicine: has the Accreditation Council for Graduate Medical Education affected how we practice and teach in the intensive care unit? Chudgar SM, Cox CE, Que LG, Andolsek K, Knudsen NW, Clay AS. Chudgar SM, et al. Crit Care Med. 2009 Jan;37(1):49-60. doi: 10.1097/CCM.0b013e31819265c8. Crit Care Med. 2009. PMID: 19050627
- Beyond the Individual: A Multidisciplinary Model for Critical Thinking in the Intensive Care Unit. Jagpal SK, Alismail A, Lin E, Blackwell L, Ahmed N, Lee MM, Chiarchiaro J. Jagpal SK, et al. Adv Med Educ Pract. 2024 May 14;15:409-417. doi: 10.2147/AMEP.S429982. eCollection 2024. Adv Med Educ Pract. 2024. PMID: 38764787 Free PMC article.
- Sleep Patterns of Premedical Undergraduate Students: Pilot Study and Protocol Evaluation. Rajput G, Gao A, Wu TC, Tsai CT, Molano J, Wu DTY. Rajput G, et al. JMIR Form Res. 2024 Feb 2;8:e45910. doi: 10.2196/45910. JMIR Form Res. 2024. PMID: 38306175 Free PMC article.
- A Pilot Standardized Simulation-Based Mechanical Ventilation Curriculum Targeting Pulmonary and Critical Care Medicine and Critical Care Medicine Fellows. Pervaiz A, Daoud A, Alchakaki A, Ganti S, Venkat D, Lee S, Sankari A. Pervaiz A, et al. Avicenna J Med. 2023 Oct 3;13(3):176-181. doi: 10.1055/s-0043-1773792. eCollection 2023 Jul. Avicenna J Med. 2023. PMID: 37799185 Free PMC article.
- Exploring Knowledge of Cognitive Disposition to Respond in Clinical Decision-Making among Early Clinical Learners. Vinaykumar N, Gugapriya TS, Kalaiselvi S. Vinaykumar N, et al. Maedica (Bucur). 2023 Jun;18(2):317-322. doi: 10.26574/maedica.2023.18.2.317. Maedica (Bucur). 2023. PMID: 37588819 Free PMC article.
- The Resident Learning Journey in the Medical Intensive Care Unit. Herzog TL, Sawatsky AP, Kelm DJ, Nelson DR, Park JG, Niven AS. Herzog TL, et al. ATS Sch. 2023 Feb 28;4(2):177-190. doi: 10.34197/ats-scholar.2022-0103OC. eCollection 2023 Jun. ATS Sch. 2023. PMID: 37533538 Free PMC article.
- Scriven M, Paul R. Critical thinking as defined by the national council for excellence in critical thinking. Presented at the 8th Annual International Conference on Critical Thinking and Education Reform; August 1987; Rohnert Park, California.
- Huang GC, Newman LR, Schwartzstein RM. Critical thinking in health professions education: summary and consensus statements of the Millennium Conference 2011. Teach Learn Med. 2014;26:95–102. - PubMed
- Croskerry P. From mindless to mindful practice--cognitive bias and clinical decision making. N Engl J Med. 2013;368:2445–2448. - PubMed
- Facione P. Critical thinking: What it is and why it counts. Millbrae, CA: The California Academic Press; 2011.
- Tversky A, Kahneman D. Judgement under uncertainty: heuristics and biases. Science. 1974;185:1124–1131. - PubMed
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Europe PubMed Central
- PubMed Central
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Who We Insure
- Insurance Products
- About Berxi
Topics on this page:
The importance of critical thinking in nursing.
Topics on this page

While not every decision is an immediate life-and-death situation, there are hundreds of decisions nurses must make every day that impact patient care in ways small and large.
“Being able to assess situations and make decisions can lead to life-or-death situations,” said nurse anesthetist Aisha Allen . “Critical thinking is a crucial and essential skill for nurses.”
The National League for Nursing Accreditation Commission (NLNAC) defines critical thinking in nursing this way: “the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief-based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research.”
Why Critical Thinking in Nursing Is Important
An eight-year study by Johns Hopkins reports that 10% of deaths in the U.S. are due to medical error — the third-highest cause of death in the country.
“Diagnostic errors, medical mistakes, and the absence of safety nets could result in someone’s death,” wrote Dr. Martin Makary , professor of surgery at Johns Hopkins University School of Medicine.
Everyone makes mistakes — even doctors. Nurses applying critical thinking skills can help reduce errors.
“Question everything,” said pediatric nurse practitioner Ersilia Pompilio RN, MSN, PNP . “Especially doctor’s orders.” Nurses often spend more time with patients than doctors and may notice slight changes in conditions that may not be obvious. Resolving these observations with treatment plans can help lead to better care.
Key Nursing Critical Thinking Skills
Some of the most important critical thinking skills nurses use daily include interpretation, analysis, evaluation, inference, explanation, and self-regulation.
- Interpretation: Understanding the meaning of information or events.
- Analysis: Investigating a course of action based on objective and subjective data.
- Evaluation: Assessing the value of information and its credibility.
- Inference: Making logical deductions about the impact of care decisions.
- Explanation: Translating complicated and often complex medical information to patients and families in a way they can understand to make decisions about patient care.
- Self-Regulation: Avoiding the impact of unconscious bias with cognitive awareness.
These skills are used in conjunction with clinical reasoning. Based on training and experience, nurses use these skills and then have to make decisions affecting care.
It’s the ultimate test of a nurse’s ability to gather reliable data and solve complex problems. However, critical thinking goes beyond just solving problems. Critical thinking incorporates questioning and critiquing solutions to find the most effective one. For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health.
8 Examples of Critical Thinking in Nursing
Here are some real-life examples of how nurses apply critical thinking on the job every day, as told by nurses themselves.
Example #1: Patient Assessments
“Doing a thorough assessment on your patient can help you detect that something is wrong, even if you're not quite sure what it is,” said Shantay Carter , registered nurse and co-founder of Women of Integrity . “When you notice the change, you have to use your critical thinking skills to decide what's the next step. Critical thinking allows you to provide the best and safest care possible.”
Example #2: First Line of Defense
Often, nurses are the first line of defense for patients.
“One example would be a patient that had an accelerated heart rate,” said nurse educator and adult critical care nurse Dr. Jenna Liphart Rhoads . “As a nurse, it was my job to investigate the cause of the heart rate and implement nursing actions to help decrease the heart rate prior to calling the primary care provider.”
Nurses with poor critical thinking skills may fail to detect a patient in stress or deteriorating condition. This can result in what’s called a “ failure to rescue ,” or FTR, which can lead to adverse conditions following a complication that leads to mortality.
Example #3: Patient Interactions
Nurses are the ones taking initial reports or discussing care with patients.
“We maintain relationships with patients between office visits,” said registered nurse, care coordinator, and ambulatory case manager Amelia Roberts . “So, when there is a concern, we are the first name that comes to mind (and get the call).”
“Several times, a parent called after the child had a high temperature, and the call came in after hours,” Roberts said. “Doing a nursing assessment over the phone is a special skill, yet based on the information gathered related to the child's behavior (and) fluid intake, there were several recommendations I could make.”
Deciding whether it was OK to wait until the morning, page the primary care doctor, or go to the emergency room to be evaluated takes critical thinking.
Example #4: Using Detective Skills
Nurses have to use acute listening skills to discern what patients are really telling them (or not telling them) and whether they are getting the whole story.
“I once had a 5-year-old patient who came in for asthma exacerbation on repeated occasions into my clinic,” said Pompilio. “The mother swore she was giving her child all her medications, but the asthma just kept getting worse.”
Pompilio asked the parent to keep a medication diary.
“It turned out that after a day or so of medication and alleviation in some symptoms, the mother thought the child was getting better and stopped all medications,” she said.
Example #5: Prioritizing
“Critical thinking is present in almost all aspects of nursing, even those that are not in direct action with the patient,” said Rhoads. “During report, nurses decide which patient to see first based on the information gathered, and from there they must prioritize their actions when in a patient’s room. Nurses must be able to scrutinize which medications can be taken together, and which modality would be best to help a patient move from the bed to the chair.”
A critical thinking skill in prioritization is cognitive stacking. Cognitive stacking helps create smooth workflow management to set priorities and help nurses manage their time. It helps establish routines for care while leaving room within schedules for the unplanned events that will inevitably occur. Even experienced nurses can struggle with juggling today’s significant workload, prioritizing responsibilities, and delegating appropriately.
Example #6: Medication & Care Coordination
Another aspect that often falls to nurses is care coordination. A nurse may be the first to notice that a patient is having an issue with medications.
“Based on a report of illness in a patient who has autoimmune challenges, we might recommend that a dose of medicine that interferes with immune response be held until we communicate with their specialty provider,” said Roberts.
Nurses applying critical skills can also help ease treatment concerns for patients.
“We might recommend a patient who gets infusions come in earlier in the day to get routine labs drawn before the infusion to minimize needle sticks and trauma,” Robert said.
Example #7: Critical Decisions
During the middle of an operation, the anesthesia breathing machine Allen was using malfunctioned.
“I had to critically think about whether or not I could fix this machine or abandon that mode of delivering nursing anesthesia care safely,” she said. “I chose to disconnect my patient from the malfunctioning machine and retrieve tools and medications to resume medication administration so that the surgery could go on.”
Nurses are also called on to do rapid assessments of patient conditions and make split-second decisions in the operating room.
“When blood pressure drops, it is my responsibility to decide which medication and how much medication will fix the issue,” Allen said. “I must work alongside the surgeons and the operating room team to determine the best plan of care for that patient's surgery.”
“On some days, it seems like you are in the movie ‘The Matrix,’” said Pompilio. “There's lots of chaos happening around you. Your patient might be decompensating. You have to literally stop time and take yourself out of the situation and make a decision.”
Example #8: Fast & Flexible Decisions
Allen said she thinks electronics are great, but she can remember a time when technology failed her.
“The hospital monitor that gives us vitals stopped correlating with real-time values,” she said. “So I had to rely on basic nursing skills to make sure my patient was safe. (Pulse check, visual assessments, etc.)”
In such cases, there may not be enough time to think through every possible outcome. Critical thinking combined with experience gives nurses the ability to think quickly and make the right decisions.
Improving the Quality of Patient Care
Nurses who think critically are in a position to significantly increase the quality of patient care and avoid adverse outcomes.
“Critical thinking allows you to ensure patient safety,” said Carter. “It’s essential to being a good nurse.”
Nurses must be able to recognize a change in a patient’s condition, conduct independent interventions, anticipate patients and provider needs, and prioritize. Such actions require critical thinking ability and advanced problem-solving skills.
“Nurses are the eyes and ears for patients, and critical thinking allows us to be their advocates,” said Allen.
Image courtesy of iStock.com/ davidf
Last updated on Jan 05, 2024 .
Originally published on Aug 25, 2021 .
The views expressed in this article are those of the author and do not necessarily reflect those of Berxi™ or Berkshire Hathaway Specialty Insurance Company. This article (subject to change without notice) is for informational purposes only, and does not constitute professional advice. Click here to read our full disclaimer
Delegation in Nursing: Steps, Skills, & Solutions for Creating Balance at Work
The 7 Most Common Nursing Mistakes (And What You Can Do If You Make One)
Resource topics.
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Critical Thinking Skills in Health Care Professional Students: A Systematic Review
Brudvig, Tracy J. PT, DPT, PhD, OCS; Dirkes, Angelique PT, DPT, MS; Dutta, Priyanka PT, MS; Rane, Kalpita PT, MS
Tracy Brudvig is a clinical associate professor in the Department of Physical Therapy in the MGH Institute of Health Professions, 36 1st Avenue, Boston, MA 02129 ( [email protected] ). Please address all correspondence to Tracy Brudvig.
Angelique Dirkes is a clinical instructor in the Department of Physical Therapy in the MGH Institute of Health Professions, Boston, Massachusetts.
Priyanka Dutta was a student in the Master of Science in Physical Therapy program at the MGH Institute of Health Professions, Boston, Massachusetts, when this study was conducted.
Kalpita Rane was a student in the Master of Science in Physical Therapy program at the MGH Institute of Health Professions, Boston, Massachusetts, when this study was conducted.
The authors declare no conflict of interest. Received January 8, 2012, and accepted August 19, 2012.
Background and Purpose.
The purpose of this systematic review is to determine if critical-thinking skills in health care professional students change as a result of participating in a health care professional education program, and to assess the quality of the evidence evaluating this change.
Method/Model Description and Evaluation.
The study design was a systematic review. Six electronic databases were searched. Articles were graded using the Evaluation Guidelines for Rating the Quality of an Intervention Study.
Outcomes.
Eighteen articles were identified as meeting the inclusion criteria. Ten articles were identified in nursing, 5 in physical therapy and occupational therapy, 2 in pharmacy, and 1 in medicine. The scores on the Evaluation Guidelines for Rating the Quality of an Intervention Study ranged from 17 to 26 out of 48. The intraclass correlation of the 2 raters on the Evaluation Guidelines for Rating the Quality of an Intervention Study was 0.87. Eight studies in nursing, 2 studies in physical therapy, 1 study each in occupational therapy, pharmacy, and medicine showed statistically significant change in criticalthinking skills.
Discussion and Conclusion.
The evidence measuring the acquisition of criticalthinking skills in the fields of physical therapy, occupational therapy, pharmacy, and medicine is scarce. In nursing, although the majority of the studies support the acquisition of critical- thinking skills, none of the studies established appropriate sample size and statistical power analysis, and the cross-sectional studies did not perform group matching beyond sex and age. In physical therapy, the results are mixed and the studies lack adequate statistical power. In occupational therapy, pharmacy, and medicine, the studies that showed a statistically significant increase in critical-thinking skills had relatively small sample sizes and weak statistical power. There is a need for additional welldesigned studies looking at the acquisition of critical-thinking skills in all health care fields.
Full Text Access for Subscribers:
Individual subscribers.

Institutional Users
Not a subscriber.
You can read the full text of this article if you:
- + Favorites
- View in Gallery
Readers Of this Article Also Read
A comparison of 2 case delivery methods: virtual and live</strong>', 'huhn karen pt phd; mcginnis, patricia q. pt, phd; wainwright, susan pt, phd; deutsch, judith e. pt, phd, fapta', 'journal of physical therapy education', 'fall 2013', '27', '3' , 'p 41-48');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link"> a comparison of 2 case delivery methods: virtual and live, tracking change in critical-thinking skills</strong>', 'huhn karen pt phd; black, lisa pt, dpt; jensen, gail m. pt, phd, fapta; deutsch, judith e. pt, phd, fapta', 'journal of physical therapy education', 'fall 2013', '27', '3' , 'p 26-31');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link"> tracking change in critical-thinking skills, pauline cerasoli lecture</strong>: <strong xmlns:mrws=\"http://webservices.ovid.com/mrws/1.0\">excellence in academic physical therapy: what is it and how do we get there</strong>', 'gordon james pt edd fapta', 'journal of physical therapy education', 'fall 2011', '25', '3' , 'p 8-13');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link"> pauline cerasoli lecture : excellence in academic physical therapy: what is it..., guide to authors</strong>', '', 'journal of physical therapy education', 'spring 2009', '23', '1' , 'p 88-89');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link"> guide to authors, critical thinking skills during a physical therapist professional education program</strong>', 'vendrely ann pt edd ocs', 'journal of physical therapy education', 'spring 2005', '19', '1' , 'p 55-59');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link"> critical thinking skills during a physical therapist professional education....
We use cookies on our website to support technical features that enhance your user experience, and to help us improve our website. By continuing to use this website, you accept our privacy policy .
- Student Login
- No-Cost Professional Certificates
- Call Us: 888-549-6755
- 888-559-6763
- Search site Search our site Search Now Close
- Request Info
Skip to Content (Press Enter)
Why Critical Thinking Skills in Nursing Matter (And What You Can Do to Develop Them)
By Hannah Meinke on 07/05/2021
The nursing profession tends to attract those who have natural nurturing abilities, a desire to help others, and a knack for science or anatomy. But there is another important skill that successful nurses share, and it's often overlooked: the ability to think critically.
Identifying a problem, determining the best solution and choosing the most effective method to solve the program are all parts of the critical thinking process. After executing the plan, critical thinkers reflect on the situation to figure out if it was effective and if it could have been done better. As you can see, critical thinking is a transferable skill that can be leveraged in several facets of your life.
But why is it so important for nurses to use? We spoke with several experts to learn why critical thinking skills in nursing are so crucial to the field, the patients and the success of a nurse. Keep reading to learn why and to see how you can improve this skill.
Why are critical thinking skills in nursing important?
You learn all sorts of practical skills in nursing school, like flawlessly dressing a wound, taking vitals like a pro or starting an IV without flinching. But without the ability to think clearly and make rational decisions, those skills alone won’t get you very far—you need to think critically as well.
“Nurses are faced with decision-making situations in patient care, and each decision they make impacts patient outcomes. Nursing critical thinking skills drive the decision-making process and impact the quality of care provided,” says Georgia Vest, DNP, RN and senior dean of nursing at the Rasmussen University School of Nursing.
For example, nurses often have to make triage decisions in the emergency room. With an overflow of patients and limited staff, they must evaluate which patients should be treated first. While they rely on their training to measure vital signs and level of consciousness, they must use critical thinking to analyze the consequences of delaying treatment in each case.
No matter which department they work in, nurses use critical thinking in their everyday routines. When you’re faced with decisions that could ultimately mean life or death, the ability to analyze a situation and come to a solution separates the good nurses from the great ones.
How are critical thinking skills acquired in nursing school?
Nursing school offers a multitude of material to master and upholds high expectations for your performance. But in order to learn in a way that will actually equip you to become an excellent nurse, you have to go beyond just memorizing terms. You need to apply an analytical mindset to understanding course material.
One way for students to begin implementing critical thinking is by applying the nursing process to their line of thought, according to Vest. The process includes five steps: assessment, diagnosis, outcomes/planning, implementation and evaluation.
“One of the fundamental principles for developing critical thinking is the nursing process,” Vest says. “It needs to be a lived experience in the learning environment.”
Nursing students often find that there are multiple correct solutions to a problem. The key to nursing is to select the “the most correct” solution—one that will be the most efficient and best fit for that particular situation. Using the nursing process, students can narrow down their options to select the best one.
When answering questions in class or on exams, challenge yourself to go beyond simply selecting an answer. Start to think about why that answer is correct and what the possible consequences might be. Simply memorizing the material won’t translate well into a real-life nursing setting.
How can you develop your critical thinking skills as a nurse?
As you know, learning doesn’t stop with graduation from nursing school. Good nurses continue to soak up knowledge and continually improve throughout their careers. Likewise, they can continue to build their critical thinking skills in the workplace with each shift.
“To improve your critical thinking, pick the brains of the experienced nurses around you to help you get the mindset,” suggests Eileen Sollars, RN ADN, AAS. Understanding how a seasoned nurse came to a conclusion will provide you with insights you may not have considered and help you develop your own approach.
The chain of command can also help nurses develop critical thinking skills in the workplace.
“Another aid in the development of critical thinking I cannot stress enough is the utilization of the chain of command,” Vest says. “In the chain of command, the nurse always reports up to the nurse manager and down to the patient care aide. Peers and fellow healthcare professionals are not in the chain of command. Clear understanding and proper utilization of the chain of command is essential in the workplace.”
How are critical thinking skills applied in nursing?
“Nurses use critical thinking in every single shift,” Sollars says. “Critical thinking in nursing is a paramount skill necessary in the care of your patients. Nowadays there is more emphasis on machines and technical aspects of nursing, but critical thinking plays an important role. You need it to understand and anticipate changes in your patient's condition.”
As a nurse, you will inevitably encounter a situation in which there are multiple solutions or treatments, and you'll be tasked with determining the solution that will provide the best possible outcome for your patient. You must be able to quickly and confidently assess situations and make the best care decision in each unique scenario. It is in situations like these that your critical thinking skills will direct your decision-making.
Do critical thinking skills matter more for nursing leadership and management positions?
While critical thinking skills are essential at every level of nursing, leadership and management positions require a new level of this ability.
When it comes to managing other nurses, working with hospital administration, and dealing with budgets, schedules or policies, critical thinking can make the difference between a smooth-running or struggling department. At the leadership level, nurses need to see the big picture and understand how each part works together.
A nurse manager , for example, might have to deal with being short-staffed. This could require coaching nurses on how to prioritize their workload, organize their tasks and rely on strategies to keep from burning out. A lead nurse with strong critical thinking skills knows how to fully understand the problem and all its implications.
- How will patient care be affected by having fewer staff?
- What kind of strain will be on the nurses?
Their solutions will take into account all their resources and possible roadblocks.
- What work can be delegated to nursing aids?
- Are there any nurses willing to come in on their day off?
- Are nurses from other departments available to provide coverage?
They’ll weigh the pros and cons of each solution and choose those with the greatest potential.
- Will calling in an off-duty nurse contribute to burnout?
- Was this situation a one-off occurrence or something that could require an additional hire in the long term?
Finally, they will look back on the issue and evaluate what worked and what didn’t. With critical thinking skills like this, a lead nurse can affect their entire staff, patient population and department for the better.
Beyond thinking
You’re now well aware of the importance of critical thinking skills in nursing. Even if you already use critical thinking skills every day, you can still work toward strengthening that skill. The more you practice it, the better you will become and the more naturally it will come to you.
If you’re interested in critical thinking because you’d like to move up in your current nursing job, consider how a Bachelor of Science in Nursing (BSN) could help you develop the necessary leadership skills.
EDITOR’S NOTE: This article was originally published in July 2012. It has since been updated to include information relevant to 2021.
- Share on Facebook
- Share on Twitter
- Share on Pinterest
- Share on LinkedIn
Request More Information
Talk with an admissions advisor today. Fill out the form to receive information about:
- Program Details and Applying for Classes
- Financial Aid and FAFSA (for those who qualify)
- Customized Support Services
- Detailed Program Plan
There are some errors in the form. Please correct the errors and submit again.
Please enter your first name.
Please enter your last name.
There is an error in email. Make sure your answer has:
- An "@" symbol
- A suffix such as ".com", ".edu", etc.
There is an error in phone number. Make sure your answer has:
- 10 digits with no dashes or spaces
- No country code (e.g. "1" for USA)
There is an error in ZIP code. Make sure your answer has only 5 digits.
Please choose a School of study.
Please choose a program.
Please choose a degree.
The program you have selected is not available in your ZIP code. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
The program you have selected requires a nursing license. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
Rasmussen University is not enrolling students in your state at this time.
By selecting "Submit," I authorize Rasmussen University to contact me by email, phone or text message at the number provided. There is no obligation to enroll. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
About the author
Hannah Meinke

Posted in General Nursing
- nursing education
Related Content

Brianna Flavin | 05.07.2024

Brianna Flavin | 03.19.2024

Robbie Gould | 11.14.2023

Noelle Hartt | 11.09.2023
This piece of ad content was created by Rasmussen University to support its educational programs. Rasmussen University may not prepare students for all positions featured within this content. Please visit www.rasmussen.edu/degrees for a list of programs offered. External links provided on rasmussen.edu are for reference only. Rasmussen University does not guarantee, approve, control, or specifically endorse the information or products available on websites linked to, and is not endorsed by website owners, authors and/or organizations referenced. Rasmussen University is accredited by the Higher Learning Commission, an institutional accreditation agency recognized by the U.S. Department of Education.

- Brooklyn, NY
- Jamaica, NY
- Phoenix, AZ
- Medical Assistant Program – Jamaica, Queens
- Medical Assistant Program – Brooklyn, NY
- Medical Assistant Program – Phoenix, AZ
- Brooklyn Campus
- Phoenix Campus
- Financial Aid
- History of the School
- Career Services
- Institution For HOPE
How Critical Thinking Skills Apply to Healthcare
Critical Thinking Includes
- The skill to draw conclusions.
- The skill to troubleshoot and problem-solve.
- The capability to use skills or knowledge in a variety of situations.
Examples of Everyday Critical Thinking
- Thinking about what steps should to be taken to avoid an accident.
- Creating a list that gives ability to accomplish every task efficiently and effectively.
- Thinking through the process and dealing with issues that might arise. (missing an ingredient needed for a dish or finding out that the vacuum cleaner is broken)
Examples of Work-Related Critical Thinking
- Deciding how to deal with a customer who is upset over service or bill to ensure a happy customer.
- Handling a disagreement with another coworker.
- Presenting an issue or proposal to the supervisor.
Examples of Work-Related Critical Thinking Situations
- If you have worked in customer service then the same critical thinking skills that are used to deal with customers will be used to deal with patients in the medical field .
- If you have worked in a fast-paced environment requiring prioritizing then you will carry that skill over to the medical field.
Leave a Reply
Click here to cancel reply.
Name (required)
Email (will not be published) (required)
XHTML: You can use these tags: <a href="" title=""> <abbr title=""> <acronym title=""> <b> <blockquote cite=""> <cite> <code> <del datetime=""> <em> <i> <q cite=""> <s> <strike> <strong>
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical Thinking in medical education: When and How?
Rapid response to:
Critical thinking in healthcare and education
- Related content
- Article metrics
- Rapid responses
Rapid Response:
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from that of general cognitive abilities [1].
People cannot think critically about topics for which they have little knowledge. Critical thinking should be viewed as a domain-specific construct that evolves as an individual acquires domain-specific knowledge [1]. For instance, most common people have no basis for prioritizing patients in the emergency department to be shifted to the only bed available in the intensive care unit. Medical professionals who could thinking critically in their own discipline would have difficulty thinking critically about problems in other fields. Therefore, ‘domain-general’ critical thinking training and evaluation could be non-specific and might not benefit the targeted domain i.e. medical profession.
Moreover, the literature does not demonstrate that it is possible to train universally effective critical thinking skills [1]. As medical teachers, we can start building up student’s critical thinking skill by contingent teaching-learning environment wherein one should encourage reasoning and analytics, problem solving abilities and welcome new ideas and opinions [2]. But at the same time, one should continue rather tapering the critical skills as one ascends towards a specialty, thereby targeting ‘domain-specific’ critical thinking.
For the benefit of healthcare, tools for training and evaluating ‘domain-specific’ critical thinking should be developed for each of the professional knowledge domains such as doctors, nurses, lab technicians and so on. As the Authors rightly pointed out, this humongous task can be accomplished only with cross border collaboration among cognitive neuroscientists, psychologists, medical education experts and medical professionals.
References 1. National Research Council. (2011). Assessing 21st Century Skills: Summary of a Workshop. J.A. Koenig, Rapporteur. Committee on the Assessment of 21st Century Skills. Board on Testing and Assessment, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. 2. Mafakheri Laleh M, Mohammadimehr M, Zargar Balaye Jame S. Designing a model for critical thinking development in AJA University of Medical Sciences. J Adv Med Educ Prof. 2016 Oct;4(4):179–87.
Competing interests: No competing interests
MINI REVIEW article
Cognitive biases in pediatric cardiac care.

- 1 CHU Nantes, Department of Pediatric Cardiology and Pediatric Cardiac Surgery, FHU PRECICARE, Nantes Université, Nantes, France
- 2 CHU Nantes, INSERM, CIC FEA 1413, Nantes Université, Nantes, France
- 3 LPPL, SFR Confluences, Nantes Université, Université d’Angers, Angers, France
- 4 CHU Nantes, Centre Référent des Troubles d’Apprentissage, Nantes Université, Nantes, France
- 5 Pediatrics Department at Filantropia Municipal Hospital of Craiova, Craiova, Romania
- 6 Department of Pediatric Cardiology, Mount Sinai Kravis Children’s Hospital, New York, NY, United States
- 7 CHU Nantes, CNRS, INSERM, l’institut du Thorax, Nantes Université, Nantes, France
- 8 INRAE, UMR 1280, PhAN, Nantes Université, Nantes, France
Medical practitioners are entrusted with the pivotal task of making optimal decisions in healthcare delivery. Despite rigorous training, our confidence in reasoning can fail when faced with pressures, uncertainties, urgencies, difficulties, and occasional errors. Day-to-day decisions rely on swift, intuitive cognitive processes known as heuristic or type 1 decision-making, which, while efficient in most scenarios, harbor inherent vulnerabilities leading to systematic errors. Cognitive biases receive limited explicit discussion during our training as junior doctors in the domain of paediatric cardiology. As pediatric cardiologists, we frequently confront emergencies necessitating rapid decision-making, while contending with the pressures of stress, fatigue, an earnest interest in “doing the right thing” and the impact of parental involvement. This article aims to describe cognitive biases in pediatric cardiology, highlighting their influence on therapeutic interventions for congenital heart disease. Whether future pediatric cardiologists or experienced professionals, understanding and actively combating cognitive biases are essential components of our ongoing medical education. Furthermore, it is our responsibility to thoroughly examine our own practices in our unwavering commitment to providing high-quality care.
1 Introduction
Type 1 processing, also known as intuitive decision-making or heuristic reasoning, refers to a rapid and automatic thinking process. It is characterized by the utilization of mental heuristics, or simple rules, to swiftly reach conclusions and make decisions without requiring in-depth analysis of available information ( 1 ). In addition to Type 1 processing, there exists Type 2 processing, characterized by slower, more deliberate analysis of information and consideration of multiple factors ( 2 ). Despite the essential nature of Type 1 processing ( 3 ), it can lead to systematic thinking errors, called cognitive biases. A cognitive bias is a systematic deviation from rationality or objectivity in judgment or decision-making, often stemming from mental shortcuts, perceptual distortions, or subjective influences. Importantly, these biases do not correlate with intelligence or cognitive ability ( 4 , 5 ). They arise from a variety of sources including acquired or inherent predispositions, societal and cultural influences, deficits in statistical understanding and mathematical reasoning and, in particular, and environmental stimuli that demand our attention ( 6 ).
Cognitive biases can impact various facets of our existence, but their significance becomes pronounced when these errors manifest within the context of medical practice. Prevalence of diagnostic error has been estimated to be as high as 10%–15% in daily clinical practice ( 7 ). Cognitive factors are the main contributor to diagnostic errors, which are associated with a proportionately higher morbidity than is the case with other types of medical error ( 8 , 9 ). Contrary to physician interviews that often identify system-related factors (organizational flaws, inadequate policies, staffing or equipment) as the main contributors to diagnostic errors, cognitive factors are more likely the primary driver of such errors ( 10 ).
Among medical specialties, paediatrics stands out as one where decisions are emotionally demanding, given the significant weight they carry for both parents and children ( 11 , 12 ). Given the high stakes involved in pediatric care, understanding, and mitigating cognitive biases is paramount.
This work aims to examine the medical reasoning and practice by highlighting several cognitive biases specifically within the field of pediatric cardiology and congenital heart disease (CHD) care.
2 Subsections relevant for the subject
Cognitive biases are prevalent in pediatric cardiology practice and can significantly impact diagnostic decision-making, multidisciplinary collaboration, and technical procedures.
2.1 Diagnostic decision-making
This section delves into cognitive biases that influence diagnostic decision-making such as the availability bias, the anchoring bias, the attrition bias, the confirmation bias, overconfidence, and search satisfying.
Cognitive biases have been identified in all steps of decision making ( 13 – 15 ), including information gathering, association triggering, context formulation, processing and verification ( 16 ). The diagnostic enterprise, construed as the distinctive characterisation of a specific disease or condition, hinges on factors including etiopathogenesis, parental interrogation, children signs, symptoms, physical examination results, diagnostic tests, and health history. Clinical expertise accrues through domain-based practice, augmented experience, enhanced knowledge and skills, and the development of domain-specific intuitive capacities. In addition to the advanced cognitive functions such as problem-solving, judgment, and decision-making mentioned earlier, formulating a diagnosis also relies on the utilization of social and emotional resources. Contemporary understanding of cognition underscores the dynamic interaction between cognitive processes and socioemotional factors in decision-making contexts. This includes the impact of emotional states, interpersonal dynamics, and cultural influences on cognitive functioning ( 17 , 18 ). Expert clinicians find it easier to effectively focus attention on and evaluate details of the infant's clinical problem. This enables them to intuitively and deliberately generate several relevant differential diagnoses and potential strategies to address the identified clinical situation.
Nonetheless, experience can be a source of bias, such as availability bias ( 19 – 21 ) or base rate neglect ( 22 ) (see Figure 1 ). Physicians often tend to perceive things as more likely if they readily come to mind: “common things are common (availability)”. They may form diagnostic hypotheses based on recent exposure to another patient with the same illness, particularly if the case was particularly notable or emotionally charged. Conversely, prolonged absence in encountering a disease tends to decrease the likelihood of considering it during diagnosis: “out of sight out of mind (non-availability)”. The bias of restricting representativeness is ingrained in the traditions of medical education ( 23 ). Our diagnostic approach often leads us to search for prototypical presentations of a disease: adhering to the adage “When you hear hoofbeats, think of horses rather than zebras”. These entrenched dogmas and mindsets tend to exclude rare diseases from consideration in the diagnostic process. This can be particularly detrimental in the field of CHD, which may present infrequently in emergency room consultations despite being relatively common, affecting 8 out of 1,000 births ( 24 ). Base rate neglect on the other hand may result in overestimates of unlikely diagnoses. This bias occurs when individuals fail to consider statistical or base rates in decision-making, instead prioritizing specific information or individual cases.
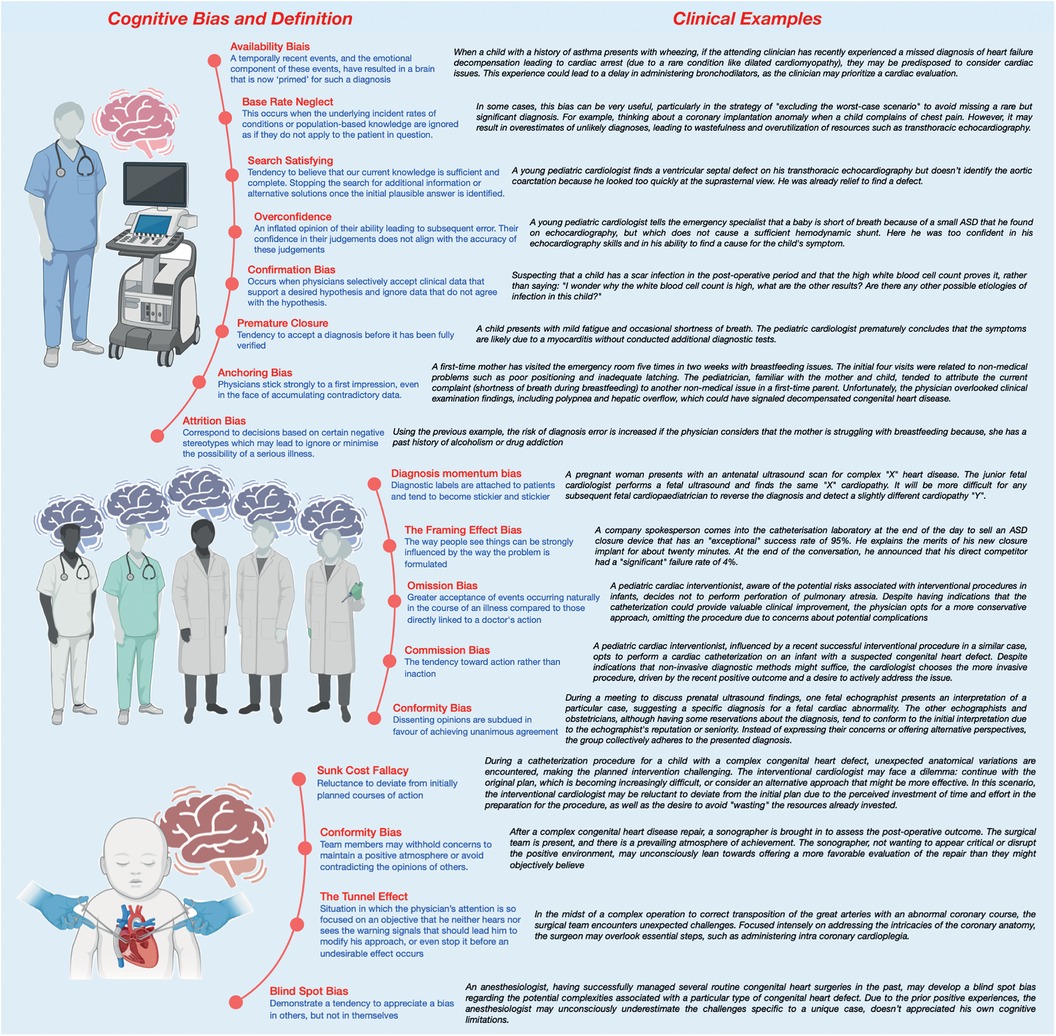
Figure 1 Clinical examples of cognitive biases during pediatric cardiac care.
Another potential bias, notably observed in emergency departments (ED), is anchoring bias whereby physicians may strongly adhere to their initial impressions, even when confronted with a substantial amount of conflicting data, particularly if they harbor certain preconceptions ( 23 , 25 ). Anchoring bias is linked to attrition bias which is attempts to discover reason for observations ( 26 ). Stereotyping and gender bias are both good examples of attrition bias. In the ED, there is often significant time pressure to make swift decisions. This urgency is particularly concerning in the context of undiagnosed CHD, where achieving accurate diagnoses may necessitate thorough and careful consideration in addition to multiple examinations such as electrocardiography, chest radiographs, echocardiography, and blood tests.
Compared with an expert, novice specialists will likely make more diagnostic errors ( 18 ). Formulating a specific diagnosis largely relies on pattern recognition, the clinician's familiarity with similar clinical scenarios, and the ease with which relevant past cases come to mind. Confirmation Bias, Overconfidence and Search Satisfying are common bias for novice specialists ( 27 ). Confirmation bias , the selective acceptance of clinical data supporting a desired hypothesis while disregarding contradictory data, significantly heightens the risk of diagnostic errors ( 28 ). Overconfidence , also known as the Dunning-Kruger effect, describes the tendency for individuals lacking expertise in a given field to overestimate their proficiency, leading them to believe they possess more knowledge than they actually do ( 29 , 30 ). This can lead to noncompliance with evidence-based guidelines. Additionally, search satisfying occurs when clinicians cease seeking additional information once they find a solution that appears satisfactory, even if it may not be the most appropriate or accurate ( 14 ). Unlike confirmation bias, where clinicians tend to seek evidence to confirm their initial hypotheses while ignoring contradictory evidence, search satisfying focuses more on the satisfaction of finding a plausible solution, even if it is not validated by additional evidence or thorough consideration. Paradoxically, qualified individuals tend to underestimate their own abilities. In other words and restated, inexperience may prevent people from recognising their own limitations and those who are more highly qualified and experienced may paradoxically underestimate the extent of their knowledge.
Another well-known bias is premature closure which is a form of bias in which we tend to be satisfied with a plausible hypothesis derived from our own experience and dismiss the possibility of uncertainty ( 31 ). Moreover, when contemplating the dynamics of the doctor-parent relationship, particularly within the nuanced context of paediatrics, a salient cognitive bias that warrants consideration is the outcome bias . This cognitive inclination manifests as a predisposition towards diagnostic decisions that are anticipated to yield positive outcomes, consciously avoiding choices associated with unfavourable consequences ( 32 ). Such a cognitive predisposition serves as a protective mechanism, strategically sidestepping the emotional distress that may be entwined with less favourable clinical outcomes. This can lead to minimizing serious diagnoses or hoping for a favourable outcome and may manifest, in pediatric cardiovascular care as the avoidance of surgery or a catheterization procedure, as two examples. Also, countertransference (positive or negative) can lead to an under-assessment of the severity of the child or adolescent's condition, to avoid breaking bad news ( 33 , 34 ). In an ideal scenario, every clinical decision would be made impartially and consistently across different patients. However, this isn't always the case. Our interactions with patients and families can evoke both favorable and unfavorable sentiments, which might influence the quality of our decisions. Within the context of the ED, instances may arise where a physician experiences positive countertransference towards a patient, potentially exerting an influence on clinical decision-making processes. This phenomenon, driven by outcome bias, could lead to underinvestigation, as decisions favoring positive outcomes may take precedence over those indicating negative outcomes. Consequently, this bias may result in the omission of diagnostic tests critical for identifying unfavorable prognostic implications for the patient.
Added to and closely linked to cognitive biases is the notion of noise which reflects errors in judgement and measurement. Some situations are more prone to biased-reasoning due to this form of error ( 17 ). The profound influence of background noise on decision-making, occasionally impeding the activation of System 2 cognition—the reflective and analytical mode of thought—is highlighted by factors including workload overload, concurrent multitasking, task interruptions, fatigue, time pressure, the broader work environment, dysfunctional team dynamics, hyperconnectivity, and various forms of distraction. These distractions may arise from external sources or be influenced by temporal factors such as the day of the week, holidays, or the time of day or night. A constant self-inquiry that warrants consideration is whether the current situation is conducive to the prevalence of biases.
2.2 Multidisciplinary collaboration
Exploring cognitive biases during multidisciplinary decision-making highlights challenges and opportunities for enhancing teamwork. These biases include memory shifting/reconstruction bias, diagnosis momentum bias, framing effect bias, order effect bias, bias of omission, commission bias, conformity bias, authority gradient effect, and hindsight bias
Multidisciplinary consultations and collaborative thinking represent effective strategies for mitigating decisions influenced by rapid reasoning with cognitive biases ( 35 – 38 ) (see Figure 1 ). However, certain inter-human factors may still be biased and affect such decision-making. Memory shifting , also called reconstruction bias , involves the inaccurate recall of information due to variations in coding of meaning and textual information, resulting in the “filling in” of details, sometimes with incorrect information, during memory recall. Diagnosis momentum bias is another concern, whereby diagnostic labels attached to patients tend to become increasingly ingrained over time, leading to the exclusion of alternative possibilities. This bias is closely related to the framing effect bias , which demonstrates how the formulation of a problem can strongly influence perception ( 39 ). Additionally, the order effect bias must be considered when presenting cases, as individuals tend to remember the beginning (primacy effect) or the end (recency effect) of a story being told, highlighting the importance of how cases are presented in such conferences ( 13 , 17 ). This holds particularly true when presenting a case of a child who has undergone multiple surgeries for a complex cardiac disease. The order in which the varied problems and interventions have been presented can have a meaningful and unintentional impact on how the case is discussed and considered.
In medical decision-making, there is a tendency toward inaction, prioritizing the principle of non-maleficence, which leads to the omission bias ( 32 , 36 , 40 ). This bias, influenced by the perceived safety of inaction, can have severe consequences despite maintaining the status quo. Conversely, commission bias , stemming from the obligation toward beneficence, involves a propensity toward action. This bias is more prevalent in overconfident physicians. Discussing these two biases in the context of pediatrics is particularly important, given the unique ethical considerations and potential consequences of either form of bias on the care of pediatric patients.
Moreover, within the intricate dynamics of medical staff discussions, the susceptibility to groupthink or false consensus effect poses a significant challenge ( 36 ). The desire for consensus may lead to a conformity bias, wherein dissenting opinions are subdued in favour of achieving unanimous agreement. This can be particularly pronounced in hierarchical medical teams, where junior members may hesitate to challenge prevailing views. Specifically, the phenomenon referred to as the authority gradient effect comes into play in such situations. The authority gradient effect describes the reluctance of junior members to challenge the opinions of senior members within hierarchical structures. Furthermore, the phenomenon of hindsight bias whereby there may be a tendency to perceive something as having been more predictable (e.g., “I knew it all along”) than it truly is while making decisions ( 41 ). This retrospective distortion may impact how post-case analyses unfold and potentially impede the recognition of avoidable errors. These behaviours may be conscious and induced by social norms, but often, they are unconscious and characteristic of cognitive biases.
2.3 Technical procedure
Exploring cognitive biases during technical procedures is essential for identifying potential errors and implementing risk-mitigation strategies. Anesthesiologists, surgeons, and cardiac interventionists, encounter various cognitive biases during medical procedures such as anchoring bias, sunk cost fallacy, social desirability bias and the tunnel effect.
Anesthesiologists confront various cognitive biases that can significantly impact decision-making ( 6 , 39 ). Anchoring bias— the tendency to fixate on specific features -, for instance, becomes pronounced when faced with unexpected challenges during surgery, including hemodynamic variation. For example, anchoring bias becomes prominent in such situations. The initial medication dosage administered acts as a cognitive anchor, disproportionately influencing subsequent decisions. This predisposition may lead to either inadequate or excessive adjustments.
Confronted with unexpected challenges in the operating room or the catheterisation laboratory, physicians (cardiac interventionists, surgeons, or anaesthesiologists) may grapple with the sunk cost fallacy , fostering a reluctance to deviate from initially planned courses of action ( 42 ). This psychological bias arises from a perceived investment of time and effort, impeding objective reassessment. Additionally, the dynamics of communication within the anesthesia/nurse/surgery team may exhibit a conformity bias , wherein team members may withhold concerns to maintain a positive atmosphere or avoid contradicting the opinions of others. Of course, physicians during technical care are also vulnerable to many of the previously described biases such as confirmation bias or overconfidence bias amongst others.
Surgeons and cardiac interventionists are highly sensitive to the tunnel effect ( 42 , 43 ). This refers to a situation in which the physician's attention is so focused on an objective (expected outcome, management of a complication) that he neither hears nor sees the warning signals that should lead him to modify his approach, or even stop it before an undesirable effect occurs. In addition, proceduralists must deal with a variable range of emotions that may influence their decision-making during procedures. For example, anger can influence decisions made by oneself or the team, regret describes the tendency to let regret about past decisions influence future decisions and anticipatory regret is the desire to avoid regret about future consequences or outcomes of decision choices. All of these may negatively impact the proceduralist.
Finally, and somewhat paradoxically, the well-known blind spot bias , whereby individuals tend to recognize biases in others but not in themselves, is observed ( 15 , 17 , 36 ). A blind spot bias may occur when a physician, while evaluating a child with cardiac symptoms, readily identifies and corrects reasoning errors in their colleagues but fails to question their own diagnostic decisions or treatments, even if they are affected by their own similar cognitive biases.
3 Discussion
Identifying physicians’ cognitive biases at an early stage is essential for optimising medical decisions, preventing errors and creating realistic expectations for patients, ultimately reducing the rising costs of healthcare ( 44 ). Most cognitive biases probably arise from overuse of System 1 or when System 1 dominates over System 2. Techniques that enhance System 2 could counteract these biases, thereby improving diagnostic accuracy and decreasing management errors ( 45 ).
Overconfidence, anchoring bias, and availability bias were prevalent, impacting diagnostic accuracy in 36.5%–77% of case scenarios ( 46 ). For example, Mamede et al. found that availability bias increased with years of training, and reflective reasoning improved diagnostic accuracy among internal medicine residents ( 21 ). Additionally, biases such as information bias, representativeness bias, and premature closure were associated with diagnostic errors in over half of the evaluated scenarios. These findings highlight the widespread presence of cognitive biases across various medical tasks, from diagnosis to treatment and management ( 46 ).
Cognitive biases not only affect diagnostic accuracy but also influence therapeutic and management decisions. For instance, Yee et al. found that better-coping strategies and higher tolerance to ambiguity among obstetricians were associated with lower rates of instrumental vaginal deliveries and fewer management errors ( 47 ). They also indicated that higher tolerance to ambiguity among physicians was associated with increased medical complications, such as postpartum hemorrhage. These studies demonstrate how cognitive biases can lead to both over-treatment and under-treatment, illustrating the necessity for balanced decision-making frameworks. This also underscores the potential severity of cognitive biases, emphasizing the need for further research to establish clear links between these biases and patient outcomes ( 48 ).
Addressing cognitive biases requires a multi-faceted approach. Increasing awareness among physicians and medical students is crucial, as is incorporating training on cognitive biases into medical education programs. Effective strategies include reflective reasoning, the use of cognitive checklists, and heuristic approaches to simplify decision-making processes. Collaborative efforts from academic institutions, healthcare organizations, and policymakers are needed to implement these strategies and improve healthcare delivery ( 49 – 51 ).
4 Conclusion
A significant portion of today's medical decision-making research evolved from studies conducted in the field of cognitive psychology in the late 20th century ( 52 ). Regrettably, despite this wealth of accumulated knowledge, medical practitioners still struggle to fully comprehend and integrate these findings into their practice. Grounded in real-world examples and informed by personal experiences, this perspective endeavors to elucidate the intricate relationship between cognitive biases and the landscape of pediatric cardiology. However, this work represents only an initial step toward grasping the complexities of human decision-making dynamics. There is a notable lack of comprehensive research in this arena in pediatrics, prompting critical inquiry into the interaction between cognitive biases and the powerful stresses and emotions experienced in pediatric care. To address these gaps, further research is imperative, along with the development of dedicated protocols and frameworks to help mitigate the impact of these biases on decision-making. Incorporating training or simulations in human factors, including the study of cognitive biases, into the curriculum of young pediatricians across all specialties should be considered as an essential component for enhancing clinical practice and patient care.
Author contributions
PP: Conceptualization, Investigation, Supervision, Writing – original draft. AR: Validation, Writing – review & editing. AG: Validation, Writing – review & editing. OC: Validation, Writing – review & editing. ML: Validation, Writing – review & editing. CMV: Validation, Writing – review & editing. RHP: Supervision, Validation, Writing – review & editing. A-EB: Conceptualization, Supervision, Writing – original draft.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
By a research grant from the French Federation of Cardiology (to PP); by a research grant from the Fondation Maladies Rares (to AE-B); by a research grant from the French Government as part of the “Investments of the future” program managed by the National Research Agency, grant reference ANR-16-IDEX-0007 (to AE-B).
Acknowledgments
We gratefully acknowledge GCS HUGO, AVIESAN and FHU PRECICARE.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Smallberg G. Bias is the nose for the story. In: Brockman J, editor. This Will Make you Smarter . New York: Harper Perennial (2012). 43–5.
Google Scholar
2. Mamede S, Schmidt HG. The structure of reflective practice in medicine. Med Educ . (2004) 38(12):1302–8. doi: 10.1111/j.1365-2929.2004.01917.x
PubMed Abstract | Crossref Full Text | Google Scholar
3. Croskerry P. Bias: a normal operating characteristic of the diagnosing brain. Diagnosis (Berl) . (2014) 1(1):23–7. doi: 10.1515/dx-2013-0028
4. Stanovich KE, West RF. On the relative independence of thinking biases and cognitive ability. J Pers Soc Psychol . (2008) 94(4):672–95. doi: 10.1037/0022-3514.94.4.672
5. Detmer DE, Fryback DG, Gassner K. Heuristics and biases in medical decision-making. J Med Educ . (1978) 53(8):682–3. doi: 10.1097/00001888-197808000-00012
6. Stiegler MP, Tung A. Cognitive processes in anesthesiology decision making. Anesthesiology . (2014) 120(1):204–17. doi: 10.1097/ALN.0000000000000073
7. Elstein A. Clinical reasoning in medicine. In: Higgs J, editor. Clinical Reasoning in the Health Professions . Oxford, England: Butterworth-Heinemann Ltd (1995). p. 49–59.
8. Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard medical practice study I. N Engl J Med . (1991) 324(6):370–6. doi: 10.1056/NEJM199102073240604
9. Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care . (2000) 38(3):261–71. doi: 10.1097/00005650-200003000-00003
10. Warrick C, Patel P, Hyer W, Neale G, Sevdalis N, Inwald D. Diagnostic error in children presenting with acute medical illness to a community hospital. Int J Qual Health Care . (2014) 26(5):538–46. doi: 10.1093/intqhc/mzu066
11. Feeks C, Chao J, Sinert R. Prevalence and risk factors for burnout in pediatric emergency medicine fellows. Pediatr Emerg Care . (2020) 36(5):236–9. doi: 10.1097/PEC.0000000000002093
12. McClafferty HH, Hubbard DK, Foradori D, Brown ML, Profit J, Tawfik DS, et al. Physician health and wellness. Pediatrics . (2022) 150(5):e2022059665. doi: 10.1542/peds.2022-059665
13. Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med . (2003) 78(8):775–80. doi: 10.1097/00001888-200308000-00003
14. Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med . (2002) 9(11):1184–204. doi: 10.1197/aemj.9.11.1184
15. Croskerry P. From mindless to mindful practice–cognitive bias and clinical decision making. N Engl J Med . (2013) 368(26):2445–8. doi: 10.1056/NEJMp1303712
16. Kassirer JP, Kopelman RI. Cognitive errors in diagnosis: instantiation, classification, and consequences. Am J Med . (1989) 86(4):433–41. doi: 10.1016/0002-9343(89)90342-2
17. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Saf . (2013) 22(Suppl 2):ii58–64. doi: 10.1136/bmjqs-2012-001712
18. Graber ML. The incidence of diagnostic error in medicine. BMJ Qual Saf . (2013) 22(Suppl 2):ii21–7. doi: 10.1136/bmjqs-2012-001615
19. Kovacs G, Croskerry P. Clinical decision making: an emergency medicine perspective. Acad Emerg Med . (1999) 6(9):947–52. doi: 10.1111/j.1553-2712.1999.tb01246.x
20. Tversky A, Kahneman D. Availability: a heuristic for judging frequency and probability. Cogn Psychol . (1973) 5(2):207–32. doi: 10.1016/0010-0285(73)90033-9
Crossref Full Text | Google Scholar
21. Mamede S, van Gog T, van den Berge K, Rikers RMJP, van Saase JLCM, van Guldener C, et al. Effect of availability bias and reflective reasoning on diagnostic accuracy among internal medicine residents. JAMA . (2010) 304(11):1198–203. doi: 10.1001/jama.2010.1276
22. Elstein AS. Heuristics and biases: selected errors in clinical reasoning. Acad Med . (1999) 74(7):791–4. doi: 10.1097/00001888-199907000-00012
23. Croskerry P. The cognitive imperative: thinking about how we think. Acad Emerg Med . (2000) 7(11):1223–31. doi: 10.1111/j.1553-2712.2000.tb00467.x
24. Liu Y, Chen S, Zühlke L, Black GC, Choy MK, Li N, et al. Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol . (2019) 48(2):455–63. doi: 10.1093/ije/dyz009
25. Croskerry P, Sinclair D. Emergency medicine: a practice prone to error? CJEM . (2001) 3(4):271–6. doi: 10.1017/S1481803500005765
26. Greenhalgh T. Narrative based medicine: narrative based medicine in an evidence based world. Br Med J . (1999) 318(7179):323–5. doi: 10.1136/bmj.318.7179.323
27. Scherer LD, de Vries M, Zikmund-Fisher BJ, Witteman HO, Fagerlin A. Trust in deliberation: the consequences of deliberative decision strategies for medical decisions. Health Psychol . (2015) 34(11):1090–9. doi: 10.1037/hea0000203
28. Kern L, Doherty ME. “Pseudodiagnosticity” in an idealized medical problem-solving environment. J Med Educ . (1982) 57(2):100–4. doi: 10.1097/00001888-198202000-00004
29. Leopold SS. Editorial: are we all better-than-average drivers, and better-than-average kissers? Outwitting the Kruger-Dunning effect in clinical practice and research. Clin Orthop Relat Res . (2019) 477(10):2183–5. doi: 10.1097/CORR.0000000000000948
30. Howell WC. Uncertainty from internal and external sources: a clear case of overconfidence. J Exp Psychol . (1971) 89(2):240–3. doi: 10.1037/h0031206
31. Voytovich AE, Rippey RM, Suffredini A. Premature conclusions in diagnostic reasoning. J Med Educ . (1985) 60(4):302–7. doi: 10.1097/00001888-198504000-00004
32. Baron J, Hershey JC. Outcome bias in decision evaluation. J Pers Soc Psychol . (1988) 54(4):569–79. doi: 10.1037/0022-3514.54.4.569
33. Andersen SM, Glassman NS, Chen S, Cole SW. Transference in social perception: the role of chronic accessibility in significant-other representations. J Pers Soc Psychol . (1995) 69(1):41–57. doi: 10.1037/0022-3514.69.1.41
34. Scarfone RJ, Nagler J. Cognitive errors in pediatric emergency medicine. Pediatr Emerg Care . (2021) 37(2):96–103. doi: 10.1097/PEC.0000000000002342
35. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 2: impediments to and strategies for change. BMJ Qual Saf . (2013) 22(Suppl 2):ii65–72. doi: 10.1136/bmjqs-2012-001713
36. Hammond MEH, Stehlik J, Drakos SG, Kfoury AG. Bias in medicine: lessons learned and mitigation strategies. JACC Basic Transl Sci . (2021) 6(1):78–85. doi: 10.1016/j.jacbts.2020.07.012
37. Croskerry P. When I say… cognitive debiasing. Med Educ . (2015) 49(7):656–7. doi: 10.1111/medu.12670
38. Eichbaum Q. Medical error, cognitive bias, and debiasing: the jury is still out. Acad Med . (2019) 94(8):1065–6. doi: 10.1097/ACM.0000000000002791
39. Stiegler MP, Neelankavil JP, Canales C, Dhillon A. Cognitive errors detected in anaesthesiology: a literature review and pilot study. Br J Anaesth . (2012) 108(2):229–35. doi: 10.1093/bja/aer387
40. Asch DA, Baron J, Hershey JC, Kunreuther H, Meszaros J, Ritov I, et al. Omission bias and Pertussis vaccination. Med Decis Making . (1994) 14(2):118–23. doi: 10.1177/0272989X9401400204
41. Fischhoff B. Hindsight ^foresight: the effect of outcome knowledge on judgment under uncertainty. J Exp Psychol Hum Percept Perform . (1975) 1(3):288–99. doi: 10.1037/0096-1523.1.3.288
42. Antonacci AC, Dechario SP, Rindskopf D, Husk G, Jarrett M. Cognitive bias and severity of harm following surgery: plan for workflow debiasing strategy. Am J Surg . (2021) 222(6):1172–7. doi: 10.1016/j.amjsurg.2021.08.035
43. Richburg CE, Dossett LA, Hughes TM. Cognitive bias and dissonance in surgical practice: a narrative review. Surg Clin North Am . (2023) 103(2):271–85. doi: 10.1016/j.suc.2022.11.003
44. Saposnik G, Redelmeier D, Ruff CC, Tobler PN. Cognitive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak . (2016) 16(1):138. doi: 10.1186/s12911-016-0377-1
45. Ely JW, Graber ML, Croskerry P. Checklists to reduce diagnostic errors. Acad Med . (2011) 86(3):307–13. doi: 10.1097/ACM.0b013e31820824cd
46. Dhillon BS. Human errors: a review. Microelectron Reliab . (1989) 29(3):299–304. doi: 10.1016/0026-2714(89)90612-4
47. Yee LM, Liu LY, Grobman WA. The relationship between obstetricians’ cognitive and affective traits and their patients’ delivery outcomes. Am J Obstet Gynecol . (2014) 211(6):692.e1–6. doi: 10.1016/j.ajog.2014.06.003
48. Baldwin RL, Green JW, Shaw JL, Simpson DD, Bird TM, Cleves MA, et al. Physician risk attitudes and hospitalization of infants with bronchiolitis. Acad Emerg Med . (2005) 12(2):142–6. doi: 10.1197/j.aem.2004.10.002
49. Balla JI, Heneghan C, Glasziou P, Thompson M, Balla ME. A model for reflection for good clinical practice. J Eval Clin Pract . (2009) 15(6):964–9. doi: 10.1111/j.1365-2753.2009.01243.x
50. Graber ML, Kissam S, Payne VL, Meyer AND, Sorensen A, Lenfestey N, et al. Cognitive interventions to reduce diagnostic error: a narrative review. BMJ Qual Saf . (2012) 21(7):535–57. doi: 10.1136/bmjqs-2011-000149
51. Raab M, Gigerenzer G. The power of simplicity: a fast-and-frugal heuristics approach to performance science. Front Psychol . (2015) 6:1672. doi: 10.3389/fpsyg.2015.01672
52. Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science . (1974) 185(4157):1124–31. doi: 10.1126/science.185.4157.1124
Keywords: congenital heart disease, cognitive biases, pediatric cardiology, diagnostic errors, medical decision-making, human factors
Citation: Padovani P, Roy A, Guerra A, Cadeau O, Ly M, Vasile CM, Pass RH and Baruteau A-E (2024) Cognitive biases in pediatric cardiac care. Front. Cardiovasc. Med. 11 :1423680. doi: 10.3389/fcvm.2024.1423680
Received: 26 April 2024; Accepted: 21 June 2024; Published: 4 July 2024.
Reviewed by:
© 2024 Padovani, Roy, Guerra, Cadeau, Ly, Vasile, Pass and Baruteau. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul Padovani, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
New 2024 Lifeguarding Program Materials are Here! Buy More, Save More with quantity discounts available. Shop Now >
10% OFF on ALL Training Supplies! Use Coupon Code LETSTRAIN0724 at checkout! Shop Now >
The 2024 Red Cross Lifeguarding Program updates are here! Learn more >
- 0 Your Cart is Empty < Continue Shopping
Your browser's Javascript functionality is turned off. Please turn it on so that you can experience the full capabilities of this site.
Pediatric Advanced Life Support Review r.21
The Pediatric Advanced Life Support (PALS) provides healthcare providers the knowledge and skills necessary to assess recognize and care for pediatric patients experiencing life threatening medical emergencies. Consistent with the American Red Cross Focused Updates and Guidelines 2020 the PALS course emphasizes providing high-quality care and integrating psychomotor skills with critical thinking and problem solving to achieve the best possible patient outcomes. This is an attenuated review couse.
Equipment Terms & Conditions
Local classes held at convenient locations and times Participate in hands-on training Provides full certification Learn from experienced instructors
Classroom / Skills Check
- Local in-person training
- Learn from experienced instructors
- Convenient locations and times for instructor-led skills check
- Satisfies OSHA workplace safety certification requirements
Certification
Red Cross courses offer Digital Certification, an online version of a Red Cross certificate, which provides anytime, anywhere access to student training history and course certificates. Digital certificates can be viewed, printed or shared online and can be accessed anytime through your Red Cross Account. Each certificate includes a unique ID and a QR code which meets employment requirements and allows employers to easily confirm your certificate is valid. There is no need to carry your printed certificate around anymore!
Once training has been successfully completed, students may also request healthcare continuing education credit. The American Red Cross is an accredited provider of continuing education by the Commission on Accreditation for Prehospital Continuing Education. For additional information on receiving continuing education credit go to www.redcross.org/CAPCE .
It is incumbent upon the healthcare professional to verify that the accredited continuing education credit provided by the American Red Cross meets the requirements of specific professional and licensing bodies.

The content of these reviews regarding the quality and value of this course is based on data collected across all American Red Cross classes with this title and does not reflect ratings of any specific instructor or provider.
Herd immunity and COVID-19: What you need to know
Understand what's known about herd immunity and what it means for illnesses like COVID-19.
Herd immunity is the name for a point in time when it's hard for a disease to spread through a group of people. The idea of herd immunity works for some diseases, such as measles. But it's a harder concept to apply to illnesses like coronavirus disease 2019 (COVID-19).
Read on to learn how herd immunity makes sense for some diseases but not others.
Why is herd immunity important?
Herd immunity is important because it defines when a whole community is protected. That includes people who haven't caught the disease, people who had the illness and recovered, and people who got a vaccine. It also includes people who can't get a vaccine.
Data on herd immunity helps guide vaccine goals set by public health agencies.
Herd immunity can't be reached for every disease, but measles is one example of the idea. Measles is a disease caused by a virus that spreads quickly among people who've never had the disease or the measles vaccine.
As people recover or get a measles vaccine, the virus has fewer new people to infect.
The virus that causes measles doesn't change much, called mutate, over time. That means once you get the vaccine for measles or recover from the illness, you are not likely to get it again.
Based on those facts, health officials estimate that herd immunity for measles is at least 94%.
That means 94 people out of 100 in a population need to be immune to stop the spread of the measles virus. That includes measles recovery or people who got both measles vaccine shots.
So keeping at least 95% of people vaccinated against the measles virus is a public health goal. At that level, people who can't get the vaccine, such as children younger than 12 months, are protected.
How is herd immunity achieved?
Herd immunity for illnesses such as measles and polio happens when you and the people around you get vaccinated.
Before the vaccine for measles, millions of people got the disease. In the U.S., hundreds died of measles each year and thousands needed care in the hospital.
After people could get the measles vaccine, the measles virus stopped spreading in the U.S. because so many people got the shots.
Each year, there are still outbreaks of measles. These are mostly among people who haven't had a vaccine, are undervaccinated or who have a breakthrough illness. But the number of people in the U.S. who get measles is in the hundreds, not millions.
But herd immunity can be lost. If people can't get a vaccine, or choose not to, the protection among a population goes down.
During the COVID-19 pandemic, children worldwide missed getting a measles vaccine. Those missed doses led to an increase in measles cases and deaths in 2022 compared with 2021.
And the idea of herd immunity doesn't work for every disease.
- Herd immunity may not be possible when viruses change a lot in a short time, as with the virus that causes COVID-19.
- Reaching herd immunity is harder if a disease can be spread by people who catch the virus but don't have symptoms.
- Herd immunity is much harder to achieve if the protection from having and recovering from the illness or getting a vaccine doesn't last a long time.
Spread of the viruses that cause COVID-19, flu and RSV are examples of when herd immunity may not be a realistic goal. With this type of illness, the goal is to control and limit the spread of the virus.
How can you slow the spread of respiratory disease, such as COVID-19?
Getting vaccinations as they are updated and on schedule helps lower the risk of getting sick. Testing when you have symptoms to know when you need to avoid other people can help prevent spreading a virus.
One key action you can take is to wash your hands.
Wash your hands well and often with soap and water for at least 20 seconds. If you can't use soap and water, use an alcohol-based hand sanitizer with at least 60% alcohol. Make sure people around you, especially children, know the importance of hand-washing and how to do it correctly.
If you can, try to avoid being in crowded, indoor spaces with poor airflow when respiratory viruses are spreading.
You also can take other actions to prevent the spread of germs:
- Cover your coughs and sneezes. Cough or sneeze into a tissue or your elbow. Then wash your hands.
- Avoid touching your face. Keeping your hands away from your eyes, nose and mouth helps keep germs from entering the body there.
- Clean surfaces. Regularly clean often-touched surfaces to prevent the spread of viruses from a surface to your face.
- Help others from afar. If you can, avoid close contact with anyone who is sick or has symptoms.
When respiratory illness germs are spreading in your area, wearing a mask can give you another layer of protection. These types of germs spread when people talk, sneeze, cough or sing, for example.
People who are at high risk of serious illness, or who are regularly around people at high risk, may choose to wear a mask. If you came in contact with a germ, are sick or are getting over sickness, wearing a mask can help protect the people around you.
In the U.S., the Centers for Disease Control and Prevention suggests wearing the most protective mask possible that you'll wear regularly, fits well and is comfortable.
If you have a chronic medical condition and may have a higher risk of serious illness, check with your healthcare professional about other ways to protect yourself.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Celentano DD, et al. The dynamics of disease transmission. In: Gordis Epidemiology. 7th ed. Elsevier; 2025. https://www.clinicalkey.com. Accessed May 6, 2024.
- What CDC is doing about global measles and rubella. Centers for Disease Control and Prevention. https://www.cdc.gov/globalhealth/measles/what/index.html. Accessed May 13, 2024.
- Child immunization schedule notes. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/schedules/hcp/imz/child-schedule-notes.html. Accessed May 13, 2024.
- Measles history. Centers for Disease Control and Prevention. https://www.cdc.gov/measles/about/history.html. Accessed May 14, 2024.
- Measles cases and outbreaks. Centers for Disease Control and Prevention. https://www.cdc.gov/measles/cases-outbreaks.html. Accessed May 14, 2024.
- Minta AA, et al. Progress toward measles elimination — Worldwide, 2000–2022. MMWR Morbidity and Mortality Weekly Report. 2023; doi:10.15585/mmwr.mm7246a3.
- Morens DM, et al. The concept of classical herd immunity may not apply to COVID-19. The Journal of Infectious Diseases. 2022; doi:10.1093/infdis/jiac109.
- Immunizations for respiratory viruses prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/immunizations.html. Accessed May 14, 2024.
- Hygiene and respiratory viruses prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/hygiene.html. Accessed May 14, 2024.
- Preventing spread of respiratory viruses when you're sick. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/precautions-when-sick.html. Accessed May 14, 2024.
- Masks and respiratory viruses prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/masks.html. Accessed May 14, 2024.
- Taking steps for cleaner air for respiratory virus prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/air-quality.html. Accessed May 14, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- COVID-19 vaccines: Get the facts - Related information COVID-19 vaccines: Get the facts
- COVID-19 and herd immunity What you need to know
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.
Main navigation
- Our Articles
- Dr. Joe's Books
- Media and Press
- Our History
- Public Lectures
- Past Newsletters
- Photo Gallery: The McGill OSS Separates 25 Years of Separating Sense from Nonsense
Subscribe to the OSS Weekly Newsletter!
There are safe sunscreens but no safe tans.

- Add to calendar
- Tweet Widget
When it comes to health matters, scientists rarely make statements that do not begin with “may.” But here is one. Excessive exposure to sunlight causes skin cancer! There’s no “may” about it. And here is another one. Chemical protection can effectively reduce exposure. Uncertainties do, however, emerge when it comes to deciding on which specific chemicals to use. Activists claim that some sunscreens are unsafe and blame regulatory agencies for not looking after the welfare of the public, while manufacturers profess that their products have been thoroughly tested for safety and efficacy. As usual, the public is left confused. Actually, when you blow away the superfluous blather emanating both from the alarmists and from industry, there is some simple advice to offer. Let’s work it out.
The challenge is clear. Find a chemical or mixture of chemicals that can be applied to the skin to reduce exposure to the full spectrum of ultraviolet light. Then make sure these chemicals do not degrade upon exposure to light, have no topical or systemic toxicity, are minimally absorbed into the body, are resistant to water, do not have a greasy feel, are cosmetically acceptable, do not stain clothing and can be incorporated into a “vehicle” that allows for easy spreading. Quite a list of demands.
The first commercial “sunscreens” appeared in the 1960s and were designed to filter out “UVB,” the shorter wavelengths of ultraviolet light (290-320 nanometers). These are the rays that cause sunburn, which was the main concern at the time. Slightly longer waves, those responsible for tanning, were deemed safe. Finding chemicals that absorb the nasty UVB rays was not particularly difficult, with para-aminobenzoic acid (PABA), octocrylene, phenylbenzimidazole sulfonic acid and various cinnamates and salicylates being up to the task.
Products with different concentrations of these ingredients were introduced for different skin types, each prominently featuring a “Sun Protection Factor (SPF),” basically a measure of the time it takes for skin to redden compared with having no protection. The SPF value is determined in the laboratory by applying 2 mg of product per square centimeter to the skin of volunteers. Using a product with an SPF of 15 means that a person who normally begins to burn in ten minutes can in theory stay in the sun for a hundred and fifty minutes before experiencing any visible effect on the skin.
It didn’t take long for this scenario to prove to be too simplistic. As a clear link between skin cancer and UVB emerged, the focus shifted from preventing sunburn to preventing skin cancer, resulting in an industry frenzy of products with higher and higher SPF values. In truth, an SPF of 15 already blocks 94% of UVB, only 3% less than one labeled as SPF 30. In any case, these numbers are only meaningful if the product is applied the same way as in the lab studies, which turns out not to be the case. Most people were applying far less than 2 mg per square centimeter and were not getting the protection they thought they were getting. What many were getting, though, were various skin reactions. And something else became apparent as well. The longer wavelengths of ultraviolet light, 320-400 nm, known as UVA, previously thought to be innocuous, were found to be more deeply penetrating than UVB and responsible for premature wrinkling and aging of the skin (“photoaging”). Unlike UVB, they can even pass through glass. Furthermore, UVA also was found to be potentially carcinogenic.
Now there was a need for a novel class of products that would protect the skin both from UVB and UVA. Ideally, not one that would just absorb some wavelengths, but one that would reduce the effects of ultraviolet light by a combination of absorption and reflection. Titanium dioxide and zinc oxide, both mineral pigments, fit the bill, but left a white residue on the skin. That was alright for lifeguards’ noses, but not for vane sunbathers. Recently, excellent products using “micronized” titanium dioxide and zinc oxide have been developed which do not leave a tell-tale white residue. Some concerns have been raised about titanium dioxide that is micronized to the extent that it contains particles smaller than 100 nanometers, known as “nanoparticles.” Ingested titanium dioxide nanoparticles can damage the genetic material in cells, but there is no evidence that such particles are absorbed through the skin. However, if they are present in spray products, inhalation could be a problem. Another issue is that on exposure to sunlight titanium dioxide reacts with water to produce tissue damaging hydroxyl radicals. Manufacturers have approached this problem by adding chemicals such as 2-(acetoacetoxy) ethyl methacrylate that coat the titanium dioxide particles and protect them from sunlight. The sunscreen needs a sunscreen!
Some organic compounds such as oxybenzone and avobenzone (Parsol 1789) can also absorb UVA but with oxybenzone there are some “buts. When oxybenzone absorbs ultraviolet light, it becomes energized, and this energy is dissipated mostly through heat. But the interaction of ultraviolet light and oxybenzone can also produce free radicals that have been linked to cancer. Oxybenzone also undergoes a reaction in the presence of ultraviolet light to form a compound called a semiquinone which in turn can inactivate some of the naturally occurring antioxidants in the skin, such as reduced glutathione. Not a good thing since antioxidants offer protection against free radicals. And if that weren't enough, it turns out that oxybenzone can also mimic the behaviour of estrogens, at least in fish exposed to high doses. It has therefore been labeled a potential "endocrine disruptor." Another concern about oxybenzone is that it can disrupt coral reefs.
But, and a big but it is, there is no evidence reported in the scientific literature of oxybenzone being linked to any human health problem, except for photodermatitis, a skin reaction triggered by exposure to sunlight. There are hundreds and hundreds of compounds, both natural and synthetic, that if scrutinized the same way as oxybenzone, could be linked to problems. Phthalates, bisphenol A, soy extracts and various pesticides are estrogenic. We live in a world full of hormone-like substances and a complete analysis of our blood would reveal hundreds of these. Nevertheless, producers now shy away from including oxybenzone in their products.
No single ingredient can protect the skin from all wavelengths of UV light. However, a combination of avobenzone, homosalate, octosalate and octocrylene is up to the task. Inclusion of tetraphalydine dicamphor sulphonic acid, which goes by the trade name “Mexoryl” increases protection from UVA. It is stable, absorbs UV light and dissipates the energy as harmless heat.
There is one more “may” about sunscreens that has been converted to fact. We no longer have to say that sunscreens may prevent skin cancer, we can say they do. A study in Australia, where skin cancer is a huge concern, involved 1600 subjects who were given sunscreen to use every day for four and a half years. They developed 40% fewer squamous cell cancers than a control group who just maintained normal skin care without being given specific instructions about the use of sunscreens.
So, there it is. Sunscreens can prevent skin cancer, which is not a rare disease. The World Health Organization estimates 48,000 deaths a year from melanoma (likely sun related but not conclusively proven) and 12,000 from other forms of skin cancer. What to do?
Look for a product with an SPF of at least 30. Rated most highly by Consumer Reports as affording the most protection is a combination of avobenzene, homosalate, octosulfate and octocrylene as found in products such as Coppertone Water Babies Lotion, Walmart’s Equate Ultra Lotion or Eucerin Advanced Hydration Lotion. Apply fifteen minutes before going out in the sun, use a shot glass full for the body and half a teaspoon for the face. Reapply frequently. Forget terms like “waterproof,” “all day protection” and “sweatproof.” They’re meaningless. And if you are buying something that is “chemical-free,” you are not getting a good deal because you’re buying a vacuum. Sunscreens should not be used to prolong sun exposure, but rather to protect the skin when exposure is unavoidable. Above all, remember that unfortunately there is no such thing as a healthy tan.
@JoeSchwarcz
What to read next
The story linking nutrition and health has unexpected twists 28 jun 2024.

A Taste of Bitter Melon 28 Jun 2024

The Blood Microbiome Is Probably Not Real 28 Jun 2024

Your Appendix May Not Be Useless After All 21 Jun 2024
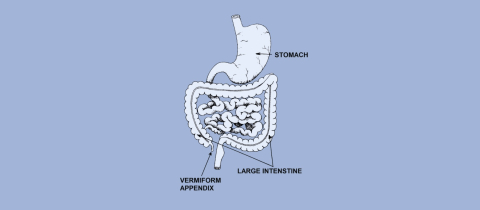
On the Trail of Chemtrail Nonsense 21 Jun 2024

Facial Creams and Lotions Offer Hope in a Jar 14 Jun 2024

Department and University Information
Office for science and society.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Med Sci Monit
- v.17(1); 2011

Evidence and its uses in health care and research: The role of critical thinking
Milos jenicek.
1 Department of Clinical Epidemiology & Biostatistics, Michael G. de Groote School of Medicine, McMaster University, Hamilton, Ontario, Canada
Pat Croskerry
2 Department of Emergency Medicine, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada
David L. Hitchcock
3 David L. Hitchcock, Department of Philosophy, Faculty of Humanities, McMaster University, Hamilton, Ontario, Canada
Obtaining and critically appraising evidence is clearly not enough to make better decisions in clinical care. The evidence should be linked to the clinician’s expertise, the patient’s individual circumstances (including values and preferences), and clinical context and settings. We propose critical thinking and decision-making as the tools for making that link.
Critical thinking is also called for in medical research and medical writing, especially where pre-canned methodologies are not enough. It is also involved in our exchanges of ideas at floor rounds, grand rounds and case discussions; our communications with patients and lay stakeholders in health care; and our writing of research papers, grant applications and grant reviews.
Critical thinking is a learned process which benefits from teaching and guided practice like any discipline in health sciences. Training in critical thinking should be a part or a pre-requisite of the medical curriculum.
Sackett et al. originally defined evidence based medicine (EBM) as ‘… the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients’, and its integration with individual clinical expertise [ 1 ].’ In the nearly two decades that have intervened, there has been significant uptake of the idea that clinical care should be based upon sound, systematically researched evidence. There has been less emphasis on how clinical expertise itself might be improved, perhaps because the concept is more amorphous and difficult to define.
Clinical expertise is an amalgam of several things: there must be a solid knowledge base, some considerable clinical experience, and an ability to think, reason, and decide in a competent and well-calibrated fashion. Our focus here is on this last component: the faculties of thinking, reasoning and decision making. Clinicians must be able to integrate the best available critically appraised evidence with insights into their patients, the clinical context, and themselves [ 2 ]. To accomplish this integration, physicians need to develop their critical thinking skills. Yet historically this need has not received explicit attention in medical training. We believe that it should.
As an illustration of the use of critical thinking in clinical care, consider the following clinical scenario from emergency medicine : A 52-year-old male presents to the emergency department of a community centre with a complaint of constipation and is triaged with a low level acuity score to a ‘minors’ area. The department is extremely busy and several hours elapse before he is seen by the emergency physician. His principal complaint is constipation; he hasn’t had a bowel movement for 4 days. His abdomen is soft and non-tender. A large amount of firm stool is evident on rectal examination. He recalls a minor back strain a few days earlier. The physician orders a soapsuds enema and continues seeing other patients. After about 30 minutes he finds the nurse who administered the enema; she reports that it was ineffective. He orders a fleet enema which again proves ineffective. The nurse expresses her opinion that the patient is taking up too much time and suggests he be given an oral laxative and another fleet enema to take home with him. She is clearly unwilling to continue investing her effort in a patient with a trivial complaint. Nevertheless, the physician decides to administer a third enema himself. The third enema is only marginally effective and he then decides to disimpact the patient. The physician notes poor rectal tone and enquires further about the patient’s urination. He says he has been unable to urinate that day. On catheterisation he is found to have 1200cc. Neurological findings are equivocal: reflexes are present in both legs and there is some subjective diminished sensation.
A diagnosis of cauda equina syndrome is made and the emergency physician calls the neurosurgery service at a tertiary care hospital. It is now late in the evening. The neurosurgeon is reluctant to accept the working diagnosis. He suggests that the loss of sphincter tone might be due to the disimpaction, and argues that there was no significant history of back injury or convincing neurological findings. When the ED physician persists, the neurosurgeon suggests transferring the patient to the tertiary hospital ED for further evaluation and asks for a CT investigation of the patient’s lower spine before seeing him. The CT reveals only some minor abnormalities and the patient is kept overnight. An MRI is done in the morning. It shows extensive disc herniation with compression of nerve roots. The patient subsequently undergoes prolonged back surgery.
This case had a good outcome, although things might have been dramatically different. The patient might have suffered permanent neurological injury requiring lifelong catheterisation for urination.
Our scenario illustrates some key points about clinical decision making. At the outset, the patient presents with an apparently benign condition – constipation. The impression of a benign condition is incorporated at triage and results in a low-level acuity score and prolonged wait. The patient’s nurse also incorporates this diagnosis and exerts coercive pressure on the physician to discharge the patient. The neurosurgeon is dismissive of a physician’s assessment in a community centre ED, creating considerable inertia against referral. Thus the ED physician faces a variety of obstacles to ensure optimal patient care. These have little to do with EBM. He must resist and overcome a variety of cognitive, affective and systemic biases, his own as well as others’, and various contextual constraints. He must continue to think critically and persist in a course that has become increasingly challenging.
Our scenario also illustrates some key points about critical thinking. The initial impression of a benign condition of constipation is not the only diagnosis compatible with the patient’s symptoms. A health care professional reaching a preliminary diagnosis must be aware of the danger of fixing prematurely on this diagnosis and ignoring (or failing to look for) subsequent evidence that tells against it, as the nurse in our scenario was inclined to do. Observational and textual studies both indicate that the most common source of errors in reasoning is to close prematurely on a favoured conclusion and then ignore evidence that argues against that conclusion [ 3 ]. It is also important to keep in mind that a patient’s signs or symptoms may have more than one cause. Data that may confirm one of the causes does not necessarily rule out all the others. Attentive listening to the patient and careful looking in the data-gathering stage are essential to good medical practice, as Groopman has recently pointed out [ 4 ]. From a logical point of view, the physician’s diagnostic task is to gather data that will determine which one (or ones) of the possible causes is (or are) responsible for the patient’s problem. This goal will guide the selection of data and of additional tests. ‘Parallel’ or ‘lateral’ thinking [ 5 ] will help with the differential diagnosis.
Critical Thinking
Dewey’s original conceptualization [ 6 ] of what he called “reflective thinking” has spawned in the intervening century a variety of definitions of critical thinking, most notably that of Ennis as “ reasonable reflective thinking that is focused on deciding what to believe or what to do” [ 7 ] . Scriven and Paul have elaborated this definition as “… the intellectually disciplined process of actively and skilfully conceptualizing, applying, synthesizing or evaluating information gathered from, or generated by observation, experience, reflection, reasoning, or communication as a guide to belief or action ” [ 8 ].
The consensus of 48 specialists in critical thinking from the fields of education, philosophy and psychology was that it should be defined as ‘ purposeful self-regulatory judgment which results in interpretation, analysis, evaluation and inference, as well as explanation of the evidential, conceptual, methodological, criteriological, or contextual considerations upon which that judgement is based ’ [ 9 ]. The list of additional definitions remains impressive [ 10 , 11 ].
Even more useful than these definitions are various lists of dispositions and skills characteristic of a “critical thinker” [ 7 , 9 , 12 ]. More useful still are criteria and standards for measuring possession of those skills and dispositions [ 13 ], criteria that have been used to develop standardized tests of critical thinking skills and dispositions [ 14 – 17 ] including some with specific reference to health sciences [ 18 ].
The elements of critical thinking subsume what has variously been described as clinical judgment [ 19 ] , logic of medicine [ 20 , 21 ] , logic in medicine [ 22 ] , philosophy of medicine [ 23 ] , causal inference [ 24 ] , medical decision making [ 25 ], clinical decision making [ 26 ], clinical decision analysis [ 27 ], and clinical reasoning [ 28 ]. An increasing number of monographs on logic and critical thinking in general have appeared [ 29 – 34 ] and their content is being adapted for medicine [ 35 – 37 ].
Everyday medical practice, whether in physicians’ offices or emergency departments or hospital wards, clearly involves “ reasonable reflective thinking that is focused on deciding what to believe (meaning the understanding of the problem) and/or what to do (i.e. deciding what to do to solve the problem)” [ 7 , 38 ]. Table 1 lists specific abilities underlying critical thinking in medical practice.
Specific abilities underlying critical thinking in medical practice.
Critical thinking is also called for in medical research and medical writing. Editors of leading medical journals have called for it. Edward Huth [ 39 , 40 ], former editor of Annals of Internal Medicine, has urged that medical articles reflect better and more organized ways of reasoning. Richard Horton [ 41 , 42 ], former editor of The Lancet , has proposed the use in medical writing of a contemporary approach to argument along the lines used by the philosopher Toulmin [ 40 , 41 ]. Subsequently, two of us have developed this approach in detail for medicine [ 43 , 44 ]. Dickinson [ 45 ] has called for an argumentative approach in medical problem solving and brought it to the attention to the world of medical informatics and beyond.
Dual Process Theory
An important component of critical thinking is being aware of one’s own thinking processes. In recent years, two general modes of thinking have been described under an approach described as dual process theory. The model is universal and has been directly applied to medicine [ 46 – 48 ] and nursing [ 49 ]. One mode is fast, reflexive, autonomous, and generally referred to as intuitive or System 1 thinking. The other is slow, deliberate, rule-based, and referred to as analytical or System 2 thinking. The mechanisms that underlie System 1 thinking are based on associative learning and innate dispositions: the latter are hard-wired, as a result of the evolutionary history of our species, to respond reflexively to certain cues in the environment. We have discrete, functionally-specialized mental programs that were selected when the brain was undergoing significant development especially spanning the last 6 million years of hominid evolution [ 50 ]. Although these programs may have served us well in our ancestral past, they may not be appropriate in some aspects of modern living. Some of this System 1 substrate also underlies various heuristics and biases in our thinking – the tendency to take mental short-cuts, or demonstrate reflexive responses in certain situations, often on the basis of past experience. Not surprisingly, most error occurs in System 1 thinking.
Contemplative , or fully reflective thinking, is System 2 thinking. It suits any practice of medicine or medical research activity where there is time to utilise the best critically appraised evidence in a step-by-step process of reasoning and argument. Contemplative, fully reflective thinking is appropriate, for example, in internal medicine, psychiatry, public health, and other specialties, in etiological research and clinical trials, and in writing up the results of such research [ 35 ].
In contrast, a shortcut or heuristic approach [ 51 ] with somehow truncated thinking is often dictated by the realities of emergency medicine, surgery, obstetrics or any situation where there is incomplete information, bounded rationality, and insufficient time to be fully reflective. The extant findings and the decision maker’s experience are all that is available. The quintessential challenge for well-calibrated decision making is to optimise performance in System 1. Hogarth [ 52 ] sees this challenge as educating our intuitive processes and has delineated a variety of strategies through which this might be accomplished.
No responsible physician would engage in reflective thinking on every occasion when a decision has to be made. Such acute emergencies as sudden complications of labour and delivery, ruptured aneurysms, multiple trauma victims and other immediately life-threatening situations generally leave no time for fully reflective thinking. A shortcut or heuristic approach is required [ 51 ], involving pattern recognition, steepest ascent reasoning, or algorithmic paths [ 21 , 53 ]. There is of course a place for reflective thinking before and after such time-constrained emergency decisions. More generally, reflective thinking is called for in any aspect of medical practice where there is time and reason for it.
The distinction should be made between the involuntary autonomous nature of System 1 thinking and a deliberate decision to use a shortcut for expediency, which is System 2 thinking. There is normally an override function of System 2 over System 1 but this may be deliberately lifted under extreme conditions.
Future Direction
Critical thinking is a learned process which benefits from teaching and guided practice like any other discipline in health sciences. It was already proposed as part of an early medical curriculum [ 54 ]. If we are to train future generations of health professionals as critical thinkers, we should do so in the spirit of critical thinking as it stands today. Clinical teachers should know how to run a Socratic discourse, and in which situations it is appropriate. They should be aware of contemporary models of argument. Clinical teachers should be trained and experienced in engaging with their interns and residents in meaningful discourse while presenting and discussing morning reports, at floor and other rounds, in morbidity and mortality conferences, or at less informal ‘hallway’, ‘elevator’ or ‘coffee-maker/drinking fountain’ teaching sites for busy clinicians. Such discourse is better than so-called “pimping”, i.e. quizzing of juniors with objectives ranging from knowledge acquisition to embarrassment and humiliation [ 37 , 55 ].
Also, somebody should point out to trainees the relevance to the health context of some basics of informal logic, critical thinking and argumentation, if those basics have been acquired as the result of studying for their first undergraduate degree.
Unquestionably, the appropriate critically appraised best evidence should be used as a foundation for reasoning and argument about how to care for patients. But, if we want to link the best available evidence to a patient’s biology, the patient’s values and preferences, the clinical or community setting, and other circumstances, we should take all these factors into account in using the best available evidence to get to the beliefs and decisions that have the best possible support.
Such a reflective integration cannot be mastered by mere exposure. A learning experience is required. Trainees in medicine need to learn how to think critically [ 56 ], just as they need to learn contemporary approaches to ‘rational’ medical decision making: how to use Bayes’ theorem in the diagnostic process, how to determine the sample size in a clinical trial, how to analyze survival curves in prognosis and outcomes studies, and how to calculate odds ratios in case control research. To understand each other, the teacher and the learner should both know the fundamentals of reasoning and argument in medicine. To achieve this understanding, we can either offer separate and distinct courses on critical thinking and decision making in medicine; or spread learning, practice and experience in critical thinking and decision making across various specialties; or do both. Only the future will show which of the alternatives is better. The integrated approach seems more promising, but harder to implement. Given the limitations on the current medical undergraduate curriculum, we might be hard-pressed to persuade a curriculum committee that precious space and time should be allocated to such concepts. The overriding rationale, however, should be that the knowledge of critical and reflective thinking is declarative knowledge (knowing how) and not simply an addition of procedural knowledge (know-how) or explicit knowledge. The old adage about it being preferable to teach someone how to fish rather than giving them fish applies. Any new additions will need to be streamlined and practical. A teaching module on critical thinking might for example include attention to how we reason and make decisions, factors that may impair decision making, the concept of critical thinking, situations where critical thinking is appropriate, some basic principles of logic and some logical fallacies. However the teaching, learning and practice of critical thinking is incorporated in the medical curriculum, it will need to include not only the contemplative, fully reflective thinking on hospital floors and in clinics but also the shortcut thinking [ 57 ] in such heuristic environments as operating theatres or emergency departments [ 46 , 48 , 58 – 60 ].
Similar education is required as a basis for framing grant applications and research reports as reasoned arguments, especially in the discussion section [ 61 , 62 ]. We may see a day when most medical journals are what Paton [ 63 ] terms “reflective journals”. If an application for a research grant, a research proposal, or a group of research findings (systematically reviewed or not) presented in a medical article are all exercises in argumentation and critical thinking, their authors, readers, and editors should find a common language for all these types of scientific and professional communication.
Almost four decades ago Feinstein [ 64 ] asked what kind of basic science clinical medicine needs. At that time, he had mostly clinical biostatistics and epidemiology in mind. Recently, Redelmeier et al. [ 65 ] proposed to add cognitive psychology as one more basic science. It is time, we think, to add critical thinking to that list.
Competing interests
None declared.
Source of support: None. Departmental support to produce the manuscript is acknowledged and appreciated

IMAGES
VIDEO
COMMENTS
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
Multiple conceptions of critical thinking likely offer educators the ability to express diverse beliefs about what 'good thinking' means in variable contexts. The findings suggest that any single definition of critical thinking in the health professions will be inherently contentious and, we argue, should be.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed. It's a dynamic process that enhances clinical reasoning, problem-solving, and overall patient outcomes.
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Critical thinking/problem-solving skills should emphasize self-examination. It should teach an individual to accomplish this using a series of steps that progress in a logical fashion, stressing that critical thinking is a progression of logical thought, not an unguided process. Pedagogy.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
Critical thinking in nursing is considered essential for delivering quality care and reflects the professional accountability of registered nurses (Chang et al., 2011 ). It is also a vital part of the clinical assignments and responsibilities nurses are expected to manage. Additionally, nurses' critical thinking has the potential to influence ...
Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).. Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught, assessed and integrated into the design and development of staff and nurse education and training ...
Higher order thinking has become one of the essential characteristic of future health care professionals and an essential attribute of medical professionalism. Hence, knowing and thinking about critical thinking and exploring the avenues for its application in medical education through appropriate means have become the need of the hour.
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care - clinical reasoning, evidence-informed decision-making, and systems thinking - and approaches to develop these skills during clinician training.
Nurses are critical thinkers. The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice.
1. Introduction. Critical thinking is defined as reflective thinking that affords individuals to decide what to believe and what to do. A critical thinker is open to alternatives, well informed and can judge the credibility of information (Ennis, 2011).In the health-care setting, critical thinking involves analysis and discrimination of evidence-based research to guide practices; synthesis of ...
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. ... Critical Thinking in Critical Care: Five Strategies to Improve Teaching and Learning in the Intensive Care Unit ... National Institutes of Health ...
Critical thinking incorporates questioning and critiquing solutions to find the most effective one. For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health. 8 Examples of Critical Thinking in Nursing
Without critical thinking, physicians, and particularly residents, are prone to cognitive errors, which can lead to diagnostic errors, especially in a high-stakes environment such as the intensive care unit. Although challenging, critical thinking skills can be taught.
Health care professional curricula need to facilitate the development of critical-thinking skills in students. This systematic review shows that there are mixed results with respect to the acquisition of critical-thinking skills in health care professional students as measured by the CCTST and the WGCTA. There are a limited number of moderate ...
Why Critical Thinking Skills in Nursing Matter (And What You Can Do to Develop Them) By Hannah Meinke on 07/05/2021. This piece of ad content was created by Rasmussen University to support its educational programs. Rasmussen University may not prepare students for all positions featured within this content.
Master Critical Thinking. Take your nursing career to the next level by learning to master critical thinking for better patient care. Learn how to pursue your degree in nursing with Carrington College. Sources [1] Papathanasiou, I. et al. "Critical Thinking: The Development of an Essential Skill for Nursing Students."
If you have worked in customer service then the same critical thinking skills that are used to deal with customers will be used to deal with patients in the medical field. If you have worked in a fast-paced environment requiring prioritizing then you will carry that skill over to the medical field. The examples listed above are just a few of ...
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from ...
However, this work represents only an initial step toward grasping the complexities of human decision-making dynamics. There is a notable lack of comprehensive research in this arena in pediatrics, prompting critical inquiry into the interaction between cognitive biases and the powerful stresses and emotions experienced in pediatric care.
The health care journey continues through interactions with payers. Thus, patient experience today is defined less as "happiness" with the provider interaction and more as appropriate and seamless care through the continuum of care. ... Responsibility for ensuring critical components of patient-centered care such as safety is shifting.
Critical thinking in nursing is an essential component of professional accountability and quality nursing care. Critical thinkers in nursing exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, openmindedness, perseverance, and reflection.
The Pediatric Advanced Life Support (PALS) provides healthcare providers the knowledge and skills necessary to assess recognize and care for pediatric patients experiencing life threatening medical emergencies. Consistent with the American Red Cross Focused Updates and Guidelines 2020 the PALS course emphasizes providing high-quality care and integrating psychomotor skills with critical ...
July Administrative Meeting for the Humphreys County Board of Commissioners.
Based on those facts, health officials estimate that herd immunity for measles is at least 94%. ... In the U.S., hundreds died of measles each year and thousands needed care in the hospital. After people could get the measles vaccine, the measles virus stopped spreading in the U.S. because so many people got the shots.
When it comes to health matters, scientists rarely make statements that do not begin with "may." But here is one. Excessive exposure to sunlight causes skin cancer! There's no "may" about it. And here is another one. Chemical protection can effectively reduce exposure. Uncertainties do, however, emerge when it comes to deciding on which specific chemicals to use. Activists claim that ...
The evidence should be linked to the clinician's expertise, the patient's individual circumstances (including values and preferences), and clinical context and settings. We propose critical thinking and decision-making as the tools for making that link. Critical thinking is also called for in medical research and medical writing, especially ...