BREAKING: Police move in to clear encampment at UCLA and detain protesters, facing stiff resistance. Follow live updates.

After decades of failures, researchers have renewed hopes for an effective HIV vaccine

The world needs an HIV vaccine if it ever hopes to beat a virus that still infects over 1 million people a year and contributes to hundreds of thousands of deaths.
Despite 20 years of failures in major HIV vaccine trials — four this decade alone — researchers say recent scientific advances have likely, hopefully, put them on the right track to develop a highly effective vaccine against the insidious virus.
But probably not until the 2030s.
“An effective vaccine is really the only way to provide long-term immunity against HIV, and that’s what we need,” Dr. Julie McElrath, the director of the vaccine and infectious disease division at the Fred Hutchinson Cancer Center in Seattle, said Monday at the Conference on Retroviruses and Opportunistic Infections in Denver.
All current HIV vaccine action is in the laboratory, animal studies or very early human trials.
Researchers at the retrovirus conference presented favorable results from two HIV vaccine studies. One found that a modification to the simian version of HIV spurred production of what are known as broadly neutralizing antibodies against the virus in monkeys. Another showed promise in the effort to coax the immune system’s B cells to make the powerful antibodies in humans.
“These trials illustrate as a proof of concept that we can train the immune system. But we need to further optimize it and test it in clinical trials,” Karlijn van der Straten, a Ph.D. student at the Academic Medical Center at Amsterdam University, who presented the human study, said at a news conference Monday.
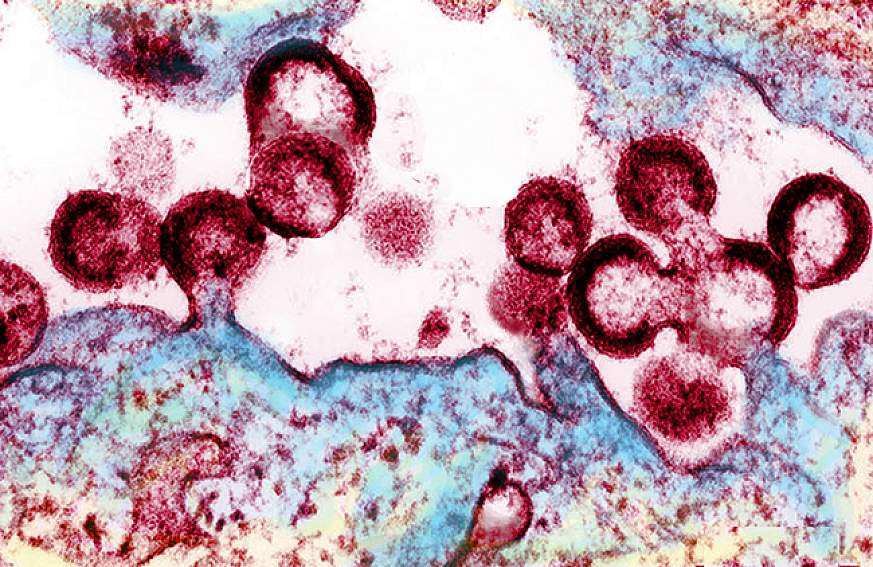
Still, the scrappy scientists in this field face a towering challenge. HIV is perhaps the most complex pathogen ever known.
“The whole field has learned from the past,” said William Schief, who leads Moderna’s HIV vaccine efforts. “We’ve learned strategies that don’t work.”
The cost has already been immense. Nearly $17 billion was spent worldwide on HIV -vaccine research from 2000 to 2021. Nearly $1 billion more is spent annually, according to the Joint United Nations Program on HIV/AIDS and the nonprofit HIV group AVAC.
“Maintaining the funding for HIV vaccines right now is really important,” said Dr. Nina Russell, who directs HIV research at the Bill & Melinda Gates Foundation. She pointed to the field’s own “progress and the excitement” and to how “HIV vaccine science and scientists continue to drive innovation and science that benefits other infectious diseases and global health in general.”
Case in point: Covid. Thanks to HIV research, the mRNA vaccine technology was already available in 2020 to speed a coronavirus vaccine to market.
Why the HIV vaccine efficacy trials failed
In strong contrast to Covid, the HIV vaccine endeavor has spanned four decades. Only one of the nine HIV vaccine trials have shown efficacy: a trial conducted in Thailand and published in 2009 that reported a modest 31% reduction in HIV risk.
HIV vaccine researchers subsequently spent years seeking to retool and improve that vaccine strategy, leading to a series of trials that launched in the late 2010s — only to fail.
Researchers have concluded those latest trials were doomed because, aside from prompting an anti-HIV response based in immune cells, they only drove the immune system to produce what are known as non-neutralizing antibodies. Those weapons just weren’t strong enough for such a fearsome foe.
Preventing HIV through vaccination remains a daunting challenge because the immune system doesn’t naturally mount an effective defense against the virus, as it does with so many other vaccine-preventable infections, including Covid. An HIV vaccine must coax from the body a supercharged immune response with no natural equivalent.
That path to victory is based on a crucial caveat: A small proportion of people with HIV do produce what are known as broadly neutralizing antibodies against the virus. They attack HIV in multiple ways and can neutralize a swath of variants of the virus.
Those antibodies don’t do much apparent good for people who develop them naturally, because they typically don’t arise until years into infection. HIV establishes a permanent reservoir in the body within about a week after infection, one that their immune response can’t eliminate. So HIV-positive people with such antibodies still require antiretroviral treatment to remain healthy.
Researchers believe that broadly neutralizing antibodies could prevent HIV from ever seeding an infection, provided the defense was ready in advance of exposure. A pair of major efficacy trials, published in 2021 , demonstrated that infusions of cloned versions of one such antibody did, indeed, protect people who were exposed to certain HIV strains that are susceptible to that antibody.
However, globally, those particular strains of the virus comprise only a small subset of all circulating HIV. That means researchers can’t simply prompt a vaccine to produce that one antibody and expect it to be effective. Importantly, from this study they got a sense of what antibody level would be required to prevent infection.
It’s a high benchmark, but at least investigators now have a clearer sense of the challenge before them.
Also frustrating the HIV vaccine quest is that the virus mutates like mad. Whatever spot on the surface of the virus that antibodies target might be prone to change through mutation, thus allowing the virus to evade their attack. Consequently, researchers search for targets on the virus’ surface that aren’t highly subject to mutation.
Experts also believe warding off the mutation threat will require targeting multiple sites on the virus. So researchers are seeking to develop a portfolio of immune system prompts that would spur production of an array of broadly neutralizing antibodies.
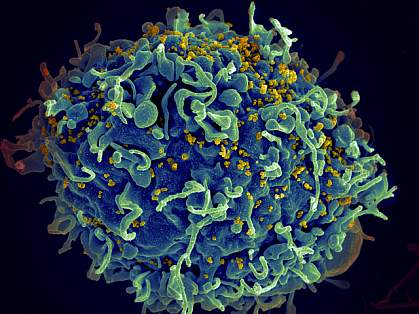
Prompting the development of such antibodies requires a complex, step-by step process of coaxing the infection-fighting B cells, getting them to multiply and then guiding their maturation into potent broadly neutralizing antibody-producing factories.
HIV vaccine development ‘in a better place’
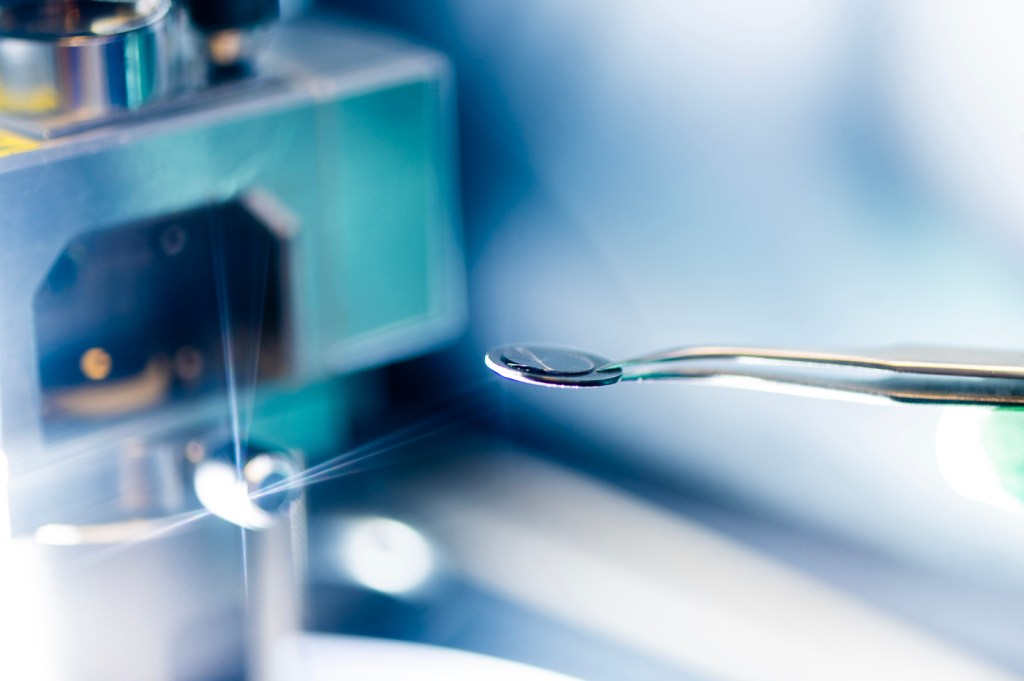
Dr. Carl Dieffenbach, the head of the AIDS division at the National Institute of Allergy and Infectious Diseases, said numerous recent technological advances — including mRNA, better animal models of HIV infection and high-tech imaging technology — have improved researchers’ precision in designing, and speed in producing, new proteins to spur anti-HIV immune responses.
Global collaboration among major players is also flourishing, researchers said. There are several early-stage human clinical trials of HIV-vaccine components underway.
Three mRNA- based early human trials of such components have been launched since 2022. Among them, they have been led or otherwise funded by the global vaccine research nonprofit group IAVI, Fred Hutch, Moderna, Scripps Research, the Gates Foundation, the National Institutes of Health, the U.S. Agency for International Development, and university teams. More such trials are in the works.
On Friday, Science magazine reported concerning recent findings that among the three mRNA trials, a substantial proportion of participants — 7% to 18%, IAVI said in a statement — experienced skin-related symptoms following injections, including hives, itching and welts.
IAVI said in its statement that it and partners are investigating the HIV trials’ skin-related outcomes, most of which were “mild or moderate and managed with simple allergy medications.”
Researchers have shown success in one of those mRNA trials in executing a particular step in the B-cell cultivation process.
That vaccine component also generated “helper” CD4 cells primed to combat HIV. The immune cells are expected to operate like an orchestra conductor for the immune system, coordinating a response by sending instructions to B cells and scaling up other facets of an assault on HIV.
A complementary strategy under investigation seeks to promote the development of “killer” CD8 cells that might be primed to kill off any immune cells that the antibodies failed to save from infection.
Crucially, investigators believe they are now much better able to discern top vaccine component candidates from the duds. They plan to spend the coming years developing such components so that when they do assemble the most promising among them into a multi-pronged vaccine, they can be much more confident of ultimate success in a trial.
“An HIV vaccine could end HIV,” McElrath said at the Denver conference. “So I say, ‘Let’s just get on with it.”
Dr. Mark Feinberg, president and CEO of IAVI, suggested that the first trial to test effectiveness of the vaccine might not launch until 2030 or later.
Even so, he was bullish.
“The field of HIV vaccine development is in a better place now than it’s ever been,” he said.
Benjamin Ryan is independent journalist specializing in science and LGBTQ coverage. He contributes to NBC News, The New York Times, The Guardian and Thomson Reuters Foundation and has also written for The Washington Post, The Nation, The Atlantic and New York.
- What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medication Every Day
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
- Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Food Safety and Nutrition
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- Ready, Set, PrEP Resources
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 27
- National African Immigrants and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
HIV Treatment Research and Key Takeaways: Dr. Dieffenbach’s Final Update from CROI 2024
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
On Wednesday as the 2024 Conference on Retroviruses and Opportunistic Infections (CROI) was winding down, HIV.gov spoke with NIH’s Dr. Carl Dieffenbach about highlights of long-acting HIV treatment research discussed at the conference. Dr. Dieffenbach is the Director of the Division of AIDS at NIH’s National Institute of Allergy and Infectious Diseases . He spoke with Brian Minalga, MSW, Deputy Director of the NIH-supported Office of HIV/AIDS Network Coordination Exit Disclaimer . Watch our conversation with Dr. Dieffenbach below:
Research Suggests Possible Expanded Options for Long-Acting HIV Treatment
Dr. Dieffenbach highlighted findings from several clinical trials and a plenary session presented at CROI about current and future options for long-acting antiretroviral treatment (ART) for HIV.
First, he discussed a NIAID-supported randomized clinical trial that found that long-acting ART with cabotegravir and rilpivirine was superior in suppressing HIV replication compared to daily oral ART in adults who had been unable to maintain viral suppression through an oral daily regimen. The LATITUDE study Exit Disclaimer enrolled participants in 31 sites in the United States. Last month, the trial’s Data and Safety Monitoring Board conducted a planned review of interim data and recommended halting randomization and offering all eligible study participants long-acting ART based on its observed superior viral suppression of HIV. At CROI, study leaders reported that the interim analysis of data from 294 participants showed that the chance of experiencing unsuppressed HIV was 7% among people taking long-acting ART compared to 25% among those taking daily oral ART . The likelihood of discontinuing the assigned regimen due to adverse events or experiencing unsuppressed HIV was 10% among people taking long-acting ART compared to 26% among those taking daily ART. These findings were statistically significant. Dr. Dieffenbach observed that these results may support expanding the use of long-acting ART among a broader population. Read the study abstract Exit Disclaimer . Read more in this NIAID news release .
Another ongoing clinical trial reported initial findings on the safety of the same long-acting injectable treatment regimen for adolescents with HIV with a suppressed viral load. The NIH-supported MOCHA study Exit Disclaimer enrolled participants aged 12 to 17 who were virally suppressed in Botswana, South Africa, Thailand, Uganda, and the United States. In what he characterized as very encouraging results, Dr. Aditya Gaur of St. Jude Children's Research Hospital, one of the trial’s co-chairs, reported that after the first six months all participants remained virally suppressed, and the level of the ART in their systems was comparable to what has been shown as efficacious in adult studies of the same drug . He also reported that, while about one-third of the participants reported an injection-site reaction, there were no surprising or unanticipated adverse events. These data support the use of cabotegravir and rilpivirine in virally suppressed adolescents, according to Dr. Gaur and colleagues. Dr. Dieffenbach noted that NIH will continue to support safety and dosing studies to determine the proper doses for adolescents and that these studies could eventually expand access to this long-acting HIV treatment to more people. Read the abstract Exit Disclaimer . Read NIAID’s news release about the study .
In addition, Dr. Dieffenbach mentioned an industry-sponsored Phase 2 trial that presented 24-week results of an oral once-weekly investigational combination of two drugs ( islatravir and lenacapavir ). Researchers reported that the investigational combination maintained a high level of viral suppression among study participants and was well tolerated. The study will continue to gather data and suggests that a weekly oral HIV treatment regimen could someday be possible . Read the abstract Exit Disclaimer .
Finally, Dr. Dieffenbach discussed Wednesday’s plenary session by Dr. Charles Flexner of The Johns Hopkins University School of Medicine, which was titled “The End of Oral? How Long-Acting Formulations Are Changing the Management of Infectious Diseases.” In his big picture, future-focused presentation exploring long-acting drug delivery, Dr. Flexner observed that there is a need for HIV products with less frequent dosing, greater convenience, and greater likelihood of viral suppression, as well as for the prevention and treatment of other diseases, including tuberculosis, malaria, and viral hepatitis. He discussed recent advances in formulation science that are going to help make available better replacements for daily oral drugs for HIV and many other infectious diseases . Dr. Dieffenbach underscored Dr. Flexner’s point that these novel products must be developed with access and equity in mind so that people who need them, especially in resource-limited settings, can use them.
Key Takeaways
Reflecting on key takeaways from the entire conference, both Dr. Dieffenbach and Brian pointed to the importance of partnership between the HIV community and scientists in all aspects of HIV research , a theme also discussed in HIV.gov’s conversation with Dr. LaRon Nelson from the conference. In terms of research highlights, Dr. Dieffenbach pointed to the results reported from the IMPAACT P1115 study in which several children who started HIV treatment within hours of birth later surpassed a year of HIV remission after a treatment pause. ( See HIV.gov’s interview with Dr. Deborah Persaud about this study .) He also noted that the additional data accumulating on the effectiveness of Doxy-PEP is encouraging and will hopefully soon be reflected in clinical guidelines that help to reduce the incidence of syphilis, chlamydia, and gonorrhea in men who have sex with men and transgender women.
Catch Up on More HIV Research Updates
HIV.gov has shared other interviews from CROI 2024 with federal HIV leaders, participating researchers, and community members. You can find all of them on HIV.gov’s social media channels and recapped here on the blog this week and next week.
More than 3,600 HIV and infectious disease researchers from 73 countries gathered in Denver and virtually from March 3-6 this year for CROI, an annual scientific meeting on the latest research that can help accelerate global progress in the response to HIV and other infectious diseases, including STIs and viral hepatitis. Over 1,000 summaries of original research were presented. Visit the conference website Exit Disclaimer for more information. Session webcasts and more information will be published there for public access in 30 days.
Related HIV.gov Blogs
- CROI Conference on Retroviruses & Opportunistic Infections
- NIAID National Institute of Allergy & Infectious Diseases
- NIH National Institutes of Health
- Treatment HIV Treatment
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Research & training, advances in hiv/aids research.
For an update on what medical science is doing to fight the global HIV/AIDS pandemic, read a Parade article by NIH Director Francis S. Collins and NIAID Director Anthony S. Fauci, AIDS in 2010: How We're Living with HIV .
Over the past several decades, researchers have learned a lot about the human immunodeficiency virus (HIV) and the disease it causes, acquired immunodeficiency syndrome (AIDS). But still more research is needed to help the millions of people whose health continues to be threatened by the global HIV/AIDS pandemic.
At the National Institutes of Health, the HIV/AIDS research effort is led by the National Institute of Allergy and Infectious Diseases (NIAID). A vast network of NIAID-supported scientists, located on the NIH campus in Bethesda, Maryland, and at research centers around the globe, are exploring new ways to prevent and treat HIV infection, as well as to better understand the virus with the goal of finding a cure. For example, in recent months, NIAID and its partners made progress toward finding a vaccine to prevent HIV infection. Check out other promising areas of NIAID-funded research on HIV/AIDS at http://www.niaid.nih.gov/topics/hivaids/Pages/Default.aspx .
Other NIH institutes, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development and National Institute on Alcohol Abuse and Alcoholism, also support research to better control and ultimately end the HIV/AIDS pandemic. Some of these researchers have found a simple, cost-effective way to cut HIV transmission from infected mothers to their breastfed infants. Others have developed an index to help measure the role of alcohol consumption in illness and death of people with HIV/AIDS.
Find out more about these discoveries and what they mean for improving the health of people in the United States and all around the globe.
This page last reviewed on August 20, 2015
Connect with Us
- More Social Media from NIH

Personalize Your Experience
Log in or create an account for a personalized experience based on your selected interests.
Already have an account? Log In
Free standard shipping is valid on orders of $45 or more (after promotions and discounts are applied, regular shipping rates do not qualify as part of the $45 or more) shipped to US addresses only. Not valid on previous purchases or when combined with any other promotional offers.
Register for an enhanced, personalized experience.
Receive free access to exclusive content, a personalized homepage based on your interests, and a weekly newsletter with topics of your choice.
Home / Innovation & Research / The innovative research behind HIV/AIDS treatment
The innovative research behind HIV/AIDS treatment
Please login to bookmark.

It’s been 40 years since the release of the first scientific report describing acquired immune deficiency syndrome (AIDS). Thanks to innovative research, scientists learned how the HIV virus that causes AIDS replicates and how the immune system responds to the virus. Today, many people with HIV take just one pill a day to suppress the virus, and treatment is continuing to evolve.
In this video, Dr. Stacey Rizza , Mayo Clinic infectious disease physician and HIV researcher, explains how dedicated innovative science contributed to where we are today and what scientists are working on for the future.
What did the early research find?
Because of truly dedicated innovative science, within a few years, the scientific community figured out that AIDS was due to HIV. It then took a few years to figure out how to test for that virus. Several years later, the scientific community was able to quantitate how much virus was in a person’s blood. During all this time, truly innovative research into how the virus replicates and how the immune system responds to the virus allowed bio pharmacy companies to develop what we call anti-retroviral drugs or medications to slow down the viral replication. How has medication to treat HIV evolved?
The first drug approved for HIV was in 1987, which was AZT (now known as zidovudine). At that time, it was the fastest drug ever approved by the FDA (Food and Drug Administration) and started the fast-track mechanism through the FDA.
Then several other drugs within that same class were approved in the early 1990s. In late 1995, very early 1996, the first HIV protease inhibitors were approved. At that point, it was possible to combine three different medications from two different classes and completely suppress the HIV replication.
In the last 20 years, we’ve gone from people taking multiple medicines with lots of side effects to many of my patients with HIV now take a single pill a day. That’s a combination of medicines coformulated into one pill a day that’s extremely well-tolerated and completely suppresses their virus. We know it does not eliminate the virus. If they were to stop taking that medicine, the virus would come back. But we now have a handful of people in the world who have been what we called functionally cured of HIV, meaning they’ve gone through some research protocols that eliminated the reservoir of HIV in their body.
The new drugs are so effective in people who have fully suppressed virus that many only need to use two medications to maintain HIV treatment and control. New research is investigating ways to deliver the medications differently, such as a shot that lasts several months, or maybe someday even implantable medication delivery mechanisms so that people don’t have to take the pill every day. It is very exciting that HIV therapy is moving that direction.
Why isn’t there a cure for HIV?
The reason why it is so difficult to cure HIV is that once HIV infects a person’s body, it integrates into the host genome of several cell types. Those cells then hide in any of the lymphoid tissue, such as the lymph nodes, the liver and the spleen. And they lay there as what we call “latent” or “hiding”, as long as the person is on HIV therapy. Anytime a virus does leave a cell, it gets taken care of by HIV therapy. But if the infected individual stops the HIV therapy, that latent virus will come back. To cure HIV, you have to eliminate those hiding viruses in the cells or that latent viral reservoir, which is the term. There are many ways you can approach eliminating the reservoir.
Where is the research now?
One of the more popular ways that have been investigated is something called — and there are many different terms for it — “prime, shock, and kill” or “kick, and kill”, which is essentially giving medications that first wake the virus up from latency and then find ways to make the cells that have the virus susceptible to dying. When the virus is awake, and the cell is susceptible to dying, it kills itself but does not kill any other cells in the body.
Essentially, it specifically targets the HIV-infected cells and eliminates them without hurting anything else. This new science is exciting. It’s getting closer and closer to understanding how to do this effectively. And if you can do that with oral medications rather than fancy therapies like gene therapy or bone marrow transplant, it’s scalable to large parts of the world, and you can touch millions of people that way. That’s where the area of research is on how to make those hiding cells wake up, how to make them sensitive to die, and how to target just the HIV-infected cell.
Will we see a vaccine for HIV?
HIV has been a very hard vaccine to develop. In the world of viruses, vaccines fall into one of three buckets. They fall into the bucket where they respond to antibodies induced by the vaccine, and the vaccines are outstanding. Such viruses include polio, mumps, and lucky for us, SARS-CoV-2. Then we have the second category, like the influenza vaccine, which is about 60% effective. It certainly saves lives and makes a difference, but it’s not perfect. And then we have the third bucket, which quite frankly is the vast majority of viruses that infect humans. And HIV is in that category, where simply forming an antibody to the virus is not adequate to prevent infection. You have to do very sophisticated engineering to induce T cell effects, as well as innate effects and antibody effects. Even then, sometimes it’s very hard to decide what is the part of the virus to target. After decades, and billions of dollars of research, we’re still not there for HIV. There have been many approaches of how to do this science. Many different scientific delivery mechanisms, many different areas of the viruses targeted, many different parts of the immune system targeted, and so far, none of them have been effective at preventing HIV infection.
What needs to happen next?
We still need to slow down the number of people getting infected through good public health measures and good education to stop the HIV epidemic. We still need to get more people who are infected on therapy.
We know we can do it with public health measures. But we also need to find out more about how we eliminate that reservoir and get people cured of the virus in a simple and effective way so that we can cure more people. And the last major hurdle we have is to develop an effective vaccine. We still don’t have a vaccine that can prevent infection, a preventive vaccine, or a therapeutic vaccine where you give it to people who already have the virus that can help them control the infection. A huge amount of research has happened, but we’re still not there yet.
This article originally appeared on Mayo Clinic News Network.

Relevant reading
Battalion Surgeon
"They call you a battalion surgeon. I didn't know surgery; really, I was simply trying to save lives." (Audio Interview) William M. McConahey graduated from medical school in 1942 and enlisted with the Army in 1943. He attended medical field service school and served as a battalion surgeon with the…

Discover more Innovation & Research content from articles, podcasts, to videos.
You May Also Enjoy

Privacy Policy
We've made some updates to our Privacy Policy. Please take a moment to review.

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Office of AIDS Research

- News and Events
Research Advances
- OAR Updates
- World AIDS Day at NIH
Tools underestimate cardiovascular event risk in people with HIV
March 4, 2024 - The elevated cardiovascular disease risk among people with HIV is even greater than predicted by a standard risk calculator in several groups, including Black people and cisgender women, according to analyses from a large international clinical trial primarily funded by NIH. The risk of having a first major cardiovascular event was also higher than previously predicted for people from high-income regions and those whose HIV replication was not suppressed below detectable levels.
New guidelines for use of statins by people with HIV to prevent cardiovascular events
February 29, 2024 - The Department of Health and Human Services Guidelines Panel for the Use of Antiretroviral Agents in Adults and Adolescents with HIV (the Panel) has developed recommendations for the use of statin therapy in people with HIV, in collaboration with representatives from the American College of Cardiology, the American Heart Association, and the HIV Medicine Association. The new guidelines, Recommendations for the Use of Statin Therapy as Primary Prevention of Atherosclerotic Cardiovascular Disease in People with HIV, were published on February 27, 2024, and can be found online at ClinicalInfo.hiv.gov
Long-acting HIV treatment demonstrates efficacy in people with challenges taking daily medicine as prescribed
February 21, 2024 - Long-acting antiretroviral therapy (ART) with cabotegravir and rilpivirine was superior in suppressing HIV replication compared to daily oral ART in people who had been unable to maintain viral suppression through an oral daily regimen, according to interim data from a randomized trial. Upon review of these findings, an independent Data and Safety Monitoring Board (DSMB) recommended halting randomization and inviting all eligible study participants to take long-acting ART.
NIH-developed HIV antibodies protect animals in proof-of-concept study: findings support the HIV fusion peptide as a promising preventive vaccine target
January 17, 2024 - Three different HIV antibodies each independently protected monkeys from acquiring simian-HIV (SHIV) in a placebo-controlled proof-of-concept study intended to inform development of a preventive HIV vaccine for people. The antibodies—a human broadly neutralizing antibody and two antibodies isolated from previously vaccinated monkeys—target the fusion peptide, a site on an HIV surface protein that helps the virus fuse with and enter cells.
Biomedical STI prevention evidence is inadequate for cisgender women
December 20, 2023 - Pivotal studies of some biomedical HIV and sexually transmitted infection (STI) prevention interventions have excluded cisgender women or demonstrated low efficacy among them, limiting their prevention options relative to other populations who experience high HIV and STI incidence. Findings from an NIH-funded study show doxycycline postexposure prophylaxis (better known as DoxyPEP) did not prevent STI acquisition in cisgender women, despite showing promising results in gay, bisexual, and other men who have sex with men and transgender women in a previous study.
NIH research identifies opportunities to improve future HIV vaccine candidates: study suggests greater CD8+ T-cell activity may increase HIV immunity
December 14, 2023 - An effective HIV vaccine may need to prompt strong responses from immune cells called CD8+ T cells to protect people from acquiring HIV, according to a new study from researchers at NIH. The study findings draw comparisons between the immune system activity of past HIV vaccine study participants and people with HIV who naturally keep the virus from replicating even in the absence of antiretroviral therapy (ART).
NIH clinical trial of tuberculous meningitis drug regimen begins: six-month multidrug regimen being evaluated against standard treatment
December 7, 2023 - A trial of a new drug regimen to treat tuberculous meningitis (TBM) has started enrolling adults and adolescents in several countries where tuberculosis (TB) is prevalent. The trial will include 330 participants aged 15 years and older who have or are likely to have TBM based on signs and symptoms, including people living with and without HIV.
Generic daily HIV prevention pill for young men who have sex with men could save lives, lower costs, NIH-funded study suggests
October 12, 2023 - Compared to annual HIV screening alone, generic daily oral HIV pre-exposure prophylaxis (PrEP) with HIV screening every three months would result in fewer HIV acquisitions, longer life expectancy, and fewer HIV-associated costs among young men who have sex with men in the United States. These predictions, which come from a simulation study supported by the National Institutes of Health, illustrate the value of promoting PrEP use in this population.
NIH-funded study finds several potential risk factors for high blood pressure disorders of pregnancy in people with HIV
September 27, 2023 - The risk for hypertensive disorders of pregnancy was higher for pregnant people with HIV if they had low CD4+ immune cell counts in the first or second trimester or if they began taking antiretroviral drug regimens after 20 weeks of pregnancy, rather than at conception, according to a study funded by the National Institutes of Health.
Clinical trial of HIV vaccine begins in United States and South Africa
September 20, 2023 - A trial of a preventive HIV vaccine candidate has begun enrollment in the United States and South Africa. The Phase 1 trial will evaluate a novel vaccine known as VIR-1388 for its safety and ability to induce an HIV-specific immune response in people.
Blocking HIV enzyme reduces infectivity and slows viral rebound
July 26, 2023 - A pair of studies funded by the National Institutes of Health showed that blocking an enzyme involved in forming HIV particles stopped the virus from becoming infectious, suggesting a possible new target for treating HIV infection.
Using content analysis to understand the usage of stigmatizing language in recent scientific literature and its harmful effect on people living with HIV
July 19, 2023 - People living with HIV and experts in the field have long advocated for the use of person-first language, which is a way to emphasize that the disorder, disease, condition, or disability as only one aspect of the whole person. Outdated terms such as “HIV-infected” and “AIDS-infected” are negative and dehumanizing, with the latter being clinically inaccurate. Recently published research supported by NIH performed a content analysis on the usage of HIV-related stigmatizing language in peer-reviewed scientific literature to understand and help address this issue.
Social support promotes HIV suppression among young adults, NIH-funded study suggests
July 17, 2023 - Young adults born with HIV who report average or high levels of social support are more likely to maintain viral suppression than peers with low social support, according to a study of U.S. young adults funded by the NIH. The findings also suggest that having sufficient social support is particularly important just prior to a young adult’s transition from pediatric to adult HIV care.
Daily statin reduces heart disease risk among adults living with HIV
July 24, 2023 – A National Institute of Health-supported study found that statins, a class of cholesterol-lowering medications, may offset the high risk of cardiovascular disease in people living with HIV by more than a third, potentially preventing one in five major cardiovascular events or premature deaths in this population. People living with HIV can have a 50-100% increased risk for cardiovascular disease. The findings are published in the New England Journal of Medicine.
Encouraging First-in-Human Results for a Promising HIV Vaccine
June 6, 2023 – The results of an early phase clinical study, published recently in the journal Science Translational Medicine and earlier in Science , showed that an experimental HIV nanoparticle vaccine is safe in people. While the vaccine alone will not offer HIV protection and is intended to be part of an eventual broader, multistep vaccination regimen, the researchers also determined that it elicited a robust immune response in nearly all 36 healthy adult volunteers.
Daily statin reduces the risk of cardiovascular disease in people living with HIV, large NIH study finds
April 11, 2023 – A National Institutes of Health (NIH) clinical trial ended ahead of schedule because of convincing findings that a daily statin medication could reduce the increased risk of cardiovascular disease among people living with HIV. It was the first large-scale clinical study to test a primary cardiovascular prevention strategy in this population.
HIV Can Persist for Years in Myeloid Cells of People on Antiretroviral Therapy
March 27, 2023 — A subset of white blood cells, known as myeloid cells, can harbor HIV in people who have been virally suppressed for years on antiretroviral therapy, according to findings from a small study supported by the National Institutes of Health.
Mixed-Race Woman Potentially Cured of HIV Using Stem Cell Transplant
March 23, 2023 — A woman with leukemia is likely cured of HIV after receiving a transplant including stem cells from banked umbilical cord blood. The result suggests a way to expand the pool of available stem cells for curing HIV in people who require transplants for other medical conditions.
Learn About the Mpox Vaccine
February 14, 2023 — Demetre Daskalakis, MD, MPH, Director, Division of HIV Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention at CDC and National Mpox Response Deputy Coordinator, answers some of the most common questions about mpox.
Long-acting antiretroviral therapy suppresses HIV among people with unstable housing, mental illnesses, substance use disorders
February 21, 2023 — A long-acting antiretroviral treatment (LA-ART) given every four to eight weeks, and delivered with comprehensive support services, suppressed HIV in people who were previously not virologically suppressed. This is according to an ongoing demonstration study of 133 people with HIV in San Francisco, funded by the National Institutes of Health. The study focused on reaching people who have historically had decreased access to antiretroviral therapy (ART), including people experiencing housing insecurity, mental illnesses, and substance use disorders. The study findings indicate that long-acting injectable ART can benefit people who face many treatment barriers and are historically underserved.
Experimental HIV Vaccine Regimen Safe but Ineffective, Study Finds
January 18, 2023 - An investigational HIV vaccine regimen tested among men who have sex with men (MSM) and transgender people was safe but did not provide protection against HIV acquisition, an independent data and safety monitoring board (DSMB) has determined. The HPX3002/HVTN 706, or “Mosaico,” Phase 3 clinical trial began in 2019 and involved 3,900 volunteers ages 18 to 60 years in Europe, North America, and South America. Based on the DSMB’s recommendation, the study will be discontinued. Participants are being notified of the findings, and further analyses of the study data are planned.
HIV Silencing and Cell Survival Signatures in Infected T Cell Reservoirs
January 5, 2023 — NIH scientists and partners developed technology to provide a genome-wide expression profile of cells harboring latent HIV, which could enable the search for new HIV cure strategies that target infected cell reservoirs.
Early HIV Diagnosis and Treatment Important for Better Long-term Health Outcomes
October 21, 2022 — Starting antiretroviral treatment (ART) early in the course of HIV infection when the immune system is stronger results in better long-term health outcomes compared with delaying ART, according to findings presented today at the IDWeek Conference in Washington, D.C. The findings are based on an extended follow-up of participants in the National Institutes of Health-funded Strategic Timing of Antiretroviral Treatment (START) study.
Three-dose Hepatitis B Vaccine Regimen Protects People with HIV
October 20, 2022 — A three-dose course of the hepatitis B vaccine HEPLISAV-B fully protected adults living with HIV who had never been vaccinated against or infected with the hepatitis B virus (HBV), according to study findings presented today at the IDWeek conference in Washington, D.C. The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, sponsors the ongoing Phase 3 ACTG A5379 clinical study.
NIH Announces Additional Funding Awards for Ending the HIV Epidemic Initiative Implementation Research Projects
October 6, 2022 — Last month, as part of their support of the Ending the HIV Epidemic in the U.S. (EHE) initiative, NIH announced 66 awards to institutions participating in the NIH-funded Centers for AIDS Research (CFAR) and the NIMH AIDS Research Centers (ARC) programs. This was the fourth year of NIH investments in EHE-focused research projects. These new awards total $26 million and will support research in 33 of the EHE priority jurisdictions to strengthen research-community collaborations and enhance the implementation science knowledge base needed to end the HIV epidemic.
White House Publishes Federal Implementation Plan for National HIV/AIDS Strategy
August 26, 2022 — The National HIV/AIDS Strategy (NHAS) Federal Implementation Plan reflects the collaborative work of representatives from 10 federal departments and details more than 380 action items they will implement individually and collaboratively. This plan documents federal agencies’ commitments to programs, policies, research, and other activities needed to meet the NHAS goals. These critical activities, which encompass work to for fiscal years 2022–2025, will move our indicators of progress in the right directions.
New Insights into HIV Latent Cells Yield Potential Cure Targets
July 27, 2022 — In a presentation today at AIDS 2022, the 24th International AIDS Conference in Montreal, scientists with the National Institute of Allergy and Infectious Diseases’ (NIAID) Vaccine Research Center (VRC) and their collaborators described how their use of cutting-edge technology revealed new insights into cellular reservoirs of HIV and what those observations could mean for the next steps in HIV cure research. NIAID is part of the National Institutes of Health.
Finding HIV’s ‘Sweet Spot’
July 22, 2022 — An NIH-funded team has found that patterns of sugars at the surface of our own human immune cells affect their vulnerability to HIV infection.
In people with HIV, treating precancerous anal lesions cuts risk of anal cancer by more than half
June 15, 2022 — Nearly all cases of anal cancer are caused by infection with cancer-causing types of HPV.
Creating a one-stop shop for HIV research
June 9, 2022 — access issue of the Journal of Acquired Immunodeficiency Syndrome (JAIDS) will highlight HIV implementation science findings, reported by scientists and implementations teams funded by the National Institutes of Health through the Ending the HIV Epidemic initiative. (JAIDS)
How Lessons From HIV Research Informed COVID-19 Vaccine Trials
May 12, 2022 — A new study shows how community engagement approaches developed by the HIV Vaccine Trials Network strengthened COVID-19 vaccine trials.
Transactional sex, HIV and health among young cisgender men and transgender women who have sex with men in Thailand
April 8, 2022 — Study examines how recent sex work is identified and the HIV risk factors and service needs among Thai cisgender men who have sex with men and transgender women who exchange sex. (Elsevier: Annals of Epidemiology)
NIH launches clinical trial of three mRNA HIV vaccines
March 14, 2022 — Phase 1 study is among first to examine mRNA technology for HIV.
Researchers document third known case of HIV remission involving stem cell transplant
February 15, 2022 — Woman has remained without detectable HIV for 14 months
First HIV Vaccines Administered in Moderna Clinical Trial
January 2022 – Moderna announces the launch of human clinical trials for an experimental HIV vaccine that uses the same kind of mRNA technology found in Moderna’s COVID-19 vaccine. (The Hill)
NIH celebrates FDA approval of long-acting injectable drug for HIV prevention
December 21, 2021 — Approval marks pivotal expansion of HIV prevention options in the United States.
Experimental mRNA HIV vaccine safe, shows promise in animals
December 9, 2021 — NIH scientists developed vaccine platform.
AIDS and Behavior: Volume 25, supplement issue 2, November 2021
November 2021 — Includes 14 articles on Innovations in Methods and Measurement Science on the Social Determinants of HIV. (AIDS and Behavior).
Too many people with HIV fail to achieve durable viral suppression
November 30, 2021 — NIH-funded study estimates global progress toward UNAIDS goal.
NIH researchers identify how two people controlled HIV after stopping treatment
October 29, 2021 — Different mechanisms suppressed the virus in each person.
NIH Awards More than $20 Million to International HIV Database Centers
July 22, 2021 — The National Institutes of Health has renewed grants to seven regional centers that compose the International epidemiology Databases to Evaluate AIDS (IeDEA), awarding $20.8 million in first-year funding. The 15-year-old IeDEA program efficiently advances knowledge about HIV by pooling and analyzing de-identified health data from more than two million people with HIV on five continents to answer research questions that individual studies cannot address. The grants are expected to last five years and to total an estimated $100 million.
NIH-funded study tests “one-stop” mobile clinics to deliver HIV, substance use care
June 9, 2021 — Mobile clinics could serve as an innovative strategy for expanding access to care.
HIV Related Stigma Research as a Priority at the National Institutes of Health
April 22, 2021 — The National Institute of Health (NIH) recognizes that ending the HIV epidemic will require eliminating HIV-related stigma, which continues to be a critical barrier to the uptake of evidence-based HIV interventions, and in this article the authors provide an overview of NIH HIV stigma research and findings. (AIDS and Behavior)
NIH experts call for accelerated research to address concurrent HIV and COVID-19 pandemics
April 8, 2021 — The COVID-19 pandemic is affecting people with or at risk for HIV indirectly and direct.
HIV/AIDS in the Era of COVID-19: A Juxtaposition of Two Pandemics
April 7, 2021 — Effective responses to concurrent COVID-19 and HIV/AIDS pandemics require a novel coordinated and collaborative global effort to accelerate biomedical research and implementation science to operationalize evidence-based interventions expeditiously. (The Journal of Infectious Diseases)
Profile: Fogarty Fellow Dr. Joseph Matovu investigates HIV self-testing in Ugandan fishing community
March/April 2021 – When social network leaders were trained to disseminate HIV self-testing kits, more than 95% were properly used and returned. (NIH Fogarty International Center Global Health Matters Newsletter, Image courtesy of Moses Mayombwe)
Scaling Up Covid-19 Vaccination in Africa – Lessons from the HIV Pandemic
March 31, 2021 — Concerns about access to Covid-19 vaccines in Africa resemble concerns raised about responding to the HIV pandemic in the mid-1990s and early 2000s, when highly active antiretroviral treatment was accessible in high-income countries but limited in African countries. (The New England Journal of Medicine)
Methodological and Measurement Advances in Social Determinants of HIV: View from NIH
March 29, 2021 — Lessons learned from a Request for Applications that called for methodological innovations around the social determinants of HIV and provided a unique opportunity to reflect on the state of the science. (AIDS and Behavior)
Final HIV Prevention & Treatment Research Highlights from CROI 2021 (video)
March 12, 2021— Dr. Carl Dieffenbach, director of the Division of AIDS at NIH’s National Institute of Allergy and Infectious Diseases, and his colleague Dr. Hillary Hoffman, joined HIV.gov for a conversation about the latest HIV prevention and treatment research presented during the 2021 Conference on Retroviruses and Opportunistic Infections. (HIV.gov)
Unique genotypic features of HIV-1 C gp41 membrane proximal external region variants during pregnancy relate to mother-to-child transmission via breastfeeding
January 2021 - Findings from a pilot study on mother-to-child transmission (MTCT) of HIV-1 through breastfeeding raise the possibility for predicting MTCT by breastfeeding based on identifying mothers with high-risk viral populations. (Journal of Clinical Pediatrics and Neonatology)
Antibody Infusions prevent acquisition of some HIV strains, NIH studies find
Tuesday, January 26, 2021 – Results of Antibody-Mediated Prevention Studies funded by the NIH’s National Institute of Allergy and Infectious Diseases will inform development of long-acting antibody-based HIV prevention tools. (Image Credit: NIAID)
To end HIV epidemic, we must address health disparities
February 19, 2021 — Expert report cites unequal progress in Southern U.S. and among marginalized groups.
NIH announces restructured HIV clinical trials networks
November 30, 2020 — Grant awards set stage for next seven years of science-driven HIV clinical research.
NIH study finds long-acting injectable drug prevents HIV acquisition in cisgender women
November 9, 2020 – Long-acting regimen more effective than daily oral pill among African women.
Implications of COVID-19 for HIV Research: data sources, indicators and longitudinal analyses
September 23, 2020 – Pandemic-driven changes in data sources, clinic activities and local policies require a new COVID-19 informed paradigm for collecting HIV cohort data. (Journal of the International AIDS Society)
NIAID – Supported Research Unveils Characteristics of Key Steps in HIV Life Cycle
October 19, 2020 – New NIAID-funded research answers longstanding questions about key steps in HIV replication. (Illustration Credit: Janet Iwasa and Devin Christensen, University of Utah Health)

NIH awards will advance HIV Implementation Research in U.S. Communities
September 24, 2020 — The National Institutes of Health has awarded approximately $10 million to support implementation science research to advance the goals of Ending the HIV Epidemic: A Plan for America
D.C. is close to ending the HIV epidemic, but covid-19 may get in the way
August 20, 2020 — Report shows that HIV infections in Washington, DC, declined by 16% in 2019. (Washington Post)
Vaginal ring for HIV prevention receives positive opinion from European regulator
July 24, 2020 — NIAID celebrates pivotal step toward expanding HIV prevention choices for women.
Kidney transplantation between people with HIV is safe, NIH study finds
July 23, 2020 — Multicenter HOPE Act study expands pool of available kidneys.
Long-acting injectable form of HIV prevention outperforms daily pill in NIH study
July 7, 2020 — Both methods highly effective at preventing HIV among men who have sex with men and transgender women.
This page last reviewed on March 19, 2024

CDC provides national leadership for HIV prevention research, including the development and evaluation of HIV biomedical and behavioral interventions to prevent HIV transmission and reduce HIV disease progression in the United States and internationally. CDC’s research efforts also include identifying those scientifically proven, cost-effective, and scalable interventions and prevention strategies to be implemented as part of a high-impact prevention approach for maximal impact on the HIV epidemic.
The AIDS epidemic, although first recognized only 20 years ago, has had a profound impact in communities throughout the United States.
The Serostatus Approach to Fighting the HIV Epidemic: Prevention Strategies for Infected Individuals R. S. Janssen, D. R. Holtgrave, and K. M. De Cock led the writing of this commentary. R. O. Valdiserri, M. Shepherd, and H. D. Gayle contributed ideas and helped with writing and reviewing the manuscript.

CDC has provided funding to HIV partners to help implement programs that will help curb the increase of HIV infections. These programs facilitated with our partners and grantees are critical in the goal of eliminating HIV infection in the United States.

CDC has researched several HIV prevention interventions that have proven effective in helping to prevent HIV infection in certain populations and communities.

CDC has worked with key cities to create effective policies and programs to curb the tide of HIV infections in those cities. These cities have higher rates of HIV due to a number of factors therefore making them key locations for studies.

The Medical Monitoring Project (MMP) is a surveillance system designed to learn more about the experiences and needs of people who are living with HIV. It is supported by several government agencies and conducted by state and local health departments along with the Centers for Disease Control and Prevention.
- Assessment of 2010 CDC-funded Health Department HIV Testing Spending and Outcomes pdf icon [PDF – 359 KB]
- HIV Testing Trends in the United States, 2000-2011 pdf icon [PDF – 1 MB]
- HIV Testing at CDC-Funded Sites, United States, Puerto Rico, and the U.S. Virgin Islands, 2010 pdf icon [PDF – 691 KB]
- HIV Prevention Funding Allocations at CDC-Funded State and Local Health Departments, 2010 pdf icon [PDF – 792 KB]
Cost-effectiveness of HIV Prevention
- The cost-effectiveness of HIV prevention efforts has long been a criterion in setting program priorities. The basic principle is straightforward: choose those options that provide the greatest outcome for the least cost.
- The fact sheet Projecting Possible Future Courses of the HIV Epidemic in the United States pdf icon compares the cost-effectiveness of three different prevention investment scenarios.
The HIV/AIDS Prevention Research Synthesis (PRS) Project identifies evidence-based HIV behavioral interventions (EBIs) listed in the Compendium of Evidence-Based HIV Behavioral Interventions to help HIV prevention planners and providers in the United States choose the interventions most appropriate for their communities.
- On January 1, 2012, CDC began a new 5-year HIV prevention funding cycle with health departments, awarding $339 million annually.
- The STD/HIV National Network of Prevention Training Centers provides training for health departments and CBOs on the HIV prevention interventions.
- HIV by Group
- HIV Risk and Prevention
- HIV Nexus: Resources for Clinicians
- HIV Public Health Partners
- HIV Resource Library
- HIV Statistics Center
- About the Division of HIV Prevention
- VIH en Español
- @StopHIVTogether
- Get Email Updates
- Send Feedback
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Healthline: New HIV variant discovered: May be more infectious and severe
Uc expert says current treatments are still effective.

New research from the University of Oxford finds a new variant of HIV, the virus that causes AIDS, that is potentially more infectious and could more seriously affect the immune system. So far, 109 people, most of whom live in the Netherlands, have the variant.
The new strain, called the VB variant, damages the immune system, weakening people’s ability to fight everyday infections and diseases much faster than the previous HIV strains, scientists say. It also means that people who contract the new variant may develop AIDS faster.
In a story published by Healthline, Carl Fichtenbaum, MD, of the Division of Infectious Diseases at the UC College of Medicine was one of the experts cited reacting to this new variant.
Carl Fichtenbaum, MD, of the Division of Infectious Diseases at the UC College of Medicine/Photo/Joe Fuqua II/UC Creative + Brand
Fichtenbaum told Healthline that it has been known for decades that some individuals get sicker quicker than others.
“The amount of virus measured in a drop of blood is a surrogate of disease progression. The higher the amount, the more likely someone will progress and become ill,” Fichtenbaum told Healthline.
“We suspect many times this is because the type of HIV they got was more aggressive or virulent,” he said. “Our practice is the same regardless of variant — get tested right away and start treatment.”
He noted that there is “no evidence” that the current treatments won’t work.
Fichtenbaum explained that reducing the risk of infection begins with sex with a condom or other barrier method.
“Know your status of HIV and those you have sex with by getting tested first; use condoms for sex; don’t share any needles or paraphernalia for injection drug use,” he said. “Those at higher risk can use PrEP or Pre-exposure prophylaxis.”
Fichtenbaum said FDA-approved treatments for people living with HIV include a tenofovir/emtricitabine combination tablet daily and cabotegravir injections every 2 months.
“Those individuals that have HIV can take their medications and be ‘undetectable’ on their viral load, which eliminates the chance of HIV transmission,” he said. “Hence the slogan U=U; undetectable equals untransmittable.”
Read the entire story here .
Lead image of HIV cell/Shutterstock
Next Lives Here
The University of Cincinnati is classified as a Research 1 institution by the Carnegie Commission and is ranked in the National Science Foundation's Top-35 public research universities. UC's medical, graduate and undergraduate students and faculty investigate problems and innovate solutions with real-world impact. Next Lives Here .
- Academic Health Center
- In The News
- Internal Medicine
- College of Medicine
Related Stories
Enquirer: salacious testimony of 1929 murder at uc rare books....
May 1, 2024
The Cincinnati Enquirer highlights a rare book found in a University of Cincinnati library that chronicled a high-profile murder trial in 1929.
WLWT: UC students experience realities of life in prison as part...
One day a week, eight UC students travel to the institution as part of the Inside-Out Prison Exchange Program, where they and eight incarcerated individuals discuss criminal justice topics such as sentencing, parole, life after prison and recidivism in a classroom setting. The program is part of a class taught by J.Z. Bennett, an assistant professor of criminal justice.
Yahoo News: Doctors see rising rates of colon cancer in younger...
Yahoo News featured comments from the University of Cincinnati's Rekha Chaudhary in a story about rising rates of diagnoses and deaths from colorectal cancers among young people.
Northeastern research on HIV infection could lead to better drugs to treat the virus
- Search Search
Northeastern physicists and National Cancer Institute researchers suggest that mechanical pressure triggers a key event in HIV infection.
- Copy Link Link Copied!
It has been more than 40 years since the beginning of the HIV/AIDS epidemic and scientists still don’t fully understand how HIV enters and replicates in human cells, which has hindered the development of treatments.
New research by a team of physicists led by Northeastern University professor Mark Williams is working on a solution.
There is no cure for HIV, the virus that causes AIDS, but there are treatments that can reduce the amount of HIV in a patient’s body and get the virus under control.
Williams’ team recently confirmed a key mechanism in the infection of cells that could lead to better drugs.
“The goal of this research is to understand the [retroviral] lifecycle much better so that better drugs for HIV can be developed,” Williams says. “And this is a great part of the lifecycle to attack with drugs.”
The study, conducted by Williams’ team in collaboration with Vinay Pathak and research biologist Ryan Burdick in his lab at the National Cancer Institute, looked at the process of “uncoating” — when the viral DNA breaks out of the original HIV capsid shell that has entered a cell.
What triggered the uncoating process was previously unknown. It was believed, Williams says, that some viral or host factors launched that process.
The new research , published in the Science Advances journal, shows that uncoating could be a natural process of mechanical pressure building up and causing the protein shell that surrounds the HIV genome to break open, a theory first proposed by collaborator Ioulia Rouzina of Ohio State University.
One of the key findings of the study is that the viral DNA must be larger than a specific minimum size in order to create sufficient pressure on the shell. Ryan Burdick observed that viruses with too little DNA cannot uncoat and infect host cells while Northeastern research associate Michael Morse showed that viral nucleocapsid protein condenses the DNA to prevent premature uncoating.
Editor’s Picks

Your guide for Northeastern University’s 2024 commencement at Fenway Park

Should you be worried about bird flu in your milk? Food safety expert explains the dangers of consuming raw dairy

From TD Garden to Fenway Park, graduate student speaker Megan Carter is a hockey and academic star

Fix it, don’t toss it. Northeastern student promotes giving new life to broken objects with Zero Waste San Diego co-op

For undergraduate commencement student speaker Rebecca Bamidele, politics and medicine are a potent mix
Understanding where and how the uncoating happens, Williams says, creates a possibility of trying to use drugs and affect the protein shell stability or the uncoating process itself.
“Because uncoating is essential for the infectivity,” he says.
HIV, or human immunodeficiency virus, is a retrovirus that causes AIDS.
As a retrovirus, HIV uses ribonucleic acid molecules, or RNA, as its genomic information carrier. This RNA converts into viral DNA that later integrates into the DNA of a host cell. The infected cell then produces more HIV retroviruses that infect other cells.
HIV is transmitted through direct contact with HIV-infected bodily fluids, such as blood, semen and vaginal fluids, or from a mother who has HIV to her child during pregnancy, labor and delivery or breastfeeding.
The virus enters a human cell as a cell-free cone-shaped viral core composed of a protein shell, called capsid.
The HIV core holds the viral genome — two copies of RNA; nucleocapsid protein, a viral protein that helps package the genome inside a closed cavity; and a few other proteins.
A viral DNA is generated by a reverse transcription of the viral RNA. Next, the newly synthesized viral DNA needs to break out of the protein shell.
Williams compares the viral RNA to a flexible string, while the viral DNA is like a stiff wire that exerts pressure on the protein shell. If the pressure created by the DNA breaks the shell too soon, the HIV genome will be released into the cytoplasm, the gelatinous liquid that fills the inside of the host cell, and destroyed by the immune system of the cell before getting to the cell nucleus that holds its DNA.
The scientists had to do a lot of experiments for the current study, he says, to figure out that nucleocapsid proteins bind not only to the viral DNA, but they also bind to the RNA once the conversion process has started.
“The RNA genome is still there when you create the DNA from that genome,” Williams says. “So you’ve increased the amount of DNA and RNA in the virus, and the fact that there’s not enough nucleocapsid protein in the capsid to condense all of the viral DNA and RNA is what seems to trigger the uncoating.”
This mechanism was pretty surprising, Williams says, but it does make physical sense.
Science & Technology

Recent Stories

Researchers find new pathway for HIV invasion of cell nucleus
The researchers also identified three proteins that are needed for the virus to carry out the invasion and have in turn synthesized molecules (potential drugs) that can target one of the proteins, potentially leading to new treatments for AIDS.
"We have revealed a protein pathway that appears to have a direct impact on diseases, which opens up a new area for potential drug development," says the study's senior author Aurelio Lorico, MD PhD, Professor of Pathology and interim Chief Research Officer at Touro University Nevada College of Osteopathic Medicine.
HIV infection requires the virus to enter a cell and gain access to the well-guarded nucleus in order for the viral components to be integrated into the healthy cell's DNA. But how the viruses get past the protective membrane is not well understood and is the subject of much debate.
The newly identified pathway begins with HIV entering a cell wrapped inside a membrane package, called an endosome. The virus-containing endosome then pushes the protective nuclear membrane inward, forming an indentation known as a nuclear invagination. The endosome then moves inside the invagination to its inner tip, where the virus then slips into the nucleus.
The study found that three proteins were critical to the invasion: One protein (Rab7) is located on the membrane of the endosome, the second (VAP-A) is on the nuclear membrane where the invagination occurs, and the third (ORP3) connects the first two proteins together. An interaction among the three proteins is needed for the invasion to be successful, so targeting any of these proteins could halt the infection. The team has synthesized and tested molecules that interrupt the interaction among the proteins. The researchers observed that, in the presence of these molecules, HIV replication does not occur.
This pathway for nuclear access was first discovered in the team's research on cancer metastasis and is likely involved in other diseases as well.
"This is an entirely new pathway and we have developed molecules (drugs) that block it," says Lorico. "Although our research is at a pre-clinical stage, it is likely that the new drugs synthesized may have therapeutic activity in AIDS, other viral diseases, and possibly metastatic cancer and other diseases where nuclear transport is involved." The team is currently looking at the pathway's role in Alzheimer's disease and metastasis of many types of cancer.
"Because the pathway we found may apply to many types of disease, there is a tremendous amount of work that needs to be done to understand the full benefits of this research," says Dr. Denis Corbeil, co-leading author of the study, research group leader at the Biotechnology Center (BIOTEC) of TUD Dresden University of Technology in Germany.
"The ground-breaking research of Dr. Lorico and his team is a testimony to the importance that Touro University gives to its mission of service to humanity. The potential therapeutic applications of this new pathway to improve patient care are immense and may help us better navigate the next pandemic," said Dr. Alan Kadish, Touro University President.
- HIV and AIDS
- Infectious Diseases
- Diseases and Conditions
- Cell Biology
- Molecular Biology
- Natural killer cell
- Somatic cell nuclear transfer
- Embryonic stem cell
- Chemotherapy
Story Source:
Materials provided by Technische Universität Dresden . Note: Content may be edited for style and length.
Journal Reference :
- Mark F. Santos, Germana Rappa, Jana Karbanová, Patrizia Diana, Girolamo Cirrincione, Daniela Carbone, David Manna, Feryal Aalam, David Wang, Cheryl Vanier, Denis Corbeil, Aurelio Lorico. HIV-1-induced nuclear invaginations mediated by VAP-A, ORP3, and Rab7 complex explain infection of activated T cells . Nature Communications , 2023; 14 (1) DOI: 10.1038/s41467-023-40227-8
Cite This Page :
Explore More
- Climate Change and Mercury Through the Eons
- Iconic Horsehead Nebula
- Sustainable Jet Fuel from Landfill Emissions
- Bacterial Spores in Bioplastic Make It 'Green'
- Genetic Signals Linked to Blood Pressure
- Double-Fangs of Adolescence Saber-Toothed Cats
- Microarray Patches for Vaccinating Children
- Virus to Save Billions of Gallons of Wastewater
- Weather Report On Planet 280 Light-Years Away
- Trotting Robots and Animal Gait Transitions
Trending Topics
Strange & offbeat.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 30, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Visa rules jeopardize HIV management, study finds
by Monash University
A Monash University sexual health expert has warned that an unintended consequence of Australia's migration rules could compromise Australia's goal to end the HIV epidemic by 2030.
Associate Professor Jason Ong, of the Melbourne Sexual Health Center (MSHC), at Monash University's School of Translational Medicine, says some people living with HIV are choosing cheaper, suboptimal antiretroviral treatment (ART) out of fear that their applications for permanent residency (PR) will be rejected.
This is because they must show their medical spending will not total more than $51,000 over 10 years—a requirement, known as the Significant Cost Threshold, designed to screen out applicants who might pose extra costs to Australia's health system.
"Being on the most effective treatments puts many people beyond that threshold , resulting in automatic rejection of their application for PR," said Associate Professor Ong, whose findings were published in the journal Sexual Health .
"Unfortunately, cheaper treatments aren't as good at controlling HIV, and they're not as safe."
Australia is a world leader in extending PrEP (an antiviral medicine that prevents HIV) to groups at risk of HIV, and is working towards elimination of HIV transmission by 2030. This does not mean zero new cases of HIV, but the absence of sustained endemic community transmission.
The study involved presenting the journeys of six patients with a mean age of 39 years living with HIV and migrating to Australia from Asian and European countries.
"We know that overseas-born gay and bisexual men are showing slower declines in transmission," Associate Professor Ong said. "It's important to bring this group with us as we work towards elimination."
"Thanks to antiretroviral therapies, HIV is now a manageable, chronic disease. It benefits everyone in the community if people living with HIV are on the right treatments."
Dash Heath-Paynter, the CEO of Health Equity Matters—the national federation for the HIV community response—urged the Federal Government to examine New Zealand's 2022 decision to raise its medical expenses threshold from NZ$41,000 to $81,000.
"There may be other options to help solve this problem, but raising the significant medical costs threshold would be a very good starting point," Mr. Heath-Paynter said.
Explore further
Feedback to editors

Study finds young adults reduced drinking during and after pandemic

Study reveals hidden diversity of innate immune cells
2 hours ago

A new form of mpox that may spread more easily found in Congo's biggest outbreak
3 hours ago

New study supports psilocybin's potential as an antidepressant
12 hours ago

Global study reveals stark differences between females and males in disease burden causes

Researcher discusses mechanism behind a birth defect affecting brain size
14 hours ago

Study indicates that cancer patients gain important benefits from genome-matched treatments

Machine learning tool identifies rare, undiagnosed immune disorders through patients' electronic health records

New technique improves T cell-based immunotherapies for solid tumors
15 hours ago

Unraveling the roles of non-coding DNA explains childhood cancer's resistance to chemotherapy
Related stories.

International migrants left behind in HIV response: Study
Jul 6, 2023

70% of Australians living with HIV report their health-related quality of life to be good
Dec 2, 2022

Research finds the most sexually adventurous gay and bisexual men are also the most vigilant with HIV prevention
Oct 30, 2023

HIV in Australia has declined by 12% in the past five years
Nov 30, 2020

HIV diagnoses in Australia remained low in 2022
Jul 20, 2023

Study finds tafenoquine is a cost-effective treatment option for malaria
Jan 11, 2024
Recommended for you

Closing the US/Mexico border during COVID-19 increased HIV transmission, study finds
21 hours ago

Study finds private equity expanding to mental health facilities
16 hours ago

Patients diagnosed with cancer in prison more likely to die from the disease, research shows
Apr 30, 2024

Early gestational diabetes treatment shown to reduce birth complications, health costs for those at higher risk

Study highlights importance of early interventions to combat HIV

Homelessness found to be a major issue for many patients in the emergency department
Apr 26, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Journal Club
- Published: 24 April 2024
Viral infection
The complex life of the HIV-1 full-length RNA
- Ricardo Soto-Rifo ORCID: orcid.org/0000-0003-0945-2970 1 , 2 , 3
Nature Reviews Microbiology ( 2024 ) Cite this article
104 Accesses
11 Altmetric
Metrics details
- Virus–host interactions
From the beginning of my career, I have been interested in studying viral replication from an RNA-centric perspective. Human immunodeficiency virus type 1 (HIV-1) attracted my attention as it offers an exquisitely and elegantly regulated model to study RNA biology, since a single viral transcript, the full-length RNA, accomplishes different functions key for a successful replication cycle. This is because it serves as a pre-mRNA template that undergoes alternative splicing to generate partially and fully spliced viral mRNAs. Additionally, it can exit the nucleus through a non-canonical nuclear export pathway (despite containing introns) to serve as the mRNA for the synthesis of the major structural proteins and viral enzymes, or as the viral genome packaged into nascent virions. How these mutually exclusive functions are coordinated during infection has intrigued researchers (including myself) for years and, despite tremendous advances, a complete understanding of these processes is far from being elucidated.
The complex regulation of the HIV-1 full-length RNA is crucial not only for efficient viral production during active replication in infected cells but also potentially impacts people living with HIV (PLWH). Viral RNA present in the cells of individuals, even those under suppressive antiretroviral therapy, has been associated with persistent immune activation, chronic inflammation and a poor clinical outcome.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Original article
Akiyama, H. et al. HIV-1 intron-containing RNA expression induces innate immune activation and T cell dysfunction. Nat. Commun. 9 , 3450 (2018)
Article PubMed PubMed Central Google Scholar
Related article
McCauley, S. M. et al. Intron-containing RNA from the HIV-1 provirus activates type I interferon and inflammatory cytokines. Nat. Commun. 9 , 5305 (2018)
Article CAS PubMed PubMed Central Google Scholar
Download references
Acknowledgements
R.S.-R. is funded by grants from ANID — Chile through the ICM Program (ANID-ICM, ICN2021_045), the Anillo Program (ATE220016) and the FONDECYT Program (no. 1230102).
Author information
Authors and affiliations.
Laboratory of Molecular and Cellular Virology, Institute of Biomedical Sciences, Faculty of Medicine, Universidad de Chile, Santiago, Chile
Ricardo Soto-Rifo
HIV/AIDS Workgroup, Faculty of Medicine, Universidad de Chile, Santiago, Chile
Millennium Institute in Immunology and Immunotherapy, Santiago, Chile
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ricardo Soto-Rifo .
Ethics declarations
Competing interests.
The author declares no competing interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Soto-Rifo, R. The complex life of the HIV-1 full-length RNA. Nat Rev Microbiol (2024). https://doi.org/10.1038/s41579-024-01049-7
Download citation
Published : 24 April 2024
DOI : https://doi.org/10.1038/s41579-024-01049-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Clients Got HIV Through 'Vampire Facial' Microneedling Treatments
Clients Got HIV Through 'Vampire Facial' Microneedling Treatments
By Ernie Mundell HealthDay Reporter

FRIDAY, April 26, 2024 (HealthDay) -- Between 2018 and the spring of 2023, a cluster of clients who had gotten 'vampire facial' microneedling skin treatments at a New Mexico spa were diagnosed with HIV , probably via poorly cleaned instruments, a new report finds.
When HIV arises among people without known risk factors, doctors "might consider cosmetic injection services as a route of HIV transmission," wrote a team led by researcher Anna Stadelman-Behar , of the U.S. Centers for Disease Control and Prevention.
The cluster of new HIV infections first came to the attention of public health officials back in the summer of 2018. That's when a woman in her 40s with no history of risk factors for HIV nonetheless tested positive for the virus while traveling abroad.
She had undergone a microneedle-based 'vampire facial' at the New Mexico spa in the spring of 2018.
U.S. Cities With the Most Homelessness

In these cosmetic procedures, a client's blood is drawn and then separated into its component cells and plasma.
Next needles -- ideally a single-use or fully sterilized multi-use needles -- are used to re-inject the "platelet-rich plasma" blood back into the face. The procedure is used to (allegedly) rejuvenate the skin.
Between 2018 and the spring of 2023, three other of the spa's female clients with no prior HIV risk factors also tested positive for HIV. Most did not even realize they carried the virus until they developed advanced AIDS-like symptoms.
The patients were all in their 40s and 50s, Stadelman-Behar's team said.
A fifth case of new HIV infection was detected in the male sexual partner of one of the infected women.
This couple had been in a long-term sexual relationship, and their HIV infection was so advanced by the time it was detected that CDC investigators believe they may have already been HIV-positive before they received their spa treatments.
Still, the exact source of the HIV involved in this cluster of cases remains unclear, the researchers said.
The spa closed in the fall of 2018, around the time that an on-site inspection revealed numerous lapses in hygiene and sterilization.
For example, a centrifuge and a rack of unlabeled tubes of blood were found on a kitchen counter; unlabeled tubes of botox and blood were stored in a household refrigerator alongside food; and unwrapped syringes were found lying on counters and drawers.
There was no autoclave (a standard steam-based sterilizer) on the premises and sterilization was substandard, the CDC team said.
The report highlights the fact that any blood-based spa treatment can be a potential source for HIV transmission, especially if proper sterilization of needles and other equipment is lacking.
"Requiring adequate infection control practices at spa facilities offering cosmetic injection services can help prevent the transmission of HIV and other blood-borne pathogens," Anna Stadelman-Behar and colleagues concluded.
The study was published April 25 in the CDC journal Morbidity and Mortality Weekly Report .
More information
Find out more about how to protect yourself against HIV at the U.S. National Institutes of Health.
SOURCE: Morbidity and Mortality Weekly Report , April 25, 2024
Copyright © 2024 HealthDay . All rights reserved.
Join the Conversation
Tags: plastic surgery
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

Fed: High Inflation Stalls Rate Cut
Tim Smart May 1, 2024

Congress Comes Down on Campus Protests
Aneeta Mathur-Ashton May 1, 2024

University Leaders in Their Own Words
Laura Mannweiler May 1, 2024

April Job Gains Above Forecasts

Nationwide Campus Protests Escalate
Laura Mannweiler April 30, 2024

What to Know: Trump Gag Order Violations
Lauren Camera April 30, 2024


COMMENTS
Your source for the latest research news. Follow: Facebook X/Twitter Subscribe: RSS Feeds. New! ... who is a Canada Research Chair in HIV Pathogenesis and Viral Control. "To live HIV-free is a ...
Blockbuster obesity drug leads to better health in people with HIV. Semaglutide reduces weight and fat accumulation associated with the antiretroviral regimen that keeps HIV at bay. Mariana ...
Nearly $17 billion was spent worldwide on HIV -vaccine research from 2000 to 2021. Nearly $1 billion more is spent annually, according to the Joint United Nations Program on HIV/AIDS and the ...
New findings offer potential breakthrough in HIV cure research. ScienceDaily . Retrieved April 30, 2024 from www.sciencedaily.com / releases / 2023 / 07 / 230726113046.htm
As new prevention tools, such as the drug cabotegravir — which protects people from HIV infection for up to two months after being injected into the body — become more widely available, health ...
More than 3,600 HIV and infectious disease researchers from 73 countries gathered in Denver and virtually from March 3-6 this year for CROI, an annual scientific meeting on the latest research that can help accelerate global progress in the response to HIV and other infectious diseases, including STIs and viral hepatitis.
The search for an HIV cure. Currently, there are approximately 38 million people living with HIV around the world and over half of them receive antiretroviral therapy. Despite the progress made in treatment, in 2021 there were an estimated 1.5 million new cases and 650,000 people died from AIDS-related illnesses worldwide, according to UNAIDS.
At the National Institutes of Health, the HIV/AIDS research effort is led by the National Institute of Allergy and Infectious Diseases (NIAID). A vast network of NIAID-supported scientists, located on the NIH campus in Bethesda, Maryland, and at research centers around the globe, are exploring new ways to prevent and treat HIV infection, as ...
An effective and scalable cure strategy is a top priority for the HIV research field; this Review discusses recent advances, knowledge gaps, and priority research areas for the next 5 years.
Interview with Dr. Anthony Fauci on progress made during the past four decades of the HIV/AIDS pandemic and ongoing efforts to end this threat. 18m 44s Download. The dramatic saga of the acquired ...
The World Health Organization (WHO) is releasing new scientific and normative guidance on HIV at the 12th International IAS (the International AIDS Society) Conference on HIV Science.New WHO guidance and an accompanying Lancet systematic review released today describe the role of HIV viral suppression and undetectable levels of virus in both improving individual health and halting onward HIV ...
The NIH supports research to better understand how the HIV reservoir forms, persists, and reactivates, as well as investigations to develop new cure treatment strategies targeting HIV reservoirs. A range of biomarkers and techniques, including single-cell and imaging technologies, are being studied to determine how to identify and describe the ...
Before the COVID-19 pandemic, the Philippines enacted a new HIV law that lowered the age of HIV testing without parental consent, incorporated HIV testing into prenatal care, and expanded public health insurance coverage to HIV treatment. 1 Although the number of new HIV infections in the Philippines decreased between 2019 and 2020, 2 officials also recorded lower rates of HIV testing ...
Nov. 1, 2023 — New research combining computer modeling and experiments with macaques shows the body's immune system helps control human immunodeficiency virus (HIV) infections largely by ...
The new drugs are so effective in people who have fully suppressed virus that many only need to use two medications to maintain HIV treatment and control. New research is investigating ways to deliver the medications differently, such as a shot that lasts several months, or maybe someday even implantable medication delivery mechanisms so that ...
New guidelines for use of statins by people with HIV to prevent cardiovascular events. February 29, 2024 - The Department of Health and Human Services Guidelines Panel for the Use of Antiretroviral Agents in Adults and Adolescents with HIV (the Panel) has developed recommendations for the use of statin therapy in people with HIV, in collaboration with representatives from the American College ...
Prevention research at CDC encompasses a provides an overview of the on-going research on HIV prevention at CDC. Skip directly to site content Skip directly to page options Skip directly to A-Z link. ... On January 1, 2012, CDC began a new 5-year HIV prevention funding cycle with health departments, awarding $339 million annually.
New research from the University of Oxford finds a new variant of HIV, the virus that causes AIDS, that is potentially more infectious and could more seriously affect the immune system. So far, 109 people, most of whom live in the Netherlands, have the variant. The new strain, called the VB variant, damages the immune system, weakening people ...
Current research into HIV aims to find a cure and eradicate the infection. Learn more about current and future research here. ... The annual number of new HIV diagnoses decreased by 7% from 2017 ...
The study highlights the importance of widespread HIV testing and treatment services, says Salim Abdool Karim, director of the Durban-based Centre for the AIDS Programme of Research in South Africa.
New research shows HIV can lie dormant in the brain. As a part of its life cycle, the human immunodeficiency virus-1 (HIV) inserts a copy of its DNA into human immune cells. Some of these newly ...
The HIV research community is led by scientists with deep personal commitments to improving the lives of people with and affected by HIV. Our collective decades of work have generated HIV testing, prevention and treatment options beyond what we could have imagined in the 1980s. Those advances enable NIAID to explore new frontiers: expanding HIV prevention and treatment modalities, increasing ...
The new research, published in the Science Advances journal, shows that uncoating could be a natural process of mechanical pressure building up and causing the protein shell that surrounds the HIV genome to break open, a theory first proposed by collaborator Ioulia Rouzina of Ohio State University.
A study has identified a new pathway that human immune deficiency virus (HIV) uses to enter the nucleus of a healthy cell, where it can then replicate and go on to invade other cells. The ...
Research finds the most sexually adventurous gay and bisexual men are also the most vigilant with HIV prevention Oct 30, 2023 HIV in Australia has declined by 12% in the past five years
Intensive research is underway on many other potential applications for this vaccine technology, which suggests a promising future. ... This technique is currently being tested against HIV and ...
Some candidates of a new circulating recombinant form (CRF) of HIV-1 were found in northern Vietnam in our previous study. We succeeded in near full-length sequencing using MinION with plasma samples from 12 people living with HIV. Three of the samples were CRF109_0107, which was recently reported in China. Three others were the newly identified CRF127_07109, while six of them were considered ...
In this Journal Club, Ricardo Soto-Rifo discusses a study on intron-containing HIV-1 RNA, revealing its role as a pathogen-associated molecular pattern in myeloid cells, which has implications for ...
Krause's acceptance into the program is a testament to the depth and excellence of HIV research at the school, as well as, the multi-level mentoring that is available, as Dr. Stephanie Shiau, another of our HIV researchers, facilitated this opportunity." ... New Brunswick: 732-235-4646; Newark: 973-972-7212; [email protected] ...
The cluster of new HIV infections first came to the attention of public health officials back in the summer of 2018. That's when a woman in her 40s with no history of risk factors for HIV ...