- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram

Pilot study shows ketogenic diet improves severe mental illness
A small clinical trial led by Stanford Medicine found that the metabolic effects of a ketogenic diet may help stabilize the brain.
April 1, 2024 - By Nina Bai

A study led by researchers at Stanford Medicine showed that diet can help those with serious mental illness. nishihata
For people living with serious mental illness like schizophrenia or bipolar disorder, standard treatment with antipsychotic medications can be a double-edged sword. While these drugs help regulate brain chemistry, they often cause metabolic side effects such as insulin resistance and obesity, which are distressing enough that many patients stop taking the medications.
Now, a pilot study led by Stanford Medicine researchers has found that a ketogenic diet not only restores metabolic health in these patients as they continue their medications, but it further improves their psychiatric conditions. The results, published March 27 in Psychiatry Research , suggest that a dietary intervention can be a powerful aid in treating mental illness.
“It’s very promising and very encouraging that you can take back control of your illness in some way, aside from the usual standard of care,” said Shebani Sethi , MD, associate professor of psychiatry and behavioral sciences and the first author of the new paper.
Making the connection
Sethi, who is board certified in obesity and psychiatry, remembers when she first noticed the connection. As a medical student working in an obesity clinic, she saw a patient with treatment-resistant schizophrenia whose auditory hallucinations quieted on a ketogenic diet.
That prompted her to dig into the medical literature. There were only a few, decades-old case reports on using the ketogenic diet to treat schizophrenia, but there was a long track record of success in using ketogenic diets to treat epileptic seizures.
“The ketogenic diet has been proven to be effective for treatment-resistant epileptic seizures by reducing the excitability of neurons in the brain,” Sethi said. “We thought it would be worth exploring this treatment in psychiatric conditions.”
A few years later, Sethi coined the term metabolic psychiatry, a new field that approaches mental health from an energy conversion perspective.

Shebani Sethi
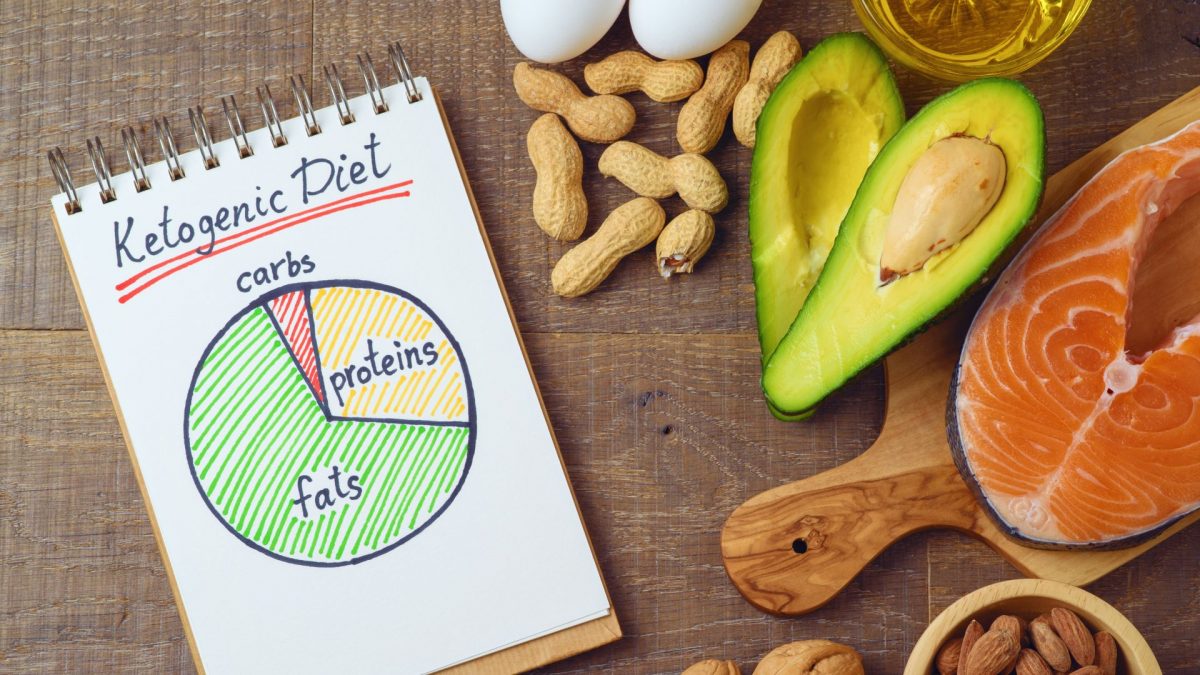
In the four-month pilot trial, Sethi’s team followed 21 adult participants who were diagnosed with schizophrenia or bipolar disorder, taking antipsychotic medications, and had a metabolic abnormality — such as weight gain, insulin resistance, hypertriglyceridemia, dyslipidemia or impaired glucose tolerance. The participants were instructed to follow a ketogenic diet, with approximately 10% of the calories from carbohydrates, 30% from protein and 60% from fat. They were not told to count calories.
“The focus of eating is on whole non-processed foods including protein and non-starchy vegetables, and not restricting fats,” said Sethi, who shared keto-friendly meal ideas with the participants. They were also given keto cookbooks and access to a health coach.
The research team tracked how well the participants followed the diet through weekly measures of blood ketone levels. (Ketones are acids produced when the body breaks down fat — instead of glucose — for energy.) By the end of the trial, 14 patients had been fully adherent, six were semi-adherent and only one was non-adherent.
The participants underwent a variety of psychiatric and metabolic assessments throughout the trial.
Before the trial, 29% of the participants met the criteria for metabolic syndrome, defined as having at least three of five conditions: abdominal obesity, elevated triglycerides, low HDL cholesterol, elevated blood pressure and elevated fasting glucose levels. After four months on a ketogenic diet, none of the participants had metabolic syndrome.
On average, the participants lost 10% of their body weight; reduced their waist circumference by 11% percent; and had lower blood pressure, body mass index, triglycerides, blood sugar levels and insulin resistance.
“We’re seeing huge changes,” Sethi said. “Even if you’re on antipsychotic drugs, we can still reverse the obesity, the metabolic syndrome, the insulin resistance. I think that’s very encouraging for patients.”
The participants reported improvements in their energy, sleep, mood and quality of life.
The psychiatric benefits were also striking. On average, the participants improved 31% on a psychiatrist rating of mental illness known as the clinical global impressions scale, with three-quarters of the group showing clinically meaningful improvement. Overall, the participants also reported better sleep and greater life satisfaction.
“The participants reported improvements in their energy, sleep, mood and quality of life,” Sethi said. “They feel healthier and more hopeful.”
The researchers were impressed that most of the participants stuck with the diet. “We saw more benefit with the adherent group compared with the semi-adherent group, indicating a potential dose-response relationship,” Sethi said.
Alternative fuel for the brain
There is increasing evidence that psychiatric diseases such as schizophrenia and bipolar disorder stem from metabolic deficits in the brain, which affect the excitability of neurons, Sethi said.
The researchers hypothesize that just as a ketogenic diet improves the rest of the body’s metabolism, it also improves the brain’s metabolism.
“Anything that improves metabolic health in general is probably going to improve brain health anyway,” Sethi said. “But the ketogenic diet can provide ketones as an alternative fuel to glucose for a brain with energy dysfunction.”
Likely there are multiple mechanisms at work, she added, and the main purpose of the small pilot trial is to help researchers detect signals that will guide the design of larger, more robust studies.
As a physician, Sethi cares for many patients with both serious mental illness and obesity or metabolic syndrome, but few studies have focused on this undertreated population.
She is the founder and director of the metabolic psychiatry clinic at Stanford Medicine.
“Many of my patients suffer from both illnesses, so my desire was to see if metabolic interventions could help them,” she said. “They are seeking more help. They are looking to just feel better.”
Researchers from the University of Michigan; the University of California, San Francisco; and Duke University contributed to the study.
The study was supported by Baszucki Group Research Fund, the Kuen Lau Fund and the Obesity Treatment Foundation.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Hope amid crisis
Psychiatry’s new frontiers

- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
July 24, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Mouse study finds increasing cardiac ketones may help treat heart failure
by American Heart Association

Increasing ketone supply to the heart in mice with heart failure with preserved ejection fraction (HFpEF) allowed their hearts to utilize more ketones and produce more energy, according to preliminary research presented today at the American Heart Association's Basic Cardiovascular Sciences Scientific Sessions 2024 . The meeting is in Chicago, July 22–25, 2024, and offers the latest research on innovations and discovery in cardiovascular science.
Heart failure with preserved ejection fraction, a common type of heart failure , occurs when there are signs and symptoms of heart failure with a high left ventricle filling pressure despite normal or a near-normal left ventricle ejection fraction of 50% or higher. Heart failure with reduced ejection fraction is when the heart's pumping power is 40% or less.
A normal ejection fraction reading is between 50 to 70%. Heart failure with reduced ejection fraction (HFrEF) is well-studied and has established management plans and therapeutic strategies; in contrast, there is no current evidence-based treatment for HFpEF.
Healthy hearts require a high rate of adenosine triphosphate (ATP) production (provides the energy to drive and support the heart) to maintain their continuous pumping action. This energy comes from a balanced use of glucose and fats to support the heart's contractile function.
"Ketones are a special energy resource," said study author Qiuyu (Violet) Sun, B.Sc., a Ph.D. candidate at the University of Alberta in Canada.
"Humans normally rely on carbohydrates and fat for energy. However, when blood glucose levels fall, such as after prolonged fasting or strenuous exercise, it poses a risk to our brain, which depends on glucose and cannot utilize fats for energy. To address this, our body has a built-in mechanism to produce this special energy substrate called ketones."
"This process is known as ketogenesis and involves breaking down fats from fat storage. The liver then converts these fats into ketone bodies , which enter the bloodstream to fuel the brain," Sun explained. "Ketones can convert the chemical energy in the form of ATP to improve the heart's pumping ability in a continuous fashion."
According to the researchers, relying on fatty acids to produce ATP could be problematic. Fatty acids are a less efficient fuel source compared to glucose because fats require more oxygen to produce the same amount of ATP as glucose.
In this study, researchers assessed mice hearts' metabolism and found that hearts with HFpEF reconstructed their metabolic profiles. Specifically, the researchers found in HFpEF hearts, ketone use was impaired, as well was also an impaired glucose oxidation rate coupled with an increase in fatty acid oxidation. These two changes balance each other, leading to overall preserved energy production.
When HFpEF hearts were given more ketones, this resulted in an increase in overall ATP production coming from ketones and glucose oxidation to ATP from 15% to 28% with preserved pumping ability. So, increasing ketone supply to the heart in HFpEF mice led to higher ATP production.
"This is crucial because this increase in ketone use by the heart did not cause any interference with glucose or fat use. In other words, ketones were not competing with glucose or fats as the energy source. As such, elevated ketone oxidation does not further aggravate the disrupted metabolic profile of the heart in HFpEF," Sun said.
According to the American Heart Association's 2024 Heart Disease and Stroke Statistics , an estimated 56.2 million people were living with heart failure across 204 countries globally in 2019. However, this estimate likely underrepresents the true rate of heart failure because of data and diagnostic gaps in low-resource regions and countries.
"The prevalence of heart failure with preserved ejection fraction is rising, driven by an aging population and increasing obesity rates. Unfortunately, there is still a lack of clinically effective treatment for this condition," Sun said.
"We hope our study can help us better understand this condition. Identifying key proteins involved in cardiac energy metabolism could potentially lead to identification of druggable targets for future development of medications to treat HFpEF."
Sun said the next steps are to investigate the precise role of ketone use by the heart in HFpEF and to assess whether increasing the ketone supply to the heart could potentially optimize heart energy production and lead to improved cardiac function.
The AHA/ACC/HFSA 2022 joint guideline for the management of heart failure calls for increased focus on preventing heart failure in people who are showing early signs of "pre-heart failure," and updated treatment strategies for people with symptomatic heart failure to include SGLT-2 inhibitor (SGLT2i) medicines. SGLT-2 inhibitors are a class of prescription medicines that are FDA-approved for use with diet and exercise to lower blood sugar in adults with Type 2 diabetes.
Study background:
- In a lab setting, two groups of mice were used. The first experimental group of mice received a 60% high-fat diet and L-NAME (an inhibitor of nitric oxide synthesis) every day for 6 weeks to induce HFpEF. The second control group (HFpEF was not induced) were fed a low-fat diet and regular drinking water.
- The mouse hearts were removed and treated with two different levels of β-hydroxybutyrate and studied for how quickly the hearts used the major energy sources, such as glucose, fatty acids and ketones.
Study limitations were that it focused on the metabolic phenotype of HFpEF. However, there are different subgroups of HFpEF that possess varied clinical presentation, such as the fibrotic type or the diastolic dysfunction phenotypes of HFpEF. Both subgroups of HFpEF are of equal importance and should be investigated further. Additionally, because mice have different physiology and metabolic profiles than humans, future research should better characterize cardiac energy metabolism in HFpEF using experimental models that more closely align and translate to humans.
Explore further
Feedback to editors

Short-term vegan diet associated with reductions in biological age estimates
11 minutes ago

Study finds big disparities in stroke services across the US
Jul 27, 2024

Study identifies biomarker that could predict whether colon cancer patients benefit from chemotherapy

New study shows 'dancing molecules' can regenerate cartilage in 3 days
Jul 26, 2024

Study uncovers key immune cells for combating aggressive Merkel cell carcinoma

Study finds unhealthy air quality from wildfires may impact fertility treatments

Higher CEO pay in large health care systems linked to hospital consolidations, study suggests

Researchers discover potential therapeutic target for degenerative eye disease

Researchers move a step closer to developing at-home test to detect dementia

Double mastectomy may offer no survival benefit to women with breast cancer
Related stories.

Weight loss drug linked with reduced need for diuretics in heart failure patients
May 13, 2024

Large geographic variation seen with heart failure phenotypes
Jul 18, 2024

Kidney dysfunction linked to heart failure with preserved ejection fraction
Dec 20, 2023

Differences identified according to ejection fraction in heart failure
Jul 20, 2023

Cause of common type of heart failure may be different for women and men
May 30, 2024

Semaglutide leads to greater weight loss in women than men with heart failure, improves symptoms
Jun 24, 2024
Recommended for you

Tiny deletion in heart muscle protein linked to long-term effects on adult atrial fibrillation
Jul 25, 2024

Mathematical method enables fast, accurate estimates of cardiovascular state to inform blood pressure management

Artificial blood vessels could improve heart bypass outcomes

High levels of a specific antibody may contribute to acute coronary syndrome, investigators say

Study shows everyday activities aren't enough to protect against stroke
Jul 24, 2024

New study identifies a key role for pharmacists in stroke risk reduction
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed
Affiliation.
- 1 New Balance Foundation Obesity Prevention Center, Boston Children's Hospital and Harvard Medical School, Boston, MA, USA.
- PMID: 31825066
- PMCID: PMC7269727
- DOI: 10.1093/jn/nxz308
For >50 y, dietary guidelines in the United States have focused on reducing intakes of saturated and total fat. However, rates of obesity and diabetes rose markedly throughout this period, with potentially catastrophic implications for public health and the economy. Recently, ketogenic diets have received substantial attention from the general public and nutrition research community. These very-low-carbohydrate diets, with fat comprising >70% of calories, have been dismissed as fads. However, they have a long history in clinical medicine and human evolution. Ketogenic diets appear to be more effective than low-fat diets for treatment of obesity and diabetes. In addition to the reductions in blood glucose and insulin achievable through carbohydrate restriction, chronic ketosis might confer unique metabolic benefits of relevance to cancer, neurodegenerative conditions, and other diseases associated with insulin resistance. Based on available evidence, a well-formulated ketogenic diet does not appear to have major safety concerns for the general public and can be considered a first-line approach for obesity and diabetes. High-quality clinical trials of ketogenic diets will be needed to assess important questions about their long-term effects and full potential in clinical medicine.
Keywords: Alzheimer disease; cancer; cardiovascular disease; diabetes; ketogenic diet; ketones; low-carbohydrate diet; low-fat diet; obesity; vegan diet.
Copyright © The Author(s) 2019.
PubMed Disclaimer
Similar articles
- Low-carbohydrate ketogenic diets, glucose homeostasis, and nonalcoholic fatty liver disease. Schugar RC, Crawford PA. Schugar RC, et al. Curr Opin Clin Nutr Metab Care. 2012 Jul;15(4):374-80. doi: 10.1097/MCO.0b013e3283547157. Curr Opin Clin Nutr Metab Care. 2012. PMID: 22617564 Free PMC article. Review.
- An isoproteic cocoa butter-based ketogenic diet fails to improve glucose homeostasis and promote weight loss in obese mice. Greenwell AA, Saed CT, Tabatabaei Dakhili SA, Ho KL, Gopal K, Chan JSF, Kaczmar OO, Dyer SA, Eaton F, Lopaschuk GD, Al Batran R, Ussher JR. Greenwell AA, et al. Am J Physiol Endocrinol Metab. 2022 Jul 1;323(1):E8-E20. doi: 10.1152/ajpendo.00435.2021. Epub 2022 May 16. Am J Physiol Endocrinol Metab. 2022. PMID: 35575232
- [The impact on metabolic and reproductive diseases of low-carbohydrate and ketogenic diets]. Moreno-Sepúlveda J, Capponi M. Moreno-Sepúlveda J, et al. Rev Med Chil. 2020 Nov;148(11):1630-1639. doi: 10.4067/S0034-98872020001101630. Rev Med Chil. 2020. PMID: 33844769 Spanish.
- Dietary carbohydrates modulate metabolic and β-cell adaptation to high-fat diet-induced obesity. Her TK, Lagakos WS, Brown MR, LeBrasseur NK, Rakshit K, Matveyenko AV. Her TK, et al. Am J Physiol Endocrinol Metab. 2020 Jun 1;318(6):E856-E865. doi: 10.1152/ajpendo.00539.2019. Epub 2020 Apr 21. Am J Physiol Endocrinol Metab. 2020. PMID: 32315211 Free PMC article.
- Ketogenic Diet: an Endocrinologist Perspective. Kuchkuntla AR, Shah M, Velapati S, Gershuni VM, Rajjo T, Nanda S, Hurt RT, Mundi MS. Kuchkuntla AR, et al. Curr Nutr Rep. 2019 Dec;8(4):402-410. doi: 10.1007/s13668-019-00297-x. Curr Nutr Rep. 2019. PMID: 31705484 Review.
- Beyond Obesity and Overweight: The Clinical Assessment and Treatment of Excess Body Fat in Children : Part 1 - Insulin Resistance as the Root Cause of Pediatric Obesity. Cucuzzella M, Bailes J, Favret J, Paddu N, Bradley AB. Cucuzzella M, et al. Curr Obes Rep. 2024 Jun;13(2):276-285. doi: 10.1007/s13679-024-00565-0. Epub 2024 May 6. Curr Obes Rep. 2024. PMID: 38709471 Review.
- Opportunities for Maximizing the Dietary Quality of Fad Diets. Phelan JM, Joyce JM, Bode K, Rosenkranz SK. Phelan JM, et al. Nutrients. 2023 Oct 25;15(21):4526. doi: 10.3390/nu15214526. Nutrients. 2023. PMID: 37960179 Free PMC article.
- The nutrient profile and cost of specialty dietary patterns: a hypothetical case study. Lenferna De La Motte KA, Zinn C. Lenferna De La Motte KA, et al. Public Health Nutr. 2023 Dec;26(12):2995-3004. doi: 10.1017/S1368980023002537. Epub 2023 Nov 13. Public Health Nutr. 2023. PMID: 37955108 Free PMC article.
- Metabolic shift toward ketosis in asocial cavefish increases social-like affinity. Iwashita M, Tran A, Garcia M, Cashon J, Burbano D, Salgado V, Hasegawa M, Balmilero-Unciano R, Politan K, Wong M, Lee RWY, Yoshizawa M. Iwashita M, et al. BMC Biol. 2023 Oct 16;21(1):219. doi: 10.1186/s12915-023-01725-9. BMC Biol. 2023. PMID: 37840141 Free PMC article.
- Brain Injury: How Dietary Patterns Impact Long-Term Outcomes. Patel PR, Armistead-Jehle P, Eltman NR, Heath KM, Cifu DX, Swanson RL. Patel PR, et al. Curr Phys Med Rehabil Rep. 2023;11(3):367-376. doi: 10.1007/s40141-023-00413-7. Epub 2023 Jul 5. Curr Phys Med Rehabil Rep. 2023. PMID: 37732170 Free PMC article. Review.
- Henderson G. Court of last appeal – the early history of the high-fat diet for diabetes. J Diabetes Metab. 2016;7(8):696.
- Ludwig DS. Lowering the bar on the low-fat diet. JAMA. 2016;316(20):2087–8. - PubMed
- Joshi S, Ostfeld RJ, McMacken M. The ketogenic diet for obesity and diabetes—enthusiasm outpaces evidence. JAMA Intern Med. 2019;179:1163–4. - PubMed
- Blundell JE, MacDiarmid JI. Fat as a risk factor for overconsumption: satiation, satiety, and patterns of eating. JADA. 1997;97(7 Suppl):S63–9. - PubMed
- Ludwig DS, Ebbeling CB. The carbohydrate-insulin model of obesity: beyond “calories in, calories out”. JAMA Intern Med. 2018;178(8):1098–103. - PMC - PubMed
- Search in MeSH
Related information
- Cited in Books
- PubChem Compound (MeSH Keyword)
LinkOut - more resources
Full text sources.
- Elsevier Science
- Europe PubMed Central
- Ovid Technologies, Inc.
- PubMed Central
- Silverchair Information Systems
Other Literature Sources
- The Lens - Patent Citations
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Ketones May Help Reverse Cognitive Decline
Summary: As we age, our brain naturally becomes more insulin resistant, disrupting neuron communication and leading to cognitive decline and neurodegeneration.
Researchers studied how acute insulin resistance impacts neuronal function before symptoms of chronic conditions like Alzheimer’s manifest. Using mice models, they found that ketones could restore impaired synaptic activity, axonal conduction, and network synchronization.
This research highlights potential ketone-based therapies for neurodegenerative diseases.
- Acute insulin resistance in the brain impairs synaptic activity, axonal conduction, and network synchronization. Administering ketones like D-βHb can restore these critical neuronal functions. This research suggests new therapeutic avenues for conditions involving insulin resistance, such as diabetes and Alzheimer’s disease.
Source: University of Rochester
As we age our brain naturally becomes more insulin resistant. This creates a breakdown in communication between neurons, causing symptoms like changes in mood, cognitive decline, and eventually neurodegeneration.
Nathan A. Smith, MS, PhD (’13), associate professor of Neuroscience, and fellow researchers studied the mechanisms in the brain that break down when insulin resistance is suddenly present, like in trauma, but before symptoms manifest into chronic conditions, like diabetes or Alzheimer’s.

“Once neuronal function is lost, there is no recovering the connection, so we need to identify when the function first becomes impaired,” said Smith, the principal investigator of this research, published in the journal PNAS Nexus .
“This study accomplishes that by bringing us closer to understanding how to rescue the function of impaired neurons and prevent or delay devastating diseases like Alzheimer’s.”
Using mice as a model system, researchers focused on the hippocampus, a well understood region of the brain responsible for learning and memory. They found acute insulin resistance impairs several aspects of neuronal function, including synaptic activity, axonal conduction, network synchronization, synaptic plasticity, and action potential properties—the processes critical to support the communication flow in and out of neurons.
Researchers then administered D-βHb, a form of ketones, a byproduct released by the liver when the body burns fat instead of glucose for energy. They found that the synaptic activity that was previously impacted by acute insulin resistance was rescued, conduction in axons increased, neurons were resynchronized, and synaptic plasticity.
“This research has implications for developing ketone-based therapies targeting specific neuronal dysfunctions in conditions involving insulin resistance/hypoglycemia like diabetes or Alzheimer’s disease,” Smith said. “We are now looking to understand the role that astrocytes and other glia cells play in acute insulin resistance.”
Additional authors include Bartosz Kula, PhD, of the Del Monte Institute for Neuroscience at the University of Rochester, Botond Antal and Lilianne Mujica-Parodi, PhD, of Stony Brook University and Harvard Medical School, Corey Weistuch, PhD, of Memorial Sloan Kettering Cancer Center, Florian Gackiere, PhD, Alexander Barre, PhD, and Jeffrey Hubbard, PhD, of Neuroservices Alliance, and Maria Kukley, PhD, of Achucarro Basque Center for Neuroscience and Basque Foundation for Science.
Funding: This research was supported by The National Institutes of Health, the National Science Foundation, and the Department of Defense.
About this neurology research news
Author: Kelsie Smith Hayduk Source: University of Rochester Contact: Kelsie Smith Hayduk – University of Rochester Image: The image is credited to Neuroscience News
Original Research: Open access. “ D-ꞵ-hydroxybutyrate stabilizes hippocampal CA3-CA1 circuit during acute insulin resistance ” by Nathan A. Smith et al. PNAS Nexus
D-ꞵ-hydroxybutyrate stabilizes hippocampal CA3-CA1 circuit during acute insulin resistance
The brain primarily relies on glycolysis for mitochondrial respiration but switches to alternative fuels such as ketone bodies (KBs) when less glucose is available. Neuronal KB uptake, which does not rely on glucose transporter 4 (GLUT4) or insulin, has shown promising clinical applicability in alleviating the neurological and cognitive effects of disorders with hypometabolic components.
However, the specific mechanisms by which such interventions affect neuronal functions are poorly understood. In this study, we pharmacologically blocked GLUT4 to investigate the effects of exogenous KB D-ꞵ-hydroxybutyrate (D-ꞵHb) on mouse brain metabolism during acute insulin resistance (AIR).
We found that both AIR and D-ꞵHb had distinct impacts across neuronal compartments: AIR decreased synaptic activity and long-term potentiation (LTP) and impaired axonal conduction, synchronization, and action potential properties, while D-ꞵHb rescued neuronal functions associated with axonal conduction, synchronization, and LTP.
Blood Tests Revolutionize Alzheimer’s Diagnosis

Epigenetics Unlocks Secrets of Memory Formation

How Size Differences in Mammals Influence Brain Evolution

Key Neurons for Maternal Bonding Identified
In 1921, a distinguished physician at the Mayo Clinic suggested trying what he called a ketogenic diet, a high-fat diet designed to be so carbohydrate-deficient it could effectively mimic the fasting state. Oddly, the success of ketogenic diets against pediatric epilepsy seems to get conflated by keto diet proponents into suggesting it is beneficial for everyone.
By eschewing carbohydrates, you force your body to burn fat. And indeed, the amount of fat you burn shoots up when you eat a keto diet. At the same time, however, the fat you take in shoots up when you eat a keto diet. What happens to our overall body-fat balance? Body fat loss slows upon switching to the ketogenic diet.
Just looking at the scale, the ketogenic diet seems like a success, but what happens inside bodies tells a different story. On the keto diet, rates of body fat loss may slow by more than half, so most of what is lost is water. The reason less fat is burned on a ketogenic diet is presumably the same reason people who start fasting may start burning less fat: Without carbohydrates, the preferred fuel, our bodies start burning more of our own protein .
Inadequate intake of 17 micronutrients has been documented in those on ketogenic diets. Children have gotten scurvy, and some have even died from deficiency of the mineral selenium , which can cause sudden cardiac death. Bone fractures disproportionately plague children on ketogenic diets, along with growth stunting and kidney stones , and constipation is a frequently cited side effect. Keto diets have also been shown to reduce the richness and diversity of our gut flora , and all of that saturated fat can have a profound impact on the heart: A meta-analysis of four cohort studies following the diets, diseases, and deaths of more than a quarter million people found that those who eat lower-carb diets suffer a significantly higher risk of all-cause mortality, meaning they live, on average, significantly shorter lives.
For substantiation of any statements of fact from the peer-reviewed medical literature, please see the associated videos below.

Subscribe to our free newsletter and receive our Care for Your Skin as You Age infographic.
Popular Videos for Keto Diet

Is Keto an Effective Cancer-Fighting Diet?

Keto Diet Theory Put to the Test

Keto Diet Results for Weight Loss

Is Weight Loss on Ketosis Sustainable?
Are Keto Diets Safe?

Keto Diets: Muscle Growth and Bone Density

Does a Ketogenic Diet Help Diabetes or Make It Worse?
All videos for keto diet.

How to Get a Good Night’s Sleep Without Sleeping Pills
Taking less than just 18 Ambien-class sleeping pills in an entire year may triple the risk of dying prematurely.

Life Extension with FGF21
What can we do to boost the longevity hormone FGF21?

The Best Diet for Fatty Liver Disease Treatment
What are the three sources of the liver fat in fatty liver disease and how do you get rid of it?

Fasting for Autoimmune Diseases
Various fasting regimens have been attempted for inflammatory autoimmune diseases such as lupus, ankylosing spondylitis, chronic urticaria, mixed connective-tissue disease, glomerulonephritis, and multiple sclerosis, as well as osteoarthritis and fibromyalgia.

Evidence-Based Weight Loss – Live Presentation
In this live presentation, Dr. Greger offers a sneak peek into his book How Not to Diet.

Highlights from the 2020 Dietary Guidelines Hearing
I was honored to testify before the US government’s Dietary Guidelines Advisory Committee. Check out the video to see my speech and a few of my favorite excerpts.

Keto diets put to the test for diabetes reversal.

Ketogenic diets found to undermine exercise efforts and lead to muscle shrinkage and bone loss.

The effects of ketogenic diets on nutrient sufficiency, gut flora, and heart disease risk.

Might the appetite-suppressing effects of ketosis improve dietary compliance?

Ketogenic diets and the $33-billion diet gimmick.

Do low-carb and ketogenic diets have a metabolic advantage for weight loss?

The clinical use of ketogenic diets for epilepsy and cancer: what does the science say?

What Causes Insulin Resistance?
Prediabetes and type 2 diabetes are caused by a drop in insulin sensitivity blamed on “intramyocellular lipid,” the buildup of fat inside our muscle cells.

What’s the “Natural” Human Diet?
What can our nutrient requirements, metabolism, and physiology tell us about what we should be eating?

The Spillover Effect Links Obesity to Diabetes
Being obese may result in as much insulin resistance as eating a high-fat diet.

The Problem with the Paleo Diet Argument
The Paleolithic period represents just the last two million years of human evolution. What did our bodies evolve to eat during the first 90% of our time on Earth?

Paleo Diets May Negate Benefits of Exercise
The deleterious effects of a Paleolithic diet appear to undermine the positive effects of a Crossfit-based high-intensity circuit training exercise program.

Low-Carb Diets and Coronary Blood Flow
Blood flow within the hearts of those eating low-carb diets was compared to those eating plant-based diets.
Plant-Based Atkins Diet
Harvard study found that men and women eating low carb diets live significantly shorter lives, but what about the “eco-Atkins diet,” a plant-based, low carbohydrate diet?

Atkins Diet: Trouble Keeping It Up
A case report in the Journal of the Academy of Nutrition and Dietetics (formerly Journal of the American Dietetic Association) of a man who went on the Atkins diet, lost his ability to have an erection—and nearly lost his life.
Pin It on Pinterest
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Metabolic Messengers
- Published: 13 December 2023
Metabolic Messengers: ketone bodies
- Alisa B. Nelson ORCID: orcid.org/0000-0001-7685-1803 1 na1 ,
- Eric D. Queathem 1 , 2 na1 ,
- Patrycja Puchalska ORCID: orcid.org/0000-0002-1875-1203 1 &
- Peter A. Crawford ORCID: orcid.org/0000-0001-8597-4426 1 , 2
Nature Metabolism volume 5 , pages 2062–2074 ( 2023 ) Cite this article
3011 Accesses
8 Citations
30 Altmetric
Metrics details
- Homeostasis
- Molecular medicine
- Nutrient signalling
- Translational research
Prospective molecular targets and therapeutic applications for ketone body metabolism have increased exponentially in the past decade. Initially considered to be restricted in scope as liver-derived alternative fuel sources during periods of carbohydrate restriction or as toxic mediators during diabetic ketotic states, ketogenesis and ketone bodies modulate cellular homeostasis in multiple physiological states through a diversity of mechanisms. Selective signalling functions also complement the metabolic fates of the ketone bodies acetoacetate and d -β-hydroxybutyrate. Here we discuss recent discoveries revealing the pleiotropic roles of ketone bodies, their endogenous sourcing, signalling mechanisms and impact on target organs, and considerations for when they are either stimulated for endogenous production by diets or pharmacological agents or administered as exogenous wellness-promoting agents.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
111,21 € per year
only 9,27 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Ketones and the cardiovascular system

A novel hepatocyte ketone production assay to help the selection of nutrients for the ketogenic diet treatment of epilepsy

Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus
Rosenbloom, J. The acetone bodies in diabetes mellitus: influence of low and high protein intake on the excretion of acetone, diacetic acid and β-oxybutyric acid. J. Am. Med. Assoc. LXV , 1715–1717 (1915).
Google Scholar
Tollens, B. Diabetic urine. Ann. Chem . 209 , 30–38 (1881).
Ewing, J. Acidosis and associated conditions. Arch. Intern. Med. II , 330–354 (1908).
Cahill, G. F. Jr Fuel metabolism in starvation. Annu. Rev. Nutr. 26 , 1–22 (2006).
CAS PubMed Google Scholar
Wilder, R. M. The effect of ketonemia on the course of epilepsy. Clin. Bull. 2 307 (1921).
Owen, O. E. et al. Brain metabolism during fasting. J. Clin. Invest. 6 , 1589–1595 (1967).
Puchalska, P. & Crawford, P. A. Multi-dimensional roles of ketone bodies in fuel metabolism, signaling, and therapeutics. Cell Metab. 25 , 262–284 (2017).
CAS PubMed PubMed Central Google Scholar
Puchalska, P. & Crawford, P. A. Metabolic and signaling roles of ketone bodies in health and disease. Annu. Rev. Nutr. 41 , 49–77 (2021).
McGarry, J., Wright, P. H. & Foster, D. Hormonal control of ketogenesis. Rapid activation of hepatic ketogenic capacity in fed rats by anti-insulin serum and glucagon. J. Clin. Invest. https://doi.org/10.1172/JCI108038 (1975).
Williamson, D., Lund, P. & Krebs, H. The redox state of free nicotinamide-adenine dinucleotide in the cytoplasm and mitochondria of rat liver. Biochem. J. https://doi.org/10.1042/bj1030514 (1967).
Williamson, D., Bates, M. W. & Krebs, H. Activity and intracellular distribution of enzymes of ketone-body metabolism in rat liver. Biochem. J. https://doi.org/10.1042/bj1080353 (1968).
Page, M., Krebs, H. A. & Williamson, D. Activities of enzymes of ketone-body utilization in brain and other tissues of suckling rats. Biochem. J. https://doi.org/10.1042/bj1210049 (1971).
Quant, P., Robin, D., Robin, P., Girard, J. & Brand, M. Control of acetoacetate production from exogenous palmitoyl-CoA in isolated rat liver mitochondria. Biochem. Soc. Trans. https://doi.org/10.1042/bst0171089 (1989).
Wakeman, A. J. D. H. D. On the decomposition of β-oxybutyric acid and aceto-acetic acid by enzymes of the liver. J. Biol. Chem. 6 , 373–389 (1909).
Lehninger, A., Sudduth, H. C. & Wise, J. D β-hydroxybutyric dehydrogenase of muitochondria. J. Biol. Chem. https://doi.org/10.1016/S0021-9258(18)64641-1 (1960).
Stagg D.B. et al. Diminished ketone interconversion, hepatic TCA cycle flux, and glucose production in D-β-hydroxybutyrate dehydrogenase hepatocyte-deficient mice. Mol. Metab. https://doi.org/10.1016/j.molmet.2021.101269 (2021).
Stern, J., Coon, M. J., Del Campillo, A. & Schneider, M. Enzymes of fatty acid metabolism. IV. Preparation and properties of coenzyme A transferase. J. Biol. Chem. https://doi.org/10.1016/S0021-9258(18)65225-1 (1956).
Kashiwaya, Y. et al. Control of glucose utilization in working perfused rat heart. J. Biol. Chem. https://doi.org/10.1016/S0021-9258(18)47278-X (1994).
Taegtmeyer, H., Hems, R. & Krebs, H. Utilization of energy-providing substrates in the isolated working rat heart. Biochem. J. https://doi.org/10.1042/bj1860701 (1980).
Randle, P., Garland, P. B., Hales, C. N. & Newsholme, E. The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet https://doi.org/10.1016/s0140-6736(63)91500-9 (1963).
Stern, J. A role of acetoacetyl-CoA synthetase in acetoacetate utilization by rat liver cell fractions. Biochem. Biophys. Res. Commun. https://doi.org/10.1016/0006-291x(71)90811-4 (1971).
Endemann, G., Goetz, P. G., Edmond, J. & Brunengraber, H. Lipogenesis from ketone bodies in the isolated perfused rat liver. Evidence for the cytosolic activation of acetoacetate. J. Biol. Chem. https://doi.org/10.1016/S0021-9258(18)34796-3 (1982).
Kang, H. et al. Metabolic rewiring by oncogenic BRAF V600E links ketogenesis pathway to BRAF-MEK1 signaling. Mol. Cell https://doi.org/10.1016/j.molcel.2015.05.037 (2015).
Henning, S. & Hird, F. Ketogenesis from butyrate and acetate by the caecum and the colon of rabbits. Biochem. J. https://doi.org/10.1042/bj1300785 (1972).
Cheng, C. et al. Ketone body signaling mediates intestinal stem cell homeostasis and adaptation to diet. Cell https://doi.org/10.1016/j.cell.2019.07.048 (2019).
Silva, B. et al. Glia fuel neurons with locally synthesized ketone bodies to sustain memory under starvation. Nat. Metab. https://doi.org/10.1038/s42255-022-00528-6 (2022).
Adijanto, J. et al. The retinal pigment epithelium utilizes fatty acids for ketogenesis. J. Biol. Chem. https://doi.org/10.1074/jbc.M114.565457 (2014).
Venable, A. et al. Fasting-induced HMGCS2 expression in the kidney does not contribute to circulating ketones. Am. J. Physiol. Renal Physiol. https://doi.org/10.1152/ajprenal.00447.2021 (2022).
Taggart, A. K. et al. D-β-hydroxybutyrate inhibits adipocyte lipolysis via the nicotinic acid receptor PUMA-G. J. Biol. Chem . https://doi.org/10.1074/jbc.C500213200 (2005).
Cahill, G. et al. Hormone-fuel interrelationships during fasting. J. Clin. Invest. https://doi.org/10.1172/JCI105481 (1966).
Miyamoto, J. et al. Ketone body receptor GPR43 regulates lipid metabolism under ketogenic conditions. Proc. Natl Acad. Sci. USA https://doi.org/10.1073/pnas.1912573116 (2019).
Kimura, I. et al. Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein-coupled receptor 41 (GPR41). Proc. Natl Acad. Sci. USA 108 , 8030–8035 (2011).
Han, Y. et al. β-Hydroxybutyrate prevents vascular senescence through hnRNP A1-mediated upregulation of Oct4. Mol. Cell https://doi.org/10.1016/j.molcel.2018.07.036 (2018).
Shimazu, T. et al. Suppression of oxidative stress by β-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science 339 , 211–214 (2013).
Xie, Z. et al. Metabolic regulation of gene expression by histone lysine β-hydroxybutyrylation. Mol. Cell 62 , 194–206 (2016).
Youm, Y.-H. et al. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome–mediated inflammatory disease. Nat. Med. 21 , 263–269 (2015).
Tsusaka, T. et al. Non-specific recognition of histone modifications by H3K9bhb antibody. iScience https://doi.org/10.1016/j.isci.2023.107235 (2023).
Puchalska, P., Nelson, A. B., Stagg, D. B. & Crawford, P. A. Determination of ketone bodies in biological samples via rapid UPLC-MS/MS. Talanta 225 , 122048 (2021).
Webber, R. & J, Edmond. Utilization of L(+)-3-hydroxybutyrate, D(-)-3-hydroxybutyrate, acetoacetate, and glucose for respiration and lipid synthesis in the 18-day-old rat. J. Biol. Chem. https://doi.org/10.1016/S0021-9258(19)63335-1 (1977).
Hsu, W.-Y. et al. Enantioselective determination of 3-hydroxybutyrate in the tissues of normal and streptozotocin-induced diabetic rats of different ages. J. Chromatogr. B 879 , 3331–3336 (2011).
CAS Google Scholar
Salomón, T. et al. Ketone body acetoacetate buffers methylglyoxal via a non-enzymatic conversion during diabetic and dietary ketosis. Cell Chem. Biol. https://doi.org/10.1016/j.chembiol.2017.07.012 (2017).
Parry-Strong, A. et al. Very low carbohydrate (ketogenic) diets in type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Obes. Metab. 24 , 2431–2442 (2022).
Hall, K. D. et al. Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake. Nat. Med. 27 , 344–353 (2021).
Saslow, L. R. et al. Comparing very low-carbohydrate vs DASH diets for overweight or obese adults with hypertension and prediabetes or type 2 diabetes: a randomized trial. Ann. Fam. Med. 21 , 256–263 (2023).
PubMed PubMed Central Google Scholar
Deemer, S. E. et al. Exogenous dietary ketone ester decreases body weight and adiposity in mice housed at thermoneutrality. Obesity 28 , 1447–1455 (2020).
Moore, M. P. et al. A dietary ketone ester mitigates histological outcomes of NAFLD and markers of fibrosis in high-fat diet fed mice. Am. J. Physiol. Gastrointest. Liver Physiol. 320 , G564–G572 (2021).
Buga, A. et al. The effects of a 6-week controlled, hypocaloric ketogenic diet, with and without exogenous ketone salts, on body composition responses. Front Nutr. 8 , 6185200 (2021).
Katsuya, S., Kawata, Y., Goto, T. & Tsubota, J. Daily intake of D-β-hydroxybutyric acid (D-BHB) reduces body fat in Japanese adult participants: a randomized, double-blind, placebo-controlled study. J. Nutr. Sci. Vitaminol. 69 , 121–128 (2023).
Stubbs, B. J. et al. A ketone ester drink lowers human ghrelin and appetite. Obesity 26 , 269–273 (2018).
Vestergaard, E. T. et al. Acute ketosis inhibits appetite and decreases plasma concentrations of acyl ghrelin in healthy young men. Diabetes Obes. Metab. 23 , 1834–1842 (2021).
Liu, Y., Bharmal, S. H., Kimita, W. & Petrov, M. S. Effect of d-β-hydroxybutyrate-(R)-1,3 butanediol on appetite regulation in people with prediabetes. Mol. Nutr. Food Res 67 , e2200615 (2023).
PubMed Google Scholar
Falkenhain, K., Daraei, A. & Little, J. P. The effect of novel exogenous ketone supplements on blood β-hydroxybutyrate and glucose. J. Diet Suppl . https://doi.org/10.1080/19390211.2023.2179152 (2023).
Satapati, S. et al. Mitochondrial metabolism mediates oxidative stress and inflammation in fatty liver. J. Clin. Invest. https://doi.org/10.1172/JCI82204 (2015).
Cunha, G. M. et al. Efficacy of a 2-month very low-calorie ketogenic diet (VLCKD) compared to a standard low-calorie diet in reducing visceral and liver fat accumulation in patients with obesity. Front. Endocrinol. 11 , 607 (2020).
Browning, J. D., Davis, J., Saboorian, M. H. & Burgess, S. C. A low-carbohydrate diet rapidly and dramatically reduces intrahepatic triglyceride content. Hepatology 44 , 487–488 (2006).
Garbow, J. R. et al. Hepatic steatosis, inflammation, and ER stress in mice maintained long term on a very low-carbohydrate ketogenic diet. Am. J. Physiol. Gastrointest. Liver Physiol. 300 , G956–967 (2011).
Luukkonen, P. K. et al. Effect of a ketogenic diet on hepatic steatosis and hepatic mitochondrial metabolism in nonalcoholic fatty liver disease. Proc. Natl Acad. Sci. USA 117 , 7347–7354 (2020).
Long, F. et al. A low-carbohydrate diet induces hepatic insulin resistance and metabolic associated fatty liver disease in mice. Mol. Metab. 69 , 101675 (2023).
Cotter, D. G. et al. Ketogenesis prevents diet-induced fatty liver injury and hyperglycemia. J. Clin. Invest . 124 , 5175–5190 (2014).
Asif, S. et al. Hmgcs2-mediated ketogenesis modulates high-fat diet-induced hepatosteatosis. Mol. Metab. 61 , 101494 (2022).
Fletcher, J. A. et al. Impaired ketogenesis and increased acetyl-CoA oxidation promote hyperglycemia in human fatty liver. JCI Insight https://doi.org/10.1172/jci.insight.127737 (2019).
Puchalska, P. et al. Hepatocyte-macrophage acetoacetate shuttle protects against tissue fibrosis. Cell Metab. 29 , 383–398 (2019).
Johnson, R., Walton, J. L., Krebs, H. A. & Williamson, D. Post-exercise ketosis. Lancet https://doi.org/10.1016/s0140-6736(69)90931-3 (1969).
Féry, F. & Balasse, E. Ketone body turnover during and after exercise in overnight-fasted and starved humans. Am. J. Physiol. https://doi.org/10.1152/ajpendo.1983.245.4.E318 (1983).
Noakes, T. D., Prins, P. J., Volek, J. S., D’Agostino, D. P. & Koutnik, A. P. Low carbohydrate high fat ketogenic diets on the exercise crossover point and glucose homeostasis. Front. Physiol. 14 , 1150265 (2023).
Chiarello, N. et al. Effect of a four-week isocaloric ketogenic diet on physical performance at very high-altitude: a pilot study. BMC Sports Sci. Med. Rehabil. 15 , 37 (2023).
Burke, L. M. et al. Adaptation to a low carbohydrate high fat diet is rapid but impairs endurance exercise metabolism and performance despite enhanced glycogen availability. J. Physiol. 599 , 771–790 (2021).
Whitfield, J. et al. Acute ketogenic diet and ketone ester supplementation impairs race walk performance. Med. Sci. Sports Exerc. 53 , 776–784 (2021).
McCarthy, D. G. et al. Effect of acute ketone monoester ingestion on cardiorespiratory responses to exercise and the influence of blood acidosis. Med Sci. Sports Exerc. https://doi.org/10.1249/mss.0000000000003141 (2023).
Article PubMed Google Scholar
Poffé, C., Robberechts, R., Van Thienen, R. & Hespel, P. Exogenous ketosis elevates circulating erythropoietin and stimulates muscular angiogenesis during endurance training overload. J. Physiol. https://doi.org/10.1113/jp284346 (2023).
Cox, P. J. et al. Nutritional ketosis alters fuel preference and thereby endurance performance in athletes. Cell Metab. 24 , 256–268, (2016).
Torres, J. A. et al. Ketosis ameliorates renal cyst growth in polycystic kidney disease. Cell Metab. 30 , 1007–1023 (2019).
Strubl, S. et al. Ketogenic dietary interventions in autosomal dominant polycystic kidney disease-a retrospective case series study: first insights into feasibility, safety and effects. Clin. Kidney J. 15 , 1079–1092 (2022).
Chakraborty, S. et al. Salt-responsive metabolite, β-hydroxybutyrate, attenuates hypertension. Cell Rep. 25 , 677–689 (2018).
Tomita, I. et al. SGLT2 inhibition mediates protection from diabetic kidney disease by promoting ketone body-induced mTORC1 inhibition. Cell Metab. 32 , 404–419 (2020).
Ang, Q. et al. Ketogenic diets alter the gut microbiome resulting in decreased intestinal Th17 cells. Cell https://doi.org/10.1016/j.cell.2020.04.027 (2020).
Article PubMed PubMed Central Google Scholar
Dmitrieva-Posocco, O. et al. β-Hydroxybutyrate suppresses colorectal cancer. Nature https://doi.org/10.1038/s41586-022-04649-6 (2022).
Suzuki, R. et al. The novel sustained 3-hydroxybutyrate donor poly-D-3-hydroxybutyric acid prevents inflammatory bowel disease through upregulation of regulatory T-cells. FASEB J. https://doi.org/10.1096/fj.202200919R (2023).
Devi, N., Madaan, P., Kandoth, N., Bansal, D. & Sahu, J. K. Efficacy and safety of dietary therapies for childhood drug-resistant epilepsy: a systematic review and network meta-analysis. JAMA Pediatr. 177 , 258–266 (2023).
Sondhi, V. et al. Efficacy of ketogenic diet, modified atkins diet, and low glycemic index therapy diet among children with drug-resistant epilepsy: a randomized clinical trial. JAMA Pediatr. https://doi.org/10.1001/jamapediatrics.2020.2282 (2020).
Hemingway, C., Freeman, J. M., Pillas, D. J. & Pyzik, P. L. The ketogenic diet: a 3- to 6-year follow-up of 150 children enrolled prospectively. Pediatrics 108 , 898–905 (2001).
Rho, J. M. How does the ketogenic diet induce anti-seizure effects? Neurosci. Lett. 637 , 4–10 (2017).
Murugan, M. & Boison, D. Ketogenic diet, neuroprotection, and antiepileptogenesis. Epilepsy Res. 167 , 106444 (2020).
McNally, M. A. & Hartman, A. L. Ketone bodies in epilepsy. J. Neurochem. 121 , 28–35 (2012).
Mu, C. et al. Targeted gut microbiota manipulation attenuates seizures in a model of infantile spasms syndrome. JCI Insight https://doi.org/10.1172/jci.insight.158521 (2022).
Kraeuter, A. K., Guest, P. C. & Sarnyai, Z. The Therapeutic potential of ketogenic diet throughout life: focus on metabolic, neurodevelopmental and neurodegenerative disorders. Adv. Exp. Med Biol. 1178 , 77–101 (2019).
Morris, J. K. et al. Cognitively impaired elderly exhibit insulin resistance and no memory improvement with infused insulin. Neurobiol. Aging 39 , 19–24 (2016).
Baker, L. D. et al. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch. Neurol. 68 , 51–57 (2011).
Shippy, D. C., Wilhelm, C., Viharkumar, P. A., Raife, T. J. & Ulland, T. K. β-Hydroxybutyrate inhibits inflammasome activation to attenuate Alzheimer’s disease pathology. J. Neuroinflammation 17 , 280 (2020).
Fortier, M. et al. A ketogenic drink improves brain energy and some measures of cognition in mild cognitive impairment. Alzheimers Dement . 15 , 625–634 (2019).
Taylor, M. K., Sullivan, D. K., Mahnken, J. D., Burns, J. M. & Swerdlow, R. H. Feasibility and efficacy data from a ketogenic diet intervention in Alzheimer’s disease. Alzheimers Dement. https://doi.org/10.1016/j.trci.2017.11.002 (2017).
Newman, J. C. et al. Ketogenic diet reduces midlife mortality and improves memory in aging mice. Cell Metab. 26 , 547–557 (2017).
Yin, J. X. et al. Ketones block amyloid entry and improve cognition in an Alzheimer’s model. Neurobiol. Aging 39 , 25–37 (2016).
Mujica-Parodi, L. R. et al. Diet modulates brain network stability, a biomarker for brain aging, in young adults. Proc. Natl Acad. Sci. USA 117 , 6170–6177 (2020).
Tieu, K. et al. D-β-Hydroxybutyrate rescues mitochondrial respiration and mitigates features of Parkinson disease. J. Clin. Invest. 112 , 892–901 (2003).
Yu, X. et al. Ketone body β-hydroxybutyric acid ameliorates dopaminergic neuron injury through modulating Zinc finger protein 36/acyl-CoA synthetase long-chain family member 4 signaling axis-mediated ferroptosis. Neuroscience https://doi.org/10.1016/j.neuroscience.2022.11.018 (2022).
Kuter, K. Z., Olech, Ł., Głowacka, U. & Paleczna, M. Increased β-hydroxybutyrate level is not sufficient for the neuroprotective effect of long-term ketogenic diet in an animal model of early Parkinson’s disease. Exploration of brain and liver energy metabolism markers. Int. J. Mol. Sci. https://doi.org/10.3390/ijms22147556 (2021).
Har-Even, M. et al. Ketogenic diet as a potential treatment for traumatic brain injury in mice. Sci. Rep. 11 , 23559 (2021).
Seira, O. et al. Ketogenesis controls mitochondrial gene expression and rescues mitochondrial bioenergetics after cervical spinal cord injury in rats. Sci. Rep. 11 , 16359 (2021).
Lin, J. et al. Neuroprotective effect of ketone metabolism on inhibiting inflammatory response by regulating macrophage polarization after acute cervical spinal cord injury in rats. Front. Neurosci. https://doi.org/10.3389/fnins.2020.583611 (2020).
Enders, J. et al. Ketolysis is required for the proper development and function of the somatosensory nervous system. Exp. Neurol. https://doi.org/10.1016/j.expneurol.2023.114428 (2023).
Nishiguchi, T. et al. Stress increases blood β-hydroxybutyrate levels and prefrontal cortex NLRP3 activity jointly in a rodent model. Neuropsychopharmacol. Rep. 41 , 159–167 (2021).
Kajitani, N. et al. Prefrontal cortex infusion of β-hydroxybutyrate, an endogenous NLRP3 inflammasome inhibitor, produces antidepressant-like effects in a rodent model of depression. Neuropsychopharmacol. Rep. 40 , 157–165 (2020).
Chen, L., Miao, Z. & Xu, X. β-hydroxybutyrate alleviates depressive behaviors in mice possibly by increasing the histone3-lysine9-β-hydroxybutyrylation. Biochem. Biophys. Res. Commun. 490 , 117–122 (2017).
Sleiman, S. F. et al. Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body β- hydroxybutyrate. eLife https://doi.org/10.7554/eLife.15092 (2016).
Marosi, K. et al. 3-Hydroxybutyrate regulates energy metabolism and induces BDNF expression in cerebral cortical neurons. J. Neurochem. 139 , 769–781 (2016).
Li, H. et al. β-hydroxybutyrate reduces reinstatement of cocaine conditioned place preference through hippocampal CaMKII-α β-hydroxybutyrylation. Cell Rep. 41 , 111724 (2022).
Bing, R. The metabolism of the heart. Harvey Lect. 50 , 27–70 (1954).
Lopaschuk, G. D., Karwi, Q. G., Tian, R., Wende, A. R. & Abel, E. D. Cardiac energy metabolism in heart failure. Circ. Res . 128 , 1487–1513 (2021).
Lommi, J. et al. Blood ketone bodies in congestive heart failure. J. Am. Coll. Cardiol. https://doi.org/10.1016/0735-1097(96)00214-8 (1996).
Bedi, K. et al. Evidence for intramyocardial disruption of lipid metabolism and increased myocardial ketone utilization in advanced human heart failure. Circulation https://doi.org/10.1161/circulationaha.115.017545 (2016).
Aubert, G. et al. The failing heart relies on ketone bodies as a fuel. Circulation https://doi.org/10.1161/circulationaha.115.017355 (2016).
Matsuura, T. R., Puchalska, P., Crawford, P. A. & Kelly, D. P. Ketones and the heart: metabolic principles and therapeutic implications. Circ. Res. 132 , 882–898 (2023).
Schugar, R. C. et al. Cardiomyocyte-specific deficiency of ketone body metabolism promotes accelerated pathological remodeling. Mol. Metab. 3 , 754–769 (2014).
Horton, J. L. et al. The failing heart utilizes 3-hydroxybutyrate as a metabolic stress defense. JCI Insight https://doi.org/10.1172/jci.insight.124079 (2019).
Uchihashi, M. et al. Cardiac-specific Bdh1 overexpression ameliorates oxidative stress and cardiac remodeling in pressure overload-induced heart failure. Circ. Heart Fail. https://doi.org/10.1161/circheartfailure.117.004417 (2017).
Yu, Y. et al. Treatment with D-β-hydroxybutyrate protects heart from ischemia/reperfusion injury in mice. Eur. J. Pharmacol. 829 , 121–128 (2018).
Yurista, S. R. et al. Therapeutic potential of ketone bodies for patients with cardiovascular disease: JACC focus seminar. J. Am. Coll. Cardiol. https://doi.org/10.1016/j.jacc.2020.12.065 (2021).
Gormsen, L. C. et al. Ketone body infusion with 3-hydroxybutyrate reduces myocardial glucose uptake and increases blood flow in humans: a positron emission tomography study. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.116.005066 (2017).
Nielsen, R. et al. Cardiovascular effects of treatment with the ketone body 3-hydroxybutyrate in chronic heart failure patients. Circulation 139 , 2129–2141 (2019).
Selvaraj, S., Kelly, D. P. & Margulies, K. B. Implications of altered ketone metabolism and therapeutic ketosis in heart failure. Circulation 141 , 1800–1812 (2020).
Wentz, A. et al. Adaptation of myocardial substrate metabolism to a ketogenic nutrient environment. J. Biol. Chem. https://doi.org/10.1074/jbc.M110.100651 (2010).
Zhang, Y. et al. Mitochondrial pyruvate carriers are required for myocardial stress adaptation. Nat. Metab. https://doi.org/10.1038/s42255-020-00288-1 (2020).
McCommis, K. et al. Nutritional modulation of heart failure in mitochondrial pyruvate carrier-deficient mice. Nat. Metab. https://doi.org/10.1038/s42255-020-00296-1 (2020).
Krebs, P. et al. Lethal mitochondrial cardiomyopathy in a hypomorphic Med30 mouse mutant is ameliorated by ketogenic diet. Proc. Natl Acad. Sci. USA https://doi.org/10.1073/pnas.1117835108 (2011).
Berg-Hansen, K. et al. Beneficial effects of ketone ester in patients with cardiogenic shock: a randomized, controlled, double-blind trial. JACC Heart Fail . https://doi.org/10.1016/j.jchf.2023.05.029 (2023).
Weis, E. M. et al. Ketone body oxidation increases cardiac endothelial cell proliferation. EMBO Mol. Med . https://doi.org/10.15252/emmm.202114753 (2022).
Garcia-Caballero, M. et al. Role and therapeutic potential of dietary ketone bodies in lymph vessel growth. Nat. Metab. 1 , 666–675 (2019).
Nakamura, M. & Sadoshima, J. Mechanisms of physiological and pathological cardiac hypertrophy. Nat. Rev. Cardiol. 15 , 387–407 (2018).
McCarthy, C. G. et al. Ketone body β-hydroxybutyrate is an autophagy-dependent vasodilator. JCI Insight https://doi.org/10.1172/jci.insight.149037 (2021).
McCarthy, C. G. et al. Low-dose 1,3-butanediol reverses age-associated vascular dysfunction independent of ketone body β-hydroxybutyrate. Am. J. Physiol. Heart Circ. Physiol. 322 , H466–H473 (2022).
Deng, Y. et al. Targeting mitochondria-inflammation circuit by β-hydroxybutyrate mitigates HFpEF. Circ. Res. 128 , 232–245 (2021).
Gopalasingam, N. et al. Stimulation of the hydroxycarboxylic acid receptor 2 with the ketone body 3-hydroxybutyrate and niacin in patients with chronic heart failure: hemodynamic and metabolic effects. J. Am. Heart Assoc. 12 , e029849 (2023).
Goldberg, E. L. et al. β-Hydroxybutyrate deactivates neutrophil NLRP3 inflammasome to relieve gout flares. Cell Rep. 18 , 2077–2087 (2017).
Kim, S. R. et al. SGLT2 inhibition modulates NLRP3 inflammasome activity via ketones and insulin in diabetes with cardiovascular disease. Nat. Commun. 11 , 2127 (2020).
Luo, S. et al. β-Hydroxybutyrate against cisplatin-induced acute kidney injury via inhibiting NLRP3 inflammasome and oxidative stress. Int. Immunopharmacol. 111 , 109101 (2022).
Fu, S. P. et al. BHBA suppresses LPS-induced inflammation in BV-2 cells by inhibiting NF-κB activation. Mediators Inflamm. 2014 , 983401 (2014).
Ferrere, G. et al. Ketogenic diet and ketone bodies enhance the anticancer effects of PD-1 blockade. JCI Insight https://doi.org/10.1172/jci.insight.145207 (2021).
Thio, C. L., Lai, A. C., Ting, Y. T., Chi, P. Y. & Chang, Y. J. The ketone body β-hydroxybutyrate mitigates ILC2-driven airway inflammation by regulating mast cell function. Cell Rep. 40 , 111437 (2022).
Zhang, L. et al. Ketogenesis acts as an endogenous protective programme to restrain inflammatory macrophage activation during acute pancreatitis. eBioMedicine 78 , 103959 (2022).
Zhang, H. et al. Ketogenesis-generated β-hydroxybutyrate is an epigenetic regulator of CD8(+) T-cell memory development. Nat. Cell Biol. 22 , 18–25 (2020).
Arima Y. et al. Murine neonatal ketogenesis preserves mitochondrial energetics by preventing protein hyperacetylation. Nat. Metab. https://doi.org/10.1038/s42255-021-00342-6 (2021).
Luda, K. et al. Ketolysis drives CD8 + T cell effector function through effects on histone acetylation. Immunity https://doi.org/10.1016/j.immuni.2023.07.002 (2023).
Adam, C. et al. Acetoacetate protects macrophages from lactic acidosis-induced mitochondrial dysfunction by metabolic reprograming. Nat. Commun. 12 , 7115 (2021).
Kaymak, I. et al. Carbon source availability drives nutrient utilization in CD8(+) T cells. Cell Metab. 34 , 1298–1311 (2022).
Goldberg, E. L. et al. Ketogenesis activates metabolically protective γδ T cells in visceral adipose tissue. Nat. Metab. 2 , 50–61 (2020).
Beylot, M., Guiraud, M., Grau, G. & Bouletreau, P. Regulation of ketone body flux in septic patients. Am. J. Physiol. 257 , E665–674 (1989).
Wannemacher, R. W. Jr et al. Role of the liver in regulation of ketone body production during sepsis. J. Clin. Invest. 64 , 1565–1572 (1979).
Paumelle, R. et al. Hepatic PPARα is critical in the metabolic adaptation to sepsis. J. Hepatol. 70 , 963–973 (2019).
Beylot, M. et al. Metabolic effects of a D-β-hydroxybutyrate infusion in septic patients: inhibition of lipolysis and glucose production but not leucine oxidation. Crit. Care Med. 22 , 1091–10987 (1994).
Goossens, C. et al. Altered cholesterol homeostasis in critical illness-induced muscle weakness: effect of exogenous 3-hydroxybutyrate. Crit. Care 25 , 252 (2021).
Bruzzone, C. et al. SARS-CoV-2 infection dysregulates the metabolomic and lipidomic profiles of serum. iScience 23 , 101645 (2020).
Hirschberger, S. et al. Ketone bodies improve human CD8(+) cytotoxic t-cell immune response during COVID-19 infection. Front. Med. 9 , 923502, (2022).
Karagiannis, F. et al. Impaired ketogenesis ties metabolism to T cell dysfunction in COVID-19. Nature 609 , 801–807 (2022).
Murashige, D. et al. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science https://doi.org/10.1126/science.abc8861 (2020).
Balasse, E. Kinetics of ketone body metabolism in fasting humans. Metab. Clin. Exp. https://doi.org/10.1016/0026-0495(79)90166-5 (1979).
Kies, C., Tobin, R. B., Fox, H. M. & Mehlman, M. A. Utilization of 1,3-butanediol and nonspecific nitrogen in human adults. J. Nutr. https://doi.org/10.1093/jn/103.8.1155 (1973).
Clarke, K. et al. Kinetics, safety and tolerability of (R)-3-hydroxybutyl (R)-3-hydroxybutyrate in healthy adult subjects. Regul. Toxicol. Pharmacol. https://doi.org/10.1016/j.yrtph.2012.04.008 (2012).
Veech, R. The therapeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism. Prostaglandins Leukot. Essent. Fatty Acids https://doi.org/10.1016/j.plefa.2003.09.007 (2004).
Poff, A. M., Koutnik, A. P. & Egan, B. Nutritional ketosis with ketogenic diets or exogenous ketones: features, convergence, and divergence. Curr. Sports Med. Rep. https://doi.org/10.1249/JSR.0000000000000732 (2020).
Kennedy, A. R. et al. A high-fat, ketogenic diet induces a unique metabolic state in mice. Am. J. Physiol. Endocrinol. Metab. 292 , E1724–E1739 (2007).
de Cabo, R. & Mattson, M. P. Effects of intermittent fasting on health, aging, and disease. N. Engl. J. Med. 381 , 2541–2551 (2019).
Caffa, I. et al. Fasting-mimicking diet and hormone therapy induce breast cancer regression. Nature 583 , 620–624 (2020).
Saris, C. G. J. & Timmers, S. Ketogenic diets and ketone suplementation: a strategy for therapeutic intervention. Front. Nutr. 9 , 947567 (2022).
Belany, P. et al. Effects of hypocaloric low-fat, ketogenic and ketogenic & ketone supplement diets on aldosterone and renin. J. Clin. Endocrinol. Metab. https://doi.org/10.1210/clinem/dgad009 (2023).
Retterstol, K., Svendsen, M., Narverud, I. & Holven, K. B. Effect of low carbohydrate high fat diet on LDL cholesterol and gene expression in normal-weight, young adults: a randomized controlled study. Atherosclerosis 279 , 52–61 (2018).
Athinarayanan, S. et al. Impact of a 2-year trial of nutritional ketosis on indices of cardiovascular disease risk in patients with type 2 diabetes. Cardiovasc. Diabetol. https://doi.org/10.1186/s12933-020-01178-2 (2020).
Hyde, P. N. et al. Dietary carbohydrate restriction improves metabolic syndrome independent of weight loss. JCI Insight https://doi.org/10.1172/jci.insight.128308 (2019).
Schugar, R. C., Huang, X., Moll, A. R., Brunt, E. M. & Crawford, P. A. Role of choline deficiency in the fatty liver phenotype of mice fed a low protein, very low carbohydrate ketogenic diet. PLOS ONE 8 , e74806 (2013).
Cai, Q. Y. et al. Safety and tolerability of the ketogenic diet used for the treatment of refractory childhood epilepsy: a systematic review of published prospective studies. World J. Pediatr. 13 , 528–536 (2017).
Stubbs, B. et al. On the metabolism of exogenous ketones in humans. Front. Physiol. https://doi.org/10.3389/fphys.2017.00848 (2017).
Ferrannini, E. et al. Shift to fatty substrate utilization in response to sodium-glucose cotransporter 2 inhibition in subjects without diabetes and patients with type 2 diabetes. Diabetes 65 , 1190–1195 (2016).
Zinman, B. et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa1504720 (2015).
Abdelgani, S. et al. Distinct mechanisms responsible for the increase in glucose production and ketone formation caused by empagliflozin in T2DM patients. Diabetes Care https://doi.org/10.2337/dc22-0885 (2023).
Saucedo-Orozco, H., Voorrips, S. N., Yurista, S. R., de Boer, R. A. & Westenbrink, B. D. SGLT2 inhibitors and ketone metabolism in heart failure. J. Lipid Atheroscler. 11 , 1–19 (2022).
Lupsa, B. C. Kibbey, R. G. & Inzucchi, S. E. Ketones: the double-edged sword of SGLT2 inhibitors? Diabetologia https://doi.org/10.1007/s00125-022-05815-1 (2023).
Falkenhain, K., Daraei, A., Forbes, S. C. & Little, J. P. Effects of exogenous ketone supplementation on blood glucose: a systematic review and meta-analysis. Adv. Nutr. 13 , 1697–1714 (2022).
Soni, S. et al. Exogenous ketone ester administration attenuates systemic inflammation and reduces organ damage in a lipopolysaccharide model of sepsis. Biochim. Biophys. Acta Mol. Basis Dis. 1868 , 166507 (2022).
Koutnik, A. P. et al. Ketone bodies attenuate wasting in models of atrophy. J. Cachexia Sarcopenia Muscle 11 , 973–996, https://doi.org/10.1002/jcsm.12554 (2020).
Download references
Acknowledgements
The authors are grateful for support from the National Institutes of Health (grants DK091538, AG069781, DK007203 and HL166142).

Author information
These authors contributed equally: Alisa B. Nelson, Eric D. Queathem.
Authors and Affiliations
Division of Molecular Medicine, Department of Medicine, University of Minnesota, Minneapolis, MN, USA
Alisa B. Nelson, Eric D. Queathem, Patrycja Puchalska & Peter A. Crawford
Department of Biochemistry, Molecular Biology and Biophysics, University of Minnesota, Minneapolis, MN, USA
Eric D. Queathem & Peter A. Crawford
You can also search for this author in PubMed Google Scholar
Contributions
A.B.N., E.D.Q., P.P. and P.A.C. generated the manuscript’s outline and drafted and revised the manuscript. E.D.Q. and P.P. generated the figures.
Corresponding authors
Correspondence to Patrycja Puchalska or Peter A. Crawford .
Ethics declarations
Competing interests.
P.A.C. has served as an external consultant for Pfizer, Abbott Laboratories, Janssen Research & Development and Selah Therapeutics. All other authors declare no competing interests.
Peer review
Peer review information.
Nature Metabolism thanks Andrew Murray and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Ashley Castellanos-Jankiewicz, in collaboration with the Nature Metabolism team.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Nelson, A.B., Queathem, E.D., Puchalska, P. et al. Metabolic Messengers: ketone bodies. Nat Metab 5 , 2062–2074 (2023). https://doi.org/10.1038/s42255-023-00935-3
Download citation
Received : 02 May 2023
Accepted : 20 October 2023
Published : 13 December 2023
Issue Date : December 2023
DOI : https://doi.org/10.1038/s42255-023-00935-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- Informatics
- Molecular Dx
- Patient Care
- Precision Medicine
- Translational Research
- Browse Issues
- Molecular Diagnostics
- Oncology/Therapeutics
- Healthcare Informatics
- Get Inside Precision Medicine Magazine
- Get Inside Precision Medicine eNewsletters
- Learning Labs
- Inside Precision Medicine Live
- Update Preferences

Mini Lungs Reveal More Cells Susceptible to COVID-19
Antimicrobial susceptibility test turnaround time slashed by novel method, new therapeutic target found for acute myeloid leukemia, fecal microbiota transplants could boost cancer immunotherapy efficacy, new research shows potential for ketone therapy in heart failure.
By IPM staff

Preliminary research presented at the American Heart Association’s Basic Cardiovascular Sciences Scientific Sessions 2024 suggests that increasing ketone supply to the heart could significantly enhance energy production in cases of heart failure with preserved ejection fraction (HFpEF).
HFpEF occurs when there are signs or symptoms of heart failure with a high left ventricle filling pressure even when there is normal or near-normal ventricle ejection fraction higher than 50%. A normal ejection fraction is between 50% and 70%. Heart failure with reduced ejection fraction (HFrEF) is when the heart’s pumping power is less than 40%. HFrEF has been meticulously studied and has well-established methods of treating it, whereas HFpEF has no current evidence-based treatment regimens.
“Humans typically rely on carbohydrates and fats for energy, but ketones become crucial when glucose levels are low, such as during fasting or intense exercise,” said study author Qiuyu (Violet) Sun, a PhD candidate at the University of Alberta, Canada. “Our study shows that increasing ketone supply in HFpEF mice improves the heart’s ability to produce adenosine triphosphate (ATP), the energy currency of cells, without disrupting glucose or fat utilization.”
For their research, the University of Alberta team induced HFpEF in mice through a high-fat diet and chemical treatment to mimic human conditions. They then administered varying levels of β-hydroxybutyrate, a major ketone body, to observe its impact on cardiac metabolism and discovered that increasing ketone supply led to a notable increase in ATP production derived from both ketones and glucose oxidation. This resulted in improved overall cardiac function.
“This increase in ketone utilization didn’t interfere with the heart’s ability to use glucose or fats, which is critical in maintaining balanced energy production,” Sun said. “This finding suggests a potential avenue for developing therapies that optimize cardiac energy metabolism in HFpEF.”
Heart failure affects millions globally, with HFpEF becoming increasingly prevalent due to aging populations and rising obesity rates. Despite these trends, effective treatments have not yet been developed. Sun noted the urgency of developing targeted therapies for HFpEF, stating, “Identifying key proteins involved in cardiac energy metabolism could pave the way for future drug development to treat this condition effectively.”
While the study is promising, the authors noted the limitation of its focus on a specific metabolic phenotype of HFpEF, while there are a range of HFpEF subtypes including fibrotic type or the diastolic dysfunction phenotypes. These are also of importance and should be studied. Future studies should also seek to develop models that more closely align with and translate to human physiology.
“The prevalence of heart failure with preserved ejection fraction is rising, driven by an aging population and increasing obesity rates. Unfortunately, there is still a lack of clinically effective treatment for this condition,” Sun said. “We hope our study can help us better understand this condition. Identifying key proteins involved in cardiac energy metabolism could potentially lead to identification of druggable targets for future development of medications to treat HFpEF.”
- News & Features
Related Content

Ohio State Researchers Nab $15M NIH Grant to Combat Long COVID

Switching Off Inflammatory Protein IL-11 Extends Lifespan and Reduces Age-Related Diseases in Mice

Weight Loss Drugs’ Effects Could Be Improved by Priming Melanocortin System

Popular Wearables Can Help Doctors Manage Medication in Patients with Heart Disease
- Terms of Service
- Cookie Policy
Immunotherapy and Cancer: Harnessing the Power of Diagnostic Assays
Rise of genomics in clinical trials, conquering cml: the breakthrough paradigm change of treatment-free remission.
Advertisement
Supported by
OpenAI Is Testing an A.I.-Powered Search Engine
The prominent A.I. start-up said it planned to eventually fold the new technology into its popular online chatbot, ChatGPT.
- Share full article

By Cade Metz
Reporting from San Francisco
OpenAI is testing an A.I.-powered search engine that can access information from across the internet in real time.
The prominent A.I. start-up revealed the new prototype, SearchGPT, in a blog post on Thursday. The company said it was testing the technology with a small group of users as well as online publishers that teamed up with OpenAI to help build the search engine.
“Getting answers on the web can take a lot of effort, often requiring multiple attempts to get relevant results,” the company said in its blog post. “We believe that by enhancing the conversational capabilities of our models with real-time information from the web, finding what you’re looking for can be faster and easier.”
OpenAI did not immediately respond to a request for additional comment.
Other companies, including tech giants like Google and Microsoft, as well as start-ups like the San Francisco-based Perplexity, have built similar technologies. These services augment traditional internet search engines with chatbot technology that generates text as a way of answering questions and summarizing online information.
OpenAI plans to integrate its new search engine technology with its existing online chatbot, ChatGPT, which launched the A.I. boom when it was released in November 2022. The company said its new technology would respond to questions with up-to-date information from the web while also providing links to relevant sources.
For instance, if someone asks when the Paris Olympics begin and SearchGPT provides a date for the opening ceremony, it might link to a news article.
OpenAI said online publishers such as Reuters are working with the company on the product. “We are committed to a thriving ecosystem of publishers and creators,” the company said, adding that the technology would highlight “high-quality content in a conversational interface with multiple opportunities for users to engage.”
The company also said it was developing ways for publishers to manage how they appeared in answers generated by the new search engine.
The New York Times has sued OpenAI and its partner, Microsoft, claiming copyright infringement of news content related to A.I. systems. The two companies have denied the suit’s claims.
Cade Metz writes about artificial intelligence, driverless cars, robotics, virtual reality and other emerging areas of technology. More about Cade Metz
Watch CBS News
Yes, money can buy happiness — the more wealth you have, the happier you get, research finds.
By Aimee Picchi
Edited By Anne Marie Lee
Updated on: July 26, 2024 / 2:38 PM EDT / CBS News
If you want to know the secret to achieving happiness, the answer might be found in your bank account — as long as it's extremely well-funded.
The link between happiness and money is getting a fresh look from economists and scientists, with new research finding multimillionaires are much happier than the merely well-to-do. In other words, the new study, from University of Pennsylvania's Wharton School senior fellow Matthew Killingsworth, indicates that the more money you have, the happier you are — and there may be no ceiling.
Killingsworth's latest research builds on his 2023 study that debunked a much-cited 2010 analysis claiming people's happiness peaked at about $75,000 in annual income, or about $110,000 in today's inflation-adjusted dollars. That 2023 research found that happiness does improve with higher earnings, but because the researchers lacked data for people earning above $500,000, it was unclear whether happiness topped out at that income.
Now, Killingsworth has found that happiness rises to even higher levels for the extremely rich, or those with assets between $3 million to $7.9 million, with their life satisfaction far exceeding that of people with mere six figure incomes. The implication is happiness continues to rise alongside one's bank account, with no clear upper limit.
"The money-happiness curve continues rising well beyond $500,000 a year," Killingsworth told CBS MoneyWatch in an email. "I think a big part of what's happening is that when people have more money, they have more control over their lives."
He added, "I suspect it's much more fundamental and psychologically deeper than simply buying more stuff."
The happiness scale
The new research is based on surveys that asked people to rate their life satisfaction from 1 to 7, with the lower end representing "not at all" happy to the top number indicating "extremely" satisfied. Low-income people earning about $30,000 or less gave their lives an average rating of about 4, while people earning about $500,000 rated their lives above 5.
But multimillionaires gave their life satisfaction an average rating closer to 6.
One question raised by the new research is whether wealth has a different impact on happiness than income. Wealth, for instance, may allow people to invest in themselves and their families, such as providing the means to fund children's college educations or buy a bigger home in a better school district.
To be sure, a high income can also help with achieving those goals, but research indicates top earners aren't immune from feeling financially stressed. For instance, one-third of people earning more than $150,000 say they are concerned about making ends meet, a higher share than those earning between $40,000 to $149,999, according to an April survey from the Federal Reserve Bank of Philadelphia.
"How wealth and income combine to explain why the wealthy people were so much happier is an open question. I'd guess that having wealth is helpful, but I can't say for sure," Killingsworth said.
Whether happiness might eventually plateau at some level of wealth or income is "hard to say," although he said he's working on additional analyses to examine that issue, he added.
Happiness and the 99%
But whether billionaires, for instance, could be even happier than multimillionaires isn't the important takeaway from his research, Killingsworth noted, pointing out that the share of people in the U.S. whose wealth exceeds those in his analysis is "pretty small."
"At some point, whether 0.1% versus 0.3% of people might be beyond some threshold becomes relevant only for a pretty small set of people, so I think showing the pattern I find here tells us a lot of what we should care about," he noted.
Most Americans earn salaries linked with lower life satisfaction, given that the U.S. median annual income stands at about $75,000. To crack the top 1% of earners in the U.S. one must earn an annual income 10 times that, about $788,000.
"It certainly doesn't look like half the population is already beyond the point where more money stops mattering, for example," Killingsworth pointed out. That could matter for policymakers who want to improve their citizens' well-being, since the research suggests there could be "huge ROI" by helping improve the financial situations of people with low incomes, he noted.
"A given amount of money appears to yield a lot more happiness for people who have less money to begin with," Killingsworth said. "Economic trends in the U.S. seems to be moving in the opposite direction — the poorest folks have gained the least in recent decades, and the richest folks have gained the most."
Is money necessary for happiness?
Absolutely not, Killingsworth said.
"One important point that isn't obvious from this paper by itself is that money is just one of many things that matter for happiness," he said. "So, I think it's important for everyone – policy makers, executives, and regular people – to keep in mind that so many things matter besides money."
And focusing solely on making money while ignoring other issues could create more harm than good, he added. Connections with friends and family may matter more to happiness, for example, given that Americans say these provide them with more meaning than material well-being, Pew Research Center has found
"It's entirely possible to be rich and miserable or poor and happy," Killingsworth noted. "The main reason is simply that lots of things matter for happiness besides money."
He added, "But, all else equal, people tend to be happier the more money they have."
- Income Inequality
Aimee Picchi is the associate managing editor for CBS MoneyWatch, where she covers business and personal finance. She previously worked at Bloomberg News and has written for national news outlets including USA Today and Consumer Reports.
More from CBS News

Park Fire evacuees in Chico look out for their neighbors

How Flashfood app has helped California residents find discounted groceries

Building accessory dwelling units in Davis just got a lot easier. Here's why.

Sacramento community discusses how best to spend Measure L funding to keep kids safe
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Sustainability
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
Large language models don’t behave like people, even though we may expect them to
Press contact :, media download.

*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."
Previous image Next image
One thing that makes large language models (LLMs) so powerful is the diversity of tasks to which they can be applied. The same machine-learning model that can help a graduate student draft an email could also aid a clinician in diagnosing cancer.
However, the wide applicability of these models also makes them challenging to evaluate in a systematic way. It would be impossible to create a benchmark dataset to test a model on every type of question it can be asked.
In a new paper , MIT researchers took a different approach. They argue that, because humans decide when to deploy large language models, evaluating a model requires an understanding of how people form beliefs about its capabilities.
For example, the graduate student must decide whether the model could be helpful in drafting a particular email, and the clinician must determine which cases would be best to consult the model on.
Building off this idea, the researchers created a framework to evaluate an LLM based on its alignment with a human’s beliefs about how it will perform on a certain task.
They introduce a human generalization function — a model of how people update their beliefs about an LLM’s capabilities after interacting with it. Then, they evaluate how aligned LLMs are with this human generalization function.
Their results indicate that when models are misaligned with the human generalization function, a user could be overconfident or underconfident about where to deploy it, which might cause the model to fail unexpectedly. Furthermore, due to this misalignment, more capable models tend to perform worse than smaller models in high-stakes situations.
“These tools are exciting because they are general-purpose, but because they are general-purpose, they will be collaborating with people, so we have to take the human in the loop into account,” says study co-author Ashesh Rambachan, assistant professor of economics and a principal investigator in the Laboratory for Information and Decision Systems (LIDS).
Rambachan is joined on the paper by lead author Keyon Vafa, a postdoc at Harvard University; and Sendhil Mullainathan, an MIT professor in the departments of Electrical Engineering and Computer Science and of Economics, and a member of LIDS. The research will be presented at the International Conference on Machine Learning.
Human generalization
As we interact with other people, we form beliefs about what we think they do and do not know. For instance, if your friend is finicky about correcting people’s grammar, you might generalize and think they would also excel at sentence construction, even though you’ve never asked them questions about sentence construction.
“Language models often seem so human. We wanted to illustrate that this force of human generalization is also present in how people form beliefs about language models,” Rambachan says.
As a starting point, the researchers formally defined the human generalization function, which involves asking questions, observing how a person or LLM responds, and then making inferences about how that person or model would respond to related questions.
If someone sees that an LLM can correctly answer questions about matrix inversion, they might also assume it can ace questions about simple arithmetic. A model that is misaligned with this function — one that doesn’t perform well on questions a human expects it to answer correctly — could fail when deployed.
With that formal definition in hand, the researchers designed a survey to measure how people generalize when they interact with LLMs and other people.
They showed survey participants questions that a person or LLM got right or wrong and then asked if they thought that person or LLM would answer a related question correctly. Through the survey, they generated a dataset of nearly 19,000 examples of how humans generalize about LLM performance across 79 diverse tasks.
Measuring misalignment
They found that participants did quite well when asked whether a human who got one question right would answer a related question right, but they were much worse at generalizing about the performance of LLMs.
“Human generalization gets applied to language models, but that breaks down because these language models don’t actually show patterns of expertise like people would,” Rambachan says.
People were also more likely to update their beliefs about an LLM when it answered questions incorrectly than when it got questions right. They also tended to believe that LLM performance on simple questions would have little bearing on its performance on more complex questions.
In situations where people put more weight on incorrect responses, simpler models outperformed very large models like GPT-4.
“Language models that get better can almost trick people into thinking they will perform well on related questions when, in actuality, they don’t,” he says.
One possible explanation for why humans are worse at generalizing for LLMs could come from their novelty — people have far less experience interacting with LLMs than with other people.
“Moving forward, it is possible that we may get better just by virtue of interacting with language models more,” he says.
To this end, the researchers want to conduct additional studies of how people’s beliefs about LLMs evolve over time as they interact with a model. They also want to explore how human generalization could be incorporated into the development of LLMs.
“When we are training these algorithms in the first place, or trying to update them with human feedback, we need to account for the human generalization function in how we think about measuring performance,” he says.
In the meanwhile, the researchers hope their dataset could be used a benchmark to compare how LLMs perform related to the human generalization function, which could help improve the performance of models deployed in real-world situations.
“To me, the contribution of the paper is twofold. The first is practical: The paper uncovers a critical issue with deploying LLMs for general consumer use. If people don’t have the right understanding of when LLMs will be accurate and when they will fail, then they will be more likely to see mistakes and perhaps be discouraged from further use. This highlights the issue of aligning the models with people's understanding of generalization,” says Alex Imas, professor of behavioral science and economics at the University of Chicago’s Booth School of Business, who was not involved with this work. “The second contribution is more fundamental: The lack of generalization to expected problems and domains helps in getting a better picture of what the models are doing when they get a problem ‘correct.’ It provides a test of whether LLMs ‘understand’ the problem they are solving.”
This research was funded, in part, by the Harvard Data Science Initiative and the Center for Applied AI at the University of Chicago Booth School of Business.
Share this news article on:
Related links.
- Ashesh Rambachan
- Laboratory for Information and Decision Systems
- Department of Electrical Engineering and Computer Science
- Department of Economics
Related Topics
- Computer science and technology
- Artificial intelligence
- Human-computer interaction
- Laboratory for Information and Decision Systems (LIDS)
- School of Humanities Arts and Social Sciences
Related Articles
Reasoning skills of large language models are often overestimated

Technique improves the reasoning capabilities of large language models

Natural language boosts LLM performance in coding, planning, and robotics
Multi-AI collaboration helps reasoning and factual accuracy in large language models
Previous item Next item
More MIT News

Edgerton Center hosts workshop for deaf high school students in STEM
Read full story →

MIT Global SCALE Network expands by adding center at Loughborough University
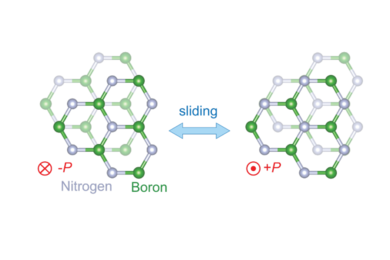
New transistor’s superlative properties could have broad electronics applications

When learning at MIT means studying thousands of miles away

Flying high to enable sustainable delivery, remote care
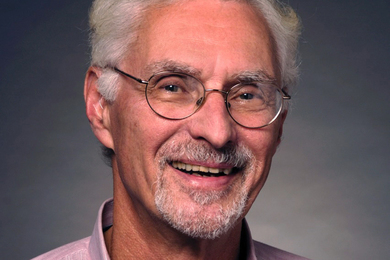
Professor Emeritus Ralph Gakenheimer, mobility planner and champion of international development, dies at 89
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Med Surg (Lond)
- v.85(6); 2023 Jun
- PMC10289692

Comprehensive review of diabetic ketoacidosis: an update
Chukwuka elendu.
a Federal Medical Center, Owerri
Johnson A. David
i VN Karazin National University, Kharkiv, Ukraine
Abasi-O. Udoyen
j Pirogov Medical University, Rossijskij nacional’nyj issledovatel’skij medicinskij universitet imeni N I Pirogova, Russia
Emmanuel O. Egbunu
d University of Ilorin Teaching Hospital
Ifeanyichukwu C. Ogbuiyi-Chima
e Babcock University
Lilian O. Unakalamba
f Rivers State University Teaching Hospital, Portharcourt
Awotoye I. Temitope
g Lagos University Teaching Hospital
Jennifer O. Ibhiedu
Amos o. ibhiedu, promise u. nwosu.
h Abia State University, Nigeria
Mercy O. Koroyin
k Bromley Healthcare
Chimuanya Eze
Adeyemo i. boluwatife, omotayo alabi.
c Redeemer’s University
Olisa S. Okabekwa
b University of Nigeria Teaching Hospital, Ituku Ozalla
John O. Fatoye
Habiba i. ramon-yusuf.
l University Hospital Lewisham, UK
Associated Data
Data will be made available by the authors upon reasonable request.
The most frequent hyperglycemic emergency and the leading cause of death in people with diabetes mellitus is diabetic ketoacidosis (DKA). DKA is common in people with type 1 diabetes, while type 2 diabetes accounts for roughly one-third of occurrences. Although DKA mortality rates have generally decreased to low levels, they are still significant in many underdeveloped nations. In industrialized countries, its mortality rate ranges from 2 to 5%, but in underdeveloped nations, it ranges from 6 to 24%. Therefore, it is always lethal if misdiagnosed or improperly treated. According to specific research, DKA can be present at the time of type 1 diabetes onset in 25 to 30% of cases and in 4 to 29% of young people with type 2 diabetes mellitus, and its features include hyperglycemia, metabolic acidosis, and ketosis with its triggering factors commonly being infections, newly discovered diabetes, and failure to start insulin therapy. Less than 20% of DKA patients present comatose, and patients with different levels of consciousness can present at other times. A close association between abnormalities found during a mental status evaluation and osmolality seems to exist. Hospital admission is necessary for vigorous intravenous fluid therapy, insulin therapy, electrolyte replacement, diagnosis and treatment of the underlying triggers, and routine monitoring of the patient’s clinical and laboratory conditions to manage DKA properly. Appropriate discharge plans should include actions to prevent a DKA recurrence and the proper selection and administration of insulin regimens.
Introduction and background
- Diabetic ketoacidosis is the most frequent hyperglycemic emergency.
- Diabetic ketoacidosis is the leading cause of death in people with diabetes mellitus.
- DKA is common in people with type 1 diabetes.
Diabetic ketoacidosis is a grievous complication of diabetes that occurs when there is a lack of insulin in the body, resulting in elevated blood glucose levels and the production of ketones. Diabetic ketoacidosis is a medical emergency that requires immediate treatment, as it can lead to life-threatening complications such as cerebral edema, acute respiratory distress syndrome, and sepsis 1 . It is becoming more prevalent worldwide, particularly among type 1 diabetic children and adolescents 1 . While insulin therapy and patient education have improved, diabetic ketoacidosis remains a common cause of hospitalization and is associated with notable morbidity and mortality 2 , 3 . Among the immediate treatment options for severe diabetic ketoacidosis is a multidisciplinary approach that emphasizes correcting fluid and electrolyte imbalances, restoring insulin sensitivity, and preventing complications. Primary care aims to prevent the progression of diabetic ketoacidosis and minimize the risk of cerebral edema, a rare but potentially fatal complication 4 , 5 . A recent publication has shed light on the pathophysiology of diabetic ketoacidosis, including the role of insulin deficiency, altered glucose metabolism, and acid-base disturbances 3 . Technological advances and monitoring techniques have also allowed for more precise management of fluid and electrolyte imbalances, insulin therapy, and other adjunctive therapies 5 . The management of severe diabetic ketoacidosis is not without challenges. For example, insulin therapy can rapidly drop blood glucose levels, increasing the risk of hypoglycemia.
Similarly, fluid therapy can lead to fluid overload and other complications, particularly in patients with underlying comorbidities 2 . To adequately address these challenges, there is a need for a comprehensive review of immediate care for severe diabetic ketoacidosis 4 . Such a review would synthesize current research findings, provide evidence-based recommendations, and highlight areas where further research is needed.
This review aims to comprehensively analyze the current state of immediate care for severe diabetic ketoacidosis. It will cover the pathophysiology, clinical manifestations, and management of diabetic ketoacidosis, focusing on evidence-based interventions. Furthermore, the study will highlight the challenges associated with immediate care for severe diabetic ketoacidosis and provide recommendations for addressing these challenges. It will be an essential resource for healthcare professionals managing severe diabetic ketoacidosis. This review can improve patient outcomes and reduce the morbidity and mortality associated with severe diabetic ketoacidosis by providing evidence-based guidance.
Methodology
This comprehensive review compiles and evaluates recurrent and dominant topics discussed in the literature regarding the epidemiology, pathophysiology, and emergent therapy for patients with diabetic ketoacidosis, a complication of type 1 diabetes (T1DM) and less frequently type 2 diabetes (T2DM). To attain the purpose of the study, the authors undertook an exhaustive and advanced Pubmed search. Pubmed is an electronic database that serves as a search engine and gives access to more than 35 million MEDLINE articles that can be cited (medical, biomedical, nursing, life sciences, etc.). We used Boolean operators to combine the search terms and phrases; epidemiology, pathophysiology, diagnosis, and emergent therapy for patients with diabetic ketoacidosis. We also entered the vital alternative terms into the search for a broader reach. The review was limited to articles published within the past decade (2012–2022) and was not restricted to a specific region. We used only English language articles from academic journals with peer review. In addition, the study included articles with both abstracts and full texts to facilitate screening. Thirty-seven articles popped up after the filters were applied. After reading through the abstracts of the initial results to screen for eligibility, six papers were eventually selected since they also provided the most recent discussions regarding the topic.
Definition and epidemiology
Diabetic ketoacidosis is a severe acute metabolic complication of diabetes mellitus characterized by hyperglycemia, hyperketonaemia, and metabolic acidosis. Patients have high insulin requirements, eventually depleting their body insulin 5 . This insulin deficiency leads to an excessive breakdown of fat, resulting in an excessive build-up of ketone bodies. Despite improvements in diabetic patients’ self-care, DKA still accounts for 14% of all hospital admissions of diabetic patients and 16% of all deaths linked to diabetes 4 . DKA commonly exists in people with type 1 diabetes, and about 3% of type 1 diabetes patients initially present with DKA; the incidence is two episodes per 100 patient-years of diabetes. Patients with type 2 diabetes can also develop it, though this is less typical 6 , 7 . Although the incidence of diabetic ketoacidosis in developing nations is unknown, it may be greater than in developed countries 8 . Whites have a greater prevalence of type 1 diabetes, contributing to the higher incidence of DKA in this racial group. For unknown causes, females are slightly more likely than males to develop DKA. Young ladies with type 1 diabetes frequently experience recurrent DKA, which is primarily brought on by failing to administer insulin therapy 6 , 9 . DKA is much more frequent in young children and teenagers than in adults among people with type 1 diabetes; however, patients with diabetes may experience DKA at any age. Intervention is feasible between the onset of symptoms and the development of DKA, although numerous factors (such as ethnic minority, lack of health insurance, lower BMI, preceding infection, delayed treatment, etc.) influence the risk of DKA among children and young people 9 .
Pathophysiology
The abnormal physiology seen in a diabetic patient with ketoacidosis is due to absolute or relative insulin deficiency with the rise in hormones that put the body in a catabolic state and cause insulin resistance leading to hyperglycemia, hyperketonemia, hyperosmolarity, and electrolyte imbalances. These hormones include; glucagon, growth hormone, and catecholamines (epinephrine and norepinephrine) 10 . The event that most commonly precipitates diabetic ketoacidosis is usually a loss of insulin activity or increased demand for insulin, which can occur due to missed insulin doses, improper administration of insulin, or the presence of infections in a diabetic patient 11 . It can lead to an inability to transport glucose intracellularly; when this occurs, most cells cannot utilize glucose for energy, so intracellular hunger and starvation begin. Most cells shift to free fatty acids (FFA) as an energy source 12 , 13 . Without insulin, there becomes a plethora of FFA in the bloodstream because insulin impedes the lipolysis of adipocytes into glycerol and FFA 8 . These abundantly circulating FFA are taken to the liver and transported to its mitochondria for oxidation; then, ketone bodies are formed, including beta-hydroxybutyrate, acetone, and acetoacetate. Insulin checks the biochemical process, but excessive ketone production results from insufficient insulin 14 . In uncomplicated diabetes or starvation, triglycerides usually predominate ketones. The ketones produced do not overwhelm the body’s ability to get rid of them, putting it in a state of ketosis 15 . Glucagon, catecholamines, cortisol, and growth hormone also significantly increase blood glucose through gluconeogenesis and glycogenolysis 15 . The release of these hormones can also be a response to stress, which can take the form of infections (i.e., urinary tract infections and respiratory tract infections, especially the lower tract); trauma; myocardial infarction; acute pancreatitis; burns; surgery; strokes; substance abuse; and so on 16 . These stressors cause a release in inflammatory cytokines that increase insulin counter-regulatory hormones like glucagon, catecholamines, cortisol, and growth hormone 17 . These hormones put the body in a catabolic state, causing more lipolysis and proteolysis to synthesize glucose, which worsens hyperglycemia 18 .
The commonest precipitants of diabetic ketoacidosis are poor compliance with insulin therapy, infections, and a new diagnosis of diabetes 19 . The most common precipitating factor of diabetic ketoacidosis in type 1 diabetes patients is nonadherence to treatment, while infections are the most common precipitant in type 2 diabetes patients 20 . Other causes are vascular events (e.g., acute coronary syndrome, cerebrovascular accidents, critical limb ischemia, bowel ischemia, and shock); excessive alcohol intake; illicit drugs such as cocaine and methamphetamine; antipsychotic drugs, for example, clozapine, risperidone, and olanzapine 19 .
Laboratory abnormalities and diagnosis
In 2003, the American Diabetes Association modified the diagnostic criteria of DKA by introducing severity categories of mild, moderate, and severe, as displayed in Table Table1 1 2 , 21 .
Diagnostic criteria and severity of diabetic ketoacidosis
| Mild | Moderate | Severe | |
|---|---|---|---|
| Plasma glucose (mmol/l) | >13.9 | >13.9 | >13.9 |
| Arterial pH | 7.25–7.30 | 7.00–7.24 | <7.00 |
| Serum bicarbonate (mmol/l) | 15–18 | 10–14.9 | <10 |
| Urine ketones | ++ | ++ | +++ |
| Serum ketones | +++ | +++ | +++ |
| Anion gap | >10 | >12 | >12 |
| Sensorium | Alert | Alert/drowsy | Stupor/coma |
| Serum sodium | Normal | Low | Low |
| Serum potassium | Normal | High | High |
| Serum phosphate | Normal | High | High |
Abnormal changes in laboratory values give a significant clue of what exactly happens in patients with suspected diabetic ketoacidosis 2 , 21 – 23 .
The diagnosis of DKA consists of a triad of hyperglycemia, ketonemia, and metabolic acidosis.
All patients with positive ketones, constitutional symptoms, or suspicion of DKA and significantly elevated blood glucose levels [>13.9 mmol/l (>250 mg/dl)] should have electrolytes and blood gases checked to look for an anion gap metabolic acidosis 2 . Significantly in type 1 diabetes, DKA can develop within hours if you stop insulin injections or an insulin pump malfunctions 21 . The new American Diabetes Association definition of DKA includes a blood glucose level of 13.9 mmol/l (250 mg/dl) 2 . Many studies show that DKA is infrequent at lower levels except in situations with poor oral intake or pregnancy 22 . It is also essential to consider DKA in differential diagnoses for patients with anion gap metabolic acidosis. Check serum glucose even when the patient has no history of diabetes 15 . Consider DKA if the serum glucose is more significant than 13.9 mmol/l (250 mg/dl), but an elevated glucose level alone is insufficient to diagnose DKA. Suspect DKA in patients with diabetes with a concurrent infection, stroke, myocardial infarction, or other serious illness 13 . These intercurrent illnesses should be sought and treated aggressively 13 . Similarly, it is vital to consider DKA when patients with diabetes experience nausea and vomiting, even if the blood sugar level is less than 13.9 mmol/l (250 mg/dl) 10 . Euglycemic DKA occurs more often in patients who have not eaten but continue taking insulin 12 . A blood sugar level of less than 13.9 mmol/l (250 mg/dl) occurs in 1–7% of reported DKA cases and seems more common in patients with hepatic dysfunction or in those who are in patients 11 . Several drugs, such as glucocorticoids or thiazides, are well-known causes of hyperglycemia that may lead to DKA. Clinicians should also consider DKA in patients taking atypical antipsychotic drugs who present with hyperglycemia 23 . Atypical antipsychotic drugs have increased the frequency of diabetes, glucose intolerance, and DKA. The healthcare provider should measure such patients’ anion gap and ketone levels. Another type of antipsychotic drug must be chosen to help resolve this complication 24 , 25 . The presentation of a patient with DKA varies substantially depending on the severity of the episode 5 . Mild or moderately ill patients may describe vague symptoms of fatigue, lethargy, poor appetite, or headache. In type 1 diabetes, the history of polyuria and polydipsia may be relatively recent, but in type 2 diabetes, these symptoms may have been building for weeks to months 8 . Nausea, vomiting, and abdominal pain are commonly seen in DKA and may be related to the combined effects of dehydration, hypokalemia, ketonemia, and delayed gastric emptying 24 . Signs of dehydration, including poor skin turgor, decreased axillary sweat, or postural hypotension, may be present on physical examination 2 . Kussmaul respirations (a pattern of deep breathing and hyperventilation in response to metabolic acidosis) may be present 5 . Patients’ breath may smell fruity due to increased acetone from ketonemia, but the absence of this finding does not rule out DKA. One examination aspect that can be confusing is abdominal tenderness, which may resolve with the treatment of DKA or reflect a more acute abdominal process that precipitates DKA 19 . Abdominal pain correlates with the level of acidosis 15 . The physical examination should identify potential precipitating factors, such as infections or cardiovascular events. Patients may have mental status changes ranging from mild lethargy to delirium or coma. The most severe cases have features like hypotension, tachycardia, and coma 20 . Capillary blood ketone measurement is a relatively new quantitative and enzymatic test that determines levels of 3-β-hydroxybutyrate, one of the three ketone bodies 13 . The equipment is similar to that patients use for home blood glucose determination, but it requires specific strips. However, checking capillary blood ketones is much more expensive than checking urine ketones, and further clinical studies are needed to define the most appropriate role for β-hydroxybutyrate monitoring 24 . If clinical suspicion of DKA is high, a negative urine dipstick for ketones does not exclude DKA. Clinicians should know that urine test sticks do not measure β-hydroxybutyrate, the predominant ketone. Acetoacetate measured on the dipstick may not be high until later during the illness 23 . Arterial blood gas assessment is generally considered the most reliable method to evaluate the degree of acidosis in DKA, but a venous pH may be a more practical alternative. The average anion gap is 7–9 mmol/l but is ~25 mmol/l in DKA 2 . Rarely do patients with DKA have mixed acidosis and alkalosis with a pH close to normal. However, this unexpected laboratory result should not affect the treatment of DKA 17 . Determination of the arterial blood gas may be optional. Most DKA guidelines indicate that hyperglycemia of more than 13.9 mmol/l is necessary for diagnosing DKA; however, this is not an absolute requirement, as there are reports about DKA without hyperglycemia 20 . DKA without hyperglycemia is reported chiefly during pregnancy and in patients with prolonged vomiting or starvation 9 . It can also occur in patients with liver failure or alcohol abusers 9 . Ketone bodies are produced in the liver from acetyl-CoA liberated during lipolysis from fatty acids. For DKA to develop, an absolute or relative insulin deficiency must be present. Three ketone bodies are produced: acetone (resulting in the fruity odor of DKA patients), acetoacetate, and β-hydroxybutyrate (β-OHB). β-OHB is the most prominent contributor to metabolic acidosis in patients with DKA 18 . Acetone does not contribute to acidosis and is not usually measured as such. Acetoacetate can be measured in the urine with a urine dipstick utilizing the nitroprusside reaction 10 . As DKA resolves, β-OHB is oxidized to acetoacetate. Therefore, if only a urine ketone dipstick procedure is done, it might give the impression that the condition is not improving. Blood ketones can be measured with a point of care (bedside) meter utilizing capillary finger prick blood 10 . This measures β-OHB directly and accurately 11 , 12 . The American Diabetic Association recommends that the blood ketone measurement of β-OHB is preferable to urine measurement for diagnosing and monitoring DKA 8 . An arterial pH of less than 7.3 should be present in diagnosing DKA. The measurement of pH or serum bicarbonate is essential for the diagnosis and estimation of the severity of DKA 4 . The pH is also an important measure to assess improvement and treatment adjustment. A venous pH determination would probably be sufficient unless respiratory function must also be evaluated 12 . The venous pH is, on average, 0.03 lower than the arterial pH 23 .
Differential diagnosis
Diabetic ketoacidosis may have a diverse and complex presentation, which makes it share many similarities in the way and manner it presents compared to other common pathologies; hence, other common pathologies may mimic diabetic ketoacidosis 1 . It is, therefore, essential to rule out other pathologies with similar presentations whenever a case of diabetic ketoacidosis is suspected. Differentials include; starvation ketoacidosis, pancreatitis, alcoholic ketoacidosis, lactic acidosis, uremia, overdose on diabetic medication, hyperosmolar hyperglycemic nonketotic syndrome, and myocardial infarction 2 .
Therapy goals in patients with hyperglycemic crises include improving the circulatory volume and tissue perfusion, gradual reduction of serum glucose and osmolality, correcting electrolyte imbalance, and identifying and promptly treating co-morbid precipitating causes. Successful treatment of DKA requires frequent monitoring of patients regarding the above goals by clinical and laboratory parameters. Table Table2 2 below illustrates the initial management of patients with diabetic ketoacidosis 2 , 26 .
Detailed management of patients with diabetic ketoacidosis
| Fluid therapy | DKA is a volume-depleted state with an estimated 6 l of total body water deficit. Initial fluid therapy aims to increase intravascular volume and ensure sufficient urine flow. We advise isotonic saline should be administered as the first beverage at 15–20 ml/kg of body weight per hour or 1–1.5 l during the first hour. The choice of the fluid for additional replenishment depends on the degree of hydration, the level of serum electrolytes, and the output of the urine. Over 12–24 h, replacing half of the expected sodium and water deficit is appropriate. Hydrating fluid in the first hour of therapy before insulin administration provides time to obtain serum potassium. Osmotic diuresis and the modulation of counter-regulatory hormone secretion are the mechanisms for lowering blood sugar. |
| Insulin therapy | Insulin administered in physiologic doses is essential for DKA treatment. Administer an IV bolus of regular insulin (0.1 U/kg body weight) followed by a 0.1 U/kg/hr constant infusion of regular insulin. The insulin rate should be reduced to 0.05 U/kg/hr when plasma glucose hits 200–250 mg/dl. The insulin infusion rate should change to maintain blood glucose levels. Regular insulin is best administered via continuous IV infusion due to its short half-life and simple titration. |
| Potassium therapy | DKA patients with acidosis and insulinopenia have mild to moderate hyperkalemia due to acidosis and insulin depletion. Insulin therapy decreases serum potassium levels. Acidosis correction, volume enlargement, and potassium replacement are commenced when serum levels drop below 5.3 mmol/l. |
| Bicarbonate therapy | Bicarbonate therapy has neither a chance of benefit nor benefit in DKA, according to a prospective randomized study of patients with a pH between 6.9 and 7.1. Adult patients with pH 6.9 should be given 100 mmol sodium bicarbonate in 400 ml sterile water with 20 mmol KCl administered at 200 ml/h for 2 h until the pH rises to 7.0. Treatment continues every 2 h if necessary. |
| Phosphate therapy | Phosphate may be used in individuals experiencing adverse effects from hypophosphatemia, but may cause hypocalcemia when administered in large doses. |
| Nursing aspects of DKA | Nursing management is essential for patients with comatose or pre-comatose states, and regular maintenance of infusions, nasogastric tubes, CVP lines, urine catheters, ECG monitors, etc. Monitor temperature, pulse, blood pressure, respiration, and cognitive state every hour to confirm progress. |
A patient with diabetic ketoacidosis might have normal potassium levels before the initiation of treatment; the medical practitioner should take caution to prevent severe hypokalemia after initiating insulin therapy. Table Table3 3 shows endocrine society’s clinical practice guideline for hospitalized patients with diabetes 2 , 26 – 29 .
Endocrine society’s clinical practice guideline for hospitalized patients with diabetes
| In patients with impaired glycemic control should be on continuous glucose monitoring devices as they effectively prevent hypoglycemic crises. |
| Scheduled insulin therapy should be administered to in patients on glucocorticoid therapy or direct enteral nutrition should they develop hyperglycemia. |
| Outpatients on regular insulin pump therapy who are psychologically and physically fit may self-manage the device with the supervision of medical personnel. |
| Education of admitted diabetic patients on essential management of the condition aids in reasonable glycemic control after discharge and decreases the chance of hospital readmission. |
| Diabetic patients being scheduled for elective surgery are desired to have a preoperative HbA1c of <8% and an immediate preoperative blood glucose of <180 mg/dl as it improves the patient’s postoperative condition. |
| Carbohydrate-containing drinks should not be given to preoperative patients with diabetes. |
| Correctional insulin can be used as the sole initial management for hospital admissions of newly recognized hyperglycemia or well-controlled diabetes. |
| In patients previously on insulin therapy with a continuous blood glucose of >180 mg/dl should be placed on scheduled insulin therapy. |
| In some patients with type 2 diabetes with milder degrees of hyperglycemia, a Dipeptidyl peptidase inhibitor can be used with correction insulin, Provided there are no contraindications to using any of them. |
This guideline addresses several crucial aspects of care precise for inpatient management of noncritically ill patients with diabetes or newly recognized hyperglycemia that can potentially improve clinical outcomes in the hospital and following discharge. This guideline addresses and updates some of the standards of care for glycemic management for noncritically ill-hospitalized adult patients with diabetes 30 .
Conclusions
Diabetic ketoacidosis is often a severe medical emergency that results in a complication of diabetes. When the diagnosis of diabetic ketoacidosis is made, the blood glucose level is higher than 250 mg/dl, the bicarbonate level is less than 15 mmol/l, the arterial pH is less than 7.3, and there is ketonuria or ketonemia. It occurs primarily in patients with type 1 diabetes. The incidence is roughly two episodes per 100 patient-years of diabetes, with about 3% of patients with type 1 diabetes initially presenting with diabetic ketoacidosis. It can occur in patients with type 2 diabetes as well; however, this is less common. Diabetic ketoacidosis usually occurs due to absolute or relative insulin lack accompanied by increased glucagon, cortisol, growth hormone, and epinephrine. This insulin deficiency enhances hepatic gluconeogenesis, glycogenolysis, and lipolysis leading to severe hyperglycemia, ketoacidosis, and ketonuria.
In most cases, there are precipitating factors, which could be: underlying infection, missed insulin treatment, previously unknown diabetes, surgical stress, etcetera. Prompt diagnosis and treatment are essential to improve patient outcomes. Treatment involves fluid resuscitation, insulin administration to correct hyperglycemia, correction of acidosis, electrolyte imbalances, and treatment of underlying causes or precipitants. The prognosis of adequately treated patients is excellent.
Ethics statement
It was exempted and waived at my institution.
Patient consent
Patient consent was waived due to the minimal risk nature of the observational chart review study.
Sources of funding
All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Authors’ contributions
The author and co-authors played important roles to actualize this article as shown below: C.E.: conceptualization, visualization, supervision, oversight and leadership, writing of the original draft; J.A.D.: conceptualization, validation, writing of the original draft, methodology; A.-O.U.: resources, software, visualization; E.O.E.: conceptualization, validation, resources, methodology; I.C.O.-C.: resource and journal review, formal analysis, writing of the original draft; L.O.U.: writing of the original draft, data creation, project administration; A.I.T.: writing of the article, data curation, leadership; J.O.I.: writing of the article, reviewing and revising the text; A.O. I.: project administration, editing, concept rephrasing; P.U.N.: literature search, writing, and editing; M.O.K.: editing, concept rephrasing, and editing; C.E.: drafting and revising the article; A.I.B.: concept rephrasing and maintenance of data research integrity; O.A.: preparation, typing, editing; O.S.O.: methodology and drafting of conclusion; F.O.J.: project administration, review, and editing; H.I.R.-Y.: editing, concept rephrasing, and editing.
Conflicts of interest
In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Research registration unique identifying number (UIN)
Chukwuka Elendu, E-mail: .moc.oohay@akuwkuhcudnele
Provenance and peer review
Commissioned, externally peer reviewed.
Data availability statement
Institutional review board statement.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Board of the Mayo Clinic (IRB ID: 21-007698).
Informed consent statement
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 23 May 2023

IMAGES
VIDEO
COMMENTS
The research team tracked how well the participants followed the diet through weekly measures of blood ketone levels. (Ketones are acids produced when the body breaks down fat — instead of glucose — for energy.) By the end of the trial, 14 patients had been fully adherent, six were semi-adherent and only one was non-adherent.
It is important to determine whether new dietary changes, such as a ketogenic diet, will positively or negatively affect overall microbiome diversity and species make-up. Some research has found that whole grains play an important role in the development of a healthy microbiome and are necessary for good health [ 21 ].
From toxic by-products of lipid metabolism during diabetic ketoacidosis to a valuable energy source for the brain and heart, emerging research in the past few years has begun to show ketones as ...
The ketogenic diet (KD) is a high-fat, adequate-protein, and very-low-carbohydrate diet regimen that mimics the metabolism of the fasting state to induce the production of ketone bodies. The KD ...
Neuroscience research suggests ketones can enhance cognitive function and protect brain networks. Researchers at the Del Monte Institute for Neuroscience at the University of Rochester have ...
Lopaschuk and Dyck review the bioenergetic and signaling effects of ketones on the cardiovascular system and discuss the potential application of ketones for treating cardiovascular diseases.
New research finds that a continuous, long-term ketogenic diet may induce senescence, or aged, cells in normal tissues, with particular implications for heart and kidney function. But planned ...
Ketones have been termed a "superfuel" for the brain ( ), upon which infants can be especially dependent ( ). Based on these pleiotropic actions, a ketogenic diet has been considered for a wide range of health conditions.
Autism, Alzheimer's and bipolar disorder: Can the development of these mental health conditions be influenced by the ketogenic diet? Increasingly, research suggests it might. "For those it helps ...
Increasing ketone supply to the heart in mice with heart failure with preserved ejection fraction (HFpEF) allowed their hearts to utilize more ketones and produce more energy, according to ...
Therefore, innovative dietary strategies with, perhaps, KD with ketone supplementation may be a favored strategy to increase circulating ketones while reducing insulin concentrations. Studies are needed to determine whether ketone supplements alone are sufficient, and at what dose and timing, to improve cancer and cancer-related outcomes. Go to:
New research finds that people on a low-carb, high-fat diet have a higher risk of developing a major cardiovascular event.
Based on available evidence, a well-formulated ketogenic diet does not appear to have major safety concerns for the general public and can be considered a first-line approach for obesity and diabetes. High-quality clinical trials of ketogenic diets will be needed to assess important questions about their long-term effects and full potential in ...
As to the most exotic claims from health and diet gurus - such as keto diets resulting in euphoria, cognitive boosts, and improvements in anything from kidney function to cancer treatment - "We just don't have the data on that yet," said Weiss. The researchers agree that the diet itself isn't inherently dangerous.
A new UC Davis Health study found that a ketogenic (keto) diet improves muscle function in older animals by preventing muscle mass loss due to age ( sarcopenia ). The lead author of the study is the molecular exercise physiologist Keith Baar, a professor in the Departments of Neurobiology, Physiology and Behavior and of Physiology and Membrane Biology.
Exploring the pleiotropic physiological and signaling properties of ketones and investigating the underlying mechanisms thereof are exciting new areas of research that promise insight into the molecular, cellular, and therapeutic effects of intermittent fasting, time-restricted feeding, ketogenic diets, and exogenous ketone supplementation. The Editors of AJP-Cell Physiology extend an ...
This research highlights potential ketone-based therapies for neurodegenerative diseases. Key Facts: Acute insulin resistance in the brain impairs synaptic activity, axonal conduction, and network synchronization. Administering ketones like D-βHb can restore these critical neuronal functions. This research suggests new therapeutic avenues for ...
Research Highlights: In mice with heart failure with preserved ejection fraction (HFpEF), increasing ketone supply to the heart allowed their hearts to utilize more ketones and produce more energy. Researchers hope this study may help to improve our ...
Just looking at the scale, the keto diet seems like a success, but what happens inside bodies tells a different story. The latest evidence-based research.
The authors present an overview of the metabolism and pleiotropic actions of ketone bodies, summarizing their endogenous sources, signalling mechanisms and systemic metabolic effects.
Increasing ketone supply to the heart could enhance energy production in cases of heart failure with preserved ejection fraction (HFpEF).
Angewandte Chemie International Edition is one of the prime chemistry journals in the world, publishing research articles, highlights, communications and reviews across all areas of chemistry.
Ingesting exogenous ketone bodies has been touted as producing ergogenic effects by altering substrate metabolism; however, research findings from recent studies appear inconsistent. This systematic review aimed to aggregate data from the current literature to examine the impact of consuming ketone supplements on enhancing physical performance.
Unlike existing azaryl-ketone-based emitters, PQMO-PXZ exhibits red-shifted emission and enhanced luminescence efficiency, due to its rigid structure and strong intramolecular charge transfer characteristics. Significantly, PQMO-PXZ demonstrates pronounced AIE properties and TADF with a short delayed lifetime.
More adults are choosing not to have children, new data shows. Experts share the reasons behind it and how to deal with the pressure from others.
Federal prosecutors in California on Friday charged prominent investor Andrew Left with multiple counts of securities fraud.
The prominent A.I. start-up said it planned to eventually fold the new technology into its popular online chatbot, ChatGPT.
Multimillionaires are much happier than the merely well off, suggesting life satisfaction continues to improve the wealthier you are.
People generalize to form beliefs about a large language model's performance based on what they've seen from past interactions. When an LLM is misaligned with a person's beliefs, even an extremely capable model may fail unexpectedly when deployed in a real-world situation.
DKA is common in people with type 1 diabetes. Diabetic ketoacidosis is a grievous complication of diabetes that occurs when there is a lack of insulin in the body, resulting in elevated blood glucose levels and the production of ketones. Diabetic ketoacidosis is a medical emergency that requires immediate treatment, as it can lead to life ...