An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Euthanasia and assisted suicide: An in-depth review of relevant historical aspects
Affiliations.
- 1 Medical and Surgical Research Center, Future Surgeons Chapter, Colombian Surgery Association, Bogotá, Colombia.
- 2 Grupo Prometheus y Biomedicina Aplicada a las Ciencias Clínicas, School of Medicine, Universidad de Cartagena, Cartagena, Colombia.
- 3 Department of Medicine, RedSalud, Santiago de Chile, Chile.
- 4 Department of Medicine, Keralty Salud, Bogotá, Colombia.
- 5 Colombian Clinical Research Group in Neurocritical Care, Latin American Council of Neurocritical Care, Bogotá, Colombia.
- 6 Department of Intensive Care, Regions Hospital, Minnesota, USA.
- 7 Independent University, Dhaka, Bangladesh.
- PMID: 35242326
- PMCID: PMC8857436
- DOI: 10.1016/j.amsu.2022.103380
End-of-life care is an increasingly relevant topic due to advances in biomedical research and the establishment of new disciplines in evidence-based medicine and bioethics. Euthanasia and assisted suicide are two terms widely discussed in medicine, which cause displeasure on many occasions and cause relief on others. The evolution of these terms and the events associated with their study have allowed the evaluation of cases that have established useful definitions for the legal regulation of palliative care and public policies in the different health systems. However, there are still many aspects to be elucidated and defined. Based on the above, this review aimed to compile relevant historical aspects on the evolution of euthanasia and assisted suicide, which will allow understanding the use and research of these terms.
Keywords: Assisted suicide; Bioethical issues; Euthanasia; History of medicine; Terminal care.
© 2022 The Authors.
PubMed Disclaimer
Conflict of interest statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
- Marín-Olalla F. Euthanasia: a 21st century right. Gac. Sanit. 2018;32(4):381–382. - PubMed
- Parreiras M., Antunes G.C., Marcon L.M.P., Andrade L.S., Rückl S., Andrade V.L.Â. Eutanásia e suicídio assistido em países ocidentais: revisão sistemática. Rev Bioét. 2016;24(2):355–367.
- Brandalise V.B., Remor A.P., Carvalho D de, Bonamigo E.L. Suicídio assistido e eutanásia na perspectiva de profissionais e acadêmicos de um hospital universitário. Rev Bioét. 2018;26(2):217–227.
- Agencia estatal Boletín Oficial del Estado Ley Orgánica 3/2021. https://www.boe.es/eli/es/lo/2021/03/24/3 de 24 de marzo, de regulación de la eutanasia [Internet]. 2021 [Cited 28 Dec 2021]. Available in:
- Á Ramis. https://www.biobiochile.cl/noticias/opinion/tu-voz/2021/01/19/libertad-y... Libertad y muerte digna en Chile [Internet]. BioBioChile. 2021 [Cited 28 Dec 2021]. Available in:
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Elsevier Science
- Europe PubMed Central
- Ovid Technologies, Inc.
- PubMed Central

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 21 May 2024
Ethical perspectives regarding Euthanasia, including in the context of adult psychiatry: a qualitative interview study among healthcare workers in Belgium
- Monica Verhofstadt 1 ,
- Loïc Moureau 2 ,
- Koen Pardon 1 &
- Axel Liégeois 2 , 3
BMC Medical Ethics volume 25 , Article number: 60 ( 2024 ) Cite this article
2125 Accesses
8 Altmetric
Metrics details
Introduction
Previous research has explored euthanasia’s ethical dimensions, primarily focusing on general practice and, to a lesser extent, psychiatry, mainly from the viewpoints of physicians and nurses. However, a gap exists in understanding the comprehensive value-based perspectives of other professionals involved in both somatic and psychiatric euthanasia. This paper aims to analyze the interplay among legal, medical, and ethical factors to clarify how foundational values shape the ethical discourse surrounding euthanasia in both somatic and psychiatric contexts. It seeks to explore these dynamics among all healthcare professionals and volunteers in Belgium.
Semi-structured interviews were conducted with 30 Dutch-speaking healthcare workers who had encountered patients requesting euthanasia for psychiatric conditions, in Belgium, from August 2019 to August 2020. Qualitative thematic analysis was applied to the interview transcripts.
Participants identified three pivotal values and virtues: religious values, professional values, and fundamental medical values encompassing autonomy, beneficence, and non-maleficence, linked to compassion, quality care, and justice. These values interwove across four tiers: the patient, the patient’s inner circle, the medical realm, and society at large. Irrespective of their euthanasia stance, participants generally displayed a blend of ethical values across these tiers. Their euthanasia perspective was primarily shaped by value interpretation, significance allocation to key components, and tier weighting. Explicit mention of varying ethical values, potentially indicating distinct stances in favor of or against euthanasia, was infrequent.
The study underscores ethical discourse’s central role in navigating euthanasia’s intricate landscape. Fostering inclusive dialogue, bridging diverse values, supports informed decision-making, nurturing justice, and empathy. Tailored end-of-life healthcare in psychiatry is essential, acknowledging all involved actors’ needs. The study calls for interdisciplinary research to comprehensively grasp euthanasia’s multifaceted dimensions, and guiding policy evolution. While contextualized in Belgium, the implications extend to the broader euthanasia discourse, suggesting avenues for further inquiry and cross-cultural exploration.
Peer Review reports
Medical assistance in dying is allowed in 27 jurisdictions in the world and if so, it is mainly restricted to the terminally ill (see BOX 1 in OSF) [ 1 ]. Medical assistance in dying entails that a patient’s death request can be granted via euthanasia , defined as the intentional termination of life by a physician at the patient’s explicit request, which is currently decriminalised in Australia, Belgium, Canada, Colombia, Luxembourg, the Netherlands, Spain, and New Zealand. In addition, it can be granted by means of assisted suicide , also defined as the intentional termination of life by a physician at the patient’s explicit request, but in these cases, the lethal drugs are provided by a physician and self-administered by the patient at a time of the latter’s own choosing (e.g., Australia, Austria, Switzerland, United States). In some countries, not only a physician, but also a nurse practitioner can be involved in the procedure (e.g., Canada, New Zealand).
Euthanasia has been legal in Belgium since 2002, positioning the country as a pioneer in this field with two decades of euthanasia practice [ 2 ]. According to Belgian legislation, individuals can be deemed eligible for euthanasia when they are, among other criteria, in a medically futile state characterized by constant and unbearable physical or psychological suffering resulting from a serious and incurable disorder caused by accident or illness [ 2 ]. Belgium is one of the few countries that does not exclude people from assisted dying who suffer predominantly from irremediable psychiatric conditions (see BOX 2 in OSF for all legal criteria in Belgium). As regards prevalence, euthanasia accounted for up to 3.1% of all registered deaths in 2023 in Belgium [ 3 ]. Whereas most registered euthanasia deaths concerned the terminally ill (approximately 84%), predominantly suffering from cancer, only 48 or 1.4% of euthanasia deaths concerned non-terminally ill adults predominantly suffering from psychiatric conditions. Since euthanasia was legalised, in total 457 such euthanasia cases have been reported, less than 1.5% of all registered euthanasia cases in Belgium [ 3 , 4 , 5 , 6 , 7 , 8 , 9 ].
However, this is only the tip of the iceberg, as there is reason to believe that the total number of requests for euthanasia in Belgium (regardless of outcome), is at least 10 times higher. For instance, recent annual reports from Vonkel, an end-of-life consultation centre in Belgium, revealed around 100 unique patients per year applying for euthanasia for psychiatric reasons. Less than 10% of those euthanasia requests were reported to be carried out [ 10 , 11 , 12 ]. Moreover, a recent survey among psychiatrists working in Flanders, Belgium, revealed that 8 out of 10 respondents had been confronted at least once throughout their career with patients requesting euthanasia for psychiatric reasons [ 13 ]. The survey also showed that, although three-quarters are supportive of not excluding the option of euthanasia for this specific patient group [ 14 ], the majority is hesitant to be actively engaged in a euthanasia procedure [ 13 , 14 ]. The literature ascribed the reluctance to the complexity of euthanasia assessment in this patient group, inherently high in professional and emotional demands [ 15 , 16 , 17 , 18 , 19 ]. The complexity was for a large part described in terms of the practical considerations surrounding euthanasia requests and assessment, e.g., whether and when these patients can meet the legal criteria.
There is thus reason to believe that healthcare workers’ overarching ethical considerations influence their attitudes on euthanasia in general and in the context of psychiatry specifically, and their practice. As empirical in-depth studies are lacking, this area is largely understudied. To date, only two recent qualitative studies among Dutch physicians emphasised the value-based reasons for euthanasia decision-making, but did not [ 20 ] or only summarily [ 21 ] scratch the specific context of psychiatry. Another recent qualitative study among Dutch physicians, including psychiatrists, emphasized the value-based reasons for supportive attitudes towards euthanasia, e.g. the value of self-determination, compassion, fairness, and suicide prevention, versus the value-based reasons for not supporting euthanasia, e.g. the mission of medicine of hope and healing [ 22 ]. Furthermore, a recent systematic review described the main ethical challenges surrounding the euthanasia practice in the context of psychiatry [ 23 ]. However, this ethical debate was mainly concentrated on the permissibility and implementation of euthanasia from a practical-clinical point of view, e.g. whether euthanasia in the context of psychiatry should be permitted, and why the legal requirements can (not) be adequately embedded in the field of psychiatric medicine. How practically and juridically relevant these considerations may be, they remain the outcome of ethical values being weighed up, which means that no single consideration can be considered ethically irrelevant, neutral, or value-free. Moreover, the review was based on articles that have been selected in a timeframe in which sound empirical data regarding euthanasia in the context of psychiatry were largely lacking.
Also, the overarching value-based views of other professionals involved in psychiatric euthanasia practice have not yet been studied. This is striking, as a recent Belgian survey study revealed that that half of the psychiatric nurses (53%) are frequently and directly confronted with such euthanasia requests [ 24 ], but in-depth insights into their value-based views are lacking. Furthermore, there are many more formal caregivers, other than psychiatric nurses, involved in euthanasia assessment procedures. End-of-life centres employ e.g., paramedical personnel such as psychologists, psychiatric nurses for intake and registration purposes, and well-trained volunteer personnel such as buddies, entrusted with the task to help these patients to cope with the euthanasia procedure. In addition, rehabilitation-oriented support groups (REAKIRO) were established to help these patients (and their relatives) in walking the tightrope of life and death [ 25 ]. All of these caregivers may also have an unacknowledged but influential role in these euthanasia assessment procedures, and therefore, an interesting perspective to reflect on euthanasia legislation and practice. Gaining insight into healthcare workers’ ethical considerations related to euthanasia in psychiatry will lay bare the ethical foundations underlying current practice and is important to inform and spark further debate around this extremely thorny issue, and to promote sound ethical analysis.
Hence, the purpose of this research is to explore healthcare workers’ ethical considerations regarding euthanasia in general and euthanasia concerning adults suffering predominantly from psychiatric conditions in particular.
Theoretical research framework
Our research was guided by the framework of ‘critical social constructionism’ [ 26 ], providing a nuanced perspective that diverges from the acknowledgment of an objective reality. This approach intricately examines the interplay of personal, social, and societal dimensions within the phenomena under study. It necessitates an acknowledgment of the layered complexities influencing our understanding of phenomena such as euthanasia, a notion supported by both our prior research [ 27 ] and additional studies [ 23 , 28 ].
Our interpretation of the data was informed by social constructionism, which recognizes the role of internalized societal norms in shaping individuals’ perceptions of reality over time. Furthermore, we embraced a contextualist epistemology [ 29 ], acknowledging the contextual influence on knowledge formation among both researchers and participants. This methodological approach aimed to capture diverse lived experiences (e.g., diversity in clinical and euthanasia trajectories) and perspectives, including varied attitudes toward euthanasia based on specific relationships (e.g., professional healthcare worker or volunteer). Consequently, we maintained a reflexive stance regarding the potential impact of our individual experiences and identities on our analyses and interpretations, as elaborated in the Ethical Considerations section.
Study design
The qualitative research design consisted of semi-structured face-to-face interviews with healthcare workers in Flanders and Brussels, Belgium.
Participants
All participants were Dutch-speaking and had at least one concrete experience with euthanasia requests and procedures concerning adults with psychiatric conditions in the period 2016–2020, either as professional or volunteer healthcare workers. We adopted a broad recruitment approach, with a particular focus on all healthcare providers directly involved in medical practice rather than in managerial or policy-making roles. No further exclusion criteria were employed.
Recruitment and interview procedure
Purposive sampling was used to ensure diversity and heterogeneity in terms of: participants’ affiliation with institutions holding different stances on ‘euthanasia and psychiatry’; being to a different extent confronted with these euthanasia procedures as regards the amount of experiences (sporadically versus regularly); the nature of the experiences (e.g. confronted with or engaged in euthanasia procedures that were still under review or that had been rejected, granted, performed or withdrawn); and their specific role as professional or volunteer healthcare worker.
Participants were recruited via assistance of our contact persons at: (1) the end-of-life consultation centre Vonkel; (2) the Brothers of Charity; (3) the rehabilitation-oriented centre REAKIRO in Louvain; and (4) the Review Belgian Euthanasia Law for psychological suffering (REBEL) group, a group of Belgian physicians (e.g. psychiatrists), therapists (e.g. psychologists) as well as academics who express their concern on euthanasia in the context of psychiatry via the media. Participants were also recruited via a notice on the sites, newsflashes and/or in the online newsletters of LEIF (Life End Information Forum), Recht op Waardig Sterven (the Flemish Right to Die with Dignity Society) and Vlaamse Vereniging voor Psychiatrie (Flemish Psychiatric Association).
Potential participants contacted MV or a study assistant by phone or mail. The patients were then given an information letter and informed consent form that consisted of 2 main parts. All interviews were conducted by MV or a study assistant, who both have experience in conducting interviews on end-of-life topics. Interviews were held at the participant’s location of choice, except for five interviews which were held online via video call by Whereby 14 due to the Covid-19 crisis lockdown regulations. Interviews lasted between 55 min and 2 h, and were audio recorded (the online video interviews were recorded by Whereby’s software and immediately transferred in an mp.3 format).
Measurements
The interview guide (see OSF) contained the following consecutive questions of importance to the present report: (1) What is your personal stance regarding euthanasia as a legalised medical end-of-life option? and (2) What is your personal stance regarding euthanasia in the context of psychiatry?
Data management and analysis
We used a model of sampling-based saturation, namely inductive thematic saturation, that relates to the emergence of new themes (defined as 7 consecutive interviews without new themes) [ 30 ]. We continued to recruit and conduct interviews so that the sample would be heterogenous in terms of socio-demographics, clinical profile, and clinical setting. In particular, our focus was on recruiting individuals with the following profiles: psychologists, male psychiatric nurses and moral consultants/spiritual caregivers employed in residential psychiatric settings ( n = 5).
All interviews were then transcribed verbatim and de-identified by the interviewers.
We made use of hybrid inductive and deductive coding and theme development by means of a 2-staged process. Stage 1 consisted of an inductive data-driven thematic coding procedure.
We made use of these four phases; (1) identification and coding of all transcripts; (2) the placing of the codes in subthemes, i.e., arguments in favour versus critical concerns; (3) the placing of these subthemes in overarching main themes, i.e., different stakeholders (patient/medicine/society); (4) the comparison and discussion of the findings (with all co-authors). In addition to the inductive approach, we also used a deductive, theory-driven template approach during stage 2. We made use of these four phases; 1) the development of an ethical interpretation framework (see OSF). The framework consists of four key concepts, each involving a multitude of ethical concepts: (a) ethical theories and methodologies, (b) ethical values, (c) basic ethical virtues, and (d) dialogue/decision making ethics; 2) the identification of codes that fit the ethical framework and the theory-driven renaming of these codes; 3) the placing of some of the subthemes in an additional main theme; and 4) the comparison and discussion of the findings (with all co-authors).
Ethical considerations
The research team comprised two experienced clinical psychologists, one specializing in euthanasia within the cancer patient population and the other skilled in conducting interviews on this sensitive topic within the adult psychiatric context. Additionally, two ethicists with expertise in assisted dying, including euthanasia, were part of the team. Some authors also have backgrounds in psychiatric practice, including outpatient and residential settings, while others bring expertise through personal experiences. Furthermore, all contributing authors have personal and/or professional connections with individuals navigating death ideation, offering diverse perspectives on euthanasia. Additionally, some authors hold religious beliefs, while others maintain a more agnostic stance. These perspectives vary depending on the predominant viewpoints adopted—whether that of the patient, a close relation, a clinician, an ethicist, or policy stances. To mitigate potential undue influence on data interpretation, three team assemblies were convened. These sessions served to share firsthand encounters from interviews and their outcomes, fostering reflection and deliberation among team members. This proactive measure was implemented to prevent both personal and professional biases from affecting the interpretation of the data.
The main characteristics of the 30 participants are listed in Table 1 . The sample consisted of 16 physicians, 7 other care professionals (ranging from psychiatric nurses to mobile support teams), and 7 volunteers, all of whom were engaged in one or more euthanasia procedures predominantly based on psychiatric conditions.
The participating physicians held various roles regarding the handling of euthanasia requests:
1 physician refused to discuss the request with the patient on principle grounds.
7 physicians managed the clarification of euthanasia requests from their own patients or referred them to colleagues for further clarification.
10 physicians provided one of the two legally required formal advices or an additional advice on the euthanasia request.
5 physicians performed the act of euthanasia.
3 physicians held a more normative, dissuasive stance against euthanasia in the context of psychiatry but were willing to explore and discuss the euthanasia request with the patient.
The sample further included 14 non-physicians, among them members holding one or more roles:
2 members were part of mobile teams providing psychiatric care and support in the patient’s home setting.
3 were psychiatric nurses working either in a general hospital or in a psychiatric residential setting.
2 were Experts by Experience, individuals with a history of mental distress trained to provide support for individuals new to the euthanasia procedure and/or rehabilitation approaches.
3 were buddies, individuals entrusted with assisting and supporting the patient throughout the euthanasia procedure.
3 were moral consultants/spiritual caregiver, tasked with offering various forms of existential guidance and support to patients considering euthanasia, including religious, moral, and/or other perspectives.
5 were consultants at end-of-life information and/or consultation centers responsible for patient intake.
Participants’ ethical considerations regarding euthanasia, in the broadest context of medicine
As can be seen from the coding structure in Table 2 , we ordered coding categories on the level of 1) the individual patient, 2) the patient’s social inner circle, 3) the (para)medical field, and 4) the society. Note that words used verbatim by the interviewees (often interview fragments instead of quotes, as to better illuminate the complexities and nuances of interviewees’ first-hand lived experiences) from the transcribed interviews are incorporated that provide both additional insightful details and reveal the at times interwoven nature of the analysed codes.”
The level of the individual patient
On the level of the individual patient, the following five ethical considerations were distinguished: (1) autonomy, (2) dignity, (3) quality of life, (4) compassion, and (5) the meaning and transformative value of suffering.
First, Autonomy was a recurrent theme in all the interviews. Some participants expressly valued individual autonomy , and more specifically its following two underpinning characteristics: (1) self-determination in terms of the fundamental right for each individual to direct the course of one’s own life, which also includes ‘taking control over the timing and circumstances of one’s end-of-life’, and (2) freedom of choice , as they strongly believed that individuals are free to choose what meaning and purpose they assign to their lives. According to them, as each individual should be enabled ‘to live according to one’s own value system’, so should the ending of one’s life also be congruent with one’s own value system. Hence, in their opinion, euthanasia should remain ‘one of the many options to die’.
Other participants called this individualistic approach of autonomy ‘unrealistic’ or even ‘delusional’, as it shies away from: (1) the relational account of autonomy, in which a true autonomous decision was seen as the outcome of a decision-making process which is shaped by individual, social and contextual components, and (2) the internalised downside of autonomy, as the feeling underpinning many euthanasia requests, namely ‘not wanting to be a burden to others’ may lead to ‘self-sacrifice’ and ‘the duty to die’ under the false pretence of autonomy. In addition, some pointed to the power of susceptibility and subliminality, as human beings are subliminal creatures whose behaviour is continuously influenced on both a subconscious and even conscious level. Consequently, internalised pressure cannot be excluded when a patient requests euthanasia. One psychiatrist even stated that ‘ there exists no such thing as a free will, as human beings are always manipulated in many areas of human life and functioning’ .
“I believe that that there should still be places in society where you could die without considering euthanasia. While many people today are facing dementia, and you almost must…. Interviewer: Yes. “Yes, like how should I deal with it? Should I exit life before it becomes inevitable dementia or something similar? Because I think that in a neo-liberal society, many people internalize the idea that at some point, it becomes a moral duty to step aside. They feel obliged to eliminate themselves. Self-elimination. In a neo-liberal model, as long as you can keep up and contribute, everything is fine. But if you can’t keep up, well, if you cannot fully exercise autonomy, then… Essentially, you should hold your honour and step aside.” (spiritual caregiver)
Second, participants mentioned euthanasia as an option to die with dignity . For those in favour of the Law, euthanasia is considered (1) a ‘dignified way of dying’ when everything that leads up to death, including individual, medical, and social needs and expectations, is consistent with one’s own sense of integrity, belief-system and lifestyle, and (2) a ‘good death’, when referring to the literal meaning of the concept ‘euthanasia’, namely ‘a soft and gentle passing’. Other participants raised concerns on the reference to euthanasia and dignified dying in the same breath, as if “ other ways of dying are not or less dignified ”.
Third, the value of quality of life underpinned the arguments made in favour of the Law on Euthanasia, as (1) life itself should not be prolonged unnecessarily, (2) meaningless suffering should be prevented, and (3) a good life should pertain to all stages in life, from the very beginning until the very end, which is feasible if quality of dying circumstances can be guaranteed. As one buddy stated: “ Living a full and good life implies dying a good death ”. Other participants made use of this value underpinning their argument against euthanasia, based on (1) the “protect-worthiness” of life itself and (2) the suffering that must be considered an inherent feature of the human condition.
Fourth, and seamlessly fitting with the former value, divergent courses also emerged regarding the aspect of how to deal with suffering . Some participants were in favour of euthanasia out of compassion in terms of (1) bringing a kind of relief to the patient when providing her the prospect of an end to the suffering and (2) ending the suffering once it has become ‘useless and meaningless’ and ‘disclosing the limits of the carrying capacity of the self’. Some participants referred to the insufficient degree of quality of life in some patients and valued euthanasia as sort of ‘ compensation for a life gone wrong’.
Others considered the option of euthanasia as compromising patients’ ability to accept, bear and cope with suffering experiences by offering the opportunity ‘to quickly resign from it’.
Some participants referred to the dynamic features and hence, the potential enriching value of suffering. They believed that one can and must revolt against the perception of pointless suffering, as suffering may offer unique opportunities to achieve personal growth through the realisation of self-actualising tendencies amidst the suffering and though all kinds of hardship and adversity in life. Therefore, the real challenge is to support the sufferer to (re)gain the ability to transform the suffering by means of redefining, accepting, and making sense of it. One psychiatrist referred to the Myth of Sisyphus and stated:
A rock that must be pushed up the mountain, which is terrible, and then Sisyphus lets the rock fall back down, and he must start all over again. And what is the purpose of that suffering? Pushing the rock up? It’s absurd, really, but still. I find it so vital, human, uh, yes. That is something that inspires me enormously and often makes me, well, yes, vitality and suffering, suffering is inherent to being, of course, and one can suffer, of course, that is very serious suffering, terrible suffering. I know that. But well, accept suffering, right? I’m not glorifying suffering, no, I don’t belong to that category. Some Catholics do that; the suffering of Christ, we must… No, not at all. Suffering is inherent to life. Interviewer: It’s just more bearable for some than for others. Interviewee: Then it’s our task to make it more bearable. Yes. (…) Look, that sets a dynamic in motion. By dynamic, I also mean movement. A euthanasia request is often rigid. I am for movement. That’s what Eastern philosophy teaches us too, that everything moves, and we must keep that movement and that the question may change or that people may also discover things. Or indeed, a suffering that is even more exposed, but on which one can then work. There is still much to do, yes, before the ultimate and final act of euthanasia, by a doctor for all sakes, should be considered. (psychiatrist)
The level of the patient’s inner circle
On the level of the social inner circle, the following three ethical considerations were distinguished: (1) involvement, (2) connectedness, and (3) attentiveness.
Some participants stressed that euthanasia can only be a soft and thus ‘good’ way of dying, if the patient’s social inner circle can be involved in the euthanasia procedure and if sufficient support to them can be provided. All participants in favour of the legal framework on euthanasia echoed the importance of the social circle being involved in an early stage of the euthanasia procedure, as the prospect of the end of life may challenge a patient’s ability of staying and feeling connected . If the euthanasia request is to be carried out, it offers a unique opportunity for both the patient and her social inner circle of consciously being present and sharing goodbyes. Other participants considered this reasoning as potentially deceiving, as concern was raised regarding the trap of false assumptions, in terms of words being left unspoken and the bottling up of one’s own needs for the sake of the other.
As the third doctor, I was asked to provide advice about someone, and the [adult child] was present, a charming [adult child]. The [adult child] was also very friendly but didn’t say much. The man explained why he himself wanted euthanasia and so on. To be honest, at first, I thought, “Well, this won’t take long,” because there were many arguments and reports I had received, but as the conversation went on, I started to feel something different. It turned into a very long conversation, during which the [adult child] also had their say. In short, the father believed that he couldn’t burden his children. He was a kind man who knew what he wanted, and his children were inclined to follow his idea, to follow his vision. However, the children thought, “Yes, we are actually going to agree with our father, and we’ll allow it,” but deep down, they still wanted to take good care of him. The father didn’t want them to take care of him, and there were many other things, but after that long conversation with the [adult child] and the father, and everything else, like, “We’ll still celebrate Christmas together,” there was a complete turnaround. The other physicians involved accepted this very well, and they said, “Okay, for us, it wasn’t clear. (physician)
In addition, concern was raised regarding the inner circle’s respect of individual patient autonomy and freedom of choice outweighing their r esponsibility and accountabilit y to take care for one another and to act according to all these subjects’ best interest.
Consequently, divergent discourses on the virtue of attentiveness emerged. Whereas for some, the euthanasia procedure may offer a unique opportunity for both the patient and her relatives to be better prepared for death and for the bereaved to better cope with grief, others pointed to the inner circle’s continued grappling with unresolved feelings and perceived helplessness after such a fast-track to death.
Yes, and sometimes I also see people, family members after such euthanasia, yeah, I’ve experienced it several times. They say things like, “Yes, I supported it, but I didn’t know it would affect me like this,” you know? They try to convince themselves, saying, “It was good, it was good, and I stand behind it.” Yeah, you are hardly allowed to do otherwise, but you feel that inner struggle in them, you know? Like, “Was it really okay?” But you can’t question it because you think, “Poor them,” but you still feel it, like, “How sad, how sad. (psychiatrist)
The level of medicine
The following five ethical considerations were distinguished: (1) professional duties, (2) responsibility to alleviate suffering, (3) subsidiarity, (4) professional integrity, and (5) monologic versus dialogic approaches.
First and as regards professional duties, it was (only) reported by some physicians that the physician’s duty is “ to provide good care, which includes good end-of-life care ”. Hence, physicians are the ones who should have euthanasia “as a tool in their end-of-life toolbox”. Others held a different stance and referred to Hippocrates’ Oath when stating that the physician’s duty is to save life at all costs.
Second, all the participants agreed that clinicians have the responsibility to alleviate the patient’s suffering . Whereas some welcomed the option of euthanasia due to the experienced limits of palliative care, that in some cases is deemed an insufficient response to intractable suffering, others stated that euthanasia is not needed as physicians have proper palliative care in their toolbox to alleviate all kinds and degrees of suffering.
Third and as regards the subsidiarity principle , opinions differed on the use of a palliative filter, i.e., whether a consultation with specialist palliative care units should precede euthanasia.
Fourth and as regards professional integrity , some participants relativized the physicians’ executive autonomy. As one psychiatrist stated “because in the end, we do not decide whether someone might die or not. We only decide whether we want to be of help and assist in it.” All the ones in favour of the current legal framework echoed that as physicians are the ones that have better access to the lethal drugs and the technical expertise to end the patient’s life in more efficacious ways than non-physicians, they should remain entrusted with euthanasia assessment procedures. Others (only physicians) criticized the Belgian legislator for placing too much power in the physicians’ hands so that the latter “ can play for God instead of using their pharmacological and technical know-how to save lives ”.
Fifth, and as regards the decision-making process, most participants valued the ethical principle of shared decision-making between the patient and her physicians, and some even preferred a triadic dialogue in which the patient, her relevant health carers and her social inner circle is involved in euthanasia assessment procedures. For most of them, this type of extended or relational autonomy is considered as best clinical euthanasia practice, especially when death is not foreseeable. According to some non-physicians, a strict dyadic patient-physician approach is to be preferred when death is reasonably foreseeable in a patient with sufficient mental competence. In this event, no intermediary should be tolerated as the medical secret is considered ‘sacred’. One participant elaborated further on this strict dyadic approach and said:
“ But actually, in my opinion, the request for euthanasia is something between two people. So…. Interviewer: The singular dialogue? “So, a relationship between the patient and the doctor, yes. That’s what I think. And I do understand that the legislation exists, primarily to protect the doctor against misuse or accusations, because euthanasia used to happen before too, but in secret. But for me as a doctor, it would be enough if a patient whom I’ve known for years, followed for years, maybe 20 years, 30 years, 40 years, and who is terminally ill, asks me in private, ‘I want it.’ For me, it doesn’t need to be more than that for me to say, ‘yes.’ So, there’s no need for a whole set of legislation, except of course to protect myself, maybe from the heirs who might have a different idea about it, yes, but I find it beautiful. And they say, you know, our legislation is such that you can write your euthanasia request on the back of a beer coaster and that’s enough, you know? But how it used to be, euthanasia happened just as well, that’s what I heard from my older colleagues. But it was done in private. Actually, that is the most beautiful sign of trust between a doctor and a patient. ” (Physician and consultant)
Others, all physicians without a favourable stance on euthanasia, considered medical paternalism morally justified in the end-of-life context, as (1) physicians have more intimate knowledge of the patient and are thus best placed to act in the patient’s best interests, (2) only the independent evaluation from well-trained and experienced physicians may rule out external or internalized pressure from the patient’s social inner circle, and (3) some patients may show impaired decision-making capacity when confronted with the end of life.
The level of society
As regards the origins and impact of euthanasia legislation on the level of society, the following four ethical themes emerged: (1) protection, (2) dignified dying, (3) solidarity, and (4) distributive justice.
First and as regards protection , some participants valued the existence of a legal framework for an ‘underground’ practice before 2002. According to them, this framework was highly needed to protect the patient against malicious practices and the physician against being charged for murder when ensuring herself that all the legal requirements are met.
So, I believe that it should be well-regulated in a state. In a country, it should be well-regulated. You can either be in favour of it, have reservations, or question it, but when it happens and many people want it or think it’s okay, then it should be regulated. And those, like me, who may be against it, have doubts about it, or wonder, “Is this really necessary?” I would say, or “Does it align with our purpose?” the existential comments that you can make about it, we must accept it because it would be terrible if it, well, it would be even worse if it happened in the underground, like before those laws were established, that’s, yeah. So, I think the laws should exist. Whether I would have made those laws is a different question, or whether I would vote for the parties in parliament that, you know, that support it, that’s another question, but apparently, here in North-western Europe, the need for those practices exists, and it should be regulated properly. And yes, it shouldn’t be left to amateurs or something like that, that’s not the intention. Yes, well, it serves to protect, both in terms of health and to ensure that it doesn’t become a business, of course. I’d prefer it to be integrated into the healthcare system rather than turning it into a profit-driven and exploitative affair for some others. So, that’s…. (psychiatric nurse)
Critical concerns were raised on the lack of protection of the most vulnerable people, i.e., the mentally ill and the elderly. Some of them referred to the amended Law in 2014, that also allowed minors to die by means of euthanasia – be it under more strict circumstances, inter alia, when based on unbearable physical suffering resulting from a medically terminal condition – and feared that the Law will be amended again, so it would no longer exclude the people suffering from dementia or for groups without serious incurable illness, e.g., the elderly with a perceived ‘completed life’.
Second, a major societal shift in thoughts regarding what constitutes dignified dying was reported. For some, the Law on Euthanasia reflects a nascent movement of death revivalism, in terms of people reclaiming control over their dying process. In this respect, euthanasia is deemed a counterreaction to the former dominant paternalistic attitude in Western society to systematically marginalise conversations on death and dying, e.g., due to the mechanisms of denial, avoidance, and postponement, and with the line between life and death increasingly held in physician’s hands, which has left many people ill-equipped to deal with dying and death. The current broad public support for euthanasia is seen as the individual patient taking back the decision-making process of dying and death in her own hands. They further considered euthanasia as a logical consequence of living an artificially prolonged life due to e.g., advances in medicine, that have not necessarily enhanced the quality of life.
“ One thing I also consider is that a part of our lives is artificially prolonged, you know. We don’t live longer because we are healthier, but because we have good pills or better surgical procedures, so we can afford to buy our health. So that part of life is still valuable to me, it’s not less valuable, but it’s artificially extended. So, I think we should keep that in mind, that we can prolong something artificially and maybe even go beyond a point where it no longer works. Interviewer: Beyond the expiration date? That’s what I was looking for (laughs). So, in that sense, I believe we should keep in mind that we can artificially extend something and then maybe, even if it’s just that artificial part, stop or be allowed to stop when the person no longer wants to, I think that makes perfect sense. ” (psychiatrist)
Others provided arguments against the increased death revivalism, referring to euthanasia as a ‘fast-track to death’ resulting in ‘the trivialisation of death’ in the face of formerly known and experienced Art of Dying. For instance, the current societal tendency to avoid suffering and the fear of dying may lead to patients (too quickly) resigning from a slow track to death, in which there is time to e.g., hold a wake.
But I won’t just grab a syringe, fill it up, and administer a lethal injection, you know? I follow the symptoms. And if they become uncomfortable, then I’ll increase the dosage so they can rest peacefully and not have to suffer. That’s what I call a dignified death. And if the family can be present, sometimes it takes a while for them to arrive, and they’ll say, “Come on, even a dog is not allowed to suffer that long.” Meanwhile, the person is just lying peacefully. But that too. Everything should, even that, should progress, and there isn’t much time left for vigil and, yes, I don’t want to romanticize it, but sometimes you see so much happening between families. There’re all kinds of things happening in those rooms, with the family, reconciliations being made. Memories being shared. “Oh, I didn’t know that about our father.“, an aunt walking in and telling a story. Well, so much still happens. I don’t want to romanticize it, but to say that all that time is useless, that’s not true either. And at the farewell, there’s always, the time, you think there’s time for it, but people are still taken aback when an infusion is given, that it can happen within a minute, even if they’re behind it and have been informed beforehand. Just a minute… and it’s done. The banality of death, it’s almost like that. (psychiatrist)
These and other participants also criticised ‘the romanticised image of euthanasia’, that masks the economics of the death system, taking financial advantage of ‘patients not wanting to be a burden to society’.
Third and consequently, divergent discourses on the value of solidarity emerged. For some, decades of civic engagement pointed to the need of death revivalism and patient empowerment, that resulted in the current legal framework. Others strongly criticised the lack of solidarity underpinning the legal framework on the following three counts: 1) the emphasis on patient autonomy is deemed a ’societal negligence in disguise’, as citizens are no longer urged to take care of others, 2) equating autonomy and dignity in euthanasia debates leads to the trap of viewing the ill or the elderly as having ‘undignified’ lives, and 3) wealth over health has become the credo of the current neoliberal society, as the Law on Euthanasia discourages further investments in health care but settles on the ‘commodification’ of health care.
“ I believe that we should take care of each other and especially care for the most vulnerable in our society. We shouldn’t just leave them to fend for themselves. I don’t think the motto should be all about autonomy, autonomy, and then the flip side, saying, “figure it out on your own.” That’s not acceptable. We have a responsibility to take care of each other. We are meant to care for one another. In biblical terms, we are each other’s keeper, right? “Am I my brother’s keeper?” Yes, I am my brother’s keeper. I must take care of each other, take care of others. So, I think in the long term, speaking maybe 100 years from now, people might say, “Sorry, that was a real mistake in the way they approached things.” I don’t know, but that’s looking at it from a meta-level, as historians call it, “longue durée,” and combining it with a neoliberal model, right? Neoliberalism and euthanasia thinking, it would be interesting to do a doctoral thesis on how they fit together perfectly. How they fit together perfectly… They are no longer patients, they are no longer clients, and I also don’t like the word ‘clients.’ They have become ‘users’. Sorry, but that’s our Dutch translation of the English word ‘consumers’ right? It’s like buying Dash detergent or a car; you buy care, just like the Personal Budget for people with disabilities. You buy your care, sorry, this goes against the very essence of what care fundamentally is. Care is a relationship between people; it’s not something you buy. It’s not something you say, “It’s a contract, and I want that.” It doesn’t work like that. [raising voice] The burden is on society. [end of raising voice] And when the money runs out, you have nothing left. If you can’t buy it, then it doesn’t come. “Here’s your little package,” that’s how it’s translated, and it’s always a hidden cost-cutting operation, let’s be very honest about it, a nice story, but it’s always a hidden cost-saving measure. I see right through that story, but well, big stories are always told, and they are always about saving money. [raising voice] It doesn’t bring anything, right? [end of raising voice] People’s self-reliance, they must stay at home, etc. How many people would benefit from going to a care centre, not at the end of their lives, but just because they feel totally lonely at home, but they can’t get in because nobody wants them there, as they don’t bring any profit. ” (spiritual caregiver)
Fourth, critical concerns were expressed concerning the lack of (distributive) justice due to the many existing misperceptions and misconceptions regarding medical end-of-life options that need to be uncovered. For instance, many people would be unaware of euthanasia and palliative sedation can both be dignified ways of dying, with euthanasia functioning as a fast-track and palliative sedation functioning as slow track to death. Also, the evolution of death literacy was contested: there was a sense that patients did not become more death literate, as many of them have insufficient knowledge of the content of the many end-of-life documents in circulation.
Yeah, I mean, you see, and I hear many people saying, “My papers are in order.” I won’t say every day, but I hear it almost every day, “My papers are in order.” That’s also something. It’s an illusion of control, right? Because what papers are they talking about? “My papers are in order.” When you ask them about it, they themselves don’t really know what that means, some kind of ‘living will’, ‘an advance care plan’, but yeah, with all… A living will or advance care plan is not that simple either, and then they think, “Oh, if I get dementia and I don’t recognize anyone anymore, they will give me an injection.” Ah yes, but then we are in a different domain, and that’s a whole other… But yeah, people are not well-informed, I find. They have totally wrong ideas and sometimes fear the wrong things, don’t know what is possible and what is not, and they also let themselves believe all kinds of things. Well, there are many misconceptions out there. (psychiatrist)
Participants’ ethical considerations regarding the additional procedural criteria for people with a non-terminal illness
As can be seen from the coding structure in Table 3 , participants made use of the principle justice to motivate their stance on additional (procedural) criteria that people with a non-terminal illness must meet before euthanasia can be carried out, in comparison with people with terminal illness. Those in favour of the additional procedural criteria referred to the differences between the terminally ill and the non-terminally ill regarding the aspect of content (i.e., the difference between general life expectancy and healthy life expectancy) and the aspect of time (i.e., the probability verging on certainty concerning the terminally ill versus the rough estimation concerning the non-terminally ill). Some of them also referred to the legal proceedings and stated that the Law was meant only for people with terminal illnesses to die by means of euthanasia. Others were of the opinion that it concerns only an arbitrary difference due to 1) the vagueness of the concept ‘naturally foreseeable’, i.e., suffering from a terminal illness, and the subjectivity of the calculated course and prognosis of e.g., degenerative somatic illnesses and dementia. A few participants said that this is beside the question, as one’s individual carrying capacity trumps the course and prognosis of an illness.
Participants’ ethical considerations regarding adults with psychiatric conditions
As can be seen from the coding structure in Table 4 , when asked about participants’ stances on euthanasia in the context of psychiatry, we distinguished value-based themes at the level of (1) the patient, (2) the field of psychiatry, and (3) society in general.
The level of the patient
Justice was the main value-based principle that emerged at the level of the patient. Participants in favour of not legally amending additional procedural criteria in the context of psychiatry stated that every patient with a non-terminal illness should receive equal end-of-life care options. The main counterargument given concerned the differences in patient profile, as some questioned whether the mentally ill can meet the legal criteria or stated that extreme caution is needed and thus additional criteria are in place due to the factor of e.g., ambiguity, impulsivity, and manipulation in the mentally ill.
“I find, the way the procedure is conducted for psychiatric suffering, I find it only natural that they handle it more cautiously because it’s indeed less… It’s not so easy to determine everything, is there really no other option left? And then I understand somewhere that time must be taken to investigate all of that. Because some of these people can be very impulsive, and that impulsivity needs to be addressed somewhere, of course. You also have people who can use their setbacks in the sense of, ‘I’ve been through all that, so I deserve euthanasia.’ And those are the people you need to single out because that’s just… I think those are also people who, with the necessary guidance, can still get out of it. Do you understand? It’s a form of self-pity, in a way. I think there might be resilience there, but they haven’t tapped into it themselves yet; it’s a kind of deflection or something. People with a history of, who say ‘I’ve experienced this and that, so I don’t need it anymore, just give me euthanasia, I deserve that. I’ve been through all that.’ While maybe, if they see, that’s still worth something to me, who knows, maybe that can still happen. They’re people who give up a little too quickly.” (Moral consultant)
Regarding the field of medicine, the following four value-based considerations emerged: (1) justice, (2) responsiveness to suffering, (3) protection, and (4) proportionality.
First, and as regards the principle of justice , participants in favour of equal procedural criteria for all non-terminally ill pointed to the indissociable unity of soma and psyche. A few physicians went one step further and reported that some psychiatric conditions can be considered terminal, e.g., suicidality, or predominantly of somatic nature, e.g., anorexia. The main counterarguments in this respect were (1) the firm belief in the inexistence of irremediableness in psychiatry (only mentioned by some physicians) or (2) that more caution is needed due to the higher level of subjectivity in terms of diagnostics, prognosis, and outcome.
Second, arguments against the distinction between the somatically versus the mentally ill were based on the attitude of responsiveness to the extreme extent and duration of mental suffering that can also render the mentally ill in a medically futile situation and the field of psychiatry empty-handed.
And many of the psychiatric patients I see suffer more than the average ALS patient who has to endure it for three years. In my experience, we’re less advanced in psychiatry compared to most other medical fields. You can easily say “we don’t know” in other areas of medicine and people will understand, but when it comes to psychiatric conditions, it’s different. Doctors might admit “it’s not working” or “there’s no trust,” and they might refer patients elsewhere or even refuse further appointments. I’ve even told a judge during a forced admission, “There’s simply no treatment available.” Yes, sometimes it’s just over and society must accept that there’s no solution. I’m not saying euthanasia is the solution for everyone, but I think it can be an option for some people. (Psychiatrist)
Other participants were not blind to the deep suffering, but strongly believed in the ground principle and core strength of psychiatry, namely the beneficial effect of hope. In addition, they pointed to the differences in the nature and course of somatic versus psychiatric illnesses when stating that considerably more time is needed in psychiatry, with inclusion of the therapeutic effect of hope to become effective.
“And I also believe that collectively, within psychiatry, we can and must provide additional support to endure profound despair. So, even in the face of seemingly endless hopelessness, we must maintain hope, look towards the future with trust, and continuously offer encouragement to those who feel hopeless. Our unwavering optimism and support convey the message that together, we can overcome. Because individuals who suffer from severe mental illness are treatable, I consider myself to be a genuinely optimistic psychiatrist. I have witnessed individuals who have harbored feelings of hopelessness and despair for extended periods, sometimes even decades, undergo profound transformations and experience significant improvement, and in some cases, complete recovery.” (Psychiatrist)
Third, participants in favour of the current legal framework reported that allowing euthanasia for the mentally ill was needed in the light of protection , as it might protect the patient against brutal suicides and also against therapeutic tenacity that more often occurs in psychiatry. Other participants in favour of, as well as participants against the current framework held a different stance on the following two counts: (1) allowing euthanasia conflicts with the aim of psychiatry to prevent suicide at all costs, and (2) the mentally ill are insufficiently protected by the Law as there are insufficient built-in safeguards against therapeutic negligence.
But usually with a psychiatric condition, death isn’t imminent. That’s the tricky part, you know? How many suicides do we have here? But anyway, I have an issue with that, using euthanasia as a kind of antidote against, well, against suicide, that’s a completely different matter. But death and psychiatry, why do we have all those government programs against suicide then? Isn’t that dying as a result of a psychiatric condition? (Psychiatrist, supportive of maintaining euthanasia option in psychiatric settings)
Fourth and as regards proportionality , a few participants with a normative stance against euthanasia in the context of psychiatry argued that psychiatric patients may not be allowed to die by means of euthanasia for as long as the field of psychiatry is under-resourced. They pointed to e.g., the lack of sufficient crisis shelters with a 24/7 availability and the lack of palliative approaches in the field of psychiatry. Instead of allowing euthanasia, they argue ‘to jolt the Belgian government’s conscience on mental health policies’. As a revolution to defeat the built-up inequalities in the field of medicine and knowing that palliative and rehabilitation initiatives in psychiatry require time.
“I oppose euthanasia in psychiatry. Compared to somatic medicine, psychiatry lags behind by 50 years. While physical pain can be managed with medication, there’s insufficient research on treatments for psychological suffering. Promising options like psilocybin and ketamine show potential in easing existential mental struggles. Magnetic stimulation can also alleviate depression, yet access remains limited. Unfortunately, these treatments are underused and under-researched. Many patients aren’t informed about these alternatives to euthanasia. It’s frustrating to see reluctance in exploring these options, especially when they offer hope to long-suffering patients. Utilizing these methods in psychiatric settings carries no risk of addiction. However, current restrictions impede access to these treatments, depriving patients of viable alternatives.” (Shortened excerpt from an interview with a psychiatrist)
When taking a societal perspective, no new arguments emerged from the respondents strongly in favour of the current euthanasia legislation, other than the main value of justice described in the subsection above. According to some, the current Law on Euthanasia busts some myths on the malleability of life and medical omnipotence, and even on psychiatric illnesses as a ‘Western phenomenon’, with e.g., depression and suicidality as a consequence of material wealth instead of a neurologic issue in the brain (only reported by some non-physicians).
There are quite a few people who consider the whole issue of the unbearable nature of psychological suffering a luxury problem, you know? They say something like, “Yeah, where are the suicide rates, to put it in equivalent terms, the lowest in the world? In Africa, because they obviously don’t have the luxury to concern themselves with that. They are already happy if they have a potato on their plate every day.” This is a viewpoint held by many, right? They call it a luxury problem, a modern, typical Western luxury problem. And perhaps there is some truth to it, right? But there are other causes of mortality there, which are much higher, such as child mortality, for example. (non-physician)
Counterarguments were also given and pointed to the value of (distributive) Justice. First, euthanasia was considered as ‘a logical but perverse consequence of systemic societal inequities’ on the one hand and the ‘further evolution towards the commodification or commercialisation of health care in individualised Western societies’ on the other. This would then lead to another vicious circle, with a rapidly growing ‘perception of vulnerable patient groups as irremediable’ and hence less likely to receive potentially beneficial treatment or other interventions. Some took a more radical stance against euthanasia in psychiatry, as they were convinced that euthanasia is nothing but ‘a perverse means to cover societal failures’. In addition, some participants with permissive stances on euthanasia in the context of psychiatry pointed to gender disparities in euthanasia requestors. This was based on the evidence that in the context of psychiatry, many more females request and die by means of euthanasia than males, and proportionally more female patient suffering from psychiatric disorders request and die by means of euthanasia compared to their fellow peers suffering from life-limiting or predominantly somatic conditions.
Finally, some respondents said that they could understand and, in some cases, even support euthanasia in some individual cases, but felt uncomfortable with its impact on the societal level. They pointed to the vicious circle of stigma and self-stigma that may impede the mentally ill to fully participate in societal encounters. In the long run, this type of societal disability may lead to vulnerable patients no longer wanting to perceive themselves a burden to society or to remain ‘socially dead’.
While considering their ethical perspectives towards euthanasia, participants weigh up various values related to and intertwining with the following levels: (1) the patient, (2) the patient’s inner circle, (3) the field of medicine, and (4) society in general. Overall, the participants shared an amalgam of ethical values on each of these four levels, regardless of their stance on euthanasia. It was mainly the interpretation of some values, the emphasis they placed on the key components underpinning each value and the importance they attach to each of the four levels, that determined their stance towards euthanasia. It was uncommon for different ethical values to be explicitly mentioned, which could distinguish distinct stances for or against euthanasia.
As regards euthanasia in the context of psychiatry, the focus has primarily been on arguments for and against euthanasia [ 23 ]. However, our study takes a more comprehensive approach, exploring the issue from a wider range of perspectives. This approach allowed us to uncover more complex insights that may have been overlooked if we had only considered it as a black-and-white issue.
Both the systematic review of Nicolini et al. [ 23 ] and our study emphasized fundamental ethical domains such as autonomy, professional duties, and the broader implications of euthanasia on mental healthcare. While our findings aligned with those of the systematic review, our inquiry delved deeper into psychiatry-specific considerations, including the influence of sudden impulses and feelings of hopelessness. This underscores the importance of healthcare professionals carefully assessing the timing and contextual aspects of such decisions within psychiatric contexts, ensuring individuals receive timely and tailored support and interventions.
Furthermore, our study extended beyond the boundaries of medical discourse, addressing broader societal ramifications. Participants engaged in discussions about ‘social death,’ a phenomenon that describes the marginalization of individuals despite their physical existence. This discussion highlighted entrenched structural inequities and societal attitudes perpetuating social alienation, particularly affecting marginalized demographics, including individuals grappling with mental health issues. Advocating for societal inclusivity and supportive measures, our study strongly emphasized the need to foster a sense of unity and respect for everyone’s worth, regardless of their circumstances.
Interpretation of the main findings
We make explicit and discuss the values corresponding to the four classical principles of biomedical ethics, in particular beneficence, non-maleficence, respect for autonomy and justice [ 31 ]. We place these values in the context of different ethical approaches, such as religious, professional, emancipatory, social, societal, and virtue-oriented approaches (see the ethical interpretation framework in OSF).
In the discussion section, therefore, the following main values and virtues are addressed: (1) the values of beneficence and non-maleficence in a religious perspective, (2) those same values in the professional context, (3) the value of autonomy in the contemporary emancipation paradigm, (4) the virtue of compassion stemming from virtue ethics theory, (5) the value of quality care in a social approach, and (6) the value of justice in societal policy contexts.
Beneficence and non-maleficence: religious perspective
In the realm of euthanasia debates, the interplay of religious beliefs and the values of ‘beneficence’ (the act of doing good) and ‘non-maleficence’ (do no harm) has emerged as a pivotal point of contention, often giving rise to divergent perspectives on this complex ethical issue [ 32 , 33 ]. Some religious traditions staunchly oppose medical end-of-life decisions, including euthanasia and abortion, viewing them as morally wrong and as disruptive to the natural order of life and death. The principle of ‘sanctity of life’ forms the bedrock of their belief system, underscoring the significance they attach to preserving life at all costs, as an embodiment of beneficence [ 34 , 35 ]. Conversely, those who argue for the ethical consideration of euthanasia emphasize the concept of beneficence in alleviating suffering and granting autonomy to individuals in their final moments. However, intriguingly, our examination of the topic has revealed a nuanced relationship between religious beliefs and attitudes toward euthanasia. While some individuals in our sample expressed strong religious convictions ( n = 5) and even considered themselves as practicing Catholics, they did not necessarily adopt a firm normative stance against euthanasia, signifying a complex balancing of beneficence and possible maleficence within their belief system. Conversely, certain participants who held steadfastly against euthanasia ( n = 3) did not identify with any religious belief system, yet their position was firmly grounded in their perception of potential maleficence associated with medical intervention in life and death decisions. This observation aligns with recent studies highlighting the intricate and multifaceted nature of religiosity, where individuals within various religious frameworks may hold diverse beliefs and values surrounding beneficence and non-maleficence [ 36 , 37 ]. Moreover, it underscores the powerful influence of societal culture on shaping personal perspectives on euthanasia, and how these views are entwined with the values of beneficence and non-maleficence [ 36 , 37 ].
Beneficence and non-maleficence: professional values
Second, a profound division arises between proponents and opponents, particularly in the field of medicine, where interpretations of the Oath of Hippocrates play a central role. At its core, the Oath emphasizes the deontological values of beneficence and non-maleficence, as physicians are bound by a prohibition against administering a deadly drug to ‘anyone,’ even at their explicit request, highlighting the reverence for the sanctity of life inherent in medical practice. This interpretation has led some to perceive active euthanasia as contrary to these sacred principles of preserving life. The notion of beneficence, understood as promoting the well-being of patients, appears to be in tension with the act of intentionally ending a life. Critics argue that euthanasia undermines the fundamental duty of physicians to protect and preserve life. Additionally, the principle of ‘non-maleficence,’ which entails not harming the patient or their life, is seen by some as being in accordance with the ‘sanctity of life’. However, the Oath also recognizes the significance of alleviating relentless suffering, opening the door to a nuanced debate on how these timeless principles align with the modern concept of euthanasia. As the discourse unfolds, perspectives emerge, with some viewing euthanasia as a compassionate form of care, that respects the autonomy and dignity of patients facing terminal illness or unbearable suffering. Advocates argue that euthanasia can be an act of beneficence, providing relief from pain and allowing individuals to die with dignity and control over their own fate. On the other hand, opponents of euthanasia steadfastly uphold the sanctity of life principle, viewing it as an ethical imperative that must not be compromised. They argue that intentionally ending a life, even in the context of relieving suffering, undermines the fundamental values of medical ethics and the intrinsic worth of every human life. For these individuals, euthanasia represents a profound ethical dilemma that conflicts with the near sanctity of medical ethics and the value of preserving life [ 38 , 39 , 40 ].
Autonomy: contemporary emancipation paradigm
The principle of autonomy emerges as one of the most prominent and contentious values in our contemporary emancipation paradigm. Autonomy, grounded in the belief in individual self-governance, is often cited as a foundational ethical principle in euthanasia legislation, emphasizing the significance of an individual’s capacity to make choices aligned with their own personal values and desires [ 31 ]. However, the discussion on autonomy extends beyond pure individualism, with considerations for relational autonomy, recognizing that individuals are not isolated entities but are shaped by their relationships, communities, and broader societal structures [ 41 ]. Within the context of euthanasia, the complexities of autonomy become evident as participants in the debate strived to find a delicate balance. On one hand, they stress the importance of respecting a patient’s individual autonomy in end-of-life decisions, ensuring that their choices are honoured and upheld. Simultaneously, they acknowledge the necessity of accounting for the patient’s social context and broader community when considering euthanasia as a compassionate option. Nevertheless, concerns are raised by some about the potential risks posed by euthanasia legislation, particularly for the most vulnerable individuals, such as the elderly and the mentally ill. These concerns centre on the negative consequences that may arise when individual autonomy is exercised without consideration for others or for societal well-being, and the concept of “social death,” which refers to the marginalization and exclusion of individuals from social relationships and networks due to illness or disability [ 42 , 43 ].
Amidst these complexities, the ethical value of autonomy stands as a paramount consideration. However, its application necessitates thoughtful consideration and balance with other values, including justice, equality, and societal responsibility. Recent reflections on “relational autonomy” have prompted critical evaluations of the idea of pure autonomy, emphasizing the need to delve deeper into the micro, meso, and macro levels that underpin autonomy and address potential conflicts between individual and relational autonomy [ 44 ]. Further, it highlights the imperative to take the broader societal context into account when grappling with the ethical challenges associated with euthanasia [ 45 ].
Compassion: virtue ethics
Our study confirms that while the value of autonomy holds importance, it is not the sole determinant in the ethical considerations surrounding euthanasia [ 46 ]. In this complex discourse, numerous other ethical values and virtues come to the fore, including the significance of compassion towards suffering individuals and the imperative of alleviating their distress. Notably, compassion is not merely a singular principle, but rather a profound ground attitude or virtue that motivates individuals to empathize with the pain of others and take actions to provide relief.
As revealed in our research, participants who opposed euthanasia did not invoke religious frameworks; instead, they explored diverse philosophical approaches to comprehend suffering and compassion. Among these, non-Western philosophies emphasized embracing suffering as an intrinsic aspect of life, acknowledging the impermanence of all things, including suffering. Additionally, the existentialist perspective of Albert Camus underscored suffering’s innate connection to human existence, leading to deeper self-understanding and comprehension of the world.
These philosophical viewpoints find relevance in the realm of ethics as well. Virtue ethics, in particular, highlights the significance of cultivating virtues such as courage and resilience, while narrative ethics emphasizes storytelling as a means to gain profound insight and reflection on experiences of suffering [ 47 , 48 ]. Such narratives foster empathy and create a shared sense of experience and community.
Our results show that, for some, suffering may hold positive value in various ways. The nature and intensity of suffering, alongside an individual’s values and virtues, beliefs, and coping capacity, significantly influence the ethics of euthanasia decision-making. An intricate approach that recognizes the multifaceted impacts of suffering becomes essential, acknowledging that various factors could potentially influence the experience of suffering as well as the interpretation of the consequences of the suffering experience. It’s possible that this approach doesn’t solely depend on the quantity of suffering or even its nature. Instead, it could be related to the delicate balance between one’s ability to endure suffering, the burden it places on them, and the (ir)remediableness of this burden, which can vary greatly among individuals as well as it might change over time. Such an approach aims to alleviate relentless suffering and, in certain cases, relieve unnecessary and enduring distress without consistently imposing interpretations upon it. Thus, acknowledging that, experiences of suffering are inherent to life and might act as drivers for personal development, fostering resilience, empathy, and a deeper apprehension of life’s essence, while it also might represent something irremediable, underscores the significance of a broader meaning of the concept of compassion as guiding principle in euthanasia discussions. These discussions further extend to the recognition of the dynamic trajectory inherent to the burden of suffering, as well as its potential for temporal evolution within the individual experiences of the afflicted. Such recognition not only fosters a more intricate understanding of the complex interplay between suffering and resilience but also highlights the acknowledgment that there may be moments when suffering becomes unendurable, surpassing the individual’s capacity to cope. This dimension introduces a layer of intricacy to the ethical considerations inherent in these discussions, thus necessitating a nuanced approach that contemplates the potentialities as well as the constraints of human endurance and the associated ethical ramifications.
Quality care: social approach
Examining euthanasia debates from a sociological perspective sheds light on the influence of societal inequalities in healthcare access and quality on the practice of euthanasia, and how it can shape personal, relational, and societal values, leading to the normalization or culturalization of euthanasia [ 49 ]. A noteworthy finding in this context is the contrasting perspectives on the evolving process of dying, transitioning from being perceived as in God’s hands to a more medical realm, where proponents of euthanasia view medicine as a catalyst for granting individuals greater control over the timing, manner, and circumstances of their own deaths. They envision the opportunity to be surrounded by loved ones and maintain consciousness while embracing the option of euthanasia, which they believe improves the quality of life at the end.
Proponents also emphasize additional benefits, such as enhanced transparency and regulation, ensuring ethical conduct through regulatory measures. They express concerns about a cultural environment where certain physicians adopt paternalistic attitudes and resist accepting death, prioritizing the extension of life as a moral imperative. In contrast, critical voices argue that death and dying have become increasingly medicalized, leading to their institutionalization. Some critics further contend that this medicalization has devalued the dying process and commodified life itself, leading patients, and families to increasingly rely on medical interventions at life’s end.
Moreover, as shared by some of the interviewees, the growing acceptance of medical assistance in dying may raise concerns. It’s conceivable that this evolving attitude could contribute to a perception of death undergoing a shift in seriousness, resulting in decisions about one’s life conclusion being made with less comprehensive thought and insufficient reflection. Consequently, this scenario could potentially lead individuals who are more susceptible to experiencing feelings of life’s insignificance, weariness, or sense of being ‘through with life’, to lean towards considering euthanasia. However, this inclination might also be driven by a lack of sufficient access to the necessary, long-term quality mental health care that would otherwise facilitate the pursuit of a life imbued with adequate significance, comfort, and dignity, achievable through appropriate (mental) healthcare.
Earlier research indicates that Belgium’s psychiatric care system has been grappling with underfunding and fragmentation, leading to individuals falling through the gaps in the mental health safety net [ 50 ]. One critical aspect is, e.g., the inadequate investment in long-term, intensive care, which is precisely the kind of support that individuals grappling with such existential questions may require.
Hence, in the context of euthanasia debates, the value of quality care emerges, encompassing the principle of beneficence, which emphasizes the obligation to provide good care and enhance the overall well-being of individuals. Ethical considerations go beyond the individual’s right to autonomy, extending to societal factors that influence healthcare practices and attitudes towards euthanasia. Addressing the impact of healthcare disparities and the medicalization of dying becomes imperative to ensure ethical and compassionate decision-making that upholds the true value of quality care and respect for human dignity.
Justice: societal policy contexts
In the context of euthanasia in somatic versus psychiatric medicine, ethical considerations regarding euthanasia often revolve around the fundamental value of justice [ 23 , 51 , 52 ]. Some respondents in our study emphasized the need for parity between somatic and psychiatric illnesses, recognizing that there should be no distinction between patients suffering from either. They argued that upholding the principle of justice demands equal treatment and recognition of the suffering experienced by individuals with psychiatric illnesses.
However, for others, achieving justice requires acknowledging and addressing the unique challenges faced by patients predominantly suffering from psychiatric illnesses. A comprehensive and integrated healthcare approach is proposed, where mental health is regarded as an integral part of overall health. This approach involves allocating the same level of attention and resources to psychiatric medicine as given to somatic illnesses, aiming to combat stigma and discrimination towards individuals with psychiatric conditions. Equitable treatment during life and at the end of life becomes the focus.
Yet, the Belgian context of psychiatry presents significant challenges. The field is characterized by underfunding and fragmented care, particularly for individuals with longstanding and complex psychiatric problems [ 53 ]. Additionally, the end-of-life care for psychiatric patients is still underdeveloped, and palliative psychiatry is in its early stages, lacking a uniformly agreed-upon definition or clear implementation guidelines [ 54 ]. In response, Belgium is exploring the “Oyster Care” model, designed to provide flexible, personalized care for individuals with severe and persistent mental illness who may be at risk of neglect or overburdened by psychiatric services [ 55 ]. This model aims to create a safe “exoskeleton” or supportive environment for patients, recognizing that recovery, reintegration, and resocialization might not be attainable for everyone with certain psychiatric conditions [ 55 ].
However, the integration of Oyster Care in today’s psychiatric practice is still limited and requires further development. Emphasizing the value of justice calls for continued efforts to enhance and refine psychiatric care, ensuring that individuals with psychiatric illnesses receive equitable treatment throughout their lives, including end-of-life care decisions [ 55 , 56 ].
Implications for future research, policy, and practice
In terms of policy and practice, our findings indicate that the discourse surrounding euthanasia extends beyond legal or medical considerations and encompasses fundamental ethical values that underpin our society. These values may not always be aligned and can create ethical dilemmas that are challenging to address. A value-centred approach to the euthanasia debate necessitates a constructive ethical dialogue among various actors involved, including patients, healthcare practitioners, and the wider community. This conversation should strive to comprehend the diverse values involved and endeavour to achieve a balance between these values. Additionally, ethical dialogue might encourage individuals to reflect on their own assumptions and beliefs, leading to more informed and thoughtful decision-making on ethical and moral issues. Ultimately, ethical dialogue can promote a more just and equitable society that prioritizes empathy, understanding, and mutual respect.
It is also crucial to acknowledge that patients with somatic illnesses and those with psychiatric illnesses may have different needs and expectations regarding the end of life. Hence, end-of life healthcare must be sensitive to the unique needs of each group. This recognition of differences does not justify unequal treatment or discrimination based on the type of illness. Instead, it involves addressing the different needs and expectations of each patient group while ensuring equitable and high-quality care for all.
As regards research, most articles on euthanasia legislation to date placed the emphasis on what other countries and states can learn from the Belgian and Dutch euthanasia practice. In addition, what can be learned is mainly restricted to the evidence and reflections on factual issues from a global practical-clinical perspective. Consequently, one of the main ethical, clinical, and societal issues remains unrequited, namely the impact of legislation and its consequences on an intrapersonal, interpersonal, medical, social, and societal level. Although cultural diversity is recently put high on the research agenda concerning general health care and mental health care, it is largely understudied in the context of end-of-life decisions and largely ignored in the context of psychiatry. Fewer articles have focused on what the latter countries may learn from those not implementing or not considering euthanasia legislation. In an increasingly diverse society, rapidly evolving in terms of fluidity and multi-ethnicity, cross-cultural research can help us learn from one another. To address the many dimensions of euthanasia, there is a need for input from a variety of academic fields, including sociology, anthropology, communication studies, and history. Further interdisciplinary research in all these areas could help inform policy and practice related to euthanasia.
Strengths and limitations
This is the first empirical in-depth interview study that uncovered the underlying ethical considerations of a variety and relatively large sample of health care professionals and volunteers in Belgium, a country with one of the most permissive legislative frameworks regarding euthanasia, as – unlike in some other countries – it does not exclude adults with psychiatric conditions per definition. Belgium is also one of the pioneering countries with such a legislative framework and can boast on two decades of euthanasia legislation and implementation.
We succeeded in providing a unique and representative sample of participants, varying in gender, work setting and expertise, and stances regarding euthanasia. Finally, and unlike former scientific studies that focused on either the somatic or psychiatric context, we now gauged for participants’ ethical perspectives on euthanasia in both fields of medicine.
There are also several limitations to our study. We may have experienced selection bias, as our sample of non-physicians had varying ages, but the sample of physicians was mostly older than 60. In addition, some interviews had to be postponed or cancelled due to COVID-19 restrictions and, potentially, due to legal and emotional concerns surrounding a high-profile euthanasia case being brought to court. Additionally, our sample exhibited heterogeneity regarding worldview (religious or non-religious), but possibly not regarding other culture-sensitive aspects, like migration background. As our qualitative research focused on exploring themes, narratives, and shared experiences rather than on ensuring high participation rates for statistical generalizability, drawing definitive conclusions regarding the prevalence of each opinion (pro/ambivalent/critical/against), the level of experience, or perspective across the entire spectrum of euthanasia practice is beyond the scope of our study.
Finally, although there is a growing number of countries and states around the globe with a legislative framework on euthanasia, all the legal frameworks differ from one another, so the results of our study cannot be generalized to the specific euthanasia context in e.g., Switzerland or Canada.
Our study illuminates the foundational values guiding perceptions of euthanasia, including autonomy, compassion, quality care, and justice, which permeate through four interconnected tiers: the patient, their inner circle, the medical community, and society at large. Despite varied stances on euthanasia, participants demonstrated a convergence of ethical principles across these tiers, shaped by nuanced interpretations and considerations. While explicit discussions of distinct ethical values were infrequent, their profound impact on euthanasia perspectives underscores the importance of ethical discourse in navigating this complex issue. By fostering inclusive dialogue and reconciling diverse values, we can promote informed decision-making, justice, and empathy in end-of-life care, particularly in psychiatric settings. Interdisciplinary research is essential for a comprehensive understanding of euthanasia’s dimensions and to inform policy development. While our study is rooted in Belgium, its implications extend to the broader euthanasia discourse, suggesting avenues for further exploration and cross-cultural understanding.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due reasons of privacy and anonymity, but are available from the corresponding author on reasonable request, following procedures from all 3 Medical Ethics Committees involved. To access the supplementary materials, see the Open Science Framework repository at https://osf.io/26gez/?view_only=af42caddb2554acfb7d1d5aabd4dec7a . Upon publication of this paper, the repository will be made public, and a shorter link will be provided.
Mroz S, Dierickx S, Deliens L, Cohen J, Chambaere K. Assisted dying around the world: a status quaestionis. Ann Palliat Med. 2021;10(3):3540–53. https://apm.amegroups.com/article/view/50986/html
Belgian Official Gazette. Wet betreffende de Euthanasie (Law on Euthanasia) (in Dutch). 2002;2002/09590, 28515. http://www.ejustice.just.fgov.be/cgi_loi/change_lg.pl?language=nl&la=N&cn=2002052837&table_name=wet
FCECE (Federal Control- and Evaluation Committee on Euthanasia). Euthanasie - Cijfers van 2023 (Press release: Euthanasia - Figures for the year 2023). 2024; https://overlegorganen.gezondheid.belgie.be/nl/documenten/persbericht-fcee-euthanasie-cijfers-van-2023
Dierickx S, Deliens L, Cohen J, Chambaere K. Euthanasia for people with psychiatric disorders or dementia in Belgium: analysis of officially reported cases. BMC Psychiatry. 2017;17(1):203. http://bmcpsychiatry.biomedcentral.com/articles/ https://doi.org/10.1186/s12888-017-1369-0
Federal Control and Evaluation Committee for Euthanasia (FCECE). Ninth Report to the Belgian Parliament, 2018–2019. 2020.
Federal Control and Evaluation Committee for Euthanasia (FCECE). Eighth Report to the Parliament (2016–2017). Brussels, Belgium. 2018. https://leif.be/data/press-articles/FCEEC_-_8_euthanasie-verslag_2016-2017-nl.pdf
Federal Control and Evaluation Committee for Euthanasia (FCECE). Seventh Report to the Belgian Parliament. Vol. 001. Brussels, Belgium. 2016. https://leif.be/data/press-articles/FCEED_-_Verslag_Wetgevende_Kamers_-_periode_2014-2015_25-10-16.pdf
FCECE (Federal Control- and Evaluation Committee on Euthanasia). EUTHANASIE – Cijfers van 2020. Vol. 64. 2021. https://overlegorganen.gezondheid.belgie.be/sites/default/files/documents/fcee-cijfers-2020_persbericht.pdf
Federal Control and Evaluation Committee for Euthanasia (FCECE). Tenth Report to the Belgian Parliament. Brussels, Belgium. 2022. https://overlegorganen.gezondheid.belgie.be/nl/documenten
Vonkel JAARVERSLAGVONKEL. 2021 (Annual Report of the end-of-life consultation center Vonkel, 2021). Ghent; 2022. https://www.vonkeleenluisterendhuis.be/teksten/jaarverslag2021.pdf
Vonkel een luisterend huis. JAARVERSLAG VONKEL. 2020. 2021; https://www.vonkeleenluisterendhuis.be/teksten/jaarverslag2020.pdf
Vonkel. JAARVERSLAG VONKEL 2019 (Annual Report of the end-of-life consultation center Vonkel, 2019). 2020. http://vonkeleenluisterendhuis.be/teksten/jaarverslag2019.pdf
Verhofstadt M, Audenaert K, Van den Broeck K, Deliens L, Mortier F, Titeca K et al. The engagement of psychiatrists in the assessment of euthanasia requests from psychiatric patients in Belgium: a survey study. BMC Psychiatry. 2020.
Verhofstadt M, Audenaert K, Van den Broeck K, Deliens L, Mortier F, Titeca K et al. Belgian psychiatrists’ attitudes towards, and readiness to engage in, euthanasia assessment procedures with adults with psychiatric conditions: a survey. BMC Psychiatry. 2020.
Dees MK, Vernooij-Dassen MJ, Dekkers WJ, Elwyn G, Vissers KC, van Weel C. Perspectives of decision-making in requests for euthanasia: A qualitative research among patients, relatives and treating physicians in the Netherlands. Palliat Med. 2013 Jan [cited 2012 Dec 26];27(1):27–37. http://www.ncbi.nlm.nih.gov/pubmed/23104511
Evenblij K, Pasman HRW, Pronk R, Onwuteaka-Philipsen BD. Euthanasia and physician-assisted suicide in patients suffering from psychiatric disorders: a cross-sectional study exploring the experiences of Dutch psychiatrists. BMC Psychiatry. 2019;1–10. https://link.springer.com/article/10.1186/s12888-019-2053-3?utm_source=researcher_app&utm_medium=referral&utm_campaign=MKEF_USG_Researcher_inbound
Verhofstadt M, Audenaert K, Van den Broeck K, Deliens L, Mortier F, Titeca K et al. Flemish Psychiatrist’s Attitudes and Readiness to Engage in Euthanasia Assessment Procedures concerning Psychiatric Patients (forthcoming).
Pronk R, Evenblij K, Willems DL, van de Vathorst S. Considerations by Dutch Psychiatrists Regarding Euthanasia and Physician-Assisted Suicide in Psychiatry. J Clin Psychiatry. 2019;80(6). https://www.psychiatrist.com/JCP/article/Pages/2019/v80/19m12736.aspx
Bolt EE, Snijdewind MC, Willems DL, van der Heide A, Onwuteaka-Philipsen BD. Can physicians conceive of performing euthanasia in case of psychiatric disease, dementia or being tired of living? J Med Ethics. 2015;41(8):592–8. http://jme.bmj.com/lookup/doi/ https://doi.org/10.1136/medethics-2014-102150
van Zwol M, de Boer F, Evans N, Widdershoven G. Moral values of Dutch physicians in relation to requests for euthanasia: a qualitative study. BMC Med Ethics. 2022;23(1):1–7. https://doi.org/10.1186/s12910-022-00834-4
Ten Cate K, van Tol DG, van de Vathorst S. Considerations on requests for euthanasia or assisted suicide; a qualitative study with Dutch general practitioners. Fam Pract. 2017;34(6):723–9.
Article Google Scholar
Pronk R, Sindram NP, van de Vathorst S, Willems DL. Experiences and views of Dutch general practitioners regarding physician-assisted death for patients suffering from severe mental illness: a mixed methods approach. Scand J Prim Health Care. 2021;39(2):166–73. https://www.tandfonline.com/doi/full/ https://doi.org/10.1080/02813432.2021.1913895
Nicolini ME, Kim SYH, Churchill ME, Gastmans C. Should euthanasia and assisted suicide for psychiatric disorders be permitted? A systematic review of reasons. Psychol Med. 2020;50(8):1241–56. https://www.cambridge.org/core/product/identifier/S0033291720001543/type/journal_article
Demedts D, Roelands M, Libbrecht J, Bilsen J. The attitudes, role & knowledge of mental health nurses towards euthanasia because of unbearable mental suffering in Belgium: a pilot study. J Psychiatr Ment Health Nurs. 2018;25(7):400–10.
Belgian Congregation of Brothers of Charity. Reakiro (in Dutch). 2020 [cited 2022 Mar 13]. https://reakiro.be/
Berger P, Luckmann T. The reality of everyday life. The social construction of reality: a treatise in the sociology of knowledge. New York: Doubleday & Company; 1966.
Google Scholar
Verhofstadt M. Euthanasia in the Context of Adult Psychiatry: Walking the Tightrope Between Life and Death [PhD-Thesis]. Vrije Universiteit Brussel & Ghent University; 2022. https://cris.vub.be/ws/portalfiles/portal/86844133/Verhofstadt_Monica_PhD_thesis_23.05.2022.pdf
Pronk R. A dialogue on death: On mental illness and physician-assisted dying. [PHD Thesis]. Universiteit van Amsterdam; 2021. https://pure.uva.nl/ws/files/65781146/Thesis_complete_.pdf
Braun V, Clarke V. Is thematic analysis used well in health psychology? A critical review of published research, with recommendations for quality practice and reporting. Health Psychol Rev. 2023;17(4):695–718. https://www.tandfonline.com/doi/full/ https://doi.org/10.1080/17437199.2022.2161594
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
Beauchamp, Childress TJ. Principles of Medical Ethics. Volume 459. Oxford Univ; 2009.
McCormack R, Clifford M, Conroy M. Attitudes of UK doctors towards euthanasia and physician-assisted suicide: A systematic literature review. Palliat Med. 2012;26(1):23–33. http://journals.sagepub.com/doi/10.1177/0269216310397688
Roelands M, Van den Block L, Geurts S, Deliens L, Cohen J. Attitudes of Belgian Students of Medicine, Philosophy, and Law Toward Euthanasia and the Conditions for Its Acceptance. Death Stud. 2015;39(3):139–50. http://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/07481187.2014.920433
Baranzke H. Sanctity-of-Life—A Bioethical Principle for a Right to Life? Ethical Theory Moral Pract. 2012;15(3):295–308. http://link.springer.com/ https://doi.org/10.1007/s10677-012-9369-0
Lockhart C, Lee CHJ, Sibley CG, Osborne D. The sanctity of life: The role of purity in attitudes towards abortion and euthanasia. Int J Psychol. 2023;58(1):16–29. https://onlinelibrary.wiley.com/doi/ https://doi.org/10.1002/ijop.12877
Muishout G, van Laarhoven HWM, Wiegers G, Popp-Baier U. Muslim physicians and palliative care: attitudes towards the use of palliative sedation. Support Care Cancer. 2018;26(11):3701–10. http://link.springer.com/ https://doi.org/10.1007/s00520-018-4229-7
Sabriseilabi S, Williams J. Dimensions of religion and attitudes toward euthanasia. Death Stud. 2022;46(5):1149–56. https://www.tandfonline.com/doi/full/10.1080/07481187.2020.1800863
Baumgartner F, Flores G. Contemporary Medical Students’ Perceptions of the Hippocratic Oath. Linacre Q. 2018;85(1):63–73. http://journals.sagepub.com/doi/10.1177/0024363918756389
Schuklenk U. The ethical case against assisted euthanasia has not been made. J Thorac Cardiovasc Surg. 2015.
Hajar R. The physician’s oath: Historical perspectives. Hear Views. 2017;18(4):154. http://www.heartviews.org/text.asp?2017/18/4/154/221224
Igel LH, Lerner BH. Moving Past Individual and Pure Autonomy: The Rise of Family-Centered Patient Care. AMA J Ethics. 2016;18(1):56–62. http://www.ncbi.nlm.nih.gov/pubmed/18733507 http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC1650661
Borgstrom E. Social Death. QJM. 2017;110(1):5–7. https://academic.oup.com/qjmed/article-lookup/doi/ https://doi.org/10.1093/qjmed/hcw183
Králová J. What is social death? Contemp Soc Sci. 2015;10(3):235–48. http://www.tandfonline.com/doi/full/10.1080/21582041.2015.1114407
Ho A. Relational autonomy or undue pressure? Family’s role in medical decision-making. Scand J Caring Sci. 2008;22(1):128–35.
Gómez-Vírseda C, de Maeseneer Y, Gastmans C. Relational autonomy: what does it mean and how is it used in end-of-life care? A systematic review of argument-based ethics literature. BMC Med Ethics. 2019;20(1):76. https://bmcmedethics.biomedcentral.com/articles/ https://doi.org/10.1186/s12910-019-0417-3
Liégeois A. Values in dialogue: Ethics in Care. Peeters Publishing; 2016. p. 138.
Nussbaum M. Upheavals of Thought. The intelligence of emotions. In Cambridge: Cambridge University Press; 2001.
Book Google Scholar
MacIntyre A. After Virtue. A study in Moral Theory. 3rd ed. Notre Dame: University of Notre Dame.; 2007.
Campbell CS. Dying well, dying badly: ethical issues at the end of life. Death and religion in a changing world. Routledge. In; 2022. pp. 226–53.
Mistiaen P, Cornelis J, Detollenaere J, Devriese S, Farfan-Portet M, Ricour C. Organisation of mental health care for adults in Belgium. Health Services Research (HSR)Brussels: Belgian Health Care Knowledge Centre (KCE). 2019. KCE Reports 318. D/2019/10. 2019. https://kce.fgov.be/sites/default/files/atoms/files/KCE_318_Mental_Health_care_Report_0.pdf
Rooney W, Schuklenk U, van de Vathorst S. Are concerns about Irremediableness, vulnerability, or competence sufficient to Justify excluding all Psychiatric patients from Medical Aid in Dying? Heal Care Anal. 2018.
Dembo J, Schuklenk U, Reggler J. For Their Own Good: A Response to Popular Arguments Against Permitting Medical Assistance in Dying (MAID) where Mental Illness Is the Sole Underlying Condition. Can J Psychiatry. 2018;63(7):451–6. http://journals.sagepub.com/doi/ https://doi.org/10.1177/0706743718766055
Hermans MHM, de Witte N, Dom G. The state of psychiatry in Belgium. Int Rev Psychiatry. 2012;24(4):286–94. http://www.tandfonline.com/doi/full/ https://doi.org/10.3109/09540261.2012.690337
Lindblad A, Helgesson G, Sjöstrand M. Towards a palliative care approach in psychiatry: do we need a new definition? J Med Ethics. 2019;45(1):26–30. https://jme.bmj.com/lookup/doi/ https://doi.org/10.1136/medethics-2018-104944
Decorte I, Verfaillie F, Moureau L, Meynendonckx S, Van Ballaer K, De Geest I et al. Oyster Care: an innovative Palliative Approach towards SPMI patients. Front Psychiatry. 2020.
De Rycke R, Sabbe S. Psychiatrie. Wat Je Moet Weten (Psychiatry. What you need to know). 4th ed. Leuven (Louvain): Uitgeverij LannooCampus; 2019. p. 304.
Download references
Acknowledgements
The authors wish to thank prof. dr. Kenneth Chambaere and prof. dr. Kurt Audenaert for their preliminary advice regarding the ethics of the research methodology, dr. Steven Vanderstichelen for his help with the interviews (i.e., conducting and transcribing) and all the participants for sharing their professional and in some cases also personal experiences during the interview. We’d also like to thank prof. dr. Kenneth Chambaere for the supervision during the conducting of the interviews and his feedback on the ‘near to final’ draft.
MV is funded by the Research Foundation Flanders via research project (G017818N) and PhD fellowship (1162618 N).
Author information
Authors and affiliations.
End-of-life Care Research Group, Vrije Universiteit Brussel (VUB) & Ghent University, Laarbeeklaan 103, Brussels, 1090, Belgium
Monica Verhofstadt & Koen Pardon
Faculty of Theology and Religious Studies, KU Leuven, Louvain, Belgium
Loïc Moureau & Axel Liégeois
Organisation Brothers of Charity, Ghent, Belgium
Axel Liégeois
You can also search for this author in PubMed Google Scholar
Contributions
The article has been developed with the following authors’ contributions: MV was responsible for the study methodology and managed ethical approval; MV conducted most of the interviews and wrote the main manuscript texts. AL drafted the ethical interpretation framework. MV, LM, KP and AL were responsible for the coding structure and data interpretation and performed a critical review and revision of the final manuscript.
Corresponding author
Correspondence to Monica Verhofstadt .
Ethics declarations
Ethics approval and consent to participate.
This research project was performed in accordance with the Declaration of Helsinki and the European rules of the General Data Protection Regulation. It received ethical approval from the Medical Ethics Committee of the Brussels University Hospital with reference BUN 143201939499, from the Medical Ethics Committee of Ghent University Hospital with reference 2019/0456, and from the Medical Ethics Committee of the Brothers of Charity with reference OG054-2019-20. The interviews were held after obtaining informed consent from all the participants.
Consent for publication
Not applicable.
Competing interests
MV has received research grants from the Research Foundation Flanders; no other relationships or activities that could appear to have influenced the submitted work were declared. All other authors declare that they do not have any competing interest.
Transparency declaration
MV is the guarantor of the manuscript and affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancy from the study have been noted and explained in the manuscript.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Verhofstadt, M., Moureau, L., Pardon, K. et al. Ethical perspectives regarding Euthanasia, including in the context of adult psychiatry: a qualitative interview study among healthcare workers in Belgium. BMC Med Ethics 25 , 60 (2024). https://doi.org/10.1186/s12910-024-01063-7
Download citation
Received : 04 September 2023
Accepted : 15 May 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s12910-024-01063-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- End-of-life
- Medical assistance in dying
- Mental disorders
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]
Euthanasia and Assisted Suicide: A Guide to the Evidence
Introduction
This evidence guide has been written to inform the debate about whether to legalise physician assisted suicide or euthanasia in the United Kingdom. Most of the sources cited here are also relevant to the debates on assisted suicide or euthanasia in other countries.
You can skim to get a sense of the different issues at stake and where to find further information, especially the most reliable information that is freely available online.
This guide aims to be useful for:
- students (especially of the medical professions, law, philosophy, and bioethics)
- research assistants to officials or parliamentarians.
More than this, it is offered to anyone who is concerned about these issues and wishes to assess the evidence.
It is important to remember, as has recently been pointed out , ‘that the medical literature is, in general, favourably disposed toward the empirical and the new [… resultantly] articles defending the ethical status quo (i.e., against PAS) tend to be shut out of the medical literature because they are not reporting anything new and, therefore, cannot have any data. The result is an impression of growing acceptance of PAS, but it really represents an artefact of a scientific bias’. It is hoped that this guide contributes to redressing this scientific bias.
Along with references for the source-data and official reports on assisted suicide and euthanasia in various countries, it identifies some useful articles that have been published in Peer Review Journals (PRJ). Publishing in a PRJ is no guarantee of the truth of an article’s conclusions, for especially in law, ethics and public policy academics frequently argue for opposite conclusions. However, being published in a PRJ is a sign that other academics have considered the argument to be well-structured and the sources of evidence to be clearly identified. This provides a good starting point for debate. Unfortunately, most PRJ material is not free to the general reader but is available only through universities or by subscription. Nevertheless, some PRJ articles are free online and sometimes there are freely available discussions based on the article. At a minimum the abstract of the article will generally be available free online. In this bibliography, all PRJ articles will be identified with an asterisk * . Where the full text of a PRJ is freely available this will be indicated by * (full text available) . Where the published version is not freely available, a pre- or post-print draft occasionally will be. This means that the full text can be read, but the article has none of the publisher’s formatting.
Many articles on euthanasia and assisted suicide have been published since the original version of this evidence guide in 2015. We have updated the guide to include new literature and the changes to legislation regarding euthanasia and assisted suicide throughout the world since that time. The guide is intended to be indicative rather than fully comprehensive, and we intend to update the resources periodically in the future.
DA Jones, R Gay and CM Wojtulewicz
Oxford, April 2022
Abbreviations
EAS = euthanasia and/or assisted suicide.
PAS / AS = physician-assisted suicide / assisted suicide
1. Parliamentary Reports
Since 1990 within the United Kingdom there have been three parliamentary reports on assisted euthanasia or suicide, each of which has been critical of such proposals. The most recent, and the most relevant to the Bills before the House of Lords and the House of Commons, is the 2015 Report of the Health and Sport Committee of the Scottish Parliament.
House of Lords Select Committee on Medical Ethics (HL Paper 21-I of 1993-4). There is no copy of the report available online, but a summary was provided by Lord Walton of Detchant (its chair) in a statement to the House of Lords recorded in Hansard.
House of Lords Assisted Dying for the Terminally Ill Committee 5 April 2005 (Mackay Committee ) On this committee’s findings see also I Finlay, VJ Wheatley, and C Izdebski. ‘The House of Lords Select Committee on the Assisted Dying for the Terminally Ill Bill: implications for specialist palliative care.’ Palliative medicine 19.6 (2005): 444-453 . *
Scottish Parliament Health and Sport Committee 6th Report, 2015 (Session 4): Stage 1 Report on Assisted Suicide (Scotland) Bill . This Committee was ‘not persuaded by the argument that the lack of certainty in the existing law on assisted suicide makes it desirable to legislate to permit assisted suicide... there are ways of responding to suffering (such as increased focus on palliative care and on supporting those with disabilities), which do not raise the kind of concerns about crossing a legal and ethical “Rubicon” that are raised by assisted suicide’. [292, 294]
The House of Lords introduced the Assisted Dying Bill 2021 [HL] , proposed by Baroness Meacher, which was given a second reading on 22 October 2021 .
House of Commons Library Debate Pack 22 January 2020, ‘The Law on Assisted Dying’ , by Elizabeth Rough and Nikki Sutherland.
Current challenges in the culture of healthcare in the UK
If legalised, assisted suicide or euthanasia would be implemented in the context of the NHS. In this regard it is important to be realistic about the current state of healthcare in the UK and failures that can occur and that have occurred, for example, in Mid Staffordshire and in the implementation of the Liverpool Care Pathway for the Dying Patient. These problems were not confined to one Trust or one Pathway but reflect cultural challenges within the NHS. How might assisted suicide or euthanasia be implemented in an environment of targets and ‘tick-boxes’ that sometimes operate to the detriment of patient care?
Mid Staffordshire NHS Foundation Trust Public Inquiry (Francis Report)
Independent Review of the Liverpool Care Pathway: More Care, Less Pathway (Neuberger Report)
2. Official Statistics from Jurisdictions with Assisted Suicide or Euthanasia
Statistics for rates and characteristics of death by assisted suicide or euthanasia are available for fifteen jurisdictions: Canada, the Netherlands, Belgium, Luxembourg, Switzerland, Victoria (Australia) , and, in the USA, the District of Columbia , and the states of California, Colorado, Hawaii, Oregon, Maine, New Jersey, Vermont and Washington . Assisted suicide is legal in Montana and New Mexico, but there are no official reports on the practice.
Such statistics are only as reliable as the questions asked and the means of data collection and in all cases rely on self-reporting. In Flanders (Belgium) it has been shown that official figures underestimate rates by approximately 50% (see section 5.4 below). Official reports tend to gloss the figures and readers should beware of ‘spin.’ Nevertheless, with these caveats, official figures remain an important source of evidence for the impact of legalising assisted suicide or euthanasia.
In Belgium euthanasia was legalised in 2002 and reports have been produced every two years. These are available (in French) here.
In Luxembourg euthanasia was legalised in 2009 and reports are produced every two years. Luxembourg has a small population (less than 1% of the UK population) and thus the number of cases is small. Nevertheless, over 6 years it is possible to see some patterns (a general increase in cases, an increase in non-cancer cases, more cases of women than men). The fifth report (for 2017-2018) is available here. The sixth report (for 2019-2020) was completed in March 2021, but is not available for download.
In the Netherlands euthanasia was effectively decriminalised by a court decision in 1984. This was the basis of a legal statute in 2001 legalising euthanasia and physician assisted suicide. Since 2002 the Netherlands has produced an annual report on the cases notified to the five regional euthanasia committees. These are available (in English once the year is selected).
In Switzerland , since 1942, inciting or assisting suicide has been illegal when it is for selfish motives (such as financial gain). Since 1982 this law has provided legal space for the organisation EXIT to promote assisted suicide for those ‘with unbearable symptoms or with unacceptable disabilities’. There are two government reports from the Federal Statistical Office, one in 2012 and latest, for 2014, published in 2016 and revised in 2017 . There are also statistics for assisted suicide by sex and age for 2003-2019 , published by the Federal Statistical Office. Dignitas has released statistics from 1998-2021 .
North America
Canada passed euthanasia and assisted suicide into law in 2016 (termed ‘medical assistance in dying’ or MAID). Further changes in the law, widening eligibility criteria, were introduced in March 2021 (though not effective until March 2023). The Second Annual Report on Medical Assistance in Dying (2020) shows that ‘MAID’ deaths increased by 34.2% from 2019.
The District of Columbia legalised assisted suicide in 2016 and has produced one statistics report in 2018.
California legalised assisted suicide in 2015 and has produced reports each year since. They can be found here.
Colorado legalised assisted suicide in 2016, and has produced reports each year since. They can be found here.
Hawaii passed assisted suicide into law in 2018, which came into effect in January 2019. The 2019 and 2020 legislative reports can be found here.
Oregon legalised physician assisted suicide in 1997 and produces annual reports. Helpfully the latest report (2021) includes data from previous years. Note that the figure for the number of deaths in the most recent year covered by the report will generally be inaccurate as deaths are recorded against the year of the lethal prescription. For example, if a lethal prescription given in 2012 were used in 2013 the death would be recorded as due to assisted suicide in the 2012 figures. Reports from all individual years can be accessed here.
Maine introduced assisted suicide in 2019 and its reports can be found here.
New Jersey also passed assisted suicide into law in 2019 and its 2019 and 2020 data summaries can be found here.
Vermont legalised physician assisted suicide in 2013 for terminally ill patients. The latest report can be seen here (issued Jan 15 2022).
Washington legalised physician assisted suicide in 2009 following the Oregon model (Washington borders Oregon and to a great extent shares a common culture and history). Washington also produces annual reports.
Victoria (Australia) legalised euthanasia and assisted suicide (under the umbrella term ‘voluntary assisted dying’ or VAD) in 2017, which came into effect in June 2019. Statistics are issued approximately every 6 months, and the data can be found here.
There are common patterns which emerge in each of these jurisdictions: in every jurisdiction numbers have increased over time and continue to do so; there has also been a shift from permitting assisted suicide for cancer victims to include other diseases. In Europe this includes non-terminal conditions such as neuro-psychiatric conditions and multiple co-morbidities (for example, those associated with old age). Supposed safeguards such as psychiatric referral have also declined in frequency (see below for further details). Essentially, the practice has become more widespread and more routine.
3. Public Opinion on Euthanasia and Assisted Suicide
Within the political debate on assisted suicide and euthanasia, both sides, but especially advocates of a change in the law, frequently appeal to surveys of public opinion. In polls, there is a consistent majority of public opinion that expresses support for legalising assisted suicide or euthanasia.
In the UK polls typically show between 70-80% support for legalising assisted suicide. Support drops to around 60% for euthanasia. See for example:
Ipsos-Mori Poll for The Economist (June 2015)
80% believe those accompanying a family member or friend abroad to receive assisted suicide should not be prosecuted. This drops to 74% when informed that current law in England and Wales is that assistance is punishable by up to 14 years in prison. 65% think the law should be changed to permit assistance in travelling abroad, see:
Ipsos-Mori Poll for Dignity in Dying (June 2009)
A 2019 poll commissioned by Dignity in Dying shows net support for assisted suicide law at 84%; but it must be noted that the procedure is referred to as ‘assisted dying’ rather than ‘assisted suicide’ (see the section below on wording of polls):
Populus Poll for Dignity in Dying (March 2019)
Gallup Poll (USA, 2013)
It should be noted that 73% think there ‘ is a difference between a terminally ill adult seeking assistance to end their life and suicide ’, see YouGov / Dignity in Dying (August 2021) . However, the proposed legislation (Assisted Dying Bill [HL] 2021) has the effect of amending the Suicide Act 1961 (as amended by the Coroners and Justice Act 2009) so that it is no longer and offence to ‘encourage or assist’ suicide.
On the issue of correct terminology and the use of euphemism, see:
David Albert Jones, ‘Defining the Terms of the Debate: Euthanasia and Euphemism’, Briefing Papers: Euthanasia and Assisted Suicide (Anscombe Bioethics Centre, Oxford: 2021)
In the UK, 78% are concerned that, as a society, as much as possible ought to be done to reduce suicide rates. 51% are concerned that people would see themselves as a burden and feel pressured into taking their own life if assisted suicide were legal, see:
ComRes Care Not Killing Assisted Suicide Poll (February 2019)
In a 2018 poll, although 75% were in favour of a change in the law, 60% did not know anyone close to them who had died who would have considered assisted suicide had it been available to them, see:
ComRes Daily Mirror Assisted Dying Poll (June 2018)
When participants are exposed to counter arguments to legislation, support wavers. In one poll from 73% to 43%:
Care Not Killing, “‘Assisted Dying’ and Public Opinion” (2014)
ComRes CARE Assisted Suicide Poll (2014)
The Mackay committee produced a very useful critical review on the state of evidence at that time (2005) in relation to public opinion on assisted suicide and euthanasia ( Chapter 6 and Appendix 7 ).
‘ The key conclusion of this report is that, although some idea of the basic attitude of the general public is available through research sources, this does not amount to an authentic picture of public opinion which is in any way comprehensive. Deliberative research techniques, unused so far for this subject, which can produce an account of informed public opinion, are recommended if a proper understanding of public opinion is to be achieved .’ ( Appendix 7 , para 17)
In 2022, it remains the case that ‘ Research sponsors frequently appear to have been more concerned to achieve statistics for media consumption than to work towards achieving a comprehensive understanding of public and health sector attitudes’ (Appendix 7, para 2).
The flaws in most yes/no polls are methodological and are not corrected merely by conducting more polls of a similar kind. Qualitative research is needed to uncover the complexities of the issue and/or the complexities of people’s attitudes to the issue. For example, a study in the Journal of Medical Ethics showed that, if people were given a range of choices (and not just one), more individuals were in favour of legal sanctions against euthanasia than were in support of it.
Hagelin, J, T Nilstun, J Hau, and H-E Carlsson. ‘Surveys on Attitudes towards Legalisation of Euthanasia: Importance of Question Phrasing’. Journal of Medical Ethics 30, no. 6 (1 December 2004): 521–23. https://doi.org/10.1136/jme.2002.002543. * (full text available).
This complexity is also shown in qualitative research with nurses and with dying cancer patients. See here:
Berghs, M, B. Dierckx de Casterlé, and C. Gastmans, ‘The Complexity of Nurses’ Attitudes toward Euthanasia: A Review of the Literature’. Journal of Medical Ethics 31, no. 8 (August 2005): 441–46. https://doi.org/10.1136/jme.2004.009092. * (full text available).
Jaklin, A., N. Olver, and I. Eliott, ‘Dying Cancer Patients Talk about Physician and Patient Roles in DNR Decision Making’. Health Expectations 14, no. 2 (2011): 147–58. https://doi.org/10.1111/j.1369-7625.2010.00630.x * (full text available).
It is worth highlighting the following conclusion from the latter study: ‘ Survey studies showing majority support for euthanasia have typically required individuals to make judgements about hypothetical and abstracted scenarios. Under such conditions, individuals are likely to draw upon the readily available and socially approved discourses of autonomy and compassion, and voice approval. To conclude that this legitimises euthanasia as social policy is to deny the import of other factors that feature when individuals have opportunity to do more than endorse or reject euthanasia ’.
These complexities are by no means peculiar to the issues of assisted suicide and euthanasia, they apply more generally to use of public opinion in ethical debates around public policy. For such reasons government engagement with the public typically employs mixed methods: public events, open online consultations, stakeholder events, and representative opinion polls. The UK government’s Code of Practice on Consultation makes it clear that consideration of public opinion should give particular weight to the views of ‘any groups or sectors... that may be disproportionately affected by the proposals ’ (3.4). [In the case of assisted suicide and euthanasia this would be people who are dying, those who are living with disabilities, their carers, and healthcare professionals, especially doctors who care for the dying.] Consultations should not just ask for conclusions but ‘ the evidence given by consultees to back up their arguments. Analysing consultation responses is primarily a qualitative rather than a quantitative exercise ’ (6.1).
These principles of good practice should apply also when judging the competing claims to how ‘the public’ thinks of assisted suicide and euthanasia.
Wording of polls
Support for euthanasia and assisted suicide in public opinion polls is subject to ‘ over 20% variation in mean support ’ where there are ‘ increasing levels of favourable wording’, and that ‘[a]llusions to hopelessness had an especially strong effect on increasing support for EPAS [euthanasia and physician-assisted suicide] ’:
Grove, Graham, Ian Hughes, Melanie Lovell, and Megan Best. ‘Content Analysis of Euthanasia Polls in Australia and New Zealand: Words Do Matter’. Internal Medicine Journal 51, no. 10 (2021): 1629–35. https://doi.org/10.1111/imj.15377. * (full text available after embargo ).
See also: L. Parkinson et al. ‘Cancer patients’ attitudes towards euthanasia and physician-assisted suicide: The influence of question wording and patients’ own definitions on responses’, Journal of Bioethical Enquiry , 2(2) (2005): 82-89 * (full text available).
Aghababaei, Naser, Hojjatollah Farahani, and Javad Hatami. ‘Euthanasia Attitude; A Comparison of Two Scales’. Journal of Medical Ethics and History of Medicine 4 (12 October 2011): 9 . * (full text available).
Another reason to be cautious of such polling (and opinion polls more generally) is that they do not necessarily reflect how people actually vote when given the opportunity. Most ballot initiatives in the USA on this issue have in fact failed , despite opinion polls seeming to show strong support. Those which have passed (Oregon, Washington, and Colorado) only secured modest majorities (51%, 58%, and 65% respectively).
4. Medical Opinion on Euthanasia and Assisted Suicide
Whereas simple yes / no public opinion polls typically find a significant majority in favour of legalising assisted suicide or euthanasia, opinion among the medical profession is generally opposed.
In March 2019, the Royal College of Physicians (RCP) adopted a position of neutrality , based on a survey of fellows’ and members’ views . 43.4% thought the RCP should be opposed to a change in the law, 31.6% thought the RCP should support such a change, and 25% thought the RCP should be neutral. While this shift was interpreted by some in the media as a move in favour of legalisation, they stated that, ‘ So that there can be no doubt, the RCP clarifies that it does not support a change in the law to permit assisted dying at the present time ’.
Although the Royal College of Radiographers (RCR) does not hold a position on ‘assisted dying’, in 2019 they polled their fellows and members , asking what they thought the RCR Faculty of Clinical Oncology’s position should be on whether or not there should be a change in the law on ‘assisted dying’. The response rate was only 34% (540 complete responses), but 42.9% thought the RCR position should be ‘opposed’, 26.9% thought ‘in favour’, and 30.3% thought ‘neutral’.
The 70th General Assembly of the World Medical Association (October 2019) stated that ‘ the WMA is firmly opposed to euthanasia and physician-assisted suicide ’.
In 2020, the Royal College of General Practitioners (RCGP) decided not to change its position of opposition to ‘assisted dying’, and would not review this for five years ‘ unless there are significant developments ’.
The decision was based on a 2019 Savanta ComRes consultation of RCGP members . Only 41% of respondents thought the RCGP should support a change in the law if ‘ there is a regulatory framework and appropriate safeguarding processes in place ’. Only 7% thought ‘ GPs should be responsible for prescribing drugs for assisted dying (provided that a formal verification process is in place) ’. There was also reluctance to the idea of referring a patient (only 46% support) or supporting/counselling whilst a decision is being made (only 42% support).
The British Medical Association (BMA) changed its position on 14th September 2021 from opposition to a position of neutrality on the subject of ‘physician-assisted dying’. This was preceded by a survey of BMA members’ views on the subject (Kantar, February 2020). The response rate was 19.35% (28,986 members out of 152,004).
50% of respondents were personally supportive of ‘physician-assisted dying’ as a practice. But the percentage of those willing to participate in some way in ‘physician-assisted dying’ was only 36%. There is stronger opposition in general to euthanasia than there is for assisted suicide.
The Association for Palliative Medicine of Great Britain and Ireland (APM) urged parliamentarians to reject the Assisted Dying Bill [HL] 2021 in a briefing statement in October 2021 . A 2021 APM member survey found that 67% of respondents thought that ‘ patients and families think they are definitely or probably practicing covert euthanasia ’, showing a prevalence of misconceptions about palliative care among the public. 87% ‘ felt there has not been good enough press coverage of good deaths ’.
A study in New Zealand showed that medical students were less likely to support euthanasia / assisted suicide towards the end of their studies compared with the beginning, which is ‘ most likely due to their time in medical education ’, see:
Nie, Luke, Kelby Smith-Han, Ella Iosua, and Simon Walker. ‘New Zealand Medical Students’ Views of Euthanasia/Assisted Dying across Different Year Levels’. BMC Medical Education 21, no. 1 (23 February 2021): 125. * (full text available).
Research in Norway in 2014 and 2016 shows that only 9.1% of doctors in the Institute for Studies of the Medical Profession ‘strongly agree’ or ‘partially agree’ with PAS:
Gaasø, Ole Marius, Karin Isaksson Rø, Berit Bringedal, and Morten Magelssen. ‘Doctors’ Attitudes to Assisted Dying’. Tidsskrift for Den Norske Laegeforening: Tidsskrift for Praktisk Medicin, Ny Raekke 139, no. 1 (15 January 2019). * (full text available).
Disparity between support and willingness to be involved
Evidence from Canada and Australia show high levels of disparity between those who support euthanasia/assisted suicide in principle, and those who are willing to participate in the procedure.
Sellars, Marcus, Mark Tacey, Rosalind McDougall, Barbara Hayes, Bridget Pratt, Courtney Hempton, Karen Detering, et al. ‘Support for and Willingness to Be Involved in Voluntary Assisted Dying: A Multisite, Cross-Sectional Survey Study of Clinicians in Victoria, Australia’. Internal Medicine Journal 51, no. 10 (2021): 1619-1628 . * ( embargoed until 01/10/2022)
Bouthillier, Marie-Eve, and Lucie Opatrny. ‘A Qualitative Study of Physicians’ Conscientious Objections to Medical Aid in Dying’. Palliative Medicine 33, no. 9 (October 2019): 1212–20. * (full text available).
The RCR poll of fellows and members in 2019 (see above) showed that 37.3% supported a change in the law to permit ‘assisted dying’, with 46.9% opposed. But when asked, regardless of support or opposition, if they would ‘participate directly’ should the law change, 56.1% said ‘no’ and 23.2% said ‘yes’.
Religious views on End-of-Life Issues
Pew Research Center, ‘Religious Groups’ Views on End-of-Life Issues’, November 21 2013.
In the UK, a study of the influence of religious beliefs on medical students’ attitudes to EAS showed that among those surveyed (with 68.5% professing belief in God), ‘ the majority of students did not agree with euthanasia and physician-assisted suicide in the study scenario. Those who had a belief in god were more likely to disagree with actions that hasten death. The findings show that this was particularly the case with students from a Muslim background ’. See:
Pomfret, Suzie, Shaya Mufti, and Clive Seale. ‘Medical Students and End-of-Life Decisions: The Influence of Religion’. Future Healthc J 5, no. 1 (1 February 2018): 25–29. https://doi.org/10.7861/futurehosp.5-1-25 . * (full text available)
5. Causes of Concern where Euthanasia and / or Assisted Suicide (EAS) is Legal (Part 1)
Euthanasia and / or assisted suicide is legal in a number of places in the world. In some cases, legalisation happened nearly 30 years ago, although there has been a rapid growth in the last 10 years in the number of jurisdictions where, in particular, assisted suicide is permitted under certain conditions.
The British Medical Association have produced a map which shows at a glance where euthanasia and / or assisted suicide is legal.
Commonly there is a requirement for reporting data and monitoring of practice in places where EAS is permitted (see section 2 above). Such reports, along with other data and analysis provides a body of evidence which highlights several aspects of the practice, including reasons for concern. This section provides information from such data which highlight problematic aspects of euthanasia and assisted.
Ever increasing number of people dying by EAS following legalisation
Belgium and the Netherlands provide data over a long period of time, and therefore are amongst the most studied jurisdictions. An obvious cause of concern from both places is that EAS have shown large incremental increases over time.
Figures 1 and 2 below show the number of deaths attributed to EAS since the early 2000s in Belgium and the Netherlands, showing the increasing numbers over time. Looking more closely, comparing the number of deaths in each country over the ten-year period between 2008 and 2018, we see significant increases, with EAS making up:
- 0.78% of deaths in Belgium in 2008, rising to 2.4% of deaths by 2018
- 1.7% of deaths in 2008 and 3.9% of deaths in 2018 in the Netherlands (4.1% in 2020)
In other jurisdictions, similar increases are seen. In Canada, for example, the increase in deaths since legalisation of PAS was very steep, rising from 1,018 in 2016 to 7,595 in 2020, a 7.5-fold increase in just four years , representing 0.38% of all deaths in 2016, increasing to 2.5% of all deaths in 2020. In Switzerland, between 2009 and 2019, the number of AS deaths increased more than 4-fold from 297 to 1,196 (see Figure 3 below).
The number of deaths due to AS in Canada in 2020 is the highest total number of deaths due to EAS reported in any country in the world at 7,595, with the Netherlands the next highest number, recording its highest ever number at 6,938 in 2020 . It should be a cause for concern that in places where EAS is legal to practice, increasing numbers of people choose to end their own lives, or to ask for others to end them for them.
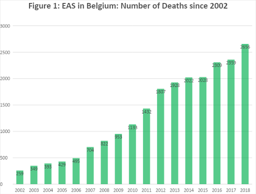
5. Causes of Concern where Euthanasia and / or Assisted Suicide (EAS) is Legal (Part 2)
Terminology of the Legislation
In many places where EAS is legally practised, the language surrounding the legislation could be argued to minimise the reality of the practices employed and the nature of the acts involved; namely a direct act by a medical practitioner with the intention of ending the life of a person (euthanasia), and the writing of a prescription for drugs knowing that they will be used by a person to bring about the end of their own life (physician-assisted suicide).
To accurately assess the ethics and effects of a particular law or practice it is important that terminology is clear and unequivocal in what it describes. ‘Assisted dying’ for example may mean PAS, or EAS. On this point see:
Jones, David Albert. ‘Defining the Terms of the Debate – Euthanasia and Euphemism’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
For an ‘ overview of the terminology, evolution and current legislative picture of assisted dying practices around the globe ’ see:
Mroz, Sarah, Sigrid Dierickx, Luc Deliens, Joachim Cohen, and Kenneth Chambaere. ‘Assisted Dying around the World: A Status Quaestionis’. Annals of Palliative Medicine 10, no. 3 (March 2021): 3540553–553. https://doi.org/10.21037/apm-20-637. * (full text available)
Figure 3 below gives the name for the legislation allowing EAS in various jurisdictions.
| Figure 3 |
|
|
| Belgian Euthanasia Act (2000) |
|
| End of Life Option Act |
|
| Medical Assistance in Dying Act (2016) |
|
| End of Life Options Act (2016) |
|
| Death With Dignity Act (2016) |
|
| Our Care, Our Choice Act (2018) |
|
| Loi sur L’Euthanasie et L’Assistance au Suicide (2009) |
|
| Death with Dignity Act (2019) |
|
| Termination of Life on Request and Assisted Suicide Act (2002) |
|
| Death with Dignity Act (2019) |
|
| Death with Dignity Act (1994) |
|
| Patient Choice and Control at End of Life Act (2013) |
|
| Death with Dignity Act (2008) |
Extension of eligibility criteria for EAS
Following legalisation, legislation can extend eligibility from those terminally ill to other non-terminal conditions (children, mentally ill, etc.), see:
Patton, Michaela, and Keith Dobson. ‘Proposal for the Extension of Rights to Medical Assistance in Dying (MAiD) to Mature Minors in Canada’. Canadian Psychology/Psychologie Canadienne 62, no. 3 (2021): 318–25. https://doi.org/10.1037/cap0000219 * (full text available).
The logic of EAS eligibility for the terminally ill can be applied in the same way both to the chronically ill, and to justify non-voluntary euthanasia ( i.e. for those incapable of requesting euthanasia). This is referred to as the ‘slippery slope’. See:
Keown, John. ‘Voluntary Euthanasia & Physician-Assisted Suicide – The Two “Slippery Slope” Arguments’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
Keown, John. ‘Euthanasia in the Netherlands: Sliding down the Slippery Slope’. Notre Dame J.L. Ethics & Pub. Pol’y 9, no. 2 (1995): 407–48. * (full text available).
These concerns, including (among others) the EAS for psychiatric indications and evidence in practice of non-voluntary euthanasia are best considered by examining evidence from the four jurisdictions which the longest history of EAS: Switzerland (1982); The Netherlands (1984); Oregon (1997); and Belgium (2002).
5.1 Switzerland
Assisted suicide in Switzerland is performed almost entirely through organisations such as EXIT and Dignitas. Since 1982 (when EXIT was founded) there have been only two official government reports, one in 2012 and another in 2014, and these are dependent on data provided by assisted suicide organisations. Media reporting of UK citizens dying in Switzerland plays a significant role in the UK debate, but it should be noted that most of those individuals would not qualify under current proposals for ‘Assisted Dying’, as they were not expected to die within six months. If the law changed in the UK either people would continue to go to Switzerland (which would have fewer restrictions) or the option of assisted suicide in Switzerland would place pressure on the UK to extend its practice to those who are not terminally ill. Research on the experience of assisted suicide in Switzerland is not reassuring.
In Switzerland, since 1942, inciting or assisting suicide has been illegal when it is for selfish motives (such as financial gain). Since 1982 this law has provided legal space for the organisation EXIT to promote assisted suicide for those ‘with unbearable symptoms or with unacceptable disabilities.’ There are two government reports from the Federal Statistical Office, one in 2012 and latest, for 2014, published in 2016 and revised in 2017 . There are also statistics for assisted suicide by sex and age for 2003-2019 , published by the Federal Statistical Office. Dignitas has released statistics from 1998-2021 .
A systematic study of 43 consecutive cases of assisted suicide in Switzerland from 1992 to 1997 found that in 10 cases (23%), the time between first contact with EXIT and the completed assisted suicide was less than a week and in 4 cases (9%) it was less than a day. In 6 cases (14%) the person had previously been treated in a psychiatric institution. In 11 cases (26%) there was no serious medical condition recorded on file, and in 5 cases (12%) the stated reason for seeking assisted suicide was bereavement. The authors of the study conclude that in the 1990s assisted suicide was ‘performed by lay-people who act without outside control and violate their own rules’.
Frei, Andreas, et al. ‘Assisted suicide as conducted by a “Right-to-Die”-society in Switzerland: a descriptive analysis of 43 consecutive cases.’ Swiss Medical Weekly 131.25-26 (2001): 375-380. * (full text available).
A later study found that between the 1990s and 2001-2004 the rate of assisted suicide for non-fatal diseases increased from 22% to 34% and concluded that ‘ weariness of life rather than a fatal or hopeless medical condition may be a more common reason for older members of Exit Deutsche Schweiz to commit suicide ’.
Fischer, S., Huber, C.A., Imhof, L., Imhof, R.M., Furter, M., Ziegler, S.J., Bosshard, G. ‘Suicide assisted by two Swiss right-to-die organisations’. Journal of Medical Ethics 34, no. 11 (2008): 810-814. * (full text available).
A study in 2014 found that assisted suicide in Switzerland was associated with living alone and divorce and was significantly more frequent among women. In 16% of deaths by assisted suicide no medical condition was listed.
Steck, Nicole, Christoph Junker, Maud Maessen, Thomas Reisch, Marcel Zwahlen, and Matthias Egger. ‘Suicide Assisted by Right-to-Die Associations: A Population Based Cohort Study’. International Journal of Epidemiology 43, no. 2 (April 2014): 614–22. * (full text available).
Research on trends from 1991 to 2008 showed ‘ a tripling of assisted suicide rates in older women, and the doubling of rates in older men ’.
Steck, Nicole, Marcel Zwahlen, and Matthias Egger. ‘Time-Trends in Assisted and Unassisted Suicides Completed with Different Methods: Swiss National Cohort’. Swiss Medical Weekly , no. 25 (14 June 2015). https://doi.org/10.4414/smw.2015.14153 . * (full text available).
Between 2009 and 2019 , the number of assisted suicide deaths increased from 297 to 1196 (an increase of over 400%).
Research showed that requests for assisted suicide were not based on symptom burden but on fear of loss of control. Moreover, those seeking assisted suicide had misconceptions about palliative care.
Gamondi, C., M. Pott, and S. Payne. ‘Families’ Experiences with Patients Who Died after Assisted Suicide: A Retrospective Interview Study in Southern Switzerland’. Annals of Oncology 24, no. 6 (1 June 2013): 1639–44. https://doi.org/10.1093/annonc/mdt033. * (full text available).
Until 2006 assisted suicide had not occurred in Switzerland in a hospital setting. The difficulties of introducing it into hospital and the concerns of the palliative care team are set out below.
Pereira, J, P Laurent, B Cantin, D Petremand, and T Currat. ‘The Response of a Swiss University Hospital’s Palliative Care Consult Team to Assisted Suicide within the Institution’. Palliative Medicine 22, no. 5 (1 July 2008): 659–67. https://doi.org/10.11 . * (full text available).
There is also research from Switzerland on the negative impact on family members of witnessing assisted suicide.
Wagner, B., J. Müller, and A. Maercker. ‘Death by Request in Switzerland: Posttraumatic Stress Disorder and Complicated Grief after Witnessing Assisted Suicide’. European Psychiatry 27, no. 7 (October 2012): 542–46. https://doi.org/10.1016/j.eurpsy.2010.1 *
Assisted suicide in Switzerland is most well known in the UK because of people travelling from the UK to die by assisted suicide. A detailed study of ‘suicide tourism’ shows numbers are increasing, the proportion of cancer is decreasing and the proportion of mental illness and multiple co-morbidities is increasing. Among reasons for assisted suicide the largest single cause, with 223 cases, was cancer, but 37 cited Parkinson’s disease, 37 gave arthritis as a reason, 14 cases were for mental illness, and 40 gave as a reason impairment of eyesight and/or hearing.
Gauthier, Saskia, Julian Mausbach, Thomas Reisch, and Christine Bartsch. ‘Suicide Tourism: A Pilot Study on the Swiss Phenomenon’. Journal of Medical Ethics 41, no. 8 (1 August 2015): 611–17. https://doi.org/10.1136/medethics-2014-102091. * (full text available).
A study from 2016 shows that there has been an increase in the practices of voluntary and non-voluntary euthanasia in Switzerland, which are both illegal. Additionally, there has been a ‘ substantial increase in the use of continuous deep sedation until death, from 4.7% of all deaths in 2001 to 17.5% in 2013 [...] this practice was therefore more common in Switzerland than in either Belgium (12.0% in 2013) or the Netherlands (12.3% in 2010) ’.
Bosshard, Georg, Ueli Zellweger, Matthias Bopp, Margareta Schmid, Samia A. Hurst, Milo A. Puhan, and Karin Faisst. ‘Medical End-of-Life Practices in Switzerland: A Comparison of 2001 and 2013’. JAMA Internal Medicine 176, no. 4 (April 2016): 555–56. * (full text available).
5.2 The Netherlands
In addition to annual reports, based on notified cases of euthanasia there have been a series of studies of end-of-life practices at 5-year intervals since 1990. These were nationwide studies of a stratified sample from the national death registry. Questionnaires were sent to physicians attending these deaths and were returned anonymously. The first is commonly termed the Remmelink Report and subsequent reports followed the same pattern. Both the annual reports and the five yearly studies show incremental increases in deaths by euthanasia over time. Deaths by assisted suicide are less frequent, in part because they are associated with complications.
In the Netherlands euthanasia was effectively decriminalised by a court decision in 1984. This was the basis of a legal statute in 2001 legalising euthanasia and physician assisted suicide. Since 2002 the Netherlands has produced an annual report on the cases notified to the five regional euthanasia committees. These are available (in English once the year is selected) .
The first two reports showed evidence of a number of deaths without explicit patient request (in other words non-voluntary euthanasia). The rates were 0.8% and 0.7% being equivalent to 1,000 and 900 deaths in per year. The reaction of supporters was generally to dismiss the significance of these figures, rather than to see them as a possible cause for concern.
Maas, Paul J. van der, Gerrit van der Wal, Ilinka Haverkate, Carmen L.M. de Graaff, John G.C. Kester, Bregje D. Onwuteaka-Philipsen, Agnes van der Heide, Jacqueline M. Bosma, and Dick L. Willems. ‘Euthanasia, Physician-Assisted Suicide, and Other Medical Practices Involving the End of Life in the Netherlands, 1990-1995’. New England Journal of Medicine 335, no. 22 (28 November 1996): 1699-1705. * (full text available).
Keown, John. ‘Euthanasia in the Netherlands: Sliding down the Slippery Slope’. Notre Dame Journal of Law, Ethics & Public Policy 9, no. 2 (1 January 2012): 407-448. * (full text available).
Van Delden, Johannes J. M., Loes Pijnenborg, and Paul J. Van Der Maas. ‘Reports from The Netherlands. DANCES WITH DATA’. Bioethics 7, no. 4 (1993): 323–29. https://doi.org/10.1111/j.1467-8519.1993.tb00222.x. *
Cohen-Almagor, Raphael. ‘Non-Voluntary and Involuntary Euthanasia in the Netherlands: Dutch Perspectives’. Issues in Law & Medicine 18 (2003): 239-257. * (full text available).
For such reasons the law and practice of euthanasia and assisted suicide in the Netherlands has been criticised several times by the United Nations Human Rights Committee.
UN Human Rights Committee (HRC), UN Human Rights Committee: Concluding Observations: Netherlands, 27 August 2001, CCPR/CO/72/NET
UN Human Rights Committee (HRC), Concluding observations of the Human Rights Committee: Netherlands, 25 August 2009, CCPR/C/NLD/CO/4
The 2019 report expresses its concern by stating ‘ The Committee is concerned, however, at the limited ex ante review of decisions to terminate life, including the legal and ethical implications of such decisions (art. 6) ’. (para. 28). See:
UN Human Rights Committee (HRC), UN Human Rights Committee: ‘Concluding Observations on the 5th Periodic Report of the Netherlands’, 126th session, 22 August 2019. CCPR/C/NLD/CO/5
Results from the most recent 5-yearly study (published in 2017 and providing data from 1990, 1995, 2001, 2005, 2010 and 2015) show that deaths classified as ‘ ending life without explicit patient request ’ have declined from 0.8% in 1990 0.3% in 2015. However, overall numbers of deaths by euthanasia have almost tripled (from 1.7% to 4.5%) Another matter of concern is the steep rise in cases of continuous deep sedation (from 8.2% in 2005to 18.3% in 2015), which is in addition to the rise in deaths by ‘ intensified alleviation of symptoms ’ (from 18.8% of deaths in 1990 to 35.8% of deaths in 2015). The presence of so many deaths with, or by, continuous deep sedation or drugs for intensified alleviations of symptoms confounds the data as either may be used as equivalent to (voluntary) euthanasia or to life ending without request. See:
Van der Heide, Agnes, Johannes JM Van Delden, and Bregje D. Onwuteaka-Philipsen. ‘End-of-life decisions in the Netherlands over 25 years.’ New England Journal of Medicine 377.5 (2017): 492-494. *
The latest annual report (for 2020) shows that the total number of deaths by euthanasia continues to increase. There were 6,938 deaths by euthanasia or assisted suicide notified in 2020, up 9.1% on the previous year, and constituting 4.1% of all deaths in the Netherlands for 2020 (which must be taken in conjunction with the fact that there was an excess of around 15,000 deaths in the Netherlands in 2020). In 2 cases, coronavirus infection was the grounds for euthanasia, and coronavirus infection plus other medical conditions in a further 4 cases.
There are no data on euthanasia for either mental illness or dementia prior to 2012 (before this they are presumably considered under ‘other conditions’). In the 2013 report the category is changed from ‘mental illness’ to ‘mental disorders’, and from 2014 on is referred to as ‘psychiatric disorders’. Figure 1 ( data source ) below shows the figures for these conditions.
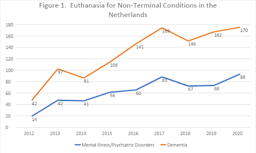
5.2 The Netherlands (cont’d)
From 2012-2020 euthanasia for psychiatric disorders has increased by over 600% and for dementia by over 400%.
This increase in euthanasia or assisted suicide for non-terminal conditions reflects opinion among professionals, with a significant number (between 24% and 39%) in favour of euthanasia or assisted suicide for individuals who experience mental suffering due to loss of control, chronic depression or early dementia. A third of doctors and 58% of nurses were in favour of euthanasia in the case of severe dementia, given the presence of an advance directive.
Kouwenhoven, Pauline SC, Natasja JH Raijmakers, Johannes JM van Delden, Judith AC Rietjens, Maartje HN Schermer, Ghislaine JMW van Thiel, Margo J Trappenburg, et al. ‘Opinions of Health Care Professionals and the Public after Eight Years of Euthanasia Leg i slation in the Netherlands: A Mixed Methods Approach’. Palliative Medicine 27, no. 3 (1 March 2013): 273-80. * (post print text available).
Other research shows a wide variation among general practitioners, consultants and members of the euthanasia committees in their judgement of whether the patient’s suffering is sufficient for euthanasia.
Rietjens, J. a. C., D. G. van Tol, M. Schermer, and A. van der Heide. ‘Judgement of Suffering in the Case of a Euthanasia Request in The Netherlands’. Journal of Medical Ethics 35, no. 8 (1 August 2009): 502–7. https://doi.org/10.1136/jme.2008.028779. *
While euthanasia is defined as ending life on request, the Netherlands has extended life ending without request to newborn infants with disabilities. A description of the protocol (known as the Groningen protocol) is given by two authors who helped develop this practice.
Verhagen, A. A. E., and P. J. J. Sauer. ‘End-of-Life Decisions in Newborns: An Approach From the Netherlands’. Pediatrics 116, no. 3 (1 September 2005): 736–39. https://doi.org/10.1542/peds.2005-0014. * (full text available).
While euthanasia and assisted suicide are requested to secure an easeful death, complications are well documented, especially in assisted suicide. A study in 2000 found that ‘ complications [such as spasm, gasping for breath, cyanosis, nausea or vomiting] occurred in 7% of cases of assisted suicide, and problems with completion [a longer-than-expected time to death, failure to induce coma, or re-awakening of the patient] occurred in 16% ’ because of which ‘ physicians who intend to provide assistance with suicide sometimes end up administering a lethal medication themselves. ’ This is not only a problem of the past; in the 2020 report there were 6,705 cases of euthanasia (‘termination of life on request’), 216 cases of assisted suicide and 17 cases involving a combination of the two ( i.e. , cases which began as assisted suicide, but had to be completed by euthanasia).
Groenewoud, Johanna H., Agnes van der Heide, Bregje D. Onwuteaka-Philipsen, Dick L. Willems, Paul J. van der Maas, and Gerrit van der Wal. ‘Clinical Problems with the Performance of Euthanasia and Physician-Assisted Suicide in the Netherlands’. New England Journal of Medicine 342, no. 8 (24 February 2000): 551–56.
https://doi.org/10.1056/NEJM200002243420805. * (full text available).
Lastly, euthanasia is possible above the age of 12 and below the age of 1. But in 2020, the Netherlands Paediatric Association (Nederlandse Vereinging voor Kindergeneeskunde) expressed the position that the law be extended to allow the termination of life of children between the ages of 1 and 12 under certain conditions. See also the letter to parliament by Hugo de Jonge, the former Minister of Health, Welfare and Sport.
The most important evidence for practice in Oregon is provided by annual reports on the Death with Dignity Act. This section also highlights some aspects that been raised in relation to Oregon practice but are not based on the reports. See also research on the impact of assisted suicide on suicide prevention (section 7, below).
According to the latest official Oregon report, the most frequent end-of-life concern cited by people requesting assisted suicide is not pain but ‘loss of autonomy’ (90.9%), followed by decreased ability ‘to engage in activities making life enjoyable’ (90.2%), ‘loss of dignity’ (73%), ‘burden on family, friends/caregivers’ (48.3%), and ‘losing control of bodily functions’ (43.7%) and only then ‘inadequate pain control or concern about it’ (27.5%), (in each case citing accumulated data for 1998-2021). Evidently, most of these concerns relate to disability and increased dependence. The concern about feeling one is a ‘burden’ on others is significant, much more so than fear of pain (which, also, should not be conflated with actual pain).
From the same report it is clear that in only 14.6% of cases was the prescribing physician present at the time of death (only 11.6% in 2020), that only 3.3% were referred for psychiatric evaluation (only 0.8% in 2021), and that in 56.7% of cases the person was dependent on Medicare/Medicaid insurance or other governmental insurance (up to 78.9% in 2021).
According to Oregon’s Prioritized List of Health Services 2022 cancer treatment is limited according to relative life expectancy, for example, ‘[t]reatment with intent to prolong survival is not a covered service for patients who have progressive metastatic cancer [...]’(Guidance Note 12, GN-5). In contrast ‘It is the intent of the Commission that services under ORS 127.800-127.897 (Oregon Death with Dignity Act) be covered for those that wish to avail themselves to those services’ (Statements of Intent, SI-1).
[N.B. The Statements of Intent and Guidance Notes come after the 160 pages of the prioritised list.]
Health Evidence Review Commission, Prioritized List of Health Services (1 January 2022) .
It should be noted that the drugs that are used for assisted suicide are also used in execution by lethal injection in the United States. This dual use is causing availability problems with supply of the drugs.
Jaquiss, Nigel. ‘Penalized By The Death Penalty’ Willamette Week 21 May 2014.
A good overview of practice in Oregon, including some case studies as well as statistical evidence, shows problems with doctor shopping, suspect coercion and lack of sufficient psychiatric evaluation.
Hendin, Herbert, and Kathleen Foley. ‘Physician-Assisted Suicide in Oregon: A Medical Perspective’. Michigan Law Review 106, no. 8 (2008): 1613–39 . * (full text available).
Kenneth Stevens has shown that from 2001 to 2007 a majority (61%, 165 out of 271) of the lethal prescriptions were written by a minority (18%, 20 out of 109) of the participating physicians. More striking still, just 3 physicians were responsible for 23% of lethal prescriptions (62 out of 271).
Stevens Jr., Kenneth R. ‘Concentration of Oregon’s Assisted Suicide Prescriptions & Deaths from a Small Number of Prescribing Physicians’. Physicians for Compassionate Care Education Foundation, 18 March 2015.
See also ‘Five Oregonians to Remember’ PCCEF, 27 December 2007.

5.4 Belgium
Though Belgium legalised euthanasia in 2002, eighteen years after the Netherlands (in 1984), its number of deaths are near that of the Netherlands. There were 5,015 reported cases in 2019 (more than six times the 822 reported cases in 2009). According to research conducted by Chambaere (see below) these official figures underreport euthanasia by around 50%. What is more worrying is that research indicates that more than 1,000 patients a year (1.7% of all deaths) have their lives ended deliberately without having requested it. This figure has not declined with time. Since legalisation in 2002, reports have been produced every two years. These are available (in French) here.
For a critical analysis of euthanasia in Belgium, see:
Jones, David Albert, Chris Gastmans, and C. MacKellar, eds. Euthanasia and Assisted Suicide: Lessons from Belgium . Cambridge Bioethics and Law. Cambridge, UK and New York, NY: Cambridge University Press, 2017. (This book can be ordered here ).
Devos, Timothy (ed.). Euthanasia: Searching for the Full Story: Experiences and Insights of Belgian Doctors and Nurses , Cham: Springer International Publishing, 2021. https://link.springer.com/book/10.1007/978-3-030-56795-8. (free e-book)
Belgian law came to prominence with the decision in February 2014 to extend euthanasia to children. This caused concern among clinicians and bioethicists in other countries.
Siegel, Andrew M., Dominic A. Sisti, and Arthur L. Caplan. ‘Pediatric Euthanasia in Belgium: Disturbing Developments’. JAMA 311, no. 19 (21 May 2014): 1963–64. https://doi.org/10.1001/jama.2014.4257. *
Carter, Brian S. ‘Why Palliative Care for Children Is Preferable to Euthanasia’. American Journal of Hospice and Palliative Medicine® 33, no. 1 (1 February 2016): 5–7. https://doi.org/10.1177/1049909114542648. * (full text available).
For background to the original 2002 law and its initial implementation see:
Cohen-Almagor, Raphael. ‘Euthanasia Policy and Practice in Belgium: Critical Observations and Suggestions for Improvement’. Issues in Law & Medicine 24, no. 3 (2009): 187–218. * (full text available)
See also a report analysing ten years of euthanasia practice in Belgium.
E de Diesbach, M de Loze, C Brochier and E Monterol. Euthanasia in Belgium: 10 years on European Institute of Bioethics (April 2012).
Research shows that the cases that are not reported are also less likely to involve a written request, less likely to involve specialist palliative care, and more likely to be performed by a nurse.
Smets, T., J. Bilsen, J. Cohen, M. L. Rurup, F. Mortier, and L. Deliens. ‘Reporting of Euthanasia in Medical Practice in Flanders, Belgium: Cross Sectional Analysis of Reported and Unreported Cases’. BMJ 341, no. oct05 2 (5 October 2010): c5174–c5174. * (full text available).
Research on nurses in Belgium in 2007 showed that cases of life-ending without request were almost as common as cases of euthanasia, and that in 12% of euthanasia cases and 45% of life-ending without request it was a nurse who administered the lethal dose, actions which went ‘beyond the legal margins of their profession’.
Inghelbrecht, E., J. Bilsen, F. Mortier, and L. Deliens. ‘The Role of Nurses in Physician-Assisted Deaths in Belgium’. Canadian Medical Association Journal 182, no. 9 (15 June 2010): 905–10. https://doi.org/10.1503/cmaj.091881. * (full text available).
On the ongoing issue of high levels of intentional life-ending without consent in Belgium see:
Cohen-Almagor, Raphael. ‘First Do No Harm: Intentionally Shortening Lives of Patients Without Their Explicit Request in Belgium’. Journal of Medical Ethics , 4 June 2015. https://papers.ssrn.com/abstract=2614587. * (full text available).
Research has also shown that, in Belgium, continuous deep sedation is used with the intention or co-intention to shorten life in 17% of cases, but that it is rarely instituted at the request of the patient (only in 12.7% of cases).
Papavasiliou, Evangelia, Kenneth Chambaere, Luc Deliens, Sarah Brearley, Sheila Payne, Judith Rietjens, Robert Vander Stichele, and Lieve Van den Block. ‘Physician-Reported Practices on Continuous Deep Sedation until Death: A Descriptive and Comparative Study’. Palliative Medicine 28, no. 6 (1 June 2014): 491-500. https://doi.org/10.1177/0269216314530768 * (full text available).
Recent research (published in 2015) shows that while rates of euthanasia increase there has been no improvement in reporting and no reduction in cases of life-ending without request.
Chambaere, Kenneth, Robert Vander Stichele, Freddy Mortier, Joachim Cohen, and Luc Deliens. ‘Recent Trends in Euthanasia and Other End-of-Life Practices in Belgium’. The New England Journal of Medicine 372, no. 12 (19 March 2015): 1179–81 . * (full text available).
In the face of evidence of widespread ending of life without request some researchers have sought to excuse these actions because a third of such patients had, ‘at some point’ in the past, either explicitly or ‘implicitly’ expressed a wish that their lives be ended. However, the very attempt to downplay concerns about deaths deliberately brought about without an explicit request itself illustrates the degree to which non-voluntary euthanasia in Belgium is tolerated and is not regarded as shocking or as a practice in urgent need of correction.
Chambaere, K., J. L. Bernheim, J. Downar, and L. Deliens. ‘Characteristics of Belgian “Life-Ending Acts without Explicit Patient Request”: A Large-Scale Death Certificate Survey Revisited’. CMAJ Open 2, no. 4 (2 December 2014): E262–67. * (full text available).
On the distinction between expressing a wish to die, a wish to hasten death, and a request, see:
Monforte-Royo, Cristina, Christian Villavicencio-Chávez, Joaquín Tomás-Sábado, and Albert Balaguer. ‘The Wish to Hasten Death: A Review of Clinical Studies’. Psycho-Oncology 20, no. 8 (2011): 795–804. https://doi.org/10.1002/pon.1839. * (full text available).
Data from the annual reports shows that an increasing percentage of those dying by euthanasia mention a combination of physical and psychical suffering (78.8% in 2018 and 82.8% in 2019), with figures for solely physical pain reducing (17.7% in 2018 and 12.8% in 2019) and suffering for solely psychic reasons increasing (3.5% in 2018 and 4.3% in 2019).
Stories of individual cases are no substitute for quantitative research, but they help show the possible human meaning behind these statistics. Some illustrative examples are given below.
‘Marc and Eddy Verbessem, Deaf Belgian Twins, Euthanized’ The World Post 15 January 2013 .
Waterfield, ‘Belgian killed by euthanasia after a botched sex change operation’ Telegraph 01 Oct 2013.
E O’Gara ‘Physically healthy 24-year-old granted right to die in Belgium’ Newsweek 29 June 2015.
Associated Press, ‘Belgian Court Acquits 3 Doctors in Landmark Euthanasia Case’ Courthouse News Service 31 January 2020.
Further example cases from Belgium are described here:
Beuselinck, Benoit. ‘Euthanasia Case Studies from Belgium: Concerns about Legislation and Hope for Palliative Care’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
6. Disability and the Impact of Assisted Suicide and Euthanasia
Groups representing people with disabilities have been at the forefront of opposition to the legalisation of assisted suicide and euthanasia. Arguments from this perspective, especially in popular publications and comment pieces, have been criticised as reflecting and/or feeding on fears without showing that these fears are reasonable. However, there is also more critical reflection from this perspective, including discussion of empirical evidence relevant to assessing these concerns.
Some opinion polls among disabled people find considerable support for legalising ‘assisted dying’ .
These results are similar to opinion polls in the general population and should be treated with the same caution (see above on the wording of polls). It is important also to take into account polls that identify concerns among disabled people that legal changes could put pressure on disabled people to end their lives prematurely .
An interesting exchange on this issue by two people with disabilities was conducted by Carol Gill and Andrew Batavia. Batavia argues that empirical data is irrelevant to the issue which, in his view, is about values, and centrally the value of autonomy. He is in favour of legalising assisted suicide.
Batavia, A. I. ‘The Relevance of Data on Physicians and Disability on the Right to Assisted Suicide: Can Empirical Studies Resolve the Issue?’ Psychology, Public Policy, and Law: An Official Law Review of the University of Arizona College of Law and the University of Miami School of Law 6, no. 2 (June 2000): 546-58. *
In response Gill presents data, which is relevant to the perception of disability and its role (implicitly or explicitly) in decisions to grant requests for assistance in suicide. For example, she cites research that shows that among 153 emergency care providers, only 18% of physicians, nurses, and technicians imagined they would be glad to be alive with a severe spinal cord injury. In contrast, 92% of a group of 128 persons with high-level spinal cord injuries said they were glad to be alive.
Gill, CJ. ‘Health professionals, disability, and assisted suicide: An examination of relevant empirical evidence and reply to Batavia (2000).’ Psychology, Public Policy, and Law 6.2 (2000): 526-45. *
Unfortunately, neither of these papers is freely available online. However, another very interesting paper by Gill provides a good sense of what a critical and empirically informed disability perspective looks like. More generally, the Disability and Health Journal (in which this paper appears) is a useful source for articles on disability and assisted suicide.
Gill, CJ. ‘No, we don't think our doctors are out to get us: Responding to the straw man distortions of disability rights arguments against assisted suicide’. Disability and Health Journal 3.1 (2010): 31-38 . * (full text available)
Probably the most influential article arguing that the evidence shows no negative impact of assisted suicide or euthanasia on vulnerable groups (including people with disabilities) is by Margaret Battin.
Battin, Margaret P, Agnes van der Heide, Linda Ganzini, and Gerrit van der Wal. ‘Legal Physician‐assisted Dying in Oregon and the Netherlands: Evidence Concerning the Impact on Patients in “Vulnerable” Groups’. Journal of Medical Ethics 33, no. 10 (October 2007):591-597. * (full text available)
The methodology and conclusions of this paper have been criticised by Ilora Finlay and Rob George.
Finlay, I. G., and R. George. ‘Legal Physician-Assisted Suicide in Oregon and The Netherlands: Evidence Concerning the Impact on Patients in Vulnerable Groups--Another Perspective on Oregon’s Data’. Journal of Medical Ethics 37, no. 3 (March 2011): 171–74 . https://doi.org/10.1136/jme.2010.037044 . *
A detailed discussion of Battin’s evidence and counter-evidence from other expert witnesses is found in the Irish Divisional Court case Fleming v Ireland [2013] IEHC 2 (especially para 67) .
‘ [T]he the expert evidence offered by Dr. O’Brien and Professor George to the effect that relaxing the ban on assisted suicide would bring about a paradigm shift with unforeseeable (and perhaps uncontrollable) changes in attitude and behaviour to assisted suicide struck the Court as compelling and deeply worrying… The Court finds the evidence of these witnesses, whether taken together or separately, more convincing than that tendered by Professor Battin, not least because of the somewhat limited nature of the studies and categories of person studied by Professor Battin… ’
Battin’s argument is also criticised by Pereira on the basis that “safeguards” are largely illusory.
Pereira, J. ‘Legalizing Euthanasia or Assisted Suicide: The Illusion of Safeguards and Controls’. Current Oncology 18, no. 2 (April 2011): e38. https://doi.org/10.3747/co.v18i2.883. * (full text available).
Similarly, a detailed discussion of the evidence from Oregon from a disability perspective concludes that ‘ Battin et al.’s interpretation that people with physical disabilities or chronic illnesses are not at increased risk for DWD does not seem to be supportable given available data’ .
CE Drum, G White, G Taitano and W Horner-Johnson, ‘The Oregon Death with Dignity Act: results of a literature review and naturalistic inquiry’. Disability and health journal , 2010, 3(1): 3-15 . * (full text available).
If disability includes mental illness, then there is clearly a group of patients who are prima facie endangered by assisted suicide. In Oregon there has been a decline in the “safeguard” of referral for psychiatric evaluation whereas in Belgium and Switzerland mental illness can itself be a basis for euthanasia or assisted suicide. A study published in the BMJ shows how far the euthanising of psychiatric patients has progressed in Belgium: of 100 patients who requested euthanasia for psychiatric reasons, 73 ‘ were medically unfit for work (they were either receiving disability living allowances or had taken early retirement) ’, i.e. most were categorised as having a disability. Of the 100, 38 were referred for further psychiatric evaluation, after which 17 were approved for euthanasia and 10 died by euthanasia during the study period. Of the 62 people not referred, 31 were approved for euthanasia and 25 died by euthanasia during the study period. These patients suffered from a variety of conditions including mood disorders (58 including 10 who were bipolar), borderline personality disorder (27), schizophrenia and other psychotic disorders (14), post-traumatic stress disorder (13), eating disorders (10), autism spectrum disorder (7), attention deficit hyperactivity (1) as well as other diagnoses, often combining diagnoses ( e.g. , a mood disorder and personality disorder). During the period of the study 6 participants died by (non-assisted) suicide, one from anorexia nervosa and one from palliative sedation. None were terminally ill.
Thienpont L, Verhofstadt M, Van Loon T, et al. ‘Euthanasia requests, procedures and outcomes for 100 Belgian patients suffering from psychiatric disorders: a retrospective, descriptive study’. BMJ Open 2015;5: e007454. doi:10.1136/bmjopen-2014-007454 * (full text available).
Disability makes assessment of ‘ decisional capacity ’ difficult. A study of cases in the Netherlands shows that the ‘ Dutch EAS due care criteria are not easily applied to people with intellectual disabilities and/or autism spectrum disorder, and do not appear to act as adequate safeguards. ’ See:
Tuffrey-Wijne, Irene et al. “Euthanasia and assisted suicide for people with an intellectual disability and/or autism spectrum disorder: an examination of nine relevant euthanasia cases in the Netherlands (2012-2016).” BMC medical ethics vol. 19,1 17. 5 Mar. 2018, doi:10.1186/s12910-018-0257-6 * (full text available).
Tuffrey-Wijne, Irene et al. “‘Because of His Intellectual Disability, He Couldn’t Cope.’ Is Euthanasia the Answer?”. Journal of Policy and Practice in Intellectual Disabilities , vol. 16, no. 2 (June 2019):113-116, https://doi.org/10.1111/jppi.12307 * (post-print draft version available).
EAS in the Netherlands for psychiatric disorders shows that patients are ‘ mostly women, of diverse ages, with complex and chronic psychiatric, medical, and psychosocial histories ’. See:
Kim, Scott Y H et al. “Euthanasia and Assisted Suicide of Patients With Psychiatric Disorders in the Netherlands 2011 to 2014.” JAMA Psychiatry vol. 73,4 (2016): 362-8. doi:10.1001/jamapsychiatry.2015.2887 * (full text available).
Concern is also expressed over safeguards for the disabled, stemming from the myriad of problems the disabled face, such as ‘ subtle pressure, despair at living in a world where their daily existence is seen as one of inevitable suffering or, exhaustion from fighting for the accommodations required to live a life of dignity and pursue their chosen lifestyle and purposes ’. See:
Stainton, Tim. “Disability, vulnerability and assisted death: commentary on Tuffrey-Wijne, Curfs, Finlay and Hollins.” BMC Medical Ethics vol. 20,1 89. 27 (Nov. 2019), doi:10.1186/s12910-019-0426-2 * (full text available).
With respect to more recent developments in Canada regarding EAS for mentally ill patients, see:
Komrad, Mark S. ‘First, Do No Harm: How Canadian Law Allows for Euthanasia and Assisted Suicide for Patients with Psychiatric Disorders’. Briefing Papers: Euthanasia and Assisted Suicide (Anscombe Bioethics Centre, Oxford: 2021).
On the changing social attitude to those living with dementia and how euthanasia poses a threat to living and dying well with dementia, see:
Matthews, Pia. ‘Dignity in Living: Addressing Euthanasia by Affirming Patient Personhood in Dementia’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
7. Suicide Prevention and the Impact of Assisted Suicide
Sometimes advocates of assisted suicide are happy to use this terminology, as for example in the ‘Assisted Suicide (Scotland) Bill’ (introduced in 2011), which was rejected by the Scottish Parliament in 2015. Other proponents avoid this language and prefer ‘dying / death with dignity’, ‘assisted dying/death’ or ‘medical aid in dying’. However, evidence indicates no sharp distinction between assisted suicide and non-assisted suicide. Evidence also suggests legalising assisted suicide ‘normalises’ suicide and is associated with increases in suicide.
Evidence from the USA shows that the legalisation of ‘ assisted suicide is associated with a significant increase in total suicide (inclusive of assisted suicide) and no reduction in non-assisted suicide .’
Jones, David Albert and David Paton ‘How does legalization of physician-assisted suicide affect rates of suicide?, Southern Medical Journal , 108.10 (2015): 599-604. * (pre-print draft available).
The association of legalising assisted suicide and a ‘ significant increase in total suicides ’ is also supported by more recent research on data from the USA. Paton and Sourafel also conclude that ‘ [i]t is possible that there is some substitution from unassisted suicide to assisted suicide but that this is balanced out by an increase in unassisted suicide arising from, for example, a reduction in societal taboos associated with suicide ’. See:
Sourafel, Girma, and David Paton. ‘Is Assisted Suicide a Substitute for Unassisted Suicide?’ European Economic Review , 9 April 2022, 104113. https://doi.org/10.1016/j.euroecorev.2022.104113. * (pre-proof text available).
In Europe, the introduction of euthanasia and assisted suicide has resulted in ‘ considerable increases in suicide (inclusive of assisted suicide) and in intentional self-initiated death ’. See:
Jones, David Albert. ‘Euthanasia, Assisted Suicide, and Suicide Rates in Europe’, Journal of the Ethics of Mental Health 11 (2022):1-35. * (full text available).
Restricting access to means of suicide appear to be ‘ particularly effective in contexts where the method is popular, highly lethal, widely available, and/or not easily substituted by other similar methods ’. See:
Sarchiapone, Marco, Laura Mandelli, Miriam Iosue, Costanza Andrisano, and Alec Roy. ‘Controlling access to suicide means.’ International journal of environmental research and public health 8, no. 12 (2011): 4550-4562, doi: 10.3390/ijerph8124550 * (full text available).
It is argued that ‘assisted death’ of a kind legalised in Oregon, is not assisted suicide because (1) with ‘assisted death’ the person is terminally ill and (2) (non-assisted) suicide is typically the result of depression. However, according to one UK study, ‘at least 10 percent of [non-assisted] suicides nationally involve[ed] some form of serious physical illness (either chronic or terminal)’. See:
Bazalgette, L., W Bradley, J Ousbey. The Truth about Suicide (London: Demos, 2011)
Similarly in Switzerland ‘ In 53% of cases, causes of death registrations for [non-assisted] suicide do not contain any information about concomitant diseases. If no information is available, this may mean various things: either no disease was present or it was unknown. If information is available, 56% of entries cite depression. In the remaining 44% of entries, a physical disease is mentioned. Physical diseases include a range similar to that of assisted suicide (G11). ’ (emphasis added)
Similarly, a report on suicide in Oregon found that 25% of men and 26% of women who died by suicide had had physical health problems, and in the over-65 cohort, 66% of men and 56% of women had physical health problems, including conditions such as cancer, heart disease, and chronic pain.
Shen, X., L Millet. Suicide in Oregon: Trends and Risk Factors 2012 Report . Oregon Health Authority, Portland, Oregon.
The vulnerability of older people, those living alone and those with physical illness was highlighted in a report by the New York Task Force in 1994. The Task Force also found that depression was prevalent in this population, but largely undiagnosed and untreated (see especially chapter 2 of the report).
New York State Task Force on Life and the Law, ‘When Death is Sought: Assisted Suicide and Euthanasia in the Medical Context’ (1994).
Similarly, in a study of 178 Compassion & Choices clients, of those who, in the study period, obtained lethal medication 3 out of 18 (17%) fulfilled the criteria for depression and of those who died by assisted suicide by the end of the study 3 out of 9 (33%) met the criteria for depression.
Ganzini, L., E. R Goy, and S. K Dobscha. ‘Prevalence of Depression and Anxiety in Patients Requesting Physicians’ Aid in Dying: Cross Sectional Survey’. BMJ 337, no. 2 (7 October 2008): a1682–a1682. https://doi.org/10.1136/bmj.a1682. * (full text available).
It has been argued that legalising assisted suicide could, paradoxically, delay or inhibit suicide. This has been argued by Lord Falconer and others, but a particularly clear statement is provided by EXIT.
However, in Oregon between 1999 (two years after PAS was introduced) and 2010 the suicide rate among those aged 35-64 increased by almost 50% (compared to 28% nationally).
See also the report on high rates of suicide in Portland, Oregon. This increase is without counting assisted suicides, which rose in Oregon by 44% in 2013 alone .
According to the Swiss government report , ‘ From 1995 to 2003, the absolute number of suicides fell considerably. Since then, it has more or less remained stable while cases of assisted suicide have increased considerably since 2008 in particular. In 2014, for 7 cases of suicide observed, 5 cases of assisted suicide were seen (G7) ’.
Determination of eligibility for EAS may also have an effect on vulnerability. Looking at the situation in Canada, Isenberg-Grzeda et al conclude that ‘ Clinicians must be vigilant and prepared for the possibility of heightened risk, including risk of self-harm, after a finding of ineligibility for assisted death ’. See:
Isenberg-Grzeda, E., S. Bean, C. Cohen, and D. Selby, ‘Suicide attempt after determination of ineligibility for assisted death: A case series’ Journal of pain and symptom management 60, no. 1 (2020): 158-163 *
It must be noted that if suicide follows on from a determination of ineligibility for EAS, that person’s death would be considered suicide. However, it would not be considered ‘suicide’ if he or she had been eligible and died as a result of the provision of EAS. This highlights the broader point that euphemistic expressions such a ‘assisted dying’ or ‘medical aid in dying’ simply rename what is correctly termed ‘suicide’.
Suicide Contagion
A Swiss study indicates evidence for suicide contagion following media reports of assisted suicide:
Frei, Andreas, Tanja Schenker, Asmus Finzen, Volker Dittmann, Kurt Kraeuchi, and Ulrike Hoffmann-Richter. ‘The Werther Effect and Assisted Suicide’. Suicide and Life-Threatening Behavior 33, no. 2 (June 2003): 192–200. https://doi.org/10.1521/suli.33.2.19 *
Research on the impact of reporting assisted suicide in Oregon has also suggested such an effect.
Stark, Paul. ‘Assisted suicide and contagion’ MCCL White Paper, May 2015 .
This evidence coheres with what is known about suicide, that it increases if the means are more widely available and if it is normalised, see for example, Euregenas (European Regions Enforcing Actions Against Suicide) Suicide Prevention Toolkit for Media Professionals .
See also Preventing Suicide: A Resource for Media Professionals, Update 2017 . Geneva: World Health Organization; 2017 (WHO/MSD/MER/17.5). Licence: CC BY-NC-SA 3.0 IGO.
Evidence of suicide rates among veterinarians (which are significantly higher than the average among the population) is generally understood to be due to access to lethal drugs.
Witte, T.K., E.G. Spitzer, N. Edwards, K.A. Fowler, and R. J. Nett. ‘Suicides and Deaths of Undetermined Intent among Veterinary Professionals from 2003 through 2014’. Journal of the American Veterinary Medical Association 255, no. 5 (2019):595-608. * (full text available).
Research also shows that positive ‘suicide role models’ reinforce high rates of suicide in a population:
Stack, Steven, and Augustine J. Kposowa. ‘The Association of Suicide Rates with Individual-Level Suicide Attitudes: A Cross-National Analysis*’. Social Science Quarterly 89, no. 1 (2008): 39–59. https://doi.org/10.1111/j.1540-6237.2008.00520.x . * (full text available).
Werther and Papageno Effects
Suicides are also associated with the way that suicide is presented in the media. The ‘Werther effect’ refers to media presentations of suicides (fictional and real) and their effect on an increase in suicide rates. The ‘Papageno effect’ refers instead to the preventative effect of media portrayals which depict people coping despite difficult life circumstances and suicidal ideation.
A survey of studies on the two effects shows that ‘ suicide contagion is more likely to occur after extensive media coverage with a content rich in positive definitions of suicide ’. Factors that increase the likelihood of imitation are, for example, ‘ the celebrity status of the suicide victim, similar demographic characteristics and the media audience, and media reports on a new suicide method’ . At the same time, different media portrayals can ‘ have an educative or preventative effect and can reduce the risk of contagion ’. See:
Domaradzki, J. ‘The Werther Effect, the Papageno Effect or No Effect? A Literature Review’. International Journal of Environmental Research and Public Health 18, no. 5 (1 March 2021): 2396. https://doi.org/10.3390/ijerph18052396 . * (full text available).
Studies of the Werther and Papageno effects focus on media portrayals of suicide, but ‘ [g]uidance is needed for media reporting of assisted suicide ’ as well. See:
Jones, David Albert. ‘Assisted dying and suicide prevention’ Journal of Disability & Religion , 22.3 (2018): 298-316 . * (pre print text available online).
A 2021 survey of members of the Association for Palliative Medicine of Great Britain and Ireland showed that ‘ There is also a significant degree of frustration at the media narrative regarding end of life care, which clinicians view as being driven by assisted suicide lobbying. There is concern that poor portrayal of palliative care in the media has led patients and families to have a skewed understanding of palliative care, and there is fear that patients are in a position of ignorance at a vulnerable moment in their lives ’.
8. Gender and the Impact of Assisted Suicide and Euthanasia
Proponents of a change in the law frequently invoke choice (for example the US organisation ‘Compassion & Choices’ or the Scottish organisation ‘My Life, My Death, My Choice’). This language is very similar to ‘pro-choice’ language in relation to abortion, and so it might seem that feminists who are in favour of increased access to legal abortion would also support legalisation of EAS. This argument is indeed accepted by some feminists; however, it has been challenged by a number of feminists who argue that EAS would have a disproportionately negative impact on women.
Wolf, SM. ‘Gender, Feminism, and Death: Physician-Assisted Suicide and Euthanasia’ in Feminism & Bioethics: Beyond Reproduction . New York: Oxford University Press, 1996, pp. 282-317.
Wolf argues that a legal right to abortion (which she supports) does not imply a legal right to assisted suicide.
Wolf, SM. ‘Physician-assisted suicide, abortion, and treatment refusal: Using gender to analyze the difference’ in R Weir, ed. Physician-Assisted Suicide . Indiana University Press, 1997, pp. 167-201 .
On this point see also:
Spindelman, Marc. ‘Are the Similarities between a Woman’s Right to Choose an Abortion and the Alleged Right to Assisted Suicide Really Compelling?’ U. Mich. J. L. Reform 29, no. 775 (1996): 775-856. * (full text available).
Whereas, in the West, the rate of suicide is much higher among men than women (roughly four times), PAS (in Oregon and Washington) is roughly equal between men and women, and rates of assisted suicide in Switzerland reveal a higher proportion of women; this is also true of the suicides assisted by Kervorkian.
Canetto, Silvia Sara, and Janet D. Hollenshead. ‘Gender and Physician-Assisted Suicide: An Analysis of the Kevorkian Cases, 1990–1997’. OMEGA - Journal of Death and Dying 40, no. 1 (2000): 165–208. *
Kohm, Lynne Marie, and Britney N. Brigner. ‘Women and Assisted Suicide: Exposing the Gender Vulnerability to Acquiescent Death’. Cardozo Women’s Law Journal 4 (1997): 241. * (full text available).
Canetto, Silvia Sara, and Janet D. Hollenshead. ‘Older Women and Mercy Killing’. OMEGA - Journal of Death and Dying 42, no. 1 (1 February 2001): 83–99. https://doi.org/10.2190/NRB4-JH8B-VBCW-WM7J. *
Canetto, Silvia Sara, and John L. McIntosh. ‘A Comparison of Physician-Assisted/Death-With-Dignity-Act Death and Suicide Patterns in Older Adult Women and Men’. The American Journal of Geriatric Psychiatry , June 2021, S1064748121003559. https://doi.org/10.1016/j.jagp.2021.06.003 *
George, Katrina. ‘A Woman’s Choice? The Gendered Risks of Voluntary Euthanasia and Physican-Assisted Suicide’. Medical Law Review 15, no. 1 (1 March 2007): 1–33. https://doi.org/10.1093/medlaw/fwl017. *
It has also been argued that a feminist account of relational autonomy gives more ground to be cautious about permitting assisted suicide.
Donchin, Anne. ‘Autonomy, Interdependence, and Assisted Suicide: Respecting Boundaries/Crossing Lines’. Bioethics 14, no. 3 (2000): 187–204. https://doi.org/10.1111/1467-8519.00190. *
Canetto, Sylvia Sara. ‘If Physician-Assisted Suicide Is the Modern Woman’s Last Powerful Choice, Why Are White Women Its Leading Advocates and Main Users?’ Professional Psychology: Research and Practice 50, no. 1 (2019): 39–50. *
For a study of the larger number of women who receive EAS for a psychiatric condition in Belgium and the Netherlands, and its relation to questions of suicide prevention, see:
Nicolini, Marie E., Chris Gastmans, and Scott Y. H. Kim. ‘Psychiatric Euthanasia, Suicide and the Role of Gender’. The British Journal of Psychiatry 220, no. 1 (January 2022): 10–13. https://doi.org/10.1192/bjp.2021.95. *
Data from Switzerland demonstrates not only an increase in total assisted suicides year on year, but also the disproportionately large number of women dying by assisted suicide.
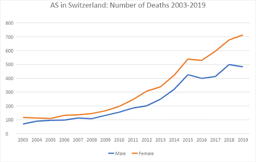
9. Links to Some Campaign Organisations and Further Resources
Whichever side of the argument you find more cogent, it is useful to look at the opposite view and the counter-arguments and evidence they produce, such as it is. Campaign organisations are, by their nature, one sided, but at the very least they raise questions and identify some relevant evidence.
Organisations in favour of legalising assisted suicide or euthanasia
In 2005 the Voluntary Euthanasia Society (founded 1935) changed its name to ‘Dignity in Dying.’ Its immediate aim is legalising physician assisted suicide for the terminally ill not, currently, euthanasia.
http://www.dignityindying.org.uk/
In 2009 Michael Irwin left the Dignity in Dying to found the Society for Old Age Rational Suicide which campaigns for assisted suicide for people who are not dying, but are tired of living. In 2015, the organisation changed its name to ‘My Death, My Decision’.
https://www.mydeath-mydecision.org.uk/
The largest organisation in the USA to campaign in favour of assisted suicide is Compassion & Choices (successor to the Hemlock Society which was founded in 1980).
http://www.compassionandchoices.org/
Also founded in 1980, The World Federation of Right to Die Societies no longer counts Dignity in Dying or Compassion & Choices as ‘members,’ but has links to them as ‘other right to die societies’.
https://wfrtds.org
EXIT founded in 1982 is the main organisation that arranges assisted suicide for Swiss citizens.
http://www.exit.ch/en/
Organisations opposed to legalising assisted suicide and euthanasia
Founded in 2005, Care Not Killing is a UK-based alliance of individuals, disability and human rights groups, healthcare providers, and faith-based bodies opposed to assisted suicide and euthanasia.
http://www.carenotkilling.org.uk/
In 2021 the Better Way campaign was founded to oppose assisted suicide and to set out a positive, alternative vision for the UK. Its website contains information about the Canadian experience of euthanasia and assisted suicide.
https://www.betterwaycampaign.co.uk/canada/
The Euthanasia Prevention Coalition (EPC) has an international scope. There is also a European arm.
https://www.epcc.ca/
https://www.epce.eu/
For a disability perspective see Not Dead Yet and the rather more British (and understated) Not Dead Yet UK.
http://www.notdeadyet.org/
http://notdeadyetuk.org/
For an American perspective critical of assisted suicide see the websites of Physicians for Compassionate Care Education Foundation, the Patients’ Rights Council and ‘Choice’ is an Illusion.
https://www.pccef.org/
https://www.patientsrightscouncil.org/site/
https://www.choiceillusion.org/
News and comment
The excellent and free bioethics news service Bioedge frequently includes stories on these issues.
https://bioedge.org/end-of-life-issues/euthanasia/
Alex Schadenberg (chair of EPC) has a blog, which is also very useful for news stories.
https://alexschadenberg.blogspot.co.uk/
Living and dying well is not a campaign organisation, but presents research and analysis of evidence relevant to (and critical of) assisted suicide and euthanasia.
https://www.livinganddyingwell.org.uk/
Further academic resources
This guide is intended only as an introduction to some of the resources for assessing the evidence and arguments for and against assisted suicide and euthanasia. It is, of necessity, selective as there are many hundreds of official reports, legal cases and journal articles on these topics. Students should research independently making use of academic indices and databases such as EBSCO, Lexis Nexis, Philosophers’ Index, PhilPapers and MEDLINE. You should also ‘follow the footnotes’ reading the sources invoked by or criticised by the article you are reading.
The search engine Pubmed gives access to the MEDLINE database, which includes very many medical journals and also journals of medical ethics, and medically related humanities and social sciences. Unlike other indices it is freely accessible and is a good place for the non-specialist to begin more serious research.
https://www.ncbi.nlm.nih.gov/pubmed
Anscombe Bioethics Centre Briefing Papers
Beuselinck, Benoit. ‘Euthanasia Case Studies from Belgium: Concerns About Legislation and Hope for Palliative Care’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
Jones, David Albert. ‘Defining the Terms of the Debate: Euthanasia and Euphemism’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
Keown, John. ‘Voluntary Euthanasia & Physician-assisted Suicide: The Two “Slippery Slope” Arguments’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2022.
Komrad, Mark. ‘First, Do No Harm: How Canadian Law Allows for Euthanasia and Assisted Suicide for Patients with Psychiatric Disorders’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
Pontifical Academy for Life. ‘Position Paper of the Abrahamic Monotheistic Religions on Matters Concerning the End of Life (28 October 2019)’.
Symons, Xavier. ‘The Principle of Autonomy – Does it Support the Legalisation of Euthanasia and Assisted Suicide?’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2022.
Most recent

Shining a Light on Gender Identity Services: How The Cass Review Shows The Need For Evidence-Based Paediatric Medicine (Dr Julie Maxwell)
22 May 2024
An account of the Cass Review into Gender Identity Services, and how it uncovers the various ways in...

Normalising Surrogacy: A Threat To Human Dignity (Dr Pia Matthews)
13 May 2024
A critique of joint proposals by the Law Commission of England and Wales, and the Scottish Law Commi...

A Briefing on the Human Fertilisation & Embryology Authority (HFEA) consultation, ‘Modernising the regulation of fertility treatment and research involving human embryos’
27 March 2023
Our Briefing on the March-April 2023 HFEA consultation into the potential revision of Human Fertilis...
The Anscombe Bioethics Centre is supported by the Catholic Church in England and Wales, Scotland, and Ireland, but has also always relied on donations from generous individuals, friends and benefactors.
FIND OUT MORE MAKE A DONATION
Cookie notice
We use cookies on our website. They help us to know a little bit about you and how you use our website. They are stored locally on your computer or mobile device. If you continue without changing your settings, we’ll assume that you are happy to receive all cookies. However, you can change your cookie settings at any time. Go to the cookie policy for more information and to update your preferences.
Your cookie preferences
We use cookies and similar technologies on our website. Cookies are text files containing small amounts of information, which your computer or mobile device downloads when you visit a website. When you return to websites, or visit websites that use the same cookies, they recognise these cookies and therefore your browsing device.
We use different types of cookies for different things, such as:
- Analysing how you use our website
- Giving you a better, more personalised experience
- Recognising when you’ve sign in
We split our cookies into three distinct categories. You can turn Functional and Performance cookies on and off right here. Strictly necessary cookies can’t be turned off.
Strictly necessary cookies
These cookies are essential in order to enable you to move around the website and use its features. Without these cookies services you have asked for cannot be provided.
Some examples of how we use these cookies are:
- Signing into our website
- Remembering previous actions such as text entered into a form when navigating back to a page in the same session
- Remembering security settings
- DOI: 10.9734/BJMMR/2015/19151
- Corpus ID: 59942719
Arguments in Support and Against Euthanasia
- Published 10 January 2015
- Philosophy, Medicine
- British journal of medicine and medical research
6 Citations
Legal application of the offence of murder and euthanasia in nigeria, right to commit suicide in india: a comparative analysis with suggestion for the policymakers, comparison of attitude of nurses and nursing students toward euthanasia, medical assistance in dying (maid): human and humanity in the study of fiqh maqașid, attitude of the nursing and midwifery students of mazandaran university of medical sciences towards euthanasia, the ethical challenge of conflicts of interest in healthcare, 78 references, what do physicians think about physician assisted suicide and voluntary euthanasia, euthanasia: right to life vs right to die, the ethics of euthanasia: advocates' perspectives., the ethics of euthanasia: advocates’ perspectives, what is the great benefit of legalizing euthanasia or physican‐assisted suicide, physician-assisted suicide: an anthropological perspective., euthanasia and suicide in antiquity: viewpoint of the dramatists and philosophers., dignity in dying should include the legalization of non-voluntary euthanasia, physician-assisted suicide, physician assisted suicide: a new look at the arguments, related papers.
Showing 1 through 3 of 0 Related Papers
- Get new issue alerts Get alerts
- Submit a Manuscript
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Euthanasia: A controversial debate
Nihal, Kanwal
Department of Medicine, Dow University of Health Sciences, Karachi, Pakistan
Address for correspondence: Dr. Kanwal Nihal, Dow Medical College, Dow University of Health Sciences, Baba-e-Urdu Road, Saddar, Karachi, Pakistan. E-mail: [email protected]
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 4.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
To the Editor,
As the word indicates, euthanasia is derived from the Greek word “euthanatos” meaning “early death.” This term has such countless debates that it has incited emotive reactions both among the clinical practicians and people in general. According to the House of Lords Select Committee on Medical Ethics, the correct definition of euthanasia is “a deliberate intervention undertaken with the express intention of ending a life, to relieve intractable sufferings.”[ 1 ] As of March 2021, active human euthanasia is legal in the Netherlands, Belgium, Colombia, Luxembourg, Western Australia, Canada, and Spain. As a matter of concern, there are many incurable diseases such as dementia and multiple sclerosis, yet my fundamental spotlight is about dementia.
People affected with dementia become unaware of their surroundings as their cognitive efficiency decreases crescively (Cheston and Bender; Kitwood), along with that they become anosognosic and adapt to a lack of decision-making capability. Thus, they live their lives through unbearable sufferings. Therefore, in the research reported by Dröes et al .[ 2 ] and Smith et al. ,[ 3 ] it is stated that the caregivers can enhance the confidence and quality of life of people with dementia by providing them access to their autonomy. Therefore, in 2004–2006 assent for geriatric care was brought in contact for cognitively impaired patients. However, in this practice, only the decision taken by the demented person before his worst condition will be taken in the subject. Thus, the result of this study showed that even after the collaborative efforts tried by the caregiver, it did not mitigate the moral dilemma; instead, it escalated the conflict.[ 4 ]
However, according to a new study, many medical organizations have accentuated to improve palliative care. The International Association for Hospice and Palliative Care stated that no country or state should consider the legalization of physician-assisted suicide-euthanasia until it ensures universal access to palliative care services and appropriate medications, including opioids for pain and dyspnea.[ 5 ]
Therefore, after going through these studies, it has raised significant concern as Pakistan is a third-world country and Islamic country where Muslims solely believe that only God should end their lives, and killing a person who is undergoing unbearable sufferings by euthanasia is forbidden.[ 6 ] As we think of Pakistan, which is a poverty-stricken country, people are confused about whether to continue treatment, which has unpredictable efficacy or to go through euthanasia that will question their lives with a moral dilemma. Thus, they live their lives between Scylla and Charybdis. Not only this, as Pakistan is an underdeveloped nation, it has very few effective therapeutics, hence we should give our prior attention to the palliative care and the conduction of rehabilitation programs to solve this issue. Therefore, the implementation of these new findings in Pakistan will surely help and improve the lives of terminally ill patients.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
- Cited Here |
- Google Scholar
- View Full Text | PubMed | CrossRef |
- View Full Text | CrossRef |
- PubMed | CrossRef |
- + Favorites
- View in Gallery
Our systems are now restored following recent technical disruption, and we’re working hard to catch up on publishing. We apologise for the inconvenience caused. Find out more: https://www.cambridge.org/universitypress/about-us/news-and-blogs/cambridge-university-press-publishing-update-following-technical-disruption
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert

- > Journals
- > Cambridge Quarterly of Healthcare Ethics
- > Volume 5 Issue 1
- > An Analysis of Arguments for and Against Euthanasia...

Article contents
An analysis of arguments for and against euthanasia and assisted suicide: part one.
Published online by Cambridge University Press: 29 July 2009
In advanced technological societies there is growing concern about the prospect of protracted deaths marked by incapacitation, intolerable pain and indignity, and invasion by machines and tubing. Life prolongation for critically ill cancer patients in the United States, for example, literally costs a fortune for very little benefit, typically from $82,845 to $189,339 for an additional year of life. Those who return home after major interventions live on average only 3 more months; the others live out their days in a hospital intensive care unit.
Access options
1. Ghosh , A . The ghosts of Mrs. Ghandi . The New Yorker 1995 ; 61 ( 20 ): 35 – 41 . Google Scholar
2. Byock , IR . The art of dying in America . American Journal of Hospice & Palliative Care 1995 ; 12 ( 2 ): 6 – 7 . CrossRef Google Scholar PubMed
3. Study puts high cost on care for dying . Chicago Tribune 1993 ; 02 10 (Sect 1): 12 . Google Scholar
4. Associated Press/Media General. Poll no. 4. Richmond, Virginia: Media General, February 1985.
5. Cohen , LM , McCue , JD , Germain , M , Kjellstrand , CM . Dialysis discontinuation: a “good” death? Archives of Internal Medicine 1995 ; 155 : 42 –7. CrossRef Google Scholar PubMed
6. Wanzer , SH , Federman , DD , Adelstein , SJ et al. , The physician's responsibility toward hopelessly ill patients: a second look . New England Journal of Medicine 1989 ; 320 : 844 –9. CrossRef Google Scholar PubMed
7. Emanuel , EJ . The history of euthanasia debates in the United States and Britain . Annals of Internal Medicine 1994 ; 121 ( 10 ): 793 – 802 . CrossRef Google Scholar PubMed
8. Brody , H . Assisted death – a compassionate response to a medical failure . New England Journal of Medicine 1992 ; 327 : 1384 –8. CrossRef Google Scholar PubMed
9. de Veber , LL , Henry , F , Nadeau , R et al. , Public Policy, Private Voices: The Euthanasia Debate . Toronto : Human Life Research Institute , 1992 . Google Scholar
10. Quill , T , Cassel , CH , Meier , D . Care of the hopelessly ill: proposed clinical criteria for physician-assisted suicide . New England Journal of Medicine 1992 ; 342 : 1380 –4. CrossRef Google Scholar
11. Ciesielski-Carlucci , C . Physician attitudes and experience with assisted suicide: results of a small opinion survey . Cambridge Quarterly of Healthcare Ethics 1993 ; 2 : 39 – 44 . CrossRef Google Scholar
12. Kushner , T . CQ Interview: Derek Humphry on death with dignity . Cambridge Quarterly of Health-care Ethics 1993 ; 2 : 57 – 62 . CrossRef Google Scholar
13. Associated Press. Oregon doctors get voters' ok to aid suicides. Chicago Tribune 1994 ; 11 11 (Sect 1): 27 . Google Scholar
14. Associated Press. U.S. judge voids assisted suicide law. Chicago Tribune 1995 ;August 4 (Sect 1): 3 . Google Scholar
15. Stevens , CA , Hassan , R . Management of death, dying and euthanasia: attitudes and practices of medical practitioners in South Australia . Journal of Medical Ethics 1994 ; 20 : 41 –6. CrossRef Google Scholar PubMed
16. McGough , PM . Washington State Initiative 119: the first public vote on legalizing physician-assisted death . Cambridge Quarterly of Healthcare Ethics 1993 ; 2 : 63 –7. CrossRef Google Scholar PubMed
17. Lee , MA , Tolle , SW . Oregon's plans to legalise suicide assisted by a doctor: how much more open will the practice become? British Medical Journal 1995 ; 310 : 613 . CrossRef Google Scholar
18. Jochemsen , H . Euthanasia in Holland: an ethical critique of the new law . Journal of Medical Ethics 1994 ; 20 ( 4 ): 212 –7. CrossRef Google Scholar PubMed
19. Netherlands eases curbs on euthanasia. Chicago Tribune 1993 ; 02 10 (Sect 1): 13 . Google Scholar
20. Los Angeles Times News Service. Euthanasia doesn't always end families' pain. Orlando Sentinel 1993 ; 03 14 :A–12. Google Scholar
21. See the entire issue of Cambridge Quarterly 1993 , Vol 2 , No 1, which is largely devoted to descriptions and analyses of the Dutch euthanasia situation. Google Scholar
22. See note 19. Chicago Tribune 1993 ; 02 10 (Sect 1): 13 . Google Scholar
23. Kimsma , GK , van Leeuwen , E . Dutch euthanasia: background, practice, and present justifications . Cambridge Quarterly of Healthcare Ethics 1993 ; 2 : 19 – 31 . CrossRef Google Scholar PubMed
24. Van der Wal , G . Euthanasie en hulp bij zelfdoding door huisartsen . Rotterdam : WYT Uitgeefgroep , 1992 . Google Scholar
25. Humphry , D . Dutch Parliament ok's euthanasia guidelines . World Right-to-Die Newsletter 1993 ; 22 : 1 . Google Scholar
26. Gomez , C . Regulating Death: Euthanasia and the case of The Netherlands . New York : Free Press , 1991 : 12 . Google Scholar
27. See note 26. Gomez , . 1991 : 16 . Google Scholar
28. Van der Wal , G , Muller , MT , Christ , LM , Ribbe , MW , van Eijk , JThM . Voluntary active euthanasia and physician-assisted suicide in Dutch nursing homes: requests and administration . Journal of the American Geriatrics Society 1994 ; 42 : 620 –3. CrossRef Google Scholar PubMed
29. Quill , TE , Cassel , CK , Meier , DE . Care of the hopelessly ill: proposed clinical criteria for physician-assisted suicide . New England Journal of Medicine 1992 ; 327 : 1380 –4. CrossRef Google Scholar PubMed
30. See note 20. Orlando Sentinel . 1993 ; 03 14 :A–12. Google Scholar
31. Report. Addressing the underlying issues of physician-assisted suicide: Kevorkian's actions fuel the debate. Issues 1994 ; 9 : 1 – 8 . Google Scholar
32. Walsh , E . “Dr. Death” is charged in suicide . Chicago Sun-Times 1993 ; 08 18 : 8 . Google Scholar
33. Associated Press. Kevorkian admits assist in 17th suicide. The Chicago Tribune , 1993 ; 08 5 (Sect 1): 20 . Google Scholar
34. New York Times News Service. Kevorkian helps woman kill herself: 1st assisted suicide in more than a year. Chicago Tribune 1994 ; 11 27 (Sect 1): 8 . Google Scholar
35. Worthington , R . Suicide doctor finally to have day in court . The Chicago Tribune 1993 ; 08 19 (Sect 1): 2 . Google Scholar
36. Castaneda , CJ . Kevorkian prosecutor under fire . USA Today 1993 ; 09 9 : 3A . Google Scholar
37. Kimsma , GK , Ciesielski-Carlucci , C . Het rapporteren van euthanasie: reflecties naar aanleiding van interviews met nabestaanden (in press). Google Scholar
38. Emanuel , EJ . Euthanasia: historical, ethical, and empiric perspectives . Archives of Internal Medicine 1994 ; 154 : 1890 – 1900 , at p. 1900 . Google Scholar PubMed
39. Callahan , D . The Troubled Dream of Life: Living with Mortality . New York : Touchstone , 1994 . Google Scholar
40. Choice in Dying News 1993 ; 2 : 1 , 5 . Google Scholar
41. This is the basis of an argument being made by Choice in Dying before the Kentucky Supreme Court in the case of Elston v DeGrella , in which a mother has requested the right to let her permanently vegetative daughter die. See note 40. Choice in Dying News . 1993 ; 2 : 1 , 4 . Google Scholar
42. Pennsylvania , Bishops . Nutrition and hydration: moral considerations . Origins: CNS Documentary Service 1992 : 21 ( 34 ): 542 –51, at p. 550 . Google Scholar
43. Bergsma , J , Thomasma , DC . Autonomy and the Doctor-Patient Relationship . Cambridge University Press (submitted). Google Scholar
44. Kimsma , GK , Ciesielski-Carlucci , C . Euthanasie – rapporteren of niet? Medisch Contact 1993 ; 48 ( 11 ): 328 –32. Google Scholar
45. Klotzko , AJ Dr . Boudewijn Chabot on assisted suicide in the absence of somatic illness . Cambridge Quarterly of Healthcare Ethics 1995 ; 4 : 239 –49. Google Scholar
46. See note 45. Klotzko , . 1995 ;4: 247 . Google Scholar
47. CeloCruz , MT . Aid-in-dying: should we decriminalize physician-assisted suicide and physician-committed euthanasia? American Journal of Law & Medicine 1994 : 18 ( 4 ): 369 –94. Google Scholar
48. US District Court, loc. cit .
49. Brandt , R . The morality and rationality of suicide. In: Rachels , J , Ed. Moral Problems . New York : Harper & Row , 1975 . Google Scholar
50. Choron , J . Suicide . New York : Scribner's Sons , 1972 : 100 . Google Scholar
51. Prado , CG . The Last Choice: Preemptive Suicide in Advanced Age . Westport, Connecticut : Greenwood Press , 1990 . Google Scholar
52. Knebel , F . Chicago Tribune 1993 ; 02 28 (Sect 2): 6 . Google Scholar
53. Osgood , NJ . Assisted-suicide and older-people – a deadly combination: ethical problems in permitted assisted suicide . Issues in Law and Medicine 1995 ; 10 ( 4 ): 415 –35. Google Scholar
54. Battin , MP . Ethical Issues in Suicide . Englewood Cliffs, New Jersey : Prentice-Hall . 1982 . Google Scholar
55. Graber , GC . The Rationality of Suicide. In: Wallace , S , Eser , A , Eds. Suicide and Euthanasia: The Rights of Personhood . Knoxville, Tennessee : University of Tennessee Press , 1981 . Google Scholar
56. Erikson , E . Childhood and Society , 2nd ed. New York : W.W. Norton , 1963 : 268 . Google Scholar
57. Moody , HR . Ethics in an Aging Society . Baltimore and London : The Johns Hopkins University Press , 1992 : 86 . Google Scholar
58. Cantor , N . Advance Directives and the Pursuit of Death With Dignity . Bloomington, Indiana : Indiana University Press , 1993 . Google Scholar
59. Bergsma , J , Thomasma , DC . Health Care: Its Psychosocial Dimensions . Pittsburgh, Pennsylvania : Duquesne University Press , 1982 . Google Scholar
60. Koop , CE , Johnson , T . Let's Talk: An Honest Conversation on Critical Issues . Grand Rapids, Michigan : Zondervaan , 1992 . Google Scholar
61. See note 1. Ghosh , . 1995 ;61(20): 41 . Google Scholar
62. Nursing homes. Consumer Reports 1995;August.

This article has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 5, Issue 1
- David C. Thomasma (a1)
- DOI: https://doi.org/10.1017/S0963180100006733
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
- Research article
- Open access
- Published: 19 February 2019
Factors associated with requesting and receiving euthanasia: a nationwide mortality follow-back study with a focus on patients with psychiatric disorders, dementia, or an accumulation of health problems related to old age
- Kirsten Evenblij ORCID: orcid.org/0000-0002-5984-4959 1 ,
- H. Roeline W. Pasman 1 ,
- Agnes van der Heide 2 ,
- Trynke Hoekstra 3 &
- Bregje D. Onwuteaka-Philipsen 1
BMC Medicine volume 17 , Article number: 39 ( 2019 ) Cite this article
45k Accesses
37 Citations
5 Altmetric
Metrics details
Recently, euthanasia and assisted suicide (EAS) in patients with psychiatric disorders, dementia, or an accumulation of health problems has taken a prominent place in the public debate. However, limited is known about this practice. The purpose of this study was threefold: to estimate the frequency of requesting and receiving EAS among people with (also) a psychiatric disorder, dementia, or an accumulation of health problems; to explore reasons for physicians to grant or refuse a request; and to describe differences in characteristics, including the presence of psychiatric disorders, dementia, and accumulation of health problems, between patients who did and did not request EAS and between patients whose request was or was not granted.
A nationwide cross-sectional survey study was performed. A stratified sample of death certificates of patients who died between 1 August and 1 December 2015 was drawn from the central death registry of Statistics Netherlands. Questionnaires were sent to the certifying physician ( n = 9351, response 78%). Only deceased patients aged ≥ 17 years and who died a non-sudden death were included in the analyses ( n = 5361).
The frequency of euthanasia requests among deceased people who died non-suddenly and with (also) a psychiatric disorder (11.4%), dementia (2.1%), or an accumulation of health problems (8.0%) varied. Factors positively associated with requesting euthanasia were age (< 80 years), ethnicity (Dutch/Western), cause of death (cancer), attending physician (general practitioner), and involvement of a pain specialist or psychiatrist. Cause of death (neurological disorders, another cause) and attending physician (general practitioner) were also positively associated with receiving euthanasia. Psychiatric disorders, dementia, and/or an accumulation of health problems were negatively associated with both requesting and receiving euthanasia.
Conclusions
EAS in deceased patients with psychiatric disorders, dementia, and/or an accumulation of health problems is relatively rare. Partly, this can be explained by the belief that the due care criteria cannot be met. Another explanation is that patients with these conditions are less likely to request EAS.
Peer Review reports
Patients suffering unbearably may wish to hasten their death. Since 2002, the Netherlands has been one of the few countries where euthanasia and assisted suicide (EAS) is allowed under strict conditions [ 1 ]. The practice of EAS is restricted to physicians who must adhere to the “statutory due care criteria,” i.e., they must (1) be satisfied that the patient’s request is voluntary and well-considered; (2) be satisfied that the patient’s suffering is unbearable and without prospect of improvement; (3) have informed the patient about his situation and prognosis; (4) have come to the conclusion, together with the patient, that there is no reasonable alternative; (5) consult at least one other, independent physician; and (6) exercise EAS with due medical care and attention. Furthermore, the cause of suffering underlying the request must have a medical dimension, either somatic or psychiatric [ 1 , 2 ], and physicians must report each case to the Regional Euthanasia Review Committees which review all EAS cases regarding whether the due care criteria were met.
In the past decade, the percentage of all deceased patients in the Netherlands who requested EAS prior to their death increased, from 5.2% in 2005, to 6.7% in 2011, and to 8.4% in 2015 [ 3 ]. Also, the percentage of requests that were carried out increased, from 37% in 2005, to 45% in 2010 and to 55% in 2015 [ 4 ]. Hence, not only is there a growing demand for EAS, requests are also more likely to result in EAS. Some evidence, however, suggests that requesting and receiving euthanasia depends, at least to some extent, on the cause of suffering. For instance patients who have cancer are more likely to request EAS compared to those with cardiovascular diseases [ 5 ]. Patients with physical symptoms, cancer, and a short life expectancy are more likely to receive EAS than others, while patients with depressive symptoms are less likely [ 6 , 7 , 8 ]. Also, demographic and care factors have been reported to influence requesting and receiving EAS [ 5 , 6 , 7 , 8 ].
Recently, EAS in patients with psychiatric disorders, dementia, or an accumulation of health problems related to old age (from now, accumulation of health problems) has taken a prominent place in the public debate [ 9 , 10 , 11 , 12 , 13 ]. In the Dutch Euthanasia Code, this last category, an accumulation of health problems, is referred to as a range of, mostly degenerative, disorders such as visual impairment, hearing impairment, osteoporosis, arthrosis, balance disorders, and cognitive decline [ 14 ]. Though the numbers are small, reports of the Euthanasia Review Committees have shown that the absolute number of EAS cases in people whose primary cause of suffering was a psychiatric disorder, dementia, or an accumulation of health problems has increased over the past 5 years [ 15 , 16 , 17 ].
Using a nationwide sample of deceased people, we studied requests for EAS in people with and without these conditions focusing on the following questions: How many deaths among people with psychiatric disorders, dementia, and accumulation of health problems were preceded by a request for EAS and how many of these requests were granted? What are the reasons to grant or refuse a request for EAS? Which patient and care characteristics, including the presence of psychiatric disorders, dementia, and an accumulation of health problems, are associated with a patient requesting EAS and with a patient receiving EAS?
Design and population
In 2015, a nationwide mortality follow-back study was performed to estimate the frequency of requesting and receiving EAS among people with (also) a psychiatric disorder, dementia, or an accumulation of health problems; to explore reasons for physicians to grant or refuse a request; and to describe differences in characteristics, including the presence of psychiatric disorders, dementia, and accumulation of health problems, between patients who did and did not request EAS and between patients whose request was or was not granted. The study was largely similar to previous mortality follow-back studies done in 1990, 1995, 2001, 2005, and 2010 [ 3 , 4 , 18 , 19 , 20 , 21 ]. A stratified sample of death certificates of persons who died between 1 of August and 1 of December 2015 was obtained from the central death registry of Statistics Netherlands. Death certificates were stratified into 10 strata based on the likelihood of the patient having made an end-of-life decision. The certifying physicians of the sampled cases received a questionnaire focusing on end-of-life decisions that might have preceded the death of the patient involved. A reminder was sent to those who had not returned the questionnaire. Of the 9351 questionnaires sent, 7277 were returned (response 78%). In this study, only those who died a non-sudden death and who were aged 17 years or older were included ( n = 5361). Ethical approval was not required for the posthumous collection of anonymous patient data [ 22 ]. Further details of the study design are described elsewhere [ 3 ].
Questionnaire
A four-page written questionnaire was sent to the physicians who signed the death certificates. The questionnaire was largely similar to the previous mortality follow-back studies [ 3 , 4 , 18 , 19 , 20 , 21 ]. It contained questions about the medical decision-making that had preceded death, whether the patient had requested for euthanasia, the reasons for granting or refusing the request, and questions about the medical care during the last month before death such as the involvement of caregivers for palliative consultation and psychosocial and spiritual issues. To obtain insight into EAS requests from people with a psychiatric disorder, dementia, and/or an accumulation of health problems (related to old age), a new question was added to the questionnaire about whether the patient had a psychiatric disorder, dementia, and/or an accumulation of health problems (yes/no). No description of these groups was provided to the physicians to classify patients; thus, physicians will most likely have interpreted these categories in the context of the Dutch euthanasia act and the current debate. The cause of death and specialty of the certifying physician were derived from the death certificate.
Statistical analyses were carried out using IBM SPSS version 22 (IBM Analytics). For presenting the frequencies of (requests for) EAS as well as the reasons for granting or refusing the requests, the results were made representative of all deaths during 2015 by weighting the data for stratification and response by patient’s sex, age, ethnic origin, and place and cause of death. This weighting procedure was similar to previous mortality follow-back studies [ 3 , 4 , 18 , 19 , 20 , 21 ]. Due to this procedure, the percentages that are reported cannot be derived from the absolute unweighted numbers.
Two multivariable logistic regression models were developed: one to identify factors associated with patients requesting EAS and one to identify factors associated with receiving EAS. The latter model was developed on a subset of the sample: patients who made an EAS request. First, the univariable association between each independent variable and the dependent variables (requesting EAS and receiving EAS) was analyzed. Next, all variables associated with requesting and receiving EAS ( p value < 0.10) were entered in a multivariable model. Subsequently, a manual backward selection procedure was applied until only variables with p < 0.10 remained. In both models, the eligible independent variables were age (17–64, 65–79, > 80 years); sex (female/male); marital status (married/unmarried); ethnicity (Dutch and Western immigrants/non-Western immigrants); cause of death (cancer, cardiovascular disorder, pulmonary disorder, neurological disorder, or other); the presence of a psychiatric disorder (yes/no), dementia (yes/no), or an accumulation of health problems (yes/no); specialty of the certifying physician (general practitioner, medical specialist, or elderly care physician); involvement (yes/no) of the following caregivers in the last month of life, namely palliative care consultant/team, specialist pain control, psychiatrist/psychologist, and pastor [ 5 , 6 , 7 , 8 ]. Results are presented as frequencies, ORs, and 95% CIs.
Extra analyses
In the multivariable model identifying factors associated with requesting EAS, the ORs and 95% CIs of cause of death changed drastically compared to the univariable model. Sensitivity analyses showed this was mainly driven by (i) collinearity between two variables, dementia and attending physicians; (ii) strong associations between cause of death, requesting EAS, and dementia and between cause of death, requesting EAS, and attending physician; and (iii) empty cells demonstrating the likelihood of unstable models. Therefore, we also performed the multivariable analyses for both requesting EAS and receiving EAS without dementia and attending physician. In these models, there was no indication for the issues described; the ORs and 95% CI of the variables did not change substantially compared to the univariable analyses. The results of the multivariable regression analyses including all independent variables (including dementia and attending physician) are reported as main outcomes.
Description of the study sample
Of the 5361 deceased patients aged ≥ 17 years and whose death was non-sudden, 183 (3.4%) had a psychiatric disorder, 803 (15.0%) dementia, and 918 (17.1%) an accumulation of health problems, possibly next to the illness that caused their death. In people with a psychiatric disorder, dementia, or an accumulation of health problems, the most frequently reported cause of death was “other.” Of the people with dementia, 25.3% died of a neurological disorder (including dementia), and of the people with an accumulation of health problems, 22.1% died of a cardiovascular disorder. Among all deceased patients who died non-suddenly, 37% died due to cancer. The characteristics of the study sample are provided in Table 1 .
Frequency of EAS requests
Figure 1 shows that 11.2% of all patients who were aged ≥ 17 years had requested EAS preceding their death. Of the people with a psychiatric disorder, 11.4% requested EAS. The prevalence of EAS requests was lower among people with an accumulation of health problems (8.0%) and people with dementia requests (2.1%). Six percent of all deceased patients had received euthanasia; this percentage was lower among people who had a psychiatric disorder (4.8%), an accumulation of health problems (3.7%), and/or dementia (0.9%).
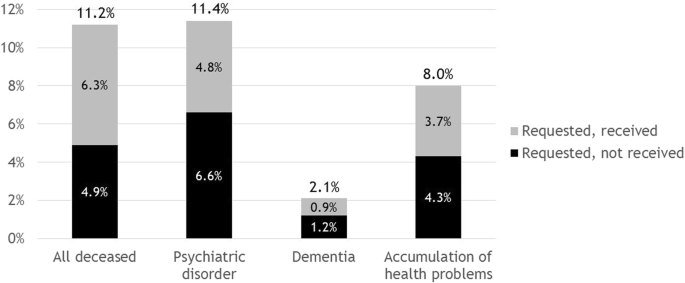
Frequency of deceased patients who did or did not receive euthanasia. Percentage of requests carried out among all deceased patients who died non-suddenly, 56% (6.3/11.2); people with psychiatric disorders, 42% (4.8/11.4); people with dementia 43% (0.9/2.1); and people with an accumulation of health problems, 46% (3.7/8.0)
Factors associated with requesting EAS
In univariable analyses, all variables showed associations ( p < 0.10) with requesting EAS, except for the presence of a psychiatric disorder (Table 2 ). In the multivariable analysis, sex, marital status, and the involvement of a palliative care consultant were no longer associated ( p < 0.10) with requesting EAS. Compared with people aged 80 years or older whose death was non-sudden, people aged between 17 and 64 years (OR 1.65 [1.33–2.04]) and between 65 and 79 (OR 1.38 [1.15–1.66]) were more likely to request EAS. Dutch and Western immigrants were 8.49 (95% CI 5.37–13.42) times more likely to request EAS compared with non-Western immigrants. Compared with people who died of cancer, people who died of cardiovascular disorders were less likely to request EAS while people who died of pulmonary disorders, neurological disorders, or another cause were more likely. People with an accumulation of health problems (OR 0.69 [0.53–0.90]) or dementia (OR (0.18 [0.12–0.28]) had lower odds of requesting EAS compared with those without these conditions. People whose attending physician was a medical specialist or an elderly care specialist had lower odds of requesting EAS (OR 0.07 [0.05–0.11] and OR 0.17 [0.13–0.23]) compared with people whose attending physician was a general practitioner. People who were supported by pain specialists (OR 2.08 [1.47–2.93]) and psychiatrists (OR 4.50 [3.15–6.41]) in the last month of life were more likely to request EAS while those supported by pastors were less likely (OR 0.77 [0.59–1.00]).
The results of the extra analysis without the variables dementia and attending physician (see the “ Methods ” section) were largely similar to the original multivariable model. However, people who died of cancer were now more likely to request EAS compared to people who died of any other cause. An accumulation of health problems dropped from the model.
Reasons to grant or refuse the request
Table 3 shows that across the full sample, the two most important reasons for the attending physician to grant the request were the lack of prospect of improvement (81.9–94.6%) and the autonomy of the patient (72.4–85.8%). In case of a psychiatric disorder, the presence of (severe) symptoms other than pain (75.4%) and expected suffering (53.5%) were also important reasons. In case of dementia, the loss of dignity (73.7%) and expected suffering of the patient (49.1%) were important. Finally, in case of an accumulation of health problems, the presence of symptoms other than pain (48.7%) and loss of dignity (54.8%) were both important reasons to grant the request. Among those with a psychiatric disorder, dementia, or an accumulation of health problems, the most important reason to refuse the request was that the due care criteria were not met, especially regarding the well-considered nature of the request. Among all deceased patients, the most important reason was that the patient died before the request was granted.
Factors associated with receiving EAS
Table 4 shows associations between receiving EAS and patient and care characteristics. In univariable analyses, age, cause of death, the presence of a psychiatric disorder and an accumulation of health problems, attending physician, and the involvement of a palliative care consultant/team and pastor showed associations ( p < 0.10) with receiving EAS. In multivariable analysis, most associations remained significant. People who died of neurological disorders or another cause had 4.70 [95% CI 2.09–10.58] and 2.38 [95% CI 1.34–4.26] times higher odds of receiving EAS compared with people who died of cancer. People with a psychiatric disorder and an accumulation of health problems had lower odds of receiving EAS compared with people without these conditions (OR 0.38 [0.18–0.82] and OR 0.62 [0.36–1.05]). People whose attending physician was a medical specialist or an elderly care specialist were less likely to receive EAS (OR 0.13 [0.06–0.27] and OR 0.16 [0.09–0.28]) compared with people whose attending physician was a general practitioner. Those who were supported by a palliative care consultant in the last month of life were also less likely to receive EAS (OR 0.70 [0.50–0.98]).
The results of the extra analysis without the variables dementia and attending physician (see the “ Methods ” section) were largely similar to the original multivariable model except for the negative association found between pastor and receiving EAS.
The frequency of EAS requests among deceased people who died non-suddenly and who had psychiatric disorders (11.4%), dementia (2.1%), and/or an accumulation of health problems (8.0%) varied. Less than half of these requests led to EAS. Factors positively associated with requesting EAS were age (< 80 years), ethnicity (Dutch/Western), cause of death (cancer), attending physician (general practitioner), and involvement of pain specialist and psychiatrist. Cause of death (neurological disorders or another cause) and attending physician (general practitioner) were also positively associated with receiving euthanasia. Psychiatric disorders, dementia, and accumulation of health problems were negatively associated with requesting and receiving EAS.
EAS in people with psychiatric disorders, dementia, and an accumulation of health problems
EAS in people with psychiatric disorders, dementia, and an accumulation of health problems is a highly debated subject, but this practice rarely occurs. Partially, this can be explained by reluctance of physicians to perform EAS in these patients [ 23 ]. Our results showed that the proportion of euthanasia requests that was carried out was lower among people with psychiatric conditions (42%), dementia (43%), and an accumulation of health problems (46%) compared to all non-sudden deceased people (56%). Moreover, having a psychiatric disorder or an accumulation of health problems was statistically significantly associated with a lower likelihood of having a request being carried out. Previous research has also shown that physicians consider it less likely to perform EAS in patients with a psychiatric disorder, dementia, and/or an accumulation of health problems compared to patients with a severe and life-limiting somatic illness such as cancer [ 23 , 24 , 25 ]. Our results suggest that the presence of a psychiatric disorder, dementia, and/or an accumulation of health problems may complicate the decision to grant a request, even if the patient also suffers from a severe and life-limiting somatic illness, such as cancer. The main reasons to refuse a request are doubts about whether the request was well-considered and about the unbearableness of the suffering. These findings corroborate previous studies [ 26 , 27 ].
This study is the first to show that people with dementia or an accumulation of health problems are less likely to request EAS compared to people without these conditions which may explain part of the lower frequency of EAS in people with these conditions. Possibly, the lower frequency of requests among people with dementia and an accumulation of health problems can be explained by the slow and gradual decline characterizing both dementia and an accumulation of health problems leading to the gradual acceptance of a declining health condition [ 28 , 29 , 30 ]. In addition, in case of advanced dementia, patients lose the ability to make a well-considered request for EAS.
Due to the aging society, associated with an increasing number of older people suffering from multimorbidity, it is likely that the number of EAS requests from patients suffering from dementia and/or an accumulation of health problems related to old age will continue to grow [ 31 , 32 ]. The question of how policy makers and care providers should respond to these requests is, therefore, highly relevant.
Characteristics associated with requesting and receiving EAS
Patient characteristics.
This study showed that younger people are more likely to request EAS which is consistent with previous studies in the Netherlands and Belgium [ 5 , 6 , 33 ]. Younger people tend to have more permissive and liberal attitudes compared to older people and are more likely to support EAS [ 34 , 35 ]. Also, a strong positive association between ethnicity and requesting EAS was found, with Dutch or Western migrants being 8.5 times more likely to request EAS compared to non-Western migrants. Cultural and religious values and beliefs have frequently been reported to profoundly influence the perceptions of death and end-of-life decision-making [ 36 , 37 , 38 , 39 , 40 ].
People who died due to a neurological disorder were almost four times more likely to receive EAS compared to people with cancer which corresponds with previous findings [ 5 , 33 , 41 ]. ALS disease, which is known for its progressive, severe physical symptoms and lack of effective treatments, probably contributes the most to this finding.
Care characteristics
The involvement of a pain specialist and the involvement of a psychiatrist/psychologist in the last month of life were associated with higher likelihood of requesting EAS. This confirms previous research in Belgium and the Netherlands [ 5 , 42 ]. Possibly, pain specialists and psychiatrists/psychologists stimulate patients to think and talk about their end-of-life wishes, including EAS, as autonomy and informed decision-making are key principles of palliative care [ 43 ]. Finally, prior to granting a request, a physician must be certain that there is no other reasonable solution; optimizing end-of-life care is one of them.
Multivariable regression analyses also showed that deceased patients who were attended by a general practitioner were more likely to request and receive EAS, supporting previous evidence [ 5 ]. The attendance of a general practitioner possibly provides more opportunity for discussing end-of-life wishes, including euthanasia, due to the long-term care relationship with the patient and the non-acute care setting.
Strengths and limitations
Major strengths of this study are the large nationwide sample which is the representative of all deaths in the Netherlands in 2015, the high response rate and few missing data. When interpreting the results, some limitations need to be considered. Physicians were asked whether the patient had either one or more of the following conditions: a psychiatric disorder, dementia, and an accumulation of health problems. Since this was a general, closed question, i.e., yes/no, it is unknown to what extent these conditions contributed to the suffering underlying the EAS request. Also, psychiatric disorders and an accumulation of health problems are very broad categories which one has to take into account when interpreting the results. Another limitation is that our sample included patients who were seriously ill after all our sample included deceased patients; patients without a life-threatening illness were not included unless their life was ended. On the one hand, this may have led to an underestimation of the number of requests since among those who request EAS are also people who are not seriously ill. On the other hand, it may have led to an overestimation of the number of requests granted among people with a psychiatric disorder, dementia, and/or an accumulation of health problems since physicians are more likely to grant requests of people with (also) a severe and life-limiting somatic condition.
A relatively small group of people who died non-suddenly received EAS but even fewer of those with (also) psychiatric disorders, dementia, or an accumulation of health problems. Partly, this can be explained by the belief that the due care criteria cannot be met. Another explanation is that patients with these conditions are less likely to request for it. Given the aging society and the related rising of the number of EAS requests from people suffering from dementia and/or an accumulation of health problems, the question of how policy makers and care providers should respond to these requests is highly relevant.
Abbreviations
Accumulation of health problems related to old age
Confidence interval
Euthanasia and assisted suicide
Wet toetsing levensbeëindiging op verzoek en hulp bij zelfdoding (Act on termination of life on request and assisted suicide) [statute on the Internet] 2001. Available from: http://wetten.overheid.nl/BWBR0012410/2014-02-15 . [Cited: 08-01-2018].
Uitspraak Hoge Raad, de zaak-Brongersma (Verdict Supreme Court, the Brongersma case) [statute on the Internet] 24-12-2002. Available from: https://uitspraken.rechtspraak.nl/inziendocument?id=ECLI:NL:PHR:2002:AE8772 .
van der Heide A, van Delden JJM, Onwuteaka-Philipsen BD. End-of-life decisions in the Netherlands over 25 years. N Engl J Med. 2017;377(5):492–4.
Article Google Scholar
Onwuteaka-Philipsen BD, Brinkman-Stoppelenburg A, Penning C, et al. Trends in end-of-life practices before and after the enactment of the euthanasia law in the Netherlands from 1990 to 2010: a repeated cross-sectional survey. Lancet. 2012;380(9845):908–15.
Onwuteaka-Philipsen BD, Rurup ML, Pasman HR, et al. The last phase of life: who requests and who receives euthanasia or physician-assisted suicide? Med Care. 2010;48(7):596–603.
Haverkate I, Onwuteaka-Philipsen BD, van Der Heide A, et al. Refused and granted requests for euthanasia and assisted suicide in the Netherlands: interview study with structured questionnaire. BMJ. 2000;321(7265):865–6.
Article CAS Google Scholar
Jansen-van der Weide MC, Onwuteaka-Philipsen BD, van der Wal G. Granted, undecided, withdrawn, and refused requests for euthanasia and physician-assisted suicide. Arch Intern Med. 2005;165(15):1698–704.
Meier DE, Emmons CA, Litke A, et al. Characteristics of patients requesting and receiving physician-assisted death. Arch Intern Med. 2003;163(13):1537–42.
‘Psychiaters te bang bij euthanasie’. Psychiaters krijgen vanuit eigen kring kritiek op hoe ze omgaan met euthanasieverzoeken. NRC [newspaper on the Internet]. 26-10-2017. Available from: https://www.nrc.nl/nieuws/2017/10/26/psychiaters-te-bang-bij-euthanasie-13691181-a1578871 . [cited 19–07-2018]
Appelbaum PS. Physician-assisted death for patients with mental disorders-reasons for concern. JAMA Psychiat. 2016;73(4):325–6.
de Beaufort ID, van de Vathorst S. Dementia and assisted suicide and euthanasia. J Neurol. 2016;263(7):1463–7.
Kouwenhoven PS, Raijmakers NJ, van Delden JJ, et al. Opinions about euthanasia and advanced dementia: a qualitative study among Dutch physicians and members of the general public. BMC Med Ethics. 2015;16:7.
Raijmakers NJ, van der Heide A, Kouwenhoven PS, et al. Assistance in dying for older people without a serious medical condition who have a wish to die: a national cross-sectional survey. J Med Ethics. 2015;41(2):145–50.
Euthanasia Code 2018. De toetsingspraktijk toegelicht. (Euthanasia Code 2018. The review procedures explained) [report at the Internet] Available from: https://www.euthanasiecommissie.nl/uitspraken/brochures/brochures/euthanasiecode/2018/euthanasiecode2018 . [Cited: 11-09-2018].
Regionale Toetsingscommissie Euthanasie. Jaarverslag 2016. (Regional Euthanasia Review Committees. Annual report 2016) [report at the Internet] Available from: https://www.euthanasiecommissie.nl/de-toetsingscommissies/uitspraken/jaarverslagen/2016/april/12/jaarverslag-2016 . [Cited: 10-01-2018].
Regionale Toetsingscommissies Euthanasie. Jaarverslag 2013. (Regional Euthanasia Review Committees. Annual report 2013) [report at the Internet] Available from: https://www.euthanasiecommissie.nl/de-toetsingscommissies/uitspraken/jaarverslagen/2013/nl-en-du-fr/nl-en-du-fr/jaarverslag-2013 . [Cited: 10-01-2018].
Regionale Toetsingscommissies Euthanasie. Jaarverslag 2010. (Regional Euthanasia Review Committees. Annual report 2010) [report at the Internet] Available from: https://www.euthanasiecommissie.nl/de-toetsingscommissies/uitspraken/jaarverslagen/2010/nl-en-du-fr/nl-en-du-fr/jaarverslag-2010 . [Cited: 10-01-2018].
Onwuteaka-Philipsen BD, van der Heide A, Koper D, et al. Euthanasia and other end-of-life decisions in the Netherlands in 1990, 1995, and 2001. Lancet. 2003;362(9381):395–9.
van der Heide A, Onwuteaka-Philipsen BD, Rurup ML, et al. End-of-life practices in the Netherlands under the Euthanasia Act. N Engl J Med. 2007;356(19):1957–65.
Van Der Maas PJ, Van Delden JJ, Pijnenborg L, et al. Euthanasia and other medical decisions concerning the end of life. Lancet. 1991;338(8768):669–74.
van der Maas PJ, van der Wal G, Haverkate I, et al. Euthanasia, physician-assisted suicide, and other medical practices involving the end of life in the Netherlands, 1990-1995. N Engl J Med. 1996;335(22):1699–705.
Wet bescherming persoonsgegevens. (Personal Data Protection Act) [statute on the Internet] Available from: http://wetten.overheid.nl/BWBR0011468/2018-05-01#Hoofdstuk1 . [Cited: 17-09-2018].
Bolt EE, Snijdewind MC, Willems DL, et al. Can physicians conceive of performing euthanasia in case of psychiatric disease, dementia or being tired of living? J Med Ethics. 2015;41(8):592–8.
Kouwenhoven PS, Raijmakers NJ, van Delden JJ, et al. Opinions of health care professionals and the public after eight years of euthanasia legislation in the Netherlands: a mixed methods approach. Palliat Med. 2013;27(3):273–80.
Snijdewind MC, Willems DL, Deliens L, et al. A study of the first year of the end-of-life clinic for physician-assisted dying in the Netherlands. JAMA Intern Med. 2015;175(10):1633–40.
Doernberg SN, Peteet JR, Kim SY. Capacity evaluations of psychiatric patients requesting assisted death in the Netherlands. Psychosomatics. 2016;57(6):556–65.
van Tol D, Rietjens J, van der Heide A. Judgment of unbearable suffering and willingness to grant a euthanasia request by Dutch general practitioners. Health Policy. 2010;97(2–3):166–72.
PubMed Google Scholar
de Boer ME, Hertogh CM, Droes RM, et al. Suffering from dementia - the patient’s perspective: a review of the literature. Int Psychogeriatr. 2007;19(6):1021–39.
van Wijmen MP, Pasman HR, Widdershoven GA, et al. Motivations, aims and communication around advance directives: a mixed-methods study into the perspective of their owners and the influence of a current illness. Patient Educ Couns. 2014;95(3):393–9.
Winter L, Parker B. Current health and preferences for life-prolonging treatments: an application of prospect theory to end-of-life decision making. Soc Sci Med. 2007;65(8):1695–707.
Onwuteaka-Philipsen B, Legemaate J, van der Heide A, et al. Derde evaluatie Wet toetsing levensbeëindiging op verzoek en hulp bij zelfdoding [Third evaluation of the Termination of Life on Request and Assisted Suicide Act]. Den Haag: ZonMw; 2017.
Google Scholar
Regionale Toetsingscommissie Euthanasie. Jaarverslag 2017. (Regional Euthanasia Review Committees. Annual report 2017) [report at the Internet] Available from: https://www.euthanasiecommissie.nl/de-toetsingscommissies/uitspraken/jaarverslagen/2017/mei/17/jaarverslag-2017 . [Cited: 12-06-2018].
Dierickx S, Deliens L, Cohen J, et al. Euthanasia in Belgium: trends in reported cases between 2003 and 2013. CMAJ. 2016;188(16):E407–E14.
Twenge, JMC, N.T.; Campbell, W.K. Time period, generational, and age differences in tolerance for controversial beliefs and lifestyles in the United States, 1972–2012. Social Forces 2015;94(1):379–399.
Lee CH, Duck IM, Sibley CG. Demographic and psychological correlates of New Zealanders support for euthanasia. N Z Med J. 2017;130(1448):9–17.
Collins JW, Zoucha R, Lockhart JS, et al. Cultural aspects of end-of-life care planning for African Americans: an integrative review of literature. J Transcult Nurs. 2018;29(6):578–90.
Manalo MF. End-of-life decisions about withholding or withdrawing therapy: medical, ethical, and religio-cultural considerations. Palliat Care. 2013;7:1–5.
PubMed PubMed Central Google Scholar
Ohr S, Jeong S, Saul P. Cultural and religious beliefs and values, and their impact on preferences for end-of-life care among four ethnic groups of community-dwelling older persons. J Clin Nurs. 2017;26(11–12):1681–9.
Portanova J, Ailshire J, Perez C, et al. Ethnic differences in advance directive completion and care preferences: what has changed in a decade? J Am Geriatr Soc. 2017;65(6):1352–7.
Sachedina A. End-of-life: the Islamic view. Lancet. 2005;366(9487):774–9.
Hedberg K, Hopkins D, Kohn M. Five years of legal physician-assisted suicide in Oregon. N Engl J Med. 2003;348(10):961–4.
Dierickx S, Deliens L, Cohen J, et al. Involvement of palliative care in euthanasia practice in a context of legalized euthanasia: a population-based mortality follow-back study. Palliat Med. 2018;32(1):114–22.
Radbruch L, Leget C, Bahr P, et al. Euthanasia and physician-assisted suicide: a white paper from the European Association for Palliative Care. Palliat Med. 2016;30(2):104–16.
Download references
Acknowledgements
Not applicable
This study was funded by the Netherlands Organisation for Health Research and Development (ZonMw, project number 3400.8003).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Department of Public and Occupational Health, Amsterdam Public Health Research Institute, Amsterdam UMC, Vrije Universiteit Amsterdam, P.O. Box 7057, 1007 MB, Amsterdam, The Netherlands
Kirsten Evenblij, H. Roeline W. Pasman & Bregje D. Onwuteaka-Philipsen
Department of Public Health, Erasmus University Medical Center, Rotterdam, The Netherlands
Agnes van der Heide
Department of Health Sciences, Amsterdam Public Health Research Institute, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands
Trynke Hoekstra
You can also search for this author in PubMed Google Scholar
Contributions
KE, HP, AH, TH, and BO designed the study. The sample was drawn from the central death registry of Statistics Netherlands. KE performed the data management and statistical analysis. KE, HP, AH, TH, and BO interpreted the data. KE prepared the initial draft of this manuscript. HP, AH, TH, and BO critically revised the manuscript for intellectual content and commented on subsequent drafts of the manuscript. KE, HP, AH, TH, and BO contributed to the final draft of the manuscript and gave the final approval for submission.
Corresponding author
Correspondence to Kirsten Evenblij .
Ethics declarations
Ethics approval and consent to participate.
Under the Dutch Medical Research Involving Human Subjects Act, ethical approval was not required for the posthumous collection of anonymous patient data [ 22 ]. Informed consent of the certifying physicians was assumed on return of the survey.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Evenblij, K., Pasman, H.R.W., van der Heide, A. et al. Factors associated with requesting and receiving euthanasia: a nationwide mortality follow-back study with a focus on patients with psychiatric disorders, dementia, or an accumulation of health problems related to old age. BMC Med 17 , 39 (2019). https://doi.org/10.1186/s12916-019-1276-y
Download citation
Received : 29 November 2018
Accepted : 31 January 2019
Published : 19 February 2019
DOI : https://doi.org/10.1186/s12916-019-1276-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Assisted suicide
- End-of-life care
- Epidemiology
- Legislation
- Medical decision-making
BMC Medicine
ISSN: 1741-7015
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Med Res
- v.136(6); 2012 Dec
Euthanasia: Right to life vs right to die
Suresh bada math.
Department of Psychiatry National Institute of Mental Health & Neuro Sciences (Deemed University) Bangalore 560 029, India
Santosh K. Chaturvedi
The word euthanasia, originated in Greece means a good death 1 . Euthanasia encompasses various dimensions, from active (introducing something to cause death) to passive (withholding treatment or supportive measures); voluntary (consent) to involuntary (consent from guardian) and physician assisted (where physician's prescribe the medicine and patient or the third party administers the medication to cause death) 2 , 3 . Request for premature ending of life has contributed to the debate about the role of such practices in contemporary health care. This debate cuts across complex and dynamic aspects such as, legal, ethical, human rights, health, religious, economic, spiritual, social and cultural aspects of the civilised society. Here we argue this complex issue from both the supporters and opponents’ perspectives, and also attempts to present the plight of the sufferers and their caregivers. The objective is to discuss the subject of euthanasia from the medical and human rights perspective given the background of the recent Supreme Court judgement 3 in this context.
In India abetment of suicide and attempt to suicide are both criminal offences. In 1994, constitutional validity of Indian Penal Code Section (IPC Sec) 309 was challenged in the Supreme Court 4 . The Supreme Court declared that IPC Sec 309 is unconstitutional, under Article 21 (Right to Life) of the constitution in a landmark judgement 4 . In 1996, an interesting case of abetment of commission of suicide (IPC Sec 306) came to Supreme Court 5 . The accused were convicted in the trial court and later the conviction was upheld by the High Court. They appealed to the Supreme Court and contended that ‘right to die’ be included in Article 21 of the Constitution and any person abetting the commission of suicide by anyone is merely assisting in the enforcement of the fundamental right under Article 21; hence their punishment is violation of Article 21. This made the Supreme Court to rethink and to reconsider the decision of right to die. Immediately the matter was referred to a Constitution Bench of the Indian Supreme Court. The Court held that the right to life under Article 21 of the Constitution does not include the right to die 5 .
Regarding suicide, the Supreme Court reconsidered its decision on suicide. Abetment of suicide (IPC Sec 306) and attempt to suicide (IPC Sec 309) are two distinct offences, hence Section 306 can survive independent of Section 309. It has also clearly stated that a person attempts suicide in a depression, and hence he needs help, rather than punishment. Therefore, the Supreme Court has recommended to Parliament to consider the feasibility of deleting Section 309 from the Indian Penal Code 3 .
Arguments against euthanasia
Eliminating the invalid : Euthanasia opposers argue that if we embrace ‘the right to death with dignity’, people with incurable and debilitating illnesses will be disposed from our civilised society. The practice of palliative care counters this view, as palliative care would provide relief from distressing symptoms and pain, and support to the patient as well as the care giver. Palliative care is an active, compassionate and creative care for the dying 6 .
Constitution of India : ‘Right to life’ is a natural right embodied in Article 21 but suicide is an unnatural termination or extinction of life and, therefore, incompatible and inconsistent with the concept of ‘right to life’. It is the duty of the State to protect life and the physician's duty to provide care and not to harm patients. If euthanasia is legalised, then there is a grave apprehension that the State may refuse to invest in health (working towards Right to life). Legalised euthanasia has led to a severe decline in the quality of care for terminally-ill patients in Holland 7 . Hence, in a welfare state there should not be any role of euthanasia in any form.
Symptom of mental illness : Attempts to suicide or completed suicide are commonly seen in patients suffering from depression 8 , schizophrenia 9 and substance users 10 . It is also documented in patients suffering from obsessive compulsive disorder 11 . Hence, it is essential to assess the mental status of the individual seeking for euthanasia. In classical teaching, attempt to suicide is a psychiatric emergency and it is considered as a desperate call for help or assistance. Several guidelines have been formulated for management of suicidal patients in psychiatry 12 . Hence, attempted suicide is considered as a sign of mental illness 13 .
Malafide intention : In the era of declining morality and justice, there is a possibility of misusing euthanasia by family members or relatives for inheriting the property of the patient. The Supreme Court has also raised this issue in the recent judgement 3 . ‘Mercy killing’ should not lead to ‘killing mercy’ in the hands of the noble medical professionals. Hence, to keep control over the medical professionals, the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002 discusses euthanasia briefly in Chapter 6, Section 6.7 and it is in accordance with the provisions of the Transplantation of Human Organ Act, 1994 14 . There is an urgent need to protect patients and also medical practitioners caring the terminally ill patients from unnecessary lawsuit. Law commission had submitted a report (no-196) to the government on this issue 15 .
Emphasis on care : Earlier majority of them died before they reached the hospital but now it is converse. Now sciences had advanced to the extent, life can be prolonged but not to that extent of bringing back the dead one. This phenomenon has raised a complex situation. Earlier diseases outcome was discussed in terms of ‘CURE’ but in the contemporary world of diseases such as cancer, Aids, diabetes, hypertension and mental illness are debated in terms best ‘CARE’, since cure is distant. The principle is to add life to years rather than years to life with a good quality palliative care. The intention is to provide care when cure is not possible by low cost methods. The expectation of society is, ‘cure’ from the health professionals, but the role of medical professionals is to provide ‘care’. Hence, euthanasia for no cure illness does not have a logical argument. Whenever, there is no cure, the society and medical professionals become frustrated and the fellow citizen take extreme measures such as suicide, euthanasia or substance use. In such situations, palliative and rehabilitative care comes to the rescue of the patient and the family. At times, doctors do suggest to the family members to have the patient discharged from the hospital wait for death to come, if the family or patient so desires. Various reasons are quoted for such decisions, such as poverty, non-availability of bed, futile intervention, resources can be utilised for other patients where cure is possible and unfortunately majority of our patient's family do accordingly. Many of the terminally ill patients prefer to die at home, with or without any proper terminal health care. The societal perception needs to be altered and also the medical professionals need to focus on care rather in addition to just cure. The motive for many euthanasia requests is unawareness of alternatives. Patients hear from their doctors that ‘nothing can be done anymore’. However, when patients hear that a lot can be done through palliative care, that the symptoms can be controlled, now and in the future, many do not want euthanasia anymore 16 .
Commercialisation of health care : Passive euthanasia occurs in majority of the hospitals across the county, where poor patients and their family members refuse or withdraw treatment because of the huge cost involved in keeping them alive. If euthanasia is legalised, then commercial health sector will serve death sentence to many disabled and elderly citizens of India for meagre amount of money. This has been highlighted in the Supreme Court Judgement 3 , 17 .
Research has revealed that many terminally ill patients requesting euthanasia, have major depression, and that the desire for death in terminal patients is correlated with the depression 18 . In Indian setting also, strong desire for death was reported by 3 of the 191 advanced cancer patients, and these had severe depression 19 . They need palliative and rehabilitative care. They want to be looked after by enthusiastic, compassionate and humanistic team of health professionals and the complete expenses need to be borne by the State so that ‘Right to life’ becomes a reality and succeeds before ‘Right to death with dignity’. Palliative care actually provides death with dignity and a death considered good by the patient and the care givers.
Counterargument of euthanasia supporters
Caregivers burden : ‘Right-to-die’ supporters argue that people who have an incurable, degenerative, disabling or debilitating condition should be allowed to die in dignity. This argument is further defended for those, who have chronic debilitating illness even though it is not terminal such as severe mental illness. Majority of such petitions are filed by the sufferers or family members or their caretakers. The caregiver's burden is huge and cuts across various domains such as financial, emotional, time, physical, mental and social. Hence, it is uncommon to hear requests from the family members of the person with psychiatric illness to give some poison either to patient or else to them. Coupled with the States inefficiency, apathy and no investment on health is mockery of the ‘Right to life’.
Refusing care : Right to refuse medical treatment is well recognised in law, including medical treatment that sustains or prolongs life. For example, a patient suffering from blood cancer can refuse treatment or deny feeds through nasogastric tube. Recognition of right to refuse treatment gives a way for passive euthanasia. Many do argue that allowing medical termination of pregnancy before 16 wk is also a form of active involuntary euthanasia. This issue of mercy killing of deformed babies has already been in discussion in Holland 20 .
Right to die : Many patients in a persistent vegetative state or else in chronic illness, do not want to be a burden on their family members. Euthanasia can be considered as a way to upheld the ‘Right to life’ by honouring ‘Right to die’ with dignity.
Encouraging the organ transplantation : Euthanasia in terminally ill patients provides an opportunity to advocate for organ donation. This in turn will help many patients with organ failure waiting for transplantation. Not only euthanasia gives ‘Right to die’ for the terminally ill, but also ‘Right to life’ for the organ needy patients.
Constitution of India reads ‘right to life’ is in positive direction of protecting life. Hence, there is an urgent need to fulfil this obligation of ‘Right to life’ by providing ‘food, safe drinking water and health care’. On the contrary, the state does not own the responsibility of promoting, protecting and fulfilling the socio-economic rights such as right to food, right to water, right to education and right to health care, which are basic essential ingredients of right to life. Till date, most of the States has not done anything to support the terminally ill people by providing for hospice care.
If the State takes the responsibility of providing reasonable degree of health care, then majority of the euthanasia supporters will definitely reconsider their argument. We do endorse the Supreme Court Judgement that our contemporary society and public health system is not matured enough to handle this sensitive issue, hence it needs to be withheld. However, this issue needs to be re-examined again after few years depending upon the evolution of the society with regard to providing health care to the disabled and public health sector with regard to providing health care to poor people.
The Supreme Court judgement to withhold decision on this sensitive issue is a first step towards a new era of health care in terminally ill patients. The Judgment laid down is to preserve harmony within a society, when faced with a complex medical, social and legal dilemma. There is a need to enact a legislation to protect terminally ill patients and also medical practitioners caring for them as per the recommendation of Law Commission Report-196 15 . There is also an urgent need to invest in our health care system, so that poor people suffering from ill health can access free health care. Investment in health care is not a charity; ‘Right to Health’ is bestowed under ‘Right to Life’ of our constitution.

COMMENTS
3. Evolution of euthanasia and assisted suicide: digging into historical events. To understand the evolution and relevance of these concepts should analyze the history of euthanasia and assisted suicide; from the emergence of the term, going through its first manifestations in antiquity; mentioning the conceptions of great thinkers such as Plato and Hippocrates; going through the role of the ...
Abstract. Euthanasia or assisted suicide—and sometimes both—have been legalized in a small number of countries and states. In all jurisdictions, laws and safeguards were put in place to prevent abuse and misuse of these practices. Prevention measures have included, among others, explicit consent by the person requesting euthanasia ...
Definition and current legal framework. Assisted dying is a general term that incorporates both physician-assisted dying and voluntary active euthanasia.Voluntary active euthanasia includes a physician (or third person) intentionally ending a person's life normally through the administration of drugs, at that person's voluntary and competent request. 2, 3 Facilitating a person's death ...
Abstract. End-of-life care is an increasingly relevant topic due to advances in biomedical research and the establishment of new disciplines in evidence-based medicine and bioethics. Euthanasia and assisted suicide are two terms widely discussed in medicine, which cause displeasure on many occasions and cause relief on others.
4 As was the case with attitudes towards euthanasia, approval towards assisted suicide increased in US from the late 1990s to the beginning of the new century, but then declined from 68 percent in 2001 to 51 percent in 2013, only to go back up again but without reaching the levels of the beginning of the century (Emanuel et al. 2016; Jones 2020).
Abstract. Euthanasia has been a subject of debate worldwide. It has brought up multiple controversies in different countries and among different societies. Over the years, euthanasia has been an ...
Abstract. Acting as the conductor on the train of impending death, a divisive turn to the left will hasten human pain and end life; while a swerve to the right will prolong human life, but also, extend unbearable human pain and suffering. One could make sound arguments that both of these grim decisions are equally acts of compassion or malice.
Assisted dying is a general term that incorporates both physician-assisted dying and voluntary active euthanasia.Voluntary active euthanasia includes a physician (or third person) intentionally ending a person's life normally through the administration of drugs, at that person's voluntary and competent request. 2,3 Facilitating a person's death without their prior consent incorporates ...
Results: A slight majority of the physicians (56, 8%) believe that active euthanasia is ethically unacceptable, while 43, 2% is for another solution (35, 2% took a viewpoint that it is completely ethically acceptable, while the remaining 8% considered it ethically acceptable in certain cases). From the other side, 56, 8% of respondents answered ...
Introduction Previous research has explored euthanasia's ethical dimensions, primarily focusing on general practice and, to a lesser extent, psychiatry, mainly from the viewpoints of physicians and nurses. However, a gap exists in understanding the comprehensive value-based perspectives of other professionals involved in both somatic and psychiatric euthanasia. This paper aims to analyze the ...
Briefing Papers: Euthanasia and Assisted Suicide (Anscombe Bioethics Centre, Oxford: 2021). On the changing social attitude to those living with dementia and how euthanasia poses a threat to living and dying well with dementia, see: Matthews, Pia. 'Dignity in Living: Addressing Euthanasia by Affirming Patient Personhood in Dementia'.
Euthanasia: An Understanding. Dharmender Kumar Nehra, Pradeep Kumar. and Sheetal Nehra. Death a friend that alone can bring the peace his treasures. cannot purchase, and remove the pain his ...
The aim of this article is to present and confront the arguments in support of euthanasia and physician assisted suicide, and the arguments against. The arguments for and against euthanasia are listed and discussed to literature cited. Euthanasia is an act of mercy, and, basically means to take a deliberate action with the express intention of ...
As the word indicates, euthanasia is derived from the Greek word "euthanatos" meaning "early death.". This term has such countless debates that it has incited emotive reactions both among the clinical practicians and people in general. According to the House of Lords Select Committee on Medical Ethics, the correct definition of ...
Conclusiones. The history and evolution of euthanasia and assisted suicide have been traumatic throughout human history. The church, politics, and biomedical research have been decisive in defining these concepts. Over the years, the legal framework and bioethical concepts on euthanasia have been strengthened.
Introduction. Regardless of the legal status of euthanasia, terminal patients cared for by palliative care teams often request from health care professionals (HCPs) that their life be terminated. 1 -9 An integral part of the definition of euthanasia adopted by the European Association for Palliative Care includes a person voluntarily and competently formulating a request themselves to a ...
An Analysis of Arguments for and Against Euthanasia and Assisted Suicide: Part One - Volume 5 Issue 1. 22 August 2024: Due to technical disruption, we are experiencing some delays to publication. We are working to restore services and apologise for the inconvenience. For further updates please visit our website: https://www.cambridge.org ...
Regardless of the legal status of euthanasia, terminal patients cared for by palliative care teams often request from health care professionals (HCPs) that their life be terminated. 1-9 An integral part of the definition of euthanasia adopted by the European Association for Palliative Care includes a person voluntarily and competently formulating a request themselves to a doctor (or other ...
In 1991, a debate at the European Parliament on euthanasia stimulated discussion at all levels in Europe. Subsequently, the European Association for Palliative Care (EAPC) produced a first statement, Regarding Euthanasia, 1 in order to clarify the position the organization should adopt towards euthanasia. In 2003, the EAPC task force on ethics published a more detailed and updated statement. 2 ...
Recently, euthanasia and assisted suicide (EAS) in patients with psychiatric disorders, dementia, or an accumulation of health problems has taken a prominent place in the public debate. However, limited is known about this practice. The purpose of this study was threefold: to estimate the frequency of requesting and receiving EAS among people with (also) a psychiatric disorder, dementia, or an ...
This study aimed at examining the approval rate of the medical students' regarding active euthanasia, passive euthanasia, and physician-assisted-suicide over the last ten years. To do so, the arguments and variables affecting students' choices were examined and a systematic review was conducted, using PubMed and Web of Science databases ...
Derived from the Greek terms eu meaning good, and thanos meaning death, euthanasia is the. act of bringing death to another person in a rela tively painless way for reasons of mercy Although euthanasia has historically been common practice in many. societies, it remains one of the most controversial topics. today.
Arguments against euthanasia. Eliminating the invalid: Euthanasia opposers argue that if we embrace 'the right to death with dignity', people with incurable and debilitating illnesses will be disposed from our civilised society.The practice of palliative care counters this view, as palliative care would provide relief from distressing symptoms and pain, and support to the patient as well ...