Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Research paper
- How to Write a Discussion Section | Tips & Examples

How to Write a Discussion Section | Tips & Examples
Published on August 21, 2022 by Shona McCombes . Revised on July 18, 2023.

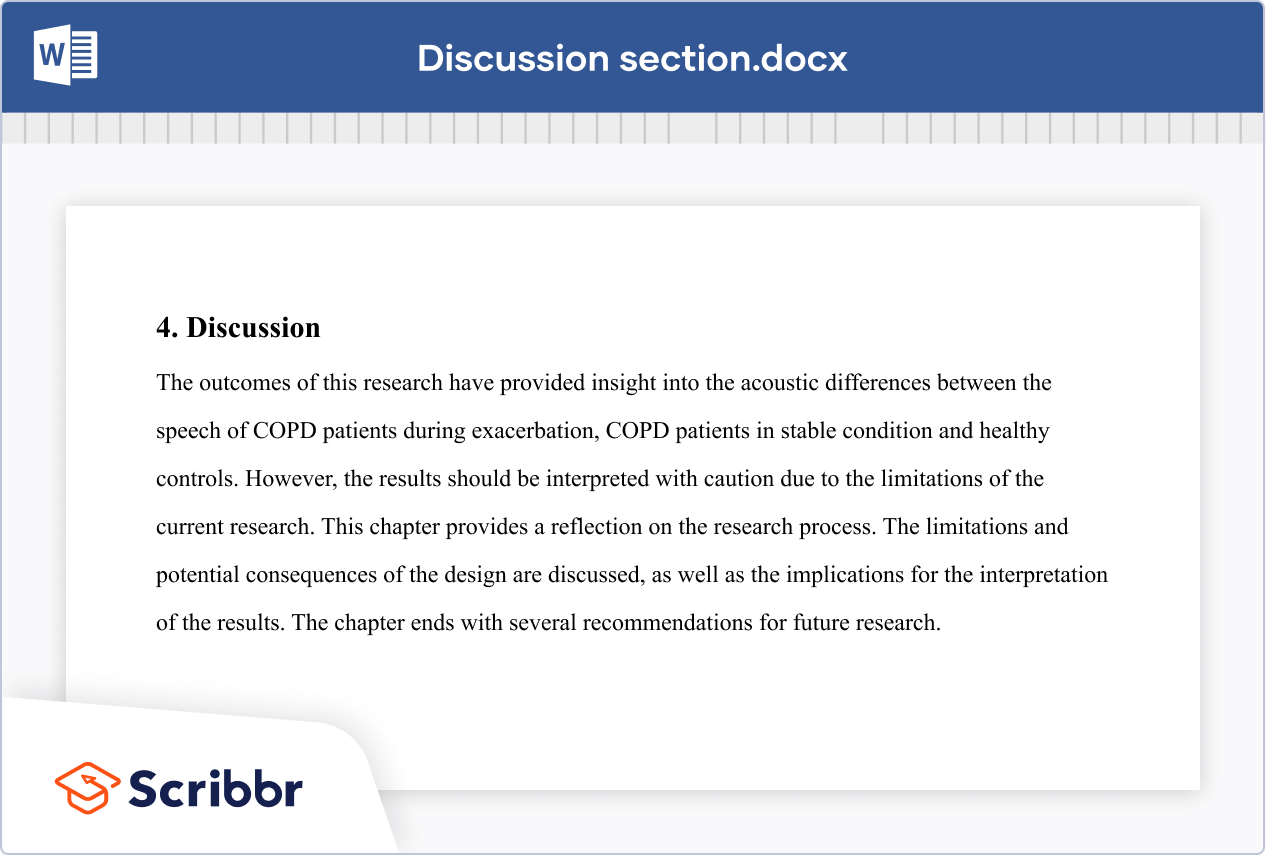
The discussion section is where you delve into the meaning, importance, and relevance of your results .
It should focus on explaining and evaluating what you found, showing how it relates to your literature review and paper or dissertation topic , and making an argument in support of your overall conclusion. It should not be a second results section.
There are different ways to write this section, but you can focus your writing around these key elements:
- Summary : A brief recap of your key results
- Interpretations: What do your results mean?
- Implications: Why do your results matter?
- Limitations: What can’t your results tell us?
- Recommendations: Avenues for further studies or analyses
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
What not to include in your discussion section, step 1: summarize your key findings, step 2: give your interpretations, step 3: discuss the implications, step 4: acknowledge the limitations, step 5: share your recommendations, discussion section example, other interesting articles, frequently asked questions about discussion sections.
There are a few common mistakes to avoid when writing the discussion section of your paper.
- Don’t introduce new results: You should only discuss the data that you have already reported in your results section .
- Don’t make inflated claims: Avoid overinterpretation and speculation that isn’t directly supported by your data.
- Don’t undermine your research: The discussion of limitations should aim to strengthen your credibility, not emphasize weaknesses or failures.
Don't submit your assignments before you do this
The academic proofreading tool has been trained on 1000s of academic texts. Making it the most accurate and reliable proofreading tool for students. Free citation check included.

Try for free
Start this section by reiterating your research problem and concisely summarizing your major findings. To speed up the process you can use a summarizer to quickly get an overview of all important findings. Don’t just repeat all the data you have already reported—aim for a clear statement of the overall result that directly answers your main research question . This should be no more than one paragraph.
Many students struggle with the differences between a discussion section and a results section . The crux of the matter is that your results sections should present your results, and your discussion section should subjectively evaluate them. Try not to blend elements of these two sections, in order to keep your paper sharp.
- The results indicate that…
- The study demonstrates a correlation between…
- This analysis supports the theory that…
- The data suggest that…
The meaning of your results may seem obvious to you, but it’s important to spell out their significance for your reader, showing exactly how they answer your research question.
The form of your interpretations will depend on the type of research, but some typical approaches to interpreting the data include:
- Identifying correlations , patterns, and relationships among the data
- Discussing whether the results met your expectations or supported your hypotheses
- Contextualizing your findings within previous research and theory
- Explaining unexpected results and evaluating their significance
- Considering possible alternative explanations and making an argument for your position
You can organize your discussion around key themes, hypotheses, or research questions, following the same structure as your results section. Alternatively, you can also begin by highlighting the most significant or unexpected results.
- In line with the hypothesis…
- Contrary to the hypothesized association…
- The results contradict the claims of Smith (2022) that…
- The results might suggest that x . However, based on the findings of similar studies, a more plausible explanation is y .
As well as giving your own interpretations, make sure to relate your results back to the scholarly work that you surveyed in the literature review . The discussion should show how your findings fit with existing knowledge, what new insights they contribute, and what consequences they have for theory or practice.
Ask yourself these questions:
- Do your results support or challenge existing theories? If they support existing theories, what new information do they contribute? If they challenge existing theories, why do you think that is?
- Are there any practical implications?
Your overall aim is to show the reader exactly what your research has contributed, and why they should care.
- These results build on existing evidence of…
- The results do not fit with the theory that…
- The experiment provides a new insight into the relationship between…
- These results should be taken into account when considering how to…
- The data contribute a clearer understanding of…
- While previous research has focused on x , these results demonstrate that y .
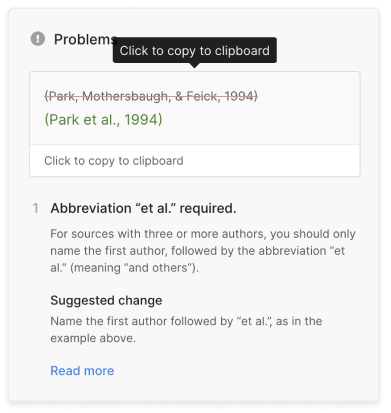
Scribbr Citation Checker New
The AI-powered Citation Checker helps you avoid common mistakes such as:
- Missing commas and periods
- Incorrect usage of “et al.”
- Ampersands (&) in narrative citations
- Missing reference entries
Even the best research has its limitations. Acknowledging these is important to demonstrate your credibility. Limitations aren’t about listing your errors, but about providing an accurate picture of what can and cannot be concluded from your study.
Limitations might be due to your overall research design, specific methodological choices , or unanticipated obstacles that emerged during your research process.
Here are a few common possibilities:
- If your sample size was small or limited to a specific group of people, explain how generalizability is limited.
- If you encountered problems when gathering or analyzing data, explain how these influenced the results.
- If there are potential confounding variables that you were unable to control, acknowledge the effect these may have had.
After noting the limitations, you can reiterate why the results are nonetheless valid for the purpose of answering your research question.
- The generalizability of the results is limited by…
- The reliability of these data is impacted by…
- Due to the lack of data on x , the results cannot confirm…
- The methodological choices were constrained by…
- It is beyond the scope of this study to…
Based on the discussion of your results, you can make recommendations for practical implementation or further research. Sometimes, the recommendations are saved for the conclusion .
Suggestions for further research can lead directly from the limitations. Don’t just state that more studies should be done—give concrete ideas for how future work can build on areas that your own research was unable to address.
- Further research is needed to establish…
- Future studies should take into account…
- Avenues for future research include…
If you want to know more about AI for academic writing, AI tools, or research bias, make sure to check out some of our other articles with explanations and examples or go directly to our tools!
Research bias
- Anchoring bias
- Halo effect
- The Baader–Meinhof phenomenon
- The placebo effect
- Nonresponse bias
- Deep learning
- Generative AI
- Machine learning
- Reinforcement learning
- Supervised vs. unsupervised learning
(AI) Tools
- Grammar Checker
- Paraphrasing Tool
- Text Summarizer
- AI Detector
- Plagiarism Checker
- Citation Generator
In the discussion , you explore the meaning and relevance of your research results , explaining how they fit with existing research and theory. Discuss:
- Your interpretations : what do the results tell us?
- The implications : why do the results matter?
- The limitation s : what can’t the results tell us?
The results chapter or section simply and objectively reports what you found, without speculating on why you found these results. The discussion interprets the meaning of the results, puts them in context, and explains why they matter.
In qualitative research , results and discussion are sometimes combined. But in quantitative research , it’s considered important to separate the objective results from your interpretation of them.
In a thesis or dissertation, the discussion is an in-depth exploration of the results, going into detail about the meaning of your findings and citing relevant sources to put them in context.
The conclusion is more shorter and more general: it concisely answers your main research question and makes recommendations based on your overall findings.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, July 18). How to Write a Discussion Section | Tips & Examples. Scribbr. Retrieved August 21, 2024, from https://www.scribbr.com/dissertation/discussion/
Is this article helpful?
Shona McCombes
Other students also liked, how to write a literature review | guide, examples, & templates, what is a research methodology | steps & tips, how to write a results section | tips & examples, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 8. The Discussion
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The purpose of the discussion section is to interpret and describe the significance of your findings in relation to what was already known about the research problem being investigated and to explain any new understanding or insights that emerged as a result of your research. The discussion will always connect to the introduction by way of the research questions or hypotheses you posed and the literature you reviewed, but the discussion does not simply repeat or rearrange the first parts of your paper; the discussion clearly explains how your study advanced the reader's understanding of the research problem from where you left them at the end of your review of prior research.
Annesley, Thomas M. “The Discussion Section: Your Closing Argument.” Clinical Chemistry 56 (November 2010): 1671-1674; Peacock, Matthew. “Communicative Moves in the Discussion Section of Research Articles.” System 30 (December 2002): 479-497.
Importance of a Good Discussion
The discussion section is often considered the most important part of your research paper because it:
- Most effectively demonstrates your ability as a researcher to think critically about an issue, to develop creative solutions to problems based upon a logical synthesis of the findings, and to formulate a deeper, more profound understanding of the research problem under investigation;
- Presents the underlying meaning of your research, notes possible implications in other areas of study, and explores possible improvements that can be made in order to further develop the concerns of your research;
- Highlights the importance of your study and how it can contribute to understanding the research problem within the field of study;
- Presents how the findings from your study revealed and helped fill gaps in the literature that had not been previously exposed or adequately described; and,
- Engages the reader in thinking critically about issues based on an evidence-based interpretation of findings; it is not governed strictly by objective reporting of information.
Annesley Thomas M. “The Discussion Section: Your Closing Argument.” Clinical Chemistry 56 (November 2010): 1671-1674; Bitchener, John and Helen Basturkmen. “Perceptions of the Difficulties of Postgraduate L2 Thesis Students Writing the Discussion Section.” Journal of English for Academic Purposes 5 (January 2006): 4-18; Kretchmer, Paul. Fourteen Steps to Writing an Effective Discussion Section. San Francisco Edit, 2003-2008.
Structure and Writing Style
I. General Rules
These are the general rules you should adopt when composing your discussion of the results :
- Do not be verbose or repetitive; be concise and make your points clearly
- Avoid the use of jargon or undefined technical language
- Follow a logical stream of thought; in general, interpret and discuss the significance of your findings in the same sequence you described them in your results section [a notable exception is to begin by highlighting an unexpected result or a finding that can grab the reader's attention]
- Use the present verb tense, especially for established facts; however, refer to specific works or prior studies in the past tense
- If needed, use subheadings to help organize your discussion or to categorize your interpretations into themes
II. The Content
The content of the discussion section of your paper most often includes :
- Explanation of results : Comment on whether or not the results were expected for each set of findings; go into greater depth to explain findings that were unexpected or especially profound. If appropriate, note any unusual or unanticipated patterns or trends that emerged from your results and explain their meaning in relation to the research problem.
- References to previous research : Either compare your results with the findings from other studies or use the studies to support a claim. This can include re-visiting key sources already cited in your literature review section, or, save them to cite later in the discussion section if they are more important to compare with your results instead of being a part of the general literature review of prior research used to provide context and background information. Note that you can make this decision to highlight specific studies after you have begun writing the discussion section.
- Deduction : A claim for how the results can be applied more generally. For example, describing lessons learned, proposing recommendations that can help improve a situation, or highlighting best practices.
- Hypothesis : A more general claim or possible conclusion arising from the results [which may be proved or disproved in subsequent research]. This can be framed as new research questions that emerged as a consequence of your analysis.
III. Organization and Structure
Keep the following sequential points in mind as you organize and write the discussion section of your paper:
- Think of your discussion as an inverted pyramid. Organize the discussion from the general to the specific, linking your findings to the literature, then to theory, then to practice [if appropriate].
- Use the same key terms, narrative style, and verb tense [present] that you used when describing the research problem in your introduction.
- Begin by briefly re-stating the research problem you were investigating and answer all of the research questions underpinning the problem that you posed in the introduction.
- Describe the patterns, principles, and relationships shown by each major findings and place them in proper perspective. The sequence of this information is important; first state the answer, then the relevant results, then cite the work of others. If appropriate, refer the reader to a figure or table to help enhance the interpretation of the data [either within the text or as an appendix].
- Regardless of where it's mentioned, a good discussion section includes analysis of any unexpected findings. This part of the discussion should begin with a description of the unanticipated finding, followed by a brief interpretation as to why you believe it appeared and, if necessary, its possible significance in relation to the overall study. If more than one unexpected finding emerged during the study, describe each of them in the order they appeared as you gathered or analyzed the data. As noted, the exception to discussing findings in the same order you described them in the results section would be to begin by highlighting the implications of a particularly unexpected or significant finding that emerged from the study, followed by a discussion of the remaining findings.
- Before concluding the discussion, identify potential limitations and weaknesses if you do not plan to do so in the conclusion of the paper. Comment on their relative importance in relation to your overall interpretation of the results and, if necessary, note how they may affect the validity of your findings. Avoid using an apologetic tone; however, be honest and self-critical [e.g., in retrospect, had you included a particular question in a survey instrument, additional data could have been revealed].
- The discussion section should end with a concise summary of the principal implications of the findings regardless of their significance. Give a brief explanation about why you believe the findings and conclusions of your study are important and how they support broader knowledge or understanding of the research problem. This can be followed by any recommendations for further research. However, do not offer recommendations which could have been easily addressed within the study. This would demonstrate to the reader that you have inadequately examined and interpreted the data.
IV. Overall Objectives
The objectives of your discussion section should include the following: I. Reiterate the Research Problem/State the Major Findings
Briefly reiterate the research problem or problems you are investigating and the methods you used to investigate them, then move quickly to describe the major findings of the study. You should write a direct, declarative, and succinct proclamation of the study results, usually in one paragraph.
II. Explain the Meaning of the Findings and Why They are Important
No one has thought as long and hard about your study as you have. Systematically explain the underlying meaning of your findings and state why you believe they are significant. After reading the discussion section, you want the reader to think critically about the results and why they are important. You don’t want to force the reader to go through the paper multiple times to figure out what it all means. If applicable, begin this part of the section by repeating what you consider to be your most significant or unanticipated finding first, then systematically review each finding. Otherwise, follow the general order you reported the findings presented in the results section.
III. Relate the Findings to Similar Studies
No study in the social sciences is so novel or possesses such a restricted focus that it has absolutely no relation to previously published research. The discussion section should relate your results to those found in other studies, particularly if questions raised from prior studies served as the motivation for your research. This is important because comparing and contrasting the findings of other studies helps to support the overall importance of your results and it highlights how and in what ways your study differs from other research about the topic. Note that any significant or unanticipated finding is often because there was no prior research to indicate the finding could occur. If there is prior research to indicate this, you need to explain why it was significant or unanticipated. IV. Consider Alternative Explanations of the Findings
It is important to remember that the purpose of research in the social sciences is to discover and not to prove . When writing the discussion section, you should carefully consider all possible explanations for the study results, rather than just those that fit your hypothesis or prior assumptions and biases. This is especially important when describing the discovery of significant or unanticipated findings.
V. Acknowledge the Study’s Limitations
It is far better for you to identify and acknowledge your study’s limitations than to have them pointed out by your professor! Note any unanswered questions or issues your study could not address and describe the generalizability of your results to other situations. If a limitation is applicable to the method chosen to gather information, then describe in detail the problems you encountered and why. VI. Make Suggestions for Further Research
You may choose to conclude the discussion section by making suggestions for further research [as opposed to offering suggestions in the conclusion of your paper]. Although your study can offer important insights about the research problem, this is where you can address other questions related to the problem that remain unanswered or highlight hidden issues that were revealed as a result of conducting your research. You should frame your suggestions by linking the need for further research to the limitations of your study [e.g., in future studies, the survey instrument should include more questions that ask..."] or linking to critical issues revealed from the data that were not considered initially in your research.
NOTE: Besides the literature review section, the preponderance of references to sources is usually found in the discussion section . A few historical references may be helpful for perspective, but most of the references should be relatively recent and included to aid in the interpretation of your results, to support the significance of a finding, and/or to place a finding within a particular context. If a study that you cited does not support your findings, don't ignore it--clearly explain why your research findings differ from theirs.
V. Problems to Avoid
- Do not waste time restating your results . Should you need to remind the reader of a finding to be discussed, use "bridge sentences" that relate the result to the interpretation. An example would be: “In the case of determining available housing to single women with children in rural areas of Texas, the findings suggest that access to good schools is important...," then move on to further explaining this finding and its implications.
- As noted, recommendations for further research can be included in either the discussion or conclusion of your paper, but do not repeat your recommendations in the both sections. Think about the overall narrative flow of your paper to determine where best to locate this information. However, if your findings raise a lot of new questions or issues, consider including suggestions for further research in the discussion section.
- Do not introduce new results in the discussion section. Be wary of mistaking the reiteration of a specific finding for an interpretation because it may confuse the reader. The description of findings [results section] and the interpretation of their significance [discussion section] should be distinct parts of your paper. If you choose to combine the results section and the discussion section into a single narrative, you must be clear in how you report the information discovered and your own interpretation of each finding. This approach is not recommended if you lack experience writing college-level research papers.
- Use of the first person pronoun is generally acceptable. Using first person singular pronouns can help emphasize a point or illustrate a contrasting finding. However, keep in mind that too much use of the first person can actually distract the reader from the main points [i.e., I know you're telling me this--just tell me!].
Analyzing vs. Summarizing. Department of English Writing Guide. George Mason University; Discussion. The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College; Hess, Dean R. "How to Write an Effective Discussion." Respiratory Care 49 (October 2004); Kretchmer, Paul. Fourteen Steps to Writing to Writing an Effective Discussion Section. San Francisco Edit, 2003-2008; The Lab Report. University College Writing Centre. University of Toronto; Sauaia, A. et al. "The Anatomy of an Article: The Discussion Section: "How Does the Article I Read Today Change What I Will Recommend to my Patients Tomorrow?” The Journal of Trauma and Acute Care Surgery 74 (June 2013): 1599-1602; Research Limitations & Future Research . Lund Research Ltd., 2012; Summary: Using it Wisely. The Writing Center. University of North Carolina; Schafer, Mickey S. Writing the Discussion. Writing in Psychology course syllabus. University of Florida; Yellin, Linda L. A Sociology Writer's Guide . Boston, MA: Allyn and Bacon, 2009.
Writing Tip
Don’t Over-Interpret the Results!
Interpretation is a subjective exercise. As such, you should always approach the selection and interpretation of your findings introspectively and to think critically about the possibility of judgmental biases unintentionally entering into discussions about the significance of your work. With this in mind, be careful that you do not read more into the findings than can be supported by the evidence you have gathered. Remember that the data are the data: nothing more, nothing less.
MacCoun, Robert J. "Biases in the Interpretation and Use of Research Results." Annual Review of Psychology 49 (February 1998): 259-287; Ward, Paulet al, editors. The Oxford Handbook of Expertise . Oxford, UK: Oxford University Press, 2018.
Another Writing Tip
Don't Write Two Results Sections!
One of the most common mistakes that you can make when discussing the results of your study is to present a superficial interpretation of the findings that more or less re-states the results section of your paper. Obviously, you must refer to your results when discussing them, but focus on the interpretation of those results and their significance in relation to the research problem, not the data itself.
Azar, Beth. "Discussing Your Findings." American Psychological Association gradPSYCH Magazine (January 2006).
Yet Another Writing Tip
Avoid Unwarranted Speculation!
The discussion section should remain focused on the findings of your study. For example, if the purpose of your research was to measure the impact of foreign aid on increasing access to education among disadvantaged children in Bangladesh, it would not be appropriate to speculate about how your findings might apply to populations in other countries without drawing from existing studies to support your claim or if analysis of other countries was not a part of your original research design. If you feel compelled to speculate, do so in the form of describing possible implications or explaining possible impacts. Be certain that you clearly identify your comments as speculation or as a suggestion for where further research is needed. Sometimes your professor will encourage you to expand your discussion of the results in this way, while others don’t care what your opinion is beyond your effort to interpret the data in relation to the research problem.
- << Previous: Using Non-Textual Elements
- Next: Limitations of the Study >>
- Last Updated: Aug 21, 2024 8:54 AM
- URL: https://libguides.usc.edu/writingguide
- Research Process
- Manuscript Preparation
- Manuscript Review
- Publication Process
- Publication Recognition
- Language Editing Services
- Translation Services

6 Steps to Write an Excellent Discussion in Your Manuscript
- 4 minute read
Table of Contents
The discussion section in scientific manuscripts might be the last few paragraphs, but its role goes far beyond wrapping up. It’s the part of an article where scientists talk about what they found and what it means, where raw data turns into meaningful insights. Therefore, discussion is a vital component of the article.
An excellent discussion is well-organized. We bring to you authors a classic 6-step method for writing discussion sections, with examples to illustrate the functions and specific writing logic of each step. Take a look at how you can impress journal reviewers with a concise and focused discussion section!
Discussion frame structure
Conventionally, a discussion section has three parts: an introductory paragraph, a few intermediate paragraphs, and a conclusion¹. Please follow the steps below:
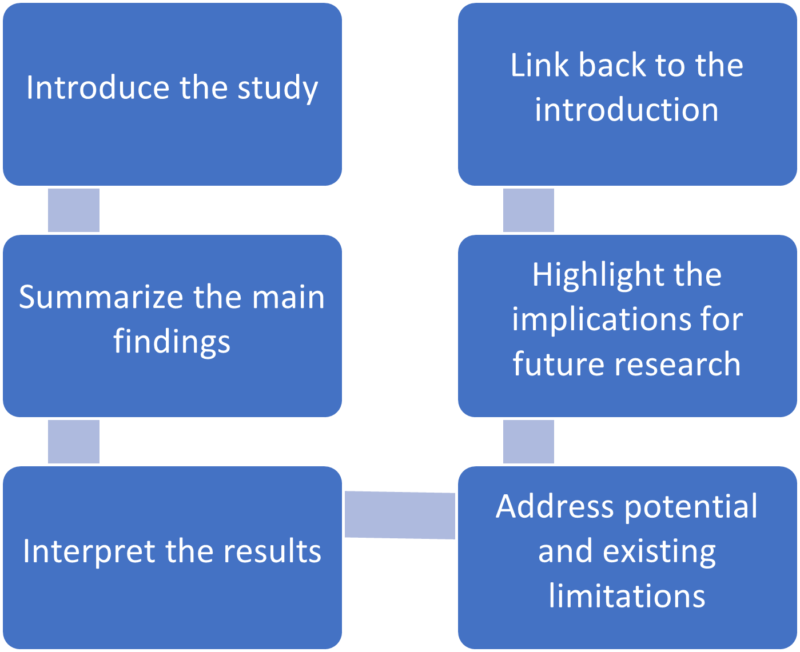
1.Introduction—mention gaps in previous research¹⁻ ²
Here, you orient the reader to your study. In the first paragraph, it is advisable to mention the research gap your paper addresses.
Example: This study investigated the cognitive effects of a meat-only diet on adults. While earlier studies have explored the impact of a carnivorous diet on physical attributes and agility, they have not explicitly addressed its influence on cognitively intense tasks involving memory and reasoning.
2. Summarizing key findings—let your data speak ¹⁻ ²
After you have laid out the context for your study, recapitulate some of its key findings. Also, highlight key data and evidence supporting these findings.
Example: We found that risk-taking behavior among teenagers correlates with their tendency to invest in cryptocurrencies. Risk takers in this study, as measured by the Cambridge Gambling Task, tended to have an inordinately higher proportion of their savings invested as crypto coins.
3. Interpreting results—compare with other papers¹⁻²
Here, you must analyze and interpret any results concerning the research question or hypothesis. How do the key findings of your study help verify or disprove the hypothesis? What practical relevance does your discovery have?
Example: Our study suggests that higher daily caffeine intake is not associated with poor performance in major sporting events. Athletes may benefit from the cardiovascular benefits of daily caffeine intake without adversely impacting performance.
Remember, unlike the results section, the discussion ideally focuses on locating your findings in the larger body of existing research. Hence, compare your results with those of other peer-reviewed papers.
Example: Although Miller et al. (2020) found evidence of such political bias in a multicultural population, our findings suggest that the bias is weak or virtually non-existent among politically active citizens.
4. Addressing limitations—their potential impact on the results¹⁻²
Discuss the potential impact of limitations on the results. Most studies have limitations, and it is crucial to acknowledge them in the intermediary paragraphs of the discussion section. Limitations may include low sample size, suspected interference or noise in data, low effect size, etc.
Example: This study explored a comprehensive list of adverse effects associated with the novel drug ‘X’. However, long-term studies may be needed to confirm its safety, especially regarding major cardiac events.
5. Implications for future research—how to explore further¹⁻²
Locate areas of your research where more investigation is needed. Concluding paragraphs of the discussion can explain what research will likely confirm your results or identify knowledge gaps your study left unaddressed.
Example: Our study demonstrates that roads paved with the plastic-infused compound ‘Y’ are more resilient than asphalt. Future studies may explore economically feasible ways of producing compound Y in bulk.
6. Conclusion—summarize content¹⁻²
A good way to wind up the discussion section is by revisiting the research question mentioned in your introduction. Sign off by expressing the main findings of your study.
Example: Recent observations suggest that the fish ‘Z’ is moving upriver in many parts of the Amazon basin. Our findings provide conclusive evidence that this phenomenon is associated with rising sea levels and climate change, not due to elevated numbers of invasive predators.
A rigorous and concise discussion section is one of the keys to achieving an excellent paper. It serves as a critical platform for researchers to interpret and connect their findings with the broader scientific context. By detailing the results, carefully comparing them with existing research, and explaining the limitations of this study, you can effectively help reviewers and readers understand the entire research article more comprehensively and deeply¹⁻² , thereby helping your manuscript to be successfully published and gain wider dissemination.
In addition to keeping this writing guide, you can also use Elsevier Language Services to improve the quality of your paper more deeply and comprehensively. We have a professional editing team covering multiple disciplines. With our profound disciplinary background and rich polishing experience, we can significantly optimize all paper modules including the discussion, effectively improve the fluency and rigor of your articles, and make your scientific research results consistent, with its value reflected more clearly. We are always committed to ensuring the quality of papers according to the standards of top journals, improving the publishing efficiency of scientific researchers, and helping you on the road to academic success. Check us out here !
Type in wordcount for Standard Total: USD EUR JPY Follow this link if your manuscript is longer than 12,000 words. Upload
References:
- Masic, I. (2018). How to write an efficient discussion? Medical Archives , 72(3), 306. https://doi.org/10.5455/medarh.2018.72.306-307
- Şanlı, Ö., Erdem, S., & Tefik, T. (2014). How to write a discussion section? Urology Research & Practice , 39(1), 20–24. https://doi.org/10.5152/tud.2013.049

Navigating “Chinglish” Errors in Academic English Writing

A Guide to Crafting Shorter, Impactful Sentences in Academic Writing
You may also like.

Submission 101: What format should be used for academic papers?

Page-Turner Articles are More Than Just Good Arguments: Be Mindful of Tone and Structure!

A Must-see for Researchers! How to Ensure Inclusivity in Your Scientific Writing

Make Hook, Line, and Sinker: The Art of Crafting Engaging Introductions

Can Describing Study Limitations Improve the Quality of Your Paper?

How to Write Clear and Crisp Civil Engineering Papers? Here are 5 Key Tips to Consider

The Clear Path to An Impactful Paper: ②
Input your search keywords and press Enter.
How to Write the Discussion Section of a Research Paper
The discussion section of a research paper analyzes and interprets the findings, provides context, compares them with previous studies, identifies limitations, and suggests future research directions.
Updated on September 15, 2023

Structure your discussion section right, and you’ll be cited more often while doing a greater service to the scientific community. So, what actually goes into the discussion section? And how do you write it?
The discussion section of your research paper is where you let the reader know how your study is positioned in the literature, what to take away from your paper, and how your work helps them. It can also include your conclusions and suggestions for future studies.
First, we’ll define all the parts of your discussion paper, and then look into how to write a strong, effective discussion section for your paper or manuscript.
Discussion section: what is it, what it does
The discussion section comes later in your paper, following the introduction, methods, and results. The discussion sets up your study’s conclusions. Its main goals are to present, interpret, and provide a context for your results.
What is it?
The discussion section provides an analysis and interpretation of the findings, compares them with previous studies, identifies limitations, and suggests future directions for research.
This section combines information from the preceding parts of your paper into a coherent story. By this point, the reader already knows why you did your study (introduction), how you did it (methods), and what happened (results). In the discussion, you’ll help the reader connect the ideas from these sections.
Why is it necessary?
The discussion provides context and interpretations for the results. It also answers the questions posed in the introduction. While the results section describes your findings, the discussion explains what they say. This is also where you can describe the impact or implications of your research.
Adds context for your results
Most research studies aim to answer a question, replicate a finding, or address limitations in the literature. These goals are first described in the introduction. However, in the discussion section, the author can refer back to them to explain how the study's objective was achieved.
Shows what your results actually mean and real-world implications
The discussion can also describe the effect of your findings on research or practice. How are your results significant for readers, other researchers, or policymakers?
What to include in your discussion (in the correct order)
A complete and effective discussion section should at least touch on the points described below.
Summary of key findings
The discussion should begin with a brief factual summary of the results. Concisely overview the main results you obtained.
Begin with key findings with supporting evidence
Your results section described a list of findings, but what message do they send when you look at them all together?
Your findings were detailed in the results section, so there’s no need to repeat them here, but do provide at least a few highlights. This will help refresh the reader’s memory and help them focus on the big picture.
Read the first paragraph of the discussion section in this article (PDF) for an example of how to start this part of your paper. Notice how the authors break down their results and follow each description sentence with an explanation of why each finding is relevant.
State clearly and concisely
Following a clear and direct writing style is especially important in the discussion section. After all, this is where you will make some of the most impactful points in your paper. While the results section often contains technical vocabulary, such as statistical terms, the discussion section lets you describe your findings more clearly.
Interpretation of results
Once you’ve given your reader an overview of your results, you need to interpret those results. In other words, what do your results mean? Discuss the findings’ implications and significance in relation to your research question or hypothesis.
Analyze and interpret your findings
Look into your findings and explore what’s behind them or what may have caused them. If your introduction cited theories or studies that could explain your findings, use these sources as a basis to discuss your results.
For example, look at the second paragraph in the discussion section of this article on waggling honey bees. Here, the authors explore their results based on information from the literature.
Unexpected or contradictory results
Sometimes, your findings are not what you expect. Here’s where you describe this and try to find a reason for it. Could it be because of the method you used? Does it have something to do with the variables analyzed? Comparing your methods with those of other similar studies can help with this task.
Context and comparison with previous work
Refer to related studies to place your research in a larger context and the literature. Compare and contrast your findings with existing literature, highlighting similarities, differences, and/or contradictions.
How your work compares or contrasts with previous work
Studies with similar findings to yours can be cited to show the strength of your findings. Information from these studies can also be used to help explain your results. Differences between your findings and others in the literature can also be discussed here.
How to divide this section into subsections
If you have more than one objective in your study or many key findings, you can dedicate a separate section to each of these. Here’s an example of this approach. You can see that the discussion section is divided into topics and even has a separate heading for each of them.
Limitations
Many journals require you to include the limitations of your study in the discussion. Even if they don’t, there are good reasons to mention these in your paper.
Why limitations don’t have a negative connotation
A study’s limitations are points to be improved upon in future research. While some of these may be flaws in your method, many may be due to factors you couldn’t predict.
Examples include time constraints or small sample sizes. Pointing this out will help future researchers avoid or address these issues. This part of the discussion can also include any attempts you have made to reduce the impact of these limitations, as in this study .
How limitations add to a researcher's credibility
Pointing out the limitations of your study demonstrates transparency. It also shows that you know your methods well and can conduct a critical assessment of them.
Implications and significance
The final paragraph of the discussion section should contain the take-home messages for your study. It can also cite the “strong points” of your study, to contrast with the limitations section.
Restate your hypothesis
Remind the reader what your hypothesis was before you conducted the study.
How was it proven or disproven?
Identify your main findings and describe how they relate to your hypothesis.
How your results contribute to the literature
Were you able to answer your research question? Or address a gap in the literature?
Future implications of your research
Describe the impact that your results may have on the topic of study. Your results may show, for instance, that there are still limitations in the literature for future studies to address. There may be a need for studies that extend your findings in a specific way. You also may need additional research to corroborate your findings.
Sample discussion section
This fictitious example covers all the aspects discussed above. Your actual discussion section will probably be much longer, but you can read this to get an idea of everything your discussion should cover.
Our results showed that the presence of cats in a household is associated with higher levels of perceived happiness by its human occupants. These findings support our hypothesis and demonstrate the association between pet ownership and well-being.
The present findings align with those of Bao and Schreer (2016) and Hardie et al. (2023), who observed greater life satisfaction in pet owners relative to non-owners. Although the present study did not directly evaluate life satisfaction, this factor may explain the association between happiness and cat ownership observed in our sample.
Our findings must be interpreted in light of some limitations, such as the focus on cat ownership only rather than pets as a whole. This may limit the generalizability of our results.
Nevertheless, this study had several strengths. These include its strict exclusion criteria and use of a standardized assessment instrument to investigate the relationships between pets and owners. These attributes bolster the accuracy of our results and reduce the influence of confounding factors, increasing the strength of our conclusions. Future studies may examine the factors that mediate the association between pet ownership and happiness to better comprehend this phenomenon.
This brief discussion begins with a quick summary of the results and hypothesis. The next paragraph cites previous research and compares its findings to those of this study. Information from previous studies is also used to help interpret the findings. After discussing the results of the study, some limitations are pointed out. The paper also explains why these limitations may influence the interpretation of results. Then, final conclusions are drawn based on the study, and directions for future research are suggested.
How to make your discussion flow naturally
If you find writing in scientific English challenging, the discussion and conclusions are often the hardest parts of the paper to write. That’s because you’re not just listing up studies, methods, and outcomes. You’re actually expressing your thoughts and interpretations in words.
- How formal should it be?
- What words should you use, or not use?
- How do you meet strict word limits, or make it longer and more informative?
Always give it your best, but sometimes a helping hand can, well, help. Getting a professional edit can help clarify your work’s importance while improving the English used to explain it. When readers know the value of your work, they’ll cite it. We’ll assign your study to an expert editor knowledgeable in your area of research. Their work will clarify your discussion, helping it to tell your story. Find out more about AJE Editing.

Adam Goulston, PsyD, MS, MBA, MISD, ELS
Science Marketing Consultant
See our "Privacy Policy"
Ensure your structure and ideas are consistent and clearly communicated
Pair your Premium Editing with our add-on service Presubmission Review for an overall assessment of your manuscript.
- Affiliate Program

- UNITED STATES
- 台灣 (TAIWAN)
- TÜRKIYE (TURKEY)
- Academic Editing Services
- - Research Paper
- - Journal Manuscript
- - Dissertation
- - College & University Assignments
- Admissions Editing Services
- - Application Essay
- - Personal Statement
- - Recommendation Letter
- - Cover Letter
- - CV/Resume
- Business Editing Services
- - Business Documents
- - Report & Brochure
- - Website & Blog
- Writer Editing Services
- - Script & Screenplay
- Our Editors
- Client Reviews
- Editing & Proofreading Prices
- Wordvice Points
- Partner Discount
- Plagiarism Checker
- APA Citation Generator
- MLA Citation Generator
- Chicago Citation Generator
- Vancouver Citation Generator
- - APA Style
- - MLA Style
- - Chicago Style
- - Vancouver Style
- Writing & Editing Guide
- Academic Resources
- Admissions Resources
How to Write a Discussion Section for a Research Paper
We’ve talked about several useful writing tips that authors should consider while drafting or editing their research papers. In particular, we’ve focused on figures and legends , as well as the Introduction , Methods , and Results . Now that we’ve addressed the more technical portions of your journal manuscript, let’s turn to the analytical segments of your research article. In this article, we’ll provide tips on how to write a strong Discussion section that best portrays the significance of your research contributions.
What is the Discussion section of a research paper?
In a nutshell, your Discussion fulfills the promise you made to readers in your Introduction . At the beginning of your paper, you tell us why we should care about your research. You then guide us through a series of intricate images and graphs that capture all the relevant data you collected during your research. We may be dazzled and impressed at first, but none of that matters if you deliver an anti-climactic conclusion in the Discussion section!
Are you feeling pressured? Don’t worry. To be honest, you will edit the Discussion section of your manuscript numerous times. After all, in as little as one to two paragraphs ( Nature ‘s suggestion based on their 3,000-word main body text limit), you have to explain how your research moves us from point A (issues you raise in the Introduction) to point B (our new understanding of these matters). You must also recommend how we might get to point C (i.e., identify what you think is the next direction for research in this field). That’s a lot to say in two paragraphs!
So, how do you do that? Let’s take a closer look.
What should I include in the Discussion section?
As we stated above, the goal of your Discussion section is to answer the questions you raise in your Introduction by using the results you collected during your research . The content you include in the Discussions segment should include the following information:
- Remind us why we should be interested in this research project.
- Describe the nature of the knowledge gap you were trying to fill using the results of your study.
- Don’t repeat your Introduction. Instead, focus on why this particular study was needed to fill the gap you noticed and why that gap needed filling in the first place.
- Mainly, you want to remind us of how your research will increase our knowledge base and inspire others to conduct further research.
- Clearly tell us what that piece of missing knowledge was.
- Answer each of the questions you asked in your Introduction and explain how your results support those conclusions.
- Make sure to factor in all results relevant to the questions (even if those results were not statistically significant).
- Focus on the significance of the most noteworthy results.
- If conflicting inferences can be drawn from your results, evaluate the merits of all of them.
- Don’t rehash what you said earlier in the Results section. Rather, discuss your findings in the context of answering your hypothesis. Instead of making statements like “[The first result] was this…,” say, “[The first result] suggests [conclusion].”
- Do your conclusions line up with existing literature?
- Discuss whether your findings agree with current knowledge and expectations.
- Keep in mind good persuasive argument skills, such as explaining the strengths of your arguments and highlighting the weaknesses of contrary opinions.
- If you discovered something unexpected, offer reasons. If your conclusions aren’t aligned with current literature, explain.
- Address any limitations of your study and how relevant they are to interpreting your results and validating your findings.
- Make sure to acknowledge any weaknesses in your conclusions and suggest room for further research concerning that aspect of your analysis.
- Make sure your suggestions aren’t ones that should have been conducted during your research! Doing so might raise questions about your initial research design and protocols.
- Similarly, maintain a critical but unapologetic tone. You want to instill confidence in your readers that you have thoroughly examined your results and have objectively assessed them in a way that would benefit the scientific community’s desire to expand our knowledge base.
- Recommend next steps.
- Your suggestions should inspire other researchers to conduct follow-up studies to build upon the knowledge you have shared with them.
- Keep the list short (no more than two).
How to Write the Discussion Section
The above list of what to include in the Discussion section gives an overall idea of what you need to focus on throughout the section. Below are some tips and general suggestions about the technical aspects of writing and organization that you might find useful as you draft or revise the contents we’ve outlined above.
Technical writing elements
- Embrace active voice because it eliminates the awkward phrasing and wordiness that accompanies passive voice.
- Use the present tense, which should also be employed in the Introduction.
- Sprinkle with first person pronouns if needed, but generally, avoid it. We want to focus on your findings.
- Maintain an objective and analytical tone.
Discussion section organization
- Keep the same flow across the Results, Methods, and Discussion sections.
- We develop a rhythm as we read and parallel structures facilitate our comprehension. When you organize information the same way in each of these related parts of your journal manuscript, we can quickly see how a certain result was interpreted and quickly verify the particular methods used to produce that result.
- Notice how using parallel structure will eliminate extra narration in the Discussion part since we can anticipate the flow of your ideas based on what we read in the Results segment. Reducing wordiness is important when you only have a few paragraphs to devote to the Discussion section!
- Within each subpart of a Discussion, the information should flow as follows: (A) conclusion first, (B) relevant results and how they relate to that conclusion and (C) relevant literature.
- End with a concise summary explaining the big-picture impact of your study on our understanding of the subject matter. At the beginning of your Discussion section, you stated why this particular study was needed to fill the gap you noticed and why that gap needed filling in the first place. Now, it is time to end with “how your research filled that gap.”
Discussion Part 1: Summarizing Key Findings
Begin the Discussion section by restating your statement of the problem and briefly summarizing the major results. Do not simply repeat your findings. Rather, try to create a concise statement of the main results that directly answer the central research question that you stated in the Introduction section . This content should not be longer than one paragraph in length.
Many researchers struggle with understanding the precise differences between a Discussion section and a Results section . The most important thing to remember here is that your Discussion section should subjectively evaluate the findings presented in the Results section, and in relatively the same order. Keep these sections distinct by making sure that you do not repeat the findings without providing an interpretation.
Phrase examples: Summarizing the results
- The findings indicate that …
- These results suggest a correlation between A and B …
- The data present here suggest that …
- An interpretation of the findings reveals a connection between…
Discussion Part 2: Interpreting the Findings
What do the results mean? It may seem obvious to you, but simply looking at the figures in the Results section will not necessarily convey to readers the importance of the findings in answering your research questions.
The exact structure of interpretations depends on the type of research being conducted. Here are some common approaches to interpreting data:
- Identifying correlations and relationships in the findings
- Explaining whether the results confirm or undermine your research hypothesis
- Giving the findings context within the history of similar research studies
- Discussing unexpected results and analyzing their significance to your study or general research
- Offering alternative explanations and arguing for your position
Organize the Discussion section around key arguments, themes, hypotheses, or research questions or problems. Again, make sure to follow the same order as you did in the Results section.
Discussion Part 3: Discussing the Implications
In addition to providing your own interpretations, show how your results fit into the wider scholarly literature you surveyed in the literature review section. This section is called the implications of the study . Show where and how these results fit into existing knowledge, what additional insights they contribute, and any possible consequences that might arise from this knowledge, both in the specific research topic and in the wider scientific domain.
Questions to ask yourself when dealing with potential implications:
- Do your findings fall in line with existing theories, or do they challenge these theories or findings? What new information do they contribute to the literature, if any? How exactly do these findings impact or conflict with existing theories or models?
- What are the practical implications on actual subjects or demographics?
- What are the methodological implications for similar studies conducted either in the past or future?
Your purpose in giving the implications is to spell out exactly what your study has contributed and why researchers and other readers should be interested.
Phrase examples: Discussing the implications of the research
- These results confirm the existing evidence in X studies…
- The results are not in line with the foregoing theory that…
- This experiment provides new insights into the connection between…
- These findings present a more nuanced understanding of…
- While previous studies have focused on X, these results demonstrate that Y.
Step 4: Acknowledging the limitations
All research has study limitations of one sort or another. Acknowledging limitations in methodology or approach helps strengthen your credibility as a researcher. Study limitations are not simply a list of mistakes made in the study. Rather, limitations help provide a more detailed picture of what can or cannot be concluded from your findings. In essence, they help temper and qualify the study implications you listed previously.
Study limitations can relate to research design, specific methodological or material choices, or unexpected issues that emerged while you conducted the research. Mention only those limitations directly relate to your research questions, and explain what impact these limitations had on how your study was conducted and the validity of any interpretations.
Possible types of study limitations:
- Insufficient sample size for statistical measurements
- Lack of previous research studies on the topic
- Methods/instruments/techniques used to collect the data
- Limited access to data
- Time constraints in properly preparing and executing the study
After discussing the study limitations, you can also stress that your results are still valid. Give some specific reasons why the limitations do not necessarily handicap your study or narrow its scope.
Phrase examples: Limitations sentence beginners
- “There may be some possible limitations in this study.”
- “The findings of this study have to be seen in light of some limitations.”
- “The first limitation is the…The second limitation concerns the…”
- “The empirical results reported herein should be considered in the light of some limitations.”
- “This research, however, is subject to several limitations.”
- “The primary limitation to the generalization of these results is…”
- “Nonetheless, these results must be interpreted with caution and a number of limitations should be borne in mind.”
Discussion Part 5: Giving Recommendations for Further Research
Based on your interpretation and discussion of the findings, your recommendations can include practical changes to the study or specific further research to be conducted to clarify the research questions. Recommendations are often listed in a separate Conclusion section , but often this is just the final paragraph of the Discussion section.
Suggestions for further research often stem directly from the limitations outlined. Rather than simply stating that “further research should be conducted,” provide concrete specifics for how future can help answer questions that your research could not.
Phrase examples: Recommendation sentence beginners
- Further research is needed to establish …
- There is abundant space for further progress in analyzing…
- A further study with more focus on X should be done to investigate…
- Further studies of X that account for these variables must be undertaken.
Consider Receiving Professional Language Editing
As you edit or draft your research manuscript, we hope that you implement these guidelines to produce a more effective Discussion section. And after completing your draft, don’t forget to submit your work to a professional proofreading and English editing service like Wordvice, including our manuscript editing service for paper editing , cover letter editing , SOP editing , and personal statement proofreading services. Language editors not only proofread and correct errors in grammar, punctuation, mechanics, and formatting but also improve terms and revise phrases so they read more naturally. Wordvice is an industry leader in providing high-quality revision for all types of academic documents.
For additional information about how to write a strong research paper, make sure to check out our full research writing series !
Wordvice Writing Resources
- How to Write a Research Paper Introduction
- Which Verb Tenses to Use in a Research Paper
- How to Write an Abstract for a Research Paper
- How to Write a Research Paper Title
- Useful Phrases for Academic Writing
- Common Transition Terms in Academic Papers
- Active and Passive Voice in Research Papers
- 100+ Verbs That Will Make Your Research Writing Amazing
- Tips for Paraphrasing in Research Papers
Additional Academic Resources
- Guide for Authors. (Elsevier)
- How to Write the Results Section of a Research Paper. (Bates College)
- Structure of a Research Paper. (University of Minnesota Biomedical Library)
- How to Choose a Target Journal (Springer)
- How to Write Figures and Tables (UNC Writing Center)

- Langson Library
- Science Library
- Grunigen Medical Library
- Law Library
- Connect From Off-Campus
- Accessibility
- Gateway Study Center

Email this link
Writing a scientific paper.
- Writing a lab report
- INTRODUCTION
Writing a "good" discussion section
"discussion and conclusions checklist" from: how to write a good scientific paper. chris a. mack. spie. 2018., peer review.
- LITERATURE CITED
- Bibliography of guides to scientific writing and presenting
- Presentations
- Lab Report Writing Guides on the Web
This is is usually the hardest section to write. You are trying to bring out the true meaning of your data without being too long. Do not use words to conceal your facts or reasoning. Also do not repeat your results, this is a discussion.
- Present principles, relationships and generalizations shown by the results
- Point out exceptions or lack of correlations. Define why you think this is so.
- Show how your results agree or disagree with previously published works
- Discuss the theoretical implications of your work as well as practical applications
- State your conclusions clearly. Summarize your evidence for each conclusion.
- Discuss the significance of the results
- Evidence does not explain itself; the results must be presented and then explained.
- Typical stages in the discussion: summarizing the results, discussing whether results are expected or unexpected, comparing these results to previous work, interpreting and explaining the results (often by comparison to a theory or model), and hypothesizing about their generality.
- Discuss any problems or shortcomings encountered during the course of the work.
- Discuss possible alternate explanations for the results.
- Avoid: presenting results that are never discussed; presenting discussion that does not relate to any of the results; presenting results and discussion in chronological order rather than logical order; ignoring results that do not support the conclusions; drawing conclusions from results without logical arguments to back them up.
CONCLUSIONS
- Provide a very brief summary of the Results and Discussion.
- Emphasize the implications of the findings, explaining how the work is significant and providing the key message(s) the author wishes to convey.
- Provide the most general claims that can be supported by the evidence.
- Provide a future perspective on the work.
- Avoid: repeating the abstract; repeating background information from the Introduction; introducing new evidence or new arguments not found in the Results and Discussion; repeating the arguments made in the Results and Discussion; failing to address all of the research questions set out in the Introduction.
WHAT HAPPENS AFTER I COMPLETE MY PAPER?
The peer review process is the quality control step in the publication of ideas. Papers that are submitted to a journal for publication are sent out to several scientists (peers) who look carefully at the paper to see if it is "good science". These reviewers then recommend to the editor of a journal whether or not a paper should be published. Most journals have publication guidelines. Ask for them and follow them exactly. Peer reviewers examine the soundness of the materials and methods section. Are the materials and methods used written clearly enough for another scientist to reproduce the experiment? Other areas they look at are: originality of research, significance of research question studied, soundness of the discussion and interpretation, correct spelling and use of technical terms, and length of the article.
- << Previous: RESULTS
- Next: LITERATURE CITED >>
- Last Updated: Aug 4, 2023 9:33 AM
- URL: https://guides.lib.uci.edu/scientificwriting
Off-campus? Please use the Software VPN and choose the group UCIFull to access licensed content. For more information, please Click here
Software VPN is not available for guests, so they may not have access to some content when connecting from off-campus.
Guide to Writing the Results and Discussion Sections of a Scientific Article
A quality research paper has both the qualities of in-depth research and good writing ( Bordage, 2001 ). In addition, a research paper must be clear, concise, and effective when presenting the information in an organized structure with a logical manner ( Sandercock, 2013 ).
In this article, we will take a closer look at the results and discussion section. Composing each of these carefully with sufficient data and well-constructed arguments can help improve your paper overall.
The results section of your research paper contains a description about the main findings of your research, whereas the discussion section interprets the results for readers and provides the significance of the findings. The discussion should not repeat the results.
Let’s dive in a little deeper about how to properly, and clearly organize each part.
How to Organize the Results Section
Since your results follow your methods, you’ll want to provide information about what you discovered from the methods you used, such as your research data. In other words, what were the outcomes of the methods you used?
You may also include information about the measurement of your data, variables, treatments, and statistical analyses.
To start, organize your research data based on how important those are in relation to your research questions. This section should focus on showing major results that support or reject your research hypothesis. Include your least important data as supplemental materials when submitting to the journal.
The next step is to prioritize your research data based on importance – focusing heavily on the information that directly relates to your research questions using the subheadings.
The organization of the subheadings for the results section usually mirrors the methods section. It should follow a logical and chronological order.
Subheading organization
Subheadings within your results section are primarily going to detail major findings within each important experiment. And the first paragraph of your results section should be dedicated to your main findings (findings that answer your overall research question and lead to your conclusion) (Hofmann, 2013).
In the book “Writing in the Biological Sciences,” author Angelika Hofmann recommends you structure your results subsection paragraphs as follows:
- Experimental purpose
- Interpretation
Each subheading may contain a combination of ( Bahadoran, 2019 ; Hofmann, 2013, pg. 62-63):
- Text: to explain about the research data
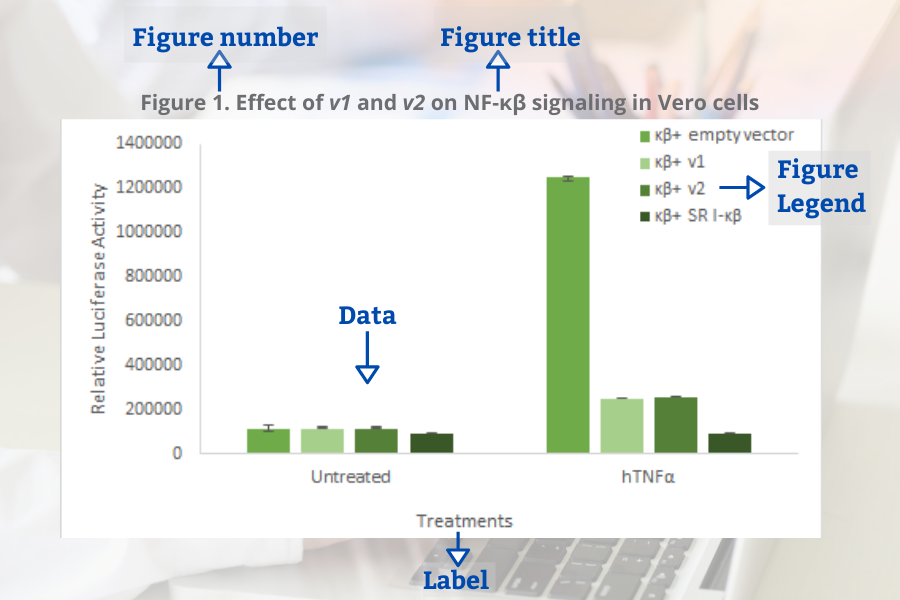
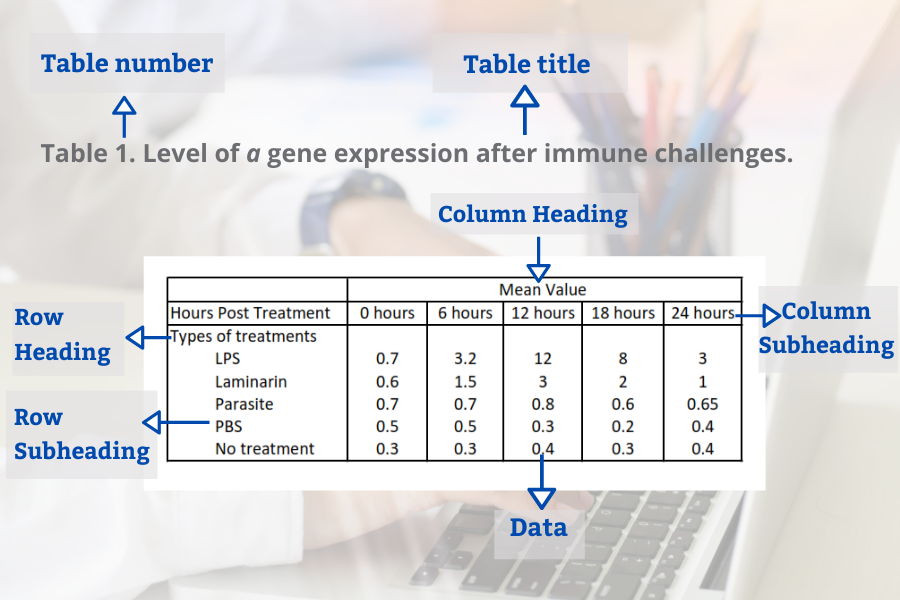
- Figures: to display the research data and to show trends or relationships, for examples using graphs or gel pictures.
- Tables: to represent a large data and exact value
Decide on the best way to present your data — in the form of text, figures or tables (Hofmann, 2013).
Data or Results?
Sometimes we get confused about how to differentiate between data and results . Data are information (facts or numbers) that you collected from your research ( Bahadoran, 2019 ).

Whereas, results are the texts presenting the meaning of your research data ( Bahadoran, 2019 ).
One mistake that some authors often make is to use text to direct the reader to find a specific table or figure without further explanation. This can confuse readers when they interpret data completely different from what the authors had in mind. So, you should briefly explain your data to make your information clear for the readers.
Common Elements in Figures and Tables
Figures and tables present information about your research data visually. The use of these visual elements is necessary so readers can summarize, compare, and interpret large data at a glance. You can use graphs or figures to compare groups or patterns. Whereas, tables are ideal to present large quantities of data and exact values.
Several components are needed to create your figures and tables. These elements are important to sort your data based on groups (or treatments). It will be easier for the readers to see the similarities and differences among the groups.
When presenting your research data in the form of figures and tables, organize your data based on the steps of the research leading you into a conclusion.
Common elements of the figures (Bahadoran, 2019):
- Figure number
- Figure title
- Figure legend (for example a brief title, experimental/statistical information, or definition of symbols).
Tables in the result section may contain several elements (Bahadoran, 2019):
- Table number
- Table title
- Row headings (for example groups)
- Column headings
- Row subheadings (for example categories or groups)
- Column subheadings (for example categories or variables)
- Footnotes (for example statistical analyses)
Tips to Write the Results Section
- Direct the reader to the research data and explain the meaning of the data.
- Avoid using a repetitive sentence structure to explain a new set of data.
- Write and highlight important findings in your results.
- Use the same order as the subheadings of the methods section.
- Match the results with the research questions from the introduction. Your results should answer your research questions.
- Be sure to mention the figures and tables in the body of your text.
- Make sure there is no mismatch between the table number or the figure number in text and in figure/tables.
- Only present data that support the significance of your study. You can provide additional data in tables and figures as supplementary material.
How to Organize the Discussion Section
It’s not enough to use figures and tables in your results section to convince your readers about the importance of your findings. You need to support your results section by providing more explanation in the discussion section about what you found.
In the discussion section, based on your findings, you defend the answers to your research questions and create arguments to support your conclusions.
Below is a list of questions to guide you when organizing the structure of your discussion section ( Viera et al ., 2018 ):
- What experiments did you conduct and what were the results?
- What do the results mean?
- What were the important results from your study?
- How did the results answer your research questions?
- Did your results support your hypothesis or reject your hypothesis?
- What are the variables or factors that might affect your results?
- What were the strengths and limitations of your study?
- What other published works support your findings?
- What other published works contradict your findings?
- What possible factors might cause your findings different from other findings?
- What is the significance of your research?
- What are new research questions to explore based on your findings?
Organizing the Discussion Section
The structure of the discussion section may be different from one paper to another, but it commonly has a beginning, middle-, and end- to the section.
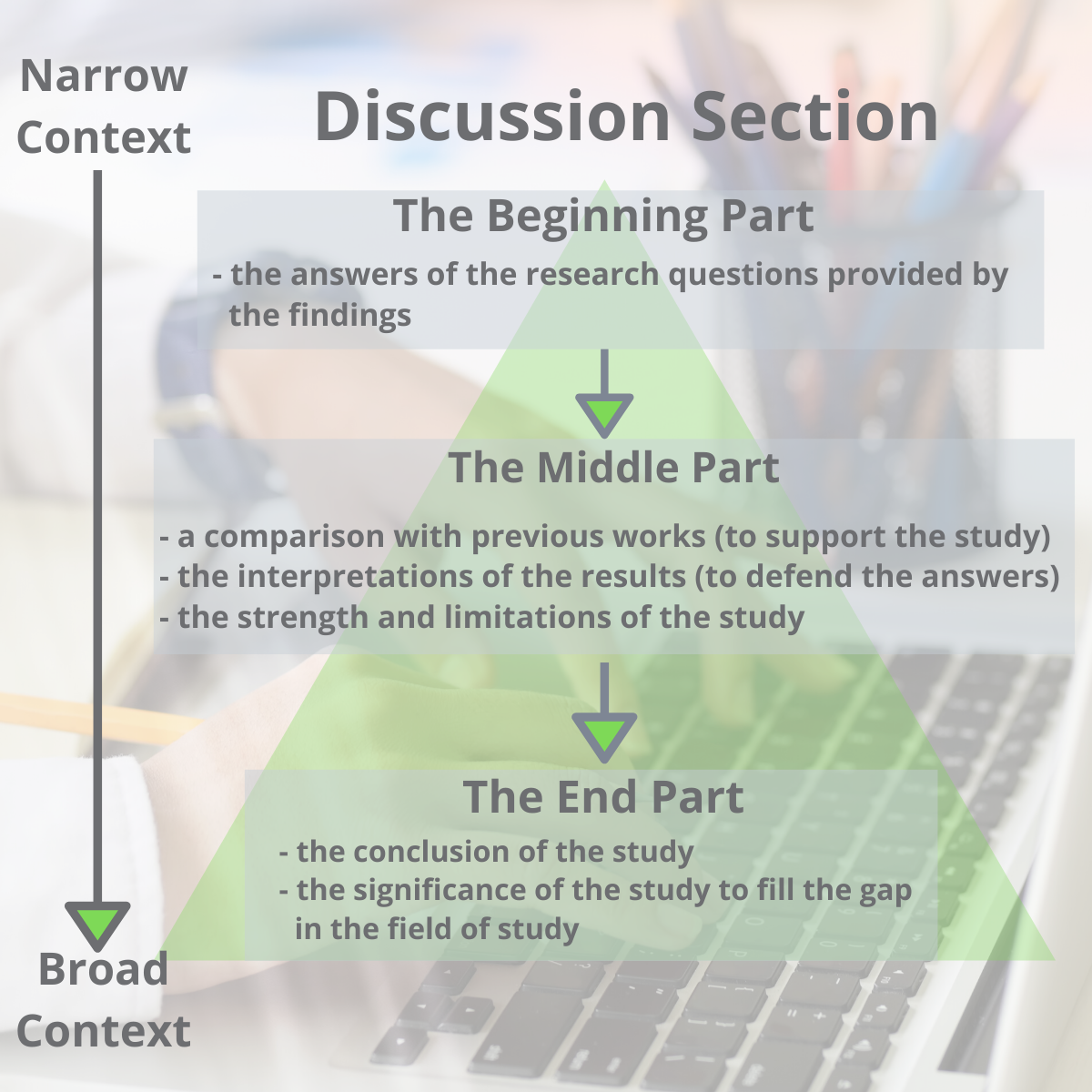
One way to organize the structure of the discussion section is by dividing it into three parts (Ghasemi, 2019):
- The beginning: The first sentence of the first paragraph should state the importance and the new findings of your research. The first paragraph may also include answers to your research questions mentioned in your introduction section.
- The middle: The middle should contain the interpretations of the results to defend your answers, the strength of the study, the limitations of the study, and an update literature review that validates your findings.
- The end: The end concludes the study and the significance of your research.
Another possible way to organize the discussion section was proposed by Michael Docherty in British Medical Journal: is by using this structure ( Docherty, 1999 ):
- Discussion of important findings
- Comparison of your results with other published works
- Include the strengths and limitations of the study
- Conclusion and possible implications of your study, including the significance of your study – address why and how is it meaningful
- Future research questions based on your findings
Finally, a last option is structuring your discussion this way (Hofmann, 2013, pg. 104):
- First Paragraph: Provide an interpretation based on your key findings. Then support your interpretation with evidence.
- Secondary results
- Limitations
- Unexpected findings
- Comparisons to previous publications
- Last Paragraph: The last paragraph should provide a summarization (conclusion) along with detailing the significance, implications and potential next steps.
Remember, at the heart of the discussion section is presenting an interpretation of your major findings.
Tips to Write the Discussion Section
- Highlight the significance of your findings
- Mention how the study will fill a gap in knowledge.
- Indicate the implication of your research.
- Avoid generalizing, misinterpreting your results, drawing a conclusion with no supportive findings from your results.
Aggarwal, R., & Sahni, P. (2018). The Results Section. In Reporting and Publishing Research in the Biomedical Sciences (pp. 21-38): Springer.
Bahadoran, Z., Mirmiran, P., Zadeh-Vakili, A., Hosseinpanah, F., & Ghasemi, A. (2019). The principles of biomedical scientific writing: Results. International journal of endocrinology and metabolism, 17(2).
Bordage, G. (2001). Reasons reviewers reject and accept manuscripts: the strengths and weaknesses in medical education reports. Academic medicine, 76(9), 889-896.
Cals, J. W., & Kotz, D. (2013). Effective writing and publishing scientific papers, part VI: discussion. Journal of clinical epidemiology, 66(10), 1064.
Docherty, M., & Smith, R. (1999). The case for structuring the discussion of scientific papers: Much the same as that for structuring abstracts. In: British Medical Journal Publishing Group.
Faber, J. (2017). Writing scientific manuscripts: most common mistakes. Dental press journal of orthodontics, 22(5), 113-117.
Fletcher, R. H., & Fletcher, S. W. (2018). The discussion section. In Reporting and Publishing Research in the Biomedical Sciences (pp. 39-48): Springer.
Ghasemi, A., Bahadoran, Z., Mirmiran, P., Hosseinpanah, F., Shiva, N., & Zadeh-Vakili, A. (2019). The Principles of Biomedical Scientific Writing: Discussion. International journal of endocrinology and metabolism, 17(3).
Hofmann, A. H. (2013). Writing in the biological sciences: a comprehensive resource for scientific communication . New York: Oxford University Press.
Kotz, D., & Cals, J. W. (2013). Effective writing and publishing scientific papers, part V: results. Journal of clinical epidemiology, 66(9), 945.
Mack, C. (2014). How to Write a Good Scientific Paper: Structure and Organization. Journal of Micro/ Nanolithography, MEMS, and MOEMS, 13. doi:10.1117/1.JMM.13.4.040101
Moore, A. (2016). What's in a Discussion section? Exploiting 2‐dimensionality in the online world…. Bioessays, 38(12), 1185-1185.
Peat, J., Elliott, E., Baur, L., & Keena, V. (2013). Scientific writing: easy when you know how: John Wiley & Sons.
Sandercock, P. M. L. (2012). How to write and publish a scientific article. Canadian Society of Forensic Science Journal, 45(1), 1-5.
Teo, E. K. (2016). Effective Medical Writing: The Write Way to Get Published. Singapore Medical Journal, 57(9), 523-523. doi:10.11622/smedj.2016156
Van Way III, C. W. (2007). Writing a scientific paper. Nutrition in Clinical Practice, 22(6), 636-640.
Vieira, R. F., Lima, R. C. d., & Mizubuti, E. S. G. (2019). How to write the discussion section of a scientific article. Acta Scientiarum. Agronomy, 41.
Related Articles

A quality research paper has both the qualities of in-depth research and good writing (Bordage, 200...
How to Survive and Complete a Thesis or a Dissertation
Writing a thesis or a dissertation can be a challenging process for many graduate students. There ar...

12 Ways to Dramatically Improve your Research Manuscript Title and Abstract
The first thing a person doing literary research will see is a research publication title. After tha...

15 Laboratory Notebook Tips to Help with your Research Manuscript
Your lab notebook is a foundation to your research manuscript. It serves almost as a rudimentary dra...
Join our list to receive promos and articles.
- Competent Cells
- Lab Startup
- Z')" data-type="collection" title="Products A->Z" target="_self" href="/collection/products-a-to-z">Products A->Z
- GoldBio Resources
- GoldBio Sales Team
- GoldBio Distributors
- Duchefa Direct
- Sign up for Promos
- Terms & Conditions
- ISO Certification
- Agarose Resins
- Antibiotics & Selection
- Biochemical Reagents
- Bioluminescence
- Buffers & Reagents
- Cell Culture
- Cloning & Induction
- Competent Cells and Transformation
- Detergents & Membrane Agents
- DNA Amplification
- Enzymes, Inhibitors & Substrates
- Growth Factors and Cytokines
- Lab Tools & Accessories
- Plant Research and Reagents
- Protein Research & Analysis
- Protein Expression & Purification
- Reducing Agents
Training videos | Faqs

Discussion Section Examples and Writing Tips
Abstract | Introduction | Literature Review | Research question | Materials & Methods | Results | Discussion | Conclusion
In this blog, we look at how to write the discussion section of a research paper. We will go through plenty of discussion examples and understand how to construct a great discussion section for your research paper.
1. What is the purpose of the discussion section?

The discussion section is one of the most important sections of your research paper. This is where you interpret your results, highlight your contributions, and explain the value of your work to your readers. This is one of the challenging parts to write because the author must clearly explain the significance of their results and tie everything back to the research questions.
2. How should I structure my discussion section?
Generally, the discussion section of a research paper typically contains the following parts.
Research summary It is a good idea to start this section with an overall summary of your work and highlight the main findings of your research.
Interpretation of findings You must interpret your findings clearly to your readers one by one.
Comparison with literature You must talk about how your results fit into existing research in the literature.
Implications of your work You should talk about the implications and possible benefits of your research.
Limitations You should talk about the possible limitations and shortcomings of your research
Future work And finally, you can talk about the possible future directions of your work.
3. Discussion Examples
Let’s look at some examples of the discussion section. We will be looking at discussion examples from different fields and of different formats. We have split this section into multiple components so that it is easy for you to digest and understand.

3.1. An example of research summary in discussion
It is a good idea to start your discussion section with the summary of your work. The best way to do this will be to restate your research question, and then reminding your readers about your methods, and finally providing an overall summary of your results.
Our aims were to compare the effectiveness and user-friendliness of different storm detection software for storm tracking. On the basis of these aims, we ran multiple experiments with the same conditions using different storm detection software. Our results showed that in both speed and accuracy of data, ‘software A’ performed better than ‘software B’. _ Aims summary _ Methodology summary _ Results summary
This discussion example is from an engineering research paper. The authors are restating their aims first, which is to compare different types of storm-tracking software. Then, they are providing a brief summary of the methods. Here, they are testing different storm-tracking software under different conditions to see which performs the best. Then, they are finally providing their main finding which is that they found ‘software A’ better than ‘software B’. This is a very good example of how to start the discussion section by presenting a summary of your work.
3.2. An example of result interpretation in discussion
The next step is to interpret your results. You have to explain your results clearly to your readers. Here is a discussion example that shows how to interpret your results.
The results of this study indicate significant differences between classical music and pop music in terms of their effects on memory recall and cognition. This implies that as the complexity of the music increases, so does its ability to facilitate cognitive processing. This finding aligns with the well-known “Mozart effect,” which suggests that listening to classical music can enhance cognitive function. _ Result _ Interpretation _ Additional evidence
The authors are saying that their results show that there is a significant difference between pop music and classical music in terms of memory recall and cognition. Now they are providing their interpretation of the findings. They think it is because there is a link between the complexity of music and cognitive processing. They are also making a reference to a well-known theory called the ‘Mozart effect’ to back up their findings. It is a nicely written passage and the author’s interpretation sounds very convincing and credible.
3.3. An example of literature comparison in discussion
The next step is to compare your results to the literature. You have to explain clearly how your findings compare with similar findings made by other researchers. Here is a discussion example where authors are providing details of papers in the literature that both support and oppose their findings.
Our analysis predicts that climate change will have a significant impact on wheat yield. This finding undermines one of the central pieces of evidence in some previous simulation studies [1-3] that suggest a negative effect of climate change on wheat yield, but the result is entirely consistent with the predictions of other research [4-5] that suggests the overall change in climate could result in increases in wheat yield. _ Result _ Comparison with literature
The authors are saying that their results show that climate change will have a significant effect on wheat production. Then, they are saying that there are some papers in the literature that are in agreement with their findings. However, there are also many papers in the literature that disagree with their findings. This is very important. Your discussion should be two-sided, not one-sided. You should not ignore the literature that doesn’t corroborate your findings.
3.4. An example of research implications in discussion
The next step is to explain to your readers how your findings will benefit society and the research community. You have to clearly explain the value of your work to your readers. Here is a discussion example where authors explain the implications of their research.
The results contribute insights with regard to the management of wildfire events using artificial intelligence. One could easily argue that the obvious practical implication of this study is that it proposes utilizing cloud-based machine vision to detect wildfires in real-time, even before the first responders receive emergency calls. _ Your finding _ Implications of your finding
In this paper, the authors are saying that their findings indicate that Artificial intelligence can be used to effectively manage wildfire events. Then, they are talking about the practical implications of their study. They are saying that their work has proven that machine learning can be used to detect wildfires in real-time. This is a great practical application and can save thousands of lives. As you can see, after reading this passage, you can immediately understand the value and significance of the work.
3.5. An example of limitations in discussion
It is very important that you discuss the limitations of your study. Limitations are flaws and shortcomings of your study. You have to tell your readers how your limitations might influence the outcomes and conclusions of your research. Most studies will have some form of limitation. So be honest and don’t hide your limitations. In reality, your readers and reviewers will be impressed with your paper if you are upfront about your limitations.
Study design and small sample size are important limitations. This could have led to an overestimation of the effect. Future research should reconfirm these findings by conducting larger-scale studies. _ Limitation _ How it might affect the results? _ How to fix the limitation?
Here is a discussion example where the author talks about study limitations. The authors are saying that the main limitations of the study are the small sample size and weak study design. Then they explain how this might have affected their results. They are saying that it is possible that they are overestimating the actual effect they are measuring. Then finally they are telling the readers that more studies with larger sample sizes should be conducted to reconfirm the findings.
As you can see, the authors are clearly explaining three things here:
3.6. An example of future work in discussion
It is important to remember not to end your paper with limitations. Finish your paper on a positive note by telling your readers about the benefits of your research and possible future directions. Here is a discussion example where the author talks about future work.
Our study highlights useful insights about the potential of biomass as a renewable energy source. Future research can extend this research in several ways, including research on how to tackle challenges that hinder the sustainability of renewable energy sources towards climate change mitigation, such as market failures, lack of information and access to raw materials. _ Benefits of your work _ Future work
The authors are starting the final paragraph of the discussion section by highlighting the benefit of their work which is the use of biomass as a renewable source of energy. Then they talk about future research. They are saying that future research can focus on how to improve the sustainability of biomass production. This is a very good example of how to finish the discussion section of your paper on a positive note.
4. Frequently Asked Questions
Sometimes you will have negative or unexpected results in your paper. You have to talk about it in your discussion section. A lot of students find it difficult to write this part. The best way to handle this situation is not to look at results as either positive or negative. A result is a result, and you will always have something important and interesting to say about your findings. Just spend some time investigating what might have caused this result and tell your readers about it.
You must talk about the limitations of your work in the discussion section of the paper. One of the important qualities that the scientific community expects from a researcher is honesty and admitting when they have made a mistake. The important trick you have to learn while presenting your limitations is to present them in a constructive way rather than being too negative about them. You must try to use positive language even when you are talking about major limitations of your work.
If you have something exciting to say about your results or found something new that nobody else has found before, then, don’t be modest and use flat language when presenting this in the discussion. Use words like ‘break through’, ‘indisputable evidence’, ‘exciting proposition’ to increase the impact of your findings.
Important thing to remember is not to overstate your findings. If you found something really interesting but are not 100% sure, you must not mislead your readers. The best way to do this will be to use words like ‘it appears’ and ‘it seems’. This will tell the readers that there is a slight possibility that you might be wrong.
Similar Posts
Figures and Tables in Research Papers – Tips and Examples
In this blog, we will look at best practices for presenting tables and figures in your research paper.
Critical Literature Review : How to Critique a Research Article?
In this blog, we will look at how to use constructive language when critiquing other’s work in your research paper.

Introduction Paragraph Examples and Writing Tips
In this blog, we will go through a few introduction paragraph examples and understand how to construct a great introduction paragraph for your research paper.

Materials and Methods Examples and Writing Tips
In this blog, we will go through many materials and methods examples and understand how to write a clear and concise method section for your research paper.

3 Costly Mistakes to Avoid in the Research Introduction
In this blog, we will discuss three common mistakes that beginner writers make while writing the research paper introduction.

Technical Terms, Notations, and Scientific Jargon in Research Papers
In this blog, we will teach you how to use specialized terminology in your research papers with some practical examples.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- 5 Share Facebook
- 7 Share Twitter
- 5 Share LinkedIn
- 10 Share Email
We apologize for any inconvenience as we update our site to a new look.

- Walden University
- Faculty Portal
General Research Paper Guidelines: Discussion
Discussion section.
The overall purpose of a research paper’s discussion section is to evaluate and interpret results, while explaining both the implications and limitations of your findings. Per APA (2020) guidelines, this section requires you to “examine, interpret, and qualify the results and draw inferences and conclusions from them” (p. 89). Discussion sections also require you to detail any new insights, think through areas for future research, highlight the work that still needs to be done to further your topic, and provide a clear conclusion to your research paper. In a good discussion section, you should do the following:
- Clearly connect the discussion of your results to your introduction, including your central argument, thesis, or problem statement.
- Provide readers with a critical thinking through of your results, answering the “so what?” question about each of your findings. In other words, why is this finding important?
- Detail how your research findings might address critical gaps or problems in your field
- Compare your results to similar studies’ findings
- Provide the possibility of alternative interpretations, as your goal as a researcher is to “discover” and “examine” and not to “prove” or “disprove.” Instead of trying to fit your results into your hypothesis, critically engage with alternative interpretations to your results.
For more specific details on your Discussion section, be sure to review Sections 3.8 (pp. 89-90) and 3.16 (pp. 103-104) of your 7 th edition APA manual
*Box content adapted from:
University of Southern California (n.d.). Organizing your social sciences research paper: 8 the discussion . https://libguides.usc.edu/writingguide/discussion
Limitations
Limitations of generalizability or utility of findings, often over which the researcher has no control, should be detailed in your Discussion section. Including limitations for your reader allows you to demonstrate you have thought critically about your given topic, understood relevant literature addressing your topic, and chosen the methodology most appropriate for your research. It also allows you an opportunity to suggest avenues for future research on your topic. An effective limitations section will include the following:
- Detail (a) sources of potential bias, (b) possible imprecision of measures, (c) other limitations or weaknesses of the study, including any methodological or researcher limitations.
- Sample size: In quantitative research, if a sample size is too small, it is more difficult to generalize results.
- Lack of available/reliable data : In some cases, data might not be available or reliable, which will ultimately affect the overall scope of your research. Use this as an opportunity to explain areas for future study.
- Lack of prior research on your study topic: In some cases, you might find that there is very little or no similar research on your study topic, which hinders the credibility and scope of your own research. If this is the case, use this limitation as an opportunity to call for future research. However, make sure you have done a thorough search of the available literature before making this claim.
- Flaws in measurement of data: Hindsight is 20/20, and you might realize after you have completed your research that the data tool you used actually limited the scope or results of your study in some way. Again, acknowledge the weakness and use it as an opportunity to highlight areas for future study.
- Limits of self-reported data: In your research, you are assuming that any participants will be honest and forthcoming with responses or information they provide to you. Simply acknowledging this assumption as a possible limitation is important in your research.
- Access: Most research requires that you have access to people, documents, organizations, etc.. However, for various reasons, access is sometimes limited or denied altogether. If this is the case, you will want to acknowledge access as a limitation to your research.
- Time: Choosing a research focus that is narrow enough in scope to finish in a given time period is important. If such limitations of time prevent you from certain forms of research, access, or study designs, acknowledging this time restraint is important. Acknowledging such limitations is important, as they can point other researchers to areas that require future study.
- Potential Bias: All researchers have some biases, so when reading and revising your draft, pay special attention to the possibilities for bias in your own work. Such bias could be in the form you organized people, places, participants, or events. They might also exist in the method you selected or the interpretation of your results. Acknowledging such bias is an important part of the research process.
- Language Fluency: On occasion, researchers or research participants might have language fluency issues, which could potentially hinder results or how effectively you interpret results. If this is an issue in your research, make sure to acknowledge it in your limitations section.
University of Southern California (n.d.). Organizing your social sciences research paper: Limitations of the study . https://libguides.usc.edu/writingguide/limitations
In many research papers, the conclusion, like the limitations section, is folded into the larger discussion section. If you are unsure whether to include the conclusion as part of your discussion or as a separate section, be sure to defer to the assignment instructions or ask your instructor.
The conclusion is important, as it is specifically designed to highlight your research’s larger importance outside of the specific results of your study. Your conclusion section allows you to reiterate the main findings of your study, highlight their importance, and point out areas for future research. Based on the scope of your paper, your conclusion could be anywhere from one to three paragraphs long. An effective conclusion section should include the following:
- Describe the possibilities for continued research on your topic, including what might be improved, adapted, or added to ensure useful and informed future research.
- Provide a detailed account of the importance of your findings
- Reiterate why your problem is important, detail how your interpretation of results impacts the subfield of study, and what larger issues both within and outside of your field might be affected from such results
University of Southern California (n.d.). Organizing your social sciences research paper: 9. the conclusion . https://libguides.usc.edu/writingguide/conclusion
- Previous Page: Results
- Next Page: References
- Office of Student Disability Services
Walden Resources
Departments.
- Academic Residencies
- Academic Skills
- Career Planning and Development
- Customer Care Team
- Field Experience
- Military Services
- Student Success Advising
- Writing Skills
Centers and Offices
- Center for Social Change
- Office of Academic Support and Instructional Services
- Office of Degree Acceleration
- Office of Research and Doctoral Services
- Office of Student Affairs
Student Resources
- Doctoral Writing Assessment
- Form & Style Review
- Quick Answers
- ScholarWorks
- SKIL Courses and Workshops
- Walden Bookstore
- Walden Catalog & Student Handbook
- Student Safety/Title IX
- Legal & Consumer Information
- Website Terms and Conditions
- Cookie Policy
- Accessibility
- Accreditation
- State Authorization
- Net Price Calculator
- Contact Walden
Walden University is a member of Adtalem Global Education, Inc. www.adtalem.com Walden University is certified to operate by SCHEV © 2024 Walden University LLC. All rights reserved.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Med Res Methodol

Writing a discussion section: how to integrate substantive and statistical expertise
Michael höfler.
1 Institute of Clinical Psychology and Psychotherapy, Technische Universität Dresden, Dresden, Germany
5 Chair of Clinical Psychology and Behavioural Neuroscience, Institute of Clinical Psychology and Psychotherapy, Technische Universität Dresden, Dresden, Germany
2 Behavioral Epidemiology, Institute of Clinical Psychology and Psychotherapy, Technische Universität Dresden, Dresden, Germany
Sebastian Trautmann
Robert miller.
3 Faculty of Psychology, Technische Universität Dresden, Dresden, Germany
4 Department of Medical Epidemiology and Biostatistics, Karolinska Institute, Stockholm, Sweden
Associated Data
Not applicable.
When discussing results medical research articles often tear substantive and statistical (methodical) contributions apart, just as if both were independent. Consequently, reasoning on bias tends to be vague, unclear and superficial. This can lead to over-generalized, too narrow and misleading conclusions, especially for causal research questions.
To get the best possible conclusion, substantive and statistical expertise have to be integrated on the basis of reasonable assumptions. While statistics should raise questions on the mechanisms that have presumably created the data, substantive knowledge should answer them. Building on the related principle of Bayesian thinking, we make seven specific and four general proposals on writing a discussion section.
Misinterpretation could be reduced if authors explicitly discussed what can be concluded under which assumptions. Informed on the resulting conditional conclusions other researchers may, according to their knowledge and beliefs, follow a particular conclusion or, based on other conditions, arrive at another one. This could foster both an improved debate and a better understanding of the mechanisms behind the data and should therefore enable researchers to better address bias in future studies.
After a research article has presented the substantive background, the methods and the results, the discussion section assesses the validity of results and draws conclusions by interpreting them. The discussion puts the results into a broader context and reflects their implications for theoretical (e.g. etiological) and practical (e.g. interventional) purposes. As such, the discussion contains an article’s last words the reader is left with.
Common recommendations for the discussion section include general proposals for writing [ 1 ] and structuring (e.g. with a paragraph on a study’s strengths and weaknesses) [ 2 ], to avoid common statistical pitfalls (like misinterpreting non-significant findings as true null results) [ 3 ] and to “go beyond the data” when interpreting results [ 4 ]. Note that the latter includes much more than comparing an article’s results with the literature. If results and literature are consistent, this might be due to shared bias only. If they are not consistent, the question arises why inconsistency occurs – maybe because of bias acting differently across studies [ 5 – 7 ]. Recommendations like the CONSORT checklist do well in demanding all quantitative information on design, participation, compliance etc. to be reported in the methods and results section and “addressing sources of potential bias”, “limitations” and “considering other relevant evidence” in the discussion [ 8 , 9 ]. Similarly, the STROBE checklist for epidemiological research demands “a cautious overall interpretation of results” and "discussing the generalizability (external validity)" [ 10 , 11 ]. However, these guidelines do not clarify how to deal with the complex bias issue, and how to get to and report conclusions.
Consequently, suggestions on writing a discussion often remain vague by hardly addressing the role of the assumptions that have (often implicitly) been made when designing a study, analyzing the data and interpreting the results. Such assumptions involve mechanisms that have created the data and are related to sampling, measurement and treatment assignment (in observational studies common causes of factor and outcome) and, as a consequence, the bias this may produce [ 5 , 6 ]. They determine whether a result allows only an associational or a causal conclusion. Causal conclusions, if true, are of much higher relevance for etiology, prevention and intervention. However, they require much stronger assumptions. These have to be fully explicit and, therewith, essential part of the debate since they always involve subjectivity. Subjectivity is unavoidable because the mechanisms behind the data can never be fully estimated from the data themselves [ 12 ].
In this article, we argue that the conjunction of substantive and statistical (methodical) knowledge in the verbal integration of results and beliefs on mechanisms can be greatly improved in (medical) research papers. We illustrate this through the personal roles that a statistician (i.e. methods expert) and a substantive researcher should take. Doing so, we neither claim that usually just two people write a discussion, nor that one person lacks the knowledge of the other, nor that there were truly no researchers that have both kinds of expertise. As a metaphor, the division of these two roles into two persons describes the necessary integration of knowledge via the mode of a dialogue. Verbally, it addresses the finding of increased specialization of different study contributors in biomedical research. This has teared apart the two processes of statistical compilation of results and their verbal integration [ 13 ]. When this happens a statistician alone is limited to a study’s conditions (sampled population, experimental settings etc.), because he or she is unaware of the conditions’ generalizability. On the other hand, a A substantive expert alone is prone to over-generalize because he or she is not aware of the (mathematical) prerequisites for an interpretation.
The article addresses both (medical) researchers educated in basic statistics and research methods and statisticians who cooperate with them. Throughout the paper we exemplify our arguments with the finding of an association in a cross-tabulation between a binary X (factor) and a binary Y (outcome): those who are exposed to or treated with X have a statistically significantly elevated risk for Y as compared to the non-exposed or not (or otherwise) treated (for instance via the chi-squared independence test or logistic regression). Findings like this are frequent and raise the question which more profound conclusion is valid under what assumptions. Until some decades ago, statistics has largely avoided the related topic of causality and instead limited itself on describing observed distributions (here a two-by-two table between D = depression and LC = lung cancer) with well-fitting models.
We illustrate our arguments with the concrete example of the association found between the factor depression (D) and the outcome lung cancer (LC) [ 14 ]. Yet very different mechanisms could have produced such an association [ 7 ], and assumptions on these lead to the following fundamentally different conclusions (Fig. (Fig.1 1 ):
- D causes LC (e.g. because smoking might constitute “self-medication” of depression symptoms)
- LC causes D (e.g. because LC patients are demoralized by their diagnosis)
- D and LC cause each other (e.g. because the arguments in both a. and b. apply)
- D and LC are the causal consequence of the same factor(s) (e.g. poor health behaviors - HB)
- D and LC only share measurement error (e.g. because a fraction of individuals that has either depression or lung cancer denies both in self-report measures).

Different conclusions about an association between D and LC. a D causes LC, b LC causes B, c D and LC cause each other, d D and LC are associated because of a shared factor (HB), e D and LC are associated because they have correlated errors
Note that we use the example purely for illustrative purposes. We do not make substantive claims on what of a. through e. is true but show how one should reflect on mechanisms in order to find the right answer. Besides, we do not consider research on the D-LC relation apart from the finding of association [ 14 ].
Assessing which of a. through e. truly applies requires substantive assumptions on mechanisms: the temporal order of D and LC (a causal effect requires that the cause occurs before the effect), shared factors, selection processes and measurement error. Questions on related mechanisms have to be brought up by statistical consideration, while substantive reasoning has to address them. Together this yields provisional assumptions for inferring that are subject to readers’ substantive consideration and refinement. In general, the integration of prior beliefs (anything beyond the data a conclusion depends on) and the results from the data themselves is formalized by Bayesian statistics [ 15 , 16 ]. This is beyond the scope of this article, still we argue that Bayesian thinking should govern the process of drawing conclusions.
Building on this idea, we provide seven specific and four general recommendations for the cooperative process of writing a discussion. The recommendations are intended to be suggestions rather than rules. They should be subject to further refinement and adjustment to specific requirements in different fields of medical and other research. Note that the order of the points is not meant to structure a discussion’s writing (besides 1.).
Recommendations for writing a discussion section
Specific recommendations.
Consider the example on the association between D and LC. Rather than starting with an in-depth (causal) interpretation a finding should firstly be taken as what it allows inferring without doubt: Under the usual assumptions that a statistical model makes (e.g. random sampling, independence or certain correlation structure between observations [ 17 ]), the association indicates that D (strictly speaking: measuring D) predicts an elevated LC risk (strictly speaking: measuring LC) in the population that one has managed to sample (source population). Assume that the sample has been randomly drawn from primary care settings. In this case the association is useful to recommend medical doctors to better look at an individual’s LC risk in case of D. If the association has been adjusted for age and gender (conveniently through a regression model), the conclusion modifies to: If the doctor knows a patient’s age and gender (what should always be the case) D has additional value in predicting an elevated LC risk.
In the above example, a substantive researcher might want to conclude that D and LC are associated in a general population instead of just inferring to patients in primary care settings (a.). Another researcher might even take the finding as evidence for D being a causal factor in the etiology of LC, meaning that prevention of D could reduce the incidence rate of LC (in whatever target population) (b.). In both cases, the substantive researcher should insist on assessing the desired interpretation that goes beyond the data [ 4 ], but the statistician immediately needs to bring up the next point.
The explanation of all the assumptions that lead from a data result to a conclusion enables a reader to assess whether he or she agrees with the authors’ inference or not. These conditions, however, often remain incomplete or unclear, in which case the reader can hardly assess whether he or she follows a path of argumentation and, thus, shares the conclusion this path leads to.
Consider conclusion a. and suppose that, instead of representative sampling in a general population (e.g. all U.S. citizens aged 18 or above), the investigators were only able to sample in primary care settings. Extrapolating the results to another population than the source population requires what is called “external validity”, “transportability” or the absence of “selection bias” [ 18 , 19 ]. No such bias occurs if the parameter of interest is equal in the source and the target population. Note that this is a weaker condition than the common belief that the sample must represent the target population in everything . If the parameter of interest is the difference in risk for LC between cases and non-cases of D, the condition translates into: the risk difference must be equal in target and source population.
For the causal conclusion b., however, sufficient assumptions are very strict. In an RCT, the conclusion is valid under random sampling from the target population, random allocation of X, perfect compliance in X, complete participation and no measurement error in outcome (for details see [ 20 ]). In practice, on the other hand, the derivations from such conditions might sometimes be modest what may produce little bias only. For instance, non-compliance in a specific drug intake (treatment) might occur only in a few individuals to little extent through a random process (e.g. sickness of a nurse being responsible for drug dispense) and yield just small (downward) bias [ 5 ]. The conclusion of downward bias might also be justified if non-compliance does not cause anything that has a larger effect on a Y than the drug itself. Another researcher, however, could believe that non-compliance leads to taking a more effective, alternative treatment. He or she could infer upward bias instead if well-informed on the line of argument.
In practice, researchers frequently use causal language yet without mentioning any assumptions. This does not imply that they truly have a causal effect in mind, often causal and associational wordings are carelessly used in synonymous way. For example, concluding “depression increases the risk of lung cancer” constitutes already causal wording because it implies that a change in the depression status would change the cancer risk. Associational language like “lung cancer risk is elevated if depression occurs”, however, would allow for an elevated lung cancer risk in depression cases just because LC and D share some causes (“inducing” or “removing” depression would not change the cancer risk here).
Often, it is unclear where the path of argumentation from assumptions to a conclusion leads when alternative assumptions are made. Consider again bias due to selection. A different effect in target and source population occurs if effect-modifying variables distribute differently in both populations. Accordingly, the statistician should ask which variables influence the effect of interest, and whether these can be assumed to distribute equally in the source population and the target population. The substantive researcher might answer that the causal risk difference between D and LC likely increases with age. Given that this is true, and if elder individuals have been oversampled (e.g. because elderly are over-represented in primary care settings), both together would conclude that sampling has led to over-estimation (despite other factors, Fig. Fig.2 2 ).

If higher age is related to a larger effect (risk difference) of D on LC, a larger effect estimate is expected in an elder sample
However, the statistician might add, if effect modification is weak, or the difference in the age distributions is modest (e.g. mean 54 vs. 52 years), selection is unlikely to have produced large (here: upward) bias. In turn, another substantive researcher, who reads the resulting discussion, might instead assume a decrease of effect with increasing age and thus infer downward bias.
In practice, researchers should be extremely sensitive for bias due to selection if a sample has been drawn conditionally on a common consequence of factor and outcome or a variable associated with such a consequence [19 and references therein]. For instance, hospitalization might be influenced by both D and LC, and thus sampling from hospitals might introduce a false association or change an association’s sign; particularly D and LC may appear to be negatively associated although the association is positive in the general population (Fig. (Fig.3 3 ).

If hospitalization (H) is a common cause of D and LC, sampling conditionally on H can introduce a spurious association between D and LC ("conditioning on a collider")
Usually, only some kinds of bias are discussed, while the consequences of others are ignored [ 5 ]. Besides selection the main sources of bias are often measurement and confounding. If one is only interested in association, confounding is irrelevant. For causal conclusions, however, assumptions on all three kinds of bias are necessary.
Measurement error means that the measurement of a factor and/or outcome deviates from the true value, at least in some individuals. Bias due to measurement is known under many other terms that describe the reasons why such error occurs (e.g. “recall bias” and “reporting bias”). In contrast to conventional wisdom, measurement error does not always bias association and effect estimates downwards [ 5 , 6 ]. It does, for instance, if only the factor (e.g. depression) is measured with error and the errors occur independently from the outcome (e.g. lung cancer), or vice versa (“non-differential misclassification”) [22 and references therein]. However, many lung cancer cases might falsely report depression symptoms (e.g. to express need for care). Such false positives (non-cases of depression classified as cases) may also occur in non-cases of lung cancer but to a lesser extent (a special case of “differential misclassification”). Here, bias might be upward as well. Importantly, false positives cause larger bias than false negatives (non-cases of depression falsely classified as depression cases) as long as the relative frequency of a factor is lower than 50% [ 21 ]. Therefore, they should receive more attention in discussion. If measurement error occurs in depression and lung cancer, the direction of bias also depends on the correlation between both errors [ 21 ].
Note that what is in line with common standards of “good” measurement (e.g. a Kappa value measuring validity or reliability of 0.7) might anyway produce large bias. This applies to estimates of prevalence, association and effect. The reason is that while indices of measurement are one-dimensional, bias depends on two parameters (sensitivity and specificity) [ 21 , 22 ]. Moreover, estimates of such indices are often extrapolated to different kinds of populations (typically from a clinical to general population), what may be inadequate. Note that the different kinds of bias often interact, e.g. bias due to measurement might depend on selection (e.g. measurement error might differ between a clinical and a general population) [ 5 , 6 ].
Assessment of bias due to confounding variables (roughly speaking: common causes of factor and outcome) requires assumptions on the entire system of variables that affect both factor and outcome. For example, D and LC might share several causes such as stressful life events or socioeconomic status. If these influence D and LC with the same effect direction, this leads to overestimation, otherwise (different effect directions) the causal effect is underestimated. In the medical field, many unfavorable conditions may be positively related. If this holds true for all common factors of D and LC, upward bias can be assumed. However, not all confounders have to be taken into account. Within the framework of “causal graphs”, the “backdoor criterion” [ 7 ] provides a graphical rule for sets of confounders to be sufficient when adjusted for. Practically, such a causal graph must include all factors that directly or indirectly affect both D and LC. Then, adjustment for a set of confounders that meets the “backdoor criterion” in the graph completely removes bias due to confounding. In the example of Fig. Fig.4 4 it is sufficient to adjust for Z 1 and Z 2 because this “blocks” all paths that otherwise lead backwards from D to LC. Note that fully eliminating bias due to confounding also requires that the confounders have been collected without measurement error [ 5 , 6 , 23 ]. Therefore, the advice is always to concede at least some “residual” bias and reflect on the direction this might have (could be downward if such error is not stronger related to D and LC than a confounder itself).

Causal graph for the effect of D on LC and confounders Z 1 , Z 2 and Z 3
Whereas the statistician should pinpoint to the mathematical insight of the backdoor criterion, its application requires profound substantive input and literature review. Of course, there are numerous relevant factors in the medical field. Hence, one should practically focus on those with the highest prevalence (a very seldom factor can hardly cause large bias) and large assumed effects on both X and Y.
If knowledge on any of the three kinds of bias is poor or very uncertain, researchers should admit that this adds uncertainty in a conclusion: systematic error on top of random error. In the Bayesian framework, quantitative bias analysis formalizes this through the result of larger variance in an estimate. Technically, this additional variance is introduced via the variances of distributions assigned to “bias parameters”; for instance a misclassification probability (e.g. classifying a true depression case as non-case) or the prevalence of a binary confounder and its effects on X and Y. Of course, bias analysis also changes point estimates (hopefully reducing bias considerably). Note that conventional frequentist analysis, as regarded from the Bayesian perspective, assumes that all bias parameters were zero with a probability of one [ 5 , 6 , 23 ]. The only exceptions (bias addressed in conventional analyses) are adjustment on variables to hopefully reduce bias due to confounding and weighting the individuals (according to variables related to participation) to take into account bias due to selection.
If the substantive investigator understands the processes of selection, measurement and confounding only poorly, such strict analysis numerically reveals that little to nothing is known on the effect of X on Y, no matter how large an observed association and a sample (providing small random error) may be [ 5 , 6 , 23 ]). This insight has to be brought up by the statistician. Although such an analysis is complicated, itself very sensitive to how it is conducted [ 5 , 6 ] and rarely done, the Bayesian thinking behind it forces researchers to better understand the processes behind the data. Otherwise, he or she cannot make any assumptions and, in turn, no conclusion on causality.
Usually articles end with statements that only go little further than the always true but never informative statement “more research is needed”. Moreover, larger samples and better measurements are frequently proposed. If an association has been found, a RCT or other interventional study is usually proposed to investigate causality. In our example, this recommendation disregards that: (1) onset of D might have a different effect on LC risk than an intervention against D (the effect of onset cannot be investigated in any interventional study), (2) the effects of onset and intervention concern different populations (those without vs. those with depression), (3) an intervention effect depends on the mode of intervention [ 24 ], and (4) (applying the backdoor criterion) a well-designed observational study may approximatively yield the same result as a randomized study would [ 25 – 27 ]. If the effect of “removing” depression is actually of interest, one could propose an RCT that investigates the effect of treating depression in a strictly defined way and in a strictly defined population (desirably in all who meet the criteria of depression). Ideally, this population is sampled randomly, and non-participants and dropouts are investigated with respect to assumed effect-modifiers (differences in their distributions between participants and non-participants can then be addressed e.g. by weighting [ 27 ]). In a non-randomized study, one should collect variables supposed to meet the backdoor-criterion with the best instruments possible.
General recommendations
Yet when considering 1) through 7); i.e. carefully reflecting on the mechanisms that have created the data, discussions on statistical results can be very misleading, because the basic statistical methods are mis-interpreted or inadequately worded.
A common pitfall is to consider the lack of evidence for the alternative hypothesis (e.g. association between D and LC) as evidence for the null hypothesis (no association). In fact, such inference requires an a-priori calculated sample-size to ensure that the type-two error probability does not exceed a pre-specified limit (typically 20% or 10%, given the other necessary assumptions, e.g. on the true magnitude of association). Otherwise, the type-two error is unknown and in practice often large. This may put a “false negative result” into the scientific public that turns out to be “unreplicable” – what would be falsely interpreted as part of the “replication crisis”. Such results are neither positive nor negative but uninformative . In this case, the wording “there is no evidence for an association” is adequate because it does not claim that there is no association.
Frequently, it remains unclear which hypotheses have been a-priori specified and which have been brought up only after some data analysis. This, of course, is scientific malpractice because it does not enable the readership to assess the random error emerging from explorative data analysis. Accordingly, the variance of results across statistical methods is often misused to filter out the analysis that yields a significant result (“ p -hacking”, [ 28 ]). Pre-planned tests (via writing a grant) leave at least less room for p-hacking because they specify a-priori which analysis is to be conducted.
On the other hand, post-hoc analyses can be extremely useful for identifying unexpected phenomena and creating new hypotheses. Verbalization in the discussion section should therefore sharply separate between conclusions from hypothesis testing and new hypotheses created from data exploration. The distinction is profound, since a newly proposed hypothesis just makes a new claim. Suggesting new hypotheses cannot be wrong, this can only be inefficient if many hypotheses turn out to be wrong. Therefore, we suggest proposing only a limited number of new hypotheses that appear promising to stimulate further research and scientific progress. They are to be confirmed or falsified with future studies. A present discussion, however, should yet explicate the testable predictions a new hypothesis entails, and how a future study should be designed to keep bias in related analyses as small as possible.
Confidence intervals address the problem of reducing results to the dichotomy of significant and non-significant through providing a range of values that are compatible with the data at the given confidence level, usually 95% [ 29 ].
This is also addressed by Bayesian statistics that allows calculating what frequentist p -values are often misinterpreted to be: the probability that the alternative (or null) hypothesis is true [ 17 ]. Moreover, one can calculate how likely it is that the parameter lies within any specified range (e.g. the risk difference being greater than .05, a lower boundary for practical significance) [ 15 , 16 ]. To gain these benefits, one needs to specify how the parameter of interest (e.g. causal risk difference between D and LC) is distributed before inspecting the data. In Bayesian statistics (unlike frequentist statistics) a parameter is a random number that expresses prior beliefs via a “prior distribution”. Such a “prior” is combined with the data result to a “posterior distribution”. This integrates both sources of information.
Note that confidence intervals also can be interpreted from the Bayesian perspective (then called “credibility interval”). This assumes that all parameter values were equally likely (uniformly distributed, strictly speaking) before analyzing the data [ 5 , 6 , 20 ].
Testing just for a non-zero association can only yield evidence for an association deviating from zero. A better indicator for the true impact of an effect/association for clinical, economic, political, or research purposes is its magnitude. If an association between D and LC after adjusting for age and gender has been discovered, then the knowledge of D has additional value in predicting an elevated LC probability beyond age and gender. However, there may be many other factors that stronger predict LC and thus should receive higher priority in a doctor’s assessment. Besides, if an association is small, it may yet be explained by modest (upward) bias. Especially large samples often yield significant results with little practical value. The p -value does not measure strength of association [ 17 ]. For instance, in a large sample, a Pearson correlation between two dimensional variables could equal 0.1 only but with a p -value <.001. A further problem arises if the significance threshold of .05 is weakened post-hoc to allow for “statistical trends” ( p between .05 and .10) because a result has “failed to reach significance” (this wording claims that there is truly an association. If this was known, no research would be necessary).
It is usually the statistician’s job to insist not only on removing the attention from pure statistical significance to confidence intervals or even Bayesian interpretation, but also to point out the necessity of a meaningful cutoff for practical significance. The substantive researcher then has to provide this cutoff.
Researchers should not draw conclusions that have not been explicitly tested for. For example, one may have found a positive association between D and LC (e.g. p = .049), but this association is not significant (e.g. p = .051), when adjusting for “health behavior”. This does not imply that “health behavior” “explains” the association (yet fully). The difference in magnitude of association in both analyses compared here (without and with adjustment on HB) may be very small and the difference in p -values (“borderline significance” after adjustment) likely to emerge from random error. This often applies to larger differences in p as well.
Investigators, however, might find patterns in their results that they consider worth mentioning for creating hypotheses. In the example above, adding the words “in the sample”, would clarify that they refer just to the difference of two point estimates . By default, “association” in hypotheses testing should mean “statistically significant association” (explorative analyses should instead refer to “suggestive associations”).
Conclusions
Some issues of discussing results not mentioned yet appear to require only substantive reasoning. For instance, Bradford Hill’s consideration on “plausibility” claims that a causal effect is more likely, if it is in line with biological (substantive) knowledge, or if a dose-response relation has been found [ 30 ]. However, the application of these considerations itself depends on the trueness of assumptions. For instance, bias might act differently across the dose of exposure (e.g. larger measurement error in outcome among those with higher dosage). As a consequence, a pattern observed across dose may mask a true or pretend a wrong dose-response relation [ 30 ]. This again has to be brought up by statistical expertise.
There are, however, some practical issues that hinder the cooperation we suggest. First, substantive researchers often feel discomfort when urged to make assumptions on the mechanisms behind the data, presumably because they fear to be wrong. Here, the statistician needs to insist: “If you are unable to make any assumptions, you cannot conclude anything!” And: “As a scientist you have to understand the processes that create your data.” See [ 31 ] for practical advice on how to arrive at meaningful assumptions.
Second, statisticians have long been skeptical against causal inference. Still, most of them focus solely on describing observed data with distributional models, probably because estimating causal effects has long been regarded as unfeasible with scientific methods. Training in causality remains rather new, since strict mathematical methods have been developed only in the last decades [ 7 ].
The cooperation could be improved if education in both fields focused on the insight that one cannot succeed without the other. Academic education should demonstrate that in-depth conclusions from data unavoidably involve prior beliefs. Such education should say: Data do not “speak for themselves”, because they “speak” only ambiguously and little, since they have been filtered through various biases [ 32 ]. The subjectivity introduced by addressing bias, however, unsettles many researchers. On the other hand, conventional frequentist statistics just pretends to be objective. Instead of accepting the variety of possible assumptions, it makes the absurd assumption of “no bias with probability of one”. Or it avoids causal conclusions at all if no randomized study is possible. This limits science to investigating just associations for all factors that can never be randomized (e.g. onset of depression). However, the alternative of Bayesian statistics and thinking are themselves prone to fundamental cognitive biases which should as well be subject of interdisciplinary teaching [ 33 ].
Readers may take this article as an invitation to read further papers’ discussions differently while evaluating our claims. Rather than sharing a provided conclusion (or not) they could ask themselves whether a discussion enables them to clearly specify why they share it (or not). If the result is uncertainty, this might motivate them to write their next discussion differently. The proposals made in this article could help shifting scientific debates to where they belong. Rather than arguing on misunderstandings caused by ambiguity in a conclusion’s assumptions one should argue on the assumptions themselves.
Acknowledgements
We acknowledge support by the German Research Foundation and the Open Access Publication Funds of the TU Dresden. We wish to thank Pia Grabbe and Helen Steiner for language editing and the cited authors for their outstanding work that our proposals build on.
John Venz is funded by the German Federal Ministry of Education and Research (BMBF) project no. 01ER1303 and 01ER1703. He has contributed to this manuscript outside of time funded by these projects.
Availability of data and materials
Abbreviations.
| D | depression |
| HB | health behavior |
| LC | lung cancer |
| RCT | randomized clinical trial |
| X | factor variable |
| Y | outcome variable |
Authors’ contributions
MH and RM had the initial idea on the article. MH has taken the lead in writing. JV has contributed to the statistical parts, especially the Bayesian aspects. RM has refined the paragraphs on statistical inference. ST joined later and has added many clarifications related to the perspective of the substantive researcher. All authors have contributed to the final wording of all sections and the article’s revision. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
How to Start a Discussion Section in Research? [with Examples]
The examples below are from 72,017 full-text PubMed research papers that I analyzed in order to explore common ways to start writing the Discussion section.
Research papers included in this analysis were selected at random from those uploaded to PubMed Central between the years 2016 and 2021. Note that I used the BioC API to download the data (see the References section below).
Examples of how to start writing the Discussion section
In the Discussion section, you should explain the meaning of your results, their importance, and implications. [for more information, see: How to Write & Publish a Research Paper: Step-by-Step Guide ]
The Discussion section can:
1. Start by restating the study objective
“ The purpose of this study was to investigate the relationship between muscle synergies and motion primitives of the upper limb motions.” Taken from the Discussion section of this article on PubMed
“ The main objective of this study was to identify trajectories of autonomy.” Taken from the Discussion section of this article on PubMed
“ In the present study, we investigated the whole brain regional homogeneity in patients with melancholic MDD and non-melancholic MDD at rest . “ Taken from the Discussion section of this article on PubMed
2. Start by mentioning the main finding
“ We found that autocracy and democracy have acted as peaks in an evolutionary landscape of possible modes of institutional arrangements.” Taken from the Discussion section of this article on PubMed
“ In this study, we demonstrated that the neural mechanisms of rhythmic movements and skilled movements are similar.” Taken from the Discussion section of this article on PubMed
“ The results of this study show that older adults are a diverse group concerning their activities on the Internet.” Taken from the Discussion section of this article on PubMed
3. Start by pointing out the strength of the study
“ To our knowledge, this investigation is by far the largest epidemiological study employing real-time PCR to study periodontal pathogens in subgingival plaque.” Taken from the Discussion section of this article on PubMed
“ This is the first human subject research using the endoscopic hemoglobin oxygen saturation imaging technology for patients with aero-digestive tract cancers or adenomas.” Taken from the Discussion section of this article on PubMed
“ In this work, we introduced a new real-time flow imaging method and systematically demonstrated its effectiveness with both flow phantom experiments and in vivo experiments.” Taken from the Discussion section of this article on PubMed
Most used words at the start of the Discussion
Here are the top 10 phrases used to start a discussion section in our dataset:
| Rank | Phrase | Percent of occurrences |
|---|---|---|
| 1 | “In this study,…” | 4.48% |
| 2 | “In the present study,…” | 1.66% |
| 3 | “To our knowledge,…” | 0.73% |
| 4 | “To the best of our knowledge,…” | 0.51% |
| 5 | “In the current study,…” | 0.38% |
| 6 | “The aim of this study was…” | 0.38% |
| 7 | “This is the first study to…” | 0.28% |
| 8 | “The purpose of this study was to…” | 0.22% |
| 9 | “The results of the present study…” | 0.14% |
| 10 | “The aim of the present study was…” | 0.11% |
- Comeau DC, Wei CH, Islamaj Doğan R, and Lu Z. PMC text mining subset in BioC: about 3 million full text articles and growing, Bioinformatics , btz070, 2019.
Further reading
- How Long Should the Discussion Section Be? Data from 61,517 Examples
- How to Write & Publish a Research Paper: Step-by-Step Guide
- “I” & “We” in Academic Writing: Examples from 9,830 Studies

Organizing Academic Research Papers: 8. The Discussion
- Purpose of Guide
- Design Flaws to Avoid
- Glossary of Research Terms
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Choosing a Title
- Making an Outline
- Paragraph Development
- Executive Summary
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tertiary Sources
- What Is Scholarly vs. Popular?
- Qualitative Methods
- Quantitative Methods
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Annotated Bibliography
- Dealing with Nervousness
- Using Visual Aids
- Grading Someone Else's Paper
- How to Manage Group Projects
- Multiple Book Review Essay
- Reviewing Collected Essays
- About Informed Consent
- Writing Field Notes
- Writing a Policy Memo
- Writing a Research Proposal
- Acknowledgements
The purpose of the discussion is to interpret and describe the significance of your findings in light of what was already known about the research problem being investigated, and to explain any new understanding or fresh insights about the problem after you've taken the findings into consideration. The discussion will always connect to the introduction by way of the research questions or hypotheses you posed and the literature you reviewed, but it does not simply repeat or rearrange the introduction; the discussion should always explain how your study has moved the reader's understanding of the research problem forward from where you left them at the end of the introduction.
Importance of a Good Discussion
This section is often considered the most important part of a research paper because it most effectively demonstrates your ability as a researcher to think critically about an issue, to develop creative solutions to problems based on the findings, and to formulate a deeper, more profound understanding of the research problem you are studying.
The discussion section is where you explore the underlying meaning of your research , its possible implications in other areas of study, and the possible improvements that can be made in order to further develop the concerns of your research.
This is the section where you need to present the importance of your study and how it may be able to contribute to and/or fill existing gaps in the field. If appropriate, the discussion section is also where you state how the findings from your study revealed new gaps in the literature that had not been previously exposed or adequately described.
This part of the paper is not strictly governed by objective reporting of information but, rather, it is where you can engage in creative thinking about issues through evidence-based interpretation of findings. This is where you infuse your results with meaning.
Kretchmer, Paul. Fourteen Steps to Writing to Writing an Effective Discussion Section . San Francisco Edit, 2003-2008.
Structure and Writing Style
I. General Rules
These are the general rules you should adopt when composing your discussion of the results :
- Do not be verbose or repetitive.
- Be concise and make your points clearly.
- Avoid using jargon.
- Follow a logical stream of thought.
- Use the present verb tense, especially for established facts; however, refer to specific works and references in the past tense.
- If needed, use subheadings to help organize your presentation or to group your interpretations into themes.
II. The Content
The content of the discussion section of your paper most often includes :
- Explanation of results : comment on whether or not the results were expected and present explanations for the results; go into greater depth when explaining findings that were unexpected or especially profound. If appropriate, note any unusual or unanticipated patterns or trends that emerged from your results and explain their meaning.
- References to previous research : compare your results with the findings from other studies, or use the studies to support a claim. This can include re-visiting key sources already cited in your literature review section, or, save them to cite later in the discussion section if they are more important to compare with your results than being part of the general research you cited to provide context and background information.
- Deduction : a claim for how the results can be applied more generally. For example, describing lessons learned, proposing recommendations that can help improve a situation, or recommending best practices.
- Hypothesis : a more general claim or possible conclusion arising from the results [which may be proved or disproved in subsequent research].
III. Organization and Structure
Keep the following sequential points in mind as you organize and write the discussion section of your paper:
- Think of your discussion as an inverted pyramid. Organize the discussion from the general to the specific, linking your findings to the literature, then to theory, then to practice [if appropriate].
- Use the same key terms, mode of narration, and verb tense [present] that you used when when describing the research problem in the introduction.
- Begin by briefly re-stating the research problem you were investigating and answer all of the research questions underpinning the problem that you posed in the introduction.
- Describe the patterns, principles, and relationships shown by each major findings and place them in proper perspective. The sequencing of providing this information is important; first state the answer, then the relevant results, then cite the work of others. If appropriate, refer the reader to a figure or table to help enhance the interpretation of the data. The order of interpreting each major finding should be in the same order as they were described in your results section.
- A good discussion section includes analysis of any unexpected findings. This paragraph should begin with a description of the unexpected finding, followed by a brief interpretation as to why you believe it appeared and, if necessary, its possible significance in relation to the overall study. If more than one unexpected finding emerged during the study, describe each them in the order they appeared as you gathered the data.
- Before concluding the discussion, identify potential limitations and weaknesses. Comment on their relative importance in relation to your overall interpretation of the results and, if necessary, note how they may affect the validity of the findings. Avoid using an apologetic tone; however, be honest and self-critical.
- The discussion section should end with a concise summary of the principal implications of the findings regardless of statistical significance. Give a brief explanation about why you believe the findings and conclusions of your study are important and how they support broader knowledge or understanding of the research problem. This can be followed by any recommendations for further research. However, do not offer recommendations which could have been easily addressed within the study. This demonstrates to the reader you have inadequately examined and interpreted the data.
IV. Overall Objectives
The objectives of your discussion section should include the following: I. Reiterate the Research Problem/State the Major Findings
Briefly reiterate for your readers the research problem or problems you are investigating and the methods you used to investigate them, then move quickly to describe the major findings of the study. You should write a direct, declarative, and succinct proclamation of the study results.
II. Explain the Meaning of the Findings and Why They are Important
No one has thought as long and hard about your study as you have. Systematically explain the meaning of the findings and why you believe they are important. After reading the discussion section, you want the reader to think about the results [“why hadn’t I thought of that?”]. You don’t want to force the reader to go through the paper multiple times to figure out what it all means. Begin this part of the section by repeating what you consider to be your most important finding first.
III. Relate the Findings to Similar Studies
No study is so novel or possesses such a restricted focus that it has absolutely no relation to other previously published research. The discussion section should relate your study findings to those of other studies, particularly if questions raised by previous studies served as the motivation for your study, the findings of other studies support your findings [which strengthens the importance of your study results], and/or they point out how your study differs from other similar studies. IV. Consider Alternative Explanations of the Findings
It is important to remember that the purpose of research is to discover and not to prove . When writing the discussion section, you should carefully consider all possible explanations for the study results, rather than just those that fit your prior assumptions or biases.
V. Acknowledge the Study’s Limitations
It is far better for you to identify and acknowledge your study’s limitations than to have them pointed out by your professor! Describe the generalizability of your results to other situations, if applicable to the method chosen, then describe in detail problems you encountered in the method(s) you used to gather information. Note any unanswered questions or issues your study did not address, and.... VI. Make Suggestions for Further Research
Although your study may offer important insights about the research problem, other questions related to the problem likely remain unanswered. Moreover, some unanswered questions may have become more focused because of your study. You should make suggestions for further research in the discussion section.
NOTE: Besides the literature review section, the preponderance of references to sources in your research paper are usually found in the discussion section . A few historical references may be helpful for perspective but most of the references should be relatively recent and included to aid in the interpretation of your results and/or linked to similar studies. If a study that you cited disagrees with your findings, don't ignore it--clearly explain why the study's findings differ from yours.
V. Problems to Avoid
- Do not waste entire sentences restating your results . Should you need to remind the reader of the finding to be discussed, use "bridge sentences" that relate the result to the interpretation. An example would be: “The lack of available housing to single women with children in rural areas of Texas suggests that...[then move to the interpretation of this finding].”
- Recommendations for further research can be included in either the discussion or conclusion of your paper but do not repeat your recommendations in the both sections.
- Do not introduce new results in the discussion. Be wary of mistaking the reiteration of a specific finding for an interpretation.
- Use of the first person is acceptable, but too much use of the first person may actually distract the reader from the main points.
Analyzing vs. Summarizing. Department of English Writing Guide. George Mason University; Discussion . The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College; Hess, Dean R. How to Write an Effective Discussion. Respiratory Care 49 (October 2004); Kretchmer, Paul. Fourteen Steps to Writing to Writing an Effective Discussion Section . San Francisco Edit, 2003-2008; The Lab Report . University College Writing Centre. University of Toronto; Summary: Using it Wisely . The Writing Center. University of North Carolina; Schafer, Mickey S. Writing the Discussion . Writing in Psychology course syllabus. University of Florida; Yellin, Linda L. A Sociology Writer's Guide. Boston, MA: Allyn and Bacon, 2009.
Writing Tip
Don’t Overinterpret the Results!
Interpretation is a subjective exercise. Therefore, be careful that you do not read more into the findings than can be supported by the evidence you've gathered. Remember that the data are the data: nothing more, nothing less.
Another Writing Tip
Don't Write Two Results Sections!
One of the most common mistakes that you can make when discussing the results of your study is to present a superficial interpretation of the findings that more or less re-states the results section of your paper. Obviously, you must refer to your results when discussing them, but focus on the interpretion of those results, not just the data itself.
Azar, Beth. Discussing Your Findings. American Psychological Association gradPSYCH Magazine (January 2006)
Yet Another Writing Tip
Avoid Unwarranted Speculation!
The discussion section should remain focused on the findings of your study. For example, if you studied the impact of foreign aid on increasing levels of education among the poor in Bangladesh, it's generally not appropriate to speculate about how your findings might apply to populations in other countries without drawing from existing studies to support your claim. If you feel compelled to speculate, be certain that you clearly identify your comments as speculation or as a suggestion for where further research is needed. Sometimes your professor will encourage you to expand the discussion in this way, while others don’t care what your opinion is beyond your efforts to interpret the data.
- << Previous: Using Non-Textual Elements
- Next: Limitations of the Study >>
- Last Updated: Jul 18, 2023 11:58 AM
- URL: https://library.sacredheart.edu/c.php?g=29803
- QuickSearch
- Library Catalog
- Databases A-Z
- Publication Finder
- Course Reserves
- Citation Linker
- Digital Commons
- Our Website
Research Support
- Ask a Librarian
- Appointments
- Interlibrary Loan (ILL)
- Research Guides
- Databases by Subject
- Citation Help
Using the Library
- Reserve a Group Study Room
- Renew Books
- Honors Study Rooms
- Off-Campus Access
- Library Policies
- Library Technology
User Information
- Grad Students
- Online Students
- COVID-19 Updates
- Staff Directory
- News & Announcements
- Library Newsletter
My Accounts
- Interlibrary Loan
- Staff Site Login
FIND US ON
How to Write an Effective Discussion
- November 2004
- Respiratory Care 49(10):1238-41
- 49(10):1238-41

- Massachusetts General Hospital
Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Huda Dawood Salman
- Jan P Vandenbroucke
- Erik von Elm
- Douglas G. Altman
- Matthias Egger

- İbrahim Sayin
- J CLIN APHERESIS
- Robert Weinstein

- Pitchai Balakumar
- Ali S. Alqahtani

- François Swart

- Johannes C Heydenreich
- Chris T Bolliger
- Antonio Antón

- Douglas K Orens
- Cynthia Fatica
- Alejandro C Arroliga
- Eleni Apostolopoulou
- Petros Bakakos

- Leonides Gregorakos
- Robert R Fluck
- Christine Schroeder
- Brenda Engbretson
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- How to Write a Discussion Section | Tips & Examples
How to Write a Discussion Section | Tips & Examples
Published on 21 August 2022 by Shona McCombes . Revised on 25 October 2022.

The discussion section is where you delve into the meaning, importance, and relevance of your results .
It should focus on explaining and evaluating what you found, showing how it relates to your literature review , and making an argument in support of your overall conclusion . It should not be a second results section .
There are different ways to write this section, but you can focus your writing around these key elements:
- Summary: A brief recap of your key results
- Interpretations: What do your results mean?
- Implications: Why do your results matter?
- Limitations: What can’t your results tell us?
- Recommendations: Avenues for further studies or analyses
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.

Table of contents
What not to include in your discussion section, step 1: summarise your key findings, step 2: give your interpretations, step 3: discuss the implications, step 4: acknowledge the limitations, step 5: share your recommendations, discussion section example.
There are a few common mistakes to avoid when writing the discussion section of your paper.
- Don’t introduce new results: You should only discuss the data that you have already reported in your results section .
- Don’t make inflated claims: Avoid overinterpretation and speculation that isn’t directly supported by your data.
- Don’t undermine your research: The discussion of limitations should aim to strengthen your credibility, not emphasise weaknesses or failures.
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Correct my document today
Start this section by reiterating your research problem and concisely summarising your major findings. Don’t just repeat all the data you have already reported – aim for a clear statement of the overall result that directly answers your main research question . This should be no more than one paragraph.
Many students struggle with the differences between a discussion section and a results section . The crux of the matter is that your results sections should present your results, and your discussion section should subjectively evaluate them. Try not to blend elements of these two sections, in order to keep your paper sharp.
- The results indicate that …
- The study demonstrates a correlation between …
- This analysis supports the theory that …
- The data suggest that …
The meaning of your results may seem obvious to you, but it’s important to spell out their significance for your reader, showing exactly how they answer your research question.
The form of your interpretations will depend on the type of research, but some typical approaches to interpreting the data include:
- Identifying correlations , patterns, and relationships among the data
- Discussing whether the results met your expectations or supported your hypotheses
- Contextualising your findings within previous research and theory
- Explaining unexpected results and evaluating their significance
- Considering possible alternative explanations and making an argument for your position
You can organise your discussion around key themes, hypotheses, or research questions, following the same structure as your results section. Alternatively, you can also begin by highlighting the most significant or unexpected results.
- In line with the hypothesis …
- Contrary to the hypothesised association …
- The results contradict the claims of Smith (2007) that …
- The results might suggest that x . However, based on the findings of similar studies, a more plausible explanation is x .
As well as giving your own interpretations, make sure to relate your results back to the scholarly work that you surveyed in the literature review . The discussion should show how your findings fit with existing knowledge, what new insights they contribute, and what consequences they have for theory or practice.
Ask yourself these questions:
- Do your results support or challenge existing theories? If they support existing theories, what new information do they contribute? If they challenge existing theories, why do you think that is?
- Are there any practical implications?
Your overall aim is to show the reader exactly what your research has contributed, and why they should care.
- These results build on existing evidence of …
- The results do not fit with the theory that …
- The experiment provides a new insight into the relationship between …
- These results should be taken into account when considering how to …
- The data contribute a clearer understanding of …
- While previous research has focused on x , these results demonstrate that y .
Prevent plagiarism, run a free check.
Even the best research has its limitations. Acknowledging these is important to demonstrate your credibility. Limitations aren’t about listing your errors, but about providing an accurate picture of what can and cannot be concluded from your study.
Limitations might be due to your overall research design, specific methodological choices , or unanticipated obstacles that emerged during your research process.
Here are a few common possibilities:
- If your sample size was small or limited to a specific group of people, explain how generalisability is limited.
- If you encountered problems when gathering or analysing data, explain how these influenced the results.
- If there are potential confounding variables that you were unable to control, acknowledge the effect these may have had.
After noting the limitations, you can reiterate why the results are nonetheless valid for the purpose of answering your research question.
- The generalisability of the results is limited by …
- The reliability of these data is impacted by …
- Due to the lack of data on x , the results cannot confirm …
- The methodological choices were constrained by …
- It is beyond the scope of this study to …
Based on the discussion of your results, you can make recommendations for practical implementation or further research. Sometimes, the recommendations are saved for the conclusion .
Suggestions for further research can lead directly from the limitations. Don’t just state that more studies should be done – give concrete ideas for how future work can build on areas that your own research was unable to address.
- Further research is needed to establish …
- Future studies should take into account …
- Avenues for future research include …
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
McCombes, S. (2022, October 25). How to Write a Discussion Section | Tips & Examples. Scribbr. Retrieved 21 August 2024, from https://www.scribbr.co.uk/thesis-dissertation/discussion/
Is this article helpful?
Shona McCombes
Other students also liked, how to write a results section | tips & examples, research paper appendix | example & templates, how to write a thesis or dissertation introduction.
- Open access
- Published: 22 August 2024
Factors influencing fidelity to guideline implementation strategies for improving pain care at cancer centres: a qualitative sub-study of the Stop Cancer PAIN Trial
- Tim Luckett 1 ,
- Jane Phillips 2 ,
- Meera Agar 1 , 3 ,
- Linda Richards 4 ,
- Najwa Reynolds 5 ,
- Maja Garcia 1 ,
- Patricia Davidson 6 ,
- Tim Shaw 7 ,
- David Currow 6 ,
- Frances Boyle 8 , 9 ,
- Lawrence Lam 10 ,
- Nikki McCaffrey 11 &
- Melanie Lovell 5 , 9
BMC Health Services Research volume 24 , Article number: 969 ( 2024 ) Cite this article
Metrics details
The Stop Cancer PAIN Trial was a phase III pragmatic stepped wedge cluster randomised controlled trial which compared effectiveness of screening and guidelines with or without implementation strategies for improving pain in adults with cancer attending six Australian outpatient comprehensive cancer centres ( n = 688). A system for pain screening was introduced before observation of a ‘control’ phase. Implementation strategies introduced in the ‘intervention’ phase included: (1) audit of adherence to guideline recommendations, with feedback to clinical teams; (2) health professional education via an email-administered ‘spaced education’ module; and (3) a patient education booklet and self-management resource. Selection of strategies was informed by the Capability, Opportunity and Motivation Behaviour (COM-B) Model (Michie et al., 2011) and evidence for each strategy’s stand-alone effectiveness. A consultant physician at each centre supported the intervention as a ‘clinical champion’. However, fidelity to the intervention was limited, and the Trial did not demonstrate effectiveness. This paper reports a sub-study of the Trial which aimed to identify factors inhibiting or enabling fidelity to inform future guideline implementation initiatives.
The qualitative sub-study enabled in-depth exploration of factors from the perspectives of personnel at each centre. Clinical champions, clinicians and clinic receptionists were invited to participate in semi-structured interviews. Analysis used a framework method and a largely deductive approach based on the COM-B Model.
Twenty-four people participated, including 15 physicians, 8 nurses and 1 clinic receptionist. Coding against the COM-B Model identified ‘capability’ to be the most influential component, with ‘opportunity’ and ‘motivation’ playing largely subsidiary roles. Findings suggest that fidelity could have been improved by: considering the readiness for change of each clinical setting; better articulating the intervention’s value proposition; defining clinician roles and responsibilities, addressing perceptions that pain care falls beyond oncology clinicians’ scopes of practice; integrating the intervention within existing systems and processes; promoting patient-clinician partnerships; investing in clinical champions among senior nursing and junior medical personnel, supported by medical leaders; and planning for slow incremental change rather than rapid uptake.
Conclusions
Future guideline implementation interventions may require a ‘meta-implementation’ approach based on complex systems theory to successfully integrate multiple strategies.
Trial registration
Registry: Australian New Zealand Clinical Trials Registry; number: ACTRN 12615000064505; data: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspxid=367236&isReview=true .
Peer Review reports
Pain is a common and burdensome symptom in people with cancer [ 1 ]. Barriers to pain care occur at all ‘levels’, including the patient and family (e.g., misconceptions regarding opioids), clinician (e.g. lack of expertise), service (e.g. inadequate referral processes) and healthcare system (e.g. lack of coordination) [ 2 , 3 , 4 , 5 , 6 , 7 , 8 ]. A recent systematic review suggests that around 40% of cancer patients with pain may not receive adequate management [ 9 ]. Research has demonstrated that routine screening and implementation of evidence-based guidelines has potential to improve quality of cancer pain care and outcomes [ 10 , 11 , 12 , 13 , 14 ]. However, experience suggests that clinicians are unlikely to utilise screening results or follow guidelines unless these are supported by targeted strategies [ 15 , 16 ].
The Stop Cancer PAIN Trial (ACTRN 12615000064505) was a phase III pragmatic stepped wedge cluster randomised controlled trial conducted between 2014 and 2019 which compared the effectiveness of screening and guidelines with or without implementation strategies for improving pain in adults with cancer attending six outpatient comprehensive cancer centres in Australia ( n = 688) [ 17 , 18 ]. A pen/paper system to screen for pain using 0–10 numerical rating scales (NRS) for worst and average intensity over the past 24 h was introduced to each centre prior to observation of a ‘control’ phase, in which clinicians were also made aware of the Australian Cancer Pain Management in Adults guidelines [ 19 ]. At the beginning of the training phase, trial investigators presented at staff meetings on the importance of better managing pain and the rationale and evidence base for the intervention components. Implementation strategies (collectively termed the ‘intervention’) were then introduced in a ‘training’ phase and maintained during an ‘intervention’ phase as follows: (1) audit of adherence to key guideline recommendations [ 19 ] and feedback delivered to clinical teams in one or two cycles; (2) health professional education via a ‘Qstream’ email-administered ‘spaced education’ module [ 20 ]; and (3) a patient education booklet and self-management resource for completion together with a clinician that included goal setting, a pain diary and pain management plan [ 21 , 22 ]. Selection of these strategies was informed by the Capability, Opportunity and Motivation Behaviour (COM-B) Model of behaviour change [ 23 ], and evidence that each strategy had been separately effective for supporting guideline implementation for other health conditions. The intervention was supported at each centre by a consultant physician who agreed to be a ‘clinical champion’ [ 24 ].
As reported previously [ 18 ], the Stop Cancer PAIN Trial found no significant differences between the intervention and the control phases on the trial’s primary outcome - the proportion of patients with moderate-severe worst pain intensity who reported a 30% decrease at 1-week follow-up. Fidelity to the intervention was lower than anticipated and variable between centres: only 2/6 centres had two audit cycles rather than one; completion rates for the health professional spaced education varied from 12% to 74% between centres; and the proportion of patients reporting receipt of written information of any kind rose to an average of only 30% (20-44%) versus 22% (2-30%) in the control phase. Unexpectedly, secondary measures of mean, worst and average pain over a 4-week follow-up period improved by 0.5 standard deviation during control as well as intervention phases. However, the lack of a comparison group with no screening system made it difficult to conclude whether improvement in the control phase was due to effects from screening, a Hawthorne effect, or some other explanation.
The current paper reports a sub-study of the Stop Cancer PAIN Trial which aimed to identify factors influencing fidelity to the intervention that might warrant consideration by similar initiatives in the future.
The intervention, methods and results of the Stop Cancer PAIN trial have been described in previous open-access articles [ 17 , 18 ]. The sub-study used a qualitative approach with pragmatic orientation to enable in-depth exploration of factors influencing success from the perspectives of clinicians at each participating centre [ 25 ]. Clinician views canvassed at interview were considered the most efficient means of identifying barriers and enablers among complex contextual factors at each centre, including personnel’s knowledge, attitudes and beliefs towards pain care and the intervention.
The sub-study was approved by the Southwestern Sydney Local Health District Human Research Ethics Committee (HREC/14/LPOOL/479) as part of the overall trial. All participants gave written informed consent to participate.
Reporting adheres to the consolidated criteria for reporting qualitative research (COREQ) [ 26 ].
Participants
Participants were eligible if they were employed on a permanent basis either full- or part-time at a participating centre in a role that provided clinical care to cancer patients or patient-focused administrative support. The clinical champion at each centre was invited to participate by the research team. Other personnel were invited by means of email circulars and verbal invitations during meetings. Given the diverse range of roles at each centre, no limit was set on sample size to canvass as many perspectives as possible.
Data collection
Data were collected by means of semi-structured interviews conducted by one of two researchers, a female pharmacist with experience of medical education for pain management (LR), and a male social scientist with a doctorate (TL). Both interviewers had prior experience in qualitative research and knew some participants through their project roles.
Participants were fully aware of the study purpose before consenting. Interviews were conducted face-to-face or by telephone, with the participant and interviewer being the only people present. Interviews began with open questions about ‘what worked’ and ‘didn’t work’ across the intervention before focusing on each implementation strategy in more detail and important contextual factors at their centre (see Table 1 for a topic guide, which was developed specifically for this study). Interviewers explicitly invited criticism, expressing a tone of open enquiry and neutrality throughout. Prompts were used as necessary to explore factors identified by participants in more detail. Factors identified at previous interviews were raised at subsequent ones for verification, inviting participants to disagree or agree as they felt appropriate. No requests were received to return transcripts to participants for comment. Interviews were audio-recorded and transcribed verbatim.
Analysis used the framework method [ 27 ] and a largely deductive approach based on the same theoretical framework used during intervention design - the COM-B Model [ 23 ]. Based on a systematic review, the COM-B Model posits that behaviour change requires three conditions, namely ‘capability’ (including both psychological and physical capacity), ‘opportunity’ (all the factors that lie outside the individual that make the behaviour possible or prompt it) and ‘motivation’ (including habitual processes, emotional responding, as well as analytical decision-making). Initial line-by-line coding categorized data against these conditions according to which best described relationships between factors and behaviours within and across implementation strategies and the levels of patient, clinician and centre. While the COM-B model originally focused directly on human behaviour, it became clear during coding that behaviour was substantially influenced by centre, specialty and disciplinary factors, so these were also considered appropriate foci for coding against COM conditions. To enhance credibility, the same data were coded in different ways where multiple interpretations seemed plausible until coding of further interviews identified consistencies to help with disambiguation. Charting of codes for data within and between centres enabled mapping between the relative contributions made by each condition, summarised as lessons learned for guiding similar initiatives in the future. Dependability was increased by ensuring coding was conducted by two members of the research team (NR, MG) who had no previous involvement in the project but were experienced in qualitative research. Review and discussion with two team members who were involved in the project throughout (TL and ML) was intended to balance ‘outsider’ and ‘insider’ perspectives to guard against bias from preconceived interpretations whilst also referencing contextual understanding. Both Excel 2019 (Microsoft) and NVivo V12 (QSR) software were used to help manage different stages of the analytic process.
Twenty-four people participated across the six centres, ranging from one to six participants. Fifteen were physicians (of whom six were clinical champions), eight were nurses, and one was a clinic receptionist. This response rate ranged from 2 to 27% of eligible personnel at each centre. See Table 2 for a more detailed summary of participant roles at each centre. Interviews were a median of 20 min long, with an inter-quartile range of 13 to 28 min.
Capability, opportunity and motivation
Coding against the COM-B Model identified ‘capability’ to be the component having most influence over intervention success, with ‘opportunity’ and ‘motivation’ playing largely subsidiary roles.
Capabilities: Pertinent capabilities were reported to include: a pre-existing, centre-level culture of continuous improvement, communication pathways between senior management and other personnel, established roles and responsibilities for pain care among disciplines and specialties, systems and processes that could readily accommodate the intervention, and a culture of involving patients as partners in care. These capabilities influenced the degree to which personnel and patients had the opportunity and motivation to fully engage with the intervention.
Opportunity and motivation: These elements were most frequently discussed by participants in terms of ‘time’ that personnel could commit to pain care relative to other responsibilities. Clinical champions were perceived to play a critical role in supporting intervention success but were under-resourced at every centre and challenged by turnover in the role at two. In addition to more systemic drivers, individual personnel’s motivation was influenced by the degree to which they accepted the intervention’s value proposition at the outset and perceived this to be demonstrated over time.
Interactions between capability, opportunity and motivation are explored below in terms of their implications for similar future initiatives. Findings suggest that fidelity could have been improved by: considering the readiness for change of each clinical setting; better articulating the intervention’s value proposition; defining clinician roles and responsibilities, addressing perceptions that pain care falls beyond oncology clinicians’ scopes of practice; integrating the intervention within existing systems and processes; promoting patient-clinician partnerships; investing in clinical champions among senior nursing and junior medical personnel, supported by medical leaders; and planning for slow incremental change rather than rapid uptake.
Consider centres’ readiness for change
The degree to which centres had a pre-existing culture of continuous improvement was considered important in providing a fertile context for the intervention. At Centre 5, there was a consensus that change of any kind was difficult to instigate, even according to the head of department: “… because it’s new - because we’re so entrenched in our ways ” (C5P04 [Centre 5, participant 04] medical oncologist, head of department and clinical champion). At another, the complex centre-level nature of the intervention was perceived to pose particular challenges compared to oncology drug trials with which they were more familiar: “ we haven’t been a principal site [in a trial of this kind] previously and I think that’s sort of opened up some gaps in knowledge for us and some opportunities for learning in the future … what kind of support we’d need to come with that trial to help it be a success in this culture ” (C3P02 palliative care physician and clinical champion).
Articulate and deliver on the intervention’s value proposition
Interviews highlighted the importance of articulating the intervention’s value proposition to every member of the workforce and maintaining engagement by demonstrating benefits over time. At Centre 5, some participants perceived that the intervention had been imposed by management rather than generated from clinical priorities: “…senior staff say [to researchers] ‘come to our clinics, but we expect everyone else to do the work’ ” (C5P05 radiation oncologist). This was compounded by a perceived lack of communication about the project, which limited personnels’ opportunity to take a more active role even when they were motivated to do so: “ I would have facilitated [the intervention] … but I didn’t know about it ” (C5P01 nurse practitioner). Eliciting and maintaining engagement was said to be additionally challenged at this centre by high staff turnover, especially among junior medical officers on rotation: “ it was very accepted by the junior medical staff [but] I think, unfortunately, when there’s a relatively high turnover of staff … ” (C5P07 radiation oncology trainee). At two other centres, turnover among personnel required a transition in the role of clinical champion, interrupting support for the intervention while the new incumbents familiarised themselves with the role.
Across centres, participants reported reservations among some of their colleagues regarding the project’s fundamental premises, including the assumption that pain care needed improving at their centre (“ they actually felt this trial was a little bit insulting for their clinical skills. There was a bit of eye rolling and ‘of course we do that already!’ ” (C3P02 palliative care physician and clinical champion)) or that pain warranted a specific focus rather than symptoms more generally: “ I find it more useful when more than one symptom is targeted ” (C5P06 palliative care physician).
More specific criticism was also levelled at each of the intervention strategies as follows.
Pain screening
In the case of screening, two participants questioned the validity of a 0–10 numerical rating scale (NRS) for different reasons: “ sometimes getting the numbers breaks the flow of the narrative” (C6P04 medical oncologist); “they [patients] would say, ‘no, I’m not in pain but I have a lot of discomfort when I swallow’ - it was in the wording ” C5P02 registered nurse). Even one of the clinical champions felt that screening was redundant where pain was very severe: “ if someone is clearly in a pain crisis, you don’t need to be asking … you kind of know what number - they might tell you it’s 15 [out of 10] ” (C6P02 palliative care physician and clinical champion). Perceptions of the value of screening were also influenced by the degree to which it led to demonstrable improvements in pain care, which was undermined by problems with establishing an efficient process at some centres: “ I think I’ve still probably got stray [pain screening] forms on my desk ” (C3P06 palliative care physician). A lack of understanding among personnel and patients about how screening might lead to better pain outcomes was said to result in “ fatigue ” (C5P03 clinical nurse consultant [clinical nurse consultant]; C1P01 palliative care physician and clinical champion), manifest as a downward spiral of effort in, and value from, screening.
Audit and feedback
The audit and feedback strategy attracted limited attention from personnel at most centres: “ I don’t think that the audit and feedback were terribly noticeable ” (C4P01 medical oncologist and clinical champion). At the centre where only the palliative care department participated, one participant perceived baseline audit results to be acceptable and therefore demotivating for change: “[ the audit results showed] we were doing a good job even ahead of time … it did sort of make you think – ‘well where do we go from here?’ ” (C6P04 pain medicine physician). At another centre, motivation among personnel to improve on less favourable audit findings was perceived to depend on whether they prioritised pain care to start with: “ people have come up to me and said, ‘Gee, we really did very badly didn’t we?’ … but they’re not necessarily the people who don’t treat pain well - that’s the problem ” (C1P01 palliative care physician and clinical champion).
Spaced education for health professionals
Participants’ opinion on the value of the online spaced education depended on discipline and seniority, with nurses and junior medical officers reporting benefits “( it gave me a bit more confidence that I was on the right track” (C5P01 nurse practitioner)) but consultant physicians perceiving the knowledge level too “basic” (C6P04 pain medicine physician) or questioning advice from online spaced education that their responses were ‘wrong’: “…some of the multiple answers could have been equally valid” (C504 medical oncologist and clinical champion). Where consultants remained engaged, motivation was said to rely on cultivating “ competition” between colleagues (C602 palliative care physician and clinical champion). Inevitably, the voluntary nature of online spaced education also meant that only motivated personnel engaged to begin with.
Patient self-management resource
All participants who had used the patient self-management resource perceived at least some value. However, its use was limited by barriers relating to role and process considered below.
Define roles and responsibilities
Among the most commonly voiced barriers was a lack of clarity about which specialties and disciplines should be responsible for pain screening, patient education and management. This was usually described in terms of a ‘lack of time’ for pain care relative to other duties afforded greater priority within their scope of practice. Perspectives on roles and responsibilities are considered separately for each aspect of pain care as follows.
While most centres allocated the clinical task of pain screening to clinic receptionists, there was widespread reflection that this had been suboptimal. The only participating clinic receptionist felt that pain screening fell outside her area of responsibility: “but I’m an administrative person - I don’t have anything to do with pain management ” (C2P03 clinic receptionist). Clinician participants across disciplines similarly perceived that pain screening required clinical expertise to assist patients with reporting their pain and triage for urgent follow-up: “ you need somebody talking to the patients, rather than just handing the form, say ‘fill this in’ ” (C2P04 clinical nurse consultant). One centre that recognised this early on reallocated screening from an administrative to a nursing role, leading to substantial improvements in the completeness and quality of data: “ it made a big difference and certainly improved our ability to recognise people who had pain and allowed access for those people who were in severe pain to medications or at least an assessment … implementation through the clerical staff was not a long-term strategy ” (C1P01 palliative care physician and clinical champion).
Patient education
There was little consensus on which disciplines should be responsible for supporting patients to use the self-management resource, with medical personnel deferring to nurses and vice-versa. Role allocation was challenged by the diverse components within the resource, with each perceived to fall within a different scope of practice: “ pain is something I always do as an assessment … [but] … I’m not managing the pain … I’ll review and make recommendations and talk about the pain diaries and discussing their diary with their palliative care doctor or their general practitioner. And I would encourage that process. [But] I wouldn’t be the one that’s setting the goals on their daily activities and stuff ” (C5P01 nurse practitioner). Some oncology nursing roles were perceived to focus on chemo- or radiotherapy protocols to the exclusion of supportive care unless symptoms arose from, or impeded, treatment. Meanwhile, oncologists tended to interpret their role as solely focused on prescribing rather than also encompassing patient education: “ junior doctors only [have] 15 minutes to take a history and everything. [They] could enter in meds [into the patient resource] if everything else is done by someone else … part of me knows it’s [patient resource] important, but the other part of me - I just - when will I have time in my clinical practice to do it? ” (C5P05 radiation oncologist).
Pain management
Some oncologists viewed even pharmacological pain management as peripheral to their scope of practice when consultation time was short, prioritising cancer treatment instead. These participants viewed their role as limited to referring to palliative medicine or pain specialists, especially where pain was believed to have causes other than cancer: “ if the pain is a complex pain where the patient doesn’t have evidence of cancer, and it may be treatment-related, then in those scenarios we tend to divert to the chronic pain team ” (C5P07 radiation oncology advanced trainee). While participants from palliative care and pain medicine welcomed referrals for complex cases, they felt that oncologists sometimes referred for pain they could have easily managed themselves: “ what about some regular paracetamol? … These are things that you’d expect any junior doctors, never mind consultants [to have provided advice on] ” (C5P06 palliative care physician).
Integrate within existing systems and processes
Participants from several centres expressed a view that the intervention’s complex nature had proven overwhelming for systems and processes at their centres. At two centres, integration was especially challenged by broader infrastructure shifts and process failures that limited receptiveness to further changes. Participants at several centres emphasised the process-driven nature of oncology services and the challenge of changing established processes: “ they have got a pro forma that they use for chemo-immunotherapy review, and pain is not part of it, and that perhaps needs more of an organisational nuance … why doesn’t pain feature as a clinical outcome as part of the chemotherapy, immunotherapy review?” (C6P01 clinical nurse consultant). Participants emphasised the need to integrate pain care into existing processes to help personnel understand what was expected of them: “…nursing staff were getting them [screening forms] in the patient’s files and going, ‘what am I supposed to do with this?’ ” (C2P04 clinical nurse consultant). Moreover, centres’ focus on cancer treatment meant that pain care struggled to gain traction even when a process could be instituted: “ unless pain is the presenting complaint and is at the forefront it goes into those, sorts of, you know, the ‘other details’ ” (C5P06 palliative care physician). For the palliative care centre, where pain care was already prioritised, there were doubts about how the proposed process improved on those already in place: “ I generally ask pretty detailed questions about pain anyway [so don’t need patients to be screened in the waiting room] ” (C6P04 pain medicine physician).
Suggestions for better integrating the intervention included “in-building” (C3P04 medical oncologist) responsibility for the strategies within new staff roles or introducing the strategies gradually by means of a “ multistep process” (C5P04 medical oncologist, head of department and clinical champion). Features of two strategies were singled out as having positive potential for supporting existing processes of care. The patient resource was said to “ facilitate communication between the oncology teams and the palliative care team ” (C5P05 radiation oncologist) and serve as a “ visual cue ” (C3P02 medical oncologist) to cover educational topics that “ they might have otherwise forgotten ” (C2P01 palliative care physician and clinical champion). Participants also found the spaced education email administration, spacing and repetition “ easy to manage ” (C2P01 palliative care physician and clinical champion) within their daily routines.
Promote patient-clinician partnership on pain care
Several participants expressed surprise at the prevalence of moderate-severe pain in screening results, and acknowledged that this revealed under-reporting of pain in usual care. Under-reporting was perceived to stem partly from patient expectations that pain from cancer was “ normal ” (C4P03 nurse practitioner) and to be especially common in the context of certain generational or cultural attitudes towards pain and opioids (“ I certainly think there’s a cultural element but there’s also your elderly patients who you know have been through the war and they’re just used to coping with things and you just suck it up … it’s like a badge of honour to be able to say ‘I’m not one of these pill-takers ’” (C3P03 registered nurse [RN])) or when patients were concerned that reporting pain might reduce their fitness for anti-cancer treatment: “[ patients might think that] if I tell them honestly how crappy I am with other symptoms and pain and everything, then they might stop my chemo” (C3P02 palliative care physician). Several participants perceived that under-reporting was also due to patients taking an overly passive role in consultations: “[clinicians assume that] if the patient doesn’t bring it up, it’s not a problem for them and … then the patient [is] thinking ‘the doctor will only talk about important things that are important for me and I won’t mention it because obviously it’s not important’ ” (C3P02 palliative care physician and clinical champion).
The screening component of the intervention was considered to address under-reporting by “ normal[ising] ” pain care, thus encouraging disclosure. The patient resource was also considered helpful for building patient capability to partner with clinicians on pain management by “ encouraging self-efficacy ” (C2P01 palliative care physician and clinical champion) through the tools it provided and its positive message that “ you can get control of your pain ” (C3P02 palliative care physician and clinical champion). It was also perceived to help patients “ keep a record ” (C5P03 clinical nurse consultant) of breakthrough pain and analgesia to discuss in their consultation. However, some participants delineated patient groups who might be less able to use the resource, including those with lower educational levels who struggled to set goals and identify an ‘acceptable’ level of pain balanced against side-effects from pharmacological management. For these patients, it was suggested that too many resources could be overwhelming rather than supportive: “ it’s almost like, the more resources they have, the less resourced there are ” (C5P06 RN). At one centre with an especially diverse demographic, patients were said to require substantial support even to understand the purpose and process of pain screening: “ most [patients] look at you going ‘oh, do I have to do anything?’ … They don’t want to read the [instruction] page which is relatively simple ” (C2P03 clinic receptionist).
Invest in clinical champions
All participants perceived the role of clinical champion to be pivotal to the intervention’s success. Champions were perceived to have two major responsibilities: advocating for the intervention among colleagues to boost motivation and providing practical support to build capability.
To be effective advocates, champions were perceived to need support from senior management ( “[leadership of change] it’s got to happen from the top ” (C5P02 RN)) as well as established, cordial relationships with colleagues they could leverage to motivate engagement: “ it also relies on the champion’s personal relationship with the staff which you’re asking to perform these roles and trying to change their management ” (C1P01 palliative care physician and clinical champion). Where champions felt under-supported by management, they relied on moral support from the project team to sustain their advocacy work: “ being the champion, and sometimes being the nagging champion, it actually felt quite nice to have the back-up of other people ” (C1P01 palliative care physician and clinical champion). Both physicians and nurses perceived the champion role might better suit the scope of practice of a junior doctor or senior nurse rather than consultants, based on their willingness to engage and approachability: “ realistically, you’re probably always going to get more engagement with registrars compared to consultants, unless it’s their own trial ” (C5P07 radiation oncologist); “ just give it [the role] to the CNCs [clinical nurse consultants] because as a general rule they’re the best at everything and have the best relationships with the patient ” (C3P04 medical oncologist).
From a practical perspective, clinical champions were expected to provide human resources for establishing and supporting pain screening and patient education: “ you need a body ” (C2P04 clinical nurse consultant). Unfortunately, however, champions across centres reported having limited time protected for the role within their usual duties: “ there just wasn’t the manpower to do that here ” (C3P02 palliative care physician and clinical champion). One suggestion for boosting capacity was to narrow the focus to one clinic and delegate practical tasks to less senior delegates than required for advocacy to render the time commitment more cost-effective: “[ it] might have been better to focus on one clinic and have full-time … junior nurse ” (C5P05 radiation oncologist). This presented an opportunity to train more than one clinical champion to provide better coverage across shifts and safeguard against the risk of losing champions to staff turnover.
Increasing pain awareness is the first step: Plan for slow incremental change rather than rapid uptake
While the barriers above meant only modest practice changes could be achieved, champions at half the centres perceived incremental progress had been made through increasing awareness among personnel regarding pain care as a focus for improvement: “ I think just trying to make pain something that people think about was probably one of the better strategies ” (C1P01 palliative care physician and clinical champion); it’s more at the top of our minds to remember, to screen the pain at every visit ” (C2P01 palliative care physician and clinical champion); “ I think it has highlighted those issues for us and we now need to take this on ” (C5P04 medical oncologist, head of department and clinical champion). Both nursing and medical participants at Centre 5 emphasized the need to be persistent in striving for continuous improvement: “ I think to get practice change, even for well-motivated people, I think it just needs to be pushed … they’ve done similar things with hand washing for doctors and it’s finally getting through ” (C504 medical oncologist and clinical champion); “ it would take more than just one of these kind of programs to get people to change ” (C5P03 clinical nurse consultant). Encouragingly, participants at this and one other centre expected some clinicians to continue using the patient education booklet and resource after the project ended: “ I’d just love to continue using these booklets ” (C5P02 RN); “[the] patient-held resource has been useful and has been taken up by people and I think they will continue to use those ” (C6P02 palliative care physician and clinical champion).
This qualitative sub-study of a cluster randomized controlled trial identified centre-level capabilities to be the most influential factors impeding or facilitating guideline implementation strategies for improving pain care for outpatients with cancer. Findings suggest that future initiatives of this kind should: consider centre readiness for change; articulate and deliver on the intervention’s value proposition; define clinician roles and responsibilities; integrate the intervention within existing systems and processes; promote patient partnership; invest in the clinical champion role, drawing from senior nurses and junior doctors, with support from medical leaders and management; and design the initiative around slow incremental change rather than rapid uptake.
Our findings are largely consistent with those from an ethnographic study exploring factors influencing implementation of cancer pain guidelines in Korean hospital cancer units, which identified a ‘lack of receptivity for change’ to be a key barrier [ 28 ]. However, observations from the Korean study suggested that a lack of centre leadership and cultural norms regarding nursing hierarchy were the most important underlying factors, whereas our Australian sample focused more on constraints imposed by centre systems and processes and a lack of clarity regarding disciplinary roles. These factors were consistently emphasized regardless of participants’ discipline and seniority, including by one centre’s head of department. Consistent with these findings, a recent Australian qualitative sub-study of anxiety/depression guideline implementation in oncology centres found greater role flexibility to be a key factor underpinning organisational readiness for change [ 29 ]. This team also provided quantitative evidence consistent with our finding that centres’ readiness for change is associated with personnel’s perception of benefit from guideline implementation [ 30 ]. Future initiatives should work harder to persuade clinicians of the intervention’s rationale and evidence base prior to commencement, given that perceptions of coherence and effectiveness are key dimensions of acceptability required for clinicians to invest time and effort [ 31 ]. Since our Trial was conducted, evidence has emerged for an impact from cancer symptom screening on survival that could be used persuasively [ 32 ]. Furthermore, the spaced education module might be more acceptable if made adjustable to the knowledge levels of a broader range of clinicians.
Other studies on implementation of cancer pain guidelines [ 11 , 13 ] suggest that structured approaches to process change tend to be more successful than less prescriptive approaches of the kind taken in the Stop Cancer PAIN Trial. We provided centres with guideline implementation strategies but no clear guidance on how to integrate these within existing contexts - i.e. implementation of the implementation, or ‘meta-implementation’. It was wrongly assumed that clinical champions could support integration with centre processes based on their knowledge of local context, but this turned out to be unreasonable given champions’ limited time for the role and lack of training in change management. Like most research to date [ 33 , 34 ], our trial focused largely on the advocacy role played by clinical champions, neglecting more practical and time consuming aspects that our interviews identified to be just as important. We join others in calling for more research on the mechanisms by which clinical champions can optimally facilitate change and ways to maximize their efficacy through training and support [ 24 ]. This should include exploration of optimal models by which different aspects of the champion role might be shared between more than one person where no-one is available with all the necessary attributes, as well as ways to ensure sustainability after support from the project team is withdrawn.
Theory-based research suggests that adding complex interventions to complex healthcare systems creates dynamic interplay and feedback loops, making consequences hard to predict [ 35 ]. In the current trial, this was likely exacerbated by our attempt to combine multiple strategies targeting patient, clinician and centre levels. We chose each strategy based on evidence for its stand-alone efficacy, and combined strategies rather than used them singly with the intent of leveraging complementary mechanisms, as recommended by the COM-B Model and US Institute of Medicine [ 36 ]. However, findings from our interviews suggest that interactions between the strategies and local processes separated their spheres of influence, precluding intended synergies. The Stop Cancer PAIN Trial is not alone in having over-estimated the value of combining guideline implementation strategies; a recent systematic review found that 8 other multi-component interventions similarly demonstrated limited effects on guideline adherence and patient outcomes [ 37 ]. Collectively, these findings suggest that future attempts at combining strategies should consider complex systems theory as well as behaviour change frameworks at each of a number of stages [ 38 ]. Alternatively, a more manageable approach for most cancer centres might be to focus on just one component at a time, periodically reviewing progress against SMART goals and, depending on results, supplementing with additional components using plan-do-study cycles [ 39 ].
Given the challenges with integrating screening into centre processes, it seems unlikely that improvements in pain scores during the control phase reported in our primary results article were due to the spontaneous use of screening data in consultations [ 18 ]. Indeed, while routine use of patient-reported outcome measures (PROMs) in oncology has been researched for more than a quarter-century [ 40 ], benefits to patient outcomes have only recently been demonstrated in the context of electronically-administered PROMs (ePROMs) that enable remote self-reporting, real-time feedback to clinicians, and clinician-patient telecommunication [ 12 ]. Further research is needed on how best to support clinician engagement with ePROMs, including training on how to use results in partnership with patients to assist shared decision-making and self-management [ 41 ].
A worrying finding from the current study was that some or all aspects of pain care were perceived to fall between the scopes of practice for oncology clinicians from each discipline. Clinical practice guidelines emphasize the need for pain care to be inter-disciplinary in recognition of the need for comprehensive assessment, non-pharmacological as well as pharmacological management, and patient education and support for self-management [ 42 ]. While the patient self-management resource included in the intervention was perceived to support communication between clinicians and patients, its potential for assisting coordination of care between disciplines was limited where roles and responsibilities were not previously established. Our findings and other research suggest that future initiatives may benefit from ‘process mapping’ with clinicians to identify where clinical workflow and roles might be reconfigured to incorporate the various aspects of pain care in the most efficient ways that do not substantially add to workload [ 41 ].
Patient education has been proven to improve pain outcomes by clinical trials [ 43 , 44 ], and we have argued previously that supporting pain self-management should be core business for all clinicians working in cancer care [ 45 ]. The ‘coaching’ approach needed to empower patients to recognize themselves as ‘experts’ on their pain and equal partners with clinicians in its management is iterative rather than a single event, and is ideally built on established and ongoing therapeutic relationships of trust with a particular team member. However, findings from patient education research more generally suggest that patient education and behaviour change is also optimally supported when key messages are reinforced by differing disciplinary perspectives [ 46 ]. Results from the current study suggest that these principles of pain care need more formal recognition within the scope of practice of oncology clinicians to ensure they are afforded sufficient time alongside anti-cancer treatment and related supportive care. Findings also indicate that clinicians may require training in the person-centred, partnership-oriented aspects of pain care beyond the educational approach used in the Stop Cancer PAIN Trial and other research [ 47 ]. Such training should be repeated regularly to ensure it reaches the majority of personnel at cancer centres, allowing for turnover.
Limitations
The current study had several limitations. Transferability even within Australia is limited by a focus on metropolitan services in only three out of eight jurisdictions. Data relied on clinician perspectives, and the response rate was less than one quarter of personnel at each centre, with the disciplines and specialties of participants being unrepresentative of centre workforces. Over-sampling of medical compared to nursing personnel likely reflects the fact that all clinical champions were medical consultants, while the predominance of palliative care physicians among medical participants presumably arises from the central focus this specialty has on pain care. Notably, our sample included no perspectives from allied health disciplines, despite the important roles these can play in non-pharmacological pain management. Confirmability was threatened by the potential for cognitive bias among researchers towards a favourable view of the intervention given their long-standing investment as members of the project team. We attempted to offset this by explicitly inviting criticism of the intervention from participants, and having the initial analysis conducted by researchers with no prior involvement in the project. A final limitation concerns reliance on the COM-B Model for analysis rather than an alternative framework or more inductive approach. While the COM-B has been widely used to explore barriers and facilitators across a wide range of healthcare interventions, we applied the model in a somewhat novel way to systems and processes as well as individuals’ behaviour after finding that participants perceived their agency to be majorly constrained by these. An implementation framework such as the integrated-Promoting Action on Research Implementation in Health Service (i-PARIHS) framework (iPARIHS) [ 48 ] or Consolidated Framework for Implementation Research (CFIR) [ 49 ] would have conceived of factors and their relationships in alternative ways that might have proven equally informative [ 50 ].
This qualitative sub-study elucidated important factors influencing the success of guideline implementation strategies at six cancer centres in the Stop Cancer PAIN Trial. Findings underscore the value that a qualitative approach offers for understanding the role of context when evaluating complex interventions [ 51 ]. Ultimately, the Stop Cancer PAIN Trial may have been overly ambitious in the scale of its intervention, especially given limited resources available at each centre. Further research is needed to understand how multi-component guideline implementation strategies can be optimally introduced within the context of local roles, systems and processes.
Availability of data and materials
The qualitative interview datasets generated and analysed during the current study are not publicly available due to the conditions of ethical approval which acknowledge the risk of participant re-identification.
Van Den Beuken-Van MH, Hochstenbach LMJ, Joosten EAJ, Tjan-Heijnen VCG, Janssen DJA. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manag. 2016;51(6):1070–90.
Article Google Scholar
Luckett T, Davidson PM, Green A, Boyle F, Stubbs J, Lovell M. Assessment and management of adult cancer pain: a systematic review and synthesis of recent qualitative studies aimed at developing insights for managing barriers and optimizing facilitators within a comprehensive framework of patient care. J Pain Symptom Manag. 2013;46(2):229–53.
Oldenmenger WH, Sillevis Smitt PAE, van Dooren S, Stoter G, van der Rijt CCD. A systematic review on barriers hindering adequate cancer pain management and interventions to reduce them: a critical appraisal. Eur J Cancer. 2009;45(8):1370–80.
Article PubMed Google Scholar
Jacobsen R, Sjogren P, Moldrup C, Christrup L. Physician-related barriers to cancer pain management with opioid analgesics: a systematic review. J Opioid Manag. 2007;3(4):207–14.
Jacobsen R, Moldrup C, Christrup L, Sjogren P. Patient-related barriers to cancer pain management: a systematic exploratory review. Scand J Caring Sci. 2009;23(1):190–208.
Jacobsen R, Liubarskiene Z, Moldrup C, Christrup L, Sjogren P, Samsanaviciene J. Barriers to cancer pain management: a review of empirical research. Medicina (Kaunas). 2009;45:427–33.
Fazeny B, Muhm M, Hauser I, Wenzel C, Mares P, Berzlanovich A, et al. Barriers in cancer pain management. Wiener Klinische Wochenschrift. 2000;112(22):978–81.
CAS PubMed Google Scholar
Makhlouf SM, Pini S, Ahmed S, Bennett MI. Managing pain in people with cancer—a systematic review of the attitudes and knowledge of professionals, patients, caregivers and Public. J Cancer Educ. 2020;35(2):214–40.
Roberto A, Greco MT, Uggeri S, Cavuto S, Deandrea S, Corli O, et al. Living systematic review to assess the analgesic undertreatment in cancer patients. Pain Pract. 2022;22(4):487–96.
Brink-Huis A, van Achterberg T, Schoonhoven L, Brink-Huis A, van Achterberg T, Schoonhoven L. Pain management: a review of organisation models with integrated processes for the management of pain in adult cancer patients. J Clin Nurs. 2008;17(15):1986–2000.
Du Pen SL, Du Pen AR, Polissar N, Hansberry J, Kraybill BM, Stillman M, et al. Implementing guidelines for cancer pain management: results of a randomized controlled clinical trial. J Clin Oncol. 1999;17(1):361–70.
Article CAS PubMed Google Scholar
Govindaraj R, Agar M, Currow D, Luckett T. Assessing patient-reported outcomes in routine cancer clinical care using electronic administration and telehealth technologies: Realist synthesis of potential mechanisms for improving health outcomes. J Med Internet Res. 2023;25:e48483.
Article PubMed PubMed Central Google Scholar
Koesel N, Tocchi C, Burke L, Yap T, Harrison A. Symptom distress: implementation of palliative care guidelines to improve pain, fatigue, and anxiety in patients with advanced cancer. Clin J Oncol Nurs. 2019;23(2):149–55.
PubMed Google Scholar
Dulko D, Hertz E, Julien J, Beck S, Mooney K. Implementation of cancer pain guidelines by acute care nurse practitioners using an audit and feedback strategy. J Am Acad Nurse Pract. 2010;22(1):45–55.
Samuelly-Leichtag G, Adler T, Eisenberg E. Something must be wrong with the implementation of cancer-pain treatment guidelines. A lesson from referrals to a pain clinic. Rambam Maimonides Med J. 2019;10(3):18.
Lopez Lopez R, Camps Herrero C, Khosravi-Shahi P, Guillem Porta V, Carrato Mena A, Garcia-Foncillas J, et al. Oncologist’s knowledge and implementation of guidelines for breakthrough cancer pain in Spain: CONOCE study. Clin Transl Oncol. 2018;20(5):613–8.
Luckett T, Phillips J, Agar M, Lam L, Davidson PM, McCaffrey N, et al. Protocol for a phase III pragmatic stepped wedge cluster randomised controlled trial comparing the effectiveness and cost-effectiveness of screening and guidelines with, versus without, implementation strategies for improving pain in adults with cancer attending outpatient oncology and palliative care services: the Stop Cancer PAIN trial. BMC Health Serv Res. 2018;18(1):1–13.
Lovell MR, Phillips JL, Luckett T, Lam L, Boyle FM, Davidson PM, et al. Effect of cancer pain guideline implementation on pain outcomes among adult outpatients with cancer-related pain: a stepped wedge cluster randomized trial. JAMA Netw Open. 2022;5(2):1–12.
Lovell M, Luckett T, Boyle F, Stubbs J, Phillips J, Davidson PM, et al. Adaptation of international guidelines on assessment and management of cancer pain for the Australian context. Asia-Pac J Clin Oncol. 2015;11(2):170–7.
Phillips JL, Heneka N, Bhattarai P, Fraser C, Shaw T. Effectiveness of the spaced education pedagogy for clinicians’ continuing professional development: a systematic review. Med Educ. 2019;53(9):886–902.
Cancer Council Australia. Overcoming cancer pain: A guide for people with cancer, their families and friends 2013 [Available from: http://www.cancercouncil.com.au/wp-content/uploads/2014/01/Can487-Overcoming-Pain-NSW-Lores2.pdf .
Luckett T, Davidson PM, Green A, Marie N, Birch MR, Stubbs J, et al. Development of a cancer pain self-management resource to address patient, provider, and health system barriers to care. Palliat Support Care. 2019;17(4):472–8.
Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. London: Silverback Publishing; 2014.
Google Scholar
Santos WJ, Graham ID, Lalonde M, Demery Varin M, Squires JE. The effectiveness of champions in implementing innovations in health care: a systematic review. Implement Sci Commun. 2022;3(1):80.
Ramanadhan S, Revette AC, Lee RM, Aveling EL. Pragmatic approaches to analyzing qualitative data for implementation science: an introduction. Implement Sci Commun. 2021;2(1):70.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):117.
Kim M, Jeong S, McMillan M, Higgins I. Translation of policy and guidelines into practice: lessons learned from implementation of the cancer pain management guideline. J Hosp Manage Health Policy. 2020;4. https://doi.org/10.21037/jhmhp.2020.02.01 .
Geerligs L, Shepherd HL, Butow P, Shaw J, Masya L, Cuddy J, et al. What factors influence organisational readiness for change? Implementation of the Australian clinical pathway for the screening, assessment and management of anxiety and depression in adult cancer patients (ADAPT CP). Support Care Cancer. 2021;29(6):3235–44.
Faris MM, Shepherd HL, Butow PN, Kelly P, He S, Rankin N, et al. Staff- and service-level factors associated with organisational readiness to implement a clinical pathway for the identification, assessment, and management of anxiety and depression in adults with cancer. BMC Health Serv Res. 2023;23(1):866.
Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):88.
Caminiti C, Maglietta G, Diodati F, Puntoni M, Marcomini B, Lazzarelli S, et al. The effects of patient-reported outcome screening on the survival of people with cancer: a systematic review and meta-analysis. Cancers. 2022;14(21):5470.
Morena AL, Gaias LM, Larkin C. Understanding the role of clinical champions and their impact on clinician behavior change: the need for causal pathway mechanisms. Front Health Serv. 2022;2:896885.
Miech EJ, Rattray NA, Flanagan ME, Damschroder L, Schmid AA, Damush TM. Inside help: an integrative review of champions in healthcare-related implementation. SAGE Open Med. 2018;6:2050312118773261.
Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 2018;16:1–14.
Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical Practice Guidelines We Can Trust. In: Graham R, Mancher M, Miller Wolman D, Greenfield S, Steinberg E, editors. Washington, D.C.: National Academies Press; 2011.
Bora A-M, Piechotta V, Kreuzberger N, Monsef I, Wender A, Follmann M, et al. The effectiveness of clinical guideline implementation strategies in oncology—a systematic review. BMC Health Serv Res. 2023;23(1):347.
McGill E, Er V, Penney T, Egan M, White M, Meier P, et al. Evaluation of public health interventions from a complex systems perspective: a research methods review. Soc Sci Med. 2021;272: 113697.
Institute for Healthcare Improvement. Quality improvement essentials toolkit. 2017.
Trowbridge RDW, Jay SJ, et al. Determining the effectiveness of a clinical-practice intervention in improving the control of pain in outpatient with cancer. Acad Med. 1997;72:798–800.
Howell D, Rosberger Z, Mayer C, Faria R, Hamel M, Snider A, et al. Personalized symptom management: a quality improvement collaborative for implementation of patient reported outcomes (PROs) in ‘real-world’ oncology multisite practices. J Patient Rep Outcomes. 2020;4(1):47.
Australian Adult Cancer Pain Management Guideline Working Party. Autralian clinical pathway for screening, assessment and management of cancer pain in adults Sydney, Australia: Cancer Council Australia. 2013. http://wiki.cancer.org.au/australia/Guidelines:Cancer_pain_management/Flowchart_overview .
Marie N, Luckett T, Davidson P, Lovell M, Lal S. Optimal patient education for cancer pain: a systematic review and theory-based meta-analysis. Support Care Cancer. 2013;21:3529–37.
Abernethy AP, Currow DC, Shelby-James T, Rowett D, May F, Samsa GP, et al. Delivery strategies to optimize resource utilization and performance status for patients with advanced life-limiting illness: results from the palliative care trial [ISRCTN 81117481]. J Pain Symptom Manage. 2013;45(3):488–505.
Lovell MR, Luckett T, Boyle FM, Phillips J, Agar M, Davidson PM. Patient education, coaching, and self-management for cancer pain. J Clin Oncol. 2014;32(16):1712–20.
Luckett T, Roberts MM, Smith T, Swami V, Cho JG, Wheatley JR. Patient perspectives on how to optimise benefits from a breathlessness service for people with COPD. NPJ Prim Care Respir Med. 2020;30(1). https://doi.org/10.1038/s41533-020-0172-4 .
Phillips JL, Heneka N, Lovell M, Lam L, Davidson P, Boyle F, et al. A phase III wait-listed randomised controlled trial of novel targeted inter-professional clinical education intervention to improve cancer patients’ reported pain outcomes (the Cancer Pain Assessment (CPAS) Trial): study protocol. Trials. 2019;20:1–12.
Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci. 2016;11(1):33.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci. 2022;17(1):1–16.
Geerligs L, Rankin NM, Shepherd HL, Butow P. Hospital-based interventions: a systematic review of staff-reported barriers and facilitators to implementation processes. Implement Sci. 2018;13(1):36.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of medical research council guidance. BMJ. 2021;374:n2061.
Download references
Acknowledgements
The authors would like to dedicate this article to the memory of Sally Fielding, who worked as a valued member of the project team throughout the Stop Cancer PAIN Trial. We would also like to acknowledge the contributions of project manager A/Prof Annmarie Hosie, data manager Dr Seong Cheah, and research assistant Layla Edwards.
This research was supported by a grant from the National Breast Cancer Foundation.
Author information
Authors and affiliations.
IMPACCT Centre—Improving Palliative, Aged and Chronic Care through Clinical Research and Translation, Faculty of Health, University of Technology Sydney (UTS), Building 10, 235 Jones St, Ultimo, Sydney, NSW, 2007, Australia
Tim Luckett, Meera Agar & Maja Garcia
School of Nursing and Centre for Healthcare Transformation, Queensland University of Technology (QUT), Brisbane, QLD, Australia
Jane Phillips
South West Sydney School of Clinical Medicine, University of New South Wales (UNSW), Sydney, NSW, Australia
The Limbic, Sydney, Australia
Linda Richards
Palliative Care Department, Greenwich Hospital, HammondCare, Sydney, NSW, Australia
Najwa Reynolds & Melanie Lovell
University of Wollongong, Wollongong, NSW, Australia
Patricia Davidson & David Currow
Charles Perkins Centre, School of Medical Sciences, The University of Sydney, Sydney, NSW, Australia
Patricia Ritchie Centre for Cancer Care and Research, The University of Sydney, Sydney, NSW, Australia
Frances Boyle
Northern Medical School, The University of Sydney, Sydney, NSW, Australia
Frances Boyle & Melanie Lovell
Macau University of Science and Technology, Macau, China
Lawrence Lam
Deakin Health Economics, Institute for Health Transformation, School of Health and Social Development, Deakin University, Melbourne, Australia
Nikki McCaffrey
You can also search for this author in PubMed Google Scholar
Contributions
TL, JP, MA, PMD, TS, DCC, FB, LL, NM and ML contributed to the concept and design of this research. TL, LR, MR, MG and ML contributed to the acquisition, analysis or interpretation of the data. TL and ML contributed to drafting of the manuscript. All authors contributed to revisions of the manuscript and approved the final version.
Corresponding author
Correspondence to Tim Luckett .
Ethics declarations
Ethics approval and consent to participate.
This research was approved by the Southwestern Sydney Local Health District Human Research Ethics Committee (HREC/14/LPOOL/479). All participants gave written informed consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Luckett, T., Phillips, J., Agar, M. et al. Factors influencing fidelity to guideline implementation strategies for improving pain care at cancer centres: a qualitative sub-study of the Stop Cancer PAIN Trial. BMC Health Serv Res 24 , 969 (2024). https://doi.org/10.1186/s12913-024-11243-1
Download citation
Received : 10 April 2024
Accepted : 25 June 2024
Published : 22 August 2024
DOI : https://doi.org/10.1186/s12913-024-11243-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Implementation
- Qualitative
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Publications
- Discussion Paper Series(English)
RIEB Discussion Paper Series No.2024-28
Industry Dynamics with Cartels: The Case of the Container Shipping Industry
I investigate how explicit cartels, known as "shipping conferences", in a global container shipping market facilitated the formation of one of the largest globally integrated markets through entry, exit, and shipbuilding investment of shipping firms. Using a novel data, I develop and construct a structural model and find that the cartels shifted shipping prices by 20-50% and encouraged firms' entry and investment. In the counterfactual, I find that cartels would increase producer surplus while slightly decreasing consumer surplus, then may increase social welfare by encouraging firms' entry and shipbuilding investment. This would validate industry policies controlling prices and quantities in the early stage of the new industry, which may not be always harmful. Investigating hypothetical allocation rules supporting large or small firms, I find that the actual rule based on tonnage shares is the best to maximize social welfare.
- Site Policy (in Japanese)
Main navigation
- Scholarships
- Interview with Miren Azkarate, visiting researcher at CIRM and holder of the Elbira-Zipitria Chair in the Basque Country
Event | Cultural safety in the context of Indigenous health research | June 6, 2024
- Tweet Widget
After extensive work over two years, Tahatikonhsontóntie' – the Quebec Network Environment in Indigenous Health Research (Qc-NEIHR), with the collaboration of Unité de Soutien SSA Québec, the Department of Family Medicine of McGill University, and the Office of Joyce’s Principle—is making public their report on cultural safety in the context of Indigenous health research.
Cultural safety has emerged as a response to systemic racism that has been experienced by Indigenous Peoples in public services, and it has been expanded to research. This report, thought to be the first on this topic in Quebec, is a follow-up to a roundtable discussion on the topic that took place in Montréal between April 26 and 28, 2023, which brought together 45 people who shared an interest in transforming Indigenous health research environments.
When : Thursday June 6, 2pm to 4pm.
Where: Hybrid. In person at: 5858 Côte-des-Neiges, the Department of Family Medicine, second-floor at the Indigenous Space, Room 218. Online via Zoom (a link will be sent to you after registration).
Contact Information
Department and university information.

- Presentation Document
- Partners and Projects
- Bylaws and Regulations
- 2022–2023 Annual Report
- Recent News
- CIRM's network 2023-2024
- Submit an announcement
- BMO Fellowship
- Newsletters

IMAGES
COMMENTS
Table of contents. What not to include in your discussion section. Step 1: Summarize your key findings. Step 2: Give your interpretations. Step 3: Discuss the implications. Step 4: Acknowledge the limitations. Step 5: Share your recommendations. Discussion section example. Other interesting articles.
Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion. Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and ...
The discussion section is often considered the most important part of your research paper because it: Most effectively demonstrates your ability as a researcher to think critically about an issue, to develop creative solutions to problems based upon a logical synthesis of the findings, and to formulate a deeper, more profound understanding of the research problem under investigation;
1.Introduction—mention gaps in previous research¹⁻². 2. Summarizing key findings—let your data speak¹⁻². 3. Interpreting results—compare with other papers¹⁻². 4. Addressing limitations—their potential impact on the results¹⁻². 5. Implications for future research—how to explore further¹⁻².
The discussion section provides an analysis and interpretation of the findings, compares them with previous studies, identifies limitations, and suggests future directions for research. This section combines information from the preceding parts of your paper into a coherent story. By this point, the reader already knows why you did your study ...
The discussion section is one of the final parts of a research paper, in which an author describes, analyzes, and interprets their findings. They explain the significance of those results and tie everything back to the research question(s). In this handout, you will find a description of what a discussion section does, explanations of how to ...
Begin the Discussion section by restating your statement of the problem and briefly summarizing the major results. Do not simply repeat your findings. Rather, try to create a concise statement of the main results that directly answer the central research question that you stated in the Introduction section.
Discussion Phrases Guide. Papers usually end with a concluding section, often called the "Discussion.". The Discussion is your opportunity to evaluate and interpret the results of your study or paper, draw inferences and conclusions from it, and communicate its contributions to science and/or society. Use the present tense when writing the ...
Point out exceptions or lack of correlations. Define why you think this is so. State your conclusions clearly. Summarize your evidence for each conclusion. "Discussion and Conclusions Checklist" from: How to Write a Good Scientific Paper. Chris A. Mack. SPIE. 2018.
Tips to Write the Results Section. Direct the reader to the research data and explain the meaning of the data. Avoid using a repetitive sentence structure to explain a new set of data. Write and highlight important findings in your results. Use the same order as the subheadings of the methods section.
This discussion example is from an engineering research paper. The authors are restating their aims first, which is to compare different types of storm-tracking software. Then, they are providing a brief summary of the methods. Here, they are testing different storm-tracking software under different conditions to see which performs the best.
Discussion Section. The overall purpose of a research paper's discussion section is to evaluate and interpret results, while explaining both the implications and limitations of your findings. Per APA (2020) guidelines, this section requires you to "examine, interpret, and qualify the results and draw inferences and conclusions from them ...
The discussion section can be written in 3 parts: an introductory paragraph, intermediate paragraphs and a conclusion paragraph. For intermediate paragraphs, a "divide and conquer" approach, meaning a full paragraph describing each of the study endpoints, can be used. In conclusion, academic writing is similar to other skills, and practice ...
After a research article has presented the substantive background, the methods and the results, the discussion section assesses the validity of results and draws conclusions by interpreting them. The discussion puts the results into a broader context and reflects their implications for theoretical (e.g. etiological) and practical (e.g ...
The Discussion section can: 1. Start by restating the study objective. Example 1: " The purpose of this study was to investigate the relationship between muscle synergies and motion primitives of the upper limb motions.". Example 2: " The main objective of this study was to identify trajectories of autonomy.". Example 3:
Discussion is mainly the section in a research paper that makes the readers understand the exact meaning of the results achieved in a study by exploring the significant points of the research, its ...
Organization and Structure. Keep the following sequential points in mind as you organize and write the discussion section of your paper: Think of your discussion as an inverted pyramid. Organize the discussion from the general to the specific, linking your findings to the literature, then to theory, then to practice [if appropriate]. Use the ...
The discussion section, a systematic critical appraisal of results, is a key part of a research paper, wherein the authors define, critically examine, describe and interpret their findings ...
Return to all guides. Results and Discussion Sections in Scientific Research Reports (IMRaD) After introducing the study and describing its methodology, an IMRaD* report presents and discusses the main findings of the study. In the results section, writers systematically report their findings, and in discussion, they interpret these findings.
Typical structure of the Discussion section in an empirical research paper: Discussion sections follow a narrow-to-broad structure. There are some variations among disciplines (for example some employ subsections in the Discussion while others do not), but most make some or all of the following moves: • Reiterate key findings (1 sentence - 1 ...
Elements to Include in the Discussion. State the study's major findings Explain the meaning and importance of the findings Relate the findings to those of similar studies Consider alternative explanations of the findings State the clinical relevance of the findings Acknowledge the study's limitations Make suggestions for further research.
Table of contents. What not to include in your discussion section. Step 1: Summarise your key findings. Step 2: Give your interpretations. Step 3: Discuss the implications. Step 4: Acknowledge the limitations. Step 5: Share your recommendations. Discussion section example.
Abstract. This guide for writers of research reports consists of practical suggestions for writing a report that is clear, concise, readable, and understandable. It includes suggestions for terminology and notation and for writing each section of the report—introduction, method, results, and discussion. Much of the guide consists of ...
This paper reports a sub-study of the Trial which aimed to identify factors inhibiting or enabling fidelity to inform future guideline implementation initiatives. ... who had no previous involvement in the project but were experienced in qualitative research. Review and discussion with two team members who were involved in the project ...
RIEB Discussion Paper Series No.2024-28 Title. Industry Dynamics with Cartels: The Case of the Container Shipping Industry Abstract. I investigate how explicit cartels, known as "shipping conferences", in a global container shipping market facilitated the formation of one of the largest globally integrated markets through entry, exit, and shipbuilding investment of shipping firms.
Cultural safety has emerged as a response to systemic racism that has been experienced by Indigenous Peoples in public services, and it has been expanded to research. This report, thought to be the first on this topic in Quebec, is a follow-up to a roundtable discussion on the topic that took place in Montréal between April 26 and 28, 2023 ...