An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry

A literature review of sleep problems and neurodevelopment disorders
Introduction.
Sleep is an incredibly complex process that goes beyond relaxing and body resting. Disturbance in sleep leads to several short-term and long-term consequences. Neurodevelopmental diseases such as “autism spectrum disorder” (ASDs), Attention-deficit hyperactivity disorder (ADHD), and intellectual disability commonly experience sleep disorders that affect their clinical presentation, daily function, and quality of life.
The incidence of sleep problems in ASD patients ranges from 32 to 71.5%, especially insomnia, while an estimated 25–50% of people with ADHD report having sleep issues in clinical settings. The incidence of sleep issues is widespread in persons with intellectual disabilities, reaching up to 86%. This article is a literature review covering the neurodevelopmental disorder interaction with sleep disorder and different management.
Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to be chronic. Recognizing and diagnosis of sleep disorders will enhance their function, response to treatment, and quality of life.
Sleep disorder
Sleeping is an incredibly complex process that goes beyond relaxing and body resting. It is a state of involuntary activity in which the brain is relatively still and responds to internal stimuli during NREM, and 20% is approximately active during REM. The exact purpose of sleep is not fully understood. Sleep has many functions, including neuronal plasticity, memory consolidation, immune function, growth, and mental health. Sympathetic overtone, an increase in the activity of hypothalamic–pituitary–adrenal axis, metabolic disorders, and inflammatory responses are factors that may cause disturbance in the sleep rhythm. Disturbance in sleep leads to several short-term consequences such as emotional disturbance, increase in stress response, mood disorder, cognitive and performance deficits, somatic pain, and reduced quality of life. Sleep disturbance influences teenagers’ mental health, academic performance, and risk-taking behaviors. Sleep disturbance in children is linked to behavioral issues and impaired cognitive performance. In those who are otherwise healthy, sleep disturbance can have long-term effects such as dyslipidemia, hypertension, cardiovascular disease, problems with weight, type 2 diabetes, metabolic syndrome, and colorectal cancer ( 1 – 3 ). The basic form of normal sleep organization is called sleep architecture. The sleep cycle is composed of two phases: non-rapid eye movement (NREM) sleep and rapid eye movement (REM). Phases 1, 2, 3, and 4 of NREM sleep form a continuum of relative depth. Every individual has distinctive characteristics of sleep, such as variations in eye movements, muscle tone, and brain wave patterns. Electroencephalogram (EEG) recordings, which monitor electrical patterns of brain activity, have been used to show sleep cycles and phases ( 4 ). The aging process has continuous and considerable effects on sleep architecture. There are noticeable differences between childhood and adulthood in sleep initiation and maintenance, the duration spent in each phase, and overall sleep efficiency. Studying age-related decreases in sleep efficiency is a general trend. Though the effects of insufficient sleep are generally well established, the causes are complicated and poorly understood. Therefore, when examining sleep stages in children of different ages, it is critical to take their unique characteristics into account. However, examining sleep characteristics according to age enables a more in-depth comprehension of how sleep contributes to effective aging and human development. Sleep disorders according to DSM-5 are insomnia, parasomnia, breath-related disorders, hypersomnolence, narcolepsy, circadian rhythm sleep–wake disorder and substance, and medication-related disorder ( 5 ).
Analysis of phenotypes for sleep disorder
There are several types of sleep assessment methods that should be customized for each child. Subjective methods including parent-reported surveys and sleep diaries are among the most frequently employed methods in the analysis of sleep disorders in human studies. They offer various advantages, including non-invasive acquisition and low costs. Children’s Sleep Habits Questionnaire (CSHQ) is considered one of the most popular parent-completed surveys. It is a tool for assessment of sleep in school-aged children based on parental reports ( 6 ). Another method is the Electroencephalography (EEG). It involves two electrodes that are attached to the patient’s scalp. It provides a recording of the brain’s electrical activity throughout sleep and weakness ( 7 ). A method known as a polysomnogram (PSG) is regarded as the benchmark for the objective assessment of sleep compared to a single-channel EEG ( 8 ). It incorporates physiological indications of normal and abnormal brain electrical activity, sleep architecture, sleep stages, and sleep quality, as well as eye movements and physical activities during sleep. Actigraphy provides a non-invasive evaluation of limb activity using an accelerometer to identify episodes of sleep and wakefulness. It enables the collection of data over several days in unstructured settings. The reliability of actigraphy with PSG was examined and revealed a strong relationship between PSG and actigraphy measures (>0.80) for sleep latency, length, and efficiency ( 9 ). Similar to actigraphy, videosomnography’s benefits come from its objective documentation over a long period ( 10 ). It can also be used to record unusual occurrences like nighttime parasomnias. However, using videosomnography in child sleep research comes with several difficulties.
Sleep problems and autism spectrum disorders
Autism spectrum disorders (ASDs) have a wide range of clinical symptoms that are connected to social communication and interaction. Restrictive, repetitive, and stereotyped behaviors and interests are common in ASD. They have persistent difficulties in reciprocal social interaction and communication across a variety of circumstances. High levels of co-occurring behavioral difficulties are frequently present in children with ASD. According to the most recent report from the United States, the incidence was 1/54 in 2020. One of the most common features of ASD is the sleep disorder that results from the interaction of several factors such as psychological, biological, family factors, environmental, and child practice methods that might not be sleep-friendly ( 11 ).
Incidence of sleep disorders in patients with ASD
The incidence of sleep problems in ASD patients ranges from 32 to 71.5%. Children and adolescents with ASD are more likely to experience sleep difficulties, especially insomnia, with incidence rates ranging from 40 to 80%. This wide range of incidence may be due to the different sleep problems assessment methods and different criteria such as different cut-off scores ( 12 ). After adjusting for family variables including poor child-rearing practices (for example, little parental supervision at bedtime), and noisy, or stressful environments, children with ASD are also more prone to experience sleep disturbances compared with their normal relatives; 47 and 16%, respectively, ( 13 ).
The causes of sleep difficulties in children with ASD
ASD is a multifactorial disease that is affected by multiple factors including neurological, genetic, immunological, and environmental factors. Several neurotransmitters like melatonin, GABA, and serotonin are required to create a regular cycle of sleep and wakefulness. Sleep may be affected by any problems with these neurotransmitters’ synthesis ( 14 ). The hormone melatonin aids in synchronizing and preserving the circadian cycle. Autism may have improper melatonin regulation. The integrity of synaptic transmissions and the control of melatonin in ASD may both be influenced by clock genes ( 15 ). Melatonin exogenous therapy has been demonstrated to improve sleep schedule in ASD kids. Children with ASD showed decreased activity of the final enzyme in the production of melatonin, indicating lower levels of melatonin. This enzyme is encoded by the N-acetylserotonin O-methyltransferase gene ( 16 ). GABA is the neurotransmitter that induces sleep by inhibiting cells that are involved in arousal functions. It is produced from the preoptic area which is the sleep area in the hypothalamus. The Bidirectional Theoretical Framework of Sleep Disturbance provides an overview of the various risk factors that can affect the development of sleep issues in people with ASD ( 12 ).
Effect of sleep disturbances in ASD patients on caregivers
Increased parental sleep problems and maternal stress have been associated with sleep abnormalities in children with ASD. Sleep issues can significantly affect a child’s quality of life, daily functioning, and family dynamics, adding stress to everyone involved. This has also been linked to more challenging behaviors in ASD children during the day, as well as an influence on the ability to control mood. Sleep quality has been linked to common medical disorders such as upper respiratory problems and vision problems. Poor appetite and a decrease in the rate of growth have been linked to increased nighttime awakening and a reduced desire to go to sleep. Sleep disturbance in ASD children has been linked to increased aggression, hyperactivity, and social issues that may be markers of poor mental health outcomes.
Sleep disorders management
It is crucial to conduct early and frequent screenings for sleep impairment and its related conditions.
Non-pharmacological management
Sleep disturbances in children and adolescents with ASD must be managed on both environmental and behavioral levels. Parents must set bedtime routines and provide a relaxing bedroom atmosphere for their children. These environmental and behavioral strategies can improve their sleep, despite the fact that they are challenging to apply ( 17 ). The Sleep Committee of the Autism Treatment Network developed the sleep tool kit (STK), which is a customized behavioral modification tool for children and adolescents with insomnia. STK advocates three approaches: visual scheduling of good evening behaviors, a supplemental relaxing module to reduce arousal levels, and a faded bedtime regimen to sleep when tired. Breathing techniques, muscular relaxation exercises, yoga, massage, mindfulness training, and warm baths are additional soothing modules that aid those patients controlling arousal and anxiety. Taking the developmental characteristics of ASD children into consideration, it is reported that positive routines, unmodified and progressive extinction, and overnight fading are more beneficial in children under 5 years, but older children and adolescents benefit more from cognitive-behavioral therapy (CBT) ( 17 ).
Pharmacological management
Medical treatment is considered if the children do not respond to behavioral therapy.
Role of melatonin
It has been suggested that a lack of sociability may be related to sleep difficulties and circadian rhythm disruptions in ASD patients. Indeed, zeitgebers (also known as timeivers) like the natural light–dark cycle, music, and social cues are necessary for the entrainment and synchronization of the circadian clock. Therefore, in ASD patients, poor social cue perception or interpretation may impair the effectiveness of systems that synchronize sleep and wakefulness ( 18 ). As an alternative, ASD patients could find it difficult to synchronize with their internal and external settings, leading to eventual rhythm and time problems which affect a variety of fields, including social interaction and circadian cycles. In other words, persons with ASD would experience circadian abnormalities due to their failure to reflect their internal clock on environmental and social rhythms ( 19 ).
Melatonin is offered in a variety of over-the-counter preparations ranging from 1 to 10 mg. Most frequently, it is advised to take a dose of 1–3 mg 30–60 min before planned bedtime (46). However, a lower dose (0.5–1 mg) given earlier (3–4 h before night) is advised if a circadian rhythm problem is found. Age or weight has no bearing on the effectiveness of a dose. Melatonin is a pineal hormone that controls the body’s circadian cycle. Melatonin appears to help shorten the time it takes to fall asleep, but its effectiveness at reducing overnight awakenings and other elements of sleep disruptions varies ( 20 ). A study included 24 ASD children aged 1–3 years who exhibited improvement in sleep latency as determined by actigraphy when given 1 mg or 3 mg. This treatment improved not just the children’s sleep patterns, but also their conduct and parental stress ( 21 ).
Antipsychotic medication
This drug class has minimal tolerability and efficacy data for the treatment of insomnia in children. Few trials on the influence on sleep architecture have found that ziprasidone, olanzapine, and risperidone increase slow-wave, although ziprasidone and risperidone reduce REM sleep. Risperidone and olanzapine are two atypical antipsychotic that have been recommended for sleep disorders in children ( 22 ). These medications are used for the treatment of insomnia off-label, and it is not advised that they be regularly prescribed for this use, particularly as a first-line pharmacotherapeutic medication. In particular, the Canadian Academy of Child and Adolescent Psychiatry has advised against using them as a first-line line treatment for insomnia in children, adults, or the elderly ( 23 ). Other countries have likewise attempted to limit the number of prescriptions that government-subsidized programs may allow.
Antidepressant
There is limited evidence on the use and effectiveness of sedative antidepressants, selective serotonin reuptake inhibitors (SSRI), and tricyclic antidepressants (TCA) for the management of sleep disturbances in ASD children. Such medications might be effective if the sleeplessness is accompanied by concomitant psychiatric disorders. Children with comorbid depression may benefit from sedative antidepressants like trazodone and mirtazapine. These antidepressants enhance sleep by reducing the effects of neurotransmitters that promote wakefulness, including acetylcholine, histamine, noradrenaline, and serotonin. As a side effect, the majority of such medications reduce REM sleep and prolong daytime sleepiness. In psychiatric practice, trazodone is widely chosen and employed. Its effectiveness has primarily been shown in people with psychiatric illnesses. Trazodone has a noticeable morning hangover effect due to the antagonism of the 5-HT2A/C and being powerful sedating antidepressant. In contrast, fluoxetine is frequently connected to insomnia. Comparatively speaking to doses used to treat mood disorders, doses used to treat insomnia are typically lower.
Alpha-adrenergic agonist
The two main alpha agonists that are frequently used off-label to treat autism-related sleep disorders are clonidine and guanfacine. Clonidine (dosing range: 0.05–0.225 mg/day) significantly reduced sleep initiation and maintenance insomnia in children and adolescents (aged 4–16 years) with autism and neurodevelopmental problems, with good tolerability and few side effects ( 24 ). Hypotension, irritability, bradycardia, dry mouth, and REM suppression are some of the side effects of clonidine that may occur, and its rapid withdrawal may result in rebound hypertension and rebound REM ( 25 ).
Sedative and hypnotics drugs
Hypnotics and sedatives benzodiazepines (BZDs) are routinely given to adults with insomnia. However, because of their side effects, which include drowsiness, headaches, cognitive impairment, dizziness and rebound sleeplessness, and physical and behavioral dependence, they are recommended less frequently to children. Clonazepam was the only benzodiazepine tested for sleep issues in autistic children. Children with developmental disabilities were found to benefit from the treatment of partial arousals, parasomnias, periodic limb movement disorder, and nocturnal biting with clonazepam, an intermediate-acting BZD ( 26 , 27 ).
Other medication
Several medications which are used in the treatment of the Alzheimer’s disease are also found to be effective in the management of ASD symptoms ( 28 ). Drugs such as donepezil and rivastigmine are cholinesterase inhibitors that increase the acetylcholine by preventing its destruction. ASD is associated with anomalies in the cholinergic system, according to previously published evidence ( 29 ). First, research looking at post-mortem brain samples from people with ASD has discovered cholinergic system anomalies ( 30 , 31 ).
According to several studies, a large percentage of children with ASD condition experience seizures. It is reported that the incidence of ASD cases that suffered from epilepsy may range from 5 to 38% which is much higher than the incidence of the epilepsy in the normal children population which is 1–2% ( 32 , 33 ). There is very limited evidence about the use of anti-epileptic drugs in ASD patients. A randomized controlled trial has been valproate in ASD cases ( 34 ). They found that valproate monotherapy reduced the irritability and repetitive behaviors in ASD cases ( 35 ).
Sleep disorder and ADHD
One of the most frequently identified illnesses in both children and adults is attention-deficit/hyperactivity disorder (ADHD). It affects 2.9% of adults and 3 to 5% of children. It continues into adolescence and adulthood. The diagnostic criteria of ADHD include symptoms of inattention or/and impulsivity that appear prior to 12 years old, and hyperactivity. Untreated ADHD patients suffer from a decrease in several critical functional domains, including the academic, social, and occupational realms ( 36 ).
Types of sleep disorders
An estimated 25–50% of people with ADHD report having sleep issues in clinical settings ( 37 ). Besides, adults who do not have enough time of sleep are more prone to have symptoms of ADHD ( 38 ). Such individuals’ sleep disruptions have been linked to concomitant primary sleep problems and/or changes brought on by ADHD drugs ( 6 ). Researchers have looked into the connections between ADHD and narcolepsy, insomnia, circadian rhythm sleep disorders (CRSDs), restless leg syndrome, and sleep-disordered breathing (SDB) ( 39 , 40 ).
Obstructive sleep apnea and ADHD
Obstructive sleep apnea (OSA) is characterized by partial or total obstruction of the upper airway, which results in interrupted sleep, while SDB is associated with unpredictable breathing rhythm during sleep ( 41 , 42 ). People with ADHD have a higher incidence of SDB, and those with a history of snoring or possible OSA throughout childhood are associated with a two-fold higher susceptibility of diagnoses with ADHD ( 43 ). Through several processes, involving negative effects of hypoxic outcomes, the inflammation that leads to brain, and/or recurrent arousal-based sleep disturbances, SDB influences psychological outcomes. These pathways may change the prefrontal cortex’s neurochemical substrates, resulting in the neurobehavioral abnormalities that underlie the symptoms of ADHD ( 44 ).
Restless leg syndrome and ADHD
Restless leg syndrome (RLS) is a common sensorimotor condition characterized by an intense need to move the legs, which is frequently accompanied by unpleasant leg or (less frequently) body-part feelings. These feelings are particularly uncomfortable in the evening or at night and get better with activity. Due to their need to walk about and the stiffness in their legs, patients frequently have sleeplessness. This comorbidity is thought to be caused by iron deficiency and dopaminergic disorders ( 45 , 46 ). Even though the incidence of RLS in children is unknown, the disorder affects 10% of adults in the United States. According to the data, up to 44% of people with ADHD have RLS or symptoms similar to it, while up to 26% of those with RLS have symptoms similar to it ( 47 , 48 ).
Circadian rhythm sleep disorder and ADHD
The timing of when a person sleeps and is awake is a concern in CRSDs. They result from changes to the circadian clock, its entrainment processes, or a misalignment of the internal circadian rhythm with the external environment. When a person routinely falls asleep and awakens more than 2 h later than is deemed normal, this condition is known as delayed sleep phase syndrome (DSPS). Changes in these processes, reductions in pineal gland volume, and/or anomalies in clock genes have all been discovered in people with ADHD. In adolescents and adults with ADHD, late chronotype and DSPS are typically co-occurring disorders. CRSD and ADHD may share a biological and behavioral etiology ( 49 , 50 ). Impulsivity control issues might impair a person’s capacity to calm down, causing resistance to going to bed and a delayed start to sleep. It is also suggested that those with ADHD might have a greater circadian preference for the evening and a potential endogenous melatonin rise delay ( 50 ).
Narcolepsy and ADHD
A persistent neurological condition called narcolepsy causes problems with sustaining constant wakefulness and sleep. A diagnosis of narcolepsy needs symptoms of rapid eye movement (REM), sleep dissociation (such as sleep paralysis, hypnagogic/hypnopompic hallucinations, and cataplexy), and disturbed nighttime sleep, regardless of how the clinical presentation manifests itself. In the past, it was discovered that adults with narcolepsy had a twice as high probability of receiving an ADHD diagnosis as children as compared to controls ( 51 ). Additionally, data points to children with ADHD experiencing hypo arousal and hypo arousal-related hyperactivity/impulsivity as possible signs of exhaustion ( 52 ). Although the relationship between the two disorders is unclear, it has been postulated that EDS in narcoleptics may cause inattention, deficient executive function, and issues with impulse control that are similar to ADHD and react well to psychiatric drugs ( 53 – 55 ). Finally, the overlap of ADHD and narcolepsy symptoms may result in diagnostic ambiguity or incorrect diagnosis of the diseases. Another theory is that the connection could be due to a common pathology in the brain ( 56 ).
ADHD medication
The effects of stimulants on sleep vary from patient to patient in those with ADHD, reflecting the intricacy of the relationships between sleep disturbance and ADHD ( 57 ). Clinical experience suggests that stimulants generate paradoxical effects, whereby symptom relief can relax patients and encourage sleep, although there is evidence linking stimulants to disturbed sleep in ADHD cases ( 58 , 59 ). Furthermore, increasing the dosage of a short-acting inducer or using a formula with prolonged action may minimize sleep disruptions caused by an increase in hyperactivity or behavioral disorders at bedtime due to the risk of symptom rebound when the concentrations of the drug in the blood is decreased ( 60 , 61 ).
Non-stimulants
The most frequent side effect associated with atomoxetine that is connected to sleep, in contrast to stimulants, is somnolence (a noradrenaline reuptake inhibitor permitted for the management of ADHD). In atomoxetine placebo-controlled trials, somnolence was observed to present in 15–17% of patients as reported by a 2009 comprehensive review ( 62 ). Atomoxetine was found to have less of an impact on subjective sleep measures than methylphenidate and was taken three times per day in a randomized, double-blind trial.
After evaluation and diagnosis, the first stage of treatment will be psychoeducation. In addition to learning about the prognosis, course, therapy, and probable functional implications of the sleep disorder, the affected individuals and their social entourage will require proper psychoeducation on ADHD symptoms and sleep problems. Additionally, educating people about healthy sleep habits and sleeping patterns will enable non-pharmacological sleep enhancement. It is common practice to use medicine to address sleep disturbances. The choice of medication can be directed to address related issues such as daytime malfunction and should be combined with behavioral techniques. Surgery to remove the tonsils or adenoids is the first line of treatment for children with ADHD and SDB, whereas oral appliances, positive airway pressure devices, or surgery are suggested treatments for adults with OSA and ADHD ( 63 ). The sleep environment may need to be changed for people with RLS and ADHD, and behavioral therapies such as iron supplements ( 64 ) (for example, ferrous sulfate) or gabapentin ( 65 ) may also be investigated, especially for a younger population. In an adults, using dopaminergic substances such as L-DOPA, ropinirole, and pramipexole, in addition to, a recently developed drug called rotigotine may also be a possibility ( 66 ).
Treatment options for people with DSPS and ADHD include scheduled melatonin therapy, light therapy ( 67 ), and chronotherapy ( 68 , 69 ). Furthermore, because treatment for DSPS differs from that for insomnia, a clear distinction between the two must be made. Treatment for ADHD and insomnia can differ depending on the age group.
People with intellectual disabilities and sleep disorders
The incidence of sleep issues in children ranges from 24 to 86%, and they are widespread in persons with intellectual disabilities ( 70 ). Adults with mental disabilities are reported to have an incidence of sleep disorders ranging from 8.5 to 34.1%, with a serious sleep problem rate of 9.2%. In one study, it was discovered that 551 older persons with intellectual disabilities had sleep issues in 72% of the cases ( 47 ). The treatment of physical and mental health issues in people with intellectual disabilities is an area that needs more study. Studies conducted on people without intellectual disabilities were often the basis for the development of diagnostic and management techniques. The same pattern is observed in persons with intellectual impairments who have sleep difficulties. There is a lack of information specifically on the causes, effects, and treatments of sleep problems in people with developmental disabilities. Assessment and treatment of sleep issues in persons with intellectual impairments can be informed by knowledge of the several types of sleep issues that these people encounter and the numerous factors that affect their sleep ( 71 ).
Adults with intellectual disabilities have a higher risk to have sleep issues, which could be due to several factors. In individuals with intellectual impairments, a systematic review of the published literature on sleep problems found links between sleep and several characteristics, such as respiratory diseases, psychoactive drugs, mental health illnesses, and challenging behavior ( 47 ). Understanding and taking into account the social, psychological, and biological aspects influencing the higher occurrence of sleep issues in persons with intellectual impairments is crucial for providing person-centered and individualized care. We have looked at several significant contributing elements that must be taken into account when evaluating sleep issues in persons with intellectual disabilities. The association between sleep disturbances and neurodevelopmental diseases like ADHD and ASD has been thoroughly studied above ( 47 ).
Genetic conditions
Our comprehension of the underlying genetic causes of intellectual impairments has recently improved ( 72 ). For example, Down’s syndrome is characterized by obesity, hypotonia, and craniofacial anomalies, all of which raise the likelihood of sleep disorders including obstructive sleep apnea (OSA). Similarly to this, those who have cri du chat syndrome have a higher risk of getting OSA ( 73 ).
Environmental and psychological factors
People with mental disorders frequently experience sleep disturbance as the first sign of a decline in their mental health, and low-quality sleep represents a common feature of many psychotic and affective diseases ( 11 ). When compared to individuals without cognitive disabilities, those with cognitive disabilities have a higher incidence of mental problems, which helps explain why sleep disturbances are so common in this population ( 12 ). When determining the etiology of sleep issues in a person with cognitive disabilities, it is crucial to take the environment’s role in the development of sleep disorders into account. According to Kerr and Wilkinson ( 13 ), staffed residential homes may not be the best places to sleep because people may check on residents at odd hours, which would result in more noise and lights that would be disruptive to sleep ( 13 ).
Diagnosis of sleep disorders
Adults with intellectual impairments are frequently given subjective sleep information by their caregivers, who may disagree with the severity of the problem or may even accept sleep disturbance as a symptom of the person’s underlying condition ( 74 ).
Because of this, sleep problems are more likely to be noticed by a physician when they induce nocturnal or daytime malfunction, including behavioral disorders, impairing a person’s subjective impression of their quality of life ( 75 ). When evaluating sleep disturbances, general population guidelines stress the significance of checking for coexisting medical diseases. This is may be even more crucial for people with intellectual impairments since they are more prone to experience physical health illness that impacts their sleep, such as OSA or epilepsy ( 76 ). For example, it is advised that everyone with Down’s syndrome be evaluated for OSA due to the condition’s high incidence in people with Down’s syndrome. When sleep–wake duration (including naps) is irregular or unpredictable, caregiver-completed sleep diaries and/or actigraphy, ideally conducted for at least 2 weeks, can be used. Individuals with intellectual impairments can be evaluated for physical sleep disorders such as OSA and nocturnal epilepsy using home or in-patient sleep examinations (such as pulse oximetry or the gold standard, polysomnography) ( 77 ). Even though these tests should always be provided when clinically indicated, if a patient is unable to endure the sleep tests, a practical therapy trial may be necessary. The variety of underlying causes of intellectual disability and the characteristics of related comorbidities make managing sleep disturbances challenging. While intellectual disability psychiatrists can easily address some problems, others will need the assistance of sleep physician and/or primary care givers. According to a study, continuous positive airway pressure therapy can significantly enhance behavior, cognitive function, and subjective drowsiness in individuals with Down’s syndrome and OSA ( 78 ). But as this study correctly notes, access to care may be difficult, and as was already said, some individuals with intellectual disabilities might find it difficult to tolerate these tests and treatments. Working together, sleep specialists and psychiatrists may be able to address these issues. For instance, sleep clinics assist the training of mental health nurses for people with intellectual disabilities in exposure treatment to aid those individuals become used to positive airway pressure masks. The initial management for persistent insomnia in the general population is multicomponent cognitive-behavioral therapy (CBT-I), and there are elements of this that can be helpful for individuals with intellectual impairments ( 74 ). Understanding the impacts of environment and lifestyle on sleep, such as caffeine use, exercise, and regular sleep schedules, along with lighting, noise, and temperature, can be achieved through education on sleep hygiene ( 75 ).
Adults with cognitive disabilities are more prone than the general population to lack appropriate daily activity and regular exposure to natural light, thus even small changes to everyday routine and the sleeping environment can be beneficial ( 75 ). The needs of the person should be taken into consideration when making such recommendations, such as lowering external noise for autistic people sensitive to sounds. The evidence is not strong enough to support the use of pharmaceuticals to treat sleep disturbances in adults with intellectual impairments. Melatonin is the drug that has drawn the most attention, maybe due to its favorable side-effect profile and the fact that several trials have demonstrated its efficacy ( 75 ). According to a meta-analysis, melatonin consumption enhances total sleep time and reduces the number of wake-ups per night in people with intellectual disabilities. Currently, the pharmacological management of illnesses other than insomnia tends to use the same routes as those for the general public ( 75 ).
Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to chronicity. Various solutions are required based on the neurodevelopmental problem, but all patients should get behavioral intervention. Understanding the distinctive characteristics of sleep disturbances in patients with neurodevelopmental disorders is critical for effective therapy.
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
A literature review of sleep problems and neurodevelopment disorders
Affiliation.
- 1 Taibah University, College of Medicine, psychiatry, Al Madinah AL Munawara, Saudi Arabia.
- PMID: 36911135
- PMCID: PMC9995546
- DOI: 10.3389/fpsyt.2023.1122344
Introduction: Sleep is an incredibly complex process that goes beyond relaxing and body resting. Disturbance in sleep leads to several short-term and long-term consequences. Neurodevelopmental diseases such as "autism spectrum disorder" (ASDs), Attention-deficit hyperactivity disorder (ADHD), and intellectual disability commonly experience sleep disorders that affect their clinical presentation, daily function, and quality of life.
Discussion: The incidence of sleep problems in ASD patients ranges from 32 to 71.5%, especially insomnia, while an estimated 25-50% of people with ADHD report having sleep issues in clinical settings. The incidence of sleep issues is widespread in persons with intellectual disabilities, reaching up to 86%. This article is a literature review covering the neurodevelopmental disorder interaction with sleep disorder and different management.
Conclusion: Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to be chronic. Recognizing and diagnosis of sleep disorders will enhance their function, response to treatment, and quality of life.
Keywords: attention-deficit hyperactivity disorder; autism spectrum disorders; electroencephalography; intellectual disabilities; sleep disorder.
Copyright © 2023 Al Lihabi.
Publication types
REVIEW article
A literature review of sleep problems and neurodevelopment disorders.

- Taibah University, College of Medicine, psychiatry, Al Madinah AL Munawara, Saudi Arabia
Introduction: Sleep is an incredibly complex process that goes beyond relaxing and body resting. Disturbance in sleep leads to several short-term and long-term consequences. Neurodevelopmental diseases such as “autism spectrum disorder” (ASDs), Attention-deficit hyperactivity disorder (ADHD), and intellectual disability commonly experience sleep disorders that affect their clinical presentation, daily function, and quality of life.
Discussion: The incidence of sleep problems in ASD patients ranges from 32 to 71.5%, especially insomnia, while an estimated 25–50% of people with ADHD report having sleep issues in clinical settings. The incidence of sleep issues is widespread in persons with intellectual disabilities, reaching up to 86%. This article is a literature review covering the neurodevelopmental disorder interaction with sleep disorder and different management.
Conclusion: Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to be chronic. Recognizing and diagnosis of sleep disorders will enhance their function, response to treatment, and quality of life.
Sleep disorder
Sleeping is an incredibly complex process that goes beyond relaxing and body resting. It is a state of involuntary activity in which the brain is relatively still and responds to internal stimuli during NREM, and 20% is approximately active during REM. The exact purpose of sleep is not fully understood. Sleep has many functions, including neuronal plasticity, memory consolidation, immune function, growth, and mental health. Sympathetic overtone, an increase in the activity of hypothalamic–pituitary–adrenal axis, metabolic disorders, and inflammatory responses are factors that may cause disturbance in the sleep rhythm. Disturbance in sleep leads to several short-term consequences such as emotional disturbance, increase in stress response, mood disorder, cognitive and performance deficits, somatic pain, and reduced quality of life. Sleep disturbance influences teenagers’ mental health, academic performance, and risk-taking behaviors. Sleep disturbance in children is linked to behavioral issues and impaired cognitive performance. In those who are otherwise healthy, sleep disturbance can have long-term effects such as dyslipidemia, hypertension, cardiovascular disease, problems with weight, type 2 diabetes, metabolic syndrome, and colorectal cancer ( 1 – 3 ). The basic form of normal sleep organization is called sleep architecture. The sleep cycle is composed of two phases: non-rapid eye movement (NREM) sleep and rapid eye movement (REM). Phases 1, 2, 3, and 4 of NREM sleep form a continuum of relative depth. Every individual has distinctive characteristics of sleep, such as variations in eye movements, muscle tone, and brain wave patterns. Electroencephalogram (EEG) recordings, which monitor electrical patterns of brain activity, have been used to show sleep cycles and phases ( 4 ). The aging process has continuous and considerable effects on sleep architecture. There are noticeable differences between childhood and adulthood in sleep initiation and maintenance, the duration spent in each phase, and overall sleep efficiency. Studying age-related decreases in sleep efficiency is a general trend. Though the effects of insufficient sleep are generally well established, the causes are complicated and poorly understood. Therefore, when examining sleep stages in children of different ages, it is critical to take their unique characteristics into account. However, examining sleep characteristics according to age enables a more in-depth comprehension of how sleep contributes to effective aging and human development. Sleep disorders according to DSM-5 are insomnia, parasomnia, breath-related disorders, hypersomnolence, narcolepsy, circadian rhythm sleep–wake disorder and substance, and medication-related disorder ( 5 ).
Analysis of phenotypes for sleep disorder
There are several types of sleep assessment methods that should be customized for each child. Subjective methods including parent-reported surveys and sleep diaries are among the most frequently employed methods in the analysis of sleep disorders in human studies. They offer various advantages, including non-invasive acquisition and low costs. Children’s Sleep Habits Questionnaire (CSHQ) is considered one of the most popular parent-completed surveys. It is a tool for assessment of sleep in school-aged children based on parental reports ( 6 ). Another method is the Electroencephalography (EEG). It involves two electrodes that are attached to the patient’s scalp. It provides a recording of the brain’s electrical activity throughout sleep and weakness ( 7 ). A method known as a polysomnogram (PSG) is regarded as the benchmark for the objective assessment of sleep compared to a single-channel EEG ( 8 ). It incorporates physiological indications of normal and abnormal brain electrical activity, sleep architecture, sleep stages, and sleep quality, as well as eye movements and physical activities during sleep. Actigraphy provides a non-invasive evaluation of limb activity using an accelerometer to identify episodes of sleep and wakefulness. It enables the collection of data over several days in unstructured settings. The reliability of actigraphy with PSG was examined and revealed a strong relationship between PSG and actigraphy measures (>0.80) for sleep latency, length, and efficiency ( 9 ). Similar to actigraphy, videosomnography’s benefits come from its objective documentation over a long period ( 10 ). It can also be used to record unusual occurrences like nighttime parasomnias. However, using videosomnography in child sleep research comes with several difficulties.
Sleep problems and autism spectrum disorders
Autism spectrum disorders (ASDs) have a wide range of clinical symptoms that are connected to social communication and interaction. Restrictive, repetitive, and stereotyped behaviors and interests are common in ASD. They have persistent difficulties in reciprocal social interaction and communication across a variety of circumstances. High levels of co-occurring behavioral difficulties are frequently present in children with ASD. According to the most recent report from the United States, the incidence was 1/54 in 2020. One of the most common features of ASD is the sleep disorder that results from the interaction of several factors such as psychological, biological, family factors, environmental, and child practice methods that might not be sleep-friendly ( 11 ).
Incidence of sleep disorders in patients with ASD
The incidence of sleep problems in ASD patients ranges from 32 to 71.5%. Children and adolescents with ASD are more likely to experience sleep difficulties, especially insomnia, with incidence rates ranging from 40 to 80%. This wide range of incidence may be due to the different sleep problems assessment methods and different criteria such as different cut-off scores ( 12 ). After adjusting for family variables including poor child-rearing practices (for example, little parental supervision at bedtime), and noisy, or stressful environments, children with ASD are also more prone to experience sleep disturbances compared with their normal relatives; 47 and 16%, respectively, ( 13 ).
The causes of sleep difficulties in children with ASD
ASD is a multifactorial disease that is affected by multiple factors including neurological, genetic, immunological, and environmental factors. Several neurotransmitters like melatonin, GABA, and serotonin are required to create a regular cycle of sleep and wakefulness. Sleep may be affected by any problems with these neurotransmitters’ synthesis ( 14 ). The hormone melatonin aids in synchronizing and preserving the circadian cycle. Autism may have improper melatonin regulation. The integrity of synaptic transmissions and the control of melatonin in ASD may both be influenced by clock genes ( 15 ). Melatonin exogenous therapy has been demonstrated to improve sleep schedule in ASD kids. Children with ASD showed decreased activity of the final enzyme in the production of melatonin, indicating lower levels of melatonin. This enzyme is encoded by the N-acetylserotonin O-methyltransferase gene ( 16 ). GABA is the neurotransmitter that induces sleep by inhibiting cells that are involved in arousal functions. It is produced from the preoptic area which is the sleep area in the hypothalamus. The Bidirectional Theoretical Framework of Sleep Disturbance provides an overview of the various risk factors that can affect the development of sleep issues in people with ASD ( 12 ).
Effect of sleep disturbances in ASD patients on caregivers
Increased parental sleep problems and maternal stress have been associated with sleep abnormalities in children with ASD. Sleep issues can significantly affect a child’s quality of life, daily functioning, and family dynamics, adding stress to everyone involved. This has also been linked to more challenging behaviors in ASD children during the day, as well as an influence on the ability to control mood. Sleep quality has been linked to common medical disorders such as upper respiratory problems and vision problems. Poor appetite and a decrease in the rate of growth have been linked to increased nighttime awakening and a reduced desire to go to sleep. Sleep disturbance in ASD children has been linked to increased aggression, hyperactivity, and social issues that may be markers of poor mental health outcomes.
Sleep disorders management
It is crucial to conduct early and frequent screenings for sleep impairment and its related conditions.
Non-pharmacological management
Sleep disturbances in children and adolescents with ASD must be managed on both environmental and behavioral levels. Parents must set bedtime routines and provide a relaxing bedroom atmosphere for their children. These environmental and behavioral strategies can improve their sleep, despite the fact that they are challenging to apply ( 17 ). The Sleep Committee of the Autism Treatment Network developed the sleep tool kit (STK), which is a customized behavioral modification tool for children and adolescents with insomnia. STK advocates three approaches: visual scheduling of good evening behaviors, a supplemental relaxing module to reduce arousal levels, and a faded bedtime regimen to sleep when tired. Breathing techniques, muscular relaxation exercises, yoga, massage, mindfulness training, and warm baths are additional soothing modules that aid those patients controlling arousal and anxiety. Taking the developmental characteristics of ASD children into consideration, it is reported that positive routines, unmodified and progressive extinction, and overnight fading are more beneficial in children under 5 years, but older children and adolescents benefit more from cognitive-behavioral therapy (CBT) ( 17 ).
Pharmacological management
Medical treatment is considered if the children do not respond to behavioral therapy.
Role of melatonin
It has been suggested that a lack of sociability may be related to sleep difficulties and circadian rhythm disruptions in ASD patients. Indeed, zeitgebers (also known as timeivers) like the natural light–dark cycle, music, and social cues are necessary for the entrainment and synchronization of the circadian clock. Therefore, in ASD patients, poor social cue perception or interpretation may impair the effectiveness of systems that synchronize sleep and wakefulness ( 18 ). As an alternative, ASD patients could find it difficult to synchronize with their internal and external settings, leading to eventual rhythm and time problems which affect a variety of fields, including social interaction and circadian cycles. In other words, persons with ASD would experience circadian abnormalities due to their failure to reflect their internal clock on environmental and social rhythms ( 19 ).
Melatonin is offered in a variety of over-the-counter preparations ranging from 1 to 10 mg. Most frequently, it is advised to take a dose of 1–3 mg 30–60 min before planned bedtime (46). However, a lower dose (0.5–1 mg) given earlier (3–4 h before night) is advised if a circadian rhythm problem is found. Age or weight has no bearing on the effectiveness of a dose. Melatonin is a pineal hormone that controls the body’s circadian cycle. Melatonin appears to help shorten the time it takes to fall asleep, but its effectiveness at reducing overnight awakenings and other elements of sleep disruptions varies ( 20 ). A study included 24 ASD children aged 1–3 years who exhibited improvement in sleep latency as determined by actigraphy when given 1 mg or 3 mg. This treatment improved not just the children’s sleep patterns, but also their conduct and parental stress ( 21 ).
Antipsychotic medication
This drug class has minimal tolerability and efficacy data for the treatment of insomnia in children. Few trials on the influence on sleep architecture have found that ziprasidone, olanzapine, and risperidone increase slow-wave, although ziprasidone and risperidone reduce REM sleep. Risperidone and olanzapine are two atypical antipsychotic that have been recommended for sleep disorders in children ( 22 ). These medications are used for the treatment of insomnia off-label, and it is not advised that they be regularly prescribed for this use, particularly as a first-line pharmacotherapeutic medication. In particular, the Canadian Academy of Child and Adolescent Psychiatry has advised against using them as a first-line line treatment for insomnia in children, adults, or the elderly ( 23 ). Other countries have likewise attempted to limit the number of prescriptions that government-subsidized programs may allow.
Antidepressant
There is limited evidence on the use and effectiveness of sedative antidepressants, selective serotonin reuptake inhibitors (SSRI), and tricyclic antidepressants (TCA) for the management of sleep disturbances in ASD children. Such medications might be effective if the sleeplessness is accompanied by concomitant psychiatric disorders. Children with comorbid depression may benefit from sedative antidepressants like trazodone and mirtazapine. These antidepressants enhance sleep by reducing the effects of neurotransmitters that promote wakefulness, including acetylcholine, histamine, noradrenaline, and serotonin. As a side effect, the majority of such medications reduce REM sleep and prolong daytime sleepiness. In psychiatric practice, trazodone is widely chosen and employed. Its effectiveness has primarily been shown in people with psychiatric illnesses. Trazodone has a noticeable morning hangover effect due to the antagonism of the 5-HT2A/C and being powerful sedating antidepressant. In contrast, fluoxetine is frequently connected to insomnia. Comparatively speaking to doses used to treat mood disorders, doses used to treat insomnia are typically lower.
Alpha-adrenergic agonist
The two main alpha agonists that are frequently used off-label to treat autism-related sleep disorders are clonidine and guanfacine. Clonidine (dosing range: 0.05–0.225 mg/day) significantly reduced sleep initiation and maintenance insomnia in children and adolescents (aged 4–16 years) with autism and neurodevelopmental problems, with good tolerability and few side effects ( 24 ). Hypotension, irritability, bradycardia, dry mouth, and REM suppression are some of the side effects of clonidine that may occur, and its rapid withdrawal may result in rebound hypertension and rebound REM ( 25 ).
Sedative and hypnotics drugs
Hypnotics and sedatives benzodiazepines (BZDs) are routinely given to adults with insomnia. However, because of their side effects, which include drowsiness, headaches, cognitive impairment, dizziness and rebound sleeplessness, and physical and behavioral dependence, they are recommended less frequently to children. Clonazepam was the only benzodiazepine tested for sleep issues in autistic children. Children with developmental disabilities were found to benefit from the treatment of partial arousals, parasomnias, periodic limb movement disorder, and nocturnal biting with clonazepam, an intermediate-acting BZD ( 26 , 27 ).
Other medication
Several medications which are used in the treatment of the Alzheimer’s disease are also found to be effective in the management of ASD symptoms ( 28 ). Drugs such as donepezil and rivastigmine are cholinesterase inhibitors that increase the acetylcholine by preventing its destruction. ASD is associated with anomalies in the cholinergic system, according to previously published evidence ( 29 ). First, research looking at post-mortem brain samples from people with ASD has discovered cholinergic system anomalies ( 30 , 31 ).
According to several studies, a large percentage of children with ASD condition experience seizures. It is reported that the incidence of ASD cases that suffered from epilepsy may range from 5 to 38% which is much higher than the incidence of the epilepsy in the normal children population which is 1–2% ( 32 , 33 ). There is very limited evidence about the use of anti-epileptic drugs in ASD patients. A randomized controlled trial has been valproate in ASD cases ( 34 ). They found that valproate monotherapy reduced the irritability and repetitive behaviors in ASD cases ( 35 ).
Sleep disorder and ADHD
One of the most frequently identified illnesses in both children and adults is attention-deficit/hyperactivity disorder (ADHD). It affects 2.9% of adults and 3 to 5% of children. It continues into adolescence and adulthood. The diagnostic criteria of ADHD include symptoms of inattention or/and impulsivity that appear prior to 12 years old, and hyperactivity. Untreated ADHD patients suffer from a decrease in several critical functional domains, including the academic, social, and occupational realms ( 36 ).
Types of sleep disorders
An estimated 25–50% of people with ADHD report having sleep issues in clinical settings ( 37 ). Besides, adults who do not have enough time of sleep are more prone to have symptoms of ADHD ( 38 ). Such individuals’ sleep disruptions have been linked to concomitant primary sleep problems and/or changes brought on by ADHD drugs ( 6 ). Researchers have looked into the connections between ADHD and narcolepsy, insomnia, circadian rhythm sleep disorders (CRSDs), restless leg syndrome, and sleep-disordered breathing (SDB) ( 39 , 40 ).
Obstructive sleep apnea and ADHD
Obstructive sleep apnea (OSA) is characterized by partial or total obstruction of the upper airway, which results in interrupted sleep, while SDB is associated with unpredictable breathing rhythm during sleep ( 41 , 42 ). People with ADHD have a higher incidence of SDB, and those with a history of snoring or possible OSA throughout childhood are associated with a two-fold higher susceptibility of diagnoses with ADHD ( 43 ). Through several processes, involving negative effects of hypoxic outcomes, the inflammation that leads to brain, and/or recurrent arousal-based sleep disturbances, SDB influences psychological outcomes. These pathways may change the prefrontal cortex’s neurochemical substrates, resulting in the neurobehavioral abnormalities that underlie the symptoms of ADHD ( 44 ).
Restless leg syndrome and ADHD
Restless leg syndrome (RLS) is a common sensorimotor condition characterized by an intense need to move the legs, which is frequently accompanied by unpleasant leg or (less frequently) body-part feelings. These feelings are particularly uncomfortable in the evening or at night and get better with activity. Due to their need to walk about and the stiffness in their legs, patients frequently have sleeplessness. This comorbidity is thought to be caused by iron deficiency and dopaminergic disorders ( 45 , 46 ). Even though the incidence of RLS in children is unknown, the disorder affects 10% of adults in the United States. According to the data, up to 44% of people with ADHD have RLS or symptoms similar to it, while up to 26% of those with RLS have symptoms similar to it ( 47 , 48 ).
Circadian rhythm sleep disorder and ADHD
The timing of when a person sleeps and is awake is a concern in CRSDs. They result from changes to the circadian clock, its entrainment processes, or a misalignment of the internal circadian rhythm with the external environment. When a person routinely falls asleep and awakens more than 2 h later than is deemed normal, this condition is known as delayed sleep phase syndrome (DSPS). Changes in these processes, reductions in pineal gland volume, and/or anomalies in clock genes have all been discovered in people with ADHD. In adolescents and adults with ADHD, late chronotype and DSPS are typically co-occurring disorders. CRSD and ADHD may share a biological and behavioral etiology ( 49 , 50 ). Impulsivity control issues might impair a person’s capacity to calm down, causing resistance to going to bed and a delayed start to sleep. It is also suggested that those with ADHD might have a greater circadian preference for the evening and a potential endogenous melatonin rise delay ( 50 ).
Narcolepsy and ADHD
A persistent neurological condition called narcolepsy causes problems with sustaining constant wakefulness and sleep. A diagnosis of narcolepsy needs symptoms of rapid eye movement (REM), sleep dissociation (such as sleep paralysis, hypnagogic/hypnopompic hallucinations, and cataplexy), and disturbed nighttime sleep, regardless of how the clinical presentation manifests itself. In the past, it was discovered that adults with narcolepsy had a twice as high probability of receiving an ADHD diagnosis as children as compared to controls ( 51 ). Additionally, data points to children with ADHD experiencing hypo arousal and hypo arousal-related hyperactivity/impulsivity as possible signs of exhaustion ( 52 ). Although the relationship between the two disorders is unclear, it has been postulated that EDS in narcoleptics may cause inattention, deficient executive function, and issues with impulse control that are similar to ADHD and react well to psychiatric drugs ( 53 – 55 ). Finally, the overlap of ADHD and narcolepsy symptoms may result in diagnostic ambiguity or incorrect diagnosis of the diseases. Another theory is that the connection could be due to a common pathology in the brain ( 56 ).
ADHD medication
The effects of stimulants on sleep vary from patient to patient in those with ADHD, reflecting the intricacy of the relationships between sleep disturbance and ADHD ( 57 ). Clinical experience suggests that stimulants generate paradoxical effects, whereby symptom relief can relax patients and encourage sleep, although there is evidence linking stimulants to disturbed sleep in ADHD cases ( 58 , 59 ). Furthermore, increasing the dosage of a short-acting inducer or using a formula with prolonged action may minimize sleep disruptions caused by an increase in hyperactivity or behavioral disorders at bedtime due to the risk of symptom rebound when the concentrations of the drug in the blood is decreased ( 60 , 61 ).
Non-stimulants
The most frequent side effect associated with atomoxetine that is connected to sleep, in contrast to stimulants, is somnolence (a noradrenaline reuptake inhibitor permitted for the management of ADHD). In atomoxetine placebo-controlled trials, somnolence was observed to present in 15–17% of patients as reported by a 2009 comprehensive review ( 62 ). Atomoxetine was found to have less of an impact on subjective sleep measures than methylphenidate and was taken three times per day in a randomized, double-blind trial.
After evaluation and diagnosis, the first stage of treatment will be psychoeducation. In addition to learning about the prognosis, course, therapy, and probable functional implications of the sleep disorder, the affected individuals and their social entourage will require proper psychoeducation on ADHD symptoms and sleep problems. Additionally, educating people about healthy sleep habits and sleeping patterns will enable non-pharmacological sleep enhancement. It is common practice to use medicine to address sleep disturbances. The choice of medication can be directed to address related issues such as daytime malfunction and should be combined with behavioral techniques. Surgery to remove the tonsils or adenoids is the first line of treatment for children with ADHD and SDB, whereas oral appliances, positive airway pressure devices, or surgery are suggested treatments for adults with OSA and ADHD ( 63 ). The sleep environment may need to be changed for people with RLS and ADHD, and behavioral therapies such as iron supplements ( 64 ) (for example, ferrous sulfate) or gabapentin ( 65 ) may also be investigated, especially for a younger population. In an adults, using dopaminergic substances such as L-DOPA, ropinirole, and pramipexole, in addition to, a recently developed drug called rotigotine may also be a possibility ( 66 ).
Treatment options for people with DSPS and ADHD include scheduled melatonin therapy, light therapy ( 67 ), and chronotherapy ( 68 , 69 ). Furthermore, because treatment for DSPS differs from that for insomnia, a clear distinction between the two must be made. Treatment for ADHD and insomnia can differ depending on the age group.
People with intellectual disabilities and sleep disorders
The incidence of sleep issues in children ranges from 24 to 86%, and they are widespread in persons with intellectual disabilities ( 70 ). Adults with mental disabilities are reported to have an incidence of sleep disorders ranging from 8.5 to 34.1%, with a serious sleep problem rate of 9.2%. In one study, it was discovered that 551 older persons with intellectual disabilities had sleep issues in 72% of the cases ( 47 ). The treatment of physical and mental health issues in people with intellectual disabilities is an area that needs more study. Studies conducted on people without intellectual disabilities were often the basis for the development of diagnostic and management techniques. The same pattern is observed in persons with intellectual impairments who have sleep difficulties. There is a lack of information specifically on the causes, effects, and treatments of sleep problems in people with developmental disabilities. Assessment and treatment of sleep issues in persons with intellectual impairments can be informed by knowledge of the several types of sleep issues that these people encounter and the numerous factors that affect their sleep ( 71 ).
Adults with intellectual disabilities have a higher risk to have sleep issues, which could be due to several factors. In individuals with intellectual impairments, a systematic review of the published literature on sleep problems found links between sleep and several characteristics, such as respiratory diseases, psychoactive drugs, mental health illnesses, and challenging behavior ( 47 ). Understanding and taking into account the social, psychological, and biological aspects influencing the higher occurrence of sleep issues in persons with intellectual impairments is crucial for providing person-centered and individualized care. We have looked at several significant contributing elements that must be taken into account when evaluating sleep issues in persons with intellectual disabilities. The association between sleep disturbances and neurodevelopmental diseases like ADHD and ASD has been thoroughly studied above ( 47 ).
Genetic conditions
Our comprehension of the underlying genetic causes of intellectual impairments has recently improved ( 72 ). For example, Down’s syndrome is characterized by obesity, hypotonia, and craniofacial anomalies, all of which raise the likelihood of sleep disorders including obstructive sleep apnea (OSA). Similarly to this, those who have cri du chat syndrome have a higher risk of getting OSA ( 73 ).
Environmental and psychological factors
People with mental disorders frequently experience sleep disturbance as the first sign of a decline in their mental health, and low-quality sleep represents a common feature of many psychotic and affective diseases ( 11 ). When compared to individuals without cognitive disabilities, those with cognitive disabilities have a higher incidence of mental problems, which helps explain why sleep disturbances are so common in this population ( 12 ). When determining the etiology of sleep issues in a person with cognitive disabilities, it is crucial to take the environment’s role in the development of sleep disorders into account. According to Kerr and Wilkinson ( 13 ), staffed residential homes may not be the best places to sleep because people may check on residents at odd hours, which would result in more noise and lights that would be disruptive to sleep ( 13 ).
Diagnosis of sleep disorders
Adults with intellectual impairments are frequently given subjective sleep information by their caregivers, who may disagree with the severity of the problem or may even accept sleep disturbance as a symptom of the person’s underlying condition ( 74 ).
Because of this, sleep problems are more likely to be noticed by a physician when they induce nocturnal or daytime malfunction, including behavioral disorders, impairing a person’s subjective impression of their quality of life ( 75 ). When evaluating sleep disturbances, general population guidelines stress the significance of checking for coexisting medical diseases. This is may be even more crucial for people with intellectual impairments since they are more prone to experience physical health illness that impacts their sleep, such as OSA or epilepsy ( 76 ). For example, it is advised that everyone with Down’s syndrome be evaluated for OSA due to the condition’s high incidence in people with Down’s syndrome. When sleep–wake duration (including naps) is irregular or unpredictable, caregiver-completed sleep diaries and/or actigraphy, ideally conducted for at least 2 weeks, can be used. Individuals with intellectual impairments can be evaluated for physical sleep disorders such as OSA and nocturnal epilepsy using home or in-patient sleep examinations (such as pulse oximetry or the gold standard, polysomnography) ( 77 ). Even though these tests should always be provided when clinically indicated, if a patient is unable to endure the sleep tests, a practical therapy trial may be necessary. The variety of underlying causes of intellectual disability and the characteristics of related comorbidities make managing sleep disturbances challenging. While intellectual disability psychiatrists can easily address some problems, others will need the assistance of sleep physician and/or primary care givers. According to a study, continuous positive airway pressure therapy can significantly enhance behavior, cognitive function, and subjective drowsiness in individuals with Down’s syndrome and OSA ( 78 ). But as this study correctly notes, access to care may be difficult, and as was already said, some individuals with intellectual disabilities might find it difficult to tolerate these tests and treatments. Working together, sleep specialists and psychiatrists may be able to address these issues. For instance, sleep clinics assist the training of mental health nurses for people with intellectual disabilities in exposure treatment to aid those individuals become used to positive airway pressure masks. The initial management for persistent insomnia in the general population is multicomponent cognitive-behavioral therapy (CBT-I), and there are elements of this that can be helpful for individuals with intellectual impairments ( 74 ). Understanding the impacts of environment and lifestyle on sleep, such as caffeine use, exercise, and regular sleep schedules, along with lighting, noise, and temperature, can be achieved through education on sleep hygiene ( 75 ).
Adults with cognitive disabilities are more prone than the general population to lack appropriate daily activity and regular exposure to natural light, thus even small changes to everyday routine and the sleeping environment can be beneficial ( 75 ). The needs of the person should be taken into consideration when making such recommendations, such as lowering external noise for autistic people sensitive to sounds. The evidence is not strong enough to support the use of pharmaceuticals to treat sleep disturbances in adults with intellectual impairments. Melatonin is the drug that has drawn the most attention, maybe due to its favorable side-effect profile and the fact that several trials have demonstrated its efficacy ( 75 ). According to a meta-analysis, melatonin consumption enhances total sleep time and reduces the number of wake-ups per night in people with intellectual disabilities. Currently, the pharmacological management of illnesses other than insomnia tends to use the same routes as those for the general public ( 75 ).
Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to chronicity. Various solutions are required based on the neurodevelopmental problem, but all patients should get behavioral intervention. Understanding the distinctive characteristics of sleep disturbances in patients with neurodevelopmental disorders is critical for effective therapy.
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1.Abbott, SM, and Videnovic, A. Chronic sleep disturbance and neural injury: links to neurodegenerative disease. Nat Sci Sleep . (2016) 8:55–61. doi: 10.2147/NSS.S78947
PubMed Abstract | CrossRef Full Text | Google Scholar
2.Kim, TW, Jeong, JH, and Hong, SC. The impact of sleep and circadian disturbance on hormones and metabolism. In. Int J Endocrinol . (2015) 2015:1–9. doi: 10.1155/2015/591729
3.Van Someren, EJW, Cirelli, C, Dijk, D-J, Van Cauter, E, Schwartz, S, and Chee, MWL. Disrupted sleep: from molecules to cognition. J Neurosci . (2015) 35:13889–95. doi: 10.1523/JNEUROSCI.2592-15.2015
4.Riemann, D, Krone, LB, Wulff, K, and Nissen, C. Sleep, insomnia, and depression. Neuropsychopharmacology . (2020) 45:74–89. doi: 10.1038/s41386-019-0411-y
5.Seow, LSE, Verma, SK, Mok, YM, Kumar, S, Chang, S, Satghare, P, et al. Evaluating DSM-5 insomnia disorder and the treatment of sleep problems in a psychiatric population. J Clin Sleep Med . (2018) 14:237–44. doi: 10.5664/jcsm.6942
6.Bhargava, S. Diagnosis and management of common sleep problems in children. Pediatr Rev . (2011) 32:91–9. doi: 10.1542/pir.32-3-91
CrossRef Full Text | Google Scholar
7.Weber, F, and Dan, Y. Circuit-based interrogation of sleep control. Nature . (2016) 538:51–9. doi: 10.1038/nature19773
8.O’donnell, S, Beaven, CM, and Driller, MW. From pillow to podium: a review on understanding sleep for elite athletes. Nat Sci Sleep . (2018) 10:243–53. doi: 10.2147/NSS.S158598
9.Bélanger, MÈ, Bernier, A, Paquet, J, Simard, V, and Carrier, J. Validating actigraphy as a measure of sleep for preschool children. Journal of Clinical Sleep Medicine . (2013) 9:701–6.
Google Scholar
10.Honomichl, RD, Goodlin-Jones, BL, Burnham, MM, Hansen, RL, and Anders, TF. Secretin and sleep in children with autism. Child Psychiatry and Human Developmen . (2002) 33:107–23.
11.Goldman, SE, Richdale, AL, Clemons, T, and Malow, BA. Parental sleep concerns in autism spectrum disorders: variations from childhood to adolescence. J Autism Dev Disord . (2012) 42:531–8. doi: 10.1007/s10803-011-1270-5
12.Hollway, JA, and Aman, MG. Sleep correlates of pervasive developmental disorders: a review of the literature. Res Dev Disabil . (2011a) 32:1399–421. doi: 10.1016/j.ridd.2011.04.001
13.Sikora, DM, Johnson, K, Clemons, T, and Katz, T. The relationship between sleep problems and daytime behavior in children of different ages with autism spectrum disorders. Pediatrics . (2012) 130 Suppl 2:S83–90. doi: 10.1542/peds.2012-0900F
14.Cortesi, F, Giannotti, F, Ivanenko, A, and Johnson, K. Sleep in children with autistic spectrum disorder. Sleep Med . (2010) 11:659–64. doi: 10.1016/j.sleep.2010.01.010
15.Bourgeron, T. The possible interplay of synaptic and clock genes in autism Spectrum disorders. Cold Spring Harb Symp Quant Biol . (2007) 72:645–54. doi: 10.1101/sqb.2007.72.020
16.Melke, J, Goubran Botros, H, Chaste, P, Betancur, C, Nygren, G, Anckarsäter, H, et al. Abnormal melatonin synthesis in autism spectrum disorders. Mol Psychiatry . (2008) 13:90–8. doi: 10.1038/sj.mp.4002016
17.Malow, BA, Adkins, KW, Reynolds, A, Weiss, SK, Loh, A, Fawkes, D, et al. Parent-based sleep education for children with autism spectrum disorders. J Autism Dev Disord . (2014) 44:216–28. doi: 10.1007/s10803-013-1866-z
18.Richdale, AL, and Prior, MR. The sleep/wake rhythm in children with autism. Eur Child Adolesc Psychiatry . (1995) 4:175–86. doi: 10.1007/BF01980456
19.Rossignol, DA, and Frye, RE. Melatonin in autism spectrum disorders: a systematic review and meta-analysis. Dev Med Child Neurol . (2011) 53:783–92. doi: 10.1111/j.1469-8749.2011.03980.x
20.Himelfarb, M, and Shatkin, JP. Pediatric insomnia. Child Adolesc Psychiatr Clin N Am . (2021) 30:117–29. doi: 10.1016/j.chc.2020.08.004
21.Goldman, SE, Adkins, KW, Calcutt, MW, Carter, MD, Goodpaste, RL, Wang, L, et al. Melatonin in children with autism Spectrum disorders: endogenous and pharmacokinetic profiles in relation to sleep. J Autism Dev Disord . (2014) 44:2525–35. doi: 10.1007/s10803-014-2123-9
22.Meltzer, LJ, Mindell, JA, Owens, JA, and Byars, KC. Use of sleep medications in hospitalized pediatric patients. Pediatrics . (2007) 119:1047–55. doi: 10.1542/peds.2006-2773
23.First-line (2015) Treatment for insomnia should not include routine use of antipsychotics, say Canadian psychiatrists - Canadian psychiatric association- association des psychiatres du Canada .
24.Wichniak, A, Wierzbicka, A, and Jernajczyk, W. Sleep and antidepressant treatment. Curr Pharm Des . (2012) 18:5802–17. doi: 10.2174/138161212803523608
25.Ingrassia, A, and Turk, J. The use of clonidine for severe and intractable sleep problems in children with neurodevelopmental disorders. Eur Child Adolesc Psychiatry . (2005) 14:34–40. doi: 10.1007/s00787-005-0424-4
26.Rossi, PG, Posar, A, and Parmeggiani, A. Niaprazine in the treatment of autistic disorder. J Child Neurol . (1999) 14:547–50. doi: 10.1177/088307389901400814
27.Hollway, JA, and Aman, MG. Pharmacological treatment of sleep disturbance in developmental disabilities: a review of the literature. Res Dev Disabil . (2011b) 32:939–62. doi: 10.1016/j.ridd.2010.12.035
28.Rossignol, DA. Novel and emerging treatments for autism spectrum disorders: a systematic review. Ann Clin Psychiatry . (2009) 21:213–36.
PubMed Abstract | Google Scholar
29.Deutsch, SI, Urbano, MR, Neumann, SA, Burket, JA, and Katz, E. Cholinergic abnormalities in autism. Clin Neuropharmacol . (2010) 33:114–20. doi: 10.1097/WNF.0b013e3181d6f7ad
30.Perry, EK, Lee, MLW, Martin-Ruiz, CM, Court, JA, Volsen, SG, Merrit, J, et al. Cholinergic activity in autism: abnormalities in the cerebral cortex and basal forebrain. Am J Psychiatr . (2001) 158:1058–66. doi: 10.1176/appi.ajp.158.7.1058
31.Ray, MA, Graham, AJ, Lee, M, Perry, RH, Court, JA, and Perry, EK. Neuronal nicotinic acetylcholine receptor subunits in autism: an immunohistochemical investigation in the thalamus. Neurobiol Dis . (2005) 19:366–77. doi: 10.1016/j.nbd.2005.01.017
32.Deykin, EY, and MacMahon, B. The incidence of seizures among children with autistic symptoms. Am J Psychiatr . (1979) 136:1310–2. doi: 10.1176/ajp.136.10.1310
33.Hara, H. Autism and epilepsy: a retrospective follow-up study. Brain Dev . (2007) 29:486–90. doi: 10.1016/j.braindev.2006.12.012
34.Hollander, E, Soorya, L, Wasserman, S, Esposito, K, Chaplin, W, and Anagnostou, E. Divalproex sodium vs. placebo in the treatment of repetitive behaviours in autism spectrum disorder. Int J Neuropsychopharmacol . (2005) 9:209–13. doi: 10.1017/S1461145705005791
35.Hollander, E, Chaplin, W, Soorya, L, Wasserman, S, Novotny, S, Rusoff, J, et al. Divalproex sodium vs placebo for the treatment of irritability in children and adolescents with autism Spectrum disorders. Neuropsychopharmacology . (2010) 35:990–8. doi: 10.1038/npp.2009.202
36.Wajszilber, D, Santiseban, JA, and Gruber, R. Sleep disorders in patients with ADHD: impact and management challenges. Nat Sci Sleep . (2018) 10:453–80. doi: 10.2147/NSS.S163074
37.Spruyt, K, and Gozal, D. Sleep disturbances in children with attention-deficit/hyperactivity disorder. In. Expert Rev Neurother . (2011) 11:565–77. doi: 10.1586/ern.11.7
38.Bogdan, AR, and Reeves, KW. Sleep duration in relation to attention deficit hyperactivity disorder in American adults. Behav Sleep Med . (2018) 16:235–43. doi: 10.1080/15402002.2016.1188391
39.Konofal, E, Lecendreux, M, and Cortese, S. Sleep and ADHD. Sleep Med . (2010) 11:652–8. doi: 10.1016/j.sleep.2010.02.012
40.Weiss, MD, Craig, SG, Davies, G, Schibuk, L, and Stein, M. New research on the complex interaction of sleep and ADHD. Curr Sleep Med Rep . (2015) 1:114–21. doi: 10.1007/s40675-015-0018-8
41.Constantin, E, Low, NCP, Dugas, E, Karp, I, and O’Loughlin, J. Association between childhood sleep-disordered breathing and disruptive behavior disorders in childhood and adolescence. Behav Sleep Med . (2015) 13:442–54. doi: 10.1080/15402002.2014.940106
42.Guilleminault, C, Korobkin, R, and Winkle, R. A review of 50 children with obstructive sleep apnea syndrome. Lung . (1981) 159:275–87. doi: 10.1007/BF02713925
43.Johnson, EO, and Roth, T. An epidemiologic study of sleep-disordered breathing symptoms among adolescents. Sleep . (2006) 29:1135–42. doi: 10.1093/sleep/29.9.1135
44.Beebe, DW, and Gozal, D. Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. In. J Sleep Res . (2002) 11:1–16. doi: 10.1046/j.1365-2869.2002.00289.x
45.Červenka, S, Pålhagen, SE, Comley, RA, Panagiotidis, G, Cselényi, Z, Matthews, JC, et al. Support for dopaminergic hypoactivity in restless legs syndrome: a PET study on D2-receptor binding. Brain . (2006) 129:2017–28. doi: 10.1093/brain/awl163
46.Wagner, ML, Walters, AS, and Fisher, BC. Symptoms of attention-deficit/hyperactivity disorder in adults with restless legs syndrome. Sleep . (2004) 27:1499–504. doi: 10.1093/sleep/27.8.1499
47.Van de Wouw, E, Evenhuis, HM, and Echteld, MA. Prevalence, associated factors and treatment of sleep problems in adults with intellectual disability: a systematic review. Res Dev Disabil . (2012) 33:1310–32. doi: 10.1016/j.ridd.2012.03.003
48.Walters, AS, Silvestri, R, Zucconi, M, Chandrashekariah, R, and Konofal, E. Review of the possible relationship and hypothetical links between attention deficit hyperactivity disorder (ADHD) and the simple sleep related movement disorders, parasomnias, hypersomnias, and circadian rhythm disorders. J Clin Sleep Med . (2008) 4:591–600. doi: 10.5664/jcsm.27356
49.Bron, TI, Bijlenga, D, Kooij, JJS, Vogel, SWN, Wynchank, D, Beekman, ATF, et al. Attention-deficit hyperactivity disorder symptoms add risk to circadian rhythm sleep problems in depression and anxiety. J Affect Disord . (2016) 200:74–81. doi: 10.1016/j.jad.2016.04.022
50.Sivertsen, B, Harvey, AG, Pallesen, S, and Hysing, M. Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. J Sleep Res . (2015) 24:11–8. doi: 10.1111/jsr.12254
51.Ohayon, MM. Narcolepsy is complicated by high medical and psychiatric comorbidities: a comparison with the general population. Sleep Med . (2013) 14:488–92. doi: 10.1016/j.sleep.2013.03.002
52.Cortese, S, Konofal, E, and Lecendreux, M. Alertness and feeding behaviors in ADHD: does the hypocretin/orexin system play a role? Med Hypotheses . (2008) 71:770–5. doi: 10.1016/j.mehy.2008.06.017
53.Nordstrand, SH, Hansen, BH, Kamaleri, Y, Nilsen, KB, Rootwelt, T, Karlsen, TI, et al. Changes in quality of life in individuals with narcolepsy type 1 after the H1N1-influenza epidemic and vaccination campaign in Norway: a two-year prospective cohort study. Sleep Med . (2018) 50:175–80. doi: 10.1016/j.sleep.2018.05.037
54.Oosterloo, M, Lammers, GJ, Overeem, S, de Noord, I, and Kooij, JJS. Possible confusion between primary hypersomnia and adult attention-deficit/hyperactivity disorder. Psychiatry Res . (2006) 143:293–7. doi: 10.1016/j.psychres.2006.02.009
55.Stores, G, Montgomery, P, and Wiggs, L. The psychosocial problems of children with narcolepsy and those with excessive daytime sleepiness of uncertain origin. Pediatrics . (2006) 118:e1116–23. doi: 10.1542/peds.2006-0647
56.Ito, W, Honda, M, Ueno, T, and Kato, N. Hypersomnia with ADHD: a possible subtype of narcolepsy type 2. Sleep Biol Rhythms . (2018) 16:205–10. doi: 10.1007/s41105-017-0139-1
57.Graham, J, Banaschewski, T, Buitelaar, J, Coghill, D, Danckaerts, M, Dittmann, RW, et al. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry . (2011) 20:17–37. doi: 10.1007/s00787-010-0140-6
58.Jerome, L. Can methylphenidate facilitate sleep in children with attention deficit hyperactivity disorder? J Child Adolesc Psychopharmacol . (2001) 11:109. doi: 10.1089/104454601750143564
59.Kratochvil, CJ, Lake, M, Pliszka, SR, and Walkup, JT. Pharmacological management of treatment-induced insomnia in ADHD. J Am Acad Child Adolesc Psychiatry . (2005) 44:499–501. doi: 10.1097/01.chi.0000155322.32500.3a
60.Carlson, GA, and Kelly, KL. Stimulant rebound: how common is it and what does it mean? J Child Adolesc Psychopharmacol . (2003) 13:137–42. doi: 10.1089/104454603322163853
61.Cortese, S, Brown, TE, Corkum, P, Gruber, R, O’Brien, LM, Stein, M, et al. Assessment and management of sleep problems in youths with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry . (2013) 52:784–96. doi: 10.1016/j.jaac.2013.06.001
62.Rae, CL, Nombela, C, Rodríguez, PV, Ye, Z, Hughes, LE, Jones, PS, et al. Atomoxetine restores the response inhibition network in Parkinson’s disease. Brain . (2016) 139:2235–48. doi: 10.1093/brain/aww138
63.Kapur, VK, Auckley, DH, Chowdhuri, S, Kuhlmann, DC, Mehra, R, Ramar, K, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American academy of sleep medicine clinical practice guideline. In. J Clin Sleep Med . (2017) 13:479–504. doi: 10.5664/jcsm.6506
64.Mohri, I, Kato-Nishimura, K, Kagitani-Shimono, K, Kimura-Ohba, S, Ozono, K, Tachibana, N, et al. Evaluation of oral iron treatment in pediatric restless legs syndrome (RLS). Sleep Med . (2012) 13:429–32. doi: 10.1016/j.sleep.2011.12.009
65.Garcia-Borreguero, D, Larrosa, O, De la Llave, Y, Verger, K, Masramon, X, and Hernandez, G. Treatment of restless legs syndrome with gabapentin: a double-blind, cross-over study. Neurology . (2002) 59:1573–9. doi: 10.1212/WNL.59.10.1573
66.Aurora, RN, Kristo, DA, Bista, SR, Rowley, JA, Zak, RS, Casey, KR, et al. The treatment of restless legs syndrome and periodic limb movement disorder in adults – an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses. Sleep . (2012) 35:1039–62. doi: 10.5665/sleep.1988
67.Lack, L, Wright, H, Kemp, K, and Gibbon, S. The treatment of early-morning awakening insomnia with 2 evenings of bright light. Sleep . (2005) 28:616–23. doi: 10.1093/sleep/28.5.616
68.Auger, RR, Burgess, HJ, Emens, JS, Deriy, LV, Thomas, SM, and Sharkey, KM. Clinical practice guideline for the treatment of intrinsic circadian rhythm sleep-wake disorders: advanced sleep-wake phase disorder (ASWPD), delayed sleep-wake phase disorder (DSWPD), Non-24-hour sleep-wake rhythm disorder (N24SWD), and irregular sleep-W. J Clin Sleep Med . (2015) 11:1199–236. doi: 10.5664/jcsm.5100
69.Weitzman, ED, Czeisler, CA, Coleman, RM, Spielman, AJ, Zimmerman, JC, Dement, W, et al. Delayed sleep phase syndrome: a Chronobiological disorder with sleep-onset insomnia. Arch Gen Psychiatry . (1981) 38:737–46. doi: 10.1001/archpsyc.1981.01780320017001
70.Richdale, AL, and Baker, EK. Sleep in individuals with an intellectual or developmental disability: recent research reports. Curr Dev Disord Rep . (2014) 1:74–85. doi: 10.1007/s40474-014-0010-x
71.Didden, R, and Sigafoos, J. A review of the nature and treatment of sleep disorders in individuals with developmental disabilities. Res Dev Disabil . (2001) 22:255–72. doi: 10.1016/S0891-4222(01)00071-3
72.Ilyas, M, Mir, A, Efthymiou, S, and Houlden, H. The genetics of intellectual disability: advancing technology and gene editing. F1000Res . (2019) 9. doi: 10.12688/f1000research.16315.1
73.Hill, EA. Obstructive sleep apnoea/hypopnoea syndrome in adults with down syndrome. Breathe . (2016) 12:e91–6. doi: 10.1183/20734735.012116
74.Surtees, ADR, Oliver, C, Jones, CA, Evans, DL, and Richards, C. Sleep duration and sleep quality in people with and without intellectual disability: a meta-analysis. Sleep Med Rev . (2018) 40:135–50. doi: 10.1016/j.smrv.2017.11.003
75.McPherson, P, Kaushal, M, and Kothapalli, V. The treatment of dually diagnosed individuals with sleep disturbances and intellectual disabilities. In: J Matson, editor. Handbook of Dual Diagnosis. Autism and Child Psychopathology Series . Cham: Springer (2020). 613–45.
76.de Carvalho, AA, Amorim, FF, Santana, LA, de Almeida, KJQ, Santana, ANC, and de Assis Rocha Neves, F. STOP-bang questionnaire should be used in all adults with down syndrome to screen for moderate to severe obstructive sleep apnea. PLoS One . (2020) 15:e0232596. doi: 10.1371/journal.pone.0232596
77.Rundo, JV, and Downey, R. Polysomnography. Handb Clin Neurol . (2019) 160:381–92. doi: 10.1016/B978-0-444-64032-1.00025-4
78.Hill, EA, Fairley, DM, Williams, LJ, Cooper, S-A, and Riha, RL. A prospective, randomised, controlled trial of CPAP in adults with down syndrome. Eur Respir J . (2015) 46:OA4754. doi: 10.1183/13993003.congress-2015.oa4754
Keywords: attention-deficit hyperactivity disorder, intellectual disabilities, electroencephalography, autism spectrum disorders, sleep disorder
Citation: Al Lihabi A (2023) A literature review of sleep problems and neurodevelopment disorders. Front. Psychiatry . 14:1122344. doi: 10.3389/fpsyt.2023.1122344
Received: 12 December 2022; Accepted: 31 January 2023; Published: 23 February 2023.
Reviewed by:
Copyright © 2023 Al Lihabi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abeer Al Lihabi, ✉ [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 12, Issue 11
- Melatonin for sleep disorders in children with neurodevelopmental disorders: protocol for a systematic review with meta-analysis and Trial Sequential Analysis of randomised clinical trials
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7756-4694 Caroline Kamp Jørgensen 1 , 2 ,
- Rikke Hermann 1 , 3 ,
- Sophie Juul 1 ,
- Pascal Faltermeier 1 , 4 ,
- Mark Horowitz 5 ,
- http://orcid.org/0000-0003-1214-6974 Joanna Moncrieff 5 , 6 ,
- Christian Gluud 1 , 2 ,
- Janus Christian Jakobsen 1 , 2
- 1 Copenhagen Trial Unit, Centre for Clinical Intervention Research , Capital Region of Denmark, Copenhagen University Hospital – Rigshospitalet , Copenhagen , Denmark
- 2 Department of Regional Health Research, Faculty of Health Sciences , University of Southern Denmark , Odense , Denmark
- 3 Centre for Children, Youth, and Families , Glostrup , Denmark
- 4 MSH Medical School Hamburg, University of Applied Sciences and Medical University , Hamburg , Germany
- 5 Research and Development Department , North East London NHS Foundation Trust (NELFT) , London , UK
- 6 Division of Psychiatry , University College London , London , UK
- Correspondence to Caroline Kamp Jørgensen; caroline.joergensen{at}ctu.dk
Introduction Neurodevelopmental disorders are a group of disorders thought to be associated with the functioning of the brain and the nervous system. Children with neurodevelopmental disorders often have sleep-related comorbidities that may negatively affect quality of life for both the children and their families. Melatonin is one of the most used interventions in children with neurodevelopmental disorders and sleep disorders. Previous reviews have investigated the effects of melatonin for sleep disorders in children with neurodevelopmental disorders, but these had important limitations, such as inadequate analysis of adverse effects, small sample sizes and short follow-up.
Methods and analysis This is a protocol for a systematic review with meta-analysis and Trial Sequential Analysis of randomised clinical trials. The protocol is reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols. We will search for published and unpublished trials in the Cochrane Central Register of Controlled Trials, MEDLINE Ovid, Embase Ovid, LILACS, Science Citation Index Expanded, Conference Proceedings Citation Index-Science, PsycINFO, ClinicalTrials.gov and the International Clinical Trials Registry Platform. We will search the databases from their inception without language restrictions. We will also request clinical study reports from regulatory authorities and pharmaceutical companies. Review authors working in pairs will screen reports, extract data and conduct risk of bias assessments using the Cochrane Risk of Bias tool. We will include randomised clinical trials comparing melatonin versus placebo or no intervention for sleep disorders in children with neurodevelopmental disorders. Primary outcomes will be total sleep time and adverse effects. Secondary outcomes will be quality of life of the child and caregivers and sleep onset latency. Data will be analysed using random-effects and fixed-effect meta-analyses. Certainty of evidence will be assessed with Grading of Recommendations, Assessment, Development and Evaluation approach.
Ethics and dissemination Ethical approval was not required for this protocol. The systematic review will be published in a peer-reviewed journal.
PROSPERO registration number CRD42022337530.
- SLEEP MEDICINE
- Paediatric neurology
- Developmental neurology & neurodisability
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2022-065520
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The methodology of our systematic review is predefined in detail to avoid data-driven biased results.
The protocol is based on the Cochrane Handbook, the eight-step procedure suggested by Jakobsen et al , Trial Sequential Analysis and the Grading of Recommendations, Assessment, Development and Evaluation approach.
This systematic review will consider the risks of random errors, systematic errors, publication bias, heterogeneity and external validity.
This systematic review will include both published and unpublished trials.
We assess multiple outcomes and subgroup analyses which increases the risks of type I errors.
Introduction
Description of the condition.
Neurodevelopmental disorders are a group of disorders thought to be associated with the functioning of the brain and the nervous system. 1 Neurodevelopmental disorders are usually diagnosed in childhood and include neurological disorders such as cerebral palsy, epilepsy, Angelman syndrome, Down’s syndrome, Fragile X syndrome, Prader-Willi syndrome, Rett syndrome, Smith-Magenis syndrome, Williams syndrome and non-specific intellectual disability, along with some psychiatric disorders including autism spectrum disorder, attention deficit hyperactivity disorder (ADHD) and attention deficit disorder (ADD). 1 2 Children with neurodevelopmental disorders may experience difficulties with learning, attention, behaviour, speech, motor skills and other neurological functions. 1
The impact of sleep disturbances was recently ranked as a top 10 research priority within the topics of children with neurodevelopmental disorders by a UK partnership of patients, carers and clinicians. 3 Children with neurodevelopmental disorders often have sleep-related comorbidities, including sleep disorders such as insomnia disorder, hypersomnolence disorder, narcolepsy, breathing-related sleep disorders, circadian rhythm sleep disorders, rapid eye movement (REM) sleep arousal disorders, non-REM sleep arousal disorders and nightmare disorders. 2 4 Studies have shown the prevalence of comorbid neurodevelopmental disorders and sleep disorders is between 25% and 86% compared with 1% and 6% in the general paediatric population. 4–8 Sleep disorders may further enhance problems with learning and behaviour in children with neurodevelopmental disorders, 4–8 and often have a negative effect on quality of life for both the children and their families. 9 10
Description of the intervention
Melatonin is a naturally occurring hormone in both humans and animals. 11 Previously, melatonin was derived from animal pineal tissue, 11 but it is now developed synthetically and distributed in different forms, including capsules, tablets, gummies and liquids. 12 Melatonin is available in many countries either sold as prescription-only medicine or as over-the-counter medicine to treat sleep disorders in both children and adults, as it is hypothesised to be associated with few adverse effects. 11 13 Furthermore, melatonin is one of the most commonly used interventions in children with neurodevelopmental disorders and sleep disorders. 14–18 The dosage recommendations vary according to country, but the UK National Health Service currently recommend treatment up to 13 weeks of 2 mg 1–2 hours before bedtime for adults with sleep problems. 19 However, there are currently no clear guidelines for prescribing melatonin for children and adolescents with neurodevelopmental disorders. 5 11
How the intervention might work
The understanding of melatonin’s underlying mechanisms has previously been extrapolated from animals to humans, but the exact physiological mechanisms of melatonin in humans remain unclear. 20–22 Melatonin is a neurohormone primarily secreted by the pineal gland. 13 Melatonin mediates dark signals, since the secretion of melatonin is related to darkness, and it is therefore associated with the circadian rhythm in humans. 13 17 The secretion of melatonin is regulated by the suprachiasmatic nucleus in the hypothalamus, and the production of melatonin depends on darkness, as the exposure to light inhibits secretion. 11 23 A decrease in the secretion of melatonin has been associated with ageing and different diseases, and synthetic melatonin may theoretically reduce sleep disturbance related to melatonin deficiency. 13 24 Previous studies have shown that melatonin improves total sleep time, sleep onset latency and sleep quality for adults with sleep disorders, but the effects seem small. 13 25 Furthermore, some studies suggest that children with autistic spectrum disorders have abnormal secretions of melatonin. 6 26 27 For these theoretical reasons, children with neurodevelopmental disorders may benefit from melatonin.
Why it is important to do this review
A systematic review published in 2018 investigated the effects of melatonin for sleep problems in children with neurodevelopmental disorders. 5 The review concluded that melatonin was safe and effective in improving sleep for children with neurodevelopmental disorders. 5 Another systematic review published in 2019 investigated the effects of oral melatonin for non-respiratory sleep disturbances in children with neurodisabilities. 28 The review concluded that there was some evidence of beneficial effects, but the extent of these effects was unclear due to the poor quality of the evidence. 28 The review also concluded that melatonin was well-tolerated, as comparable adverse effects were found in the melatonin and placebo groups. 28
These previous reviews had important limitations. The conclusions were affected by a high degree of heterogeneity, high and unclear risk of bias in the included trials and small sample sizes. 5 28 Furthermore, the duration of treatment was limited to a maximum of 13 weeks, and adverse events were not adequately reported or analysed in either of the reviews. 5 28
In recent studies, it has been questioned whether higher levels of melatonin are associated with delayed puberty, and other adverse effects of melatonin are also theoretically possible. 29–31 In 2021, a 2-year follow-up of a trial investigating the treatment with melatonin in 119 children with autism spectrum disorder was published. 32 This trial concluded that melatonin was safe and effective for long-term treatment in children. 32 Other, new randomised clinical trials might have been published since the last published systematic reviews, and on-going trials have been identified on ClinicalTrials.gov. 33 34 These trials may contribute important information about the use of melatonin in children with neurodevelopmental disorders, including adverse effects. Therefore, there is a need for a systematic review to shed light on this important topic and to assess whether the beneficial effects outweigh any harmful effects. Our systematic review will take risks of systematic errors (‘bias’), risks of random errors (‘play of chance’) and the certainty of the evidence into consideration when assessing the effects of melatonin for sleep disorders in children with neurodevelopmental disorders.
Methods and analysis
The present protocol has been registered in the PROSPERO database and is reported according to the guidance suggested in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) statement (please find the checklist in online supplemental material 1 ). 35 36
Supplemental material
Criteria for considering studies for this review, types of studies.
We will include randomised clinical trials irrespective of trial design (including crossover trials), setting, publication status, publication year and language. We will use online translation services to translate foreign abstracts and reach out to our international colleagues (who will be thanked in the acknowledgements) for help with data extraction of relevant trials. We will not include quasi-randomised trials, cluster-randomised trials or observational studies.
Types of participants
We will include trials randomising children and adolescents (below 18 years of age) with neurodevelopmental disorders, such as cerebral palsy, epilepsy, Angelman syndrome, Down’s syndrome, Fragile X syndrome, Prader-Willi syndrome, Rett syndrome, Smith-Magenis syndrome, Williams syndrome, non-specific intellectual disability, autism spectrum disorder, ADHD and ADD. 1 2 Trials will be included if the disorders of the participants are diagnosed by standardised diagnostic criteria, such as the Diagnostic and Statistical Manual of Mental Disorders 37 or International Classification of Diseases 38 or where the diagnosis or designation of neurodevelopmental disorder is made by a clinician. The participants also need to have a diagnosis of any type of sleep disorder (as defined by trialists), such as insomnia disorder, hypersomnolence disorder, narcolepsy, breathing-related sleep disorder, circadian rhythm sleep disorders, REM sleep arousal disorder, non-REM sleep arousal disorder, and nightmare disorders.
We will include participants irrespective of sex, comorbidities, demographic factors, the stage of their condition and the care setting. If a trial reports data where only a subset of participants is eligible (eg, a combination of children and adults), we will only include data from those participants that fulfil the inclusion criteria, and we will therefore require subset data for the specific group to be available.
Types of interventions
We will include trials where participants in the experimental group are given melatonin at any dose, form (eg, tablet, capsules, gummies, liquids), duration of administration, type of administration (eg, oral), timing of administration and setting. We will include trials where participants receive a co-intervention (eg, pharmacological interventions, such as methylphenidate, or non-pharmacological interventions, such as exercise), providing it is delivered equally (in any aspect, eg, same dose, equal subset of population receiving co-intervention) in the experimental group and the control group.
Comparators
As control intervention we will accept placebo or ‘no intervention’.
Types of outcome measures
Primary outcomes.
Total sleep time (in minutes using any type of measurement, eg, polysomnography, actigraphy, self-report or parent-report).
Adverse effects
The proportion of participants with one or more serious adverse events. We will use the International Conference on Harmonisation of technical requirements for registration of pharmaceuticals for human use—Good Clinical Practice (ICH-GCP) definition of a serious adverse event, which is any untoward medical occurrence that resulted in death, was life-threatening, required hospitalisation or prolonging of existing hospitalisation, resulted in persistent or significant disability or jeopardised the participant. 39 If the trialists do not use the ICH-GCP definition, we will include the data if the trialists use the term ‘serious adverse event’. If the trialists do not use the ICH-GCP definition nor use the term serious adverse event, then we will also include the data provided the event clearly fulfils the ICH-GCP definition for a serious adverse event. We will also analyse each type of serious adverse event separately.
The proportion of participants with one or more non-serious adverse events (any adverse event not classified as serious). We will also analyse each type of adverse event separately.
Secondary outcomes
Quality of life of the child (any valid continuous scale, eg, Child Quality of Life Questionnaire). 40
Quality of life of the parents/caregivers (any valid continuous scale, eg, 36-Item Short Form Survey (SF-36)). 41
Sleep onset latency (in minutes using any type of measurement, eg, polysomnography, actigraphy, self-report or parent-report).

Exploratory outcomes
Quality of sleep (any valid continuous scale), such as the Pittsburgh Sleep Quality Index. 42
Delayed puberty or any reports of hormonal changes.
Any continuous scale assessing adverse effects (eg, Paediatric Adverse Event Rating Scale). 43
Timing of outcome assessment
We will include outcome data recorded at the end of the treatment period primarily and at maximum follow-up secondarily.
Search methods for identification of studies
Electronic searches.
We will search the following:
Cochrane Central Register of Controlled Trials (CENTRAL; current issue) in The Cochrane Library.
MEDLINE Ovid (1946 onwards).
Embase Ovid (1974 onwards).
LILACS (Latin American and Caribbean Health Science Information database; 1982 onwards).
Science Citation Index Expanded (Web of Science; 1964 onwards).
Conference Proceedings Citation Index-Science (Web of Science; 1990 onwards).
PsycINFO (1967 onwards).
ClinicalTrials.gov.
International Clinical Trials Registry Platform (ICTRP).
Please see online supplemental material 2 for the search strategy.
Searching other resources
We will check reference lists of all included trials and any relevant systematic reviews to identify additional trials. We will also search for errata and retraction statements for the included trials. We will search websites of pharmaceutical companies (eg, Natrol, Neurim Pharmaceuticals, Takeda Pharma), websites of US Food and Drug Administration (FDA) and European Medicines Agency (EMA) to identify relevant trials. We will request FDA, EMA and national medicines agencies to provide all publicly releasable information about relevant studies that were submitted for marketing approval, including clinical study reports. We will contact authors of eligible trials and other experts to identify any relevant trials (published or unpublished).
Data collection and analysis
We will perform and report the review based on the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions. 44 Analyses will be performed using Stata V.17 45 and Trial Sequential Analysis. 46 47
Selection of studies
Two review authors will independently screen titles and abstracts using Covidence. 48 We will mark articles that clearly do not meet the eligibility criteria as excludes, while potentially eligible articles will go through to the next phase. We will retrieve all relevant full-text study reports/publications, and two review authors will independently screen the full text to identify and record reasons for exclusion of the ineligible trials. The two review authors will resolve any disagreement through discussion, or, if required, they will consult with a third author (JCJ). We will illustrate the selection process of the trials in a PRISMA flow diagram. 49 If multiple reports are available for a single trial, all reports will be grouped under a single reference ID.
Data extraction and management
Review authors in pairs will independently extract data from the included trials using a pilot tested data extraction form. Disagreements will be resolved through internal discussion or, if required, by discussion with a third author (JCJ). The two review authors will assess all publications of a trial together to evaluate all available data simultaneously. We will contact trial authors by email to obtain any additional data, which may not have been reported sufficiently in the publication. We will extract the following data:
Methods: trial setting, trial location, trial design, trial duration, duration of follow-ups, date of the trial, estimation of sample size, inclusion criteria and exclusion criteria.
Participants: number randomised, number analysed for each outcome, number lost to follow-up, age (mean and SD), sex ratio and diagnostic criteria.
Interventions: type, dose, timing and duration of intervention.
Control: type, dose, timing and duration of comparison.
Co-intervention: type, dose, timing and duration of co-interventions.
Outcomes: primary, secondary and exploratory outcomes at the reported time points.
Notes: trial funding and conflicts of interest of the trial authors.
One review author will transfer the data to Stata. We will double-check the data by comparing the data presented in the review to the data extraction form.
Assessment of risk of bias in included studies
Our bias risk assessment will be based on the Cochrane Risk of Bias tool—version 2 (RoB 2) as recommended in the Cochrane Handbook of Systematic Reviews of Interventions. 44 We will evaluate the methodology in respect of the following bias domains:
Bias arising from the randomisation process.
Bias due to deviations from the intended interventions (effect of assignment to intervention).
Bias due to missing outcome data.
Bias in measurement of the outcome.
Bias in selection of the reported result.
Review authors in pairs will independently assess the risk of bias using a template (available at https://www.riskofbias.info/ ). Disagreements will be resolved through internal discussion or, if required, by discussion with a third author (JCJ). We will use the signalling questions in the RoB 2 tool to rate each domain at either ‘low risk of bias’, ‘some concerns’ or ‘high risk of bias’. We will assess all domains of risk of bias for each outcome in each trial. The overall risk of bias of a result will be judged to be low if all domains are assessed at low risk of bias. If one or more domains are assessed at either some concerns or high risk of bias, the overall risk of bias will be assessed at high. We will assess the risk of bias for the outcomes of the included trials presented in the ‘Summary of findings’ table (primary and secondary outcomes at end of treatment). The risk of bias assessments will be illustrated in a table (using https://www.riskofbias.info/ ), and the assessments will be used to conduct subgroup analyses. The risk of bias assessment will also be used to inform the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) and the ‘Summary of findings’ table. For trials using crossover design, only data from the first period will be assessed.
Measures of treatment effect
Continuous outcomes.
We will calculate mean differences (MDs) and consider calculating standardised mean differences (SMDs) with 95% CIs for continuous outcomes. We will enter data presented as a scale with a consistent direction of effect. We will primarily analyse scores assessed at single time points. If only changes from baseline scores are reported, we will analyse the results together with follow-up scores for MD (not for SMD). 44 If SDs are not reported, we will calculate the SDs using trial data, if possible, or request such data from the authors.
Dichotomous outcomes
We will calculate risk ratios with 95% CIs for dichotomous outcomes.
Unit of analysis issues
We will only include randomised clinical trials. Trials using a crossover design will be treated as parallel trials, since only data from the first period will be included. 44 Where multiple trial arms are reported in a single trial, we will include only the relevant arms. For trials with multiple relevant experimental or control groups, we will combine the groups as appropriate. 44
Dealing with missing data
We will, as the first option, contact all trial authors to obtain information on missing data (ie, for data extraction and for assessment of risk of bias, as specified above). We will use intention-to-treat data if provided by the trialists. 50
We will not impute missing values for any outcomes in our primary analysis. In our sensitivity analyses (see below), we will impute data.
We will not impute missing values for any outcomes in our primary analysis. In our sensitivity analysis (see below) for continuous outcomes, we will impute data.
Assessment of heterogeneity
We will investigate forest plots to visually assess for signs of heterogeneity. We will also estimate the presence of statistical heterogeneity by a χ 2 test (threshold p<0.05) and measure the quantities of heterogeneity by the I² statistic. 51 52 We will investigate possible heterogeneity through subgroup analyses. We may ultimately decide that a meta-analysis should be avoided. 44 We will interpret I² heterogeneity as suggested by the Cochrane Handbook for Systematic Reviews of Interventions. 44 If we identify substantial heterogeneity (I²>50%), we will report it, and explore the possible causes by prespecified subgroup analyses. We will carefully investigate trial characteristics and report if we find unexpected heterogeneity due to clinical or methodological factors. Ultimately it will be decided if meta-analysis should be avoided.
Assessment of reporting biases
We will use funnel plots to assess reporting bias if 10 or more trials are included in an outcome. 44 We will visually inspect funnel plots to assess the risk of small trial effects that could potentially reflect publication bias. We are aware of the limitations of a funnel plot (ie, a funnel plot assesses bias due to small sample size). From this information, we will assess possible risk of publication bias. For dichotomous outcomes, we will test asymmetry with the Harbord test 53 if τ 2 is <0.1 and with the Rücker test if τ 2 is >0.1. For continuous outcomes, we will use the regression asymmetry test 54 and the adjusted rank correlation. 55
Data synthesis
Meta-analysis.
We will undertake this meta-analysis according to the recommendations stated in the Cochrane Handbook for Systematic Reviews of Interventions, 44 Keus et al 56 and our eight-step procedure suggested by Jakobsen et al . 57 We will assess our intervention effects with both random-effects meta-analyses (Hartung-Knapp-Sidik-Jonkman) 58 and fixed-effect meta-analyses (Mantel-Haenszel for dichotomous outcomes and inverse variance for continuous outcomes), 44 59 and report both meta-analysis results. 57 We will primarily report the most conservative result (widest CI and highest p value), and report the less conservative result as a sensitivity analysis. 57 As two primary outcomes are specified, we will consider a p value of 0.025 or less as the threshold for statistical significance for all outcomes. 57 Our primary analyses will include all trials. Where data are only available from one trial, we will use Fisher’s exact test for dichotomous data and Student’s t-test for continuous data. 60 61
Trial Sequential Analysis
Traditional meta-analysis runs the risk of random errors due to sparse data and repetitive testing of accumulating data when updating reviews. We wish to control for the risks of type I and type II errors. We will therefore perform Trial Sequential Analysis on all outcomes, in order to calculate the required information size (ie, the number of participants needed in a meta-analysis to detect or reject a certain intervention effect) and the cumulative Z-curve’s breach of relevant trial sequential monitoring boundaries. 47 62–67 A more detailed description of Trial Sequential Analysis can be found in the manual 47 and at www.ctu.dk/tsa/ . For dichotomous outcomes, we will estimate the required information size based on the observed proportion of patients with an outcome in the control group (the cumulative proportion of patients with an event in the control groups relative to all patients in the control groups), a relative risk reduction or a relative risk increase of 25%, an alpha of 2.5% for all our outcomes, a beta of 10% and the observed diversity as suggested by the trials in the meta-analysis. For continuous outcomes, we will use the observed SD in the control group, a mean difference of 30 min when assessing total sleep time; otherwise, a mean difference of the observed SD/2, an alpha of 2.5% for all outcomes, a beta of 10% and the observed diversity of the trials in the meta-analysis. We will only use the diversity-adjusted required information size (DARIS) for random-effects Trial Sequential Analyses.
Subgroup analysis and investigation of heterogeneity
We will perform the following subgroup analyses on the primary outcomes:
Type of neurodevelopmental disorder: this subgroup analysis will assess whether the effects of melatonin are different depending on the neurodevelopmental disorder of the child.
Age (below 12 years compared with above 12 years and preschool-age children compared with school-age children (as defined by trialists)): this will assess whether the effects of melatonin vary depending on the age of the participants.
Type of comparator (placebo or no intervention): this subgroup analysis will assess whether the effects of melatonin vary depending on the comparator.
Timing of the melatonin administration: if data are available, we will use the following comparisons: <2 hours before bedtime, 2–4 hours before bedtime or 4–8 hours before bedtime. If not, we will use definitions by trialists. This subgroup analysis is relevant, because the timing of administration may affect the outcomes. 68–70
Formulation of medication: this subgroup analysis will assess whether the effects of melatonin vary depending on the formulation of melatonin.
Type of sleep disorder: this subgroup analysis will assess whether the effects of melatonin vary depending on the type of sleep disorder.
Trials at high risk of bias compared with trials at low risk of bias: this subgroup analysis will assess whether the effects of melatonin vary depending on the risk of bias of the included trials.
Duration of trials: this subgroup analysis will assess whether the effects of melatonin vary depending on the duration of the included trials.
Post-hoc subgroup analyses might be warranted if unexpected clinical or statistical heterogeneity is identified during the analysis of the review results. 57 We will disclose any new subgroup analyses not reported in this protocol in the ‘Differences between protocol and review’ section of the systematic review.
Sensitivity analysis
To assess the potential impact of the missing data, we will perform the two following sensitivity analyses on the primary outcomes:
‘Best-worst-case’ scenario: we will assume that all participants lost to follow-up in the experimental group had beneficial outcomes (no serious adverse events/improved quality of sleep defined as the group mean plus two SDs). 57 We will accordingly assume that all participants lost to follow-up in the control group had poor outcomes (serious adverse events/deteriorated quality of sleep defined as the group mean plus two SDs). 57
‘Worst-best-case’ scenario: we will assume that all participants lost to follow-up in the experimental group had poor outcomes (serious adverse events/deteriorated quality of sleep defined as the group mean plus two SDs). 57 We will accordingly assume that all participants lost to follow-up in the control group had beneficial outcomes (no serious adverse events/improved quality of sleep defined as the group mean plus two SDs). 57
We will present the results of both scenarios in our review.
We will assess the potential impact of missing SDs for quality of sleep as follows: when SDs are missing, and it is not possible to calculate them, we will impute SDs from trials with similar populations and low risk of bias. If we find no such trials, we will impute SDs from trials with a similar population. As the final option, we will impute SDs from all trials. We will present results of this scenario in our review.
Summary of findings and assessment of the certainty of the evidence
Review authors in pairs will use GRADE to assess the certainty of the body of evidence associated with each of the primary and secondary outcomes at the end of treatment in our review. We will construct ‘Summary of findings’ tables using the GRADEpro GDT. 71 The GRADE approach appraises the certainty of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. We will assess the GRADE levels of evidence as either high, moderate, low or very low certainty on the following quality measures: risk of bias (the overall risk of bias will be used for each outcome), directness of the evidence, heterogeneity of the data, precision of effect estimates (assessed by Trial Sequential Analysis) and risk of publication bias. 71 We will downgrade the evidence by one or two levels due to serious or very serious issues. We will downgrade imprecision in GRADE by two levels if the accrued number of participants is below 50% of the DARIS, and one level if between 50% and 100% of DARIS. We will not downgrade if the cumulative Z-curve crosses the monitoring boundaries for benefit, harm or futility, or DARIS is reached. Two review authors will assess the certainty of evidence independently and decide on downgrading. If no agreement can be reached, a third review author (JCJ) will resolve the discussion. We will justify all decisions to downgrade the certainty of evidence using footnotes, and we will make comments to aid the reader’s understanding of the review where necessary. The ‘Summary of findings’ table will also report the anticipated absolute effects, relative effects, number of participants, type of participants and setting.
Differences between the protocol and the review
We will conduct the review according to this published protocol and report any deviations from it in the ‘differences between the protocol and the review’ section of the systematic review.
Patient and public involvement
Ethics and dissemination.
Ethical approval was not required for this protocol and systematic review. The results of the systematic review will be published in a peer-reviewed journal to help inform future research and clinical practice.
Ethics statements
Patient consent for publication.
Not applicable.
Acknowledgments
We thank Sarah Louise Klingenberg (Information Specialist, The Cochrane Hepato-Biliary Group, Copenhagen Trial Unit, Centre for Clinical Intervention Research, Copenhagen University Hospital—Rigshospitalet, Denmark) for the help with developing the search strategy.
- United States Environmental Protection Agency
- Morris-Rosendahl DJ ,
- Simkiss D ,
- Busk M , et al
- Robinson-Shelton A ,
- Abdelgadir IS ,
- Gordon MA ,
- Gringras P ,
- Breddy J , et al
- Hollway JA ,
- Jones AP , et al
- Devnani PA ,
- Esposito S ,
- D'Alonzo R , et al
- Li WA , et al
- Greenham S ,
- Sullivan M , et al
- Kimland EE ,
- Bardage C ,
- Collin J , et al
- Mindell JA , et al
- Rzepka-Migut B ,
- Schwichtenberg AJ ,
- National Health Service
- Cipolla-Neto J ,
- Amaral FGdo
- Guillaume J-L , et al
- Ferracioli-Oda E ,
- Qawasmi A ,
- Rossignol DA ,
- Tordjman S ,
- Anderson GM ,
- Pichard N , et al
- Beresford B ,
- Dawson V , et al
- Alenezi S , et al
- Kennaway DJ
- Abdallah N ,
- Findling RL ,
- Schroder CM , et al
- ClinicalTrials.gov
- Shamseer L ,
- Clarke M , et al
- American Psychiatric Association
- World Health Organization
- International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use
- Stevenson J ,
- Sherbourne CD
- Buysse DJ ,
- Reynolds CF ,
- Monk TH , et al
- Wehmeier PM ,
- Schacht A ,
- Lehmann M , et al
- Higgins J ,
- Chandler J , et al
- Copenhagen Trial Unit
- Thorlund K ,
- Engstrøm J ,
- Wetterslev J , et al
- McKenzie JE ,
- Bossuyt PM , et al
- Jakobsen JC ,
- Higgins JPT ,
- Thompson SG
- Thompson SG ,
- Deeks JJ , et al
- Harbord RM ,
- Davey Smith G ,
- Schneider M , et al
- Wetterslev J ,
- Gluud C , et al
- Winkel P , et al
- IntHout J ,
- Ioannidis JPA ,
- Imberger G ,
- Devereaux PJ ,
- Brok J , et al
- Benloucif S ,
- Harsanyi K , et al
- Guyatt GH ,
- Vist GE , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
Twitter @joannamoncrieff
Contributors CKJ, RH, SJ, PF, MH, JM, CG and JCJ contributed to the conceptualisation and design of the study. CKJ and JCJ wrote the original draft. All authors commented and approved the final manuscript. JCJ is the guarantor of the review.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Behavioural Treatments for Sleep Problems in Children with Autism Spectrum Disorder: a Review of the Recent Literature
- Sleep Disorders (P Gehrman, Section Editor)
- Published: 13 July 2020
- Volume 22 , article number 46 , ( 2020 )
Cite this article
- Emily Pattison 1 ,
- Nicole Papadopoulos 1 ,
- Deborah Marks 1 , 2 ,
- Jane McGillivray 1 &
- Nicole Rinehart 1
2091 Accesses
15 Citations
11 Altmetric
Explore all metrics
Purpose of Review
Behavioural sleep problems in children with autism spectrum disorder (ASD) are common and burdensome for both the child and their family. We provide an up-to-date review on behavioural sleep interventions and their core features and conclude with expert recommendations regarding the modification of interventions for children with ASD.
Recent Findings
In the past 3 years, four original research studies ( n ≥ 10) have evaluated behavioural sleep interventions for children with ASD (one RCT, three pre-post studies). All four studies reported significant improvements across various sleep outcomes and daytime behaviours. The interventions varied, however, in assessment comprehensiveness, nature of implementation support, length and delivery of intervention, outcome measurements, and follow-up periods.
Clinically, behavioural sleep interventions are regarded as the first-line of treatment for sleep problems experienced by children with ASD. However, there is still much to be learnt regarding their clinical effectiveness.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price excludes VAT (USA) Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Sleep Disorders in Children and Adolescents with Autism Spectrum Disorder: Diagnosis, Epidemiology, and Management
Samuele Cortese, Fang Wang, … Oliviero Bruni
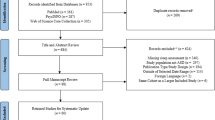
Sleep in Children with Autism Spectrum Disorder: A Narrative Review and Systematic Update
A. J. Schwichtenberg, Amy Janis, … Jane Kinkus Yatcilla
The relationship between sleep and behavior in autism spectrum disorder (ASD): a review
Simonne Cohen, Russell Conduit, … Kim M Cornish
Papers of particular interest, published recently, have been highlighted as: • Of importance
Association AP. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub; 2013.
Cortesi F, Giannotti F, Ivanenko A, Johnson K. Sleep in children with autistic spectrum disorder. Sleep Med. 2010;11:659–64.
PubMed Google Scholar
Richdale AL, Schreck KA. Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies. Sleep Med Rev. 2009;13:403–11.
Owens J. Classification and epidemiology of childhood sleep disorders. Prim Care Clin Off Pract. 2008;35:533–46.
Google Scholar
Hodge D, Carollo TM, Lewin M, Hoffman CD, Sweeney DP. Sleep patterns in children with and without autism spectrum disorders: developmental comparisons. Res Dev Disabil. 2014;35:1631–8.
Taylor MA, Schreck KA, Mulick JA. Sleep disruption as a correlate to cognitive and adaptive behavior problems in autism spectrum disorders. Res Dev Disabil. 2012;33:1408–17.
Delahaye J, Kovacs E, Sikora D, Hall TA, Orlich F, Clemons TE, et al. The relationship between health-related quality of life and sleep problems in children with autism spectrum disorders. Res Autism Spectr Disord. 2014;8:292–303.
Cohen S, Conduit R, Lockley SW, Rajaratnam SM, Cornish KM. The relationship between sleep and behavior in autism spectrum disorder (ASD): a review. J Neurodev Disord. 2014;6:44.
PubMed PubMed Central Google Scholar
Martin CA, Papadopoulos N, Chellew T, Rinehart NJ, Sciberras E. Associations between parenting stress, parent mental health and child sleep problems for children with ADHD and ASD: systematic review. Res Dev Disabil. 2019;93:103463.
1 Recommendations | Autism spectrum disorder in under 19s: support and management | Guidance | NICE. https://www.nice.org.uk/guidance/cg170/chapter/1-Recommendations . Accessed 27 Oct 2019.
• Williams Buckley A, Hirtz D, Oskoui M, et al. Practice guideline: treatment for insomnia and disrupted sleep behavior in children and adolescents with autism spectrum disorder: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2020;94:392–404 This systematic review provides evidence-based practice recommendations for treating sleep disturbances in children and adolescents with ASD.
Rigney G, Ali NS, Corkum PV, Brown CA, Constantin E, Godbout R, et al. A systematic review to explore the feasibility of a behavioural sleep intervention for insomnia in children with neurodevelopmental disorders: a transdiagnostic approach. Sleep Med Rev. 2018;41:244–54.
Adkins KW, Molloy C, Weiss SK, Reynolds A, Goldman SE, Burnette C, et al. Effects of a standardized pamphlet on insomnia in children with autism spectrum disorders. Pediatrics. 2012;130:S139–44.
Johnson CR, Turner KS, Foldes E, Brooks MM, Kronk R, Wiggs L. Behavioral parent training to address sleep disturbances in young children with autism spectrum disorder: a pilot trial. Sleep Med. 2013;14:995–1004.
Malow BA, Adkins KW, Reynolds A, Weiss SK, Loh A, Fawkes D, et al. Parent-based sleep education for children with autism spectrum disorders. J Autism Dev Disord. 2014;44:216–28.
Beresford B, McDaid C, Parker A, Scantlebury A, Spiers G, Fairhurst C, et al. Pharmacological and non-pharmacological interventions for non-respiratory sleep disturbance in children with neurodisabilities: a systematic review. Health Technol Assess. 2018;22:1–296.
Scantlebury A, Mcdaid C, Dawson V, Elphick H, Fairhurst C, Hewitt C, et al. Non-pharmacological interventions for non-respiratory sleep disturbance in children with neurodisabilities: a systematic review. Dev Med Child Neurol. 2018;60:1076–92.
• Keogh S, Bridle C, Siriwardena NA, Nadkarni A, Laparidou D, Durrant SJ, et al. Effectiveness of non-pharmacological interventions for insomnia in children with autism spectrum disorder: a systematic review and meta-analysis. PLOS ONE. 2019;14:e0221428 This systematic review and meta-analysis synthesises three RCTs and provides preliminary quantitative evidence on the effectiveness of behavioural interventions for treating sleep disturbances in children with ASD.
CAS PubMed PubMed Central Google Scholar
Cortesi F, Giannotti F, Sebastiani T, Panunzi S, Valente D. Controlled-release melatonin, singly and combined with cognitive behavioural therapy, for persistent insomnia in children with autism spectrum disorders: a randomized placebo-controlled trial. J Sleep Res. 2012;21:700–9.
• Papadopoulos N, Sciberras E, Hiscock H, Mulraney M, McGillivray J, Rinehart N. The efficacy of a brief behavioral sleep intervention in school-aged children with ADHD and comorbid autism spectrum disorder. J Atten Disord. 2019;23:341–50 This study is one of the largest RCTs with a rigorous methodology to demonstrate the efficacy of a brief behavioural sleep intervention in improving sleep problems and behavioural functioning in children with comorbid ASD-ADHD .
• Phillips NL, Moore T, Teng A, Brookes N, Palermo TM, Lah S. Behavioral interventions for sleep disturbances in children with neurological and neurodevelopmental disorders: a systematic review and meta-analysis of randomized controlled trials. Sleep. 2020;40:1–18 This systematic review and meta-analysis provides evidence of the effectiveness of behavioural interventions in improving sleep disturbances for children with neurological and neurodevelopmental disorders in the short term. It also appraises any functional improvements in behaviour.
Loring WA, Johnston RL, Shui AM, Malow BA. Impact of a brief behavioral intervention for insomnia on daytime behaviors in adolescents with autism spectrum disorders. J Contemp Psychother. 2018;48:165–77.
• McCrae CS, Chan WS, Curtis AF, et al. Cognitive behavioral treatment of insomnia in school-aged children with autism spectrum disorder: a pilot feasibility study. Autism Res. 2020;13:167–76 This pilot study demonstrates that CBT-I can be used by parents and their primary school-aged children with ASD to improve child and parent outcomes.
• Roberts CA, Smith KC, Sherman AK. Comparison of online and face-to-face parent education for children with autism and sleep problems. J Autism Dev Disord. 2019;49:1410–22 The findings of this study show promise that online interventions can improve sleep disturbances in children with ASD.
Sutton JE, Huws JC, Burton CR. Experiences of sleep hygiene education as an intervention for sleep problems in children with developmental disabilities: findings from an exploratory study. Br J Learn Disabil. 2019;47:165–73.
Arbelle S, Ben-Zion IZ. Sleep problems in autism. In: Schopler E, Yirmiya N, Shulman C, Marcus LM, editors. Res. Basis Autism Interv. Boston: Springer US; 2001. p. 219–27.
Moore M, Evans V, Hanvey G, Johnson C. Assessment of sleep in children with autism spectrum disorder. Children. 2017;4:72.
PubMed Central Google Scholar
Allik H, Larsson J-O, Smedje H. Insomnia in school-age children with Asperger syndrome or high-functioning autism. BMC Psychiatry. 2006;6:18.
Souders MC, Mason TBA, Valladares O, Bucan M, Levy SE, Mandell DS, et al. Sleep behaviors and sleep quality in children with autism spectrum disorders. 2009;32:13.
Prata J, Lawson W, Coelho R. Parent training for parents of children on the autism spectrum: a review. Int J Clin Neurosci Ment Health. 2018;3:1–8.
Kirkpatrick B, Louw JS, Leader G. Efficacy of parent training incorporated in behavioral sleep interventions for children with autism spectrum disorder and/or intellectual disabilities: a systematic review. Sleep Med. 2019;53:141–52.
Beresford B, Stuttard L, Clarke S, Maddison J. Parents’ experiences of psychoeducational sleep management interventions: a qualitative study of parents of children with neurodevelopmental disabilities. Clin Pract Pediatr Psychol. 2016;4:164–75.
McLay L, Sutherland D, Machalicek W, Sigafoos J. Systematic review of telehealth interventions for the treatment of sleep problems in children and adolescents. J Behav Educ. 2020;29:222–45. https://doi.org/10.1007/s10864-020-09364-8 .
Article Google Scholar
Telehealth delivery of treatment for sleep disturbances in young children with autism spectrum disorder - Full Text View - ClinicalTrials.gov . https://clinicaltrials.gov/ct2/show/NCT03668873 . Accessed 5 May 2020.
Goldman SE, Richdale AL, Clemons T, Malow BA. Parental sleep concerns in autism spectrum disorders: variations from childhood to adolescence. J Autism Dev Disord. 2012;42:531–8.
Liu X, Hubbard JA, Fabes RA, Adam JB. Sleep disturbances and correlates of children with autism spectrum disorders. Child Psychiatry Hum Dev. 2006;37:179–91.
Vivanti G, Prior M, Williams K, Dissanayake C. Predictors of outcomes in autism early intervention: why don’t we know more? Front Pediatr. 2014;2. https://doi.org/10.3389/fped.2014.00058 .
McMahon CM, Vismara LA, Solomon M. Measuring changes in social behavior during a social skills intervention for higher-functioning children and adolescents with autism spectrum disorder. J Autism Dev Disord. 2013;43:1843–56.
Williams BT, Gray KM, Tonge BJ. Teaching emotion recognition skills to young children with autism: a randomised controlled trial of an emotion training programme. J Child Psychol Psychiatry. 2012;53:1268–76.
Herbrecht E, Poustka F, Birnkammer S, Duketis E, Schlitt S, Schmötzer G, et al. Pilot evaluation of the Frankfurt Social Skills Training for children and adolescents with autism spectrum disorder. Eur Child Adolesc Psychiatry. 2009;18:327–35.
Pellecchia M, Connell JE, Kerns CM, Xie M, Marcus SC, Mandell DS. Child characteristics associated with outcome for children with autism in a school-based behavioral intervention. Autism. 2016;20:321–9.
Sallows GO, Graupner TD. Intensive behavioral treatment for children with autism: four-year outcome and predictors. Am J Ment Retard. 2005;110:417–38.
Sciberras E, Mulraney M, Mensah F, Oberklaid F, Efron D, Hiscock H. Sustained impact of a sleep intervention and moderators of treatment outcome for children with ADHD: a randomised controlled trial. Psychol Med. 2019;18:1–10.
Lord C. Taking sleep difficulties seriously in children with neurodevelopmental disorders and ASD. Pediatrics. 2019;143:e20182629.
Weiskop S, Richdale A, Matthews J. Behavioural treatment to reduce sleep problems in children with autism or fragile X syndrome. Dev Med Child Neurol. 2005;47:94–104.
Richdale AL, Baglin CL. Self-report and caregiver-report of sleep and psychopathology in children with high-functioning autism spectrum disorder: a pilot study. Dev Neurorehabil. 2015;18:272–9.
Mazurek MO, Petroski GF. Sleep problems in children with autism spectrum disorder: examining the contributions of sensory over-responsivity and anxiety. Sleep Med. 2015;16:270–9.
Cuomo BM, Vaz S, Lee EAL, Thompson C, Rogerson JM, Falkmer T. Effectiveness of sleep-based interventions for children with autism spectrum disorder: a meta-synthesis. Pharmacother J Hum Pharmacol Drug Ther. 2017;37:555–78.
Abdelgadir IS, Gordon MA, Akobeng AK. Melatonin for the management of sleep problems in children with neurodevelopmental disorders: a systematic review and meta-analysis. Arch Dis Child. 2018;103:1155–62.
Gringras P, Nir T, Breddy J, Frydman-Marom A, Findling RL. Efficacy and safety of pediatric prolonged-release melatonin for insomnia in children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2017;56:948–957.e4.
Papadopoulos N, Sciberras E, Hiscock H, Williams K, McGillivray J, Mihalopoulos C, et al. Sleeping sound with autism spectrum disorder (ASD): study protocol for an efficacy randomised controlled trial of a tailored brief behavioural sleep intervention for ASD. BMJ Open. 2019;9:e029767.
Download references
Author information
Authors and affiliations.
Deakin Child Study Centre, School of Psychology, Faculty of Health, Deakin University, Geelong, VIC, Australia
Emily Pattison, Nicole Papadopoulos, Deborah Marks, Jane McGillivray & Nicole Rinehart
The Royal Children’s Hospital, Parkville, VIC, Australia
Deborah Marks
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nicole Papadopoulos .
Ethics declarations
Conflict of interest.
Emily Pattison and Deborah Marks declare that they have no conflict of interest. The Deakin Child Study Centre (Nicole Rinehart, Nicole Papadopoulous, Jane McGillivray) receives philanthropic funding from the Moose Toys, Ferrero Group Australia as part of its Kinder + Sport pillar of Corporate Social Responsibility initiatives, MECCA Brands, Wenig Family, Geelong Community Foundation, and Grace & Emilio Foundation; and industry partner funding from the Victorian Department of Education, to conduct research in the field of neurodevelopmental disorders and inclusion. The Deakin Child Study Centre (NR, NP, JM) has also previously received scholarship funding from the Australian Football League and industry partner funding from the NDIS. NR has received donations from Vic Health and Bus Association Victoria and previous speaker honorarium from Novartis (2002), Pfizer (2006) and Nutricia (2007) and is a Director of the Amaze Board (Autism Victoria).
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards and international/national/institutional guidelines).
None of the companies, industry partners or organisational bodies listed above had a role in this research including the collection, analysis, and interpretation of data; in writing of the manuscript; and/or in the decision to submit the article for publication.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
Reprints and permissions
About this article
Pattison, E., Papadopoulos, N., Marks, D. et al. Behavioural Treatments for Sleep Problems in Children with Autism Spectrum Disorder: a Review of the Recent Literature. Curr Psychiatry Rep 22 , 46 (2020). https://doi.org/10.1007/s11920-020-01172-1
Download citation
Published : 13 July 2020
DOI : https://doi.org/10.1007/s11920-020-01172-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Behavioural sleep intervention
- Sleep problems
Advertisement
- Find a journal
- Publish with us
- Track your research
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,905,756 articles, preprints and more)
- Free full text
- Citations & impact
- Similar Articles
A literature review of sleep problems and neurodevelopment disorders.
Author information, affiliations.
- Al Lihabi A 1
Frontiers in Psychiatry , 23 Feb 2023 , 14: 1122344 https://doi.org/10.3389/fpsyt.2023.1122344 PMID: 36911135 PMCID: PMC9995546
Abstract
Introduction, free full text , a literature review of sleep problems and neurodevelopment disorders.
Sleep is an incredibly complex process that goes beyond relaxing and body resting. Disturbance in sleep leads to several short-term and long-term consequences. Neurodevelopmental diseases such as “autism spectrum disorder” (ASDs), Attention-deficit hyperactivity disorder (ADHD), and intellectual disability commonly experience sleep disorders that affect their clinical presentation, daily function, and quality of life.
The incidence of sleep problems in ASD patients ranges from 32 to 71.5%, especially insomnia, while an estimated 25–50% of people with ADHD report having sleep issues in clinical settings. The incidence of sleep issues is widespread in persons with intellectual disabilities, reaching up to 86%. This article is a literature review covering the neurodevelopmental disorder interaction with sleep disorder and different management.
Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to be chronic. Recognizing and diagnosis of sleep disorders will enhance their function, response to treatment, and quality of life.
- Sleep disorder
Sleeping is an incredibly complex process that goes beyond relaxing and body resting. It is a state of involuntary activity in which the brain is relatively still and responds to internal stimuli during NREM, and 20% is approximately active during REM. The exact purpose of sleep is not fully understood. Sleep has many functions, including neuronal plasticity, memory consolidation, immune function, growth, and mental health. Sympathetic overtone, an increase in the activity of hypothalamic–pituitary–adrenal axis, metabolic disorders, and inflammatory responses are factors that may cause disturbance in the sleep rhythm. Disturbance in sleep leads to several short-term consequences such as emotional disturbance, increase in stress response, mood disorder, cognitive and performance deficits, somatic pain, and reduced quality of life. Sleep disturbance influences teenagers’ mental health, academic performance, and risk-taking behaviors. Sleep disturbance in children is linked to behavioral issues and impaired cognitive performance. In those who are otherwise healthy, sleep disturbance can have long-term effects such as dyslipidemia, hypertension, cardiovascular disease, problems with weight, type 2 diabetes, metabolic syndrome, and colorectal cancer ( 1 – 3 ). The basic form of normal sleep organization is called sleep architecture. The sleep cycle is composed of two phases: non-rapid eye movement (NREM) sleep and rapid eye movement (REM). Phases 1, 2, 3, and 4 of NREM sleep form a continuum of relative depth. Every individual has distinctive characteristics of sleep, such as variations in eye movements, muscle tone, and brain wave patterns. Electroencephalogram (EEG) recordings, which monitor electrical patterns of brain activity, have been used to show sleep cycles and phases ( 4 ). The aging process has continuous and considerable effects on sleep architecture. There are noticeable differences between childhood and adulthood in sleep initiation and maintenance, the duration spent in each phase, and overall sleep efficiency. Studying age-related decreases in sleep efficiency is a general trend. Though the effects of insufficient sleep are generally well established, the causes are complicated and poorly understood. Therefore, when examining sleep stages in children of different ages, it is critical to take their unique characteristics into account. However, examining sleep characteristics according to age enables a more in-depth comprehension of how sleep contributes to effective aging and human development. Sleep disorders according to DSM-5 are insomnia, parasomnia, breath-related disorders, hypersomnolence, narcolepsy, circadian rhythm sleep–wake disorder and substance, and medication-related disorder ( 5 ).
Analysis of phenotypes for sleep disorder
There are several types of sleep assessment methods that should be customized for each child. Subjective methods including parent-reported surveys and sleep diaries are among the most frequently employed methods in the analysis of sleep disorders in human studies. They offer various advantages, including non-invasive acquisition and low costs. Children’s Sleep Habits Questionnaire (CSHQ) is considered one of the most popular parent-completed surveys. It is a tool for assessment of sleep in school-aged children based on parental reports ( 6 ). Another method is the Electroencephalography (EEG). It involves two electrodes that are attached to the patient’s scalp. It provides a recording of the brain’s electrical activity throughout sleep and weakness ( 7 ). A method known as a polysomnogram (PSG) is regarded as the benchmark for the objective assessment of sleep compared to a single-channel EEG ( 8 ). It incorporates physiological indications of normal and abnormal brain electrical activity, sleep architecture, sleep stages, and sleep quality, as well as eye movements and physical activities during sleep. Actigraphy provides a non-invasive evaluation of limb activity using an accelerometer to identify episodes of sleep and wakefulness. It enables the collection of data over several days in unstructured settings. The reliability of actigraphy with PSG was examined and revealed a strong relationship between PSG and actigraphy measures (>0.80) for sleep latency, length, and efficiency ( 9 ). Similar to actigraphy, videosomnography’s benefits come from its objective documentation over a long period ( 10 ). It can also be used to record unusual occurrences like nighttime parasomnias. However, using videosomnography in child sleep research comes with several difficulties.
- Sleep problems and autism spectrum disorders
Autism spectrum disorders (ASDs) have a wide range of clinical symptoms that are connected to social communication and interaction. Restrictive, repetitive, and stereotyped behaviors and interests are common in ASD. They have persistent difficulties in reciprocal social interaction and communication across a variety of circumstances. High levels of co-occurring behavioral difficulties are frequently present in children with ASD. According to the most recent report from the United States, the incidence was 1/54 in 2020. One of the most common features of ASD is the sleep disorder that results from the interaction of several factors such as psychological, biological, family factors, environmental, and child practice methods that might not be sleep-friendly ( 11 ).
Incidence of sleep disorders in patients with ASD
The incidence of sleep problems in ASD patients ranges from 32 to 71.5%. Children and adolescents with ASD are more likely to experience sleep difficulties, especially insomnia, with incidence rates ranging from 40 to 80%. This wide range of incidence may be due to the different sleep problems assessment methods and different criteria such as different cut-off scores ( 12 ). After adjusting for family variables including poor child-rearing practices (for example, little parental supervision at bedtime), and noisy, or stressful environments, children with ASD are also more prone to experience sleep disturbances compared with their normal relatives; 47 and 16%, respectively, ( 13 ).
The causes of sleep difficulties in children with ASD
ASD is a multifactorial disease that is affected by multiple factors including neurological, genetic, immunological, and environmental factors. Several neurotransmitters like melatonin, GABA, and serotonin are required to create a regular cycle of sleep and wakefulness. Sleep may be affected by any problems with these neurotransmitters’ synthesis ( 14 ). The hormone melatonin aids in synchronizing and preserving the circadian cycle. Autism may have improper melatonin regulation. The integrity of synaptic transmissions and the control of melatonin in ASD may both be influenced by clock genes ( 15 ). Melatonin exogenous therapy has been demonstrated to improve sleep schedule in ASD kids. Children with ASD showed decreased activity of the final enzyme in the production of melatonin, indicating lower levels of melatonin. This enzyme is encoded by the N-acetylserotonin O-methyltransferase gene ( 16 ). GABA is the neurotransmitter that induces sleep by inhibiting cells that are involved in arousal functions. It is produced from the preoptic area which is the sleep area in the hypothalamus. The Bidirectional Theoretical Framework of Sleep Disturbance provides an overview of the various risk factors that can affect the development of sleep issues in people with ASD ( 12 ).
Effect of sleep disturbances in ASD patients on caregivers
Increased parental sleep problems and maternal stress have been associated with sleep abnormalities in children with ASD. Sleep issues can significantly affect a child’s quality of life, daily functioning, and family dynamics, adding stress to everyone involved. This has also been linked to more challenging behaviors in ASD children during the day, as well as an influence on the ability to control mood. Sleep quality has been linked to common medical disorders such as upper respiratory problems and vision problems. Poor appetite and a decrease in the rate of growth have been linked to increased nighttime awakening and a reduced desire to go to sleep. Sleep disturbance in ASD children has been linked to increased aggression, hyperactivity, and social issues that may be markers of poor mental health outcomes.
Sleep disorders management
It is crucial to conduct early and frequent screenings for sleep impairment and its related conditions.
Non-pharmacological management
Pharmacological management.
Medical treatment is considered if the children do not respond to behavioral therapy.
Role of melatonin
It has been suggested that a lack of sociability may be related to sleep difficulties and circadian rhythm disruptions in ASD patients. Indeed, zeitgebers (also known as timeivers) like the natural light–dark cycle, music, and social cues are necessary for the entrainment and synchronization of the circadian clock. Therefore, in ASD patients, poor social cue perception or interpretation may impair the effectiveness of systems that synchronize sleep and wakefulness ( 18 ). As an alternative, ASD patients could find it difficult to synchronize with their internal and external settings, leading to eventual rhythm and time problems which affect a variety of fields, including social interaction and circadian cycles. In other words, persons with ASD would experience circadian abnormalities due to their failure to reflect their internal clock on environmental and social rhythms ( 19 ).
Antipsychotic medication
This drug class has minimal tolerability and efficacy data for the treatment of insomnia in children. Few trials on the influence on sleep architecture have found that ziprasidone, olanzapine, and risperidone increase slow-wave, although ziprasidone and risperidone reduce REM sleep. Risperidone and olanzapine are two atypical antipsychotic that have been recommended for sleep disorders in children ( 22 ). These medications are used for the treatment of insomnia off-label, and it is not advised that they be regularly prescribed for this use, particularly as a first-line pharmacotherapeutic medication. In particular, the Canadian Academy of Child and Adolescent Psychiatry has advised against using them as a first-line line treatment for insomnia in children, adults, or the elderly ( 23 ). Other countries have likewise attempted to limit the number of prescriptions that government-subsidized programs may allow.
Antidepressant
There is limited evidence on the use and effectiveness of sedative antidepressants, selective serotonin reuptake inhibitors (SSRI), and tricyclic antidepressants (TCA) for the management of sleep disturbances in ASD children. Such medications might be effective if the sleeplessness is accompanied by concomitant psychiatric disorders. Children with comorbid depression may benefit from sedative antidepressants like trazodone and mirtazapine. These antidepressants enhance sleep by reducing the effects of neurotransmitters that promote wakefulness, including acetylcholine, histamine, noradrenaline, and serotonin. As a side effect, the majority of such medications reduce REM sleep and prolong daytime sleepiness. In psychiatric practice, trazodone is widely chosen and employed. Its effectiveness has primarily been shown in people with psychiatric illnesses. Trazodone has a noticeable morning hangover effect due to the antagonism of the 5-HT2A/C and being powerful sedating antidepressant. In contrast, fluoxetine is frequently connected to insomnia. Comparatively speaking to doses used to treat mood disorders, doses used to treat insomnia are typically lower.
Alpha-adrenergic agonist
Sedative and hypnotics drugs.
Hypnotics and sedatives benzodiazepines (BZDs) are routinely given to adults with insomnia. However, because of their side effects, which include drowsiness, headaches, cognitive impairment, dizziness and rebound sleeplessness, and physical and behavioral dependence, they are recommended less frequently to children. Clonazepam was the only benzodiazepine tested for sleep issues in autistic children. Children with developmental disabilities were found to benefit from the treatment of partial arousals, parasomnias, periodic limb movement disorder, and nocturnal biting with clonazepam, an intermediate-acting BZD ( 26 , 27 ).
Other medication
Several medications which are used in the treatment of the Alzheimer’s disease are also found to be effective in the management of ASD symptoms ( 28 ). Drugs such as donepezil and rivastigmine are cholinesterase inhibitors that increase the acetylcholine by preventing its destruction. ASD is associated with anomalies in the cholinergic system, according to previously published evidence ( 29 ). First, research looking at post-mortem brain samples from people with ASD has discovered cholinergic system anomalies ( 30 , 31 ).
According to several studies, a large percentage of children with ASD condition experience seizures. It is reported that the incidence of ASD cases that suffered from epilepsy may range from 5 to 38% which is much higher than the incidence of the epilepsy in the normal children population which is 1–2% ( 32 , 33 ). There is very limited evidence about the use of anti-epileptic drugs in ASD patients. A randomized controlled trial has been valproate in ASD cases ( 34 ). They found that valproate monotherapy reduced the irritability and repetitive behaviors in ASD cases ( 35 ).
- Sleep disorder and ADHD
Types of sleep disorders
An estimated 25–50% of people with ADHD report having sleep issues in clinical settings ( 37 ). Besides, adults who do not have enough time of sleep are more prone to have symptoms of ADHD ( 38 ). Such individuals’ sleep disruptions have been linked to concomitant primary sleep problems and/or changes brought on by ADHD drugs ( 6 ). Researchers have looked into the connections between ADHD and narcolepsy, insomnia, circadian rhythm sleep disorders (CRSDs), restless leg syndrome, and sleep-disordered breathing (SDB) ( 39 , 40 ).
Obstructive sleep apnea and ADHD
Obstructive sleep apnea (OSA) is characterized by partial or total obstruction of the upper airway, which results in interrupted sleep, while SDB is associated with unpredictable breathing rhythm during sleep ( 41 , 42 ). People with ADHD have a higher incidence of SDB, and those with a history of snoring or possible OSA throughout childhood are associated with a two-fold higher susceptibility of diagnoses with ADHD ( 43 ). Through several processes, involving negative effects of hypoxic outcomes, the inflammation that leads to brain, and/or recurrent arousal-based sleep disturbances, SDB influences psychological outcomes. These pathways may change the prefrontal cortex’s neurochemical substrates, resulting in the neurobehavioral abnormalities that underlie the symptoms of ADHD ( 44 ).
Restless leg syndrome and ADHD
Restless leg syndrome (RLS) is a common sensorimotor condition characterized by an intense need to move the legs, which is frequently accompanied by unpleasant leg or (less frequently) body-part feelings. These feelings are particularly uncomfortable in the evening or at night and get better with activity. Due to their need to walk about and the stiffness in their legs, patients frequently have sleeplessness. This comorbidity is thought to be caused by iron deficiency and dopaminergic disorders ( 45 , 46 ). Even though the incidence of RLS in children is unknown, the disorder affects 10% of adults in the United States. According to the data, up to 44% of people with ADHD have RLS or symptoms similar to it, while up to 26% of those with RLS have symptoms similar to it ( 47 , 48 ).
Circadian rhythm sleep disorder and ADHD
Narcolepsy and adhd.
A persistent neurological condition called narcolepsy causes problems with sustaining constant wakefulness and sleep. A diagnosis of narcolepsy needs symptoms of rapid eye movement (REM), sleep dissociation (such as sleep paralysis, hypnagogic/hypnopompic hallucinations, and cataplexy), and disturbed nighttime sleep, regardless of how the clinical presentation manifests itself. In the past, it was discovered that adults with narcolepsy had a twice as high probability of receiving an ADHD diagnosis as children as compared to controls ( 51 ). Additionally, data points to children with ADHD experiencing hypo arousal and hypo arousal-related hyperactivity/impulsivity as possible signs of exhaustion ( 52 ). Although the relationship between the two disorders is unclear, it has been postulated that EDS in narcoleptics may cause inattention, deficient executive function, and issues with impulse control that are similar to ADHD and react well to psychiatric drugs ( 53 – 55 ). Finally, the overlap of ADHD and narcolepsy symptoms may result in diagnostic ambiguity or incorrect diagnosis of the diseases. Another theory is that the connection could be due to a common pathology in the brain ( 56 ).
ADHD medication
The effects of stimulants on sleep vary from patient to patient in those with ADHD, reflecting the intricacy of the relationships between sleep disturbance and ADHD ( 57 ). Clinical experience suggests that stimulants generate paradoxical effects, whereby symptom relief can relax patients and encourage sleep, although there is evidence linking stimulants to disturbed sleep in ADHD cases ( 58 , 59 ). Furthermore, increasing the dosage of a short-acting inducer or using a formula with prolonged action may minimize sleep disruptions caused by an increase in hyperactivity or behavioral disorders at bedtime due to the risk of symptom rebound when the concentrations of the drug in the blood is decreased ( 60 , 61 ).
Non-stimulants
The most frequent side effect associated with atomoxetine that is connected to sleep, in contrast to stimulants, is somnolence (a noradrenaline reuptake inhibitor permitted for the management of ADHD). In atomoxetine placebo-controlled trials, somnolence was observed to present in 15–17% of patients as reported by a 2009 comprehensive review ( 62 ). Atomoxetine was found to have less of an impact on subjective sleep measures than methylphenidate and was taken three times per day in a randomized, double-blind trial.
After evaluation and diagnosis, the first stage of treatment will be psychoeducation. In addition to learning about the prognosis, course, therapy, and probable functional implications of the sleep disorder, the affected individuals and their social entourage will require proper psychoeducation on ADHD symptoms and sleep problems. Additionally, educating people about healthy sleep habits and sleeping patterns will enable non-pharmacological sleep enhancement. It is common practice to use medicine to address sleep disturbances. The choice of medication can be directed to address related issues such as daytime malfunction and should be combined with behavioral techniques. Surgery to remove the tonsils or adenoids is the first line of treatment for children with ADHD and SDB, whereas oral appliances, positive airway pressure devices, or surgery are suggested treatments for adults with OSA and ADHD ( 63 ). The sleep environment may need to be changed for people with RLS and ADHD, and behavioral therapies such as iron supplements ( 64 ) (for example, ferrous sulfate) or gabapentin ( 65 ) may also be investigated, especially for a younger population. In an adults, using dopaminergic substances such as L-DOPA, ropinirole, and pramipexole, in addition to, a recently developed drug called rotigotine may also be a possibility ( 66 ).
Treatment options for people with DSPS and ADHD include scheduled melatonin therapy, light therapy ( 67 ), and chronotherapy ( 68 , 69 ). Furthermore, because treatment for DSPS differs from that for insomnia, a clear distinction between the two must be made. Treatment for ADHD and insomnia can differ depending on the age group.
- People with intellectual disabilities and sleep disorders
The incidence of sleep issues in children ranges from 24 to 86%, and they are widespread in persons with intellectual disabilities ( 70 ). Adults with mental disabilities are reported to have an incidence of sleep disorders ranging from 8.5 to 34.1%, with a serious sleep problem rate of 9.2%. In one study, it was discovered that 551 older persons with intellectual disabilities had sleep issues in 72% of the cases ( 47 ). The treatment of physical and mental health issues in people with intellectual disabilities is an area that needs more study. Studies conducted on people without intellectual disabilities were often the basis for the development of diagnostic and management techniques. The same pattern is observed in persons with intellectual impairments who have sleep difficulties. There is a lack of information specifically on the causes, effects, and treatments of sleep problems in people with developmental disabilities. Assessment and treatment of sleep issues in persons with intellectual impairments can be informed by knowledge of the several types of sleep issues that these people encounter and the numerous factors that affect their sleep ( 71 ).
Adults with intellectual disabilities have a higher risk to have sleep issues, which could be due to several factors. In individuals with intellectual impairments, a systematic review of the published literature on sleep problems found links between sleep and several characteristics, such as respiratory diseases, psychoactive drugs, mental health illnesses, and challenging behavior ( 47 ). Understanding and taking into account the social, psychological, and biological aspects influencing the higher occurrence of sleep issues in persons with intellectual impairments is crucial for providing person-centered and individualized care. We have looked at several significant contributing elements that must be taken into account when evaluating sleep issues in persons with intellectual disabilities. The association between sleep disturbances and neurodevelopmental diseases like ADHD and ASD has been thoroughly studied above ( 47 ).
Genetic conditions
Our comprehension of the underlying genetic causes of intellectual impairments has recently improved ( 72 ). For example, Down’s syndrome is characterized by obesity, hypotonia, and craniofacial anomalies, all of which raise the likelihood of sleep disorders including obstructive sleep apnea (OSA). Similarly to this, those who have cri du chat syndrome have a higher risk of getting OSA ( 73 ).
Environmental and psychological factors
People with mental disorders frequently experience sleep disturbance as the first sign of a decline in their mental health, and low-quality sleep represents a common feature of many psychotic and affective diseases ( 11 ). When compared to individuals without cognitive disabilities, those with cognitive disabilities have a higher incidence of mental problems, which helps explain why sleep disturbances are so common in this population ( 12 ). When determining the etiology of sleep issues in a person with cognitive disabilities, it is crucial to take the environment’s role in the development of sleep disorders into account. According to Kerr and Wilkinson ( 13 ), staffed residential homes may not be the best places to sleep because people may check on residents at odd hours, which would result in more noise and lights that would be disruptive to sleep ( 13 ).
Diagnosis of sleep disorders
Adults with intellectual impairments are frequently given subjective sleep information by their caregivers, who may disagree with the severity of the problem or may even accept sleep disturbance as a symptom of the person’s underlying condition ( 74 ).
Adults with cognitive disabilities are more prone than the general population to lack appropriate daily activity and regular exposure to natural light, thus even small changes to everyday routine and the sleeping environment can be beneficial ( 75 ). The needs of the person should be taken into consideration when making such recommendations, such as lowering external noise for autistic people sensitive to sounds. The evidence is not strong enough to support the use of pharmaceuticals to treat sleep disturbances in adults with intellectual impairments. Melatonin is the drug that has drawn the most attention, maybe due to its favorable side-effect profile and the fact that several trials have demonstrated its efficacy ( 75 ). According to a meta-analysis, melatonin consumption enhances total sleep time and reduces the number of wake-ups per night in people with intellectual disabilities. Currently, the pharmacological management of illnesses other than insomnia tends to use the same routes as those for the general public ( 75 ).
Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to chronicity. Various solutions are required based on the neurodevelopmental problem, but all patients should get behavioral intervention. Understanding the distinctive characteristics of sleep disturbances in patients with neurodevelopmental disorders is critical for effective therapy.
- Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
- Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Full text links
Read article at publisher's site: https://doi.org/10.3389/fpsyt.2023.1122344
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Article citations
Developmental alcohol exposure is exhausting: sleep and the enduring consequences of alcohol exposure during development..
Wilson DA , Sullivan RM , Smiley JF , Saito M , Raineki C
Neurosci Biobehav Rev , 158:105567, 01 Feb 2024
Cited by: 0 articles | PMID: 38309498
Associations between Milk Intake and Sleep Disorders in Chinese Adults: A Cross-Sectional Study.
Xu J , Lao J , Jiang Q , Lin W , Chen X , Zhu C , He S , Xie W , Wang F , Yang B , Liu Y
Nutrients , 15(18):4079, 21 Sep 2023
Cited by: 0 articles | PMID: 37764862 | PMCID: PMC10536886
Natural Course of IQSEC2 -Related Encephalopathy: An Italian National Structured Survey.
Leoncini S , Boasiako L , Lopergolo D , Altamura M , Fazzi C , Canitano R , Grosso S , Meloni I , Baldassarri M , Croci S , Renieri A , Mastrangelo M , De Felice C
Children (Basel) , 10(9):1442, 24 Aug 2023
Cited by: 0 articles | PMID: 37761403 | PMCID: PMC10528631
Efficacy and safety of electroacupuncture for secondary sleep disorders: A meta-analysis and systematic review.
Liu S , Liu J , Su J , Zhang F
Medicine (Baltimore) , 102(26):e34150, 01 Jun 2023
Cited by: 0 articles | PMID: 37390293 | PMCID: PMC10313263
Correlations between Sleep Features and Iron Status in Children with Neurodevelopmental Disorders: A Cross-Sectional Study.
Giambersio D , Marzulli L , Margari L , Matera E , Nobili L , De Grandis E , Cordani R , Barbieri A , Peschechera A , Margari A , Petruzzelli MG
J Clin Med , 12(15):4949, 27 Jul 2023
Cited by: 0 articles | PMID: 37568350 | PMCID: PMC10420017
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Inattention and hyperactivity/impulsivity among children with attention-deficit/hyperactivity-disorder, autism spectrum disorder, and intellectual disability.
McClain MB , Hasty Mills AM , Murphy LE
Res Dev Disabil , 70:175-184, 26 Sep 2017
Cited by: 17 articles | PMID: 28957735
DSM-5 Changes in Attention Deficit Hyperactivity Disorder and Autism Spectrum Disorder: Implications for Comorbid Sleep Issues.
Ramtekkar UP
Children (Basel) , 4(8):E62, 27 Jul 2017
Cited by: 8 articles | PMID: 28749421 | PMCID: PMC5575584
Sleep EEG oscillations in neurodevelopmental disorders without intellectual disabilities.
Gorgoni M , Scarpelli S , Reda F , De Gennaro L
Sleep Med Rev , 49:101224, 30 Oct 2019
Cited by: 18 articles | PMID: 31731102
Efficacy and Safety of Melatonin Treatment in Children with Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder-A Review of the Literature.
Rzepka-Migut B , Paprocka J
Brain Sci , 10(4):E219, 07 Apr 2020
Cited by: 15 articles | PMID: 32272607 | PMCID: PMC7226342
[Intellectual developmental disability overlapping with autism spectrum disorder and attention deficit-hyperactivity disorder].
Mulas F , Rojas M
Medicina (B Aires) , 78 Suppl 2:63-68, 01 Jan 2018
Cited by: 1 article | PMID: 30199368
Europe PMC is part of the ELIXIR infrastructure

IMAGES
VIDEO
COMMENTS
The incidence of sleep problems in ASD patients ranges from 32 to 71.5%, especially insomnia, while an estimated 25-50% of people with ADHD report having sleep issues in clinical settings. The incidence of sleep issues is widespread in persons with intellectual disabilities, reaching up to 86%. This article is a literature review covering the ...
The incidence of sleep issues is widespread in persons with intellectual disabilities, reaching up to 86%. This article is a literature review covering the neurodevelopmental disorder interaction with sleep disorder and different management. Conclusion: Disorders of sleep are key concerns in children with neurodevelopmental disorders.
This article is a literature review covering the neurodevelopmental disorder interaction with sleep disorder and different management. Conclusion: Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to be chronic. Recognizing and diagnosis of sleep ...
This article is a literature review covering the neurodevelopmental disorder interaction with sleep disorder and different management. Conclusion: Disorders of sleep are key concerns in children ...
Prior to reviewing specific sleep problems experienced by individuals with IDD, a review of common sleep problems and their definitions is warranted. Prior classification systems for sleep disorders varied, contributing to the use of different terms to describe sleep problems in the research literature.
This review provides an introduction to the types of sleep disturbance experienced by children with neurodevelopmental conditions and a checklist for assessment of sleep and possible co-occurring physiological or psychological symptoms (Table 1).It focuses on children with common neurodevelopmental conditions autism spectrum disorder, attention-deficit and hyperactivity disorder, Down syndrome ...
Sleep problems are common among children with neurodevelopmental disorders (NDDs). We review sleep disturbance in three major NDDs: autism spectrum disorder, Down syndrome, and fetal alcohol spectrum disorder (FASD). We review associations with functional impairment, discuss how patterns of sleep disturbance inform understanding of etiology, and theorize about mechanisms of impairment. Sleep ...
A systematic review published in 2018 investigated the effects of melatonin for sleep problems in children with neurodevelopmental disorders.5 The review concluded that melatonin was safe and effective in improving sleep for children with neurodevelopmental disorders.5 Another systematic review published in 2019 investigated the effects of oral ...
Sleep problems are more frequent in children with neurodevelopmental disorders [].A recent systematic review by Petruzzelli et al. investigated literature data on polysomnography, sleep electroencephalography, and sleep-related questionnaires in children with autism spectrum disorders.
assessment of psychiatric disorders [3]. Sleep problems are more frequent in children with neurodevelopmental disorders [4]. A recent systematic review by Petruzzelli et al. investigated literature data on polysomnog-raphy, sleep electroencephalography, and sleep-related questionnaires in children with autism spectrum disorders.
Prior to reviewing specific sleep problems experienced by individuals with IDD, a review of common sleep problems and their definitions is warranted. Prior classification systems for sleep disorders varied, contributing to the use of different terms to describe sleep problems in the research literature.
A total of 22 scientific articles were selected using a systematic literature review following the criteria established using the PRISMA model. ... is a neurodevelopmental disorder that typically begins in the first 30 months ... To assess sleep problems in children with ASD and their correlation with attention deficit hyperactivity disorder ...
The article presents a review of the relationships between melatonin and neurodevelopmental disorders. First, the antioxidant properties of melatonin and its physiological effects are considered to understand better the role of melatonin in typical and atypical neurodevelopment. Then, several neurodevelopmental disorders occurring during infancy, such as autism spectrum disorder or ...
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterised by impairments in social interaction and communication, and restricted and repetitive patterns of interests, behaviours, and activities [].Sleep problems are one of the most common comorbid disorders experienced by children with ASD and include difficulties initiating and maintaining sleep, frequent and prolonged ...
Melatonin for the management of sleep problems in children with neurodevelopmental disorders: a systematic review and meta-analysis. Melatonin appeared safe and effective in improving sleep in the studied children, and the overall quality of the evidence was limited due to heterogeneity and inconsistency. Expand.
This article is a literature review covering the neurodevelopmental disorder interaction with sleep disorder and different management. Conclusion Disorders of sleep are key concerns in children with neurodevelopmental disorders. In this group of patients, sleep disorders are common and tend to be chronic.
The literature review was conducted using the PubMed database. Publications were selected from 2002 to 2023 using the following keywords and their combinations: Sotos syndrome and psychiatric symptoms, psychiatric disorders, cognitive profile, behavioral phenotype, intellectual disability, autism spectrum disorder, sleep disorder ...