

Down Syndrome Clinical Presentation
- Author: Gratias Tom Mundakel, MD, FAAP; Chief Editor: Maria Descartes, MD more...
- Sections Down Syndrome
- Practice Essentials
- Pathophysiology
- Epidemiology
- Patient Education
- Physical Examination
- Complications
- Approach Considerations
- Laboratory Studies
- Radiography and Ultrasonography
- Prenatal Screening and Diagnosis
- Other Tests
- Surgical Care
- Diet and Activity
- Consultations
- Genetic Counseling
- Pharmacologic Therapy and Supportive Care
- Special Considerations in Adolescents
- Medication Summary
- Analgesics, Other
- Antidysrhythmics, Ia
- Diuretics, Other
- Questions & Answers
- Media Gallery
When recording the history from the parents of a child with Down syndrome, the clinician should include the following [ 21 ] :
Parental concern about hearing, vision, developmental delay, respiratory infections, and other problems
Feeding history to ensure adequate caloric intake
Prenatal diagnosis of Down syndrome
Vomiting secondary to GI tract blockage by duodenal web or atresia
Absence of stools secondary to Hirschsprung disease
Delay in cognitive abilities, motor development, language development (specifically expressive skills), and social competence
Arrhythmia, fainting episodes, palpitations, or chest pain secondary to heart lesion
Symptoms of sleep apnea, including snoring, restlessness during sleep, difficulty awaking, daytime somnolence, behavioral changes, and school problems
A history of possible physical or sexual abuse
Symptoms of atlantoaxial instability include the following:
About 13-14% of patients have radiographic evidence of atlantoaxial instability but no symptoms
Only 1-2% of patients have symptoms that require treatment
Symptoms include easy fatigability, neck pain, limited neck mobility or head tilt, torticollis, difficulty walking, change in gait pattern, loss of motor skills, incoordination, clumsiness, sensory deficits, spasticity, hyperreflexia, clonus, extensor-plantar reflex, loss of upper-body strength, abnormal neurologic reflexes, change in bowel and bladder function, increased muscle tone in the legs, and changes in sensation in the hands and feet
These symptoms often remain relatively stable for months or years
In rare cases, the symptoms progress to paraplegia, hemiplegia, quadriplegia, or death
On physical examination, patients with trisomy 21 have characteristic craniofacial findings, such as the following:
Flat occiput and a flattened facial appearance
Small brachycephalic head
Epicanthal folds
Flat nasal bridge
Upward-slanting palpebral fissures
Brushfield spots
Small nose and small mouth
Protruding tongue
Small and dysplastic ears
Generous nuchal skin
General physical features in patients with Down syndrome may include the following [ 22 , 23 , 24 , 25 , 26 , 27 ] :
Shortened extremities
Short, broad hands, with short fifth finger with hypoplasia of the middle phalanx and clinodactyly, along with single transverse palmar creases (~60% of patients)
Joint hyperextensibility or hyperflexibility
A wide space between the first and second toes (sandal gap)
Neuromuscular hypotonia
Diastasis recti
Premature aging
Wide range of intelligence quotients (IQs)
Congenital heart defects
These findings and features are described more fully below.
Central nervous system
Moderate to severe intellectual disability occurs as a constant feature, with IQs ranging from 20 to 85 (mean, approximately 50). Muscle hypotonia is seen in newborns with decreased response to normal stimuli; this improves with age. Articulatory problems are present. Sleep apnea occurs when inspiratory airflow from the upper airway to the lungs is impeded for 10 seconds or longer; it often results in hypoxemia or hypercarbia.
Seizure disorders are present in 5-10% or patients. Infantile spasms are the most common seizures observed in infancy, whereas tonic-clonic seizures are most common in older patients.
Behavior and psychiatric status
In general, natural spontaneity, genuine warmth, cheerfulness, gentleness, patience, and tolerance are characteristics of patients with Down syndrome. A few patients exhibit anxiety and stubbornness.
Most children with Down syndrome do not have a coexisting psychiatric or behavioral disorder. The available estimates of psychiatric comorbidity range from 18-38%. The disorders include attention-deficit/hyperactivity disorder, oppositional defiant disorder, nonspecific disruptive disorder, autism spectrum disorders, and stereotypical movement disorder in prepubertal children with Down syndrome and depressive illness, obsessive-compulsive disorder, and psychosislike disorder in adolescents and adults with Down syndrome.
Decreased skin tone, early graying or loss of hair, hypogonadism , cataracts, hearing loss, age-related increase in hypothyroidism, seizures, neoplasms, degenerative vascular disease, loss of adaptive abilities, and increased risk of senile dementia of Alzheimer type are observed.
For more detailed information on this topic, please consult the following article: Zigman WB. Atypical aging in Down syndrome. Dev Disabil Res Rev. 2013;18(1):51-67. PMID: 23949829 [ 28 ]
Brachycephaly, microcephaly, a sloping forehead, a flat occiput, large fontanels with late closure, a patent metopic suture, absent frontal and sphenoid sinuses, and hypoplasia of the maxillary sinuses occur.
Up-slanting palpebral fissures, bilateral medial epicanthal folds, Brushfield spots (speckled iris), refractive errors (50%), strabismus (44%), nystagmus (20%), blepharitis (33%), conjunctivitis, tearing from stenotic nasolacrimal ducts, congenital cataracts (3%), pseudopapilledema, spasm nutans (a type of nystagmus associated with head bobbing), acquired lens opacity (30-60%), retinal detachment, and keratoconus in adults are observed (see the images below). [ 29 ]

A flat facies with increased interocular distance (hypertelorism), hypoplastic nasal bone, and a flat nasal bridge is characteristic (see the image below).

Mouth and teeth
Characteristic features include a (relatively) small mouth with a tendency for tongue protrusion, a fissured and furrowed tongue, mouth breathing with drooling, a chapped lower lip, angular cheilitis, partial anodontia (50%), tooth agenesis, malformed teeth, delayed tooth eruption, microdontia (35-50%) in both the primary and secondary dentition (see the image below), hypoplastic and hypocalcified teeth, malocclusion, taurodontism (0.54-5.6%), and increased periodontal destruction. Cleft lip or palate may occur but is rare.

The ears are small with an overfolded helix (see the images below). Chronic otitis media and hearing loss are common. About 66-89% of children have hearing loss of greater than 15-20 dB in at least 1 ear, as assessed by means of the auditory brainstem response (ABR).

The neck is typically broad and short, with excess skin on the back. Atlantoaxial instability (14%) can result from laxity of transverse ligaments that ordinarily hold the odontoid process close to the anterior arch of the atlas. Laxity can cause backward displacement of the odontoid process, leading to spinal cord compression in about 2% of children with Down syndrome.
Chest and abdomen
The internipple distance is decreased. The abdomen is frequently protuberant. Diastasis recti and umbilical hernia (see the image below) may occur.

Skin disorders occur in up to 80% of children with Down syndrome. Xerosis, localized hyperkeratotic lesions, elastosis serpiginosa, alopecia areata (< 10%), vitiligo, folliculitis (especially common in adolescents), abscess formation, and recurrent skin infections are observed. [ 30 , 31 ] Distal axial triradius in the palms, transverse palmar creases, a single flexion crease in the fifth finger, ulnar loops (often 10), a pattern in hypothenar, and interdigital III regions are observed. [ 32 ]
Heart defects
Congenital heart defects are common (40-50%); they are frequently observed in patients with Down syndrome who are hospitalized (62%) and are a common cause of death in this aneuploidy in the first 2 years of life.
The most common congenital heart defects are the following:
Endocardial cushion defect (43%), which results in atrioventricular septal defect (AVSD)/AV canal defect
Ventricular septal defect (32%)
Secundum atrial septal defect (10%)
Tetralogy of Fallot (6%)
Isolated patent ductus arteriosus (4%).
About 30% of patients have more than one cardiac defect. The most common secondary lesions are patent ductus arteriosus (16%), atrial septal defect, and pulmonic stenosis (9%). About 70% of all endocardial cushion defects are associated with Down syndrome.
Valve abnormalities, such as mitral valve prolapse or aortic regurgitation may develop in up to 40-50% of adolescents and adults who were born without structural heart disease. [ 33 ]
Gastrointestinal tract abnormalities
Newborns with Down syndrome may often have initial difficulty in establishing successful breastfeeding.
GI abnormalities occur in approximately 12% of patients. Duodenal atresia or stenosis (occasionally associated with annular pancreas) may be seen in 2.5% of newborns with Down syndrome. Hirschsprung disease (< 1%), tracheoesophageal fistula, Meckel diverticulum , imperforate anus , and omphalocele are also observed. About 25% of infants with duodenal atresia, stenosis, or annular pancreas have Down syndrome.
An increased incidence of celiac disease has been reported in Down syndrome. Signs and symptoms include growth failure, abdominal pain, and loose stools. Prevalence in individuals with Down syndrome is reportedly 5-15% in different European and US studies. Celiac disease occurs in genetically susceptible individuals, specifically those who have the human leukocyte antigen (HLA) heterodimers DQ2 (observed in 86-100% of individuals with celiac disease) and DQ8. These are strong linkages with high sensitivity and poor specificity.
Gastroesophageal reflux and swallowing difficulties are also common in individuals with Down syndrome.
Genitourinary tract abnormalities
Renal malformations, hypogenitalism ( micropenis or small scrotum and testes), hypospadias , cryptorchidism , and delayed and incomplete puberty may occur.
A study by Postolache et al indicated that children with Down syndrome tend to have smaller kidneys (by length and volume) than sex-and-age–matched controls. There is also evidence that kidney function is reduced in children with Down syndrome. Forty-three percent of the children with Down syndrome in the study had an estimated glomerular filtration rate (eGFR) of below 90 mL/min/1.73 m 2 . [ 34 ]
Growth and skeletal anomalies
Newborns with Down syndrome have lower birth weight, length, and head circumference compared with control newborns. Growth parameters continue to be low up to puberty. Growth charts for children with Down syndrome have been published. [ 35 ] Failure to thrive is common in infancy, especially in patients with cardiac and gastrointestinal problems. Short stature occurs during adolescence and may be especially severe in patients with congenital heart disease. The exact etiology of growth retardation in Down syndrome is unknown; however, a deficiency of insulinlike growth factor 1 (IGF-1) has been described in some studies. [ 36 ] Obesity usually starts in early childhood, and up to 50% of adults may be obese. Obesity is thought to be related to a reduced metabolic rate. [ 37 ]
Broad, short hands, feet, and digits; a short curved fifth finger (dysplasia and shortening of the midphalanx) or clinodactyly of the fifth finger with a single flexion crease; dysplasia of the pelvis (a shallow acetabular angle with small iliac wings); joint laxity; a wide gap between the first and second toes (see the image below); and atlanto-occipital instability are typical presentations.

Endocrine abnormalities
Hypothyroidism is common in Down syndrome, occurring in about 1% of newborns, 10% of children, and up to 50% of adults. Causes include congenital hypothyroidism, as well as acquired hypothyroidism secondary to Hashimoto thyroiditis.
Hashimoto thyroiditis that causes hypothyroidism is by far the most common acquired thyroid disorder in patients with Down syndrome. [ 38 ] The onset is usually from school age onwards, but onset in infancy is reported. [ 39 ] More rarely, Hashimoto thyroiditis can cause hyperthyroidism; [ 40 ] the incidence of Graves disease is also increased. [ 41 ]
Individuals with Down syndrome are at higher risk of developing type I diabetes mellitus. In addition, infertility is nearly universal in males and can occur in up to 50% of females.
Hematologic abnormalities
The most important hematologic abnormality in Down syndrome involves the white blood cells. Children with Down syndrome have an increased risk of developing leukemias, including acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). [ 42 ] AML is as common as ALL in these individuals. Acute megakaryocytic leukemia is the most common form of AML in affected children and is uncommon in children who do not have Down syndrome.
The relative risk of acute leukemia in the first 5 years of life is 56 times that of individuals without Down syndrome. Approximately one in 150 patients develops leukemia. (Neonatal leukemoid reactions [ie, pseudoleukemia] are common, and distinguishing these from true leukemia frequently poses a diagnostic challenge.) [ 43 ]
Approximately 10% of newborns with Down syndrome develop a preleukemic clone, originating from myeloid progenitors in the fetal liver that are characterized by a somatic mutation in GATA1 , which is localized on the X-chromosome. Mutations in this transcription factor lead to a truncated mutant protein, GATA1short or GATA1s. [ 44 , 45 ] This preleukemia is referred to as transient leukemia (TL), transient myeloproliferative disease (TMD), or transient abnormal myelopoiesis (TAM). [ 46 , 47 , 48 ]
TMD is a hematologic abnormality that primarily affects infants with Down syndrome in the neonatal period. [ 49 , 50 ] It is characterized by an excessive proliferation of myeloblast cells in the infant’s blood and bone marrow. [ 51 ]
An estimated 25% of infants with Down syndrome who present with TMD develop megakaryocytic leukemia 1-3 years later. [ 52 ] TMD is associated with pancytopenia, hepatosplenomegaly, and circulating immature white blood cells (WBCs). TMD spontaneously regresses within the first 3 months of life. In some children, however, it can be life-threatening. [ 53 , 54 ]
Although the risk for leukemia is higher in children with Down syndrome, this risk normalizes by the age of 20 years. By age 30 years, the risk of developing leukemia is 2.7%. On the other hand, the risk of developing most solid tumors, such as cervical, lung, and prostate cancer, is lower; however, there is an increased risk for ovarian and testicular germ cell tumors and, perhaps, retinoblastomas and lymphomas. [ 55 , 56 , 57 ]
Another hematologic abnormality, polycythemia, is common in the newborn period.
Immunodeficiency
Patients have about a 12-fold increased risk of infectious diseases, especially pneumonia , because of impaired cellular immunity. Chemotactic defects, as well as decreased immunoglobulin levels, have also been reported in studies of Down syndrome.
Tumor profile
The tumor profile of patients with Down syndrome is different from that of other people. Syringomas occur more often in patients with Down syndrome than in other patients. These benign appendiceal tumors are observed in 18.5-39% of patients with this disease. Females are affected more than twice as often as males. Lesions are usually limited to regions around the eyes, but disseminated syringomas are also observed. The presence of tumors is not related to IQ or any other manifestation of the disorder.
Trisomy 21 mosaicism
Trisomy 21 mosaicism can present with absent or minimal manifestations of Down syndrome and may be underdiagnosed as a cause of early onset Alzheimer disease. [ 58 ] The phenotype of persons having mosaicism for trisomy 21 and Down syndrome reflects the percentage of trisomic cells present in different tissues. [ 59 ]
Complications of Down syndrome involve almost every organ system of the body. [ 60 ]
Cardiac and cardiovascular complications
Cardiovascular complications are important in Down syndrome. [ 24 , 61 ] Children who seem asymptomatic at birth and do not have a murmur may have a significant cardiac defect. Children who have left-to-right shunts, such as atrioventricular septal defects, may develop signs of heart failure at age 1-2 months, manifested by tachypnea, poor feeding, and failure to thrive. If increased pulmonary vascular resistance is noted, the left-to-right shunt may be minimized, thus preventing early heart failure. However, if left undetected, this condition may lead to persistent pulmonary hypertension with irreversible pulmonary vascular changes.
Generally, surgery to correct the heart defect is delayed until the infant is larger and is strong enough to tolerate the operation, which is usually performed at age 6-9 months. Most children do very well and thrive after the procedure.
In patients with an atrioventricular septal defect (AVSD), symptoms usually occur in infancy as a result of systemic-to-pulmonary shunting, high pulmonary blood flow, and an increased risk of pulmonary arterial hypertension. Increased pulmonary resistance may lead to a reversal of the systemic-to-pulmonary shunt accompanied by cyanosis (ie, Eisenmenger syndrome). To reduce the risk of this complication, children with a large AVSD without pulmonary obstruction should have their defect repaired before the age of 4 months. [ 2 ]
Patients with Down syndrome are considered to be at higher risk for pulmonary arterial hypertension than patients without Down syndrome. This is because of the diminished number of alveoli, the thinner media of pulmonary arterioles, and the impaired endothelial function in these patients.
Early corrective cardiac surgery is warranted to prevent irreversible pulmonary vascular lung damage. Moreover, new medical treatment strategies (eg, prostacyclin, endothelin receptor antagonist and phosphodiesterase-5-inhibitor) have been demonstrated to substantially improve clinical status and life expectancy of patients with pulmonary arterial hypertension.
Coronary artery disease–related mortality is surprisingly low. Pathologic studies have revealed decreased levels of atherosclerosis in Down syndrome. Individuals with Down syndrome also have a decreased risk of hypertension.
Acquired heart valve disease is common in Down syndrome and includes mitral valve prolapse and aortic regurgitation. [ 33 ]
Respiratory complications
Respiratory problems are among the most common reasons for hospital admissions and mortality in children and adults with Down syndrome. [ 61 ] Hypotonia, developmental delay, obstructive sleep apnea, craniofacial anomalies, immune deficiency, and cardiac problems, as well as gastroesophageal reflux, all contribute to the increased risk of developing respiratory complications, such as lung infection, aspirations, and cor pulmonale. [ 57 , 62 ]
A French study, by Alimi et al, indicated that Down syndrome is a risk factor for pulmonary hemosiderosis and that the condition appears to be more severe in the presence of Down syndrome. Of 34 patients under age 20 years with pulmonary hemosiderosis, nine (26.5%) presented with Down syndrome. Pulmonary hemosiderosis in patients with Down syndrome was more likely to have earlier onset and to be associated with greater dyspnea at diagnosis, a higher incidence of secondary pulmonary hypertension, and a greater risk of fatal evolution. [ 63 ]
Gastrointestinal complications
Gastroesophageal reflux is commonly seen in children with Down syndrome and can be severe enough to result in aspiration of stomach contents, causing respiratory symptoms such as persistent coughing, wheezing, and pneumonia. Infants with oral-motor difficulties may present with choking and gagging on feedings, as well as the respiratory symptoms mentioned. Dysphagia may affect children as well as adults. Celiac disease is more common in patients with Down syndrome than in those without it. Chronic constipation is frequently seen.
Obesity is common. Patients need to have specific dietary guidelines on caloric needs and portion sizes. An active lifestyle with routine exercises is recommended for the whole family. Children should be encouraged to participate in recreational activities, such as swimming, dancing, walking, and playing outdoors.
Ophthalmologic complications
Eye disorders affect a majority of patients with Down syndrome. [ 64 ] Refractive errors, such as myopia, hyperopia, and astigmatism, occur in 35-75% of individuals and can be corrected with glasses. [ 65 ] Other common eye disorders include strabismus and nystagmus. Congenital cataracts may affect 5% of newborns and can lead to blindness if left untreated. Additional serious eye disorders include glaucoma and keratoconus. Blockage of tear ducts (nasolacrimal duct stenosis) is common and can lead to increased tear stasis and conjunctivitis.
Otolaryngologic complications
Hearing loss can occur in 40-75% of individuals with Down syndrome. Newborns with Down syndrome have a high incidence of congenital hearing loss. Many children experience recurrent ear infections or persistent middle ear effusions, probably caused by midfacial hypoplasia. Early and aggressive treatment of chronic ear disease can greatly reduce hearing loss in children with Down syndrome. Sinusitis and nasopharyngitis may occur secondary to narrow nasal passages and sinuses. Obstructive sleep apnea may develop secondary to enlarged tonsils or to other causes of upper airway obstruction.
Endocrine complications
Thyroid dysfunction, particularly acquired hypothyroidism, is relatively common in Down syndrome. Because of the increased risk, thyroid function tests should be performed in the newborn, repeated at ages 6 and 12 months, and then performed annually. Hyperthyroidism can also develop. In addition, type I diabetes mellitus occurs with higher frequency in Down syndrome.
Hematologic complications
Patients with Down syndrome exhibit a unique pattern of malignancies, yielding intriguing insights into cancer biology. [ 66 ] These patients also pose distinctive challenges to the oncologist because of their particular profile of treatment-related toxicities. Individuals with Down syndrome have a higher risk for leukemia, experiencing three distinct disease entities (ie, TMD, AML, and ALL), and have a lower risk for solid tumors. [ 67 ]
Childhood leukemia is relatively common; AML is more common in infants, whereas ALL is more common in children older than 1 year. Newborn infants with Down syndrome are prone to TMD (also known as transient abnormal myelopoiesis or transient leukemia). In some cases, TMD can progress to more severe disease, such as AML, within the first 4 years of life.
Immunologic complications
Children are more prone to recurrent respiratory and systemic infections secondary to deficiencies in some immunoglobulin levels. B cells are reduced in number and function. Reduction in immune function has been shown to be secondary to overexpression of immunity-related genes on chromosome 21. [ 68 ] Immunoglobulin (Ig) A deficiency, as well as deficiencies of IgG subclasses, can be seen in individuals with Down syndrome. Individuals with Down syndrome are also more susceptible to autoimmune diseases, such as thyroid disease (hypothyroidism more often than hyperthyroidism), diabetes, and celiac disease. [ 61 ]
Orthopedic complications
Approximately 20% of all patients with Down syndrome experience orthopedic problems. [ 69 ] Upper cervical spine instability has the most potential for morbidity and consequently requires close monitoring. Other conditions (eg, scoliosis, hip instability, patellar instability, and foot problems) can cause disability if left untreated. In some of these conditions, early diagnosis can prevent severe disability.
Atlantoaxial instability, defined as increased mobility of the cervical spine at the level of the first and second vertebrae, can lead to subluxation of the cervical spine. Approximately 10-30% of individuals with Down syndrome have this condition. [ 70 ] Most are asymptomatic; however, 10% of individuals with atlantoaxial instability have symptoms, including neck pain, torticollis, changes in gait, changes in bowel or bladder control, or other signs of paralysis or weakness. [ 71 ]
Joint dislocations due to ligamentous laxity and hypotonia are observed. Other orthopedic conditions include genu valgus, overpronation of the ankle, and flat feet.
There is an increased risk of juvenile idiopathic arthritis in Down syndrome. [ 72 ] Down syndrome is also associated with a greater risk of osteoporosis, and the incidence of fractures is high, especially in patients over age 50 years. [ 57 ]
Psychiatric and behavioral complications
Psychiatric disorders are reported in 13-17.6% of children with Down syndrome [ 73 ] ; these conditions include common psychiatric disorders such as depression , anxiety, obsessive-compulsive disorder , schizophrenia , and anorexia nervosa .
Other disruptive behavior disorders, such as attention-deficit/hyperactivity disorder , oppositional defiant disorder , and conduct disorder , can also be present. Children with Down syndrome have autism more often than expected. [ 74 ] In one Down syndrome study, the incidence of autism was 7%. [ 75 ] Current evidence indicates that autism affects 1 of every 150 children. [ 76 ]
A study by Foley et al indicated that while behavioral and psychiatric difficulties in persons with Down syndrome tend to improve with age, depressive symptoms, as well as problems in social relating behavior, can persist into adulthood. The investigators, who conducted the questionnaire study over 8 years, suggested that persistence of depressive symptoms in persons with Down syndrome may increase their chances of developing depressive illness in adulthood. [ 77 ]
Alzheimer disease
Alzheimer disease develops in about 50% of individuals with Down syndrome, often arising at a relative early age. Autopsy studies have shown that the characteristic plaques and tangles associated with Alzheimer disease are present in almost all individuals with Down syndrome by age 40 years. [ 78 , 19 ] The increased risk of Alzheimer disease in Down syndrome is thought to be related to the presence of an extra copy of the APP gene, which codes for the amyloid precursor protein. Too much of this protein leads to accumulation of amyloid plaques in the brain, which impairs brain cell function. Alzheimer disease is characterized by memory loss, inability to learn new information, and a decline in intellectual skills. [ 79 , 80 ] Behavioral changes in patients with Down syndrome diagnosed with Alzheimer dementia include the following [ 22 ] :
Episodic noisy excitement
Irritability
Wandering and confusion
Destructive, aggressive, or difficult behavior
Lethargy, withdrawal, loss of interest
Limited response to people
Social inadequacy, isolation
Extreme changes in appetite (typically leading to weight loss)
Restlessness
Sleep disturbance
Incontinence
Excessive uncooperativeness
Anxiety and fearfulness
Stealing and general regressive behavior
Personality changes
Increased dependence
Individuals with Down syndrome are at high risk for physical and sexual abuse. Physicians taking care of Down syndrome patients should be alert to this risk and parents and patients should be appropriately educated about it.
Karmiloff-Smith A, Al-Janabi T, D'Souza H, et al. The importance of understanding individual differences in Down syndrome. F1000Res . 2016. 5: [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Bull MJ. Health supervision for children with Down syndrome. Pediatrics . 2011 Aug. 128(2):393-406. [QxMD MEDLINE Link] . [Full Text] .
Lejeune J. Le mongolisme. Premier example d'aberration autosomique humaine. Ann Genet . 1959. 1:41-9.
Jacobs PA, Baikie AG, Court Brown WM, Strong JA. The somatic chromosomes in mongolism. Lancet . 1959 Apr 4. 1(7075):710. [QxMD MEDLINE Link] .
Peterson MB, Mikkelsen M. Nondisjunction in trisomy 21: origin and mechanisms. Cytogenet Cell Genet . 2000. 91:199-203.
Down JL. Observations on an ethnic classification of idiots. 1866. Ment Retard . 1995 Feb. 33(1):54-6. [QxMD MEDLINE Link] .
LEJEUNE J, GAUTIER M, TURPIN R. [Study of somatic chromosomes from 9 mongoloid children]. C R Hebd Seances Acad Sci . 1959 Mar 16. 248(11):1721-2. [QxMD MEDLINE Link] .
Levenson D. Talking about Down syndrome. Am J Med Genet A . 2009 Feb 15. 149A(4):vii-viii. [QxMD MEDLINE Link] .
[Guideline] Hartway S. A parent's guide to the genetics of Down syndrome. Adv Neonatal Care . 2009 Feb. 9(1):27-30. [QxMD MEDLINE Link] .
Ranweiler R. Assessment and care of the newborn with Down syndrome. Adv Neonatal Care . 2009 Feb. 9(1):17-24; Quiz 25-6. [QxMD MEDLINE Link] .
Reeves RH, Baxter LL, Richtsmeier JT. Too much of a good thing: mechanisms of gene action in Down syndrome. Trends Genet . 2001 Feb. 17(2):83-8. [QxMD MEDLINE Link] .
Cheon MS, Shim KS, Kim SH, Hara A, Lubec G. Protein levels of genes encoded on chromosome 21 in fetal Down syndrome brain: Challenging the gene dosage effect hypothesis (Part IV). Amino Acids . 2003 Jul. 25(1):41-7. [QxMD MEDLINE Link] .
Baksh RA, Strydom A, Pape SE, Chan LF, Gulliford MC. Susceptibility to COVID-19 Diagnosis in People with Down Syndrome Compared to the General Population: Matched-Cohort Study Using Primary Care Electronic Records in the UK. J Gen Intern Med . 2022 Apr 6. [QxMD MEDLINE Link] . [Full Text] .
Tarani L, Carito V, Ferraguti G, et al. Neuroinflammatory Markers in the Serum of Prepubertal Children with Down Syndrome. J Immunol Res . 2020. 2020:6937154. [QxMD MEDLINE Link] . [Full Text] .
Romano A, Cornia R, Moraschi M, et al. Age-Related Cortical Thickness Reduction in Non-Demented Down's Syndrome Subjects. J Neuroimaging . 2015 May 21. [QxMD MEDLINE Link] .
[Guideline] Practice Bulletin No. 163: Screening for Fetal Aneuploidy. Obstet Gynecol . 2016 May. 127 (5):e123-37. [QxMD MEDLINE Link] . [Full Text] .
Canfield MA, Honein MA, Yuskiv N, Xing J, Mai CT, Collins JS. National estimates and race/ethnic-specific variation of selected birth defects in the United States, 1999-2001. Birth Defects Res A Clin Mol Teratol . 2006 Nov. 76(11):747-56. [QxMD MEDLINE Link] .
Coppus AM, Evenhuis HM, Verberne GJ, et al. Survival in elderly persons with Down syndrome. J Am Geriatr Soc . 2008 Dec. 56(12):2311-6. [QxMD MEDLINE Link] .
Hartley D, Blumenthal T, Carrillo M, et al. Down syndrome and Alzheimer's disease: common pathways, common goals. Alzheimers Dement . 2015 Jun. 11 (6):700-9. [QxMD MEDLINE Link] . [Full Text] .
Matthews TJ, Allain DC, Matthews AL, Mitchell A, Santoro SL, Cohen L. An assessment of health, social, communication, and daily living skills of adults with down syndrome. Am J Med Genet A . 2018 Apr 25. [QxMD MEDLINE Link] .
[Guideline] Cohen WI, ed. Health care guidelines for individuals with Down syndrome (Down syndrome preventative medical check list). Down Syndrome Q . 1996. 1(2):1-10. [Full Text] .
Nieuwenhuis-Mark RE. Diagnosing Alzheimer’s dementia in Down syndrome: Problems and possible solutions. Res Dev Disabil . 2009. 30(5):827-838.
Kusters MA, Verstegen RH, Gemen EF, de Vries E. Intrinsic defect of the immune system in children with Down syndrome: a review. Clin Exp Immunol . 2009 May. 156(2):189-93. [QxMD MEDLINE Link] . [Full Text] .
Vis JC, Duffels MG, Winter MM, Weijerman ME, Cobben JM, Huisman SA. Down syndrome: a cardiovascular perspective. J Intellect Disabil Res . 2009 May. 53(5):419-25. [QxMD MEDLINE Link] .
Lanfranchi S, Carretti B, Spanò G, Cornoldi C. A specific deficit in visuospatial simultaneous working memory in Down syndrome. J Intellect Disabil Res . 2009 May. 53(5):474-83. [QxMD MEDLINE Link] .
Levorato MC, Roch M, Beltrame R. Text comprehension in Down syndrome: the role of lower and higher level abilities. Clin Linguist Phon . 2009 Apr. 23(4):285-300. [QxMD MEDLINE Link] .
Salomon LJ, Bernard M, Amarsy R, Bernard JP, Ville Y. The impact of crown-rump length measurement error on combined Down syndrome screening: a simulation study. Ultrasound Obstet Gynecol . 2009 May. 33(5):506-11. [QxMD MEDLINE Link] .
Zigman WB. Atypical aging in Down syndrome. Dev Disabil Res Rev . 2013. 18 (1):51-67. [QxMD MEDLINE Link] .
Scherbenske JM, Benson PM, Rotchford JP, James WD. Cutaneous and ocular manifestations of Down syndrome. J Am Acad Dermatol . 1990 May. 22(5 Pt 2):933-8. [QxMD MEDLINE Link] .
Wilms A, Dummer R. [Elastosis perforans serpiginosa in Down syndrome]. Hautarzt . 1997 Dec. 48(12):923-5. [QxMD MEDLINE Link] .
Daneshpazhooh M, Nazemi TM, Bigdeloo L, Yoosefi M. Mucocutaneous findings in 100 children with Down syndrome. Pediatr Dermatol . 2007 May-Jun. 24(3):317-20. [QxMD MEDLINE Link] .
Masjkey D, Bhattacharya S, Dhungel S, Jha CB, Shrestha S, Ghimire SR, et al. Utility of phenotypic dermal indices in the detection of Down syndrome patients. Nepal Med Coll J . 2007 Dec. 9(4):217-21. [QxMD MEDLINE Link] .
Geggel RL, O'Brien JE, Feingold M. Development of valve dysfunction in adolescents and young adults with Down syndrome and no known congenital heart disease. J Pediatr . 1993 May. 122 (5 Pt 1):821-3. [QxMD MEDLINE Link] .
Postolache L, Parsa A, Simoni P, et al. Widespread kidney anomalies in children with Down syndrome. Pediatr Nephrol . 2022 Feb 3. [QxMD MEDLINE Link] .
Zemel BS, Pipan M, Stallings VA, et al. Growth Charts for Children With Down Syndrome in the United States. Pediatrics . 2015 Nov. 136 (5):e1204-11. [QxMD MEDLINE Link] . [Full Text] .
Annerén G, Gustavson KH, Sara VR, Tuvemo T. Growth retardation in Down syndrome in relation to insulin-like growth factors and growth hormone. Am J Med Genet Suppl . 1990. 7:59-62. [QxMD MEDLINE Link] .
Bertapelli F, Pitetti K, Agiovlasitis S, Guerra-Junior G. Overweight and obesity in children and adolescents with Down syndrome-prevalence, determinants, consequences, and interventions: a literature review. Res Dev Disabil . 2016 Oct. 57:181-92. [QxMD MEDLINE Link] .
Popova G, Paterson WF, Brown A, Donaldson MD. Hashimoto's thyroiditis in Down's syndrome: clinical presentation and evolution. Horm Res . 2008. 70(5):278-84. [QxMD MEDLINE Link] .
Shalitin S, Phillip M. Autoimmune thyroiditis in infants with Down’s syndrome. J Pediatr Endocrinol . 2002. 15:649-652.
Idris I, O’Malley BP. Thyrotoxicosis in Down’s and Turner’s syndromes: the likelihood of Hashimoto’s thyroiditis as the underlying aetiology. Int J Clin Pract . 2000. 54:272-273.
Rudberg C, Johansson H, Akerstrom G, Tuvema T, Karlsson FA. Graves’ disease in children and adolescents. Late results of surgical treatment. Eur J Endocrinol . 1996. 134:710-7.
Zwaan MC, Reinhardt D, Hitzler J, Vyas P. Acute leukemias in childrenwith Down syndrome. Pediatr Clin N Am . 2008. 55:53-70.
Lerner LH, Wiss K, Gellis S, Barnhill R. An unusual pustular eruption in an infant with Down syndrome and a congenital leukemoid reaction. J Am Acad Dermatol . 1996 Aug. 35(2 Pt 2):330-3. [QxMD MEDLINE Link] .
Hitzler JK, Zipursky A. Origins of leukaemia in children with Down syndrome. Nat Rev Cancer . 2005 Jan. 5(1):11-20. [QxMD MEDLINE Link] .
Li Z, Godinho FJ, Klusmann JH, Garriga-Canut M, Yu C, Orkin SH. Developmental stage-selective effect of somatically mutated leukemogenic transcription factor GATA1. Nat Genet . 2005 Jun. 37(6):613-9. [QxMD MEDLINE Link] .
Magalhaes IQ, Splendore A, Emerenciano M, et al. Transient neonatal myeloproliferative disorder without Down syndrome and detection of GATA1 mutation. J Pediatr Hematol Oncol . 2005 Jan. 27(1):50-2. [QxMD MEDLINE Link] .
Ahmed M, Sternberg A, Hall G, et al. Natural history of GATA-1 mutations in Down syndrome. Blood . 2004. 103:2480-2489.
Bhatt S, Schreck R, Graham JM, Korenberg JR, Hurvitz CG, Fischel-Ghodsian N. Transient leukemia with trisomy 21: description of a case and review of the literature. Am J Med Genet . 1995 Sep 25. 58(4):310-4. [QxMD MEDLINE Link] .
Roderick JA, Bradshaw WT. Transient myeloproliferative disorder in a newborn with Down syndrome. Adv neonat Care . 2008. 8:208-218.
Gamis A, Hilden J. Transient myleoproliferative disorder with too few data and many unanswered questions: does it contain an important piece of the puzzle to understanding hemataopoiesis and acute myelogenous leukemia?. J Pediatr Hematol Oncol . 2002. 24:2-5.
Ma SK, Wan TS, Chan GC, Ha SY, Fung LF, Chan LC. Relationship between transient abnormal myelopoiesis and acute megakaryoblastic leukaemia in Down's syndrome. Br J Haematol . 2001 Mar. 112(3):824-5. [QxMD MEDLINE Link] .
Taub J. Down syndrome and megakaryocytic leukemia/transient myeloproliferative disorder: when does it begin?. Blood . 2003. 101:4228-4300.
Al Kasim F, Doyle JJ, Massey GV, et al. Incidence and treatment of potentially lethal diseasesin transient leukemia of Down syndrome: Pediatric Oncology Group Study. J Pediatr Hematol Oncol . 2002. 24:9-13.
Massey GV, Zipursky A, Chang MN, Doyle JJ, Nasim S, Taub JW. A prospective study of the natural history of transient leukemia (TL) in neonates with Down syndrome (DS): Children's Oncology Group (COG) study POG-9481. Blood . 2006 Jun 15. 107(12):4606-13. [QxMD MEDLINE Link] .
Krivit W, Good RA. The simultaneous occurrence of leukemia and mongolism; report offour cases. AMA J Dis Child . 1956. 91:218-222.
Hasle H, Clemmensen IH, Mikkelsen M. Risks of leukaemia and solid tumours in individuals with Down's syndrome. Lancet . 2000 Jan 15. 355(9199):165-9. [QxMD MEDLINE Link] .
Jensen KM, Bulova PD. Managing the care of adults with Down's syndrome. BMJ . 2014 Sep 30. 349:g5596. [QxMD MEDLINE Link] .
Ringman JM, Rao N, Lu PH, Cederbaum S. Mosaicism for trisomy 21 in a patient with young-onset dementia. A case report and brief literature review. Arch Neurol . 2008. 65:412-415.
Papavassiliou P, York TP, Gursoy N, Hill G, Nicely LV, Sundaram U. The phenotype of persons having mosaicism for trisomy 21/Down syndrome reflects the percentage of trisomic cells present in different tissues. Am J Med Genet A . 2009 Feb 15. 149A(4):573-83. [QxMD MEDLINE Link] .
Baum RA, Nash PL, Foster JE, Spader M, Ratliff-Schaub K, Coury DL. Primary care of children and adolescents with down syndrome: an update. Curr Probl Pediatr Adolesc Health Care . 2008 Sep. 38(8):241-61. [QxMD MEDLINE Link] .
Colvin KL, Yeager ME. What people with Down Syndrome can teach us about cardiopulmonary disease. Eur Respir Rev . 2017 Jan. 26 (143): [QxMD MEDLINE Link] . [Full Text] .
McDowell KM, Craven DI. Pulmonary complications of Down syndrome during childhood. J Pediatr . 2011 Feb. 158 (2):319-25. [QxMD MEDLINE Link] .
Alimi A, Taytard J, Abou Taam R, et al. Pulmonary hemosiderosis in children with Down syndrome: a national experience. Orphanet J Rare Dis . 2018 Apr 20. 13 (1):60. [QxMD MEDLINE Link] . [Full Text] .
Liyanage S, Barnes J. The eye and Down's syndrome. Br J Hosp Med (Lond) . 2008 Nov. 69(11):632-4. [QxMD MEDLINE Link] .
Miyazaki EA. The orthoptics of Down syndrome. Am Orthopt J . 2014. 64:12-6. [QxMD MEDLINE Link] .
Rabin KR, Whitlock JA. Malignancy in children with trisomy 21. Oncologist . 2009 Feb. 14(2):164-73. [QxMD MEDLINE Link] . [Full Text] .
Bhatnagar N, Nizery L, Tunstall O, Vyas P, Roberts I. Transient Abnormal Myelopoiesis and AML in Down Syndrome: an Update. Curr Hematol Malig Rep . 2016 Oct. 11 (5):333-41. [QxMD MEDLINE Link] . [Full Text] .
Martinez E, Castaneda D, Jaramillo S, et al. Altered immune parameters correlate with infection-related hospitalizations in children with Down syndrome. Hum Immunol . 2016 Jul. 77 (7):594-9. [QxMD MEDLINE Link] .
Mik G, Gholve PA, Scher DM, Widmann RF, Green DW. Down syndrome: orthopedic issues. Curr Opin Pediatr . 2008 Feb. 20(1):30-6. [QxMD MEDLINE Link] .
Rogers PT, Roizen NJ, Capone GT. Down syndrome. Capute AJ, Accardo PJ. Developmental disabilities in infancy and childhood . 2nd. 1996. 221-224.
Pueschel SM, Scola FH. Atlantoaxial instability in individuals with Down Syndrome: epidemiologic, radiographic, and clinical studies. Pediatrics . 1987. 80:555-560.
Juj H, Emery H. The arthropathy of Down syndrome: an underdiagnosed and under-recognized condition. J Pediatr . 2009 Feb. 154 (2):234-8. [QxMD MEDLINE Link] .
Myers BA, Pueschel SM. Psychiatric disorders in persons with Down syndrome. J Nerv Ment Dis . 1991 Oct. 179(10):609-13. [QxMD MEDLINE Link] .
Miles JH. Autism spectrum disorders--a genetics review. Genet Med . 2011 Apr. 13(4):278-94. [QxMD MEDLINE Link] .
Kent L, Evans J, Paul M, Sharp M. Comorbidity of autistic spectrum disorders in children with Down syndrome. Dev Med Child Neurol . 1999 Mar. 41(3):153-8. [QxMD MEDLINE Link] .
Rice C. Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders—autism and developmental disabilities monitoring network, 14 sites, United States,2002. MMWR CDC Surveill Summ . 2007. 56:12-28.
Foley KR, Bourke J, Einfeld SL, Tonge BJ, Jacoby P, Leonard H. Patterns of depressive symptoms and social relating behaviors differ over time from other behavioral domains for young people with Down syndrome. Medicine (Baltimore) . 2015 May. 94 (19):1-7. [QxMD MEDLINE Link] .
Wisniewski KE, Wisniewski HM, Wen GY. Occurrence of neuropathological changes and dementia of Alzheimer's disease in Down's syndrome. Ann Neurol . 1985 Mar. 17 (3):278-82. [QxMD MEDLINE Link] .
Fonseca LM, Yokomizo JE, Bottino CM, Fuentes D. Frontal Lobe Degeneration in Adults with Down Syndrome and Alzheimer's Disease: A Review. Dement Geriatr Cogn Disord . 2016. 41 (3-4):123-36. [QxMD MEDLINE Link] . [Full Text] .
Esbensen AJ, Johnson EB, Amaral JL, Tan CM, Macks R. Differentiating Aging Among Adults With Down Syndrome and Comorbid Dementia or Psychopathology. Am J Intellect Dev Disabil . 2016 Jan. 121 (1):13-24. [QxMD MEDLINE Link] . [Full Text] .
Driscoll DA, Morgan MA, Schulkin J. Screening for Down syndrome: changing practice of obstetricians. Am J Obstet Gynecol . 2009 Apr. 200(4):459.e1-9. [QxMD MEDLINE Link] .
Summerfield P. Prenatal screening for Down's syndrome: balanced debate needed. Lancet . 2009 Feb 28. 373(9665):722. [QxMD MEDLINE Link] .
Fransen MP, Hajo Wildschut, Vogel I, Mackenbach J, Steegers E, Essink-Bot ML. Information about prenatal screening for Down syndrome: ethnic differences in knowledge. Patient Educ Couns . 2009 Nov. 77(2):279-88. [QxMD MEDLINE Link] .
Cuckle H. Biochemical screening for Down syndrome. Eur J Obstet Gynecol Reprod Biol . 2000 Sep. 92(1):97-101. [QxMD MEDLINE Link] .
Nicolaides KH, Spencer K, Avgidou K, Faiola S, Falcon O. Multicenter study of first-trimester screening for trisomy 21 in 75 821 pregnancies: results and estimation of the potential impact of individual risk-orientated two-stage first-trimester screening. Ultrasound Obstet Gynecol . 2005 Mar. 25(3):221-6. [QxMD MEDLINE Link] .
Kagan KO, Wright D, Baker A, Sahota D, Nicolaides KH. Screening for trisomy 21 by maternal age, fetal nuchal translucency thickness, free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A. Ultrasound Obstet Gynecol . 2008 Jun. 31(6):618-24. [QxMD MEDLINE Link] .
Nicolaides KH. Nuchal translucency and other first-trimester sonographic markers of chromosomal abnormalities. Am J Obstet Gynecol . 2004 Jul. 191(1):45-67. [QxMD MEDLINE Link] .
Spencer K, Souter V, Tul N, Snijders R, Nicolaides KH. A screening program for trisomy 21 at 10-14 weeks using fetal nuchal translucency, maternal serum free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A. Ultrasound Obstet Gynecol . 1999 Apr. 13(4):231-7. [QxMD MEDLINE Link] .
Dreux S, Olivier C, Dupont JM, Leporrier N, Oury JF. Maternal serum screening in cases of mosaic and translocation Down syndrome. Prenat Diagn . 2008 Aug. 28(8):699-703. [QxMD MEDLINE Link] .
Natoli JL, Ackerman DL, McDermott S, Edwards JG. Prenatal diagnosis of Down syndrome: a systematic review of termination rates (1995-2011). Prenat Diagn . 2012 Feb. 32 (2):142-53. [QxMD MEDLINE Link] .
Snijders RJ, Noble P, Sebire N, Souka A, Nicolaides KH. UK multicentre project on assessment of risk of trisomy 21 by maternal age and fetal nuchal-translucency thickness at 10-14 weeks of gestation. Fetal Medicine Foundation First Trimester Screening Group. Lancet . 1998 Aug 1. 352(9125):343-6. [QxMD MEDLINE Link] .
Norton ME, Brar H, Weiss J, Karimi A, Laurent LC, Caughey AB, et al. Non-Invasive Chromosomal Evaluation (NICE) Study: results of a multicenter prospective cohort study for detection of fetal trisomy 21 and trisomy 18. Am J Obstet Gynecol . 2012 Jun 1. [QxMD MEDLINE Link] .
Barclay L. Maternal blood test may detect trisomy in first trimester. Medscape Medical News. June 7, 2013. Available at http://www.medscape.com/viewarticle/805519 . Accessed: July 8, 2013.
Gil MM, Quezada MS, Bregant B, Ferraro M, Nicolaides KH. Implementation of maternal blood cell-free DNA testing in early screening for aneuploidies. Ultrasound Obstet Gynecol . 2013 Jul. 42(1):34-40. [QxMD MEDLINE Link] .
Nicolaides KH, Wright D, Poon LC, Syngelaki A, Gil MM. First-trimester contingent screening for trisomy 21 by biomarkers and maternal blood cell-free DNA testing. Ultrasound Obstet Gynecol . 2013 Jul. 42(1):41-50. [QxMD MEDLINE Link] .
Palomaki GE, Kloza EM, Lambert-Messerlian GM, et al. DNA sequencing of maternal plasma to detect Down syndrome: An international clinical validation study. Genet Med . 2011 Nov. 13(11):913-920. [QxMD MEDLINE Link] .
Barclay L. Maternal blood test may detect trisomy in first trimester. Medscape Medical News, June 7, 2013. Available at http://www.medscape.com/viewarticle/805519 . Accessed: July 8, 2013.
Rupela V, Velleman SL, Andrianopoulos MV. Motor speech skills in children with Down syndrome: A descriptive study. Int J Speech Lang Pathol . 2016 Jan 11. 1-10. [QxMD MEDLINE Link] .
Bunt CW, Bunt SK. Role of the family physician in the care of children with Down syndrome. Am Fam Physician . 2014 Dec 15. 90 (12):851-8. [QxMD MEDLINE Link] . [Full Text] .
Tassone JC, Duey-Holtz A. Spine concerns in the Special Olympian with Down syndrome. Sports Med Arthrosc . 2008 Mar. 16 (1):55-60. [QxMD MEDLINE Link] .
Diaz KM. Physical Activity and Sedentary Behavior Among U.S. Children With and Without Down Syndrome: The National Survey of Children's Health. Am J Intellect Dev Disabil . 2020 May. 125 (3):230-42. [QxMD MEDLINE Link] .
Warburton D, Dallaire L, Thangavelu M, Ross L, Levin B, Kline J. Trisomy recurrence: a reconsideration based on North American data. Am J Hum Genet . 2004 Sep. 75(3):376-85. [QxMD MEDLINE Link] .
Nussbaum RL, McInnes RR, Willard HF. Thompson and Thompson genetics in medicine. 6th Revised Reprint Edition . Philadelphia: W.B. Saunders; 2004.
Tolmie J. Down syndrome and other autosomal trisomies. Rimoin DL, Connor JM, Pyeritz RE, Korf BR. Emery and Rimoin’s Principles and Practice of Medical Genetics . 4th edition. 2002. 1129-1183.
Galleguillos C, Galleguillos B, Larios G, Menchaca G, Bont L, Castro-Rodriguez JA. Down's syndrome is a risk factor for severe lower respiratory tract infection due to respiratory syncytial virus. Acta Paediatr . 2016 Nov. 105 (11):e531-5. [QxMD MEDLINE Link] .
Sugimoto D, Bowen SL, Meehan WP 3rd, Stracciolini A. Effects of Neuromuscular Training on Children and Young Adults with Down Syndrome: Systematic Review and Meta-Analysis. Res Dev Disabil . 2016 Apr 25. 55:197-206. [QxMD MEDLINE Link] .
- Infant with Down syndrome. Note up-slanting palpebral fissures, bilateral epicanthal folds, flat nasal bridge, open mouth with tendency for tongue protrusion, and small ear with overfolded helix.
- Child with Down syndrome. Note up-slanting palpebral fissures, bilateral epicanthal folds, small nose with flat nasal bridge, open mouth with tendency for tongue protrusion, and small ears with overfolded helix.
- G-banded karyotype showing trisomy 21 (47,XY,+21).
- G-banded karyotype showing trisomy 21 of isochromosome arm 21q type [46,XY,i(21)(q10)].
- Hand of infant with Down syndrome. Note transverse palmar crease and clinodactyly of fifth finger.
- Ear of infant with Down syndrome. Note characteristic small ear with overfolded helix.
- Characteristic flat facies with hypertelorism, depressed nasal bridge, and protrusion of tongue, as well as single palmar simian crease in 2-year-old girl with Down syndrome. Image courtesy of L. Dourmishev, MD, PhD, DSc.
- Small auricle and anomalies of folds in patient with Down syndrome. Image courtesy of L. Dourmishev, MD, PhD, DSc.
- Palmar simian crease in patient with Down syndrome. Image courtesy of L. Dourmishev, MD, PhD, DSc.
- Patient with Down syndrome with protuberant abdomen and umbilical hernia. Image courtesy of L. Dourmishev, MD, PhD, DSc.
- Wide gap between first and second toes and onychomycosis in patient with Down syndrome. Image courtesy of L. Dourmishev, MD, PhD, DSc.
- Hypodontia in patient with Down syndrome. Image courtesy of L. Dourmishev, MD, PhD, DSc.
Contributor Information and Disclosures
Gratias Tom Mundakel, MD, FAAP Clinical Associate Professor, Neonatologist, Division of Neonatology, Department of Pediatrics, Kings County Hospital Center, State University of New York Downstate Medical Center Gratias Tom Mundakel, MD, FAAP is a member of the following medical societies: American Academy of Pediatrics Disclosure: Nothing to disclose.
Purushottam Lal, MD Resident Physician, Department of Pediatrics, Children's Hospital at SUNY Downstate Purushottam Lal, MD is a member of the following medical societies: Delhi Medical Council , Indian Academy of Pediatrics Disclosure: Nothing to disclose.
Lois J Starr, MD, FAAP Assistant Professor of Pediatrics, Clinical Geneticist, Munroe Meyer Institute for Genetics and Rehabilitation, University of Nebraska Medical Center Lois J Starr, MD, FAAP is a member of the following medical societies: American Academy of Pediatrics , American College of Medical Genetics and Genomics Disclosure: Nothing to disclose.
Maria Descartes, MD Medical Geneticist, Miami Cancer Institute, Baptist Health South Florida Maria Descartes, MD is a member of the following medical societies: American Academy of Pediatrics , American College of Medical Genetics and Genomics , American Medical Association , American Society of Human Genetics , International Skeletal Dysplasia Society , Society for Inherited Metabolic Disorders , Southeastern Regional Genetics Group Disclosure: Nothing to disclose.
Harold Chen, MD, MS, FAAP, FACMG Professor, Department of Pediatrics, Louisiana State University Medical Center Harold Chen, MD, MS, FAAP, FACMG is a member of the following medical societies: American Academy of Pediatrics , American College of Medical Genetics and Genomics , American Medical Association , American Society of Human Genetics Disclosure: Nothing to disclose.
Michael M Henry, MD Fellow in Neonatal/Perinatal Medicine, Children’s Hospital at SUNY Downstate Medical Center Michael M Henry, MD is a member of the following medical societies: Brooklyn Pediatric Society Disclosure: Nothing to disclose.
James Bowman, MD Senior Scholar of Maclean Center for Clinical Medical Ethics, Professor Emeritus, Department of Pathology, University of Chicago
James Bowman, MD is a member of the following medical societies: Alpha Omega Alpha , American Society for Clinical Pathology , American Society of Human Genetics , Central Society for Clinical Research , and College of American Pathologists
Disclosure: Nothing to disclose.
David Flannery, MD, FAAP, FACMG Vice Chair of Education, Chief, Section of Medical Genetics, Professor, Department of Pediatrics, Medical College of Georgia
David Flannery, MD, FAAP, FACMG is a member of the following medical societies: American Academy of Pediatrics and American College of Medical Genetics
Mary L Windle, PharmD, Adjunct Associate Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- Childhood Cancer Genetics
- Fast Five Quiz: Genomic Medicine — CRISPR Gene Editing
- Pathologic Findings in Small Cell Bladder Carcinoma
- HIV Testing Overview
- Pervasive Developmental Disorder
- Fast Five Quiz: Precision Medicine in Cancer
- Genetics of Asthma
- Oncologists Voice Financial Concerns of Genomic Testing
- Blood Biomarkers with Genomic Information May Predict Common Diseases
- Food an Effective Medicine in Diabetes?

- Drug Interaction Checker
- Pill Identifier
- Calculators

A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Talking with Your Healthcare Provider
- Birth Defects Statistics
- Birth Defects Resources
- Birth Defects Awareness Month
- Living with Down Syndrome
- Conversation Tips
- Growth Charts for Down Syndrome
- Accessing NBDPS and BD-STEPS Data
- Birth Defects Awareness Month Social Media Resources
Related Topics:
- View All Home
- About Alcohol Use During Pregnancy
Down Syndrome
- Down syndrome is a genetic condition where a person is born with an extra chromosome.
- This can affect how their brain and body develop.
- People diagnosed with Down syndrome can lead healthy lives with supportive care.
Down syndrome is a condition in which a person has an extra copy of chromosome 21. Chromosomes are small "packages" of genes in the body's cells, which determine how the body forms and functions.
When babies are growing, the extra chromosome changes how their body and brain develop. This can cause both physical and mental challenges.
People with Down syndrome often have developmental challenges, such as being slower to learn to speak than other children.
Distinct physical signs of Down syndrome are usually present at birth and become more apparent as the baby grows. They can include facial features, such as:
- A flattened face, especially the bridge of the nose
- Almond-shaped eyes that slant up
- A tongue that tends to stick out of the mouth
Other physical signs can include:
- A short neck
- Small ears, hands, and feet
- A single line across the palm of the hand (palmar crease)
- Small pinky fingers
- Poor muscle tone or loose joints
- Shorter-than-average height
Some people with Down syndrome have other medical problems as well. Common health problems include:
- Congenital heart defects
- Hearing loss
- Obstructive sleep apnea
Down syndrome is the most common chromosomal condition diagnosed in the United States. Each year, about 5,700 babies born in the US have Down syndrome. 1
There are three types of Down syndrome. The physical features and behaviors are similar for all three types.
With Trisomy 21, each cell in the body has three separate copies of chromosome 21. About 95% of people with Down syndrome have Trisomy 21.
Translocation Down syndrome
In this type, an extra part or a whole extra chromosome 21 is present. However, the extra chromosome is attached or "trans-located" to a different chromosome rather than being a separate chromosome 21. This type accounts for about 3% of people with Down syndrome.
Mosaic Down syndrome
Mosaic means mixture or combination. In this type, some cells have three copies of chromosome 21, but other cells have the typical two copies. People with mosaic Down syndrome may have fewer features of the condition. This type accounts for about 2% of people with Down syndrome.
Risk factors
We don't know for sure why Down syndrome occurs or how many different factors play a role. We do know that some things can affect your risk of having a baby with Down syndrome.
One factor is your age when you get pregnant. The risk of having a baby with Down syndrome increases with age, especially if you are 35 years or older when you get pregnant. 2 3 4
However, the majority of babies with Down syndrome are still born to mothers less than 35 years old. This is because there are many more births among younger women. 5 6
Regardless of age, parents who have one child with Down syndrome are at an increased risk of having another child with Down syndrome. 7
Screening and diagnosis
There are two types of tests available to detect Down syndrome during pregnancy: screening tests and diagnostic tests. A screening test can tell you if your pregnancy has a higher chance of being affected Down syndrome. Screening tests don't provide an absolute diagnosis.
Diagnostic tests can typically detect if a baby will have Down syndrome, but they carry more risk. Neither screening nor diagnostic tests can predict the full impact of Down syndrome on a baby.
The views of these organizations are their own and do not reflect the official position of CDC.
Down Syndrome Resource Foundation (DSRF) : The DSRF supports people living with Down syndrome and their families with individualized and leading-edge educational programs, health services, information resources, and rich social connections so each person can flourish in their own right.
GiGi's Playhouse : GiGi's Playhouse provides free educational, therapeutic-based, and career development programs for individuals with Down syndrome, their families, and the community, through a replicable playhouse model.
Global Down Syndrome Foundation : This foundation is dedicated to significantly improving the lives of people with Down syndrome through research, medical care, education and advocacy.
National Association for Down Syndrome : The National Association for Down Syndrome supports all persons with Down syndrome in achieving their full potential. They seek to help families, educate the public, address social issues and challenges, and facilitate active participation.
National Down Syndrome Society (NDSS) : NDSS seeks to increase awareness and acceptance of those with Down syndrome.
- Stallings, E. B., Isenburg, J. L., Rutkowski, R. E., Kirby, R. S., Nembhard, W.N., Sandidge, T., Villavicencio, S., Nguyen, H. H., McMahon, D. M., Nestoridi, E., Pabst, L. J., for the National Birth Defects Prevention Network. National population-based estimates for major birth defects, 2016–2020. Birth Defects Research. 2024 Jan;116(1), e2301.
- Allen EG, Freeman SB, Druschel C, et al. Maternal age and risk for trisomy 21 assessed by the origin of chromosome nondisjunction: a report from the Atlanta and National Down Syndrome Projects. Hum Genet. 2009 Feb;125(1):41-52.
- Ghosh S, Feingold E, Dey SK. Etiology of Down syndrome: Evidence for consistent association among altered meiotic recombination, nondisjunction, and maternal age across populations. Am J Med Genet A. 2009 Jul;149A(7):1415-20.
- Sherman SL, Allen EG, Bean LH, Freeman SB. Epidemiology of Down syndrome. Ment Retard Dev Disabil Res Rev. 2007;13(3):221-7.
- Olsen CL, Cross PK, Gensburg LJ, Hughes JP. The effects of prenatal diagnosis, population ageing, and changing fertility rates on the live birth prevalence of Down syndrome in New York State, 1983-1992. Prenat Diagn. 1996 Nov;16(11):991-1002.
- Adams MM, Erickson JD, Layde PM, Oakley GP. Down's syndrome. Recent trends in the United States. JAMA. 1981 Aug 14;246(7):758-60.
- Morris JK, Mutton DE, Alberman E. Recurrences of free trisomy 21: analysis of data from the National Down Syndrome Cytogenetic Register. Prenatal Diagnosis: Published in Affiliation With the International Society for Prenatal Diagnosis. 2005 Dec 15;25(12):1120-8.
Birth Defects
About one in every 33 babies is born with a birth defect. Although not all birth defects can be prevented, people can increase their chances of having a healthy baby by managing health conditions and adopting healthy behaviors before becoming pregnant.
For Everyone
Health care providers, public health.
- Patient Care & Health Information
- Diseases & Conditions
- Down syndrome
The American College of Obstetricians and Gynecologists recommends offering the option of screening tests and diagnostic tests for Down syndrome to all pregnant women, regardless of age.
- Screening tests can indicate the likelihood or chances that a mother is carrying a baby with Down syndrome. But these tests can't tell for sure or diagnose whether the baby has Down syndrome.
- Diagnostic tests can identify or diagnose whether your baby has Down syndrome.
Your health care provider can discuss the types of tests, advantages and disadvantages, benefits and risks, and the meaning of your results. If appropriate, your provider may recommend that you talk to a genetics counselor.
Screening tests during pregnancy
Screening for Down syndrome is offered as a routine part of prenatal care. Although screening tests can only identify your risk of carrying a baby with Down syndrome, they can help you make decisions about more-specific diagnostic tests.
Screening tests include the first trimester combined test and the integrated screening test.
The first trimester combined test
The first trimester combined test, which is done in two steps, includes:
- Blood test. This blood test measures the levels of pregnancy-associated plasma protein-A (PAPP-A) and the pregnancy hormone known as human chorionic gonadotropin (HCG). Abnormal levels of PAPP-A and HCG may indicate a problem with the baby.
- Nuchal translucency test. During this test, an ultrasound is used to measure a specific area on the back of your baby's neck. This is known as a nuchal translucency screening test. When abnormalities are present, more fluid than usual tends to collect in this neck tissue.
Using your age and the results of the blood test and the ultrasound, your doctor or genetic counselor can estimate your risk of having a baby with Down syndrome.
Integrated screening test
The integrated screening test is done in two parts during the first and second trimesters of pregnancy. The results are combined to estimate the risk that your baby has Down syndrome.
- First trimester. Part one includes a blood test to measure PAPP-A and an ultrasound to measure nuchal translucency.
- Second trimester. The quad screen measures your blood level of four pregnancy-associated substances: alpha fetoprotein, estriol, HCG and inhibin A.
Diagnostic tests during pregnancy
If your screening test results are positive or worrisome, or you're at high risk of having a baby with Down syndrome, you might consider more testing to confirm the diagnosis. Your health care provider can help you weigh the pros and cons of these tests.
Diagnostic tests that can identify Down syndrome include:
- Chorionic villus sampling (CVS). In CVS, cells are taken from the placenta and used to analyze the fetal chromosomes. This test is typically performed in the first trimester, between 10 and 13 weeks of pregnancy. The risk of pregnancy loss (miscarriage) from a CVS is very low.
- Amniocentesis. A sample of the amniotic fluid surrounding the fetus is withdrawn through a needle inserted into the mother's uterus. This sample is then used to analyze the chromosomes of the fetus. Doctors usually perform this test in the second trimester, after 15 weeks of pregnancy. This test also carries a very low risk of miscarriage.
Preimplantation genetic diagnosis is an option for couples undergoing in vitro fertilization who are at increased risk of passing along certain genetic conditions. The embryo is tested for genetic abnormalities before it's implanted in the womb.
Diagnostic tests for newborns
After birth, the initial diagnosis of Down syndrome is often based on the baby's appearance. But the features associated with Down syndrome can be found in babies without Down syndrome, so your health care provider will likely order a test called a chromosomal karyotype to confirm diagnosis. Using a sample of blood, this test analyzes your child's chromosomes. If there's an extra chromosome 21 in all or some cells, the diagnosis is Down syndrome.
More Information
- Amniocentesis
- Genetic testing
Early intervention for infants and children with Down syndrome can make a major difference in improving their quality of life. Because each child with Down syndrome is unique, treatment will depend on individual needs. Also, different stages of life may require different services.
If your child has Down syndrome, you'll likely rely on a team of specialists that can provide medical care and help him or her develop skills as fully as possible. Depending on your child's particular needs, your team may include some of these experts:
- Primary care pediatrician to coordinate and provide routine childhood care
- Pediatric cardiologist
- Pediatric gastroenterologist
- Pediatric endocrinologist
- Developmental pediatrician
- Pediatric neurologist
- Pediatric ear, nose and throat (ENT) specialist
- Pediatric eye doctor (ophthalmologist)
- Audiologist
- Speech pathologist
- Physical therapist
- Occupational therapist
You'll need to make important decisions about your child's treatment and education. Build a team of health care providers, teachers and therapists you trust. These professionals can help evaluate the resources in your area and explain state and federal programs for children and adults with disabilities.
Coping and support
When you learn your child has Down syndrome, you may experience a range of emotions, including anger, fear, worry and sorrow. You may not know what to expect, and you may worry about your ability to care for a child with a disability. The best antidote for fear and worry is information and support.
Consider these steps to prepare yourself and to care for your child:
- Ask your health care provider about early intervention programs in your area. Available in most states, these special programs offer infants and young children with Down syndrome stimulation at an early age (typically until age 3) to help develop motor, language, social and self-help skills.
- Learn about educational options for school. Depending on your child's needs, that may mean attending regular classes (mainstreaming), special education classes or both. With your health care team's recommendations, work with the school to understand and choose appropriate options.
- Seek out other families who are dealing with the same issues. Most communities have support groups for parents of children with Down syndrome. You can also find internet support groups. Family and friends can also be a source of understanding and support.
- Participate in social and leisure activities. Take time for family outings and look in your community for social activities such as park district programs, sports teams or ballet classes. Although some adaptations may be required, children and adults with Down syndrome can enjoy social and leisure activities.
- Encourage independence. Your child's abilities may be different from other children's abilities, but with your support and some practice your child may be able to perform tasks such as packing lunch, managing hygiene and dressing, and doing light cooking and laundry.
- Prepare for the transition to adulthood. Opportunities for living, working, and social and leisure activities can be explored before your child leaves school. Community living or group homes, and community employment, day programs or workshops after high school require some advance planning. Ask about opportunities and support in your area.
Expect a bright future. Most people with Down syndrome live with their families or independently, go to mainstream schools, read and write, participate in the community, and have jobs. People with Down syndrome can live fulfilling lives.
- What is Down syndrome? National Down Syndrome Society. http://www.ndss.org/down-syndrome/what-is-down-syndrome/. Accessed Dec. 16, 2016.
- Down syndrome fact sheet. National Down Syndrome Society. http://www.ndss.org/Down-Syndrome/Down-Syndrome-Facts/. Accessed Dec. 16, 2016.
- Messerlian GM, et al. Down syndrome: Overview of prenatal screening. http://www.uptodate.com/home. Accessed Dec. 16, 2016.
- National Library of Medicine. Down syndrome. Genetics Home Reference. https://ghr.nlm.nih.gov/condition/down-syndrome. Accessed Dec. 16, 2016.
- Facts about Down syndrome. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/birthdefects/downsyndrome.html. Accessed Dec. 16, 2016.
- Down syndrome. Eunice Kennedy Shriver National Institute of Child Health and Human Development. https://www.nichd.nih.gov/health/topics/down/conditioninfo/Pages/default.aspx. Accessed Dec. 16, 2016.
- Frequently asked questions. Prenatal genetic diagnostic tests. FAQ164. Pregnancy. American College of Obstetricians and Gynecologists. https://www.acog.org/-/media/For-Patients/faq164.pdf?dmc=1&ts=20161216T1208042192. Accessed Dec. 16, 2016.
- Ostermaier KK. Down syndrome: Management. http://www.uptodate.com/home. Accessed Dec. 22, 2016.
- Ostermaier KK. Down syndrome: Clinical features and diagnosis. http://www.uptodate.com/home. Accessed Jan. 10, 2017.
- Gabbe SG, et al., eds. Genetic screening and prenatal genetic diagnosis. In: Obstetrics: Normal and Problem Pregnancies. 7th ed. Philadelphia, Pa.: Saunders Elsevier; 2017.
- Rink BD, et al. Screening for fetal aneuploidy. Seminars in Perinatology. 2016;40:35.
- Bunt CW, et al. The role of the family physician in the care of children with Down syndrome. American Family Physician. 2014;90:851.
- Butler Tobah YS (expert opinion). Mayo Clinic, Rochester, Minn. Jan. 26, 2017.
- The genetic basis of Down syndrome
Associated Procedures
Products & services.
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Double your impact on fighting cancer
Make a gift before July 31 and it can go twice as far to fight cancer.
Skip to content
Trisomy 21 (Down Syndrome)
Trisomy 21 program, what is trisomy 21 (down syndrome).
Trisomy 21 is the most common chromosomal anomaly in humans, affecting about 5,000 babies born each year and more than 350,000 people in the United States.
Also known as Down syndrome, trisomy 21 is a genetic condition caused by an extra chromosome. Most babies inherit 23 chromosomes from each parent, for a total of 46 chromosomes. Babies with Down syndrome however, end up with three chromosomes at position 21, instead of the usual pair.
Other examples of trisomies occur at position 13 and 18. Trisomy 21 is the most common of the three, occurring in 1 out of every 691 births. The disorder was first identified in 1866 by John Langdon Down, a British physician, and later named after him.
As your child with Down syndrome grows, he is at greater risk for certain medical problems and may develop:
- Congenital heart disease
- Gastrointestinal abnormalities
- Musculoskeletal and movement problems
- Spine disorders such as scoliosis, kyphosis or lordosis
- Endocrinologic disorders
- Hearing loss
- Speech apraxia (difficulty making speech sounds)
- Sleep disorders
- Feeding disorders
- Developmental disabilities (learning disabilities, intellectual disabilities and autism)
Problems in any of these areas can affect your child's development and behavior.
Down syndrome occurs because of the extra copy of chromosome 21, which can cause the body and brain to develop differently than a child without the syndrome.
The risk of having a baby with Down syndrome increases as a woman ages — women older than 35 are often encouraged to have prenatal genetic testing done of their unborn babies — but, because younger women have more babies, they give birth to 80 percent of babies with Down syndrome.
Signs and symptoms
Symptoms of Down syndrome may include:
- Distinctive facial features
- Mild to moderate intellectual disabilities
- Heart, kidney and thyroid issues
- Numerous respiratory infections, from colds to bronchitis and pneumonia
- Skeletal abnormalities, including spine, hip, foot and hand disorders
- Flexible joints and weak, floppy muscles
- Overly quiet baby
- Less responsive to stimuli
- Vision and hearing impairment
- Inwardly curved little finger
- Wide space between the great and second toe
- Single, deep crease on the soles of the feet and one or both hands
Testing and diagnosis
Tests to confirm Down syndrome are often done before a baby is born through amniocentesis or chorionic villus sampling (CVS). For amniocentesis, a needle is inserted through the mother’s abdominal wall into the amniotic sac and a small sample of amniotic fluid is drawn out and tested in a laboratory.
If your child was not prenatally diagnosed with Down syndrome, diagnosis usually begins at birth based on your child’s physical appearance. Doctors will ask you for a thorough family medical history, do a physical exam of your child, and analyze your child’s chromosomes. Once a diagnosis is made, additional testing may be ordered to help clinicians better understand how Down syndrome may affect your child and help spot any early complications from the disorder.
Tests may include:
- Genetic testing , in which a sample of your child’s saliva is used to identify your child’s DNA.
- Blood tests , which can help determine drug usage and effectiveness, biochemical diseases and organ function.
- X-rays , which produce images of bones.
- Magnetic resonance imaging (MRI) , which uses a combination of large magnets, radiofrequencies and a computer to produce detailed images of organs and structures within the body.
- Computed tomography (CT) scan , which uses a combination of X-rays and computer technology to produce cross-sectional images ("slices") of the body.
- EOS imaging , an imaging technology that creates 3-dimensional models from two planar images. Unlike a CT scan, EOS images are taken while the child is in an upright or standing position, enabling improved diagnosis — for some conditions — due to weight-bearing positioning.
There is no cure for Down syndrome. Treatment is ordered when certain issues — such as heart problems, muscle weaknesses or spinal curvatures — occur and need to be treated.
At Children’s Hospital of Philadelphia (CHOP), we practice collaborative, family-centered care. A team of expert clinicians — including world-class surgeons and physicians, pediatric nurses, physical and occupational therapists, psychologists and other specialists — will partner with you in the care of your child.
Many children with Down syndrome are also diagnosed with a variety of secondary conditions that are present at birth and can be treated when your child is young. This is often true for conditions such as heart issues, hand and foot anomalies.
In other cases, the complications from Down syndrome may only become evident — or problematic — as your child grows. This is often true for spinal deformities such as scoliosis and hip conditions that might require surgical correction.
Every child’s condition is different, so treatment is determined on a case-by-case basis. Depending on your child’s needs, specialists from cardiology, orthopaedics, endocrinology and others will treat your child. Treatment may include therapy, surgery or additional support services for your child and family.
A Care Binder can help you organize the most important information about your child's care in a central place.
Follow-up care
Your child with Down syndrome should continue to be monitored by a physician into adulthood. Experts in the Trisomy 21 Program at CHOP are available to help you manage the care of your child with Down syndrome at all stages of growth. The Trisomy 21 Program is one of the few programs at Children's Hospital that treats patients beyond age 18 and into old age.
Tips for the Transition to Adulthood

This toolkit outlines steps for individuals with Down syndrome who are transitioning from pediatric to adult healthcare.
If your child had surgery, she will need to follow up with her surgeon about one to two weeks after surgery, then again at three and six months post-surgery. After that, annual monitoring by trained clinicians is strongly encouraged to ensure any problems are spotted and treated as soon as possible.
During follow-up visits, your child may need additional X-rays and other diagnostic testing done. The goal of continued monitoring is to help spot any irregularities in growth or development and to address health issues as they develop.
Follow-up care and ongoing support and services are available at our Main Campus and throughout our CHOP Care Network. Our team is committed to partnering with parents and referring physicians to provide the most current, comprehensive and specialized care possible for your child.
In addition, physicians may recommend your child see several different specialists because so many body systems can be involved in a diagnosis of Down syndrome.
For example, your child may see:
- An orthopaedic physician for any bone- and muscle-related issues, particularly to diagnose and manage instability of the cervical spine, hip instability and the possibility of hip dislocation.
- A cardiologist for any heart-related issues. An echocardiogram may be ordered to create pictures of your baby’s heart to help diagnose or rule out heart defects.
- A pediatric audiologist, who is trained to identify, diagnose, treat and monitor hearing problems.
- A pediatric ophthalmologist (eye doctor), who can assess your child’s vision and diagnosis and treat eye or vision problems.
- A pediatric endocrinologist for a thyroid function test. Thyroid hormones play an important role in your child’s growth, development and metabolism. Thyroid levels are checked with a blood test.
- A geneticist for individual or family counseling.
- A pulmonologist for any breathing issues.
- A neurologist for any nerve and brain-related issues.
- Physical therapists and occupational therapists to expand your child’s physical dexterity and skill.
In 1983, the life expectancy for people with Down syndrome was 25 years; however today, it is 60 years. Advances in cardiology have significantly contributed to this rapid increase. As science and technology continue to improve and the intricacies of Down syndrome are explored and discovered, it is expected that the life expectancy for people with Down syndrome will continue to increase too.
Today, children with Down syndrome are included in regular academic classrooms in schools across the country. In some instances they are integrated into specific courses, while in other situations students are fully included in the regular classroom for all subjects. The degree of mainstreaming is based in the abilities of the child.
Many people with Down syndrome have gone to college, live independently and hold jobs. These individuals are hard workers and dedicated employees. A stimulating home environment, positive support from family and friends, quality educational programs and good healthcare enable people with Down syndrome to develop their full potential and lead fulfilling lives. Be creative, persistent and set high expectations.
Despite the advances, children with Down syndrome continue to have a higher risk of developing certain health conditions, such as heart disease, gastrointestinal abnormalities and dementia. Early diagnosis and treatment of these associated conditions leads to better outcomes.
With regular medical care and a solid support system, children with Down syndrome can lead long, full and happy lives.
Providers Who Treat Trisomy 21 (Down Syndrome)

Kathy Abel, DNP, RN APNC

Jason B. Anari, MD

Paul D. Bradford, MEd, MMS, PA-C

Richard S. Davidson, MD

Malcolm L. Ecker, MD

John M. Flynn, MD

B. David Horn, MD

Michela Mansfield, MSN, CRNP

Wudbhav N. Sankar, MD

David A. Spiegel, MD

Jessica C. Staschak, MSN, CRNP, CPNP-PC

Jennifer Winell, MD
You might also like.

Evan's Story
Born with Down syndrome, Evan has been treated at CHOP since he was a baby. His family shares how that care has made a difference in Evan’s life.

Your Child's Trisomy 21 Program Visit
Learn more about what to expect at your first appointment with the Trisomy 21 Program clinic.

John and Sara's Story
John and Sara have been coming to CHOP's Trisomy 21 Program all of their lives. Learn about how their care transitioned as they grew up.
About Down Syndrome
In every cell in the human body there is a nucleus, where genetic material is stored in genes. Genes carry the codes responsible for all of our inherited traits and are grouped along rod-like structures called chromosomes. Typically, the nucleus of each cell contains 23 pairs of chromosomes, half of which are inherited from each parent. Down syndrome occurs when an individual has a full or partial extra copy of chromosome 21.
This additional genetic material alters the course of development and causes the characteristics associated with Down syndrome. A few of the common physical traits of Down syndrome are low muscle tone, small stature, an upward slant to the eyes, and a single deep crease across the center of the palm – although each person with Down syndrome is a unique individual and may possess these characteristics to different degrees, or not at all.
On this page:
Your donation will help people with Down syndrome, their families, and their caregivers.

How common is Down syndrome?
According to the Centers for Disease Control and Prevention, approximately one in every 775 babies in the United States is born with Down syndrome, making Down syndrome the most common chromosomal condition. About 5,000 babies with Down syndrome are born in the United States each year.
-De Graaf, G., Buckley, F., & Skotko, B. (2024, May 3). People living with Down syndrome in the USA: Births and Population . https://go.downsyndromepopulation.org/usa-factsheet
When was Down syndrome discovered?
For centuries, people with Down syndrome have been alluded to in art, literature, and science. It wasn’t until the late nineteenth century, however, that John Langdon Down, an English physician, published an accurate description of a person with Down syndrome. It was this scholarly work, published in 1866, that earned Down the recognition as the “father” of the syndrome. Although other people had previously recognized the characteristics of the syndrome, it was Down who described the condition as a distinct and separate entity.
In recent history, advances in medicine and science have enabled researchers to investigate the characteristics of people with Down syndrome. In 1959, the French physician Jérôme Lejeune identified Down syndrome as a chromosomal condition. Instead of the usual 46 chromosomes present in each cell, Lejeune observed 47 in the cells of individuals with Down syndrome. It was later determined that an extra partial or whole copy of chromosome 21 results in the characteristics associated with Down syndrome. In the year 2000, an international team of scientists successfully identified and catalogued each of the approximately 329 genes on chromosome 21. This accomplishment opened the door to great advances in Down syndrome research.
Are there different types of Down syndrome?
Trisomy 21 (nondisjunction).
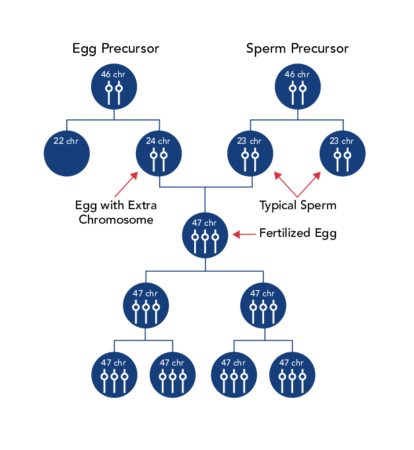
Down syndrome is usually caused by an error in cell division called “nondisjunction.” Nondisjunction results in an embryo with three copies of chromosome 21 instead of the usual two. Prior to or at conception, a pair of 21st chromosomes in either the sperm or the egg fails to separate. As the embryo develops, the extra chromosome is replicated in every cell of the body. This type of Down syndrome, which accounts for 95% of cases, is called trisomy 21.
Mosaicism (or mosaic Down syndrome) is diagnosed when there is a mixture of two types of cells, some containing the usual 46 chromosomes and some containing 47. Those cells with 47 chromosomes contain an extra chromosome 21.
Mosaicism is the least common form of Down syndrome and accounts for only about 2% of all cases of Down syndrome (Facts about Down syndrome, 2021). Research has indicated that individuals with mosaic Down syndrome may have fewer characteristics of Down syndrome than those with other types of Down syndrome. However, broad generalizations are not possible due to the wide range of abilities people with Down syndrome possess.
Translocation
In translocation, which accounts for about 3% of cases of Down syndrome, the total number of chromosomes in the cells remains 46; however, an additional full or partial copy of chromosome 21 attaches to another chromosome, usually chromosome 14 (Facts and Down syndrome, 2021). The presence of the extra full or partial chromosome 21 causes the characteristics of Down syndrome.
What causes Down syndrome?
Regardless of the type of Down syndrome, a person may have, all people with Down syndrome have an extra, critical portion of chromosome 21 present in all or some of their cells.
The cause of the extra full or partial chromosome is still unknown. Age is the only factor that has been linked to an increased chance of having a baby with Down syndrome resulting from nondisjunction or mosaicism. However, due to higher birth rates in younger women, 51% of children with Down syndrome are born to women under 35 years of age. (De Graaf et al., 2022).
There is no definitive scientific research that indicates that Down syndrome is caused by environmental factors or the parents’ activities before or during pregnancy.
The additional partial or full copy of the 21st chromosome which causes Down syndrome can originate from either parent. Approximately 5% of the cases have been traced to the father.
A Promising Future Together
This booklet includes sections on healthy starts, early intervention therapies, how to find support and care for your family, and what the future holds for your child.

What is the likelihood of having a child with Down syndrome?
Down syndrome occurs in people of all races and economic levels, though older women have an increased chance of having a child with Down syndrome. A 35-year-old woman has about a one in 350 chance of conceiving a child with Down syndrome, and this chance increases gradually to 1 in 100 by age 40. At age 45 the incidence becomes approximately 1 in 30. The age of the mother, or birthing parent, does not seem to be linked to the risk of translocation.
Since many couples are postponing parenting until later in life, the incidence of Down syndrome conceptions is expected to increase. Therefore, genetic counseling for parents is becoming increasingly important. Still, many physicians are not fully informed about advising their patients about the incidences of Down syndrome, advancements in diagnosis, and the protocols for care and treatment of babies born with Down syndrome.
Does Down syndrome run in families?
All three types of Down syndrome are genetic conditions (relating to the genes), but only 1% of all cases of Down syndrome have a hereditary component (passed from parent to child through the genes). Heredity is not a factor in trisomy 21 (nondisjunction) and mosaicism. However, in one-third of cases of Down syndrome resulting from translocation, there is a hereditary component – accounting for about 1% of all cases of Down syndrome (Facts about Down syndrome, 2021).
The age of the parent does not seem to be linked to the risk of translocation. Most cases are sporadic – chance – events. However, in about one-third of cases, one parent is a carrier of a translocated chromosome.
What is the likelihood of having a second child with Down syndrome?
Once a parent has given birth to a baby with trisomy 21 (nondisjunction) or translocation, it is estimated that the chances of having another baby with trisomy 21 is 1 in 100 up until age 40.
The risk of recurrence of translocation is about 3% if the father is the carrier and 10-15% if the mother is the carrier. Genetic counseling can determine the origin of translocation.
| Maternal Age | Incidence of Down syndrome |
|---|---|
| 20 | 1 in 2,000 |
| 21 | 1 in 1,700 |
| 22 | 1 in 1,500 |
| 23 | 1 in 1,400 |
| 24 | 1 in 1,300 |
| 25 | 1 in 1,200 |
| 26 | 1 in 1,100 |
| 27 | 1 in 1,050 |
| 28 | 1 in 1,000 |
| 29 | 1 in 950 |
| 30 | 1 in 900 |
| 31 | 1 in 800 |
| 32 | 1 in 720 |
| 33 | 1 in 600 |
| 34 | 1 in 450 |
| 35 | 1 in 350 |
| 36 | 1 in 300 |
| 37 | 1 in 250 |
| 38 | 1 in 200 |
| 39 | 1 in 150 |
| 40 | 1 in 100 |
| 41 | 1 in 80 |
| 42 | 1 in 70 |
| 43 | 1 in 50 |
| 44 | 1 in 40 |
| 45 | 1 in 30 |
| 46 | 1 in 25 |
| 47 | 1 in 20 |
| 48 | 1 in 15 |
| 49 | 1 in 10 |
How is Down syndrome diagnosed?
There are two categories of tests for Down syndrome that can be performed before a baby is born: screening tests and diagnostic tests. Prenatal screens estimate the chance of the fetus having Down syndrome. These tests do not tell you for sure whether your fetus has Down syndrome; they only provide a probability. Diagnostic tests, on the other hand, can provide a definitive diagnosis with almost 100% accuracy.
There is an extensive menu of prenatal screening tests now available for pregnant parents. Most screening tests involve a blood test and an ultrasound (sonogram). The blood tests (or serum screening tests) measure quantities of various substances in the blood of the parent. Together with age, these are used to estimate the chance of having a child with Down syndrome. These blood tests are often performed in conjunction with a detailed sonogram to check for “markers” (characteristics that some researchers feel may have a significant association with Down syndrome). New advanced prenatal screens are now able to detect chromosomal material from the fetus that is circulating in the maternal blood. These tests are not invasive (like the diagnostic tests below), but they provide a high accuracy rate. Still, all of these screens will not definitively diagnose Down syndrome. Prenatal screening and diagnostic tests are now routinely offered to all ages.
The diagnostic procedures available for prenatal diagnosis of Down syndrome are chorionic villus sampling (CVS) and amniocentesis. These procedures, which carry up to a 1% risk of causing a spontaneous termination (miscarriage), are nearly 100% accurate in diagnosing Down syndrome. Amniocentesis is usually performed in the second trimester between 15 and 20 weeks of gestation, CVS in the first trimester between 11 and 14 weeks (Chrionic villus sampling, 2020).
Down syndrome is usually identified at birth by the presence of certain physical traits: low muscle tone, a single deep crease across the palm of the hand, a slightly flattened facial profile, and an upward slant to the eyes. Because these features may be present in babies without Down syndrome, a chromosomal analysis called a karyotype is done to confirm the diagnosis. To obtain a karyotype, doctors draw a blood sample to examine the baby’s cells. They photograph the chromosomes and then group them by size, number, and shape. By examining the karyotype, doctors can diagnose Down syndrome. Another genetic test called fluorescence in situ hybridization (FISH) can confirm a diagnosis in a shorter amount of time by visualizing and mapping the genetic material in an individual's cells.

What impact does Down syndrome have on society?
Individuals with Down syndrome are becoming increasingly integrated into society and community organizations, such as schools, health care systems, work forces, and social and recreational activities. Individuals with Down syndrome possess varying degrees of cognitive delays, from very mild to severe. Most people with Down syndrome have cognitive delays that are mild to moderate.
Due to advances in medical technology, individuals with Down syndrome are living longer than ever before. In 1910, children with Down syndrome were expected to survive to age nine. With the discovery of antibiotics, the average survival age increased to 19 or 20. Now, with recent advancements in clinical treatment, most particularly corrective heart surgeries, as many as 80% of adults with Down syndrome reach age 60, and many live even longer (Down syndrome, 2018). More and more Americans are interacting with individuals with Down syndrome, increasing the need for widespread public education and acceptance.
Preferred Language Guide
Use this language when referring to down syndrome and people who have down syndrome:.
- People with Down syndrome should always be referred to as people first.
- Instead of “a Down syndrome child,” it should be “a child with Down syndrome.” Also avoid “Down’s child” and describing the condition as “Down’s,” as in, “He has Down’s.”
- Down syndrome is a condition or a syndrome, not a disease.
- People “have” Down syndrome, they do not “suffer from” it and are not “afflicted by” it.
- “Typically developing” or “typical” is preferred over “normal.”
- “Intellectual disability” or “cognitive disability” has replaced “mental retardation” as the appropriate term.
- NDSS strongly condemns the use of the word “retarded” in any derogatory context. Using this word is hurtful and suggests that people with disabilities are not competent.
Down vs. Down’s
- NDSS uses the preferred spelling, Down syndrome, rather than Down’s syndrome.
- Down syndrome is named for the English physician John Langdon Down, who characterized the condition, but did not have it. An “apostrophe s” connotes ownership or possession.
- While Down syndrome is listed in many dictionaries with both popular spellings (with or without an apostrophe s), the preferred usage in the United States is Down syndrome. The AP Stylebook recommends using “Down syndrome,” as well.
A downloadable version of the Preferred Language Guide is available to print and distribute.
Citations:
Chorionic villus sampling. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/chorionic-villus-sampling/a… . Published November 12, 2020. Accessed June 28, 2022.
de Graaf G, Buckley F, Skotko B. People living with Down syndrome in the USA: BIRTHS AND POPULATION. May 2022. https://go.dselink.net/us-population-factsheet.  ;
Down syndrome. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/down-syndrome/symptoms-c… . Published March 8, 2018. Accessed June 28, 2022.
Facts about Down syndrome. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/birthdefects/downsyndrome.html . Published April 6, 2021. Accessed June 28, 2022.
- Introduction to Genomics
- Educational Resources
- Policy Issues in Genomics
- The Human Genome Project
- Funding Opportunities
- Funded Programs & Projects
- Division and Program Directors
- Scientific Program Analysts
- Contact by Research Area
- News & Events
- Research Areas
- Research investigators
- Research Projects
- Clinical Research
- Data Tools & Resources
- Genomics & Medicine
- Family Health History
- For Patients & Families
- For Health Professionals
- Jobs at NHGRI
- Training at NHGRI
- Funding for Research Training
- Professional Development Programs
- NHGRI Culture
- Social Media
- Broadcast Media
- Image Gallery
- Press Resources
- Organization
- NHGRI Director
- Mission & Vision
- Policies & Guidance
- Institute Advisors
- Strategic Vision
- Leadership Initiatives
- Diversity, Equity, and Inclusion
- Partner with NHGRI
- Staff Search
About Down Syndrome
Down syndrome is a chromosomal condition related to chromosome 21. It affects 1 in 800 to 1 in 1000 live born infants.
What are the symptoms of Down syndrome?
People who have Down syndrome have learning difficulties, mental disability, a characteristic facial appearance, and poor muscle tone (hypotonia) in infancy.
Individuals with Down syndrome also have an increased risk for having heart defects, digestive problems such as gastroesophageal reflux or celiac disease, and hearing loss. Some people who have Down syndrome have low activity of the thyroid gland (hypothyroidism) - an organ in the lower neck that produces hormones.
How is Down syndrome diagnosed?
Down syndrome can be diagnosed in infancy based on the characteristic clinical findings. When Down syndrome is suspected in a person, a genetic test called a chromosome analysis is performed on a blood or skin sample to look for an extra chromosome 21 (trisomy 21). Trisomy 21 means that each cell in the body has three copies of chromosome 21 instead of the usual two copies.
Having an extra number 21 chromosome interrupts the normal course of development, causing the characteristic clinical features of Down syndrome. Some people who have Down syndrome have an extra number 21 chromosome in only some of their body's cells. This type of Down syndrome is called mosaic Down syndrome.
A small number of individuals have Down syndrome because part of chromosome 21 becomes attached (translocated) to another chromosome before or at the time of conception. These individuals have two copies of chromosome 21, and additional material from chromosome 21 that is attached to another chromosome. The chromosomes of parents of a child with Down Syndrome caused by a translocation are studied to see whether the translocation was inherited.
What is the treatment for Down syndrome?
Treatment for Down syndrome is based on the person's physical problems and intellectual challenges. Many babies who have Down syndrome do not have good muscle tone, which makes it harder for them to roll over and walk. Physical therapy can help with these problems.
About 40 - 60 percent of babies born with Down syndrome have a heart defect. Therefore, all newborns with Down syndrome have their heart checked with an electrocardiogram and an echocardiogram. When there is a heart defect present in an infant with Down syndrome, the infant is referred to a pediatric cardiologist for medical management or to a pediatric cardiac surgeon for early surgical repair.
Some infants with Down syndrome have difficulties with swallowing or they may have blockages in their bowels. Surgery can be performed to correct these problems. Once corrected, they usually cause no further health issues.
Children with Down syndrome may have frequent colds and sinus and ear infections. These are treated early and aggressively to prevent hearing loss and chronic infections.
Low thyroid levels are more common in infants who have Down syndrome. It is recommended that thyroid level testing be performed at least yearly.
Some infants with Down syndrome have eye problems such as cataracts (cloudy lenses) or crossed eyes (strabismus). Surgery can help with these problems.
Sucking problems related to low muscle tone or heart problems may make breast feeding difficult initially. Occupational therapists, speech therapists, breast feeding consultants and support groups usually have specific resources for the mothers of infants with Down syndrome.
Intelligence in individuals with Down syndrome ranges from low normal to very slow to learn. At birth it is not possible to tell the level of intelligence a baby with Down syndrome will have. All areas of development including motor skills, language, intellectual abilities, and social and adaptive skills are followed closely in children with Down syndrome. Early referral, beginning at birth, to an early intervention program will help enhance development. Preschool programs for children with Down syndrome include physical, occupational, speech and educational therapies.
Many adults with Down syndrome have jobs and live independently.
Is Down syndrome inherited?
Most cases of Down syndrome are not inherited, but occur as random events during the formation of reproductive cells (eggs and sperm). An error in cell division called nondisjunction results in reproductive cells with an abnormal number of chromosomes. For example, an egg or sperm cell may gain an extra copy of chromosome 21. If one of these atypical reproductive cells contributes to the genetic makeup of a child, the child will have an extra chromosome 21 in each of the body's cells.
Mosaic Down syndrome is also not inherited. It occurs as a random error during cell division early in fetal development. As a result, some of the body's cells have the usual two copies of chromosome 21, and other cells have three copies of the chromosome. Translocation Down syndrome can be inherited. An unaffected person can carry a rearrangement of genetic material between chromosome 21 and another chromosome. This rearrangement is called a balanced translocation because there is no extra material from chromosome 21. Although they do not have signs of Down syndrome, people who carry this type of balanced translocation are at an increased risk of having children with the condition.
Additional Resources for Down Syndrome
The Genetics Home Reference: Down Syndrome
National Institute of Child Health and Human Development th and Human Development.
MedlinePlus
National Down Syndrome Society
National Down Syndrome Congress
MUMS National Parent-to-Parent Network
Facts About Down Syndrome
Genetics and Rare Diseases Information Center
Finding Reliable Health Information Online
Last updated: June 29, 2017
- Children's Health
- Common Symptoms
- Common Conditions
- Chronic Conditions
- View Full Guide
Down Syndrome

- What Is Down Syndrome?
Down syndrome is a genetic condition that causes mild to significant physical and developmental problems.
People with Down syndrome (DS) are born with an extra chromosome. Chromosomes are bundles of genes, and your body relies on having just the right number of them. With Down syndrome, this extra chromosome leads to a range of issues that affect you both mentally and physically.
Down syndrome is named after John Langdon Down, an English doctor who was the first person to publish an accurate description of the condition in the 1860s.
Down syndrome is a lifelong condition. Although it can’t be cured, doctors know more about it now than ever. If your child has it, getting the right care early on can make a big difference in helping them live a full and meaningful life.
How many people have Down syndrome?
No one knows for sure. It could be as high as 6 million people worldwide, according to the Global Down Syndrome Foundation. The CDC estimated there were around 250,700 children, teens, and adults living with Down syndrome in the U.S. in 2008. It also said 1 in every 700 babies in the U.S. are born with Down syndrome. This makes it the most common chromosomal condition in America.
Down syndrome vs. autism
There are some similarities and differences between the two conditions. First, we'll look at the differences.
Down syndrome : Genetic disorder, usually with physical traits. People with this condition are often social and friendly. Their language development is similar to that of more typical children.
Autism: Neurological disorder (dysfunction in the brain and nervous system) with no physical characteristics. People with this condition often prefer to be alone and not socialize. Their language skills might be delayed or not develop.
Similarities: Both groups may:
- Prefer routine
- Have developmental delays
- Avoid eye contact
- Enjoy repetitive play
- Show challenging behaviors (trouble managing feelings when frustrated, lack of impulse control, etc.)
About 18% of children with Down syndrome also have autism, but sometimes children with DS might show these behaviors without having autism.
Types of Down Syndrome
There are three types of Down syndrome : trisomy 21, translocation Down syndrome, and mosaic Down syndrome.
This is the most common type of Down syndrome, with 95% of people with DS having trisomy 21. Here, all your body's cells have three copies of chromosome 21 instead of two.
Translocation Down syndrome
About 3% of people with Down syndrome have this type, where there's an extra part or whole chromosome 21, but it's attached to another chromosome instead of being a separate chromosome 21.
Mosaic Down syndrome
This type of Down syndrome, which affects about 2% of people with the condition, happens when only some cells in your body have an extra chromosome 21.
You can’t tell what type of Down syndrome someone has by how they look. The effects of all three types are very similar, but someone with mosaic Down syndrome may not have as many symptoms because fewer cells have the extra chromosome. So it's possible to have undiagnosed mosaic Down syndrome.
Down Syndrome Symptoms
Down syndrome can have many effects, and it’s different for each person. Some will grow up to live almost entirely on their own, while others will need more help taking care of themselves.
Mental abilities vary, but most people with Down syndrome have mild to moderate issues with thinking, reasoning, and understanding. They’ll learn and pick up new skills their whole lives, but they may take longer to reach important goals like walking, talking, and developing social skills.
People with Down syndrome may also have trouble with behavior – they may not pay attention well, or can be obsessive about some things. That’s because it’s harder for them to control their impulses , relate to others, and manage their feelings when they get frustrated.
As adults, people with Down syndrome may learn to decide many things on their own but will likely need help with more complex issues, like birth control or managing money. Some may go to a college that can provide accommodations and modifications tailored to developmental and intellectual delays and may go on to live independently, while others will need more day-to-day care.
Down syndrome features
People with Down syndrome tend to have certain physical features in common. These may include:
- Eyes that slant up at the outer corner
- A flat nose
- Tongue that sticks out
- Tiny white spots in the colored part of the eyes
- Short neck and overall height
- Small hands and feet
- Short stature
- Loose joints
- Weak muscle tone and joints
- Small pinky fingers that curve in
- One crease across the palm of the hand
Many people with Down syndrome don’t have any other health issues, but others do. They may have eye diseases , vision problems, hearing loss and ear infections, sleep apnea, and heart problems.
What Causes Down Syndrome?
For most people, each cell in the body has 23 pairs of chromosomes. One chromosome in each pair comes from your mother and the other comes from your father.
But with Down syndrome, you get an extra copy of chromosome 21. That means you have three copies instead of two, which leads to the symptoms of Down syndrome. Doctors aren’t sure why this happens. There’s no link to anything in the environment or anything the parents did or didn’t do.
Is Down syndrome genetic?
It’s not common, but it's possible to pass Down syndrome from parent to child. Sometimes, a parent has what experts call “translocated” genes. That means some of their genes aren’t in their normal place, perhaps on a different chromosome from where they’d usually be found.
The parent doesn’t have Down syndrome because they have the right number of genes, but their child may have translocation Down syndrome, where they have an extra chromosome 21. Not everyone with translocation Down syndrome gets it from their parents – it may also happen by chance.

Down Syndrome Risk Factors
While doctors don’t know what causes it, they do know that women (or people with female anatomy) ages 35 and older have a higher chance of having a baby with Down syndrome. If you’ve already had a child with Down syndrome, you’re more likely to have another one who also has it. But most babies who have Down syndrome are born to mothers under 35 because most children are born to younger women.
Men (or people with male anatomy) over 40 at the time of conception also have an increased risk of having a child with Down, particularly if the mother is also over 35.
Down Syndrome Tests
Routine tests done during pregnancy can check to see if it’s likely your baby has Down syndrome. If those results are positive, or if you’re at high risk, you may choose to have some more invasive tests to be sure.
Prenatal genetic testing
Screening tests are usually done first and are considered to pose no risk to you and your growing baby. These normally include a combination of blood tests and ultrasounds, which show images of your baby.
In the first trimester , you may have:
- Blood tests. Your doctor measures the levels of a protein called PAPP-A and a hormone called hCG in your blood. Anything out of the normal range could mean a problem with the baby.
- Cell-free DNA test . This blood test checks the baby's DNA circulating in your blood via the placenta. It can tell if your unborn baby is at a higher risk of a chromosomal abnormality like Down syndrome or another condition.
- Ultrasound (nuchal translucency test). Your doctor looks at a picture of your baby and measures the folds of tissue at the back of their neck. The extra tissue is called the nuchal fold. Babies with Down syndrome tend to have extra fluid there. Since this fluid buildup can be due to a number of genetic conditions, this test is usually combined with a blood test.
In the second trimester, you may have:
- Blood tests. Either a triple or quad-screen test measures other substances in your blood, including the protein AFP and the hormone estriol. Those levels, combined with the results from the first-trimester tests, give your doctor a good estimate of the chances your baby has Down syndrome.
- Ultrasound. When your baby is more developed, an ultrasound can show some of the physical features of Down syndrome.
Screening tests don't tell you for certain that your baby has Down syndrome. They only tell you if your baby is at high or low risk for DS. For confirmation, you have to do a diagnostic test. These d iagnostic tests usually happen after screening test results are positive, as they carry a small risk that you could miscarry after having them. They include :
- Chorionic villus sampling (CVS). This can be done during the first trimester, using cells taken from the placenta.
- Amniocentesis. Fluid is taken from the amniotic sac surrounding the baby, usually during the second trimester.
- Percutaneous umbilical blood sampling (PUBS). This is also done in the second trimester using blood removed from the umbilical cord.
Down Syndrome Diagnosis
After a baby is born, a doctor may suspect Down syndrome in a newborn based on the baby’s appearance. But some babies without DS may have similar physical features to a baby with Down syndrome.
A diagnosis can be confirmed by a blood test called a karyotype test that lines up the chromosomes and will show if there’s an extra chromosome 21.
Down Syndrome Complications
Babies with Down syndrome may be born with other physical problems, and they’re at a higher risk of certain health issues later in life.
Possible complications of Down syndrome include:
- Heart problems. About half of babies with Down syndrome are born with a heart defect that may need surgery.
- Hearing and vision problems, including crossed eyes and cataracts
- Gastrointestinal disorders like blockages, reflux, and celiac disease
- Weight issues
- Breathing issues, including sleep apnea, asthma, and pulmonary hypertension
- Underactive thyroid
- Childhood leukemia
- Early-onset dementia
They’re also more likely to have:
- Blood conditions like anemia, where you have low iron. It’s not as common, but they also have a higher chance of getting leukemia, a type of blood cancer.
- Infections. People with Down syndrome may get sick more often because they tend to have weaker immune systems.
As they age, adults with Down syndrome are at a higher risk of depression and Alzheimer's dementia, which are conditions that will also affect their behavior.
Treatments for Down Syndrome
There’s no specific treatment for Down syndrome. But there is a wide range of physical and developmental therapies designed to help people with Down syndrome reach their full potential.
The earlier you start treatment, the better. Children with Down syndrome can usually hit the same milestones as other children but at later stages. So, therapy is key to help children with the disorder meet those milestones.
Each child will have different needs. Yours may benefit from:
- Physical, occupational, and speech therapy. Physical and speech therapists can help your child with sitting and walking properly, developing speech, and learning to communicate. Occupational therapists teach everyday skills like how to get dressed, eat, or use a computer.
- Behavioral counseling . Children with Down syndrome may also have conditions like ADHD, autism, or compulsive behaviors that need to be addressed.
- Specialized education services . By law in the U.S., children with Down syndrome can get free educational services and devices to help with learning. This assistance lasts until age 21 or when they finish high school, whichever comes first.
- Social and recreation activities
- Programs that offer job training and teach self-care skills
You’ll also work closely with your child’s doctor to watch for and manage any health problems that come with the condition.
Individualized education program (IEP)
This is a legal written document required for each child who needs special educational services in the U.S. The IEP is written by school personnel (teachers, school psychologist, etc.) after meeting with you and setting developmental goals for your child for the year. This also helps you decide whether to place your child in a school for kids with special needs or in one where most of the kids don't have special needs. A new IEP is written each year.
Raising a Child With Down Syndrome
When your child has Down syndrome, one of the most useful things you can do is learn as much about it as you can. You might search online for programs and resources to help your child.
Along the way, talk with other parents whose children have Down syndrome so you can learn tips and find out what to expect. And as your child grows, you can work with doctors, therapists, teachers, and other specialists.
Beyond these big-picture tasks, it can help to know what you can do day to day, not only to support your child, but also to take care of yourself.
Down syndrome support
Every family has their joys, stresses, and challenges, but when you have a child with Down syndrome, things look a little different. Besides juggling school, music lessons, sports, and jobs, you typically have a lot of extra visits with doctors and therapists.
Your needs and the needs of your child make it even more important to accept help when it’s offered. Here are a few ideas:
- Build a support system. Invite your friends and family to take part in caregiving . They can let you have a little time to yourself to walk, read a book, or just zone out for a while. A break, even a small one, can help you be a better parent and partner.
- Talk about your challenges. People want to help but don’t always know how. A simple, “It’s hard to get a healthy dinner on the table with all these appointments” opens a door and gives them ideas of what they can do.
- Keep a list of things you need. And don’t be afraid to use it. Next time someone says, “Just let me know how I can help,” you’ll be ready.
- Find time for friends. Even if it’s just a small moment after the kids go to bed, friends can help you laugh and recharge.
- Consider therapy. You might think about seeing a therapist. They can help you work through your feelings and give you tools to handle everyday stresses.
- Take care of your health. Exercise and eat well, even when you feel burned out. Try to make a plan and stick to it as best you can.
Everyday tips
Like most children, kids with Down syndrome tend to do well with routine. They also respond better to positive support than discipline. Keep both of those things in mind as you try the following daily tips:
- Give your child chores around the house, but break them up into small steps and be patient.
- Have your child play with other kids who do and don’t have Down syndrome.
- Keep your expectations high as your child tries and learns new things.
- Make time to play, read, have fun, and go out together.
- Support your child in doing day-to-day tasks on their own.
For everyday tasks, you can try to:
- Create a daily schedule and stick to it as best you can. For example, the morning might be getting up, eating breakfast, brushing teeth , and getting dressed.
- Help your child change from one activity to the next with very clear signals. For younger kids, seeing a picture or singing a song can help.
- Use pictures to make a daily plan your child can see.
- Use simple terms when talking to your child, with fewer steps.
- Encourage your child to repeat directions back to you. This helps to make sure they understand.
- Name and talk about things your child seems excited about.
To help your child with school, you might:
- Avoid saying “That’s wrong” to correct mistakes. Instead, say, “Try it again.” Offer help if it’s needed.
- As you work with doctors, therapists, and teachers, focus on your child’s needs rather than on the condition.
- Look at what your child is learning at school and see if you can work those lessons into your home life.
It's also important for all kids to feel like they have some control over their lives. It’s even more important for kids with Down syndrome, and it’s one way to help them live a fulfilling life. To do this, you can:
- Let your child make choices when it makes sense to. This can be as simple as letting them choose what clothes to wear.
- Allow them to take reasonable risks. This is a challenge every parent faces. You need to protect your children, but you should also let them see what they can handle.
- Support them in solving problems, like how to deal with an issue with friends or approach a problem at school. You don’t have to fix it for them, but you can help them do it themselves.
People with Down syndrome are born with an extra chromosome . This can lead to a range of issues that affect them mentally and physically. Nowadays, there are a lot of interventions to help people with DS lead fulfilling and productive lives.
Down Syndrome FAQs
What is the life expectancy of someone with Down syndrome ?
The lifespan for people with Down syndrome has increased over the years. In the 1980s, the lifespan was about 25 years. Now, it's around 60 years.
Can Down syndrome be diagnosed later in life?
Yes. Most people with DS are either diagnosed before birth through genetic testing or at birth based on physical appearance. But people with the rare mosaic Down syndrome may grow to adulthood without being aware they have it. This is probably because they may not have the typical physical features of someone with Down syndrome. Only some of their body cells have three copies of chromosome 21, while with the more common trisomy 21, every cell has three copies of chromosome 21.
Can people with Down syndrome have children?
About half the women with Down syndrome are fertile, but most of the men with this condition are infertile. The few children born to men who had DS didn't inherit the condition. But for women with DS, about a third gave birth to children who also had it.
- Parenting a Child With Down Syndrome
- Tips for Adults With Down Syndrome
Top doctors in ,
Find more top doctors on, related links.
- Children's Health News
- Children's Health Reference
- Children's Health Slideshows
- Children's Health Quizzes
- Children's Health Videos
- Find a Pediatrician
- ADHD in Children
- Baby Development
- BMI Calculator for Parents
- Children's Vaccines
- Kids' Dental Care
- Newborn & Baby
- Teen Health
- More Related Topics
- Type 2 Diabetes
Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Signs and Symptoms of Down Syndrome
Understanding the Physical, Mental, Developmental, and Medical Challenges
- Physical Symptoms
- Mental Symptoms
- Medical Symptoms
Life Expectancy
Down syndrome is a genetic disorder caused by having an extra copy of chromosome 21. It affects one of every 700 babies born in the United States each year, causing distinctive physical and facial features (such as a flattened face and almond-shaped eyes).
Down syndrome is also associated with developmental delays and mild to moderate intellectual disability, although the severity can vary from one individual to the next. People with Down syndrome are also faced with many health challenges, including high rates of infertility , heart disease , epilepsy , and leukemia .
This article describes the signs and symptoms of Down syndrome, including physical, developmental, and medical challenges faced by those living with the disorder. It also looks at current life expectancy rates.
Physical and Facial Features of Down Syndrome
Down syndrome is characterized by distinctive facial and physical features. These features are often apparent at birth, but, in some cases, they may only become apparent as the baby grows.
Facial features characteristic in people with Down syndrome include:
- A somewhat smaller head with a flattened back ( brachycephaly )
- A round face with a flattened nose
- A small chin
- A small nose
- A flattened bridge of the nose
- Upward-slanting, almond-shaped eyes
- A narrow roof of the mouth
- Crowded, missing, or malformed teeth
- A tongue with deep lines and crevices (furrowed tongue)
- A tongue that tends to stick out (due to having a proportionally larger tongue)
- Light-colored spots in their eyes (called Brushfield spots)
Other physical signs include:
- A shorter stature
- A stocky build
- Shorter limbs
- A short neck
- Small ears, hands, and feet
- Stubby fingers
- Pinky fingers that bend inward at the middle joint
- A single line across the palm ( clinodactyly )
- Increased skin on the back of the neck
- Poor muscle tone ( hypotonia )
- Loose joints (due to flexible ligaments )
- A bulging naval (due to an umbilical hernia )
- A large space between the big toe and the second toe
- Very fine, straight hair
Down Syndrome Doctor Discussion Guide
Get our printable guide for your next doctor's appointment to help you ask the right questions.
Sign up for our Health Tip of the Day newsletter, and receive daily tips that will help you live your healthiest life.
Thank you, {{form.email}}, for signing up.
There was an error. Please try again.
Intellectual and Developmental Symptoms of Down Syndrome
Most individuals with Down syndrome have mild to moderate intellectual disability. Mild intellectual disability is defined as an intelligence quotient (IQ) of between 50 and 69, while moderate intellectual disability is defined as an IQ between 35 and 50. Some people with Down syndrome have severe intellectual disability with an IQ of 25 to 30.
The degree of disability is important in that people with mild to moderate intellectual disability can often learn to take care of themselves, while those with severe intellectual disability cannot live independently.
As a result of this and other factors, key developmental milestones in children with Down syndrome are often delayed compared to neurotypical children in the general population.
| Differences in Development Milestones | ||
|---|---|---|
| Children with Down syndrome | Neurotypical children | |
| Smiles responsively | 1 to 5 months | 1 to 3 months |
| Sits independently | 6 to 36 months | 5 to 9 months |
| Crawls | 8 to 22 months | 6 to 12 months |
| Stands | 12 to 40 months | 8 to 17 months |
| Walks independently | 12 to 48 months | 9 to 18 months |
| First word | 12 to 48 months | 12 to 24 months |
| First two-word phrases | 24 to 90 months | 15 to 32 months |
| Uses a spoon | 13 to 39 months | 12 to 20 months |
| Drinks from a cup alone | 12 to 32 months | 12 to 24 months |
| Dresses independently | 42 to 106 months | 40 to 60 months |
| Is potty trained | 14 to 84 months | 16 to 42 months |
Depending on the child, the differences in development are sometimes incidental and not noteworthy. But, at the later stages, beginning at around 26 months, the gap between the children with Down syndrome and neurotypical children tends to widen.
From a social standpoint, older children with Down syndrome generally engage in social exchanges that are more like neurotypical kids in the 36- to 40-month age range. Children with Down syndrome tend to be happy and do fairly well with social skills, albeit with some delays.
Studies have shown that some of these delays can be reduced with early interventions from one or several specialists, such as speech therapists and physical therapists. This should start shortly after birth and usually continue until the child reaches age 3.
Medical and Health Problems in Down Syndrome
Children with Down syndrome have a higher risk of developing certain medical problems involving the teeth, eyes, ears, heart, brain, thyroid gland, and reproductive system. They are also vulnerable to certain cancers.
Tooth and Gum Disease
Congenital problems with the teeth, tongue, and mouth can contribute to oral diseases in people with Down syndrome.
Features like crowded teeth, an enlarged tongue, and crowded, missing, or malformed teeth can promote tooth and gum diseases (in part by increasing the risk of mouth-breathing and altering the acidity of saliva). Poor oral hygiene can also contribute.
Oral conditions commonly seen in people with Down syndrome include:
- Bruxism (tooth-grinding), causing severe tooth wear
- Gingivitis (a form of gum disease associated with tooth plaque and bacteria)
- Necrotizing ulcerative gingivitis (non-infectious gum disease associated with tooth loss)
Vision Problems
Vision problems are common with Down syndrome, the likelihood of which increases with age. Among the conditions commonly seen in children with Down syndrome (and often developing as early as six months of age) are:
- Myopia (nearsightedness)
- Hyperopia (farsightedness)
- Strabismus (crossed eyes)
- Nystagmus (uncontrollable, jerky eye movements)
- Keratonocus (thinning of the cornea)
Neurological Disorders
Children and adults with Down syndrome are at increased risk of epileptic seizures . Between 5% and 10% of children are affected, increasing to around 50% by adulthood. Around 40% of those who develop epilepsy do so by the age of one year.
The majority of seizures are partial (focal) seizures affecting one side of the brain, while around 20% are generalized (tonic-clonic) seizures affecting both sides.
Alzheimer's disease is another concern among people with Down syndrome. For reasons that are not clear, 15% of people with Down syndrome who live past 40 will develop the neurodegenerative disorder. (By contrast, only around 5% of people in the general population between 65 and 74 develop Alzheimer's.)
Hearing Loss
Hearing problems are common with Down syndrome. Around 15% of newborns are born with hearing loss, while 50% to 90% will develop hearing problems sometime during childhood. This can contribute to developmental delays as well as problems with learning and social interactions.
Between 10% and 70% of adults with Down syndrome will experience hearing loss later in life.
Causes of hearing loss with Down syndrome include:
- Congenital hearing loss (hearing loss at birth associated with nerve dysfunction or defects)
- Otitis media with effusion (middle ear infection associated with deformity of the ear canal)
- Acquired sensorineural hearing loss (potentially linked to the high rates of epilepsy among people with Down syndrome)
About 50% of babies with Down syndrome are born with heart defects, referred to as congenital heart disease . Some of these defects are mild and may correct themselves on their own. Others are severe and require surgery or medications. Adults with Down syndrome are at increased risk of heart disease as they age.
Heart diseases most commonly seen with Down syndrome include:
- Atrial septal defect (a congenital defect that causes a hole between the upper chambers of the heart)
- Ventricular septal defect (a congenital defect that causes a hole between the lower chambers of the heart)
- Mitral valve prolapse (the bulging of the valve between the upper and lower chambers of the heart)
Gastrointestinal Problems
Nearly half of all people with Down syndrome experience chronic constipation , which can affect their moods and general well-being.
There are many possible reasons for this including:
- Duodenal atresia (a congenital malformation of the opening of the first part of the small intestine, called the duodenum)
- Hirschsprung's disease (the congenital lack of nerve cells in the colon)
- Imperforate colon (the congenital malformation of the rectum and anus)
Most of these malformations can be fixed with surgery.
Thyroid Disease
Between 20% and 50% of people with Down syndrome have problems with their thyroid gland . The most common problem is hypothyroidism (low thyroid function). The condition may be congenital or occur later in life due to Graves' disease (an autoimmune form of hypothyroidism).
Some people with Down syndrome may also experience hyperthyroidism (overactive thyroid), most commonly an autoimmune form called Hashimoto's thyroiditis .
The rate of leukemia , a type of blood cancer, is 10 to 15 times greater among children with Down syndrome than the rate seen in the general population. Certain types of leukemia are even more common, including:
- Acute lymphoblastic leukemia (20 times greater)
- Acute myeloid leukemia (up 500 times greater)
Interestingly, people with Down syndrome have a lower risk of many solid tumor cancers including breast cancer, lung cancer, and cervical cancer.
Infertility
Down syndrome is directly and indirectly associated with low rates of fertility. According to the American Pregnancy Association, between 70% to 85% of females with Down syndrome are infertile, and those able to conceive have a 50/50 chance of having a child with Down syndrome.
Further lowering the conception rate is the early onset of menopause commonly seen in females with Down syndrome.
As for males, the current medical literature suggests that few with Down syndrome have ever conceived a child. This is thought to be due to problems with spermatogenesis (the creation of sperm cells in the testicles ) along with a general lack of sexual activity.
Down syndrome is associated with a lowered life expectancy. According to the Centers for Disease Control and Prevention (CDC), the current life expectancy for a person living with Down syndrome in the United States is 47 years.
While this is a vast improvement from the 1960s when someone with Down syndrome lived to age 10, significant barriers stand in the way of increasing the rate among those living with the disease today.
Among the concerns, congenital heart defects kill many babies with Down syndrome. Those who survive run a high risk of premature heart disease and early heart disease-related death.
Racial disparities also play a role wherein Black babies with Down syndrome are more likely to die during infancy than infants of other ethnic or racial groups.
Down syndrome is a genetic disorder characterized by distinctive facial and physical features, developmental delays, mild to moderate intellectual disability, and an increased risk of many diseases and disorders, including heart disease, epilepsy, Alzheimer's disease, and infertility. The types and severity of symptoms can vary from one person to the next.
The current life expectancy of someone with Down syndrome is 47 years. Heart disease is one of the major factors contributing the shortened life expectancy, but others contribute.
Centers for Disease Control and Prevention. Down syndrome .
Asim A, Kumar A, Muthuswamy S, Jain S, Agarwal S. Down syndrome: an insight of the disease . J Biomed Sci . 2015;22:41. doi:10.1186/s12929-015-0138-y
Onnivello S, Pulina F, Locatelli C, et al. Cognitive profiles in children and adolescents with Down syndrome . Sci Rep. 2022;12:1936. doi:10.1038/s41598-022-05825-4
National Down Syndrome Society. Early intervention .
Down Syndrome Association of Central California. Developmental scale for children with Down syndrome .
Ghaffarpour M, Karami-Zarandi M, Rahdar HA, Feyisa SG, Taki E. Periodontal disease in Down syndrome: predisposing factors and potential non‐surgical therapeutic approach . J Clin Lab Anal. 2024 Jan;38(1-2):e25002. doi:10.1002/jcla.25002
Haseeb A, Huynh E, ElSheikh RH, et al. Down syndrome: a review of ocular manifestations . Ther Adv Ophthalmol. 2022 Jan-Dec;14:25158414221101718. doi:10.1177/25158414221101718
Rahmann MM, Fatema K. Seizures in Down syndrome: an update . Mymensingh Med J. 2019 Jul;28(3):712-715.
Nixon DW. Down syndrome, obesity, Alzheimer's disease, and cancer: a brief review and hypothesis . Brain Sciences. 2018;8(4):53. doi:10.3390/brainsci8040053
Kreicher KL, Weir FW, Nguyen SA, Meyer TA. Characteristics and progression of hearing loss in children with Down syndrome . J Pediatr . 2018 Feb:193:27-33.e2. doi:10.1016/j.jpeds.2017.09.053
Benhaourech S, Drighil A, Hammiri AE. Congenital heart disease and Down syndrome: various aspects of a confirmed association . Cardiovasc J Afr . 2016;27(5):287-290. doi:10.5830/CVJA-2016-019
Holmes G. Gastrointestinal disorders in Down syndrome . Gastroenterol Hepatol Bed Bench . 2014;7(1):6-8.
Amr NH. Thyroid disorders in subjects with Down syndrome: an update . Acta Biomed. 2018;89(1):132-139. doi:10.23750/abm.v89i1.7120
Mateos MK, Barbaric D, Byatt SA, Sutton R, Marshall GM. Down syndrome and leukemia: insights into leukemogenesis and translational targets . Transl Pediatr . 2015;4(2):76-92. doi: 10.3978/j.issn.2224-4336.2015.03.03
American Pregnancy Association. Down syndrome/trisomy 21 .
Parizot E, Dard R, Janel N, Vialard F. Down syndrome and infertility: what support should we provide? J Assist Reprod Genet. 2019 Jun;36(6):1063–1067. doi:10.1007/s10815-019-01457-2
Centers for Disease Control and Prevention. Living with Down syndrome .
By Kathleen Fergus Kathleen Fergus, MS, LCGC, is a board-certified genetic counselor who has worked extensively with families affected by Down syndrome.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Down syndrome
Stylianos e. antonarakis.
1 Department of Genetic Medicine and Development, University of Geneva Medical School, Geneva, Switzerland.
Brian G. Skotko
2 Down Syndrome Program, Division of Medical Genetics, Department of Pediatrics, Massachusetts General Hospital, Boston, MA, USA.
3 Department of Pediatrics, Harvard Medical School, Boston, MA, USA.
Michael S. Rafii
4 Keck School of Medicine of University of Southern California, California, CA, USA.
Andre Strydom
5 Department of Forensic and Neurodevelopmental Sciences, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK.
Sarah E. Pape
Diana w. bianchi.
6 Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, MD, USA.
7 National Human Genome Research Institute, National Institutes of Health, Bethesda, MD, USA.
Stephanie L. Sherman
8 Department of Human Genetics, Emory University School of Medicine, Atlanta, GA, USA.
Roger H. Reeves
9 Department of Physiology, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
10 McKusick-Nathans Department of Genetic Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Author contributions
Trisomy 21, the presence of a supernumerary chromosome 21, results in a collection of clinical features commonly known as Down syndrome (DS). DS is among the most genetically complex of the conditions that are compatible with human survival post-term, and the most frequent survivable autosomal aneuploidy. Mouse models of DS, involving trisomy of all or part of human chromosome 21 or orthologous mouse genomic regions, are providing valuable insights into the contribution of triplicated genes or groups of genes to the many clinical manifestations in DS. This endeavour is challenging, as there are >200 protein-coding genes on chromosome 21 and they can have direct and indirect effects on homeostasis in cells, tissues, organs and systems. Although this complexity poses formidable challenges to understanding the underlying molecular basis for each of the many clinical features of DS, it also provides opportunities for improving understanding of genetic mechanisms underlying the development and function of many cell types, tissues, organs and systems. Since the first description of trisomy 21, we have learned much about intellectual disability and genetic risk factors for congenital heart disease. The lower occurrence of solid tumours in individuals with DS supports the identification of chromosome 21 genes that protect against cancer when overexpressed. The universal occurrence of the histopathology of Alzheimer disease and the high prevalence of dementia in DS are providing insights into the pathology and treatment of Alzheimer disease. Clinical trials to ameliorate intellectual disability in DS signal a new era in which therapeutic interventions based on knowledge of the molecular pathophysiology of DS can now be explored; these efforts provide reasonable hope for the future.
Down syndrome (DS) is the most common genomic disorder of intellectual disability and is caused by trisomy of Homo sapiens chromosome 21 (HSA21). The eponym of the syndrome is from Down, who described the clinical aspects of the syndrome in 1866 (REF. 1 ). The DS phenotype involves manifestations that affect multiple bodily systems, in particular the musculoskeletal, neurological and cardiovascular systems. Individuals with DS commonly have short stature, muscle hypotonia, atlantoaxial instability, reduced neuronal density, cerebellar hypoplasia, intellectual disability and congenital heart defects (CHDs; particularly atrioventricular septal defects (AVSDs)). Individuals with DS are also more likely to develop certain health conditions, including hypothyroidism, autoimmune diseases, obstructive sleep apnoea, epilepsy, hearing and vision problems, haematological disorders (including leukaemia), recurrent infections, anxiety disorders and early-onset Alzheimer disease (AD) ( FIG. 1 ). Other conditions, such as most solid tumour types, show inverse comorbidity and seem to be less common in individuals with DS than in the general population 2 .

Individuals with trisomy 21 (the presence of a supernumerary chromosome 21; also known as Down syndrome (DS)) present with a distinct collection of symptoms and manifestations that affect multiple body systems, although variation exists between individuals. Individuals with DS are generally of short stature, with short fingers, hypotonia and atlantoaxial instability. Facial characteristics include the presence of epicanthic folds, flat nasal bridge and occiput, small mouth and ears, and up-slanting palpebral fissures. Congenital heart defects are common, particularly atrioventricular septal defect (AVSD). Individuals with DS are also more likely to develop certain health conditions compared with the general population, including hypothyroidism, obstructive sleep apnoea, epilepsy, hearing and vision problems, haematological disorders (including leukaemia), recurrent infections, anxiety disorders, and early-onset Alzheimer disease.
The discovery of a link between a supernumerary chromosome 21 and the DS phenotype was first reported in 1959 (REF. 3 ) and was an important landmark for the development of genetic medicine. Mouse models for the study of DS were first developed in 1990 (REF. 4 ), and the complete nucleotide sequence of the long arm of HSA21 was published in 2000 by a multinational consortium of investigators 5 . Substantial progress has been made in the ensuing 19 years in understanding the molecular pathophysiology of the different phenotypic manifestations of DS, which is currently considered a disorder of gene expression dysregulation. In addition, widely used screening methods have been introduced for the prenatal detection of DS. The management of the different symptoms and the quality of life of individuals with DS have improved. However, enormous challenges remain, including understanding the precise biological mechanism of each phenotypic component of the syndrome; treatment of the different symptoms, including cognitive dysfunction; and integration of individuals with DS into society in different parts of the world. Furthermore, studies in animal models to unravel the effects of triplication of the >200 protein-coding genes on HSA21, not to mention the triplicated non-coding genes and the downstream and indirect effects of these alterations, are extremely challenging.
In this Primer, we discuss the epidemiology of DS, current understanding of genetics and pathophysiology resulting from the extra chromosome 21, and advances in the diagnosis of trisomy 21. Furthermore, we review the management of the syndrome and the quality of life of individuals with DS, and offer an outlook for the future. Several reviews of DS and trisomy 21 have been published elsewhere and provide additional details about this common and challenging syndrome 6 – 9 .
Epidemiology
The lifetime prevalence of DS is increasing substantially as the global population grows. For example, in the USA, the population prevalence of DS increased from ~50,000 in 1950 (3.3 per 10,000 individuals) to ~212,000 in 2013 (6.7 per 10,000 individuals; based on unpublished data 10 ), mostly due to improvements in childhood survival of individuals with DS 11 ( FIG. 2 ). The life expectancy of individuals with DS in the USA increased from an estimated mean of 26 years and median of 4 years in 1950 to 53 years and 58 years, respectively, in 2010 (REF. 11 ). As of 2015, estimates of DS population prevalence have been reported for Europe (4.9 per 10,000 individuals) 12 , Europe excluding former Eastern Bloc countries (6.0 per 10,000 individuals), and former Eastern Bloc countries (3.3 per 10,000 individuals) 12 . However, a precise global estimate cannot be reliably calculated until more birth registries are created within countries and more data are available on historical and current survival of individuals with DS in different parts of the world.

a | Prevalence of Down syndrome (DS) in the USA for the period 1950–2013. This graph combines the prevalence data for 1950–2010 in the USA 9 with unpublished prevalence data for 2011–2013 for the same region 10 . b | Pregnancy outcomes in the USA for the period 1974–2013. This graph combines estimates of live births, natural losses and elective terminations in women carrying a fetus with DS after 10 weeks gestation for the period 1974–2010 in the USA 17 with unpublished data for 2011–2013 (REF. 10 ). GA, gestational age. Part a adapted from REF. 11 , Springer Nature Limited. Part b adapted with permission from REF. 17 , Wiley-VCH.
DS occurs in all populations, but differences in maternal age at conception between countries and ethnicities influence the number of live births 13 – 16 . As of 2013 in the USA, unpublished data suggest that ~1 in every 779 babies born had DS 10 (~12.8 per 10,000 live births) ( FIG. 2a ). The prevalence of DS is influenced by maternal age at conception, which varies among countries, and is estimated to be ~1 in 365 fetuses at 10 weeks gestation 17 ( FIG. 2b ). Some of these pregnancies will result in spontaneous miscarriage, ~32% between 10 weeks gestation and the expected date of birth and ~25% between 16 weeks gestation and the expected date of birth, the risk depending on maternal age, as estimated from reports from England and Wales 18 . The number of pregnancies that are electively terminated is influenced by the availability and accuracy of screening tests within each country, the number of people choosing prenatal screening and subsequently prenatal testing, and parental decisions once a prenatal diagnosis of DS is made. In 2013, an estimated 3,400 DS-related elective terminations were carried out in the USA, resulting in a 33% reduction in the number of babies with DS that would have been born that year. By comparison, the estimated percentage reduction was 55% in Australia for 2004 (REF. 19 ), and 54% in Europe, 66% in Europe excluding the former Eastern Bloc countries and 32% in former Eastern Bloc countries, for the period 2010–2015 (REF. 12 ). In China, during the period 2003–2011, the termination rate for fetuses with DS led to a 55% reduction in the overall perinatal prevalence 20 .
Studies from England and Wales 21 , Slovenia 22 , Australia 19 , 23 and EUROCAT regions 24 have shown that increasing maternal age has counterbalanced the uptake in prenatal screening, resulting in a stable or slightly decreasing prevalence of DS in live births from the 1990s until now. In Europe, DS prevalence in live births has been decreasing slightly since the 1990s, although there are substantial regional differences 12 . In southern Europe, DS prevalence in live births almost halved in the period 1980–2015 (REF. 12 ). By contrast, in the Netherlands, the live birth prevalence increased slightly in the period 1980–2000 but seems to have been decreasing slightly since 2005 (REF. 25 ). In the USA, the increased prevalence of DS in live births began in the 1980s and levelled off after 2005 (REF. 17 ). Sequencing cell-free placental DNA in maternal plasma, termed noninvasive prenatal screening (NIPS) or noninvasive prenatal testing (NIPT), has been available since 2011 in many countries; however, not enough time has elapsed for the full impact of surveillance programmes on birth rates to be measured. Furthermore, variability in access to prenatal care is also expected to affect the uptake of surveillance programmes.
Risk factors
Advanced maternal age at conception is a major risk factor for trisomy 21, as is true for all human autosomal trisomies 26 . This risk is associated with non-disjunction of homologous chromosomes or chromatids occurring during the meiotic divisions that occur in the formation of oocytes 27 . Advanced maternal age has been associated with HSA21 segregation errors in both maternal meiosis I and meiosis II 28 – 32 . In addition, specific altered recombination patterns have been observed for these types of maternal errors, only some of which are associated with maternal age 33 .
Meiotic processes, such as recombination, involve the action of many genes. Thus, there is a clear rationale for examining whether genetic variants predispose to meiotic nondisjunction in humans. A study including a candidate gene analysis and an untargeted genome-wide association study (GWAS) of HSA21 nondisjunction in mothers who gave birth to an infant with trisomy 21 derived from a maternal error was conducted using the mothers as cases and the fathers as controls 34 . These analyses were stratified by maternal MI or MII errors. Results from this study emphasize the heterogeneity of risk factors based on type of error. For example, variants in candidate genes coding for components of the synaptonemal complex showed an association limited to meiosis I errors (for example, SYCE2 ) while others were associated with MII errors (for example, SYCP2 ) 34 .
Environmental factors also influence the risk of non-disjunction but are difficult to identify due to the inherent problem of defining the exposure, dosage and timing of each factor. Again, studies must define the type of error (parental origin and the type of meiotic or mitotic error) leading to trisomy 21 due to their heterogeneous aetiology. Environmental factors that influence the risk of trisomy 21 include tobacco use, folic acid supplementation, oral contraceptive use and several others (the studies investigating environmental risk factors and their limitations, and possible biomarkers of exposure such as telomere length, have been reviewed elsewhere 35 ).
For example, maternal socioeconomic status (SES) is associated only with maternal meiosis II errors 36 – 39 . As SES is a proxy for specific exposures, a follow-up study examined maternal occupation as a risk factor and found that some job classification categories were more prevalent in mothers of infants with DS than in mothers of infants with no chromosomal abnormality or major birth defect, and were associated with specific types of meiotic errors 40 . A preliminary analysis revealed that these occupations involved exposure to solvents in the work environment. Further studies of this kind are needed to examine specific exposures to toxic agents in the work and home environments and their relationship with maternal and paternal HSA21 nondisjunction. This is emphasized by the finding that exposure to endocrine-disrupting chemicals affects meiosis and increases the prevalence of aneuploidy 41 . For example, exposure to the ubiquitous environmental contaminant bisphenol A (BPA) and other endocrine-disrupting chemicals affects the reproductive system in both sexes (including the ovaries, testes and reproductive tract) 41 , 42 .
It is important to point out that not only do different types of meiotic and mitotic errors leading to aneuploidy most likely have different susceptibility to specific environmental exposures but that exposures of multiple generations (for example, grandmother and mother) must also be considered 35 , 43 . For example, there is now mounting evidence of transgenerational effects of BPA exposure on sperm and oocytes in experimental models 42 .
Mechanisms/pathophysiology
Genetics of ds.
Partial or complete trisomy 21 (that is, the presence of part of or a complete supernumerary HSA21) is the genomic cause of DS 3 . A free trisomy 21 is present in 95% of individuals with DS and results from an error in maternal meiosis I (~66%) or meiosis II (~21%); paternal meiosis I (~3%) or meiosis II (5%); or mitosis, after the formation of the zygote (5%) 15 , 44 , 45 . Translocation accounts for trisomy 21 in ~5% of affected individuals, usually t(14;21) or t(21;21) 46 , 47 . Mosaicism for trisomy 21 occurs in ~2% of individuals with DS. Partial trisomy 21 is rare 48 , 49 and is associated with a range of symptoms that vary according to the length of the partial triplication of HSA21.
The first published sequence of HSA21 annotated 225 genes on chromosome 21q 5 . With increased knowledge of the elements of coding and non-coding genes and regulatory motifs, the number of gene structures recognized on HSA21 has increased considerably. The strengths and limitations of genome annotations available in existing public databases have been reviewed elsewhere 50 . The current version of GENCODE/ENSEMBL (GENCODE release 32) lists 233 protein-coding genes, 423 non-protein-coding genes (69 small, 330 long and 24 miscellaneous non-coding genes) and 188 pseudogenes. Of note, 48% of HSA21 has not been annotated 6 , the vast majority of which contains repetitive elements (as is the case for all human chromosomes).
Understanding the genetic aetiology of the increased susceptibility of individuals with DS to the multiple manifestations or conditions that are associated with the DS phenotype is an enormous challenge 51 . Compounding the difficulty of identifying the specific genetic and other effects of trisomy 21, studies of DS in humans are restricted to those conceptuses that survive to term; among pregnancies with a confirmed prenatal diagnosis of DS at 9–14 weeks, ~30–40% subsequently spontaneously miscarry 18 , 52 . Extrapolating to all pregnancies, ~80% of trisomy 21 conceptuses are lost during pregnancy 53 . Thus, it is essential to acknowledge that in studying any DS-associated condition, only the combinations of genetic variants that allow the conceptus to survive to term and to manifest the phenotype of interest are being considered.
Two main hypotheses have been proposed to explain the biological perturbations that underlie the phenotypic manifestations of DS: first, a specific HSA21 gene-dosage effect, which includes both the direct effects of overexpressed HSA21 genes and the downstream consequences of this overexpression; and second, developmental instability, in which nonspecific global disturbance of gene expression from the extra HSA21 results in disruption of overall biological homeostasis 54 , 55 . It is likely that the aetiology of DS-associated phenotypes involves both proposed mechanisms. Single-cell transcriptome analyses in trisomy 21 and other trisomies have suggested that the gene dosage effect for trisomic genes with low-to-average expression is mainly due to the higher fraction of trisomic cells expressing these genes 56 . This results in the expected 1.5-fold higher average expression of trisomic genes in the various tissues of individuals with trisomy 21.
Gene dosage effects.
The simplest effect of HSA21 trisomy is the direct effect of an increased dosage of a single HSA21 gene. For example, an increased dosage of APP , an HSA21 gene that encodes amyloid precursor protein (APP), increases susceptibility to early-onset AD in individuals with DS. Although APP is clearly an ‘effector’ gene, whether only the direct and downstream effects of APP overexpression affect the penetrance and severity of AD, or whether other aspects of trisomy 21 also have a role, remains to be determined. Of note, returning the App copy number to two copies in a mouse model of trisomy 21 (Ts65Dn) alleviates some but not all of the effects of App dosage 57 .
To define the direct and indirect consequences of increasing gene dosage, many studies have characterized the expression profile of HSA21 genes and the effect of overexpressing these genes on the rest of the genome. Common findings among these studies emerge. First, the expression of most but not all HSA21 genes is increased. It will be important to identify the mechanisms that underlie these discordant expression levels, which may include negative feedback, dosage compensation and epigenetic alterations. Second, in many affected individuals, the expression of some non-HSA21 genes is also altered, which suggests that trisomy 21 leads to perturbation of downstream transcription and signalling networks. A meta-analysis compared the expression profiles of trisomy 21 and euploid samples from various human tissues (such as brain and thymus) or cells (such as lymphoblastoid cell lines (LCLs), blood cells, fibroblasts and induced pluripotent stem cells (iPSCs)) 58 . This analysis found that the trisomy 21:euploid expression ratio was typically close to 3:2 for dysregulated genes and close to 1:1 for unaffected genes. These data are consistent with the hypothesis that upregulation of effector genes (that is, those that enhance or suppress gene expression) on HSA21 leads to similar changes in the expression of associated downstream genes, resulting in a similar altered ratio of 3:2 or 2:3 for these genes. There are exceptions to this pattern, with more extreme ratios that may result from gene–gene interactions or other types of chain effects that amplify the final expression levels. For example, JAKMIP3 is highly upregulated (256.13:1 ratio) in the thymus transcriptome map, whereas BEX5 is highly downregulated (0.07:1 ratio) in the brain transcriptome map.
Finally, as expected, the expression patterns of both HSA21 genes and non-HSA21 genes in trisomy 21 cells differ depending on the tissue being examined. For example, the interferon response is highly upregulated in trisomy 21 fibroblasts and LCLs, most likely due to increased expression of four interferon receptor genes ( IFNAR1 , IFNAR2 , INGR2 and IL10RB ) that are located on HSA21 (REF. 59 ). An increased interferon response was also present in iPSCs generated from trisomy 21 fibroblasts but not in neuronal cultures derived from these iPSCs 60 .
Disruption of homeostasis by genome-wide effects on transcription regulation.
Trisomy 21 may also affect global transcription, either directly if an HSA21 gene functions in transcription regulation or indirectly as a by-product of the additional genetic material 61 , 62 . For example, at least three HSA21 genes encode proteins involved in transcription regulation: ADARB1 (one of two proteins involved in adenosine-to-inosine RNA editing), the constitutive splicing factor U2AF1, and DYRK1A, a dual specificity kinase that phosphorylates splicing factors 60 . Altered ADARB1 transcript levels did not change global adenosine-to-inosine editing levels in trisomy 21 iPSC-derived neuronal cells, whereas trisomy 21-dependent splicing changes were observed in both iPSCs and the neuronal cultures derived from them 60 .
The possibility that increased genetic material could lead to altered genome-wide gene expression was suggested based on the observation that genes whose expression is similarly altered (that is, upregulated or downregulated) are clustered in regions termed gene expression dysregulation domains (GEDDs) in trisomic iPSCs and fibroblasts 61 . However, other studies using a range of methods found no evidence for the existence of GEDDs specifically in trisomy 21 cells 63 , 64 .
Studies of nuclear genome organization using three-dimensional fluorescence in situ hybridization (3D-FISH) have shown that chromosomes are preferentially localized to discrete regions within the nucleus, termed chromosome territories (reviewed elsewhere 65 ). Homeostasis in trisomic cells can be disrupted by the alteration of chromosome territories. Although studies of chromosome territories in trisomy 21 cells and their effects on cellular processes are just beginning, initial studies have found that an extra HSA21 does not change the overall organization of chromosome territories in the interphase nucleus 66 but does alter chromosome compaction and displaces other chromosome territories from their usual nuclear position 66 .
Trisomy 21 also alters regional and/or global methylation patterns (reviewed elsewhere 62 ), although the methylation changes are evenly distributed on all chromosomes and are not specifically enriched on HSA21. One observed pattern is an overall bias towards hypermethylation in DS cells compared with euploid cells, particularly in brain samples 67 – 69 . Furthermore, differential methylation in trisomy 21 cells seems to be localized to discrete regulatory regions of single genes and not to domain-like regions. A meta-analysis identified a small set of genes for which the methylation patterns were different between trisomy 21 and euploid cells in all tissues examined, suggesting that these altered methylation patterns are established early in development and thereby persist in multiple tissue types in DS 62 .
Two mechanisms have been proposed for the globally altered methylation patterns in trisomy 21. First, some triplicated HSA21 genes might function directly in methylation pathways, including SLC19A1 , FTCD , GART , CBS , PRMT2 , N6AMT1 , MIS18A and DNMT3L . SLC19A1 , FTCD , GART and CBS all have a role in the one-carbon metabolism pathway, which is central to DNA methylation. PRMT2 encodes a protein arginine methyltransferase with multiple targets, including histones 70 . N6AMT1 encodes a methyltransferase responsible for DNA N 6 -adenosine methylation 71 . The protein encoded by MIS18A is involved in maintaining the heterochromatic state of centromeres by recruiting the DNA methyltransferases DNMT3A and DNMT3B, thereby repressing the production of non-coding transcripts from centromeric satellite repeats 72 . DNMT3L also interacts with DNMT3A and DNMT3B and enhances their de novo methylation activity, but lacks DNA methyltransferase activity itself 73 . DNMT3L is overexpressed in DS neuroprogenitors, which leads to increased expression of APP and PSD95 in differentiating neurons 74 . These examples illustrate the various mechanisms by which overexpression of these HSA21 genes may lead to trans-epigenetic changes in DS.
The second proposed mechanism is that differential methylation is a result of altered transcription factor occupancy of their binding sites. For example, RUNX1, an HSA21-encoded transcription factor, is overexpressed in trisomy 21 T lymphocytes and differentially methylated sites in trisomy 21 cells are enriched for the RUNX1 binding motif 67 . Thus, the higher occupancy of RUNX1 binding sites in trisomy 21 cells affects CpG methylation at these sites. Additional support for this hypothesis comes from the observation that several types of sequence motifs, including the binding site for CTCF (an insulator protein that blocks the interaction between enhancers and promoters), are enriched at loci that are differentially methylated in all trisomy 21 tissues examined 67 , 75 . Because CTCF binding to its recognition site is sensitive to methylation, the pattern of CTCF occupancy may be particularly affected by DS-associated epigenetic perturbations, which may result in altered 3D conformation of chromatin in the nucleus.
Histone deacetylation and acetylation are other epigenetic mechanisms that are potentially influenced by triplication of some HSA21 genes. For example, DYRK1A , which is overexpressed in trisomy 21, promotes histone deacetylation by phosphorylation and activation of the deacetylase SIRT1 (REF. 76 ). Furthermore, DYRK1A affects chromatin remodelling through its interaction with the transcription repressor REST (also known as NRSF) 77 , resulting in neuronal gene dysregulation that might contribute to the neural phenotypic changes associated with DS.
Although genomic and transcriptomic data are important for understanding the consequences of trisomy 21 and how they relate to interindividual variation in clinical manifestations, integration with other ‘omics’ datasets is necessary to obtain a complete picture of the effects of trisomy 21. For example, in a proteomic study 78 using a method that analysed a large fraction of the proteome 79 of fibroblasts from a pair of monozygotic twins discordant for DS (with follow up on samples from 11 unrelated individuals with DS and matched controls), extensive changes were detected in the levels of proteins encoded by HSA21 genes and non-HSA21 genes. In transcriptome data from both of these twins 61 , steady-state transcript levels were moderately correlated with protein levels. However, the trisomy 21:euploid ratios for gene expression and protein levels were only weakly correlated (Spearman rank correlation ρ = 0.34–0.51), which was mostly due to incongruence of transcript and protein levels for non-HSA21 genes. Thus, substantial post-transcriptional regulation has a role in the differential effect of trisomy 21 on the expression levels of different genes. For example, for HSA21-encoded proteins that are components of heteromeric protein complexes with non-HSA21-encoded proteins, protein degradation seems to buffer against increased transcript levels. Gene enrichment set analyses have shown that protein levels are substantially altered for cell cycle-related functions, cell morphogenesis, lipoprotein metabolism and cellular respiration in mitochondria 78 .
In another study 80 using a proteomics method focused primarily on secreted proteins and those with extracellular domains 81 , plasma samples from 165 individuals with DS and 98 euploid individuals were compared. Among the proteins that were dysregulated in trisomy 21 samples, many are involved in immune control, the complement cascade and growth factor signalling. However, no clear link exists between the identity or levels of dysregulated proteins and specific clinical manifestations of DS.
Indicators of mitochondrial dysfunction have been observed in trisomy 21 cells (for example, fibroblasts) and organs, including the heart (their properties and consequences have been reviewed elsewhere 82 – 84 ). The mitochondrial phenotype in DS includes reduced ATP production by oxidative phosphorylation; decreased respiratory capacity; impaired generation of mitochondrial membrane potential; and alterations in mitochondrial structure. These altered functions result in perturbed mitochondrial energy metabolism and oxidative stress, which in turn could increase susceptibility of individuals with DS to a wide range of conditions, including intellectual disability and AD. The molecular basis for mitochondrial dysfunction involves effector HSA21 genes and key regulatory signalling pathways (reviewed elsewhere 82 ). Of 77 HSA21 genes consistently dysregulated identified by a meta-analysis of 45 DS gene expression studies 85 , NRIP1 , SUMO3 , DYRK1A , RCAN1 , SOD1 , APP and CBS are directly or indirectly involved in mitochondrial function and thus represent candidates for the observed DS-associated mitochondrial phenotypes.
Animal models
Animal models of DS, especially mouse models, have been instrumental in advancing DS research. However, a caveat when studying these models is that DS is a human condition that cannot be precisely replicated in other species. Nonetheless, insights into the mechanisms that underlie the developmental and functional consequences of trisomy 21 have been obtained by overexpression of groups of HSA21 genes or orthologues of HSA21 genes from other species. Important questions about the usefulness of animal models for studying trisomy 21 pathophysiology include the question as to what types of studies are informative in mice, whether results in mice are relevant to understanding human outcomes of trisomy 21 and whether mouse models of DS can be used as a translational platform for drug testing.
Mouse models have transformed basic research in DS, beginning with development of the Ts65Dn mouse, which contains a partial trisomy of Mus musculus chromosome 16 (MMU16) 4 , 86 . Prior to the introduction of this mouse model, the identification, cloning and expression of individual genes in transgenic mouse models was laborious, and studies using these approaches led to wide-ranging conclusions about individual genes that could ‘cause’ DS. However, overexpression of dozens or hundreds of genes simultaneously, supported by more precisely defined terminal phenotypes, has enabled a more realistic interpretation of studies of development, function and genome-wide perturbations in gene expression.
To understand the challenges of using mouse models, it is necessary to understand the complexity of trisomy 21. Trisomy 21 has profound phenotypic effects, as HSA21 contains >200 protein-coding genes and ~400 additional transcripts of known or presumed importance, which are present in an extra copy in every cell from conception onwards. Conversely, the gene overexpression changes in trisomy 21 are subtle, with an average increase in expression of ~1.5-fold in trisomic cells compared with euploid cells. Expression levels of individual genes vary widely and mRNA levels do not always correlate with the levels of the corresponding protein 78 . For genes expressed at a low level, this difference cannot be reliably measured with precision in many high-throughput assays. The consequences of this modest overexpression are substantial, as up to 80% of conceptuses with trisomy 21 do not survive to term 15 .
Relevance of mouse phenotypes to DS.
Several phenotypic features of DS manifest (to varying extents) in all individuals with trisomy 21, including cerebellar hypoplasia, retrusion of the midface skeleton and mandible, Alzheimer-disease-type histopathology at an early age, and intellectual impairment. The risk of CHDs is greatly increased in individuals with DS. Whereas adults with DS show an overall lower risk of developing solid tumour cancers, including breast cancers, when compared to the general population, children with DS have an increased incidence of leukaemia 2 . All of these features are present in some form in the animal models of DS that have been generated to date. For example, whereas the overt histopathology of AD (plaques and tangles) does not occur in mouse models of trisomy 21, accumulation of tau protein and endosomal changes have been reported in these mice 51 .
An overall finding from animal models of DS is that the penetrance (occurrence) and expressivity (severity) of a given phenotype is a function of overexpression of multiple genes; DS is not a collection of independent single gene effects. However, many mouse models that are trisomic for different subsets of mouse orthologues of HSA21 genes have been used effectively — especially in combination with individual gene knockouts that allow specific genes to be returned to the normal two copies in a trisomic background — to identify genes with major effects that are important for understanding a number of phenotypes 57 , 87 , 88 . Rather than asking the simplistic question of whether a gene causes DS, different mouse models provide information about whether altered expression of a specific gene or genes is necessary and/or sufficient to contribute to a phenotype. Interpretation is then limited by the ability to quantify the effects of trisomy in an animal model. Saying that a given model has incompletely penetrant CHDs is of little use in understanding the contributions of specific genes to specific outcomes; failure of ventricular or atrial septum development, AVSDs or outflow tract anomalies all occur in different developmental fields involving different cells at different stages of heart development with the contribution of different genes.
Genetic basis of animal models.
The extent of the triplicated region of HSA21 or the orthologous mouse genomic regions (that is, a segment of a mouse chromosome) is an important consideration in determining the relevance of a mouse model of DS. Trisomy for mouse genomic regions orthologous to HSA21 has the advantage that these regions are subject to endogenous transcription regulation, whereas genetic variation in, for example, promoter or enhancer sequences between mouse and human might be expected to affect transcription. Similarly, any normal human-specific variation in processing signals in DNA and RNA, or amino acid substitutions in proteins, could affect the stoichiometry of interactions between HSA21-encoded proteins and non-HSA21-encoded proteins. Data from GWAS and RNA sequencing suggest that these effects are small, but their potential importance cannot be dismissed. Conversely, although the gene content of HSA21 and the orthologous segments on MMU16, MMU17 and MMU10 are similar, they are not identical ( FIG. 3 ). Of the 233 predicted protein-coding genes on HSA21, only 168 are well conserved in mice. Furthermore, the difference in number and sequence between human and mouse in the non-coding transcripts of presumed function is even greater. The limitations of individual mouse models are emphasized in a comparative study of three of these models, Ts65Dn, Ts1Cje and Ts1Yey 89 .

Down syndrome (DS) results from the presence of a supernumerary Homo sapiens chromosome 21 (HSA21). More than 20 mouse models of DS have been created, which are designed to overexpress part of or a complete HSA21, or the orthologous mouse genomic regions 7 , 91 , 246 . Mouse orthologues of HSA21 genes occur on Mus musculus chromosome 16 (MMU16), MMU17 and MMU10. Tc1 mice carry a mutated HSA21 and are mosaic animals, with a mix of trisomic and euploid cells that is unique to each individual, apparently due to suboptimal function of the human centromere in mice. Ts65Dn animals contain a duplication of ~140 genes on MMU16, some of which are not orthologous to HSA21 247 , 248 (dashed line). TcMAC21 animals contain the long arm of HSA21 (HSA21q) as a mouse artificial chromosome (that is, with a mouse centromere to ensure that the chromosome is retained in every cell); however, this artificial chromosome contains deletions that affect ~8% of HSA21q genes. All of these models except Ts65Dn are direct duplications; that is, the genes in each are trisomic but they do not contain an extra chromosome or centromere. Ts1Rhr, Ts1Cje, Ts1Yey and Ts65Dn mouse models are discussed in the text.
These differences have not been emphasized in the past, as only one mouse model (Tc1) that contained a freely segregating HSA21 existed. To date, Ts65Dn is the only reported mouse model of DS that segregates an extra mouse chromosome; all other models are made by direct duplication of a mouse chromosome segment that is orthologous to HSA21 (detailed mapping of the partial mouse trisomies of segments orthologous to HSA21 has been reviewed elsewhere 6 , 7 ). Genome sequencing in Tc1 mice has revealed substantial deletions, mutations and duplications of HSA21 that compromise the expression of >20% of HSA21 genes in these mice 90 . However, the biggest drawback of Tc1 is the spontaneous loss of the entire HSA21 in a substantial proportion of cells, resulting in mosaic trisomy (that is, each animal is a unique mosaic of trisomic and euploid cells). As development is driven and regulated through cell–cell communication, many aspects of an individual are liable to vary if neighbouring cells suddenly change ploidy. As the loss of HSA21 is random, the development of every animal is unique. Consequently, these rearrangements and mosaicism necessitate cautious interpretation of studies using Tc1 mice. A new model containing 92% of the protein-coding genes on the long arm of HSA21 as a mouse artificial chromosome avoids the problem of mosaicism and has many of the DS manifestations of trisomy 21 that have been observed in previous mouse models 91 .
The demonstration that directed interchromosomal recombination could be achieved using the Cre–Lox system paved the way for the creation of new mouse models for dosage imbalance studies 92 , 93 . To date, >20 mouse models that are trisomic for different HSA21-homologous portions of MMU16, MMU17 and MMU10 have been created 7 ( FIG. 3 ). A set of three mouse strains that together contain a complete duplication of all mouse genomic regions orthologous to HSA21 has been described 94 . In theory, a three-way cross of these mouse strains should produce ‘full trisomy’ in one out of eight offspring. Although this low frequency is only acceptable for some applications, in practice, the frequency of full trisomy is far lower than the predicted Mendelian frequencies, making models such as Tc1 or the MAC21 mice the most viable options for maximum gene representation.
Whereas 95% of individuals with DS have an extra freely segregating HSA21 and therefore an extra centromere and telomeres, the segmental duplication mouse models of DS do not. In these models, trisomy occurs through direct intrachromosomal duplications so that chromosome (and centromere) number is unchanged. One effect of an extra centromere in mammals is reduced male fertility, which is observed in human males with DS and in mouse models of DS. The exact mechanism of this is not well understood 95 . Furthermore, trisomic cells seem to proliferate more slowly and/or have a prolonged cell cycle compared with euploid cells 96 , 97 . Although the results of many of these studies are contradictory, it is feasible that very small changes in the cell cycle could have a major effect on development. As human development requires 43 population doublings to progress from a single cell to the estimated one trillion cells in a fetus (if all of the cells survived — the actual number is clearly much higher), a very small increase in cell cycle length could result in recognizable phenotypes, such as small stature, short fingers, skeletal retrusion, decreased neuronal density in the brain and hypocellular tissues.
Pathophysiological insights from animal models.
In bio-medical research, mouse models provide an important translational tool to identify and prioritize therapeutic approaches to ameliorate the effects of a condition. Efforts to correlate DS-like phenotypes in mice with trisomy of specific genes (and groups of genes) have led to the development of more than 20 mouse models with partial trisomy 7 ( FIG. 3 ). Although the mouse provides a good mammalian genetic model for understanding DS pathogenetic mechanisms, it is important to keep in mind that mice do not develop DS. However, mouse models do illustrate several fundamental principles of gene effects in trisomy and preclinical pharmacological amelioration seems promising, especially for cognitive effects. Trisomic genes that contribute to a deleterious phenotype are targets for drug development to ameliorate features of DS. To illustrate the application of mouse models, examples of the use of mouse models to identify the genetic basis of trisomy effects in brain function, heart development and cancer risk are discussed.
Many preclinical studies emphasize improving cognitive function, possibly the most difficult target for pharmacological intervention. Ts65Dn and many subsequent models exhibit learning and memory deficits and electrophysiological changes consistent with altered synaptic function in the hippocampus 86 , 98 , 99 . Interestingly, Ts65Dn mice showed a significant learning deficit compared with Ts1Cje mice in a standard memory test 57 . Ts65Dn is trisomic for a larger number of genes than Ts1Cje ( FIG. 3 ), one of which is APP . Returning APP copy number to two by crossing a null allele of APP into the Ts65Dn background substantially improved the performance of these mice, although not to the level of a euploid mouse.
CHDs are present in ~50% of babies born with DS and mouse models display some analogous developmental deficits, albeit at a lower frequency than in human babies 100 . To identify a gene or genes that cause CHDs when present in three copies, seven (partial or complete) trisomies of the ~23 Mb region of MMU16 orthologous to HSA21 were studied 101 , which narrowed down the region responsible for causing CHDs (especially septal defects reminiscent of those in DS) to a 4.9 Mb portion of MMU16. However, three smaller trisomies subdividing the 4.9 MB segment did not have heart defects, suggesting that at least two genes must be trisomic to cause CHDs. In a different approach, interactions between trisomy and disomic modifiers of CHD risk were examined. A mouse hemizygous for Creld1 (a gene implicated in familial AVSD) was crossed with Ts65Dn and Ts1Cje mice 102 . Whereas Creld1 +/− mice had normal heart development, the occurrence of septal defects was markedly increased in Creld1 +/− Ts65Dn mice but not in Creld1 +/− Ts1Cje mice. Of the genes that are trisomic in Ts65Dn but not in Ts1Cje, 14 are expressed in heart development, including junctional adhesion molecule 2 ( Jam2 ), which consistently increases the frequency of heart abnormalities when overexpressed in zebrafish 103 . Restoration of two copies of Jam2 in Creld1 +/− Ts65Dn mice blocked the increased occurrence of CHD in these mice. Thus, trisomy for Jam2 is required for the disomic risk factor gene Creld1 to affect heart development.
Animal models have also been important in understanding cancer risk in individuals with DS. Epidemiological studies provide strong evidence that the incidence of many cancers is reduced in adults with DS 104 . Importantly, studies in mouse models of DS have confirmed these results, showing that partial trisomy 21 protects against various cancers. For example, familial adenomatous polyposis (FAP) is a congenital condition involving the formation of precancerous adenomatous polyps (predominantly in the colon) at an early age, and is caused by mutations in the tumour suppressor adenomatous polyposis coli ( APC ). Interestingly, Ts65Dn mice carrying an Apc mutation found in patients with FAP ( Apc Min ) develop 50% fewer adenomatous polyps than euploid mice 87 . Ts1Rhr mice, which are trisomic for just 33 of the genes triplicated in Ts65Dn, have a similar reduction in adenomatous polyp formation. This reduction is substantially reversed by restoring just one of these 33 genes, the proto-oncogene Ets2 , to two copies. Furthermore, Apc Min mice monosomic for these 33 genes (including Ets2 ) develop more tumours than euploid Apc Min mice. Thus, assessment in mouse models of trisomy and monosomy has uncovered a protective effect of Ets2 overexpression and a tumorigenesis-permissive effect of reduced Ets2 expression.
Preclinical studies and drug development.
Several clinical trials of pharmaceutical and nutraceutical agents to improve cognition in individuals with DS were initiated on the basis of preclinical observations in mouse models of DS (for example, {"type":"clinical-trial","attrs":{"text":"NCT00748007","term_id":"NCT00748007"}} NCT00748007 for rivastigmine, {"type":"clinical-trial","attrs":{"text":"NCT02484703","term_id":"NCT02484703"}} NCT02484703 and {"type":"clinical-trial","attrs":{"text":"NCT02024789","term_id":"NCT02024789"}} NCT02024789 for RG1662, and {"type":"clinical-trial","attrs":{"text":"NCT01112683","term_id":"NCT01112683"}} NCT01112683 for memantine). Although in-depth discussion of all of these trials is beyond the scope of this Primer, for illustrative purposes we discuss preclinical studies that led to phase I and II trials of RG1662 (also known as basmisanil or RO5186582), an inverse agonist of GABA A α5 receptors. Cognitive tests in Ts65Dn mice showed that these mice have deficits in learning and memory in tasks that depend on hippocampal function 86 , 105 , 106 , prompting electrophysiological studies demonstrating that long-term potentiation (LTP) is reduced in hippocampal slices from Ts65Dn mice 98 , 99 , 107 . The reduced LTP stemmed from excess GABA-mediated inhibition, which could be reversed by treatment with the GABA A inhibitor pentylenetetrazol (PTZ), restoring the inhibitory–excitatory balance and thereby improving performance in cognitive tests, even in young adult mice 108 .
These studies profoundly changed the understanding of cognitive dysfunction in DS and its treatment, by showing not only that treatment of cognitive deficits in DS is possible but that it is effective in adults, when previously it was widely thought that cognitive improvements could only be made during a small window early in life. Furthermore, this treatment had long-lasting effects, as the improved LTP was measured 3 months after cessation of PTZ treatment 108 . Thus, treatment for cognitive deficits is not a nebulous goal far in the future but can and should be addressed immediately. An inverse agonist of GABA A α5 receptors restores LTP and improves performance in cognitive tests in Ts65Dn mice 109 , 110 . RG1662 was assessed for safety and tolerability in individuals with DS in a successful phase I trial ( {"type":"clinical-trial","attrs":{"text":"NCT01436955","term_id":"NCT01436955"}} NCT01436955 ) that concluded in 2013. However, a phase II trial begun in 2014 was stopped prematurely in 2016 because RG1662 did not show efficacy.
Although the lack of efficacy in this specific trial design was disappointing, the trial represented several advances. First, it demonstrated that the pharmaceutical industry now had the confidence to treat intellectual disability, a first for the DS community. Second, the ability to enlist multiple centres throughout the USA and Europe that were capable of the complex measurements used in the trials, combined with strong support from the DS community in recruiting individuals for the trials, was a clear statement of interest by researchers, clinicians and individuals with DS. Finally, the application of cognitive tests designed specifically for DS was an important part of the trial. Although the official summary of results from this trial have not yet been published, the principles involved in treating individuals with DS have been reported by a number of the investigators involved in the trial 111 . Overall, the disappointment of the trial result was overlaid with optimism for improved treatment and trial design approaches in the future, and informed further trials such as a recent phase II trial using green tea extract containing epigallocatechin-3-gallate (EGCG) to improve cognitive outcomes 112 .
Mechanisms of Alzheimer disease
Almost all adults with DS develop AD-like neuropathology by 40 years of age. AD is characterized by a long asymptomatic preclinical stage in which amyloid pathology develops, ~15–20 years before any cognitive impairment is observed 113 . This preclinical stage is present in autosomal dominant forms of AD 114 and in early-onset AD associated with DS 115 . The evidence is compelling that an increased dosage of APP in trisomy 21 is necessary for increased risk of AD in individuals with DS, although the underlying mechanisms that link APP dosage to neurodegeneration are unknown. However, at least three molecular mechanisms have been proposed to explain the increased risk of AD in individuals with DS ( FIG. 4 ).

The increased gene dosage of APP (encoding amyloid precursor protein (APP)) and DYRK1A (encoding dual-specificity tyrosine-phosphorylation-regulated kinase 1A (DYRK1A)) on Homo sapiens chromosome 21 (HSA21) in individuals with Down syndrome (DS; trisomy 21) increases their risk of developing Alzheimer disease (AD). APP can undergo non-amyloidogenic processing (not shown) and amyloidogenic processing by β-secretase 1 (β-sec) and γ-secretase (γ-sec) to produce the neurotoxic Aβ42 peptide. The increased APP levels result in higher levels of Aβ42, and phosphorylation of APP at Thr668 by DYRK1A increases the amyloidogenic processing of APP. DYRK1A has other targets in the cell, including splicing factors and the microtubule-binding protein tau. DYRK1A phosphorylation of splicing factors alters the splicing of the MAPT mRNA (encoding tau), resulting in increased levels of tau containing three microtubule-binding domains (three-repeat (3R) tau) and reduced levels of 4R tau. This imbalance leads to neurofibrillary tangle (NFT) formation, possibly due to the lower binding affinity of 3R tau for microtubules. Furthermore, DYRK1A phosphorylation of Thr212 in tau alters the conformation of the protein, reducing the affinity of tau for microtubules and leading to NFT formation. The presence of the ε4 allele of APOE ( APOE ⋆ ε4 ) alters the processing, deposition and clearance of Aβ 249 , and is therefore a major risk allele for AD. AICD, APP intracellular domain; APOE, apolipoprotein E; CNS, central nervous system; P i , inorganic phosphate; sAPP, soluble amyloid precursor protein.
APP and A β 42.
Increased APP expression resulting from the presence of an additional copy of the APP gene is strongly correlated with early-onset AD 116 , 117 . Genomic duplication of the APP locus is the cause of some cases of familial, early-onset AD 118 , 119 . In individuals with DS with complete HSA21 trisomy, the extra copy of HSA21-located APP results in increased levels of APP and its cleavage products, including the neurotoxic Aβ42 peptide, in the brain 120 . However, individuals with partial trisomy of HSA21 who are disomic for APP do not develop early-onset AD and have normal APP expression levels 121 .
A second mechanism involves multiple neuropathological effects of DYRK1A overexpression. HSA21-encoded DYRK1A phosphorylates APP at Thr668, resulting in increases phosphoAPP levels in cells from a mouse model of DS that overexpresses the human DYRK1A gene 122 . This phosphorylation facilitates the amyloidogenic processing of APP by β-secretase and γ-secretase, leading to increased production of neurotoxic Aβ42 peptide 123 , 124 . The levels of phosphoAPP and Aβ42 are increased in the brain of these mice, and phosphoAPP, DYRK1A and Aβ42 levels are increased in the brain of individuals with DS.
DYRK1A also has effects on another molecule implicated in the pathophysiology of AD, the microtubule-stabilizing protein tau. DYRK1A phosphorylates tau at Thr212, a residue that is hyperphosphorylated in individuals with AD 125 . Abnormal hyperphosphorylation of tau changes its conformation, leading to a reduced affinity for microtubules 126 and resulting in microtubule instability, neurofibrillary tangle (NFT) formation and cell death 127 . Furthermore, DYRK1A also phosphorylates splicing factors and thereby alters the splicing of the mRNA of the tau-encoding gene MAPT . Alternative splicing of MAPT results in the production of tau protein isoforms with three or four microtubule-binding domains (three-repeat (3R) tau and 4R tau, respectively). Equal levels of 3R tau and 4R tau are required for maintaining normal brain function and an imbalance in their levels has been detected in sporadic tauopathies 128 . DYRK1A overexpression increases the abundance of 3R tau at the expense of 4R tau, which is thought to lead to the formation of NFTs, as 3R tau has lower affinity for microtubules than 4R tau 129 , 130 .
Endosomal dysfunction.
An extra copy of APP is sufficient to cause endosomal enlargement and intracellular trafficking defects by an Aβ-independent mechanism 131 . RAB5 mediates the endocytosis of cell-surface proteins and the homotypic fusion of early endosomes 132 . Enlargement of RAB5-positive early endosomes, a phenotype consistent with excessive activation of RAB5 (REF. 133 ), is present in neurons in the brain of individuals with sporadic or familial AD 134 , 135 and in individuals with DS who develop AD 136 . In fact, endosomal size in circulating peripheral blood mononuclear cells might serve as a blood-based biomarker of AD-related endosomal pathology 137 .
Endosomal function is also affected by other factors in DS. The ε4 allele of APOE ( APOE ⋆ ε4 ) is the most important genetic risk factor for late-onset AD, as ~80% of all patients with AD have at least one APOE ⋆ ε4 allele 138 . APOE ⋆ ε4 is also thought to increase the risk of dementia in older adults with DS, albeit to a lower extent than for sporadic AD in euploid individuals 139 . Endosomal enlargement in trisomic neurons is thought to cause axonal trafficking defects that contribute to neuronal degeneration 140 . Furthermore, APOE regulates the endosomal trafficking of amyloid fibrils 141 and early endosomal enlargement is present in the brain of mice carrying APOE ⋆ ε4 (REF. 142 ). APP gene dose, Aβ42 and the C-terminal fragment of APP, C99 (also known as βCTF), also have important roles in the development of endosome dysfunction. An increased level of C99 is the only APP-related alteration associated with abnormal endosome enlargement and proliferation that is common to all forms of AD 143 – 146 .
As APP gene dosage is an important determinant of AD risk in individuals with DS, various therapies to reduce APP levels in individuals with DS might have efficacy in treating AD, including reducing APP expression (using anti-sense approaches) and APP production (using translational inhibitors such as Posiphen), blocking APP cleavage (such as by BACE or DYRK1A inhibition or using γ-secretase modulators) or removing Aβ (by active or passive Aβ immunization).
Diagnosis, screening and prevention
Prenatal screening.
In developed countries, laboratory-based prenatal screening for DS is offered as part of routine antenatal care. Screening is a way to identify pregnancies at high risk, thereby limiting diagnostic procedures to minimize the risk of an iatrogenic miscarriage. Since the 1980s, the primary prenatal screening approach has involved a combination of measuring maternal serum biochemical analytes and, more recently, the size of the fetal nuchal translucency (NT; a pouch of fluid behind the neck) in the first trimester 147 . Initially, levels of α-fetoprotein in maternal serum and amniotic fluid in the second trimester were measured and a level ~70% of that in a normal pregnancy indicated an elevated risk of a DS conceptus. More recently, additional maternal serum analytes have been measured, including β-human chorionic gonado-tropin, unconjugated oestriol, inhibin A and pregnancy-associated plasma protein A. The levels of all of these markers change with gestational age, and some are better at distinguishing between trisomy 21 and euploid fetuses in the first trimester and others in the second trimester. Thus, correct dating of the pregnancy by ultrasonography examination is needed for accurate interpretation of serum analyte test results. For each woman, the risk of DS in the fetus is calculated using a computer algorithm with inputs of raw analyte values, gestational age and demographic information, such as maternal age, geo-ethnic background, smoking status and whether or not she has diabetes. The numerical risk cut-off values used in clinical practice differ in their reference points (that is, the risk of an affected fetus versus a liveborn infant). The chance of having a liveborn infant with DS is lower than the chance of having a fetus with DS in the second trimester because some of the fetuses will spontaneously miscarry in the second trimester 18 . Professional guidelines recommend that pregnant women with positive screening results are offered post-test counselling and a diagnostic test, such as amniocentesis or chorionic villus sampling followed by genetic analysis.
In the late 1980s and early 1990s, prenatal ultrasonography was incorporated into routine care, and some abnormalities were demonstrated to be associated with DS. Of note, no fetal anatomical findings are diagnostic of DS and, in fact, many neonates with DS have apparently normal prenatal sonograms. First-trimester ultrasonography features that may indicate DS include an increased NT measurement for gestational age and four other first trimester markers: absent nasal bone, increased frontomaxillary angle, tricuspid valve regurgitation and absent or reduced flow in the ductus venosus 147 . A second trimester anomaly scan has become routine at 18–20 weeks of gestation and includes quantifiable markers, such as a thickened nuchal skin fold and femoral and humeral length measurements. Additional so-called ‘soft’ ultrasonography markers include cystic hygroma, prominent tongue, choroid plexus cysts, mild ventriculomegaly, heart defects, echogenic bowel, duodenal atresia, pyelectasis, bilateral fifth finger clinodactyly and a wide space between the great and second toes 148 .
Using a combination of either first or second trimester maternal serum analyte quantification and NT measurement, the positive predictive values (PPV) for positive screening results are ~3–5% (refs 149 , 150 ). Because of these low PPVs, there has been longstanding interest in a more precise NIPS for fetal chromosome aneuploidies. In 2011, sequencing of cell-free DNA in maternal serum became clinically available 151 . Using massively parallel sequencing, the DNA fragments are counted, mapped to specific areas of the genome, and compared to a reference value; an excess number of fragments that map to HSA21 is suggestive (but not diagnostic) of DS 151 . Within a very short time, NIPS has become the most clinically implemented example of genomic medicine, with ~10 million tests performed to date 152 . Currently, in the USA, a pregnant woman at high risk of having a fetus with DS (maternal age >35 years, positive family history, positive serum analyte and/or NT measurements, suggestive ultrasonographic abnormalities) is offered NIPS as a primary screen. In many countries in Europe, NIPS is beginning to be offered as a secondary test following a positive primary screen. At present, only in Belgium and the Netherlands is NIPS offered as a primary screen for all pregnant women, regardless of a priori risk.
A meta-analysis examined the PPV of NIPS in pregnant women at high or low risk of having a fetus with DS 153 . For DS, the PPVs were 91% and 82% for high-risk and low-risk pregnant women, respectively. Studies that directly compared the predictive performance of analyte and/or NT measurement to that of NIPS in the same pregnant woman have demonstrated a 10–20-fold increase in PPVs using sequencing 149 , 150 . Importantly, NIPS is not dependent on gestational age and can be performed at any time between 10 weeks of gestation and delivery. Because NIPS performs better than current standards of care, in some countries with nationalized health systems there is a move towards providing NIPS as a primary screen for DS 151 .
Because NIPS is noninvasive and has a very good PPV, there have been concerns about what effect this testing will have on the live birth rates of infants with DS. A preliminary study found no difference in the number of live births of babies with DS before and after NIPS became available in eight countries 154 . However, without access to all prenatal testing results, it is unclear how many more babies with DS would have been born during this time period. More extensive studies are needed to assess the effect of NIPS on the incidence of DS. Although many women choose not to have prenatal testing because it would not influence their reproductive decisions, in one study, women who knew prenatally that their babies had DS had better results on psychological tests than women who discovered at birth that their baby had DS 155 . A prenatal diagnosis of DS has been reported to have several benefits, including opportunity for parental education, meetings with paediatric subspecialists ahead of delivery, and change of the location of delivery so that qualified paediatric subspecialists are available for care, thereby enabling mother and baby to remain in the same hospital together 155 . A future benefit of accurate prenatal screening could include the opportunity to initiate treatment during fetal life to improve cognition (discussed later).
Each individual with DS has a distinct set of strengths and challenges that can change throughout his or her life 156 . Some individuals will require high levels of medical input from birth, whereas others may have few health complications. Similarly, some individuals will require social care and support throughout adulthood, whereas others live independently. Several health problems are more common in individuals with DS than in the general population, including CHDs, obstructive sleep apnoea, thyroid disease, dementia, epilepsy, gastrointestinal disease, hearing and vision problems, intellectual disability and developmental disorders, mental illness, immunological dysfunction, haematological disorders and musculoskeletal issues. Screening for these manifestations should be carried out regularly and there are consensus screening guidelines for children with DS (such as the guidelines of the American Academy of Pediatrics 157 ) but not yet for adults 158 – 160 . Services for adults are often more specialized than those for children, and care usually needs to be managed by a number of different medical teams. No consensus currently exists about who should oversee care in adults with DS, but primary care physicians often take on this role 100 ; occasionally, paediatricians may remain involved until early adulthood, and in some countries, such as the UK, intellectual disability psychiatrists are most likely to provide medical support within community teams. Due to the lack of consensus, adults with DS may miss out on regular screening and proactive treatments, with interventions only occurring when difficulties are clinically apparent 161 .
Illness and disease may present differently in people with DS. There is a risk of diagnostic overshadowing and misattribution of symptoms, which can be compounded by the high prevalence of communication difficulties in individuals with DS. Due to the multisystem involvement in DS, care requires multidisciplinary input from a range of medical, social care and educational teams.
Perinatal management
Pregnant women carrying a fetus with a confirmed DS diagnosis require regular monitoring and support throughout the perinatal period. Pregnant women carrying a fetus with DS are at increased risk of miscarriage, with an estimated rate of spontaneous fetal death after 12 weeks of 30%, which increases with maternal age 18 . Monitoring recommendations suggest that a detailed ultrasonography examination and fetal echocardiography should be performed at 18–20 weeks gestation, with further ultrasonography examinations at 28–30, 34–36 and 38 weeks to assess for evidence of upper gastrointestinal obstruction, chylothorax, fetal hydrops and intra-uterine growth restriction. If abnormalities are detected, then increased fetal surveillance is recommended. Local paediatric teams should be informed if abnormalities are detected so that they can be involved in planning postnatal care and treatment (for guidance see, for example, the Down’s Syndrome Association and the Down Syndrome Medical Interest Group fact sheet).
Congenital heart defects
CHDs occur in ~50% of individuals with DS, most commonly AVSD (42% of CHDs in individuals with DS), ventricular septal defect (22%) and atrial septal defect (16%) 162 . Although the frequency of the specific type of CHD depends on age and ethnicity, the primary point is that CHDs have a severe effect on the quality of life of the individual. During pregnancy, a fetal echocardiography examination is recommended. A cardiology examination should take place postnatally, and another echocardiography examination should be performed within the first month after birth. Management is the same as for the general population, including surgical repair 163 . The mortality rate after surgery in children with DS is equal to or lower than that in the general population 164 . All individuals with DS should have annual screening throughout life for signs of acquired valve disease and heart failure.
Sleep apnoea
Obstructive sleep apnoea is common in individuals with DS, with an estimated prevalence of 54–90% 159 , 165 . Screening for symptoms should be carried out at every health check; these symptoms include loud snoring, heavy breathing, restless nights and daytime sleepiness, as well as neurocognitive symptoms, such as irritability, depression, paranoia, cognitive decline and behavioural problems 166 . Overnight polysomnography is recommended for all children with DS before 4 years of age, regardless of symptoms 157 , 167 . Alternative approaches, such as home oximetry, have been suggested to enable identification of at-risk individuals and to reduce the number of children that require full diagnostic studies 168 . Management of sleep apnoea includes the use of continuous positive airway pressure (CPAP), mandibular advancement devices and weight loss. Surgical interventions, including tonsillectomy and adenoidectomy, can be considered, although sleep apnoea may persist after surgery 165 , 169 .
Thyroid dysfunction
Congenital hypothyroidism is present in ~1% of individuals with DS, and abnormal thyroid function tests have been reported in >50% of neonates with DS 170 – 172 . An increased risk of developing thyroid disease remains throughout life, and the risk of developing autoimmune-related thyroid dysfunction increases with age 173 . As clinical diagnosis can be difficult, it is important to perform regular blood screening. Thyroid-stimulating hormone (TSH) and thyroxine (T4) levels should be obtained postnatally and at 6 months and 12 months of age. Measurements of TSH should then be repeated annually 157 .
Alzheimer disease
A substantial proportion of individuals with DS develop early-onset AD, which is related to APP overproduction 120 , 174 , and dementia is the proximal cause of death in 70% of older adults with DS 175 . Clinical symptoms appear after 40 years of age, and 77% of individuals with DS aged 60–69 years, and up to 100% of those aged >70 years, will develop cognitive decline 176 – 178 ( FIG. 5 ). The cognitive decline needs to be understood in the context of the existing cognitive phenotype and individual risk, including APOE genotype, as the presence of the APOE ⋆ ε4 allele seems to increase the risk of earlier cognitive decline due to AD and of mortality 179 ( FIG. 5b ).

a | Distribution of age at dementia diagnosis in individuals with Down syndrome (DS). The risk of developing Alzheimer disease in individuals with DS is closely related to age. The mean age of dementia diagnosis is 55 years, although some individuals already show cognitive decline starting from 40 years of age, whereas others are not diagnosed until after 60 years of age. b | Cognitive decline in individuals with DS, measured by performance ( z score) in a memory test. Cross-sectional data from the London Down Syndrome Consortium showing the distribution of test scores on an object memory task by age and apolipoprotein E ( APOE ) genotype in individuals with DS. The task is a measure of short-term and delayed memory, adapted for individuals with DS. Participants are instructed to name and recall seven objects with two immediate recall trials, and one delayed recall trial after 5 minutes 250 . The data are split by APOE genotype to compare the effect of the ε4 allele of APOE ( APOE ⋆ ε4 ; which increases the risk of late-onset sporadic Alzheimer disease) with that of the APOE ⋆ ε2 allele (which decreases AD risk) and APOE ⋆ ε3 allele (which has a neutral effect on AD risk) on cognitive performance. Cognitive performance in individuals with an APOE ⋆ ε3 / APOE ⋆ ε4 or APOE ⋆ ε4 / APOE ⋆ ε4 genotype declines from 40 years of age, noticeably earlier than the average age of dementia diagnosis and earlier than in individuals with an APOE ⋆ ε2 / APOE ⋆ ε2 , APOE ⋆ ε2 / APOE ⋆ ε3 , APOE ⋆ ε2 / APOE ⋆ ε4 or APOE ⋆ ε3 / APOE ⋆ ε3 genotype. Part a is adapted from REF. 251 , CC-BY-4.0 ( https://creativecommons.org/licenses/by/4.0/ ). Part b adapted with permission from REF. 115 , Elsevier.
Deficits in memory and attention occur early in DS, as in individuals with sporadic AD 180 , but often go unnoticed until behavioural changes appear 181 . Some individuals with DS and dementia may present with seizures and, as the disease progresses, the development of neurological symptoms, such as myoclonus and seizures, is commonly seen 182 .
A baseline assessment of cognitive and adaptive functioning at 30 years of age is recommended in all individuals with DS, to aid future monitoring and diagnosis 183 . Management should focus on early detection and supportive measures. Positive benefit may be obtained from the use of acetylcholinesterase inhibitors 184 , 185 , although some individuals may develop a reduced heart rate and other adverse effects. Individuals with DS and dementia should have access to adequate support, as their needs will increase as the disease progresses. Efforts should be made to keep individuals within their familiar homes, and transfer to other providers should be based on individual circumstances and needs 186 .
Epilepsy is present in 8% of children with DS, with a bimodal age of onset (one peak before 3 years of age and the other after 30 years of age 160 ). Infant onset, most frequently infantile spasms, has been associated with a severe form of epilepsy termed West syndrome, which includes psychomotor regression and hypsarrhythmia (an abnormal pattern of activity between convulsions) on electroencephalography, and occurs in ~6–32% of seizures reported in infants 187 . Later onset of epilepsy is linked to the development of AD 136 . The management of epilepsy depends on the aetiology, but usually involves anticonvulsant medication, which is generally effective in reducing seizure activity 156 , 178 , 188 .
Hearing and vision
Conductive hearing loss is common in individuals with DS, with a high prevalence of otitis media with effusion 189 , 190 . Baseline hearing tests should be performed postnatally using, for example, brainstem auditory acoustic response, and then every 6 months until school age and at least annually thereafter 157 . Early recognition and treatment can reduce the risk of later hearing loss 191 . Sensorineural loss becomes increasingly common in adulthood. Treatment with hearing aids and cochlear implantation has been successful. The use of speech therapy, communication aids and sign language, including the language programme Makaton, can also be beneficial 160 .
Because there is increased risk of refractive errors, cataracts (congenital and developmental), keratoconus and amblyopia in individuals with DS, ophthalmological examination should be performed at birth and regularly throughout life, ideally every 1–2 years 157 . Treatment and corrective aids should be given promptly 157 . Cataract surgery is routinely performed, usually with good outcomes 192 , 193 .
Atlantoaxial instability
Atlantoaxial subluxation (misalignment of the first and second cervical vertebrae) develops in ~1–2% of children with DS 194 . If the condition is present, parents should be advised that participation in sports increases the risk of spinal cord injury in the child. Symptoms such as neck pain, weakness, spasticity, gait difficulties and hyperreflexia should be evaluated with cervical spine radiography 157 .
Mental health
Individuals with DS have increased prevalence of behavioural and mental health problems compared with the general population 195 , in particular, depressive and anxiety disorders 196 , 197 . A small proportion of adolescents and young adults with DS undergo acute regression (also known as Down syndrome disintegrative disorder), which involves a loss of skills and independence compared with their previous levels of functioning. At present, the cause of this decline is unknown, although it often seems to occur after exposure to emotional stressors 198 . To date, there is no definitive treatment for this presentation.
Diagnosis of mental health issues in individuals with DS can be complicated by the presence of intellectual disability, communication difficulties and atypical symptoms 199 . The effect of psychological stressors should not be underestimated, including transitions in accommodation, school or care arrangements, and bereavement 166 , 200 . Treatment for mental illness should be based on standard clinical guidelines, and individuals with DS show positive responses to behavioural interventions, psychotropic medication and psychological therapy.
Neurodevelopment
DS is the most common genetic cause of intellectual disability, with the majority of individuals with DS classified as having mild–moderate disability. Their cognitive profile demonstrates strengths in visual learning, but weaknesses in expressive language, verbal working memory, and episodic memory 201 . However, there is a wide range in cognitive function, with variations in IQ, language, attention, memory and functional abilities.
Individuals with DS often have autism spectrum disorder (~10–15%) and attention-deficit–hyperactivity disorder (ADHD; ~6%) and appropriate screens for these should be performed 160 , 202 . Clinical presentations may differ from those of the general population and assessments may require input from specialists. Standard treatments for ADHD are recommended, although there can be a less marked response to stimulant medication in individuals with intellectual disability than in those without intellectual disability 203 .
Prenatal therapy to improve neurocognition.
Increasing attention has been paid to using prenatal diagnosis of DS as an opportunity to provide antenatal therapy to improve neurocognition 204 , 205 . Impairment of neurogenesis in individuals with DS begins prenatally 206 – 208 and is one of several factors 209 that result in abnormalities in fetal brain growth and shape that are recognizable in third trimester prenatal ultrasound and MR images 210 . Thus, treatment initiated in fetal or early neonatal life is hypothesized to have maximal effect 211 (the ethical issues posed by treatment of fetuses with DS are discussed elsewhere 212 ).
To date, most experiments involving fetal therapy have been performed using mouse models of DS. Antenatal treatments that have resulted in postnatal improvement in learning and neurobehaviour in Ts65Dn mice include dosing with the vasoactive intestinal pep-tides NAPVSIPQ (NAP) and SALLRSIPA (SAL) 213 , maternal dietary choline supplementation 214 , and inhibition of DYRK1A. For example, prenatal treatment with the DYRK1A inhibitor EGCG, which crosses both the placental and blood–brain barriers in mice, improved some aspects of the cranial vault morphological defects in Ts65Dn mice 215 . Furthermore, oral administration of the novel DYRK1A inhibitor ALGERNON (altered generation of neurons) to pregnant Ts1Cje dams from embryonic day 10 (E10) to E15 improved neurogenesis, corticogenesis and behavioural performance of their pups, possibly by enhancing the proliferation of neural stem cells 216 .
Other potential therapeutic targets have been identified from studies of mouse models. For example, mitochondrial dysfunction in fibroblasts from human fetuses with DS is reversed by activation of the PGC1α pathway using metformin 217 . The mRNA and protein levels of PGC1α are markedly reduced in fibroblasts from fetuses with DS, and metformin treatment increased oxygen consumption and cellular ATP concentration, improved respiratory activity, increased mitochondrial membrane potential and reversed mitochondrial ultrastructural abnormalities in these cells 217 . Metformin already has FDA regulatory approval for the treatment of maternal gestational diabetes, so its use in clinical trials in pregnant women carrying fetuses with DS would potentially face fewer regulatory hurdles. Studies in mouse models of DS have also shown that prenatal treatment with the selective serotonin reuptake inhibitor fluoxetine restores hippocampal neurogenesis and connectivity, granule cell number and dendritic patterns, and hippocampus-dependent memory functions 218 . A clinical trial of high-dose fluoxetine in pregnant women (without psychiatric disorders) is ongoing at the University of Texas (USA) 211 , although no information about the trial is publicly available. However, fluoxetine use in the first trimester may have adverse effects, such as increasing the risk of congenital heart disease and other malformations 219 .
Apigenin, a natural flavone found in citrus fruits and leafy green vegetables, also shows promise in reducing oxidative stress and improving total oxidative capacity in human cells from fetuses with trisomy 21, as well as improving some behaviours in neonatal and adult Ts1Cje mice treated prenatally 204 . The recognition of the possibilities for improving fetal brain development, and testing of an increasing number of compounds for eventual use in clinical trials, make this a very exciting time in DS research, although recommendations for supplementation cannot be made owing to a paucity of evidence.
Immune and haematological systems
Individuals with DS are more prone to infections, especially of the respiratory tract 220 – 222 . Infections should be recognized and treated promptly 157 . There is no contraindication to immunizations, and the standard childhood schedule should be followed.
Individuals with DS also show a predisposition to autoimmune diseases, particularly coeliac disease 160 , 223 . Testing the levels of immunoglobulin A antibodies to tissue transglutaminase 2 is recommended if symptoms of coeliac disease are present 157 , but screening of asymptomatic individuals has not proved cost-effective 224 . Type 1 diabetes mellitus, alopecia areata and Addison disease have also been reported in individuals with DS at higher rates than in the general population.
Children with DS are at a markedly increased risk of developing acute leukaemia, compared with children without DS. Transient myeloproliferative disorder (TMD), also referred to as transient leukaemia of DS, is observed in 5–30% of individuals with DS before 3 months of age, and a blood count and film should be performed within 3 days of birth to enable the identification and monitoring of this disorder 225 . Although TMD usually resolves without treatment in the first few months of life, it seems to increase the risk of developing leukaemia by 5 years of age, and it is estimated that 20–30% of individuals with TMD will go on to develop myeloid leukaemia of DS 157 , 226 , 227 .
Quality of life
Research into the quality of life of individuals with DS is limited, although it is recognized that stigma and cultural norms can be barriers to the active participation of individuals with DS in the community. If adequately supported during their life, many individuals with DS can live fairly independently. The perspectives of family members of individuals with DS have been somewhat studied 228 . Support groups and DS networks can provide valuable input, and individuals with DS and their families should be aware of local and national organizations.
Children with DS are now regularly educated within mainstream schools, often with additional one-to-one or specific Special Educational Needs support 229 . Some children with DS can gain additional benefits in terms of language and literacy skills when educated in inclusion classrooms rather than in substantially separate classrooms, whereas others may require a specialist school 230 .
Many individuals with DS are employed and report fairly high levels of satisfaction, and many have become successful professionals, including artists, speakers and actors. However, there is a disparity between the number of individuals with DS who wish to work and those who have secured employment. They may access voluntary work and this seems to be more common than in the general adult population. Cultural assumptions, social care cuts and inadequate adjustments in work can make it difficult for individuals with DS to access employment 231 , 232 .
Quality of life can be affected by physical health, and proactive screening programmes and early intervention can reduce the negative effect of prolonged hospitalizations and ill health. Recognition and correction of hearing and vision problems can reduce the negative effect on communication and development 233 . Obesity, cervical spine abnormalities and muscular difficulties may contribute to the exclusion of individuals with DS from physical activity, and in the USA, children with DS have lower levels of physical activity than their peers 234 . However, the majority would be able to participate in exercise programmes if available, which can have a positive effect on health and wellbeing 235 .
Owing to early cognitive decline, many adults with DS have increased support needs as they age. Adequate proactive support, with regular reassessment of needs and services set up to anticipate functional impairments, is crucial for their quality of life.
Although the lives of individuals with DS have been much improved by the evolution of medical care and the benefits of societal changes, there is no treatment for DS at present that is based on the current understanding of the molecular pathophysiology of DS. Therefore, to design effective therapies, further research is needed to improve understanding of the biology of each symptom and feature of the syndrome. The most important topics for further research are discussed below.
Understanding the contribution of genetic variation to the different and variable phenotypic characteristics and manifestations of DS is an important goal that could be achieved by genome sequencing of thousands of individuals with DS, and linking the genetic variation with the detailed phenotypic characterization of each individual 6 . This effort is based on the reasonable hypothesis that genomic differences are major determinants of the extensive phenotypic variation. Furthermore, genes and other functional genomic elements that in three copies contribute to the phenotype of DS need to be identified. There is supportive evidence that genes causing disease states with haploinsufficiency, in which one functional copy is not sufficient, may also be important when present in three copies, as is the case with DS. For example, DYRK1A is haploinsufficient (probability of loss-of-function intolerant (pLI) score of 1), and the loss of one copy of DYRK1A causes intellectual disability 236 . Several studies have also shown that an extra copy of DYRK1A is involved in the biological dysfunction that results from trisomy 21 (REF. 237 ). However, the pLI score may not be an absolute discriminator of genes involved in the pathophysiology of DS. For example, APP has been strongly linked to AD in individuals with DS 120 but has a pLI score of 0.06, which is compatible with a haplosufficient gene. Furthermore, HMGN1 , a gene that is linked to the transcriptional dysregulation in trisomy 21(REF. 238 ), has a pLI score of 0.22. In addition to the causative contribution of specific genes on HSA21, the phenotypic contribution of the extra-chromosomal material, regardless of its gene content, needs to be investigated.
Experimental models, such as the mouse and other organisms 7 , need to be used to study the brain and other organs in the different stages of development. Advances in single-cell technologies 239 that enable study of the genome, transcriptome, histone modifications, chromatin contacts and protein levels in individual cells will certainly provide insights into the cellular mechanisms of the altered developmental pathways in DS and the effect of chromatin conformation on the dysregulation of gene expression.
Experimental efforts to modify the dysregulated expression of genes on HSA21 and other chromosomes may result in novel therapeutic approaches that should be explored further. For example, experimental silencing of large chromosomal regions by introducing the X chromosome-inactivation effector XIST on one copy of HSA21, or silencing one of the three alleles of HMGN1 , DYRK1A or APP , may rescue some phenotypic characteristics of DS.
Early-onset AD in individuals with DS is genetically analogous to some forms of autosomal dominant AD, and the amyloid pathway is strongly implicated in AD pathology due to APP triplication. Therefore, amyloid-targeting drugs should be trialled in individuals with DS, as they are at very high risk of early-onset AD, preferably before any symptoms develop in order to prevent or delay the onset of dementia 115 . PET imaging of amyloid or tau deposits in the brain 240 , 241 or measures of Aβ peptide ratios in cerebrospinal fluid 242 have been shown to be feasible biomarkers for patient stratification, whereas plasma levels of the neurodegeneration markers neurofilament light chain and neuronal pentraxin 2 show promise as biomarkers of treatment response 243 – 245 .
Population-based, longitudinal, large-scale cohort studies following individuals with DS would be helpful to the further understanding of the co-occurring medical conditions, family attitudes, educational achievement, individual experiences, and societal successes that now exist for individuals with DS. Increasingly sophisticated analytical methods combined with improved genetic models offer hope for more translation of promising therapies.
Acknowledgements
The authors thank the members of the London Down Syndrome (LonDownS) Consortium, G. de Graaf of the Dutch Down Syndrome Foundation and F. Buckley of Down Syndrome Education International for their review of the epidemiology section of this article. Work in the authors’ laboratories and clinics was supported by grants from the SNF, EU, ERC, Jerome Lejeune, and ChildCare Foundations to S.E.A.; a Wellcome Trust Strategic Award (grant number 098330/Z/12/Z) conferred upon the LonDownS Consortium, an MRC project grant (LonDownsPREVENT MR/S011277/1), and grants from the EU Joint Programme - Neuro-degenerative Disease Research (MR/R024901/1, as part of the HEROES consortium), Network of Centres of Excellence in Neurodegeneration (COEN) (MR/S005145/1), Lumind Foundation and Jerome Lejeune Foundation to A.S.; the Jerome Lejeune Foundation USA, Anna and John Sie Foundation, US National Institutes of Health (NIH; HD42053-10, UL1TR001064, ZIA HG200399-04) to D.W.B.; NIH and Lumind Foundation to S.L.S.; HD038384-20, HD098540 and the Lumind Foundation to R.H.R.; and the Alzheimer’s Society and BRC to S.P. The authors thank all past and present members of their laboratories, their collaborators and the patients and their families for their inspiration and support.
Competing interests
S.E.A. is the co-founder and CEO of MediGenome, a clinical and laboratory diagnostic company. B.G.S. occasionally consults on the topic of Down syndrome through Gerson Lehrman Group. B.G.S. receives remuneration from Down syndrome non-profit organizations for speaking engagements and associated travel expenses. B.G.S. receives annual royalties from Woodbine House, Inc., for the publication of his book, Fasten Your Seatbelt: A Crash Course on Down Syndrome for Brothers and Sisters . Within the past 2 years, B.G.S. has received research funding from F. Hoffmann-La Roche, Inc., and LuMind IDSC Down Syndrome Foundation to conduct clinical trials for people with Down syndrome. B.G.S. is occasionally asked to serve as an expert witness in legal cases where Down syndrome is discussed. B.G.S. serves in a non-paid capacity on the Honorary Board of Directors for the Massachusetts Down Syndrome Congress and the Professional Advisory Committee for the National Center for Prenatal and Postnatal Down Syndrome Resources. B.G.S. has a sister with Down syndrome. M.S.R. is a consultant to AC Immune SA. A.S. has consulted for Roche Pharmaceuticals, ONO Pharma, Aelis Farma and AC Immune, and he serves on the Scientific Advisory Board of ProMIS Neurosciences. A.S. and S.E.P. provide clinical services within the UK National Health Service to individuals with Down syndrome. The remaining authors declare no competing interests.

Down’s Syndrome
- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE , Medicine , Surgery , Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Table of Contents
Suggest an improvement
- Hidden Post Title
- Hidden Post URL
- Hidden Post ID
- Type of issue * N/A Fix spelling/grammar issue Add or fix a link Add or fix an image Add more detail Improve the quality of the writing Fix a factual error
- Please provide as much detail as possible * You don't need to tell us which article this feedback relates to, as we automatically capture that information for you.
- Your Email (optional) This allows us to get in touch for more details if required.
- Which organ is responsible for pumping blood around the body? * Enter a five letter word in lowercase
- Comments This field is for validation purposes and should be left unchanged.
Introduction
Down’s syndrome (DS), also known as trisomy 21, is the most common congenital chromosomal abnormality, occurring in about 1 in 800 to 1 in 1000 live births. 1,2 The presence of additional genetic material from chromosome 21 results in characteristic phenotypic features and increased morbidity through its effect on multiple organ systems. The major cause of early mortality in Down’s syndrome is congenital heart disease. 3,4 Despite this, many people with Down’s syndrome live happy and fulfilling lives, developing at their own pace and receiving coordinated care to manage comorbidities.
Trisomy 21 typically occurs via one of the following mechanisms: 4,5
- Meiotic non-disjunction of the maternal chromosome 21 (95%)
- Robertsonian translocation of unbalanced chromosomal material, usually between chromosome 14 and chromosome 21 (4%)
- Mosaicism (1%)
Risk factors
Maternal age is the strongest risk factor for Down’s syndrome. 23
Table 1. Risk of Down’s syndrome (live births) in relation to maternal age at delivery, prior to screening in pregnancy. 4
|
|
|
| All ages | 1 in 650 |
| 20 | 1 in 1530 |
| 30 | 1 in 900 |
| 35 | 1 in 385 |
| 37 | 1 in 240 |
| 40 | 1 in 110 |
| 45 | 1 in 37 |
Clinical features
Dysmorphic features.
Dysmorphic features which may be noted in neonates with Down’s syndrome are described below. 2,7
- Hypotonia: this may cause difficulties with feeding
- Hyperflexibility
- Oblique palpebral fissures
- Epicanthic folds
- Flat nasal bridge
- Brachycephaly (flat occiput)
- Dysplastic, low-set, small ears
- Open mouth with protruding or furrowed tongue
- High arched palate
- Short neck with excessive skin at the nape of the neck
- Transverse palmar crease (Simian crease)
- Short and incurved little finger
- Large gap between the first and second toes (“sandal toe deformity”)

Congenital heart defects
Approximately 50% of neonates with DS will have associated congenital heart disease .
The most common forms of congenital heart disease are: 2-4,7,10
- Complete atrioventricular septal defect (37%)
- Ventricular septal defect (31%)
- Atrial septal defect (15%)
Neurological disease
Developmental delay and intellectual disability.
Developmental milestones are frequently delayed in Down’s syndrome.
Intellectual disability is an almost universal feature of Down’s syndrome which can vary significantly in severity.
Autism , attention deficit hyperactivity disorder (ADHD) and aggressive behaviour are also more prevalent in Down’s syndrome. 20
Alzheimer’s disease
Alzheimer’s disease develops in up to 75% of DS patients by the sixth decade of life. 8,9,20.
Respiratory disease
Asthma and obstructive sleep apnoea are more common in Down’s syndrome. 1
Gastrointestinal disease
Gastrointestinal tract anomalies requiring surgery occur in about 12% of patients with Down’s syndrome. 1 The most characteristic anomaly is duodenal atresia caused by a failure of the intestine to recanalize during development. 7,11 Other structural gastrointestinal anomalies may include imperforate anus and/or tracheo-oesophageal fistula .
Down’s syndrome is also associated with an increased risk of Hirschsprung disease . 7
Endocrine disease
Endocrine diseases most commonly associated with Down’s syndrome include hypothyroidism and type 1 diabetes mellitus .
Haematological disease
Down’s syndrome is associated with an increased risk of developing several different haematological disorders including: 1,7,14,15
- Immunodeficiency
- Transient myeloproliferative disorder
- Polycythaemia
- Acute megakaryoblastic leukaemia
- Acute lymphoblastic leukaemia
Other clinical features
Other clinical features associated with Down’s syndrome include (but are not limited to):
- Short stature and obesity
- Ophthalmological disorders including cataracts, refractive disorders, nystagmus, strabismus and glaucoma
- Orthopaedic disorders such as atlanto-axial instability, hyperflexibility, hip dislocation and foot deformities
- Recurrent acute otitis media 1
- Benign skin disorders such as hyperkeratosis and seborrhoeic dermatitis
- Urological abnormalities such as hypospadias and cryptorchism
- Juvenile idiopathic arthritis
Differential diagnosis
Differential diagnosis of Down’s syndrome includes, but is not limited to: 5,24
- Congenital hypothyroidism
- 49 XXXXY chromosome and high-order X chromosome disorders
- Zellweger syndrome (or other peroxisomal disorders)
- Aymé-Gripp syndrome
Investigations
Prenatal investigations, screening for down’s syndrome.
Pre-natal screening is currently the most common means through which Down’s syndrome is identified and eventually diagnosed. Screening tests along with other data such as maternal age, weight, family origin and gestation are combined in software to calculate the probability of a fetus having Down’s syndrome. The screening test is considered positive if the risk of a fetus having Down’s syndrome is greater than 1 in 150 . If the screening test returns a positive result, women are offered diagnostic testing .
Down’s syndrome screening most commonly involves:
- Serum screening : assessment of a range of biomarkers in the serum between 10-14 weeks + 1 day of gestation.
- Nuchal translucency scanning : ultrasound is used to assess the translucency of the nuchal pad at the nape of the fetal neck between 11 weeks + 2 days and 14 weeks + 1 day gestation. Increased nuchal translucency is associated with Down’s syndrome.
Serum screening and nuchal translucency scanning are typically used in combination (known as ‘ the combined test ‘).
The standard serum screen measures the following biomarkers:
- Beta-hCG : raised in Down’s syndrome
- PAPPA-A : decreased in Down’s syndrome
If a woman engages with antenatal care later in pregnancy when nuchal translucency scanning is less reliable, a different set of biomarkers are assessed (known as ‘ the quadruple test ‘):
- AFP : low in Down’s syndrome
- Inhibin A : raised in Down’s syndrome
- Unconjugated estriol (uE3) : low in Down’s syndrome
The quadruple test is less reliable than the combined test.
Non-invasive prenatal testing (NIPT)
During pregnancy, the placenta sheds cell-free DNA (cfDNA) into the mother’s bloodstream. As a result, the mother’s blood contains a mixture of placental and maternal cfDNA . By evaluating the cfDNA in the blood and combining this with the mother’s background chance of a trisomy (mother’s age or the combined test results), a likelihood ratio is obtained to predict whether or not the baby is more likely to have a chromosomal condition such as Down’s , Edward’s or Patau’s syndrome. It is possible from around 10 weeks gestation and has a sensitivity of around 99% . 17-20
This test is not currently part of the routine screening pathway.
Confirming the diagnosis of Down’s syndrome
Karyotype analysis of fetal cells via chorionic villus sampling (9–12 weeks gestation) or amniocentesis (15–19 weeks gestation) is the gold standard for diagnosing Down’s syndrome, with equal detection rates of around 99%. There is a higher risk of pregnancy loss with chorionic villus sampling compared to amniocentesis. 19
Post-natal investigations
Given the association of Down’s syndrome with a wide range of pathologies, it is essential that comprehensive screening is performed in the post-natal period to allow early identification and management of these complications.
Some examples of post-natal investigations include:
- Echocardiography: to screen for congenital cardiovascular abnormalities
- Red reflex testing: to screen for congenital cataracts
- TFTs: to screen for congenital thyroid disease
- FBC: to screen for myeloproliferative disorders and polycythaemia
- Hearing assessment: to screen for congenital hearing issues
- Radiographic swallowing assessment: performed if feeding difficulties are present to screen for gastrointestinal abnormalities (e.g. duodenal atresia)
Management of Down’s syndrome requires a tailored multidisciplinary approach to screen , diagnose and treat complications . Patients with Down’s syndrome often require ongoing regular review from relevant specialists.
Genetic counselling
If a newborn is diagnosed with Down’s syndrome, parents should be referred for genetic counselling to discuss the risk of further children having Down’s syndrome.
- Down’s syndrome is caused by the presence of additional genetic material from chromosome 21 .
- Clinical features of Down’s syndrome are wide-ranging including dysmorphic features, cognitive impairment and a multitude of other medical conditions.
- The biggest risk factor for Down’s syndrome is maternal age.
- Prenatal screening provides a method for assessing the risk of Down’s syndrome through the assessment of serum biomarkers and nuchal translucency.
- Prenatal diagnosis of Down’s syndrome can be achieved through chorionic villus sampling or amniocentesis.
- Post-natal screening investigations are essential to allow early identification of Down’s syndrome complications.
- Management of Down’s syndrome requires a tailored multidisciplinary approach to screen, diagnose and treat complications.
- Center for Disease Control. Data and statistics on Down syndrome. Reviewed December 5, 2019. Available from: [ LINK ]
- The University of Chicago Pediatrics Clerkship. Trisomy 21 (Down). 2013. Available from: [ LINK ]
- O’Learly, L et al. Early death and causes of death of people with Down syndrome: A systematic review . Published September 2018. Available from: [ LINK ]
- Illustrated textbook of pediatrics with STUDENT CONSULT online. Genetics . Published in 2015. Available from: [ LINK ]
- Orphanet. Down syndrome . Reviewed in September 2019. Available from: [ LINK ]
- Halliday, Jacquelyn V et al. Patient education: Should I have a screening test for Down syndrome during pregnancy? (Beyond the Basics). Reviewed in February 2020. Available from: [ LINK ]
- Kathryn K. Ostermaier. UpToDate.com. Down syndrome: Clinical features and diagnosis . Reviewed January 2020. Available from: [ LINK ]
- Alzheimer’s society. Down Syndrome and Alzheimer’s Disease. Available from: [ LINK ]
- Hill, DA et al. Mortality and cancer incidence among individuals with Down syndrome. March, 2003. Available from: [ LINK ]
- Freeman, SB et al. Population-based study of congenital heart defects in Down syndrome. Published in 1998. Available from: [ LINK ]
- Orphanet. Duodenal atresia. February 2009. Available from: [ LINK ]
- Celiac Disease Foundation. What is celiac disease? Available from: [ LINK ]
- Gillespie, Kath et al. The Down Syndrome Medical Interest Group. Down Syndrome Association: Health series . PDF. Reviewed in 2018. Available from: [ LINK ]
- Manivannan et al. Down Syndrome with Different Hematological Manifestations: A Short Series of 3 Cases with Review of Literature . March 2013. Available from: [ LINK ]
- Rabin, Karen and James A. Whitlock. Malignancy in Children with Trisomy 21. February 2009. Available from: [ LINK ]
- Lacy, Jordan et al. Atlantoaxial instability. January 2020. Available from: [ LINK ]
- Palomaki GE et al. A summary analysis of Down syndrome markers in the late first trimester. Published in 2007. Available from: [ LINK ]
- Alldred SK et al. Cochrane Database System Review. Second trimester serum tests for Down’s Syndrome screening. Published in 2012. Available from: [ LINK ]
- Hall, Justin and Azra Premji. Essential Med Notes 2015 Obstetrics. Page OB6. PDF. Published 2015.
- Bunt, Christopher W. Role of the Family Physician in the Care of Children with Down Syndrome . AAFP. December 15, 2014. Available from: [ LINK ]
- NHS. What is Down Syndrome? Reviewed in October 2019. Available from: [ LINK ]
- Benn, Peter. Advances in prenatal screening for Down syndrome: II first trimester testing, integrated testing, and future directions . 2002. Available from: [ LINK ]
- Stanford Children’s Health. Risks of Pregnancy Over Age 30. 2020. Available from: [ LINK ]
- Gratias Tom Mundakel. Down Syndrome Questions & Answers: Differential diagnosis. April 30, 2018. Available from: [ LINK ]

Other pages
- Product Bundles 🎉
- Join the Team 🙌
- Institutional Licence 📚
- OSCE Station Creator Tool 🩺
- Create and Share Flashcards 🗂️
- OSCE Group Chat 💬
- Newsletter 📰
- Advertise With Us
Join the community
TRISOMY 21- DOWN SYNDROME
Jan 15, 2011
350 likes | 1.54k Views
TRISOMY 21- DOWN SYNDROME. Dr. Gupta PL-II. Incidence. Approximately one in 1000 live births. Genetics. Trisomy 21 (47, +21), - 94 %, The frequency of trisomy increases with increasing maternal age.
Share Presentation
- obstructive sleep apnea
- less common
- reduced growth rate
- thyroid disease

Presentation Transcript
TRISOMY 21- DOWN SYNDROME Dr. Gupta PL-II
Incidence Approximately one in 1000 live births.
Genetics • Trisomy 21 (47, +21), - 94 %, The frequency of trisomy increases with increasing maternal age. • Robertsonian translocation involving chromosome 21- Approx. 3-4 %, not related to maternal age. • Trisomy 21 mosaicism – 2 to 3 % cases
Head and neck Brachycephaly Up-slanting palpebral fissures Epicanthal folds Brushfield spots Flat nasal bridge Folded or dysplastic ears Open mouth Protruding tongue Short neck Excessive skin at the nape of neck Extremities Shortbroad hands Short fifth finger Incurved fifth finger Transverse palmer crease Space between first and second toe Hyper flexibility of joints Clinical Features
Flat facial profile Poor Moro reflex Excessive skin at the nape of neck Slanted palpebral fissures Hypotonia Hyper flexibility of joints Dysplasia of pelvis Anomalous ears Dysplasia of midphalanx of fifth finger Transverse palmer crease Neonatal features
Mental Retardation • Almost all DS babies have MR. • Mildly to moderately retarded . • Starts in the first year of life. • Average age of sitting(11 mon), and walking (26 mon) is twice the typical age. • First words at 18 months. • IQ declines through the first 10 years of age, reaching a plateau in adolescence that continues into adulthood.
Heart Disease • 50 % of Down Syndrome pts have heart disease • Atrioventricular septal defect • VSD • Secundum ASD • PDA • Tetrology of Fallot • Mitral valve prolapse • AR, MR
GI abnormalities • 5% of cases • Duodenal atresia or stenosis, sometimes assoc with annular pancreas in 2.5 % of cases • Imperforate anus • Esophageal atresia with TE fistula is less common • Hirschsprung’s disease • Strong assoc with celiac disease b/w 5 – 16 % , 5 – 16 fold increase as compared to general population
Growth • BW, length and HC are less in DS • Reduced growth rate • Prevalence of obesity is greater in DS • Weight is less than expected for length in infants with DS, and then increases disproportion ally so that they are obese by age 3-4 yrs
Eye problems Most common disorders are Refractory error – 35 to 76 percent Strabismus – 25 to 57 percent Nystagmus – 18 to 22 percent Cataract occur in 5 % of newborns. Frequency increases with age.
Hearing loss • Unilateral or bilateral • Conductive, sensorineural or mixed • Otitis media is a frequent problem
Hematologic disorders • The risk of leukemia is 1 to 1.5 percent. • 65% of newborn have polycythemia resulting in hypoglycemia. • Risk of AML and ALL is also much higher than the general population. • Transient leukemia – exclusively affects NB. - It is asymptomatic with spontaneous resolution in 2-3 months. - Vesiculopustular skin eruptions are common and resolve with disorder.
Endocrine disorder • Thyroid disease – Hypothyroidism occurs more frequently than hyperthyroidism. • Diabetes – The risk of type 1 diabetes is three times greater than that of the general population.
Reproduction • Women with DS are fertile and may become pregnant. • Nearly all males with DS are infertile. The mechanism is impairment of spermatogenesis
Atlantoaxial instability • Excessive mobility of atlas (C1) and the axis (C2), may lead to subluxation of the cervical spine. • Diagnosis made by lateral neck radiograph. • Patients are advised to avoid contact sports.
Sleep apnea • Obstructive sleep apnea is more common.
Skin disorder • Palmoplantar hyperkeratosis • Seborreic dermatitis • Fissured tongue • Cutis marmorata • Geographical tongue • Xerosis
Diagnosis • Prenatal screening • If no screening – It is recognized from the characteristic phenotypic features. • Confirmed by Karyotype.
Management 1. Growth – Measurements should be plotted on the appropriate growth chart for children with DS. • This will help in prevention of obesity and early diagnosis of celiac disease and hypothyroidism. 2. Cardiac disease – All newborns should be evaluated by cardiac ECHO for CHD in consultation with pediatric cardiologist. 3. Hearing – Screening to be done in the newborn period, every 6 months until 3 yrs of age and then annually.
Management (cont.) 4. Eye disorders - An eye exam should be performed in the newborn period or at least before 6 months of age to detect strabismus, nystagmus, and cataracts. 5. Thyroid Function – Should be done in newborn period and should be repeated at six and 12 months , and then annually. 6. Celiac Disease – Screening should begin at 2 yrs. Repeat screening if signs/Sx develop.
Management ( cont) • Hematology – CBC with differential at birth to evaluate for polycythemia as well as WBC. • Atlanto-axial instability – X ray for evidence of AAI or sub-luxation at 3 to 5 years of age. • Alzheimer’s disease – Adult with a Down Syndrome has earlier onset of symptoms. When diagnosis is considered, thyroid disease and possible depression should be excluded.
Mortality Median age of death has increased from 25 yrs in 1983 to 49 yrs in 1997, an average of 1.7 yrs increase per year. Most likely cause of death is CHD, Dementia, Hypothyroidism and Leukemia. Improved survival is because of increased placements of infants in homes and changes in treatment for common causes of death. Survival is better for males and blacks.
Counseling • May begin when a prenatal diagnosis is made. • Discuss the wide range of variability in manifestation and prognosis. • Medical and educational treatments and interventions should be discussed. • Initial referrals for early intervention, informative publications, parent groups, and advocacy groups.
- More by User
Trisomy 18 or Edward's Syndrome
Trisomy 18 or Edward's Syndrome. By Austin Scharfstein. How does the disorder occur?. Trisomy 18, or Edward's syndrome, is the second most common trisomy after Down's syndrome. Edward's syndrome occurs when three sets (trisomy) of chromosome 18 occur.
3.54k views • 10 slides
Edwards Syndrome- Trisomy 18
Edwards Syndrome- Trisomy 18. Katie Coker 6 th period. Effects.
1.98k views • 9 slides
Down Syndrome
Down Syndrome. Down Syndrome… What is it?. (1) Down Syndrome ( trisomy 21) is a chromosomal condition caused by the presence of all or part of an extra 21 st chromosome.
633 views • 8 slides
Down Syndrome. We have developed a website http://specialededuc3026.wikispaces.com/. The website provides information about Key characteristics of a child with Down Syndrome Useful resources Useful teaching/management strategies Useful websites with links (references)
624 views • 20 slides
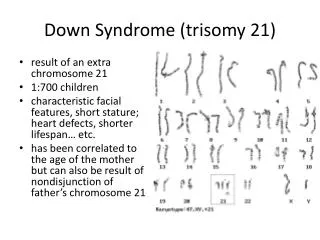
Down Syndrome ( trisomy 21)
Down Syndrome ( trisomy 21). result of an extra chromosome 21 1:700 children characteristic facial features, short stature; heart defects, shorter lifespan… etc. has been correlated to the age of the mother but can also be result of nondisjunction of father’s chromosome 21. Down Syndrome.
1.89k views • 7 slides

Down syndrome
Down syndrome. Megan Rogg ED 243 April 13, 2012. The Basics of Down Syndrome. Genetic Condition: Chromosome deficiency Most common cause of human birth defects There are different levels of severity Screenings and tests are available to determine if an unborn baby has Down Syndrome.
655 views • 22 slides
Trisomy 21: Down Syndrome
Trisomy 21: Down Syndrome. By: Taylor Kresge. Down syndrome occurs in about 1 in every 740 newborns . Type of Genetic Disorder . Down Syndrome is chromosomal disorder (autosomal) caused by an error in cell division that causes an extra 21 st chromosome.
2.14k views • 9 slides
Trisomy 21. By: Cindy Lam. What is it?. Also known as Down syndrome Down syndrome is when a person has 47 chromosomes instead of 46. In Trisomy 21, they have an extra chromosome 21. History. An essay was published in 1866 by John Langdon Down. Originally called “Mongoloids”
541 views • 9 slides
Down Syndrome. Claire Zhang Arjun Rao AP Biology-7 th. Symptoms. Physical development is often slower than normal and most children never reach their average adult height. Flat face Small broad nose Abnormally shaped ears Large tongue
728 views • 13 slides
TRISOMY 21 . Haniyeh Khorramnezhad. trisomy 21.
722 views • 26 slides
Trisomy 21 Down Syndrome
Trisomy 21 Down Syndrome. Marissa Lazenby Comm 1010 . Just ONE extra chromosome!. There’s an extra number 21 chromosome, which makes the child have Down Syndrome. Do parents know their child has down syndrome before birth?.
557 views • 19 slides
Down Syndrome. What is it? __________________________________ _____________________________________________ DS affects 1/________ babies born in the US What causes it? ______________________________ ______________________________________________
196 views • 8 slides
Down Syndrome. By: Colleen Hybl. Chromosomal Abnormalities. 3 Types of Down Syndrome, but all of them occur on the 21 st chromosome as an extra chromosome. 1. Trisomy 21: An entire extra chromosome 21 in all cells, so each one has 47 chromosomes in each body cell.
491 views • 5 slides
Down Syndrome. By: DeAna G. What is the Genetic cause of Down Syndrome?.
950 views • 7 slides

DOWN SYNDROME
By: Ralph Gomez. DOWN SYNDROME. DOWN SYNDROME IN THE 21ST CENTURY. WHAT IS DOWN SYNDROME ?. A chromosomal disorder caused by an error in cell division that results in an extra 21st chromosome
503 views • 11 slides
Down Syndrome. Taylor Arp Emily Payton Monica Tate. Definition/Genetic Cause of Down Syndrome. MT. There are three genetic variations of Down Syndrome: Trisomy 21 Mosaic Down syndrome Translocation Down syndrome. Trisomy 21. MT.
3.65k views • 31 slides
Down syndrome. By: Leah Stavely Issues in Special Education. Silver Metal Winner!!. Special Olympics. Bilingual: English & Spanish speaker. Mi amigita. hhmmm …. Down’s syndrome OR Down syndrome Why?. Down syndrome. “apostrophe s” connotes ownership or possession
1.15k views • 25 slides
Trisomy 21 Down Syndrome. Defining Down Syndrome: *A genetic, chromosomal disorder, specifically involving a third, extra copy of the 21 st chromosome. *Causes mental retardation and slower physical development.
628 views • 14 slides
Trisomy 18 Edwards Syndrome
Trisomy 18 Edwards Syndrome. Trisomy 18, also known as Edwards syndrome, it is caused by a chromosome defect. A trisomy is when a person is born with three chromosomes instead of the normal two chromosomes. So Trisomy 18 is when there is three 18 chormosomes. Three number 18 Chromosomes.
1.33k views • 9 slides
Down Syndrome. By Janet Sobczyk. Strategies and Considerations For Helping Students with DS in the Classroom.
409 views • 17 slides
Down Syndrome (Trisomy 21 ( Trisomy 13 & 18
Down Syndrome (Trisomy 21 ( Trisomy 13 & 18. Dr Pupak Derakhshandeh, PhD Ass Prof Medical Science of Tehran University. What are chromosomes?. Chromosomes are the structures that hold our genes Genes are the individual instructions that tell our bodies how to develop and function
1.35k views • 72 slides

COMMENTS
Down syndrome (DS) is the most common chromosome abnormality among liveborn infants. It is the most frequent form of intellectual disability caused by a microscopically demonstrable chromosomal aberration. DS is characterized by a variety of dysmorphic features, congenital malformations, and other health problems and medical conditions.
Down syndrome is a genetic disorder caused when abnormal cell division results in an extra full or partial copy of chromosome 21. This extra genetic material causes the developmental changes and physical features of Down syndrome. Down syndrome varies in severity among individuals, causing lifelong intellectual disability and developmental delays.
Down syndrome was first described by an English physician, John Langdon Down, in 1866, but its association with chromosome 21 was established almost 100 years later by Dr. Jerome Lejeune in Paris. It is the presence of all or part of the third copy of chromosome 21 that causes Down syndrome, the most common chromosomal abnormality occurring in humans.[1] It is also found that the most ...
A history of possible physical or sexual abuse. Symptoms of atlantoaxial instability include the following: About 13-14% of patients have radiographic evidence of atlantoaxial instability but no symptoms. Only 1-2% of patients have symptoms that require treatment. Symptoms include easy fatigability, neck pain, limited neck mobility or head tilt ...
What it is. Down syndrome is a condition in which a person has an extra copy of chromosome 21. Chromosomes are small "packages" of genes in the body's cells, which determine how the body forms and functions. When babies are growing, the extra chromosome changes how their body and brain develop. This can cause both physical and mental challenges.
The integrated screening test is done in two parts during the first and second trimesters of pregnancy. The results are combined to estimate the risk that your baby has Down syndrome. First trimester. Part one includes a blood test to measure PAPP-A and an ultrasound to measure nuchal translucency. Second trimester.
Trisomy 21 is the most common chromosomal anomaly in humans, affecting about 5,000 babies born each year and more than 350,000 people in the United States. Also known as Down syndrome, trisomy 21 is a genetic condition caused by an extra chromosome. Most babies inherit 23 chromosomes from each parent, for a total of 46 chromosomes.
According to the Centers for Disease Control and Prevention, approximately one in every 775 babies in the United States is born with Down syndrome, making Down syndrome the most common chromosomal condition. About 5,000 babies with Down syndrome are born in the United States each year. -De Graaf, G., Buckley, F., & Skotko, B. (2024, May 3).
People who have Down syndrome have learning difficulties, mental disability, a characteristic facial appearance, and poor muscle tone (hypotonia) in infancy. Individuals with Down syndrome also have an increased risk for having heart defects, digestive problems such as gastroesophageal reflux or celiac disease, and hearing loss.
People with Down syndrome have an extra chromosome that impacts their looks and their ability to think, learn, and reason. Discover the type, causes, and kinds of effects it can have.
Trisomy 21: In this type of Down syndrome, each cell in the body has three separate copies of chromosome 21 instead of the usual 2 copies. About 95% of people with Down syndrome have this type. Translocation Down syndrome: This occurs when an extra part or a whole extra chromosome 21 is present, but it is attached to a different chromosome ("trans-located") rather than being a separate ...
Down's syndrome is the most common genetic cause of cognitive or intellectual disability, with a prevalence of 1 in 800 births worldwide. Characteristic physical features include brachycephaly with a flat occiput; epicanthal folds and upslanting palpebral fissures; Brushfield spots in the iris; low nasal bridge; low-set ears; broad neck; and small hands with transverse crease.
Down syndrome is a genetic disorder characterized by distinctive facial and physical features, developmental delays, mild to moderate intellectual disability, and an increased risk of many diseases and disorders, including heart disease, epilepsy, Alzheimer's disease, and infertility. The types and severity of symptoms can vary from one person ...
Down syndrome (DS) is the most common genomic disorder of intellectual disability and is caused by trisomy of Homo sapiens chromosome 21 (HSA21). The eponym of the syndrome is from Down, who described the clinical aspects of the syndrome in 1866 (REF. 1).The DS phenotype involves manifestations that affect multiple bodily systems, in particular the musculoskeletal, neurological and ...
Down syndrome (DS) is a genetic condition caused by an extra chromosome 21. It causes delays in physical and intellectual development. The document defines DS, discusses its etiology and pathophysiology, risk factors, clinical manifestations, diagnostic tests, treatments, nursing management, nursing diagnoses and interventions, and prevention and education strategies.
Down syndrome is a genetic disorder caused by the presence of all or part of a third copy of chromosome 21. It causes delays in physical and intellectual development and is the most common chromosome abnormality in humans, affecting approximately 1 in 800 live births. The signs and symptoms include cognitive impairment and characteristic facial ...
Down syndrome is a genetic condition that occurs in 1 of every 750 live births in Canada. affects people of all ages, races, and economic levels and is the most frequently occurring chromosomal abnormality. More than 45,000 people have Down syndrome in Canada. The most common form of Down syndrome, Trisomy 21, occurs when there are three ...
Down syndrome (DS) is a genetic condition caused by an extra chromosome 21. It causes delays in physical and intellectual development. The document defines DS, discusses its etiology and pathophysiology, risk factors, clinical manifestations, diagnostic tests, treatments, nursing management, nursing diagnoses and interventions, and prevention and education strategies.
Presentation Transcript. Trisomy 21 MT • A child with Trisomy 21 has three copies of chromosome 21 — instead of the usual two copies — in all of his or her cells. • This form of Down syndrome is caused by abnormal cell division during the development of the sperm cell or the egg cell. Mosaic Down syndrome MT • Rare form of Down ...
Introduction. Down's syndrome (DS), also known as trisomy 21, is the most common congenital chromosomal abnormality, occurring in about 1 in 800 to 1 in 1000 live births. 1,2 The presence of additional genetic material from chromosome 21 results in characteristic phenotypic features and increased morbidity through its effect on multiple organ ...
Down Syndrome PPT - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Introduction to Down's Syndrome types, clinical manifestations, diagnosis, medical and detailed Physiotherapy Management of Down's Syndrome.
Presentation Transcript. TRISOMY 21- DOWN SYNDROME Dr. Gupta PL-II. Incidence Approximately one in 1000 live births. Genetics • Trisomy 21 (47, +21), - 94 %, The frequency of trisomy increases with increasing maternal age. • Robertsonian translocation involving chromosome 21- Approx. 3-4 %, not related to maternal age.
1 INTRODUCTION. Down syndrome (DS) is a congenital chromosomal anomaly caused by trisomy 21 (þ21) and is associated with various complications such as infections, congenital heart or digestive tract diseases, mental retardation, and developmental delays. 1, 2 Individuals with DS have a significantly higher risk (10-30 times higher) of developing hematological malignancies compared to those ...
Scans of a Neanderthal child's inner ear revealed anomalies consistent with Down syndrome. Mercedes Conde-Valverde et al.. Because the child was born with its condition, the findings at Cova Negra suggest something different: that the Neanderthals looked after members of the group simply because they cared for them, not because they expected to be repaid in material terms.
When Amanda Vellon opened the Inclusion Coffee Shop — the only café in the small borough of Elmer in Salem County — her goal was to live up to the restaurant's name and welcome the community.