An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection


Impact of COVID-19 pandemic on mental health in the general population: A systematic review
Jiaqi xiong.
a Department of Pharmacology and Toxicology, University of Toronto, Toronto, ON
Orly Lipsitz
c Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, Ontario
Flora Nasri
Leanna m.w. lui, hartej gill, david chen-li, michelle iacobucci.
e Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
f Institute for Health Innovation and Technology (iHealthtech), National University of Singapore, Singapore
Amna Majeed
Roger s. mcintyre.
b Department of Psychiatry, University of Toronto, Toronto, Ontario
d Brain and Cognition Discovery Foundation, Toronto, ON
Associated Data
As a major virus outbreak in the 21st century, the Coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented hazards to mental health globally. While psychological support is being provided to patients and healthcare workers, the general public's mental health requires significant attention as well. This systematic review aims to synthesize extant literature that reports on the effects of COVID-19 on psychological outcomes of the general population and its associated risk factors.
A systematic search was conducted on PubMed, Embase, Medline, Web of Science, and Scopus from inception to 17 May 2020 following the PRISMA guidelines. A manual search on Google Scholar was performed to identify additional relevant studies. Articles were selected based on the predetermined eligibility criteria.
Results: Relatively high rates of symptoms of anxiety (6.33% to 50.9%), depression (14.6% to 48.3%), post-traumatic stress disorder (7% to 53.8%), psychological distress (34.43% to 38%), and stress (8.1% to 81.9%) are reported in the general population during the COVID-19 pandemic in China, Spain, Italy, Iran, the US, Turkey, Nepal, and Denmark. Risk factors associated with distress measures include female gender, younger age group (≤40 years), presence of chronic/psychiatric illnesses, unemployment, student status, and frequent exposure to social media/news concerning COVID-19.
Limitations
A significant degree of heterogeneity was noted across studies.
Conclusions
The COVID-19 pandemic is associated with highly significant levels of psychological distress that, in many cases, would meet the threshold for clinical relevance. Mitigating the hazardous effects of COVID-19 on mental health is an international public health priority.
1. Introduction
In December 2019, a cluster of atypical cases of pneumonia was reported in Wuhan, China, which was later designated as Coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) on 11 Feb 2020 ( Anand et al., 2020 ). The causative virus, SARS-CoV-2, was identified as a novel strain of coronaviruses that shares 79% genetic similarity with SARS-CoV from the 2003 SARS outbreak ( Anand et al., 2020 ). On 11 Mar 2020, the WHO declared the outbreak a global pandemic ( Anand et al., 2020 ).
The rapidly evolving situation has drastically altered people's lives, as well as multiple aspects of the global, public, and private economy. Declines in tourism, aviation, agriculture, and the finance industry owing to the COVID-19 outbreak are reported as massive reductions in both supply and demand aspects of the economy were mandated by governments internationally ( Nicola et al., 2020 ). The uncertainties and fears associated with the virus outbreak, along with mass lockdowns and economic recession are predicted to lead to increases in suicide as well as mental disorders associated with suicide. For example, McIntyre and Lee (2020b) have reported a projected increase in suicide from 418 to 2114 in Canadian suicide cases associated with joblessness. The foregoing result (i.e., rising trajectory of suicide) was also reported in the USA, Pakistan, India, France, Germany, and Italy ( Mamun and Ullah, 2020 ; Thakur and Jain, 2020 ). Separate lines of research have also reported an increase in psychological distress in the general population, persons with pre-existing mental disorders, as well as in healthcare workers ( Hao et al., 2020 ; Tan et al., 2020 ; Wang et al., 2020b ). Taken together, there is an urgent call for more attention given to public mental health and policies to assist people through this challenging time.
The objective of this systematic review is to summarize extant literature that reported on the prevalence of symptoms of depression, anxiety, PTSD, and other forms of psychological distress in the general population during the COVID-19 pandemic. An additional objective was to identify factors that are associated with psychological distress.
Methods and results were formated based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines ( Moher et al., 2010 ).
2.1. Search strategy
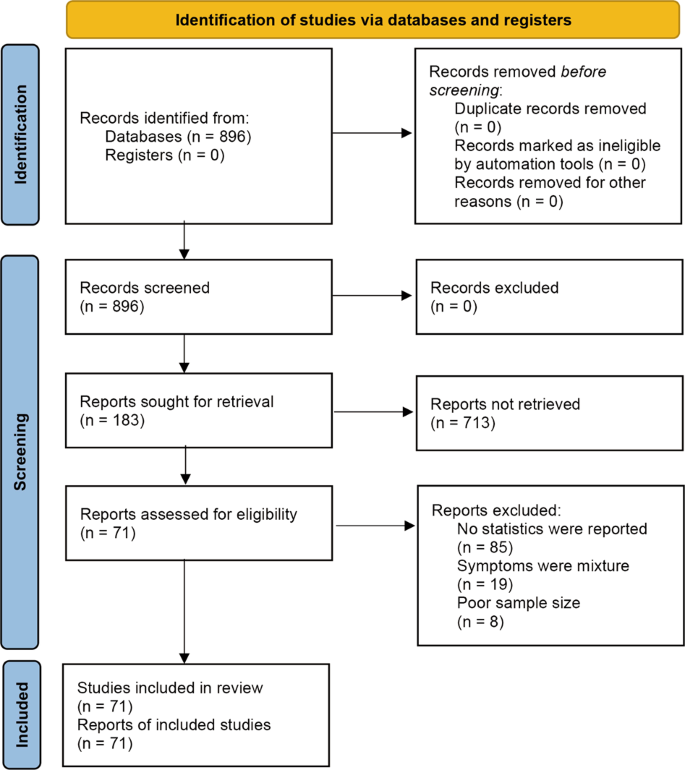
A systematic search following the PRISMA 2009 flow diagram ( Fig. 1 ) was conducted on PubMed, Medline, Embase, Scopus, and Web of Science from inception to 17 May 2020. A manual search on Google Scholar was performed to identify additional relevant studies. The search terms that were used were: (COVID-19 OR SARS-CoV-2 OR Severe acute respiratory syndrome coronavirus 2 OR 2019nCoV OR HCoV-19) AND (Mental health OR Psychological health OR Depression OR Anxiety OR PTSD OR PTSS OR Post-traumatic stress disorder OR Post-traumatic stress symptoms) AND (General population OR general public OR Public OR community). An example of search procedure was included as a supplementary file.

Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) study selection flow diagram. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
2.2. Study selection and eligibility criteria
Titles and abstracts of each publication were screened for relevance. Full-text articles were accessed for eligibility after the initial screening. Studies were eligible for inclusion if they: 1) followed cross-sectional study design; 2) assessed the mental health status of the general population/public during the COVID-19 pandemic and its associated risk factors; 3) utilized standardized and validated scales for measurement. Studies were excluded if they: 1) were not written in English or Chinese; 2) focused on particular subgroups of the population (e.g., healthcare workers, college students, or pregnant women); 3) were not peer-reviewed; 4) did not have full-text availability.
2.3. Data extraction
A data extraction form was used to include relevant data: (1) Lead author and year of publication, (2) Country/region of the population studied, (3) Study design, (4) Sample size, (5) Sample characteristics, (6) Assessment tools, (7) Prevalence of symptoms of depression/anxiety/ PTSD/psychological distress/stress, (8) Associated risk factors.
2.4 Quality appraisal
The Newcastle-Ottawa Scale (NOS) adapted for cross-sectional studies was used for study quality appraisal, which was modified accordingly from the scale used in Epstein et al. (2018) . The scale consists of three dimensions: Selection, Comparability, and Outcome. There are seven categories in total, which assess the representativeness of the sample, sample size justification, comparability between respondents and non-respondents, ascertainments of exposure, comparability based on study design or analysis, assessment of the outcome, and appropriateness of statistical analysis. A list of specific questions was attached as a supplementary file. A total of nine stars can be awarded if the study meets certain criteria, with a maximum of four stars assigned for the selection dimension, a maximum of two stars assigned for the comparability dimension, and a maximum of three stars assigned for the outcome dimension.
3.1. Search results
In total, 648 publications were identified. Of those, 264 were removed after initial screening due to duplication. 343 articles were excluded based on the screening of titles and abstracts. 41 full-text articles were assessed for eligibility. There were 12 articles excluded for studying specific subgroups of the population, five articles excluded for not having a standardized/ appropriate measure, three articles excluded for being review papers, and two articles excluded for being duplicates. Following the full-text screening, 19 studies met the inclusion criteria.
3.2. Study characteristics
Study characteristics and primary study findings are summarized in Table 1 . The sample size of the 19 studies ranged from 263 to 52,730 participants, with a total of 93,569 participants. A majority of study participants were over 18 years old. Female participants ( n = 60,006) made up 64.1% of the total sample. All studies followed a cross-sectional study design. The 19 studies were conducted in eight different countries, including China ( n = 10), Spain ( n = 2), Italy ( n = 2), Iran ( n = 1), the US ( n = 1), Turkey ( n = 1), Nepal ( n = 1), and Denmark ( n = 1). The primary outcomes chosen in the included studies varied across studies. Twelve studies included measures of depressive symptoms while eleven studies included measures of anxiety. Symptoms of PTSD/psychological impact of events were evaluated in four studies while three studies assessed psychological distress. It was additionally observed that four studies contained general measures of stress. Three studies did not explicitly report the overall prevalence rates of symptoms; notwithstanding the associated risk factors were identified and discussed.
Summary of study sample characteristics, study design, assessment tools used, prevalence rates and associated risk factors.
3.3. Quality appraisal
The result of the study quality appraisal is presented in Table 2 . The overall quality of the included studies is moderate, with total stars awarded varying from four to eight. There were two studies with four stars, two studies with five stars, seven studies with six stars, seven studies with seven stars, and one study with eight stars.
Results of study quality appraisal of the included studies.
3.4. Measurement tools
A variety of scales were used in the studies ( n = 19) for assessing different adverse psychological outcomes. The Beck Depression Inventory-II (BDI-II), Patient Health Questionnaire-9/2 (PHQ-9/2), Self-rating Depression Scales (SDS), The World Health Organization-Five Well-Being Index (WHO-5), and Center for Epidemiologic Studies Depression Scale (CES-D) were used for measuring depressive symptoms. The Beck Anxiety Inventory (BAI), Generalized Anxiety Disorder 7/2-item (GAD-7/2), and Self-rating Anxiety Scale (SAS) were used to evaluate symptoms of anxiety. The Depression, Anxiety, and Stress Scale- 21 items (DASS-21) was used for the evaluation of depression, anxiety, and stress symptoms. The Hospital Anxiety and Depression Scale (HADS) was used for assessing anxiety and depressive symptoms. Psychological distress was measured by The Peritraumatic Distress Inventory (CPDI) and the Kessler Psychological Distress Scale (K6/10). Symptoms of PTSD were assessed by The Impact of Event Scale-(Revised) (IES(-R)), PTSD Checklist (PCL-(C)-2/5). Chinese Perceived Stress Scale (CPSS-10) was used in one study to evaluate symptoms of stress.
3.5. Symptoms of depression and associated risk factors
Symptoms of depression were assessed in 12 out of the 19 studies ( Ahmed et al., 2020 ; Gao et al., 2020 ; González-Sanguino et al., 2020 ; Huang and Zhao, 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Olagoke et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ; Özdin and S.B. Özdin, 2020 ; Sønderskov et al., 2020 ; Wang et al., 2020a ; Wang et al., 2020b ). The prevalence of depressive symptoms ranged from 14.6% to 48.3%. Although the reported rates are higher than previously estimated one-year prevalence (3.6% and 7.2%) of depression among the population prior to the pandemic ( Huang et al., 2019 ; Lim et al., 2018 ), it is important to note that presence of depressive symptoms does not reflect a clinical diagnosis of depression.
Many risk factors were identified to be associated with symptoms of depression amongst the COVID-19 pandemic. Females were reported as are generally more likely to develop depressive symptoms when compared to their male counterparts ( Lei et al., 2020 ; Mazza et al., 2020 ; Sønderskov et al., 2020 ; Wang et al., 2020a ). Participants from the younger age group (≤40 years) presented with more depressive symptoms ( Ahmed et al., 2020 ; Gao et al., 2020 ; Huang and Zhao, 2020 ; Lei et al., 2020 ; Olagoke et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ;). Student status was also found to be a significant risk factor for developing more depressive symptoms as compared to other occupational statuses (i.e. employment or retirement) ( González et al., 2020 ; Lei et al., 2020 ; Olagoke et al., 2020 ). Four studies also identified lower education levels as an associated factor with greater depressive symptoms ( Gao et al., 2020 ; Mazza et al., 2020 ; Olagoke et al., 2020 ; Wang et al., 2020a ). A single study by Wang et al., 2020b reported that people with higher education and professional jobs exhibited more depressive symptoms in comparison to less educated individuals and those in service or enterprise industries.
Other predictive factors for symptoms of depression included living in urban areas, poor self-rated health, high loneliness, being divorced/widowed, being single, lower household income, quarantine status, worry about being infected, property damage, unemployment, not having a child, a past history of mental stress or medical problems, having an acquaintance infected with COVID-19, perceived risks of unemployment, exposure to COVID-19 related news, higher perceived vulnerability, lower self-efficacy to protect themselves, the presence of chronic diseases, and the presence of specific physical symptoms ( Gao et al., 2020 ; González-Sanguino et al., 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Olagoke et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ; Özdin and Özdin, 2020 ; Wang et al., 2020a ).
3.6. Symptoms of anxiety and associated risk factors
Anxiety symptoms were assessed in 11 out of the 19 studies, with a noticeable variation in the prevalence of anxiety symptoms ranging from 6.33% to 50.9% ( Ahmed et al., 2020 ; Gao et al., 2020 ; González-Sanguino et al., 2020 ; Huang and Zhao, 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Moghanibashi-Mansourieh, 2020 ; Ozamiz-Etxebarria et al., 2020 ; Özdin and Özdin, 2020 ; Wang et al., 2020a ; Wang et al., 2020b ).
Anxiety is often comorbid with depression ( Choi et al., 2020 ). Some predictive factors for depressive symptoms also apply to symptoms of anxiety, including a younger age group (≤40 years), lower education levels, poor self-rated health, high loneliness, female gender, divorced/widowed status, quarantine status, worry about being infected, property damage, history of mental health issue/medical problems, presence of chronic illness, living in urban areas, and the presence of specific physical symptoms ( Ahmed et al., 2020 ; Gao et al., 2020 ; González-Sanguino et al., 2020 ; Huang and Zhao, 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Moghanibashi-Mansourieh, 2020 ; Ozamiz-Etxebarria et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ; Wang et al., 2020a ; Wang et al., 2020b ).
Additionally, social media exposure or frequent exposure to news/information concerning COVID-19 was positively associated with symptoms of anxiety ( Gao et al., 2020 ; Moghanibashi-Mansourieh, 2020 ). With respect to marital status, one study reported that married participants had higher levels of anxiety when compared to unmarried participants ( Gao et al., 2020 ). On the other hand, Lei et al. (2020) found that divorced/widowed participants developed more anxiety symptoms than single or married individuals. A prolonged period of quarantine was also correlated with higher risks of anxiety symptoms. Intuitively, contact history with COVID-positive patients or objects may lead to more anxiety symptoms, which is noted in one study ( Moghanibashi-Mansourieh, 2020 ).
3.7. Symptoms of PTSD/ psychological distress/stress and associated risk factors
With respect to PTSD symptoms, similar prevalence rates were reported by Zhang and Ma (2020) and N. Liu et al. (2020) at 7.6% and 7%, respectively. Despite using the same measurement scale as Zhang and Ma (2020) (i.e., IES), Wang et al. (2020a) noted a remarkably different result, with 53.8% of the participants reporting moderate-to-severe psychological impact. González et al. ( González-Sanguino et al., 2020 ) noted 15.8% of participants with PTSD symptoms. Three out of the four studies that measured the traumatic effects of COVID-19 reported that the female gender was more susceptible to develop symptoms of PTSD. In contrast, the research conducted by Zhang and Ma (2020) found no significant difference in IES scores between females and males. Other risk factors included loneliness, individuals currently residing in Wuhan or those who have been to Wuhan in the past several weeks (the hardest-hit city in China), individuals with higher susceptibility to the virus, poor sleep quality, student status, poor self-rated health, and the presence of specific physical symptoms. Besides sex, Zhang and Ma (2020) found that age, BMI, and education levels are also not correlated with IES-scores.
Non-specific psychological distress was also assessed in three studies. One study reported a prevalence rate of symptoms of psychological distress at 38% ( Moccia et al., 2020 ), while another study from Qiu et al. (2020) reported a prevalence of 34.43%. The study from Wang et al. (2020) did not explicitly state the prevalence rates, but the associated risk factors for higher psychological distress symptoms were reported (i.e., younger age groups and female gender are more likely to develop psychological distress) ( Qiu et al., 2020 ; Wang et al., 2020 ). Other predictive factors included being migrant workers, profound regional severity of the outbreak, unmarried status, the history of visiting Wuhan in the past month, higher self-perceived impacts of the epidemic ( Qiu et al., 2020 ; Wang et al., 2020 ). Interestingly, researchers have identified personality traits to be predictive of psychological distresses. For example, persons with negative coping styles, cyclothymic, depressive, and anxious temperaments exhibit greater susceptibility to psychological outcomes ( Wang et al., 2020 ; Moccia et al., 2020 ).
The intensity of overall stress was evaluated and reported in four studies. The prevalence of overall stress was variably reported between 8.1% to over 81.9% ( Wang et al., 2020a ; Samadarshi et al., 2020 ; Mazza et al., 2020 ). Females and the younger age group are often associated with higher stress levels as compared to males and the elderly. Other predictive factors of higher stress levels include student status, a higher number of lockdown days, unemployment, having to go out to work, having an acquaintance infected with the virus, presence of chronic illnesses, poor self-rated health, and presence of specific physical symptoms ( Wang et al., 2020a ; Samadarshi et al., 2020 ; Mazza et al., 2020 ).
3.8. A separate analysis of negative psychological outcomes
Out of the nineteen included studies, five studies appeared to be more representative of the general population based on the results of study quality appraisal ( Table 1 ). A separate analysis was conducted for a more generalizable conclusion. According to the results of these studies, the rates of negative psychological outcomes were moderate but higher than usual, with anxiety symptoms ranging from 6.33% to 18.7%, depressive symptoms ranging from 14.6% to 32.8%, stress symptoms being 27.2%, and symptoms of PTSD being approximately 7% ( Lei et al., 2020 ; Liu et al., 2020 ; Mazza et al., 2020 ; Wang et al., 2020b ; Zhang et al., 2020 ). In these studies, female gender, younger age group (≤40 years), and student population were repetitively reported to exhibit more adverse psychiatric symptoms.
3.9. Protective factors against symptoms of mental disorders
In addition to associated risk factors, a few studies also identified factors that protect individuals against symptoms of psychological illnesses during the pandemic. Timely dissemination of updated and accurate COVID-19 related health information from authorities was found to be associated with lower levels of anxiety, stress, and depressive symptoms in the general public ( Wang et al., 2020a ). Additionally, actively carrying out precautionary measures that lower the risk of infection, such as frequent handwashing, mask-wearing, and less contact with people also predicted lower psychological distress levels during the pandemic ( Wang et al., 2020a ). Some personality traits were shown to correlate with positive psychological outcomes. Individuals with positive coping styles, secure and avoidant attachment styles usually presented fewer symptoms of anxiety and stress ( Wang et al., 2020 ; Moccia et al., 2020 ). ( Zhang et al. 2020 ) also found that participants with more social support and time to rest during the pandemic exhibited lower stress levels.
4. Discussion
Our review explored the mental health status of the general population and its predictive factors amid the COVID-19 pandemic. Generally, there is a higher prevalence of symptoms of adverse psychiatric outcomes among the public when compared to the prevalence before the pandemic ( Huang et al., 2019 ; Lim et al., 2018 ). Variations in prevalence rates across studies were noticed, which could have resulted from various measurement scales, differential reporting patterns, and possibly international/cultural differences. For example, some studies reported any participants with scores above the cut-off point (mild-to-severe symptoms), while others only included participants with moderate-to-severe symptoms ( Moghanibashi-Mansourieh, 2020 ; Wang et al., 2020a ). Regional differences existed with respect to the general public's psychological health during a massive disease outbreak due to varying degrees of outbreak severity, national economy, government preparedness, availability of medical supplies/ facilities, and proper dissemination of COVID-related information. Additionally, the stage of the outbreak in each region also affected the psychological responses of the public. Symptoms of adverse psychological outcomes were more commonly seen at the beginning of the outbreak when individuals were challenged by mandatory quarantine, unexpected unemployment, and uncertainty associated with the outbreak ( Ho et al., 2020 ). When evaluating the psychological impacts incurred by the coronavirus outbreak, the duration of psychiatric symptoms should also be taken into consideration since acute psychological responses to stressful or traumatic events are sometimes protective and of evolutionary importance ( Yaribeygi et al., 2017 ; Brosschot et al., 2016 ; Gilbert, 2006 ). Being anxious and stressed about the outbreak mobilizes people and forces them to implement preventative measures to protect themselves. Follow-up studies after the pandemic may be needed to assess the long-term psychological impacts of the COVID-19 pandemic.
4.1. Populations with greater susceptibility
Several predictive factors were identified from the studies. For example, females tended to be more vulnerable to develop the symptoms of various forms of mental disorders during the pandemic, including depression, anxiety, PTSD, and stress, as reported in our included studies ( Ahmed et al., 2020 ; Gao et al., 2020 ; Lei et al., 2020 ). Greater psychological distress arose in women partially because they represent a higher percentage of the workforce that may be negatively affected by COVID-19, such as retail, service industry, and healthcare. In addition to the disproportionate effects that disruption in the employment sector has had on women, several lines of research also indicate that women exhibit differential neurobiological responses when exposed to stressors, perhaps providing the basis for the overall higher rate of select mental disorders in women ( Goel et al., 2014 ; Eid et al., 2019 ).
Individuals under 40 years old also exhibited more adverse psychological symptoms during the pandemic ( Ahmed et al., 2020 ; Gao et al., 2020 ; Huang and Zhao, 2020 ). This finding may in part be due to their caregiving role in families (i.e., especially women), who provide financial and emotional support to children or the elderly. Job loss and unpredictability caused by the COVID-19 pandemic among this age group could be particularly stressful. Also, a large proportion of individuals under 40 years old consists of students who may also experience more emotional distress due to school closures, cancelation of social events, lower study efficiency with remote online courses, and postponements of exams ( Cao et al., 2020 ). This is consistent with our findings that student status was associated with higher levels of depressive symptoms and PTSD symptoms during the COVID-19 outbreak ( Lei et al., 2020 ; Olagoke et al., 2020 , Wang et al., 2020a ; Samadarshi et al., 2020 ).
People with chronic diseases and a history of medical/ psychiatric illnesses showed more symptoms of anxiety and stress ( Mazza et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ; Özdin and Özdin, 2020 ). The anxiety and distress of chronic disease sufferers towards the coronavirus infection partly stem from their compromised immunity caused by pre-existing conditions, which renders them susceptible to the infection and a higher risk of mortality, such as those with systemic lupus erythematosus ( Sawalha et al., 2020 ). Several reports also suggested that a substantially higher death rate was noted in patients with diabetes, hypertension and other coronary heart diseases, yet the exact causes remain unknown ( Guo et al., 2020 ; Emami et al., 2020 ), leaving those with these common chronic conditions in fear and uncertainty. Additionally, another practical aspect of concern for patients with pre-existing conditions would be postponement and inaccessibility to medical services and treatment as a result of the COVID-19 pandemic. For example, as a rapidly growing number of COVID-19 patients were utilizing hospital and medical resources, primary, secondary, and tertiary prevention of other diseases may have unintentionally been affected. Individuals with a history of mental disorders or current diagnoses of psychiatric illnesses are also generally more sensitive to external stressors, such as social isolation associated with the pandemic ( Ho et al., 2020 ).
4.2. COVID-19 related psychological stressors
Several studies identified frequent exposure to social media/news relating to COVID-19 as a cause of anxiety and stress symptoms ( Gao et al., 2020 ; Moghanibashi-Mansourieh, 2020 ). Frequent social media use exposes oneself to potential fake news/reports/disinformation and the possibility for amplified anxiety. With the unpredictable situation and a lot of unknowns about the novel coronavirus, misinformation and fake news are being easily spread via social media platforms ( Erku et al., 2020 ), creating unnecessary fears and anxiety. Sadness and anxious feelings could also arise when constantly seeing members of the community suffering from the pandemic via social media platforms or news reports ( Li et al., 2020 ).
Reports also suggested that poor economic status, lower education level, and unemployment are significant risk factors for developing symptoms of mental disorders, especially depressive symptoms during the pandemic period ( Gao et al., 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Olagoke et al., 2020 ;). The coronavirus outbreak has led to strictly imposed stay-home-order and a decrease in demands for services and goods ( Nicola et al., 2020 ), which has adversely influenced local businesses and industries worldwide. Surges in unemployment rates were noted in many countries ( Statistics Canada, 2020 ; Statista, 2020 ). A decrease in quality of life and uncertainty as a result of financial hardship can put individuals into greater risks for developing adverse psychological symptoms ( Ng et al., 2013 ).
4.3. Efforts to reduce symptoms of mental disorders
4.3.1. policymaking.
The associated risk and protective factors shed light on policy enactment in an attempt to relieve the psychological impacts of the COVID-19 pandemic on the general public. Firstly, more attention and assistance should be prioritized to the aforementioned vulnerable groups of the population, such as the female gender, people from age group ≤40, college students, and those suffering from chronic/psychiatric illnesses. Secondly, governments must ensure the proper and timely dissemination of COVID-19 related information. For example, validation of news/reports concerning the pandemic is essential to prevent panic from rumours and false information. Information about preventative measures should also be continuously updated by health authorities to reassure those who are afraid of being infected ( Tran, et al., 2020a ). Thirdly, easily accessible mental health services are critical during the period of prolonged quarantine, especially for those who are in urgent need of psychological support and individuals who reside in rural areas ( Tran et al., 2020b ). Since in-person health services are limited and delayed as a result of COVID-19 pandemic, remote mental health services can be delivered in the form of online consultation and hotlines ( Liu et al., 2020 ; Pisciotta et al., 2019 ). Last but not least, monetary support (e.g. beneficial funds, wage subsidy) and new employment opportunities could be provided to people who are experiencing financial hardship or loss of jobs owing to the pandemic. Government intervention in the form of financial provisions, housing support, access to psychiatric first aid, and encouragement at the individual level of healthy lifestyle behavior has been shown effective in alleviating suicide cases associated with economic recession ( McIntyre and Lee, 2020a ). For instance, declines in suicide incidence were observed to be associated with government expenses in Japan during the 2008 economic depression ( McIntyre and Lee, 2020a ).
4.3.2. Individual efforts
Individuals can also take initiatives to relieve their symptoms of psychological distress. For instance, exercising regularly and maintaining a healthy diet pattern have been demonstrated to effectively ease and prevent symptoms of depression or stress ( Carek et al., 2011 ; Molendijk et al., 2018 ; Lassale et al., 2019 ). With respect to pandemic-induced symptoms of anxiety, it is also recommended to distract oneself from checking COVID-19 related news to avoid potential false reports and contagious negativity. It is also essential to obtain COVID-19 related information from authorized news agencies and organizations and to seek medical advice only from properly trained healthcare professionals. Keeping in touch with friends and family by phone calls or video calls during quarantine can ease the distress from social isolation ( Hwang et al., 2020 ).
4.4. Strengths
Our paper is the first systematic review that examines and summarizes existing literature with relevance to the psychological health of the general population during the COVID-19 outbreak and highlights important associated risk factors to provide suggestions for addressing the mental health crisis amid the global pandemic.
4.5. Limitations
Certain limitations apply to this review. Firstly, the description of the study findings was qualitative and narrative. A more objective systematic review could not be conducted to examine the prevalence of each psychological outcome due to a high heterogeneity across studies in the assessment tools used and primary outcomes measured. Secondly, all included studies followed a cross-sectional study design and, as such, causal inferences could not be made. Additionally, all studies were conducted via online questionnaires independently by the study participants, which raises two concerns: 1] Individual responses in self-assessment vary in objectivity when supervision from a professional psychiatrist/ interviewer is absent, 2] People with poor internet accessibility were likely not included in the study, creating a selection bias in the population studied. Another concern is the over-representation of females in most studies. Selection bias and over-representation of particular groups indicate that most studies may not be representative of the true population. Importantly, studies in inclusion were conducted in a limited number of countries. Thus generalizations of mental health among the general population at a global level should be made cautiously.
5. Conclusion
This systematic review examined the psychological status of the general public during the COVID-19 pandemic and stressed the associated risk factors. A high prevalence of adverse psychiatric symptoms was reported in most studies. The COVID-19 pandemic represents an unprecedented threat to mental health in high, middle, and low-income countries. In addition to flattening the curve of viral transmission, priority needs to be given to the prevention of mental disorders (e.g. major depressive disorder, PTSD, as well as suicide). A combination of government policy that integrates viral risk mitigation with provisions to alleviate hazards to mental health is urgently needed.
Authorship contribution statement
JX contributed to the overall design, article selection , review, and manuscript preparation. LL and JX contributed to study quality appraisal. All other authors contributed to review, editing, and submission.
Declaration of Competing Interest
Acknowledgements.
RSM has received research grant support from the Stanley Medical Research Institute and the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/National Natural Science Foundation of China and speaker/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.jad.2020.08.001 .
Appendix. Supplementary materials
- Ahmed M.Z., Ahmed O., Zhou A., Sang H., Liu S., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 2020; 51 doi: 10.1016/j.ajp.2020.102092. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Anand K.B., Karade S., Sen S., Gupta R.M. SARS-CoV-2: camazotz's curse. Med. J. Armed Forces India. 2020; 76 :136–141. doi: 10.1016/j.mjafi.2020.04.008. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brosschot J.F., Verkuil B., Thayer J.F. The default response to uncertainty and the importance of perceived safety in anxiety and stress: an evolution-theoretical perspective. J. Anxiety Disord. 2016; 41 :22–34. doi: 10.1016/j.janxdis.2016.04.012. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020; 287 doi: 10.1016/j.psychres.2020.112934. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carek P.J., Laibstain S.E., Carek S.M. Exercise for the treatment of depression and anxiety. Int. J. Psychiatry Med. 2011; 41 (1):15–28. doi: 10.2190/PM.41.1.c. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Choi K.W., Kim Y., Jeon H.J. Comorbid Anxiety and Depression: clinical and Conceptual Consideration and Transdiagnostic Treatment. Adv. Exp. Med. Biol. 2020; 1191 :219–235. doi: 10.1007/978-981-32-9705-0_14. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eid R.S., Gobinath A.R., Galea L.A.M. Sex differences in depression: insights from clinical and preclinical studies. Prog. Neurobiol. 2019; 176 :86–102. doi: 10.1016/j.pneurobio.2019.01.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of Underlying Diseases in Hospitalized Patients. Arch. Acad. Emerg. Med. 2020; 8 (1):e35. doi: 10.22037/aaem.v8i1.600.g748. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Epstein S., Roberts E., Sedgwick R., Finning K., Ford T., Dutta R., Downs J. Poor school attendance and exclusion: a systematic review protocol on educational risk factors for self-harm and suicidal behaviours. BMJ Open. 2018; 8 (12) doi: 10.1136/bmjopen-2018-023953. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Erku D.A., Belachew S.W., Abrha S., Sinnollareddy M., Thoma J., Steadman K.J., Tesfaye W.H. When fear and misinformation go viral: pharmacists' role in deterring medication misinformation during the 'infodemic' surrounding COVID-19. Res. Social. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.032. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020; 15 (4) doi: 10.1371/journal.pone.0231924. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gilbert P. Evolution and depression: issues and implications. Psycho. Med. 2006; 36 (3):287–297. doi: 10.1017/S0033291705006112. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goel N., Workman J.L., Lee T.F., Innala L., Viau V. Sex differences in the HPA axis. Compr. Physiol. 2014; 4 (3):1121‐1155. doi: 10.1002/cphy.c130054. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- González-Sanguino C., Ausín B., Castellanos M.A., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.040. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guo W., Li M., Dong Y., Zhou H., Zhang Z., Tian C., Qin R., Wang H., Shen Y., Du K., Zhao L., Fan H., Luo S., Hu D. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab. Res. Rev. 2020 doi: 10.1002/dmrr.3319. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.069. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ho C.S.H., Chee C.Y., Ho R.C.M. Mental health strategies to combat the psychological impact of coronavirus disease (COVID-19) beyond paranoia and panic. Ann. Acad. Med. Singapore. 2020; 49 (3):155–160. [ PubMed ] [ Google Scholar ]
- Huang Y., et al. . Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiat. 2019; 6 (3):211–224. doi: 10.1016/S2215-0366(18)30511-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020; 288 doi: 10.1016/j.psychres.2020.112954. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hwang T., Rabheru K., Peisah C., Reichman W., Ikeda M. Loneliness and social isolation during COVID-19 pandemic. Int. Psychogeriatr. 2020:1–15. doi: 10.1017/S1041610220000988. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lassale C., Batty G.D., Baghdadli A., Jacka F., Sánchez-Villegas A., Kivimäki M., Akbaraly T. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol. Psychiatry. 2019; 24 :965–986. doi: 10.1038/s41380-018-0237-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the covid-19 epidemic in southwestern China. Med. Sci. Monit. 2020; 26 doi: 10.12659/MSM.924609. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Li Z., et al. . Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immum. 2020 doi: 10.1016/j.bbi.2020.03.007. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lim G.Y., Tam W.W., Lu Y., Ho C.S., Zhang M.W., Ho R.C. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 2018; 8 (1):2861. doi: 10.1038/s41598-018-21243-x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020; 287 doi: 10.1016/j.psychres.2020.112921. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu S., Yang L., Zhang C., Xiang Y., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiat. 2020; 7 (4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mamun M.A., Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty?—The forthcoming economic challenges for a developing country. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.028. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020; 17 :3165. doi: 10.3390/ijerph17093165. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McIntyre R.S., Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020; 19 (2):250–251. doi: 10.1002/wps.20767. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McIntyre R.S., Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020; 290 doi: 10.1016/j.psychres.2020.113104. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., Martin V.D., Chieffo D., Janiri L., Fiorillo A., Sani G., Nicola M.D. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.048. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19. Asian J. Psychiatr. 2020; 51 doi: 10.1016/j.ajp.2020.102076. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. Int. J. Surg. 2010; 8 (5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Molendijk M., Molero P., Sánchez-Pandreño F.O., Van der Dose W., Martínez-González M.A. Diet quality and depression risk: a systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 2018; 226 :346–354. doi: 10.1016/j.jad.2017.09.022. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ng K.H., Agius M., Zaman R. The global economic crisis: effects on mental health and what can be done. J. R. Soc. Med. 2013; 106 :211–214. doi: 10.1177/0141076813481770. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 2020; 78 :185–193. doi: 10.1016/j.ijsu.2020.04.018. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Olagoke A.A., Olagoke O.O., Hughes A.M. Exposure to coronavirus news on mainstream media: the role of risk perceptions and depression. Br. J. Health Psychol. 2020 doi: 10.1111/bjhp.12427. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saude. Publica. 2020; 36 (4) doi: 10.1590/0102-311X00054020. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Özdin S., Özdin S.B. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatry. 2020:1–8. doi: 10.1177/0020764020927051. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pisciotta M., Denneson L.M., Williams H.B., Woods S., Tuepker A., Dobscha S.K. Providing mental health care in the context of online mental health notes: advice from patients and mental health clinicians. J. Ment. Health. 2019; 28 (1):64–70. doi: 10.1080/09638237.2018.1521924. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 2020; 33 doi: 10.1136/gpsych-2020-100213. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Samadarshi S.C.A., Sharma S., Bhatta J. An online survey of factors associated with self-perceived stress during the initial stage of the COVID-19 outbreak in Nepal. Ethiop. J. Health Dev. 2020; 34 (2):1–6. [ Google Scholar ]
- Sawalha A.H., Zhao M., Coit P., Lu Q. Epigenetic dysregulation of ACE2 and interferon-regulated genes might suggest increased COVID-19 susceptibility and severity in lupus patients. J. Clin. Immunol. 2020; 215 doi: 10.1016/j.clim.2020.108410. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sønderskov K.M., Dinesen P.T., Santini Z.I., Østergaard S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020:1–3. doi: 10.1017/neu.2020.15. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Statista, 2020. Monthly unemployment rate in the United States from May 2019 to May 2020. https://www.statista.com/statistics/273909/seasonally-adjusted-monthly-unemployment-rate-in-the-us/ (Accessed June 12 2020,).
- Statistic Canada, 2020. Labour force characteristics, monthly, seasonally adjusted and trend-cycle, last 5 months. https://doi.org/10.25318/1410028701-eng(Accessed June 12 2020,).
- Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Zhang Z., Lai A., Ho R., Tran B., Ho C., Tam W. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.055. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thakur V., Jain A. COVID 2019-Suicides: a global psychological pandemic. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.062. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ] Retracted
- Tran B.X., et al. Coverage of Health Information by Different Sources in Communities: implication for COVID-19 Epidemic Response. Int. J. Environ. Res. Public Health. 2020; 17 (10):3577. doi: 10.3390/ijerph17103577. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tran B.X., Phan H.T., Nguyen T.P.T., Hoang M.T., Vu G.T., Lei H.T., Latkin C.A., Ho C.S.H., Ho R.C.M. Reaching further by Village Health Collaborators: the informal health taskforce of Vietnam for COVID-19 responses. J. Glob. Health. 2020; 10 (1) doi: 10.7189/jogh.10.010354. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020; 17 (5):1729. doi: 10.3390/ijerph17051729. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.028. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang H., Xia Q., Xiong Z., Li Z., Xiang W., Yuan Y., Liu Y., Li Z. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: a web-based survey. PLoS ONE. 2020; 15 (5) doi: 10.1371/journal.pone.0233410. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang Y., Di Y., Ye J., Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2020:1–10. doi: 10.1080/13548506.2020.1746817. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yaribeygi H., Panahi Y., Sahraei H., Johnston T.P., Sahebkar A. The impact of stress on body function: a review. EXCLI J. 2017; 16 :1057–1072. doi: 10.17179/excli2017-480. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Environ. Res. Public Health. 2020; 17 (7):2381. doi: 10.3390/ijerph17072381. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Downloadable Content
A Study on Students' Mental Health During the COVID-19 Pandemic Through the Perspective of Mental Health Professionals
- Masters Thesis
- Hightower, Shelby
- Navarro, Richard
- Olson, Peter
- Lim, Andrew
- Education & Integrative Studies
- California State Polytechnic University, Pomona
- pandemic lockdown 2020
- mental health
- http://hdl.handle.net/20.500.12680/9306t488f
Relationships
- CPP Education

Items in ScholarWorks are protected by copyright, with all rights reserved, unless otherwise indicated.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 10, Issue 12
- Impact of the COVID-19 pandemic on mental health and well-being of communities: an exploratory qualitative study protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-0180-0213 Anam Shahil Feroz 1 , 2 ,
- Naureen Akber Ali 3 ,
- Noshaba Akber Ali 1 ,
- Ridah Feroz 4 ,
- Salima Nazim Meghani 1 ,
- Sarah Saleem 1
- 1 Community Health Sciences , Aga Khan University , Karachi , Pakistan
- 2 Institute of Health Policy, Management and Evaluation , University of Toronto , Toronto , Ontario , Canada
- 3 School of Nursing and Midwifery , Aga Khan University , Karachi , Pakistan
- 4 Aga Khan University Institute for Educational Development , Karachi , Pakistan
- Correspondence to Ms Anam Shahil Feroz; anam.sahyl{at}gmail.com
Introduction The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. In addition, with the widespread use of social media, rumours, myths and inaccurate information about the virus are spreading rapidly, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes of community members towards COVID-19 and its impact on their daily lives and mental well-being.
Methods and analysis This formative research will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews with community members. The study will be conducted in the Karimabad Federal B Area and in the Garden (East and West) community settings in Karachi, Pakistan. The community members of these areas have been selected purposively for the interview. Study data will be analysed thematically using NVivo V.12 Plus software.
Ethics and dissemination Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The results of the study will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
- mental health
- public health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-041641
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The mental health impact of the COVID-19 pandemic is likely to last much longer than the physical health impact, and this study is positioned well to explore the perceptions and attitudes of community members towards the pandemic and its impact on their daily lives and mental well-being.
This study will guide the development of context-specific innovative mental health programmes to support communities in the future.
One limitation is that to minimise the risk of infection all study respondents will be interviewed online over Zoom and hence the authors will not have the opportunity to build rapport with the respondents or obtain non-verbal cues during interviews.
The COVID-19 pandemic has affected almost 180 countries since it was first detected in Wuhan, China in December 2019. 1 2 The COVID-19 outbreak has been declared a public health emergency of international concern by the WHO. 3 The WHO estimates the global mortality to be about 3.4% 4 ; however, death rates vary between countries and across age groups. 5 In Pakistan, a total of 10 880 cases and 228 deaths due to COVID-19 infection have been reported to date. 6
The worldwide COVID-19 pandemic has not only incurred massive challenges to the global supply chains and healthcare systems but also has a detrimental effect on the overall health of individuals. 7 The pandemic has led to lockdowns and has created destructive impact on the societies at large. Most company employees, including daily wage workers, have been prohibited from going to their workplaces or have been asked to work from home, which has caused job-related insecurities and financial crises in the communities. 8 Educational institutions and training centres have also been closed, which resulted in children losing their routine of going to schools, studying and socialising with their peers. Delay in examinations is likewise a huge stressor for students. 8 Alongside this, parents have been struggling with creating a structured milieu for their children. 9 COVID-19 has hindered the normal routine life of every individual, be it children, teenagers, adults or the elderly. The crisis is engendering burden throughout populations and communities, particularly in developing countries such as Pakistan which face major challenges due to fragile healthcare systems and poor economic structures. 10
The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. 8 Further, the highly contagious nature of COVID-19 has also escalated confusion, fear and panic among community residents. Moreover, social distancing is often an unpleasant experience for community members and for patients as it adds to mental suffering, particularly in the local setting where get-togethers with friends and families are a major source of entertainment. 9 Recent studies also showed that individuals who are following social distancing rules experience loneliness, causing a substantial level of distress in the form of anxiety, stress, anger, misperception and post-traumatic stress symptoms. 8 11 Separation from family members, loss of autonomy, insecurity over disease status, inadequate supplies, inadequate information, financial loss, frustration, stigma and boredom are all major stressors that can create drastic impact on an individual’s life. 11 Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. 12 With the widespread use of social media, 13 rumours, myths and inaccurate information about COVID-19 are also spreading rapidly, not only among adults but are also carried on to children, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. 9 The psychological symptoms associated with COVID-19 at the community level are also manifested as anxiety-driven panic buying, resulting in exhaustion of resources from the market. 14 Some level of panic also dwells in the community due to the unavailability of essential protective equipment, particularly masks and sanitisers. 15 Similarly, mental health issues, including depression, anxiety, panic attacks, psychotic symptoms and even suicide, were reported during the early severe acute respiratory syndrome outbreak. 16 17 COVID-19 is likely posing a similar risk throughout the world. 12
The fear of transmitting the disease or a family member falling ill is a probable mental function of human nature, but at some point the psychological fear of the disease generates more anxiety than the disease itself. Therefore, mental health problems are likely to increase among community residents during an epidemic situation. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes towards COVID-19 among community residents and the impact of these perceptions and attitude on their daily lives and mental well-being.
Methods and analysis
Study design.
This study will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews (IDIs) with community members. The IDIs aim to explore perceptions of community members towards COVID-19 and its impact on their mental well-being.
Study setting and study participants
The study will be conducted in two communities in Karachi City: Karimabad Federal B Area Block 3 Gulberg Town, and Garden East and Garden West. Karimabad is a neighbourhood in the Karachi Central District of Karachi, Pakistan, situated in the south of Gulberg Town bordering Liaquatabad, Gharibabad and Federal B Area. The population of this neighbourhood is predominantly Ismailis. People living here belong mostly to the middle class to the lower middle class. It is also known for its wholesale market of sports goods and stationery. Garden is an upmarket neighbourhood in the Karachi South District of Karachi, Pakistan, subdivided into two neighbourhoods: Garden East and Garden West. It is the residential area around the Karachi Zoological Gardens; hence, it is popularly known as the ‘Garden’ area. The population of Garden used to be primarily Ismailis and Goan Catholics but has seen an increasing number of Memons, Pashtuns and Baloch. These areas have been selected purposively because the few members of these communities are already known to one of the coinvestigators. The coinvestigator will serve as a gatekeeper for providing entrance to the community for the purpose of this study. Adult community members of different ages and both genders will be interviewed from both sites, as mentioned in table 1 . Interview participants will be selected following the eligibility criteria.
- View inline
Study participants for indepth interviews
IDIs with community members
We will conduct IDIs with community members to explore the perceptions and attitudes of community members towards COVID-19 and its effects on their daily lives and mental well-being. IDI participants will be identified via the community WhatsApp group, and will be invited for an interview via a WhatsApp message or email. Consent will be taken over email or WhatsApp before the interview begins, where they will agree that the interview can be audio-recorded and that written notes can be taken. The interviews will be conducted either in Urdu or in English language, and each interview will last around 40–50 min. Study participants will be assured that their information will remain confidential and that no identifying features will be mentioned on the transcript. The major themes will include a general discussion about participants’ knowledge and perceptions about the COVID-19 pandemic, perceptions on safety measures, and perceived challenges in the current situation and its impact on their mental well-being. We anticipate that 24–30 interviews will be conducted, but we will cease interviews once data saturation has been achieved. Data saturation is the point when no new themes emerge from the additional interviews. Data collection will occur concurrently with data analysis to determine data saturation point. The audio recordings will be transcribed by a transcriptionist within 24 hours of the interviews.
An interview guide for IDIs is shown in online supplemental annex 1 .
Supplemental material
Eligibility criteria.
The following are the criteria for inclusion and exclusion of study participants:
Inclusion criteria
Residents of Garden (East and West) and Karimabad Federal B Area of Karachi who have not contracted the disease.
Exclusion criteria
Those who refuse to participate in the study.
Those who have experienced COVID-19 and are undergoing treatment.
Those who are suspected for COVID-19 and have been isolated/quarantined.
Family members of COVID-19-positive cases.
Data collection procedure
A semistructured interview guide has been developed for community members. The initial questions on the guide will help to explore participants’ perceptions and attitudes towards COVID-19. Additional questions on the guide will assess the impact of these perceptions and attitude on the daily lives and mental health and well-being of community residents. All semistructured interviews will be conducted online via Zoom or WhatsApp. Interviews will be scheduled at the participant’s convenient day and time. Interviews are anticipated to begin on 1 December 2020.
Patient and public involvement
No patients were involved.
Data analysis
We will transcribe and translate collected data into English language by listening to the audio recordings in order to conduct a thematic analysis. NVivo V.12 Plus software will be used to import, organise and explore data for analysis. Two independent researchers will read the transcripts at various times to develop familiarity and clarification with the data. We will employ an iterative process which will help us to label data and generate new categories to identify emergent themes. The recorded text will be divided into shortened units and labelled as a ‘code’ without losing the main essence of the research study. Subsequently, codes will be analysed and merged into comparable categories. Lastly, the same categories will be grouped into subthemes and final themes. To ensure inter-rater reliability, two independent investigators will perform the coding, category creation and thematic analyses. Discrepancies between the two investigators will be resolved through consensus meetings to reduce researcher bias.
Ethics and dissemination
Study participants will be asked to provide informed, written consent prior to participation in the study. The informed consent form can be submitted by the participant via WhatsApp or email. Participants who are unable to write their names will be asked to provide a thumbprint to symbolise their consent to participate. Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The study results will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
The findings of this study will help us to explore the perceptions and attitudes towards the COVID-19 pandemic and its impact on the daily lives and mental well-being of individuals in the community. Besides, an indepth understanding of the needs of the community will be identified, which will help us develop context-specific innovative mental health programmes to support communities in the future. The study will provide insights into how communities are managing their lives under such a difficult situation.
- World Health Organization
- Nielsen-Saines K , et al
- Worldometer
- Ebrahim SH ,
- Gozzer E , et al
- Snoswell CL ,
- Harding LE , et al
- Nargis Asad
- van Weel C ,
- Qidwai W , et al
- Brooks SK ,
- Webster RK ,
- Smith LE , et al
- Tripathy S ,
- Kar SK , et al
- Schwartz J ,
- Maunder R ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
ASF and NAA are joint first authors.
Contributors ASF and NAA conceived the study. ASF, NAA, RF, NA, SNM and SS contributed to the development of the study design and final protocols for sample selection and interviews. ASF and NAA contributed to writing the manuscript. All authors reviewed and approved the final version of the paper.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 09 July 2021
Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence
- Xuerong Liu ORCID: orcid.org/0000-0002-9236-5773 1 ,
- Mengyin Zhu ORCID: orcid.org/0000-0001-5561-9570 1 ,
- Rong Zhang ORCID: orcid.org/0000-0003-4516-4116 2 ,
- Jingxuan Zhang ORCID: orcid.org/0000-0002-8979-5107 1 ,
- Chenyan Zhang ORCID: orcid.org/0000-0002-2945-6584 3 ,
- Peiwei Liu ORCID: orcid.org/0000-0003-2660-1106 4 ,
- Zhengzhi Feng ORCID: orcid.org/0000-0001-6144-5044 1 &
- Zhiyi Chen ORCID: orcid.org/0000-0003-1744-4647 1 , 2
Translational Psychiatry volume 11 , Article number: 384 ( 2021 ) Cite this article
19k Accesses
99 Citations
46 Altmetric
Metrics details
- Psychiatric disorders
- Scientific community
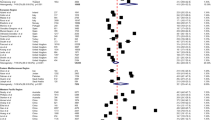
The coronavirus disease 2019 (COVID-19) pandemic has exposed humans to the highest physical and mental risks. Thus, it is becoming a priority to probe the mental health problems experienced during the pandemic in different populations. We performed a meta-analysis to clarify the prevalence of postpandemic mental health problems. Seventy-one published papers ( n = 146,139) from China, the United States, Japan, India, and Turkey were eligible to be included in the data pool. These papers reported results for Chinese, Japanese, Italian, American, Turkish, Indian, Spanish, Greek, and Singaporean populations. The results demonstrated a total prevalence of anxiety symptoms of 32.60% (95% confidence interval (CI): 29.10–36.30) during the COVID-19 pandemic. For depression, a prevalence of 27.60% (95% CI: 24.00–31.60) was found. Further, insomnia was found to have a prevalence of 30.30% (95% CI: 24.60–36.60). Of the total study population, 16.70% (95% CI: 8.90–29.20) experienced post-traumatic stress disorder (PTSD) symptoms during the COVID-19 pandemic. Subgroup analysis revealed the highest prevalence of anxiety (63.90%) and depression (55.40%) in confirmed and suspected patients compared with other cohorts. Notably, the prevalence of each symptom in other countries was higher than that in China. Finally, the prevalence of each mental problem differed depending on the measurement tools used. In conclusion, this study revealed the prevalence of mental problems during the COVID-19 pandemic by using a fairly large-scale sample and further clarified that the heterogeneous results for these mental health problems may be due to the nonstandardized use of psychometric tools.
Similar content being viewed by others
Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis

Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review
Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis
Introduction.
Since the end of 2019, the coronavirus disease 2019 (COVID-19) outbreak has continued to spread worldwide. Researchers rapidly identified the cause of COVID-19 to be the transmission of serious acute respiratory syndrome by a novel coronavirus (SARS-CoV-2) [ 1 ]. Unfortunately, due to the lack of effective cures and vaccines, the ability of public medical systems to guard against COVID-19 is deteriorating rapidly. Although approved vaccines are now available, their safety is still a concern [ 2 , 3 ]. Further, because of reports regarding the potential to be reinfected with COVID-19, public panic is still spreading even though COVID-19 transmission has been contained substantially [ 4 ]. To date, projections regarding the end of the COVID-19 pandemic around the world are still far from optimistic. There were more than 158.95 million confirmed cases and 3.30 million deaths by May 11, 2021 (supported by Johns Hopkins University), a situation that has led to unprecedented losses and stress.
COVID-19 not only threatens physical health but has also led to mental health sequelae (i.e., loss of family, job loss, social constraints and uncertainty, and fear about the future) [ 5 , 6 , 7 ]. In general, mental health problems, including depression and anxiety, have had major negative impacts on the public during the COVID-19 pandemic [ 8 , 9 ]. Previous studies showed that mental health problems, such as depression, anxiety, insomnia, and post-traumatic stress disorder (PTSD), suddenly increased after the COVID-19 outbreak: 53.8% of respondents rated the psychological impact of the outbreak as moderate or severe; 16.5% of participants reported moderate to severe depressive symptoms; 28.8% of participants reported moderate to severe anxiety symptoms; and 24.5% of participants showed psychological stress [ 10 ]. Moreover, such mental health problems were worse in confirmed patients and healthcare workers. As a typical example, one early study revealed acute anxiety symptoms in 98.84% of confirmed patients and depression symptoms in 79.07% of confirmed cases [ 11 ]. In addition, an early investigation concerning the mental health status of 400 public health workers found that 31% of public health workers had anxiety symptoms, and 24.5% of them had depressive symptoms [ 12 ]. In this vein, it seems that the mental health sequelae of the COVID-19 pandemic warrant more attention. In addition, with the development of the epidemic situation, long-term isolation due to the increasing number of confirmed and suspected patients has caused losses to life and property, which has not only caused considerable psychological stress in the population but has also had physiological effects, such as insomnia and PTSD.
In brief, the COVID-19 pandemic has exposed public health to dramatic risks and resulted in unacceptable mental and physiological stresses. Despite considerable research, two critical concerns regarding mental health problems during the COVID-19 pandemic remain. One concern in previous studies is that the conclusions regarding the prevalence of these mental health problems are highly heterogeneous, irrespective of whether they are derived from original investigations or meta-analyses [ 13 , 14 ]. Another is that early investigations were almost all done during the peak of the COVID-19 pandemic and thus may overestimate the scale of mental health problems. Thus, the main purpose of this study is to provide comprehensive statistical results regarding the impact of COVID-19 on individual mental health through a large-scale meta-analysis of the existing research in this field and to provide an evidence-based reference for the prevention and control of psychological crises during this pandemic. It is noteworthy that this study employs a larger data pool than any of the existing meta-analyses to date. Further, much effort has been made to perform an in-depth investigation of the patterns of mental health problems triggered by the COVID-19 pandemic, including population-, region-, and measurement-specific patterns.
Materials and methods
To improve reproducibility and standardization, all the pipelines and protocols were in line with the Cochrane Handbook and were double-checked by using the PRISMA checklist [ 15 ]. This meta-analysis has been preregistered on OSF for open access ( https://doi.org/10.17605/OSF.IO/A5VMK ).
Search strategy and selection criteria
A systematic search was conducted for studies published from January 1, 2020 to July 1, 2020 (the period from the commencement of the outbreak to its initial control in China) in PubMed, EMBASE, the Cochrane Library, EBSCO, Web of Science, CNKI (Chinese database), WANGFANG DATA, the Chinese Biomedical Literature Service System, and public information release platforms (WeChat Subscription or microblogs). According to the indices of the various databases, keywords, including “2019 novel coronavirus,” “COVID-19,” “novel coronavirus pneumonia,” “NPC,” “2019-nCoV,” “mental health,” “anxiety,” “depression,” “psychological health,” “sleep,” “insomnia,” “Posttraumatic stress disorder,” and “PTSD,” were adopted to retrieve published surveys of psychological status during the COVID-19 epidemic from January 1, 2020 to July 1, 2020. In addition to identifying any target studies that may have been missed, we checked the reference list of each selected paper. The population was divided into three categories according to the probable psychological stress intensity experienced: public health workers, confirmed patients, and the general population (see Fig. 1 , Supplemental information, and Table S1 ).
This flowchart is coincide with the broad-certified 2020 PRISMAstatement. Small sample size was predefined as < 30 participants.
Data extraction and quality assessment
The following data were extracted from each article by two researchers independently: study type; total number of participants; participation rate; region; percentage of physicians, nurses, and other healthcare workers screened in the survey; number of male and female participants; assessment methods used and their cutoffs; and the total number and percentage of participants who screened positive for depression, anxiety, insomnia or PTSD. If any of this information was not reported, the necessary calculations (e.g., transforming the percentage of healthcare workers to the number of healthcare workers) were performed. The accuracy of the extracted or calculated data was confirmed by comparing the collection forms of the two investigators.
In addition, two authors independently evaluated the risk of bias of the included cross-sectional studies using a modified form of the Newcastle-Ottawa scale. Potential disagreements were resolved by a third author. Specifically, the quality assessment criteria were as follows: sample representativeness and size; comparability between respondents and nonrespondents; ascertainment of depression, anxiety, and insomnia; and adequacy of the descriptive statistics. The total quality scores ranged between 0 and 5; studies scoring ≥3 points were regarded as having a low risk of bias, while studies scoring <3 points were regarded as having a high risk of bias (see Table S1 ).
Encoding and statistical analysis
The two investigators (XL and MZ), who performed the literature search, also extracted the data from the included studies independently. Disagreements were resolved with the third investigator (ZC) or by consensus. Then, the following variables were extracted: author, date of publication, age, gender, region, sample size, method, number of positive cases, and positivity rate. All these analytical procedures were performed with the CMA software (V3). In particular, given the heterogeneity within and between studies, random-effects models were used to estimate the average effect and its precision, which would give a more conservative estimate of the 95% confidence intervals (CIs). The I 2 statistic and Cochran’s Q test were conducted to assess statistical heterogeneity.
Prior researchers held that the fixed-effects model is ideally suited to the meta-analysis of a nonheterogeneous data pool ( I 2 < 50%, P value ≥0.1) [ 16 ]. Conversely, the random-effects model should be used when there is heterogeneity between the studies ( I 2 > 50%). According to the factors that may affect the heterogeneity between studies, moderation analysis was further carried out for distinct cohorts (i.e., health workers, confirmed and suspected patients, the general population) and distinct sample sources (China, other countries). A funnel chart was created for visual inspection to determine whether the included studies showed publication bias; Egger’s test and Kendall’s test for the quantitative analysis of publication bias were also used, with p > 0.05 indicating no publication bias.
In the current study, 896 Chinese and English studies were initially retrieved. According to the inclusion and exclusion criteria, 71 papers were eligible for inclusion in the data pool for the meta-analysis, and the total number of respondents reached 146,139 (see Table 1 and Table S2 ).
Heterogeneity test
The results of the heterogeneity test on the prevalence of mental problems in patients with COVID-19 showed that the heterogeneity across studies was large ( I 2 > 98%, P < 0.05), which suggested that the random-effects model was needed to analyze the total effect. Importantly, to increase the robustness of the results and reduce the heterogeneity between studies, population, nationality, and subgroup were analyzed as possible moderators.
Prevalence of mental problems
Four symptoms related to stress were selected as the mental problems, and the related symptoms and symptom groups were analyzed according to the definitions given in each study. The prevalence of anxiety was 32.6% (95% CI: 29.1–36.3; N = 86,035, see Fig. 2 ). In addition, the prevalence of depression was 27.60% (95% CI: 24.0–31.6; N = 90,156, see Fig. 3 ). Likewise, insomnia prevalence during the COVID-19 pandemic was 30.30% (95% CI: 24.6–36.6; N = 62,202, see Fig. 4A ). Finally, 16.70% of participants were found to meet the criteria for PTSD during the COVID-19 pandemic in this meta-analysis (95% CI: 8.9–29.2; N = 17,169, see Fig. 4B ).
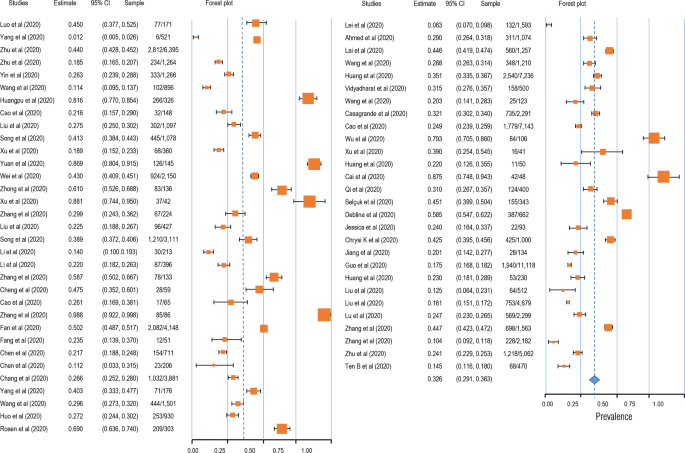
The squares colored by orange represent the point estimation foreffect towards corresponding study, with the large square size for high effect size. The orange diamond represent meta-analytic effect size.
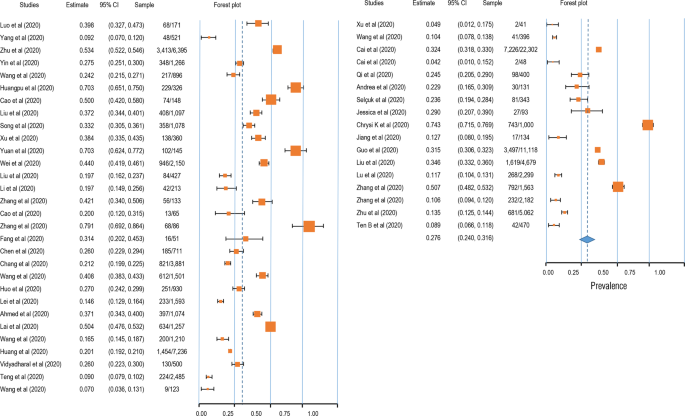
The squares colored by orange represent the point estimation for effect towards corresponding study, with the large square size for high effect size. The orange diamond represent meta-analytic effect size.
Moderation analysis
Given the high heterogeneity, we assumed that there were some potential moderators, including the cohort (confirmed patients, healthcare workers, and the general population), region (China and other countries), and measurement tool. The results demonstrated a significantly higher prevalence of mental health problems in confirmed patients than in others (see Table S3 ). Further, the prevalence of mental health problems was found to be lower in China than in other countries. In addition, these findings derived from the moderation analysis revealed the moderating role of the measurement tool, with the results varying significantly across different scales (see Table S3 and Figs. S1–3).
Publication bias assessment
A funnel plot was first used for qualitative analysis of the publication bias. As shown in Figure S4 , a symmetrical distribution was found for the four psychological symptoms. In addition, Begg’s rank test was performed to quantitatively analyze the publication bias. The results showed that there was no publication bias in the studies regarding anxiety (Kendall’s tau = 0.044, p = 0.614), depression (Kendall’s tau = −0.046, p = 0.647), insomnia (Kendall’s tau = −0.096, p = 0.592), or PTSD (Kendall’s tau = −0.145, p = 0.533).
In this study, a meta-analysis was performed to clarify the mental health situation in the population during the COVID-19 pandemic with respect to anxiety, depression, sleep problems, and PTSD. The results showed that the detection rate of anxiety symptoms in a total of 86,035 cases was 32.6% (95% CI: 29.1–363); the detection rate of depression symptoms in a total of 90,156 cases was 27.6% (95% CI: 24.0–31.6); the detection rate of insomnia symptoms in a total of 62,202 cases was 30.3% (95% CI: 24.6–36.6); and the detection rate of PTSD symptoms was 16.7% in a total of 17,169 cases (95% CI: 8.9–29.2). Furthermore, the moderator analysis showed that mental health problems (i.e., anxiety and depression) had the highest prevalence in COVID-19 patients, and fewer anxiety, depression, and sleep problems were observed in healthcare workers than in the general population. Overall, this study provided solid evidence of the mental health situation during the COVID-19 pandemic and indicated the potential heterogeneity across cohorts, regions, and measurement tools.
Furthermore, regarding anxiety symptoms, health workers accounted for 32.7% (95% CI: 27.9–38.2) of the detection rate; the general population accounted for 29.5% (95% CI: 25.2–34.3). A total of 25.8% (95% CI: 20.4–31.0), and 25.3% (95% CI: 20.4–32.0) of depressive symptoms were found in health workers and the general population, respectively. The highest detection rate of insomnia, which was 37.3% (95% CI: 32.1–42.8%), was found in health workers, and the general population represented 26.1% of cases (95% CI: 18.2–36.1). The detection rate of PTSD was 30.6% (95% CI: 9.1–65.9) in health workers and just 9.3% (95% CI: 4–19.8) in the general population. Moving beyond previous studies, this meta-analysis covered the latest COVID-19-related articles and examined more publications than its predecessors. In contrast to the existing research conclusions, this study found that the mental health problems of healthcare workers are the same as those of the general population, suggesting that the existing research may overestimate the mental health problems of healthcare workers (i.e., one study showed that 50.4% of healthcare workers reported symptoms of depression, 44.6% symptoms of anxiety, and 34.0% insomnia) [ 17 ]. This may be because in the early stage of COVID-19, the pressures experienced by healthcare workers were considerable due to the sudden workload and lack of adequate understanding of the COVID-19 pandemic. However, in later stages, as an understanding of COVID-19 improved, healthcare workers became familiar with the situation and gained a more comprehensive understanding of the disease. This led to higher self-regulation ability under the circumstance of the epidemic even though the stress level of the first-line workers was high. Therefore, a very important conclusion of this study is that the mental health problems of healthcare workers are not as serious as previously thought, and lagging research conclusions may lead to label effects, which in turn worsen the mental health status of healthcare workers. In addition, we found that the detection rate of mental health problems in infected patients is higher in the COVID-19 pandemic than it was during the SARS outbreak [ 18 ]. For example, during SARS, the detection rate of anxiety symptoms was 35.7% (95% CI: 27.6–44.2), and that of depressed mood was 32.6% (95% CI: 24.7–40.9); in contrast, we found anxiety and depression rates of 63.9% (95% CI: 29.6–88.2) and 55.4% (95% CI: 32.8–76.0), respectively, in the COVID-19 context. During the outbreak of SARS in 2003, information dissemination was less developed than at present, and the public understanding of the virus was based on official information, which made the spread of rumors and concomitant psychological distress less likely. This shows that we should pay attention not only to the spread of the virus but also to the spread of false/fake information about the virus.
The second core finding of this study is that the detection rates of anxiety, depression, insomnia, and PTSD in other countries are higher than those in China. Existing study demonstrated the higher anxiety and depression symptoms in overseas Chinese lived in Italy than do of overseas Chinese lived in mainland China [ 19 ]. This may be because China was the first country to have an outbreak of the diseases and has taken a series of effective measures. Civil society organizations took responsibility for isolating residents in every community and helped solve practical life difficulties. At the individual level, home isolation, social distancing, and the wearing of personal protective equipment such as face masks were implemented to prevent community transmission nationwide. Due to the development of advanced technology, residents have had easy access to reliable information and medical guidance, which can reduce misinformation and the impact of rumors. The public was well educated on the seriousness of COVID-19 complied cooperatively with the national approach of hand washing, mask wearing, social distancing, and universal temperature monitoring. All citizens were keenly aware of their roles in preventing the virus from spreading. To strike a balance between epidemic control and normal social and economic operations, industrial activities have gradually resumed in phases and batches since February 8, 2020 [ 20 ]. The supply of daily necessities was kept stable in every stage of the outbreak to ensure the smooth operation of society. The WHO-China Joint Mission report said that China has rolled out perhaps the most ambitious, agile, and aggressive disease containment efforts in history [ 21 ]. By striking contrast, the number of confirmed cases outside China is quickly climbing following an exponential growth trend. The total number of COVID-19 cases outside China has reached 333,706,43, including 999,603 deaths as of September 29, 2020. Furthermore, we also conjecture that the reason why fewer pandemic impacts were seen in mainland China is that the well-established psychological rescue system strongly guards against the potential panic arising from the COVID-19 pandemic. Specifically, Chinese governmental intervention agencies provide professional psychological intervention services for patients with confirmed diseases or mental disorders, front-line medical staff, and other key groups in special places such as designated hospitals and isolated hospitals. In addition, public psychological rescue organizations offer free 24/7 on-call professional psychological advice to the public. Ultimately, massive open online courses were released to enrich the Chinese public’s understanding of the COVID-19 pandemic, which has significantly strengthened belief in the ability to control this disaster [ 22 ]. In addition, the comparative analysis of the results obtained with different measurement tools showed heterogeneity and poor consistency across the tools. Therefore, it is suggested that reliable measurement tools should be established in future research to avoid deviation in research results caused by measurement tools.
This study adjusted the prevalence of mental health problems reported in previous studies by analyzing more recent studies and thus provided a more accurate picture of the mental health status of the population. Previous studies have provided very timely and important evidence to prove that the COVID-19 pandemic is a threat to individual mental health. However, most of the surveys were performed in the early and peak periods and may overestimate the prevalence of these problems. Moreover, for the sake of timeliness in sharing research findings, low-quality articles were published in some journals. Therefore, this study also adopts the method of quality control evaluation to exclude articles with lower quality and obtain more accurate and unbiased conclusions. In general, the detection rate of mental health problems found in this study was lower than that in previous studies. There may be two reasons for this. First, stricter quality control was adopted in this study, making the analysis results more accurate and unbiased. Second, more new studies were included in this study; that is, the investigation time extended from the initial stage to the peak of the pandemic and then to the later stage of COVID-19 pandemic in the present study. Therefore, the results of this study may reflect that, with better control and understanding of the epidemic situation, people’s mental health status has improved, which is a good sign.
This study has several limitations. First, the sample sizes were not matched well, with the number of healthcare workers being smaller than the number of people from the general population. Second, the international sample was insufficient, and the research on Chinese people significantly exceeded than that on people from other countries. Third, the impact of specific epidemic status was not taken into account. In future studies, covariates can be added to the meta-analysis to control the epidemic situation of samples in different regions.
In conclusion, our systematic review and meta-analysis provide a timely and comprehensive synthesis of existing evidence, confirming the presence of mental health problems in patients (including suspected patients) as well as insomnia and PTSD in medical staff. The findings help to quantify staff support in the context of a pandemic when stratified and customized interventions are needed to enhance resilience and reduce vulnerability. With the continuous emergence of new evidence, we can further update the meta-analysis and perform follow-ups to analyze the factors related to the epidemic situation to facilitate national-level planning, improve the hierarchical intervention of the mental health security system, and address similar public health events in the future.
Data and code availability
Study protocols and hypotheses were preregistered on the Open Science Framework (OSF) ( https://osf.io/a5vmk/ ). Raw data, protocols, and analysis scripts are available openly at the OSF ( https://osf.io/a5vmk/ ).
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus:implications for virus origins and receptor binding. Lancet. 2020;395:565–74.
Article CAS PubMed PubMed Central Google Scholar
Hotez PJ, Corry BD, Bottazzi ME. COVID-19 vaccine design: the Janus face of immune enhancement. Nat Rev Immun. 2020;20:347–8. https://doi.org/10.1038/s41577-020-0323-4 .
Article CAS Google Scholar
Lurie N, Sharfstein JM, Goodman JL. The development of COVID-19 vaccines: safeguards needed. JAMA. 2020;324:439–40. https://doi.org/10.1001/jama.2020.12461 .
Article CAS PubMed Google Scholar
Deng W, et al. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Science. 2020;369:818–23. https://doi.org/10.1126/science.abc5343 .
Berg-Weger M, Morley JE. Editorial: loneliness and social isolation in older adults during the COVID-19 pandemic: implications for gerontological social work. J Nutr Health Aging. 2020;24:456–8. https://doi.org/10.1007/s12603-020-1366-8 .
Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D. Family violence and COVID-19: increased vulnerability and reduced options for support. Int J Ment Health Nurs. 2020;29:549–52. https://doi.org/10.1111/inm.12735 .
Article PubMed Google Scholar
Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes & metabolic syndrome, 2020;14,779–88. https://doi.org/10.1016/j.dsx.2020.05.035 .
Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020;17:10. https://doi.org/10.3390/ijerph17103740.
Article Google Scholar
Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang YT. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e19. https://doi.org/10.1016/S2215-0366(20)30079-1 .
Article PubMed PubMed Central Google Scholar
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during theInitial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020; 17:1729. https://doi.org/10.3390/ijerph17051729 .
Jinglong Z, Rong S, Juan Y. Anxiety and depression in elderly patients during epidemic of coronavirus disease 2019 and its influencing factors. J Clin Med Pract. 2020;04:246–50.
Google Scholar
Jing Q, et al. The evaluation of sleep disturbances for chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 2020;72:1–4.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7. https://doi.org/10.1016/j.bbi.2020.05.026 .
Wei L, Caidi Z, Jin JL, Huijuan Z, Hui W, Bixi Y, et al. Meta analysis of mental state of different groups of people during the outbreak of new coronavirus pneumonia. J Tongji Univ. 2020;02:147–54. https://doi.org/10.16118/j.1008-0392.2020.02.002 .
Page MJ. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3:486–504.
Lai J, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3:e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 .
Jonathan PR, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:7.
Chen W, Zhan H, Hong YLJY. COVID-19 epidemic survey of mental state of overseas Chinese in Italy abstract. Psychol Mon. 2020;17:46–47+50. 10.19738/j.cnki. psy.2020.17.014.
The State Council of the People’s Republic of China. The notice on orderly resuming production and resuming production in enterprises. 2020. http://www.gov.cn/xinwen/2020-02/09/content_5476550.htm (in Chinese). Accessed 7 Mar 2020.
WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-fifinal-report.pdf . Accessed 7 Mar 2020.
Chen LL, Du MJ. Research on the improvement of psychological counseling mechanism for major public emergencies in Hubei Province during the 14th Five Year Plan period. Soc Sci Trends. 2020;8:110–8.
Qianyi L, et al. Investigation of mental health status of frontline medical staff in COVID-19 treatment hospital in Guangdong Province. Guangdong Med. 2020;41:984–90. https://doi.org/10.13820/j.cnki.gdyx.20200920 .
Yang L, Zhang Y, Xu Y, Zheng J, Lin CQ. investigation on psychological stress in fighting against corona virus disease 2019 among community residents. Nurs Res. 2020;34:1140–5.
Xiaolin Z, et al. Psychological status of school students and employees during the COVID-19 epidemic. Chin J Ment Health. 2020;34:549–54.
Kaiheng Z, et al. Anxiety symptom and its associates among primary school students in Hubei province during 2019 novel coronavirus diseases epidemic. Chin Public Health. 2020;36:673–6.
Jiao Y, et al. Psychological investigation and analysis on mental care personnel in designated hospitals of coronavirus disease 2019. Med Philos. 2020;41:38–42+67.
Wang Z, Chen L, Li L, Zhang X, Wang YM, Xu X. Influence of COVID-2019 on mental health of medical students. J Changchun Univ Tradit Chin Med. 2020;36:1015–8. https://doi.org/10.13463/j.cnki.cczyy.2020.05.051 .
Huangfu M, Fu X, Wang LH. Investigation on psychological stress of frontline nurses in novel coronavirus pneumonia prevention. Chongqing Med. 2020;19:3172–6.
Cao J, Wen M, Shi Y, Wu Y, He Q. Prevalence and factors associated with anxiety and depression in patients with Coronavirus disease 2019 (COVID-19). J Nurs. 2020;35:15–17.
Xiaolei L, et al. Psychological state of nursing staff in a large scale of general hospital during COVID-19 epidemic. Chin J Hosp Infect. 2020;30:1641–6.
Song F, Wang X, Ju Z, Liu A, Junjie L, Wang T. Mental health status and related influencing factors during the epidemic of coronavirus disease 2019(COVID-19). Public Health Prev Med. 2020;31:23–27.
Xu Y, Zhao M, Tang X, Zhu X, Chen J. Correlation study between mental health and coping style of medical staff during COVID-19 epidemic. Anhui Med. 2020;41:368–71.
Yuan J, Du Y, Xu W, Chen Y. Study on the anxiety and depression levels and influencing factors in patients with suspected corona virus disease 2019 in isolation. Chongqing Med. 2020;19:3156–60.
Wei L, Shi L, Cao J. Psychological status of primary care workers during the COVID-19 epidemic in Shanghai. J Tongji Univ. 2020;41:155–60. https://doi.org/10.16118/j.1008-0392.2020.02.003 .
Zhong Y, Song X, Li J, Luo X, Chen W. Survey on the mental health of medical staffs in Emergency Department and Fever Clinic in Guiyang City under the Epidemic Situation of COVID-19. J Guizhou Univ Tradit Chin Med. 2020;42:16–22. https://doi.org/10.16588/j.cnki.issn1002-1108.2020.02.004 .
Xu Y. Investigation and analysis of the psychological status of the first batch of military nurses in “aiding Hubei to fight epidemic disease” and protection suggestions. Mil Med. 2020;04:313–5.
Zhang Y, Zhang X, Peng J, Fang P. A survey on mental of medical staff fighting 2019 Novel Coronavirus Disease in Wuhan. J Trop Med. 2020;10:1371–4.
Liu H, Liu Q, Li J. Investigation on the participation of mental health workers fighting against COVID-19 pandemic. Int J Psychiatry. 2020;02:201–4+209. https://doi.org/10.13479/j.cnki.jip.2020.02.003 .
Sun M, Li S, Yue HY, Li X, Li W, Xu S. analysis of Internet users’ anxiety and its influencing factors during the period of new crown pneumonia in China. World Sci Technol Modernization Chin Med. 2020;03:686–91.
Li X. novel coronavirus pneumonia isolation ward hope level, mental health and influencing factors. Gen Nurs. 2020;10:1203–6.
Li S, Wang Y, Yang Y, Lei X, Yang Y. Investigation on the influencing factors for anxiety related emotional disorders of children and adolescents with home quarantine during the prevalence of coronavirus disease 2019. China J Child Health. 2020;28:407–10.
Zhang X, et al. Survey of psychological status of front-line nurses staff during the period of epidemic and intervention measures. Nurs Pract Res. 2020;17:11–14.
Cheng J, Tan X, Zhang L, Zhu S, Yao H, Liu B. Research on the psychological status and influence factor of novel coronavirus pneumonia patients and people under medical observation. J Nurs Manag. 2020;20:247–51.
Cao X, Tang X, Xue JY. Knowledge Investigation,prevention and psychological analysis of patients with suspected coronavirus disease 2019. J Med Univ Chongqing. 2020. https://doi.org/10.13406/j.cnki.cyxb.002460 .
Fan Y, Wang J, Jia X, Liu X, Song YL, Zhang L. The role of mental problem evaluation and intervention in the university or college students kept at the home due to serious Corona Virus Disease-2019 epidemic during high education. Pharm Serv Res. 2020;20:81–85+91.
Fang X, et al. The mental health status of the close contacts of the new coronavirus pneumonia during the epidemic period. Chin J Crit Care Med. 2020;31:60–62.
Chen Y, Sun J, Hu J, Chen PL, Chen S. Analysis of mental health status of residents during COVID-19 epidemic. Clin Educ Gen Pract. 2020;18:237–9+244. https://doi.org/10.13558/j.cnki.issn1672-3686.2020.003.013 .
Chen J, Yin X, Luo J, Chen F, Ren J, Gong W. investigation and analysis of psychological anxiety status of medical staff in Qingbaijiang District of Chengdu city under new epidemic situation of coronavirus pneumonia. Shandong Med. 2020;60:70–72.
Chang J, Yuan Y, Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. J South Med Univ. 2020;40:171–6.
Yang Y, Qi Ling Z, Zhang H. The anxiety and social support of the spouses of front-line medical staff in Suining under the new coronavirus pneumonia situation. Gen Nurs. 2020;18:940–4.
Wang M, Liu X, Guo H, Fan HZ, Jiang R, Tan S. Mental health of middle-aged and elderly population during outbreak of coronavirus disease 2019. J Chin Geriatr Multi Organ Dis. 2020;19:241–5.
Fang P, et al. Analysis on psychological characteristics of the public in the epidemic of COVID-19. Infect Dis Inf. 2020;33:30–35.
Li C, et al. Investigation and analysis of post-traumatic stress disorder in front-line nursing staff of new coronavirus. Nurse’s Continuing Educ J. 2020;35:615–8. https://doi.org/10.16821/j.cnki.hsjx.2020.25.003 .
Mei J, et al. Analysis of psychological and sleep state of medical staff with novel coronavirus pneumonia. Med. Guidance. 2020;39:345–9.
Huo M, Yin Y, Jiang L, Duan X. Survey on the mental status of inhabitants living in Wuhan, Huanggang, Kunming and Yuxi epidemic outbreak stage of COVID-19. Int J Psychiatry. 2020;47:197–200.
Lei L. et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 eEpidemic in Southwestern China. Med Sci Monit. 2020;26:e924609. https://doi.org/10.12659/MSM.924609 .
Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatry. 2020;51:102092. https://doi.org/10.1016/j.ajp.2020.102092 .
Huang, Y, Zhao, N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group?. Psychol Health Med. 2020;1–12. https://doi.org/10.1080/13548506.2020.1754438 .
Vidyadhara S, Chakravarthy A, Pramod Kumar A, Sri Harsha C, Rahul R. Mental health status among the South Indian Pharmacy students during Covid-19 pandemic’s quarantine period: a cross-sectional study. MedRxiv. May 12, 2020. https://doi.org/10.1101/2020.05.08.20093708 .
Tang W, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020;274:1–7. https://doi.org/10.1016/j.jad.2020.05.009 .
Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med. 2020;70:364–9. https://doi.org/10.1093/occmed/kqaa074 .
Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. https://doi.org/10.1016/j.sleep.2020.05.011 .
Cao W. et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. https://doi.org/10.1016/j.psychres.2020.112934 .
Wu J, et al. Sleep quality survey and its influencing factors of clinical nurses in the first class of new coronavirus pneumonia. Chin Nurs Res. 2020;34:558–62.
Xu M, Zhang Y. Psychological survey of the first line supporting nurses who fight the new coronavirus pneumonia. Clin Nurs Res. 2020;34:368–70.
Kuang Z, Guo K, Liu Y, Li J, Kuang YF. investigation on cognition and psychological status of new university coronavirus pneumonia in Wuhan. J. Trop Med. 2020;03:283–5+288.
Wang Y, Yang Y, Li S, Lei X, Yang Y. Investigation on the status and influencing factors for depression symptom of children and adolescents with home quarantine during the prevalence of novel coronavirus pneumonia. Chin J Child Health. 2020;28:277–80.
Cai H, et al. Novel coronavirus pneumonia epidemic-related knowledge, behaviors and psychology status among college students and their family members and. China Public Health. 2020;36:152–5.
Tian Y, Zhang Y, Qian ZL. Investigation on the emotional status of villagers in a rural area of Hangzhou after the implementation of closure measures during the prevention and control of 2019–nCoV infection. Health Res. 2020;40:16–18+21.
Huang X, Ke P. Effect of standardized training novel coronavirus pneumonia on the anxiety level of the central sterile supply center. Gen Nurs. 2020;8:548–50.
Cai F, Yuan Q. The psychological status of the first line medical staff in combating new coronavirus pneumonia and intervention measures. Gen Nurs. 2020;18:827–8.
Amerio A, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Bio Med. 2020;91:83–88. https://doi.org/10.23750/abm.v91i2.9619 .
Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry. 2020;66:504–11. https://doi.org/10.1177/0020764020927051 .
Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatry. 2020;51:102083. https://doi.org/10.1016/j.ajp.2020.102083 .
Goodman-Casanova JM, Dura-Perez E, Guzman-Parra J, Cuesta-Vargas A, Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: survey study. J Med Internet Res. 2020;22:e19434. https://doi.org/10.2196/19434 .
Kaparounaki CK, Patsali ME, Mousa DV, Papadopoulou E, Papadopoulou K, Fountoulakis KN. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020;290:113111. https://doi.org/10.1016/j.psychres.2020.113111 .
Zohn R, Weinberger-Litman SL, Cheskie R, Rosmarin DH, Leib L. Anxiety and distress among the first community quarantined in the U.S due to COVID-19: Psychological implications for the unfolding crisis. 2020. https://doi.org/10.31234/osf.io/7eq8c .
Du J, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. 2020;20. https://doi.org/10.1016/j.genhosppsych.2020.03.011 .
Guo J, Liao L, Wang B, Li X, Guo L, Tong Z, et al. Psychological effects of covid-19 on hospital staff: a national cross-sectional survey in mainland China. Vasc Invest Ther. 2021;4:6–11.
Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of novel coronavirus pneumonia patients receiving medical treatment in hospitals. Chin J Ind Hyg Occup Dis. 2020;38:192–5. https://doi.org/10.3760/cma.j.cn121094-20200219-00063 .
Liu C, Yang Y, Zhang XM, Xu X, Dou QL, Zhang WW. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiology and infection, 2020;148:e98. https://doi.org/10.1017/S0950268820001107 .
Liu Z, et al. Mental health status of doctors and nurses during COVID-19 epidemic in China. SSRN Electron J. 2020. https://doi.org/10.2139/ssrn.3551329 .
Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936.
Qi J, Xu J, Li BZ, Huang JS, Yang Y, Zhang ZT, et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep medicine, 2020;72:1–4. https://doi.org/10.1016/j.sleep.2020.05.023 .
Zhang C, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 Novel Coronavirus Disease outbreak. Front Psychiatry. 2020;11:306.
Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychotherapy and psychosomatics. 2020;89:242–50. https://doi.org/10.1159/000507639 .
Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, et al. COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine, 2020;24:100443. https://doi.org/10.1016/j.eclinm.2020.100443 .
Tan BYQ, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020. https://doi.org/10.7326/M20-1083 .
Download references
Acknowledgements
Special appreciations to Dr. Yancheng Tang (Peking University, Beijing, China; School of Business and Management, Shanghai International Studies University, Shanghai, China) for his comments on scientific contexts. Many thanks to Xi Luo and Ke Xu (Army Medical University, Chongqing, China) for their contributions to English writing. This study was supported by the People’s Liberation Army of China (PLA) Key Researches Foundation (CWS20J007).
Author information
Authors and affiliations.
Department of Medical Psychology, Army Medical University, Chongqing, China
Xuerong Liu, Mengyin Zhu, Jingxuan Zhang, Zhengzhi Feng & Zhiyi Chen
School of Psychology, Southwest University, Chongqing, China
Rong Zhang & Zhiyi Chen
Cognitive Psychology Unit, The Institute of Psychology, Faculty of Social and Behavioural Sciences, Leiden University, Leiden, Netherlands
Chenyan Zhang
Department of Psychology, University of Florida, Gainesville, FL, USA
You can also search for this author in PubMed Google Scholar
Contributions
XL and ZC: conceptualization, methodology, software, writing—original draft and visualization; MZ, JZ, and RZ: writing—review and editing, methodology, or validation; PL and CZ: writing—revision; RZ and XL: replication analysis and validation; ZC: formal analysis and validation; ZC and ZF: conceptualization, supervision, project administration, and funding acquisition.
Corresponding authors
Correspondence to Zhengzhi Feng or Zhiyi Chen .
Ethics declarations
Competing interests.
The authors declare no competing interests
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplemental material, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions

About this article
Cite this article.
Liu, X., Zhu, M., Zhang, R. et al. Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence. Transl Psychiatry 11 , 384 (2021). https://doi.org/10.1038/s41398-021-01501-9
Download citation
Received : 09 October 2020
Revised : 07 June 2021
Accepted : 21 June 2021
Published : 09 July 2021
DOI : https://doi.org/10.1038/s41398-021-01501-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Work-related problems and the psychosocial characteristics of individuals with irritable bowel syndrome: an updated literature review.
- Nagisa Sugaya
BioPsychoSocial Medicine (2024)
An in-person survey of the influence of the COVID-19 pandemic on physical function, functional capacity, cognitive function, and mental health among community-dwelling older adults in Japan from 2016 to 2022
- Yuko Fukase
- Naoto Kamide
- Hirokuni Tagaya
BMC Geriatrics (2024)
A 2-year longitudinal study examining the change in psychosocial factors under the COVID-19 pandemic in Japan
- Tetsuya Yamamoto
- Chigusa Uchiumi
Scientific Data (2024)
Measuring various aspects of coronavirus anxiety: a psychometric evaluation of Pandemic anxiety and Coronophobia scales from the latent and network perspective
- Lenka Vargová
- Pavol Kačmár
- Gabriel Baník
Current Psychology (2024)
Symptoms and risk factors of depression and PTSD in the prolonged COVID-19 pandemic: a longitudinal survey conducted from 2020 to 2022 in Japan
- Kanako Ichikura
BMC Psychiatry (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 11 April 2023
Effects of the COVID-19 pandemic on mental health, anxiety, and depression
- Ida Kupcova 1 ,
- Lubos Danisovic 1 ,
- Martin Klein 2 &
- Stefan Harsanyi 1
BMC Psychology volume 11 , Article number: 108 ( 2023 ) Cite this article
9747 Accesses
14 Citations
38 Altmetric
Metrics details
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact. According to the World Health Organization (WHO), anxiety and depression prevalence increased by 25% globally. In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population.
A cross-sectional study using an anonymous online-based 45-question online survey was conducted at Comenius University in Bratislava. The questionnaire comprised five general questions and two assessment tools the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS). The results of the Self-Rating Scales were statistically examined in association with sex, age, and level of education.
A total of 205 anonymous subjects participated in this study, and no responses were excluded. In the study group, 78 (38.05%) participants were male, and 127 (61.69%) were female. A higher tendency to anxiety was exhibited by female participants (p = 0.012) and the age group under 30 years of age (p = 0.042). The level of education has been identified as a significant factor for changes in mental state, as participants with higher levels of education tended to be in a worse mental state (p = 0.006).
Conclusions
Summarizing two years of the COVID-19 pandemic, the mental state of people with higher levels of education tended to feel worse, while females and younger adults felt more anxiety.
Peer Review reports
Introduction
The first mention of the novel coronavirus came in 2019, when this variant was discovered in the city of Wuhan, China, and became the first ever documented coronavirus pandemic [ 1 , 2 , 3 ]. At this time there was only a sliver of fear rising all over the globe. However, in March 2020, after the declaration of a global pandemic by the World Health Organization (WHO), the situation changed dramatically [ 4 ]. Answering this, yet an unknown threat thrust many countries into a psycho-socio-economic whirlwind [ 5 , 6 ]. Various measures taken by governments to control the spread of the virus presented the worldwide population with a series of new challenges to which it had to adjust [ 7 , 8 ]. Lockdowns, closed schools, losing employment or businesses, and rising deaths not only in nursing homes came to be a new reality [ 9 , 10 , 11 ]. Lack of scientific information on the novel coronavirus and its effects on the human body, its fast spread, the absence of effective causal treatment, and the restrictions which harmed people´s social life, financial situation and other areas of everyday life lead to long-term living conditions with increased stress levels and low predictability over which people had little control [ 12 ].
Risks of changes in the mental state of the population came mainly from external risk factors, including prolonged lockdowns, social isolation, inadequate or misinterpreted information, loss of income, and acute relationship with the rising death toll. According to the World Health Organization (WHO), since the outbreak of the COVID-19 pandemic, anxiety and depression prevalence increased by 25% globally [ 13 ]. Unemployment specifically has been proven to be also a predictor of suicidal behavior [ 14 , 15 , 16 , 17 , 18 ]. These risk factors then interact with individual psychological factors leading to psychopathologies such as threat appraisal, attentional bias to threat stimuli over neutral stimuli, avoidance, fear learning, impaired safety learning, impaired fear extinction due to habituation, intolerance of uncertainty, and psychological inflexibility. The threat responses are mediated by the limbic system and insula and mitigated by the pre-frontal cortex, which has also been reported in neuroimaging studies, with reduced insula thickness corresponding to more severe anxiety and amygdala volume correlated to anhedonia as a symptom of depression [ 19 , 20 , 21 , 22 , 23 ]. Speaking in psychological terms, the pandemic disturbed our core belief, that we are safe in our communities, cities, countries, or even the world. The lost sense of agency and confidence regarding our future diminished the sense of worth, identity, and meaningfulness of our lives and eroded security-enhancing relationships [ 24 ].
Slovakia introduced harsh public health measures in the first wave of the pandemic, but relaxed these measures during the summer, accompanied by a failure to develop effective find, test, trace, isolate and support systems. Due to this, the country experienced a steep growth in new COVID-19 cases in September 2020, which lead to the erosion of public´s trust in the government´s management of the situation [ 25 ]. As a means to control the second wave of the pandemic, the Slovak government decided to perform nationwide antigen testing over two weekends in November 2020, which was internationally perceived as a very controversial step, moreover, it failed to prevent further lockdowns [ 26 ]. In addition, there was a sharp rise in the unemployment rate since 2020, which continued until July 2020, when it gradually eased [ 27 ]. Pre-pandemic, every 9th citizen of Slovakia suffered from a mental health disorder, according to National Statistics Office in 2017, the majority being affective and anxiety disorders. A group of authors created a web questionnaire aimed at psychiatrists, psychologists, and their patients after the first wave of the COVID-19 pandemic in Slovakia. The results showed that 86.6% of respondents perceived the pathological effect of the pandemic on their mental status, 54.1% of whom were already treated for affective or anxiety disorders [ 28 ].
In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population. This study aimed to assess the symptoms of anxiety and depression in the general public of Slovakia. After the end of epidemiologic restrictive measures (from March to May 2022), we introduced an anonymous online questionnaire using adapted versions of Zung Self-Rating Anxiety Scale (SAS) and Zung Self-Rating Depression Scale (SDS) [ 29 , 30 ]. We focused on the general public because only a portion of people who experience psychological distress seek professional help. We sought to establish, whether during the pandemic the population showed a tendency to adapt to the situation or whether the anxiety and depression symptoms tended to be present even after months of better epidemiologic situation, vaccine availability, and studies putting its effects under review [ 31 , 32 , 33 , 34 ].
Materials and Methods
This study utilized a voluntary and anonymous online self-administered questionnaire, where the collected data cannot be linked to a specific respondent. This study did not process any personal data. The questionnaire consisted of 45 questions. The first three were open-ended questions about participants’ sex, age (date of birth was not recorded), and education. Followed by 2 questions aimed at mental health and changes in the will to live. Further 20 and 20 questions consisted of the Zung SAS and Zung SDS, respectively. Every question in SAS and SDS is scored from 1 to 4 points on a Likert-style scale. The scoring system is introduced in Fig. 1 . Questions were presented in the Slovak language, with emphasis on maintaining test integrity, so, if possible, literal translations were made from English to Slovak. The questionnaire was created and designed in Google Forms®. Data collection was carried out from March 2022 to May 2022. The study was aimed at the general population of Slovakia in times of difficult epidemiologic and social situations due to the high prevalence and incidence of COVID-19 cases during lockdowns and social distancing measures. Because of the character of this web-based study, the optimal distribution of respondents could not be achieved.
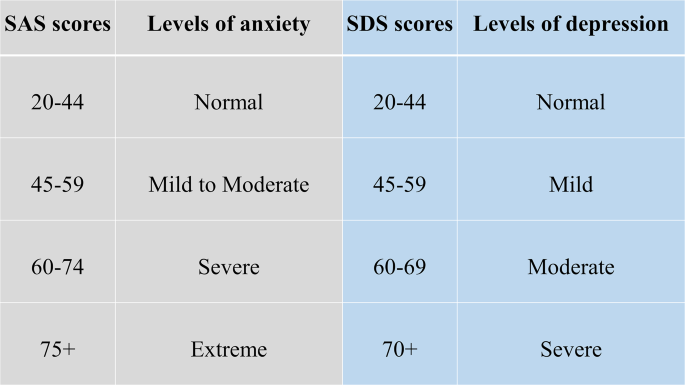
Categories of Zung SAS and SDS scores with clinical interpretation
During the course of this study, 205 respondents answered the anonymous questionnaire in full and were included in the study. All respondents were over 18 years of age. The data was later exported from Google Forms® as an Excel spreadsheet. Coding and analysis were carried out using IBM SPSS Statistics version 26 (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY, USA). Subject groups were created based on sex, age, and education level. First, sex due to differences in emotional expression. Second, age was a risk factor due to perceived stress and fear of the disease. Last, education due to different approaches to information. In these groups four factors were studied: (1) changes in mental state; (2) affected will to live, or frequent thoughts about death; (3) result of SAS; (4) result of SDS. For SAS, no subject in the study group scored anxiety levels of “severe” or “extreme”. Similarly for SDS, no subject depression levels reached “moderate” or “severe”. Pearson’s chi-squared test(χ2) was used to analyze the association between the subject groups and studied factors. The results were considered significant if the p-value was less than 0.05.
Ethical permission was obtained from the local ethics committee (Reference number: ULBGaKG-02/2022). This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines. Due to the anonymous design of the study and by the institutional requirements, written informed consent for participation was not required for this study.
In the study, out of 205 subjects in the study group, 127 (62%) were female and 78 (38%) were male. The average age in the study group was 35.78 years of age (range 19–71 years), with a median of 34 years. In the age group under 30 years of age were 34 (16.6%) subjects, while 162 (79%) were in the range from 31 to 49 and 9 (0.4%) were over 50 years old. 48 (23.4%) participants achieved an education level of lower or higher secondary and 157 (76.6%) finished university or higher. All answers of study participants were included in the study, nothing was excluded.
In Tables 1 and 2 , we can see the distribution of changes in mental state and will to live as stated in the questionnaire. In Table 1 we can see a disproportion in education level and mental state, where participants with higher education tended to feel worse much more than those with lower levels of education. Changes based on sex and age did not show any statistically significant results.
In Table 2 . we can see, that decreased will to live and frequent thoughts about death were only marginally present in the study group, which suggests that coping mechanisms play a huge role in adaptation to such events (e.g. the global pandemic). There is also a possibility that living in times of better epidemiologic situations makes people more likely to forget about the bad past.
Anxiety and depression levels as seen in Tables 3 and 4 were different, where female participants and the age group under 30 years of age tended to feel more anxiety than other groups. No significant changes in depression levels based on sex, age, and education were found.
Compared to the estimated global prevalence of depression in 2017 (3.44%), in 2021 it was approximately 7 times higher (25%) [ 14 ]. Our study did not prove an increase in depression, while anxiety levels and changes in the mental state did prove elevated. No significant changes in depression levels go in hand with the unaffected will to live and infrequent thoughts about death, which were important findings, that did not supplement our primary hypothesis that the fear of death caused by COVID-19 or accompanying infections would enhance personal distress and depression, leading to decreases in studied factors. These results are drawn from our limited sample size and uneven demographic distribution. Suicide ideations rose from 5% pre-pandemic to 10.81% during the pandemic [ 35 ]. In our study, 9.3% of participants experienced thoughts about death and since we did not specifically ask if they thought about suicide, our results only partially correlate with suicidal ideations. However, as these subjects exhibited only moderate levels of anxiety and mild levels of depression, the rise of suicide ideations seems unlikely. The rise in suicidal ideations seemed to be especially true for the general population with no pre-existing psychiatric conditions in the first months of the pandemic [ 36 ]. The policies implemented by countries to contain the pandemic also took a toll on the population´s mental health, as it was reported, that more stringent policies, mainly the social distancing and perceived government´s handling of the pandemic, were related to worse psychological outcomes [ 37 ]. The effects of lockdowns are far-fetched and the increases in mental health challenges, well-being, and quality of life will require a long time to be understood, as Onyeaka et al. conclude [ 10 ]. These effects are not unforeseen, as the global population suffered from life-altering changes in the structure and accessibility of education or healthcare, fluctuations in prices and food insecurity, as well as the inevitable depression of the global economy [ 38 ].
The loneliness associated with enforced social distancing leads to an increase in depression, anxiety, and posttraumatic stress in children in adolescents, with possible long-term sequelae [ 39 ]. The increase in adolescent self-injury was 27.6% during the pandemic [ 40 ]. Similar findings were described in the middle-aged and elderly population, in which both depression and anxiety prevalence rose at the beginning of the pandemic, during the pandemic, with depression persisting later in the pandemic, while the anxiety-related disorders tended to subside [ 41 ]. Medical professionals represented another specific at-risk group, with reported anxiety and depression rates of 24.94% and 24.83% respectively [ 42 ]. The dynamic of psychopathology related to the COVID-19 pandemic is not clear, with studies reporting a return to normal later in 2020, while others describe increased distress later in the pandemic [ 20 , 43 ].
Concerning the general population, authors from Spain reported that lockdowns and COVID-19 were associated with depression and anxiety [ 44 ]. In January 2022 Zhao et al., reported an elevation in hoarding behavior due to fear of COVID-19, while this process was moderated by education and income levels, however, less in the general population if compared to students [ 45 ]. Higher education levels and better access to information could improve persons’ fear of the unknown, however, this fact was not consistent with our expectations in this study, as participants with university education tended to feel worse than participants with lower education. A study on adolescents and their perceived stress in the Czech Republic concluded that girls are more affected by lockdowns. The strongest predictor was loneliness, while having someone to talk to, scored the lowest [ 46 ]. Garbóczy et al. reported elevated perceived stress levels and health anxiety in 1289 Hungarian and international students, also affected by disengagement from home and inadequate coping strategies [ 47 ]. Wathelet et al. conducted a study on French University students confined during the pandemic with alarming results of a high prevalence of mental health issues in the study group [ 48 ]. Our study indicated similar results, as participants in the age group under 30 years of age tended to feel more anxious than others.
In conclusion, we can say that this pandemic changed the lives of many. Many of us, our family members, friends, and colleagues, experienced life-altering events and complicated situations unseen for decades. Our decisions and actions fueled the progress in medicine, while they also continue to impact society on all levels. The long-term effects on adolescents are yet to be seen, while effects of pain, fear, and isolation on the general population are already presenting themselves.
The limitations of this study were numerous and as this was a web-based study, the optimal distribution of respondents could not be achieved, due to the snowball sampling strategy. The main limitation was the small sample size and uneven demographic distribution of respondents, which could impact the representativeness of the studied population and increase the margin of error. Similarly, the limited number of older participants could significantly impact the reported results, as age was an important risk factor and thus an important stressor. The questionnaire omitted the presence of COVID-19-unrelated life-changing events or stressors, and also did not account for any preexisting condition or risk factor that may have affected the outcome of the used assessment scales.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to compliance with institutional guidelines but they are available from the corresponding author (SH) on a reasonable request.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Article PubMed PubMed Central Google Scholar
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Liu Y-C, Kuo R-L, Shih S-R. COVID-19: the first documented coronavirus pandemic in history. Biomed J. 2020;43:328–33.
Advice for the public on COVID-19 – World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . Accessed 13 Nov 2022.
Osterrieder A, Cuman G, Pan-Ngum W, Cheah PK, Cheah P-K, Peerawaranun P, et al. Economic and social impacts of COVID-19 and public health measures: results from an anonymous online survey in Thailand, Malaysia, the UK, Italy and Slovenia. BMJ Open. 2021;11:e046863.
Article PubMed Google Scholar
Mofijur M, Fattah IMR, Alam MA, Islam ABMS, Ong HC, Rahman SMA, et al. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustainable Prod Consum. 2021;26:343–59.
Article Google Scholar
Vlachos J, Hertegård E, Svaleryd B. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A. 2021;118:e2020834118.
Ludvigsson JF, Engerström L, Nordenhäll C, Larsson E, Open Schools. Covid-19, and child and teacher morbidity in Sweden. N Engl J Med. 2021;384:669–71.
Miralles O, Sanchez-Rodriguez D, Marco E, Annweiler C, Baztan A, Betancor É, et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six european countries. Eur Geriatr Med. 2021;12:193–204.
Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: a review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104:368504211019854.
The Lancet null. India under COVID-19 lockdown. Lancet. 2020;395:1315.
Lo Coco G, Gentile A, Bosnar K, Milovanović I, Bianco A, Drid P, et al. A cross-country examination on the fear of COVID-19 and the sense of loneliness during the First Wave of COVID-19 outbreak. Int J Environ Res Public Health. 2021;18:2586.
COVID-19 pandemic. triggers 25% increase in prevalence of anxiety and depression worldwide. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide . Accessed 14 Nov 2022.
Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int J Clin Health Psychol. 2021;21:100196.
Hajek A, Sabat I, Neumann-Böhme S, Schreyögg J, Barros PP, Stargardt T, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the european COvid Survey (ECOS). J Affect Disord. 2022;299:517–24.
Piumatti G, Levati S, Amati R, Crivelli L, Albanese E. Trajectories of depression, anxiety and stress among adults during the COVID-19 pandemic in Southern Switzerland: the Corona Immunitas Ticino cohort study. Public Health. 2022;206:63–9.
Korkmaz H, Güloğlu B. The role of uncertainty tolerance and meaning in life on depression and anxiety throughout Covid-19 pandemic. Pers Indiv Differ. 2021;179:110952.
McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290:113104.
Funkhouser CJ, Klemballa DM, Shankman SA. Using what we know about threat reactivity models to understand mental health during the COVID-19 pandemic. Behav Res Ther. 2022;153:104082.
Landi G, Pakenham KI, Crocetti E, Tossani E, Grandi S. The trajectories of anxiety and depression during the COVID-19 pandemic and the protective role of psychological flexibility: a four-wave longitudinal study. J Affect Disord. 2022;307:69–78.
Holt-Gosselin B, Tozzi L, Ramirez CA, Gotlib IH, Williams LM. Coping strategies, neural structure, and depression and anxiety during the COVID-19 pandemic: a longitudinal study in a naturalistic sample spanning clinical diagnoses and subclinical symptoms. Biol Psychiatry Global Open Sci. 2021;1:261–71.
McCracken LM, Badinlou F, Buhrman M, Brocki KC. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. J Context Behav Sci. 2021;19:28–35.
Talkovsky AM, Norton PJ. Negative affect and intolerance of uncertainty as potential mediators of change in comorbid depression in transdiagnostic CBT for anxiety. J Affect Disord. 2018;236:259–65.
Milman E, Lee SA, Neimeyer RA, Mathis AA, Jobe MC. Modeling pandemic depression and anxiety: the mediational role of core beliefs and meaning making. J Affect Disorders Rep. 2020;2:100023.
Sagan A, Bryndova L, Kowalska-Bobko I, Smatana M, Spranger A, Szerencses V, et al. A reversal of fortune: comparison of health system responses to COVID-19 in the Visegrad group during the early phases of the pandemic. Health Policy. 2022;126:446–55.
Holt E. COVID-19 testing in Slovakia. Lancet Infect Dis. 2021;21:32.
Stalmachova K, Strenitzerova M. Impact of the COVID-19 pandemic on employment in transport and telecommunications sectors. Transp Res Procedia. 2021;55:87–94.
Izakova L, Breznoscakova D, Jandova K, Valkucakova V, Bezakova G, Suvada J. What mental health experts in Slovakia are learning from COVID-19 pandemic? Indian J Psychiatry. 2020;62(Suppl 3):459–66.
Rabinčák M, Tkáčová Ľ, VYUŽÍVANIE PSYCHOMETRICKÝCH KONŠTRUKTOV PRE, HODNOTENIE PORÚCH NÁLADY V OŠETROVATEĽSKEJ PRAXI. Zdravotnícke Listy. 2019;7:7.
Google Scholar
Sekot M, Gürlich R, Maruna P, Páv M, Uhlíková P. Hodnocení úzkosti a deprese u pacientů se zhoubnými nádory trávicího traktu. Čes a slov Psychiat. 2005;101:252–7.
Lipsitch M, Krammer F, Regev-Yochay G, Lustig Y, Balicer RD. SARS-CoV-2 breakthrough infections in vaccinated individuals: measurement, causes and impact. Nat Rev Immunol. 2022;22:57–65.
Accorsi EK, Britton A, Fleming-Dutra KE, Smith ZR, Shang N, Derado G, et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta Variants. JAMA. 2022;327:639–51.
Barda N, Dagan N, Cohen C, Hernán MA, Lipsitch M, Kohane IS, et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. 2021;398:2093–100.
Magen O, Waxman JG, Makov-Assif M, Vered R, Dicker D, Hernán MA, et al. Fourth dose of BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2022;386:1603–14.
Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301:113998.
Kok AAL, Pan K-Y, Rius-Ottenheim N, Jörg F, Eikelenboom M, Horsfall M, et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in dutch case-control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J Affect Disord. 2022;305:85–93.
Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve J-E, et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. The Lancet Public Health. 2022;7:e417–26.
Prochazka J, Scheel T, Pirozek P, Kratochvil T, Civilotti C, Bollo M, et al. Data on work-related consequences of COVID-19 pandemic for employees across Europe. Data Brief. 2020;32:106174.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239e3.
Zetterqvist M, Jonsson LS, Landberg Ã, Svedin CG. A potential increase in adolescent nonsuicidal self-injury during covid-19: a comparison of data from three different time points during 2011–2021. Psychiatry Res. 2021;305:114208.
Mooldijk SS, Dommershuijsen LJ, de Feijter M, Luik AI. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. 2022;149:274–80.
Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110247.
Stephenson E, O’Neill B, Kalia S, Ji C, Crampton N, Butt DA, et al. Effects of COVID-19 pandemic on anxiety and depression in primary care: a retrospective cohort study. J Affect Disord. 2022;303:216–22.
Goldberg X, Castaño-Vinyals G, Espinosa A, Carreras A, Liutsko L, Sicuri E et al. Mental health and COVID-19 in a general population cohort in Spain (COVICAT study).Soc Psychiatry Psychiatr Epidemiol. 2022;:1–12.
Zhao Y, Yu Y, Zhao R, Cai Y, Gao S, Liu Y, et al. Association between fear of COVID-19 and hoarding behavior during the outbreak of the COVID-19 pandemic: the mediating role of mental health status. Front Psychol. 2022;13:996486.
Furstova J, Kascakova N, Sigmundova D, Zidkova R, Tavel P, Badura P. Perceived stress of adolescents during the COVID-19 lockdown: bayesian multilevel modeling of the Czech HBSC lockdown survey. Front Psychol. 2022;13:964313.
Garbóczy S, Szemán-Nagy A, Ahmad MS, Harsányi S, Ocsenás D, Rekenyi V, et al. Health anxiety, perceived stress, and coping styles in the shadow of the COVID-19. BMC Psychol. 2021;9:53.
Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors Associated with Mental Health Disorders among University students in France Confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2025591.
Download references
Acknowledgements
We would like to provide our appreciation and thanks to all the respondents in this study.
This research project received no external funding.
Author information
Authors and affiliations.
Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Ida Kupcova, Lubos Danisovic & Stefan Harsanyi
Institute of Histology and Embryology, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Martin Klein
You can also search for this author in PubMed Google Scholar
Contributions
IK and SH have produced the study design. All authors contributed to the manuscript writing, revising, and editing. LD and MK have done data management and extraction, SH did the data analysis. Drafting and interpretation of the manuscript were made by all authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Stefan Harsanyi .
Ethics declarations
Ethics approval and consent to participate.
Ethical permission was obtained from the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava (Reference number: ULBGaKG-02/2022). The need for informed consent was waived by the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava due to the anonymous design of the study. This study did not process any personal data and the dataset does not contain any direct or indirect identifiers of participants. This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kupcova, I., Danisovic, L., Klein, M. et al. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol 11 , 108 (2023). https://doi.org/10.1186/s40359-023-01130-5
Download citation
Received : 14 November 2022
Accepted : 20 March 2023
Published : 11 April 2023
DOI : https://doi.org/10.1186/s40359-023-01130-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Departments
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Mental Health and COVID-19
- Mental Health Diversity, Equity, and Inclusion
- Origins of Mental Health
- Job Openings
- Faculty Profiles
- PET Alumni Profiles - Postdocs
- PET Alumni Profiles - Predocs
- Trainee Profiles
- NIMH T32 Mental Health Services and Systems Training Grant
- Funded Training Program in Data Integration for Causal Inference in Behavioral Health
- Aging and Dementia Funded Training Program
- COVID-19 and Mental Health Research
- Mental Health Resources During COVID-19
- News and Media
- Social Determinants of Mental and Behavioral Health
Our Work in Action
- Global Mental Health
- Related Faculty
- Courses of Interest
- Training and Funding Opportunities
- Mental Health in the Workplace: A Public Health Summit
- Autism and Developmental Disabilities
- Alumni Newsletters
- Alumni Updates
- Postdoctoral Fellows
- Doctor of Philosophy (PhD) Students in Mental Health
- Master of Health Science (MHS) Students in Mental Health
- In the News
- Past Seminars 2020-21 AY: Wednesday Seminar Series
- Make a Gift
- Available Datasets
The COVID-19 pandemic has had a huge impact on public health around the globe in terms of both physical and mental health, and the mental health implications of the pandemic may continue long after the physical health consequences have resolved. This research area aims to contribute to our understanding of the COVID-19 pandemics implications for mental health, building on a robust literature on how environmental crises, such as SARS or natural disasters, can lead to mental health challenges, including loneliness, acute stress, anxiety, and depression. The social distancing aspects of the COVID-19 pandemic may have particularly significant effects on mental health. Understanding how mental health evolves as a result of this serious global pandemic will inform prevention and treatment strategies moving forward, including allocation of resources to those most in need. Critically, these data can also serve as evidence-based information for public health organizations and the public as a whole.
Understanding the Mental Health Implications of a Pandemic

Introduction
The world is entering into a new phase with COVID-19 spreading rapidly. People will be studying various consequences of the COVID-19 pandemic and mental and behavioral health should be a core part of that effort. There is a robust literature on how environmental crises, such as SARS or natural disasters, can lead to mental health challenges, including loneliness, acute stress, anxiety, and depression. The social distancing aspects of the current pandemic may have particularly significant effects on mental health. Understanding how mental health evolves as a result of this serious global outbreak will inform prevention and treatment strategies moving forward, including allocation of resources to those most in need. Critically, these data can also serve as evidence-based information for public health organizations and the public as a whole.
The data will be leveraged to address many questions, such as:
- Which individuals are at greatest risk for high levels of mental health distress during a pandemic?
- As individuals spend more time inside and isolated, how does their mental health distress evolve?
- How do different behaviors (such as media consumption) relate to mental health?
Read more about how our experts are measuring mental distress amid a pandemic.
We have been working to ensure that measurement of mental health measures is a key part of large-scale national and international data collections relative to COVID-19.
Read more about conducting research studies on mental health during the pandemic.
Mental Health Resources
See our resources guide here.
Members of the COVID-19 Mental Health Measurement Working Group
- M. Daniele Fallin, JHSPH
- Calliope Holingue, Kennedy Krieger Institute, JHSPH
- Renee M. Johnson, JHSPH
- Luke Kalb, Kennedy Krieger Institute, JHSPH
- Frauke Kreuter, University of Maryland, University of Mannheim
- Courtney Nordeck, JHSPH
- Kira Riehm, JHSPH
- Emily J. Smail, JHSPH
- Elizabeth Stuart, JHSPH
- Johannes Thrul, JHSPH
- Cindy Veldhuis, Columbia University School of Nursing
The Johns Hopkins COVID-19 Mental Health Measurement Working Group developed key questions to add to existing large domestic and international surveys to measure the mental health impact of the pandemic.


Societal and biological factors both contribute to mental health issues in the wake of COVID-19

Even as classrooms, offices, concerts and weddings have begun to look more like their pre-2020 counterparts, marks of the global pandemic remain visible in new norms and long-term issues.
“COVID-19 affected a whole generation of individuals at every level,” said Khalid Afzal, MD , a pediatric psychiatrist at the University of Chicago Medicine.
In conversations on social media and in other forums, many people share a general sense that COVID-19 had a significant impact on mental health — that it represents a collective trauma from which we will be healing for years. Now that researchers have a few years’ worth of data to analyze, they’re beginning to unpack that mental impact more fully from an empirical standpoint.
The toll of upheaval
According to Afzal, attempted suicide and suicide-related emergency department visits for both children and adults went up significantly within a few months of the pandemic’s onset, as did completed suicide rates. Data from the CDC and researchers across the country also show a jump in rates of disorders like anxiety and depression, and psychiatric treatment centers have reported longer wait times as demand exceeded capacity.
“After a few months, the reality hit people that the situation wasn’t going to change anytime soon,” Afzal said. “And the more they became isolated, the more that isolation compounded with other stressors like financial worries and fear of dying. It’s pretty disheartening to see the toll it took on people.”
He said the interruption of major life milestones like graduations was especially traumatizing for children and adolescents, as were the lack of privacy and relational tensions caused by families being cooped up in close quarters.
How a respiratory virus can affect the brain
It makes sense that the pandemic’s massive societal disruptions triggered mental distress. Less obvious — but still important — are the direct impacts of biological changes from COVID-19 that affect the brain and behavior.
Although COVID-19 is first and foremost a respiratory virus, it attacks many systems in the body and can cause dangerous inflammation. Health experts quickly realized that adults with particularly serious psychiatric disorders, such as schizophrenia and bipolar disorder, were uniquely vulnerable to COVID-19 infection — their cases were more likely to be medically severe, and many experienced worsening of their psychiatric disorders. “It wasn’t necessarily an intuitive outcome, but the trend became clear very early on,” said Royce Lee, MD , a psychiatrist and researcher at UChicago Medicine.
People who didn’t have psychiatric diagnoses before contracting COVID-19 weren’t invulnerable to neurological effects, either. Many wound up with “long COVID” symptoms like pain, mental cloudiness, lack of sustained attention, difficulty with memory, depression, anxiety, fatigue and irritability.
“There are causal pathways in both directions between immune activation and brain function, which affect behavior and emotions,” said Lee, whose research often focuses on those pathways. “In particular, there’s a very strong connection between immune activation and regulating anger.” Immune activation can come directly from the virus itself or be triggered indirectly by stress and fear.
Lee pointed out that even people who don’t notice brain fog or have detectable “long COVID” may still experience subtler symptoms like increased irritability, so it’s important to continue the destigmatization of mental health and encourage awareness to help people take back control of their emotions.
“If abrupt shifts in mental health show up, it’s still relevant to ask yourself, ‘When was my last COVID-19 infection? And how does the timing of that align with my change in mental state?’” Lee said.
Staying proactive about mental health and safety
Elevated rates of suicide and psychiatric disorders make mental health safety an especially high priority in the wake of COVID-19. A group of UChicago researchers recently published a study highlighting safety concerns related to a substance found in countless homes: acetaminophen.
“It's important to think about how something that's so easily accessible could be used for something very dangerous,” said first author Wendy Luo, a third-year student at the UChicago Pritzker School of Medicine. “As the pandemic unfolded and kids started to struggle even more with mental health, it makes sense that they’ve often turned to what's available in the home.”
Even before 2020, researchers had noticed an increase in calls to poison control hotlines related to suspected attempted suicide by acetaminophen overdose. Experts also documented higher suicide rates among students during the academic year compared to the summer months. Luo and her collaborators set out to investigate whether COVID-19 exacerbated these trends even further.
They compared acetaminophen-related hospital admissions from the pre-COVID-19 era (January 2016–February 2020) to the COVID-19 era (March 2020-December 2022). They found that intentional acetaminophen ingestion became much more frequent during the COVID-19 era among children ages 8-18, and the rates remained highest during the school year even though many schools were at least partially remote during that time period.
“We're hoping these results send a message that we need to have more resources in schools because we consistently see the highest rates of self-harm during the months students spend in school,” Luo said. “And when there are major disruptions in school like the shift from in-person to virtual and hybrid during the pandemic, some children struggle even more with the uncertainty and isolation.”
Moving forward as COVID-19 lingers
“As a society, we need to educate ourselves, recognize that these mental effects are very real, and provide individualized support and accommodations for people as they recover,” Afzal said. “It’s important to view people as survivors rather than victims. I think people are naturally resilient, but the way we talk about things affects the way we move forward.”
Like Luo, Afzal pointed out the need for more resources in multiple settings. He said some hopeful trends have already emerged, such as an increase in the number of medical students choosing to specialize in psychiatry, but added that there is plenty of room for various decision-makers to increase mental healthcare capacity and provide a wider range of solutions and support.
Lee likes to refer back to the Spanish flu as a good teaching case for understanding some of the effects of a worldwide pandemic. Fortunately, the past may have some hope to offer:
“There was kind of a delayed response: in the two or three years following that viral outbreak, psychiatric disorders increased in prevalence and some new ones emerged, probably as a result of immune activation,” he said. “It was almost like a neuropsychiatric second wave of the pandemic. But then it got quiet again and more or less went back to normal. I think it’s possible we’ll see similar trends with this pandemic.”
“ COVID-19 and Intentional Toxic Pediatric Acetaminophen Ingestions: A Research Brief ” was published in Hospital Pediatrics , the journal of the American Academy of Pediatrics, in April 2024. Authors included Wendy Luo, Isabella Zaniletti, Sana J. Said and Jason M. Kane.

Khalid Afzal, MD
Khalid Afzal, MD, is an Associate Professor of Psychiatry and Behavioral Neuroscience and the Director of the Child and Adolescent Psychiatry Consult-Liaison Service.

Royce Lee, MD
Royce Lee, MD, is a psychiatrist who specializes in treating patients who suffer from depression, personality disorders and post traumatic stress disorder (PTSD).
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Public Health, College of Science and Health, William Paterson University, Wayne, NJ, United States of America
Roles Conceptualization, Data curation, Methodology, Writing – review & editing
Roles Methodology, Writing – review & editing
Affiliation Department of Environmental Science, College of Science and Health, William Paterson University, Wayne, NJ, United States of America
- Aleksandar Kecojevic,
- Corey H. Basch,
- Marianne Sullivan,
- Nicole K. Davi

- Published: September 30, 2020
- https://doi.org/10.1371/journal.pone.0239696
- Reader Comments
The COVID-19 pandemic has been a period of upheaval for college students. The objective of this study was to assess the factors associated with the increased levels of mental health burden among a sample of undergraduate college students in Northern New Jersey, the region of the U.S. severely impacted by the outbreak of COVID-19.
College students (N = 162) enrolled in an introductory core curriculum course completed a cross-sectional survey. The survey collected information on demographics, knowledge levels and sources of COVID-19 information, behavior changes, academic and everyday difficulties, and mental health measurements (depression, anxiety, somatization, and stress). Multivariable regression analysis was performed to identify factors associated with mental health outcomes.
Descriptive findings indicate that students have a fundamental knowledge of COVID-19 transmission and common symptoms. Students tend to use and trust the official sources and have changed their behaviors in accordance with public health recommendations (i.e., increased hand washing, wearing mask). However, students reported a number of academic and everyday difficulties and high levels of mental health distress. High levels of depression were associated with difficulties in focusing on academic work and with employment losses, while higher levels of anxiety were more likely to be reported by students other than freshmen and those who spend more than one hour per day looking for information on COVID-19. Inability to focus on academic work and an elevated concern with COVID-19 were more likely to be associated with higher levels of somatization, while trusting news sources was associated with lower levels of somatization. Those with higher levels of perceived stress were more likely to be females, unable to focus on academic work, and report difficulties in obtaining medications and cleaning supplies.
Conclusions
The COVID-19 pandemic is making a significant negative impact on mental health of college students. Proactive efforts to support the mental health and well-being of students are needed.
Citation: Kecojevic A, Basch CH, Sullivan M, Davi NK (2020) The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS ONE 15(9): e0239696. https://doi.org/10.1371/journal.pone.0239696
Editor: Kristin Vickers, Ryerson University, CANADA
Received: April 29, 2020; Accepted: September 12, 2020; Published: September 30, 2020
Copyright: © 2020 Kecojevic et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The novel coronavirus (COVID-19) pandemic has rapidly spread across the globe, causing massive disruptions to everyday life, including in the United States (U.S.). According to the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University [ 1 ], as of April 27 th , there were close to a million of confirmed cases with a total of 55,952 deaths in the U.S., with New Jersey among the hardest hit states in the country reporting 111,188 confirmed cases and 6,044 deaths [ 2 ]. At the time of this study, the counties in Northern New Jersey, where this study took place, have some of the highest confirmed case counts in the state.
The pandemic has the potential to affect college students physically, academically, financially and psychologically. Some colleges and universities in New Jersey have reported that a number of students have tested positive for COVID-19 [ 3 – 6 ]. In order to prevent widespread transmission of the COVID-19 virus among staff and the young adult population, higher-education institutions across the country have rapidly switched from in-person to online learning [ 7 ]. In a short period of time, college students’ lives have dramatically changed as they have been asked to leave campus, adjust to new living circumstances, and adapt to online learning platforms. The switch to online learning, particularly in courses that were not originally designed for on-line delivery likely has increased stress among students. Courses designed to include high levels of interaction and hands-on experiences such as practicums, labs, and/or artistic performance have a clear disadvantage in regards to the evaluation of students [ 8 ]. Some students may have difficulties with access to computers and the internet at home [ 8 , 9 ]. Additional challenges include concerns about their health, health of family members, and worry about finances, particularly among those who support themselves by working in industries severely impacted by prolonged closures such as retail or the service industry. According to a survey by the loan management website Student Loan Hero [ 10 ] 4 out of 5 college students are facing financial difficulties due to the COVID-19 pandemic. Further, most college students are not eligible for immediate financial relief under the Coronavirus Aid, Relief and Economic Security (CARES) Act [ 11 ].
College students’ mental health has been rising concern with a significant number of students experiencing psychological distress [ 12 ]. Mental health issues can significantly impair students’ academic success and social interactions affecting their future career and personal opportunities. The rapid spread of COVID-19 and social distancing measures imposed across the country are expected to further affect the mental health of the population, including college students. Several studies have examined the psychological impact of the pandemic on the general public [ 13 – 15 ], health care workers [ 16 ], or older adults [ 17 ]. These surveys revealed greater concerns about social isolation, and increased stress, anxiety, and depression among respondents. Interestingly, a study of Chinese general public [ 13 ] also reported that exposure to accurate content of health information during the epidemic was associated with lower stress levels. Conversely, the studies of previous epidemics show that inaccurate information, particularly prevalent in online discussion boards or social media, was associated with anxiety and fear [ 18 ]. Accurate information, knowledge and perceptions of risk can contribute to behavioral changes [ 19 ], such as social distancing, which is currently one of the few ways to mitigate the spread of COVID-19. The current evidence also shows that taking prescribed precautionary measures (i.e. hand hygiene, mask wearing) to prevent the spread of COVID-19 may reduce negative psychological impacts by providing a sense of security to those engaging in these preventative actions [ 13 ]. While many colleges and universities provide students with information related to COVID-19 from reliable sources [ 20 ], there is a high potential for misinformation and disinformation to spread through online sources and social media often used by young adults [ 21 – 23 ] further contributing to stress, anxiety and depression among students.
Available literature examining the impact of the COVID-19 epidemic on students in the U.S. is primarily focused on the role of medical and other health profession students during the current COVID-19 epidemic [ 24 – 26 ]. Limited research examining the impact of the COVID-19 epidemic on the psychological health of students has primarily focused on students outside the U.S. Furthermore, little is known about factors contributing to psychological distress related to COVID-19 among college students. One study of undergraduates of Changzhi medical college in China, indicated that a quarter of those surveyed have experienced anxiety due to COVID-19 [ 27 ]. Having a relative or an acquaintance infected with COVID-19, economic stressors and academic delays were all positively associated with an increased level of anxiety symptoms. A previous study investigating adverse psychological reactions to the Middle East Respiratory Syndrome Corona Virus (MERS-CoV) outbreak in 2014 among medical students in Saudi Arabia indicated that increased hygienic habits and social distancing were positively associated with the psychological well-being of students [ 28 ]. Additionally, a study of Iranian medical students found a high level of COVID-19 related knowledge, engagement in self-reported preventive behaviors, and moderate risk perception among respondents [ 29 ].
Current study
In light of growing concerns related to the impact of COVID-19 on the mental health of vulnerable groups [ 30 ], there is an urgent need for research to address mental health burden of the COVID-19 pandemic on college students. At the time of writing we were unable to identify published research on the impact of the COVID-19 pandemic on the mental health of undergraduate college students in the US. Therefore, the current investigation had two primary aims. First, we sought to determine the levels of mental health distress among undergraduate college students during a time period when the significant number of people in Northern New Jersey were testing positive and dying due to COVID-19. Second, we sought to examine whether factors such as knowledge, sources of information, and academic and everyday difficulties are associated with mental health distress among college students during the COVID-19 pandemic.
This cross-sectional survey was administered at a suburban public university in Northern New Jersey, U.S., in April of 2020. All students (n = 450) taking an introductory core curriculum course focusing on personal health and delivered by the Department of Public Health were invited to participate in this study. While completion of this course is required for admission to a Public Health program, students from other majors may take either this course or other courses focused on personal well-being. The instructors of 17 course sections were provided with a description of the study and were asked to alert their students about the forthcoming invitation. A link to the survey was delivered to students via e-mail, and two reminders were sent in the subsequent week following the initial invitation. Participants provided informed consent to participate in an anonymous survey by completing and submitting the questionnaire electronically in Qualtrics software (Qualtrics, Provo, UT). All data were self-reported. A total of 162 students completed the survey, resulting in a response rate of 36.0%. Students were given an opportunity to enter a raffle to win one of five $20 gift cards. The University Institutional Review Board (IRB) approved the study.
Demographics.
Demographic information included age (recorded as continuous variable), sex (male, female, other), ethnicity (Hispanic/non-Hispanic), race, class level (freshman, sophomore, junior, senior), and whether the student is a health major—public health or nursing (yes/no).
Knowledge related to COVID-19.
A total of 10 knowledge questions were asked, 7 of which were True/False (e.g., “Those who are elderly and have chronic illnesses are more likely to be severe cases”), while 3 questions assessed the level of agreement with the statements (e.g. “To prevent infection with COVID-19, people should avoid going to crowded places”) on a 5-point scale (0 = “ strongly disagree ” to 4 = “ strongly agree ”). All knowledge questions were based on Centers for Disease Control and Prevention (CDC) fact sheets [ 31 ].
Sources of information on COVID-19.
Students were asked what information sources (i.e. news websites, doctors, friends) they trust to provide accurate COVID-19 information (check all that apply). Additionally, students were asked how often do they use these sources to get health information on COVID-19 on a 5-point scale that ranges from 0 =“ never ” to 4 =“ always ”. Values were dichotomized to 0 (never, rarely, sometimes) and 1 (often, always). In addition, they were asked to indicate the average number of hours per day they spend looking for information on COVID-19.
Engagement in precautionary behaviors.
Using 5-point scale (0 = “ not at all ” to 4 = “ extremely ”), participants were asked whether they engaged in precautionary changes of behaviors related to their personal hygiene (e.g. “I have increased hand washing”) or social habits (e.g. “I have limited going outside only to essential trips”) since the start of the pandemic. The statements were formed based on previous literature [ 13 ]. Values were dichotomized to 0 (did not engage in precautionary behaviors at all) and 1 (engaged in in precautionary behaviors even a little bit).
Hardships experienced during the pandemic.
Students were asked to indicate whether they experienced various academic (i.e. difficulties with online learning, ability to focus on academic work, etc.), or life (i.e. losing job, getting food, etc.) difficulties. Some values were combined for easiness of presentation (i.e. difficulties with online learning and inadequate WiFi/Internet access).
Mental health burden
Level of concern with the current pandemic was assessed by a single question asking how concerned the respondent feels about COVID-19. Responses were recorded on a 5-point scale that ranges from 0 =“ not at all ” to 4 =“ extremely ”. Values were dichotomized to 0 (not at all to moderately concerned), and 1 (very to extremely concerned).
To assess levels of depression, anxiety and somatic distress, we used the Brief Symptom Inventory, BSI-18, [ 32 ]. The assessment measures self-reported psychological distress in the prior week. Participants were queried about the extent to which something has distressed or bothered them in the past 7 days (e.g., “In the past 7 days, how much were you distressed by feeling lonely?”) on a 5-point scale ranging from 0 =“ not at all ” to 4 =“ extremely ”. As per the BSI-18 scoring instructions, raw scores were converted to T scores using gender specific community norms. Higher scores signify greater levels of depression, anxiety, or distress arising from perceptions of bodily dysfunctions, i.e. somatization. Because the BSI clinical case cutoff likely has a low positive predictive value in this population [ 33 ], we are not reporting on prevalence of psychological distress in our sample. Cronbach’s alpha for the overall scale was 0.94 (α = 0.89, 0.89, 0.84 for the depression, anxiety, and somatization subscales, respectively).
The Perceived Stress Scale (PSS), a 10-item self-report questionnaire with strong reliability and validity [ 34 ], was used to assess general stress appraisal. Respondents were asked to specify how often they have felt or thought a certain way in the past month (e.g., “In the last month, how often have you been upset because of something that happened unexpectedly?”) on a 5-point scale ranging from 0 =“ never ” to 4 =“ very often ”. Some of the items were scored in reverse. Responses were then summed to indicate the level of perceived stress. It should be noted that the PSS is not a diagnostic instrument and there are no score cut-offs. Nevertheless, higher scores signify a greater perceived stress. Cronbach’s alpha was 0.84.
Data analysis
Statistical analyses were conducted using the Statistical Package for Social Sciences, SPSS, 26.0 (IBM). Descriptive analyses examined the distribution of all variables of interest. Eleven participants did not complete questions about mental health burden and stress; hence they were not included in bivariate and regression analyses. Using t-tests for means we then examined unadjusted bivariate associations between the independent variables and the four variables describing mental health burden. Next, we entered all bivariate correlates that achieved significance of less than 0.05 into multivariable linear regression models to evaluate the predictive nature of independent variables on depression, anxiety, somatization and stress while controlling for the potentially confounding effects of other variables in models. To ensure that covariates were not collinear, we examined the variance inflation factors for each variable, none of which were greater than two, indicating low levels of collinearity. Standardized β regression coefficient, 95% confidence intervals (CIs), and p -values are reported, together with the test-statistic for each of four models.
Descriptive findings
As shown in Table 1 , the median age of our sample was 19 years (range 18–37). Study participants were predominantly female (71.0%) and non-White (63.0%). Two-thirds of the participants were freshman, while approximately one third were health majors.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0239696.t001
As indicated in Table 2 , participants generally had a very good knowledge of the main modes of COVID-19 transmission and common symptoms of the disease. Close to two-thirds identified correct answers to all knowledge questions in the survey. Additionally, to a great extent students agreed with, and were following social distancing measures currently instituted. The most trusted sources of information were official sources: government (77.8%), followed by medical professionals (58.0%). These were also the most commonly used sources of information about the COVID-19 pandemic. Only 12.3% said they trusted social media as a source of information. Almost universally, students had changed their behaviors in response to the pandemic, including by increasing hand washing and limiting social contacts (100%), and starting to wear masks (97.5%).
https://doi.org/10.1371/journal.pone.0239696.t002
A majority of students reported experiencing academic difficulties since the start of the pandemic. Ability to focus on academic work (73.5%) and difficulties with online learning (58.6%) were the most commonly cited issues related to academics. With respect to difficulties in everyday life, obtaining hygiene supplies and medications (59.3%), and losing job/work hours/reduced wages (56.8%) were the most common life difficulties. A number of students (22.2%) also reported difficulties in getting food. Two-thirds of participants (66.7%) were greatly concerned about COVID-19 epidemic. Finally we report levels of depression, anxiety, somatization, and perceived stress reported by the study participants.
3.2. Bivariate Associations with mental health burden variables.
Bivariate associations between demographic characteristics, knowledge and concerns, precautionary behaviors, and hardships experienced during the pandemic and mental health burden variables are presented in Table 3 . With respect to demographic characteristics, non-freshmen (sophomores, juniors, and seniors) were more likely to exhibit increased levels of anxiety compared to freshmen, and female students reported significantly higher levels of stress than their male counterparts. Spending a greater amount of time looking for COVID-19 information on news sites was associated with increased level of anxiety and somatization, while increased level of anxiety was also associated with spending greater hours looking for information on social media. Interestingly, the number of hours spent on news sites looking for information on COVID-19 was significantly correlated with the amount of time spent on social media looking for COVID-19 information (ρ = 0.77, p<0.001). Those who reported trust in the news media were less likely to exhibit increased levels of somatization.
https://doi.org/10.1371/journal.pone.0239696.t003
Academic difficulties (the ability to focus on academic work and online learning) were associated with the increased levels of all four mental health burden measures. Those with increased levels of depression and anxiety were also more likely to report having lost job, wages, or work hours, and difficulties in obtaining medications and hygiene supplies. Increased levels of stress were also associated with difficulties in obtaining medications and hygiene supplies. Finally, those participants who expressed higher levels of concern about COVID-19 were more likely to report higher levels of anxiety and somatization.
Multivariable associations
Table 4 presents results from the linear regression models for each of mental health burden outcomes. Analyses indicated that economic hardship was the most significant predictor of depression among respondents, followed by difficulties with focusing on academics (see Table 4 for test statistics). Anxiety levels were significantly higher among non-freshmen, those who spent more than one hour per day looking for COVID-19 information on news sites, and ability to focus on academic work. Ability to focus on academic work was also a significant predictor of somatic problems, together with being very to extremely concerned about COVID-19. Interestingly, those who exhibited trust in news media were less likely to exhibit somatic problems. Finally, male sex was significantly associated with lower levels of stress, while inability to focus on academic work, and difficulties with obtaining medicine and hygiene supplies were significant predictors of higher levels of stress among undergraduate students.
https://doi.org/10.1371/journal.pone.0239696.t004
Previous studies have shown that public health emergencies have a significant impact on mental health of college students [ 28 , 35 ]. Since the COVID-19 outbreak, a few studies have emerged describing higher levels of anxiety and increased risk perception among college students during COVID-19 pandemic [ 26 , 27 ]. The current study is among the first to examine the impact of the COVID-19 pandemic on mental health among undergraduate college students in the U.S. Northern New Jersey has been one of the most severely affected regions in the U.S. by the current pandemic, creating uncertainty, anxiety and stress among a wider population. The pandemic has also elevated concerns about well-being of the members of the university community, including students. While previous studies have indicated that the current pandemic may have widespread impacts on students’ learning experiences [ 8 , 36 ], our results indicate that college students who are experiencing considerable number of academic and everyday difficulties during the COVID-19 pandemic also report increased levels of mental health burden. This is of potential concern as the pandemic is occurring against the backdrop of increasing mental health issues among college students [ 37 ]. Additional stress may lead to further detrimental effects on the learning experiences and mental health of undergraduates.
Most of our participants were females, which is not surprising considering that the student body at the university is approximately 60% female. As this was an introductory personal health course, the majority of participants were freshmen. The racial composition of the sample was also reflective of the University’s diverse undergraduate student body. In multivariable models, students other than freshmen were more likely to report higher levels of anxiety. A possible explanation for this could be that students in upper classes may be more concerned about the impact of the pandemic on their post-graduation plans and the economy. Additionally, male students were less likely to report higher levels of stress. This is similar to previous studies’ findings that, in general, female students report higher perceived stress levels than their male counterparts [ 38 , 39 ]. Traditional self-concepts of masculinity and femininity can lead to differential expression of attitudes and emotions towards life experiences [ 40 ]. Therefore, it is possible that in circumstances surrounding COVID-19 pandemic female students were more likely to express internalized disorders such as stress.
Change of behavior in response to the pandemic was pervasive. In accordance with the current recommendations, our respondents almost universally increased hand washing, limited social outings, and started wearing masks. This is contrary to the findings of a recent study of adults in the U.S. with chronic conditions [ 41 ], but similar to behavior changes observed in two population studies in Hong Kong [ 42 ] and China [ 43 ]. While some of the changes in behavior may be the result of mandatory requirements (i.e. lockdowns, mandatory mask wearing), it is also possible that students taking a personal health course are more conscious of the way virus spreads and are more likely to adapt to behaviors that would prevent the spread of the virus.
While we found no significant association of knowledge levels with mental health burden variables, the descriptive findings of this study indicate that undergraduate students possessed an adequate level of knowledge related to COVID-19 at the time of the survey administration. Nearly all respondents correctly identified how the virus spreads, clinical symptoms of the infection, or the most vulnerable populations to an infection. Information surrounding COVID-19 pandemic has been characterized as an “infodemic” [ 44 ] with an unprecedented amount of information but also misinformation, particularly present on social media. Yet, participants in this study were more likely to report use of “formal” sources of information as opposed to “informal” or news sites, resulting in higher correct knowledge of COVID-19. Additionally, students who are enrolled in personal health course may be more likely to be attuned to correct information related to COVID-19. The most common misconception was that those with COVID-19 cannot transmit the virus to others when a fever is not present (35.8% of participants endorsed this statement). Another misconception exhibited by a smaller number (18.5%) of participants was that young people do not necessarily need to take measures to prevent infection with COVID-19. Educating students on the role that asymptomatic and pre-symptomatic individuals play in transmission of COVID-19 should be a priority for college health educators, as returning to campus may necessitate limits on students’ gathering in confined settings, or institute mask-wearing to mitigate spread of the virus.
Overall, official sources, such as health professionals (64.8%) and government sites (55.6%), were the most common sources of information regarding COVID-19 among undergraduate students. Furthermore, official sites were the most trusted sources of information (87.0%). Similar to the study of adult U.S. population [ 45 ], social media was the least trusted source of COVID-19 information in this sample (12.3%), which is encouraging as social media platforms may have a high potential for spreading misinformation [ 44 ]. It is also possible that users searching for information on social media are directed to reliable sources such as the CDC [ 46 ]. In multivariable regression models, spending a greater amount of time looking for COVID-19 information on the news sites was associated higher levels of anxiety. This is consistent with previous studies which have found that increased time spent using social media per day was associated with increased odds of reporting high levels of anxiety [ 47 ]. While we did not test for possible exposure to COVID-19 virus, it is possible that those who perceived as being exposed to virus were more likely to search for information. It is also possible that highly anxious individuals may engage in more information-seeking as an adaptive coping strategy [ 48 ]. However, trusting news media was associated with decreased levels of perceptions of bodily dysfunctions. News sites presenting substantiated and accurate COVID-related information may have the potential to create a positive environment that is conducive to easing somatic distress in response to psychosocial stress.
Academic difficulties, such as ability to focus on academic work, were significantly associated with increased levels of depression, anxiety, somatization, and stress. It is also important to note that, at the bivariate level, all four forms of mental health burden were significantly associated with online learning difficulties. However, once the effects of other covariates were considered, difficulty with online learning was no longer a significant predictor of mental health burden. Higher level of depression were also significantly associated with loss of job, reduced wages or work hours, while difficulties in obtaining medicine and hygiene supplies were significantly associated with increased stress levels. Students who are dependent on jobs to support themselves and/or families may be particularly vulnerable to depression and worry due to economic hardship. As uncertainties about the future continue this may lead to worsening mental health status, particularly among young individuals [ 49 ]. The current pandemic has shifted students’ priorities. Many are worried about their own health, health of their families, or struggling financially, perhaps making them less focused on academics, and increasing academic difficulties. An abrupt migration of traditional face-to-face courses to the on-line mode may be particularly difficult for students who are used to in person classes and to those from academically marginal undergraduate student groups [ 50 ], or in courses that are poorly suited for online learning [ 51 ]. Struggling academically with online courses may further exacerbate mental health distress among students. All of this may have implications for students’ retention rate, leaving college administrators and instructors with the task to create innovative solutions to the unexpected challenge the pandemic has created. College support services may have a crucial role in helping students navigate the life challenges associated with the pandemic may help to improve their mental health.
Limitations
This study has several limitations worth noting. The study design is cross-sectional. Therefore, the causality cannot be established, as data represents a single moment in time. Given the limited resources available and time-sensitivity of the COVID-19 outbreak, the sample is comprised of undergraduates who are enrolled in one introductory core curriculum course. While the course is university-wide, our results may not generalize to other students. Participation in the study may have been influenced by various difficulties students found themselves in. The data are based on self-report and may be subject to social desirability bias. Our questions captured only fundamental knowledge, attitudes, and a limited set of behaviors. It is possible that our questions tapped into personal beliefs and/or endorsement of health promotion guidelines by the authorities. Future studies should also capture whether direct or indirect exposure to COVID-19 virus added to mental health distress. Additionally, self-reported levels of mental health distress are not confirmed by the mental health professionals’ assessments.
Our findings support the notion that the current COVID-19 pandemic is making a significant negative impact on mental health of college students. College students who exhibit greater academic and life difficulties may be particularly vulnerable to higher mental health distress. The current pandemic may further exacerbate already existing problems. The timeline of the pandemic is uncertain further impacting students’ academics, lives, and mental health. With a host of negative consequences associated with poor mental health, further research is needed to address additional risk factors (i.e., substance use, coping mechanisms, social support, family and peer relationships dynamics) that are associated with mental health in this population. Additional studies investigating the effect of pandemic on mental health of faculty may provide a better understanding of the impact of COVID-19 on higher education. Our findings suggest that college health service providers and administrators need to consider proactive measures to support the mental health and well-being of students. Mental health interventions and professionally trained counselors could help students address academic and financial concerns, which may alleviate mental health burden of the COVID-19 pandemic. In public health emergencies like this, many students will have special needs and emerging challenges that will require responsive programming by colleges.
Supporting information
https://doi.org/10.1371/journal.pone.0239696.s001
https://doi.org/10.1371/journal.pone.0239696.s002
- 1. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Vol. 0, The Lancet Infectious Diseases. Lancet Publishing Group; 2020.
- 2. New Jersey Department of Health. New Jersey COVID-19 Information Hub. 2020 [cited 2020 Apr 18]. Available from: https://covid19.nj.gov/
- 3. Bloomfield College. Important Update On COVID-19 At Bloomfield College, Student Tests Positive | TAPinto. 2020 [cited 2020 Apr 18]. Available from: https://www.tapinto.net/towns/nutley/articles/important-update-on-covid-19-at-bloomfield-college-student-tests-positive
- 4. Princeton University. COVID-19: Coronavirus Information | Princeton University. 2020 [cited 2020 Apr 18]. Available from: https://www.princeton.edu/content/covid-19-coronavirus-information
- 5. Saint Peters University. Coronavirus Updates. 2020 [cited 2020 Apr 18]. Available from: https://www.saintpeters.edu/?post_type=notification&p=13327
- 6. College R. Coronavirus (COVID-19) Information and Updates—Health Services. 2020 [cited 2020 Apr 23]. Available from: https://www.ramapo.edu/health/coronavirus-covid-19/#s1
- View Article
- PubMed/NCBI
- Google Scholar
- 9. Lederman D. How the shift to remote learning might affect students, instructors and colleges. 2020 [cited 2020 Apr 29]. Available from: https://www.insidehighered.com/digital-learning/article/2020/03/25/how-shift-remote-learning-might-affect-students-instructors-and
- 10. Student Loan Hero. 4 Out of 5 College Students Face Troubles Due to Coronavirus Pandemic | Student Loan Hero. 2020 [cited 2020 Apr 18]. Available from: https://studentloanhero.com/featured/college-students-financial-coronavirus-survey/
- 12. American College Health Association. American College Health Association-National College Health Assessment III: Reference Group Executive Summary Fall 2019. Silver Spring, MD; 2020.
- 14. Ipsos MORI. COVID-19 and Mental Wellbeing. 2020 [cited 2020 Apr 18]. Available from: https://www.ipsos.com/ipsos-mori/en-uk/Covid-19-and-mental-wellbeing
- 20. Centers for Disease Control and Prevention C. Guidance for Institutes of Higher Education | CDC. 2020 [cited 2020 Apr 18]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/colleges-universities/index.html
- 31. Centers for Disease Control and Prevention C. Coronavirus Disease 2019 (COVID-19) | CDC. [cited 2020 Apr 18]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/index.html
- 32. Derogatis LR. BSI 18, Brief Symptom Inventory 18: administration, scoring and procedures manual. NCS Pearson, Inc. 2001;
- 35. López, Ruth M.; Carales VD. Supporting College Students Through a Public Health Crisis: Lessons Learned from Hurricane Harvey—Higher Education Today. 2020 [cited 2020 Apr 26]. Available from: https://www.higheredtoday.org/2020/04/20/supporting-college-students-public-health-crisis-lessons-learned-hurricane-harvey/
- 37. American College Health Association. American College Health Association-national college health assessment II: undergraduate student reference group executive summary fall 2018]. Hanover, MD; 2018. Available from: www.acha-ncha.org .

- < Previous
Home > School of Health and Natural Sciences > Nursing > Senior Theses > 48
Nursing | Senior Theses
An exploration of covid-19 impact on healthcare workers’ mental health in china.
Jenny Yang , Dominican University of California Follow
Graduation Year
Document type.
Senior Thesis
Bachelor of Science in Nursing
Primary Major
Primary minor, second minor.
Leadership Studies
Thesis Advisor
Patricia Harris, PhD, RN, CNS
A literature review will be conducted, including research articles that discuss different psychiatric conditions from healthcare workers related to COVID-19, healthcare workers’ mental state in two specialized units, and various interventions to improve mental health. Additionally, a proposal for further research will be mentioned on what best methods to help alleviate healthcare workers’ symptoms of depression and anxiety?
I would like to express my gratitude to Dr. Patricia Harris, who guided and supported me during my first research thesis. I would also like to dedicate this thesis to the brave healthcare workers who helped out during the COVID-19 pandemic. Lastly, the thesis inspiration came from my beloved grandparents who are currently living in China.
Since December 13, 2021
Included in
Critical Care Commons , Critical Care Nursing Commons , Emergency Medicine Commons , Other Nursing Commons , Psychiatric and Mental Health Nursing Commons , Psychiatry Commons
https://doi.org/10.33015/dominican.edu/2022.NURS.ST.04
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
- Expert Gallery
Author Corner
- Thesis Style Guides
- Submission Guidelines
- Deposit Your Research
- School of Health and Natural Sciences at Dominican University of California
- Dominican Scholar Feedback
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Frontiers in Psychiatry
- Mood Disorders
- Research Topics
Impact of the Coronavirus Pandemic (COVID-19) on Mood Disorders and Suicide
Total Downloads
Total Views and Downloads
About this Research Topic
Beyond the unprecedented health emergency, the COVID 19 pandemic represents a new big challenge for mental health researchers and clinical practitioners. During the coronavirus COVID-19 pandemic, a large number of people have been severely impacted in terms of development of mood disorders. On top of that, ...
Keywords : COVID-19, Coronavirus, mental health, psychopathology
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
High school bans use of phones next academic year to address student mental health concerns
DES MOINES, Iowa (KCCI) – A high school in Des Moines, Iowa is banning students from using their phones, headphones, and air pods during the school day.
The new policy at Hoover High School aims to improve students’ mental health. It will take effect at the start of the next school year.
Student Caden Walker admits to scrolling Instagram a lot during the day.
“I feel like a lot of my mental issues were definitely amplified by the use of my phone because it provides distractions,” Walker said.
Gen Z is more digitally connected than ever. Most teenagers like Walker have access to smartphones and use social media for more than eight hours a day.
That is causing concern for school administrators at Hoover High School about students’ well-being.
This fall, they are ditching digital distractions to improve mental health. The plan is part of the Hoover Mental Health Movement.
Associate Principal Rob Randazzo is spearheading the change after seeing the rise of anxiety and depression in his students.
“One thing that we are needing to do for students, we are needing to re-imagine school for them – without a phone,” Randazzo said.
Randazzo said during the pandemic, there was a higher level of anxiety and depression in students.
However, he said there’s evidence that shows students began showing signs and symptoms of mental health issues as far back as 2012 when smartphones became more commonplace.
In addition to the phone and headphone bans inside the classroom, Hoover High School is encouraging parents to not give phones to their kids until age 14 and to not allow social media use until age 16.
School leaders know this will be difficult, but they believe it will help students reconnect themselves to their families, community, and school.
“We’re going to see not just grades increase, but the quality of the students’ work, the creativity, the invention. That’s what we’re even more excited for,” Randazzo said.
Copyright 2024 KCCI via CNN Newsource. All rights reserved.

Ginnie Springs closed as deputies search for attempted murder suspect

8 dead, dozens injured in Marion County farm worker bus crash, truck driver arrested

Power lines, trees down as thunderstorms move through North Central Florida

Brothers arrested for deadly Ginnie Springs shooting, FDLE investigates 2nd shooting

Pro-wrestler Ric Flair blasts Gainesville restaurant for ‘disrespect’ after spending $1,500
Latest news.

Teacher on leave after holding mock slave auction in class

One person hospitalized after officer involved shooting

Police officer killed, another hurt after disturbance call leads to shooting in Arizona

Alachua Conservation Trust hosts nature themed family fest

Alachua County commissioners declare June 1 as ‘The Gate of the Muses for Ray Charles at Dreamer Garden Day’

IMAGES
VIDEO
COMMENTS
The COVID-19 pandemic represents an unprecedented threat to mental health in high, middle, and low-income countries. In addition to flattening the curve of viral transmission, priority needs to be given to the prevention of mental disorders (e.g. major depressive disorder, PTSD, as well as suicide).
The thesis focuses on students' mental health during the COVID-19 pandemic and zooms in on how distance learning is impacting students. The thesis first provides a background of mental health with previous studies surrounding the effects of loneliness, anxiety and depression.
This thesis explores how the COVID-19 pandemic affects the mental health of adolescents through a review of the research literature. This paper also assesses the interventions ... concerns about the mental health during the pandemic, more specifically, relating to the mental health of adolescents. Although many have concerns for the mental ...
The aim of this research is to identify any existing correlations between the COVID-19. pandemic and negative mental health outcomes in younger populations. This paper examines the. impact of the COVID-19 pandemic on the mental health of those younger than 25 years of age, specifically focusing on students.
Introduction The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. In addition, with the widespread use of social media, rumours ...
Existing literature on the mental health crisis among college students before and during the COVID-19 pandemic (12-14) suggests that there is a gap in understanding how these different experiences impacted college students. This gap is particularly salient for young adults, who were perceived to be "healthier" and at lower risk for COVID-19 ...
The coronavirus disease 2019 (COVID-19) pandemic has exposed humans to the highest physical and mental risks. Thus, it is becoming a priority to probe the mental health problems experienced during ...
To determine the facilitators or stressors among college students that modified their mental health status during the COVID-19 pandemic, quarantine, and subsequent shift to online learning. ... Zhou G. Social media use and mental health during the COVID‐19 pandemic: Moderator role of disaster stressor and mediator role of negative affect ...
Background The COVID-19 pandemic has led to dramatic social and economic changes in daily life. First studies report an impact on mental health of the general population showing increased levels of anxiety, stress and depression. In this study, we compared the impact of the pandemic on two culturally and economically similar European countries: the UK and Germany. Methods Participants (UK ...
This study assessed nearly 10,000 participants across many countries to examine the impact of the pandemic and resultant governmental lockdown measures on mental health. During the height of the lockdown, the pandemic was experienced as at least moderately stressful for most people, and 11% reported the highest levels of stress.
Background Although research shows that the Covid-19 pandemic has led to declines in mental health, the existing research has not identified the pathways through which this decline happens. Aims The current study identifies the distinct pathways through which COVID-induced stressors (i.e., social distancing, disease risk, and financial stressors) trigger mental distress and examines the causal ...
To minimize the mental health consequences of the COVID-19 pandemic, WHO also recommends that countries: Apply a whole of society approach to promote, protect and care for mental health, including through social and financial protection to safeguard people from domestic violence or impoverishment, and by communicating widely about COVID-19 to ...
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact.
Additionally, apart from the physical effects of. COVID-19, significant psychological effects such as anxiety, depression, and loneliness. are shown to affect individuals of all ages including the older adult population, individuals aged 65 years and older (Wang et al., 2020). In a prevalence study of the rates.
In this section. The COVID-19 pandemic has had a huge impact on public health around the globe in terms of both physical and mental health, and the mental health implications of the pandemic may continue long after the physical health consequences have resolved. This research area aims to contribute to our understanding of the COVID-19 ...
Shofner, Ashley D., "Exploring Mental Health & COVID-19: How a Pandemic Could Become America's Next Mental Health Crisis" (2021). ... This Open Access Thesis is brought to you for free and open access by the Student Scholarship at Encompass. It has been accepted for inclusion in Honors Theses by an authorized administrator of Encompass. For ...
school can have on student mental health. Following the onset of the coronavirus pandemic, research revealed negative effects on mental health for a variety of populations across the globe; however, comprehensive reviews about the effect that the pandemic had on the mental health of. American K-12 students are limited.
Lee said. Staying proactive about mental health and safety. Elevated rates of suicide and psychiatric disorders make mental health safety an especially high priority in the wake of COVID-19. A group of UChicago researchers recently published a study highlighting safety concerns related to a substance found in countless homes: acetaminophen.
Introduction. During the early months of the COVID-19 pandemic, there was concern about the effects on the mental health of healthcare work. Citation 1, Citation 2 Early reports suggested that those working with patients known or suspected to be infected with the SARS-CoV-2 virus were anxious and depressed. Citation 3-7 Given the uncertainties about the length and intensity of the pandemic ...
Objective The COVID-19 pandemic has been a period of upheaval for college students. The objective of this study was to assess the factors associated with the increased levels of mental health burden among a sample of undergraduate college students in Northern New Jersey, the region of the U.S. severely impacted by the outbreak of COVID-19. Methods College students (N = 162) enrolled in an ...
Background In December 2019, the first confirmed human case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or COVID-19 occurred in Wuhan, China. By March 2020, the World Health Organization (WHO) had classified the COVID-19 outbreak as a pandemic due to the rapid spread of the virus to other countries. Many people have been affected by the COVID-19 pandemic in various aspects ...
symptoms of insomnia, stress, anxiety, and depression during the pandemic. Further, some turned to substance abuse to cope with stress about the pandemic (World Health Organization, 2022; American Psychological Association, 2020). As the national prevalence of mental illness rose, professionals pushed to meet the growing needs of many communities.
Beyond the unprecedented health emergency, the COVID 19 pandemic represents a new big challenge for mental health researchers and clinical practitioners. During the coronavirus COVID-19 pandemic, a large number of people have been severely impacted in terms of development of mood disorders. On top of that, many people have suffered anxiety, depression, sadness, sleep problems and perceived ...
The new policy at Hoover High School aims to improve students' mental health. It will take effect at the start of the next school year. Student Caden Walker admits to scrolling Instagram a lot during the day. "I feel like a lot of my mental issues were definitely amplified by the use of my phone because it provides distractions," Walker said.