
Glaucoma Case Studies
Nov 18, 2014
380 likes | 2.63k Views
Glaucoma Case Studies. James C. Tsai, M.D. Associate Professor of Ophthalmology Director, Glaucoma Division Edward S. Harkness Eye Institute Columbia University. LD: Clinical History & Exam. 78 y/o woman with glaucoma x 7 months PMHx: hypothyroid; Meds: Synthroid, Premarin
Share Presentation
- va 20 200 od

Presentation Transcript
Glaucoma Case Studies James C. Tsai, M.D. Associate Professor of Ophthalmology Director, Glaucoma Division Edward S. Harkness Eye Institute Columbia University
LD: Clinical History & Exam • 78 y/o woman with glaucoma x 7 months • PMHx: hypothyroid; Meds: Synthroid, Premarin • Ocular Hx: negative; on Xalatan qhs OU • Va: 20/40 OU, Ta: 17 OD, 22 OS (9:25 AM) • SLE: 2+ NSC OU (+ PXE flakes), A/C D&Q • Gonio: Grade II-III OU; CCT: 518 OD, 533 OS • C/D ratio: 0.75 OD, 0.85 OS; thin temporally OU
LD: Clinical Assessment • HVF: OD: WNL, OS: inf. arcuate defect/nasal step • OCT3: OD: 88.0 microns, OS: 74.75 microns • Imp: PXF glaucoma w/ uncontrolled IOP (OS>OD) ? Thin CCT OU a risk factor Target IOP: mid-teens OU • Treatment Plan: ??
Patient: J.D. • 47 y.o. M w/ COAG & recurrent erosions • FHx of POAG, Myopia (-4 to -6 D) • Va 20/20 OU; IOP 18 OD, 16 OS • cc: grayer & darker vision (OD > OS) • C/D = 0.8 OD, 0.7 OS (cupped temporally) • Meds: Betaxolol, Propine
Patient: J.D. • Initial ALT OD, followed by ALT OS • 1 year later: c/o worse vision (OS > OD) • Va 20/20 OU; IOP 10 OD, 11 OS • Diurnal curve: peak of 13 OU • HVF: worse OU • C/D = 0.9 OD; 0.85 OS
Patient: J.D. • Neuro-ophthalmology consult: B-12 and folate: WNL CT of orbits: WNL • 3 months later: IOP 16 OU; cc: OS dimmer • TBX w/ MMC OS & OD 2 months later • 5 year F/U: Va 20/20 OU; IOP 10 OD, 9 OS HVF stable OU; No visual loss
Visual Fields Pre-Surgery
Visual Fields Post-Surgery
Case Presentation • 15 year old boy S/P trauma OD (tennis ball) • Cc: Blurred vision OD x 3 months • PMHx: negative • Va: 20/200 OD, 20/20 OS • IOP: 4 mm Hg OD, 15 mm OS • SLE (OD): deep A/C, trace RBCs
Anterior Ultrasound
Assessment • Ocular hypotony OD (with maculopathy) • Cyclodialysis cleft with concomitant angle recession • Treatment:1. Argon laser closure of cleft2. Surgical closure of cleft • Need to monitor for post-op IOP spike(? Concurrent Stage 1 glaucoma tube)
Followed in glaucoma clinic for COAG Noted progressive ↓ invision Referred to retina clinic to evaluate macula VA: 20/50 OD 20/80 OS 0.6 log unit RAPD OS Color 1/15 OU 74 Year Old Female
Optic Disc Exam
Humphrey Visual Fields
Neuroimaging
- More by User
Case Studies
Case Studies. Direct Energy. Company Overview: Client is one of North America’s leading integrated energy companies and part of the Centrica Group (British Gas). Scope: Inbound and Outbound services Systems Used: Inbound/Outbound blended Asterisk based ACD/Dialer. Business Needs:
293 views • 7 slides
Case studies
By Mr Daniel Hansson. Case studies. What Is a Case Study?. Originated in clinical psychology to diagnose and treat patients An in-depth investigation of one single case ( person, group, organization etcetera )
825 views • 16 slides
Case studies. How to do them. Case studies. Definition A comprehensive, in-depth investigation of a situation, a sequence of activities, or a procedure within its natural setting Purpose
610 views • 12 slides

Case Studies. Source of Information. MEET MARY. Age: 20 Primary: Mild MR (Downs Syndrome) Secondary: Seizure Disorder (infrequent), Speech Difficulties Behavioral: None Medical: Infrequent Seizures Desires: Independence (be at home alone) Living Situation: Family Home.
127 views • 0 slides
Case-studies
Case-studies. Irish Medical Technology Industry Compliance Training Workshop January 26, 2011, Dublin Karen Leyshon , Convatec ;; Alphie Moran, Cook & Aline Lautenberg, Eucomed. Organisation: Instructions. Please sit at your respective tables.
284 views • 8 slides

Case Studies. March 2013. Massive Overstocks & Out-of-Stocks Discovered Thru Visibility and Big-Data Analysis. CHALLENGE:. PCG developed a systematic process that supports efficient analysis of over 1,600 items in over 4,000 locations that have 8-12 attributes
279 views • 15 slides
CASE STUDIES
CASE STUDIES. IMS 423 BLOCK. Dr. Shaikh Mujeeb Ahmed Assistant Professor AlMaarefa College. CASE -1 . An 18 –year- old female reported to the physician for consultation. She complained of generalized weakness, lethargy and inability to do the routine work from the previous few months. .
703 views • 15 slides

Case Studies . To learn to analyse each activity at each stage of the sporting development. 5 Case Studies. Bathing/ Swimming Athletics Football Cricket Tennis. Case Study 1: Bathing/ Swimming. Using the format of your choice
214 views • 5 slides

Case Studies . To learn to analyse each activity at each stage of the sporting development. 5 Case Studies. Bathing/ Swimming Athletics Football Cricket Tennis. Case Study 2: Mob Football. Using the format of your choice
242 views • 5 slides

Case Studies:
Case Studies:. A MODEL RESPONSE TO DOMESTIC VIOLENCE GAP INC. Julie East , Gap Inc. Global Senior Employee Relations Manager Dan Schlosser , Banana Republic Regional Loss Prevention Manager David Harris , Banana Republic Field Human Resources Manager. Who is Gap Inc.?.
677 views • 42 slides

Case Studies:. A MODEL RESPONSE TO DOMESTIC VIOLENCE CIGNA CORPORATION. Marjorie Stein, CIGNA Corp. Director of Employee Relations T om Healy, CIGNA Corp. Director of Corporate Security & Investigations Dan Fallon, CIGNA Corp. Health Promotion and Wellness Consultant.
306 views • 9 slides
CASE STUDIES:
Interoperability Clearing House IT Acquisition Advisory Council. CASE STUDIES:. Dedicated to maximizing the utilization of COTS/Open Solutions and leveraging of existing implementation/testing best practices. “Assuring the business value of technology”. Robert Babiskin , Chief Engineer
395 views • 11 slides
CASE STUDIES.
260 views • 17 slides
Case Studies. Cases Covered. Design methodology Simple aritmetic opperations boundary-control Without database connection Pizza order boundary – control – entity Without database connection Human resource monitoring boundary – control – entity With database conection ATM
1.07k views • 94 slides
Case Studies. BlueCross Blue Shield.
160 views • 6 slides
Case Studies. AFIX Decision-makers’ Workshop Session 2. Outline of Content. Mozambique - MOZIX Kenya - South Africa - JINX Lessons. MOZIX. Handling local traffic today Option A: Bypassing ISPs Option B: Bi-lateral peering Option C: The IXP. Kenya. ISP Models
210 views • 7 slides
Case Studies. November 19-20, 2009 Medical Legal Issues in Obstetrics Practice Ronald S. Gibbs, MD Professor, Department of Obstetrics and Gynecology Associate Dean, Continuing Medical Education. Case Study 1 – Neonatal Brain Injury, Neonatal Encephalopathy and Cerebral Palsy.
450 views • 6 slides
Landmark Glaucoma Studies
WHICH Patients ARE AT Risk for the PROGRESSION?. TARIQ ALASBALI. Landmark Glaucoma Studies. ``Doctor is my glaucoma likely to get worse?``. ``Doctor will my eye condition get worse?``. What is the diagnosis (OHT vs NTG vs POAG early or late ?)
1.17k views • 57 slides
Case Studies. Case Study #1: Patient with Controlled Hypertension. Patient Information. 52 year old African American female Presented in September 2004 for 1 yr minimum lifestyle change intervention Referred by PCP. Patient Information. Measurements Height: 5’ 3” Weight: 215 lbs
704 views • 54 slides

MS Relapse Management: Team Approaches Colleen Harris MN NP MSCN. Case Studies. Case Study #1.
132 views • 9 slides
Case Studies. SYSTEMC. Abstraction Layers for Hardware Design. TRANSACTION-LEVEL MODELS (TLM). TLMs have a common feature: they implement communication among processes via function calls !. Abstraction Layers for Hardware Design. Purpose of Abstraction Layers. Algorithmic model.
292 views • 25 slides
Case Studies. Class 4. LAM/MPI.
187 views • 16 slides

- Current Issue
- Supplements
- Digital Supplements
- Angle-Closure Glaucoma
- Congenital Glaucoma
- Exfoliation Glaucoma
- Low-Tension Glaucoma
- Diagnosis & Monitoring
- Glaucoma Medications
- Implant Surgery
- Clinical Videos
- Product Videos
- Article Reprints
- Societies and Associations
- Submission Guidelines
- Calendar of Events
- Corneal Physician Symposium
- Glaucoma Physician Symposium
PentaVision
- Ophthalmology Management
- Contact Lens Spectrum
- Corneal Physician
- Eyecare Business
Glaucoma Physician
- New Retinal Physician
- Ophthalmic Professional
- Optometric Management
- Presbyopia Physician
- Retinal Physician
- News & Reviews

Diagnosing & Managing Glaucoma: A Case Study
The importance of imaging the macula in glaucoma and its effects on patient education
T his case study is an example of how meticulously and elegantly we can identify structural and functional defects by incorporating more than one imaging modality when diagnosing glaucoma patients. Although nerve fiber layer OCT imaging is often the most useful to detect early glaucoma, in some instances, the defect can be so localized that it is easy to miss when surrounded by healthy nerve fiber layer (NFL).
In this case study, however, the lesson is two-fold. Not only are images of the macula useful for clinical knowledge and decision making for individual patient management, but there is also considerable value in imaging the NFL and macula connected to patient education. A large part of the challenge associated with managing glaucoma patients is convincing them to comply with their treatment regimens. This case study also serves as an example of how imaging allows me to educate patients about their condition and progression. These visuals are easily understood by patients and encourage them to adhere to their treatment and, ultimately, improve their disease.
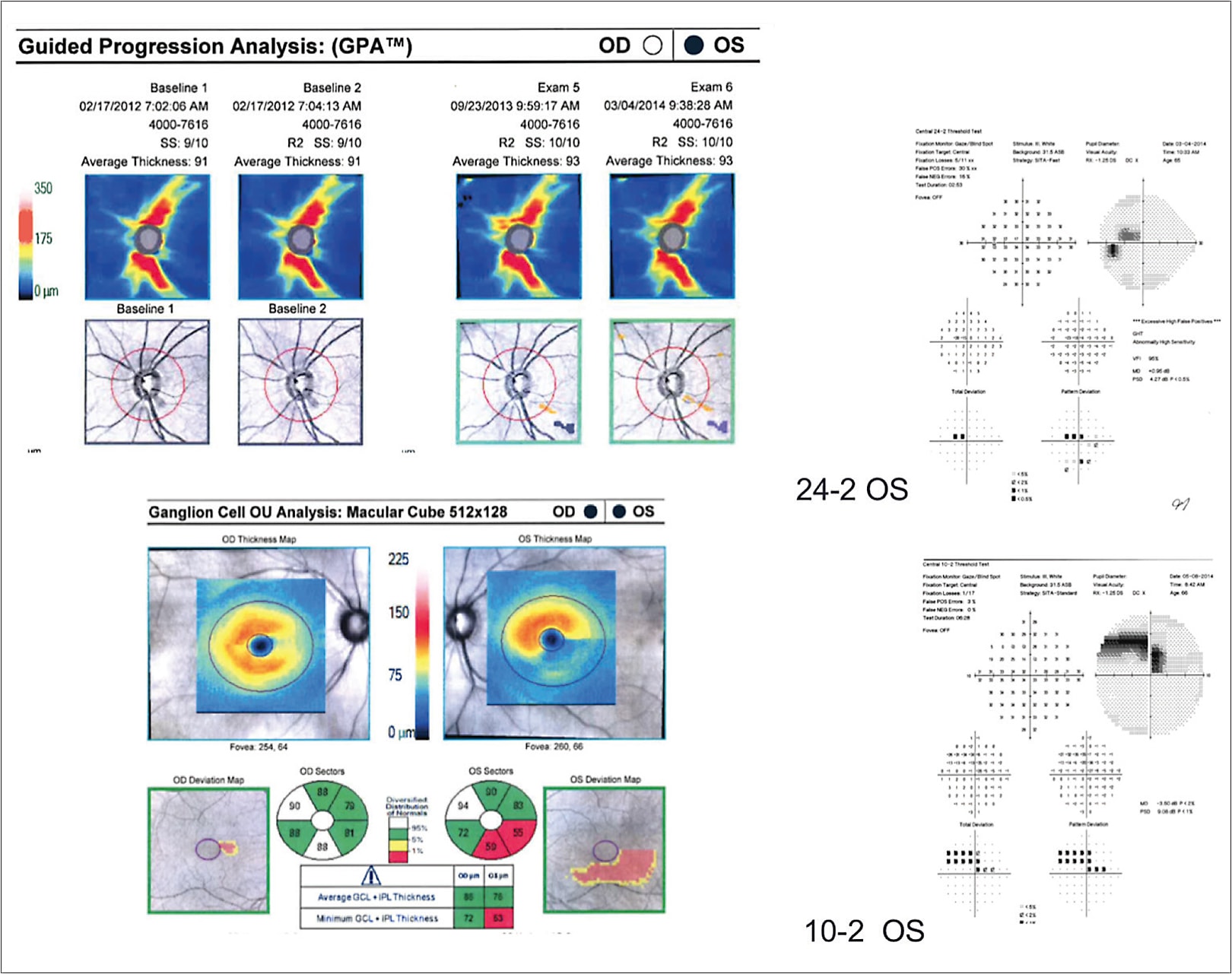
A 66-year-old female presented to my clinic for glaucoma consultation. The highest IOP that had been recorded throughout her prior history was 22 mmHg. Her risk factors were minimal. She had normal central corneal thickness, no significant familial risk factors, an angle open, and an unremarkable slit-lamp examination with OCT (Cirrus HD-OCT, Carl Zeiss Meditec) showed that she had a robust nerve fiber layer, which is typically reassuring ( Figure 1 ).

However, upon completing visual field testing (Humphrey Visual Field Analyzer, Carl Zeiss Meditec), I was surprised that the patient had a definite localized paracentral scotoma ( Figure 2 ).When I compared the visual field results with the OCT result, there was a disconnect. On OCT, the NFL appeared to be quite healthy, thus, the definite and reproducible visual field defect was unexpected.
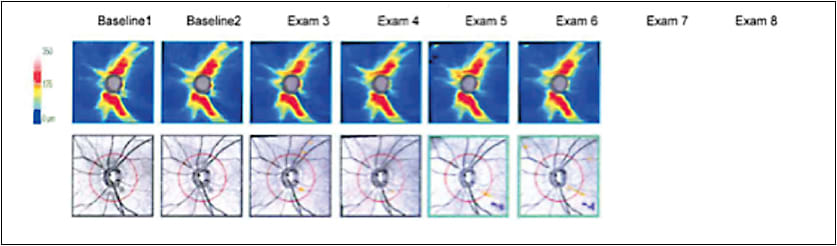
Next, I administered a macular cube scan, which showed that the right eye was normal, but the left was quite abnormal and consistent with the visual field imaging. The very pronounced defect inferiorly on the macular cube correlated perfectly with the visual field images. I then reviewed the nerve fiber layer again on the OCT images, and I could see the defect on the left NFL at the 4 o’clock position on the optic nerve ( Figure 3 ). If I had only relied on OCT imaging, it would have been very easy to overlook the abnormality in the left eye. I used the images and the visual fields to demonstrate the well-defined structural and functional defects to the patient. The study results had a clear impact on the patient, so her resolve to follow the suggested treatment regimen was enhanced significantly.
An Important Lesson
This case confirms that we should not rely only on just one parameter. It would have been easy to analyze the OCT NFL image and deem it to be a normal scan, but, by also taking a macular scan, in addition to a visual field, the abnormality was clearly apparent. This is a rare example in which the NFL OCT misses glaucoma and the visual field picks it up. It was only when I imaged the macula that it became obvious that there was an abnormality in the NFL as well.
In many similar cases, I might only take images of the NFL and not request a visual field if the images of the NFL looked normal, because in such cases, the likelihood of finding a field defect is small, but we also know from the Ocular Hypertension Treatment Study (OHTS) trial 1 and others that abnormalities don’t always show up on the first attempt at diagnostic testing. In the OHTS trial, 2,304 patients underwent at least two visual field examinations in both eyes to determine whether they were at risk for developing open-angle glaucoma to be deemed eligible for the trial. The study was designed to evaluate the safety and efficacy of a topical ocular hypotensive medication. On patients whose prior test was abnormal, questionable, or unreliable, researchers performed a third test.
Seventy-nine percent of the patients were eligible based on their initial visual field tests. The third eligibility test was required for 11% of the patients. Researchers reported that by repeating the test one time after an initial unreliable test, they could identify an additional 560 patients as being at risk for developing primary open-angle glaucoma. The practical implications of the OHTS trial’s findings are that there are many instances in our clinics every day where we may be missing an opportunity to properly diagnose a patient by failing to incorporate additional testing.
As a result, many patients benefit from imaging of the macula and NFL in my practice. I perform both types of imaging routinely for patients who have early-to-moderate glaucoma. In some instances, I also image patients with more advanced glaucoma because they’re often far advanced in one eye and only moderate or mild in their fellow eye.
In addition to diagnosis, I use macula and NFL imaging in glaucoma patients to determine if they’re stable or progressing. When progression is identified, it presets an opportunity to review compliance to be certain that patients comprehend the potential severity of their disease. I’ve found that many poorly compliant patients become more compliant when their imaging studies are shared with them and they can clearly see the structural changes.
Furthermore, I’ve found that imaging of the NFL and macula as an educational tool is useful for patients who are at a crossroads in their treatment. When I have patients who need surgery, have had a change in their treatment regimen, or are not complying, I show them their imaging results, because glaucoma is relatively asymptomatic — until it isn’t. Once it’s symptomatic and the patient becomes aware of his visual deficit, he can never turn back the clock.
When I show images, I can point out the structural defect and how it correlates to the visual field to show patients their defects in terrific detail. I also find it useful for family members caring for loved ones who have glaucoma. Imaging helps them better understand the physiology and the seriousness of the disease.
IT TAKES TWO
In this example, the macular scan in conjunction with the visual field and NFL was more useful than the visual field or NFL alone. As a bonus, demonstrating the patient’s abnormality to them, visually and graphically, improves disease education and compliance, especially in patients who need to improve their compliance with recommended therapies.
- Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701-713;discussion 829-830.

Dr. Samuelson is an attending surgeon at Minnesota Eye Consultants in Minneapolis and an adjunct professor at the University of Minnesota in Minneapolis. Dr. Samuelson may be reached at (612) 813-3628; [email protected] . He is a consultant to Carl Zeiss Meditec, Inc.
Recommendations
What to read next.
FROM THE EDITOR
When is glaucoma “controlled”, outliers & moving targets, iop at-home monitoring.
- Current Issue

June 2011 Supplement
Challenging glaucoma cases, jonathan s. myers, md, case 1: low-tension glaucoma.
A 40-year-old woman received a diagnosis of glaucoma and was referred for further evaluation. She has a history of low blood pressure and migraine headaches. She has multiple disc hemorrhages. Her highest IOP was 19 mm Hg, and central corneal thickness is average. Figure 1 shows scans of both eyes taken with optical coherence tomography (OCT). The thickness profile of the right eye shows a definite reduction inferiorly. The quality of the scan of the left eye is not quite as good, but it clearly shows thinning of the nerve fiber layer. The cup is large compared to the surrounding rim, and little rim tissue remains. In the right eye, the border of the retinal pigment epithelium (RPE) does not reach the edge of the optic nerve's scleral canal. The OCT uses the RPE edge as the limit of the optic nerve. In the right eye, the OCT sets the optic nerve border more peripherally than as seen on clinical examination, and the cupping that was seen clinically is less evident.
Visual fields (Figure 2) correlate closely to the OCT findings. There is a dense superior arcuate defect with nasal step in the right eye, whereas in the left eye, there is a dense superior and inferior arcuate defect similar to a central island. How would you manage this patient with apparent open-angle glaucoma?
In young patients with myopic discs and less pronounced visual field losses, suspicious optic nerves, even with visual field loss, could be physiologic in nature, and clinicians might opt to observe. In this case, however, with the more advanced visual field changes, this patient should be treated.
Because this patient may have advanced disease and her highest pressure was 19 mm Hg, fairly aggressive treatment is appropriate. In the Collaborative Normal Tension Glaucoma Study (CNTGS), the goal of treatment was a 30% reduction in IOP. 1 For this patient, a pressure of 13 mm Hg would be a reasonable goal. In the CNTGS, reducing pressures by 30% reduced the progression rate from 35% to 12%. Even with that aggressive pressure reduction, however, 12% of the treated patients in that study progressed. Furthermore, only about half of the patients were able to achieve those pressure goals with only medications or laser treatment. By committing to an aggressive pressure goal, you may be committing to a more aggressive form of treatment.
Various first-line treatment options are available. Topical ß-blockers have been shown to be effective pressure- reducing agents for most patients, and once-a-day dosing is usually sufficient. Some clinicians may avoid a topical ß-blocker as a first choice in patients with lowtension glaucoma because of hemodynamic considerations. 2 Specifically, there are concerns that a reduced heart rate or, possibly, reduced blood pressure may lead to reduced perfusion of the optic nerve in patients with abnormal autoregulation of blood flow, which may be associated with low-tension glaucoma and migraines. The literature is complex and varied, but there may be reductions in some of the hemodynamic parameters in the retrobulbar and intrabulbar circulation.
Another option for this patient is a topical prostaglandin analogue. Prostaglandin analogues offer once-daily dosing, have a safe systemic profile, and often achieve good reductions in IOP.
A twice-daily α-agonist, such as brimonidine, is also an option for this patient. In the Low-Pressure Glaucoma Treatment Study (LoGTS), patients with low-tension glaucoma were randomized to either timolol or brimonidine and observed for 4 years. 3 Both groups had similar reductions in IOP. Interestingly, after 4 years, visual field progression was statistically less frequent in the brimonidinetreated patients (9%) than in the timolol-treated patients (31%). These findings were seen with three different field grading algorithms. The research does not directly answer the question of why brimonidine proved more effective than timolol in preserving visual field. Possible explanations include a neuroprotective effect of brimonidine or a deleterious effect of timolol on the optic nerve directly or via hemodynamic effects.
Many studies show that laser trabeculoplasty, even in low-tension glaucoma, can achieve pressure reduction. Its safety and efficacy have been shown to be equal to that of topical medications, 4,5, and it takes compliance out of the equation. Laser trabeculoplasty is effective initially in about 80% of patients, however, and the effect persists for only 2 to 4 years. 6 Selective laser trabeculoplasty reduces mean IOP and IOP variation in normal-tension glaucoma patients. Although it can be a helpful adjunct, it often does not replace topical therapy.
As we think about our goal pressure of 13 mm Hg, we must acknowledge it may take more than one of these treatments to achieve that goal for this patient.
CASE 2: ADVANCED GLAUCOMA
A 70-year-old man has open-angle glaucoma. His initial IOPs were 20 mm Hg in the right eye and 42 mm Hg in the left eye. He recalls having a severe impact to his left eye from a tennis ball at age 40. His pressures have been well controlled with various medications (9 mm Hg to 17 mm Hg). His central corneal thickness is markedly reduced in both eyes (< 500 μm). He has had trabeculectomies in both eyes and a tube shunt in the left eye. Figure 3 shows advanced cupping of both optic nerves, and Figure 4 shows advanced field loss, with a central island in the right eye and a small central island in the left eye. The patient feels his vision has been worsening in recent years despite the pressure control. What should be done for this patient?
In certain patients, it may be advisable to measure pressures in the office throughout the day, as this may reveal pressure spikes that put the patient at a greater risk of progression. Serologies would not be unreasonable in this case. Although the patient clearly has open-angle glaucoma, he could also have an autoimmune-related or infectious retinopathy or optic neuropathy.
With progressive glaucoma, in the absence of explanations for visual field progression, some practice guidelines suggest magnetic resonance imaging to look for tumors or other compressive lesions. This patient has had all of these tests, which were normal.
This patient has a history of hypertension, requiring multiple medications. We instructed him to monitor his blood pressure at home and found, with his current medication regimen, his blood pressure was fluctuating from very high in the morning to extremely low overnight. We consulted with the patient's cardiologist, who adjusted the medication regimen. The patient's overall blood pressure stabilized to a level that was safe for his heart and, at the same time, would maintain a more even perfusion to his optic nerve. We have evidence from the Los Angeles Latino Eye Study (LALES) 7 and others that uncontrolled or very low blood pressure may lead to greater risk of progressive optic neuropathy in glaucoma. Additionally, studies have shown that patients taking multiple blood pressure medications may be at greater risk for optic nerve cupping. 8
CASE 3: COMPLEMENTARY THERAPIES FOR PRIMARY OPEN-ANGLE GLAUCOMA
A 71-year-old man with open-angle glaucoma has a history of myopia and combined cataract and glaucoma surgery. His central corneal thicknesses are 538 and 531 μm. His pressures had been 15 mm Hg or lower for years, but he had visual field progression in recent years and started taking dorzolamide and timolol. His pressures ranged from 8 mm Hg to 12 mm Hg with this regimen. On examination at this visit, his optic nerves are tilted with peripapillary atrophy, consistent with his history of myopia before cataract surgery. Glaucomatous optic neuropathy in the form of cupping is evident. As shown by the disc drawings (Figure 5), the clinician believed the glaucomatous cupping, not the tilt, was problematic. The patient said his vision was deteriorating almost on a weekly basis, making it more difficult to participate in activities he enjoys. At the top of the series of visual fields for the right eye (Figure 6), a central island is visible. Although there is a great deal of variation field to field, the last field in the series has almost the same mean deviation as the first field in the series. Visual fields for the left eye (Figure 7) show a dense paracentral scotoma with nasal extension consistent with glaucoma. In patients with myopia, we often see these paracentral scotomas earlier in the course of glaucoma. Although there may be an increased paracentral scotoma inferiorly early in this series of fields, significant progressive changes to match the patient's complaints are not obvious. On the 10-2 field from the left eye (Figure 8), we can see a dense defect approaching fixation that was also fairly stable on follow-up. When considering stability in such a scenario, we should remember that points registering “0” on the field are not necessarily blind to all stimuli but are beyond what the machine can test. Thus, real changes may not be evident. On the other hand, most clinicians are reluctant to consider aggressive interventions without objective evidence.
This patient has read just about everything there is to read about glaucoma, including information on alternative therapies that do not rely on pressure reduction. He asks what else can be done for him.
Many patients have heard that bilberry was used by pilots during World War II to improve night vision and ocular health. There is little evidence, however, that bilberry changes the course of glaucoma or improves visual function in patients who have glaucoma.
Eyebright is another popular supplement purported to aid vision. Perhaps it is helpful, but there are no controlled, randomized studies showing improvement in glaucoma.
Ginkgo biloba has been used to improve neuronal function in various diseases. In one study, 27 subjects with normal-tension glaucoma and established field loss had baseline visual field testing on gingko biloba and placebo in a masked, randomized, crossover study. 9 Half the subjects took placebo and half ginkgo for 4 weeks and then underwent field testing. After washout, each group took the other treatment for 4 weeks and underwent field testing again. In this study, the patients' visual fields were better while they were taking ginkgo than placebo, with a more than 20% reduction in mean deviation. This was a limited study, and there have been no repeat or long-term studies. This study provides at least some reasonably scientific evidence, however, that ginkgo may be helpful for selected patients. At the same time, ginkgo can thin the blood, so it may not be a safe choice for patients with clotting disorders or patients taking blood thinners or high-dose vitamin E.
In a prospective, multicenter trial, patients with lowtension glaucoma were randomized to placebo or memantine. Although findings from this study have not been published, the company that funded the study reported the primary endpoint of better preservation of vision was not met with memantine. So, although it is used in other neurodegenerative diseases, we have no evidence to date that memantine is neuroprotective in glaucoma.
In the LoGTS, brimonidine was shown to be potentially neuroprotective in low-tension glaucoma. This patient is not currently taking brimonidine, so we could discuss those findings with him and consider adding that agent to his regimen or possibly substituting it for dorzolamide or timolol.
- The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Collaborative Normal-Tension Glaucoma Study Group. Am J Ophthalmol. 1998;126:498-505.
- Hayreh SS, Podhajsky P, Zimmerman MB. ß-blocker eyedrops and nocturnal arterial hypotension. Am J Ophthalmol. 1999;128:301-309.
- Krupin T, Liebmann JM, Greenfield DS, et al.; Low-Pressure Glaucoma Study Group. A randomized trial of brimonidine versus timolol in preserving visual function: results from the Low-Pressure Glaucoma Treatment Study. Am J Ophthalmol. 2011;151:671-681.
- Barkana Y, Belkin M. Selective laser Trabeculoplasty. Surv Ophthalmol. 2007;52:634-654.
- Katz LJ, Steinmann WC, Kabir A, Molineaux J, Wizov SS, Marcellino G. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma. 2011 May 3. [Epub ahead of print].
- El Mallah MK, Walsh MM, Stinnett SS, Asrani SG. Selective laser trabeculoplasty reduces mean IOP and IOP variation in normal tension glaucoma patients. Clin Ophthalmol. 2010;4:889-893.
- Varma R, Ying-Lai M, Francis BA, et al; Los Angeles Latino Eye Study Group. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004;111:1439-1448.
- Topouzis F, Coleman AL, Harris A, et al. Association of blood pressure status with the optic disk structure in non-glaucoma subjects: the Thessaloniki eye study. Am J Ophthalmol. 2006;142:60-67.
- Quaranta L, Bettelli S, Iva MG, et al. Effect of ginkgo biloba extract on preexisting visual field damage in normal tension glaucoma. Ophthalmology. 2003;110:359-362.
Identifying and Managing Early Glaucoma
RONALD L. GROSS, MD
Within this issue
Evidence-based Best Practices for Glaucoma Care
Why do patients with glaucoma go blind.
L. JAY KATZ, MD
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Case Rep

Case Report
Managing advanced unilateral pseudoexfoliative glaucoma.
The only proven therapy for glaucoma is intraocular pressure (IOP) reduction, which can be accomplished by different means. Each should be properly discussed with patients in order to best preserve visual function and quality of life. We report a case of unilateral pseudoexfoliative glaucoma, treated for years with triple topical IOP-lowering drugs. The patient presented with advanced optic neuropathy and important ocular side effects secondary to the treatment. Having discussed his options and prognosis, laser trabeculoplasty was performed while maintaining the remaining therapy considering the advanced stage of glaucoma. His IOP was effectively reduced and no progression was noted after 1-year follow-up. Although medical therapy is the mainstream in glaucoma management, its side effects should not be ignored, especially in unilateral cases. Surgery might have been a better solution, but we chose to perform laser trabeculoplasty, an effective and safer alternative, considering the unlikely but serious risk of the “wipe-out phenomenon” in this case.
Glaucomatous optic neuropathy, or simply glaucoma, remains the most commonly acquired optic neuropathy and a leading cause of blindness. Its overall estimated prevalence varies widely across population-based studies: primary open-angle glaucoma (POAG) is believed to affect between 1.1% and 2.1% of whites aged 40 years and older, with a higher prevalence in some ethnic groups such as African Americans (who are 3−4 times more likely to suffer from it and at least four times more likely to become blind by it), while primary angle-closure glaucoma affects around 0.1% of white populations in Europe and the USA. 1 Secondary open-angle or angle-closure glaucoma may be caused by a variety of different pathologies and their overall prevalence is harder to estimate.
Several risk factors contribute to and increase the likelihood of developing glaucoma, but high intraocular pressure (IOP) remains the most important and, notably, one of the few (if not truly the only) we can target for treatment. 1–4 There are three main strategies for lowering the IOP: medical, laser therapy and surgery. Most patients are treated medically with topical eye drops or gels, with a number of available agents to choose from: β-blockers, prostaglandins analogues, carbonic anhydrase inhibitors and others. Although most drugs are relatively well tolerated, one cannot forget there are some important side effects for each of these medications, not only ocular but possibly also systemic. In addition, the use of some excipients and the chronicity of glaucoma treatment come as a probably overlooked problem to the ocular surface, with many patients presenting dysfunction of the ocular tear film and the ocular surface integrity and reporting a wide range of ophthalmic symptoms and signs which may include discomfort, burning, ulceration, scarring and possibly vision loss in severe cases.
A relatively common cause of chronic open-angle glaucoma is the pseudoexfoliative (PXF) syndrome, or more correctly, pseudoexfoliative glaucoma (PXG), accounting for approximately 15–20% of all open-angle glaucoma diagnosis. 2 It tends to be more frequent in women aged over 50 (although male patients appear to be at a higher risk of developing glaucoma), 3 with an estimated overall prevalence between 0.6% (age 52–64) and 5% (age 75–85). 2 Thought to be an ocular manifestation of a systemic disease, in the eye it is characterised by deposition on the trabecular meshwork and other structures of the anterior segment of a grey–white fibrillar extracellular material produced by abnormal basement membranes of ageing epithelial cells. 1–4 Classically, it leads to unilateral glaucoma, but the ‘uninvolved’ eye most likely has subclinical PXF syndrome, so it may be more adequate to call it an asymmetrical disease. 2 It also tends to present a higher incidence of late medical therapy failure than POAG. 5 6 with patients having to be submitted to laser therapy or surgery more often. These two particular aspects—unilateral or asymmetric disease and poorer response to medical treatment—mean that PXG may constitute a truly difficult form of glaucoma to manage in some cases, making us weigh the potential side effects of prescribing eye drops only for one eye (often in associations and for a long period of time) versus the risk of disease progression or more invasive treatment modalities, namely surgery. Laser trabeculoplasty may, therefore, be a powerful adjunct in the treatment of many patients with PXG, making it possible in some cases to lower the medical therapy or even avoid the risks of surgery.
Case presentation
We report a case of a Caucasian male patient, 64 years old, with no relevant medical history, who presented to our ophthalmology department with a glaucoma diagnosis. He had been followed in a private setting by another doctor for many years who had prescribed two different eye drops for his right eye: a combination of a prostaglandine analogue (latanoprost) with timolol and brinzolamide, a carbonic anhydrase inhibitor. His doctor did no treatment whatsoever in the left eye and did not use any other eye drops, such as lubricants, although the patient experienced some burning and foreign body sensation since he started the medication. He also referred non-complicated cataract surgery by phacoemulsification in the right eye 2 years earlier due to diminished visual acuity (VA).
During initial examination, his best corrected VA was 20/20 in both eyes. On closer look, there was an obvious difference in his eyelashes’ length and width between both eyes, with hypertrichosis on the right side, and heterochromia with the right iris presenting a more brownish hue in comparison to the greyish-blue colour of the left eye ( figure 1 ). The patient and his wife were concerned about the pigmentary changes but decided to continue the prescribed prostaglandin analogue for fear of worsening his sight if he did not do so.

Hypertrichosis and heterochromia. Hypertrichosis and heterochromia induced by chronic therapy with a prostaglandin analogue (latanoprost). Note the darker iris on the right eye, treated for glaucoma.
On slit-lamp examination, a decrease in tear meniscus height as well as in break-up time (<5 sec) was noticed, on his right eye, upon fluorescein instillation, which also revealed a punctate keratitis on the cornea's lower one-third ( figure 2 ). Pseudophakic status was confirmed on the right, with a posterior chamber intraocular lens well centred and with no posterior capsular opacification. A careful look at the pupillary margin ( figure 3 ) revealed “moth-eaten” transillumination defects and deposition of a greyish material, non-existent on his left eye, suggestive of PSX. His IOP was 22 mm Hg on the right and 16 mm Hg on the left. According to the Spaeth grading system, gonioscopy ( figure 4 ) revealed, in his right eye, an open anterior chamber angle (approximately 45°), with a deep iris insertion and a clearly visible ciliary body, a regular peripheral iris and moderate pigmentation of the trabecular meshwork (most marked inferiorly) with an accompanying Sampaolesi line; gonioscopy findings were similar in his left eye, although the angle was somewhat narrower (due to phakic status) and less pigmented. Fundus examination confirmed a generalised compromise of the neuroretinal rim in his right eye, with a diffuse concentric enlargement of the cup (estimated cup-disk ratio of 0.9), suggestive of advanced glaucoma ( figure 5 ); his left eye was unremarkable, with a healthy-looking optic nerve head.

Punctate keratitis. Slit-lamp examination with fluorescein showing punctate keratitis on the cornea's lower one-third in the right eye.

Transillumination defects and deposition of pseudoexfoliative material in the pupillary margin. Slit-lamp examination showing transillumination defects and deposition of pseudoexfoliative material in the pupillary margin (right eye). Note pseudophakic status.

Gonioscopy using Goldmann three-mirror lens. Gonioscopic appearance of the anterior chamber angle (right eye): open anterior chamber angle (approximately 45°), with a deep iris insertion with the ciliary body clearly visible, a regular peripheral iris and moderate pigmentation (+3) of the trabecular meshwork, with an accompanying Sampaolesi line.

Optic nerve head appearance. Retinography detailing the optic discs. Right eye: diffuse compromise of the neuroretinal rim with a cup-disc ratio of 0.9. Left eye: normal, non-suspicious looking disc.
Investigations
Time-domain optical coherence tomography, to assess disc morphology and peripapillary retinal nerve fibre layer (RNFL) thickness, and automated static perimetry (using Octopus Perimeter), for visual field (VF) testing, were requested to evaluate glaucoma severity. In the right eye, OCT revealed a generalised decrease in the RNFL thickness and a disc morphology compatible with the fundoscopic findings ( figure 6 ). Perimetry showed severe changes of the VF with a mean deviation of −20.6 dB compatible with end-stage unilateral glaucoma with a small island of central vision accompanied by a temporal island ( figure 7 ).

Retinal nerve fibre (RNF) evaluation by optical coherence tomography (OCT). OCT revealed in the right eye an important diffuse reduction of the RNF thickness compared to the left eye, with an average thickness of 39.48 and 78.41 μm, respectively.

Visual field (VF) assessment by the Octopus Perimeter (right eye). VF of the right eye, showing severe changes with a mean deviation of −20.6 dB compatible with end-stage glaucoma with only a small island of central vision accompanied by a temporal island remaining.

Differential diagnosis
In summary, the patient presented with unilateral PXG in an advanced stage, for which he was being treated with three different topical IOP-lowering agents. Despite this approach, his IOP was far from being controlled (22 mm Hg) and he also presented with some important side effects, namely hypertrichosis, heterochromia and keratitis.
After discussing his treatment options, and fearing losing his remaining vision with surgery, we decided to perform double-frequency Nd:YAG laser trabeculoplasty in the right eye, around 50 spots (with a spot size of 50 μm, 0.1 s duration and power ranging from 950 to 1100 mW) aimed at the junction of the pigmented and non-pigmented lower 180° trabecular meshwork. No complications were registered; prophylactic apraclonidine 1% was instilled before and after the procedure to avoid early postlaser IOP rise and a short course of topical fluorometholone was also prescribed to treat laser-induced inflammation.
Outcome and follow-up
Owing to the glaucoma severity, we decided to maintain the current medical therapy. Lubricants were added, however, to treat the keratitis which resolved with success, leading to a significant symptomatic improvement. His postlaser IOP ranged from 10 to 12 mm Hg and no deterioration was seen in his OCTs and VF after a follow-up of 1 year.
The reported case is a clear example of how glaucoma (or any other) treatment must be thoroughly planned and balanced. Although the patient’s complete previous medical and ocular history was unavailable, making it impossible to have a clear idea of the disease progression, it is fair to say that it was not under good control despite triple therapy, prescribed for some years now. In fact, it was severely advanced with almost total cupping of the disc and only a small island of central vision with accompanying temporal island remaining.
It is well known that PXG has a worse prognosis than POAG, often showing rapid progression and poor response to medical therapy. 1–6 In most patients, this makes using more than one IOP-lowering drug avoidable. Many cases of PXG are also unilateral, at least at the time of diagnosis (although 25% of patients develop PXF signs in the fellow eye within 10 years) 2 such as in the reported case, which makes therapy decisions even harder. So how should we treat these patients?
β-Blockers are an excellent first-line therapy option, although most need to be used twice a day and have potential systemic side effects that have to be taken into account (this, however, was not a major issue with this patient, who was otherwise healthy with no heart problems, asthma or other relevant illnesses). Prostaglandin analogues are another good choice, with a once-daily dosing regimen that may be easier for patients to follow and fewer systemic adverse events, but with important potential secondary ocular changes 1–4 7 8 such as eyelash lengthening, thickening and hyperpigmentation, and irreversible iris hyperpigmentation (in 11–23% of patients in 6 months) 3 which can obviously lead to heterochromia when one eye is not under treatment. Both drug classes (and their associated excipients) can also lead to ocular surface dysfunction, decreasing aqueous tear secretion (β-blockers), causing corneal staining, 9 inducing inflammation 10 and causing symptoms such as foreign body or burning sensation and hyperaemia, all of which can be a concern to patients’ compliance. α-2 Agonists (such as brimonidine), topical carbonic anhydrase inhibitors (such as brinzolamide, also prescribed to our patient) and other now less commonly used drugs (namely miotics—which are, however, associated with an increased risk of induced angle-closure and development of posterior synechiae in PXG 2 ) are also available, but are usually used as second-line therapy options.
Another problem which needs to be taken into account when discussing glaucoma therapy is the surgery failure related to chronic exposure to preservatives present in many of these eye drops. In fact, considering surgery as an “if all else fails” option may not be the wisest choice; earlier, better IOP control may possibly be achieved with trabeculectomy (and probably other surgical approaches), preventing glaucoma progression while avoiding years of ocular exposure to eye drops, which can ultimately make the surgery harder and reduce its success rate. 1–4 11 12 This is even more worrying in patients with end-stage glaucoma whose options are running out and who cannot afford having uncontrolled IOP for much longer and be submitted to repeated invasive procedures in an attempt to lower it. Only by knowing our patient’s full previous history could we discuss the possible best course of action; maybe an earlier surgery could have delayed the disease progression and avoided most mentioned side effects thus decreasing risk of failure if surgery became clearly necessary.
Although recent data seem not to support the traditional idea of “wipe-out phenomenon” with sudden visual loss following surgery in end-stage glaucoma (which can occur in approximately 6% of these cases), 13–15 due to the patient’s concern of losing his remaining vision we decided to perform laser trabeculoplasty hoping to lower his IOP to more acceptable values and slow down his progression. We appear to have been successful in doing so (at least with a 1-year follow-up), although only time will tell if the laser effect is long-lasting and sufficient enough or not. Published data, 1–4 unfortunately, tells us that in resemblance to what happens with topical therapy, laser trabeculoplasty also presents higher failure rates in PXG than in POAG. Retreatment is, nevertheless, an option (especially since we only treated the lower 180°), and a safe one.
In conclusion, glaucoma remains one of the most important and usually preventable or more easily manageable causes of blindness worldwide. Thankfully, every day new advances in its therapy are registered, contributing to the healthcare and quality of life of these patients. Topical IOP-lowering agents are still the mainstay of glaucoma treatment and efficient in most cases in preventing its progression, and are usually well tolerated. One must not forget, however, that this is a chronic therapy and although probably surpassed by their benefits, all of these drugs have some side effects which should not be disregarded. Ocular surface integrity is essential to the eye’s normal physiology and health and its compromise is a well-known cause of potential serious diseases and many discomforting symptoms, which in turn may lead to poor patient compliance and ultimately glaucoma progression. Hence our responsibility in choosing the best treatment options for our patients and not overlooking what may seem “minor” and “acceptable” adverse effects. Laser treatments such as trabeculoplasty, available and easily performed by most ophthalmologists, stand as good adjunct therapies, in some cases making it possible to avoid multiple topical agents while also being safer than surgery.
Learning points
- Chronic therapy with topical intraocular pressure-lowering drugs can have a serious impact on ocular surface integrity, affecting patients’ quality of life and potentially their treatment compliance.
- Surgery may be a better alternative when dealing with unilateral glaucoma, especially in cases which tend to respond poorly to medical therapy such as pseudoexfoliative glaucoma.
- In addition to being an easy and fast procedure, laser trabeculoplasty remains an effective and safe alternative or adjunctive therapy option when treating open-angle glaucoma.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.

- Biosimilars
- Cataract Therapeutics
- Gene Therapy
- Optic Relief
- Geographic Atrophy
- Ocular Surface Disease
- Practice Management
- Therapeutics
- Understanding Antibiotic Resistance
- Ocular Allergy
- Clinical Diagnosis
Patient Case #1: 58-year-old patient with open angle glaucoma utilizing minimally invasive glaucoma surgery procedure
Ehsan Sadri, MD, FACS, reviews the case of a 58-year-old male with open angle glaucoma utilizing minimally invasive glaucoma surgery procedure.

EP: 1 . Patient Case #1: 58-year-old patient with open angle glaucoma utilizing minimally invasive glaucoma surgery procedure
Ep: 2 . impressions and take away points from patient case #1, ep: 3 . patient case #2: 67-year-old white female with open angle glaucoma benefits from minimally invasive glaucoma surgery, ep: 4 . impressions and take away points from patient case #2.
Ehsan Sadri, MD, FACS: Hi everybody, my name is Dr Ehsan Sadri. I’m a board-certified ophthalmologist, fellowship trained in glaucoma, practicing in lovely Newport Beach, California. I am the founder and medical director of Visionary Eye Institute. I’m also the co-founder of Visionary Ventures, also located in Southern California. It’s absolutely my delight to be here with you, and an honor and a pleasure.
Our first case is a 58-year-old practicing vascular surgeon who had LASIK surgery in 1995. He was referred in for a glaucoma and cataract evaluation. He’s on maximal medical therapies, intolerant to other medications, as you can see, he’s on latanoprost and Combigan. His best-corrected visual acuity is 20/50; he does have dense arcus, which we’ll show in the next couple of slides. He presents with intraocular pressure of 16 mm Hg. We don’t know his range in the past, but presumably, it was higher. The corneal thickness test is 490 μm, and you can see the cup/disc ratio is 0.85 in the right eye and 0.9 in the left eye.
This is a startling example of his right optic nerve, and he is obviously, again, status post-LASIK. We don’t know his pre-LASIK, preoperative measurements and refractive error, but you can see from a physical examination that he obviously has high myopia, and it’s very tough to delineate where the disc vs the rest of the tissue is. But there’s a circle that I put there for us to be able to delineate where the cup-to-disc is.
This is visual field progressive loss; you can see it’s pretty remarkable and disconcerting that he’s presenting this way because he has loss of visual field functionality in both eyes. And he’s obviously a very reliable patient on examination. For this patient, you can see he underwent cataract extraction surgery with monofocal lens implants. We did an OMNI trabeculotomy, goniotomy, and eye stents in both eyes. His intraocular pressures now are pretty steady, between 10 and 12 mm Hg, which is actually the target for this patient, and his best-corrected visual acuity is 20/20. He’s still practicing.
Transcript Edited for Clarity

New World Medical receives 510k clearance for device for reduction of IOP in patients with POAG

EyePod: Transforming the MIGS pipeline into clinical reality

Alcon to acquire Belkin Vision in deal estimated at $335 million

Modifying and optimizing a new era of glaucoma surgeries

iStent MIGS devices associated with less visual field progression in glaucoma compared with medical therapy

Video Journal of Cataract, Refractive, and Glaucoma Surgery: 40 years and counting
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

- Departments /
- Ophthalmology and Visual Sciences /
- Education /
- Ophthalmic Case Studies /
Ophthalmic Case Study 17
Case study 17 - cc: routine eye exam.
Patient History
HPI: The patient, a 61 year-old female retired school teacher, has not had an eye exam in 10 years. She reports no problems with driving, watching TV, computer or reading. She uses over-the-counter readers for close work. She admits to mild eye burning feeling after reading for long periods of time or in the afternoons. She denies any flashes, floaters, pain, redness or double vision.
Past Ocular History: Presbyopia. No prior eye surgeries, hx of eye trauma, amblyopia or strabismus.
Ocular Medications: None
Past Medical History: Hypertension
Surgical History: Cesarean delivery x 1
Past Family Ocular History: Cataract surgery in her mother and father. Negative for macular degeneration, glaucoma or blindness.
Social History: Never smoked
Medications: Hydrochlorothiazide
Allergies: None
ROS: Denies any recent illness or any new CNS, heart, lungs, GI, skin or joint symptoms.
Ocular Exam
Visual Acuity (cc): OD: 20/20 OS: 20/20
IOP (tonoapplantation):} OD: 21 mmHg OS: 23 mmHg
Pupils: Equal, round and reactive to light, no APD
Extraocular Movements: Full OU, no nystagmus
Confrontational Visual Fields: Full to finger counting OU
External: Normal, both sides
Dilated Fundus Examination:
Other: Gonioscopy: Open angles with minimal pigmentation in the trabecular meshwork, no synechiae OU
Automated visual field test: superior arcuate defect in both eyes
Pachymetry: 560 OD; 551 OS (within normal range)
Diagnosis: Primary open-angle glaucoma
Discussion: Differential Diagnosis: This patient is presenting with primary open-angle glaucoma (POAG). The diagnosis is supported by evidence of increased IOP (normal is 8 to 21 mmHg), optic nerve head abnormality, open anterior chamber angle, visual field deficits and no history to suggest a secondary glaucoma (glaucoma due to an identifiable cause). Differential diagnosis would include steroid-induced glaucoma, pigmentary glaucoma, pseudoexfoliation glaucoma, trauma-induced glaucoma or other identifiable causes of glaucoma associated with high intraocular pressure, intermittent angle-closure glaucoma or an optic neuropathy (to explain the optic nerve head changes and visual field defects).
Definition: Primary open-angle glaucoma is an optic neuropathy associated with high IOP and a characteristic visual field loss. The primary problem in open-angle glaucoma is a defect in the trabecular meshwork. This leads to a disruption in the normal draining process of the aqueous humor which causes a rise in intraocular pressure (IOP). Over the course of months or years, the increased pressure leads to a thinned, damaged optic disc. This results in vision loss initially in the periphery. Patients may not notice any vision loss for years, as their central vision remains intact. In primary open-angle glaucoma there is no identifiable cause to the IOP elevation or optic nerve head changes and visual field deficits. Risk factors for open angle glaucoma include central corneal thickness measured with pachymetry (risk is increased the thinner the cornea), race, age and family history (10x the risk in siblings of patients with POAG).
Examination: Because the condition is asymptomatic until the late stages, it is usually diagnosed in a routine eye exam. It is important to inquire about ocular trauma, systemic steroid use and family history of glaucoma. Typical findings are elevated IOP and increased cup-to-disc ratio on funduscopic exam. A visual field examination shows defects that are consistent with the state of the optic nerve. Measurements of the nerve fiber layer over the optic nerve can confirm an abnormally thin nerve.
Treatment: Topical medications are used as first-line therapy to decrease the intraocular pressure (the only modifiable risk factor). Medication categories include prostaglandins, adrenergic agonists, beta blockers, and carbonic anhydrase inhibitors. The target is a 30% reduction of the baseline intraocular pressure (ideally an IOP of less than 21 mmHg). Other options for treatment include argon laser trabeculoplasty, trabeculectomy, or a tube shunt procedure. The purpose of these treatments is to increase aqueous outflow from the anterior chamber, lowering the intraocular pressure. Regular follow-up with IOP monitoring, visual field assessment and optic nerve examination are important to ensure no glaucoma progression or the need to modify therapy.
- enlarged cup-to-disc ratio
- visual acuity loss
- family history of glaucoma
- african american race
- loss of central visual acuity
- shallowing of the anterior chamber angle
- thinning of the optic nerve cup-to-disc space
- corneal endothelial cell loss
- steroid use
- history of eye trauma
- congenital iris malformation
References/Resources:
1. What findings are needed for the diagnosis of POAG?
a. enlarged cup-to-disc ratio Patients with primary open angle glaucoma usually have an enlarged cup-to-disc ratio, which signifies loss of optic nerve tissue. 2. What are the consequences of untreated POAG disease?
c. thinning of the optic nerve cup-to-disc space If untreated, patients with POAG will have continued loss of nerves and enlargement of the optic nerve cup-to-disc ratio.
3. What is a common risk factor for POAG?
a. age The other answers are risk factors for development of: steroid-induced glaucoma, trauma-induced glaucoma, or congenital glaucoma.
Medical College of Wisconsin Ophthalmology and Visual Sciences Case Studies
Ophthalmic case study 1, ophthalmic case study 10, ophthalmic case study 2, ophthalmic case study 11, ophthalmic case study 3, ophthalmic case study 12, ophthalmic case study 4, ophthalmic case study 13, ophthalmic case study 5, ophthalmic case study 14, ophthalmic case study 6, ophthalmic case study 15, ophthalmic case study 7, ophthalmic case study 16, ophthalmic case study 8, ophthalmic case study 9, ophthalmic case study 18, contact ophthalmology.
For patient care inquires, call us at (414) 955-2020 or use MyChart. Email is for research and education inquiries only.
Eye Institute Location
925 N. 87th St.
Milwaukee, WI 53226
Appointments
(414) 955-2020
(414) 955-6166 (fax)
Continuing Medical Education
Taylor Schmidt
(414) 955-2088
Medical Education Coordinator
Associate Director of Development - Ophthalmology
Sarah Walker
Refer to Us - Consultation requests
Patient Referral Form (PDF)
Fax to (414) 955-0136
Emergent Requests
Within 48 hours call
Vesper Williams
(414) 955-7862
Advanced Ocular Imaging Program
(414) 955-2647
Eye Institute Executive Director (Administrator)
Shannon Dreier

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 06 May 2024
Medications for attention deficit hyperactivity disorder associated with increased risk of developing glaucoma
- Rami Darwich ORCID: orcid.org/0000-0001-7125-230X 1 ,
- Mahyar Etminan 2 ,
- Bonnie He 1 &
- Brennan D. Eadie 1
Eye ( 2024 ) Cite this article
247 Accesses
1 Citations
50 Altmetric
Metrics details
- Risk factors
Attention deficit hyperactivity disorder (ADHD) therapies including atomoxetine, methylphenidate, and amphetamines are some of the most prescribed medications in North America. Due to their sympathomimetic action, these drugs are contraindicated in patients with a history of angle closure glaucoma (ACG). This study aims to determine the risk of ACG and open angle glaucoma (OAG) among users of these treatments.
This is a retrospective cohort study with a case control analysis using the PharMetrics Plus Database (IQVIA, USA). We created a cohort of new users of atomoxetine, methylphenidate, and amphetamines and they were followed to the first diagnosis of (1) ACG or OAG; or (2) end of follow up. For each case, four age-matched controls were selected. A conditional logistic regression model was used to adjust for confounders and to calculate adjusted incidence-rate-ratios (aIRRs).
A total of 240,257 new users of the ADHD medications were identified. The mean age was 45.0 ± 19.4 years and 55% of the cohort was female. Regular users of atomoxetine and amphetamines had a higher aIRR for developing ACG compared with non-users (aIRR = 2.55 95% CI [1.20–5.43] and 2.27 95% CI [1.42–3.63], respectively); while users of methylphenidate had a higher aIRR for developing OAG (aIRR = 1.23 95% CI [1.05–1.59]).
Conclusions
Use of amphetamines and atomoxetine had a higher risk for ACG, while use of methylphenidate was associated with a higher risk for OAG. Given the prevalence of ADHD medication use (medically and recreationally), our current data on their associated risk of glaucoma have profound public health implications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
251,40 € per year
only 13,97 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Risk factors for low adherence to methylphenidate treatment in pediatric patients with attention-deficit/hyperactivity disorder

ADHD medications use and risk of mortality and unintentional injuries: a population-based cohort study

Attention-deficit hyperactivity disorder medication use is associated with testosterone hypofunction–results from a national claims database analysis
Data availability.
Data can be provided upon a reasonable request. The authors can share the complete data set creation plan and the analytic code upon request; please contact Dr. Mahyar Etminan. The data sets utilized in this study are accessible with permission from IQVIA. However, there are restrictions on the availability of this data, as it was used under license for this study and is not publicly accessible.
Ayyıldız D, Ayyıldız T. Ophthalmological findings in children and adolescents with attention deficit and hyperactivity disorder. Int Phys Med Rehabil J. 2019;4:276–9.
Guvenmez O, Cubuk M, Gunes S. The effects of medication on intraocular pressure in children with attention deficit hyperactivity disorder: a prospective study. J Popul Ther Clin Pharm. 2020;27:e45–50.
Google Scholar
Mechler K, Banaschewski T, Hohmann S, Häge A. Evidence-based pharmacological treatment options for ADHD in children and adolescents. Pharm Ther. 2021;23:107940.
Faraone SV. The pharmacology of amphetamine and methylphenidate: relevance to the neurobiology of attention-deficit/hyperactivity disorder and other psychiatric comorbidities. Neurosci Biobehav Rev. 2018;87:255–70.
Article CAS PubMed PubMed Central Google Scholar
Bradley C. The behavior of children receiving benzedrine. Am J Psychiatry. 1937;94:577–85.
Article Google Scholar
McCabe SE, Schulenberg JE, Wilens TE, Schepis TS, McCabe VV, Veliz PT. Prescription stimulant medical and nonmedical use among US secondary school students, 2005 to 2020. JAMA Netw Open. 2023;6:e238707–07.
Article PubMed PubMed Central Google Scholar
McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100:96–106.
Article PubMed Google Scholar
Chen LY, Crum RM, Strain EC, Alexander GC, Kaufmann C, Mojtabai R. Prescriptions, nonmedical use, and emergency department visits involving prescription stimulants. J Clin Psychiatry. 2016;77:e297–304.
Lu C-K, Kuang T-M, Chou JC-K. Methylphenidate (Ritalin)-associated cataract and glaucoma. J Chin Med Assoc. 2006;69:589–90.
Article CAS PubMed Google Scholar
Bartlik B, Harmon G, Kaplan P. Use of methylphenidate in a patient with glaucoma and attention-deficit hyperactivity disorder: a clinical dilemma. Arch Gen Psychiatry. 1997;54:188–89.
Julien RG, Vincendeau J. Fuchs heterochromy, glaucoma and sympathomimetics. Bulletin des societes d’ophtalmologie de France 1956:187-8.
Karabulut M, Karabulut S, Kocatürk T, Ozkan SB. Is the treatment of attention deficit hyperactivity disorder a new cause of cataract? Open J Ophthalmol 2018;8. https://doi.org/10.4236/ojoph.2018.81004
Bymaster FP, Katner JS, Nelson DL, Hemrick-Luecke SK, Threlkeld PG, Heiligenstein JH, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27:699–711.
Upadhyaya HP, Desaiah D, Schuh KJ, Bymaster FP, Kallman MJ, Clarke DO, et al. A review of the abuse potential assessment of atomoxetine: a nonstimulant medication for attention-deficit/hyperactivity disorder. Psychopharmacology. 2013;226:189–200.
Eadie B, Etminan M, Mikelberg FS. Risk for uveitis with oral moxifloxacin: a comparative safety study. JAMA Ophthalmol. 2015;133:81–84.
Eadie BD, Etminan M, Carleton BC, Maberley DA, Mikelberg FS. Association of repeated intravitreous bevacizumab injections with risk for glaucoma surgery. JAMA Ophthalmol. 2017;135:363–68.
Hussein M, Wei W, Mastey V, Sanchez RJ, Wang D, Murdock DJ, et al. Real-world effectiveness of casirivimab and imdevimab among patients diagnosed with COVID-19 in the ambulatory setting: a retrospective cohort study using a large claims database. BMJ Open. 2022;12:e064953.
Essebag V, Genest J Jr, Suissa S, Pilote L. The nested case-control study in cardiology. Am Heart J. 2003;146:581–90.
İzci F, göde öğüten E. Methylphenidate induced increase in intraocular pressure, Dusunen Adam . J Psychiatry Neurol Sci. 2016;29. https://doi.org/10.5350/dajpn2016290413 .
Larrañaga-Fragoso P, Noval S, Rivero J, Boto-de-los-Bueis A. The effects of methylphenidate on refraction and anterior segment parameters in children with attention deficit hyperactivity disorder. J AAPOS . 2015;19. https://doi.org/10.1016/j.jaapos.2015.04.005
Duman NS, Duman R, Sarı Gökten E, Duman R. Lens opacities in children using methylphenidate hydrochloride. Cutan Ocul Toxicol. 2017;36:362–65.
Kong N, Bao Y, Zhao H, Kang X, Tai X, Shen Y. Methylphenidate causes cytotoxicity on photoreceptor cells via autophagy. Hum Exp Toxicol. 2020;40:71–80.
Corona JC. Role of oxidative stress and neuroinflammation in attention-deficit/hyperactivity disorder. Antioxidants. 2020;9:1039.
Corona JC, Carreón-Trujillo S, González-Pérez R, Gómez-Bautista D, Vázquez-González D, Salazar-García M. Atomoxetine produces oxidative stress and alters mitochondrial function in human neuron-like cells. Sci Rep. 2019;9:13011.
Izzotti A, Bagnis A, Saccà SC. The role of oxidative stress in glaucoma. Mutat Res. 2006;612:105–14.
de la Torre R, Farré M, Navarro M, Pacifici R, Zuccaro P, Pichini S. Clinical pharmacokinetics of amfetamine and related substances: monitoring in conventional and non-conventional matrices. Clin Pharmacokinet. 2004;43:157–85.
Kelly RP, Yeo KP, Teng C-H, Smith BP, Lowe S, Soon D, et al. Hemodynamic effects of acute administration of atomoxetine and methylphenidate. J Clin Pharmacol. 2005;45:851–55.
Lowe RF. Primary creeping angle-closure glaucoma. Br J Ophthalmol. 1964;48:544–50.
Enoch J, Jones L, Taylor DJ, Bronze C, Kirwan JF, Jones PR, et al. How do different lighting conditions affect the vision and quality of life of people with glaucoma? A systematic review. Eye. 2020;34:138–54.
D’Alli RE. Chapter 90 - Child And Adolescent Psychopharmacology. In: Carey WB, Crocker AC, Coleman WL, et al., eds. Developmental-Behavioral Pediatrics (Fourth Edition). Philadelphia: W.B. Saunders 2009:885-910.
Cui YM, Teng CH, Pan AX, Yuen E, Yeo KP, Zhou Y, et al. Atomoxetine pharmacokinetics in healthy Chinese subjects and effect of the CYP2D6*10 allele. Br J Clin Pharmacol. 2007;64:445–9.
Trzepacz PT, Williams DW, Feldman PD, Wrishko RE, Witcher JW, Buitelaar JK. CYP2D6 metabolizer status and atomoxetine dosing in children and adolescents with ADHD. Eur Neuropsychopharmacol. 2008;18:79–86.
Download references
Acknowledgements
This study was funded by the Glaucoma Research Society of Canada Project Grant.
Author information
Authors and affiliations.
Department of Ophthalmology and Visual Sciences, Dalhousie University, Halifax, NS, Canada
Rami Darwich, Bonnie He & Brennan D. Eadie
Department of Ophthalmology and Visual Sciences, University of British Columbia, Vancouver, BC, Canada
Mahyar Etminan
You can also search for this author in PubMed Google Scholar
Contributions
RD was responsible for designing the study, conducting the search, analysing, and interpreting results, and writing the report. BH contributed to the design of the research and provided feedback on the report. ME and BE supervised the design of the study, writing the report, extracting and analysing data, interpreting the results, and provided feedback on the report.
Corresponding author
Correspondence to Mahyar Etminan .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplemental table 1: icd-9 and icd-10 of the angle closure subtypes., supplemental table 2: icd-9 and icd-10 of the open angle subtypes., rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Darwich, R., Etminan, M., He, B. et al. Medications for attention deficit hyperactivity disorder associated with increased risk of developing glaucoma. Eye (2024). https://doi.org/10.1038/s41433-024-03100-6
Download citation
Received : 29 May 2023
Revised : 31 March 2024
Accepted : 18 April 2024
Published : 06 May 2024
DOI : https://doi.org/10.1038/s41433-024-03100-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
VIDEO
COMMENTS
glaucoma case presentation. Apr 8, 2019 • Download as PPTX, PDF •. 47 likes • 24,373 views. AI-enhanced description. S. sakib_lostvalley. A 60-year-old female presented with pain, redness and dimming of vision in her left eye for 3 days. On examination, her left eye showed high intraocular pressure, hazy cornea, shallow anterior chamber ...
6 likes • 1,384 views. Lyndon Woytuck. A review of juvenile glaucoma including screening, diagnostic approach, and management. Patient details have been anonymised to protect the individual. Health & Medicine. 1 of 9. Download now. Juvenile glaucoma: a case study and disease review - Download as a PDF or view online for free.
Glaucoma Case Studies James C. Tsai, M.D. Associate Professor of Ophthalmology Director, Glaucoma Division Edward S. Harkness Eye Institute Columbia University. LD: Clinical History & Exam • 78 y/o woman with glaucoma x 7 months • PMHx: hypothyroid; Meds: Synthroid, Premarin • Ocular Hx: negative; on Xalatan qhs OU • Va: 20/40 OU, Ta: 17 OD, 22 OS (9:25 AM) • SLE: 2+ NSC OU (+ PXE ...
2. DEFINITION • It is a group of disorders characterized by an abnormally high intra ocular pressure (IOP), optic nerve dystrophy (weakness) and peripheral visual field loss (tunnel vision.) • It is a symptomatic condition of the eye where the IOP is more than normal (above 25mm Hg). • Untreated of glaucoma leads to permanent damage of ...
Glaucoma. A group of eye disorders, glaucoma is characterized by high intraocular pressure (IOP) that damages the optic nerve. Glaucoma is one of the leading causes of irreversible blindness in the world and is the leading cause of blindness among adults in the United States. Glaucoma may occur as primary or congenital disease or secondary to ...
This case study is an example of how meticulously and elegantly we can identify structural and functional defects by incorporating more than one imaging modality when diagnosing glaucoma patients.Although nerve fiber layer OCT imaging is often the most useful to detect early glaucoma, in some instances, the defect can be so localized that it is easy to miss when surrounded by healthy nerve ...
Glaucoma - Download as a PDF or view online for free. ... This SlideShare presentation covers the procedure, benefits, and considerations for using VCE in children. Learn how this non-invasive diagnostic tool is revolutionizing the detection and treatment of gastrointestinal conditions in young patients, offering a safer and more comfortable ...
A Case Presentation on GLAUCOMA. - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Glaucoma is a group of eye conditions that damage the optic nerve and can lead to vision loss. There are four main types: open-angle, angle-closure, congenital, and secondary glaucoma.
Glaucoma is a leading cause of blindness and visual impairment for Americans, affecting as many as 2.2 million people nationwide. Most studies show that at least half of all persons with glaucoma do not know that they have this potentially blinding condition. Anyone can get glaucoma, but some people are at higher risk. They include the following:
The exam is simple and painless — your eye doctor will give you some eye drops to dilate (widen) your pupil and then check your eyes for glaucoma and other eye problems. The exam includes a visual field test to check your side vision. Remember, a basic eye exam for glasses or contacts can't catch glaucoma.
Case presentation. Mr AA is a 48-year-old shop attendant who presented at the eye unit of a teaching hospital with a history of gradual, painless vision loss. His presenting (unaided) visual acuity was counting fingers at 1 metre in the right eye and 6/60 in the left eye. Both corneas were clear, and the pupils had a slow reaction to light.
Case 1. Man With Diabetes Who Has Glaucoma, Cataracts, and Newly Diagnosed Dry Eye Disease From the Files of Elizabeth Yeu, MD • 83-year-old white man was referred by a community optometrist for evaluation of coexisting cataract and OAG • He reported eyes were gritty and red, and vision was blurred, particularly in the
CET OCT in Glaucoma Case Studies - Viewpoint
Abstract. This review article summarizes four key case reports published in the field of glaucoma in the year 2014. The first article describes successful early drainage of delayed suprachoroidal hemorrhage in 7 patients who underwent glaucoma surgery. The second describes the use of a corneal patch graft to repair leaking or hypotonous blebs ...
Signs of glaucoma optic neuropathy include abnormal neural retinal rim configuration (the absence of ISNT sign and/or notching), abnormal cup configuration (cup size for disc size), blood vessel changes and compromises, peripapillary atrophy, retinal nerve fiber layer loss, and function. loss typical of glaucoma of the eye.
the Accreditation Council for Continuing Medical Education. (ACCME) to provide continuing medical education for physicians. Evolve is an approved COPE Administrator. Case Presentations. in Medical ...
In the Collaborative Normal Tension Glaucoma Study (CNTGS), the goal of treatment was a 30% reduction in IOP. 1 For this patient, a pressure of 13 mm Hg would be a reasonable goal. In the CNTGS, reducing pressures by 30% reduced the progression rate from 35% to 12%. Even with that aggressive pressure reduction, however, 12% of the treated ...
Background. Glaucoma is one of the most common causes of blindness and patterns of visual field loss due to retinal ganglion cell degeneration. 1 Risk factors for the two main types of glaucoma, (i.e., open-angle and closed-angle glaucoma disease) with different patterns of disease occurrence include increasing age, high intraocular pressure (IOP), family history of glaucoma, race and ...
Abstract. The only proven therapy for glaucoma is intraocular pressure (IOP) reduction, which can be accomplished by different means. Each should be properly discussed with patients in order to best preserve visual function and quality of life. We report a case of unilateral pseudoexfoliative glaucoma, treated for years with triple topical IOP ...
Ehsan Sadri, MD, FACS, reviews the case of a 58-year-old male with open angle glaucoma utilizing minimally invasive glaucoma surgery procedure. News. All News. Contributors. Money Matters. Media. Expert Interviews. Medical World News. Podcasts. Case Based Roundtable Series. EyeView. Grand Rounds.
Ophthalmic Case Study 17. Case Study 17 - CC: Routine eye exam. all. Patient Visit. Patient History. HPI: The patient, a 61 year-old female retired school teacher, has not had an eye exam in 10 years. She reports no problems with driving, watching TV, computer or reading. She uses over-the-counter readers for close work.
This study aims to determine the risk of ACG and open angle glaucoma (OAG) among users of these treatments. This is a retrospective cohort study with a case control analysis using the PharMetrics ...