Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- JME Commentaries
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 44, Issue 12
- How to read an ethics paper
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-4609-9179 Melanie Jansen 1 , 2 ,
- Peter Ellerton 3
- 1 Paediatric Intensive Care Unit & Centre for Children’s Health Ethics and Law , Children’s Health Queensland Hospital and Health Service , South Brisbane , Queensland , Australia
- 2 Faculty of Medicine , University of Queensland , Herston , Queensland , Australia
- 3 Faculty of Humanities and Social Sciences , University of Queensland , Brisbane , Queensland , Australia
- Correspondence to Dr Melanie Jansen, Paediatric Intensive Care Unit & Centre for Children’s Health Ethics and Law, Children’s Health Queensland Hospital and Health Service, Brisbane, QLD 4101, Australia; doctormjansen{at}gmail.com
In recent decades, evidence-based medicine has become one of the foundations of clinical practice, making it necessary that healthcare practitioners develop keen critical appraisal skills for scientific papers. Worksheets to guide clinicians through this critical appraisal are often used in journal clubs, a key part of continuing medical education. A similar need is arising for health professionals to develop skills in the critical appraisal of medical ethics papers. Medicine is increasingly ethically complex, and there is a growing medical ethics literature that modern practitioners need to be able to use in their practice. In addition, clinical ethics services are commonplace in healthcare institutions, and the lion’s share of the work done by these services is done by clinicians in addition to their usual roles. Education to support this work is important. In this paper, we present a worksheet designed to help busy healthcare practitioners critically appraise ethics papers relevant to clinical practice. In the first section, we explain what is different about ethics papers. We then describe how to work through the steps in our critical appraisal worksheet: identifying the point at issue; scrutinising definitions; dissecting the arguments presented; considering counterarguments; and finally deciding on relevance. Working through this reflective worksheet will help healthcare practitioners to use the ethics literature effectively in clinical practice. We also intend it to be a shared evaluative tool that can form the basis of professional discussion such as at ethics journal clubs. Practising these critical reasoning skills will also increase practitioners’ capacity to think through difficult ethical decisions in daily clinical practice.
- clinical ethics
- education for health care professionals
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/medethics-2018-104997
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Evidence-based medicine is a foundation of clinical practice, necessitating that healthcare practitioners develop keen critical appraisal skills for scientific papers. Many excellent resources exist, including the paper by Sackett et al 1 and a reference book by Greenhalgh. 2 In 1992, the Medical Journal of Australia published a paper titled ‘How to read a journal article’ . 3 The authors’ goal was to give a step-by-step guide to critically appraising scientific papers. Journal clubs using this worksheet, or similar, are now commonplace in teaching hospitals and are a key part of medical education. A similar need is arising for health professionals to develop skills in the critical appraisal of ethics papers. The reasons for this are twofold. First, healthcare grows increasingly ethically complex. Just as clinicians must keep abreast of the scientific literature, they should also keep up to date with the ethics literature relevant to their practice. Second, clinical ethics services (CES) have become commonplace in hospitals in developed nations. The lion’s share of the work of these services is done by healthcare professionals in addition to their clinical roles 4–6 and who have highly variable levels of training. 4–8 There is an urgent need to equip these and other clinical staff with skills to appraise papers relevant to these aspects of practice.
In this paper, we present the critical appraisal worksheet developed at the Centre for Children’s Health Ethics and Law (CCHEL), Children’s Health Queensland, Brisbane, Australia ( table 1 ). The worksheet was developed for our ethics journal club and has proved useful both for the critical appraisal of ethics papers and for the development of critical thinking skills that can be applied in clinical practice and in clinical ethics consultation work. The goal of this paper is to provide a tool for clinicians without extensive philosophical training to critically appraise ethics papers relevant to clinical practice. We also intend it to be a shared evaluative tool that can form the basis of professional discussion such as at ethics journal clubs. In the first section, we explain what is different about ethics papers. We then describe the steps in our critical appraisal worksheet.
- View inline
Ethics critical appraisal worksheet
What is different about ethics papers? A discussion of arguments, facts and values
It is important to recognise that ethics is a philosophical, not a scientific, discipline. Healthcare professionals are accustomed to critically appraising scientific data, and to constructing an argument based on that data for why a particular clinical decision is justified. Note that we use the word argument in the philosophical sense, meaning a set of reasons that justify a position. For example, if a patient presents with clinical signs consistent with bacterial pneumonia, the doctor will prescribe an antibiotic regimen based on their knowledge of the likely pathogens and the efficacy of particular antibiotics against these. That oral amoxicillin is an effective treatment for mild community-acquired pneumonia is a factual claim supported by scientific evidence. In contrast, ethical claims are claims of value and must be justified with an ethical argument. For example, the claim that life-sustaining therapy (LST) should be withdrawn from a patient with end-stage cancer is a value claim. Prescriptive words such as ‘should’ and ‘ought’ are useful signposts for value claims. An argument that may justify the claim that LST should be withdrawn is that the patient had previously stated that they did not want to be maintained on LST, and therefore to respect their autonomy the treatment should be withdrawn.
Note that matters of fact and matters of value coexist in clinical medicine (as they do in life) and that rationales for ethical and medical decisions are usually made up of both fact and value claims. Take the example just given of the argument that therapy should be stopped to respect the patient’s autonomy. That the patient had previously expressed wishes not to be maintained on life support is a factual claim. The claim that we should respect autonomy is a value claim. Likewise, when deciding on antibiotics for the patient with pneumonia, the claim that amoxicillin is effective is a factual claim. That we should treat the patient with amoxicillin is a value claim—the implicit argument for which is that the right thing to do is to treat patients with the most effective therapy for their disease. This seems so plainly reasonable that it does not need to be stated; however, it is important to recognise implicit value judgements in clinical decisions, as these are often at issue when there is conflict. The important skill is to be able to differentiate fact and value claims and to understand how the two can interact to form a set of reasons that support a particular conclusion. To do this, it is important to understand how arguments are constructed.
Understanding arguments is important for clinical practice, because ethical decision making threads through everything healthcare practitioners do. High-level skills in this area are especially important for those providing clinical ethics consultation. The UK Clinical Ethics Network and the American Society for Bioethics and Humanities have each published core competencies for clinical ethics consultation. 9 10 Both specify the need for consultants to understand ethical theory and reasoning, to analyse ethical conflicts, and to be able to elicit values and assumptions. Understanding argumentation is fundamental to these skills. The ethics critical appraisal worksheet provides a framework through which to appraise arguments and, by guiding practitioners to read ethics papers actively, aims to deepen understanding of ethical argumentation. We acknowledge that there is a growing literature in empirical ethics—this critical appraisal worksheet is not intended for these papers, as they are scientific papers and can be appraised as such. This worksheet is intended for papers that discuss ethical issues, not those that present scientific data relevant to an ethical issue.
The ethics critical appraisal worksheet
We have structured the worksheet in a similar way to the one by Darzins et al , 3 as a matrix of questions arranged in three columns ( table 1 ). In the first column are questions that prompt the reader to look for important types of information in the article. The second column contains questions that help the reader to decide whether there are problems with these. The third column poses questions to help the reader decide if any problems identified threaten the quality of the paper. Using this worksheet should assist clinicians to more rapidly identify problems with the paper, making the reading of ethics papers more time-efficient.
Critical appraisal questions
What is the point at issue.
The point at issue is the ethical question that the paper is addressing. Well-written ethics papers will explicitly state the point, or points, at issue in the introduction and will go on to address them. Poorly written ethics papers will shift between points at issue, which clouds reasoning and precludes systematic appraisal of all the relevant arguments. Shifting the point at issue happens often in ethical discussions. For example, we may be discussing the issue of whether we should continue providing LST to a child with a very poor prognosis. One person believes that the LST is causing suffering to the child, another person questions the truth of this. A third person points out that we cannot over-ride the parents’ autonomy. This third person is shifting the point at issue. The ethicality of over-riding parental autonomy is important, but concerns a different point at issue. Whether the LST is causing suffering or not is a point that needs to be explored and clarified before moving onto the question of whether it is of a magnitude that makes it reasonable to interfere with parental autonomy.
Has the author defined all of the terms they use?
Defining key terms is critical to avoid confusion. For example, in a paper discussing the rights of adolescents to autonomy in medical decision making, the author needs to define what persons they are referring to with the word ‘adolescent’; exactly what range of decisions they are referring to within the phrase ‘medical decision making’; and exactly how autonomy is conceived in this context. Failing to define key terms used in an argument sacrifices clarity, and defining key terms in an unusual or unreasonable way may have implications for the generalisability of the argument.
Dissect the argument: What are the premises of the author’s argument? What is/are the author’s conclusion/s?
This section of the worksheet requires explanation of the anatomy of an argument and clarification of the difference between truth and validity.
Arguments consist of premises and a conclusion, for example:
Premise 1: Human suffering is undesirable.
Premise 2: Medically extending life in case X prolongs human suffering.
Conclusion: Medically extending life in case X is undesirable.
This is a valid argument because the conclusion follows logically from the premises; that is, it is impossible for the premises to be true and the conclusion false. Whether the conclusion (or a premise) is true or not is a separate issue. Refuting this argument requires proving one or both of the premises to be false—finding evidence that suffering is not always undesirable, or making a case that this particular medical intervention does not prolong suffering. There are no errors of reasoning in this argument, but there may be factual errors which will prove the argument to be a bad one. Consider another argument:
Premise 1: Lucy has a chronic cough.
Premise 2: Lung cancer can present with a chronic cough.
Conclusion: Lucy has lung cancer.
In this case, the argument is invalid. The premises are true but the reasoning is flawed. It is true that Lucy has a chronic cough, and that lung cancer can present with a chronic cough, but it does not follow that Lucy necessarily has lung cancer. Her chronic cough may be from asthma or chronic bronchitis. Lucy may even have lung cancer, although it could be of a type that would not usually cause coughing. So, even if all the information given is true, the conclusion that she must have lung cancer does not necessarily follow.
Another important phenomenon to be aware of is the ‘hidden assumption’. A hidden assumption is a premise that is not explicitly stated. For example, a person may claim that homosexuality is morally wrong because it is unnatural. The hidden premise here is that things that are unnatural are morally wrong, as follows:
Premise 1: (Hidden) Things that are unnatural are morally wrong.
Premise 2: Homosexuality is unnatural.
Conclusion: Homosexuality is morally wrong.
To refute this argument one needs to either show the premises are false or that the reasoning is invalid. The reasoning is valid because it is impossible for the premises to be true and the conclusion false. However, even if one were to accept premise 2—in ignorance of the natural occurrence of homosexuality in many animals—the hidden premise 1 ignores that many things that are unnatural are considered morally good (or at least morally neutral), such as medicines, clothing or the telephone. Identifying the hidden premise is necessary to fully represent the argument, and hence to properly evaluate it.
In ethics papers, deciding whether premises are true will often require recourse to the scientific literature. Good ethics papers have well-researched references for factual premises. Appraising the validity of reasoning can be more difficult and requires practice. A full and rich account of logical fallacies is outside the scope of this paper; however, there are excellent, accessible resources available to hone these skills. 11 It is also worth noting that the overall position of an ethics paper is likely to be made up of a complex argument, with the conclusions of initial arguments making up the premises of further arguments. For example, some may claim that premise 1 (above) is a claim about the existence of ethical laws of nature. To support this claim, the person must develop an argument for the existence of ethical laws of nature and the definition of ‘unnatural’, ending with premise 1—things that are unnatural are morally wrong—as the conclusion. The analytical framework we present here is applicable to each constituent argument of a complex argument.
Does the author address all relevant counterarguments?
When making a case for an ethical position, it is imperative that authors address counterarguments to their position. If an author has not addressed relevant counterarguments, or has done so unconvincingly, this significantly decreases the strength of their case, or at least suggests a shallow investigation of the issue.
Is the argument or exploration of the issue relevant to your practice?
Some ethics papers will address a specific ethical question arising in the reader’s own practice and assist them in navigating this scenario. Other papers will change the way practitioners think, affecting practice in myriad but subtle ways. There will be papers that, while of good internal quality, are not relevant to the reader’s practice. Explicitly deciding on the relevance of a paper prompts practitioners to contextualise new ethical information within their own practice.
Working through this reflective worksheet will aid healthcare practitioners in actively reading and critically appraising ethics papers, enabling them to use the ethics literature more effectively. Developing these critical reasoning skills will also increase capacity to think through difficult ethical decisions in day-to-day practice. It is of particular importance that clinicians working within CES develop these skills to a high level. In the future, we hope to empirically evaluate the ethics critical appraisal worksheet.
Key messages
Healthcare is increasingly ethically complex, and so there is a growing need for clinicians to keep up to date with the ethics literature relevant to clinical practice.
Clinical ethics services have become commonplace, and the majority of the work of these services is done by clinicians in addition to their clinical roles.
Ethics papers differ in important ways from scientific papers, requiring a different set of critical appraisal skills.
We have developed a worksheet to assist clinicians in the critical appraisal of ethics papers, which can also be used as a shared evaluative tool, such as at ethics journal clubs.
Acknowledgments
The authors would like to acknowledge all CCHEL Clinical Ethics Response Pool members who have participated in the ethics journal club, and in so doing have helped to refine this critical appraisal worksheet.
- Sackett DL ,
- Rosenberg WM ,
- Gray JA , et al
- Greenhalgh T
- Darzins PJ ,
- Pearlman RA
- Slowther AM ,
- McClimans L ,
- Irving H , et al
- Godkin MD ,
- Upshur RE , et al
- Kesselheim JC ,
- Johnson J ,
- Larcher V ,
- Richardson J ,
- Meaden S , et al
Contributors MJ conceived the idea of the critical appraisal worksheet for clinicians. PE assisted in developing the idea and refining the worksheet. MJ wrote the initial draft of the manuscript. PE and MJ were both involved in draft review and development of the final version of the manuscript. MJ is the guarantor of this article.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer The views expressed in this paper are the authors’ own and do not necessarily reflect the views of their institutions.
Competing interests None declared.
Patient consent Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement No additional data are available.
Author note MJ is a medical doctor in intensive care medicine and has additional qualifications and experience in clinical ethics. She co-led the working group to establish the Centre for Children’s Health Ethics and Law at Children’s Health Queensland, and was the centre’s inaugural Clinical Ethics Fellow. MJ recently completed a Churchill Fellowship in clinical ethics. She has published both empirical research and analysis pieces on healthcare ethics issues. PE is a science educator and philosopher, and is the Curriculum Director of the University of Queensland Critical Thinking Project. He is an expert in critical thinking and argumentation and has published on these topics in a number of contexts.
Correction notice This article has been made Open Access since it was published Online First.
Read the full text or download the PDF:
Other content recommended for you.
- Ethical climate in contemporary paediatric intensive care Katie M. Moynihan et al., Journal of Medical Ethics, 2021
- Paediatric clinical ethics in Australia and New Zealand: a survey Emma Cottle et al., BMJ Paediatrics Open, 2017
- What kinds of cases do paediatricians refer to clinical ethics? Insights from 184 case referrals at an Australian paediatric hospital Rosalind J McDougall et al., Journal of Medical Ethics, 2016
- Development of clinical ethics services in the UK: a national survey Anne Marie Slowther et al., Journal of Medical Ethics, 2011
- Project Examining Effectiveness in Clinical Ethics (PEECE): phase 1—descriptive analysis of nine clinical ethics services M D Godkin et al., Journal of Medical Ethics, 2005
- Clinical bioethics integration, sustainability, and accountability: the Hub and Spokes Strategy S MacRae et al., Journal of Medical Ethics, 2005
- Taking the burden off: a study of the quality of ethics consultation in the time of COVID-19 Lulia Kana et al., Journal of Medical Ethics, 2021
- Evaluating interventions to improve ethical decision making in clinical practice: a review of the literature and reflections on the challenges posed Agnieszka Ignatowicz et al., Journal of Medical Ethics, 2022
- Objectives and outcomes of clinical ethics services: a Delphi study Leah McClimans et al., Journal of Medical Ethics, 2019
- Clinical ethicists’ perspectives on organisational ethics in healthcare organisations D S Silva et al., Journal of Medical Ethics, 2008
- Open access
- Published: 18 April 2024
Research ethics and artificial intelligence for global health: perspectives from the global forum on bioethics in research
- James Shaw 1 , 13 ,
- Joseph Ali 2 , 3 ,
- Caesar A. Atuire 4 , 5 ,
- Phaik Yeong Cheah 6 ,
- Armando Guio Español 7 ,
- Judy Wawira Gichoya 8 ,
- Adrienne Hunt 9 ,
- Daudi Jjingo 10 ,
- Katherine Littler 9 ,
- Daniela Paolotti 11 &
- Effy Vayena 12
BMC Medical Ethics volume 25 , Article number: 46 ( 2024 ) Cite this article
641 Accesses
5 Altmetric
Metrics details
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice. In this paper we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town, South Africa in November 2022.
The GFBR is an annual meeting organized by the World Health Organization and supported by the Wellcome Trust, the US National Institutes of Health, the UK Medical Research Council (MRC) and the South African MRC. The forum aims to bring together ethicists, researchers, policymakers, research ethics committee members and other actors to engage with challenges and opportunities specifically related to research ethics. In 2022 the focus of the GFBR was “Ethics of AI in Global Health Research”. The forum consisted of 6 case study presentations, 16 governance presentations, and a series of small group and large group discussions. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics. In this paper, we highlight central insights arising from GFBR 2022.
We describe the significance of four thematic insights arising from the forum: (1) Appropriateness of building AI, (2) Transferability of AI systems, (3) Accountability for AI decision-making and outcomes, and (4) Individual consent. We then describe eight recommendations for governance leaders to enhance the ethical governance of AI in global health research, addressing issues such as AI impact assessments, environmental values, and fair partnerships.
Conclusions
The 2022 Global Forum on Bioethics in Research illustrated several innovations in ethical governance of AI for global health research, as well as several areas in need of urgent attention internationally. This summary is intended to inform international and domestic efforts to strengthen research ethics and support the evolution of governance leadership to meet the demands of AI in global health research.
Peer Review reports
Introduction
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice [ 1 , 2 , 3 ]. Beyond the growing number of AI applications being implemented in health care, capabilities of AI models such as Large Language Models (LLMs) expand the potential reach and significance of AI technologies across health-related fields [ 4 , 5 ]. Discussion about effective, ethical governance of AI technologies has spanned a range of governance approaches, including government regulation, organizational decision-making, professional self-regulation, and research ethics review [ 6 , 7 , 8 ]. In this paper, we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health research, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town, South Africa in November 2022. Although applications of AI for research, health care, and public health are diverse and advancing rapidly, the insights generated at the forum remain highly relevant from a global health perspective. After summarizing important context for work in this domain, we highlight categories of ethical issues emphasized at the forum for attention from a research ethics perspective internationally. We then outline strategies proposed for research, innovation, and governance to support more ethical AI for global health.
In this paper, we adopt the definition of AI systems provided by the Organization for Economic Cooperation and Development (OECD) as our starting point. Their definition states that an AI system is “a machine-based system that can, for a given set of human-defined objectives, make predictions, recommendations, or decisions influencing real or virtual environments. AI systems are designed to operate with varying levels of autonomy” [ 9 ]. The conceptualization of an algorithm as helping to constitute an AI system, along with hardware, other elements of software, and a particular context of use, illustrates the wide variety of ways in which AI can be applied. We have found it useful to differentiate applications of AI in research as those classified as “AI systems for discovery” and “AI systems for intervention”. An AI system for discovery is one that is intended to generate new knowledge, for example in drug discovery or public health research in which researchers are seeking potential targets for intervention, innovation, or further research. An AI system for intervention is one that directly contributes to enacting an intervention in a particular context, for example informing decision-making at the point of care or assisting with accuracy in a surgical procedure.
The mandate of the GFBR is to take a broad view of what constitutes research and its regulation in global health, with special attention to bioethics in Low- and Middle- Income Countries. AI as a group of technologies demands such a broad view. AI development for health occurs in a variety of environments, including universities and academic health sciences centers where research ethics review remains an important element of the governance of science and innovation internationally [ 10 , 11 ]. In these settings, research ethics committees (RECs; also known by different names such as Institutional Review Boards or IRBs) make decisions about the ethical appropriateness of projects proposed by researchers and other institutional members, ultimately determining whether a given project is allowed to proceed on ethical grounds [ 12 ].
However, research involving AI for health also takes place in large corporations and smaller scale start-ups, which in some jurisdictions fall outside the scope of research ethics regulation. In the domain of AI, the question of what constitutes research also becomes blurred. For example, is the development of an algorithm itself considered a part of the research process? Or only when that algorithm is tested under the formal constraints of a systematic research methodology? In this paper we take an inclusive view, in which AI development is included in the definition of research activity and within scope for our inquiry, regardless of the setting in which it takes place. This broad perspective characterizes the approach to “research ethics” we take in this paper, extending beyond the work of RECs to include the ethical analysis of the wide range of activities that constitute research as the generation of new knowledge and intervention in the world.
Ethical governance of AI in global health
The ethical governance of AI for global health has been widely discussed in recent years. The World Health Organization (WHO) released its guidelines on ethics and governance of AI for health in 2021, endorsing a set of six ethical principles and exploring the relevance of those principles through a variety of use cases. The WHO guidelines also provided an overview of AI governance, defining governance as covering “a range of steering and rule-making functions of governments and other decision-makers, including international health agencies, for the achievement of national health policy objectives conducive to universal health coverage.” (p. 81) The report usefully provided a series of recommendations related to governance of seven domains pertaining to AI for health: data, benefit sharing, the private sector, the public sector, regulation, policy observatories/model legislation, and global governance. The report acknowledges that much work is yet to be done to advance international cooperation on AI governance, especially related to prioritizing voices from Low- and Middle-Income Countries (LMICs) in global dialogue.
One important point emphasized in the WHO report that reinforces the broader literature on global governance of AI is the distribution of responsibility across a wide range of actors in the AI ecosystem. This is especially important to highlight when focused on research for global health, which is specifically about work that transcends national borders. Alami et al. (2020) discussed the unique risks raised by AI research in global health, ranging from the unavailability of data in many LMICs required to train locally relevant AI models to the capacity of health systems to absorb new AI technologies that demand the use of resources from elsewhere in the system. These observations illustrate the need to identify the unique issues posed by AI research for global health specifically, and the strategies that can be employed by all those implicated in AI governance to promote ethically responsible use of AI in global health research.
RECs and the regulation of research involving AI
RECs represent an important element of the governance of AI for global health research, and thus warrant further commentary as background to our paper. Despite the importance of RECs, foundational questions have been raised about their capabilities to accurately understand and address ethical issues raised by studies involving AI. Rahimzadeh et al. (2023) outlined how RECs in the United States are under-prepared to align with recent federal policy requiring that RECs review data sharing and management plans with attention to the unique ethical issues raised in AI research for health [ 13 ]. Similar research in South Africa identified variability in understanding of existing regulations and ethical issues associated with health-related big data sharing and management among research ethics committee members [ 14 , 15 ]. The effort to address harms accruing to groups or communities as opposed to individuals whose data are included in AI research has also been identified as a unique challenge for RECs [ 16 , 17 ]. Doerr and Meeder (2022) suggested that current regulatory frameworks for research ethics might actually prevent RECs from adequately addressing such issues, as they are deemed out of scope of REC review [ 16 ]. Furthermore, research in the United Kingdom and Canada has suggested that researchers using AI methods for health tend to distinguish between ethical issues and social impact of their research, adopting an overly narrow view of what constitutes ethical issues in their work [ 18 ].
The challenges for RECs in adequately addressing ethical issues in AI research for health care and public health exceed a straightforward survey of ethical considerations. As Ferretti et al. (2021) contend, some capabilities of RECs adequately cover certain issues in AI-based health research, such as the common occurrence of conflicts of interest where researchers who accept funds from commercial technology providers are implicitly incentivized to produce results that align with commercial interests [ 12 ]. However, some features of REC review require reform to adequately meet ethical needs. Ferretti et al. outlined weaknesses of RECs that are longstanding and those that are novel to AI-related projects, proposing a series of directions for development that are regulatory, procedural, and complementary to REC functionality. The work required on a global scale to update the REC function in response to the demands of research involving AI is substantial.
These issues take greater urgency in the context of global health [ 19 ]. Teixeira da Silva (2022) described the global practice of “ethics dumping”, where researchers from high income countries bring ethically contentious practices to RECs in low-income countries as a strategy to gain approval and move projects forward [ 20 ]. Although not yet systematically documented in AI research for health, risk of ethics dumping in AI research is high. Evidence is already emerging of practices of “health data colonialism”, in which AI researchers and developers from large organizations in high-income countries acquire data to build algorithms in LMICs to avoid stricter regulations [ 21 ]. This specific practice is part of a larger collection of practices that characterize health data colonialism, involving the broader exploitation of data and the populations they represent primarily for commercial gain [ 21 , 22 ]. As an additional complication, AI algorithms trained on data from high-income contexts are unlikely to apply in straightforward ways to LMIC settings [ 21 , 23 ]. In the context of global health, there is widespread acknowledgement about the need to not only enhance the knowledge base of REC members about AI-based methods internationally, but to acknowledge the broader shifts required to encourage their capabilities to more fully address these and other ethical issues associated with AI research for health [ 8 ].
Although RECs are an important part of the story of the ethical governance of AI for global health research, they are not the only part. The responsibilities of supra-national entities such as the World Health Organization, national governments, organizational leaders, commercial AI technology providers, health care professionals, and other groups continue to be worked out internationally. In this context of ongoing work, examining issues that demand attention and strategies to address them remains an urgent and valuable task.
The GFBR is an annual meeting organized by the World Health Organization and supported by the Wellcome Trust, the US National Institutes of Health, the UK Medical Research Council (MRC) and the South African MRC. The forum aims to bring together ethicists, researchers, policymakers, REC members and other actors to engage with challenges and opportunities specifically related to research ethics. Each year the GFBR meeting includes a series of case studies and keynotes presented in plenary format to an audience of approximately 100 people who have applied and been competitively selected to attend, along with small-group breakout discussions to advance thinking on related issues. The specific topic of the forum changes each year, with past topics including ethical issues in research with people living with mental health conditions (2021), genome editing (2019), and biobanking/data sharing (2018). The forum is intended to remain grounded in the practical challenges of engaging in research ethics, with special interest in low resource settings from a global health perspective. A post-meeting fellowship scheme is open to all LMIC participants, providing a unique opportunity to apply for funding to further explore and address the ethical challenges that are identified during the meeting.
In 2022, the focus of the GFBR was “Ethics of AI in Global Health Research”. The forum consisted of 6 case study presentations (both short and long form) reporting on specific initiatives related to research ethics and AI for health, and 16 governance presentations (both short and long form) reporting on actual approaches to governing AI in different country settings. A keynote presentation from Professor Effy Vayena addressed the topic of the broader context for AI ethics in a rapidly evolving field. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics. The 2-day forum addressed a wide range of themes. The conference report provides a detailed overview of each of the specific topics addressed while a policy paper outlines the cross-cutting themes (both documents are available at the GFBR website: https://www.gfbr.global/past-meetings/16th-forum-cape-town-south-africa-29-30-november-2022/ ). As opposed to providing a detailed summary in this paper, we aim to briefly highlight central issues raised, solutions proposed, and the challenges facing the research ethics community in the years to come.
In this way, our primary aim in this paper is to present a synthesis of the challenges and opportunities raised at the GFBR meeting and in the planning process, followed by our reflections as a group of authors on their significance for governance leaders in the coming years. We acknowledge that the views represented at the meeting and in our results are a partial representation of the universe of views on this topic; however, the GFBR leadership invested a great deal of resources in convening a deeply diverse and thoughtful group of researchers and practitioners working on themes of bioethics related to AI for global health including those based in LMICs. We contend that it remains rare to convene such a strong group for an extended time and believe that many of the challenges and opportunities raised demand attention for more ethical futures of AI for health. Nonetheless, our results are primarily descriptive and are thus not explicitly grounded in a normative argument. We make effort in the Discussion section to contextualize our results by describing their significance and connecting them to broader efforts to reform global health research and practice.
Uniquely important ethical issues for AI in global health research
Presentations and group dialogue over the course of the forum raised several issues for consideration, and here we describe four overarching themes for the ethical governance of AI in global health research. Brief descriptions of each issue can be found in Table 1 . Reports referred to throughout the paper are available at the GFBR website provided above.
The first overarching thematic issue relates to the appropriateness of building AI technologies in response to health-related challenges in the first place. Case study presentations referred to initiatives where AI technologies were highly appropriate, such as in ear shape biometric identification to more accurately link electronic health care records to individual patients in Zambia (Alinani Simukanga). Although important ethical issues were raised with respect to privacy, trust, and community engagement in this initiative, the AI-based solution was appropriately matched to the challenge of accurately linking electronic records to specific patient identities. In contrast, forum participants raised questions about the appropriateness of an initiative using AI to improve the quality of handwashing practices in an acute care hospital in India (Niyoshi Shah), which led to gaming the algorithm. Overall, participants acknowledged the dangers of techno-solutionism, in which AI researchers and developers treat AI technologies as the most obvious solutions to problems that in actuality demand much more complex strategies to address [ 24 ]. However, forum participants agreed that RECs in different contexts have differing degrees of power to raise issues of the appropriateness of an AI-based intervention.
The second overarching thematic issue related to whether and how AI-based systems transfer from one national health context to another. One central issue raised by a number of case study presentations related to the challenges of validating an algorithm with data collected in a local environment. For example, one case study presentation described a project that would involve the collection of personally identifiable data for sensitive group identities, such as tribe, clan, or religion, in the jurisdictions involved (South Africa, Nigeria, Tanzania, Uganda and the US; Gakii Masunga). Doing so would enable the team to ensure that those groups were adequately represented in the dataset to ensure the resulting algorithm was not biased against specific community groups when deployed in that context. However, some members of these communities might desire to be represented in the dataset, whereas others might not, illustrating the need to balance autonomy and inclusivity. It was also widely recognized that collecting these data is an immense challenge, particularly when historically oppressive practices have led to a low-trust environment for international organizations and the technologies they produce. It is important to note that in some countries such as South Africa and Rwanda, it is illegal to collect information such as race and tribal identities, re-emphasizing the importance for cultural awareness and avoiding “one size fits all” solutions.
The third overarching thematic issue is related to understanding accountabilities for both the impacts of AI technologies and governance decision-making regarding their use. Where global health research involving AI leads to longer-term harms that might fall outside the usual scope of issues considered by a REC, who is to be held accountable, and how? This question was raised as one that requires much further attention, with law being mixed internationally regarding the mechanisms available to hold researchers, innovators, and their institutions accountable over the longer term. However, it was recognized in breakout group discussion that many jurisdictions are developing strong data protection regimes related specifically to international collaboration for research involving health data. For example, Kenya’s Data Protection Act requires that any internationally funded projects have a local principal investigator who will hold accountability for how data are shared and used [ 25 ]. The issue of research partnerships with commercial entities was raised by many participants in the context of accountability, pointing toward the urgent need for clear principles related to strategies for engagement with commercial technology companies in global health research.
The fourth and final overarching thematic issue raised here is that of consent. The issue of consent was framed by the widely shared recognition that models of individual, explicit consent might not produce a supportive environment for AI innovation that relies on the secondary uses of health-related datasets to build AI algorithms. Given this recognition, approaches such as community oversight of health data uses were suggested as a potential solution. However, the details of implementing such community oversight mechanisms require much further attention, particularly given the unique perspectives on health data in different country settings in global health research. Furthermore, some uses of health data do continue to require consent. One case study of South Africa, Nigeria, Kenya, Ethiopia and Uganda suggested that when health data are shared across borders, individual consent remains necessary when data is transferred from certain countries (Nezerith Cengiz). Broader clarity is necessary to support the ethical governance of health data uses for AI in global health research.
Recommendations for ethical governance of AI in global health research
Dialogue at the forum led to a range of suggestions for promoting ethical conduct of AI research for global health, related to the various roles of actors involved in the governance of AI research broadly defined. The strategies are written for actors we refer to as “governance leaders”, those people distributed throughout the AI for global health research ecosystem who are responsible for ensuring the ethical and socially responsible conduct of global health research involving AI (including researchers themselves). These include RECs, government regulators, health care leaders, health professionals, corporate social accountability officers, and others. Enacting these strategies would bolster the ethical governance of AI for global health more generally, enabling multiple actors to fulfill their roles related to governing research and development activities carried out across multiple organizations, including universities, academic health sciences centers, start-ups, and technology corporations. Specific suggestions are summarized in Table 2 .
First, forum participants suggested that governance leaders including RECs, should remain up to date on recent advances in the regulation of AI for health. Regulation of AI for health advances rapidly and takes on different forms in jurisdictions around the world. RECs play an important role in governance, but only a partial role; it was deemed important for RECs to acknowledge how they fit within a broader governance ecosystem in order to more effectively address the issues within their scope. Not only RECs but organizational leaders responsible for procurement, researchers, and commercial actors should all commit to efforts to remain up to date about the relevant approaches to regulating AI for health care and public health in jurisdictions internationally. In this way, governance can more adequately remain up to date with advances in regulation.
Second, forum participants suggested that governance leaders should focus on ethical governance of health data as a basis for ethical global health AI research. Health data are considered the foundation of AI development, being used to train AI algorithms for various uses [ 26 ]. By focusing on ethical governance of health data generation, sharing, and use, multiple actors will help to build an ethical foundation for AI development among global health researchers.
Third, forum participants believed that governance processes should incorporate AI impact assessments where appropriate. An AI impact assessment is the process of evaluating the potential effects, both positive and negative, of implementing an AI algorithm on individuals, society, and various stakeholders, generally over time frames specified in advance of implementation [ 27 ]. Although not all types of AI research in global health would warrant an AI impact assessment, this is especially relevant for those studies aiming to implement an AI system for intervention into health care or public health. Organizations such as RECs can use AI impact assessments to boost understanding of potential harms at the outset of a research project, encouraging researchers to more deeply consider potential harms in the development of their study.
Fourth, forum participants suggested that governance decisions should incorporate the use of environmental impact assessments, or at least the incorporation of environment values when assessing the potential impact of an AI system. An environmental impact assessment involves evaluating and anticipating the potential environmental effects of a proposed project to inform ethical decision-making that supports sustainability [ 28 ]. Although a relatively new consideration in research ethics conversations [ 29 ], the environmental impact of building technologies is a crucial consideration for the public health commitment to environmental sustainability. Governance leaders can use environmental impact assessments to boost understanding of potential environmental harms linked to AI research projects in global health over both the shorter and longer terms.
Fifth, forum participants suggested that governance leaders should require stronger transparency in the development of AI algorithms in global health research. Transparency was considered essential in the design and development of AI algorithms for global health to ensure ethical and accountable decision-making throughout the process. Furthermore, whether and how researchers have considered the unique contexts into which such algorithms may be deployed can be surfaced through stronger transparency, for example in describing what primary considerations were made at the outset of the project and which stakeholders were consulted along the way. Sharing information about data provenance and methods used in AI development will also enhance the trustworthiness of the AI-based research process.
Sixth, forum participants suggested that governance leaders can encourage or require community engagement at various points throughout an AI project. It was considered that engaging patients and communities is crucial in AI algorithm development to ensure that the technology aligns with community needs and values. However, participants acknowledged that this is not a straightforward process. Effective community engagement requires lengthy commitments to meeting with and hearing from diverse communities in a given setting, and demands a particular set of skills in communication and dialogue that are not possessed by all researchers. Encouraging AI researchers to begin this process early and build long-term partnerships with community members is a promising strategy to deepen community engagement in AI research for global health. One notable recommendation was that research funders have an opportunity to incentivize and enable community engagement with funds dedicated to these activities in AI research in global health.
Seventh, forum participants suggested that governance leaders can encourage researchers to build strong, fair partnerships between institutions and individuals across country settings. In a context of longstanding imbalances in geopolitical and economic power, fair partnerships in global health demand a priori commitments to share benefits related to advances in medical technologies, knowledge, and financial gains. Although enforcement of this point might be beyond the remit of RECs, commentary will encourage researchers to consider stronger, fairer partnerships in global health in the longer term.
Eighth, it became evident that it is necessary to explore new forms of regulatory experimentation given the complexity of regulating a technology of this nature. In addition, the health sector has a series of particularities that make it especially complicated to generate rules that have not been previously tested. Several participants highlighted the desire to promote spaces for experimentation such as regulatory sandboxes or innovation hubs in health. These spaces can have several benefits for addressing issues surrounding the regulation of AI in the health sector, such as: (i) increasing the capacities and knowledge of health authorities about this technology; (ii) identifying the major problems surrounding AI regulation in the health sector; (iii) establishing possibilities for exchange and learning with other authorities; (iv) promoting innovation and entrepreneurship in AI in health; and (vi) identifying the need to regulate AI in this sector and update other existing regulations.
Ninth and finally, forum participants believed that the capabilities of governance leaders need to evolve to better incorporate expertise related to AI in ways that make sense within a given jurisdiction. With respect to RECs, for example, it might not make sense for every REC to recruit a member with expertise in AI methods. Rather, it will make more sense in some jurisdictions to consult with members of the scientific community with expertise in AI when research protocols are submitted that demand such expertise. Furthermore, RECs and other approaches to research governance in jurisdictions around the world will need to evolve in order to adopt the suggestions outlined above, developing processes that apply specifically to the ethical governance of research using AI methods in global health.
Research involving the development and implementation of AI technologies continues to grow in global health, posing important challenges for ethical governance of AI in global health research around the world. In this paper we have summarized insights from the 2022 GFBR, focused specifically on issues in research ethics related to AI for global health research. We summarized four thematic challenges for governance related to AI in global health research and nine suggestions arising from presentations and dialogue at the forum. In this brief discussion section, we present an overarching observation about power imbalances that frames efforts to evolve the role of governance in global health research, and then outline two important opportunity areas as the field develops to meet the challenges of AI in global health research.
Dialogue about power is not unfamiliar in global health, especially given recent contributions exploring what it would mean to de-colonize global health research, funding, and practice [ 30 , 31 ]. Discussions of research ethics applied to AI research in global health contexts are deeply infused with power imbalances. The existing context of global health is one in which high-income countries primarily located in the “Global North” charitably invest in projects taking place primarily in the “Global South” while recouping knowledge, financial, and reputational benefits [ 32 ]. With respect to AI development in particular, recent examples of digital colonialism frame dialogue about global partnerships, raising attention to the role of large commercial entities and global financial capitalism in global health research [ 21 , 22 ]. Furthermore, the power of governance organizations such as RECs to intervene in the process of AI research in global health varies widely around the world, depending on the authorities assigned to them by domestic research governance policies. These observations frame the challenges outlined in our paper, highlighting the difficulties associated with making meaningful change in this field.
Despite these overarching challenges of the global health research context, there are clear strategies for progress in this domain. Firstly, AI innovation is rapidly evolving, which means approaches to the governance of AI for health are rapidly evolving too. Such rapid evolution presents an important opportunity for governance leaders to clarify their vision and influence over AI innovation in global health research, boosting the expertise, structure, and functionality required to meet the demands of research involving AI. Secondly, the research ethics community has strong international ties, linked to a global scholarly community that is committed to sharing insights and best practices around the world. This global community can be leveraged to coordinate efforts to produce advances in the capabilities and authorities of governance leaders to meaningfully govern AI research for global health given the challenges summarized in our paper.
Limitations
Our paper includes two specific limitations that we address explicitly here. First, it is still early in the lifetime of the development of applications of AI for use in global health, and as such, the global community has had limited opportunity to learn from experience. For example, there were many fewer case studies, which detail experiences with the actual implementation of an AI technology, submitted to GFBR 2022 for consideration than was expected. In contrast, there were many more governance reports submitted, which detail the processes and outputs of governance processes that anticipate the development and dissemination of AI technologies. This observation represents both a success and a challenge. It is a success that so many groups are engaging in anticipatory governance of AI technologies, exploring evidence of their likely impacts and governing technologies in novel and well-designed ways. It is a challenge that there is little experience to build upon of the successful implementation of AI technologies in ways that have limited harms while promoting innovation. Further experience with AI technologies in global health will contribute to revising and enhancing the challenges and recommendations we have outlined in our paper.
Second, global trends in the politics and economics of AI technologies are evolving rapidly. Although some nations are advancing detailed policy approaches to regulating AI more generally, including for uses in health care and public health, the impacts of corporate investments in AI and political responses related to governance remain to be seen. The excitement around large language models (LLMs) and large multimodal models (LMMs) has drawn deeper attention to the challenges of regulating AI in any general sense, opening dialogue about health sector-specific regulations. The direction of this global dialogue, strongly linked to high-profile corporate actors and multi-national governance institutions, will strongly influence the development of boundaries around what is possible for the ethical governance of AI for global health. We have written this paper at a point when these developments are proceeding rapidly, and as such, we acknowledge that our recommendations will need updating as the broader field evolves.
Ultimately, coordination and collaboration between many stakeholders in the research ethics ecosystem will be necessary to strengthen the ethical governance of AI in global health research. The 2022 GFBR illustrated several innovations in ethical governance of AI for global health research, as well as several areas in need of urgent attention internationally. This summary is intended to inform international and domestic efforts to strengthen research ethics and support the evolution of governance leadership to meet the demands of AI in global health research.
Data availability
All data and materials analyzed to produce this paper are available on the GFBR website: https://www.gfbr.global/past-meetings/16th-forum-cape-town-south-africa-29-30-november-2022/ .
Clark P, Kim J, Aphinyanaphongs Y, Marketing, Food US. Drug Administration Clearance of Artificial Intelligence and Machine Learning Enabled Software in and as Medical devices: a systematic review. JAMA Netw Open. 2023;6(7):e2321792–2321792.
Article Google Scholar
Potnis KC, Ross JS, Aneja S, Gross CP, Richman IB. Artificial intelligence in breast cancer screening: evaluation of FDA device regulation and future recommendations. JAMA Intern Med. 2022;182(12):1306–12.
Siala H, Wang Y. SHIFTing artificial intelligence to be responsible in healthcare: a systematic review. Soc Sci Med. 2022;296:114782.
Yang X, Chen A, PourNejatian N, Shin HC, Smith KE, Parisien C, et al. A large language model for electronic health records. NPJ Digit Med. 2022;5(1):194.
Meskó B, Topol EJ. The imperative for regulatory oversight of large language models (or generative AI) in healthcare. NPJ Digit Med. 2023;6(1):120.
Jobin A, Ienca M, Vayena E. The global landscape of AI ethics guidelines. Nat Mach Intell. 2019;1(9):389–99.
Minssen T, Vayena E, Cohen IG. The challenges for Regulating Medical Use of ChatGPT and other large Language models. JAMA. 2023.
Ho CWL, Malpani R. Scaling up the research ethics framework for healthcare machine learning as global health ethics and governance. Am J Bioeth. 2022;22(5):36–8.
Yeung K. Recommendation of the council on artificial intelligence (OECD). Int Leg Mater. 2020;59(1):27–34.
Maddox TM, Rumsfeld JS, Payne PR. Questions for artificial intelligence in health care. JAMA. 2019;321(1):31–2.
Dzau VJ, Balatbat CA, Ellaissi WF. Revisiting academic health sciences systems a decade later: discovery to health to population to society. Lancet. 2021;398(10318):2300–4.
Ferretti A, Ienca M, Sheehan M, Blasimme A, Dove ES, Farsides B, et al. Ethics review of big data research: what should stay and what should be reformed? BMC Med Ethics. 2021;22(1):1–13.
Rahimzadeh V, Serpico K, Gelinas L. Institutional review boards need new skills to review data sharing and management plans. Nat Med. 2023;1–3.
Kling S, Singh S, Burgess TL, Nair G. The role of an ethics advisory committee in data science research in sub-saharan Africa. South Afr J Sci. 2023;119(5–6):1–3.
Google Scholar
Cengiz N, Kabanda SM, Esterhuizen TM, Moodley K. Exploring perspectives of research ethics committee members on the governance of big data in sub-saharan Africa. South Afr J Sci. 2023;119(5–6):1–9.
Doerr M, Meeder S. Big health data research and group harm: the scope of IRB review. Ethics Hum Res. 2022;44(4):34–8.
Ballantyne A, Stewart C. Big data and public-private partnerships in healthcare and research: the application of an ethics framework for big data in health and research. Asian Bioeth Rev. 2019;11(3):315–26.
Samuel G, Chubb J, Derrick G. Boundaries between research ethics and ethical research use in artificial intelligence health research. J Empir Res Hum Res Ethics. 2021;16(3):325–37.
Murphy K, Di Ruggiero E, Upshur R, Willison DJ, Malhotra N, Cai JC, et al. Artificial intelligence for good health: a scoping review of the ethics literature. BMC Med Ethics. 2021;22(1):1–17.
Teixeira da Silva JA. Handling ethics dumping and neo-colonial research: from the laboratory to the academic literature. J Bioethical Inq. 2022;19(3):433–43.
Ferryman K. The dangers of data colonialism in precision public health. Glob Policy. 2021;12:90–2.
Couldry N, Mejias UA. Data colonialism: rethinking big data’s relation to the contemporary subject. Telev New Media. 2019;20(4):336–49.
Organization WH. Ethics and governance of artificial intelligence for health: WHO guidance. 2021.
Metcalf J, Moss E. Owning ethics: corporate logics, silicon valley, and the institutionalization of ethics. Soc Res Int Q. 2019;86(2):449–76.
Data Protection Act - OFFICE OF THE DATA PROTECTION COMMISSIONER KENYA [Internet]. 2021 [cited 2023 Sep 30]. https://www.odpc.go.ke/dpa-act/ .
Sharon T, Lucivero F. Introduction to the special theme: the expansion of the health data ecosystem–rethinking data ethics and governance. Big Data & Society. Volume 6. London, England: SAGE Publications Sage UK; 2019. p. 2053951719852969.
Reisman D, Schultz J, Crawford K, Whittaker M. Algorithmic impact assessments: a practical Framework for Public Agency. AI Now. 2018.
Morgan RK. Environmental impact assessment: the state of the art. Impact Assess Proj Apprais. 2012;30(1):5–14.
Samuel G, Richie C. Reimagining research ethics to include environmental sustainability: a principled approach, including a case study of data-driven health research. J Med Ethics. 2023;49(6):428–33.
Kwete X, Tang K, Chen L, Ren R, Chen Q, Wu Z, et al. Decolonizing global health: what should be the target of this movement and where does it lead us? Glob Health Res Policy. 2022;7(1):3.
Abimbola S, Asthana S, Montenegro C, Guinto RR, Jumbam DT, Louskieter L, et al. Addressing power asymmetries in global health: imperatives in the wake of the COVID-19 pandemic. PLoS Med. 2021;18(4):e1003604.
Benatar S. Politics, power, poverty and global health: systems and frames. Int J Health Policy Manag. 2016;5(10):599.
Download references
Acknowledgements
We would like to acknowledge the outstanding contributions of the attendees of GFBR 2022 in Cape Town, South Africa. This paper is authored by members of the GFBR 2022 Planning Committee. We would like to acknowledge additional members Tamra Lysaght, National University of Singapore, and Niresh Bhagwandin, South African Medical Research Council, for their input during the planning stages and as reviewers of the applications to attend the Forum.
This work was supported by Wellcome [222525/Z/21/Z], the US National Institutes of Health, the UK Medical Research Council (part of UK Research and Innovation), and the South African Medical Research Council through funding to the Global Forum on Bioethics in Research.
Author information
Authors and affiliations.
Department of Physical Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, Canada
Berman Institute of Bioethics, Johns Hopkins University, Baltimore, MD, USA
Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA
Department of Philosophy and Classics, University of Ghana, Legon-Accra, Ghana
Caesar A. Atuire
Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Mahidol Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
Phaik Yeong Cheah
Berkman Klein Center, Harvard University, Bogotá, Colombia
Armando Guio Español
Department of Radiology and Informatics, Emory University School of Medicine, Atlanta, GA, USA
Judy Wawira Gichoya
Health Ethics & Governance Unit, Research for Health Department, Science Division, World Health Organization, Geneva, Switzerland
Adrienne Hunt & Katherine Littler
African Center of Excellence in Bioinformatics and Data Intensive Science, Infectious Diseases Institute, Makerere University, Kampala, Uganda
Daudi Jjingo
ISI Foundation, Turin, Italy
Daniela Paolotti
Department of Health Sciences and Technology, ETH Zurich, Zürich, Switzerland
Effy Vayena
Joint Centre for Bioethics, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
You can also search for this author in PubMed Google Scholar
Contributions
JS led the writing, contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. JA contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. CA contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. PYC contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. AE contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. JWG contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. AH contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. DJ contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. KL contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. DP contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. EV contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper.
Corresponding author
Correspondence to James Shaw .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shaw, J., Ali, J., Atuire, C.A. et al. Research ethics and artificial intelligence for global health: perspectives from the global forum on bioethics in research. BMC Med Ethics 25 , 46 (2024). https://doi.org/10.1186/s12910-024-01044-w
Download citation
Received : 31 October 2023
Accepted : 01 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12910-024-01044-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Machine learning
- Research ethics
- Global health
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]
- Log In Username Enter your ACP Online username. Password Enter the password that accompanies your username. Remember me Forget your username or password ?
- Privacy Policy
- Career Connection
- Member Forums
© Copyright 2024 American College of Physicians, Inc. All Rights Reserved. 190 North Independence Mall West, Philadelphia, PA 19106-1572 800-ACP-1915 (800-227-1915) or 215-351-2600
If you are unable to login, please try clearing your cookies . We apologize for the inconvenience.
Medical Ethics Issues: Position Papers & Resources
In addition to the ACP Ethics Manual, ACP publishes ethics position papers on a broad range of health care ethics issues including clinical ethics, professionalism, the delivery of health care, teaching, medical research, human rights and other topics. ACP ethics policy is approved by the Board of Regents and serves as the basis for the development of ACP ethics education and practice resources and legislative, regulatory and policy implementation activities.
Current ACP Ethics Policies and Resources
New determination of death and organ transplantation, position papers.
- Standards and Ethics Issues in the Determination of Death: A Position Paper From the American College of Physicians (September 4, 2023)
- Ethics, Determination of Death, and Organ Transplantation in Normothermic Regional Perfusion (NRP) with Controlled Donation after Circulatory Determination of Death (cDCD): American College of Physicians Statement of Concern (April 17, 2021)
Comments and Letters
- ACP letter to the Uniform Law Commission Committee about updating the Uniform Determination of Death Act (UDDA) (June 7, 2023)
- Does Normothermic Regional Perfusion Violate the Ethical Principles Underlying Organ Procurement? Yes. (Chest. 2022;162(2):288-90)
- Rebuttal From Dr. DeCamp et al. (Chest. 2022;162(2):292-3)
NEW Disability
- ACP Letter Regarding Discrimination on Basis of Disability in Health and Human Service Programs Proposed Rule 2023 (November 13, 2023)
NEW Electronic and Online Professionalism
Ethics manual, electronic patient-physician communication, electronic health records, telemedicine, and online professionalism.
- Initiating and Discontinuing the Patient–Physician Relationship
- The Medical Record
- Boundaries and Privacy
Case Studies
- Lab Results Reporting, Ethics, and the 21st Century Cures Act Rule on Information Blocking CME/MOC
Ethics, Electronic Health Record Integrity and the Patient-Physician Relationship CME/MOC (ACP Ethics Case Studies Series. CME and MOC by Medscape. 2021)
Ethics, Professionalism, and the Physician Social Media Influencer CME/MOC (ACP Ethics Case Studies Series. CME and MOC by Medscape. 2020)
”Doctor, Can’t You Just Phone a Prescription In?” and Other Ethical Challenges of Telemedicine Encounters CME/MOC (ACP Ethics Case Studies Series. MOC and CME by Medscape. 2019)
Maintaining Medical Professionalism Online: Posting of Patient Information CME (ACP Ethics Case Studies Series. CME by Medscape. 2018)
Addressing a Colleague's Sexually Explicit Facebook Post CME (ACP Ethics Case Studies Series. CME by Medscape. 2017)
Copied and Pasted and Misdiagnosed (or Cloned Notes and Blind Alleys) CME (ACP Ethics Case Studies Series. CME by Medscape. 2015)
American College of Physicians Ethical Guidance for Electronic Patient-Physician Communication: Aligning Expectations (J Gen Intern Med. published online 22 June 2020)
Ethical Implications of the Electronic Health Record: In the Service of the Patient (J Gen Intern Med. 2017;32:935-9)
Policy Recommendations to Guide the Use of Telemedicine in Primary Care Settings (Ann Intern Med. 2015;163:787-9)
Online Medical Professionalism: Patient and Public Relationships (Ann Intern Med. 2013;158:620-7)
NEW End-of-Life Care
- Care of Patients Near the End of Life
- Show Codes, Slow Codes, Full Codes, or No Codes: What Is a Doctor to Do? CME/MOC (ACP Ethic Case Studies Series, MOC and CME by Medsape. 2023)
2011 Letter and 2009 letter to Congressman Blumenauer regarding ACP’s support for legislation to pay for voluntary end-of-life care consultations (see H.R. 1898, the Life Sustaining Treatment Preferences Act of 2009).
- Ethics, Determination of Death, and Organ Transplantation in Normothermic Regional Perfusion (NRP) with Controlled Donation after Circulatory Determination of Death (cDCD): American College of Physicians Statement of Concern
End-of-Life (PEACE) Brochures (ACP. 2014) The PEACE brochures were developed by the Patient Education Work Group, which was convened in conjunction with the Consensus Panel project. Order copies of printed brochures
- Improving Your End-of-Life Care Practice
- Living with a Serious Illness: Talking with Your Doctor When the Future is Uncertain
- When You Have Pain at the End of Life
- Making Medical Decisions for a Loved One at the End of Life
ACP-ASIM End-of-Life Care Consensus Panel Papers (1999-2001) ACP convened this Greenwall Foundation supported consensus panel to develop ethical, policy, and clinical recommendations for physicians and other clinicians on end-of-life decisions.
Physician's Guide to End-of-Life Care Edited by Lois Snyder, JD, and Timothy Quill, MD, FACP (ACP Books. 2001)
Advance Directive Forms for Your State Contact Caring Connections, a program of the National Hospice and Palliative Care Organization (NHPCO).
National Healthcare Decisions Day, April 16 Details and resources on NHDD and the importance of advance care planning.
- Expert Witnesses
To Be or Not to Be: Should I Serve as an Expert Witness? CME (ACP Ethics Case Studies Series. CME by Medscape. 2014)
Guidelines for the Physician Expert Witness (Ann Intern Med. 1990;113:789)
NEW Family Caregivers
Ethical Guidance on Family Caregiving, Support, and Visitation in Hospitals and Residential Health Care Facilities, Including During Public Health Emergencies (J Gen Intern Med. 2023 Mar 20:1–8)
Family Caregivers, Patients and Physicians: Ethical Guidance to Optimize Relationships (J Gen Intern Med. 2010;25:255-60)
Family Caregivers, Patients and Physicians: Ethical Guidance to Optimize Relationships (ACP. 2009) (This publication is a longer version of the position paper above.)
Information Resources for Physicians Supporting Family Caregivers (ACP. 2010) This appendix of resources was developed in conjunction with the ACP position paper to help physicians manage relationships with patients and caregivers.
When the Family Caregiver Is a Physician: Negotiating the Ethical Boundaries CME/MOC (ACP Ethics Case Studies Series. CME and MOC by Medscape. 2020)
Genetic Testing and Precision Medicine
- Precision Medicine, Genetic Testing, Privacy, and Confidentiality
ACP Comments on privacy protection and human genome sequencing (May 24, 2012) ACP provided comments to the Presidential Commission for the Study of Bioethical Issues regarding the ethical implications of evolving notions of privacy and access in relation to the integration of large-scale human genome sequencing into research and clinical care.
Position Papers and Statements
Ethical Considerations in Precision Medicine and Genetic Testing in Internal Medicine Practice Ann Intern Med.2022;175:1322-1323
Genetic Testing and Reuniting Families (July 10, 2018)
Global Health Clinical Experiences
- Cultural Humility and Volunteerism
Ethical Obligations Regarding Short-Term Global Health Clinical Experiences (Ann Intern Med. 2018;168:651-7)
NEW Health and Human Rights
"Health and human rights are interrelated. When human rights are promoted, health is promoted ... Physicians have important roles in promoting health and human rights and addressing social inequities." (Ethics Manual, seventh edition).
- Obligations of the Physician to Society
Health as a Human Right (Ann Intern Med. doi:10.7326/M23-1900)
ACP's Human Rights Page : ACP policy statements and letters of support, as well as documents related to College advocacy for the humane treatment of prisoners and detainees.
NEW Health Information Privacy, Protection, and Use
- Confidentiality
- Research Sections within the Research chapter include “Use of Human Biological Materials in Research” and “Internet and Social Media Research”.
Maintaining Medical Professionalism Online: Posting of Patient Information (ACP Ethics Case Studies Series. CME by Medscape. 2018)
Confidentiality and Privacy: Beyond HIPAA to Honey, Can We Talk? (ACP Ethics Case Studies Series. CME by Medscape. 2018)
Ethical Guidance for Physicians and Health Care Institutions on Grateful Patient Fundraising: A Position Paper From the American College of Physicians (Ann Intern Med.doi:10.7326/M23-1691)
Health Information Privacy, Protection, and Use in the Expanding Digital Health Ecosystem: A Position Paper of the American College of Physicians (Ann Intern Med.2021;174:994-998)
NEW Pandemics and Ethics -->
Health care system catastrophes.
- The Patient-Physician Relationship and Health Care System Catastrophes
- Medical Risk to Physician and Patient
When Resources Are Limited During a Public Health Catastrophe: Nondiscrimination and Ethical Allocation Guidance CME/MOC (ACP Ethics Case Studies Series. MOC and CME by Medscape. 2023)
Pandemic Treatment Resource Allocation Ethics and Nondiscrimination (ACP Ethics Case Studies Series. CME and MOC by Medscape. 2020)
Stewardship of Health Care Resources: Allocating Mechanical Ventilators During Pandemic Influenza (ACP Ethics Case Studies Series. 2017)
ACP supports ACIP recommendation for additional mRNA COVID-19 vaccine dose and WHO call for equitable global vaccine distribution (August 17, 2021)
ACP Statement on Global COVID-19 Vaccine Distribution and Allocation: On Being Ethical and Practical (June 8, 2021)
ACP's Policy Statement on the Ethical Allocation of Vaccines During Pandemics Including COVID-19 (November 23, 2020)
A Wake-up Call for Healthcare Emerging Ethical Lessons from Covid-19 (Modern Healthcare, June 16, 2020)
Non-Discrimination in the Stewardship of Healthcare Resources in Health System Catastrophes, including COVID-19 Pandemic (March 26, 2020)
Internists Say Harassment Based on Race or Ethnic Origin is Never Okay (March 31, 2020)
Universal Do-Not-Resuscitate Orders, Social Worth, and Life-Years: Opposing Discriminatory Approaches to the Allocation of Resources During the COVID-19 Pandemic and Other Health System Catastrophes (Ann Intern Med.2020;173:230-232)
NEW Patient–Physician Relationship
Patient-physician relationship.
- The Physician and the Patient
- Initiating and Discontinuing the Patient-Physician Relationship
- Third-Party Evaluations
- Providing Medical Care to One’s Self; Persons With Whom the Physician has a Preexisting Close Nonprofessional Relationship or a Reporting Relationship; and VIPs
- Sexual Contact between Physician and Patient
- Gifts from Patients
Confidentiality and privacy, disclosure of medical errors, and informed and surrogate decision making
- Informed Decision Making and Consent
- Making Decisions Near the End of Life
The Doctor Will See You Shortly. The Ethical Significance of Time for the Patient–Physician Relationship (J Gen Intern Med. 2005;20:1057-62)
Ethics and Time, Time Perception, and the Patient–Physician Relationship (ACP. March 2003) (This publication is a longer version of the position paper above.)
- Patient Prejudice? The Patient Said What?... and What Comes Next CME (ACP Ethics Case Studies Series. CME by Medscape. 2022)
Confidentiality and Privacy: Beyond HIPAA to Honey, Can We Talk? CME (ACP Ethics Case Studies Series. CME by Medscape. 2018)
Preventive Health Screening, Ethics, and the Cognitively Impaired Patient CME (ACP Ethics Case Studies Series. CME by Medscape. 2015)
The Difficult Patient: Should You End the Relationship? What Now? An Ethics Case Study CME (ACP Ethics Case Studies Series. CME by Medscape. 2014)
Must You Disclose Mistakes Made by Other Physicians? CME (ACP Observer. November 2003)
Physicians and Society
- Relation of the Physician to Government
- Strikes and Other Joint Actions by Physicians
Physician Work Stoppages and Political Demonstrations—Economic Self-Interest or Patient Advocacy? Where Is the Line? CME (ACP Ethics Case Studies Series. CME by Medscape. 2010)
- Physician-Assisted Suicide and Euthanasia
- Toolkit on Issues in Delivering Patient-Centered End-of-Life Care and Responding to a Request for Physician-Assisted Suicide (Member login)
Ethics and the Legalization of Physician-Assisted Suicide (Ann Intern Med. 2017;167:576-8)
Physician–Industry Relations
- Conflicts of Interest
- Sponsored Research
Physician Open Payments (Sunshine Rule) This ACP webpage provides guidance and related tools for physicians on the Physician Payment Sunshine Rule (also referred to as the National Physician Payment Transparency Program, or Open Payments). The Open Payments system, implemented by the Centers for Medicare and Medicaid Services (CMS) in 2015, provides a mechanism for the public reporting of physician and teaching hospital financial relationships with industry.
Physician–Industry Relations. Part 1: Individual Physicians (Ann Intern Med. 2002;136:396-402)
Physician–Industry Relations. Part 2: Organizational Issues (Ann Intern Med. 2002;136:403-6)
NEW Practice Models, the Business of Medicine and the Changing Practice Environment
- The Changing Practice Environment
- Financial Arrangements
Ethics, Professionalism, Physician Employment and Health Care Business Practices CME/MOC
Banning Harmful Health Behaviors as a Condition of Employment: Where There's Smoke There's Fired? CME (ACP Ethics Case Studies Series. CME by Medscape. 2018)
Wellness Programs and Patient Goals of Care CME (ACP Ethics Case Studies Series. CME by Medscape. 2017)
Obligations and Opportunities: The Role of Clinical Societies in the Ethics of Managed Care (J Am Geriatr Soc. 1998;46:378-80)
Ethical and Professionalism Implications of Physician Employment and Health Care Business Practices CME (Ann Intern Med. published online 15 March 2021)
Assessing the Patient Care Implications of “Concierge” and Other Direct Patient Contracting Practices (Ann Intern Med. 2015;163:949-52)
The Patient-Centered Medical Home: An Ethical Analysis of Principles and Practice (J Gen Intern Med. 2013;28:141-6)
Ethical Considerations for the Use of Patient Incentives to Promote Personal Responsibility for Health: West Virginia Medicaid and Beyond (ACP. 2010)
Pay-for-Performance Principles That Promote Patient-Centered Care: An Ethics Manifesto (Ann Intern Med. 2007;147:792-4)
Pay-for-Performance Principles that Ensure the Promotion of Patient Centered Care—An Ethics Manifesto (ACP. 2007) (This publication is a longer version of the position paper above.)
Medical Professionalism in the Changing Health Care Environment: Revitalizing Internal Medicine by Focusing on the Patient–Physician Relationship (ACP. 2005)
Ethics in Practice: Managed Care and the Changing Health Care Environment (Ann Intern Med. 2004;141:131-6)
Selling Products Out of the Office (Ann Intern Med. 1999;131:863-4)
Prescription Drug Abuse
Prescription Drug Abuse (Ann Intern Med. 2014;160:198-200)
NEW Professionalism
American College of Physicians Pledge (ACP. 1982 [updated; original 1924]) The ACP Pledge is taken by new Fellows at Convocation at each Internal Medicine annual meeting. The Pledge affirms the physician’s membership in an ethical and moral community dedicated to healing, comfort, and altruism.
Physician Charter on Professionalism
Medical Professionalism in the New Millennium: A Physician Charter (Ann Intern Med. 2002;136:243-6)
- Professionalism
Ethical and Professionalism Implications of Physician Employment and Health Care Business Practices (Ann Intern Med. published online 15 March 2021)
- ACP Professional Accountability Principles (ACP. March 2018)
Professional Attire and the Patient-Physician Relationship CME/MOC (ACP Ethics Case Studies Series. CME and MOC by Medscape. 2020)
Addressing a Colleague's Unprofessional Behavior During Sign-Out CME (ACP Ethics Case Studies Series. CME by Medscape. 2018)
Dealing with the "Disruptive" Physician Colleague CME (ACP Ethics Case Studies Series. CME by Medscape. 2009)
Professional Well-being and Ethics
- The Impaired Physician
Physician Suicide Prevention: The Ethics and Role of the Physician Colleague and the Healing Community CME/MOC
When an Aging Colleague Seems Impaired CME (ACP Ethics Case Studies Series. CME by Medscape. 2017)
Physician Suicide Prevention and the Ethics and Role of a Healing Community: An American College of Physicians Policy Paper (J Gen Intern Med. 2021 Sep;36(9):2829-2835)
Physician Impairment and Rehabilitation: Reintegration Into Medical Practice While Ensuring Patient Safety (Ann Intern Med. 2019;170(12):871-879.)
ACP’s Physician Well-being and Professional Satisfaction initiative aims to foster a culture of wellness, reduce administrative burdens on physicians, improve practice efficiency and enhance individual physician well-being. The project website includes tools and programs for individual members, their practices, and ACP Chapters.

Research Ethics and Human Subjects
Research Sections within the chapter include “Protection of Human Subjects,” “Use of Human Biological Materials in Research,” “Placebo Controls,” “Innovative Medical Therapies,” “Scientific Publication,” “Sponsored Research” and “Public Announcement of Research Discoveries.”
Responsible Conduct of Research (RCR) Project
Under a grant from the Association of American Medical Colleges and the DHHS Office of Research Integrity, ACP Ethics staff has implemented member education and support programs on the responsible conduct of office-based research. Workshops have been presented at ACP's annual meeting as well as at several ACP chapter meetings.
Research in the Physician's Office: Navigating the Ethical Minefield (Hastings Cent Rep. 2008)
Volunteering for a Research Study? Talk with Your Doctor About What You Should Know This patient education brochure provides information and guidance to patients who are considering volunteering for a research study. The brochures are designed to facilitate conversations between doctors and their patients. They are intended for distribution in doctors’ offices and come in packages of 50. Access the brochure order form .
Author! Author! Who Should Be Named in a Published Study? An Ethics Case Study CME (ACP Ethics Case Studies Series. CME by Medscape. 2014)
When are Industry-Sponsored Trials a Good Match for Community Doctors? CME (ACP-ASIM Observer. 2001)
Research Ethics Training Resources
- Revised Common Rule Educational Materials , Department of Health and Human Services
- The Research Clinic , Office of Research Integrity, Department of Health and Human Services
- Responsible Conduct of Research (RCR) , Research Ethics and Compliance Training, CITI Program
- Responsible Conduct of Research Training , Office of Intramural Research, National Institutes of Health
- HIPAA Training and Resources , Department of Health and Human Services
- Online Ethics Center for Engineering and Science , Center for Engineering Ethics and Society, National Academy of Engineering
- World Association of Medical Editors (WAME)
- Council of Science Editors (CSE)
- European Association of Science Editors (EASE)
ACP supports National Academies’ call for withdrawal of Notice of Proposed Rulemaking (NPRM) for ‘Common Rule’ and for appointing a new commission (Dec. 31, 2015) ACP issued a statement in support of the National Academies' call for withdrawal of the Common Rule NPRM and for appointing a new research ethics commission.
ACP Comments on Notice of Proposed Rule Making (NPRM) (Dec. 31, 2015) ACP submitted comments to the Office for Human Research Protections of the U.S. Department of Health and Human Services on the Notice of Proposed Rule Making, "Federal Policy for the Protection of Human Subjects," also known as the Common Rule. ACP also submitted an earlier round of comments on the proposed rule making on Oct. 25, 2011.
Stewardship of Health Care Resources
"Physicians have a responsibility to practice effective and efficient health care and to use health care resources responsibly in practicing high-value care. Parsimonious care that utilizes the most efficient means to effectively diagnose a condition and treat a patient puts the patient first but also respects the need to use resources wisely and to help ensure that resources are equitably available" (Ethics Manual, seventh edition).
Conflicting duties? The physician's primary duty, first and foremost, is to the individual patient. She or he must advocate for the patient—in a health care system that grows more and more complex by the year—based on the best interests of the patient. But the physician also should use health care resources responsibly and efficiently. Are these duties in conflict? The Ethics Manual and ethics case studies explore these issues and provide help in sorting them out.
Is it rationing? Parsimonious care is not rationing. The goal of medical parsimony is to provide the care necessary for the patient's good on the basis primarily of evidence-based medicine. Although this may have the welcome side effect of preserving resources, reducing resource use is not the intent. It is this difference in intent and action that helps provide a foundation for the ethical distinction between parsimonious medicine and rationing.
- Resource Allocation
ACP’s High Value Care Project aims to improve health, avoid harms, and eliminate wasteful practices. The project website offers learning resources for clinicians and medical educators, clinical guidelines, best practice advice, case studies and patient resources on a wide variety of related topics.
Patient Requests for Specific Care: 'Surely You Can Explain to My Insurer That I Need Boniva?' CME (ACP Ethics Case Studies Series. CME by Medscape. 2018)
Who Should Get What? Mammography and the Stewardship of Health Care Resources CME (ACP Ethics Case Studies Series. CME by Medscape. 2012)
The following ethics case studies were developed through an award from the ABIM Foundation's Putting the Charter into Practice project. Watch a video report of the ACP's work on this project presented by Dr. David Fleming, former President of the College.
Stewardship of Health Care Resources: Allocating Mechanical Ventilators During Pandemic Influenza CME (ACP Ethics Case Studies Series. CME by Medscape. 2017)
Stewardship of Health Care Resources: Responding to a Patient's Request for Antibiotics (ACP Ethics Case Studies Series. CME by Medscape. 2014)
Teaching, Training and the Hidden Curriculum
- Attending Physicians and Physicians-in-Training
Resident Duty Hours: To Hand Over or Gloss Over? CME (ACP Ethics Case Studies Series. CME by Medscape. 2017)
Hidden Curricula, Ethics, and Professionalism: Optimizing Clinical Learning Environments in Becoming and Being a Physician (Ann Intern Med. 2018;168:506-8)
CME/MOC activities based on this ACP position paper are available:
Annals offers two CME/MOC activities:
Ethics, Professionalism, and the Hidden Curriculum (Click on “CME/MOC” on the left sidebar.)
Annals On Call – Hidden Curriculum
In this Curbsiders Podcast , Sanjay Desai, MD, coauthor of ACP’s position paper and Internal Medicine program director at Johns Hopkins, reviews several cases that illustrate how institutional norms can shape the practice of medicine. Detailed summaries of the cases discussed are available here .
Archived Ethics Position Papers
Health Information Technology & Privacy (July 2011)
Cognitively Impaired Subjects (November 1989)
- Ethics Position Papers by Publication Date
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
- We're Hiring!
- Help Center
Medical Ethics
- Most Cited Papers
- Most Downloaded Papers
- Newest Papers
- Save to Library
- Last »
- Bioethics Follow Following
- Applied Ethics Follow Following
- Ethics Follow Following
- Medical Law Follow Following
- Medical Ethics & Law Follow Following
- Bioethics Reproductive Technology Follow Following
- Moral Philosophy Follow Following
- Research Ethics Follow Following
- Bioethics, Death, Life extension Follow Following
- Public Health Ethics Follow Following
Enter the email address you signed up with and we'll email you a reset link.
- Academia.edu Publishing
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

“The Doctor as a Humanist”: The Viewpoint of the Students
Conference Report and Reflection by Poposki Ognen (University Pompeu Fabra); Castillo Gualda Paula (University of Balearic Islands); Barbero Pablos Enrique (University Autonoma de Madrid); Pogosyan Mariam (Sechenov University); Yusupova Diana (Sechenov University); and Ahire Akash (Sechenov University)

The practice of Medicine as a profession has become very technical; doctors rely on fancy investigations, treatment algorithms and standardized guidelines in treating patients. In a lot of universities, medical students and residents are trained without appreciating the importance of art and the humanities in delivering good care to patients and their families. Factual knowledge is imposed on us, as students, from scientific evidence delivered by highly specialized professionals: those who know more and more about niche subjects.
As a result, when someone decides to become a doctor , it seems that scientific training is the sole priority, with most attention being given to the disease-treatment model. As medical students, we are taught very specific subjects, leaving little or no space or time for any cultural enrichment programs. And yet, Personal growth as a doctor and a human being cannot be achieved unless one is exposed to the whole range of human experience. Learning from art and artists can be one such means of gaining these enriching experiences. We can learn from historians, and from eminent painters, sculptors, and writers, as well as from great scientists. How do we achieve these ends? The following essay summarizes and reviews one attempt at providing answers. The 2nd “Doctor as a Humanist” Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment.
To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference. Culture is a complex phenomenon that includes knowledge, beliefs, artistic production, morals, customs and skills acquired by being part of a society, which can be transmitted consciously or unconsciously, by individuals to others and through different generations.
The humanities are academic disciplines that study the cultural aspects and frailties of being human, and use methods that are primarily analytical, critical, or speculative, which distinguish them from the approaches of the natural sciences. Humanism is the practice of making the human story central. Consequently, the studies of humanities, so invested in human stories, is one aspect of practicing humanism.
Technological and practical progress in medicine has been impressive in the past fifty years. Nevertheless, patients still suffer from chronic conditions such as heart failure, chronic lung disease, depression, and many others. These are conditions where technology cannot significantly change the outcomes or reverse the underlying condition. One of the ways to alleviate suffering is through compassion and empathy where the doctor is a professional who listens to, understands and comforts the patient, as well as engaging the patient as a fellow human being. We need arts and humanities as doctors’ tools to comfort and, perhaps, even to heal. We also need them to remind us that we are ‘merely human’ ourselves, and that we share our humanity with our patients, as equals.
Unquestionably, there are fundamental requirements that every physician must internalize; the conference goal was to explain that one such requirement is the humanistic view. Opera, poetry, philosophy, history, the study of dialectics, biographical readings, and even volunteering abroad can be means of engaging the world for positive change. Sometimes called “soft” skills, these are in fact necessary and valuable qualities to empower ourselves as persons, as well as doctors. The 2nd The Doctor as a Humanist Symposium placed the corner stone in a global project that aims to understand medicine as a multidisciplinary subject, and to establish the concept of humanistic medicine both as a science and an art where the patient and the doctor are human beings working together.

STUDENT PARTICIPATION
The event united experts in Medicine and the Humanities from all over the world. The speakers (doctors, nurses and students) were from Russia, the USA, the UK, Spain, Italy, Germany, Mexico and more. Each day’s program was both intense and diverse, and included plenary lectures and panel sessions. Medical students were highly involved in all parts of the conference, offering us a great chance to introduce our projects, share our opinions on various topics, and discuss our questions connected with the role of the humanities in medicine.We participated in roundtable discussions, which were chaired by experts from different countries. Even though this made us nervous, at the same time it was very important for us, as students, to be a part of it. We discussed the future of medical humanities from various perspectives, and above all our thoughts and ideas were listened to and commented on, on an equal basis with the world’s experts. For once, we could see that our views were being taken into consideration, and we hope that in the future this will be the norm and NOT the exception. We are the future of medicine, and our voices should be heard, too.
At the end of the first day there was a students’ session, where we gave our opinions on the relative importance of the medical humanities from a multicultural viewpoint, and on this particular roundtable there were students from Russia, Spain, Iran, Mexico, Italy, as well as a Nursing resident. One of the students during the session shared her view that “I would like to see medicine through the lens of humanism and empathy, and also implement all its principles in my professional life on a daily basis”. All participants agreed, and although we were representing different countries and cultures there was no disagreement about this. Even though we have not yet faced many of the obstacles of the world of medicine, we can see the role of compassion in clinical practice better perhaps than our seniors. We shared our points of view about this question and its relevance in the different countries. It was an incredible moment, as experts and professors demonstrated a great interest in our ideas.
The program was extremely diverse; however, the main idea that most speakers expressed was how to find, sustain and not lose humanist goals. Brandy Schillace gave an impressive presentation entitled “Medical Humanities today: a publisher’s perspective”, which studied the importance of writing and publishing not only clinical trials, but also papers from historians, literary scholars, sociologists, and patients with personal experiences. The nurses Pilar d’Agosto and Maria Arias made a presentation on the topic of the Nursing Perspective that is one of the main pillars of medical practice. Professor Jacek Mostwin (Johns Hopkins University) shared his thoughts on patients’ memoirs. An Italian student, Benedetta Ronchi presented the results of an interview on medical humanities posed to the participants and speakers during the symposium. The plurality of perspectives made this conference an enriching event and showed us how diverse ideas can help us become better doctors. More importantly, it reminded us of our common humanity.
A significant part of the symposium was dedicated to Medicine and Art. Prof Josep Baños and Irene Canbra Badii spoke about the portrayal of physicians in TV medical dramas during the last fifty years. The book “The role of the humanities in the teaching of medical students” was presented by these authors and then given to participants as gifts. Dr Ourania Varsou showed how Poetry can influence human senses through her own experience in communicating with patients. She believed that many of the opinions and knowledge that we have internalized should be unlearned in order to have a better understanding of the human mind. The stimulus of poetry makes this possible. Poetry allows us to find new ways to express ourselves, and thus increase our emotional intelligence and understanding of other people’s feelings.
One of the most impressive lectures was by Dr Joan.B Soriano, who spoke about “Doctors and Patients in Opera” and showed how the leading roles of physicians in opera have changed over the centuries. People used to consider the doctor as the antihero, but with time this view has transformed into a positive one that plays a huge role in history.
It is important to be professional in your medical career, but also to be passionate about the life surrounding you; for instance, Dr Soriano is also a professional baritone singer. For students, this Symposium was full of obvious and hidden messages, which gave us much lot of food for thought. As Edmund Pellegrino, the founding editor of the Journal of Medicine and Philosophy , said: “Medicine is the most humane of sciences, the most empiric of arts, and the most scientific of humanities.”

CHOOSING ONE WORD
To conclude our summary of the students’ viewpoint each of us chose One word to encapsulate our thoughts about the symposium.
The Doctor as a Humanist is a multicultural event where everyone can learn and contribute to this global necessity to put the heart and soul back into medicine. Of course, we are aware and delighted that other organizations are championing the cause of the Humanities in Medicine, and in some cases, such as https://www.dur.ac.uk/imh/ , they have been doing so for many years.
As medical students, we appreciate how we have been placed at the centre of the symposium, which we believe has made this new initiative rather special. We hope that students of Medicine and from other disciplines come and participate in future symposia.
If you want to learn more, and see how you can participate, please contact the International student representatives, Mariam ( [email protected] ) and David ( [email protected] ).
Acknowledgements
Assistance provided by Jonathan McFarland (c) and Joan B. Soriano (University Autonoma de Madrid) was greatly appreciated during the planning and the development of the article.
Analysis and discussion of research | Updates on the latest issues | Open debate
All BMJ blog posts are published under a CC-BY-NC licence
BMJ Journals
- Introduction
- Article Information
NA indicates not available.
Data Sharing Statement
- Errors in Introduction JAMA Network Open Correction January 5, 2024
- Navigating the Intersection of Physician Mental Health and Medical Licensing JAMA Network Open Invited Commentary September 12, 2023 John B. Herman, MD
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Douglas RN , Sharpe EE , Kraus M , Saddawi-Konefka D , Hanson AC , Pulos B. Mental Health Questions on State Medical License Applications and Evaluation of Updates. JAMA Netw Open. 2023;6(9):e2333360. doi:10.1001/jamanetworkopen.2023.33360
Manage citations:
© 2024
- Permissions
Mental Health Questions on State Medical License Applications and Evaluation of Updates
- 1 Department of Anesthesiology and Perioperative Medicine, Mayo Clinic, Rochester, Minnesota
- 2 Department of Anesthesiology and Perioperative Medicine, Mayo Clinic, Phoenix, Arizona
- 3 Department of Anesthesia, Critical Care, and Pain Medicine, Massachusetts General Hospital, Boston
- 4 Division of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, Minnesota
- Invited Commentary Navigating the Intersection of Physician Mental Health and Medical Licensing John B. Herman, MD JAMA Network Open
- Correction Errors in Introduction JAMA Network Open
Many physicians avoid mental health care, fearing it could lead to the loss of their medical license. 1 - 3 In 2014, the US Department of Justice found that to be compliant with the Americans with Disabilities Act (ADA) professional licensing boards must limit mental health questions to current diagnoses impairing the applicant’s ability to perform professional duties. 4 In 2018, the Federation of State Medical Boards (FSMB) released 4 recommendations for medical boards to be compliant with the ADA and promote physician wellness on medical license applications: (1) ask only if impaired, (2) ask only current, (3) allow for safe haven nonreporting, and (4) include supportive language normalizing physician wellness. 5 , 6
The main objective of this study is to evaluate consistency with FSMB recommendations for state or territory medical license renewal applications. Secondary objectives include assessing the consistency between initial and renewal applications and examining the progress made in following FSMB guidelines for initial licensing applications since 2020. To our knowledge, this is the first study assessing the FSMB recommendation consistency on renewal applications.
This cross-sectional study follows the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline. The Mayo Clinic institutional review board waived informed consent because data were publicly available.
Between March and December 2022, initial and renewal applications from 55 US state and territory allopathic medical licensing boards were collected and scored by 2 authors (R.D. and B.P.) using previously described methods. 6 Disagreements were resolved through group consensus. The number of applications meeting each recommendation was summarized. Differences between initial and renewal applications and 2020 and 2022 initial applications 6 were summarized with absolute differences. Because the analysis covers nearly the entire finite population, no formal hypothesis testing was warranted. Data were summarized using R version 4.1.2 (R Foundation for Statistical Computing) between February and April 2023.
Initial and renewal medical license applications were obtained from all 50 states, Washington DC, and 4 US territories. For renewal applications, only 3 states or territories (5%) met all 4 recommendations, 28 (51%) met 3 recommendations, 12 (22%) met 2 recommendations, 9 (16%) met 1 recommendation, and 3 (5%) met no recommendations ( Figure ).
In 2022, fewer renewal applications met the only if impaired criteria compared with initial applications (40 of 55 [73%] vs 47 of 55 [85%]), but renewal applications more often met criteria for safe haven nonreporting (33 of 55 [60%] vs 23 of 55 [42%]), and only current (49 of 55 [89%] vs 46 of 55 [84%]) compared with initial applications ( Figure and Table ).
Compared with 2020 initial applications, more 2022 initial applications met the criteria for only if impaired (47 of 55 [85%] vs 39 of 54 [72%]) and only current (46 of 55 [84%] vs 41 of 54 [76%]) recommendations. However, the 2022 initial applications met safe haven nonreporting (23 of 55 [42%] vs 25 of 54 [46%]) and supportive language criteria less frequently (7 of 55 [13%] vs 8 of 54 [15%]) ( Figure and Table ).
The findings of this cross-sectional study suggest that the consistency of renewal applications with FSMB guidelines is notably low, particularly for safe haven nonreporting and supportive language. Notably, the renewal application of only 3 states or territories met all recommendations, suggesting that substantial work is needed to fully support our health care workforce in an era marked by rising physician burnout and mental health issues.
There was also marked heterogeneity between initial and renewal applications within the same state. Notably, renewal applications fared far better in safe haven nonreporting. Addressing these within-state discrepancies offers a straightforward and meaningful opportunity to support physician mental health care.
Progress since 2020 has been mixed. Initial applications demonstrated an improvement in meeting the only if impaired and only current recommendations, which may suggest an emphasis on ADA compliance. It is concerning that consistency with safe haven nonreporting and supportive language has not improved because reducing stigma is critical to removing barriers to care access. A paradigm shift is needed, where boards see supporting physician mental health as crucial to safeguarding public health.
This study had limitations. One limitation was potential changes to applications within the review period. Future research should investigate the association of safe haven nonreporting and supportive language with physicians mental health and their awareness of treatment options.
Accepted for Publication: August 2, 2023.
Published: September 12, 2023. doi:10.1001/jamanetworkopen.2023.33360
Correction: This article was corrected on January 5, 2024, to fix an error in the introduction.
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Douglas RN et al. JAMA Network Open .
Corresponding Author: Bridget Pulos, MD, Department of Anesthesiology and Perioperative Medicine, Mayo Clinic Minnesota, 200 First St SW, Rochester, MN 55902 ( [email protected] ).
Author Contributions: Drs Douglas and Pulos had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Douglas, Sharpe, Kraus, Hanson, Pulos.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Douglas, Sharpe, Kraus, Pulos.
Critical review of the manuscript for important intellectual content: Douglas, Kraus, Saddawi-Konefka, Hanson, Pulos.
Statistical analysis: Douglas, Saddawi-Konefka, Hanson.
Obtained funding: Pulos.
Administrative, technical, or material support: Douglas, Kraus, Pulos.
Supervision: Sharpe, Kraus, Saddawi-Konefka, Pulos.
Conflict of Interest Disclosures: Dr Saddawi-Konefka reported being the president and cofounder of The Emotional PPE Project oustide the submitted work. No other disclosures were reported.
Data Sharing Statement: See the Supplement .
Additional Contributions: The authors acknowledge Becky J. Erickson (Mayo Clinic Rochester Department of Anesthesiology and Perioperative Medicine) for assistance gathering applications.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Center Staff
This Week at the Center
Research Projects
Winning with Character
Recommended Reading
Conferences
Online Store
Affiliate Organizations
CENTER FOR ETHICS* University of Idaho Center for ETHICS 500 Memorial Gym Moscow, ID 83844-3080 Phone: (208) 885-2103 Fax: (208) 885-2108 Email: [email protected]
The Center for ETHICS*
(ethical theory and honor in competition and sport), the challenge... to think beyond the norm,, the goal... to gain clear thinking,, the purpose... to become better people..

The Center for ETHICS* at the University of Idaho offers study, intervention, outreach, consultation, and leadership in developing and advancing the theory, knowledge and understanding of character education including moral and ethical reasoning, moral development, ethical leadership, and ethical application.
Competing With Honor: To Dope or Not To Dope This project was supported through funding of the World Anti-Doping Agency ( WADA )
Now you can Subscribe to the Center for ETHICS* Newsletters .
Character is the life of right conduct ~ Aristotle
Home | About Us | Center Staff | Conferences | Contact Us | Affiliated Organizations | Online Store | Recommended Reading | This Week at the Center | Winning with Character
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Latest science news, discoveries and analysis
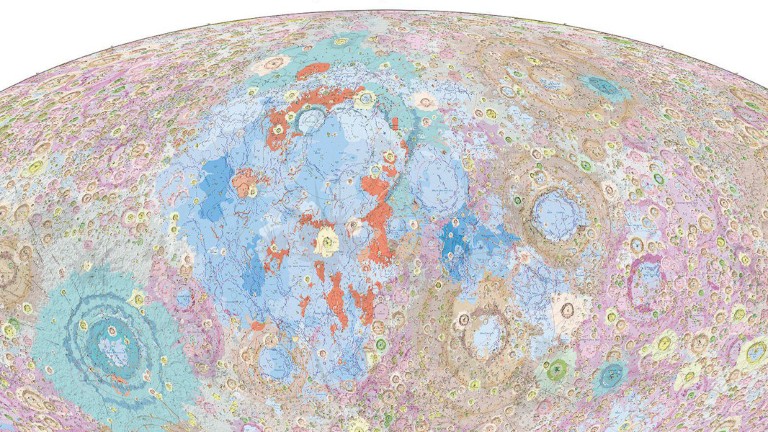
China's Moon atlas is the most detailed ever made
‘Shut up and calculate’: how Einstein lost the battle to explain quantum reality
Rat neurons repair mouse brains — and restore sense of smell

Mini-colon and brain 'organoids' shed light on cancer and other diseases
Scientists urged to collect royalties from the ‘magic money tree’, first glowing animals lit up the oceans half a billion years ago, plastic pollution: three numbers that support a crackdown, the maldives is racing to create new land. why are so many people concerned, ecologists: don’t lose touch with the joy of fieldwork chris mantegna.

Should the Maldives be creating new land?

Lethal AI weapons are here: how can we control them?

Algorithm ranks peer reviewers by reputation — but critics warn of bias

How gliding marsupials got their ‘wings’
Bird flu in us cows: is the milk supply safe, nato is boosting ai and climate research as scientific diplomacy remains on ice, hello puffins, goodbye belugas: changing arctic fjord hints at our climate future, nih pay raise for postdocs and phd students could have us ripple effect.
Retractions are part of science, but misconduct isn’t — lessons from a superconductivity lab

Any plan to make smoking obsolete is the right step

Citizenship privilege harms science
European ruling linking climate change to human rights could be a game changer — here’s how charlotte e. blattner, will ai accelerate or delay the race to net-zero emissions, current issue.

Surprise hybrid origins of a butterfly species
Stripped-envelope supernova light curves argue for central engine activity, optical clocks at sea, research analysis.

Ancient DNA traces family lines and political shifts in the Avar empire
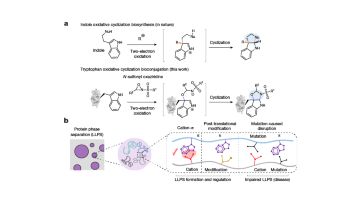
A chemical method for selective labelling of the key amino acid tryptophan

Robust optical clocks promise stable timing in a portable package
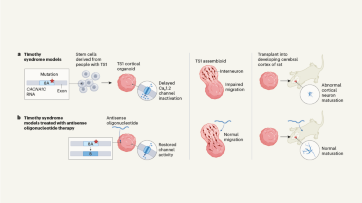
Targeting RNA opens therapeutic avenues for Timothy syndrome
Bioengineered ‘mini-colons’ shed light on cancer progression, galaxy found napping in the primordial universe, tumours form without genetic mutations, marsupial genomes reveal how a skin membrane for gliding evolved.

Breaking ice, and helicopter drops: winning photos of working scientists

Shrouded in secrecy: how science is harmed by the bullying and harassment rumour mill
How ground glass might save crops from drought on a caribbean island, londoners see what a scientist looks like up close in 50 photographs, books & culture.

How volcanoes shaped our planet — and why we need to be ready for the next big eruption
Dogwhistles, drilling and the roots of Western civilization: Books in brief

Cosmic rentals
Las borinqueñas remembers the forgotten puerto rican women who tested the first pill, dad always mows on summer saturday mornings, nature podcast.

Latest videos
Nature briefing.
An essential round-up of science news, opinion and analysis, delivered to your inbox every weekday.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
This paper is in the following e-collection/theme issue:
Published on 24.4.2024 in Vol 26 (2024)
The Costs of Anonymization: Case Study Using Clinical Data
Authors of this article:

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Indian Assoc Pediatr Surg
- v.25(6); Nov-Dec 2020
Ethics in Research and Publication
Pradyumna pan.
Ashish Hospital and Research Centre, Pediatric Surgery Unit, Jabalpur, Madhya Pradesh, India
Published articles in scientific journals are a key method for knowledge-sharing. Researchers can face the pressures to publish and this can sometimes lead to a breach of ethical values, whether consciously or unconsciously. The prevention of such practices is achieved by the application of strict ethical guidelines applicable to experiments involving human subjects or biological tissues. Editors too are faced with ethical problems, including how best to handle peer-review bias, and find reviewers with experience, probity, and professionalism. This article emphasizes that authors and their sponsoring organizations need to be informed of the importance of upholding the guidelines in research and ethical rules when disclosing scientific work.
I NTRODUCTION
Accurate reporting of results of research depends on the integrity of the authors, their application of and compliance with guidelines relating to the assurance of an ethical approach throughout and also on robust institutional research governance protocols ensuring that study design, conduct, and analysis of research and the publishing process all comply to an ethical framework. There is a growing concern that research misconduct over the past two decades has become more common.[ 1 ] It is challenging to determine whether this apparent increase is a true increase in the number of misconducts committed or detection has increased during this period.[ 2 ]
W HAT IS P UBLICATION E THICS ?
It is important that persons involved in the research must be compliant with the ethical framework in which they should function. The Committee on Publication Ethics (COPE) published guidelines on Good Publication Practice in 1999[ 3 ] and continues to update these regularly.[ 4 ]
Study design
The design of the study is a collection of methods and procedures used to gather and analyze the data on variables defined in a research. A poorly designed study can never be recovered, whereas an inadequately analyzed study can be re-analyzed to reach a meaningful conclusion.[ 5 ] The study design should be clearly expressed in a written protocol. In clinical studies, the number of participants to be included in the analysis should be sufficiently large to give a definitive result. Local ethical research committees should hold back approval until the deficiencies in the design of the study have been corrected. All investigators should agree on the final protocol, and their contributions should be clearly defined.
Ethical approval
For all studies involving individuals or medical records, approval from a duly appointed research ethics committee is necessary. The research protocol should adhere strictly to the international standards such as those of the Council for International Medical Science Organizations.[ 6 ]
When human tissues or body fluids have been collected for one project for which ethical authorization and consent has been obtained, these preserved specimens cannot be used again without further permission. It should be presumed that no author can publish research of humans or animals that do not follow the ethical standards of the country where the article is published.[ 2 ]
Data analysis
The data analysis methodology should be clearly stated in the protocol. The variations such as post hoc analysis or data omission should be agreed upon and reported in the paper by all investigators.[ 7 ] The capacity for manipulating data electronically now is enormous. Original images should always be retained and any alteration should be revealed.
The International Committee of Medical Editors (the Vancouver Group) has developed authorship guidelines that allow each writer to make a substantial contribution throughout the process.[ 8 ] In the past honorary authorship had been employed widely. However, the concept that the professor or department head should inevitably find his/her way to a paper is no longer acceptable. Each contributor should be able to mention clearly how they took part in the study. Each author must take public responsibility for the work published in the journal, and it is desirable to have one senior author, to serve as a guarantor. Participation in fundraising, data collection, or general supervision of the research is insufficient for authorship. Authorship acknowledgment should be based on substantial contributions to: (1) concept and design, (2) interpretation of data, (3) drafts and critical revisions of intellectual content, and (4) final approval of the version to be published.[ 2 ]
There is a possible conflict of interest when an investigator, writer, publisher, or reviewer has a financial, personal interest, or opinion that may impair their objectivity, or improperly influence their behavior. Financial ties are the most visible competing interests. As a result of personal relationships, academic rivalry, and intellectual zeal, competing interests can also exist. Competing interests are not unethical as long as they are revealed. They should be disclosed to the ethics committee and to the editor of the journal to which a article is submitted.
P EER R EVIEW
Peer review is the method used to evaluate the quality of articles submitted to a journal. COPE has developed ethical guidelines for peer reviewers.[ 9 ] The affiliation between the author, the editor, and the peer reviewer is a confidential collaboration. It is only with the editor's permission the manuscript should be passed on to a colleague or other individuals. A reviewer or editor should not use the information contained in the paper for their benefit.[ 2 ] Journals should have clearly defined and communicated policies on the type of peer review used, for example, single-blinded, double-blinded, open, or postpublication.[ 10 ] Peer reviewers can play a vital function in figuring out data fabrication, falsification, plagiarism, image manipulation, unethical research, biased reporting, authorship abuse, redundant or duplicate publication, and undeclared conflicts of interest.[ 11 ]
D UTIES OF E DITORS
Editors are the wardens of the scientific literature and are responsible for maintaining high research and publishing ethics standards. There may be competing interests among participants, and it is the responsibility of the editor to ensure that they do not affect the journal. They should not be hesitant to publish work that challenges previously published studies in their journal, and they should not reject studies with negative results.[ 2 ] Editors must act promptly if a published paper is found to have publication misconduct.[ 12 ]
R ESEARCH AND P UBLICATION M ISCONDUCT
Research misconduct represents a spectrum ranging from the errors of judgment (mistakes made in good faith) to deliberate fraud, usually categorized as fabrication, falsification, and plagiarism.[ 13 ]
Falsification is the changing or omission of research results (data) or manipulation of images or representations in a manner that distorts the data to support claims or hypotheses.[ 13 ]
Fabrication is the construction or addition of data, observations, or characterizations that never occurred in the gathering of data or running of experiments.[ 13 ]
Plagiarism is the use of another individual or group's published work or unpublished ideas, language, thoughts, ideas, or expressions and makes the representation of them as one's original work.[ 14 ] The advent of digital material and its ease of accessibility have accelerated the use of plagiarism.[ 15 ] In some instances, plagiarism is used as a tool to cover up language problems for those whom English is not their first language. Where language is a problem, the authors should always be encouraged to obtain help in preparing their manuscript and not resort to using other people's words. It is unacceptable to republish a paper with minor changes, without referring to the primary publication, and to present it to the readership as a new source.[ 16 ]
R EDUNDANT P UBLICATION
Redundant publication (sometimes referred to as duplicate or triplicate publication) is the term used when two or more papers that overlap in a significant way are published in different journals without cross-reference.[ 17 ] It is not uncommon for two or more papers involving the same or similar patient database to be published in sequence. The authors should disclose this to the editor and make a cross-reference to previous papers. It is permissible to publish a paper in another language as long as this is disclosed.
Motives for misconduct
The motives why investigators fabricate records are not understood. Improving understanding of why researchers commit misconduct and detrimental research practices (DRPs) is essential. A range of possible reasons are: (1) career and funding pressures, (2) institutional failures of oversight, (3) commercial conflicts of interest, (4) inadequate training, (5) erosion of standards of mentoring, and (6) part of a larger pattern of social deviance.[ 18 ]
Prevention of misconduct
The widespread nature of research and publication misconduct indicates that existing control measures are inadequate. Enhanced methods for detecting misconduct are required. Even if research policing were made more effective, the fundamental question of why certain individuals violate their duties as a scientist or medical researcher intentionally or unintentionally would not be addressed. Clear guidance on ethics should be emphasized during research training in all institutions actively involved in research.[ 19 ] Training is a crucial step in avoiding publication misconduct. All researchers should be presented with organizational guidance and publishing ethics when they join a new organization. Misconduct in the study may be more common when investigators are alone with an inadequate review of data by a project supervisor. Research integrity depends on excellent communication between contributors, with frequent discussion of project progress and openness to any difficulties in adhering to the research protocol. Everyone should agree with the changes to the protocol. Maintaining documents must be of the highest quality. The law requires data and photographic record of experimental results to be maintained for 15 years. The records of laboratory experiments should be held in the department where the study is carried out and should be available for review for at least 15 years.
Strategies to support research integrity
- Ensure policies governing academic research not only are in place but are followed
- Enforce expectations for process rigor
- Communicate expectations for accurate accounting of time spent on research activities
- Evaluate the grant accounting function
- Establish an office of research integrity.[ 20 ]
C ONCLUSION
Accurate and ethical reporting is crucial to the quality of scientific research that is published. Unethical practices such as falsification of data and plagiarism cause long-term damage to the dependability of published literature. Whilst such practices do still exist, these can be prevented by having robust institutional ethical processes in place, regular training, and editorial vigilance.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
R EFERENCES

IMAGES
VIDEO
COMMENTS
Our hope is that the Fundamentals of Medical Ethics series will suggest broad lessons to keep in mind as physicians, patients, research participants, families, and communities struggle with new ...
Bioethics and Clinical (Medical) Ethics. A number of deplorable abuses of human subjects in research, medical interventions without informed consent, experimentation in concentration camps in World War II, along with salutary advances in medicine and medical technology and societal changes, led to the rapid evolution of bioethics from one ...
Journal of Medical Ethics is a leading international journal that reflects the whole field of medical ethics. Validation period: 4/23/2024, 10:31:42 AM - 4/23/2024, 4:31:42 PM. Subscribe Login. ... promoting ethical reflection and conduct in scientific research and medical practice. Impact Factor: 4.2 ... Author information Submit a paper ...
BMC Medical Ethics is an open access journal publishing original peer-reviewed research articles in relation to the ethical aspects of biomedical research and clinical practice, including professional choices and conduct, medical technologies, healthcare systems and health policies. We are recruiting new, international Editorial Board Members.
To present the basic principles and standards of Ethics in medical research and publishing, as well as the need for continuing education in the principles and ethics in science and publication in biomedicine. ... Authors of research papers should state whether they had complete access to the study data that support the publication. Contributors ...
Ethics of medical research on human subjects must be clinically justified and scientifically sound. Informed consent is a mandatory component of any clinical research. Investigators are obligated to design research protocols that establish standards of scientific integrity, safeguard ethical and legislative issues of the human subjects, and ...
This paper describes the basic principles of Western research ethics - respect for persons, beneficence, and justice - and how the principles may be contextualized in different settings, by researchers of various backgrounds with different funding streams. Examples of lapses in ethical practice of research are used to highlight best practices.
It is a standpoint for deciding how to act in a given situation or analyze a complex problem. Medical ethics focuses on moral conduct and principles to apply toward patients, doctor-patient relationship, and communication in the practice of medicine. However, the span of medical ethics is wider and includes research ethics and publication ethics.
This paper reports on the findings of an international workshop organised by the UK-France+ Genomics and Ethics Network (UK-FR + GENE) in 2022. The focus of the workshop were the ethical and ...
The top 10 most-read medical ethics articles in 2021. Dec 29, 2021 . 3 MIN READ. By. Kevin B. O'Reilly , Senior News Editor. Print Page. Each month, the AMA Journal of Ethics® ( @JournalofEthics) gathers insights from physicians and other experts to explore issues in medical ethics that are highly relevant to doctors in practice and the future ...
The fundamentals of ethical research are steadfast, even for vaccine trials in a pandemic. Opinions from the AMA Code of Medical Ethics outline top-level concerns. Trial design and informed consent take on ethical significance when developing vaccines, even during the urgency of a pandemic such as COVID-19.
In recent decades, evidence-based medicine has become one of the foundations of clinical practice, making it necessary that healthcare practitioners develop keen critical appraisal skills for scientific papers. Worksheets to guide clinicians through this critical appraisal are often used in journal clubs, a key part of continuing medical education. A similar need is arising for health ...
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice. In this paper we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town ...
In addition to the ACP Ethics Manual, ACP publishes ethics position papers on a broad range of health care ethics issues including clinical ethics, professionalism, the delivery of health care, teaching, medical research, human rights and other topics. ACP ethics policy is approved by the Board of Regents and serves as the basis for the ...
For example, a "medical ethicist" is someone who studies ethical standards in medicine. One may also define ethics as a method ... She has just published a paper on the relationship between pesticide exposure and PD in a prestigious journal. ... education in research ethics should be able to help researchers grapple with the ethical dilemmas ...
Ethics of embryonic stem cell research according to Buddhist, Hindu, Catholic, and Islamic religions: perspective from Malaysia. Background: The use of embryos in embryonic stem cell research (ESCR) has elicited ethical controversies as it entails the destruction of 5-day old human embryos to harvest stem cells.
To the authors' knowledge, this is the first rapid review to examine the use of the term 'ethical challenge (s)' in empirical healthcare research literature. Notably, only 12/72 (17%) of included studies published in the last 5 years contained a definition for 'ethical challenge (s)', despite this being the focus of the research being ...
The World Medical Association believes that medical ethics is identical in times of armed conflict to those in times of peace. In stating this the WMA recognizes that the tensions within the ... The ICRC has published a research paper (include reference) explaining the pressures that individuals caring for patients face. While the major ...
The 2nd "Doctor as a Humanist" Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment. To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference.
This paper is in the following e-collection/theme issue: Peer-to-Peer Support and Online Communities (557) Virtual Communities and Communities of Practice for Healthcare Providers (41) Physician and Health Services Rating by Consumers (124) Quality/Credibility of eHealth Information and Trust Issues (471) Health Care Quality and Health Services Research (221) Clinical Communication, Electronic ...
Abstract. Ethics, an essential dimension of human research, is considered both as discipline and practice. For clinical research, ethically justified criteria for the design, conduct, and review ...
Many physicians avoid mental health care, fearing it could lead to the loss of their medical license. 1-3 In 2014, the US Department of Justice found that to be compliant with the Americans with Disabilities Act (ADA) professional licensing boards must limit mental health questions to current diagnoses impairing the applicant's ability to perform professional duties. 4 In 2018, the ...
The Independent Interdisciplinary Ethics Committee on Ethical Review for Clinical Studies (hereinafter referred to as the ''Committee'') is the independent local research ethic committee. ... ethic committee. It was established in 2000 by Moscow State University of Medicine and Dentistry, Russian Academy of Medical Sciences, Society for ...
CENTER FOR ETHICS* University of Idaho Center for ETHICS 500 Memorial Gym Moscow, ID 83844-3080 Phone: (208) 885-2103 Fax: (208) 885-2108 Email: [email protected]
Find breaking science news and analysis from the world's leading research journal.
Ethics in medical research deals with the conflicts of interest across various levels. Guidelines have been proposed for standardized ethical practice throughout the globe. The four fundamental principles of ethics which are being underscored are autonomy, non-maleficence, beneficence, and justice. Some special ethical issues have particular ...
As the health care industry increasingly embraces large language models (LLMs), understanding the consequence of this integration becomes crucial for maximizing benefits while mitigating potential pitfalls. This paper explores the evolving relationship among clinician trust in LLMs, the transition of data sources from predominantly human-generated to artificial intelligence (AI)-generated ...
Background: Sharing data from clinical studies can accelerate scientific progress, improve transparency, and increase the potential for innovation and collaboration. However, privacy concerns remain a barrier to data sharing. Certain concerns, such as reidentification risk, can be addressed through the application of anonymization algorithms, whereby data are altered so that it is no longer ...
Centre for Digital Ethics (CEDE) Research Paper Series. Subscribe to this free journal for more curated articles on this topic FOLLOWERS. 653. PAPERS. 287. This Journal is curated by: Luciano Floridi at Yale University - Digital Ethics Center, Mariarosaria Taddeo at University of Oxford - Oxford Internet Institute. Feedback. Feedback to SSRN ...
Keywords: Ethics, guidelines, medical research, scientific misconduct. ... The variations such as post hoc analysis or data omission should be agreed upon and reported in the paper by all investigators. The capacity for manipulating data electronically now is enormous. Original images should always be retained and any alteration should be revealed.