Nursing Care for Transgender Patients: Tips and Resources

NurseJournal.org is committed to delivering content that is objective and actionable. To that end, we have built a network of industry professionals across higher education to review our content and ensure we are providing the most helpful information to our readers.
Drawing on their firsthand industry expertise, our Integrity Network members serve as an additional step in our editing process, helping us confirm our content is accurate and up to date. These contributors:
- Suggest changes to inaccurate or misleading information.
- Provide specific, corrective feedback.
- Identify critical information that writers may have missed.
Integrity Network members typically work full time in their industry profession and review content for NurseJournal.org as a side project. All Integrity Network members are paid members of the Red Ventures Education Integrity Network.
Explore our full list of Integrity Network members.

Are you ready to earn your online nursing degree?

One responsibility of healthcare providers involves creating a welcoming and nonjudgmental environment for every patient. Still, transgender individuals — people whose gender is different than the one assigned at birth — and gender nonconforming (GNC) patients continue to face challenges and prejudice in healthcare settings.
Nurses have an especially important role in providing an affirming space for transgender people. Many patients confide in nurses, sometimes finding them more trustworthy than physicians. In fact, nursing has consistently ranked as the most honest and ethical profession for the past two decades, according to Gallup polls .
More and more nurses wish to provide a comfortable environment for all their patients, including those who are transgender or GNC. However, this can feel challenging for nurses without a great deal of experience caring for this community, especially because they have not had adequate or appropriate educational resources.
This guide aims to help nurses better understand the transgender and GNC community, the hurdles they might face in healthcare, and helpful steps on working with transgender and GNC patients.
Healthcare Barriers to Transgender Patients
For many transgender patients, healthcare can be an intimidating — and often inaccessible — environment.
Transgender people are more likely to be uninsured than cisgender patients, those who are gendered correctly at birth or those who are not transgender. This can restrict their access to healthcare with high costs. According to an analysis by the Kaiser Family Fund , 19% of transgender adults reported not possessing health insurance compared to 12% of the cisgender population. Another 19% reported encountering cost-related barriers to receiving care. Only 13% of cisgender adults encountered these barriers.
For instance, without the sensitivity and consideration needed to communicate concerns relating to transgender patients, some healthcare providers may accidentally out transgender patients to their families and friends, risking the patient’s health and safety.
In addition to emotional and financial barriers, transgender people also face outdated polices and processes modeled for heterosexual and cisgender patients.
According to Desiree Díaz, Ph.D., associate professor at University of Central Florida’s College of Nursing , these distressing experiences can lead to transgender people avoiding necessary appointments and procedures.
“Transgender patients often delay care due to past experiences when attempting to access care,” Díaz says.
Healthcare Biases and Discrimination
Often healthcare providers do not intentionally or maliciously misgender patients or make them feel alienated. The problem roots from broader systemic issues, meaning, among many things, that some nurses and other healthcare professionals have been socialized or taught to believe that being transgender or GNC is wrong so they might not want to treat or support trans and GNC patients.
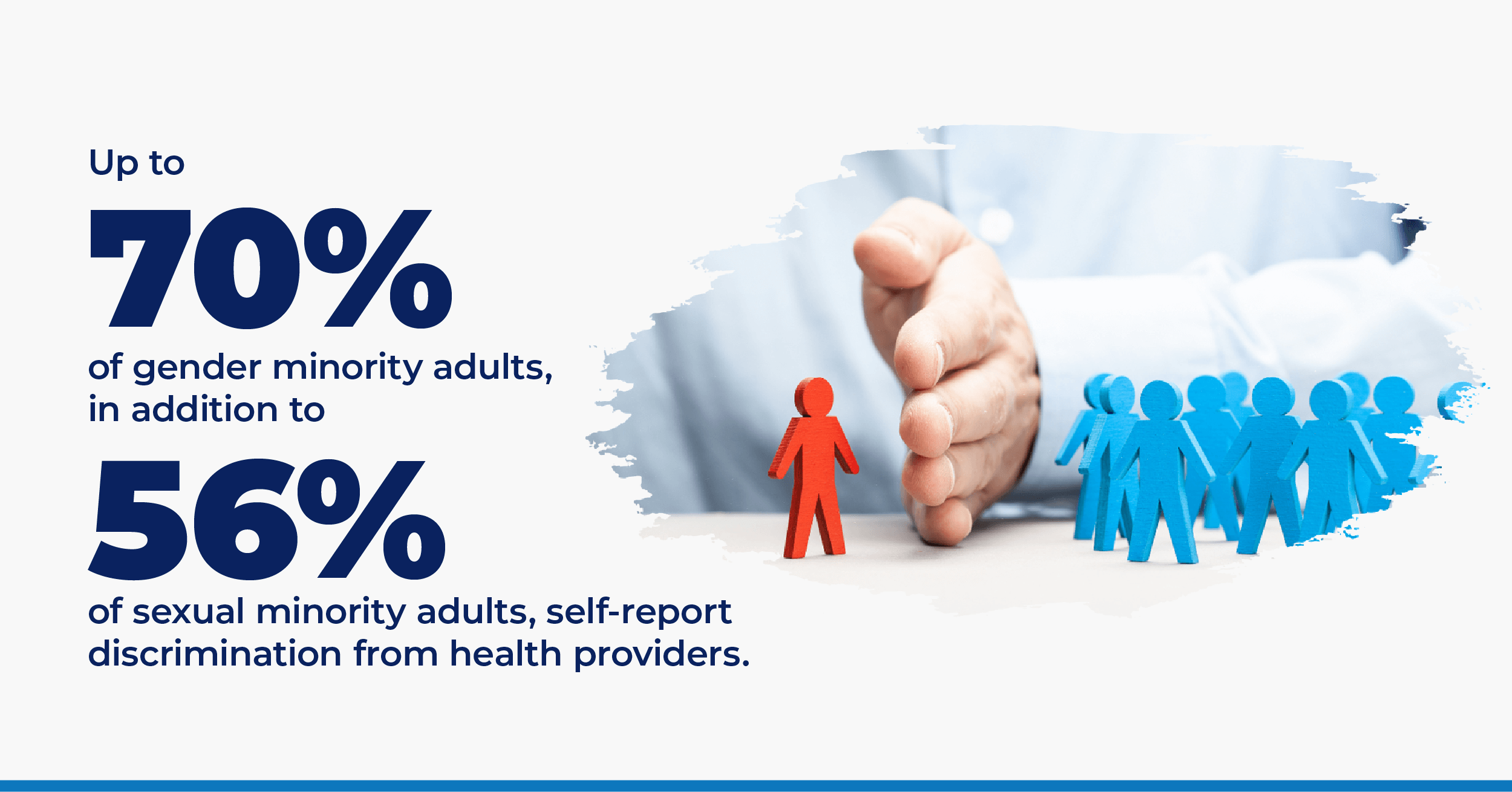
Another systemic issue is that the healthcare system can disproportionately harm trans and GNC patients due to biases, stigmatization, and outdated policies. Even those who do wish to provide competent care do not necessarily have the training to adequately care for transgender patients.
Additionally, broad-based hostility and discrimination can limit the number of transgender and GNC people who pursue a nursing career which would bring lived experience to the field. Systemic issues have also resulted in a lack of research on transgender patients in healthcare.
— “I believe that there are many nurses and providers who want to do the right thing and provide affirming care, but don’t have the support of their organization for training,” says Kristie Overstreet, Ph.D., who works as a clinical sexologist, psychotherapist, and LGBTQIA+ healthcare expert.
Greater education and training for working with transgender and GNC people is one solution to this problem. Another is acknowledging biases, then taking action to eliminate or lessen the potential harm those biases can cause.
For example, healthcare providers may make assumptions because of internal biases that can lead to mistakes about medical transitioning or taking sex and gender as the same. Some transgender people face more direct discrimination, such as providers refusing to treat them or calling them by a legal name they do not use because of the providers’ personal beliefs.
Considerations for Creating a More Supportive Environment
Once nurses understand their own biases and learn more about transgender and GNC individuals, they can take steps to provide affirming healthcare spaces for people in these communities. Remember: Each person and their individual situation is unique, so consider these considerations as general guidelines.
“In general, it is not acceptable to ask about people’s genitals or gender-affirming surgeries or hormone therapy or other details about medical or nonmedical transition, or lack of transition,” explains Dasuqi.
If these details are directly relevant to a patient’s care, ask in a careful and sensitive manner. Do not share this information with other healthcare staff unless it is medically necessary.
“Healthcare staff should assume this information is very personal and should inform patients ahead of time when it will be necessary to share information about their body to other healthcare providers for the purpose of medical treatment,” Dasqui says.
Ask open-ended questions, but make sure you do so in a direct but sensitive way. You can ask about a person’s gender, but be mindful how you ask about their sex.
“More direct questions that are relevant are often more appropriate,” Dasuqi advises, “such as ‘can you tell me more about what kind of genitalia you have and the symptoms you are experiencing there.'”
If you are unsure about something regarding a person’s gender, seek clarification instead of making assumptions.
Make note of your patient’s pronouns.
Use the terms your patient uses when referring to themselves and their partner(s). Your patient may use he/him/his, she/her/hers, they/them/theirs — even if they present more stereotypically feminine or masculine. Others may use less common pronouns like ze/hir/hirs or ze/zir/zirs, so always ask before addressing them.
You can also make transgender and GNC patients feel more comfortable by introducing yourself with your own pronouns.
“Because most forms still require healthcare workers to fill out the sex of an individual, they should know that this question can be painful or triggering for transgender and gender nonconforming individuals to answer,” says Dasuqi, adding that nurses and healthcare workers should be ready to offer support and understanding in these situations.
Sometimes, a patient’s name and gender may not match what is listed on their insurance or medical records. Should you need to cross-check a patient’s identification information, never ask what their “real” or given name is. Instead, the LGBT National Health Education Center recommends asking the patient what the name on their insurance is and confirming their date of birth and address, then continuing to address them by the name they originally provided.
You can find a guide on how to do so here , and templates here from the National LGBT Health Education Center.
As Overstreet says, “A patient’s gender identity is one part of them, so be sure to care for them as a whole person and not inflate or narrow their identity.”
In other words, consider a patient’s transgender or GNC identity within their larger cultural, emotional, physical, and psychological being.
“Cultural congruence is important when caring for all people but specifically the LGBTQ+ population,” Díaz adds. “This means understanding how culture pertains to … respecting the intersection.”
If you hear your coworkers misgendering patients or making transphobic comments, do not be afraid to speak up. You can also be a patient advocate on issues like gender confirmation surgery and fertility treatments.
Key Terms and Concepts
Keep some key terms and concepts in mind when working with members of the LGBTQ+ community. The following list comes from Overstreet who has trained healthcare practitioners on best practices in LGBTQIA+ wellness and care. The list is not exhaustive, and terms may vary across communities and cultures. To learn about more terms, visit this resource from the Human Rights Campaign .
- Cisgender: Someone who is not transgender (‘cis’)
- Transgender: Someone who does not identify with their sex assigned at birth (‘trans’)
- Nonbinary: Someone who does not identify as exclusively a man or woman, identifies as a mix of genders, or has no gender at all; does not conform to gender expectations
- Crossdresser: Someone who wears clothing typical for a different gender
- Drag king or queen: Someone who performs for entertainment purposes (may or may not be transgender)
- Agender or genderless: No gender identity or expression (sometimes interchangeable with gender-neutral)
- Genderqueer: Someone who does not identify within the gender binary
- Bigender: Having two gender identities or expressions, either simultaneously, at different times, or in different situations
- Intersex: An “umbrella” term for someone who is born with general sex characteristics (genitals, gonads, and chromosome patterns) that do not fit typical binary male or female bodies; they have a wide range of bodily variations, which do not always show up at birth
- Lesbian: Female of any gender identity who is emotionally, romantically, or sexually attracted to other females
- Gay: A person who is emotionally, romantically, or sexually attracted to members of the same gender identity or expression (for example, a gay male or gay person)
- Bisexual: A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity; capacity for attraction for all genders (note: do not get confused with ‘bi’ which reinforces the binary)
- Queer: A multifaceted word that is used in different ways and has different definitions, including sexual and gender identities other than straight and cisgender
- Asexual: Lack of sexual attraction or desire for other people; may have romantic attraction
- Pansexual: Someone who has the potential for emotional, romantic, or sexual attraction to people of any gender identity or expression; this is a more inclusive term (note: “bisexual” and “pansexual” are not interchangeable for all people)
- Gender Dysphoria: A distressed state arising from the conflict between a person’s gender identity and the sex the person has or was assigned at birth
For more information, see our guide to LGBTQIA2S+ Key Terms and Definitions for Nurses and Healthcare Providers .
Creating More Equitable and Gender-Affirming Care in Nursing
“Health equity is the most important concept. It is about providing safe care to all people regardless of sexual preference, orientation, or identity,” Díaz says.
Equity within the healthcare space requires buidling a safe, nonthreatening environment for all patients, including those who are transgender. The ultimate goal, according to Dasuqi, is creating a healthcare system in which transgender patients would not have to worry about being treated like special cases.
“It is about shifting the systems and social conditioning on wider levels to include the trans and GNC experience as part of what is normal, rather than always an exception,” Dasuqi concludes.
Helpful Resources for Nurses
National lgbtqia+ health education center, centers for disease control and prevention, national clinician consultation center, university of california, san francisco – transgender care, glma – health professionals advancing lgbtq equality, meet our contributors.

Kristie Overstreet, Ph.D.
Kristie Overstreet, Ph.D., is a clinical sexologist, psychotherapist, LGBTQIA+ healthcare expert, host of the “Fix Yourself First” podcast, and author of “Fix Yourself First: 25 Tips to Stop Ruining Your Relationships.” She is the creator of The Transgender Dignity Model , which provides LGBTQIA+ training for healthcare professionals.
She has been featured in Forbes, Huffington Post, Cosmopolitan, New York Magazine, Oprah Magazine, The Washington Post, on CNN, and various other media outlets.

Ash Dasuqi, CPM, RN
Ash Dasuqi, CPM, RN, is a trans genderqueer midwife, childbirth educator, critical care nurse, and parent. They created a trauma-informed, evidence-based childbirth preparation curriculum called the Embodied Birth Class that is open to all people while centering the experience of first-time pregnant and birthing queer/transgender individuals.

Desiree Díaz, Ph.D.
Desiree Díaz, Ph.D., is an associate professor of the University of Central Florida’s College of Nursing . One of the world’s first 22 certified advanced healthcare simulation educators, Díaz focuses her research on using the cutting-edge technology of simulation to improve the care for underserved patient populations in an effort to reduce healthcare disparities. Recognizing her contributions to nursing science and education, she has been inducted as a fellow of both the American Academy of Nursing and the Academy of Nursing Education.
Reviewed by:

Angelique Geehan
A queer Asian gender-binary nonconforming parent, Angelique Geehan founded Interchange , a consulting group that offers anti-oppression support through materials and process assessments, staff training, and community building. Geehan works to support and repair the connections people have to themselves and their families, communities, and cultural practices.
She organizes as a part of National Perinatal Association’s Health Equity Workgroup, the Health and Healing Justice Committee of the National Queer and Trans Asian and Pacific Islander Alliance, the Houston Community Accountability and Transformative Justice Collective, the Taking Care Study Group, QTPOC+ Family Circle, and Batalá Houston.
Geehan is a paid member of our Healthcare Review Partner Network. Learn more about our review partners .
Related LGBTQ+ Resources

LGBTQIA2S+ Key Terms & Definitions for Nurses & Healthcare Providers
Nurses can use this glossary of terms to help improve their ability to communicate with LGBTQIA2S+ patients and their families. Excellent nursing care requires practitioners to learn about their patients, so while knowing terms does not guarantee excellence, it can help build toward that.

LGBTQ+ Care: Training and Resources for Nurses
Expand your skill set and cultural competency working with LGBTQ+ patients with these free or low-cost continuing education and training courses.

Scholarships for LGBTQ+ College Students
Several public and private organizations offer scholarships for LGBTQ+ college students. Use this guide to help you research undergraduate and graduate funding opportunities for LGBTQ+ applicants.
Feature Image: FG Trade / E+ / Getty Images
Whether you’re looking to get your pre-licensure degree or taking the next step in your career, the education you need could be more affordable than you think. Find the right nursing program for you.
You might be interested in

HESI vs. TEAS Exam: The Differences Explained
Nursing schools use entrance exams to make admissions decisions. Learn about the differences between the HESI vs. TEAS exams.

10 Nursing Schools That Don’t Require TEAS or HESI Exam

For Chiefs’ RB Clyde Edwards-Helaire, Nursing Runs in the Family
Nursing Care For Transgender Patients
The transgender dilemma, create a supportive environment.
- Patient-Led Care
- Understand the Process
- Understand the Patient
- Community Support

Laverne Cox. Caitlyn Jenner. Amazon’s series Transparent .
Transgender issues are becoming more visible in pop culture, and in real life and healthcare, too.
The New York Times reported that the number of people who identify as transgender has doubled since 2011.
Those numbers are already showing up in healthcare facilities nationwide.
So don’t be surprised if a transgender male seeks an appointment for his annual pap smear.
As healthcare providers , a recent challenge is providing equal and unbiased care to transgender patients.
Historically, that hasn’t happened.
As a nurse, how will you handle your next patient’s mammogram if she was born a man?
Oncology Nurses are in high demand. Search open positions now.
Transgender patients often avoid care.
The fear of discrimination, lower quality of care, and lack of insurance access can be paralyzing.
Just entering your doors takes courage.
Ask yourself how you could reward that courage with an open and nonjudgmental attitude.
Act like you’ve been here before, even if you haven’t. Make the patient believe this is an everyday occurrence for you and nothing to be ashamed of.
We go into more depth in a recent article about caring for LGBTQ individuals. But first and foremost, remember that:
1. A transgender patient is a person with a health concern.
2. Our job as nursing professionals is to provide equitable care
Nurses who are firmly grounded in these two tenets are on their way to providing quality care for these patients.
Make the best career decision ever.
To a transgender patient, how they identify is more important than their sexual equipment.
Use the pronoun the person prefers. He or she knows which one s/he prefers before using one.
If all else fails, “you” and “your” work great.
On that subject, ask the patient the name s/he prefers. A patient’s legal name may be Michael, but she prefers Debra.
But verbal language is not the only kind of communication.
Does the healthcare space offer symbols of inclusivity? A rainbow flag or poster about World AIDS Day can go a long way.
Ensure that forms cater to transgender individuals. There should be a section for preferred name, sexual orientation, gender identity, and “partner” information.
Rework assessment questions with hetero-preferential word choices. Even LGBTQ members on your team can set the stage for open interaction.
Need more advice? Read 10 Tips For Caring for LGBTQ Patients.
Setting the Pace for Self-Disclosure: Let the Transgender Patient Lead
Transgender patients may be slow to reveal much about themselves. Negative experiences can do that to a person.
Cultivate patience. Over time, the individual will feel assured that the environment is safe for self-disclosure.
Gender Transitions Happen Slowly
Transgender identity is a process. Individuals may fall at different points along the transition spectrum.
A transgender man is a person assigned female at birth but who identifies as male. A transgender male patient may have taken hormones and/or had breast reduction surgery, but may or may not have female genitalia.
A transgender woman is a person assigned male at birth but who identifies as female. A transgender woman may have a female voice and breasts, and also the male genitalia that genetics gave her.
Don’t assume she will use a bedpan. Instead, ask “ Is there anything else you need for your physical comfort? ”
Put Yourself In His High Heels
Transgender individuals often avoid or postpone preventive screenings.
Many can’t endure the thought of a repeat of a past experience. And, some fear the looks when others assess that they are walking into the “wrong” type of clinic.
A transgender male may be stressed by having to sit in a mammography waiting room with women.
He has a right to be there, though. His residual female breast tissue warrants a mammogram.
Likewise, a transgender woman still has a prostate needing an annual check.
Nonetheless, quality care includes good information to help patients protect their health and life through early screening and detection.
Get familiar with recommended screenings for transgender men and women. Be ready with the correct information and protocol.
Don’t act surprised or flustered. This heightens tension and can shut down any chances you had at having an open discussion.
Employers are looking for qualified Registered Nurses like you.
See who’s hiring now. Get Started Today!
Tap Your Community For Help
Consult with your organization’s social work or patient navigation department. Familiarize yourself with local and national community resources.
But don’t just rely on organizations. Ask your nurse friends from other units or facilities about their most awkward situations and how they handled them.
Their triumphs and mistakes can make your next encounter with a transgender patient a smooth one.
Beyond that, stay abreast of health concerns and risks. Know the appropriate terminology, and any additions to the LGBTQ spectrum. People are not defined by acronyms.
Lastly, don’t be afraid to ask the tough, awkward questions in a non-judgmental fashion.
- Can you give information about your sexual preferences?
- With whom are a few of your supportive relationships?
- Are you engaged in high-risk behaviors?
- Anything else I should know that could impact your health?
Sensitivity is key when administering care to your transgender patient. But, don’t shy away from relevant information that can protect and prolong his or her health.
Your patient will thank you in the long run, and so will his or her loved ones.
Next Up: Guaranteed Moments of Happiness In Hospital Corridors
1. Judge rules doctors can refuse trans patients and women who have had abortions. Marie Solis, Mic.com. mic.com/articles/164234/judge-rules-doctors-can-refuse-trans-patients-and-women-who-have-had-abortions (accessed March 3, 2017).
2. Estimate of US Transgender Population Doubles to 1.4 Million Adults . Jan Hoffman, New York Times. www.nytimes.com/2016/07/01/health/transgender-population.html?_r=0 (accessed March 3, 2017).
3. About LGBT Health. Centers for Disease Control and Prevention, www.cdc.gov/lgbthealth/about.htm (accessed February 11, 2017)
4. Gay and Lesbian Medical Association. Guidelines for Care of Lesbian, Gay, Bisexual, and Transgender Patients. www.outforhealth.org/files/all/glma_guidelines_providers.pdf (accessed February 11, 2017)
5. Gay and lesbian Medical Association. Ten Things Transgender Persons Should Discuss with Their Healthcare Care Provider. www.glma.org/index.cfm?fuseaction=Page.viewPage&pageID=692 (accessed February 11, 2017).
6. Green J, et al. Lesbian, Gay, Bisexual, and Transgender Health Disparities, and President Obama’s Commitment for Change in Health Care . Race, Gender & Class: Vol. 17 No. 3-4, 2010 (272-287).
7. More Than Pink: LGBTQ Breast Health – LGBTQ Health Care Experiences in Western Washington . Susan G. Komen, Puget Sound: http://komenpugetsound.org/wp-content/uploads/2016/11/More-Than-Pink-LGBTQ-Breast-Health_web.pdf (accessed February 11, 2017)
8. The Joint Commission. Advancing Effective Communication, Cultural Competence, and Patient-and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community – A Field Guide. 2011. www.jointcommission.org/assets/1/18/LGBTFieldGuide.pdf (accessed February 11, 2017)
9. Women’sHealth.gov: www.womenshealth.gov/publications/our-publications/fact-sheet/lesbian-bisexual-health.html (accessed February 11, 2017).

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

Supporting the Transgender Community: Gender Affirming Care Resources
Home / Nursing Articles / Supporting the Transgender Community: Gender Affirming Care Resources
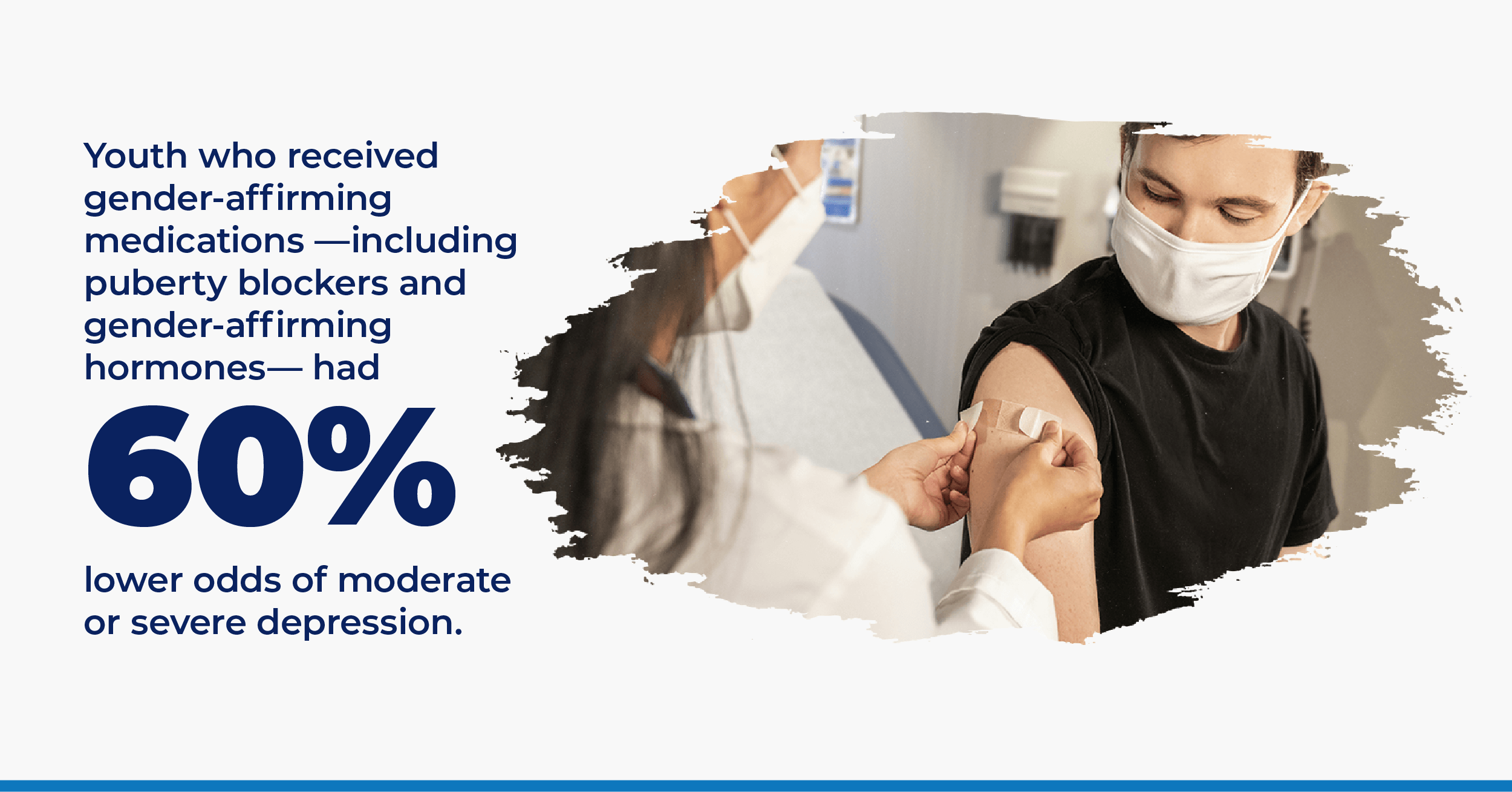
For transgender and nonbinary individuals, early and continued access to gender-affirming care is critical to improving confidence and allowing people to use their focus for transitioning socially while navigating the complex and sometimes unwelcoming healthcare system. Gender-affirming care can include social affirmation, puberty blockers, hormone therapy, and gender-affirming surgeries. This care can be life-saving , as it improves the mental health and overall well-being of gender-diverse children, adolescents, and adults.
Gender non-conforming students can find access to gender-affirming treatment at many colleges in the United States and abroad, and healthcare providers working in these schools receive training on gender-affirming, patient-centered care. For younger students, school nurses play an important role in supporting gender non-conforming students by directing them to resources and assuring them that their identities and feelings are valid and meaningful. For adults, healthcare provider education is crucial since many gender diverse individuals report discrimination within the healthcare system.
These resources are made available to anyone in the healthcare field, preparing as a student to work with diverse populations, including gender non-conforming youth, allies, educators, the transgender community, and more. You'll find research articles, helpful websites, links to organizations, and even legal and healthcare resources here. We hope you find these resources informative and helpful, no matter what part of your journey.
Gender-Affirming Care is Trauma-Informed Care
The National Child Trauma Stress Network released this article, which looks at how gender-affirming care in children can reduce future stress.
Supporting Safe and Healthy Schools for Lesbian, Gay, Bisexual, Transgender, and Queer Students
In this article, you’ll see the results of a major survey that talked with school professionals about the changes needed to support LGBTQ+ students .
Mental Health Outcomes in Transgender and Nonbinary Youths Receiving Gender-Affirming Care
Published in February 2022, this article looks at whether mental health support and gender-affirming care can reduce the suicide numbers among LGBTQ+ youths.
Gender-Affirming Care of Transgender and Gender-Diverse Youth: Current Concepts
Read this recent article to learn more about gender-affirming care, the field’s current concepts, and what needs to change.
Mental Health and Timing of Gender-Affirming Care
Available for free, this article focuses on whether the age at which an individual receives gender-affirming care relates to their mental health.
Factors Associated with Experiences of Gender-Affirming Health Care: A Systematic Review
This systematic review looks at youths’ experiences with gender-affirming care and what factors impacted them in getting it.
Barriers to Gender-Affirming Care for Transgender and Gender Nonconforming Individuals
Discover the barriers that keep transgender and non-binary people from getting the care and treatment they need in this article from 2017.
Experiences of Transgender and Non-Binary Youth Accessing Gender-Affirming Care: A Systematic Review and Meta-Ethnography
The authors reviewed current and past studies to examine the experiences associated with gender-affirming care among youth.
Understanding Community Member and Health Care Professional Perspectives on Gender-Affirming Care—A Qualitative Study
This article examines the barriers to seeking gender-affirming care and addresses some possible solutions.
"It's Kind of Hard to go to the Doctor's Office if You're Hated There." A Call for Gender-Affirming Care from Transgender and Gender Diverse Adolescents in the United States
This article examines barriers to health care and delves into how some patients feel their doctors hate them or dislike them.
Association Between Gender-Affirming Surgeries and Mental Health Outcomes
Released in 2021, this journal article focuses on the link between mental health and when patients received gender-affirming care.
Gender-Affirming Care for Transgender Patients
Learn more about the disparities between transgender patients and others in this study that came out in June 2022 and looked at modern treatments.
Psychosocial Characteristics of Transgender Youth Seeking Gender-Affirming Medical Treatment: Baseline Findings From the Trans Youth Care Study
This study looked at two groups of trans youths to see the impact of gender-affirming medical treatment on their development over time.
Helpful Websites
The Gender Unicorn
The Gender Unicorn takes a fun approach to gender and shows how it can fluctuate along with what each term means.
Learning Resources – Transgender Health
This is a great website to visit if you have questions about getting health care as a transgender person or you want to know about the available treatments.
National Center for Transgender Equality
This website offers a range of helpful resources for transgender youths and links to resources in different states.
The Trans Hub is a fantastic place for transgender students, and it offers social, legal, and medical help to you and your allies.
TransActual
Please read through the research studies done by this organization on its website, which also features stories and experiences of transgender people.
Trans Lifeline
This organization was launched to help people whom others look down on and provide them a lifeline in the modern world through free resources.
You can read through the stories on this website to learn from people who are trans or watch some of the videos that cover exciting and challenging topics.
Transgender Map
If you feel alone in the world, this website acts as your map with its resources for transgender youths who are in the closet or recently out.
TransFamilies
Designed for the loved ones of transgender youths, this site features a range of resources, such as frequently asked questions and local events.
National Black Trans Advocacy Coalition
Members of the black community who are also transgender will find lots of help on this site, such as resources for getting medical help and finding a job.
Trans Student Educational Resources
Also known as TSER, this organization has a website with press releases and offers services such as scholarships, policies, and workshops.
TransLatin Coalition
Designed for transgender and Latin people for people in the same community, this organization offers a training course for professionals and services in the LA area.
Transgender Aging Network
The Transgender Aging Network offers support for the loved ones of elderly people, including training programs and products to make their lives easier.
Movement Advancement Project
Known as MPA, this organization offers information about new and upcoming transgender equality projects and programs nationwide.
Global Action for Trans Equality
GATE is an organization that runs campaigns designed to improve equality for transgender youth as well as those who are intersex or non-binary.
TransAthlete
Turn to this website if you have questions about transgender athletes or if you want to learn about the policies used by schools and states.
Puberty and Transgender Youth
Amaze released this short video to discuss some of the changes that happen to their bodies during puberty among transgender youth.
El Camino College – TimelyCare Provides Gender-Affirming Care for Student
In this El Camino College video, you’ll see how TimelyCare supports students who need gender-affirming care when they go to college.
Best Practices for Supporting Transgender College Students | Building Bridges
Building Bridges spends nearly an hour reviewing what colleges can do to support transgender students and help them feel comfortable and confident.
Trans Health: What is Gender-Affirming Care?
York University uses this video to review the fundamentals of gender-affirming care, such as what it means and how to get it.
HRC Explains Gender-Affirming Care
In this video, the Human Rights Campaign details gender-affirming care to help viewers find answers to their questions.
Population Healthy S5 Ep02: Gender Affirming Care
From Michigan Public Health, this video offers a good explanation of gender-affirming care and the benefits it has for transgender youth today.
How Gender-Affirming Care Improves Mental Health
In just over a minute, an expert speaks about the positive impacts that gender-affirming care has on both transgender youth and their loved ones.
Education and Training for Gender-Affirming Health Care
Created by a medical organization, this video examines why education and training are essential for healthcare professionals and their patients.
What to Expect on Hormones
Planned Parenthood offers videos in both English and Spanish to ensure transgender youth understand what hormones will do to their bodies and the overall benefits.
Basics of Gender-Affirming Care for Health Professionals
Designed for medical professionals, this video helps medical professionals understand how to treat transgender patients and provide gender-affirming care.
Podcast: An Introduction to Transgender Health
This podcast serves as an introduction to transgender health issues and is suitable for members of the community as well as healthcare providers.
Exclusively Inclusive
Tune in every week to listen as professional and everyday people discuss what it means to be inclusive in today’s world.
Gender Affirming Care
The School of Public Health at the University of Michigan designed this podcast to inform listeners about the importance of gender-affirming care.
Podcast: Medical Care and Emotional Support for Transgender Youth
This episode from Kids Health Cast focuses on why transgender kids need both emotional support and medical care from their doctors and others.
The Gender GP Podcast
Two women use The Gender GP Podcast to discuss identity and other issues in the trans community with others.
Listen Now: Transgender Health Care Today
Listen Now is one of the best podcasts if you are interested in transgender health care and want to know more about its challenges.
The Trans Narrative
The Trans Narrative offers a safe space for transgender youths and others to talk and hear about some of the most significant issues in the community.
A Health Podyssey
Though not entirely about transgender issues, this podcast uses each episode to discuss the common problems affecting the healthcare industry.
Gender Stories
The author of a book about gender identity hosts this podcast, which gives listeners a safe space to share their gender experiences and stories.
PFLAG: Our Trans Loved Ones
Download a copy of this guide from PFLAG organizers to find some ways you can support a trans loved one after they come out.
PFLAG: Find Resources
PFLAG offers many resources for those in need that you’ll find here, including how to become or be a better ally and what you can do to help others.
Straight for Equality: Trans & Non-Binary
Straight for Equality, which was launched in 2007, now offers helpful online guides and resources on creating an inclusive workplace and other topics.
Be an Ally – Support Trans Equality
Join the Human Rights Campaign to watch online videos and discover tips on being a better ally to those in the trans community.
Guide to Being an Ally to Transgender and Nonbinary Young People
This resource is free and introduces how to treat and act around young people who identify as non-binary or transgender.
Tips for Allies of Transgender People
This guide offers many useful tips, such as when to use pronouns, what coming out means, and how to discuss gender topics.
Supporting the Transgender People in Your Life: A Guide to Being a Good Ally
This guide explains what it means to be an excellent transgender ally, including when to step up and how to change the world.
This PDF explains what transgender and non-binary mean, how to avoid common mistakes, and what to do when you make a mistake.
Straight for Equality: Becoming a Trans Ally
PFLAG offers this toolkit that includes information on what pronouns mean and when to use them, worksheets, and tips on becoming an ally.
Legal Resources
Clinicians in Court: A Guide to Subpoenas, Depositions, Testifying, and Everything Else You Need to Know
Students and professionals worldwide use this guide to learn the basics of case law and how they should act in the courtroom.
Supporting the Rights of Transgender Students and Their Families
In this piece, Heather Godsey addresses some issues facing transgender students today and discusses what they and their families can do.
Freedom for All Americans
Please read this letter from the organization of the same name to see some of the changes it helped fund and its plans for the future.
Transgender Rights
The ACLU looks at the rights of transgender people here and includes links to articles about big policy changes and legal challenges.
Your Rights
Work with GLAD to learn more about your legal rights and to get help finding a lawyer willing to fight for you and defend your rights.
Healthcare is Caring
Please read through the open letter to learn about the positive impacts of gender-affirming care and then sign it at the bottom to show your support.
Transgender Law Center
This organization offers a range of resources to help transgender individuals learn about their rights and find legal help.
Trans Agenda
The Trans Agenda believes that everyone deserves the right to legal help, which is why it funds cases and provides resources to those in need.
Transgender Resources
This website, available from the American Bar Association (ABA), offers information about the Legal Resistance Network and highlights resistance groups.
SRLP Legal Intake
See how you can get help from the SRLP on its official website and learn how to get involved and help others in need.
Transgender Legal Services Network
If you or someone you know is transgender and needs legal help, turn to this organization to find lawyers working across the country.
Transgender Legal Defense & Education Fund
This fund offers financial support for transgender people who need help paying for school or mounting a legal defense.
Lambda Legal
Lambda Legal defends non-binary and transgender people worldwide through financial support and free legal resources.
Health Education for Healthcare Providers and Educators
Transgender & Gender Diverse Inclusive Resources for Your Practice
If you work in the healthcare field, this page is perfect because it offers resources, such as how to examine and help transgender patients.
Pubertal Suppression for Youth with Gender Dysphoria/Gender Incongruence
This article is available as a PDF and looks at how hormone blockers and other treatments that prevent puberty can help transgender patients.
Standards of Care for the Health of Transgender and Gender Diverse People, Version 8
Version 8 is an updated version of this guide that helps doctors and other medical providers understand the standards of transgender care.
Transgender and Gender Diverse Services
Outside, In is a weekday clinic that helps transgender and non-binary patients receive health care they can’t get anywhere else.
Provider Directory
WPATH offers a free directory to search for gender-affirming care doctors based on your location or their name.
Creating Safer Spaces for LGBTQ Youth
Though this PDF toolkit is just a few pages, it covers many helpful topics for community organizations like creating a safe space.
Transgender Health in Medical Education
Created by the Bull World Health Organization, this piece goes over the changes it hopes to see by 2030 and what those changes will mean for the community.
National LGBTQIA+ Health Education Center
Discover free resources, educational programs, and much more on this website of an organization dedicated to helping LGBTQIA+ people with their health care needs.
The Power to Help or Harm: Student Perceptions of Transgender Health Education Using a Qualitative Approach
The authors of this piece look at how students think and feel about gender-affirming care based on whether they can access it.
Transgender Health Care: Improving Medical Students’ and Residents’ Training and Awareness
This article, released in 2018, examines the best practices and methods for raising residents’ and students’ awareness of transgender topics.
Patient-Centered Care for Transgender People: Recommended Practices for Health Care Settings
The CDC addresses how to put transgender patients first and how to understand their unique needs and the challenges in helping them.
Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People
Recently revised, this guide from UCSF looks at what doctors and other medical professionals should do when caring for non-binary and transgender patients.
Standards of Care for the Health of Transgender and Gender Diverse People
Get a free version of this book in a PDF form that helps you learn about and understand the standards of care for today’s patients.
Compulsory Transgender Health Education: The Time Has Come
Family Medicine published this article by a medical doctor to explain that complete care for transgender is necessary in the modern world.
Fair Use Statement: Please share our content for editorial or discussion purposes. Please link back to this page and give proper credit to RegisteredNursing.org.
Latest Articles & Guides
One of the keys to success as a registered nurse is embracing lifelong learning. Our articles and guides address hot topics and current events in nursing, from education to career mobility and beyond. No matter where you are on your nursing journey, there’s an article to help you build your knowledge base.
Browse our latest articles, curated specifically for modern nurses.
See All Articles


DAVID A. KLEIN, MD, MPH, SCOTT L. PARADISE, MD, AND EMILY T. GOODWIN, MD
Am Fam Physician. 2018;98(11):645-653
Related editorial: The Responsibility of Family Physicians to Our Transgender Patients
See related article from Annals of Family Medicine : Primary Care Clinicians' Willingness to Care for Transgender Patients
Patient information: A handout on this topic is available at https://familydoctor.org/lgbtq-mental-health-issues/
Author disclosure: No relevant financial affiliations.
Persons whose experienced or expressed gender differs from their sex assigned at birth may identify as transgender. Transgender and gender-diverse persons may have gender dysphoria (i.e., distress related to this incongruence) and often face substantial health care disparities and barriers to care. Gender identity is distinct from sexual orientation, sex development, and external gender expression. Each construct is culturally variable and exists along continuums rather than as dichotomous entities. Training staff in culturally sensitive terminology and transgender topics (e.g., use of chosen name and pronouns), creating welcoming and affirming clinical environments, and assessing personal biases may facilitate improved patient interactions. Depending on their comfort level and the availability of local subspecialty support, primary care clinicians may evaluate gender dysphoria and manage applicable hormone therapy, or monitor well-being and provide primary care and referrals. The history and physical examination should be sensitive and tailored to the reason for each visit. Clinicians should identify and treat mental health conditions but avoid the assumption that such conditions are related to gender identity. Preventive services should be based on the patient's current anatomy, medication use, and behaviors. Gender-affirming hormone therapy, which involves the use of an estrogen and antiandrogen, or of testosterone, is generally safe but partially irreversible. Specialized referral-based surgical services may improve outcomes in select patients. Adolescents experiencing puberty should be evaluated for reversible puberty suppression, which may make future affirmation easier and safer. Aspects of affirming care should not be delayed until gender stability is ensured. Multidisciplinary care may be optimal but is not universally available.
A = consistent, good-quality patient-oriented evidence; B = inconsistent or limited-quality patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, expert opinion, or case series. For information about the SORT evidence rating system, go to https://www.aafp.org/afpsort .
eTable A provides definitions of terms used in this article. Transgender describes persons whose experienced or expressed gender differs from their sex assigned at birth. 5 , 6 Gender dysphoria describes distress or problems functioning that may be experienced by transgender and gender-diverse persons; this term should be used to describe distressing symptoms rather than to pathologize. 7 , 8 Gender incongruence, a diagnosis in the International Classification of Diseases , 11th revision (ICD-11), 9 describes the discrepancy between a person's experienced gender and assigned sex but does not imply dysphoria or a preference for treatment. 10 The terms transgender and gender incongruence generally are not used to describe sexual orientation, sex development, or external gender expression, which are related but distinct phenomena. 5 , 7 , 8 , 11 It may be helpful to consider the above constructs as culturally variable, nonbinary, and existing along continuums rather than as dichotomous entities. 5 , 8 , 12 , 13 For clarity, the term transgender will be used as an umbrella term in this article to indicate gender incongruence, dysphoria, or diversity.
Optimal Clinical Environment
It is important for clinicians to establish a safe and welcoming environment for transgender patients, with an emphasis on establishing and maintaining rapport ( Table 1 ) . 5 , 6 , 8 , 11 , 12 , 14 – 21 Clinicians can tell patients, “Although I have limited experience caring for gender-diverse persons, it is important to me that you feel safe in my practice, and I will work hard to give you the best care possible.” 22 Waiting areas may be more welcoming if transgender-friendly materials and displayed graphics show diversity. 5 , 12 , 14 , 15 Intake forms can be updated to include gender-neutral language and to use the two-step method (two questions to identify chosen gender identity and sex assigned at birth) to help identify transgender patients. 5 , 16 , 23 Training clinicians and staff in culturally sensitive terminology and transgender topics, as well as cultural humility and assessment of personal internal biases, may facilitate improved patient interactions. 5 , 21 , 24 Clinicians may also consider advocating for transgender patients in their community. 12 , 14 , 15 , 21
MEDICAL HISTORY
When assessing transgender patients for gender-affirming care, the clinician should evaluate the magnitude, duration, and stability of any gender dysphoria or incongruence. 8 , 12 Treatment should be optimized for conditions that may confound the clinical picture (e.g., psychosis) or make gender-affirming care more difficult (e.g., uncontrolled depression, significant substance use). 6 , 11 , 17 The support and safety of the patient's social environment also warrants evaluation as it pertains to gender affirmation. 6 , 8 , 11 This is ideally accomplished with multidisciplinary care and may require several visits to fully evaluate. 5 , 6 , 8 , 17 Depending on their comfort level and the availability of local subspecialty support, primary care clinicians may elect to take an active role in the patient's gender-related care by evaluating gender dysphoria and managing hormone therapy, or an adjunctive role by monitoring well-being and providing primary care and referrals ( Figure 1 ) . 5 , 6 , 8 , 11 – 15 , 17 , 19 , 21 , 22
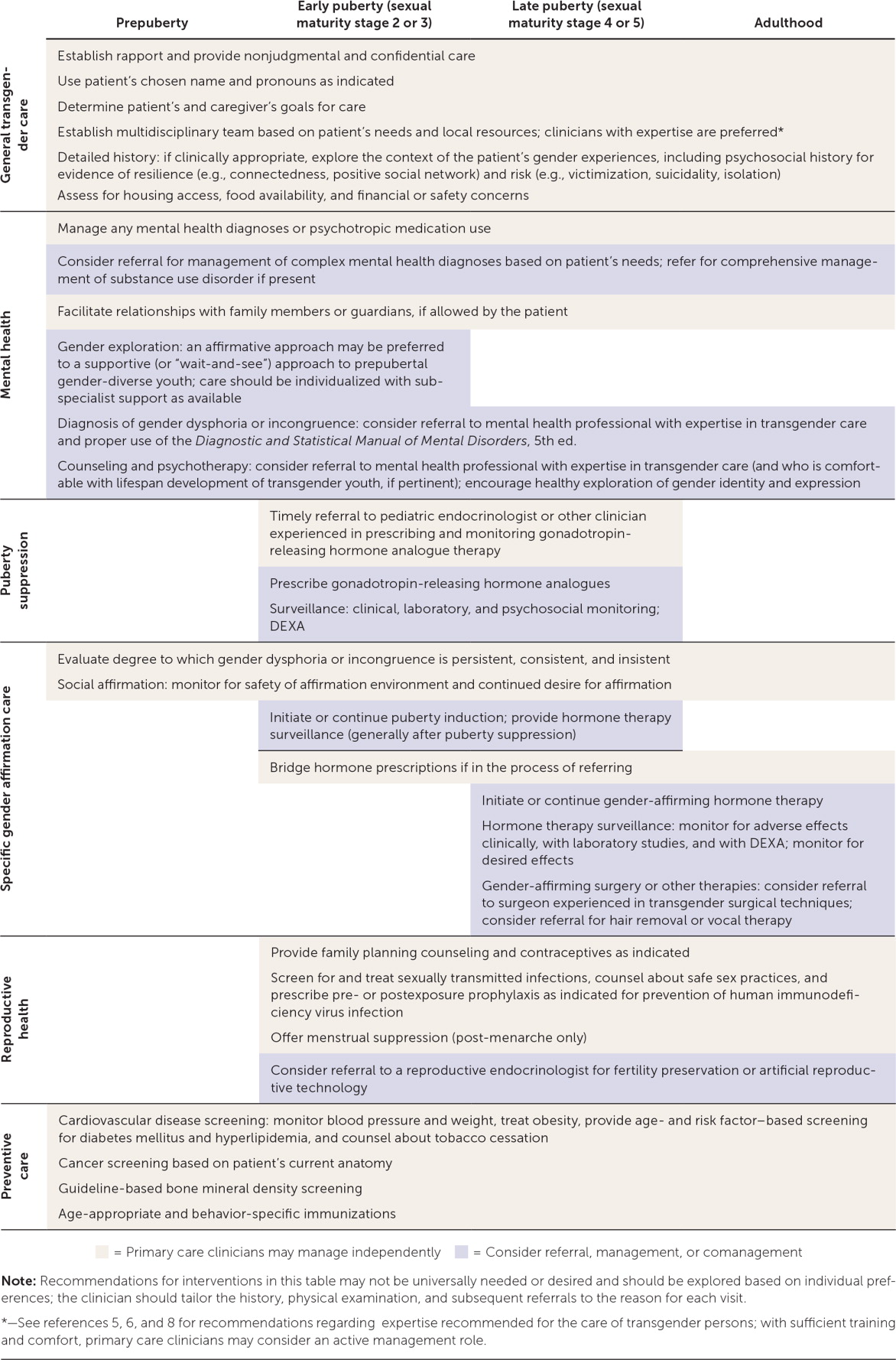
Clinicians should not consider themselves gatekeepers of hormone therapy; rather, they should assist patients in making reasonable and educated decisions about their health care using an informed consent model with parental consent as indicated. 5 , 17 Based on expert opinion, the Endocrine Society recommends that clinicians who diagnose gender dysphoria or incongruence and who manage gender-affirming hormone therapy receive training in the proper use of the Diagnostic and Statistical Manual of Mental Disorders , 5th ed., and the ICD; have the ability to determine capacity for consent and to resolve psychosocial barriers to gender affirmation; be comfortable and knowledgeable in prescribing and monitoring hormone therapies; attend relevant professional meetings; and, if applicable, be familiar with lifespan development of transgender youth. 6
PHYSICAL EXAMINATION
Transgender patients may experience discomfort during the physical examination because of ongoing dysphoria or negative past experiences. 4 , 5 , 8 Examinations should be based on the patient's current anatomy and specific needs for the visit, and should be explained, chaperoned, and stopped as indicated by the patient's comfort level. 5 Differences of sex development are typically diagnosed much earlier than gender dysphoria or gender incongruence. However, in the absence of gender-affirming hormone therapy, an initial examination may be warranted to assess for sex characteristics that are incongruent with sex assigned at birth. Such findings may warrant referral to an endocrinologist or other subspecialist. 6 , 25
Mental Health
Transgender patients typically have high rates of mental health diagnoses. 11 , 18 However, it is important not to assume that a patient's mental health concerns are secondary to being transgender. 5 , 12 , 15 Primary care clinicians should consider routine screening for depression, anxiety, posttraumatic stress disorder, eating disorders, substance use, intimate partner violence, self-injury, bullying, truancy, homelessness, high-risk sexual behaviors, and suicidality. 5 , 11 , 14 , 15 , 19 , 26 – 29 Clinicians should be equipped to handle the basic mental health needs of transgender persons (e.g., first-line treatments for depression or anxiety) and refer patients to subspecialists when warranted. 5 , 8 , 15
Because of the higher prevalence of traumatic life experiences in transgender persons, care should be trauma-informed (i.e., focused on safety, empowerment, and trustworthiness) and guided by the patient's life experiences as they relate to their care and resilience. 5 , 15 , 30 Efforts to convert a person's gender identity to align with their sex assigned at birth—so-called gender conversion therapy—are unethical and incompatible with current guidelines and evidence, including policy from the American Academy of Family Physicians. 6 , 8 , 11 , 12 , 14 , 15 , 17 , 31
Health Maintenance
Preventive services are similar for transgender and cisgender (i.e., not transgender) persons. Nuanced recommendations are based on the patient's current anatomy, medication use, and behaviors. 5 , 6 , 32 Screening recommendations for hyperlipidemia, diabetes mellitus, tobacco use, hypertension, and obesity are available from the U.S. Preventive Services Task Force (USPSTF). 33 Clinicians should be vigilant for signs and symptoms of venous thromboembolism (VTE) and metabolic disease because hormone therapy may increase the risk of these conditions. 5 , 6 , 34 Screening for osteoporosis is based on hormone use. 6 , 35
Cancer screening recommendations are determined by the patient's current anatomy. Transgender females with breast tissue and transgender males who have not undergone complete mastectomy should receive screening mammography based on guidelines for cisgender persons. 6 , 36 Screening for cervical and prostate cancers should be based on current guidelines and the presence of relevant anatomy. 5 , 6
Recommendations for immunizations (e.g., human papillomavirus) and screening and treatment for sexually transmitted infections (including human immunodeficiency virus) are provided by the Centers for Disease Control and Prevention and USPSTF based on sexual practices. 32 , 33 , 37 , 38 Pre- and postexposure prophylaxis for human immunodeficiency virus infection should be considered for patients who meet treatment criteria. 32 , 38
Hormone Therapy
Feminizing and masculinizing hormone therapies are partially irreversible treatments to facilitate development of secondary sex characteristics of the experienced gender. 6 Not all gender-diverse persons require or seek hormone treatment; however, those who receive treatment generally report improved quality of life, self-esteem, and anxiety. 5 , 6 , 39 – 44 Patients must consent to therapy after being informed of the potentially irreversible changes in physical appearance, fertility potential, and social circumstances, as well as other potential benefits and risks.
Feminizing hormone therapy includes estrogen and antiandrogens to decrease the serum testosterone level below 50 ng per dL (1.7 nmol per L) while maintaining the serum estradiol level below 200 pg per mL (734 pmol per L). 6 Therapy may reduce muscle mass, libido, and terminal hair growth, and increase breast development and fat redistribution; voice change is not expected. 5 , 6 The risk of VTE can be mitigated by avoiding formulations containing ethinyl estradiol, supraphysiologic doses, and tobacco use. 34 , 45 – 47 Additional risks include breast cancer, prolactinoma, cardiovascular or cerebrovascular disease, cholelithiasis, and hypertriglyceridemia; however, these risks are rare (yet clinically significant), indolent, or incompletely studied. 5 , 6 , 36 , 48 Spironolactone use requires monitoring for hypotension, hyperkalemia, and changes in renal function. 5 , 6
Masculinizing hormone therapy includes testosterone to increase serum levels to 320 to 1,000 ng per dL (11.1 to 34.7 nmol per L). 6 Anticipated changes include acne, scalp hair loss, voice deepening, vaginal atrophy, clitoromegaly, weight gain, facial and body hair growth, and increased muscle mass. Patients receiving masculinizing hormone therapy are at risk of erythrocytosis, as determined by male-range reference values (e.g., hematocrit greater than 50%). 5 , 6 , 45 , 49 Data on patient-oriented outcomes (e.g., death, thromboembolic disease, stroke, osteoporosis, liver toxicity, myocardial infarction) are sparse. Despite possible metabolic effects, few serious events have been identified in meta-analyses. 6 , 34 , 35 , 45 , 46 , 49
Active hormone-sensitive malignancy is an absolute contraindication to gender-affirming hormone treatment. 5 Patients who are older, use tobacco, or have severe chronic disease, current or previous VTE, or a history of hormone-sensitive malignancy may benefit from individualized dosing regimens and subspecialty consultation. 5 The benefits and risks of treatment should be weighed against the risks of inaction, such as suicidality. 5 The use of low-dose transdermal estradiol-17 β (Climara) may reduce the risk of VTE. 5
Some patients without coexisting conditions may prefer a lower dose or individualized regimen. 5 All patients should be offered referral to discuss fertility preservation or artificial reproductive technology. 5 , 20 Table 2 5 , 6 , 17 , 22 , 50 and eTable B present surveillance guidelines and dosing recommendations for patients receiving gender-affirming hormone therapy.
Surgery and Other Treatments
Gender-affirming surgical treatments may not be required to minimize gender dysphoria, and care should be individualized. 6 Mastectomy (i.e., chest reconstruction surgery) may be performed for transmasculine persons before 18 years of age, depending on consent, duration of applicable hormone treatment, and health status. 6 Breast augmentation for transfeminine persons may be timed to maximal breast development from hormone therapy. 5 , 6 Mastectomy or breast augmentation generally costs less than $10,000, and insurance coverage varies. 51 Patients may also request referral for facial and laryngeal surgery, voice therapy, or hair removal. 5 , 6 , 8
The Endocrine Society recommends that persons who seek fertility-limiting surgeries reach the legal age of majority, optimize treatment for coexisting conditions, and undergo social affirmation and hormone treatment (if applicable) continuously for 12 months. 6 Adherence to hormone therapy after gonadectomy is paramount for maintaining bone mineral density. 6 Despite associated costs, varying insurance coverage, potential complications, and the potential for prolonged recovery, 6 , 8 , 51 gender-affirming surgeries generally have high satisfaction rates. 6 , 42
Transgender Youth
Most, but not all, transgender adults report stability of their gender identity since childhood. 17 , 52 However, some gender-diverse prepubertal children subsequently identify as gay, lesbian, or bisexual adolescents, or have other identities instead of transgender, 8 , 11 , 17 , 53 – 55 as opposed to those in early adolescence, when gender identity may become clearer. 5 , 8 , 11 , 17 , 43 , 44 , 53 , 55 There is no universally accepted treatment protocol for prepubertal gender-diverse children. 6 , 12 , 17 Clinicians may preferentially focus on assisting the child and family members in an affirmative care strategy that individualizes healthy exploration of gender identity (as opposed to a supportive, “wait-and-see” approach); this may warrant referral to a mental health clinician comfortable with the lifespan development of transgender youth. 6 , 12 , 13 , 21
Transgender adolescents should have access to psychological therapy for support and a safe means to explore their gender identity, adjust to socioemotional aspects of gender incongruence, and discuss realistic expectations for potential therapy. 6 , 8 , 12 , 17 The clinician should advocate for supportive family and social environments, which have been shown to confer resilience. 14 , 18 , 21 , 40 , 56 , 57 Unsupportive environments in which patients are bullied or victimized can have adverse effects on psychosocial functioning and well-being. 21 , 58 , 59
Transgender adolescents may experience distress at the onset of secondary sex characteristics. Clinicians should consider initiation of or timely referral for a gonadotropin-releasing hormone (GnRH) to suppress puberty when the patient has reached stage 2 or 3 of sexual maturity. 5 , 6 , 8 , 17 , 21 , 40 , 44 This treatment is fully reversible, may make future affirmation easier and safer, and allows time to ensure stability of gender identity. 6 , 17 No hormonal intervention is warranted before the onset of puberty. 6 , 8 , 17
Consent for treatment with GnRH analogues should include information about benefits and risks 5 , 6 , 8 , 15 , 50 ( eTable B ) . Before therapy is initiated, patients should be offered referral to discuss fertility preservation, which may require progression through endogenous puberty. 5 , 6
Some persons prefer to align their appearance (e.g., clothing, hairstyle) or behaviors with their gender identity. The risks and benefits of social affirmation should be weighed. 5 , 6 , 8 , 13 , 17 , 56 Transmasculine postmenarcheal youth may undergo menstrual suppression, which typically provides an additional contraceptive benefit (testosterone alone is insufficient). 5 Breast binding may be used to conceal breast tissue but may cause pain, skin irritation, or skin infections. 5
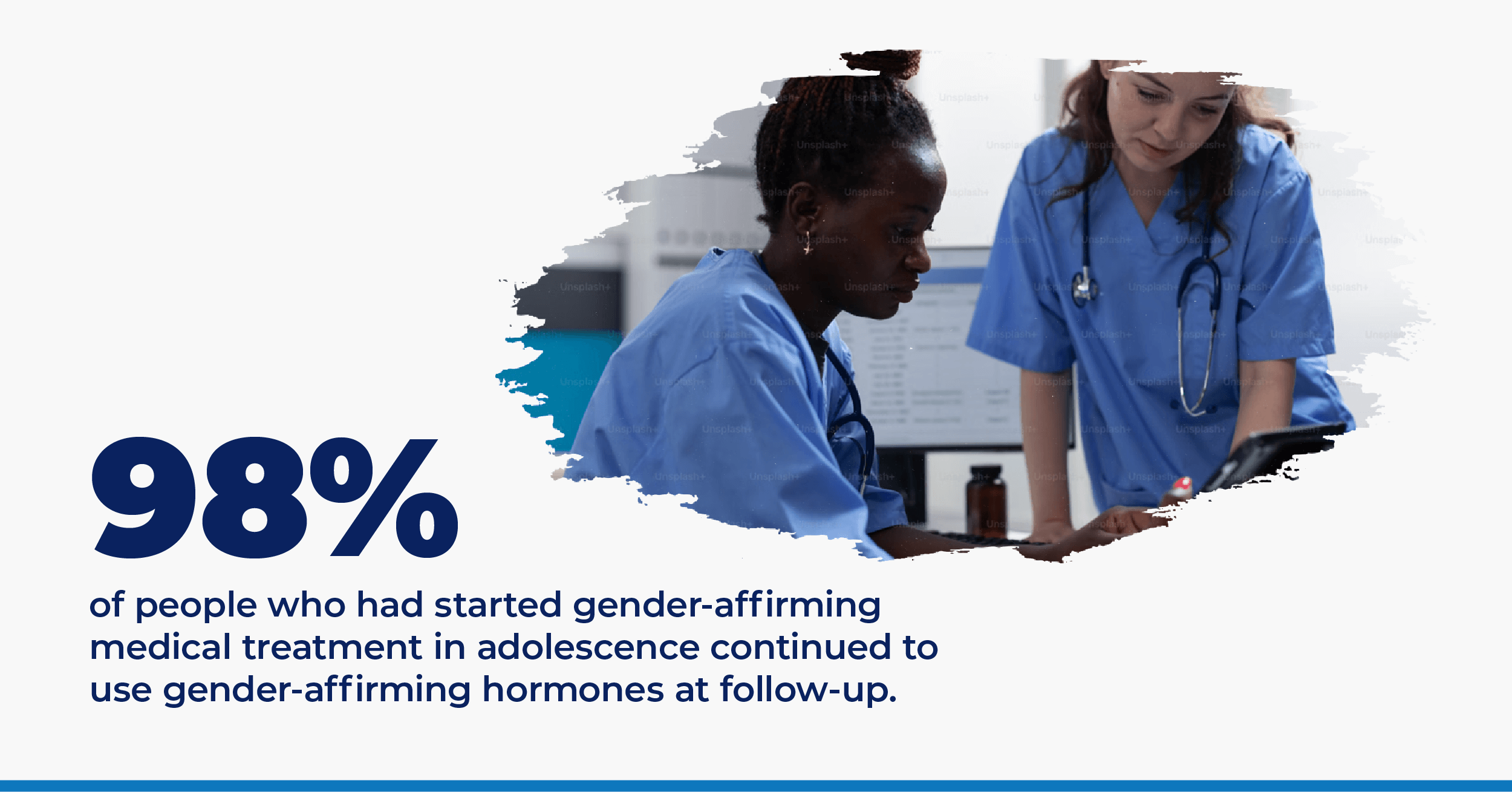
Multiple studies report improved psychosocial outcomes after puberty suppression and subsequent gender-affirming hormone therapy. 39 – 42 , 44 , 60 Delayed treatment may potentiate psychiatric stress and gender-related abuse; therefore, withholding gender-affirming treatment in a wait-and-see approach is not without risk. 8 Additional resources for transgender persons, family members, and clinicians are presented in eTable C .
Data Sources: PubMed searches were completed using the MeSH function with the key phrases transgender, gender dysphoria, and gender incongruence. The reference lists of six cited manuscripts were searched for additional studies of interest, including three relevant reviews and guidelines by the World Professional Association for Transgender Health; the Center of Excellence for Transgender Health at the University of California, San Francisco; and the Endocrine Society. Other queries included Essential Evidence Plus and the Cochrane Database of Systematic Reviews. Search dates: November 1, 2017, to September 18, 2018.
The views expressed in this publication are those of the authors and do not reflect the official policy or position of the Departments of the Army, Navy, or Air Force; the Department of Defense; or the U.S. government.
Conron KJ, Scott G, Stowell GS, Landers SJ. Transgender health in Massachusetts: results from a household probability sample of adults. Am J Public Health. 2012;102(1):118-122.
Herman JL, Flores AR, Brown TN, Wilson BD, Conron KJ. Age of individuals who identify as transgender in the United States. January 2017. https://williamsinstitute.law.ucla.edu/wp-content/uploads/TransAgeReport.pdf . Accessed July 5, 2018.
Meerwijk EL, Sevelius JM. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health. 2017;107(2):e1-e8.
Grant JM, Mottet LA, Tanis J, Harrison J, Herman JL, Keisling M. Injustice at every turn: a report of the National Transgender Discrimination Survey. http://www.thetaskforce.org/static_html/downloads/reports/reports/ntds_full.pdf . Accessed July 5, 2018.
Deutsch MB. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2nd ed. June 17, 2016. http://transhealth.ucsf.edu/protocols . Accessed July 5, 2018.
Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline [published correction appears in J Clin Endocrinol Metab . 2018;103(2):699]. J Clin Endocrinol Metab. 2017;102(11):3869-3903.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders . 5th ed. Washington, DC: American Psychiatric Association; 2013.
Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism. 2012;13(4):165-232.
World Health Organization. ICD-11: classifying disease to map the way we live and die. Coding disease and death. June 18, 2018. http://www.who.int/health-topics/international-classification-of-diseases . Accessed August 25, 2018.
Reed GM, Drescher J, Krueger RB, et al. Disorders related to sexuality and gender identity in the ICD-11: revising the ICD-10 classification based on current scientific evidence, best clinical practices, and human rights considerations [published correction appears in World Psychiatry . 2017;16(2):220]. World Psychiatry. 2016;15(3):205-221.
Adelson SL American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI). Practice parameter on gay, lesbian, or bisexual sexual orientation, gender nonconformity, and gender discordance in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2012;51(9):957-974.
American Psychological Association. Guidelines for psychological practice with transgender and gender nonconforming people. Am Psychol. 2015;70(9):832-864.
de Vries AL, Klink D, Cohen-Kettenis PT. What the primary care pediatrician needs to know about gender incongruence and gender dysphoria in children and adolescents. Pediatr Clin North Am. 2016;63(6):1121-1135.
Levine DA Committee on Adolescence. Office-based care for lesbian, gay, bisexual, transgender, and questioning youth. Pediatrics. 2013;132(1):e297-e313.
Klein DA, Malcolm NM, Berry-Bibee EN, et al. Quality primary care and family planning services for LGBT clients: a comprehensive review of clinical guidelines. LGBT Health. 2018;5(3):153-170.
Deutsch MB, Buchholz D. Electronic health records and transgender patients—practical recommendations for the collection of gender identity data. J Gen Intern Med. 2015;30(6):843-847.
Olson J, Forbes C, Belzer M. Management of the transgender adolescent. Arch Pediatr Adolesc Med. 2011;165(2):171-176.
Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103(5):943-951.
Marcell AV, Burstein GR Committee on Adolescence. Sexual and reproductive health care services in the pediatric setting. Pediatrics. 2017;140(5):e20172858.
Klein DA, Berry-Bibee EN, Keglovitz Baker K, Malcolm NM, Rollison JM, Frederiksen BN. Providing quality family planning services to LGBTQIA individuals: a systematic review. Contraception. 2018;97(5):378-391.
Rafferty J Committee on Psychosocial Aspects of Child and Family Health; Committee on Adolescence; Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents. Pediatrics. 2018;142(4):e20182162.
Klein DA, Ellzy JA, Olson J. Care of a transgender adolescent. Am Fam Physician. 2015;92(2):142-148.
Tate CC, Ledbetter JN, Youssef CP. A two-question method for assessing gender categories in the social and medical sciences. J Sex Res. 2013;50(8):767-776.
Keuroghlian AS, Ard KL, Makadon HJ. Advancing health equity for lesbian, gay, bisexual and transgender (LGBT) people through sexual health education and LGBT-affirming health care environments. Sex Health. 2017;14(1):119-122.
Lee PA, Nordenström A, Houk CP, et al. Global DSD Update Consortium. Global disorders of sex development update since 2006: perceptions, approach and care [published correction appears in Horm Res Paediatr 2016;85(3):180]. Horm Res Paediatr. 2016;85(3):158-180.
de Vries AL, Doreleijers TA, Steensma TD, Cohen-Kettenis PT. Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry. 2011;52(11):1195-1202.
Olson J, Schrager SM, Belzer M, Simons LK, Clark LF. Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. J Adolesc Health. 2015;57(4):374-380.
Becerra-Culqui TA, Liu Y, Nash R, et al. Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics. 2018;141(5):e20173845.
Downing JM, Przedworski JM. Health of transgender adults in the U.S., 2014–2016. Am J Prev Med. 2018;55(3):336-344.
Richmond KA, Burnes T, Carroll K. Lost in translation: interpreting systems of trauma for transgender clients. Traumatology. 2012;18(1):45-57.
American Academy of Family Physicians. Reparative therapy. 2016. https://www.aafp.org/about/policies/all/reparative-therapy.html . Accessed July 5, 2018.
Edmiston EK, Donald CA, Sattler AR, Peebles JK, Ehrenfeld JM, Eckstrand KL. Opportunities and gaps in primary care preventative health services for transgender patients: a systemic review. Transgend Health. 2016;1(1):216-230.
U.S. Preventive Services Task Force. USPSTF A and B recommendations. June 2018. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations . Accessed July 5, 2018.
Maraka S, Singh Ospina N, Rodriguez-Gutierrez R, et al. Sex steroids and cardiovascular outcomes in transgender individuals: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2017;102(11):3914-3923.
Singh-Ospina N, Maraka S, Rodriguez-Gutierrez R, et al. Effect of sex steroids on the bone health of transgender individuals: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2017;102(11):3904-3913.
Brown GR, Jones KT. Incidence of breast cancer in a cohort of 5,135 transgender veterans. Breast Cancer Res Treat. 2015;149(1):191-198.
Centers for Disease Control and Prevention. Immunization schedules. https://www.cdc.gov/vaccines/schedules/hcp/index.html . Accessed July 5, 2018.
Workowski KA, Bolan GA Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015 [published correction appears in MMWR Recomm Rep . 2015;64(33):924]. MMWR Recomm Rep. 2015;64(RR-03):1-137.
Costa R, Colizzi M. The effect of cross-sex hormonal treatment on gender dysphoria individuals' mental health: a systematic review. Neuropsychiatr Dis Treat. 2016;12:1953-1966.
de Vries AL, McGuire JK, Steensma TD, Wagenaar EC, Doreleijers TA, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134(4):696-704.
Gómez-Gil E, Zubiaurre-Elorza L, Esteva I, et al. Hormone-treated transsexuals report less social distress, anxiety and depression. Psychoneuroendocrinology. 2012;37(5):662-670.
Murad MH, Elamin MB, Garcia MZ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol (Oxf). 2010;72(2):214-231.
Steensma TD, Biemond R, de Boer F, Cohen-Kettenis PT. Desisting and persisting gender dysphoria after childhood: a qualitative follow-up study. Clin Child Psychol Psychiatry. 2011;16(4):499-516.
de Vries AL, Steensma TD, Doreleijers TA, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med. 2011;8(8):2276-2283.
Meriggiola MC, Gava G. Endocrine care of transpeople part I. A review of cross-sex hormonal treatments, outcomes and adverse effects in transmen. Clin Endocrinol (Oxf). 2015;83(5):597-606.
Weinand JD, Safer JD. Hormone therapy in transgender adults is safe with provider supervision; A review of hormone therapy sequelae for transgender individuals. J Clin Transl Endocrinol. 2015;2(2):55-60.
Asscheman H, T'Sjoen G, Lemaire A, et al. Venous thrombo-embolism as a complication of cross-sex hormone treatment of male-to-female transsexual subjects: a review. Andrologia. 2014;46(7):791-795.
Joint R, Chen ZE, Cameron S. Breast and reproductive cancers in the transgender population: a systematic review [published online ahead of print April 28, 2018]. BJOG . https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/1471-0528.15258 . Accessed August 25, 2018.
Jacobeit JW, Gooren LJ, Schulte HM. Safety aspects of 36 months of administration of long-acting intramuscular testosterone undecanoate for treatment of female-to-male transgender individuals. Eur J Endocrinol. 2009;161(5):795-798.
Carel JC, Eugster EA, Rogol A, et al. ; ESPE-LWPES GnRH Analogs Consensus Conference Group. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics. 2009;123(4):e752-e762.
Kailas M, Lu HM, Rothman EF, Safer JD. Prevalence and types of gender-affirming surgery among a sample of transgender endocrinology patients prior to state expansion of insurance coverage. Endocr Pract. 2017;23(7):780-786.
Landén M, Wålinder J, Lundström B. Clinical characteristics of a total cohort of female and male applicants for sex reassignment: a descriptive study. Acta Psychiatr Scand. 1998;97(3):189-194.
Steensma TD, McGuire JK, Kreukels BP, Beekman AJ, Cohen-Kettenis PT. Factors associated with desistence and persistence of childhood gender dysphoria: a quantitative follow-up study. J Am Acad Child Adolesc Psychiatry. 2013;52(6):582-590.
Drummond KD, Bradley SJ, Peterson-Badali M, Zucker KJ. A follow-up study of girls with gender identity disorder. Dev Psychol. 2008;44(1):34-45.
Wallien MS, Cohen-Kettenis PT. Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry. 2008;47(12):1413-1423.
Olson KR, Durwood L, DeMeules M, McLaughlin KA. Mental health of transgender children who are supported in their identities [published correction appears in Pediatrics . 2016;137(3):e20153223]. Pediatrics. 2016;137(3):e20153223.
Johns MM, Beltran O, Armstrong HL, Jayne PE, Barrios LC. Protective factors among transgender and gender variant youth: a systematic review by socioecological level. J Prim Prev. 2018;39(3):263-301.
Toomey RB, Ryan C, Diaz RM, Card NA, Russell ST. Gender-nonconforming lesbian, gay, bisexual, and transgender youth: school victimization and young adult psychosocial adjustment. Dev Psychol. 2010;46(6):1580-1589.
de Vries AL, Steensma TD, Cohen-Kettenis PT, VanderLaan DP, Zucker KJ. Poor peer relations predict parent- and self-reported behavioral and emotional problems of adolescents with gender dysphoria: a cross-national, cross-clinic comparative analysis. Eur Child Adolesc Psychiatry. 2016;25(6):579-588.
Chew D, Anderson J, Williams K, May T, Pang K. Hormonal treatment in young people with gender dysphoria: a systematic review. Pediatrics. 2018;141(4):e20173742.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2018 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Preparing for Gender Affirmation Surgery: Ask the Experts
Featured Expert:

Romy Smith, LMSW
Preparing for your gender affirmation surgery can be daunting. To help provide some guidance for those considering gender affirmation procedures, our team from the Johns Hopkins Center for Transgender and Gender Expansive Health (JHCTGEH) answered some questions about what to expect before and after your surgery.
What kind of care should I expect as a transgender individual?
What kind of care should I expect as a transgender individual? Before beginning the process, we recommend reading the World Professional Association for Transgender Health Standards Of Care (SOC). The standards were created by international agreement among health care clinicians and in collaboration with the transgender community. These SOC integrate the latest scientific research on transgender health, as well as the lived experience of the transgender community members. This collaboration is crucial so that doctors can best meet the unique health care needs of transgender and gender-diverse people. It is usually a favorable sign if the hospital you choose for your gender affirmation surgery follows or references these standards in their transgender care practices.
Can I still have children after gender affirmation surgery?
Many transgender individuals choose to undergo fertility preservation before their gender affirmation surgery if having biological children is part of their long-term goals. Discuss all your options, such as sperm banking and egg freezing, with your doctor so that you can create the best plan for future family building. JHCTGEH has fertility specialists on staff to meet with you and develop a plan that meets your goals.
Are there other ways I need to prepare?
It is very important to prepare mentally for your surgery. If you haven’t already done so, talk to people who have undergone gender affirmation surgeries or read first-hand accounts. These conversations and articles may be helpful; however, keep in mind that not everything you read will apply to your situation. If you have questions about whether something applies to your individual care, it is always best to talk to your doctor.
You will also want to think about your recovery plan post-surgery. Do you have friends or family who can help care for you in the days after your surgery? Having a support system is vital to your continued health both right after surgery and long term. Most centers have specific discharge instructions that you will receive after surgery. Ask if you can receive a copy of these instructions in advance so you can familiarize yourself with the information.
An initial intake interview via phone with a clinical specialist.
This is your first point of contact with the clinical team, where you will review your medical history, discuss which procedures you’d like to learn more about, clarify what is required by your insurance company for surgery, and develop a plan for next steps. It will make your phone call more productive if you have these documents ready to discuss with the clinician:
- Medications. Information about which prescriptions and over-the-counter medications you are currently taking.
- Insurance. Call your insurance company and find out if your surgery is a “covered benefit" and what their requirements are for you to have surgery.
- Medical Documents. Have at hand the name, address, and contact information for any clinician you see on a regular basis. This includes your primary care clinician, therapists or psychiatrists, and other health specialist you interact with such as a cardiologist or neurologist.
After the intake interview you will need to submit the following documents:
- Pharmacy records and medical records documenting your hormone therapy, if applicable
- Medical records from your primary physician.
- Surgical readiness referral letters from mental health providers documenting their assessment and evaluation
An appointment with your surgeon.
After your intake, and once you have all of your required documentation submitted you will be scheduled for a surgical consultation. These are in-person visits where you will get to meet the surgeon. typically include: The specialty nurse and social worker will meet with you first to conduct an assessment of your medical health status and readiness for major surgical procedures. Discussion of your long-term gender affirmation goals and assessment of which procedures may be most appropriate to help you in your journey. Specific details about the procedures you and your surgeon identify, including the risks, benefits and what to expect after surgery.
A preoperative anesthesia and medical evaluation.
Two to four weeks before your surgery, you may be asked to complete these evaluations at the hospital, which ensure that you are healthy enough for surgery.
What can I expect after gender affirming surgery?
When you’ve finished the surgical aspects of your gender affirmation, we encourage you to follow up with your primary care physician to make sure that they have the latest information about your health. Your doctor can create a custom plan for long-term care that best fits your needs. Depending on your specific surgery and which organs you continue to have, you may need to follow up with a urologist or gynecologist for routine cancer screening. JHCTGEH has primary care clinicians as well as an OB/GYN and urologists on staff.
Among other changes, you may consider updating your name and identification. This list of resources for transgender and gender diverse individuals can help you in this process.
The Center for Transgender and Gender Expansive Health Team at Johns Hopkins
Embracing diversity and inclusion, the Center for Transgender and Gender Expansive Health provides affirming, objective, person-centered care to improve health and enhance wellness; educates interdisciplinary health care professionals to provide culturally competent, evidence-based care; informs the public on transgender health issues; and advances medical knowledge by conducting biomedical research.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
Find Additional Treatment Centers at:

Request an Appointment

Facial Feminization Surgery (FFS)

Gender Affirmation: Do I Need Surgery?

Gender Affirmation Nonsurgical Services
Related Topics
Registered Nurses as Optimizers of Gender-Affirming Care Within a Transgender and Intersex Specialty Care Clinic
- PMID: 32321797
- DOI: 10.1891/CRNR-D-20-00005
An estimated 1.4 million transgender adults live in the United States; this equates to approximately 0.6% of the U.S. population (Lane et al., 2018). Clinical focus on gender dysphoria has significantly increased over the past 30 years (MacCarthy, Reisner, Nunn, Perez-Brumer, & Operario, 2015), with burgeoning evidence from across disciplines documenting the positive outcomes associated with gender-affirming interventions. The purpose of this article is to illustrate how RNs optimize psychosocial, hormonal, and surgical gender-affirming care through performing comprehensive assessments, coordinating care, and providing education and health coaching.
Keywords: RNs; gender-affirming care; gender-affirming surgery; transgender clinic.
© Copyright 2020 Creative Health Care Management.
- Attitude of Health Personnel*
- Gender Identity*
- Middle Aged
- Nurse's Role / psychology*
- Nurses / psychology*
- Nursing Care / psychology*
- Sex Reassignment Procedures / nursing*
- Sexual and Gender Minorities / psychology*
- United States
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Gender Confirmation Surgery (GCS)
What is Gender Confirmation Surgery?
- Transfeminine Tr
Transmasculine Transition
- Traveling Abroad
Choosing a Surgeon
Gender confirmation surgery (GCS), known clinically as genitoplasty, are procedures that surgically confirm a person's gender by altering the genitalia and other physical features to align with their desired physical characteristics. Gender confirmation surgeries are also called gender affirmation procedures. These are both respectful terms.
Gender dysphoria , an experience of misalignment between gender and sex, is becoming more widely diagnosed. People diagnosed with gender dysphoria are often referred to as "transgender," though one does not necessarily need to experience gender dysphoria to be a member of the transgender community. It is important to note there is controversy around the gender dysphoria diagnosis. Many disapprove of it, noting that the diagnosis suggests that being transgender is an illness.
Ellen Lindner / Verywell
Transfeminine Transition
Transfeminine is a term inclusive of trans women and non-binary trans people assigned male at birth.
Gender confirmation procedures that a transfeminine person may undergo include:
- Penectomy is the surgical removal of external male genitalia.
- Orchiectomy is the surgical removal of the testes.
- Vaginoplasty is the surgical creation of a vagina.
- Feminizing genitoplasty creates internal female genitalia.
- Breast implants create breasts.
- Gluteoplasty increases buttock volume.
- Chondrolaryngoplasty is a procedure on the throat that can minimize the appearance of Adam's apple .
Feminizing hormones are commonly used for at least 12 months prior to breast augmentation to maximize breast growth and achieve a better surgical outcome. They are also often used for approximately 12 months prior to feminizing genital surgeries.
Facial feminization surgery (FFS) is often done to soften the lines of the face. FFS can include softening the brow line, rhinoplasty (nose job), smoothing the jaw and forehead, and altering the cheekbones. Each person is unique and the procedures that are done are based on the individual's need and budget,
Transmasculine is a term inclusive of trans men and non-binary trans people assigned female at birth.
Gender confirmation procedures that a transmasculine person may undergo include:
- Masculinizing genitoplasty is the surgical creation of external genitalia. This procedure uses the tissue of the labia to create a penis.
- Phalloplasty is the surgical construction of a penis using a skin graft from the forearm, thigh, or upper back.
- Metoidioplasty is the creation of a penis from the hormonally enlarged clitoris.
- Scrotoplasty is the creation of a scrotum.
Procedures that change the genitalia are performed with other procedures, which may be extensive.
The change to a masculine appearance may also include hormone therapy with testosterone, a mastectomy (surgical removal of the breasts), hysterectomy (surgical removal of the uterus), and perhaps additional cosmetic procedures intended to masculinize the appearance.
Paying For Gender Confirmation Surgery
Medicare and some health insurance providers in the United States may cover a portion of the cost of gender confirmation surgery.
It is unlawful to discriminate or withhold healthcare based on sex or gender. However, many plans do have exclusions.
For most transgender individuals, the burden of financing the procedure(s) is the main difficulty in obtaining treatment. The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed.
A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019.
Traveling Abroad for GCS
Some patients seek gender confirmation surgery overseas, as the procedures can be less expensive in some other countries. It is important to remember that traveling to a foreign country for surgery, also known as surgery tourism, can be very risky.
Regardless of where the surgery will be performed, it is essential that your surgeon is skilled in the procedure being performed and that your surgery will be performed in a reputable facility that offers high-quality care.
When choosing a surgeon , it is important to do your research, whether the surgery is performed in the U.S. or elsewhere. Talk to people who have already had the procedure and ask about their experience and their surgeon.
Before and after photos don't tell the whole story, and can easily be altered, so consider asking for a patient reference with whom you can speak.
It is important to remember that surgeons have specialties and to stick with your surgeon's specialty. For example, you may choose to have one surgeon perform a genitoplasty, but another to perform facial surgeries. This may result in more expenses, but it can result in a better outcome.
A Word From Verywell
Gender confirmation surgery is very complex, and the procedures that one person needs to achieve their desired result can be very different from what another person wants.
Each individual's goals for their appearance will be different. For example, one individual may feel strongly that breast implants are essential to having a desirable and feminine appearance, while a different person may not feel that breast size is a concern. A personalized approach is essential to satisfaction because personal appearance is so highly individualized.
Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review . Transgend Health . 2018;3(1):159-169. doi:10.1089/trgh.2018.0014
Morrison SD, Vyas KS, Motakef S, et al. Facial Feminization: Systematic Review of the Literature . Plast Reconstr Surg. 2016;137(6):1759-70. doi:10.1097/PRS.0000000000002171
Hadj-moussa M, Agarwal S, Ohl DA, Kuzon WM. Masculinizing Genital Gender Confirmation Surgery . Sex Med Rev . 2019;7(1):141-155. doi:10.1016/j.sxmr.2018.06.004
Dowshen NL, Christensen J, Gruschow SM. Health Insurance Coverage of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information . Transgend Health . 2019;4(1):131-135. doi:10.1089/trgh.2018.0055
American Society of Plastic Surgeons. Rhinoplasty nose surgery .
Rights Group: More U.S. Companies Covering Cost of Gender Reassignment Surgery. CNS News. http://cnsnews.com/news/article/rights-group-more-us-companies-covering-cost-gender-reassignment-surgery
The Sex Change Capital of the US. CBS News. http://www.cbsnews.com/2100-3445_162-4423154.html
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
This Policy Statement was reaffirmed August 2023.
Introduction, definitions, epidemiology, mental health implications, gender-affirmative care, developmental considerations, medical management, clinical setting, pubertal suppression, gender affirmation, health disparities, family acceptance, safe schools and communities, medical education, recommendations, acknowledgments, lead author, contributor, committee on psychosocial aspects of child and family health, 2017–2018, committee on adolescence, 2017–2018, section on lesbian, gay, bisexual, and transgender health and wellness executive committee, 2016–2017, former executive committee members, ensuring comprehensive care and support for transgender and gender-diverse children and adolescents.
POTENTIAL CONFLICT OF INTEREST: The author has indicated he has no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The author has indicated he has no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Jason Rafferty , COMMITTEE ON PSYCHOSOCIAL ASPECTS OF CHILD AND FAMILY HEALTH , COMMITTEE ON ADOLESCENCE , SECTION ON LESBIAN, GAY, BISEXUAL, AND TRANSGENDER HEALTH AND WELLNESS , Michael Yogman , Rebecca Baum , Thresia B. Gambon , Arthur Lavin , Gerri Mattson , Lawrence Sagin Wissow , Cora Breuner , Elizabeth M. Alderman , Laura K. Grubb , Makia E. Powers , Krishna Upadhya , Stephenie B. Wallace , Lynn Hunt , Anne Teresa Gearhart , Christopher Harris , Kathryn Melland Lowe , Chadwick Taylor Rodgers , Ilana Michelle Sherer; Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents. Pediatrics October 2018; 142 (4): e20182162. 10.1542/peds.2018-2162
Download citation file:
- Ris (Zotero)
- Reference Manager
As a traditionally underserved population that faces numerous health disparities, youth who identify as transgender and gender diverse (TGD) and their families are increasingly presenting to pediatric providers for education, care, and referrals. The need for more formal training, standardized treatment, and research on safety and medical outcomes often leaves providers feeling ill equipped to support and care for patients that identify as TGD and families. In this policy statement, we review relevant concepts and challenges and provide suggestions for pediatric providers that are focused on promoting the health and positive development of youth that identify as TGD while eliminating discrimination and stigma.
In its dedication to the health of all children, the American Academy of Pediatrics (AAP) strives to improve health care access and eliminate disparities for children and teenagers who identify as lesbian, gay, bisexual, transgender, or questioning (LGBTQ) of their sexual or gender identity. 1 , 2 Despite some advances in public awareness and legal protections, youth who identify as LGBTQ continue to face disparities that stem from multiple sources, including inequitable laws and policies, societal discrimination, and a lack of access to quality health care, including mental health care. Such challenges are often more intense for youth who do not conform to social expectations and norms regarding gender. Pediatric providers are increasingly encountering such youth and their families, who seek medical advice and interventions, yet they may lack the formal training to care for youth that identify as transgender and gender diverse (TGD) and their families. 3
This policy statement is focused specifically on children and youth that identify as TGD rather than the larger LGBTQ population, providing brief, relevant background on the basis of current available research and expert opinion from clinical and research leaders, which will serve as the basis for recommendations. It is not a comprehensive review of clinical approaches and nuances to pediatric care for children and youth that identify as TGD. Professional understanding of youth that identify as TGD is a rapidly evolving clinical field in which research on appropriate clinical management is limited by insufficient funding. 3 , 4
To clarify recommendations and discussions in this policy statement, some definitions are provided. However, brief descriptions of human behavior or identities may not capture nuance in this evolving field.
“Sex,” or “natal gender,” is a label, generally “male” or “female,” that is typically assigned at birth on the basis of genetic and anatomic characteristics, such as genital anatomy, chromosomes, and sex hormone levels. Meanwhile, “gender identity” is one’s internal sense of who one is, which results from a multifaceted interaction of biological traits, developmental influences, and environmental conditions. It may be male, female, somewhere in between, a combination of both, or neither (ie, not conforming to a binary conceptualization of gender). Self-recognition of gender identity develops over time, much the same way as a child’s physical body does. For some people, gender identity can be fluid, shifting in different contexts. “Gender expression” refers to the wide array of ways people display their gender through clothing, hair styles, mannerisms, or social roles. Exploring different ways of expressing gender is common for children and may challenge social expectations. The way others interpret this expression is referred to as “gender perception” ( Table 1 ). 5 , 6
Relevant Terms and Definitions Related to Gender Care
This list is not intended to be all inclusive. The pronouns “they” and ”their” are used intentionally to be inclusive rather than the binary pronouns “he” and “she” and “his” and “her.” Adapted from Bonifacio HJ, Rosenthal SM. Gender variance and dysphoria in children and adolescents. Pediatr Clin North Am . 2015;62(4):1001–1016. Adapted from Vance SR Jr, Ehrensaft D, Rosenthal SM. Psychological and medical care of gender nonconforming youth. Pediatrics . 2014;134(6):1184–1192. DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition ; FTM, female to male; MTF, male to female.
These labels may or may not be congruent. The term “cisgender” is used if someone identifies and expresses a gender that is consistent with the culturally defined norms of the sex that was assigned at birth. “Gender diverse” is an umbrella term to describe an ever-evolving array of labels that people may apply when their gender identity, expression, or even perception does not conform to the norms and stereotypes others expect of their assigned sex. “Transgender” is usually reserved for a subset of such youth whose gender identity does not match their assigned sex and generally remains persistent, consistent, and insistent over time. These terms are not diagnoses; rather, they are personal and often dynamic ways of describing one’s own gender experience.
Gender identity is not synonymous with “sexual orientation,” which refers to a person’s identity in relation to the gender(s) to which they are sexually and romantically attracted. Gender identity and sexual orientation are distinct but interrelated constructs. 8 Therefore, being transgender does not imply a sexual orientation, and people who identify as transgender still identify as straight, gay, bisexual, etc, on the basis of their attractions. (For more information, The Gender Book , found at www.thegenderbook.com , is a resource with illustrations that are used to highlight these core terms and concepts.)
In population-based surveys, questions related to gender identity are rarely asked, which makes it difficult to assess the size and characteristics of the population that is TGD. In the 2014 Behavioral Risk Factor Surveillance System of the Centers for Disease Control and Prevention, only 19 states elected to include optional questions on gender identity. Extrapolation from these data suggests that the US prevalence of adults who identify as transgender or “gender nonconforming” is 0.6% (1.4 million), ranging from 0.3% in North Dakota to 0.8% in Hawaii. 9 On the basis of these data, it has been estimated that 0.7% of youth ages 13 to 17 years (∼150 000) identify as transgender. 10 This number is much higher than previous estimates, which were extrapolated from individual states or specialty clinics, and is likely an underestimate given the stigma regarding those who openly identify as transgender and the difficulty in defining “transgender” in a way that is inclusive of all gender-diverse identities. 11
There have been no large-scale prevalence studies among children and adolescents, and there is no evidence that adult statistics reflect young children or adolescents. In the 2014 Behavioral Risk Factor Surveillance System, those 18 to 24 years of age were more likely than older age groups to identify as transgender (0.7%). 9 Children report being aware of gender incongruence at young ages. Children who later identify as TGD report first having recognized their gender as “different” at an average age of 8.5 years; however, they did not disclose such feelings until an average of 10 years later. 12
Adolescents and adults who identify as transgender have high rates of depression, anxiety, eating disorders, self-harm, and suicide. 13 , – 20 Evidence suggests that an identity of TGD has an increased prevalence among individuals with autism spectrum disorder, but this association is not yet well understood. 21 , 22 In 1 retrospective cohort study of 180 trans youth and matched cisgender peers, 56 youth who identified as transgender reported previous suicidal ideation, and 31 reported a previous suicide attempt, compared with 20 and 11 among matched youth who identified as cisgender, respectively. 13 Some youth who identify as TGD also experience gender dysphoria, which is a specific diagnosis given to those who experience impairment in peer and/or family relationships, school performance, or other aspects of their life as a consequence of the incongruence between their assigned sex and their gender identity. 23
There is no evidence that risk for mental illness is inherently attributable to one’s identity of TGD. Rather, it is believed to be multifactorial, stemming from an internal conflict between one’s appearance and identity, limited availability of mental health services, low access to health care providers with expertise in caring for youth who identify as TGD, discrimination, stigma, and social rejection. 24 This was affirmed by the American Psychological Association in 2008 25 (with practice guidelines released in 2015 8 ) and the American Psychiatric Association, which made the following statement in 2012:
Being transgender or gender variant implies no impairment in judgment, stability, reliability, or general social or vocational capabilities; however, these individuals often experience discrimination due to a lack of civil rights protections for their gender identity or expression.… [Such] discrimination and lack of equal civil rights is damaging to the mental health of transgender and gender variant individuals . 26
Youth who identify as TGD often confront stigma and discrimination, which contribute to feelings of rejection and isolation that can adversely affect physical and emotional well-being. For example, many youth believe that they must hide their gender identity and expression to avoid bullying, harassment, or victimization. Youth who identify as TGD experience disproportionately high rates of homelessness, physical violence (at home and in the community), substance abuse, and high-risk sexual behaviors. 5 , 6 , 12 , 27 , – 31 Among the 3 million HIV testing events that were reported in 2015, the highest percentages of new infections were among women who identified as transgender 32 and were also at particular risk for not knowing their HIV status. 30
In a gender-affirmative care model (GACM), pediatric providers offer developmentally appropriate care that is oriented toward understanding and appreciating the youth’s gender experience. A strong, nonjudgmental partnership with youth and their families can facilitate exploration of complicated emotions and gender-diverse expressions while allowing questions and concerns to be raised in a supportive environment. 5 In a GACM, the following messages are conveyed:
transgender identities and diverse gender expressions do not constitute a mental disorder;
variations in gender identity and expression are normal aspects of human diversity, and binary definitions of gender do not always reflect emerging gender identities;
gender identity evolves as an interplay of biology, development, socialization, and culture; and
if a mental health issue exists, it most often stems from stigma and negative experiences rather than being intrinsic to the child. 27 , 33
The GACM is best facilitated through the integration of medical, mental health, and social services, including specific resources and supports for parents and families. 24 Providers work together to destigmatize gender variance, promote the child’s self-worth, facilitate access to care, educate families, and advocate for safer community spaces where children are free to develop and explore their gender. 5 A specialized gender-affirmative therapist, when available, may be an asset in helping children and their families build skills for dealing with gender-based stigma, address symptoms of anxiety or depression, and reinforce the child’s overall resiliency. 34 , 35 There is a limited but growing body of evidence that suggests that using an integrated affirmative model results in young people having fewer mental health concerns whether they ultimately identify as transgender. 24 , 36 , 37
In contrast, “conversion” or “reparative” treatment models are used to prevent children and adolescents from identifying as transgender or to dissuade them from exhibiting gender-diverse expressions. The Substance Abuse and Mental Health Services Administration has concluded that any therapeutic intervention with the goal of changing a youth’s gender expression or identity is inappropriate. 33 Reparative approaches have been proven to be not only unsuccessful 38 but also deleterious and are considered outside the mainstream of traditional medical practice. 29 , 39 , – 42 The AAP described reparative approaches as “unfair and deceptive.” 43 At the time of this writing, * conversion therapy was banned by executive regulation in New York and by legislative statutes in 9 other states as well as the District of Columbia. 44
Pediatric providers have an essential role in assessing gender concerns and providing evidence-based information to assist youth and families in medical decision-making. Not doing so can prolong or exacerbate gender dysphoria and contribute to abuse and stigmatization. 35 If a pediatric provider does not feel prepared to address gender concerns when they occur, then referral to a pediatric or mental health provider with more expertise is appropriate. There is little research on communication and efficacy with transfers in care for youth who identify as TGD, particularly from pediatric to adult providers.
Acknowledging that the capacity for emerging abstract thinking in childhood is important to conceptualize and reflect on identity, gender-affirmation guidelines are being focused on individually tailored interventions on the basis of the physical and cognitive development of youth who identify as TGD. 45 Accordingly, research substantiates that children who are prepubertal and assert an identity of TGD know their gender as clearly and as consistently as their developmentally equivalent peers who identify as cisgender and benefit from the same level of social acceptance. 46 This developmental approach to gender affirmation is in contrast to the outdated approach in which a child’s gender-diverse assertions are held as “possibly true” until an arbitrary age (often after pubertal onset) when they can be considered valid, an approach that authors of the literature have termed “watchful waiting.” This outdated approach does not serve the child because critical support is withheld. Watchful waiting is based on binary notions of gender in which gender diversity and fluidity is pathologized; in watchful waiting, it is also assumed that notions of gender identity become fixed at a certain age. The approach is also influenced by a group of early studies with validity concerns, methodologic flaws, and limited follow-up on children who identified as TGD and, by adolescence, did not seek further treatment (“desisters”). 45 , 47 More robust and current research suggests that, rather than focusing on who a child will become, valuing them for who they are, even at a young age, fosters secure attachment and resilience, not only for the child but also for the whole family. 5 , 45 , 48 , 49
Pediatric primary care providers are in a unique position to routinely inquire about gender development in children and adolescents as part of recommended well-child visits 50 and to be a reliable source of validation, support, and reassurance. They are often the first provider to be aware that a child may not identify as cisgender or that there may be distress related to a gender-diverse identity. The best way to approach gender with patients is to inquire directly and nonjudgmentally about their experience and feelings before applying any labels. 27 , 51
Many medical interventions can be offered to youth who identify as TGD and their families. The decision of whether and when to initiate gender-affirmative treatment is personal and involves careful consideration of risks, benefits, and other factors unique to each patient and family. Many protocols suggest that clinical assessment of youth who identify as TGD is ideally conducted on an ongoing basis in the setting of a collaborative, multidisciplinary approach, which, in addition to the patient and family, may include the pediatric provider, a mental health provider (preferably with expertise in caring for youth who identify as TGD ), social and legal supports, and a pediatric endocrinologist or adolescent-medicine gender specialist, if available. 6 , 28 There is no prescribed path, sequence, or end point. Providers can make every effort to be aware of the influence of their own biases. The medical options also vary depending on pubertal and developmental progression.
In the past year, 1 in 4 adults who identified as transgender avoided a necessary doctor’s visit because of fear of being mistreated. 31 All clinical office staff have a role in affirming a patient’s gender identity. Making flyers available or displaying posters related to LGBTQ health issues, including information for children who identify as TGD and families, reveals inclusivity and awareness. Generally, patients who identify as TGD feel most comfortable when they have access to a gender-neutral restroom. Diversity training that encompasses sensitivity when caring for youth who identify as TGD and their families can be helpful in educating clinical and administrative staff. A patient-asserted name and pronouns are used by staff and are ideally reflected in the electronic medical record without creating duplicate charts. 52 , 53 The US Centers for Medicare and Medicaid Services and the National Coordinator for Health Information Technology require all electronic health record systems certified under the Meaningful Use incentive program to have the capacity to confidentially collect information on gender identity. 54 , 55 Explaining and maintaining confidentiality procedures promotes openness and trust, particularly with youth who identify as LGBTQ. 1 Maintaining a safe clinical space can provide at least 1 consistent, protective refuge for patients and families, allowing authentic gender expression and exploration that builds resiliency.
Gonadotrophin-releasing hormones have been used to delay puberty since the 1980s for central precocious puberty. 56 These reversible treatments can also be used in adolescents who experience gender dysphoria to prevent development of secondary sex characteristics and provide time up until 16 years of age for the individual and the family to explore gender identity, access psychosocial supports, develop coping skills, and further define appropriate treatment goals. If pubertal suppression treatment is suspended, then endogenous puberty will resume. 20 , 57 , 58
Often, pubertal suppression creates an opportunity to reduce distress that may occur with the development of secondary sexual characteristics and allow for gender-affirming care, including mental health support for the adolescent and the family. It reduces the need for later surgery because physical changes that are otherwise irreversible (protrusion of the Adam’s apple, male pattern baldness, voice change, breast growth, etc) are prevented. The available data reveal that pubertal suppression in children who identify as TGD generally leads to improved psychological functioning in adolescence and young adulthood. 20 , 57 , – 59
Pubertal suppression is not without risks. Delaying puberty beyond one’s peers can also be stressful and can lead to lower self-esteem and increased risk taking. 60 Some experts believe that genital underdevelopment may limit some potential reconstructive options. 61 Research on long-term risks, particularly in terms of bone metabolism 62 and fertility, 63 is currently limited and provides varied results. 57 , 64 , 65 Families often look to pediatric providers for help in considering whether pubertal suppression is indicated in the context of their child’s overall well-being as gender diverse.
As youth who identify as TGD reflect on and evaluate their gender identity, various interventions may be considered to better align their gender expression with their underlying identity. This process of reflection, acceptance, and, for some, intervention is known as “gender affirmation.” It was formerly referred to as “transitioning,” but many view the process as an affirmation and acceptance of who they have always been rather than a transition from 1 gender identity to another. Accordingly, some people who have gone through the process prefer to call themselves “affirmed females, males, etc” (or just “females, males, etc”), rather than using the prefix “trans-.” Gender affirmation is also used to acknowledge that some individuals who identify as TGD may feel affirmed in their gender without pursuing medical or surgical interventions. 7 , 66
Supportive involvement of parents and family is associated with better mental and physical health outcomes. 67 Gender affirmation among adolescents with gender dysphoria often reduces the emphasis on gender in their lives, allowing them to attend to other developmental tasks, such as academic success, relationship building, and future-oriented planning. 64 Most protocols for gender-affirming interventions incorporate World Professional Association of Transgender Health 35 and Endocrine Society 68 recommendations and include ≥1 of the following elements ( Table 2 ):
The Process of Gender Affirmation May Include ≥1 of the Following Components
Note that the provided age range and reversibility is based on the little data that are currently available.
There is limited benefit to starting gonadotropin-releasing hormone after Tanner stage 5 for pubertal suppression. However, when cross-sex hormones are initiated with a gradually increasing schedule, the initial levels are often not high enough to suppress endogenous sex hormone secretion. Therefore, gonadotropin-releasing hormone may be continued in accordance with the Endocrine Society Guidelines. 68
The effect of sustained puberty suppression on fertility is unknown. Pubertal suppression can be, and often is indicated to be, followed by cross-sex hormone treatment. However, when cross-sex hormones are initiated without endogenous hormones, then fertility may be decreased. 68
Eligibility criteria for gender-affirmative surgical interventions among adolescents are not clearly defined between established protocols and practice. When applicable, eligibility is usually determined on a case-by-case basis with the adolescent and the family along with input from medical, mental health, and surgical providers. 68 , – 71
Social Affirmation: This is a reversible intervention in which children and adolescents express partially or completely in their asserted gender identity by adapting hairstyle, clothing, pronouns, name, etc. Children who identify as transgender and socially affirm and are supported in their asserted gender show no increase in depression and only minimal (clinically insignificant) increases in anxiety compared with age-matched averages. 48 Social affirmation can be complicated given the wide range of social interactions children have (eg, extended families, peers, school, community, etc). There is little guidance on the best approach (eg, all at once, gradual, creating new social networks, or affirming within existing networks, etc). Pediatric providers can best support families by anticipating and discussing such complexity proactively, either in their own practice or through enlisting a qualified mental health provider.
Legal Affirmation: Elements of a social affirmation, such as a name and gender marker, become official on legal documents, such as birth certificates, passports, identification cards, school documents, etc. The processes for making these changes depend on state laws and may require specific documentation from pediatric providers.
Medical Affirmation: This is the process of using cross-sex hormones to allow adolescents who have initiated puberty to develop secondary sex characteristics of the opposite biological sex. Some changes are partially reversible if hormones are stopped, but others become irreversible once they are fully developed ( Table 2 ).
Surgical Affirmation: Surgical approaches may be used to feminize or masculinize features, such as hair distribution, chest, or genitalia, and may include removal of internal organs, such as ovaries or the uterus (affecting fertility). These changes are irreversible. Although current protocols typically reserve surgical interventions for adults, 35 , 68 they are occasionally pursued during adolescence on a case-by-case basis, considering the necessity and benefit to the adolescent’s overall health and often including multidisciplinary input from medical, mental health, and surgical providers as well as from the adolescent and family. 69 , – 71
For some youth who identify as TGD whose natal gender is female, menstruation, breakthrough bleeding, and dysmenorrhea can lead to significant distress before or during gender affirmation. The American College of Obstetrics and Gynecology suggests that, although limited data are available to outline management, menstruation can be managed without exogenous estrogens by using a progesterone-only pill, a medroxyprogesterone acetate shot, or a progesterone-containing intrauterine or implantable device. 72 If estrogen can be tolerated, oral contraceptives that contain both progesterone and estrogen are more effective at suppressing menses. 73 The Endocrine Society guidelines also suggest that gonadotrophin-releasing hormones can be used for menstrual suppression before the anticipated initiation of testosterone or in combination with testosterone for breakthrough bleeding (enables phenotypic masculinization at a lower dose than if testosterone is used alone). 68 Masculinizing hormones in natal female patients may lead to a cessation of menses, but unplanned pregnancies have been reported, which emphasizes the need for ongoing contraceptive counseling with youth who identify as TGD. 72
In addition to societal challenges, youth who identify as TGD face several barriers within the health care system, especially regarding access to care. In 2015, a focus group of youth who identified as transgender in Seattle, Washington, revealed 4 problematic areas related to health care:
safety issues, including the lack of safe clinical environments and fear of discrimination by providers;
poor access to physical health services, including testing for sexually transmitted infections;
inadequate resources to address mental health concerns; and
lack of continuity with providers. 74
This study reveals the obstacles many youth who identify as TGD face in accessing essential services, including the limited supply of appropriately trained medical and psychological providers, fertility options, and insurance coverage denials for gender-related treatments. 74
Insurance denials for services related to the care of patients who identify as TGD are a significant barrier. Although the Office for Civil Rights of the US Department of Health and Human Services explicitly stated in 2012 that the nondiscrimination provision in the Patient Protection and Affordable Care Act includes people who identify as gender diverse, 75 , 76 insurance claims for gender affirmation, particularly among youth who identify as TGD, are frequently denied. 54 , 77 In 1 study, it was found that approximately 25% of individuals who identified as transgender were denied insurance coverage because of being transgender. 31 The burden of covering medical expenses that are not covered by insurance can be financially devastating, and even when expenses are covered, families describe high levels of stress in navigating and submitting claims appropriately. 78 In 2012, a large gender center in Boston, Massachusetts, reported that most young patients who identified as transgender and were deemed appropriate candidates for recommended gender care were unable to obtain it because of such denials, which were based on the premise that gender dysphoria was a mental disorder, not a physical one, and that treatment was not medically or surgically necessary. 24 This practice not only contributes to stigma, prolonged gender dysphoria, and poor mental health outcomes, 77 but it may also lead patients to seek nonmedically supervised treatments that are potentially dangerous. 24 Furthermore, insurance denials can reinforce a socioeconomic divide between those who can finance the high costs of uncovered care and those who cannot. 24 , 77
The transgender youth group in Seattle likely reflected the larger TGD population when they described how obstacles adversely affect self-esteem and contribute to the perception that they are undervalued by society and the health care system. 74 , 77 Professional medical associations, including the AAP, are increasingly calling for equity in health care provisions regardless of gender identity or expression. 1 , 8 , 23 , 72 There is a critical need for investments in research on the prevalence, disparities, biological underpinnings, and standards of care relating to gender-diverse populations. Pediatric providers who work with state government and insurance officials can play an essential role in advocating for stronger nondiscrimination policies and improved coverage.
There is a lack of quality research on the experience of youth of color who identify as transgender. One theory suggests that the intersection of racism, transphobia, and sexism may result in the extreme marginalization that is experienced among many women of color who identify as transgender, 79 including rejection from their family and dropping out of school at younger ages (often in the setting of rigid religious beliefs regarding gender), 80 increased levels of violence and body objectification, 81 3 times the risk of poverty compared with the general population, 31 and the highest prevalence of HIV compared with other risk groups (estimated as high as 56.3% in 1 meta-analysis). 30 One model suggests that pervasive stigma and oppression can be associated with psychological distress (anxiety, depression, and suicide) and adoption of risk behaviors by such youth to obtain a sense of validation toward their complex identities. 79
Research increasingly suggests that familial acceptance or rejection ultimately has little influence on the gender identity of youth; however, it may profoundly affect young people’s ability to openly discuss or disclose concerns about their identity. Suppressing such concerns can affect mental health. 82 Families often find it hard to understand and accept their child’s gender-diverse traits because of personal beliefs, social pressure, and stigma. 49 , 83 Legitimate fears may exist for their child’s welfare, safety, and acceptance that pediatric providers need to appreciate and address. Families can be encouraged to communicate their concerns and questions. Unacknowledged concerns can contribute to shame and hesitation in regard to offering support and understanding, 84 which is essential for the child’s self-esteem, social involvement, and overall health as TGD. 48 , 85 , – 87 Some caution has been expressed that unquestioning acceptance per se may not best serve questioning youth or their families. Instead, psychological evidence suggests that the most benefit comes when family members and youth are supported and encouraged to engage in reflective perspective taking and validate their own and the other’s thoughts and feelings despite divergent views. 49 , 82
In this regard, suicide attempt rates among 433 adolescents in Ontario who identified as “trans” were 4% among those with strongly supportive parents and as high as 60% among those whose parents were not supportive. 85 Adolescents who identify as transgender and endorse at least 1 supportive person in their life report significantly less distress than those who only experience rejection. In communities with high levels of support, it was found that nonsupportive families tended to increase their support over time, leading to dramatic improvement in mental health outcomes among their children who identified as transgender. 88
Pediatric providers can create a safe environment for parents and families to better understand and listen to the needs of their children while receiving reassurance and education. 83 It is often appropriate to assist the child in understanding the parents’ concerns as well. Despite expectations by some youth with transgender identity for immediate acceptance after “coming out,” family members often proceed through a process of becoming more comfortable and understanding of the youth’s gender identity, thoughts, and feelings. One model suggests that the process resembles grieving, wherein the family separates from their expectations for their child to embrace a new reality. This process may proceed through stages of shock, denial, anger, feelings of betrayal, fear, self-discovery, and pride. 89 The amount of time spent in any of these stages and the overall pace varies widely. Many family members also struggle as they are pushed to reflect on their own gender experience and assumptions throughout this process. In some situations, youth who identify as TGD may be at risk for internalizing the difficult emotions that family members may be experiencing. In these cases, individual and group therapy for the family members may be helpful. 49 , 78
Family dynamics can be complex, involving disagreement among legal guardians or between guardians and their children, which may affect the ability to obtain consent for any medical management or interventions. Even in states where minors may access care without parental consent for mental health services, contraception, and sexually transmitted infections, parental or guardian consent is required for hormonal and surgical care of patients who identify as TGD. 72 , 90 Some families may take issue with providers who address gender concerns or offer gender-affirming care. In rare cases, a family may deny access to care that raises concerns about the youth’s welfare and safety; in those cases, additional legal or ethical support may be useful to consider. In such rare situations, pediatric providers may want to familiarize themselves with relevant local consent laws and maintain their primary responsibility for the welfare of the child.
Youth who identify as TGD are becoming more visible because gender-diverse expression is increasingly admissible in the media, on social media, and in schools and communities. Regardless of whether a youth with a gender-diverse identity ultimately identifies as transgender, challenges exist in nearly every social context, from lack of understanding to outright rejection, isolation, discrimination, and victimization. In the US Transgender Survey of nearly 28 000 respondents, it was found that among those who were out as or perceived to be TGD between kindergarten and eighth grade, 54% were verbally harassed, 24% were physically assaulted, and 13% were sexually assaulted; 17% left school because of maltreatment. 31 Education and advocacy from the medical community on the importance of safe schools for youth who identify as TGD can have a significant effect.
At the time of this writing, * only 18 states and the District of Columbia had laws that prohibited discrimination based on gender expression when it comes to employment, housing, public accommodations, and insurance benefits. Over 200 US cities have such legislation. In addition to basic protections, many youth who identify as TGD also have to navigate legal obstacles when it comes to legally changing their name and/or gender marker. 54 In addition to advocating and working with policy makers to promote equal protections for youth who identify as TGD, pediatric providers can play an important role by developing a familiarity with local laws and organizations that provide social work and legal assistance to youth who identify as TGD and their families.
School environments play a significant role in the social and emotional development of children. Every child has a right to feel safe and respected at school, but for youth who identify as TGD, this can be challenging. Nearly every aspect of school life may present safety concerns and require negotiations regarding their gender expression, including name/pronoun use, use of bathrooms and locker rooms, sports teams, dances and activities, overnight activities, and even peer groups. Conflicts in any of these areas can quickly escalate beyond the school’s control to larger debates among the community and even on a national stage.
The formerly known Gay, Lesbian, and Straight Education Network (GLSEN), an advocacy organization for youth who identify as LGBTQ, conducts an annual national survey to measure LGBTQ well-being in US schools. In 2015, students who identified as LGBTQ reported high rates of being discouraged from participation in extracurricular activities. One in 5 students who identified as LGBTQ reported being hindered from forming or participating in a club to support lesbian, gay, bisexual, or transgender students (eg, a gay straight alliance, now often referred to as a genders and sexualities alliance) despite such clubs at schools being associated with decreased reports of negative remarks about sexual orientation or gender expression, increased feelings of safety and connectedness at school, and lower levels of victimization. In addition, >20% of students who identified as LGBTQ reported being blocked from writing about LGBTQ issues in school yearbooks or school newspapers or being prevented or discouraged by coaches and school staff from participating in sports because of their sexual orientation or gender expression. 91
One strategy to prevent conflict is to proactively support policies and protections that promote inclusion and safety of all students. However, such policies are far from consistent across districts. In 2015, GLSEN found that 43% of children who identified as LGBTQ reported feeling unsafe at school because of their gender expression, but only 6% reported that their school had official policies to support youth who identified as TGD, and only 11% reported that their school’s antibullying policies had specific protections for gender expression. 91 Consequently, more than half of the students who identified as transgender in the study were prevented from using the bathroom, names, or pronouns that aligned with their asserted gender at school. A lack of explicit policies that protected youth who identified as TGD was associated with increased reported victimization, with more than half of students who identified as LGBTQ reporting verbal harassment because of their gender expression. Educators and school administrators play an essential role in advocating for and enforcing such policies. GLSEN found that when students recognized actions to reduce gender-based harassment, both students who identified as transgender and cisgender reported a greater connection to staff and feelings of safety. 91 In another study, schools were open to education regarding gender diversity and were willing to implement policies when they were supported by external agencies, such as medical professionals. 92
Academic content plays an important role in building a safe school environment as well. The 2015 GLSEN survey revealed that when positive representations of people who identified as LGBTQ were included in the curriculum, students who identified as LGBTQ reported less hostile school environments, less victimization and greater feelings of safety, fewer school absences because of feeling unsafe, greater feelings of connectedness to their school community, and an increased interest in high school graduation and postsecondary education. 91 At the time of this writing, * 8 states had laws that explicitly forbade teachers from even discussing LGBTQ issues. 54
One of the most important ways to promote high-quality health care for youth who identify as TGD and their families is increasing the knowledge base and clinical experience of pediatric providers in providing culturally competent care to such populations, as recommended by the recently released guidelines by the Association of American Medical Colleges. 93 This begins with the medical school curriculum in areas such as human development, sexual health, endocrinology, pediatrics, and psychiatry. In a 2009–2010 survey of US medical schools, it was found that the median number of hours dedicated to LGBTQ health was 5, with one-third of US medical schools reporting no LGBTQ curriculum during the clinical years. 94
During residency training, there is potential for gender diversity to be emphasized in core rotations, especially in pediatrics, psychiatry, family medicine, and obstetrics and gynecology. Awareness could be promoted through the inclusion of topics relevant to caring for children who identify as TGD in the list of core competencies published by the American Board of Pediatrics, certifying examinations, and relevant study materials. Continuing education and maintenance of certification activities can include topics relevant to TGD populations as well.
The AAP works toward all children and adolescents, regardless of gender identity or expression, receiving care to promote optimal physical, mental, and social well-being. Any discrimination based on gender identity or expression, real or perceived, is damaging to the socioemotional health of children, families, and society. In particular, the AAP recommends the following:
that youth who identify as TGD have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space;
that family-based therapy and support be available to recognize and respond to the emotional and mental health needs of parents, caregivers, and siblings of youth who identify as TGD;
that electronic health records, billing systems, patient-centered notification systems, and clinical research be designed to respect the asserted gender identity of each patient while maintaining confidentiality and avoiding duplicate charts;
that insurance plans offer coverage for health care that is specific to the needs of youth who identify as TGD, including coverage for medical, psychological, and, when indicated, surgical gender-affirming interventions;
that provider education, including medical school, residency, and continuing education, integrate core competencies on the emotional and physical health needs and best practices for the care of youth who identify as TGD and their families;
that pediatricians have a role in advocating for, educating, and developing liaison relationships with school districts and other community organizations to promote acceptance and inclusion of all children without fear of harassment, exclusion, or bullying because of gender expression;
that pediatricians have a role in advocating for policies and laws that protect youth who identify as TGD from discrimination and violence;
that the health care workforce protects diversity by offering equal employment opportunities and workplace protections, regardless of gender identity or expression; and
that the medical field and federal government prioritize research that is dedicated to improving the quality of evidence-based care for youth who identify as TGD.
American Academy of Pediatrics
gender-affirmative care model
Gay, Lesbian, and Straight Education Network
lesbian, gay, bisexual, transgender, or questioning
transgender and gender diverse
Dr Rafferty conceptualized the statement, drafted the initial manuscript, reviewed and revised the manuscript, approved the final manuscript as submitted, and agrees to be accountable for all aspects of the work.
For more information regarding state-specific laws, please contact the AAP Division of State Government Affairs at stgov@ aap.org.
This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
Policy statements from the American Academy of Pediatrics benefit from expertise and resources of liaisons and internal (AAP) and external reviewers. However, policy statements from the American Academy of Pediatrics may not reflect the views of the liaisons or the organizations or government agencies that they represent.
The guidance in this statement does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All policy statements from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
FUNDING: No external funding.
We thank Isaac Albanese, MPA, and Jayeson Watts, LICSW, for their thoughtful reviews and contributions.
Jason Richard Rafferty, MD, MPH, EdM, FAAP
Robert Garofalo, MD, FAAP
Michael Yogman, MD, FAAP, Chairperson
Rebecca Baum, MD, FAAP
Thresia B. Gambon, MD, FAAP
Arthur Lavin, MD, FAAP
Gerri Mattson, MD, FAAP
Lawrence Sagin Wissow, MD, MPH, FAAP
Sharon Berry, PhD, LP – Society of Pediatric Psychology
Ed Christophersen, PhD, FAAP – Society of Pediatric Psychology
Norah Johnson, PhD, RN, CPNP-BC – National Association of Pediatric Nurse Practitioners
Amy Starin, PhD, LCSW – National Association of Social Workers
Abigail Schlesinger, MD – American Academy of Child and Adolescent Psychiatry
Karen S. Smith
James Baumberger
Cora Breuner, MD, MPH, FAAP, Chairperson
Elizabeth M. Alderman, MD, FSAHM, FAAP
Laura K. Grubb, MD, MPH, FAAP
Makia E. Powers, MD, MPH, FAAP
Krishna Upadhya, MD, FAAP
Stephenie B. Wallace, MD, FAAP
Laurie Hornberger, MD, MPH, FAAP – Section on Adolescent Health
Liwei L. Hua, MD, PhD – American Academy of Child and Adolescent Psychiatry
Margo A. Lane, MD, FRCPC, FAAP – Canadian Paediatric Society
Meredith Loveless, MD, FACOG – American College of Obstetricians and Gynecologists
Seema Menon, MD – North American Society of Pediatric and Adolescent Gynecology
CDR Lauren B. Zapata, PhD, MSPH – Centers for Disease Control and Prevention
Karen Smith
Lynn Hunt, MD, FAAP, Chairperson
Anne Teresa Gearhart, MD, FAAP
Christopher Harris, MD, FAAP
Kathryn Melland Lowe, MD, FAAP
Chadwick Taylor Rodgers, MD, FAAP
Ilana Michelle Sherer, MD, FAAP
Ellen Perrin, MD, MA, FAAP
Joseph H. Waters, MD – AAP Section on Pediatric Trainees
Renee Jarrett, MPH

Competing Interests
Sex isn't "assigned" , it's determined.
Please change the word "assigned" to "determined".
The policy states:
"Sex,” or “natal gender,” is a label, generally “male” or “female,” that is typically assigned at birth on the basis of genetic and anatomic characteristics, such as genital anatomy, chromosomes, and sex hormone levels.
This is unscientific and illogical. Sex is a REALITY. It's DETERMINED by observed biology. Not "assigned".
Your use of the word "assigned" demonstrates an anti-science position of denying biological reality.
A health and science professional group like AAP betrays it's professional and scientific credibility by replacing science with politics.
Regards, John Weiss
RE: Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents
Dr. Johnson and Dr. Sax make clear and compelling arguments against some over-reach and mischaracterizations found in this policy statement. I strongly recommend that the committee consider the arguments presented and update the policy statement accordingly.
In addition, I wish to point out the overly broad way in which this committee defined reparative therapy. Not only are physically aversive and shock therapies contained in this committee's definition or repeative therapy, but also non-aversive talk therapies all based around the nebulous idea that the therapist's intentions define the type of therapy.
What type of therapy is it if the child's intentions are to attempt to align her gender with her biological sex, while the therapist remains neutral? Is any amount of challenging considered reparative therapy? If so has the therapist's role changed from being a therapist to being a facilitator? Is there such a thing as therapy without a certain amount of challenging?
Clearly this definition of "reparative therapy" is overly broad, and cumbersome. This type of definition leads to a constraint of legitimate therapy due to the spectre that someone may perceive appropriate therapy to be "reparative" because of the faulty way in which "reparative" therapy is defined.
On a separate note, the citation about the inefficacy of "reparative therapy" for adult gay men has no place in a policy statement for TGD children and adolescents. As stated in the article, sexual orientation and gender are not the same. Likewise, adults are not the same as children or adolescents. When there is not evidence to support the idea put forth, let the idea stand on its own merits. Adding a citation that does not apply draws false parallels and is disengenous.
Thank you for this opportunity to comment on this policy statement. I strongly recommend the revisions mentioned.
Sincerely, Dr. Brown
Thank you for the opportunity to submit a comment on the article mentioned above. Upon reading what I submitted initially, I realize that one salient point was not included in my comments. I would like to submit my comments in their entirety as below:
The excellent points made by Dr. Sax (see comment from 23 Oct 2018 below) encompass many of my concerns about this AAP statement. His clear writing and references clearly call for amendments to this policy statement. Two other important considerations regarding this policy statement are as follows: 1) This AAP statement clearly mischaracterizes watchful waiting as unsupportive and a way of pathologizing. This could not be further from the truth. A watchful waiting approach acknowledges that changes happen as the brain develops and humbly realizes that the ultimate outcome is unknown at an early age. It allows the child self-expression without strict adherence to a label that may not fit in the future. Watchful waiting is both compassionate and flexible; there is no reason to demonize this legitimate clinical approach. Please revise the statement to provide a more accurate description of watchful waiting. 2) The 4th bullet of gender-affirming care states "if a mental health issue exists, it most often stems from stigma and negative experiences rather than being intrinsic to the child". However, the policy statement reports that 20% of matched controls have experienced suicidality and 11% have attempted suicide which is not due to gender-related issues. We have no reason to believe that TGD children would be immune from non gender-related mental health conditions that are often intrinsic to other children and adults. This statement makes this dangerous and often repeated assertion that causes some of the mental health needs of TGD children to be overlooked and under treated. Please revise this bullet.
Sincerely, Paul Johnson MD
What is best practice, when a 7-year-old boy announces that he is really a girl? We do have longitudinal cohort studies which provide useful evidence. Wallien and Cohen-Kettenis (2008) reported on 45 boys and 14 girls who presented with gender dysphoria with a mean age of 8.4 years. Ten years later, 28 of those boys, and 5 of the girls, were no longer gender dysphoric. In other words, of 45 boys followed over ten years, 28 boys, or 62%, did not persist in gender dysphoria. In another study (Singh 2012), 139 boys with gender dysphoria were enrolled at an average age of 7.5 years; at follow-up, averaging 13 years later, only 17 boys out of 139 (12.7%) were still gender-dysphoric. These studies, and others like them (see Zucker 2008 for review), suggest that the majority of boys who identify as gender-dysphoric prior to the onset of puberty will not persist in gender dysphoria after the onset of puberty.
Suppose parents consult a physician regarding their 7-year-old son who has said that he is really a girl. Suppose the physician, mindful of Wallien & Cohen-Kettenis (2008), Singh (2012), and Zucker et al. (2012), advises a cautious wait-and-see approach. The 7-year-old wants to study ballet? Excellent. But he will study ballet as a boy, not a girl, at least for the next year.
Rafferty & Committee (2018) savagely denounce such an approach as “outdated.” Even worse: that physician is trying “to prevent children and adolescents from identifying as transgender”. Such an approach they label “reparative therapy.” They then assert that reparative therapies have been shown to be unsuccessful. In support of that assertion they provide one citation, citation #38, a 1994 report of the lack of success of strategies intended to change the sexual orientation of homosexual men and women. Outdated, indeed. A report documenting the failure of efforts to change the sexual orientation of adults is of doubtful relevance to the question of whether a 5-year-old boy who says that he is a girl should be encouraged to transition.
Rafferty & Committee assert that “more robust and current research” has proven that the old strategy of “watchful waiting” is harmful, and that gender-affirmative strategies should be deployed in prepubertal children. They set no lower age limit for the age at which a child can decide that the child should be reassigned to a different gender. They provide no longitudinal cohort study documenting any outcomes significantly different from those cited above. However, if a clinician were to conclude from studies such as Wallien & Cohen-Kettenis (2008) that watchful waiting is a reasonable approach, Rafferty & Committee harshly reject such an approach, without providing any more recent longitudinal cohort study documenting different outcomes.
Common sense suggests that a 3-year-old boy who says that he is a girl should be subject to some degree of watchful waiting before the boy is put in a dress and has his name legally changed. But such common sense is notably lacking from Rafferty & Committee.
Leonard Sax MD PhD
References:
Singh D. A follow-up study of boys with gender identity disorder. Ph.D. Dissertation, University of Toronto, 2012. Online at http://images.nymag.com/images/2/daily/2016/01/SINGH-DISSERTATION.pdf . Wallien MS, & Cohen-Kettenis PT. Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry. 2008;47(12):1413–1423
Zucker KJ. On the ‘natural history’ of gender identity disorder in children. J Am Acad Child Adolesc Psychiatry. 2008;47(12):1361-1363.
Zucker KJ. A developmental, biopsychosocial model for the treatment of children with gender identity disorder. J Homosexuality 2012:59(3):369-397.
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Login / Register

‘Let’s hear it for the midwives and everything they do’
STEVE FORD, EDITOR
- You are here: Clinical content
Gender identity
The role of specialist nurses in gender identity services
13 December, 2012 By NT Contributor
Nurse specialists can support patients through the gender dysphoria care pathway
Citation: Noble, Vanessa (2012) The role of specialist nurses in gender identity services. Nursing Times ; 108; online issue.
Author : Vanessa Noble is clinical nurse specialist at Leeds Gender Identity Service, Leeds and York Partnership Foundation Trust
- Scroll down to read the article or download a print-friendly PDF including any tables and figures
Introduction
The Leeds Gender Identity Service provides assessment and treatment for people diagnosed with gender dysphoria, which occurs when people believe their biological gender is not consistent with how they feel inside. Many people with this condition express a wish to transition and live full time in their true gender. In some cases, if left untreated, gender dysphoria can lead to deterioration in mental, physical and social health.
The care pathway
After a period of assessment, if appropriate, clients follow a care pathway, which was implemented to standardise care and maintain safe practice for those wishing to transition into the new gender.
The care pathway is as follows:
- Social gender transition;
- First opinion before referral for surgery;
- Referral for a second opinion;
- Referral for gender reassignment surgery;
- Post-surgery follow-up.
Other interventions may include: referral for voice coaching; laser hair removal; breast augmentation; access to the service-user peer-support group; and one-to;-one support with people who have already moved through the care pathway.
The team is made up of seven clinical nurse specialists (CNSs), an occupational therapist, two consultant psychiatrists, a sessional voice coach, a clinical team manager, a pharmacist, a practitioner with special interest and a team administrator.
The CNSs use a range of skills, by continually assessing and evaluating clients who wish to transition. For clients to be accepted onto the care pathway, the following factors must be considered: physical health; social health; mental health; persistent discomfort of the biological gender; identifying with the opposite gender; and whether clients have made a self-diagnosis of gender dypshoria. Finally, the specialist team needs to provide a confirmed diagnosis of gender dysphoria with transsexualism during the assessment process so that clients can move forward to the care pathway.
Social gender transition
During the social gender transition, CNSs work collaboratively with clients to support them through this crucial stage, in which they change their name, engage in meaningful activity in the true gender and change personal details including passport and driving licence. Clients need ongoing support from nurses at this stage as they will have lived in their true gender for 3-6 months on a full-time basis. If clients are unable to do this at this point of the care pathway, they could be discharged from the service until they are ready to move forward.
During this stage a care plan is devised which looks at clients’ individual needs in relation to successful transition.
Ways of working
The service adopts the bio-psychosocial model and provides the following: fact finding; family work; counselling skills; a cognitive behaviour therapy approach; health promotion; practical support; and brief solution-focused therapy.
During the first two parts of the care pathway, it is vital to adopt socratic questioning styles, which seek to get people to answer their own questions by making them think and drawing out the answer from them.
For example: What does it mean to you to change gender? How will you tell others about your gender change? How do you think people will respond? At this point it is crucial that the client-nurse relationship is well established to ensure the client feels supported psychologically. CNSs explore the consequences of the life choices clients choose to take, which may be challenging at times.
A key skill is being able to identify whether clients are eligible and ready to move through to each stage of the care pathway. It is important to understand timescales and to work at a safe pace for each individual. CNSs also discuss clients’ expectations, allowing them to understand possible outcomes of surgery and feelings after surgery.
Advice for nurses
Nurses working with a patient who they think may have gender dysphoria should consider the following points:
- Is the person willing to discuss their gender issues?
- Suggest they carry out as much research as possible on gender dysphoria;
- Can they speak to other transgender people?
- Suggest that the person speaks to their GP for further advice.
Box 1. Resources
● World Professional Association for Transgender Health ● Gender Identity Research and Education Society ● Leeds Gender Identity Service
- Gender dysphoria is not about sexuality; it is about the person and their gender
- Treatment and surgery is available to those clients who are ready and eligible
- Transition to the opposite gender can be a lengthy process. The length of time taken from assessment to post surgery is on average three years
- Funding for treatment and surgery needs to be requested from local primary care trusts unless commissioning arrangements are in place
- There are a number of gender services across the UK; to find the nearest one ask local GPs
Related files
181212 the role of specialist nurses in gender identity services.
- Add to Bookmarks
Have your say
Sign in or Register a new account to join the discussion.
What to Know About the Gender-Affirming-Care Bans Spreading Across the Country

O nly six states in the U.S. have not introduced a bill restricting LGBTQ rights during this legislative session, including Delaware and Illinois. Bathroom bills, measures that would limit the ability to update identity and gender information on records and IDs, sports bans, and bans on gender-affirming care are all up for consideration in states across America.
That last category of bills is growing. On Thursday, Iowa prohibited gender-reassignment procedures and prescriptions, and two of Florida’s State Senate committees passed Senate Bill 254, which would add onto the existing gender-affirming-care restrictions by prohibiting entities from using state funds to cover gender-affirming care, among other things.
Just this year, five states—Mississippi, Utah, South Dakota, Iowa, and Tennessee—have passed bans on gender-affirming care for minors, and nearly 90 other bills targeting access to gender-affirming health care, including Florida’s, are being considered in the U.S.
Proponents of these measures often claim these laws will protect young Americans from what they portray as risky medical experimentation. “We need to let kids be kids, and our laws need to set appropriate boundaries that respect the rights and responsibilities of parents, while protecting children from the serious health, safety, and welfare consequences of social agendas that are totally inconsistent with how the overwhelming majority of parents want to raise their children,” says Florida State Sen. Yarborough, the sponsor of a gender-affirming-care ban in the state, in a press release.
But every major medical organization—including the American Medical Association, American Academy of Pediatrics, American Psychiatric Association, and more— agrees that gender-affirming care for transgender patients , which can range from social interventions, to hormonal treatments, to surgery, is both safe and medically appropriate. For transgender people, who face unemployment at twice the rate of the general population and have a suicide rate nearly nine times that of the broader U.S. population, the prospect of losing access to such care is harrowing.
“Many adolescents with gender dysphoria have severe negative psychological reactions to their bodies developing in ways that do not align with who they are, and [hormonal treatments] can temporarily put these changes on pause,” Dr. Jack Turban, Assistant Professor of Child & Adolescent Psychiatry at The University of California, San Francisco, tells TIME.
Here’s what to know about some of the gender-affirming-care bans being considered across the U.S.
Where have bans been passed already?
Eight states already have gender-affirming-care bans in place for people under the age of 18, and states like Tennessee and Iowa, which both passed legislation this year, are part of the rise in anti-trans legislation being considered more broadly.
They join states like Arkansas, which passed similar legislation two years ago. (Ongoing lawsuits in Arkansas have delayed the program from rolling out, though legislators passed a measure that would criminalize medical practitioners for providing gender- affirming care for minors in March 2023.) Arizona and Alabama also passed gender-care bans in 2022, though the latter’s law is temporarily blocked by legal challenges.
Most laws in this category, like that of Tennessee, would ban puberty blockers and hormone treatment from being used to treat gender dysphoria. Patients would also be unable to undergo surgery.
Healthcare providers who violate the Tennessee law can be sued in civil court within 30 years of the violation. They could also face a fine of up to $25,000 and have their license restricted.
The Tennessee law, which could face lawsuits, is set to go into effect in the summer, though minors who are currently undergoing treatment have until March 31, 2024 to stop treatment.
Where are gender-affirming-care bans being considered?
While the many restrictions on gender-affirming care being considered in state houses across the country do share some similarities, state lawmakers are trying a range of tactics to control access to such medical treatment.
In Oklahoma, for example, state senators are advancing Senate Bill 613 , which would revoke doctors’, nurse practitioners’, or advanced practice nurses’ licenses if they offer gender-transition services to people under the age of 18. (Legislators did add a measure that says the bill would not prevent mental health counseling, depression and anxiety medication or “medications prescribed, dispensed, or administered specifically for the purpose of treating precocious puberty or delayed puberty in that patient.”)
Another bill being considered in the state, Senate Bill 129, adds onto the restrictions by banning transgender medical care at hospitals that indirectly receive public funding. This includes hospitals that are on land that is owned by a state or local government, according to the Oklahoman . House Bill 2177, meanwhile, would prohibit insurance from covering some gender-affirming care, including puberty blockers for minors, is also being considered.
“[People said] we need to protect sports…and then [legislators] didn’t and we knew it wasn’t going to stop there,” Eddie Hefner, a 22-year-old trans, nonbinary Oklahoma resident says. “That’s not what this is about. This is trans-affirming care across the board. And trans health care is essential for saving [lives] because, [for] a lot of the people that I know, to them it is just normal health care.”
Hefner, who plans on getting one gender-affirming surgery in the future, fears that legislators will make age restrictions increasingly strict—and, they say, 18 is already too late for some care. Under previous medical guidelines, UC San Francisco’s Turban tells TIME, most doctors did not allow patients to use gender-affirming hormones until age 16. (Doctors and mental health providers now work with parents to assess the best time frame for a patient to start estrogen or testosterone, which in some cases may be before 16.) But puberty blockers, which stop processes like voice changes or breast growth, are often used in the earlier stages of puberty.“Forcing [patients] to undergo a puberty that doesn’t align with who they are,” he says, “can be horrifying and traumatic.”
In Florida, a ban took effect on March 16 after the Florida Board of Medicine voted in favor of banning gender-affirming care including puberty blockers, cross-sex hormones, and surgery for minors in November.
Doctors who violate the law could face fines and the potential to have their licenses revoked. Legislators are attempting to make that ban law through Senate Bill 254, which would also mean that any healthcare paid for by the state, like Medicaid or state-employee plans, would not cover gender-affirming care.
Devon Ojeda, the Senior National Organizer at the National Center for Transgender Equality, notes that despite the rhetoric used to attack this form of healthcare, cisgender people could also be affected by these types of bans. “Cancer survivors who get breast implants, regardless if they’re cisgender or not, [are getting surgeries that are] affirming their gender,” Ojeda says. “Gender affirming care is for everyone.”
The bill would also allow Florida courts “to enter, modify, or stay a child custody determination relating to a child present in this state to the extent necessary to protect the child from being subjected to sex-reassignment prescriptions or procedures in another state.”
Two Senate committees have passed the bill. It will now head to the Senate floor for a vote.
In Missouri, the State Senate voted to advance their gender-affirming ban after a series of back-door negotiations in which Republican lawmakers agreed they would not prohibit people who are already transitioning from doing so, according to the Associated Press . (Florida’s medical rule has a similar provision.) Missouri’s Attorney General Andrew Bailey also announced on Monday that he would pass an emergency rule that would limit gender-affirming care for minors.
Bailey’s plan would require minors endure 15 hour-long therapy sessions and get a full psychiatric evaluation over the course of 18 months before accessing gender-affirming care.
“I am dedicated to using every legal tool at my disposal to stand in the gap and protect children from being subject to inhumane science experiments,” Bailey tweeted .
Organizations like the ACLU, however, contend that these bills will not protect kids, but are instead “harmful and exploitative.”
“There’s nothing extraordinary about this care except that it saves lives,” Harper Seldin, Staff Attorney for the ACLU’s LGBTQ and HIV Project, tells TIME. “I think it’s important to realize that this is not just an attack on this small group of people but is in fact, part of an ongoing attack on the bodily autonomy of people in every state.”
Correction, April 3
The original version of this story misstated when patients may start gender-affirming hormones. Previous medical guidelines instructed doctors not to begin these treatments before patients turned 16, but those guidelines have been updated.
More Must-Reads from TIME
- The New Face of Doctor Who
- Putin’s Enemies Are Struggling to Unite
- Women Say They Were Pressured Into Long-Term Birth Control
- Scientists Are Finding Out Just How Toxic Your Stuff Is
- Boredom Makes Us Human
- John Mulaney Has What Late Night Needs
- The 100 Most Influential People of 2024
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Rev Bras Enferm
- v.76(Suppl 3); 2023
- PMC10695030

Language: English | Spanish | Portuguese
The ethics of nursing care for transgender people
A ética do cuidado de enfermagem às pessoas transgênero, la ética de la atención de enfermería a las personas transgénero, enrique oltra-rodríguez.
I Facultad de Enfermería de Gijón. Gijón, Asturias, Spain
Eva González-López
II Facultad de Enfermería de Gijón. Hospital de Cruz Roja de Gijón. Gijón, Asturias, Spain
Sofía Osorio-Álvarez
Andrea rodríguez-alonso, objectives:.
to discuss ethical aspects in nursing care for transgender people.
reflective study based on the dilemmas that emerges in nursing care for transgender people. The report was structured around the four bioethical principles.
health care for trans people is complex, transversal to many devices and specialties and longitudinal in time, that is why it requires coordinated action. There is an ethical framework in which the nursing care must be observed in the care of this group.
Final Considerations:
the nurse as a health worker can assume several general lines in the care of transgender patients. So, complementary training should be provided not only to professionals, but also to students of nursing and other health sciences.
debatir sobre aspectos éticos en la atención de enfermería a personas transgénero.
Métodos:
estudio reflexivo fundamentado sobre los dilemas que se plantean en los cuidados de enfermería a personas transgénero. El relato se ha estructurado en torno a los cuatro principios bioéticos.
Resultados:
la atención sanitaria a las personas trans es compleja, transversal a muchos dispositivos y especialidades y longitudinal en el tiempo por lo que precisa de la actuación coordinada. Existe un marco ético en el que se encuadran los cuidados de enfermería que se precisan en la atención a este colectivo.
Consideraciones Finales:
la enfermera como agente de salud puede asumir diversas líneas generales en la atención a pacientes transgénero. Para ello, se debe brindar formación adicional no solo a los profesionales, también a los estudiantes de enfermería y de las demás ciencias de la salud.
discutir aspectos éticos na assistência de enfermagem às pessoas transgênero.
estudo reflexivo a partir dos dilemas que surgem no cuidado de enfermagem às pessoas transgênero. O relato foi estruturado em torno dos quatro princípios bioéticos.
a atenção à saúde de pessoas trans é complexa, transversal a muitos dispositivos e especialidades e longitudinal no tempo, por isso requer ação coordenada. Existe um referencial ético no qual se enquadram os cuidados de enfermagem que devem ser observados no atendimento a esse grupo.
Considerações Finais:
o enfermeiro como agente de saúde pode assumir diversas linhas gerais no atendimento a pacientes transgênero. Para tal, deve ser proporcionada formação complementar não só aos profissionais, mas também aos estudantes de enfermagem e outras ciências da saúde.
INTRODUCTION
In the human species, the genetic determination of gender is chromosomal, homogametic for the female and heterogametic for the male, which conditions gonadal development, with some possible and infrequent variations. In a complex process mediated by the consecutive secretion of gender hormones (fundamentally androgens) in a proportional, meticulous and sensitive way in each gender and at each moment of prenatal development, secondary differentiations are produced. This impregnation and sexual differentiation affect all cells, tissues and organs, both structurally and biochemically. It is very important to note that the brain is also affected in the sexual process, and although at the beginning of the 20th century the endocrinologist and sexologist Dr. Gregorio Marañón said that “The brain is the most important sexual organ of the human being”, it is only very recently, mainly due to the contributions of neuroimaging and genetic analysis techniques, among others, that solid knowledge has been acquired about the sexuation process and more specifically on brain sexuation and, consequently, on the perception of differences in sexual identity. As with gonadal differentiation, in the internal and external genitalia, in the hormonal characteristics and even secondary sexual characteristics, there are cases that deviate from the majority process or statistical normality, it also seems that brain differentiation occurs, and this has consequences for self-perception of identity, which may differ from the biological gender ( 1 ) .
One of the results of the whole process of sexual differentiation is the acquisition of sexual identity, ego sexuation, that is, how everyone perceives themselves as a man or a woman. For most people, ego sexuation coincides with the sex assigned or designated by their environment at birth, allosexuality, and which is based fundamentally on the observation of the external genitalia. After this initial sexing, the whole gender construction process begins, male or female, starting with the attribution of the name, treatment in creation and education, etc. ( 2 ) .
If the two perceptions, ego sexuation and allosexuation, coincided, it would be a situation of cissexuality or cisgender, while if they did not coincide, it would be transsexuality or transgender ( 2 ) . From here, the concept “trans” will be used, since it is quite complex and goes beyond the objectives of this article - to explain the difference between the concepts of transsexuality and transgender.
Both in mythology and in classical cultures, as well as in various ethnic groups and current cultures, sexual identities emerged that could be similar to those that in our society today is known as transsexuals, people who do not accept their biological gender or their assigned gender, or even those who do not fit into the male/female dichotomous categories. These people are known in various fields as the third gender: hijra in Pakistan, khanith in Oman, fa’afafine in Samoa, muxes in Mexico...; they are generally not considered a problem and are even seen socially as a positive value.
It is not easy to know the magnitude of the trans phenomenon because studies are few and those that exist are partial and generally cannot be compared because they are based on different registers, definitions and methodologies. According to a meta-analysis carried out in 2015, based on 250 studies carried out in 9 countries, the overall prevalence of transsexuality was 4.6 in 100000 people: 6.8 for trans women and 2.6 for trans men ( 3 ) . Over the past 50 years, there has been an increase in prevalence. These data are related to people who resort to health systems and, therefore, it can be expected that the social reality is greater, although the value is unknown. This increase in prevalence that seems to be accelerating in recent times raises a debate about its interpretation, some argue that, due to the current greater social permissiveness, cases arise that some time ago did not dare, while other authors are very critical and attribute to other factors such as personal dissatisfactions, personality crises, typical of adolescence, and even a certain social fashion induced by the Queer movement ( 4 ) .
There are two aspects in which a high level of consensus is observed. The first one is that trans people tend to suffer from a worse quality of life, physical and mental health than the general population, related to the situation of vulnerability they suffer. The second one is that they often maintain a relationship with the health systems, either because of health problems or because of the endocrinological and surgical techniques that health care offers them to adjust their body appearance to the perceived gender pattern and the corresponding gender ( 5 - 6 ) .
Currents of thought are also emerging within the trans movement that disagree with the general essentialist approach and that question the relevance of having to redesign or transform the body of those who present incongruence with the perception of their gender, attributing this incongruence to the social sclerosis of the concepts of sex-gender ( 7 ) .
The health needs of transgender people and the care that health systems and professionals provide or deny them mean that several dilemmas are constantly raised and open up debates ranging from ideological to operational and even legislative, and those debates are not alien to nursing as a care profession, accompaniment and defense of people who suffer or need help.
As a guideline for the professional positioning of nurses, an attempt will be made to ethically analyze some of the dilemmas that arise when caring for transgender people, using the model of four principles established by Beauchamp and Childress in Principles of Biomedical Ethics ( 8 ) , which was later qualified by Professor Diego Gracia, hierarchizing these principles ( 9 ) .
To discuss ethical aspects in nursing care for transgender people.
Reflective study in which the most common dilemmas encountered when carrying out a narrative bibliographic review on nursing care for transgender people are analyzed. The analysis will be carried out around the four bioethical principles that constitute the so-called “Hierarchical Principle-ism”, which are: the two principles of minimum requirement that must be fulfilled in all actions to be considered ethical; non-maleficence and justice; while the two principles considered as maximum or of bioethical excellence are: beneficence and autonomy.
As indicated in article 1.2 of the Code of Ethics for Nurses of the International Council of Nursing (ICN) (2021): “Nurses promote an environment in which everyone recognizes and respects the human rights, values, customs, religious and spiritual beliefs of the person, families and communities” ( 10 ) . It is within this ethical framework that the nursing care required in the care of transgender people will be framed.
Non-maleficence
This principle, essential for any action to be considered ethical, stems from the Latin aphorism primum non nocere (first do no harm). In the care of trans people, it has a transcendent application both at the care level and at the community preventive level.
Care must be oriented to avoid the damage that any type of discrimination can cause and that can range from stereotyping these people when they declare themselves trans, making assumptions about their sexual practices or ways of life, to derogatory reactions or disrespect to the name or pronoun with which they are identified. Likewise, sanitary facilities must be adapted to ensure the necessary privacy and dignified treatment.
Transgender people, who so need it, should receive the most appropriate and safe hormone treatments and forms of administration, as indicated by the World Health Organization in its Guidelines on self-care interventions for health and well-being (2022 revision).
No less important are the community health education interventions in schools and families aimed at accepting sexual diversity and, within it, the underage trans. Acceptance is the first necessary step to protect and avoid situations of marginalization or mistreatment, which are the direct cause of the so-called gender dysphoria. Transcendent for the acceptance is the early detection of underage trans within the family and that they understand the nature of the phenomenon so that they can deal with it in a positive way.
This principle is based on providing more care to those who need it the most. The health inequities of this group are recognized, related to the laws and rights recognized in different countries. These inequities occur both in those who start the transition process and in the collective in general, considering the health conditions to which they are forced on multiple occasions, such as socioeconomic and labor situations, mental health and marginality.
It should be part of nurses’ advocacy to encourage public health initiatives involving transgender people, ensure the competence of health professionals for this group and monitor compliance with non-discriminatory policies both in health systems and in society in general.
When carrying out an economic assessment of the transition process, not only the direct costs of health care, basically surgical and hormonal, should be considered, but a rigorous Assessment of Health Technologies should be carried out in which direct, indirect, health and non-sanitary costs are considered, as well as those of difficult tangibility.
Beneficence
As health professionals and if they intend to provide excellent care, they have an ethical obligation to do good if it does not imply a risk to their way of life or coexistence.
Both the process of adaptation and acceptance by families in the case of underage people, and the process of transition or gender reassignment in adults involve a complex and sometimes tortuous and labyrinthine journey.
It is beneficial to monitor and advise families in the community, promoting support and self-help services and networks, in addition to bringing the population closer to knowledge of the trans phenomenon based on science so that citizens can understand it and, consequently, accept and respect it.
People who decide to go through a process of harmonizing their sexual characteristics must go through an intricate journey through the different services of the health systems, simplify it and implement strategies aimed at the specific health care of this population and offer follow-up through figures as a case manager nurse or similar also supposes a beneficial action.
This principle of bioethical excellence is also transcendent, it means facilitating people to make decisions according to their way of being in the world, it implies allowing the right to recognition of the trans condition that is neither volitional, nor apprehensible, nor teachable, nor ephemeral, nor capricious. Therefore, conditions and support are necessary, but also understandable and true information, especially when decisions will condition actions that are difficult or impossible to reverse.
Nurses who capture situations of need, in their role as advocates for patients, should have the responsibility of putting those who need it in contact with specialized professionals or with solvent organizations that provide this information. According to article 1.3 of the ICN code of ethics ( 10 ) , “nurses ensure that the person and the family receive understandable, accurate, sufficient and timely information, in a way that is appropriate to the cultural, linguistic, cognitive and physical needs of the patient, in addition to their psychological state, on which to base their consent to care and corresponding treatment”.
In the case of underage people, although the perception of sexuality corresponds to the individual, autonomy in decision-making corresponds to their legal representatives. It will be necessary to guide the family unit towards early detection, follow up by providing references, contribute to the authentication of the story, rule out interference, respect the process and even accept evanescence situations, if they occur, and encourage prudence, delaying irreversible interventions as much as possible, that is, to provide underage people with as much time as possible for personal maturation so that they can experience and establish the relationship they deem most appropriate with their sexual identity, their body and their gender role, protecting them and always avoiding situations of suffering or marginalization.
FINAL CONSIDERATIONS
Currently, the increase in the prevalence of trans people is worrying, contemplating several hypotheses and requiring more consistent studies. Therefore, especially in childhood and adolescence, the processes must be respected, but acting with prudence.
Hormonal and surgical techniques for sex reassignment have advanced a lot, but they are not free of risks and undesirable side effects, especially regarding the genitals. For this reason and for the options of living fully without assuming the normative conditions of gender in force, the debate is increasingly open and the need to completely transform and, in all cases, the sexual characteristics is questioned. Metaphorically, one can question whether people who experience an inconsistency between their self-perception of gender and their body characteristics should admit that they “were born in the wrong body” or that “they must conquer the body based on their identity” ( 4 , 7 ) .
Nurses as health workers, and from their role as advocates for users of the health system, can assume several general lines of action in the face of the trans phenomenon:
Monitoring and facilitating those who carry out the transition process in their passage through the complex labyrinth of the health system.
Accompanying and advising families and the educational community with doubts about the identity of their children, out of respect, but also out of prudence.
Dissemination of scientific knowledge about the trans phenomenon in society to promote respect for sexual diversity and their rights.
For all these reasons, complementary training should be provided to professionals and students of nursing and other health sciences, with the involvement of both university centers, as well as collegiate entities and professional scientific societies.
In the article “The ethics of nursing care for transgender people”, with DOI number: https://doi.org/10.1590/0034-7167-2022-0797 , published in Revista Brasileira de Enfermagem, 2023;76(Suppl 3):e20220797, in authorship:
Where it read:
Enrique Oltra Rodríguez I
ORCID: 0000-0002-9124-5550
Eva González López II
ORCID: 0000-0001-7653-0110
Sofía Osorio Álvarez I
ORCID: 0000-0002-0624-9259
Andrea Rodríguez Alonso I
ORCID: 0000-0002-5722-2662
How to cite this article:
Rodríguez EO, López EG, Álvarez SO, Alonso AR. The ethics of nursing care for transgender people. Rev Bras Enferm. 2023;76(Suppl 3):e20220797. https://doi.org/10.1590/0034-7167-2022-0797
Corresponding author: Enrique Oltra Rodríguez E-mail: moc.liamg@artloekik
Enrique Oltra-Rodríguez I
Eva González-López II
Sofía Osorio-Álvarez I
Andrea Rodríguez-Alonso I
Oltra-Rodríguez E, González-López E, Osorio-Álvarez S, Rodríguez-Alonso A. The ethics of nursing care for transgender people. Rev Bras Enferm. 2023;76(Suppl 3):e20220797. https://doi.org/10.1590/0034-7167-2022-0797
Corresponding author: Enrique Oltra-Rodríguez E-mail: moc.liamg@artloekik

Gillian Keegan changes transgender stance and agrees men can sometimes become women
Gillian Keegan has said men who undergo gender reassignment are women.
Last month, the Education Secretary told The Telegraph that she would no longer say that trans women were women, and her understanding of the issue had “evolved”.
But in an interview with Radio 4’s Today programme, she said it depended whether the person was self-identifying as the opposite sex or whether they had actually obtained a gender reassignment certificate from a doctor.
To gain a gender recognition certificate, a person must have a signed report from a specialist doctor showing they have “ gender dysphoria ”, which means they are distressed because of the mismatch between their biological sex and their gender identity.
In the first instance, that person was not a woman, but in the second the person was, if only in a legal sense, indicated Ms Keegan.
Grilled on the subject by new Today presenter Emma Barnett , Ms Keegan said she had “always known that trans women aren’t women”.
She said there was a “huge difference between self-identification, people who want to identify but still have a male body, biologically are male: and then there are a very, very small number of people … who do have and have had gender reassignment and reassignment surgery”.
Asked if she would say that people who had gone through gender reassignment were women, she said: “Well, this is what we should say. I personally believe if you have gone to that level of, you have got the gender recognition, you have got the reassignment, then you are legally and medically allowed to say that you are a woman.”
Ms Barnett put it to her: “Those who’ve had their bodies changed, you would say are women, those trans women are women, that’s what you’re delineating between.”
Ms Keegan replied: “I think that’s a sensitive way to handle it.”
She was also asked how widespread the teaching of “inappropriate” material about gender identity was in schools.
“I don’t think it’s widespread, I mean, I don’t know because you know, it’s not something that we’ve gone and done a particular survey of,” she said.
In an at-times-tense exchange, Ms Barnett put it to Ms Keegan that it was “staggering” that the education secretary did not know how widespread the issue was.
Ms Barnett said: “It’s staggering that you are across education but you have no idea how widespread this problem is. It matters because teachers, some of them say, this isn’t an issue at all. You’ve even almost just said that yourself and you’ve just created silence around one of these issues.”
Later on Thursday, Ms Keegan unveiled her department’s new guidance on relationships, sex and health education (RSHE) in the Commons.
It says children must not be given sex education before the age of nine , and that gender ideology should not be treated as fact.
The Education Secretary said gender identity “should not be taught in schools at any age”.
“Following disturbing reports from parents of pupils being taught inappropriate content in schools, and requests from schools who wanted more clarity on when to teach certain topics, the Prime Minister and I decided to bring forward the review into RSHE,” she said.
Core values
Ms Keegan said the guidance was “underpinned by three core values”.
She said: “One, parents have a right to know what their children are being taught . Two, teachers are there to teach children facts, not push the agendas of campaign groups. Three, schools should not teach about the contested issue of gender identity, including that gender is a spectrum.”
Catherine McKinnell, Labour’s shadow education minister, said: “Teaching children about the facts of the world in which they grow up must include an understanding that there are people who are transgender, that people can go through a process of change of their gender, and that the law provides for that.”
Sir John Hayes, the Conservative former minister, told the Commons: “Darkness falls when very young children are forced to know too much too early and their innocence is stolen.
“Will the secretary of state look again at the third-party organisations often invited into schools – sometimes witlessly, sometimes carelessly – for they steal children’s innocence in the name, very often, of diversity and inclusion, and in so doing promote, promulgate and perpetuate every kind of horror?”
Ms Keegan’s comments on trans women differ from the view she expressed in 2020 , when she said: “Trans women are women and trans people deserve equal and fair access to healthcare, safe spaces, and opportunities, as well as to live their life with dignity.”
The statement was made in response to a question from an LGBT forum in her constituency of Chichester.
She told The Telegraph that she had changed her position.
“Since becoming an MP and later a minister I have learnt a huge amount more about this complex and challenging subject,” she said.
“At the time of writing that response, I didn’t have any direct experience of this topic and took advice on how best to respond, given the complexities surrounding individual cases. Having now spoken to experts and professionals, like many, my understanding has evolved.
“I have since been crystal clear about my concerns that women are being erased in this debate, and have always been clear that women do not have, nor have ever had, a penis.”
Play The Telegraph’s brilliant range of Puzzles - and feel brighter every day. Train your brain and boost your mood with PlusWord, the Mini Crossword, the fearsome Killer Sudoku and even the classic Cryptic Crossword.

Florida's transgender affirming care ban is now law. Here's what SB 254 does:

Florida Gov. Ron DeSantis signed a new bill into law Wednesday that restricts gender-affirming care for transgender adults and children .
Critics of the bill, SB 254, refer to it as the Florida “abduction” bill because they claim it allows children to be “legally kidnapped” by disagreeing parents — even if the opposing parent lives across state lines — if the child is subject to or “threatened” with sex-reassignment prescriptions or procedures.
Senator Clay Yarborough, who introduced the bill, said the bill is meant to protect children from “drastic life-altering gender dysphoria therapies and surgeries” that he said are being prescribed for children. He argued that both parents should have a say in whether their child receives gender-affirming care.
Florida's anti-LGBTQ bills: A rundown of Florida bills causing 'massive panic' in transgender, LGBTQ communities
SB 254 lands on DeSantis' desk: Restrictions on transgender health care pass Florida Legislature, head to DeSantis
The Tallahassee Democrat reported that while the legislation was not as wide-reaching as House members wanted it to be, it will still restrict care for both transgender children and adults. Along with the ban for new youth patients, the bill requires that a physician administer gender affirming care to adult patients in person, barring the use of telehealth and other health care workers, like nurse practitioners and physicians' assistants, to begin care. Doctors who violate those sections could face a first-degree misdemeanor.
Gender-affirming care for youth has support from nearly every mainstream medical organization, including the American Academy of Pediatrics, the World Health Organization, the Endocrine Society and the American Psychiatric Association. Politifact has determined that while the state cannot kidnap children, the law can affect custody disputes.
LGBTQ advocacy groups said last week they plan to ask a judge to block the law as part of an ongoing lawsuit against the Board of Medicine ban.
Here’s a breakdown of what’s in the bill:
Florida courts can receive temporary emergency jurisdiction
The bill would grant Florida courts temporary emergency jurisdiction if a child present in the state has been abandoned; it’s deemed necessary if the child, a sibling or the parent of a child is subjected to or “threatened” with mistreatment or abuse; or if the child is subjected to or “threatened” with sex-reassignment prescriptions or procedures.
Parents can apply for a warrant to receive physical custody of a child
Section 2 of the bill allows parents to file a petition seeking enforcement of a child custody determination. If a parent believes that their child is likely to “imminently suffer serious physical harm or removal of the state,” they can file a verified issuance of a warrant to take physical custody of the child.
The section explicitly states that serious physical harm “includes, but is not limited to,” being subjected to sex-reassignment prescriptions and procedures.
Florida diversity, pronoun bills: Florida bills targeting diversity programs and pronouns in schools heads to DeSantis
Censoring drag shows, Pride events: In one day, three bills targeting transgender Floridians pass House
State funds are prohibited from being used for gender-affirming care
Another section of the bill prohibits any “governmental entity” from expending state funds for sex-reassignment prescriptions or procedures.
State is erasing trans options: What can I do if I'm a transgender person living in Florida?
People under 18 can no longer receive gender-affirming care unless they qualify for an exception
Section 5 of the bill prohibits sex-reassignment prescriptions and procedures for patients younger than 18 years old. The Board of Medicine and the Board of Osteopathic Medicine will have 60 days to adopt emergency rules pertaining to standards of practice where a minor could continue to be treated with a prescription consistent with those defined in Florida Statute 456.001.
That transition-related medical care includes puberty blockers, hormones and surgery. Despite claims by DeSantis that medical care amounts to child mutilation, gender-affirmation surgery is generally only recommended for adults. For children, care doesn't begin until the onset of puberty.
Physicians must be in the room with adults receiving gender-affirming care, barring the use of telehealth services
The same section also requires that physicians prescribing, administering a pharmaceutical product or performing a procedure must be, at minimum, physically present in the same room as the patient.
Further restrictions require that only physicians can administer and perform these procedures, barring other health care workers, like nurse practitioners and physicians' assistants, to begin care.
The Tallahassee Democrat reported that at least one Florida clinic that provides gender-affirming care is staffed only by nurse practitioners, leaving care for those patients uncertain under the bill. SPEKTRUM Health serves patients in Central Florida with locations in Orlando and Melbourne.
"Absolutely gutted," CEO Joey Knoll told the Democrat on Thursday. "I've spent the last year trying to raise awareness, get help, and avoid a catastrophe ... that is now imminent."
- Newsletters
- Instapundit
- News & Politics
Appeals Court Finds a Constitutional Right to Gender Reassignment Surgery

The 14th Amendment to the Constitution is truly a magical amendment. It was used to justify attempts to kick Donald Trump off the 2024 ballot. Through the decades, judges who want to play at social engineering have used it frequently to justify questionable law.
It's even been invoked to bypass Congress to raise the debt limit.
Now, the Fourth Circuit Court of Appeals has decided that the amendment's "equal protection" clause means that state Medicaid programs have to cover gender reassignment surgeries.
The appeals court ruled that West Virginia's Medicaid rules on mastectomies are unconstitutional because they violate the "equal protection standard" by not covering mastectomies for gender dysphoria.
Yes, really.
The ruling also includes a North Carolina Medicaid case that the state government won't cover "sex changes." The Fourth Circuit nullified the state ban on gender change surgeries, citing the 14th Amendment’s guarantee of “equal protection of the laws.”
This was a court looking for an excuse to make law.
Judge Roger Gregory who wrote the majority opinion in Kadel v. Folwell (8-6) asked, “Is removing a patient’s breasts to treat cancer the same procedure as removing a patient’s breasts to treat gender dysphoria?” He continued, “There is no case law to ground this discussion nor obvious first principles.”
Wall Street Journal:
He is undeterred, and he concludes that gender dysphoria and transgender status are intertwined, so that such insurance exclusions are nothing more than a proxy for discriminating against gender identity. Then he goes further, finding that West Virginia’s and North Carolina’s policies also unconstitutionally discriminate based on sex. How so? Imagine, Judge Gregory says, an unidentified patient seeking a vaginoplasty. Is this a biological female with a rare birth defect? Is it a transgender patient? “By virtue of the fact that they are seeking a vaginoplasty, we know that they were born without a vagina,” he writes. “But we do not know what sex they were assigned at birth. Without that information, we cannot say whether the Plan or Program will cover the surgery.” Ergo, sex discrimination.
Gregory gets even nuttier.
The differences in coverage "is rooted in a gender stereotype: the assumption that people who have been assigned female at birth are supposed to have breasts, and that people assigned male at birth are not."
It's not a "gender stereotype." It's a biological fact.
"No doubt, the majority of those assigned female at birth have breasts, and the majority of those assigned male at birth do not. But we cannot mistake what is for what must be.”
Not just a "majority." It's a universal biological fact with a tiny number of exceptions.
Treating different things differently doesn’t violate the 14th Amendment’s Equal Protection Clause, and jurists aren’t supposed to ignore the obvious. Writing in dissent at the Fourth Circuit, Judge Julius Richardson struggles to contain his exasperation. “The states,” he says, “have chosen to cover alterations of a person’s breasts or genitalia only if the person experiences physical injury, disease, or (in West Virginia) congenital absence of genitalia.” That determination does not turn on the patient’s sex or gender. “Christopher Fain—one of the plaintiffs below—received coverage for a hysterectomy based on a diagnosis unrelated to Fain’s transgender status,” the dissent says. Likewise, males with gynecomastia qualify for surgery coverage in West Virginia only “if they have physical symptoms, like breast pain,” meaning that isn’t a procedure done merely “to affirm a patient’s biological sex.”
The ruling that opened this can of worms was Bostock v. Clayton County, a case that "held that Title VII of the Civil Rights Act of 1964 protects employees against discrimination because of sexuality or gender identity." Now, as a dissenting judge in Kadel v. Folwell, Judge J. Harvie Wilkinson III is saying that this ruling could be a Roe v Wade ruling for the transgender community.
“This is imperial judging at its least defensible,” he says, “What plaintiffs propose is nothing less than to use the Constitution to establish a nationwide mandate that States pay for emerging gender dysphoria treatments.”
He's not wrong. But getting the ruling past this Supreme Court would be a stretch.

Rick Moran has been writing for PJ Media for 18 years. His work has appeared in dozens of media outlets including the Washington Times and ABC News. He was an editor at American Thinker for 14 years. His own blog is Right Wing Nut House . For media inquiries, please contact [email protected] .
Recommended

Trending on PJ Media Videos
- Michael Cohen Gets Destroyed During Cross Examination, Leaving Anderson Cooper Stunned
- Trump Attorney Delivers a Perry Mason Moment Against Michael Cohen
- Time for the Bud Light Treatment: NFL Denounces Player for Advocating Traditional Values
Assistant Manager, Nurse - Proton Therapy Center
- Requisition #: 167823
- Department: Radiation Therapeutic Nursing
- Location: Houston, TX
- Posted Date: 5/14/2024
- Requisition ID: 167823
- Employment Status: Full-Time
- Employee Status: Regular
- Work Week: Day/Evening, Evenings
- Minimum Salary: US Dollar (USD) 86,000
- Midpoint Salary: US Dollar (USD) 115,500
- Maximum Salary : US Dollar (USD) 144,500
- FLSA: exempt and eligible for overtime, paid at a straight rate
- Fund Type: Hard
- Work Location: Onsite
- Pivotal Position: No
- Referral Bonus Available?: Yes
- Relocation Assistance Available?: Yes
- Science Jobs: No
Be more at MD Anderson
- Applicant Rights & Notices
- EEO / Accessibility
- mdanderson.org
© 2024 The University of Texas MD Anderson Cancer Center
School of Nursing
- Which Program is Right for Me Overview
- Comparing the PhD & DNP
- Technical Standards
- Bachelor of Science in Nursing
- Master of Nursing
- PhD in Nursing
- Doctor of Nursing Practice
- Certificate Overview
- Adult Gerontological Acute Care Nurse Practitioner Certificate
- Leadership in Health Information Technology for Health Professionals Certificate
- Population Health Informatics and Technology (PHIT) Certificate
- Post-Graduate Certificate Program Overview
- Meet Our Students
- Current Student Resources
- Office of Student & Career Advancement Services
- Research Overview
- Research Projects
- Research Day
- Faculty Grants
- Faculty Experts
- Laboratory of Clinical Exercise Physiology
- Publications Overview
- Books by Faculty
- Research Seminars
- Student Research Resources
- About the Office of Nursing Research and Scholarship
- News & Events Overview
- Minnesota Nursing Magazine Overview
- Current Issue
- Magazine Issue Archive
- Clinical Preceptors Overview
- BSN/MN (Prelicensure) Preceptor Information
- DNP Preceptor Information
- Clinical Preceptor e-Toolkit
- Nurse-midwifery specialty
- DNP Project Ideas
- Nurse Practitioners Clinic
- School of Nursing at a Glance
- School of Nursing Leadership
- Our Faculty
- Faculty Emeriti & Faculty Ad Honorem
- Cooperatives
- Faculty Honors and Awards
- Employment Opportunities
- Our Facilities Overview
- Bentson Health Communities Innovation Center
- Bakken Center for Spirituality and Healing
- Global Health Overview
- Visiting Scholars
- Global Collaborations
- Global Health Faculty Scholars
- Opportunities for Students
- Inclusivity, Diversity & Equity
- Professional Development
- Giving to Nursing Overview
- Areas of Need
- Scholarships
- Impact Stories
- Ways to Give
- Board of Trustees
- History Overview
- Heritage Committee
- History of Our School Leadership
- Program Histories
- Historical Videos and Photos
- Sigma Theta Tau International Overview
- Zeta Chapter Board
- Grants & Awards
- Volunteer Opportunities
- Alumni Overview
- Submit a Class Note
- Alumni Society Awards Overview
- Rising Star Award
- Distinguished Alumni Humanitarian Award
- Excellence in Practice Award
- Board of Directors
- Degree Verification
- Volunteering
- Centers Overview
- Center for Adolescent Nursing Overview
- Center Projects
- Learning Opportunities
- Publications
- Center for Aging Science & Care Innovation Overview
- Center for Child and Family Health Promotion Research Overview
- Center for Children with Special Health Care Needs Overview
- Contact form
- Center projects
- Center for Nursing Informatics Overview
- 2024 Nursing Knowledge: Big Data Science Conference
- Previous Conferences
- Nursing Knowledge Big Data Science Initiative
- Center for Planetary Health and Environmental Justice Overview
- Katharine J. Densford International Center for Nursing Leadership Overview
- Leadership Model
- Directorate
- Initiatives
- Contact the Center
- 2024 Planting Seeds of Innovation Colloquium
Leveraging generative AI to modernize nursing education
May 13, 2024 Brett Stursa

Martin Michalowski
The proliferation of new generative artificial intelligence (AI) tools can be challenging for nurse educators and clinicians to keep up with, as the potential benefits also come with new challenges.
Associate Professor Martin Michalowski, PhD, FAMIA, examines generative AI in nursing education and provides recommendations for nurse educators to optimize its use in recent publications.
Michalowski’s most recent article, The ChatGPT Effect: Nursing Education and Generative Artificial Intelligence, published in the February issue of the Journal of Nursing Education, examines generative AI in nursing education more broadly and urges nurse educators to harness its potential.
Prompt engineering when using generative AI in nursing education, published in the January issue of Nurse Education in Practice, makes recommendations to integrate prompt engineering — the process of refining questions to get better results — in nursing education.
“Generative AI is one of the key required competencies and it needs to be integrated into the education nurses receive both as concepts to understand and as tools to use,” says Michalowski. “Similar to concepts in machine learning, natural language processing, automated reasoning, and other AI subfields, generative AI is transforming the provision of care. Therefore, it is important that nurses understand how to use it, and how its use impacts health care systems, providers and patients.”
Currently, he says that the most effective uses of generative AI in nursing classrooms is creating mock patient-related data and providing patient scenarios for practice.
“When applying learned theories or tools where patient-related data is needed, generative AI models are very useful for building synthetic data in different formats, like tables, free text notes, etc.,” says Michalowski.
“Additionally, generative AI enables critical thinking through the creation of patient use cases/scenarios. This application is one of the few where hallucinations — presenting output patterns as fact while they are clinically or factually incorrect — is acceptable. Students need to apply what they learned and use critical thinking to identify inaccuracies and contradictions in the use case. The instructor can also tailor the output use cases by providing important context for the learning exercise.”
Michalowski says it’s imperative nurse educators integrate AI competencies into their classrooms to ensure students are well equipped as future clinicians.
“Nurses have an incredible opportunity to lead health care’s transformation of clinical care with AI. They touch all aspects of the care process, understand the clinical problems and interface with patients. They are positioned to be the bridge between AI developers, health care practitioners and stakeholders,” says Michalowski. “However, to fully realize this potential they need basic AI competencies that aren’t currently part of their education.”
Categories: Research
In this Issue: Spring-Summer 2024
Building collaborations with Tribal Nations, health care and higher ed
Nursing informatics, innovation empower nurses.

We celebrate 115 years of ‘the educated spirit of the nurse’
- Admission Requirements
- Required Courses
- Admissions Requirements
- How to Apply
- Post-Graduate Certificate Program Plans by Specialty
- Message from the Dean
- Board of Visitors
- Adult & Gerontological Health
- Child & Family Health
- Population Health & Systems
- Tenured Faculty Opportunities
- Tenure-Track Faculty
- Clinical Track Faculty Opportunities
- Postdoctoral Fellowship Program
- Guidance for Applicants for faculty positions
- Marie Manthey Endowed Professorship
- Leaving a Nursing Legacy
- 100 Distinguished Nursing Alumni (A-E)
- 100 Distinguished Nursing Alumni (F-J)
- 100 Distinguished Nursing Alumni (K-O)
- 100 Distinguished Nursing Alumni (P-T)
- 100 Distinguished Nursing Alumni (U-Z)
- Distinguished Faculty Alumni
- Program Histories Overview
- Adult-Gero Nurse Practitioner Programs
- DNP Program
- Geriatric Nurse Practitioner/Geriatric Clinical Nurse Specialist
- Health Innovation and Leadership
- Integrative Health and Healing
- Master of Nursing Administration
- Nurse Anesthesia
- Nurse Midwifery
- Nursing Informatics
- Pediatric Primary Care Nurse Practitioner
- PhD Program
- Practical Nursing Program
- Pre-licensure programs
- Psychiatric-Mental Health
- Public Health Nursing
- Women's Health Nurse Practitioner
- Evidence-based Practice Grants
- Research Grants
- Travel Grants
- Summer Institute in Adolescent Health
- Past Summer Institutes in Adolescent Health
- Clinical Teaching in Nursing Homes
- Resources for Clinical Teaching in Nursing Homes
- Competencies for Public Health Nursing Practice Instrument
- Families as Teachers
- Doctoral Education Pathway for American Indian/Alaska Native Nurses
- Accreditation
- Call for Abstracts
- Registration
- Online Teaching Resources
- 2022 Nursing Knowledge: Big Data Science Conference
- 2020 Nursing Knowledge: Big Data Science Conference
- 2019 Workgroups
- 2018 Workgroups
- 2017 Nursing Knowledge: Big Data Science Conference
- 2016 Workgroups
- 2015 Workgroups
- 2014 Nursing Knowlege: Big Data Science Conference
- 2013 Nursing Knowledge: Pre-conference Materials
- Vision and Mission
- Five-Year Strategic Plan
- Steering committee
- Resources for Workgroup Members
- Nursing Knowledge: Big Data Science Conference
- Nursing Big Data Repository
- Contact information and social media
- Foresight Leadership
Education Secretary Gillian Keegan says gender identity 'should not be taught in schools at any age'
The education secretary, who oversaw draft statutory sex education guidance published on Thursday, said while gender reassignment should be taught in school, gender 'ideology' shouldn't be presented as fact. The NSPCC responded by criticising age limits in the guidance.
By Claire Gilbody Dickerson, news reporter
Thursday 16 May 2024 16:22, UK
Please use Chrome browser for a more accessible video player

Gender identity "should not be taught in schools at any age", the education secretary has said after new draft guidance on relationships, sex and health education (RSHE) was published on Thursday.
The draft guidance for schools in England was compiled following concerns that children were being exposed to "inappropriate" content. It states that sex education should be taught no earlier than year five, when pupils are aged nine, and what is described as the "contested topic of gender identity" should not be taught at all.
In her foreword on the document, Gillian Keegan said the guidance is about giving children the "right information at the right time" but also ensuring "childhood innocence" isn't taken away by being taught "too much too soon".

The NSPCC criticised imposing age limits, saying children and young people must be empowered to "recognise when something isn't right and seek help when it's needed".
The children's charity added now should be the time to "embed" lessons on life-enhancing skills rather than "back-track on RSE in schools".
Ms Keegan said while gender reassignment should be taught, "schools should not teach about the contested issue of gender identity, including that gender is a spectrum".
"Whilst protected characteristics such as gender reassignment should be taught, they must be done so on a factual basis, at an appropriate age and not based on contested ideology," she added.
Read more: The gender treatments currently available to children PM urges 'extreme caution' on gender treatments

Keep up with all the latest news from the UK and around the world by following Sky News
'Evidence pupils being taught there could be 72 genders'
Ms Keegan launched the review after there had been "some evidence from some people" that pupils were being taught that there could be "72 genders" and gender could "change daily" as facts.
Speaking in the House of Commons after the guidance was published, Labour's shadow education minister Catherine McKinnell said: "Teaching children about the facts of the world in which they grow up must include an understanding that there are people who are transgender, that people can go through a process of change of their gender, and that the law provides for that."
Be the first to get Breaking News
Install the Sky News app for free

Guidance on harmful sexual behaviour published
Subjects around what constitutes harmful sexual behaviour in relationships, the concepts and laws relating to sexual harassment, revenge porn, sexual exploitation and abuse, grooming, stalking and forced marriage should not be taught before year seven (age 11), the guidance states.
While the risks of inappropriate online content such as pornography can be discussed "in an age-appropriate way" from year seven, the details of sexual acts should not be discussed before year nine (age 13) it adds.
When it comes to laws relating to sexual violence, including rape and sexual assault, the guidance sets out it is important for pupils to understand the key principles around such offences including what consent means, but says "schools should not teach about this in any sexually explicit way before year nine".
Related Topics
- Weird But True
- Sex & Relationships
- Viral Trends
- Human Interest
- Fashion & Beauty
- Food & Drink
trending now in Lifestyle

Bride calls out wedding guest's 'ridiculous' RSVP: 'Nothing I can...

Doctor cancer-free one year after using own revolutionary...

McDonald's adds sad option to replace Happy Meal smile

I'm a dermatologist — this is the one nail sign you should...

Gen Z daughter tries to explain what she does at family steel...

'Anti-sex' beds have arrived at Paris Olympics — after horny...

McDonald's is getting rid of free drink refills — and more...

Hoka just launched a new 'illegal' running shoe that's worth the...
Breaking news, university apologizes after wildly mispronouncing graduates’ names: ‘she made a graduation entertaining’.
- View Author Archive
- Follow on Twitter
- Get author RSS feed
Thanks for contacting us. We've received your submission.
How em-bar-uhs-ing.
A Thomas Jefferson University presenter utterly butchered students’ names during the Jefferson College of Nursing commencement ceremony on May 9 .
“My apologies for the phonetic spelling or pronunciation of the names that was on the cards,” the speaker said during the graduation. “I would have been better just reading from the book. My apologies, graduates.”
Thomas Jefferson University explained that the odd delivery was due to the way phonetic spellings were shown on the speaker’s name cards.
She incorrectly pronounced several nursing students’ names, such as Jessica, Allison, Sarah, Louise, Virginia, Stephanie, Maeve, Molly and Elizabeth.

Instead of saying “Molly Elizabeth Camp,” the speaker said “Mollina—zabeth—cap.” For Maeve Elizabeth, she blurted out “May-vee Lee Zu-beth.” And Sarah Virginia Brennan’s name was pronounced as “Sayer Oo-voon Geen-goo Bree-none.”
But one name took many attendees by surprise, and that name was “Tha-mo-may,” also known as Thomas Michael Canevari Jr.

As the presenter says, “Tha-mo-may,” many audience members sigh in disappointment, and the student frustratedly corrects her, saying, “It’s Thomas.”
Many people found it odd that the presenter needed help pronouncing Thomas correctly, even though the institution is named Thomas Jefferson University.
The university located in Philadelphia, Pennsylvania, apologized to graduates for the embarrassing name mispronunciations that went viral over the weekend.
“Leadership and faculty of Thomas Jefferson University extend our sincerest apologies for the mispronunciations of the names of several of our graduating nursing students during our recent commencement ceremony,” the university said in a statement posted on Facebook.

The viral moment had people roasting the university online for such a major flop.
“It’s the fact that the college itself is Thomas Jefferson University and the person calling out the graduate’s names couldn’t pronounce Thomas… it’s literally the schools name lol,” one person tweeted on X.
“As a parent, I would be [mad] if it was my kids,” a parent commented.
“Hysterical!! Glad our profs know what they’re doing!!” tweeted another.
Even comedian Jimmy Fallon joined in on the roast, sharing the clip on his late night show , claiming “she did the impossible, she made a graduation entertaining.”
However with three more commencement ceremonies scheduled on May 21 and 22 at the university, graduations can’t anticipate no muh-stayks.
Share this article:

Advertisement
- Skip to main content
- Keyboard shortcuts for audio player
My Unsung Hero
After a serious car accident, a man pulled over — and continued to help for days.
Laura Kwerel

Apryle Oswald. Apryle Oswald hide caption
Apryle Oswald.
This story is part of the My Unsung Hero series from the Hidden Brain team. It features stories of people whose kindness left a lasting impression on someone else.
In 1997, Apryle Oswald was on a road trip with her boyfriend and two dogs, driving through a wide-open stretch of Nevada. Suddenly, one of the dogs tried to jump in the front seat. Oswald swerved and lost control of the car.
"I can picture it very, very clearly," she remembered. "The car did a somersault, back-over-front, for nearly a hundred yards."
Once it stopped, she unfastened her seatbelt and got out of the car, yelling for her boyfriend, John Williams, who had disappeared.
"All of a sudden I see him come running towards me, and then I collapse," she said. She learned later she had bruised lungs and splintered ribs. "And I remember laying on the ground, and I just couldn't get up ... I remember being cold — really, really cold."

They had 3 suitcases and faced 5 flights of stairs. That's when a stranger appeared

A funeral home worker tracked down a family — and uncovered a decades-old secret
At that point it was around midnight, with below-freezing temperatures. One of their dogs was badly injured, and needed attention. Williams tried to flag down the cars driving by, but no one slowed down. They started to panic.
"I ... remember him coming back and saying, 'Nobody's stopping, nobody's stopping,'" she said.
Williams eventually took off his coat and threw it at a truck coming by. "He got the guy to stop," Oswald said. "And that guy's ... the unsung hero."
Oswald doesn't recall his name, or what he looked like. But she remembers his deep voice, and how he wrapped her in a blanket.
"I recall in my mind ... this scratchy wool plaid blanket, and covering me up to make sure I was warm," she said.
Luckily the man had an emergency radio in his truck, so he called for help. An air medical helicopter arrived and evacuated Oswald to the hospital.
If her unsung hero had left after that, it would have been enough. She believes that if not for him, she might have died of hypothermia. But his generosity didn't end there.

The way a dying baby girl was cared for in 1980 helped shape her approach to nursing

No one could figure out the cause of her cough. Then a nurse practitioner had an idea
For the next three nights, the man drove Williams back and forth between his motel and the hospital, so Williams could visit her. He even drove their injured dog, Digby, to the veterinary clinic for blood transfusions.
"He just really cared," she said. "And he just went above and beyond."
She wishes she had gotten his phone number, to thank him again for saving her life — and for sticking around to help.
"I mean, who does that?" she said. "What an amazing person ... what an amazing thing for a stranger to do in the middle of a cold Nevada night."
After that, Oswald never saw the man again. But now, whenever she sees a person having car troubles, or who looks cold or hungry, she always stops. It's her way of paying the favor forward.
"If I go by somebody that needs help, I always think, 'Is there something I can do?'" Oswald said. "I feel compelled to help when I can."
My Unsung Hero is also a podcast — new episodes are released every Tuesday.
- car accident

IMAGES
COMMENTS
Still, transgender individuals — people whose gender is different than the one assigned at birth — and gender nonconforming (GNC) patients continue to face challenges and prejudice in healthcare settings. Nurses have an especially important role in providing an affirming space for transgender people. Many patients confide in nurses ...
1. A transgender patient is a person with a health concern. 2. Our job as nursing professionals is to provide equitable care. Nurses who are firmly grounded in these two tenets are on their way to providing quality care for these patients. Make the best career decision ever.
However, all nurses can be prepared to provide affirming care, which is a step toward building safer, more inclusive practice. Affirming care recognizes the significant impact of sexual/gender minority status on a person's health. The health assessment course is a natural place to begin discussions of LGBTQ affirming care; for example, when ...
Nurses are important in primary care for transgender people. One of the main challenges was the lack of education, but mentoring and collaboration contributed to skills development. Ensuring the workplace provided gender-affirming care was key to a safe and inclusive environment. Conclusion.
Gender dysphoria refers to the distress experienced by an individual when one's gender identity and sex are not completely congruent. ... Sobralske M. Primary care needs of patients who have undergone gender reassignment. J Am Acad Nurse Pract. 2005; 17 (4):133-138. [Google Scholar] 5. Unger CA. Hormone therapy for transgender patients.
For transgender and nonbinary individuals, early and continued access to gender-affirming care is critical to improving confidence and allowing people to use their focus for transitioning socially while navigating the complex and sometimes unwelcoming healthcare system. Gender-affirming care can include social affirmation, puberty blockers ...
In the United States, approximately 150,000 youth and 1.4 million adults identify as transgender. 1, 2 As sociocultural acceptance patterns evolve, clinicians will likely care for an increasing ...
These treatments can include a combination of medical (cross-sex hormone therapy), surgical (genital reassignment surgery and non-genital surgical procedures), mental health and other related treatments and services (e.g. speech and voice therapy). 2, 6, 7 However, delayed treatment initiation and barriers to access are common, because the ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. To help provide guidance for those considering gender affirmation surgery, two experts from the Johns Hopkins Center for Transgender Health answer questions about what to expect before and after your surgery.
Gender reassignment procedures sought by transgender patients are costly, and more insurance companies have begun to provide coverage for transgender individuals who meet the criteria for gender reassignment surgery. 40 For example, insurance companies such as Aetna, Cigna, and Blue Cross Blue Shield have expanded transgender-related coverage ...
An estimated 1.4 million transgender adults live in the United States; this equates to approximately 0.6% of the U.S. population (Lane et al., 2018). Clinical focus on gender dysphoria has significantly increased over the past 30 years (MacCarthy, Reisner, Nunn, Perez-Brumer, & Operario, 2015), …
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
This Policy Statement was reaffirmed August 2023.. As a traditionally underserved population that faces numerous health disparities, youth who identify as transgender and gender diverse (TGD) and their families are increasingly presenting to pediatric providers for education, care, and referrals. The need for more formal training, standardized treatment, and research on safety and medical ...
As nurses, it is important to be culturally sensitive to all patients, respective of diversity, and appropriate care. As social acceptance has grown, awareness of gender identity and sexual preferences has increased. The term "transgender" is used for individuals who don't identify with the gender they were assigned at birth.
Gender dysphoria can occur at any age, although young children often explore gender identity through dress-up and play at age 3. Youth experiencing gender incongruence need access to health care providers who are aware of medical interventions for gender reassignment and the importance of follow-up care. Nurse practitioners (NPs) need to be well versed on issues surrounding gender identity ...
Nurses, nurse practitioners, physician assistants. Trainees (residents and fellows). Advertisement. ... Gender reassignment is an outdated term for gender affirmation surgery. The new language, "gender affirmation," is more accurate in terms of what the surgery does (and doesn't) do. ...
Nurse specialists can support patients through the gender dysphoria care pathway. Citation: Noble, Vanessa(2012) The role of specialist nurses in gender identity services. Nursing Times; 108; online issue. Author: Vanessa Noble is clinical nurse specialist at Leeds Gender Identity Service, Leeds and York Partnership Foundation Trust.
7 minutes. June 17, 2015. With the current media frenzy about Caitlyn Jenner,aka Bruce Jenner, questions about the transgender cohort have been moved to the forefront of society. Nurses sometimes struggle with the care and management of transgender patients. Recent studies have documented the need for inclusion of the care of the LGBT ...
On Thursday, Iowa prohibited gender-reassignment procedures and prescriptions, and two of Florida's State Senate committees passed Senate Bill 254, which would add onto the existing gender ...
The questions are usually very specific, but the principles tend to be broadly applicable. Today's question is from an anonymous woman. She writes, "Pastor John, hello! I am a nurse in surgery pre-op and recovery for a hospital that performs gender-reassignment surgeries. I play no role in the decisions made to undergo these surgeries.
Hormonal and surgical techniques for sex reassignment have advanced a lot, but they are not free of risks and undesirable side effects, especially regarding the genitals. For this reason and for the options of living fully without assuming the normative conditions of gender in force, the debate is increasingly open and the need to completely ...
Among the patients receiving psychiatric care, women who received psychiatric care from men providers reported that they felt misunderstood (42.2%) and dismissed or patronized (47.4%). These ...
Gillian Keegan has said men who undergo gender reassignment are women. Last month, the Education Secretary told The Telegraph that she would no longer say that trans women were women, and her ...
2:53. Florida Gov. Ron DeSantis signed a new bill into law Wednesday that restricts gender-affirming care for transgender adults and children. Critics of the bill, SB 254, refer to it as the ...
The Fourth Circuit nullified the state ban on gender change surgeries, citing the 14th Amendment's guarantee of "equal protection of the laws." This was a court looking for an excuse to make ...
Assistant Nurse Manager Proton Therapy Center: Services - Head & Neck, GI, Thoracic, Pediatrics/CNS. ... Ensures scheduling and assignment/reassignment of staff meet the needs of the patient. Participates in hiring and performance management of employees. ... religion, age, national origin, sex, gender, sexual orientation, gender identity ...
The NP of sex and drugs. As a rural nurse practitioner, Emily Carroll, DNP '20, shows where there's a will, there's a way. Briefly. See all Spring-Summer 2024 Stories. School of Nursing Sitewide Footer. 5-140 Weaver-Densford Hall 308 Harvard Street SE Minneapolis, MN 55455
Gender identity "should not be taught in schools at any age", the education secretary has said after new draft guidance on relationships, sex and health education (RSHE) was published on Thursday.
4. Thomas Jefferson University commencement presenter mispronounced nursing gradutes names horribly. Thomas Jefferson University. Instead of saying "Molly Elizabeth Camp," the speaker said ...
In 1997, Apryle Oswald got in a car accident. The man who responded went on to help for three more days — driving her dog to the vet and Oswald's boyfriend back and forth to the hospital.