

Introduction to qualitative nursing research
This type of research can reveal important information that quantitative research can’t.
- Qualitative research is valuable because it approaches a phenomenon, such as a clinical problem, about which little is known by trying to understand its many facets.
- Most qualitative research is emergent, holistic, detailed, and uses many strategies to collect data.
- Qualitative research generates evidence and helps nurses determine patient preferences.
Research 101: Descriptive statistics
Differentiating research, evidence-based practice, and quality improvement
How to appraise quantitative research articles
All nurses are expected to understand and apply evidence to their professional practice. Some of the evidence should be in the form of research, which fills gaps in knowledge, developing and expanding on current understanding. Both quantitative and qualitative research methods inform nursing practice, but quantitative research tends to be more emphasized. In addition, many nurses don’t feel comfortable conducting or evaluating qualitative research. But once you understand qualitative research, you can more easily apply it to your nursing practice.
What is qualitative research?
Defining qualitative research can be challenging. In fact, some authors suggest that providing a simple definition is contrary to the method’s philosophy. Qualitative research approaches a phenomenon, such as a clinical problem, from a place of unknowing and attempts to understand its many facets. This makes qualitative research particularly useful when little is known about a phenomenon because the research helps identify key concepts and constructs. Qualitative research sets the foundation for future quantitative or qualitative research. Qualitative research also can stand alone without quantitative research.
Although qualitative research is diverse, certain characteristics—holism, subjectivity, intersubjectivity, and situated contexts—guide its methodology. This type of research stresses the importance of studying each individual as a holistic system (holism) influenced by surroundings (situated contexts); each person develops his or her own subjective world (subjectivity) that’s influenced by interactions with others (intersubjectivity) and surroundings (situated contexts). Think of it this way: Each person experiences and interprets the world differently based on many factors, including his or her history and interactions. The truth is a composite of realities.
Qualitative research designs
Because qualitative research explores diverse topics and examines phenomena where little is known, designs and methodologies vary. Despite this variation, most qualitative research designs are emergent and holistic. In addition, they require merging data collection strategies and an intensely involved researcher. (See Research design characteristics .)
Although qualitative research designs are emergent, advanced planning and careful consideration should include identifying a phenomenon of interest, selecting a research design, indicating broad data collection strategies and opportunities to enhance study quality, and considering and/or setting aside (bracketing) personal biases, views, and assumptions.
Many qualitative research designs are used in nursing. Most originated in other disciplines, while some claim no link to a particular disciplinary tradition. Designs that aren’t linked to a discipline, such as descriptive designs, may borrow techniques from other methodologies; some authors don’t consider them to be rigorous (high-quality and trustworthy). (See Common qualitative research designs .)
Sampling approaches
Sampling approaches depend on the qualitative research design selected. However, in general, qualitative samples are small, nonrandom, emergently selected, and intensely studied. Qualitative research sampling is concerned with accurately representing and discovering meaning in experience, rather than generalizability. For this reason, researchers tend to look for participants or informants who are considered “information rich” because they maximize understanding by representing varying demographics and/or ranges of experiences. As a study progresses, researchers look for participants who confirm, challenge, modify, or enrich understanding of the phenomenon of interest. Many authors argue that the concepts and constructs discovered in qualitative research transcend a particular study, however, and find applicability to others. For example, consider a qualitative study about the lived experience of minority nursing faculty and the incivility they endure. The concepts learned in this study may transcend nursing or minority faculty members and also apply to other populations, such as foreign-born students, nurses, or faculty.
Qualitative nursing research can take many forms. The design you choose will depend on the question you’re trying to answer.
| Action research | Education | Conducted by and for those taking action to improve or refine actions | What happens to the quality of nursing practice when we implement a peer-mentoring system? |
| Case study | Many | In-depth analysis of an entity or group of entities (case) | How is patient autonomy promoted by a unit? |
| Descriptive | N/A | Content analysis of data | |
| Discourse analysis | Many | In-depth analysis of written, vocal, or sign language | What discourses are used in nursing practice and how do they shape practice? |
| Ethnography | Anthropology | In-depth analysis of a culture | How does Filipino culture influence childbirth experiences? |
| Ethology | Psychology | Biology of human behavior and events | What are the immediate underlying psychological and environmental causes of incivility in nursing? |
| Grounded theory | Sociology | Social processes within a social setting | How does the basic social process of role transition happen within the context of advanced practice nursing transitions? |
| Historical research | History | Past behaviors, events, conditions | When did nurses become researchers? |
| Narrative inquiry | Many | Story as the object of inquiry | How does one live with a diagnosis of scleroderma? |
| Phenomenology | Philosophy Psychology | Lived experiences | What is the lived experience of nurses who were admitted as patients on their home practice unit? |
A sample size is estimated before a qualitative study begins, but the final sample size depends on the study scope, data quality, sensitivity of the research topic or phenomenon of interest, and researchers’ skills. For example, a study with a narrow scope, skilled researchers, and a nonsensitive topic likely will require a smaller sample. Data saturation frequently is a key consideration in final sample size. When no new insights or information are obtained, data saturation is attained and sampling stops, although researchers may analyze one or two more cases to be certain. (See Sampling types .)
Some controversy exists around the concept of saturation in qualitative nursing research. Thorne argues that saturation is a concept appropriate for grounded theory studies and not other study types. She suggests that “information power” is perhaps more appropriate terminology for qualitative nursing research sampling and sample size.
Data collection and analysis
Researchers are guided by their study design when choosing data collection and analysis methods. Common types of data collection include interviews (unstructured, semistructured, focus groups); observations of people, environments, or contexts; documents; records; artifacts; photographs; or journals. When collecting data, researchers must be mindful of gaining participant trust while also guarding against too much emotional involvement, ensuring comprehensive data collection and analysis, conducting appropriate data management, and engaging in reflexivity.

Data usually are recorded in detailed notes, memos, and audio or visual recordings, which frequently are transcribed verbatim and analyzed manually or using software programs, such as ATLAS.ti, HyperRESEARCH, MAXQDA, or NVivo. Analyzing qualitative data is complex work. Researchers act as reductionists, distilling enormous amounts of data into concise yet rich and valuable knowledge. They code or identify themes, translating abstract ideas into meaningful information. The good news is that qualitative research typically is easy to understand because it’s reported in stories told in everyday language.
Evaluating a qualitative study
Evaluating qualitative research studies can be challenging. Many terms—rigor, validity, integrity, and trustworthiness—can describe study quality, but in the end you want to know whether the study’s findings accurately and comprehensively represent the phenomenon of interest. Many researchers identify a quality framework when discussing quality-enhancement strategies. Example frameworks include:
- Trustworthiness criteria framework, which enhances credibility, dependability, confirmability, transferability, and authenticity
- Validity in qualitative research framework, which enhances credibility, authenticity, criticality, integrity, explicitness, vividness, creativity, thoroughness, congruence, and sensitivity.
With all frameworks, many strategies can be used to help meet identified criteria and enhance quality. (See Research quality enhancement ). And considering the study as a whole is important to evaluating its quality and rigor. For example, when looking for evidence of rigor, look for a clear and concise report title that describes the research topic and design and an abstract that summarizes key points (background, purpose, methods, results, conclusions).
Application to nursing practice
Qualitative research not only generates evidence but also can help nurses determine patient preferences. Without qualitative research, we can’t truly understand others, including their interpretations, meanings, needs, and wants. Qualitative research isn’t generalizable in the traditional sense, but it helps nurses open their minds to others’ experiences. For example, nurses can protect patient autonomy by understanding them and not reducing them to universal protocols or plans. As Munhall states, “Each person we encounter help[s] us discover what is best for [him or her]. The other person, not us, is truly the expert knower of [him- or herself].” Qualitative nursing research helps us understand the complexity and many facets of a problem and gives us insights as we encourage others’ voices and searches for meaning.

When paired with clinical judgment and other evidence, qualitative research helps us implement evidence-based practice successfully. For example, a phenomenological inquiry into the lived experience of disaster workers might help expose strengths and weaknesses of individuals, populations, and systems, providing areas of focused intervention. Or a phenomenological study of the lived experience of critical-care patients might expose factors (such dark rooms or no visible clocks) that contribute to delirium.
Successful implementation
Qualitative nursing research guides understanding in practice and sets the foundation for future quantitative and qualitative research. Knowing how to conduct and evaluate qualitative research can help nurses implement evidence-based practice successfully.
When evaluating a qualitative study, you should consider it as a whole. The following questions to consider when examining study quality and evidence of rigor are adapted from the Standards for Reporting Qualitative Research.
| o What is the report title and composition of the abstract? o What is the problem and/or phenomenon of interest and study significance? o What is the purpose of the study and/or research question? | → Clear and concise report title describes the research topic and design (e.g., grounded theory) or data collection methods (e.g., interviews) → Abstract summarizes key points including background, purpose, methods, results, and conclusions → Problem and/or phenomenon of interest and significance is identified and well described, with a thorough review of relevant theories and/or other research → Study purpose and/or research question is identified and appropriate to the problem and/or phenomenon of interest and significance |
| o What design and/or research paradigm was used? o Is there evidence of researcher reflexivity? o What is the setting and context for the study? o What is the sampling approach? How and why were data selected? Why was sampling stopped? o Was institutional review board (IRB) approval obtained and were other issues relating to protection of human subjects outlined? | → Design (e.g., phenomenology, ethnography), research paradigm (e.g., constructivist), and guiding theory or model, as appropriate, are identified, along with well-described rationales → Design is appropriate to research problem and/or phenomenon of interest → Researcher characteristics that may influence the study are identified and well described, as well as methods to protect against these influences (e.g., journaling, bracketing) → Settings, sites, and contexts are identified and well described, along with well-described rationales |
| o What data collection and analysis instruments and/or technologies were used? o What is the method for data processing and analysis? o What is the composition of the data? o What strategies were used to enhance quality and trustworthiness? | → Sampling approach and how and why data were selected are identified and well described, along with well-described rationales; participant inclusion and exclusion criteria are outlined and appropriate → Criteria for deciding when sampling stops is outlined (e.g., saturation) and rationale is provided and appropriate → Documentation of IRB approval or explanation of lack thereof provided; consent, confidentiality, data security, and other protection of human subject issues are well described and thorough → Description of instruments (e.g., interview scripts, observation logs) and technologies (e.g., audio-recorders) used is provided, including how instruments were developed; description of if and how these changed during the study is given, along with well-described rationales → Types of data collected, details of data collection, analysis, and other processing procedures are well described and thorough, along with well-described rationales → Number and characteristics of participants and/or other data are described and appropriate → Strategies to enhance quality and trustworthiness (e.g., member checking) are identified, comprehensive, and appropriate, along with well-described rationales; trustworthiness framework, if identified, is established from experts (e.g., Lincoln and Guba, Whittemore et al.) and strategies are appropriate to this framework |
| o Were main study results synthesized and interpreted? If applicable, were they developed into a theory or integrated with prior research? o Were results linked to empirical data? | → Main results (e.g., themes) are presented and well described and a theory or model is developed and described, if applicable; results are integrated with prior research → Adequate evidence (e.g., direct quotes from interviews, field notes) is provided to support main study results |
| o Are study results described in relation to prior work? o Are study implications, applicability, and contributions to nursing identified? o Are study limitations outlined? | → Concise summary of main results are provided and thorough, including relation to prior works (e.g., connection, support, elaboration, challenging prior conclusions) → Thorough discussion of study implications, applicability, and unique contributions to nursing is provided → Study limitations are described thoroughly and future improvements and/or research topics are suggested |
| o Are potential or perceived conflicts of interest identified and how were these managed? o If applicable, what sources of funding or other support did the study receive? | → All potential or perceived conflicts of interest are identified and well described; methods to manage potential or perceived conflicts of interest are identified and appear to protect study integrity → All sources of funding and other support are identified and well described, along with the roles the funders and support played in study efforts; they do not appear to interfere with study integrity |
Jennifer Chicca is a PhD candidate at the Indiana University of Pennsylvania in Indiana, Pennsylvania, and a part-time faculty member at the University of North Carolina Wilmington.
Amankwaa L. Creating protocols for trustworthiness in qualitative research. J Cult Divers. 2016;23(3):121-7.
Cuthbert CA, Moules N. The application of qualitative research findings to oncology nursing practice. Oncol Nurs Forum . 2014;41(6):683-5.
Guba E, Lincoln Y. Competing paradigms in qualitative research . In: Denzin NK, Lincoln YS, eds. Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications, Inc.;1994: 105-17.
Lincoln YS, Guba EG. Naturalistic Inquiry . Thousand Oaks, CA: SAGE Publications, Inc.; 1985.
Munhall PL. Nursing Research: A Qualitative Perspective . 5th ed. Sudbury, MA: Jones & Bartlett Learning; 2012.
Nicholls D. Qualitative research. Part 1: Philosophies. Int J Ther Rehabil . 2017;24(1):26-33.
Nicholls D. Qualitative research. Part 2: Methodology. Int J Ther Rehabil . 2017;24(2):71-7.
Nicholls D. Qualitative research. Part 3: Methods. Int J Ther Rehabil . 2017;24(3):114-21.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med . 2014;89(9):1245-51.
Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice . 10th ed. Philadelphia, PA: Wolters Kluwer; 2017.
Thorne S. Saturation in qualitative nursing studies: Untangling the misleading message around saturation in qualitative nursing studies. Nurse Auth Ed. 2020;30(1):5. naepub.com/reporting-research/2020-30-1-5
Whittemore R, Chase SK, Mandle CL. Validity in qualitative research. Qual Health Res . 2001;11(4):522-37.
Williams B. Understanding qualitative research. Am Nurse Today . 2015;10(7):40-2.

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Increasing diversity in nursing with support from Nurses on Boards Coalition

Adventures in lifelong learning

The power of language

Making peace with imperfection

When laws and nursing ethics collide

Taking on health disparities

Medication safety and pediatric health

Confidence is in

Tailored falls prevention plans

Men in nursing

FAQs: AI and prompt engineering

Caring for adults with autism spectrum disorder

Known fallers

Florence Nightingale overcame the limits set on proper Victorian women – and brought modern science and statistics to nursing

Bird flu is bad for poultry and dairy cows. It’s not a dire threat for most of us — yet.
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Qualitative Research
The “what,” “why,” “who,” and “how”.
Cypress, Brigitte S. EdD, RN, CCRN
Brigitte S. Cypress, EdD, RN, CCRN, is assistant professor at Lehman College and The Graduate Center, City University of New York.
The author has disclosed that she has no significant relationships with, or financial interest in, any commercial companies pertaining to this article.
Address correspondence and reprint requests to: Brigitte S. Cypress, EdD, RN, CCRN, PO Box 2205, Pocono Summit, PA 18346 ( [email protected] ).
There has been a general view of qualitative research as a lower level form of inquiry and the diverse conceptualizations of what it is, its use or utility, its users, the process of how it is conducted, and its scientific merit. This fragmented understanding and varied ways in which qualitative research is conceived, synthesized, and presented have a myriad of implications in demonstrating and enhancing the utilization of its findings and the ways and skills required in transforming knowledge gained from it. The purpose of this article is to define qualitative research and discuss its significance in research, the questions it addresses, its characteristics, methods and criteria for rigor, and the type of results it can offer. A framework for understanding the “what,” “why,” “who,” and “how” of qualitative research; the different approaches; and the strategies to achieve trustworthiness are presented. Qualitative research provides insights into health-related phenomena and seeks to understand and interpret subjective experience and thus humanizes health care and can enrich further research inquiries and be made clearer and more rigorous as it is relevant to the perspective and goals of nursing.
Qualitative research methods began to appear in nursing in 1960s and 1970s amid cautious and reluctant acceptance. In the 1980s, qualitative health research emerged as a distinctive domain and mode of inquiry. 1 Qualitative research refers to any kind of research that produces findings not arrived at by means of statistical analysis or other means of quantification. 2,3 It uses a naturalistic approach that seeks to understand phenomena about persons’ lives, stories, and behavior including those related to health, organizational functioning, social movements, or interactional relationships. Qualitative research is underpinned by several theoretical perspectives, namely, constructivist-interpretive, critical, postpositivist, poststructural/postmodern, and feminism. 4 One conducts a qualitative study to uncover the nature of the person’s experiences with a phenomenon in context-specific conditions such as illness (acute and chronic), addiction, loss, disability, and end of life. Qualitative research is used to explore, uncover, describe, and understand what lies behind any phenomenon about which maybe little is known. This deeper understanding of the phenomenon in its specific context can be attained only through a qualitative inquiry than mere numbers and statistical models could provide using a quantitative approach. Qualitative inquiry represents a legitimate mode of social and human science exploration, without apology or comparisons to quantitative research. 5
This article describes what is qualitative research methodology, the “what,” “why,” “who,” and “how,” including its components. The aim is to simplify the terminology and process of qualitative inquiry to enable novice readers of research to better understand the concepts involved.
WHY DO QUALITATIVE RESEARCH?
The tradition of using qualitative methods to study human phenomena is grounded in the social sciences. 6 This methodological revolution has made way for a more interpretative approach because aspects of human values, culture, and relationships are not described fully using quantitative research methods. Unlike quantitative researchers who seek causal determination, prediction, and generalization of findings, qualitative researchers allow for the phenomenon of interest to unfold naturally, 7 strive to explore, describe and understand it, and delve into a colorful, deep, contextual world of interpretations. 8 Thus, the practice of qualitative research has expanded to clinical settings because empirical approaches have proven to be inadequate in answering questions related to human subjectivity where interpretation is involved. 9 Consequently, qualitative health research is a research approach to exploring health and illness as they are perceived by the people themselves rather than from the researcher’s perspective. 10 Morse 10 further stated that “Researchers use qualitative research methods to illicit emotions and perspectives, beliefs and values, actions, and behaviors and to understand the participant’s responses to health and illness and the meanings they construct about the experience.” 10 (p21) It provides a rich inductive description that necessitates interpretations. Researchers in the health care arena, practitioners, and policy makers are increasingly pressed to translate these findings for practice, put them to use, and evaluate how useful they actually are in effecting desired change with goal of improving public health and reducing disparities in health care delivery. 1 Even though qualitative research has been used for many decades, and it is in fact flourishing, it is not free of criticisms from experts with impoverished view of the methodology.
Despite the current urgency of the utilization of qualitative methodologies in research studies, questions are raised for its lack of objectivity, generalizability, utility, and its tendency to be anecdotal. 1 Critics continue to make these charges related to their limited understanding of qualitative designs, approaches, and methods. Sandelowski 1 asserted that the current urgency about the utility of qualitative research findings is the result of several converging trends in health care research that include the elevation of practical over basic knowledge as the highest form of knowledge, the proliferation of qualitative health research studies, and the rise of evidence-based practice as a paradigm and methodology for health care. 1 Consequently, these events have, in turn, contributed to the growing interest of incorporating qualitative health research findings into evidence-based practice.
Morse 10 asserted that there are other reasons for conducting a qualitative inquiry. Others believe that the role of qualitative inquiry is to provide hypothesis and research questions that can be posed from the findings of qualitative research studies. Qualitative research can also serve as a foundation from which surveys and questionnaires could be developed, thus increasing its validity that would produce models for quantitative testing. But, what is really the most important function of qualitative inquiry? According to Morse, 10 this key function is the moral imperative of qualitative inquiry to humanize health care. She stated, “The social justice agenda of qualitative health research is one that humanizes health care.” 10 (p52) So, what is humanizing health care? Morse 10 stated, “Humanizing encompasses a perspective on attitudes, beliefs, expectations, practices, and behaviors that influence the quality of care, administration of that care, conditions judged to warrant (or not warrant) empathetic care, responses to care and therapeutics, and anticipated and actual outcomes of patient or community care.” 10 (pp54,55)
Conducting research should be sort of a social justice project. 10 Denzin 11 recognizes making social justice a public agenda within qualitative inquiry. He emphasized that qualitative inquiry can contribute to social justice through ( a ) identifying different definitions of a problem and/or situation that is being evaluated with some agreement that change is required; ( b ) the assumptions that are held by policy makers, clients, welfare workers, online professionals, and other interested parties can be located and shown to be correct or incorrect; ( c ) strategic points of interventions can be identified and thus evaluated and improved; ( d ) suggest alternative moral points of view from which the problem, the policy, and the program can be interpreted and assessed; and ( e ) the limits of statistics and statistical evaluations can be exposed with the more qualitative materials furnished by this approach. 11
WHO DOES QUALITATIVE RESEARCH?
Qualitative research is done by researchers in the social sciences as well as by practitioners in fields that concern themselves with issues related to human behavior and functioning. 3 They are also health professionals who are able to identify a research question and able to recognize the particular context and situation that would achieve the best answers. 10 According to Morse, 10 the qualitative health researcher should be an expert methodologist who should have the understanding of illness, the patient’s condition, and the staff roles and relationships and able to balance the clinical situation from different perspectives. 10 (p23) A qualitative researcher also requires theoretical and social sensibility, interactional skills, and the ability to maintain analytical distance while drawing upon past experience and theoretical knowledge to interpret what is seen or observed. 3
WHAT ARE THE CHARACTERISTICS OF QUALITATIVE RESEARCH?
Creswell 12 discussed that qualitative research studies today involve closer attention to the interpretive nature of inquiry and situating the study within the political, social, and cultural context of the researchers, participants, and readers of the study. He presented several characteristics of qualitative research, which are ( a ) natural setting: data are collected face-to-face in the field at the site where participants experience the phenomenon under study; the inquiry should be conducted in a way that does not disturb the natural context of the phenomenon; ( b ) researcher as key instrument: the researchers collect the data themselves rather than relying on instruments developed by others; ( c ) multiple sources of data: researchers gather multiple forms of data including interviews, observations, and examining documents rather than rely on a single source; ( d ) inductive data analysis: data are organized into abstract units of information (“bottom-up” or moving from specific to general), working back and forth between the themes and the database until a comprehensive set of themes is established and ending up with general conclusions or theories; ( e ) participant’s meanings: the researchers keep a focus on learning the meaning that the participants hold about the phenomenon, not the meaning that the researchers bring to the study; ( f ) emergent design: the initial plan for the study cannot be tightly prescribed; rather, it is emergent, and all phases of the process may change or shift after the researchers enter the field and begin to collect the data; ( g ) theoretical lens: use of a “lens” to view the study such as the concept of culture, gender, race or class differences, and social, political, or historical context of the problem under study; ( h ) interpretive inquiry: a form of inquiry in which researchers make interpretation of what they see, hear, and understand that cannot be separated from their own background, history, context, and prior understanding; ( i ) holistic account: reporting multiple perspectives, identifying the many factors involved in a situation, and sketching the larger picture that emerges. 12
WHAT ARE THE METHODS FREQUENTLY USED IN QUALITATIVE RESEARCH?
The research question dictates the method to be used for a qualitative study. Qualitative and quantitative questions are distinct and serve different purposes. 10 Some of the different types of qualitative research that will be discussed in this article are phenomenology, grounded theory, ethnography, case study, and narrative research. Researchers from different disciplines use these approaches depending on what the purpose of the study is.
Narrative research begins with the experiences as expressed in lived and told stories of individuals. Narrative is a spoken word or written text giving an account of an event/action chronologically connected. Some examples of this approach are biographical studies, autobiographies, and life stories. Kvangarsnes et al 13 explored the patient perceptions of chronic obstructive pulmonary disease exacerbation and their experiences of their relations with health personnel during care and treatment using narrative research design. Ten in-depth qualitative interviews were conducted with patients who had been admitted to 2 intensive care units (ICUs) in Western Norway during the autumn of 2009 and the spring of 2010. Narrative analysis and theories on trust and power were used to analyze the interviews. The patients perceived that they were completely dependent on others during the acute phase. Some stated that they had experienced an altered perception of reality and had not understood how serious their situation was. Although the patients trusted the health personnel in helping them breathe, they also told stories about care deficiencies and situations in which they felt neglected. This study shows that patients with an acute exacerbation of chronic obstructive pulmonary disease often feel wholly dependent on health personnel during the exacerbation and, as a result, experience extreme vulnerability.
Whereas a narrative approach explores the life of a single person, a phenomenological study describes the meaning for several individuals of their lived experiences of a phenomenon. 12 Phenomenology is the most inductive of all qualitative methods. 10 The philosophical assumptions of phenomenology rest on some common grounds: the study of the lived experiences of persons, the view that these experiences are conscious ones and the development of descriptions of the essences of these experiences, not explanations or analysis. 12 There are different types of phenomenological approaches, namely, descriptive-transcendental (Husserl, Giorgi), interpretive/hermeneutic (Heidegger, Gadamer, Jen-Luc Nancy), descriptive-hermeneutic (van Manen), empirical-transcendental (Moustakas), and existential (Sarte, Heidegger, Merleau-Ponty). A phenomenological study conducted by Cypress 14 explored the lived experiences of nurses, patients, and family members during critical illness in the emergency department (ED). Data were collected over a 6-month period by means of in-depth interviews, and thematic analysis was done using van Manen’s 15 hermeneutic-phenomenological approach. The findings of this qualitative phenomenological study indicate that the patient’s and family member’s perception of the nurses in the ED relates to their critical thinking skills, communication, sensitivity, and caring abilities. Nurses of this study identified that response to the patient’s physiological deficit is paramount in the ED, and involving the patients and families in the human care processes will help attain this goal.
While phenomenology aims to illuminate themes and describe the meaning of lived experiences of a number of individuals, grounded theory has the intent to move beyond description and to generate or discover a theory, an abstract analytical schema of a process, or interaction shaped by the views of a large number of participants. 12 This qualitative method was developed by Glaser and Strauss 16 in 1967. Other grounded theorists followed, including Clarke, 17 who relies on postmodern perspectives, and Charmaz, 18 on constructivist approach. Gallagher et al 19 collected and analyzed qualitative data using grounded theory to understand nurses’ end-of-life (EOL) decision-making practices in 5 ICUs in different cultural contexts. Interviews were conducted with 51 experienced ICU nurses in university or hospital premises in 5 countries. The comparative analysis of the data within and across data generated by the different research teams enabled researchers to develop a deeper understanding of EOL decision-making practices in the ICU. The core category that emerged was “negotiated reorienting.” Gallagher et al 19 stated, “Whilst nurses do not make the ‘ultimate’ EOL decisions, they engage in 2 core practices: consensus seeking (involving coaxing, information cuing and voice enabling) and emotional holding (creating time-space and comfort giving).” 19 (p794)
Although a grounded theory approach examines a number of individuals to develop a theory, participants are not studied as 1 unit. Ethnography uses a larger number of individuals and focuses on an entire cultural group as 1 unit of analysis. This qualitative approach describes and interprets the shared and learned patters of values, behaviors, beliefs, and language of a cultural-sharing group. 12 There are many forms of ethnography, namely, confessional, life history, autoethnography, feminist, ethnographic novels, visual ethnography found in photography and video, and electronic media. Price 20 explored what aspects affect registered health care professionals’ ability to care for patients within the technological environment of a critical care unit. Ethnography was utilized to focus on the cultural elements within a situation. Data collection involved participant observation, document review, and semistructured interviews. Nineteen participants took part in the study. An overarching theme of the “crafting process” was developed with subthemes of “vigilance,” “focus of attention,” “being present,” and “expectations,” with the ultimate goal of achieving the best interests for the individual patient.
A culture-sharing group in ethnography can be considered a case, but its aim is to ascertain how the culture works rather than understanding 1 or more specific cases within a bounded system. Creswell 12 defines case study research as an approach in which the researcher explores a bounded system (a case) or multiple bounded systems (cases) over time through detailed in-depth data collection involving multiple sources of information and reports a case description and case-based themes. 12 (p73) In terms of intent, there are 3 types of case study: single instrumental, collective or multiple, and the intrinsic case study. Hyde-Wyatt 21 studied spinally injured patients on sedation in the ICU. A reflection-on-action exercise was carried out when a spinally injured patient became physically active during a sedation hold. This was attributed to hyperactive delirium. Reflection on this incident led to a literature search for guidance on the likelihood of delirium causing secondary spinal injury in patients with unstable fractures. Through a case study approach, the research was reviewed in relation to a particular patient. This case study illustrated that there was a knowledge deficit when it came to managing the combination of the patient’s spinal injury and delirium. Sedation cessation episodes are an essential part of patient care on intensive care. For spinally injured patients, these may need to be modified to sedation reductions to prevent sudden wakening and uncontrolled movement should the patient be experiencing hyperactive delirium.
WHAT IS THE PROCESS OF CONCEPTUALIZING AND DESIGNING A QUALITATIVE RESEARCH?
Designing a qualitative is not a fully structured, rigid process. Even books and experts vary in their understanding and guides in the “how to” perspective of a qualitative inquiry. Conducting a qualitative study is also extremely difficult. 10 Sometimes there is concern about access and the qualitative procedures involved in data collection including disclosure of participant’s identity and confidentiality of data. Nevertheless, qualitative research involves a rigorous and scientific process that serves as guide for researchers who are planning to embark on a journey and complete a naturalistic inquiry.
Unlike quantitative research that involves a fairly linear process, qualitative studies have a flexible approach and flow of activities, and the researchers do not know in advance exactly how the study will unfold. 22 The process of designing a qualitative study does not begin with the methods—which in fact is the easiest part of naturalistic research. 12 Qualitative researchers usually begin with a broad topic focusing on 1 aspect or a phenomenon of which little is known. The phenomenon may be one in the “real world,” a gap in the literature, or past findings of investigations, for example, in the area of social and human sciences. 12 A fairly broad question is then posed to be able to allow the focus to be delineated and sharpened once the study is underway.
Once the research question is posed, the researchers should conduct a brief literature review to inform the question asked and to help establish the significance of the problem. There is a continuous debate about the value of doing a literature review prior to collecting of data and how much of it should be done. Some believe that knowledge about findings of previous studies might influence the conceptualization of the phenomenon of interest, which ideally should be illuminated from the participants rather than on prior findings. 22 A grounded theory investigator, for example, may make a point of not conducting a review of literature before beginning the study to avoid “contamination” of the data with preconceived concepts and notions about what might be relevant. 2 After the review of literature, the researchers must identify an appropriate site for the study to be conducted.
Selecting and gaining entry to the site require knowledge of settings in which participants in their lifeworld are experiencing the phenomenon under study. For example, research in the area of health is a very broad topic. A researcher should determine definitions, concepts, scope, and theories about health that will be used for the proposed qualitative inquiry. Health can be perceived as absence or presence of illness, physical, psychosocial, psychological, and spiritual health of individuals, families, or groups. 10 Morse 10 further stated that “Research into the intimate, experiential and interpersonal aspects of illness, into caring for the ill, and into seeking and maintaining wellness introduces extraordinary methodological challenges.” 10 (p89) Thus, knowledge about the characteristics of participants who will be recruited for the study and the specific context of the settings (ie, hospital/institution, community/outpatient) where they are at the time when research will be conducted is important. To be able to gain entry to the site, the ethical aspect of the study should also be addressed. Approval from the institution’s institutional review board and informed consent from the participants must be obtained. Qualitative studies have special ethical concerns involved because of the more intimate nature of the relationship that typically develop between researchers and participants. 22 The researchers must develop specific plans addressing these issues. After addressing the ethical concerns and gaining entry to the site, an overall approach should be planned and developed.
It has been previously addressed that even though the researchers plan for a specific approach to be used, the design can be emergent during the course of data collection. Modifications are made as the need arises. It is rare that a qualitative study has rigidly structured design that will prohibit changes while in the field, 22 but being aware that the purposes, questions, and methods of research are all interconnected and interrelated so that the study appears as a cohesive whole rather than fragmented isolated parts. 5 For example, patients in hospitals have limited abilities related to their medical condition and the contextual features of a hospital. A patient’s condition may demand a different method be used because of patient fatigue, the interruptions of data collection for treatments, or physician’s rounds and visitors. In this context, the study requires modifications of methods, and participation in a research study has the lowest priority at this specific moment and time. 10
In qualitative studies, sampling, data collection, and analysis including interpretation take place repetitively. The sampling method usually used is purposive. Qualitative researchers use rigorous data collection procedures by talking to participants face-to-face, interviewing, and observing them (individual, focus groups, or an entire culture) to be able to explore the phenomenon under study. The discussions and observations are loosely structured, allowing participants full range of beliefs, feelings, and behaviors. 22 Other types of information that can be collected are documents, photographs, audiovisual materials, sounds, e-mail massages, digital text messages, and computer software. The backbone of qualitative research is extensive collection of data from multiple sources of information. 12 After organizing and storing the data, the researcher will try to make sense of the data, working inductively from particulars to more general perspectives until categories, codes, and themes emerge and are illuminated, which are used to build a rich description of the phenomenon. 12,22 The researcher analyzes data using multiple levels of abstraction. Analysis and interpretation are ongoing concurrent activities that guide the researchers about the kinds of questions to ask or observations to make. The kinds of data gathered become increasingly meaningful as the theory emerges. When themes and categories become repetitive and redundant and no new information can be gleaned, the researcher has reached data saturation and thus stops collecting data and recruitment of participants. 22 Trustworthiness of the data and rigor have to be then established. Steps have to be taken to confirm that the findings accurately reflect the experiences and perceptions of participants rather than the researcher’s viewpoints. Some of the strategies that can be used are validation techniques that include confirming and triangulating data from several sources, going back to participants, sharing preliminary interpretations with them, asking them whether the researcher’s thematic analysis is consistent with their experiences, 22 (p55) and having other expert researchers review the procedures undertaken and interpretations made. 12
FINAL THOUGHTS
Qualitative research uses a naturalistic approach that seeks to understand phenomena in context-specific settings, attempting to make sense of it and interpreting in terms of meaning people bring to them. It contributes to the humanizing of health care as it addresses content about health and illness. Qualitative research does not have firm or rigid guidelines and takes time to conduct. Some of the methods for a qualitative inquiry are narrative research, phenomenology, grounded theory, case study, and ethnography. Although the study design emerges during the inquiry, it follows the pattern of scientific research. Researchers collect data rigorously in natural settings over a period and analyze them inductively to establish patterns or themes. Ethical decisions and considerations for rigor and trustworthiness are also continuously threaded throughout the study. The final report presents the active voices of participants and the description and interpretation of the meaning of the phenomenon including the reflexivity of the researcher.
Goals of nursing; Health care; Qualitative research
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Qualitative research: challenges and dilemmas, data analysis software in qualitative research: preconceptions, expectations,..., qualitative research methods: a phenomenological focus, generational diversity.
The purpose of qualitative research
Cite this chapter.

- Janice M. Morse 3 &
- Peggy Anne Field 4
717 Accesses
5 Citations
Research fills a vital and important role in society: it is the means by which discoveries are made, ideas are confirmed or refuted, events controlled or predicted and theory developed or refined. All of these functions contribute to the development of knowledge. However, no single research approach fulfills all of these functions, and the contribution of qualitative research is both vital and unique to the goals of research in general. Qualitative research enables us to make sense of reality, to describe and explain the social world and to develop explanatory models and theories. It is the primary means by which the theoretical foundations of social sciences may be constructed or re-examined.
Research is to see what everybody has seen and to think what nobody has thought. (Albert Szent-Gyorgy)
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Unable to display preview. Download preview PDF.
Bohannan, L. (1956/1992) Shakespeare in the bush, in Qualitative Health Research , (ed. J.M. Morse), Sage, Newbury Park, CA, pp. 20–30.
Google Scholar
Brace, C.L., Gamble, G.R. and Bond, J.T. (eds) (1971) Race and Intelligence: Anthropological Studies Number 8 , American Anthropological Association, Washington, DC.
Burton, A. (1974) The nature of personality theory, in Operational Theories of Personality , (ed. A. Burton), Brunner/Mazel, New York, pp. 1–19.
Chapman, C.R. (1976) Measurement of pain: problems and issues. Advances in Pain Research and Therapy , 1 , 345.
Corbin, J. (1986) Coding, writing memos, and diagramming, in From Practice to Grounded Theory , (eds W.C. Chenitz and J.M. Swanson), Addison-Wesley, Menlo Park, CA, pp. 91–101.
Duffy, M.E. (1985) Designing nursing research: the qualitative — quantitative debate. Journal of Advanced Nursing , 10 , 225–32.
Article PubMed CAS Google Scholar
Elliott, M.R. (1983) Maternal infant bonding. Canadian Nurse , 79 (8), 28–31.
PubMed CAS Google Scholar
Engelhardt, H.T. (1974/1992) The disease of masturbation: values and the concept of disease, in Qualitative Health Research , (ed. J.M. Morse), Sage, Newbury Park, CA, pp. 5–19.
Feyerabend, P. (1978) Against Method , Varo, London.
Geertz, C. (1973) The Interpretation of Cultures , Basic Books, New York.
Glaser, B.G. (1978) Theoretical Sensitivity , The Sociology Press, Mill Valley, CA.
Glaser, B.G. and Strauss, A.L. (1967) The Discovery of Grounded Theory: Strategies for Qualitative Research , Aldine, Chicago.
Goodwin, L.D. and Goodwin, W.L. (1984) Qualitative vs. quantitative research or qualitative and quantitative research? Nursing Research , 33 (6), 378–80.
Hinds, P.S., Chaves, D.E. and Cypess, S.M. (1992) Context as a source of meaning and understanding, in Qualitative Health Research , (ed. J.M. Morse), Sage, Newbury Park, CA, pp. 31–49.
Klaus, M.H. and Kennel, J.H. (1976) Parent Infant Bonding: The Impact of Early Separation or Loss on Family Development , Mosby, St Louis.
Morse, J.M. (1989/1992) ‘Euch, those are for your husband!’: examination of cultural values and assumptions associated with breastfeeding, in Qualitative Health Research , (ed. J.M. Morse), Sage, Newbury Park, CA, pp. 50–60.
Morse, J.M. (1992) If you believe in theories.... Qualitative Health Research , 2 (3), 259–61.
Article Google Scholar
Morse, J.M., Harrison, M. and Prowse, M. (1986) Minimal breastfeeding. Journal of Obstetric Gynecologic and Neonatal Nursing , 15 (4), 333–8.
Article CAS Google Scholar
Pelto, P.J. and Pelto, G.H. (1978) Anthropological Research: The Structure of Inquiry , Cambridge University Press, Cambridge.
Book Google Scholar
Scheper-Hughes, N. (1992) Death Without Weeping , University of California Press, Berkeley, CA.
Smith, J.K. (1983) Quantitative versus qualitative research: an attempt to clarify the issue. Educational Researcher , 12 (3), 6–13.
Smith, J.K. and Heshusius, L. (1986) Closing down the conversation: the end of the quantitative — qualitative debate among educational inquirers. Educational Researcher , 15 , 4–12.
Strauss, A. and Corbin, J. (1990) Basics of Qualitative Research: Grounded Theory Procedures and Techniques , Sage, Newbury Park, CA.
Tesch, S. (1981) Disease causality and politics. Journal of Health Politics, Policy and Law , 6 (1), 369–89.
Vidich, A.J. and Lyman, S.M. (1994) Qualitative methods: their history in sociology and anthropology, in Handbook of Qualitative Research , (eds N.K. Denzin and Y.S. Lincoln), Sage, Newbury Park, CA, pp. 23–59.
Wolcott, H.F. (1992) Posturing in qualitative research, in The Handbook of Qualitative Research in Education , (eds M.D. LeCompte, W.L. Millroy and J. Preissle), Academic Press, San Diego, CA, pp. 3–52.
Further Reading
Atkinson, P. (1994) Some perils of paradigms. Qualitative Health Research , 5 (1).
Denzin, N.K. and Lincoln, Y.S. (eds) (1994) Part II: Major paradigms and perspectives, in Handbook of Qualitative Research , Sage, Thousand Oaks, CA, pp. 99–198.
Filstead, W.J. (ed.) (1970) Qualitative Methodology: Firsthand Involvement with the Social World , Rand McNally, Chicago.
Gilbert, N. (ed.) (1993) Researching Social Life , Sage, London.
Glassner, B. and Moreno, J.D. (eds) (1989) The Qualitative-Quantitative Distinction in the Social Sciences , Kluwer, Dordrecht, The Netherlands.
Hammersley, M. (ed) (1993) Social Research: Philosophy, Politics and Practice , Sage, London.
Morse, J.M. (ed.) (1992) Part I: The characteristics of qualitative research, in Qualitative Health Research , Sage, Newbury Park, CA, pp. 69–90.
Morse, J.M., Bottorff, J.L., Neander, W. et al. (1991/1992) Comparative analysis of conceptualizations and theories of caring, in Qualitative Health Research , (ed. J.M. Morse), Sage, Newbury Park, CA, pp. 69–90.
Noblit, G.W. and Engel, J.D. (1991/1992) The holistic injunction: an ideal and a moral imperative for qualitative research, in Qualitative Health Research , (ed. J.M. Morse), Sage, Newbury Park, CA, pp. 43–63.
Rabinow, P. and Sullivan, W.M. (eds) (1979) Interpretive Social Science: A Reader , University of California Press, Berkeley, CA.
Smith, R.B. and Manning, P.K. (eds) (1982) A Handbook of Social Science Methods , Ballinger, Cambridge, MA.
Download references
Author information
Authors and affiliations.
School of Nursing, Pennsylvania State University, USA
Janice M. Morse ( Professor of Nursing and Behavioural Science )
Faculty of Nursing, University of Alberta, Canada
Peggy Anne Field ( Professor Emeritus )
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
Copyright information
© 1996 Janice M. Morse and Peggy Anne Field
About this chapter
Morse, J.M., Field, P.A. (1996). The purpose of qualitative research. In: Nursing Research. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-4471-9_1
Download citation
DOI : https://doi.org/10.1007/978-1-4899-4471-9_1
Publisher Name : Springer, Boston, MA
Print ISBN : 978-0-412-60510-9
Online ISBN : 978-1-4899-4471-9
eBook Packages : Springer Book Archive
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Library Research Guides - University of Wisconsin Ebling Library
Uw-madison libraries research guides.
- Course Guides
- Subject Guides
- University of Wisconsin-Madison
- Research Guides
- Nursing Resources
- Types of Research within Qualitative and Quantitative
Nursing Resources : Types of Research within Qualitative and Quantitative
- Definitions of
- Professional Organizations
- Nursing Informatics
- Nursing Related Apps
- EBP Resources
- PICO-Clinical Question
- Types of PICO Question (D, T, P, E)
- Secondary & Guidelines
- Bedside--Point of Care
- Pre-processed Evidence
- Measurement Tools, Surveys, Scales
- Types of Studies
- Table of Evidence
- Qualitative vs Quantitative
- Cohort vs Case studies
- Independent Variable VS Dependent Variable
- Sampling Methods and Statistics
- Systematic Reviews
- Review vs Systematic Review vs ETC...
- Standard, Guideline, Protocol, Policy
- Additional Guidelines Sources
- Peer Reviewed Articles
- Conducting a Literature Review
- Systematic Reviews and Meta-Analysis
- Writing a Research Paper or Poster
- Annotated Bibliographies
- Levels of Evidence (I-VII)
- Reliability
- Validity Threats
- Threats to Validity of Research Designs
- Nursing Theory
- Nursing Models
- PRISMA, RevMan, & GRADEPro
- ORCiD & NIH Submission System
- Understanding Predatory Journals
- Nursing Scope & Standards of Practice, 4th Ed
- Distance Ed & Scholarships
- Assess A Quantitative Study?
- Assess A Qualitative Study?
- Find Health Statistics?
- Choose A Citation Manager?
- Find Instruments, Measurements, and Tools
- Write a CV for a DNP or PhD?
- Find information about graduate programs?
- Learn more about Predatory Journals
- Get writing help?
- Choose a Citation Manager?
- Other questions you may have
- Search the Databases?
- Get Grad School information?
Aspects of Quantative (Empirical) Research
♦ Statement of purpose—what was studied and why.
♦ Description of the methodology (experimental group, control group, variables, test conditions, test subjects, etc.).
♦ Results (usually numeric in form presented in tables or graphs, often with statistical analysis).
♦ Conclusions drawn from the results.
♦ Footnotes, a bibliography, author credentials.
Hint: the abstract (summary) of an article is the first place to check for most of the above features. The abstract appears both in the database you search and at the top of the actual article.
Types of Quantitative Research
There are four (4) main types of quantitative designs: descriptive, correlational, quasi-experimental, and experimental.
samples.jbpub.com/9780763780586/80586_CH03_Keele.pdf
Types of Qualitative Research
|
http://wilderdom.com/OEcourses/PROFLIT/Class6Qualitative1.htm
Log in using your username and password
You are here
https://doi.org/10.1136/eb-2018-102939 Statistics from Altmetric.comRequest permissions. If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways. Qualitative research methods allow us to better understand the experiences of patients and carers; they allow us to explore how decisions are made and provide us with a detailed insight into how interventions may alter care. To develop such insights, qualitative research requires data which are holistic, rich and nuanced, allowing themes and findings to emerge through careful analysis. This article provides an overview of the core approaches to data collection in qualitative research, exploring their strengths, weaknesses and challenges. Collecting data through interviews with participants is a characteristic of many qualitative studies. Interviews give the most direct and straightforward approach to gathering detailed and rich data regarding a particular phenomenon. The type of interview used to collect data can be tailored to the research question, the characteristics of participants and the preferred approach of the researcher. Interviews are most often carried out face-to-face, though the use of telephone interviews to overcome geographical barriers to participant recruitment is becoming more prevalent. 1 A common approach in qualitative research is the semistructured interview, where core elements of the phenomenon being studied are explicitly asked about by the interviewer. A well-designed semistructured interview should ensure data are captured in key areas while still allowing flexibility for participants to bring their own personality and perspective to the discussion. Finally, interviews can be much more rigidly structured to provide greater control for the researcher, essentially becoming questionnaires where responses are verbal rather than written. Deciding where to place an interview design on this ‘structural spectrum’ will depend on the question to be answered and the skills of the researcher. A very structured approach is easy to administer and analyse but may not allow the participant to express themselves fully. At the other end of the spectrum, an open approach allows for freedom and flexibility, but requires the researcher to walk an investigative tightrope that maintains the focus of an interview without forcing participants into particular areas of discussion. Example of an interview schedule 3What do you think is the most effective way of assessing a child’s pain? Have you come across any issues that make it difficult to assess a child’s pain? What pain-relieving interventions do you find most useful and why? When managing pain in children what is your overall aim? Whose responsibility is pain management? What involvement do you think parents should have in their child’s pain management? What involvement do children have in their pain management? Is there anything that currently stops you managing pain as well as you would like? What would help you manage pain better? Interviews present several challenges to researchers. Most interviews are recorded and will need transcribing before analysing. This can be extremely time-consuming, with 1 hour of interview requiring 5–6 hours to transcribe. 4 The analysis itself is also time-consuming, requiring transcriptions to be pored over word-for-word and line-by-line. Interviews also present the problem of bias the researcher needs to take care to avoid leading questions or providing non-verbal signals that might influence the responses of participants. Focus groupsThe focus group is a method of data collection in which a moderator/facilitator (usually a coresearcher) speaks with a group of 6–12 participants about issues related to the research question. As an approach, the focus group offers qualitative researchers an efficient method of gathering the views of many participants at one time. Also, the fact that many people are discussing the same issue together can result in an enhanced level of debate, with the moderator often able to step back and let the focus group enter into a free-flowing discussion. 5 This provides an opportunity to gather rich data from a specific population about a particular area of interest, such as barriers perceived by student nurses when trying to communicate with patients with cancer. 6 From a participant perspective, the focus group may provide a more relaxing environment than a one-to-one interview; they will not need to be involved with every part of the discussion and may feel more comfortable expressing views when they are shared by others in the group. Focus groups also allow participants to ‘bounce’ ideas off each other which sometimes results in different perspectives emerging from the discussion. However, focus groups are not without their difficulties. As with interviews, focus groups provide a vast amount of data to be transcribed and analysed, with discussions often lasting 1–2 hours. Moderators also need to be highly skilled to ensure that the discussion can flow while remaining focused and that all participants are encouraged to speak, while ensuring that no individuals dominate the discussion. 7 ObservationParticipant and non-participant observation are powerful tools for collecting qualitative data, as they give nurse researchers an opportunity to capture a wide array of information—such as verbal and non-verbal communication, actions (eg, techniques of providing care) and environmental factors—within a care setting. Another advantage of observation is that the researcher gains a first-hand picture of what actually happens in clinical practice. 8 If the researcher is adopting a qualitative approach to observation they will normally record field notes . Field notes can take many forms, such as a chronological log of what is happening in the setting, a description of what has been observed, a record of conversations with participants or an expanded account of impressions from the fieldwork. 9 10 As with other qualitative data collection techniques, observation provides an enormous amount of data to be captured and analysed—one approach to helping with collection and analysis is to digitally record observations to allow for repeated viewing. 11 Observation also provides the researcher with some unique methodological and ethical challenges. Methodologically, the act of being observed may change the behaviour of the participant (often referred to as the ‘Hawthorne effect’), impacting on the value of findings. However, most researchers report a process of habitation taking place where, after a relatively short period of time, those being observed revert to their normal behaviour. Ethically, the researcher will need to consider when and how they should intervene if they view poor practice that could put patients at risk. The three core approaches to data collection in qualitative research—interviews, focus groups and observation—provide researchers with rich and deep insights. All methods require skill on the part of the researcher, and all produce a large amount of raw data. However, with careful and systematic analysis 12 the data yielded with these methods will allow researchers to develop a detailed understanding of patient experiences and the work of nurses.
Competing interests None declared. Patient consent Not required. Provenance and peer review Commissioned; internally peer reviewed. Read the full text or download the PDF:An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Save citation to fileEmail citation, add to collections.
Add to My BibliographyYour saved search, create a file for external citation management software, your rss feed.
Maintaining reflexivity in qualitative nursing researchAffiliation.
Aims: Reflexivity is central to the construction of knowledge in qualitative research. This purpose of this paper was to outline one approach when using reflexivity as a strategy to ensure quality of the research process. Design: In this exploratory research, reflexivity was established and maintained by using repeated questionnaires, completed online. Using the approach presented by Bradbury-Jones (2007) and Peshkin's I's, the aim of the research was to identify the researcher's values, beliefs, perspectives and perceptions prevalent in the research. Methods: Qualitative data were collected in online reflexive questionnaires, completed monthly by the researcher from January 2017 to December 2018. Data analysis used interpretive and reflective reading and inductive processes. Results: Seventeen questionnaires were analysed. Data indicated use of questionnaires enabled and detailed development of specific strategies to ensure trustworthiness. Importantly, reflexivity, supported by questionnaires, brought about transformation through self-awareness and enlightenment. Keywords: nursing research; qualitative research; reflexivity; trustworthiness. © 2021 The Authors. Nursing Open published by John Wiley & Sons Ltd. PubMed Disclaimer Conflict of interest statementNo conflict of interest has been declared by the author. Similar articles
LinkOut - more resourcesFull text sources.

NCBI Literature Resources MeSH PMC Bookshelf Disclaimer The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
The needs and experiences of critically ill patients and family members in intensive care unit of a tertiary hospital in Malaysia: a qualitative study
BMC Health Services Research volume 23 , Article number: 627 ( 2023 ) Cite this article 3469 Accesses Metrics details Admission to an intensive care unit (ICU) is a stressful experience for patients and their family members. While the focus of management is primarily on medical care, there can be other areas which are overlooked. The purpose of this study was to investigate the needs and experiences of ICU patients and family members. This qualitative study involved four trained researchers conducting in-depth interviews (IDI) based on a semi-structured interview guide. The participants were ICU patients and family members. All IDIs were audio-recorded and transcribed verbatim. Four researchers independently analyzed the data via thematic analysis with the aid of QDA Miner Lite®. The themes and subthemes were generated and confirmed by literature and expert opinion. Six IDIs were conducted with three patients and three family members, whose ages ranged from 31 to 64 years old. One pair of participants consisted of a patient and his respective family member, while the other four participants did not have a familial relationship with each other. Three main themes emerged from the analysis: (I) critical care services; (II) physical spaces; and (III) monitoring technology. Medical, psychological, physical, and social needs for critical care services were expressed by both patients and family members. Patients’ needs in clinical spaces were highlighted as a conducive ICU environment with ambient temperature and controlled noise levels. In non-clinical spaces, family members expressed a need for more chairs in the waiting area. Participants expressed the need for call bells as well as patients’ negative perceptions of medical equipment alarms in the ICU when it pertained to monitoring technology. This study provides an in-depth view at the needs and experiences of ICU patients and family members who have a variety of unmet needs. This understanding is critical for guiding ICU personnel and stakeholders in their efforts to humanize ICU care. Peer Review reports Critical care is a multidisciplinary and inter-professional specialty that manages patients with acute, and life-threatening organ dysfunction. Admission to the intensive care unit (ICU) causes distress to both patients and their families [ 1 ]. ICU patient care emphasizes a holistic approach that not merely focuses on medical care but also aims to fulfill patients’ and families’ needs [ 2 , 3 ]. The needs identified by the patients warded in ICUs across different countries are broadly categorized as physical, medical, psychological, and social needs [ 4 ]. Generally, ICU patients desire individualized care from the medical personnel and prompt medical attention when the need arises. The patients also need to understand their medical conditions to make decisions on treatment priorities and at the same time to alleviate fear, anxiety, and panic attacks. A secure environment that creates a sense of security, fosters self-worth and motivation toward recovery is essential [ 5 , 6 , 7 , 8 ]. A sense of hope is an important need for family members of patients who are admitted to the ICU. Additionally, they require reassurance from the ICU personnel that the care provided is in the patient’s best interest [ 1 ]. Having an adequate understanding and attempting to meet the families’ needs would improve their ability to cope with the ICU admissions of their loved ones [ 9 ]. There is a slight geographical variation in family member’s needs. In Hong Kong and Malaysia, family members needed assurance that the patients were adequately cared for [ 10 , 11 , 12 ]. The primary concerns in Saudi Arabia were information, reassurance, spiritual healing, and support [ 13 ]. Moving west, in the United Kingdom, the needs were access to maintain proximity to patients; a positive and supportive environment; information; and hope [ 14 ]. An open communication and regular updates build mutual trust between the ICU personnel and the family members. In Ireland, families expressed their needs for truthful updates on the patient’s condition; understanding ICU admission is a dynamic and continuous process; being with their relatives; having the nurses’ assurances; and support for coping [ 15 ]. The difference in priorities and needs globally reflect disparities in culture, religion, and healthcare. In Malaysia, the challenge in providing culturally sensitive intensive care is further compounded due to its multiracial composition with diverse cultural and religious backgrounds. Patient experience is defined as interactions that patients have with the healthcare system, including their management plan, the providers, and the providers’ practices in the healthcare institution [ 16 ]. Their experience in the ICU affects them physically and psychologically. The common physical discomforts experienced include pain, sleepiness, discomfort, inactivity or over-activity, noise, thirst, headache, discomfort associated with endotracheal tubes, and swallowing difficulties. Psychologically, they are affected by their disease progression, medical treatment, and perception of care concerning the manner and behavior of the ICU personnel. Patients reported hallucinations, fear, worry, anxiety, melancholy, loneliness, death thoughts, panic, uneasiness, uncertainty and despair [ 17 ]. These areas of patient experience can be easily overlooked when their critical illnesses are the primary focus of the managing team. Family members experience distress when they learn that their loved ones have been admitted to the ICU. Emotional helplessness is experienced by family members when their need for information, reassurance, help, and support have not been met. They experience a lack of control, uncertainty, and loneliness. They undergo intense emotional changes whenever there is a morbid change in the status of their relatives. Family members are frustrated when their experiences deviate from their expectations, which are affected by their cultural background [ 18 ]. Gauging the needs and experiences of patients and their family members is a crucial step forward in establishing humanized ICU care. This study aims to learn about the needs and experiences of critically ill patients and their family members in a local setting. Study design and settingThis exploratory qualitative study was conducted from February to March 2020 in a multidisciplinary ICU of a tertiary government hospital in Malaysia. The ICU had two wards with a total of 23 beds, with 1200 to 1400 admissions per year. A multi-disciplinary team of 150 to 160 personnel in the ICU includes two consultant intensivists, ICU trainees, anaesthesiologists, anaesthesia-trained medical officers, staff nurses, physiotherapists, pharmacists and attendants. The staff nurses in the ICU worked in shifts, and the medical doctors were subject to an on-call arrangement. The patients’ families were permitted to visit them twice a day, one at a time, between 1 pm and 2 pm and again between 5 pm and 6.30 pm. Due to the lack of a waiting room, family members were compelled to wait in the corridor outside the ICU during visiting hours. The corridor was furnished with seats for ten to fifteen individuals. During non-visiting hours, family members were called by phone if medical doctors wished to discuss the patient’s medical condition with family members. Family conferences were often held in the nursing manager’s office or the Intensivist’s office, while daily patient updates to family members were typically delivered at the bedside. Sample and recruitmentInclusion criteria. Patients who were 18 and above, Malaysian, able to read and speak English, Malay or Mandarin, had their first ICU encounter, admitted to the ICU for at least 72 h to make sure there was enough time to establish their needs [ 11 , 19 ], had a Glasgow Coma Scale (GCS) of 15, a Richmond Agitation-Sedation Scale (RASS) of 0, a negative Confusion Assessment Method for the ICU (CAM-ICU), and an overall stable health condition at the discretion of consultant intensivists, were fit to participate in a 60-minute interview. Patients were recruited based on different characteristics such as age, gender, and the types of specialty care they received in order to enrich the data. Family members, not limited to first-degree relatives, who had been the main person interacting with critical care personnel and were willing to share their experience were invited for interviews. The patients and the family members invited to the study were not necessarily related or paired as certain patients may not fit the eligibility criteria to participate in this study while their family members were. Exclusion criteriaPatients with language or communication barriers, with underlying psychiatric disorders or newly diagnosed psychiatric disorders during ICU admission and those with intellectual impairment were excluded. Family members of critically ill patients with unstable vital signs or whose death was considered imminent were not included in this study out of respect for the grieving needs of the family members [ 19 ]. InterviewersThere were a total of four interviewers (ELL, SLL, CCC and JYA), all of whom were trained in qualitative research. Two of the interviewers held graduate degrees in medicine, while the other two held graduate degrees in pharmacy. Prior to the interview, the interviewers did not know the participants nor did they establish a relationship with them. Interviewers were guided by a semi-structured interview guide, which ensured consistency in the domains covered during each IDI. Additionally, prior to the actual data collection, trial interviews were conducted among the interviewers. These trial interviews served the purpose of establishing a shared understanding of the interview guide and techniques, thereby ensuring a more uniform approach across the IDIs. Sample size and sampling methodPatients and their family members were recruited through purposive sampling. The potential patients were identified during daily ward rounds, and the family members were identified via prior interaction for patients’ updates by the treating intensivist. The participants who agreed to participate were then referred to the interviewers for a scheduled face-to-face interview. A semi-structured interview guide in English was created separately for patients and family members based on existing literature that reported patients’ and families’ needs in ICU [ 20 , 21 , 22 , 23 ], as well as expert opinion. The domains were perception of the ICU, the experience of interacting with the health care personnel working in the ICU, information required, perspectives on medical care, the need for privacy (only applicable for patients), types of support needed, and requirements of facilities in the ICU. Subsequently, these guides were translated into Malay and Mandarin by native speakers of Malay and Chinese. Each language’s interview guide was pre-tested to ensure the comprehensibility of terms and phrases used in the interview guide. Data collectionApproval to conduct this study was obtained from the Medical Research and Ethics Committee, Ministry of Health Malaysia with the protocol number NMRR-19-3358-51827 (IIR) prior to data collection. Each participant signed a written informed consent form before data collection. The sociodemographic information of the participants was collected prior to the IDIs. The IDI sessions with the patients were conducted at the bedside, with curtains or blinds drawn to provide privacy. IDI sessions for family members were held in a private office room inside the ICU. Only two interviewers and a participant were present during each IDI. The IDIs lasted 40 to 60 min and were all audio-recorded. There were no additional interviews conducted. This study was terminated after the sixth IDI due to the prohibition on visitors and researchers entering the ICU, as well as possible changes in participants’ perspectives during the COVID-19 pandemic. All IDIs in this study were conducted before the implementation of pandemic-related movement restrictions in Malaysia [ 24 ]. Despite this, the last two consecutive IDIs did not yield any new themes, indicating that data saturation had been reached. Data analysisThree patients and three family members participated in this study. Coincidentally, there was only one pair of patient-family members who took part in this study. The remaining four participants were not patient-family members paired. The data collected from the patient-family member pair were analyzed separately. The audio recordings were transcribed verbatim and the transcripts were not returned to the participants for verification. Data management was conducted using QDA Miner Lite®, and data analysis was performed following the six steps of thematic analysis established by Braun and Clark [ 25 ]. All researchers (ELL, SLL, CCC, and JYA) familiarized themselves with the transcript, and each transcript was independently coded by two researchers, with any disputes of coding being resolved by discussion and consensus between researchers. Emerging themes were later categorized based on the five domains of care for critically ill patients, reported by the World Federation of Societies of Intensive and Critical Care Medicine. The domains are (I) critical care services, (II) physical space, (III) monitoring technology, (IV) human resources, and (V) research and quality improvement [ 26 ]. Relevant sub-themes were grouped under respective themes. Study findings were further validated by the literature and expert opinion. Non-English quotes were translated into English by one researcher and were cross-checked by another researcher to ensure the accuracy of the translation. The participants’ age ranged from 31 to 64 years old. The patients’ median age was 42 (IQR = 15.5) while the family members’ median age was 60 (IQR = 14.5). There were three Malay and three Chinese. Four of them were females and were all married. Four of the six participants had completed secondary school, one had completed primary school, and the other had completed university education. ICU stays ranged from 6 to 182 days (Table 1 ). A total of three themes emerged in this study: (I) critical care services, (II) physical space, (III) monitoring technology; with several subthemes identified under each of them (Table 2 ). Theme 1: critical care servicesCritical care services needs and what the participants had experienced were not limited to the immediate need for the treatment of individual patients, but also the services that extend beyond basic care. The patients’ and family members’ need for critical services were further classified into medical, physical, psychological and social needs. Medical needsThe medical needs of patients and their family members were identified based on their experience during the patients’ ICU stay. The needs include continuous pain relief management, effective ICU communication, a decision-making process, the provision of continuity of care and culturally competent care. Continuous pain relief managementPain experience was one of the concerns of ICU patients, the continuous need for pain relief has been reiterated by the patients in this study. Necessary analgesics that could not be provided on time have been a concern of ICU patients. … if I need the medication to alleviate toothache, he (staff) could not give [the pain medication] immediately, [he will] delay in giving [the pain medication]. (Patient #3) Effective communication in the ICUThis is part of the essential medical need that occurred between “patient-critical care personnel,“ “family members-patient” and “family members-critical care personnel”. “Patient-critical care personnel”: The patients described that they were unable to communicate their needs to the critical care personnel due to endotracheal tube barriers. Like that time when I was inserted with the [breathing] tube, [and] my urine catheter was blocked, I was unable to call people [for help]. (Patient #3) “Family member-patient”: the family members had difficulties learning about the needs of the intubated patients. We (family members) could not guess what he (intubated patient) was saying. (Family member #2) “Family members-critical care personnel”: Ineffective communication was seen in the non-synchronized conveying of patient information among ICU personnel. Family members were confused by the disparities in the information provided by different ICU personnel. When I came in [to ICU], I told [the nurse that] Dr. XXX allowed me to come in [to see my wife] (family member presumed wife’s condition worsened)… I was taken aback (when the nurse responded that), “No, her condition is improving. Why do you want to come (for a visit)?“ (Family member #1) Besides, a lack of designated communication channels in the ICU by having specific personnel and allocation of a specific time that allows the family members to get patients’ updates has been raised. The family members were uncertain about who and how to obtain patients’ information updates. We could not find a suitable person to ask [regarding patients’ condition], [and] we do not know who to ask [for patients’ condition]. (Family member #2) While some family members attempted to obtain information from the nurse, they were instructed to meet the doctors for updates. In contrast, doctors were perceived as rarely seen in the ward during family visiting hours, making it difficult for family members to obtain information. But initially, we could not differentiate between who was a doctor and who was a nurse. Sometimes when I asked the nurse, she would say, “you [have to] wait for [the] doctor.” But we hardly saw the doctor when we were here [in ICU during family visiting hours]. (Family member #2) Owing to the difficulty in locating the person in charge, a form of communication channel was suggested. The family members preferred bedside name tags that identified the person in charge of a specific patient, allowing them to directly request patient information from that individual. Unless the name [of staff in charge] is stated, [then] I will find the person [directly]. That is [one of the] possible [solutions]. (Family member #3) Cultural competence careThe ability of ICU personnel to provide culturally competent care to patients from diverse backgrounds that take into account language, communication styles, beliefs, attitudes, values, and behavioural diversity was identified as a need in critical care services [ 27 ]. The inadequacy of providing cultural competence care was recognised as an issue where some patients encounter language barriers when seeking medical care, necessitating the search for native-speaking critical care personnel to communicate their needs. [About] Communication… because I am not very fluent in Bahasa Melayu (Malay language) … So when I see [a] Chinese nurse, I will ask her to help to translate. (Patient #2) Cultural competent care has not been confined to medical care; addressing the beliefs of family members in terms of patients’ nutrition intake was notably a need. A few family members were unsatisfied with the food provided by the hospital to the patients, believing it to be less nutritious for patients. Yes, sometimes I see one piece of chicken and some porridge with some squash, [which is] not suitable [for patients]. (Family member #2) Participation in patient careThis study revealed that family members were willing to learn and perform simple care for their loved ones in the ICU. A family member articulated her willingness to acquire basic skills from the healthcare providers in order to ensure the sustenance of patient care. Then, my son-in-law (who is a healthcare professional) taught me something easier, like how to help him (patient) to do phlegm suction (…) so when we see him (visit the patient in ICU), we will do [phlegm suction] by ourselves. (Family Member #2) Decision makingThe lack of medical treatment knowledge among the participants made them follow the decision of the medical doctors to receive critical care for the patients. [We] listen to the doctors regarding all [medical treatment]. We totally have no idea [on medical treatment]. (Family member #2) Psychological needsThe principal psychological needs in the ICU evolve around the elements, making them feel safe in the ICU. The elements include “knowing”, “hoping”, “trusting” and “regaining control”. These elements are greatly influenced by family and friends, ICU personnel, and religion [ 28 ]. This study identified that ICU personnel and religious support were highlighted by the family members as perceived psychological needs of the patients. Patient counselling service was mentioned as an important psychological need for patients in the ICU. ICU personnel supportThe ICU personnel is regarded as crucial in terms of providing patients with support and encouragement to live [ 28 ]. Some family members believed that the doctors’ encouragement would be more effective in motivating the patients than the families themselves. [When] Dr. XXX passed by, he will encourage him (patient) [by saying]: “Uncle [you have] improved a lot over these few days.” (Family member #2) The impact of ICU personnel on the patients’ psychological needs is perceived as substantial, including in a negative way. The family members believed that negative words would harm the patients. Therefore, they requested the doctor in charge to be cautious when disclosing information to patients. Doctors’ words (information on patient’s condition) will affect patients (…) Hope [that we] can know [about the patient’s condition], but [we preferred that the doctor] do not disclose [the negative information] in front of the patient. (Family member #2) Religious supportSome of the patients expressed a need for religious support while in the ICU. Maybe listening to the radio. My husband helped on the radio and played verses from Al-Quran. (Patient #1) Patient counsellingThe family members agreed that patient counselling service would be one of the best ways to support the patients psychologically. It is even better to counsel the patient because the patients need encouragement. (Family member #3) Physical needsComfortable bed-bath. Some of the patients had negative experiences with bed-bath by having to take late-night showers in cold water. There was a need to use warm water for bathing among the ICU patients. [It was] eleven (o’clock at night) that [the staff] helped me to shower using … cold water. How [could I] bear with this (showering at night with cold water)? I told them (the staff) that … I would like to use warm water [instead]. He (the staff) agreed [to bring warm water], but what he brought over was cold water. He (staff) told me that … he (staff) would help me to shower at a faster speed. That time I was suffering. (Patient #2)  Social needsLonger visiting hours. The patients needed longer visiting hours to meet each of their loved ones during hospitalization in the ICU. Because they (family members) only [had] one hour [of visiting time]. If it can be extended, [then] we (patient and family member) can talk [longer]… A lot of people (visitors) come [to visit me], [I have] not get to talk to each visitor (within the visiting hour) … So [it will be good] to have longer visiting hours. (Patient #2) Theme 2: physical spacesThe physical spaces in the ICU are divided into clinical and non-clinical spaces. The clinical space includes the presence of a discrete location where it accommodates the beds, devices, and rooms; a nursing station; and multiple computer stations that are essential in patient care. The pantry, a room for medical personnel to rest, seminar rooms close by, and a place for families to wait are all part of the non-clinical space, which is outside of the physical boundaries of the patient care area [ 29 ]. The experience of physical space in the clinical area was described by the patients as a cold and noisy environment. Unmet needs for non-clinical spaces included a lack of visitor chairs in the waiting area. Clinical spacesConducive ward. Some patients complained of the cold environment in the ICU which resulted in the need to cover themselves with thick layers of blankets. The air conditioner was too cold. I needed to cover three layers of blankets, yet [I was] still feeling cold. (Patient #3) Family members were concerned about patients who were unable to sleep at night owing to the noisy environment in the ICU. My husband (patient) complained to me that there were a few nights he could not sleep because they (the staff) kept talking loudly. (Family member #3) Non-clinical spacesConducive waiting area. Meanwhile, the participants raised the issue of insufficient chairs for family members in the waiting area, suggesting that the situation could be improved by adding a few additional chairs, especially for elderly visitors. I thought that a few more chairs could be added outside the ICU because there were too many people (visitors). Sometimes, some elderly [visitors] do not have chairs to sit on and they need to climb up [the stairs to reach ICU]; yet there was only one row of chairs … I thought it (ICU) should have been equipped with few more chairs. (Family member #3) Theme 3: monitoring technologyOne of the aspects that distinguish critical care from traditional hospital treatment would be the availability of devices with advanced technologies that provide continuous monitoring of a patient’s physiologic status in an ICU [ 29 ]. The monitoring technology identified by the participants could be classified into medical devices and non-medical devices. The medical devices in the ICU frequently emitted alarms that startled the patients. On the other hand, the family members were concerned about malfunctioning call bells, which is an important non-medical device. Perception of medical equipment alarmsThe ICU was thought to be well-equipped with a variety of medical devices by the majority of the participants. Some were unconcerned about the devices that were attached, while others perceived a sense of hopelessness and fear hearing the alarms and seeing the lights emitted by the medical devices. All sorts of sounds (from the devices), [it was] scary (…) [I felt] like no hope [in the ICU]. (Patient #1) One of the family members believed it was dangerous to leave a patient in an isolated room without a functioning emergency call bell, especially if the patient has a health condition that causes breathing difficulties. Yes, [you are] right. Sometimes they may be in danger, such as having breathing problems or any other condition, [it is] better to have the bell for them to press, otherwise it is very dangerous [in such a situation]. (Family member #3) Discussions and recommendationsThis study uncovered the needs and experiences of critically ill patients and their families in the ICU concerning the critical care services, physical environment, and equipment in the ICU. While previous local studies have focused on the family members of ICU patients [ 11 , 12 ], this qualitative study in Malaysia investigates the needs and experiences of critically ill patients as well as their family members. The main medical need that is deemed unmet for the ICU patients in this study would be insufficient pain treatment. This inadequacy was attributed to difficulties in assessing and accurately locating pain, as well as poor awareness among healthcare personnel, particularly among patients who did not undergo any surgical procedures [ 30 ]. However, a culture of addressing pain in critically ill patients should be fostered, as dealing with pain complaints promptly has been shown to result in a less stressful stay [ 17 , 31 ]. One step forward could be reinforcing adherence to the appropriate pain management strategy supported by the Malaysia Ministry of Health [ 32 ]. Effective communication in the ICU is reiterated as an essential need of patients and family members. Critically ill patients who received invasive mechanical ventilation experienced communication difficulties. At the same time, ICU personnel and families reported difficulties in understanding patients’ needs as well [ 33 , 34 ]. The utilization of aided or unaided augmentative and alternative communication systems could assist in meeting this demand, and this should be implemented according to the local culture and setting [ 35 ]. The family members in this study had a great desire for up-to-date patients’ information, as identified as a fundamental need of family members [ 9 ]. They needed to know about the patients’ progress and prognosis, why certain activities were conducted for the patients, and who to call when they were away [ 36 , 37 ]. In Malaysia, patients’ information is disclosed by medical doctors and reinforced by nurses to the family members [ 38 ]. However, the medical doctors in the ICU tend to prioritise patients’ care, which may result in insufficient time for communication or difficulty locating them when they are managing other patients [ 34 ]. Hence, to establish family-centered care in the ICU and obtain standardised patient information promptly, a consensus for a point person, frequency and types of contact should be made between ICU personnel and family members [ 39 ]. However, these proposals should be addressed further among the ICU team in order to better adapt to the local system. Family members’ participation in various patient care activities has been reported, ranging from massage, bathing, eye and mouth care, to positioning and adjusting equipment [ 40 ]. This study captured family members’ willingness to learn and participate in patient care. Such a desire to assist the patient, who is their loved one, stems from the kinship and relationship between family members and the patient, precipitating their desire to assist the patient [ 41 ]. Also, being able to get involved in patient care reduces family members’ fear and helplessness when their loved ones are critically ill. Family members’ involvement in patient care during the ICU stay also provides an opportunity for them to acquire relevant skills that enables them to care for the patient after discharge [ 26 ]. Nonetheless, such involvement necessitates additional attention and careful supervision from healthcare providers, which adds to their workload and may cause task delays [ 41 , 42 ]. Concerns about poor quality patient care, accidental extubation, and failure to adhere to infectious control measures have also been raised when family members are involved in patient care [ 43 ]. Hence, a clear policy is formed in the local ICU to direct the selection of patients and family members, the level of their involvement in patient care, and to offer ongoing supervision while they are involved in patient care. In terms of the psychological needs of the patients, family members acknowledged the ICU personnel as vital individuals for providing psychological support to the patients. This involves requesting that ICU personnel selectively share information with patients to offer hope to patients. Typically, the Asian family culture wishes to shield their loved ones from unpleasant news. However, this request violates the medical ethics of patient autonomy [ 44 ]. Therefore, the ICU personnel has to be trained with strong communication and negotiation skills when challenged with a need for selective non-disclosure [ 45 ]. Apart from that, patients’ need of religious support and counselling have also been articulated in this study. Spiritual distress is common among ICU patients, and thus religious support (such as praying with the patient, discussing religious topics, and fostering religious growth) is regarded as a source of encouragement and hope [ 46 ]. Meanwhile, psychological support (such as counselling, stress management, and coping strategies) provided during ICU stay has been shown to reduce post-traumatic stress disorder and the need for psychiatric medication among patients [ 47 ]. In the local ICU, spiritual support is always offered to the family based on the patients’ religious beliefs. Such effort in supporting patients’ religious and counselling needs is thus to be applauded and should be more proactively offered to those who are in need, although identifying spiritual needs is rather difficult. The unmet physical need highlighted by the ICU patients would be an unpleasant experience during bed-bath with cold water late at night. This finding is similar to a study in Istanbul that found bed-bath was prevalent between midnight and five o’clock in the morning [ 48 ]. This practice could be due to a less busy schedule during midnight for the nurses to conduct bed-baths. Aside from the timing of bed-baths, the water temperature should be ideal. It is recommended that bed-bathing timing be based on individual patient preference [ 49 ], with the water temperature set at 40 to 42.5 o C [ 50 ]. Though bed-bath may cause some discomfort to patients, it is vital in preserving patients’ hygiene and improving health outcomes [ 51 ]. Patients’ social needs, including seeing their family members [ 17 ], cannot be met due to the restricted visiting hours. Permission for flexible visiting hours to accommodate family members who have other commitments or different working schedules can facilitate family involvement in patient care. However, this has to be carefully considered taking into consideration the consequences on nursing care and disturbance to other patients [ 52 ]. Developing defined yet flexible visiting policies by tailoring visiting hours based on the needs of patients, families, and healthcare personnel may be more feasible and acceptable to all [ 53 ]. Currently, extended visiting hours in the ICU have been offered to family members of selected patients, particularly patients requiring long-term care. The provision of flexible visiting hours allows family members to engage in patient care with the assistance of the nurses. Intolerable cold environments emerged as a negative experience for ICU patients when they were asked about the need for clinical spaces in the ICU. As part of the infection control recommendations, the Centers for Disease Control and Prevention (CDC) recommends that hospital wards maintain a temperature of 21-24 o C [ 54 ]. However, the cold environment may not be well tolerated by patients [ 55 ]. To strike a balance between CDC recommendations and patients’ comfort, patients could be reassured and given extra blankets to assist them to cope with the cold environment in the ICU. In the aspect of non-clinical space, family members expressed the need for additional waiting chairs to be placed outside the ICU. Driving this need is the desire of families for reassurance and to be in close proximity with their loved ones during the critical phase [ 11 , 56 ]. In the United States, family members desired a comfortable waiting area where they could find solace in the company of other relatives of critically ill patients [ 57 ]. Unfortunately, at the ICU where the study was conducted, there was no designated ICU waiting room for family members. A hospital waiting-lounge facility is available within a five-minute walking distance from the ICU, but not all of the family members were aware of this facility [ 58 ]. They should be informed of the availability of the facility during the initial meeting with the ICU personnel. The need for functioning call bells was raised by the participants, especially for patients who were placed in the isolated unit in the ICU. In case of an emergency, this medical device facilitates communication and connectivity of patients with healthcare providers. Patients felt safer knowing that they could reach healthcare providers for care or assistance when needed [ 59 , 60 ]. It is important for the ICU personnel to monitor the function of the call bell and to set up a call bell response system. However, due to structural limitations in this ICU, functional call bells were unable to be installed, and the team was continually exploring alternatives. Consistent with the reports of other studies, some of the devices in the ICU emit sounds and alarms, which are a source of distress for the patients [ 55 , 61 , 62 ]. The alarms may trigger anxiety in patients, which, when combined with the patients’ lack of familiarity with the meaning of the sounds and alarms, causes them to perceive them as a threat [ 63 , 64 ]. This situation can be improved by minimizing the effects of the alarms by providing earplugs or setting “quiet times” [ 65 , 66 ]. Practicing light down and reducing alarms to create “quiet times” at night have been implemented in this ICU. Strengths, limitations and recommendationsThis research was undertaken just before the COVID-19 epidemic. The pandemic resulted in policy adjustments, including modifications to the visiting policy. Therefore, the data collection was stopped at the sixth participant when the Malaysian government declared a “Movement Controlled Order” on March 18, 2020, in response to the health emergency. Nonetheless, data from all six IDIs revolved around the same themes and no new themes emerged, data for the themes is thus saturated. Additionally, this study provides a baseline understanding of the needs and experiences of both critically ill patients and their families in Malaysia. Future research should focus on the disparities between the needs and experiences of critically ill patients and family members before and after the pandemic, and if the policy changes implemented during the COVID-19 pandemic affected their needs and experiences. This study provides a comprehensive look at the needs and experiences of critically ill patients and their families. Some of the concerns are acknowledged as having no immediate solution. The study’s findings, on the other hand, would aid ICU professionals in recognising and communicating the needs of patients and families in order to foster mutual understanding. Addressing the challenges outlined in this study could provide insights into organisational and systemic reforms to humanise ICU care. Availability of data and materialsThe datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request. AbbreviationsIntensive Care Unit Molter NC, Leske JS. Critical Care Family Needs Inventory. Heart and Lung. 1995. https://doi.org/10.1037/t37619-000 . Holden J, Harrison L, Johnson M. Families, nurses and intensive care patients: a review of the literature. J Clin Nurs. 2002;11(2):140–8. Article PubMed Google Scholar Pattison N. Psychological implications of admission to critical care. Br J Nurs Mark Allen Publ. 2005;14:708–14. Article Google Scholar Stein-Parbury J, McKinley S. Patients’ experiences of being in an intensive care unit: a select literature review. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses. 2000;9(1):20–7. CAS Google Scholar Wåhlin I, Ek AC, Idvall E. Patient empowerment in intensive care–an interview study. Intensive Crit Care Nurs. 2006;22(6):370–7. Hofhuis JGM, Spronk PE, van Stel HF, Schrijvers AJP, Rommes JH, Bakker J. Experiences of critically ill patients in the ICU. Intensive Crit Care Nurs. 2008;24(5):300–13. Aro I, Pietilä AM, Vehviläinen-Julkunen K. Needs of adult patients in intensive care units of estonian hospitals: a questionnaire survey. J Clin Nurs. 2012;21(13–14):1847–58. Wåhlin I, Samuelsson P, Ågren S. What do patients rate as most important when cared for in the ICU and how often is this met? - an empowerment questionnaire survey. J Crit Care. 2017;40:83–90. Scott P, Thomson P, Shepherd A. Families of patients in ICU: A Scoping review of their needs and satisfaction with care. Nurs Open. 2019;6(3):698–712. Lee LYK, Lau YL. Immediate needs of adult family members of adult intensive care patients in Hong Kong. J Clin Nurs. 2003;12(4):490–500. Dharmalingam TK, Kamaluddin MR, Hassan SK, Zaini RHM. The needs of malaysian family members of critically ill patients treated in Intensive Care Unit. Hosp Universiti Sains Malaysia. 2016;12:8. Google Scholar Mohamed Z, Sasikala M, Nurfarieza M, Siew Eng H. Needs of Family Members of Critically Ill Patients in a Critical Care Unit at Universiti Kebangsaan Malaysia Medical Centre. Med Health. 2016;11(1):11–21. Al-Mutair AS, Plummer V, Clerehan R, O’Brien A. Needs and experiences of intensive care patients’ families: a saudi qualitative study. Nurs Crit Care. 2014;19(3):135–44. Wilkinson P. A qualitative study to establish the self-perceived needs of family members of patients in a general intensive care unit. Intensive Crit Care Nurs. 1995;11(2):77–86. Article CAS PubMed Google Scholar McKiernan M, McCarthy G. Family members’ lived experience in the intensive care unit: A phemenological study. Intensive Crit Care Nurs. 2010;26(5):254–61. Agency for Healthcare Research and Quality. What Is Patient Experience?. 2022 [cited 2022 Sep 23]. Available from: https://www.ahrq.gov/cahps/about-cahps/patient-experience/index.html . Topçu S, Ecevit Alpar Ş, Gülseven B, Kebapçı A. Patient experiences in intensive care units: a systematic review. Patient Exp J. 2017;4(3):115–27. Hirshberg EL, Butler J, Francis M, Davis FA, Lee D, Tavake-Pasi F et al. Persistence of patient and family experiences of critical illness. BMJ Open. 2020;10(4):e035213. Coulter MA. The needs of family members of patients in intensive care units. Intensive Care Nurs. 1989;5(1):4–10. Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of critical Care Medicine Task Force 2004–2005: Crit Care Med. 2007;35(2):605–22. Khalaila R. Meeting the needs of patients’ families in intensive care units. Nurs Stand R Coll Nurs G B. 1987. 2014;28(43):37–44. Novaes MAFP, Aronovich A, Ferraz MB, Knobel E. Stressors in ICU: patients’ evaluation. Intensive Care Med. 1997;23(12):1282–5. Leung K, Chien WT, Mackenzie AE. Needs of chinese families of critically ill patients. West J Nurs Res. 2000;22(7):826–40. Shah AUM, Safri SNA, Thevadas R, Noordin NK, Rahman AA, Sekawi Z et al. COVID-19 outbreak in Malaysia: Actions taken by the Malaysian government. Int J Infect Dis. 2020;97:108–16. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. Marshall JC, Bosco L, Adhikari NK, Connolly B, Diaz JV, Dorman T, et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of intensive and critical Care Medicine. J Crit Care. 2017;37:270–6. Butler M, McCreedy E, Schwer N, et al. Improving Cultural Competence to Reduce Health Disparities [Internet]. Rockville: Agency for Healthcare Research and Quality (US); 2016. (Comparative Effectiveness Reviews, No. 170.). https://www.ncbi.nlm.nih.gov/books/NBK361126/ . Accessed 23 Sept 2022. Hupcey JE. Feeling safe: the psychosocial needs of ICU patients. J Nurs Scholarsh Off Publ Sigma Theta Tau Int Honor Soc Nurs. 2000;32(4):361–7. Marshall JC, Bosco L, Adhikari NK, Connolly B, Diaz JV, Dorman T et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2017;37:270–6. Hasegawa R. Consideration of pain felt by patients in the ICU. J Intensive Care. 2017;5(1):73. Article PubMed PubMed Central Google Scholar Rotondi AJ, Chelluri L, Sirio C, Mendelsohn A, Schulz R, Belle S, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002;30(4):746–52. Ministry of Health. Pain as the 5th vital sign. 2018. https://www.moh.gov.my/moh/resources/Penerbitan/Program%20Bebas%20Kesakitan/Garis%20Panduan/2_in_1_P5VS_Guideline_3rd_Edition_Corrected_2020.pdf . Accessed 30 Sept 2022. Martinho CIF, Rodrigues ITRM. Communication of mechanically ventilated patients in intensive care units. Rev Bras Ter Intensiva. 2016;28(2):132–40. Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: a qualitative study. PLoS ONE. 2020;15(7):e0235694. Article CAS PubMed PubMed Central Google Scholar Salem A, Ahmad MM. Communication with invasive mechanically ventilated patients and the use of alternative devices: integrative review. J Res Nurs JRN. 2018;23(7):614–30. Alsharari AF. The needs of family members of patients admitted to the intensive care unit. Patient Prefer Adherence. 2019;13:465–73. Al-Akash H, Maabreh R, AbuRuz M, Khader K, Shajrawi A. Jordanian Patients’ Family Members Need Perceptions in the Critical Care Settings: Nurses’ Perspectives versus Family Members’ Perspectives in the Context of Health Informatics. J Healthc Eng. 2021;2021:4071523. Hussin R, Hashim F. Communication needs of family members with a relative in Intensive Care Unit. J ASIAN Behav Stud. 2017;2:19. Schwartz AC, Dunn SE, Simon HFM, Velasquez A, Garner D, Tran DQ, et al. Making family-centered care for adults in the ICU a reality. Front Psychiatry. 2022;24:13:837708. Liput SA, Kane-Gill SL, Seybert AL, Smithburger PL. A review of the perceptions of Healthcare Providers and Family Members toward Family involvement in active adult patient care in the ICU. Crit Care Med. 2016;44(6):1191–7. Fateel EE, O’Neill CS. Family members’ involvement in the care of critically ill patients in two intensive care units in an acute hospital in Bahrain: the experiences and perspectives of family members’ and nurses’ - a qualitative study. Clin Nurs Stud. 2015;30(1):p57. Hsiao PR, Redley B, Hsiao YC, Lin CC, Han CY, Lin HR. Family needs of critically ill patients in the emergency department. Int Emerg Nurs. 2017;30:3–8. Azoulay E, Pochard F, Chevret S, Arich C, Brivet F, Brun F, et al. Family participation in care to the critically ill: opinions of families and staff. Intensive Care Med. 2003;29(9):1498–504. McCabe MS, Wood WA, Goldberg RM. When the Family Requests Withholding the Diagnosis: Who Owns the Truth? J Oncol Pract. 2010;6(2):94–6. Hallenbeck J, Arnold R. A request for nondisclosure: don’t tell mother. J Clin Oncol Off J Am Soc Clin Oncol. 2007;25(1):5030–4. Ho JQ, Nguyen CD, Lopes R, Ezeji-Okoye SC, Kuschner WG. Spiritual care in the Intensive Care Unit: a narrative review. J Intensive Care Med. 2018;33(5):279–87. Peris A, Bonizzoli M, Iozzelli D, Migliaccio ML, Zagli G, Bacchereti A, et al. Early intra-intensive care unit psychological intervention promotes recovery from post traumatic stress disorders, anxiety and depression symptoms in critically ill patients. Crit Care. 2011;15(1):R41. Celik S, Oztekin D, Akyolcu N, Issever H. Sleep disturbance: the patient care activities applied at the night shift in the intensive care unit. J Clin Nurs. 2005;14:102–6. American Association of Critical-Care Nurses. AACN Updates Patient Bathing Practices Protocol. 2013. https://www.infectioncontroltoday.com/view/aacn-updates-patient-bathing-practices-protocol . Accessed 30 Sept 2022. da Silva CJB, Silva M, dos Reis S, Miranda FF, de Santos GCO. L dos, Lima DVM de. Bed bath for infarcted patients: crossover of the hydrothermal control 40 o C versus 42.5 o C. Online Braz J Nurs. 2016;15(3):341–50. El-Soussi A, Abd El Hamid H. Examining bed-bath practices of critically ill patients. J Nurs Educ Pract. 2016;6(12):1–11. Khaleghparast S, Joolaee S, Ghanbari B, Maleki M, Peyrovi H, Bahrani N. A review of visiting policies in Intensive Care Units. Glob J Health Sci. 2015;8(6):267–76. Berwick DM, Kotagal M. Restricted visiting hours in ICUs: time to change. JAMA. 2004;11(6):736–7. U.S. Department of Health and Human Services Centers for Disease Control and Prevention (CDC). Guidelines for Environmental Infection Control in Health-Care Facilities. 2003. https://www.cdc.gov/infectioncontrol/guidelines/environmental/index.html . Accessed 30 Sept 2022. Krampe H, Denke C, Gülden J, Mauersberger VM, Ehlen L, Schönthaler E et al. Perceived Severity of Stressors in the Intensive Care Unit: A Systematic Review and Semi-Quantitative Analysis of the Literature on the Perspectives of Patients, Health Care Providers and Relatives. J Clin Med. 2021;10(17):3928. Plakas S, Taket A, Cant B, Fouka G, Vardaki Z. The meaning and importance of vigilant attendance for the relatives of intensive care unit patients. Nurs Crit Care. 2014;19(5):243–54. Kutash M, Northrop L. Family members’ experiences of the intensive care unit waiting room. J Adv Nurs. 2007;60(4):384–8. “Anjung Kasih” Meets the Needs of the Target Group. Perak Today. 2017. https://peraktoday.com.my/2017/04/anjung-kasih-penuhi-keperluan-golongan-sasar/ . Accessed 30 Sept 2022. Lasiter S. The button”: initiating the patient-nurse interaction. Clin Nurs Res. 2014;23(2):188–200. Montie M, Shuman C, Galinato J, Patak L, Anderson CA, Titler MG. Conduits to care: call lights and patients’ perceptions of communication. J Multidiscip Healthc. 2017;10:359–66. Ma P, Wang Y, Xi X, ming, Lin H yuan, Xu Y, Du B et al. [Epidemiology of unpleasant experiences in conscious critically ill patients during intensive care unit stay]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue Chin Crit Care Med Zhongguo Weizhongbing Jijiuyixue. 2008;20(9):553–7. Soh KL, Soh KG, Ahmad Z, Raman RA, Japar S. Perception of intensive care unit stressors by patients in Malaysian Federal Territory hospitals. Contemp Nurse. 2008;31(1):86–93. Johansson L, Bergbom I, Lindahl B. Meanings of Being Critically Ill in a Sound-Intensive ICU Patient Room - A Phenomenological Hermeneutical Study. Open Nurs J. 2012;6:108–16. Darbyshire JL. Excessive noise in intensive care units. BMJ. 2016;353:i1956. Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit Care. 2013;17(5):R187. Burdick KJ, Callahan CJ. Sleeping Soundlessly in the Intensive Care Unit. Multimodal Technol Interact. 2020;4(1):6. Download references AcknowledgementsThe team thanks all staff in ICU Hospital Raja Permaisuri Bainun Ipoh for facilitating the interview sessions conducted in ICU. The team would also like to thank the Director General of Health, Malaysia, for his permission to publish this article. The authors received no funding for conducting this research. Author informationAuthors and affiliations. Clinical Research Centre, Hospital Raja Permaisuri Bainun, Ministry of Health, 30450, Ipoh, Perak, Malaysia E-Li Leong, Chii-Chii Chew, Ju-Ying Ang, Sharon-Linus Lojikip & Philip-Rajan Devesahayam Otolaryngology Department, Hospital Raja Permaisuri Bainun, Ministry of Health, Ipoh, Malaysia Philip-Rajan Devesahayam Anaesthesiology and Intensive Care Department, Hospital Raja Permaisuri Bainun, Ministry of Health, Ipoh, Malaysia Kit-Weng Foong You can also search for this author in PubMed Google Scholar ContributionsAll authors contributed to the idea and drafting of the study protocol. CCC, JYA, ELL and SLL were involved in in-depth interviews and thematic analysis. KWF and PRD were involved in the final confirmation of the thematic analysis. ELL, CCC, JYA and SLL contributed to the writing of the manuscript. KWF and PRD contributed to the critical revision of the manuscript. All authors read, reviewed and approved the final version. Corresponding authorCorrespondence to E-Li Leong . Ethics declarationsEthics approval and consent to participate. Approval to conduct this study was obtained from the Medical Research and Ethics Committee, Ministry of Health Malaysia with the protocol number NMRR-19-3358-51827 (IIR). The study was adhere to the Declaration of Helsinki. Informed consent was obtained from participants prior to the initiation of the in-depth interview. Consent for publicationNot applicable. Competing interestsThe authors declare that they have no competing interests. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsOpen Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data. Reprints and permissions About this articleCite this article. Leong, EL., Chew, CC., Ang, JY. et al. The needs and experiences of critically ill patients and family members in intensive care unit of a tertiary hospital in Malaysia: a qualitative study. BMC Health Serv Res 23 , 627 (2023). https://doi.org/10.1186/s12913-023-09660-9 Download citation Received : 03 January 2023 Accepted : 06 June 2023 Published : 13 June 2023 DOI : https://doi.org/10.1186/s12913-023-09660-9 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
BMC Health Services ResearchISSN: 1472-6963
Expanding the non-technical skills vocabulary of operating room nurses: a qualitative study
BMC Nursing volume 22 , Article number: 323 ( 2023 ) Cite this article 1991 Accesses 2 Altmetric Metrics details Operating room nurses have specialised technical and non-technical skills and are essential members of the surgical team. The profession’s dependency of tacit knowledge has made their non-technical skills difficult to access for researchers, thus, creating limitations in the identification of the non-technical skills of operating room nurses. Non-technical skills are categorised in the crew resource management framework, and previously, non-technical skills of operating room nurses have been identified within the scope of the framework. The purpose of this study is to explore operating room nurses’ descriptions of their practices in search for non-technical skills not included in the crew resource management framework. This study has a qualitative design. An expert panel of experienced operating room nurses (N = 96) in Norway provided qualitative descriptions of their practice in a Delphi survey. The data were analysed in an inductive thematic analysis. This study was conducted and reported in line with Standards for Reporting Qualitative Research (SRQR). The inductive thematic analysis developed two themes, ‘Ethical competence’ and ‘Professional accountability’, that encompass operating room nurses’ novel descriptions of their non-technical skills. The participants take pride in having the patients’ best interest as their main objective even if this may threaten their position in the team. ConclusionsThis study has identified novel non-technical skills that are not described in the crew resource management framework. These findings will contribute to the development of a new behavioural marker system for the non-technical skills of operating room nurses. This system will facilitate verbalisation of tacit knowledge and contribute to an increased knowledge about the operating room nursing profession. Peer Review reports Operating room (OR) nursing as a profession originates from the early days of surgery on anaesthetised patients [ 1 ]. Since then, it has developed from attending the surgeon and providing ‘household’ of the OR, to a profession with advanced specialised skills. Traditionally, OR nursing relied on historical legacy, with tacit and unspoken knowledge developed within the OR, rather than theoretical principles and evidence-based knowledge [ 1 ]. The main issue with tacit and unspoken knowledge lies in the name; it is difficult to verbalise. Tacit knowledge has been described as knowledge nurses are aware of but struggle to explain [ 2 ]. With the requirements of modern healthcare and formalised OR nursing education, all relevant skills-sets must be verbalizable. Sirevåg et al. [ 3 ] found that the use of non-technical skills (NTS) vocabulary helped the OR nurses verbalise their tacit knowledge. By using the term NTS, defined as ‘the cognitive, social and personal resource skills that complement technical skills, and contribute to safe and efficient task performance’ p.1 [ 4 ], we gain a common vocabulary for the former ‘tacit skills’ [ 3 ]. When relying on NTS developing over time, as have traditionally been the case, we accept a higher risk of adverse events until novice and student OR nurses have developed their NTS. Therefore, to ensure safe surgery independent of staff experience, systematic training and, subsequently, assessment of NTS are necessary [ 5 ]. The Crew Resource Management (CRM) coursework was initially developed for training NTS in aviation [ 6 ]. Requirements from the aviation authorities led to the development of a behavioural marker system for the assessment of pilot’s NTS [ 6 ]. Subsequently, Flin et al. have constructed a CRM framework of the main NTS categories and elements based on CRM courses and NTS lists from various organisations (Table 1 , Columns 1 and 2) [ 4 ]. Several behavioural marker systems for individual skills training and assessment have been developed based on the CRM system. According to Flin et al. [ 4 ], these tools must be customised with user specific behavioural markers, and the developers of such tools must define the context and identify all relevant NTS of the target users. OR nursing is practiced by scrub and circulating nurses behind closed doors. The lack of verbalisation of their competence results in hospital administration, and even other members of the surgical team, being unaware of their full competencies and responsibilities [ 1 , 7 ]. These issues may have contributed to ‘outsiders’ defining OR nursing in relation to the surgeons [ 7 ]. When examining the development of an existing NTS assessment tool, the Scrub Practitioners’ List of Intraoperative Non-Technical Skills (SPLINTS) [ 8 ], we detect that some limitations were made which may decrease the usability of the instrument. Firstly, in SPLINTS, the intraoperative timespan is defined as ‘knife-to-skin to close’ (p. 826) [ 9 ], which corresponds with the period the surgeon is present. However, the OR nursing profession defines the intraoperative timespan as the time from when the patient arrives at the OR until they are transferred to the recovery unit after surgery [ 10 ]. Furthermore, the development of the SPLINTS instrument was based exclusively on the scrub nurse’s skills, thus dismissing the NTS of the circulating nursing role [ 11 ]. The first step in developing a customised taxonomy of skills for OR nursing is to identify the nurses’ skills and behaviours that are considered to influence their safe performance [ 4 ]. Literature searches in the CINAHL and Medline databases (operating room nurs*/perioperative nurs* and non-technical skills/nontechnical skills) identified two reviews and seven empirical studies, where the NTS of OR nurses were identified to some degree with OR nurses as informants/participants. The most frequently identified NTS for scrub and circulating nurses were in the ‘communication’, ‘situation awareness’, and ‘teamwork’ categories [ 12 , 13 , 14 , 15 , 16 , 17 , 18 ]. Two studies identified the ‘task management’ category for scrub and circulating nurses [ 13 , 15 ]. However, the ‘decision making’ and ‘leadership’ categories were only identified for circulating nurses [ 13 , 15 , 16 ]. Two studies found that ethical aspects influence OR nurses’ NTS [ 18 , 19 ]. The research shows that the NTS of scrub nurses are more widely explored than those of circulating nurses [ 13 , 14 , 15 , 16 , 17 ]. However, the circulating nurses’ NTS are more advanced and autonomous than those of scrub nurses [ 13 , 15 , 16 ]. While most studies on NTS are based on the CRM framework; Hanssen et al. [ 19 ] shows that there may be other aspects of NTS not yet captured by the literature. To improve the education, and promote life-long learning, regarding NTS for OR nurses we want to construct a new behavioural marker tool for NTS observation and assessment that includes the NTS of both the circulating and the scrub OR nursing role during the entire intra-operative timespan. To generate an item pool of NTS descriptions for our tool development we must include the identified NTS of scrub and circulating nurses and further explore whether there are NTS outside the CRM framework which should be included to create a customised tool. This study aims to explore OR nurses’ descriptions of their practices in search for NTS not covered by the CRM framework. We have used an exploratory design with an inductive thematic analysis to explores the dimensions of NTS [ 20 ]. The Delphi technique is considered suitable for capturing collective knowledge within a group, and for researching areas that lack empirical data [ 21 , 22 ] Thus, the Delphi technique was chosen to open the ‘closed doors’ of OR nursing and exploring its NTS. Although a three-round Delphi technique was conducted, the data for this study is limited to the qualitative elaborations of the second round. This study was conducted and reported in line with Standards for Reporting Qualitative Research (SRQR). Population and sampleThe success of the Delphi technique depends upon an ‘expert’ panel [ 23 ]; thus, we defined eligible experts as being OR nurses with a minimum of 2 years post-training experience. In Norway, the qualifications required for OR nurses include being registered nurses and to have completed additional post graduate education (18 months) or Masters’ degree (24 months) specialising in OR nursing where the main difference between the educations are the writing of a master’s thesis. Furthermore, the OR nurses alternate between the scrub and circulating role throughout the day. The Norwegian Association of Operating Room Nurses distributed our invitations containing survey links to 1640 members, and we performed the convenience sampling through self-recruitment. The inclusion criteria were: OR nurse in active duty. Minimum 2-years post-training experience. Completion of previous Delphi round. Scholars have discussed the proper sample size for Delphi studies in the methodological literature. For example, Keeney et al. [ 23 ] suggests balancing the ability to generate conclusions with practical management of the panel size. Therefore, we considered a panel size of approximately 100 participants to be sufficient yet feasible, and 106 participants were recruited. We expected some attrition to occur between rounds; hence, 96 OR nurses participated in the second round. Data collectionThe Delphi survey was conducted between May and August 2020. We created and implemented the surveys in Norwegian using online survey software (SurveyXact 12.9; Ramboll Management Consulting, Copenhagen, Denmark) based on the categories and elements presented in the CRM framework [ 4 ] (Table 1 ). The Delphi survey was pre-tested by three fellow academics before it was piloted by 10 OR nurses meeting our inclusion criteria. A full description of the surveys for all three rounds is presented in a separate article [ 16 ]. Based on the first-round analysis we realised there were some misinterpretations of the elements; thus, we constructed the qualitative questions to operationalise and adapt the contents to the perioperative context (Table 1 ). In order to maintain a reasonable completion time in the second-round survey, the participants were asked to select the three most important categories of NTS. Subsequently they received follow-up questions about the selected categories and their respective elements. The panel were encouraged to write freely without limitations regarding word-count or content. We collected approximately 32,500 words of rich content from 490 text field answers. Table 1 presents the distribution of the answers. Data analysisFollowing the initial deductive (theory-driven, CRM framework) analysis, the selective coding resulted in a large amount of uncoded, content rich data. For this study, these residual qualitative data were analysed (all authors) using inductive thematic analysis to explore the NTS in OR nursing not covered by the CRM framework [ 24 ]. The open questions led to lengthy answers and rich data, which allowed an inductive (data-driven) approach in the analyses. As the data was written, the initial transcription step recommended by Braun and Clarke was redundant [ 24 ]. The contents of all text fields were exported from SurveyXact into Microsoft Word (Microsoft, Redmond, WA, USA), and were thoroughly read and controlled for their relevance and sensitive contents. The edited Norwegian text was imported to Nvivo 12 Pro (Alfasoft, Göteborg, Sweden) where we re-read the text and annotated areas of particular interest. We searched for descriptions of OR nursing practice which were in line with the previously mentioned definition of NTS and performed a complete coding. We then revised the codes, merging similar codes. We searched for patterns across the codes and developed candidate sub-themes containing NTS descriptions. The candidate sub-themes were then reviewed, and some were merged. Sub-themes with similar contents were grouped into themes. We reviewed the codes belonging to each theme and ensured that all theme names represent their contents. Illustrative citations were translated into English by the first author. We developed a thematic map (Fig. 1) and finalised our analysis in writing up the results and discussing the findings [ 24 ]. The inductive thematic analysis developed two themes answering our aim. Thus, the OR nurses’ NTS outside CRM are organised into the themes ‘Ethical competence’ and ‘Professional accountability’. Ethical considerationsWe conducted this research study according to the ethical principles of the Declaration of Helsinki and the Norwegian National Research Legislation [ 25 , 26 ]. The study was approved by the Norwegian Centre for Research Data (ref.#: 155,726). All participants were asked to read the provided information prior to confirming their informed consent and activating the survey. The participants could withdraw at any time without ramifications. Anonymity was ensured between the panel members. However, the iteration process of the Delphi technique hinders the anonymity between researchers and participants. We treated e-mail addresses as personal information and stored them accordingly. We removed any identifying characteristics from the submitted text before analysis to provide confidentiality in the absence of anonymity [ 20 ]. All data storage protocols adhered to the requirements of the Norwegian Centre for Research Data. Researcher characteristics and reflexivityTwo of the authors (IS and IT) are experienced OR nurses, which provided some preconceptions during the planning of the research and the construction of the Delphi survey. Our prior understanding of the OR nursing profession, and its areas of responsibility, provided insights and facilitated a deeper understanding of the situations described by our participants. By collecting data through a survey, we did not influence the participants’ contributions. We took great care not to insert our own experiences into the data. We develop the trustworthiness of the qualitative aspects of the Delphi study by demonstrating the credibility, dependability, confirmability, transferability, and authenticity of our findings according to Lincoln and Guba’s framework [ 27 , 28 ]. We enhanced the credibility of the sub-study’s results by providing transparency in our expert panel selection and provided the reader with the survey questions in relation to the CRM framework. Two of the authors (IS and IT) are OR nurses and are familiar with the ‘tribal’ language in the OR. This familiarity should establish confidence in the truth of the data and their interpretations [ 20 ]. The dependability of our data refers to its stability over time and different conditions [ 20 ]. The demographic data confirm the representativeness of the expert sample in our panel [ 29 ]. The anonymity between panel members in a Delphi approach removes group bias. In addition, the panel size should ensure that a single opinion did not overpower the group. Therefore, the study findings could be repeated if our study is to be replicated with comparable participants and context. The confirmability of our results refers to their objectivity or that the data is a good representation of the participants’ information [ 20 ]. All authors actively participated in the interpretations and analysis. We ensured that no data were invented by the authors by repeatedly revisiting the original statements. The presentation of the findings includes quotes from the participants to illustrate that the interpretations are not invented by the authors. The transferability of our results refers to the extent our findings can have applicability in other settings [ 20 ]. To aid the reader in determining the level of transferability to their context, we aimed for transparency in all study steps. The inclusion criteria are presented, and the researchers did not control the self-inclusion of the participants. The authenticity of the text is enhanced by the citations which convey the mood of the participants’ experiences [ 20 ]. Following our exploration of the OR nurses’ narratives of their practices we developed two themes, ‘Ethical competence’ and ‘Professional accountability’, which illustrates their NTS outside the CRM framework. The findings will be presented according to themes and subthemes developed in our thematic analysis guided by Braun and Clarke (Fig. 1) [ 24 ]. Due to the nature of the data collection, we are unable to pair participant numbers with citations. 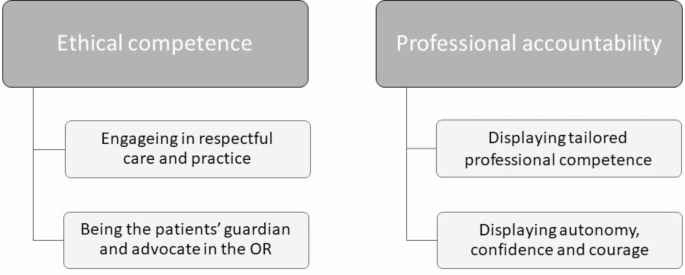 Thematic map: Themes and sub-themes Participants96 OR nurses completed the second Delphi round, which provided the qualitative data for this study. The expert panel members had a mean post-training experience of 24.4 years. Norwegian hospitals conduct three shifts in 24 h, and the work schedules for more than half of the panel members included evening or night shifts. Most of our participants were employed full time (35,5 h/week for shift-workers); however, half of these participants worked more than full time. Table 2 provides the participants’ demographics in detail. Ethical competenceThe OR nurses take pride in having the patients’ best interest as their main objective throughout their work, thus displaying their ‘Ethical competence’. This theme includes two sub-themes: ‘Engaging in respectful care and practice’ and ‘Being the patients guardian and advocate in the OR’. Engaging in respectful care and practiceA core function of the OR nurse is to maintain a sterile field to prevent infections, even when it may be perceived as disrespectful by the surgeon: ‘I have asked the surgeon to take a break to allow me to reinforce the draping, or for the surgeon to change gloves. Often, they are not interested in taking this break, but I refuse to give them instruments until we have re-established sterility’. The panel members consider all their actions as aspects of care, even when their patient is asleep or otherwise incapacitated. During surgery, the scrub nurses inspect every instrument for damage or residue, and they segregate all instruments contaminated by bowel, abscesses, or cysts from other instruments. All these aspects of managing asepticism illustrates how the OR nurse cares for patients by preventing surgical site infections. Another aspect of respectful care is thoughtful positioning of patients on the operating table. Nurses mainly perform this when the patient has no, or reduced, awareness of their body or surroundings. However, the OR nurses are conscious of positioning the patient with care to prevent nerve damage, decubitus, and malignant hypothermia: ‘ As the circulating nurse, I monitor the positioning of the patient throughout the surgery. Is everything OK? Maybe their leg has slipped off the table? ’ As experienced team workers, the OR nurses recognise that each profession has their own responsibilities and that respectful cooperation is needed to reach the goal of successful surgery for their patients: ‘ This cooperation is amazing, and the joy of the work rubs off onto the patient’. The expert panel agreed that cooperation strengthens the surgical team. However, this requires effort from all team members. Some panel members experienced a lack of understanding and respect of their work, and that they were not allowed enough time to perform their job according to their professional standards: ‘I have experienced that a patient tried to free herself from the leg supports and almost fell off the operating table […] and it was difficult to keep her safe. This happened because the anaesthesia was terminated before I had secured the patient’. A well-functioning team depends on respect between team members. Some of the OR nurses showed their respect by ‘lifting others up’ through providing support and positive feedback. Being the patients’ guardian and advocate in the ORWhen engaging with the patients prior to anaesthesia, the OR nurse safeguards that all the information is correct and that the patient understands what will happen to them. This creates an opportunity for discovering and rectifying issues like wrong surgical site or procedure: ’The patient was scheduled with amputation … Luckily, I knew them from their actual amputation earlier that week and knew that the correct plan for today was wound revision and change of vacuum bandages. The surgeon had copied the previous requisition.’ Panel members also described advocating for their patients during surgery: ‘ I have urged the surgeon to administer more local anaesthetics during surgery on an awake patient with unsatisfactory pain relief. The surgeon was reluctant because they were focusing on the procedure. Sometimes, when I advocate for my patient, no one listens… ’. Hence, OR nurses serve as guardians and advocates for the patient before and during their surgical procedure. Professional accountabilityThe panel members note that they have the competence to organise and manage individual procedures as well as surgical schedules. Furthermore, they must maintain their awareness of the patient, technical equipment, procedures, and the coordination needed to ensure that the patient receives safe and efficient treatment. With this professional accountability, the OR nurse contributes to minimising the risk of adverse events. Two sub-themes, ‘Displaying tailored professional competence’ and ‘Displaying autonomy, confidence, and courage’, comprise this theme. Displaying tailored professional competenceThe panel members value their competence as highly educated health-care practitioners. They use their advanced knowledge to decide which OR is appropriate, which operating table and equipment meets the requirement for the patient’s safe positioning, and what medical or technical equipment is compatible with the surgeon’s needs and the patient’s conditions. Through extensive experience, they develop the competence to consider the consequences of their choices for the patient and the health-care personnel. Although our panel comprised experienced OR nurses, they are aware of their responsibility in training new colleagues. The novice OR nurses build competence by being supported by their experienced colleagues: ‘To see them, listen to them, and give them advice when needed. Learning is promoted when they feel safe and have a sense of coping, instead of feeling anxious’. The panel members’ tailored competence is also visible in their interactions with other team members. The Safe Surgery checklist is implemented in Norway [ 30 ]. However, some panel members have experienced that team members do not pay attention during ‘time-outs’ because of their simultaneous work or parallel conversations. They may miss essential information, which results in the lack of shared understanding, repetition of information, and prolonged anaesthesia time. A panel member shared an extreme consequence of not having a proper ‘time-out’: ‘ I have taken part in doing the wrong surgery on a patient after a poorly executed ‘time out’ ’. Several panel members have experienced that some surgeons rush out when surgery is completed, leaving the rest of the team responsible for completing the ‘after surgery’ part of the checklist. The absence of the surgeon’s point of view may compromise the accuracy of the information passed on during the patient’s transfer into postoperative care. Displaying autonomy, confidence, and courageThe OR nurses position themselves as autonomous members of the surgical team who act independently rather than just following task lists and answering their colleagues’ demands: ‘ We decide when to move the patient into the OR. We decide when to call the surgeon. We decide which infection control routines to implement. We decide how to arrange the equipment. […] The OR nurses have a wide range of responsibilities’. The panel members describe that they regularly take responsibility on behalf of others: ‘I once refused to give the cardiac surgeon his sutures because a gauze was missing. The surgeon was grumpy, but eventually he found a gauze that was used for cooling behind the heart. He thanked me later’. One OR nurse described the frustration of having to police their colleagues and the consequences it had on a personal level: ‘ I am fed up with surgeons not adhering to the standards of preoperative hand hygiene and masks, but I am even more fed up with fellow OR nurses who don’t make sure the team follows the rules. They become more popular than me because I want to keep up my professional standards and follow the rules’. This illustrates how the OR nurses use their professional confidence and personal courage to do the right thing for their patient, despite the hierarchical authority within the OR and the potential risk of being disfavoured by the surgeon. Our findings show that the International Council of Nurses’ code of ethics are embedded in the participants’ performance. Their respect for the first code: ‘Nurses’ primary professional responsibility is to people requiring nursing care…’ [ 31 ] is illustrated by participants repeatedly stating that ‘the patient always comes first’ even when it damages their own position in the surgical team. Norms such as ethical competence and professional accountability has not previously been discussed in relation to CRM based behavioural marker tools, and it might be timely to raise the question why such rich norms for core skills are not captured by existing frameworks and tools. Ethical competence as non-technical skillsFrom an outsider’s perspective, the technical expertise of OR nurses is often perceived as the antithesis of caring with nursing and technology representing two opposing paradigms [ 32 ]. However, from within the closed doors of the OR, it is apparent that being technologically competent is perceived as being caring. Our findings illustrate that nursing in a technological environment requires the interweaving of caring and technology [ 33 ], and the tension between nursing and technology described by Barnard and Sandelowski [ 34 ] is not recognised in our data. Furthermore, while Locsin [ 35 ] theorise over the relationship between technological competency and caring, our participants considers correct handling of technical equipment and smooth instrumentation when serving the surgeon as acts of caring, which is similar to the findings of Bull and FitzGerald [ 33 ]. Intraoperative nursing care is characterised by constantly being present throughout the surgery and personalising nursing care procedures for each patient [ 10 ]. The participating OR nurses emphasised the importance of establishing a connection with their patients. However, the level of connection varies according to time allowances, with ample time given during preparation for elective surgery but only time for eye contact and maybe a reassuring touch during acute situations. In some instances, the patient may already be anaesthetised upon arrival in the OR; however, the OR nurses still care for these patients through their prevention of positioning-related injuries, surgical site infections, malignant hypothermia, or other undesired outcomes. The OR nurse’s care is mostly invisible to the patient. However, similarly to Bull and FitzGerald [ 33 ], our findings show that the OR nurses took pride in providing excellent patient care even when the patient is unaware. Thus, while Nordström & Wihlborg [ 36 ] highlight the OR nurses’ advocacy for awake patients, our study, along with Levesque et al. [ 37 ], found that the advocacy continues when the patients are unable to advocate for themselves. Our findings illustrate that value conflicts are created between requirements for efficiency and the desire to do the best for the patients. According to Blomberg et al. [ 38 ], these value conflicts are particularly common when the surgical team do not consider the OR nurse to be competent. In these situations, our participants portrayed moral courage in their efforts to protect their patients, even if they end up being perceived as bossy or difficult by the surgical team. Blomberg et al. [ 38 ] described this moral courage as acting according to one’s conviction despite criticism from others. When the OR nurse discovers threats to their patient’s safety, such as wrongly marked surgical sites or missing surgical objects, they consult with the surgeon to rectify the issue. Therefore, they contribute to a shared risk awareness among the surgical team [ 39 ]. Such incidents may seem minor, but if not ameliorated, they may lead to major harm for the patients. Few researchers have explored the OR nurses’ error-preventing ability; however, Yang et al. [ 40 ] found that the circulating nurse play a significant role in identifying and addressing potential harmful incidents. When our panel members make decisions, they have the patients’ best interests as their guidance. Therefore, ethical considerations regarding the patients influence the OR nurses’ NTS. Few previous studies have identified the ethical aspects of NTS [ 18 , 19 ]. However, Kelvered et al. [ 10 ] also found that OR nurses portrayed their ethical views and moral approach through their desire to promote their patients’ well-being. According to their descriptions of their work, the panel members position themselves as safeguards and advocates in the OR, or as Voight [ 41 ] commented, they are ‘the last line of defence for patient safety’ (p. 822). Professional accountability as non-technical skillsAll surgical team members are experts with specialised skills that are inaccessible to someone without their training and experience. They are members of established professions that declare their responsibility for certain tasks [ 42 ]. There is some degree of division of labour within the team, which requires the knowledge of other team members’ competence and trust in their abilities [ 42 ]. Traditionally, OR nurses were trained in situ while working in the OR [ 1 ]. Following an increase in educational level, OR nurses now have more autonomous functions. However, they still have an underdeveloped language for verbalising their competence to the surgical team. Thus, OR nursing can be described similarly to an iceberg, where only the ‘above-water’ work is visible to the other professions in the perioperative team while their ‘under-water’ work is unverbalised. The lack of verbalisation results in OR nursing competence being invisible to the surgical team and also hospital administration, which is comparable to ‘the invisible work of nurses’ described by Allen [ 43 ]. This may explain why several study participants experience that their competence is underestimated, and the importance of their work underrated. Furthermore, they are not allowed sufficient time to perform their responsibilities according to the required standards. Both experienced and new OR nurses in other contexts have described this feeling of invisibility, being underrated, and not given enough time to provide quality care [ 36 , 37 , 44 ]. Therefore, the pursuit of efficiency to complete surgical task may cause a spiral effect, where the efficiency may hinder the surgical team’s recognition of the OR nurses’ contribution to the team [ 7 ]. The safety of the OR environment relies on procedures and standards; however, the team members adherence to these standards varies. The participating OR nurses display a sense of responsibility on behalf of other professions when they must argue with other team members to convince them to meet the given standards. Similarly, Nordström et al. [ 36 ] found that OR nurses and nurse anaesthetists took responsibility to remind other team members to do their tasks, while Flin et al. [ 11 ] underestimates the autonomy of the OR nurses and reduces their ability to ‘adhering to codes of good practice and guidelines’ (p.11). The OR nurses’ sense of responsibility on behalf of others originates from a professional obligation to keep the patient safe. However, if the corrected team members perceive this as a disturbance, the correction comes at a professional cost for OR nurses. Successful treatments depend on the establishment of a shared understanding among the surgical team. However, the communication among team members before the patient arrives and the suspension of activities during surgical time-outs are the two most frequently missed nursing care areas in the OR [ 45 ]. Our results show that gathering the teams’ attention during time-outs is challenging. Neuhaus et al. [ 39 ] noted that the time-outs are considered burdensome by surgeons and anaesthetists. In addition, time-outs are often combined with tasks like scrubbing and draping. However, Freundlich et al. [ 46 ] found fewer disruptions and mainly full-team attendance during time-out when they were initiated by the circulating OR nurse. Levesque et al. [ 37 ] found that although the circulating nurse is in a good position to lead the surgical team in some situations, they did not receive the organisational support to lead. A core responsibility for OR nurses is to establish and maintain an aseptic field; therefore, when they notify a team member of a breach of sterility, it is usually respected. However, some of our participants portrayed great courage and professional confidence when contesting their surgeons about missing gauzes or retained items during counting procedures. The extensive experience of our participants (mean, 23 years), and their high level of education, may influence this courage. Furthermore, the OR nurses become trusted members of the surgical team through building their experience, and thus become more comfortable speaking up [ 37 ]. Our results show that ethical competence and professional accountability are cognitive and personal resource NTS essential to patients’ safety. Similarly, Hanssen et al. (2020) identified respecting and caring for the patient in a rushed environment, and respect within the perioperative nursing team as ethical NTS. Previously, Agha et al. [ 47 ] have identified that such personal and professional values are required, along with technical and non-technical skills, for creating good surgical practices. Strengths and limitations of the workThe Delphi technique for data collection in this study provides both strengths and limitations. The Delphi survey was conducted during the initial months of the COVID-19 pandemic, which highly influenced data collection from healthcare workers. Face-to-face interviews were not an option during this period; however, the survey’s free text fields proved to be a robust substitute. We collected rich data from a larger and more representative group of OR nurses. However, we had limited opportunities for clarification and further elaboration. The online survey software enabled the inclusion of participants representing all Norwegian health regions and allowed the participants to use their preferred device for the survey and take breaks at their own convenience. Recommendations for further researchConsidering the variety of qualifications required for OR nursing in different countries, our findings might not be representative in contexts where OR nurses have less education and experience than our panel members. We recommend further qualitative research studies to explore the NTS of OR nurses over different contexts. We will also recommend an exploration of NTS outside the CRM framework for other professions within the surgical team. The participants of this study have opened the closed doors to the OR. By exploring their narratives, we have identified that ‘Ethical competence’ and ‘Professional accountability’ are descriptors of OR nurses’ NTS that are essential for safe and efficient OR nursing without being included in the CRM framework. After more than a decade of constructing NTS behavioural marker systems for healthcare within the borders of the CRM framework, it may be timely to acknowledge that not all NTS in OR nursing, and the surgical team, can be drawn from those of the pilots. Our findings illustrate that not only behavioural marker systems, but also the CRM framework itself may need adaptation to allow for successful implementation into healthcare. In a time with a global outcry over the lack of qualified OR nurses, and the threat of less qualified personnel taking over OR nursing responsibilities, verbalisation of the competence of the profession is paramount to inform hospital management and funding bodies of OR nurses’ contribution to safe and efficient surgical treatment. The authors are developing a new behavioural marker system for the NTS of OR nurses. By including these novel NTS, or (formerly) tacit skills, in a new behavioural marker system, the verbalisation of OR nursing skills will be facilitated. Data AvailabilityThe datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. AbbreviationsOperating Room
Crew Resource Management The Scrub Practitioners List of Interoperative Non-Technical Skills McGarvey HE, Chambers MGA, Boore JRP. Development and definition of the role of the operating department nurse: a review. J Adv Nurs. 2000;32(5):1092–100. Article CAS PubMed Google Scholar Benner P, Kyriakidis PH, Stannard D. Clinical wisdom and interventions in Acute and critical care: a thinking-in-Action Approach. 2nd ed. New York, USA: Springer Publishing Company, LLC; 2011. Book Google Scholar Sirevåg I, Aamodt KH, Mykkeltveit I, Bentsen SB. Student supervision using the Scrub Practitioners’ list of intraoperative non-technical skills (SPLINTS-no): a qualitative study. Nurse Educ Today. 2021;97. Flin O, Connor C. Safety at the Sharp End. 1st ed. Boca Raton, Florida: CRC Press; 2008. Google Scholar Flin R, Patey R. Improving patient safety through training in non-technical skills. BMJ. 2009;339(7728). Flin R, Lynne M, Goeters K-M, Hörmann H-J, Amalberti R, Valot C, et al. Development of the NOTECHS (non-technical skills) system for assessing pilots’ CRM skills. Hum Factors Aerosp Saf. 2003;3(2):22. Bull RM, Fitzgerald M. The invisible nurse—behind the Scenes in an australian OR. AORN J. 2004;79(4):810. ,8,21-,6,8,23. Article PubMed Google Scholar Flin R, Mitchell L. Scrub practitioners’ list of intra-operative non-technical skills - SPLINTS. Safer surgery, Analysing Behavior in the Operating Theatre. Boca Raton: CRC Press; 2017. Mitchell L, Flin R, Yule S, Mitchell J, Coutts K, Youngson G. Thinking ahead of the surgeon. An interview study to identify scrub nurses’ non-technical skills. Int J Nurs Stud. 2011;48(7):818–28. Kelvered M, Öhlén J, Gustafsson BÃ. Operating theatre nurses’ experience of patient-related, intraoperative nursing care. Scand J Caring Sci. 2012;26(3):449–57. Flin R, Mitchell L, Coutts K, Youngson G, Mitchell J. Scrub Practitioners’ List of Intraoperative Non-Technical Skills (SPLINTS): University of Aberdeen; 2010 [Available from: https://research.abdn.ac.uk/wp-content/uploads/sites/14/2019/03/SPLINTS-V1-0-Handbook-1.pdf . Gillespie BM, Gwinner K, Chaboyer W, Fairweather N. Team communications in surgery - creating a culture of safety. J Interprof Care. 2013;27:387–93. Kang E, Gillespie BM, Massey D. What are the non-technical skills used by scrub nurses? An integrated review. ACORN. 2014;27(4):16–25. Mitchell L, Flin R. Non-technical skills of the operating theatre scrub nurse: literature review. J Adv Nurs. 2008;63:15–24. Redaelli I. Nontechnical skills of the operating theatre circulating nurse: an ethnographic study. J Adv Nurs. 2018;74:2851–9. Sirevåg I, Tjoflåt I, Hansen BS. A Delphi study identifying operating room nurses’ non-technical skills. J Adv Nurs. 2021;77(12):4935–49. Skråmm SH, Smith Jacobsen IL, Hanssen I. Communication as a non-technical skill in the operating room: a qualitative study. Nurs Open. 2021. Mundt AS, Spanager L, Lyk-Jensen HT, Østergaard D. Adaptation of a tool to assess non-technical skills of scrub practitioners in Denmark. J Perioper Pract. 2017;27(9):180–5. PubMed Google Scholar Hanssen I, Smith Jacobsen IL, Skråmm SH. Non-technical skills in operating room nursing: ethical aspects. Nurs Ethics. 2020;27(5):1364–72. Polit DF, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. 10 ed. Philadelphia: Wolters Kluwer; 2017. Foth T, Efstathiou N, Vanderspank-Wright B, Ufholz L-A, Dütthorn N, Zimansky M, et al. The use of Delphi and Nominal Group technique in nursing education: a review. Int J Nurs Stud. 2016;60:112–20. McKenna HP. The Delphi technique: a worthwhile research approach for nursing? J Adv Nurs. 1994;19(6):1221–5. Keeney S, Hasson F, McKenna H. The Delphi technique in nursing and Health Research. West Sussex, United Kingdom: Wiley-Blackwell; 2011. Braun V, Clarke V. Successful qualitative research. London: SAGE Publications Ltd; 2013. The Norwegian National Research Ethics Committees. General Guidelines for research ethics 2019 [Available from: https://www.forskningsetikk.no/en/guidelines/general-guidelines/ . World Medical Association. WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects The World Medical Association, Inc. ; 2013 [Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ . Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, Calif: Sage; 1985. Guba EG, Lincoln YS. Competing paradigms in qualitative research. SAGE; 2006. pp. 216–36. Hasson F, Keeney S. Enhancing rigour in the Delphi technique research. Technological Forecast Social Change. 2011;78(9):1695–704. Article Google Scholar World Alliance for Patient Safety. WHO surgical safety checklist and implementation manual: WHO; 2008 [Available from: https://www.who.int/teams/integrated-health-services/patient-safety/research/safe-surgery/tool-and-resources . ICN. The ICN code of ethics for nurses 2021 [Available from: https://www.icn.ch/sites/default/files/inline-files/ICN_Code-of-Ethics_EN_Web.pdf . Sandelowski M. Troubling distinctions: a semiotics of the nursing/technology relationship. Nurs Inq. 1999;6(3):198–207. Bull R, FitzGerald M. Nursing in a technological environment: nursing care in the operating room. Int J Nurs Pract. 2006;12(1):3–7. Barnard A, Sandelowski M. Technology and humane nursing care: (ir)reconcilable or invented difference? J Adv Nurs. 2001;34(3):367–75. Locsin RC. Rozzano Locsin’s Technological Competency as Caring in nursing. In: Smith MC, editor. Nursing theories and nursing practice. Philadelphia: F.A. Davis Company; 2020. Nordström AMRN, Wihlborg MPRN. A phenomenographic study of swedish nurse anesthetists’ and OR Nurses’ work experiences. AORN J. 2019;109(2):217–26. Levesque MJ, Etherington C, Lalonde M, Stacey D. Interprofessional collaboration in the OR: a qualitative study of Nurses’ perspectives. AORN J. 2022;116(4):300–11. Blomberg A-C, Bisholt B, Lindwall L. Value conflicts in perioperative practice. Nurs Ethics. 2019;26(7–8):2213–24. Neuhaus C, Spies A, Wilk H, Weigand MA, Lichtenstern C. Attention everyone, Time Out! Safety Attitudes and Checklist Practices in Anesthesiology in Germany. A cross-sectional study. J Patient Saf. 2017;17(6):467–71. Yang YT, Henry L, Dellinger M, Yonish K, Emerson B, Seifert PC. The circulating nurse’s role in Error Recovery in the Cardiovascular OR. AORN J. 2012;95(6):8. Voight PE. Our value as nurses. AORN J. 2009;89(5):821–2. Abbott A. The system of professions : an essay on the division of expert labor. Chicago: University of Chicago Press; 1988. Allen D. The invisible work of nurses: hospitals, Organisation and Healthcare. London: London: Routledge; 2015. Eriksson J, Lindgren BM, Lindahl E. Newly trained operating room nurses’ experiences of nursing care in the operating room. Scand J Caring Sci. 2020;34(4):1074–82. Marsh V, Kalisch B, McLaughlin M, Nguyen L. Nurses’ perceptions of the extent and type of missed perioperative nursing care. AORN J. 2020;112(3):237–47. Freundlich RE, Bulka CM, Wanderer JP, Rothman BS, Sandberg WS, Ehrenfeld JM. Prospective investigation of the operating room time-out process. Anesth Analg. 2020;130(3):725–9. Article PubMed PubMed Central Google Scholar Agha RA, Fowler AJ, Sevdalis N. The role of non-technical skills in surgery. Ann Med Surg (Lond). 2015;4(4):422–7. Download references AcknowledgementsNot applicable. This study received no external funding. Author informationAuthors and affiliations. Faculty of Health Sciences, Department of Caring and Ethics, University of Stavanger, Postboks 8600, Stavanger, 4036, Norway Irene Sirevåg Faculty of Health Sciences, Department of Quality and Health Technology, University of Stavanger, Stavanger, Norway Ingrid Tjoflåt & Britt Sætre Hansen You can also search for this author in PubMed Google Scholar ContributionsIrene Sirevåg: Project administrator. Conceptualisation and methodology of the study. Investigation and data collection. Analysis of the data. Design of tables and figures and drafting of the original manuscript. Editing of the manuscript. Approval of the final version of the manuscript. Ingrid Tjoflåt: Conceptualisation and methodology of the study. Analysis of the data. Review and editing of the manuscript. Approval of the final version of the manuscript. Britt Sætre Hansen: Conceptualisation and methodology of the study. Analysis of the data. Review and editing of the manuscript. Approval of the final version of the manuscript. Corresponding authorCorrespondence to Irene Sirevåg . Ethics declarationsCompeting interests. The authors declare that they have no competing interests. Ethics approval and consent to participateWe conducted this research study according to the ethical principles of the Declaration of Helsinki and the Norwegian National Research Legislation. In Norway, the ethical approval is divided between the Norwegian centre for research data (data protection) and the Regional Ethical Committees (Medical and Health related research). The Norwegian Centre for Research Data (ref.#: 155726) has approved that the data protection plan of the study complies with Norwegian legislation ( https://lovdata.no/dokument/NL/lov/2018-06-15-38 ) and the European General Data Protection Regulation (GDPR). Our study does not qualify for consideration by the Regional Ethical Committee since it does not involve human intervention or invasive studies, human biological material or health information, and thus does not fall under the jurisdiction of the Law of medical and health related research ( https://lovdata.no/dokument/NL/lov/2008-06-20-44 ). Written informed concent was obtained from all participants, and they were informed about the rigth to withdraw from the study at any point. Consent for publicationAdditional information, publisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsOpen Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data. Reprints and permissions About this articleCite this article. Sirevåg, I., Tjoflåt, I. & Hansen, B.S. Expanding the non-technical skills vocabulary of operating room nurses: a qualitative study. BMC Nurs 22 , 323 (2023). https://doi.org/10.1186/s12912-023-01500-9 Download citation Received : 22 May 2023 Accepted : 12 September 2023 Published : 19 September 2023 DOI : https://doi.org/10.1186/s12912-023-01500-9 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
BMC NursingISSN: 1472-6955
Migraine self-management at work: a qualitative study
Journal of Occupational Medicine and Toxicology volume 19 , Article number: 22 ( 2024 ) Cite this article 120 Accesses Metrics details Migraine is common and can be highly disabling. Adequate migraine self-management (SM) can mitigate the potentially adverse health effects of migraine. However, adequate SM can be challenging to implement in everyday life, for instance, at the workplace. We aimed to explore how migraine SM is carried out at work and which occupational factors may determine effective implementation according to employees with migraine. We also explored the potential impact of the COVID-19 pandemic and the associated re-arrangement of working conditions on migraine SM at work. We conducted semi-structured qualitative interviews (08/2020–01/2021). Participants were eligible if they have worked for at least six months with a minimum of twenty hours per week and with a migraine diagnosis. The interviews were transcribed and content-analyzed using MAXQDA. Migraine SM was perceived to be influenced by social interactions at work (e.g., in terms of understanding vs. stigmatization), the level of job decision latitude (JDL, i.e., the extent to which one is able to influence work processes, e.g., when working from home), and workplace design (e.g., in terms of opportunities to withdraw from work). During the COVID-19 pandemic, especially increased JDL appeared to favorably influence migraine SM. ConclusionsMigraine SM at work is fostered or complicated by various psychosocial working conditions. By considering these facilitators and barriers, more migraine-friendly workplaces can be created. Migraine is associated with a considerable burden in terms of its prevalence, related disability, and cost. The prevalence is especially high among people between the age of 36 and 46, who are in the midst of their occupational life [ 1 ]. It has been estimated that the European Union loses € 111 billion annually due to migraine [ 2 ]. As much as 93% of this amount is considered to be attributable to indirect cost, i.e., cost resulting from lost and reduced productivity at work [ 2 ]. To successfully manage their condition, individuals with migraine need to acquire and apply various skills (i.e., self-management [SM]). Five major areas of migraine self-management activities have been identified in prior studies: (1) utilizing the healthcare system, (2) taking medication adequately, (3) using alternative therapies (such as osteopathy, herbal, and homeopathic remedies), (4) requesting social support, and (5) self-care (e.g., trigger detection and avoidance, stress management, and a healthy lifestyle) [ 3 , 4 , 5 ]. Migraine SM can be hampered or facilitated by external factors in everyday life, for instance, at the workplace. With regard to the latter, the European Federation of Neurological Associations (EFNA) conducted a survey in 2020 inquiring individuals with migraine or other types of headaches ( n = 167) from 20 European countries what their company should do to help them cope better with the effects of their health condition [ 6 ]. Proposed areas of improvement included (but were not limited to): more understanding by managers, more opportunities to work from home, private workspace, less social interaction, part-time work, and noise-cancelling headphones [ 6 ]. In the same vein, Scaratti et al. [ 7 ] used an online questionnaire to examine the needs of headache patients in Europe ( n = 103) related to staying at or returning to work. Here, too, physical environment adaptions (such as single offices, rest rooms), work-related aspects (e.g., longer, and flexible breaks), and support at work (among other things, social support by supervisors and human resources) were mentioned [ 7 ]. While there is thus confirmatory preliminary evidence regarding headache SM, there is still a need to examine in depth if and how working conditions may affect successful implementation of specifically migraine SM (rather than headache management in general) at work. Migraine cannot be equated with headache, as headache is only one symptom of migraine, which is also usually accompanied by other symptoms such as nausea, vomiting, or sensitivity to light, and thus likely to lead to more impairment. We aimed to gain detailed insights into the types of working conditions that may facilitate or hamper the ability to self-manage migraine. Work arrangements have changed swiftly and dramatically for many employees during the COVID-19 pandemic and we therefore also sought to explore the potential effects of these re-arrangements on SM strategies. We conducted a qualitative study using semi-structured interviews. Our report adheres to the Consolidated Criteria for Reporting Qualitative Research (COREQ) statement [ 8 ]. The primary researcher (CK) was a medical student at the time of our study. Qualitative research skills are usually not acquired during medical studies in Germany. CK conducted the study to obtain a German Doctor of Medicine (Dr. med.) degree, which is comparable (in terms of its scope and quality) with a master thesis rather than with a PhD degree. The general choice of self-management at work as the research topic was due to the foci of the research group headed by AL, who acted as CK’s thesis supervisor. It was CK’s wish to relate her research project to migraine, as she had several migraine patients in her personal environment. CK familiarized herself extensively with the methodology of qualitative research (especially through self-studies and online tutorials) and in particular with the coding process. Prior to the interviews and the analysis, CK was trained (e.g., in interviewing techniques) by KH who is an experienced qualitative researcher [ 9 , 10 ] (female, degrees in psychology and public health). Also, detailed feedback and opportunities for reflection were provided during the actual interviewing and subsequent analysis (see below). Study populationWe sought to recruit participants who met the following inclusion criteria: (1) participant-report that migraine has ever been diagnosed by a physician and (2) employment with the migraine diagnosis for at least six months with a minimum of 20 working hours per week. Study participants were recruited via three different pathways: an inpatient rehabilitation clinic for headache disorders (Berolina Klinik, Löhne, Germany), migraine self-help groups from different regions in Germany, and private contacts of members of the study team. In the run-up to the interviews all potential participants received information on the objectives of the study, the professional background of the interviewer (CK) and the inclusion criteria (either via a flyer or from CK in person). This information was presented again later at the start of the interviews. It was also ensured at the beginning of the interviews that the inclusion criteria were met. All participants provided written informed consent prior to the interviews. In line with participants’ preferences, interviews were either conducted face-to-face or by telephone. Face-to-face interviews took place in the clinic or at the participants’ homes. We did not gather any information from non-participants, that is, from those who were exposed to our recruitment efforts (e.g., members of the self-help groups), but decided not to participate. Our study was approved by the Institutional Review Board of the Faculty of Medicine of the University of Düsseldorf, Germany (# 2019 − 627). Data collectionBased on previous qualitative research by our group [ 9 , 11 ], we designed a topic guide [see Additional File 1 ]. After three interviews, the topic guide was discussed and adjusted by the study team. In particular, we then decided to add one question about migraine SM at work specifically during the COVID-19 pandemic, as this was an issue frequently referred to in the first interviews. Prior to the interviews, participants were asked to complete a standardized questionnaire collecting information on socio-demographics and the health status (see Results – Table 1 ). Data collection took place from August 2020 to January 2021. All interviews were conducted in German by one researcher (CK), who took field notes during the interviews. Besides the interviewer and the participant, no one was present. Follow-up interviews were not conducted. All interviews were digitally recorded and transcribed. CK received detailed feedback on the way she conducted the interviews after three interviews from AL, who is an experienced qualitative researcher [ 9 , 10 , 11 , 13 ] (male, degrees in epidemiology and health sciences). These three interviews were initially supposed to serve as test interviews, but as they contained valuable information we decided to include these interviews in the analysis. There were also no major concerns from AL regarding CK’s interview style except that CK should be even more careful not to ask too closed questions. Data collection was terminated when thematic saturation was reached, which implies that no new information was expected to be delivered by additional interviews [ 14 ]. To verify that saturation had been reached, the data analysis already started during data collection. As the interviews and the analysis were carried out by the same person (CK), she was able to pay close attention to when no new aspects were mentioned in the interviews. The interviews were then terminated after consultation with AL. Study participants were not given access to the transcripts, nor could they provide feedback on the findings. Qualitative data analysisTranscripts were content-analyzed [ 15 ] using the software MAXQDA 2020. The coding was based closely on the topic guide and the research questions of the study. Consequently, the questions of our topic guide [see Additional File 1 ] served as main categories (deductive coding). For example, the question ‘Are there conditions at work that help you deal with your migraine?’ served as one main category, labelled ‘Facilitators of migraine self-management’. Subcategories were then developed based on the interview content (inductive coding). After CK had coded five interviews, the coding framework was carefully reviewed by two experienced qualitative researchers (KH and AL). Once everyone approved the initial coding framework, CK applied the code system to all interviews and expanded it by adding further categories. After this first round of coding was completed, AL reviewed the codes again. For instance, AL checked the structure of the coding tree level by level to see whether the codes may be overlapping or seemed ordered logically (e.g., according to the same criteria) within each level. He read all text passages included into each code to explore whether the respective text passages relate to the same phenomenon (and thus can be grouped into a single code) or whether codes may be merged or could be further sub-divided. Based on this, he suggested changes and other inductive categories and discussed them with CK. Based on this discussion, CK re-coded all interviews. Afterwards, the codes were re-discussed with AL and the framework was marginally adjusted. Finally, CK carried out a third and final round of coding. The analysis was carried out using German-language transcripts. The quotes presented in this paper were translated from German into English by a researcher who is familiar with health research and has a Master’s degree in English studies (see acknowledgments). Description of the sampleIn total, 24 interviews were conducted with a mean duration of 31.8 min (range: 17.6–55.3, standard deviation [SD] = 11.4). Twelve interviews were carried out face-to-face and twelve by telephone. Ten participants were recruited in the rehabilitation clinic, nine through self-help groups, and five were private contacts of study team members. Table 1 shows characteristics of our sample: our study population was mainly female (88%), and the mean age was 49.5 years (SD = 9.0). More than half of the participants ( n = 14) were classified as having a job that was mainly characterized by cognitive or psychosocial demands (e.g., librarian, social worker, pastoral counsellor). The remainder of participants had jobs with mixed requirements (e.g., teacher, nurse, shop assistant). The mean time since the diagnosis of migraine was 20.6 years and varied from five to 40 years (SD = 8.5). On average, participants reported to have had 10.0 days of migraine during the last month, but the variation was considerable (range: 2–26, SD = 6.6). Qualitative interviewsA broad range of psychosocial facilitators and barriers of migraine SM at work emerged from our data which are described in the following. Our results indicated that the COVID-19 pandemic affected workplace SM both favorably and adversely. All quotes referenced below can be found in the appendix [see Additional File 2 ]. If there is an interest in the shared migraine self-management strategies at work, a description of these can also be found in the appendix [see Additional File 3 ]. These are not explained in more detail below however, as the specification of the strategies is beyond the scope of our main research questions. Which psychosocial working conditions influence migraine self-management at work?Facilitators : The following working conditions were perceived to be helpful in managing migraine at work: (1) high social support, (2) high job decision latitude (JDL; i.e., the degree of an employee’s control over tasks and how and when they are addressed), and (3) a suitable workplace design. Receiving social support at work from colleagues, supervisors, or in form of company or government policies was reported. Support by colleagues included the understanding for the illness, especially from colleagues with the same disease. It was frequently expressed that some colleagues could – without words – sense when the individual with migraine was not feeling well. Relevant support-related activities by colleagues that made migraine SM easier included support in avoiding triggers (e.g., by ensuring a good air supply), encouragement to withdraw during acute migraine attacks, and taking over tasks (quote 1). According to the participants, social support by supervisors was effective by creating flexible arrangements regarding tasks, working times, and locations, for example the option to work from home (quote 2). Overall, it seemed that understanding for the disease and the social support from colleagues and supervisors facilitated the SM strategy communication. In Germany, people with chronic illness (including migraine) can apply for a so-called “degree of disability”. This entails entitlement to – amongst other things – more holidays and better protection against dismissal from the job. This legal possibility was perceived as helpful, also in the way that these official degrees simplified the justification of the disease and certified its seriousness (quote 3). Furthermore, one participant shared that she has approached the staff council (in her case the teachers’ council). By disclosing her migraine in front of the council, she gained the understanding of her colleagues (quote 4). In addition to social support, the study participants described a high JDL – that is, a high degree of control over their tasks – as beneficial. Influence on the order of tasks was perceived as allowing for flexibility in planning and carrying out SM during migraine attacks. Control over the type and number of tasks (e.g., working independently instead of attending meetings [quote 5] or the possibility to avoid screen work during the acute attack [quote 6]) were relevant in managing migraine attacks. Another important factor in terms of JDL was the possibility of working from home. The latter provided the opportunity to organize the working day according to one’s own preferences and to take flexible breaks. For example, one participant reported that one had the option of starting one’s working day later at home if one had a headache in the morning (quote 7). The improved opportunities of stopping work at home was also considered to be beneficial because, according to one participant, the threshold to stop working when experiencing complaints is lower when one works at home than at the workplace (quote 8). A suitable workplace design, which referred mainly to a single rather than a multi-person office, was also experienced as helpful. In a single office, one had the opportunity to retreat and control air supply and light. As many individuals with migraine are sensitive to light during an attack, this can be beneficial (quote 9). In addition to the office situation, the provision of appropriate work equipment such as flicker-free screens, noise-cancelling headphones, and height-adjustable desks was also reported to have a positive effect on one’s migraine. The latter had been reported to reduce cramping in the shoulders and neck and thereby easing headaches (quote 10). Barriers : The reported barriers represented in certain respects the opposites of the above-mentioned facilitators. Yet as these were explored separately and several aspects were not overlapping, they are described independently. The following aspects were mentioned: (1) poor social interactions, (2) unfavorable working time arrangements, (3) unfavorable workplace arrangements, and (4) other working conditions. Poor social interactions included interactions with colleagues, supervisors, and service users. Several participants felt that migraine as a disease was often not taken seriously by others and stigmatized at their workplace. For example, this led to migraine being dismissed as a trifle or lack of understanding for staying at home in case of complaints (quote 11). One participant also emphasized the lack of empathy at the workplace: if one was present at work, one was expected to be fully functioning (quote 12). In this context, participants also found it bothering that migraine is “an invisible condition” (quote 13). During contact with service users (e.g., customers, patients, clients), it was reported to be disturbing that there were often high expectations that could not be met during a migraine attack and the associated impairments (quote 14). Some workplace and working time arrangements were also considered as detrimental. In workplaces where migraine triggers were present (such as heavy noise, little air supply, bright light), migraine SM and especially the preventive strategy of trigger avoidance was reported to be negatively affected. For example, one participant reported the problem of sharing an office and not being able to adapt it to one’s own need, for example not having control over room temperature (quote 15). Visual display unit (VDU) work was also described to be a migraine trigger (quote 16). Another mentioned problem in workplace design was the lack of opportunities to retreat – physically (e.g., due to lack of break rooms, open-plan offices) and mentally (in terms of being permanently approachable). One participant, for example, shared that it was very difficult to deal with migraine if one always had to be approachable on business trips and thus has no possibility to retreat (quote 17). The lack of opportunities to retreat from challenging situations was believed to worsen symptoms and delay recovery from an attack. In terms of unfavorable working time arrangements, irregularity was mentioned as it implies an interruption of one’s usual circadian rhythm, which may trigger a migraine attack. This could be unscheduled client appointments due to public traffic (quote 18), shift work or exceptional weekend work (quote 19), but also business trips (including school trips as a teacher), missing or insufficient breaks, and time pressure at work (quote 20). Other working conditions that were considered as barriers included, for example, a lack of staff and therefore a lack of replacement hampering one to go home when experiencing an acute migraine attack (quote 21) as well as poor contract conditions. Regarding the latter, one participant shared that she did not call in sick despite symptoms because then she did not get paid (quote 22). It should also be mentioned that one study participant did not see any connection between migraine and the workplace and thus could not name any facilitators or barriers to SM (quote 23). How was migraine self-management at work affected by the COVID-19 pandemic?In Germany, the first two COVID-19-related lockdowns began in March 2020 (until May 2020) and in December 2020. As we gathered our data between August 2020 and January 2021, experiences during the COVID-19 pandemic were an important topic in the interviews. One positive aspect for migraine SM during the pandemic was reported to be increased JDL. This was mainly due to new opportunities (and in some cases the obligation) to work remotely (quote 24) providing the advantage of more flexibility (e.g., the arrangement of breaks), a lower noise level, and an elimination of travel times. The fact that many employees took the opportunity to work from home also meant that the office was less busy and therefore more quiet (quote 25). This increased quietness also seemed to be beneficial for employees with migraine. One study participant reported that it was easier to close the office door to do a few stretching exercises (quote 26). The increased structuring of the working day and thus increased regularity as a facilitator for migraine SM (e.g., through stricter appointment policy [quote 27]), and the partial reduction of the workload also appeared to be positive. Furthermore, one study participant had more of a feeling of being needed in one’s work at a nursing home. The increased job satisfaction was reported to lower the frequency of migraine complaints (quote 28). The stress caused by the additional hygienic measures, the mouth-to-nose covering, and the increased amount of screen work were perceived as negative for migraine SM. Coming in contact with COVID-19-positive people often necessitated use of additional stressful measures such as the application of hygiene or personal protective measures. This was, for example, reported by a study participant that worked as a nurse in a hospital (quote 29). The mouth-to-nose covering seemed to make it difficult not only to breathe but also to speak, which in turn was perceived to trigger migraine (quote 30). A final migraine trigger in the pandemic was the fear of the end of the pandemic and thus the loss of the possibility to work from home (quote 31). Summary of main findingsAccording to our participants migraine SM at work is affected by social interactions (e.g., understanding as a facilitator vs. stigmatization as a barrier), the extent of JDL (e.g., in terms of working hours and localization) as well as the workplace design (e.g., regarding opportunities to retreat or to avoid VDU work). During the COVID-19 pandemic, it was considered positive for migraine SM that the daily structure was associated with more predictability and planning (e.g., through stricter appointment scheduling). It was also emphasized that there were more opportunities to work from home and thus better conditions for appropriate migraine SM through more JDL. A negative aspect associated with the COVID-19 pandemic was increased work-related screen time. Participants also shared that the novel hygiene measures (e.g., after contact with a COVID-19-positive person) and the mouth-to-nose covering triggered migraine complaints. Findings in light of earlier researchIn terms of barriers and facilitators, our findings are in line with prior research. A qualitative study on migraine and chronic daily headache management by Peters et al. [ 4 ] highlighted the importance of social support. The authors concluded that social support, especially from peers with the same conditions, can lead to better understanding from colleagues. The lack of social support and the feeling of stigmatization was an important aspect in another qualitative study by Heidari et al. [ 16 ], focusing on common themes of migraine patients. In that study one participant reported going to work despite migraine, because the supervisor seemed not to take migraine seriously [ 16 ]. One study – in accordance with our findings – linked stigmatization to migraine being an invisible disease, limiting the understanding for the condition [ 17 ]. Other factors influencing migraine SM that emerged from our study were factors related to workplace design. This is in keeping with findings from a cross-sectional study on the burden and impact of migraine on work productivity and quality of life that also addressed job-related migraine triggers and coping strategies: Looking at computer screens for too long was one of the two most frequently mentioned migraine triggers at the workplace [ 18 ]. Having control of light, noise and smells was under the top five coping strategies [ 18 ]. In the context of the EFNA study [ 6 ], individuals with migraine and other headache type patients were asked what their company should do to help them cope better with their condition. The wishes mentioned included a greater understanding for the disease, less social interaction, the possibility to work from home, flexible working hours, and more opportunities to withdraw if needed [ 6 ]. These aspects overlap with the facilitators that emerged from our study, in particular regarding social support and JDL. Regarding the COVID-19 pandemic, our results are consistent with findings from other studies that found a link between personal protective equipment, especially the wearing of masks, and a worsening of migraine [ 19 , 20 , 21 ]. There is also further evidence that the increased screen time, for example due to remote working or online lessons during the pandemic, served as a trigger for migraine, in particular in young adults and adolescents [ 22 , 23 ]. However, remote working during the pandemic was generally considered to have a positive impact on migraine (e.g., reduced migraine attack duration) [ 24 ]. In a qualitative study by Buse et al. [ 20 ], examining the general impact of the COVID-19 pandemic on patients with migraine, participants reported that working from home was associated with more control, e.g., over the work environment. This reflects the importance of JDL for migraine SM. Notably, some factors that were mentioned to influence SM in general (e.g., social support) played little or no role in the COVID-19 pandemic and associated SM. The pandemic served as a kind of natural experiment elucidating which factors – when modified – influence migraine and its SM. Based on this, it can be hypothesized that the facilitator “JDL,” which played an important role in general and during the pandemic, has the utmost relevance on migraine SM at work. To our knowledge, no previous qualitative study on migraine or chronic headache has yet highlighted the high relevance of JDL for SM. Methodological considerationsThe interviews were conducted face-to-face or by telephone, depending on the preference of the participants. This provided us with the opportunity to include participants nationwide and despite restrictions due to COVID-19. We did not notice considerable differences regarding the contents between the two interview modes, which is supported by earlier research [ 25 ]. To reduce a potential healthy worker bias (i.e., the assumption that the working population is healthier than the non-working population), we recruited migraine patients who had ever worked for six months with a diagnosis of migraine and not only patients who were currently working. This allowed us to include patients who might have had to leave their job due to severe migraine or who attempted to regain their workability through rehabilitation. We relied on the patients’ report of being diagnosed with migraine by a physician, and we did not apply the International Classification of Headache Disease [ 26 ] for diagnoses. However, those participants who were recruited from the rehabilitation clinic for migraine ( n = 10) had received a medical diagnosis of migraine and their condition was severe enough to threaten their employment status. Further, as we interviewed mainly patients from this rehabilitation clinic and from self-help groups, however, we cannot exclude the possibility of a selection bias: those patients interact with other individuals with migraine, a are usually well-informed about their condition, and their experiences and perspectives may differ to some extent from the broader patient population. Moreover, only three out of 24 participants were male. This may have limited the scope of views that emerged from male participants regarding migraine SM. Also, our study especially included patients who worked in a job with mainly cognitive and social demands. It is well conceivable that their experiences differ from that of migraine patients who work in a job with mainly physical demands (e.g., individuals working in transportation or farming). We were able to cover a broad distribution regarding the average number of migraine days per month (mean = 10.0, SD = 6.6, range: 2–26 days). These observations increase the confidence that we covered a large range of potential views and experiences. Another methodological weakness is that the coding was carried out by only one single person who had no previous experience in coding (CK). The intense involvement of additional individuals in the coding process (e.g., more experienced coders, people with migraine, occupational physicians, and/or neurologists), would likely have led to a richer analysis and additional insights, but this was beyond the resources of our study (i.e., time and financial means). Finally, due to the limited experience with qualitative research methods of the first author, who was also the primary analyst, and due to the fact that it was not feasible to substantially involve additional analysists in the coding, the depth of our analyses may have been limited. Accordingly, our study may be classified as a ‘topical survey’ with aspects of a ‘thematic survey’ – according to the classification of findings in qualitative studies suggested by Sandelowski & Barroso [ 27 ]. A topical survey stays close to the data collected and is primarily a description of it, whereas a thematic survey provides a higher level of transformation of data [ 27 ]. The purpose of thematic surveys were only achieved to a limited extent. However, Sandelowski & Barroso state that a topical survey is not necessarily inferior in terms of the quality of its value [ 27 ]. Implications for practice and researchBased on our findings, interventions could be devised to improve migraine SM at work. Regarding social support, it is important to reduce stigma of migraine to create a working environment in which patients feel comfortable to talk openly about their migraine without it being dismissed as a trifle. Our study thus calls attention to the fact that migraine healthcare professionals should offer support for improving patients’ social communication skills in the workplace leading to greater acceptance of the condition. One health care sector that seems particularly suitable for this endeavor is rehabilitation. Treatment in rehabilitation clinics in Germany involves patient education, which can help to raise awareness among migraine patients for the potential influence of their working conditions on their opportunities to manage their migraine at work. Also, patients can be empowered (e.g., by improving knowledge about legal frameworks and practicing communication skills) to modify their working conditions to some extent. Similar concepts are currently tested for other conditions than migraine [ 28 ]. To increase JDL, employers should try to give migraine patients as much freedom as possible. For example, for office jobs the possibility of expanding remote working should be explored. Here, the experience gained during the COVID-19 pandemic can be used. If working from home is not possible, care can be taken to create a migraine-friendly workplace, for example by providing single offices, noise-cancelling headphones, height-adjustable desks, and places of retreat. VDU work could also be designed to be as gentle as possible, e.g., by using flicker-free screens. If available and needed, occupational physicians should support all these interventions by educating workers with migraine and by serving as mediators between supervisors and employees with migraine. All these interventions should be carefully developed and evaluated prior to their implementation in routine care. We believe that more preparatory research is needed. Firstly, as mentioned above, our analysis may be limited in depth. It therefore seems promising to carry out additional qualitative studies that involve analysts with more diverse professional backgrounds and employees with migraine as co-researchers. In the next step, the scope of the problem could be confirmed, and possible interventions may be explored. Quantitative research (e.g., surveys) would be suitable to examine, amongst others, the proportion of workers with migraine that find self-management at work to be challenging, to prioritize areas for intervention, and to examine what types of interventions would be acceptable to those receiving them and those potentially delivering them. Also, working life in the post-COVID-19 era has further evolved since our study to arrive at a “new normal” (e.g., allowing for more home office working hours than in the pre-COVID-era), which our study does not reflect, and which follow-up qualitative studies could explore. Furthermore, quantitative studies could test hypotheses that can be deduced from our qualitative study (e.g., “The ability to perform migraine SM at work is associated with the level of experienced JDL”). Such research could move beyond self-management as an outcome to include symptoms and occupational outcomes (e.g. workability, presenteeism and absenteeism) and may explore whether improved migraine SM at work curtails the considerable cost associated with migraine-related impairment. Migraine SM at work is influenced positively and negatively by various occupational factors. By considering these facilitators and barriers, a more migraine-friendly workplace can be created to reduce a burden not only for patients but also for society. Further research is needed before interventions can be implemented. Data availabilityData cannot be shared publicly because the transcripts may contain sensitive information. The data may be obtained from the corresponding author upon reasonable request and provided that legal frameworks are not violated and that responsibilities and confidentially have been clarified. AbbreviationsChronic migraine
Job decision latitude European Federation of Neurological Associations Visual display unit Headache disorders. World Health Organization. 2016. https://www.who.int/news-room/fact-sheets/detail/headache-disorders . Accessed February 13, 2024. Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, de la Ruiz E, Tassorelli C, Andrée C. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19(5):703–11. Article CAS PubMed Google Scholar Peters M, Abu-Saad HH, Vydelingum V, Dowson A, Murphy M. Patients’ decision-making for migraine and chronic daily headache management. A qualitative study. Cephalalgia. 2003;23(8):833–41. Peters M, Abu-Saad HH, Vydelingum V, Dowson A, Murphy M. Migraine and chronic daily headache management: a qualitative study of patients’ perceptions. Scand J Caring Sci. 2004;18(3):294–303. Article PubMed Google Scholar Peters M, Abu-Saad HH, Robbins I, Vydelingum V, Dowson A, Murphy M. Patients’ management of migraine and chronic daily headache: a study of the members of the Migraine Action Association (United Kingdom). Headache. 2005;45(5):571–81. Results of EFNA’s survey on stigma and neurological disorder. European Federation of Neurological Associations. 2020. https://www.efna.net/survey2020/ . Accessed January 13, 2023. Scaratti C, Foitzek N, Grignani E, Leonardi M, Raggi A, Coenen M. The employment needs and the factors having a negative or positive impact on work of people with chronic diseases in Europe: the case of headache. Neurol Sci. 2018;39(Suppl 1):121–3. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. Heinrichs K, Vu-Eickmann P, Hummel S, Gholami J, Loerbroks A. What are the perceived influences on asthma self-management at the workplace? A qualitative study. BMJ Open. 2018;8(8):e022126. Article PubMed PubMed Central Google Scholar Heinrichs K, Hermülheim V, Pilz González L, Loerbroks A. When in doubt … Career Indecision,Mental Wellbeing, and Consultation-seeking Behaviour-A qualitative interview study among students and counsellors. Int J Environ Res Public Health. 2021;18(23):12604. Loerbroks A, Nguyen XQ, Vu-Eickmann P, Krichbaum M, Kulzer B, Icks A, Angerer P. Psychosocial working conditions and diabetes self-management at work: a qualitative study. Diabetes Res Clin Pract. 2018;140:129–38. Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–21. PubMed Google Scholar Scharf J, Angerer P, Müting G, Loerbroks A. Return to work after Common Mental disorders: a qualitative study exploring the expectations of the involved stakeholders. Int J Environ Res Public Health. 2020;17(18):6635. Corbin JM, Strauss AL. Basics of qualitative research: Techniques and procedures for developing grounded theory. Fourth edition. SAGE Publications. 2014. Mayring P. Qualitative Content Analysis [Qualitative Inhaltsanalyse: Grundlagen und Techniken. 12., überarb. Aufl.]. Weinheim, Beltz. 2015. Heidari E, Rao D, Pfalzgraf AR, Lobo C, Giannetti V. An explorative study of common themes of patient experiences with migraine. Prim Care Companion CNS Disord. 2022;24(2):21m02939. Basoglu Koseahmet F, Polat B, Gozubatik-Celik RG, Baytekin I, Soylu MG, Ceyhan Dirican A, Ozturk M. An invisible cause of disability: stigma in migraine and epilepsy. Neurol Sci. 2022;43(6):3831–8. Haw NJ, Cabaluna IT, Kaw GE, Cortez JF, Chua MP, Guce K. A cross-sectional study on the burden and impact of migraine on work productivity and quality of life in selected workplaces in the Philippines. J Headache Pain. 2020;21(1):125. Yuksel H, Kenar SG, Gursoy GT, Bektas H. The impacts of masks and disinfectants on migraine patients in the COVID-19 pandemic. J Clin Neurosci. 2022;97:87–92. Article CAS PubMed PubMed Central Google Scholar Buse DC, Gerstein MT, Houts CR, McGinley JS, Uzumcu AA, McCarrier KP, Cooke A, Touba NM, Nishida TK, Wirth RJ, Lipton RB. Impact of the COVID-19 pandemic on people living with migraine: results of the MiCOAS qualitative study. Headache. 2022;62(3):284–93. Ong JJY, Bharatendu C, Goh Y, Tang JZY, Sooi KWX, Tan YL, Tan BYQ, Teoh HL, Ong ST, Allen DM, Sharma VK. Headaches Associated with Personal Protective Equipment - A cross-sectional study among Frontline Healthcare workers during COVID-19. Headache. 2020;60(5):864–77. Wehbe AT, Costa TE, Abbas SA, Costa JE, Costa GE, Wehbe TW. The effects of the COVID-19 confinement on screen time, headaches, stress and Sleep disorders among adolescents: A Cross Sectional Study. Chronic Stress (Thousand Oaks). 2022;6:24705470221099836. Abou Hashish EA, Baatiah NY, Bashaweeh AH, Kattan AM. The online learning experience and reported headaches associated with screen exposure time among Saudi health sciences students during the COVID-19 pandemic. BMC Med Educ. 2022;22(1):226. Currò CT, Ciacciarelli A, Vitale C, Vinci ES, Toscano A, Vita G, Trimarchi G, Silvestri R, Autunno M. Chronic migraine in the first COVID-19 lockdown: the impact of sleep, remote working, and other life/psychological changes. Neurol Sci. 2021;42(11):4403–18. Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note. Qualitative Res. 2004;4(1):107–18. Article Google Scholar IHS Classification ICHD-3. International Headache Society. https://ichd-3.org/classification-outline/ . Accessed February 13, 2024. Sandelowski M, Barroso J. Classifying the findings in qualitative studies. Qual Health Res. 2003;13(7):905–23. Salandi J, Hayden MC, Heinrichs K, Limbach M, Schultz K, Schwarzl G, Neumeister W, Loerbroks A. Can an educational intervention in the context of inpatient pulmonary rehabilitation improve asthma self-management at work? A study protocol of a randomized controlled trial. BMC Pulm Med. 2024;24(1):40. Download references AcknowledgementsThe authors would like to thank Prof. Dr. Scott Stock Gissendanner for his support related to participant recruitment (Berolina Klinik, Löhne). For her translation of the quotes, we are grateful to Lisa Guthardt (Institute of Occupational, Social and Environmental Medicine, Faculty of Medicine, University of Düsseldorf). The authors would also like to thank the participants for taking their time to share their experiences with respect to working with migraine. Open Access funding enabled and organized by Projekt DEAL. This research did not receive any funding. Open Access funding enabled and organized by Projekt DEAL. Author informationAuthors and affiliations. Institute of Occupational, Social and Environmental Medicine, Centre for Health and Society, Faculty of Medicine, University of Düsseldorf, Moorenstr. 5, Düsseldorf, 40225, Germany Clara Knauf & Adrian Loerbroks Institute of Health and Nursing Science, Charité – Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany Katherina Heinrichs Berolina Klinik, Löhne, Germany Rolf Süllwold Institute of Health Services Research and Health Economics, Centre for Health and Society, Faculty of Medicine, University of Düsseldorf, Düsseldorf, Germany Andrea Icks You can also search for this author in PubMed Google Scholar ContributionsC.K., K.H., A.I. and A.L. contributed to the conception and design of the study. C.K. and R.S. contributed to the acquisition of the data. The interviews were conducted by C.K. C.K. performed the analysis and interpretation of the data supported by K.H. and A.L. C.K. drafted the manuscript and all authors revised it for intellectual content. All authors read and approved the final version of the manuscript. All authors agreed to be accountable for all aspects of the work. Corresponding authorCorrespondence to Adrian Loerbroks . Ethics declarationsEthics approval and consent to participate. This study was approved by the Institutional Review Board of the Faculty of Medicine of the University of Düsseldorf, Germany (no 2019 − 627). All participants provided written informed consent prior to the interviews. Consent for publicationNot applicable. Competing interestsThe authors declare no competing interests. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Electronic supplementary materialBelow is the link to the electronic supplementary material. Supplementary Material 1Supplementary material 2, supplementary material 3, rights and permissions. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data. Reprints and permissions About this articleCite this article. Knauf, C., Heinrichs, K., Süllwold, R. et al. Migraine self-management at work: a qualitative study. J Occup Med Toxicol 19 , 22 (2024). https://doi.org/10.1186/s12995-024-00421-w Download citation Received : 26 February 2024 Accepted : 22 May 2024 Published : 04 June 2024 DOI : https://doi.org/10.1186/s12995-024-00421-w Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
Journal of Occupational Medicine and ToxicologyISSN: 1745-6673
An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
 Evidence-Based Practice and Nursing ResearchEvidence-based practice is now widely recognized as the key to improving healthcare quality and patient outcomes. Although the purposes of nursing research (conducting research to generate new knowledge) and evidence-based nursing practice (utilizing best evidence as basis of nursing practice) seem quite different, an increasing number of research studies have been conducted with the goal of translating evidence effectively into practice. Clearly, evidence from research (effective innovation) must be accompanied by effective implementation, and an enabling context to achieve significant outcomes. As mentioned by Professor Rita Pickler, “nursing science needs to encompass all manner of research, from discovery to translation, from bench to bedside, from mechanistic to holistic” ( Pickler, 2018 ). I feel that The Journal of Nursing Research must provide an open forum for all kind of research in order to help bridge the gap between research-generated evidence and clinical nursing practice and education. In this issue, an article by professor Ying-Ju Chang and colleagues at National Cheng Kung University presents an evidence-based practice curriculum for undergraduate nursing students developed using an action research-based model. This “evidence-based practice curriculum” spans all four academic years, integrates coursework and practicums, and sets different learning objectives for students at different grade levels. Also in this issue, Yang et al. apply a revised standard care procedure to increase the ability of critical care nurses to verify the placement of nasogastric tubes. After appraising the evidence, the authors conclude that the aspirate pH test is the most reliable and economical method for verifying nasogastric tube placement at the bedside. They subsequently develop a revised standard care procedure and a checklist for auditing the procedure, conduct education for nurses, and examine the effectiveness of the revised procedure. I hope that these two studies help us all better appreciate that, in addition to innovation and new breakthrough discoveries, curriculum development and evidence-based quality improvement projects, though may not seem so novel, are also important areas of nursing research. Translating evidence into practice is sound science and merits more research. Cite this article as: Chien, L. Y. (2019). Evidence-based practice and nursing research. The Journal of Nursing Research, 27 (4), e29. https://doi.org/10.1097/jnr.0000000000000346
 | |||||||||||||
IMAGES
VIDEO
COMMENTS
Qualitative research is valuable because it approaches a phenomenon, such as a clinical problem, about which little is known by trying to understand its many facets. Most qualitative research is emergent, holistic, detailed, and uses many strategies to collect data. Qualitative research generates evidence and helps nurses determine patient ...
Qualitative Research Questions and Purpose Statements. Qualitative questions are exploratory and are open-ended. A well-formulated study question forms the basis for developing a protocol, guides the selection of design, and data collection methods. Qualitative research questions generally involve two parts, a central question and related ...
Qualitative research aims to collect data multi-dimensionally and provide in-depth explanations of the phenomenon being researched. Ultimately, the purpose of qualitative research is set to help researchers gain an understanding of the research topic and reveal the implications of the research findings.
As the use of qualitative research methods proliferates throughout health care, and specifically nursing research studies, there is a need for Clinical Nurse Specialists (CNSs) to become informed regarding the potential utility of qualitative research findings in practice. In this column, the questions of what qualitative findings mean, how the ...
Title, keywords, authors and abstract. In a previous paper, we discussed how the title, keywords, authors' positions and affiliations and abstract can influence the authenticity and readability of quantitative research papers,4 the same applies to qualitative research. However, other areas such as the purpose of the study and the research question, theoretical and conceptual frameworks ...
Qualitative research methods began to appear in nursing in 1960s and 1970s amid cautious and reluctant acceptance. In the 1980s, qualitative health research emerged as a distinctive domain and mode of inquiry. 1 Qualitative research refers to any kind of research that produces findings not arrived at by means of statistical analysis or other means of quantification. 2,3 It uses a naturalistic ...
The purpose of qualitative research Download book PDF ... Duffy, M.E. (1985) Designing nursing research: the qualitative — quantitative debate. Journal of Advanced Nursing, 10, 225-32. Article PubMed CAS Google Scholar Elliott, M.R. (1983) Maternal infant bonding. Canadian Nurse, 79(8), 28-31 ...
Qualitative inquiry requires more than merely a lack of knowledge or information about a given phenomenon. The methodology and methodological choices should arise from the research question. 5 The selected methodology should help the researcher arrive at new knowledge while uncovering the meaning within the phenomenon.
Abstract. Background: The use of qualitative research methods in nursing research is common. There is a need for Clinical Nurse Specialists (CNSs) to become informed regarding how such qualitative findings can serve as evidence for nursing practice changes. Purpose: To inform CNSs of the meaning and utility of qualitative research findings.
Good qualitative research uses a systematic and rigorous approach that aims to answer questions concerned with what something is like (such as a patient experience), what people think or feel about something that has happened, and it may address why something has happened as it has. Qualitative data often takes the form of words or text and can include images. Qualitative research covers a ...
In addition, contributors also examine the importance of funding, institutional review, and peer reviews. Qualitative Nursing Research is a vital resource for all nursing researchers and their advanced students. "The book is a valuable contribution grounded in the current state of qualitative research.
It is so easy to confuse the words "quantitative" and "qualitative," it's best to use "empirical" and "qualitative" instead. Hint: An excellent clue that a scholarly journal article contains empirical research is the presence of some sort of statistical analysis. See "Examples of Qualitative and Quantitative" page under "Nursing Research" for ...
♦ Statement of purpose—what was studied and why.. ♦ Description of the methodology (experimental group, control group, variables, test conditions, test subjects, etc.).. ♦ Results (usually numeric in form presented in tables or graphs, often with statistical analysis).. ♦ Conclusions drawn from the results.. ♦ Footnotes, a bibliography, author credentials.
Qualitative descriptive designs are common in nursing and healthcare research due to their inherent simplicity, flexibility and utility in diverse healthcare contexts. However, the application of descriptive research is sometimes critiqued in terms of scientific rigor. Inconsistency in decision making within the research process coupled with a ...
The three core approaches to data collection in qualitative research—interviews, focus groups and observation—provide researchers with rich and deep insights. All methods require skill on the part of the researcher, and all produce a large amount of raw data. However, with careful and systematic analysis 12 the data yielded with these ...
Data analysis. Data collection and inductive thematic analysis took place iteratively [45, 53].The first author coded the data (i.e. observation reports, interview and focus group transcripts), basing the codes on the research question and theoretical notions on nursing role development and distinctions.
Qualitative thematic analysis is a commonly used and widely applicable form of qualitative analysis, though it can be challenging to implement. Due to its use across research questions, qualitative traditions, and fields, thematic analysis is also prevalent in mixed methods studies.
506 Journal of Research in Nursing 27(6) Methods Design This qualitative, interview study drew upon interpretive description (ID) (Thorne, 2008) to un-derstand nurses' work. Research in ID describes and interprets a phenomenon, considers the meaning of related behaviours, and formulates a valuable clinical response (Thorne, 2008). The
While many books and articles guide various qualitative research methods and analyses, there is currently no concise resource that explains and differentiates among the most common qualitative approaches. We believe novice qualitative researchers, students planning the design of a qualitative study or taking an introductory qualitative research course, and faculty teaching such courses can ...
Qualitative research is critical for studies about regulatory issues in nursing and across all health professions. When in-depth stakeholder perspectives are needed, qualitative approaches are often the best methodological choice to ensure their viewpoints and experiences are captured when evaluating the consequences of policy implementation or when informing regulation design.
Qualitative research is a type of research that explores and provides deeper insights into real-world problems.[1] Instead of collecting numerical data points or intervening or introducing treatments just like in quantitative research, qualitative research helps generate hypothenar to further investigate and understand quantitative data. Qualitative research gathers participants' experiences ...
Abstract. Aims: Reflexivity is central to the construction of knowledge in qualitative research. This purpose of this paper was to outline one approach when using reflexivity as a strategy to ensure quality of the research process. Design: In this exploratory research, reflexivity was established and maintained by using repeated questionnaires ...
Purpose. This study aimed to investigate the final year nursing students' experiences of pursuing competency in nursing amidst the COVID-19 pandemic. ... associate professor in mental health nursing with a PhD in a university and the second author is a PhD in mental health nursing and a research assistant at a university. ... qualitative and ...
Admission to an intensive care unit (ICU) is a stressful experience for patients and their family members. While the focus of management is primarily on medical care, there can be other areas which are overlooked. The purpose of this study was to investigate the needs and experiences of ICU patients and family members. This qualitative study involved four trained researchers conducting in ...
This study has a qualitative design. An expert panel of experienced operating room nurses (N = 96) in Norway provided qualitative descriptions of their practice in a Delphi survey. The data were analysed in an inductive thematic analysis. This study was conducted and reported in line with Standards for Reporting Qualitative Research (SRQR).
The development of research questions and the subsequent hypotheses are prerequisites to defining the main research purpose and specific objectives of a study. ... Hypotheses in qualitative research are stated in the form of a clear statement concerning the problem to be investigated. ... Weak nursing and midwifery management contribute to the ...
We conducted a qualitative study using semi-structured interviews. Our report adheres to the Consolidated Criteria for Reporting Qualitative Research (COREQ) statement . The primary researcher (CK) was a medical student at the time of our study. Qualitative research skills are usually not acquired during medical studies in Germany.
Evidence-based practice is now widely recognized as the key to improving healthcare quality and patient outcomes. Although the purposes of nursing research (conducting research to generate new knowledge) and evidence-based nursing practice (utilizing best evidence as basis of nursing practice) seem quite different, an increasing number of research studies have been conducted with the goal of ...