- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support

What Is Problem-Solving Therapy?
Verywell / Madelyn Goodnight
Problem-Solving Therapy Techniques
How effective is problem-solving therapy, things to consider, how to get started.
Problem-solving therapy is a brief intervention that provides people with the tools they need to identify and solve problems that arise from big and small life stressors. It aims to improve your overall quality of life and reduce the negative impact of psychological and physical illness.
Problem-solving therapy can be used to treat depression , among other conditions. It can be administered by a doctor or mental health professional and may be combined with other treatment approaches.
At a Glance
Problem-solving therapy is a short-term treatment used to help people who are experiencing depression, stress, PTSD, self-harm, suicidal ideation, and other mental health problems develop the tools they need to deal with challenges. This approach teaches people to identify problems, generate solutions, and implement those solutions. Let's take a closer look at how problem-solving therapy can help people be more resilient and adaptive in the face of stress.
Problem-solving therapy is based on a model that takes into account the importance of real-life problem-solving. In other words, the key to managing the impact of stressful life events is to know how to address issues as they arise. Problem-solving therapy is very practical in its approach and is only concerned with the present, rather than delving into your past.
This form of therapy can take place one-on-one or in a group format and may be offered in person or online via telehealth . Sessions can be anywhere from 30 minutes to two hours long.
Key Components
There are two major components that make up the problem-solving therapy framework:
- Applying a positive problem-solving orientation to your life
- Using problem-solving skills
A positive problem-solving orientation means viewing things in an optimistic light, embracing self-efficacy , and accepting the idea that problems are a normal part of life. Problem-solving skills are behaviors that you can rely on to help you navigate conflict, even during times of stress. This includes skills like:
- Knowing how to identify a problem
- Defining the problem in a helpful way
- Trying to understand the problem more deeply
- Setting goals related to the problem
- Generating alternative, creative solutions to the problem
- Choosing the best course of action
- Implementing the choice you have made
- Evaluating the outcome to determine next steps
Problem-solving therapy is all about training you to become adaptive in your life so that you will start to see problems as challenges to be solved instead of insurmountable obstacles. It also means that you will recognize the action that is required to engage in effective problem-solving techniques.
Planful Problem-Solving
One problem-solving technique, called planful problem-solving, involves following a series of steps to fix issues in a healthy, constructive way:
- Problem definition and formulation : This step involves identifying the real-life problem that needs to be solved and formulating it in a way that allows you to generate potential solutions.
- Generation of alternative solutions : This stage involves coming up with various potential solutions to the problem at hand. The goal in this step is to brainstorm options to creatively address the life stressor in ways that you may not have previously considered.
- Decision-making strategies : This stage involves discussing different strategies for making decisions as well as identifying obstacles that may get in the way of solving the problem at hand.
- Solution implementation and verification : This stage involves implementing a chosen solution and then verifying whether it was effective in addressing the problem.
Other Techniques
Other techniques your therapist may go over include:
- Problem-solving multitasking , which helps you learn to think clearly and solve problems effectively even during times of stress
- Stop, slow down, think, and act (SSTA) , which is meant to encourage you to become more emotionally mindful when faced with conflict
- Healthy thinking and imagery , which teaches you how to embrace more positive self-talk while problem-solving
What Problem-Solving Therapy Can Help With
Problem-solving therapy addresses life stress issues and focuses on helping you find solutions to concrete issues. This approach can be applied to problems associated with various psychological and physiological symptoms.
Mental Health Issues
Problem-solving therapy may help address mental health issues, like:
- Chronic stress due to accumulating minor issues
- Complications associated with traumatic brain injury (TBI)
- Emotional distress
- Post-traumatic stress disorder (PTSD)
- Problems associated with a chronic disease like cancer, heart disease, or diabetes
- Self-harm and feelings of hopelessness
- Substance use
- Suicidal ideation
Specific Life Challenges
This form of therapy is also helpful for dealing with specific life problems, such as:
- Death of a loved one
- Dissatisfaction at work
- Everyday life stressors
- Family problems
- Financial difficulties
- Relationship conflicts
Your doctor or mental healthcare professional will be able to advise whether problem-solving therapy could be helpful for your particular issue. In general, if you are struggling with specific, concrete problems that you are having trouble finding solutions for, problem-solving therapy could be helpful for you.
Benefits of Problem-Solving Therapy
The skills learned in problem-solving therapy can be helpful for managing all areas of your life. These can include:
- Being able to identify which stressors trigger your negative emotions (e.g., sadness, anger)
- Confidence that you can handle problems that you face
- Having a systematic approach on how to deal with life's problems
- Having a toolbox of strategies to solve the issues you face
- Increased confidence to find creative solutions
- Knowing how to identify which barriers will impede your progress
- Knowing how to manage emotions when they arise
- Reduced avoidance and increased action-taking
- The ability to accept life problems that can't be solved
- The ability to make effective decisions
- The development of patience (realizing that not all problems have a "quick fix")
Problem-solving therapy can help people feel more empowered to deal with the problems they face in their lives. Rather than feeling overwhelmed when stressors begin to take a toll, this therapy introduces new coping skills that can boost self-efficacy and resilience .
Other Types of Therapy
Other similar types of therapy include cognitive-behavioral therapy (CBT) and solution-focused brief therapy (SFBT) . While these therapies work to change thinking and behaviors, they work a bit differently. Both CBT and SFBT are less structured than problem-solving therapy and may focus on broader issues. CBT focuses on identifying and changing maladaptive thoughts, and SFBT works to help people look for solutions and build self-efficacy based on strengths.
This form of therapy was initially developed to help people combat stress through effective problem-solving, and it was later adapted to address clinical depression specifically. Today, much of the research on problem-solving therapy deals with its effectiveness in treating depression.
Problem-solving therapy has been shown to help depression in:
- Older adults
- People coping with serious illnesses like cancer
Problem-solving therapy also appears to be effective as a brief treatment for depression, offering benefits in as little as six to eight sessions with a therapist or another healthcare professional. This may make it a good option for someone unable to commit to a lengthier treatment for depression.
Problem-solving therapy is not a good fit for everyone. It may not be effective at addressing issues that don't have clear solutions, like seeking meaning or purpose in life. Problem-solving therapy is also intended to treat specific problems, not general habits or thought patterns .
In general, it's also important to remember that problem-solving therapy is not a primary treatment for mental disorders. If you are living with the symptoms of a serious mental illness such as bipolar disorder or schizophrenia , you may need additional treatment with evidence-based approaches for your particular concern.
Problem-solving therapy is best aimed at someone who has a mental or physical issue that is being treated separately, but who also has life issues that go along with that problem that has yet to be addressed.
For example, it could help if you can't clean your house or pay your bills because of your depression, or if a cancer diagnosis is interfering with your quality of life.
Your doctor may be able to recommend therapists in your area who utilize this approach, or they may offer it themselves as part of their practice. You can also search for a problem-solving therapist with help from the American Psychological Association’s (APA) Society of Clinical Psychology .
If receiving problem-solving therapy from a doctor or mental healthcare professional is not an option for you, you could also consider implementing it as a self-help strategy using a workbook designed to help you learn problem-solving skills on your own.
During your first session, your therapist may spend some time explaining their process and approach. They may ask you to identify the problem you’re currently facing, and they’ll likely discuss your goals for therapy .
Keep In Mind
Problem-solving therapy may be a short-term intervention that's focused on solving a specific issue in your life. If you need further help with something more pervasive, it can also become a longer-term treatment option.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
Shang P, Cao X, You S, Feng X, Li N, Jia Y. Problem-solving therapy for major depressive disorders in older adults: an updated systematic review and meta-analysis of randomized controlled trials . Aging Clin Exp Res . 2021;33(6):1465-1475. doi:10.1007/s40520-020-01672-3
Cuijpers P, Wit L de, Kleiboer A, Karyotaki E, Ebert DD. Problem-solving therapy for adult depression: An updated meta-analysis . Eur Psychiatry . 2018;48(1):27-37. doi:10.1016/j.eurpsy.2017.11.006
Nezu AM, Nezu CM, D'Zurilla TJ. Problem-Solving Therapy: A Treatment Manual . New York; 2013. doi:10.1891/9780826109415.0001
Owens D, Wright-Hughes A, Graham L, et al. Problem-solving therapy rather than treatment as usual for adults after self-harm: a pragmatic, feasibility, randomised controlled trial (the MIDSHIPS trial) . Pilot Feasibility Stud . 2020;6:119. doi:10.1186/s40814-020-00668-0
Sorsdahl K, Stein DJ, Corrigall J, et al. The efficacy of a blended motivational interviewing and problem solving therapy intervention to reduce substance use among patients presenting for emergency services in South Africa: A randomized controlled trial . Subst Abuse Treat Prev Policy . 2015;10(1):46. doi:doi.org/10.1186/s13011-015-0042-1
Margolis SA, Osborne P, Gonzalez JS. Problem solving . In: Gellman MD, ed. Encyclopedia of Behavioral Medicine . Springer International Publishing; 2020:1745-1747. doi:10.1007/978-3-030-39903-0_208
Kirkham JG, Choi N, Seitz DP. Meta-analysis of problem solving therapy for the treatment of major depressive disorder in older adults . Int J Geriatr Psychiatry . 2016;31(5):526-535. doi:10.1002/gps.4358
Garand L, Rinaldo DE, Alberth MM, et al. Effects of problem solving therapy on mental health outcomes in family caregivers of persons with a new diagnosis of mild cognitive impairment or early dementia: A randomized controlled trial . Am J Geriatr Psychiatry . 2014;22(8):771-781. doi:10.1016/j.jagp.2013.07.007
Noyes K, Zapf AL, Depner RM, et al. Problem-solving skills training in adult cancer survivors: Bright IDEAS-AC pilot study . Cancer Treat Res Commun . 2022;31:100552. doi:10.1016/j.ctarc.2022.100552
Albert SM, King J, Anderson S, et al. Depression agency-based collaborative: effect of problem-solving therapy on risk of common mental disorders in older adults with home care needs . The American Journal of Geriatric Psychiatry . 2019;27(6):619-624. doi:10.1016/j.jagp.2019.01.002
By Arlin Cuncic, MA Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.

- Presidential Message
- Nominations/Elections
- Past Presidents
- Member Spotlight
- Fellow List
- Fellowship Nominations
- Current Awardees
- Award Nominations
- SCP Mentoring Program
- SCP Book Club
- Pub Fee & Certificate Purchases
- LEAD Program
- Introduction
- Find a Treatment
- Submit Proposal
- Dissemination and Implementation
- Diversity Resources
- Graduate School Applicants
- Student Resources
- Early Career Resources
- Principles for Training in Evidence-Based Psychology
- Advances in Psychotherapy
- Announcements
- Submit Blog
- Student Blog
- The Clinical Psychologist
- CP:SP Journal
- APA Convention
- SCP Conference
DIAGNOSIS: Depression TREATMENT: Problem-Solving Therapy for Depression
2015 est status : treatment pending re-evaluation very strong: high-quality evidence that treatment improves symptoms and functional outcomes at post-treatment and follow-up; little risk of harm; requires reasonable amount of resources; effective in non-research settings strong: moderate- to high-quality evidence that treatment improves symptoms or functional outcomes; not a high risk of harm; reasonable use of resources weak: low or very low-quality evidence that treatment produces clinically meaningful effects on symptoms or functional outcomes; gains from the treatment may not warrant resources involved insufficient evidence: no meta-analytic study could be identified insufficient evidence: existing meta-analyses are not of sufficient quality treatment pending re-evaluation, 1998 est status : strong research support strong: support from two well-designed studies conducted by independent investigators. modest: support from one well-designed study or several adequately designed studies. controversial: conflicting results, or claims regarding mechanisms are unsupported., strength of research support.
Find a Therapist specializing in Problem-Solving Therapy for Depression List your practice
Brief Summary
- Basic premise: the manner in which people historically and currently cope with extant stressful events via effective social problem solving may affect the degree to which they will experience psychological distress
- Essence of therapy: Contemporary Problem-Solving Therapy, or PST, is a transdiagnostic intervention, generally considered to be under a cognitive-behavioral umbrella, that increases adaptive adjustment to life problems and stress by training individuals in several affective, cognitive, and behavioral tools. The training is aimed at several barriers to effective problem solving. Through experiential practice, PST helps people to train their brains to overcome common barriers to the way they react to and attempt to solve real-life problems.
- Length : approx. 12 sessions; however, effective changes have been observed in PST programs with as few as 4 sessions and may extend to long-term intervention when individuals have long-term and inflexible problem-solving styles or a high degree of emotional dysregulation.
Treatment Resources
Editors: Alexandra Greenfield, MS
Note: The resources provided below are intended to supplement not replace foundational training in mental health treatment and evidence-based practice
Treatment Manuals / Outlines
Treatment manuals.
Treatment manuals available upon request for patients with depression and breast cancer, depression and heart failure, depression and hypertension, and veterans with housing instability (contact Dr. Arthur Nezu )
Books Available for Purchase Through External Sites
- Problem-Solving Therapy: A Treatment Manual (Nezu, Nezu, & D’Zurilla)
Measures, Handouts and Worksheets
- Problem-Solving Therapy Instructional Materials and Patient Handouts (Nezu, Nezu, & D’Zurilla)
- Social Problem-Solving Inventory-Revised (SPSI-R; D’Zurilla, Nezu, & Maydeu-Olivares)
Self-help Books
- Solving Life’s Problems: A 5-Step Guide to Enhanced Well-Being (Nezu, Nezu, & D’Zurilla)
Smartphone Apps
- Moving Forward (US Dept of Veterans Affairs & US Dept of Defense)
Video Demonstrations
Videos available for purchase through external sites.
- Problem-Solving Therapy (APA/Nezu & Nezu)
Clinical Trials
- Efficacy of a social problem-solving therapy approach for unipolar depression (Nezu, 1986)
- Improving depression outcomes in older adults with comorbid medical illness (Harpole et al., 2005)
- Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial (Unützer et al., 2002)
- Behavioral activation and problem-solving therapy for depressed breast cancer patients: Preliminary support for decreased suicidal ideation (Hopko et al., 2013)
- Effects of problem solving therapy on mental health outcomes in family caregivers of persons with a new diagnosis of mild cognitive impairment or early dementia: A randomized controlled trial (Garand et al., 2013)
- Problem-solving training for family caregivers of persons with traumatic brain injuries: A randomized controlled trial (Rivera et al., 2008)
- Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction: Effect on disability (Alexopoulos et al., 2011)
- Six-month postintervention depression and disability outcomes of in-home telehealth problem-solving therapy for depressed, low-income, homebound older adults (Choi et al., 2014)
- Randomized controlled trial of collaborative care management of depression among low-income patients with cancer (Ell et al., 2008)
- The Pathways Study: A randomized trial of collaborative care in patients with diabetes and depression (Katon et al., 2004)
- Problem solving treatment and group psychoeducation for depression: Multicentre randomised controlled trial (Dowrick et al., 2000)
- Escitalopram and problem-solving therapy for prevention of poststroke depression: A randomized controlled trial (Robinson et al., 2000)
- Problem-solving therapy for relapse prevention in depression (Nezu & Nezu, 2010)
- Social problem-solving therapy for unipolar depression: An initial dismantling investigation (Nezu & Perri, 1989)
- Project Genesis: Assessing the efficacy of problem-solving therapy for distressed adult cancer patients (Nezu et al., 2003)
Meta-analyses and Systematic Reviews
- The efficacy of problem solving therapy in reducing mental and physical health problems: A meta-analysis (Malouff, Thorsteinsson, & Schutte, 2007)
- Problem solving therapies for depression: A meta-analysis (Cuijpers, van Straten, & Warmerdam, 2007)
- Problem-solving therapy for depression: A meta-analysis (Bell & D’Zurilla, 2009)
- Brief psychological therapies for anxiety and depression in primary care: Meta-analysis and meta-regression (Cape et al., 2010)
- Brief psychotherapy for depression: A systematic review and meta-analysis (Nieuwsma et al., 2012)
- Comparative efficacy of seven psychotherapeutic interventions for patients with depression: A network meta-analysis (Barth et al., 2013)
- Problem-solving therapy for depression in adults: A systematic review (Gellis & Kenaley, 2008)
Other Treatment Resources
- Moving Forward (free, interactive, 6-hour web program; US Dept of Veterans Affairs & US Dept of Defense)
- Social problem solving as a risk factor for depression (Nezu, Nezu, & Clark, 2008)
- Depression treatment for homebound medically ill older adults: Using evidence-based problem-solving therapy (Gellis & Nezu, 2011)
Thank you for supporting the Society of Clinical Psychology. To enhance our membership benefits, we are requesting that members fill out their profile in full. This will help the Division to gather appropriate data to provide you with the best benefits. You will be able to access all other areas of the website, once your profile is submitted. Thank you and please feel free to email the Central Office at [email protected] if you have any questions
Join our Newsletter
Get helpful tips and the latest information
Problem-Solving Therapy: How It Works & What to Expect
Author: Lydia Antonatos, LMHC
Lydia Angelica Antonatos LMHC
Lydia has over 16 years of experience and specializes in mood disorders, anxiety, and more. She offers personalized, solution-focused therapy to empower clients on their journey to well-being.
Problem-solving therapy (PST) is an intervention with cognitive and behavioral influences used to assist individuals in managing life problems. Therapists help clients learn effective skills to address their issues directly and make positive changes. PST is used in various settings to address mental health concerns such as depression, anxiety, and more.
Find the perfect therapist for you, with BetterHelp.
If you don’t click with your first match, you can easily switch therapists. BetterHelp has over 20,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you.
What Is Problem-Solving Therapy?
Problem-solving therapy (PST) is based on a model that the body, mind, and environment all interact with each other and that life stress can interact with a person’s predisposition for developing a mental condition. 2 Within this context, PST contends that mental, emotional, and behavioral struggles stem from an ongoing inability to solve problems or deal with everyday stressors. Therefore, the key to preventing health consequences and improving quality of life is to become a better problem-solver. 3 , 4
The problem-solving model has undergone several revisions but upholds the value of teaching people to become better problem-solvers. Overall, the goal of PST is to provide individuals with a set of rational problem-solving tools to reduce the impact of stress on their well-being.
The two main components of problem-solving therapy include: 3 , 4
- Problem-solving orientation: This focuses on helping individuals adopt an optimistic outlook and see problems as opportunities to learn from, allowing them to believe they can solve problems.
- Problem-solving style: This component aims to provide people with constructive problem-solving tools to deal with different life stressors by identifying the problem, generating/brainstorming solution ideas, choosing a specific option, and implementing and reviewing it.
Techniques Used in Problem-Solving Therapy
PST emphasizes the client, and the techniques used are merely conduits that facilitate the problem-solving learning process. Generally, the individual, in collaboration and support from the clinician, leads the problem-solving work. Thus, a strong therapeutic alliance sets the foundation for encouraging clients to apply these skills outside therapy sessions. 4
Here are some of the most relevant guidelines and techniques used in problem-solving therapy:
Creating Collaboration
As with other psychotherapies, creating a collaborative environment and a healthy therapist-client relationship is essential in PST. The role of a therapist is to cultivate this bond by conveying a genuine sense of commitment to the client while displaying kindness, using active listening skills, and providing support. The purpose is to build a meaningful balance between being an active and directive clinician while delivering a feeling of optimism to encourage the client’s participation.
This tool is used in all psychotherapies and is just as essential in PST. Assessment seeks to gather facts and information about current problems and contributing stressors and evaluates a client’s appropriateness for PST. The problem-solving therapy assessment also examines a person’s immediate issues, problem-solving attitudes, and abilities, including their strengths and limitations. This sets the groundwork for developing an individualized problem-solving plan.
Psychoeducation
Psychoeducation is an integral component of problem-solving therapy and is used throughout treatment. The purpose of psychoeducation is to provide a client with the rationale for problem-solving therapy, including an explanation for each step involved in the treatment plan. Moreover, the individual is educated about mental health symptoms and taught solution-oriented strategies and communication skills.
This technique involves verbal prompting, like asking leading questions, giving suggestions, and providing guidance. For example, the therapist may prompt a client to brainstorm or consider alternatives, or they may ask about times when a certain skill was used to solve a problem during a difficult situation. Coaching can be beneficial when clients struggle with eliciting solutions on their own.
Shaping intervention refers to teaching new skills and building on them as the person gradually improves the quality of each skill. Shaping works by reinforcing the desired problem-solving behavior and adding perspective as the individual gets closer to their intended goal.
In problem-solving therapy, modeling is a method in which a person learns by observing. It can include written/verbal problem-solving illustrations or demonstrations performed by the clinician in hypothetical or real-life situations. A client can learn effective problem-solving skills via role-play exercises, live demonstrations, or short-film presentations. This allows individuals to imitate observed problem-solving skills in their own lives and apply them to specific problems.
Rehearsal & Practice
These techniques provide opportunities to practice problem-solving exercises and engage in homework assignments. This may involve role-playing during therapy sessions, practicing with real-life issues, or imaginary rehearsal where individuals visualize themselves carrying out a solution. Furthermore, homework exercises are an important aspect when learning a new skill. Ongoing practice is strongly encouraged throughout treatment so a client can effectively use these techniques when faced with a problem.
Positive Reinforcement & Feedback
The therapist’s task in this intervention is to provide support and encouragement for efforts to apply various problem-solving skills. The goal is for the client to continue using more adaptive behaviors, even if they do not get it right the first time. Then, the therapist provides feedback so the client can explore barriers encountered and generate alternate solutions by weighing the pros and cons to continue working toward a specific goal.
Use of Analogies & Metaphors
When appropriate, analogies and metaphors can be useful in providing the client with a clearer vision or a better understanding of specific concepts. For example, the therapist may use diverse skills or points of reference (e.g., cooking, driving, sports) to explain the problem-solving process and find solutions to convey that time and practice are required before mastering a particular skill.
What Can Problem-Solving Therapy Help With?
Although problem-solving therapy was initially developed to treat depression among primary care patients, PST has expanded to address or rehabilitate other psychological problems, including anxiety , post-traumatic stress disorder , personality disorders , and more.
PST theory asserts that vulnerable populations can benefit from receiving constructive problem-solving tools in a therapeutic relationship to increase resiliency and prevent emotional setbacks or behaviors with destructive results like suicide. It is worth noting that in severe psychiatric cases, PST can be effectively used when integrated with other mental health interventions. 3 , 4
PST can help individuals challenged with specific issues who have difficulty finding solutions or ways to cope. These issues can involve a wide range of incidents, such as the death of a loved one, divorce, stress related to a chronic medical diagnosis, financial stress , marital difficulties, or tension at work.
Through the problem-solving approach, mental and emotional distress can be reduced by helping individuals break down problems into smaller pieces that are easier to manage and cope with. However, this can only occur as long the person being treated is open to learning and able to value the therapeutic process. 3 , 4
Lastly, a large body of evidence has indicated that PST can positively impact mental health, quality of life, and problem-solving skills in older adults. PST is an approach that can be implemented by different types of practitioners and settings (in-home care services, telemedicine, etc.), making mental health treatment accessible to the elderly population who often face age-related barriers and comorbid health issues. 1 , 5, 6
Top Rated Online Therapy Services
BetterHelp – Best Overall
“BetterHelp is an online therapy platform that quickly connects you with a licensed counselor or therapist and earned 4 out of 5 stars.” Take a Free Assessment
Talkspace - Best For Insurance
Talkspace accepts many insurance plans including Optum, Cigna, and Aetna. Typical co-pay is $30, but often less. Visit Talkspace
Problem-Solving Therapy Examples
Due to the versatility of problem-solving therapy, PST can be used in different forms, settings, and formats. Following are some examples where the problem-solving therapeutic approach can be used effectively. 4
People who suffer from depression often evade or even attempt to ignore their problems because of their state of mind and symptoms. PST incorporates techniques that encourage individuals to adopt a positive outlook on issues and motivate individuals to tap into their coping resources and apply healthy problem-solving skills. Through psychoeducation, individuals can learn to identify and understand their emotions influence problems. Employing rehearsal exercises, someone can practice adaptive responses to problematic situations. Once the depressed person begins to solve problems, symptoms are reduced, and mood is improved.
The Veterans Health Administration presently employs problem-solving therapy as a preventive approach in numerous medical centers across the United States. These programs aim to help veterans adjust to civilian life by teaching them how to apply different problem-solving strategies to difficult situations. The ultimate objective is that such individuals are at a lower risk of experiencing mental health issues and consequently need less medical and/or psychiatric care.
Psychiatric Patients
PST is considered highly effective and strongly recommended for individuals with psychiatric conditions. These individuals often struggle with problems of daily living and stressors they feel unable to overcome. These unsolved problems are both the triggering and sustaining reasons for their mental health-related troubles. Therefore, a problem-solving approach can be vital for the treatment of people with psychological issues.
Adherence to Other Treatments
Problem-solving therapy can also be applied to clients undergoing another mental or physical health treatment. In such cases, PST strategies can be used to motivate individuals to stay committed to their treatment plan by discussing the benefits of doing so. PST interventions can also be utilized to assist patients in overcoming emotional distress and other barriers that can interfere with successful compliance and treatment participation.
Benefits of Problem-Solving Therapy
PST is versatile, treating a wide range of problems and conditions, and can be effectively delivered to various populations in different forms and settings—self-help manuals, individual or group therapy, online materials, home-based or primary care settings, as well as inpatient or outpatient treatment.
Here are some of the benefits you can gain from problem-solving therapy:
- Gain a sense of control over your life
- Move toward action-oriented behaviors instead of avoiding your problems
- Gain self-confidence as you improve the ability to make better decisions
- Develop patience by learning that successful problem-solving is a process that requires time and effort
- Feel a sense of empowerment as you solve your problems independently
- Increase your ability to recognize and manage stressful emotions and situations
- Learn to focus on the problems that have a solution and let go of the ones that don’t
- Identify barriers that may hinder your progress
How to Find a Therapist Who Practices Problem-Solving Therapy
Finding a therapist skilled in problem-solving therapy is not any different from finding any qualified mental health professional. This is because many clinicians often have knowledge in cognitive-behavioral interventions that hold similar concepts as PST.
As a general recommendation, check your health insurance provider lists, use an online therapist directory , or ask trusted friends and family if they can recommend a provider. Contact any of these providers and ask questions to determine who is more compatible with your needs. 3 , 4
Are There Special Certifications to Provide PST?
Therapists do not need special certifications to practice problem-solving therapy, but some organizations can provide special training. Problem-solving therapy can be delivered by various healthcare professionals such as psychologists, psychiatrists, physicians, mental health counselors, social workers, and nurses.
Most of these clinicians have naturally acquired valuable problem-solving abilities throughout their career and continuing education. Thus, all that may be required is fine-tuning their skills and familiarity with the current and relevant PST literature. A reasonable amount of understanding and planning will transmit competence and help clients gain insight into the causes that led them to their current situation. 3 , 4
Questions to Ask a Therapist When Considering Problem-Solving Therapy
Psychotherapy is most successful when you feel comfortable and have a collaborative relationship with your therapist. Asking specific questions can simplify choosing a clinician who is right for you. Consider making a list of questions to help you with this task.
Here are some key questions to ask before starting PST:
- Is problem-solving therapy suitable for the struggles I am dealing with?
- Can you tell me about your professional experience with providing problem-solving therapy?
- Have you dealt with other clients who present with similar issues as mine?
- Have you worked with individuals of similar cultural backgrounds as me?
- How do you structure your PST sessions and treatment timeline?
- How long do PST sessions last?
- How many sessions will I need?
- What expectations should I have in working with you from a problem-solving therapeutic stance?
- What expectations are required from me throughout treatment?
- Does my insurance cover PST? If not, what are your fees?
- What is your cancellation policy?
How Much Does Problem-Solving Therapy Cost?
The cost of problem-solving therapy can range from $25 to $150 depending on the number of sessions required, severity of symptoms, type of practice, geographic location, and provider’s experience level. However, if your insurance provider covers behavioral health, the out-of-pocket costs per session may be much lower. Medicare supports PST through professionally trained general health practitioners. 1
What to Expect at Your First PST Session
During the first session, the therapist will strive to build a connection and become familiar with you. You will be assessed through a clinical interview and/or questionnaires. During this process, the therapist will gather your background information, inquire about how you approach life problems, how you typically resolve them, and if problem-solving therapy is a suitable treatment for you. 3 , 4
Additionally, you will be provided psychoeducation relating to your symptoms, the problem-solving method and its effectiveness, and your treatment goals. The clinician will likely guide you through generating a list of the current problems you are experiencing, selecting one to focus on, and identifying concrete steps necessary for effective problem-solving. Lastly, you will be informed about the content, duration, costs, and number of therapy sessions the therapist suggests. 3 , 4
Would you like to try therapy?
Find a supportive and compassionate therapist ! BetterHelp has over 20,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you.
Is Problem-Solving Therapy Effective?
Extensive research and studies have shown the efficacy of problem-solving therapy. PST can yield significant improvements within a short amount of time. PST is also useful for addressing numerous problems and psychological issues. Lastly, PST has shown its efficacy with different populations and age groups.
One meta-analysis of PST for depression concluded that problem-solving therapy was as efficient for reducing symptoms of depression as other types of psychotherapies and antidepressant medication. Furthermore, PST was significantly more effective than not receiving any treatment. 7 However, more investigation may be necessary about PST’s long-term efficacy in comparison to other treatments. 5,6
How Is PST Different From CBT & SFT?
Problem-solving, cognitive-behavioral, and solution-focused therapy belong to the cognitive-behavioral framework, sharing a common goal to modify thoughts, aptitudes, and behaviors to improve mental health and quality of life.
Problem-Solving Therapy Vs. Cognitive-Behavioral Therapy
Cognitive behavioral therapy (CBT) is a short-term psychosocial treatment developed under the premise that how we think affects how we feel and behave. CBT addresses problems arising from maladaptive thought patterns and seeks to challenge and modify these to improve behavioral responses and overall well-being. CBT is the most researched approach and preferred treatment in psychotherapy due to its effectiveness in addressing various problems like anxiety, sleep disorders, substance abuse, and more.
Like CBT, PST addresses mental, emotional, and behavioral issues. However, PST may provide a better balance of cognitive and behavioral elements.
Another difference between these two approaches is that PST mostly focuses on faulty thoughts about problem-solving orientation and modifying maladaptive behaviors that specifically interfere with effective problem-solving. Usually, PST is used as an integrated approach and applied as one of several other interventions in CBT psychotherapy sessions.
Problem-Solving Therapy Vs. Solution-Focused Therapy
Solution-focused therapy (SFT) , like PST, is a goal-directed, evidence-based brief therapeutic approach that encourages optimism, options, and self-efficacy. Similarly, it is also grounded on cognitive behavioral principles. However, it differs from problem-solving therapy because SFT is a semi-structured approach that does not follow a step-by-step sequential format. 8
SFT mainly focuses on solution-building rather than problem-solving, specifically looking at a person’s strengths and previous successes. SFT helps people recognize how their lives would differ without problems by exploring their current coping skills. Community mental health, inpatient settings, and educational environments are increasing the use of SFT due to its demonstrated efficacy. 8
Final Thoughts
Problem-solving therapy can be an effective treatment for various mental health concerns. If you are considering treatment, ask your doctor for recommendations or conduct your own research to learn more about this approach and other options available.
Additional Resources
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below.
Online Therapy
BetterHelp – Get support and guidance from a licensed therapist. BetterHelp has over 20,000 therapists who provide convenient and affordable online therapy. Take A Free Online Assessment and get matched with the right therapist for you. Free Assessment
Online Psychiatry
Hims / Hers If you’re living with anxiety or depression, finding the right medication match may make all the difference. Connect with a licensed healthcare provider in just 12 – 48 hours. Explore FDA-approved treatment options and get free shipping, if prescribed. No insurance required. Get Started
Medication + Therapy
Brightside Health – Together, medication and therapy can help you feel like yourself, faster. Brightside Health treatment plans start at $95 per month. United Healthcare, Anthem, Cigna, and Aetna accepted. Following a free online evaluation and receiving a prescription, you can get FDA approved medications delivered to your door. Free Assessment
Starting Therapy Newsletter
A free newsletter for those interested in learning about therapy and how to get the most benefits out of therapy. Get helpful tips and the latest information. Sign Up
Choosing Therapy Directory
You can search for therapists by specialty, experience, insurance, or price, and location. Find a therapist today .
For Further Reading
- 12 Strategies to Stop Using Unhealthy Coping Mechanisms
- Depression Therapy: 4 Effective Options to Consider
- CBT for Depression: How It Works, Examples, & Effectiveness
Best Online Therapy Services
There are a number of factors to consider when trying to determine which online therapy platform is going to be the best fit for you. It’s important to be mindful of what each platform costs, the services they provide you with, their providers’ training and level of expertise, and several other important criteria.
Best Online Psychiatry Services
Online psychiatry, sometimes called telepsychiatry, platforms offer medication management by phone, video, or secure messaging for a variety of mental health conditions. In some cases, online psychiatry may be more affordable than seeing an in-person provider. Mental health treatment has expanded to include many online psychiatry and therapy services. With so many choices, it can feel overwhelming to find the one that is right for you.
Problem-Solving Therapy Infographics
A free newsletter for those interested in starting therapy. Get helpful tips and the latest information.
Choosing Therapy strives to provide our readers with mental health content that is accurate and actionable. We have high standards for what can be cited within our articles. Acceptable sources include government agencies, universities and colleges, scholarly journals, industry and professional associations, and other high-integrity sources of mental health journalism. Learn more by reviewing our full editorial policy .
Beaudreau, S. A., Gould, C. E., Sakai, E., & Terri Huh, J. W. (2017). Problem-Solving Therapy. In N. A. Pachana (Ed.), Encyclopedia of geropsychology : with 148 figures and 100 tables . Singapore: Springer.
Broerman, R. (2018). Diathesis-Stress Model. In T. Shackleford & V. Zeigler-Hill (Eds.), Encyclopedia of Personality and Individual Differences (Living Edition, pp. 1–3). Springer, Cham. https://doi.org/10.1007/978-3-319-28099-8_891-1
Mehmet Eskin. (2013). Problem solving therapy in the clinical practice . Elsevier.
Nezu, A. M., Nezu, C. M., & D’Zurilla, T. J. (2013). Problem-Solving Therapy A Treatment Manual . Springer Publishing Company.
Cuijpers, P., et al. (2018). Problem-solving therapy for adult depression: An updated meta-analysis. European Psychiatry 48 , 27–37. https://doi.org/10.1016/j.eurpsy.2017.11.006
Kirkham, J. G., Choi, N., & Seitz, D. P. (2015). Meta-analysis of problem-solving therapy for the treatment of major depressive disorder in older adults. International Journal of Geriatric Psychiatry , 31 (5), 526–535. https://doi.org/10.1002/gps.4358
Bell, A. C., & D’Zurilla, T. J. (2009). Problem-solving therapy for depression: A meta-analysis. Clinical Psychology Review , 29 (4), 348–353. https://doi.org/10.1016/j.cpr.2009.02.003
Proudlock, S. (2017). The Solution Focused Way Incorporating Solution Focused Therapy Tools and Techniques into Your Everyday Work . Routledge.
Nezu, A. M., Nezu, C. M., & Gerber, H. R. (2019). (Emotion‐centered) problem‐solving therapy: An update. Australian Psychologist , 54 (5), 361–371. https://doi.org/10.1111/ap.12418
We regularly update the articles on ChoosingTherapy.com to ensure we continue to reflect scientific consensus on the topics we cover, to incorporate new research into our articles, and to better answer our audience’s questions. When our content undergoes a significant revision, we summarize the changes that were made and the date on which they occurred. We also record the authors and medical reviewers who contributed to previous versions of the article. Read more about our editorial policies here .
Your Voice Matters
Can't find what you're looking for.
Request an article! Tell ChoosingTherapy.com’s editorial team what questions you have about mental health, emotional wellness, relationships, and parenting. The therapists who write for us love answering your questions!
Leave your feedback for our editors.
Share your feedback on this article with our editors. If there’s something we missed or something we could improve on, we’d love to hear it.
Our writers and editors love compliments, too. :)
FOR IMMEDIATE HELP CALL:
Medical Emergency: 911
Suicide Hotline: 988
© 2024 Choosing Therapy, Inc. All rights reserved.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Types of Therapy Are Helpful for Depression?
What is psychotherapy, psychotherapy for depression.
- Therapy Approaches
- How Long Does It Take to Work?
- Choosing a Therapist
Depression is more than feeling sad or unmotivated for a few days; it’s an ongoing and persistent feeling of extreme sadness or despair affecting every aspect of a person’s life. Data from 2020 shows 18.4% of U.S. adults have received a diagnosis of depression.
Fortunately, treatment options like psychotherapy can be effective. The key is finding out what type of psychotherapy is right for you, depending on the severity of your symptoms, personal preferences, and therapy goals.
This article covers the most effective evidence-based psychotherapy treatments for depression.
The Good Brigade / Getty Images
Psychotherapy is talk therapy . It takes place in outpatient settings (i.e., therapy offices) and inpatient settings (i.e., hospitals). Its purpose is to help relieve symptoms and prevent them from returning.
Each form of psychotherapy is unique, but typical sessions help a person identify the thought patterns, learned behaviors, or personal circumstances that may be contributing to their depression. The focus then shifts to building healthy coping strategies for managing negative thoughts, unwanted behaviors, and difficult emotions or experiences.
The following are the most common types of psychotherapy for depression.
Cognitive Therapy
Cognitive therapy (also called cognitive processing therapy) is a type of cognitive behavioral therapy shown to be effective in helping people challenge and change unhelpful or unwanted beliefs or attitudes that result from traumatic experiences such as sexual assault or natural disaster.
Cognitive therapy involves learning about symptoms like intrusive thoughts resulting from traumatic experiences and working on processing the experience and questioning and reframing negative self-thinking.
Behavioral Therapy
Behavioral therapy (also called behavioral activation) focuses on how certain behaviors influence or trigger symptoms of depression. It works by helping a person identify and understand specific behavioral triggers and then providing behavioral activation exercises that encourage behavioral modifications or changes where possible, resulting in more positive mood outcomes.
Cognitive Behavioral Therapy (CBT)
CBT is considered the best-researched technique and the "gold standard" of psychotherapy. It's been shown effective in reducing depression symptoms and helping patients build skills to change thought patterns and behaviors to break them out of depression. It also encourages greater adherence to medications and other treatments.
CBT when combined with medication for depression has been shown more effective in treating symptoms and preventing relapse than pharmacology alone.
Dialectical Behavior Therapy (DBT)
DBT is a skilled-focused technique centered on acceptance and change. It involves acceptance-oriented skills, such as mindfulness and increasing tolerance to distress. It also uses change-oriented skills, emotional regulation (keeping emotions in check), and interpersonal development (i.e., saying no, asking for what you want, and establishing interpersonal boundaries).
Research suggests DBT is particularly beneficial for people experiencing chronic suicidal thinking .
Suicide Prevention Hotline
If you or someone you know is having suicidal thoughts, dial 988 to contact the 988 Suicide & Crisis Lifeline and connect with a trained counselor. For more mental health resources, see our National Helpline Database.
Psychodynamic Therapy
Psychodynamic therapy is based on the theory that moods and behaviors are directly but unconsciously related to childhood and past experiences. It involves building self-awareness of these experiences and their influence on a person while empowering them to change unwanted patterns.
Treatment with psychodynamic therapy has been shown to be as effective as other treatments in reducing depressive symptoms in depressive disorders.
Interpersonal Therapy (IPT)
IPT focuses on how relationships impact mental health. It helps people manage and strengthen current relationships, as well as looking at how different environments influence thinking and behavior. Numerous studies support the effectiveness of ITP for depression treatment and symptom relapse prevention.
Problem-Solving Therapy (PST)
PST is about strengthening a person’s ability to cope with stressful events by enhancing problem-solving skills. Several studies support the effectiveness of problem-solving therapy for people with depression, depressive disorders, and other mental health conditions.
Approaches to Therapy for Depression
Therapy is not one-size-fits-all. The best approach will depend on severity of symptoms and overall therapy goals, and may include a combination of individual therapy, group therapy , family therapy , or couples therapy . Someone experiencing ongoing depression may benefit from the one-on-one support of individual therapy, but also from a family-based approach and peer support groups .
How Long Does Therapy for Depression Take?
The length of time therapy takes to experience results will vary depending on factors such as:
- Depression type: Acute depression (i.e. depression that does not persist over a long period of time) will typically take fewer sessions to show results than chronic depression.
- Symptom severity: More severe symptoms like suicidal thinking may require longer or more intensive treatment.
- Therapy goals: Focused goals are reached more quickly than broader-based goals.
- Session frequency: People are typically advised to attend as often as they feel comfortable, but more frequent sessions typically result in quicker results.
- Technique: Some types of therapy like cognitive behavioral therapy are more goal-focused and generally quicker than other types.
- Trust: Higher levels of trust between client and therapist often yield quicker results.
- Personal circumstances: A new or ongoing traumatic life experience or other health condition like substance use disorder may prolong how long treatment takes.
General Timeline
Psychotherapy can be short-term and last a few weeks to months (for situational acute depression) or long-term and last a few months to years (for persistent or chronic depression).
How to Choose a Technique and Therapist
Consider which types of therapy best align with your goals and seek a therapist who offers that type of therapy. Bear in mind that therapists may offer more than one technique and can help you determine which techniques may be most suitable.
When choosing a therapist, you may consider their credentials, such as if they have a medical degree and can prescribe medication for depression , as a psychiatrist can. It's crucial to choose a therapist whom you feel comfortable working with. It’s OK to attend a few sessions before deciding if they're the right therapist for you.
A Word From Verywell
Making sure you feel comfortable and have rapport with your therapist is one of the most important determinants for effective therapy. Set up short introductions or consultations with a few therapists so you can pick one you feel you can build the most rapport with.
There are many types of evidence-based therapy that are suitable for treating depression. Some involve working one-on-one with a therapist, and others may include family members, spouses, or peer groups experiencing depression. Making the correct choice includes determining your therapy goals and finding a therapist you feel comfortable working with.
Centers for Disease Control and Prevention. National, state-level, and county-level prevalence estimates of adults aged ≥18 years self-reporting a lifetime diagnosis of depression — United States, 2020 .
Informed Health. Depression: How effective is psychological treatment?
American Psychological Association. Cognitive processing therapy (CPT) .
University of Michigan. Behavioral activation for depression .
Gautam M, Tripathi A, Deshmukh D, Gaur M. Cognitive behavioral therapy for depression . Indian J Psychiatry . 2020;62( 2):S223-S229. doi:10.4103/psychiatry.IndianJPsychiatry_772_19
Wersen AD, Meiser-Stedman R, Laidlaw K. A meta-analysis of CBT efficacy for depression comparing adults and older adults . Journal of Affective Disorders . 2022;319:189-20. doi:10.1016/j.jad.2022.09.020
University of Washington. Dialectical behavioral therapy .
American Psychiatric Association. What is psychotherapy?
Steinert C, Munder T, Rabung S, Hoyer J, Leichsenring F. Psychodynamic therapy: as efficacious as other empirically supported treatments? A meta-analysis testing equivalence of outcomes . AJP . 2017;174(10):943-953. doi:10.1176/appi.ajp.2017.17010057
American Psychological Association. APA dictionary of psychology: interpersonal psychotherapy (ITP) .
Cuijpers P, Donker T, Weissman MM, Ravitz P, Cristea IA. Interpersonal psychotherapy for mental health problems: A comprehensive meta-analysis. Am J Psychiatry . 2016;173(7):680-687. doi:10.1176/appi.ajp.2015.15091141
Zhang A, Park S, Sullivan JE, Jing S. The effectiveness of problem-solving therapy for primary care patients' depressive and/or anxiety disorders: A systematic review and meta-analysis . J Am Board Fam Med . 2018;31(1):139-150. doi:10.3122/jabfm.2018.01.170270
American Psychological Association. How long will it take for treatment to work?
By Michelle Pugle Michelle Pugle, MA is a freelance writer and reporter focusing on mental health and chronic conditions. As seen in Verywell, Healthline, Psych Central, Everyday Health, and Health.com, among others.
- CLASSIFIEDS
- Advanced search

American Board of Family Medicine
Advanced Search
The Effectiveness of Problem-Solving Therapy for Primary Care Patients' Depressive and/or Anxiety Disorders: A Systematic Review and Meta-Analysis
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- Figures & Data
- Info & Metrics
Background: There is increasing demand for managing depressive and/or anxiety disorders among primary care patients. Problem-solving therapy (PST) is a brief evidence- and strength-based psychotherapy that has received increasing support for its effectiveness in managing depression and anxiety among primary care patients.
Methods: We conducted a systematic review and meta-analysis of clinical trials examining PST for patients with depression and/or anxiety in primary care as identified by searches for published literature across 6 databases and manual searching. A weighted average of treatment effect size estimates per study was used for meta-analysis and moderator analysis.
Results: From an initial pool of 153 primary studies, 11 studies (with 2072 participants) met inclusion criteria for synthesis. PST reported an overall significant treatment effect for primary care depression and/or anxiety ( d = 0.673; P < .001). Participants' age and sex moderated treatment effects. Physician-involved PST in primary care, despite a significantly smaller treatment effect size than mental health provider only PST, reported an overall statistically significant effect ( d = 0.35; P = .029).
Conclusions: Results from the study supported PST's effectiveness for primary care depression and/or anxiety. Our preliminary results also indicated that physician-involved PST offers meaningful improvements for primary care patients' depression and/or anxiety.
- Anxiety Disorders
- Depressive Disorder
- Mental Health
- Primary Health Care
- Problem Solving
- Psychotherapy
Depressive and anxiety disorders are the 2 leading global causes of all nonfatal burden of disease 1 and the most prevalent mental disorders in the US primary care system. 2 ⇓ – 4 The proportion of primary care patients with a probable depressive and/or anxiety disorder ranges from 33% to 80% 2 , 5 , 6 ; primary care patients also have alarmingly high levels of co-/multi-morbidity of depressive, anxiety, and physical disorders. 7 Depression and anxiety among primary care patients contribute to: poor compliance with medical advice and treatment 8 ; deficits in patient–provider communication 9 ; reduced patient engagement in healthy behaviors 10 ; and decreased physical wellbeing. 11 , 12 Given the high prevalence of primary care depression and anxiety, and their detrimental effects on the qualities of primary care treatments and patients' wellbeing, it is important to identify effective interventions suitable to address primary care depression and anxiety.
Primary care patients with depression and/or anxiety are often referred out to specialty mental health care. 13 , 14 However, outcomes from these referrals are usually poor due to patients' poor adherence and their resistance to mental health treatment 15 , 16 . Therefore, it is critical to identify effective mental health interventions that can be delivered in primary care for patients' depression and/or anxiety. 17 , 18 During the past decade, a plethora of clinical trials have investigated different mental health interventions for depression and anxiety delivered in primary care. One of the most promising interventions that has received increasing support for managing depression and anxiety in primary care is Problem-Solving Therapy (PST).
Holding that difficulties with problem solving make people more susceptible to depression, PST is a nonpharmacological, competence-based intervention that involves a step-by-step approach to constructive problem solving. 19 , 20 Developed from cognitive-behavioral-therapy, PST is a short-term psychotherapy approach delivered individually or in group settings. The generic PST manual 19 contains 14 training modules that guides PST providers working with patients from establishing a therapeutic relationship to identifying and understanding patient-prioritized problems; from building problem-solving skills to eventually solving the problems. Focused on patient problems in the here-and-now, a typical PST treatment course ranges from 7 to 14 sessions and can be delivered by various health care professionals such as physicians, clinical social workers or nurse practitioners. Because the generic PST manual outlines the treatment formula in detail, providers may deliver PST after receiving 1 month of training. For example, 1 feasibility study on training residents in PST found that residents can provide fidelious PST after 7 weeks' training and reach moderate to high competence after 3 years of practicing PST. 21 PST also has a self-help manual available to clients when needed.
PST is a well-established, evidence-based intervention for depression in specialty mental health care and is receiving greater recognition for its effectiveness in treating depression and anxiety in primary care. Systematic and meta-analytic reviews of PST for depression consistently reported moderate to large treatment effects, ranging from d = 0.4 to d = 1.15. 22 ⇓ – 24 Several clinical trials indicated PST's clinical effectiveness in alleviating anxiety as well. 25 , 26 Most importantly, PST has been adapted for primary care settings (PST-PC) and can be delivered by a variety of health care providers with fewer number of sessions and shorter session length. These unique features make PST(-PC) an ideal psychotherapy for depressive and/or anxiety disorders in primary care.
Previous reviews of PST focused on its effectiveness for depression care, but with little attention to PST's effect on anxiety or comorbid depression anxiety. In addition, to our knowledge, no previous reviews of PST have focused on managing depressive and/or anxiety disorders in primary care. Although research demonstrates that PST has a strong evidence base for treating depression and/or anxiety in specialty mental health care settings, more research is needed to determine whether PST remains effective for treating depressive and/or anxiety disorders when delivered in primary care. To address this gap, we conducted a systematic review and meta-analysis on the effectiveness of PST for treating depressive and/or anxiety disorders with primary care patients.
Search Strategies
This review included searches in 6 electronic databases (Academic Search Complete, CINAHL, Medline, PsychINFO, PUBMED, and the Cochrane Library/Database) and 3 professional Web sites (Academy of Cognitive Therapy, IMPACT, Anxiety and Depression Association of America) for primary care depression and anxiety studies published between January 1900 and September 2016. We also E-mailed major authors of PST studies for feedback and input. Search terms of title and/or abstract searches included: [“PST” or “Problem-Solving Therapy” or “Problem Solving Therapy” or “Problem Solving”] AND [“Depression” or “Depressive” or “Anxiety” or “Panic” or “Phobia”] AND [“primarycare” or “primary care” or “PCP” or “Family Medicine” or “Family Doctor”]. We supplemented the procedure described above with a manual search of study references.
Eligibility Criteria
For inclusion in analyses, a study needed to be 1) a randomized-controlled-trial of 2) PST for 3) primary care patients' 4) depressive and/or anxiety disorders. For studies that examined face-to-face, in-person PST, the intervention must be delivered in primary care for inclusion. If studies examined tele-PST (eg, telephone delivery, video conferencing, computer-based), the intervention must be connected to patients' primary care services for a study to be included. For example, when a primary care physician prescribed computer-based PST at home for their patients, the study met inclusion criteria (as it was still considered managing depression “in primary care” in the present review). However, studies would be excluded if a primary care physician referred patients to an external mental health intervention. Finally, studies must document and report sufficient statistical information for calculating effect size for inclusion in the final analysis.
Data Abstraction and Coding
Two authors (AZ and JES) reviewed an initial pool of 153 studies and agreed to remove 65 studies based on title and 68 studies based on abstract, resulting in 20 studies for full-text review. To develop the final list, we excluded 6 studies after closer review of full-text and consultation with a third reviewer who is an established PST researcher. Lastly, we excluded 2 studies due to 1) a study with a design that blurred the effect of PST with other treatments and 2) unsuccessful contact with a study author to request data needed for calculating effect size. We used a final sample of 11 studies for meta-analysis. The PRISMA chart is presented in Figure 1 .
- Download figure
- Open in new tab
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) chart of literature search for Problem-solving therapy (PST) studies for treating primary care patients' depression and/or anxiety.
Statistical Analysis
This study conducted meta-analysis with the following procedures: 1) calculated a weighted average of effect size estimates per study for depression and anxiety separately (to ensure independence) 27 ; 2) synthesized an overall treatment effect estimate using fixed- or random-effects model based on a heterogeneity statistic (Q-statistic) 28 ; and 3) performed univariate meta-regression with a mixed-effects model for moderator analysis. 29 Although other more advanced statistical approaches allow inclusion of multiple treatment effect size estimates per study for data synthesis, like the Generalized Least Squares method 30 or the Robust Variance Estimation method 31 , this study employed a typical approach because of the relatively small sample and absence of study information required to conduct more advanced methods. Following procedures outlined by Cooper and colleagues 32 , we conducted all analyses with R software. 33 We chose to conduct analyses in R, rather than software specific to meta-analysis (eg, RevMan), because R allowed for more flexibility in statistical modeling (eg, small sample size correction). 34 Sensitivity analysis using Robust Variance Estimation did not significantly alter results estimated with the typical approach. And so this study presents results from only the typical approach for purposes of parsimony and clarity.
Publication Bias, Risk of Bias and Quality of Studies
To detect publication bias, we used a funnel plot of effect size estimates graphed against their standard errors for visual investigation. To evaluate risk of bias, we used the Cochrane Collaboration's tool for assessing risk of bias in randomized trials 35 and the Quality Assessment of Controlled Intervention Studies to evaluate study quality. 36
Primary Studies
Eleven PST studies for primary care depression and/or anxiety reported a total sample size of 2072 participants. Participants' age averaged 50.1 and ranged from 24.5 to 71.8 years old. Ten studies reported participants' sex with an average of 35.6% male participants across all studies. Seven studies (63.6%) reported participants' racial background with most identified as non-Hispanic white (83.6%). Other racial/ethnic groups were poorly reported for meaningful summary. Five studies used active medication as a comparison, including 3 studies that used both active medication and placebo medication. The rest compared PST with treatment-as-usual while 2 studies used active control group (eg, video education material). Four studies involved physicians in some component of intervention delivery. PCPs provided PST in 2 studies; supervised and collaborated with depression care manager in 1 study, and collaborated with a primary care nurse in another. Ten studies reported an average of 6 PST sessions ( M = 6.1) ranging from 3 to 12 sessions. All but 1 study (n = 10) used individual PST and 2 studies used tele-health modalities to provide PST. All studies used standardized measures of depression and anxiety. Examples of the most common measures included: PHQ-9, CES-D, HAM-D, and BDI-II. Table 1 presents a detailed description of study characteristics.
- View inline
Study Characteristics for Problem-Solving Therapy as Intervention for Treating Depression and/or Anxiety Among Primary Care Patients ( n = 11)
Publication Bias, Risk of Bias, and Quality of Studies
The funnel plot ( Figure 2 ) did not indicate any clear sign of publication bias. Risk of bias ( Table 4 ) indicated an overall acceptable risk across studies included for review with blinding of participants and personnel, blinding of outcome assessment and incomplete outcome data most vulnerable to risk of bias. Quality of study assessment ( Table 5 ) indicated an overall satisfactory study quality with over half of studies (n = 6) achieving ratings of “Good” study quality.
Funnel Plot for Publication Bias in Problem-solving therapy (PST) Studies for Treating Primary Care Patients' Depression an/or Anxiety.
Meta-analysis and moderator analysis
Figure 3 presents a forest plot of treatment effects per study, including depression and anxiety measures. Table 3 presents subgroup analysis of overall treatment effect by moderator and Table 2 presents the results of meta-analysis and moderator analysis. Meta-analysis revealed an overall significant treatment effect of PST for primary care depression and/or anxiety ( d = 0.67; P < .001). Further investigation revealed no significant difference between the mean treatment effect of PST for depression versus anxiety in primary care ( d ( diff .) = −0.25; P = .317) while subgroup analysis revealed the overall treatment effect for anxiety was not significant ( d = 0.35; P = .226). Age was found to be a significant moderator (β 1 = 0.02; P = .012) for treatment outcomes, indicating that for each unit increase in participants' age, the overall treatment effect for primary are depression and/or anxiety are expected to increase by 0.02 (standard deviations). Neither participants' ethnic or racial backgrounds nor marital status significantly moderated the overall treatment outcome.
Forest Plot of PST Treatment Effect Size Estimates for Treating Primary Care Patients' Depression and/or Anxiety per Study.
PST for Treating Primary Care Patients' Depression and/or Anxiety; Results of Univariate Meta-regression
Results of Subgroup Analysis of Overall Treatment Effect (by Moderator) of PST for Treating Primary Care Patients' Depression and/or Anxiety
PST for Treating Primary Care Patients' Depression and/or Anxiety; Results of the Cochrane Collaboration's Tool for Assessing Risk of Bias *
Quality Assessment of Controlled PST Intervention Studies for Primary Care Patients' Depression and/or Anxiety ( n =11)
The overall treatment effect was not moderated by any treatment characteristics including: treatment modality (individual vs group PST), delivery methods (face-to-face vs tele-health PST), number of PST sessions and length of individual PST sessions. Subgroup analysis indicated an overall significant treatment effect of in-person PST ( d = 0.72; P < .001) but not of tele-PST ( d = 0.53; P = .097). However, the difference between the 2 was not statistically significant.
PST providers background and primary care physician's involvement significantly moderated the overall treatment effect size. Master's-level providers reported an overall treatment effect ( d = 1.57; P < .001) significantly higher than doctoral-level providers ( d = −1.33; P = .007). Both physician-involved and nonphysician involved PST reported significant overall treatment effect of PST for depression and/or anxiety in primary care ( d = 1.06; P < .001 and d = 0.35; P = .029, respectively). Moderator analysis further revealed that PST without physician involvement reported significantly greater treatment effects compared with physician-involved PST in primary care ( d = −0.71; P = .005). Results of subgroup and moderator analyses indicated that while the difference (in treatment effect) between physician and nonphysician involved PST in primary care were statistically significant, physician-involved PST was also statistically significant, thus practically meaningful.
Results of the study demonstrated a statistically significant overall treatment effect in outcomes of depression and/or anxiety for primary care patients receiving PST compared with patients in control groups. The outcome type—depression versus anxiety—failed to moderate treatment effect; only PST for depression reported a significant overall effect size. This could indicate that many studies primarily targeted depression and included anxiety measures as secondary outcomes. For this reason, we expect to find a greater treatment effect for primary care depression. It was unsurprising that treatment characteristics failed to moderate treatment effect size because most primary studies used PST-PC or its modified version; there was insufficient variation between studies (and moderators), yielding insignificant moderating coefficients.
Although delivery method did not moderate treatment effect reported in studies included in this review, significant effect was only reported by studies using face-to-face in-person PST but not by those with tele-PST modalities (n = 2). Although evidence for the effectiveness of tele-PST is established or increasing in a variety of settings 37 ⇓ – 39 most PST studies for primary care patients have used face-to-face, in-person PST. Our study further supported the use of face-to-face in-person PST for treating depression and anxiety among primary care patients. We recognize, however, that current and projected shortages in specialty mental health care provision, felt acutely in subspecialties such as geriatric mental health, necessitate more trials with PST tele-health modalities. 40
It is salient to note that, while nonphysician-involved PST studies reported significantly greater treatment effect than those involving physicians, PCP-involved studies also reported an overall significant effect size. Closer examination indicated that studies with physician-involved PST were either delivered by physicians or other nonmental health professionals (eg, registered nurses or depression care managers). Lack of sufficient PST training might explain the difference in treatment effect sizes being statistically significant. Yet, the fact that physician-involved PST studies reported an overall statistically significant effect size for primary care depression and/or anxiety suggested a meaningful treatment effect for clinical practice. When faced with a shortage of mental health professionals (eg, psychologists, clinical social workers, licensed professional counselors), our findings suggest physician-led or -supervised PST interventions could still improve primary care patients' depression and/or anxiety. Researchers are encouraged to further examine the treatment effect of PST delivered by mental health professionals in collaboration with primary care physicians.
This study has several weaknesses that are inherent to meta-analyses. There is no way to assure we included all studies despite adopting a comprehensive search and coding strategy (ie, file drawer problem). Second, while all studies in this meta-analysis seemed to have satisfactory methodological rigor, it is possible that internal biases within some studies may influence results. This study takes a quantitative meta-analysis approach which inherently neglects other study designs and methodologies that also provide valuable information about the effectiveness, feasibility, and acceptability of PST for treating primary care patients with depression. To ensure independence of data, this study used a weighted average of effect size estimates per study in synthesizing an overall treatment effect and conducting moderator analysis. While sensitivity analysis did not reveal significant differences from the reported results, we will not know for sure how our choice of statistical method might affect the results.
- Acknowledgments
The authors are grateful to Dr. Namkee Choi, Professor and the Louis and Ann Wolens Centennial Chair in Gerontology at the University of Texas at Austin Steve Hicks School of Social Work, for her mentorship and insightful comments during preparation of the manuscript.
This article was externally peer reviewed.
Funding: none.
Conflict of interest: none declared.
Ethics Review: This is a systematic review and meta-analysis based on de-identified aggregate study data. No human participants or animals were involved in this study. No ethics review was required.
To see this article online, please go to: http://jabfm.org/content/31/1/139.full .
- Received for publication July 5, 2017.
- Revision received September 14, 2017.
- Accepted for publication September 27, 2017.
- Whiteford HA ,
- Degenhardt L ,
- Kroenke K ,
- Spitzer RL ,
- Williams JB ,
- Monahan PO ,
- Verhaak PF ,
- Hilbink-Smolders M ,
- Mitchell AJ ,
- Sherbourne CD ,
- Mussell M ,
- Schellberg D ,
- Clarke DM ,
- Schenker Y ,
- Stewart A ,
- Vander Weg MW
- Salovey P ,
- Rothman AJ ,
- Detweiler JB ,
- Williams JW
- Hunkeler EM ,
- Pincus HA ,
- Thielke S ,
- Richards D ,
- Gilbody S ,
- Grimshaw J ,
- Maguth Nezu C ,
- D'Zurilla TJ
- D'Zurilla TJ ,
- Dietrich AJ ,
- Seville JL ,
- Cuijpers P ,
- van Straten A ,
- Warmerdam L
- Kirkham JG ,
- Kleiboer A ,
- Seekles W ,
- Higgins JP ,
- Thompson SG
- Raudenbush SW
- Hedges LV ,
- Valentine JC
- Gleser LJ ,
- Harris LV ,
- Valentine ,
- 33. ↵ R Development Core Team . R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria . Vienna, Austria : R Foundation for Statistical Computing 2015 .
- Pustejovsky JE
- Altman DG ,
- Gøtzsche PC ,
- 36. ↵ National Heart, Lung, and Blood Institute . Quality assessment of controlled intervention studies . Systematic evidence reviews and clinical practice guideline . Available from: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/rct .
- Marinucci ML ,
- Sirrianni L ,
- Wilson NL ,
- Cartreine JA ,
- Buckey JC ,
- Sandoval L ,
- Yarborough BJ
- Barret JE ,
- Williams JW ,
- Chibanda D ,
- Shetty AK ,
- Tshimanga M ,
- Stranix-Chibanda L ,
- Rusakaniko S
- Von Korff M ,
- Tamburrino M ,
- McCusker J ,
- Mynors-Wallis LM ,
- Dietrich AJ
- Reynolds CF III . ,
- Thomas SB ,
- Schmaling KB ,
- Dimidjian S ,
- Williams JW Jr . ,
- Barrett J ,
- Sullivan M ,
- Cornell J ,
In this issue

- Table of Contents
- Table of Contents (PDF)
- Cover (PDF)
- Index by author
Thank you for your interest in spreading the word on American Board of Family Medicine.
NOTE: We only request your email address so that the person you are recommending the page to knows that you wanted them to see it, and that it is not junk mail. We do not capture any email address.
Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager

- Tweet Widget
- Facebook Like
- Google Plus One
Jump to section
Related articles.
- No related articles found.
- Google Scholar
Cited By...
- Global health reciprocal innovation to address mental health and well-being: strategies used and lessons learnt
- Psychologic Treatment of Depression Compared With Pharmacotherapy and Combined Treatment in Primary Care: A Network Meta-Analysis
- Brief behaviour change strategies for distressed patients in primary care
- Interventions Must Be Realistic to Be Useful and Completed in Family Medicine
More in this TOC Section
- Perinatal Depression: A Guide to Detection and Management in Primary Care
- Denosumab versus Bisphosphonates for Reducing Fractures in Postmenopausal Women with Osteoporosis: A Meta-Analysis
- An Evidence-Based Review of Vitamin D for Common and High-Mortality Conditions
Similar Articles
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Numismatics
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Social History
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Legal System - Costs and Funding
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Restitution
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Social Issues in Business and Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Management of Land and Natural Resources (Social Science)
- Natural Disasters (Environment)
- Pollution and Threats to the Environment (Social Science)
- Social Impact of Environmental Issues (Social Science)
- Sustainability
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Politics of Development
- Public Policy
- Public Administration
- Qualitative Political Methodology
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Disability Studies
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

Problem-Solving Treatment for Anxiety and Depression: a practical guide
- Cite Icon Cite
- Permissions Icon Permissions
Problem-solving treatment is a well researched, practical psychological intervention. The treatment is very much a here and now treatment, focusing on current difficulties and setting future goals. It does not dwell on past relationships and past mistakes. Patients are helped to gain a sense of mastery over their difficulties. There is good evidence to support the use of problem-solving in treatment of patients with depression, emotional disorders, and after episodes of deliberate self-harm. Problem-solving has been developed as a brief, feasible, psychological treatment that can be delivered by non-specialists. Much of the evidence supporting the use of problem-solving treatment has been undertaken in primary care. This definitive guide provides a 'hands-on' manual to assist potential therapists in understanding the background and rationale for problem-solving. The first chapter of the book provides a brief description of the theory which lead to the development of problem-solving treatment. The research trials underpinning the effectiveness of treatment are discussed in chapter two. Chapters three to seven provide a detailed manual for potential therapists. The structure of problem-solving is set out supported by many relevant clinical examples. Detailed advice is given as to how to structure a course of problem-solving. Case examples of how problem-solving develops over a course of treatment are set out. Advice for would-be practitioners as to how best to deliver problem-solving and also guidance as to potential pitfalls are given. Chapter eight sets out the content of a two day course suitable for teaching problem-solving.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995-.

Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet].
Problem-solving therapy for depression in adults: a systematic review.
ZD Gellis and B Kenaley .
Review published: 2008 .
- CRD summary
This review concludes that problem-solving therapy (PST) combined with antidepressant treatment is associated with more favourable outcomes than PST alone for the treatment of non-institutionalised adults with depression. Overall, given the differences between studies, the methodological flaws in some studies and the potential for publication bias, the authors' findings should be interpreted with caution.
- Authors' objectives
To determine whether problem-solving therapy (PST) reduces depression in non-institutionalised adults.
PubMed, PsycINFO, and PsycLit were searched from 1967 to March 2006. AgeLine (up to February 2006), Social Work Abstracts (up to December 2005) and Social Science Abstracts (up to January 2006) were also searched. Search terms were reported. Relevant journals were handsearched to identify further trials. Only published studies written in English were eligible for inclusion in the review.
- Study selection
Randomised controlled trials (RCTs) assessing the effects of PST on symptoms of depression in depressed non-institutionalised adults (at least 18 years) were eligible for inclusion in the review. Eligible control groups included placebo and other treatments including both pharmacological and psychosocial treatments.
The majority of included studies assessed individual PST therapy. The remainder assessed the effects of group or telephone-based PST. Most interventions lasted at least 12 weeks (range 4 to 52 weeks), with an average of eight sessions delivered over 10 weeks (median 6; standard deviation (SD) 10.24). The majority of interventions were compared with usual care/treatment or placebo; others were compared with waiting-list control, medication (paroxetine, fluvoxamine, amitriptyline), a psychosocial intervention (supportive or reminiscence therapy or psychoeducation) or other interventions such as home-based hospice care. Included participants were mainly Caucasian females. Participant age ranged between 18 and 90 years. The most frequently reported outcome measure was depression severity, usually reported using the Beck Depression Inventory (BDI) or the Hamilton Rating Scale for Depression (HAM-D). Outcomes were most commonly assessed over a period of 52 weeks (range 8 to 52 weeks).
Two reviewers independently assessed studies for inclusion.
- Assessment of study quality
Study validity was assessed by two independent reviewers using criteria recommended by the Cochrane Collaboration: use of random allocation; use of a power calculation; adequate description of intervention methods; use of an intention-to-treat (ITT) analysis; description of interventionist training; and description of outcome measures. Each study was awarded either 0 or 1 point per criterion, with the exception of the assessment of study power, where studies were awarded 1 to 3 points. Overall scores ranged from 0 to 10; with studies scoring 6 or more points judged to be of above average quality.
- Data extraction
Two reviewers independently extracted the study data. Data were extracted for the main outcome measures along with the time of follow-up assessment and the statistical significance of any differences between intervention and control groups, where reported. Data relating to the inclusion of any minority groups of participants were also extracted.
- Methods of synthesis
Due to the variation in interventions and outcome measures, the studies were discussed using a narrative synthesis.
- Results of the review
Twenty-two RCTs (n=5,550) were included in the review. Sample sizes ranged from 20 to 1,801 (mean 238.68; SD 371.06). Fifteen out of 22 studies were rated as having above average quality. The most common reason for failing to meet the quality criteria was a lack of ITT data.
Seven studies demonstrated that PST was significantly superior to control (waiting list, usual care or treatment) in reducing depressive symptoms, with effects persisting up to 52 weeks in some cases. Two of the six studies comparing PST with antidepressant therapy (amitriptyline or paroxetine) and placebo found a combination of PST and paroxetine to significantly reduce depressive symptoms at two and 11 weeks. No significant differences were reported between multifaceted PST interventions, paroxetine and placebo therapy. Three of the five studies comparing PST with alternative interventions reported that PST was significantly superior, but one study comparing PST provided to a significant other such as a spouse (PST-SO) and another comparing it with hospice care did not. All five studies assessing multifaceted PST reported significant reductions in depressive symptoms in favour of the intervention group. Significant effects were found in most cases to be maintained for up to 12 months.
- Authors' conclusions
PST combined with antidepressant treatment for non-institutionalised adults with depression is associated with more favourable outcomes in comparison with PST alone.
- CRD commentary
This review answers a clear research question supported by appropriate, but sometimes wide inclusion criteria, particularly for participants and outcomes. A number of databases and additional sources were searched, but publication and language bias may be present as only published studies written in English were eligible for inclusion. Attempts were made to reduce the risk of reviewer error and bias when selecting studies, assessing their quality and extracting the data. Criteria used to assess the quality of the studies were reported along with details of the scores for individual studies. The quality of the studies was graded as above average for more than half of the studies and the authors described the evidence as rigorous. However, at least a third of studies had methodological flaws that may have affected the reliability of their findings. The sometimes wide inclusion criteria led to wide variations between the studies, most notably in terms of outcomes and the way in which interventions were performed. This justifiably led the authors to restrict their findings to a narrative synthesis based on overall effects and their statistical significance, although actual effect sizes were rarely reported and the data reported in the text and tables did not always agree. The study data were also mainly restricted to female Caucasians, which the authors rightly suggest may limit the overall generalisability of their findings to other populations. Overall, given the differences between studies, the methodological flaws in some studies and the potential for publication bias, the authors' findings should be interpreted with caution.
- Implications of the review for practice and research
Research: the authors did not state any implications for practice.
Practice: the authors stated that future studies should evaluate the effects of PST in other health disorders and in older depressed adults and different ethnic and cultural groups, and compare effects with newer alternative treatments and in settings where social workers are employed.
The review was supported by a grant from the National Institute of Mental Health (Grant no. K01 MH071253).
- Bibliographic details
Gellis Z D, Kenaley B. Problem-solving therapy for depression in adults: a systematic review. Research on Social Work Practice 2008; 18(2): 117-131.
- Indexing Status
Subject indexing assigned by CRD
Depression /therapy; Humans; Problem Solving; Psychotherapy /methods
- AccessionNumber
12008102854
- Database entry date
- Record Status
This is a critical abstract of a systematic review that meets the criteria for inclusion on DARE. Each critical abstract contains a brief summary of the review methods, results and conclusions followed by a detailed critical assessment on the reliability of the review and the conclusions drawn.
- Cite this Page Gellis ZD, Kenaley B. Problem-solving therapy for depression in adults: a systematic review. 2008. In: Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995-.
In this Page
Recent activity.
- Problem-solving therapy for depression in adults: a systematic review - Database... Problem-solving therapy for depression in adults: a systematic review - Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
10 Best Problem-Solving Therapy Worksheets & Activities

Cognitive science tells us that we regularly face not only well-defined problems but, importantly, many that are ill defined (Eysenck & Keane, 2015).
Sometimes, we find ourselves unable to overcome our daily problems or the inevitable (though hopefully infrequent) life traumas we face.
Problem-Solving Therapy aims to reduce the incidence and impact of mental health disorders and improve wellbeing by helping clients face life’s difficulties (Dobson, 2011).
This article introduces Problem-Solving Therapy and offers techniques, activities, and worksheets that mental health professionals can use with clients.
Before you continue, we thought you might like to download our three Positive Psychology Exercises for free . These science-based exercises explore fundamental aspects of positive psychology, including strengths, values, and self-compassion, and will give you the tools to enhance the wellbeing of your clients, students, or employees.
This Article Contains:
What is problem-solving therapy, 14 steps for problem-solving therapy, 3 best interventions and techniques, 7 activities and worksheets for your session, fascinating books on the topic, resources from positivepsychology.com, a take-home message.
Problem-Solving Therapy assumes that mental disorders arise in response to ineffective or maladaptive coping. By adopting a more realistic and optimistic view of coping, individuals can understand the role of emotions and develop actions to reduce distress and maintain mental wellbeing (Nezu & Nezu, 2009).
“Problem-solving therapy (PST) is a psychosocial intervention, generally considered to be under a cognitive-behavioral umbrella” (Nezu, Nezu, & D’Zurilla, 2013, p. ix). It aims to encourage the client to cope better with day-to-day problems and traumatic events and reduce their impact on mental and physical wellbeing.
Clinical research, counseling, and health psychology have shown PST to be highly effective in clients of all ages, ranging from children to the elderly, across multiple clinical settings, including schizophrenia, stress, and anxiety disorders (Dobson, 2011).

Can it help with depression?
PST appears particularly helpful in treating clients with depression. A recent analysis of 30 studies found that PST was an effective treatment with a similar degree of success as other successful therapies targeting depression (Cuijpers, Wit, Kleiboer, Karyotaki, & Ebert, 2020).
Other studies confirm the value of PST and its effectiveness at treating depression in multiple age groups and its capacity to combine with other therapies, including drug treatments (Dobson, 2011).
The major concepts
Effective coping varies depending on the situation, and treatment typically focuses on improving the environment and reducing emotional distress (Dobson, 2011).
PST is based on two overlapping models:
Social problem-solving model
This model focuses on solving the problem “as it occurs in the natural social environment,” combined with a general coping strategy and a method of self-control (Dobson, 2011, p. 198).
The model includes three central concepts:
- Social problem-solving
- The problem
- The solution
The model is a “self-directed cognitive-behavioral process by which an individual, couple, or group attempts to identify or discover effective solutions for specific problems encountered in everyday living” (Dobson, 2011, p. 199).
Relational problem-solving model
The theory of PST is underpinned by a relational problem-solving model, whereby stress is viewed in terms of the relationships between three factors:
- Stressful life events
- Emotional distress and wellbeing
- Problem-solving coping
Therefore, when a significant adverse life event occurs, it may require “sweeping readjustments in a person’s life” (Dobson, 2011, p. 202).

- Enhance positive problem orientation
- Decrease negative orientation
- Foster ability to apply rational problem-solving skills
- Reduce the tendency to avoid problem-solving
- Minimize the tendency to be careless and impulsive
D’Zurilla’s and Nezu’s model includes (modified from Dobson, 2011):
- Initial structuring Establish a positive therapeutic relationship that encourages optimism and explains the PST approach.
- Assessment Formally and informally assess areas of stress in the client’s life and their problem-solving strengths and weaknesses.
- Obstacles to effective problem-solving Explore typically human challenges to problem-solving, such as multitasking and the negative impact of stress. Introduce tools that can help, such as making lists, visualization, and breaking complex problems down.
- Problem orientation – fostering self-efficacy Introduce the importance of a positive problem orientation, adopting tools, such as visualization, to promote self-efficacy.
- Problem orientation – recognizing problems Help clients recognize issues as they occur and use problem checklists to ‘normalize’ the experience.
- Problem orientation – seeing problems as challenges Encourage clients to break free of harmful and restricted ways of thinking while learning how to argue from another point of view.
- Problem orientation – use and control emotions Help clients understand the role of emotions in problem-solving, including using feelings to inform the process and managing disruptive emotions (such as cognitive reframing and relaxation exercises).
- Problem orientation – stop and think Teach clients how to reduce impulsive and avoidance tendencies (visualizing a stop sign or traffic light).
- Problem definition and formulation Encourage an understanding of the nature of problems and set realistic goals and objectives.
- Generation of alternatives Work with clients to help them recognize the wide range of potential solutions to each problem (for example, brainstorming).
- Decision-making Encourage better decision-making through an improved understanding of the consequences of decisions and the value and likelihood of different outcomes.
- Solution implementation and verification Foster the client’s ability to carry out a solution plan, monitor its outcome, evaluate its effectiveness, and use self-reinforcement to increase the chance of success.
- Guided practice Encourage the application of problem-solving skills across multiple domains and future stressful problems.
- Rapid problem-solving Teach clients how to apply problem-solving questions and guidelines quickly in any given situation.
Success in PST depends on the effectiveness of its implementation; using the right approach is crucial (Dobson, 2011).
Problem-solving therapy – Baycrest
The following interventions and techniques are helpful when implementing more effective problem-solving approaches in client’s lives.
First, it is essential to consider if PST is the best approach for the client, based on the problems they present.
Is PPT appropriate?
It is vital to consider whether PST is appropriate for the client’s situation. Therapists new to the approach may require additional guidance (Nezu et al., 2013).
Therapists should consider the following questions before beginning PST with a client (modified from Nezu et al., 2013):
- Has PST proven effective in the past for the problem? For example, research has shown success with depression, generalized anxiety, back pain, Alzheimer’s disease, cancer, and supporting caregivers (Nezu et al., 2013).
- Is PST acceptable to the client?
- Is the individual experiencing a significant mental or physical health problem?
All affirmative answers suggest that PST would be a helpful technique to apply in this instance.
Five problem-solving steps
The following five steps are valuable when working with clients to help them cope with and manage their environment (modified from Dobson, 2011).
Ask the client to consider the following points (forming the acronym ADAPT) when confronted by a problem:
- Attitude Aim to adopt a positive, optimistic attitude to the problem and problem-solving process.
- Define Obtain all required facts and details of potential obstacles to define the problem.
- Alternatives Identify various alternative solutions and actions to overcome the obstacle and achieve the problem-solving goal.
- Predict Predict each alternative’s positive and negative outcomes and choose the one most likely to achieve the goal and maximize the benefits.
- Try out Once selected, try out the solution and monitor its effectiveness while engaging in self-reinforcement.
If the client is not satisfied with their solution, they can return to step ‘A’ and find a more appropriate solution.

Download 3 Free Positive Psychology Exercises (PDF)
Enhance wellbeing with these free, science-based exercises that draw on the latest insights from positive psychology.
Download 3 Free Positive Psychology Tools Pack (PDF)
By filling out your name and email address below.
Positive self-statements
When dealing with clients facing negative self-beliefs, it can be helpful for them to use positive self-statements.
Use the following (or add new) self-statements to replace harmful, negative thinking (modified from Dobson, 2011):
- I can solve this problem; I’ve tackled similar ones before.
- I can cope with this.
- I just need to take a breath and relax.
- Once I start, it will be easier.
- It’s okay to look out for myself.
- I can get help if needed.
- Other people feel the same way I do.
- I’ll take one piece of the problem at a time.
- I can keep my fears in check.
- I don’t need to please everyone.

Prefer Uninterrupted Reading? Go Ad-free.
Get a premium reading experience on our blog and support our mission for $1.99 per month.
✓ Pure, Quality Content
✓ No Ads from Third Parties
✓ Support Our Mission
PST practitioners have many different techniques available to support clients as they learn to tackle day-to-day or one-off trauma.
5 Worksheets and workbooks
Problem-solving self-monitoring form.

Ask the client to complete the following:
- Describe the problem you are facing.
- What is your goal?
- What have you tried so far to solve the problem?
- What was the outcome?
Reactions to Stress
It can be helpful for the client to recognize their own experiences of stress. Do they react angrily, withdraw, or give up (Dobson, 2011)?
The Reactions to Stress worksheet can be given to the client as homework to capture stressful events and their reactions. By recording how they felt, behaved, and thought, they can recognize repeating patterns.
What Are Your Unique Triggers?
Helping clients capture triggers for their stressful reactions can encourage emotional regulation.
When clients can identify triggers that may lead to a negative response, they can stop the experience or slow down their emotional reaction (Dobson, 2011).
The What Are Your Unique Triggers ? worksheet helps the client identify their triggers (e.g., conflict, relationships, physical environment, etc.).
Problem-Solving worksheet
Imagining an existing or potential problem and working through how to resolve it can be a powerful exercise for the client.
Use the Problem-Solving worksheet to state a problem and goal and consider the obstacles in the way. Then explore options for achieving the goal, along with their pros and cons, to assess the best action plan.
Getting the Facts
Clients can become better equipped to tackle problems and choose the right course of action by recognizing facts versus assumptions and gathering all the necessary information (Dobson, 2011).
Use the Getting the Facts worksheet to answer the following questions clearly and unambiguously:
- Who is involved?
- What did or did not happen, and how did it bother you?
- Where did it happen?
- When did it happen?
- Why did it happen?
- How did you respond?
2 Helpful Group Activities
While therapists can use the worksheets above in group situations, the following two interventions work particularly well with more than one person.
Generating Alternative Solutions and Better Decision-Making
A group setting can provide an ideal opportunity to share a problem and identify potential solutions arising from multiple perspectives.
Use the Generating Alternative Solutions and Better Decision-Making worksheet and ask the client to explain the situation or problem to the group and the obstacles in the way.
Once the approaches are captured and reviewed, the individual can share their decision-making process with the group if they want further feedback.
Visualization
Visualization can be performed with individuals or in a group setting to help clients solve problems in multiple ways, including (Dobson, 2011):
- Clarifying the problem by looking at it from multiple perspectives
- Rehearsing a solution in the mind to improve and get more practice
- Visualizing a ‘safe place’ for relaxation, slowing down, and stress management
Guided imagery is particularly valuable for encouraging the group to take a ‘mental vacation’ and let go of stress.
Ask the group to begin with slow, deep breathing that fills the entire diaphragm. Then ask them to visualize a favorite scene (real or imagined) that makes them feel relaxed, perhaps beside a gently flowing river, a summer meadow, or at the beach.
The more the senses are engaged, the more real the experience. Ask the group to think about what they can hear, see, touch, smell, and even taste.
Encourage them to experience the situation as fully as possible, immersing themselves and enjoying their place of safety.
Such feelings of relaxation may be able to help clients fall asleep, relieve stress, and become more ready to solve problems.
We have included three of our favorite books on the subject of Problem-Solving Therapy below.
1. Problem-Solving Therapy: A Treatment Manual – Arthur Nezu, Christine Maguth Nezu, and Thomas D’Zurilla
This is an incredibly valuable book for anyone wishing to understand the principles and practice behind PST.
Written by the co-developers of PST, the manual provides powerful toolkits to overcome cognitive overload, emotional dysregulation, and the barriers to practical problem-solving.
Find the book on Amazon .
2. Emotion-Centered Problem-Solving Therapy: Treatment Guidelines – Arthur Nezu and Christine Maguth Nezu
Another, more recent, book from the creators of PST, this text includes important advances in neuroscience underpinning the role of emotion in behavioral treatment.
Along with clinical examples, the book also includes crucial toolkits that form part of a stepped model for the application of PST.
3. Handbook of Cognitive-Behavioral Therapies – Keith Dobson and David Dozois
This is the fourth edition of a hugely popular guide to Cognitive-Behavioral Therapies and includes a valuable and insightful section on Problem-Solving Therapy.
This is an important book for students and more experienced therapists wishing to form a high-level and in-depth understanding of the tools and techniques available to Cognitive-Behavioral Therapists.
For even more tools to help strengthen your clients’ problem-solving skills, check out the following free worksheets from our blog.
- Case Formulation Worksheet This worksheet presents a four-step framework to help therapists and their clients come to a shared understanding of the client’s presenting problem.
- Understanding Your Default Problem-Solving Approach This worksheet poses a series of questions helping clients reflect on their typical cognitive, emotional, and behavioral responses to problems.
- Social Problem Solving: Step by Step This worksheet presents a streamlined template to help clients define a problem, generate possible courses of action, and evaluate the effectiveness of an implemented solution.
If you’re looking for more science-based ways to help others enhance their wellbeing, check out this signature collection of 17 validated positive psychology tools for practitioners. Use them to help others flourish and thrive.
17 Top-Rated Positive Psychology Exercises for Practitioners
Expand your arsenal and impact with these 17 Positive Psychology Exercises [PDF] , scientifically designed to promote human flourishing, meaning, and wellbeing.
Created by Experts. 100% Science-based.
While we are born problem-solvers, facing an incredibly diverse set of challenges daily, we sometimes need support.
Problem-Solving Therapy aims to reduce stress and associated mental health disorders and improve wellbeing by improving our ability to cope. PST is valuable in diverse clinical settings, ranging from depression to schizophrenia, with research suggesting it as a highly effective treatment for teaching coping strategies and reducing emotional distress.
Many PST techniques are available to help improve clients’ positive outlook on obstacles while reducing avoidance of problem situations and the tendency to be careless and impulsive.
The PST model typically assesses the client’s strengths, weaknesses, and coping strategies when facing problems before encouraging a healthy experience of and relationship with problem-solving.
Why not use this article to explore the theory behind PST and try out some of our powerful tools and interventions with your clients to help them with their decision-making, coping, and problem-solving?
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free .
- Cuijpers, P., Wit, L., Kleiboer, A., Karyotaki, E., & Ebert, D. (2020). Problem-solving therapy for adult depression: An updated meta-analysis. European P sychiatry , 48 (1), 27–37.
- Dobson, K. S. (2011). Handbook of cognitive-behavioral therapies (3rd ed.). Guilford Press.
- Dobson, K. S., & Dozois, D. J. A. (2021). Handbook of cognitive-behavioral therapies (4th ed.). Guilford Press.
- Eysenck, M. W., & Keane, M. T. (2015). Cognitive psychology: A student’s handbook . Psychology Press.
- Nezu, A. M., & Nezu, C. M. (2009). Problem-solving therapy DVD . Retrieved September 13, 2021, from https://www.apa.org/pubs/videos/4310852
- Nezu, A. M., & Nezu, C. M. (2018). Emotion-centered problem-solving therapy: Treatment guidelines. Springer.
- Nezu, A. M., Nezu, C. M., & D’Zurilla, T. J. (2013). Problem-solving therapy: A treatment manual . Springer.
Share this article:
Article feedback
What our readers think.
Thanks for your information given, it was helpful for me something new I learned
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

The Empty Chair Technique: How It Can Help Your Clients
Resolving ‘unfinished business’ is often an essential part of counseling. If left unresolved, it can contribute to depression, anxiety, and mental ill-health while damaging existing [...]

29 Best Group Therapy Activities for Supporting Adults
As humans, we are social creatures with personal histories based on the various groups that make up our lives. Childhood begins with a family of [...]
47 Free Therapy Resources to Help Kick-Start Your New Practice
Setting up a private practice in psychotherapy brings several challenges, including a considerable investment of time and money. You can reduce risks early on by [...]
Read other articles by their category
- Body & Brain (55)
- Coaching & Application (59)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (27)
- Meditation (21)
- Mindfulness (44)
- Motivation & Goals (46)
- Optimism & Mindset (35)
- Positive CBT (30)
- Positive Communication (23)
- Positive Education (48)
- Positive Emotions (32)
- Positive Leadership (20)
- Positive Parenting (16)
- Positive Psychology (34)
- Positive Workplace (37)
- Productivity (18)
- Relationships (46)
- Resilience & Coping (40)
- Self Awareness (22)
- Self Esteem (38)
- Strengths & Virtues (33)
- Stress & Burnout Prevention (37)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)

The Latest on the Medications and Therapies That Treat Depression
New research highlights the most effective treatments for depression..
Posted July 15, 2024 | Reviewed by Devon Frye
- What Is Depression?
- Take our Depression Test
- Find a therapist to overcome depression
- Both antidepressants and behavioral treatments improve symptoms of depression.
- Antidepressants appear to have small/medium-sized effects (amitriptyline having the largest impact).
- Psychotherapies seem to have medium-sized effects (behavioral activation having the largest impact).
Published in June 2024, a recent paper in The Journal of the American Medical Association (JAMA) reviews the latest research on managing depression in adults.
What is Major Depression?
In everyday language, the word depression is used in diverse ways and can refer to anything from passing feelings of sadness and unhappiness to chronic grief and deep despair. When clinicians and therapists use the term depression, however, they usually mean major depression , which is a serious mental illness.
Major depression is a mood disorder defined by persistent feelings of sadness and/or a loss of pleasure and interest in regular activities. It is often accompanied by a variety of symptoms including excessive guilt , lack of energy, concentration difficulties, recurrent thoughts of death or suicide , and significant changes in sleep, appetite /weight, and psychomotor behavior (e.g., agitation).
The lifetime prevalence of depression—which refers to the proportion of the population that will at some point develop this mood disorder—is high, especially among women: Roughly one in six men and one in three women will eventually develop depression.
Some researchers, however, have suggested masculine depression is much more common in men.
Effective Treatments for Depression
First-line treatments for depression consist of antidepressant medications and psychotherapy . But which ones are most effective?
Based on their review of previous meta-analyses of randomized clinical trials, Simon et al. (the authors of the recent paper in JAMA) offer the following conclusions:
Effective psychotherapeutic interventions for depression include behavioral activation, brief psychodynamic therapy, cognitive therapy, interpersonal therapy, mindfulness -based therapy, and problem-solving therapy.
Compared with usual care but without psychotherapy, the above psychological treatments had at least medium-sized effects. The standardized mean differences ranged from 0.50 (for short-term dynamic psychotherapy) to 0.73 (for behavioral activation).
Medications for depression were also effective. Compared to placebo , 21 antidepressants had either small or medium effects.
These medications consisted of bupropion (Wellbutrin), citalopram (Celexa), duloxetine (Cymbalta), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft), venlafaxine (Effexor), fluvoxamine (Luvox), amitriptyline (Elavil), desvenlafaxine (Pristiq), levomilnacipran (Fetzima), milnacipran (Savella), mirtazapine (Remeron), nefazodone (Serzone), vilazodone (Viibryd), Agomelatine (Valdoxan), clomipramine (Anafranil), vortioxetine (Brintellix), reboxetine (Edronax), and trazodone (Desyrel).
The standardized mean differences ranged from 0.23 (for fluoxetine) to 0.48 (for amitriptyline).
The research also showed that for more severe or chronic depression, a combination of antidepressants and psychotherapy was more effective than either modality alone. The standardized mean differences were approximately 0.3. This corresponds to “typical response rates of 50 percent with psychotherapy or medication alone,” but “65 percent for combined treatment.”
What if the first antidepressant prescribed fails to improve symptoms? Then, the following options should be considered: switching medications, adding another antidepressant, or augmenting with a different type of medication (e.g., stimulants, antipsychotics , thyroid hormones ). According to the data, these three approaches have a nearly equal likelihood of success.

If you have low mood, excessive shame and guilt, concentration difficulties, and other symptoms of depression, you may have major depression. So please see a qualified mental health professional for assessment and treatment options.
Your healthcare provider will evaluate your symptoms to determine the presence of depression or another condition that shares some symptoms with depression; for example, bipolar disorder , borderline personality disorder , drug withdrawal, post- traumatic stress disorder ( PTSD ), or attention-deficit/hyperactivity disorder ( ADHD ).

In terms of treatments for depression, both psychotherapy and medications have been shown to help.
Commonly prescribed antidepressants have small- to medium-sized effects, with amitriptyline having the largest effect. (I have discussed the best antidepressants for depression in more detail in a previous article.
Behavioral and psychological interventions can also alleviate depression. These include:
- Behavioral activation
- Brief psychodynamic psychotherapy
- Cognitive therapy
- Interpersonal therapy
- Mindfulness-based therapy
- Problem-solving therapy
(To learn more about the above psychological treatments for depression, see my article here .)
Sadly, despite the benefits of medications and psychotherapy, there are multiple barriers to treatment for depression. Some examples are cost, availability, access, and stigma . As a result, many individuals with depression do not receive the help they need.
Telehealth and telemedicine (e.g., videoconferencing, telephone modalities) may hold the key to eliminating a number of these barriers without sacrificing quality of care. Indeed, preliminary research shows that telehealth tends to produce “similar outcomes as face-to-face provision of psychotherapy and psychiatry services.”

Arash Emamzadeh attended the University of British Columbia in Canada, where he studied genetics and psychology. He has also done graduate work in clinical psychology and neuropsychology in U.S.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Last updated 10th July 2024: Online ordering is currently unavailable due to technical issues. We apologise for any delays responding to customers while we resolve this. For further updates please visit our website https://www.cambridge.org/news-and-insights/technical-incident
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert

- > Journals
- > The British Journal of Psychiatry
- > Volume 155 Issue 5
- > Problem-Solving Therapy for Depression: Theory, Research...

Article contents
Problem-solving therapy for depression: theory, research and clinical guidelines. by arthur m. nezu, christine m. nezu and michael g. perri. chichester: john wiley. 1989. 274 pp. £19.15..
Published online by Cambridge University Press: 02 January 2018

Access options

No CrossRef data available.
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 155, Issue 5
- Rhinedd Toms (a1)
- DOI: https://doi.org/10.1192/S000712500001850X
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
No bias. No misinformation. No spin. Just what you need!
The Mental Elf
Problem solving therapy: is it an effective ingredient for treating depression #activeingredientsmh.
“All life is problem solving” suggested the philosopher Karl Popper (Popper & Camiller, 2013).
In mental health, we might say, “all psychotherapy is problem solving.” For example, problem solving is part and parcel of many psychotherapies for depression, including cognitive behavioural therapy (CBT), interpersonal psychotherapy (IPT), family therapy, and dialectical behaviour therapy (DBT).
Problem solving therapy (PST) is also a therapeutic approach in its own right with roots in Social Learning Theory that was developed by Thomas D’Zurilla and Marvin Goldfried in the 1970s (D’Zurilla & Goldfried, 1971).
Problem solving training typically builds self-efficacy and teaches rational problem solving skills, based on the idea that effective and rational problem solving protects from the negative effects of chronic or sudden stress, while ineffective problem solving (e.g., avoiding problems, leaving them for others to solve, or jumping on the first solution that comes to mind) does not. Problem-solving training can be brief (i.e., fewer than 10 sessions) and be delivered by trained clinicians, general practitioners, lay counsellors, or online. It is a versatile treatment ingredient that deserves greater scrutiny as a means to tackle depression.
In this blog, I review findings from an updated meta-analysis published in 2018 by Pim Cuijpers and colleagues (Cuijpers et al., 2018). The meta-analysis assessed the effectiveness of stand-alone PST for adults with depression, compared with control conditions and with other evidence-based therapies.
I also talk about my own recent Wellcome Trust-funded review of problem solving for young people with depression.

Problem-solving training is an active treatment ingredient of many evidence-based therapies for depression in adulthood.
Randomised controlled trials were retrieved from an existing database that was compiled through systematic searches in PubMed, PsycInfo, Embase and the Cochrane Library, and databases specifically cataloguing trials from lower- and middle-income countries. For inclusion, studies had to be randomised controlled trials (RCTs) comparing problem solving therapy (PST) for adult depression (established via a diagnostic interview or above-threshold self-report score) with a control group (e.g., waitlist, treatment as usual, placebo, etc.) or with another active treatment. Maintenance studies or those using inpatient samples were excluded. RCTs for other types of psychotherapy for depression were also retrieved to compare their effectiveness to that of PST. Two reviewers independently screened abstracts and full texts.
All included studies underwent a risk of bias assessment using the Cochrane Collaboration’s assessment tool, and reviewers coded suspected “researcher allegiance” in favour of PST (e.g., where PST was mentioned as the principal intervention to be tested in a paper’s introduction). A random effects meta-analysis assessed the difference in depression scores between intervention and control groups post treatment, using Hedge’s g and a correction for small sample bias. Subgroup and multivariate meta-regression analysis aimed to identify causes of heterogeneity, and publication bias was also examined.
The meta-analysis considered 30 PST trials and 264 trials of other therapies for comparison. Close to two thirds of PST trials had been done in North America, one third in Europe, and one trial in Africa. There was considerable risk of bias in most PST trials, with only seven out of 30 meeting all Cochrane criteria of high quality.
Key findings
- When considering only studies with low risk of bias , the effect size was smaller (g = 0.34; 95% CI: 0.22 to 0.46), and heterogeneity was low ( I 2 = 32).
- Several study characteristics were significantly related to effect size in a subgroup analysis (see Table 1 below), but only low risk of bias remained significant in a multivariate meta-regression (associated with smaller effect sizes).
- PST versus another type of psychotherapy (12 direct comparisons): PST was slightly superior (g = 0.18; 95% CI: 0.01 to 0.35), with low heterogeneity ( I 2 = 27), but there was researcher allegiance pro PST in most studies.
- PST versus antidepressants (6 comparisons): No statistically significant effect was found (g = 0.09; 95% CI: -0.13 to 0.30).
When comparing the effect size for PST with those achieved by other psychotherapies (compared with control groups), there was no statistically significant difference in effectiveness.
Table 1. Findings about possible causes of heterogeneity
| Study characteristic | Initial subgroup analysis | Subgroup analysis after removing studies with very high effect sizes to avoid distortion | Multivariate regression analysis—full model | Multivariate regression analysis—parsimonious model |
| Participants recruited from the community (vs. clinical settings) | ✔️ | ✔️ | ||
| Group-based PST (vs. individual) | ✔️ | ✔️ | ||
| Done in North America (vs. Europe or Africa) | ✔️ | |||
| Using a wait-list control (vs. treatment as usual or other comparison group) | ✔️ | ✔️ | ||
| Low risk of bias (vs. high risk) | ✔️ | ✔️ | ✔️ | |
| Target group (adults; older adults) | ||||
| Diagnosis (diagnosed disorder or above cut-off) | ||||
| Type of PST (extended, brief, self-directed) |
Conclusions
The authors concluded that despite some limitations, this meta-analysis showed that:
PST is probably an effective treatment of [adult] depression, with effect sizes that are small, but comparable to those found for other psychological treatments of depression (p. 35).

The effect sizes for problem-solving therapy (PST) as a treatment approach for adult depression were found to be comparable to those of other evidence-based psychotherapies.
Strengths and limitations
The authors provide a thorough and systematic approach to assessing the evidence, controlling for possible sources of bias (e.g., publication bias, researcher allegiance, distorting influence of very high effect sizes), and investigating causes of heterogeneity.
The sample of studies was too small to examine the influence of factors such as treatment length or delivery format on PST effectiveness, with a lack of high-quality studies (k = 9) in particular. Publication bias, and researcher allegiance in over half of the included studies were additional barriers to drawing credible conclusions. The authors could have further enhanced the strength of their review by using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system to appraise the overall quality of the evidence and of the clinical recommendations that can be made on their basis (Guyatt et al., 2008).
Implications for practice
Problem solving therapy is not currently recommended as a stand-alone treatment for adult depression by the NICE guidelines, but this meta-analysis found it could be offered as an alternative to CBT or IPT, with similar expected benefits.
Problem solving training for young people with depression: our Active Ingredients review
We were inspired by this finding from Cuijpers et al (2018) that problem solving therapy (PST) is as effective as evidence-based therapy packages (including CBT), because problem solving is one of the coping skills that youth most frequently use in their daily lives (Ng et al., 2016). Learning coping and self-management skills is also a key desired outcome of depression treatment in the eyes of youth with lived experience (Krause et al., 2020a; Krause et al., 2020b). This got us interested in looking at problem-solving as an active ingredient of treatment for youth depression.
We conducted a scoping review that considered four clinical trials of stand-alone PST for youth depression; four secondary analyses of trial data looking at problem solving as a predictor, moderator, or mediator of treatment response; and 24 clinical practice guidelines for youth depression.
Our findings suggest that there is currently no strong evidence in favour of PST as a stand-alone treatment for reducing youth depression symptoms. Stand-alone PST may be beneficial for youth who face stress from challenging events or daily hassles and who struggle with problem solving, but whose mental health difficulties are relatively mild. In turn, the current evidence base suggests that youth who struggle with low mood and other depression symptoms may require broader psychotherapeutic support to recover from their depression. More high-quality research is needed to investigate the effective of problem-solving training for youth.
We had the chance of having two youth advisors work with us as co-researchers. They consulted a larger panel of youth research advisors at the Centre for Addiction and Mental Health in Toronto, Ontario to help us contextualize our review findings. From our youth advisors we learned that in order to be meaningful, problem-solving training should be:
- youth-driven (with youth rather than therapists defining the problem)
- strengths-based (avoiding deficit-focused language)
- comprehensive (by considering the root causes of superficial problems) and
- personalised (by embracing people’s individual problem solving styles).
In order to be acceptable to youth, problem-solving training needs to be youth-driven, strengths-based, comprehensive, and personalised.
Statement of interests
Karolin’s team at the Cundill Centre for Child and Youth Depression (Centre for Addiction and Mental Health) received funding through the Wellcome Trust Mental Health Priority Area ‘Active Ingredients’ commission to conduct their review of problem solving training as an active ingredient for treating youth depression.
Primary paper
Cuijpers, P., de Wit, L., Kleiboer, A., Karyotaki, E., & Ebert, D. D. (2018). Problem-solving therapy for adult depression: An updated meta-analysis. European Psychiatry, 48, 27–37. https://doi.org/10.1016/j.eurpsy.2017.11.006
Other references
Cuijpers, P., de Wit, L., Kleiboer, A., Karyotaki, E., & Ebert, D. D. (2018). Problem-solving therapy for adult depression: An updated meta-analysis. European Psychiatry , 48 , 27–37. https://doi.org/10.1016/j.eurpsy.2017.11.006
D’Zurilla, T. J., & Goldfried, M. R. (1971). Problem solving and behaviour modification. Journal of Abnormal Psychology , 78 (1), 107–126. https://doi.org/10.1037/h0031360
Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., & Schünemann, H. J. (2008). GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ , 336 (7650), 924–926. https://doi.org/10.1136/bmj.39489.470347.AD
Krause, K., Midgley, N., Edbrooke-Childs, J., & Wolpert, M. (2020a). A comprehensive mapping of outcomes following psychotherapy for adolescent depression: The perspectives of young people, their parents and therapists. European Child & Adolescent Psychiatry . https://doi.org/10.1007/s00787-020-01648-8
Krause, K. R., Edbrooke-Childs, J., Bear, H. A., Calderón, A., & Wolpert, M. (2020b). What Treatment Outcomes Matter Most? A Q-study of Outcome Priority Profiles Among Youth with Lived Experience of Depression. MedRxiv , 2020.10.12.20210468. https://doi.org/10.1101/2020.10.12.20210468
Ng, M. Y., Eckshtain, D., & Weisz, J. R. (2016). Assessing Fit Between Evidence-Based Psychotherapies for Youth Depression and Real-Life Coping in Early Adolescence. Journal of Clinical Child and Adolescent Psychology , 45 (6), 732–748. https://doi.org/10.1080/15374416.2015.1041591
Popper, K., & Camiller, P. (2013). All life is problem solving. In All Life is Problem Solving . Psychology Press. https://doi.org/10.4324/9780203431900
Profile cancel
Email Not published

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Problem solving therapies for depression: a meta-analysis
Affiliation.
- 1 Department of Clinical Psychology, Vrije Universiteit Amsterdam, Van der Boechorststraat 1, 1081 BT Amsterdam, The Netherlands. [email protected]
- PMID: 17194572
- DOI: 10.1016/j.eurpsy.2006.11.001
Purpose: In the past decades, the effects of problem-solving therapy (PST) for depression have been examined in several randomized controlled studies. However, until now no meta-analysis has tried to integrate the results of these studies.
Methods: We conducted a systematic literature search and identified 13 randomized studies examining the effects of PST, with a total of 1133 subjects. The quality of studies varied.
Results: The mean standardized effect size was 0.34 in the fixed effects model and 0.83 in the random effects model, with very high heterogeneity. Subgroup analyses indicated significantly lower effects for individual interventions in studies with subjects who met criteria for major depression, studies in which intention-to-treat analyses were conducted instead of completers-only analyses, and studies with pill placebo and care-as-usual control groups. Heterogeneity was high, and the subgroup analyses did not result in clear indications of what caused this high heterogeneity. This indicates that PST has varying effects on depression, and that it is not known to date what determines whether PST has larger of smaller effects.
Conclusion: Although there is no doubt that PST can be an effective treatment for depression, more research is needed to ascertain the conditions and subjects in which these positive effects are realized.
PubMed Disclaimer
Similar articles
- Problem-solving therapy for adult depression: An updated meta-analysis. Cuijpers P, de Wit L, Kleiboer A, Karyotaki E, Ebert DD. Cuijpers P, et al. Eur Psychiatry. 2018 Feb;48:27-37. doi: 10.1016/j.eurpsy.2017.11.006. Epub 2018 Jan 10. Eur Psychiatry. 2018. PMID: 29331596
- Relative efficacy of psychotherapy and combined therapy in the treatment of depression: a meta-analysis. de Maat SM, Dekker J, Schoevers RA, de Jonghe F. de Maat SM, et al. Eur Psychiatry. 2007 Jan;22(1):1-8. doi: 10.1016/j.eurpsy.2006.10.008. Epub 2006 Dec 27. Eur Psychiatry. 2007. PMID: 17194571
- Problem-solving treatment and coping styles in primary care for minor depression. Oxman TE, Hegel MT, Hull JG, Dietrich AJ. Oxman TE, et al. J Consult Clin Psychol. 2008 Dec;76(6):933-43. doi: 10.1037/a0012617. J Consult Clin Psychol. 2008. PMID: 19045962 Free PMC article. Clinical Trial.
- Characteristics of psychological interventions that improve depression in people with coronary heart disease: a systematic review and meta-regression. Dickens C, Cherrington A, Adeyemi I, Roughley K, Bower P, Garrett C, Bundy C, Coventry P. Dickens C, et al. Psychosom Med. 2013 Feb;75(2):211-21. doi: 10.1097/PSY.0b013e31827ac009. Epub 2013 Jan 16. Psychosom Med. 2013. PMID: 23324874 Review.
- Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents (Review). Gillies D, Taylor F, Gray C, O'Brien L, D'Abrew N. Gillies D, et al. Evid Based Child Health. 2013 May;8(3):1004-116. doi: 10.1002/ebch.1916. Evid Based Child Health. 2013. PMID: 23877914 Review.
- Enhancing Efficiency and Reach Using Facebook to Recruit Breast Cancer Survivors for a Telephone-Based Supportive Care Randomized Trial During the COVID-19 Pandemic. Ejem DB, Wechsler S, Gallups S, Khalidi S, Coffee-Dunning J, Montgomery AP, Stevens CJ, Keene K, Rocque GB, Chamberlin M, Hegel MT, Azuero A, Pisu M, Ellis D, Ingram SA, Lawhon VM, Gilbert T, Morrissette K, Morency J, Thorp K, Codini M, Newman R, Echols J, Cloyd D, Dos Anjos S, Muse C, Goedeken S, Laws KE, Herbert J, Bakitas M, Lyons KD. Ejem DB, et al. JCO Oncol Pract. 2023 Nov;19(11):1020-1030. doi: 10.1200/OP.23.00117. Epub 2023 Sep 21. JCO Oncol Pract. 2023. PMID: 37733975 Clinical Trial.
- Effects of M-DEPTH Model of Depression Care on Maternal HIV Viral Suppression and Adherence to the PMTCT Care Continuum Among HIV-Infected Pregnant Women in Uganda: Results from a Cluster Randomized Controlled Trial at Pregnancy Completion. Wagner GJ, Gwokyalya V, Faherty L, Akena D, Nakigudde J, Ngo V, McBain R, Ghosh-Dastidar B, Beyeza-Kashesya J, Nakku J, Kyohangirwe L, Nabitaka LK, Lukwata H, Mukasa B, Wanyenze RK. Wagner GJ, et al. AIDS Behav. 2023 Sep;27(9):2902-2914. doi: 10.1007/s10461-023-04014-2. Epub 2023 Mar 13. AIDS Behav. 2023. PMID: 36907945 Free PMC article. Clinical Trial.
- In the here and now: Future thinking and social problem-solving in depression. Noreen S, Dritschel B. Noreen S, et al. PLoS One. 2022 Jun 30;17(6):e0270661. doi: 10.1371/journal.pone.0270661. eCollection 2022. PLoS One. 2022. PMID: 35771846 Free PMC article.
- Peer-led family-centred problem management plus for immigrants (PMP-I) for mental health promotion among immigrants in USA: protocol for a pilot, randomised controlled feasibility trial. Poudel-Tandukar K, Jacelon CS, Martell CR, Poudel KC, Rai S, Ramdam R, Laws H, Meyer JS, Bertone-Johnson ER, Hollon SD. Poudel-Tandukar K, et al. BMJ Open. 2022 May 3;12(5):e061353. doi: 10.1136/bmjopen-2022-061353. BMJ Open. 2022. PMID: 35504635 Free PMC article.
- Residual posttraumatic stress disorder symptoms after provision of brief behavioral intervention in low- and middle-income countries: An individual-patient data meta-analysis. Akhtar A, Koyiet P, Rahman A, Schafer A, Hamdani SU, Cuijpers P, Sijbrandij M, Bryant RA. Akhtar A, et al. Depress Anxiety. 2022 Jan;39(1):71-82. doi: 10.1002/da.23221. Epub 2021 Nov 9. Depress Anxiety. 2022. PMID: 34752690 Free PMC article.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Elsevier Science
- Genetic Alliance
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Research article
- Open access
- Published: 26 October 2011
Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV
- Dixon Chibanda 1 ,
- Petra Mesu 2 ,
- Lazarus Kajawu 1 , 2 ,
- Frances Cowan 3 , 4 ,
- Ricardo Araya 5 &
- Melanie A Abas 6
BMC Public Health volume 11 , Article number: 828 ( 2011 ) Cite this article
28k Accesses
206 Citations
174 Altmetric
Metrics details
There is limited evidence that interventions for depression and other common mental disorders (CMD) can be integrated sustainably into primary health care in Africa. We aimed to pilot a low-cost multi-component 'Friendship Bench Intervention' for CMD, locally adapted from problem-solving therapy and delivered by trained and supervised female lay workers to learn if was feasible and possibly effective as well as how best to implement it on a larger scale.
We trained lay workers for 8 days in screening and monitoring CMD and in delivering the intervention. Ten lay workers screened consecutive adult attenders who either were referred or self-referred to the Friendship Bench between July and December 2007. Those scoring above the validated cut-point of the Shona Symptom Questionnaire (SSQ) for CMD were potentially eligible. Exclusions were suicide risk or very severe depression. All others were offered 6 sessions of problem-solving therapy (PST) enhanced with a component of activity scheduling. Weekly nurse-led group supervision and monthly supervision from a mental health specialist were provided. Data on SSQ scores at 6 weeks after entering the study were collected by an independent research nurse. Lay workers completed a brief evaluation on their experiences of delivering the intervention.
Of 395 potentially eligible, 33 (8%) were excluded due to high risk. Of the 362 left, 2% (7) declined and 10% (35) were lost to follow-up leaving an 88% response rate (n = 320). Over half (n = 166, 52%) had presented with an HIV-related problem. Mean SSQ score fell from 11.3 (sd 1.4) before treatment to 6.5 (sd 2.4) after 3-6 sessions. The drop in SSQ scores was proportional to the number of sessions attended. Nine of the ten lay workers rated themselves as very able to deliver the PST intervention.
We have found preliminary evidence of a clinically meaningful improvement in CMD associated with locally adapted problem-solving therapy delivered by lay health workers through routine primary health care in an African setting. There is a need to test the effectiveness of this task-shifting mental health intervention in an appropriately powered randomised controlled trial.
Trial registration
ISRCTN: ISRCTN25476759
Peer Review reports
Mental disorders cause considerable suffering, disability and social exclusion in Africa, and are poorly recognised and undertreated [ 1 , 2 ]. In Zimbabwe, common mental disorders, such as depression mixed with anxiety, are found in over 25% of those attending primary health care services or maternal services, and in up to 30% of females in the community [ 3 – 5 ]. In the Zimbabwean Shona language, thinking too much ( kufungisisa ), along with deep sadness ( kusuwisisa ), and painful heart (moyo unorwadza) are terms in common use for emotional distress being close to European and American categories of common forms of depression and anxiety [ 3 , 6 ]
There is increasing evidence, mainly from other world regions but also rapidly growing evidence from within low income countries, that improving mental health is a low cost approach to improve quality of life and reduce disability [ 7 , 8 ]. Very little of this evidence, however, is from Africa. In Chile, low intensity low-cost treatments for depression have been integrated into primary health care [ 9 ]. These include, for example, psycho education, problem-solving therapy and self-help approaches [ 10 , 11 ]. Problem-solving therapy has been shown to be effective for depression and common mental health problems [ 12 , 13 ]. Previous attempts to deliver care for common mental disorders through primary care clinics in Zimbabwe although promising in the short-term had shown little long-term success due to reliance on overstretched nursing staff and lack of supervision [ 14 ]. In 2005, a government operation in Mbare , a township in Harare, resulted in many people becoming homeless or losing their livelihoods [ 15 ] and was perceived by the Mbare community to lead to high rate of emotional distress. Local stakeholders identified the need for a community mental health intervention. This had to be at no extra cost to the primary health care clinic, to utilise space outside the overcrowded clinic rooms, and to use methods already tested locally. A pilot intervention based on a problem-solving approach was identified [ 16 ]. It was suggested this be delivered by lay health workers via a 'Friendship Bench' ( Chigaro Chekupanamazano ) placed in the clinic grounds, and that a system of supervision and stepped care be part of the package. A team comprising psychologists, a primary care nurse and a psychiatrist adapted existing training materials on problem solving therapy [ 16 , 17 ] in the light of experience working with lay workers and general nurses in primary care. Adaptations included at least one home visit by the lay workers early in the therapy given it is normal practice for lay workers to visit clients in their homes, and encouraging clients to schedule some positive activities that really mattered to them to make life more rewarding. The training and the intervention were pre-tested in 5 lay workers and 143 primary care clients and found to be acceptable to them and to the lay workers. The aim of this pilot was to gather preliminary data on the effectiveness of this intervention and to see if the intervention would be feasible, and if so to gather ideas about how best to implement it on a larger scale.
Mbare is a high density suburb or township in the south of Harare. It is characterized by ethnic diversity and high unemployment with most residents relying on informal trading. The literacy rate is estimated to be over 90%. There are three government run Primary Health Care (PHC) clinics, staffed almost exclusively by general nurses, for a population of approximately 200 000. The study took place in all three clinics.
Twenty lay workers, locally termed health promoters, support the nurses at these three clinics. The lay workers are a respected group of primary health care providers, commonly referred to as ambuya utano (grandmother health provider) (Figure 1 ). In Mbare , all lay workers are female, literate, have at least primary school education, and have lived locally for at least 15 years. Their mean age is 58 years. Their main role is in community health outreach, which includes supporting people living with HIV/AIDS and Tuberculosis by providing individual and family support (practical, psychological and spiritual) and encouraging medication adherence. They also deliver community health education and promotion e.g. through encouraging immunisation and methods to control disease outbreaks. Lay workers report weekly to the environmental health officer and a nurse-manager. The lay workers cover geographical patches, which are sections of the community demarcated by the City of Harare according to street grids. Each geographical patch has approximately 3000 inhabitants. Ten lay workers were selected at random for this pilot: three from two of the clinics and four from the largest clinic.

Some of the lay health workers involved in the Friendship Bench project, sitting in front of one of the Benches .
Participants
Inclusion criteria: aged 18 and over; residents of geographical patches in Mbare , Harare, covered by the ten selected lay workers; score > 7 on Shona Symptom Questionnaire screen for common mental disorders. Exclusion criteria: requiring acute medical attention such that they cannot participate; severe psychiatric symptoms and/or risk to self or others requiring specialist referral as assessed by primary care research nurse
Ethical approval was obtained from the Medical Research Council of Zimbabwe and written informed consent was sought from all participants. The study was registered as a non-controlled trial http://www.controlled-trials.com/ISRCTN25476759
Recruitment
We aimed to recruit from the clinic staff, from the community, and from the lay workers themselves. The psychiatrist (DC) and psychologists (PM, KJ) presented to the clinic nursing staff and to all 20 lay workers the rationale for the project and referral methods to the friendship Bench. Notices written in the local vernacular language explaining the location and uses of the benches were placed at six different points within the entrance hall and waiting area of each clinic.
The lay workers introduced and publicised the Friendship Bench to the community through community stakeholders' meetings and during visits to people's homes, churches, schools and police stations. They introduced it as an adjunct to their normal daily community health outreach activity. They described the Friendship Bench approach as aimed at addressing common mental health issues such as kufungisisa (thinking too much) as a result of, among other things, HIV infection, AIDS, domestic violence, family sickness and poverty.
Clients were either referred or could self refer to the Friendship Bench, which was available Mon-Friday 9.00 am to 12.00 pm at each clinic. Those referred or who self-referred were directed by nursing or reception staff to sit on the Friendship Bench which in each clinic was a large wooden bench located under a tree within sight of the lay workers' office. One duty lay worker was responsible for the Bench each day on rotation and would approach the Bench after a potential client sat on it. The duty lay worker was responsible for collecting data on inclusion criteria including residential and basic demographic information and on psychological symptoms using the Shona Symptom Questionnaire (SSQ) [ 4 ]. She also gathered information on recent stressors using a brief life events screen based on one used previously in Harare [ 18 ]. Everyone was offered some education, advice and often sign-posted to support services. Those meeting inclusion criteria were referred to a research nurse for assessment of risk to self or to others (e.g. suicidal ideation, history of deliberate self harm, very severe symptoms). She referred those excluded on these grounds to the visiting psychiatrist (DC). She invited those meeting eligibility criteria to participate in the pilot and took written informed consent. She then referred them back to the lay worker who made arrangements for their first Friendship Bench session within 2-5 days with a lay worker that covered their geographical patch.
Outcome measure
The main outcome measure was the Shona Symptom Questionnaire (SSQ). The SSQ is a 14-item screening tool for common mental disorders, integrating local idioms and internationally recognised items for emotional distress. It was developed and validated in Zimbabwe using exemplary cross-cultural methods [ 4 ]. It is self-administered and has a reliable internal consistency (r = 0.85) and satisfactory sensitivity and specificity, with a score of > = 8 being the cut-point. It is based on a yes/no response and asks about symptoms such as thinking too much, failing to concentrate, work lagging behind, insomnia, suicidal ideation, unhappiness and so on, over a 1 week period. All participants were approached six to eight weeks after their first treatment session to complete a self-administered SSQ which was collected by the research nurse in the absence of the attending lay worker.
The Intervention
The intervention consisted of brief individual talking therapy based on problem-solving therapy delivered by a lay worker. Most sessions took place sitting on a bench termed "The Friendship Bench" ( Chigaro Chekupanamazano ). The Friendship Benches were made for the project by local craftsmen (see Figure 1 ). They are located within the grounds of each of the three participating clinics in a discrete area under the trees in the clinic gardens.
Table 1 shows the activities involved in the delivery of the Friendship Bench. The lay worker would initially explain to all participants how to self-administer the screening tool, the Shona Symptom Questionnaire. Problem-solving therapy (PST) included identification and exploration of problems, and identification and implementation of solutions, based on prior principles [ 19 ]. Our PST was a locally developed seven-step plan previously used in partnership with government, lay and traditional care providers [ 16 ]. Up to a maximum of 6 sessions on the Bench were offered with the second session taking place at the client's home and sometimes also one of the later sessions. Those most in financial need were referred to two local income-generating projects (peanut butter making; recycling). The problem solving therapy was enhanced with a component of activity scheduling in that clients were also encouraged to carry out activities that really mattered to them to make life more rewarding. Home visits included prayer. Prayer was already a well recognised part of the support provided by LW in their community health outreach role in Mbare , which has a 98% Christian population with more than 70 Christian faith groups. On average each prayer lasts 15-30 minutes and is delivered by one lay worker together with the family. The aim of the prayer is to comfort the sick and the family. The use of prayer in formal gatherings related to health is a common practice in Zimbabwe. The existing prayer format used prior to the introduction of the Friendship Bench was incorporated in the six sessions without any alterations.
Training, selection and supervision of facilitators
All 20 lay workers were trained.
We provided an 8-day training run by two clinical psychologists (PM and LK), a general nurse trained in systemic counselling (ST) and a psychiatrist (DC). This covered didactic lectures on common mental disorders (CMD), including kufungisisa (thinking too much) but particularly focussed on skills to identify CMD using the Shona Symptoms Questionnaire [ 4 ], and to manage CMD using simple psycho-education and problem-solving therapy [ 16 – 19 ]. Lay workers then took part in two days of pre-testing including screening, identification, and referral processes within the clinic, and referral of 'red flags' (critical case-situations such as suicidal risk). We made use of practise with clients on the Friendship Bench and in clients' homes'. We developed a client referral manual, which included a list of NGO's, private and public institutions, and church organizations to be used by lay workers or patients.
Ten lay workers were selected at random for the pilot: three from two of the clinics and four from the largest clinic.
A daily peer-support group for lay workers was introduced. The peer group meetings were facilitated by one of the lay workers who would then present during weekly group supervision where all lay workers participated. A clinic staff nurse trained in counseling provided weekly group supervision at the largest clinic. The clinical psychologist and the psychiatrist provided further supervision every fortnightly and monthly, respectively.
We developed a brief 6-item questionnaire with a 4-point Likert scale for the lay workers to evaluate the PST intervention. For instance, we asked them to rate the ease with which they had learned the problem-solving therapy approach, the ease with which they delivered the intervention and the proportion of clients who appeared to benefit from the PST approach. We asked the lay workers to complete this once 6 weeks after the study has begun. We also carried out one focus group with 6 of the 10 workers and asked them to describe their experiences of delivering the intervention. Their responses were recorded in writing and analysed for content and themes by two of the authors.
Data analysis
Descriptive statistics (means and standard deviations and proportions) were estimated for those who participated, who declines, who were lost to follow, and who were excluded due to psychiatric risk. We used t-tests and regression models to test changes in SSQ scores before and after completion of the treatment, adjusting for SSQ scores at baseline. Data were entered and analysed using EpiInfo 2002 and STATA 10.0 (Release 10, College Station, TX: Stata Corporation. 2003) after range checks and double entry of all questionnaires.
Recruitment and attrition at follow-up
Between July and November 2007, 948 persons visited the Bench. Of these 948 persons who visited the Bench, 395 (42%) scored above the cut-point of the Shona Symptom Questionnaire (SSQ). Among these, 33 (8%) with a mean SSQ score of 11.8 (sd 1.2) were excluded from the pilot study due to being severely depressed and/or suicidal and were referred to the psychologist or psychiatrist (see Figure 2 ). Of the 362 invited to take part, 2% (7) declined and 10% (35) were lost to follow-up leaving an 88% response rate (320 participants). Of the 395, 188 (48%) presented with an HIV-related problem of whom 166 (88%) participated.
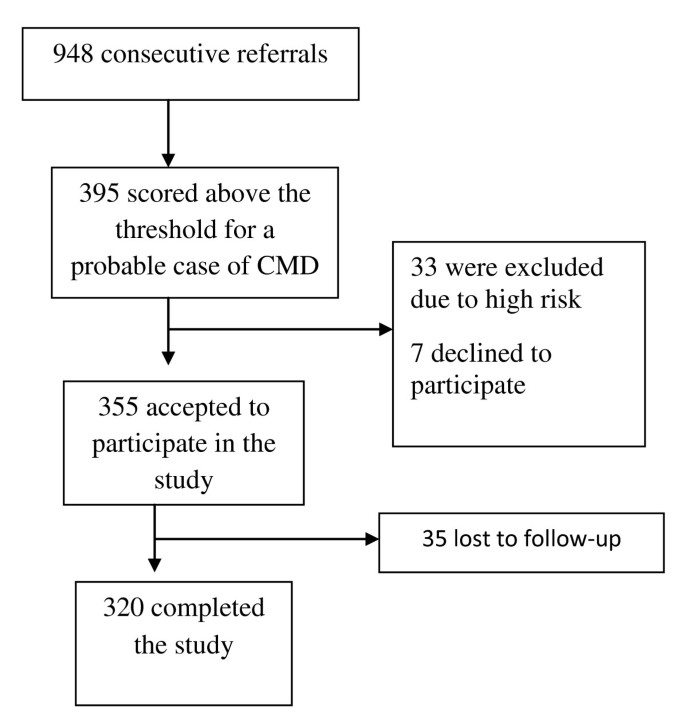
Flow diagram of recruitment into the study .
Table 2 shows the characteristics of the 395 who scored above the cut-point of the SSQ, according to whether or not they entered the study. Participants were more likely to be female. More of those who participated were female and married (70% female, 57% married) compared to those who declined (42% female, 43% married) or who were those lost to follow-up (40% female, 41% married). Those with less than eight years of education were more likely to be lost to follow-up than to participate. The primary reasons presented for visiting the Bench among those who participated were HIV-related, somatic complaints and domestic violence.
Most of those who participated were referred to the Friendship Bench by clinic staff (35%) and lay workers (24%). Other common forms of referral were: friend/relative (13%), self-referral (12%) or police (9%).
Psychological symptoms scores before and after the six-week intervention period
All participants completed a minimum of 3 sessions over a six week period with 20%, 30%, 21% and 30% completing 3, 4, 5 or 6 sessions respectively.
The mean SSQ score for the 320 cases was 11.3 (sd 1.4) before treatment. After receiving between 3 to 6 sessions the mean score dropped by 4.8 points to 6.5 (sd 2.4) [t = 13.6 (p = 0.0087)]. For those completing 3 or more sessions, 66% recovered to below case level on the SSQ at 6-8 weeks
Table 3 shows the drop in SSQ scores according to the number of sessions attended, adjusting for baseline SSQ score. The more sessions attended the larger the drop in SSQ scores with a drop of more than 3 points observed among those who attended all six sessions.
Lay workers evaluation
Nine of the ten lay workers rated themselves as very able to deliver the PST intervention. All of them rated at least half of their clients as benefiting from PST with 7/10 rating 'more than half' of their clients benefiting from the intervention. Themes emerging from the focus group suggested that the lay workers viewed effective ingredients of the Friendship Bench to include:
Their position of trust in the community-clients viewed them as wise and confidential. The clients viewed them as 'persons who would not gossip' which was 'reassuring in a small community'
Being able to visit clients in their homes which they felt instilled hope
Minimising stigma associated with having a mental health problem. The lay workers heard from their clients that as they were already connected with public health work (rather than psychiatry) and carried out home visits routinely as part of their work on public health promotion and that it was not stigmatising for clients with kufungisisa (thinking too much) to be visited.
The structured 'talk therapy' helped them to monitor the progress and challenges that clients were facing.
Breaking down the problems into specific and manageable steps
Giving feedback to clients.
In the focus group, the lay workers reported several case histories of their clients. These included the following:
A female client who had been to the bench with a score of 12/14 on the SSQ at baseline and subsequently received 2 home visits described the lay health workers as 'bringing peace' in her home, and 'less agitation' from her partner. Her score dropped to 7/14 after six sessions.
ii) A female client with an SSQ of 11/14 dropped to 6/14 after five sessions which included a home visit after she presented with being unable to come to terms with her HIV status.
iii) A female senior member of the local protestant church described the home visits as 'hope for those of us who are unable to open up in a church congregation about our HIV status'. Her score went down to 5/14 from 10/14 after 6 sessions.
This is the first example of lay health workers in Africa delivering a low intensity mental health intervention, using locally adapted tools, for common mental disorders in primary care. We have shown that it is feasible for lay workers to deliver this intervention for depression and common mental disorders, and that recruitment to the intervention from primary care, community agencies and self-referral was also feasible (Figure 2 ). The treatment appeared acceptable to the community and the lay workers were able to integrate the intervention into their routine work. Preliminary findings also show that the intervention is efficacious in reducing psychological morbidity, with a drop in score of nearly 5 points on the 14-item psychological outcome scale after 3-6 sessions, and efficacy proportional to the number of sessions attended. Over half of those who participated had presented with a problem related to HIV.
Chance does not seem a likely explanation for our finding as the significance value for the drop in score after 3-6 sessions was at p < 0.01 level. Bias may explain some of the results in that women and married participants were more likely to participate than to decline or to be lost to follow-up and those with lower education were more likely to be lost to follow-up than to participate. However, overall, the response rate of 88% was extremely high so it appears unlikely that bias is playing a major role in explaining the results. Measurement error is also unlikely to explain the findings. The Shona Symptom Questionnaire was developed using optimal cross-cultural methods and has been validated against an international diagnostic interview with most of those scoring at or above the recommended cut-off having mixed depression and anxiety or pure depression using ICD criteria [ 4 ].
We do not have a comparison group from the same study who did not receive the intervention. However, a prospective study in primary care in Harare showed that a mean drop in score of 4.7 (sd 6.3) on the SSQ was associated with recovery from 'case' to 'non-case' and with significantly less disability [ 20 ] (see Table 3 of the Patel paper). These authors further report that those who experienced a drop in score of 4 or more points on the SSQ were more likely to self-report an improvement in health than those who remained at case-level on the SSQ. Our crude mean drop in score of 4.8 points thus appears to represent a meaningful drop in score indicating efficacy of the Friendship Bench intervention. Furthermore, our finding that drop in score was significantly correlated with the number of sessions attended, even after adjusting for baseline SSQ score, adds weight to our assertion that the intervention appears to be efficacious. In our pilot, 34% remained cases at 6-8 weeks follow-up after the intervention, whereas in the Patel et al study [ 20 ], where there was no specific intervention, 48% of primary health care attenders remained cases.
The quantitative findings are supported by the lay workers evaluation. All of them rated at least half of their clients as benefiting from problem-solving therapy with 7/10 rating 'more than half' of their clients benefiting from the intervention. Themes that emerged from qualitative work support the argument that implementing this intervention through an existing public health intervention and by mature women with a position of trust in the community, helps explain its apparent efficacy. The lay workers-or 'grandmother health providers' are viewed as wise, confidential, authoritative and not prone to gossip. As the lay workers were already respected for their public health work, participants said they did not find it not stigmatising to be visited.
The intervention is theoretically closely linked to problem-solving therapy, which has been shown to be effective for depression and common mental health problems [ 12 , 13 ], together with an activity scheduling component [ 21 ]. It incorporates local adaptations that are integral to the routine work of the therapists who are culturally sanctioned lay health workers, known and respected as 'grandmother health providers'. For instance, the inclusion of Christian prayer for 15 minutes during 1 or 2 of the 6 sessions was part of the existing practice of the lay workers and it would have been inappropriate to remove that normal practice. While there is no evidence from randomised controlled trials that prayer is an effective treatment for depression in Christians, there is some suggestion from non-randomised studies with small samples that religious activities may benefit depression [ 22 ].
In 1994 we showed that major barriers to up-scaling mental health care in this setting include lack of supervision, and lack of recording systems for common mental disorders. We provided evidence that problems in improving primary mental health care may be less with the attitudes (or even the training) of primary care staff and more with bureaucratic limitations such as the inadequacy of the diagnostic codes, absence of mental health supervision, lack of protocol for following-up CMD patients, lack of medicines, and lack of incentives to see patients with CMD [ 23 ]. The Friendship Bench has managed to address some of these challenges, especially through making use of lay workers and providing a system for them of peer and nurse-led supervision, with an available step up to specialist care which has been used in less than 10% of cases screening positive for CMD. An emphasis on local concepts and terms helped to reduce stigma of mental disorders. The local knowledge of the lay workers facilitated linkage with two local income-generating projects (peanut butter making; recycling) for those in most financial need.
Our decision to use problem-solving therapy was anchored in earlier evidence that kufungisisa and common mental disorders were associated with everyday social and health problems [ 16 , 24 ], and that the community trusted the lay health workers to aid them in resolving these problems using culturally accepted methods, which sometimes included prayer. This is consistent with the traditionally accepted rationale for using problem-solving therapy [ 19 ]. We found that those who used a greater number of sessions benefited more. Thus in future work it will be important to optimise adherence to the intervention and to follow-up clients. Given the value found in Western settings of written materials for clients in low-intensity psychological treatments, we wish to develop these for clients in Zimbabwe, with the aim of increasing the efficacy of the therapy. We will also add training in more collaborative structured approaches to activity scheduling for clients who remain depressed despite problem-solving therapy.
Of the 320 participants in this pilot, just over half had presented with an HIV-related problem. There is need to evaluate whether treatment for depression might improve physical health outcomes such as medication adherence in those who have depression co-morbid with physical illness [ 25 ].
With the large treatment gap that currently exists in low and middle income countries for mental health care, lay workers may be able to play a pivotal role [ 26 ]. In Zimbabwe, earlier work has shown the feasibility of using lay workers to prevent mother to child transmission of HIV, and to screen for psychological morbidity [ 5 , 27 , 28 ]. While there is evidence supporting the effectiveness of task-shifting in HIV [ 29 ], immunization, malaria prevention, and management of upper respiratory infections [ 30 ], ours is an important study given the dearth of evidence on lay workers addressing depression and common mental health problems in Africa.
Limitations of the study include the short follow-up period of 6 weeks. Also, the observed drop in SSQ score after six sessions of problem-solving therapy was not controlled for potential confounding factors such as socio-economic position [ 31 ]. The fundamental limitation to this study is the absence of a comparison group receiving 'usual care' or a placebo intervention, if one could be found. Furthermore, the lay workers were not observed during the course of their work and what they did in practice could have differed from their training. The low level of attrition among the participants is unusual; however, this could be attributed to the short follow up period, the close proximity of participants to the local study area, and the ability of the lay workers and research nurse to physically follow up participants in the community, and is consistent with high follow-up rates found in previous research in Harare [ 20 ]. The City of Harare Health Department continued the Friendship Bench after the pilot. In the 14 months from January 2008 to February 2009, 2348 clients had visited the Friendship Bench with 973 having received the problem-solving intervention. In view of this it is imperative to rigorously test this intervention.
We have found preliminary evidence that lay primary health care workers can deliver locally adapted problem-solving therapy in Harare, Zimbabwe and that this can be associated with a meaningful reduction in symptoms of depression and common mental disorders. The problem solving therapy was integrated into the routine work load of the community based lay workers whose roles include supporting people living with HIV and carrying out health promotion activities. There is need to carry out appropriately powered randomised controlled trials to test if this task-shifting mental health intervention is effective compared to usual care in reducing psychological symptoms and also in improving physical health outcomes in those who have depression co-morbid with physical illness.
No external funding
Bolton P, et al: Group Interpersonal Psychotherapy for Depression in Rural Uganda: A Randomized Controlled Trial. Journal of the American Medical Association. 2003, 289 (23): 3117-10.1001/jama.289.23.3117.
Article PubMed Google Scholar
Saxena S, et al: Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007, 370 (9590): 878-89. 10.1016/S0140-6736(07)61239-2.
Abas MA, Broadhead JC: Depression and anxiety among women in an urban setting in Zimbabwe. Psychological Medicine. 1997, 27: 59-10.1017/S0033291796004163.
Article CAS PubMed Google Scholar
Patel V, et al: The Shona Symptom Questionnaire: the development of an indigenous measure of common mental disorders in Harare. Acta Psychiatrica Scandinavica. 1997, 95 (6): 469-10.1111/j.1600-0447.1997.tb10134.x.
Stranix-Chibanda L, et al: Screening for psychological morbidity in HIV-infected and HIV-uninfected pregnant women using community counselors in Zimbabwe. Journal of the International Association of Physicians in AIDS Care. 2005, 4 (4): 83-8. 10.1177/1545109706286555.
Patel V, et al: The explanatory models and phenomenology of common mental disorders in primary care in Harare. Psychological Medicine. 1995, 25: 1191-10.1017/S003329170003316X.
Lancet Global Mental Health Group, et al: Scale up services for mental disorders: a call for action. Lancet. 2007, 370 (9594): 1241-52.
Article Google Scholar
Hyman S, et al: Mental Disorders. Disease control priorities in Developing Countries). 2006, New York: Oxford University Press, 605-626.
Google Scholar
Araya R, et al: Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet. 2003, 361 (9362): 995-1000. 10.1016/S0140-6736(03)12825-5.
Araya R, et al: Cost-effectiveness of a primary care treatment program for depression in low-income women in Santiago, Chile. American Journal of Psychiatry. 2006, 163 (8): 1379-87. 10.1176/appi.ajp.163.8.1379.
Richards DA, et al: Improving access to psychological therapies: phase IV prospective cohort study. British Journal of Clinical Psychology. 2009, 48 (Pt 4): 377-96.
Cuijpers P, et al: Problem Solving Therapies For Depression: A meta-analysis. European Psychiatry. 2007, 22 (1): 9-15. 10.1016/j.eurpsy.2006.11.001.
Malouff JM, et al: The efficacy of problem solving therapy in reducing mental and physical health problems: A meta-analysis. Clinical Psychology Review. 2007, 27 (1): 46-57. 10.1016/j.cpr.2005.12.005.
Abas M, et al: Primary care services for depression in Harare, Zimbabwe. Harvard Review of Psychiatry. 2003, 11 (3): 157-10.1080/10673220303952.
Tibaijuka AK: Report of the Fact-Finding Mission to Zimbabwe to assess the Scope and Impact of Operation Murambatsvina by the UN Special Envoy on Human Settlements Issues In Zimbabwe. UN Habitat. 2005
Abas M, et al: Defeating depression in the developing world: a Zimbabwean model. British Journal of Psychiatry. 1994, 164 (3): 293-10.1192/bjp.164.3.293.
Amani Trust: The Chiweshe Nurse-Counsellor Programme: Trainer's Manual (revised). Harare. 1994
Broadhead J, Abas M: Life events, difficulties and depression among women in an urban setting in Zimbabwe. Psychological Medicine. 1998, 28: 29-10.1017/S0033291797005618.
Mynors-Wallis L: Problem-solving treatment in general psychiatric practice. Advances in psychiatric treatment. 2001, 417-425.
Patel V, et al: Outcome of common mental disorders in Harare, Zimbabwe. British Journal of Psychiatry. 1998, 157: 53-57.
Mazzucchelli T, et al: Behavioral Activation Treatments for Depression in Adults: A Meta-analysis and Review. Clinical Psychology: Science and Practice. 16 (4): 383-411.
Townsend M, et al: Systematic Review of Clinical Trials Examining the Effects of Religion on Health. Southern Medical Journal. 2002, 95 (12): 142929-
Abas M, et al: Common mental disorders and primary health care: Current practice in low-income countries. Harvard Review of Psychiatry. 2003, 11 (3): 166-10.1080/10673220303954.
Patel V, et al: Women, poverty and common mental disorders in four restructuring societies. Social Science & Medicine. 1999, 49 (11): 1461-10.1016/S0277-9536(99)00208-7.
Article CAS Google Scholar
Sikkema K, et al: Mental Health Treatment to Reduce HIV transmission Risk Behaviour: A Positive Prevention Model. Aids and Behaviour. 2010, 14 (2): 252-10.1007/s10461-009-9650-y.
Patel V, et al: Improving the outcomes of primary care attenders with common mental disorders in developing countries: a cluster randomized controlled trial of a collaborative stepped care intervention in Goa, India. Trials. 2008, 9 (1): 4-10.1186/1745-6215-9-4.
Article PubMed PubMed Central Google Scholar
Shetty A, et al: The feasibility of preventing mother-to-child transmission of HIV using peer counselors in Zimbabwe. AIDS Research and Therapy. 2008, 5 (1): 17-10.1186/1742-6405-5-17.
Chibanda D, et al: Validation of the Edinburgh Postnatal Depression Scale among women in a high HIV prevalence area in urban Zimbabwe. Archives of Women's Mental Health. 2009
Zachariah N, et al: Task shifting in HIV/AIDS: opportunities, challenges and proposed actions for sub-Saharan Africa Royal Society of Tropical Medicine and Hygiene. 2009, 103: 549-558.
Lewin S, et al: Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database of Systematic Reviews. 2009, 3
Abas MA, et al: Socioeconomic Deprivation and Extended hospitalization in severe mental disorder; A two year follow-up study. Psychiatric Services. 2008, 59 (3): 322-325. 10.1176/appi.ps.59.3.322.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/11/828/prepub
Download references
Acknowledgements
We thank Dr. F Lovemore Director of the Counselling Services Unit (CSU), and Dr. P Chonzi and Dr S Mungofa, Directors of The City of Harare Health Department, Harare hospital psychiatric unit and the Mbare community; Shirly Tshimanga (ST), nursing staff at the three clinics, Church groups, Local police, Schools, NGO's and the health promoters for their continued support of the Friendship Bench. Written consent was provided by the lay health workers for the photograph shown in Figure 1 .
Author information
Authors and affiliations.
Department of Psychiatry, University of Zimbabwe, Harare, Zimbabwe
Dixon Chibanda & Lazarus Kajawu
Counselling Services Unit, Harare, Zimbabwe
Petra Mesu & Lazarus Kajawu
Centre for Sexual Health and HIV Research, University College London, London, UK
Frances Cowan
Department of Community Medicine, University of Zimbabwe, Harare, Zimbabwe
School of Social and Community Medicine, Bristol, UK
Ricardo Araya
King's College London, Institute of Psychiatry, London, UK
Melanie A Abas
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Dixon Chibanda .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
DC was responsible for study design, data collection, writing manuscript and analysis of the data. PM and LK responsible for study design and review of second draft. FC reviewed second draft. RA assisted with analysing data and editing manuscripts.
MA developed Multiple Symptoms Card, made comments on first draft of manuscript, responsible for second draft of manuscript, contributed to revisions following referees comments and to writing of final draft. All authors read and approved the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Chibanda, D., Mesu, P., Kajawu, L. et al. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health 11 , 828 (2011). https://doi.org/10.1186/1471-2458-11-828
Download citation
Received : 06 June 2010
Accepted : 26 October 2011
Published : 26 October 2011
DOI : https://doi.org/10.1186/1471-2458-11-828
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Primary Health Care
- Common Mental Disorder
- Common Mental Health Problem
- Primary Mental Health Care
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
depression.org.nz
Start the conversation, reaching out can be hard, but it is worth it..

Is it depression or anxiety?
Understanding mental health, he āhuatanga taumaha.
Learn about mental wellbeing.

Mahia i runga i te rangimārie me te ngākau māhaki
With a peaceful mind and respectful heart, we will always get the best results.
Hear from others
You’re not alone..
Listen to the stories of many in Aotearoa who've walked this path.

Seeking support
Poutokomanawa.
Find out about the people and services that are there to support you.

Staying well
Explore ways to look after yourself and your whānau.

Welcome to depression.org.nz, lovingly managed by the dedicated team at Te Whatu Ora – Health Promotion.
We have a number of options available free and 24/7.
Alo i ou faiva, give us strength as we embark on a journey that maps out our aspirations in life..
Samoan blessing
No data? No worries
This website is available through the zero data initiative, so it won't use up any data on a mobile device.
This website is lovingly managed by the dedicated team at Te Whatu Ora | Health Promotion. We've collaborated with those who've bravely navigated life's challenges, skilled health practitioners and community leaders to craft this website.
We're here to offer understanding, validation and practical advice for those navigating depression and anxiety. Our mission is to lessen the impact of these challenges on New Zealanders' lives by promoting early recognition, encouraging help seeking and fostering supportive communities.
- depression.org.nz privacy policy
- . Copyright
- . Accessibility
- . Disclaimer

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Understanding the Link Between Chronic Disease and Depression
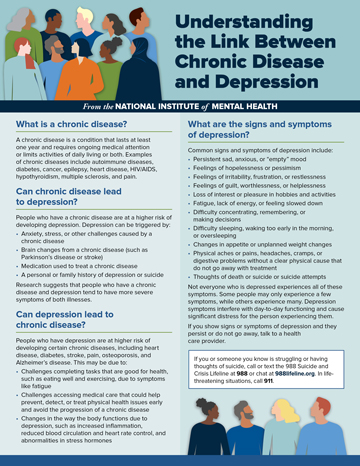
- Download PDF
What is a chronic disease?
A chronic disease is a condition that lasts at least one year and requires ongoing medical attention or limits activities of daily living or both. Examples of chronic diseases include autoimmune diseases, diabetes, cancer, epilepsy, heart disease, HIV/AIDS, hypothyroidism, multiple sclerosis, and pain.
Can chronic disease lead to depression?
People who have a chronic disease are at a higher risk of developing depression. Depression can be triggered by:
- Anxiety, stress, or other challenges caused by a chronic disease
- Brain changes from a chronic disease (such as Parkinson’s disease or stroke)
- Medication used to treat a chronic disease
- A personal or family history of depression or suicide
Research suggests that people who have a chronic disease and depression tend to have more severe symptoms of both illnesses.
Can depression lead to chronic disease?
People who have depression are at higher risk of developing certain chronic diseases, including heart disease, diabetes, stroke, pain, osteoporosis, and Alzheimer’s disease. This may be due to:
- Challenges completing tasks that are good for health, such as eating well and exercising, due to symptoms like fatigue
- Challenges accessing medical care that could help prevent, detect, or treat physical health issues early and avoid the progression of a chronic disease
- Changes in the way the body functions due to depression, such as increased inflammation, reduced blood circulation and heart rate control, and abnormalities in stress hormones
What are the signs and symptoms of depression?
Common signs and symptoms of depression include:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness or pessimism
- Feelings of irritability, frustration‚ or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Fatigue, lack of energy, or feeling slowed down
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking too early in the morning, or oversleeping
- Changes in appetite or unplanned weight changes
- Physical aches or pains, headaches, cramps, or digestive problems without a clear physical cause that do not go away with treatment
- Thoughts of death or suicide or suicide attempts
Not everyone who is depressed experiences all of these symptoms. Some people may only experience a few symptoms, while others experience many. Depression symptoms interfere with day-to-day functioning and cause significant distress for the person experiencing them.
If you show signs or symptoms of depression and they persist or do not go away, talk to a health care provider.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911.
How is depression treated?
Depression is treatable—even if you have a chronic disease.
Depression treatment typically involves psychotherapy (in person or virtual), medication, or both.
A health care provider can help you choose the right treatment plan based on your needs, preferences, and existing medical conditions. Tell the provider about the medications you take and treatments you undergo to avoid multiple medications interfering with one another.
If you cannot or do not wish to take antidepressant medication, other evidence-based treatments are available, including psychotherapy, brain stimulation therapy, and light therapy.
You may have to try a few treatments to find the best one for you. With treatment, you can feel better. Learn more about treatments for depression .
Research suggests that a “collaborative care approach” can improve the overall health of people with depression. In this approach, primary care providers, care managers, and psychiatric consultants work together to provide mental and physical health care at the same location. Collaborative care is not yet available in all primary care offices or clinics—ask your health care provider if it’s an option for you.
How can I find help?
If you have concerns about your mental health, talk to a primary care provider. They can refer you to a qualified mental health professional, such as a psychologist, psychiatrist, or clinical social worker, who can help you figure out the next steps. Find tips for talking with a health care provider about your mental health.
You can learn more about getting help on the NIMH website. You can also learn about finding support and locating mental health services in your area on the Substance Abuse and Mental Health Services Administration (SAMHSA) website.
What are clinical trials and why are they important?
Clinical trials are research studies that look at ways to prevent, detect, or treat diseases and conditions. These studies help show whether a treatment is safe and effective in people. Some people join clinical trials to help doctors and researchers learn more about a disease and improve health care. Other people, such as those with health conditions, join to try treatments that aren’t widely available.
NIMH supports clinical trials across the United States. Talk to a health care provider about clinical trials and whether one is right for you. Learn more about participating in clinical trials .
The information in this publication is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health NIH Publication No. 24-MH-8015 Revised 2024

COMMENTS
Problem-solving therapy is a short-term treatment used to help people who are experiencing depression, stress, PTSD, self-harm, suicidal ideation, and other mental health problems develop the tools they need to deal with challenges. This approach teaches people to identify problems, generate solutions, and implement those solutions.
Problem-Solving Therapy for Depression. 1998 EST Status: Strong Research Support Strong: Support from two well-designed studies conducted by independent investigators. Modest: Support from one well-designed study or several adequately designed studies. Controversial: Conflicting results, or claims regarding mechanisms are unsupported.
Problem-solving therapy (PST) is an intervention with cognitive and behavioral influences used to assist individuals in managing life problems. Therapists help clients learn effective skills to address their issues directly and make positive changes. PST is used in various settings to address mental health concerns such as depression, anxiety, and more.
Problem-Solving Therapy (PST) PST is about strengthening a person's ability to cope with stressful events by enhancing problem-solving skills. Several studies support the effectiveness of problem-solving therapy for people with depression, depressive disorders, and other mental health conditions.
PST. Holding that difficulties with problem solving make people more susceptible to depression, PST is a nonpharmacological, competence-based intervention that involves a step-by-step approach to constructive problem solving. 19,20 Developed from cognitive-behavioral-therapy, PST is a short-term psychotherapy approach delivered individually or in group settings.
Problem-Solving Therapy (PST) is a cognitive-behavioral intervention that focuses on training in adaptive problem-solving attitudes and skills. The purpose of this paper was to conduct a meta-analysis of controlled outcome studies on efficacy of PST for reducing depressive symptomatology. Based on results involving 21 independent samples, PST ...
There is good evidence to support the use of problem-solving in treatment of patients with depression, emotional disorders, and after episodes of deliberate self-harm. Problem-solving has been developed as a brief, feasible, psychological treatment that can be delivered by non-specialists.
Problem-solving therapy (PST) In some cases, depression can cause people to view problems as threats or believe they're incapable of solving the problem. In PST, your therapist may help you:
Her current areas of interest include the treatment of depression in medical patients, the integration of cognitive and behavioral therapies with patients' spiritual beliefs and practices, interventions directed toward stress, coping, and health, and cognitive behavior therapy and problem-solving therapy for individuals with personality disorders.
One of the interventions that has been tested as a treatment of adult depression in a considerable number of randomized trials is problem-solving therapy (PST). PST was developed in the 1970s as one of the first treatments of depression Reference D'zurilla and Goldfried [21] , and was first tested in the 1980s [ Reference Nezu 22 , Reference ...
The effortful-automatic perspective has implications for understanding the nature of the clinical features of major depressions. The aim of this study was to investigate the influence of problem solving therapy (PST) on effortful cognition in major depression (MD). Methods: The participants included an antidepressant treatment (AT) group ( n ...
This review concludes that problem-solving therapy (PST) combined with antidepressant treatment is associated with more favourable outcomes than PST alone for the treatment of non-institutionalised adults with depression. Overall, given the differences between studies, the methodological flaws in some studies and the potential for publication bias, the authors' findings should be interpreted ...
Problem-solving therapy (PST) is an evidence-based psychotherapy for depression, with particularly robust evidence for use among older adults. It is based on the premise that depression is maintained by ineffective problem-solving and resultant poor coping, low self-efficacy, and negative emotions. Problem-solving therapy aims to reduce ...
This book presents a pluralistic model of depression that utilizes a problem-solving framework. Adoption of such a model provides a heuristic metaphor that describes how various current cognitive-behavioral theories of depression interact with each other. Research supportive of the problem-solving model will be described throughout. This book was written to facilitate empirical inquiries by ...
Background: Problem-solving therapy (PST) is one of the best examined types of psychotherapy for adult depression. No recent meta-analysis has examined the effects of PST compared to control groups or to other treatments. We wanted to verify whether PST is effective, whether effects are comparable to those of other treatments, and whether we could identify the possible sources of high ...
We have included three of our favorite books on the subject of Problem-Solving Therapy below. 1. Problem-Solving Therapy: A Treatment Manual - Arthur Nezu, Christine Maguth Nezu, and Thomas D'Zurilla. This is an incredibly valuable book for anyone wishing to understand the principles and practice behind PST.
Problem-solving therapy (To learn more about the above psychological treatments for depression, see my article here .) Sadly, despite the benefits of medications and psychotherapy, there are ...
Problem-Solving Therapy (PST) is a brief, psychosocial treatment for patients experiencing depression and distress related to inefficient problem-solving skills. The PST model instructs patients on problem identification, efficient problem solving, and managing associated depressive symptoms. PST was originally developed in
Problem-Solving Therapy for Depression: Theory, Research and Clinical Guidelines. By Arthur M. Nezu, Christine M. Nezu and Michael G. Perri. Chichester: John Wiley. 1989. 274 pp. £19.15. - Volume 155 Issue 5
For example, problem solving is part and parcel of many psychotherapies for depression, including cognitive behavioural therapy (CBT), interpersonal psychotherapy (IPT), family therapy, and dialectical behaviour therapy (DBT). Problem solving therapy (PST) is also a therapeutic approach in its own right with roots in Social Learning Theory that ...
Purpose: In the past decades, the effects of problem-solving therapy (PST) for depression have been examined in several randomized controlled studies. However, until now no meta-analysis has tried to integrate the results of these studies. Methods: We conducted a systematic literature search and identified 13 randomized studies examining the effects of PST, with a total of 1133 subjects.
There is limited evidence that interventions for depression and other common mental disorders (CMD) can be integrated sustainably into primary health care in Africa. We aimed to pilot a low-cost multi-component 'Friendship Bench Intervention' for CMD, locally adapted from problem-solving therapy and delivered by trained and supervised female lay workers to learn if was feasible and possibly ...
Problem-Solving Therapy (PST) PST is a therapy for Veterans who are experiencing depression or suicidal thoughts. PST can help you recover from the effects of experiencing difficult situations and learn skills for coping with challenging life circumstances and chronic daily stressors.
We're here to offer understanding, validation and practical advice for those navigating depression and anxiety. Our mission is to lessen the impact of these challenges on New Zealanders' lives by promoting early recognition, encouraging help seeking and fostering supportive communities.
Depression treatment typically involves psychotherapy (in person or virtual), medication, or both. A health care provider can help you choose the right treatment plan based on your needs, preferences, and existing medical conditions. Tell the provider about the medications you take and treatments you undergo to avoid multiple medications ...