Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches


free template
97 templates
32 templates
cell biology
45 templates

welcome back to school
110 templates
11 templates
sunday school
65 templates
Diabetes Presentation templates
Here at slidesgo, we would like to help you raise awareness about diabetes, a metabolic disorder related to insulin and the levels of glucose in our blood. with these google slides & powerpoint templates, you can make sure that the audience will pay attention to your speech, as these slides will keep them focused on the screen and your explanations..
It seems that you like this template!
Register for free and start downloading now
Diabetes infographics.
Information on health issues requires pedagogical resources to make it understandable to others. At Slidesgo we have created this diabetes infographic template so that you can easily and entertainingly report on this disease. It contains numerous icons and illustrations to make the data more visual and easier to remember. With...

World Diabetes Day
Diabetes is a serious illness that affects millions of people all around the world, and making proper treatment, care and information accessible to everyone who needs it is an unresolved issue that needs more awareness. For reasons like these, the United Nations decided to establish November 14th as the World...

Type 2 Diabetes Breakthrough
Type 2 diabetes is a metabolic disorder with a high prevalence in the world. Hundreds of millions of people suffer from it every year. Basically, a person cannot produce enough insulin, which can cause very severe consequences. Are there news on the treatment of type 2 diabetes? Waste no time...

Premium template
Unlock this template and gain unlimited access
Diabetes Devices and Technology Breakthrough
This modern and cool template is the perfect way to showcase the amazing breakthroughs in diabetes technologies and devices. With this template, you can easily present the latest developments to help treat and control diabetes. It features modern visuals and graphics that provide insight into the technology, as well as...

Diabetes Breakthrough: Insulin Increase
This is a modern template full of illustrations and resources that gives medical presentations a visual and creative touch. This design focuses on diabetes: a medical issue that affects the lives of millions of people. If you have investigated on this and have come up with a new treatment, these...

Diabetic Mastopathy Clinical Case
Download the Diabetic Mastopathy Clinical Case presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...

Gestational Diabetes
Gestational diabetes is diabetes that first appears during pregnancy. It usually occurs in the middle of the gestation period and it is necessary to take care of it so that it does not cause problems. For this, information is key, so we have created this beautiful pink template, with creative...

Diabetes Mellitus Breakthrough
Diabetes mellitus refers to a group of diseases that affects the way the body uses blood glucose. Many people in the world suffer from this disease, and we are sure that your breakthrough will give a new perspective to its diagnosis and treatment. Present it with this complete and impressive...

World Diabetes Day Infographics
Slidesgo is aware of how healthcare professionals love to have extra help when sharing information about diseases, treatments or breakthroughs. Today, we're releasing a series of infographic designs for presentations about diabetes, a serious illness that affects millions of people. Check them out! The main color used is blue, a...

Kidney Diseases: Diabetic Nephropathy
Download the Kidney Diseases: Diabetic Nephropathy presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking...

Download the "Gestational Diabetes" presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking medical attention....

Treatment of Hypoglycemia Breakthrough
When the glucose levels in our blood drop below normal, our body can experience symptoms such as shakiness, confusion, sweating, and fatigue. A more correct name for this condition is hypoglycemia, but there's treatment (usually, ingesting sugar and carbohydrates), but perhaps there's more to it. Any new breakthrough in this...

Labor Induction for Gestational Diabetes Breakthrough
Download the Labor Induction for Gestational Diabetes Breakthrough presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news. Should...

Type 2 Diabetes Disease
Type 2 diabetes is a chronic condition that affects the way the body processes glucose. With this disease, the patient's body does not produce enough insulin or is resistant to it. Share your research on this important disease using this modern and minimalist template designed in pastel colors, with which...

Diabetes Education Center
Running a medical center specialized on diabetes involves lots of organization and management. What is the admission procedure? How are patients going to be allocated? What fun/free time activities do you offer? That’s an important question to think about, because offering your patients activities to disconnect can improve their mental...

Happy World Diabetes Day!
Celebrate World Diabetes Day in style with our fully editable Google Slides and PowerPoint template. Complete with illuminating light green design and vivid photographs, it provides a perfect platform to give an informative presentation about diabetes, its varied types, and summarize significant research. It also offers a fantastic opportunity to...

Gestational Diabetes Breakthrough
Download the Gestational Diabetes Breakthrough presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news. Should there be a...

Diabetes Mellitus Disease
Diabetes mellitus refers to a group of diseases that affects the way the body uses blood glucose. Glucose is vital for health, as it is an important source of energy for the cells that make up muscles and tissues. Understanding a disease thoroughly is the first step to being able...
- Page 1 of 2
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Encore Presentation, The National Diabetes Prevention Program — Changing Lifestyles to Prevent Type 2 Diabetes
Originally presented on Tuesday, November 13, 2018 . Encore presentation on Tuesday, March 17, 2020 .
Diabetes is a serious public health problem. About 34 million Americans have diabetes, and more than 88 million American adults have prediabetes. People with prediabetes have blood sugar levels that are higher than normal, but not high enough to be diagnosed with type 2 diabetes. They are at risk for type 2 diabetes, heart attack and stroke, but lifestyle changes, such as losing weight and increasing physical activity, can reduce their risk and may even prevent the onset of type 2 diabetes.
Learn how participating in the CDC-led National Diabetes Prevention Program lifestyle change program can help prevent or delay type 2 diabetes in those at high risk.

Dr. John Iskander & Dr. Ann Albright discuss how participating in the CDC-led National Diabetes Prevention Program can help prevent or delay type 2 diabetes in those at high risk.

The National Diabetes Prevention Program — Changing Lifestyles to Prevent Type 2 Diabetes
Drs. Phoebe Thorpe and Ann Albright discuss the serious public health problem of diabetes and the CDC-led National Diabetes Prevention Program .
Get notified about the latest updates from Public Health Grand Rounds right in your inbox by setting up an alert today!
Get notified about the latest updates from Public Health Grand Rounds right in your inbox by setting up an alert today! Sign Up
- Presentation Slide Deck [3.9MB, 67 Pages, HTML]
- Could You Have Prediabetes? Take the Risk Test.

CDC Course Code: PHGR10 CPE UAN: JA4008229-0000-20-070-H04-P
For more information, see Grand Rounds Continuing Education.
ALS is a rapidly progressive, fatal neurological disease. Researchers don’t know what causes ALS and there is no cure. The National ALS Registry was created in 2010 to help scientists learn who gets ALS and what causes it. Learn about research, drug development, and patient care options and the role of the ALS Registry.

The risk factors for cancer are many and varied. Inherited genetic mutations play a major role in 5 to 10 % of all cancers. When genetic mutations are identified early, patients are able to work with their healthcare providers. Find out how public health agencies are evolving in the rapidly growing field of genomics.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Collections
Free Diabetes Presentation Templates
Struggling with boring diabetes presentations download free diabetes powerpoint templates and google slides themes that are easy to use and understand. bright colors, creative visuals, and helpful infographics - make your message clear spread awareness about diabetes mellitus, including causes, symptoms, diets, etc. the best choice for doctors.

- Diverse themes: Explore slides dedicated to diabetic ketoacidosis, case studies, diet plans, and even captivating backgrounds for your chosen topic.
- World Diabetes Day: Celebrate this special day with slides that everyone will understand! It will help you raise awareness and make people want to learn more about keeping their sugar in check.
- Let creativity flow: Infographics, multicolor palettes, and a variety of layouts give your presentation a unique and impactful edge.
- Customization: All slides are 100% editable, allowing you to tailor them to your specific needs and add your own touch.
- Multiple formats: Choose from 4:3 or 16:9 aspect ratios, portrait or landscape orientations, and find slides that work seamlessly with any presentation platform.
- Free options to explore: A collection of diabetes PPT presentation free downloads available to let you experience the quality before investing further.
- Doctors, nurses, and teachers: Explain things clearly to patients, friends, and everyone else.
- People who spread the word about diabetes: Teach people how to stay healthy and avoid problems with sugar.
- People living with diabetes: Share your story and help others, or fight for better care with powerful pictures. It will help to share your experiences and make a difference!
- Conferences and workshops: Deliver impactful presentations at medical gatherings, community events, and educational seminars.
- Patient education sessions: Use clear visuals to explain complex topics to patients and families in an accessible and engaging way.
- Awareness campaigns: Create presentations that raise awareness about diabetes , its impact, and steps for prevention and management.
- Online presentations and webinars: Share your knowledge with a wider audience through online platforms using visually compelling slides.
We're here to help you!
What types of diabetes presentation templates are available.
We offer a variety of templates for different topics, including awareness campaigns, patient education, research presentations, and more.
Do I have to be good at design to use these templates?
Not at all! Our templates are made for everyone, even if you're just starting. Just put in your content and change the look with a few clicks – it's that easy!
Are the templates free to download?
Yes, we offer a collection of free slides to download and use.
Can I edit the templates after downloading them?
Yes, you can fully customize the templates with your own content, images, and colors. You can edit them from PowerPoint or Google Slides.
Can I use these templates for commercial purposes?
Yes, you can use our templates for personal and commercial use.
Can I share your templates with others?
Yes, you can share our templates with your friends, colleagues, and anyone else who needs to create a diabetes presentation.
How can I get help if I have trouble using the templates?
We're happy to help! Contact our 24/7 customer support team.
Do you offer any premium diabetes presentation templates?
Yes, we also offer a selection of premium templates.
Diabetes Presentation Template
Customize the Diabetes presentation template for PowerPoint & Google Slides to present your diabetes awareness presentations comprehensively. Diabetes is a chronic disease that alters the normal glucose level of the body and can lead to various complications. The major cause of diabetes is the decreased production of insulin. The prevalence of this disease is more than ever, and it’s crucial to understand the causes and risk factors associated with diabetes. We have specifically designed this interactive PowerPoint template for social workers, healthcare experts, and doctors. So that they can create useful presentations for the audience while accomplishing diabetes awareness campaigns. November is National Diabetes Month, and it is important to educate the public about diabetes.
Our Diabetes presentation template can also be used in executive sessions to present support for diabetes funding, research, and awareness. The title slide contains the diagram of a glucometer connected with a blue diabetes support ribbon. The further slides contain human illustrations with a diagram of the glucometer, pricker, and test strips, which can help the audience understand safe sugar levels and risky conditions. Moreover, in the following slide, a weighing balance shows that the significance of fruits is higher than fast food. Some other slides are:
- Symptoms slide to describe the signs of the poor health condition
- Horizontal timeline slide with editable textboxes to demonstrate the history of diabetes and its futuristic details.
- Data-driven charts slide and column chart slides to mention the relevant data about the prevalence and occurrence of diabetes patients and the increasing number of patients.
This creative diabetes template is compatible with all versions of Microsoft PowerPoint, Google Slides, and Keynote. The users can change the slides’ colors, relevant graphical elements, icons, and theme according to their preferences. So, download this useful PPT template and make amazing presentations in the diabetes month of November. Alternatively, you can download the Diabetes PPT template design with other useful slides that you can use in your presentation on diabetes topics.
You must be logged in to download this file.
Favorite Add to Collection

Subscribe today and get immediate access to download our PowerPoint templates.
Related PowerPoint Templates

Healthcare Market Analysis PowerPoint Template

Volleyball PowerPoint Template
5-Level Swiss Cheese Model PowerPoint Template
Incident Report PowerPoint Template
Dec 20, 2019
2.01k likes | 3.66k Views
Diabetes. Nhung H. Nguyen. Definition:. “A metabolic disease in which the body’s inability to produce any or enough insulin causes elevated levels of glucose in the blood.”. Types of diabetes:. Type 1 Type 2 Gestational diabetes Prediabetes. Type 1 diabetes:.
Share Presentation


Presentation Transcript
Diabetes Nhung H. Nguyen
Definition: • “A metabolic disease in which the body’s inability to produce any or enough insulin causes elevated levels of glucose in the blood.”
Types of diabetes: • Type 1 • Type 2 • Gestational diabetes • Prediabetes
Type 1 diabetes: • Also known as juvenile diabetes • Usually diagnosed in children and young adults • When body’s own immune system destroys the insulin producing cells of the pancreas – beta cells – which produce insulin • Only 5% of people have this disease • Body does not produce insulin • Is not preventable • No primary intervention • Causes? • Predisposition to diabetes – genetics - and something (i.e. weather, virus ... etc ) in environment triggers the disease
Symptoms of Diabetes:
Type 2 diabetes: • Most common form of diabetes – about 90% of cases • Used to be called adult onset, non insulin dependent diabetes • Body produces insulin, but does not use it properly • glucose doesn’t move into cells, they pile up in the bloodstream • sx’s when they do occur are often ignored because they may not seem serious
Risk factors: • Genetics • Family pmHx • Polycystic ovary syndrome • Irregular menses • Race • African Americans, Hispanics and Asians > whites • Age • After age 45, but increases in younger adults and children • Environmental factors • Inactivity • Weight gain
Gestational diabetes mellitus (GDM): • Having diabetes during pregnancy • Family Hx of diabetes, overweight prior to pregnancy? • Having gestational diabetes puts you at risk for diabetes type 2 • Giving birth to a baby >9 lbs also puts you at risk for type 2 • 18 out of every 100 pregnant females will develop GDM
Complications for uncontrolled diabetes:
How to monitor your diabetes:
Preventions: • Type 1: • Not preventable, as of right now. • Studies on ways to possible prevent further destruction of the beta cells • Maintain and control sugar levels, insulin injection • Healthy life style – exercise and diet • Islet transplantation?
Preventions: • Type 2: • Primary: maintain a healthy lifestyle • Secondary: check HgA1c, adjust diet • HgA1c – blood sugar avg over span of 3 months • Measures what % of your Hg is coated with sugar • Nl = 4 % - 5.6%, pre diabetes = 5.7% -6.4% and diabetes = 6.5% + • Tertiary: exercise and eat well • Foot exam?
Preventions: • Gestational diabetes: • Physical activity • Researchers found being physically active before and after their pregnancy reduced their risk of GDM by about 70% or more • Diet • A study showed that each 10 gram increase in fiber a day reduced their risk of GDM by 26%
U.S. Prevalence:
Diabetes and Obesity:
Cost of Diabetes (US):
Global prevalence: http://www.idf.org/atlasmap/atlasmap
Global prevalence:
Prediabetes:
Prediabetes: • Diabetes prevention program • Lifestyle intervention group vs medicated group with Metformin vs placebo group • 3,243 participants were overweight and had prediabetes • Lifestyle intervention reduced diabetes by 58% • Metformin reduced diabetes by 31% • Effective in both sexes ages 25-44 yoa and BMI of 30 + Summary: Type 2 diabetes can be prevented/delayed with activity and diet.
Twin study:
The Future:
Websites: • http://www.idf.org/about-diabetes • global • http://www.diabeteseducator.org/ • http://www.cdc.gov/diabetes/home/ • http://www.diabetes.org/ • U.S.
- More by User
DIABETES Gross Anatomy Endocrine Gland Hormone Blood Target tissues Anatomy of Pancreas Microscopic Pancreas Islet of Langerhans Protein Hormone Control of Hormone Secretion What is Diabetes?
914 views • 25 slides
Diabetes. Prepared by: Nadia jradi Masri , m.D. Definition. A group of metabolic diseases in which a person has high blood sugar because : The body does not produce enough insulin or The receptor cells do not respond to the produced insulin. Pancreas. Diabetes - types.
1.03k views • 26 slides
Diabetes. By: Tanesha Haynes. A disease in which the body does not produce or properly use insulin Insulin is a hormone that is needed to convert sugar, starches, and other food into energy needed for daily life. The causes of Diabetes. A mystery
437 views • 11 slides
DIABETES. Presentation by DR.VIOLET (de Sa) PINTO Lecturer, Department of PSM. Objectives. At the end of the session the student shall have knowledge of : Diabetes - definition, types and problem statement Factors involved in causation
815 views • 23 slides
Diabetes Mellitus. Trastorno metab
1.01k views • 56 slides
Diabetes. Normal Anatomy and Physiology. Pancreas : abdominal organ responsible for exocrine secretion of digestive enzymes into the gut And Endocrine secretion of hormones of glucose control: insulin and glucagon. Pancreas : Exocrine And Endocrine: Islets of Langerhans.
474 views • 37 slides
Diabetes. Diabetes mellitus (DM) is a common syndrome and caused by lack or decreased effectiveness of endogenous insulin Insulin is needed to facilitate entrance of glucose from blood to cells to be used in different metabolic processes.
403 views • 23 slides

*Diabetes*. By: Katie Garnett, Brittany Vereen , Brandon Lacks, & Jason Moorehead. ~Description of Diabetes~.
246 views • 7 slides
Diabetes. How much do you really know? . What is Diabetes. A chronic lifelong illness that effects the major the bodies ability to regulate blood sugar properly. Broken down into two types. Type 1. Type 2. Type 1 Diabetes. Formally known as juvenile diabetes.
340 views • 9 slides
Diabetes. What is it?.
334 views • 7 slides

Diabetes. Practice Nurses SA www.cdprogramdevelopment.com.au [email protected]. Chronic Disease Management Good chronic disease management requires : awareness of your patient demographics, ‘ what’s affecting who? ’
490 views • 15 slides
Mentoring in Medicine Virtual Camp Final project 22 nd August, 2013 By Poojitha Kolluri. DIABETES. Symptoms of Diabetes. Type 1 Excessively thirsty Frequent urination Type 2 – symptoms appear gradually Mild thirst Frequent urination Mild fatigue Blurred vision
302 views • 10 slides
Diabetes. Diabetes Prevalence in U.S., 1994 (CDC). Diabetes Prevalence in U.S., 1995 (CDC). Diabetes Prevalence in U.S., 1996 (CDC). Diabetes Prevalence in U.S., 1997 (CDC). Diabetes Prevalence in U.S., 1998 (CDC). Diabetes Prevalence in U.S., 1999 (CDC).
786 views • 42 slides

Diabetes. Julia von Oettingen, MD. History. Insulin Regimen: □ Twice a day 70/30 Insulin (Mixtard) □ AM breakfast dose_________IU □ PM dinner dose________IU □ Total Daily Dose per kg = ______(total Units per day) ÷ ______ (weight in kg) = ______U/kg/day. Review of blood sugars:
506 views • 18 slides
Diabetes. U.S.-Mexico Border Diabetes Project. Pan American Health Organization U.S. Mexico Border Field Office (915) 845-5950 [email protected]/[email protected]. Diabetes definition.
502 views • 20 slides
Diabetes. “ blood sugar problem”. Definitions. Diabetes. disease in which there is inadequate insulin produced by the body. Glucose. source of energy required by all cells for normal functioning. Insulin. hormone secreted by pancreas - it allows cells to use glucose. Hypoglycemia.
762 views • 24 slides
About Diabetes.Types, Reasons, Causes and prevention.
264 views • 16 slides
Diabetes. By Anthony. What is diabetes. Diabetes is when your body doesn’t make enough insulin. The insulin is a hormone that convert foods and sugar starches into energy for everyday.
154 views • 7 slides
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 20 July 2024
Risk of chronic kidney disease in patients with a hyperglycemic crisis as the initial presentation of type 2 diabetes
- Chun-Ta Huang 1 , 2 ,
- Chih-Hsin Muo 3 ,
- Fung-Chang Sung ORCID: orcid.org/0000-0003-3542-8552 3 , 4 , 5 &
- Pei-Chun Chen 6
Scientific Reports volume 14 , Article number: 16746 ( 2024 ) Cite this article
137 Accesses
Metrics details
- Chronic kidney disease
- Outcomes research
- Type 2 diabetes
Limited data exist on long-term renal outcomes in patients with hyperglycemic crisis (HC) as initial type 2 diabetes presentation. We evaluated the risk of chronic kidney disease (CKD) development in those with concurrent HC at diagnosis. Utilizing Taiwan’s insurance claims from adults newly diagnosed with type 2 diabetes during 2006–2015, we created HC and matched non-HC cohorts. We assessed incident CKD/diabetic kidney disease (DKD) by 2018’s end, calculating the hazard ratio (HR) with the Cox model . Each cohort comprised 13,242 patients. The combined CKD and DKD incidence was two-fold higher in the HC cohort than in the non-HC cohort (56.47 versus 28.49 per 1000 person-years) with an adjusted HR (aHR) of 2.00 (95% confidence interval [CI] 1.91–2.10]). Risk increased from diabetic ketoacidosis (DKA) (aHR:1.69 [95% CI 1.59–1.79]) to hyperglycemic hyperosmolar state (HHS) (aHR:2.47 [95% CI 2.33–2.63]) and further to combined DKA-HHS (aHR:2.60 [95% CI 2.29–2.95]). Subgroup analysis in individuals aged ≥ 40 years revealed a similar trend with slightly reduced incidences and HRs. Patients with HC as their initial type 2 diabetes presentation face a higher CKD risk than do those without HC. Enhanced medical attention and customized interventions are crucial to reduce this risk.
Similar content being viewed by others
Prevalence and Risk Factors of Chronic Kidney Disease among Type 2 Diabetes Patients: A Cross-Sectional Study in Primary Care Practice
Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes
Hypoglycemia risk with inappropriate dosing of glucose-lowering drugs in patients with chronic kidney disease: a retrospective cohort study
Introduction.
Diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS) represent life-threatening hyperglycemic crises (HC) in patients with diabetes 1 . Although commonly seen in patients with preexisting diabetes, up to 20% of cases occur in those newly diagnosed 2 , 3 , 4 . Individuals with HC episodes face higher risks of subsequent morbidity and mortality compared with those without such episodes 5 , 6 , 7 . However, limited research explores the risk of chronic complications in patients experiencing HC during diabetes diagnosis, underscoring the need for further investigation.
Previous studies have reported an increased risk of subsequent stroke 8 , 9 , cardiovascular events 10 , long-term mortality 11 , 12 , and end-stage renal disease 13 in patients with diabetes who have experienced an HC. Nevertheless, these studies overlook the confounding effect of glycemic control on the development of diabetes-related chronic complications. Moreover, type 1 and type 2 diabetes possess distinct pathophysiologies and should not be considered as a single entity; however, only two studies exclusively included patients with type 2 diabetes 8 , 9 , and none were conducted in patients with newly diagnosed diabetes. In contrast, an Italian multicenter cohort study demonstrated that patients with DKA upon type 1 diabetes onset were not at an increased risk of diabetic retinopathy or albuminuria 14 . The reasons behind these conflicting findings and the impact of HC that occurs in patients newly diagnosed with type 2 diabetes remain to be elucidated.
Therefore, in this study, we aimed to examine the risk of developing chronic kidney disease (CKD), one of the major chronic complications of diabetes, in patients experiencing HC upon type 2 diabetes diagnosis. We hypothesized that HC occurring upon type 2 diabetes diagnosis is associated with a higher risk of developing CKD. Our findings could hold significance if this unique initial presentation of type 2 diabetes can be utilized to identify patients at increased risk of developing CKD; moreover, it could facilitate the implementation of preventive interventions to reduce CKD risk in this population.
Data sources
In this study, we utilized Taiwan’s insurance claims data to identify adults newly diagnosed with type 2 diabetes between 2006 and 2015. We used the Taiwan National Health Insurance Research Database (NHIRD), a comprehensive repository established in 1995 that covers over 99% of the nation’s residents 15 , 16 . The NHIRD comprises encrypted records encompassing sociodemographic information, household income, residency, outpatient/inpatient care, and prescribed medications. Diseases in the NHIRD are coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) before 2016 and Tenth Revision (ICD-10-CM). Previous investigations have validated the NHIRD’s accuracy and reliability for population-based studies 17 , 18 .
Design setting and study cohorts
From the NHIRD, we used the ICD-9-CM or ICD-10-CM and Anatomical Therapeutic Chemical Codes (Tables S1 and Table S2 ) to identify newly diagnosed cases with type 2 diabetes (ICD-9-CM codes: 250. X0 or 250. × 2) during the study period (Fig. 1 ). We excluded individuals who were diagnosed with diabetes or using glucose-lowering drugs before the study period, younger than 20 years of age, had a history of kidney disease including benign or malignant neoplasms of the kidney, chronic kidney disease of any cause, glomerulonephritis, nephrotic syndrome, urolithiasis, and congenital renal anomalies, or were deceased at baseline. Individuals with concurrent HC at the time of their type 2 diabetes diagnosis (first-time type 2 diabetes diagnosis appeared with at least one of the following ICD-9-CM codes: 250.10, 250.12, 250.20, or 250.22) were categorized into the HC cohort. The clinical diagnostic criteria for HC were based on previous guidelines 19 , 20 , and our data were based on diagnostic codes from all medical facilities regardless of inpatient/outpatient care or emergency department visits. Regarding individuals without HC, we selected a control (non-HC) cohort with the same sample size frequency matched by diagnosis year and propensity score. The propensity scores were calculated using multivariable logistic regression for each person at baseline, including sex, age, type of residence, enrollment category, monthly income, comorbidities, and use of angiotensin-converting enzyme inhibitors ( ACEis) or angiotensin II receptor blockers (ARBs) . Comorbidities were diseases with at least two outpatient claims or one inpatient claim within 1 year of the index date and included hypertension, heart failure, coronary artery disease, ischemic stroke, transient ischemic attack, peripheral arterial disease, hyperlipidemia, obesity, and malignancy. Variables with a between-group standardized mean difference of < 0.1 were considered well-balanced 21 . Sodium-glucose cotransporter-2 inhibitors were not included due to their unavailability in Taiwan during the enrollment period.
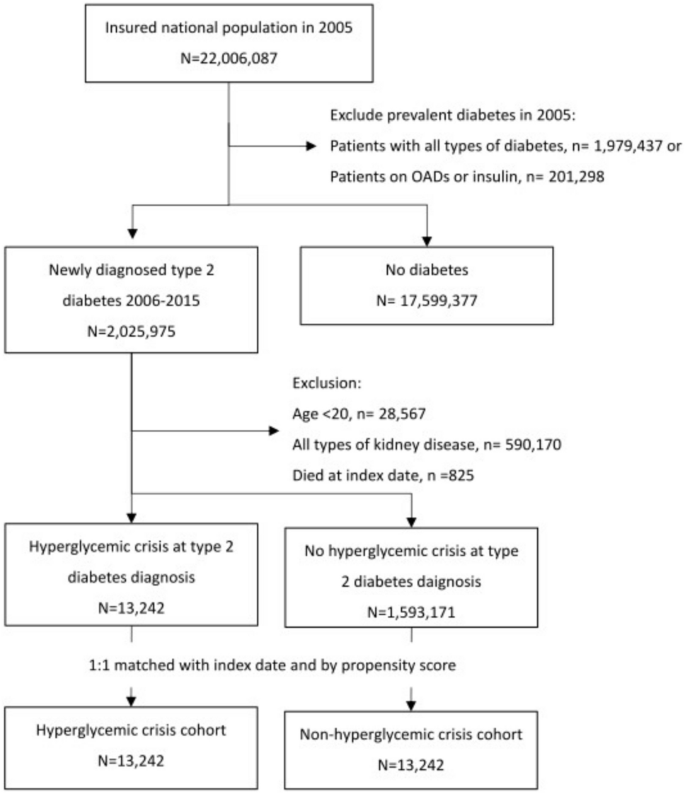
Flow chart showing the establishment of the hyperglycemic crisis cohort and propensity score matched non-hyperglycemic crisis cohort from the National Health Insurance Research Database, Taiwan, 2006–2018. OAD, oral anti-diabetic agent.
The two cohorts were followed up until the end of 2018. Our outcome of interest was the combined incidence of CKD (ICD-9-CM codes: 585–586; ICD-10-CM code: N184–N186, N189–N19) or diabetic kidney disease (DKD) (ICD-9-CM codes: 250.40 or 250.42; ICD-10-CM: E112), or both. In Taiwan, it is generally accepted that CKD is characterized by a decreased glomerular filtration rate of less than 60 mL/min per 1.73 m 2 and/or markers of kidney damage that persist for longer than 3 months. DKD is a clinical diagnosis that refers to those cases with CKD presumed to be caused by diabetes. Clinicians are free to use whichever code is appropriate based on their judgment. Hence, the data of patients with diabetes and CKD may be coded using CKD, DKD, or both. As DKD is within the spectrum of CKD and our aim was to explore the risk of CKD, we used both codes to maximize the probability of capturing our main outcome of interest.
Institutional review board statement
This study was approved by the Institutional Review Board of Mackay Memorial Hospital (approval number: 22MMHIS382e). Our study was performed in accordance with the Declaration of Helsinki and all our methods were carried out under relevant guidelines and regulations. As all personal identifications in the database were encrypted and unidentifiable, the requirement for informed consent from the insured individuals was waived.
Statistical analysis
Baseline characteristics and comorbidities were compared between the HC and non-HC cohorts using Pearson’s χ 2 test for categorical variables and Student’s t -test for continuous variables. The HC cohort comprised three sub-cohorts: patients with DKA (ICD-9-CM codes: 250.10 or 250.12), HHS (ICD-9-CM codes: 250.20 or 250.22), and combined DKA and HHS (DKA-HHS). The cumulative incidence rate of combined CKD and DKD between the HC and non-HC cohorts, as well as between the HC sub-cohorts, was estimated and plotted using the Kaplan–Meier method. Inter-group differences were examined using the log-rank test. Cox proportional hazards regression analysis was used to calculate the crude hazard ratio comparing the HC and non-HC cohorts; moreover, the adjusted hazard ratio (aHR), along with its corresponding 95% confidence interval (CI), was used for the combined occurrence of CKD and DKD. The aHR was estimated after adjusting for age, sex, socioeconomic factors, and significant comorbidities. As patients who died before the event occurred will never be coded with CKD and/or DKD, the competing risk of death was managed using the Fine-Grey analysis model to estimate the sub-distribution hazard ratio (sHR) 22 . To address potential misclassification and pollution bias from claims data, where type 1 diabetes might have been incorrectly recorded as type 2 diabetes, we performed a subgroup analysis to estimate the combined incidence rates of CKD and DKD for individuals aged 40 years and older. We selected this cutoff because the incidence of type 1 diabetes drops significantly after age 40 years and remains relatively low in this age group. This approach helps to minimize the risk of pollution bias in our results 23 . To validate that the incident events were not the result of undiagnosed preexisting CKD or DKD, a supplementary sensitivity analysis was performed by excluding outcomes that occurred within 6 months after the diagnosis of type 2 diabetes. Finally, we conducted a nested case–control analysis to explore the risk factors for CKD or DKD, including DKA, HHS, acute kidney injury, nonsteroidal anti-inflammatory drug use, and ACEi or ARB use. Medication use was stratified based on the prescription length into three categories: no exposure (0 days), 90 days or less, and more than 90 days. Statistical analyses were performed using the Statistical Package for SAS V. 9.4 (SAS Institute, Cary, North Carolina, USA), and a two-sided P -value of less than 0.05 was considered statistically significant.
Ethics-approval and consent to participate
This study was approved by the Institutional Review Board of Mackay Memorial Hospital (approval number: 22MMHIS382e) and informed consent was waived.
Presentation at a meeting
The current study was presented as an e-poster at the IDF 2022 Congress in Lisbon, Portugal, on December 5–8.
Cohort characteristics
There were 13,242 participants in each cohort (Fig. 1 ), and their baseline characteristics are shown in Table 1 . The mean age of the study participants was approximately 54 years (men: 62%). Compared with the non-HC cohort, the HC cohort had a lower income and higher prevalence of malignancy (6.24% vs. 2.99%, respectively); however, they had a lower prevalence of hypertension (32.7% vs. 37.5%, respectively) and hyperlipidemia (13.2% vs. 20.7%, respectively). The two cohorts did not differ in the proportion of patients who received either ACEis or ARBs.
Combined incidence of CKD and DKD
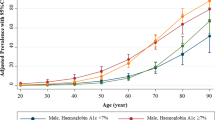
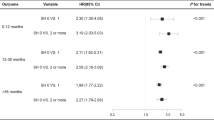
Table 2 depicts the combined incidence of CKD and DKD in the HC cohort, its sub-cohorts, and in the non-HC cohort. The HC cohort comprised mainly patients with DKA (55.1%) and HHS (39.2%), with a few cases of combined DKA-HHS (5.7%). There were 4106 (31%) and 2735 (20.7%) events observed in the HC and non-HC cohorts during median follow-ups of 4.97 years and 7.15 years, respectively. This corresponded to incidence rates of 56.47 and 28.49 per 1000 person-years, respectively. The cumulative incidence of CKD and DKD was significantly greater in the HC cohort than in the non-HC cohort (Fig. 2 A). Within the HC cohort, the cumulative incidence was higher in patients with HHS and combined DKA-HHS than in those with DKA (Fig. 2 B). The aHR among the HC sub-cohorts increased from 1.69 (95% CI 1.59–1.79) for DKA to 2.47 (95% CI 2.33–2.63) for HHS and 2.60 (95% CI 2.29–2.95) for combined DKA-HHS. In the sub-distribution hazard models, the sHRs were attenuated but remained significantly higher in the main HC cohort and its sub-cohorts.

Group comparisons of the Kaplan–Meier estimated cumulative incidence of combined chronic kidney disease and diabetic kidney disease between hyperglycemic crisis (HC) and non-hyperglycemic crisis (non-HC) cohorts ( A ), and among hyperglycemic hyperosmolar state (HHS), diabetic ketoacidosis (DKA), combined DKA-HHS sub-cohorts and non-HC cohorts ( B ), from the National Health Insurance Research Database, Taiwan, 2006–2018.
Subgroup analysis in individuals aged 40 years and older
There were 10,266 (77.5%) and 10,419 (78.7%) individuals aged 40 years and older in the HC and non-HC cohorts, respectively (Table 3 ). This subgroup comprised 5104 (49.7%) individuals with DKA and 4591 (44.7%) with HHS in the HC cohort. A similar increase in the HR between the HC and non-HC cohorts, compatible with the result in our primary analysis, was observed in this age group. The aHR among the HC sub-cohorts also showed a stepwise escalation from 1.62 (95% CI 1.51–1.72) for DKA to 2.33 (95% CI 2.19–2.49) for HHS and 2.59 (95% CI 2.25–2.98) for combined DKA-HHS.
Sensitivity analysis
The sensitivity analysis demonstrated that the patterns of CKD or DKD development 6 months after the diagnosis of type 2 diabetes were consistent with the findings of the primary analysis (Table S3 ).
Nested case–control analyses
The nested case–control analysis showed that the risk of developing CKD or DKD was significantly higher for patients with a history of hyperlipidemia (adjusted odds ratio [aOR] 1.22; 95% CI 1.15–1.30), acute kidney injury (aOR 1.33; 95% CI 1.18–1.50), DKA (aOR 1.56; 95% CI 1.47–1.66), and HHS (aOR 1.75; 95% CI 1.64–1.86). Compared with patients who did not receive ACEis or ARBs, those who had received treatment with ACEis or ARBs also had a higher risk, with an aOR of 1.93 (95% CI 1.75–2.13) for those treated for 90 days or less and an aOR of 1.69 (95% CI 1.57–1.82) for those who were treated for more than 90 days (Table S4 ).
This population-based cohort study revealed a higher risk of incident CKD and/or DKD in patients with HC as their initial presentation of type 2 diabetes than in patients who present type 2 diabetes without HC. This association remained consistent across all HC sub-cohorts and stayed significant in the subgroup analysis for those aged 40 years and older. The risk was higher in patients with HHS and in those with both DKA and HHS than in those with DKA. This association remained robust after excluding cases that appeared within 6 months of diabetes diagnosis. Our nested case–control analysis corroborates that, compared with patients with type 2 diabetes who did not develop CKD or DKD, those who did were more likely to have experienced HC upon diabetes diagnosis.
The surprisingly high proportion of patients having DKA instead of HHS on the initial presentation of their type 2 diabetes in our cohort may raise concerns of pollution bias by the presence of patients with type 1 diabetes. Although there is currently no data reporting the proportion of DKA versus HHS in patients with HC as the initial presentation of type 2 diabetes, we believe that our findings are valid because previous studies have also reported a high percentage of newly diagnosed type 2 diabetes among patients with DKA. In an early study of 141 episodes of DKA in a tertiary referral center in Taiwan, 32 (22.7%) episodes were caused by newly diagnosed diabetes 24 . Twenty-five of the newly diagnosed patients were followed for at least 12 months, and 11 (44%) of them were not using insulin and exhibited metabolic features of type 2 diabetes. A recent study that retrospectively reviewed the medical records of consecutive patients with index DKA in four general hospitals in Qatar showed that 442 (48%) of them had type 2 diabetes 25 . Of the 324 patients with DKA and newly diagnosed diabetes, 176 (54.3%) had type 2 diabetes, and 93 (52.8%) were Asian. We speculate that the excessive DKA cases observed in our study and previous studies may be attributed to ‘ketosis-prone diabetes (KPD)’ 26 . This syndrome is characterized by the acute onset of severe hyperglycemia with ketoacidosis, necessitating hospital admission and treatment. However, it often undergoes spontaneous remission, with patients maintaining long-term insulin independence several weeks after discharge 27 . Initially identified in individuals of African descent and African Americans 28 , KPD is now recognized as a significant clinical entity in Asian populations 27 . Patients with KPD are typically young or middle-aged and predominantly male 29 , consistent with the clinical characteristics of our study population. Another reason we believe that we secured the cases of type 2 diabetes in our study is due to the unique characteristics of the NHIRD. In Taiwan, type 1 diabetes is classified as a catastrophic illness by the National Health Insurance Administration. When a physician diagnoses a patient with such a condition, the patient can apply for a catastrophic illness certificate by submitting the necessary documentation. Upon issuance, this certification is recorded on the patient’s National Health Insurance Card. During the validity period of this certificate, patients are exempt from co-payment of outpatient or inpatient care related to the certified illness 30 . However, this exemption is contingent upon the physician using the correct ICD codes, as is the case with type 1 diabetes. An incorrect ICD coding that misclassifies type 1 diabetes as type 2 diabetes would prevent patients with type 1 diabetes from receiving exemptions for medical expenses, a scenario which is unlikely to occur in real-world practice or in the NHIRD. Moreover, the result of our subgroup analysis for those aged 40 years and older, which comprised nearly 78% of all patients, did not differ from our main findings. As the incidence of type 2 diabetes increases with age in Taiwan, and the incidence of type 1 diabetes over 40 years of age is remarkably low (0.02 per 100,000 population) 23 , the possibility that our findings are biased due to the presence of patients with type 1 diabetes is negligibly low.
Our findings align with those of previous Taiwan NHIRD studies demonstrating the detrimental effects of HC in patients with diabetes 8 , 9 , 10 , 11 , 12 , 13 . The present research adds value to the previous literature in several aspects. First, unlike previous studies that examined diabetes as a single entity 10 , 11 , 12 , 13 , we focused exclusively on type 2 diabetes and examined the individual effects of different types of HC. Given the distinct pathophysiologies underlying DKA and HHS, as well as those underlying type 1 and type 2 diabetes, our study design may ensure a more robust association between HC and CKD. The higher risk of CKD and/or DKD observed in patients with HHS or those with combined DKA-HHS than in patients with isolated DKA also aligns with previous studies reporting worse in-hospital outcomes in patients with combined DKA-HHS than in those with isolated DKA or HHS 31 . Second, HC typically signifies uncontrolled diabetes 32 , which is a well-recognized risk factor for diabetic complications 33 . Studies not adjusting for patients’ glycemic control may confound the impact of HC on long-term outcomes. We minimized such confounding by focusing on patients newly diagnosed with diabetes, where subsequent glycemic control acts as a mediator or effect modifier that requires no adjustment. Third, this pioneering study investigates the impact of HC on patients newly diagnosed with type 2 diabetes without prior kidney disease, offering potential insights for future clinical practice. Given their increased risk of CKD, patients experiencing HC upon type 2 diabetes diagnosis should receive proactive early preventive measures to mitigate such risk.
Several mechanisms may explain our findings. A longitudinal study on type 2 diabetes in Taiwan highlighted that individuals with lower income levels were more likely to have hospitalization-diagnosed diabetes, although it did not report how many of these patients were diagnosed via HC 34 . Patients with type 2 diabetes who are not diagnosed until hospitalization may be less likely to receive early detection screenings or may lack sufficient awareness of diabetes-related symptoms to seek appropriate healthcare 34 . Although the two study groups in our study did not differ in most baseline characteristics after propensity-score matching, individuals in the HC group exhibited significantly lower income levels than those in the non-HC group. Such difference may suggest that our HC group, compared with the non-HC group, included more individuals facing healthcare inequality, potentially resulting in worse renal outcomes. Furthermore, common risk factors for CKD, such as hypertension and hyperlipidemia, often remain undiagnosed among underprivileged individuals 35 . The paradoxically higher risk of CKD despite a lower prevalence of hypertension and hyperlipidemia in the HC group than in the non-HC group may be a result of more undiagnosed rather than healthier cases in the former group. As our propensity score considered only established comorbidities, the true risk difference of CKD at baseline between the two groups may be unbalanced. This could explain the remaining two-fold higher risk of CKD in the HC group, even after adjusting for income level, comorbidities, and other covariates.
From a biological perspective, our finding may be a consequence of initial priming by hyperglycemia, as the onset of diabetes followed by subsequent insults from acute kidney injury (AKI) during HC ultimately leads to persistent nephron damage. Hyperglycemia-induced epigenetic change can lead to progressive and irreversible renal injury, a phenomenon known as the “metabolic memory of DKD” 36 . Following exposure to hyperglycemia, vascular endothelial cells continue to increase oxidative stress and elicit inflammation even after normalization of blood glucose levels 37 . Owing to the slow progression of type 2 diabetes, the exact duration between disease onset and diagnosis is difficult to ascertain. Previous studies have suggested that the interval between the onset and diagnosis of type 2 diabetes is at least 5 years 38 , 39 . Moreover, low income is significantly associated with delayed diagnosis and inadequate diabetes care and management 34 . We speculate that patients experiencing HC upon diabetes diagnosis had a longer duration from diabetes onset to diagnosis compared with those who had diabetes diagnosed without HC. Such a latent period aggravates metabolic memory and leads to an increased risk of CKD. Moreover, AKI is a known risk factor for CKD 40 , 41 , 42 and is common in patients with DKA due to volume depletion 7 , 43 . Despite this, there is a paucity of data reporting the incidence of AKI during HHS. A higher rate of AKI in patients with HHS is expected as patients with HHS are more likely to be dehydrated than patients with DKA. The occurrence of AKI during HC may exacerbate renal damage and increase the risk of CKD. A recent study revealed a higher incidence of AKI in patients with HHS and combined DKA-HHS than in those with DKA 44 , which may also explain the greater risk of CKD in patients with HHS and combined DKA-HHS than in those with DKA in our study. Nevertheless, we cannot exclude the possibility that our findings result from surveillance bias between the two cohorts. As patients experiencing HC upon diabetes diagnosis have more severe disease compared with those without HC at diagnosis, clinicians should provide more vigilant follow-ups for earlier detection of CKD.
This study had some limitations. First, relying solely on claims data may have led to the misclassification of diseases. However, the accuracy and validity of the NHIRD claims data have been demonstrated previously 15 , 17 , 18 , minimizing the impact of misclassification on our results. Second, we could not adjust for covariates unavailable in the NHIRD, including laboratory tests, blood pressure, waist circumference, body mass index, and lifestyle. The potential impact of this missing data remains unassessed. Furthermore, the inherent limitations of the NHIRD also restricted us from determining the severity of DKA and the stage of CKD, which may also have affected our results. Third, in large-sample studies, even minor differences can achieve statistical significance, warranting cautious interpretation. Because we established our study cohorts using a propensity score-matched design and conducted the analysis using stratification, we believe that the observed risk differences between the two cohorts were not a result of overpowering. Finally, the generalizability of our findings may be limited to populations with similar characteristics.
Conclusions
Patients who experience HC upon type 2 diabetes diagnosis have a higher risk of developing CKD compared with those without HC at diagnosis. As type 2 diabetes and end-stage renal disease are highly prevalent in Taiwan, proactive preventive measures are imperative to mitigate risks in this vulnerable population. These interventions should include early introduction of ACEis or ARBs and sodium-glucose cotransporter-2 inhibitors, stringent control of diabetes and the reduction of other risk factors, and educational programs for continuous diabetes self-care management. Furthermore, healthcare authorities should reinforce government-subsidized diabetes screening programs, especially for the underprivileged, to facilitate early recognition of undiagnosed diabetes and prevent HC incidents.
Data availability
No original data were generated or collected as part of this study. The NHIRD used in this study is available from the Taiwan National Health Insurance Administration, Ministry of Health and Welfare.
Gosmanov, A. R. et al. Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State (Endotext, 2021).
Google Scholar
Misra, S. et al. Temporal trends in emergency admissions for diabetic ketoacidosis in people with diabetes in England before and during the COVID-19 pandemic: A population-based study. Lancet Diabetes Endocrinol. 9 , 671–680 (2021).
Article CAS PubMed PubMed Central Google Scholar
Wachtel, T. J., Tetu-Mouradjian, L. M., Goldman, D. L., Ellis, S. E. & O’Sullivan, P. S. Hyperosmolarity and acidosis in diabetes mellitus: A three-year experience in Rhode Island. J. Gen. Intern. Med. 6 , 495–502 (1991).
Article CAS PubMed Google Scholar
Fourtner, S. H., Weinzimer, S. A. & Levitt Katz, L. E. Hyperglycemic hyperosmolar non-ketotic syndrome in children with type 2 diabetes*. Pediatr. Diabetes 6 , 129–135 (2005).
Article PubMed Google Scholar
Desai, R. et al. Temporal trends in the prevalence of diabetes decompensation (diabetic ketoacidosis and hyperosmolar hyperglycemic state) among adult patients hospitalized with diabetes mellitus: A nationwide analysis stratified by age, gender, and race. Cureus 11 , e4353 (2019).
PubMed PubMed Central Google Scholar
Lawrence, S. E., Cummings, E. A., Gaboury, I. & Daneman, D. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. J. Pediatr. 146 , 688–692 (2005).
Orban, J. C., Maizière, E. M., Ghaddab, A., Van Obberghen, E. & Ichai, C. Incidence and characteristics of acute kidney injury in severe diabetic ketoacidosis. PLOS One 9 , e110925 (2014).
Article ADS PubMed PubMed Central Google Scholar
Wang, J. Y. et al. Increased risk of ischemic stroke after hyperosmolar hyperglycemic state: A population-based follow-up study. PLOS One 9 , e94155 (2014).
Chen, Y. L., Weng, S. F., Yang, C. Y., Wang, J. J. & Tien, K. J. Long-term risk of stroke in type 2 diabetes patients with diabetic ketoacidosis: A population-based, propensity score-matched, longitudinal follow-up study. Diabetes Metab. 43 , 223–228 (2017).
Chang, L. H. et al. Association between hyperglycaemic crisis and long-term major adverse cardiovascular events: a nationwide population-based, propensity score-matched, cohort study. BMJ Open. 6 , e012233 (2016).
Article PubMed PubMed Central Google Scholar
Kao, Y. et al. Subsequent mortality after hyperglycemic crisis episode in the non-elderly: A national population-based cohort study. Endocrine 51 , 72–82 (2016).
Huang, C. C. et al. Long-term mortality risk after hyperglycemic crisis episodes in geriatric patients with diabetes: A national population-based cohort study. Diabetes Care 38 , 746–751 (2015).
Kao, Y. et al. Association of hyperglycemic crisis with an increased risk of end-stage renal disease: A nationwide population-based cohort study. Diabetes Res. Clin. Pract. 138 , 106–112 (2018).
Salardi, S. et al. Ketoacidosis at diagnosis in childhood-onset diabetes and the risk of retinopathy 20years later. J. Diabetes Complicat. 30 , 55–60 (2016).
Article Google Scholar
Lin, L. Y., Warren-Gash, C., Smeeth, L. & Chen, P. C. Data resource profile: The National Health Insurance Research Database (NHIRD). Epidemiol. Health 40 , e2018062 (2018).
Wang, T. H., Tsai, Y. T. & Lee, P. C. Health big data in Taiwan: A national health insurance research database. J. Formos. Med. Assoc. 122 , 296–298 (2023).
Lin, C. C., Lai, M. S., Syu, C. Y., Chang, S. C. & Tseng, F. Y. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J. Formos. Med. Assoc. 104 , 157–163 (2005).
PubMed Google Scholar
Hsieh, M. T., Hsieh, C. Y., Tsai, T. T., Wang, Y. C. & Sung, S. F. Performance of ICD-10-CM diagnosis codes for identifying acute ischemic stroke in a national health insurance claims database. Clin. Epidemiol. 12 , 1007–1013 (2020).
Kitabchi, A. E., Umpierrez, G. E., Murphy, M. B. & Kreisberg, R. A. Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association. Diabetes Care 29 , 2739–2748 (2006).
Kitabchi, A. E., Umpierrez, G. E., Miles, J. M. & Fisher, J. N. Hyperglycemic crises in adult patients with diabetes. Diabetes Care 32 , 1335–1343 (2009).
Nguyen, T. L. et al. Double-adjustment in propensity score matching analysis: Choosing a threshold for considering residual imbalance. BMC Med. Res. Methodol. 17 , 78 (2017).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94 , 496–509 (1999).
Article MathSciNet Google Scholar
Sheen, Y. J. et al. Trends in prevalence and incidence of diabetes mellitus from 2005 to 2014 in Taiwan. J. Formos. Med. Assoc. 118 (suppl 2), S66–S73 (2019).
Yan, S. H., Sheu, W. H., Song, Y. M. & Tseng, L. N. The occurrence of diabetic ketoacidosis in adults. Intern. Med. 39 , 10–14 (2000).
Ata, F. et al. Differential evolution of diabetic ketoacidosis in adults with pre-existent versus newly diagnosed type 1 and type 2 diabetes mellitus. BMC Endocr. Disord. 23 , 193 (2023).
Gaba, R., Mehta, P. & Balasubramanyam, A. Evaluation and management of ketosis-prone diabetes. Expert. Rev. Endocrinol. Metab. 14 , 43–48 (2019).
Lebovitz, H. E. & Banerji, M. A. Ketosis-prone diabetes (flatbush diabetes): An emerging worldwide clinically important entity. Curr. Diabetes Rep. 18 , 120 (2018).
Banerji, M. A. et al. GAD antibody negative NIDDM in adult black subjects with diabetic ketoacidosis and increased frequency of human leukocyte antigen DR3 and DR4. Flatbush diabetes. Diabetes 43 , 741–745 (1994).
Wang, X. & Tan, H. Male predominance in ketosis-prone diabetes mellitus. Biomed. Rep. 3 , 439–442 (2015).
National Health Insurance Administration, Ministry of Health and Welfare, Taiwan: Policies and Services: Care for Special Groups (Accessed 15 June 2024). https://www.nhi.gov.tw/en/cp-90-d4e0a-18-2.html
Pasquel, F. J. et al. Clinical outcomes in patients with isolated or combined diabetic ketoacidosis and hyperosmolar hyperglycemic state: A retrospective, hospital-based cohort study. Diabetes Care 43 , 349–357 (2020).
Chou, W. et al. Clinical characteristics of hyperglycemic crises in patients without a history of diabetes. J. Diabetes Investig. 5 , 657–662 (2014).
An, J. et al. Prevalence and incidence of microvascular and macrovascular complications over 15 years among patients with incident type 2 diabetes. BMJ Open Diabetes Res. Care 9 , e001847 (2021).
Hsu, C. C. et al. Poverty increases type 2 diabetes incidence and inequality of care despite universal health coverage. Diabetes Care 35 , 2286–2292 (2012).
Ayanian, J. Z., Zaslavsky, A. M., Weissman, J. S., Schneider, E. C. & Ginsburg, J. A. Undiagnosed hypertension and hypercholesterolemia among uninsured and insured adults in the Third National Health and Nutrition Examination Survey. Am. J. Public Health 93 , 2051–2054 (2003).
Kato, M. & Natarajan, R. Epigenetics and epigenomics in diabetic kidney disease and metabolic memory. Nat. Rev. Nephrol. 15 , 327–345 (2019).
El-Osta, A. et al. Transient high glucose causes persistent epigenetic changes and altered gene expression during subsequent normoglycemia. J. Exp. Med. 205 , 2409–2417 (2008).
Harris, M. I., Klein, R., Welborn, T. A. & Knuiman, M. W. Onset of NIDDM occurs at least 4–7 yr before clinical diagnosis. Diabetes Care 15 , 815–819 (1992).
Porta, M. et al. Estimating the delay between onset and diagnosis of type 2 diabetes from the time course of retinopathy prevalence. Diabetes Care 37 , 1668–1674 (2014).
Thakar, C. V., Christianson, A., Himmelfarb, J. & Leonard, A. C. Acute kidney injury episodes and chronic kidney disease risk in diabetes mellitus. Clin. J. Am. Soc. Nephrol. 6 , 2567–2572 (2011).
Coca, S. G., Singanamala, S. & Parikh, C. R. Chronic kidney disease after acute kidney injury: A systematic review and meta-analysis. Kidney Int. 81 , 442–448 (2012).
Hsu, R. K. & Hsu, C. Y. The role of acute kidney injury in chronic kidney disease. Semin. Nephrol. 36 , 283–292 (2016).
Myers, S. R. et al. Frequency and risk factors of acute kidney injury during diabetic ketoacidosis in children and association with neurocognitive outcomes. JAMA Netw. Open 3 , e2025481 (2020).
Schmitt, J., Rahman, A. F. & Ashraf, A. Concurrent diabetic ketoacidosis with hyperosmolality and/or severe hyperglycemia in youth with type 2 diabetes. Endocrinol. Diabetes Metab. 3 , e00160 (2020).
Download references
Acknowledgements
We are grateful to the Health Data Science Center of China Medical University Hospital for providing administrative, technical, and funding support.
This work was supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial Center (Grant Number: MOHW110-TDU-B-212-124004), the Ministry of Science and Technology (grant number: MOST 110-2321-B-039-003), and China Medical University Hospital (Grant Numbers: DMR-111-228 and CMU110-MF-63). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Division of Endocrinology and Metabolism, Department of Internal Medicine, Mackay Memorial Hospital, Taipei City, 104217, Taiwan
Chun-Ta Huang
Department of Medicine, Mackay Medical College, New Taipei City, 252005, Taiwan
Management Office for Health Data, China Medical University Hospital, Taichung City, 404328, Taiwan
Chih-Hsin Muo & Fung-Chang Sung
Department of Health Services Administration, China Medical University College of Public Health, 100 Jingmao Road Section 1, Beitun Dist., Taichung, 406040, Taiwan
Fung-Chang Sung
Department of Food Nutrition and Health Biotechnology, Asia University, Taichung, 413305, Taiwan
International Master Program for Public Health, China Medical University, Taichung, 406040, Taiwan
Pei-Chun Chen
You can also search for this author in PubMed Google Scholar
Contributions
Conception and design: CT, FC. Acquisition, analysis, and interpretation of data: all authors. Drafting of the manuscript: CT. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: CH. Obtained funding: FC, PC. All authors had full access to all the study data and take responsibility for its integrity and the accuracy of data analysis. All authors have read and approved the final version of the manuscript submitted for publication.
Corresponding author
Correspondence to Fung-Chang Sung .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Huang, CT., Muo, CH., Sung, FC. et al. Risk of chronic kidney disease in patients with a hyperglycemic crisis as the initial presentation of type 2 diabetes. Sci Rep 14 , 16746 (2024). https://doi.org/10.1038/s41598-024-67678-3
Download citation
Received : 15 March 2024
Accepted : 15 July 2024
Published : 20 July 2024
DOI : https://doi.org/10.1038/s41598-024-67678-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Diabetic ketoacidosis
- Diabetic kidney disease
- Hyperglycemic crisis
- Hyperglycemic hyperosmolar state
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Special Edition: Oral Health and Diabetes Podcasts

In partnership with Haleon , the American Diabetes Association is excited to present two special episodes dedicated to exploring the vital connection between oral health and diabetes management. Join host Dr. Neil Skolnik as he delves into expert interviews revealing the often underappreciated yet crucial link between oral health and diabetes. These episodes provide an invaluable resource for healthcare professionals, offering insights and practical advice to enhance the care of patients with diabetes. By emphasizing the importance of integrated health strategies, this series aims to foster better collaboration between dentists and primary care doctors, ultimately improving patient outcomes.
The two-episode program will be presented between July and October 2024. Thank you for listening!
Please listen to each episode by clicking on the podcast players below or by freely subscribing to Diabetes Core Update via Apple Podcasts , Amazon Music , Spotify , or your preferred podcast platform.
July 18, 2024
Special Edition: Oral Health and Diabetes, Part 1
Play Episode
Total Time: 34:53 | File Size: 48.2 MB
In this special episode on Oral Health our host, Dr. Neil Skolnik, will discuss the bidirectional relationship between oral health and diabetes with Dr. Wenche Borgnakke. This special episode is supported by an independent educational grant from Haleon .
Presented by:
Neil Skolnik, M.D., Professor of Family and Community Medicine, Sidney Kimmel Medical College, Thomas Jefferson University; Associate Director, Family Medicine Residency Program, Abington Jefferson Health
Dr. Wenche Borgnakke. Dr Borgnakke DDS, MPH, PhD, Adjunct Clinical Assistant Professor of Dentistry in the department of Periodontics and Oral Medicine at the University of Michigan School of Dentistry.
Diabetes Core Update is a monthly audio podcast devoted to presenting and discussing the latest clinically relevant articles from ADA’s four scholarly journals: Diabetes , Diabetes Care , Clinical Diabetes , and Diabetes Spectrum . Users can freely access previous episodes of Diabetes Core Update here .
For previous episodes, please visit:

- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Patient Education Library
Types of Physical Activity
Plan Your Plate
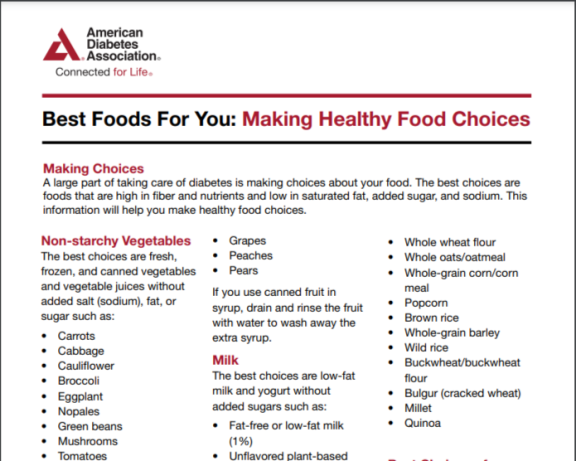
Best Foods For You: Making Healthy Food Choices
Your Mental Health and Diabetes
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Risk of chronic kidney disease in patients with a hyperglycemic crisis as the initial presentation of type 2 diabetes
Affiliations.
- 1 Division of Endocrinology and Metabolism, Department of Internal Medicine, Mackay Memorial Hospital, Taipei City, 104217, Taiwan.
- 2 Department of Medicine, Mackay Medical College, New Taipei City, 252005, Taiwan.
- 3 Management Office for Health Data, China Medical University Hospital, Taichung City, 404328, Taiwan.
- 4 Management Office for Health Data, China Medical University Hospital, Taichung City, 404328, Taiwan. [email protected].
- 5 Department of Health Services Administration, China Medical University College of Public Health, 100 Jingmao Road Section 1, Beitun Dist., Taichung, 406040, Taiwan. [email protected].
- 6 Department of Food Nutrition and Health Biotechnology, Asia University, Taichung, 413305, Taiwan. [email protected].
- 7 International Master Program for Public Health, China Medical University, Taichung, 406040, Taiwan.
- PMID: 39033190
- DOI: 10.1038/s41598-024-67678-3
Limited data exist on long-term renal outcomes in patients with hyperglycemic crisis (HC) as initial type 2 diabetes presentation. We evaluated the risk of chronic kidney disease (CKD) development in those with concurrent HC at diagnosis. Utilizing Taiwan's insurance claims from adults newly diagnosed with type 2 diabetes during 2006-2015, we created HC and matched non-HC cohorts. We assessed incident CKD/diabetic kidney disease (DKD) by 2018's end, calculating the hazard ratio (HR) with the Cox model. Each cohort comprised 13,242 patients. The combined CKD and DKD incidence was two-fold higher in the HC cohort than in the non-HC cohort (56.47 versus 28.49 per 1000 person-years) with an adjusted HR (aHR) of 2.00 (95% confidence interval [CI] 1.91-2.10]). Risk increased from diabetic ketoacidosis (DKA) (aHR:1.69 [95% CI 1.59-1.79]) to hyperglycemic hyperosmolar state (HHS) (aHR:2.47 [95% CI 2.33-2.63]) and further to combined DKA-HHS (aHR:2.60 [95% CI 2.29-2.95]). Subgroup analysis in individuals aged ≥ 40 years revealed a similar trend with slightly reduced incidences and HRs. Patients with HC as their initial type 2 diabetes presentation face a higher CKD risk than do those without HC. Enhanced medical attention and customized interventions are crucial to reduce this risk.
Keywords: Chronic kidney disease; Diabetic ketoacidosis; Diabetic kidney disease; Hyperglycemic crisis; Hyperglycemic hyperosmolar state.
© 2024. The Author(s).
PubMed Disclaimer
- Gosmanov, A. R. et al. Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State (Endotext, 2021).
- Misra, S. et al. Temporal trends in emergency admissions for diabetic ketoacidosis in people with diabetes in England before and during the COVID-19 pandemic: A population-based study. Lancet Diabetes Endocrinol. 9, 671–680 (2021). - PubMed - PMC - DOI
- Wachtel, T. J., Tetu-Mouradjian, L. M., Goldman, D. L., Ellis, S. E. & O’Sullivan, P. S. Hyperosmolarity and acidosis in diabetes mellitus: A three-year experience in Rhode Island. J. Gen. Intern. Med. 6, 495–502 (1991). - PubMed - DOI
- Fourtner, S. H., Weinzimer, S. A. & Levitt Katz, L. E. Hyperglycemic hyperosmolar non-ketotic syndrome in children with type 2 diabetes*. Pediatr. Diabetes 6, 129–135 (2005). - PubMed - DOI
- Desai, R. et al. Temporal trends in the prevalence of diabetes decompensation (diabetic ketoacidosis and hyperosmolar hyperglycemic state) among adult patients hospitalized with diabetes mellitus: A nationwide analysis stratified by age, gender, and race. Cureus 11, e4353 (2019). - PubMed - PMC
- Search in MeSH
Grants and funding
- MOHW110-TDU-B-212-124004/Ministry of Health and Welfare
- MOST 110-2321-B-039-003/Ministry of Science and Technology, Taiwan
- DMR-111-228/China Medical University Hospital
- CMU110-MF-63/China Medical University Hospital
LinkOut - more resources
Full text sources.
- Nature Publishing Group
- Genetic Alliance
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
VIDEO
COMMENTS
Type 2 Diabetes Warning Signs. Warning Signs and Symptoms - Can occur slowly over time. Blurred vision. Tingling or numbness in legs, feet or fingers. Recurring skin, gum or urinary tract infections. Drowsiness. Slow healing of cuts and bruises. Any symptoms that occur with Type 1 diabetes.
This comprehensive slide deck of ADA's 2023 Standards of Care contains content created, reviewed, and approved by the American Diabetes Association. You are free to use the slides in presentations without further permission as long as the slide content is not altered in any way and appropriate attribution is made to the American Diabetes Association (the Association name and logo on the slides ...
This topic will review the clinical presentation, diagnosis, and initial evaluation of diabetes in nonpregnant adults. Screening for and prevention of diabetes, the etiologic classification of diabetes mellitus, the treatment of diabetes, as well as diabetes during pregnancy are discussed separately. (See "Screening for type 2 diabetes mellitus" .)
Type 1 Diabetes. Previously called "insulin dependent diabetes" or "juvenile-onset diabetes". Develops when the immune system destroys pancreatic beta cells and the rate of beta cell destruction is variable. 5-10% of the U.S. population diagnosed with Diabetes have type 1 (CDC 2018)1. Multiple genetic predispositions.
This comprehensive slide deck of ADA's 2024 Standards of Care (.PPTX) contains content created, reviewed, and approved by the ADA. You are free to use the slides in presentations without further permission as long as the slide content is not altered in any way and appropriate attribution is made to the American Diabetes Association (the ADA name and logo on the slides constitutes appropriate ...
Happy World Diabetes Day! Celebrate World Diabetes Day in style with our fully editable Google Slides and PowerPoint template. Complete with illuminating light green design and vivid photographs, it provides a perfect platform to give an informative presentation about diabetes, its varied types, and summarize significant research.
Download the latest ADA's Standards of Care slide deck for diabetes professionals and educators.
The Diabetes PowerPoint Template has 13 slides of high-quality vector graphics. This is a presentation tool to discuss diabetes and related topics in ways that are most appealing to the audience. Such as shapes and graphics demonstrating a body diagram, test device, and data charts. Furthermore, the diabetes PowerPoint presentation is a ...
People with prediabetes have blood sugar levels that are higher than normal, but not high enough to be diagnosed with type 2 diabetes. They are at risk for type 2 diabetes, heart attack and stroke, but lifestyle changes, such as losing weight and increasing physical activity, can reduce their risk and may even prevent the onset of type 2 diabetes.
Free Canva presentation template. Elevate your health seminar with this bold, illustrated Diabetes Mellitus Disease template. Crafted specifically for health professionals, its dominant colors of black and red create a corporate yet engaging look. Ideal for presenting complex information about diabetes management, research findings or awareness ...
Older People and Diabetes Stats. 26% of Americans age 65 or older have diabetes (11.8 million seniors) 50% of people with diabetes, 65 yrs plus. 50% of older adults have prediabetes Rate of older population with diabetes growing rapidly due to increasing life expectancy. Diabetes prevalence to double in next 20 years, in part due to the aging ...
Download FREE Diabetes PowerPoint templates and Google Slides themes that are easy to use and understand. Bright colors, creative visuals, and helpful infographics - make your message clear! Spread awareness about diabetes mellitus, including causes, symptoms, diets, etc. The best choice for doctors! Diabetes PPT Presentation Template and ...
This creative diabetes template is compatible with all versions of Microsoft PowerPoint, Google Slides, and Keynote. The users can change the slides' colors, relevant graphical elements, icons, and theme according to their preferences. So, download this useful PPT template and make amazing presentations in the diabetes month of November ...
Screening and Monitoring for Diabetes. A1C Blood Draw: average blood sugar over the past two to three months. 1. Can Diagnose Prediabetes. 2. Monitors Diabetes. If A1C level is between 5.7 and less than 6.5%, levels are in the prediabetes range. If A1C level of 6.5% or higher, levels are in the diabetes range. 26.
Diabetes Mellitus. Dr Ibrahim Bashaireh, RN, PhD. Diabetes Mellitus Definition. A multisystem disease related to: Chronic disorder Abnormal metabolism of fuels glucose and fat An endocrine disorder causes Abnormal insulin production Impaired insulin utilization Slideshow 6596402 by alvin-solis.
Presentation Transcript. Definition: • "A metabolic disease in which the body's inability to produce any or enough insulin causes elevated levels of glucose in the blood.". Type 1 diabetes: • Also known as juvenile diabetes • Usually diagnosed in children and young adults • When body's own immune system destroys the insulin ...
Limited data exist on long-term renal outcomes in patients with hyperglycemic crisis (HC) as initial type 2 diabetes presentation. We evaluated the risk of chronic kidney disease (CKD) development ...
This is especially true when a chronic illness like diabetes is involved. According to Mental Health America, people who have diabetes are more likely to have depression, anxiety, and eating disorders. Stress from managing diabetes and changes in blood sugar levels have a direct and immediate impact on mood and cognition, called diabetes distress.
Special Edition: Oral Health and Diabetes Podcasts. In partnership with Haleon, the American Diabetes Association is excited to present two special episodes dedicated to exploring the vital connection between oral health and diabetes management. Join host Dr. Neil Skolnik as he delves into expert interviews revealing the often underappreciated yet crucial link between oral health and diabetes.
What is Diabetes? What is diabetes? •Lifelong disease affecting body's ability to make or use insulin. •Diabetes causes blood glucose (blood sugar) levels to go up higher than normal. -People without diabetes have blood sugars between approx. 70-125 mg/dLwhen fasting •We refer to people living with diabetes as PWD
over time, you are less likely to develop any diabetes-related eye conditions. Type 1 diabetes: You need to have a dilated eye exam within five years of being diagnosed and every year after that. Your first exam should include a dilated eye exam. Depending on the results, your doctor may approve waiting one to two years before you need another.
View presentations from the 83 rd Scientific Sessions. Why Attend Scientific Sessions. Tools to help with planning your attendance. ... Learn about ADA's work with the National Diabetes Prevention Program. Consumer Guide. Explore products for diabetes management. Clinical References. Browse the ShopDiabetes store. bold.
Limited data exist on long-term renal outcomes in patients with hyperglycemic crisis (HC) as initial type 2 diabetes presentation. We evaluated the risk of chronic kidney disease (CKD) development in those with concurrent HC at diagnosis. Utilizing Taiwan's insurance claims from adults newly diagnosed with type 2 diabetes during 2006-2015, we ...