Melanoma and Other Skin Cancers Research Results and Study Updates
See Advances in Melanoma and Other Skin Cancers Research for an overview of recent findings and progress, plus ongoing projects supported by NCI.
In an event more than three decades in the making, FDA has approved lifileucel (Amtagvi), the first cancer treatment that uses immune cells called tumor-infiltrating lymphocytes, or TILs.
People with desmoplastic melanoma, a rare form of skin cancer, are likely to benefit from treatment with a single immunotherapy drug, pembrolizumab (Keytruda), according to new results from a small clinical trial.
For melanoma that can be treated with surgery, a few doses of pembrolizumab (Keytruda) beforehand looks to be a good choice. In a clinical trial, people who got the presurgical immunotherapy were much less likely to have their cancer come back than those who only received it after surgery.
Male patients with metastatic melanoma don’t live as long as females, and their tumors are more likely to become resistant to commonly used treatments. A new study may help explain why: the androgen receptor.
Regular skin cancer screening leads to many diagnoses of very early-stage melanomas, results from a new study suggest. The results add to a debate about whether screening is fueling an overdiagnosis of melanoma in the United States.
The immunotherapy treatment, which combines the LAG-3 inhibitor relatlimab and PD-1 inhibitor nivolumab, becomes the first new immune checkpoint inhibitor approved in 8 years. Both drugs are given to patients via a single infusion to treat advanced melanoma.
Melanoma cells that travel to the brain produce their own amyloid beta, helping the cells survive and form metastases, a new study in mice shows. The Alzheimer’s-linked proteins appear to tamp down the brain’s immune response to the cancer cells.
NCI researchers have found that a diet rich in fiber may help some people being treated for melanoma respond to immunotherapy treatment by influencing the gut microbiome. The new findings come from an analysis of people with melanoma and mouse models of the disease.
Clinical trial finds that ipilimumab (Yervoy) and nivolumab (Opdivo) combo is superior to a combination of the targeted therapies dabrafenib (Tafinlar) and trametinib (Mekinist) as the first treatment for metastatic BRAF-positive melanoma.
Trial results show patients who received the immunotherapy pembrolizumab (Keytruda) after surgery to remove high-risk stage II melanomas were less likely to have the cancer come back than those who received no treatment after surgery.
People with advanced melanoma treated with two immunotherapy drugs—nivolumab (Opdivo) and a new drug called relatlimab—lived longer without their cancer getting worse than those treated only with nivolumab, results from a large clinical trial show.
While doctors are familiar with the short-term side effects of immune checkpoint inhibitors, less is known about potential long-term side effects. A new study details the chronic side effects of these drugs in people who received them as part of treatment for melanoma.
In a large trial, tebentafusp helped patients with uveal melanoma live longer than patients who received other treatments for the disease. Uveal melanoma is an aggressive cancer of the eye, and many patients do not survive for a year once it has spread.
For patients with cancers that do not respond to immunotherapy drugs, the use of fecal transplants to modify the gut microbiome may help some of these patients respond to the immunotherapy drugs.
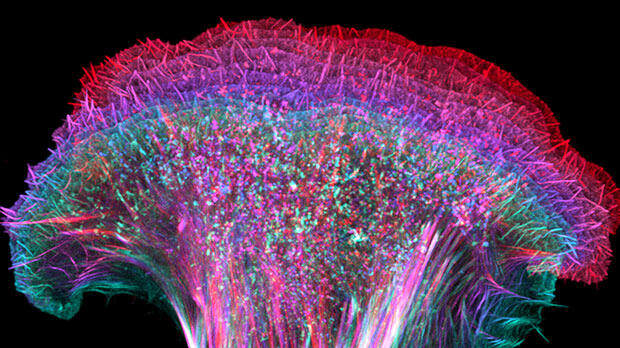
Melanoma cells that pass through the lymphatic system before entering the bloodstream are more resistant to cell death and spread more readily than cells that enter the bloodstream directly. The finding could lead to new treatment approaches.
After rising steadily for decades, the number of people in the United States who die each year from the skin cancer melanoma has dramatically dropped in recent years, results from a new study show. Learn what has contributed to the dramatic decline.
Melanoma cells that metastasize to other parts of the body produce high levels of a protein called MCT1, a new study in mice has found. Blocking MCT1 with an investigational drug, AZD3965, led to fewer and smaller metastatic tumors.
Researchers have developed a device that uses lasers and sound waves to scan circulating blood for melanoma cells. In a small study, the device accurately detected and reduced the amount of cancer cells in participants’ blood.
FDA has approved pembrolizumab (Keytruda) to treat people with Merkel cell carcinoma, a rare and deadly form of skin cancer. The approval covers use of the drug to treat locally advanced or metastatic forms of the disease.
The Food and Drug Administration approved the immunotherapy drug cemiplimab (Libtayo) for an advanced form of cutaneous squamous cell carcinoma (SCC), a common type of skin cancer. It is the first agent to be approved specifically for advanced SCC.
Results from a clinical trial show that the combination of nivolumab (Opdivo) and ipilimumab (Yervoy) halted the growth of or shrank metastatic brain tumors in more than half of participants with melanoma that had spread to the brain.
In a new study, NCI-led researchers developed a gene expression predictor that can indicate whether melanoma in a specific patient is likely to respond to treatment with immune checkpoint inhibitors, a type of immunotherapy.
A new study has linked age with how well patients with melanoma responded to treatment with immune checkpoint inhibitors. Experiments in mice suggested that the response pattern may be due to an age-related shift in the kinds of immune cells in tumors.
FDA recently approved the targeted-drug combination to treat patients with advanced melanoma and a subset of patients with a rare and aggressive form of thyroid cancer whose tumors have a specific mutation in the BRAF gene.
A new study suggests that patients with a rare form of melanoma, called desmoplastic melanoma, may be particularly likely to benefit from treatments known as immune checkpoint inhibitors. An NCI-sponsored clinical trial is already testing one such drug in patients with this cancer.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts

Skin cancer articles within Nature Reviews Clinical Oncology
Research Highlight | 14 June 2024
Neoadjuvant ipilimumab–nivolumab superior to adjuvant nivolumab
- Peter Sidaway
Research Highlight | 01 February 2024
Personalized neoantigen mRNA vaccine mitigates melanoma recurrence
- David Killock
Review Article | 26 January 2024
BRAF — a tumour-agnostic drug target with lineage-specific dependencies
Various BRAF alterations are found and function as oncogenic drivers across diverse cancer types. BRAF inhibitor-based therapy has improved outcomes for patients with cancers harbouring BRAF V600 mutations, although resistance develops in most, and the current inhibitors are not effective against other types of BRAF alterations. In this Review, the authors describe the mechanisms underlying oncogenic BRAF signalling, as well as pan-cancer and lineage-specific mechanisms of intrinsic, adaptive and acquired resistance to BRAF inhibitors. They also discuss novel RAF inhibitors and drug combinations designed to overcome these resistance mechanisms and/or expand the applicability of molecularly targeted therapy to a broader range of BRAF -mutant cancers.
- Aphrothiti J. Hanrahan
- , Ziyu Chen
- & David B. Solit
Review Article | 08 January 2024
Tumour-infiltrating lymphocyte therapy for patients with advanced-stage melanoma
Despite dramatic progress over the past decade, only around 50% of patients with advanced-stage melanoma derive durable benefit from immune-checkpoint inhibitors (ICIs) and/or BRAF and MEK (BRAF/MEK) inhibitors. Over the past few years, adoptive cell therapy with tumour-infiltrating lymphocytes (TILs) has demonstrated encouraging efficacy including in patients with disease progression on ICIs or BRAF/MEK inhibitors. In this Review, the authors summarize the role of TIL therapies in the management of these patients and describe future research strategies that might improve safety or efficacy.
- Sebastian Klobuch
- , Tom T. P. Seijkens
- & John B. A. G. Haanen
Research Highlight | 28 July 2023
Adjuvant nivolumab shows promise in MCC
Review Article | 05 May 2023
Personalizing neoadjuvant immune-checkpoint inhibition in patients with melanoma
Neoadjuvant immune-checkpoint inhibition is a promising emerging treatment strategy that potentially enables patients with a good response to initial therapy to avoid further treatment and the associated toxicity risks, while also identifying those who might require treatment escalation. In this Review, the authors describe treatment personalization strategies based on the initial response to one or more neoadjuvant immune-checkpoint inhibitors and consider the potential to expand this approach beyond patients with melanoma.
- Minke W. Lucas
- , Judith M. Versluis
- & Christian U. Blank
Research Highlight | 10 March 2023
Neoadjuvant pembrolizumab improves outcomes
Review Article | 11 January 2023
Therapy with oncolytic viruses: progress and challenges
Oncolytic viruses (OVs) provide a novel cancer treatment strategy, with a mechanism of action and toxicity profiles that are distinctly different to those of more traditional therapies. Thus far, four OVs have entered clinical use globally, yet only talimogene laherparepvec (T-VEC) has entered widespread clinical use. In this Review, the authors describe the clinical and regulatory experience with T-VEC thus far, and how this can guide the development of novel OVs. Discussions of a range of novel OVs with the potential for clinical implementation in the near future are also provided.
- Sophia Z. Shalhout
- , David M. Miller
- & Howard L. Kaufman
Review Article | 04 January 2023
Advances in the clinical management of uveal melanoma
Although almost all patients with uveal melanoma have localized disease at diagnosis, and despite effective treatment of the primary tumour, metastatic recurrence is common and holds a dismal prognosis. Unlike its cutaneous counterpart, therapeutic advances for uveal melanoma have not been forthcoming, although the recent approval of the first systemic therapy for this disease has ushered in a new era of hope. This Review summarizes the biology of uveal melanoma and the management of primary disease, including molecular risk classification, adjuvant therapy and follow-up strategies. The discussion is then focused on the established and emerging regional and systemic treatments for metastatic uveal melanoma.
- Richard D. Carvajal
- , Joseph J. Sacco
- & Sophie Piperno-Neumann
Research Highlight | 23 December 2022
Efficacy of TILs confirmed
Research Highlight | 09 November 2022
DREAMseq of therapy for BRAF -mutant melanoma
News & Views | 30 August 2022
Personalizing the approach to neoadjuvant therapy: a promising path to improving outcomes of resectable melanoma
Clinical trials of neoadjuvant therapy for melanoma have expanded rapidly over the past several years. Preliminary data demonstrate the prognostic value of pathological response, which might have clinical implications for refining the roles of surgery and adjuvant therapy. These clinical questions are under active investigation across many ongoing clinical trials.
- Giorgos C. Karakousis
- & Tara C. Mitchell
Research Highlight | 23 May 2022
Tiragolumab active in PD-L1 + NSCLC
Viewpoint | 25 April 2022
Optimal systemic therapy for high-risk resectable melanoma
Immune-checkpoint inhibitors and BRAF-targeted therapy have revolutionized the treatment of advanced-stage, unresectable melanoma and have been successfully transitioned into the resectable disease setting as (neo)adjuvant treatments. The expanding range of treatment options available for resectable high-risk melanoma raises questions over selection of the optimal therapeutic strategy and agents for each individual. Furthermore, the use of perioperative therapy has potentially important implications for the management of patients who have disease recurrence. In this Viewpoint, we asked four expert investigators who have been involved in the key studies of perioperative systemic therapies for their perspectives on the optimal management of patients with high-risk melanoma.
- Alexander M. M. Eggermont
- , Omid Hamid
- & Jason J. Luke
News & Views | 21 April 2022
Gut microbes as biomarkers of ICI response — sharpening the focus
Two recent large-cohort studies reinforce the potential predictive capability of gut microbiota for immune-checkpoint inhibitor response and toxicities in patients with melanoma. However, additional investigations are required to understand the mechanistic underpinnings of this complex multifaceted relationship, and how it can be exploited for personalized cancer care.
- Neal Bhutiani
- & Jennifer A. Wargo
Research Highlight | 19 April 2022
Pembrolizumab reduces recurrence risk in stage II melanoma
Review Article | 23 March 2022
The emerging role of photoacoustic imaging in clinical oncology
Photoacoustic imaging is a novel imaging technique that provides scalably high levels of spatial resolution at rapid acquisition speed, without the need for radiation or exogenous contrast agents. In this Review, the authors describe the emerging role of this technology in the screening, diagnosis and management of patients with cancer, and provide an overview of the future implementation of this technology.
- & Lihong V. Wang
Review Article | 26 January 2022
Immune-checkpoint inhibitors: long-term implications of toxicity
Immune-checkpoint inhibitors (ICIs) have dramatically improved the outcomes of patients with advanced-stage solid tumours, including the potential for long-term remission in a subset. However, long-term follow-up data reveal a risk of chronic toxicities from these agents, which can have important quality-of-life implications. In this Review, the authors describe the current level of evidence of chronic toxicities of ICIs and their implications for patients
- Douglas B. Johnson
- , Caroline A. Nebhan
- & Justin M. Balko
Research Highlight | 14 January 2022
LAG3 inhibition improves outcomes
Research Highlight | 16 November 2021
Early ICI uptake on PET predicts response
Research Highlight | 08 October 2021
Tebentafusp for uveal melanoma
Research Highlight | 22 June 2021
From the 2021 ASCO Annual Meeting
Research Highlight | 25 May 2021
Cemiplimab is a new option in BCC
- Diana Romero
News & Views | 19 March 2021
First clinical proof-of-concept that FMT can overcome resistance to ICIs
An unfavourable gut bacterial composition has been shown to reduce the likelihood of clinical benefit from immune-checkpoint inhibitors (ICIs). The results of two first-in-human studies of faecal microbiota transplantation in patients with melanoma refractory to anti-PD-1 antibodies validate preclinical evidence that this approach can improve the gut microbiota and overcome resistance to ICIs; however, many questions remain.
- Arielle Elkrief
- & Bertrand Routy
Research Highlight | 24 February 2021
Pathological correlates and predictive biomarkers for neoadjuvant ICIs in melanoma
News & Views | 25 September 2020
Cancer vaccine induces potent T cell responses — but is it enough?
Tumour-associated antigens are an attractive therapeutic target in immuno-oncology. Here, the exploratory analyses of T cell responses and preliminary clinical outcomes of the Lipo-MERIT trial of a melanoma vaccine are discussed in the context of prior efforts to harness the immunogenicity of such antigens for antitumour immunity.
- Anjali Rohatgi
- & John M. Kirkwood
Research Highlight | 29 May 2020
ICI for resected stage IV melanoma
News & Views | 23 January 2020
Biology confirmed but biomarkers elusive in melanoma immunotherapy
Liu et al. report data from the largest sequencing analysis of tumour material from patients with metastatic melanoma receiving immune-checkpoint inhibitors. These data confirm the correlations between baseline immune infiltrate and treatment response, but also demonstrate inconsistent associations of tumour mutational burden, specific gene mutations and previously described gene expression patterns with clinical outcomes.
- Jason J. Luke
- & Paolo A. Ascierto
Research Highlight | 11 October 2019
Combinations provide sustained benefit
Research Highlight | 27 September 2019
Paradoxical roles of mutational load as a determinant of anticancer immunity
Research Highlight | 25 June 2019
BRAF+MEKi and ICI triplets show promise in melanoma
Comment | 20 May 2019
No other interest can take precedence — a patient’s perspective on oncology drug development
My husband’s diagnosis with melanoma and our struggle to access effective therapy challenged what I had learnt about medical research. I have since founded a patient network, becoming a vocal advocate for patient-centric drug development. Herein, I discuss some of the lessons I have learnt.
- Bettina Ryll
Review Article | 15 May 2019
Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance
Immune-checkpoint inhibitors (ICIs) have dramatically improved the survival of patients with certain forms of cancer; however, these agents also have adverse effects that are often quite different to those of more traditional cancer therapies. In this Review, the authors describe the epidemiology, treatment and management of the various immune-related adverse events that can occur in patients receiving ICIs.
- Filipe Martins
- , Latifyan Sofiya
- & Michel Obeid
Review Article | 09 April 2019
Cell-state dynamics and therapeutic resistance in melanoma from the perspective of MITF and IFNγ pathways
The authors of this Review propose a new model in which dynamic fluctuations of protein expression at the single-cell level and longitudinal reshaping of the cellular state at the cell-population level explain the process of therapeutic resistance development in patients with melanoma.
- , David E. Fisher
- & Keith T. Flaherty
Research Highlight | 05 March 2019
Early responses indicate remission
Research Highlight | 08 November 2018
New window of opportunity with ICIs in melanoma
In Brief | 06 November 2018
Interferon enhances immune-checkpoint inhibition
Research Highlight | 01 November 2018
Long-term benefits in COMBI-AD
Research Highlight | 23 October 2018
BCC identity switch breaks restraints of Hedgehog pathway inhibition
Consensus Statement 04 October 2018 | Open Access
The biology and treatment of Merkel cell carcinoma: current understanding and research priorities
Merkel cell carcinoma (MCC) is a rare and aggressive form of nonmelanoma skin cancer. The availability of immune checkpoint inhibition has improved the outcomes of a subset of patients with MCC, although many unmet needs continue to exist. In this Consensus Statement, the authors summarize developments in our understanding of MCC while also providing consensus recommendations for future research.
- Paul W. Harms
- , Kelly L. Harms
- & Isaac Brownell
Research Highlight | 07 September 2018
What’s new under the Sun for ICIs?
Research Highlight | 31 August 2018
Signatures IMPRES and might turn the TIDE in predicting responses
Research Highlight | 07 August 2018
MHC expression predicts response
Research Highlight | 09 July 2018
Sequencing cells of the immune TME
Research Highlight | 19 June 2018
Cemiplimab effective in cutaneous SCC
News & Views | 30 May 2018
The new era of adjuvant therapies for melanoma
New treatment options for patients with resected stage III melanoma have been established with the publication of the results of four pivotal randomized clinical trials, resulting in three drug approvals, with a forth expected, all within only 4 years. Herein, we put these advances into context.
- , Caroline Robert
- & Antoni Ribas
In Brief | 18 April 2018
Combination effective against brain metastases
Research Highlight | 12 April 2018
Encorafenib — a new agent for advanced-stage disease
Research Highlight | 13 March 2018
Time for adjuvant vemurafenib?
Research Highlight | 06 February 2018
Local chemotherapy synergizes with CTLA-4 inhibition
Browse broader subjects
- Skin diseases
Browse narrower subjects
- Basal cell carcinoma
- Squamous cell carcinoma
Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
Melanoma Skin Cancer
- What Is Melanoma Skin Cancer?
- Key Statistics for Melanoma Skin Cancer
What’s New in Melanoma Skin Cancer Research?
- Risk Factors for Melanoma Skin Cancer
- What Causes Melanoma Skin Cancer?
- Can Melanoma Skin Cancer Be Prevented?
- Genetic Counseling and Testing for People at High Risk of Melanoma
- Can Melanoma Skin Cancer Be Found Early?
- Signs and Symptoms of Melanoma Skin Cancer
- Tests for Melanoma Skin Cancer
- Questions to Ask About Melanoma Skin Cancer
- Melanoma Skin Cancer Stages
- Survival Rates for Melanoma Skin Cancer
- Surgery for Melanoma Skin Cancer
- Immunotherapy for Melanoma Skin Cancer
- Targeted Therapy Drugs for Melanoma Skin Cancer
- Chemotherapy for Melanoma Skin Cancer
- Radiation Therapy for Melanoma Skin Cancer
- Treatment of Melanoma Skin Cancer, by Stage
- Living as a Melanoma Skin Cancer Survivor
- If You Have Melanoma Skin Cancer
Research into the causes, prevention, diagnosis, and treatment of melanoma is being done in medical centers throughout the world.
Causes and prevention
Melanoma genetics, early detection and diagnosis, lab tests to help determine prognosis (outlook), sunlight and ultraviolet (uv) radiation.
Some research suggests there are 2 main ways that exposure to UV rays is linked to melanoma, but there is likely some overlap.
The first link is to sun exposure as a child and teenager. People with melanoma often have an early history of sunburns or other intense sun exposures, although not everyone does. This early sun exposure may damage the DNA (genes) in skin cells called melanocytes, which starts them on a path to becoming melanoma cells many years later. This might help explain why melanomas often occur on the thighs (in women) and trunk (in men), areas that generally aren’t exposed to the sun as much in adulthood.
The second link is to chronic sun exposure. This type of exposure may be the cause of many melanomas that occur on the arms, neck, and face – areas that often get a lot of sun.
Researchers are studying if melanomas that develop from these different patterns of UV exposure have different gene changes that might require them to be treated differently.
Public education
Most melanomas (and other skin cancers) can be prevented . The best way to lower the number of skin cancers and the serious problems they can cause is to educate people, especially parents, about risk factors and warning signs and symptoms . It’s important for health care professionals and skin cancer survivors to remind everyone about the dangers of too much UV exposure (both from the sun and from man-made sources such as tanning beds) and about the ways you can protect your skin from UV rays .
Along with recommending staying in the shade, the American Cancer Society uses a slogan popularized in Australia as part of our skin cancer prevention message in the United States. Slip! Slop! Slap! ® and Wrap! is a catchy way to remember when going outdoors to slip on a shirt, slop on sunscreen, slap on a hat, and wrap on sunglasses to protect your eyes and the sensitive skin around them.
Scientists have made a great deal of progress in understanding how some of the DNA (gene) changes inside normal skin cells can lead them to become melanoma cells.
Some people inherit gene changes (mutations) from their parents that raise their risk of melanoma. For example, changes in the CDKN2A ( p16 ) gene cause some melanomas that run in certain families. People who have a strong family history of melanoma might want to speak with a cancer genetic counselor or a doctor experienced in cancer genetics to discuss the possible benefits, limits, and downsides of testing for changes in this gene (and others) that can increase melanoma cancer risk.
Researchers are also looking at other gene changes (or even patterns of gene changes) in melanoma cells to learn more about how they grow and how best to treat them. For example:
- Melanoma cells with certain gene changes might be more likely to spread, and therefore might need more intensive testing or treatment.
- Some gene changes make it more likely that the cancer will respond to certain treatments, such as targeted drugs or immunotherapy.
These topics are discussed in more detail below.
Melanoma can often be found early , when it is most likely to be cured. Monthly skin self-exams and awareness of the possible warning signs may be helpful in finding most melanomas when they are at an early, curable stage.
The American Academy of Dermatology (AAD) sponsors annual free skin cancer screenings throughout the country. Many local American Cancer Society offices work closely with the AAD to provide volunteers for registration, coordination, and education efforts related to these free screenings. Look for information in your area about these screenings or contact the American Academy of Dermatology for more information.
Smartphone apps
In recent years, many smartphone apps have been developed that claim to help identify skin cancers, including melanomas. Recent advances in artificial intelligence (AI) may help make these apps better at identifying concerning areas on the skin that need to be looked at by a doctor.
While these tools may eventually prove to be helpful, it’s not yet clear how accurate they are, and more research is needed before expert groups would recommend them. For now, it’s best to have any area you’re concerned about looked at by a trained health professional.
Newer approaches to help determine if a tumor is a melanoma
Sometimes it can be hard for health care providers – even dermatologists – to tell if an abnormal area is likely to be a melanoma (and therefore should be biopsied) just based on how it looks. Because of this (and because of how dangerous melanomas can be), many skin biopsies are done on areas that turn out not to be melanomas.
Some newer devices can be placed over the skin to help health care providers get a better idea if an abnormal area is likely to be a melanoma, without needing to remove it.
For example, dermatologists sometimes use a technique known as reflectance confocal microscopy (RCM) , in which a low-powered laser is aimed at the suspicious area. The light from the laser enters the upper layers of the skin and reflects off the structures there. This can be used to create a very detailed, three-dimensional image of the area, which can help the doctor determine if the area needs to be biopsied.
Other handheld devices might be especially helpful for primary care providers and other health professionals who don’t usually see as many skin cancers as dermatologists do. These types of devices are typically placed over the skin, and the tip of the device sends out beams of light or electrical signals, which then bounce off the skin cells and are detected by the device. The patterns of signals from cancer cells tend to be different from those of normal cells. The device can analyze the pattern coming from the area and let the provider know if it’s likely to be a melanoma (and therefore further testing is needed).
Another newer technique is adhesive patch testing . Instead of cutting into the skin to get a biopsy sample, a sticky patch is placed over the suspicious area. When it’s removed it takes some of the top layers of skin with it, which can then be tested for certain gene changes that are often linked with melanoma. If one of those gene changes is found, a standard biopsy of the area can then be done. If no gene changes are found, a biopsy isn’t needed, and the area can be watched instead.
Most melanomas found at an early stage can be cured with surgery. But a small portion of these cancers eventually spread to other parts of the body, where they can be hard to treat.
Some research has shown that certain gene expression patterns in melanoma cells can help predict if early-stage melanomas are likely to spread or to come back after treatment. A lab test based on this research, known as DecisionDx-Melanoma , is now available. This test can be used to divide stage I to III melanomas into 3 main groups, based on their gene expression patterns:
- Class 1A melanomas have a lower risk of spreading or coming back.
- Class 1B or 2A melanomas have an intermediate risk of spreading or coming back.
- Class 2B melanomas have a higher risk of spreading or coming back.
This test might be used (along with other information about the melanoma) to help tell if someone with early-stage melanoma should get a sentinel lymph node biopsy (SLNB) or additional treatment, or if they need to be followed more closely after treatment to look for signs of recurrence.
Tests of other genes and gene patterns are now being studied as well.
While early-stage melanomas can often be cured with surgery , more advanced melanomas can be harder to treat. In recent years, newer types of immunotherapy and targeted therapy drugs have changed the treatment of this disease.
Immunotherapy
This type of treatment helps the body’s immune system attack melanoma cells more effectively. Some forms of immune therapy are now used to treat some melanomas (see Immunotherapy for Melanoma Skin Cancer ), and others are now being studied.
Immune checkpoint inhibitors: Some newer drugs block “checkpoint” proteins that normally suppress the T-cell immune response against melanoma cells. These drugs are now one of the mainstays of treatment for advanced melanomas. Researchers are now looking for ways to make these drugs work even better. One way to do this might be by combining different checkpoint inhibitors, or using them with other treatments, such as other types of immunotherapy or targeted drugs.
Researchers are also studying how useful these drugs can be for earlier-stage melanomas, as an adjuvant (additional) treatment after surgery. Some have already been shown to be useful after surgery for melanomas that have reached the lymph nodes, where they can help lower the chance that the cancer will come back. Researchers are now studying to see if these drugs might be helpful for even earlier-stage melanomas, or if they might be helpful if used before surgery (called neoadjuvant treatment) for some people.
Newer immune checkpoint inhibitors with slightly different targets are now being studied as well.
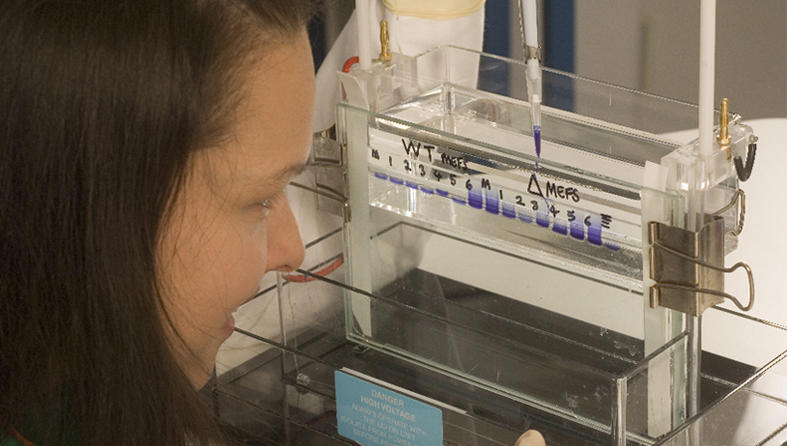
Adoptive cell therapy with tumor-infiltrating lymphocytes (TILs): Some studies have shown that treating advanced melanomas with tumor-infiltrating lymphocytes (TILs) can shrink tumors and possibly prolong a person’s life as well. This treatment is now an option for some people with advanced melanomas, if other treatments are no longer working.
TILs are immune system cells that have entered (infiltrated) a tumor to attack the cancer cells. Once a tumor is removed with surgery, the TILs can be separated out and then multiplied in the lab, after which they can be given back to the person as an IV infusion. In studies done so far, people are usually given chemotherapy before this treatment to help the body accept the TILs. After getting the TILs, people might also be given another type of immunotherapy such as interleukin-2 (IL-2) , which might help these immune cells better attack the cancer.
Newer studies are looking at changing certain genes in the TILs before they are given to see if this can make them more effective at fighting the cancer. This approach looks promising in early studies.
Melanoma vaccines: Vaccines to treat melanoma are being studied in clinical trials .
These vaccines are, in some ways, like the vaccines used to prevent diseases such as polio, measles, and mumps that are caused by viruses. Such vaccines usually contain weakened viruses or parts of a virus that can’t cause the disease. The vaccine stimulates the body’s immune system to destroy the more harmful type of virus.
In the same way, killed melanoma cells or parts of cells (antigens) can be used as a vaccine to try to stimulate the body’s immune system to destroy other melanoma cells in the body. Usually, the cells or antigens are mixed with other substances that help boost the immune response. But unlike vaccines that are meant to prevent infections, these vaccines are meant to treat an existing disease.
Making an effective vaccine against melanoma has proven to be harder than making a vaccine to fight a virus. The results of studies using vaccines to treat melanoma have been mixed so far, but many newer vaccines are now being studied and may hold more promise.
Other immunotherapies: Other new forms of immunotherapy are also being studied. In addition, many studies are now looking at combining different types of immunotherapy, which may be more effective than any single treatment for advanced melanoma.
Targeted drugs
Targeted therapy drugs are designed to attack parts of melanoma cells that make them different from normal cells. These drugs work differently from standard chemotherapy drugs. As researchers have learned more about some of the changes in melanoma cells that make them different from normal cells, they’ve developed drugs that target these changes. Some of these drugs are now commonly used to treat melanomas with certain gene changes, while others are still being studied.
Drugs that target cells with BRAF gene changes: About half of all melanomas have changes in the BRAF gene, which helps the cells grow. Drugs that target the BRAF protein or the related MEK proteins have been shown to shrink many of these tumors, especially when BRAF and MEK inhibitors are combined.
Drugs that target cells with changes in the C-KIT gene: A small number of melanomas have changes in the C-KIT gene. This is more likely in melanomas that start on the palms of the hands, soles of the feet, under the nails, or in certain other places. Drugs that target cells with changes in C-KIT can often be helpful in treating these melanomas.
Drugs that target other gene or protein changes: Several drugs that target other abnormal genes or proteins are now being studied in clinical trials as well.
Researchers are also looking at combining some of these targeted drugs with other types of treatments, such as chemotherapy or immunotherapy.
Skin Cancer ACS Research Highlights
See latest examples of how the Society conducts & funds research to help prevent, find, diagnose, treat, and live with skin cancers.

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
American Academy of Dermatology. Health and Wellness Apps that Dermatologists Do and Don’t Recommend. 2023. Accessed at https://www.aad.org/public/fad/digital-health/apps on September 28, 2023.
Mitchell TC, Karakousis G, Schuchter L. Chapter 66: Melanoma. In: Niederhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, eds. Abeloff’s Clinical Oncology . 6th ed. Philadelphia, Pa: Elsevier; 2020.
National Comprehensive Cancer Network (NCCN). Practice Guidelines in Oncology: Cutaneous Melanoma. Version 2.2023. Accessed at https://www.nccn.org/professionals/physician_gls/pdf/cutaneous_melanoma.pdf on September 28, 2023.
Ribas A, Read P, Slingluff CL. Chapter 92: Cutaneous Melanoma. In: DeVita VT, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology . 11th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2019.
Robbins PF, Morgan RA, Feldman SA, et al. Tumor regression in patients with metastatic synovial cell sarcoma and melanoma using genetically engineered lymphocytes reactive with NY-ESO-1. J Clin Oncol . 2011;29:917-924.
Rohaan MW, Borch TH, van den Berg JH, et al. Tumor-infiltrating lymphocyte therapy or ipilimumab in advanced melanoma. N Engl J Med . 2022;387(23):2113-2125.
Sosman JA. Interleukin-2 and experimental immunotherapy approaches for advanced melanoma. UpToDate. 2023. Accessed at https://www.uptodate.com/contents/interleukin-2-and-experimental-immunotherapy-approaches-for-advanced-melanoma on September 28, 2023.
Sosman JA. Overview of the management of advanced cutaneous melanoma. UpToDate. 2023. Accessed at https://www.uptodate.com/contents/overview-of-the-management-of-advanced-cutaneous-melanoma on September 28, 2023.
Sosman JA. Systemic treatment of metastatic melanoma lacking a BRAF mutation. UpToDate. 2023. Accessed at https://www.uptodate.com/contents/systemic-treatment-of-metastatic-melanoma-lacking-a-braf-mutation on September 28, 2023.
Last Revised: February 21, 2024
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy .
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.
More in Melanoma Skin Cancer
- About Melanoma Skin Cancer
- Causes, Risk Factors, and Prevention
- Early Detection, Diagnosis, and Staging
- After Treatment
Help us end cancer as we know it, for everyone.

If this was helpful, donate to help fund patient support services, research, and cancer content updates.
Together we are beating cancer
About cancer
Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
Cancers in general
- Clinical trials
Causes of cancer
Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
Get involved
- Make a donation
By cancer type
- Leave a legacy gift
- Donate in Memory
Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay For Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our We Are campaign
Our research
- Brain tumours
- Skin cancer
- All cancer types
By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
Funding for researchers
Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
Applying for funding
- Start your application online
- How to make a successful application
- Funding committees
- Successful applicant case studies
How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
- Recently funded awards
- Manage your research grant
- Notify us of new publications
Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
Shop online
- Wedding favours
- Cancer Care
- Flower Shop
Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
Our organisation
Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
Cancer news
- Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
ABOUT CANCER
GET INVOLVED
NEWS & RESOURCES
FUNDING & RESEARCH
You are here

Our research into skin cancer

For the past 120 years, we’ve been making discoveries that have saved countless lives. But we have so much more to do. Our strategy sets out how we'll accelerate progress towards a better future.
Our research is saving lives
Today, 9 in 10 people diagnosed with malignant melanoma (the most serious type of skin cancer) survive their disease for 10 years or more. Advances like immunotherapy have brought hope to many people with advanced skin cancer, but there is still much more to do for people whose cancers don't respond to these cutting edge treatments.
Current research

From studying the biology of skin cancer cells in the lab to leading clinical trials testing cutting-edge treatments, our researchers are working hard to ensure more people survive skin cancer.
Past research
Thanks to research, we’ve helped change the outlook for people with skin cancer.
Patients' stories

Meet people like Tracey who have experienced first-hand how our research is making a difference. The life-saving research we do wouldn’t be possible without your support.
From cutting edge science and debunking myths to patient stories, read the latest news, analysis and opinion on our news site.
Further information
Over the last 40 years, cancer survival in the UK has doubled. In the 1970s just 1 in 4 people survived their disease for 10 years or more. Today 2 in 4 survive.
We want to accelerate progress and see 3 in 4 patients surviving the disease by 2034.
Rate this page:
- Frontiers in Immunology
- Cancer Immunity and Immunotherapy
- Research Topics
Immunology and Immunotherapy of Skin Cancer
Total Downloads
Total Views and Downloads
About this Research Topic
Skin cancer originates from the different cell types residing in the skin. Its most common forms include melanoma, squamous cell carcinoma, and basal cell carcinoma. Moreover, there are several rare cancer entities such as Merkel cell carcinoma, cutaneous sarcoma, and epithelial cancers of the skin adnexa. ...
Keywords : Skin Cancer, Immune Surveillance, Vaccines, Adoptive Cell Transfer, Cytokine Therapy, Immune Checkpoint Inhibitors, Tumor Antigens, Tumor Microenvironment
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
| Manuscript |
Participating Journals
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.

Home › Press Room › Skin Cancer Issues and Research
Skin Cancer Issues & Research
The skin cancer foundation's position statements on controversial topics with supporting evidence-based research studies.
The Skin Cancer Foundation receives many questions about sun protection and skin cancer prevention. The safety of certain sunscreen ingredients, the link between indoor tanning and skin cancer, and the role of vitamin D are among the most popular — and debated —subjects for our readers and members of the media. Here, we share our positions on some common controversies.
Our position statements are supported by scientific research that has been published in medical journals after review by experts in the field. We’ve include references to relevant studies and articles, which you can find under “Related Reading and Evidence-Based Research Studies.”
The link between sun exposure and melanoma
Skin Cancer Foundation Statement : It’s estimated that 86 percent of all melanomas are caused by exposure to ultraviolet (UV) radiation from the sun. While genetics and family history also play a role, a pattern of sun exposure is a definite factor in the majority of melanomas.
More Information:
Intense UV radiation exposure (the kind you may get on a sun-drenched holiday after spending many months indoors) is linked with an increased risk of melanoma, research has shown. Intense UV exposure often causes sunburn, and just one blistering burn in childhood or adolescence (or a total of five sunburns sustained by any age) more than doubles a person’s chances of developing melanoma later in life.
Related Reading and Evidence-Based Research Studies:
Parkin DM, Mesher D, Sasieni P. Cancers attributable to solar (ultraviolet) radiation exposure in the UK in 2010 . Br J Cancer 2011; 105:566-69.
Pleasance ED, Cheetham RK, Stephens PJ, et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nature 2010; 463:191-96.
Chang YM, Barrett JH, Bishop DT, et al. Sun exposure and melanoma risk at different latitudes: a pooled analysis of 5700 cases and 7216 controls . Int J Epidemiol 2009; 38(3):814-30. Epub 2009 Apr 8.
Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: II. sun exposure . Eur J Cancer 2005; 41(1):45-60.
Pfahlberg A, Kolmel KF, Gefeller O. Timing of excessive ultraviolet radiation and melanoma: epidemiology does not support the existence of a critical period of high susceptibility to solar ultraviolet radiation-induced melanoma . Brit J Dermatol 2001; 144:3:471.
Lew RA, Sober AJ, Cook N, Marvell R, Fitzpatrick TB. Sun exposure habits in patients with cutaneous melanoma: a case study . J Dermatol Surg Onc 1983; 12:981-6.
The link between indoor tanning use and melanoma
Skin Cancer Foundation Statement : Studies offer dramatic evidence that indoor tanning bed use increases the risk of melanoma, the deadliest form of skin cancer. Those who begin tanning before age 35 increase their risk by almost 75 percent. Any suggestion that tanning beds are safe is putting people’s lives in danger.
The International Agency for Research on Cancer, affiliated with the World Health Organization, has determined that UV radiation-emitting tanning devices are cancer-causing in humans. While many members of the medical community had long believed that UV radiation from indoor tanning is carcinogenic, it had been difficult to verify the association between indoor tanning and melanoma incidence until recently. Additionally, those who have ever tanned indoors have a 69 percent risk of developing basal cell carcinoma before age 40.
Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis . Brit Med J 2012; 345:e4757. Doi: 10.1136/bmj.e4757.
Zhang M, Qureshi AA, Geller AC, Frazier L, Hunter DJ, Han J. Use of tanning beds and incidence of skin cancer . J Clin Oncol 2012; 30(14):1588-93.
National Toxicology Program. Report on Carcinogens, Twelfth Edition . U.S. Department of Health and Human Services, Public Health Service, National Toxicology Program. 2011: 429-430. Accessed February 12, 2012.
Cust AE, Armstrong BK, Goumas C, et al. Sunbed use during adolescence and early adulthood is associated with increased risk of early-onset melanoma . Int J Cancer 2011; 128(10):2425-35. doi: 10.1002/ijc.25576.
Ferrucci LM, Cartmel B, Molinaro AM, Leffell DJ, Bale AE, Mayne ST. Indoor tanning and risk of early-onset basal cell carcinoma. Journal of American Academy of Dermatology. 2011.
The International Agency for Research on Cancer Working Group. The association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: a systematic review. Int J Canc 2006; 120:1116-1122.
World Health Organization. Sunbeds, tanning and UV exposure Fact sheet N°287. Interim revision April 2010. Accessed Oct 7, 2011.
El Ghissassi F, Baan R, Straif K, et al. WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens–part D: radiation. Lancet Oncol 2009; 10(8):751-2.
Karagas MR, Stannard VA, Mott LA, Slattery MJ, Spencer SK, Weinstock MA. Use of tanning devices and risk of basal cell and squamous cell skin cancers . J Natl Cancer Inst 2002; 94:224. doi:10.1093/jnci/94.3.224.
Swerdlow AJ, Weinstock, MA. Do tanning lamps cause melanoma? An epidemiologic assessment . JAM Acad Derm 1998; 38(1):89-98.
U.S. Food and Drug Administration (FDA) final order to reclassify tanning beds
The Skin Cancer Foundation supports any effort to raise awareness about the hazards of indoor tanning and applauds the FDA for taking the important step to reclassify ultraviolet (UV) tanning devices from class I (low to moderate risk) to class II (moderate to high risk) devices, which is a major step in skin cancer prevention.
More Information :
On May 29, 2014 the FDA issued a final order, reclassifying ultraviolet (UV) tanning devices from class I (low to moderate risk) to class II (moderate to high risk) devices. In addition, the FDA will require warning labels on these tanning devices, noting that they should not be used on persons under the age of 18. The order follows a March 2013 proposed order to reclassify ultraviolet (UV) tanning devices from class I medical devices (the same designation given to elastic bandages and tongue depressors) to class II devices.
Studies offer alarming evidence that indoor tanning bed use increases the risk of melanoma, the deadliest form of skin cancer. In fact, those who begin tanning before age 35 increase their risk by almost 75 percent.
Related Reading and Evidence-Based Research Studies :
Cust AE, Armstrong BK, Goumas C, et al. Sunbed use during adolescence and early adulthood is associated with increased risk of early-onset melanoma. Int J Cancer 2011 May 1; 128(10):2425-35. doi: 10.1002/ijc.25576
Lazovich D, Vogel RI, Berwick M, Weinstock MA, Anderson KE, Warshaw EM. Indoor tanning and risk of melanoma: a case-control study in a highly exposed population. Cancer Epidemiol Biomarkers Prev 2010 Jun; 19(6):1557-68. Epub 2010 May 26.
El Ghissassi F, Baan R, Straif K, et al. WHO International Agency for Research on Cancer Monograph Working Group . A review of human carcinogens–part D: radiation. Lancet Oncol 2009 Aug; 10(8):751-2.
Karagas MR, Stannard VA, Mott LA, Slattery MJ, Spencer SK, Weinstock MA. Use of tanning devices and risk of basal cell and squamous cell skin cancers. J Natl Cancer Inst 2002; 94:224; doi:10.1093/jnci/94.3.224.
Swerdlow AJ, Weinstock, MA. Do tanning lamps cause melanoma? An epidemiologic assessment. J Am Acad Derm 1998 Jan; 38(1):89-98.
U.S. Department of Health and Human Services. Report on Carcinogens twelfth edition, 2011. p.429-434. http://ntp.niehs.nih.gov/ntp/roc/twelfth/profiles/UltravioletRadiationRelatedExposures.pdf . Accessed Oct 7, 2011.
World Health Organization. Sunbeds, tanning and UV exposure Fact sheet N°287. Interim revision April 2010. http://www.who.int/mediacentre/factsheets/fs287/en/ . Accessed Oct 7, 2011.
The role of sunscreen in the prevention of premature skin aging
A June 2013 study reveals strong evidence that daily sunscreen use significantly slows skin aging, even in middle-aged men and women. Specifically, the findings show that subjects who applied an SPF of 15+ broad-spectrum (UVA/UVB) sunscreen every morning (and reapplied sunscreen after sweating, bathing or spending more than a few hours outdoors), reduced their skin aging by 24 percent.
More than 90 percent of the visible skin changes associated with aging are caused by the sun’s ultraviolet rays.
Skin Cancer Foundation Statement : This study makes the case even stronger for daily sunscreen use as part of a complete sun protection regimen that also includes seeking shade and covering up with protective clothing including wide-brimmed hats and UV-blocking sunglasses.
Hughes MCB, Williams GM, Baker P, Green AC. Sunscreen and prevention of skin aging: a randomized trial. Ann Intern Med 2013 June; 158 (11):781-790.
Gilchrest BA. Skin and aging process. CRC Press . 1984; 124.
Godar DE, Urbach F, Gasparro FP, Van der Leun JC. UV doses of young adults. Photochem Photobiol 2003; 77(4):453-457.
Vitamin D deficiency and the sun
Skin Cancer Foundation Statement : There are three sources of vitamin D: exposure to the sun’s UVB radiation, certain foods, and supplements. The Skin Cancer Foundation recommends that everyone obtain the recommended daily 600 International Units (IU) through a combination of diet and supplements. The limited benefits of exposure to UVB radiation cannot be separated from the sun’s harmful effects, including an increased risk of skin cancers, premature skin aging and a weakened immune system.
Vitamin D is essential for strong bones and a healthy immune system, and the Institute of Medicine recommends that people ages 1-70 receive 600 IU a day. There has been much speculation on the other benefits vitamin D may offer, but after a review of more than 1,000 studies, in 2010 the Institute determined that evidence about the vitamin’s ability to prevent other health problems was inconclusive.
Vitamin D can be obtained from oily fish (salmon, mackerel, sardines) and cod liver oil as well as from fortified orange juice and milk, yogurts, and cereals such as Kashi® U™, Grape-Nuts and Total®. Supplements are readily available and inexpensive.
While obtaining vitamin D from the sun’s UVB rays may at first sound simpler, in fact it is not. Overexposure to UVB actually contributes to the breakdown of vitamin D in the body. After limited UVB exposure (determined by season, time of day, skin type and latitude; approximately five minutes daily for a Caucasian in New York City at 12 PM in the summer), the body’s vitamin D production reaches its maximum. Further UV exposure will not result in more vitamin D, but will instead prompt its disintegration into inactive compounds.
Office of Dietary Supplements. Dietary supplement fact sheet: vitamin D . National Institutes of Health. Reviewed June 24, 2011. Accessed Oct. 24, 2011.
Balk SJ. Council on Environmental Health; Section on Dermatology. Ultraviolet radiation: a hazard to children and adolescents . Pediatrics 2011; 127(3):e791-817. Epub 2011 Feb 28.
Institute of Medicine of the National Academies. Report brief: dietary reference intakes for calcium and vitamin D . Nov. 30, 2010. Accessed Oct. 10, 2011.
Brightman L, Hamann G, Geronemus R. The vitamin D dilemma . The Skin Cancer Foundation J 2008; (26):29-31.
The role of sunscreen in preventing skin cancers, including melanoma
Skin Cancer Foundation Statement : Landmark research has provided evidence of the value of sunscreen use in helping to prevent melanoma and squamous cell carcinoma. The Skin Cancer Foundation considers sunscreen one vital part of a comprehensive sun safety strategy, along with seeking shade and covering up with clothing, wide-brimmed hats, and UV-blocking sunglasses.
For years there has been strong evidence that daily sunscreen use plays a role in lowering the risk of actinic keratosis, the most common skin precancer, and squamous cell carcinoma. In 2011, a rigorous study of more than 1,600 adults over the course of a decade found that daily sunscreen use also plays a role in melanoma prevention. The researchers determined that subjects who applied sunscreen with an SPF of 15 or higher daily reduced their risk of melanoma by 50 percent.
Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol 2011; 29(3):257-63.
Green AC, Williams GM. Point: sunscreen use is a safe and effective approach to skin cancer prevention . Cancer Epidem Biomar Prev 2007; 16(10):1921-22.
van der Pols JC, Williams GM, Pandeya N, Logan V, Green AC. Prolonged prevention of squamous cell carcinoma of the skin by regular sunscreen use . Cancer Epidemiol Biomar Prev 2006; 15(12):2546-8. Epub 2006 Nov 28.
Green A, Williams G, Neale R, et al. Daily sunscreen application and betacarotene supplementation in prevention of basal-cell and squamous-cell carcinomas of the skin: a randomised controlled trial . Lancet 1999; 354(9180):723-9.
Jolley D, Marks R, Thompson SC. Reduction of Solar Keratoses by Regular Sunscreen Use. New England Journal of Medicine 1993.
The safety of nanotechnology
Skin Cancer Foundation Statement: By reducing the particles of the sunscreen ingredients titanium dioxide and zinc oxide to tiny, “micronized” or “nanosize” particles, sunscreen manufacturers are able to eliminate the white, pasty look associated with these ingredients, making sunscreen products appear more natural on the skin. The concern is that nano-sized sunscreen particles could penetrate the skin and damage living tissue. However, this is not the case: sunscreens are applied to the outermost layer of skin, which is made up of dead skin cells. Several studies have shown that nanoparticles do not penetrate intact living skin. Therefore they pose no risk to human health.
Wang SQ, Tooley IR. Photoprotection in the era of nanotechnology . Semin Cutan Med Surg 2011; 30(4):210-3.
Mavon A, Miquel C, Lejeune O, Payre B, Moretto P. In vitro percutaneous absorption and in vivo stratum corneum distribution of an organic and a mineral sunscreen . Skin Pharmacol Physiol 2007; 20:10-20.
Gamer AO, Leibold E, van Ravenzwaay B. The in vitro absorption of microfine zinc oxide and titanium dioxide through porcine skin . Toxicol In Vitro 2006; 20:301-307.
Schulz J, Hohenberg H, Pflücker F, et al. Distribution of sunscreens on skin . Adv Drug Deliv Rev 2002; 54 (Suppl. 1): S157-S163.
Pflucker F, Wendel V, Hohenberg H, et al. The human stratum corneum layer: an effective barrier against dermal uptake of different forms of topically applied micronised titanium dioxide . Skin Pharmacol Appl Skin Physiol 2001; 14 (Suppl. 1): 92-97
Laderman J, et al. Penetration of titanium dioxide microparticles in a sunscreen formulation into the horny layer and the follicular orifice . Skin Pharmacol Appl Skin Physiol 1999; 12:247-256.
Lansdown AB, Taylor A. Zinc and titanium oxides: promising UV-absorbers but what influence do they have on the intact skin? Int J Cosmet Sci 1997; 19:167-172.
SCF Statement on Sunscreen Ingredient Bans
Skin Cancer Foundation Statement: At a time when skin cancer is occurring at the highest levels in decades, any legislation that limits options for effective sun protection is cause for concern. Laws banning products containing oxybenzone and other ultraviolet (UV) filters will undermine years of education and awareness about the importance of sun protection and create another hurdle for anyone trying to make sunscreen use a priority. The Skin Cancer Foundation encourages legislators to consider established science showing that UV rays increase the risk of skin cancer before making decisions to limit sun protection options.
The Skin Cancer Foundation plays a major role in educating the public about effective sun protection for skin cancer prevention, including the daily use of sunscreen. Hawaii, the U.S. Virgin Islands and Key West, Florida, are among several places that have proposed or enacted bans on sunscreen products containing ingredients permitted under the current FDA monograph. (However, in March, Florida legislation was introduced that, if the governor signs, will prohibit local governments from regulating sunscreens or other over-the-counter drugs. That would mean the law won’t go into effect in January 2021 as scheduled.) Still, several additional local governments have legislation in the works, adding to the number of people who could find their sunscreen choices limited. The Foundation offers the following recommendations to residents of areas that have enacted bans on oxybenzone and other organic ingredients:
Everyone needs sunscreen, every day and everywhere. Even incidental exposure damages skin and can lead to skin cancer. There is well-established evidence that regular daily use of an SPF 15 or higher sunscreen reduces the risk of developing melanoma and nonmelanoma skin cancer.
Places near the equator, like Hawaii, receive more intense UV rays than most other regions. This makes sun protection even more important, especially for tourists. Periodic, concentrated exposure to UV radiation (such as the kind received on a tropical vacation) frequently causes sunburn and severely damages the skin, increasing the risk of developing melanoma.
Anyone who will experience extended exposure to the sun should apply a broad-spectrum, SPF 30 or higher sunscreen. Look for water-resistant formulas, which are labeled to protect for up to 40 or 80 minutes while swimming or sweating before needing reapplication. If you are in an area that has banned products with oxybenzone and octinoxate, your options may be limited, but it is important that you find products that achieve the guidelines above. You can do it.
Sunscreen alone isn’t enough. Since its inception in 1979, the Foundation has recommended following a complete sun protection regimen that includes seeking shade and covering up with clothing, including a wide-brimmed hat and UV-blocking sunglasses, in addition to daily sunscreen use. Clothing is the most effective form of sun protection, and swim shirts, rash guards and wet suits offer great protection during water activities, especially in intense UV environments like Hawaii. Look for clothing and hats labeled with an ultraviolet protection factor (UPF) rating of 30 or higher to ensure effective protection. For more information about skin cancer prevention and sun protection, visit SkinCancer.org.
Is Oxybenzone Safe? What to Know About the FDA’s Latest Proposed Rule on Sunscreens
Skin Cancer Foundation Statement: Promoting sun protection has been a high priority for The Skin Cancer Foundation since it was founded in 1979, and the Foundation has always made recommendations based on the latest scientific evidence available. Sunscreen has been a central part of the Foundation’s sun safety recommendations. All sunscreen ingredients that are currently FDA-approved, including oxybenzone, have been used in the U.S. for many years, and there is no evidence that sunscreens with these ingredients are harmful to humans. The FDA’s recent calls for further research on the effects of absorption of certain ingredients are welcomed by The Skin Cancer Foundation. While we encourage further research on this topic, it is important that people continue to practice complete sun protection, including the use of sunscreens, as there is already substantial evidence showing that UV exposure is harmful and that sunscreen helps reduce skin cancer risk.
In February 2019, the Food and Drug Administration (FDA) issued a proposed rule that updated regulatory requirements for sunscreens. Of the 16 currently marketed active ingredients, zinc oxide and titanium dioxide were generally recognized as safe and effective (GRASE) for use in sunscreens. PABA and trolamine salicylate were deemed NOT GRASE for use in sunscreens due to safety issues. There was insufficient safety data for the FDA to make a positive GRASE determination on the remaining 12 ingredients. To address those 12 ingredients, the FDA asked industry and other interested parties for additional data.
This declaration was alarming for many in the media and in the public, but the FDA itself pointed out that its “request for more data about these ingredients doesn’t mean the agency believes these products are ineffective or unsafe, or that these products should be removed from the marketplace. Rather, the agency asked for more data to help assess whether these products are safe and effective for regular use.”
More specifically, the proposed rule outlined concerns about the safety of sunscreen absorption into the body. While the FDA was not concerned about a small amount of absorption, if the amount of sunscreen absorbed was above a certain threshold (0.5ng/ml), it would need more detailed information about the safety of that ingredient.
The FDA published two studies, one in May 2019 and the other in January 2020, showing evidence that certain sunscreen ingredients (including avobenzone, oxybenzone and octocrylene) are absorbed into the body and exceed the minimal threshold for absorption. But in an editorial accompanying the research, the study authors note: “It is critical to recognize that these two studies conducted by the FDA do not provide any evidence that chemical sunscreens cause harm.”
The Skin Cancer Foundation encourages further research on the 12 sunscreen ingredients that have not yet been deemed GRASE, in hopes that additional data can help the FDA come to a conclusion about the safety of these UV filters. In the meantime, The Skin Cancer Foundation urges the FDA to take action in approving new sunscreen ingredients that could help diversify consumer choices.
While many sunscreen ingredients protect against damage from the sun’s UVB rays, which cause sunburn, oxybenzone is one of the few available in the U.S. that provides effective broad-spectrum protection against both UVB and the sun’s UVA rays, which can also cause sunburn as well as tanning, wrinkles and skin aging. Several ingredients available in other countries for years provide better UVA protection. However, they are not commercially available in the U.S., as they have been stuck in FDA review for nearly two decades. Since 2000, not a single new sunscreen ingredient has been added to the FDA’s approved list.
The Skin Cancer Foundation supported the federal Sunscreen Innovation Act (SIA), which was passed in 2014. The intention of SIA was to encourage the FDA to step up its process for reviewing new sunscreen ingredients, but the FDA has still not approved any to date. Innovation in sunscreen formulation will provide the public with more choices for sun protection, potentially leading to a decrease in the incidence of skin cancer.
Consumers who choose not to use products with oxybenzone or other chemical UV filters can purchase sunscreen products containing only the ingredients deemed GRASE by the FDA, zinc oxide and titanium dioxide. It should be noted that products only containing zinc oxide and titanium dioxide are not a perfect solution for everyone, as some may not achieve high SPF (sun protection factor) and broad-spectrum protection. Others may leave a whitish cast, especially on darker skin tones.
Americans deserve more choices, which is why the Foundation continues to support efforts to encourage the FDA to approve the use of new UV filters that are currently available outside the U.S. The Over-the-Counter Monograph Safety, Innovation and Reform Act, signed into law by President Trump in March 2020, is a promising first step toward making the approval process more efficient.
Finally, it’s important to keep in mind that sunscreen is just one part of a complete sun protection strategy. There are many ways to protect yourself from the sun, including seeking shade and covering up with clothing, wide-brimmed hats and UV-blocking sunglasses.
Last updated: October 2023
- Skin Cancer Prevention
- Recommended Products
- Eye Protection
- Sun Protective Clothing
- Seal of Recommendation
- Skin Cancer Information
- Skin Cancer Facts & Statistics
- Newly Diagnosed with Skin Cancer
- Skin Cancer Pictures
- Skin Cancer in People of Color
- Actinic Keratosis Risk Factors
- Actinic Keratosis Warning Signs and Images
- Actinic Keratosis Treatment
- Basal Cell Carcinoma Risk Factors
- Basal Cell Carcinoma Warning Signs and Images
- Basal Cell Carcinoma Treatment
- Melanoma Risk Factors
- Melanoma Warning Signs and Images
- Melanoma Stages
- Melanoma Treatment
- Merkel Cell Carcinoma Risk Factors
- Merkel Cell Carcinoma Warning Signs and Images
- Merkel Cell Carcinoma Stages
- Merkel Cell Carcinoma Treatment
- Merkel Cell Carcinoma Patient Support Center
- Squamous Cell Carcinoma Risk Factors
- Squamous Cell Carcinoma Warning Signs and Images
- Squamous Cell Carcinoma Treatment
- Advanced Squamous Cell Carcinoma Treatment
- Rare Skin Cancers
- Risk Factors
- Atypical Moles
- UV Radiation
- Photosensitivity
- Early Detection
- Annual Exams
- Find a Dermatologist
- Destination Healthy Skin
- Save Destination Healthy Skin
- The Big See
- Treatment & Resources
- Mohs Surgery
- Treatment Glossary
- Robins Nest
- COVID-19 and You
- Get Involved
- Ways to Give
- Your Donation at Work
- Connect With Us
- Sign Up for Newsletter
- Sign the Petition
- Skin Cancer Awareness Toolkit
- Skin Cancer Awareness Month
- Share Your Story
- Create a Fundraiser
- Host an Event
- Champions for Change Gala
- Research Grants
- Publications
- Corporate Council
- Education Programs

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

Common types of skin cancer
Share this:.
By Deb Balzer
Skin cancer is the most common cancer in the U.S., affecting millions worldwide. This cancer comes in two main types: melanoma , which is less common but more deadly, and nonmelanoma skin cancers, which include basa l cell carcinoma and squamous cell carcinoma .
Collin Costello, M.D. , a Mayo Clinic dermatologist , says these nonmelanoma skin cancers are more prevalent – and with early diagnosis and treatment, the prognosis is good.
Watch this Mayo Clinic Minute video:
"Both basal and squamous cell carcinoma are often slow-growing skin cancers. They're both caused mostly by the sun," says Dr. Costello.
These cancers are predominantly found on sun-exposed areas, like the face, scalp, neck and ears.
Basal cell carcinoma often appears as a change in the skin, such as a growth or a sore that won't heal, or a slightly transparent bump on the skin.

"For basal cells, they're often a pink bump that slowly enlarges with time. And sometimes they can bleed and be a little tender," Dr. Costello says.

Squamous cell carcinoma may look like a skin-colored bump and can start anywhere on the skin. It’s typically found on sun-exposed areas in sunburn-prone people. However, in those with darker skin tones, it can appear on sun-protected areas, including the genitals or toes.
"Sometimes they can get painful and ulcerated or be almost like a nonhealing wound," he says.
Early diagnosis and treatment for these nonmelanoma cancers are crucial. See a dermatologist if you notice spots changing or growing.
"The majority of the time both basal cell and squamous cell carcinoma are treated with Mohs surgery , particularly when it's on the face, scalp and neck," Dr. Costello says.

Reduce your risk of skin cancer
Use sunscreen daily to help prevent exposure to dangerous ultraviolet rays.
- Wear sunscreen of at least 30 SPF.
- Perform regular skin self-exams.
- See a healthcare professional for abnormal growths or warts.
- Wear protective clothing.
Learn more about skin cancer and find a clinical trial at Mayo Clinic.
Join the Skin Health Support Group on Mayo Clinic Connect , an online community moderated by Mayo Clinic for patients and caregivers.
Also, read these articles:
- Removing skin cancer with Mohs surgery
- Who should be screened for skin cancer?
- Melanoma in darker skin tones: Race and sex play a role, Mayo study finds
A version of this article was originally published on the Mayo Clinic News Network .
Related Posts

Dr. John Kohorst, a dermatologist and Mohs surgeon, discusses Mohs surgery, an outpatient surgical treatment for removing skin cancer.

Dr. Collin Costello, a Mayo Clinic dermatologist, explains who should see a healthcare professional for an annual skin exam.

Mayo Clinic study suggests added vigilance in early melanoma screening is particularly needed for Black men.
Recent Blog Articles
Want to cool down? 14 ideas to try
A fresh look at risks for developing young-onset dementia
Are you getting health care you don't need?
Weighing in on weight gain from antidepressants
Dengue fever: What to know and do
How do trees and green spaces enhance our health?
Testosterone-blocking drugs boost heart disease risk when given in combination
Parenting isn't easy: Two important skills can help
Does sleeping with an eye mask improve learning and alertness?
Do tattoos cause lymphoma?
.jpg)
On this page you'll discover
What is skin cancer?
What are the symptoms of skin cancer, types of skin cancer, what is melanoma, how can you prevent skin cancer, how is skin cancer treated, skin cancer.
- Reviewed by Mallika Marshall, MD , Contributing Editor
Skin cancer is the most common cancer in the United States. An estimated one in five Americans will develop skin cancer in their lifetime. The single most important thing you can do to protect your skin is to reduce sun exposure.
Skin cancer occurs when skin cells are damaged by ultraviolet (UV) rays from repeated sun exposure and sunburns. Exposure to UV radiation from tanning beds and sunlamps can also increase skin cancer risk.
The two most common skin cancers are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). They are slow-growing and seldom spread to other parts of the body. Both can be treated, but they can be disfiguring.
Melanoma is the most dangerous skin cancer. Though less common—accounting for about 1% of skin cancers—melanoma is responsible for the majority of skin cancer deaths. Melanoma is fast-growing and more likely to spread than BCC and SCC.
Skin cancer develops primarily on areas of sun-exposed skin , such as the scalp, face, ears, neck, lips, chest, arms, hands, and legs. But it also can form in other areas like the palms, beneath the fingernails and toenails, and genitals.
Besides overexposure to UV rays, other factors that increase one’s risk for skin cancer include having:
- blond or red hair
- blue, green, or gray eyes
- skin that burns easily
- a family history of skin cancer
- a tendency to develop moles or abnormal appearing or large moles
- previous bad sunburns
The best way to lower your risk for skin cancer is to protect your skin from UV light. Use sunscreen on exposed skin whenever outside and wear protective clothing, including wrap-around sunglasses and a wide-brim hat.
Skin cancers commonly appear on the most sun-exposed areas of the body, like the face, ears, neck, lips, and backs of the hands. They can also develop in scars, skin sores, or rashes elsewhere on the body. Here is what common skin cancers look like.
Basal cell carcinoma (BCC) . BCCs usually appear as tiny, painless bumps with a pink, pearly surface. As it slowly grows, the center of the bump may become sore and develop into a crater that bleeds, crusts, or forms a scab. Although it is commonly located on the face, basal cell cancer can develop on the ears, back, and neck.
Squamous cell carcinoma (SCC). SCCs usually begin as a small, red, painless lump or skin patch that slowly grows and may develop into a non-healing sore. It usually occurs on the head, ears, and hands.
Melanoma. Melanoma is usually visible as a single dark skin spot. It may appear anywhere on the body, but it most commonly develops on the back, chest, and legs. Most of the time, melanoma develops on normal-looking skin, but it can grow out of an existing mole. Following the ABCDE guideline is a good way to recognize the warning signs for possible melanoma.
- A: Asymmetry: One half of a mole or spot does not match the other.
- B: Border irregularity: The edges are ragged, notched, or blurred.
- C: Color: The pigmentation is not uniform; the coloring may include shades of tan, brown, or black; dashes of red, white, or blue can add to the mottled appearance.
- D: Diameter: A mole or spot is greater than ¼ inch in diameter or about the width of a pencil eraser. However, melanomas can be smaller.
- E: Evolving: A mole or spot looks different from others and/or changes size, shape, or color; or begins to itch, hurt, or bleed. A mole that bleeds, feels numb, or has a crusty surface also may indicate a melanoma.
The most common types of skin cancer are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Less common are melanoma and the even more rare Merkel cell carcinoma, the two leading causes of death from skin cancer.
Most skin cancers start in the top layer of the skin, called the epidermis. The main difference between skin cancers is the type of cell from which each originates.
Basal cell carcinoma (BCC). BCC is the most common type of skin cancer, accounting for approximately 80% of cases. It starts in basal cells located deep in the epidermis. BCCs tend to grow slowly, and it’s rare for a BCC to spread to other parts of the body. But if left untreated, BCCs can grow into nearby areas, deep into the skin, and destroy bone and tissue. If not fully eradicated during treatment, BCCs can return to the same place. People with BCCs are also more likely to get new ones elsewhere.
Squamous cell carcinoma (SCC). About 20% of skin cancers are SCC . They begin in the squamous cells in the middle and outer parts of the epidermis. SCC sometimes develop from a precancerous skin growth called an actinic keratosis, a rough, scaly patch on the skin that usually affects older adults after years of sun exposure. SCCs also are slow-growing, although they are more likely than BCCs to grow into deeper layers of the skin and spread to other parts of the body.
Melanoma. This type of skin cancer forms from melanocytes, skin cells in the bottom layer of the epidermis. Melanoma only makes up about 1% of skin cancers but it’s the deadliest because affected melanocytes can multiply and spread quickly.
Merkel cell carcinoma. This skin cancer is 40 times more rare than melanoma and forms from Merkel cells found in the layer of basal cells. It also tends to grow and spread quickly and is the second most common cause of skin cancer death after melanoma.
Melanoma (also known as malignant melanoma) is the deadliest form of skin cancer. It occurs when melanocytes (the cells that give skin its color) begin to reproduce uncontrollably. Melanoma can grow quickly and spread to other parts of the body.
Melanoma is usually visible as a single dark skin spot, often larger than 6 millimeters (mm) in diameter (about the size of a pencil eraser) but sometimes smaller. Melanoma can form from an existing mole or develop on normal-looking skin. Certain features of moles can raise the risk of melanoma, such as:
- A new mole appearing after age 30
- A new mole at any age if it is in an area rarely exposed to the sun
- A change in an existing mole
- One or more atypical moles—moles that resemble a fried egg, that are darker than others, or have an irregular shape.
- 20 or more moles on the body larger than 2 mm across
- Five or more moles each larger than 5 mm across
The most common sites for melanoma are the face (especially in older people), upper trunk (primarily in men), and legs (mostly in women). Melanoma can also appear on other parts of the body, such as under fingernails or toenails, the genitals, and inside the eye.
Melanoma is often easy to spot early. Regularly check your skin to look for new moles and for changes in existing ones.
People at increased risk for melanoma need regular checkups from their doctor or dermatologist. Because some melanomas can arise from existing moles, a doctor or dermatologist may remove atypical moles as they may be more likely to become cancerous.
Determining whether a mole or other spot is melanoma usually involves removing a small piece and some of the surrounding tissue and examining it for cancer.
There are five stages of melanoma—zero to four—with each stage defined by the melanoma’s thickness, how deep it has penetrated the skin, and whether it has spread. The higher the number, the more extensive the disease and, generally, the worse the prognosis.
Tumors on the skin's surface can usually be cured, but deeper cancers are more difficult and sometimes impossible to treat.
If treatment begins when the tumor is less than 0.75 mm deep, the chance of a cure is excellent. More than 95% of people with small melanomas are cancer-free as long as eight years later. However, for deeper melanomas, the survival rate is poor.
To help prevent skin cancer, follow standard sun protection guidelines. For example:
Sunscreen. The mantra for sunscreen is to use it early and often. Apply sunscreen 15 to 20 minutes before heading outside then reapply every two hours. Use at least two tablespoons to cover exposed areas of the face and body, with a nickel-sized dollop to the face alone. And don’t forget the ears, the tops of the feet, and the backs of the legs.
When choosing a sunscreen, focus on broad-spectrum coverage, SPF number, and water resistance.
Broad-spectrum coverage. This means the sunscreen protects against UVB sun rays—the leading cause of sunburns—and UVA, which penetrates deeper into the skin and contributes to skin aging and wrinkles. Both types of UV rays can damage DNA, raising the risk of skin cancer. Other terms you might see on labels that mean the same thing are “multi-spectrum” or “UVA/UVB protection.”
SPF. This stands for sun protection factor. The higher the SPF number, the greater the protection. For instance, SPF 30 blocks 97% of the UVB rays, and SPF 50 blocks 98%. Anything higher than 70 SPF does not provide much extra protection. Stick with sunscreen with a 30 to 50 SPF.
Water resistance. No sunscreen is waterproof, but water-resistant sunscreen withstands water and sweat for a limited time. It’s best to reapply sunscreen after getting out of the water or if you’ve been sweating a lot.
Attire. Wear a hat with at least a four-inch brim all around and sunglasses that block sunlight from the sides. As for clothing, opt for synthetic fibers, such as polyester, Lycra, nylon, and acrylic. These have elastic threads that pull the fibers close together, which reduces the spaces between them and thus blocks more of the sun’s UV rays. Color matters, too. Darker colors are better at protecting the skin against UV rays than lighter colors.
Some clothing brands offer specially designed sun protection clothing, which is marked with a UPF (ultraviolet protection factor) label and number. The number indicates what fraction of the sun’s UV rays can penetrate the fabric and reach your skin. For example, a shirt with a UPF of 50 allows only one-fiftieth of the sun’s rays through, according to the Skin Cancer Foundation.
Time. Avoid the sun from 10 a.m. to 2 p.m., when ultraviolet (UV) radiation exposure is at its peak.
Check your skin. Get a professional skin check from a dermatologist every one to two years. Those with previous skin cancer or strong family history should be checked more often. Also, keep an eye on your skin. Routinely check your body in the mirror for unusual spots, growths, or suspicious moles. Ask your spouse, partner, or a family member to look at your back and other areas you can’t see, like the scalp and the backs of the thighs and ears. Consult your doctor or dermatologist if you notice any suspicious spots, growths, or moles that get larger, become darker, or change shape.
Many skin cancers are treatable if caught early. Your dermatologist may recommend various treatments depending on the type of skin cancer, its size and location, how far it's spread, and whether a treated skin cancer has returned.
Melanoma. Surgery is the initial treatment for melanoma that appears in just one spot. The doctor removes the visible tumor along with 0.5 to 2 centimeters of healthy skin around the tumor, depending on its size.
In some cases, the doctor may perform Mohs surgery, a specialized procedure in which the tumor is shaved away one thin layer at a time and examined under the microscope. If any cancer cells remain, another layer of tissue is removed, and the process is repeated until no cancer cells appear in the removed sample. This technique helps the doctor remove as little healthy skin as possible.
If the melanoma is more than 1 millimeter deep, your doctor must determine if it has spread to nearby lymph nodes. If cancer is found, most often all of the lymph nodes in the area will be removed. However, it has not been absolutely proven that removing all lymph nodes improves the chances of survival. When a cancer has spread to only one or two other sites, surgical removal can improve survival.
Additional therapies can often help people with thicker tumors that have grown deep into the skin, spread to other areas of the body, or both. Most often, patients are treated with immunotherapy and/or drugs designed to block major pathways that allow cancers to grow. Radiation therapy and chemotherapy are less effective but can be used when other treatments stop working.
Basal cell carcinoma and squamous cell carcinoma. BCC and SCC share similar treatments. These include:
- cutting away the cancer and a small amount of healthy tissue around it. A skin graft may be necessary if a large area of skin is removed.
- scraping away the cancer with a surgical tool then using an electric probe to kill any remaining cancer cells.
- freezing cancer cells with liquid nitrogen.
- destroying the tumor with radiation.
- Mohs surgery.
- applying drugs directly to the skin or injecting them into the tumor.
- using a narrow laser beam to destroy the cancer.
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Thanks for visiting. Don't miss your FREE gift.
The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School
Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more.
Health Alerts from Harvard Medical School
Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss ...from exercises to build a stronger core to advice on treating cataracts . PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts.
BONUS! Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness

Stay on top of latest health news from Harvard Medical School.
Plus, get a FREE copy of the Best Diets for Cognitive Fitness .
- Cancer Topics
- Research Branches and Programmes
- Research Teams
- Knowledge Transfer
Research Project Websites
- International Research Collaborations
- Useful Links
Press Releases
- Featured News
- Videos and Podcasts
- Infographics and Photos
- Questions and Answers
- WHO Classification of Tumours
- IARC Monographs Programme
- IARC Handbooks of Cancer Prevention
- IARC Staff Journal Articles
- Scientific Meetings and Lectures
- IARC Seminar Series
- IARC/NCI Tumour Seminars
- Medals of Honour
- Professional Staff
- General service Staff
- Talent Pools
- Visiting Scientist and Postdoctoral Opportunities
- Postdoctoral Fellowships
- Call for Tenders
- Office of the Director
- Organization and Management
- Supporters and Friends
- IARC Newsletter
- Visitor Information
- Terms of use
- Privacy Policy
- iarc newsletter
Skin cancer

Introduction
News & events, iarc marks global non-melanoma skin cancer awareness day, multi-ethnic study uncovers unique origins of melanoma types and actionable molecular targets, infographics, global non-melanoma skin cancer awareness day: social media tiles.
Kathmandu, Nepal
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 8, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Study shows a distinct pattern in protein production can predict severe side effects from skin cancer treatment
by NYU Langone Health
An activity pattern in certain genes responsible for building proteins known as spleen tyrosine kinases can predict which melanoma patients are likely to have severe side effects from immunotherapy designed to treat the most deadly skin cancer, a study, publishing in the journal Clinical Cancer Research online Aug. 8, shows.
Led by researchers at NYU Langone Health and its Perlmutter Cancer Center, the experiments focused on checkpoint inhibitors, drugs that have in the last decade become a mainstay of treating melanoma. This form of skin cancer kills nearly 10,000 Americans annually.
The drugs work by blocking molecules (checkpoints) that sit on the surface of immune T cells and stop them from attacking cancer cells like they would invading viruses or bacteria.
While the immune system normally uses checkpoints to recognize and protect healthy cells , cancer cells are able to hijack and turn off immune cell surveillance, evading detection.
Immunotherapy drugs like nivolumab and ipilimumab are designed to block checkpoints, making cancer cells more "visible" again to T cells.
However, more than a third of melanoma patients given checkpoint inhibitors develop side effects so severe that they compromise their quality of life and ability to continue therapy.
Side effects most often involve some form of inflammation, a sign of an overactive immune response. Patients can experience severe skin rashes, diarrhea, or hyperthyroidism. More severe side effects can include liver toxicity, colitis, and rheumatoid arthritis.
In the study researchers found that even before treatment began in their test subjects , the activity of genes controlling the production of spleen tyrosine kinases predicted 83% of melanoma patients who eventually developed severe side effects from combined immunotherapy with nivolumab and ipilimumab.
Moreover, the researchers found that this heightened gene signature, as evidenced by the production of spleen tyrosine kinases, or the SYK pathway, did not interfere with the effectiveness of therapies in preventing recurrence of melanoma. The impact was connected only to side effects.
"Our study results show that increased gene activity in the spleen tyrosine kinase pathway could be the basis of a possible blood test that identifies melanoma patients most susceptible to having severe side effects from immunotherapy, and well before they start treatment," said study co-lead investigator Kelsey Monson, Ph.D.
"Predictive information of this kind is critically important to oncologists and patients to help guide their immunotherapy decisions, to either minimize these side effects by taking additional precautions or choose alternative immunotherapies," said study co-senior investigator Tomas Kirchhoff, Ph.D. Kirchhoff is an associate professor in the Department of Population Health at NYU Grossman School of Medicine and a member of Perlmutter Cancer Center.
For the study, researchers analyzed immune system cell samples from 212 men and women with melanoma participating in a national multicenter trial called CheckMate-915.
The trial was designed to test whether combined therapy with nivolumab and ipilimumab worked better than single therapy with nivolumab in preventing postsurgical recurrence of melanoma.
All immune cell samples were taken prior to the start of immunotherapy. Both drugs are manufactured by the pharmaceutical company Bristol Myers Squibb, which sponsored the CheckMate-915 trial, and provided the patient specimens and data used in the analysis.
When researchers looked at what genes were more active than others in patients who experienced side effects from their immunotherapy, they found a specific pattern among 24 genes tied to the production of spleen tyrosine kinases.
Further statistical analyses showed that increased or decreased activity (transcription) of only five of these genes—CD22, PAG1, CD33, HNRNPU, and FCGR2C—along with age and stage severity of their melanoma served as the best predictors of who would experience immunotherapy side effects.
Study co-senior investigator Jeffrey Weber, MD, Ph.D., says that the SYK pathway has previously been linked to other autoimmune diseases , including lupus, rheumatoid arthritis, and colitis, disorders marked by immune system attack on healthy cells. He also points out that immunotherapy side effects were also most common in areas affected by these autoimmune diseases, including the skin, colon, and liver.
Weber, the Laura and Isaac Perlmutter Professor of Oncology in the Department of Medicine at NYU Grossman School of Medicine, says the team next plans to investigate if an activated SYK pathway is predictive of side effects in patients treated with ipilimumab alone or with other combination immunotherapies. Weber also serves as deputy director of NYU Langone's Perlmutter Cancer Center.
"If our future research can explain how an activated spleen tyrosine kinase pathway leads to increased risk of side effects from immunotherapy , then it could also potentially help us to design better cancer immunotherapies and potentially other treatments for autoimmune diseases," said Kirchhoff.
Explore further
Feedback to editors

US health regulator rejects MDMA treatment for PTSD, for now
Aug 10, 2024

Study finds baked potatoes can improve heart health for diabetics
Aug 9, 2024

National study shows how internal medicine chief residency has changed over 20 years

Vegan diet better than Mediterranean, finds new research

Memory problems in old age linked to a key enzyme, study in mice finds

Key factor found in drug-context links, relapse

Researchers outline promises, challenges of understanding AI for biological discovery

The dengue vaccine is effective and safe: Confirmation from the first global meta-analysis

'PTNM' system provides new classification for Peyronie's disease and penile curvature

Researchers crack a key celiac mystery: Where the gluten reaction begins
Related stories.

Clinical trial: Immunotherapy drug combo helps extend the lives of patients with metastatic melanoma
Aug 17, 2023

Experimental test promises to predict side-effects and cancer's return in patients treated with immunotherapy
Sep 15, 2022

From immunotherapy to mRNA vaccines—the latest science on melanoma treatment explained
Jun 5, 2024

Adding new vaccine type to leading immunotherapy dramatically reduced melanoma recurrence
Apr 16, 2023

Team presents promising results from first clinical trial of next-gen antibody in patients with advanced solid tumors
Jun 3, 2024
Immunotherapy drug made available for some NHS patients with advanced skin cancer after surgery
Nov 30, 2018
Recommended for you

Epigenetic change to DNA associated with cancer risk in 'multi-omics' study

Feedback loop promotes cancer cells' adaption to molecular stress

Unmasking hidden potential: LMO4 enhances T cell cancer-fighting abilities

Cannabis use tied to head and neck cancer
Aug 8, 2024

Drug shows promise for treating brain tumors resulting from breast cancer, trial reports
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dermatol Ther (Heidelb)
- v.7(Suppl 1); 2017 Jan

Skin Cancer: Epidemiology, Disease Burden, Pathophysiology, Diagnosis, and Therapeutic Approaches
1 First Department of Dermatology, Aristotle University of Thessaloniki, Thessaloniki, Greece
Dorothée Nashan
2 Teaching Hospital of the University of Münster, Münster, Germany
Richard B. Weller
3 University of Edinburgh, Edinburgh, UK
Xavier Castellsagué
4 Catalan Institute of Oncology (ICO), L’Hospitalet de Llobregat, Catalonia, Spain
Associated Data
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Skin cancer, including both melanoma and non-melanoma, is the most common type of malignancy in the Caucasian population. Firstly, we review the evidence for the observed increase in the incidence of skin cancer over recent decades, and investigate whether this is a true increase or an artefact of greater screening and over-diagnosis. Prevention strategies are also discussed. Secondly, we discuss the complexities and challenges encountered when diagnosing and developing treatment strategies for skin cancer. Key case studies are presented that highlight the practic challenges of choosing the most appropriate treatment for patients with skin cancer. Thirdly, we consider the potential risks and benefits of increased sun exposure. However, this is discussed in terms of the possibility that the avoidance of sun exposure in order to reduce the risk of skin cancer may be less important than the reduction in all-cause mortality as a result of the potential benefits of increased exposure to the sun. Finally, we consider common questions on human papillomavirus infection.
Evolving Epidemiology and Burden of Skin Cancer
The increasing incidence of skin cancer, overall skin cancer.
Skin cancer, including both malignant melanoma (MM) and non-melanoma skin cancer (NMSC), represents the most common malignancy in Caucasians [ 1 – 10 ]. The incidence of both MM and NMSC is on the rise, with an annual increase in MM of 0.6% among adults over 50 years [ 11 ]. The estimated number of new cases of skin melanoma in 2016 is 76,380, which represents 4.5% of all new cancer cases [ 12 ]. Deviations in reported incidence rates exist and are attributed to varying risk factors amongst different populations, as well as discrepancies in national registration systems. Furthermore, the incidence of melanoma may be even higher than indicated, as the National Cancer Registries has reported an underestimation of its incidence in certain countries [ 13 ].
The increased incidence of melanoma has not been accompanied by a corresponding increase in mortality rates [ 12 ]. This has led to the question of whether there is a true melanoma epidemic, or if the increased incidence represents an epiphenomenon attributable to over-diagnosis resulting from intense screening and more biopsies.
The increased incidence of melanoma in the USA involves all thickness groups (American Joint Committee on Cancer tumor categories) and is independent of socio-economic status (a surrogate marker for access to care and screening), suggesting that increased screening and biopsy alone cannot account for the dramatic change observed [ 14 , 15 ]. This finding is in agreement with the results reported by Shaikh et al., who showed that thickness increased in T3/T4 tumors and nodular melanoma [ 16 ]. These observations together “suggest that the melanoma epidemic is real and not simply an artefact of increased detection pressure of earlier-stage T1/T2 lesions” [ 16 ].
Conversely, there is evidence that over-diagnosis may have a part to play. Recent epidemiologic studies indicate that melanoma in situ, with an annual incidence of 9.5% [ 12 ], occupies a disproportionately high percentage of the overall increase in MM incidence [ 17 ]. From the dermatopathologic point of view, there are studies suggesting a current trend towards reclassification of prior non-malignant diagnoses as ΜΜ [ 18 ]. Furthermore, in a population-based study correlating the number of skin biopsies and the incidence of MM, the investigators noted that there was a parallel increase during a 15-year period, suggesting that the MM epidemic may also be related to increased scrutiny and number of biopsies [ 19 ].
Non-Melanoma Skin Cancer
NMSC includes, amongst others, Bowen’s disease, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC). In Caucasians, the incidence of NMSC is higher (by as much as 18–20 times) than that of MM [ 20 – 22 ]. However, there are significant limitations to NMSC epidemiology, mainly attributed to marked geographic variations in incidence rates, as well as to exclusion of NMSC by large cancer registries due to low mortality rates. Even secondary analyses, whereby incidence data are extracted from administrative healthcare databases, are comparatively limited [ 23 ].
NMSC carries a substantial economic burden [ 24 , 25 ]. In Australia, it is the most costly cancer, accounting for expenditure of AUS$511 million in 2010 [ 24 ]. In the USA, it has been estimated that total annual NMSC-related expenditure is US$650 million, with Medicare costs 6–7 times greater than those for treating melanoma [ 26 ].
Reasons for Increased Incidence of Skin Cancer
The observed increases in skin cancer rates are associated with several factors, including the transition toward significantly older populations that are associated with a higher risk of NMSC [ 27 ]. However, research has also revealed the important role of increased occupational and recreational UV light exposure [ 22 , 28 ]. For example, women <40 years exhibited a constant linear increase in BCC incidence rates of 6.3% between 1973 and 2009 [ 29 ], and studies have shown that indoor tanning is associated with a significantly increased risk of BCC and SCC, with a higher risk with use in early life (<25 years) [ 30 ].
Diagnostic and Therapeutic Approaches to Skin Cancer: Challenging Clinical Cases
Skin cancer diagnosis.
A diagnosis of skin cancer needs consideration of alternative diagnoses. Concerning actinic keratosis, benign conditions include seborrheic keratosis, verruca vulgaris, actinic porokeratosis, O’Brien’s actinic granuloma, eczema, lentigo solaris, lichen planus, or psoriasis (Figs. 1 , ,2, 2 , ,3), 3 ), whereas malignant conditions include SCC, Bowen’s disease, BCC, lentigo maligna, keratoacanthoma, or extramammary Paget’s disease.

Case studies: 80-year-old woman presenting with field cancerization, and 45-year-old woman presenting with lupus erythematodes (forehead and cheek shown)

Case study: lichen planus complicating diagnosis in a 78-year-old man with actinic keratosis on his hand

Case study: psoriasis complicating diagnosis in a 47-year-old man with actinic keratosis on his hand
Clinicians should ideally perform total body skin examination (see Fig. 4 as an example case of actinic keratosis appearing on the back of the hand, as is often overlooked), at least for high-risk individuals [ 31 , 32 ]. The use of non-invasive optical technologies, such as optical coherence tomography (non-invasive imaging test of the retina using light waves) or dermatoscopy (imaging of the skin, allowing statements concerning thickening of layers, epidermal organization, and borders of a lesion—in the case of actinic keratosis, the typical honeycomb pattern may be observed), may be helpful to improve diagnostic accuracy in some skin cancers [ 33 – 37 ] (the case presented in Fig. 5 may have benefitted from such technologies, for example). Photodynamic visualization (fluorescent visualization of skin cancerization extension after preparation with 5-aminolaevulinic acid and subjection to photodynamic therapy [light exposure]) might also be beneficial for identification of actinic keratosis, with histologic confirmation also being necessary in cases in which invasive skin cancer is suspected [ 38 ].

Case study: cheilitis actinica versus actinic keratosis (mouth and cheek shown)

Case study: 89-year-old woman presenting with multiple comorbidities (leg shown)
Treatment Challenges
Treatment strategies for skin cancers require careful consideration, and there are many challenges to overcome. However, with increasing treatment choices, in terms of both therapy combinations and sequences, we can achieve better outcomes for patients with fewer recurrences and longer treatment-free periods.
Field Cancerization and Non-Melanoma Skin Cancer
Field cancerization of the skin, by which large areas are affected by carcinogenic alternations, presents various therapeutic challenges (Fig. 6 ). Owing to the difficulty in determining which actinic keratosis lesions may progress to invasive SCC, European guidelines recommend that all lesions, or the affected field, are treated [ 39 ]. For a patient with actinic keratosis, there are three evolutionary possibilities: spontaneous clearing; persistence; or progression to invasive SCC [ 40 ]. Approximately 60–65% of primary SCCs are believed to have arisen from lesions previously diagnosed clinically as actinic keratosis [ 41 , 42 ], and the rate at which a specific lesion may become SCC is estimated to be a fraction of a percent over the course of a year [ 43 ]. Even when actinic keratosis lesions are classified according to their clinical appearance, there is little correlation with their histologic classification, thereby reinforcing the need to treat all actinic keratosis lesions and field cancerization [ 44 ] (see “Cyclooxygenase in Cancer Prevention and Treatments for Actinic Keratosis”, by Gareth Thomas and Colin Morton, published in this Supplement, for further details on actinic keratosis treatment). While long-term efficacy and tolerance of treatments are key considerations for clinicians, comorbidities may impact treatment success.

Case study: field cancerization in an 80-year-old patient (head and shoulder/neck shown)
The broad actinic keratosis spectrum characterized by age, localization, medication, co-dermatoses, and exogenous factors (Figs. 1 , ,5) 5 ) requires an individualized treatment approach for each patient. Figures 1 , ,2, 2 , ,3, 3 , ,4, 4 , ,5, 5 , ,6, 6 , ,7 7 and and8 8 show examples of clinical cases. Patients who have received a kidney transplant represent a particularly challenging population. Skin tumors are a major problem in these patients, and key challenges for the clinician include treatment of the whole integument, sequential therapies, and achievement of long-term success when the patient is immunosuppressed (where inflammatory and immunomodulatory approaches are restricted). Figure 7 shows an example of a transplant patient in whom there was a suspicion of actinic keratoses in an extended field, with treatment choices being operative or destructive.

Case study: Treatment of a patient who had received a kidney transplant (leg shown)

Case study: 85-year-old woman with multiple basal cell carcinomas (forehead shown)
Many more therapeutic options are available for non-immunosuppressed patients. However, there is still limited availability of some medications as they are not approved for all NMSC types and localizations (Table 1 ). Furthermore, when extensive field cancerization encompassing the whole integument is evident, treatment must occur over a very large area of affected skin.
Table 1
Recommended topical treatments for actinic keratosis
| Drug | EMA approval date | Approved for localization | Area |
|---|---|---|---|
| 5% 5-FU [ ] | 1998 | All localizations | 500 cm |
| 5-FU 0.5% with 10% salicylic acid [ ] | 2011 | All localizations | 25 cm (maximum of 10 lesions) |
| 3% diclofenac with 2.5% hyaluronic acid [ ] | 2000 | All localizations | Maximum of 8 g/day |
| 5% imiquimod [ ] | 1998 | Head | 25 cm |
| 3.75% imiquimod [ ] | 2012 | Head | 25 cm |
| 0.05% ingenol mebutate [ ] | 2012 | Body, extremities | 25 cm |
| 0.015% ingenol mebutate [ ] | 2012 | Head | 25 cm |
Please refer to your local prescribing information
a MEDA ( http://www.meda.co.za/ )
b Almirall ( http://www.almirall.com/en/ )
c LEO ( http://www.leo-pharma.co.uk/ )
Basal Cell Carcinoma
Though the majority of patients with BCC have a good prognosis, some patients develop a more complex, advanced disease with relatively few treatment options; indeed, no formal treatment algorithms are available. However, the recent development of hedgehog signaling pathway inhibitors, such as vismodegib, has been significant, providing an effective treatment option for some patients. In particular, vismodegib treatment may be appropriate if the tumor is considered inoperable and radiation therapy is declined; complete remission is achieved in 21% of locally advanced BCC [ 45 ], even in those infiltrating adjacent muscle and bone structures. Many more cases with partial remission and shrinking tumors may be considered for operation (Fig. 8 ).
Malignant Melanoma Stage IV
Treatment approaches for melanoma encompass two main strategies: targeted therapies (e.g., BRAF- and MEK-inhibitors); and immunotherapies (e.g., anti-CTLA-4 and anti-PD-1).
The combination of BRAF- and MEK-inhibitors is well established in patients with tumors harboring the BRAF mutation, primarily owing to the development of tumor resistance with BRAF-inhibitor monotherapy [ 46 ]. Although this combination represents an effective option with an acceptable toxicity profile [ 47 ], questions still remain as to whether sequential or cyclic application of BRAF- and MEK-inhibitors would be more beneficial, and whether immunotherapies may represent equally useful alternatives [ 48 ].
With regard to immunotherapies, anti-PD-1 monotherapy may be preferable to anti-CLTA-4 monotherapy [ 49 ]: combining anti-PD-1 and anti-CTLA-4 therapies may increase response and remission rates. However, this may be at the risk of higher toxicity (with predominantly gastrointestinal, hepatic, and cutaneous adverse events) [ 50 ] and therefore would be most appropriate in patients with progressive disease or lower PD-L1 expression. Further studies on sequential/cyclic combinations of these immunotherapies with consideration of immunologically relevant parameters (e.g., PD-L1 expression levels, BRAF/NRAS/cKIT mutation analysis), tumor typing and staging, and patient characteristics (e.g., age, comorbidities, treatment history) are ongoing [ 48 ].
The Sun: Friend or Foe?
The impact of sunlight exposure on health.
The impact of sunlight exposure on health is subject to debate—here, we present our views on the available evidence. Several epidemiologic studies have provided evidence for the beneficial effect of sun exposure on overall health status. All-cause mortality (death due to any cause) was inversely correlated with increased sun exposure in several studies, with a particular reduction in cardiovascular mortality. A nationwide Danish case–control study showed that having a diagnosis of skin cancer, a marker for sun exposure, was associated with a lower incidence of myocardial infarction, fewer hip fractures in those below the age of 90 years, and fewer deaths from any cause [ 51 ]. Similarly, among Swedish women, habits indicating avoidance of sun exposure were a risk factor for all-cause mortality; the mortality rate among such ‘avoiders’ was approximately two-fold higher compared with the highest sun exposure group [ 52 ]. It is possible that severely restricting sun exposure, particularly at locations with low solar intensity, might in fact have a negative effect on health [ 52 ].
In addition, studies have shown that blood pressure and the incidence of ischemic heart disease correlate with the latitude of a person’s country of residence [ 53 , 54 ]. It is also known that blood pressure is lower during summer compared with winter [ 55 ]. This is of great significance as high blood pressure is the leading cause of disease and premature death in the world [ 56 , 57 ].
Meta-analyses of several studies indicate that serum vitamin D levels are inversely correlated with blood pressure and the incidence of cardiovascular disease, diabetes, and hypertension [ 58 , 59 ]. Furthermore, observational studies indicate that the risk of death from any cause is correlated with circulating 25-hydroxyvitamin D [ 60 ]. However, extensive studies, comprising meta-analyses of several clinical trials, have conclusively shown that oral vitamin D supplementation has no effect on blood pressure, ischemic heart disease, or stroke [ 58 , 61 ], although vitamin D3 supplementation may reduce all-cause mortality [ 60 ]. Although vitamin D may account for some of the beneficial effects observed with sunlight exposure, it may be considered a marker of the person’s occupational or recreational sun exposure.
Nitric Oxide and the Skin as a Mechanism Behind the Positive Effects of Sunlight
It has been proposed that many of the documented beneficial effects of exposure to sunlight, particularly those related to cardiovascular health, involve mechanisms unrelated to melatonin, vitamin D, and exposure to UVB [ 62 ]. Recent studies suggest that stores of nitric oxide (NO)-related species in the skin may be particularly important in this respect. Both the skin and the dermal vasculature contain biologically significant stores of bound NO species [ 63 ]. Upon exposure of the skin to UVA, photodecomposition of these NO stores takes place and NO species are released into the circulation, resulting in arterial vasodilation, with cardioprotective and antihypertensive effects [ 62 , 64 ]. This mechanism has also been shown to suppress the development of diabetes and metabolic syndrome in a mouse model [ 65 ]. Long-term suberythemal and erythemal UV light significantly suppressed weight gain, glucose intolerance, and insulin resistance in mice fed a high-fat diet, an effect that was not reproduced by vitamin D supplementation. Importantly, skin induction of NO reproduced many of the effects of UV radiation [ 65 ].
What Should a Dermatologist Know About HPV?
There are several key areas in which knowledge of HPV natural history and vaccination status is important for dermatologists. Table 2 provides examples of common questions, along with evidence-based responses for each question.
Table 2
What should the dermatologist know about HPV? Key questions and answers
| Question | Answer |
|---|---|
| Does every patient develop genital warts after HPV infection? | Even though HPV infection is very common, very few patients will develop genital warts after infection |
| How long can HPV infections last? | Up to 90% of HPV infections will clear within 2 years |
| Is a patient with subclinical infection contagious? | Yes, but we should distinguish between subclinical and latent infections (we know very little about latent infections). subclinical infections do exist and can last for years, but they are probably only contagious when there is viral replication and shedding |
| Is the patient no longer infectious once genital warts have been treated? | Patients can be infectious even after removal/treatment of genital warts |
| Is there a rationale for treating subclinical HPV infections? | No, what is important is the lesions, not the infection itself |
| What should be the advice for patients who have been treated for genital warts, but who may still have subclinical infection? | The important thing to focus on is the lesions; screening for early lesions, and subsequent treatment Although there is no formal recommendation, HPV vaccination is advised among patients with a history of HPV-related lesions |
| What advice should patients receive for their sexual partners concerning infection? | The important thing to focus on is the lesions; screening for early lesions, and subsequent treatment Although there is no formal recommendation, HPV vaccination is advised among patients with a history of HPV-related lesions |
| Is there any risk of HPV-related cancer in male patients? | Only patients who do not resolve HPV infections are at a higher risk of HPV persistence and subsequent HPV-related diseases, including pre-cancer and cancer |
| Do HPV vaccines protect against other HPV genotypes that may cause genital warts? | Yes, they protect against HPV types 6 and 11 that cause 90% of genital warts and recurrent respiratory papillomatosis |
| Considering the cost of the vaccine, is there enough evidence for vaccination of already infected patients? And for their sexual partners? | The current cost of HPV vaccines in national immunization programs has been reduced threefold Yes, the vaccine will not cure current active infections but will block new infections as well as auto-inoculated virions |
| Is there a rationale for HPV vaccination in young males? | Yes, very strong, and threefold: 1. To reduce transmission and circulation in the population 2. To protect themselves (male burden is now considerable) 3. For gender equality |
Human Papillomavirus and Cancer
More than 150 human papillomavirus (HPV) types have so far been identified. HPV falls into five genera, with the Alpha and Beta/Gamma genera representing the largest groups [ 66 ]. Mucosal HPV types from the Alpha genus are the ones associated with neoplastic disease and the most common viral infections of the reproductive tract; the World Health Organization acknowledges that most sexually active men and women will be infected at some point in their lives [ 67 ]. Twelve Alpha HPVs are classified as carcinogenic to humans and fifteen as probably/possibly carcinogenic [ 68 ]. Two HPVs, HPV 16 and 18, stand out for their carcinogenicity and contribute to approximately 70% of all HPV-related cancers worldwide [ 69 – 74 ]. Although most infections resolve spontaneously and the majority of women with infection do not develop cancer, a small proportion of HPV infections will persist and progress to pre-cancer and cancer [ 75 ]. Protective risk factors that reduce the risk of HPV infection and subsequent cancer include consistent condom use [ 76 ], male circumcision [ 77 ], and use of an intrauterine device [ 78 ].
The impact of the estimated contribution of HPV to cancer from an epidemiologic point of view is larger than previously thought. Indeed, HPV infection can be considered a pandemic disease for several reasons [ 79 ]. Firstly, it is universal and widespread, occurring on all continents, in both women and men, among young people and adults, and across most races and socioeconomic groups. Secondly, it is extensive, as it causes a variety of related diseases, both pre-cancerous and cancerous, involving a wide range of anatomic sites. Finally, the epidemiology of HPV is dynamic, as opposed to stable, with increasing rates of infection and disease.
The Role of HPV in Skin Cancer
Some studies suggest that a particular genus, the β HPVs, may play a role in the pathogenesis of NMSC [ 80 ], though this role has not been well studied. However, the association of β HPV infection with NMSC in patients with a very rare, genetically determined condition, epidermodysplasia verruciformis, has been well established [ 81 ]. In stark contrast to α HPV-associated cancers (such as cervical cancer, as discussed above), the presence of β-HPV DNA does not appear to be essential for the maintenance of the malignant phenotype [ 82 ].
Prevention Through Vaccination Strategies
Three HPV vaccines are commercially available including a bivalent form against HPV types 16 and 18, a quadrivalent form against HPV types 6, 11, 16 and 18, and a 9-valent form against types 6, 11, 16, 18, 31, 33, 45, 52 and 58 [ 83 ]. Persistent infection with high-risk HPV types 16 and 18 is responsible for the majority of cervical cancer worldwide, whereas low-risk types 6 and 11 are responsible for most genital warts [ 84 ]. The vaccines are highly efficacious, immunogenic and safe in the prevention of pre- and neoplastic cervical-, vulvar-, vaginal- or anal-related disease in women [ 85 – 87 ]. The quadrivalent HPV vaccine has been shown to be effective against genital warts [ 88 , 89 ] and anal precancerous lesions [ 90 ]. As well as being associated with wart formation, cutaneous papillomaviruses can lead to the development of NMSC, but further research with HPV vaccines is needed to assess their efficacy in preventing NMSC.
Data from multiple countries have shown a clear impact in the reduction of HPV infections and related conditions within a few years of vaccine introduction [ 91 ], and pediatricians, gynecologists, primary healthcare professionals, clinicians, and public health officials, as well as dermatologists, have all played a key role in achieving this wide vaccination coverage.
This article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors.
Acknowledgements
Sponsorship and article processing charges for this supplement were funded by Almirall S.A. This article is based on presentations from the 9th Skin Academy Symposium, April 9–10, 2016, Barcelona, Spain, sponsored by Almirall S.A. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. We thank Dr Laia Bruni for her advice and contribution to this manuscript, on behalf of Dr Castellsagué, upon his passing. All images (figures) provided courtesy of Dorothée Nashan with full patient consent. Medical writing support was provided by Chrissie Kouremenou of Complete Medical Communications, funded by Almirall S.A.
Disclosures
Zoe Apalla has received honoraria from Almirall S.A. and Leo Pharma. Dorothée Nashan has received honoraria from Almirall S.A., BMS, MEDA, MSD, Novartis, and Roche. Richard B Weller has acted as a consultant for AOBiome and Novartis; has been on the Speakers’ Bureaux for Almirall S.A. and Johnson and Johnson; has received honoraria from Johnson and Johnson and Novartis; and is an employee and stockholder of Relaxsol Ltd. Xavier Castellsagué has received occasional honoraria for lecturing from Almirall S.A., Merck, SPMSD, and Vianex, and has received funding for institutional research from Genticel, GSK, Merck, and SPMSD.
Compliance with Ethics Guidelines
This article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors. Informed consent was obtained from all patients for which identifying information is included in this article.
Data Availability
Open access.
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License ( http://creativecommons.org/licenses/by-nc/4.0/ ), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Dr Castellsagué very sadly passed away during the development of this article. However, given his involvement in the preparation and delivery of his presentation at the 9th Skin Academy Symposium, and his initial guidance on the content of this article, he has been included as a posthumous author at the request of his co-authors and Professor Blume-Peytavi.
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/6C47F0600685C21C .
Watch CBS News
Black men have lowest melanoma survival rate compared to other races, study finds
By Sara Moniuszko
Edited By Paula Cohen
Updated on: August 7, 2023 / 7:43 PM EDT / CBS News
Men with melanoma, particularly Black men, are more likely to die than women with melanoma, according to a new study published in the Journal of the American Academy of Dermatology.
Comparing data from the National Cancer Database from 2004 to 2018, the analysis of more than 200,000 people found the 5-year survival rate in men with melanoma was highest for White men, at around 75%, compared to Black men, who ranked the lowest, with a survival rate of 52%. American Indian/Alaskan Native (69%), Asian (68%) and Hispanic (66%) men fell in between.
The study also showed that men of color were more likely to have melanoma diagnosed at an advanced stage, making it more difficult to treat. Even when adjusted for factors like income level and insurance coverage, Black race alone increased mortality risk compared to the White population, the study found.
Melanoma causes more than 9,000 deaths per year in the U.S., according to the Centers for Disease Control and Prevention. CDC data also show rates of male mortality for melanoma, of all races, are more than double that of females of all races.
"We know that men may be less likely to seek medical care than women, so they can be diagnosed with melanoma at later stages," dermatologist and co-author of the study Ashley Wysong, founding chair of the Department of Dermatology at the University of Nebraska Medical Center, said in a news release . "However, even after accounting for later stages at diagnosis, men still have worse overall survival rates than women with melanoma, so we suspect that there are some unmeasured social, genetic, tumor-specific and potentially biological factors at play, such as hormones and the way the immune system responds to melanoma tumors."
Dr. Alix Charles, chairman of dermatology at Duly Health and Care, told CBS News, "Unfortunately Black Americans are less likely to carry private insurance. They're less likely to be able to have access to quality healthcare in their neighborhoods and in their communities."
If detected early, the five-year survival rate for melanoma is 99%, according to the American Cancer Society. But that figure drops down to 32% once the melanoma has spread to other organs.
While it has been known that skin cancer is increasing among all Americans , with specific rises in men and people of color, this is the largest study to date to look specifically at the role of race among men with melanoma.
"We hope our research can lay the foundation for future studies to determine why there's such a gap in survival rates, and to make headway to reduce these survival rate gaps," Wysong said.
Steps to protect yourself from skin cancer
The American Academy of Dermatology says to reduce your risk, wear sunscreen and sun-protective clothing and watch for changes to your skin.
"If you have a spot on your skin that has looked the same your whole life and suddenly the edges might look different or the color changes, if the size changes, that's an important factor," Dr. Maral Kibarian Skelsey, dermatologist and director of the Dermatologic Surgery Center of Washington, previously told CBS News.
It's also recommended that everyone above age 18 get an annual skin examination.
Detroit Lions defensive lineman Josh Paschall was a sophomore playing for the University of Kentucky when he saw a strange mark on the bottom of his foot. It turned out to be a rare form of melanoma, and Paschall needed multiple surgeries and immunotherapy to remove it.
"If you see anything that's abnormal, get that checked out," he told CBS News.
"The thing that's unique about skin cancer — it's so common, but it's also so preventable," Dr. Elizabeth Hale, associate professor of dermatology at NYU Langone and senior vice president of the Skin Cancer Foundation previously told CBS News.
About 90% of skin cancers are associated with sun exposure, which makes protection important, Hale added.
"We recommend a broad spectrum SPF 30 or higher, and it's important to think about sunscreen every single day. It's not just enough when going to the beach or pool because we know that some damage is cumulative," she says. "When you're outside, you want to reapply every two hours — even more if you're sweating or swimming. Getting people to wear it every day is the real goal."
— Errol Barnett contributed reporting.
Sara Moniuszko is a health and lifestyle reporter at CBSNews.com. Previously, she wrote for USA Today, where she was selected to help launch the newspaper's wellness vertical. She now covers breaking and trending news for CBS News' HealthWatch.
More from CBS News

Ferguson officer injured, 5 charged at protest over Michael Brown's death

Ferguson marks 10 years since Michael Brown's death

Indian airline tests feature that lets women book seats not next to men

Dozens dead after Israeli airstrike on Gaza mosque, health ministry says
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
- Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- All Summits
- STATUS List
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
Rising rates of skin cancer: The cost of FDA’s inaction on novel sunscreen products
By Darrell Rigel Aug. 1, 2024

A decade after Sen. Jack Reed (D-R.I.) authored the Sunscreen Innovation Act , which became law in 2014, Americans are still waiting for newer, more effective sunscreen products due to the Food and Drug Administration’s chronic inaction.
Ten years ago, Republicans and Democrats came together to pass this legislation with the promise of overcoming regulatory obstacles and ushering in a new era of sun protection. As Reed stated , “Americans shouldn’t have to wait decades for access to the most advanced, effective sunscreens as they try to better protect themselves from skin cancer.”
advertisement
But the FDA has failed to deliver on that promise. Bureaucratic red tape continues to leave Americans without access to the most innovative sun protection that is widely available to consumers in other parts of the world.
For more than two decades, people across Europe, Asia, and Canada have had access to sunscreens that provide protection against the full spectrum of ultraviolet rays, while older versions here in the U.S. often fail to efficiently block out ultraviolet A (UVA) rays that are known to cause cancer and age the skin. Newer agents also help produce more cosmetically elegant sunscreens that don’t leave a white cast, which encourages people of all skin tones to utilize this lifesaving preventative tool.
Related: In ‘landmark’ study, cell therapy exceeds expectations in melanoma patients
The result of these delays is that skin cancer rates in the U.S. remain stubbornly high . In fact, skin cancer is the most common type of cancer — with more diagnosed in the U.S. than all other cancers combined. The country now has some of the highest skin cancer incidence globally.
One of the most disheartening aspects of these statistics is that it’s one of the few cancers where the direct cause is known, and the risk of developing it can easily be lowered by protection from the sun’s ultraviolet rays. The sun’s UV intensity has also been increasing over the past 20 years , making for an even greater need for better protection.
Despite this, over this past decade of FDA inaction, the U.S. has continued to see one American die every hour from melanoma .
It doesn’t have to be this way. Other countries now empower their citizens with the latest tools to combat rising skin cancer rates, including nearly twice as many sunscreen ingredients that better absorb or block UV radiation. Governments in these countries remain focused on the core issue: protecting the body’s largest organ — skin — against a known carcinogen – UV radiation.
The U.S. somehow has it backward. The FDA has not approved a single new sunscreen ingredient since the 1990s . Instead of approving new ingredients, the agency has befuddlingly chosen to move in the other direction. It insists on testing and retesting existing ingredients that have been used for decades for hypothetical and unproven risks, even though tens of millions of Americans have used sunscreen daily for decades with none of those hypothetical problems ever seen.
In addition, the FDA also relies on tests that lack common sense and bear no resemblance to real-world conditions, like feeding rats sunscreen ingredients and exposing them to levels that any human being wouldn’t reach even after applying sunscreen every day for 277 years.
The FDA needs to return to the facts and real-world evidence. Using sunscreen lowers the risk of getting skin cancer. Nearly all dermatologists agree that sunscreen is safe , and research demonstrates its ability to cut melanoma rates by more than half when used as directed. To put it simply, Americans need better access to the newer safe and effective sunscreens, and not be limited to the products currently available to them.
With one in five Americans being diagnosed with a largely preventable cancer , it is essential to safeguard and increase access to the most effective sun protection available. The FDA needs to align itself with the efforts of the major national medical and scientific organizations to combat skin cancer by advancing — not hindering — innovation that can help save lives.
Darrell Rigel, M.D., is a clinical professor of dermatology at the NYU Grossman School of Medicine, a consultant dermatologist at the Cooper Clinic in Dallas, and the former president of the American Academy of Dermatology, the American Academy of Dermatology Association, the American Society for Dermatologic Surgery, and the American Dermatological Association. These views expressed here are the author’s alone and not necessarily official positions of these organizations.
LETTER TO THE EDITOR
Have an opinion on this essay submit a letter to the editor here ., about the author reprints, darrell rigel.
STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect
To submit a correction request, please visit our Contact Us page .

Recommended

Recommended Stories

Getting to ‘Plan B’ for psychedelic medicine: Lessons from reproductive health

Controlling obesity is a noble goal. Controlling mpox is a far more urgent one

STAT Plus: Health Care's Colossus: How UnitedHealth turned a questionable artery-screening program into a gold mine

STAT Plus: Health Care's Colossus: How UnitedHealth harnesses its physician empire to squeeze profits out of patients

STAT Plus: ‘Jerking families around’: Canceled Roche rare disease trial devastates parents, angers researchers
Meteorin-like protein drains energy from T cells, limiting immune system's power to fight cancer
A protein called Meteorin-like (METRNL) in the tumor microenvironment saps energy from T cells, thereby severely limiting their ability to fight cancer, according to new research directed by investigators at the Johns Hopkins University School of Medicine and the Johns Hopkins Kimmel Cancer Center and its Bloomberg~Kimmel Institute for Cancer Immunotherapy. Finding ways to block the effects of METRNL signaling on tumor-infiltrating T cells may allow these immune cells to regain the energy necessary to eliminate tumors.
A report about the work was published Aug. 6 in the journal Immunity .
METRNL has been described in the medical literature before -- initially as playing a role in helping keep cold or exercising animals (and people) warm by poking holes in the mitochondria (energy factory) of fat cells so they produce heat. However, it had not previously been known to be active in cancer or in T cells, says lead study author Christopher Jackson, M.D., an assistant professor of neurosurgery at Johns Hopkins.
When T cells try to eliminate a tumor, the state of chronic stimulation/stress causes them to secrete METRNL, Jackson explains. Once METRNL is secreted, it interacts with the mitochondria and pokes holes in the electron transport chain, a cluster of proteins participating in a process to create energy. When T cells can no longer keep up with their energy requirements, they stop trying to kill cancer cells, which enables cancer cells to multiply and spread.
"Others have shown that metabolic dysfunction limits T cells' ability to fight cancer, but we are among the first to describe a discrete signaling pathway that causes that to happen," Jackson says. "Most of the previous work has looked at how the lack of specific nutrients in tumors limits a T cell's ability to function. The problem is this is difficult to modify because it's hard to get the right nutrients into a tumor and direct them to T cells. We potentially can do much better by targeting a signaling pathway because we can block it or turn it on or off, but until now, nobody had identified such a pathway that restores the metabolic health of T cells in tumors."
In a series of laboratory investigations, researchers first studied T cells from the tumor tissue and blood of patients with previously untreated brain tumors (glioblastomas), prostate cancer, bladder cancer and renal cell/kidney cancer, and performed RNA sequencing to try to identify genes responsible for dysfunction in the tumor. METRNL was the gene most highly expressed.
Next, they wanted to find out what makes T cells secrete METRNL in the first place, discovering that the reason was chronic stimulation. Normally, the immune system activates when stimulated to fight an infection and then diminishes when that illness resolves. But in the setting of cancer, T cells are chronically stimulated, which causes them to become dysfunctional. METRNL also was found to be secreted by other immune cells in tumors such as macrophages and dendritic cells, but it acts specifically on T cells.
Additional study determined that METRNL acts directly on the mitochondria, and decouples the electron transport chain. As T cells lose energy and start to fail, they increase their attempts to use glucose (natural sugar) as a backup source of energy. But, because the tumor environment is low in glucose, they continue to flounder and eventually die. This is one of the ways that tumors can continue to grow. Deleting METRNL in models of different cancer types in the researchers' investigations universally delayed tumor growth.
Finally, researchers observed that METRNL is activated through a family of transcription factors (proteins that control the rate of transcription of genetic information from DNA to RNA) called E2F, that it is dependent on signaling by a receptor called PPAR delta, and that modulating these factors downstream can block the effects of METRNL.
The next steps are to determine how this can help patients, Jackson says. He and his colleagues are actively working on different means to target the METRNL-E2F-PPAR delta pathway or to combine targeted treatment with other immunotherapies.
"We think that one of the reasons that some current immunotherapies fail is they require more energy from immune cells that already are functioning at decreased capacity," he says. "Blocking the pathway may allow these immunotherapies that maybe have not been effective in the past to be more effective because there will be enough fuel for the T cells to meet that increased demand."
Study co-authors were Ayush Pant, Aanchal Jain, Eli Yazigi, Liang Zhao, Thomas Nirschl, Christina Kochel, Denis Routkevitch, Kisha Patel, Stephany Tzeng, Sarah Neshat, Barbara Smith, Jordan Green, Chetan Bettegowda, Henry Brem and Drew Pardoll of Johns Hopkins. Additional study co-authors who were at Johns Hopkins at the time the research was conducted were Wikum Dinalankara and Luigi Marchionni of Weill Cornell Medicine in New York, Charles Drake of Janssen Research and Michael Lim of Stanford School of Medicine in Palo Alto, California. Other investigators from Stanford and Asan Medical Center in Seoul, South Korea, contributed to the project.
RNA sequencing was supported by grants through the Bristol Myers Squibb International Immuno-Oncology Network and Janssen Pharmaceuticals. Dinalankara and Marchionni were supported by the National Institutes of Health-National Cancer Institute award R01CA200859.
Jackson is a consultant for Egret Therapeutics with equity interests in the company. He is an inventor on a patent filed by The Johns Hopkins University for using immune checkpoint agonists to treat cerebrovascular disorders. He receives research support from Biohaven, InCephalo and Grifols. His work is funded by philanthropy and the Goldhirsh-Yellin Foundation. The Johns Hopkins University has filed a provisional patent on METRNL blockade for cancer treatment, on which Jackson, Pant, Brem and others are inventors.
Additionally, Bettegowda is a consultant for Depuy-Synthes and Bionaut Labs. Brem is a consultant for Perosphere, AsclepiX Therapeutics, StemGen, Accelerating Combination Therapies, Catalio Nexus Fund II LLC, LikeMinds Inc., Acuity Bio Corp., InSightec, Galen Robotics and Nurami Medical. These relationships are managed by The Johns Hopkins University in accordance with its conflict-of-interest policies.
- Brain Tumor
- Prostate Cancer
- Lung Cancer
- Colon Cancer
- Skin Cancer
- Immune System
- Immune system
- Monoclonal antibody therapy
- Prostate cancer
- Renal cell carcinoma
Story Source:
Materials provided by Johns Hopkins Medicine . Note: Content may be edited for style and length.
Journal Reference :
- Christopher M. Jackson, Ayush Pant, Wikum Dinalankara, John Choi, Aanchal Jain, Ryan Nitta, Eli Yazigi, Laura Saleh, Liang Zhao, Thomas R. Nirschl, Christina M. Kochel, Brandon Hwa-Lin Bergsneider, Denis Routkevitch, Kisha Patel, Kwang Bog Cho, Stephany Tzeng, Sarah Y. Neshat, Young-Hoon Kim, Barbara J. Smith, Maria Cecilia Ramello, Elena Sotillo, Xinnan Wang, Jordan J. Green, Chetan Bettegowda, Gordon Li, Henry Brem, Crystal L. Mackall, Drew M. Pardoll, Charles G. Drake, Luigi Marchionni, Michael Lim. The cytokine Meteorin-like inhibits anti-tumor CD8+ T cell responses by disrupting mitochondrial function . Immunity , 2024; DOI: 10.1016/j.immuni.2024.07.003
Cite This Page :
Explore More
- Creating Unique Molecular Building Blocks
- Artificial Compound Eye for Robotic Vision
- Breakthrough in Molecular Control
- Glimpse Into the Nanoworld: New Microscope
- Easy Continual Measurement of Blood Pressure
- Biomaterial Regrows Damaged Cartilage
- Using WiFi Signals as Energy for Electronics
- More Fruits and Veggies for Kidneys and Heart
- Warming: Millions of Years for Plants to Recover
- Enhancing Stem-Cell Transplants
Trending Topics
Strange & offbeat.
Log in to our secure, personalized website to manage your care (formerly myMDAnderson).
Request an Appointment
If you are ready to make an appointment, select a button on the right. If you have questions about MD Anderson’s appointment process, our information page may be the best place to start.
- Donate Today

- Clinical Trials
- Our Doctors
‘How I knew I had inflammatory breast cancer’: 6 survivors' symptoms
August 08, 2024
BY Cynthia DeMarco
Inflammatory breast cancer symptoms tend to appear very quickly.
“At first, patients might complain of a spot-like rash , or of their bra not fitting like it used to or suddenly feeling tight,” explains Bora Lim, M.D.. , a medical oncologist who specializes in the treatment of inflammatory breast cancer . “Then, in a matter of months, weeks or even days, more than half of their breast — or their entire breast — is involved.”
That was the case for Terry Arnold , who was diagnosed with inflammatory breast cancer at age 49.
“For me, the symptoms literally appeared overnight,” recalls the stay-at-home mom of five from Sealy. “I woke up one morning, and it looked as if someone had drawn a circle around my right breast. It was red and puffy and very sudden.”
Swelling and ‘peau d’orange’
One-sided breast swelling is another classic sign of inflammatory breast cancer. So is a subtle dimpling of the skin called “peau d’orange,” named for the surface of orange peel it resembles.
“My left breast was extremely tender one morning,” remembers Jenée Bobbora , who was 32 when she was diagnosed with inflammatory breast cancer. “The skin was pink and very swollen.”
“It just kept getting bigger and more painful,” notes the licensed professional counselor associate from Houston. “And it pitted when squeezed.”
A rash or a change in skin color
A rash or a change in skin color on the breast is another sign of inflammatory breast cancer. But this symptom often gets mistaken for insect bites or contact dermatitis, a type of skin irritation caused by additives in laundry detergent, body lotion and other products.
“I noticed a rash about the size of a quarter on my upper left breast on New Year’s Day,” says Valerie Fraser . “I thought it might be chafing from a new bra.” But four weeks later, after an MRI and biopsy, the retired paralegal from Michigan was diagnosed with inflammatory breast cancer.
“The rash was a very subtle pink and not alarming at all,” she adds. “But the next day, my breast was swollen. And every day after that, it felt thicker and denser. By the ninth or tenth day, my left breast was noticeably larger than my right, and the skin had a dimpled appearance.”
One reason for the discoloration and enlargement is that IBC forms clusters of cells called emboli that can impair circulation.
“That’s why you get the swelling and thickening,” notes Lim. “Emboli block the lymphatic ducts , which normally drain excess fluid from the breast.”
Pain and lumps: the inconsistent inflammatory breast cancer symptoms
Pain and lumps are not always symptoms of inflammatory breast cancer, but they can be. Tiffany Honken , for instance, had pain at both her initial diagnosis at age 49 and when she had a recurrence a few years later.
“I don’t believe I ever had a rash,” says the private home health aide from Nebraska. “But I did have a lump the size of my fist, and my left breast got huge and very red and painful.”
A few years after finishing treatment, Tiffany went to an emergency room because she started feeling pain in her sternum. “I thought I was having a gallbladder attack,” she says.
But a CT scan showed that the inflammatory breast cancer had returned, and it was in her left lung and the lymph nodes around her collar bone.
Nipple inversion
Stephanie Cobb ’s first symptoms of inflammatory breast cancer were a little different. She was still nursing her five-month-old daughter when she was diagnosed at age 35.
“One day, I was pumping breastmilk at work and noticed I wasn’t getting anything out of the left side,” recalls the corporate accountant from Minnesota. “I remember thinking, ‘What’s going on? Am I doing this wrong?’ But the right side was totally normal. My left breast kept getting harder and harder, and a few months later, the nipple inverted. Shortly after that, I noticed a rash, and my breast developed a leathery texture.”
‘Red flag’ inflammatory breast cancer symptoms: nipple inversion and sudden nodules
Nipple inversion is one of two inflammatory breast cancer symptoms that Lim says warrants an immediate call to your doctor.
“It’s totally normal for someone’s breasts to vary in size and shape from one side to the other,” she notes. “But nipples usually look the same. So, any significant architectural change, such as a sudden shifting to one side or an inversion, is a big red flag.”
The other “red flag” IBC symptom is a lump or a nodule popping up around your neck, collar bone or armpit.
“Those can be signs that the breast cancer has already spread to nearby lymph nodes ,” explains Lim, “so you really need to insist on having imaging done in those two situations.”
JoAnn Hill found a hard spot in her left arm pit when she was diagnosed at age 33. She first noticed it on her honeymoon, about six months before her diagnosis.
“But I didn’t find out that’s what it was until I had a biopsy ,” says the IT operations manager from Cypress, Texas. “My left breast had gotten so big overnight that I literally couldn’t wear any bra I owned. Other changes included redness and peau d’orange. The skin also felt thicker and very warm to the touch.”
When to push for a second opinion
Inflammatory breast cancer is frequently misdiagnosed as mastitis, clogged milk ducts, and abscesses, among other things. But a quick and accurate diagnosis is essential because the disease is also very aggressive.
“Inflammatory breast cancer is advanced by its very nature,” notes Lim. “Even at its earliest, it’s already considered at least stage III .”
That’s why Lim strongly recommends having an alternate plan in place if you suspect you might have inflammatory breast cancer but get told it’s something else.
“If your symptoms improve significantly after you’re prescribed antibiotics or steroids , it’s very unlikely you had cancer,” says Lim. “But talk to your provider about scheduling a diagnostic mammogram or ultrasound, or even a breast biopsy , before starting the medication. You don’t want to wait any longer for an accurate diagnosis, if you see no changes in your symptoms after two weeks.”
Request an appointment at MD Anderson online or call 1-877-632-6789.
My left breast got huge and very red and painful.
Tiffany Honken
Share Your Story
Coronavirus precautions, help #endcancer, donate blood.
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.

IMAGES
COMMENTS
The Skin SPORE program's main focus is on melanoma research activities, but it also includes projects in other skin cancer types, such as cutaneous T-cell lymphoma. NCI's National Clinical Trials Network (NCTN) is a collection of organizations and clinicians that coordinates and supports cancer clinical trials at more than 3,000 sites across ...
Skin cancer can involve melanocytes, leading to melanoma, but there are other non-melanoma skin cancers. These include basal cell carcinoma, squamous cell carcinoma and, less commonly, Merkel cell ...
Study Adds to Debate about Screening for Melanoma. Posted: May 4, 2022. Regular skin cancer screening leads to many diagnoses of very early-stage melanomas, results from a new study suggest. The results add to a debate about whether screening is fueling an overdiagnosis of melanoma in the United States. Opdualag Becomes First FDA-Approved ...
Melanoma skin cancer death rates have dropped steeply because of advances in treatment. Melanoma accounts for only about 1% of skin cancers but causes a large majority of skin cancer deaths. About 99,780 Americans are expected to be diagnosed with melanoma in 2022. About 7,650 are expected to die from it.
According to the annual status report from the International Agency for Research on Cancer, there were approximately 9.6 million cancer-related fatalities and 18.1 million new instances of cancer globally in 2018. ... Skin cancer progression involves a complex interplay of genetic, molecular, and environmental factors that lead to the ...
This paper presents a detailed systematic review of deep learning techniques for the early detection of skin cancer. Research papers published in well-reputed journals, relevant to the topic of skin cancer diagnosis, were analyzed. Research findings are presented in tools, graphs, tables, techniques, and frameworks for better understanding.
1. Introduction. Skin cancer is one of the most common types of malignancy in the United States and the world, with rising incidence [1,2].It is estimated that one out of five Americans will develop skin cancer by the age of 70, with Caucasians displaying the highest incidence [].Non-melanoma skin cancer (NMSC), including basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), is the ...
A systematic evaluation of the value of AI-based decision support in skin tumor diagnosis demonstrates the superiority of human-computer collaboration over each individual approach and supports ...
The biology and treatment of Merkel cell carcinoma: current understanding and research priorities. Merkel cell carcinoma (MCC) is a rare and aggressive form of nonmelanoma skin cancer. The ...
This editorial initiative of particular relevance, led by Dr. Vladimir Spiegelman and Dr. Mohammad Athar, Specialty Chief Editors of the Skin Cancer section, is focused on new insights, novel developments, current challenges, latest discoveries, recent advances, and future perspectives in the field of Skin Cancer. The Research Topic solicits ...
Our current researchers. Investigating a new molecule. Professor Victoria Sanz-Moreno is investigating a particular molecule called ROCK in melanoma. She is looking at how ROCK works as cancer grows, spreads and becomes resistant to treatments. This will suggest whether it is a good target for future melanoma treatments. Learn more about Prof ...
The goal of this special edition Research Topic is to shed light on the progress made in the past decade in the Skin Cancer field, and on its future challenges to provide a thorough overview of the field. This article collection will inspire, inform and provide direction and guidance to researchers in the field.Manuscripts consisting solely of ...
Research into the causes, prevention, detection, and treatment of basal and squamous cell skin cancer is going on in many medical centers throughout the world. Basic skin cancer research Scientists have made a great deal of progress in recent years in learning how ultraviolet (UV) light damages the DNA (genes) inside normal skin cells, and how ...
Causes and prevention Sunlight and ultraviolet (UV) radiation. Some research suggests there are 2 main ways that exposure to UV rays is linked to melanoma, but there is likely some overlap.. The first link is to sun exposure as a child and teenager. People with melanoma often have an early history of sunburns or other intense sun exposures, although not everyone does.
Our research is saving lives. Today, 9 in 10 people diagnosed with malignant melanoma (the most serious type of skin cancer) survive their disease for 10 years or more. Advances like immunotherapy have brought hope to many people with advanced skin cancer, but there is still much more to do for people whose cancers don't respond to these ...
This Research Topic addresses novel clinical, translational, and basic research on Immunology and Immunotherapy of Skin Cancer. Despite significant progress, challenges remain, such as understanding resistance mechanisms and managing immune-related adverse events. Ongoing research aims to identify new targets, refine existing therapies, and ...
Skin cancer has been the leading type of cancer worldwide. Melanoma and non-melanoma skin cancers are now the most common types of skin cancer that have been reached to epidemic proportion. Based on the rapid prevalence of skin cancers, and lack of efficient drug delivery systems, it is essential to surge the possible ways to prevent or cure ...
We suggest focusing future research on skin cancer epidemiology on the following areas, accounting for the information gaps that have been identified to facilitate comparisons across studies and populations (1) establish standardized reporting guidelines for skin cancer prevalence and incidence rates; (2) conduct additional research on the ...
An interesting short report described an inverse association between Alzheimer's disease and both melanoma and non-melanoma skin cancer in a large urban patient population. 5 Regarding the mechanisms of this descriptive finding, the authors speculate about the effect of pathways promoting survival and favouring cancer contrary to pathways ...
The Skin Cancer Foundation's position statements on controversial topics with supporting evidence-based research studies. The Skin Cancer Foundation receives many questions about sun protection and skin cancer prevention. The safety of certain sunscreen ingredients, the link between indoor tanning and skin cancer, and the role of vitamin D are ...
By Deb Balzer. Skin cancer is the most common cancer in the U.S., affecting millions worldwide. This cancer comes in two main types: melanoma, which is less common but more deadly, and nonmelanoma skin cancers, which include basa l cell carcinoma and squamous cell carcinoma. Collin Costello, M.D., a Mayo Clinic dermatologist, says these nonmelanoma skin cancers are more prevalent - and with ...
Skin cancer occurs when skin cells are damaged by ultraviolet (UV) rays from repeated sun exposure and sunburns. Exposure to UV radiation from tanning beds and sunlamps can also increase skin cancer risk. The two most common skin cancers are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). They are slow-growing and seldom spread to ...
Summary. Skin cancers are the most common groups of cancers diagnosed worldwide, with more than 1.5 million new cases estimated in 2022. In 2022, an estimated 330 000 new cases of melanoma were diagnosed worldwide and almost 60 000 people died from the disease. There are large geographical variations in melanoma incidence rates across countries ...
Basal and squamous cell skin cancers are the most common forms of skin cancer and are not tracked by cancer registries. Melanoma is the least common but most serious form of skin cancer, and it is ...
In the study researchers found that even before treatment began in their test subjects, the activity of genes controlling the production of spleen tyrosine kinases predicted 83% of melanoma ...
Overall Skin Cancer . Skin cancer, including both malignant melanoma (MM) and non-melanoma skin cancer (NMSC), represents the most common malignancy in Caucasians [1-10].The incidence of both MM and NMSC is on the rise, with an annual increase in MM of 0.6% among adults over 50 years [].The estimated number of new cases of skin melanoma in 2016 is 76,380, which represents 4.5% of all new ...
Black men at higher risk of dying from skin cancer, study finds 01:54. Men with melanoma, particularly Black men, are more likely to die than women with melanoma, according to a new study ...
A decade after Sen. Jack Reed (D-R.I.) authored the Sunscreen Innovation Act, which became law in 2014, Americans are still waiting for newer, more effective sunscreen products due to the Food and ...
A protein called Meteorin-like (METRNL) in the tumor microenvironment saps energy from T cells, thereby severely limiting their ability to fight cancer, according to new research directed by ...
Inflammatory breast cancer symptoms tend to appear very quickly. "At first, patients might complain of a spot-like rash, or of their bra not fitting like it used to or suddenly feeling tight," explains Bora Lim, M.D.., a medical oncologist who specializes in the treatment of inflammatory breast cancer.. "Then, in a matter of months, weeks or even days, more than half of their breast ...