

The top 10 journal articles of 2020
In 2020, APA’s 89 journals published more than 5,000 articles—the most ever and 25% more than in 2019. Here’s a quick look at the 10 most downloaded to date.
Vol. 52 No. 1 Print version: page 24

1. Me, My Selfie, and I: The Relations Between Selfie Behaviors, Body Image, Self-Objectification, and Self-Esteem in Young Women
Veldhuis, j., et al..
Young women who appreciate their bodies and consider them physical objects are more likely to select, edit, and post selfies to social media, suggests this study in Psychology of Popular Media (Vol. 9, No. 1). Researchers surveyed 179 women, ages 18 to 25, on how often they took selfies, how they selected selfies to post, how often they used filters and editing techniques, and how carefully they planned their selfie postings. They also assessed participants’ levels of body appreciation and dissatisfaction, self-objectification, and self-esteem. Higher levels of self-objectification were linked to more time spent on all selfie behaviors, while body appreciation was related to more time spent selecting selfies to post, but not frequency of taking or editing selfies. Body dissatisfaction and self-esteem were not associated with selfie behaviors. DOI: 10.1037/ppm0000206
2. A Closer Look at Appearance and Social Media: Measuring Activity, Self-Presentation, and Social Comparison and Their Associations With Emotional Adjustment
Zimmer-gembeck, m. j., et al..
This Psychology of Popular Media (online first publication) article presents a tool to assess young people’s preoccupation with their physical appearance on social media. Researchers administered a 21-item survey about social media to 281 Australian high school students. They identified 18 items with strong inter-item correlation centered on three categories of social media behavior: online self-presentation, appearance-related online activity, and appearance comparison. In a second study with 327 Australian university students, scores on the 18-item survey were found to be associated with measures of social anxiety and depressive symptoms, appearance-related support from others, general interpersonal stress, coping flexibility, sexual harassment, disordered eating, and other factors. The researchers also found that young women engaged in more appearance-related social media activity and appearance comparison than did young men. DOI: 10.1037/ppm0000277
3. The Novel Coronavirus (COVID-2019) Outbreak: Amplification of Public Health Consequences by Media Exposure
Garfin, d. r., et al..
Repeated media exposure to the COVID-19 pandemic may be associated with psychological distress and other public health consequences, according to this commentary in Health Psychology (Vol. 39, No. 5). The authors reviewed research about trends in health behavior and psychological distress as a response to media coverage of crises, including terrorist attacks, school shootings, and disease outbreaks. They found that repeated media exposure to collective crises was associated with increased anxiety and heightened acute and post-traumatic stress, with downstream effects on health outcomes such as new incidence of cardiovascular disease. Moreover, misinformation can further amplify stress responses and lead to misplaced or misguided health-protective and help-seeking behaviors. The authors recommended public health agencies use social media strategically, such as with hashtags, to keep residents updated during the pandemic. They also urged the public to avoid sensationalism and repeated coverage of the same information. DOI: 10.1037/hea0000875
4. Barriers to Mental Health Treatment Among Individuals With Social Anxiety Disorder and Generalized Anxiety Disorder
Goetter, e. m., et al..
This study in Psychological Services (Vol. 17, No. 1) indicates that 3 in 4 people who suffer from anxiety do not receive proper care. Researchers recruited 226 participants in the United States who were previously diagnosed with social anxiety disorder or generalized anxiety disorder and assessed their symptom severity and asked them to self-report any barriers to treatment. Shame and stigma were the highest cited barriers, followed by logistical and financial barriers and not knowing where to seek treatment. Participants with more severe symptoms reported more barriers to treatment than those with milder symptoms. Racial and ethnic minorities reported more barriers than racial and ethnic majorities even after controlling for symptom severity. The researchers called for increased patient education and more culturally sensitive outreach to reduce treatment barriers. DOI: 10.1037/ser0000254
5. The Construction of “Critical Thinking”: Between How We Think and What We Believe
This History of Psychology (Vol. 23, No. 3) article examines the emergence of “critical thinking” as a psychological concept. The author describes how, between World War I and World War II in the United States, the concept emerged out of growing concerns about how easily people’s beliefs could be changed and was constructed in a way that was independent of what people believed. The author delves into how original measurements of critical thinking avoided assumptions about the accuracy of specific real-world beliefs and details how subsequent critical thinking tests increasingly focused on logical abilities, often favoring outcome (what we believe) over process (how we think). DOI: 10.1037/hop0000145
6. Treatment of Alcohol Use Disorder: Integration of Alcoholics Anonymous and Cognitive Behavioral Therapy
Breuninger, m. m., et al..
This article in Training and Education in Professional Psychology (Vol. 14, No. 1) details how to work with alcohol use disorder patients who are participating in both cognitive behavioral therapy (CBT) and Alcoholics Anonymous (AA). The authors point to distinctions between AA and CBT: The goal of AA is total abstinence and the primary therapeutic relationship is with a peer in recovery, while CBT takes a less absolute approach and the primary relationship is with a psychotherapist. The authors also point to commonalities: both approaches emphasize identifying and replacing dysfunctional beliefs and place value in social support. The authors recommend clinicians and trainees become more educated about AA and recommend a translation of the 12-step language into CBT terminology to bridge the gap. DOI: 10.1037/tep0000265
7. Positivity Pays Off: Clients’ Perspectives on Positive Compared With Traditional Cognitive Behavioral Therapy for Depression
Geschwind, n., et al..
Positive cognitive behavioral therapy, a version of CBT focused on exploring exceptions to the problem rather than the problem itself, personal strengths, and embracing positivity, works well to counter depressive symptoms and build well-being, according to this study in Psychotherapy (Vol. 57, No. 3). Participants received a block of eight sessions of traditional CBT and a block of eight sessions of positive CBT. Researchers held in-depth interviews with 12 of these participants. Despite initial skepticism, most participants reported preferring positive CBT but indicated experiencing a steeper learning curve than with traditional CBT. Researchers attributed positive CBT’s favorability to four factors: feeling empowered, benefiting from effects of positive emotions, learning to appreciate baby steps, and rediscovering optimism as a personal strength. DOI: 10.1037/pst0000288
8. Targeted Prescription of Cognitive-Behavioral Therapy Versus Person-Centered Counseling for Depression Using a Machine Learning Approach
Delgadillo, j., & gonzalez salas duhne, p..
Amachine learning algorithm can identify which patients would derive more benefit from cognitive behavioral therapy (CBT) versus counseling for depression, suggests research in this Journal of Consulting and Clinical Psychology (Vol. 88, No. 1) article. Researchers retrospectively explored data from 1,085 patients in the United Kingdom treated with either CBT or counseling for depression and discovered six patient characteristics—age, employment status, disability, and three diagnostic measures of major depression and social adjustment—relevant to developing an algorithm for prescribing the best approach. The researchers then used the algorithm to determine which therapy would work best for an additional 350 patients with depression. They found that patients receiving their optimal treatment type were twice as likely to improve significantly. DOI: 10.1037/ccp0000476
9. Traumatic Stress in the Age of COVID-19: A Call to Close Critical Gaps and Adapt to New Realities
Horesh, d., & brown, a. d..
This article in Psychological Trauma: Theory, Research, Practice, and Policy (Vol. 12, No. 4) argues that COVID-19 should be examined from a post-traumatic stress perspective. The authors call for mental health researchers and clinicians to develop better diagnoses and prevention strategies for COVID-related traumatic stress; create guidelines and talking points for the media and government officials to use when speaking to an anxious, and potentially traumatized, public; and provide mental health training to professionals in health care, education, childcare, and occupational support in order to reach more people. DOI: 10.1037/tra0000592
10. Emotional Intelligence Predicts Academic Performance: A Meta-Analysis
Maccann, c., et al..
Students with high emotional intelligence get better grades and score higher on standardized tests, according to the research presented in this article in Psychological Bulletin (Vol. 146, No. 2). Researchers analyzed data from 158 studies representing more than 42,529 students—ranging in age from elementary school to college—from 27 countries. The researchers found that students with higher emotional intelligence earned better grades and scored higher on achievement tests than those with lower emotional intelligence. This finding was true even when controlling for intelligence and personality factors, and the association held regardless of age. The researchers suggest that students with higher emotional intelligence succeed because they cope well with negative emotions that can harm academic performance; they form stronger relationships with teachers, peers, and family; and their knowledge of human motivations and socialinteractions helps them understand humanities subject matter. DOI: 10.1037/bul0000219
5 interviews to listen to now
Psychology’s most innovative thinkers are featured on APA’s Speaking of Psychology podcast , which highlights important research and helps listeners apply psychology to their lives. The most popular episodes of 2020, as measured by the number of downloads in the first 30 days, were:
- How to have meaningful dialogues despite political differences , with Tania Israel, PhD
- Canine cognition and the survival of the friendliest , with Brian Hare, PhD
- The challenges faced by women in leadership , with Alice Eagly, PhD
- How to choose effective, science-based mental health apps , with Stephen Schueller, PhD
- Psychedelic therapy , with Roland Griffiths, PhD
Listen to all of the Speaking of Psychology episodes .
Contact APA
You may also like.
Science News
These are the most-read science news stories of 2020.

When squeezed to high pressure between two diamonds (shown), a material made of carbon, sulfur and hydrogen can transmit electricity without resistance at room temperature. The discovery ranked among Science News ' most popular in 2020.
Adam Fenster
Share this:
By Cassie Martin
December 31, 2020 at 8:00 am
Science News drew over 22 million visitors to our website this year. Our COVID-19 coverage was most popular. Here’s a recap of the other most-read news stories and long reads of 2020.
Top news stories
1. In a first, a person’s immune system fought HIV — and won
Scientists analyzed billions of cells from two people with HIV who don’t require medication to keep the virus under control. What the team found was astonishing: One person had no working copies of HIV in any of the cells, while the other person had just one working copy. What’s more, that one copy was imprisoned in tightly wound DNA.
2. The first room-temperature superconductor has finally been found
Up to 15° Celsius, a material made of carbon, sulfur and hydrogen can conduct electricity without resistance. While the room-temperature superconductor works only at high pressures, the discovery brings scientists a step closer to realizing a more energy-efficient future .
3. Astronomers have found the edge of the Milky Way at last
Computer simulations and observations of nearby galaxies have revealed that the Milky Way stretches 1.9 million light-years across. The measurement could help tease out how massive the galaxy is and exactly how many galaxies orbit it .
4. More ‘murder hornets’ are turning up. Here’s what you need to know
An invasion of Asian giant hornets into North America could spell trouble for honeybees. But the threat that the world’s largest hornet species poses to people is minimal .
5. A star orbiting the Milky Way’s black hole validates Einstein
The odd orbit of a star around the supermassive black hole at the Milky Way’s center confirms Albert Einstein’s general theory of relativity. Rather than tracing out a single ellipse, the star’s orbit rotates over time — the result of the black hole warping spacetime .
Favorite visualization
“ A new 3-D map illuminates the ‘little brain’ within the heart ” ( SN: 6/2/20 ) enthralled online readers. An unprecedented view of the heart’s nerve cell cluster could help scientists better understand what those cells do and perhaps lead to targeted therapies for heart diseases.

Top feature stories
1. After the Notre Dame fire, scientists get a glimpse at the cathedral’s origins
A fire that ripped through Paris’ Notre Dame cathedral in April 2019 gave scientists the opportunity to dig into the cathedral’s history and study the building’s materials , including to learn more about climate change.
2. New fleets of private satellites are clogging the night sky
SpaceX and other private companies are planning to launch thousands of internet satellites into orbit around Earth. Hundreds of the satellites already in outer space are obstructing the view of ground-based telescopes and interfering with astronomers’ research .
3. It’s time to stop debating how to teach kids to read and follow the evidence
Research has identified the most effective approaches for teaching children how to read. Those findings could help resolve a long-standing debate that pits phonics against methods that emphasize understanding the meaning of words .
4. To fight discrimination, the U.S. census needs a different race question
The U.S. census has failed to accurately count certain minority groups. As a result, some sociologists are calling for more nuanced census questions that better reflect how respondents view themselves, as well as how society views them — a clearer metric for measuring discrimination .
5. What lifestyle changes will shrink your carbon footprint the most?
Individual actions around shelter, transportation and food can create ripple effects in society to help mitigate the effects of climate change. But to have the most impact, people need to tailor their efforts to their own circumstances .
Pandemic post
Science News has reported on the COVID-19 pandemic since it began, but none of those stories were included in our most-read lists of 2020. That’s because we think the coverage is in a league of its own.
Stories about when, during an infection, the coronavirus is most contagious and debunking the claim that the virus was made in a lab are among our most-read stories of all time. Readers also were drawn to stories about how the coronavirus spreads and COVID-19 vaccines .
As Feedback editor, I review every e-mail we receive from Science News readers. In 2020, more than a third of the thousands of e-mails that filled our inbox were about COVID-19. Hunger for information, for certainty in an uncertain time, has been insatiable.
We’ve strived to answer readers’ pandemic-related questions accurately, given the rapid pace of scientific research into the coronavirus and its effects. Some of those questions have been featured in the pages of this magazine, as well as in the Science News Coronavirus Update newsletter — a weekly e-mail that highlights the latest research, data and articles on the coronavirus and COVID-19.
Everyone at Science News thanks you, our readers, for your sharp, insightful comments and your continued support. We look forward to answering your many science questions, coronavirus-related and not, in the year ahead.
“ Radiation measurement could help guide lengthy lunar missions ” ( SN: 11/7/20, p. 5 ) incorrectly stated that the average daily exposure to cosmic radiation on the moon is 1.5 million times as high as the average daily exposure on Earth. The average daily exposure on the moon is 1,500 times as high as the average daily exposure on Earth.
Subscribers, enter your e-mail address for full access to the Science News archives and digital editions.
Not a subscriber? Become one now .
2020 year in review: Highlights from our publishing
Top 10 lists of most popular insights, overall top 10 for the year, mckinsey quarterly, mckinsey global institute, editors’ picks, diversity & inclusion, marketing, consumer, and retail, organization, strategy & corporate finance, sustainability.

A tale of 2020 in 20 McKinsey charts

Twenty images that offer a lens on 2020
Top reports this year.

Women in the Workplace 2022

State of Fashion report archive (2017-2023)
McKinsey’s Global Banking Annual Review archive: 2014 to 2022

Diversity wins: How inclusion matters

How executives can help sustain value creation for the long term

McKinsey’s Private Markets Annual Review: 2017 to 2022
New features this year, we are mckinsey, the mckinsey crossword, mckinsey’s annual reading list, 2020 favorites from gen z colleagues, new experiences this year, what now decisive actions to emerge stronger in the next normal, mckinsey for kids, do you know your life’s purpose, popular special collections this year.

The Next Normal: Emerging stronger from the coronavirus pandemic
COVID Response Center

McKinsey and the World Economic Forum

McKinsey on Books

The graduate’s guide to the world of work
Popular podcasts this year.
In this year of lockdowns, listeners tuned in to reflect and learn—how to be more productive, more inclusive, and more resilient in the face of adversity. Here are some of our most streamed podcasts of 2020.
Listen to more McKinsey Podcasts

Uncovering the state of fashion

The future of air travel

The mass personalization of change: Large-scale impact, one individual at a time

Building a business within a business: How to power continual organic growth

Getting the measure of corporate Asia

Meet Generation Z: Shaping the future of shopping
Newsletters.
The editors of our four most-read email newsletters and multimedia series chose their favorite issues of the year to share with you. Whether daily, weekly, or monthly, our newsletter offerings span functional, industry, and news-based topics—and we’re adding more in 2021.
The Shortlist
The Next Normal

The Five Fifty
Popular webinars from mckinsey live.
The COVID-19 pandemic has created and exacerbated countless challenges for leaders, organizations, and communities. In our most popular McKinsey Live webinars, McKinsey experts brought these issues to the forefront and offered perspectives on navigating beyond the crisis to shape the next normal.
Learn more about McKinsey Live
New at McKinsey blog: 2020 year in review
Mckinsey global institute: twelve highlights from our 2020 research, covid response center’s year in review.

Building a stronger, more inclusive US workforce

Leading voices on the pandemic

The emotional toll of COVID-19
Acknowledgments.
McKinsey Global Publishing would like to thank, first and foremost, the many authors of these articles and other insights for their contributions and analysis.
And we want to acknowledge the many direct contributors who offered vital energy and expertise—under extraordinary personal and professional circumstances—to the development, editing, risk review, copyediting, fact checking, data visualization, design, production, and dissemination of all of McKinsey’s content over the past year.
McKinsey Global Publishing
Raju Narisetti
Global Editorial Director
Lucia Rahilly
Julia Arnous, Diane Brady, Richard Bucci, Lang Davison, Tom Fleming, Roberta Fusaro, Eileen Hannigan, Heather Hanselman, Justine Jablonska, Bill Javetski, Jason Li, Cait Murphy, Josh Rosenfield, Astrid Sandoval, David Schwartz, Daniella Seiler, Mark Staples, Rick Tetzeli, Barbara Tierney, and Monica Toriello
Digital innovation and audience development
Nicole Adams, Heather Andrews, Mike Borruso, Sherri Capers, Torea Frey, Mary Halpin, Eleni Kostopoulos, and Philip Mathew
Vanessa Burke, Heather Byer, Nancy Cohn, Roger Draper, Drew Holzfeind, Julie Macias, LaShon Malone, Pamela Norton, Kanika Punwani, and Sarah Thuerk
Visual storytelling
Victor Cuevas, Nicole Esquerre, Richard Johnson, Maya Kaplun, Stephen Landau, Janet Michaud, Matthew Perry, Dan Redding, Jonathon Rivait, Dan Spector, and Nathan Wilson
Editorial and digital production
Michael Allen, Matt Baumer, Elana Brown, Andrew Cha, Paromita Ghosh, Gwyn Herbein, Chris Konnari, Milva Mantilla, Katrina Parker, Charmaine Rice, Dana Sand, Katie Shearer, Venetia Simcock, Chandan Srivastava, Sean Stebner, Sneha Vats, Pooja Yadav, and Belinda Yu
Social media/video
Devin Brown, Chelsea Bryan, Mona Hamouly, Lauren Holmes, Simon London, Puneet Mishra, Kathleen O’Leary, Elizabeth Schaub, and Rita Zonius
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
December 22, 2020
2020 Research Highlights — Promising Medical Findings
Results with potential for enhancing human health.
With NIH support, scientists across the United States and around the world conduct wide-ranging research to discover ways to enhance health, lengthen life, and reduce illness and disability. Groundbreaking NIH-funded research often receives top scientific honors. In 2020, these honors included one of NIH’s own scientists and another NIH-supported scientist who received Nobel Prizes . Here’s just a small sample of the NIH-supported research accomplishments in 2020.
Full 2020 NIH Research Highlights List
20200929-covid.jpg

New approaches to COVID-19
As the global pandemic unfolded, researchers worked at unprecedented speed to develop new treatments and vaccines. Scientists studied antibodies from the blood of people who recovered from COVID-19 and identified potent, diverse ones that neutralize SARS-CoV-2 . Some antibody treatments have now been given emergency use authorization by the FDA, with many others in development . However, such antibodies—called monoclonal antibodies—are difficult to produce and must be given intravenously. NIH-researchers have been pursuing other approaches, including using antibodies from llamas , which are only about a quarter of the size of a typical human antibody and could be delivered directly to the lungs using an inhaler. Computer-designed “miniproteins” and other antiviral compounds are also under investigation.
20200622-mosquito.jpg

Universal mosquito vaccine tested
Most mosquito bites are harmless. But some mosquitoes carry pathogens, like bacteria and viruses, that can be deadly. A small trial showed that a vaccine against mosquito saliva—designed to provide broad protection against mosquito-borne diseases—is safe and causes a strong immune response in healthy volunteers. More studies are needed to test its effectiveness against specific diseases.
20201006-knee-stock.jpg

Machine learning detects early signs of osteoarthritis
Osteoarthritis is the most common type of arthritis. It results when cartilage, the tissue that cushions the ends of the bones, breaks down. People with osteoarthritis can have joint pain, stiffness, and swelling. Some develop serious pain and disability from the disease. Using artificial intelligence and MRI scans, scientists identified signs of osteoarthritis three years before diagnosis. The results suggest a way to identify people who may benefit from early interventions.
20201103-eye.jpg

Advances in restoring vision
Several common eye diseases, such as age-related macular degeneration and retinitis pigmentosa, damage the retina, the light-sensitive tissue in the eye. They can eventually lead to vision loss. Two studies looked at ways to restore vision in mouse models. Researchers reprogrammed skin cells into light-sensing eye cells that restored sight in mice. The technique may lead to new approaches for modeling and treating eye diseases. Other scientists restored vision in blind mice by using gene therapy to add a novel light-sensing protein to cells in the retina. The therapy will soon be tested in people.
20200107-aging.jpg

Blood protein signatures change across lifespan
The bloodstream touches all the tissues of the body. Because of the constant flow of proteins through the body, some blood tests measure specific proteins to help diagnose diseases. Researchers determined that the levels of nearly 400 proteins in the blood can be used to determine people’s age and relative health. More research is needed to understand if these protein signatures could help identify people at greater risk of age-related diseases.
20201027-hiv-thumb.jpg

Understanding HIV’s molecular mechanisms
More than a million people nationwide are living with HIV, the virus that causes AIDS. HIV attacks the immune system by destroying immune cells vital for fighting infection. Researchers uncovered key steps in HIV replication by reconstituting and watching events unfold outside the cell. The system may be useful for future studies of these early stages in the HIV life cycle. In other work, experimental treatments in animal models of HIV led to the viruses emerging from their hiding places inside certain cells—a first step needed to make HIV vulnerable to the immune system.
20200225-parkinsons.jpg
Test distinguishes Parkinson’s disease from related condition
A protein called alpha-synuclein plays a major role in Parkinson’s disease as well as other brain disorders. Early symptoms of Parkinson’s disease and another disease involving alpha-synuclein, multiple system atrophy, can be similar. Researchers created a test using cerebrospinal fluid that can distinguish between these two diseases with 95% accuracy. The results have implications for the early diagnosis and treatment of these conditions and may help in the development of new targeted therapies.
20200114-cream.jpg

Understanding allergic reactions to skin care products
Personal care products like makeup, skin cream, and fragrances commonly cause rashes called allergic contact dermatitis. It’s not well understood how chemical compounds in personal care products trigger such allergic reactions. Scientists gained new insight into how personal care products may cause immune responses that lead to allergic responses in some people. Understanding how compounds in these products trigger immune reactions could lead to new ways to prevent or treat allergic contact dermatitis.
Connect with Us
- More Social Media from NIH
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Older Adults and the Mental Health Effects of COVID-19
- 1 McLean Hospital, Belmont, Massachusetts
- 2 Harvard Medical School, Boston, Massachusetts
- 3 University of California, San Diego, La Jolla
- 4 University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
- Viewpoint Mental Health Disorders Related to COVID-19–Related Deaths Naomi M. Simon, MD, MSc; Glenn N. Saxe, MD; Charles R. Marmar, MD JAMA
- Viewpoint Addressing the Long-term Effects of the COVID-19 Pandemic on Children and Families Tumaini R. Coker, MD, MBA; Tina L. Cheng, MD, MPH; Marci Ybarra, MSW, PhD JAMA
- Viewpoint The Mental Health Consequences of COVID-19 and Physical Distancing Sandro Galea, MD; Raina M. Merchant, MD; Nicole Lurie, MD JAMA Internal Medicine
- Viewpoint Meeting the Care Needs of Older Adults Isolated at Home During the COVID-19 Pandemic Michael A. Steinman, MD; Laura Perry, MD; Carla M. Perissinotto, MD, MHS JAMA Internal Medicine
- Original Investigation Delirium in Older Patients With COVID-19 Presenting to the Emergency Department Maura Kennedy, MD, MPH; Benjamin K. I. Helfand, MSc; Ray Yun Gou, MA; Sarah L. Gartaganis, MSW, MPH; Margaret Webb, BA; J. Michelle Moccia, DNP, ANP-BC, GS-C; Stacey N. Bruursema, LMSW-C; Belinda Dokic, MHA; Brigid McCulloch, DO; Hope Ring, MD; Justin D. Margolin, BS; Ellen Zhang, BA; Robert Anderson, MD; Rhonda L. Babine, MS, APRN, ACNS-BC; Tammy Hshieh, MD, MPH; Ambrose H. Wong, MD, MSEd; R. Andrew Taylor, MD, MHS; Kathleen Davenport, MD; Brittni Teresi, BA; Tamara G. Fong, MD, PhD; Sharon K. Inouye, MD, MPH JAMA Network Open
- Viewpoint The Coronavirus Disease 2019 (COVID-19) Outbreak and Mental Health Doron Amsalem, MD; Lisa B. Dixon, MD; Yuval Neria, PhD JAMA Psychiatry
As the coronavirus disease 2019 (COVID-19) began to spread in the US in early 2020, older adults experienced disproportionately greater adverse effects from the pandemic including more severe complications, higher mortality, concerns about disruptions to their daily routines and access to care, difficulty in adapting to technologies like telemedicine, and concerns that isolation would exacerbate existing mental health conditions. Older adults tend to have lower stress reactivity, and in general, better emotional regulation and well-being than younger adults, 1 but given the scale and magnitude of the pandemic, there was concern about a mental health crisis among older adults. The concern pertained to older adults both at home and in residential care facilities, where contact with friends, family, and caregivers became limited. The early data suggest a much more nuanced picture. This Viewpoint summarizes evidence suggesting that, counter to expectation, older adults as a group may be more resilient to the anxiety, depression, and stress-related mental health disorders characteristic of younger populations during the initial phase of the COVID-19 pandemic.
Approximately 8 months into the pandemic, multiple studies have indicated that older adults may be less negatively affected by mental health outcomes than other age groups. In August 2020, the Centers for Disease Control and Prevention (CDC) published a survey, conducted June 24-30, 2020, of 5412 community-dwelling adults across the US, 2 noting that the 933 participants aged 65 years or older reported significantly lower percentages of anxiety disorder (6.2%), depressive disorder (5.8%), or trauma- or stress-related disorder (TSRD) (9.2%) than participants in younger age groups. According to the report, of the 731 participants aged 18 through 24 years, 49.1% reported anxiety disorder; 52.3%, depressive disorder; and 46%, TSRD. Of the 1911 participants aged 25 through 44 years, 35.3% reported anxiety disorder; 32.5%, depressive disorder; and 36% for TSRD. Of the 895 participants aged 45 through 64 years, 16.1% reported anxiety disorder; 14.4%, depressive disorder; and 17.2%, TSRD. Older adults, compared with other age groups, also reported lower rates of new or increased substance use and suicidal ideation in the preceding 30 days, with rates of 3% and 2%, respectively.
These findings are similar to other reports from high-income countries. A cross-sectional study involving 3840 community-dwelling older adults aged 18 through 80 years from Spain noted that older age (60-80 years) compared with younger age (40-59 years) was associated with lower rates of anxiety, depression, and posttraumatic stress disorder (PTSD). 3 In this study, women had higher prevalence of anxiety, PTSD, and depressive symptoms than men. A study involving 776 community-dwelling US and Canadian adults who used a 7-day daily diary to track affect and stress found that older adults (>60 years; n = 193), compared with younger adults (18-39 years; n = 330) and middle-aged adults (40-59 years; n = 253) had less negative affect and more positive affect and more often reported positive daily events than the younger groups, despite similar level of perceived stress. 4 A longitudinal study involving 1679 community-dwelling older adults (65-102 years) in the Netherlands found that although loneliness increased after the pandemic, mental health levels remained unchanged before and after the start of the pandemic. 5
There are several caveats to consider about these data. The findings represent the experience during the first few months of the pandemic. The longer-term effects of COVID-19, especially in countries like the US with very high rates of disease, remain unclear. Long-term population-level stressors can increase the rates of mental health conditions such as prolonged grief disorder, depression, and anxiety. Positive short-term outcomes among older adults at the population level may not necessarily capture the heterogeneity of outcomes at the level of individuals or circumscribed communities or environments (eg, nursing homes, assisted living facilities). According to the CDC report, 2 even though older adults may have better mental health outcomes than expected, those from underrepresented minorities or with lower household incomes or who are serving as unpaid caregivers are at disproportionally elevated risk of experiencing negative health outcomes. The currently available data also do not provide perspectives on subgroups of older adults like those with dementia, those caring for persons with dementia, or those residing in assisted living facilities or nursing homes. The effect of comorbid chronic medical or psychiatric conditions also remains unclear thus far.
Despite these caveats, the early findings suggest higher resilience to the mental health effects of COVID-19 at least in a proportion of community-dwelling older adults. This resilience may reflect an interaction among internal factors (eg, biological stress response, cognitive capacity, personality traits, physical health) and external resources (eg, social status, financial stability). 6
Much of the initial concern related to how older adults would respond to COVID-19 was based on how loneliness and isolation would be exacerbated as lockdown measures were implemented. The negative influence of loneliness among older adults has been well documented. However, this reaction might have been partially countered by a range of coping mechanisms. In a mixed-methods study involving 73 older adults 7 (mean age, 69.2 years) with known depression or anxiety who had demonstrated resilience (ie, no worsening of symptoms) 2 months after the start of the pandemic, investigators noted that study participants appeared to withstand the influence of isolation, especially with social connectedness and access to mental health care. However, despite this early resilience, older adults expressed concerns about their longer-term physical and financial well-being.
A cross-sectional study of 515 community-dwelling adults (20-79 years) in the US noted that the use of proactive precautionary measures such as avoiding people who cough, unnecessary travel, and use of public transportation or public places 8 was associated with lower COVID-related anxiety among older adults. The quality rather than the number of social connections may also be a factor. Thus, for older adults experiencing isolation, having more close or meaningful relationships may be protective, rather than just having more interactions with others. 5 Maintaining these connections during the pandemic may require better ability to use technology to connect with loved ones.
An additional factor to consider is wisdom, a complex personality trait comprised of specific components, including prosocial behaviors like empathy and compassion, emotional regulation, the ability to self-reflect, decisiveness while accepting uncertainty and diversity of perspectives, social advising, and spirituality. 9 Several recent studies involving various groups of people across the adult lifespan (25-≥100 years) have shown a significant inverse correlation between loneliness and wisdom, based on validated scales for measuring these constructs. The component of wisdom that is correlated most strongly (and inversely) with loneliness is compassion. Other data also suggest that enhancing compassion may reduce loneliness and promote greater well-being. 10 Cross-sectional studies show higher levels of wisdom, especially the compassion component, in older than in younger adults. Additional studies are needed to shed more light on risk and protective factors as well as the nature of mediating and moderating relationships among these factors with respect to the mental health consequences of COVID-19 among older adults. There should also be more longitudinal studies on mental health trajectories among specific high-risk populations like older individuals in assisted living facilities and nursing homes.
The data from various studies contrast the numerous personal stories about how difficult the pandemic has been for the older population. This divergence likely represents the heterogeneity that is a hallmark of aging. Also, resilience captured at the population level may not translate to individuals in specific circumstances. Thus far, there is not a clear understanding of which risk factors and protective factors are the strongest determinants of mental health outcomes, although these may vary from person to person.
Many older adults do not have the resources required to deal with the stress of COVID-19. This may include material (eg, lack of access to smart technology), social (eg, few family members or friends), or cognitive or biological (eg, inability to engage in physical exercise or participate in activities or routines) resources. Clinicians and caregivers must estimate resource availability and consider how the absence of resources can be mitigated for a given individual and family. Of particular importance is the role of technology, which has emerged as an important factor for maintaining social connection as well as accessing mental health services.
Moreover, clinicians must recognize the importance of nonpharmacological approaches, which are more effective than pharmacotherapy in the treatment of chronic stress, anxiety, and prolonged grief. Such approaches include manualized therapies such as cognitive behavior therapy, as well as promoting physical activity, greater connectedness, compassion training, and engaging in spirituality as appropriate. These approaches have also been shown to enhance coping, promote resilience, and reduce loneliness. 9
The great pandemic of 2020 has been a unique stressor that has affected communities all around the world. Yet it is noteworthy that some individual studies from different countries have shown that at least some older adults are not experiencing disproportionately increased negative mental health consequences commensurate with the elevated risks they faced during the first few months of the COVID-19 pandemic. Understanding the factors and mechanisms that drive this resilience can guide intervention approaches for other older people and for other groups whose mental health may be more severely affected— eg, increasing components of wisdom like emotional regulation, empathy, and compassion. 10 It would also be useful to consider how technology may be leveraged to this end. However, it is critical to recognize that these apparently positive early findings notwithstanding, careful monitoring and additional research will be needed to understand the psychological and mental health effects of the ongoing COVID-19 pandemic among the older population.
Corresponding Author: Ipsit V. Vahia, MD, McLean Hospital, 115 Mill St, Mail Stop 234, Belmont, MA 02478 ( [email protected] ; [email protected] ).
Published Online: November 20, 2020. doi:10.1001/jama.2020.21753
Conflict of Interest Disclosures: Drs Vahia and Reynolds reported receiving honorarium, respectively, as editor and editor in chief of the American Journal of Geriatric Psychiatry . Dr Jeste reported receiving a stipend as editor-in-chief of International Psychogeriatrics . No other disclosures were reported.
Additional Contributions: We thank Hailey Cray, BA, McLean Hospital, Belmont, Massachusetts, for her assistance in preparing this manuscript, for which she received no compensation.
See More About
Vahia IV , Jeste DV , Reynolds CF. Older Adults and the Mental Health Effects of COVID-19. JAMA. 2020;324(22):2253–2254. doi:10.1001/jama.2020.21753
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Durvalumab Extends Lives of People with Early-Stage Small Cell Lung Cancer
June 25, 2024 , by Nadia Jaber
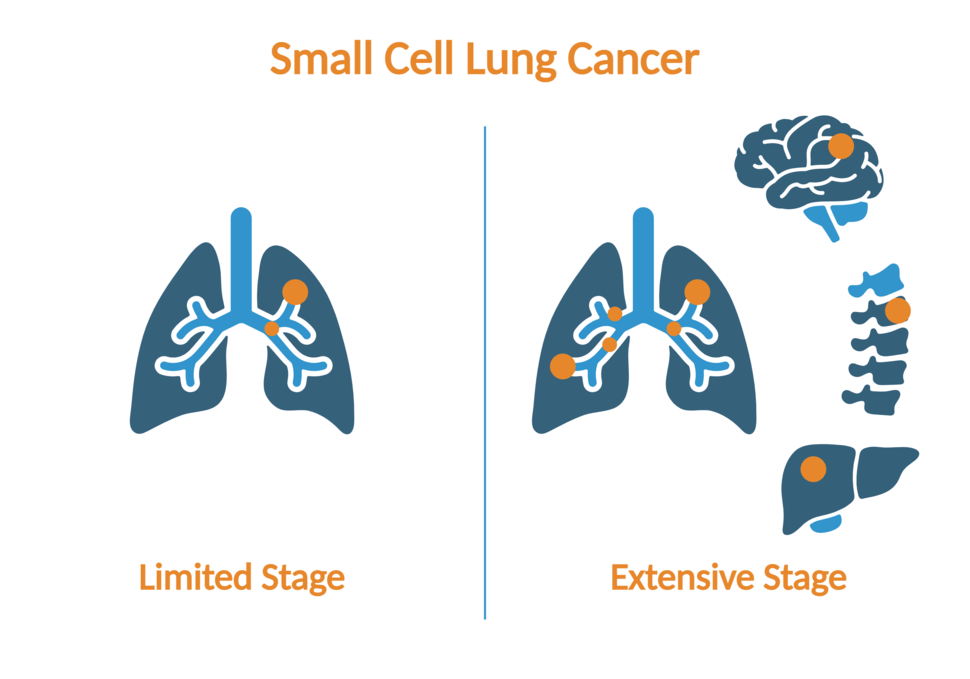
A clinical trial has shown that durvalumab (Imfinzi) helps people with limited-stage small cell lung cancer live longer. Durvalumab is already used to treat people with extensive-stage small cell lung cancer.
The immunotherapy drug durvalumab (Imfinzi) helped people with early-stage small cell lung cancer live longer, according to initial results from a large clinical trial. Durvalumab is a type of immunotherapy called an immune checkpoint inhibitor .
The standard initial treatment for early-stage (also called limited-stage) small cell lung cancer—cancer that is confined to one lung or one side of the chest—is chemotherapy and radiation given at the same time. Although this treatment tends to work well at first, the cancer often comes back quickly, at which point it has typically spread throughout the body.
“There really have not been any major advances in the treatment of limited-stage small cell lung cancer for several decades,” said the study’s leader, David Spigel, M.D., of Sarah Cannon Research Institute in Nashville, Tennessee.
In the new trial, dubbed ADRIATIC, more than 500 people with limited-stage small cell lung cancer who had finished chemotherapy and radiation were randomly assigned to receive durvalumab or a placebo for up to 2 years.
People who received durvalumab stayed in remission longer and lived substantially longer than those treated with placebo. Three years after starting the treatment, 57% of people in the durvalumab group were still alive , compared with 48% in the placebo group, Dr. Spigel reported at the annual meeting of the American Society of Clinical Oncology on June 2.
“The ADRIATIC trial is a landmark study and provides a new standard of care for patients with early-stage small cell lung cancer,” said Lauren Byers, M.D., professor of thoracic head and neck medical oncology at the University of Texas MD Anderson Cancer Center, at a press briefing where the study was discussed. Dr. Byers was not involved in the trial.
The findings are “definitely practice changing,” said Anish Thomas, M.D., of NCI’s Center for Cancer Research , who studies small cell lung cancer but wasn’t involved in the new trial.
“This is really encouraging for patients as well as people who are working on this cancer,” Dr. Thomas said.
Durvalumab extends overall survival and progression-free survival
Small cell lung cancer grows quickly and often spreads beyond the lungs before it is even diagnosed. While targeted therapies have had less success for small cell than for non-small cell lung cancer, immunotherapy is a somewhat different story.
Over the past 5 years, durvalumab and two other immunotherapies— atezolizumab (Tecentriq) and tarlatamab (Imdelltra) —have been approved for the treatment of people with advanced, or extensive-stage, small cell lung cancer.
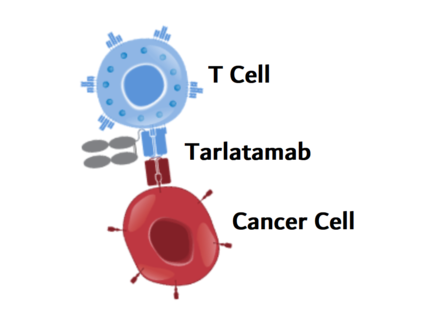
New Immunotherapy Drug Shows Promise for Small Cell Lung Cancer
In an early-stage clinical trial, tarlatamab shrank tumors that had progressed after previous treatments.
Spurred by the improvements seen with durvalumab for extensive-stage small cell lung cancer and non-small cell lung cancer, Dr. Spigel and his colleagues launched the ADRIATIC trial to see if durvalumab could improve outcomes of people with limited-stage small cell lung cancer.
All participants in the trial had cancer that had responded to standard chemotherapy and radiation.
Durvalumab was given after the standard treatment to help kill any leftover cancer cells—a strategy known as consolidation therapy . The trial was funded by AstraZeneca, the company that makes durvalumab.
Participants in the durvalumab group lived longer without their cancer growing back. Two years after the start of the trial, 46% of those in the durvalumab group and 34% in the placebo group didn’t have any sign of the cancer returning.
Durvalumab also extended the median overall survival by nearly 2 years, Dr. Spigel noted, from 33 months with placebo to 56 months with durvalumab.
That is in stark contrast to the magnitude of benefit seen in extensive-stage small cell lung cancer, Dr. Thomas emphasized. In that setting, atezolizumab and durvalumab each extended median overall survival by only 2 or 3 months, he explained.
“ADRIATIC is the first phase 3 study to establish the role of immunotherapy in [treating] limited-stage small cell lung cancer,” Dr. Spigel concluded.
However, the findings haven’t yet been peer-reviewed—meaning, evaluated for scientific quality and accuracy by other experts in the field.
Side effects of durvalumab consolidation therapy
Durvalumab, which is given every 4 weeks as an infusion, didn’t cause any unexpected side effects, Dr. Spigel noted. The side effects were typical of those seen with durvalumab and other immunotherapies, which rev up the immune system.
In particular, those in the durvalumab group experienced inflammatory conditions in the lungs, skin, and thyroid. Serious immune-related side effects occurred in 5% of people in the durvalumab group and 2% of those in the placebo group.
Durvalumab can also cause a serious and sometimes fatal lung inflammation called pneumonitis . This condition also develops frequently in people who have just received chest radiation, like the patients in this study.
In the ADRIATIC trial, 38% of people in the durvalumab group and 30% of those in the placebo group developed pneumonitis, including one participant in the durvalumab group who died of pneumonitis.
About a quarter of participants in both groups experienced a serious side effect of any kind. Side effects led 16% of patients in the durvalumab group and 11% of those in the placebo group to stop the treatment.
Next steps for small cell lung cancer research
The ADRIATIC trial is ongoing and more will be learned about durvalumab treatment, Dr. Spigel said.
In addition, another arm of the trial is evaluating the combination of durvalumab and another immunotherapy drug, tremelimumab (Imjudo) . Results from that group of 200 patients are still being collected.
Drug Combination Shrinks Small Cell Lung Cancers
When given together, topotecan and berzosertib produced lasting responses in some patients.
In the meantime, small cell lung cancer researchers are already thinking about what questions to investigate next.
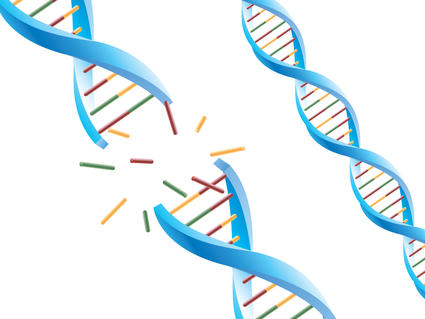
“One important next step will be to understand who is benefitting the most from the addition of durvalumab and how we can start thinking about personalizing treatment for the different subtypes of small cell lung cancer,” Dr. Byers said.
Like many other kinds of cancer, small cell lung cancer can be separated into subtypes based on the molecular characteristics of the cancer cells, she explained. Some subtypes are more easily recognized by cancer-killing immune cells and may have better responses to immunotherapy, she added.
As for Dr. Thomas, his mind is on earlier detection because most small cell lung cancers are found when the disease is already widespread. If more of these cancers could be found when the disease is at an early stage, he said, patients could potentially get more benefit from durvalumab treatment.
The challenge is that low-dose CT scans , which are used to screen people at risk for lung cancer, don’t pick up small cell lung cancers early enough.
“Can we come up with methods to identify small cell [lung cancer] earlier than CT scans [can]?” Dr. Thomas asked. Given the recent progress with blood tests for early cancer detection , he said he’s hopeful that such a test will someday be developed for small cell lung cancer.
Featured Posts
June 5, 2024, by Linda Wang
May 3, 2024, by Carmen Phillips
May 1, 2024, by Edward Winstead
- Biology of Cancer
- Cancer Risk
- Childhood Cancer
- Clinical Trial Results
- Disparities
- FDA Approvals
- Global Health
- Leadership & Expert Views
- Screening & Early Detection
- Survivorship & Supportive Care
- February (6)
- January (6)
- December (7)
- November (6)
- October (7)
- September (7)
- February (7)
- November (7)
- October (5)
- September (6)
- November (4)
- September (9)
- February (5)
- October (8)
- January (7)
- December (6)
- September (8)
- February (9)
- December (9)
- November (9)
- October (9)
- September (11)
- February (11)
- January (10)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Dementia prevention, intervention, and care: 2020 report of the Lancet Commission
Gill livingston.
a Division of Psychiatry, University College London, London, UK
d Camden and Islington NHS Foundation Trust, London, UK
Jonathan Huntley
Andrew sommerlad.
f National Ageing Research Institute and Academic Unit for Psychiatry of Old Age, University of Melbourne, Royal Melbourne Hospital, Parkville, VIC, Australia
Clive Ballard
g University of Exeter, Exeter, UK
Sube Banerjee
h Faculty of Health: Medicine, Dentistry and Human Sciences, University of Plymouth, Plymouth, UK
Carol Brayne
i Cambridge Institute of Public Health, University of Cambridge, Cambridge, UK
Alistair Burns
j Department of Old Age Psychiatry, University of Manchester, Manchester, UK
Jiska Cohen-Mansfield
k Department of Health Promotion, School of Public Health, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
l Heczeg Institute on Aging, Tel Aviv University, Tel Aviv, Israel
m Minerva Center for Interdisciplinary Study of End of Life, Tel Aviv University, Tel Aviv, Israel
Claudia Cooper
Sergi g costafreda.
n Department of Preventive and Social Medicine, Goa Medical College, Goa, India
b Dementia Research Centre, UK Dementia Research Institute, University College London, London, UK
o Institute of Neurology, National Hospital for Neurology and Neurosurgery, University College London Hospitals NHS Foundation Trust, London, UK
Laura N Gitlin
p Center for Innovative Care in Aging, Johns Hopkins University, Baltimore, MA, USA
Robert Howard
Helen c kales.
r Department of Psychiatry and Behavioral Sciences, UC Davis School of Medicine, University of California, Sacramento, CA, USA
Mika Kivimäki
c Department of Epidemiology and Public Health, University College London, London, UK
Eric B Larson
s Kaiser Permanente Washington Health Research Institute, Seattle, WA, USA
Adesola Ogunniyi
t University College Hospital, Ibadan, Nigeria
Vasiliki Orgeta
Karen ritchie.
u Inserm, Unit 1061, Neuropsychiatry: Epidemiological and Clinical Research, La Colombière Hospital, University of Montpellier, Montpellier, France
v Centre for Clinical Brain Sciences, University of Edinburgh, Edinburgh, UK
Kenneth Rockwood
w Centre for the Health Care of Elderly People, Geriatric Medicine Dalhousie University, Halifax, NS, Canada
Elizabeth L Sampson
e Barnet, Enfield, and Haringey Mental Health Trust, London, UK
Quincy Samus
q Department of Psychiatry and Behavioral Sciences, Johns Hopkins University, Baltimore, MA, USA
Lon S Schneider
x Department of Psychiatry and the Behavioural Sciences and Department of Neurology, Keck School of Medicine, Leonard Davis School of Gerontology of the University of Southern California, Los Angeles, CA, USA
Geir Selbæk
y Norwegian National Advisory Unit on Ageing and Health, Vestfold Hospital Trust, Tønsberg, Norway
z Institute of Clinical Medicine, Faculty of Medicine, University of Oslo, Oslo, Norway
aa Geriatric Department, Oslo University Hospital, Oslo, Norway
ab Department Psychosocial and Community Health, School of Nursing, University of Washington, Seattle, WA, USA
Naaheed Mukadam
Associated data, executive summary.
The number of older people, including those living with dementia, is rising, as younger age mortality declines. However, the age-specific incidence of dementia has fallen in many countries, probably because of improvements in education, nutrition, health care, and lifestyle changes. Overall, a growing body of evidence supports the nine potentially modifiable risk factors for dementia modelled by the 2017 Lancet Commission on dementia prevention, intervention, and care: less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, and low social contact. We now add three more risk factors for dementia with newer, convincing evidence. These factors are excessive alcohol consumption, traumatic brain injury, and air pollution. We have completed new reviews and meta-analyses and incorporated these into an updated 12 risk factor life-course model of dementia prevention. Together the 12 modifiable risk factors account for around 40% of worldwide dementias, which consequently could theoretically be prevented or delayed. The potential for prevention is high and might be higher in low-income and middle-income countries (LMIC) where more dementias occur.
Our new life-course model and evidence synthesis has paramount worldwide policy implications. It is never too early and never too late in the life course for dementia prevention. Early-life (younger than 45 years) risks, such as less education, affect cognitive reserve; midlife (45–65 years), and later-life (older than 65 years) risk factors influence reserve and triggering of neuropathological developments. Culture, poverty, and inequality are key drivers of the need for change. Individuals who are most deprived need these changes the most and will derive the highest benefit.
Policy should prioritise childhood education for all. Public health initiatives minimising head injury and decreasing harmful alcohol drinking could potentially reduce young-onset and later-life dementia. Midlife systolic blood pressure control should aim for 130 mm Hg or lower to delay or prevent dementia. Stopping smoking, even in later life, ameliorates this risk. Passive smoking is a less considered modifiable risk factor for dementia. Many countries have restricted this exposure. Policy makers should expedite improvements in air quality, particularly in areas with high air pollution.
We recommend keeping cognitively, physically, and socially active in midlife and later life although little evidence exists for any single specific activity protecting against dementia. Using hearing aids appears to reduce the excess risk from hearing loss. Sustained exercise in midlife, and possibly later life, protects from dementia, perhaps through decreasing obesity, diabetes, and cardiovascular risk. Depression might be a risk for dementia, but in later life dementia might cause depression. Although behaviour change is difficult and some associations might not be purely causal, individuals have a huge potential to reduce their dementia risk.
In LMIC, not everyone has access to secondary education; high rates of hypertension, obesity, and hearing loss exist, and the prevalence of diabetes and smoking are growing, thus an even greater proportion of dementia is potentially preventable.
Amyloid-β and tau biomarkers indicate risk of progression to Alzheimer's dementia but most people with normal cognition with only these biomarkers never develop the disease. Although accurate diagnosis is important for patients who have impairments and functional concerns and their families, no evidence exists to support pre-symptomatic diagnosis in everyday practice.
Our understanding of dementia aetiology is shifting, with latest description of new pathological causes. In the oldest adults (older than 90 years), in particular, mixed dementia is more common. Blood biomarkers might hold promise for future diagnostic approaches and are more scalable than CSF and brain imaging markers.
Wellbeing is the goal of much of dementia care. People with dementia have complex problems and symptoms in many domains. Interventions should be individualised and consider the person as a whole, as well as their family carers. Evidence is accumulating for the effectiveness, at least in the short term, of psychosocial interventions tailored to the patient's needs, to manage neuropsychiatric symptoms. Evidence-based interventions for carers can reduce depressive and anxiety symptoms over years and be cost-effective.
Keeping people with dementia physically healthy is important for their cognition. People with dementia have more physical health problems than others of the same age but often receive less community health care and find it particularly difficult to access and organise care. People with dementia have more hospital admissions than other older people, including for illnesses that are potentially manageable at home. They have died disproportionately in the COVID-19 epidemic. Hospitalisations are distressing and are associated with poor outcomes and high costs. Health-care professionals should consider dementia in older people without known dementia who have frequent admissions or who develop delirium. Delirium is common in people with dementia and contributes to cognitive decline. In hospital, care including appropriate sensory stimulation, ensuring fluid intake, and avoiding infections might reduce delirium incidence.
Key messages
- • New evidence supports adding three modifiable risk factors—excessive alcohol consumption, head injury, and air pollution—to our 2017 Lancet Commission on dementia prevention, intervention, and care life-course model of nine factors (less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, and infrequent social contact).
- • Modifying 12 risk factors might prevent or delay up to 40% of dementias.
- • Prevention is about policy and individuals. Contributions to the risk and mitigation of dementia begin early and continue throughout life, so it is never too early or too late. These actions require both public health programmes and individually tailored interventions. In addition to population strategies, policy should address high-risk groups to increase social, cognitive, and physical activity; and vascular health.
- • Aim to maintain systolic BP of 130 mm Hg or less in midlife from around age 40 years (antihypertensive treatment for hypertension is the only known effective preventive medication for dementia).
- • Encourage use of hearing aids for hearing loss and reduce hearing loss by protection of ears from excessive noise exposure.
- • Reduce exposure to air pollution and second-hand tobacco smoke.
- • Prevent head injury.
- • Limit alcohol use, as alcohol misuse and drinking more than 21 units weekly increase the risk of dementia.
- • Avoid smoking uptake and support smoking cessation to stop smoking, as this reduces the risk of dementia even in later life.
- • Provide all children with primary and secondary education.
- • Reduce obesity and the linked condition of diabetes. Sustain midlife, and possibly later life physical activity.
- • Addressing other putative risk factors for dementia, like sleep, through lifestyle interventions, will improve general health.
- • Many risk factors cluster around inequalities, which occur particularly in Black, Asian, and minority ethnic groups and in vulnerable populations. Tackling these factors will involve not only health promotion but also societal action to improve the circumstances in which people live their lives. Examples include creating environments that have physical activity as a norm, reducing the population profile of blood pressure rising with age through better patterns of nutrition, and reducing potential excessive noise exposure.
- • Dementia is rising more in low-income and middle-income countries (LMIC) than in high-income countries, because of population ageing and higher frequency of potentially modifiable risk factors. Preventative interventions might yield the largest dementia reductions in LMIC.
For those with dementia, recommendations are:
- • Post-diagnostic care for people with dementia should address physical and mental health, social care, and support. Most people with dementia have other illnesses and might struggle to look after their health and this might result in potentially preventable hospitalisations.
- • Specific multicomponent interventions decrease neuropsychiatric symptoms in people with dementia and are the treatments of choice. Psychotropic drugs are often ineffective and might have severe adverse effects.
- • Specific interventions for family carers have long-lasting effects on depression and anxiety symptoms, increase quality of life, are cost-effective and might save money.
Acting now on dementia prevention, intervention, and care will vastly improve living and dying for individuals with dementia and their families, and thus society.

Introduction
Worldwide around 50 million people live with dementia, and this number is projected to increase to 152 million by 2050, 1 rising particularly in low-income and middle-income countries (LMIC) where around two-thirds of people with dementia live. 1 Dementia affects individuals, their families, and the economy, with global costs estimated at about US$1 trillion annually. 1
We reconvened the 2017 Lancet Commission on dementia prevention, intervention, and care 2 to identify the evidence for advances likely to have the greatest impact since our 2017 paper and build on its work. Our interdisciplinary, international group of experts presented, debated, and agreed on the best available evidence. We adopted a triangulation framework evaluating the consistency of evidence from different lines of research and used that as the basis to evaluate evidence. We have summarised best evidence using, where possible, good- quality systematic reviews, meta-analyses, or individual studies, where these add important knowledge to the field. We performed systematic literature reviews and meta-analyses where needed to generate new evidence for our analysis of potentially modifiable risk factors for dementia. Within this framework, we present a narrative synthesis of evidence including systematic reviews and meta-analyses and explain its balance, strengths, and limitations. We evaluated new evidence on dementia risk in LMIC; risks and protective factors for dementia; detection of Alzheimer's disease; multimorbidity in dementia; and interventions for people affected by dementia.
Nearly all the evidence is from studies in high-income countries (HIC), so risks might differ in other countries and interventions might require modification for different cultures and environments. This notion also underpins the critical need to understand the dementias related to life-course disadvantage—whether in HICs or LMICs.
Our understanding of dementia aetiology is shifting. A consensus group, for example, has described hippocampal sclerosis associated with TDP-43 proteinopathy, as limbic-predominant age-related TDP-43 encephalopathy (LATE) dementia, usually found in people older than 80 years, progressing more slowly than Alzheimer's disease, detectable at post-mortem, often mimicking or comorbid with Alzheimer's disease. 3 This situation reflects increasing attention as to how clinical syndromes are and are not related to particular underlying pathologies and how this might change across age. More work is needed, however, before LATE can be used as a valid clinical diagnosis.
The fastest growing demographic group in HIC is the oldest adults, those aged over 90 years. Thus a unique opportunity exists to focus on both human biology, in this previously rare population, as well as on meeting their needs and promoting their wellbeing.
Prevention of dementia
The number of people with dementia is rising. Predictions about future trends in dementia prevalence vary depending on the underlying assumptions and geographical region, but generally suggest substantial increases in overall prevalence related to an ageing population. For example, according to the Global Burden of Diseases, Injuries, and Risk Factors Study, the global age-standardised prevalence of dementia between 1990 and 2016 was relatively stable, but with an ageing and bigger population the number of people with dementia has more than doubled since 1990. 4
However, in many HIC such as the USA, the UK, and France, age-specific incidence rates are lower in more recent cohorts compared with cohorts from previous decades collected using similar methods and target populations 5 ( figure 1 ) and the age-specific incidence of dementia appears to decrease. 6 All-cause dementia incidence is lower in people born more recently, 7 probably due to educational, socio-economic, health care, and lifestyle changes. 2 , 5 However, in these countries increasing obesity and diabetes and declining physical activity might reverse this trajectory. 8 , 9 In contrast, age-specific dementia prevalence in Japan, South Korea, Hong Kong, and Taiwan looks as if it is increasing, as is Alzheimer's in LMIC, although whether diagnostic methods are always the same in comparison studies is unclear. 5 , 6 , 7

Incidence rate ratio comparing new cohorts to old cohorts from five studies of dementia incidence 5
IIDP Project in USA and Nigeria, Bordeaux study in France, and Rotterdam study in the Netherlands adjusted for age. Framingham Heart Study, USA, adjusted for age and sex. CFAS in the UK adjusted for age, sex, area, and deprivation. However, age-specific dementia prevalence is increasing in some other countries. IID=Indianapolis–Ibadan Dementia. CFAS=Cognitive Function and Ageing Study. Adapted from Wu et al, 5 by permission of Springer Nature.
Modelling of the UK change suggests a 57% increase in the number of people with dementia from 2016 to 2040, 70% of that expected if age-specific incidence rates remained steady, 10 such that by 2040 there will be 1·2 million UK people with dementia. Models also suggest that there will be future increases both in the number of individuals who are independent and those with complex care needs. 6
In our first report, the 2017 Commission described a life-course model for potentially modifiable risks for dementia. 2 Life course is important when considering risk, for example, obesity and hypertension in midlife predict future dementia, but both weight and blood pressure usually fall in later life in those with or developing dementia, 9 so lower weight and blood pressure in later life might signify illness, not an absence of risk. 11 , 12 , 13 , 14 We consider evidence on other potential risk factors and incorporate those with good quality evidence in our model.
Figure 2 summarises possible mechanisms of protection from dementia, some of which involve increasing or maintaining cognitive reserve despite pathology and neuropathological damage. There are different terms describing the observed differential susceptibility to age-related and disease-related changes and these are not used consistently. 15 , 16 A consensus paper defines reserve as a concept accounting for the difference between an individual's clinical picture and their neuropathology. It, divides the concept further into neurobiological brain reserve (eg, numbers of neurones and synapses at a given timepoint), brain maintenance (as neurobiological capital at any timepoint, based on genetics or lifestyle reducing brain changes and pathology development over time) and cognitive reserve as adaptability enabling preservation of cognition or everyday functioning in spite of brain pathology. 15 Cognitive reserve is changeable and quantifying it uses proxy measures such as education, occupational complexity, leisure activity, residual approaches (the variance of cognition not explained by demographic variables and brain measures), or identification of functional networks that might underlie such reserve. 15 , 16 , 17 , 18 , 19 , 20

Possible brain mechanisms for enhancing or maintaining cognitive reserve and risk reduction of potentially modifiable risk factors in dementia
Early-life factors, such as less education, affect the resulting cognitive reserve. Midlife and old-age risk factors influence age-related cognitive decline and triggering of neuropathological developments. Consistent with the hypothesis of cognitive reserve is that older women are more likely to develop dementia than men of the same age, probably partly because on average older women have had less education than older men. Cognitive reserve mechanisms might include preserved metabolism or increased connectivity in temporal and frontal brain areas. 17 , 18 , 19 , 20 , 21 People in otherwise good physical health can sustain a higher burden of neuropathology without cognitive impairment. 22 Culture, poverty, and inequality are important obstacles to, and drivers of, the need for change to cognitive reserve. Those who are most deprived need these changes the most and will derive the highest benefit from them.
Smoking increases air particulate matter, and has vascular and toxic effects. 23 Similarly air pollution might act via vascular mechanisms. 24 Exercise might reduce weight and diabetes risk, improve cardiovascular function, decrease glutamine, or enhance hippocampal neurogenesis. 25 Higher HDL cholesterol might protect against vascular risk and inflammation accompanying amyloid-β (Aβ) pathology in mild cognitive impairment. 26
Dementia in LMIC
Numbers of people with dementia in LMIC are rising faster than in HIC because of increases in life expectancy and greater risk factor burden. We previously calculated that nine potentially modifiable risk factors together are associated with 35% of the population attributable fraction (PAFs) of dementia worldwide: less education, high blood pressure, obesity, hearing loss, depression, diabetes, physical inactivity, smoking, and social isolation, assuming causation. 2 Most research data for this calculation came from HIC and there is a relative absence of specific evidence of the impact of risk factors on dementia risk in LMIC, particularly from Africa and Latin America. 27
Calculations considering country-specific prevalence of the nine potentially modifiable risk factors indicate PAF of 40% in China, 41% in India and 56% in Latin America with the potential for these numbers to be even higher depending on which estimates of risk factor frequency are used. 28 , 29 Therefore a higher potential for dementia prevention exists in these countries than in global estimates that use data predominantly from HIC. If not currently in place, national policies addressing access to education, causes and management of high blood pressure, causes and treatment of hearing loss, socio-economic and commercial drivers of obesity, could be implemented to reduce risk in many countries. The higher social contact observed in the three LMIC regions provides potential insights for HIC on how to influence this risk factor for dementia. 30 We could not consider other risk factors such as poor health in pregnancy of malnourished mothers, difficult births, early life malnutrition, survival with heavy infection burdens alongside malaria and HIV, all of which might add to the risks in LMIC.
Diabetes is very common and cigarette smoking is rising in China while falling in most HIC. 31 A meta-analysis found variation of the rates of dementia within China, with a higher prevalence in the north and lower prevalence in central China, estimating 9·5 million people are living with dementia, whereas a slightly later synthesis estimated a higher prevalence of around 11 million. 30 , 32 These data highlight the need for more focused work in LMIC for more accurate estimates of risk and interventions tailored to each setting.
Specific potentially modifiable risk factors for dementia
Risk factors in early life (education), midlife (hypertension, obesity, hearing loss, traumatic brain injury, and alcohol misuse) and later life (smoking, depression, physical inactivity, social isolation, diabetes, and air pollution) can contribute to increased dementia risk ( table 1 ). Good evidence exists for all these risk factors although some late-life factors, such as depression, possibly have a bidirectional impact and are also part of the dementia prodrome. 33 , 34
PAF for 12 dementia risk factors
| Less education | 1·6 (1·3–2·0) | 40·0% | 61·2% | 19·4% | 7·1% |
| Hearing loss | 1·9 (1·4–2·7) | 31·7% | 45·6% | 22·2% | 8·2% |
| Traumatic brain injury | 1·8 (1·5–2·2) | 12·1% | 55·2% | 9·2% | 3·4% |
| Hypertension | 1·6 (1·2–2·2) | 8·9% | 68·3% | 5·1% | 1·9% |
| Alcohol (>21 units/week) | 1·2 (1·1–1·3) | 11·8% | 73·3% | 2·1% | 0·8% |
| Obesity (body-mass index ≥30) | 1·6 (1·3–1·9) | 3·4% | 58·5% | 2·0% | 0·7% |
| Smoking | 1·6 (1·2–2·2) | 27·4% | 62·3% | 14·1% | 5·2% |
| Depression | 1·9 (1·6–2·3) | 13·2% | 69·8% | 10·6% | 3·9% |
| Social isolation | 1·6 (1·3–1·9) | 11·0% | 28·1% | 4·2% | 3·5% |
| Physical inactivity | 1·4 (1·2–1·7) | 17·7% | 55·2% | 9·6% | 1·6% |
| Diabetes | 1·5 (1·3–1·8) | 6·4% | 71·4% | 3·1% | 1·1% |
| Air pollution | 1·1 (1·1–1·1) | 75·0% | 13·3% | 6·3% | 2·3% |
Data are relative risk (95% CI) or %. Overall weighted PAF=39·7%. PAF=population attributable fraction.
In the next section, we briefly describe relevant newly published and illustrative research studies that add to the 2017 Commission's evidence base, including risks and, for some, mitigation. We have chosen studies that are large and representative of the populations, or smaller studies in areas where very little evidence exists. We discuss them in life-course order and within the life course in the order of magnitude of population attributable factor.
Education and midlife and late-life cognitive stimulation
Education level reached.
Higher childhood education levels and lifelong higher educational attainment reduce dementia risk. 2 , 35 , 36 , 37 New work suggests overall cognitive ability increases, with education, before reaching a plateau in late adolescence, when brain reaches greatest plasticity; with relatively few further gains with education after age 20 years. 38 This suggests cognitive stimulation is more important in early life; much of the apparent later effect might be due to people of higher cognitive function seeking out cognitively stimulating activities and education. 38 It is difficult to separate out the specific impact of education from the effect of overall cognitive ability, 38 , 39 and the specific impact of later-life cognitive activity from lifelong cognitive function and activity. 39 , 40
Cognitive maintenance
One large study in China tried to separate cognitive activity in adulthood from activities for those with more education, by considering activities judged to appeal to people of different levels of education. 40 It found people older than 65 years who read, played games, or bet more frequently had reduced risk of dementia (n=15 882, odds ratio [OR]=0·7, 95% CI 0·6–0·8). The study excluded people developing dementia less than 3 years after baseline to reduce reverse causation.
This finding is consistent with small studies of midlife activities which find them associated with better late-life cognition; so for example, in 205 people aged 30–64 years, followed up until 66–88 years, travel, social outings, playing music, art, physical activity, reading, and speaking a second language, were associated with maintaining cognition, independent of education, occupation, late-life activities, and current structural brain health. 41 Similarly, engaging in intellectual activity as adults, particularly problem solving, for 498 people born in 1936, was associated with cognitive ability acquisition, although not the speed of decline. 42
Cognitive decline
The use it or lose it hypothesis suggests that mental activity, in general, might improve cognitive function. People in more cognitively demanding jobs tend to show less cognitive deterioration before, and sometimes after retirement than those in less demanding jobs. 43 , 44 One systematic review of retirement and cognitive decline found conflicting evidence. 45 Subsequently, a 12-year study of 1658 people found older retirement age but not number of years working, was associated with lower dementia risk. 46 Those retiring because of ill health had lower verbal memory and fluency scores than those retiring for other reasons. 47 Another study found a two-fold increase in episodic memory loss attributable to retirement (n=18 575, mean age 66 years), compared to non-retirees, adjusting for health, age, sex, and wealth. 48 Similarly, in a cohort of 3433 people retiring at a mean age of 61 years, verbal memory declined 38% (95% CI 22–60) faster than before retirement. 44 In countries with younger compared to higher retirement ages, average cognitive performance drops more. 49
Cognitive interventions in normal cognition and mild cognitive impairment
A cognitive intervention or cognition-orientated treatment comprises strategies or skills to improve general or specific areas of cognition. 50 Computerised cognitive training programmes have increasingly replaced tasks that were originally paper-and-pencil format with computer-based tasks for practice and training. 51
Three systematic reviews in the general population found no evidence of generalised cognition improvement from specific cognitive interventions, including computerised cognitive training, although the domain trained might improve. 52 , 53 , 54
A meta-analysis of 17 controlled trials of at least 4 hours of computerised cognitive training, (n=351, control n=335) for mild cognitive impairment, found a moderate effect on general cognition post-training (Hedges' g=0·4, 0·2–0·5); 55 however few high quality studies and no long-term high quality evidence about prevention of dementia currently exists. A meta-analysis of 30 trials of computerised, therapy-based and multimodal interventions for mild cognitive impairment found an effect on activities of daily living (d=0·23) and metacognitive outcomes (d=0·30) compared to control. 56 A third systematic review identified five high quality studies, four group-delivered and one by computer, and concluded the evidence for the effects of cognitive training in mild cognitive impairment was insufficient to draw conclusions. 53 A comprehensive, high quality, systematic overview of meta-analyses of cognitive training in healthy older people, those with mild cognitive impairment and those with dementia, found that most were of low standard, were positive and most reached statistical significance but it was unclear whether results were of clinical value because of the poor standard of the studies and heterogeneity of results ( figure 3 ). 51

Pooled results of meta-analyses investigating objective cognitive outcomes of cognition-oriented treatment in older adults with and without cognitive impairment
K represents the number of primary trials included in the analysis. If a review reported several effect sizes within each outcome domain, a composite was created and k denotes the range of the number of primary trials that contributed to the effect estimate. AMSTAR=A MeaSurement Tool to Assess systematic Reviews (max score 16). Adapted from Gavelin et al, 51 by permission of Springer Nature.
In the only randomised controlled trial (RCT) of behavioural activation (221 people) for cognition in amnestic mild cognitive impairment, behavioural activation versus supportive therapy was associated with a decreased 2-year incidence of memory decline (relative risk [RR] 0·12, 0·02–0·74). 57
Hearing impairment
Hearing loss had the highest PAF for dementia in our first report, using a meta-analysis of studies of people with normal baseline cognition and hearing loss present at a threshold of 25 dB, which is the WHO threshold for hearing loss. In the 2017 Commission, we found an RR of 1·9 for dementia in populations followed up over 9–17 years, with the long follow-up times making reverse causation bias unlikely. 2 A subsequent meta-analysis using the same three prospective studies measuring hearing using audiometry at baseline, found an increased risk of dementia (OR 1·3, 95% CI 1·0–1·6) per 10 dB of worsening of hearing loss. 58 A cross-sectional study of 6451 individuals designed to be representative of the US population, with a mean age of 59·4 years, found a decrease in cognition with every 10 dB reduction in hearing, which continued to below the clinical threshold so that subclinical levels of hearing impairment (below 25 dB) were significantly related to lower cognition. 59
Although the aetiology still needs further clarification, a small US prospective cohort study of 194 adults without baseline cognitive impairment, (baseline mean age 54·5 years), and at least two brain MRIs, with a mean of 19 years follow-up, found that midlife hearing impairment measured by audiometry, is associated with steeper temporal lobe volume loss, including in the hippocampus and entorhinal cortex. 60
Hearing aids
A 25-year prospective study of 3777 people aged 65 years or older found increased dementia incidence in those with self-reported hearing problems except in those using hearing aids. 61 Similarly, a cross–sectional study found hearing loss was only associated with worse cognition in those not using hearing aids. 62 A US nationally representative survey of 2040 people older than 50 years, tested every two years for 18 years, found immediate and delayed recall deteriorated less after initiation of hearing aid use, adjusting for other risk factors. 63 Hearing aid use was the largest factor protecting from decline (regression coefficient β for higher episodic memory 1·53; p<0·001) adjusting for protective and harmful factors. The long follow-up times in these prospective studies suggest hearing aid use is protective, rather than the possibility that those developing dementia are less likely to use hearing aids. Hearing loss might result in cognitive decline through reduced cognitive stimulation.
Traumatic brain injury (TBI)
The International Classification of Disease (ICD) defines mild TBI as concussion and severe TBI as skull fracture, oedema, brain injury or bleed. Single, severe TBI is associated in humans, and mouse models, with widespread hyperphosphorylated tau pathology, and mice with APOE ε4 compared to APOE ε3 allele have more hippocampal hyper-phosphorylated tau after TBI. 64 , 65 TBI is usually caused by car, motorcycle, and bicycle injuries; military exposures; boxing, horse riding, and other recreational sports; firearms; and falls. 66 A nationwide Danish cohort study of nearly 3 million people aged 50 years or older, followed for a mean of 10 years, found an increased dementia (HR 1·2, 95% CI 1·2–1·3) and Alzheimer's disease risk (1·2, 1·1–1·2). 67 Dementia risk was highest in the 6 months after TBI (4·1, 3·8–4·3) and increased with number of injuries in people with TBI (one TBI 1·2, 1·2–1·3; ≥5 TBIs 2·8, 2·1–3·8). Risk was higher for TBI than fractures in other body areas (1·3, 1·3–1·3) and remained elevated after excluding those who developed dementia within 2 years after TBI, to reduce reverse causation bias. 67
Similarly, a Swedish cohort of over 3 million people aged 50 years or older, found TBI increased 1-year dementia risk (OR 3·5, 95% CI 3·2–3·8); and risk remained elevated, albeit attenuated over 30 years (1·3, 1·1–1·4). 68 ICD defined single mild TBI increased the risk of dementia less than severe TBI and multiple TBIs increased the risk further (OR 1·6, 95% CI 1·6–1·7 for single TBI; 2·1, 2·0–2·2 for more severe TBI; and 2·8, 2·5–3·2 for multiple TBI). A nested case control study of early onset clinically diagnosed Alzheimer's disease within an established cohort also found TBI was a risk factor, increasing with number and severity. 69 A stronger risk of dementia was found nearer the time of the TBI, leading to some people with early-onset Alzheimer's disease.
Military veterans have a high risk of occupational TBI, and formal record keeping allows long-term follow-up. A study of 178 779 veterans with TBI with propensity-matched veterans without TBI found dementia risk was associated with TBI severity (HR 2·4, 95% CI 2·1–2·7 for mild TBI without loss of consciousness; 2·5, 2·3–2·8 for mild TBI with loss of consciousness; and 3·8, 3·6–3·9 for moderate to severe TBI). 70 Similarly women veterans with TBI had increased risk of dementia compared to those without TBI (1·5, 1·0–2·2). 71
A cohort study of 28 815 older adults with concussion, found the risk of dementia doubled, with 1 in 6 developing dementia over a mean follow-up of 3·9 years, although those taking statins had a 13% reduced risk of dementia compared to those who were statin-free. They suggest future RCTs as statins might mitigate injury-related brain oedema, oxidative stress, amyloid protein aggregation, and neuroinflammation. 72
The term chronic traumatic encephalopathy describes sports head injury, which is not yet fully characterised and covers a broad range of neuropathologies and outcomes, with current views largely conjecture. 73 The evidence has subsequently been strengthened by a study on Scottish former soccer players reporting that they are more likely than controls to have Alzheimer's disease specified on their death certificates (HR 5·1, 95% CI 2·9–8·8) and to have been prescribed any dementia-related medications (OR 4·9, 95% CI 3·8–6·3) but not on medical records. 74 The study controlled for socio-economic class based on residential address, which in footballers might be less linked to level of education.
Hypertension
Persistent midlife hypertension is associated with increased risk of a late life dementia. In the Framingham Offspring cohort comprising 1440 people, elevated systolic blood pressure (≥140 mm Hg in midlife; mean age 55 years) was associated with an increased risk of developing dementia (HR 1·6, 95% CI 1·1–2·4) over an 18 year follow-up period. 12 In this study risk increased further if hypertension persisted into later life (mean age 69 years; HR 2·0, 95% CI 1·3–3·1). In the same cohort, people in late midlife (mean age 62 years) with ideal cardiovascular parameters (current non-smoker, body mass index [BMI] 18·5–25 kg/m 2 , regular physical activity, healthy diet, optimum blood pressure <120/<80 mm Hg, cholesterol, and normal fasting blood glucose) were compared to people with at least one of these risks. 75 Those with ideal cardiovascular parameters had a lower 10-year risk of all-cause dementia (HR 0·8, 95% CI 0·1–1·0), vascular dementia (0·5, 0·3–0·8) and clinically diagnosed Alzheimer's disease (0·8, 0·6–1·0). In a UK cohort study of 8639 civil servants, a single measure of systolic blood pressure of 130 mm Hg or higher at age 50 years but not at age 60 or 70 years was associated with increased risk of dementia (1·4, 1·1–1·7). 13 In those with persistent systolic blood pressure of 130 mm Hg or higher, from mean age 45 to 61 years, dementia risk is increased even if free of cardiovascular disease relative to those without hypertension (1·3, 1·0–1·7).
A further cohort study has provided potential insights into mechanisms, reporting that midlife hypertension, defined as from age 40 years, was associated with reduced brain volumes and increased white matter hyperintensity volume but not amyloid deposition. 76 Of note, blood pressure declines in later life and this decline is associated with and, potentially caused by, dementia development (HR 2·4, 95% CI 1·4–4·2). 12 , 13 , 77
Antihypertensive drugs, aspirin, and statins
The US and Puerto Rico Systolic Blood Pressure Intervention Trial (SPRINT) in 9361 hypertensive adults aged 50 years and older, was stopped early because of significantly fewer cardiovascular events and deaths occurring in the intensive treatment arm (aiming for systolic <120 mm Hg, n=4678) in comparison with standard treatment (systolic <140 mm Hg, n=4683). 78 Cognitive assessment continued after stopping the trial intervention in SPRINT MIND. 79 In the intensive compared with the standard treatment group, there were 7·2 dementia cases as opposed to 8·6 cases/1000 person-years (HR 0·8; 95% CI 0·7–1·0) within on average 2 years from the end of the intervention period and 5 years after baseline. Pre-specified secondary outcomes were also reduced in the intensive arm for mild cognitive impairment (14·6 vs 18·3 cases/1000 person-years; HR 0·8, 95% CI 0·7–1·0), combined mild cognitive impairment or dementia (20·2 vs 24·1 cases/1000 person-years; HR 0·9, 95% CI 0·7–1·0) 79 making this the first trial to suggest reduction of risk for mild cognitive impairment. Those who were lost to follow-up were at greater risk of dementia than those who continued but follow-up rates did not differ according to intervention group. 80
Four meta-analyses of blood pressure medications to lower high blood pressure with six studies overlap have provided combined estimates of effects. All meta-analyses suggest reduced dementia in those in the interventions arms for outcomes of any dementia as well as clinically diagnosed Alzheimer's disease. The first included randomised controlled trials (RCTs) of any drug to lower blood pressure and reported a reduction in risk of around 10% at marginal significance (RR 0·9, 95% CI 0·9–1·0). 81 Meta-regression showed risk lowered more if the achieved systolic pressure differential was larger between the intervention and control group. The second included 15 trials and observational studies of diuretics involving 52 599 people (median age 76 years) with 6·1 years median follow-up (dementia HR 0·8, 95% CI 0·8–0·9 and Alzheimer's disease 0·8, 0·7–0·9). 82 The third included used individual participant data from six observational studies; (dementia 0·9, 0·8–1·0 and Alzheimer's disease 0·8, 0·7–1·0; figure 4 ). 83 The fourth focused on people prescribed calcium channel blocker only, included 10 RCTs and observational studies comprising 75 239 hypertensive older adults (median age 72 years, median follow-up 8·2 years) found lowered dementia risk (RR 0·7, 95% CI 0·6–0·9). 84 A 2019 meta-analysis addressing which class of anti-hypertensive drug to use to lower risk of either incident dementia or cognitive decline, found over 50 000 participants in 27 studies and reported no consistent difference in effect according to which class of drug was used. 85

Associations of antihypertensive medication use with incident dementia in those with high blood pressure
Adapted from Ding et al, 83 by permission of Elsevier.
A Cochrane review reported good evidence that statins given to older people at risk of vascular disease do not prevent cognitive decline or dementia. 86 One RCT found 100 mg aspirin versus placebo in 19 114 healthy adults older than 65 years did not reduce dementia (HR 1·0, 95% CI 0·8–1·2), death, physical disability, or cardiovascular disease over a period of 4·7 years. 87
Physical inactivity, exercise, and fitness
Studies of physical activity are complex. Patterns of physical activity change with age, generation, and morbidity and are different across sex, social class, and cultures. The studies suggest a complicated relationship with the potential for both risk reduction and reverse causation.
Meta-analyses of longitudinal observational studies of 1–21 years duration showed exercise to be associated with reduced risk of dementia. 2 A further overview of systematic reviews concluded that there is convincing evidence for physical activity protecting against clinically diagnosed Alzheimer's disease. 88
Since the 2017 Commission, the HUNT study of 28 916 participants aged 30–60 years has been published, reinforcing the previous literature in this area. At least weekly midlife moderate-to-vigorous physical activity (breaking into a sweat) was associated with reduced dementia risk over a 25-year period of follow-up (HR 0·8, 95% CI 0·6–1·1) but the confidence intervals were wide. 89 In contrast the Whitehall Study reporting on the 28-year follow-up of 10 308 people, found that more than 2·5 hours of self-reported moderate-to-vigorous physical activity per week, lowered dementia risk over 10, but not 28 years. 33 Very long-term studies are unusual; however, one 44-year study recruited 191 women (mean age 50) purposively to be representative of the Swedish population and reported that 32% of the participants with low baseline peak fitness, 25% with medium, and 5% with high fitness developed dementia (high vs medium HR 0·1, 95% CI 0·03–0·5, low vs medium 1·4, 0·7–2·8). 90
An individual-level meta-analysis of 19 observational studies of relatively younger adults included 404 840 participants' data (mean baseline age 45·5 years; mean follow-up duration 14·9 years), reporting an increased incidence of all-cause dementia (HR 1·4, 95% CI 1·2–1·7) and clinically diagnosed Alzheimer's disease (1·4, 1·1–1·7) in those who were physically inactive in the 10-year period before diagnosis. 91 Notably, however, no difference in dementia risk measured 10–15 years before time of dementia incidence was found except in those with comorbid cardio-metabolic disease (RR 1·3, 95% CI 0·8–2·1).
People might stop exercising due to prodromal dementia so inactivity might be either a consequence or a cause or both in dementia and might be more of a risk in those with cardiovascular morbidity. As with other outcomes, exercise might be required to be sustained and continue nearer the time of risk. 92
Trials of exercise
Since the 2017 Commission several meta-analyses and systematic reviews have been published with three high quality meta-analyses which we include. The first included 39 RCTs with an unclear total number of participants examining moderate or vigorous exercise of any frequency lasting 45–60 min per session in cognitively normal adults aged older than 50 years. This analysis reported global cognitive improvements (standard mean difference [SMD]=0·3, 95% CI 0·2–0·4) for moderate or vigorous resistance (13 studies) or aerobic exercise (18 studies) lasting 45–60 min per session with no difference between them but no effect found for yoga. 93 A second meta-analysis of RCTs in people with mild cognitive impairment found global cognition improved in the intervention group (0·3, 0·1–0·5) with aerobic exercise having a higher effect (0·6, 0·5–0·6). 94 This study did not have dementia as an outcome measure. A third meta-analysis of RCTs of longer term exercise found five studies (four lasting 12 months and one 24 months) with 2878 participants with normal baseline cognition. 95 The incidence of dementia was 3·7% (n=949) for exercisers and 6·1% (n=1017) for controls (random effect RR 0·6, 95% CI 0·3–1·1; fixed effect as no evidence of heterogeneity 0·7, 0·4–1·0). The authors concluded that the study showed no significant effect of exercise for reducing dementia, mild cognitive impairment, or clinically significant cognitive decline but was underpowered. WHO guidelines have been published since the 2017 Commission, suggesting specific activity levels drawing on these, and one further systematic review which considered sex differences on the effect of exercise. 96 , 97 It concluded the evidence points towards physical activity having a small, beneficial effect on normal cognition, with a possible effect in mild cognitive impairment, mostly due to aerobic exercise. 97 Evidence about the effect of specific types of exercise, such as progressive muscle resistance training, on dementia risk is scarce.
In the 2017 Commission we reported on diabetes as a risk factor for dementia. Distinguishing between treated and untreated diabetes as a risk factor for dementia is challenging in observational studies. In a pooled meta-analysis from over 2·3 million individuals with type 2 diabetes across 14 cohort studies, including 102 174 with dementia, diabetes was associated with an increased risk of any dementia (RR 1·6, 95% CI 1·5–1·8 for women and 1·6, 1·4–1·8 for men). 98 The risk of dementia increased with the duration and severity of diabetes. The effect of different diabetic medications on cognition or dementia outcomes remains unclear as few studies have investigated this area. 99 However, one meta-analysis of cohort studies of diabetes reported that, cross sectionally, people with diabetes taking metformin had lower prevalence of cognitive impairment (three studies OR 0·6, 95% CI 0·4–0·8) and, longitudinally, reduced dementia incidence (six studies HR 0·8, 95% CI 0·4–0·9) compared with those taking other medications or no medication. 100 However another analysis did not find a protective effect of metformin for incident dementia (three studies, RR 1·1, 95% CI 0·5–2·4) with possible harm with insulin therapy (1·2, 1·1–1·4); but this did not account for severity of diabetes of those with type 2 diabetes on insulin. 99 A Cochrane review reported intensive compared to standard diabetes control trials with 5 year follow up (n=11 140), showing no impact on cognitive decline (1·0, 95% CI 0·9–1·1) or dementia (1·3, 0·9–1·9). 101
Overall type 2 diabetes is a clear risk factor for development of future dementia; however, whether any particular medication ameliorates this risk is unclear. Intensive diabetic control does not decrease the risk of dementia.
Combined cardiovascular risk factors
Studies of individual cardiovascular risk factors usually control for other cardiovascular risks, which cluster in individual people. This does not take into account the combinations and contexts in which risk occurs. A UK study of 7899 people aged 50 years followed up for 25 years, calculated a cardiovascular health score based on four behaviour-related (smoking, diet, physical activity, BMI) and three biological (fasting glucose, blood cholesterol, blood pressure) metrics each coded on a three-point scale (0, 1, 2). 100 A better score was associated with a lower risk of dementia (HR 0·9, 95% CI 0·9–1·0 per 1 point scale increment), for both behaviour-related (HR/1 point increment in subscales 0·9, 95% CI 0·8–0·9) and biological subscales (0·9, 0·8–1·0), maintained in people free of cardiovascular disease over the follow-up (0·9, 95% CI 0·8–1·0). These authors also reported an association of the score on the scale with hippocampal atrophy and total brain volume but not white matter hyperintensities. This finding underlines the importance of clustering of cardiovascular risk factors in midlife, as studies of individual risk factors in this sample had not shown a significant association, when controlling for other individual risks. 33
Excessive alcohol consumption
Heavy drinking is associated with brain changes, cognitive impairment, and dementia, a risk known for centuries. 102 An increasing body of evidence is emerging on alcohol's complex relationship with cognition and dementia outcomes from a variety of sources including detailed cohorts and large-scale record based studies. Alcohol is strongly associated with cultural patterns and other sociocultural and health-related factors, making it particularly challenging to understand the evidence base.
A French 5-year longitudinal study of over 31 million people admitted to hospital, found alcohol use disorders (harmful use or dependence as defined in ICD) were associated with increased dementia risk, calculated separately for men and women (women HR 3·3, 95% CI 3·3–3·4, men 3·4, 3·3–3·4). 103 The relationship of dementia with alcohol use disorders was particularly clear in the earlier onset dementias (age less than 65 years) in which 56·6% had an alcohol use disorder noted in their records (n=57 353; 5·2% all dementias).
A systematic review incorporating 45 studies of light to moderate drinking using a variety of definitions reported a reduced risk of dementia compared with not drinking (RR 0·7; 95% CI 0·6–0·91). 104 Risk was not reported separately for men and women. Drinking less than 21 units of alcohol per week (1 unit of alcohol=10 mL or 8 g pure alcohol) might be associated with a lower risk of dementia. 105 , 106 A 5-year follow-up study of 13 342 men and women volunteers from UK biobank aged 40–73 years who drank, included few heavy drinkers and did not analyse abstainers. 106 The study reported that those who drank more than 12 units per week declined slightly more in reaction time in a perceptual matching task than those who drank less (β2=−0·07, 95% CI −0·09 to −0·04). 106 The UK Whitehall study with 23 years follow-up, included 9087 participants aged 35–55 years at baseline. 107 Drinking more than 21 units per week and long-term abstinence were both associated with a 17% (95% CI 4–32 and 13–23 respectively) increase in dementia compared to drinking less than 14 units. Drinking more than 14 units was also associated with right sided hippocampal atrophy on MRI. 108
Weight control and obesity
Overweight is an emerging concern, given the changing BMI across the world's ageing population. New evidence supports the relationship between increased BMI and dementia from a review of 19 longitudinal studies including 589 649 people aged 35 to 65 years, followed up for up to 42 years. It reported obesity (BMI ≥30; RR 1·3, 95% CI 1·1–1·6) but not being overweight (BMI 25–30; 1·1, 1·0–1·2) was associated with late-life dementia. 109 In a further meta-analysis of individual level data from 1·3 million adults (aged ≥18 years), which included two studies from the meta-analysis cited above, 109 higher body mass measured before probable preclinical and prodromal dementia was associated with increased dementia risk (RR 1·3, 1·1–1·7/5-unit increase in BMI). 11
Weight loss in midlife and dementia risk
A meta-analysis of seven RCTs (468 participants) and 13 longitudinal studies (551 participants) of overweight and obese adults without dementia, mean age 50 years, found weight loss of 2 kg or more in people with BMI greater than 25 was associated with a significant improvement in attention and memory. All but one of the studies included participants aged younger than 65 years. The RCTs reported memory improvement over 8–48 weeks (SMD=0·4, 95% CI 0·2–0·6) and short-term longitudinal studies found improvement over a median of 24 weeks (SMD=0·7, 95% CI 0·5–0·8); however, data about the long-term effects or the effect of weight loss in preventing dementia are absent. 110
Smokers are at higher risk of dementia than non-smokers, 2 and at a higher risk of premature death before the age at which they might have developed dementia, introducing some bias and uncertainty in the association between smoking and risk of dementia. 111 , 112 Stopping smoking, even when older, reduces this risk. Among 50 000 men aged older than 60 years, stopping smoking for more than 4 years, compared to continuing, substantially reduced dementia risk over the subsequent 8 years (HR 0·9; 95% CI 0·7–1·0). 113 Worldwide, 35% of non-smoking adults and 40% of children are estimated to be exposed to second-hand smoke; 114 although literature on the impact of this exposure and dementia risk is scarce. One study indicated that in women aged 55–64 years, second-hand smoke exposure was associated with more memory deterioration and the risk increased with exposure duration even after controlling for other confounding factors. 115
Depression is associated with dementia incidence, with a variety of possible psychological or physiological mechanisms. It is also part of the prodrome and early stages of dementia. Reverse causation is possible whereby depressive symptoms result from dementia neuropathology that occurs years before clinical dementia onset. These explanations are not mutually exclusive. As in diabetes, few studies considering depression as a risk factor for dementia have distinguished between treated and untreated depression. In a meta-analysis of 32 studies, with 62 598 participants, with follow-up from 2 to 17 years, a depressive episode was a risk factor for dementia (pooled effect size 2·0, 95% CI 1·7–2·3). 116 Meta-regression analysis revealed a non-significant trend for the association between depression and incident dementia to be weaker when the length of follow-up was longer. The Norwegian HUNT study, suggested that symptoms of psychological distress predicted dementia 25 years later however with wide bounds of uncertainty (HR 1·3, 95% CI 1·0–1·7). 89 Two further studies differentiate between late-life and earlier life depressive symptoms. The UK Whitehall study, in a follow-up of 10 189 people, reports that in late life these symptoms increase dementia risk but not at younger ages (follow-up 11 years HR 1·7; 95% CI 1·2–2·4; follow-up 22 years 1·0, 0·7–1·4). 34 , 117 A 14-year longitudinal study of 4922 initially cognitively healthy men, aged 71–89 years, found depression was associated with 1·5 (95% CI 1·2- 2·0) times the incidence of dementia but this association was accounted for by people developing dementia within 5 years of depression. 118 The use of antidepressants did not decrease this risk.
A study of 755 people with mild cognitive impairment and with a history of depression from the Australian longitudinal Alzheimer's Disease Neuroimaging Initiative, considered the effect of selective serotonin-reuptake inhibitor (SSRI) treatment, such as citalopram, known to reduce amyloid plaque generation and plaque formation in animal models. 119 The study found that more than 4 years of such treatment was associated with delayed progression to clinically diagnosed Alzheimer's disease. People treated with antidepressants seem likely to differ from those who are not treated. Thus, the question of whether antidepressant treatment mitigates dementia risk remains open.
Social contact
Social contact, now an accepted protective factor, enhances cognitive reserve or encourages beneficial behaviours, although isolation might also occur as part of the dementia prodrome. Several studies suggest that less social contact increases the risk of dementia. Although most people in mid and later life are married, by the time they reach older age, disproportionate numbers of women are widowed as they outlive their husbands, thus reducing their social contact. In these generations, marital status is therefore an important contributor to social engagement. Additionally, most marriages are in the relatively young, and married people usually have more interpersonal contact than do single people—this gives a long-term estimate of the effect of social contact. A systematic review and meta-analysis including 812 047 people worldwide found dementia risk to be elevated in lifelong single (RR 1·4, 95% CI 1·1–1·9) and widowed people (1·2, 1·0–1·4), compared with married people and the association was consistent in different sociocultural settings. 120 Studies adjusted for sex and we do not know if a differential risk between men and women exists. Differences persisted in studies that adjusted for education and physical health so might be attributable to married people having more social contact, rather than solely because they tend to have better physical health and more education, although residual confounding is possible. A systematic review and meta-analysis of 51 longitudinal cohort studies of social isolation and cognition included 102 035 participants aged 50 or more years at baseline, with follow-up of 2–21 years. 121 High social contact (measured through either or both of social activity and social network) was associated with better late-life cognitive function (r=0·05, 95% CI: 0·04–0·065) and no differences according to sex or length of time followed up.
A new meta-analysis found that in long-term studies (≥10 years), good social engagement was modestly protective (n=8876, RR=0·9, 95% CI 0·8–1·0); but loneliness was not associated with dementia risk. 122 No long term (>10 years) studies of loneliness and dementia outcomes have been done.
A UK 28-year follow-up study of 10 308 people found that more frequent social contact at age 60 years was associated with lower dementia risk over 15 years of follow-up (HR for one standard deviation social contact frequency 0·9, 95% CI 0·8–1·0). This finding suggests more frequent social contact during late middle age is associated with a modest reduction in dementia risk, independent of socio-economic and other lifestyle factors. 123 A Japanese longitudinal cohort study of 13 984 adults aged older than 65 years with a mean of 10 years follow-up calculated a five-point social contact scale based on: marital status; exchanging support with family members; having contact with friends; participating in community groups; and engaging in paid work. It found the score to be linearly associated with reduced dementia risk; those who scored highest on the five-point scale were 46% less likely to develop incident dementia compared with those in the lowest category. 124
Despite clear cultural variation in the meaning and perception of social isolation, findings of protective effect of more social contact are largely consistent in different settings and for either sex across the studies and meta-analyses. 118 , 120 , 121
Social interventions
Little evidence of the effects of social interventions on dementia exists but a systematic review of low quality RCTs of 576 adults aged 60 or more years with normal cognition found facilitated meeting and discussion groups were associated with improved global cognition and increased brain volume at follow-up. 118
Air pollutants
Air pollution and particulate pollutants are associated with poor health outcomes, including those related to non-communicable diseases. Attention has turned to their potential effect on the brain. Animal models suggest airborne particulate pollutants accelerate neurodegenerative processes through cerebrovascular and cardiovascular disease, Aβ deposition, and amyloid precursor protein processing. 125 , 126 Although the higher levels of dementia from air pollutants are still subject to the potential for residual confounding, the effects on animal models are evidence of physiological effects over and above those driven by life-course deprivation.
High nitrogen dioxide (NO 2 ) concentration (>41·5 μg/m 3 ; adjusted HR 1·2, 95% CI 1·0–1·3), fine ambient particulate matter (PM) 2·5 from traffic exhaust (1·1, 1·0–1·2) 127 , 128 , 129 and PM 2·5 from residential wood burning (HR=1·6, 95% CI 1·0–2·4 for a 1 μg/m 3 increase) are associated with increased dementia incidence. Traffic often produces NO 2 and PM 2·5 and it is hard to separate their effects, although evidence for additive effects of different pollutants exists. 127 , 128 , 129 A systematic review of studies until 2018 including 13 longitudinal studies with 1–15 years follow-up of air pollutants exposure and incident dementia, found exposure to PM 2·5, NO 2 , and carbon monoxide were all associated with increased dementia risk. 24 The attributable burden of dementia and excess death from PM 2·5 in one large 10-year US study was particularly high in Black or African American individuals and socio-economically disadvantaged communities and related to particulate PM 2·5 concentrations above the US guidelines. 130
Mechanisms by which sleep might affect dementia remain unclear, but sleep disturbance has been linked with β-amyloid (Aβ) deposition, 131 , 132 reduced glymphatic clearance pathways activation, 133 low grade inflammation, increased Tau, hypoxia 132 , 134 and cardiovascular disease. 135 Sleep disturbance is hypothesised to increase inflammation which raises Aβ burden, leading to Alzheimer's disease and further sleep disturbance. 136
Two meta-analyses showed similar findings. The first was a synthesis of longitudinal studies with an average of 9·5 years follow-up and the second reported cross-sectional and prospective cohort studies of mixed quality with different methods of measuring sleep. Sleep disturbances were defined broadly, often self-reported and including short and long sleep duration, poor sleep quality, circadian rhythm abnormality, insomnia, and obstructive sleep apnoea. All these disturbances were associated with a higher risk of all-cause dementia (RR 1·2; 95% CI 1·1–1·3) 137 and clinically diagnosed Alzheimer's disease (1·6, 1·3–1·9) compared with no sleep disturbance, although not all cohort studies excluded those with cognitive impairment or dementia at baseline from their analyses. 138 A U-shaped association has been reported between sleep duration and risk of mild cognitive impairment or dementia with higher risks of dementia with less than 5 hours (HR=2·6; 95% CI 1·4–5·1) compared with more than 5 and less than 7 and more than 10 hours sleep (2·2, 1·4–3·5) and risks for all-cause dementia and clinically diagnosed Alzheimer's disease being similar. 135 , 139 , 140 , 141
The postulated mechanisms of reduced sleep leading to accumulation of Alzheimer's type pathology is inconsistent with the evidence that both more sleep and less sleep are associated with increased risk of dementia. New onset late-life sleep disturbance, a few years before clinical dementia, might be part of the natural history of the dementia syndrome, appearing to be a risk factor, or reflect other disorders, for example, mood disturbances or cardiovascular disease. 135 , 142 Hypnotic use might increase risks although this is unclear and a 2018 study 139 suggests that findings of a connection were related to reverse causality and confounders. 143 When benzodiazepine use was considered, in one study, sleep length was no longer significant 139 but not in all studies. 135 Those taking hypnotics were at greater risk of dementia than those who did not regardless of sleep duration. 139 Medication for sleep disturbance might be harmful and benzodiazepines are associated with falls, hospital admissions, and possibly dementia. 139 , 144
Nutrition and dietary components are challenging to research with controversies still raging around the role of many micronutrients and health outcomes in dementia. Observational studies have focused on individual components ranging from folate and B vitamins, Vitamin C, D, E, and selenium amongst others as potential protective factors. 88 There has been a move towards considering the evidence base for whole diets in the last 5 years, particularly high plant intake such as in the Mediterranean diet (high intake of vegetables, legumes, fruits, nuts, cereals, and olive oil; low intake of saturated lipids and meat) or the similar Nordic diet, rather than individual nutrients, which might reduce cognitive decline and dementia. 145 One example is a longitudinal cohort study of 960 participants, ages 58–99 years, in which those reporting the highest intake of green leafy vegetables, equivalent to 1·3 servings per day, had less cognitive decline over 4·7 years than those reporting the lowest intake (β=0·05 standardised units 95% CI 0·02–0·07). 146 The authors report this difference as being equivalent to being 11 years younger. A further prospective cohort study with three midlife dietary assessments in 8255 people, followed up for a mean of nearly 25 years, found neither healthy dietary pattern nor Mediterranean diet protected from dementia, except in those with cardiovascular disease, suggesting that diet might influence dementia risk by protecting from the excess risk of cardiovascular risk factors. 147
Dietary interventions
As well as whole diets, there has been some interest in multi-nutrient interventions. A systematic review and a Cochrane review including RCTs of supplements (A, B, C, D, and E; calcium, zinc, copper, and multivitamins trials, n-3 fatty acids, antioxidant vitamins, and herbs) found a lack of evidence for supplement use to preserve cognitive function or prevent dementia in middle-aged (45–64 years) or older people (aged 65 years and older). 148 , 149 Cochrane reviews found no evidence for beneficial effects on cognition of those with mild cognitive impairment of supplementation with B vitamins for 6 to 24 months 150 or with vitamin E in preventing progression from mild cognitive impairment to dementia. 151 A 24-month RCT of 311 people of a multi-nutrient drink containing docosahexaenoic acid, vitamins B12, B6, folic acid, and other nutrients; found no significant effect on preventing cognitive deterioration in prodromal Alzheimer's disease. 152 The authors comment that the control group's cognitive decline was much lower than expected, leading to an inadequately powered trial.
Meta-analysis of two RCTs with 471 participants with normal cognition found the Mediterranean diet improved global cognition compared to controls (SMD 0·2, 95% CI 0·0–0·4). 153 A further meta-analysis identified five RCTs (n=1888) with a weak effect on global cognition (SMD 0·2, 95% Cl 0·0–0·5) 154 but no benefit of Mediterranean diet for incident cognitive impairment or dementia.
The WHO guidelines recommend a Mediterranean diet to reduce the risk of cognitive decline or dementia, as it might help and does not harm, but conclude Vitamins B and E, polyunsaturated fatty acid, and multicomplex supplementation should not be recommended. 97
Trials of combination strategies to prevent dementia
The FINGER RCT was a 2-year multidomain intervention to prevent cognitive decline and dementia in 1260 people with cardiovascular risk factors aged 60–77 years, recruited from a Finnish national survey. Similar multidomain studies were discussed in the 2017 Commission. 2 FINGER found a small group reduction in cognitive decline in the intervention group compared with control (comprehensive neuropsychological test battery Z score 0·02, 95% Cl 0·00–0·04) regardless of baseline sociodemographic, socio-economic, cognitive, or cardiovascular status. 155 However, in a subgroup analysis, greater beneficial effects were observed on processing speed in individuals with higher baseline cortical thickness in Alzheimer's disease areas. 156
The Healthy Ageing Through Internet Counselling in the Elderly (HATICE) study recruited 2724 older people (≥65 years) in the Netherlands, Finland, and France with two or more cardiovascular risk factors. 157 , 158 It compared an interactive internet platform plus remote support by a coach, aiming to improve self-management of vascular risk factors, with a non-interactive control platform with basic health information. A small improvement in the cardiovascular risk composite primary outcome was observed in the intervention group compared with the control group at 18 months, mainly through weight loss, and the dementia risk score was slightly lower in those who received the intervention (mean difference −0·15, 95% CI −0·3 to −0·0). A larger effect was observed in the younger age group (65–70 years) and those with the lowest level of education, who had a higher baseline risk, suggesting that targeting high-risk populations might be more effective. Several multidomain preventive trials are ongoing—for example, World Wide FINGERS .
Total PAF calculation
We incorporated excessive alcohol consumption, TBI, and air pollution into our life-course model of dementia, as well as the original nine risk factors, because of the updated evidence. To calculate new RRs for excessive alcohol consumption, TBI and air pollution, we systematically reviewed the literature and did new meta-analyses for excessive alcohol consumption and TBI. For the other nine factors, we used values for RR and risk factors prevalence from our previous analysis and calculated communality using the same method as in the 2017 Commission. 2
PAF calculation
We used a representative sample of over 10 000 UK community-dwelling adults, to calculate communality (clustering of risk factors) of 11 risk factors for which data existed, 159 to allow calculation of each factor's unique risk. As we could find no datasets measuring TBI, with the other 11 risk factors of interest, we could not calculate its communality. We therefore used the mean of the other 11 communalities to calculate a weighted PAF, so we could include TBI. We used cohabitation as a proxy measure for social contact, and urbanicity for air pollution exposure. Our analysis found four principal components, explaining 55% of the total variance between the eleven risk factors, suggesting substantial overlap. The appendix (p 2) shows the PAF formula and the steps in calculating communality and we detail our new meta-analyses next, which we used to update the figure and perform our new calculations.
Incorporation of the new chosen risks in new systematic reviews
We searched, from inception to Oct 29, 2019, Embase, Allied, and Complementary Medicine, MEDLINE, and PsycINFO terms “dementia” OR “dement*” OR “AD” OR “VaD”, “Alzheimer*” AND “alcohol” OR “ethanol” OR “alcohol*” OR “drink*” OR “drunk*” to update an earlier review. 160 We used inclusion criteria: original population-based cohort studies measuring drinking during midlife, as alcohol intake tends to fall with age; 161 alcohol consumption quantified at baseline by units or number of drinks (one drink, 1·5 units) per week; and all-cause dementia ascertained at follow-up using validated clinical measures. We contacted authors for additional data. 162 Three studies met our inclusion criteria. 107 , 162 , 163 We converted HRs to RRs 164 and used raw data 162 to calculate RR, 165 for our random effects meta-analysis using Generic Inverse Variance Methods. The RR associated with drinking—more than 21 units (168 g) of alcohol weekly—compared with lighter drinking was 1·18 (95% Cl 1·06–1·31; figure 5 ). We used Health Survey England figures for heavier drinking prevalence to calculate PAF as we could not find a worldwide estimate. The weighted PAF was 0·8.

Meta-analysis of relative risk of dementia associated with drinking more than 21 units of alcohol per week in midlife compared to lighter consumption of alcohol
To estimate the RR of TBI of all severities for all cause dementia, we searched Embase, Medline, and PsycINFO from Jan 1, 2016, to Oct 21, 2019, updating an earlier search, 166 using terms (“traumatic brain injury” or “head injury” or “brain injury” or TBI) AND (neurodegeneration or “cognitive dysfunction” or dementia or “Alzheimer's disease” or “Parkinson's disease” or “frontotemporal dementia”). We converted HR figures to RR. 164 , 167 We used inclusion criteria: original population-based cohort studies, baseline TBI of all severities reported, and all-cause dementia ascertained at follow-up using validated clinical measures. We combined four new studies meeting inclusion criteria 67 , 68 , 71 , 168 with the four studies meeting criteria from the original review in a random effects meta-analysis. 166 The pooled RR was 1·84 (95% CI 1·54–2·20) for all cause dementia from all severities of TBI ( figure 6 ) although there was heterogeneity in study-specific estimates, possibly because of different populations. We used the TBI adult population prevalence of 12·1% from a meta-analysis to calculate PAF. 173 The weighted PAF was 3·4.

Meta-analysis of relative risk of all-cause dementia associated with all severity midlife traumatic brain injury
A 2019 systematic review synthesised observational studies, finding consistently increased risk of dementia from air pollution, but heterogeneous comparator groups precluded meta-analysis. 24 We updated the search, using the same search terms and searching MEDLINE, Embase, and PsycINFO from Sept 20, 2018, (the end date of the last search) to Oct 22, 2019. We included longitudinal studies with assessment of all cause air pollution exposure; use of formal assessment of cognitive function at baseline; report of incident all-cause dementia, data from adults (age ≥18 years); and a minimum follow-up of 6 months. As meta-analysis was not possible, we used data from the only study of all-cause air pollution with the outcome of all-cause dementia, with low-moderate risk of bias. This population-based, observational cohort was from Canada, where pollutant concentrations are among the lowest in the world and examined 2 066 639 people, with a mean baseline age of 67 years. 174 We calculated the RR of dementia for those in the three highest quartiles compared to the lowest was 1·09 (1·07–1·11). The attributable fraction for exposure to the highest three quartiles versus the lowest quartile of PM 2·5 and NO 2 was 6·1% (4·8–7·5). The weighted PAF was 2·3.
Table 1 displays the prevalence, communality, relative risk, unweighted and weighted PAFs adjusted for communality. Figure 7 shows the updated life-course model of potentially modifiable risk factors for dementia, including the three new risk factors.

Population attributable fraction of potentially modifiable risk factors for dementia
Strengths and limitations
This Commission is the most comprehensive analysis to date and updates the 2017 Commission with emerging risk factor evidence convincing enough to calculate PAF for potentially reversible risk factors. We reviewed the literature systematically for the chosen risk factors and provided illustrative new literature to update our synthesis and identify data to calculate communality. We find a hopeful picture with an estimate of around 40% of all cases of dementia being associated with 12 potentially modifiable risk factors.
We have made assumptions to calculate this new model. We used global figures for dementia risk although we know the risk factors prevalence varies between countries and most global research is from HIC, so LMIC are under-represented because of lack of data. We have assumed a causal relationship between risk factors and dementia, although we have been cautious and not included risk factors with less good evidence. No single database exists with all 12 risk factors together, but we found 11 of the factors in a UK database and used the mean figure for communality calculations for TBI. We calculated communality for the other 11. We do not know how far findings of communality in other geographical populations might differ, or in those with a differing distribution of age groups or sex. We found that social isolation was not explicitly measured and had to use proxies, such as cohabitation when considering prevalence, which are approximate.
Specifically, evidence for the association of alcohol misuse with dementia comes from HIC and future studies from LMIC are needed to complete the picture. Exposure to air pollution changes over a lifetime and is inextricably linked to poverty and deprivation. However, the effects on animal models suggests specific physiological effects over and above those driven by life-course deprivation. We also considered the overlap with education for this and other risk factors and the correction for education, strongly inversely linked to deprivation, will address at least some of the confounding. However, the results in one study which reported the effect of air pollution on incident dementia showed very little difference in estimates before and after adjustment for education and other risk factors, suggesting little residual confounding exists. 174 We were also unable to meta-analyse data on pollution and thus unlike the other relative risks, the figure comes from only one study, from an area of low pollution so is likely to be an underestimate.
The longitudinal evidence linking potentially modifiable risk factors to dementia generally fulfils causality criteria in observational data (strength, consistency, biological plausibility, temporality, dose–response, coherence, and quasi-experimental studies, for example, more education or using hearing aids). When measuring a risk nearer to the age of dementia onset, then it is more likely that prodromal change affects, or even causes it. Alternatively, a risk factor might act on preclinical pathology or even cause dementia near the time of exposure. Thus, excessive alcohol, and TBI are particularly important in young-onset dementia, although many early onset dementias relate to genetic risks. Risk factors might also matter more at a time of higher biological vulnerability, which the studies we have drawn on cannot establish. The length of exposure required for risk or protection effect, and their inter-relationships as they change across life is unclear—it seems probable that longer or more intense exposure has stronger effects. Additionally, as our communality figures show, risk factors overlap. We cannot establish from these data if having multiple risk factors has an additive or synergistic effect. Association does not prove causation, however, as already noted, the reductions in prevalence and incidence in several HIC suggests that at least some of the risk factors estimated here do have a causal relationship with the clinical expression of dementia.
Key points and recommendations
We judge that sufficient new evidence supports adding three additional modifiable risk factors for dementia to our 2017 Commission model (excessive alcohol, traumatic brain injury, and air pollution). We have been able to add updated evidence on the nine risk factors implicated in the 2017 Commission (education, hypertension, hearing impairment, smoking, obesity, depression, inactivity, diabetes, and social contact). Reduction of these risk factors might be protective for people with or without a genetic risk, although study findings have not been entirely consistent. 175 , 176 , 177 , 178 As we noted in the 2017 Commission, others have previously calculated an estimate of the risk associated with APOε4 at 7% taking into account some other risk factors and this estimate highlights how relatively important potentially modifiable risk factors are in dementia. 2 , 179
For some risk factors, the pattern of risk and the individual's other health, both physical and mental, might be especially important. Currently, the evidence suggests a Mediterranean or Scandinavian diet might have value in preventing cognitive decline in people with intact cognition, particularly as one component of a healthy lifestyle, although how long the exposure has to be or during which ages is unclear. We do not recommend taking additional vitamins, oils, or mixed dietary supplements as a means of preventing dementia as extensive testing in trials has not led to signals of beneficial effects.
Data from RCTs on interventions to prevent cognitive decline, all-cause dementia, or Alzheimer's disease are few. For some key life influences, only observational data, particularly related to natural experiments such as changing the statutory education age, are possible. These influences should be investigated systematically wherever possible. Others can theoretically be investigated but the long follow-up required for midlife risk and protective factors and non-random attrition in longer studies are challenging. Using intermediate endpoints, such as cognition, and dementia onset in research remains uncertain because no intermediate markers with such a close relationship to dementia outcomes exist that it would be possible to predict with certainty for any given individual, age, and sex. Overall, the evidence for treating hypertension is strongest and high blood pressure throughout midlife increases the risk of dementia even without stroke.
Although a need for more evidence is apparent, recommendations should not wait, as clear indications of ways to reduce the chances of developing dementia without causing harm will also lead to other health and wellbeing benefits.
Our recommended strategies for dementia risk reduction include both population-wide and targeted interventions ( panel ). It is important to remember that more socially disadvantaged groups, including Black, Asian, and minority ethnic groups, are particularly at risk.
Recommended strategies for dementia risk reduction
Risks are particularly high in more socially disadvantaged populations including in Black, Asian, and minority ethnic groups.
Population-wide
- • Prioritise childhood education for all, worldwide
- • Implement social public health policies that reduce hypertension risk in the entire population
- • Develop policies that encourage social, cognitive, and physical activity across the life course for all (with no evidence for any specific activities being more protective)
- • Scrutinise the risks for hearing loss throughout the life course, to reduce the risk of exposure to this risk factor
- • Reduce the risk of serious brain trauma in relevant settings, including occupational and transport
- • National and international policies to reduce population exposure to air pollution
- • Continue to strengthen national and international efforts to reduce exposure to smoking, both for children and adults, and to reduce uptake and encourage cessation
Targeted on individuals
- • Treat hypertension and aim for SBP <130 mm Hg in midlife
- • Use hearing aids for hearing loss; we need to help people wear hearing aids as many find them unacceptable, too difficult to use, or ineffective
- • Avoid or discourage drinking 21 or more units of alcohol per week
- • Prevent head trauma where an individual is at high risk
- • Stopping smoking is beneficial regardless of age
- • Reduce obesity and the linked condition of diabetes by healthy food availability and an environment to increase movement
- • Sustain midlife, and possibly late-life physical activity
Although we have more to learn about effectiveness, avoiding or delaying even a proportion of potentially modifiable dementias should be a national priority for all.
Interventions and care in dementia
Not all dementia will be preventable and we present the latest evidence on intervention and care for dementia. To date the emphasis has been on specific subtypes of dementia, most notably on Alzheimer's disease, which has been conceptualised over the years in a variety of changing diagnostic criteria—eg, DSM IV and DSM V. 180 , 181 Intense efforts have been put into biomarkers for early preclinical detection of the disease process before it becomes dementia. Biomarkers need to show reliability and validity, and for dementias they also need to be very closely and clearly related to clinical syndrome outcomes in the way that, for example, human papillomavirus is for cervical cancer, and hypertension has been for stroke.
Biomarkers and detection of Alzheimer's disease
Markers of neurodegeneration linked to clinical dementia include brain volume loss—ie, hippocampal volume loss and entorhinal cortex and medial temporal cortical thinning—seen in structural imaging. The most studied molecular markers are in Alzheimer's disease and are amyloid and tau, which PET and CSF detect clinically. The prevalence of particular pathologies at different ages is important in interpretation of such studies. So, for example, population derived studies show increases in plaques in the population from less than 3% at age 50–59 years to around 40% at age 80–89 years. 182
Amyloid imaging
Amyloid imaging detects amyloid in the brain with high sensitivity and specificity in both cognitively normal and people with Alzheimer's disease when the gold-standard comparison is either neuropathology or clinical diagnosis, distinguishing Alzheimer's disease from other neurodegenerative conditions. 183 Amyloid imaging is not a diagnostic test for dementia. A US study of randomly selected older people from the community recruited 1671 people (mean age of 71 years). 182 The prevalence of PET detected amyloid positivity increased from 2·7% (95% CI 0·5–4·9) of people without cognitive impairment aged 50–59 years to 41·3% (95% CI 33·4–49·2%) aged 80–89 years. 182 In 10-year follow-up PET positivity was associated with a higher probability of developing Alzheimer's disease compared with those who were amyloid negative (HR 2·6, 95% CI 1·4–4·9). In participants with mild cognitive impairment who were amyloid positive the probability (HR 1·9, 95% CI 0·9–3·9) was not very different to those who were amyloid negative (1·6, 0·8–3·4).
Similarly, an 8-year follow-up study of 599 volunteers (average age 70 years) in Australia found that cognitively normal PET amyloid-positive people had an elevated risk of developing Alzheimer's disease compared with amyloid negative (17·7% vs 8·1%; OR 2·4, 95% CI 1·5–4·0). 184 Over 80% of the 266 people who were PET amyloid-positive did not go onto develop a cognitive impairment within 8 years, showing positive status does not predict impairment for most people in a timeframe that might be a useful prognostic window. Follow-up at 5 years of amyloid-positive participants with normal cognition or mild cognitive impairment versus amyloid negative people found the same pattern of increased risk (2·6, 1·4–4·9). Risk also increases per 1 year of age (HR 1·05, 95% CI 0·55–2·0/year), and APOEε4 status (2·6, 1·4–5·0). 184
Most people who are amyloid positive with no other markers have not developed Alzheimer's disease dementia during their lifetime. A model of lifetime risks of people who are amyloid positive without any other biomarkers finds it to be 8·4% for a 90-year-old woman who is cognitively normal at baseline, 23·5% for a 75-year-old woman and 29·3% for a 65-year-old woman. 185 The 10-year risk is considerably less, so a 65-year-old woman with only amyloid biomarkers but who is cognitively normal and has no neurodegeneration has a 10-year Alzheimer's disease risk of 2·5% and a man 2·3%, but the risk is higher with accompanying neurodegeneration ( table 2 ). 185
Ten-year risks by age of developing Alzheimer's disease for women based on amyloidosis alone and in the presence of neurodegeneration and mild cognitive impairment
| 60 years | 0·2 (0·06–0·8) | 1·3 (0·6–2·5) | 3·6 (1·1–14·2) | 7·1 (4·5–10·9) | 93·5 (91·1–95·0) | 57·2 (48·2–67·9) |
| 65 years | 0·5 (0·14–1·8) | 2·5 (1·2–4·9) | 4·3 (1·4–15·0) | 10·7 (6·8–16·2) | 91·7 (89·2–93·5) | 55·4 (46·6–65·8) |
| 70 years | 1·1 (0·34–3·5) | 4·7 (2·4–8·7) | 5·5 (2·0–16·6) | 15·5 (10·0–22·8) | 88·6 (85·8–90·6) | 52·2 (43·8–62·4) |
| 75 years | 2·2 (0·74–6·5) | 7·8 (4·1–14·0) | 7·3 (2·9–19·0) | 20·8 (13·7–29·7) | 83·8 (80·7–86·2) | 47·4 (39·6–57·0) |
| 80 years | 3·7 (1·3–9·8) | 11·1 (6·0–18·7) | 9·3 (3·9–20·9) | 24·4 (16·4–33·8) | 75·8 (72·2–78·7) | 40·0 (33·1–48·6) |
| 85 years | 4·7 (1·8–11·0) | 11·5 (6·5–18·5) | 9·7 (4·3–19·3) | 23·1 (15·8–31·2) | 63·7 (59·6–67·2) | 30·0 (24·5–37·2) |
| 90 years | 3·8 (1·5–8·2) | 8·2 (4·7–12·9) | 7·1 (3·3–13·3) | 16·8 (11·5–22·6) | 46·7 (42·7–50·2) | 19·1 (15·3–24·3) |
Data are relative risk (95% CI) or %. Reproduced from Brookmeyer and Abdalla 185 by permission of Elsevier.
Overall, the knowledge of PET-measured amyloid and tau status and MRI-derived cortical thickness in a general population derived sample, only adds a small improvement, which might not be clinically important for predicting memory decline over a model with clinical and genetic variables. 186
Using amyloid PET in patients with cognitive impairment of uncertain causes, results in changes to the clinical diagnosis of Alzheimer's disease 187 and sometimes to medication prescription. We do not know whether PET use improves patient care or decreases care costs. Many people have a mixed cause of dementia and a positive result does not indicate only Alzheimer's disease.
Fluid biomarkers
PET imaging is very costly (US$3000 in the USA) and although used in some clinical settings remains the topic of research to understand its usefulness in broader populations. Fluid biomarkers—ie, blood and cerebrospinal fluid tests—have become a more practical focus of interest since it has become possible to measure specific proteins linked to the proteins associated with the neuropathologies of Alzheimer's disease. 188 A composite blood biomarker for amyloid tested in a discovery dataset and then a validation cohort of participants aged 60–90 years who were already taking part in studies in Japan or Australia had areas under the receiver operating characteristic curves of 96·7% for discovery and 94·1% for validation. The blood biomarker had sensitivity and specificity above 80% against amyloid PET measurement 188 and correlated with CSF concentrations of Aβ1–42. These results are similar to other amyloid blood biomarkers 189 , 190 and harmonisation to a common reference standard is now vital. Although CSF Aβ1–42/1–40 ratio and amyloid PET are now considered interchangeable, 191 CSF tau biomarkers have only correlated weakly with brain tau as currently measured by radioligands. 192 Neurofilament light protein is measured in many cohorts; however, it is non-specific. People with Huntington's disease, multiple sclerosis, mild cognitive impairment, and Alzheimer's disease might have raised blood neurofilament light concentrations, which are a marker of neurodegeneration. 193 , 194 , 195
Key points and conclusions
To be useful in clinical practice biomarkers must be well understood in the populations to which they are going to be applied, including the effects of age and sex on results. There is now reasonable evidence that amyloid and tau measured by PET or in fluid indicate increased risk for development of cognitive impairment in older adults but at the individual level prognostication is not possible as most cognitively normal people with these markers do not develop dementia within a clinically relevant timeframe. Negative amyloid results can be useful for ruling out current Alzheimer's pathology in people with cognitive impairment when the cause is uncertain and show an individual is unlikely to develop Alzheimer's disease during the next few years. High neurofilament light concentrations indicate a neurodegenerative process but not its cause. The value of biomarkers, in terms of diagnostic value, has not been addressed in different representative populations and particularly not in those from LMIC. The potential advantages of blood biomarkers are their low cost and their wider acceptability and applicability in many settings. In many areas of medicine more reliable diagnostic tests have improved research, including epidemiological and public health research and trials, to help distinguish cause from symptom (tuberculosis from a fever) or assess risk factor and disease (hypercholesterolaemia and ischaemic heart disease). Those biomarkers developed for the underlying biology of the dementia syndrome are subject to the same assessment of value.
Principles of intervention in people with dementia
In the 2017 Commission, we discussed that when concerns are raised by patients or family, an accurate diagnosis is helpful. Such a diagnosis provides a gateway to intervention and services where available, for planning for possible futures, and support for family, as well as to research. Unfortunately, these services are not always available. National plans for dementia support timely diagnosis and offer help to individuals and their families.
We did not address screening of those not presenting with concerns but rigorous systematic reviews by the US Task Force on Prevention have found an absence of evidence of benefit and harm. 196 The first trial of population screening took place in the USA, screening 4005 primary care patients aged 65 years or older. No clear benefit or harm in terms of quality of life, mood, or increasing diagnostic rates was found. 197 Other strategies might become more valuable in time such as sensitive awareness of risk factors, when routine records suggest an individual might be deteriorating cognitively. 198
People with dementia have complex problems with symptoms in many domains. Those providing support and any interventions must consider the person as a whole, as well as their context and their close carers, whether family or friends. Individuals' medical, cognitive, psychological, environmental, cultural, and social needs must be given consideration. 2 In the context of under provision of services, this notion is and will continue to be a challenge. Dementia, as an illness which affects cognition by definition, affects the ability to organise activities and people with dementia often need help to do what they enjoy—for example, listen to music, or go to gardens and parks. Wellbeing is one of the goals of dementia care.
Interventions once a diagnosis has been made
Cholinesterase inhibitors have a useful, modest role in improving cognition and activities of daily living in patients with mild-to-moderate Alzheimer's disease and memantine can be prescribed in combination or each drug used separately for moderate and severe Alzheimer's disease. 2 , 199 , 200 However, although available in most countries these drugs are no longer remunerated in France because it is felt that they offer only a small benefit while shifting clinician's attention from other interventions. Whether non-prescribing of this drug will help patients by removing an intervention with known benefit or be detrimental to them is unknown. 201 No advances have been reported in Aβ therapeutics, with negative results from phase 3 trials of monoclonal antibodies (eg, solanezumab, crenezumab) and inhibitors of β-secretase, a protease involved in the production of Aβ peptides. 202 Aducanumab previously abandoned as futile now has further unpublished results. Three 5HT6 antagonists and the calcium channel blocker nilvadipine 203 , 204 have also been ineffective. These drugs also show substantial impact during treatments at so-called therapeutic concentrations on the leakiness of blood vessels. The long-term impact of such side-effects is unknown. Anti-tau, anti-amyloid, and anti-inflammatory drugs continue to be in focus and some argue that pre-symptomatic interventions are necessary, especially if targeting Aβ production, but no evidence of efficacy 205 and some evidence of worsening target symptoms currently exists. 206
Cognitive training in people with dementia
A meta-analysis of 12 controlled trials of 389 people with mild dementia, completing 4 or more hours of group-based computerised cognitive training (mean age 66–81 years, 63·5% female participants), found a small, statistically significant beneficial effect on overall cognition, driven by two trials of virtual reality or Video games (SMD=0·3, 95% CI 0·0–0·5), one with a low and one with a high risk of bias. 55
A Cochrane review 207 found 33 trials of cognitive training, only one of which overlapped with the study above, with around 2000 participants with mild-to-moderate dementia, most with a high or uncertain risk of bias. 207 People completing cognitive training, compared with usual treatment or non-specific activities, had small-to-moderate effects on overall cognition (SMD 0·4, 95% CI 0·2–0·6) and specific cognitive abilities such as verbal fluency and improvements lasted for a few months to 1 year. No direct evidence was observed to suggest that cognitive training was better than cognitive stimulation therapy.
Exercise and physical activity
The Dementia and Physical Activity RCT 208 found moderate-to-high intensity aerobic and strength exercise training did not slow cognitive impairment in people with mild-to-moderate dementia but improved physical fitness. The US Reducing Disability in Dementia study 209 implemented an at-home multicomponent intervention including exercise education, training to increase pleasant events, and activator-behaviour-consequence problem-solving approach over 6 weeks by case managers in 255 community dwelling people with dementia older than 60 years and their family carer and were able to follow up 140 (54·9%). The study found increased physical activity; days of taking 30 or more minutes of exercise (effect size 0·6, 95% CI 0·4–0·8 after the treatment and 0·3, 0·1–0·5 at 13 months) in a before and after intervention comparison.
Interventions for neuropsychiatric symptoms of dementia
Neuropsychiatric symptoms are common and often clustered in people with dementia. These symptoms might precede dementia and are associated with tau and amyloid neuropathology. 210 This suggests that underlying neurobiological mechanisms might underpin neuropsychiatric symptoms. However, other drivers relating to the personal history and the environment of the person with dementia are also likely to exist. Neurodegeneration could lead to increased vulnerability to stressors or triggers. Genetics, cognitive reserve, resilience, medical comorbidities, and environment including responses of carers might modify these relationships. Needs and responses will also be individual and relate to a person's own social, cultural, and historical context. First-line assessment and management of neuropsychiatric symptoms should focus on basic health: describe and diagnose symptoms; look for causes such as pain (using validated pain assessments might help), illness, discomfort, hunger, loneliness, boredom, lack of intimacy and worry that could cause the behaviours and alleviate these while considering risks of harm. 2
No new evidence of medication effectiveness for these symptoms exists; risperidone in low doses (0·5 mg daily) and some other antipsychotics are sometimes effective but often ineffective and have adverse effects. 2 Specific initiatives have led to a decrease in antipsychotic prescriptions for people with dementia, although often replaced with other psychotropics ( figure 8 ), such as benzodiazepines, antidepressants, and mood stabilisers. 211 These psychotropics lack evidence of efficacy for neuropsychiatric symptoms but show clear evidence of possible harm; for example, trazodone and benzodiazepines increase fall-related injuries. 144 Major policy changes should be assessed carefully, within and across countries for unintended consequences (and perhaps unexpected benefits) and their costs.

Proportion of patients with a diagnosis of dementia prescribed an antipsychotic drug (A) and those prescribed an anxiolytic, hypnotic, or antidepressant (B)
CPRD=Clinical Practice Research Datalink. Reproduced from Donegan et al, 211 by permission of Elsevier.
Evidence is slowly accumulating for the effectiveness, at least in the short term, of person-centred evidence-based psychosocial interventions. In Germany, a 6-month cluster RCT of nurse-delivered, supervised dementia care management used a computer-assisted nurse assessment to determine personalised intervention modules, then a multi-disciplinary team discussion and agreement with the physician for 634 people (mean age 80 years) with dementia living at home with a primary carer or alone. 212 The mean mini mental state examination (MMSE) was 23, only 38% had a formal diagnosis of dementia; the majority of participants (51%) had mild dementia but some had moderate and some severe dementia. The intervention consisted of psychosocial management of treatment and care, medication management and carer support, and education and discussion with a psychiatrist or neurologist. The intervention, compared with care as usual, was associated with better outcomes for neuropsychiatric symptoms (Neuropsychiatric Inventory [NPI] score −7·5, 95% CI −11·1 to −3·8), however this effect could be because of deterioration in care as usual (in the care as usual group NPI increased from 7·2 to 15·2; in the intervention group NPI increased from 7·6 to 8·2). This between-group reduction in neuropsychiatric symptoms was greater than that expected, extrapolating from other study results, with antipsychotic medication. Effects on quality of life were only apparent for those people living with a carer.
An eight-session home-based tailored activity programme RCT, tailored both to the person with dementia living at home and to a family member compared with eight telephone-based education sessions, recruited 160 participants with 64% follow-up, imputing values for the rest. 213 The study reported a large reduction in overall neuropsychiatric symptoms immediately after the intervention, which were better in the group receiving home-based tailored activity programme on the neuropsychiatric inventory (mean difference in score 24·3, 95% CI 3·1–45·6), and on functional dependence and pain but this was not sustained 4 months later. Non-completers had more severe neuropsychiatric symptoms.
Since the 2017 Commission two new systematic reviews of antidepressants to treat depression in dementia reported moderate quality evidence that antidepressant treatment for people with dementia does not lead to better control of symptomatology compared with placebo. 214 , 215
Agitation is distressing for people with dementia and those around them, and contributes substantially to the overall costs as the level of agitation increases. 216 The body of evidence on this key behaviour is growing, mostly focused on care-home settings. These findings are valuable as these populations are most affected; however, because many people with dementia reside at home a major gap in knowledge remains.
Care home residents with agitation often find sitting still difficult and therefore might not be included in activities. 217 , 218 Two new cluster RCTs of professionals delivering multicomponent, interdisciplinary, interventions in care homes successfully reduced agitation. The WHELD study 219 included participants with or without neuropsychiatric symptoms and provided person-centred care, aiming to improve communication with people with dementia. It implemented social, sensory experiences or other activities; educated about antipsychotic review; and addressed physical problems, finding lower Cohen Mansfield Agitation Inventory (CMAI) at 9 months (MD −4·3 points, 95% CI −7·3 to −1·2). 219 The TIME study 220 for people with moderate-to-high levels of agitation consisted of a manual-based comprehensive assessment of the resident and structured case conference for the staff and doctor, to create a tailored plan, and then implement it. This intervention led to reduced agitation at 8 weeks (NPI −1·1 points, 95% CI −0·1 to −2·1; CMAI −4·7 points, −0·6 to −8·8) and 12 weeks (NPI −1·6, −0·6 to −2·7; CMAI −5·9, −1·7 to −10·1). 220 These effect sizes are similar to those seen for medications, but without harmful side-effects. 2 , 221 A further RCT studied a six-session intervention with staff in groups, teaching staff to understand agitation as related to medical, psychological, or social unmet needs and to implement strategies to meet these needs, using the describe, investigate, create, and evaluate approach. 222 The intervention did not reduce agitation symptoms, although it was cost-effective, improving quality of life. 223 Overall, the current evidence for agitation in care homes favours multi-component interventions by clinical staff, including considering if drugs might harm, and not drug interventions. Thus a major gap remains in knowledge about people living at home who comprise the majority of those with dementia.
Psychotic symptoms in dementia
People with dementia might be wrongly thought to have delusions when they misremember, and new psychotic symptoms are often due to delirium, thus thorough assessment of symptoms is essential. 2 Management of psychosis in dementia should start with non-pharmacological interventions; however, evidence for effectiveness of these interventions for psychosis in dementia is weaker than for agitation. 224 Antipsychotics for psychosis in dementia should be prescribed in as low a dose and for the shortest duration possible. 2 However, a Cochrane review of antipsychotics withdrawal found two trials with participants with dementia who had responded to antipsychotic treatment. These reported that stopping antipsychotics was associated with symptomatic relapse 225 suggesting the need for caution in any medication withdrawal in this group. There was low-quality evidence that, in general, discontinuation might make little or no difference to overall neuropsychiatric symptoms, adverse events, quality of life or cognitive function. 226
Apathy might be conceptualised as the opposite of engagement, comprising reduced interest, initiative, and activity. Like people without dementia, those with dementia engage more in preferred activities, but require additional support to do so. 227 A study in care homes observed engagement increased during activities in those who attended the groups. 228 A Cochrane review of the few people who had been in drug RCTs of methylphenidate versus placebo for apathy in dementia found small improvements on the apathy evaluation scale (MD −5·0, 95% CI −9·6 to−0·4, n=145, three studies, low-quality evidence) but not on the NPI apathy subscale (MD −0·1, 95% CI −3·9 to 3·7, n=85, two studies). 229
There is no evidence that medication for sleep in dementia is effective 230 and considerable evidence for harm—ie, earlier death, increased hospitalisation, and falls—exists. 139 , 144 Testing of non-pharmacological interventions is ongoing. 231
Carer distress related to neuropsychiatric symptoms rather than the dementia symptoms was associated in one study with increased use and costs of health services, 232 highlighting the need for effectively identifying, educating, and supporting distressed carers. An RCT 233 reporting 6-year follow-up after the eight session STrAtegies for RelaTives intervention—manual-based coping intervention delivered by supervised psychology graduates—found continuing effectiveness for depressive symptoms in carers (adjusted MD −2·00; 95% CI −3·4 to −0·6) and risk of case-level depression, with patient-related cost being approximately 3 times lower than those who did not receive the intervention (median £5759 vs £16 964 in the final year; p=0·07). 233 Another US study 234 followed up 663 people, mean age 77 years, 55% women. Caregiver depression rather than symptoms of people with dementia predicted emergency department use for people with dementia, with a 73% (RR 1·73, 95% CI 1·3–2·3) increase. 234
Functioning
A UK RCT of 14 sessions of cognitive rehabilitation focused on individual goal attainment with therapy delivered at home by an occupational therapist or nurse to 475 participants with mild-to-moderate dementia (MMSE ≥18 for inclusion; mean 24) and a family carer. 235 Individuals had two or three goals; the most common was engaging in activities (21% of goals). The intervention group reported increased goal attainment over 3 and 9 months compared with usual treatment (effect size 0·8, 95% CI 0·6–1·0 at both 3 and 9 months). 235 The treatment did not improve participants' quality of life, mood, self-efficacy, cognition, carer stress, or health status and was not cost-effective. A systematic review 236 of RCTs without meta-analysis for overall effect size, concluded that all interventions which had improved functioning in people living with dementia in the community have been individual rather than group interventions. These were: in-home physiotherapist delivered aerobic exercise (two studies, larger one positive, 140 people with Alzheimer's disease; smaller study negative, 30 people with Alzheimer's disease), individualised cognitive rehabilitation (mild or moderate dementia; two studies; 257 cognitive reserve intervention groups and 255 controls), and in-home activities-focused occupational therapy (people with mild to moderate dementia, three studies, 201 intervention, 191 controls) reduced functional decline compared to controls but group-exercise and reminiscence therapies were ineffective. 236
People with dementia have other illnesses
Multimorbidity is a huge challenge in dementia, not only because people with dementia have increased rates of other illnesses, but also because they often find it particularly difficult to organise care. People with dementia might forget to tell their family or health professionals of symptoms, struggle to understand or follow agreed plans, and are more likely to forget to drink and eat, increasing falling and infection rates. 237 People with dementia consult primary care less often 238 and have fewer dental visits 239 than those without dementia and their family members, if involved, often feel they lack knowledge to assist. 240 Health-care professionals need education to be more comfortable, understanding, and positive in communicating with people with dementia. 241
Around 70–80% of people diagnosed with dementia in primary care have at least two other chronic illnesses. 242 , 243 People who are physically more frail are more likely to have dementia, but the relationship between pathology and symptoms in these people is comparatively weak suggesting that dementia might be from other causes. 22 Compared to the general older population, people with dementia have increased rates of cerebrovascular disease, 243 , 244 , 245 , 246 stroke, 247 Parkinson's disease, 243 , 245 diabetes, 245 , 247 skin ulcers, anxiety and depression, 243 , 245 pneumonia, incontinence, and electrolyte disturbance. 245 Multimorbidity in people with dementia is associated with faster functional decline 248 and worse quality of life for people with dementia and their family carers. 249
Dementia and COVID-19
Severe acute respiratory syndrome coronavirus 2, was first identified in patients with viral pneumonia in Hubei province, China. 250 Severity and mortality of the associated disease (COVID-19) worsen with increasing age 251 and with pre-existing illnesses such as hypertension and diabetes, 252 and thus many people with dementia are at particular risk. Death certificates from the UK indicate that dementia and Alzheimer's disease were the most common underlying conditions, specified in 11 950 deaths (25·6% of all deaths involving COVID-19) in March to May, 2020. 253 Many charities, practitioners, and academics supporting people with dementia have issued guidance based on current evidence and best practice, including advance consideration of whether people would wish to be hospitalised if they develop severe COVID-19. Concern has been expressed that the illness and consequent distancing might increase family carer stress, loneliness, neuropsychiatric symptoms and use of psychotropic medication, and lead to complications, including future dementia. Interventions delivered remotely through technology have also been implemented in some places. 254 , 255 , 256 , 257
People with dementia might struggle to adhere to measures to reduce virus transmission, as they might not understand or remember about required changes to behaviour, such as physical distancing and hygiene, leading to increased risk to themselves and their carers. 258 They might additionally be vulnerable if they depend on others for daily activities or personal care, as this necessitates close personal contact.
This situation is particularly concerning in those care homes, where many residents have dementia and where many COVID-19 deaths have occurred in many countries 259 , 260 , 261 with reports of more than half of residents being admitted to hospital. In US nursing homes, among 10 576 people with confirmed COVID-19, residents living with dementia made up 52% of COVID-19 cases; yet, accounted for 72% of all deaths (an increased risk of 1·7). 262 The number of people living together in care homes means that the infection of an individual, either staff or resident, could endanger more people than in traditional or family households. Although evidence exists that if staff are sufficiently and rigorously protected they are unlikely to develop COVID-19, many staff have become unwell and some have died. 263 , 264 Illness means that there are fewer people to care for residents at a time when they need particularly high levels of care. This situation is particularly relevant in the care of residents with dementia, if they are expected to remain in their own rooms, rather than eating and participating in activities with others. Staff or residents might also be moved between care homes and increase risk in other homes. 261 Restrictions on visitors to private homes, care homes, and hospitals might cause greater distress for people with dementia and they might not understand why people are wearing masks, recognise who is behind it, or understand speech when lips are covered. Lack of restrictions means that the visitors might also be at elevated risk. 261
The impacts of COVID-19 on people with dementia might be particularly severe in LMICs, due to smaller health budgets for testing and protective equipment, capacity of health-care systems, quality of care home provision and patterns of workforce mobility. 264
Thus, people with dementia are particularly vulnerable to COVID-19 because of their age, multimorbidity, and difficulties in maintaining physical distancing. 250 , 251 , 252
We recommend rigorous public health measures of protective equipment and hygiene, including not moving staff or residents between care homes or admitting new residents when their COVID-19 status is unknown, should mitigate impacts on people with dementia. It is also imperative that there is frequent and regular testing of staff in care homes for infection, ensuring staff have sick pay so that they do not come in when symptomatic and interim care is being set up for people discharged from hospital so that only those who are COVID-19 free come to live in care homes. Resident testing should encompass asymptomatic as well as symptomatic people, when there is exposure within the home to COVID-19. In the future, many homes might be able to start to provide oxygen therapy so that those who do not want to be admitted to hospital are still able to access oxygen therapy. In addition, it is also important to reduce isolation by providing the necessary equipment and a brief training to relatives on how to protect themselves and others from COVID-19; so that they can visit their relatives with dementia in nursing homes safely when it is allowed. Further evidence is needed to inform responses to this and future public health emergencies.
Hospital admissions
Hospitalisation in people with dementia is associated with adverse, unintended consequences, including distress, functional and cognitive decline, and high economic costs. 265 , 266 , 267 People with dementia have 1·4 to 4 times more hospital admissions than others with similar illnesses. 266 , 268 , 269 , 270
A systematic review and meta-analysis including 34 studies of 277 432 people with dementia found that in the six studies which compared the two groups, people with dementia had increased hospital admissions compared with those without dementia, after adjusting for age, sex, and physical comorbidity (RR 1·4, 95% CI 1·2–1·7; figure 9 ). 271 Hospitalisation rates in people with dementia ranged from 0·37 to 1·26 per person-year in high-quality studies. Admissions are often for conditions that might be manageable in the community (potentially preventable hospitalisations). 268 People with dementia experience longer and more frequent admissions and readmissions; health-care expenditure for people with moderate-severe dementia is around double that of people without dementia. 269 , 272 , 273 Early detection and management of physical ill-health in people with dementia, particularly of pain, falls, diabetes, incontinence, and sensory impairment, is important. 199 , 274 , 275 However, no intervention has successfully reduced number of hospital admissions of community-dwelling people with dementia, 276 although education, exercise, rehabilitation, and telemedicine have reduced admissions for older people without dementia. 277

Systematic review and meta-analysis of hospitalisation rates of people with dementia compared to those without dementia controlled for age and sex
Reproduced from Shepherd et al, 271 by permission of Springer Nature.
High-quality care for people with dementia takes longer than caring for others with the same condition. 278 Recognition of dementia in hospital inpatients is necessary for optimum care, 279 but dementia is often undetected or unrecorded. 280 In the UK however, detection rates have increased over the past 10 years. 281
Physical illness, delirium, and dementia
Dementia and delirium frequently occur together. In one hospital inpatients' survey nearly 35% of those older than 80 years experienced delirium; those with prior cognitive impairment had 15 times the risk of developing delirium than those without (OR 15·3, 95% CI 5·2–45·4). 282 People with delirium without known dementia are more likely to be diagnosed with dementia in the future than others, either because of pre-existing undiagnosed dementia or cognitive impairment, present in 20·7% (95% CI 11·9–29·5) and 37·8% (27·3–88·3) respectively of one cohort, or because delirium has neurotoxic effects and so precipitates dementia. 283 People with similar neuropathology show faster cognitive decline if they develop delirium than if they do not. 284 Additionally, older people without dementia declined cognitively more than twice as fast after an emergency hospital admission for any cause, compared with those not admitted, suggesting any severe illness is associated with cognitive decline. 285 Risk factors for delirium in dementia include sensory impairment, pain, polypharmacy, dehydration, intercurrent illnesses, such as urinary tract infections or faecal impaction, and an unfamiliar or changing environment. 286 Delirium in older people should prompt consideration of underlying dementia.
Most research on delirium prevention has been in people without dementia. It suggests targeting hydration, stopping medication predisposing to delirium, monitoring the depth of anaesthesia, and sleep promotion. However, no evidence for medication efficacy, including cholinesterase inhibitors, antipsychotic medication, or melatonin exists. 287 , 288 , 289 The Hospital Elder Life Program 290 —an intervention to prevent delirium in those admitted to hospital—reduces delirium incidence and includes people who are cognitively impaired. This multidisciplinary treatment consists of daily visits, orientation, therapeutic activities, sleep enhancement, early mobilisation, vision and hearing adaptation, fluid repletion, infection prevention and management of constipation, pain, and hypoxia, and feeding assistance. 290
A network meta-analysis of drugs for prevention and treatment of delirium did not include studies of people with dementia, thus we cannot use this to recommend drugs for people with dementia and delirium as this research might be inapplicable to them. 291
Little high-quality research exists on managing delirium in dementia. One RCT compared care at a specialist medical and mental health unit to usual care for 600 confused people older than 65 years, acutely admitted to hospital and found no difference in the primary outcome of days spent at home or in hospital, but increased family satisfaction. 292 A further RCT of cognitively stimulating activities for people with delirium in dementia did not improve the delirium. 293 No definitive evidence that any medication improves delirium in people with dementia exists: cholinesterase inhibitors, antipsychotics, and sedating benzodiazepines are ineffective and antipsychotics and benzodiazepines are associated with mortality and morbidity. 265 , 288 , 294 , 295 , 296 , 297 Given the risk of dementia in people who develop delirium, its prevention, and possibly advances in its management, might offer a means for dementia prevention. 298
Link between very old age, frailty, and dementia
The fastest growing demographic group in most advanced countries are people aged 90 years and older. One well characterised post-mortem cohort of the oldest old (n=1079; mean age 90 years) dying with dementia, found that neuropathological features of Alzheimer's disease account for about half of the cognitive decline seen as people diagnosed with Alzheimer's disease had mixed causes of dementia. 299 Although Alzheimer's disease neuropathology was the commonest cause of dementia, Alzheimer's disease changes rarely occurred on their own, so only 9% of people with dementia had pure Alzheimer's disease pathology. 300 People who have Alzheimer's disease pathology without developing dementia tend to have fewer age-related health deficits than those who develop it with even low concentrations of plaques and tangles. 301 A moderation analysis showed that the relationship between Alzheimer's disease pathology and dementia status differed according to level of frailty (adjusted for age, sex, and education) with increasing frailty weakening the relationship between Alzheimer's disease pathology and dementia ( figure 10 ). 22 As with delirium, some of this additional health risk might be modifiable. This approach suggests a new type of therapy focus on specific age-related processes that underpin many diseases of late life might reduce the incidence or severity of dementia.

Moderation analyses of the relationship between Alzheimer's disease pathology and clinical diagnosis of Alzheimer's dementia (adjusted for age, sex, and education)
As frailty increased, the odds of a neuropathological diagnosis of Alzheimer disease corresponding to a clinical diagnosis decreased. Reproduced from Wallece et al, 22 by permission of Elsevier.
End-of-life care in dementia
The numbers of people dying with dementia are increasing but the evidence for the best end-of-life care is scarce. Trends in age-standardised death rates (3·6%) for dementia increased slightly between 1990–2016, with pronounced increases in the USA and Japan and decreases in western Europe and central Latin America. 4 Dementia is more readily being included on death certificates, which accounts for some of the rise. The increase might be related to dementia manifesting at later ages, with higher physical frailty 22 leading to a faster decline.
Most people with dementia might die while still in the mild-to-moderate stages whereas only about a quarter of those dying with dementia have severe dementia. 302 , 303 The trajectory of dementia is often unpredictable 304 and palliative care initiation should reflect need not prognosis.
Decision making about end of life is complex and simple rules of thumb, co-designed with staff and carers, provided clarity in some small studies. 304 One RCT testing decision-aids about families' and doctors' goals of care for people with advanced dementia led to increased palliative care content in care plans. 305 , 306 In a 9-month UK prospective study, 85 care home residents with advanced dementia from 14 homes were likely to be living with distressing symptoms, specifically agitation (54%) or pain (61% on movement). 304
Capacity to make abstract decisions, including about the future, might be lost early in dementia. 307 Therefore, advance care planning, designed to empower people with dementia and improve quality of dying, might theoretically be something everyone should do before developing dementia. 308 However, people might not be able to predict their future wishes. This might explain why family carer proxies show only low-to-moderate agreement with stated end-of-life treatment preferences of people with dementia. 309 Advance care planning might, however, reduce carers' uncertainty in decision making and improve perceptions of quality of care. 310
Partners of people dying with dementia experience poorer mental health than those facing bereavement from other causes 311 possibly because of long and difficult caring responsibilities. This might be ameliorated through sensitive and timely information, particularly regarding the progression of dementia, 312 individually or through family and staff case-conferencing. 313 , 314
Conclusions
Knowledge about risk factors and potential prevention, detection, and diagnosis of dementia is improving although significant gaps remain. 315 In this Commission report, we have specified policy and individual changes to delay the onset of cognitive impairment and dementia and better ways to support and treat people with dementia and their families and to improve their quality of life.
Interventions, including organisation of the complex physical illness and social needs, to support people affected by dementia can have a huge effect when taken as a whole. Our ambition is for worldwide provision of resources for an adequate level of wellbeing to people with dementia and their carers with a better evidence base to guide individual care and policy making alike. With good quality care, people can live well with dementia and families can feel supported.
Acknowledgments
We are partnered by University College London (UCL), the Alzheimer's Society, UK, the Economic and Social Research Council, and Alzheimer's Research UK, and would like to thank them for financial help. These organisations funded the fares, accommodation, and food for the Commission meeting but had no role in the writing of the manuscript or the decision to submit it for publication. We would like to thank Bernadette Courtney, Jacques Gianino, and Nuj Monowari, from UCL, London, UK, for their administrative help, including managing finances, booking rooms and food, and setting up a website supported by the University College London Hospitals National Institute for Health Research Biomedical Research Centre. We would like thank Henrik Zetterberg for advice on biomarkers and dementia.
Contributors
GL, JH, AS, and NM contributed to literature searches and quality assessments for systematic reviews. JH and NM performed meta-analyses. GL, JH, AS, and NM conceived the new PAF calculation and NM led the statistical analysis. GL, JH, AS, NM, DA, CLB, SB, AB, JC-M, CC, SGC, NF, RH, HCK, EBL, VO, KRi, KRo, ELS, QS, LSS, and GS attended the conference to discuss the content. GL, JH, EBL, AS, DA, and ELS wrote first drafts of sections of the paper. GL wrote the first draft of the whole paper and revisions of drafts. CBa reviewed and contributed to revision of the final drafts. All authors contributed to sections of the reports and all revised the paper for important intellectual content.
Declaration of interests
AS reports grants from Wellcome Trust (200163/Z/15/Z), outside the submitted work. DA reports grants from Eli Lilly, during the conduct of the study. CBa reports grants and personal fees from Aca-dia and Lundbeck; and personal fees from Roche, Otsuka, Biogen, Eli Lilly, and Pfizer, outside the sub-mitted work. SB reports grants and personal fees from AbbVie, personal fees and non-financial sup-port from Eli Lilly, and personal fees from Eleusis, Daval International, Boehringer Ingelheim, Axovant Sciences, Lundbeck, and Nutricia, outside the submitted work; and he has been employed by the Department of Health for England. NF reports non-financial support from Eli Lilly, outside the submitted work. LNG and her institutions (Johns Hopkins University, Baltimore, MD, USA, Drexel University, Philadelphia, PA, USA, and Thomas Jefferson University, Philadelphia, PA, USA) are entitled to receive royalties from fees associated with online training for the tailored activity program, which is an evidence-based program referenced in the Review. RH reports grants from Department of Health, NIHR HTA Programme, outside the submitted work; and he is a Scientific Trustee of the charity Alzheimer's Research UK. MK reports grants from the UK Medical Research Council (S011676, R024227), NordForsk (the Nordic Programme on Health and Welfare, 75021) and the Academy of Finland (311492), outside the submitted work. EBL reports other (royalties) from UpToDate, outside the submitted work. KRo reports personal fees from Clinical Cardio Day-Cape Breton University, Sydney, NS, Canada, CRUIGM-Montreal, Jackson Laboratory, Bar Harbor, MA, USA (speaker fees), MouseAge, Rome, Italy (speaker fees), Lundbeck, Frontemporal Dementia Study-Group, SunLife Insurance, Japan, outside the submitted work. He is a President and Chief Science Officer of DGI Clinical, which in the last 5 years has contracts with pharma and device manufacturers (Baxter, Baxalta, Shire, Hollister, Nutricia, Roche, Otsuka) on individualised outcome measurement. In 2017, he attended an advisory board meeting with Lundbeck. He is also Associate Director of the Canadian Consortium on Neurodegeneration in Aging, which is funded by the Canadian Institutes of Health Research, and with additional funding from the Alzheimer Society of Canada and several other charities, as well as, in its first phase (2013-2018), from Pfizer Canada and Sanofi Canada. He receives career support from the Dalhousie Medical Research Foundation as the Kathryn Allen Weldon Professor of Alzheimer Research, and research support from the Canadian Institutes of Health Research, the QEII Health Science Centre Foundation, the Capital Health Research Fund and the Fountain Family Innovation Fund of the QEII Health Science Centre Foundation. LSS reports grants and personal fees from Eli Lilly, Merck, and Roche/Genentech; personal fees from Avraham, Boehringer Ingelheim, Neurim, Neuronix, Cognition, Eisai, Takeda, vTv, and Abbott; and grants from Biogen, Novartis, Biohaven, and Washington University DIAN-TU, outside the submitted work. The remaining authors declare no conflict of interests.
Supplementary Material
Uncited references.
Retraction Note: It is time to control the worst: testing COVID-19 outbreak, energy consumption and CO2 emission
- Retraction Note
- Published: 03 July 2024
Cite this article

- Sajid Iqbal ORCID: orcid.org/0000-0001-7729-8464 1 ,
- Ahmad Raza Bilal ORCID: orcid.org/0000-0001-9471-7093 2 ,
- Mohammad Nurunnabi 3 ,
- Wasim Iqbal 4 ,
- Yazeed Alfakhri 4 &
- Nadeem Iqbal 5
The Original Article was published on 12 November 2020
Avoid common mistakes on your manuscript.
Retraction Note: Environmental Science and Pollution Research (2020) 28:19008-19020
https://doi.org/10.1007/s11356-020-11462-z
The Publisher has retracted this article in agreement with the Editor-in-Chief. An investigation by the publisher found a number of articles, including this one, with a number of concerns, including but not limited to compromised peer review process, inappropriate or irrelevant references, containing nonstandard phrases or not being in scope of the journal. Based on the investigation's findings the publisher, in consultation with the Editor-in-Chief therefore no longer has confidence in the results and conclusions of this article.
Authors Mohammad Nurunnabi and Yazeed Alfakhri disagree with the retraction. The Publisher has not been able to obtain a current email address for author Ahmad Raza Bilal. Authors Wasim Iqbal, Nadeem Iqbal and Sajid Iqbal have not responded to correspondence regarding this retraction.
Author information
Authors and affiliations.
KUBEAC, University of Management & Technology, Sialkot, 51310, Pakistan
Sajid Iqbal
School of Business, Sohar University, 311, Sohar, Oman
Ahmad Raza Bilal
College of Business Administration, Prince Sultan University, Riyadh, Saudi Arabia
Mohammad Nurunnabi
Department of Management Science, College of Management, Shenzhen University, Shenzhen, China
Wasim Iqbal & Yazeed Alfakhri
Department of Business Administration, Ghazi University, Dera Ghazi Khan, Pakistan
Nadeem Iqbal
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Wasim Iqbal .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Iqbal, S., Bilal, A.R., Nurunnabi, M. et al. Retraction Note: It is time to control the worst: testing COVID-19 outbreak, energy consumption and CO2 emission. Environ Sci Pollut Res (2024). https://doi.org/10.1007/s11356-024-34253-2
Download citation
Published : 03 July 2024
DOI : https://doi.org/10.1007/s11356-024-34253-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
- As Partisan Hostility Grows, Signs of Frustration With the Two-Party System
Nearly half of younger adults say they ‘wish there were more parties to choose from’
Table of contents.
- Leaners’ ratings of the opposing party are quite negative, but ratings of their ‘own’ party are lukewarm
- A rise in the share of Americans with unfavorable views of both parties
- The partisan gap in presidential approval ratings has grown over time
- About half of Republicans like leaders who contend Trump won 2020 election
- Views of political leaders’ approach to the other party
- Does support for a political party reflect on a person’s character?
- Majority of public sees a great deal of difference between Republican and Democratic parties
- Most Americans say at least one candidate for office shares their views
- Why partisan leaners lean – and why they don’t identify with a party
- Non-college adults are more likely than college graduates to cite the party ‘sticking up for people like them’ as a major reason for identifying with it
- Few voters say it is likely they will vote for the other party
- Leaners hold fewer negative stereotypes about the other party than partisans, but rising shares attribute negative traits
- Most Democrats view those in their party as more open-minded than other Americans; most GOP see co-partisans as more hardworking
- Across the political spectrum, a rise in the number of negative traits attributed to opposing partisans
- Acknowledgments
- Methodology
Pew Research Center conducted this study to better understand Americans’ feelings about the country’s major political parties and the reasons why they choose to affiliate with or lean toward a party. For this analysis, we surveyed 6,174 U.S. adults between June 27 and July 4, 2022. Everyone who took part in this survey is a member of the Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Here are the questions used for the report and its methodology .
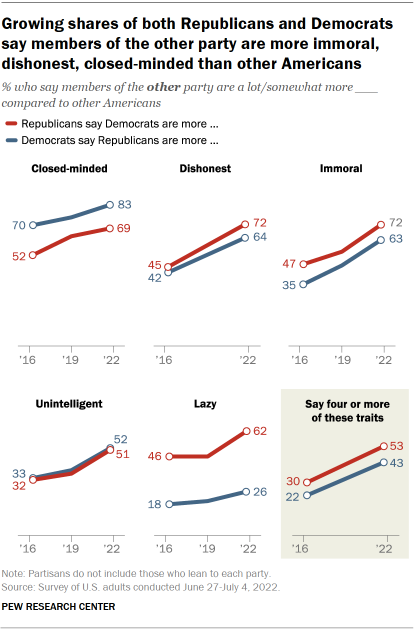
Partisan polarization has long been a fact of political life in the United States. But increasingly, Republicans and Democrats view not just the opposing party but also the people in that party in a negative light. Growing shares in each party now describe those in the other party as more closed-minded, dishonest, immoral and unintelligent than other Americans.
Perhaps the most striking change is the extent to which partisans view those in the opposing party as immoral. In 2016, about half of Republicans (47%) and slightly more than a third of Democrats (35%) said those in the other party were a lot or somewhat more immoral than other Americans. Today, 72% of Republicans regard Democrats as more immoral, and 63% of Democrats say the same about Republicans.
The pattern is similar with other negative partisan stereotypes: 72% of Republicans and 64% of Democrats say people in the opposing party are more dishonest than other Americans. Fewer than half in each party said this six years ago. Large majorities in both parties also describe those in the other party as more closed-minded than other Americans (83% of Democrats and 69% of Republicans say this), and this sentiment also has increased in recent years.
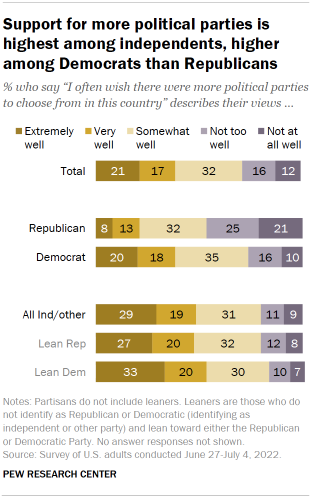
Yet there is one negative trait that Republicans are far more likely than Democrats to link to their political opponents. A 62% majority of Republicans say Democrats are “more lazy” than other Americans, up from 46% in previous studies in 2019 and 2016 . Only about a quarter of Democrats (26%) say Republicans are lazier than others, and this has changed only modestly since 2016.
The new survey on parties and partisanship by Pew Research Center, conducted among 6,174 Americans between June 27 and July 4, 2022, on the nationally representative American Trends Panel, finds that negative sentiment – the belief that the opposing party’s policies are harmful to the country – remains a major factor in why Republicans and Democrats choose to affiliate with their party.
In fact, nearly equal shares of Republicans cite the harm caused by Democratic policies (78%) and the positive impact of GOP policies (76%) as major reasons why they identify with their party. This also is the case for Democrats, with identical shares (68% each) citing these negative and positive reasons for their decision to affiliate with the Democratic Party.
The belief that the opposing party’s policies are harmful to the country is a particularly prominent factor in why independents lean toward the Republican and Democratic parties. It is the only one, among the five included on this survey, cited by majorities of both Republican-leaning (57%) and Democratic-leaning independents (55%) as a major reason why they lean toward their parties.
The survey finds that while negative partisanship remains extensive – and in many cases is increasing – there also are signs of frustration with the two-party system and the parties themselves. This frustration is more evident among partisan leaners – who tend to be younger and less politically engaged than partisans – than among those who identify as Republicans or Democrats.
Among the public overall, 39% say the following describes their views extremely or very well: “I often wish there were more political parties to choose from in this country.” Another 32% say the statement describes their views somewhat well, while 28% say it describes their views not too well or not at all well.
Notably, Democrats are more likely than Republicans to express a desire for more political parties: 38% of those who identify with the Democratic Party say this describes their views extremely or very well, compared with 21% of Republicans. Yet it is among independents and others who do not identify with a party that the sentiment is most pronounced: 48% say it describes their views extremely or very well, including 48% of those who lean Republican and 53% of those who lean Democratic.
Overall, interest in having more political parties is higher among younger Americans than older adults. Nearly half of those ages 18 to 49 say they often wish there were more parties to choose from (47% say it describes their views extremely or very well); that compares with 35% of those ages 50 to 64 and just 23% of those 65 and older.
Neither party is very popular with the public : Roughly four-in-ten Americans (41%) have a very or somewhat favorable view of the Democratic Party, while even fewer (37%) have a favorable impression of the Republican Party.
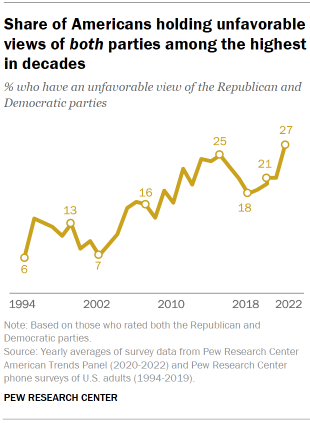
Over the past several decades, the share of Americans who express unfavorable opinions of both major parties has grown: In 1994, just 6% of the public had an unfavorable view of the Republican and Democratic parties. Today, about a quarter (27%) have negative views of both parties. This view is especially pronounced among partisan leaners: 44% of Republican-leaning independents – and an identical share of Democratic leaners – currently have negative views of both parties.
The Democratic Party has advantages over the GOP on several traits and attributes, particularly when it comes to tolerance for different types of people and not making excuses for hateful views among members of their own party. About six-in-ten adults (57%) say the phrase “respectful and tolerant of different types of people” describes the Democratic Party very or somewhat well, compared with 38% who say it describes the Republican Party.
And while 61% say the phrase “too often makes excuses for party members who have hateful views” describes the Republican Party, a smaller share (51%) say it describes the Democratic Party.
At the same time, there are more modest differences in views of the parties’ respect for the nation’s democratic institutions. About half of adults (51%) say “respects the country’s democratic institutions and traditions” describes the Democratic Party very or somewhat well, while 45% say it applies to the GOP. And neither party gets high ratings for honesty: 43% say the phrase “governs in an honest and ethical way” describes the Democratic Party, compared with 37% who characterize the Republican Party this way.
Other important findings from the survey
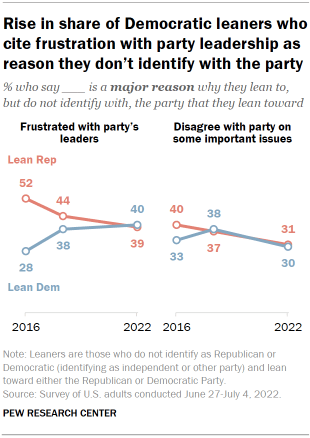
Those who lean to the Democratic Party have become more critical of Democratic leaders. When asked why they lean toward a party – rather than identify with it – many leaners say they do not want to put a political label on their views, while nearly as many offer that they are frustrated with the leadership of the party they lean toward. The share of Democratic leaners who cite frustration with the party’s leaders as a major reason for why they do not more closely associate with the party has risen from 28% in 2016 to 40% currently. Over the same period, the share of Republican leaners who express frustration with GOP leadership has declined from 52% to 39%.
The GOP is divided over leaders who endorse Trump’s unproven election claims. About half of Republicans (51%) say they like political leaders who publicly assert that Donald Trump was the legitimate winner of the 2020 presidential election; 17% say they do not like such leaders, while 31% neither like nor dislike them. Those who identify strongly with the GOP – strong Republicans, who make up 70% of all Republicans – are far more likely than those who identify with the party less strongly or Republican leaners to express positive views of such leaders. About six-in-ten strong Republicans (59%) express positive views of leaders who say Trump won in 2020, compared with 31% of less strong Republicans and 24% of Republican-leaning independents.
Republicans and Democrats express increasingly positive views of themselves . While Republicans and Democrats express increasingly negative views of those in the other party, they have become more positive about the people in their party. For example, a majority of Republicans (63%) now say that members of their party are a lot or somewhat more moral than other Americans; about half of Republicans (51%) said that in 2016 and 2019. The share of Democrats who say their fellow Democrats are more moral than other Americans has increased from 38% in 2016 to 51% currently.
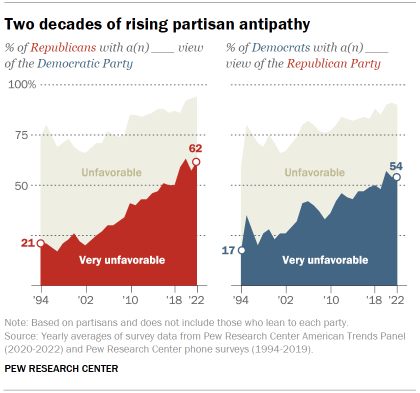
Deeply negative views of the opposing party are far more widespread than in the past. About six-in ten Republicans (62%) and more than half of Democrats (54%) have a very unfavorable view of the other party in Pew Research Center surveys conducted this year. While these highly negative views of the opposing party are little changed in the last few years, the share expressing this level of antipathy is higher than it was even five years ago, and considerably higher than it was a few decades ago. In 1994, fewer than a quarter in both parties rated the other party very unfavorably.
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Political Animosity
- Political Parties
- Political Polarization
Most Americans say elected officials should avoid heated or aggressive speech
Americans’ dismal views of the nation’s politics, partisan antipathy: more intense, more personal, most popular, report materials.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
© 2024 Pew Research Center

In-Person Time
In the Changing Role of the Office, It’s All about Moments That Matter
New research highlights three key times when bringing employees and teams together in person creates lasting connection
Illustration by Zara Picken
T Three years into flexible work, we’re entering a new phase: structured flexible work. While every organization approaches flexibility differently, leaders are looking to establish norms and best practices with their employees, particularly around when—and how much—to come into the office. At Microsoft, our structured flexible work model empowers individuals and teams to intentionally decide what works for them, within company and team guidelines. “We enable managers and employees to do what they believe is best for each individual’s unique needs, as well as each team’s success,” says Karen Kocher, global general manager, Future of Work, Workforce of the Future, and talent & learning experiences at Microsoft. Study after study shows that employees want the best of both worlds—flexible work and in-person connection. Back in 2021, the Work Trend Index uncovered what we call the hybrid paradox: over 70% of workers wanted flexible work to stay, and over 65% were craving more in-person time with their teams. While the amount of flexibility might differ by role—data center employees or hardware engineers might spend more time on-site, for example—we’ve seen this trend persist in both our external research and in our Microsoft employee surveys. How can leaders bring structure to flexible work and help employees get the in-person connection they crave? New research shows it’s not about the number of days people are in the office, it’s about creating moments that matter. hree years into flexible work, we’re entering a new phase: structured flexible work. While every organization approaches flexibility differently, leaders are looking to establish norms and best practices with their employees, particularly around when—and how much—to come into the office. At Microsoft, our structured flexible work model empowers individuals and teams to intentionally decide what works for them, within company and team guidelines. “We enable managers and employees to do what they believe is best for each individual’s unique needs, as well as each team’s success,” says Karen Kocher, global general manager, Future of Work, Workforce of the Future, and talent & learning experiences at Microsoft. Study after study shows that employees want the best of both worlds—flexible work and in-person connection. Back in 2021, the Work Trend Index uncovered what we call the hybrid paradox: over 70% of workers wanted flexible work to stay, and over 65% were craving more in-person time with their teams. While the amount of flexibility might differ by role—data center employees or hardware engineers might spend more time on-site, for example—we’ve seen this trend persist in both our external research and in our Microsoft employee surveys. How can leaders bring structure to flexible work and help employees get the in-person connection they crave? New research shows it’s not about the number of days people are in the office, it’s about creating moments that matter.
Our internal data points to three specific moments when in-person time is most beneficial:
Strengthening team cohesion
Onboarding to a new role, team, or company
Kicking off a project
1. Strengthening team cohesion
There’s no going back to 2019. Over the past four years, organizations have become increasingly distributed, and for many of them, a large-scale return to the office is no longer a feasible way to create meaningful connections between individuals and teams. This is certainly true of Microsoft. “We’re not the same company that we were prior to the pandemic,” says Dawn Klinghoffer, head of people analytics at Microsoft. Back then, 61% of teams at the company were all in the same location; today that number is 27%. And research shows that 70% of managers at Fortune 100 companies have at least one remote team member.
Fewer Teams Are Fully Co-Located Than in 2020
New research shows that teams are more geographically dispersed than before the pandemic, and fewer teammates all live within the same city.*
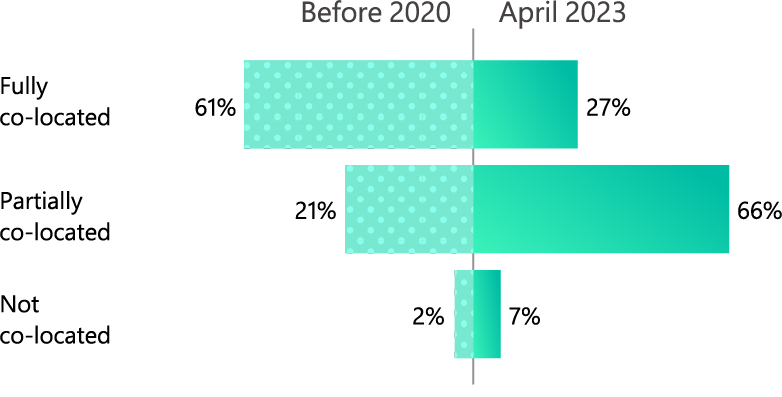
And employees say that flexibility is going well: In our latest Microsoft employee engagement survey, 92% of our employees say they believe the company values flexibility and allows them to work in a way that works best for them. An even higher 93% are confident in their ability to work together as a team, regardless of location. At the same time, the survey shows people are craving more connection. When we looked at the comments from employees who did not rate their quality of connection with co-workers as favorable (only neutral or unfavorable), 29% of those comments said that remote work has made it difficult to create meaningful connections and relationships. We know that people come into an office for each other—whether it’s once a week or once a year—and in the same engagement survey, employees made it clear they’re looking for time together spent connecting, not just co-working. When asked what in-person activities Microsoft should offer to support teams’ success, 37% of comments were about social and team-building activities—the number one theme overall.
Just ask Maryleen Emeric, who organized a recent team week for the Microsoft Modern Work and Business Applications group. (Team week brings together far-flung colleagues who would otherwise rarely see each other.) And after a long day of meetings and workshops during team week, she brought down the house with a karaoke cover of Bonnie Tyler’s “Total Eclipse of the Heart.” “Those sorts of social connections are not something that you can create over a screen,” she says. “Allowing people to get to know each other and find those common interests outside of work—I don’t think that can happen if you don’t bring people together once in a while.”
We see this sentiment in our external surveys too. According to the September 2022 Work Trend Index report , about 85% of people were motivated to go into the office for socializing with co-workers; just as many also said they’d be motivated by a desire to rebuild team bonds.
“You have to think of your social capital like a battery,” Emeric says. “The longer you go without having in-person interaction, the lower the charge gets on your battery. These moments that matter—like a team week—allow us to recharge the battery.” In fact, Microsoft employees who spent six days or more a month in the office with their team had a slightly higher thriving score than those who did not spend any time in the office. (Thriving is our outcome for engagement at Microsoft, defined by a combination of three tenets: being “ empowered and energized to do meaningful work .”) While even more days together raises scores for feeling energized and for alignment on goals, it also starts to push down scores for flexibility and satisfaction.
In-person time can also remind the individual employee of the role they play in the success of the broader team and the organization. Team week culminated in an “ask me anything” style conversation with organization leader Jared Spataro, CVP of Modern Work & Business Applications, during which he spoke openly about the company’s vigorous focus on AI. “It made people feel very connected to our mission, very connected to our goals, and very connected to our culture,” Emeric says. “It got people very energized. And it felt like people were recommitting to the cause. Like, ‘Yeah, we’re all in.’” We know from the Work Trend Index report that high-quality connections pay off for both people and businesses: Employees who have positive relationships with their immediate team members report better wellbeing than those with poor relationships. They also report higher productivity, and are less likely to change employers in the year ahead. Strengthening networks outside of the immediate team matters, too, according to the Work Trend Index. Employees with positive relationships beyond their immediate team members say they’re more satisfied with their employer, more fulfilled by work, and have a more positive outlook on workplace stress than those with weak organizational networks. Or, in the immortal words of Ms. Bonnie Tyler: “ Together we can take it to the end of the line …”
2. Onboarding to a new role, team, or company
Our research showed that when starting a new role—whether at a new company or in an internal switch—meeting your manager or onboarding buddy in person makes certain things easier. Compared with employees who didn’t meet their managers in person within the first 90 days, employees who did were more likely to seek feedback, be asked for input by their team, build strong relationships with colleagues, feel supported when discussing tough issues with their manager, and get effective coaching and feedback. (However, there are no differences in how these new hires feel about other outcomes in the survey, including driving impact, finding the support they need, being supported by their colleagues and feeling included, knowing their stakeholders, and getting to know the culture.) Meeting your onboarding “buddy”—a teammate assigned to support your transition to the new team—in person within 90 days makes a difference too. Those who did were more likely to seek feedback, feel included, feel trusted by their team, and report they had clarity about how to drive impact—and have the necessary tools to do so. (But meeting their onboarding buddy in person did not meaningfully affect new hires’ scores in other areas, such as finding the support they need, understanding their organization’s vision, or knowing their stakeholders.) The quicker that new hires develop trust with their managers and teammates, the quicker they can become productive contributors and collaborators with the team and the company. “Understanding the priorities and feeling a sense of belonging is just really a goodness for both the organization and the individual,” Kocher says.
Meeting In Person Has Clear Benefits for New Hires
For new employees, connecting with their manager or onboarding “buddy“ in person has a measurable short-term effect on how well they integrate with their new teams.
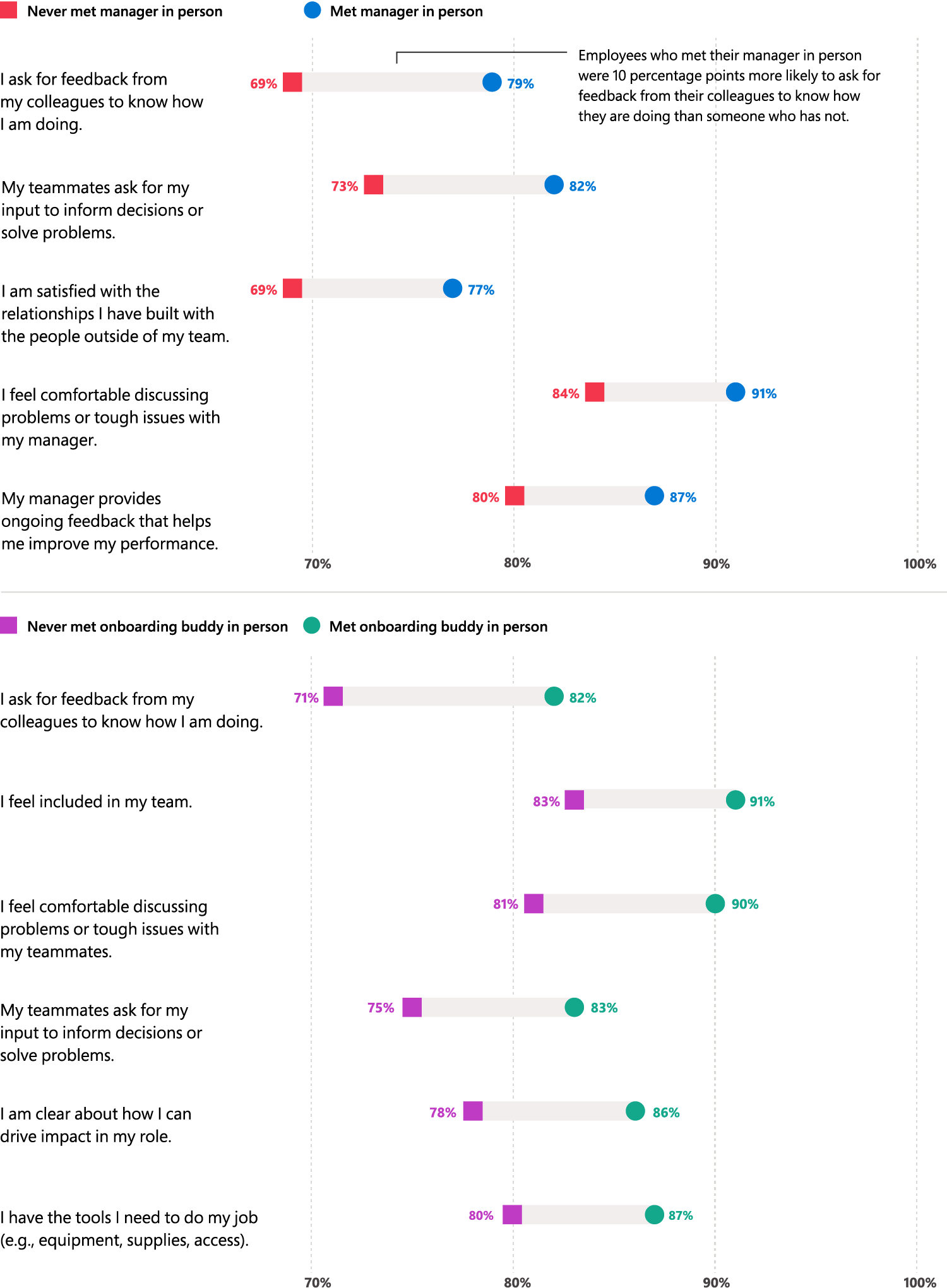
Source: Onboarding Research Survey at 90 Days, Microsoft, Sept. 7 to Dec. 31, 2022
Stretches of in-person training also help new hires understand their tasks and priorities with less friction. They can receive close guidance and immediate feedback, with easy access to assistance, clarification, and tacit knowledge. “It helps you get more quickly up to speed,” Kocher says. “And when you can deliver at your maximum capacity much more quickly, it helps you become more intrinsically motivated and energized.” Another internal survey showed that early-in-career employees felt slightly more energized when they worked regularly in the same building with their team members. In-person time also gives employees the opportunity to observe company norms and team dynamics—subtleties that are difficult to pick up on virtually and that can be especially important for early-in-career employees. All that said, as Klinghoffer notes, once you’ve onboarded, in-person one-on-one meetings are not necessarily mission critical, which is good news for distributed teams. It’s a balance: “Meeting one’s manager early on is a moment that matters and has some great outcomes, but down the road, you don’t necessarily have to be in person regularly.”
3. Kicking off a project
In-person time is useful in the earliest stages of a project life cycle for the same reason it’s useful during the onboarding process: getting people on the same page. When respondents of our employee engagement survey shared specific examples of moments that matter to be in person for, they included initial customer engagements and planning sessions—one respondent even said it “would be a significant boost to team collaboration, culture, and execution.” The Microsoft 365 Copilot project kickoff , which assembled teams from diverse departments for the company’s most ambitious project in a decade, happened in person, for example. Physical proximity simply helps people feel like their colleagues understand them. “Everyone likes to feel heard by others,” Kocher says. “And it’s easier to feel heard when you’re right next to somebody having a conversation.” With mutual trust and alignment in place, the creative juices can start flowing. In-person time helps spark innovation and outside-the-box thinking. In fact, studies show that while it’s easiest to choose the best idea virtually, in-person pairs generated 18% more creative ideas and 14% more ideas overall compared with virtual pairs in the same hour—so you can have better choices to pick from. “If you want the best and most ideas, you do it in person,” Kocher says. “When you’re in a big room with a lot of people, your mind perceives an expansion. Compare that to when you’re at a computer and you’re talking to people online: your mind goes very narrow very quickly.” Aside from boosting brainstorming power, being together in person at the beginning of a project allows a team to more efficiently share tacit knowledge, get clarity, establish individual roles, and coordinate their efforts. “Get to know people, build the trust, have some initial brainstorming sessions,” Klinghoffer says. “Then, once you’ve built that social capital, go back to your home offices or separate locations and keep on moving the project forward.”
Key Takeaway
While flexible work looks different for every organization, it’s clear that it’s here to stay. As organizations embrace this transformative model, they unlock their capacity to increase productivity, enhance employee satisfaction, and create a more inclusive workforce. Remote work has benefits, and in-person time does too. Every team is different, but one thing is clear: finding this balance must be approached with intentionality. Rather than considering the office as a one-size-fits-all solution, teams should consider the type of work they do and determine key points in time or reasons to gather in person. What’s more, the benefits of in-person time—whether it’s for a weeklong on-site or a day here and there—should be weighed against things like travel and expenses, commuting, and creating space for deep work. As Klinghoffer says, “Ask yourself and your team: What are the moments that matter for us?”
Stay in the AI know with WorkLab
Sign up for the WorkLab newsletter to get the latest AI research, insights, and trends delivered straight to your inbox.

Better Meetings
How to Get Hybrid Meetings Right

3 Ways Hybrid Collaboration Can Bridge Both Space and Time
- At least 10% of research may already be co-authored by AI
That might not be a bad thing

Your browser does not support the <audio> element.
“C ERTAINLY, HERE is a possible introduction for your topic...” began a recent article in Surfaces and Interfaces , a scientific journal. Attentive readers might have wondered who exactly that bizarre opening line was addressing. They might also have wondered whether the ensuing article, on the topic of battery technology, was written by a human or a machine .
It is a question ever more readers of scientific papers are asking. Large language models ( LLM s) are now more than good enough to help write a scientific paper. They can breathe life into dense scientific prose and speed up the drafting process, especially for non-native English speakers. Such use also comes with risks: LLM s are particularly susceptible to reproducing biases, for example, and can churn out vast amounts of plausible nonsense. Just how widespread an issue this was, though, has been unclear.
In a preprint posted recently on arXiv, researchers based at the University of Tübingen in Germany and Northwestern University in America provide some clarity. Their research, which has not yet been peer-reviewed, suggests that at least one in ten new scientific papers contains material produced by an LLM . That means over 100,000 such papers will be published this year alone. And that is a lower bound. In some fields, such as computer science, over 20% of research abstracts are estimated to contain LLM -generated text. Among papers from Chinese computer scientists, the figure is one in three.
Spotting LLM -generated text is not easy. Researchers have typically relied on one of two methods: detection algorithms trained to identify the tell-tale rhythms of human prose, and a more straightforward hunt for suspicious words disproportionately favoured by LLM s, such as “pivotal” or “realm”. Both approaches rely on “ground truth” data: one pile of texts written by humans and one written by machines. These are surprisingly hard to collect: both human- and machine-generated text change over time, as languages evolve and models update. Moreover, researchers typically collect LLM text by prompting these models themselves, and the way they do so may be different from how scientists behave.

The latest research by Dmitry Kobak, at the University of Tübingen, and his colleagues, shows a third way, bypassing the need for ground-truth data altogether. The team’s method is inspired by demographic work on excess deaths, which allows mortality associated with an event to be ascertained by looking at differences between expected and observed death counts. Just as the excess-deaths method looks for abnormal death rates, their excess-vocabulary method looks for abnormal word use. Specifically, the researchers were looking for words that appeared in scientific abstracts with a significantly greater frequency than predicted by that in the existing literature (see chart 1). The corpus which they chose to analyse consisted of the abstracts of virtually all English-language papers available on PubMed, a search engine for biomedical research, published between January 2010 and March 2024, some 14.2m in all.
The researchers found that in most years, word usage was relatively stable: in no year from 2013-19 did a word increase in frequency beyond expectation by more than 1%. That changed in 2020, when “ SARS ”, “coronavirus”, “pandemic”, “disease”, “patients” and “severe” all exploded. (Covid-related words continued to merit abnormally high usage until 2022.)

By early 2024, about a year after LLM s like Chat GPT had become widely available, a different set of words took off. Of the 774 words whose use increased significantly between 2013 and 2024, 329 took off in the first three months of 2024. Fully 280 of these were related to style, rather than subject matter. Notable examples include: “delves”, “potential”, “intricate”, “meticulously”, “crucial”, “significant”, and “insights” (see chart 2).
The most likely reason for such increases, say the researchers, is help from LLM s. When they estimated the share of abstracts which used at least one of the excess words (omitting words which are widely used anyway), they found that at least 10% probably had LLM input. As PubMed indexes about 1.5m papers annually, that would mean that more than 150,000 papers per year are currently written with LLM assistance.

This seems to be more widespread in some fields than others. The researchers’ found that computer science had the most use, at over 20%, whereas ecology had the least, with a lower bound below 5%. There was also variation by geography: scientists from Taiwan, South Korea, Indonesia and China were the most frequent users, and those from Britain and New Zealand used them least (see chart 3). (Researchers from other English-speaking countries also deployed LLM s infrequently.) Different journals also yielded different results. Those in the Nature family, as well as other prestigious publications like Science and Cell , appear to have a low LLM- assistance rate (below 10%), while Sensors (a journal about, unimaginatively, sensors), exceeded 24%.
The excess-vocabulary method’s results are roughly consistent with those from older detection algorithms, which looked at smaller samples from more limited sources. For instance, in a preprint released in April 2024, a team at Stanford found that 17.5% of sentences in computer-science abstracts were likely to be LLM -generated. They also found a lower prevalence in Nature publications and mathematics papers ( LLM s are terrible at maths). The excess vocabulary identified also fits with existing lists of suspicious words.
Such results should not be overly surprising. Researchers routinely acknowledge the use of LLM s to write papers. In one survey of 1,600 researchers conducted in September 2023, over 25% told Nature they used LLM s to write manuscripts. The largest benefit identified by the interviewees, many of whom studied or used AI in their own work, was to help with editing and translation for those who did not have English as their first language. Faster and easier coding came joint second, together with the simplification of administrative tasks; summarising or trawling the scientific literature; and, tellingly, speeding up the writing of research manuscripts.
For all these benefits, using LLM s to write manuscripts is not without risks. Scientific papers rely on the precise communication of uncertainty, for example, which is an area where the capabilities of LLM s remain murky. Hallucination—whereby LLM s confidently assert fantasies—remains common, as does a tendency to regurgitate other people’s words, verbatim and without attribution.
Studies also indicate that LLM s preferentially cite other papers that are highly cited in a field, potentially reinforcing existing biases and limiting creativity. As algorithms, they can also not be listed as authors on a paper or held accountable for the errors they introduce. Perhaps most worrying, the speed at which LLM s can churn out prose risks flooding the scientific world with low-quality publications.
Academic policies on LLM use are in flux. Some journals ban it outright. Others have changed their minds. Up until November 2023, Science labelled all LLM text as plagiarism, saying: “Ultimately the product must come from—and be expressed by—the wonderful computers in our heads.” They have since amended their policy: LLM text is now permitted if detailed notes on how they were used are provided in the method section of papers, as well as in accompanying cover letters. Nature and Cell also allow its use, as long as it is acknowledged clearly.
How enforceable such policies will be is not clear. For now, no reliable method exists to flush out LLM prose. Even the excess-vocabulary method, though useful at spotting large-scale trends, cannot tell if a specific abstract had LLM input. And researchers need only avoid certain words to evade detection altogether. As the new preprint puts it, these are challenges that must be meticulously delved into. ■
Curious about the world? To enjoy our mind-expanding science coverage, sign up to Simply Science , our weekly subscriber-only newsletter.
Explore more
This article appeared in the Science & technology section of the print edition under the headline “Scientists, et ai”
Science & technology June 29th 2024
The race to prevent satellite armageddon.
- A deadly new strain of mpox is raising alarm

From the June 29th 2024 edition
Discover stories from this section and more in the list of contents
More from Science and technology

New yeast strains can produce untapped flavours of lager
One Chilean hybrid has a spicy taste, with hints of clove

A new technique could analyse tumours mid-surgery
It would be fast enough to guide the hands of neurosurgeons

The world’s most studied rainforest is still yielding exciting new insights
Even after a century of research, a tropical rainforest in Panama continues to shed valuable light on the world’s abundance of natural life
A new bionic leg can be controlled by the brain alone
Those using the prosthetic can walk as fast as those with intact lower limbs
How the last mammoths went extinct
Small genetic mutations accumulated through inbreeding may have made them vulnerable to disease
Fears of a Russian nuclear weapon in orbit are inspiring new protective tech
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- NATURE PODCAST
- 17 December 2020
Coronapod: The big COVID research papers of 2020
- Benjamin Thompson ,
- Noah Baker &
- Traci Watson
You can also search for this author in PubMed Google Scholar
Benjamin Thompson, Noah Baker and Traci Watson discuss some of 2020's most significant coronavirus research papers.
In the final Coronapod of 2020, we dive into the scientific literature to reflect on the COVID-19 pandemic. Researchers have discovered so much about SARS-CoV-2 – information that has been vital for public health responses and the rapid development of effective vaccines. But we also look forward to 2021, and the critical questions that remain to be answered about the pandemic.
Papers discussed
A Novel Coronavirus from Patients with Pneumonia in China, 2019 - New England Journal of Medicine, 24 January
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China - The Lancet , 24 January
A pneumonia outbreak associated with a new coronavirus of probable bat origin - Nature , 3 February
A new coronavirus associated with human respiratory disease in China - Nature , 3 February
Temporal dynamics in viral shedding and transmissibility of COVID-19 - Nature Medicine , 15 April
Spread of SARS-CoV-2 in the Icelandic Population - New England Journal of Medicine , 11 June
High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice — Skagit County, Washington, March 2020 - Morbidity & Mortality Weekly Report , 15 August
Respiratory virus shedding in exhaled breath and efficacy of face masks - Nature Medicine , 3 April
Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1 - New England Journal of Medicine , 13 April
Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period - Science , 22 May
Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe - Nature, 8 June
The effect of large-scale anti-contagion policies on the COVID-19 pandemic - Nature , 8 June
Retraction—Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis - The Lancet, 20 June
A Randomized Trial of Hydroxychloroquine as Postexposure Prophylaxis for Covid-19 - New England Journal of Medicine , 3 June
Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19 - JAMA , 2 September
Immunological memory to SARS-CoV-2 assessed for greater than six months after infection - bioRxiv, 16 November
Coronavirus Disease 2019 (COVID-19) Re-infection by a Phylogenetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2 Strain Confirmed by Whole Genome Sequencing - Clinical Infectious Diseases , 25 August
Nature’s COVID research updates – summarising key coronavirus papers as they appear
Never miss an episode: Subscribe to the Nature Podcast on Apple Podcasts , Google Podcasts , Spotify or your favourite podcast app. Head here for the Nature Podcast RSS feed .
doi: https://doi.org/10.1038/d41586-020-03609-2
Related Articles
- Public health

Spike deep mutational scanning helps predict success of SARS-CoV-2 clades
Article 03 JUL 24

First encounter with SARS-CoV-2: immune portraits of COVID susceptibility
News & Views 19 JUN 24
What causes long COVID? Case builds for rogue antibodies
News 13 JUN 24
Streamlined collaboration can boost CRISPR gene therapies for rare diseases
Correspondence 02 JUL 24

Combined COVID-flu vaccines are coming: Moderna jab clears major test
News 28 JUN 24

‘Vindicated’: Embattled misinformation researchers celebrate key US Supreme Court decision
News 26 JUN 24
‘Epigenome editor’ silences gene that causes deadly brain disorders
News 27 JUN 24

How blockbuster obesity drugs create a full feeling — even before one bite of food

Ketamine for depression: slow-release pills could make treatment more accessible
Global Faculty Recruitment of School of Life Sciences, Tsinghua University
The School of Life Sciences at Tsinghua University invites applications for tenure-track or tenured faculty positions at all ranks (Assistant/Ass...
Beijing, China
Tsinghua University (The School of Life Sciences)
Sales Executive, Nature Careers
If you're customer-focused, thrive in sales, and want to impact Europe's job market, join our Nature Careers team !
London - hybrid working model
Springer Nature Ltd
Junior Group Leader
The Imagine Institute is a leading European research centre dedicated to genetic diseases, with the primary objective to better understand and trea...
Paris, Ile-de-France (FR)
Imagine Institute
[DGIST] 2024 Tenure-Track Faculty Public Invitation
South Korea (KR)
Postdoctoral / Research Scientist / Research Assistant positions in Molecular Immunology
Postdoctoral / Research Scientist / Research Assistant positions in Molecular Immunology / Cancer Immunology
Dallas, Texas (US)
The University of Texas Southwestern Medical Center (UT Southwestern Medical Center)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
How Electric Vehicles Could Affect State Transportation Budgets
Pew-supported study urges states to identify potential future shortfalls.
- Data File The Emerging Highway And Roads Revenue Gap (XLSX)
Navigate to:
- Table of Contents

Federal and state incentives, combined with changing consumer preferences, have helped to boost sales of electric vehicles (EVs) in the United States at a time of growing concerns about climate change. Although EVs only make up 1.3% of current vehicle registrations nationwide, sales grew by 57% year over year in the first half of 2023, reaching over 9% of all vehicle sales by the end of 2023, up from around 2% in 2020.
At this point, the EV transition is inevitable and necessary to limit the effects of a changing climate—the transportation sector is responsible for the largest share of greenhouse gases in the U.S. and a central focus of the Biden administration’s efforts to meet international targets for reducing emissions . But it will also present unique challenges to states, which traditionally rely on fuel tax revenues to fund expenses for state transportation infrastructure such as roads, highways, and bridges.
With these compounding changes in mind, state policymakers need to take a closer look at how the EV transition could affect their transportation budgets. Diminishing fuel tax revenue, combined with growing expenses for road maintenance and charging infrastructure will have a profound effect on how states are able to fund critical transportation infrastructure.
With support from The Pew Charitable Trusts, the Dynamic Sustainability Lab at Syracuse University recently examined the potential impact of the EV transition on state transportation revenues and expenditures . Because EV adoption rates and fuel tax revenue vary greatly by state, the impact to state budgets will also vary (see map). Still, each state will need to prepare for the unique budgetary challenges that this change will bring. The key findings from the white paper are summarized below.
Source: Dynamic Sustainability Lab, “The Emerging Highway and Roads Revenue Gap” (2024)
1. The EV transition will exacerbate existing fuel tax revenue declines and boost demand for infrastructure funding.
States fund initiatives to support their highways and roads in several ways, but the primary source is per gallon fuel excise taxes. In 2021, revenue from state and local motor fuel tax revenue exceeded $53 billion nationwide. However, as EVs become a greater share of total vehicle registrations and the demand for fuel slows, the lab’s white paper predicts that the revenue streams from these taxes will become less reliable. As seen in Figure 1, fuel consumption has already been slowing as new vehicles have become more fuel efficient.
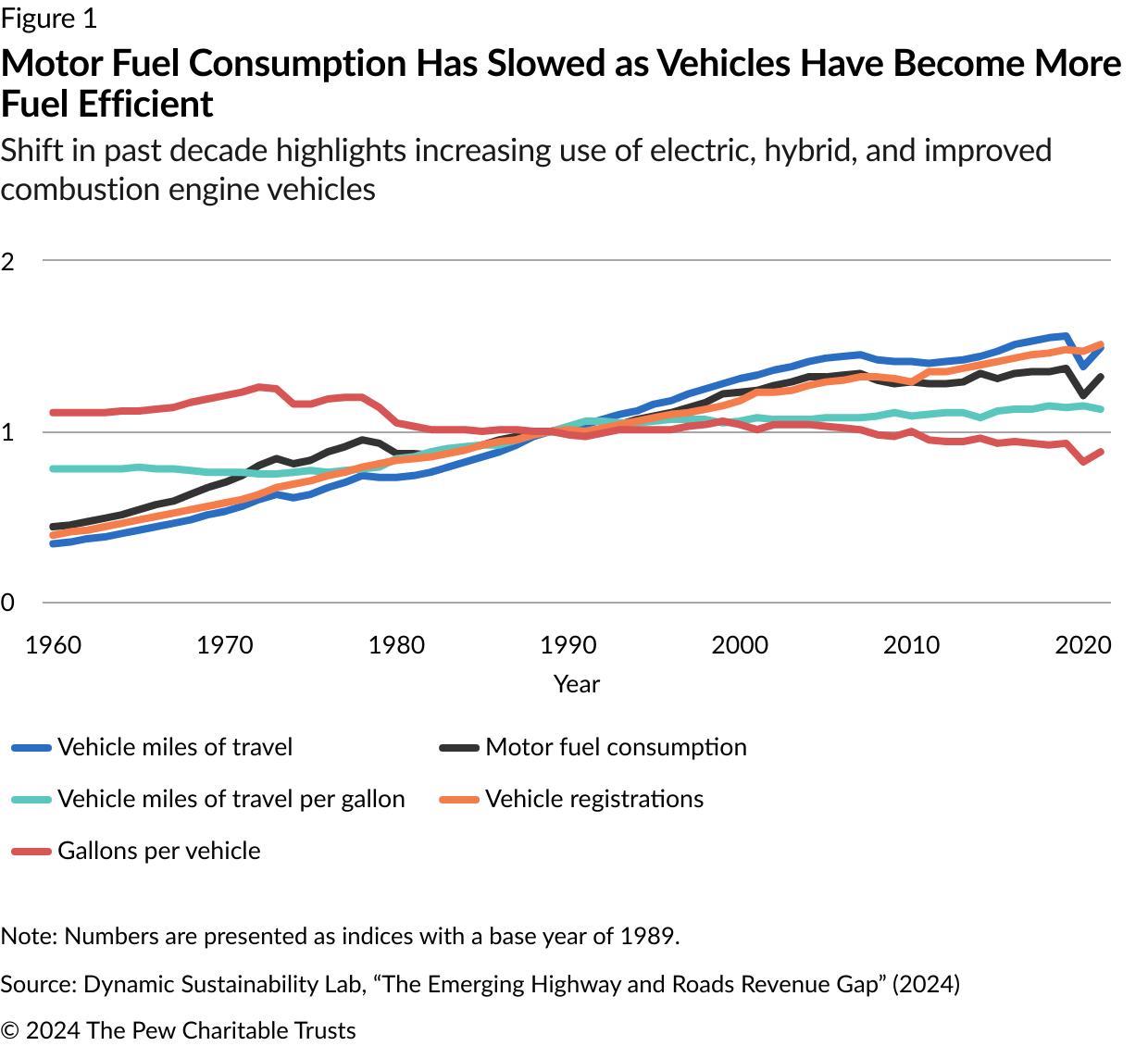
Additionally, the federal Highway Trust Fund, which provides grants to states and local governments for maintaining highways and roads, faces its own challenges. In recent years, spending from the fund has exceeded revenues; in fact, the Congressional Budget Office estimates that it could be depleted by 2028 if spending increases at the rate of inflation and taxes remain the same.
These challenges come at a time when years of underinvestment in critical transportation infrastructure has already resulted in a large gap between needed maintenance and available funding for roads, bridges, and highways. Additionally, climate change is having noticeable effects on these infrastructure systems already because of the increase in more severe storms, altered precipitation patterns, and sea-level rise.
2. EVs could present long-term revenue challenges, beyond reduced fuel tax revenue.
Although the EV transition will undoubtedly primarily affect fuel tax revenues, the Sustainability Lab’s report highlights several other possible long-term revenue considerations. For example, if fewer people frequent gas stations and convenience stores, states could see some decreases in sales tax revenue—gas stations and convenience stores generated more than $200 billion in taxes nationwide in 2022.
Similarly, lottery sales could decrease if EVs lead to lower foot traffic in gas stations and convenience stores. In 2020, convenience stores accounted for 70% of all lottery sales in the U.S. These sales are an important source of revenue in many states; for example, in Delaware, lottery revenue is the state’s fifth largest revenue source. Although less significant, other considerations highlighted in the report include losses in sales tax revenue from EVs having lower maintenance costs and property tax losses if gas stations are sold or abandoned.
3. EVs will increase necessary transportation expenditures.
In addition to creating unique revenue challenges, the EV transition will also have expenditure implications. First and foremost, the Sustainability Lab white paper highlights that the weight of EVs—EVs weigh about 30% more than gas-powered vehicles— will increase maintenance costs for roads, highways, and bridges.
Additionally, states will need to install and maintain EV charging stations, upgrade utilities to support charging infrastructure, develop new revenue streams to offset fuel tax revenue losses, and manage abandoned underground storage tanks as gas stations decrease in number. All of these actions will put a strain on already stretched state transportation budgets.
4. States should model transportation budget shortfalls and plan for the future.
Because decreasing fuel tax revenues and increasing expenditures will create a budget gap, the Sustainability Lab recommends that states model their transportation budget shortfalls. This could include, for example, an analysis of how different EV adoption rates would reduce fuel tax revenues and increase expenditures. Only a handful of states—California, Michigan, Rhode Island, and New York—have modeled the budgetary impact of the EV transition.
The white paper also proposes several strategies that states can use to offset budget shortfalls, which are summarized in Table 1. Emerging strategies include imposing road user charges (also called distance-based user fees, vehicle-miles traveled taxes, or mileage-based user fees), which charge travelers based on how far they travel on a road or highway, instituting EV registration fees, or charging an electricity sales tax.

State Infrastructure Financing
Collected resources on federal funding opportunities, metrics, and financing tools
State and local governments spend roughly half a trillion dollars annually on America’s roads, bridges, transit, and water systems, but still struggle to keep pace with needed repairs or make the significant upfront investments required to modernize public infrastructure. Most states lack the tools to track maintenance, repair, and investment needs for critical public infrastructure and, as a result, create unmonitored, long-term liabilities that could pose significant fiscal burdens in the future.
The EV Transition Will Require States to Find New Ways to Fund Transportation Infrastructure
Emerging strategies can help counter budget shortfalls
Assessing the fiscal landscape
| Most states have not modeled how EVs will impact revenues (primarily through decreases in fuel tax revenue) or expenditures, an important first step in identifying future budget shortfalls. | |||
| Some policy strategies do not account for nonresident usage of state highways, roads, and bridges. Therefore, all states should quantify the current percentage of fuel tax revenues obtained from nonresident vehicles. Tennessee provides an example of why quantifying this variable is important; 30% to 40% of Tennessee’s fuel tax revenue comes from nonresident truckers and drivers. | |||
Revenue-raising options
| These states are piloting projects or have implemented programs: | |||
| Thirty-two states have some form of annual EV additional fees. | |||
| Source: Dynamic Sustainability Lab, “The Emerging Highway and Roads Revenue Gap” (2024) |
Although the exact budgetary impact of EVs is unknown, they will continue to become more prevalent, which will force states to adapt to changing revenue sources and expenditures. And while there are drawbacks to all the emerging budget strategies to reduce shortfalls, the Sustainability Lab’s white paper highlights why it is important that states quantify and plan for the potential impacts of this ongoing transition.
Mollie Mills is a principal associate, Susan Banta is a project director, and Fatima Yousofi is a senior officer with The Pew Charitable Trusts’ state fiscal policy project.

More Federal Funding Needed to Improve Drinking Water
Water utilities throughout the United States will need to spend $625 billion over the next 20 years to fix, maintain, and improve the country’s drinking water infrastructure, according to preliminary results of a periodic assessment done by the Environmental Protection Agency (EPA).

Long-Term Liabilities Weigh on State Finances
If not effectively managed, long-term liabilities can squeeze state budgets and constrain future public investments. Of the three liabilities that states regularly report on, unfunded pension obligations are the biggest in most states, ahead of unfunded retiree health care and outstanding debt. In recent years, states have narrowed the gap between promised pension benefits and money set aside to pay for them, but the shortfall still amounts to nearly half of states’ own-source revenue—$836 billion in fiscal year 2021.
Exclusive state-policy research, infographics, and stats every two weeks.
ADDITIONAL RESOURCES

MORE FROM PEW


COMMENTS
Students with high emotional intelligence get better grades and score higher on standardized tests, according to the research presented in this article in Psychological Bulletin (Vol. 146, No. 2). Researchers analyzed data from 158 studies representing more than 42,529 students—ranging in age from elementary school to college—from 27 countries.
Articles in 2020. Filter By: Article Type. All. All; Article (1002) Author Correction (75) ... Research articles News Opinion Research Analysis Careers ...
Sensory capability and information integration independently explain the cognitive status of healthy older adults. Jonas Misselhorn. Florian Göschl. Andreas K. Engel. Article Open Access 31 Dec 2020.
Browse the 50 most downloaded Nature Communications articles across life and biological sciences published in 2020. ... these papers highlight valuable research from an international community.
Google Scholar provides a simple way to broadly search for scholarly literature. Search across a wide variety of disciplines and sources: articles, theses, books, abstracts and court opinions.
Lancet 2020;395:912-920. Crossref. PubMed. ISI. ... (B.P.); and the Altshuler Center for Education and Research, Metrocare Services, and the Division of Trauma and Disaster, Department of ...
A two-dose regimen of BNT162b2 (30 μg per dose, given 21 days apart) was found to be safe and 95% effective against Covid-19. The vaccine met both primary efficacy end points, with more than a 99 ...
But the threat that the world's largest hornet species poses to people is minimal. 5. A star orbiting the Milky Way's black hole validates Einstein. The odd orbit of a star around the ...
Research Letter. February 21, 2020. Interpreting Diagnostic Tests for SARS-CoV-2. JAMA. Viewpoint. May 6, 2020. Turbulent Gas Clouds and Respiratory Pathogen Emissions: Potential Implications for Reducing Transmission of COVID-19. JAMA. JAMA Insights.
The number of older people, including those living with dementia, is rising, as younger age mortality declines. However, the age-specific incidence of dementia has fallen in many countries, probably because of improvements in education, nutrition, health care, and lifestyle changes. Overall, a growing body of evidence supports the nine potentially modifiable risk factors for dementia modelled ...
As 2020 draws to a close, here are 20 striking findings from Pew Research Center's studies this year, covering the pandemic, race-related tensions, the presidential election and other notable trends that emerged during the year. Since the very beginning of the U.S. coronavirus outbreak, Democrats have been far more likely than Republicans to ...
Bethesda, MD 20892-2094. Editor: Harrison Wein, Ph.D. Assistant Editors: Vicki Contie and Brian Doctrow, Ph.D. NIH Research Matters is a weekly update of NIH research highlights reviewed by NIH's experts. It's published by the Office of Communications and Public Liaison in the NIH Office of the Director. ISSN 2375-9593.
The year 2020 saw tremendous change and suffering—not only because of the pandemic but also due to heightened concerns over racial justice and climate change. From the start of what turned out to be a year filled with crises and heroic responses, McKinsey produced a record stream of articles, reports, and new features to help the world come ...
The analysis of the field and suggestions for future research in this positional article is primarily based on (a) ... Citation 2020) the results of the school subsequently declined and in 2014 the school appeared to be an average Swedish school as regards learning and social aspects. Studying what appears to be a development away from ...
NIH Research Matters is a weekly update of NIH research highlights reviewed by NIH's experts. It's published by the Office of Communications and Public Liaison in the NIH Office of the Director. ISSN 2375-9593. NIH findings with potential for enhancing human health include new approaches to COVID-19, a universal mosquito vaccine, and advances ...
Research articles. Filter By: Article Type. All. All; Analysis (2) Article (1001) Matters Arising (34) ... Article 23 Dec 2020. Pairing of segmentation clock genes drives robust pattern formation.
The COVID-19 pandemic has mobilized the world scientific community in 2020, especially in the life sciences [ 1, 2 ]. In the first three months after the pandemic, the number of scientific papers about COVID-19 was fivefold the number of articles on H1N1 swine influenza [ 3 ]. Similarly, the number of clinical trials related to COVID-19 ...
Introduction. The National Institutes of Health (NIH) is the world's largest funder of biomedical research, employing over 20 000 people with a US$45.3 billion budget in 2020, 41.7 billion appropriated by Congress with an additional 3.6 billion in COVID-19 supplementary funding.1-3 Prior research suggested that the NIH research funding has not been proportionately aligned with disease ...
As the coronavirus disease 2019 (COVID-19) began to spread in the US in early 2020, older adults experienced disproportionately greater adverse effects from the pandemic including more severe complications, higher mortality, concerns about disruptions to their daily routines and access to care, difficulty in adapting to technologies like telemedicine, and concerns that isolation would ...
1. To Teach Vocabulary, Let Kids Be Thespians. When students are learning a new language, ask them to act out vocabulary words. It's fun to unleash a child's inner thespian, of course, but a 2020 study concluded that it also nearly doubles their ability to remember the words months later. Researchers asked 8-year-old students to listen to ...
Next steps for small cell lung cancer research. The ADRIATIC trial is ongoing and more will be learned about durvalumab treatment, Dr. Spigel said. In addition, another arm of the trial is evaluating the combination of durvalumab and another immunotherapy drug, tremelimumab (Imjudo). Results from that group of 200 patients are still being ...
Overall, a growing body of evidence supports the nine potentially modifiable risk factors for dementia modelled by the 2017 Lancet Commission on dementia prevention, intervention, and care: less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, and low social contact.
Retraction Note: Environmental Science and Pollution Research (2020) 28:19008-19020. ... An investigation by the publisher found a number of articles, including this one, with a number of concerns, including but not limited to compromised peer review process, inappropriate or irrelevant references, containing nonstandard phrases or not being in ...
The new survey on parties and partisanship by Pew Research Center, conducted among 6,174 Americans between June 27 and July 4, 2022, ... say they like political leaders who publicly assert that Donald Trump was the legitimate winner of the 2020 presidential election; 17% say they do not like such leaders, while 31% neither like nor dislike them ...
Research Highlight 25 Nov 2020 The crystalline armour that protects ants in battle A species of leaf-cutter ant is the first known example of an insect with mineralized armour, which shields them ...
Fewer Teams Are Fully Co-Located Than in 2020. New research shows that teams are more geographically dispersed than before the pandemic, and fewer teammates all live within the same city.* ... Our research showed that when starting a new role—whether at a new company or in an internal switch—meeting your manager or onboarding buddy in ...
They might also have wondered whether the ensuing article, on the topic of battery technology, was written by a human or a machine. It is a question ever more readers of scientific papers are asking.
Download MP3. In the final Coronapod of 2020, we dive into the scientific literature to reflect on the COVID-19 pandemic. Researchers have discovered so much about SARS-CoV-2 - information that ...
Federal and state incentives, combined with changing consumer preferences, have helped to boost sales of electric vehicles (EVs) in the United States at a time of growing concerns about climate change. Although EVs only make up 1.3% of current vehicle registrations nationwide, sales grew by 57% year over year in the first half of 2023, reaching over 9% of all vehicle sales by the end of 2023 ...
WASHINGTON (Reuters) -Rudy Giuliani lost his New York law license on Tuesday, after a state appeals court found he had lied in arguing that the 2020 presidential election was stolen from his ...