An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Iran J Med Sci
- v.45(4); 2020 Jul

A Narrative Review of COVID-19: The New Pandemic Disease
Kiana shirani, md.
1 Infectious Diseases and Tropical Medicine Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Erfan Sheikhbahaei, MD
2 Student Research Committee, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
Zahra Torkpour, MD
Mazyar ghadiri nejad, phd.
3 Industrial Engineering Department, Girne American University, Kyrenia, TRNC, Turkey
Bahareh Kamyab Moghadas, PhD
4 Department of Chemical Engineering, Shiraz Branch, Islamic Azad University, Shiraz, Iran
Matina Ghasemi, PhD
5 Faculty of Business and Economics, Business Department, Girne American University, Kyrenia, TRNC, Turkey
Hossein Akbari Aghdam, MD
6 Department of Orthopedic Surgery, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
Athena Ehsani, PhD
7 Department of Biomedical Engineering, Science and Research Branch, Islamic Azad University, Tehran, Iran
Saeed Saber-Samandari, PhD
8 New Technologies Research Center, Amirkabir University of Technology, Tehran, Iran
Amirsalar Khandan, PhD
9 Department of Electrical Engineering, Isfahan (Khorasgan) Branch, Islamic Azad University, Isfahan, Iran
10 0Technology Incubator Center, Isfahan (Khorasgan) Branch, Islamic Azad University, Isfahan, Iran
Nearly every 100 years, humans collectively face a pandemic crisis. After the Spanish flu, now the world is in the grip of coronavirus disease 2019 (COVID-19). First detected in 2019 in the Chinese city of Wuhan, COVID-19 causes severe acute respiratory distress syndrome. Despite the initial evidence indicating a zoonotic origin, the contagion is now known to primarily spread from person to person through respiratory droplets. The precautionary measures recommended by the scientific community to halt the fast transmission of the disease failed to prevent this contagious disease from becoming a pandemic for a whole host of reasons. After an incubation period of about two days to two weeks, a spectrum of clinical manifestations can be seen in individuals afflicted by COVID-19: from an asymptomatic condition that can spread the virus in the environment, to a mild/moderate disease with cold/flu-like symptoms, to deteriorated conditions that need hospitalization and intensive care unit management, and then a fatal respiratory distress syndrome that becomes refractory to oxygenation. Several diagnostic modalities have been advocated and evaluated; however, in some cases, diagnosis is made on the clinical picture in order not to lose time. A consensus on what constitutes special treatment for COVID-19 has yet to emerge. Alongside conservative and supportive care, some potential drugs have been recommended and a considerable number of investigations are ongoing in this regard
What’s Known
- Substantial numbers of articles on COVID-19 have been published, yet there is controversy among clinicians and confusion among the general population in this regard. Furthermore, it is unreasonable to expect physicians to read all the available literature on this subject.
What’s New
- This article reviews high-quality articles on COVID-19 and effectively summarizes them for healthcare providers and the general population.
Introduction
A pathogen from a human-animal virus family, the coronavirus (CoV), which was identified as the main cause of respiratory tract infections, evolved to a novel and wild kind in Wuhan, a city in Hubei Province of China, and spread throughout the world, such that it created a pandemic crisis according to the World Health Organization (WHO). CoV is a large family of viruses that were first discovered in 1960. These viruses cause such diseases as common colds in humans and animals. Sometimes they attack the respiratory system, and sometimes their signs appear in the gastrointestinal tract. There have been different types of human CoV including CoV-229E, CoV-OC43, CoV-NL63, and CoV-HKU1, with the latter two having been discovered in 2004 and 2005, respectively. These types of CoV regularly cause respiratory infections in children and adults. 1 There are also other types of these viruses that are associated with more severe symptoms. The new CoV, scientifically known as “SARS-CoV-2”, causes severe acute respiratory syndrome (SARS). 2 A newer type of the virus was discovered in September 2012 in a 60-year-old man in Saudi Arabia who died of the disease; the man had traveled to Dubai a few days earlier. The second case was a 49-year-old man in Qatar who also passed away. The discovery was first confirmed at the Health Protection Agency’s Laboratory in Colindale, London. The outbreak of this CoV is known as the Middle East Respiratory Syndrome (MERS), commonly referred to as “MERS-CoV”. The virus has infected 2260 people and has killed 912, most of them in the Middle East. 3 - 5 Finally, in December 2019, for the first time in Wuhan, in Hubei Province of China, a new type of CoV was identified that caused pneumonia in humans. 6 SARS-CoV-2 has affected 5404512 people and killed more than 343514 around the world according to the WHO situation report-127 (May 26, 2020). 3 , 7 - 10 The WHO has officially termed the disease “COVID-19”, which refers to corona, the virus, the disease, the year 2019, and its etiology (SARS-CoV-2). This type of CoV had never been seen in humans before. The initial estimates showed a mortality rate ranging from between 1% and 3% in most countries to 5% in the worst-hit areas ( Figure 1 ). 9 Some Chinese researchers succeeded in determining how SARS-CoV-2 affects human cells, which could help to develop techniques of viral detection and had antiviral therapy potential. Via a process termed “cryogenic electron microscopy (cryo-EM)”, these scientists discovered that CoV enters human cells utilizing a kind of cell membrane glycoprotein: angiotensin-converting enzyme 2 (ACE2). Then, the S protein is split into two sub-units: S1 and S2. S1 keeps a receptor-binding domain (RBD); accordingly, SARS-CoV-2 can bind to the peptidase domain of ACE2 directly. It appears that S2 subsequently plays a role in cellular fusion. Chinese researchers used the cryo-EM technique to provide ACE2 when it is linked to an amino acid transporter called “B0AT1”. They also discovered how to connect SARS-CoV-2 to ACE2-B0AT1, which is another complex structure. Given that none of these molecular structures was previously known, the researchers hoped that these studies would lead to the development of an antiviral or vaccine that would help to prevent CoV. Along the way, scientists found that ACE2 has to undergo a molecular process in which it binds to another molecule to be activated. The resulting molecule can bind two SARS-CoV-2 protein molecules simultaneously. The scientists also studied different SARS-CoV-2 RBD binding methods compared with other SARS-CoV-RBDs, which showed how subtle changes in the molecular binding sequence make the coronal structure of the virus stronger.

Most cases with SARS-CoV-2 are asymptomatic or have mild clinical pictures such as influenza and colds. This group of patients should be detected and isolated in their homes to break the transmission chain of the disease and adhere to the precautionary recommendations in order not to infect other people. The screening process will help this group and suppress the outbreak in the community. Patients with the confirmed disease who are admitted to hospitals can contaminate this environment, which should be borne in mind by healthcare providers and policymakers.
Transmission
While the first mode of the transmission of COVID-19 to humans is still unknown, a seafood market where live animals were sold was identified as a potential source at the beginning of the outbreak in the epidemiologic investigations that found some infected patients who had visited or worked in that place. The other viruses in this family, namely MERS and SARS, were both confirmed to be zoonotic viruses. Afterward, the person-to-person spread was established as the main mode of transmission and the reason for the progression of the outbreak. 11 Similar to the influenza virus, SARS-CoV-2 spreads through the population via respiratory droplets. When an infected person coughs, sneezes, or talks, the respiratory secretions, which contain the virus, enter the environment as droplets. These droplets can reach the mucous membranes of individuals directly or indirectly when they touch an infected surface or any other source; the virus, thereafter, finds its ways to the eyes, nose, or mouth as the first incubation places. 11 - 15 It has been reported that droplets cannot travel more than two meters in the air, nor can they remain in the air owing to their high density. Nonetheless, given the other hitherto unknown modes of transmission, routine airborne transmission precautions should be considered in high-risk countries and during high-risk procedures such as manual ventilation with bags and masks, endotracheal intubation, open endotracheal suctioning, bronchoscopy, cardiopulmonary resuscitation, sputum induction, lung surgery, nebulizer therapy, noninvasive positive pressure ventilation (eg, bilevel positive airway pressure and continuous positive airway pressure ), and lung autopsy. In the early stages of the disease, the chances of the spread of the virus to other persons are high because the viral load in the body may be high despite the absence of any symptoms ( Figure 2 ). 11 - 13 The person-to-person transmission rates can be different depending on the location and the infection control intervention; still, according to the latest reports, the secondary COVID-19 infection rate ranges from 1% to 5%. 13 - 23 Although the RNA of the virus has been detected in blood and stool, fecal-oral and blood-borne transmissions are not regarded as significant modes of transmission yet. 19 - 26 There have been no reports of mother-to-fetus transmission in pregnant women. 27

SARS-CoV-2 mode of transmission and clinical manifestations are illustrated in this figure. The potential source of this outbreak was identified to be from animals, similar to MERS and SARS, in epidemiologic studies; nonetheless, person-to-person transmission through droplets is currently the important mode. After reaching mucous membranes by direct or indirect close contact, the virus replicates in the cells and the immune system attacks the body due to its nature. Afterward, the clinical pictures appear, which are much more similar to influenza. However, different patients will have a spectrum of signs and symptoms.
Source Investigation
Recently, the appearance of SARS-CoV-2 in society shocked the healthcare system. 28 - 32 Veterinary corona virologists reported that COVID-19 was isolated from wildlife. Several studies have shown that bats are receptors of the CoV new version in 2019 with variants and changes in the environment featuring various biological characteristics. 33 - 36 The aforementioned mammals are a major source of CoV, which causes mild-to-severe respiratory illness and can even be deadly. In recent years, the virus has killed several thousands of people of all ages. 37 - 39 The mutated alternative of the virus can be transmitted to humans and cause acute respiratory distress. 40 , 41 One of the main causes of the spread of the virus is the exotic and unusual Chinese food in Wuhan: CoV is a direct result of the Chinese food cycle. The virus is found in the body of animals such as bats, 42 and snake or bat soup is a favorite Chinese food. Therefore, this sequence is replicated continuously. Almost everyone who was infected for the first time was directly in the local Wuhan market or had indirectly tried snake or bat soup in a Chinese restaurant. An investigation stated that the Malayan pangolin (Manis javanica) was a possible host for SARS-CoV-2 and recommended that it be removed from the wet market to prevent zoonotic transmissions in the future. 43 , 44
Pathogenesis
The important mechanisms of the severe pathogenesis of SARS-CoV-2 are not fully understood. Extensive lung injury in SARS-CoV-2 has been related to increased virus titers; monocyte, macrophage, and neutrophil infiltrations into the lungs; and elevated levels of pro-inflammatory cytokines and chemokines. Thus, the clinical exacerbation of SARS-CoV-2 infection may be in consequence of a combination of direct virus-induced cytopathic and immunopathological effects due to excessive cytokinesis. Changes in the cytokine/chemokine profile during SARS infection showed increased levels of circulating cytokines such as tumor necrosis factor-α (TNF-α), C–X–C motif chemokine 10 (CXCL10), interleukin (IL)-6, and IL-8 levels, in conjunction with elevated levels of serum pro-inflammatory cytokines such as IL-1, IL-6, IL-12, interferon-gamma (IFN-γ), and transforming growth factor-β (TGF-β). Nevertheless, constant stimulation by the virus creates a cytokine storm that has been related to acute respiratory distress syndrome (ARDS) and multiple organ dysfunction syndromes (MODS) in patients with COVID-19, which may ultimately lead to diminished immunity by lowering the number of CD4+ and CD8+ T cells and natural killer cells (crucial in antiviral immunity) and decreasing cytokine production and functional ability (exhaustion). It has been shown that IL-10, an inhibitory cytokine, is a major player and a potential target for therapeutic aims. 45 - 51 Severe cases of COVID-19 have respiratory distress and failure, which has been linked to the altered metabolism of heme by SARS-CoV-2. Some virus proteins can dissociate iron from porphyrins by attacking the 1-β chain of hemoglobin, which decreases the oxygen-transferring ability of hemoglobin. Research has also indicated that chloroquine and favipiravir might inhibit this process. 52
Clinical Manifestations
SARS-CoV-2, which attacks the respiratory system, has a spectrum of manifestations; nonetheless, it has three main primary symptoms after an incubation period of about two days to two weeks: fever and its associated symptoms such as malaise/fatigue/weakness; cough, which is nonproductive in most of the cases but can be productive indeed; and shortness of breath (dyspnea) due to low blood oxygenation. Although these symptoms appear in the body of the affected person over two to 14 days, patients may refer to the clinic with gastrointestinal symptoms (nausea/vomiting-diarrhea) or decreased sense of smell and/or taste. More devastatingly, however, patients may refer to the emergency room with such coagulopathies as pulmonary thromboembolism, cerebral venous thrombosis, and other related manifestations. The WHO has stated that dry throat and dry cough are other symptoms detected in the early stages of the infection. 53 , 54 The estimations of the severity of the disease are as follows: mild (no or mild pneumonia) in 81%, severe (eg, with dyspnea, hypoxia, or >50% lung involvement on imaging within 24 to 48 hours) in 14%, and critical (eg, with respiratory failure, shock, or multiorgan dysfunction) in 5%. In the early stages, the overall mortality rate was 2.3% and no deaths were observed in non-severe patients. Patients with advanced age or underlying medical comorbidities have more mortality and morbidity. 55 Although adults of middle age and older are most commonly affected by SARS-CoV-2, individuals at any age can be infected. A few studies have reported symptomatic infection in children; still, when it occurs, it has mild symptoms. The vast majority of cases have the infection with no signs and symptoms or mild clinical pictures; they are called “the asymptomatic group”. These patients do not seek medical care and if they come into close contact with others, they can spread the virus. Therefore, quarantine in their home is the best option for the population to break the transmission of the virus. It should be considered that some of these asymptomatic patients have clinical signs such as chest computed tomography scan (CT-Scan) infiltrations. Similar to bacterial pneumonia, lower respiratory signs and symptoms are the most frequent manifestations in serious cases of COVID-19, characterized by fever, cough, dyspnea, and bilateral infiltrates on chest imaging. In a study describing pneumonia in Wuhan, the most common clinical signs and symptoms at the onset of the illness were fever in 99% (although fever might not be a universal finding), fatigue in 70%, dry cough in 59%, anorexia in 40%, myalgia in 35%, dyspnea in 31%, and sputum production in 27%. Headache, sore throat, and rhinorrhea are less common, and gastrointestinal symptoms (eg, nausea and diarrhea) are relatively rare. 7 , 42 , 43 , 45 - 48 , 56 , 57 According to our clinical experience in Iran, anosmia, atypical chest pain, diarrhea, nausea/vomiting, and hemoptysis are other presenting symptoms in the clinic. It should be noted that COVID-19 has some unexplained potential complications such as secondary bacterial infections, myocarditis, central nervous system injury, cerebral edema, MODS, acute demyelinating encephalomyelitis (ADEM), kidney injury, liver injury, new-onset seizure, coagulopathy, and arrhythmias.
Laboratory data : Complete blood counts, which constitute a routine laboratory test, have shown different results in terms of the white blood cell count: from leukopenia and lymphopenia to leukocytosis, although lymphopenia appears to be the most common. Fatal cases have exhibited severe lymphopenia accompanied by an increased level of D-dimer. Liver function enzymes can be increased; however, it is not sufficient to diagnose a disease. The serum procalcitonin level is a marker of infection, especially in bacterial diseases. Patients with COVID-19 who require intensive care unit (ICU) management may have elevated procalcitonin. Increased urea and creatinine, creatinine-phosphokinase, lactate dehydrogenase, and C-reactive protein are other findings in some cases. 7 , 56 , 57
Imaging studies : Routine chest X-ray (CXR) is widely deemed the first-step management to evaluate any respiratory involvement. Although negative findings in CXR do not rule out the viral disease, patients without common findings do not have severe disease and can, consequently, be managed in the outpatient setting. 58 , 59 Another modality is chest CT-Scan. It can be ordered in suspected cases with typical symptoms at the first step, or it can be performed after the detection of any abnormalities in CXR. The most common demonstrations in CT-Scan images are ground-glass opacification, round opacities, and crazy paving with or without bilateral consolidative abnormalities (multilobar involvement) in contrast to most cases of bacterial pneumonia, which have locally limited involvement. Pleural thickening, pleural effusion, and lymphadenopathy are less common. 58 - 61 Tree-in-bud, peribronchial distribution, nodules, and cavity are not in favor of common COVID-19 findings. Although reverse transcriptase-polymerase chain reaction (RT-PCR) is used to confirm the diagnosis, it is a time-consuming procedure and has high false-negative/false-positive findings; hence, in the emergency clinical setting, CT-Scan findings can be a good approach to make the diagnosis. It is deserving of note, however, that false-positive/false-negative cases were reported by one study to be high and other differential diagnoses should be in mind in order not to miss any other cases such as acute pulmonary edema in patients with heart disease.
Suspected cases should be diagnosed as soon as possible to isolate and control the infection immediately. COVID-19 should be considered in any patient with fever and/or lower respiratory tract symptoms with any of the following risk factors in the previous 2 weeks: close contact with confirmed or suspected cases in any environment, especially at work in healthcare places without sufficient protective equipment or long-time standing in those places, and living in or traveling from well-known places where the disease is an epidemic. 61 - 66 Patients with severe lower respiratory tract disease without alternative etiologies and a clear history of exposure should be considered having COVID-19 unless confirmed otherwise. According to the Centers for Disease Control and Prevention (CDC), sending tests to check SARS-CoV-2 in suspected cases is based on physicians’ clinical judgment. Although there are some positive cases without clinical manifestations (ie, fever and/or symptoms of acute respiratory illness such as cough and dyspnea), infectious disease and control centers should take action in society to limit the exposure of such patients to other healthy individuals. The CDC prioritizes the use of the specific test for hospitalized patients, symptomatic patients who are at risk of fatal conditions (eg, age ≥65 y, chronic medical conditions, and immunocompromising conditions) and those who have exposure risks (recent travel, contact with patients with COVID-19, and healthcare workers). 61 - 66 Although treatment should be started after the confirmation of the disease, RT-PCR for highly suspected cases is a time-consuming test; accordingly, a considerable number of clinicians favor the use of a combination of clinical manifestations with imaging modalities (eg, CT-Scan findings) and their clinical judgment regarding the probability of the disease in order not to lose more time. 61 - 66
Treatment of COVID-19
There is no confirmed recommended treatment or vaccine for SARS-CoV-2; prevention is, therefore, better than treatment. Nevertheless, the high contagiousness of COVID-19, combined with the fact that some individuals fail to adhere to precautionary measures or they have significant risk factors, means that this infectious disease is inevitable in some people. Beside supportive treatments, many types of medications have been introduced. These medications come from previous experimental studies on SARS, MERS, influenza, or human immunodeficiency virus (HIV); hence, their efficacy needs further experimental and clinical approval. Patients with mild symptoms who do not have significant risk factors should be managed in their home like a self-made quarantine (in an isolated room); still, prompt hospital admission is required if patients exhibit signs of disease deterioration. 25 , 67 , 68 Isolation from other family members is an important prevention tip. Patients should wear face masks, eat healthy and warm foods similar to when struggling with influenza or colds, do the handwashing process, dispose of the contaminated materials cautiously, and disinfect suspicious surfaces with standard disinfectants. 69 Patients with severe symptoms or admission criteria should be hospitalized with other patients who have the same disease in an isolated department. When the disease is progressed, ICU care is mandatory. 25 , 67 , 68 SARS-CoV-2 attacks the respiratory system, diminishing the oxygenation process and forcing patients with low blood oxygen saturation to take extra oxygen from different modalities. Nasal cannulae, face masks with or without a reservoir, intubation in severe cases, and then extracorporeal membrane oxygenation in refractory hypoxia have been used; however, the safety and efficacy of these measures should be evaluated. As was mentioned above, impaired coagulation is one of the major complications of the disease; consequently, alongside all recommended supportive care and drugs, anticoagulants such as heparin should be administered prophylactically ( Table 1 ). Although it is said that all the clinical signs and symptoms of COVID-19 are induced by the immune system, as other research on influenza and MERS has revealed, glucocorticoids are not recommended in COVID-19 pneumonia unless other indications are present (eg, exacerbation of chronic obstructive pulmonary disease and refractory septic shock) due to the high risk of mortality and delayed viral clearance. Earlier in the national and international guidelines, nonsteroidal anti-inflammatory drugs such as naproxen were recommended on the strength of their antipyretic and anti-inflammatory components; however, the guideline has been revised recently and acetaminophen with or without codeine is currently the favored drug in patients with COVID-19. 25 , 67 , 68 According to the pathogenesis of the disease, whereby cytokine storm and immune-cell exhaustion can be seen in severe cases, selective antibodies against harmful interleukins such as IL-6 and IL-10 or other possible agents can be therapeutic for fatal complications. Tocilizumab, an IL-6 inhibitor, albeit with limited clinical efficacy, has been introduced in China’s National Health Commission treatment guideline for severe infection with profound pulmonary involvement (ie, white lung). 70 , 87
Summary of possible anti-COVID-19 drugs
mg, Milligrams; BD, Every 12 hours; RdRP, RNA-dependent RNA polymerase; TDS, Every 8 hours; IV, Intravenous; IL, Interleukin; μg, Micrograms
RNA synthesis inhibitors (eg, tenofovir disoproxil fumarate and 2’-deoxy-3’-thiacytidine [3TC]), neuraminidase inhibitors (NAIs), nucleoside analogs, lopinavir/ritonavir, atazanavir, remdesivir, favipiravir, INF-β, and Chinese traditional medicine (eg, Shufeng Jiedu and Lianhuaqingwen capsules) are the major candidates for COVID-19. 26 , 70 , 85 , 88 - 96 Antiviral drugs have been investigated for various diseases, but their efficacy in the treatment of COVID-19 is under investigation and several randomized clinical trials are ongoing to release a consensus result on the treatment of this infectious disease. Moderate-to-severe SARS-CoV-2 disease needs drug therapy. Favipiravir, a previously validated drug for influenza, is a drug that has shown promising results for COVID-19 in experimental and clinical studies, but it is under further evaluation. 70 , 79 , 80 Remdesivir, which was developed for Ebola, is an antiviral drug that is under evaluation for moderate-to-severe COVID-19 owing to its promising results in in vitro investigations. 70 , 73 - 75 , 81 Remdesivir was shown to have reduced the virus titer in infected mice with MERS-CoV and improved lung tissue damage with more efficiency compared with a group treated with lopinavir/ritonavir/INF-β. 67 , 70 Another investigation studied the potential efficacy of INF-β-1 in the early stages of COVID-19 as a potential antiviral drug. 86 Although there is some hope, an evidence-based consensus requires further clinical trials. 70 , 77 A combined protease inhibitor, lopinavir/ritonavir, is used for HIV infection and has shown interesting results for SARS and MERS in in vitro studies. 73 - 75 The clinical effectiveness of lopinavir/ritonavir for SARS-CoV-2 was also reported in a case report. 70 , 71 , 74 , 76 Atazanavir, another protease inhibitor, with or without ritonavir is another possible anti-COVID-19 treatment. 77 , 78 NAIs, including oseltamivir, zanamivir, and peramivir, are recommended as antiviral treatment in influenza. 68 Oral oseltamivir was tried for COVID-19 in China and was first recommended in the Iranian guideline for COVID-19 treatment; nevertheless, because of the absence of strong evidence indicating its efficacy for SARS-CoV-2, it was eliminated from the subsequent updates of the guideline. 85 RNA-dependent RNA polymerase inhibitors with anti-hepatitis C effects such as ribavirin have shown satisfactory results against SARS-CoV-2 RNA polymerase; however, they have limited clinical approval. 82 - 84 The well-known drugs for rheumatoid arthritis, systemic lupus erythematosus, and an antimalarial drug, chloroquine 71 and hydroxychloroquine 21 are other potential drugs for moderate-to-severe COVID-19 but with limited or no clinical appraisal. Hydroxychloroquine has exhibited better safety and fewer side effects than chloroquine, which makes it the preferred choice. 70 Furthermore, the immunomodulatory effects of hydroxychloroquine can be used to control the cytokine precipitation in the late phases of SARS-CoV-2 infections. There are numerous mechanisms for the antiviral activity of hydroxychloroquine. A weak base drug, hydroxychloroquine concentrates on such intracellular sections as endosomes and lysosomes, thereby halting viral replication in the phase of fusion and uncoating. Additionally, this immunosuppressive and antiparasitic drug is capable of altering the glycosylation of ACE2 and inhibiting both S-protein binding and phagocytosis. 72 A recent multicenter study showed that regarding the risks of cardiovascular adverse effects and mortality rates, hydroxychloroquine or chloroquine with or without a macrolide (eg, azithromycin) was not beneficial for hospitalized patients, although further research is needed to end such controversies. 97
Disease Duration
It is not easy to quarantine the patients who have fully recovered because there is evidence that they are highly infectious. 81 The recovery time for confirmed cases based on the National Health Commission reports of China’s government was estimated to range between 18 and 22 days. 73 As indicated by the WHO, the healing time seems to be around two weeks for moderate infections and 3 to 6 weeks for the severe/ serious disease. 75 Pan Feng and others studied 21 confirmed cases with COVID-19 pneumonia with about 82 CT-Scan images with a mean interval of four days. Lung abnormalities on chest CT showed the highest severity approximately 10 days after the initial onset of symptoms. All patients became clear after 11 to 26 days of hospitalization. From day zero to day 26, four stages of lung CT were defined as follows: Stage 1 (first 4 days): ground-glass opacities; Stage 2 (second 4 days): crazy-paving patterns; Stage 3 (days 9–13): maximum total CT scores in the consolidations; and Stage 4 (≥14 d): steady improvements in the consolidations with a reduction in the total CT score without any crazy-paving pattern. 74 Nevertheless, there are also rare cases reported from some studies that show the recurrence of COVID-19 after negative preliminary RT-PCR results. For example, Lan and othersstudied one hospitalized and three home-quarantined patients with COVID-19 and evaluated them with RT-PCR tests of the nucleic acid. All the patients with positive RT-PCR test results had CT imaging with ground-glass opacification or mixed ground-glass opacification and consolidation with mild-to-moderate disease. After antiviral treatments, all four patients had two consecutive negative RT-PCR test results within 12 to 32 days. Five to 13 days after hospital discharge or the discontinuation of the quarantine, RT-PCR tests were repeated, and all were positive. An additional RT-PCR test was performed using a kit from a different manufacturer, and the results were also positive. Their findings propose that a minimum percentage of recovered patients may still be infection carriers. 76
Supplements for COVID-19
Since the appearance of SARS-CoV-2 in Wuhan, China, there have been reports of the unreliable and unpredictable use of mysterious therapies. Some recommendations such as the use of certain herbs and extracts including oregano oil, mulberry leaf, garlic, and black sesame may be safe as long as people do not utilize their hands for instance. 98 According to data released by the CDC, vitamin C (VitC) supplements can decrease the risk of colds in people besides preventing CoV from spreading. The aforementioned organization states that frequent consumption of VitC supplements can also decrease the duration of the cold; however, if used only after the cold has risen, its consumption does not influence the disease course. VitC also plays an important role in the body. One of the main reasons for taking VitC is to strengthen the immune system because this vitamin plays a significant part in the immune system. Firstly, VitC can increase the production of white blood cells (lymphocytes and phagocytes) in the bone marrow, which can support and protect the body against infections. Secondly, VitC helps immune cells to function better while preserving white blood cells from damaging molecules such as free oxidative radicals and ions. Thirdly, VitC is an essential part of the skin’s immune system. This vitamin is actively transported to the skin surface, where it serves as an antioxidant and helps to strengthen the skin barrier by optimizing the collagen synthesis process. Patients with pneumonia have lower levels of VitC and have been revealed to have a longer recovery time. 69 , 99 In a randomized investigation, 200 mg/d of VitC was applied to older patients and resulted in improvements in the respiratory symptoms. Another investigation reported 80% fewer mortalities in a controlled group of VitC takers. 73 However, for effective immune system improvement, VitC should be consumed alongside adequate doses of several other supplements. Although VitC plays an important role in the body, often a balanced diet and the consumption of fresh fruits and vegetables can quickly fill the blanks. While taking high amounts of VitC is less risky because it is water-soluble and its waste is eliminated in the urine, it can induce diarrhea, nausea, and abdominal spasms at higher concentrations. Too much VitC may cause calcium-oxalate kidney stones. People with genetic hemochromatosis, an iron deficiency disorder, should consult a physician before taking any VitC supplements as high levels of VitC can lead to tissue damage. Some studies have evaluated the different doses of oral or intravenous VitC for patients admitted to the hospital for COVID-19. Although they used different regimens, all of them demonstrated satisfactory results regarding the resolution of the compilations of the disease, decreased mortality, and shortened lengths of stay in the ICU and/or the hospital. 100 , 101 Immunologists have also recommended 6 000 units of vitamin A (VitA) per day for two weeks, more than twice the recommended limit for VitA, which can create a poisoning environment over time. According to the guidance of the National Institutes of Health (NIH), middle-aged men and women should take 1 and 2 mg of VitA every day, respectively. The safe upper limit of this vitamin is 6000 mg or 5000 units, and overdose can have serious outcomes such as dizziness, nausea, headache, coma, and even death. Extreme consumption of VitA throughout pregnancy can lead to birth anomalies.
Similar to VitC, vitamin D (VitD) has antioxidant, anti-inflammatory, and immune-modulatory effects in our body such as reducing pro-inflammatory cytokines and inhibiting viral replication according to experimental studies. 83 The VitD state of our body is checked through 25 (OH) VitD in the serum. VitD deficiency is pandemic around the world due to multifactorial reasons. It has been shown that VitD deficient patients are prone to SARS-CoV-2 and, accordingly, treating VitD deficiency is not without benefits. Grant and others recommended 10 000 units per day for two weeks and then 5 000 units per day as the maintenance dose to keep the level between 40 and 100 ng/mL. 102 VitD toxicity causes gastrointestinal discomfort (dyspepsia), congestion, hypercalcemia, confusion, positional disorders, dysrhythmia, and kidney dysfunction.
James Robb, 103 a researcher who detected CoV for the first time as a consultant pathologist with the National Cancer Institute of America, suggested the influence of zinc consumption. Oral zinc supplements can be dissolved in the nback of the throat. Short-term therapy with oral zinc can decrease the duration of viral colds in adults. Zinc intake is also associated with the faster resolution of nasal congestion, nasal drainage, sore throats, and coughs. Researchers 104 , 105 have warned that the consumption of more than 1 mg of zinc a day can lead to zinc poisoning and have side effects such as lowered immune function. Children and old people with zinc insufficiency in developing nations are extremely vulnerable to pneumonia and other viral infections. It has also been determined that zinc has a major role in the production and activation of T-cell lymphocytes. 106 , 107
And finally, for high-risk people or those who work in high-risk places such as healthcare providers, hydroxychloroquine has been mentioned to be effective as a prophylactic regimen ( Table 2 ). Although different doses have been investigated so far, Pourdowlat and others recommended 200 mg daily before exposure, and for the post-exposure scenario, a loading dose of 600-800 mg followed by a maintenance dose of 200 mg daily. 74
Possible prophylactic regimens against SARS-CoV-2 infection
IU, International unit; mg, Milligrams; kg, Kilograms; ICU, Intensive care unit; g, Grams; IV, Intravenous; Vit, Vitamin; ng, Nanograms; mL, Milliliter
COVID-19 Kits and Deep Learning
COVID-19 has threatened public health, and its fast global spread has caught the scientific community by surprise. 108 Hence, developing a technique capable of swiftly and reliably detecting the virus in patients is vital to prevent the spreading of the virus. 109 , 110 One of the ways to diagnose this new virus is through RT-PCR, a test that has previously demonstrated its efficacy in detecting such CoV infections as MERS-CoV and SARS-CoV. Consequently, increasing the availability of RT-PCR kits is a worldwide concern. The timing of the RT-PCR test and the type of strain collected are of vital importance in the diagnosis of COVID-19. One of the characteristics of this new virus is that the serum is negative in the early stage, while respiratory specimens are positive. The level of the virus at the early stage of the illness is also high, even though the infected individual experiences mild symptoms. 111 For the management of the emerging situation of COVID-19 in Wuhan, various effective diagnostic kits were urgently made available to markets. While a few different diagnostics kits are used merely for research endeavors, only a single kit developed by the Beijing Genome Institute (BGI) called “Real-Time Fluorescent PCR” has been authenticated for clinical diagnostics. Fluorescent RT-PCR is reliable and able to offer fast results probably within a few hours (usually within two hours). Besides RT-PCR, China has successfully developed a metagenomic-sequencing kit based on combinatorial probe-anchor synthesis that can identify virus-related bacteria, allowing observation and evaluation during the transmission of the virus. Furthermore, the metagenomic-sequencing kit based on combinatorial probe-anchor synthesis is far faster than the abovementioned fluorescent RT-PCR kit. Apart from China, a Singapore-based laboratory, Veredus, developed a virus detection kit (Vere-CoV) in late January. It is a portable Lab-On-Chip used to detect MERS-CoV, SARS-CoV, and SARS-CoV-2, in a single examination. This kit works based on the VereChip™ technology, the lines of code (LOC) program incorporating two different influential molecular biological functions (microarray and PCR) precisely. Several studies have focused on SARS-CoV diagnostic testing. These papers have presented investigative approaches to the identification of the virus using molecular testing (ie, RT-PCR). Researchers probed into the use of a nested PCR technique that contains a pre-amplification step or integrating the N gene as an extra subtle molecular marker to improve on the sensitivity. 112 - 115 CT-Scan is very useful for diagnosing, evaluating, and screening infections caused by COVID-19. One recommendation for scanning the disease is to take a scan every three to five days. According to researchers, most CT-Scan images from patients with COVID-19 are bilateral or peripheral ground-glass opacification, with or without stabilization. Nowadays, because of a paucity of computerized quantification tools, only qualitative reports and sometimes inaccurate analyses of contaminated areas are drawn upon in radiology reports. A categorization system based on the deep learning approach was proposed by a study to automatically measure infected parts and their volumetric ratios in the lung. The functionality of this system was evaluated by making some comparisons between the infected portions and the manually-delineated ones on the CT-Scan images of 300 patients with COVID-19. To increase the manual drawing of training samples and the non-interference in the automated results, researchers adopted a human-based approach in collaboration with radiologists so as to segment the infected region. This approach shortens the time to about four minutes after 3-time updating. The mean Dice similarity coefficient illustrated that the automatically detected infected parts were 91.6% similar to the manually detected ones, and the average of the percentage estimated error was 0.3% for the whole lung. 116 , 117
Prevention Considerations
In the healthcare setting, any individual with the manifestations of COVID-19 (eg, fever, cough, and dyspnea) should wear a face mask, have a separate waiting area, and keep the distance of at least two meters. Symptomatic patients should be asked about recent travel or close contact with a patient in the preceding two weeks to find other possible infected patients. The CDC and WHO have announced special precautions for healthcare providers in the hospital and during different procedures. Wearing tight-fitting face masks with special filters and impermeable face shields is necessary for all of them. 11 , 18 , 65 , 66 , 76 , 118 - 124 Other people should pay attention to the CDC and WHO preventive strategies, which recommend that individuals not touch their eyes, mouth, and nose before washing or disinfecting their hands; wash their hands regularly according to the standard protocol; use effective disinfection solutions (ie, containing at least 60% ethylic alcohol) for contaminated surfaces; cover their mouth when coughing and sneezing; avoid waiting or walking in crowded areas, and observe isolation protocols in their home. Postponing elective work and decreasing non-urgent visits and traveling to areas in the grip of COVID-19 may be useful to lessen the risk of exposure. If suspected individuals with mild symptoms are managed in outpatient settings, an isolated room with minimal exposure to others should be designed. Patients and their caregivers should wear tight-fitting face masks. 11 , 18 , 65 , 66 , 76 , 118 - 124 Substantial numbers of individuals with COVID-19 are asymptomatic with potential exposure; accordingly, a screening tool should be employed to evaluate these cases. In addition to passport checks, corona checks have been incorporated into the protocols in airports and other crowded places. The use of a remote thermometer to measure body temperature leads to an increase in the number of false-negative cases. It is, thus, essential that everyone pay sufficient heed to the WHO and CDC recommendations in their daily life. Traveling is not prohibited, but it should be restricted and passengers from any country should be monitored. 11 , 18 , 65 , 66 , 76 , 118 - 124
SARS-CoV-2 is the new highly contagious CoV, which was first reported in China. While it had a zoonotic origin in the beginning, it subsequently spread throughout the world by human contact. COVID-19 has a spectrum of manifestations, which is not lethal most of the time. To diagnose this condition, physicians can avail themselves of laboratory and imaging findings besides signs and symptoms. RT-PCR is the gold standard, but it lacks sufficient sensitivity and specificity. Although there are some potential drugs for COVID-19 and some vitamins or minerals for prophylaxis, the best preventive strategies are quarantine (staying at home) and the use of personal protective equipment and disinfectants.
Acknowledgement
The authors express their gratitude toward the Supporting Organizations for Foreign Iranian Students, Islamic Azad University Isfahan (Khorasgan) Branch, and Isfahan University of Medical Sciences.
Conflict of Interest: None declared.
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
by Alissa Wilkinson

The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
- The Vox guide to navigating the coronavirus crisis
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
- A syllabus for the end of the world
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
- What day is it today?
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
- Vox is starting a book club. Come read with us!
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Most Popular
The hottest place on earth is cracking from the stress of extreme heat, the backlash against children’s youtuber ms rachel, explained, take a mental break with the newest vox crossword, an artist snuck an anti-semitic message into marvel’s newest x-men comic book, openai insiders are demanding a “right to warn” the public, today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
More in Culture

Kate Middleton’s cancer diagnosis, explained

Why are we so obsessed with morning routines?

Here are all 50+ sexual misconduct allegations against Kevin Spacey

Is TikTok breaking young voters’ brains?

Backgrid paparazzi photos are everywhere. Is that such a big deal?

Modi won the Indian election. So why does it seem like he lost?

Baby Reindeer’s “Martha” is, inevitably, suing Netflix

Where AI predictions go wrong

The failure of the college president

Trump’s felony conviction has hurt him in the polls
How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.
Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College
You May Also Like
Mental health on college campuses.
Sarah Wood June 6, 2024

Advice From Famous Commencement Speakers
Sarah Wood June 4, 2024

The Degree for Investment Bankers
Andrew Bauld May 31, 2024

States' Responses to FAFSA Delays
Sarah Wood May 30, 2024

Nonacademic Factors in College Searches
Sarah Wood May 28, 2024

Takeaways From the NCAA’s Settlement
Laura Mannweiler May 24, 2024

New Best Engineering Rankings June 18
Robert Morse and Eric Brooks May 24, 2024

Premedical Programs: What to Know
Sarah Wood May 21, 2024

How Geography Affects College Admissions
Cole Claybourn May 21, 2024

Q&A: College Alumni Engagement
LaMont Jones, Jr. May 20, 2024

- Current Issue
- Journal Archive
- Current Call
Search form

Coronavirus: My Experience During the Pandemic
Anastasiya Kandratsenka George Washington High School, Class of 2021
At this point in time there shouldn't be a single person who doesn't know about the coronavirus, or as they call it, COVID-19. The coronavirus is a virus that originated in China, reached the U.S. and eventually spread all over the world by January of 2020. The common symptoms of the virus include shortness of breath, chills, sore throat, headache, loss of taste and smell, runny nose, vomiting and nausea. As it has been established, it might take up to 14 days for the symptoms to show. On top of that, the virus is also highly contagious putting all age groups at risk. The elderly and individuals with chronic diseases such as pneumonia or heart disease are in the top risk as the virus attacks the immune system.
The virus first appeared on the news and media platforms in the month of January of this year. The United States and many other countries all over the globe saw no reason to panic as it seemed that the virus presented no possible threat. Throughout the next upcoming months, the virus began to spread very quickly, alerting health officials not only in the U.S., but all over the world. As people started digging into the origin of the virus, it became clear that it originated in China. Based on everything scientists have looked at, the virus came from a bat that later infected other animals, making it way to humans. As it goes for the United States, the numbers started rising quickly, resulting in the cancellation of sports events, concerts, large gatherings and then later on schools.
As it goes personally for me, my school was shut down on March 13th. The original plan was to put us on a two weeks leave, returning on March 30th but, as the virus spread rapidly and things began escalating out of control very quickly, President Trump announced a state of emergency and the whole country was put on quarantine until April 30th. At that point, schools were officially shut down for the rest of the school year. Distanced learning was introduced, online classes were established, a new norm was put in place. As for the School District of Philadelphia distanced learning and online classes began on May 4th. From that point on I would have classes four times a week, from 8AM till 3PM. Virtual learning was something that I never had to experience and encounter before. It was all new and different for me, just as it was for millions of students all over the United States. We were forced to transfer from physically attending school, interacting with our peers and teachers, participating in fun school events and just being in a classroom setting, to just looking at each other through a computer screen in a number of days. That is something that we all could have never seen coming, it was all so sudden and new.
My experience with distanced learning was not very great. I get distracted very easily and find it hard to concentrate, especially when it comes to school. In a classroom I was able to give my full attention to what was being taught, I was all there. However, when we had the online classes, I could not focus and listen to what my teachers were trying to get across. I got distracted very easily, missing out on important information that was being presented. My entire family which consists of five members, were all home during the quarantine. I have two little siblings who are very loud and demanding, so I’m sure it can be imagined how hard it was for me to concentrate on school and do what was asked of me when I had these two running around the house. On top of school, I also had to find a job and work 35 hours a week to support my family during the pandemic. My mother lost her job for the time being and my father was only able to work from home. As we have a big family, the income of my father was not enough. I made it my duty to help out and support our family as much as I could: I got a job at a local supermarket and worked there as a cashier for over two months.
While I worked at the supermarket, I was exposed to dozens of people every day and with all the protection that was implemented to protect the customers and the workers, I was lucky enough to not get the virus. As I say that, my grandparents who do not even live in the U.S. were not so lucky. They got the virus and spent over a month isolated, in a hospital bed, with no one by their side. Our only way of communicating was through the phone and if lucky, we got to talk once a week. Speaking for my family, that was the worst and scariest part of the whole situation. Luckily for us, they were both able to recover completely.
As the pandemic is somewhat under control, the spread of the virus has slowed down. We’re now living in the new norm. We no longer view things the same, the way we did before. Large gatherings and activities that require large groups to come together are now unimaginable! Distanced learning is what we know, not to mention the importance of social distancing and having to wear masks anywhere and everywhere we go. This is the new norm now and who knows when and if ever we’ll be able go back to what we knew before. This whole experience has made me realize that we, as humans, tend to take things for granted and don’t value what we have until it is taken away from us.
Articles in this Volume
[tid]: dedication, [tid]: new tools for a new house: transformations for justice and peace in and beyond covid-19, [tid]: black lives matter, intersectionality, and lgbtq rights now, [tid]: the voice of asian american youth: what goes untold, [tid]: beyond words: reimagining education through art and activism, [tid]: voice(s) of a black man, [tid]: embodied learning and community resilience, [tid]: re-imagining professional learning in a time of social isolation: storytelling as a tool for healing and professional growth, [tid]: reckoning: what does it mean to look forward and back together as critical educators, [tid]: leader to leaders: an indigenous school leader’s advice through storytelling about grief and covid-19, [tid]: finding hope, healing and liberation beyond covid-19 within a context of captivity and carcerality, [tid]: flux leadership: leading for justice and peace in & beyond covid-19, [tid]: flux leadership: insights from the (virtual) field, [tid]: hard pivot: compulsory crisis leadership emerges from a space of doubt, [tid]: and how are the children, [tid]: real talk: teaching and leading while bipoc, [tid]: systems of emotional support for educators in crisis, [tid]: listening leadership: the student voices project, [tid]: global engagement, perspective-sharing, & future-seeing in & beyond a global crisis, [tid]: teaching and leadership during covid-19: lessons from lived experiences, [tid]: crisis leadership in independent schools - styles & literacies, [tid]: rituals, routines and relationships: high school athletes and coaches in flux, [tid]: superintendent back-to-school welcome 2020, [tid]: mitigating summer learning loss in philadelphia during covid-19: humble attempts from the field, [tid]: untitled, [tid]: the revolution will not be on linkedin: student activism and neoliberalism, [tid]: why radical self-care cannot wait: strategies for black women leaders now, [tid]: from emergency response to critical transformation: online learning in a time of flux, [tid]: illness methodology for and beyond the covid era, [tid]: surviving black girl magic, the work, and the dissertation, [tid]: cancelled: the old student experience, [tid]: lessons from liberia: integrating theatre for development and youth development in uncertain times, [tid]: designing a more accessible future: learning from covid-19, [tid]: the construct of standards-based education, [tid]: teachers leading teachers to prepare for back to school during covid, [tid]: using empathy to cross the sea of humanity, [tid]: (un)doing college, community, and relationships in the time of coronavirus, [tid]: have we learned nothing, [tid]: choosing growth amidst chaos, [tid]: living freire in pandemic….participatory action research and democratizing knowledge at knowledgedemocracy.org, [tid]: philly students speak: voices of learning in pandemics, [tid]: the power of will: a letter to my descendant, [tid]: photo essays with students, [tid]: unity during a global pandemic: how the fight for racial justice made us unite against two diseases, [tid]: educational changes caused by the pandemic and other related social issues, [tid]: online learning during difficult times, [tid]: fighting crisis: a student perspective, [tid]: the destruction of soil rooted with culture, [tid]: a demand for change, [tid]: education through experience in and beyond the pandemics, [tid]: the pandemic diaries, [tid]: all for one and 4 for $4, [tid]: tiktok activism, [tid]: why digital learning may be the best option for next year, [tid]: my 2020 teen experience, [tid]: living between two pandemics, [tid]: journaling during isolation: the gold standard of coronavirus, [tid]: sailing through uncertainty, [tid]: what i wish my teachers knew, [tid]: youthing in pandemic while black, [tid]: the pain inflicted by indifference, [tid]: education during the pandemic, [tid]: the good, the bad, and the year 2020, [tid]: racism fueled pandemic, [tid]: coronavirus: my experience during the pandemic, [tid]: the desensitization of a doomed generation, [tid]: a philadelphia war-zone, [tid]: the attack of the covid monster, [tid]: back-to-school: covid-19 edition, [tid]: the unexpected war, [tid]: learning outside of the classroom, [tid]: why we should learn about college financial aid in school: a student perspective, [tid]: flying the plane as we go: building the future through a haze, [tid]: my covid experience in the age of technology, [tid]: we, i, and they, [tid]: learning your a, b, cs during a pandemic, [tid]: quarantine: a musical, [tid]: what it’s like being a high school student in 2020, [tid]: everything happens for a reason, [tid]: blacks live matter – a sobering and empowering reality among my peers, [tid]: the mental health of a junior during covid-19 outbreaks, [tid]: a year of change, [tid]: covid-19 and school, [tid]: the virtues and vices of virtual learning, [tid]: college decisions and the year 2020: a virtual rollercoaster, [tid]: quarantine thoughts, [tid]: quarantine through generation z, [tid]: attending online school during a pandemic.
Report accessibility issues and request help
Copyright 2024 The University of Pennsylvania Graduate School of Education's Online Urban Education Journal

- < Previous
Home > History Community Special Collections > Remembering COVID-19 Community Archive > Community Reflections > 21

Community Reflections
My life experience during the covid-19 pandemic.
Melissa Blanco Follow
Document Type
Class Assignment
Publication Date
Affiliation with sacred heart university.
Undergraduate, Class of 2024
My content explains what my life was like during the last seven months of the Covid-19 pandemic and how it affected my life both positively and negatively. It also explains what it was like when I graduated from High School and how I want the future generations to remember the Class of 2020.
Class assignment, Western Civilization (Dr. Marino).
Recommended Citation
Blanco, Melissa, "My Life Experience During the Covid-19 Pandemic" (2020). Community Reflections . 21. https://digitalcommons.sacredheart.edu/covid19-reflections/21
Creative Commons License

Since September 23, 2020
Included in
Higher Education Commons , Virus Diseases Commons
To view the content in your browser, please download Adobe Reader or, alternately, you may Download the file to your hard drive.
NOTE: The latest versions of Adobe Reader do not support viewing PDF files within Firefox on Mac OS and if you are using a modern (Intel) Mac, there is no official plugin for viewing PDF files within the browser window.
Advanced Search
- Notify me via email or RSS
- Expert Gallery
- Collections
- Disciplines
Author Corner
- SelectedWorks Faculty Guidelines
- DigitalCommons@SHU: Nuts & Bolts, Policies & Procedures
- Sacred Heart University Library
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright

Coronavirus Disease 2019
Defining the covid-19 narrative, the story we tell about this pandemic will shape our preparedness for the next..
Posted July 6, 2021 | Reviewed by Vanessa Lancaster
- The core narrative of the pandemic, and arguably the central one, is the presence of inequities.
- COVID-19 exposed inequities in morbidity and mortality, who bears the burden of steps we have taken to mitigate the virus, and vaccine uptake.
- The effects of these inequities will likely be with us for some time, shaping the story of the pandemic and the lives of those who lived it.

What story will we tell about COVID-19 ? The events of the past year and a half were more than just a story of the emergence and behavior of a virus. It was also a story of the social, economic, scientific, and political context into which the virus emerged and the intersection of these forces within complex, dynamic systems. Given this complexity, it can be challenging to predict which stories will rise to the surface of the overarching story of the pandemic. Yet, we need to try. The stories we tell about health shape how we engage with the present moment to support a better future—or how we fail to do so.
With this in mind, I suggest four critical narratives that emerged from the broader story of the pandemic and which can help define the overall COVID-19 narrative in the years to come. Next week, I will address the perhaps deeper issue of why we remember what we remember.
The first narrative which has come to define the COVID-19 moment is that of scientific excellence. The speed with which a COVID-19 vaccine was developed, supported by mRNA technology, reflects a new era in cutting -edge science. This narrative of scientific excellence is powerful for two key reasons.
First, because this latest vaccine technology is unique and impressive and has begun the long-awaited process of helping return us to our families, friends, colleagues, lives. Second, it is powerful because of how closely it aligns with how we already think about health. We often think about health in terms of treatment—doctors and medicines—which can cure us when we are sick, rather than in terms of the structural forces in society which shape whether or not we get sick, to begin with. We tend to confuse health (the state of not being sick) with healthcare (what we turn to once sickness strikes), which has led us to invest vast sums in healthcare at the expense of the core forces that shape health. The success of vaccines reflects that this investment is indeed core to supporting scientific excellence. Still, our story of health and COVID-19 is incomplete if it is confined to science and treatment alone.
This leads to the following core narrative of the pandemic and arguably the central one—the presence of inequities. These include, centrally, inequities in morbidity and mortality, who bears the burden of the steps we have taken to mitigate the virus and vaccine uptake. When COVID-19 struck, it quickly became apparent that certain groups—such as Black Americans, people over 65, and people with underlying health conditions—were more vulnerable to the virus than others. This vulnerability was shaped by longstanding health inequities informed by marginalization, social and economic injustice, and other foundational forces in our society. The story of COVID-19 is, in large part, the level of these forces.
These inequities have also come to define who has most felt the consequences of our efforts to mitigate the pandemic. COVID-19 caused us to embrace extraordinary measures, shut down society, and incur severe economic costs in the process. The pandemic led to significant job losses , which most affected low-income, minority workers. When the economy began to recover, with higher-wage workers bouncing back relatively quickly, lower-wage minority workers recovered at a far slower rate. The effects of this inequity will likely be with us for some time, shaping the story of the pandemic and the lives of those who lived it.
Third, the story of COVID-19 would be incomplete without an honest reckoning with widespread loss of trust in institutions and the consequences of this for public health. The most prominent example of this was how the inconsistent, often dishonest, words of former President Trump informed a lack of trust in guidance from the White House throughout the crisis. It is also true that seeming inconsistencies occasionally characterized public health efforts, perhaps most clearly in our field’s widespread embrace of civic protests last summer, in apparent contrast with our guidance on social distancing and masks. Given that COVID-19 emerged at a time when trust in institutions was already declining , the story of the pandemic may well be, in large part, a story of how this trend accelerated, making it harder for anyone to speak with a widely-heeded, authoritative voice on matters core to health.
Finally, a core narrative of the pandemic, one which could well characterize our future memory of this time, is that, as bad as COVID-19 was, it could have been far worse. I realize that this may seem strange, even unfeeling, in the context of mass death and suffering. But it is nevertheless true. COVID-19 has been a disaster. Yet, the virus itself, compared to past pandemics, is nowhere near as lethal as it might have been. A future pandemic could combine the high transmissibility of COVID-19 with the lethality of, say, SARS or even of the Black Death. While the latter may seem historically remote, there is no reason why we could not see something as deadly strike in our own time. The better we understand this, the more the story we tell about COVID-19 can help inform our efforts to build a world that is no longer vulnerable to contagion.
Each of these stories represents a vital part of the broader narrative of COVID-19. It is also the case that one or two of these narratives may rise even further to the top of our minds to conclusively define this era. Only time will tell for sure what will happen. However, I would argue several factors contribute to making stories stick when we think back on critical events, which increases the chance that the stories I have presented here will long outlast this moment. I will explore these factors and how we come to believe what we believe in our narratives next week.
This piece was also posted on Substack.

Sandro Galea, M.D., is the Robert A. Knox professor and dean of the Boston University School of Public Health
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- How covid-19 spreads:...
How covid-19 spreads: narratives, counter narratives, and social dramas
Read our covid inquiry series.
- Related content
- Peer review
This article has a correction. Please see:
- How covid-19 spreads: narratives, counter narratives, and social dramas - September 06, 2022
- Trisha Greenhalgh , professor of primary care health sciences 1 ,
- Mustafa Ozbilgin , professor of organisational behaviour 2 ,
- David Tomlinson , consultant cardiologist and electrophysiologist 3
- 1 Nuffield Department of Primary Care Health Sciences, University of Oxford, UK
- 2 Brunel University London, Uxbridge, UK
- 3 University Hospitals Plymouth NHS Trust, Plymouth, UK
- Correspondence to: T Greenhalgh trish.greenhalgh{at}phc.ox.ac.uk
Trisha Greenhalgh and colleagues explore why inaccurate narratives about the mode of transmission of SARS-CoV-2 emerged early in the pandemic and shaped a flawed policy response, with tragic consequences
Key messages
A flawed narrative that SARS-CoV-2 was transmitted by droplets rather than being airborne became entrenched early in the pandemic
Measures aimed at an assumed droplet pathogen (handwashing, surface cleansing, physical distancing) were over-emphasised
Measures to reduce airborne transmission (improving indoor air quality, reducing indoor crowding and time spent indoors, and high-grade respiratory protection) were under-emphasised
UK policy makers seemed to favour narratives from a narrow group of scientific advisers
Consequences included care home deaths, mission critical delays in public masking, and avoidable infections of healthcare workers
The draft terms of reference for the UK covid-19 inquiry encompass not just what decisions were made but also how and why. 1 As Dyani Lewis has argued in Nature , the World Health Organization overlooked—and at times explicitly denied—airborne transmission of SARS-CoV-2 for over two years, despite early evidence indicating that this was an important, and perhaps the dominant, route of transmission. 2 UK policy makers likewise adhered to an assumed droplet mode of transmission and prioritised interventions accordingly, neglecting the key topic of indoor air quality. 3
We consider how flawed narratives about SARS-CoV-2 transmission arose and became entrenched, leading to misplaced policies and avoidable deaths, focusing mainly on the UK. We invite the inquiry to consider not just those specific flawed decisions but also the culture of premature scientific conclusions and reluctance to engage with uncertainty.
Policy making as a struggle between narratives
Policy making involves competing narratives (about problems, how they arose, and how they will be resolved), institutions (especially government and its bureaucratic machinery), and interests (financial, political, ideological). 4 Policy might ideally “follow science,” but whose science and why? Science shapes policy narratives through an “inside track” (such as official advisory committees) and, to a lesser extent, through an “outside track” (such as less mainstream scientists and citizen movements). 4 Pandemic policy making has been characterised not by clearly identified knowledge gaps that science obligingly fills but by toxic clashes between competing scientific and moral narratives.
Getting the mode of SARS-CoV-2 transmission right matters, because preventive strategies follow ( box 1 ). 5 6 Being honest about scientific uncertainty also matters, because—among other reasons—it is hard to backtrack after declaring a policy to be “evidence based.” 7
Droplet versus airborne transmission: implications for public health and healthcare worker protection
Droplet transmission.
If an infectious pathogen spreads predominantly through large respiratory droplets that fall quickly, the most important public health measures are:
respiratory hygiene (eg, sneezing into tissues)
disinfecting surfaces and objects (fomites) onto which droplets might have fallen
reducing direct contact (eg, do not shake hands with others or touch one’s own face)
staying physically apart from others at a distance that reflects the effect of gravity on droplets (1-2 m)
wearing face masks within that droplet distance
physical barriers (such as visors or plastic screens)
providing respirator grade facial protection to healthcare staff who undertake “aerosol generating” procedures
These contact, droplet, and fomite precautions do not distinguish between indoor and outdoor settings, because a gravity driven mechanism for transmission would operate similarly in both.
Airborne transmission
If an infectious pathogen is mainly airborne, a person could be infected by inhaling aerosols emitted in the breath of an infected person. These aerosols might remain suspended in the air for many hours. Reducing airborne transmission requires measures to avoid inhalation of infectious aerosols, including:
engineering controls in indoor spaces (ventilation, air filtration)
reducing crowding (eg, by encouraging people to work from home if possible)
reducing time spent indoors (eg, frequent breaks for school classes)
maximising physical distance between people indoors (even beyond 2 m)
wearing masks whenever indoors
careful attention to mask quality (to maximise filtration) and fit (to avoid air getting in through gaps)
taking particular care during indoor activities that generate aerosols (eg, speaking, singing, exercising)
providing respirator grade facial protection to healthcare staff and others that work directly with patients
Competing narratives around transmission
“covid is droplet, not airborne, spread”.
At a press conference on 11 February 2020, WHO’s director general announced that covid-19 was airborne. 8 After a prompt, he corrected himself and declared that the virus was transmitted by droplets (coughs, sneezes, and contaminated objects). The reasons for this hasty correction are not fully known but might have included a desire to prevent public panic and to avoid exacerbating a major supply chain issue with personal protective equipment 9 in the face of known international shortages. 10
WHO’s early public information campaign promoted droplet measures—handwashing, respiratory hygiene, and disinfection of surfaces and objects ( box 1 )—and firmly reassured the public that the virus was not airborne ( fig 1 ). This stance reflected the dominance of infection prevention and control clinicians—whose day jobs included enforcing controls against droplet-borne infections in hospitals—on key committees. 11 Airborne precautions for airborne diseases are, of course, a legitimate component of infection prevention and control science, but in practice this professional group has focused historically on droplet precautions. 12

Tweet from WHO on 28 March 2020 denying airborne transmission of SARS-CoV-2
- Download figure
- Open in new tab
- Download powerpoint
The UK government’s narrative ( box 2 ) was similar to WHO’s. It did not reflect nuanced discussions in the Scientific Advisory Group on Emergencies (SAGE), some members of which had raised the possibility of other transmission routes on 18 February 2020. 15 Rather, it reflected advice from a small group of infection prevention and control experts from Public Health England, Public Health Wales, NHS Scotland, and Public Health Agency Northern Ireland (see supplementary file on bmj.com) who favoured a droplet-but-not-airborne narrative.
Contrasting early announcements about preventing transmission of SARS-CoV-2 from England and Japan
From public health england.
“There are general principles you can follow to help prevent the spread of respiratory viruses, including:
washing your hands more often—with soap and water for at least 20 seconds or use a hand sanitiser when you get home or into work, when you blow your nose, sneeze or cough, eat or handle food
avoid touching your eyes, nose, and mouth with unwashed hands
avoid close contact with people who have symptoms
cover your cough or sneeze with a tissue, then throw the tissue in a bin and wash your hands
clean and disinfect frequently touched objects and surfaces in the home”
Posted 3 March 2020, updated 30 March 2020, withdrawn 1 May 2020. 13
This narrative assumes a droplet mode of transmission and implies a high level of certainty.
From the Japanese Prime Minister’s office
“The locations where mass infections were confirmed so far are places where the following three conditions were met simultaneously: closed space with poor ventilation, crowded with many people, and conversations and vocalisation in close proximity (within arm’s reach of one another). It is believed that more people were infected in such places. Therefore, we ask that you predict locations and settings where these three conditions could occur simultaneously and avoid them. We do not have enough scientific evidence yet on how significantly such actions can reduce the risk of spreading infection. However, since places with poor ventilation and crowded places are increasing infections, we ask that you take precautions even before scientific evidence for clear standards is found.”
Posted 9 March 2020. 14
This narrative assumes the possibility of airborne transmission and asks citizens to share the uncertainty and act in a precautionary way.
The droplet-but-not-airborne narrative emphasised randomised controlled trials (see supplementary file on bmj.com), 16 drawing implicitly on the hierarchy of evidence—a formalisation of the assumed superiority of randomised trials, which “typically serve[s] the needs and realities of clinical medicine, but not necessarily public policy.” 17 It did not acknowledge the hierarchy of controls—a public health framework incorporating system level interventions to eliminate pathogens, environmental controls aimed at making air and water safe, and behavioural interventions. 18 This mindset seems to have led policy makers to reject a wealth of evidence on the science of how to optimise indoor air quality. 6
“Covid is unequivocally airborne”
Aerosol scientists study how fluids and particles travel in the air. Some specialise in how respiratory pathogens—including tuberculosis, influenza, and other coronaviruses such as SARS and MERS—travel. They have shown, using laboratory studies, real world case studies, and computer modelling, that these pathogens are transmitted by aerosols and require airborne mitigation measures ( box 1 ) and that coughs and sneezes generate turbulent gas clouds of different sized particles that can travel long distances. 19
Since early 2020, evidence has accumulated from a range of study designs to support the hypothesis that, like most other respiratory pathogens and perhaps more so than other coronaviruses, SARS-CoV-2 is transmitted through the air ( box 3 ). 5 34 35 36
10 Streams of evidence that support airborne transmission of SARS-CoV-2
Superspreading events: the virus is often transmitted at mass events from one or a few people to many people 20 21
Long range transmission: the virus spreads in shared air among people who have never physically met or touched any common surface 22
Asymptomatic and pre-symptomatic transmission: a high proportion of people who pass on the virus have no symptoms at the time 23
Indoor dominance: transmission is many times greater indoors than outdoors, and ventilation reduces transmission 24
Nosocomial infections occur despite strict contact and droplet precautions and reduce when airborne precautions are added 25
Although SARS-CoV-2 is difficult to isolate from air, viable SARS-CoV-2 was detected early in the pandemic in real world settings where infected people had been 26 27 28
SARS-CoV-2 has been detected in air filters in building ducts 29
Transmission between animals has occurred when their cages are connected with air ducts 30
The virus exhibits overdispersion (one person with covid-19 might infect no-one; another might infect dozens) 31
Empirical evidence supporting droplet or fomite transmission is sparse 32 33
Adapted from Greenhalgh et al. 34
Countries such as Japan, 14 where “inside track” aerosol scientists had the ear of government, 11 introduced airborne precautions early in the pandemic ( box 2 ). But in most western countries the aerosol narrative initially fell on deaf policy ears. By July 2020, aerosol scientists were alarmed that official advice was based on oversimplistic and incorrect models of transmission (which had perpetuated for decades in the infection control literature 37 ) and wrote an open letter to WHO offering to help. 5
“Covid is ‘situationally’ airborne”
From the outset, WHO’s guidance on protecting healthcare workers from covid-19 recommended a standard level of protection for most activities but a higher level for “aerosol generating” ones, 38 reflecting a long established (but flawed) medical research tradition. WHO’s Infection Prevention and Control Research and Development Expert Group for Covid-19 did not initially include any aerosol scientists and seemed to ignore the offer of help. A new scientific brief was quickly published, reiterating the dominance of droplet transmission in most circumstances but acknowledging airborne transmission in certain situations—aerosol generating medical procedures and crowded, poorly ventilated indoor settings. 39
Some parts of WHO subsequently welcomed the input of aerosol scientists and changed the guidance in December 2021 to recommend higher grade personal protective equipment (including N95 respirators) for all covid-19 patient care. 40 But the expert group dissented from this overall view, as noted in a footnote (page 1): “WHO provides this interim recommendation independent of the covid-19 infection prevention and control guidelines development group.” That group continued to promote the “situationally airborne” narrative, which has persisted despite evidence against it and has far reaching implications. If aerosols transmit only when certain procedures are being performed, only a small fraction of healthcare staff need higher grade protection and only when performing particular procedures. If that assumption is incorrect, staff (especially non-medical and less senior ones) and patients in most healthcare facilities are under protected.
“Everyone generates aerosols; everyone is vulnerable”
A systematic review found wide disagreement among guideline panels about which procedures and activities should count as aerosol generating (and hence earn respirator grade protection for the person doing them). 41 Many procedures, such as taking a nasopharyngeal swab, were inconsistently classified; some acts, such as coughing, were not procedures; and several procedures were classified as aerosol generating only because they induced coughing. 41 A review of the physiology and aerodynamics of respiratory acts concluded that coughing, sneezing, breathing (especially if laboured), speaking, and singing generated substantial amounts of aerosol and that well documented superspreading events for covid-19 involved a critical triad of poor ventilation, crowding, and loud vocalisation. 42
These findings raise some paradigm challenging questions. Should respirator grade protection be worn by everyone—including other patients—whenever patients are coughing? Should more attention be paid to measures higher up the hierarchy of controls, such as ventilation or filtration of air or ensuring that fewer people share air and for shorter periods?
Social dramas
Droplet precautions became ritualised.
The official droplet-but-not-airborne narrative materialised as artefacts (such as posters, disinfectant dispensers, and 2 metre distancing markers) and social practices (actions accepted and expected in particular contexts). Droplet directed practices became ubiquitous, as people washed hands and forearms assiduously for 20 seconds, quarantined and disinfected their post, and stayed a measured distance apart, and institutions installed and policed the various artefacts and practices.
These rituals of purification 43 powerfully reinforced the official narrative. “Clean” and “contaminated” came to be demarcated in terms of how recently and thoroughly hands had been sanitised and how far a droplet was assumed to travel ( box 1 ). The same rituals served to downplay or obscure the narrative of aerosol transmission—which demarcated clean and contaminated in terms of air purity, with practices oriented to controlling indoor crowding and time spent indoors, ventilating or filtering air, and optimising quality and fit of masks ( box 1 ). These material and enacted features of policy discourse served to silence further the narrative that SARS-CoV-2 is airborne.
Care home residents died in their thousands
On 23 March 2020, with up to 500 000 deaths and an overwhelmed NHS predicted, the UK’s prime minister announced a national lockdown. Hospitals had switched into urgent discharge mode on 19 March, sending patients back to care homes without routine pre-discharge testing. Between March and June 2020, 18 104 deaths involving covid-19 and 11 169 additional deaths above the five year UK average occurred among care home residents. 44
Amnesty International depicted the UK’s care home crisis as a gross breach of human rights in which thousands of vulnerable people had been treated as expendable. 45 The crisis was largely avoidable. Public Health England’s guidance for care homes emphasised a situationally airborne narrative. 46 Because aerosol generating procedures are rarely undertaken in care homes, these settings were low priority for personal protective equipment. Under-emphasis of the importance of ventilation and no routine use of masks are likely to have greatly amplified transmission between infectious residents and care home staff. In Hong Kong, by contrast, surgical masks were mandated for all care home staff by late January 2020, and no excess care home deaths occurred in the first wave of covid-19 (March to June 2020). 47
Public masking became a libertarian lightning rod
Libertarianism is a political ideology that favours individual choice, freedom, and a retreat from state and institutional control. Libertarians resist imposed rules and like to do their own research rather than trust scientists or government. Uncertainty and conflict about the value and place of public masking allowed libertarian messages and practices to flourish.
At its 4 February 2020 meeting, SAGE advised masks for patients with symptomatic covid-19 to reduce transmission “if tolerated.” 15 This group had acknowledged the potential for asymptomatic transmission of SARS-CoV-2 on 28 January 2020 15 but did not make the logical leap to recommend that asymptomatic people should wear masks as source control. In official meetings between January and April 2020, either public masking was not mentioned or arguments against it—lack of efficacy, harm, wastage—were tabled (see supplementary file on bmj.com). 15 Public announcements and professional videos 48 issued by Public Health England between February and June 2020 presented masking as ineffective and potentially harmful on the grounds that people might take compensatory risks or self-contaminate while putting on or removing their mask (the “donning” and “doffing” of infection control jargon). They provided no evidence to support these claims.
The confusion about masking in key decision making committees was due partly to confusion about mode of transmission. Asymptomatic transmission reflects a predominantly airborne route (because asymptomatic people are not coughing or sneezing), but the preoccupation with self-contamination and donning and doffing rituals reflected a predominantly droplet model ( box 1 ). Wearing a cloth or surgical mask protects others (imperfectly) from transmission by droplets and (to some extent) aerosols; wearing a well fitting respirator grade mask also provides strong protection for the wearer against aerosol transmission. 49 A presumption of droplet transmission explains the limited attention paid to the type of mask and the excessive concern about self-contamination.
An influential inside track narrative seemed to conflate the absence of relevant randomised controlled trial evidence with evidence that masking was ineffective. 16 Outside track scientists argued for the precautionary principle, on the grounds that there was—as early as March 2020—indirect and mechanistic evidence (notably, around asymptomatic transmission) and strong theoretical arguments for public masking and huge potential risks associated with delay. 50 Mask mandates were finally introduced in England on 15 June (public transport) and 24 July 2020 (all public places). By then, public opinion was polarised, and many thought it was ineffective. 51 Most Asian countries had high public compliance with early masking policies and very low death rates; many western countries introduced masking late and had many more deaths, although causal links are complex and confounders many. 52
Masking policies in the United States, and to a lesser extent the UK, were met with a strong libertarian backlash aligned with populist political leaders, right wing Christianity, anti-authoritarian social media groups, and, latterly, anti-vaccination groups. 53 In this context, masks came to symbolise pointless restriction of individual freedom, mindless compliance with authoritarian governments, and even blasphemy. 54
Healthcare settings became occupational health battlegrounds
As documented in the 9 January minutes of the New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG)—an expert committee of the Department of Health and Social Care that advises the UK government, SARS-CoV-2 was initially classified as an airborne high consequence infectious disease by the four nations’ public health agencies. 55 Consequently, staff caring for patients with suspected or confirmed covid-19 required filtering facepiece respirators (FFP3) or equivalent. This reflected guidance from the UK Health Security Agency (previously Public Health England) and Health and Safety Executive on other coronaviruses and avian influenza and legal requirements for employers to protect their workers against airborne biohazards. The Health and Safety Executive had concluded in 2008 that surgical masks “should not be used in situations where close exposure to infectious aerosols is likely.” 56
NERVTAG minutes from 13 March 2020, however, show growing concern about shortages of respirator masks and the Department of Health and Social Care’s request for “adapted” guidance that recommended surgical masks in most circumstances. 55 The deputy chief medical officer agreed to meet with the chair of the government’s Advisory Committee on Dangerous Pathogens, whose members “were unanimous in supporting the declassification of covid-19 [as a high consequence infectious disease].” 55
The declassification of covid-19 in early March 2020 had profound implications for the protection of healthcare workers. The following sentence, for example, was present in version 8.1 of Health Protection Scotland’s guidance for clinicians on infectious pathogens (dated 5 March 2020): “The precautionary principle should be applied for all novel or emerging respiratory pathogens of high consequence when the mode of transmission is incompletely determined. Airborne precautions (including the use of correctly fitted FFP3 respirators) should be applied for all patients admitted with suspected or confirmed covid-19.” 57
But this entire paragraph was removed from version 9.0 of the guidance (dated 10 March 2020). 58 Notes in a marked-up version 8.1 obtained by us under the Freedom of Information Act reveal a comment against the paragraph as follows: “subject to change based on NERVTAG PPE decisions.”
Although NERVTAG minutes from 6 March 2020 allude to severe shortages of respirator grade protective equipment, this was not made explicit in communications to either healthcare organisations or the public. A letter to UK healthcare organisations dated 28 March 2020 from NHS England and NHS Improvement, Public Health England, and the Academy of Medical Royal Colleges stated that, because of rising covid-19 cases and because “more was understood about the behaviour of the virus and its clinical outcomes,” 59 respirator grade protection would now be restricted to aerosol generating procedures. 59
The number of UK health and care workers infected with SARS-CoV-2 at work is not officially documented. The secretary of state for health and social care reported that by mid-2021, around 1500 had died of covid-19 and 120 000 had developed long covid (some of whom remained on long term sick leave). 60 In April 2020, excess deaths were noted among healthcare staff (especially men and ethnic minority groups) working outside intensive care units, and this impression was confirmed in subsequent academic publications. 61 In early 2021, the British Medical Association and Royal College of Nursing demanded respirator grade protection for all staff working with patients with covid-19.
The latest guidance from the UK Health Security Agency, introduced in April 2022 but withdrawn in May 2022 when all jurisdictions were asked to revert to their respective national guidance, continued to promote a situationally airborne narrative and restrict respirator use to aerosol generating procedures. 62 It did not recommend respirator masks for all covid-19 patient care. But the document glossary states, “Airborne particles can be released when a person coughs or sneezes, and during [aerosol generating procedures].” There remains wide variation in infection control policies in different NHS trusts (perhaps because some interpret the guidance as mandatory); those that provide respirator grade protection seem to have much lower nosocomial infection rates for covid-19. 63
At the root of the UK’s limited success in controlling transmission of SARS-CoV-2 lie flawed droplet-but-not-airborne and situationally airborne narratives. These narratives, and the false certainty with which they were conveyed, produced ineffective public health measures, contributed to shocking levels of care home deaths, exacerbated toxic discourse on masking, and justified withholding adequate protection from most health and care staff.
Why did the flawed narratives prevail? We consider four complementary hypotheses. The first is psychological. Social representation theory holds that people faced with new information show two tendencies: anchoring (grounding the new in an existing framework of concepts, ideas, and values) and concretisation (in which something abstract is made meaningful by making it physical and tangible). 64 People are unlikely to change their beliefs in light of complex and contravening evidence because this requires effort and causes aversion. 65 Policy makers are known to exhibit “satisficing” — meaning they narrow the parameters within which their decisions must make sense and be accountable, especially when threats are complex and urgent. 66 These well documented psychological tendencies might underpin the tendency for business and policy decisions to show what has been termed “escalation of commitment to a failing course of action.” 7
Our second hypothesis is scientific elitism. Scientists in infection control have amassed considerable scientific capital (influence, status, accolades); their favoured methods (randomised controlled trials) are greatly valued; and they have much to lose if they discard their long held droplet narrative and concede the importance of other kinds of evidence. 11 The inside track for pandemic policy making in the UK and WHO was narrow and partisan, 11 67 enabling an unusual degree of power to be wielded against outside track scientific voices, imposing a narrow and rigid set of acceptable scientific methods (what Danziger called “methodolatry” 68 ), and precluding the kind of interdisciplinary deliberation that might have allowed a full and fair consideration of important competing narratives. The low status of aerosol science in policy circles was perhaps compounded by the relative youth of this scientific field and the inherent technical difficulties of isolating viable virus from the air (resulting in inconsistent findings in air sampling studies, especially when undertaken by non-experts). 35 The science of indoor air quality (for example, how and when to open windows, what kinds of filters to use) might be (wrongly) viewed as unsophisticated compared with much of modern biomedicine. 3
Our third hypothesis is practical and logistical. As confirmed in official minutes, the national shortage of high grade respiratory protective equipment was a live discussion topic in UK policy advisory groups at the beginning of the pandemic. Although adherence to a droplet-but-not-airborne narrative was not consciously undertaken purely because of this shortage, it certainly helped to make existing stocks go further.
Our fourth hypothesis is political. Droplet precautions are, at least to some extent, under the control of individuals and hence resonate with neoliberal discourses about individual freedom, personal responsibility, and restraint of the state (although the “choice” to distance physically, for example, presupposes sufficient space in which to do so). Airborne precautions require a paradigm shift in policy making, with strategic actions from those responsible for public safety; this approach aligns with a more socialist leaning political discourse and requires considerable up-front investment in the built environment whose benefits may take years to accrue. 6 WHO’s tweet ( fig 1 ) emphasises how to protect yourself rather than what to expect of your employer, your child’s school, or your government. Relatedly, we hypothesise a role for populism, the modus operandi of which is cherry picking evidence that supports the policy drive and validating anti-science sentiment under the guise of bringing power to people. 69 Populism drew on public desires to return to normalcy and further marginalised aerosol science by depicting its recommended measures 6 as obscure, unaffordable, and an enemy of the public interest.
The narratives and dramas presented in this paper are not exhaustive. The framing of protection as a matter of individual responsibility, for example, also accommodates the current political narrative of “learning to live with covid-19,” in which good citizens stoically accept the endemicity of a—hopefully attenuating—virus in exchange for greater individual freedoms.
The covid-19 pandemic can be framed as what Marcel Mauss (cited in Chaunlat 70 ) calls a “total social fact,” a phenomenon that affects all domains and layers of society (economic, legal, political, religious) and requires us to draw evidence from across multiple scientific and other fields. In such circumstances, the combination of the cognitive biases and satisficing behaviour of policy makers, scientists’ desire to protect their interests, and politicians’ alignment with individualist values and populist sentiment proved perilous.
As the pandemic continues to cause death and long term illness more than 30 months after the first case, airborne transmission of SARS-CoV-2 and the mitigations needed to tackle it ( box 1 ) remain misunderstood and under-recognised. Extraordinarily, a recent UK inquiry into errors made in the pandemic did not mention masks or ventilation at all. 71 Although we acknowledge that solutions are always much more evident in retrospect, we think that the inquiry should ask hard questions about policy makers’ accountability in relation to past and ongoing omissions in this regard. We have 10 specific questions for the inquiry ( box 4 ).
Questions for the inquiry
1. Why were early indications that this virus could be airborne overlooked by policy makers, resulting in public health measures that over-emphasised handwashing, surface cleansing, and 2 m distancing? What checks and balances might have helped policy makers keep a more open mind about mode of transmission rather than seeing it as a settled issue from an early stage?
2. Why did policy makers convey an unjustified level of scientific certainty about the mode of transmission and measures to prevent transmission, rather than sharing with the public that the mode was not yet known, as other countries did? How might the culture of UK policy bodies change to foster greater intellectual engagement with scientific uncertainty and how to handle it?
3. What were (and are) the membership and terms of reference of the UK’s “infection prevention and control cell”? Who appoints them? Who checks their work? Does this group include any experts on airborne transmission and the delivery of safe indoor air? Why did (and does) this group have such a high degree of influence on policy? Why are its activities (at least partly) hidden from the public? Where are the minutes of its meetings?
4. Why did policy makers continue to de-emphasise the evidence base on the airborne mode of transmission for so long, even as strong and consistent empirical evidence was accumulating? To what extent were cognitive biases operating at either individual or group level? How might such biases have been minimised or overcome?
5. Why did policy makers continue to place so much emphasis on droplet precautions even after they had accepted that the virus was likely airborne? Why was indoor air quality given so little attention not just at the beginning of the pandemic but two years (and counting) into it?
6. To what extent were policy decisions adversely influenced (either consciously or unconsciously) by the shortage of high grade personal protective equipment? Who made these decisions and what is the chain of accountability?
7. To what extent was the limited public confidence in the efficacy of masks influenced by negative policy announcements on this subject early in the pandemic? Why were early statements that masks were likely ineffective and could be harmful not corrected as evidence to refute them accumulated? What lessons might specific public health leaders be encouraged to learn from this error?
8. Why are UK health and care workers still not fully protected against airborne infections in the workplace? Why is a premature and false narrative that the pandemic is over being used to justify not supplying workers with personal protective equipment designed to protect against airborne pathogens?
9. Are experts in aerosol science now adequately represented on all key science advisory bodies and are measures in place to ensure that their advice is sought and heeded?
10. Why have policy makers put prime responsibility for preventive measures on individuals given that many effective preventive measures for airborne transmission are located at institutional and national policy levels?
Bold action is now needed to ensure that the science of SARS-CoV-2 transmission is freed from the shackles of historical errors, scientific vested interests, ideological manipulation, and policy satisficing. Policy makers should actively seek to broaden the scientific inside track to support interdisciplinarity and pluralism as a route to better policies, greater accountability, and a reduction in the huge inequities that the pandemic has generated.
Acknowledgments
Thanks to Alex Hunt of News EU for permission to reproduce the timeline of mask policy decisions in the supplementary file, to Birgitte Nerlich for additional background material, and to Stephen Reicher for helpful comments on an earlier draft and suggestions of additional references on psychological theories. The research on which it was based is funded from the following sources for TG: UK Research and Innovation via ESRC and NIHR (ES/V010069/1) and Wellcome Trust (WT104830MA).
Contributors and sources: The interdisciplinary author team was from secondary care medicine (DT), primary care and public health (TG), and critical social science (MO). All authors drafted sections of the manuscript. TG produced an initial synthesis which was then improved by iteration and discussion. All authors approved the final manuscript. TG is guarantor.
Patient involvement: The article relates to a public health issue that affects everyone. As such, we are all potential patients. TG lost her mother to hospital acquired covid-19 so brings a user perspective on nosocomial transmission.
Competing interests: We have read and understood BMJ policy on declaration of interests and have the following interests to declare: in November 2020, DT contacted Public Health England, the chair of NERVTAG, the Department of Health and Social Care, and NHS England to request improved personal protective equipment for healthcare staff. In February 2021, TG added her signature to a letter from the Royal College of Nursing to the UK prime minister making a similar request. She is a member of Independent Sage. MO declares no conflicts of interest.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a series commissioned, peer reviewed, and edited by The BMJ . The advisory group for the series was chaired by Kara Hanson and included Martin McKee, although he was not involved in the decision making on the papers that he co-authored. Kamran Abbasi was the lead editor for The BMJ .
- ↵ Cabinet Office. UK covid-19 inquiry: draft terms of reference. 22 March 2022. https://www.gov.uk/government/publications/uk-covid-19-inquiry-draft-terms-of-reference
- Dancer SJ ,
- Bluyssen PM ,
- Morawska L ,
- Bahnfleth W ,
- ↵ World Health Organization. Coronavirus press conference 11 February (transcript). WHO, 2020. https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-full-press-conference-11feb2020-final.pdf
- ↵ World Health Organization. Public health response to biological and chemical weapons: WHO guidance. 2004. https://www.who.int/publications/i/item/public-health-response-to-biological-and-chemical-weapons-who-guidance-(2004)
- Kerbache L ,
- Greenhalgh T ,
- Ozbilgin M ,
- Contandriopoulos D
- Jimenez JL ,
- Randall K ,
- ↵ Public Health England. Guidance on social distancing for everyone in the UK. PHE, 2020. [Withdrawn]. https://www.gov.uk/government/publications/covid-19-guidance-on-social-distancing-and-for-vulnerable-people/guidance-on-social-distancing-for-everyone-in-the-uk-and-protecting-older-people-and-vulnerable-adults
- ↵ Government of Japan. Expert meeting on the novel coronavirus disease control. Views on the novel coronavirus disease control (summary version). 9 Mar 2020. https://www.mhlw.go.jp/content/10900000/000608425.pdf 2020.
- ↵ Scientific Advisory Group on Emergencies. SAGE minutes archive London: UK Government Transparency and Freedom of Information Releases 2020. https://www.gov.uk/search/transparency-and-freedom-of-information-releases?organisations%5B%5D=scientific-advisory-group-for-emergencies&parent=scientific-advisory-group-for-emergencies
- Jefferson T ,
- Del Mar CB ,
- Parkhurst JO ,
- Abeysinghe S
- Bourouiba L
- Miller SL ,
- Nazaroff WW ,
- Eichler N ,
- Thornley C ,
- Johansson MA ,
- Quandelacy TM ,
- Bulfone TC ,
- Malekinejad M ,
- Rutherford GW ,
- Klompas M ,
- van Doremalen N ,
- Bushmaker T ,
- Morris DH ,
- Lednicky JA ,
- Shankar SN ,
- Elbadry MA ,
- Lauzardo M ,
- Krambrich J ,
- Akaberi D ,
- Kutter JS ,
- de Meulder D ,
- Bestebroer TM ,
- Kucharski AJ ,
- Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group
- Prather KA ,
- Tufekci Z ,
- Sznitman J ,
- Bahnfleth WP ,
- Jimenez J ,
- ↵ World Health Organization. Infection prevention and control during health care when coronavirus disease (covid-19) is suspected or confirmed [withdrawn]. https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2020.4
- ↵ World Health Organization. Transmission of SARS-CoV-2: implications for infection prevention precautions. Scientific brief. 9 July 2020. https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions
- ↵ World Health Organization. WHO recommendations on mask use by health workers, in light of the Omicron variant of concern: WHO interim guidelines. 22 Dec 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC_Masks-Health_Workers-Omicron_variant-2021.1
- Jackson T ,
- Deibert D ,
- Stadnytskyi V ,
- Anfinrud P ,
- ↵ Office for National Statistics. Deaths involving COVID-19 in the care sector, England and Wales: deaths registered between week ending 20 March 2020 and week ending 2 April 2021. https://www.ons.gov.uk/releases/deathsinvolvingcovid19inthecaresectorenglandandwales
- ↵ Amnesty International. As if expendable: The UK government’s failure to protect older people in care homes during the COVID-19 pandemic. 2020. https://www.amnesty.org.uk/files/2020-10/Care%20Homes%20Report.pdf
- ↵ Public Health England. COVID-19 Infection Prevention and Control London: UK Government 2021. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control
- ↵ Health and Social Care Committee. Oral evidence from Professor Terry Lum: Management of The Coronavirus Outbreak, HC36. 2020. https://committees.parliament.uk/oralevidence/407/pdf/
- ↵ Public Health England. Covid-19: donning and doffing of personal protective equipment in health and social care settings. 2020. https://www.youtube.com/watch?v=-GncQ_ed-9w
- Czypionka T ,
- Bassler D ,
- Schmid MB ,
- Asmundson GJG
- Leffler CT ,
- Lykins JD ,
- McKeown CA ,
- Grzybowski A
- ↵ Lee C, Yang T, Inchoco GD, et al. Viral visualizations: how coronavirus skeptics use orthodox data practices to promote unorthodox science online. Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems 2021:1-18.
- Southerton C ,
- ↵ New and Emerging Respiratory Virus Threats Advisory Group. NERVTAG minutes archive. 2020. https://app.box.com/s/3lkcbxepqixkg4mv640dpvvg978ixjtf/folder/49329372034
- ↵ Health and Safety Laboratory. An Agency of the Health and Safety Executive. Evaluating the protection afforded by surgical masks against influenza bioaerosols London: HSE 2008. https://www.hsl.gov.uk/media/50561/evaluating%20the%20protection%20offered%20by_layout%201.pdf
- ↵ Health Protection Scotland. Infection prevention and control advice for acute care settings: acute respiratory illness from novel or emerging pathogens (coronavirus (covid-19), Middle East respiratory syndrome coronavirus (MERS-CoV), avian influenza (eg, A/H7N9, A/H5N1). Version 8.1. 5 Mar 2020. https://www.hps.scot.nhs.uk/media/1950/infection-control-acute-care-v81.pdf
- ↵ Health Protection Scotland. Infection prevention and control advice for acute care settings: acute respiratory illness from novel or emerging pathogens (coronavirus (covid-19), Middle East respiratory syndrome coronavirus (MERS-CoV), avian influenza (eg, A/H7N9, A/H5N1). Version 9.0. 10 Mar 2020. https://www.hps.scot.nhs.uk/media/1951/infection-control-acute-care-v90.pdf . 2020.
- ↵ England NHS, Improvement NHS. Letter to chief executives of all NHS trusts (publication reference 001559), 28 Mar 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0113-reducing-burden-and-releasing-capacity-at-nhs-providers-and-commissioners.pdf
- ↵ Hancock M. Formal meeting (oral evidence session): Coronavirus: lessons learnt. Oral Evidence to Science and Technology Committee. 10 Jun 2021. https://committees.parliament.uk/event/4400/formal-meeting-oral-evidence-session/
- Gribben C ,
- ↵ UK Health Security Agency. Infection prevention and control for seasonal respiratory infections in health and care settings (including SARS-CoV-2) for winter 2021 to 2022 Updated 14 Apr 2022. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-guidance-for-maintaining-services-within-health-and-care-settings-infection-prevention-and-control-recommendations
- Moscovici S
- Lewandowsky S ,
- Seifert CM ,
- Schwarz N ,
- Gigerenzer G
- Chanlat J-F
- ↵ House of Commons Health and Social Care and Science and Technology Committees. Coronavirus: lessons learned to date. Sixth report of the Health and Social Care Committee and Third Report of the Science and Technology Committee of Session 2021-22. 12 Oct 2021. https://committees.parliament.uk/publications/7496/documents/78687/default/
Home — Essay Samples — Nursing & Health — Covid 19 — My Experience during the COVID-19 Pandemic
My Experience During The Covid-19 Pandemic
- Categories: Covid 19
About this sample

Words: 440 |
Published: Jan 30, 2024
Words: 440 | Page: 1 | 3 min read
Table of contents
Introduction, physical impact, mental and emotional impact, social impact.
- World Health Organization. (2021). Coronavirus (COVID-19) Dashboard. https://covid19.who.int/
- American Psychiatric Association. (2020). Mental health and COVID-19. https://www.psychiatry.org/news-room/apa-blogs/apa-blog/2020/03/mental-health-and-covid-19
- The New York Times. (2020). Coping with Coronavirus Anxiety. https://www.nytimes.com/2020/03/11/well/family/coronavirus-anxiety-mental-health.html

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 563 words
2 pages / 850 words
1 pages / 603 words
3 pages / 1280 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Covid 19
The COVID-19 pandemic, which swept across the globe, brought about profound changes in our daily routines and lifestyles. In this essay, we will explore the ways in which the pandemic has transformed the way we live, work, and [...]
The COVID-19 pandemic has highlighted the indispensable role of accurate information and scientific advancements in managing public health crises. In a time marked by uncertainty and fear, access to reliable data and ongoing [...]
The Black Death, a devastating pandemic that swept through Europe in the 14th century, and COVID-19, the ongoing global pandemic caused by the novel coronavirus, have left indelible marks on history. This essay seeks to analyze [...]
The COVID-19 pandemic, which has swept across the globe, has not only caused physical health concerns but has also had a profound impact on mental health. This essay, titled "How Does COVID-19 Affect Mental Health," delves [...]
As a Computer Science student who never took Pre-Calculus and Basic Calculus in Senior High School, I never realized that there will be a relevance of Calculus in everyday life for a student. Before the beginning of it uses, [...]
According to the World Health Organization, 'Mental health is a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Quick Links
Tools & Resources
- Events Calendar
- Strauss Health Sciences Library
- Department A-Z Directory
- Campus Directory
- Faculty & Staff Resources
- Supporter & Alumni Resources
- Student Resources
- Mental Health Resources
- University Policies
CU Campuses
Cu anschutz medical campus.
- CU Colorado Springs
- School of Dental Medicine
- Graduate School
School of Medicine
- College of Nursing
- Skaggs School of Pharmacy and Pharmaceutical Sciences
- Colorado School of Public Health
Department of Physical Medicine and Rehabilitation
News & media, tell your story with covid-19 narratives.

Physical Medicine and Rehabilitation (SOM)
CU Anschutz
Academic Office One
12631 East 17th Avenue
Aurora, CO 80045
- Clinical Services
- Residency & Fellowship
- Medical Student Rotation
- Doctorate in Physical Therapy
- PhD in Clinical Services
- News and Media

Home > LIBRARIES > Archives and Special Collections > Personal Narratives of COVID-19

Together Again: Personal Narratives of COVID-19 Uniting the Seton Hall Community
The COVID-19 pandemic has disrupted life at Seton Hall as it has for millions of others around the country and the world. In the name of saving lives, the social distancing needed to slow the spread of the virus has scattered us into our homes around the region and the country. Although we are now physically distant from one another, we remain united as Setonians through our connection to Seton Hall.
To reconnect as a community, we seek your stories of what this time has been like for you. How has it changed your experience at Seton Hall, as a student, faculty, staff member, or alum? We hope that sharing these stories with one another will bring us back together in a new way, through sharing our personal experiences of this moment. When we move forward, because there will be a time when we move forward, we plan to listen to these stories together as a community, reflect on what we have learned, and let them guide us into the future.
Questions to guide your response:
● What is your day to day life like? What would you want people the future to know about what life is like for us now?
● What has been most challenging about this time? What do you miss about your life before COVID-19? Are there specific places or things on campus that you miss?
● Essential is a word we are hearing a lot right now. What does essential mean to you? Who is essential? What are we learning about what is essential?
● What is COVID-19 making possible that never existed before? What good do you see coming out of this moment? How can we re-frame this moment as an opportunity?
● What is it you want to remember about this time? What have you learned?
● After this pandemic ends, will things go back to the way they were? What kinds of changes would you like to see? How will you contribute to rebuilding the world? What will you do differently?
Please submit your 1-3 minute audio or video recording to our portal. Please view submission instructions.
Need an Accessible transcript of this submission? Please email [email protected] to request.
With thanks to the scholars and librarians who came together to create this project: Professors Angela Kariotis Kotsonis, Sharon Ince, Marta Deyrup, Lisa DeLuca, and Alan Delozier, Technical Services Archivist Sheridan Sayles and Assistant Deans Elizabeth Leonard and Sarah Ponichtera.

Simple but Not Easy
Alexis Kuterka

Meredith Elliott Response
Meredith Elliott

Be Grateful and Make The Days Count
Vincent Tamburro

Life during a pandemic
Cecilie Webb


Covid-19 personal narrative
Daisy Kaloshi

Christian Sigua

Life During COVID-19
Justin Oosterwyk

COVID-19 Personal narrative

Isabella M. Solano

What Essential means to me
Marina Michael

COVID-19 Personal Response
John Zabriskie

Adriana Sanguinetti

Life At Home During The Pandemic
Brett Raichel

Day to Day Life in Quarantine
Kyle Reasor

Covid-19 Challenges
Juliana Spector

Mackenzie Tamburro

Changes and Opportunities during COVID-19
Giovanna Dabbagh

A Day in My Life
Brynne Cave

COVID 19 Personal Narrative Project
Olivia Scro

COVID-19 Personal Narrative Story

Julia Wilkins

Theo's Quarantine Story
Theo Schoenfeld

Something Called History
Chelsea Basedow
COVID-19 Response
Aashish Singh

Life in Quarantine
Gianna Vento
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
- Submit Contribution
- University Libraries
- Seton Hall Law
- eRepository Services
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 48, Issue 2
- COVID-19 narratives and layered temporality
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Jessica Howell
- English , Texas A&M University , College Station , Texas , USA
- Correspondence to Dr Jessica Howell, English, Texas A&M University, College Station, TX 77843, USA; jmhowell{at}tamu.edu
The essay outlines the ways in which narrative approaches to COVID-19 can draw on imaginative literature and critical oral history to resist the ‘closure’ often offered by cultural representations of epidemics. To support this goal, it analyses science and speculative fiction by Alejandro Morales and Tananarive Due in terms of how these works create alternative temporalities, which undermine colonial and racist medical discourse. The essay then examines a new archive of emerging autobiographical illness narratives, namely online Facebook posts and oral history samples by 'long COVID' survivors, for their alternate temporalities of illness.
- literature and medicine
- patient narratives
- medical humanities
Data availability statement
No data are available.
This article is made freely available for personal use in accordance with BMJ’s website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
https://doi.org/10.1136/medhum-2021-012258
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
At the time of writing (July 2020), the current COVID-19 pandemic has infected more than thirteen million people and claimed more than 580 000 lives worldwide.
At the time of revision (May 2021), the COVID-19 pandemic has infected more than one hundred sixty-five million people and claimed more than 3.42 million lives worldwide.
At the time of second revision (October 2021), the COVID-19 pandemic has infected more than 242 million people and has claimed more than 4.93 million lives worldwide.
Due to the timescale of academic publication, over a year separates my writing and second revision of this article. I have chosen to include the three versions of my first sentence, because it shows that, while I have been working on this piece, 4.35 million human beings have died. I want to begin this article by acknowledging that there is no narrative, whether epidemiological, sociological, or literary, that can adequately emplot the three versions of my first sentence. There is no story that can make sense of this progression. Instead, current Health Humanities scholarship is created in the breach between three versions of one sentence—in the suffering, and in the becoming.
While the three versions of this first sentence are desperately inadequate, they are also, inescapably, a form of representation. The sentence harkens back to the early beginnings of the essay as genre: a written meditation on a subject, which shows its own process of thought. In terms of content, the sentence presents my own time of writing, embedding me in a historical moment; it names the disease and it documents that disease’s spread by stating in stark terms the growing fatalities from COVID-19. During the first review, this manuscript was sent back with the comment to remove the strike-throughs, which the editorial team understandably assumed were a typographical error. With the use of typography, the strike-throughs try to make legible our necessary re-evaluations and revisions throughout the pandemic. These revisions also reflect the temporal ‘layering’ of COVID-19 narratives. Each declarative statement has within it its own future overwriting. Nothing feels stable. By the time you are reading this article, holding either the print copy of the journal or scrolling online, the numbers will have shifted, inevitably higher. Your moment overwrites my most recent revision. Finally, the last version makes us circle back to the first, continually trying and failing to make sense of the progression. The reader is trapped in a recursive time.
The most obvious gap, which the sentences do not address, is the human impact of the pandemic. The repetition of the sentence shows the impossibility of capturing loss with these facts. Visual and written art forms can creatively reframe medical and historical data to show how human experience is ‘layered’ with facts and figures. For example, the image below is a reproduction of artist Anatol Bologan’s painting ‘Viral 01’. It is the first in a series of multimedia works dealing with the human cost of COVID-19. The painting is a visual meditation on loss, as a patient with COVID-19 reaches to embrace a loved one who has died ( figure 1 , Bologan 2020 ). Furthermore, by digitally layering pandemic data visualisations behind and on top of the central couple, the artist illustrates the human pain that is not fully captured by discussions of disease ‘rates’ and ‘curves.' The medical image of the patient’s lungs, taken from a computer rendering of a CT scan, shows an active COVID-19 infection with an uncertain outcome. The viewer assumes that the central figure may become part of one of the bars on the graph, and that his body may continue to fragment and dissolve, as it does on the left edge of the artwork. The red line across the bottom third of the image provides the base for the graph, and could represent a flatlining heart monitor ( figure 1 , Bologan 2020 ).
- Download figure
- Open in new tab
- Download powerpoint
Anatol Bologan, ‘Viral 01’ ( Bologan 2020 ).
The painting is a vivid portrayal of what I call the layered temporalities of the COVID-19 pandemic. While epidemiology offers one model for how to trace the spread of COVID-19 (geographically, spreading outwards from one or multiple epicentres) and public health offers another (as with the graphs of infection and mortality), these models do not capture the multiply unfolding temporalities of people’s lived experience of the pandemic. Each of us is a distinct nodal point in terms of the timing of this disease outbreak. Our stories of growing awareness about the disease, travel, work, social distancing and perhaps illness, healing and loss, all unfold on different patterns. These temporalities may be anchored by some shared news cycles and social media conversations, or may echo one another in terms of the how infection and symptoms manifest on the body. However, they are also distinct. By placing the human figures in the centre of these graphs and charts, overlaid but not determined by them, the painting demonstrates that artistic and creative works can engage the distinctiveness of the lived experience of this time.
The painting also invokes the people permanently missing from our lives and communities, and makes one wonder about their stories. Jay Baruch and his coauthors, in their article about art and patients’ stories, recount an exercise with medical students where the students are asked to contemplate Cy Twombly’s Untitled (1968). The leaders ask the students to look for negative space in the abstract artwork, relating this negative space to understanding patient experience: “When you’re listening to stories, are you sensitive to the gaps, mindful of what was unsaid—perhaps even unsayable?” ( Baruch et al 2020, 430 ). Though representational and not abstract, the painting ‘Viral 01’ uses negative space—the around and between—to show loss that defies full comprehension.
Currently, the Centers for Disease Control (CDC) has rescinded the mask order. In spite of surges in Delta-variant hospitalisations and deaths, schools and universities have opened to in-person instruction. More Americans flew home to see their families for Memorial Day, 2021, than have flown since the beginning of the pandemic. Understandably, the public is focusing on new ‘firsts’, new beginnings and reunions. However, when public discourse focuses on the ending to disease outbreaks it can also conveniently overlook ongoing health inequities.
In this article, I focus on stories that represent the lived experience of epidemic disease, specifically those that defy the temporal closure offered by popular disease rhetoric. Specifically, I suggest that the affective engagement or embodied reading practices encouraged by Health Humanities allows us to remain sensitised to the COVID-19 stories that might be otherwise unnoticed. I propose a narrative investigation that takes up the layered temporalities of COVID-19 stories, specifically focusing on chronicity, erasure, fragmentation, revision, and repetition. This article first demonstrates how postcolonial speculative and science fiction, such as works by Tananarive Due and Alberto Morales, nuance our understanding of the lived experience of epidemics. These works highlight injustices perpetrated on those blamed for the outbreak and offer different imaginative possibilities for how we could relate to one another during a time of crisis.
The article then turns to excerpts from oral histories and life-writing by COVID-19 survivors. Studying the ‘unknowingness’ in postcolonial science fiction can inform the way in which one engages COVID-19 narratives and how they resist temporal closure. Especially for those struggling with long COVID, or for those mourning the loss of loved ones to COVID-19, triumphalist, chronological narratives of ‘flattening the curve’ or putting the pandemic behind us ring false. These first-hand stories follow different narrative arcs than crisis to cure, or pandemic’s start to pandemic’s end. In fact, more possibilities may be offered from narratives of endemicity and chronic illness than the structure of climax and resolution of traditional plague narratives. Understanding COVID-19 as both epidemic and endemic allows different critical approaches to emerge, such as allowing us to address systemic health inequities as ongoing 1 . In addition, as I have shown elsewhere, those living in an environment with endemic disease can also use this status to gain authority and make demands on medical systems ( Howell 2014 ). Furthermore, Health Humanities scholarship that engages with chronic pain acknowledges that ‘reading less in search of narrative coherence or self-authorship’ allows a heightened appreciation for the ‘value of textual fragments, episodes and moments’ ( Wasson 2018 , 106). By examining COVID-19 narratives using the methods of postcolonial studies and critical oral history, Health Humanities scholars can resist the stories’ instrumentalisation within national and medical discourses.
Defying closure and cure: postcolonial and speculative fiction
We have never lived through this pandemic. However, we have talked about epidemics before. Written and visual narratives of epidemics may consolidate a chaotic series of events, give a sense of purpose and directionality and also to attempt to capture for the reader the experience of the disease. Such methods are a way to engage our attention and to create or direct readers’ anxiety about future epidemics, or, conversely, to comfort us that the epidemic is safely over. However, to write and to read a story set during an epidemic is to work within a set of expectations and constraints. Our cultural values, scientific knowledge base and previously established disease discourse all play a role in how we discuss the current moment. For example, Patricia Wald identifies a certain ‘vocabulary of disease outbreaks’ as beginning during the AIDS crisis in the 1980s and being reinterpreted within the outbreak films and science writing of the 90s ( Wald 2008, 2 ). In this case, the vocabulary of ‘emerging infections’ which many of us now use in fact originated within a particular set of political, biological and cultural circumstances (heteronormative, middle-class, 1980s white America and its imagined others).
Within the realm of illness narrative in particular, critical medical humanities scholarship has begun to examine why certain stories of pain and healing are validated while others are not. Within the edited volume by Angela Whitehead et al. (2016) , scholars examine why certain subjects’ experiences are more often discounted: the ‘obese’ (Evans and Cooper), black Americans (Andrews and Metzl), disabled individuals (Tilley and Olsén) and the neurodivergent (Herman). These studies assume that our idea of what constitutes a coherent narrative, and thus our receptivity towards what we read, is influenced by our own cultural and political values. This holds true with our reading of epidemic narratives as well, the structures of which are deeply intertwined with the history of colonialism. We may assume that one writes a story to consolidate a sense of self. However, the concept of ‘self’ which narrative supposedly consolidates, as Sylvia Wynter and others have shown, is at base a colonial construct: the ‘(Western bourgeois) conception of the human’ ‘over-represents itself as if it were the human itself’ ( Wynter 2003, 260 ). In other words, the ways in which certain subjects’ narratives are recognised as human experience while others are not, are influenced by histories of colonial exploitation and racism. 2
One key subject of analysis for Global Health Humanities scholarship is how the legacies of colonial medicine influence which stories of illness are read and in what manner. Colonial medical politics de-authorised the illness experience of indigenous populations, privileging instead white subjects’ perceptions of the health threats posed by foreign lands. For example, as Megan Vaughn (1991) has demonstrated in Curing Their Ills , medical discourse in late 19th and early 20th century Africa worked to undermine indigenous knowledge formations and to construct the ‘African’ as a subject in need of health intervention. Publications as diverse as cartoons, medical journals and public health posters worked to stereotype local health practices and depict the colonial doctor as heroic. John and Jean Comaroff engage the ‘ideology of colonial healing’ that depicted colonialism as driven by humanitarianism ( Comaroff and Comaroff 1992 ). This ideology does not acknowledge whether or not a health intervention is desired by local populations.
Colonialist narratives of cure rest on specific conventions: an exoticised location is pathologised, its inhabitants blamed for their current state of ill health. Western-trained doctors and nurses are depicted as providing a heroic intervention, benefitting local populations and inspiring their gratitude. If the health crisis is not eradicated by the end of the narrative, at the least the worst is averted. Contemporary global health organisations currently draw on similar rhetoric when they depict local populations as suffering from abject poverty and ill health and in need of top-down interventions. As Nicholas King explains, both former colonial medical and contemporary global public health discourses justify the control of disease for protection of western economic growth ( King 2002, 776 ). Postcolonial science fiction or speculative fiction disrupts specific colonialist underpinnings of medical narrative: geographies are interdependent rather than separable; Western forms of medical knowledge are fallible. Most important for my purposes, postcolonial fiction de-stabilises the very assumptions about disease outbreaks as following a specific chronology or temporal progression through presenting instead alternate or recursive temporalities. 3
Works such as Tananarive Due’s ‘Patient Zero’ and Alejandro Morales’s The Rag Doll Plagues both use the structures of science fiction to question the traditional temporal unfolding of an outbreak. Historically, scientists such as Ronald Ross tested indigenous bodies as the ‘source’ of disease. 4 Both Due and Morales craft characters who are subject to experimentation, ostensibly in the name of solving the epidemic. These postcolonial science/speculative fictions draw on these histories by using the affective response of the reader to engage the colonial and settler colonial medical practice of experimenting on bodies of colour during a time of disease outbreak.
Postcolonial fiction disrupts or nuances certain Western assumptions about the relationship between temporality and narrative. Paul Ricœur has claimed that narrative and time are inextricable, and that narrative reflects a ‘temporal experience’ ( Ricœur 1984, 3 ) . The work by Patricia Tobin highlights the gendered nature of this narrative structure. She argues that the ‘genealogical imperative’ in Western narrative structures—the way in which language is structured to show cause and effect and seriality—is influenced by its cultural context, namely patriarchal structures of lineage ( Tobin 1978, 8 ) . Subsequent generations of critics have shown that such 20th-century theories of narrative and time were greatly influenced by the structures of 19th-century writing, which manifested a ‘belief in progress’ ( Gomel 2010, 8 ), or ‘linear industrial time’ ( Henrikson and Kullberg 2021, 12 ). Medical Humanities scholars such as Laura Salisbury show that ‘linear narratives that stress deep psychological continuities across time’ might ‘privilege and render problematically universal modes of subjectivity and self-expression that are, in fact, culturally and historically contingent’ ( Salisbury 2016, 444 ).
Critics Elana Gomel, Randall Stevenson and Russell West-Pavlov have suggested that these earlier theoretical assumptions about time and narrative be revised to acknowledge their capitalist-colonialist underpinnings. 5 West-Pavlov claims, ‘Time’s attributes of linearity (“what’s past is past”), universality, quantifiability and commodifiability (“time is money”), and finally contemporaneity and modernity (“newer is better”) all work to structure human existence according to the restrictive but profitable mechanisms of late capitalism’ ( West-Pavlov 2012, 5 ). Rather, he suggests that one cultivate an awareness of reading as ‘digressive’ and an understanding of literature as a ‘playful re-working of the putatively factual givens of reality’, which gestures towards a ‘plethora of temporalities subsisting under the threshold of an all-embracing and coercive time’ (9).
One example of the ‘coercive time’ that West-Pavlov discusses is temporality ‘inculcated’ by colonial education, which embodied a ‘forward vector of progress and incremental acquisition of civilization’ (159). What would happen, he asks, if one were to ‘abandon the sequence’ this time ‘relies on altogether’, taking up instead ‘a notion of overlapping, non-segmented temporal planes’ with ‘many actants with agency’ (166)—what Dipesh Chakrabarty calls ‘ interlocking of presents, pasts and futures’ ( Chakrabarty 2000 )? Postcolonial authors experiment with temporality in their works to unmoor narrative from its colonialist associations with progress. In speaking about Salman Rushdie’s Midnight’s Children (1981), Randall Stevenson (2019, 211 ) demonstrates that the literary text ‘illustrates a range of tensions between imperially imposed temporality and influences indigenous to countries colonialism sought to subjugate’. Time is ‘an unsteady affair’ (citing Rushdie, 1981, 79), whereby postcolonial fiction ‘magnifies and valorises unsteady, divergent temporalities’.
For the purposes of the current analysis, the most important aspect of narrative structure and time is its inter-relationship with science. Tobin observes that science follows an ‘arrow of time’ similar to that of traditional chronological narration in stressing causation and effect, hypothesis and proof (8). I would add that this assumption about science is similarly influenced by colonial and national consolidation of the scientific process—recent scholarship has shown that there are narrative multiplicities possible in indigenous scientific knowledge as well. If colonial science ‘instrumentalises nature’, then critics like Masood Raja, Jason Ellis and Swaralipi Nandi suggest that postcolonial science fiction can, by stressing incomprehensibility, ‘magic’ and the unknowable, call into question these scientific logics underpinning narrative ( Raja, Ellis, and Nandi 2011, 5 ). This is not just a theoretical practice, but an embodied one. As Michel Foucault has shown, biopower inscribes control of the life course through social expectations. Arne de Boever, following Edward Said, claims that ‘historically, the rise of the novel coincides with the rise of what Foucault calls governmentality and biopower’ ( De Boever 2013, 9 ). By changing the colonial-scientific temporal logic of narrative, one can attempt to redefine the stakes of one’s own life course. Elizabeth Freeman argues that ‘temporality is a mode of implantation through which institutional forces come to seem like somatic facts’ ( Freeman 2007 ), cited in ( West-Pavlov 2012, 5 ). In the case of an epidemic, the ‘somatic facts’ of infection, illness and healing, on both a national and personal level, are quickly identified according to a normative timeline, which may or may not align with an individual’s lived experience. Instead, as Paula Henrikson and Christina Kullberg observe, ‘lived time is contextually dependent’ (citing Hartog 2003 , 14).
Questioning the narrative patterns of science, and particularly colonial science, does not lead one to an antiscience or antimedicine stance. To argue that disease treatment is not equally available to all, and that this inequality both reflects pre-existing colonial priorities as well as reinforces existing racial and national disparities, is not to argue against medical research or treatment. Medical research and treatment are needed. Rather, the critique focuses on two aspects of medical narrative logic: one which claims that Western medical science is the apex of modernity, and that this modernity is offered or given to others, and the other that depicts disease eradication in a chronological and definitive arc. By understanding these logical assumptions as constructed rather than inherently ‘true’, one may approach stories of chronic illness, or stories of repeated or ongoing outbreaks, not as unusual but as endemic to a global system of medical inequality.
Furthermore, reading literary descriptions of physical symptoms and suffering causes an embodied reaction in the reader specific to the disease being invoked. In Postcolonial Poetics , Elleke Boehmer claims that reading “sets off a cascading set of inferences, which the reader processes at different simultaneously unfolding cognitive (semantic, sensory, kinaesthetic) levels, their responses modifying and adjusting as the communication develops” ( Boehmer 2018, 8 ) . When considering the multisensorial experience of reading about illness, one must assume that in specific scenes of suffering, and throughout the work, we are plunged into the space-time of disease particular to that disease itself. The structure of illness from disease (acute vs chronic) is also embedded in the chronology and structure of literary texts (for more, see Howell 2018 ). By creating this affective response in relationship to a fictional disease, these following literary works invite the reader to reflect on how we behave towards one another during times of health crisis, without the specific anchor of a named plague. I suggest that critical engagement with specific literary works about epidemics allows us to practice the radical, speculative exercise of imagining a more equitable present as well as future. These works subvert the Patient Zero myth and disease stigmatisation; encourage us to consider what a decolonised medical praxis would look like and allow us to be aware of our own experiences of embodied reading.
The Rag Doll Plagues by Alejandro Morales (1992) explicitly critiques colonial medicine’s exploitation of Mexican bodies during a fictional, mysterious illness called La Mona in 1788 Mexico City. The book directly engages the colonial value systems that are embedded with the treatment of epidemic disease. The novel self-consciously invokes the tradition of colonial judgmentalism towards ‘uncivilised’ populations, in order to turn this stereotype on its head. Morales’s narrator, Don Gregorio, the First Professor of Medicine, Anatomy and Surgery in his Majesty’s Empire, is a Spaniard who visits colonial Mexico to ‘implement these new [medical] procedures’. In addition to improving sanitation, the ‘new procedures’ he introduces ‘to the native population’ includes a great deal of cauterisation, surgery and amputation, as if seeking to quite literally cut out all that is rotten and diseased in the colonies, including the ‘hedonistic carnal acts’ he witnesses (28).
Each section of this tripartite novel shifts locations and times, thus disrupting colonial narratives of progress. This ‘collapsing of linear time’ is emphasised by the ‘phantasmic atemporal characters Gregory and Papa Damian, who appear in each of the three books of the novel’ ( Joyce and Garay 2013, 141 ). Morales’s novel follows a tradition, as with the work of Gabriel García Márquez (1988) , which undermines colonial assumptions of medical progress. When García Márquez’s character Juvenal Urbino returns to his Caribbean home from medical training in Europe, he brings back all the disparaging assumptions about indigenous subjects’ inadequate hygiene and backwardness with him. The novel describes Urbino as arriving home with ‘the beard of a young Pasteur’ (106).
The clearest articulation of The Rag Doll Plagues’ critique of colonial medical legacies can be found in its last section. Don Gregorio’s descendants discover that residents of Mexico City, who are called ‘Mexico City Mexicans’, have a uniquely healing property to their blood that perhaps has been caused by their survival of La Mona in the 18th century. These Mexican citizens become valued and commodified, their blood used for infusions to cure people during a ‘major plague’ (183). Through reverse-colonisation via transfusion, ‘Mexican blood would gain control of the land it lost almost two hundred and fifty years ago’ (195). Morales’s novel points towards the double-edged sword of biological essentialism: whether being decimated or valued for their blood, disparaged or fetishised for their relationship to place, the colonised subject’s body is commodified by the dominant political power. Finally, as Joyce and Garay demonstrate, the The Rag Doll Plagues ’ focus on the male doctor/scientist, on a quest for self-improvement and discovery, is not unproblematic in its gender politics, as could be said of other famous pandemic fiction such as Michael Crichton’s Andromeda Strain .
By showing the breakdown in social relationships, pandemic fiction can inspire the readers to imagine a different world, where we choose to relate to one another during a time of crisis with more humanity. Tananarive Due’s short story ‘Patient Zero’ (2010) engages the harvesting of immune groups’ blood or body parts for study or the development of antibodies, with or without their consent. ‘Patient Zero’ is narrated by a 10-year-old boy, Jay, who is the subject of study in a research facility during a future pandemic. Jay has recovered from ‘Virus-J’, while everyone else around him dies. He is thus labelled the ‘Patient Zero’, and made both the subject of study as well as the recipient of hostility and misunderstanding.
Due uses the innocent voice of a child narrator to undermine the stigmatisation that occurs during a pandemic. The Patient Zero is a mythic figure who reassures us that pandemics have a traceable beginning. Jay questions his label at the first patient: “that was when I first learned how people tell lies, because that wasn’t true. Somebody on my dad’s oil rig caught it first, and then he gave it to my dad. And my dad gave it to me, my mom and my brother” ( Due 2001, 9 ). His sense of injustice highlights the uncertain timeframe and geography of pandemics. Jay’s own temporality is different from the official timeline. This official timeline has the goal of certainty rather than truth.
This work of speculative fiction also plunges the reader into the experience of being experimented on. Jay recounts that the doctors and nurses at the containment facility “take so much blood from me all the time, until they make purple bruises on my arms and I feel dizzy” (12). He continues,
“I think they have even taken out parts of me, but I’m not really sure. …I had surgery on my belly a year ago, and sometimes when I’m climbing the play-rope hanging from the ceiling in my room, I feel like it hasn’t healed right, like I’m still cut open. … I don’t hate anything like I hate operations” (12).
Jay’s physical symptoms are not from the virus but from his doctors’ search for the virus’s cause. These are described in visceral detail, so that the reader can imagine being dizzy from multiple blood draws, or aching from multiple surgeries. The story invites us to balance the cost of specific individuals’ pain against the larger goals of scientific discovery, especially during times of uncertain and emerging knowledge when that pain may or may not lead to a cure.
The text is important in terms of Health Humanities’ critical engagement with scale—if one is the only person who suffers from an undiagnosed illness, does that make one’s suffering less legitimate? If someone recovers from an illness that kills many, which community will welcome them? As a story by a black American author about one boy being blamed for a pandemic, ‘Patient Zero’ also invites us to read within the framework of America’s historical and present medical abuse of bodies of colour. From Tuskegee to COVID-19, black Americans have received inadequate or abusive medical treatment. The erroneous creation of race as a biologic category has been used to justify medical experimentation on groups of black people since the times of slavery (see Roberts 1997 , 2011 ; Hogarth 2017 ).
It is outside the scope of this article to fully address the continuities and divergences between colonial medicine practised by Britain in India, for example, with colonial medicine in Mexico, alongside medical exploitation of black Americans. 6 Narrative experimentations also will reflect authors’ distinctive cultural and historical associations with time and the body. However, while different national literatures invoke distinctive histories of medical treatment, reading these works in conjunction offers specific insights. One becomes more aware of the political stakes of aggrandising medical ‘modernity’, and one can see more clearly the power differentials that relate to who lives and who dies during a pandemic (see discussion of biopolitics and the right to ‘make live and let die’, in Society Must be Defended by Michel Foucault 1976; 2003 ). This practice encourages reading disease, not as an inherent manifestation of biological and historical circumstances, but also as a symptom of longstanding injustice.
These conversations are unfortunately timely due to the racial disparities exemplified by COVID-19 illness and death rates ( Chowkwanyun and Reed 2020 ). In a recent article, authors Yoshiko Iwai, Zahra Khan and Sayantani DasGupta exhort medical professionals to practice what they term ‘abolition medicine’: ‘imagining… ourselves into a more racially just future invested in enriching communities’ and (thereby) working ‘toward a future of health and social justice’ ( Iwai, Khan, and DasGupta 2020, 158 ). As of 12 June 2020, the Centers for Disease Control (2020) showed that ‘age-adjusted hospitalisation rates’ for ‘American Indian or Alaska Native’ as well as black people are approximately five times, and Hispanic or Latino people four times, that of non-Hispanic white people. According to the CDC, this is due to factors such as dense population, caused by housing segregation; proportionately higher risk of living in a food desert and depending on public transport or being an essential worker and having no sick leave. The devastating effects of COVID-19 on communities of colour are exacerbated because ‘racism, stigma and systemic inequities undermine prevention efforts, increase levels of chronic and toxic stress and ultimately sustain health and healthcare inequities’ ( Centers for Disease Control 2021 ). This moment is revealing the faultlines within our systems and making clear the impact of ongoing stress and violence on the bodies of people of colour. Health Humanities research is engaging the overlapping categories of systemic violence that have caused unnecessary and avoidable human suffering.
Examining postcolonial pandemic fiction is relevant to our current moment. The ‘Patient Zero’ is a temporal trope used to exoticise and blame racialised subjects, whether in a formerly colonised country such as Guinea or in an American context. This individual is often identified with marginalised groups, an easy scapegoat to protect normative group identity. One observes the Patient Zero myth uncritically reproduced within contemporary scholarship. For example, in a preface to the newest edition of Epidemics and Society: From the Black Death to the Present , seminal medical historian Frank Snowden (2020) connects COVID-19 with Ebola through the image of human-non-human transmission in an ‘exotic’ locale: in 2013, “a small child played in the hollow of a tree near the garden of his home in Guinea…The misfortune of the four year-old boy was to inhale viruses shed in the dejecta of the displaced bats” (ix). Guinea in 2013 becomes Wuhan in 2019: ‘this sequence of events, transposed to an urban context, probably recurred at a bushmeat “wet market” in Wuhan, China’, where ‘unhygienic passageways’ become a ‘giant petri dish’ (ix–x).
This new preface to Epidemics and Society risks invoking the same colonialist judgmentalism critiqued by García Márquez and Morales, and risks ‘othering’ the Patient Zero as in Due’s short story. In fact, as Kelly, Keck, and Lynteris (2020, 1 ) demonstrate in Anthropology of Epidemics, ‘While the viruses that spill over from wild animals to remote village populations occupy pride of place in these end-of-the-world fantasies, today the pathogens that could spark global pandemics might as easily evolve in antimicrobial-rich hospital environments in Europe and the United States’. Both histories and works of fiction about pandemics ask us to project ourselves into a disease’s beginnings; however, popular disease rhetoric is often based on the assumption of the self as inviolate, threatened by external forces. ‘Patient Zero’ invites us to enter into the experience of vulnerability, not only of the uninfected but of the ‘carrier’ by employing the voice of a child. Therefore, even as our physical bodies are in quarantine from pandemic illness, or to avoid pandemic illness, we can recognise the ways in which our stories are embedded in embodied experience, and how affective reading practice connects our own bodies to others’.
Plague has its own vocabulary. The texts by Due and Morales use a haemorrhagic framework of metaphors and images to describe the effects of disease on the body. The images are drawn from bacterial infections causing acute and immediate suffering. When reading COVID-19 narratives, whether first-person accounts written by sufferers, health practitioners, family members or fictionalised accounts, Health Humanities scholars must engage with this disease’s unique descriptive lexicon. Patients’ narratives offer experiences of respiratory distress and isolation; technologically-mediated communication; neurological and cognitive aftereffects. Healthcare practitioners find themselves cast in roles they did not audition for. 7 The study of postcolonial science fiction and speculative fiction suggests that one keep in mind the ways in which authors can portray health injustice by subverting the linear temporality offered by medical discourses.
Furthermore, postcolonial and social justice scholars stress the importance of oral history as a critical methodology that can complicate official narratives. Historian Indira Chowdhury argues for the practice of oral history to understand science in the postcolonial context, specifically the ways ‘scientific practice has adapted to local and contingent factors’ ( Chowdhury 2013 ). Quoting writer Chimamanda Adichie, Christine Lemley argues that critical oral history can subvert the ‘danger of a single story’: in the case of Adichie’s experience, the dominance of a Western-centric, stereotypical viewpoint of her upbringing in Nigeria. According to Lemley, critical oral history ‘exists to contextualise story and create spaces through which people who are underrepresented in dominant systems use agency to identify and act on struggles to build new possibilities’ ( Lemley 2013, 7 ). In the context of a pandemic, critical oral history offers diversity in terms of venue, perspective, and positionality to stories of illness and healing. Genres of study include interviews, as well as drawings, documentaries and material objects. In the section that follows, I draw on social media postings, emails and interviews in order to demonstrate how critical oral history about COVID-19 can contribute to postcolonial Health Humanities scholarship.
COVID-19 stories and layered temporality: healthcare workers and long COVID survivors
Text message, 11 February 2021: Why did you come [to the home] when you knew you had a known COVID-19 exposure and no negative test? Reply: It had been 10 days. Email sent to all faculty and students, from Texas A&M University, received 6 September 2021: Close contact is defined as being within six feet for a cumulative 15 minutes over 24 hours with someone who tested positive for COVID-19. Vaccinated individuals do not have to quarantine, while unvaccinated must quarantine. Oral history excerpt, ‘B’: I said, I am going to be walking and I’m going to leave (the hospital) at the date in which you [the doctors] prescribe, which I believe was the 21st of January. If I remember correctly. […] All these difficult, very difficult things but I wasn’t going to take any other sort of answer and I left on January 21st. ( B, interview 2021 )
During a pandemic, official time and personal lived time diverge. COVID-19 is morphic, variable, emerging; both respiratory and neurological in its effects; both acute and chronic in manifestation. However, the guidance set by public health entities such as the CDC must by necessity be standardised, in order to provide individuals guidance on how to behave to curb the spread of disease. Our success as a nation is then measured by how well we have followed official time and its interlocking health guidelines; our individual success is measured by how well we have avoided illness or progressed towards healing on a specific timeline. We exercise bodily autonomy in the individual interpretation of that time, and our body’s relationship to it. We create space for alternate temporalities through narrative and art, as well as through other means.
In the first excerpt above, the speaker reminds someone of his individual responsibility and how he had broken a social contract by not heeding that responsibility. In the official email, Texas A&M University leadership places responsibility on the teacher or student for calculating the minutes they have been exposed to someone who is COVID-19 positive within 24 hours, in order to determine if they should quarantine. In the third excerpt, oral history participant ‘B’ sets his own goal for his discharge date after 3 months in the hospital with acute COVID-19, as a motivation to get well. The very length of his hospitalisation belies the CDC’s implied average timeline of illness: even ‘severely ill’ people can expect to re-enter society after 20 days, the website reads ( https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html ).
One may form an appreciation for alternate and divergent illness temporalities through studying narratives of COVID-19. By so doing, one may also bear witness to the ongoing human impact of the pandemic. This analysis in no way undermines quarantine, masking or self-monitoring practices. Rather, it stresses that individual lived time is very different from official guidance, and official guidance insistently overlooks systemic inequalities. For example, 2 weeks’ quarantine (during the pre-vaccine era of COVID-19) for someone who is self-employed might be a hardship that pushes that person closer to financial precarity. Racism and xenophobia can make the time one waits for equitable and humane medical treatment interminable. Time spent away from one’s small children due to an exposure; time spent away from one’s beloved in hospital; time spent asking one’s body to perform tasks that used to come easily; time spent waiting for a referral to a specialist to study a little-known symptom: these minutes, hours and days are agonisingly slow. Trauma and post-traumatic stress disorder can cause someone to revisit the same time again and again, compounded by lack of widespread understanding and acknowledgement of one’s illness.
Our temporalities are acutely distinct, and also shared; fractured, and also continuous. Historically important, but not yet historical. The disease is both personally isolating, and creates global interconnection, as patients read others’ narratives from Italy, China or New York online, predicting what might be their future symptoms. Stories from the COVID-19 pandemic reflect this unique temporality: they capture something of the world in which they occurred, emerging as photo essays, texts, vlogs, Facebook posts, Tweets, scraps of paper slid under the door within a shared household, or notes written by practitioners on the glass separating a hospitalised patient from the hallway.
Some of the first overtures at narrating hospitalised patients with COVID-19 suffering were performed by their healthcare practitioners. Rafael Campo, a poet and medical internist, has spoken about the challenge of communicating with and hearing the stories of severely sick patients with COVID-19. He says “some patients living with this disease are literally silenced. When that tube goes in someone’s throat to support their breathing, it physically takes away the voice” ( Gibson 2020 ). In response, he has turned to writing poetry as “a kind of a channel for some of the experiences that I’m having and that we’re having”. He says that healthcare practitioners’ writing can “shed light on what people are actually experiencing who have this illness and who are dying from it and who don’t have that voice, which is so necessary for us to hear”.
In his poem-in-draft ‘The Doctor’s Song’, Campo incorporates some of the foregoing imagery in the first few lines: ‘The ventilator’s rise and fall/The yellow gown’s swish down the hall’. These are markers of embodied time: one imagines oneself in the setting of the hospital, seeing the rhythm of the ventilator and hearing the sound of the gowns. It is implied that these are repeated, ongoing sounds. Even while an individual’s case comes to a crisis, leading to discharge or death, the healthcare practitioner’s experience is of inexorable time, where case after case succeeds the other. Campo captures the doctor’s own frustration:
The stethoscope won’t be an instrument of hope: It merely amplifies the gallop, makes audible the broken heart.
The space that a poem creates between each line emphasises the gaps in the doctor’s knowledge. The speaker’s stethoscope amplifies the patient’s ‘broken heart’, but also, by implication, the doctor’s own, facing that which cannot be controlled.
In a poem about cardiac and respiratory symptoms, the poem as a form also makes us mindful of these symptoms through our embodied reading. We breathe in the pauses between lines, or feel the scansion’s echo in the rhythm of our own heartbeats. Finally, with the line ‘The Doctor’s Song is not heroic’, Campo undercuts the expectation that doctors’ heroism in the face of a pandemic should be the focus of COVID-19 narration. From the comment in Campo’s interview that his patients are ‘silenced’, one assumes he agrees that it is important to hear more stories by patients themselves.
Therefore, in addition to literary works like poetry, first-person narratives of COVID-19 illness are necessary to understand the ongoing and debilitating temporality of the disease. The following narratives were collected under a grant-funded, cross-disciplinary oral history project titled ‘Global Health and the Humanities’ (IRB2018-1513M). My collaborators included Violet Showers Johnson and Laura Dague, as well as graduate researcher Michelle Yeoman and undergraduate assistant Trinity Buchanan. We are following the Oral History Association ethical guidelines, including gathering informed consent, performing advance training for interviewers, including diverse voices, using open-ended questioning methods within interviews, recording and transcribing the oral histories, identifying an open-access repository for anonymised transcripts, and making research publications available to interviewees ( https://www.oralhistory.org/oha-statement-on-ethics/ ). Oral histories were conducted from 2018 to 2019 with participants in Sierra Leone and Sierra Leonean diasporic communities in Dallas, Texas. These interviewees were asked questions about their experiences with the 2014–2016 Ebola outbreak in West Africa and with endemic malaria.
The follow-on project included COVID-19 oral histories collected via an online video conferencing platform, with subjects based across the USA. Future research outputs will engage from a comparative perspective the role of oral histories in illuminating global health crises. However, for the purpose of this article, only the COVID-19 oral histories are excerpted and analysed. Participants for these interviews were recruited using social media networks and posting boards related to COVID-19, and selected to represent diversity of perspectives. All excerpts used in publication are anonymised to the level that the participant should not be identifiable. Readers who have certain first-hand experiences of COVID-19 may find the following descriptions difficult to read. If a reader were to wish to avoid this section, the conclusion to this article’s argument appears with the paragraph beginning ‘Often, psychology’.
First, SurvivorCorps Facebook Group Posts (2020) provide a platform for patient advocacy and social justice work. They also provide an opportunity to study how illness narratives of chronic debility can be used as a form of protest against those who might suggest that falling numbers marks a tapering off of the pandemic’s human impact ( SurviviorCorps ). As ‘a grassroots solution-based movement’, the online support group SurvivorCorps seeks ‘to mobilise the sharply increasing number of people affected by COVID-19 to come together, support and participate in the medical and scientific research community efforts’. The Facebook group is open membership, which means that anyone can join and post. It provides a venue for those who have never received formal medical treatment to commiserate, and for those who have received medical treatment to compare diagnoses and interventions. Members post pictures and ask questions about their own symptoms, drawing on the shared knowledge of the group; they post one-line or two-line obituaries of loved ones who have died. The moderator publicises survivors’ interviews in news outlets and opportunities for members to participate in academic research studies. As the public group grows and gains more recognition, the experiences shared by this group are also driving science and social science policy and research. Punctuation and spelling have been kept verbatim in the examples that follow.
‘Long COVID’ sufferers use the forum to validate each-others’ experiences, using a form of collective as well as individual story-telling. They are co-constituting a narrative of chronic illness within a sociohistorical context that instead encourages closure and healing. One of the methods through which they do this is by stating how long their symptoms have persisted at the beginning of their narratives. One poster writes, “I was a firefighter/paramedic at the time of infection. I am on day 130. I have a collapsed lung—was never hospitalised, and have experienced about 70 symptoms” ( SurvivorCorps Facebook Group Posts 2020 ).
Many posters document their difficulty receiving proper treatment. One poster received a false negative test, and spent months suffering without adequate medical support: “after 4 lung x-rays 3 EKGs and 3 C Scans, and one new primary Doctor later… visit to a lung specialist…it was determined that the negative COVID-19 test administered was a false negative…next step for me a scheduled Bronchoscopy which allows doctor to visualize scar tissue and nodules that have formed in my lungs” ( SurvivorCorps Facebook Group Posts 2020 ). Another says that when she started feeling ill she “called my doctor’s office and they said I should be given a test because of my asthma and to call the walk in. I called, was asked a bunch of questions, and told i didn’t qualify”. A final poster shares, “I have not been able to receive any medical care due to lack of belief and insurance and workers comp issues”. For some of these individuals, a timeline of COVID-19 illness never officially ‘began’ on their medical records. Their stories are only available in private diaries and through social media. In order to provide ongoing treatment, their future practitioners will need to piece together a health history invisible to digital patient charts and laboratory results. This process of recreation will be a narrative one, whereby patients craft their own timeline and causality in reporting the long-term impact of their illness. Finally, the number of long COVID-19 survivors who are uninsured or underinsured needs further investigation—oftentimes these sufferers may have avoided hospitalisation and tried to cope at home. This economic inequality directly impacts how the data about their suffering, whether medical or narrative, will be accessed and analysed in the future.
Common descriptions emerge across narratives, which capture the cyclical and inexorable temporality of illness with COVID-19. Specifically, many call the illness a rollercoaster, with the associations of a frightening and unexpected ride that ends up where one began. On a roller coaster, emotions are intensified, but movement is circular. A further example reads, “107 days later I still continue to fight off this horrific rollercoaster of a virus. This virus is relentless…” ( SurvivorCorps Facebook Group Posts 2020 ). Many keep a log or journal of exactly how many days they have been sick. Another poster is still suffering after 4 months: “It was a roller coaster for about 2 weeks in isolation of my room”. A final poster says, “Hi, I am ___ and I have been riding the Coranacoaster for 16 straight weeks”.
Taken together, the ‘long haulers’’ experiences are being studied as emerging medical knowledge. Neurological and psychiatric symptoms, less well understood by the medical community, are being documented by symptom surveys based on members’ experiences ( Lambert, Natalie and SurvivorCorps 2020 ). Some symptoms, like hair loss and sadness, were not previously represented on the CDC list. These posts are also developing a new lexicon for illness narratives. Metaphors such as ‘coronacoaster’, as well as precise physical descriptions, offer their fellow sufferers, as well as interested readers, a new way to understand the lived experience of the disease.
Although this creation of new knowledge and community is a mobilising and unifying experience for many members, some are also experiencing mental distress from not feeling supported adequately medically or not understood within wider discussions of the disease. They express a drastic shift in physical ability and sometimes feeling alienated from their pre-COVID identity. One poster says, “I feel like I’ll never be the same again” and another says, “I’m praying that we all eventually make it back to who we were before this”. Notable is the language of identification—not I’ll never feel the same again but I’ll never be the same again; not we can make it back to where we were (in terms of lifestyle) before this but to who we were.
This demonstrates what chronic illness scholars have pointed out is a risk in terms of a balance between one’s ambition for one’s life and one’s daily ability: ‘The tension within the experience of chronic conditions lies in the uncertainty whether this separation or alienation [with the world one inhabited before] can be reduced’ ( Barnard 1995, 42 ). Added to the uncertainty inherent in all chronic illnesses is the extra uncertainty for COVID-19 survivors because they are infected with or recovering from a disease about which much is still unknown. However, scholars of chronic illness and literature also have pointed towards the creative potential offered when authors create a ‘chronic poetics’. Hillary Gravendyk claims that chronic poetics provides a mode through which the reader co-constitutes meaning with the text. She defines chronic poetics as the ‘perception and artistic practice that allows the shared conditions of embodiment to emerge from the text’ (cited in Day 2017, 95 ), especially the work’s focus on ‘simultaneity, chronicity, duration and other forms of embodied perception’ ( Day 2017, 95 ).
Online forums and groups provide a particularly promising avenue to study COVID-19 narratives, because the real-time and communal nature of the storytelling that occurs in these settings can capture the temporality of pain in new and multifaceted ways. Social media can make pain visible, by incorporating photos, screen shots and condensed stories; it also creates ‘networks of voices engaging and reinterpreting pain’ through ‘multimodal communications’ ( Gonzalez-Polledo and Tarr 2014, 1467 ). In the process of ‘sharing pain experiences and meanings’, participants create new kinds of storytelling, where the ‘teller and audience’ meet within the story. Thus, ‘new forms of patient expertise emerge through communicating about chronic illness online’. As the SurvivorCorps community demonstrates, patients can use storytelling (and information sharing, and grassroots campaigning) to exercise ‘transformative agency’ to affect “not only their own health care, but also the quality of health care for others” ( Hinson and Sword 2019, 106 ).
This article began by introducing, and then intentionally revising, a ‘global’, or ‘public health’ chronology of the SARS-CoV-2 pandemic, to show the constant changes in our current temporality. It then created a framework for analysis of temporal innovations in pandemic literature by analysing examples from late-20th-century-postcolonial and speculative fiction. This final section has examined online COVID-19 narratives from 2020, and now turns to very recently gathered and transcribed oral histories from October 2021. Articles have their own internal chrono-logic. By ending with these recent oral histories, I am both introducing emerging original Health Humanities research, as well as illustrating the ongoingness of COVID-19 survivors’ own stories. Specifically, the genre of recorded and transcribed oral history offers unique opportunities to understand the stories of COVID-19 as full of nuance and multiplicity. Oral histories are digressive and capacious narratives, originating before editing and streamlining have imposed a chronology of illness. Interviewees return to a specific moment of significance multiple times; their stories wind through and around difficult experiences. Audio recordings include the patter of conversation that one engages in to feel at ease. They also show the mundane temporality of chronic illness as it impacts daily life.
The extracts that follow are from an interview with a middle-aged father and former army medic, who was working in a prison when he contracted COVID-19. He was hospitalised from October 2020 through January 2021, and is seeking medical retirement due to the ongoing physical effects of his illness. When asked if he could think of one moment that illustrates living during the time of COVID-19, ‘B’ (alias) responds with a historically significant mortality marker before turning to a brief encapsulation of his own illness. The interviewee first says, “we just surpassed the deaths for the Spanish flu, which is just crazy” ("B. Interview," Global Health and the Humanities project, 2021). Both this marker, as well as his narrative of symptoms that follows, stresses the ongoing nature of the pandemic, in both its national and personal impact. B explains,
So for the rest of my life, I’m going to be dealing with permanent issues, including pulmonary fibrosis, scar[s] on my heart. I had a heart attack during my period when I was in my medication-induced coma. I have vision loss. I have to wear glasses now, prior to COVID, I had 20/15, 20/20 vision. So I have to wear actually prism glasses because my balance was affected. Also, I have significant memory loss, short- and long-term memory loss. ("B. Interview," Global Health and the Humanities project, 2021)
This list is matter-of-fact and declarative. However, timing shifts between past crises (“I had a heart attack”), present condition (“I have vision loss”) and future predictions (“for the rest of my life”). The final sentence, regarding B’s memory loss, implies what an effort it may be to deal with the physical symptoms, and to recall and organise these symptoms into a recognisable order. The embodied effort of telling a story—the mental exhaustion, thirst and sadness that come with the telling—are integral to the texture of this recording. Temporal layering and fragmentation are part of the unique quality of COVID-19 storytelling.
B’s story is interrupted at one point when the sensory memory and trauma of his extended hospitalisation causes him to be overcome with emotion. His story is a necessary companion to Rafael Campo’s poem. While the doctors treating patients with COVID-19 may be wrestling with uncertainty and loss as they see the rhythmic rise and fall of the ventilator, it becomes apparent that for at least some of their patients, the sensory memories of the hospital’s temporal rhythm (especially procedures done repeatedly) are not rhythmic but intrusive and traumatic. B says,
I have a lot of problems with … I recently had to go into the emergency room for chest pain…When I got there, there were many triggers that occurred when I was there. So be it the smell of the deodorizer disinfectant cleaner that they use on the floor to the fluorescent lights, to the Hoyer lift that was above me, that they used to have to transfer me when I couldn’t move, when I was bedridden. All those things came back to me and I’m sorry, I… Interviewer: No, please. Yeah. Take your time and I understand, this is difficult. BB: It still affects me emotionally.
This transcript shows a dialogue that unfolded as a lived conversation via Zoom. Therefore, in reading it, one is immersed in the temporality of the interview: not the same temporality as the recording, but an individual reading of that temporality as reflected in text. When B breaks off, it is a temporal as well as spatial break for the reader. However, one does not know if the pause was 3 seconds or 3 minutes. Therefore, one does not know how long to hold one’s breath out of concern for the speaker’s well-being. Perhaps our eyes need to leave the page for a moment. Perhaps our heartbeats quicken. The next line, “it still affects me emotionally,” registers as a thunderclap through its very understatement. These are just some possible embodied responses to reading—however, they are meant to suggest that it will be important to reproduce first-person narratives of COVID-19 illness in their original form. One must be attuned to the way the genre influences how one reads, and to how one’s own embeddedness in this moment influences interpretation.
Often, psychology and brain sciences presuppose that trauma disrupts the teller’s access to ‘natural’ narrative ordering: ‘an essential dimension of psychological trauma is the breaking up of the unifying thread of temporality’ ( Stolorow 2003, 158 ). However, postmodern and postcolonial criticism, as previously demonstrated, offer us the possibility that time is co-constituted between physical and cultural realities. Narrative shows us, not the ‘reality’ of a universal time, but how disparate one person’s experience of lived time can be to another’s. That is to say, the same chronological time of hospital staff, organised by shift changes, regular cleaning of the floors and daily functions performed for the patient’s body, are registered by the patient’s subjectivity as acutely traumatic and recursive time.
More work needs to be done understanding COVID-19 survivors’ experiences from a disability studies perspective. Rebecca Garden argues that ‘narrative, particularly first-person accounts, provide a critical resource by representing the point of view of people with disabilities and by offering a means of examining the social context and social determinants of disability’ ( Garden 2010, 70 ). One goal of disability studies is increased accessibility for disabled persons. Accommodating disabled and chronically ill ‘long haulers’ may mean reconfiguring our understanding of the pervasiveness of chronic COVID-19, and encouraging communities to understand these long-term effects.
One of the challenges of oral history and auto/biographical scholarship is discussing the import of others’ experiences in terms they have not used themselves. Not all posters or interviewees cited herein associate themselves with antiracist or disability rights activism. Instead, this article means to use critical oral history in order open up analytical frameworks useful to analyse the emerging stories of COVID-19, making space for the multiplicity of these speakers’ own experiences. This is an important intervention, as many of the patient stories thus far have been curated by the organisation publishing them—whether this is a public health organisation using the story for educational purposes, or a hospital advertising the quality of its care. For example, a story titled ‘Grateful to be Alive’ represents the experience of Ernesto Castro, a patient at UC Health, Greeley, Colorado. Castro’s experience is framed using illness narrative clichés such as “he fought for his life”. The article stresses the heroic nature of the hospital workers (“Health workers greeted him and jumped into action”). His interviewer encouraged a specific kind of testimonial storytelling, so that when he is directly quoted it is to commend his practitioners: “If it wasn’t for the UC Health staff, I don’t think I’d be here” ( UC Health 2020 ).
Postcolonial and disability studies can help one to focus on the lack of health access and health inequity during a time of pandemic, and to help us to envision radical new ways of storytelling that do not impose closure on narratives of illness with COVID-19. Health Humanities scholarship regarding chronic pain and chronic illness narratives demonstrates the importance of cultivating an aesthetic appreciation for non-linear or fragmented narrative structures. In uniting these approaches, the project is to create discursive space, and interpretive flexibility, around these narratives. By so doing, one may help resist their instrumentalisation within medical or nationalist discourse.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
Texas A&M University IRB2018-1513M. Participants gave informed consent to participate in the study before taking part.
Acknowledgments
The author acknowledges the contribution of the Global Health and the Humanities oral history project collaborators and interviewees for collecting the oral histories. Thanks to Violet Showers Johnson, Laura Dague, Michelle Yeoman, Trinity Buchanan, Lise Saffran and the oral history interviewees who shared their stories.
1. For more on the cultural values of endemic and epidemic disease in narrative, see The Endemic Pandemic by Larsen (2020) and Endemic: Essays in Contagion Theory by Nixon and Servitje (2016) . Specifically, Nixon and Servitje claim that “Epidemic discourse so thoroughly structures our world that it is endemic to our processes of social construction” (2).
2. We may assume, based on Western norms of storytelling, that human subjects seek to unify their sense of self through narrative. However, as Angela Woods has demonstrated, some of us do not have ‘the propensity or orientation towards narrativity: the feeling of deep psychological continuity with one’s past self, married with the desire to frame experience, tell stories and revise the past’ ( Woods 2011, 73 ).
3. Rosemary Jolly has pointed towards the importance of self-questioning in memoirs by Western subjects: the doctor-writer’s misunderstanding, she suggests, demonstrates the ‘limits of colonial diagnostic knowledge’ and ‘works against the narrator-as-doctor enacting the colonialist fantasy of remedying, or ministering to, the chronically ill indigenous subject’ ( Jolly 2016, 528 ). These works make visible in a specific way how colonialist medical practices do harm.
4. For more on medical experimentation in colonial settings, see Africa as Living Laboratory by Tilley (2011) and Bacteriology in British India: Laboratory Medicine and the Tropics by Chakravarty (2012) .
5. Recently, Elaine Freedgood also questions our assumptions about 19th century realism. Freedgood suggests that our perceptions of this literary past rests on post-1970s aesthetic valuation and that we thereby overlook 19th century novels’ ‘oddness’. She also questions the ‘aesthetic racism’ that has valued realism in the novel ( Freedgood 2019 ).
6. ‘The logics of dispossession and elimination, which are key tenets of a settler colonial model, were not isolated to British imperialism; they were also central to Spanish and Portuguese imperial projects’ ( Castellanos 2017, 778 ).
7. Rishi Goyal’s recent work stresses how the label of healthcare workers as ‘heroes’ serves to distract from the ‘deep institutional betrayal’ they were subjected (inadequate supplies, protections and support) during the pandemic ( Goyal 2020 ).
Bibliography
- B, interview
- Baruch J. ,
- Springs S. ,
- Poterack A. , and
- Blythe S. G.
- Castellanos M. B
- Centers for Disease Control
- Chakrabarty D
- Chakravarty P
- Chowdhury I
- Chowkwanyun M. , and
- Comaroff J. , and
- Comaroff J.
- De Boever A
- Freedgood E
- García Márquez G
- Gonzalez-Polledo E. , and
- Henrikson P. , and
- Kullberg C.
- Hinson K. , and
- Hogarth R. A
- Khan Z. H. , and
- DasGupta S.
- Joyce R. , and
- Kelly A. H. ,
- Keck F. , and
- Lynteris C.
- Lambert, Natalie and SurvivorCorps
- Lemley C. K
- Nixon K. , and
- Servitje L.
- Ellis J. , and
- Salisbury L
- Snowden F. M
- Stevenson R
- Stolorow R. D
- SurviviorCorps
- SurvivorCorps Facebook Group Posts
- West-Pavlov R
- Whitehead A. ,
- Atkinson S. ,
- Macnaughton J. , and
- Richards J.
Contributors JH is the sole author.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the 'Methods' section for further details.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, covid issue: visual narratives about covid-19 improve message accessibility, self-efficacy, and health precautions.

- 1 LifeOmic, Baton Rouge, LA, United States
- 2 LSU, College of Science, Communications, Baton Rouge, LA, United States
- 3 Charles H. Sandage Department of Advertising, University of Illinois at Urbana-Champaign, Champaign, IL, United States
- 4 Freelance, Taipei City, Taiwan
- 5 Freelance, Washington, DC, United States
Visual narratives are promising tools for science and health communication, especially for broad audiences in times of public health crisis, such as during the COVID-19 pandemic. In this study, we used the Lifeology illustrated “flashcard” course platform to construct visual narratives about COVID-19, and then assessed their impact on behavioral intentions. We conducted a survey experiment among 1,775 health app users. Participants viewed illustrated (sequential art) courses about: 1) sleep, 2) what COVID-19 is and how to protect oneself, 3) mechanisms of how the virus works in the body and risk factors for severe disease. Each participant viewed one of these courses and then answered questions about their understanding of the course, how much they learned, and their perceptions and behavioral intentions toward COVID-19. Participants generally evaluated “flashcard” courses as easy to understand. Viewing a COVID-19 “flashcard” course was also associated with improved self-efficacy and behavioral intentions toward COVID-19 disease prevention as compared to viewing a “flashcard” course about sleep science. Our findings support the use of visual narratives to improve health literacy and provide individuals with the capacity to act on health information that they may know of but find difficult to process or apply to their daily lives.
Introduction
The COVID-19 (Coronavirus Disease 2019) pandemic is a serious global health threat. COVID-19 has spread quickly and unrelentingly since its emergence in Wuhan, China in December 2019. The pandemic has had devastating impacts on human lives, public health, and the global economy. But it has also unified the scientific community in a mission to educate and engage the public in solutions such as public health precautions, including social distancing, testing, masks, engagement in clinical trials for vaccine candidates, and vaccination with approved vaccines. Educational resources about COVID-19 have subsequently exploded. However, communication efforts have left out large segments of the population with low health literacy skills ( Frieden, 2020 ).
Health information has historically been presented such that it is not accessible to most Americans [“Health Literacy” by CDC (2021) ]. Nearly a third of Americans have low general health literacy ( Paasche-Orlow et al., 2005 ). While in this study we focused on developing and assessing health literate COVID-19 materials in a U.S. context, low health literacy and a lack of health literate materials are also problems globally. Nearly half of all Europeans have inadequate and problematic health literacy skills according to a WHO report ( Kickbusch et al., 2013 ). Further, nine out of 10 adults in the U.S. struggle to understand and use personal and public health information that doesn’t follow health literacy guidelines [“Health Literacy” by CDC (2021) ]. Much of the information about COVID-19 has fallen into this trap and is not accurate, trustworthy, and understandable by most people ( Caballero et al., 2020 ). Many experts have pointed out that health literacy has been underestimated as a public health problem during the COVID-19 pandemic ( Abdel-Latif, 2020 ; Paakkari and Okan, 2020 ).
Health-related educational resources designed for broad audiences, especially for adults with low levels of formal education, adults with mental health issues or disabilities ( Kamalakannan et al., 2021 ), non-English speakers, or children, should follow health literacy best practices ( CDC, 2021 ). They should be accurate, accessible, and actionable ( CDC, 2021 ). They should make effective use of plain language, narrative, and visuals or multimedia to improve accessibility. But COVID-19 educational resources incorporating all of these elements remain rare as of the writing of this manuscript. Caballero and colleagues (2020) found that only 39% of assessed COVID-19 consumer materials from the internet included visual images that would have helped readers understand the information. Most of the materials failed to use plain language. Other experts have pointed out similar problems, including infectious disease specialist Benjamin P. Linas, MD. In late March, Linas observed an “absence of COVID-19 health education materials that could speak across language, literacy levels, and cultural norms” ( Bailey, 2020 ).
Broadly accessible resources increased in availability in the months following the outbreak of COVID-19 and stay-at-home orders in the U.S. People produced simple cartoon-like patient factsheets in multiple languages ( Bailey, 2020 ), kids’ visual storybooks, and other accessible resources 1 . Yet, these resources remained limited and urgently needed in more languages and on more topics, such as updated information on COVID-19, immune system responses, and vaccine candidates.
Early in the outbreak of COVID-19 in the U.S., we observed few educational materials or graphics that were accessible and actionable. We observed few resources that helped people understand how they should prepare, how and when they should self-isolate, what they could expect if they got sick, how their bodies would fight the virus, and who should seek emergency care and when. Such actionable information is critical given the devastating potential impact of COVID-19 for people with any risk factors, and every person’s role in helping limit the spread of COVID-19.
Park and colleagues (2020) found that among more than 1,000 U.S. adults recruited to a survey via Amazon’s Mechanical Turk, many people expressed uncertainty about length of quarantine and social distancing requirements. In another study from Germany, up to 52% of just over 1,000 participants reported difficulty accessing, understanding and applying information about how to recognize infection, when and how to find professional help upon infection, and risk factors of disease ( Okan et al., 2020 ). Although these findings don’t necessarily mean that there weren’t educational materials available on these topics, materials on these topics may not have been accessible, easy to understand or health literate.
In addition, while stories of people’s COVID-19 infection experiences did start to appear in the local news media once COVID-19 began to spread in their communities, we didn’t see these stories within the educational resources of government and healthcare institutions. Most resources (especially visual ones) that we saw focused on the history and science of SARS-CoV-2 and the respiratory disease it causes, or abstract concepts such as “flatten the curve”. Meanwhile, there were mixed messages about mask wearing, risk factors and airborne infection risks. There seemed to be a gap in visual and broadly accessible educational materials covering the COVID-19 experience and how people should navigate the disease from prevention to treatment.
More accessible COVID-19 educational resources on a variety of topics are critical for the one in five U.S. adults with low literacy skills 2 and the nearly one-third with low health literacy. But they are also important for people who may be experiencing isolation-exacerbated feelings of fear, stress, anxiety, and/or depression ( Park et al., 2020 ). Stress and mental health issues can make it more difficult for people to process technical health-related information ( CDC, 2021 ) and adhere to public health recommendations ( Middleton et al., 2013 ; Beutel et al., 2018 ). Stress can lower health literacy or an individual’s capacity to put recommended preventative health behaviors into action.
In this study, we started to evaluate the impact of educational resources designed to address the audience and COVID-19 education gaps highlighted above. To do this, we leveraged a new visual science communication format developed by the science-art platform Lifeology.io. In March 2020, Lifeology published two expert-created illustrated “flashcard” courses about COVID-19 that contained plain language visual narratives suitable for broad audiences and people with low health literacy. The courses featured visuals created by professional artists. They were available in 20 + languages and addressed the topic gaps we identified above. One course (“Prevention Primer”) covered the basics of COVID-19 prevention and care, through the story of a family learning to navigate the pandemic. The other course (“Mechanism”) was more technical and covered the mechanisms of COVID-19 inside the body, risk factors and medical considerations for at-risk individuals.
The goal of this study was to test the impact of these two different “flashcard” courses on people’s self-reported self-efficacy, perceived threat, and behavioral intentions toward COVID-19, based on the Extended Parallel Process Model (EPPM). Another goal was to evaluate the ability of these courses to improve health literacy by helping people understand and use information about COVID-19. We did this through self-reported data of people’s experiences with and takeaways from the course content. We conducted an online survey experiment via Qualtrics. We were particularly interested to see any differences in impact between a course with more basic information about COVID-19, a course with more technical information about the mechanisms and risk factors of SARS-CoV-2 infection, and a control course about the general health benefits of sleep.
This study also represents a collaborative effort to put evidence-based science communication into practice ( Jensen and Gerber, 2020 ) and then to measure some outcomes of that practice. We (the authors of this study) are a team of science communication researchers, health writers, industry science communicators, artists and designers. Evidence in science and health communication research, including literature in the field of health literacy reviewed below, informed the creation of the COVID-19 “flashcard” courses evaluated herein. These courses were viewed by over 24,000 people in 3 months; one course was translated into 20 + languages by community volunteers who wanted to share the courses with audiences in their own languages/countries/communities. While the courses were still highly relevant, we began collecting data via survey experiment to evaluate their impact on people’s self-efficacy and behavioral intentions, plugging practice back into research.
Literature Review
Covid-19 pandemic and educational interventions.
The necessity of clear, actionable, and broadly accessible health education ( CDC, 2021 ) has never been more apparent than during the COVID-19 pandemic. According to the World Health Organization (WHO), risk communication and community engagement “is integral to the success of responses to health emergencies” ( WHO, 2020a ). Risk communication and community engagement “helps prevent “infodemics”; (an excessive amount of information about a problem that makes it difficult to identify a solution), builds trust in the response, and increases the probability that health advice will be followed” ( WHO, 2020b , p. 1). Effective communication around COVID-19 should translate scientific information to improve understanding, make it relatable, and deliver it in an accessible manner to diverse populations and communities.
WHO has also provided specific recommendations for communication materials intended for community engagement during the pandemic. They have recommended that countries translate materials into relevant languages, adapt them to appropriate literacy levels, and create shareable (online) visuals/multimedia pieces that present key information. They have encouraged the creation of materials that “explain the disease etiology, symptoms, transmission, how to protect oneself, and what to do if someone gets sick” ( WHO, 2020a ). The United Nations and WHO even launched an unprecedented global call to creators 3 to help stop the spread of COVID-19 through artwork, encouraging creativity and “empathetic communication” to promote the adoption of public health precautions across age groups, affiliations, geographies, and languages.
But despite these recommendations, there has been a dearth of COVID-19 educational materials in the U.S. that make information accessible to most adults and that are inclusive of different people and cultures. This has been despite the disproportionate impact of COVID-19 and related serious illness among racial and ethnic minority groups who are more likely to experience low health literacy ( Eichler et al., 2009 ), including Hispanic/Latino and Black/African American persons ( CDC, 2020 ).
Health Literacy and Models of Health Behavior Change
Health literacy has been defined as “the degree to which individuals have the capacity to obtain, process, and understand the basic health information and services needed to make appropriate health decisions” (Wagner et al., 2009, p. 860; Institute of Medicine, 2004). Modern definitions also focus on the capacity to process and understand health information and use and apply it. Health literacy “entails people’s knowledge, motivation and competencies to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course” ( Sorensen et al., 2012 ). Low health literacy is associated with poorer health outcomes (Institute of Medicine, 2004). Health literacy can impact health-related knowledge, beliefs, motivations, self-efficacy, and ability to problem-solve with regard to self-care as well as using healthcare services ( Paasche-Orlow and Wolf, 2007 ). Health-related knowledge, beliefs, motivations, and self-efficacy (and fear) are critical in determining health behaviors according to theories of health behavior action and change. These theories include the Health Belief Model and the Extended parallel process model ( Jones et al., 2015 ; Sheeran et al., 2016 ).
Difficult-to-read health information and an overabundance of conflicting media health messages (as seen in the COVID-19 “infodemic”) exacerbate health literacy issues. They also contribute to poor health outcomes ( Paasche-Orlow and Wolf, 2007 ). However, educational materials that are accessible and promote experiential learning, i.e., learning through a transforming experience ( Kolb, 1984 ), can improve health literacy ( Day, 2009 ). Improving health literacy can, in turn, improve beliefs, attitudes, and motivations toward health behaviors (Wagner et al., 2009). Educational materials that improve health literacy and address determinants of health behavior change are most likely to drive better health outcomes. Educational materials about COVID-19 should improve health literacy and help people turn their perceived threat from COVID-19 into action by helping them believe that they can act in ways that make a difference.
Educational materials that follow guidelines for improving health literacy are easier to read, digest, understand, and act upon. Health literacy guidelines focus on plain language, actionable information, resources that include visuals such as pictures and drawings, and an audience-centered approach that includes culturally appropriate messages ( CDC, 2021 ). A growing body of research also focuses on the positive impact of visual narratives or storytelling, as seen in the body of research on Graphic Medicine. Storytelling and visual narratives with relatable human characters provide a fun and experiential way of learning that allows people to reflect on information and relate to it on a personal level ( Day, 2009 ).
With this study, we sought to evaluate the impact of health literate visual narratives (Lifeology “flashcard” courses) on content experiences, attitudes and behavioral intentions toward COVID-19. Below, we review relevant literature on the potential impact of visuals and storytelling on health literacy and determinants of health behavior.
Research Question RQ1 : To what extent do people report visual narratives (about COVID-19 or another health topic) as being easy to understand, informative and engaging?
Role of Visuals in Science and Health Education
People typically enjoy content that is visual or that includes illustrations and sequential art (e.g., comics) more than they do content that is not visual (Z. Dayan, 2018 ). In a recent study, medical and healthcare students indicated enjoying multimedia (a mix of images and text, and sometimes sound) as a practical learning tool ( Vagg et al., 2020 ). Visuals can also aid learning among students with different learning styles and preferences ( Aisami, 2015 ). Visuals can improve people’s motivation to learn ( Aisami, 2015 ), increase their engagement with message content ( Lazard and Atkinson, 2015 ), and improve information processing and retention: “Words are abstract and rather difficult for the brain to retain, whereas visuals are concrete and, as such, more easily remembered” ( Aisami, 2015 , p. 542). Scientific concepts, like words, are also abstract. Visuals can make them more concrete and easier to grasp.
Visuals can also stimulate critical thinking. Visual representations draw more attention than text-only messages. Visuals facilitate information processing and enhance message elaboration ( Cvijikj and Michahelles, 2013 ; Kim et al., 2015 ; Lazard and Atkinson, 2015 ). Townsend et al. (2008) found that text with color photographs increases understanding and learning of a food behavior checklist most when compared with text alone, text with line drawings, and text with grayscale photographs. This highlights the positive potential of colorful artwork in improving people’s engagement with science and health information.
People with limited literacy or language skills in particular “benefit from illustrations, not just words” ( Osborne, 2012 p. 214). Visuals “can help people take in information faster and more accurately, and remember it better” ( Osborne, 2012 , p. 214), improving attention to, comprehension of, and recall of technical and health information ( Houts, et al., 2006 ). People with low literacy skills are especially likely to benefit from visuals accompanying text ( Houts et al., 2006 ).
Healthcare providers are encouraged to use visuals and multimedia resources when communicating with people with low health literacy ( Hart et al., 2015 ) to improve patient knowledge ( Nova et al., 2019 ). Empathetic and positively framed visuals and data visualizations in health education materials may help reduce anxiety ( Demircelik et al., 2016 ) and minimize emotional stress associated with risk communication and getting negative prognostic information ( Kim et al., 2020 ). Visuals may even improve behavioral intentions and behaviors, especially among low literacy audiences ( Houts et al., 2006 ). These impacts are observed when viewers have a positive emotional response to visuals in health education materials ( Delp and Jones, 1996 ).
Visual Storytelling for Science and Health Communication
There is a growing field of research around the use of narrative visual formats, sequential art, or visual storytelling for science and health communication. These formats combine the power of visuals with the power of storytelling ( Green and Brock, 2002 ; Leung et al., 2014 ; Wang X. et al., 2019 ) to aid information processing and recall, enhance understanding, and increase engagement. For example, comics are a form of sequential art that combines visuals and plain language storytelling. Comics are preferred over other types of visual narratives because they often include characters readers can relate to, short text that is easy to read, and a story arc that keeps their attention ( Wang Z. et al., 2019 ).
In school and healthcare settings, comics are effective at increasing knowledge and awareness of health issues/conditions ( Ohyama et al., 2015 ; Tekle-Haimanot et al., 2016 ). In one study, a comic about pediatric anesthesia helped reduce preoperative anxiety in children ( Kassai et al., 2016 ). In another study, Leung and colleagues (2014) found that exposure to relatable characters in a detailed artwork comic can capture imagination and influence health behaviors. A comic combining concise text and detailed artwork that encouraged fruit intake increased self-reported self-efficacy and snack selection in urban minority youth ( n = 57). This happened regardless of changes in knowledge. The youth who read the comic were also more absorbed in the content (they reported paying attention without getting distracted) than youth who read a newsletter. The researchers surmise that greater transportation into the narrative of the comic lead to the observed changes in health-related outcomes: “(N)arratives that transport readers have been shown to change beliefs and motivate behavior change” ( Leung et al., 2014 ).
Most studies have investigated the impact of visual narratives among younger audiences. However, there is early evidence that they can also help people of all ages. Health professionals are being encouraged to apply similar mediums—illustrated stories or comic strips—to communicate with older patients and their caregivers. According to behavioral science expert and RN Sarah Kagan, “(m)uch of what we provide as educational material lacks interest, overshoots reading level, and necessarily includes an enormous level of detail” ( Kagan, 2018 ). Some researchers and science communicators have used visual narratives to engage people in preventing the spread of COVID-19. Igarashi et al. (2020) found that manga comics, as a form of visual storytelling steeped in culture and lived experience, can “provide the public with a deeper understanding of (scientific) messages through … characters and their “real-life” situations” (2020, p. 1).
Visual narratives in health education may be especially appropriate for individuals with low health literacy or limited prior knowledge about the topic being communicated ( Mayer, 1997 ; Schnotz and Bannert, 2003 ). According to comic research expert Matteo Farinella, “the visual language of comics might make information, not only more accessible, but also help to overcome linguistic barriers” ( Farinella and Mbakile-Mahlanza, 2020 ). The cartoon-like visual nature of comics and other visual narratives may also make scientific information less daunting and more approachable for people. When it comes to the communication of sensitive health topics or complex, unfamiliar, or scary topics like vaccines ( Muzumdar and Pantaleo, 2017 ), people often prefer simplified, stylized, conceptual, or interpretational illustrations over photographs and realistic art ( Haragi et al., 2019 ; Farinella and Mbakile-Mahlanza, 2020 ).
Despite the burgeoning research field around comics and other narrative visual formats, visual storytelling remains poorly studied in terms of its efficacy for health and risk communication among broader publics in real-world settings ( Farinella, 2018 ). Lifeology “flashcard” courses provide opportunities for further research in this area. They are similar to graphic novels or comics in combining short text with relevant detailed visuals in cards that tell a story and often include characters. We wanted to see when or for whom the visuals in these courses mattered, which we explored through participants’ self-reported content experiences.
Research Question RQ2 : Which factors are correlated/associated with self-reported attention to the visuals in a visual narrative about COVID-19 or another health topic?
Heuristic-Systematic Model of Information Processing
Developed by Chaiken (1980) , the heuristic-systematic model (HSM) stated that information can be processed via two approaches: systematic and heuristic. Systematic processing often occurs when an information seeker is highly motivated and capable of digesting data; thus, the individual pays more attention to message content ( Metzger et al., 2010 ; Katz et al., 2018 ). Conversely, when an individual lacks motivation or the ability to comprehend information, they may rely on contextual factors such as visual or vocal cues to make judgments ( Wang X. et al., 2019 ; Kim, 2018 ; Lahuerta-Otero et al., 2018 ). Additionally, some researchers have found that heuristic processing is more dominant than systematic processing, because the former requires less cognitive effort ( Chan and Park, 2015 ; Lahuerta-Otero et al., 2018 ).
In this study, we use HSM as a framework to investigate the impacts of visual narratives on health-related perceptions (attitudes and beliefs) and behavioral intentions. For example, individuals with lower health literacy or education (lower education is related to lower health literacy) may rely on and pay greater attention to the visuals in an illustrated flashcard course about COVID-19 to process the message. But even highly educated individuals could rely on and pay greater attention to the visuals in a more technical course about the mechanisms of COVID-19 in the body, because technical science and health information can be difficult for anyone to understand and apply in their own lives. Regardless, we would expect greater attention to visuals to result in improved engagement with the content/message and improved outcomes.
This idea—that greater attention to visuals in educational materials improves engagement and outcomes - is related to the concept of absorption ( Oh et al., 2015 ), immersion, or transportation with content being related to associated outcomes. Absorption is defined as “the degree to which users experience temporal dissociation, focused immersion, heightened enjoyment, curiosity, and control over the computer interaction” ( Agarwal and Karahanna, 2000 ; Oh et al., 2015 , p. 740) when interacting with media. Greater absorption can improve behavioral intentions. Both attention and absorption can be conceptualized as components of content engagement. But in this study, we were particularly interested in attention to visuals as a key component of engagement—consisting of qualities like attention, focus, curiosity, interest ( Webster and Ho, 1997 )—with illustrated flashcard courses.
Research Question RQ3 : Is greater self-reported attention to the visuals in a visual narrative about COVID-19 associated with increased self-efficacy, perceived threat, and protective behavioral intentions toward COVID-19?
Health Communication and the Extended Parallel Process Model
In this study, we also explored whether and how understandable and engaging visual narratives about COVID-19 can drive behavior change, either directly and by activating perceived threat and self-efficacy ( Witte, 1994 ). According to the EPPM, external stimuli that increase perceived efficacy and perceived threat (including severity of the threat and one’s susceptibility to it) along with fear can increase protection motivation, message acceptance, and behavioral intentions. People can respond to risk messages and fear appeals in one of three ways: 1) through danger control, for instance in the form of behavioral intentions in line with the message recommendations; 2) fear control (e.g., denial, avoidance); 3) no response.
It is important to note that during the global spread of SARS-CoV-2, fear and perceived threat from COVID-19 have generally been high, especially among older adults. In May 2020, Pew Research found that in the U.S., 38% of adults total, 43% of adults between the ages of 50 and 64, and 49% of adults over the age of 65 see COVID-19 as a major threat to their personal health ( Schaeffer and Rainie, 2020 ). Younger adults also tended to report high levels of emotional distress. In light of this, we expected that educational content that delivered empowering information about COVID-19 prevention and care would improve protective behavioral intentions through improvements in self-efficacy in particular. While perceived threat is key to motivating behavior change according to the EPPM, self-efficacy is key to a positive response. Some researchers have also proposed that “as perceived threat increases when perceived efficacy is low, people will do the opposite of what is advocated” ( Popova, 2012 , p. 463).
Based on the EPPM, risk messages that increase people’s self-efficacy in the face of a health threat can help to drive positive behaviors that may protect them from that threat. Based on research we’ve reviewed above related to health literacy, highly health literate educational content (which is understandable, visual, engaging, actionable) should be best able to help improve people’s understanding of the health threat, and their self-efficacy or knowledge of how to protect themselves and confidence in their ability to do so. We explore this idea through our final research question and corresponding hypotheses, which we analyze in Means of Self-Efficacy, Perceived Threat and Behavioral Intentions Across Course Conditions and Course Impacts on Behavioral Intentions .
Research Question RQ4 : Can understandable and engaging visual narratives about COVID-19 improve self-efficacy and protective behavioral intentions?
Hypothesis H1 : People who view a visual narrative about COVID-19 will have increased self-efficacy toward protecting themselves from COVID-19 than people who view a control narrative.
Hypothesis H2 : People who view a visual narrative about COVID-19 will have improved protection behavioral intentions toward COVID-19 than people who view a control narrative.
Hypothesis H3 : Self-efficacy and perceived threat will mediate the impact of viewing a visual narrative about COVID-19 on protection behaviors.
For all hypotheses, we planned to look at the impact of two illustrated flashcard courses about COVID-19 separately.
We did not predict that viewing an illustrated flashcard course about COVID-19 would increase viewers’ perceived threat from COVID-19 compared to a control course. We did not predict this because we thought that perceived threat would already be high in general among study participants given the state of the pandemic in the U.S. at the time (late March). However, we did plan to explore whether the more technical “Mechanisms” COVID-19 course would raise perceived threat, as this course discussed risk factors of severe COVID-19 illness.
Educational Platform—Lifeology “Flashcard” Courses
Lifeology’s illustrated flashcard courses are self-contained digital and interactive online card decks, where each card contains a small amount of text (one to three short sentences) along with a custom illustration. The cards contain sequential art that, along with bite-sized text, tells a story. The course viewer allows users to swipe or click through the course flashcards. It also allows users to toggle between different language options, tap/click to see information sources, tap/click to learn more about the course creators, and submit feedback. The course viewer is optimized for mobile devices but is responsive and works in any smart-device or desktop web browser. Courses are free and often published under a CC-BY-SA Creative Commons license.
Each course is the product of a collaboration between one or more technical experts, one or more plain-language writers, and an artist. It is becoming increasingly important to incorporate diverse, creative, and non-technical voices in the creation of science and health educational materials. Diverse perspectives improve the accessibility and relatability of science and health information for broad audiences. Every course also goes through a collaborative creation process 4 that conforms to established health literacy strategies ( Osborne, 2012 ). The process includes collaborative identification of one or a few key messages, card script-writing by a plain-language writer, visual storyboarding, fact-checking by external scientists, and listening to early audience feedback.
The courses evaluated in this study incorporate features that meet modern recommendations of health literacy experts ( Osborne, 2012 ; “Principle: Understandable”; WHO, 2020a ; Simmons et al., 2017 ; Mayer, 2003 ). These include: plain language and succinct sentences; definition of technical terms; conversational and positive tone; actionable information; narrative elements including characters and a story-arc; text in close proximity to related visuals. The visuals also incorporate features important for health literacy including: high detail but not hyper-realistic visuals; informative visuals that show characters/people at their best modeling desired behaviors; illustrations that communicate scale and context, as for cells or virus particles; storytelling.
Study Procedure
We conducted an online survey experiment. Participants were randomly assigned to one of three stimulus (flashcard course) conditions: a course about sleep; a Prevention Primer course about the basics of COVID-19 prevention and self-care; a Mechanism course about how the novel coronavirus impacts our body. The study was approved for IRB exemption by Louisiana State University (IRB# E11953).
Study participants first answered questions about whether their state of residence was under a stay at home order, their perceived knowledge about COVID-19, and attention to news about it. Participants were then instructed to open and swipe/click through “a series of health-related flashcards organized into a mini-course” and answer some questions about it. We used an opened-ended question asking participants what the course was about and what they had learned, to ensure that participants had opened and browsed through the course cards. Finally, participants answered questions related to their perceptions of the course they had viewed, their perceptions of COVID-19 as a threat to their health, their self-efficacy and their behavioral intentions toward COVID-19 protection and care, and demographics.
Stimulus Content
The control flashcard course 5 covered why we sleep, sleep patterns of humans and animals, and sleep hygiene tips for brain health. It was illustrated in a storybook style by artist Ariella Abolaffio.
The COVID-19 Prevention Primer course 6 titled “What do I need to know about the 2019 novel coronavirus?” focused on explaining and clarifying basic information about COVID-19. It introduced and explained the viral cause of COVID-19 and the lifestyle and environmental changes that are recommended to keep people healthy and safe from infection. The content addressed what people could expect during the outbreak and what they might do if a family member were to get sick. The course used a detailed cartoon-like visual style and pictorial/representation visuals ( Haragi et al., 2019 ) to illustrate preventative behaviors and processes people could adopt such as handwashing and social distancing ( Figure 1 ). The course was illustrated by science artist Elfy Chiang.
FIGURE 1 . Above we’ve reproduced three of the “cards” contained within the COVID-19 Primer Prevention course, as they would be seen on a mobile device. The first is the title card of the course, while the others are example cards to demonstrate the visual style, informational content, and amount of text.
The COVID-19 Mechanism course 7 titled “What does the coronavirus do in my body?” covered how the virus SARS-CoV-2 infects cells, infection mechanisms at the cellular level, how the body fights back, why some people are at risk for more severe illness and when they should seek care. This course followed a character from the Primer course but focused on providing a basic understanding of how viruses cause symptoms, how people recover from infection, and why there are differences in disease severity. This course used more interpretational ( Haragi et al., 2019 ), metaphor-communicating visuals in a hand-drawn but digitized watercolor style to enhance understanding of the technical information about virology and the immune response ( Figure 2 ). The course was illustrated by science artist Elfy Chiang.
FIGURE 2 . Above we’ve reproduced three of the “cards” contained within the COVID-19 Mechanism course, as they would be seen on a mobile device. The first is the title card of the course, while the others are example cards to demonstrate the visual style, informational content, and amount of text.
We assessed whether the courses were health literate based on validated external tools including the SMOG ( McLaughlin, 1969 ) online calculator, a tool for assessing reading level, and the PEMAT for printable materials ( Shoemaker et al., 2014 ) 8 .
The SMOG index was 9.2 for the Primer course and 9.3 for the Mechanism course, meaning they were both at a sixth grade reading level and “easy to read”.
We evaluated PEMAT understandability and actionability scores for our COVID-19 courses, and we also had an independent reviewer submit scores—the independently derived scores matched our own. We evaluated the Primer course to have a 95% Understandability Score (14 out of 15 points 9 ) and an 80% Actionability Score (4 out of 5 points 10 ). We deducted one point for not providing a “tangible tool” for taking action, although we linked to WHO and CDC guidance and resources on home care and prevention for COVID-19. We evaluated the Mechanism course to have an 87% Understandability Score (13 out of 15 points) and a 60% Actionability Score (3 out of 5 points). We took a point away on Understandability for the Mechanism course for some technical terms like cytokines and antibodies, even though we defined them. We also took a point away on Actionability for “steps to action”—this course was more focused on informing people about COVID-19 risk factors.
Variables and Scales
Following news about covid-19.
We measured (pre-stimulus) how closely participants were following news about COVID-19 on traditional news media outlets in print, on TV, or online, on a 5-point scale from not at all closely to very closely .
Perceived Knowledge About COVID-19
We Asked Participants “ How informed would you say you are about COVID-19? ”, measured (pre-stimulus) on a 5-point scale from not at all to very .
Understanding and Learning
We measured perceived learning or the degree to which people found courses informative (“ I learned a lot ”), and understanding (“ It was easy for me to understand the information ”), as single items on 5-point scales, based on level of agreement. We also explored how relatable the course was to people (“ The mini-course was created with people like me in mind ”) as a single item on a 5-point scale.
We assessed basic COVID-19 knowledge with a 4-item quiz (Sum of items, mean score = 3.87, SD = 0.38). Its usefulness was limited by a low Chronbach’s alpha of 0.21. Although Chronbach’s alpha is not always a useful characteristic of knowledge instruments ( Taber, 2018 ), we’ve only used the sum of knowledge items related to information presented across the two COVID-19 courses as an informal check and context for our self-reported learning measure.
The quiz consisted of true/false statements for the following: Scientists are working on developing potential vaccines for COVID-19 (true); Coronaviruses are found only in humans (false); Some people with COVID-19 have no symptoms (true); When practicing social distancing , 3 feet is the recommended distance (false).
Attention and Absorption
We measured self-reported attention to the visuals and absorption in the content of the course based on items taken from Agarwal Karahanna (2000) and Oh et al. (2015) . Participants were asked to indicate their level of agreement on a 5-point scale ( strongly disagree to strongly agree ) to statements “ I paid close attention to the graphics and visuals in the mini-course ” and “ The mini-course held my attention all the way through to the end ”. These two variables are moderately correlated (Correlation = 0.48, p < 0.001) and used separately.
Perceived Threat
We evaluated COVID-19 risk perceptions as a 4-item scale (Chronbach’s alpha = 0.67) based on level of agreement on a 5-point scale to statements reflecting participants’ belief that they could get COVID-19, that they could get very sick, and that COVID-19 is serious; personal feelings of risk because of COVID-19; belief that COVID-19 is serious. This measure and items represent threat in the EPPM and were taken from Witte et al. (1996) and Popova (2012) .
Self-Efficacy
We evaluated self-efficacy for COVID-19 prevention and care as a 3-item scale (Cronbach’s Alpha = 0.68) based on level of agreement on a 5-point scale to the following statements: “ I feel confident in my ability to protect myself from getting COVID-19 ”, “ I know how to protect myself from getting COVID-19 ”, “ I know what to do if I get COVID-19 and when to seek emergency care if necessary ”. This measure incorporates both knowledge about COVID prevention and self-care and belief about one’s ability to act on that knowledge. This measure represents self-efficacy in the EPPM.
Behavioral Intentions
We evaluated behavioral intentions as an 8-item scale (Chronbach’s Alpha = 0.87). We measured participants’ likelihood to engage in the following behaviors during the COVID-19 pandemic, on a 5-point scale from extremely unlikely to extremely likely : Stay 6 feet from others in public spaces, wash hands often, limit visits to public places or crowds, wear a face mask/covering in public, avoid visits with people I don’t live with, follow government recommendations, stay at home as much as possible. All behavioral items were derived from official public health recommendations published by the CDC and other official sources.
Demographics
We measured demographic and other personal information including age, gender, formal education level, location (state), and existence of a stay-at-home order in the participant’s state. Participants represented all 50 states and DC.
Data Collection, Cleaning, and Analysis
We collected data via a Qualtrics online questionnaire, which linked participants out to the courses in a new window that automatically closed upon course completion. Participants were recruited from two mobile health tracking apps—the LIFE Fasting Tracker (185k users received a study email) and the LIFE Extend mobile health applications (4,616 received a study email). To avoid recruiting too many participants, we recruited only participants that had 1) used the app at least one time within the previous 30 days, 2) a valid email address linked to their mobile application account, and 3) country of residence was the United States. An invitation to participate was sent to the eligible participant pool using an industry-standard mobile application data and analytics platform (MixPanel). The email outlined the study with a button/link to participate, the estimated time to complete, and a random reward for completion. All participants who clicked to participate received a follow-up “thank you” email and reminder to complete the questionnaire.
By May 22, 2020 (first email sent on May 8), 1,890 users completed and submitted the questionnaire, while 1,670 users had responses in progress. The completion rate was 53%. Based on emails opened ( n = 37,581), the response rate for partial completions was 9.5% (1.8% based on total emails sent), while the rate of study invite emails open to completion was 5% (0.97% based on total emails sent).
We processed and analyzed all anonymous survey responses in SPSS. For data analysis, we only included partial responses where respondents completed more than half of the questionnaire and answered at least some of the post-stimulus dependent variables (starting with risk perceptions) ( n = 65). We also removed responses ( n = 115) where participants didn’t correctly answer an attention filter question correctly or incorrectly answered what the course was about (responded “flu” as opposed to sleep or the novel coronavirus). We ended up with a total of 1,775 responses. The minimum time for questionnaire completion among these was 4.5 min.
To explore our research questions, we used ANOVA or ANCOVA tests to evaluate the impact of stimulus condition (categorical variable) as well as covariates that were not substantially correlated (typically age, gender and level of education) on interval data dependent variables. We assumed linearity, and normal distribution on dependent variables which we confirmed with histogram plots (understanding and behavioral intentions were most left skewed). We used conservative Bonferroni post hoc tests to adjust for multiple pairwise comparisons between stimulus conditions. Because Levene’s test was sometimes significant in our ANOVA tests, we report the Welch F statistic (does not assume equal variances) for these tests.
White test for heteroskedasticity was positive in univariate tests predicting learning, absorption, and quiz scores. However, parameter estimates with robust standard errors (HC3 method) revealed no differences in significant results or differences between standard errors and robust standard errors ( Hayes and Cai, 2007 ). Therefore, we report the standard statistics for ANOVA, ANCOVA and linear regression tests below. For ANCOVA tests, we report effect size as R 2 .
We used linear regression to test our hypotheses with continuous interval outcome variables. In these regression tests, residuals for outcome variables (self-efficacy, threat, behavioral intentions) were normally distributed.
Demographics and Descriptives
Our final data analysis included 1,775 participants: 637 participants (36%) saw the control course about sleep, 546 (31%) saw the COVID-19 Prevention Primer course, and 592 (33%) saw the COVID-19 Mechanism course. Randomization was successful - there were no significant differences in participant age, education level, stay at home order status, self-reported previous knowledge about COVID-19, or attention to COVID-19 in the news across stimulus conditions.
Participants’ age range was 18 to 90 years (Mean = 44.0, SD = 11.7). A majority of participants were female (80%, n = 1,423), reflecting the demographics of LIFE Apps users; 67% ( n = 1,195) identified as White, 9% ( n = 153) identified as Hispanic/Latino, 8% ( n = 135) as Black; 4% ( n = 68) as Asian. Participants were highly educated with 30% ( n = 528) having a graduate degree, 33% ( n = 587) having a Bachelor’s/4-year degree, 27% having some college education ( n = 487) and only 6% ( n = 108) having a high school GED or less. These demographics reflected the self-reported data we had for all LIFE Apps users, suggesting our survey respondents were representative of the eligible study population.
A majority of the participants (81%, n = 1,442) indicated that their state was under a stay at home order at the time of study participation. On 5-point scales, most participants reported feeling quite or very informed about COVID-19 (M = 3.99, SD = 0.91), and that they were following news about COVID-19 on traditional news outlets quite or very closely (M = 3.44, SD = 1.12).
Looking only at participants randomized to the control group ( n = 637) as a baseline (these individuals had no exposure to COVID-19 information within this study), participants generally expressed moderate to high self-efficacy (M = 4.16, SD = 0.63), high behavioral intentions toward COVID-19 (M = 4.41, SD = 0.722), and moderate perceived threat (M = 3.67, SD = 0.81). According to their self-reports, a majority (> 70%) of participants said they were extremely likely to wash their hands often and practice social distancing. Fewer, but still many, were extremely likely to wear a face mask in public (68%) avoid visiting people they don’t live with (46%), clean and disinfect frequently touched surfaces (49%), or follow government recommendations such as stay-at-home orders (59%). (For all but handwashing, the “extremely likely” intentions for these behaviors went up four to five percentage points among participants who saw a COVID-19 course.) While most participants (53%) somewhat agreed that they feel confident in their ability to protect themselves from COVID-19, only 23% strongly agreed; 38% strongly agreed that they know how to protect themselves. (These percentages increased substantially in the Primer course group, where 29% strongly agreed they feel confident in their ability to protect themselves and 53% strongly agreed they know how to protect themselves.) While most participants in the control group strongly agreed that COVID-19 is serious (60%), only 11% strongly agreed and 35% somewhat agreed that they personally feel at risk because of COVID-19.
Content Experiences—Course Understanding, Learning, and Absorption
To address RQ1, we looked at participants’ experiences with the “flashcard” course content. We specifically looked at self-reported understanding of, learning from, and absorption in the courses. Participants generally reported that all the courses were very easy to understand (M = 4.59, SD = 0.67). See Mean results per course in Table 1 . In an ANCOVA, course condition, age, gender, and level of education had no significant impacts on course understanding.
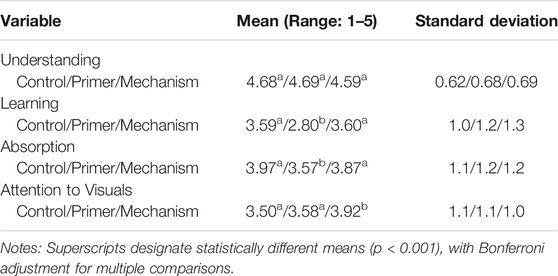
TABLE 1 . Mean values of courses for Understanding, Learning, and Absorption.
Participants who saw the control or Mechanism courses indicated learning (“ I learned a lot ”) significantly more (Bonferroni post hoc test p < 0.001) than those who saw the Primer course (ANOVA, Welch F(2, 1,154.04) = 83.11, p < 0.001). See Mean results per course in Table 1 . The Primer course was designed and written for broad audiences to learn the basics of COVID-19; it contained information that many participants observed in open-ended post-course reflections that they were already aware of through information sources such as the CDC. The Mechanism course was also written for broad audiences but covered more technical information related to COVID-19 and how it works in the body. However, participants with lower levels of education indicated learning more from both of the COVID-19 courses (ANCOVA for COVID-19 conditions only with covariates age, education and gender; R 2 (effect size) = 0.14; Stimulus F(1, 1,083) = 137.18, p < 0.001; Education covariate F(1, 1,083) = 28.59, p < 0.001).
Although we focused on evaluating self-reported content experiences for RQ1, we did conduct a basic 4-item quiz of basic COVID-19 information following stimulus exposure. The quiz scores were generally very high, with over 90% of participants across all conditions answering correctly for each question. However, participants who viewed the Primer course scored slightly but significantly higher (M = 3.92, SD = 0.31; Bonferonni post hoc test p < 0.05) than did those who viewed the control (M = 2.84, SD = 0.44) or Mechanism (M = 3.87, SD = 0.38) courses (ANCOVA across all conditions with covariates age, education and gender; R 2 (effect size) = 0.02; Stimulus F(2, 1,680) = 6.6; p < 01). This result was largely driven by scores for the question of whether coronaviruses are only found in humans or not (significant differences were found across stimulus conditions for this question alone, which was covered in the Primer course), as well as the question about COVID-19 symptoms. Higher education also predicted higher quiz scores (Education covariate F(1, 1,680) = 24.80, p < 0.001).
Participants indicated significantly (Bonferroni post hoc test p < 0.001) greater absorption in the control and Mechanism courses compared to the Primer course (ANOVA, Welch F (2, 1,154.25) = 17.72, p < 0.001). See Mean results per course in Table 1 . Absorption in the course and perceived learning are significantly and moderately correlated (Pearson Correlation = 0.58, p < 0.001).
We also explored whether participants found the course they viewed to be relatable (“ The mini-course was created with people like me in mind .”) (M = 3.53, SD = 1.21). Most people agreed (55%) or neither agreed nor disagreed (26%) that the course was created with people like them in mind. The Mechanism course was evaluated as more relatable (M = 3.73, SD = 1.17), significantly more so (Bonferroni host hoc test p < 0.001) than the Primer course (M = 3.26, SD = 1.30; ANOVA across all stimulus conditions, Welch F (2, 1,156.51) = 21.40, p < 0.001). However, as with perceived learning, lower levels of education were associated with greater evaluation of relatability (ANCOVA across all conditions with covariates age, education and gender; R 2 (effect size) = 0.06; Education covariate F (1, 1,680) = 28.96, p < 0.001). Perceived relatability was significantly and strongly correlated with perceived learning (Pearson Correlation = 0.65, p < 0.001) and absorption (Pearson Correlation = 0.50, p < 0.001). It was weakly but negatively correlated with level of education (Pearson Correlation = −0.12, p < 0.001). The strongest correlation between relatability and level of education existed for those viewing the Primer course, suggesting that this course was particularly well suited to meet the informational needs of people with lower levels of education.
Based on these findings, the illustrated flashcard course format appears to make information about COVID-19 easy to understand for people with high and low levels of education alike. Individuals with lower levels of education indicated learning more from the course they viewed and perceiving it to be created with people like them in mind to a greater extent.
We relied on self-reported data of learning and absorption in the content, which limits robustness of the results. However, data on the time participants spent on the page that linked out to the Lifeology course can provide some context. Participants spent, on average, 3.3 min on the page linking to the sleep course (36 cards), 4 min on the page linking to the Primer course (49 cards), and 4.3 min on the page linking to the Mechanism course (47 cards). A minority (less than 1 out of 5) of participants spent less than a minute, and few spent more than 13 min. Based on previous user testing, a 30-card Lifeology courses takes around 4–6 min for a reader to read aloud. Most participants who completed the survey were engaged enough to spend a few minutes on the content, but didn’t spend so much time that distracted reading (e.g., browsing off) was likely. Time spent was weakly but positively correlated with absorption (Pearson Correlation = 0.10, p < 0.001).
Attention to Visuals
Participants indicated paying significantly closer attention (Bonferroni post hoc test p < 0.001) to the visuals in the Mechanism course compared to the control or Primer courses (ANOVA, Welch F (2, 1,168.41) = 27.89, p < 0.001).
We were also interested in exploring predictors of attention to visuals (RQ2), so we ran a linear regression test predicting this variable with stimulus condition dummy variables, demographic variables, previous knowledge, and following of COVID-19 news (R 2 (effect size) = 0.06; F (8, 1,677) = 13.53, p < 0.001). See results in Table 2 . People who viewed the Mechanism course, people with lower education levels, and people following COVID-19 news closely on traditional media paid closer attention to the course visuals.
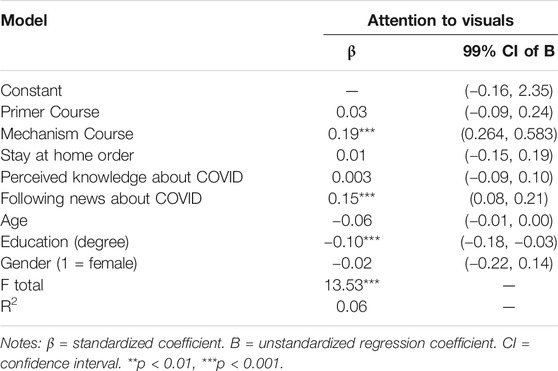
TABLE 2 . Results of linear regression analysis predicting attention to visuals.
Attention to visuals is significantly correlated with absorption in the course content (Pearson Correlation = 0.48, p < 0.001), perceived learning (Pearson Correlation = 0.38, p < 0.001) and relatability (Pearson Correlation = 0.35, p < 0.001).
Means of Self-Efficacy, Perceived Threat and Behavioral Intentions Across Course Conditions
We conducted a series of simple ANOVA tests with Bonferonni post hoc tests for multiple comparisons, followed by a serial mediation analysis, to explore RQ3 and RQ4, and to test our hypotheses H1, H2, and H3. We hypothesized that people who view an illustrated flashcard course about COVID-19 will have increased self-efficacy and behavioral intentions than people who view a control course, and that self-efficacy and perceived threat will mediate course impacts on behavioral intentions. As a reminder, the self-efficacy measure was based on participants self-reported feelings of confidence in their ability to protect themselves from COVID-19, knowledge of how to do so, knowledge of what to do if they got COVID-19 and knowledge of when to seek emergency care. Perceived threat was based on participants’ belief that they could get COVID-19, that they could get very sick, and that COVID-19 is serious; personal feelings of risk because of COVID-19; belief that COVID-19 is serious.
Participants who saw the Primer course (M = 4.35, SD = 0.56) had significantly (p < 0.001) higher self-efficacy for personal COVID-19 prevention and care than did participants who saw either the Mechanism course (M = 4.21, SD = 0.63) or the control course (M = 4.14, SD = 0.63). The means were significantly different overall: Welch F(2, 1,177.80) = 15.62, p < 0.001.
Perceived threat was slightly lower for the Primer course (M = 3.57, SD = 0.79) than for the Mechanism course (M = 3.68, SD = 0.78) or the control course (M = 3.67, SD = 0.81). But the means were not significantly different overall.
Participants who saw the Primer course reported slightly greater behavioral intentions (M = 4.51, SD = 0.64), followed by those who saw the Mechanism course (M = 4.47, SD = 0.69) and those who saw the control course (M = 4.41, SD = 0.72). But the means were not significantly different overall.
Course Impacts on Behavioral Intentions
Analytical approach.
We used the PROCESS macro add-on ( Hayes and Cai, 2007 ) to conduct a serial mediation analysis 11 to test whether and how course viewing was causally linked ( Hayes, 2012 ) to COVID-19 preventive behavioral intentions, both directly and indirectly through attention to visuals, self-efficacy, and perceived threat. Preventive behavioral intentions was the primary outcome variable, course condition was the primary predictor entered as a multi-categorical variable 12 , and self-efficacy and perceived threat were entered as serial mediators. We also included attention to course visuals as a mediator between course viewing and all other outcomes. Given the large sample size used in the present study, we opted for a more stringent level of significance ( α = 0.01). The results are presented in Table 3 .
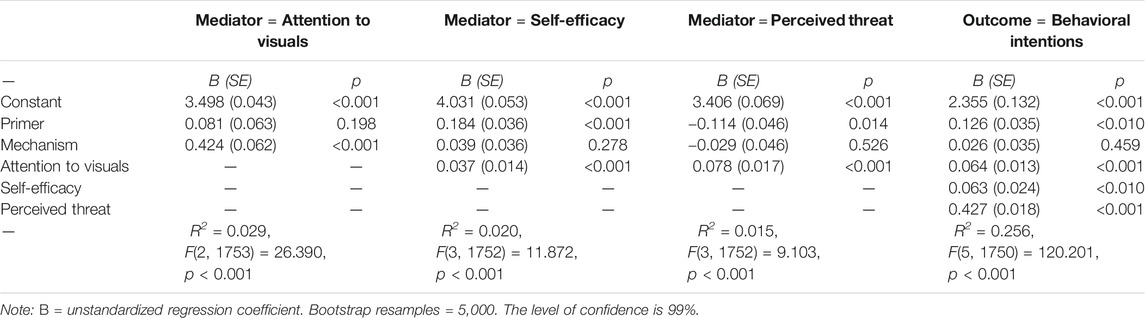
TABLE 3 . The serial mediation model of the effects of course types on preventive behavioral intentions via attention to visuals, self-efficacy, and perceived threat.
Attention to visuals was a significant predictor ( p < 0.01) in a series of regression tests predicting all other mediators and outcomes—self-efficacy (B = 0.037, SE = 0.014), perceived threat (B = 0.078, SE = 0.017) and behavioral intentions (B = 0.064, SE = 0.013). (Effect sizes are generally small; R 2 between 0.5% and 2%.) As we noted previously, people paid significantly closer attention to visuals embedded in the Mechanism course (B = 0.424, SE = 0.061, p < 0.001) compared to the control course (Model R = 0.17, F(2, 1753) = 26.39, p < 0.001). This addresses RQ3 and shows that greater attention to visuals in COVID-19 visual narratives predicts improved outcomes. See arrows connecting attention to visuals and outcomes in Figure 3 .
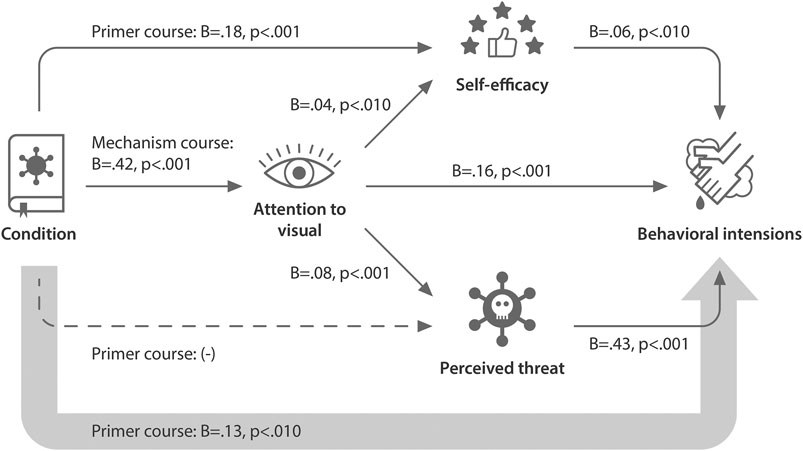
FIGURE 3 . Path diagram illustrating the relative direct and indirect effects of illustrated flashcard course viewing on behavioral intentions toward COVID-19. This path diagram visually represents a serial mediation model of the effects of viewing three different courses on behavioral intentions via attention to the course visuals, self-efficacy, and perceived threat. Solid thin arrows represent significant links between variables ( p < 0.01), dashed thin arrows represent marginally significant links ( p < 0.05). B, unstandardized coefficients showing relationship between variables. The larger arrow connecting condition directly to behavioral intentions denotes the path from predictor to outcome controlling for all mediators. See Table 3 for full results of the regression analyses that this path diagram represents.
We hypothesized in H1 that people who saw a course about COVID-19 would have a greater sense of self-efficacy. Course viewing did have a significant relative direct effect on self-efficacy. Specifically, people who saw the Primer (B = 0.184, SE = 0.036, p < 0.001) as compared to a control course about sleep had improved self-efficacy in terms of protecting themselves from COVID-19. We controlled for attention to visuals (Model R = 0.141, F(3, 1752) = 11.87, p < 0.001). Attention to visuals was also a significant predictor in this regression model (B = 0.036, SE = 0.0136, p < 0.01). We found partial support for H1, based on the relative impacts of a COVID-19 Prevention Primer course. See arrows connecting the course stimulus condition to self-efficacy in Figure 3 .
Course viewing did not have a significant relative direct effect on perceived threat. However, attention to the course visuals was a significant predictor (Model R = 0.124, F(3, 1752) = 9.10, p < 0.001; B = 0.078, SE = 0.017, p < 0.001).
As hypothesized in H2, people who saw a COVID-19 course as compared to a control course about sleep had greater behavioral intentions toward COVID-19. There was a significant relative direct effect of Primer course viewing on behavioral intentions, controlling for attention to visuals, self-efficacy, and perceived threat (Model R = 0.51, R 2 (effect size) = 0.26, F(5, 1750) = 120.20, p < 0.001). See the large arrow directly connecting course condition to behavioral intentions in Figure 3 . People who viewed the Primer course had greater behavioral intentions toward protecting themselves from COVID-19 compared to those who viewed a control course (B = 0.126, SE = 0.035, p < 0.001, 99% bootstrap confidence interval: 0.035, 0.217). Attention to visuals (B = 0.064, p < 0.001), self-efficacy (B = 0.063, p < 0.01) and perceived threat (B = 0.427, p < 0.001) were all significant predictors in this regression model. We found partial support for H2, based on the relative impacts of a COVID-19 Prevention Primer course.
There was a significant indirect effect from Primer course → self-efficacy → behavioral intentions (B = 0.011, SE = 0.005, 99% bootstrap confidence interval: 0.000, 0.027). The bootstrap confidence intervals were based on 5,000 bootstrap samples.
There was a significant indirect effect from Mechanism course → attention to visuals → behavioral intentions (B = 0.027, SE = 0.007, 99% bootstrap confidence interval: 0.011, 0.047). The indirect effect from Mechanism course → attention to visuals → perceived threat → behaviors was also significant (B = 0.014, SE = 0.004, 99% bootstrap confidence interval: 0.005, 0.026).
As hypothesized in H3, both self-efficacy and perceived threat mediated the impact of course viewing on behavioral intentions. Self-efficacy was a key mediator of the impact of viewing a COVID-19 Prevention Primer course on behavioral intentions, while perceived threat was a key mediator of the impact of viewing a COVID-19 Mechanism course on behavioral intentions.
Visual narratives are a useful tool for engaging broad audiences in risk messages and public health precautions for COVID-19. We found that illustrated flashcard courses (visual narratives) about COVID-19 were perceived as understandable and engaging for a relatively broad audience, regardless of level of education. The effect sizes for these relationships were typically small but robust, where stimulus condition and other key independent variables often explained 1–6% of the variance in outcome metrics.
We also found that viewing an illustrated flashcard course about COVID-19 resulted in improved perceptions of self-efficacy and behavioral intentions. The stimulus condition, attention to the visuals, self-efficacy and perceived threat explained a substantial amount of the variance in behavioral intentions (over 25%). Visual narratives may improve health literacy, or capacity to understand and act on health information.
Interestingly, the COVID-19 Primer course impacted self-efficacy and behavioral intentions even though, on average, people indicated not necessarily learning anything new from the content. Participants viewing our COVID-19 courses had most likely come across similar information in other formats based on their existing knowledge of COVID-19, but these formats may not have made the information as accessible and relatable to their daily lives. Our results also suggest that visual narratives may improve health outcomes and disease prevention.
While both of the courses about COVID-19 had positive outcomes compared to a control course, they impacted self-efficacy and perceived threat to different extents. The Prevention Primer course was particularly effective in improving self-efficacy and behavioral intentions directly. This course visually told a story of a family’s journey through a COVID-19 outbreak in their city and their experience when a younger family member got sick. The course visuals showed characters expressing concern but ultimately modeling preventative behaviors such as handwashing for at least 20 s, social distancing, and safely caring for a sick family member. It also provided actionable takeaways. All of these features likely contributed to the course’s impact on self-reported self-efficacy and behavioral intentions. On the other hand, the impact of the COVID-19 Mechanism course on behavioral intentions was primarily mediated by greater self-reported attention to the course visuals and perceived threat from COVID-19. This course explained how the coronavirus works in the body and why some people are at greater risk of severe illness, again with actionable takeaways.
Across both COVID-19 courses, greater self-reported attention to the visuals mediated the impacts of course viewing on self-efficacy, perceived threat, and behavioral intentions. We also found support for the idea that people with lower levels of formal education rely to a greater extent on visuals in these educational materials. This seems to be particularly true when the materials contain more technical science and health information. The more technical Mechanism course received slightly lower ease of understanding scores than the Primer and control courses. Participants who saw this course also reported paying significantly greater attention to the course visuals than did participants who saw the Primer course or the control course. Greater self-reported attention to the visuals in the Mechanism course in turn mediated a significant impact on perceived threat, and thus protective behavioral intentions.
Other factors beyond the level of technical content in the Mechanism course could also have contributed to the self-reported attention to the visuals in this course. The course contained more interpretational visuals, defined as representing information associated with as opposed to directly representing the textual referents ( Haragi et al., 2019 ). These types of visuals have previously been found to invite interpretation and elaboration of content, and to improve self-reported understanding, memorability, and interest ( Haragi et al., 2019 ). However, future research is needed to explore whether it was the greater level of difficulty of this course that truly drove greater attention to visuals, or some other aspect of the visuals in this course.
Implications
This study fills a gap in literature looking at the real-world, holistic impact of health education materials that combine text, narrative, and visuals. The lack of research in this area may stem from the lack of health education materials that make effective, data-driven use of stories and visuals. But why are these materials missing from the media landscape? One of the reasons may be a dearth of collaboration between scientific and art communities. There are a growing number but still few resources and spaces that make it easy for scientists, artists, and communication experts to work together on such materials. However, calls for collaboration between scientists and creatives are increasing ( Khoury et al., 2019 ; Botsis et al., 2020 ; Murchie and Diomede, 2020 ). Art-science platforms including Art The Science, Lifeology, the SciArt Initiative, and others are facilitating this collaboration through nascent online spaces that bring people from STEM and art fields together.
It is difficult today to assess visual quality or exactly how “good” illustrations improve information processing ( McGrath and Brown, 2005 ). Different people have different tastes in the aesthetics of artwork that may stem from their cultural or social background. For this reason, it is important that the public have diverse options in terms of illustrated educational content available to them, created by diverse artists in diverse styles and cultural contexts.
Limitations
Participants in this study represented U.S. users of popular health tracking apps (the LIFE Apps). These apps have a broad user base with over 2.5 million users. Users of these apps are likely to be motivated to improve their health and adopt positive health behaviors; however, many join the app because they are struggling to achieve their health and weight loss goals. Most of the participants were highly educated. This does not necessarily mean that they had high health literacy levels, as even highly educated people can struggle to understand and apply technical health information. However, the results of our study are limited by this sample and the fact that we did not directly assess the health literacy level of our participants. While we did confirm that our courses were broadly understandable and had positive outcomes for a subset of our participants who had less than a high school education, outcomes could be different for people facing more substantial language, reading level, and internet access barriers.
Creators of visual narrative educational materials for science and health communication should always design their messages and content with target audiences in mind and evaluate their materials early among those target audiences. Future studies could target evaluation of visual narratives and illustrated flashcard courses in different languages within low-literacy populations, non-English-speaking populations, rural populations, racial and ethnic minorities, etc.
This study is also limited by not comparing the flashcard courses to the same messages presented in non-visual and/or non-narrative formats. We don’t know how much the narrative elements of the courses (story, characters, emotions, etc.) distinctly contributed to the outcomes, separately from the visual elements and factual information presented. However, this would have been difficult to test in practice, as both the visuals and the text of the courses contained narrative as well as informational elements.
Another important limitation of this study is self-reported data. To measure learning outcomes, we would have needed to assess knowledge before and after viewing the courses ( Jensen, 2014 ). However, we note that the COVID-19 courses had positive outcomes even though participants generally reported being quite informed beforehand. Self-reported behavioral intentions also do not fully predict behaviors ( Sheeran and Webb, 2016 ). However, the self-reported data can still tell us a lot about people’s experiences of the content and how prepared and motivated it helped them feel to protect themselves and others from COVID-19. Measures of enjoyment and absorption in content often rely on self-reports related to how much people enjoyed the content, whether it held their attention or if they were distracted by other things while viewing the content. However, real-world measured data for these variables would provide greater insight.
There was the possibility of bias in people’s responses to experiences of the content. To try to prevent this, we assured survey respondents that their responses were anonymous, and we asked for honest evaluation to help us create better content for others. None of the content was branded by LifeOmic or LIFE Apps to avoid eliciting any identity with or loyalty to the LIFE Apps brand. LIFE Apps users also do not pay to use their apps and are often invited to join various other health research projects where strict privacy and HIPAA regulations apply. The risk that they joined this study because of any social pressure or experienced pressure to “like” the educational content displayed is no more likely than in other survey experiments, in our opinion.
Finally, we also acknowledge that we did not fully test or directly manipulate all factors of the EPPM in this study, particularly fear. We leveraged materials that had already been created and designed survey questions around the messages contained in these materials, with a focus on practical takeaways. While this approach has its strengths in terms of evaluating new educational resources at a high level in a real-world setting, it is limited when it comes to pinpointing effect mechanisms.
Takeaways and Recommendations
New visual narrative formats have the potential to substantially improve engagement on issues of pressing public health concern. These formats are also ripe for future research.
In the process of conducting this study, starting with the collaborative creation the “flashcard” courses evaluated herein, we learned a lot about how to create effective visual educational materials science and health. We’ve curated some of what we learned into actionable tips below. (We are also leveraging lessons learned into a series of Lifeology SciComm “flashcard” courses 13 that help scientists and communicators learn evidence-based science and health communication practices.) This advice is based on our own process for and experiences in creating the materials evaluated in this study. It is based on factors that we think may have contributed to the impact of our materials. Future research should pin-point the role of these different strategies in making health education materials more effective.
1) Use plain language and non-clinical, narrative illustrations to improve understanding and relatability of science and health messages.
2) Assemble interdisciplinary teams in the creation of visual narrative materials. Collaborate with local professional artists and storytellers.
3) Use visuals that complement text. Avoid decorative visuals or ones that are either exact visual representations or conversely are unrelated to the text. Visuals might communicate helpful metaphors or help the viewer interpret or create accurate mental models of abstract concepts or hidden processes.
4) Include empowering stories of characters who face struggles, express relatable emotions, and achieve ultimately positive outcomes or a change in perspective through desired behaviors. Be compassionate when visualizing characters.
5) Be inclusive and illustrate a diversity of characters to engage a diverse audience.
Data Availability Statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Alex Cohen, Louisiana State University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
PJ, DA, and MF are full-time employees of LifeOmic, a private health software company that owns and operates Lifeology, the platform being used and evaluated in this study. PJ, DA, and MF have received management incentive units (a form of equity compensation) in LifeOmic. Survey participants were recruited from the LifeOmic LIFE health tracking apps and incentives (e.g., free LifeOmic t-shirts) were randomly provided for 5 participants.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2021.712658/full#supplementary-material
1 https://education.gsu.edu/research-outreach/alrc/adult-literacy-coronavirus-resource-links/
2 https://www.oecd.org/skills/piaac/ ; https://nces.ed.gov/datapoints/2019179.asp
3 https://www.talenthouse.com/i/united-nations-global-call-out-to-creatives-help-stop-the-spread-of-covid-19 . The call has been controversial among artists on account of asking for free labor in exchange for “exposure”.
4 https://app.us.lifeology.io/viewer/lifeology/default/how-is-a-lifeology-course-created
5 https://app.us.lifeology.io/viewer/lifeology/default/why-do-we-sleep
6 https://app.us.lifeology.io/viewer/lifeology/default/2019-novel-coronavirus
7 https://app.us.lifeology.io/viewer/lifeology/default/what-does-the-coronavirus-do-in-my-body
8 https://www.ahrq.gov/health-literacy/patient-education/pemat-p.html
9 N/A scores given to items on headers and narration
10 N/A scores given to calculations and charts
11 The sample size for the PROCESS analysis was 1765, the custom seed was 20200617
12 Entered as dummy variables relative to the control group
13 https://lifeology.io/lifeology-univ-scicomm/
Abdel-Latif, M. M. M. (2020). The enigma of Health Literacy and COVID-19 Pandemic. Public Health 185, 95–96. doi:10.1016/j.puhe.2020.06.030
PubMed Abstract | CrossRef Full Text | Google Scholar
Agarwal, R., and Karahanna, E. (2000). Time Flies when You're Having Fun: Cognitive Absorption and Beliefs about Information Technology Usage. MIS Q. 24, 665–694. doi:10.2307/3250951
CrossRef Full Text | Google Scholar
Aisami, R. S. (2015). Learning Styles and Visual Literacy for Learning and Performance. Procedia Soc. Behav. Sci. 176, 538–545.
Bailey, Meryl. (2020). COVID-19 in Translation: Making Patient Education Accessible . Boston: HealthCity . Available at: https://www.bmc.org/healthcity/policy-and-industry/covid-19-translation-making-patient-education-accessible (Accessed on June 22, 2020).
Beutel, T. F., Zwerenz, R., and Michal, M. (2018). Psychosocial Stress Impairs Health Behavior in Patients with Mental Disorders. BMC psychiatry 18 (1), 375. doi:10.1186/s12888-018-1956-8
Botsis, T., Fairman, J. E., Moran, M. B., and Anagnostou, V. (2020). Visual Storytelling Enhances Knowledge Dissemination in Biomedical Science. J. Biomed. Inform. 103458.
Caballero, A., Leath, K., and Watson, J. (2020). COVID-19 Consumer Health Information Needs Improvement to Be Readable and Actionable by High-Risk Populations. Front. Commun. 5, 56. doi:10.3389/fcomm.2020.00056
CDC (2020). COVID-19 in Racial and Ethnic Minority Groups. COVID-19 . Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html (Accessed on June 22, 2020).
CDC (2021). Understanding Health Literacy. Health Literacy . Available at: https://www.cdc.gov/healthliteracy/learn/Understanding.html (Accessed on June 22, 2021).
Chaiken, S. (1980). Heuristic versus Systematic Information Processing and the Use of Source versus Message Cues in Persuasion. J. Personal. Soc. Psychol. 39 (5), 752–766. doi:10.1037/0022-3514.39.5.752
Chan, C. S. R., and Park, H. D. (2015). How Images and Color in Business Plans Influence Venture Investment Screening Decisions. J. business Venturing 30 (5), 732–748. doi:10.1016/j.jbusvent.2014.12.002
Cvijikj, I. P., and Michahelles, F. (2013). Online Engagement Factors on Facebook Brand Pages. Social Netw. Anal. mining 3 (4), 843–861.
Google Scholar
Day, V. (2009). Promoting Health Literacy through Storytelling. OJIN: Online J. Issues Nurs. 14 (3), 6.
Dayan, Z. (2018). Visual Content: The Future of Storytelling. Forbes. Available at: https://www.forbes.com/sites/forbestechcouncil/2018/04/02/visual-content-the-future-of-storytelling/?sh=288d4afd3a46 (Accessed on July 3, 2021). doi:10.33107/ubt-ic.2018.360
Delp, C., and Jones, J. (1996). Communicating Information to Patients: the Use of Cartoon Illustrations to Improve Comprehension of Instructions. Acad. Emerg. Med. 3 (3), 264–270. doi:10.1111/j.1553-2712.1996.tb03431.x
Demircelik, M. B., Cakmak, M., Nazli, Y., Şentepe, E., Yigit, D., Keklik, M., et al. (2016). Effects of Multimedia Nursing Education on Disease-Related Depression and Anxiety in Patients Staying in a Coronary Intensive Care Unit. Appl. Nurs. Res. 29, 5–8. doi:10.1016/j.apnr.2015.03.014
Eichler, K., Wieser, S., and Brügger, U. (2009). The Costs of Limited Health Literacy: a Systematic Review. Int. J. Public Health 54, 313–324. doi:10.1007/s00038-009-0058-2
Farinella, M., and Mbakile-Mahlanza, L. (2020). Making the Brain Accessible with Comics. World Neurosurg. 133, 426–430. doi:10.1016/j.wneu.2019.10.168
Farinella, M. (2018). The Potential of Comics in Science Communication. Jcom 17 (01), Y01. doi:10.22323/2.17010401
Frieden, Joyce. (2020). Lack of Health Literacy a Barrier to Grasping COVID-19. MedPage Today . Available at: https://www.medpagetoday.com/infectiousdisease/covid19/87002 (Accessed on June 22, 2020).
Green, M. C., and Brock, T. C. (2002). “In the Mind's Eye: Transportation-Imagery Model of Narrative Persuasion,” in Narrative Impact: Social and Cognitive Foundations . Editors M. C. Green, J. J. Strange, and T. C. Brock ( Lawrence Erlbaum Associates Publishers ), 315–341.
Haragi, M., Ishikawa, H., and Kiuchi, T. (2019). Investigation of Suitable Illustrations in Medical Care. J. Vis. Commun. Med. 42 (4), 158–168. doi:10.1080/17453054.2019.1633237
Hart, T. L., Blacker, S., Panjwani, A., Torbit, L., and Evans, M. (2015). Development of Multimedia Informational Tools for Breast Cancer Patients with Low Levels of Health Literacy. Patient Educ. Couns. 98 (3), 370–377. doi:10.1016/j.pec.2014.11.015
Hayes, A. F., and Cai, L. (2007). Using Heteroskedasticity-Consistent Standard Error Estimators in OLS Regression: An Introduction and Software Implementation. Behav. Res. Methods 39 (4), 709–722. doi:10.3758/bf03192961
Hayes, J. R., and Process, (2012). A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling. [White paper] 2012. Available at: http://www.afhayes.com/public/process2012.pdf (Accessed on June 22, 2020). doi:10.1037/e533652013-424
Houts, P. S., Doak, C. C., Doak, L. G., and Loscalzo, M. J. (2006). The Role of Pictures in Improving Health Communication: a Review of Research on Attention, Comprehension, Recall, and Adherence. Patient Educ. Couns. 61 (2), 173–190. doi:10.1016/j.pec.2005.05.004
Igarashi, Y., Mizushima, N., and Yokoyama, H. M. (2020). Manga-based Risk Communication for the COVID-19 Pandemic: a Case Study of Storytelling that Incorporates a Cultural Context. Jcom 19 (7), N02. doi:10.22323/2.19070802
Jensen, E. A., and Gerber, A. (2020). Evidence-based Science Communication. Front. Commun. 4, 78. doi:10.3389/fcomm.2019.00078
Jensen, E. (2014). The Problems with Science Communication Evaluation. Jcom 13 (1), C04. doi:10.22323/2.13010304
Jones, C. L., Jensen, J. D., Scherr, C. L., Brown, N. R., Christy, K., and Weaver, J. (2015). The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation. Health Commun. 30 (6), 566–576. doi:10.1080/10410236.2013.873363
Kagan, S. H. (2018). Using story and Art to Improve Education for Older Patients and Their Caregivers. Geriatr. Nurs. 39 (1), 119–121. doi:10.1016/j.gerinurse.2017.12.008
Kahneman, D. (2003). Maps of Bounded Rationality: Psychology for Behavioral Economics. Am. Econ. Rev. 93, 1449–1475. doi:10.1257/000282803322655392
Kamalakannan, S., Bhattacharjya, S., Bogdanova, Y., Papadimitriou, C., Arango-Lasprilla, J., Bentley, J., et al. (2021). Health Risks and Consequences of a COVID-19 Infection for People with Disabilities: Scoping Review and Descriptive Thematic Analysis. Ijerph 18 (8), 4348. doi:10.3390/ijerph18084348
Kassai, B., Rabilloud, M., Dantony, E., Grousson, S., Revol, O., Malik, S., et al. (2016). Introduction of a Paediatric Anaesthesia Comic Information Leaflet Reduced Preoperative Anxiety in Children. Br. J. Anaesth. 117 (1), 95–102. doi:10.1093/bja/aew154
Katz, S. J., Erkkinen, M., Lindgren, B., and Hatsukami, D. (2018). Assessing the Impact of Conflicting Health Warning Information on Intentions to Use E-Cigarettes-An Application of the Heuristic-Systematic Model. J. Health Commun. 23 (10-11), 874–885. doi:10.1080/10810730.2018.1533052
Khoury, C. K., Kisel, Y., Kantar, M., Barber, E., Ricciardi, V., Klirs, C., et al. (2019). Science–graphic Art Partnerships to Increase Research Impact. Commun. Biol. 2 (1), 1–5. doi:10.1038/s42003-019-0516-1
Kickbusch, I., Pelikan, J. M., and Apfel, F. (2013). Health Literacy: The Solid Facts . Editors A. D. Tsouros World Health Organization .
Kim, D. H., Spiller, L., and Hettche, M. (2015). Analyzing media Types and Content Orientations in Facebook for Global Brands. J. Res. Interactive Marketing . doi:10.14257/astl.2015.113.06
Kim, J. W. (2018). They Liked and Shared: Effects of Social media Virality Metrics on Perceptions of Message Influence and Behavioral Intentions. Comput. Hum. Behav. 84, 153–161. doi:10.1016/j.chb.2018.01.030
Kim, S., Trinidad, B., Mikesell, L., and Aakhus, M. (2020). Improving Prognosis Communication for Patients Facing Complex Medical Treatment: A User-Centered Design Approach. Int. J. Med. Inform. , 104147. doi:10.1109/cbms49503.2020.00075
Kolb, D. A. (1984). Experiential Learning: Experience as the Source of Learning and Development . Englewood Cliffs, NJ: Prentice-Hall .
Lahuerta-Otero, E., Cordero-Gutiérrez, R., and De la Prieta-Pintado, F. (2018). Retweet or like? that Is the Question. Oir 42 (5), 562–578. doi:10.1108/oir-04-2017-0135
Lazard, A., and Atkinson, L. (2015). Putting Environmental Infographics Center Stage. Sci. Commun. 37 (1), 6–33. doi:10.1177/1075547014555997
Leung, M. M., Tripicchio, G., Agaronov, A., and Hou, N. (2014). Manga Comic Influences Snack Selection in Black and Hispanic New York City Youth. J. Nutr. Education Behav. 46 (2), 142–147. doi:10.1016/j.jneb.2013.11.004
Mayer, R. E. (1997). Multimedia Learning: Are We Asking the Right Questions? Educ. Psychol. 32 (1), 1–19. doi:10.1207/s15326985ep3201_1
Mayer, R. E. (2003). The Promise of Multimedia Learning: Using the Same Instructional Design Methods across Different media. Learn. instruction 13 (2), 125–139. doi:10.1016/s0959-4752(02)00016-6
McGrath, M. B., and Brown, J. R. (2005). Visual Learning for Science and Engineering. IEEE Comput. Grap. Appl. 25 (5), 56–63. doi:10.1109/mcg.2005.117
McLaughlin, G. H. (1969). SMOG Grading-A New Readability Formula. J. reading 12 (8), 639–646.
Metzger, M. J., Flanagin, A. J., and Medders, R. B. (2010). Social and Heuristic Approaches to Credibility Evaluation Online. J. Commun. 60 (3), 413–439. doi:10.1111/j.1460-2466.2010.01488.x
Middleton, K. R., Anton, S. D., and Perri, M. G. (2013). Long-term Adherence to Health Behavior Change. Am. J. lifestyle Med. 7 (6), 395–404. doi:10.1177/1559827613488867
Murchie, K. J., and Diomede, D. (2020). Fundamentals of Graphic Design-Essential Tools for Effective Visual Science Communication. FACETS 5, 409–422. doi:10.1139/facets-2018-0049
Muzumdar, J. M., and Pantaleo, N. L. (2017). Comics as a Medium for Providing Information on Adult Immunizations. J. Health Commun. 22 (10), 783–791. doi:10.1080/10810730.2017.1355418
Nova, F., Allenidekania, A., and Agustini, N. (2019). The Effect of Multimedia-Based Nutrition Education on Parents' Knowledge and Body Weight Change in Leukemia Children. Enfermería Clínica 29, 229–233. doi:10.1016/j.enfcli.2019.04.027
Oh, J., Bellur, S., and Sundar, S. S. (2015). Clicking, Assessing, Immersing, and Sharing: An Empirical Model of User Engagement with Interactive media. Commun. Res. 45 (5), 737–763. doi:10.1177/0093650215600493
Ohyama, S., Yokota, C., Miyashita, F., Amano, T., Inoue, Y., Shigehatake, Y., et al. (2015). Effective Education Materials to advance Stroke Awareness without Teacher Participation in Junior High School Students. J. Stroke Cerebrovasc. Dis. 24 (11), 2533–2538. doi:10.1016/j.jstrokecerebrovasdis.2015.07.001
Okan, O., Bollweg, T. M., Berens, E.-M., Hurrelmann, K., Bauer, U., and Schaeffer, D. (2020). Coronavirus-related Health Literacy: A Cross-Sectional Study in Adults during the COVID-19 Infodemic in Germany. Ijerph 17 (15), 5503. doi:10.3390/ijerph17155503
Osborne, M. E. (2012). Health Literacy from A to Z . Lake Placid: Jones & Bartlett Publishers . doi:10.30965/9783846752746
CrossRef Full Text
Paakkari, L., and Okan, O. (2020). COVID-19: Health Literacy Is an Underestimated Problem. The Lancet Public Health 5 (5), e249–e250. doi:10.1016/s2468-2667(20)30086-4
Paasche-Orlow, M. K., and Wolf, M. S. (2007). The Causal Pathways Linking Health Literacy to Health Outcomes. Am. J. Health Behav. 31 (Suppl. 1), 19–26. doi:10.5993/ajhb.31.s1.4
Paasche-Orlow, M. K., Parker, R. M., Gazmararian, J. A., Nielsen-Bohlman, L. T., and Rudd, R. R. (2005). The Prevalence of Limited Health Literacy. J. Gen. Intern. Med. 20 (2), 175–184. doi:10.1111/j.1525-1497.2005.40245.x
Park, C. L., Russell, B. S., Fendrich, M., Finkelstein-Fox, L., Hutchison, M., and Becker, J. (2020). Americans' COVID-19 Stress, Coping, and Adherence to CDC Guidelines. J. Gen. Intern. Med. 35 (8), 2296–2303. doi:10.1007/s11606-020-05898-9
Popova, L. (2012). The Extended Parallel Process Model. Health Educ. Behav. 39 (4), 455–473. doi:10.1177/1090198111418108
Schaeffer, K., and Rainie, L. (2020). Experiences with the COVID-19 Outbreak Can Vary for Americans of Different Age s . Pew Research Center. Available at: https://www.pewresearch.org/fact-tank/2020/06/16/experiences-with-the-covid-19-outbreak-can-vary-for-americans-of-different-ages/ (Accessed on June 22, 2020).
Schnotz, W., and Bannert, M. (2003). Construction and Interference in Learning from Multiple Representation. Learn. Instruction 13 (2), 141–156. doi:10.1016/s0959-4752(02)00017-8
Sheeran, P., Maki, A., Montanaro, E., Avishai-Yitshak, A., Bryan, A., Klein, W. M. P., et al. (2016). The Impact of Changing Attitudes, Norms, and Self-Efficacy on Health-Related Intentions and Behavior: A Meta-Analysis. Health Psychol. 35 (11), 1178–1188. doi:10.1037/hea0000387
Sheeran, P., and Webb, T. L. (2016). The Intention-Behavior Gap. Social Personal. Psychol. Compass 10 (9), 503–518. doi:10.1111/spc3.12265
Shoemaker, S. J., Wolf, M. S., and Brach, C. (2014). Development of the Patient Education Materials Assessment Tool (PEMAT): a New Measure of Understandability and Actionability for Print and Audiovisual Patient Information. Patient Education Couns. 96 (3), 395–403. doi:10.1016/j.pec.2014.05.027
Simmons, R. A., Cosgrove, S. C., Romney, M. C., Plumb, J. D., Brawer, R. O., Gonzalez, E. T., et al. (2017). Health Literacy: Cancer Prevention Strategies for Early Adults. Am. J. Prev. Med. 53 (3), S73–S77. doi:10.1016/j.amepre.2017.03.016
Sørensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., et al. (2012). Health Literacy and Public Health: a Systematic Review and Integration of Definitions and Models. BMC public health 12 (1), 80–13. doi:10.1186/1471-2458-12-80
Taber, K. S. (2018). The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 48 (6), 1273–1296.
Tekle-Haimanot, R., Preux, P. M., Gerard, D., Worku, D. K., Belay, H. D., and Gebrewold, M. A. (2016). Impact of an Educational Comic Book on Epilepsy-Related Knowledge, Awareness, and Attitudes Among School Children in Ethiopia. Epilepsy Behav. 61, 218–223. doi:10.1016/j.yebeh.2016.05.002
Townsend, M. S., Sylva, K., Martin, A., Metz, D., and Wooten-Swanson, P. (2008). Improving Readability of an Evaluation Tool for Low-Income Clients Using Visual Information Processing Theories. J. Nutr. Education Behav. 40 (3), 181–186. doi:10.1016/j.jneb.2007.06.011
Vagg, T., Balta, J. Y., Bolger, A., and Lone, M. (2020). Multimedia in Education: What Do the Students Think?. Health Prof. Educ. 6 (3), 325–333.
Wang, X., Chen, L., Shi, J., and Peng, T.-Q. (2019). What Makes Cancer Information Viral on Social media? Comput. Hum. Behav. 93, 149–156. doi:10.1016/j.chb.2018.12.024
Wang, Z., Wang, S., Farinella, M., Murray-Rust, D., Henry Riche, N., and Bach, B. (2019). Comparing Effectiveness and Engagement of Data Comics and Infographics. Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems , 1–12.
Webster, J., and Ho, H. (1997). Audience Engagement in Multimedia Presentations. SIGMIS Database 28, 63–77. doi:10.1145/264701.264706
WHO, (2020a). Risk Communication and Community Engagement Readiness and Response to Coronavirus Disease (COVID-19): Interim Guidance . World Health Organization , 19. Available at: https://apps.who.int/iris/handle/10665/331513 (Accessed on June 22, 2020).
WHO, (2020b). Principle: Understandable . Available at: https://www.who.int/about/communications/understandable Accessed on June, 22, 2020.
Witte, K., Cameron, K. A., McKeon, J. K., and Berkowitz, J. M. (1996). Predicting Risk Behaviors: Development and Validation of a Diagnostic Scale. J. Health Commun. 1, 317–342. doi:10.1080/108107396127988
Witte, K. (1994). Fear Control and Danger Control: A Test of the Extended Parallel Process Model (EPPM). Commun. Monogr. 61 (2), 113–134. doi:10.1080/03637759409376328
Zhao, M., Zhao, D., Wei, J., and Wang, F. (2015). The Effects of Firm Action Messages on the Information Processing and Risk Perception of Customers. Risk Manag. 17 (4), 205–225. doi:10.1057/rm.2015.13
Keywords: COVID-19, visual narratives, public engagement, visual communication, storytelling
Citation: Jarreau PB, Su LY-F, Chiang EC-L, Bennett SM, Zhang JS, Ferguson M and Algarra D (2021) COVID ISSUE: Visual Narratives About COVID-19 Improve Message Accessibility, Self-Efficacy, and Health Precautions. Front. Commun. 6:712658. doi: 10.3389/fcomm.2021.712658
Received: 20 May 2021; Accepted: 26 July 2021; Published: 18 August 2021.
Reviewed by:
Copyright © 2021 Jarreau, Su, Chiang, Bennett, Zhang, Ferguson and Algarra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paige Brown Jarreau, [email protected]
This article is part of the Research Topic
Evidence-Based Science Communication in the COVID-19 Era
Why the Pandemic Probably Started in a Lab, in 5 Key Points

By Alina Chan
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “Viral: The Search for the Origin of Covid-19.”
This article has been updated to reflect news developments.
On Monday, Dr. Anthony Fauci returned to the halls of Congress and testified before the House subcommittee investigating the Covid-19 pandemic. He was questioned about several topics related to the government’s handling of Covid-19, including how the National Institute of Allergy and Infectious Diseases, which he directed until retiring in 2022, supported risky virus work at a Chinese institute whose research may have caused the pandemic.
For more than four years, reflexive partisan politics have derailed the search for the truth about a catastrophe that has touched us all. It has been estimated that at least 25 million people around the world have died because of Covid-19, with over a million of those deaths in the United States.
Although how the pandemic started has been hotly debated, a growing volume of evidence — gleaned from public records released under the Freedom of Information Act, digital sleuthing through online databases, scientific papers analyzing the virus and its spread, and leaks from within the U.S. government — suggests that the pandemic most likely occurred because a virus escaped from a research lab in Wuhan, China. If so, it would be the most costly accident in the history of science.
Here’s what we now know:
1 The SARS-like virus that caused the pandemic emerged in Wuhan, the city where the world’s foremost research lab for SARS-like viruses is located.
- At the Wuhan Institute of Virology, a team of scientists had been hunting for SARS-like viruses for over a decade, led by Shi Zhengli.
- Their research showed that the viruses most similar to SARS‑CoV‑2, the virus that caused the pandemic, circulate in bats that live r oughly 1,000 miles away from Wuhan. Scientists from Dr. Shi’s team traveled repeatedly to Yunnan province to collect these viruses and had expanded their search to Southeast Asia. Bats in other parts of China have not been found to carry viruses that are as closely related to SARS-CoV-2.

The closest known relatives to SARS-CoV-2 were found in southwestern China and in Laos.
Large cities
Mine in Yunnan province
Cave in Laos
South China Sea

The closest known relatives to SARS-CoV-2
were found in southwestern China and in Laos.
philippines

The closest known relatives to SARS-CoV-2 were found
in southwestern China and Laos.
Sources: Sarah Temmam et al., Nature; SimpleMaps
Note: Cities shown have a population of at least 200,000.

There are hundreds of large cities in China and Southeast Asia.

There are hundreds of large cities in China
and Southeast Asia.

The pandemic started roughly 1,000 miles away, in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away,
in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away, in Wuhan,
home to the world’s foremost SARS-like virus research lab.
- Even at hot spots where these viruses exist naturally near the cave bats of southwestern China and Southeast Asia, the scientists argued, as recently as 2019 , that bat coronavirus spillover into humans is rare .
- When the Covid-19 outbreak was detected, Dr. Shi initially wondered if the novel coronavirus had come from her laboratory , saying she had never expected such an outbreak to occur in Wuhan.
- The SARS‑CoV‑2 virus is exceptionally contagious and can jump from species to species like wildfire . Yet it left no known trace of infection at its source or anywhere along what would have been a thousand-mile journey before emerging in Wuhan.
2 The year before the outbreak, the Wuhan institute, working with U.S. partners, had proposed creating viruses with SARS‑CoV‑2’s defining feature.
- Dr. Shi’s group was fascinated by how coronaviruses jump from species to species. To find viruses, they took samples from bats and other animals , as well as from sick people living near animals carrying these viruses or associated with the wildlife trade. Much of this work was conducted in partnership with the EcoHealth Alliance, a U.S.-based scientific organization that, since 2002, has been awarded over $80 million in federal funding to research the risks of emerging infectious diseases.
- The laboratory pursued risky research that resulted in viruses becoming more infectious : Coronaviruses were grown from samples from infected animals and genetically reconstructed and recombined to create new viruses unknown in nature. These new viruses were passed through cells from bats, pigs, primates and humans and were used to infect civets and humanized mice (mice modified with human genes). In essence, this process forced these viruses to adapt to new host species, and the viruses with mutations that allowed them to thrive emerged as victors.
- By 2019, Dr. Shi’s group had published a database describing more than 22,000 collected wildlife samples. But external access was shut off in the fall of 2019, and the database was not shared with American collaborators even after the pandemic started , when such a rich virus collection would have been most useful in tracking the origin of SARS‑CoV‑2. It remains unclear whether the Wuhan institute possessed a precursor of the pandemic virus.
- In 2021, The Intercept published a leaked 2018 grant proposal for a research project named Defuse , which had been written as a collaboration between EcoHealth, the Wuhan institute and Ralph Baric at the University of North Carolina, who had been on the cutting edge of coronavirus research for years. The proposal described plans to create viruses strikingly similar to SARS‑CoV‑2.
- Coronaviruses bear their name because their surface is studded with protein spikes, like a spiky crown, which they use to enter animal cells. T he Defuse project proposed to search for and create SARS-like viruses carrying spikes with a unique feature: a furin cleavage site — the same feature that enhances SARS‑CoV‑2’s infectiousness in humans, making it capable of causing a pandemic. Defuse was never funded by the United States . However, in his testimony on Monday, Dr. Fauci explained that the Wuhan institute would not need to rely on U.S. funding to pursue research independently.

The Wuhan lab ran risky experiments to learn about how SARS-like viruses might infect humans.
1. Collect SARS-like viruses from bats and other wild animals, as well as from people exposed to them.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of human cells.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of
human cells.

In Defuse, the scientists proposed to add a furin cleavage site to the spike protein.
3. Create new coronaviruses by inserting spike proteins or other features that could make the viruses more infectious in humans.

4. Infect human cells, civets and humanized mice with the new coronaviruses, to determine how dangerous they might be.

- While it’s possible that the furin cleavage site could have evolved naturally (as seen in some distantly related coronaviruses), out of the hundreds of SARS-like viruses cataloged by scientists, SARS‑CoV‑2 is the only one known to possess a furin cleavage site in its spike. And the genetic data suggest that the virus had only recently gained the furin cleavage site before it started the pandemic.
- Ultimately, a never-before-seen SARS-like virus with a newly introduced furin cleavage site, matching the description in the Wuhan institute’s Defuse proposal, caused an outbreak in Wuhan less than two years after the proposal was drafted.
- When the Wuhan scientists published their seminal paper about Covid-19 as the pandemic roared to life in 2020, they did not mention the virus’s furin cleavage site — a feature they should have been on the lookout for, according to their own grant proposal, and a feature quickly recognized by other scientists.
- Worse still, as the pandemic raged, their American collaborators failed to publicly reveal the existence of the Defuse proposal. The president of EcoHealth, Peter Daszak, recently admitted to Congress that he doesn’t know about virus samples collected by the Wuhan institute after 2015 and never asked the lab’s scientists if they had started the work described in Defuse. In May, citing failures in EcoHealth’s monitoring of risky experiments conducted at the Wuhan lab, the Biden administration suspended all federal funding for the organization and Dr. Daszak, and initiated proceedings to bar them from receiving future grants. In his testimony on Monday, Dr. Fauci said that he supported the decision to suspend and bar EcoHealth.
- Separately, Dr. Baric described the competitive dynamic between his research group and the institute when he told Congress that the Wuhan scientists would probably not have shared their most interesting newly discovered viruses with him . Documents and email correspondence between the institute and Dr. Baric are still being withheld from the public while their release is fiercely contested in litigation.
- In the end, American partners very likely knew of only a fraction of the research done in Wuhan. According to U.S. intelligence sources, some of the institute’s virus research was classified or conducted with or on behalf of the Chinese military . In the congressional hearing on Monday, Dr. Fauci repeatedly acknowledged the lack of visibility into experiments conducted at the Wuhan institute, saying, “None of us can know everything that’s going on in China, or in Wuhan, or what have you. And that’s the reason why — I say today, and I’ve said at the T.I.,” referring to his transcribed interview with the subcommittee, “I keep an open mind as to what the origin is.”
3 The Wuhan lab pursued this type of work under low biosafety conditions that could not have contained an airborne virus as infectious as SARS‑CoV‑2.
- Labs working with live viruses generally operate at one of four biosafety levels (known in ascending order of stringency as BSL-1, 2, 3 and 4) that describe the work practices that are considered sufficiently safe depending on the characteristics of each pathogen. The Wuhan institute’s scientists worked with SARS-like viruses under inappropriately low biosafety conditions .

In the United States, virologists generally use stricter Biosafety Level 3 protocols when working with SARS-like viruses.
Biosafety cabinets prevent
viral particles from escaping.
Viral particles
Personal respirators provide
a second layer of defense against breathing in the virus.
DIRECT CONTACT
Gloves prevent skin contact.
Disposable wraparound
gowns cover much of the rest of the body.

Personal respirators provide a second layer of defense against breathing in the virus.
Disposable wraparound gowns
cover much of the rest of the body.
Note: Biosafety levels are not internationally standardized, and some countries use more permissive protocols than others.

The Wuhan lab had been regularly working with SARS-like viruses under Biosafety Level 2 conditions, which could not prevent a highly infectious virus like SARS-CoV-2 from escaping.
Some work is done in the open air, and masks are not required.
Less protective equipment provides more opportunities
for contamination.

Some work is done in the open air,
and masks are not required.
Less protective equipment provides more opportunities for contamination.
- In one experiment, Dr. Shi’s group genetically engineered an unexpectedly deadly SARS-like virus (not closely related to SARS‑CoV‑2) that exhibited a 10,000-fold increase in the quantity of virus in the lungs and brains of humanized mice . Wuhan institute scientists handled these live viruses at low biosafet y levels , including BSL-2.
- Even the much more stringent containment at BSL-3 cannot fully prevent SARS‑CoV‑2 from escaping . Two years into the pandemic, the virus infected a scientist in a BSL-3 laboratory in Taiwan, which was, at the time, a zero-Covid country. The scientist had been vaccinated and was tested only after losing the sense of smell. By then, more than 100 close contacts had been exposed. Human error is a source of exposure even at the highest biosafety levels , and the risks are much greater for scientists working with infectious pathogens at low biosafety.
- An early draft of the Defuse proposal stated that the Wuhan lab would do their virus work at BSL-2 to make it “highly cost-effective.” Dr. Baric added a note to the draft highlighting the importance of using BSL-3 to contain SARS-like viruses that could infect human cells, writing that “U.S. researchers will likely freak out.” Years later, after SARS‑CoV‑2 had killed millions, Dr. Baric wrote to Dr. Daszak : “I have no doubt that they followed state determined rules and did the work under BSL-2. Yes China has the right to set their own policy. You believe this was appropriate containment if you want but don’t expect me to believe it. Moreover, don’t insult my intelligence by trying to feed me this load of BS.”
- SARS‑CoV‑2 is a stealthy virus that transmits effectively through the air, causes a range of symptoms similar to those of other common respiratory diseases and can be spread by infected people before symptoms even appear. If the virus had escaped from a BSL-2 laboratory in 2019, the leak most likely would have gone undetected until too late.
- One alarming detail — leaked to The Wall Street Journal and confirmed by current and former U.S. government officials — is that scientists on Dr. Shi’s team fell ill with Covid-like symptoms in the fall of 2019 . One of the scientists had been named in the Defuse proposal as the person in charge of virus discovery work. The scientists denied having been sick .
4 The hypothesis that Covid-19 came from an animal at the Huanan Seafood Market in Wuhan is not supported by strong evidence.
- In December 2019, Chinese investigators assumed the outbreak had started at a centrally located market frequented by thousands of visitors daily. This bias in their search for early cases meant that cases unlinked to or located far away from the market would very likely have been missed. To make things worse, the Chinese authorities blocked the reporting of early cases not linked to the market and, claiming biosafety precautions, ordered the destruction of patient samples on January 3, 2020, making it nearly impossible to see the complete picture of the earliest Covid-19 cases. Information about dozens of early cases from November and December 2019 remains inaccessible.
- A pair of papers published in Science in 2022 made the best case for SARS‑CoV‑2 having emerged naturally from human-animal contact at the Wuhan market by focusing on a map of the early cases and asserting that the virus had jumped from animals into humans twice at the market in 2019. More recently, the two papers have been countered by other virologists and scientists who convincingly demonstrate that the available market evidence does not distinguish between a human superspreader event and a natural spillover at the market.
- Furthermore, the existing genetic and early case data show that all known Covid-19 cases probably stem from a single introduction of SARS‑CoV‑2 into people, and the outbreak at the Wuhan market probably happened after the virus had already been circulating in humans.

An analysis of SARS-CoV-2’s evolutionary tree shows how the virus evolved as it started to spread through humans.
SARS-COV-2 Viruses closest
to bat coronaviruses
more mutations

Source: Lv et al., Virus Evolution (2024) , as reproduced by Jesse Bloom

The viruses that infected people linked to the market were most likely not the earliest form of the virus that started the pandemic.

- Not a single infected animal has ever been confirmed at the market or in its supply chain. Without good evidence that the pandemic started at the Huanan Seafood Market, the fact that the virus emerged in Wuhan points squarely at its unique SARS-like virus laboratory.
5 Key evidence that would be expected if the virus had emerged from the wildlife trade is still missing.

In previous outbreaks of coronaviruses, scientists were able to demonstrate natural origin by collecting multiple pieces of evidence linking infected humans to infected animals.
Infected animals
Earliest known
cases exposed to
live animals
Antibody evidence
of animals and
animal traders having
been infected
Ancestral variants
of the virus found in
Documented trade
of host animals
between the area
where bats carry
closely related viruses
and the outbreak site

Infected animals found
Earliest known cases exposed to live animals
Antibody evidence of animals and animal
traders having been infected
Ancestral variants of the virus found in animals
Documented trade of host animals
between the area where bats carry closely
related viruses and the outbreak site

For SARS-CoV-2, these same key pieces of evidence are still missing , more than four years after the virus emerged.

For SARS-CoV-2, these same key pieces of evidence are still missing ,
more than four years after the virus emerged.
- Despite the intense search trained on the animal trade and people linked to the market, investigators have not reported finding any animals infected with SARS‑CoV‑2 that had not been infected by humans. Yet, infected animal sources and other connective pieces of evidence were found for the earlier SARS and MERS outbreaks as quickly as within a few days, despite the less advanced viral forensic technologies of two decades ago.
- Even though Wuhan is the home base of virus hunters with world-leading expertise in tracking novel SARS-like viruses, investigators have either failed to collect or report key evidence that would be expected if Covid-19 emerged from the wildlife trade . For example, investigators have not determined that the earliest known cases had exposure to intermediate host animals before falling ill. No antibody evidence shows that animal traders in Wuhan are regularly exposed to SARS-like viruses, as would be expected in such situations.
- With today’s technology, scientists can detect how respiratory viruses — including SARS, MERS and the flu — circulate in animals while making repeated attempts to jump across species . Thankfully, these variants usually fail to transmit well after crossing over to a new species and tend to die off after a small number of infections. In contrast, virologists and other scientists agree that SARS‑CoV‑2 required little to no adaptation to spread rapidly in humans and other animals . The virus appears to have succeeded in causing a pandemic upon its only detected jump into humans.
The pandemic could have been caused by any of hundreds of virus species, at any of tens of thousands of wildlife markets, in any of thousands of cities, and in any year. But it was a SARS-like coronavirus with a unique furin cleavage site that emerged in Wuhan, less than two years after scientists, sometimes working under inadequate biosafety conditions, proposed collecting and creating viruses of that same design.
While several natural spillover scenarios remain plausible, and we still don’t know enough about the full extent of virus research conducted at the Wuhan institute by Dr. Shi’s team and other researchers, a laboratory accident is the most parsimonious explanation of how the pandemic began.
Given what we now know, investigators should follow their strongest leads and subpoena all exchanges between the Wuhan scientists and their international partners, including unpublished research proposals, manuscripts, data and commercial orders. In particular, exchanges from 2018 and 2019 — the critical two years before the emergence of Covid-19 — are very likely to be illuminating (and require no cooperation from the Chinese government to acquire), yet they remain beyond the public’s view more than four years after the pandemic began.
Whether the pandemic started on a lab bench or in a market stall, it is undeniable that U.S. federal funding helped to build an unprecedented collection of SARS-like viruses at the Wuhan institute, as well as contributing to research that enhanced them . Advocates and funders of the institute’s research, including Dr. Fauci, should cooperate with the investigation to help identify and close the loopholes that allowed such dangerous work to occur. The world must not continue to bear the intolerable risks of research with the potential to cause pandemics .
A successful investigation of the pandemic’s root cause would have the power to break a decades-long scientific impasse on pathogen research safety, determining how governments will spend billions of dollars to prevent future pandemics. A credible investigation would also deter future acts of negligence and deceit by demonstrating that it is indeed possible to be held accountable for causing a viral pandemic. Last but not least, people of all nations need to see their leaders — and especially, their scientists — heading the charge to find out what caused this world-shaking event. Restoring public trust in science and government leadership requires it.
A thorough investigation by the U.S. government could unearth more evidence while spurring whistleblowers to find their courage and seek their moment of opportunity. It would also show the world that U.S. leaders and scientists are not afraid of what the truth behind the pandemic may be.
More on how the pandemic may have started

Where Did the Coronavirus Come From? What We Already Know Is Troubling.
Even if the coronavirus did not emerge from a lab, the groundwork for a potential disaster had been laid for years, and learning its lessons is essential to preventing others.
By Zeynep Tufekci

Why Does Bad Science on Covid’s Origin Get Hyped?
If the raccoon dog was a smoking gun, it fired blanks.
By David Wallace-Wells

A Plea for Making Virus Research Safer
A way forward for lab safety.
By Jesse Bloom
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Alina Chan ( @ayjchan ) is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “ Viral : The Search for the Origin of Covid-19.” She was a member of the Pathogens Project , which the Bulletin of the Atomic Scientists organized to generate new thinking on responsible, high-risk pathogen research.
- Share full article
Advertisement
Things you buy through our links may earn Vox Media a commission.
The Lab-Leak Hypothesis
For decades, scientists have been hot-wiring viruses in hopes of preventing a pandemic, not causing one. but what if ….

This article was featured in One Great Story , New York’ s reading recommendation newsletter. Sign up here to get it nightly.
When Nicholson Baker published “The Lab-Leak Hypothesis” in early January, the subject itself was still deeply taboo across the American political and journalistic landscape. A year later, the hypothesis has been revived and reconsidered not just by major investigations by the New York Times , The Wall Street Journal , the Washington Post , and The Atlantic , but also by the WHO and the U.S. Intelligence Community. Nearly everything that would later serve as the basis for this public reconsideration of pandemic origins was contained in Baker’s original story, the first of its kind to break the ice.
Flask Monsters
What happened was fairly simple, I’ve come to believe. It was an accident. A virus spent some time in a laboratory, and eventually it got out. SARS-CoV-2, the virus that causes COVID-19, began its existence inside a bat, then it learned how to infect people in a claustrophobic mine shaft, and then it was made more infectious in one or more laboratories, perhaps as part of a scientist’s well-intentioned but risky effort to create a broad-spectrum vaccine. SARS-2 was not designed as a biological weapon. But it was, I think, designed. Many thoughtful people dismiss this notion , and they may be right. They sincerely believe that the coronavirus arose naturally, “zoonotically,” from animals, without having been previously studied, or hybridized, or sluiced through cell cultures, or otherwise worked on by trained professionals. They hold that a bat, carrying a coronavirus, infected some other creature, perhaps a pangolin, and that the pangolin may have already been sick with a different coronavirus disease, and out of the conjunction and commingling of those two diseases within the pangolin, a new disease, highly infectious to humans, evolved. Or they hypothesize that two coronaviruses recombined in a bat, and this new virus spread to other bats, and then the bats infected a person directly — in a rural setting, perhaps — and that this person caused a simmering undetected outbreak of respiratory disease, which over a period of months or years evolved to become virulent and highly transmissible but was not noticed until it appeared in Wuhan.
There is no direct evidence for these zoonotic possibilities, just as there is no direct evidence for an experimental mishap — no written confession, no incriminating notebook, no official accident report. Certainty craves detail, and detail requires an investigation. It has been a full year, 80 million people have been infected , and, surprisingly, no public investigation has taken place. We still know very little about the origins of this disease.
Nevertheless, I think it’s worth offering some historical context for our yearlong medical nightmare. We need to hear from the people who for years have contended that certain types of virus experimentation might lead to a disastrous pandemic like this one. And we need to stop hunting for new exotic diseases in the wild, shipping them back to laboratories, and hot-wiring their genomes to prove how dangerous to human life they might become.
Over the past few decades, scientists have developed ingenious methods of evolutionary acceleration and recombination, and they’ve learned how to trick viruses, coronaviruses in particular, those spiky hairballs of protein we now know so well, into moving quickly from one species of animal to another or from one type of cell culture to another. They’ve made machines that mix and mingle the viral code for bat diseases with the code for human diseases — diseases like SARS, severe acute respiratory syndrome, for example, which arose in China in 2003, and MERS, Middle East respiratory syndrome, which broke out a decade later and has to do with bats and camels. Some of the experiments — “gain of function” experiments — aimed to create new, more virulent, or more infectious strains of diseases in an effort to predict and therefore defend against threats that might conceivably arise in nature. The term gain of function is itself a euphemism; the Obama White House more accurately described this work as “experiments that may be reasonably anticipated to confer attributes to influenza, MERS, or SARS viruses such that the virus would have enhanced pathogenicity and/or transmissibility in mammals via the respiratory route.” The virologists who carried out these experiments have accomplished amazing feats of genetic transmutation, no question, and there have been very few publicized accidents over the years. But there have been some.
And we were warned, repeatedly. The intentional creation of new microbes that combine virulence with heightened transmissibility “poses extraordinary risks to the public,” wrote infectious-disease experts Marc Lipsitch and Thomas Inglesby in 2014. “A rigorous and transparent risk-assessment process for this work has not yet been established.” That’s still true today. In 2012, in Bulletin of the Atomic Scientists , Lynn Klotz warned that there was an 80 percent chance, given how many laboratories were then handling virulent viro-varietals, that a leak of a potential pandemic pathogen would occur sometime in the next 12 years.
A lab accident — a dropped flask, a needle prick, a mouse bite, an illegibly labeled bottle — is apolitical. Proposing that something unfortunate happened during a scientific experiment in Wuhan — where COVID-19 was first diagnosed and where there are three high-security virology labs, one of which held in its freezers the most comprehensive inventory of sampled bat viruses in the world — isn’t a conspiracy theory. It’s just a theory. It merits attention, I believe, alongside other reasoned attempts to explain the source of our current catastrophe.
“A Reasonable Chance”

From early 2020, the world was brooding over the origins of COVID-19. People were reading research papers, talking about what kinds of live animals were or were not sold at the Wuhan seafood market — wondering where the new virus had come from.
Meanwhile, things got strange all over the world. The Chinese government shut down transportation and built hospitals at high speed. There were video clips of people who’d suddenly dropped unconscious in the street. A doctor on YouTube told us how we were supposed to scrub down our produce when we got back from the supermarket. A scientist named Shi Zhengli of the Wuhan Institute of Virology published a paper saying that the novel coronavirus was 96 percent identical to a bat virus, RaTG13, found in Yunnan province in southern China. On March 13, I wrote in my journal that there seemed to be something oddly artificial about the disease: “It’s too airborne — too catching — it’s something that has been selected for infectivity. That’s what I suspect. No way to know so no reason to waste time thinking about it.”
This was just a note to self — at the time, I hadn’t interviewed scientists about SARS-2 or read their research papers. But I did know something about pathogens and laboratory accidents; I published a book last year, Baseless , that talks about some of them. The book is named after a Pentagon program, Project Baseless, whose goal, as of 1951, was to achieve “an Air Force–wide combat capability in biological and chemical warfare at the earliest possible date.”
A vast treasure was spent by the U.S. on the amplification and aerial delivery of diseases — some well known, others obscure and stealthy. America’s biological-weapons program in the ’50s had A1-priority status, as high as nuclear weapons. In preparation for a total war with a numerically superior communist foe, scientists bred germs to be resistant to antibiotics and other drug therapies, and they infected lab animals with them, using a technique called “serial passaging,” in order to make the germs more virulent and more catching.
And along the way, there were laboratory accidents. By 1960, hundreds of American scientists and technicians had been hospitalized, victims of the diseases they were trying to weaponize. Charles Armstrong, of the National Institutes of Health, one of the consulting founders of the American germ-warfare program, investigated Q fever three times, and all three times, scientists and staffers got sick. In the anthrax pilot plant at Camp Detrick, Maryland, in 1951, a microbiologist, attempting to perfect the “foaming process” of high-volume production, developed a fever and died. In 1964, veterinary worker Albert Nickel fell ill after being bitten by a lab animal. His wife wasn’t told that he had Machupo virus, or Bolivian hemorrhagic fever. “I watched him die through a little window to his quarantine room at the Detrick infirmary,” she said.
In 1977, a worldwide epidemic of influenza A began in Russia and China; it was eventually traced to a sample of an American strain of flu preserved in a laboratory freezer since 1950. In 1978, a hybrid strain of smallpox killed a medical photographer at a lab in Birmingham, England; in 2007, live foot-and-mouth disease leaked from a faulty drainpipe at the Institute for Animal Health in Surrey. In the U.S., “more than 1,100 laboratory incidents involving bacteria, viruses and toxins that pose significant or bioterror risks to people and agriculture were reported to federal regulators during 2008 through 2012,” reported USA Today in an exposé published in 2014. In 2015, the Department of Defense discovered that workers at a germ-warfare testing center in Utah had mistakenly sent close to 200 shipments of live anthrax to laboratories throughout the United States and also to Australia, Germany, Japan, South Korea, and several other countries over the past 12 years. In 2019, laboratories at Fort Detrick — where “defensive” research involves the creation of potential pathogens to defend against — were shut down for several months by the Centers for Disease Control and Prevention for “breaches of containment.” They reopened in December 2019.
High-containment laboratories have a whispered history of near misses. Scientists are people, and people have clumsy moments and poke themselves and get bitten by the enraged animals they are trying to nasally inoculate. Machines can create invisible aerosols, and cell solutions can become contaminated. Waste systems don’t always work properly. Things can go wrong in a hundred different ways.
Hold that human fallibility in your mind. And then consider the cautious words of Alina Chan, a scientist who works at the Broad Institute of MIT and Harvard. “There is a reasonable chance that what we are dealing with is the result of a lab accident,” Chan told me in July of last year. There was also, she added, a reasonable chance that the disease had evolved naturally — both were scientific possibilities. “I don’t know if we will ever find a smoking gun, especially if it was a lab accident. The stakes are so high now. It would be terrifying to be blamed for millions of cases of COVID-19 and possibly up to a million deaths by year end, if the pandemic continues to grow out of control. The Chinese government has also restricted their own scholars and scientists from looking into the origins of SARS-CoV-2. At this rate, the origin of SARS-CoV-2 may just be buried by the passage of time.”
I asked Jonathan A. King, a molecular biologist and biosafety advocate from MIT, whether he’d thought lab accident when he first heard about the epidemic. “Absolutely, absolutely,” King answered. Other scientists he knew were concerned as well. But scientists, he said, in general were cautious about speaking out. There were “very intense, very subtle pressures” on them not to push on issues of laboratory biohazards. Collecting lots of bat viruses, and passaging those viruses repeatedly through cell cultures, and making bat-human viral hybrids, King believes, “generates new threats and desperately needs to be reined in.”
“All possibilities should be on the table, including a lab leak,” a scientist from the NIH, Philip Murphy — chief of the Laboratory of Molecular Immunology — wrote me recently. Nikolai Petrovsky, a professor of endocrinology at Flinders University College of Medicine in Adelaide, Australia, said in an email, “There are indeed many unexplained features of this virus that are hard if not impossible to explain based on a completely natural origin.” Richard Ebright, a molecular biologist at Rutgers University, wrote that he’d been concerned for some years about the Wuhan laboratory and about the work being done there to create “chimeric” (i.e., hybrid) SARS-related bat coronaviruses “with enhanced human infectivity.” Ebright said, “In this context, the news of a novel coronavirus in Wuhan ***screamed*** lab release.”
“No Credible Evidence”
The new disease , as soon as it appeared, was intercepted — stolen and politicized by people with ulterior motives. The basic and extremely interesting scientific question of what happened was sucked up into an ideological sharknado.
Some Americans boycotted Chinese restaurants; others bullied and harassed Asian Americans . Steve Bannon, broadcasting from his living room, in a YouTube series called War Room , said that the Chinese Communist Party had made a biological weapon and intentionally released it. He called it the “CCP virus.” And his billionaire friend and backer, Miles Guo, a devoted Trump supporter, told a right-wing website that the communists’ goal was to “use the virus to infect selective people in Hong Kong, so that the Chinese Communist Party could use it as an excuse to impose martial law there and ultimately crush the Hong Kong pro-democracy movement. But it backfired terribly.”
In The Lancet , in February, a powerful counterstatement appeared, signed by 27 scientists. “We stand together to strongly condemn conspiracy theories suggesting that COVID-19 does not have a natural origin,” the statement said. “Scientists from multiple countries have published and analyzed genomes of the causative agent, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and they overwhelmingly conclude that this coronavirus originated in wildlife, as have so many other emerging pathogens.”
The behind-the-scenes organizer of this Lancet statement, Peter Daszak, is a zoologist and bat-virus sample collector and the head of a New York nonprofit called EcoHealth Alliance — a group that (as veteran science journalist Fred Guterl explained later in Newsweek ) has channeled money from the National Institutes of Health to Shi Zhengli’s laboratory in Wuhan, allowing the lab to carry on recombinant research into diseases of bats and humans. “We have a choice whether to stand up and support colleagues who are being attacked and threatened daily by conspiracy theorists or to just turn a blind eye,” Daszak said in February in Science magazine.
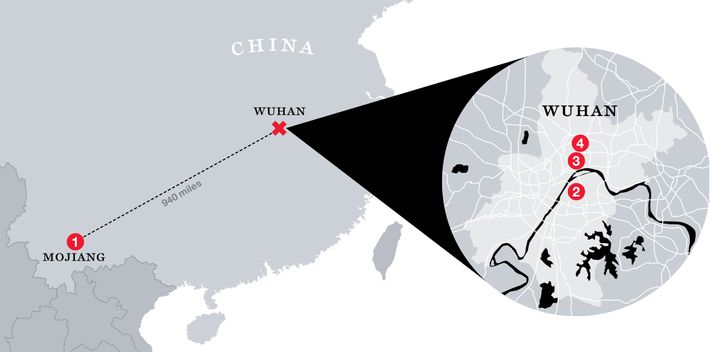
Vincent Racaniello, a professor at Columbia and a co-host of a podcast called This Week in Virology , said on February 9 that the idea of an accident in Wuhan was “complete bunk.” The coronavirus was 96 percent similar to a bat virus found in 2013, Racaniello said. “It’s not a man-made virus. It wasn’t released from a lab.”
Racaniello’s dismissal was seconded by a group of scientists from Ohio State, the University of Pennsylvania, and the University of North Carolina, who put out a paper in Emerging Microbes and Infections to quiet the “speculations, rumors, and conspiracy theories that SARS-CoV-2 is of laboratory origin.” There was “currently no credible evidence” that SARS-2 leaked from a lab, these scientists said, using a somewhat different argument from Racaniello’s. “Some people have alleged that the human SARS-CoV-2 was leaked directly from a laboratory in Wuhan where a bat CoV (RaTG13) was recently reported,” they said. But RaTG13 could not be the source because it differed from the human SARS-2 virus by more than a thousand nucleotides. One of the paper’s authors, Susan Weiss, told the Raleigh News & Observer , “The conspiracy theory is ridiculous.”
The most influential natural-origin paper , “The Proximal Origin of SARS-CoV-2,” by a group of biologists that included Kristian Andersen of Scripps Research, appeared online in a preliminary version in mid-February. “We do not believe any type of laboratory-based scenario is plausible,” the scientists said. Why? Because molecular-modeling software predicted that if you wanted to optimize an existing bat virus so that it would replicate well in human cells, you would arrange things a different way than how the SARS-2 virus actually does it — even though the SARS-2 virus does an extraordinarily good job of replicating in human cells. The laboratory-based scenario was implausible, the paper said, because, although it was true that the virus could conceivably have developed its unusual genetic features in a laboratory, a stronger and “more parsimonious” explanation was that the features came about through some kind of natural mutation or recombination. “What we think,” explained one of the authors, Robert F. Garry of Tulane University, on YouTube , “is that this virus is a recombinant. It probably came from a bat virus, plus perhaps one of these viruses from the pangolin.” Journalists, for the most part, echoed the authoritative pronouncements of Daszak, Racaniello, Weiss, Andersen, and other prominent natural-originists. “The balance of the scientific evidence strongly supports the conclusion that the new coronavirus emerged from nature — be it the Wuhan market or somewhere else,” said the Washington Post ’s “Fact Checker” column. “Dr. Fauci Again Dismisses Wuhan Lab As Source of Coronavirus,” said CBS News , posting a video interview of Anthony Fauci by National Geographic . “If you look at the evolution of the virus in bats, and what’s out there now,” Fauci said, “it’s very, very strongly leaning toward ‘This could not have been artificially or deliberately manipulated’ — the way the mutations have naturally evolved.”
Everyone took sides; everyone thought of the new disease as one more episode in an ongoing partisan struggle. Think of Mike Pompeo, that landmass of Cold War truculence; think of Donald Trump himself. They stood at their microphones saying, in a winking, I-know-something-you-don’t-know sort of way, that this disease escaped from a Chinese laboratory. Whatever they were saying must be wrong. It became impermissible, almost taboo, to admit that, of course, SARS-2 could have come from a lab accident. “The administration’s claim that the virus spread from a Wuhan lab has made the notion politically toxic, even among scientists who say it could have happened,” wrote science journalist Mara Hvistendahl in the Intercept .
“Is It a Complete Coincidence?”
Even so, in January and February of 2020, there were thoughtful people who were speaking up, formulating their perplexities.
One person was Sam Husseini, an independent journalist. He went to a CDC press conference at the National Press Club on February 11, 2020. By then, 42,000 people had gotten sick in China and more than a thousand had died. But there were only 13 confirmed cases in the U.S. Halfway through the Q&A period, Husseini went to the microphone and asked the CDC’s representative, Anne Schuchat, where the virus had come from. His head was spinning, he told me later.
“Obviously the main concern is how to stop the virus,” Husseini said; nonetheless, he wanted to know more about its source. “Is it the CDC’s contention,” he asked, “that there’s absolutely no relation to the BSL-4 lab in Wuhan? It’s my understanding that this is the only place in China with a BSL-4 lab. We in the United States have, I think, two dozen or so, and there have been problems and incidents.” (A BSL-4 laboratory is a maximum-security biosafety-level-four facility, used to house research on the most dangerous known pathogens. New York has confirmed there are at least 11 BSL-4 facilities currently operating in the U.S.) Husseini hastened to say that he wasn’t implying that what happened in Wuhan was in any way intentional. “I’m just asking, Is it a complete coincidence that this outbreak happened in the one city in China with a BSL-4 lab?”
Schuchat thanked Husseini for his questions and comments. Everything she’d seen was quite consistent with a natural, zoonotic origin for the disease, she said.
That same month, a group of French scientists from Aix-Marseille University posted a paper describing their investigation of a small insertion in the genome of the new SARS-2 virus. The virus’s spike protein contained a sequence of amino acids that formed what Etienne Decroly and colleagues called a “peculiar furin-like cleavage site” — a chemically sensitive region on the lobster claw of the spike protein that would react in the presence of an enzyme called furin, which is a type of protein found everywhere within the human body, but especially in the lungs. When the spike senses human furin, it shudders, chemically speaking, and the enzyme opens the protein, commencing the tiny morbid ballet whereby the virus burns a hole in a host cell’s outer membrane and finds its way inside.
The code for this particular molecular feature — not found in SARS or any SARS-like bat viruses, but present in a slightly different form in the more lethal MERS virus — is easy to remember because it’s a roar: “R-R-A-R.” The letter code stands for amino acids: arginine, arginine, alanine, and arginine. Its presence, so Decroly and his colleagues observed, may heighten the “pathogenicity” — that is, the god-awfulness — of a disease.
Botao Xiao, a professor at the South China University of Technology, posted a short paper on a preprint server titled “The Possible Origins of 2019-nCoV Coronavirus.” Two laboratories, the Wuhan Center for Disease Control and Prevention (WHCDC) and the Wuhan Institute of Virology, were not far from the seafood market, which was where the disease was said to have originated, Xiao wrote — in fact, the WHCDC was only a few hundred yards away from the market — whereas the horseshoe bats that hosted the disease were hundreds of miles to the south. (No bats were sold in the market, he pointed out.) It was unlikely, he wrote, that a bat would have flown to a densely populated metropolitan area of 15 million people. “The killer coronavirus probably originated from a laboratory in Wuhan,” Xiao believed. He urged the relocation of “biohazardous laboratories” away from densely populated places. His article disappeared from the server.
And late in the month, a professor at National Taiwan University, Fang Chi-tai, gave a lecture on the coronavirus in which he described the anomalous R-R-A-R furin cleavage site. The virus was “unlikely to have four amino acids added all at once,” Fang said — natural mutations were smaller and more haphazard, he argued. “From an academic point of view, it is indeed possible that the amino acids were added to COVID-19 in the lab by humans.” When the Taiwan News published an article about Fang’s talk, Fang disavowed his own comments, and the video copy of the talk disappeared from the website of the Taiwan Public Health Association. “It has been taken down for a certain reason,” the association explained. “Thank you for your understanding.”
“A Serious Shortage of Appropriately Trained Technicians”
In the spring , I did some reading on coronavirus history. Beginning in the 1970s, dogs, cows, and pigs were diagnosed with coronavirus infections; dog shows were canceled in 1978 after 25 collies died in Louisville, Kentucky. New varieties of coronaviruses didn’t start killing humans, though, until 2003 — that’s when restaurant chefs, food handlers, and people who lived near a live-animal market got sick in Guangzhou, in southern China, where the shredded meat of a short-legged raccoonlike creature, the palm civet, was served in a regional dish called “dragon-tiger-phoenix soup.” The new disease, SARS, spread alarmingly in hospitals, and it reached 30 countries and territories. More than 800 people died; the civet-borne virus was eventually traced to horseshoe bats .
Later, smaller outbreaks of SARS in Taiwan, Singapore, and China’s National Institute of Virology in Beijing were all caused by laboratory accidents. Of the Beijing Virology Institute, the World Health Organization’s safety investigators wrote , in May 2004, that they had “serious concerns about biosafety procedures.” By one account, a SARS storage room in the Beijing lab was so crowded that the refrigerator holding live virus was moved out to the hallway. “Scientists still do not fully understand exactly where or how SARS emerged 18 months ago,” wrote Washington Post reporter David Brown in June 2004. “But it is clear now that the most threatening source of the deadly virus today may be places they know intimately — their own laboratories.”
MERS arose in 2012, possibly spread by camels that had contracted the disease from bats or bat guano, then passed it to human drinkers of raw camel milk and butchers of camel meat. It was an acute sickness, with a high fatality rate, mostly confined to Saudi Arabia. Like SARS, MERS ebbed quickly — it all but disappeared outside the Middle East, except for an outbreak in 2015 at the Samsung Medical Center in South Korea, where a single case of MERS led to more than 180 infections, many involving hospital workers.
In January 2015, the brand-new BSL-4 lab in Wuhan, built by a French contractor, celebrated its opening, but full safety certification came slowly. According to State Department cables from 2018 leaked to the Washington Post , the new BSL-4 lab had some start-up problems, including “a serious shortage of appropriately trained technicians and investigators needed to safely operate this high-containment laboratory.” The staff had gotten some training at a BSL-4 lab in Galveston, Texas, but they were doing potentially dangerous work with SARS-like viruses, the memo said, and they needed more help from the U.S.
In November or December of 2019, the novel coronavirus began to spread. Chinese scientists initially named it “Wuhan seafood market pneumonia virus,” but soon that idea went away. The market, closed and decontaminated by Chinese officials on January 1, 2020, was an amplifying hub, not the source of the outbreak, according to several studies by Chinese scientists. Forty-five percent of the earliest SARS-2 patients had no link with the market.
Now let’s take a step back. AIDS, fatal and terrifying and politically charged, brought on a new era in government-guided vaccine research, under the guidance of Anthony Fauci. A virologist at Rockefeller University, Stephen S. Morse, began giving talks on “emerging viruses” — other plagues that might be in the process of coming out of nature’s woodwork. In 1992, Richard Preston wrote a horrific account of one emergent virus, Ebola, in The New Yorker , which became a best-selling book in 1994; Laurie Garrett’s The Coming Plague: Newly Emerging Diseases in a World Out of Balance appeared that same year and was also a best seller. The idea seemed to be everywhere: We were on the verge of a wave of zoonotic, emergent plagues.
This new, useful term, emerging , began to glow in the research papers of some coronavirologists, who were out of the spotlight, working on common colds and livestock diseases. The term was useful because it was fluid. An emerging disease could be real and terrifying, as AIDS was — something that had just arrived on the medical scene and was confounding our efforts to combat it — or it could be a disease that hadn’t arrived, and might never arrive, but could be shown in a laboratory to be waiting in the wings, just a few mutations away from a human epidemic. It was real and unreal at the same time — a quality that was helpful when applying for research grants.
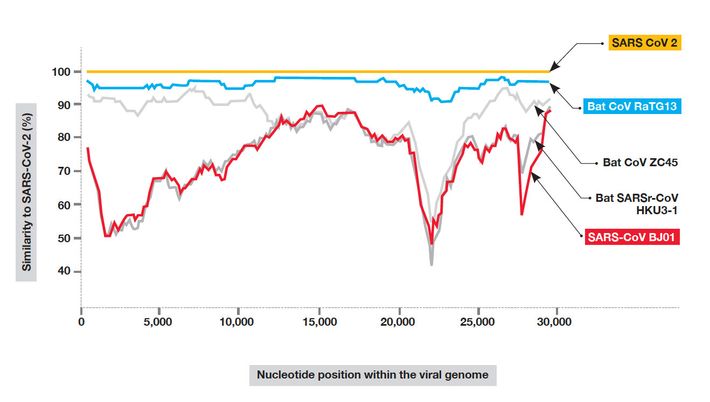
Take, for instance, this paper from 1995: “High Recombination and Mutation Rates in Mouse Hepatitis Viruses Suggest That Coronaviruses May Be Potentially Important Emerging Viruses.” It was written by Dr. Ralph Baric and his bench scientist, Boyd Yount, at the University of North Carolina. Baric, a gravelly voiced former swim champion, described in this early paper how his lab was able to train a coronavirus, MHV, which causes hepatitis in mice, to jump species, so that it could reliably infect BHK (baby-hamster kidney) cell cultures. They did it using serial passaging: repeatedly dosing a mixed solution of mouse cells and hamster cells with mouse-hepatitis virus, while each time decreasing the number of mouse cells and upping the concentration of hamster cells. At first, predictably, the mouse-hepatitis virus couldn’t do much with the hamster cells, which were left almost free of infection, floating in their world of fetal-calf serum. But by the end of the experiment, after dozens of passages through cell cultures, the virus had mutated: It had mastered the trick of parasitizing an unfamiliar rodent. A scourge of mice was transformed into a scourge of hamsters. And there was more: “It is clear that MHV can rapidly alter its species specificity and infect rats and primates,” Baric said. “The resulting virus variants are associated with demyelinating diseases in these alternative species.” (A demyelinating disease is a disease that damages nerve sheaths.) With steady prodding from laboratory science, along with some rhetorical exaggeration, a lowly mouse ailment was morphed into an emergent threat that might potentially cause nerve damage in primates. That is, nerve damage in us.
A few years later, in a further round of “interspecies transfer” experimentation, Baric’s scientists introduced their mouse coronavirus into flasks that held a suspension of African-green-monkey cells, human cells, and pig-testicle cells. Then, in 2002, they announced something even more impressive: They’d found a way to create a full-length infectious clone of the entire mouse-hepatitis genome. Their “infectious construct” replicated itself just like the real thing, they wrote .
Not only that, but they’d figured out how to perform their assembly seamlessly, without any signs of human handiwork. Nobody would know if the virus had been fabricated in a laboratory or grown in nature. Baric called this the “no-see’m method,” and he asserted that it had “broad and largely unappreciated molecular biology applications.” The method was named, he wrote, after a “very small biting insect that is occasionally found on North Carolina beaches.”
In 2006, Baric, Yount, and two other scientists were granted a patent for their invisible method of fabricating a full-length infectious clone using the seamless, no-see’m method. But this time, it wasn’t a clone of the mouse-hepatitis virus — it was a clone of the entire deadly human SARS virus, the one that had emerged from Chinese bats, via civets, in 2002. The Baric Lab came to be known by some scientists as “the Wild Wild West.” In 2007, Baric said that we had entered “the golden age of coronavirus genetics.”
“I would be afraid to look in their freezers,” one virologist told me.
Baric and Shi Zhengli of the Wuhan Institute of Virology, the two top experts on the genetic interplay between bat and human coronaviruses, began collaborating in 2015.
“I Had Not Slept a Wink”

Early in the pandemic, Scientific American profiled Shi Zhengli, known in China as the “bat woman.” Shi trapped hundreds of bats in nets at the mouths of caves in southern China, sampled their saliva and their blood, swabbed their anuses, and gathered up their fecal pellets. Several times, she visited and sampled bats in a mine in Mojiang, in southern China, where, in 2012, six men set to work shoveling bat guano were sickened by a severe lung disease, three of them fatally. Shi’s team took the samples back to Wuhan and analyzed whatever fragments of bat virus she could find. In some cases, when she found a sequence that seemed particularly significant, she experimented with it in order to understand how it might potentially infect humans. Some of her work was funded by the National Institutes of Health and some of it by the U.S. Defense Threat Reduction Agency of the Department of Defense via Peter Daszak’s EcoHealth Alliance.
As Shi explained to Scientific American , late in December 2019, she heard from the director of the Wuhan Institute that there was an outbreak of a new disease in the city. Medical samples taken from hospital patients arrived at her lab for analysis. Shi determined that the new virus was related to SARS but even more closely related to a bat disease that her own team had found on a virus-hunting trip: the now-famous RaTG13. Shi was surprised that the outbreak was local, she said: “I had never expected this kind of thing to happen in Wuhan, in central China.” The bat hiding places that she’d been visiting were, after all, as far away as Orlando, Florida, is from New York City. Could this new virus, she wondered, have come from her own laboratory? She checked her records and found no exact matches. “That really took a load off my mind,” she said. “I had not slept a wink for days.”
If one of the first thoughts that goes through the head of a lab director at the Wuhan Institute of Virology is that the new coronavirus could have come from her lab, then we are obliged to entertain the scientific possibility that it could indeed have come from her lab. Right then, there should have been a comprehensive, pockets-inside-out, fully public investigation of the Virology Institute, along with the other important virus labs in Wuhan, including the one close by the seafood market, headquarters of the Wuhan CDC. There should have been interviews with scientists, interviews with biosafety teams, close parsings of laboratory notebooks, freezer and plumbing and decontamination systems checks — everything. It didn’t happen. The Wuhan Institute of Virology closed down its databases of viral genomes, and the Chinese Ministry of Education sent out a directive: “Any paper that traces the origin of the virus must be strictly and tightly managed.”
Shi made some WeChat posts early in 2020. “The novel 2019 coronavirus is nature punishing the human race for keeping uncivilized living habits,” she wrote. “I, Shi Zhengli, swear on my life that it has nothing to do with our laboratory.” She advised those who believed rumors, and gave credence to unreliable scientific papers, to “shut their stinking mouths.”
“ ‘Bug to Drug’ in 24 Hours”
It wasn’t only AIDS that changed the way the NIH funded research. The War on Terror also influenced which diseases got the most attention. In the late ’90s, under Bill Clinton and then George W. Bush, biodefense specialists became interested — again — in anthrax. The Defense Threat Reduction Agency built a small anthrax factory in Nevada, using simulants, to demonstrate how easy it would be for a terrorist to build a small anthrax factory. And in the first year of the Bush presidency, the Defense Intelligence Agency wrote up plans to create a vaccine-resistant form of anthrax using state-of-the-art gene-splicery. A front-page article describing these initiatives, “U.S. Germ Warfare Research Pushes Treaty Limits,” appeared in the New York Times on September 4, 2001, one week before 9/11. “Pentagon Says Projects Are Defense, Is Pressing Ahead,” was the subtitle.
After the 9/11 attacks, and the mysterious anthrax mailings that began a week later (which said, “TAKE PENACILIN [ sic ] NOW / DEATH TO AMERICA / DEATH TO ISRAEL / ALLAH IS GREAT”), the desire for biopreparedness became all consuming. Now there were emerging biothreats from humans as well as from the evolving natural world. Fauci’s anti-terror budget went from $53 million in 2001 to $1.7 billion in 2003. Setting aside his work toward an AIDS vaccine, which was taking longer than he’d foreseen, Fauci said he would be going all out to defend against a suite of known Cold War agents, all of which had been bred and perfected in American weapons programs many years before — brucellosis, anthrax, tularemia, and plague, for instance. “We are making this the highest priority,” Fauci said. “We are really marshaling all available resources.”
Vaccine development had to progress much faster, Fauci believed; he wanted to set up “vaccine systems” and “vaccine platforms,” which could be quickly tailored to defend against a particular emergent strain some terrorist with an advanced biochemistry degree might have thrown together in a laboratory. “Our goal within the next 20 years is ‘bug to drug’ in 24 hours,” Fauci said. “This would specifically meet the challenge of genetically engineered bioagents.” The first Project BioShield contract Fauci awarded was to VaxGen, a California pharmaceutical company, for $878 million worth of shots of anthrax vaccine.
By 2005, so much money was going toward biothreat reduction and preparedness that more than 750 scientists sent a protest letter to the NIH. Their claim was that grants to study canonical biowar diseases — anthrax, plague, brucellosis, and tularemia, all exceptionally rare in the U.S. — had increased by a factor of 15 since 2001, whereas funds for the study of widespread “normal” diseases, of high public-health importance, had decreased.
Fauci was firm in his reply: “The United States through its leaders made the decision that this money was going to be spent on biodefense,” he said. “We disagree with the notion that biodefense concerns are of ‘low public-health significance.’ ”
In 2010, by one count, there were 249 BSL-3 laboratories and seven BSL-4 laboratories in the U.S., and more than 11,000 scientists and staffers were authorized to handle the ultralethal germs on the government’s select pathogen list. And yet the sole bioterrorist in living memory who actually killed American citizens, according to the FBI — the man who sent the anthrax letters — turned out to be one of the government’s own researchers. Bruce Ivins , an eccentric, suicidal laboratory scientist from Ohio who worked in vaccine development at Fort Detrick, allegedly wanted to boost the fear level so as to persuade the government to buy more of the patented, genetically engineered anthrax VaxGen vaccine, of which he was a co-inventor. (See David Willman’s fascinating biography of Ivins, Mirage Man .) Fauci’s staff at NIH funded Ivins’s vaccine laboratory and gave $100 million to VaxGen to accelerate vaccine production. (The NIH’s $878 million contract with VaxGen, however, was quietly canceled in 2006; Ivins, who was never charged, killed himself in 2008.)
“The whole incident amounted to a snake eating its own tail,” wrote Wendy Orent in an August 2008 piece titled “Our Own Worst Bioenemy” in the Los Angeles Times . “No ingenious biowarrior from Al Qaeda sent the lethal envelopes through the U.S. postal system. An American scientist did.” What confirmed Ivins’s guilt, according to the FBI, was that there was a genetic match between the anthrax used in the killings and the strain held at Fort Detrick.
“Weapons of Mass Disruption”
After SARS appeared in 2003, Ralph Baric’s laboratory moved up the NIH funding ladder. SARS was a “dual use” organism — a security threat and a zoonotic threat at the same time. In 2006, Baric wrote a long, fairly creepy paper on the threat of “weaponizable” viruses. Synthetic biology had made possible new kinds of viral “weapons of mass disruption,” he wrote, involving, for example, “rapid production of numerous candidate bioweapons that can be simultaneously released,” a scattershot terror tactic Baric called the “ ‘survival of the fittest’ approach.”
Baric hoped to find a SARS vaccine, but he couldn’t; he kept looking for it, year after year, supported by the NIH, long after the disease itself had been contained. It wasn’t really gone, Baric believed. Like other epidemics that pop up and then disappear, as he told a university audience some years later, “they don’t go extinct. They are waiting to return.” What do you do if you run a well-funded laboratory, an NIH “center of excellence,” and your emergent virus is no longer actually making people sick? You start squeezing it and twisting it into different shapes. Making it stand on its hind legs and quack like a duck, or a bat. Or breathe like a person.
Baric’s safety record is good — although there was a minor mouse-bite incident in 2016, uncovered by ProPublica — and his motives are beyond reproach: “Safe, universal, vaccine platforms are needed that can be tailored to new pathogens as they emerge, quickly tested for safety, and then strategically used to control new disease outbreaks in human populations,” he wrote in a paper on public health. But the pioneering work he did over the past 15 years — generating tiny eager single-stranded flask monsters and pitting them against human cells, or bat cells, or gene-spliced somewhat-human cells, or monkey cells, or humanized mice — was not without risk, and it may have led others astray.
In 2006, for instance, Baric and his colleagues, hoping to come up with a “vaccine strategy” for SARS, produced noninfectious virus replicon particles (or VRPs) using the Venezuelan-equine-encephalitis virus (another American germ-warfare agent), which they fitted with various SARS spike proteins. Then, wearing Tyvek suits and two pairs of gloves each, and working in a biological safety cabinet in a BSL-3-certified laboratory, they cloned and grew recombinant versions of the original SARS virus in an incubator in a medium that held African-green-monkey cells. When they had grown enough virus, the scientists swapped out one kind of spike protein for a carefully chosen mutant, and they challenged their prototype vaccine with it in mice.
The scientists also tried their infectious SARS clones in something called an air-liquid interface, using a relatively new type of cell culture developed by Raymond Pickles of the University of North Carolina’s Cystic Fibrosis Center. Pickles had perfected a method of emulating the traits of human airway tissue by cultivating cells taken from lung-disease patients — nurturing the culture over four to six weeks in such a way that the cells differentiated and developed a crop of tiny moving hairs, or cilia, on top and goblet cells within that produced real human mucus. In fact, before infecting these HAE (human airway epithelial) cells with a virus, the lab worker must sometimes rinse off some of the accumulated mucus, as if helping the lab-grown tissue to clear its throat. So Baric was exposing and adapting his engineered viruses to an extraordinarily true-to-life environment — the juicy, sticky, hairy inner surface of our breathing apparatus.
SARS-2 seems almost perfectly calibrated to grab and ransack our breathing cells and choke the life out of them. “By the time SARS-CoV-2 was first detected in late 2019, it was already pre-adapted to human transmission,” Alina Chan and her co-authors have written, whereas SARS, when it first appeared in 2003, underwent “numerous adaptive mutations” before settling down. Perhaps viral nature hit a bull’s-eye of airborne infectivity, with almost no mutational drift, no period of accommodation and adjustment, or perhaps some lab worker somewhere, inspired by Baric’s work with human airway tissue, took a spike protein that was specially groomed to colonize and thrive deep in the ciliated, mucosal tunnels of our inner core and cloned it onto some existing viral bat backbone. It could have happened in Wuhan, but — because anyone can now “print out” a fully infectious clone of any sequenced disease — it could also have happened at Fort Detrick, or in Texas, or in Italy, or in Rotterdam, or in Wisconsin, or in some other citadel of coronaviral inquiry. No conspiracy — just scientific ambition, and the urge to take exciting risks and make new things, and the fear of terrorism, and the fear of getting sick. Plus a whole lot of government money.
“Risky Areas for Spillover”
Project Bioshield began to fade by the end of the Bush administration, although the expensive high-containment laboratories, controversial preservers and incubators of past and future epidemics, remain. By 2010, some BioShield projects had dissolved into Obama’s Predict program, which paid for laboratories and staff in 60 “risky areas for spillover” around the world. Jonna Mazet, a veterinary scientist from the University of California, Davis, was in charge of Predict, which was a component of USAID’s “Emerging Pandemic Threats” program. Her far-flung teams collected samples from 164,000 animals and humans and claimed to have found “almost 1,200 potentially zoonotic viruses, among them 160 novel coronaviruses, including multiple SARS- and MERS-like coronaviruses.” The fruits of Predict’s exotic harvest were studied and circulated in laboratories worldwide, and their genetic sequences became part of GenBank , the NIH’s genome database, where any curious RNA wrangler anywhere could quickly synthesize snippets of code and test out a new disease on human cells.
Baric, Jonna Mazet, and Peter Daszak of EcoHealth worked together for years — and Daszak also routed Predict money to Shi Zhengli’s bat-surveillance team in Wuhan through his nonprofit, mingling it with NIH money and money from the U.S. Defense Threat Reduction Agency. In 2013, Mazet announced that Shi Zhengli’s virus hunters, with Predict’s support, had, for the first time, isolated and cultured a live SARS-like virus from bats and demonstrated that this virus could bind to the human ACE2, or “angiotensin-converting enzyme 2,” receptor, which Baric’s laboratory had determined to be the sine qua non of human infectivity. “This work shows that these viruses can directly infect humans and validates our assumption that we should be searching for viruses of pandemic potential before they spill over to people,” Mazet said .
Daszak, for his part, seems to have viewed his bat quests as part of an epic, quasi-religious death match. In a paper from 2008, Daszak and a co-author described Bruegel’s painting The Fall of the Rebel Angels and compared it to the contemporary human biological condition. The fallen angels could be seen as pathogenic organisms that had descended “through an evolutionary (not spiritual) pathway that takes them to a netherworld where they can feed only on our genes, our cells, our flesh,” Daszak wrote . “Will we succumb to the multitudinous horde? Are we to be cast downward into chthonic chaos represented here by the heaped up gibbering phantasmagory against which we rail and struggle?”
“Lab-Made?”
There are, in fact, some helpful points of agreement between zoonoticists — those who believe in a natural origin of the SARS-2 virus — and those who believe that it probably came from a laboratory. Both sides agree, when pressed, that a lab origin can’t be conclusively ruled out and a natural origin can’t be ruled out either — because nature, after all, is capable of improbable, teleological-seeming achievements. Both sides also agree, for the most part, that the spillover event that began the human outbreak probably happened only once, or a few times, quite recently, and not many times over a longer period. They agree that bat virus RaTG13 (named for the Rinolophus affinus bat, from Tongguan, in 2013) is the closest match to the human virus that has yet been found, and that although the two viruses are very similar, the spike protein of the bat virus lacks the features the human spike protein possesses that enable it to work efficiently with human tissue.
Zoonoticists hold that SARS-2’s crucial features — the furin cleavage site and the ACE2 receptor — are the result of a recombinant event involving a bat coronavirus (perhaps RaTG13 or a virus closely related to it) and another, unknown virus. Early on, researchers proposed that it could be a snake sold at the seafood market — a Chinese cobra or a banded krait — but no: Snakes don’t typically carry coronaviruses. Then there was a thought that the disease came from sick smuggled pangolins, because there existed a certain pangolin coronavirus that was, inexplicably, almost identical in its spike protein to the human coronavirus — but then, no: There turned out to be questions about the reliability of the genetic information in that diseased-pangolin data set, on top of which there were no pangolins for sale at the Wuhan market. Then a group from China’s government veterinary laboratory at Harbin tried infecting beagles, pigs, chickens, ducks, ferrets, and cats with SARS-2 to see if they could be carriers. (Cats and ferrets got sick; pigs, ducks, and most dogs did not.)
In September, some scientists at the University of Michigan, led by Yang Zhang, reported that they had created a “computational pipeline” to screen nearly a hundred possible intermediate hosts, including the Sumatran orangutan, the Western gorilla, the Olive baboon, the crab-eating macaque, and the bonobo. All these primates were “permissive” to the SARS-2 coronavirus and should undergo “further experimentational investigation,” the scientists proposed.
Despite this wide-ranging effort, there is at the moment no animal host that zoonoticists can point to as the missing link. There’s also no single, agreed-upon hypothesis to explain how the disease may have traveled from the bat reservoirs of Yunnan all the way to Wuhan, seven hours by train, without leaving any sick people behind and without infecting anyone along the way.
The zoonoticists say that we shouldn’t find it troubling that virologists have been inserting and deleting furin cleavage sites and ACE2-receptor-binding domains in experimental viral spike proteins for years: The fact that virologists have been doing these things in laboratories, in advance of the pandemic, is to be taken as a sign of their prescience, not of their folly. But I keep returning to the basic, puzzling fact: This patchwork pathogen, which allegedly has evolved without human meddling, first came to notice in the only city in the world with a laboratory that was paid for years by the U.S. government to perform experiments on certain obscure and heretofore unpublicized strains of bat viruses — which bat viruses then turned out to be, out of all the organisms on the planet, the ones that are most closely related to the disease. What are the odds?
In July, I discovered a number of volunteer analysts who were doing a new kind of forensic, samizdat science, hunched over the letter code of the SARS-2 genome like scholars deciphering the cuneiform impressions in Linear B tablets. There were the anonymous authors of Project Evidence, on GitHub, who “disavow all racism and violent attacks, including those which are aimed at Asian or Chinese people,” and there was Yuri Deigin, a biotech entrepreneur from Canada, who wrote a massive, lucid paper on Medium, “Lab-Made?,” which illumined the mysteries of the spike protein. Jonathan Latham of the Bioscience Resource Project, with his co-author Allison Wilson, wrote two important papers: one a calm, unsparing overview of laboratory accidents and rash research and the other a close look at the small outbreak of an unexplained viral pneumonia in a bat-infested copper mine in 2012. I corresponded with Alina Chan (now the subject of a nicely turned piece in Boston magazine by Rowan Jacobsen) and with the pseudonymous Billy Bostickson, a tireless researcher whose Twitter photo is a cartoon of an injured experimental monkey, and Monali Rahalkar, of the Agharkar Research Institute in Pune, India, who wrote a paper with her husband, Rahul Bahulikar, that also sheds light on the story of the bat-guano-shoveling men whose virus was remarkably like SARS-2, except that it was not nearly as catching. I talked to Rossana Segreto, a molecular biologist at the University of Innsbruck, whose paper , “Is Considering a Genetic-Manipulation Origin for SARS-CoV-2 a Conspiracy Theory That Must Be Censored?,” co-authored with Yuri Deigin, was finally published in November under a milder title; it argued that SARS-2’s most notable features, the furin site and the human ACE2-binding domain, were unlikely to have arisen simultaneously and “might be the result of lab manipulation techniques such as site directed mutagenesis.” Segreto is also the person who first established that a bat-virus fragment named BtCoV/4991, identified in 2013, was 100 percent identical to the closest known cousin to SARS-CoV-2, the bat virus RaTG13, thereby proving that the virus closest to the SARS-2-pandemic virus was linked back not to a bat cave but to a mine shaft, and that this same virus had been stored and worked on in the Wuhan Institute for years. This made possible the first big investigative piece on SARS-2’s origins, in the Times of London, in July: “Nobody can deny the bravery of scientists who risked their lives harvesting the highly infectious virus,” the Times authors write. “But did their courageous detective work lead inadvertently to a global disaster?”
“A New, Non-Natural Risk”
In 2011, a tall , confident Dutch scientist, Ron Fouchier, using grant money from Fauci’s group at NIH, created a mutant form of highly pathogenic avian influenza, H5N1, and passaged it ten times through ferrets in order to prove that he could “force” (his word) this potentially fatal disease to infect mammals, including humans, “via aerosols or respiratory droplets.” Fouchier said his findings indicated that these avian influenza viruses, thus forced, “pose a risk of becoming pandemic in humans.”
This experiment was too much for some scientists: Why, out of a desire to prove that something extremely infectious could happen, would you make it happen? And why would the U.S. government feel compelled to pay for it to happen? Late in 2011, Marc Lipsitch of the Harvard School of Public Health got together with several other dismayed onlookers to ring the gong for caution. On January 8, 2012, the New York Times published a scorcher of an editorial , “An Engineered Doomsday.” “We cannot say there would be no benefits at all from studying the virus,” the Times said. “But the consequences, should the virus escape, are too devastating to risk.”
These gain-of-function experiments were an important part of the NIH’s approach to vaccine development, and Anthony Fauci was reluctant to stop funding them. He and Francis Collins, director of the National Institutes of Health, along with Gary Nabel, NIAID director of vaccine research, published an opinion piece in the Washington Post in which they contended that the ferret flu experiments, and others like them, were “a risk worth taking.” “Important information and insights can come from generating a potentially dangerous virus in the laboratory,” they wrote; the work can “help delineate the principles of virus transmission between species.” The work was safe because the viruses were stored in a high-security lab, they believed, and the work was necessary because nature was always coming up with new threats. “Nature is the worst bioterrorist,” Fauci told a reporter. “We know that through history.”
Soon afterward, there followed some distressing screwups in secure federal laboratories involving live anthrax, live smallpox, and live avian influenza. These got attention in the science press. Then Lipsitch’s activists (calling themselves the Cambridge Working Group) sent around a strong statement on the perils of research with “Potential Pandemic Pathogens,” signed by more than a hundred scientists. The work might “trigger outbreaks that would be difficult or impossible to control,” the signers said. Fauci reconsidered, and the White House in 2014 announced that there would be a “pause” in the funding of new influenza, SARS, and MERS gain-of-function research.
Baric, in North Carolina, was not happy. He had a number of gain-of-function experiments with pathogenic viruses in progress. “It took me ten seconds to realize that most of them were going to be affected,” he told NPR . Baric and a former colleague from Vanderbilt University wrote a long letter to an NIH review board expressing their “profound concerns.” “This decision will significantly inhibit our capacity to respond quickly and effectively to future outbreaks of SARS-like or MERS-like coronaviruses, which continue to circulate in bat populations and camels,” they wrote. The funding ban was itself dangerous, they argued. “Emerging coronaviruses in nature do not observe a mandated pause.”
Hoping to smooth over controversy by showing due diligence, the National Science Advisory Board for Biosecurity, founded in the BioShield era under President Bush, paid a consulting firm, Gryphon Scientific, to write a report on gain-of-function research, which by now was simply referred to as GoF. In chapter six of this thousand-page dissertation, published in April 2016, the consultants take up the question of coronaviruses. “Increasing the transmissibility of the coronaviruses could significantly increase the chance of a global pandemic due to a laboratory accident,” they wrote.
The Cambridge Working Group continued to write letters of protest and plead for restraint and sanity. Steven Salzberg, a professor of biomedical engineering at Johns Hopkins, said, “We have enough problems simply keeping up with the current flu outbreaks — and now with Ebola — without scientists creating incredibly deadly new viruses that might accidentally escape their labs.” David Relman of Stanford Medical School said, “It is unethical to place so many members of the public at risk and then consult only scientists — or, even worse, just a small subset of scientists — and exclude others from the decision-making and oversight process.” Richard Ebright wrote that creating and evaluating new threats very seldom increases security: “Doing so in biology — where the number of potential threats is nearly infinite, and where the asymmetry between the ease of creating threats and the difficulty of addressing threats is nearly absolute — is especially counterproductive.” Lynn Klotz wrote, “Awful as a pandemic brought on by the escape of a variant H5N1 virus might be, it is SARS that now presents the greatest risk. The worry is less about recurrence of a natural SARS outbreak than of yet another escape from a laboratory researching it to help protect against a natural outbreak.” Marc Lipsitch argued that gain-of-function experiments can mislead, “resulting in worse not better decisions,” and that the entire gain-of-function debate as overseen by the NIH was heavily weighted in favor of scientific insiders and “distinctly unwelcoming of public participation.”
Nariyoshi Shinomiya, a professor of physiology and nano-medicine at the National Defense Medical College in Japan, offered this warning: “Similar to nuclear or chemical weapons there is no going back once we get a thing in our hands.”
But in the end, Baric was allowed to proceed with his experiments, and the research papers that resulted, showered with money, became a sort of Anarchist’s Cookbook for the rest of the scientific world. In November 2015, Baric and colleagues published a collaboration paper with Shi Zhengli titled “A SARS-like Cluster of Circulating Bat Coronaviruses Shows Potential for Human Emergence.” Into a human SARS virus that they had adapted so that it would work in mice, Baric and Shi et al. inserted the spike protein of a bat virus, SHC014, discovered by Shi in southern China. They dabbed the mice nasally with virus and waited, looking for signs of sickness: “hunching, ruffled fur.” They also infected human airway cells with the mouse-adapted bat-spike-in-a-human-virus backbone. In both mice and human airway cells, the chimeric virus caused a “robust infection.”
This proved, Baric and Shi believed, that you did not need civets or other intermediate hosts in order for bats to cause an epidemic in humans and that therefore all the SARS-like viruses circulating in bat populations “may pose a future threat.” Peter Daszak, who had used Predict funds to pay Shi for her work on the paper, was impressed by this conclusion; the findings, he said, “move this virus from a candidate emerging pathogen to a clear and present danger.”
Richard Ebright was trenchantly unenthusiastic. “The only impact of this work,” he said , “is the creation, in a lab, of a new, non-natural risk.”
Early in 2016, Baric and Shi again collaborated. Shi sent Baric a fresh bat virus spike protein, and Baric inserted it into the backbone of a human SARS virus and then used that infectious clone to attack human airway cells. “The virus readily and efficiently replicated in cultured human airway tissues, suggesting an ability to potentially jump directly to humans,” reported the UNC’s website. This time, they also used the bat-human hybrid virus to infect transgenic humanized mice that grew human ACE2 protein. The mice, young and old, lost weight and died, proving, again, that this particular bat virus was potentially “poised to emerge in human populations.” It was “an ongoing threat,” Baric wrote. But was it? Civets and camels that are exposed to a lot of bat-guano dust may be an ongoing threat and a manageable one. But the bats themselves just want to hang in their caves and not be bothered by frowning sightseers in spacesuits who want to poke Q-tips in their bottoms. This 2016 “poised for human emergence” paper was supported by eight different NIH grants. In 2015, Baric’s lab received $8.3 million from the NIH; in 2016, it received $10.5 million.
Gain-of-function research came roaring back under Trump and Fauci. “The National Institutes of Health will again fund research that makes viruses more dangerous,” said an article in Nature in December 2017. Carrie Wolinetz of the NIH’s office of science policy defended the decision. “These experiments will help us get ahead of viruses that are already out there and pose a real and present danger to human health,” she told The Lancet . The NIH, Wolinetz said, was committed to a leadership role with gain-of-function research internationally. “If we are pursuing this research in an active way, we will be much better positioned to develop protection and countermeasures should something bad happen in another country.”
A reporter asked Marc Lipsitch what he thought of the resumption of NIH funding. Gain-of-function experiments “have done almost nothing to improve our preparedness for pandemics,” he said, “yet they risked creating an accidental pandemic.”
“Proximity Is a Problem”
In April , four months into the coronavirus emergency, a deputy director at the NIH wrote an email to EcoHealth Alliance. “You are instructed to cease providing any funds to Wuhan Institute of Virology,” it said. In response, Daszak and the chief scientific officer of New England Biolabs (a company that sells seamless gene-splicing products to laboratories, among other things) got 77 Nobel Prize winners to sign a statement saying that the cancellation deprived the “nation and the world of highly regarded science that could help control one of the greatest health crises in modern history and those that may arise in the future.” Later, as a condition of further funding, the NIH wrote to say it wanted Daszak to arrange an outside inspection of the Wuhan lab and to procure from Wuhan’s scientists a sample of whatever they’d used to sequence the SARS-2 virus. Daszak was outraged (“I am not trained as a private detective”), and again he fought back. He was reluctant to give up his own secrets, too. “Conspiracy-theory outlets and politically motivated organizations have made Freedom of Information Act requests on our grants and all of our letters and emails to the NIH,” he told Nature . “We don’t think it’s fair that we should have to reveal everything we do.”
But Daszak has survived — even prospered. Recently, The Lancet made him the lead investigator in its inquiry into the origins of the pandemic, and the World Health Organization named him to its ten-person origins investigation. (“We’re still close enough to the origin to really find out more details about where it has come from,” Daszak told Nature .)
The NIH has also set up an ambitious new international program, called CREID, which stands for Centers for Research in Emerging Infectious Diseases, and it has put Daszak’s EcoHealth in charge of trapping animals and looking for obscure bat viruses in Singapore, Malaysia, and Thailand. Baric is one of Daszak’s partners in CREID. The virus hunting and collecting, which Richard Ebright likens to “looking for a gas leak with a lighted match,” will continue and widen with U.S. funding. “We’re going to work in remote parts of Malaysia and Thailand to get to the front line of where the next pandemic is going to start,” Daszak told NPR.
In May, an interviewer from the People’s Pharmacy website asked Baric if he had any thoughts on whether the coronavirus began with a natural bat-to-human transfer. “Or was there something a little bit more, perhaps, insidious involved?”
“Well, of course the answers to those questions are in China,” Baric replied. “Exactly how they work in that facility is something that would be very difficult for a Westerner to know,” he said. “The main problems that the Institute of Virology has is that the outbreak occurred in close proximity to that Institute. That Institute has in essence the best collection of virologists in the world that have gone out and sought out, and isolated, and sampled bat species throughout Southeast Asia. So they have a very large collection of viruses in their laboratory. And so it’s — you know — proximity is a problem. It’s a problem.”
Over the course of the fall, and especially after the election muffled Donald Trump’s influence over the country’s public-health apparatus, that proximity problem — and the uncomfortable questions of origins it raised — began to grow somewhat more discussable. The BBC, Le Monde , and Italy’s RAI have all recently taken seriously the scientific possibility of a lab leak. In late October, the World Health Organization convened the first meeting of its second inquiry into the origins of the disease. The WHO’s effort is perhaps the world’s best chance to satisfy its curiosity about goings-on at the Wuhan Institute of Virology and at the Wuhan CDC’s virus lab near the Wuhan seafood market. But, as the New York Times has reported , the WHO’s information gathering has been hindered by Chinese secretiveness since February, when an initial investigative team sent to Beijing was told its members’ access to scientists would be restricted and that it couldn’t visit the seafood market, then considered a hub of the pandemic.
When a BBC video team tried to inspect the Yunnan mine shaft, they found the road to the mine blocked by a strategically parked truck that had “broken down” shortly before they arrived. Reporter John Sudworth asked Daszak, one of the ten members of the second WHO investigative team, whether he would push for access to the Wuhan Institute of Virology. “That’s not my job to do that,” Daszak replied.
In November, David Relman, the Stanford microbiologist, one of the most thoughtful of the voices warning against gain-of-function research, published a paper in Proceedings of the National Academy of Sciences on the urgent need to unravel the origins of COVID-19. “If SARS-CoV-2 escaped from a lab to cause the pandemic,” he wrote, “it will become critical to understand the chain of events and prevent this from happening again.” Conflicts of interest by researchers and administrators will need to be addressed, Relman wrote; to reach the truth, the investigation must be transparent, international, and, as much as possible, unpolitical. “A more complete understanding of the origins of COVID-19 clearly serves the interests of every person in every country on this planet.”
“The world is sitting on a precedent-setting decision right now,” wrote Alina Chan on December 8. “It is unclear if SARS2 is 100 percent natural or emerged due to lab/research activities. If we walk away from this, demonstrating that we cannot effectively investigate its origins, it will pave the way for future COVIDS.”
Just before this issue of New York went to press, I reached Ralph Baric by phone and asked him where he now believed SARS-2 came from. (Anthony Fauci, Shi Zhengli, and Peter Daszak didn’t respond to emails, and Kristian Andersen said he was busy with other things.) Baric said he still thought the virus came from bats in southern China, perhaps directly, or possibly via an intermediate host, although the smuggled pangolins, in his view, were a red herring. The disease evolved in humans over time without being noticed, he suspected, becoming gradually more infectious, and eventually a person carried it to Wuhan “and the pandemic took off.” Then he said, “Can you rule out a laboratory escape? The answer in this case is probably not.”
Transmission
So how did we actually get this disease?
Here’s what I think happened. In April 2012, in a copper mine in Mojiang, China, three men were given an awful job — they were told to shovel bat guano out of a mine shaft. They went to work and shoveled guano for seven hours a day in the confined, insufficiently ventilated space of the mine shaft, and by the end of the week, they were sick with a viral pneumonia of unknown etiology. Three more, younger shovelers were hired to replace the ones who were out sick.
The viral load in their lungs was so huge, because of all the guano dust, that their lungs became a kind of accelerated laboratory passaging experiment, as Jonathan Latham and Allison Wilson have written, forcing the virus to switch its allegiance from bats to humans. SARS experts were consulted, and the disease was judged to be SARS-like but not SARS. It was something new. (Shi Zhengli told Scientific American that the guano shovelers had died of a fungal disease, but, as Monali Rahalkar pointed out, they were treated with antivirals, and their symptoms were consistent with viral pneumonia with attendant secondary fungal infections.)
Although it was a severe disease, and in the end three of the shovelers died, there was no resultant epidemic. It was actually a case of industrial overexposure to an infectious substance — what we might call a massive OSHA violation. The bat disease that the men encountered wasn’t necessarily all that dangerous except in an environment of immunosuppressive overload.
Peter Daszak and Shi Zhengli were interested, of course, because this unidentified coronavirus disease involved bats and people. Of the fragmentary bits of virus Shi retrieved from the mine shaft, one was SARS-like, and Shi sequenced it and called it BtCoV/4991 and published a paper about it. Several times — in 2016 and 2018 and 2019 — this most interesting sample, a portion of what we now know as RaTG13, was taken out of the freezers in Shi’s lab and worked on in undisclosed ways. (Peter Daszak claims that these samples have disintegrated and can’t be validated or studied.) Samples of the nameless human disease also traveled back to the Wuhan Institute of Virology — few specifics about these valuable specimens have been released by Chinese sources, however.
This is the period in the story that demands a very close investigation, when chimeric assemblages may have been created and serially passaged, using BtCoV/4991, a.k.a. RaTG13, and other bat viruses, perhaps along with forms of the human virus. It’s when Shi and Baric both published papers that were about what happened when you hot-swapped mutant spike proteins between bat viruses and human viruses.
The link, via the renamed sample BtCoV/4991, to the copper mine is of exceptional importance because of the one huge difference between the unnamed guano shovelers’ virus and the SARS-2 virus that is now ravaging, for example, California: transmissibility. Airborne human-to-human transmissibility — the kind of thing that gain-of-functioneers like Ron Fouchier and Ralph Baric were aiming at, in order to demonstrate what Baric called “lurking threats” — is COVID-19’s crucial distinguishing feature. If six men had gotten extremely sick with COVID-19 back in 2012 in southern China, doctors and nurses in the hospital where they lay dying would likely have gotten sick as well. There might have been hundreds or thousands of cases. Instead, only the shovelers themselves, who had breathed a heavy concentration of guano dust for days, got it.
The existence of bat virus RaTG13 is therefore not necessarily evidence of a natural bat origin. In fact, it seems to me to imply the opposite: New functional components may have been overlaid onto or inserted into the RaTG13 genome, new Tinkertoy intermolecular manipulations, especially to its spike protein, which have the effect of making it unprecedentedly infectious in human airways.
This is where the uniquely peculiar furin insert and/or the human-tuned ACE2-receptor-binding domain may come in — although it’s also possible that either of these elements could have evolved as part of some multistep zoonotic process. But in the climate of gonzo laboratory experimentation, at a time when all sorts of tweaked variants and amped-up substitutions were being tested on cell cultures and in the lungs of humanized mice and other experimental animals, isn’t it possible that somebody in Wuhan took the virus that had been isolated from human samples, or the RaTG13 bat virus sequence, or both (or other viruses from that same mine shaft that Shi Zhengli has recently mentioned in passing), and used them to create a challenge disease for vaccine research — a chopped-and-channeled version of RaTG13 or the miners’ virus that included elements that would make it thrive and even rampage in people? And then what if, during an experiment one afternoon, this new, virulent, human-infecting, furin-ready virus got out?
For more than 15 years, coronavirologists strove to prove that the threat of SARS was ever present and must be defended against, and they proved it by showing how they could doctor the viruses they stored in order to force them to jump species and go directly from bats to humans. More and more bat viruses came in from the field teams, and they were sequenced and synthesized and “rewired,” to use a term that Baric likes. In this international potluck supper of genetic cookery, hundreds of new variant diseases were invented and stored. And then one day, perhaps, somebody messed up. It’s at least a reasonable, “parsimonious” explanation of what might have happened.
This may be the great scientific meta-experiment of the 21st century. Could a world full of scientists do all kinds of reckless recombinant things with viral diseases for many years and successfully avoid a serious outbreak? The hypothesis was that, yes, it was doable. The risk was worth taking. There would be no pandemic.
I hope the vaccine works.
- coronavirus
- investigations
- new york magazine
- one great story
Most Viewed Stories
- Hunter Biden Is Probably Guilty. But His Prosecution Doesn’t Make Sense.
- Alex Jones Is Finally Screwed
- It’s Good That Caitlin Clark Is Getting Pushed Around in the WNBA
- Conservatives Angry at Biden’s Anti-Nazi D-Day Speech
- Who’s the Trump VP Pick? Latest Odds for Every Shortlist Candidate.
- The Problem With Darling 58
- The Scam at the Heart of the Mysterious Epoch Times
Editor’s Picks
Most Popular
- Hunter Biden Is Probably Guilty. But His Prosecution Doesn’t Make Sense. By Elie Honig
- Alex Jones Is Finally Screwed By Matt Stieb
- It’s Good That Caitlin Clark Is Getting Pushed Around in the WNBA By Will Leitch
- Conservatives Angry at Biden’s Anti-Nazi D-Day Speech By Jonathan Chait
- Who’s the Trump VP Pick? Latest Odds for Every Shortlist Candidate. By Margaret Hartmann
- The Problem With Darling 58 By Kate Morgan
- The Scam at the Heart of the Mysterious Epoch Times By Matt Stieb

What is your email?
This email will be used to sign into all New York sites. By submitting your email, you agree to our Terms and Privacy Policy and to receive email correspondence from us.
Sign In To Continue Reading
Create your free account.
Password must be at least 8 characters and contain:
- Lower case letters (a-z)
- Upper case letters (A-Z)
- Numbers (0-9)
- Special Characters (!@#$%^&*)
As part of your account, you’ll receive occasional updates and offers from New York , which you can opt out of anytime.

Stanford reinstates ACT/SAT requirements for university admissions process
O n Friday, Stanford University said they will once again require ACT or SAT scores for all future applicants , starting with the class of 2030.
They're following suit behind other Ivy League schools such as Harvard, Yale and Dartmouth.
"The pendulum has swung all the way in the other direction, and the narrative once again is, doggonit, I guess we need those tests," Adam Ingersoll, co-founder of Compass Education Group said.
Ingersoll is a co-founder of Compass Education, a national provider for test prep and academic tutoring.
He says the school first went test-optional in 2020 because public health concerns during the COVID-19 pandemic.
MORE: UC system officially drops SAT, ACT scores from use in admissions and scholarships
The university said in a statement on Friday, "The renewed testing requirement will allow Stanford to consider the fullest array of information in support of each student's application."
They add a review of their policy also found test scores are an important predictor of academic performance at Stanford.
"They're simply saying that we think more information is better, and we want to be trusted to consider everything that is available about a student's academic preparedness," Ingersoll said.
Though many students say that explanation isn't good enough.
"I feel like they need to say why because if you have data that suggests, like if you're mad because you think the quality of students is getting worse, then like you can say that and say why you think that," Alan Deloera, A Stanford senior said.
MORE: College Board will no longer offer SAT's optional essay and subject tests amid COVID-19 pandemic
Deloera is a first-generation college student coming from a low-income family.
He was part of Stanford's first class of students that weren't required to submit test scores.
"I myself was a test-optional student, and I've had plenty of success here at Stanford so I think that you don't really need to do good on that test to be able to do good in school," he said.
Carmen Davalos was part of the last class of students required to submit test scores.
"I don't see that there's this huge like need for it given that the classes that have been here afterwards with no requirement are clearly very capable, very smart," Davalos said.
Still, he doesn't think it's fair to add the requirement back in.
"I'm pretty confused about it to be honest because I have heard a lot of like the criticism that ACT and SAT act as a further barrier of entry for certain populations like people of color," he said.
Stanford says this applies to all students currently finishing 10th grade and going into 11th grade in the fall.
They will continue to be test-optional for the future class of 2029 applying this fall.

Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Integrating Clinical Trials and Practice : A New JAMA Series and Call for Papers
- 1 Executive Editor, JAMA
- Special Communication The Integration of Clinical Trials With the Practice of Medicine Derek C. Angus, MD, MPH; Alison J. Huang, MD, MAS; Roger J. Lewis, MD, PhD; Amy P. Abernethy, MD, PhD; Robert M. Califf, MD; Martin Landray, PhD; Nancy Kass, ScD; Kirsten Bibbins-Domingo, PhD, MD, MAS; JAMA Summit on Clinical Trials Participants; Ali B Abbasi; Kaleab Z Abebe; Amy P Abernethy; Stacey J. Adam; Derek C Angus; Jamy Ard; Rachel A Bender Ignacio ; Scott M Berry; Deepak L. Bhatt; Kirsten Bibbins-Domingo; Robert O. Bonow; Marc Bonten; Sharon A. Brangman; John Brownstein; Melinda J. B. Buntin; Atul J Butte; Robert M. Califf; Marion K Campbell; Anne R. Cappola; Anne C Chiang; Deborah Cook; Steven R Cummings; Gregory Curfman; Laura J Esserman; Lee A Fleisher; Joseph B Franklin; Ralph Gonzalez; Cynthia I Grossman; Tufia C. Haddad; Roy S. Herbst; Adrian F. Hernandez; Diane P Holder; Leora Horn; Grant D. Huang; Alison Huang; Nancy Kass; Rohan Khera; Walter J. Koroshetz; Harlan M. Krumholz; Martin Landray; Roger J. Lewis; Tracy A Lieu; Preeti N. Malani; Christa Lese Martin; Mark McClellan; Mary M. McDermott; Stephanie R. Morain; Susan A Murphy; Stuart G Nicholls; Stephen J Nicholls; Peter J. O'Dwyer; Bhakti K Patel; Eric Peterson; Sheila A. Prindiville; Joseph S. Ross; Kathryn M Rowan; Gordon Rubenfeld; Christopher W. Seymour; Rod S Taylor; Joanne Waldstreicher; Tracy Y. Wang JAMA
- Viewpoint Why Should the FDA Focus on Pragmatic Clinical Research? Ali B. Abbasi, MD; Lesley H. Curtis, PhD; Robert M. Califf, MD JAMA
Randomized clinical trials remain the cornerstone of evidence-based medicine. As a leading medical journal publishing the science that advances the clinical care of patients and the health of the public, JAMA is committed to the publication of clinical trials, as well as promoting the discourse on how clinical trial evidence can best serve the needs of patients and clinicians.
In autumn of 2023, JAMA hosted its inaugural in-person JAMA Summit 1 on the topic of randomized clinical trials and the challenges and opportunities to improve their design and conduct to be most responsive to the needs of clinical practice. The Special Communication published in JAMA, 2 “The Integration of Clinical Trials With the Practice of Medicine: Repairing a House Divided,” was written on behalf of the participants in the JAMA Summit and outlines many of the themes discussed during this provocative 2-day meeting.
A central theme of the JAMA Summit, which is elaborated on in the Special Communication in this issue, is how best to integrate clinical trials with clinical practice. Traditionally, clinical trialists and clinicians have worked independently, and, as the authors of the Special Communication underscore, their separate missions, incentives, and infrastructures have been siloed. The result is inefficiency in the performance of trials and limitations in their scope and impact. The authors offer solutions, including advances in implementation science, novel approaches to statistical analysis of trial data, and integration of trials with the electronic health record as a very rich source of clinical data. The clinical trial and health care delivery disciplines have functioned as a house divided. The authors proffer an approach to bridging the gap.
The future of clinical medicine will be greatly influenced by the data derived from randomized clinical trials, and trials will need to be accomplished more quickly, efficiently, and cheaply than they are today. A recent example is the platform trials 3 that were conducted during the COVID-19 pandemic. 4 - 6 These trials were embedded within clinical care and permitted the study of multiple therapeutic interventions simultaneously, with the results applicable to patient care in short order. The platform trials are exemplary of the types of novel approaches to clinical trials that are needed to realign the house divided.
With this Special Communication and an accompanying Viewpoint, 7 we launch a new series in JAMA— Integrating Clinical Trials and Practice. JAMA invites submissions that explore innovations in clinical trial design, implementation, funding, regulation, education, and application that may bring randomized trial evidence to more effectively address the needs in clinical practice. Our goal is to engage the research community in a significant publishing project to advance clinical trials and better align them with clinical practice. We welcome articles of any type, and we are happy to hear from you with presubmission inquiries. We are eager to chart a new path for randomized clinical trials and the delivery of health care, and we hope you will participate in navigating the road ahead.
Published Online: June 3, 2024. doi:10.1001/jama.2024.10266
Corresponding Author: Greg Curfman, MD, JAMA, Editorial Office, 330 N Wabash Ave, Chicago, IL 60611 ( [email protected] ).
Conflict of Interest Disclosures: None reported.
See More About
Curfman G. Integrating Clinical Trials and Practice : A New JAMA Series and Call for Papers . JAMA. Published online June 03, 2024. doi:10.1001/jama.2024.10266
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

IMAGES
VIDEO
COMMENTS
Nearly every 100 years, humans collectively face a pandemic crisis. After the Spanish flu, now the world is in the grip of coronavirus disease 2019 (COVID-19). First detected in 2019 in the Chinese city of Wuhan, COVID-19 causes severe acute respiratory distress syndrome. Despite the initial evidence indicating a zoonotic origin, the contagion ...
Read these 12 moving essays about life during coronavirus. Artists, novelists, critics, and essayists are writing the first draft of history. A woman wearing a face mask in Miami. Alissa Wilkinson ...
Together Again: Personal Narratives of COVID-19 Uniting the Seton Hall Community. The COVID-19 pandemic has disrupted life at Seton Hall as it has for millions of others around the country and the world. In the name of saving lives, the social distancing needed to slow the spread of the virus has scattered us into our homes around the region ...
Writing About COVID-19 in College Essays. Experts say students should be honest and not limit themselves to merely their experiences with the pandemic. The global impact of COVID-19, the disease ...
The coronavirus is a virus that originated in China, reached the U.S. and eventually spread all over the world by January of 2020. The common symptoms of the virus include shortness of breath, chills, sore throat, headache, loss of taste and smell, runny nose, vomiting and nausea. As it has been established, it might take up to 14 days for the ...
My content explains what my life was like during the last seven months of the Covid-19 pandemic and how it affected my life both positively and negatively. It also explains what it was like when I graduated from High School and how I want the future generations to remember the Class of 2020. Class assignment, Western Civilization (Dr. Marino).
The core narrative of the pandemic, and arguably the central one, is the presence of inequities. COVID-19 exposed inequities in morbidity and mortality, who bears the burden of steps we have taken ...
Introduction. This narrative review overviews a selection of 22 papers from among those concerning coronavirus disease 2019 (COVID-19) and healthcare that BJPsych Open has published during the pandemic. We draw them together in this thematic series to illustrate the huge volume of literature that has been presented to many journals in the last 18 months.
Trisha Greenhalgh and colleagues explore why inaccurate narratives about the mode of transmission of SARS-CoV-2 emerged early in the pandemic and shaped a flawed policy response, with tragic consequences ### Key messages The draft terms of reference for the UK covid-19 inquiry encompass not just what decisions were made but also how and why.1 As Dyani Lewis has argued in Nature , the World ...
Xiang Zhao. This is a narrative reflection about my experience of the ongoing coronavirus (COVID-19) outbreaks across countries between January and early March 2020. My recalled memories showed the shifting and contingent thoughts and emotions. Contextual factors such as my ethnic identity and local anti-coronavirus policies also constructed my ...
Conclusion. In conclusion, the COVID-19 pandemic has had a profound impact on my life. It affected me physically, mentally, and emotionally and challenged my ability to cope with adversity. However, it also taught me valuable lessons and allowed me to grow as an individual. This is only a sample.
COVID-19 Narratives is a series of five online writing sessions offered at no cost to all University of Colorado staff. Participants respond to writing prompts that are designed to allow expression of their thoughts and feelings about distressing experiences. Between sessions, participants receive feedback from a licensed Mental Health ...
Together Again: Personal Narratives of COVID-19 Uniting the Seton Hall Community. The COVID-19 pandemic has disrupted life at Seton Hall as it has for millions of others around the country and the world. In the name of saving lives, the social distancing needed to slow the spread of the virus has scattered us into our homes around the region ...
During the COVID-19 pandemic, medicine and public health have grappled with challenges related to individual behaviour and decision making, both in terms of infection and more recently concerning the uptake of COVID-19 vaccines. Social theory has long pointed to the role of narrative when trying to grasp the complexity of understanding and decision making in times of crisis.
Love came up in 286 essays; science in 128; art in 110; music in 109; and honor in 32. Personal tragedy also loomed large, with 30 essays about cancer alone. ... Covid-19 has taken a lot from me ...
Data Analysis. The analysis aimed to map the main dimensions of meanings underpinning the set of contents of the narratives collected and defining the SUs through which respondents make sense of their COVID-19 experiences. Each dimension of meaning can be conceived of as a generalized meaning component that was highlighted by the interviewees to talk about the time of COVID-19 and that ...
The essay outlines the ways in which narrative approaches to COVID-19 can draw on imaginative literature and critical oral history to resist the 'closure' often offered by cultural representations of epidemics. To support this goal, it analyses science and speculative fiction by Alejandro Morales and Tananarive Due in terms of how these works create alternative temporalities, which ...
Future historians may look back on the journals, essays and art that ordinary people are creating now to tell the story of life during the coronavirus. But writing can also be deeply therapeutic.
NARRATIVE ESSAY: COVID-19 PANDEMIC changed the life of the people. Covid-19 or also known as Corona Virus Disease, is an infectious disease caused by newly discovered virus and because this virus that is spreading all over the world, all the government officials around the world decided to start lockdown or quarantine, where all places and establishments are closed like malls, shops ...
Visual narratives are promising tools for science and health communication, especially for broad audiences in times of public health crisis, such as during the COVID-19 pandemic. In this study, we used the Lifeology illustrated "flashcard" course platform to construct visual narratives about COVID-19, and then assessed their impact on behavioral intentions. We conducted a survey experiment ...
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of "Viral: The Search for the Origin of Covid-19." This article has been updated to reflect news ...
The best clinical response to Favipiravir is shown in COVID-19 patients with mild-to-moderate early symptoms, and the most frequently reported ADE and elevated alanine aminotransferase levels were hyperuricemia and elevated alanine aminotransferase levels. COVID-19 is an acute respiratory disease resulting from the infection of SARS-COV-2 viruses and causes high morbidity, which requires ...
From early 2020, the world was brooding over the origins of COVID-19. People were reading research papers, talking about what kinds of live animals were or were not sold at the Wuhan seafood ...
Erratum to "Effects of Narrative Messages on Key COVID-19 Protective Responses: Findings from a Randomized Online Experiment"
MORE: College Board will no longer offer SAT's optional essay and subject tests amid COVID-19 pandemic Deloera is a first-generation college student coming from a low-income family. He was part of ...
Narrative Medicine; Nephrology; Neurology; Neuroscience and Psychiatry ... A New JAMA Series and Call for Papers. Gregory Curfman, MD 1. Author Affiliations Article ... A recent example is the platform trials 3 that were conducted during the COVID-19 pandemic. 4-6 These trials were embedded within clinical care and permitted the study of ...
When COVID-19 was first introduced to the United States, state and local governments enacted a variety of policies intended to mitigate the virulence of the epidemic. At the time, the most effective measures to prevent the spread of COVID-19 included stay-at-home orders, closing of nonessential businesses, and mask mandates. Although it was well known that regions with high population density ...