Essay on Smoking
500 words essay on smoking.
One of the most common problems we are facing in today’s world which is killing people is smoking. A lot of people pick up this habit because of stress , personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them. It has many ill-effects on the human body which we will go through in the essay on smoking.


Ill-Effects of Smoking
Tobacco can have a disastrous impact on our health. Nonetheless, people consume it daily for a long period of time till it’s too late. Nearly one billion people in the whole world smoke. It is a shocking figure as that 1 billion puts millions of people at risk along with themselves.
Cigarettes have a major impact on the lungs. Around a third of all cancer cases happen due to smoking. For instance, it can affect breathing and causes shortness of breath and coughing. Further, it also increases the risk of respiratory tract infection which ultimately reduces the quality of life.
In addition to these serious health consequences, smoking impacts the well-being of a person as well. It alters the sense of smell and taste. Further, it also reduces the ability to perform physical exercises.
It also hampers your physical appearances like giving yellow teeth and aged skin. You also get a greater risk of depression or anxiety . Smoking also affects our relationship with our family, friends and colleagues.
Most importantly, it is also an expensive habit. In other words, it entails heavy financial costs. Even though some people don’t have money to get by, they waste it on cigarettes because of their addiction.
How to Quit Smoking?
There are many ways through which one can quit smoking. The first one is preparing for the day when you will quit. It is not easy to quit a habit abruptly, so set a date to give yourself time to prepare mentally.
Further, you can also use NRTs for your nicotine dependence. They can reduce your craving and withdrawal symptoms. NRTs like skin patches, chewing gums, lozenges, nasal spray and inhalers can help greatly.
Moreover, you can also consider non-nicotine medications. They require a prescription so it is essential to talk to your doctor to get access to it. Most importantly, seek behavioural support. To tackle your dependence on nicotine, it is essential to get counselling services, self-materials or more to get through this phase.
One can also try alternative therapies if they want to try them. There is no harm in trying as long as you are determined to quit smoking. For instance, filters, smoking deterrents, e-cigarettes, acupuncture, cold laser therapy, yoga and more can work for some people.
Always remember that you cannot quit smoking instantly as it will be bad for you as well. Try cutting down on it and then slowly and steadily give it up altogether.
Get the huge list of more than 500 Essay Topics and Ideas
Conclusion of the Essay on Smoking
Thus, if anyone is a slave to cigarettes, it is essential for them to understand that it is never too late to stop smoking. With the help and a good action plan, anyone can quit it for good. Moreover, the benefits will be evident within a few days of quitting.
FAQ of Essay on Smoking
Question 1: What are the effects of smoking?
Answer 1: Smoking has major effects like cancer, heart disease, stroke, lung diseases, diabetes, and more. It also increases the risk for tuberculosis, certain eye diseases, and problems with the immune system .
Question 2: Why should we avoid smoking?
Answer 2: We must avoid smoking as it can lengthen your life expectancy. Moreover, by not smoking, you decrease your risk of disease which includes lung cancer, throat cancer, heart disease, high blood pressure, and more.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App


Essay on No Smoking
Students are often asked to write an essay on No Smoking in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on No Smoking
What is no smoking.
No Smoking means not using cigarettes or other tobacco products. It’s a choice to stay away from smoke that harms our bodies. When we say No Smoking, we protect our health and the air around us.
Why is Smoking Bad?
Smoking is bad because it can make you very sick. It hurts our lungs and heart. People who smoke can get diseases like cancer. It’s also expensive and makes your clothes and breath smell bad.
Benefits of Not Smoking
Not smoking keeps you healthy and full of energy. Your body feels better, and you can breathe easier. It saves money and keeps your teeth white. Plus, you set a good example for others.
Helping Others Quit
If someone you know smokes, you can help them quit. Tell them about the good things that come from not smoking. Be supportive and kind. They might need a friend to help them stop.
250 Words Essay on No Smoking
Smoking is bad for health. It can cause diseases like cancer, heart problems, and breathing issues. The smoke from cigarettes has chemicals that are dangerous. When people breathe in this smoke, it can make them sick, even if they are not the ones smoking.
Not smoking has many good points. People who do not smoke have better health. They can breathe easier, have more energy, and are less likely to get sick. Also, they save money because cigarettes are expensive.
Helping Smokers Quit
Quitting smoking is not easy, but it’s important. There are many ways to help smokers stop. They can use patches, gum, or medicine. Support from family and friends can also make a big difference.
No Smoking is important for everyone’s health. It keeps our air clean and our bodies healthy. By saying no to smoking, we can all live better and longer lives. Let’s encourage everyone to stop smoking and help those who are trying to quit. This way, we make our world a safer place for all.
500 Words Essay on No Smoking
No Smoking means not using cigarettes, pipes, or any other tool that burns tobacco and lets people inhale its smoke. This idea is important for keeping our bodies healthy and protecting the air everyone breathes. The smoke from cigarettes is not only bad for the person smoking but also for those around them, known as secondhand smoke.
Why People Start Smoking
Health risks of smoking.
Smoking is harmful and can cause a lot of health problems. It can damage the heart, lungs, and other parts of the body. Smokers can get sick with diseases like cancer, especially in the lungs, throat, and mouth. It also makes it hard to breathe and can ruin teeth, making them yellow and causing bad breath. For kids, it’s crucial to understand that starting to smoke can lead to a lifetime of health issues.
Choosing not to smoke has many good points. People who don’t smoke have better health, live longer, and have more energy for fun activities. They also save a lot of money because cigarettes are expensive. Not smoking means clothes and hair won’t smell bad, and it keeps teeth whiter. Plus, it sets a good example for friends and family.
How to Say No to Smoking
If someone knows a person who smokes, they can help them quit. They can tell them about the health risks and how much better life can be without cigarettes. It’s important to be supportive and patient because quitting is a big challenge. There are also many programs and products designed to help smokers give up the habit.
No Smoking is a choice that leads to a healthier life, not just for the person who decides not to smoke, but also for those around them. By understanding why people start, the risks involved, and the benefits of living smoke-free, it’s easier to say no to smoking. Encouraging others to quit and supporting them through the process can make a big difference in their lives and the health of the community. Remember, it’s never too late to stop smoking or to choose not to start at all.
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Importance of Quitting Smoking Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Smoking is a practice which involves the burning of a substance, for instance tobacco or cannabis, and later the smoke that emanates from it is inhaled. When referring to smoking, many people refer to tobacco smoking or cigarette smoking. The most widely used substance for smoking is tobacco, which is manufactured as cigarettes or hand-rolled tobacco. Smoking is an addictive habit and most smokers would attest that they wish they were able to stop the habit.
As much as it may seem to be a comfortable habit, smoking is in its actual sense not pleasurable and in any case it does not bring any relief. It is therefore the desire of many smokers to quit smoking. The knowledge that smoking can lead to serious health problems is one that is conscious in every smoker. This may make the smoker stay worried yet overcoming the addiction is a problem.
As such, quitting smoking is important since it helps relief the worry and the fear associated with possibility of developing cancer among other smoking-related illnesses. The smell that comes with smoking is very embarrassing and most people hate it.
Quitting smoking is therefore an important way of regaining self confidence by doing away with the embarrassing smell of cigarette smoke. Quitting smoking is an important way of shedding off the worry of the constant coughs and short breath brought about by smoking (Quit Smoking Review para 2-3).
Quitting smoking comes with a myriad of benefits which place more weight on the importance of quitting this addictive habit. If one quits smoking, it is no doubt that someone else is also saved from the problem of chain smoking. It is important that smokers reconsider their actions and identify that they spread the negative effects of smoking to persons who would not like to smoke.
It is therefore important to quit smoking if the problems associated with chain smoking are to be solved. The unborn are also beneficiaries of quitting smoking, especially among pregnant mothers. The elimination of very dangerous chemicals from the body motivates many people to avoid the practice. Most smokers thus find the health benefits as an encouraging gesture to quit smoking.
Quitting smoking is important since it leads to saving of monies that would have been used to buy cigarettes. These daily savings resulting from quitting smoking can be put into wiser and productive ways such as helping the family to settle bills as well as saving the money for investing. The fact that every individual’s lifestyle seems to influence another person’s life is an important reason why it is advisable to quit smoking. For instance, parents can act as good role models to their children by choosing to quit smoking.
In such a case, children are able to appreciate that smoking is a harmful habit and they will view the parent as a proactive parent as far as achieving good health is concerned. Additionally, quitting smoking gives the individual whiter and good looking teeth coupled with a fresh breath (Quit Smoking Review para 4-5). Most smokers are prone to gum diseases among other mouth diseases in comparison to non-smokers.
The individual’s health is also greatly improved as the breathing system that was once clogged with tobacco particles becomes clear and the lung capacity improves generally by about 10% (Gilman & Xun 45). Young smokers may not experience the negative effects of smoking until their later years but lung capacity generally weakens and diminishes with age.
Further, quitting smoking increases the individual’s life span, as Gilman and Xun (51) notes that half of all long-term smokers die from smoking related diseases such as heart attacks, lung cancer and others such as chronic bronchitis.
Those who quit smoking at age 30 are at an advantage as they add almost 10 years of their life span. As earlier mentioned stress levels are lower after one quits smoking since one has overcome the annoying habit. Most smokers suffer from withdrawal effects especially from nicotine, and the pleasant feeling of satisfying a craving is very temporary. Thus, non-smokers can concentrate better than smokers.
The body senses are also improved to a great extent as the system gets rid of many toxic chemicals found in the body as a result of cigarette smoke. Additionally, the individual experiences more energy as two weeks after quitting smoking, the circulation improves making many physical activities much easier. Additionally, the immune system is improved as mild diseases such as flu, colds and headaches can be easily fought.
In general, quitting smoking is an important step towards realizing an overall improvement in quality of life. Quitting smoking is also an important measure of ensuring cleanliness in one’s environment (American Academy of Family Physicians para 6).
Once one has quit smoking, the cigarette butts and ashes that are common in houses or cars of the smoker are no longer seen. This leads to greater happiness to the individual as well as those who live with the smoker. In addition, there is no need to worry much over the possible fire outbreaks brought about by careless disposal of burning cigarette butts.
Works Cited
American Academy of Family Physicians. Do I want to quit smoking ? 2000. Web.
Gilman, Sander and Xun, Zhou. Smoke: A global history of smoking . London, UK: Reaktion Books. 2004. Print.
Quit Smoking Review. The importance of quitting smoking . Web.
- The Social Contract Aspects
- Respect and Its Significance
- The Moral Dilemma: Nephrologist's Choices
- Quitting Smoking and Related Health Benefits
- Psychosocial Smoking Rehabilitation
- Women in the Contemporary Society
- Sexuality and Masculinity in Adolescents
- The Challenges and Advantages of Facebook
- Stay-At-Home Dads
- Social Article About Websites' Problem by Jenna Wortham
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, April 27). Importance of Quitting Smoking. https://ivypanda.com/essays/importance-of-quitting-smoking/
"Importance of Quitting Smoking." IvyPanda , 27 Apr. 2020, ivypanda.com/essays/importance-of-quitting-smoking/.
IvyPanda . (2020) 'Importance of Quitting Smoking'. 27 April.
IvyPanda . 2020. "Importance of Quitting Smoking." April 27, 2020. https://ivypanda.com/essays/importance-of-quitting-smoking/.
1. IvyPanda . "Importance of Quitting Smoking." April 27, 2020. https://ivypanda.com/essays/importance-of-quitting-smoking/.
Bibliography
IvyPanda . "Importance of Quitting Smoking." April 27, 2020. https://ivypanda.com/essays/importance-of-quitting-smoking/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .
Harms of Cigarette Smoking and Health Benefits of Quitting
What harmful chemicals does tobacco smoke contain.
Tobacco smoke contains many chemicals that are harmful to both smokers and nonsmokers. Breathing even a little tobacco smoke can be harmful ( 1 - 4 ).
Of the more than 7,000 chemicals in tobacco smoke, at least 250 are known to be harmful, including hydrogen cyanide , carbon monoxide , and ammonia ( 1 , 2 , 5 ).
Among the 250 known harmful chemicals in tobacco smoke, at least 69 can cause cancer. These cancer-causing chemicals include the following ( 1 , 2 , 5 ):
- Acetaldehyde
- Aromatic amines
- Beryllium (a toxic metal)
- 1,3–Butadiene (a hazardous gas)
- Cadmium (a toxic metal)
- Chromium (a metallic element)
- Ethylene oxide
- Formaldehyde
- Nickel (a metallic element)
- Polonium-210 (a radioactive chemical element)
- Polycyclic aromatic hydrocarbons (PAHs)
- Tobacco-specific nitrosamines
- Vinyl chloride
What are some of the health problems caused by cigarette smoking?
Smoking is the leading cause of premature, preventable death in this country. Cigarette smoking and exposure to tobacco smoke cause about 480,000 premature deaths each year in the United States ( 1 ). Of those premature deaths, about 36% are from cancer, 39% are from heart disease and stroke , and 24% are from lung disease ( 1 ). Mortality rates among smokers are about three times higher than among people who have never smoked ( 6 , 7 ).
Smoking harms nearly every bodily organ and organ system in the body and diminishes a person’s overall health. Smoking causes cancers of the lung, esophagus, larynx, mouth, throat, kidney, bladder, liver, pancreas, stomach, cervix, colon, and rectum, as well as acute myeloid leukemia ( 1 – 3 ).
Smoking also causes heart disease, stroke, aortic aneurysm (a balloon-like bulge in an artery in the chest), chronic obstructive pulmonary disease (COPD) ( chronic bronchitis and emphysema ), diabetes , osteoporosis , rheumatoid arthritis, age-related macular degeneration , and cataracts , and worsens asthma symptoms in adults. Smokers are at higher risk of developing pneumonia , tuberculosis , and other airway infections ( 1 – 3 ). In addition, smoking causes inflammation and impairs immune function ( 1 ).
Since the 1960s, a smoker’s risk of developing lung cancer or COPD has actually increased compared with nonsmokers, even though the number of cigarettes consumed per smoker has decreased ( 1 ). There have also been changes over time in the type of lung cancer smokers develop – a decline in squamous cell carcinomas but a dramatic increase in adenocarcinomas . Both of these shifts may be due to changes in cigarette design and composition, in how tobacco leaves are cured, and in how deeply smokers inhale cigarette smoke and the toxicants it contains ( 1 , 8 ).
Smoking makes it harder for a woman to get pregnant. A pregnant smoker is at higher risk of miscarriage, having an ectopic pregnancy , having her baby born too early and with an abnormally low birth weight, and having her baby born with a cleft lip and/or cleft palate ( 1 ). A woman who smokes during or after pregnancy increases her infant’s risk of death from Sudden Infant Death Syndrome (SIDS) ( 2 , 3 ). Men who smoke are at greater risk of erectile dysfunction ( 1 , 9 ).
The longer a smoker’s duration of smoking, the greater their likelihood of experiencing harm from smoking, including earlier death ( 7 ). But regardless of their age, smokers can substantially reduce their risk of disease, including cancer, by quitting.
What are the risks of tobacco smoke to nonsmokers?
Secondhand smoke (also called environmental tobacco smoke, involuntary smoking, and passive smoking) is the combination of “sidestream” smoke (the smoke given off by a burning tobacco product) and “mainstream” smoke (the smoke exhaled by a smoker) ( 4 , 5 , 10 , 11 ).
The U.S. Environmental Protection Agency, the U.S. National Toxicology Program, the U.S. Surgeon General, and the International Agency for Research on Cancer have classified secondhand smoke as a known human carcinogen (cancer-causing agent) ( 5 , 11 , 12 ). Inhaling secondhand smoke causes lung cancer in nonsmoking adults ( 1 , 2 , 4 ). Approximately 7,300 lung cancer deaths occur each year among adult nonsmokers in the United States as a result of exposure to secondhand smoke ( 1 ). The U.S. Surgeon General estimates that living with a smoker increases a nonsmoker’s chances of developing lung cancer by 20 to 30% ( 4 ).
Secondhand smoke causes disease and premature death in nonsmoking adults and children ( 2 , 4 ). Exposure to secondhand smoke irritates the airways and has immediate harmful effects on a person’s heart and blood vessels. It increases the risk of heart disease by an estimated 25 to 30% ( 4 ). In the United States, exposure to secondhand smoke is estimated to cause about 34,000 deaths from heart disease each year ( 1 ). Exposure to secondhand smoke also increases the risk of stroke by 20 to 30% ( 1 ). Pregnant women exposed to secondhand smoke are at increased risk of having a baby with a small reduction in birth weight ( 1 ).
Children exposed to secondhand smoke are at an increased risk of SIDS, ear infections, colds, pneumonia, and bronchitis. Secondhand smoke exposure can also increase the frequency and severity of asthma symptoms among children who have asthma. Being exposed to secondhand smoke slows the growth of children’s lungs and can cause them to cough, wheeze, and feel breathless ( 2 , 4 ).
Is smoking addictive?
Smoking is highly addictive. Nicotine is the drug primarily responsible for a person’s addiction to tobacco products, including cigarettes. The addiction to cigarettes and other tobacco products that nicotine causes is similar to the addiction produced by using drugs such as heroin and cocaine ( 13 ). Nicotine is present naturally in the tobacco plant. But tobacco companies intentionally design cigarettes to have enough nicotine to create and sustain addiction.
The amount of nicotine that gets into the body is determined by the way a person smokes a tobacco product and by the nicotine content and design of the product. Nicotine is absorbed into the bloodstream through the lining of the mouth and the lungs and travels to the brain in a matter of seconds. Taking more frequent and deeper puffs of tobacco smoke increases the amount of nicotine absorbed by the body.
Are other tobacco products, such as smokeless tobacco or pipe tobacco, harmful and addictive?
Yes. All forms of tobacco are harmful and addictive ( 4 , 11 ). There is no safe tobacco product.
In addition to cigarettes, other forms of tobacco include smokeless tobacco , cigars , pipes , hookahs (waterpipes), bidis , and kreteks .
- Smokeless tobacco : Smokeless tobacco is a type of tobacco that is not burned. It includes chewing tobacco , oral tobacco, spit or spitting tobacco, dip, chew, snus, dissolvable tobacco, and snuff. Smokeless tobacco causes oral (mouth, tongue, cheek and gum), esophageal, and pancreatic cancers and may also cause gum and heart disease ( 11 , 14 ).
- Cigars : These include premium cigars, little filtered cigars (LFCs), and cigarillos. LFCs resemble cigarettes, but both LFCs and cigarillos may have added flavors to increase appeal to youth and young adults ( 15 , 16 ). Most cigars are composed primarily of a single type of tobacco (air-cured and fermented), and have a tobacco leaf wrapper. Studies have found that cigar smoke contains higher levels of toxic chemicals than cigarette smoke, although unlike cigarette smoke, cigar smoke is often not inhaled ( 11 ). Cigar smoking causes cancer of the oral cavity, larynx, esophagus, and lung. It may also cause cancer of the pancreas. Moreover, daily cigar smokers, particularly those who inhale, are at increased risk for developing heart disease and other types of lung disease.
- Pipes : In pipe smoking, the tobacco is placed in a bowl that is connected to a stem with a mouthpiece at the other end. The smoke is usually not inhaled. Pipe smoking causes lung cancer and increases the risk of cancers of the mouth, throat, larynx, and esophagus ( 11 , 17 , 18 ).
- Hookah or waterpipe (other names include argileh, ghelyoon, hubble bubble, shisha, boory, goza, and narghile): A hookah is a device used to smoke tobacco (often heavily flavored) by passing the smoke through a partially filled water bowl before being inhaled by the smoker. Although some people think hookah smoking is less harmful and addictive than cigarette smoking ( 19 ), research shows that hookah smoke is at least as toxic as cigarette smoke ( 20 – 22 ).
- Bidis : A bidi is a flavored cigarette made by rolling tobacco in a dried leaf from the tendu tree, which is native to India. Bidi use is associated with heart attacks and cancers of the mouth, throat, larynx, esophagus, and lung ( 11 , 23 ).
- Kreteks : A kretek is a cigarette made with a mixture of tobacco and cloves. Smoking kreteks is associated with lung cancer and other lung diseases ( 11 , 23 ).
Is it harmful to smoke just a few cigarettes a day?
There is no safe level of smoking. Smoking even just one cigarette per day over a lifetime can cause smoking-related cancers (lung, bladder, and pancreas) and premature death ( 24 , 25 ).
What are the immediate health benefits of quitting smoking?
The immediate health benefits of quitting smoking are substantial:
- Heart rate and blood pressure , which are abnormally high while smoking, begin to return to normal.
- Within a few hours, the level of carbon monoxide in the blood begins to decline. (Carbon monoxide reduces the blood’s ability to carry oxygen.)
- Within a few weeks, people who quit smoking have improved circulation, produce less phlegm , and don’t cough or wheeze as often.
- Within several months of quitting, people can expect substantial improvements in lung function ( 26 ).
- Within a few years of quitting, people will have lower risks of cancer, heart disease, and other chronic diseases than if they had continued to smoke.
What are the long-term health benefits of quitting smoking?
Quitting smoking reduces the risk of cancer and many other diseases, such as heart disease and COPD , caused by smoking.
Data from the U.S. National Health Interview Survey show that people who quit smoking, regardless of their age, are less likely to die from smoking-related illness than those who continue to smoke. Smokers who quit before age 40 reduce their chance of dying prematurely from smoking-related diseases by about 90%, and those who quit by age 45-54 reduce their chance of dying prematurely by about two-thirds ( 6 ).
Regardless of their age, people who quit smoking have substantial gains in life expectancy, compared with those who continue to smoke. Data from the U.S. National Health Interview Survey also show that those who quit between the ages of 25 and 34 years live about 10 years longer; those who quit between ages 35 and 44 live about 9 years longer; those who quit between ages 45 and 54 live about 6 years longer; and those who quit between ages 55 and 64 live about 4 years longer ( 6 ).
Also, a study that followed a large group of people age 70 and older ( 7 ) found that even smokers who quit smoking in their 60s had a lower risk of mortality during follow-up than smokers who continued smoking.
Does quitting smoking lower the risk of getting and dying from cancer?
Yes. Quitting smoking reduces the risk of developing and dying from cancer and other diseases caused by smoking. Although it is never too late to benefit from quitting, the benefit is greatest among those who quit at a younger age ( 3 ).
The risk of premature death and the chances of developing and dying from a smoking-related cancer depend on many factors, including the number of years a person has smoked, the number of cigarettes smoked per day, and the age at which the person began smoking.
Is it important for someone diagnosed with cancer to quit smoking?
Quitting smoking improves the prognosis of cancer patients. For patients with some cancers, quitting smoking at the time of diagnosis may reduce the risk of dying by 30% to 40% ( 1 ). For those having surgery, chemotherapy, or other treatments, quitting smoking helps improve the body’s ability to heal and respond to therapy ( 1 , 3 , 27 ). It also lowers the risk of pneumonia and respiratory failure ( 1 , 3 , 28 ). In addition, quitting smoking may lower the risk that the cancer will recur, that a second cancer will develop, or that the person will die from the cancer or other causes ( 27 , 29 – 32 ).
Where can I get help to quit smoking?
NCI and other agencies and organizations can help smokers quit:
- Visit Smokefree.gov for access to free information and resources, including Create My Quit Plan , smartphone apps , and text message programs
- Call the NCI Smoking Quitline at 1–877–44U–QUIT ( 1–877–448–7848 ) for individualized counseling, printed information, and referrals to other sources.
- See the NCI fact sheet Where To Get Help When You Decide To Quit Smoking .
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Commentaries /
Quit tobacco to be a winner
World no tobacco day 2021 campaign - commit to quit.
The saying goes that “quitters never win,” but in the case of tobacco, quitters are the real winners.
When the news came out that smokers were more likely to develop severe disease with COVID-19 compared to non-smokers, it triggered millions of smokers to want to quit tobacco. But without adequate support, quitting can be incredibly challenging.
The nicotine found in tobacco is highly addictive and creates dependence. The behavioural and emotional ties to tobacco use – like having a cigarette with your coffee, craving tobacco, feelings of sadness or stress – make it hard to kick the habit.
With professional support and cessation services, tobacco users double their chances of quitting successfully.
Currently, over 70% of the 1.3 billion tobacco users worldwide lack access to the tools they need to quit successfully. This gap in access to cessation services is only further exacerbated in the last year as the health workforce has been mobilized to handle the pandemic.
That’s why WHO launched a year-long campaign for World No Tobacco Day’s – “Commit to Quit” theme. The campaign aims to empower 100 million tobacco users to make a quit attempt by creating networks of support and increasing access to services proven to help tobacco users quit successfully.
This will be achieved by scaling-up existing services such as brief advice from health professionals and national toll free quit lines, as well as launching innovative services like Florence, WHO’s first digital health worker, and chatbot support programmes on WhatsApp and Viber.
To truly help tobacco users quit, they need to be supported with tried and tested policies and interventions to drive down the demand for tobacco.
The WHO Framework Convention on Tobacco Control (WHO FCTC) provides a strong, concerted response to the global tobacco epidemic and its enormous health, social, environmental and economic costs. To help countries implement the WHO FCTC, WHO introduced the MPOWER technical package to support implementation of key strategies, such as raising tobacco taxes, creating smoke-free environments and offering help to quit.
E-cigarettes are not proven cessation aids
The tobacco industry has continuously attempted to subvert these life-saving public health measures. Over the last decade, the tobacco industry has promoted e-cigarettes as cessation aids under the guises of contributing to global tobacco control. Meanwhile, they have employed strategic marketing tactics to hook children on this same portfolio of products, making them available in over 15,000 attractive flavours.
The scientific evidence on e-cigarettes as cessation aids is inconclusive and there is a lack of clarity as to whether these products have any role to play in smoking cessation. Switching from conventional tobacco products to e-cigarettes is not quitting.
"We must be guided by science and evidence, not the marketing campaigns of the tobacco industry – the same industry that has engaged in decades of lies and deceit to sell products that have killed hundreds of millions of people”, said WHO Director-General Dr Tedros Adhanom Ghebreyesus. “E-cigarettes generate toxic chemicals, which have been linked to harmful health effects such as cardiovascular disease & lung disorders."
Why does the UN prohibit partnerships with the tobacco industry and their front groups?
The tobacco industry is the single greatest barrier to reducing deaths caused by tobacco use. Their interests are irreconcilably opposed to promoting public health, and point to a critical need to keep them out of global tobacco control efforts.
WHO FCTC Article 5.3 aims to do just that. WHO established a firewall in 2007 to protect policies from commercial and other vested interests of the tobacco industry. The United Nations Global Compact followed suit, banning the tobacco industry from participation in 2017, flagging the problematic and irreconcilable conflicts between the goals of the UN and an industry that is responsible for more than 8 million deaths per year. In line with Article 5.3, industry has been entirely excluded from the UN system and its agencies have been urged to devise strategies to prevent industry interference.
The United Nations Inter-Agency Task Force on the Prevention and Control of NCDs , which has both the WHO and the Secretariat of the WHO FCTC as leading participants, has crafted a Model policy for agencies of the United Nations system on preventing tobacco industry interference , a strong policy to prevent industry tactics operating in the UN and then ensured its implementation at the intergovernmental level.
In 2008, the United Nations General Assembly adopted a Resolution for Smoke-free United Nations Premises, and in 2012, the United Nations Economic and Social Council called for “system-wide coherence on tobacco control”. The creation of smoke-free campuses puts into practice the United Nations smoke-free workplace policy, which aims to protect approximately 100,000 UN staff members from second-hand tobacco smoke.
WHO and the Secretariat of the WHO FCTC have stated that no partnerships should be forged with tobacco industry front groups such as the Foundation for a Smoke Free World. PMI has committed to spending one billion USD over 12 years funding a new captive organization, the Foundation for a Smoke Free World (FSFW) – Philip Morris International (PMI) is its sole funder – to reproduce and launder its harm-reduction messages.
The importance of tobacco duties and taxes and smoke-free workplaces
Despite these challenges brought on by the tobacco industry, the world has seen significant progress in tobacco control.
Since the MPOWER technical package was introduced more than a decade ago, 5 billion people have now been covered by at least one of these best-practice tobacco control measures, has more than quadrupled since 2007.Over the last two decades, global tobacco use has fallen by 60 million people. But the decrease varies by region and we are now seeing the tobacco industry vigorously target low-and middle-income countries with traditional cigarettes, while pushing its new and emerging products in higher income countries.
WHO urges governments to help tobacco users quit by providing the support, services, policies and tobacco taxes that enable people to quit.
Smoke-free policies have the potential to protect non-smokers, including over 65,000 children and adolescents who die every year from exposure to second-hand smoke.
Tobacco costs economies over US$ 1.4 trillion in health expenditures and lost productivity, which is equivalent to 1.8% of annual global GDP. Increasing tobacco taxes helps make these lethal products less affordable and helps cover health-care costs for the diseases they create.
There has never been a better time to quit tobacco, and commitment to helping tobacco users quit is critical to improving health and saving lives.
Dr Ruediger Krech
Director Health Promotion World Health Organization
World No Tobacco Day 2021
WHO Framework Convention on Tobacco Control

Alonzo Mourning, Prostate Cancer Survivor
Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
Cancer Risk and Prevention
- Common Questions About Causes of Cancer
- Is Cancer Contagious?
- Lifetime Risk of Developing or Dying From Cancer
- How to Interpret News About Cancer Causes
- Determining if Something Is a Carcinogen
- Known and Probable Human Carcinogens
- Cancer Clusters
- Cancer Warning Labels Based on California's Proposition 65
- Cancer Facts for Men
- Cancer Facts for Gay and Bisexual Men
- Cancer Facts for Women
- Cancer Facts for Lesbian and Bisexual Women
- How to Interpret News About Ways to Prevent Cancer
Reasons to Quit Smoking
- Health Benefits of Quitting Smoking Over Time
- Making a Plan to Quit and Planning Your Quit Day
- Quitting Smoking or Smokeless Tobacco
- Quitting E-cigarettes
- Nicotine Replacement Therapy to Help You Quit Tobacco
- Dealing with the Mental Part of Tobacco Addiction
- Prescription Medicines to Help You Quit Tobacco
- Ways to Quit Tobacco Without Using Medicines
- Staying Tobacco-free After You Quit
- Help for Cravings and Tough Situations While You're Quitting Tobacco
- How to Help Someone Quit Smoking
- Why People Start Smoking and Why It’s Hard to Stop
- Health Risks of Smoking Tobacco
- Health Risks of Smokeless Tobacco
- Health Risks of Secondhand Smoke
- Health Risks of E-cigarettes
- Harmful Chemicals in Tobacco Products
- Is Any Type of Tobacco Product Safe?
- ACS Position Statement on Electronic Cigarettes
- What Do We Know About E-cigarettes?
- Keeping Your Kids Tobacco-free
- History of the Great American Smokeout
- Great American Smokeout Event Tools and Resources
Empowered to Quit
- American Cancer Society Guideline for Diet and Physical Activity
- Effects of Diet and Physical Activity on Risks for Certain Cancers
- Common Questions About Diet, Activity, and Cancer Risk
- Infographic: Diet and Activity Guidelines to Reduce Cancer Risk
- Diet and Physical Activity: What’s the Cancer Connection?
- Stock Your Kitchen with Healthy Ingredients
- Tips for Eating Healthier
- Find Healthy Recipes
- Quick Entrees: Healthy in a Hurry
- Snacks and Dashboard Dining
- Tips for Eating Out
- Calorie Counter
- Controlling Portion Sizes
- Cut Calories and Fat, Not Flavor
- Low-Fat Foods
- Understanding Food Terms
- Fitting in Fitness
- Kids on the Move
- Community Actions for a Healthful Life
- Exercise Activity Calculator
- Target Heart Rate Calculator
- Find Your Body Mass Index (BMI)
- Alcohol Use and Cancer
- Nutrition and Activity Quiz
- Healthy Eating, Active Living Videos
- What Is HPV (Human Papillomavirus)?
- Types of HPV
- Cancers Linked with HPV
- HPV Signs and Symptoms
- How to Protect Against HPV
- HPV Testing
- HPV Vaccines
- HPV Vaccine in Texas
- Understanding Family Cancer Syndromes
- Ataxia-telangiectasia (A-T)
- Birt-Hogg-Dubé syndrome (BHD)
- Carney Complex (CNC)
- Cowden Syndrome
- Familial GIST Syndrome
- Hereditary Breast and Ovarian Cancer Syndrome (HBOC)
- Li-Fraumeni Syndrome (LFS)
- Lynch Syndrome
- Understanding Genetic Testing for Cancer Risk
- What Should I Know Before Getting Genetic Testing?
- What Happens During Genetic Testing for Cancer Risk?
- What Are X-rays and Gamma Rays?
- How Are People Exposed to X-rays and Gamma Rays?
- Do X-rays and Gamma Rays Cause Cancer?
- Do X-rays and Gamma Rays Cause Health Problems Other than Cancer?
- Can I Avoid or Limit My Exposure to X-rays and Gamma Rays?
- Radiofrequency (RF) Radiation
- Power Lines, Electrical Devices, and Extremely Low Frequency Radiation
- Cellular (Cell) Phones
- Cell Phone Towers
- Smart Meters
- Agent Orange
- Antiperspirants
- Diesel Exhaust
- Firefighting
- Formaldehyde
- Military Burn Pits
- Recombinant Bovine Growth Hormone (rBGH)
- PFOA, PFOS, and Related PFAS Chemicals
- Talcum Powder
- Water Fluoridation
- Can Infections Cause Cancer?
- Viruses that Can Lead to Cancer
- Bacteria that Can Lead to Cancer
- Parasites that Can Lead to Cancer
- What Are HIV and AIDS?
- HIV and Cancer
- Abortion and Breast Cancer Risk
- DES Exposure: Questions and Answers
- Menopausal Hormone Therapy and Cancer Risk
- UV (Ultraviolet) Radiation and Cancer Risk
- Sun Safety and Vitamin D
- What Factors Affect UV Risk?
- Is It Safe to Get a Fake (Sunless) Tan?
- How to Protect Your Skin from UV Rays
- How to Use Sunscreen
- How to Do a Skin Self-Exam
- Sun Safety Quiz
- Sun Safety Videos
Lots of studies have been done about the benefits of quitting smoking. Decades of research have found several good reasons to quit, including health and financial benefits that can save lives and money. While it’s best to quit as early in life as possible, quitting at any age can lead to a better health and lifestyle.
Quitting can make you look, feel, and be healthier
- Quitting can help you save money
Quitting can improve self-confidence and lead to a better lifestyle
- Using tobacco leads to disease and disability and harms nearly every organ of the body.
- Smoking is the leading cause of preventable death.
- Secondhand smoke is dangerous and can harm the health of your friends and family.
Quitting can help you save money
- Cigarettes and other tobacco products are expensive.
- The risk for getting colds and other respiratory problems is lower, meaning fewer doctor visits, less money spent on medicines, and fewer sick days off work.
- Cleaning and home repairs could cost less since clothes, furniture, curtains, and the car won’t smell like tobacco.
- Not using tobacco products helps keep your family safe.
- Your may have more energy, helping you have more quality family and leisure time.
- Quitting can set a good example for others who might need help quitting.
- Others will be proud of your progress and willpower to quit and stay quit.

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
This content has been developed by the American Cancer Society in collaboration with the Smoking Cessation Leadership Center to help people who want to learn about quitting tobacco.
Smokefree.gov Reasons to quit. Available at https://smokefree.gov/quit-smoking/why-you-should-quit/reasons-to-quit. Accessed October 10, 2020.
US Department of Health and Human Services. What you need to know about quitting smoking: Advice from the Surgeon General. Available at https://www.hhs.gov/sites/default/files/2020-cessation-sgr-consumer-guide.pdf. Accessed October 10, 2020.
Last Revised: October 10, 2020
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy .
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.
Related Resources
A free, email-based smoking cessation program from the American Cancer Society.
Help us end cancer as we know it, for everyone.


An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Tobacco, Nicotine, and E-Cigarettes Research Report How can we prevent tobacco use?

The medical consequences of tobacco use—including secondhand exposure—make tobacco control and smoking prevention crucial parts of any public health strategy. Since the first Surgeon General’s Report on Smoking and Health in 1964, states and communities have made efforts to reduce initiation of smoking, decrease exposure to smoke, and increase cessation. Researchers estimate that these tobacco control efforts are associated with averting an estimated 8 million premature deaths and extending the average life expectancy of men by 2.3 years and of women by 1.6 years. 18 But there is a long way yet to go: roughly 5.6 million adolescents under age 18 are expected to die prematurely as a result of an illness related to smoking. 13
Prevention can take the form of policy-level measures, such as increased taxation of tobacco products; stricter laws (and enforcement of laws) regulating who can purchase tobacco products; how and where they can be purchased; where and when they can be used (i.e., smoke-free policies in restaurants, bars, and other public places); and restrictions on advertising and mandatory health warnings on packages. Over 100 studies have shown that higher taxes on cigarettes, for example, produce significant reductions in smoking, especially among youth and lower-income individuals. 217 Smoke-free workplace laws and restrictions on advertising have also shown benefits. 218
Prevention can also take place at the school or community level. Merely educating potential smokers about the health risks has not proven effective. 218 Successful evidence-based interventions aim to reduce or delay initiation of smoking, alcohol use, and illicit drug use, and otherwise improve outcomes for children and teens by reducing or mitigating modifiable risk factors and bolstering protective factors. Risk factors for smoking include having family members or peers who smoke, being in a lower socioeconomic status, living in a neighborhood with high density of tobacco outlets, not participating in team sports, being exposed to smoking in movies, and being sensation-seeking. 219 Although older teens are more likely to smoke than younger teens, the earlier a person starts smoking or using any addictive substance, the more likely they are to develop an addiction. Males are also more likely to take up smoking in adolescence than females.
Some evidence-based interventions show lasting effects on reducing smoking initiation. For instance, communities utilizing the intervention-delivery system, Communities that Care (CTC) for students aged 10 to14 show sustained reduction in male cigarette initiation up to 9 years after the end of the intervention. 220
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Health Effects of Cigarette Smoking
- Secondhand Smoke
- E-cigarettes (Vapes)
- Menthol Tobacco Products
- Morbidity and Mortality Weekly Reports (MMWR)
- About Surveys
- Other Tobacco Products
- Smoking and Tobacco Use Features
- Patient Care Settings and Smoking Cessation
- Patient Care
- Funding Opportunity Announcements
- State and Community Work
- National and State Tobacco Control Program
- Multimedia and Tools
Related Topics:
- View All Home
- Tobacco - Health Equity
- Tobacco - Surgeon General's Reports
- State Tobacco Activities Tracking and Evaluation (STATE) System
- Global Tobacco Control
World No Tobacco Day: Protect Our Youth
At a glance.
Learn what individuals and communities can do to help keep young people tobacco-free, or help them quit for good, on this World No Tobacco Day.

Why observe World No Tobacco Day?
Using any kind of tobacco product is unsafe, especially for kids, teens, and young adults. But worldwide, at least 14 million young people aged 13 to 15 currently use tobacco products, according to CDC's 2006–2017 Global Youth Tobacco Survey .
Tobacco companies, meanwhile, spend billions of dollars every year on marketing tobacco products, including cigarettes, cigars, and e-cigarettes.
Since 1988, the World Health Organization (WHO) has used World No Tobacco Day to highlight the harmful effects of cigarettes and other tobacco products on a person's overall health. This year, WHO is focusing on preventing youth tobacco product use and the tobacco industry's attempts to attract youth.
This World No Tobacco Day, learn what individuals and communities can do to help keep young people tobacco-free, or help them quit for good.
U.S. youth and tobacco: the numbers
In 2019, about 40% of U.S. middle and high school students reported ever using any kind of tobacco product—including e-cigarettes —and 23% said they had used a tobacco product in the past 30 days.
Studies show that most adults in the United States who regularly use tobacco products started before the age of 18. Using any tobacco product, including e-cigarettes, is unsafe for young people .
Tobacco products—including cigarettes, smokeless tobacco, and most e-cigarettes—contain nicotine, which is an addictive drug. Being exposed to nicotine can also harm brain development. A young person's brain is still developing up to age 25. Exposure to nicotine during these important years can harm the parts of the brain that control attention, learning, mood, and impulse control.
Secondhand smoke: a danger at home and abroad
At least 500 million people younger than 15 in 21 countries are exposed to secondhand smoke .
It's a problem in the United States:
- 1 in 4 Americans, or about 58 million people, are exposed to secondhand smoke.
- Children aged 3 to 11 have the highest exposure to secondhand smoke compared to any other age group.
- African American children are more likely to be exposed to secondhand smoke than children of other racial or ethnic groups.
Quitting smoking and adopting smokefree policies help protect the health of people who do not smoke.
Targeting young people
The younger a person is when they start using tobacco products, the more likely they are to become dependent on nicotine. The tobacco industry uses this information to attract youth and young people to their products through ads and sponsorships in stores, online, in media, and at cultural events.
Studies in the United States and other countries have shown that the more ads for tobacco products a young person sees, the more likely they are to use tobacco products. The U.S. Surgeon General has also said that seeing people smoke in movies makes youth more likely to smoke. Although the number of movies rated PG-13 or lower that feature smoking has gone down in the past 15 years, the films that do show smoking show it more often.
Tobacco flavors
The flavors in tobacco products, including e-cigarettes, make these products appealing to kids and teens. Since 2009, tobacco companies have not been allowed to sell cigarettes in flavors other than menthol in the United States. Still, youth are more likely than adults to smoke menthol cigarettes .
Flavoring is also a major driver of e-cigarette use among young people. More than 2 out of 3 youth who currently use e-cigarettes use flavored e-cigarettes, and flavors are a major reason they report starting to use e-cigarettes.
The danger of e-cigarettes for youth
Since 2014, most U.S. youth who said they had ever used tobacco products reported using e-cigarettes. This percentage has grown over time. E-cigarettes typically contain nicotine. Newer e-cigarettes use a new form of nicotine called nicotine salts, which make it easier to inhale higher levels of nicotine.
Because of the recent rise in e-cigarette use by U.S. middle and high school students, CDC offers resources for parents , teachers , and health care providers to help them talk to kids about e-cigarettes.
What you can do
Everyone—from individuals who influence youth directly to whole communities—can help prevent kids, teens, and young adults from trying and using tobacco products.

Parents and other caregivers can:
- Set a good example by being tobacco-free. They can call 1-800-QUIT-NOW or visit smokefree.gov for help with quitting.
- Talk to kids about the harms of tobacco products, including e-cigarettes.
- Know what kids watch on screen and talk to them about tobacco use.
- Tell kids you expect them not to use tobacco products or tell them to stop using them.
- Refuse to give tobacco products to kids, teens, or young adults.
The Office of the Surgeon General has more tips for parents and caregivers to help keep young people tobacco-free.
Health care providers can:
- Talk to their patients about the dangers of tobacco use. In a 2015 survey, only 1 out of 3 U.S. high schoolers said their doctor brought up smoking during a visit.
- Ask patients if they use tobacco products and advise them to quit.
CDC offers resources and tools to help providers start the conversation about tobacco and quitting.
States and communities can:
- Fund state tobacco control programs at the level CDC recommends.
- Work to limit tobacco product advertising.
- Use science-based strategies to prevent and reduce tobacco use. For example, states and communities can increase tobacco prices, conduct hard-hitting media campaigns, adopt comprehensive smoke-free laws, require licenses for tobacco sellers, and limit where tobacco products can be sold.
- Provide barrier-free access to treatments proven to help people quit.
If everyone works together to keep youth safe from the harms of tobacco use, we can move further toward a healthier, smokefree world.
Quitting resources for youth
In 2019, more than half of U.S. young people who reported currently using tobacco products said they were seriously thinking about quitting. Quitting as soon as possible is the healthiest choice for mind and body.
State quitlines can connect people to resources like text support, counseling, and web-based chat. People who want to quit can call 1-800-QUIT-NOW to find out what their state offers. Quitlines are also available in Spanish, Chinese (Cantonese and Mandarin), Korean, and Vietnamese.
- 1-855-DÉJELO-YA (Spanish)
- 1-800-838-8917 (Cantonese & Mandarin)
- 1-800-556-5564 (Korean)
- 1-800-778-8440 (Vietnamese)
SmokefreeTXT for Teens is a free mobile text messaging program for youth aged 13 to 19.
The quitSTART phone app offers custom tips, inspiration, and challenges.
Quitting resources for adults
At any age, it's never too late to quit. U.S. adults who want to quit can call 1-800-QUIT-NOW or
- 1-800-838-8917 (Cantonese and Mandarin)
They can also visit CDC.gov/Quit or Smokefree.gov to sign up for texting programs and download mobile apps.
Smoking and Tobacco Use
Commercial tobacco use is the leading cause of preventable disease, disability, and death in the United States.
For Everyone
Health care providers, public health.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2012.

Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General.
1 introduction, summary, and conclusions.
- Introduction
Tobacco use is a global epidemic among young people. As with adults, it poses a serious health threat to youth and young adults in the United States and has significant implications for this nation’s public and economic health in the future ( Perry et al. 1994 ; Kessler 1995 ). The impact of cigarette smoking and other tobacco use on chronic disease, which accounts for 75% of American spending on health care ( Anderson 2010 ), is well-documented and undeniable. Although progress has been made since the first Surgeon General’s report on smoking and health in 1964 ( U.S. Department of Health, Education, and Welfare [USDHEW] 1964 ), nearly one in four high school seniors is a current smoker. Most young smokers become adult smokers. One-half of adult smokers die prematurely from tobacco-related diseases ( Fagerström 2002 ; Doll et al. 2004 ). Despite thousands of programs to reduce youth smoking and hundreds of thousands of media stories on the dangers of tobacco use, generation after generation continues to use these deadly products, and family after family continues to suffer the devastating consequences. Yet a robust science base exists on social, biological, and environmental factors that influence young people to use tobacco, the physiology of progression from experimentation to addiction, other health effects of tobacco use, the epidemiology of youth and young adult tobacco use, and evidence-based interventions that have proven effective at reducing both initiation and prevalence of tobacco use among young people. Those are precisely the issues examined in this report, which aims to support the application of this robust science base.
Nearly all tobacco use begins in childhood and adolescence ( U.S. Department of Health and Human Services [USDHHS] 1994 ). In all, 88% of adult smokers who smoke daily report that they started smoking by the age of 18 years (see Chapter 3 , “The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide”). This is a time in life of great vulnerability to social influences ( Steinberg 2004 ), such as those offered through the marketing of tobacco products and the modeling of smoking by attractive role models, as in movies ( Dalton et al. 2009 ), which have especially strong effects on the young. This is also a time in life of heightened sensitivity to normative influences: as tobacco use is less tolerated in public areas and there are fewer social or regular users of tobacco, use decreases among youth ( Alesci et al. 2003 ). And so, as we adults quit, we help protect our children.
Cigarettes are the only legal consumer products in the world that cause one-half of their long-term users to die prematurely ( Fagerström 2002 ; Doll et al. 2004 ). As this epidemic continues to take its toll in the United States, it is also increasing in low- and middle-income countries that are least able to afford the resulting health and economic consequences ( Peto and Lopez 2001 ; Reddy et al. 2006 ). It is past time to end this epidemic. To do so, primary prevention is required, for which our focus must be on youth and young adults. As noted in this report, we now have a set of proven tools and policies that can drastically lower youth initiation and use of tobacco products. Fully committing to using these tools and executing these policies consistently and aggressively is the most straight forward and effective to making future generations tobacco-free.
The 1994 Surgeon General’s Report
This Surgeon General’s report on tobacco is the second to focus solely on young people since these reports began in 1964. Its main purpose is to update the science of smoking among youth since the first comprehensive Surgeon General’s report on tobacco use by youth, Preventing Tobacco Use Among Young People , was published in 1994 ( USDHHS 1994 ). That report concluded that if young people can remain free of tobacco until 18 years of age, most will never start to smoke. The report documented the addiction process for young people and how the symptoms of addiction in youth are similar to those in adults. Tobacco was also presented as a gateway drug among young people, because its use generally precedes and increases the risk of using illicit drugs. Cigarette advertising and promotional activities were seen as a potent way to increase the risk of cigarette smoking among young people, while community-wide efforts were shown to have been successful in reducing tobacco use among youth. All of these conclusions remain important, relevant, and accurate, as documented in the current report, but there has been considerable research since 1994 that greatly expands our knowledge about tobacco use among youth, its prevention, and the dynamics of cessation among young people. Thus, there is a compelling need for the current report.
Tobacco Control Developments
Since 1994, multiple legal and scientific developments have altered the tobacco control environment and thus have affected smoking among youth. The states and the U.S. Department of Justice brought lawsuits against cigarette companies, with the result that many internal documents of the tobacco industry have been made public and have been analyzed and introduced into the science of tobacco control. Also, the 1998 Master Settlement Agreement with the tobacco companies resulted in the elimination of billboard and transit advertising as well as print advertising that directly targeted underage youth and limitations on the use of brand sponsorships ( National Association of Attorneys General [NAAG] 1998 ). This settlement also created the American Legacy Foundation, which implemented a nationwide antismoking campaign targeting youth. In 2009, the U.S. Congress passed a law that gave the U.S. Food and Drug Administration authority to regulate tobacco products in order to promote the public’s health ( Family Smoking Prevention and Tobacco Control Act 2009 ). Certain tobacco companies are now subject to regulations limiting their ability to market to young people. In addition, they have had to reimburse state governments (through agreements made with some states and the Master Settlement Agreement) for some health care costs. Due in part to these changes, there was a decrease in tobacco use among adults and among youth following the Master Settlement Agreement, which is documented in this current report.
Recent Surgeon General Reports Addressing Youth Issues
Other reports of the Surgeon General since 1994 have also included major conclusions that relate to tobacco use among youth ( Office of the Surgeon General 2010 ). In 1998, the report focused on tobacco use among U.S. racial/ethnic minority groups ( USDHHS 1998 ) and noted that cigarette smoking among Black and Hispanic youth increased in the 1990s following declines among all racial/ethnic groups in the 1980s; this was particularly notable among Black youth, and culturally appropriate interventions were suggested. In 2000, the report focused on reducing tobacco use ( USDHHS 2000b ). A major conclusion of that report was that school-based interventions, when implemented with community- and media-based activities, could reduce or postpone the onset of smoking among adolescents by 20–40%. That report also noted that effective regulation of tobacco advertising and promotional activities directed at young people would very likely reduce the prevalence and onset of smoking. In 2001, the Surgeon General’s report focused on women and smoking ( USDHHS 2001 ). Besides reinforcing much of what was discussed in earlier reports, this report documented that girls were more affected than boys by the desire to smoke for the purpose of weight control. Given the ongoing obesity epidemic ( Bonnie et al. 2007 ), the current report includes a more extensive review of research in this area.
The 2004 Surgeon General’s report on the health consequences of smoking ( USDHHS 2004 ) concluded that there is sufficient evidence to infer that a causal relationship exists between active smoking and (a) impaired lung growth during childhood and adolescence; (b) early onset of decline in lung function during late adolescence and early adulthood; (c) respiratory signs and symptoms in children and adolescents, including coughing, phlegm, wheezing, and dyspnea; and (d) asthma-related symptoms (e.g., wheezing) in childhood and adolescence. The 2004 Surgeon General’s report further provided evidence that cigarette smoking in young people is associated with the development of atherosclerosis.
The 2010 Surgeon General’s report on the biology of tobacco focused on the understanding of biological and behavioral mechanisms that might underlie the pathogenicity of tobacco smoke ( USDHHS 2010 ). Although there are no specific conclusions in that report regarding adolescent addiction, it does describe evidence indicating that adolescents can become dependent at even low levels of consumption. Two studies ( Adriani et al. 2003 ; Schochet et al. 2005 ) referenced in that report suggest that because the adolescent brain is still developing, it may be more susceptible and receptive to nicotine than the adult brain.
Scientific Reviews
Since 1994, several scientific reviews related to one or more aspects of tobacco use among youth have been undertaken that also serve as a foundation for the current report. The Institute of Medicine (IOM) ( Lynch and Bonnie 1994 ) released Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youths, a report that provided policy recommendations based on research to that date. In 1998, IOM provided a white paper, Taking Action to Reduce Tobacco Use, on strategies to reduce the increasing prevalence (at that time) of smoking among young people and adults. More recently, IOM ( Bonnie et al. 2007 ) released a comprehensive report entitled Ending the Tobacco Problem: A Blueprint for the Nation . Although that report covered multiple potential approaches to tobacco control, not just those focused on youth, it characterized the overarching goal of reducing smoking as involving three distinct steps: “reducing the rate of initiation of smoking among youth (IOM [ Lynch and Bonnie] 1994 ), reducing involuntary tobacco smoke exposure ( National Research Council 1986 ), and helping people quit smoking” (p. 3). Thus, reducing onset was seen as one of the primary goals of tobacco control.
As part of USDHHS continuing efforts to assess the health of the nation, prevent disease, and promote health, the department released, in 2000, Healthy People 2010 and, in 2010, Healthy People 2020 ( USDHHS 2000a , 2011 ). Healthy People provides science-based, 10-year national objectives for improving the health of all Americans. For 3 decades, Healthy People has established benchmarks and monitored progress over time in order to encourage collaborations across sectors, guide individuals toward making informed health decisions, and measure the impact of prevention activities. Each iteration of Healthy People serves as the nation’s disease prevention and health promotion roadmap for the decade. Both Healthy People 2010 and Healthy People 2020 highlight “Tobacco Use” as one of the nation’s “Leading Health Indicators,” feature “Tobacco Use” as one of its topic areas, and identify specific measurable tobacco-related objectives and targets for the nation to strive for. Healthy People 2010 and Healthy People 2020 provide tobacco objectives based on the most current science and detailed population-based data to drive action, assess tobacco use among young people, and identify racial and ethnic disparities. Additionally, many of the Healthy People 2010 and 2020 tobacco objectives address reductions of tobacco use among youth and target decreases in tobacco advertising in venues most often influencing young people. A complete list of the healthy people 2020 objectives can be found on their Web site ( USDHHS 2011 ).
In addition, the National Cancer Institute (NCI) of the National Institutes of Health has published monographs pertinent to the topic of tobacco use among youth. In 2001, NCI published Monograph 14, Changing Adolescent Smoking Prevalence , which reviewed data on smoking among youth in the 1990s, highlighted important statewide intervention programs, presented data on the influence of marketing by the tobacco industry and the pricing of cigarettes, and examined differences in smoking by racial/ethnic subgroup ( NCI 2001 ). In 2008, NCI published Monograph 19, The Role of the Media in Promoting and Reducing Tobacco Use ( NCI 2008 ). Although young people were not the sole focus of this Monograph, the causal relationship between tobacco advertising and promotion and increased tobacco use, the impact on youth of depictions of smoking in movies, and the success of media campaigns in reducing youth tobacco use were highlighted as major conclusions of the report.
The Community Preventive Services Task Force (2011) provides evidence-based recommendations about community preventive services, programs, and policies on a range of topics including tobacco use prevention and cessation ( Task Force on Community Preventive Services 2001 , 2005 ). Evidence reviews addressing interventions to reduce tobacco use initiation and restricting minors’ access to tobacco products were cited and used to inform the reviews in the current report. The Cochrane Collaboration (2010) has also substantially contributed to the review literature on youth and tobacco use by producing relevant systematic assessments of health-related programs and interventions. Relevant to this Surgeon General’s report are Cochrane reviews on interventions using mass media ( Sowden 1998 ), community interventions to prevent smoking ( Sowden and Stead 2003 ), the effects of advertising and promotional activities on smoking among youth ( Lovato et al. 2003 , 2011 ), preventing tobacco sales to minors ( Stead and Lancaster 2005 ), school-based programs ( Thomas and Perara 2006 ), programs for young people to quit using tobacco ( Grimshaw and Stanton 2006 ), and family programs for preventing smoking by youth ( Thomas et al. 2007 ). These reviews have been cited throughout the current report when appropriate.
In summary, substantial new research has added to our knowledge and understanding of tobacco use and control as it relates to youth since the 1994 Surgeon General’s report, including updates and new data in subsequent Surgeon General’s reports, in IOM reports, in NCI Monographs, and in Cochrane Collaboration reviews, in addition to hundreds of peer-reviewed publications, book chapters, policy reports, and systematic reviews. Although this report is a follow-up to the 1994 report, other important reviews have been undertaken in the past 18 years and have served to fill the gap during an especially active and important time in research on tobacco control among youth.
- Focus of the Report
Young People
This report focuses on “young people.” In general, work was reviewed on the health consequences, epidemiology, etiology, reduction, and prevention of tobacco use for those in the young adolescent (11–14 years of age), adolescent (15–17 years of age), and young adult (18–25 years of age) age groups. When possible, an effort was made to be specific about the age group to which a particular analysis, study, or conclusion applies. Because hundreds of articles, books, and reports were reviewed, however, there are, unavoidably, inconsistencies in the terminology used. “Adolescents,” “children,” and “youth” are used mostly interchangeably throughout this report. In general, this group encompasses those 11–17 years of age, although “children” is a more general term that will include those younger than 11 years of age. Generally, those who are 18–25 years old are considered young adults (even though, developmentally, the period between 18–20 years of age is often labeled late adolescence), and those 26 years of age or older are considered adults.
In addition, it is important to note that the report is concerned with active smoking or use of smokeless tobacco on the part of the young person. The report does not consider young people’s exposure to secondhand smoke, also referred to as involuntary or passive smoking, which was discussed in the 2006 report of the Surgeon General ( USDHHS 2006 ). Additionally, the report does not discuss research on children younger than 11 years old; there is very little evidence of tobacco use in the United States by children younger than 11 years of age, and although there may be some predictors of later tobacco use in those younger years, the research on active tobacco use among youth has been focused on those 11 years of age and older.
Tobacco Use
Although cigarette smoking is the most common form of tobacco use in the United States, this report focuses on other forms as well, such as using smokeless tobacco (including chew and snuff) and smoking a product other than a cigarette, such as a pipe, cigar, or bidi (tobacco wrapped in tendu leaves). Because for young people the use of one form of tobacco has been associated with use of other tobacco products, it is particularly important to monitor all forms of tobacco use in this age group. The term “tobacco use” in this report indicates use of any tobacco product. When the word “smoking” is used alone, it refers to cigarette smoking.
- Organization of the Report
This chapter begins by providing a short synopsis of other reports that have addressed smoking among youth and, after listing the major conclusions of this report, will end by presenting conclusions specific to each chapter. Chapter 2 of this report (“The Health Consequences of Tobacco Use Among Young People”) focuses on the diseases caused by early tobacco use, the addiction process, the relation of body weight to smoking, respiratory and pulmonary problems associated with tobacco use, and cardiovascular effects. Chapter 3 (“The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide”) provides recent and long-term cross-sectional and longitudinal data on cigarette smoking, use of smokeless tobacco, and the use of other tobacco products by young people, by racial/ethnic group and gender, primarily in the United States, but including some worldwide data as well. Chapter 4 (“Social, Environmental, Cognitive, and Genetic Influences on the Use of Tobacco Among Youth”) identifies the primary risk factors associated with tobacco use among youth at four levels, including the larger social and physical environments, smaller social groups, cognitive factors, and genetics and neurobiology. Chapter 5 (“The Tobacco Industry’s Influences on the Use of Tobacco Among Youth”) includes data on marketing expenditures for the tobacco industry over time and by category, the effects of cigarette advertising and promotional activities on young people’s smoking, the effects of price and packaging on use, the use of the Internet and movies to market tobacco products, and an evaluation of efforts by the tobacco industry to prevent tobacco use among young people. Chapter 6 (“Efforts to Prevent and Reduce Tobacco Use Among Young People”) provides evidence on the effectiveness of family-based, clinic-based, and school-based programs, mass media campaigns, regulatory and legislative approaches, increased cigarette prices, and community and statewide efforts in the fight against tobacco use among youth. Chapter 7 (“A Vision for Ending the Tobacco Epidemic”) points to next steps in preventing and reducing tobacco use among young people.
- Preparation of the Report
This report of the Surgeon General was prepared by the Office on Smoking and Health (OSH), National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention (CDC), USDHHS. In 2008, 18 external independent scientists reviewed the 1994 report and suggested areas to be added and updated. These scientists also suggested chapter editors and a senior scientific editor, who were contacted by OSH. Each chapter editor named external scientists who could contribute, and 33 content experts prepared draft sections. The draft sections were consolidated into chapters by the chapter editors and then reviewed by the senior scientific editor, with technical editing performed by CDC. The chapters were sent individually to 34 peer reviewers who are experts in the areas covered and who reviewed the chapters for scientific accuracy and comprehensiveness. The entire manuscript was then sent to more than 25 external senior scientists who reviewed the science of the entire document. After each review cycle, the drafts were revised by the chapter and senior scientific editor on the basis of the experts’ comments. Subsequently, the report was reviewed by various agencies within USDHHS. Publication lags prevent up-to-the-minute inclusion of all recently published articles and data, and so some more recent publications may not be cited in this report.
- Evaluation of the Evidence
Since the first Surgeon General’s report in 1964 on smoking and health ( USDHEW 1964 ), major conclusions concerning the conditions and diseases caused by cigarette smoking and the use of smokeless tobacco have been based on explicit criteria for causal inference ( USDHHS 2004 ). Although a number of different criteria have been proposed for causal inference since the 1960s, this report focuses on the five commonly accepted criteria that were used in the original 1964 report and that are discussed in greater detail in the 2004 report on the health consequences of smoking ( USDHHS 2004 ). The five criteria refer to the examination of the association between two variables, such as a risk factor (e.g., smoking) and an outcome (e.g., lung cancer). Causal inference between these variables is based on (1) the consistency of the association across multiple studies; this is the persistent finding of an association in different persons, places, circumstances, and times; (2) the degree of the strength of association, that is, the magnitude and statistical significance of the association in multiple studies; (3) the specificity of the association to clearly demonstrate that tobacco use is robustly associated with the condition, even if tobacco use has multiple effects and multiple causes exist for the condition; (4) the temporal relationship of the association so that tobacco use precedes disease onset; and (5) the coherence of the association, that is, the argument that the association makes scientific sense, given data from other sources and understanding of biological and psychosocial mechanisms ( USDHHS 2004 ). Since the 2004 Surgeon General’s report, The Health Consequences of Smoking , a four-level hierarchy ( Table 1.1 ) has been used to assess the research data on associations discussed in these reports ( USDHHS 2004 ). In general, this assessment was done by the chapter editors and then reviewed as appropriate by peer reviewers, senior scientists, and the scientific editors. For a relationship to be considered sufficient to be characterized as causal, multiple studies over time provided evidence in support of each criteria.
Four-level hierarchy for classifying the strength of causal inferences based on available evidence.
When a causal association is presented in the chapter conclusions in this report, these four levels are used to describe the strength of the evidence of the association, from causal (1) to not causal (4). Within the report, other terms are used to discuss the evidence to date (i.e., mixed, limited, and equivocal evidence), which generally represent an inadequacy of data to inform a conclusion.
However, an assessment of a casual relationship is not utilized in presenting all of the report’s conclusions. The major conclusions are written to be important summary statements that are easily understood by those reading the report. Some conclusions, particularly those found in Chapter 3 (epidemiology), provide observations and data related to tobacco use among young people, and are generally not examinations of causal relationships. For those conclusions that are written using the hierarchy above, a careful and extensive review of the literature has been undertaken for this report, based on the accepted causal criteria ( USDHHS 2004 ). Evidence that was characterized as Level 1 or Level 2 was prioritized for inclusion as chapter conclusions.
In additional to causal inferences, statistical estimation and hypothesis testing of associations are presented. For example, confidence intervals have been added to the tables in the chapter on the epidemiology of youth tobacco use (see Chapter 3 ), and statistical testing has been conducted for that chapter when appropriate. The chapter on efforts to prevent tobacco use discusses the relative improvement in tobacco use rates when implementing one type of program (or policy) versus a control program. Statistical methods, including meta-analytic methods and longitudinal trajectory analyses, are also presented to ensure that the methods of evaluating data are up to date with the current cutting-edge research that has been reviewed. Regardless of the methods used to assess significance, the five causal criteria discussed above were applied in developing the conclusions of each chapter and the report.
- Major Conclusions
- Cigarette smoking by youth and young adults has immediate adverse health consequences, including addiction, and accelerates the development of chronic diseases across the full life course.
- Prevention efforts must focus on both adolescents and young adults because among adults who become daily smokers, nearly all first use of cigarettes occurs by 18 years of age (88%), with 99% of first use by 26 years of age.
- Advertising and promotional activities by tobacco companies have been shown to cause the onset and continuation of smoking among adolescents and young adults.
- After years of steady progress, declines in the use of tobacco by youth and young adults have slowed for cigarette smoking and stalled for smokeless tobacco use.
- Coordinated, multicomponent interventions that combine mass media campaigns, price increases including those that result from tax increases, school-based policies and programs, and statewide or community-wide changes in smoke-free policies and norms are effective in reducing the initiation, prevalence, and intensity of smoking among youth and young adults.
- Chapter Conclusions
The following are the conclusions presented in the substantive chapters of this report.
Chapter 2. The Health Consequences of Tobacco Use Among Young People
- The evidence is sufficient to conclude that there is a causal relationship between smoking and addiction to nicotine, beginning in adolescence and young adulthood.
- The evidence is suggestive but not sufficient to conclude that smoking contributes to future use of marijuana and other illicit drugs.
- The evidence is suggestive but not sufficient to conclude that smoking by adolescents and young adults is not associated with significant weight loss, contrary to young people’s beliefs.
- The evidence is sufficient to conclude that there is a causal relationship between active smoking and both reduced lung function and impaired lung growth during childhood and adolescence.
- The evidence is sufficient to conclude that there is a causal relationship between active smoking and wheezing severe enough to be diagnosed as asthma in susceptible child and adolescent populations.
- The evidence is sufficient to conclude that there is a causal relationship between smoking in adolescence and young adulthood and early abdominal aortic atherosclerosis in young adults.
- The evidence is suggestive but not sufficient to conclude that there is a causal relationship between smoking in adolescence and young adulthood and coronary artery atherosclerosis in adulthood.
Chapter 3. The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide
- Among adults who become daily smokers, nearly all first use of cigarettes occurs by 18 years of age (88%), with 99% of first use by 26 years of age.
- Almost one in four high school seniors is a current (in the past 30 days) cigarette smoker, compared with one in three young adults and one in five adults. About 1 in 10 high school senior males is a current smokeless tobacco user, and about 1 in 5 high school senior males is a current cigar smoker.
- Among adolescents and young adults, cigarette smoking declined from the late 1990s, particularly after the Master Settlement Agreement in 1998. This decline has slowed in recent years, however.
- Significant disparities in tobacco use remain among young people nationwide. The prevalence of cigarette smoking is highest among American Indians and Alaska Natives, followed by Whites and Hispanics, and then Asians and Blacks. The prevalence of cigarette smoking is also highest among lower socioeconomic status youth.
- Use of smokeless tobacco and cigars declined in the late 1990s, but the declines appear to have stalled in the last 5 years. The latest data show the use of smokeless tobacco is increasing among White high school males, and cigar smoking may be increasing among Black high school females.
- Concurrent use of multiple tobacco products is prevalent among youth. Among those who use tobacco, nearly one-third of high school females and more than one-half of high school males report using more than one tobacco product in the last 30 days.
- Rates of tobacco use remain low among girls relative to boys in many developing countries, however, the gender gap between adolescent females and males is narrow in many countries around the globe.
Chapter 4. Social, Environmental, Cognitive, and Genetic Influences on the Use of Tobacco Among Youth
- Given their developmental stage, adolescents and young adults are uniquely susceptible to social and environmental influences to use tobacco.
- Socioeconomic factors and educational attainment influence the development of youth smoking behavior. The adolescents most likely to begin to use tobacco and progress to regular use are those who have lower academic achievement.
- The evidence is sufficient to conclude that there is a causal relationship between peer group social influences and the initiation and maintenance of smoking behaviors during adolescence.
- Affective processes play an important role in youth smoking behavior, with a strong association between youth smoking and negative affect.
- The evidence is suggestive that tobacco use is a heritable trait, more so for regular use than for onset. The expression of genetic risk for smoking among young people may be moderated by small-group and larger social-environmental factors.
Chapter 5. The Tobacco Industry’s Influences on the Use of Tobacco Among Youth
- In 2008, tobacco companies spent $9.94 billion on the marketing of cigarettes and $547 million on the marketing of smokeless tobacco. Spending on cigarette marketing is 48% higher than in 1998, the year of the Master Settlement Agreement. Expenditures for marketing smokeless tobacco are 277% higher than in 1998.
- Tobacco company expenditures have become increasingly concentrated on marketing efforts that reduce the prices of targeted tobacco products. Such expenditures accounted for approximately 84% of cigarette marketing and more than 77% of the marketing of smokeless tobacco products in 2008.
- The evidence is sufficient to conclude that there is a causal relationship between advertising and promotional efforts of the tobacco companies and the initiation and progression of tobacco use among young people.
- The evidence is suggestive but not sufficient to conclude that tobacco companies have changed the packaging and design of their products in ways that have increased these products’ appeal to adolescents and young adults.
- The tobacco companies’ activities and programs for the prevention of youth smoking have not demonstrated an impact on the initiation or prevalence of smoking among young people.
- The evidence is sufficient to conclude that there is a causal relationship between depictions of smoking in the movies and the initiation of smoking among young people.
Chapter 6. Efforts to Prevent and Reduce Tobacco Use Among Young People
- The evidence is sufficient to conclude that mass media campaigns, comprehensive community programs, and comprehensive statewide tobacco control programs can prevent the initiation of tobacco use and reduce its prevalence among youth.
- The evidence is sufficient to conclude that increases in cigarette prices reduce the initiation, prevalence, and intensity of smoking among youth and young adults.
- The evidence is sufficient to conclude that school-based programs with evidence of effectiveness, containing specific components, can produce at least short-term effects and reduce the prevalence of tobacco use among school-aged youth.
- Adriani W, Spijker S, Deroche-Gamonet V, Laviola G, Le Moal M, Smit AB, Piazza PV. Evidence for enhanced neurobehavioral vulnerability to nicotine during peri-adolescence in rats. Journal of Neuroscience. 2003; 23 (11):4712–6. [ PMC free article : PMC6740776 ] [ PubMed : 12805310 ]
- Alesci NL, Forster JL, Blaine T. Smoking visibility, perceived acceptability, and frequency in various locations among youth and adults. Preventive Medicine. 2003; 36 (3):272–81. [ PubMed : 12634018 ]
- Anderson G. Chronic Care: Making the Case for Ongoing Care. Princeton (NJ): Robert Wood Johnson Foundation; 2010. [accessed: November 30, 2011]. < http://www .rwjf.org/files /research/50968chronic .care.chartbook.pdf >.
- Bonnie RJ, Stratton K, Wallace RB, editors. Ending the Tobacco Problem: A Blueprint for the Nation. Washington: National Academies Press; 2007.
- Cochrane Collaboration. Home page. 2010. [accessed: November 30, 2010]. < http://www .cochrane.org/ >.
- Community Preventive Services Task Force. First Annual Report to Congress and to Agencies Related to the Work of the Task Force. Community Preventive Services Task Force. 2011. [accessed: January 9, 2012]. < http://www .thecommunityguide .org/library /ARC2011/congress-report-full.pdf >.
- Dalton MA, Beach ML, Adachi-Mejia AM, Longacre MR, Matzkin AL, Sargent JD, Heatherton TF, Titus-Ernstoff L. Early exposure to movie smoking predicts established smoking by older teens and young adults. Pediatrics. 2009; 123 (4):e551–e558. [ PMC free article : PMC2758519 ] [ PubMed : 19336346 ]
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ (British Medical Journal). 2004; 32 :1519. [ PMC free article : PMC437139 ] [ PubMed : 15213107 ] [ CrossRef ]
- Fagerström K. The epidemiology of smoking: health consequences and benefits of cessation. Drugs. 2002; 62 (Suppl 2):1–9. [ PubMed : 12109931 ]
- Family Smoking Prevention and Tobacco Control Act, Public Law 111-31, 123 U.S. Statutes at Large 1776 (2009)
- Grimshaw G, Stanton A. Tobacco cessation interventions for young people. Cochrane Database of Systematic Reviews. 2006;(4):CD003289. [ PubMed : 17054164 ] [ CrossRef ]
- Kessler DA. Nicotine addiction in young people. New England Journal of Medicine. 1995; 333 (3):186–9. [ PubMed : 7791824 ]
- Lovato C, Linn G, Stead LF, Best A. Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database of Systematic Reviews. 2003;(4):CD003439. [ PubMed : 14583977 ] [ CrossRef ]
- Lovato C, Watts A, Stead LF. Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database of Systematic Reviews. 2011;(10):CD003439. [ PMC free article : PMC7173757 ] [ PubMed : 21975739 ] [ CrossRef ]
- Lynch BS, Bonnie RJ, editors. Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youths. Washington: National Academies Press; 1994. [ PubMed : 25144107 ]
- National Association of Attorneys General. Master Settlement Agreement. 1998. [accessed: June 9, 2011]. < http://www .naag.org/back-pages /naag/tobacco /msa/msa-pdf/MSA%20with %20Sig%20Pages%20and%20Exhibits .pdf/file_view >.
- National Cancer Institute. Changing Adolescent Smoking Prevalence. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 2001. Smoking and Tobacco Control Monograph No. 14. NIH Publication. No. 02-5086.
- National Cancer Institute. The Role of the Media in Promoting and Reducing Tobacco Use. Bethesda (MD): U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2008. Tobacco Control Monograph No. 19. NIH Publication No. 07-6242.
- National Research Council. Environmental Tobacco Smoke: Measuring Exposures and Assessing Health Effects. Washington: National Academy Press; 1986. [ PubMed : 25032469 ]
- Office of the Surgeon General Reports of the Surgeon General, U.S. Public Health Service. 2010. [accessed: November 30, 2010]. < http://www .surgeongeneral .gov/library/reports/index.html >.
- Perry CL, Eriksen M, Giovino G. Tobacco use: a pediatric epidemic [editorial] Tobacco Control. 1994; 3 (2):97–8.
- Peto R, Lopez AD. Future worldwide health effects of current smoking patterns. In: Koop CE, Pearson CE, Schwarz MR, editors. Critical Issues in Global Health. San Francisco: Wiley (Jossey-Bass); 2001. pp. 154–61.
- Reddy KS, Perry CL, Stigler MH, Arora M. Differences in tobacco use among young people in urban India by sex, socioeconomic status, age, and school grade: assessment of baseline survey data. Lancet. 2006; 367 (9510):589–94. [ PubMed : 16488802 ]
- Schochet TL, Kelley AE, Landry CF. Differential expression of arc mRNA and other plasticity-related genes induced by nicotine in adolescent rat forebrain. Neuroscience. 2005; 135 (1):285–97. [ PMC free article : PMC1599838 ] [ PubMed : 16084664 ]
- Sowden AJ. Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews. 1998;(4):CD001006. [ PubMed : 10796581 ] [ CrossRef ]
- Sowden AJ, Stead LF. Community interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews. 2003;(1):CD001291. [ PubMed : 12535406 ] [ CrossRef ]
- Stead LF, Lancaster T. Interventions for preventing tobacco sales to minors. Cochrane Database of Systematic Reviews. 2005;(1):CD001497. [ PubMed : 15674880 ] [ CrossRef ]
- Steinberg L. Risk taking in adolescence: what changes, and why? Annals of the New York Academy of Sciences. 2004; 1021 :51–8. [ PubMed : 15251873 ]
- Task Force on Community Preventive Services. Recommendations regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. American Journal of Preventive Medicine. 2001; 20 (2 Suppl):S10–S15. [ PubMed : 11173214 ]
- Task Force on Community Preventive Services. Tobacco. In: Zaza S, Briss PA, Harris KW, editors. The Guide to Preventive Services: What Works to Promote Health? New York: Oxford University Press; 2005. pp. 3–79. < http://www .thecommunityguide .org/tobacco/Tobacco.pdf >.
- Thomas RE, Baker PRA, Lorenzetti D. Family-based programmes for preventing smoking by children and adolescents. Cochrane Database of Systematic Reviews. 2007;(1):CD004493. [ PubMed : 17253511 ] [ CrossRef ]
- Thomas RE, Perera R. School-based programmes for preventing smoking. Cochrane Database of Systematic Reviews. 2006;(3):CD001293. [ PubMed : 16855966 ] [ CrossRef ]
- US Department of Health and Human Services. Preventing Tobacco Use Among Young People A Report of the Surgeon General. Atlanta (GA): US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994.
- US Department of Health and Human Services. Tobacco Use Among US Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998.
- U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington: U.S. Government Printing Office; 2000.
- US Department of Health and Human Services. Reducing Tobacco Use: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000.
- US Department of Health and Human Services. Women and Smoking A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001.
- US Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004.
- US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [ PubMed : 20669524 ]
- US Department of Health and Human Services. How Tobacco Smoke Causes Disease—The Biology and Behavioral Basis for Tobacco-Attributable Disease: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [ PubMed : 21452462 ]
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. 2011. [accessed: November 1, 2011]. < http://www .healthypeople .gov/2020/default.aspx >.
- US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Center for Disease Control; 1964. PHS Publication No. 1103.
- Cite this Page National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2012. 1, Introduction, Summary, and Conclusions.
- PDF version of this title (18M)

In this Page
Other titles in these collections.
- Reports of the Surgeon General
- Health Services/Technology Assessment Text (HSTAT)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Introduction, Summary, and Conclusions - Preventing Tobacco Use Among Youth and ... Introduction, Summary, and Conclusions - Preventing Tobacco Use Among Youth and Young Adults
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Home — Essay Samples — Nursing & Health — Smoking — The Challenges of Quitting Smoking
The Challenges of Quitting Smoking
- Categories: Smoking Tobacco
About this sample

Words: 509 |
Published: Mar 1, 2019
Words: 509 | Page: 1 | 3 min read
Cite this Essay
To export a reference to this article please select a referencing style below:
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 789 words
1 pages / 514 words
2 pages / 783 words
2 pages / 1129 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Smoking
Initial impressions of a person smoking Association of smoking with wealth and maturity Irony of anti-smoking education Relaxation and stress reduction Taking breaks and social interactions Life skills [...]
In the "should smoking be illegal argumentative" debate, one of the primary concerns is the well-known harmful effects of cigarettes on the human body. Many people are aware that smoking cigarettes is detrimental. Cigarettes [...]
While the idea of making tobacco illegal may seem like a definitive solution to the smoking epidemic, it is crucial to consider the broader implications and potential unintended consequences. Prohibition would undoubtedly have [...]
Smoking is a prevalent practice in many societies, with approximately 1 billion people engaging in this habit. The act of smoking involves burning substances, such as tobacco or cannabis, and inhaling the resulting smoke into [...]
Vaping is not a traditional smoking. Many of us don’t even consider it as a substitute of smoking. That’s why a large chunk of non-smokers get attracted towards vaping because it’s harmless, flavored, aromatic and obviously [...]
For years there has been conflicting research whether smoking should be banned or not and it is a significant issue today. Many people have given up smoking while others still continue to smoke. Smoking is the inhalation and [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Summary of Recommendations
- Introduction
- USPSTF Assessment of Magnitude of Net Benefit
- Practice Considerations
- Update of Previous USPSTF Recommendation
- Supporting Evidence
- Research Needs and Gaps
- Recommendations of Others
- Article Information
See the Figure for a more detailed summary of the recommendations for clinicians. See the Practice Considerations section for more information on recommended behavioral interventions and pharmacotherapy and for suggestions for practice regarding the I statements. USPSTF indicates US Preventive Services Task Force.
USPSTF indicates US Preventive Services Task Force.
eFigure. US Preventive Services Task Force (USPSTF) Grades and Levels of Evidence
- USPSTF Review: Interventions for Tobacco Cessation in Adults, Including Pregnant Persons JAMA US Preventive Services Task Force January 19, 2021 This systematic review to support the 2021 US Preventive Services Task Force Recommendation Statement on interventions for tobacco cessation in adults summarizes published evidence on the benefits and harms of interventions for tobacco cessation in adults, including pregnant persons. Carrie D. Patnode, PhD, MPH; Jillian T. Henderson, PhD, MPH; Erin L. Coppola, MPH; Joy Melnikow, MD, MPH; Shauna Durbin, MPH; Rachel G. Thomas, MPH
- A Comprehensive Approach to Increase Adult Tobacco Cessation JAMA Editorial January 19, 2021 Brenna VanFrank, MD, MSPH; Letitia Presley-Cantrell, PhD
- Initiating Pharmacologic Treatment in Tobacco-Dependent Adults JAMA JAMA Clinical Guidelines Synopsis January 19, 2021 This JAMA Clinical Guidelines Synopsis summarizes the American Thoracic Society’s 2020 recommendations for treating tobacco dependence with pharmacologic therapy in adults. Atul Jain, MD, MS; Andrew M. Davis, MD, MPH
- USPSTF Recommendation: Interventions to Promote Tobacco Cessation JAMA JAMA Patient Page January 19, 2021 This JAMA Patient Page summarizes the USPSTF 2020 guideline recommending that physicians ask all adults about tobacco use, advise them to stop using tobacco, and provide behavioral interventions and drugs shown effective for stopping cigarette and other tobacco use. Jill Jin, MD, MPH
- COVID-19 and the “Lost Year” for Smokers Trying to Quit JAMA Medical News & Perspectives May 18, 2021 This Medical News article describes a reduction in smoking cessation attempts during the COVID-19 pandemic. Mary Chris Jaklevic, MSJ
- Considerations of Sex and Gender in FDA Tobacco Regulation JAMA Viewpoint June 20, 2023 This Viewpoint discusses how sex and gender subpopulations may be differentially affected by tobacco products and suggests that the FDA formulate regulations in clinically meaningful ways. Danielle R. Davis, PhD; Suchitra Krishnan-Sarin, PhD; Carolyn M. Mazure, PhD
- Varenicline or Nicotine Replacement After Initial Treatment Failure JAMA Original Investigation May 28, 2024 This sequential, multiple assignment randomized trial compares treatment strategies and dosages after abstinence from smoking was not achieved after 6 weeks of first-line therapies. Paul M. Cinciripini, PhD; Charles E. Green, PhD; Sanjay Shete, PhD; Jennifer A. Minnix, PhD; Jason D. Robinson, PhD; Yong Cui, PhD; Seokhun Kim, PhD; George Kypriotakis, PhD; Diane Beneventi, PhD; Janice A. Blalock, PhD; Francesco Versace, PhD; Maher Karam-Hage, MD
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
US Preventive Services Task Force. Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Persons : US Preventive Services Task Force Recommendation Statement . JAMA. 2021;325(3):265–279. doi:10.1001/jama.2020.25019
Manage citations:
© 2024
- Permissions
Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Persons : US Preventive Services Task Force Recommendation Statement
- Editorial A Comprehensive Approach to Increase Adult Tobacco Cessation Brenna VanFrank, MD, MSPH; Letitia Presley-Cantrell, PhD JAMA
- US Preventive Services Task Force USPSTF Review: Interventions for Tobacco Cessation in Adults, Including Pregnant Persons Carrie D. Patnode, PhD, MPH; Jillian T. Henderson, PhD, MPH; Erin L. Coppola, MPH; Joy Melnikow, MD, MPH; Shauna Durbin, MPH; Rachel G. Thomas, MPH JAMA
- JAMA Clinical Guidelines Synopsis Initiating Pharmacologic Treatment in Tobacco-Dependent Adults Atul Jain, MD, MS; Andrew M. Davis, MD, MPH JAMA
- JAMA Patient Page USPSTF Recommendation: Interventions to Promote Tobacco Cessation Jill Jin, MD, MPH JAMA
- Medical News & Perspectives COVID-19 and the “Lost Year” for Smokers Trying to Quit Mary Chris Jaklevic, MSJ JAMA
- Viewpoint Considerations of Sex and Gender in FDA Tobacco Regulation Danielle R. Davis, PhD; Suchitra Krishnan-Sarin, PhD; Carolyn M. Mazure, PhD JAMA
- Original Investigation Varenicline or Nicotine Replacement After Initial Treatment Failure Paul M. Cinciripini, PhD; Charles E. Green, PhD; Sanjay Shete, PhD; Jennifer A. Minnix, PhD; Jason D. Robinson, PhD; Yong Cui, PhD; Seokhun Kim, PhD; George Kypriotakis, PhD; Diane Beneventi, PhD; Janice A. Blalock, PhD; Francesco Versace, PhD; Maher Karam-Hage, MD JAMA
Importance Tobacco use is the leading preventable cause of disease, disability, and death in the US. In 2014, it was estimated that 480 000 deaths annually are attributed to cigarette smoking, including second hand smoke exposure. Smoking during pregnancy can increase the risk of numerous adverse pregnancy outcomes (eg, miscarriage and congenital anomalies) and complications in the offspring (including sudden infant death syndrome and impaired lung function in childhood). In 2019, an estimated 50.6 million US adults (20.8% of the adult population) used tobacco; 14.0% of the US adult population currently smoked cigarettes and 4.5% of the adult population used electronic cigarettes (e-cigarettes). Among pregnant US women who gave birth in 2016, 7.2% reported smoking cigarettes while pregnant.
Objective To update its 2015 recommendation, the USPSTF commissioned a review to evaluate the benefits and harms of primary care interventions on tobacco use cessation in adults, including pregnant persons.
Population This recommendation statement applies to adults 18 years or older, including pregnant persons.
Evidence Assessment The USPSTF concludes with high certainty that the net benefit of behavioral interventions and US Food and Drug Associated (FDA)–approved pharmacotherapy for tobacco smoking cessation, alone or combined, in nonpregnant adults who smoke is substantial. The USPSTF concludes with high certainty that the net benefit of behavioral interventions for tobacco smoking cessation on perinatal outcomes and smoking cessation in pregnant persons is substantial. The USPSTF concludes that the evidence on pharmacotherapy interventions for tobacco smoking cessation in pregnant persons is insufficient because few studies are available, and the balance of benefits and harms cannot be determined. The USPSTF concludes that the evidence on the use of e-cigarettes for tobacco smoking cessation in adults, including pregnant persons, is insufficient, and the balance of benefits and harms cannot be determined. The USPSTF has identified the lack of well-designed, randomized clinical trials on e-cigarettes that report smoking abstinence or adverse events as a critical gap in the evidence.
Recommendations The USPSTF recommends that clinicians ask all adults about tobacco use, advise them to stop using tobacco, and provide behavioral interventions and FDA-approved pharmacotherapy for cessation to nonpregnant adults who use tobacco. (A recommendation) The USPSTF recommends that clinicians ask all pregnant persons about tobacco use, advise them to stop using tobacco, and provide behavioral interventions for cessation to pregnant persons who use tobacco. (A recommendation) The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of pharmacotherapy interventions for tobacco cessation in pregnant persons. (I statement) The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of e-cigarettes for tobacco cessation in adults, including pregnant persons. The USPSTF recommends that clinicians direct patients who use tobacco to other tobacco cessation interventions with proven effectiveness and established safety. (I statement)
Tobacco use is the leading preventable cause of disease, disability, and death in the US. In 2014, it was estimated that 480 000 deaths annually are attributed to cigarette smoking, including second hand smoke. 1 Smoking during pregnancy can increase the risk for miscarriage, congenital anomalies, stillbirth, fetal growth restriction, preterm birth, placental abruption, and complications in the offspring, including sudden infant death syndrome and impaired lung function in childhood. 1 - 4 In 2019 (the most recent data currently available), an estimated 50.6 million US adults (20.8% of the adult population) used tobacco; 14.0% of the US adult population currently smoked cigarettes; and 4.5% of the US adult population used electronic cigarettes (e-cigarettes). 5 According to data from the National Vital Statistics System, in 2016, 7.2% of women who gave birth smoked cigarettes during pregnancy. 6 There are disparities in smoking behaviors associated with certain sociodemographic factors: smoking rates are particularly high in non-Hispanic American Indian/Alaska Native persons; lesbian, gay, or bisexual adults; adults whose highest level of educational attainment is a General Educational Development certificate; persons who are uninsured and those with Medicaid; adults with a disability; and persons with mild, moderate, or severe generalized anxiety symptoms. 5 According to the 2015 National Health Interview Survey, which reported responses from 33,672 adults, 68% of adults who smoked reported that they wanted to stop smoking and 55% attempted quitting in the past year 7 ; only 7% reported having recently quit smoking and 31% reported having used cessation counseling, medication, or both when trying to quit. 7
Quiz Ref ID The USPSTF concludes with high certainty that the net benefit of behavioral interventions and US Food and Drug Administration (FDA)–approved pharmacotherapy for tobacco smoking cessation, alone or combined, in nonpregnant adults who smoke is substantial .
Quiz Ref ID The USPSTF concludes with high certainty that the net benefit of behavioral interventions for tobacco smoking cessation on perinatal outcomes and smoking cessation in pregnant persons is substantial .
Quiz Ref ID The USPSTF concludes that the evidence on pharmacotherapy interventions for tobacco smoking cessation in pregnant persons is insufficient because few studies are available, and the balance of benefits and harms cannot be determined.
Quiz Ref ID The USPSTF concludes that the evidence on the use of e-cigarettes for tobacco smoking cessation in adults, including pregnant persons, is insufficient , and the balance of benefits and harms cannot be determined. The USPSTF has identified the lack of well-designed, randomized clinical trials (RCTs) on e-cigarettes that report smoking abstinence or adverse events as a critical gap in the evidence.
See the Figure , Table 1 , and the eFigure in the Supplement for more information on the USPSTF recommendation rationale and assessment. For more details on the methods the USPSTF uses to determine net benefit, see the USPSTF Procedure Manual. 8
This recommendation applies to adults 18 years or older, including pregnant persons. The USPSTF has issued a separate recommendation statement on primary care interventions for the prevention and cessation of tobacco use in children and adolescents. 9
Key definitions related to tobacco use are reported in the Box . Although tobacco use refers broadly to the use of any tobacco product, cigarette smoking has historically been the most prevalent form of tobacco use in the US, and most of the evidence surrounding cessation of tobacco products relates to quitting combustible cigarette smoking. Thus, the current USPSTF recommendations focus on interventions for tobacco smoking cessation. Additionally, although e-cigarettes are considered a tobacco product that should also be the focus of tobacco prevention and cessation efforts, for this recommendation statement, the evidence on e-cigarettes as a potential cessation aid for cigarette smoking was also evaluated.
Key Definitions Related to Tobacco Use
Tobacco use.
Tobacco use refers to use of any tobacco product. As defined by the US Food and Drug Administration, tobacco products include any product made or derived from tobacco intended for human consumption (except products that meet the definition of drugs), including, but not limited to, cigarettes, cigars (including cigarillos and little cigars), dissolvables, hookah tobacco, nicotine gels, pipe tobacco, roll-your-own tobacco, smokeless tobacco products (including dip, snuff, snus, and chewing tobacco), vapes, electronic cigarettes (e-cigarettes), hookah pens, and other electronic nicotine delivery systems. 10
Smoking generally refers to the inhaling and exhaling of smoke produced by combustible tobacco products such as cigarettes, cigars, and pipes.
Vaping refers to the inhaling and exhaling of aerosols produced by e-cigarettes. 11 Vaping products (ie, e-cigarettes) usually contain nicotine, which is the addictive ingredient in tobacco. Substances other than tobacco can also be used to smoke or vape. While the 2015 USPSTF recommendation statement used the term “electronic nicotine delivery systems” or “ENDS,” the USPSTF recognizes that the field has shifted to using the term “e-cigarettes” (or “e-cigs”) and uses the term e-cigarettes in the current recommendation statement. e-Cigarettes can come in many shapes and sizes, but generally they heat a liquid that contains nicotine (the addictive drug in tobacco) to produce an aerosol (or “vapor”) that is inhaled (“vaped”) by users. 11
USPSTF indicates US preventive Services Task Force.
All patients should be asked about their tobacco use, whether or not risk factors for use are present, and encouraged to stop using tobacco. When smoking is identified, all patients should be provided interventions to quit smoking. Higher smoking prevalence has been observed in men; persons younger than 65 years; non-Hispanic American Indian/Alaska Native persons; persons who are lesbian, gay, or bisexual; persons whose highest level of educational attainment is a General Educational Development certificate; persons with an annual household income less than $35 000; persons with a disability; and persons with mild, moderate, or severe anxiety symptoms. 5
Common approaches for clinicians to assess patients’ tobacco use include the following.
The 5 As: (1) Ask about tobacco use; (2) Advise to quit through clear, personalized messages; (3) Assess willingness to quit; (4) Assist in quitting; and (5) Arrange follow-up and support. 12
“Ask, Advise, Refer,” which encourages clinicians to ask patients about tobacco use, advise them to quit, and refer them to telephone quit lines, other evidence-based cessation interventions, or both. 12
Vital Sign: Treating smoking status as a vital sign and recording smoking status at every health visit are also frequently used to assess smoking status. 12
Because many pregnant women who smoke do not report it, using multiple choice questions to assess smoking status in this group may improve disclosure. 12
Effective tobacco smoking cessation interventions for nonpregnant adults include behavioral counseling and pharmacotherapy, either individually or in combination. 13 , 14
Combining behavioral and pharmacotherapy interventions has been shown to increase tobacco smoking cessation rates compared with either usual care/brief cessation interventions alone or pharmacotherapy alone. 13 Most combination interventions include behavioral counseling involving several sessions (≥4), with planned total contact time usually ranging from 90 to 300 minutes. 13 The largest effect was found in interventions that provided 8 or more sessions, although the difference in effect among the number of sessions was not significant. 13
Many behavioral counseling interventions are available to increase tobacco smoking cessation in adults. These interventions can be delivered in the primary care setting or can be referred to community settings with feedback to the primary care clinician. Effective behavioral interventions include physician advice, nurse advice, individual counseling with a cessation specialist, group behavioral interventions, telephone counseling, and mobile phone–based interventions. 13 Behavioral counseling interventions used in studies typically targeted individuals who were motivated to quit tobacco smoking. 13 For additional information about behavioral counseling interventions in nonpregnant adults, see Table 2 .
Quiz Ref ID The current pharmacotherapy interventions approved by the FDA for the treatment of tobacco smoking dependence in adults are nicotine replacement therapy (NRT) (including nicotine transdermal patches, lozenges, gum, inhalers, or nasal spray), bupropion hydrochloride sustained-release (SR), and varenicline. 46 All 3 types of pharmacotherapy increase tobacco smoking cessation rates. Using a combination of NRT products (in particular, combining short-acting plus long-acting forms of NRT) has been found to be more effective than using a single form of NRT. 13 Based on a smaller number of studies, varenicline appears to be more effective than NRT or bupropion SR. 13 Information on dosing regimens is available in the package inserts of individual medications or in the 2020 Surgeon General Report on Smoking Cessation. 47
Providing any psychosocial intervention to pregnant persons who smoke tobacco can increase smoking cessation. The behavioral counseling intervention type most often studied in pregnant persons who smoke was counseling. Behavioral interventions were more effective when they provided more intensive counseling, were augmented with messages and self-help materials tailored for pregnant persons, and included messages about the effects of smoking on both maternal and fetal health and strong advice to quit as soon as possible. 12 , 13 Although smoking cessation at any point during pregnancy yields substantial health benefits for the expectant mother and infant, quitting early in pregnancy provides the greatest benefit to the fetus. 12 , 13 Other interventions included feedback, incentives, health education, and social support, although provision of health education alone, without counseling, was not found to be effective. For additional information about behavioral counseling interventions in pregnant persons, see Table 2 .
Primary care clinicians may find the following resources useful in talking with adults and pregnant persons about tobacco smoking cessation.
Centers for Disease Control and Prevention
Health care clinician resources for treatment of tobacco use and dependence https://www.cdc.gov/tobaccoHCP
Tips From Former Smokers https://www.cdc.gov/tobacco/campaign/tips/partners/health/index.html
US Department of Health and Human Services
SmokeFree.Gov Health Professionals Page https://smokefree.gov/help-others-quit/health-professionals
SmokeFreeWomen http://women.smokefree.gov/pregnancy-motherhood
In addition, the following resources may be useful to primary care clinicians and practices trying to implement interventions for tobacco smoking cessation.
Million Hearts tools for clinicians for tobacco cessation https://millionhearts.hhs.gov/tools-protocols/tools/tobacco-use.html
Centers for Disease Control and Prevention state and community resources for tobacco control programs https://www.cdc.gov/tobacco/stateandcommunity/index.htm
The US Department of Veterans Affairs (VA) Primary Care & Tobacco Cessation Handbook https://www.mentalhealth.va.gov/quit-tobacco/docs/IB_10-565-Primary-Care-Smoking-Handbook-PROVIDERS-508.pdf
World Health Organization’s toolkit for delivering brief smoking interventions in primary care http://www.who.int/tobacco/publications/smoking_cessation/9789241506953/en/
In 2020, the Surgeon General issued a Report on Smoking Cessation. 47 The report’s findings were largely similar to that of the USPSTF. The Surgeon General’s report issued some additional findings regarding internet-based interventions for cessation and describes some suggestive but not sufficient evidence about specific e-cigarette use behaviors and increased cessation. Overall, the Surgeon General’s report found that there is inadequate evidence to conclude that e-cigarettes increase smoking cessation. More information on the Surgeon General’s Report on Smoking Cessation is available at https://www.cdc.gov/tobacco/data_statistics/sgr/2020-smoking-cessation/#fact-sheets .
According to data from the National Vital Statistics System, in 2016, 7.2% of women who gave birth smoked cigarettes during pregnancy, 6 and among 1071 pregnant women aged 18 to 44 years, 3.6% reported using e-cigarettes. 48 Smoking during pregnancy reduces fetal growth, increases the risk of preterm birth, and doubles the risk for delivering an infant with low birth weight. It also increases the relative risk for stillbirth death by 25% to 50%. 1 , 2 Quitting smoking early in pregnancy can reduce or eliminate the adverse effects of smoking on fetal growth. 47 For pregnant persons for whom behavioral counseling alone does not work, evidence to support other options to increase smoking cessation during pregnancy are limited. Few clinical trials have evaluated the effectiveness of NRT for smoking cessation in pregnant women. Although most studies were in the direction of benefit, no statistically significant increase in cessation was seen. 13 There is limited evidence on harms of NRT from trials in pregnant persons. Potential adverse maternal events reported in studies of NRT include slightly increased diastolic blood pressure and skin reactions to the patch. 13 Potential adverse events reported in nonpregnant adults include higher rates of low-risk cardiovascular events, such as tachycardia. 13 It has been suggested that NRT may be safer than smoking during pregnancy given that cigarette smoke contains harmful substances in addition to nicotine. The USPSTF identified no studies on bupropion SR or varenicline pharmacotherapy for tobacco smoking cessation during pregnancy.
In the absence of clear evidence on the balance of benefits and harms of pharmacotherapy in pregnant women, clinicians are encouraged to consider the severity of tobacco dependence in each patient and engage in shared decision-making to determine the best individual treatment course.
No tobacco product use is risk-free, including the use of e-cigarettes. Tobacco smoking cessation can be difficult for many individuals; thus, having a variety of tools available to help persons quit smoking would potentially be helpful. Findings from small surveys and qualitative data report mixed findings on whether physicians are recommending e-cigarettes to patients to help them quit smoking. 13 , 49 - 51 Few randomized trials have evaluated the effectiveness of e-cigarettes to increase tobacco smoking cessation in nonpregnant adults, and no trials have evaluated e-cigarettes for tobacco smoking cessation in pregnant persons. 13 Overall, results were mixed on whether smoking cessation increased with e-cigarettes; however, continued e-cigarette use after the intervention phase of trials remained high, indicating continued nicotine dependence. Trial evidence on harms of e-cigarettes used for smoking cessation is also limited. The most commonly reported adverse effects from e-cigarette use reported in trials included coughing, nausea, throat irritation, and sleep disruption. 13 Generally, no significant difference in short-term serious adverse events associated with e-cigarette use was reported. 13 Evidence on potential harms of e-cigarette use in general (whether for tobacco smoking cessation or not) has been reviewed in the National Academies of Science, Engineering, and Medicine report Public Health Consequences of E-Cigarettes. 52 For example, the report found conclusive evidence that in addition to nicotine, most e-cigarette products contain and emit numerous potentially toxic substances. Additionally, an outbreak of e-cigarette, or vaping product, use–associated lung injury (EVALI) that occurred in the US in late 2019 also suggests potential harms of e-cigarette use. The vast majority of cases have been associated with tetrahydrocannabinol (THC)–containing e-cigarettes. 53
Given the high rates of e-cigarette use in children and adolescents currently in the US, 54 the USPSTF recognizes that an overall public health question remains on whether the potential use of e-cigarettes as a tobacco smoking cessation aid (if ever proven effective) could be balanced with the high rates of e-cigarette use in youth as a driver for increasing overall tobacco use. The USPSTF has issued a separate recommendation statement on the prevention of tobacco use, including e-cigarettes, in children and adolescents. 9 The current USPSTF recommendation statement for adults evaluated the evidence on the benefits and harms of e-cigarettes to increase tobacco cessation; the USPSTF found this evidence to be insufficient. Given the proven effectiveness of behavioral counseling interventions in both nonpregnant and pregnant adults, and of pharmacotherapy in nonpregnant adults, the USPSTF recommends that clinicians focus on offering behavioral counseling and pharmacotherapy to increase smoking cessation in nonpregnant adults, and behavioral counseling to increase smoking cessation in pregnant persons.
In 2020, the USPSTF recommended that primary care clinicians provide interventions, including education or brief counseling, to prevent the initiation of tobacco use (including e-cigarettes) in school-aged children and adolescents. 9 The USPSTF found the evidence on primary care interventions for the cessation of tobacco use in youth to be insufficient.
This recommendation statement replaces the 2015 USPSTF recommendation statement on behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women. 55 The current recommendation statement has been updated to reflect newer evidence and language in the field of tobacco cessation and includes a description of the 2019 EVALI outbreak in the US. However, the recommendations on the services primary care clinicians should provide for tobacco cessation are the same as in 2015.
The USPSTF commissioned a systematic review to evaluate the benefits and harms of primary care interventions on tobacco use cessation in adults, including pregnant persons. 13 , 14 The USPSTF considered evidence on the benefits and harms of behavioral counseling interventions, pharmacotherapy interventions, and e-cigarettes in nonpregnant adults and pregnant persons. The vast majority of evidence identified focused on cigarette smoking cessation.
The USPSTF reviewed evidence on the benefits of behavioral counseling interventions on tobacco use cessation in general adults primarily from 20 systematic reviews that covered approximately 830 RCTs and more than 500 000 participants. 13 The evidence almost exclusively evaluated interventions for cessation of cigarette smoking. Physician advice, nurse advice, individual counseling with a cessation specialist, group behavioral interventions, telephone counseling, and mobile phone–based interventions have all been found to be effective to increase cessation of cigarette smoking. 13
Based on a 2013 systematic review that pooled 26 trials (n = 22 239), rates of smoking cessation at 6 months or more were an average of 8.0% in groups that received physician advice compared with 4.8% in groups that received no advice or usual care (risk ratio [RR], 1.76 [95% CI, 1.58-1.96]). 13 , 56 When stratified by intensity level, both minimal advice (defined as a single session lasting <20 minutes with ≤1 follow-up sessions) and intensive advice (defined as a single session lasting ≥20 minutes or >1 follow-up session) from a physician was associated with significantly increased cessation rates compared with no advice. Although not definitive, some subgroup analyses suggest that more intensive physician counseling (>20 minutes for initial consult, use of additional materials, or >1 follow-up visit) may be associated with an increase in cessation rates, particularly in patients who have smoking-related disease. 13 , 56
Based on a 2017 systematic review that pooled 44 trials evaluating nurse advice, 14.2% of participants who received interventions from nurses achieved smoking cessation at 6 months or more compared with 12.2% of those who received usual care or minimal intervention (RR, 1.29 [95% CI, 1.21-1.38]). 13 , 57 No evidence of effect modification was found when comparing higher- or lower-intensity counseling provided by nurses.
A systematic review from 2017 that pooled 33 trials (n = 13 762) found that an average of 11.4% of participants who received individual counseling with a cessation specialist achieved smoking cessation, compared with 7.7% of those who received minimal contact of less than 15 minutes of advice (RR, 1.48 [95% CI, 1.34-1.64]). 13 , 58 The review found some evidence suggesting that more intensive counseling was associated with higher cessation rates. Another systematic review published in 2017 that pooled 13 trials (n = 4395) also found that participants receiving group behavioral interventions had higher cessation rates compared with those who received a self-help program (10.4% cessation rate in intervention group vs 5.8% cessation rate in control group; RR, 1.88 [95% CI, 1.52-2.33]). 13 , 59
A 2019 review on telephone counseling interventions found that proactive telephone counseling (where telephone counselors called participants directly either to initiate counseling or in response to a participant calling a quitline) was associated with increased cessation rates. 13 , 60 If the telephone counseling was a “cold call” from telephone counselors to initiate counseling, smoking cessation rates were 11.0% in control participants and 13.9% in telephone counseling recipients (RR, 1.25 [95% CI, 1.15-1.35]; 65 trials; n = 41 233). 13 , 60 If telephone counseling occurred in response to a participant contacting a quitline, cessation rates were 7.8% in control participants and 10.8% in intervention recipients (RR, 1.38 [95% CI, 1.19-1.61]; 14 trials; n = 32 484). 13 , 60
A 2019 review that pooled 13 trials (n = 14 133) found higher cessation rates associated with mobile phone–based interventions. 13 , 61 All studies primarily used text messaging as the main intervention component, although a limited number of studies looked at individual mobile phone applications. Smoking cessation rates were an average of 5.6% in participants receiving usual or minimal care and 9.5% in those receiving mobile phone–based interventions (RR, 1.54 [95% CI, 1.19-2.00]).
The USPSTF considered evidence on other behavioral counseling interventions such as print-based, nontailored self-help materials, internet-based interventions, motivational interviewing, biofeedback, exercise, acupuncture, and hypnotherapy 13 ; however, limited evidence was available on these interventions.
The USPSTF reviewed evidence from 4 systematic reviews on pharmacotherapy that reported smoking cessation at 6 months or more. 13
A 2018 review on NRT (133 studies; n = 64 640) 62 found that 16.9% of participants taking any form of NRT achieved smoking abstinence at 6 months or more compared with 10.5% of participants receiving placebo or taking no NRT (RR, 1.55 [95% CI, 1.49-1.61]). All forms of NRT (patch, gum, inhaler, intranasal, and tablets) were found to be effective. Another review found that using combination NRT (patch plus a fast-acting form) was associated with higher smoking cessation rates than using a single form of NRT (16.9% vs 13.9%; RR, 1.25 [95% CI, 1.15-1.36]). 63
A 2020 systematic review on the use of antidepressants for smoking cessation (46 studies; n = 17 866) found that bupropion SR was associated with a significantly higher rate of smoking abstinence at 6 months or more than placebo or no bupropion SR (19.0% vs 11.0%; RR, 1.64 [95% CI, 1.52-1.77]). 64
Based on pooled analyses of 27 studies (n = 12 625), a 2016 systematic review found that varenicline was associated with higher rates of smoking cessation over placebo (25.6% vs 11.1%; RR, 2.24 [95% CI, 2.06-2.43]). 65
Smaller subsets of studies from these reviews directly compared types of pharmacotherapy for smoking cessation. Eight studies (n = 6264) compared varenicline and NRT and found that varenicline was associated with a greater smoking cessation rate over any form of NRT. 65 Six studies (n = 6286) evaluated varenicline vs bupropion SR and found that varenicline was associated with a higher cessation rate. 64 , 65 Smoking cessation rates among participants using NRT vs bupropion SR at 6 months or more did not significantly differ (10 studies; n = 9230). 64
Combinations of behavioral counseling and pharmacotherapy for smoking cessation were also effective, and potentially more effective than behavioral counseling or pharmacotherapy alone. 13 A 2016 systematic review (52 studies; n = 19 488) 66 found that participants who received combination pharmacotherapy and intensive behavioral counseling had a higher abstinence rate at 6 months or more compared with control participants who received usual care, self-help materials, or brief advice on quitting (which was less intensive than the counseling or support given to the intervention groups) (15.2% vs 8.6%; RR, 1.83 [95% CI, 1.68-1.98]). These combination interventions often have behavioral components delivered by specialized smoking cessation counselors or trained staff; however, no difference in effectiveness was seen in studies in which a nonspecialist provided the counseling. 13 Most studies used NRT as the pharmacotherapy. The intensity and format of the behavioral counseling component of the intervention varied greatly, with the majority of studies offering at least 4 behavioral counseling sessions, with a total planned contact time generally ranging from 90 to 300 minutes. Most of the behavioral counseling was delivered by a specialized smoking cessation counselor or trained trial staff.
Another systematic review, 67 which pooled analyses of 65 studies (n = 23 331), found that cessation rates at 6 months or more were modestly higher in participants who received behavioral support as an adjunct to pharmacotherapy than in those who received pharmacotherapy alone. Most studies offered NRT as the pharmacotherapy. Participants in the control group may have also received some counseling or support, but it was less intensive than in the intervention group. The addition of behavioral support to pharmacotherapy was associated with significantly higher cessation rates, approximately 17% in persons using pharmacotherapy alone vs 20% in those using a combination of pharmacotherapy and behavioral support (RR, 1.15 [95% CI, 1.08-1.22]). 13
For benefits of tobacco use cessation interventions in pregnant persons, the USPSTF reviewed evidence from an existing systematic review on behavioral counseling interventions 68 and from primary studies of pharmacotherapy. As with the evidence base in nonpregnant adults, the available evidence primarily addressed smoking cessation.
Based on a systematic review from 2017, 68 the USPSTF found that behavioral counseling interventions in pregnant women were effective at improving rates of smoking cessation as well as some perinatal health outcomes. Pooled analyses from 97 studies (n = 26 637) found that use of any psychosocial intervention was associated with higher smoking cessation rates in late pregnancy relative to control groups (an average quit rate of 12.2% in control groups and 16.4% in intervention groups) (RR, 1.35 [95% CI, 1.23-1.48]). The majority of studies used counseling interventions, and analyses of only counseling interventions (51 studies; n = 18 276) found a significant increase in smoking cessation rates late in pregnancy, from 10.8% in control groups to 14.5% in intervention groups (RR, 1.31 [95% CI, 1.16-1.47]). Studies of other intervention types (health education, feedback, incentives, social support, and exercise) were much fewer, with fewer total participants. Findings of smoking cessation effectiveness by intervention type were all in the direction of benefit, although not all were statistically significant. No subgroup differences by intervention type were found. The same systematic review also assessed the association of behavioral counseling interventions with perinatal outcomes and found lower rates of low birth weight (RR, 0.83 [95% CI, 0.72-0.94]; 18 trials; n = 9402) and increased mean birth weight (mean difference, 55.6 g [95% CI, 29.82-81.38]; 26 trials; n = 11 338). No statistically significant difference in rates of preterm births or stillbirths was found.
The USPSTF identified 5 placebo-controlled trials on NRT during pregnancy. 13 All 5 trials included behavioral counseling or support in addition to NRT. One trial used NRT gum as the intervention, one used an inhaler, while the other 3 trials used a NRT patch. Adherence to NRT in studies was low (<10% in 1 study). Findings of the 5 trials were all generally in the direction of benefit with NRT; however, none of the studies, either individually or when pooled, found a statistically significant difference in smoking cessation (11.9% in NRT intervention groups vs 10.1% in control groups; RR, 1.11 [95% CI, 0.79-1.56]; 5 trials; n = 2033). 13 Seven trials (the 5 placebo-controlled trials previously mentioned plus 2 additional non–placebo-controlled trials) reported on perinatal and health outcomes with NRT during pregnancy 13 ; findings were inconsistent and imprecise. No studies on bupropion SR or varenicline for smoking cessation during pregnancy were identified.
The FDA classifies e-cigarettes as a tobacco product and to date, no e-cigarettes have been approved as a smoking cessation aid. Approximately 4.5% of adults 5 , 69 and 3.6% of pregnant women 48 report using e-cigarettes. Higher e-cigarette use is reported among young adults aged 18 to 24 years (7.6%) 70 and has been increasing in recent years. 70 In addition to young adults, e-cigarette use among adults is higher in men; non-Hispanic White adults and other non-Hispanic adults; lesbian, gay, or bisexual 5 persons; and persons with chronic illnesses (such as cardiovascular disease, diabetes, cancer, asthma, chronic obstructive pulmonary disease, chronic kidney disease, and depression). 13 , 71 Most adult e-cigarette users report that quitting smoking and health improvement are major reasons why they started using e-cigarettes. 72 , 73 This is in contrast to youth, where it has been found that e-cigarette use increases risk of ever smoking cigarettes. 52 Nineteen percent of tobacco users use 2 or more tobacco products, the most common combination being cigarettes and e-cigarettes. 74
The USPSTF identified 5 RCTs (n = 3117) on e-cigarettes for smoking cessation in nonpregnant adults 13 , 75 - 80 and no studies in pregnant persons. 13 All 5 studies were conducted outside of the US (2 in New Zealand, 1 in Italy, 1 in Korea, and 1 in the UK). Four of the studies included participants who either wanted to stop smoking or were attending a stop smoking service. The type of e-cigarette interventions (nicotine content, whether NRT was also given, nicotine cartridge vs e-liquid, and whether behavioral support was also provided) and control interventions (NRT vs nonnicotine e-cigarette) varied across studies, making comparisons difficult. Only 3 of the e-cigarettes used in the studies are currently available in the US. Study size ranged from 150 to 1124 participants.
Reported trial findings were mixed. The 2 largest and most recent trials reported a statistically significant increase in smoking cessation at 6 months; 1 study reported smoking cessation rates of 4% in control groups vs 7% 79 in intervention groups; the second trial reported smoking cessation rates of 25% in control groups vs 35% 78 in intervention groups. The 3 remaining trials reported no statistically significant differences in smoking cessation rates. Three of the studies reported on continued e-cigarette use after achievement of smoking cessation in intervention groups at 6 months to 1 year, with continued e-cigarette use ranging from 38% to 80%. One study reported that 26.9% of all study participants were using e-cigarettes at 1 year. 77
The USPSTF identified limited evidence on harms from behavioral counseling interventions for tobacco cessation. Three systematic reviews (1 on internet-based interventions, another on incentives, and 1 on hypnotherapy) did not find evidence of serious adverse events associated with interventions. 13
The USPSTF identified 4 systematic reviews on NRT that reported on harms 13 : 3 reviews compared harms of NRT vs placebo 62 , 81 , 82 and 1 compared harms from various types of NRT. 63 Twelve to 21 studies (n = 10 234 to 11 647) reported on cardiovascular harms. Statistically significantly more cardiovascular adverse events (in particular, heart palpitations and chest pain) were found for participants randomized to NRT vs placebo (RR, 1.81 [95% CI, 1.35-2.43]; 21 trials; n = 11 647). 82 However, when analyses focused on major cardiovascular adverse events (combined outcome of cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke), findings were no longer statistically significant (RR, 1.38 [95% CI, 0.58-3.26]; 21 trials; n = 11 647). 82 Other reported harms associated with NRT included nausea, vomiting, gastrointestinal symptoms, and insomnia. Localized increased skin irritation at the NRT patch site has also been reported. No statistically significant increase in headaches, dizziness, anxiety, or depression were found. Cardiac adverse events and other serious adverse events did not differ by type of NRT. 63
The USPSTF considered evidence on harms from bupropion SR for tobacco smoking cessation from 4 systematic reviews. 13 No difference in serious adverse events (RR, 1.30 [95% CI, 1.00-1.69]; 33 trials; n = 9631), 83 cardiovascular adverse events (RR, 1.03 [95% CI, 0.71-1.50]; 27 trials; n = 10 402), 82 or major cardiovascular events (RR, 0.57 [95% CI, 0.31-1.04]; 27 trials; n = 10 402) 82 were found with bupropion SR (compared with placebo or no bupropion SR). No difference in moderate and severe neuropsychiatric events, including rates of suicidal behavior and ideation, were found with bupropion SR (compared with varenicline or NRT) in the recent Evaluating Adverse Events in a Global Smoking Cessation Study (EAGLES) trial. 84 , 85
Evidence on harms of varenicline for tobacco cessation are available from 3 systematic reviews on varenicline in unselected smokers, 4 systematic reviews of varenicline among persons with severe mental illness, and 1 review on varenicline for cessation of smokeless tobacco. 13 Common adverse effects reported with varenicline include nausea, insomnia, abnormal dreams, headache, and fatigue. 13 One review found an increase in serious adverse events with varenicline in unselected smokers (RR, 1.25 [95% CI, 1.04-1.49]; 29 trials; n = 15 370); however, many of these events included comorbidities that were mostly considered by the study authors to be unrelated to the treatments. 65 Across 3 systematic reviews (encompassing 18 to 38 studies; n = 8587 to 12 706), no statistically significant difference in cardiovascular adverse events or cardiovascular severe adverse events was found. 13 Additionally, no statistically significant increase in neuropsychiatric adverse events (including depression, suicidal ideation, and suicide attempt) was found across several systematic reviews. 13
The USPSTF did not identify any reports of adverse events related to combinations of behavioral counseling interventions and pharmacotherapy. Any harms of combined therapy are assumed to be similar to those of the pharmacotherapy being used.
The primary review that informed the USPSTF on the benefits of behavioral counseling interventions for smoking cessation during pregnancy also summarized evidence on harms of behavioral counseling interventions. 68 Based on analyses of 13 trials (n = 5831), no increase in adverse effects from psychosocial interventions was seen.
Nicotine in general has been shown in animal studies to cause fetal harms. However, NRT does not contain many harmful substances, such as hydrogen cyanide and carbon monoxide, that are present in cigarette smoke. 86 Evidence on harms of NRT during pregnancy is limited; the USPSTF identified 5 placebo-controlled trials (n = 3117), 2 non–placebo-controlled trials (n = 233), and 3 cohort studies (n = 306 721). 13 Findings on potential harms of NRT on birth outcomes from trial evidence is mixed, although most studies reported findings in the direction of benefit rather than harm. Observational evidence from cohort studies generally did not indicate an increase in stillbirth or low birth weight with NRT. Based on observational evidence, there was no evidence of increased risk of premature delivery, small for gestational age, stillbirth, or congenital anomalies associated with the use of NRT, bupropion, and varenicline vs smoking. According to FDA labeling, some fetal harms with bupropion were noted in animal studies, but currently, no adequate, well-controlled studies of bupropion SR use during pregnancy (for any indication) in humans are available. 87 Labeling for varenicline states that available studies cannot definitively establish or exclude varenicline-associated risk during pregnancy. 88
The USPSTF identified 9 RCTs (n = 3942) that reported on harms of e-cigarette interventions for tobacco smoking cessation in nonpregnant adults 13 (the 5 trials previously described that reported cessation rates at 6 months or more, as well as an additional 4 trials that reported on cessation rates at less than 6 months). No trials on harms of e-cigarettes for smoking cessation in pregnant persons was identified. The most commonly reported adverse effects from e-cigarette use reported in trials include coughing, nausea, throat irritation, and sleep disruption. 13 Generally, no significant difference in short-term serious adverse events associated with e-cigarette use was reported. 13 Data on potential long-term harms of e-cigarette use are currently lacking.
Additional evidence on harms from e-cigarette use (whether used for tobacco cessation or not) considered by the USPSTF included data of the 2019 EVALI outbreak in the US 53 and the 2018 report Public Health Consequences of E-Cigarettes by the National Academies of Sciences, Engineering, and Medicine. 52 In late 2019, an outbreak of EVALI occurred in the US. Symptoms of EVALI include cough, shortness of breath, chest pain, nausea, vomiting, stomach pain, diarrhea, fever, chills, and weight loss. As of February 2020, more than 2800 cases of EVALI were reported, with 68 deaths. 53 Based on testing of bronchoalveolar lavage fluid samples of patients with EVALI 89 and testing of products used by patients with EVALI, 53 vitamin E acetate (an additive in some THC-containing e-cigarettes) was found to be strongly linked to EVALI. 53 However, evidence is not sufficient to rule out the contribution of other chemicals of concern, including chemicals in either THC- or non–THC–containing products, in some reported EVALI cases. 53
The National Academies of Sciences, Engineering, and Medicine report found that in youth and young adults, there is substantial evidence that e-cigarette use increases risk of ever using combustible tobacco and moderate evidence that e-cigarette use increases the frequency and intensity of subsequent cigarette smoking. 52 The report also found conclusive evidence that e-cigarettes contain and emit potentially toxic substances, although substantial evidence shows that other than nicotine, there is significantly lower exposure to potentially toxic substances from e-cigarettes compared with combustible tobacco cigarettes. 52
A draft version of this recommendation statement was posted for public comment on the USPSTF website from June 2, 2020, to June 29, 2020. Several comments expressed concern about the insufficient evidence statement on e-cigarettes for cessation. Some respondents wanted the USPSTF to recommend against e-cigarettes for tobacco cessation, while others wanted the USPSTF to recommend in favor of e-cigarettes. Based on the evidence reviewed, the USPSTF could not determine whether e-cigarettes are effective in helping persons to quit smoking cigarettes, nor could it determine what the potential long-term harms of e-cigarette use are; thus, it cannot recommend for or against their use. Some comments were also received requesting that the USPSTF recommend NRT for smoking cessation during pregnancy. Too few trials were identified for the USPSTF to determine whether NRT during pregnancy provides overall more benefits or harms, and the USPSTF calls for more research on NRT and other pharmacotherapy to help pregnant persons quit using tobacco. Last, edits to clarify language, as well as additional information from the recent 2020 Surgeon General’s Report on Smoking Cessation, have been provided in response to comments.
Because of the well-established health benefits of smoking cessation, 1 , 12 , 47 most of the research on interventions for smoking cessation focuses on cessation (rather than health outcomes) as a primary outcome. The current review identified 1 study 90 of middle-aged men at high risk for cardiorespiratory disease that found lower (although not statistically significant) total mortality, fatal coronary disease, and lung cancer death at 20 years of follow-up in participants who received advice from medical practitioners. 91 The study also found some reduction in all-cause mortality, coronary disease mortality, and lung cancer incidence and mortality at 20 years of follow-up, although these outcomes were not significant. 91
Although not zero, less toxins have been found to be released by e-cigarettes than by cigarettes. It is hypothesized that health outcomes may be improved in adults who completely switch from cigarette smoking to e-cigarette use, although long-term data are not available yet to support this. Evidence on long-term harms of e-cigarette use in general is lacking and is needed. Additionally, emerging evidence suggests that toxicant levels in dual users of e-cigarettes and cigarettes may be higher than in conventional cigarette–only users. 92
The greatest research needs are to gain a better understanding of the effectiveness of e-cigarettes for smoking cessation, as well as potential short- and long-term harms of e-cigarette use, and to understand whether there are effective pharmacotherapy options for pregnant persons.
e-Cigarettes: Given the potential negative effect that increasing e-cigarette use in youth is having on overall tobacco control efforts, there is an urgent need for research that provides both a clearer understanding of whether e-cigarettes may increase adult tobacco smoking cessation, as well as the potential harms of e-cigarette use as a tobacco product. Future research on e-cigarettes for smoking cessation in adults should address the following:
Studies must be well-designed RCTs that compare e-cigarette interventions with placebo, as well as established, effective combinations of pharmacotherapy and behavioral support.
Studies should be adequately powered to detect differences in continued smoking abstinence rates at 6 months or more.
Given the high rate of continued e-cigarette use after smoking cessation, research on both the short- and long-term harms of e-cigarette use is needed, as well as the harms in dual users of e-cigarettes and conventional cigarettes. More research is needed on smoking relapse rates in adults who have used e-cigarettes for smoking cessation and how to help with cessation of e-cigarette use once smoking abstinence has been achieved.
Given the rapidly evolving landscape of e-cigarettes, trials should include current generations of e-cigarettes. Additionally, to successfully conduct these types of studies, standardization of how to quantify e-cigarette use and levels of nicotine exposure from e-cigarettes is needed.
More research is needed to understand the patterns of e-cigarette use in youth and the risk factors for their transition from e-cigarette use to conventional cigarette smoking.
More research is also needed to better understand patterns of e-cigarette use in pregnant persons and potential harms of e-cigarette use to both pregnant persons and their offspring.
More research is needed on understanding how to help adults quit e-cigarettes.
Pharmacotherapy in pregnant persons: Although behavioral counseling interventions have been found to be effective in improving smoking cessation during pregnancy, additional research is needed on pharmacotherapy options, in particular NRT, for pregnant persons for whom behavioral counseling interventions alone are not effective.
Larger studies adequately powered to detect an effect on both smoking cessation rates (during pregnancy and postpartum) and changes in perinatal and child health outcomes are needed.
A better understanding of why adherence rates to NRT during pregnancy is so low would also be helpful.
Although the benefits of behavioral counseling interventions and pharmacotherapy in nonpregnant adults and the benefits of behavioral counseling interventions in pregnant adults are well established, additional research on effective components of behavioral counseling and who to target specific interventions to would be informative. More research on newer modalities and remotely delivered interventions (mobile phone apps, internet-based interventions) would also be helpful. Additionally, the effectiveness of interventions for cessation of other forms of tobacco and whether interventions need to be tailored to individual tobacco product types are also needed. Last, more research is needed on interventions to prevent relapse of tobacco use.
Numerous professional societies and health organizations, including the American Academy of Family Physicians, 93 American College of Physicians, 94 and American College of Obstetricians and Gynecologists (ACOG), 95 recommend that clinicians screen for tobacco use and provide interventions to patients who smoke.
For pregnant persons, ACOG recommends brief behavioral counseling and the use of evidence-based smoking cessation aids as effective strategies for achieving smoking cessation, even for very heavy smokers. 96 ACOG also recommends that NRT should be considered only after a detailed discussion with the patient of the known risks of continued smoking, the possible risks of NRT, and need for close supervision. 95
The American Academy of Pediatrics also has a policy statement recommending that pediatricians screen for the tobacco exposure of children during pediatric care visits and recommend nicotine dependence treatment, including behavioral interventions and pharmacotherapy, to tobacco-dependent parents. 97
More recently some organizations have addressed e-cigarette use in their tobacco use guidelines. The American Academy of Family Physicians, 98 the American College of Preventive Medicine, 99 and the American Heart Association 100 recommend that clinicians screen for e-cigarette use. Organizations vary somewhat in terms of whether they recommend e-cigarettes for smoking cessation. ACOG recommends against use of e-cigarettes in pregnant and postpartum individuals. 95 , 101 The American Cancer Society does not recommend e-cigarettes as a smoking cessation method, 102 and the American Heart Association 100 states that there is not enough evidence for clinicians to counsel patients on using e-cigarettes as a primary smoking cessation aid.
Corresponding Author: Alex H. Krist, MD, MPH, Virginia Commonwealth University, One Capitol Square, 6th Flr, 830 E Main St, Richmond, Virginia 23219 ( [email protected] )).
Accepted for Publication: December 4, 2020.
The US Preventive Services Task Force (USPSTF) members: Alex H. Krist, MD, MPH; Karina W. Davidson, PhD, MAS; Carol M. Mangione, MD, MSPH; Michael J. Barry, MD; Michael Cabana, MD, MA, MPH; Aaron B. Caughey, MD, PhD; Katrina Donahue, MD, MPH; Chyke A. Doubeni, MD, MPH; John W. Epling Jr, MD, MSEd; Martha Kubik, PhD, RN; Gbenga Ogedegbe, MD, MPH; Lori Pbert, PhD; Michael Silverstein, MD, MPH; Melissa A. Simon, MD, MPH; Chien-Wen Tseng, MD, MPH, MSEE; John B. Wong, MD.
Affiliations of The US Preventive Services Task Force (USPSTF) members: Fairfax Family Practice Residency, Fairfax, Virginia (Krist); Virginia Commonwealth University, Richmond (Krist); Feinstein Institute for Medical Research at Northwell Health, Manhasset, New York (Davidson); University of California, Los Angeles (Mangione); Harvard Medical School, Boston, Massachusetts (Barry); University of California, San Francisco (Cabana); Oregon Health & Science University, Portland (Caughey); University of North Carolina at Chapel Hill (Donahue); Mayo Clinic, Rochester, Minnesota (Doubeni); Virginia Tech Carilion School of Medicine, Roanoke (Epling Jr); George Mason University, Fairfax, Virginia (Kubik); New York University, New York, New York (Ogedegbe); University of Massachusetts Medical School, Worcester (Pbert); Boston University, Boston, Massachusetts (Silverstein); Northwestern University, Evanston, Illinois (Simon); University of Hawaii, Honolulu (Tseng); Pacific Health Research and Education Institute, Honolulu, Hawaii (Tseng); Tufts University School of Medicine, Boston, Massachusetts (Wong).
Author Contributions: Dr Krist had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The USPSTF members contributed equally to the recommendation statement.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Authors followed the policy regarding conflicts of interest described at https://www.uspreventiveservicestaskforce.org/Page/Name/conflict-of-interest-disclosures . All members of the USPSTF receive travel reimbursement and an honorarium for participating in USPSTF meetings. Dr Barry reported receiving grants and personal fees from Healthwise.
Funding/Support: The USPSTF is an independent, voluntary body. The US Congress mandates that the Agency for Healthcare Research and Quality (AHRQ) support the operations of the USPSTF.
Role of the Funder/Sponsor: AHRQ staff assisted in the following: development and review of the research plan, commission of the systematic evidence review from an Evidence-based Practice Center, coordination of expert review and public comment of the draft evidence report and draft recommendation statement, and the writing and preparation of the final recommendation statement and its submission for publication. AHRQ staff had no role in the approval of the final recommendation statement or the decision to submit for publication.
Disclaimer: Recommendations made by the USPSTF are independent of the US government. They should not be construed as an official position of AHRQ or the US Department of Health and Human Services.
Additional Contributions: We thank Tina Fan, MD, MPH (AHRQ), who contributed to the writing of the manuscript, and Lisa Nicolella, MA (AHRQ), who assisted with coordination and editing.
Additional Information: The US Preventive Services Task Force (USPSTF) makes recommendations about the effectiveness of specific preventive care services for patients without obvious related signs or symptoms. It bases its recommendations on the evidence of both the benefits and harms of the service and an assessment of the balance. The USPSTF does not consider the costs of providing a service in this assessment. The USPSTF recognizes that clinical decisions involve more considerations than evidence alone. Clinicians should understand the evidence but individualize decision-making to the specific patient or situation. Similarly, the USPSTF notes that policy and coverage decisions involve considerations in addition to the evidence of clinical benefits and harms.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Appointments at Mayo Clinic
- Quit smoking
Quitting smoking: 10 ways to resist tobacco cravings
Tobacco cravings can wear you down when you're trying to quit. Use these tips to reduce and resist cravings.
For most people who use tobacco, tobacco cravings or smoking urges can be strong. But you can stand up against these cravings.
When you feel an urge to use tobacco, keep in mind that even though the urge may be strong, it will likely pass within 5 to 10 minutes whether or not you smoke a cigarette or take a dip of chewing tobacco. Each time you resist a tobacco craving, you're one step closer to stopping tobacco use for good.
Here are 10 ways to help you resist the urge to smoke or use tobacco when a craving strikes.
1. Try nicotine replacement therapy
Ask your health care provider about nicotine replacement therapy. The options include:
- Prescription nicotine in a nasal spray or inhaler
- Nicotine patches, gum and lozenges you can buy without a prescription
- Prescription non-nicotine stop-smoking drugs such as bupropion (Wellbutrin SR, Wellbutrin XL, others) and varenicline
Short-acting nicotine replacement therapies — such as nicotine gum, lozenges, nasal sprays or inhalers — can help you overcome intense cravings. These short-acting therapies are usually safe to use along with long-acting nicotine patches or one of the non-nicotine stop-smoking drugs.
Electronic cigarettes (e-cigarettes) have had a lot of interest recently as a replacement for smoking traditional cigarettes. But e-cigarettes haven't proved to be safer or more effective than nicotine-replacement medications in helping people stop smoking.
2. Avoid triggers
Tobacco urges are likely to be strongest in the places where you smoked or chewed tobacco most often, such as at parties or bars, or at times when you were feeling stressed or sipping coffee. Find out your triggers and have a plan in place to avoid them or get through them without using tobacco.
Don't set yourself up for a smoking relapse. If you usually smoked while you talked on the phone, for instance, keep a pen and paper nearby to keep busy with doodling rather than smoking.
If you feel like you're going to give in to your tobacco craving, tell yourself that you must first wait 10 more minutes. Then do something to distract yourself during that time. Try going to a public smoke-free zone. These simple tricks may be enough to move you past your tobacco craving.
4. Chew on it
Give your mouth something to do to resist a tobacco craving. Chew on sugarless gum or hard candy. Or munch on raw carrots, nuts or sunflower seeds — something crunchy and tasty.
5. Don't have 'just one'
You might be tempted to have just one cigarette to satisfy a tobacco craving. But don't fool yourself into thinking that you can stop there. More often than not, having just one leads to one more. And you may end up using tobacco again.
6. Get physical
Physical activity can help distract you from tobacco cravings. Even short bursts of activity — such as running up and down the stairs a few times — can make a tobacco craving go away. Get out for a walk or jog.
If you're at home or in the office, try squats, deep knee bends, pushups, running in place, or walking up and down a set of stairs. If you don't like physical activity, try prayer, sewing, woodwork or writing in a journal. Or do chores for distraction, such as cleaning or filing papers.
7. Try relaxation techniques
Smoking may have been your way to deal with stress. Fighting back against a tobacco craving can itself be stressful. Take the edge off stress by trying ways to relax, such as deep breathing, muscle relaxation, yoga, visualization, massage or listening to calming music.
8. Call for reinforcements
Connect with a family member, friend or support group member for help in your effort to resist a tobacco craving. Chat on the phone, go for a walk, share a few laughs, or meet to talk and support each other. Counseling can be helpful too. A free telephone quit line — 800-QUIT-NOW (800-784-8669) — provides support and counseling.
9. Go online for support
Join an online stop-smoking program. Or read a quitter's blog and post encouraging thoughts for someone else who might be dealing with tobacco cravings. Learn from how others have handled their tobacco cravings.
10. Remind yourself of the benefits
Write down or say out loud why you want to stop smoking and resist tobacco cravings. These reasons might include:
- Feeling better
- Getting healthier
- Sparing your loved ones from secondhand smoke
- Saving money
Keep in mind that trying something to beat the urge to use tobacco is always better than doing nothing. And each time you resist a tobacco craving, you're one step closer to being tobacco-free.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Rigotti NA. Overview of smoking cessation management in adults. https://www.uptodate.com/contents/search. Accessed March 23, 2022.
- How to manage cravings. Smokefree.gov. https://smokefree.gov/challenges-when-quitting/cravings-triggers/how-manage-cravings. Accessed March 23, 2022.
- Know your triggers. Smokefree.gov. https://smokefree.gov/challenges-when-quitting/cravings-triggers/know-your-triggers. Accessed March 23, 2022.
- AskMayoExpert. Tobacco use (adult). Mayo Clinic; 2021.
- Broaddus, VC. Smoking cessation. In: Murray & Nadel's Textbook of Respiratory Medicine. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 23, 2022.
- Rigotti NA. Pharmacotherapy for smoking cessation in adults. https://www.uptodate.com/contents/search. Accessed March 23, 2022.
- Park ER. Behavioral approaches to smoking cessation. https://www.uptodate.com/contents/search. Accessed March 23, 2022.
- Making your plan to quit and planning your quit day. American Cancer Society. https://www.cancer.org/healthy/stay-away-from-tobacco/guide-quitting-smoking/deciding-to-quit-smoking-and-making-a-plan.html. Accessed March 23, 2022.
- US Preventive Services Task Force. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force Recommendation Statement. JAMA. 2021; doi:10.1001/jama.2020.25019.
Products and Services
- A Book: Live Younger Longer
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Guide to Home Remedies
- A Book: Mayo Clinic on High Blood Pressure
- A Book: Mayo Clinic Family Health Book
- Cancer-prevention strategies
- Cigar smoking
- Hookah smoking
- Quit-smoking products
- Skin care tips
- Chewing tobacco
- Nicotine addiction
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Quitting smoking 10 ways to resist tobacco cravings
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 24 March 2022
Tobacco and nicotine use
- Bernard Le Foll 1 , 2 ,
- Megan E. Piper 3 , 4 ,
- Christie D. Fowler 5 ,
- Serena Tonstad 6 ,
- Laura Bierut 7 ,
- Lin Lu ORCID: orcid.org/0000-0003-0742-9072 8 , 9 ,
- Prabhat Jha 10 &
- Wayne D. Hall 11 , 12
Nature Reviews Disease Primers volume 8 , Article number: 19 ( 2022 ) Cite this article
40k Accesses
96 Citations
107 Altmetric
Metrics details
- Disease genetics
- Experimental models of disease
- Preventive medicine
Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will die prematurely from tobacco-related complications. In addition, people who smoke have a significant reduction in their quality of life. Neurobiological findings have identified the mechanisms by which nicotine in tobacco affects the brain reward system and causes addiction. These brain changes contribute to the maintenance of nicotine or tobacco use despite knowledge of its negative consequences, a hallmark of addiction. Effective approaches to screen, prevent and treat tobacco use can be widely implemented to limit tobacco’s effect on individuals and society. The effectiveness of psychosocial and pharmacological interventions in helping people quit smoking has been demonstrated. As the majority of people who smoke ultimately relapse, it is important to enhance the reach of available interventions and to continue to develop novel interventions. These efforts associated with innovative policy regulations (aimed at reducing nicotine content or eliminating tobacco products) have the potential to reduce the prevalence of tobacco and nicotine use and their enormous adverse impact on population health.
Similar content being viewed by others

Associations between classic psychedelics and nicotine dependence in a nationally representative sample
Nicotine dependence and incident psychiatric disorders: prospective evidence from us national study, use of electronic cigarettes and heated tobacco products during the covid-19 pandemic, introduction.
Tobacco is the second most commonly used psychoactive substance worldwide, with more than one billion smokers globally 1 . Although smoking prevalence has reduced in many high-income countries (HICs), tobacco use is still very prevalent in low-income and middle-income countries (LMICs). The majority of smokers are addicted to nicotine delivered by cigarettes (defined as tobacco dependence in the International Classification of Diseases, Tenth Revision (ICD-10) or tobacco use disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)). As a result of the neuro-adaptations and psychological mechanisms caused by repeated exposure to nicotine delivered rapidly by cigarettes, cessation can also lead to a well-characterized withdrawal syndrome, typically manifesting as irritability, anxiety, low mood, difficulty concentrating, increased appetite, insomnia and restlessness, that contributes to the difficulty in quitting tobacco use 2 , 3 , 4 .
Historically, tobacco was used in some cultures as part of traditional ceremonies, but its use was infrequent and not widely disseminated in the population. However, since the early twentieth century, the use of commercial cigarettes has increased dramatically 5 because of automated manufacturing practices that enable large-scale production of inexpensive products that are heavily promoted by media and advertising. Tobacco use became highly prevalent in the past century and was followed by substantial increases in the prevalence of tobacco-induced diseases decades later 5 . It took decades to establish the relationship between tobacco use and associated health effects 6 , 7 and to discover the addictive role of nicotine in maintaining tobacco smoking 8 , 9 , and also to educate people about these effects. It should be noted that the tobacco industry disputed this evidence to allow continuing tobacco sales 10 . The expansion of public health campaigns to reduce smoking has gradually decreased the use of tobacco in HICs, with marked increases in adult cessation, but less progress has been achieved in LMICs 1 .
Nicotine is the addictive compound in tobacco and is responsible for continued use of tobacco despite harms and a desire to quit, but nicotine is not directly responsible for the harmful effects of using tobacco products (Box 1 ). Other components in tobacco may modulate the addictive potential of tobacco (for example, flavours and non-nicotine compounds) 11 . The major harms related to tobacco use, which are well covered elsewhere 5 , are linked to a multitude of compounds present in tobacco smoke (such as carcinogens, toxicants, particulate matter and carbon monoxide). In adults, adverse health outcomes of tobacco use include cancer in virtually all peripheral organs exposed to tobacco smoke and chronic diseases such as eye disease, periodontal disease, cardiovascular diseases, chronic obstructive pulmonary disease, stroke, diabetes mellitus, rheumatoid arthritis and disorders affecting immune function 5 . Moreover, smoking during pregnancy can increase the risk of adverse reproductive effects, such as ectopic pregnancy, low birthweight and preterm birth 5 . Exposure to secondhand cigarette smoke in children has been linked to sudden infant death syndrome, impaired lung function and respiratory illnesses, in addition to cognitive and behavioural impairments 5 . The long-term developmental effects of nicotine are probably due to structural and functional changes in the brain during this early developmental period 12 , 13 .
Nicotine administered alone in various nicotine replacement formulations (such as patches, gum and lozenges) is safe and effective as an evidence-based smoking cessation aid. Novel forms of nicotine delivery systems have also emerged (called electronic nicotine delivery systems (ENDS) or e-cigarettes), which can potentially reduce the harmful effects of tobacco smoking for those who switch completely from combustible to e-cigarettes 14 , 15 .
This Primer focuses on the determinants of nicotine and tobacco use, and reviews the neurobiology of nicotine effects on the brain reward circuitry and the functioning of brain networks in ways that contribute to the difficulty in stopping smoking. This Primer also discusses how to prevent tobacco use, screen for smoking, and offer people who smoke tobacco psychosocial and pharmacological interventions to assist in quitting. Moreover, this Primer presents emerging pharmacological and novel brain interventions that could improve rates of successful smoking cessation, in addition to public health approaches that could be beneficial.
Box 1 Tobacco products
Conventional tobacco products include combustible products that produce inhaled smoke (most commonly cigarettes, bidis (small domestically manufactured cigarettes used in South Asia) or cigars) and those that deliver nicotine without using combustion (chewing or dipping tobacco and snuff). Newer alternative products that do not involve combustion include nicotine-containing e-cigarettes and heat-not-burn tobacco devices. Although non-combustion and alternative products may constitute a lesser risk than burned ones 14 , 15 , 194 , no form of tobacco is entirely risk-free.
Epidemiology
Prevalence and burden of disease.
The Global Burden of Disease Project (GBDP) estimated that around 1.14 billion people smoked in 2019, worldwide, increasing from just under a billion in 1990 (ref. 1 ). Of note, the prevalence of smoking decreased significantly between 1990 and 2019, but increases in the adult population meant that the total number of global smokers increased. One smoking-associated death occurs for approximately every 0.8–1.1 million cigarettes smoked 16 , suggesting that the estimated worldwide consumption of about 7.4 trillion cigarettes in 2019 has led to around 7 million deaths 1 .
In most populations, smoking prevalence is much higher among groups with lower levels of education or income 17 and among those with mental health disorders and other co-addictions 18 , 19 . Smoking is also more frequent among men than women (Figs 1 – 3 ). Sexual and/or gender minority individuals have disproportionately high rates of smoking and other addictions 17 , 20 . In addition, the prevalence of smoking varies substantially between regions and ethnicities; smoking rates are high in some regions of Asia, such as China and India, but are lower in North America and Australia. Of note, the prevalence of mental health disorders and other co-addictions is higher in individuals who smoke compared with non-smokers 18 , 19 , 21 . For example, the odds of smoking in people with any substance use disorder is more than five times higher than the odds in people without a substance use disorder 19 . Similarly, the odds of smoking in people with any psychiatric disorder is more than three times higher than the odds of smoking in those without a psychiatric diagnosis 22 . In a study in the USA, compared with a population of smokers with no psychiatric diagnosis, subjects with anxiety, depression and phobia showed an approximately twofold higher prevalence of smoking, and subjects with agoraphobia, mania or hypomania, psychosis and antisocial personality or conduct disorders showed at least a threefold higher prevalence of smoking 22 . Comorbid disorders are also associated with higher rates of smoking 22 , 23 .
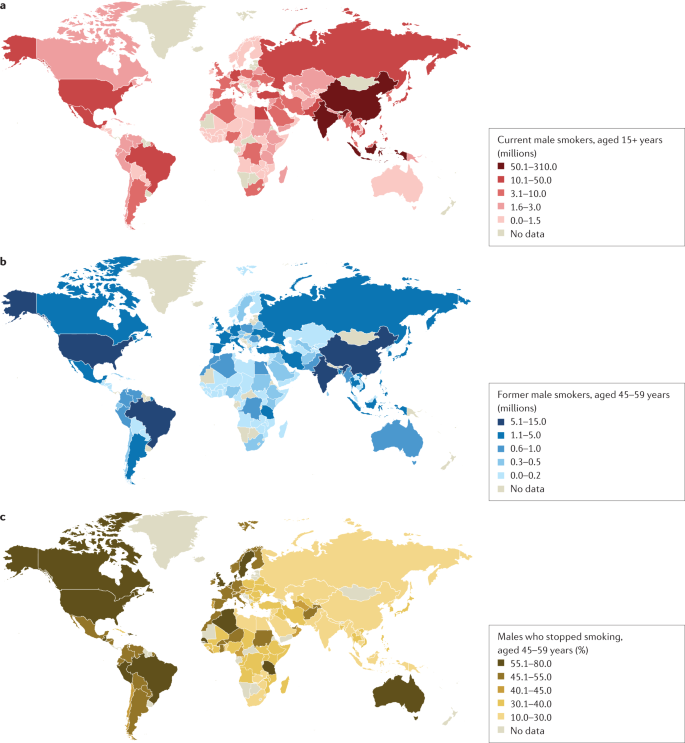
a | Number of current male smokers aged 15 years or older per country expressed in millions. b | Former male smokers aged 45–59 years per country expressed in millions. c | Former male smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for male smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among males is less variable than among females. Data from ref. 1 .
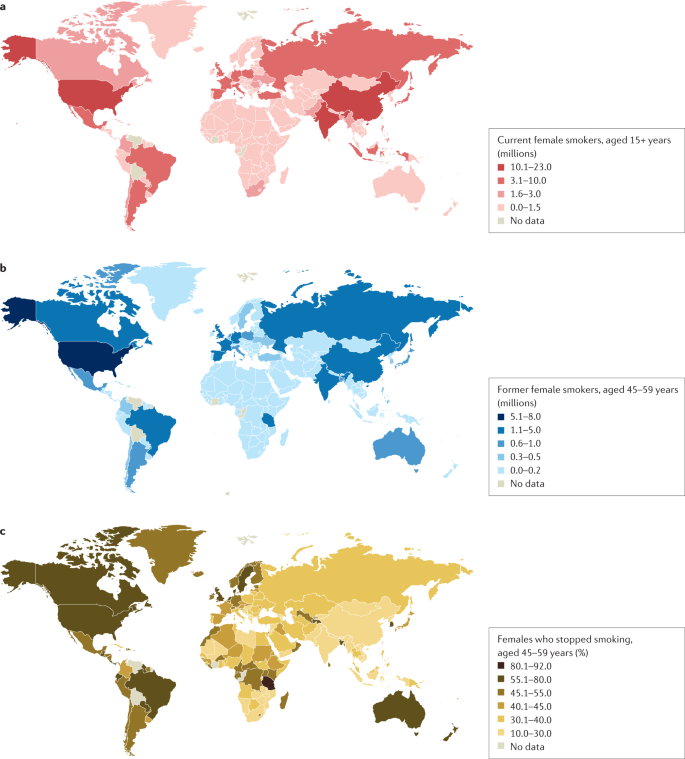
a | Number of current female smokers aged 15 years or older per country expressed in millions. b | Former female smokers aged 45–59 years per country expressed in millions. c | Former female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for female smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among females is much lower in East and South Asia than in Latin America or Eastern Europe. Data from ref. 1 .
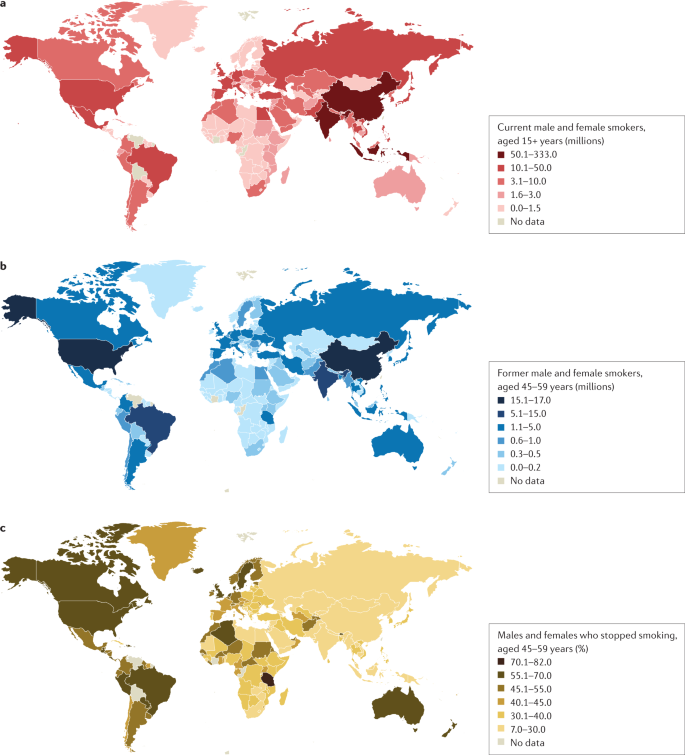
a | Number of current male and female smokers aged 15 years or older per country expressed in millions. b | Former male and female smokers aged 45–59 years per country expressed in millions. c | Former male and female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for the period 2015–2019 from countries with direct smoking surveys. Cessation rates are higher in high-income countries, but also notably high in Brazil. Cessation is far less common in South and East Asia and Russia and other Eastern European countries, and also low in South Africa. Data from ref. 1 .
Age at onset
Most smokers start smoking during adolescence, with almost 90% of smokers beginning between 15 and 25 years of age 24 . The prevalence of tobacco smoking among youths substantially declined in multiple HICs between 1990 and 2019 (ref. 25 ). More recently, the widespread uptake of ENDS in some regions such as Canada and the USA has raised concerns about the long-term effects of prolonged nicotine use among adolescents, including the possible notion that ENDS will increase the use of combustible smoking products 25 , 26 (although some studies have not found much aggregate effect at the population level) 27 .
Smoking that commences in early adolescence or young adulthood and persists throughout life has a more severe effect on health than smoking that starts later in life and/or that is not persistent 16 , 28 , 29 . Over 640 million adults under 30 years of age smoke in 22 jurisdictions alone (including 27 countries in the European Union where central efforts to reduce tobacco dependence might be possible) 30 . In those younger than 30 years of age, at least 320 million smoking-related deaths will occur unless they quit smoking 31 . The actual number of smoking-related deaths might be greater than one in two, and perhaps as high as two in three, long-term smokers 5 , 16 , 29 , 32 , 33 . At least half of these deaths are likely to occur in middle age (30–69 years) 16 , 29 , leading to a loss of two or more decades of life. People who smoke can expect to lose an average of at least a decade of life versus otherwise similar non-smokers 16 , 28 , 29 .
Direct epidemiological studies in several countries paired with model-based estimates have estimated that smoking tobacco accounted for 7.7 million deaths globally in 2020, of which 80% were in men and 87% were current smokers 1 . In HICs, the major causes of tobacco deaths are lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas and bladder cancer 28 , 29 . In some lower income countries, tuberculosis is an additional important cause of tobacco-related death 29 , 34 , which could be related to, for example, increased prevalence of infection, more severe tuberculosis/mortality and higher prevalence of treatment-resistant tuberculosis in smokers than in non-smokers in low-income countries 35 , 36 .
Despite substantial reductions in the prevalence of smoking, there were 34 million smokers in the USA, 7 million in the UK and 5 million in Canada in 2017 (ref. 16 ), and cigarette smoking remains the largest cause of premature death before 70 years of age in much of Europe and North America 1 , 16 , 28 , 29 . Smoking-associated diseases accounted for around 41 million deaths in the USA, UK and Canada from 1960 to 2020 (ref. 16 ). Moreover, as smoking-associated diseases are more prevalent among groups with lower levels of education and income, smoking accounts for at least half of the difference in overall mortality between these social groups 37 . Any reduction in smoking prevalence reduces the absolute mortality gap between these groups 38 .
Smoking cessation has become common in HICs with good tobacco control interventions. For example, in France, the number of ex-smokers is four times the number of current smokers among those aged 50 years or more 30 . By contrast, smoking cessation in LMICs remains uncommon before smokers develop tobacco-related diseases 39 . Smoking cessation greatly reduces the risks of smoking-related diseases. Indeed, smokers who quit smoking before 40 years of age avoid nearly all the increased mortality risks 31 , 33 . Moreover, individuals who quit smoking by 50 years of age reduce the risk of death from lung cancer by about two-thirds 40 . More modest hazards persist for deaths from lung cancer and emphysema 16 , 28 ; however, the risks among former smokers are an order of magnitude lower than among those who continue to smoke 33 .
Mechanisms/pathophysiology
Nicotine is the main psychoactive agent in tobacco and e-cigarettes. Nicotine acts as an agonist at nicotinic acetylcholine receptors (nAChRs), which are localized throughout the brain and peripheral nervous system 41 . nAChRs are pentameric ion channels that consist of varying combinations of α 2 –α 7 and β 2 –β 4 subunits, and for which acetylcholine (ACh) is the endogenous ligand 42 , 43 , 44 . When activated by nicotine binding, nAChR undergoes a conformational change that opens the internal pore, allowing an influx of sodium and calcium ions 45 . At postsynaptic membranes, nAChR activation can lead to action potential firing and downstream modulation of gene expression through calcium-mediated second messenger systems 46 . nAChRs are also localized to presynaptic membranes, where they modulate neurotransmitter release 47 . nAChRs become desensitized after activation, during which ligand binding will not open the channel 45 .
nAChRs with varying combinations of α-subunits and β-subunits have differences in nicotine binding affinity, efficacy and desensitization rate, and have differential expression depending on the brain region and cell type 48 , 49 , 50 . For instance, at nicotine concentrations found in human smokers, β 2 -containing nAChRs desensitize relatively quickly after activation, whereas α 7 -containing nAChRs have a slower desensitization profile 48 . Chronic nicotine exposure in experimental animal models or in humans induces an increase in cortical expression of α 4 β 2 -containing nAChRs 51 , 52 , 53 , 54 , 55 , but also increases the expression of β 3 and β 4 nAChR subunits in the medial habenula (MHb)–interpeduncular nucleus (IPN) pathway 56 , 57 . It is clear that both the brain localization and the type of nAChR are critical elements in mediating the various effects of nicotine, but other factors such as rate of nicotine delivery may also modulate addictive effects of nicotine 58 .
Neurocircuitry of nicotine addiction
Nicotine has both rewarding effects (such as a ‘buzz’ or ‘high’) and aversive effects (such as nausea and dizziness), with the net outcome dependent on dose and others factors such as interindividual sensitivity and presence of tolerance 59 . Thus, the addictive properties of nicotine involve integration of contrasting signals from multiple brain regions that process reward and aversion (Fig. 4 ).
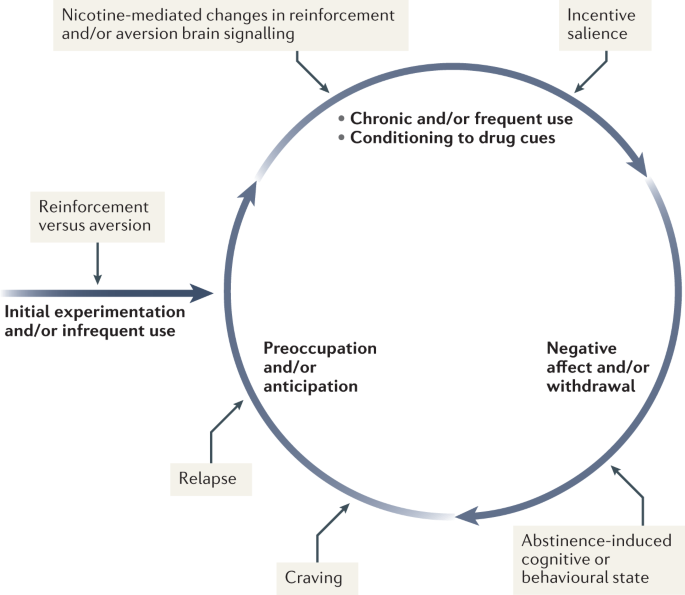
During initial use, nicotine exerts both reinforcing and aversive effects, which together determine the likelihood of continued use. As the individual transitions to more frequent patterns of chronic use, nicotine induces pharmacodynamic changes in brain circuits, which is thought to lead to a reduction in sensitivity to the aversive properties of the drug. Nicotine is also a powerful reinforcer that leads to the conditioning of secondary cues associated with the drug-taking experience (such as cigarette pack, sensory properties of cigarette smoke and feel of the cigarette in the hand or mouth), which serves to enhance the incentive salience of these environmental factors and drive further drug intake. When the individual enters into states of abstinence (such as daily during sleep at night or during quit attempts), withdrawal symptomology is experienced, which may include irritability, restlessness, learning or memory deficits, difficulty concentrating, anxiety and hunger. These negative affective and cognitive symptoms lead to an intensification of the individual’s preoccupation to obtain and use the tobacco/nicotine product, and subsequently such intense craving can lead to relapse.
The rewarding actions of nicotine have largely been attributed to the mesolimbic pathway, which consists of dopaminergic neurons in the ventral tegmental area (VTA) that project to the nucleus accumbens and prefrontal cortex 60 , 61 , 62 (Fig. 5 ). VTA integrating circuits and projection regions express several nAChR subtypes on dopaminergic, GABAergic, and glutamatergic neurons 63 , 64 . Ultimately, administration of nicotine increases dopamine levels through increased dopaminergic neuron firing in striatal and extrastriatal areas (such as the ventral pallidum) 65 (Fig. 6 ). This effect is involved in reward and is believed to be primarily mediated by the action of nicotine on α 4 -containing and β 2 -containing nAChRs in the VTA 66 , 67 .
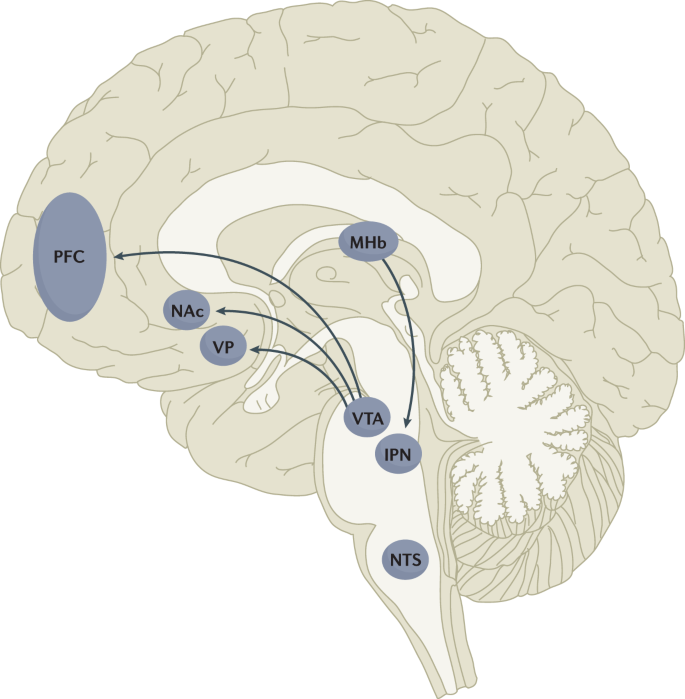
Multiple lines of research have demonstrated that nicotine reinforcement is mainly controlled by two brain pathways, which relay predominantly reward-related or aversion-related signals. The rewarding properties of nicotine that promote drug intake involve the mesolimbic dopamine projection from the ventral tegmental area (VTA) to the nucleus accumbens (NAc). By contrast, the aversive properties of nicotine that limit drug intake and mitigate withdrawal symptoms involve the fasciculus retroflexus projection from the medial habenula (MHb) to the interpeduncular nucleus (IPN). Additional brain regions have also been implicated in various aspects of nicotine dependence, such as the prefrontal cortex (PFC), ventral pallidum (VP), nucleus tractus solitarius (NTS) and insula (not shown here for clarity). All of these brain regions are directly or indirectly interconnected as integrative circuits to drive drug-seeking and drug-taking behaviours.
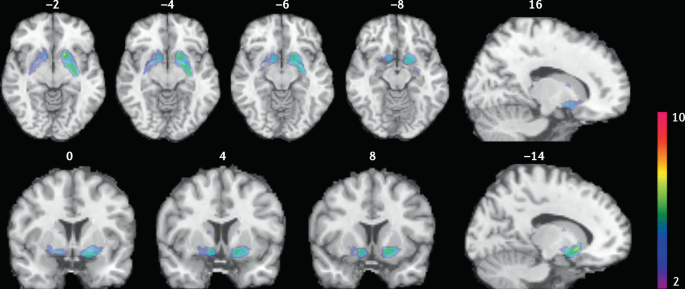
Smokers received brain PET scans with [ 11 C]PHNO, a dopamine D 2/3 PET tracer that has high sensitivity in detecting fluctuations of dopamine. PET scans were performed during abstinence or after smoking a cigarette. Reduced binding potential (BP ND ) was observed after smoking, indicating increased dopamine levels in the ventral striatum and in the area that corresponds to the ventral pallidum. The images show clusters with statistically significant decreases of [ 11 C]PHNO BP ND after smoking a cigarette versus abstinence condition. Those clusters have been superimposed on structural T1 MRI images of the brain. Reprinted from ref. 65 , Springer Nature Limited.
The aversive properties of nicotine are mediated by neurons in the MHb, which project to the IPN. Studies in rodents using genetic knockdown and knockout strategies demonstrated that the α 5 -containing, α 3 -containing and β 4 -containing nAChRs in the MHb–IPN pathway mediate the aversive properties of nicotine that limit drug intake, especially when animals are given the opportunity to consume higher nicotine doses 68 , 69 , 70 , 71 , 72 . In addition to nAChRs, other signalling factors acting on the MHb terminals in the IPN also regulate the actions of nicotine. For instance, under conditions of chronic nicotine exposure or with optogenetic activation of IPN neurons, a subtype of IPN neurons co-expressing Chrna5 (encoding the α 5 nAChR subunit) and Amigo1 (encoding adhesion molecule with immunoglobulin-like domain 1) release nitric oxide from the cell body that retrogradely inhibits MHb axon terminals 70 . In addition, nicotine activates α 5 -containing nAChR-expressing neurons that project from the nucleus tractus solitarius to the IPN, leading to release of glucagon-like peptide-1 that binds to GLP receptors on habenular axon terminals, which subsequently increases IPN neuron activation and decreases nicotine self-administration 73 . Taken together, these findings suggest a dynamic signalling process at MHb axonal terminals in the IPN, which regulates the addictive properties of nicotine and determines the amount of nicotine that is self-administered.
Nicotine withdrawal in animal models can be assessed by examining somatic signs (such as shaking, scratching, head nods and chewing) and affective signs (such as increased anxiety-related behaviours and conditioned place aversion). Interestingly, few nicotine withdrawal somatic signs are found in mice with genetic knockout of the α 2 , α 5 or β 4 nAChR subunits 74 , 75 . By contrast, β 2 nAChR-knockout mice have fewer anxiety-related behaviours during nicotine withdrawal, with no differences in somatic symptoms compared with wild-type mice 74 , 76 .
In addition to the VTA (mediating reward) and the MHb–IPN pathway (mediating aversion), other brain areas are involved in nicotine addiction (Fig. 5 ). In animals, the insular cortex controls nicotine taking and nicotine seeking 77 . Moreover, humans with lesions of the insular cortex can quit smoking easily without relapse 78 . This finding led to the development of a novel therapeutic intervention modulating insula function (see Management, below) 79 , 80 . Various brain areas (shell of nucleus accumbens, basolateral amygdala and prelimbic cortex) expressing cannabinoid CB 1 receptors are also critical in controlling rewarding effects and relapse 81 , 82 . The α 1 -adrenergic receptor expressed in the cortex also control these effects, probably through glutamatergic afferents to the nucleus accumbens 83 .
Individual differences in nicotine addiction risk
Vulnerability to nicotine dependence varies between individuals, and the reasons for these differences are multidimensional. Many social factors (such as education level and income) play a role 84 . Broad psychological and social factors also modulate this risk. For example, peer smoking status, knowledge on effect of tobacco, expectation on social acceptance, exposure to passive smoking modulate the risk of initiating tobacco use 85 , 86 .
Genetic factors have a role in smoking initiation, the development of nicotine addiction and the likelihood of smoking cessation. Indeed, heritability has been estimated to contribute to approximatively half of the variability in nicotine dependence 87 , 88 , 89 , 90 . Important advances in our understanding of such genetic contributions have evolved with large-scale genome-wide association studies of smokers and non-smokers. One of the most striking findings has been that allelic variation in the CHRNA5 – CHRNA3 – CHRNB4 gene cluster, which encodes α 5 , α 3 and β 4 nAChR subunits, correlates with an increased vulnerability for nicotine addiction, indicated by a higher likelihood of becoming dependent on nicotine and smoking a greater number of cigarettes per day 91 , 92 , 93 , 94 , 95 . The most significant effect has been found for a single-nucleotide polymorphism in CHRNA5 (rs16969968), which results in an amino acid change and reduced function of α 5 -containing nAChRs 92 .
Allelic variation in CYP2A6 (encoding the CYP2A6 enzyme, which metabolizes nicotine) has also been associated with differential vulnerability to nicotine dependence 96 , 97 , 98 . CYP2A6 is highly polymorphic, resulting in variable enzymatic activity 96 , 99 , 100 . Individuals with allelic variation that results in slow nicotine metabolism consume less nicotine per day, experience less-severe withdrawal symptoms and are more successful at quitting smoking than individuals with normal or fast metabolism 101 , 102 , 103 , 104 . Moreover, individuals with slow nicotine metabolism have lower dopaminergic receptor expression in the dopamine D2 regions of the associative striatum and sensorimotor striatum in PET studies 105 and take fewer puffs of nicotine-containing cigarettes (compared with de-nicotinized cigarettes) in a forced choice task 106 . Slower nicotine metabolism is thought to increase the duration of action of nicotine, allowing nicotine levels to accumulate over time, therefore enabling lower levels of intake to sustain activation of nAChRs 107 .
Large-scale genetic studies have identified hundreds of other genetic loci that influence smoking initiation, age of smoking initiation, cigarettes smoked per day and successful smoking cessation 108 . The strongest genetic contributions to smoking through the nicotinic receptors and nicotine metabolism are among the strongest genetic contributors to lung cancer 109 . Other genetic variations (such as those related to cannabinoid, dopamine receptors or other neurotransmitters) may affect certain phenotypes related to smoking (such as nicotine preference and cue-reactivity) 110 , 111 , 112 , 113 , 114 , 115 .
Diagnosis, screening and prevention
Screening for cigarette smoking.
Screening for cigarette smoking should happen at every doctor’s visit 116 . In this regard, a simple and direct question about a person’s tobacco use can provide an opportunity to offer information about its potential risks and treatments to assist in quitting. All smokers should be offered assistance in quitting because even low levels of smoking present a significant health risk 33 , 117 , 118 . Smoking status can be assessed by self-categorization or self-reported assessment of smoking behaviour (Table 1 ). In people who smoke, smoking frequency can be assessed 119 and a combined quantity frequency measure such as pack-year history (that is, average number of cigarettes smoked per day multiplied by the number of years, divided by 20), can be used to estimate cumulative risk of adverse health outcomes. The Association for the Treatment of Tobacco Use and Dependence recommends that all electronic health records should document smoking status using the self-report categories listed in Table 1 .
Owing to the advent of e-cigarettes and heat-not-burn products, and the popularity of little cigars in the US that mimic combustible cigarettes, people who use tobacco may use multiple products concurrently 120 , 121 . Thus, screening for other nicotine and tobacco product use is important in clinical practice. The self-categorization approach can also be used to describe the use of these other products.
Traditionally tobacco use has been classified according to whether the smoker meets criteria for nicotine dependence in one of the two main diagnostic classifications: the DSM 122 (tobacco use disorder) and the ICD (tobacco dependence) 123 . The diagnosis of tobacco use disorder according to DSM-5 criteria requires the presence of at least 2 of 11 symptoms that have produced marked clinical impairment or distress within a 12-month period (Box 2 ). Of note, these symptoms are similar for all substance use disorder diagnoses and may not all be relevant to tobacco use disorder (such as failure to complete life roles). In the ICD-10, codes allow the identification of specific tobacco products used (cigarettes, chewing tobacco and other tobacco products).
Dependence can also be assessed as a continuous construct associated with higher levels of use, greater withdrawal and reduced likelihood of quitting. The level of dependence can be assessed with the Fagerström Test for Nicotine Dependence, a short questionnaire comprising six questions 124 (Box 2 ). A score of ≥4 indicates moderate to high dependence. As very limited time may be available in clinical consultations, the Heaviness of Smoking Index (HSI) was developed, which comprises two questions on the number of cigarettes smoked per day and how soon after waking the first cigarette is smoked 125 . The HSI can guide dosing for nicotine replacement therapy (NRT).
Other measures of cigarette dependence have been developed but are not used in the clinical setting, such as the Cigarette Dependence Scale 126 , Hooked on Nicotine Checklist 127 , Nicotine Dependence Syndrome Scale 128 , the Wisconsin Inventory of Smoking Dependence Motives (Brief) 129 and the Penn State Cigarette Dependence Index 130 . However, in practice, these are not often used, as the most important aspect is to screen for smoking and encourage all smokers to quit smoking regardless of their dependence status.
Box 2 DSM-5 criteria for tobacco use disorder and items of the Fagerström Test for nicotine dependence
DSM-5 (ref. 122 )
Taxonomic and diagnostic tool for tobacco use disorder published by the American Psychiatric Association.
A problematic pattern of tobacco use leading to clinically significant impairment or distress as manifested by at least two of the following, occurring within a 12-month period.
Tobacco often used in larger amounts or over a longer period of time than intended
A persistent desire or unsuccessful efforts to reduce or control tobacco use
A great deal of time spent in activities necessary to obtain or use tobacco
Craving, or a strong desire or urge to use tobacco
Recurrent tobacco use resulting in a failure to fulfil major role obligations at work, school or home
Continued tobacco use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of tobacco (for example, arguments with others about tobacco use)
Important social, occupational or recreational activities given up or reduced because of tobacco use
Recurrent tobacco use in hazardous situations (such as smoking in bed)
Tobacco use continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco use
Tolerance, defined by either of the following.
A need for markedly increased amounts of tobacco to achieve the desired effect
A markedly diminished effect with continued use of the same amount of tobacco
Withdrawal, manifesting as either of the following.
Withdrawal syndrome for tobacco
Tobacco (or a closely related substance, such as nicotine) taken to relieve or avoid withdrawal symptoms
Fagerström Test for Nicotine Dependence 124
A standard instrument for assessing the intensity of physical addiction to nicotine.
How soon after you wake up do you smoke your first cigarette?
Within 5 min (scores 3 points)
5 to 30 min (scores 2 points)
31 to 60 min (scores 1 point)
After 60 min (scores 0 points)
Do you find it difficult not to smoke in places where you should not, such as in church or school, in a movie, at the library, on a bus, in court or in a hospital?
Yes (scores 1 point)
No (scores 0 points)
Which cigarette would you most hate to give up; which cigarette do you treasure the most?
The first one in the morning (scores 1 point)
Any other one (scores 0 points)
How many cigarettes do you smoke each day?
10 or fewer (scores 0 points)
11 to 20 (scores 1 point)
21 to 30 (scores 2 points)
31 or more (scores 3 points)
Do you smoke more during the first few hours after waking up than during the rest of the day?
Do you still smoke if you are so sick that you are in bed most of the day or if you have a cold or the flu and have trouble breathing?
A score of 7–10 points is classified as highly dependent; 4–6 points is classified as moderately dependent; <4 points is classified as minimally dependent.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Young people who do not start smoking cigarettes between 15 and 25 years of age have a very low risk of ever smoking 24 , 131 , 132 . This age group provides a critical opportunity to prevent cigarette smoking using effective, evidence-based strategies to prevent smoking initiation and reduce escalation from experimentation to regular use 131 , 132 , 133 , 134 , 135 .
Effective prevention of cigarette uptake requires a comprehensive package of cost-effective policies 134 , 136 , 137 to synergistically reduce the population prevalence of cigarette smoking 131 , 135 . These policies include high rates of tobacco taxation 30 , 134 , 137 , 138 , widespread and rigorously enforced smoke-free policies 139 , bans on tobacco advertising and promotions 140 , use of plain packaging and graphic warnings about the health risks of smoking 135 , 141 , mass media and peer-based education programmes to discourage smoking, and enforcement of laws against the sale of cigarettes to young people below the minimum legal purchase age 131 , 135 . These policies make cigarettes less available and affordable to young people. Moreover, these policies make it more difficult for young people to purchase cigarettes and make smoking a much less socially acceptable practice. Of note, these policies are typically mostly enacted in HICs, which may be related to the declining prevalence of smoking in these countries, compared with the prevalence in LMICs.
Pharmacotherapy
Three evidence-based classes of pharmacotherapy are available for smoking cessation: NRT (using nicotine-based patches, gum, lozenges, mini-lozenges, nasal sprays and inhalers), varenicline (a nAChR partial agonist), and bupropion (a noradrenaline/dopamine reuptake inhibitor that also inhibits nAChR function and is also used as an antidepressant). These FDA-approved and EMA-approved pharmacotherapies are cost-effective smoking cessation treatments that double or triple successful abstinence rates compared with no treatment or placebo controls 116 , 142 .
Combinations of pharmacotherapies are also effective for smoking cessation 116 , 142 . For example, combining NRTs (such as the steady-state nicotine patch and as-needed NRT such as gum or mini-lozenge) is more effective than a single form of NRT 116 , 142 , 143 . Combining NRT and varenicline is the most effective smoking cessation pharmacotherapy 116 , 142 , 143 . Combining FDA-approved pharmacotherapy with behavioural counselling further increases the likelihood of successful cessation 142 . Second-line pharmacotherapies (for example, nortriptyline) have some potential for smoking cessation, but their use is limited due to their tolerability profile.
All smokers should receive pharmacotherapy to help them quit smoking, except those in whom pharmacotherapy has insufficient evidence of effectiveness (among adolescents, smokeless tobacco users, pregnant women or light smokers) or those in whom pharmacotherapy is medically contraindicated 144 . Table 2 provides specific information regarding dosing and duration for each FDA-approved pharmacotherapy. Extended use of pharmacotherapy beyond the standard 12-week regimen after cessation is effective and should be considered 116 . Moreover, preloading pharmacotherapy (that is, initiating cessation medication in advance of a quit attempt), especially with the nicotine patch, is a promising treatment, although further studies are required to confirm efficacy.
Cytisine has been used for smoking cessation in Eastern Europe for a long time and is available in some countries (such as Canada) without prescription 145 . Cytisine is a partial agonist of nAChRs and its structure was the precursor for the development of varenicline 145 . Cytisine is at least as effective as some approved pharmacotherapies for smoking cessation, such as NRT 146 , 147 , 148 , and the role of cytisine in smoking cessation is likely to expand in the future, notably owing to its much lower cost than traditional pharmacotherapies. E-cigarettes also have the potential to be useful as smoking cessation devices 149 , 150 . The 2020 US Surgeon General’s Report concluded that there was insufficient evidence to promote cytisine or e-cigarettes as effective smoking cessation treatments, but in the UK its use is recommended for smoking cessation (see ref. 15 for regularly updated review).
Counselling and behavioural treatments
Psychosocial counselling significantly increases the likelihood of successful cessation, especially when combined with pharmacotherapy. Even a counselling session lasting only 3 minutes can help smokers quit 116 , although the 2008 US Public Health Service guidelines and the Preventive Services Task Force 151 each concluded that more intensive counselling (≥20 min per session) is more effective than less intensive counselling (<20 min per session). Higher smoking cessation rates are obtained by using behavioural change techniques that target associative and self-regulatory processes 152 . In addition, behavioural change techniques that will favour commitment, social reward and identity associated with changed behaviour seems associated with higher success rates 152 . Evidence-based counselling focuses on providing social support during treatment, building skills to cope with withdrawal and cessation, and problem-solving in challenging situations 116 , 153 . Effective counselling can be delivered by diverse providers (such as physicians, nurses, pharmacists, social workers, psychologists and certified tobacco treatment specialists) 116 .
Counselling can be delivered in a variety of modalities. In-person individual and group counselling are effective, as is telephone counselling (quit lines) 142 . Internet and text-based intervention seem to be effective in smoking cessation, especially when they are interactive and tailored to a smoker’s specific circumstances 142 . Over the past several years, the number of smoking cessation smartphone apps has increased, but there the evidence that the use of these apps significantly increases smoking cessation rates is not sufficient.
Contingency management (providing financial incentives for abstinence or engagement in treatment) has shown promising results 154 , 155 but its effects are not sustained once the contingencies are removed 155 , 156 . Other treatments such as hypnosis, acupuncture and laser treatment have not been shown to improve smoking cessation rates compared with placebo treatments 116 . Moreover, no solid evidence supports the use of conventional transcranial magnetic stimulation (TMS) for long-term smoking cessation 157 , 158 .
Although a variety of empirically supported smoking cessation interventions are available, more than two-thirds of adult smokers who made quit attempts in the USA during the past year did not use an evidence-based treatment and the rate is likely to be lower in many other countries 142 . This speaks to the need to increase awareness of, and access to, effective cessation aids among all smokers.
Brain stimulation
The insula (part of the frontal cortex) is a critical brain structure involved in cigarette craving and relapse 78 , 79 . The activity of the insula can be modulated using an innovative approach called deep insula/prefrontal cortex TMS (deep TMS), which is effective in helping people quit smoking 80 , 159 . This approach has now been approved by the FDA as an effective smoking cessation intervention 80 . However, although this intervention was developed and is effective for smoking cessation, the number of people with access to it is limited owing to the limited number of sites equipped and with trained personnel, and the cost of this intervention.
Quality of life
Generic instruments (such as the Short-Form (SF-36) Health Survey) can be used to evaluate quality of life (QOL) in smokers. People who smoke rate their QOL lower than people who do not smoke both before and after they become smokers 160 , 161 . QOL improves when smokers quit 162 . Mental health may also improve on quitting smoking 163 . Moreover, QOL is much poorer in smokers with tobacco-related diseases, such as chronic respiratory diseases and cancers, than in individuals without tobacco-related diseases 161 , 164 . The dimensions of QOL that show the largest decrements in people who smoke are those related to physical health, day-to-day activities and mental health such as depression 160 . Smoking also increases the risk of diabetes mellitus 165 , 166 , which is a major determinant of poor QOL for a wide range of conditions.
The high toll of premature death from cigarette smoking can obscure the fact that many of the diseases that cause these deaths also produce substantial disability in the years before death 1 . Indeed, death in smokers is typically preceded by several years of living with the serious disability and impairment of everyday activities caused by chronic respiratory disease, heart disease and cancer 2 . Smokers’ QOL in these years may also be adversely affected by the adverse effects of the medical treatments that they receive for these smoking-related diseases (such as major surgery and radiotherapy).
Expanding cessation worldwide
The major global challenge is to consider individual and population-based strategies that could increase the substantially low rates of adult cessation in most LMICs and indeed strategies to ensure that even in HICs, cessation continues to increase. In general, the most effective tools recommended by WHO to expand cessation are the same tools that can prevent smoking initiation, notably higher tobacco taxes, bans on advertising and promotion, prominent warning labels or plain packaging, bans on public smoking, and mass media and educational efforts 29 , 167 . The effective use of these policies, particularly taxation, lags behind in most LMICs compared with most HICs, with important exceptions such as Brazil 167 . Access to effective pharmacotherapies and counselling as well as support for co-existing mental health conditions would also be required to accelerate cessation in LMICs. This is particularly important as smokers living in LMICs often have no access to the full range of effective treatment options.
Regulating access to e-cigarettes
How e-cigarettes should be used is debated within the tobacco control field. In some countries (for example, the UK), the use of e-cigarettes as a cigarette smoking cessation aid and as a harm reduction strategy is supported, based on the idea that e-cigarette use will lead to much less exposure to toxic compounds than tobacco use, therefore reducing global harm. In other countries (for example, the USA), there is more concern with preventing the increased use of e-cigarettes by youths that may subsequently lead to smoking 25 , 26 . Regulating e-cigarettes in nuanced ways that enable smokers to access those products whilst preventing their uptake among youths is critical.
Regulating nicotine content in tobacco products
Reducing the nicotine content of cigarettes could potentially produce less addictive products that would allow a gradual reduction in the population prevalence of smoking. Some clinical studies have found no compensatory increase in smoking whilst providing access to low nicotine tobacco 168 . Future regulation may be implemented to gradually decrease the nicotine content of combustible tobacco and other nicotine products 169 , 170 , 171 .
Tobacco end games
Some individuals have proposed getting rid of commercial tobacco products this century or using the major economic disruption arising from the COVID-19 pandemic to accelerate the demise of the tobacco industry 172 , 173 . Some tobacco producers have even proposed this strategy as an internal goal, with the idea of switching to nicotine delivery systems that are less harmful ( Philip Morris International ). Some countries are moving towards such an objective; for example, in New Zealand, the goal that fewer than 5% of New Zealanders will be smokers in 2025 has been set (ref. 174 ). The tobacco end-game approach would overall be the best approach to reduce the burden of tobacco use on society, but it would require coordination of multiple countries and strong public and private consensus on the strategy to avoid a major expansion of the existing illicit market in tobacco products in some countries.
Innovative interventions
The COVID-19 pandemic has shown that large-scale investment in research can lead to rapid development of successful therapeutic interventions. By contrast, smoking cessation has been underfunded compared with the contribution that it makes to the global burden of disease. In addition, there is limited coordination between research teams and most studies are small-scale and often underpowered 79 . It is time to fund an ambitious, coordinated programme of research to test the most promising therapies based on an increased understanding of the neurobiological basis of smoking and nicotine addiction (Table 3 ). Many of those ideas have not yet been tested properly and this could be carried out by a coordinated programme of research at the international level.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 397 , 2337–2360 (2021). This study summarizes the burden of disease induced by tobacco worldwide .
Google Scholar
West, R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol. Health 32 , 1018–1036 (2017).
PubMed PubMed Central Google Scholar
West, R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD 6 , 277–283 (2009).
PubMed Google Scholar
Fagerström, K. Determinants of tobacco use and renaming the FTND to the Fagerström test for cigarette dependence. Nicotine Tob. Res. 14 , 75–78 (2012).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Doll, R. & Hill, A. B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 2 , 739–748 (1950).
CAS PubMed PubMed Central Google Scholar
Royal College of Physicians. Smoking and health. Summary of a report of the Royal College of Physicians of London on smoking in relation to cancer of the lung and other diseases (Pitman Medical Publishing, 1962).
Henningfield, J. E., Smith, T. T., Kleykamp, B. A., Fant, R. V. & Donny, E. C. Nicotine self-administration research: the legacy of Steven R. Goldberg and implications for regulation, health policy, and research. Psychopharmacology 233 , 3829–3848 (2016).
Le Foll, B. & Goldberg, S. R. Effects of nicotine in experimental animals and humans: an update on addictive properties. Hand. Exp. Pharmacol. https://doi.org/10.1007/978-3-540-69248-5_12 (2009).
Article Google Scholar
Proctor, R. N. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll. Tob. Control. 21 , 87–91 (2012).
Hall, B. J. et al. Differential effects of non-nicotine tobacco constituent compounds on nicotine self-administration in rats. Pharmacol. Biochem. Behav. 120 , 103–108 (2014).
Musso, F. et al. Smoking impacts on prefrontal attentional network function in young adult brains. Psychopharmacology 191 , 159–169 (2007).
CAS PubMed Google Scholar
Goriounova, N. A. & Mansvelder, H. D. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb. Perspect. Med. 2 , a012120 (2012).
Fagerström, K. O. & Bridgman, K. Tobacco harm reduction: the need for new products that can compete with cigarettes. Addictive Behav. 39 , 507–511 (2014).
Hartmann-Boyce, J. et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 9 , CD010216 (2021).
Jha, P. The hazards of smoking and the benefits of cessation: a critical summation of the epidemiological evidence in high-income countries. eLife https://doi.org/10.7554/eLife.49979 (2020).
Article PubMed PubMed Central Google Scholar
Palipudi, K. M. et al. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS ONE 7 , e33466 (2012).
Goodwin, R. D., Pagura, J., Spiwak, R., Lemeshow, A. R. & Sareen, J. Predictors of persistent nicotine dependence among adults in the United States. Drug Alcohol. Depend. 118 , 127–133 (2011).
Weinberger, A. H. et al. Cigarette use is increasing among people with illicit substance use disorders in the United States, 2002-14: emerging disparities in vulnerable populations. Addiction 113 , 719–728 (2018).
Evans-Polce, R. J., Kcomt, L., Veliz, P. T., Boyd, C. J. & McCabe, S. E. Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. Am. J. Psychiatry 177 , 1073–1081 (2020).
Hassan, A. N. & Le Foll, B. Survival probabilities and predictors of major depressive episode incidence among individuals with various types of substance use disorders. J. Clin. Psychiatry https://doi.org/10.4088/JCP.20m13637 (2021).
Article PubMed Google Scholar
Smith, P. H., Mazure, C. M. & McKee, S. A. Smoking and mental illness in the U.S. population. Tob. Control. 23 , e147–e153 (2014).
Bourgault, Z., Rubin-Kahana, D. S., Hassan, A. N., Sanches, M. & Le Foll, B. Multiple substance use disorders and self-reported cognitive function in U.S. adults: associations and sex-differences in a nationally representative sample. Front. Psychiatry https://doi.org/10.3389/fpsyt.2021.797578 (2022).
Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990-2019. Lancet Public Health 6 , e472–e481 (2021).
Warner, K. E. How to think–not feel–about tobacco harm reduction. Nicotine Tob. Res. 21 , 1299–1309 (2019).
Soneji, S. et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 171 , 788–797 (2017).
Levy, D. T. et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob. Control. 28 , 629–635 (2019).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking — 50 years of progress: a report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Jha, P. & Peto, R. Global effects of smoking, of quitting, and of taxing tobacco. N. Engl. J. Med. 370 , 60–68 (2014). This review covers the impact of tobacco, of quitting smoking and the importance of taxation to impact prevalence of smoking .
Jha, P. & Peto., R. in Tobacco Tax Reform: At the Crossroads of Health and Development . (eds Marquez, P. V. & Moreno-Dodson, B.) 55–72 (World Bank Group, 2017).
Jha, P. et al. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 368 , 341–350 (2013).
Banks, E. et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 13 , 38 (2015).
Pirie, K. et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381 , 133–141 (2013).
Jha, P. et al. A nationally representative case-control study of smoking and death in India. N. Engl. J. Med. 358 , 1137–1147 (2008).
Chan, E. D. et al. Tobacco exposure and susceptibility to tuberculosis: is there a smoking gun? Tuberculosis 94 , 544–550 (2014).
Wang, M. G. et al. Association between tobacco smoking and drug-resistant tuberculosis. Infect. Drug Resist. 11 , 873–887 (2018).
Jha, P. et al. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 368 , 367–370 (2006).
Jha, P., Gelband, H, Irving, H. & Mishra, S. in Reducing Social Inequalities in Cancer: Evidence and Priorities for Research (eds Vaccarella, S et al.) 161–166 (IARC, 2018).
Jha, P. Expanding smoking cessation world-wide. Addiction 113 , 1392–1393 (2018).
Jha, P. Avoidable global cancer deaths and total deaths from smoking. Nat. Rev. Cancer 9 , 655–664 (2009).
Wittenberg, R. E., Wolfman, S. L., De Biasi, M. & Dani, J. A. Nicotinic acetylcholine receptors and nicotine addiction: a brief introduction. Neuropharmacology 177 , 108256 (2020).
Boulter, J. et al. Functional expression of two neuronal nicotinic acetylcholine receptors from cDNA clones identifies a gene family. Proc. Natl Acad. Sci. USA 84 , 7763–7767 (1987).
Couturier, S. et al. A neuronal nicotinic acetylcholine receptor subunit (α7) is developmentally regulated and forms a homo-oligomeric channel blocked by α-BTX. Neuron 5 , 847–856 (1990).
Picciotto, M. R., Addy, N. A., Mineur, Y. S. & Brunzell, D. H. It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog. Neurobiol. 84 , 329–342 (2008).
Changeux, J. P. Structural identification of the nicotinic receptor ion channel. Trends Neurosci. 41 , 67–70 (2018).
McKay, B. E., Placzek, A. N. & Dani, J. A. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem. Pharmacol. 74 , 1120–1133 (2007).
Wonnacott, S. Presynaptic nicotinic ACh receptors. Trends Neurosci. 20 , 92–98 (1997).
Wooltorton, J. R., Pidoplichko, V. I., Broide, R. S. & Dani, J. A. Differential desensitization and distribution of nicotinic acetylcholine receptor subtypes in midbrain dopamine areas. J. Neurosci. 23 , 3176–3185 (2003).
Gipson, C. D. & Fowler, C. D. Nicotinic receptors underlying nicotine dependence: evidence from transgenic mouse models. Curr. Top. Behav. Neurosci. 45 , 101–121 (2020).
Hamouda, A. K. et al. Potentiation of (α4)2(β2)3, but not (α4)3(β2)2, nicotinic acetylcholine receptors reduces nicotine self-administration and withdrawal symptoms. Neuropharmacology 190 , 108568 (2021).
Lallai, V. et al. Nicotine acts on cholinergic signaling mechanisms to directly modulate choroid plexus function. eNeuro https://doi.org/10.1523/ENEURO.0051-19.2019 (2019).
Benwell, M. E., Balfour, D. J. & Anderson, J. M. Evidence that tobacco smoking increases the density of (-)-[3H]nicotine binding sites in human brain. J. Neurochem. 50 , 1243–1247 (1988).
Perry, D. C., Davila-Garcia, M. I., Stockmeier, C. A. & Kellar, K. J. Increased nicotinic receptors in brains from smokers: membrane binding and autoradiography studies. J. Pharmacol. Exp. Ther. 289 , 1545–1552 (1999).
Marks, M. J. et al. Nicotine binding and nicotinic receptor subunit RNA after chronic nicotine treatment. J. Neurosci. 12 , 2765–2784 (1992).
Le Foll, B. et al. Impact of short access nicotine self-administration on expression of α4β2* nicotinic acetylcholine receptors in non-human primates. Psychopharmacology 233 , 1829–1835 (2016).
Meyers, E. E., Loetz, E. C. & Marks, M. J. Differential expression of the beta4 neuronal nicotinic receptor subunit affects tolerance development and nicotinic binding sites following chronic nicotine treatment. Pharmacol. Biochem. Behav. 130 , 1–8 (2015).
Zhao-Shea, R., Liu, L., Pang, X., Gardner, P. D. & Tapper, A. R. Activation of GABAergic neurons in the interpeduncular nucleus triggers physical nicotine withdrawal symptoms. Curr. Biol. 23 , 2327–2335 (2013).
Jensen, K. P., Valentine, G., Gueorguieva, R. & Sofuoglu, M. Differential effects of nicotine delivery rate on subjective drug effects, urges to smoke, heart rate and blood pressure in tobacco smokers. Psychopharmacology 237 , 1359–1369 (2020).
Villanueva, H. F., James, J. R. & Rosecrans, J. A. Evidence of pharmacological tolerance to nicotine. NIDA Res. Monogr. 95 , 349–350 (1989).
Corrigall, W. A., Coen, K. M. & Adamson, K. L. Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res. 653 , 278–284 (1994).
Nisell, M., Nomikos, G. G., Hertel, P., Panagis, G. & Svensson, T. H. Condition-independent sensitization of locomotor stimulation and mesocortical dopamine release following chronic nicotine treatment in the rat. Synapse 22 , 369–381 (1996).
Rice, M. E. & Cragg, S. J. Nicotine amplifies reward-related dopamine signals in striatum. Nat. Neurosci. 7 , 583–584 (2004).
Mameli-Engvall, M. et al. Hierarchical control of dopamine neuron-firing patterns by nicotinic receptors. Neuron 50 , 911–921 (2006).
Picciotto, M. R., Higley, M. J. & Mineur, Y. S. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 76 , 116–129 (2012).
Le Foll, B. et al. Elevation of dopamine induced by cigarette smoking: novel insights from a [11C]-+-PHNO PET study in humans. Neuropsychopharmacology 39 , 415–424 (2014). This brain imaging study identified the brain areas in which smoking elevates dopamine levels .
Maskos, U. et al. Nicotine reinforcement and cognition restored by targeted expression of nicotinic receptors. Nature 436 , 103–107 (2005). This article discusses the implication of the β 2 - containing nAChRs in the VTA in mammalian cognitive function .
Picciotto, M. R. et al. Acetylcholine receptors containing the beta2 subunit are involved in the reinforcing properties of nicotine. Nature 391 , 173–177 (1998). This article discusses the implication of the β 2 - containing nAChRs in addictive effects of nicotine .
Fowler, C. D., Lu, Q., Johnson, P. M., Marks, M. J. & Kenny, P. J. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature 471 , 597–601 (2011). This article discusses the implication of the α5 nicotinic receptor located in the MHb in a mechanism mediating the aversive effects of nicotine .
Elayouby, K. S. et al. α3* Nicotinic acetylcholine receptors in the habenula-interpeduncular nucleus circuit regulate nicotine intake. J. Neurosci. https://doi.org/10.1523/JNEUROSCI.0127-19.2020 (2020).
Ables, J. L. et al. Retrograde inhibition by a specific subset of interpeduncular α5 nicotinic neurons regulates nicotine preference. Proc. Natl Acad. Sci. USA 114 , 13012–13017 (2017).
Frahm, S. et al. Aversion to nicotine is regulated by the balanced activity of β4 and α5 nicotinic receptor subunits in the medial habenula. Neuron 70 , 522–535 (2011).
Jackson, K. J. et al. Role of α5 nicotinic acetylcholine receptors in pharmacological and behavioral effects of nicotine in mice. J. Pharmacol. Exp. Ther. 334 , 137–146 (2010).
Tuesta, L. M. et al. GLP-1 acts on habenular avoidance circuits to control nicotine intake. Nat. Neurosci. 20 , 708–716 (2017).
Salas, R., Pieri, F. & De Biasi, M. Decreased signs of nicotine withdrawal in mice null for the β4 nicotinic acetylcholine receptor subunit. J. Neurosci. 24 , 10035–10039 (2004).
Salas, R., Sturm, R., Boulter, J. & De Biasi, M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J. Neurosci. 29 , 3014–3018 (2009).
Jackson, K. J., Martin, B. R., Changeux, J. P. & Damaj, M. I. Differential role of nicotinic acetylcholine receptor subunits in physical and affective nicotine withdrawal signs. J. Pharmacol. Exp. Ther. 325 , 302–312 (2008).
Le Foll, B. et al. Translational strategies for therapeutic development in nicotine addiction: rethinking the conventional bench to bedside approach. Prog. Neuropsychopharmacol. Biol. Psychiatry 52 , 86–93 (2014).
Naqvi, N. H., Rudrauf, D., Damasio, H. & Bechara, A. Damage to the insula disrupts addiction to cigarette smoking. Science 315 , 531–534 (2007). This article discusses the implication of the insular cortex in tobacco addiction .
Ibrahim, C. et al. The insula: a brain stimulation target for the treatment of addiction. Front. Pharmacol. 10 , 720 (2019).
Zangen, A. et al. Repetitive transcranial magnetic stimulation for smoking cessation: a pivotal multicenter double-blind randomized controlled trial. World Psychiatry 20 , 397–404 (2021). This study validated the utility of deep insula/prefrontal cortex rTMS for smoking cessation .
Le Foll, B., Forget, B., Aubin, H. J. & Goldberg, S. R. Blocking cannabinoid CB1 receptors for the treatment of nicotine dependence: insights from pre-clinical and clinical studies. Addict. Biol. 13 , 239–252 (2008).
Kodas, E., Cohen, C., Louis, C. & Griebel, G. Cortico-limbic circuitry for conditioned nicotine-seeking behavior in rats involves endocannabinoid signaling. Psychopharmacology 194 , 161–171 (2007).
Forget, B. et al. Noradrenergic α1 receptors as a novel target for the treatment of nicotine addiction. Neuropsychopharmacology 35 , 1751–1760 (2010).
Garrett, B. E., Dube, S. R., Babb, S. & McAfee, T. Addressing the social determinants of health to reduce tobacco-related disparities. Nicotine Tob. Res. 17 , 892–897 (2015).
Polanska, K., Znyk, M. & Kaleta, D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health 22 , 72 (2022).
Volkow, N. D. Personalizing the treatment of substance use disorders. Am. J. Psychiatry 177 , 113–116 (2020).
Li, M. D., Cheng, R., Ma, J. Z. & Swan, G. E. A meta-analysis of estimated genetic and environmental effects on smoking behavior in male and female adult twins. Addiction 98 , 23–31 (2003).
Carmelli, D., Swan, G. E., Robinette, D. & Fabsitz, R. Genetic influence on smoking–a study of male twins. N. Engl. J. Med. 327 , 829–833 (1992).
Broms, U., Silventoinen, K., Madden, P. A. F., Heath, A. C. & Kaprio, J. Genetic architecture of smoking behavior: a study of Finnish adult twins. Twin Res. Hum. Genet. 9 , 64–72 (2006).
Kendler, K. S., Thornton, L. M. & Pedersen, N. L. Tobacco consumption in Swedish twins reared apart and reared together. Arch. Gen. Psychiat 57 , 886–892 (2000).
Saccone, N. L. et al. The CHRNA5-CHRNA3-CHRNB4 nicotinic receptor subunit gene cluster affects risk for nicotine dependence in African-Americans and in European-Americans. Cancer Res. 69 , 6848–6856 (2009).
Bierut, L. J. et al. Variants in nicotinic receptors and risk for nicotine dependence. Am. J. Psychiatry 165 , 1163–1171 (2008). This study demonstrates that nAChR gene variants are important in nicotine addiction .
Bierut, L. J. et al. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum. Mol. Genet. 16 , 24–35 (2007).
Berrettini, W. et al. α-5/α-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol. Psychiatry 13 , 368–373 (2008).
Sherva, R. et al. Association of a single nucleotide polymorphism in neuronal acetylcholine receptor subunit alpha 5 (CHRNA5) with smoking status and with ‘pleasurable buzz’ during early experimentation with smoking. Addiction 103 , 1544–1552 (2008).
Thorgeirsson, T. E. et al. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat. Genet. 42 , 448–453 (2010).
Ray, R., Tyndale, R. F. & Lerman, C. Nicotine dependence pharmacogenetics: role of genetic variation in nicotine-metabolizing enzymes. J. Neurogenet. 23 , 252–261 (2009).
Bergen, A. W. et al. Drug metabolizing enzyme and transporter gene variation, nicotine metabolism, prospective abstinence, and cigarette consumption. PLoS ONE 10 , e0126113 (2015).
Mwenifumbo, J. C. et al. Identification of novel CYP2A6*1B variants: the CYP2A6*1B allele is associated with faster in vivo nicotine metabolism. Clin. Pharmacol. Ther. 83 , 115–121 (2008).
Raunio, H. & Rahnasto-Rilla, M. CYP2A6: genetics, structure, regulation, and function. Drug Metab. Drug Interact. 27 , 73–88 (2012).
CAS Google Scholar
Patterson, F. et al. Toward personalized therapy for smoking cessation: a randomized placebo-controlled trial of bupropion. Clin. Pharmacol. Ther. 84 , 320–325 (2008).
Rodriguez, S. et al. Combined analysis of CHRNA5, CHRNA3 and CYP2A6 in relation to adolescent smoking behaviour. J. Psychopharmacol. 25 , 915–923 (2011).
Strasser, A. A., Malaiyandi, V., Hoffmann, E., Tyndale, R. F. & Lerman, C. An association of CYP2A6 genotype and smoking topography. Nicotine Tob. Res. 9 , 511–518 (2007).
Liakoni, E. et al. Effects of nicotine metabolic rate on withdrawal symptoms and response to cigarette smoking after abstinence. Clin. Pharmacol. Ther. 105 , 641–651 (2019).
Di Ciano, P. et al. Influence of nicotine metabolism ratio on [11C]-(+)-PHNO PET binding in tobacco smokers. Int. J. Neuropsychopharmacol. 21 , 503–512 (2018).
Butler, K. et al. Impact of Cyp2a6 activity on nicotine reinforcement and cue-reactivity in daily smokers. Nicotine Tob. Res. https://doi.org/10.1093/ntr/ntab064 (2021).
Benowitz, N. L., Swan, G. E., Jacob, P. 3rd, Lessov-Schlaggar, C. N. & Tyndale, R. F. CYP2A6 genotype and the metabolism and disposition kinetics of nicotine. Clin. Pharmacol. Ther. 80 , 457–467 (2006).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51 , 237–244 (2019).
McKay, J. D. et al. Large-scale association analysis identifies new lung cancer susceptibility loci and heterogeneity in genetic susceptibility across histological subtypes. Nat. Genet. 49 , 1126–1132 (2017).
Chukwueke, C. C. et al. The CB1R rs2023239 receptor gene variant significantly affects the reinforcing effects of nicotine, but not cue reactivity, in human smokers. Brain Behav. 11 , e01982 (2021).
Ahrens, S. et al. Modulation of nicotine effects on selective attention by DRD2 and CHRNA4 gene polymorphisms. Psychopharmacology 232 , 2323–2331 (2015).
Harrell, P. T. et al. Dopaminergic genetic variation moderates the effect of nicotine on cigarette reward. Psychopharmacology 233 , 351–360 (2016).
Lerman, C. et al. Role of functional genetic variation in the dopamine D2 receptor (DRD2) in response to bupropion and nicotine replacement therapy for tobacco dependence: results of two randomized clinical trials. Neuropsychopharmacology 31 , 231–242 (2006).
Le Foll, B., Gallo, A., Le Strat, Y., Lu, L. & Gorwood, P. Genetics of dopamine receptors and drug addiction: a comprehensive review. Behav. Pharmacol. 20 , 1–17 (2009).
Chukwueke, C. C. et al. Exploring the role of the Ser9Gly (rs6280) dopamine D3 receptor polymorphism in nicotine reinforcement and cue-elicited craving. Sci. Rep. 10 , 4085 (2020).
The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. Public Health Service report. Am. J. Prev. Med. 35 , 158–176 (2008).
Hackshaw, A., Morris, J. K., Boniface, S., Tang, J. L. & Milenković, D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 360 , j5855 (2018).
Qin, W. et al. Light cigarette smoking increases risk of all-cause and cause-specific mortality: findings from the NHIS cohort study. Int. J. Env. Res. Public Health https://doi.org/10.3390/ijerph17145122 (2020).
Rodu, B. & Plurphanswat, N. Mortality among male smokers and smokeless tobacco users in the USA. Harm Reduct. J. 16 , 50 (2019).
Kasza, K. A. et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 376 , 342–353 (2017).
Richardson, A., Xiao, H. & Vallone, D. M. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob. Res. 14 , 927–932 (2012).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental disorders 5th edn (American Psychiatric Association, 2013).
World Health Organization. Tobacco fact sheet. WHO https://www.who.int/news-room/fact-sheets/detail/tobacco (2021).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C. & Fagerström, K. O. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br. J. Addict. 86 , 1119–1127 (1991).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W. & Robinson, J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 84 , 791–799 (1989).
Etter, J. F., Le Houezec, J. & Perneger, T. V. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology 28 , 359–370 (2003).
DiFranza, J. R. et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Arch. Pediatr. Adolesc. Med. 156 , 397–403 (2002).
Shiffman, S., Waters, A. & Hickcox, M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 6 , 327–348 (2004).
Smith, S. S. et al. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob. Res. 12 , 489–499 (2010).
Foulds, J. et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob. Res. 17 , 186–192 (2015).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing tobacco use among youth and young adults: a report of the Surgeon General (Centers for Disease Control and Prevention, 2012).
World Health Organization. Tobacco control to improve child health and development. Thematic brief (WHO, 2021).
Lantz, P. M. et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob. Control. 9 , 47–63 (2000).
Leão, T., Kunst, A. E. & Perelman, J. Cost-effectiveness of tobacco control policies and programmes targeting adolescents: a systematic review. Eur. J. Public Health 28 , 39–43 (2018).
Royal College of Physicians. Smoking and health 2021: a coming of age for tobacco control? (RCP, 2021).
Higashi, H. et al. Cost effectiveness of tobacco control policies in Vietnam: the case of population-level interventions. Appl. Health Econ. Health Policy 9 , 183–196 (2011).
Ranson, M. K., Jha, P., Chaloupka, F. J. & Nguyen, S. N. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tob. Res. 4 , 311–319 (2002).
International Agency for Research on Cancer. I ARC Handbooks of Cancer Prevention: Tobacco control Vol. 14 (IARC, 2011).
Frazer, K. et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2 , CD005992 (2016).
Hoffman, S. J. & Tan, C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health 15 , 744 (2015).
McNeill, A. et al. Tobacco packaging design for reducing tobacco use. Cochrane Database Syst. Rev. 4 , CD011244 (2017).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General (Department of Health and Human Services, 2020).
Lindson, N. et al. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 4 , CD013308 (2019).
Krist, A. H. et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA 325 , 265–279 (2021).
Tutka, P. & Zatonski, W. Cytisine for the treatment of nicotine addiction: from a molecule to therapeutic efficacy. Pharmacol. Rep. 58 , 777–798 (2006).
Courtney, R. J. et al. Effect of cytisine vs varenicline on smoking cessation: a randomized clinical trial. JAMA 326 , 56–64 (2021).
Walker, N. et al. Cytisine versus nicotine for smoking cessation. N. Engl. J. Med. 371 , 2353–2362 (2014). This study validated the utility of cytisine for smoking cessation .
West, R. et al. Placebo-controlled trial of cytisine for smoking cessation. N. Engl. J. Med. 365 , 1193–1200 (2011).
Hajek, P. et al. E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technol. Assess. 23 , 1–82 (2019).
Walker, N. et al. Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. Lancet Respir. Med. 8 , 54–64 (2020).
Siu, A. L., U.S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 163 , 622–634 (2015).
Black, N. et al. Behaviour change techniques associated with smoking cessation in intervention and comparator groups of randomized controlled trials: a systematic review and meta-regression. Addiction 115 , 2008–2020 (2020).
Center for Substance Abuse and Treatment. Detoxification and Substance Abuse Treatment (Center for Substance Abuse and Treatment, 2006).
Cahill, K., Hartmann-Boyce, J. & Perera, R. Incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub5 (2015).
Secades-Villa, R., Aonso-Diego, G., García-Pérez, Á. & González-Roz, A. Effectiveness of contingency management for smoking cessation in substance users: a systematic review and meta-analysis. J. Consult. Clin. Psychol. 88 , 951–964 (2020).
Cahill, K. & Perera, R. Competitions and incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub4 (2011).
Trojak, B. et al. Transcranial magnetic stimulation combined with nicotine replacement therapy for smoking cessation: a randomized controlled trial. Brain Stimul. 8 , 1168–1174 (2015).
Wing, V. C. et al. Brain stimulation methods to treat tobacco addiction. Brain Stimul. 6 , 221–230 (2013).
Dinur-Klein, L. et al. Smoking cessation induced by deep repetitive transcranial magnetic stimulation of the prefrontal and insular cortices: a prospective, randomized controlled trial. Biol. Psychiatry 76 , 742–749 (2014).
Goldenberg, M., Danovitch, I. & IsHak, W. W. Quality of life and smoking. Am. J. Addict. 23 , 540–562 (2014).
Heikkinen, H., Jallinoja, P., Saarni, S. I. & Patja, K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicotine Tob. Res. 10 , 1199–1207 (2008).
Moayeri, F., Hsueh, Y. A., Dunt, D. & Clarke, P. Smoking cessation and quality of life: insights from analysis of longitudinal Australian data, an application for economic evaluations. Value Health 24 , 724–732 (2021).
Taylor, G. M. et al. Smoking cessation for improving mental health. Cochrane Database Syst. Rev. 3 , CD013522 (2021).
López-Nicolás, Á., Trapero-Bertran, M. & Muñoz, C. Smoking, health-related quality of life and economic evaluation. Eur. J. Health Econ. 19 , 747–756 (2018).
Morris, A. Linking nicotine addiction and T2DM. Nat. Rev. Endocrinol. 16 , 6 (2020).
Willi, C., Bodenmann, P., Ghali, W. A., Faris, P. D. & Cornuz, J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama 298 , 2654–2664 (2007).
World Health Organization. WHO report on the global tobacco epidemic (WHO, 2019).
Donny, E. C. et al. Randomized trial of reduced-nicotine standards for cigarettes. N. Engl. J. Med. 373 , 1340–1349 (2015). This study tested the impact of reducing the quantity of nicotine present in cigarettes on smoking .
Benowitz, N. L. & Henningfield, J. E. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N. Engl. J. Med. 331 , 123–125 (1994).
Benowitz, N. L. & Henningfield, J. E. Reducing the nicotine content to make cigarettes less addictive. Tob. Control. 22 , i14–i17 (2013).
Gottlieb, S. & Zeller, M. A nicotine-focused framework for public health. N. Engl. J. Med. 377 , 1111–1114 (2017).
Hall, W. & West, R. Thinking about the unthinkable: a de facto prohibition on smoked tobacco products. Addiction 103 , 873–874 (2008).
Ioannidis, J. P. A. & Jha, P. Does the COVID-19 pandemic provide an opportunity to eliminate the tobacco industry? Lancet Glob. Health 9 , e12–e13 (2021).
Smokefree. Smokefree 2025. Smokefree https://www.smokefree.org.nz/smokefree-in-action/smokefree-aotearoa-2025 (2021).
Morgan, C. J., Das, R. K., Joye, A., Curran, H. V. & Kamboj, S. K. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict. Behav. 38 , 2433–2436 (2013).
Elsaid, S., Kloiber, S. & Le Foll, B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog. Mol. Biol. Transl. Sci. 167 , 25–75 (2019).
Butler, K. & Le Foll, B. Novel therapeutic and drug development strategies for tobacco use disorder: endocannabinoid modulation. Expert Opin. Drug Discov. 15 , 1065–1080 (2020).
D’Souza, D. C. et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2a single-site randomised controlled trial. Lancet Psychiatry 6 , 35–45 (2019).
Robinson, J. D. et al. Pooled analysis of three randomized, double-blind, placebo controlled trials with rimonabant for smoking cessation. Addict. Biol. 23 , 291–303 (2018).
Gueye, A. B. et al. The CB1 neutral antagonist AM4113 retains the therapeutic efficacy of the inverse agonist rimonabant for nicotine dependence and weight loss with better psychiatric tolerability. Int. J. Neuropsychopharmacol. https://doi.org/10.1093/ijnp/pyw068 (2016).
Yammine, L. et al. Exenatide adjunct to nicotine patch facilitates smoking cessation and may reduce post-cessation weight gain: a pilot randomized controlled trial. Nicotine Tob. Res. 23 , 1682–1690 (2021).
Eren-Yazicioglu, C. Y., Yigit, A., Dogruoz, R. E. & Yapici-Eser, H. Can GLP-1 be a target for reward system related disorders? A qualitative synthesis and systematic review analysis of studies on palatable food, drugs of abuse, and alcohol. Front. Behav. Neurosci. 14 , 614884 (2020).
Vanderkam, P. et al. Effectiveness of drugs acting on adrenergic receptors in the treatment for tobacco or alcohol use disorders: systematic review and meta-analysis. Addiction 116 , 1011–1020 (2021).
Sokoloff, P. & Le Foll, B. The dopamine D3 receptor, a quarter century later. Eur. J. Neurosci. 45 , 2–19 (2017).
David, S. P., Lancaster, T., Stead, L. F., Evins, A. E. & Prochaska, J. J. Opioid antagonists for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003086.pub3 (2013).
Ray, L. A. et al. Efficacy of combining varenicline and naltrexone for smoking cessation and drinking reduction: a randomized clinical trial. Am. J. Psychiatry 178 , 818–828 (2021).
Mooney, M. E. et al. Bupropion and naltrexone for smoking cessation: a double-blind randomized placebo-controlled clinical trial. Clin. Pharmacol. Ther. 100 , 344–352 (2016).
Justinova, Z., Le Foll, B., Redhi, G. H., Markou, A. & Goldberg, S. R. Differential effects of the metabotropic glutamate 2/3 receptor agonist LY379268 on nicotine versus cocaine self-administration and relapse in squirrel monkeys. Psychopharmacology 233 , 1791–1800 (2016).
Le Foll, B., Wertheim, C. E. & Goldberg, S. R. Effects of baclofen on conditioned rewarding and discriminative stimulus effects of nicotine in rats. Neurosci. Lett. 443 , 236–240 (2008).
Franklin, T. R. et al. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol. Depend. 103 , 30–36 (2009).
Lotfy, N., Elsawah, H. & Hassan, M. Topiramate for smoking cessation: systematic review and meta-analysis. Tob. Prev. Cessat. 6 , 14 (2020).
Shanahan, W. R., Rose, J. E., Glicklich, A., Stubbe, S. & Sanchez-Kam, M. Lorcaserin for smoking cessation and associated weight gain: a randomized 12-week clinical trial. Nicotine Tob. Res. 19 , 944–951 (2017).
Higgins, G. A., Fletcher, P. J. & Shanahan, W. R. Lorcaserin: a review of its preclinical and clinical pharmacology and therapeutic potential. Pharmacol. Ther. 205 , 107417 (2020).
Stead, L. F. & Lancaster, T. Interventions to reduce harm from continued tobacco use. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD005231.pub2 (2007).
Download references
Acknowledgements
B.Le F. is supported by a clinician-scientist award from the Department of Family and Community Medicine at the University of Toronto and the Addiction Psychiatry Chair from the University of Toronto. The funding bodies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The authors thank H. Fu (University of Toronto) for assistance with Figs 1–3.
Author information
Authors and affiliations.
Translational Addiction Research Laboratory, Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada
Bernard Le Foll
Departments of Family and Community Medicine, Psychiatry, Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada
Department of Medicine, University of Wisconsin, Madison, WI, USA
Megan E. Piper
University of Wisconsin Center for Tobacco Research and Intervention, Madison, WI, USA
Department of Neurobiology and Behaviour, University of California Irvine, Irvine, CA, USA
Christie D. Fowler
Section for Preventive Cardiology, Department of Endocrinology, Morbid Obesity and Preventive Medicine, Oslo University Hospital, Oslo, Norway
Serena Tonstad
Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, USA
Laura Bierut
Institute of Mental Health, Peking University Sixth Hospital, Peking University, Beijing, China
National Institute on Drug Dependence, Peking University Health Science Center, Beijing, China
Centre for Global Health Research, Unity Health Toronto, University of Toronto, Toronto, Ontario, Canada
- Prabhat Jha
National Centre for Youth Substance Use Research, The University of Queensland, St Lucia, Queensland, Australia
Wayne D. Hall
Queensland Alliance for Environmental Health Sciences, The University of Queensland, Woolloongabba, Queensland, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (B.Le F.); Epidemiology (P.J. and W.D.H.); Mechanisms/pathophysiology (C.D.F., L.B., L.L. and B.Le F.); Diagnosis, screening and prevention (P.J., M.E.P., S.T. and B.Le F.); Management (M.E.P., S.T., W.D.H., L.L. and B.Le F.); Quality of life (P.J. and W.D.H.); Outlook (all); Conclusions (all). All authors contributed substantially to the review and editing of the manuscript.
Corresponding author
Correspondence to Bernard Le Foll .
Ethics declarations
Competing interests.
B.Le F. has obtained funding from Pfizer (GRAND Awards, including salary support) for investigator-initiated projects. B.Le F. has received some in-kind donations of cannabis product from Aurora and medication donation from Pfizer and Bioprojet and was provided a coil for TMS study from Brainsway. B.Le F. has obtained industry funding from Canopy (through research grants handled by CAMH or the University of Toronto), Bioprojet, ACS, Indivior and Alkermes. B.Le F. has received in-kind donations of nabiximols from GW Pharma for past studies funded by CIHR and NIH. B.Le F. has been an advisor to Shinoghi. S.T. has received honoraria from Pfizer the manufacturer of varenicline for lectures and advice. All other authors declare no competing interests.
Peer review
Peer reviewer information.
Nature Reviews Disease Primers thanks Jamie Brown, Elisardo Iglesias and Ming Li for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
CTRI website: https://d3futrf33lk36a.cloudfront.net/wp-content/uploads/sites/240/2019/04/Meds-Chart.pdf
Philip Morris International: https://www.pmi.com/
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Le Foll, B., Piper, M.E., Fowler, C.D. et al. Tobacco and nicotine use. Nat Rev Dis Primers 8 , 19 (2022). https://doi.org/10.1038/s41572-022-00346-w
Download citation
Accepted : 07 February 2022
Published : 24 March 2022
DOI : https://doi.org/10.1038/s41572-022-00346-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrated mrna- and mirna-sequencing analyses unveil the underlying mechanism of tobacco pollutant-induced developmental toxicity in zebrafish embryos.
- Jiasheng Chen
- Xiaoping Zhong
Journal of Translational Medicine (2024)
Influence of substance use on male reproductive health and offspring outcomes
- Jamie O. Lo
- Jason C. Hedges
- Charles A. Easley
Nature Reviews Urology (2024)
Reductions in smoking due to ratification of the Framework Convention for Tobacco Control in 171 countries
- Guillermo Paraje
- Mauricio Flores Muñoz
Nature Medicine (2024)
Impact of benzoic acid and 2,2’-methylenebis (6-tert-butyl-4-methylphenol) on the metabolome of flue-cured tobacco and rhizosphere microbial communities: implications for continuous cropping obstacles
- Qiulian Peng
- Jiayan Zhang
Plant and Soil (2024)
Nicotinic regulation of microglia: potential contributions to addiction
- Alexa R. Soares
- Marina R. Picciotto
Journal of Neural Transmission (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
VIDEO
COMMENTS
500 Words Essay On Smoking. One of the most common problems we are facing in today's world which is killing people is smoking. A lot of people pick up this habit because of stress, personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them.
Introduction. Tobacco use, including smoking, has become a universally recognized issue that endangers the health of the population of our entire planet through both active and second-hand smoking. Pro-tobacco arguments are next to non-existent, while its harm is well-documented and proven through past and contemporary studies (Jha et al., 2013).
500 Words Essay on Stop Smoking ... The production of tobacco also contributes to deforestation and loss of biodiversity. The Social Aspect of Smoking. Smoking can also strain relationships. The smell of smoke can be off-putting to non-smokers, and the health risks associated with secondhand smoke can cause tension. Additionally, the time spent ...
Within 20 minutes, your heart rate and blood pressure drop. 12 hours, the carbon monoxide level in your blood drops to normal. 2-12 weeks, your circulation improves and your lung function increases. 1-9 months, coughing and shortness of breath decrease. 1 year, your risk of coronary heart disease is about half that of a smoker's.
No Smoking means not using cigarettes, pipes, or any other tool that burns tobacco and lets people inhale its smoke. This idea is important for keeping our bodies healthy and protecting the air everyone breathes. The smoke from cigarettes is not only bad for the person smoking but also for those around them, known as secondhand smoke.
Argumentative Essay on Smoking Cigarettes. The dangers of smoking cigarettes have been well-documented, yet millions of people continue to engage in this harmful habit. The debate over the impact of smoking on public health is ongoing, with some arguing for stricter regulations and others advocating for personal freedom.
Here we've gathered a range of catchy titles for research papers about smoking together with smoking essay examples. Get inspired with us! We will write a custom essay specifically for you by our professional experts. 186 writers online. Learn More. Smoking is a well-known source of harm yet popular regardless, and so smoking essays should ...
Quitting smoking is therefore an important way of regaining self confidence by doing away with the embarrassing smell of cigarette smoke. Quitting smoking is an important way of shedding off the worry of the constant coughs and short breath brought about by smoking (Quit Smoking Review para 2-3). Quitting smoking comes with a myriad of benefits ...
Persuasive Essay: Similar to an argumentative essay, this type of essay aims to persuade the reader to quit smoking. It presents facts, statistics, and other relevant information to convince the reader to stop smoking. ... Tobacco is a nicotine, cellulose, ammonia, and protein-containing plant whose leaves are dried and fermented to make it ...
Smoking is the leading cause of premature, preventable death in this country. Cigarette smoking and exposure to tobacco smoke cause about 480,000 premature deaths each year in the United States ().Of those premature deaths, about 36% are from cancer, 39% are from heart disease and stroke, and 24% are from lung disease (). Mortality rates among smokers are about three times higher than among ...
Stopping smoking reduces the future risk of tobacco-related diseases, slows the progression of existing tobacco-related disease, and improves life expectancy by an average of 10 years [5]. Quitting can bring immediate health benefits at any age, regardless of how long one has smoked. It is never too late to quit.
The saying goes that "quitters never win," but in the case of tobacco, quitters are the real winners. When the news came out that smokers were more likely to develop severe disease with COVID-19 compared to non-smokers, it triggered millions of smokers to want to quit tobacco. But without adequate support, quitting can be incredibly ...
Quitting can improve self-confidence and lead to a better lifestyle. Not using tobacco products helps keep your family safe. Your may have more energy, helping you have more quality family and leisure time. Quitting can set a good example for others who might need help quitting. Others will be proud of your progress and willpower to quit and ...
Prevention can also take place at the school or community level. Merely educating potential smokers about the health risks has not proven effective. 218 Successful evidence-based interventions aim to reduce or delay initiation of smoking, alcohol use, and illicit drug use, and otherwise improve outcomes for children and teens by reducing or ...
1-855-DÉJELO-YA (Spanish) 1-800-838-8917 (Cantonese and Mandarin) 1-800-556-5564 (Korean) 1-800-778-8440 (Vietnamese) They can also visit CDC.gov/Quit or Smokefree.gov to sign up for texting programs and download mobile apps. Using any kind of tobacco product is unsafe, especially for kids, teens, and young adults.
Introduction. Tobacco use is a global epidemic among young people. As with adults, it poses a serious health threat to youth and young adults in the United States and has significant implications for this nation's public and economic health in the future (Perry et al. 1994; Kessler 1995).The impact of cigarette smoking and other tobacco use on chronic disease, which accounts for 75% of ...
The act of smoking involves burning substances, such as tobacco or cannabis, and inhaling the resulting smoke into [...] The Dangers of Vaping: An In-Depth Analysis Essay Vaping, once hailed as a safer alternative to traditional smoking, has now come under scrutiny due to its potential health risks and widespread usage among young people.
Decades after its ill effects on human health were first documented, tobacco smoking remains one of the major global drivers of premature death and disability. In 2017, smoking was responsible for ...
Persuasive Essay On Stop Smoking. Smoking is a huge problem in today's society. Many people don't understand the consequences that come with smoking. Cigarettes and marijuana are very common uses of smoking. As a college student I am able to the effects these two drugs have on students mental and physical abilities.
Importance Tobacco use is the leading preventable cause of disease, disability, and death in the US. In 2014, it was estimated that 480 000 deaths annually are attributed to cigarette smoking, including second hand smoke exposure. Smoking during pregnancy can increase the risk of numerous adverse pregnancy outcomes (eg, miscarriage and congenital anomalies) and complications in the offspring ...
4. Chew on it. Give your mouth something to do to resist a tobacco craving. Chew on sugarless gum or hard candy. Or munch on raw carrots, nuts or sunflower seeds — something crunchy and tasty. 5. Don't have 'just one'. You might be tempted to have just one cigarette to satisfy a tobacco craving.
Tobacco is the second most commonly used psychoactive substance worldwide, with more than one billion smokers globally 1.Although smoking prevalence has reduced in many high-income countries (HICs ...
Friday's papers cover a mix of stories, including Zelensky's urge for Western support and Sven-Goran Eriksson's funeral.