

PLOS Mental Health, a new Open Access journal for research that leads to healthier lives by improving discussion, interdisciplinary collaboration and understanding of all aspects of mental health in individual, societal, and community contexts.
Get new content from plos mental health in your inbox, thank you you have successfully subscribed to the plos mental health newsletter., sorry, an error occurred while sending your subscription. please try again later..

Meet our Editors-in-Chief

Apply to join the PLOS Mental Health Editorial Board
Sign up for information and updates from plos mental health, be among the first to know when plos mental health opens for submissions, receive editorial board updates and more by joining our email list., publish with plos.
- Submission Instructions
- Submit Your Manuscript
Connect with Us
- PLOS Mental Health on Twitter
- PLOS on Facebook

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years
Research. discovery. hope..
Explore our Events and Stories
Health Topics
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder
- Autism Spectrum Disorder
- Bipolar Disorder
- Borderline Personality Disorder
- Eating Disorders
- Obsessive-Compulsive Disorder
- Post-Traumatic Stress Disorder
- Schizophrenia
- Suicide Prevention
- More Topics
Featured Topics

Director’s Message: The Importance of Lived Experience Perspectives – Insights From the IACC

FY 2024 Budget Fact Sheet

Autism Acceptance Month
Science updates.

Gene-Based Therapy for Timothy Syndrome

Accelerating Science to Improve Early Autism Screening

Novel Treatment Helps Children With Severe Irritability
Meetings and events, facebook live: brain stimulation therapies, workshop: neurofeedback intervention development, nimh research and science track at 2024 apa annual meeting.

Director of NIMH
Joshua A. Gordon, M.D., Ph.D.

NIMH Strategic Plan
Read about our plan for the institute's research priorities.
Inside NIMH
Funding News for Current and Future NIMH Awardees.

Find NIMH funding opportunities and announcements, including those specific to clinical research and training, and learn more about NIMH funding strategies, the application process, and grants management.

Finding Treatment
If you or someone you know has a mental illness, there are ways to get help. Use these resources to find help for yourself, a friend, or a family member.

Join A Study
Learn more about how to participate in outpatient and inpatient studies at the NIH Clinical Center, a hospital dedicated to the highest quality research.
Featured Resources

Brochures and Fact Sheets
Explore NIMH brochures and fact sheets. En español .
Learn more about our research areas, policies, resources, and initiatives.

Investigators
Learn more about scientists, physicians, and clinicians in NIMH’s Division of Intramural Research Programs (IRP).
Learn more about Research Domain Criteria Initiative (RDoC), a research framework that supports new ways of studying mental disorders.

Social Media
Connect with Us on Twitter, Facebook, YouTube, and LinkedIn.

Support for Clinical Trials
Learn more about clinical trials and funding opportunity announcements.
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Research and Practice
- Mental Health Diversity, Equity, and Inclusion
- Origins of Mental Health
- Job Openings
- Faculty Profiles
- PET Alumni Profiles - Postdocs
- PET Alumni Profiles - Predocs
- Trainee Profiles
- NIMH T32 Mental Health Services and Systems Training Grant
- Funded Training Program in Data Integration for Causal Inference in Behavioral Health
- Aging and Dementia Funded Training Program
- COVID-19 and Mental Health Research
- Mental Health Resources During COVID-19
- News and Media
Social Determinants of Mental and Behavioral Health
- Our Work in Action
- Global Mental Health
- Related Faculty
- Courses of Interest
- Training and Funding Opportunities
- Mental Health in the Workplace: A Public Health Summit
Autism and Developmental Disabilities
- Alumni Newsletters
- Alumni Updates
- Postdoctoral Fellows
- Doctor of Philosophy (PhD) Students in Mental Health
- Master of Health Science (MHS) Students in Mental Health
- In the News
- Past Seminars 2020-21 AY: Wednesday Seminar Series
- Make a Gift
- Available Datasets
Research Areas
The Department of Mental Health covers a wide array of topics related to mental health, mental illness, and substance abuse. We emphasize ongoing research that enriches and stimulates the teaching programs. All students and fellows are encouraged to participate in at least one research group. Faculty and students from multiple disciplines work together within and across several major research areas:
Faculty are working to understand the distribution, causes and consequences of autism and developmental disabilities as well as the impact of public health policy on children and families.
Global Mental Health faculty develop, implement and evaluate measures and interventions to assess and meet mental health needs of communities around the world, with a focus on developing nations.
Mental Health and Aging
Faculty in the Mental Health and Aging Research Area conduct observational and intervention research aimed at enhancing cognitive and mental well being in older adults.
Mental Health and COVID-19
Understanding how mental health evolves as a result of this serious global pandemic will inform prevention and treatment strategies moving forward.
Mental Health in the Workplace
At the Bloomberg School of Public Health, which houses the only department of mental health in a school of public health, we have a unique ability to define both the problems and potential solutions.
Mental Health Services and Policy
Faculty in this area study mental health and behavioral health services and supports in communities, educational institutions and employment settings. They aim to reduce risk, and provide effective long-term treatment.
The Methods program area develops and applies innovative qualitative and quantitative methods for public mental health research, with a focus on statistical methods and economic models.
Prevention Research
The Prevention Research faculty develop, test, refine and bring to scale prevention programs directed at a range of mental health and behavioral problems in children, adolescents, adults and the elderly.
Psychiatric and Behavioral Genetic Epidemiology
Faculty in this area research genetic factors and how they interact with the physical and social environment to affect the risk for mental disorders.
Psychiatric Epidemiology
Faculty in this area study the occurrence and distribution of mental and behavioral disorders across people, space and time, and examine the causes to develop support and treatment strategies.
School-based Mental Health
The Department of Mental Health views the education and schools as a key public health context. Multiple faculty members partner with local school systems to develop, refine, and test preventive interventions for school-aged children and aim to promote mental health as well as positive social, emotional, and behavioral development.
Social Determinants of Mental & Behavioral Health Area emphasizes the role of multilevel social and structural factors in shaping mental and behavioral health, such as stigma, social networks, structural racism and policies on housing, drug control, and criminal justice domestically and internationally.
Substance Use Epidemiology
Faculty in this area study the etiology and natural history of substance use, and develop and evaluate interventions to prevent and control substance use disorders.
The Department of Mental Health has projects focused on various aspects of violence such as suicide, intimate partner violence , and youth violence. Faculty and students from multiple disciplines work together within and across several major research areas.
Centers and Institutes
The department houses several school-based centers, and has a significant role in many others across the school. These are described below. Centers help bring together faculty, students, and community partners across multiple departments and schools to meet their particular missions in pursuit of improving public mental health.
- Moore Center for the Prevention of Child Sexual Abuse
- Wendy Klag Center for Autism and Developmental Disabilities
- Center on Aging and Health
- Center for Mental Health and Addiction Policy Research
- Suicide Prevention
Our Students and Faculty Work in Action
The Johns Hopkins COVID-19 Mental Health Measurement Working Group developed key questions to add to existing large domestic and international surveys to measure the mental health impact of the pandemic.

Mental Health Research News
Top headlines, latest headlines.
- Low Intensity Exercise: Less Depression
- Detecting Stress Levels During Sleep
- Heart Disease, Depression Linked by Inflammation
- A Welcome Hug Is Good for Your Health
- Feeding the Lonely Brain
- Prairie Voles Display Human-Like Depression
- How the Brain Regulates Emotions
- Detecting and Evaluating ADHD
- Ketogenic Diet for Severe Mental Illness
- Younger Women: Mental Health, Heart Health
Earlier Headlines
Thursday, april 11, 2024.
- Study Finds Increased Anxiety and PTSD Among People Who Remained in Ukraine
Thursday, March 28, 2024
- Positive Associations Between Premenstrual Disorders and Perinatal Depression
Wednesday, March 27, 2024
- People With Depression See No Immediate Change from Common GP Assessment, Study Shows
Tuesday, March 26, 2024
- Large-Scale Animal Study Links Brain pH Changes to Wide-Ranging Cognitive Issues
Wednesday, March 20, 2024
- Treating Anxiety, Depression in People With Heart Disease Reduced ER Visits, Hospitalizations
Monday, March 18, 2024
- Study Eases Concern at Antipsychotics Use in Pregnancy
Thursday, March 14, 2024
- How Fear Unfolds Inside Our Brains
Wednesday, March 13, 2024
- Researchers Identify Brain Connections Associated With ADHD in Youth
Monday, March 11, 2024
- 'Study Drugs' Set the Stage for Other Drug Use and Mental Health Decline
Wednesday, March 6, 2024
- New Study May Broaden the Picture of the Consequences of Childhood Adversity
Monday, March 4, 2024
- It's Not Just You: Young People Look, Feel Older When They're Stressed
Friday, March 1, 2024
- Link Between Adversity, Psychiatric and Cognitive Decline
- Study Paves the Way for Better Diagnosis and Treatment of Endocrine Diseases
Tuesday, February 27, 2024
- Teens Benefit from 'forest Bathing' -- Even in Cities
Monday, February 26, 2024
- Gut-Brain Communication Turned on Its Axis
- Intervention Reduces Likelihood of Developing Postpartum Anxiety and Depression by More Than 70%
- Yoga Provides Unique Cognitive Benefits to Older Women at Risk of Alzheimer's Disease
Wednesday, February 21, 2024
- Maternal Mental Conditions Drive Climbing Death Rate in U.S., Evidence Review Finds
Tuesday, February 20, 2024
- Wildfires Linked to Surge in Mental Health-Related Emergency Department Visits
- Stress During Pregnancy Can Lead to Early Maturation of First-Born Daughters
Monday, February 19, 2024
- Understanding the Relationship Between Our Sleep, Body Clock and Mental Health
Thursday, February 15, 2024
- Burnout: Identifying People at Risk
Tuesday, February 13, 2024
- A Closer Look at Cannabis Use and Binge Eating
Thursday, February 8, 2024
- Benefits of Resistance Exercise Training in Treatment of Anxiety and Depression
- Ketamine's Promise for Severe Depression Grows, but Major Questions Remain
Wednesday, February 7, 2024
- Researchers Make Progress Toward Developing Blood Tests for Psychiatric and Neurological Disorders
- Stress Influences Brain and Psyche Via Immune System
Tuesday, February 6, 2024
- Bullied Teens' Brains Show Chemical Change Associated With Psychosis
Monday, February 5, 2024
- Are Body Temperature and Depression Linked? Science Says, Yes
Thursday, February 1, 2024
- Psychological Care Delivered Over the Phone Is an Effective Way to Combat Loneliness and Depression, According to a Major New Study
Wednesday, January 31, 2024
- Potential Link Between High Maternal Cortisol, Unpredicted Birth Complications
Tuesday, January 30, 2024
- Researchers Find Early Symptoms of Psychosis Spectrum Disorder in Youth Higher Than Expected
Wednesday, January 24, 2024
- Mood Interventions May Reduce Inflammation in Crohn's and Colitis
Thursday, January 18, 2024
- Relationships With Caring Adults Provide a Buffer Against Depression, Anxiety, Regardless of Adverse Childhood Experiences
Wednesday, January 17, 2024
- Therapy Versus Medication: Comparing Treatments for Depression in Heart Disease
Friday, January 12, 2024
- Psychotherapy Effective in Treating Post-Traumatic Stress Disorder Following Multiple Traumatic Events, Meta-Study Finds
- Stress, Via Inflammation, Is Linked to Metabolic Syndrome
Wednesday, January 10, 2024
- Feeling Depressed Linked to Short-Term Increase in Bodyweight
- Newly Identified Genes for Depression May Lead to New Treatments
- Reduced Drug Use Is a Meaningful Treatment Outcome for People With Stimulant Use Disorders, Study Shows
Monday, January 8, 2024
- Clear Link Between Autoimmune Disease and Perinatal Depression
Thursday, January 4, 2024
- Bipolar Disorder Linked to Early Death
Thursday, December 21, 2023
- Psychologist Publishes Most Thorough Compilation of Sleep and Emotion Research to Date
- Connection Between Light Levels and Mental Health -- Climate Change Could Also Have an Impact in the Future
Thursday, December 14, 2023
- Genetic 'protection' Against Depression Was No Match for Pandemic Stress
Wednesday, December 13, 2023
- Unravelling the Association Between Neonatal Proteins and Adult Health
- Body Dissatisfaction Linked With Depression Risk in Children
Tuesday, December 12, 2023
- Caregiving Can Be Stressful, but It Could Also Lower Risk of Depression
Thursday, December 7, 2023
- Discrimination During Pregnancy May Alter Circuits in Infants' Brains
Tuesday, December 5, 2023
- Depression, Constipation, and Urinary Tract Infections May Precede MS Diagnosis
Monday, December 4, 2023
- New Study Maps Ketamine's Effects on Brain
Wednesday, November 29, 2023
- AI May Aid in Diagnosing Adolescents With ADHD
- Mindfulness-Based Intervention Shows Promise for PTSD in Cardiac Arrest Survivors
Tuesday, November 28, 2023
- Understanding Subjective Beliefs Could Be Vital to Tailoring More Effective Treatments for Depression and ADHD
Monday, November 27, 2023
- Discrimination During Pregnancy Can Affect Infant's Brain Circuitry
Thursday, November 16, 2023
- A Small Molecule Blocks Aversive Memory Formation, Providing a Potential Treatment Target for Depression
- High Levels of Maternal Stress During Pregnancy Linked to Children's Behavior Problems
- New Studies of Brain Activity Explain Benefits of Electroconvulsive Therapy
Tuesday, November 14, 2023
- US Men Die 6 Years Before Women, as Life Expectancy Gap Widens
- Genetic Testing Could Greatly Benefit Patients With Depression, Save Health System Millions
- Reducing 'vivid Imagery' That Fuels Addiction Cravings
Monday, November 13, 2023
- Early-Life Stress Changes More Genes in Brain Than a Head Injury
Thursday, November 9, 2023
- Brain Imaging Identifies Biomarkers of Mental Illness
- Study Shows Link Between Mental and Physical Health
Monday, November 6, 2023
- Location of Strong Sense of Discomfort in Brain Found
Friday, November 3, 2023
- Paid Family Leave Boosted Postpartum Wellbeing, Breastfeeding Rates
Thursday, November 2, 2023
- New Clues to the Mechanism Behind Treatment-Resistant Depression

Wednesday, November 1, 2023
- Contraceptive Pill Users Less Likely to Report Depression
Monday, October 30, 2023
- The Genetic Heritage of the Denisovans May Have Left Its Mark on Our Mental Health
Thursday, October 26, 2023
- Youngest Children in Class With ADHD as Likely to Keep Diagnosis in Adulthood as Older Pupils, Find Scientists
Wednesday, October 25, 2023
- New Distractibility 'd Factor' May Be Linked With ADHD
Monday, October 23, 2023
- Researchers Use Pioneering New Method to Unlock Brain's Noradrenaline System
- Heated Yoga May Reduce Depression Symptoms, According to Recent Clinical Trial
Friday, October 20, 2023
- Pupil Response May Shed Light on Who Responds Best to Transcranial Magnetic Stimulation for Depression
- Consistent Lack of Sleep Is Related to Future Depressive Symptoms
Thursday, October 19, 2023
- Researchers Confirm Postpartum Depression Heritability, Home in on Treatment Mechanism
- Ketamine's Effect on Depression May Hinge on Hope
- Study Finds Men's Antidepressant Use Did Not Negatively Impact IVF Success
Tuesday, October 17, 2023
- Adults With ADHD Are at Increased Risk for Developing Dementia
- Study Reveals Health Impact of Eating Disorders
- Depression, Anxiety Common Among College Students
Thursday, October 5, 2023
- Psychedelics Improve Mental Health, Cognition in Special Ops Veterans
Wednesday, October 4, 2023
- Strong Link Between ADHD and Car Crashes in Older Adult Drivers
- Should Fathers Be Screened for Postpartum Depression? Pilot Study
Monday, October 2, 2023
- Study Indicates Possible Link Between Chronic Stress and Alzheimer's Disease
Friday, September 29, 2023
- Increased Risk of Depression and Anxiety When in Higher Education, Study Finds
Thursday, September 28, 2023
- Grandparent Childcare May Not Help the Wellbeing of Mums or Reduce Mother-Child Conflict, Study Suggests
Monday, September 25, 2023
- Depression, Anxiety May Be Among Early Signs of MS
Friday, September 22, 2023
- Study Shows Millions of People Live With Co-Occuring Chronic Pain and Mental Health Symptoms
Thursday, September 21, 2023
- Posttraumatic Brain Activity Predicts Resilience to PTSD
Monday, September 18, 2023
- Study Shows Nearly 300% Increase in ADHD Medication Errors
Wednesday, September 13, 2023
- Inflammatory Signs for Adolescent Depression Differ Between Boys and Girls
Tuesday, September 12, 2023
- Older Adults With Digestive Diseases Experience Higher Rates of Loneliness, Depression
- Your Body's Own Cannabinoid Molecules Calm You During Stress
Monday, September 11, 2023
- Healthy Lifestyle Can Help Prevent Depression -- And New Research May Explain Why
- Antidepressants May Reduce Negative Memories While Improving Overall Memory
Friday, September 8, 2023
- Sleep-Wake Therapy Gives New Hope for Teens With Depression
Thursday, September 7, 2023
- Antidepressant Use in People With Both Physical Health Problems and Depression
Tuesday, September 5, 2023
- Active Children Are More Resilient
Wednesday, August 30, 2023
- Stress and Insomnia Linked to Irregular Heart Rhythms After Menopause
- LATEST NEWS
- Health & Medicine
- Diseases & Conditions
- Alzheimer's Research
- Amyotrophic Lateral Sclerosis
- Attention Deficit Disorder
- Back and Neck Pain
- Birth Defects
- Bladder Disorders
- Blood Clots
- COVID and SARS
- Cervical Cancer
- Bladder Cancer
- Multiple Myeloma
- Pancreatic Cancer
- Brain Tumor
- Colon Cancer
- Breast Cancer
- Ovarian Cancer
- Lung Cancer
- Mesothelioma
- Skin Cancer
- Prostate Cancer
- Cerebral Palsy
- Chikungunya
- Chronic Fatigue Syndrome
- Cold and Flu
- Crohn's Disease
- Cystic Fibrosis
- Dengue Fever
- Down Syndrome
- Eating Disorder Research
- Encephalitis
- Epilepsy Research
- Erectile Dysfunction
- Fibromyalgia
- Gastrointestinal Problems
- HIV and AIDS
- Headache Research
- Hearing Loss
- Heart Health
- Cholesterol
- Stroke Prevention
- Heart Disease
- Hormone Disorders
- Hypertension
- Infectious Diseases
- Insomnia Research
- Irritable Bowel Syndrome
- Kidney Disease
- Liver Disease
- Lung Disease
- Lyme Disease
- Mental Health Research
- Multiple Sclerosis Research
- Mumps, Measles, Rubella
- Muscular Dystrophy
- Osteoporosis
- Parkinson's Research
- Prostate Health
- Restless Leg Syndrome
- Sickle Cell Anemia
- Sleep Disorder Research
- Thyroid Disease
- Triglycerides
- Tuberculosis
- Medical Topics
- Accident and Trauma
- Alternative Medicine
- Birth Control
- Bone and Spine
- Chronic Illness
- Controlled Substances
- Dietary Supplements and Minerals
- Epigenetics
- Food Additives
- Foodborne Illness
- Foot Health
- Gene Therapy
- Health Policy
- Human Biology
- Immune System
- Joint Health
- Medical Imaging
- Nervous System
- Pain Control
- Personalized Medicine
- Pharmacology
- Psychology Research
- Wounds and Healing
- PHYSICAL/TECH
- ENVIRONMENT
- SOCIETY & EDUCATION
- Humans and Earth's Deep Subsurface Fluid Flow
- Holographic Displays: An Immersive Future
- Harvesting Energy Where River Meets Sea
- Making Diamonds at Ambient Pressure
- Eruption of Mega-Magnetic Star
- Clean Fuel Generation With Simple Twist
- Bioluminescence in Animals 540 Million Years Ago
- Fossil Frogs Share Their Skincare Secrets
- Fussy Eater? Most Parents Play Short Order Cook
- Precise Time Measurement: Superradiant Atoms
Trending Topics
Strange & offbeat.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
In CDC survey, 37% of U.S. high school students report regular mental health struggles during COVID-19 pandemic

Many high school students have reported experiencing mental health challenges during the coronavirus outbreak, according to recently published survey findings from the Centers for Disease Control and Prevention (CDC). High school students who are gay, lesbian or bisexual, as well as girls, were especially likely to say their mental health has suffered during the pandemic.
This analysis explores U.S. high school students’ self-reported mental health challenges during the COVID-19 pandemic. It expands on Pew Research Center surveys that have explored U.S. adults’ mental health difficulties during this time. Not all of the survey questions asked specifically about mental health during the pandemic.
This analysis relies on the Center for Disease Control and Prevention’s Adolescent Behaviors and Experiences Survey (ABES), which was conducted from January to June 2021 to assess students’ health-related behaviors and experiences during the COVID-19 pandemic. ABES surveyed high school students in grades 9-12 attending U.S. public and private schools. More information about the survey and its methodology can be found on the CDC’s website.
The results from this one-time survey are not directly comparable to previous CDC surveys on these topics.
Overall, 37% of students at public and private high schools reported that their mental health was not good most or all of the time during the pandemic, according to the CDC’s Adolescent Behaviors and Experiences Survey , which was fielded from January to June 2021. In the survey, “poor mental health” includes stress, anxiety and depression. About three-in-ten high school students (31%) said they experienced poor mental health most or all of the time in the 30 days before the survey. In addition, 44% said that, in the previous 12 months, they felt sad or hopeless almost every day for at least two weeks in a row such that they stopped doing some usual activities. (Not all of the survey questions asked specifically about mental health during the pandemic.)
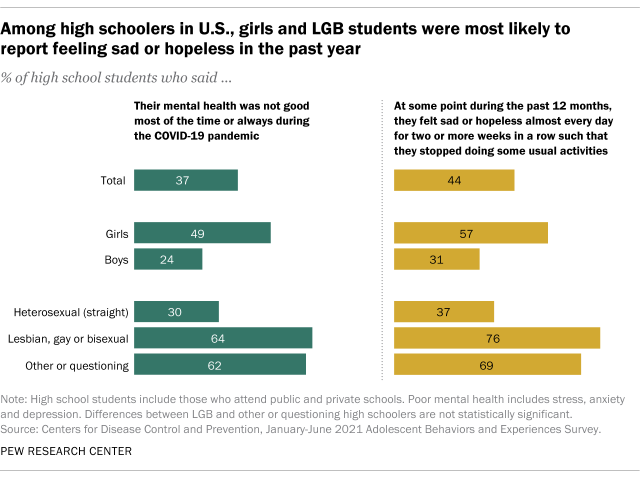
High school students who are gay, lesbian or bisexual reported higher rates of mental health stresses than their heterosexual (straight) peers. The share of LGB high schoolers who said their mental health was not good most of the time or always during the pandemic was more than double that of heterosexual students (64% vs. 30%). More than half of LGB students (55%) said they experienced poor mental health at least most of the time in the 30 days before the survey, while 26% of heterosexual teens said the same. And about three-quarters of LGB high schoolers (76%) said they felt sad or hopeless almost daily for at least two weeks such that they stopped doing some of their usual activities, compared with 37% of heterosexual students.
There were also differences by gender. About half of high school girls (49%) said their mental health was not good most of the time or always during the COVID-19 outbreak – roughly double the share of boys who said this (24%). And roughly four-in-ten girls (42%) reported feeling this way in the 30 days before the survey; 20% of boys said the same. About six-in-ten high school girls (57%) reported that at some point in the 12 months before taking the survey (in the first half of 2021) they felt sad or hopeless almost every day for at least two weeks in a row such that they stopped doing some usual activities, compared with 31% of high school boys who said this.
LGB high schoolers were also more likely than their heterosexual peers to have sought mental health care – including treatment or counseling for alcohol or drug use – via telemedicine during the COVID-19 pandemic. Around one-in-five LGB students (19%) said they received treatment this way at some point during the pandemic, compared with 6% of heterosexual students. Girls were more likely than boys to have received mental health care through telemedicine (10% vs. 7%, respectively).
Pandemic-related disruptions to schooling, socializing and family life have created a situation that the U.S. surgeon general has described as a “ youth mental health crisis ,” with high rates of teens experiencing distress. But public health experts had called attention to teen mental health even before the coronavirus outbreak. For instance, a separate CDC survey conducted in 2015 found that LGB teens were at greater risk of depression than their heterosexual peers. And a Pew Research Center analysis of pre-pandemic data from the National Survey for Drug Use and Health showed teenage girls were more likely than their male peers to report recent experiences with depression , as well as to receive treatment for it.
- Coronavirus (COVID-19)
- Generation Z
- Happiness & Life Satisfaction
- LGBTQ Attitudes & Experiences
- Teens & Youth

Katherine Schaeffer is a research analyst at Pew Research Center
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, mental health and the pandemic: what u.s. surveys have found, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Research: More People Use Mental Health Benefits When They Hear That Colleagues Use Them Too
- Laura M. Giurge,
- Lauren C. Howe,
- Zsofia Belovai,
- Guusje Lindemann,
- Sharon O’Connor

A study of 2,400 Novartis employees around the world found that simply hearing about others’ struggles can normalize accessing support at work.
Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager for the training, uptake of the program remains low. To understand why, a team of researchers conducted a randomized controlled trial with 2,400 Novartis employees who worked in the UK, Ireland, India, and Malaysia. Employees were shown one of six framings that were designed to overcome two key barriers: privacy concerns and usage concerns. They found that employees who read a story about their colleague using the service were more likely to sign up to learn more about the program, and that emphasizing the anonymity of the program did not seem to have an impact. Their findings suggest that one way to encourage employees to make use of existing mental health resources is by creating a supportive culture that embraces sharing about mental health challenges at work.
“I almost scheduled an appointment about a dozen times. But no, in the end I never went. I just wasn’t sure if my problems were big enough to warrant help and I didn’t want to take up someone else’s time unnecessarily.”
- Laura M. Giurge is an assistant professor at the London School of Economics, and a faculty affiliate at London Business School. Her research focuses on time and boundaries in organizations, workplace well-being, and the future of work. She is also passionate about translating research to the broader public through interactive and creative keynote talks, workshops, and coaching. Follow her on LinkedIn here .
- Lauren C. Howe is an assistant professor in management at the University of Zurich. As head of research at the Center for Leadership in the Future of Work , she focuses on how human aspects, such as mindsets, socioemotional skills, and leadership, play a role in the changing world of work.
- Zsofia Belovai is a behavioral science lead for the organizational performance research practice at MoreThanNow, focusing on exploring how employee welfare can drive KPIs.
- Guusje Lindemann is a senior behavioral scientist at MoreThanNow, in the social impact and organizational performance practices, working on making the workplace better for all.
- Sharon O’Connor is the global employee wellbeing lead at Novartis. She is a founding member of the Wellbeing Executives Council of The Conference Board, and a guest lecturer on the Workplace Wellness postgraduate certificate at Trinity College Dublin.
Partner Center
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 10 May 2023
Mental health awareness: uniting advocacy and research
Nature Mental Health volume 1 , pages 295–296 ( 2023 ) Cite this article
3440 Accesses
6 Altmetric
Metrics details
Mental Health Month has been observed to reduce the stigma that is associated with mental illness and to educate the public and encourage individuals to make their mental health and wellbeing a priority. It is an important moment to bring the strengths of advocacy groups and researchers together to promote mental health awareness and to improve equity.
Observances have become a popular tool to garner media and notice for topics deserving attention, from medical conditions to public health concerns, commemoration of notable events, or celebration of cultural groups. Codifying the scope and needs connected to an issue or illness through awareness campaigns can provide opportunities for imparting useful information, reducing stigma and marshalling support for policy change. The impact of awareness campaigns can be difficult to measure beyond tallying social media mentions or news stories. Effective advocacy, however, extends beyond traffic and paves the way for the creation of knowledge and partnerships among allies and with those whose interests are being represented. When the magnitude of an issue and the potential for improvement are great and are matched by broad involvement and recognition by stakeholders, the possibility for impact is also great.

Held annually in May, Mental Health Month , also called Mental Health Awareness Month, is an observance with such reach, resonating with many people. Nearly everyone has experience with the challenges that are associated with mental health, either first-hand or through loved ones or in their community. There is a need for education, support and initiative to improve our understanding of the causes of mental health disorders and to increase the availability of resources for prevention and treatment. Mental Health Month also offers the possibility of bringing together groups who often work in parallel, such as mental health advocates and mental health research organizations, that can mutually benefit from each other’s functions and expertise.
Mental Health Month was first established in the US in 1949 by the National Mental Health Association, now known as Mental Health America . At a time more often associated with the outset of the Cold War and Marshall Plan than setting an agenda for domestic mental health and wellbeing advocacy, in the more than 70 years since, Mental Health Month has grown into an international event designed to reduce exclusion, stigma and discrimination against people with mental health conditions or disorders. Mental Health America are joined by other prominent mental health advocacy groups to sponsor related observances: Mental Health Awareness Week Canada (1–7 May, 2023) and Europe (22–28 May, 2023); and federal agencies such as the Substance Use Abuse and Mental Health Services Administration ( SAMSHA ) in the US, promoting related public education platforms, including National Prevention Week (7–13 May, 2023).
Observances and awareness campaigns also provide occasions to put mental health in context. Increasing acknowledgment of the role of social determinants, for example, as mechanisms that can increase vulnerability for developing disorders and that drive disparities in mental health are an important framework to underscore as part of promoting mental health awareness. Given the complex and broad scope of people, disorders, conditions and issues under the umbrella of mental health, observances also give us the chance to focus more closely on specific problems or experiences. The theme for Mental Health Month in 2023 is ‘Look Around, Look Within’, which emphasizes the interdependence of mental health and wellness with an individual’s internal and external experiences and environments.
“The ‘Look Around, Look Within’ theme builds on the growing recognition that all humans have mental health needs and that our available resources to build resilience and heal come in many forms — including in the natural world,” explains Jennifer Bright, Mental Health America Board Chair and President of Momentum Health Strategies. “Mental Health America’s strategic plan, focused on NextGen Prevention, carries a similar theme — that the social factors supporting mental health are essential building blocks. These encompass basic needs like healthy food, stable housing, and access to treatment and supports, but they also include spirituality, connection with peers with lived experience, and safe and natural spaces.”
Overlapping with Mental Health Month, Mental Health Foundation sponsors Mental Health Week in the UK (15–21 May, 2023), dedicating this year to raising awareness around anxiety. It shares an individual-centered approach to advocacy. In addition to providing toolkits and resources that point to how prevalent stress and anxiety can be to reduce stigma, it also promotes the accessibility of coping strategies for managing anxiety. As part of the Mental Health Awareness Week campaign, Mental Health Foundation and others use the international symbol of wearing a green ribbon or clothing to physically raise awareness around mental health. Nature Mental Health also incorporates the symbol of the green ribbon on the cover of this month’s issue and as our journal theme color. Green evokes the ideas of vitality, growth, new beginnings and hope — powerful imagery in mental health awareness.
Alongside stories, sponsorships and social media resources, mental health advocacy toolkits and strategy documents include fact sheets and messaging that are shaped and informed by research. Yet, there is often a perception that a divide exists between the mental health advocacy and research spaces, but observances such as Mental Health Month can bridge the two.
According to Lea Milligan, Chief Executive Officer of MQ: Transforming Mental Health , an international mental health research organization, there are complementary approaches and priorities in advocacy and research: “Mental health research can be used to bolster awareness by providing evidence-based information and resources that can help individuals and communities better understand mental health and the factors that contribute to mental health problems. This can include information on risk factors, prevention strategies, and available treatments.”
In addition, increased efforts to involve people with lived experience of mental illness in the research enterprise is a goal that is well-served through connection with advocacy. “While MQ is primarily focused on promoting mental health research, it also recognizes the importance of advocacy in advancing the mental health agenda” suggests Milligan. “MQ advocates for increased funding and support for mental health research, as well as policies that promote mental health and wellbeing. Additionally, MQ seeks to empower individuals with lived experience of mental health conditions to be involved in research and advocacy efforts, and to have their voices heard in the development of policies and programs that affect their lives. MQ provides resources and support for individuals with lived experience who wish to be involved in research or advocacy efforts, including training programs, research grants, and opportunities to participate in research studies.”
Involvement or engagement is certainly one of the most important metrics of advocacy. By strengthening collaboration between advocacy and research organizations and identifying the mutual areas of benefit, such as engagement and increased funding, we may find new ways to green light mental health awareness and action toward mental health equity.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mental health awareness: uniting advocacy and research. Nat. Mental Health 1 , 295–296 (2023). https://doi.org/10.1038/s44220-023-00072-6
Download citation
Published : 10 May 2023
Issue Date : May 2023
DOI : https://doi.org/10.1038/s44220-023-00072-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Header menu - Mobile | United Kingdom
Header menu - drawer | united kingdom.
We are passionate about the transformative power of mental health research to create change in people’s lives, their communities and workplaces regarding services and policy.
We aim to contribute to the mental health evidence base by:
- undertaking original research
- synthesising existing knowledge
- translating this research to further understanding of what works, transferring interventions to other populations and places at a scale that maximises benefit and impact, and including mental health in all policies
Our research covers work in England, Scotland, Wales and Northern Ireland. We have offices in London, Glasgow, Cardiff and Belfast and conduct various evaluations and research in these areas.

Mental health A-Z
Explore our A to Z topics on mental health, where you can find more information on specific mental health problems and some of the things that can have an impact –good and bad – on our mental health.

Our Personal Experience Network (OPEN)
OPEN is a diverse online community of people we ask to inform us what we do, through anything from quick feedback on a social media post to fully participating in a research project.
Featured reports
Uncertain times: anxiety in the uk and how to tackle it.
This briefing looks at the prevalence and rates of anxiety amongst different groups of people, and the current key drivers and risk factors for anxiety. It also considers the main ways of coping with anxiety and provides recommendations to governments across the UK for preventing anxiety.
The economic case for investing in the prevention of mental health conditions in the UK
Our report with the London School of Economics and Political Science provides evidence from the UK and around the world that proves prevention interventions work.
Surviving or Thriving? The state of the UK's mental health
This report aims to understand the prevalence of self-reported mental health problems, levels of positive and negative mental health in the population, and the actions people take to deal with the stressors in their lives.
Supporting and expanding green social prescribing to address mental health inequalities in London
London has lots of green space, but not everyone can get to it. Our report suggests ways to expand green social prescribing across London to help people benefit from green spaces.
Prevention and mental health report
This report provides an understanding of the evidence for prevention and mental health so that we can address the greatest health challenge of our times.
Tackling social inequalities to reduce mental health problems
This report describes the extent of inequalities contributing to poor mental health in the UK today. It explains how certain circumstances interact with our own risks and discusses communities that are facing vulnerabilities.
Fundamental facts about mental health 2016
A comprehensive summary of mental health research, providing a unique handbook of key facts and figures, covering all key areas of mental health.
Relationships in the 21st century: the forgotten foundation of mental health and well-being
This report explores relationships across the life course, why they matter and the importance of being part of a community.
The impact of traumatic events on mental health
This report explores the impact traumatic events have on our mental health and provides advice on coping with trauma.
See more research reports
Our research projects
Thriving learners.
This research study is one of the largest of its kind, looking into student mental health across Scotland.
See Me Scotland
See Me is Scotland's national programme to tackle mental health stigma across Scotland, with the Mental Health Foundation providing the research and evaluation for the programme.
The Mental Health Foundation is the evaluation and learning partner for Barnardo’s Core Priority Programme in mental health and wellbeing.
Gaming and Mental Health
Using funding from Jingle Jam, we conducted an exciting new study exploring the link between video games and mental well-being.
Coronavirus: Mental Health in the Pandemic Study
Between 2020-2022, working with partners, the Mental Health Foundation led a ground-breaking, long-term, UK-wide research study of how the pandemic affected people’s mental health.
Coronavirus: Mental Health in the Pandemic Study in Scotland
Explore the Scotland Research team’s work as part of the UK-wide study.
Coronavirus and Adolescent Mental Health Study
The Mental Health Foundation and Swansea University led a repeated cross-sectional study of how the COVID-19 pandemic affected adolescents' mental health (people aged 13 to 19) across Great Britain.
Was this content useful?

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
2024 National Strategy for Suicide Prevention
Suicide is an urgent and growing public health crisis. More than 49,000 people in the United States died by suicide in 2022. That’s one death every 11 minutes.
National Strategy for Suicide Prevention
The 2024 National Strategy for Suicide Prevention is a bold new 10-year, comprehensive, whole-of-society approach to suicide prevention that provides concrete recommendations for addressing gaps in the suicide prevention field. This coordinated and comprehensive approach to suicide prevention at the national, state, tribal, local, and territorial levels relies upon critical partnerships across the public and private sectors. People with lived experience are critical to the success of this work.
The National Strategy seeks to prevent suicide risk in the first place; identify and support people with increased risk through treatment and crisis intervention; prevent reattempts; promote long-term recovery; and support survivors of suicide loss.
Four strategic directions guide the National Strategy:
Strategic Direction 1: Community-Based Suicide Prevention
Goal 1: Establish effective, broad-based, collaborative, and sustainable suicide prevention partnerships.
Goal 2: Support upstream comprehensive community-based suicide prevention.
Goal 3: Reduce access to lethal means among people at risk of suicide.
Goal 4: Conduct postvention and support people with suicide-centered lived experience.
Goal 5: Integrate suicide prevention into the culture of the workplace and into other community settings.
Goal 6: Build and sustain suicide prevention infrastructure at the state, tribal, local, and territorial levels.
Goal 7: Implement research-informed suicide prevention communication activities in diverse populations using best practices from communication science.
Strategic Direction 2: Treatment and Crisis Services
Goal 8: Implement effective suicide prevention services as a core component of health care.
Goal 9: Improve the quality and accessibility of crisis care services across all communities.
Strategic Direction 3: Surveillance, Quality Improvement, and Research
Goal 10: Improve the quality, timeliness, scope, usefulness, and accessibility of data needed for suicide-related surveillance, research, evaluation, and quality improvement.
Goal 11: Promote and support research on suicide prevention.
Strategic Direction 4: Health Equity in Suicide Prevention
Goal 12: Embed health equity into all comprehensive suicide prevention activities.
Goal 13: Implement comprehensive suicide prevention strategies for populations disproportionately affected by suicide, with a focus on historically marginalized communities, persons with suicide-centered lived experience, and youth.
Goal 14: Create an equitable and diverse suicide prevention workforce that is equipped and supported to address the needs of the communities they serve.
Goal 15: Improve and expand effective suicide prevention programs for populations disproportionately impacted by suicide across the life span through improved data, research, and evaluation.
Federal Action Plan
The Federal Action Plan identifies more than 200 actions across the federal government to be taken over the next three years in support of those goals. These actions include:
- Evaluating promising community-based suicide prevention strategies
- Identifying ways to address substance use/overdose and suicide risk together in the clinical setting
- Funding a mobile crisis locator for use by 988 crisis centers
- Increasing support for survivors of suicide loss and others whose lives have been impacted by suicide
These actions will be monitored and evaluated regularly to determine progress and success, and to further identify barriers to suicide prevention.
Get Involved
Join the conversation. Everyone has a role to play in preventing the tragedy of suicide. Find social media material, templates, and other resources to support and participate in the shared effort.
Read the press release
* This content is undergoing Section 508 remediation. For immediate assistance, contact [email protected] .
WHAT ARE YOU LOOKING FOR?
Key searches.
Mental Health Award: applying neuroscience to understand symptoms in anxiety, depression and psychosis
- Application due July 23, 2024
- £2 million to £5 million (15% indirects)
- Three to five years
The award is for a team of researchers.
This award will fund innovative projects that combine computational and experimental neuroscience approaches to improve understanding of symptoms of anxiety, depression and psychosis. Research must take a symptom-based approach rather than looking solely at diagnostic categories. Mental health conditions to be studied can include:
- All types of anxiety and depressive disorders (including obsessive compulsive disorder and post-traumatic stress disorder)
- All forms of psychotic disorders (including schizophrenia, postpartum psychosis and bipolar disorder).
Research must include a computational component and an experimental component. The team should include mental health practitioners and neuroscientists.
More information: https://wellcome.org/grant-funding/schemes/mental-health-award-applying-neuroscience-understand-symptoms-anxiety
- External Opportunities
Building and construction workers are reporting mental health issues in high numbers, but some are trying to make a difference
Like many people in construction, James Knight is feeling the pressure his industry is under.
In recent times, his Canberra electrical business has been left unpaid for work due to other construction companies collapsing.
"It's affected my kids seeing my wife and I stressed about it," Mr Knight said.
"It's affected our employees with the uncertainty and just having to go by our word that that we'll pull through and we'll be okay."
Mental health challenges among tradies have been common for years, if not always talked about.
The charity MATES in Construction estimates someone from the industry is lost to suicide every two days.
High interest rates, increased costs and a shortage of labour and materials are now adding an extra mental burden.
Mr Knight lives with depression and anxiety, and said the issues the industry is facing have not helped.
"I notice I'm not running at optimum performance, mentally speaking," he said.
"The guys notice it and notice the self-esteem is not always there.
"I've actually been diagnosed with ADHD, which lends itself to [depression and anxiety]"
But his experiences have prompted Mr Knight to take action to prevent others going through the same thing.
He and his wife Nikki run their business a little differently.
They reimburse staff for health-related costs such as gym memberships and supplements to help them maintain positive mental health.
He said he also encouraged his staff to be open about their problems.
"Their general health is very important to us, both mental and physical," Mr Knight said.
"My wife Nikki and I have got an open-door policy. We've definitely had a range of different things brought to us and some surprising, some straight down what we were expecting.
"But I think holistically, everyone is in a lot better place for it."
Industry wide problems
Research conducted by Central Queensland University indicates people who work in the building and construction industry are at a significantly higher risk of mental health problems.
MATES in Construction chief executive Chris Lockwood said it was a combination of long hours and work that could be both dangerous and lonely.
"That's why we do see significantly higher rates of poor mental health and tragically, even suicide in the industry," Mr Lockwood said.
The cost-of-living crisis overlaid on the current problems in the industry has compounded those dangers.
"Those sorts of pressures in terms of the finances that already were an issue for people working construction," Mr Lockwood said.
"[With] the cost of living, the impacts on top of it, we've seen some very direct impacts.
"Some months our call volumes have almost more than doubled, [from] people that are actually calling in distress needing support."
Building in a fix
Like a lot of male-dominated industries, Mr Knight said in decades past there has been a culture of silence when it comes to mental health.
He said things had changed in the industry.
"[It used to be] just go to the pub and write yourself off," he said.
"I think it's a lot easier these days, there's a lot more education around the mental health space and it being okay to not be okay."
Across the industry, mental health charities are improving mental health culture one job site at a time.
Canberra's The Healthy Tradie Project speaks to workers on site about mental health, incorporating breath work and yoga into their outreach.
OzHelp has been helping people in blue collar "high risk and hard to reach" jobs for 20 years.
David Lockwood said the mental health outreach sessions that MATES in Construction have on-site can save lives.
"The blokes and the women are all comfortable to step forward and actually say 'we should look out for our mates and have those honest conversations'."
- X (formerly Twitter)
Related Stories
'bang there goes $120,000': subcontractors struggling to stay afloat after building companies collapse.
Construction workers are more likely to die by suicide than a work accident. Joel wants to change that statistic
Jeff was having suicidal thoughts. Then he met John
- Construction and Real Estate Industry
- Mental Health
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- SSM Popul Health
- v.15; 2021 Sep
Barriers to healthcare access among U.S. adults with mental health challenges: A population-based study
Nicholas c. coombs.
a School of Public & Community Health Sciences, University of Montana, 32 Campus Dr, Missoula, MT, 59812, USA
Wyatt E. Meriwether
b VA Heartland Network 15, Kansas City VA Medical Center, 4801 E. Linwood Blvd., Kansas City, MO, 64128, USA
James Caringi
Sophia r. newcomer.
Having sufficient healthcare access helps individuals proactively manage their health challenges, leading to positive long-term health outcomes. In the U.S., healthcare access is a public health issue as many Americans lack the physical or financial resources to receive the healthcare services they need. Mental healthcare is especially difficult due to lingering social stigmas and scarcity of services. Subsequently, those with mental health impairment tend to be complex patients, which may convolute delivery of services.
To quantify the prevalence of barriers to healthcare access among U.S. adults with and without mental health challenges (MHC) and evaluate the relationship between MHC and no usual source of care (NUSC).
A cross-sectional study was conducted with data from the 2017–2018 National Health Interview Survey. MHC was categorized into three levels: no (NPD), moderate (MPD) and severe (SPD) psychological distress. Eight barriers were quantified; one was used as the primary outcome: NUSC. Multivariable logistic regression was used to quantify associations between these characteristics.
The sample included 50,103 adults. Most reported at least one barrier to healthcare access (95.6%) while 13.3% reported NUSC. For each barrier, rates were highest among those with SPD and lowest for those with NPD. However, in the multivariable model, SPD and MPD were not associated with NUSC (OR, 0.92; 95% CI, 0.83–1.01; 0.88; 0.73–1.07). Male sex (1.92; 1.78–2.06), Hispanic race/ethnicity (1.59; 1.42–1.77), and worry to afford emergent (1.38; 1.26–150) or normal (1.60; 1.46–1.76) healthcare were associated with NUSC. Having a current partner (0.88; 0.80–0.96), dependent(s) (0.77; 0.70–0.85) and paid sick leave (0.60; 0.56–0.65) were protective.
Conclusions
The most prevalent barriers to healthcare access link to issues with affordability, and MHC exist more often when any barrier is reported. More work is needed to understand the acuity of burden as other social and environmental factors may hold effect.
- • The most prevalent barriers to healthcare access link to issues with affordability.
- • The prevalence of barriers was higher among people with MHC.
- • Deficiencies in access may be influenced by other social and environmental factors.
1. Introduction
Access to healthcare services has a considerable impact on overall health at all stages of life ( Gu et al., 2009 ; Jerant et al., 2012 ). When healthcare services are sufficiently utilized, this allows for earlier detection and diagnosis of health problems so they may be addressed more proactively ( Mesquita-Neto et al., 2020 ; Papastergiou et al., 2020 ; Smith & Fader, 2018 ). This, in turn, results in positive effects on chronic illness and life expectancy ( Winkelman et al., 2016 ; World Health Organization News, 2019 ). Most healthcare systems around the world emphasize minimizing barriers to healthcare access for its citizens, but a multitude of barriers systematically complicate such an objective ( Agency for Healthcare Research and Quality, 2019 ; Corscadden et al., 2018 ). A few notable barriers involve services being inadequately approachable, physically available or affordable ( Levesque et al., 2013 ).
To add further complication, “access” has not been conceptualized with uniformity within or across health systems, which often directs policy without considering all relevant issues ( Oliver & Mossialos, 2004 ). In reality, access revolves around a spectrum of characteristics, all of which require consideration to adequately determine one's level of access. This involves interface between characteristics of individuals, households, and social and physical environments with characteristics of health systems, organizations, and healthcare providers. It encapsulates both supply- and demand-features with the ultimate objective to have healthcare needs fulfilled. A conceptual framework by Levesque and colleagues synthesized each of these characteristics and define access as “the opportunity to identify healthcare needs, to seek healthcare services, to reach, to obtain or use health care services, and to actually have the need for services fulfilled” ( Levesque et al., 2013 ). This framework composites five dimensions of accessibility: approachability (the ability to perceive), availability (the ability to reach), affordability (the ability to pay), acceptability (the ability to seek) and appropriateness (the ability to engage).
Revisions are frequently made to health policy to improve healthcare access. Most recently in the United States, the 2010 Affordable Care Act (ACA) was enacted with the intent to improve access and quality of healthcare services for U.S. citizens. Over the next decade, the ACA expanded Medicaid eligibility to persons earning up to 138% of the federal poverty level, which marked the largest expansion of coverage to non-elderly adults in over fifty years. As of June 2021, 38 U.S. states and the District of Columbia have either moved forward with expansion or are in the process of implementation ( Kaiser Family Foundation, 2020 ).
In the years following Medicaid expansion, levels of healthcare access showed remarkable improvements. States that expanded reported reduced out-of-pocket spending, fewer skipped medications and increased utilization of healthcare services ( Sommers et al., 2016 ). Collectively, rates of those with health insurance coverage and a usual source of care increased while concerns of barriers to healthcare access decreased ( McMorrow et al., 2017 ; Schmittdiel et al., 2018 ). These improvements were found at most levels of age, sex, socioeconomic status, and among those with a disability or pre-existing condition ( Daw and Sommers, 2019 ; Hill & Hyde, 2020 ). Noteworthy improvements were shown in affordability, but there remains issues with longer wait times, scheduling conflicts and transportation ( Alcala et al., 2018 ; Miller and Wherry, 2017 ).
The ACA did not affect all persons equally. Certain vulnerable populations, like those with mental health challenges (MHC), remain disproportionately susceptible to barriers to healthcare access. One study found increasing levels of psychological distress, a proxy measure of MHC, associated with an increased rate of forgoing medical care due to cost, although this rate has decreased in recent years ( Dedania & Gonzales, 2019 ; Fry and Sommers, 2018 ). In a sample of emergency department patients, one study found a three-fold increase in the total number of perceived barriers reported from those positively screened for depression and anxiety ( Abar et al., 2017 ). Persons with MHC face a range of multifaceted complications when navigating healthcare services as evidenced by increased risk of the onset, persistence and severity of a wide range of physical disorders, which may convolute the delivery of mental healthcare ( Ortega et al., 2006 ). Additionally, persons with MHC contend with perceptions of stigma amongst healthcare professionals, making it difficult to navigate healthcare systems ( Knaak et al., 2017 ; Vistorte et al., 2018 ; Thornicroft et al., 2007 ). Stigma continues to play an influential role in affecting patient perception and in some cases creates moral injury, either introducing or exacerbating MHC ( Brondani et al., 2017 ). A large multi-country comparison found the U.S. has a wider gap in healthcare access barriers between persons with and without MHC than several other countries ( Corscadden et al., 2018 ). The investigators who conducted the aforementioned study adopted Levesque's framework and mapped dozens of characteristics to each dimension of healthcare access, one of the few studies to aggregately evaluate all five dimensions, rather than a predetermined subset of dimensions, in the same population.
Post-ACA reforms, approximately one-fifth of U.S. adults with MHC still lack a usual source of care, and more than half report affordability-related barriers to accessing healthcare ( Sherrill & Gonzales, 2017 ; Thomas et al., 2018 ). Despite improvements made, the cost of healthcare in the U.S. continues to rise, un- and under insurance rates remain elevated, and there is speculation that improvements will be negated if the ACA is repealed in the future ( Lorenzoni et al., 2019 ; Winkelman et al., 2016 ). As challenges to healthcare access persist, research efforts must be made to observe the magnitude of effect healthcare access disparities have on populations who experience a range of MHC. The aims of this study were two-fold: quantify the prevalence of barriers to healthcare access among U.S. adults with and without MHC, and evaluate the relationship between the presence of MHC with not having a usual source of care (NUSC) while adjusting for demographic and lifestyle characteristics as well as other barriers to healthcare access.
2. Material and methods
2.1. study design.
We employed a cross-sectional study design with data from the 2017–2018 National Health Interview Survey (NHIS), choosing the two most recent consecutive years of data because a new sampling design was implemented in 2016. NHIS is a principal source of information on the health of the civilian noninstitutionalized population of the U.S., overseen by the National Center for Health Statistics (NCHS) at the Centers for Disease Control and Prevention ( National Center for Health Statistics, 2020 ). The in-person survey is administered annually to approximately 35,000 households across the U.S. and records basic demographic, health, and disability information for each household member. One random adult in each household is then selected for a detailed interview on more specific health information, which includes mental health status and healthcare access; we used these interviews to composite our study sample.
2.2. Mental health challenges (MHC)
MHC was treated as the primary independent variable of interest for this study and the classification of “mental health challenges” was purposeful. Mental health issues can occur along a wide spectrum and include formal illness/diagnostic disease but also comprise problems related to moral injury and distress. Additionally, there is current precedent to support the use of “mental health challenges” when describing a variety of mental health related problems in populations who experience inadequate access to healthcare ( Wang et al., 2020 ). For our study, we defined MHC using the 6-item Kessler Psychological Distress Scale (K6), which was developed with support from the NCHS for its specific use in the NHIS ( Kessler et al., 2003 ). The K6 measures non-specific psychological distress over the 30-day period prior to interview by assessing the frequency with which participants experienced feelings of sadness, nervousness, restlessness, hopelessness, worthlessness and everything being an effort. Validation of the K6 confirmed the measure's sensitivity around the threshold for the clinically significant range of the distribution of psychological distress, which expanded use and analysis of the K6 into three levels. Scores range from 0 to 24; scores ≤4 were classified as having no psychological distress (NPD), scores 5–12 were classified as having moderate psychological distress (MPD), and scores ≥13 were classified as having severe psychological distress (SPD) ( Prochaska et al., 2012 ).
2.3. Conceptual framework
We adopted Levesque's conceptual framework to synthesize the variety of healthcare access-related question items used in the NHIS. Upon reviewing survey content, we selected only items that inquired on a general function of access, that is, a barrier to healthcare access that may have potential impact on any U.S. adult. A participant's ‘inability to afford prescription medication,’ for example, was an item that we did not use as it limits the population of respondents to those who are or have been prescribed pharmacological forms of treatment. A total of eight question items were selected as shown in Table 1 . One item linked to the dimension of Approachability, five items to Availability and two items to Affordability.
NHIS question items used to measure healthcare access.
2.4. No usual source of care
The selection of these items directed the methodological construction for how to best analyze barriers to healthcare access for our study. Through synthesis of the literature, we found studies that investigated determinants of healthcare access used a variety of self-reported indicators, and among the items we selected, one seemed to appear most frequently: whether an individual has a usual source of care when they are sick or need advice about their health (Item 1) ( Brown et al., 2010 ; Choi, 2011 ; Gonzales et al., 2019 ; Farietta et al., 2018 ; Jones et al., 2014 ; Pullen et al., 2014 ; Sherrill & Gonzales, 2017 ). In some cases, this question item was used exclusively and acknowledged as one of the most protective factors to accessing healthcare services for any standard or emergent medical need as the perennial starting point to ensure all U.S. citizens have a medical home ( Blewett et al., 2008 ; Jerant et al., 2012 ; Manuel, 2017 ). For these reasons, not having a usual source of care was used as the primary outcome for this study, which we abbreviated as NUSC. NHIS participants who reported “Yes” or “There is more than one place” to this question were classified as having a usual source of care. Those who answered “There is no place” were classified as NUSC and, subsequently, have the approachability-related barrier to care (Approachability: relates to that fact that people facing health needs can actually identify that some form of services exist and have an impact on one's health).
2.5. Other indicators of barriers to healthcare access
As noted earlier, ‘access’ is a multi-dimensional concept and although we designated NUSC as our primary outcome measure of healthcare access, we were interested in exploring a range of other barriers as well because a consensus in the literature suggests that a variety of factors may influence one's level of access. Items 2 through 8 in Table 1 highlight specific characteristics of access as they relate to availability (the ability to reach healthcare services both physically and in a timely manner) and affordability (the economic capacity for people to spend resources without catastrophic expenditure to compromise access for basic necessities). The phrasing of these items enabled their temporal relationship with NUSC to be fluid, even though approachability (as measured by NUSC) is acknowledged as the initial stage of achieving access. Issues with wait time (Item 4) or worry affording normal healthcare services (Item 8), for instance, may both occur as either a cause or result from lacking a usual source of care. Additionally, these question items and the dimensions they represent are infrequently measured alongside approachability-related barriers in health services research. For these reasons, we decided to employ them as independent variables in our study, allowing us to adjust for the effect of availability- and affordability-related barriers when investigating the relationship between MHC and NUSC. Participants who reported “Yes” to Items 2 through 6 were classified as having that respective availability-related barrier to care and those who answered “No” were not. Participants who reported “Very worried” or “Somewhat worried” to Items 7 and 8 were classified as having that respective affordability-related barrier to care and those who answered “Not at all worried” were not. No items from the NHIS were linked to the acceptability or appropriateness dimensions (the ability to seek; the ability to engage) which consider a) the social and cultural factors that determine the possibility for a patient to accept aspects of the services for which they are to receive and b) the fit between those services and the patient's specific healthcare needs, respectively ( Levesque et al., 2013 ).
2.6. Statistical analysis
Descriptive statistics were used to characterize the study sample, and binary logistic regression analyses were used to explore the relationship between MHC and NUSC. To control for confounding and more thoroughly understand other factors among U.S. adults that are associated with NUSC, models adjusted for demographic characteristics [age (18–25, 26–34, 34–49, 50–64, 85+), sex (male, female) and race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Non-Hispanic other races, Hispanic)], lifestyle characteristics [current partner (yes: ‘Married – spouse in household’, ‘Married – spouse not in household’, ‘Married – spouse in household unknown’, ‘Living with partner’; no: ‘Widowed’, ‘Divorced’, ‘Separated’, ‘Never married’), at least one dependent living at home (yes: ‘Yes, the Sample Adult is a parent of a child residing in the family’, ‘There are minor children residing in the family but the Sample Adult is not their parent’, no: ‘There are no minor children residing in the family’), current source of income (yes: ‘Working for pay at a job or business’, ‘With a job or business but not at work’; no: ‘Looking for work’, ‘Working not for pay at a family-owned job or business’, ‘Not working at a job or business and not looking for work’), working multiple jobs (yes, no) and paid sick leave at a current or most recent job (yes, no)], and other barriers to healthcare access (Items 2–8 from Table 1 as defined in section 2.5 ). Additionally, we used a Chi-square test to analyze the association between MHC and each barrier to healthcare access (Items 1–8). We followed up this test with the Cramer's V strength statistic, the most common strength test used when a Chi-square test produces a significant test statistic and is particularly useful when said statistic is suspected to result from a large sample size ( McHugh, 2013 ). Analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC). All reported results incorporated NHIS provided survey weights and accounted for the complex survey design. Results were presented by a stepwise inclusion of variables from the unadjusted model containing only the main independent variable of interest (MHC, as measured by psychological distress: NPD, MPD, and SPD) then adjusting for demographic, lifestyle, and healthcare access barrier variables separately. Model adequacy was evaluated with the max-rescaled R-Squared statistic and the receiving operating characteristic (ROC) curve.
A total of 52,159 U.S. adults participated in the 2017 and 2018 NHIS. We excluded 2,056 participants who did not report complete information on mental health status or healthcare access or those who had a physical or mental condition that prohibited their ability to respond and did not have a knowledgeable proxy. After meeting exclusion criteria, our study sample consisted of 50,103 participants. Based on responses to the K6, 37,895 (76.0%) participants were classified as having NPD, 10,324 (20.4%) were classified as having MPD and 1,884 (3.6%) were classified as having SPD. The majority of participants were female (51.6%), White (78.2%) and Non-Hispanic (83.8%) with a mean age of 47.4 years (±0.10 S.E.). Over 60% reported having a current partner and close to one-quarter had at least one dependent living in their home at the time of completing the survey. More details are included in Table 2 .
Descriptive statistics of 2017–2018 NHIS participants by those who reported having and not having a usual source of care.
Note : Weighted means and percentages are reported; S.E. = standard error; no. = number; Race was not obtained for 111 participants; Current employment was not obtained for 17 participants.
Approximately 13.3% (n = 6,060) of participants reported NUSC with comparable rates at each level of psychological distress (SPD: 14.4%, MPD: 14.1%, NPD: 13.0%). The average number of self-reported barriers to healthcare access by participants was 1.8. Most reported having at least one barrier (95.6%), the most prevalent being Item 7 (worried one would be able to pay medical bills if they were to get sick or have an accident). For all availability- and affordability-related barriers, rates were highest among participants with SPD and lowest among participants with NPD as shown in Table 3 . Although each chi-square test produced a significant result, the most substantive relationships between MHC and barriers to healthcare access were shown for Items 7 and 8, the affordability-related barriers (Cramer's V: 0.19, 0.22, respectively).
Barriers to healthcare access across all levels of psychological distress.
Note : Weighted means and percentages are reported; NPD = No Psychological Distress, MPD = Moderate Psychological Distress, SPD = Severe Psychological Distress; All eight barriers produced a Chi-square test result of P ≤ 0.01.
A complete list of results from the logistic regression models is included in Table 4 beginning with the unadjusted model (Model #1), then controlling for demographic (Model #2), lifestyle (Model #3 & Model #4, personal and employment characteristics added separately), availability-related (Model #5) and affordability-related (Model #6) variables. In the final multivariable model where all variables were controlled for (Model #6), male sex, Hispanic race/ethnicity, no partner, no dependent(s), no paid sick leave from a current or recent job, having a source of income, and worried one is able to pay for both a) medical bills if they get sick or have an accident and b) medical costs for normal healthcare were all significantly associated with NUSC. The primary independent variable (psychological distress) was not significant in neither the unadjusted (Model #1) nor final model (Model #6). Compared to their designated reference groups, male sex (OR, 1.92; 95% CI, 1.78–2.06, vs. females) and Hispanic persons (OR, 1.59; 95% CI, 1.42–1.77, vs. Non-Hispanic White) were associated with NUSC. Those with paid sick leave were 40% less likely to have NUSC (OR, 0.60; 95% CI, 0.56–0.65, vs. those without paid sick leave) while at least some worry of affording emergent (OR, 1.38; 95% CI, 1.26–1.50, vs. no worry) or normal medical costs (OR, 1.60; 95% CI, 1.46–1.76, vs. no worry) increased risk. A suggestive dose response was found between age brackets. Compared to persons ages 18–25 years, all age groups older than 35 reported having a lower risk of NUSC with the strongest protective effect reported in the oldest age group (85+). None of the five availability-related barriers were associated with an increased risk of NUSC. The final model (Model #6) explained 15.9% of the overall variance, with the area under the ROC curve (0.75) indicating a fair level of discrimination.
Regression results for not having a usual source of care for NHIS participants.
Note : Results are displayed by the following: OR (lower 95% CI, upper 95% CI), OR = Odds Ratio, CI = Confidence Interval. NPD = No Psychological Distress, MPD = Moderate Psychological Distress, SPD = Severe Psychological Distress, *P ≤ 0.05, **P ≤ 0.01.
4. Discussion
Our descriptive results highlighted increased self-reported barriers to accessing healthcare services across dimensions of approachability, availability and affordability among individuals with MHC compared to individuals without MHC. In multivariable models, we identified several determinants of NUSC independent from MHC. Many significant findings were consistent with that of previous studies, namely identifying lower rates of usual source of care among males, younger adults and Hispanic persons ( Choi, 2011 ; Manuel, 2017 ; Singh & Wilk, 2019 ). Having a usual source of care is likely associated with one's perceived level of need and desire of services, of which older persons are likely to have. The effect found in Hispanic persons signals continued disparities in healthcare access for minority ethnic populations ( Rangel Gomez et al., 2019 ). In addition, those without employer-provided benefits of paid sick leave were disproportionately impacted by reduced healthcare access; this is evident in their increased risk of NUSC, foregoing medical care for themselves or their family, and continuing to attend work when ill ( Derigne et al., 2016 ). In times of a pandemic due to the 2019 novel coronavirus (SARS-CoV-2; COVID-19), this relationship is particularly disconcerting and may be exacerbated. Future studies should illustrate that this propensity to work while ill has hindered efforts to mitigate the spread of coronavirus in the U.S.
Although the main effect of MHC was not statistically significant in multivariable models, its direction shifted when considering the two affordability-related barriers to care. Issues affording normal healthcare and unanticipated medical bills remained significant signifying that one's mental health status does not impede on the consistent burden of affordability when accessing healthcare services. On the contrary, only one of the availability-related barriers produced a significant effect, which may have been attributed to lower prevalence rates. The most common barrier (Item 7) was reported over three times more than the primary outcome (NUSC) and over five times more than the most frequently reported availability-related barrier (Item 3: couldn't get an appointment soon enough). In any case, the elevated prevalence estimates of affordability-related barriers to care suggest that certain dimensions of healthcare access may be more impactful than others when considering a generalizable population of non-institutionalized U.S. adults. It may also be suspected that barriers within or across different dimensions affect one another. For instance, if one worries about affording normal medical costs, they may likely be concerned about cost should they get sick or have an accident, and general concerns related to cost may also interfere with the ability to physically make it to services as taking off work and dealing with long wait times, for example, may prove more burdensome.
However, the true prevalence of availability-related barriers may be better understood when considering geographic determinants, such as urban-rural classification. With a disproportionate allocation of healthcare resources spread out over larger physical areas for rural inhabitants, it may be assumed that those living in those regions of the U.S. face more burden with travel distances and time, a concern that has already produced a rural-based federal initiative to serve counterpart to recognizing national health objectives in the general population ( Bolin et al., 2015 ). Our study ascertained data from publicly-available NHIS records, which do not include information on participants’ geographic characteristics. Thus, geographic determinants of healthcare access were not explored.
Using NHIS data, we were able to examine three dimensions of healthcare access: approachability, availability, and affordability. However, we were not able to study acceptability and appropriateness, which are the ability to seek and engage in healthcare services, respectively. No NHIS question items linked to these dimensions as they are not traditionally captured through quantitatively driven data collection mechanisms. Occasionally in research, stigma serves as a comparable indicator for these dimensions. One study that examined factors associated with difficulty in receiving medical care among a sample of adults with mental illness found its comorbid existence with a chronic physical health condition posed additional challenges ( Ostrow et al., 2014 ). The implications this has on healthcare access link to several considerations. First, it is suspected that healthcare providers are often influenced by the perceived stigma objectified by the patients they serve. Navigating the U.S. healthcare system requires an informative and authoritative approach, which places a great deal of responsibility on the patient. Those who lack empowerment in these areas, which may include those with MHC, are met with a disadvantage. Second, evidence suggests that a majority of persons who seek mental healthcare services in the U.S. do so through a general practitioner rather than one who specializes in mental health treatment. This demands healthcare providers to expand their services across mental and physical health issues, of which some generalists are not properly trained and equipped to effectively address more serious mental health issues and complications. It is particularly in rural areas that providers have become make-shift mental healthcare specialists out of the necessity for treating the geographic population ( Chipp et al., 2011 ; Cunningham, 2009 ). It is due to these missing resources that rural healthcare organizations can be further burdened by the needs of their populations. Third, fewer than half of those in need of mental healthcare actually seek out services ( National Alliance on Mental Illness, 2019 ). This casts an additional layer of complication over the representativeness of MHC on U.S. citizens and how best to treat. For this reason, this study was methodical in capturing MHC broadly by including those who both have and have not navigated the U.S.‘s healthcare system. This population is both larger and more representative of true mental health impairment on U.S. adults. Follow up research efforts should aim to include these more abstract dimensions through qualitative or mixed approaches as to gain a more complete understanding of healthcare access barriers among persons with MHC.
We believe it is important to address the study's limitations. First and foremost, the cross-sectional design of the study prevents any ability to infer temporality or causality with characteristics associated with persons lacking a usual source of care. We also recognize that our multi-dimensional approach to investigate healthcare access does not definitely measure one's true level of access. In conjunction with the three dimensions and eight barriers explored, there are many other factors that influence the identification, reachability, utilization and fulfillment of healthcare services. The NHIS survey used, although incredibly comprehensive, does not come without its own limitations. The NHIS omits institutionalized individuals, thus missing such segments of the population as military personnel or older adults in nursing homes and other long-term care facilities. The annual survey sample for each year, because of the cross-sectional design, represents a changing cohort of subjects, although this concern is mitigated with only two consecutive years used over the same sampling design period ( Backinger et al., 2008 ). We must also acknowledge the limitations inherent with self-reported data, as this may influence participants willingness to report undesirable feelings of psychological distress. If so, the effects shown in this study may be attenuated. Finally, we must consider the changing landscape to healthcare systems that resulted from the COVID-19 pandemic, preceded by the time period of the data used for this study. Systems throughout the U.S. have modified practices to mitigate face-to-face encounters by providing telehealth as a more widespread modality. For this reason, future studies should consider the impact of COVID-19, and subsequent adjustments to healthcare delivery, when evaluating healthcare access. Although tele-mental health may become more common, future research efforts must still evaluate all dimensions of healthcare access to ensure comprehensive recovery for future generations.
5. Conclusion
The most prevalent barriers to healthcare access link to issues with affordability, and MHC exist more often when any barrier to healthcare access is reported. Ideally, all five dimensions of healthcare access should be considered when evaluating healthcare systems, particularly when studying complex populations with unique health challenges. It is important not to undermine the influence this has on persons with MHC or how having MHC impacts the maneuvering of such challenges. In doing so, public policy may be directed from more complete framing of the issues at hand.
This study emphasizes the need to continue monitoring disparities of healthcare access among persons experiencing MHC. More work is needed to understand the acuity of mental health burden on U.S. adults as other social and environmental factors may be of importance.
Ethical statement
Authorship of the paper: CRediT authorship contribution statement
Nicholas C. Coombs : Conceptualization, Methodology, Software, Formal analysis, Writing – original draft, Writing – review & editing. Wyatt E Meriwether : Writing – review & editing, Supervision, the views and opinions expressed in this article are the authors’ and do not express the views of the Department of Veterans Affairs or the federal government. James Caringi : Writing – review & editing, Supervision, first author’s advisory chair. Sophia R. Newcomer : Methodology, Software, Writing – review & editing, Supervision.
Originality and plagiarism
We ensure that this manuscript is an entirely original work. All work and/or words of others have been appropriately cited.
Data access and retention
We have provided the raw data and analytic code in our supplemental materials.
Multiple, redundant or concurrent publication
We confirm that this work is original and has not been published elsewhere, nor is it currently under consideration for publication elsewhere.
Disclosure and conflicts of interest
Declarations of interest, statement of funding.
This research did not receive any specific grant from funding agencies in the public, commercial, and not-for-profit sectors.
Acknowledgements
This research was supported by a Center for Biomedical Research Excellence award (P20GM130418) from the National Institute of General Medical Sciences of the National Institutes of Health. The first author was also supported by the University of Montana Burnham Population Health Fellowship. The contents are solely the responsibility of the authors and do not necessarily represent the official views of NIGMS or NIH.
- Abar B., Holub A., Lee J., Derienzo V., Nobay F. Depression and anxiety among emergency department patients: Utilization and barriers to care. Academic Emergency Medicine. 2017; 24 (10):1286–1289. doi: 10.1111/acem.13261. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Agency for Healthcare Research and Quality . Agency for Healthcare Research and Quality; Rockville, MD: 2019. 2015 national healthcare quality and disparities report and 5th anniversary update on the national quality strategy. Content last reviewed july 2019. https://archive.ahrq.gov/research/findings/nhqrdr/nhqdr15/index.html Retrieved from. [ Google Scholar ]
- Alcalá H.E., Roby D.H., Grande D.T., Mckenna R.M., Ortega A.N. Insurance type and access to health care providers and appointments under the affordable care Act. Medical Care. 2018; 56 (2):186–192. doi: 10.1097/mlr.0000000000000855. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Backinger C.L., Lawrence D., Swan J., Winn D.M., Breen N., Hartman A., Grana R., Tran D., Farrell S. Using the national health interview survey to understand and address the impact of tobacco in the United States: Past perspectives and future considerations. Epidemiologic Perspectives & Innovations. 2008; 5 :8. doi: 10.1186/1742-5573-5-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blewett L.A., Johnson P.J., Lee B., Scal P.B. When a usual source of care and usual provider matter: Adult prevention and screening services. Journal of General Internal Medicine. 2008; 23 (9):1354–1360. doi: 10.1007/s11606-008-0659-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bolin J.N., Bellamy G.R., Ferdinand A.O., Vuong A.M., Kash B.A., Schulze A., Helduser J.W. Rural healthy people 2020: New decade, same challenges. The Journal of Rural Health. 2015:326–333. doi: 10.1111/jrh.12116. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brondani M.A., Alan R., Donnelly L. Stigma of addiction and mental illness in healthcare: The case of patients' experiences in dental settings. PloS One. 2017; 12 (5) doi: 10.1371/journal.pone.0177388. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown R.T., Kimes R.V., Guzman D., Kushel M. Health care access and utilization in older versus younger homeless adults. Journal of Health Care for the Poor and Underserved. 2010; 21 (3):1060–1070. doi: 10.1353/hpu.0.0344. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chipp C., Dewane S., Brems C., Johnson M.E., Warner T.D., Roberts L.W. “If only someone had told me…”: Lessons from rural providers. The Journal of Rural Health. 2011; 27 (1):122–130. doi: 10.1111/j.1748-0361.2010.00314.x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Choi S. Longitudinal changes in healthcare access by immigrant status among older adults: The importance of health insurance as a mediator. The Gerontologist. 2011; 51 (2):156–169. doi: 10.1093/geront/gnq064. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Corscadden L., Callander E.J., Topp S.M. International comparisons of disparities in access to care for people with mental health conditions. The International Journal of Health Planning and Management. 2018; 33 (4):967–995. doi: 10.1002/hpm.2553. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cunningham P.J. Beyond parity: Primary care physicians' perspectives on access to mental health care. Health Affairs. 2009; 28 (3):w490–501. doi: 10.1377/hlthaff.28.3.w490. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Daw J.R., Sommers B.D. The affordable care Act and access to care for reproductive-aged and pregnant women in the United States, 2010–2016. American Journal of Public Health. 2019; 109 (4):565–571. doi: 10.2105/AJPH.2018.304928. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dedania R., Gonzales G. Disparities in access to health care among US-born and foreign-born US adults by mental health status, 2013–2016. American Journal of Public Health. 2019; 109 (S3):S221–S227. doi: 10.2105/AJPH.2019.305149. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Derigne L., Stoddard-Dare P., Quinn L. Workers without paid sick leave less likely to take time off for illness or injury compared to those with paid sick leave. Health Affairs. 2016; 35 (3):520–527. doi: 10.1377/hlthaff.2015.0965. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Farietta T.P., Lu B., Tumin R. Ohio's Medicaid expansion and unmet health needs among low-income women of reproductive age. Maternal and Child Health Journal. 2018; 22 (12):1771–1779. doi: 10.1007/s10995-018-2575-1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fry C.E., Sommers B.D. Effect of Medicaid expansion on health insurance coverage and access to care among adults with depression. Psychiatric Services. 2018; 69 (11):1146–1152. doi: 10.1176/appi.ps.201800181. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gonzales G., Dedania R., Driscoll R. Health insurance coverage and access to care among US-born and foreign-born sexual minorities. Journal of Immigrant and Minority Health. 2019; 21 (3):540–548. doi: 10.1007/s10903-018-0774-x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gu D., Zhang Z., Zeng Y. Healthcare access services makes a difference in healthy longevity among older Chinese adults. Social Science & Medicine. 2009; 68 (2):210–219. doi: 10.1016/j.socscimed.2008.10.025. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hill A., Hyde J.S. Insurance coverage and access to care for workers with disabilities, 2001–2017. Disability and Health Journal. 2020; 13 (1):100843. doi: 10.1016/j.dhjo.2019.100843. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jerant A., Fenton J.J., Franks P. Primary care attributes and mortality: A national person-level study. The Annals of Family Medicine. 2012; 10 (1):34–41. doi: 10.1370/afm.1314. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jones E., Lebrun-Harris L.A., Sripipatana A., Ngo-Metzger Q. Access to mental health services among patients at health Centers and factors associated with unmet needs. Journal of Health Care for the Poor and Underserved. 2014; 25 (1):425–436. doi: 10.1353/hpu.2014.0056. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaiser Family Foundation . 2020. Status of state action on the Medicaid expansion decision. Content last reviewed november 2020. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ Retrieved from. [ Google Scholar ]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., Howes M.J., Horman S.T., Manderscheid R.W., Walter E.E., Zaslavsky A.M. Screening for serious mental illness in the general population. JAMA Psychiatry. 2003; 60 (2):184–189. doi: 10.1001/archpsyc.60.2.184. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Knaak S., Mantler E., Szeto A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthcare Management Forum. 2017; 30 (2):111–116. doi: 10.1177/0840470416679413. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levesque J., Harris M.F., Russell G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. International Journal for Equity in Health. 2013; 12 :18. doi: 10.1186/1475-9276-12-18. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lorenzoni L., Marino A., Morgan D., James C. Vol. 110. OECD Publishing; Paris: 2019. (Health spending projections to 2030: New results based on a revised OECD methodology, OECD health working papers). [ CrossRef ] [ Google Scholar ]
- Manuel J.I. Racial/ethnic and gender disparities in health care use and access. Health Services Research. 2017; 53 (3):1407–1429. doi: 10.1111/1475-6773.12705. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McHugh M.L. The Chi-square test of independence. Biochemical Medicine. 2013; 23 (2):143–149. doi: 10.11613/bm.2013.018. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McMorrow S., Gates J.A., Long S.K., Kenney G.M. Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Affairs. 2017; 36 (5):808–818. doi: 10.1377/hlthaff.2016.1650. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mesquita-Neto J.W., Cmorej P., Mouzaihem H., Weaver D., Kim S., Macedo F.I. Disparities in access to cancer surgery after Medicaid expansion. The American Journal of Surgery. 2020; 219 (1):181–184. doi: 10.1016/j.amjsurg.2019.06.023. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller S., Wherry L.R. Health and access to care during the first 2 Years of the ACA Medicaid expansions. New England Journal of Medicine. 2017; 376 (10):947–956. doi: 10.1056/nejmsa1612890. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Alliance on Mental Illness Mental health by the numbers. Content last reviewed: September 2019. 2019. https://www.nami.org/mhstats Retrieved from.
- National Center for Health Statistics Centers for disease control and prevention. About the national health interview survey. 2020. https://www.cdc.gov/nchs/nhis/about_nhis.htm Page last reviewed: September 16, 2020. Retrieved from.
- Oliver A., Mossialos E. Equity of access to health care: Outlining the foundations for action. Journal of Epidemiology & Community Health. 2004; 58 (8):655–658. doi: 10.1136/jech.2003.017731. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ortega A.N., Feldman J.M., Canino G., Steinman K., Alegría M. Co-occurrence of mental and physical illness in US Latinos. Social Psychiatry and Psychiatric Epidemiology. 2006; 41 (12):927–934. doi: 10.1007/s00127-006-0121-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ostrow L., Manderscheid R., Mojtabai R. Stigma and difficulty accessing medical care in a sample of adults with serious mental illness. Journal of Health Care for the Poor and Underserved. 2014; 25 (4):1956–1965. doi: 10.1353/hpu.2014.0185. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Papastergiou J., Donnelly M., Li W., Sindelar R.D., Bemt B.V. Community pharmacy-based eGFR screening for early detection of CKD in high risk patients. Canadian Journal of Kidney Health and Disease. 2020; 7 doi: 10.1177/2054358120922617. 205435812092261. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prochaska J.J., Sung H., Max W., Shi Y., Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. International Journal of Methods in Psychiatric Research. 2012; 21 (2):88–97. doi: 10.1002/mpr.1349. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pullen E., Perry B., Oser C. African American women's preventative care usage: The role of social support and racial experiences and attitudes. Sociology of Health & Illness. 2014; 36 (7):1037–1053. doi: 10.1111/1467-9566.12141. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rangel Gomez M.G., Lopez Jaramillo A.M., Svarch A., Tonda J., Lara J., Anderson E.J., Rosales C.B. Together for health: An initiative to access health services for the hispanic/Mexican population living in the United States. Frontiers in Public Health. 2019; 7 :273. doi: 10.3389/fpubh.2019.00273. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schmittdiel J.A., Barrow J.C., Wiley D., Ma L., Sam D., Chau C.V., Shetterly S.M. Improvements in access and care through the affordable care Act. American Journal of Managed Care. 2018; 23 (3):E95–E97. PMID: 28385029. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sherrill E., Gonzales G. Recent changes in health insurance coverage and access to care by mental health status, 2012-2015. JAMA Psychiatry. 2017; 74 (10):1076–1079. doi: 10.1001/jamapsychiatry.2017.2697. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Singh K.A., Wilk A.S. Affordable care Act Medicaid expansion and racial and ethnic disparities in access to primary care. Journal of Health Care for the Poor and Underserved. 2019; 30 (4):1543–1559. doi: 10.1353/hpu.2019.0088. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith A.J., Fader A.N. Effects of the affordable care Act on young women with gynecologic cancers. Obstetrics & Gynecology. 2018; 131 (6):966–976. doi: 10.1097/aog.0000000000002592. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sommers B.D., Blendon R.J., Orav E.J., Epstein A.M. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Internal Medicine. 2016; 176 (10):1501. doi: 10.1001/jamainternmed.2016.4419. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thomas K.C., Shartzer A., Kurth N.K., Hall J.P. Impact of ACA health reforms for people with mental health conditions. Psychiatric Services. 2018; 69 (2):231–234. doi: 10.1176/appi.ps.201700044. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thornicroft G., Rose D., Kassam A. Discrimination in health care against people with mental illness. International Review of Psychiatry. 2007; 19 (2):113–122. doi: 10.1080/09540260701278937. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vistorte A.O.R., Ribeiro W.S., Jaen D., Jorge M.R., Evans-Lacko S., Mari J.D.J. Stigmatizing attitudes of primary care professionals towards people with mental disorders: A systematic review. The International Journal of Psychiatry in Medicine. 2018; 53 (4):317–338. doi: 10.1177/0091217418778620. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang Y., Pan B., Liu Y., Wilson A., Ou J., Chen R. Health care and mental health challenges for transgender individuals during the COVID-19 pandemic. Lancet Diabetes Endocrinology. 2020; 8 (7):564–565. doi: 10.1016/S2213-8587(20)30182-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Winkelman T.N., Kieffer E.C., Goold S.D., Morenoff J.D., Cross K., Ayanian J.Z. Health insurance trends and access to behavioral healthcare among justice-involved individuals—United States, 2008–2014. Journal of General Internal Medicine. 2016; 31 (12):1523–1529. doi: 10.1007/s11606-016-3845-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization News . World Health Organization; 2019. Uneven access to health services drives life expectancy gaps. Content last reviewed April 2019. https://www.who.int/news/item/04-04-2019-uneven-access-to-health-services-drives-life-expectancy-gaps-who Retrieved from. [ Google Scholar ]

COMMENTS
The National Institute of Mental Health (NIMH) is the Nation's leader in research on mental disorders, supporting research to transform the understanding and treatment of mental illnesses. Below you can learn more about NIMH funded research areas, policies, resources, initiatives, and research conducted by NIMH on the NIH campus.
All WHO Member States are committed to implementing the Comprehensive mental health action plan 2013-2030, which aims to improve mental health by strengthening governance, providing community-based care, implementing promotion and prevention strategies, and strengthening information systems, evidence and research.. WHO's World mental health report: transforming mental health for all called ...
PLOS Mental Health is an inclusive, peer-reviewed, journal that aims to address challenges and gaps in the field of mental health research, treatment, and care in ways that put the lived experience of individuals and communities first. By uniting all stakeholders through rigorous, open research, and increased visibility of the experiences of individuals and societies we aim to serve, we can ...
The COVID-19 pandemic has profoundly influenced the world. In wave after wave, many countries suffered from the pandemic, which caused social instability, hindered global growth, and harmed mental health. Although research has been published on various mental health issues during the pandemic, some profound effects on mental health are ...
Mental health is a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community. It is an integral component of health and well-being that underpins our individual and collective abilities to make decisions, build relationships and shape ...
Mental health is a focus of NIH research during the COVID-19 pandemic. Researchers at NIH and supported by NIH are creating and studying tools and strategies to understand, diagnose, and prevent mental illnesses or disorders and improve mental health care for those in need.
Although most mental-health disorders arise during adolescence, UNICEF says that only one-third of investment in mental-health research is targeted towards young people. Moreover, the research ...
D2/D3 dopamine supports the precision of mental state inferences and self-relevance of joint social outcomes. In this article, the authors demonstrate that haloperidol D2/D3 dopamine antagonism ...
Three years into the COVID-19 outbreak in the United States, Pew Research Center published this collection of survey findings about Americans' challenges with mental health during the pandemic.All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
Open for Submissions Publishing high-quality research on mental health and well-being npj Mental Health Research is a new open-access, online-only journal ...
Impact on mental health. Mental health is defined as a state of well-being in which people understand their abilities, solve everyday life problems, work well, and make a significant contribution to the lives of their communities [].There is debated presently going on regarding the benefits and negative impacts of social media on mental health [9,10].
An overview of statistics for mental illnesses. Mental illnesses are common in the United States. One in six U.S. adults lives with a mental illness (43.4 million in 2015). Mental illnesses include many different conditions that vary in degree of severity, ranging from mild to moderate to severe.
This study aimed to establish what is known about the mental health of researchers based on the existing literature. The literature identified focuses mainly on stress in the academic workforce and contributory factors in the academic workplace. Keywords: Depression, Scientific Professions, Workforce Management, Workplace Wellness Programs.
The Division of Intramural Research Programs (IRP) is the internal research division of the NIMH. Over 40 research groups conduct basic neuroscience research and clinical investigations of mental illnesses, brain function, and behavior at the NIH campus in Bethesda, Maryland. Learn more about research conducted at NIMH.
Research. One of the most important commitments of an academic department of psychiatry is research and scholarship. Research pushes back the barriers of ignorance about the causes of mental disorders, brings to bear on patient care scientifically informed treatment, and creates an environment of critical thinking essential for clinical training.
Research Areas. The Department of Mental Health covers a wide array of topics related to mental health, mental illness, and substance abuse. We emphasize ongoing research that enriches and stimulates the teaching programs. All students and fellows are encouraged to participate in at least one research group. Faculty and students from multiple ...
Read the latest research as well as in-depth information on clinical depression, schizophrenia, bipolar disorder, ADHD and other mental health disorders in adults, teens, and children.
Overall, 37% of students at public and private high schools reported that their mental health was not good most or all of the time during the pandemic, according to the CDC's Adolescent Behaviors and Experiences Survey, which was fielded from January to June 2021.In the survey, "poor mental health" includes stress, anxiety and depression.
Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager for the training, uptake of the program ...
The COVID-19 pandemic represents an unprecedented threat to mental health in high, middle, and low-income countries. In addition to flattening the curve of viral transmission, priority needs to be given to the prevention of mental disorders (e.g. major depressive disorder, PTSD, as well as suicide).
Adolescence (10-19 years) is a unique and formative time. Multiple physical, emotional and social changes, including exposure to poverty, abuse, or violence, can make adolescents vulnerable to mental health problems. Promoting psychological well-being and protecting adolescents from adverse experiences and risk factors that may impact their potential to thrive are critical for their well-being ...
Mental Health America are joined by other prominent mental health advocacy groups to sponsor related observances: Mental Health Awareness Week Canada (1-7 May, 2023) and Europe (22-28 May ...
Research. We are passionate about the transformative power of mental health research to create change in people's lives, their communities and workplaces regarding services and policy. We aim to contribute to the mental health evidence base by: undertaking original research. synthesising existing knowledge. translating this research to ...
Goal 12: Embed health equity into all comprehensive suicide prevention activities. Goal 13: Implement comprehensive suicide prevention strategies for populations disproportionately affected by suicide, with a focus on historically marginalized communities, persons with suicide-centered lived experience, and youth.
America's mental health woes essentially serve as an annual economic downturn for the nation, a new study says. Mental illness costs the U.S. economy $282 billion every year, equivalent to the ...
Scope of Mental Health Promotion and Prevention in the Current Situation. Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses (18, 36-42).There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe ...
This award will fund innovative projects that combine computational and experimental neuroscience approaches to improve understanding of symptoms of anxiety, depression and psychosis. Research must take a symptom-based approach rather than looking solely at diagnostic categories. Mental health conditions to be studied can include:
Research conducted by Central Queensland University indicates people who work in the building and construction industry are at a significantly higher risk of mental health problems.
Mental health issues can occur along a wide spectrum and include formal illness/diagnostic disease but also comprise problems related to moral injury and distress. ... items and the dimensions they represent are infrequently measured alongside approachability-related barriers in health services research. For these reasons, we decided to employ ...
Professor in Mental Health at Trinity College Dublin, Professor Agnes Higgins who led the research team, said the findings continued to highlight that a significant proportion of those under 25 ...