- Search Menu
- Sign in through your institution
- Volume 2024, Issue 6, June 2024 (In Progress)
- Volume 2024, Issue 5, May 2024
- Bariatric Surgery
- Breast Surgery
- Cardiothoracic Surgery
- Colorectal Surgery
- Colorectal Surgery, Upper GI Surgery
- Gynaecology
- Hepatobiliary Surgery
- Interventional Radiology
- Neurosurgery
- Ophthalmology
- Oral and Maxillofacial Surgery
- Otorhinolaryngology - Head & Neck Surgery
- Paediatric Surgery
- Plastic Surgery
- Transplant Surgery
- Trauma & Orthopaedic Surgery
- Upper GI Surgery
- Vascular Surgery
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Submit
- About Journal of Surgical Case Reports
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic


Senior Editors
Mr Julien Al Shakarchi
Mr Tariq Ali
Mr Varun Dewan
Mr Khalid Hussain
Case Report of the Year
Reveal the latest Case Report of the Year, as selected by our expert panel, to inform your research and practice.
Latest articles

Browse by specialty
JSCR publishes surgical techniques, case reports, and series across all surgical specialties. Browse collections including orthopaedics , vascular surgery , and urology .
Explore more

‘ A rare case of inflammatory breast cancer with delayed auto-amputation in modern times ’ has been selected as this years' winning case report, following a review by our expert panel.
Read the winning case report now

Benefits of publishing with JSCR
Time from submission to first decision: 21 days Article Processing Charges (APC):
- Case Report/Surgical Technique $849
- Case Series $970

Email alerts
Register to receive table of contents email alerts as soon as new issues of Journal of Surgical Case Reports are published online.
Register now

Why submit to JSCR ?
JSCR publishes original surgical techniques, case reports, and series that expand the field of surgery. Discover our top reasons why you should submit your manuscript.
- Find out more
- Submit your case

Enhanced discoverability
JSCR deposits all cases in PubMed Central . Surgeons, physicians, dentists and researchers can find your work through PubMed , helping you reach the widest possible audience.
The journal is also indexed in the Web of Science Core Collection .
Related Titles

Affiliations
- Online ISSN 2042-8812
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Recent Search Keywords
- Surgical Case Reports
Review Time
Publish time, about journal scr.

Surgical Case Reports (SCR) the renowned official journal. Dive into a comprehensive collection of gastroenterological surgery, cardiovascular surgery, thoracic surgery, and more. Our open-access platform, supported by rigorous peer-review processes, showcases novel treatments and unique surgical experiences from around the globe.
The journal aims to develop and uphold the highest research standards, to provide a scope for evidence-based treatments through the publication of quick review papers and special issues, and to contextualise the findings through the publication of editorials, commentaries, and letters from the surgical community. We enforce reporting guidelines and require that all research involving human participants be registered in a public access research database.
From transplant surgery insights to rare breast and endocrine surgery tales, SCR is committed to advancing the realm of surgical science. By encapsulating unique cases and innovative treatments, we aim to foster a rich educational forum for clinicians and researchers alike.
Scope of Journal
Surgical Case Reports (SCR) is a dedicated platform aiming to advance the understanding and practice of surgery. Our principal goal is to provide a global forum where clinicians, surgeons, and researchers can share, learn, and discuss novel surgical techniques, treatments, and patient case studies that contribute to the field's progress.
Submit Manuscript
For submission authors can directly submit manuscript to [email protected] . If you want to proceed with online submission you can follow the below link. You will need to be a register user to submit your manuscript.
Submit Online
General Information
Manuscripts number will be provided to the corresponding author within 72 hours for the respective manuscript submitted.
- • 14 days review process with international peer-review standards
- • Timeline of processing from Submission to Publication is 30 days
- • Manuscript will be published within 7 days of acceptance
Open Access
All the work at Surgical Case Reports is licensed under a Creative Commons Attribution 4.0 International License. Authors at Surgical Case Reports retain copyright to their work and allow others to copy, distribute, transmit, and adapt their work, provided proper attribution is given.
We follow Creative Commons 'Attribution' licence (CC BY) . This license lets others distribute, remix, tweak, and build upon your work, even commercially, as long as they credit you for the original creation. View License Deed | View Legal Code
Indexing and Abstract
All articles are made open access to maximise the long-term visibility, impact and influence of our content.
- • AcademicPub
- • The British Library
- • Cancerlit
- • Google Scholar
- • Medline/PubMed
- • Science Citation Index Expanded
- • Scisearch
- • Web of Science
- • Emerging Sources Science Citation Index
About Journal
Peer review process, editorial board, article processing charge, article in press, current issue.
Peer Review
Highest quality of international peer review standard
Initial submission.
Select the right journal and submit your manuscript.
Manuscript Number
Our editors will communicate and send you the manuscript number. We officially begin processing your manuscript.
First Decision
Based on the outcome of the peer-review you would receive review comments from the international experts on your subject.
APC Invoicing
We will share the invoice that can be paid online using credit card or bank transfer. We also have option to convert the invoice in the desired currency.
Proofing & Correction
Once you are aware of the review comments then you can make minor changes based on the inputs and any corrections that should be done before we move ahead.
Indexing & Archiving
If your research is not easy to find, it cannot help advance science or scientific society. Post-publication of your research, indexing is the most important things we do at Surgical Case Reports. We aim to make all articles published with Surgical Case Reports easy to find by the widest audience and also work with search engines, social media platforms and scholarly communication networks.

Case Reports
Preparing your manuscript.
The title page should:
- "A versus B in the treatment of C: a randomized controlled trial", "X is a risk factor for Y: a case control study", "What is the impact of factor X on subject Y: A systematic review, A case report etc."
- or, for non-clinical or non-research studies: a description of what the article reports
- if a collaboration group should be listed as an author, please list the Group name as an author. If you would like the names of the individual members of the Group to be searchable through their individual PubMed records, please include this information in the “Acknowledgements” section in accordance with the instructions below
- indicate the corresponding author
The abstract should not exceed 350 words. Please minimize the use of abbreviations and do not cite references in the abstract. The abstract must include the following separate sections:
- Background: why the case should be reported and its novelty
- Case presentation: a brief description of the patient’s clinical and demographic details, the diagnosis, any interventions and the outcomes
- Conclusions: a brief summary of the clinical impact or potential implications of the case report
Three to ten keywords representing the main content of the article.
The Background section should explain the background to the case report or study, its aims, a summary of the existing literature.
Case presentation
This section should include a description of the patient’s relevant demographic details, medical history, symptoms and signs, treatment or intervention, outcomes and any other significant details.
Discussion (optional)
Author may add this section to discuss the implications of the outcomes from the case, any practical issues involved or any other issues not covered in other sections.
Conclusions
This should state clearly the main conclusions and include an explanation of their relevance or importance to the field.
Declarations
List of abbreviations
If abbreviations are used in the text they should be defined in the text at first use, and a list of abbreviations should be provided.
Ethics approval and consent to participate
Manuscripts reporting studies involving human participants, human data or human tissue must:
- include a statement on ethics approval and consent (even where the need for approval was waived)
- include the name of the ethics committee that approved the study and the committee’s reference number if appropriate
Studies involving animals must include a statement on ethics approval.
See our editorial policies for more information.
If your manuscript does not report on or involve the use of any animal or human data or tissue, this section is not applicable to your submission. Please state “Not applicable” in this section.
Consent for publication
If your manuscript contains any individual person’s data in any form, consent to publish must be obtained from that person, or in the case of children, their parent or legal guardian. All presentations of case reports must have consent to publish.
If your manuscript does not contain any individual persons data, please state “Not applicable” in this section.
Availability of data and materials
For all journals, SpringerOpen strongly encourages all datasets on which the conclusions of the manuscript rely to be either deposited in publicly available repositories (where available and appropriate) or presented in the main paper or additional supporting files, in machine-readable format (such as spreadsheets rather than PDFs) whenever possible. Please see the list of recommended repositories in our editorial policies.
For some journals, deposition of the data on which the conclusions of the manuscript rely is an absolute requirement. Please check the Criteria section for this article type (located at the top of this page) for journal specific policies.
For all journals, authors must include an “Availability of data and materials” section in their article detailing where the data supporting their findings can be found. If you do not wish to share your data, please state that data will not be shared, and state the reason.
For instructions on how to cite your data and format this section see preparation/style and formatting.
Competing interests
All financial and non-financial competing interests must be declared in this section. A competing interests form is available here . All authors of the manuscript should compete this form and return it to the corresponding author, who should upload these to the submission system along with the main manuscript.
See our editorial policies for a full explanation of competing interests. If you are unsure whether you or any of your co-authors have a competing interest please contact the editorial office.
All sources of funding for the research reported should be declared. The role of the funding body in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript should be declared.
Authors' contributions
The individual contributions of authors to the manuscript should be specified in this section.
Acknowledgements
Please acknowledge anyone who contributed towards the article who does not meet the criteria for authorship including anyone who provided professional writing services or materials.
Authors should obtain permission to acknowledge from all those mentioned in the Acknowledgements section.
See our editorial policies for a full explanation of acknowledgements and authorship criteria.
Group authorship: if you would like the names of the individual members of a collaboration Group to be searchable through their individual PubMed records, please ensure that the title of the collaboration Group is included on the title page and in the submission system and also include collaborating author names as the last paragraph of the “Acknowledgements” section. Please add authors in the format First Name, Middle initial(s) (optional), Last Name. You can add institution or country information for each author if you wish, but this should be consistent across all authors.
Please note that individual names may not be present in the PubMed record at the time a published article is initially included in PubMed as it takes PubMed additional time to code this information.
Authors' information
You may choose to use this section to include any relevant information about the author(s) that may aid the reader's interpretation of the article, and understand the standpoint of the author(s). This may include details about the authors' qualifications, current positions they hold at institutions or societies, or any other relevant background information. Please refer to authors using their initials. Note this section should not be used to describe any competing interests.
Endnotes should be designated within the text using a superscript lowercase letter and all notes (along with their corresponding letter) should be included in the Endnotes section. Please format this section in a paragraph rather than a list.
Examples of the Vancouver reference style are shown below.
See our editorial policies for author guidance on good citation practice.
Web links and URLs: All web links and URLs, including links to the authors' own websites, should be given a reference number and included in the reference list rather than within the text of the manuscript. They should be provided in full, including both the title of the site and the URL, as well as the date the site was accessed, in the following format: The Mouse Tumor Biology Database. http://tumor.informatics.jax.org/mtbwi/index.do . Accessed 20 May 2013. If an author or group of authors can clearly be associated with a web link, such as for weblogs, then they should be included in the reference.
Example reference style:
Article within a journal
Smith JJ. The world of science. Am J Sci. 1999;36:234-5.
Article within a journal (no page numbers)
Rohrmann S, Overvad K, Bueno-de-Mesquita HB, Jakobsen MU, Egeberg R, Tjønneland A, et al. Meat consumption and mortality - results from the European Prospective Investigation into Cancer and Nutrition. BMC Medicine. 2013;11:63.
Article within a journal by DOI
Slifka MK, Whitton JL. Clinical implications of dysregulated cytokine production. Dig J Mol Med. 2000; doi:10.1007/s801090000086.
Article within a journal supplement
Frumin AM, Nussbaum J, Esposito M. Functional asplenia: demonstration of splenic activity by bone marrow scan. Blood 1979;59 Suppl 1:26-32.
Book chapter, or an article within a book
Wyllie AH, Kerr JFR, Currie AR. Cell death: the significance of apoptosis. In: Bourne GH, Danielli JF, Jeon KW, editors. International review of cytology. London: Academic; 1980. p. 251-306.
OnlineFirst chapter in a series (without a volume designation but with a DOI)
Saito Y, Hyuga H. Rate equation approaches to amplification of enantiomeric excess and chiral symmetry breaking. Top Curr Chem. 2007. doi:10.1007/128_2006_108.
Complete book, authored
Blenkinsopp A, Paxton P. Symptoms in the pharmacy: a guide to the management of common illness. 3rd ed. Oxford: Blackwell Science; 1998.
Online document
Doe J. Title of subordinate document. In: The dictionary of substances and their effects. Royal Society of Chemistry. 1999. http://www.rsc.org/dose/title of subordinate document. Accessed 15 Jan 1999.
Online database
Healthwise Knowledgebase. US Pharmacopeia, Rockville. 1998. http://www.healthwise.org. Accessed 21 Sept 1998.
Supplementary material/private homepage
Doe J. Title of supplementary material. 2000. http://www.privatehomepage.com. Accessed 22 Feb 2000.
University site
Doe, J: Title of preprint. http://www.uni-heidelberg.de/mydata.html (1999). Accessed 25 Dec 1999.
Doe, J: Trivial HTTP, RFC2169. ftp://ftp.isi.edu/in-notes/rfc2169.txt (1999). Accessed 12 Nov 1999.
Organization site
ISSN International Centre: The ISSN register. http://www.issn.org (2006). Accessed 20 Feb 2007.
Dataset with persistent identifier
Zheng L-Y, Guo X-S, He B, Sun L-J, Peng Y, Dong S-S, et al. Genome data from sweet and grain sorghum (Sorghum bicolor). GigaScience Database. 2011. http://dx.doi.org/10.5524/100012 .
General formatting information
Manuscripts must be written in concise English. For help on scientific writing, or preparing your manuscript in English, please see Springer's Author Academy .
Quick points:
- Use double line spacing
- Include line and page numbering
- Use SI units: Please ensure that all special characters used are embedded in the text, otherwise they will be lost during conversion to PDF
- Do not use page breaks in your manuscript
File formats
The following word processor file formats are acceptable for the main manuscript document:
- Microsoft word (DOC, DOCX)
- Rich text format (RTF)
- TeX/LaTeX
Please note: editable files are required for processing in production. If your manuscript contains any non-editable files (such as PDFs) you will be required to re-submit an editable file if your manuscript is accepted.
For more information, see ' Preparing figures ' below.
Additional information for TeX/LaTeX users
You are encouraged to use the Springer Nature LaTeX template when preparing a submission. A PDF of your manuscript files will be compiled during submission using pdfLaTeX and TexLive 2021. All relevant editable source files must be uploaded during the submission process. Failing to submit these source files will cause unnecessary delays in the production process.
Style and language
For editors and reviewers to accurately assess the work presented in your manuscript you need to ensure the English language is of sufficient quality to be understood. If you need help with writing in English you should consider:
- Getting a fast, free online grammar check .
- Visiting the English language tutorial which covers the common mistakes when writing in English.
- Asking a colleague who is proficient in English to review your manuscript for clarity.
- Using a professional language editing service where editors will improve the English to ensure that your meaning is clear and identify problems that require your review. Two such services are provided by our affiliates Nature Research Editing Service and American Journal Experts . SpringerOpen authors are entitled to a 10% discount on their first submission to either of these services. To claim 10% off English editing from Nature Research Editing Service, click here . To claim 10% off American Journal Experts, click here .
Please note that the use of a language editing service is not a requirement for publication in Surgical Case Reports and does not imply or guarantee that the article will be selected for peer review or accepted. 为便于编辑和评审专家准确评估您稿件中陈述的研究工作,您需要确保文稿英语语言质量足以令人理解。如果您需要英文写作方面的帮助,您可以考虑:
- 获取快速、免费的在线 语法检查 。
- 查看一些有关英语写作中常见语言错误的 教程 。
- 请一位以英语为母语的同事审阅您的稿件是否表意清晰。
- 使用专业语言编辑服务,编辑人员会对英语进行润色,以确保您的意思表达清晰,并提出需要您复核的问题。例如我们的附属机构 Nature Research Editing Service 以及合作伙伴 American Journal Experts 都可以提供此类专业服务。SpringerOpen作者享受首次订单10%优惠,该优惠同时适用于两家公司。您只需点击以下链接即可开始。使用 Nature Research Editing Service的编辑润色10%的优惠服务,请点击 这里 。使用 American Journal Experts的10%优惠服务,请点击 这里 。
请注意,使用语言编辑服务并非在期刊上发表文章的必要条件,这也并不意味或保证文章将被选中进行同行评议或被接受。 エディターと査読者があなたの論文を正しく評価するには、使用されている英語の質が十分であることが必要とされます。英語での論文執筆に際してサポートが必要な場合には、次のオプションがあります:
- 高速なオンライン 文法チェック を無料で受ける。
- 英語で執筆する際のよくある間違いに関する 英語のチュートリアル を参照する。
- 英語を母国語とする同僚に、原稿内の英語が明確であるかをチェックしてもらう。
- プロの英文校正サービスを利用する。校正者が原稿の意味を明確にしたり、問題点を指摘し、英語を向上させます。 Nature Research Editing Service と American Journal Experts の2つは弊社と提携しているサービスです。SpringerOpenのジャーナルの著者は、いずれかのサービスを初めて利用する際に、10%の割引を受けることができます。Nature Research Editing Serviceの10%割引を受けるには、 こちらをクリックしてください 。. American Journal Expertsの10%割引を受けるには、 こちらをクリックしてください 。
英文校正サービスの利用は、このジャーナルに掲載されるための条件ではないこと、また論文審査や受理を保証するものではないことに留意してください。 영어 원고의 경우, 에디터 및 리뷰어들이 귀하의 원고에 실린 결과물을 정확하게 평가할 수 있도록, 그들이 충분히 이해할 수 있을 만한 수준으로 작성되어야 합니다. 만약 영작문과 관련하여 도움을 받기를 원하신다면 다음의 사항들을 고려하여 주십시오:
- 영어 튜토리얼 페이지 에 방문하여 영어로 글을 쓸 때 자주하는 실수들을 확인합니다.
- 귀하의 원고의 표현을 명확히 해줄 영어 원어민 동료를 찾아서 리뷰를 의뢰합니다
- 리뷰에 대비하여, 원고의 의미를 명확하게 해주고 리뷰에서 요구하는 문제점들을 식별해서 영문 수준을 향상시켜주는 전문 영문 교정 서비스를 이용합니다. Nature Research Editing Service 와 American Journal Experts 에서 저희와 협약을 통해 서비스를 제공하고 있습니다. SpringerOpen에서는 위의 두 가지의 서비스를 첫 논문 투고를 위해 사용하시는 경우, 10%의 할인을 제공하고 있습니다. Nature Research Editing Service이용시 10% 할인을 요청하기 위해서는 여기 를 클릭해 주시고, American Journal Experts 이용시 10% 할인을 요청하기 위해서는 여기 를 클릭해 주십시오.
영문 교정 서비스는 게재를 위한 요구사항은 아니며, 해당 서비스의 이용이 피어 리뷰에 논문이 선택되거나 게재가 수락되는 것을 의미하거나 보장하지 않습니다.
Data and materials
For all journals, SpringerOpen strongly encourages all datasets on which the conclusions of the manuscript rely to be either deposited in publicly available repositories (where available and appropriate) or presented in the main paper or additional supporting files, in machine-readable format (such as spread sheets rather than PDFs) whenever possible. Please see the list of recommended repositories in our editorial policies.
For some journals, deposition of the data on which the conclusions of the manuscript rely is an absolute requirement. Please check the Instructions for Authors for the relevant journal and article type for journal specific policies.
For all manuscripts, information about data availability should be detailed in an ‘Availability of data and materials’ section. For more information on the content of this section, please see the Declarations section of the relevant journal’s Instruction for Authors. For more information on SpringerOpen's policies on data availability, please see our editorial policies .
Formatting the 'Availability of data and materials' section of your manuscript
The following format for the 'Availability of data and materials section of your manuscript should be used:
"The dataset(s) supporting the conclusions of this article is(are) available in the [repository name] repository, [unique persistent identifier and hyperlink to dataset(s) in http:// format]."
The following format is required when data are included as additional files:
"The dataset(s) supporting the conclusions of this article is(are) included within the article (and its additional file(s))."
For databases, this section should state the web/ftp address at which the database is available and any restrictions to its use by non-academics.
For software, this section should include:
- Project name: e.g. My bioinformatics project
- Project home page: e.g. http://sourceforge.net/projects/mged
- Archived version: DOI or unique identifier of archived software or code in repository (e.g. enodo)
- Operating system(s): e.g. Platform independent
- Programming language: e.g. Java
- Other requirements: e.g. Java 1.3.1 or higher, Tomcat 4.0 or higher
- License: e.g. GNU GPL, FreeBSD etc.
- Any restrictions to use by non-academics: e.g. licence needed
Information on available repositories for other types of scientific data, including clinical data, can be found in our editorial policies .
What should be cited?
Only articles, clinical trial registration records and abstracts that have been published or are in press, or are available through public e-print/preprint servers, may be cited.
Unpublished abstracts, unpublished data and personal communications should not be included in the reference list, but may be included in the text and referred to as "unpublished observations" or "personal communications" giving the names of the involved researchers. Obtaining permission to quote personal communications and unpublished data from the cited colleagues is the responsibility of the author. Either footnotes or endnotes are permitted. Journal abbreviations follow Index Medicus/MEDLINE.
Any in press articles cited within the references and necessary for the reviewers' assessment of the manuscript should be made available if requested by the editorial office.
Preparing figures
When preparing figures, please follow the formatting instructions below.
- Figure titles (max 15 words) and legends (max 300 words) should be provided in the main manuscript, not in the graphic file.
- Tables should NOT be submitted as figures but should be included in the main manuscript file.
- Multi-panel figures (those with parts a, b, c, d etc.) should be submitted as a single composite file that contains all parts of the figure.
- Figures should be numbered in the order they are first mentioned in the text, and uploaded in this order.
- Figures should be uploaded in the correct orientation.
- Figure keys should be incorporated into the graphic, not into the legend of the figure.
- Each figure should be closely cropped to minimize the amount of white space surrounding the illustration. Cropping figures improves accuracy when placing the figure in combination with other elements when the accepted manuscript is prepared for publication on our site. For more information on individual figure file formats, see our detailed instructions.
- Individual figure files should not exceed 10 MB. If a suitable format is chosen, this file size is adequate for extremely high quality figures.
- Please note that it is the responsibility of the author(s) to obtain permission from the copyright holder to reproduce figures (or tables) that have previously been published elsewhere. In order for all figures to be open access, authors must have permission from the rights holder if they wish to include images that have been published elsewhere in non open access journals. Permission should be indicated in the figure legend, and the original source included in the reference list.
Figure file types
We accept the following file formats for figures:
- EPS (suitable for diagrams and/or images)
- PDF (suitable for diagrams and/or images)
- Microsoft Word (suitable for diagrams and/or images, figures must be a single page)
- PowerPoint (suitable for diagrams and/or images, figures must be a single page)
- TIFF (suitable for images)
- JPEG (suitable for photographic images, less suitable for graphical images)
- PNG (suitable for images)
- BMP (suitable for images)
- CDX (ChemDraw - suitable for molecular structures)
Figure size and resolution
Figures are resized during publication of the final full text and PDF versions to conform to the SpringerOpen standard dimensions, which are detailed below.
Figures on the web:
- width of 600 pixels (standard), 1200 pixels (high resolution).
Figures in the final PDF version:
- width of 85 mm for half page width figure
- width of 170 mm for full page width figure
- maximum height of 225 mm for figure and legend
- image resolution of approximately 300 dpi (dots per inch) at the final size
Figures should be designed such that all information, including text, is legible at these dimensions. All lines should be wider than 0.25 pt when constrained to standard figure widths. All fonts must be embedded.
Figure file compression
Vector figures should if possible be submitted as PDF files, which are usually more compact than EPS files.
- TIFF files should be saved with LZW compression, which is lossless (decreases file size without decreasing quality) in order to minimize upload time.
- JPEG files should be saved at maximum quality.
- Conversion of images between file types (especially lossy formats such as JPEG) should be kept to a minimum to avoid degradation of quality.
If you have any questions or are experiencing a problem with figures, please contact the customer service team at [email protected] .
Preparing tables
When preparing tables, please follow the formatting instructions below.
- Tables should be numbered and cited in the text in sequence using Arabic numerals (i.e. Table 1, Table 2 etc.).
- Tables less than one A4 or Letter page in length can be placed in the appropriate location within the manuscript.
- Tables larger than one A4 or Letter page in length can be placed at the end of the document text file. Please cite and indicate where the table should appear at the relevant location in the text file so that the table can be added in the correct place during production.
- Larger datasets, or tables too wide for A4 or Letter landscape page can be uploaded as additional files. Please see [below] for more information.
- Tabular data provided as additional files can be uploaded as an Excel spreadsheet (.xls ) or comma separated values (.csv). Please use the standard file extensions.
- Table titles (max 15 words) should be included above the table, and legends (max 300 words) should be included underneath the table.
- Tables should not be embedded as figures or spreadsheet files, but should be formatted using ‘Table object’ function in your word processing program.
- Color and shading may not be used. Parts of the table can be highlighted using superscript, numbering, lettering, symbols or bold text, the meaning of which should be explained in a table legend.
- Commas should not be used to indicate numerical values.
If you have any questions or are experiencing a problem with tables, please contact the customer service team at [email protected] .
Preparing additional files
As the length and quantity of data is not restricted for many article types, authors can provide datasets, tables, movies, or other information as additional files.
All Additional files will be published along with the accepted article. Do not include files such as patient consent forms, certificates of language editing, or revised versions of the main manuscript document with tracked changes. Such files, if requested, should be sent by email to the journal’s editorial email address, quoting the manuscript reference number.
Results that would otherwise be indicated as "data not shown" should be included as additional files. Since many web links and URLs rapidly become broken, SpringerOpen requires that supporting data are included as additional files, or deposited in a recognized repository. Please do not link to data on a personal/departmental website. Do not include any individual participant details. The maximum file size for additional files is 20 MB each, and files will be virus-scanned on submission. Each additional file should be cited in sequence within the main body of text.
Submit manuscript
- Editorial Board
- Sign up for article alerts and news from this journal
Affiliated with

Home » Case Studies » Knee » Case Study: Left Total Knee Replacement in a 62-year-old Male
Case Study: Left Total Knee Replacement in a 62-year-old Male
A 62-year-old male presented for evaluation of his left knee. Over the last seven months, he has had increasing knee pain and discomfort. He stated that in April he got up from a seated position and felt a “crack” within his knee.
He had earlier seen another physician who diagnosed him with a torn meniscus . He underwent a surgical arthroscopy, and following the procedure, his pain increased in severity. He saw another physician in August and was treated with a gel injection. He still had persistent pain and discomfort diffusely about his left knee joint.
He stated that he also gets some swelling in the back of the knee. The pain was sharp with weight-bearing and activities. He got a buckling sensation, clicking and limited range of motion. He described pain with transfers, his walking tolerance was less than a block. He used a cane as an assistive device.
He negotiated stairs one at a time with the use of the banister. He was on Percocet as well as Mobic. He also had a prior right total knee replacement a few years ago. He developed an infection three years after the procedure and underwent a two-staged revision with final reimplantation by an outside physician.
Currently, the right knee was minimally symptomatic, but he did develop a postoperative DVT (deep vein thrombosis) and pulmonary embolism requiring placement of an inferior vena cava filter three years ago. He had been on Coumadin therapy which was recently discontinued by her vascular surgeon. He had a history of low back pain and was going to pain management.
He was a retired school bus driver and currently lives with his wife. The patient was dismayed with the left knee pain and limited mobility secondary to pain. He was unable to do even basic tasks without pain and was apprehensive about climbing stairs. He was exploring the possibility of total knee replacement.
He was a past smoker having quit 30 years ago. Earlier he also had a trial of conservative management in the form of physical therapy and gel injections with minimal relief. He had a known drug allergy to Biaxin.
On his office visit, he was calm, conscious, cooperative and well oriented to time place and person. He walked with an antalgic gait with a reduced stance phase on the left side. The skin overlying the left skin demonstrated a well-healed scar suggestive of prior arthroscopic surgery.
There was mild swelling in the left knee. Pain and crepitus were present throughout the arch of motion. The range of movements was present from 10 degrees to 90 degrees. There was tenderness on the medial and lateral joint lines. Tenderness was also present on patellar facets.
There was mild genu varum deformity. There were no signs of instability or laxity in coronal, sagittal, and axial planes. The examination of the right knee revealed a well-healed anterior scar. The range of motion was full with no pain or stiffness.
The examination of the bilateral hip and ankle was normal. The neurological examination of the lower extremities was normal. The bulk and tone of both lower limbs were normal. The bilateral lower extremity pulses were palpable and comparable.
Imaging revealed severe tricompartmental osteoarthritis of the left knee with joint space reduction and osteophytes.
Considering the lifestyle limiting left knee pain, the patient was advised left knee total replacement. Risks, benefits, and alternatives were discussed with the patient at length. He agreed to undergo left total knee arthroplasty .

Anteroposterior and lateral view of the left knee
OPERATION: Left total knee replacement .
IMPLANTS USED: Posterior stabilized 8 left standard femoral component left-sided with tibia E left cemented with 14 x 30 stem with poly 16 mm with a 29-mm diameter poly patella.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent, signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure.
The patient, as well as the family, understood that he had increased risk of complications including, but not limited to infection and deep vein thrombosis and pulmonary embolism.
Anesthesia was obtained by the anesthesiologist. The patient was then definitely positioned, and the left knee was then draped and prepped in the usual sterile manner. A straight incision centered over the patella was used for the arthrotomy.
Skin and subcutaneous tissues were then incised. A medial parapatellar arthrotomy was then performed. The knee was then exposed and the femoral cutting guide was then placed into position. The distal cut was then performed. The anterior, posterior, and then the chamfer cuts were then performed.
Attention was then turned towards the tibia. The tibial cut was then performed. Lamina spreaders were used medially and laterally, and the remainder of the meniscus was then debrided. The notch cut was then performed and the femur was then placed into position followed by the tibia.
The tibia was then broached and the trial poly was then placed into position. The gap balancing was performed before the final broaching and was found to be correct. The patella was then resected. The drill holes were made in the patella and then the trial patella was then placed into position.
The knee was then reduced. The knee was then ranged through a full range of motion and the patellar tracking was found to be normal, and the gap balancing was then again checked and was found to be satisfactory.
The trial components were then removed. Thorough lavage was given. The femur was cemented into position. Excess cement was then removed. The tibia was then cemented into position. Excess cement was then removed. Poly was then placed over the tibia. The knee was then reduced.
The knee was then held in full extension and then the patella was cemented into position and held in position with a patellar clamp. The excess cement was removed after the cement hardened. The knee was injected with intraarticular injection and thorough lavage was given.
Medial parapatellar arthrotomy was closed with Ethibond, cutaneous tissues were closed with 0 Vicryl, subcuticular tissues were closed with 2-0 Vicryl, and skin was closed using staples. Sterile dressing was then applied, and the patient was then transferred to the postoperative care unit in stable condition.

Postoperative X-ray of the left showing the anteroposterior and lateral view with total knee prosthesis in position.
The patient had an excellent recovery post-op , his pain was managed well with medications. He was started on Aspirin 325 mg BID for deep vein thrombosis prophylaxis. He was able to walk 100 feet on the same day of the procedure. He was discharged the following day.
The sutures were taken off 14th-day post-op with no complications. There was no swelling of the calves and no neurological deficit of the lower extremities. The patient underwent physical therapy to strengthen muscles and increase range of motion of the joint.
Three months post-op , the patient was able to walk with no pain and a full range of motion. He was extremely happy with the outcome of the procedure and was back to his baseline activities.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
Call Us Now!
(631) 981-2663.
On your phone? Tap here to text us!
- Knee Cartilage Damage
- Posterior Cruciate Ligament
- Post Operative Knee Arthroscopy
- Patellofemoral Pain
- Patellofemoral Instability
- Meniscal Tear of the Knee
- Anterior Cruciate Ligament
- Knee Bursitis
- Medial & Lateral Collateral Ligament of the Knee
- Unicompartmental Knee Replacement
- Meniscus Tear
- 3D Knee Implant
Knee Services
- Total Knee Replacement
- Custom Knee Replacement
- Cartilage Injury & Management
- KneeCap Maltracking and Management
- High Tibial Osteotomy
- Subchondroplasty
- Total Knee Replacement Recovery Guide
- Cemented and Cementless Knee Replacement
- Knee Anatomy
- Achilles Tendon Injuries
- Revision Total Knee Replacement Surgery
- Cortisone Injection
- Knee Arthroplasty Implants
- Bilateral Knee Replacement (Simultaneous)
- Unstable Knee
- Knee Viscosupplementation
- Adjacent Segment Disease after Cervical Fusion
- Anterior Lumbar Interbody Fusion Surgery
- Cauda Equina Syndrome
- Hinged Knee Replacement
- Patient-Specific Knee Replacement – Customized Implants Vs Customized Cutting Blocks
- Iliotibial Band Syndrome
- Gender-Specific Knee Replacement
- Outpatient Knee Replacement
- Posterior Cruciate Ligament Injury
- Smart Total Knee Replacement for Healthcare Professionals
- Smart Total Knee Replacement
Knee Case Studies
- Left Total Knee Arthroplasty – 66 year old male
- Right Total Knee Arthroplasty – 51 year old male
- Custom Left Total Knee Replacement in a 66-year-old male
- Custom Total Knee Replacement in Left Knee Arthritis with prior Hardware on the Lateral Tibial Plateau
- Left Total Knee Replacement – 63 year old Female
- Case Study: Bilateral Custom Total Knee Replacement in a 72-year-old Male
- Customized Total Knee Replacement in a 59-year-old male
- Customized Total Knee Replacement in a 58-year-old female with Arthritis
- Left Custom Total Knee Arthroplasty in a 68-year-old male
- Custom Right Total Knee Arthroplasty – 62-year-old male
- Right Total Knee Replacement with Custom Instruments in a 67-year-old female
- Left Total Knee Replacement in a 68-year-old male
- Left Total Knee Replacement in a 62-year-old Male
- Right Total Knee Replacement in a 72-year-old female with Arthritis
- Right Total Knee Replacement with Custom Instruments in a 66-year-old male
- Right Custom Total Knee Replacement in a 68-year-old female
- Right Total Knee Replacement with Custom Instruments in a 60-year-old female with Avascular Necrosis of the Knee
- Left Custom Total Knee Replacement in a 74-year-old female
- Bilateral Customized Total Knee Replacement in a 72-year-old female
- Custom Right Total Knee Replacement in a 55-year-old Female with Prior ACL Reconstruction
- Bilateral Customized Total Knee Replacement in a 72-year-old patient with Arthritis
- Customized Left Total Knee Replacement in a 73-year-old Male
- Revision Total Knee Replacement in a 68-year-old male with prior Unicondylar Knee Replacement
- Bilateral Custom Total Knee Replacement in a 61-year-old male with Knee Arthritis & Genu Valgum Deformity
- Customized Left Knee Total Replacement in a 66-year-old female
- Customized Right Total Knee Replacement in a 73-year-old Male with Arthritis
- Custom Left Knee Total Replacement in a 68-year-old Female

My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
- Español ( Spanish )
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 36 wrong-site surgery: a preventable medical error.
Deborah F. Mulloy ; Ronda G. Hughes .
Affiliations
Surgery is one area of health care in which preventable medical errors and near misses can occur. However, until the 1999 Institute of Medicine report, To Err Is Human , 1 clinicians were unaware of the number of surgery-associated injuries, deaths, and near misses because there was no process for recognizing, reporting, and tracking these events. 2 Of great concern is wrong-site surgery (WSS), which encompasses surgery performed on the wrong side or site of the body, wrong surgical procedure performed, and surgery performed on the wrong patient. 3 This definition also includes “any invasive procedure that exposes patients to more than minimal risk, including procedures performed in settings other than the OR [operating room], such as a special procedures unit, an endoscopy unit, and an interventional radiology suite” 4 (p. 11). WSS is also defined as a sentinel event (i.e., an unexpected occurrence involving death or serious physical or psychological injures, or the risk thereof) by the Joint Commission (formerly called the Joint Commission on Accreditation of Healthcare Organizations), which found WSSs to be the third-highest-ranking event. 5
- Causes and Consequences of Wrong-Site Surgery
WSS can be a devastating experience for the patient and have a negative impact on the surgical team. 6 , 7 State licensure boards are imposing penalties on surgeons for WSS, 8 and some insurers have decided to no longer pay providers for WSS or wrong-person surgery, nor for leaving a foreign object in a patient’s body after surgery. 9 Surgery performed on the wrong site or wrong person has also often been held compensable under malpractice claims. Indeed, 79 percent of wrong-site eye surgery and 84 percent of wrong-site orthopedic claims resulted in malpractice awards. 10 , 11
WSSs are rare events, but we are learning more about their prevalence. Because reporting of sentinel events to the Joint Commission is voluntary, it could be that only 10 percent of actual WSSs are reported. 12 Researchers have confirmed that the Joint Commission’s numbers are low, finding wide variations in the number of WSSs: 1 out of 27,686 cases, 6 or 1 out of every 112,994 surgeries, 13 or 1 in 5 hand surgeons during their career, 7 or 1 out of 4 orthopedic surgeons with 25 years’ experience. 14 Regardless of the exact number of WSSs, they are seen as a preventable medical error if certain steps are taken and standardized procedures are implemented in the perioperative setting. 15 , 16
The incidence of reported WSS has increased in recent years. From the inception of the Joint Commission’s Sentinel Event program, the number of WSSs reported has increased from 15 cases in 1998, to a total of 592 cases reported by June 30, 2007. 17 Of these, WSSs most commonly occur in orthopedic or podiatric procedures, 5 general surgery, and urological and neurosurgical procedures. 17 In response to the occurrence of these preventable errors, the Joint Commission issued two National Patient Safety Goals on January 1, 2003 to target wrong-site surgery:
Goal 1 —to improve the accuracy of patient identification by using two patient identifiers and a “time-out” procedure before invasive procedures.
Goal 4 —to eliminate wrong-site, wrong-patient, and wrong-procedure surgery using a preoperative verification process to confirm documents, and to implement a process to mark the surgical site and involve the patient/family. 40
Both of these goals continue to be an ongoing priority for the Joint Commission. Yet with many surgical procedures traditionally performed only in acute care settings now being performed in freestanding surgical centers and physician offices—not necessarily all under the purview of the Joint Commission—surgeons, surgical teams, and patients need to be vigilant with all surgeries, particularly when the level of oversight and scrutiny may not be as high as in hospitals.
WSS is generally caused by a lack of a formal system to verify the site of surgery or a breakdown of the system that verifies the correct site of surgery. 18 In using root-cause analysis, a process that determines the underlying organizational causes or factors that contributed to an event, the Joint Commission found the top root causes of WSS to be communication failure (70 percent), procedural noncompliance (64 percent), and leadership (46 percent). 16 Other system and process causes are listed in Table 1 . Risk factors associated with WSS were identified as emergency cases, multiple surgeons, multiple procedures, obesity, deformities, time pressures, unusual equipment or setup, and room changes. 17
Causes of Wrong-Site Surgeries
- Universal Protocol for Preventing Wrong-Site Surgery
Early attempts to address the occurrence of WSS started with the American Academy of Orthopedic Surgeons (AAOS) and the North American Spine Society (NASS). After reviewing of 10 years of malpractice claims and polling its members, 21 AAOS developed an awareness campaign to encourage the marking of the right surgical site, called “Sign Your Site.” 22 But in practice, adding an additional warning such as “No” on the incorrect site and having the surgical team work together to verify the correct site helped the Sign Your Site program to be effective. 23 The NASS further refined the Sign Your Site process by adding more detail for the appropriate level and site of the spine in its “Sign, Mark, and X-ray” program, calling for marking the exact site and side of the spine with a radiopaque indicator, and put forth a checklist for patient and procedure verification. 24
In 2003, the Joint Commission convened a summit, including the AAOS and leaders from 23 other organizations, to address the continued escalation of reported WSS cases (i.e., sentinel events reported to the Joint Commission); and the impact of WSS on patients, their families, and health care professionals; and associated health care costs. The summit was specifically designed to bring health care professionals and others together to address and develop strategies to lessen or eliminate WSS. 14 A major outcome of the summit was creation of a protocol, The Universal Protocol for Preventing Wrong Site, Wrong Procedure, and Wrong Person Surgery TM (see Text Box 1 ). 20 This protocol was designed to be used in all areas where invasive procedures are performed within health care organizations, including nonoperating-room settings. The goal was to drastically reduce or eliminate completely the incidence of WSS by using a standardized routine and acceptable preoperative process of verifying the patient and the correct site, as well as the physician marking the site with his or her initials before the patient is sedated.
Wrong site, wrong procedure, wrong person surgery can be prevented. This Universal Protocol is intended to achieve that goal. It is based on the consensus of experts from the relevant clinical specialties and professional disciplines and is endorsed by (more...)
The Universal Protocol for WSS is based on prevention theories that drive safety practice in high-risk industries, such as aviation and development of nuclear weapons. The operating room is complex with “tight coupling” of processes that happen very quickly and cannot be turned off once started; failed parts cannot be isolated from other parts—resulting in an unsafe process. A model most often used to demonstrate this is the one described by Reason 25 as the Swiss cheese model, where error defenses breakdown or are not in place, resulting in patient harm. (See the chapter on human factors for more information on Reason’s model.)
By implementing a systems change required by the WSS protocol, the possibility of a WSS should be prevented. The three key elements of the Universal Protocol for WSS are (1) preoperative verification process, (2) marking the operative site, and (3) taking a time out. The Universal Protocol is to be used in ambulatory care, hospitals, critical access hospitals, and office-based settings. 20 Implementing and adhering to this protocol should eliminate WSS errors that can be attributable to interruptions, distractions, and too many forms or procedures. On July 1, 2004, the Joint Commission began to include these three key Universal Protocol elements in its accreditation process for health care organizations and also provided further guidance on its implementation (see Text Box 2 ).
These guidelines provide detailed implementation requirements, exemptions, and adaptations for special situations. Preoperative verification process
The Association of periOperative Registered Nurses (AORN), realizing the importance of the Universal Protocol for WSS, worked collaboratively with the Joint Commission to develop a Correct Site Surgery Tool Kit. The tool kit, designed to assist health care providers to implement the Universal Protocol for WSS in their facilities, was endorsed by the American College of Surgeons, American Society of Anesthesiologists, American Society for Healthcare Risk Management, American Hospital Association, and the American Association of Ambulatory Surgery Centers.
The AORN Correct Site Surgery Tool Kit contains a variety of resources to educate health care providers about the Universal Protocol for WSS and to assist them with its implementation. The resources include (1) an educational program on CD-ROM; (2) a pocket reference card outlining the steps necessary to promote patient identification, site marking, and the time out; (3) a template to facilitate development of a facility policy to implement the Universal Protocol for WSS; (4) a copy of the Universal Protocol for WSS and Guidelines for Implementing the Universal Protocol; (5) frequently asked questions of the Joint Commission and AORN; (6) letters to nurses, physicians, facility chief executive officers, and health care risk managers encouraging standard implementation of the Universal Protocol across all facilities; and (7) information for patients about the Universal Protocol for WSS and health care safety. This tool kit is available from AORN at http://www.aorn.org/PracticeResources/ToolKits/CorrectSiteSurgeryToolKit . In addition, AORN Standards, Recommended Practices, and Guidelines has a position statement on Correct Site Surgery that has additional information on preventing wrong site surgery. 39
Several other organizations have set forth tools and policies to prevent WSS. The Veterans Affairs National Center for Patient Safety put forth the Ensuring Correct Surgery and Invasive Procedures directive, based on root-cause analysis, that adds two steps to the Joint Commission’s Universal Protocol: ensuring the consent form is administered and used properly, and having two members of the surgical team review patient information and radiological images prior to the start of the surgery. 26 The OR briefing tool used at Johns Hopkins Hospital expands the time-out part of the Universal Protocol by prompting additional dialogue between the anesthesia care team, nursing, and the surgical team. 27 Additionally, the British National Patient Safety Agency has introduced a risk management tool, setting forth a process for double-checking and identifying who is accountable at each stage for ensuring surgical markings on the right site to avoid WSS. 28
- Research Evidence
There is limited research on wrong-site surgery. The majority of studies have been retrospective, chart reviews, case studies, and surveys of various professional organizations. The evidence table summarizes the most recent evidence related to WSS, specifically the three components of the Universal Protocol.
Evidence Table
Summary of Evidence Related to Wrong-Site Surgery
In two of the retrospective studies that investigated WSS broadly, Meinberg and Stern, 7 in a study relating to the Universal Protocol, found that nearly half of surgeons changed their preoperative practices in response to the Sign Your Site campaign. Since the campaign targeted orthopedic surgeons, they were more knowledgeable about the campaign and were more likely to have changed their practices. Kwaan and colleagues 6 identified 62 percent of WSS cases that could have been prevented had providers adhered to the Universal Protocol. In this study, the authors concluded that the Universal Protocol would not have prevented the remaining one-third of WSS documented cases because of errors initiated in weeks before surgery (e.g., wrong documentation, inaccurate labeling of radiological reports). In an analysis of quality improvement efforts, similar findings also indicated implementation challenges associated with staff nonadherence because the issue of laterality was not addressed in the policy and the process was vulnerable to communication failures during handoffs. 29
Preoperative Verification
In verifying that the right patient is to have the right surgery in the right location, one study found that when discrepancies occurred among clinicians, a review of the patient’s information could resolve the discrepancy. 30 Published guidelines assert the need for a checklist to itemize exactly what should be checked, but do not specify what should happen if a discrepancy occurs. 31
Marking the Site
Three different studies and one quality improvement project assessed aspects of site marking, included two different approaches in who actually marks the right site. All found challenges in ensuring that each surgical patient had the right site marked, therefore exposing patients to possible WSS. One study that surveyed a small number of surgeons on their site-marking practices following the establishment of national guidelines, found that their practices ranged from no marking to marking every patient, with some relationship to the type of surgery. 32 In approaching site marking from the point of view that it is the patient’s responsibility, instead of the surgeon having complete responsibility, DiGiovanni and colleagues 33 sought to have patients mark the right site after being given a set of instructions. They found that when patients (instead of someone from the surgical team) were asked preoperatively to mark “no” on the wrong foot or ankle, 60 percent of patients marked the site correctly.
The last study and quality improvement project assessed whether marking would cause other errors, because of the permanence of the ink, thereby discouraging site marking. The study found that marking the surgical site with a pen marker did not affect sterility or place a patient at a higher risk for infection. 34 The quality improvement project found that staff were not marking the right site because the ink upset breast cancer patients and was indelible on premature infants, and the policy did not address laterality. 29
Two studies found that the time out component can prevent the majority of WSS, but not all. 6 , 13 , 35 Another study found that when surgeons, anesthesiologists, and nurses were trained in doing a standardized 2-minute briefing prior to surgery, there were specific improvements in communication on the surgical site and side operated on. 36
- Evidence-Based Practice Implications
In response to continued WSS sentinel event reports, one of the Joint Commission’s National Patient Safety Goals continues to be to eliminate wrong-site, wrong-patient, and wrong-procedure surgery. Eliminating WSS errors requires a systems approach, institutionalizing robust systems to verify the correct site that adequately addresses potential causes of breakdowns in the system. Hospital and surgery center leaders and managers should evaluate their policies and procedures regarding WSS and marking the right site to ensure that no WSSs occur under any circumstances.
Adoption of the Universal Protocol standardizes preoperative preparations, improves function of the health care team, and should avert any potential for WSS. All health care personnel must be knowledgeable about the Universal Protocol and consistently adhere to the three key elements—patient identification, site mark, and time out—as outlined in the Universal Protocol to reduce the number of WSSs occurring in the United States.
The Universal Protocol for WSS should be adhered to on all applicable cases, as the operating room and procedural areas are highly coupled and complex areas that would be unlikely to be completely error proof. Measures should be taken that require less reliance on memory. For example, a surgical site mark is a measure to prevent reliance on memory. However, when involving patients in marking the surgical site, one needs to assess their physical, cognitive, and emotional ability. 31
All health care professionals have an obligation to comply with the Universal Protocol and to speak up if they feel patient safety is being compromised in any way. 37 Nurses, specifically perianesthesia nurses, should function as the patient’s advocate and foster procedures that ensure right-site surgery. 38
- Research Implications
There is little empirical evidence regarding prevention of WSS or quantitative evaluation of implementation of strategies to prevent WSS. Part of the problem with research in this area has been that the medical-error data are not easy to extract, and error data are often transferred to medical claims data and medical liability, further preventing the sharing of such data. Mandatory reporting of these data has just recently been required in some States. Consequently, there are gaps in the current evidence on wrong-site surgery. For example, there were no randomized controlled studies to evaluate the effect of the Universal Protocol on WSS. Research is needed to determine whether the patient’s risk for WSS is associated with the organization following the Joint Commission’s Universal Protocol or other standardized process, or with the effectiveness of the surgical team in communicating with each other. It is unknown how effective surgical teams are in complying with the protocol on a daily basis, and it is unknown what factors or barriers exist to implementing the Universal Protocol for WSS in facilities across the country.
The reported number of WSS cases continues to increase as health care organizations become more transparent to medical error. Many health care organizations, drawing on error-prevention theories and the experience of the aviation industry, recognize that through such transparencies, systems can change and result in better patient outcomes. However, it is unlikely that WSS will fully be reported because of industrywide report cards, fear of litigation, and difference of opinions. Although absolute numbers of WSS may not be striking, the consequences to the patient on whom it occurs are dire.
- Search Strategy
Both PUBMED® and CINAHL® databases between 1990 and March 2007 were searched, using wrong site surgery[keyword] OR wrong site surgery[subject heading]. This identified 239 citations. Citations were excluded for the following reasons: non-English, dealt only with disclosing errors or patient preferences, opinion/editorial pieces, news articles, or announcements. This left 68 articles for consideration in this review, 10 of which were considered as evidence.
- Cite this Page Mulloy DF, Hughes RG. Wrong-Site Surgery: A Preventable Medical Error. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 36.
- PDF version of this page (123K)
In this Page
Other titles in this collection.
- Advances in Patient Safety

Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Wrong-site craniotomy: analysis of 35 cases and systems for prevention. [J Neurosurg. 2010] Review Wrong-site craniotomy: analysis of 35 cases and systems for prevention. Cohen FL, Mendelsohn D, Bernstein M. J Neurosurg. 2010 Sep; 113(3):461-73.
- Prevention training of wrong-site spine surgery. [J Surg Educ. 2015] Prevention training of wrong-site spine surgery. Mesfin A, Canham C, Okafor L. J Surg Educ. 2015 Jul-Aug; 72(4):680-4. Epub 2015 Apr 15.
- Concept analysis: wrong-site surgery. [AORN J. 2015] Concept analysis: wrong-site surgery. Watson DS. AORN J. 2015 Jun; 101(6):650-6.
- Incidence of neurosurgical wrong-site surgery before and after implementation of the universal protocol. [Neurosurgery. 2013] Incidence of neurosurgical wrong-site surgery before and after implementation of the universal protocol. Vachhani JA, Klopfenstein JD. Neurosurgery. 2013 Apr; 72(4):590-5; discussion 595.
- Review [Wrong site surgery : Incidence, risk factors and prevention]. [Chirurg. 2015] Review [Wrong site surgery : Incidence, risk factors and prevention]. Ambe PC, Sommer B, Zirngibl H. Chirurg. 2015 Nov; 86(11):1034-40.
Recent Activity
- Wrong-Site Surgery: A Preventable Medical Error - Patient Safety and Quality Wrong-Site Surgery: A Preventable Medical Error - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Introduction
- Conclusions
- Article Information
Data are from the Michigan Surgical Quality Collaborative from January 1, 2012, through June 30, 2018. These data reflect practices at all hospitals included in the study.
Proportional use of robotic, laparoscopic, and open approaches for general surgical procedures are shown in the 4 years before and after hospitals began performing robotic general surgery. From 2012 to 2018, 23 of 73 hospitals (31.5%) in the Michigan Surgical Quality Collaborative started performing robotic general surgery. These data are restricted to those hospitals.
eTable 1. Trends in the Use of Open Surgery for Specific Procedures, 2012-2018
eTable 2. Trends in the Use of Laparoscopic Surgery for Specific Procedures, 2012-2018
eFigure. Proportion of Hospitals and Surgeons Performing Any Robotic General Surgery in Michigan, 2012-2018
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Sheetz KH , Claflin J , Dimick JB. Trends in the Adoption of Robotic Surgery for Common Surgical Procedures. JAMA Netw Open. 2020;3(1):e1918911. doi:10.1001/jamanetworkopen.2019.18911
Manage citations:
© 2024
- Permissions
Trends in the Adoption of Robotic Surgery for Common Surgical Procedures
- 1 Department of Surgery, University of Michigan, Ann Arbor
- 2 Center for Healthcare Outcomes and Policy, University of Michigan School of Medicine, Ann Arbor
- 3 currently a medical student at University of Michigan School of Medicine, Ann Arbor
Question Given concerns that robotic surgery is increasing for common surgical procedures with limited evidence and unclear clinical benefit, how is the use of robotic surgery changing over time?
Findings In this cohort study of 169 404 patients in 73 hospitals, the use of robotic surgery for all general surgery procedures increased from 1.8% to 15.1% from 2012 to 2018. Hospitals that launched robotic surgery programs had a broad and immediate increase in the use of robotic surgery, which was associated with a decrease in traditional laparoscopic minimally invasive surgery.
Meaning These findings highlight a need to continually monitor the adoption of robotic surgery to ensure that enthusiasm for new technology does not outpace the evidence needed to use it in the most effective clinical contexts.
Importance Increasing use of robotic surgery for common surgical procedures with limited evidence and unclear clinical benefit is raising concern. Analyses of population-based trends in practice and how hospitals’ acquisition of robotic surgical technologies is associated with their use are limited.
Objective To characterize trends in the use of robotic surgery for common surgical procedures.
Design, Setting, and Participants This cohort study used clinical registry data from Michigan from January 1, 2012, through June 30, 2018. Trends were characterized in the use of robotic surgery for common procedures for which traditional laparoscopic minimally invasive surgery was already considered a safe and effective approach for most surgeons when clinically feasible. A multigroup interrupted time series analysis was performed to determine how procedural approaches (open, laparoscopic, and robotic) change after hospitals launch a robotic surgery program. Data were analyzed from March 1 through April 19, 2019.
Exposures Initiation of robotic surgery.
Main Outcomes and Measures Procedure approach (ie, robotic, open, or laparoscopic).
Results The study cohort included 169 404 patients (mean [SD] age, 55.4 [16.9] years; 90 595 women [53.5%]) at 73 hospitals. The use of robotic surgery increased from 1.8% in 2012 to 15.1% in 2018 (8.4-fold increase; slope, 2.1% per year; 95% CI, 1.9%-2.3%). For certain procedures, the magnitude of the increase was greater; for example, for inguinal hernia repair, the use of robotic surgery increased from 0.7% to 28.8% (41.1-fold change; slope, 5.4% per year; 95% CI, 5.1%-5.7%). The use of robotic surgery increased 8.8% in the first 4 years after hospitals began performing robotic surgery (2.8% per year; 95% CI, 2.7%-2.9%). This trend was associated with a decrease in laparoscopic surgery from 53.2% to 51.3% (difference, −1.9%; 95% CI, −2.2% to −1.6%). Before adopting robotic surgery, hospitals’ use of laparoscopic surgery increased 1.3% per year. After adopting robotic surgery, the use of laparoscopic surgery declined 0.3% (difference in trends, −1.6%; 95% CI, −1.7% to −1.5%).
Conclusions and Relevance These results suggest that robotic surgery has continued to diffuse across a broad range of common surgical procedures. Hospitals that launched robotic surgery programs had a broad and immediate increase in the use of robotic surgery, which was associated with a decrease in traditional laparoscopic minimally invasive surgery.
Robotic surgery continues to diffuse across an increasingly broad range of surgical procedures. However, concerns have been raised that robotic surgery is more costly 1 , 2 and may be no more effective 3 , 4 than other established operative approaches, such as traditional laparoscopic minimally invasive and open surgery. With respect to costs, for example, robotic surgery has been associated with episode costs as much as 25% higher compared with laparoscopic surgery. There are also concerns about the rapid growth of robotic surgery in areas with limited evidence to support its use and little theoretical benefit or clinical rationale (eg, inguinal hernia repair). The US Food and Drug Administration (FDA) recently issued a warning against the use of robotic surgery for the treatment of breast and cervical cancers. 5 In their communication, they expressed concerns about the lack of epidemiologic data characterizing the use of robotic surgery in real-world practice settings. Current estimates are limited to single-center studies, 6 - 8 device manufacturers’ financial statements, 9 and claims data, which may be inaccurate owing to unreliable coding. 10 , 11 We used population-based data from a manually abstracted statewide clinical registry to characterize contemporary trends in the adoption of robotic surgery across a range of general surgical procedures, which now represent the largest market for the technology in the United States.
This cohort study used data from the Michigan Surgical Quality Collaborative (MSQC), an Agency for Healthcare Research and Quality–recognized patient safety organization. The MSQC represents a voluntary partnership between 73 Michigan hospitals and Blue Cross/Blue Shield of Michigan that focuses on clinical quality improvement for surgical care. Hospitals participating in the MSQC perform more than 90% of all surgical procedures in Michigan. The MSQC maintains a clinical registry using a standardized data collection platform, validated case-sampling methods, and trained nurse data abstractors at each participating site. Data accuracy is maintained through rigorous training, internal data audits, and annual site visits by MSQC program staff. This data source allowed us to identify robotic procedures with greater precision and accuracy than is possible using claims data. This study was approved by the University of Michigan institutional review board, which deemed the study exempt from informed consent owing to use of secondary data. This study was designed and reported in adherence to the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We used data from the complete MSQC clinical registry file to identify all inpatient and outpatient general surgical episodes from January 1, 2012, through June 30, 2018. Procedures were identified and categorized by Current Procedural Terminology codes. We focused on general surgical procedures, which represent the clinical domain with the largest growth in robotic surgery. These files include additional information on patient age, demographic characteristics, and comorbid conditions in addition to detailed procedural information (eg, operative approach and anesthesia type), postoperative complications, death, and resource use (readmissions and emergency department visits).
Our primary outcome of interest was the surgical approach—robotic, laparoscopic, or open. The MSQC data were manually abstracted, and data on surgical approach were derived directly from the operative reports rather than procedural codes. Procedures were considered robotic if surgeons reported using the surgical robot in their operative report. Cases in which a robotic procedure was unexpectedly converted to another approach (eg, conversion to open procedure for bleeding) were characterized as robotic because this was the original approach chosen by the surgeon.
Data were analyzed from March 1 through April 19, 2019. The purpose of this analysis was to characterize trends in the use of surgical approaches over time for common general surgical procedures. We first reported raw proportions that were not adjusted for patient or hospital characteristics. We evaluated trends by calculating the fold change in each approach over time by dividing the proportional use of robotic surgery in 2018 by the proportional use in 2012. We also calculated the annual increase or decrease in the proportional use of each approach using linear regression. The coefficient for study years, modeled as a continuous variable, is reported as the annual trend. We then replicated the overall analysis stratified by specific procedures to determine whether overall trends were influenced by changes in practice for certain procedures.
To determine how hospitals change their practices after they begin performing robotic surgery, we performed a multigroup interrupted time series analysis. During the study period, 23 of the 73 MSQC participating hospitals (31.5%) began performing robotic surgery (32 hospitals were already performing robotic surgery at the time that MSQC began collecting data on this approach in 2012). We determined the date of the first robotic general surgery procedure within each of the hospitals that adopted robotic surgery during the study period. We then centered all hospitals on this date and evaluated the trends in the proportional use of each approach in the years before and after the hospital performed its first robotic operation. We used linear splines to model absolute levels and trends in the periods before and after introduction of robotic surgery. This analysis was designed to test the incremental association of adopting robotic surgery with trends in surgical practice but not to make assumptions about what would have happened had the hospital not begun performing robotic surgery. Our primary analysis was not adjusted for specific procedures, but we generated estimates for each procedure group in a sensitivity analysis. We estimated cluster-robust standard errors to account for repeated observations within hospitals. We performed all statistical analyses using Stata, version 14.2 statistical software (StataCorp LLC).
Characteristics for the 169 404 patients and 73 hospitals are included in Table 1 . The mean (SD) age for all patients was 55.4 (16.9) years; 90 595 (53.5%) were women and 78 809 (46.5%) were men. Cholecystectomy was the most common operation (62 854 [37.1%]). Of the 73 hospitals included in the study, 31 (42.5%) had fewer than 200 beds and 11 (15.1%) had at least 500 beds. Sixty-two hospitals (84.9%) were teaching hospitals, and the mean (SD) total surgical volume was 12 068 (10 933) cases.
From January 2012 through June 2018, the use of robotic surgery for all general surgery procedures increased from 1.8% to 15.1% (8.4-fold change; slope, 2.1% per year; 95% CI, 1.9%-2.3%) ( Figure 1 and Table 2 ). During the same period, the use of both laparoscopic and open surgery declined. For example, the proportional use of open surgery was 42.4% in 2012 compared with 32.4% in 2018 (0.8-fold change; slope, −1.5% per year; 95% CI, −1.8% to −1.2%) (eTable 1 and eTable 2 in the Supplement ). Trends in robotic surgery use were similar for specific procedures, although for some, the magnitude of the increase was greater. For example, the use of robotic surgery for inguinal hernia repair increased from 0.7% to 28.8% from January 2012 through June 2018 (41.1-fold change; slope, 5.4% per year; 95% CI, 5.1%-5.7%).
The proportion of hospitals and surgeons performing robotic surgery increased from January 2012 through June 2018. For example, 8.7% of surgeons performed robotic general surgery in 2012 compared with 35.1% in 2018 (eFigure in the Supplement ). During the study period, 23 hospitals (31.5%) began performing robotic surgery. In those hospitals, the use of robotic surgery increased from 3.1% in the first year to 13.1% in the fourth year after hospitals began performing robotic general surgery operations (overall mean in first 4 years, 8.8%; slope, 2.8% per year; difference, 2.8% [95% CI, 2.7%-2.9%]) ( Figure 2 and Table 3 ). The use of laparoscopic surgery decreased from 53.2% to 51.3% after hospitals began performing robotic surgery (difference, −1.9%; 95% CI, −2.2% to −1.6%) ( Table 3 ). Before hospitals performed robotic surgery, a trend toward greater use of laparoscopic surgery occurred (slope, 1.3% per year). A trend toward less laparoscopic surgery after hospitals began performing robotic surgery occurred (slope, −0.3% per year; difference, −1.6%; 95% CI, −1.7% to −1.5%). Results remained the same when stratified across specific procedures.
This study used a unique, clinically oriented, and manually abstracted data source to characterize the use of robotic surgery across a wide range of common general surgical procedures. These data identify the correct procedure approach with greater precision and accuracy than claims. We found that the use of robotic surgery increased dramatically from 2012 to 2018. Although the use of robotic surgery increased across all procedures, for certain operations, such as inguinal hernia repair, practice patterns shifted by an order of magnitude toward greater use of robotics. We also found that the use of robotic surgery increased rapidly and diffused widely across numerous different procedures in the years after hospitals begin performing robotic surgery. This trend was associated with a decrease in the use of open and laparoscopic minimally invasive procedures, which for most surgeons was already considered a safe and effective approach when clinically feasible.
Recent work suggests that the United States now performs more robotic surgery than any other country in the world, although overall trends in other specialties (eg, urology) toward greater use of robotic surgery have been present for many years. 9 Based on robotic device manufacturers’ financial statements, procedure volumes exceeded 600 000 in 2017, with the largest and fastest growing contributor being the field of general surgery. 9 This finding suggests that the clinical footprint for robotic surgery will continue to increase as it has for more than a decade already. However, accurate data on how robotic surgery is being applied in contemporary practice is lacking. Prior studies are limited to single-center reports and claims-based analyses that may be inaccurate owing to unreliable coding. 6 - 8 , 10 , 11 This inaccuracy is problematic because it may limit our ability to understand the clinical implications of this rapid change in practice. It also limits the ability of policy makers and regulators to scope oversight or, more broadly, the public health implications of rapid changes in surgical practice.
Within this context, regulators from the FDA recently expressed safety concerns about the rapidly growing use of robotic approaches for certain cancer operations. 5 These concerns stem from the limited evidence of benefit (eg, fewer complications or better oncologic resection quality) for robotic surgery. For example, randomized clinical trials have failed to demonstrate the benefits of robotic surgery over other approaches in the treatment of rectal cancer 12 and have shown even potentially worse outcomes in procedures for cervical cancer. 4 Observational studies that compared robotic surgery with more established laparoscopic or open approaches have also failed to demonstrate superior outcomes after inguinal hernia repair, 8 kidney resections, 1 colectomy, 13 - 16 or cholecystectomy. 7 The discrepancy between the ongoing rapid adoption of robotic surgery and unclear clinical benefit highlights why accurate information on how it is being applied in contemporary surgical practice is necessary.
This study expands on prior work in several ways. We used manually abstracted data from a statewide surgical registry to ensure that our estimates reflect the true incidence of robotic surgery across a wide range of procedures, hospitals, and surgeons. Making further use of these unique data, we estimated how the initiation of robotic surgery within hospitals had broad associations with surgical practice for numerous procedures that differed in complexity, anatomical location, and surgical indications (eg, repair of a hernia vs removal of an organ). This investigation builds on existing literature, which has shown similar associations of an increase in robotic prostatectomy with hospital acquisitions of robotic systems. 17 We also demonstrate that increasing use of robotic surgery changed existing trends toward greater use of laparoscopic surgery. For many common and low-risk procedures, such as cholecystectomy, conventional laparoscopic surgery is already the accepted standard of care. Laparoscopic approaches are also less expensive and can be performed by most general surgeons without robotics. 18 This situation highlights a questionable trend: robotic surgery is replacing conventional laparoscopic approaches for procedures that may not be complex enough to warrant the consideration of an advanced, expensive, and unproven minimally invasive platform.
This study suggests that regulators and the surgical community can take additional steps to monitor the ongoing diffusion of robotic surgery and ensure that this trend does not lead to diminished patient safety. Because accurate data are necessary to inform the creation of appropriate safeguards, the FDA and the Centers for Medicare & Medicaid Services should consider providing coverage for robotic surgery with provisions for evidence development. 19 This process has been previously used by the Centers for Medicare & Medicaid Services to create registries of patients treated with new and unproven surgical technologies (eg, carotid artery stenting). Use of these provisions would facilitate greater understanding of how robotic procedures are being used in real-world practice. Akin to postmarket surveillance of pharmaceuticals, such provisions would also create a common data resource from which the comparative safety and effectiveness of robotic operations can be evaluated by numerous investigators.
This action would also allow hospitals, which provide credentials to perform robotic surgery, to better understand where sufficient evidence suggests plausible benefit. At present, surgeons are largely able to use robotic surgery for any procedure at their professional discretion. As has been shown in the FDA warning and through prior studies, this discretionary use may place patients at risk for poor outcomes. 3 Facilitating transparency around the allocation of robotic surgery would allow patients to make better collaborative decisions with their surgeons. After all, for many of the procedures we report in this study, little to no evidence suggests that robotic surgery increases patient safety or treatment effectiveness compared with other approaches.
Our results should be interpreted within the context of several limitations. Our clinical registry only captures data from Michigan and therefore may not be generalizable to the country as a whole. However, the MSQC represents a heterogeneous group of hospitals, surgeons, and practice settings. Furthermore, we report on the most common general surgery procedures performed in the United States. Changes in patient factors, such as obesity, may influence trends in procedure choice. Our estimates may therefore be limited by a lack of adjustment for patient characteristics. That said, adjusting for patient factors may introduce its own biases because no clinical consensus exists around how robotic procedures should be allocated. Much of this decision-making is based on case-by-case surgeon assessments and clinical nuance not captured in any registry. Our results are consistent across multiple different procedures, which also suggests that these trends are independent of unique clinical domains or disease processes. Our study is unable to account for how other nonclinical factors, such as marketing, may influence the adoption of robotic surgery. However, others have found that the chances of receiving robotic surgery were 2- to 5-fold greater in highly competitive vs noncompetitive health care markets. 20 Moreover, evidence suggests that hospitals immediately begin advertising their acquisition of robotic surgical services through web-based and conventional health system marketing campaigns. 21 These data are complementary to ours and suggest that the greatest forces driving robotic surgery adoption may be the technological imperative and economic pressures experienced by hospitals in certain health care markets.
This study found that robotic surgery is rapidly diffusing across a broad range of common general surgical procedures. Trends toward greater use of the robotic platform appeared to occur rapidly after hospitals begin performing robotic surgery and were associated with a decrease in the use of established minimally invasive techniques, such as laparoscopic surgery. This trend was consistent across numerous specific procedures, even those for which conventional laparoscopic surgery is already considered standard of care and for which robotic surgery offers little theoretical clinical benefit to the patient. These findings highlight a need to continually monitor the diffusion of robotic surgery to ensure that enthusiasm for a new technology does not outpace the evidence needed to use it in the most effective clinical contexts.
Accepted for Publication: November 14, 2019.
Published: January 10, 2020. doi:10.1001/jamanetworkopen.2019.18911
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2020 Sheetz KH et al. JAMA Network Open .
Corresponding Author: Kyle H. Sheetz, MD, MSc, Center for Healthcare Outcomes & Policy, University of Michigan School of Medicine, 2800 Plymouth Rd, NCRC Bldg 16, Room 100N-11, Ann Arbor, MI 48109 ( [email protected] ).
Author Contributions: Drs Sheetz and Dimick had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All authors.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: Sheetz, Dimick.
Statistical analysis: All authors.
Obtained funding: Dimick.
Administrative, technical, or material support: Dimick.
Supervision: Dimick.
Conflict of Interest Disclosures: Dr Dimick reported receiving personal fees from ArborMetrix, Inc, outside the submitted work and being an equity owner of ArborMetrix, Inc. No other disclosures were reported.
Funding/Support: This study was supported grants 2T32HS000053-27 (Dr Sheetz) and R01HS023597 (Dr Dimick) from the Agency for Healthcare Research and Quality and grant R01AG039434 from the National Institute on Aging, National Institutes of Health.
Role of the Funder/Sponsor: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Case Studies in Surgery International Peer-Reviewed and Open Access Journal for Surgical Specialists
Journal Metrics
Google-based Impact Factor (2019): 0.24
h-index (August 2019): 2
i10-index (August 2019): 0
h5-index (August 2019): N/A
h5-median (August 2019): N/A
Editor-in-Chief
- Other Journals
- For Readers
- For Authors
- For Librarians
Announcements
- Recruitment
Case Studies in Surgery
Authors are encouraged to submit complete, unpublished, original works that are not under review in any other journals. The journal is published in both print and online versions. The online version is free access and download.
Areas include but are not limited to:
- Head and Neck Surgery
- General Surgery
- Surgical Oncology
- Neurosurgery
- Cardiovascular Surgery
- Gastrointestinal Surgery
- Thoracic Surgery
- Emergency Surgery
- Gynecologic surgery
- Oral and Maxillofacial Surgery
- Ophthalmology
- Otolaryngology
- Orthopedics Surgery
- Plastic Surgery
- Minimally Invasive Surgery
- Microsurgery
Original Articles, Case Reports, Case Studies, Reviews.
2023: Articles Received: 0; Accepted: 1; Rejected: 0; Published: 1; Retracted: 0
2022: Articles Received: 2; Accepted: 1; Rejected: 1; Published: 1; Retracted: 0
2021: Articles Received: 4; Accepted: 1; Rejected: 0; Published: 2; Retracted: 0
2020: Articles Received: 2; Accepted: 2; Rejected: 0; Published: 1; Retracted: 0
2019: Articles Received: 11; Accepted: 10; Rejected: 0; Published: 10; Retracted: 0
2018: Articles Received: 22; Accepted: 16; Rejected: 6; Published: 15; Retraced: 0
2017: Articles Received: 39; Accepted: 22; Rejected: 3; Published: 22; Retraced: 0
2016: Articles Received: 56; Accepted: 35; Rejected: 10; Published: 35; Retraced: 0
---------------------------------------------------------------------
What is e-Version First TM
e-Version First is a feature offered through our journal platform. It allows PDF version of manuscripts that have been peer reviewed and accepted, to be hosted online prior to their inclusion in a final printed journal. Readers can freely access or cite the article. We aim to publish accepted manuscripts in e-Version First in two weeks' time after the final draft completed.
Paper Selection and Publication Process
a) Upon receipt of a submission, the editorial assistant sends an e-mail of confirmation to the submission’s author within one to three working days. If you fail to receive this confirmation, your submission e-mail may have been missed.
b) Peer review. We use a double-blind system for peer review; both reviewers’ and authors’ identities remain anonymous. The paper will be reviewed by at least two experts: one editorial staff member and at least one external reviewer. The review process may take four to ten weeks.
c) Notification of the result of review by e-mail.
d) If the submission is accepted, the authors revise paper and pay the Article Processing Charge.
e) A PDF version of the journal is available for download on the journal’s website, free of charge.
The publisher and journal have a policy of “ Zero Tolerance on the Plagiarism ”. We check the plagiarism issue through two methods: reviewer check and plagiarism prevention tool ( ithenticate.com ).
All submissions will be checked by iThenticate before being sent to reviewers.
Vol 9, No 1 (2023)
Table of contents, case report.
Case Studies in Surgery ISSN 2377-7311(Print) ISSN 2377-732X(Online)
Copyright © Sciedu Press
Post-Processing Applied to Brain Tumor Surgery: Case studies
- Conference paper
- First Online: 31 May 2024
- Cite this conference paper

- Fernando Icazatti 10 ,
- Juan Pablo Graffigna 10 ,
- Pablo Barceló 11 ,
- Rocio Buenamaizon 10 , 11 &
- Ricardo Berjano 11
Part of the book series: IFMBE Proceedings ((IFMBE,volume 106))
Included in the following conference series:
- Congreso Argentino de Bioingeniería
This paper introduces the implementation of post-processing techniques applied to the fusion, segmentation, and 3D reconstruction of studies involving patients with brain tumors. The objective of this study is to emphasize the interdisciplinary collaboration that facilitates synergy between the academic and clinical environments, involving various medical specialties and bioengineering. Two cases are presented where a coordinated generation of clinically relevant scenes has been achieved to visualize key regions for surgery. The employed studies and the obtained results regarding surgical planning are described for each case.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Barrow, D.L., Bendok, B.R.: Introduction: what is neurosurgery? Operative Neurosurg. 17 (Supplement_1), S1–S2 (2019). https://doi.org/10.1093/ons/opz071
Article Google Scholar
Snell, R.S.: Clinical neuroanatomy. Lippincott Williams & Wilkins (2010)
Google Scholar
Bear, M., Connors, B., Paradiso, M.A.: Neuroscience: exploring the brain, enhanced edition: exploring the brain. Jones & Bartlett Learning (2020)
Greenberg, M.S.: Handbook of Neurosurgery, 7th edn. Greenberg Graphics, Tampa, FL (2010)
Miner, R.C.: Image-guided neurosurgery. J. Med. Imag. Radiat. Sci. 48 (4), 328–335 (2017)
Ayache, Nicholas, et al. (eds.) Medical Image Computing and Computer-Assisted Intervention--MICCAI 2012: 15th International Conference, Nice, France, October 1–5, 2012, Proceedings, Part III. vol. 7512. Springer (2012)
Chowdhary, C.L., Acharjya, D.P.: Segmentation and feature extraction in medical imaging: a systematic review. Procedia Comput. Sci. 167 , 26–36 (2020)
Mikhail, M., Mithani, K., Ibrahim, G.M.: Presurgical and intraoperative augmented reality in neuro-oncologic surgery: clinical experiences and limitations. World Neurosurg. 128 , 268–276 (2019). https://doi.org/10.1016/j.wneu.2019.04.256
Hainc, N., Reinhardt, J., Stippich, C.: Functional Magnetic Resonance Imaging. Neuroimaging Techniques in Clinical Practice: Physical Concepts and Clinical Applications (2020)
Pieper, S., Halle, M., Kikinis, R.: 3D slicer. In 2004 2nd IEEE international symposium on biomedical imaging: nano to macro (IEEE Cat No. 04EX821), pp. 632–635. IEEE (2004)
Liu, X., Wang, M., Song, Z.: Multi-modal image registration based on multi-feature mutual information. J. Med. Imag. Hlth. Inform. 9 (1), 153–158 (2019)
Pinter, C., Lasso, A., Fichtinger, G.: Polymorph segmentation representation for medical image computing. Comput. Methods Programs Biomed. 171 , 19–26 (2019). https://doi.org/10.1016/j.cmpb.2019.02.011
Download references
Author information
Authors and affiliations.
Instituto de Bioingeniería, Facultad de Ingeniería, Universidad Nacional de San Juan, San Juan, Argentina
Fernando Icazatti, Juan Pablo Graffigna & Rocio Buenamaizon
Hospital Descentralizado Dr. Guillermo Rawson, San Juan, Argentina
Pablo Barceló, Rocio Buenamaizon & Ricardo Berjano
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Rocio Buenamaizon .
Editor information
Editors and affiliations.
Instituto de Ingeniería y Agronomía, National University Arturo Jauretche, Florencio Varela, Buenos Aires, Argentina
Fernando Emilio Ballina
EMBS IEEE technical committee on Cardiopulmonary Systems and Physiology-based Engineering, Piscataway, NJ, USA
Ricardo Armentano
Facultad de Ingeniería, Universidad Nacional de Entre Ríos, Oro Verde, Argentina
Rubén Carlos Acevedo
Instituto de Investigaciones Científicas y Tecnológicas en Electrónica, Universidad Nacional de Mar del Plata, Mar del Plata, Argentina
Gustavo Javier Meschino
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper.
Icazatti, F., Graffigna, J.P., Barceló, P., Buenamaizon, R., Berjano, R. (2024). Post-Processing Applied to Brain Tumor Surgery: Case studies. In: Ballina, F.E., Armentano, R., Acevedo, R.C., Meschino, G.J. (eds) Advances in Bioengineering and Clinical Engineering. SABI 2023. IFMBE Proceedings, vol 106. Springer, Cham. https://doi.org/10.1007/978-3-031-61960-1_58
Download citation
DOI : https://doi.org/10.1007/978-3-031-61960-1_58
Published : 31 May 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-61959-5
Online ISBN : 978-3-031-61960-1
eBook Packages : Engineering Engineering (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Venovenous bypass in adult liver transplant recipients: A single-center observational case series
Roles Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Department of Anaesthesia, Austin Health, Heidelberg, Australia, Department of Critical Care, Austin Health, The University of Melbourne, Heidelberg, Australia
Roles Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Anaesthesia, Austin Health, Heidelberg, Australia
Roles Data curation, Visualization, Writing – review & editing
Roles Data curation, Writing – review & editing
Roles Conceptualization, Formal analysis, Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Anesthesiology and Pain Medicine, Dongguk University Ilsan Hospital, Goyang, Republic of Korea
Roles Data curation, Validation, Writing – review & editing
Roles Data curation, Validation, Writing – original draft
Affiliation Department of Surgery, Austin Health, The University of Melbourne, Heidelberg, Australia
Roles Visualization, Writing – original draft
Roles Conceptualization, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing
- Laurence Weinberg,
- Rebecca Caragata,
- Riley Hazard,
- Jarryd Ludski,
- Dong-Kyu Lee,
- Hugh Slifirski,
- Patrick Nugraha,
- Daniel Do,
- Wendell Zhang,

- Published: May 31, 2024
- https://doi.org/10.1371/journal.pone.0303631
- Peer Review
- Reader Comments
Very little information is currently available on the use and outcomes of venovenous bypass (VVB) in liver transplantation (LT) in adults in Australia. In this study, we explored the indications, intraoperative course, and postoperative outcomes of patients who underwent VVB in a high-volume LT unit.
The study was a single-center, retrospective observational case series of adult patients who underwent VVB during LT at Austin Health in Melbourne, Australia between March 2008 and March 2022. Information on baseline preoperative status and intraoperative variables, including specific VVB characteristics as well as postoperative and VVB-related complications was collected. The lengths of intensive care unit and hospital stays as well as intraoperative and in-hospital mortality were recorded.
Of the 900 LTs performed at this center during the aforementioned 14-year period, 27 (3%) included a VVB procedure. VVB was performed electively in 16 of these 27 patients (59.3%) and as a rescue technique to control massive bleeding in the other 11 (40.1%). The median (interquartile range [IQR]) age of those who underwent VVB procedures was 48 (39–55) years; the median age was 56 (47–62) years in the non-VVB group ( p <0.0001). The median model for end-stage liver disease (MELD) scores were similar between the two patient groups. Complete blood data was available for 622 non-VVB patients. Twenty-six VVB (96.3%) and 603 non-VVB (96.9%) patients required intraoperative blood transfusions. The median (IQR) number of units of packed red blood cells transfused was 7 (4.8–12.5) units in the VVB group compared to 3.0 units (1.0–6.0) in the non-VVB group ( p <0.0001). Inpatient mortality was 18.5% and 1.1% for the VVB and non-VVB groups, respectively ( p <0.0001). There were no significant differences in length of hospital stay or incidence of acute kidney injury, primary graft dysfunction, or long-term graft failure between the two groups. Patients in the VVB group experienced a higher rate of postoperative non-anastomotic biliary stricture compared to patients in the non-VVB group (33% and 7.9%, respectively; p = 0.0003).
Conclusions
VVB continues to play a vital role in LT. This case series highlights the heightened risk of major complications linked to VVB. However, the global transition to selective use of VVB underscores the urgent need for collaborative multi-center studies designed to address outstanding questions and parameters related to the safe implementation of this procedure.
Citation: Weinberg L, Caragata R, Hazard R, Ludski J, Lee D-K, Slifirski H, et al. (2024) Venovenous bypass in adult liver transplant recipients: A single-center observational case series. PLoS ONE 19(5): e0303631. https://doi.org/10.1371/journal.pone.0303631
Editor: Robert Jeenchen Chen, Stanford University School of Medicine, UNITED STATES
Received: August 21, 2023; Accepted: April 29, 2024; Published: May 31, 2024
Copyright: © 2024 Weinberg et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Traditional surgical techniques used for liver transplantation (LT) procedures involve full cross-clamping and resection of the retrohepatic inferior vena cava (IVC) and temporary clamping of the portal vein. This can result in significant hemodynamic perturbations, including a reduction in venous return and cardiac output, distal venous congestion, and organ hypoperfusion [ 1 ]. Veno-venous bypass (VVB) was first popularized in the 1980s in an attempt to minimize these physiologic insults and maintain intraoperative hemodynamic stability [ 2 ]. Many variations in VVB set-up and technique as well as numerous approaches to vascular access have been developed [ 3 , 4 ].
The performance of caval anastomoses with or without VVB continues to be a subject of debate. A rigorous Cochrane analysis examined the advantages and disadvantages of this procedure and reported that there was insufficient evidence available to support or dismiss the use of VVB in LT [ 5 ]. As part of this analysis, the authors evaluated the evidence that directly compared LT procedures performed with or without VVB. Of note, no significant differences in renal failure or blood transfusion requirements were identified. However, all trials identified featured a high risk of bias, and none reported on patient or graft survival.
More recently, an expert panel at a consensus conference on Enhanced Recovery for Liver Transplantation evaluated the routine application of VVB during LT and identified length of hospital stay, duration of surgery, units of packed red blood cells (PRBCs) transfused, early complication rates and mortality, and renal dysfunction as critical significant outcomes for patients undergoing VVB [ 6 ]. A comprehensive re-evaluation of the current literature and assessments focused on VVB during LT revealed that the quality of evidence for all outcomes of significance was extremely poor. The authors reported that most of the studies that compared outcomes of LT procedures involving VVB to those with no VVB reported no significant differences in duration of surgery [ 7 – 13 ], units of PRBCs transfused [ 7 – 14 ], early postoperative mortality [ 9 , 12 , 14 ], postoperative acute kidney injury [ 7 – 9 , 11 – 13 , 15 , 16 ], early complication rates [ 10 , 12 , 16 ], or length of hospital stay [ 8 , 11 , 12 ]. The expert panel advised against the routine implementation of VVB, but acknowledged that there are specific circumstances in which its use may be justified.
The potential benefits of VVB in a select patient cohort include improved hemodynamic stability during the anhepatic phase secondary to preservation of venous return, decreased blood loss associated with portal hypertension, and preservation of blood flow to other vital organs [ 17 , 18 ]. Furthermore, some patients with metabolic or cholestatic liver disease, even in the absence of portal hypertension, are at an increased risk of portal congestion and may require VVB or a temporary portocaval shunt. VVB can promote diversion of blood flow in cases with complex anatomy and/or difficult surgical exposure (i.e., massive hepatomegaly), facilitate decompression of the portal-mesenteric circulation to reduce bacterial translocation secondary to intestinal congestion [ 19 ], and limit diffuse abdominal bleeding from venous collaterals [ 20 ]. Finally, VVB can also be considered in cases of fulminant hepatic failure as a means to maintain venous return, thereby reducing the need for excess fluids that can exacerbate intracranial hypertension and potential cerebral edema.
VVB has many associated disadvantages, with reported complication rates ranging from 10% to 30% [ 21 ]. Complications associated with vascular access include hematomas, wound infections, and lymphoceles as well as injuries to the brachial plexus and major vasculature. Additionally, the use of extracorporeal circuits may lead to hypothermia, air emboli, and thromboembolic complications. Overall, there is little to no high-quality evidence regarding the benefits and risks of VVB [ 6 ].
Advances in surgical methodology, notably, the increased use of caval-sparing surgical techniques (e.g., piggyback or cavo-cavostomy), had led to a gradual global decline in the routine use of VVB [ 22 ]. However, significant inter-institutional variations remain [ 23 ]. Recent surveys suggest that 42% of transplant centers across the United States and up to 38% of centers within European networks still offer selective use of VVB [ 24 , 25 ].
At this time, there is little information regarding the uptake, safety, and outcomes of VVB in LT centers in Australia. This observational study was designed to characterize contemporary practices at a major Australian center and describe baseline characteristics, intraoperative course, specific VVB complications, and postoperative outcomes experienced by patients who have undergone LTs with VVB. As part of this case series, we aimed to explore ongoing indications for this procedure as well as the practicalities of VVB use in this modern era of selective use.
Ethical approval
This case series was registered retrospectively with the Australian New Zealand Clinical Trials Registry (no. 12623000499684) on May 16, 2023. Ethical approval was obtained from the Austin Health Human Research Ethics Committee on July 27, 2023 (HREC: 545–2022). The Ethics Committee waived the requirement for informed consent because the study was limited to the retrospective collection of de-identified data. There were no changes to the original study protocol at any stage of the work. Data analysis was performed only after obtaining ethical approval. Data were collected for research purposes on July 27, 2023. All data were de-identified and data analysis was completed on August 15, 2023.
Study population, data sources, and variables
The study features a single-center retrospective, observational case series of patients who underwent a LT procedure at Austin Health between March 2008 and March 2022. Austin Health is a university teaching hospital located in Melbourne, Australia, and the site of the Victorian Liver Transplant Unit. More than 1,600 LTs have been performed to date at this unit. The unit currently performs ~100 LTs per year. The adult recipient program at this LT unit uses only deceased donor grafts. Inclusion criteria included adult patients (i.e., those ≥18 years of age) who received VVB as part of their LT procedure for any indication, including redo LTs, and patients who received elective (planned) or emergent (rescue) VVB. Patients who did not receive VVB were included as controls. Paediatric LT recipients (i.e., those <18 years of age) were excluded.
Data were collected from the hospital’s electronic medical record system and the prospectively maintained database of the transplant unit. Information was extracted regarding the prevalence of VVB, baseline patient characteristics and comorbidities, and preoperative biochemical, hematological, and coagulation profiles. Intraoperative variables included surgical time, indications for VVB use, nature of the bypass circuits, vascular access sites, laboratory findings, anesthesia management, administration of blood products, and fluid management. With respect to postoperative outcomes, we extracted information related to a broad range of perioperative complications, which were stratified by severity using the Clavien-Dindo classification system [ 26 ]. Finally, we evaluated the lengths of intensive care unit and hospital stays as well as intraoperative and in-hospital mortality. The study was conducted in accordance with Surgical CAse REport (SCARE) guidelines [ 27 ].
VVB management
The decision to implement planned or emergency use of VVB for intraoperative rescue was made contemporaneously by the treating surgical and anesthesiology teams based on clinician preferences and clinical concerns. Planned VVB was considered in patients with severe portal hypertension in which a difficult hepatectomy was anticipated (i.e., total portal vein thrombosis with the need for vascular grafts or previous liver procedures in which decompression of the portal system had been performed to prevent excessive blood loss). Planned VVB was also considered for patients with massive livers, in which IVC clamping would be necessary for vascular occlusion needed to facilitate surgery (i.e., polycystic liver disease). In cases in which the diseased liver was so large that it would be difficult to access the major hepatic vasculature in the absence of portal hypertension, VVB was used to divert blood from the infrarenal IVC (and therefore the kidneys, lower limbs, and pelvis) to the right heart to facilitate decompression of the portal circulation and reduced congestion of the intestinal and splanchnic circulation.
Implementation of VVB was also considered in patients with pre-existing cardiac conditions, such as aortic stenosis or severe left ventricular outflow obstruction as a means to maintain adequate venous return to the right heart, thereby reducing the risk of cardiac decompensation and collapse with subsequent organ hypoperfusion. VVB was also employed as an “on-table” rescue intervention in patients who had undergone massive blood loss to facilitate vascular access needed to control bleeding while maintaining hemodynamic stability by ensuring adequate venous return to the right heart.
Likewise, the use of specific vascular access sites and techniques (cutdown versus percutaneous) were at the discretion of the treatment teams. When employed, the percutaneous approach was performed under ultrasound guidance; transesophageal echocardiography was used for the placement of all upper-body venous return lines. Cannulation was achieved using 16–18 Fr FemFlex cannulae (Edwards Lifesciences). A Cardiohelp ™ (Maquet) extracorporeal membrane oxygenation (ECMO) console with an integrated centrifugal pump, oxygenator, and heat exchanger (HLS Module Advanced 7.0) was used at flow rates between 1–3 L/min. Heparin-bonded circuits were employed; systemic heparin was administered if required to target activated clotting time between 180 and 220 seconds. All VVB procedures were supervised by a dedicated clinical perfusionist.
Statistical analysis
All statistical analysis was performed with GraphPad Prism version 10.2.2 for macOS (GraphPad Software, Boston, Massachusetts USA). Continuous variables were evaluated for normality assumption using Shapiro’s test and visual check of Q-Q plots. Data are presented with mean ± standard deviation (SD), median (1 st – 3 rd quartiles) [minimun:maximum], or number of cases (percentile) for the descriptive statistics. Both the (single) t test (and nonparametric) analysis was used to compare two groups of values. Fishers exact test or the Chi-Square test was used to determine whether a statistically significant association existed between two categorical variables. A 2-sided P value below 0.05 was considered statistical significance based on the null hypothesis significance testing.
Of the 900 LT procedures performed at our center between March 2008 and March 2023, 27 (3%) included VVB. The information presented in Table 1 outlines the preoperative characteristics of these 900 patients. Patients who underwent LTs with VVB (VVB group) were younger and had lower body mass indexes (BMIs) than LT patients who did not undergo VVBs (non-VVB group); the median (IQR) ages were 48 (39–55) years versus 56 years (47–62) years (p <0.0001), respectively, and the median BMIs were 25.0 (21.4–28.9) kg/m 2 versus 27 (24.1–31.2) kg/m 2 ( p = 0.001). The underlying primary liver pathologies are also summarized in Table 1 . The median (IQR) model for end-stage liver disease (MELD) scores were similar between the two groups, at 20 (9–26) versus 8 (13–24) for the VVB and non-VVB groups, respectively ( p = 0.868). We observed no significant changes in the yearly median MELD scores of all patients in these groups over the entire 14-year period ( p = 0.329).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Data are presented as number s (percentages) or medians (interquartile ranges) [minimum and maximum].
https://doi.org/10.1371/journal.pone.0303631.t001
Most of the VVB patients underwent caval-sparing surgical procedures (93%); only two patients (7%) were treated with conventional caval interposition. Table 2 summarizes the intraoperative course of this cohort, including the surgical and anesthetic management used in these cases. VVB was instituted as a planned procedure in 16 of 27 patients (59.3%); the remaining 11 (40.7%) required rescue VVB intraoperatively. Elective indications for VVB predominantly reflected anatomic complexity, including polycystic liver disease, massive hepatomegaly (from other causes), tumor proximity to the IVC (a large segment one lesion), and a previous transjugular intrahepatic portosystemic shunt procedure. In one case, VVB was initiated electively because of pre-existing cardiac disease (mixed aortic regurgitation and stenosis in a patient with a unicuspid valve). All 11 emergency cases underwent VVB to address massive intraoperative bleeding.
Data are presented as numbers (proportions), medians (interquartile ranges), and [minimum and maximum].
https://doi.org/10.1371/journal.pone.0303631.t002
The different types of VVB circuits used at our center are shown in Figs 1 and 2 . Most of the VVB procedures (85%) were performed with double-limb venous bypass circuits with concurrent systemic and portal venous drainage lines. Three patients were treated with single-limb circuits with either portal or systemic venous drainage alone (7% and 4%, respectively). Systemic venous drainage was achieved using an open surgical cut-down approach in 78% of the patients, most commonly via a groin incision targeting the femoral-saphenous veins or, in one case, via the infrahepatic IVC (within the operative field). Return venous cannulae were most commonly positioned in the internal jugular veins (63%) using a percutaneous approach. Surgical cut-downs of the left axillary vein were performed less frequently (33%). Detailed data related to the VVB circuit setup were missing from the handwritten operative report included in one patient record.
https://doi.org/10.1371/journal.pone.0303631.g001
https://doi.org/10.1371/journal.pone.0303631.g002
Use of blood and blood products
The use of blood and blood products is summarized in Table 3 . A similar proportion of patients received an intraoperative PRBC transfusion. However, the median (IQR) number of PRBCs transfused was 7 (4.8–12.5) units in the VVB group versus 3.0 (1.0–6.0) units in the non-VVB group ( p <0.0001). While similar proportions of patients in each group received platelets and cryoprecipitate, a higher fraction of the patients in the VVB group (81.5%) received fresh frozen plasma compared to the non-VVB group (58%, p = 0.016). Of the patients who required blood or blood products, patients in the VVB group received significantly more units than those in the non-VVB group ( Table 3 ). Intraoperative and postoperative arterial blood gas data are presented in the S1 File .
Only patients with complete medical records were included. Data are presented as number (proportion), median (interquartile ranges), and [minimum and maximum].
https://doi.org/10.1371/journal.pone.0303631.t003
Length of stay and complications
The perioperative complications and postoperative outcomes of patients in both the VVB and non-VVB groups are presented in Table 4 . Two patients (7.4%) in the VVB group died during the procedure; both of these patients required emergency rescue VVB. Four other patients experienced complications that were directly attributed to the VVB procedure. One patient sustained a guidewire injury to the right heart that resulted in cardiac tamponade (Clavien Dindo Grade 3b), while another experienced an injury to the left subclavian artery that led to hemothorax and significant blood loss (Clavien Dindo Grade 3b). Both complications occurred during the percutaneous insertion of the return cannula into the internal jugular veins. There was also a single case of a groin wound seroma related to a saphenous cut-down site, which did not require further management. One patient experienced a small-volume air embolism which resulted in transient intraoperative hypoxia and right heart dysfunction albeit with no long-term sequelae.
Data are presented as numbers (proportions) and medians (interquartile ranges [IQRs]).
https://doi.org/10.1371/journal.pone.0303631.t004
While a substantially higher proportion of patients in the VVB group needed to return to the operating room for treatment of postoperative bleeding (85.2% versus 13.6%, p <0.0001), the incidence of hepatic artery thrombosis, major neurological complications, acute kidney injury, and postoperative sepsis were similar between the two groups ( Table 4 ). Although the inpatient mortality was 18.5% in the VVB group, compared to 1.1% in the non-VVB group ( p <0.0001). we observed no significant differences in length of hospital stay, primary graft nonfunction, or long-term graft failure. Interestingly, patients in the VVB group had a higher rate of postoperative non-anastomotic biliary stricture compared to patients in the non-VVB group (33% versus 7.9%; p = 0.0003).
In this retrospective single-center study, 3% of patients undergoing LT experienced an intraoperative VVB procedure. While no significant differences were observed between the VVB and non-VVB groups with respect to length of hospital stay, acute kidney injury, primary graft nonfunction, or long-term graft failure, VVB use was associated with a higher long-term incidence of non-anastomotic strictures and a greater need for blood products. The inpatient mortality of patients who underwent a VVB procedure was 18.5%. Our findings suggest that while VVB continues to play a vital role in LT in our center, the high rate of postoperative complications and perioperative mortality underscore an urgent need for collaborative multi-center studies that address appropriate implementation and patient selection.
There has been a global trend away from routine use of VVB, largely due to the absence of high-quality evidence supporting its benefit. An earlier Cochrane review [ 5 ] and a more recent systematic review [ 6 ] highlighted the limited evidence available that could be interpreted as supporting or opposing the routine use of VVB in LT, noting specifically the small number of published trials and the high risk of bias. Many of the technical aspects of LT procedures are based largely on individual institutional protocols and preferences, and recent survey data suggest that VVB continues to be employed selectively in up to 38–42% of transplant centers across Europe and the United States [ 24 , 25 ].
Among our most noteworthy findings, our results revealed that nearly one in five patients who underwent VVB procedures died in the immediate perioperative period. One alternative to VVB is the use of a temporary portocaval shunt (PCS). A PCS involves an end-to-side connection between the portal vein and infrahepatic IVC to reduce portal venous pressure, alleviate congestion in the splanchnic bed, and prevent intestinal edema. In our practice, the utilization of portocaval shunt (PCS) is not a standard procedure. In our institution, PCSs are employed in patients who do not have portal hypertension, for example, those with fulminant liver failure and no collateral blood vessels. This approach facilitates and optimizes hemodynamics during the anhepatic phase and helps prevent bowel edema. With VVB, we routinely place a cannula in the femoral vein and portal veins, obviating the necessity for a portocaval shunt. However, there is currently a contentious debate over the effectiveness of PCS in improving the outcomes of LT procedures. A recent systematic review with expert panel recommendations concluded that the routine use of PCS during LT procedures should be discouraged [ 6 ]. However, the expert panel did recognize a temporary PCS might be beneficial in certain rare cases and reiterated the need for multicenter, prospective randomized trials designed to delineate the immediate and short-term outcomes associated with its routine use. The results of several studies revealed that the implementation of PCSs is associated with a lower requirement for blood transfusion [ 7 , 28 – 32 ] and reduced hospital lengths of stay [ 32 ].
Our case series provides important insight into the selective use of VVB during LT during the modern era at a major Australian transplant center. Among the unique features of our study, the indications for VVB at our center differ subtly from the broader range featured in previous reports. Within our cohort, elective VVB was performed nearly exclusively in patients with complex surgical anatomy; our series included only one case in which this procedure was performed in a patient with cardiac disease and concerns regarding hemodynamic stability. Furthermore, at its inception, VVB was described as an alternative to complete caval clamping. As such, traditional indications for this procedure focused on clinical scenarios in which impaired venous return would be poorly tolerated, including pre-existing ventricular impairment, pulmonary hypertension, proven instability after test-clamping, and limited venous collateralization (i.e., fulminant liver failure and/or non-cirrhotic metabolic disease) [ 21 , 33 ]. At our center, we predominantly employ methods that support caval preservation; thus, these indications are arguably less relevant.
Of note, our series included one patient with Budd-Chiari syndrome, which is historically described as a contraindication to VVB, given the potential increase in thromboembolic risk [ 2 ]. Shaw et al. [ 2 ] previously reported a case of fatal pulmonary embolism during the initiation of a bypass procedure in a patient with polycystic liver disease and massive hepatomegaly with IVC obstruction. They attributed the fatality to the contributions of a pre-existing thrombus and advocated for caution when performing VVB procedures in these patients. Interestingly, 40% of our case cohort (n = 12) included nine patients with polycystic liver disease and an additional three patients with massive hepatomegaly secondary to other causes. While we observed no intraoperative thrombotic complications during VVB, one patient experienced a postoperative pulmonary embolus on day 6 that did not result in hemodynamic compromise. The optimal approach to anticoagulation during VVB also remains to be determined. There is very little high-quality evidence supporting or refuting current systemic anticoagulation practices or the choice of different circuit types (i.e., heparin-bonded) [ 5 ].
Potentially life-threatening complications associated with vascular access needed for VVB are clearly documented in the literature [ 4 , 34 ]. Two patients in our series sustained significant access-associated vascular injuries. One patient sustained a guidewire injury to the right heart which led to cardiac tamponade that required intraoperative evacuation. The patient ultimately recovered uneventfully. A second case involved an injury to the left subclavian artery that resulted in a massive hemothorax. A large-gauge venous “return” cannula was inserted into the left internal jugular vein. Although the left axillary vein can be used for venous access via a surgical cut-down on an elective basis, it was not considered in this case because of ongoing massive bleeding. The right internal jugular vein was also not suitable for cannulation as it was the access site used for the delivery of fluids and high-dose vasoconstrictor agents. In this case, VVB was attempted as a rescue technique during uncontrollable abdominal bleeding from collateral vessels. Line insertion was technically difficult due to concurrent hypovolemia and venous collapse. Ultimately, the patient experienced an asystolic arrest secondary to hemorrhagic shock and died intraoperatively. This case emphasizes the amplified risks of vascular complications while establishing rescue bypass from the left internal jugular vein, even while using ultrasound and transesophageal echocardiography to guide the cannulation and catheter placement. For these reasons, the right internal jugular vein is our institution’s preferred access site for the VVB "return" cannulae. Compared to the left internal jugular vein, the right jugular vein runs more superficially and has a larger diameter [ 35 ] with an unhindered straight passage to the right atrium. Although transesophageal echocardiography is invaluable for guiding line insertion [ 36 ], as demonstrated in this case, its use does not completely preclude the development of vascular complications.
Clinical scenarios prompting the consideration of emergency bypass inherently involve co-existing physiologic insults, including hemorrhagic shock, prolonged vascular clamping, and organ hypoperfusion. Of the five in-hospital deaths included in our series, four were emergency rescue VVB cases. The issue of selection bias in VVB cohort studies has been acknowledged (38); this phenomenon may be further intensified when addressing the subset of patients who underwent bypass procedures as a rescue intervention. For example, results from previous studies revealed that patients who underwent VVB procedures had significantly higher MELD scores compared to those who did not [ 13 , 37 ]. By contrast, the VVB patients featured in our case series exhibit a relatively modest median MELD score of 20. The comparatively low MELD score reported for patients in our series reflects the large proportion of polycystic cases. However, in isolation, MELD scores may not fully characterize predicted surgical complexity, which was an overriding issue in our VVB cohort and a potential contributor to patient morbidity.
Overall, our complication rates were comparable to those reported in other VVB studies [ 21 ]. Apart from the major vascular access complications described above, our cohort also included one case of non-fatal air embolism, which presented as self-limiting hypoxia and transient right ventricular dysfunction. Although air emboli as a complication of VVB have been documented in previous studies [ 3 ], its overall incidence may be underestimated. Of note, we demonstrated a comparatively low rate of local complications that develop due to open vascular access. While 78% of systemic venous drainage lines at our center were achieved via femoral-saphenous cut-downs, nine patients (33%) underwent open axillary access for the placement of venous return cannulae. Nonetheless, we identified only one case of a wound-site seroma, which required no further management. Similarly, the median number of PRBCs transfused in patients in the VVB group was 7 units, which is consistent with the transfusion rates reported in other studies [ 20 ]. Finally, the use of VVB procedures was previously associated with the development of hypothermia [ 34 ]. Although 31% of our cohort experienced hypothermia (body temperature <35 °C at any point during the procedure), the median low temperature was a relatively robust 35.5 °C. This result may reflect the incorporation of a heat exchanger within the extracorporeal circuit.
Our study features several important strengths. The data collected for this study included a detailed exploration of baseline characteristics, intraoperative management, and postoperative outcomes. This enabled us to provide a comprehensive description of the pre- and perioperative state and evaluate how and for whom the practitioners at our center chose to implement VVB. Secondly, we have compared the preoperative characteristics and major outcomes of VVB patients to those who did not undergo this procedure.
The study also includes several limitations. Firstly, the findings reflect adult surgical practice at a single center and thus cannot be generalized to other institutions or pediatric LT recipients. Furthermore, the retrospective approach may have prevented us from capturing data from patients in whom VVB was deemed indicated but not initiated (e.g., due to inadequate vascular access or lack of an available perfusionist). It would be useful to identify these patients and explore the reasons why a planned VVB procedure was aborted as this would permit us to assess issues that affect the utilization of this resource. Finally, our case series is derived from a contemporary era with only a limited collection of long-term mortality data.
In conclusion, VVBs were used in 3% of the LT procedures performed at a single center in Australia over a 14-year period. While elective indications predominantly reflected unique anatomical and surgical factors, emergency use was universally precipitated by massive intraoperative bleeding. The complications associated with VVB use were comparable to those reported in other studies. While inpatient mortality of patients who underwent VVB was significantly higher than in LT patients who did not undergo this procedure, we observed no significant differences in length of hospital stay as well as rates of acute kidney injury, primary graft nonfunction, and long-term graft failure. Patients who underwent a VVB procedure exhibited a higher rate of postoperative non-anastomotic biliary stricture. While VVB continues to play a vital role in LT in general, the global transition to selective VVB use underscores the urgent need for collaborative multi-center studies designed to address outstanding questions related to patient selection and the safe implementation of this procedure.
Supporting information
S1 file. intra and postoperative arterial blood gas data for veno-venous bypass patients..
Data are presented as median (interquartile range) and [minimum maximum].
https://doi.org/10.1371/journal.pone.0303631.s001
- View Article
- PubMed/NCBI
- Google Scholar
- Open access
- Published: 01 June 2024
Risk factors of pneumothorax in computed tomography guided lung nodule marking using autologous blood: a retrospective study
- Shaohang Wu 1 na1 ,
- Jianyang Wu 1 na1 ,
- Junkai Xiong 1 ,
- Chengbin Huang 1 ,
- Yiwei Lin 1 ,
- Jun Guan 1 &
- Jianxin Xu 1
Journal of Cardiothoracic Surgery volume 19 , Article number: 317 ( 2024 ) Cite this article
Metrics details
To investigate the risk factors of pneumothorax of using computed tomography (CT) guidance to inject autologous blood to locate isolated lung nodules.
In the First Hospital of Putian City, 92 cases of single small pulmonary nodules were retrospectively analyzed between November 2019 and March 2023. Before each surgery, autologous blood was injected, and the complications of each case, such as pneumothorax and pulmonary hemorrhage, were recorded. Patient sex, age, position at positioning, and nodule type, size, location, and distance from the visceral pleura were considered. Similarly, the thickness of the chest wall, the depth and duration of the needle-lung contact, the length of the positioning procedure, and complications connected to the patient’s positioning were noted. Logistics single-factor and multi-factor variable analyses were used to identify the risk factors for pneumothorax. The multi-factor logistics analysis was incorporated into the final nomogram prediction model for modeling, and a nomogram was established.
Logistics analysis suggested that the nodule size and the contact depth between the needle and lung tissue were independent risk factors for pneumothorax.
The factors associated with pneumothorax after localization are smaller nodules and deeper contact between the needle and lung tissue.
Peer Review reports
Lung cancer is the most common cause of cancer death in men and women. Owing to the widespread use of lung cancer screening programs, thoracic surgeons currently encounter an increasing number of patients with isolated nodules in the lungs. The widespread use of high-resolution and thin-layer computed tomography (CT) has enabled the detection of significantly small lung nodules [ 1 ]. CT reveals early lung tumors usually as pulmonary nodules (PNs) [ 2 , 3 , 4 ]. Early diagnosis and treatment of this PN type are usually performed through video-assisted thoracoscopic surgery (VATS) [ 5 , 6 , 7 ]. Many small nodules are pathologically confirmed to be cancerous during removal [ 8 ]. The accurate localization of small PNs and ground glass nodules remains challenging in thoracoscopic surgery, and effective preoperative positioning can help thoracic surgeons quickly locate tumor nodules during surgery [ 9 ]. In addition, liquid material (methylene blue, iodide oil, medical glue, barium sulfate, radionuclide, and autologous blood), solid material, and other (ultrasonic positioning and near-infrared scanning) positioning technologies can be effective [ 10 , 11 ]. Regarding the preoperative positioning technology for PN, the most reported invasive preoperative positioning methods are CT-guided Hook-wire and micro-spring ring positioning [ 12 ]. Menginghua et al. [ 13 ] reported that the total incidence of complications was 48.04% in the Hook-wire group and 33.85% in the micro-coil group, including pneumothorax, pulmonary hemorrhage, and chest pain. Previous studies [ 14 ] and Wu Gao’s report [ 15 ] demonstrated CT-guided injection of autologous blood to locate small PNs as a simple, intuitive, effective, and economical method. In this study, autologous blood was used for preoperative PN localization, and the complications and risk factors associated with CT-guided autoblood localization of small PNs were analyzed. The complications usually included pneumothorax, pulmonary hemorrhage, hemoptysis, and pain.
General information
This is a retrospective cohort study. Patients with isolated PNs located through the injection of autologous blood before VAST between November 2019 and March 2023 in the First Hospital of Putian City were included. There is no current unified standard for indicating PN puncture location; the process is primarily based on the comprehensive deduction of the nodule type and the distance from the pleura. Participants met the following criteria: ① solid nodule with a major axis diameter ≤ 1.5 cm and distance from visceral pleura ≥ 0.5 cm; ② pure ground glass nodules; and ③ the diameter of the main axis of the mixed grinding glass nodule was ≤ 2 cm and the distance from the pleura was ≥ 0.5 cm. The exclusion criteria were as follows: presence of ① pulmonary vascular lesions or lesions close to pulmonary large vessels; and ② severe cardiopulmonary insufficiency or bleeding tendency. Finally, 92 patients (44 males and 48 females) were enrolled in this study and were aged 54 ± 12 (range: 23–80) years. This study was approved by the Institutional Ethics Committee. All patients signed informed consent before positioning and VATS.
The data collected included demographic information, imaging features of the nodules (nodule nature, nodule size, nodule location, shortest distance from visceral pleura, and pleural depression sign), laboratory indicators before localization (forced vital capacity[FVC], forced expiratory volume in the first second/forced vital capacity[FEV1/FVC], maximal voluntary ventilation[MVV], white blood cell[WBC], and emphysema), position at localization, depth of needle insertion, depth of needle to lung tissue contact, contact time, the duration of localization surgery, the complications of localization surgery, operation mode, operation time, and pathological diagnosis.
Successful definition of the marker is the presence of a visible autoblood stain on the visceral pleura at the time of thoracoscopy. Successful localization was defined as the localization of nodules using staining marks with/without autoblood stains or the guidance of pinholes on the visceral pleura, dissection, and radiographic excision in excised specimens.
CT-guided autologous blood localization
According to the preoperative imaging examination, the appropriate position was selected, and the distance between the nodules and the chest wall and parietal pleura was measured using chest CT thin-slice scanning(GE Healthcare, USA). Subsequently, the puncture site, needle insertion level, and needle insertion path were determined. Next, 5 mL of the patient’s autologous blood was extracted before using a puncture. After local lidocaine anesthesia, A percutaneous lung puncture was performed with a 20G puncture needle produced by CareFusion(address: Zona France las Americas, km,22-E-1. Santo Domingo. Dominican Republic) under the cooperation and guidance of radiology technicians. The shape path of the needle tip was adjusted according to timely CT 3D guidance, and it was finally located in the normal lung parenchyma approximately 1 cm around the small nodule. Autologous blood was injected next to the lesion, and the needle was gradually withdrawn. Furthermore, autologous blood was injected into the lung parenchyma through the path to the subpleural area (distance from pleura < 1 cm). After completion, CT was repeated to confirm the positioning effect and rule out complications such as pneumothorax and hemothorax (Fig. 1 a). After localization, the patient returned to the ward and underwent thoracoscopic surgery the same day or the next day.

Computed tomography (CT)-guided autologous blood injection to locate isolated pulmonary nodules and intraoperative images. A . Chest CT shows a pure ground-glass nodule with a diameter of 0.7 cm in the left inferior lobe of the lungs (black arrow). In the patient’s lateral position, a CT-guided lung puncture was performed to inject autologous blood within 1 cm of the lesion (red arrow). B . Intraoperative pinholes (yellow arrows) and focal blood stains (white arrows) are seen under thoracoscopy
Statistical analysis
Demographic information, imaging features of nodules, and data related to localization surgery of small PNs in thoracic surgery before autologous blood localization were retrospectively analyzed, and the complications of localization surgery in each group were recorded, including pneumothorax, pulmonary hemorrhage, hemoptysis, and pain. SPSS25.0 software was used for the statistical analysis. The Shapiro–Wilk test was used to evaluate normality. Continuous variables are expressed as mean and standard deviation (SD) or median and interquartile range(IQR), and counting data are expressed as frequency (n) and percentage (%). Logistics regression was used for single-factor analysis, and potential risk factors with P < 0.2 were obtained. Multivariate analysis was conducted using logistics regression to determine independent risk factors for pneumothorax. P < 0.05 was considered to be a statistically significant difference. The multi-factor logistics analysis was incorporated into the final nomogram prediction model for modeling. The identification and calibration of the model were evaluated. The bootstrap method was applied for further internal verification, and a nomogram was established.
Ethical review
This study was reviewed by the Ethics Committee of Putian First Hospital. All patients signed informed consent before the surgery.
PN localization was successful in 89 cases (96.7%), Such as Fig. 1 b, and failed in 3. All PNs were successfully removed by VATS without any conversion to thoracotomy. The general clinical data of patients are shown in Table 1 . There were 92 nodules (44 males and 48 females; age 54 ± 12 [range: 23–80] years). There were 62 and 30 nodules in the non-inferior and inferior lobes, respectively. There were 12 solid, 77 ground glass, and 3 cystic nodules. The median nodule diameter was 0.9 cm (range: 0.5–2.0 cm). The median vertical distance between the nodules and the nearest pleura was 1.2 (range: 0–4.0) cm. FVC was 3.042 ± 0.772 L, FEV1/FVC was 85.755 ± 10.265%, MVV was 92.847 ± 26.403 L/min, and the median WBC was 6.01 (range: 3.15–10.74) E9/L. The median needle tip distances from the skin and the pleura were 6.3 (range: 3.6–11.2) and 2.2 (range: 0.9–4.6) cm, respectively. The median contact time between the puncture needle and lung tissue was 5 (range: 2–26) min, and the median total positioning time was 18 (range: 7–51) min. Sixteen cases (17.3%) had mild pneumothorax (the lung collapse rate in patients with pneumothorax was less than 20%) and no dyspnea; therefore, no indignant chest tube was placed. Two cases (2.0%) had mild pulmonary hemorrhage (found under thoracoscopic vision). However, there were no evident manifestations of hemoptysis; therefore, it was not identified before VAST, and there was no special treatment. All patients walked back to the ward without significant pain. The overall complication rate was 17.3% (16 of 92) (two patients had concurrent mild pneumothorax and pulmonary hemorrhage), and there were no serious complications.
Single-factor analysis showed that FVC, MVV, WBC, depth of needle-to-lung tissue contact, tumor size, and nodule nature were the risk factors of pneumothorax in PNs located using autologous blood. Multivariate logistic regression analysis was used to study the risk factors for pneumothorax. The results showed that the depth of needle-to-lung tissue contact (odds ratio (OR) = 2.80; 95% confidence interval (Cl): 1.04–7.56; P = 0.042) and nodule size (OR = 0.04; 95%Cl: 0.00–0.51; P = 0.014) are the independent risk factors for locating isolated PNs complicated by pneumothorax induced by injecting autologous blood under CT guidance (Table 2 ). Receiver operating characteristic (ROC) curve analysis was performed using puncture needle penetration depth and nodule size as independent variables and pneumothorax as the dependent variable. Subsequently, a nomogram prediction model was established, and the area under the curve (AUC) was 0.713 (95% confidence interval = 0.618–0.750) (Fig. 2 ), indicating that the prediction ability of the model was acceptable. The bootstrap method was applied for internal verification. The AUC was 0.713 (95% confidence interval = 0.603–0.720) (Fig. 3 ), and a column graph was drawn (Fig. 4 ). The calibration diagram shows that the model has good prediction accuracy (Fig. 5 ).

Receiver operating characteristic curve analysis was performed using puncture needle penetration depth and nodule size as independent variables and pneumothorax as dependent variables. The area under the curve was 0.713 (95% confidence interval = 0.618–0.750)

Receiver operating characteristic curve analysis was performed with internal validation (bootstrap method), and the area under the curve was 0.713 (95% CI = 0.603–0.720)
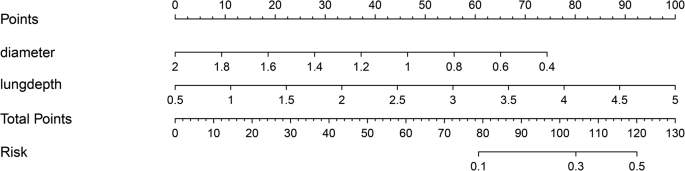
Nomogram for predicting the probability of autologous blood localization of isolated pulmonary nodules with pneumothorax. A score is assigned to the depth of needle contact with lung tissue and the diameter of the nodule by drawing a line upward from the corresponding value to the “dot line.” The “total score” is calculated as the sum of the individual scores for each of the two variables included in the column chart

Calibration diagram of nomogram prediction model. The first dotted line represents the curve of the model, the second solid line is the corrected curve of the model, and the third dotted line represents the reference line where the ideal model is located
PN localization was successful in 89 cases (96.7%) and failed in 3. Owing to extensive pulmonary adhesion, there were no evident blood stains on the surface of the visceral pleura after autologous blood injection, and no evident pinholes on the parietal and visceral pleura were observed in these three patients. In the other four cases, owing to extensive anthrax pigmentation, no evident blood stain was observed; however, the nodules could be resected successfully by guiding the pinholes in the parietal and visceral pleura. The operation time was 190.6 ± 78.2 min. Postoperative pathology showed that among the 92 nodules, six cases were inflammatory lesions, 1 was tuberculosis, 1 was alveolar epithelial hyperplasia, 1 was sclerosing pulmonary cell tumor, 1 was leiomyoma, 1 was a hamartoma, 4 were atypical adenomatoid hyperplasia, 3 were in situ adenocarcinoma, 31 were micro-invasive adenocarcinoma, 42 were invasive adenocarcinoma, and one was poorly differentiated.
Herein, we investigated the risks and side effects of using CT guidance to inject autologous blood to locate isolated lung nodules. Smaller nodules and deeper contact between the needle and lung tissue were found to be the factors associated with pneumothorax after localization.
In thoracoscopic surgery, the absence of preoperative localization increases the possibility of failed direct palpation of small PN. Therefore, locating such lesions is essential. Common localization methods include CT-guided indentation of locators in the lungs, such as wire with hooks, micro coils, methylene blue, and glue. Each method has its advantages and disadvantages. The hook wire is the most used and easy to operate. However, patients experience pain, a high incidence of complications, such as pneumothorax and intrapulmonary hemorrhage, and superficial lesions are prone to dislocation [ 16 ]. Microcoil has fewer complications and a good positioning effect [ 17 , 18 ]; however, its operation is slightly complicated, and its consumables are more expensive. Biogel injections can cause coughing. If the injection site is too close to or within the lesion, Biogel may overwhelm the lesion and affect the pathological Sect. [ 19 ]. Injection of methylene blue and other liquid dyes is simple and economical. Its limitation is that the dye diffuses easily, resulting in poor positioning accuracy [ 20 ]. Prompt surgery should be performed after dye localization to avoid expanding the excision scope. The injection of iodide and barium provides a cheap and safe labeling method; however, fluoroscopic guidance is required during VATS, during which special equipment and radiation protection are required [ 21 ], increasing the radiation dose to patients and medical staff [ 22 , 23 ]. Furthermore, barium may cause inflammation of surrounding lung tissue and affect the pathological diagnosis of nodules. Therefore, the above positioning methods have certain limitations.
Pneumothorax and pulmonary hemorrhage are common complications of CT-guided lung puncture [ 24 , 25 ]. The overall complication rate of CT-guided lung puncture is reportedly 9–54% (average, 20%). Pneumothorax and intrapulmonary hemorrhage are common, and the incidence of critical complications requiring surgical treatment is less than 5% [ 26 , 27 ]. Ye et al. reported that the incidence of pneumothorax was 31.9% while using medical glue to locate PN, compared with 51.4% during hook wire positioning. In addition, pulmonary parenchymal hemorrhage occurred in 13.9% of PNs treated with medical glue, compared with 13.5% of those treated with hook wire placement [ 28 ]. In this study, the incidence of pneumothorax was 17.3% and that of pulmonary hemorrhage was 2.2%. Among them, the degree of pulmonary collapse in 10 cases was 5–20% (two were found in VATS combined with a small amount of thoracic hemorrhagic fluid, two were owing to needle compression, and four were less than 5%), all of which were minor, required no special treatment, and exhibited no critical complications. Considering that the autologous blood coagulation rate is fast, it can effectively block the puncture site and reduce complications such as lung leakage and bleeding. According to Filippo’s study, an autologous blood clot is used as a blood patch, in which fine needle aspiration of PNs has a lower incidence of pneumothorax when there is bleeding around the needle path or high local bleeding (> 6 mm) [ 29 ]. In this study, the maximum diameter of blood distribution on CT images after autologous blood injection was 15.5 ± 5.7 mm, which may reduce the possibility of pneumothorax occurrence. Notably, because autologous blood is not added with anticoagulants, the infusion of autologous blood during the positioning process should be conducted promptly to prevent blocking the positioning needle tip and increasing the number of positioning punctures. All patients experienced good localization under local anesthesia, no hemoptysis, and no evident pain after localization.
Logistics analysis suggested that the puncture depth into the lung and the nodule size are independent risk factors for pneumothorax. A deep puncture depth into the lung and a small nodule size increased the possibility of the occurrence of pneumothorax. The reasons may be as follows: ① When the distance between the lesion and the pleura is long, the puncture needle passes through more tissues, increasing the severity of the induced injury. Ineffective control of the injection depth causes the injection direction to be adjusted repeatedly, increasing the possibility of pneumothorax. ② Small lesions are greatly affected by the patient’s respiratory movement during puncture and are easy to deviate from the target. The area under the ROC curve was 0.713, and after further internal validation with bootstrap 1000, the area under the ROC curve was 0.713 (0.6026–0.7196), indicating that the ability of this model to distinguish between patients with pneumothorax after positioning with this technology was acceptable.
The risk factors for the diameter of pulmonary nodules could not be changed in this study. Compared with it, shortening the distance of the puncture needle into lung tissue is a feasible and effective strategy. The judgment of the location of pulmonary nodules mainly depends on the blood tattoos formed on the pleural surface of the visceral layer of the lung tissue after localization by autologous blood, thus reducing the circumference of target nodules palpated by fingers in VATS. After the initial confirmation of the location of the pulmonary nodule, the marked point was sutured with a thread crochet. After taking out the resected lung tissue specimen, carefully palpating the fingers according to the marked point to find the lesion, using the hook needle again to suture the target nodule, sending the rapid frozen pathological section during the operation to the pathologist for pathological diagnosis, but injecting about 5–10 mm of autologous blood around the target nodule has little effect on this process.
CT-guided injection of autologous blood as a novel localization technology for PNs was underreported both locally and internationally. It is convenient, simple and effective, economical and practical, can effectively reduce costs, has fewer side effects and complications, and can improve the success rate of thoracoscopic pulmonary wedges. However, reports on risk factors related to pneumothorax after localization using this technique were not investigated. In this study, smaller nodules and deeper contact between the needle and lung tissue were related to pneumothorax after CT-guided localization using autologous blood. The predictive model provides a useful tool for assessing the risk of PNs with pneumothorax owing to autologous blood localization and may help patients and clinicians select the best risk reduction strategy based on individual risks, which has certain significance for clinical guidance and diagnosis.
Our study had limitations because it lacked randomness and was a retrospective analysis conducted at a single site, making it susceptible to potential bias. In addition, the sample size of this study is relatively small and might have influenced the conclusion of the safety and effectiveness of the autologous blood localization method; therefore, it may need to be studied in a larger population size.
Conclusions
In conclusion, The factors associated with pneumothorax after localization are smaller nodules and deeper contact between the needle and lung tissue.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Computed tomography
Pulmonary nodule
Video-assisted thoracoscopic surgery
Forced vital capacity
Forced expiratory volume in the first second/forced vital capacity
Maximal voluntary ventilation
White blood cell
Ground-glass nodule
Raad RA, Suh J, Harari S, et al. Nodule character-ization: subsolid nodules, Radiol. Clin. 2014;52:47–67.
Google Scholar
Groheux D, Quere G, Blanc E, et al. FDG PET-CT for solitary pulmo–nary nodule and lung cancer: literature review. Diagn Interv Imaging. 2016;97:1003–17.
Article CAS PubMed Google Scholar
Godoy MCB, Odisio EGLC, Truong MT, de Groot PM, Shroff GS. ErasmusJJ. Pulmonary nodule management in lung cancer screening: a pictorial review of lung-RADS version 1.0. Radiol Clin. N Am. 2018;56:353–63.
McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancerin pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369:910–9.
Article CAS PubMed PubMed Central Google Scholar
Fu YF, Zhang M, Wu WB, Wang T. Coil localization-guided video-assisted thoracoscopic surgery for lung nodules. J Laparoendosc Adv Surg Tech A. 2018;28:292–7.
Article PubMed Google Scholar
Teng F, Wang ZS, Wu AL, Fu YF, Yang S. Computed tomography-guided coil localization for video-assisted thoracoscopic surgery of sub-solid lung nodules: a retrospective study. ANZ J Surg. 2019;89:E514–8.
Nardini M, Dunning J. Pulmonary nodules precision localization tech–niques. Future Oncol. 2020;16:15–9.
Shrager JB. Approach to the patient with multiple lung nodules. Thorac Surg Clin. 2013;23:257–66.
Iqbal SI, Molgaard C, Williamson C, et al. Purposeful creation of a pneumothorax and chest tube placement to facilitate CT-guided coil localization of lung nodules before video-assisted thoracoscopic surgical wedge resection. J Vasc Interv Radiol. 2014;25:1133–8.
Liu L, Zhang LJ, Chen B, et al. Novel CT-guided coil localization of peripheral pulmonary nodules prior to video-assisted thoracoscopic surgery: a pilot study. Acta Radiol. 2014;55:699–706.
Almousa O, Mayo J, English J, et al. Microcoil-guided video-assisted thoracoscopic excision of nodules suspicious for metastasis in patients with extra- thoracic malignancies. Semin Thorac Cardiovasc Surg. 2019;31:129–34.
Shen Cheng LI, Pengfei LI, Jue, et al. Research progress on common localization methods of pulmonary nodules under thoracoscopic surgery. Chin J Lung Cancer. 2018;21(8):628–34.
CAS Google Scholar
Meng Qinghua Z, Mei H, Xiaokun. Application of CT-guided microspring ring and Hookwire in puncture localization of pulmonary nodules. Imaging Res Med Appl. 2002;6(2):179–81.
Xu Jianxin X, Zhiyang G, Jun, et al. Application of preoperative autologous blood localization under CT guidance in thoracoscopic resection of small pulmonary nodules. J Clin Pulmonol. 2019;25(3):469–71.
Wu Gao J, Xianliang L. Preliminary study on the application of autologous blood in the positioning of pulmonary nodules under the guidance of CT. Chin J Interventional Radiol. 2019;8(2):155–9.
Ichinose J, Kohno T, Fujimori S, et al. Efficacy and complications of computed tomography–guided hook wire localization. Ann Thorac Surg. 2013;96(4):1203–8. https://doi.org/10.1016/j.athoracsur.2013.05.026 .
Sui Xichao Y, Feng Z, Hui et al. Thoracoscope surgery small lung nodules ground glass shadow micro spring coil position. Journal of the chest Tube surg. 2014;30 (12): 711 714. doi: 10.3760 / cma. J.issn. 1001 4497.2014.12.002.
Sui X, Zhao H, Yang F, et al. Computed tomography guided microcoil localization for pulmonary small nodules and ground–glass opacity prior to thoracoscopic resection. J Thorac Dis. 2015;7(9):1580–7. https://doi.org/10.3978/j.issn.2072-1439.2015.09.02 .
Article PubMed PubMed Central Google Scholar
Qian Kun Z, Xiuyi Z, Yi et al. Application of CT-guided injection of medical glue in thoracoscopic preoperative localization of pulmonary nodules. J Capital Med Univ, 2015; 4 (4): 529 532. doi: 10.3969 / j.i SSN. 1006 7795.2015.04.003.
Tseng YH, Lee YF, Hsieh MS, et al. Preoperative com-puted tomography-guided dye injection to localize multiple lung nodules for video-assisted thoracoscopic surgery. J Thorac Dis. 2016;8:S666–71.
Nardini M, Bilancia R, Paul I, et al. 99mTechnetium and methylene blue guided pulmonary nodules resections: preliminary British experience. J Thorac Dis. 2018;10:1015–21.
Miura H, Yamagami T, Tanaka O, et al. CT findings after lipiodol marking performed before video-assisted thoracoscopic surgery for small pulmonary nodules. Acta Radiol. 2016;57:303–10.
Lee NK, Park CM, Kang CH, et al. CT-guided percutaneous transthoracic localization of pulmonary nodules prior to video-assisted thoracoscopic surgery using barium suspension. Korean J Radiol. 2012;13:694–701.
Ichinose J, Kohno T, Fujimori S, Harano T, Suzuki S. Efficacy and complications of computed tomography-guided hook wire localization. Ann Thorac Surg. 2013;96:1203–8.
Horan TA, Pinheiro PM, Araújo LM, Santiago FF, Rodrigues MR. Massive gas embolism during pulmonary nodule hook wire localization. Ann Thorac Surg. 2002;73:1647–9.
Hiraki T, Mimura H, Gobara H, et al. Incidence of and risk factors for pneumothorax and chest tube placement after CT fluoroscopy–guided percutaneous lung biopsy: retrospective analysis of the procedures conducted over a 9–year period.AJR. Am J Roentgenol. 2010;194(3):809–14. https://doi.org/10.2214/AJR.09.3224 .
Article Google Scholar
Boskovic T, Stanic J, Pena–Karan S, et al. Pneumothorax after transthoracic needle biopsy of lung lesions under CT guidance. J Thorac Dis. 2014;6(1):S99–107. https://doi.org/10.3978/j.issn.2072-1439.2013.12.08 .
Ye W, Dong C, Lin C, Wu Q, Li J, Zhou Z, et al. Medical adhesive vs hookwire for computed tomography-guided preoperative localization and risk factors of major complications. Br J Radiol. 2021;94:20201208. https://doi.org/10.1259/bjr.20201208 .
De Filippo M, Saba L, Silva M, et al. CT-guided biopsy of pulmonary nodules: is pulmonary hemorrhage a complication or an advantage? Diagn Interv Radiol. 2014;20:421–5.
Download references
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Supported by The Research Project of Putian College (No. 2022093).
Author information
Shaohang Wu and Jianyang Wu contributed equally to this work.
Authors and Affiliations
Department of Thoracic Surgery, The First Hospital of Putian, The School of Clinical Medicine, Fujian Medical University, No. 449 Nanmenxi Road, Putian, Fujian, 351100, China
Shaohang Wu, Jianyang Wu, Junkai Xiong, Chengbin Huang, Yiwei Lin, Jun Guan & Jianxin Xu
You can also search for this author in PubMed Google Scholar
Contributions
SHW, JKX, CBH and YWL collected the data; JG and JXX performed the localization and VATS procedure; SHW and JYW analyzed these data; SHW wrote and revised thispaper; JXX and JG participated in the study design and draft the manuscript.
Corresponding authors
Correspondence to Jun Guan or Jianxin Xu .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the ethics committee of The First Hospital of Putian and waived the requirement for informed consent for the use of the patients’medical data.
Consent for publication
All the authors agree to the publication of this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wu, S., Wu, J., Xiong, J. et al. Risk factors of pneumothorax in computed tomography guided lung nodule marking using autologous blood: a retrospective study. J Cardiothorac Surg 19 , 317 (2024). https://doi.org/10.1186/s13019-024-02810-y
Download citation
Received : 28 December 2023
Accepted : 25 May 2024
Published : 01 June 2024
DOI : https://doi.org/10.1186/s13019-024-02810-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pulmonary nodules
- Autologous blood localization
- Complications
Journal of Cardiothoracic Surgery
ISSN: 1749-8090
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Bouveret's syndrome: a rare presentation of a common surgical enigma. Cyst of the Canal of Nuck: a case report. Heterotopic pancreas in Meckel's diverticulum causing perforation in an infant: a case report. Immunoglobulin G4-related sclerosing mastitis: an unexpected diagnosis for a breast mass. Stump appendicitis: challenging diagnosis ...
Wrong-site surgery occurs in all surgical specialties but is most common among orthopedic surgeons and neurosurgeons, 4 with 68% of claims in the United States related to orthopedic surgery. 5 In ...
ACS Case Reviews in Surgery is a unique, peer-reviewed, open access, online-only case report journal published six times a year that presents high-quality, in-depth analyses of actual surgical cases. The journal boasts an exceptional editorial and reviewer board comprised of distinguished surgeon leaders from around the world.
In the TransNEOS study, among patients who received neoadjuvant letrozole, the incidence of disease progression was low if the score on the 21-gene recurrence-score assay was below 31 (<1% among ...
Surgical Case Reports is an official journal of the Japan Surgical Society. This open access, peer-reviewed, online journal will consider any original case reports in the fields of gastroenterological surgery, cardiovascular surgery, thoracic surgery, breast and endocrine surgery, pediatric surgery, transplant surgery, and acute care surgery ...
Case Reports in Surgery publishes case reports and case series related to all aspects of surgery. Topics include but are not limited to oncology, trauma, gastrointestinal, vascular, and transplantation surgery. ... More documented cases and their management and ultimately longitudinal cohort studies will help facilitate the creation of ...
Surgical Case Reports (SCR) is a dedicated platform aiming to advance the understanding and practice of surgery. Our principal goal is to provide a global forum where clinicians, surgeons, and researchers can share, learn, and discuss novel surgical techniques, treatments, and patient case studies that contribute to the field's progress.
Dr. John Conte performed the coronary bypass surgery. Of interest is the fact that in 1999, Dr. Conte published a case report of the first ever successful bloodless lung transplant in a Jehovah's Witness patient. In this case presented here, he decided the patient would be best served by performing an "off-pump" cardiac surgery where the ...
Here we report a case of De Garengeot's hernia that occurred in a male patient who had a history of inguinal hernia surgery ... Shiro Fujihata, Hiromasa Kuzuya, Masaaki Kurimoto, Tadashi Shibata, Hirozumi Sawai and Shuji Takiguchi. Surgical Case Reports 2024 10 :132. Case Report Published on: 29 May 2024. Full Text.
Surgery Case Reports: Advances and Techniques is an open access, peer-reviewed journal. The journal publishes case reports and case series on all surgical specialties from all regions of the world. Submissions to the journal should report unusual or unexpected situations in the clinical setting. Case reports should be practice-based resources ...
Case Study 1: Revision Surgery for Thoracic and Abdominal Aortic Aneurysm Using a Minimally Invasive Endovascular Fenestrated Stent Graft. An 81-year old female patient (Jehovah's Witness) presented with an expanding aortic aneurysm in the thoraco-abdominal (chest and abdomen) region that had enlarged from 5 to 7 centimeters.
Oral and Maxillofacial Surgery Cases is a surgical journal dedicated to publishing case reports and case series only which must be original, educational, rare conditions or findings, or clinically interesting to an international audience of surgeons and clinicians. Case series can be prospective or retrospective and examine the outcomes of management or mechanisms in more than one patient.
The Background section should explain the background to the case report or study, its aims, a summary of the existing literature. Case presentation. This section should include a description of the patient's relevant demographic details, medical history, symptoms and signs, treatment or intervention, outcomes and any other significant details
Journal of Vascular Surgery Cases, Innovations and Techniques is a surgical journal dedicated to publishing peer reviewed and high-quality case reports, vascular images, and innovative techniques related to all aspects of arterial, venous, and lymphatic diseases and disorders, including vascular trauma, malformations, wound care, and the ...
The 2020 Best Practices Case Studies were selected from a bank of more than 450 abstracts submitted for the 2020 ACS Quality and Safety Conference. All abstracts were reviewed and vetted by a panel of program experts, and the authors of the studies chosen were asked to further develop their case study and share their accomplishments.
Case Study: Left Total Knee Replacement. in a 62-year-old Male. A 62-year-old male presented for evaluation of his left knee. Over the last seven months, he has had increasing knee pain and discomfort. He stated that in April he got up from a seated position and felt a "crack" within his knee. He had earlier seen another physician who ...
The majority of studies have been retrospective, chart reviews, case studies, and surveys of various professional organizations. The evidence table summarizes the most recent evidence ... In verifying that the right patient is to have the right surgery in the right location, one study found that when discrepancies occurred among ...
Case Studies. In this section we report a variety of clinical cases in an effort to share our experience with healthcare providers and with patients who may benefit. The cases are categorized into a wide variety of different medical and surgical specialties listed under subheadings. The main objective is to share our knowledge and experience ...
Gastroesophageal Surgery Case FIGURE 1. Image from upper endoscopic examination of the stomach. of electrolytes and tests of kidney and liver ... DISCUSSION OF MANAGEMENT This patient has a stomach cancer that appears to be locoregionally advanced on imaging studies. The first decision regarding management is whether to resect it immediately or ...
Previous NSQIP studies in plastic surgery use data derived from a single procedure with a narrow focus. ... Weiler J, Taggart P, Khoobehi K. A case for the safety and efficacy of lipoabdominoplasty: a single surgeon retrospective review of 173 consecutive cases. Aesthet Surg J. 2010;30(5):702-713.
Robotic-assisted surgery for complicated and non-complicated diverticulitis: a single-surgeon case series. ... This study found that robotic surgery is rapidly diffusing across a broad range of common general surgical procedures. Trends toward greater use of the robotic platform appeared to occur rapidly after hospitals begin performing robotic ...
Despite advancement in surgical innovation, C1-C2 fixation remains challenging due to risks of screw malposition and vertebral artery (VA) injuries. Traditional image-based navigation, while useful, often demands that surgeons frequently shift their attention to external monitors, potentially causing distractions. In this article, we introduce a microscope-based augmented reality (AR ...
Case Studies in Surgery (CSS) is an international, peer-reviewed, open-access journal, published by the Sciedu Press. It publishes original research, applied, and educational articles in all areas of surgery. All the publications can be searched from Google Scholar Citations. Authors are encouraged to submit complete, unpublished, original ...
Home Bloodless medicine surgery Case studies. Case Study: Neurosurgery. Pediatric Neurosurgery Patient with a Paraspinous S1 Nerve Sheath Tumor. An 11-year old girl who was a member of a Jehovah's Witness family, presented to an outside hospital with progressive right leg weakness and right lower abdominal pain of one-month duration. The MRI ...
From the a Department of Plastic and Reconstructive Surgery, Seoul National University College of Medicine, Seoul. b Department of Plastic and Reconstructive Surgery, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.. Received September 20, 2023, and accepted for publication, after revision January 2, 2024. J.-Y.K. and S.M. contributed equally to this study.
Abstract. This paper introduces the implementation of post-processing techniques applied to the fusion, segmentation, and 3D reconstruction of studies involving patients with brain tumors. The objective of this study is to emphasize the interdisciplinary collaboration that facilitates synergy between the academic and clinical environments ...
Background Very little information is currently available on the use and outcomes of venovenous bypass (VVB) in liver transplantation (LT) in adults in Australia. In this study, we explored the indications, intraoperative course, and postoperative outcomes of patients who underwent VVB in a high-volume LT unit. Methods The study was a single-center, retrospective observational case series of ...
To investigate the risk factors of pneumothorax of using computed tomography (CT) guidance to inject autologous blood to locate isolated lung nodules. In the First Hospital of Putian City, 92 cases of single small pulmonary nodules were retrospectively analyzed between November 2019 and March 2023. Before each surgery, autologous blood was injected, and the complications of each case, such as ...
Experts analysed 68 transgender men who were taking the cross-sex hormone to change their identity from female to male and found that 95 per cent had developed pelvic floor dysfunction. The ...