- Open access
- Published: 19 May 2020

The mediating effect of social support on uncertainty in illness and quality of life of female cancer survivors: a cross-sectional study
- Insook Lee ORCID: orcid.org/0000-0001-6090-7999 1 &
- Changseung Park 2
Health and Quality of Life Outcomes volume 18 , Article number: 143 ( 2020 ) Cite this article
2934 Accesses
19 Citations
Metrics details
Cancer survivors have been defined as those living more than 5 years after cancer treatment with no signs of recurrence or further growth; however, the National Coalition for Cancer Survivorship of the United States defined cancer survivors as those undergoing treatment after being diagnosed with cancer or those considered to be fully cured. The National Cancer Institute of the United States established the Office of Cancer Survivorship, with the American Society of Clinical Oncology including “patient and survivor management” as its 2006 annual objective [ 1 ], indicating the importance of cancer survivor management as a major agenda item.
Typically, breast and thyroid cancer diagnoses occur among women in their 40s and 50s, and patients who receive treatment have high survival rates. The majority of breast and thyroid cancer survivors return to their daily lives within a relatively short timeframe [ 2 ], making quality of life after treatment and important factor in cancer treatment [ 3 , 4 , 5 ].
Cancer survivors have reported experiencing a variety of physical difficulties during or after treatment, including fatigue, pain, loss of energy, sleeping disorders, and constipation [ 6 , 7 ]. They also have psychological concerns, such as fear of the cancer spreading, concerns about treatment results, and uncertainty about the future [ 8 ], as well as financial difficulties, issues with their sex lives, decreased body image, difficulties in interpersonal relationships, role disorders, and difficulty returning to work [ 7 ]. Thus, cancer patients require a diverse range of healthcare services, plus emotional and socioeconomic support, with an international study of the quality of life and symptoms of cancer survivors reporting that the quality of life among Asian patients to be the lowest of those than other country [ 6 ]. Survivors of breast cancer have reported low quality of life after treatment [ 9 , 10 ], which is influenced by emotional and psychological factors such as uncertainty, body image, lack of self-respect, and depression [ 9 , 10 , 11 ], as well as social factors including social, family, and spouse support [ 10 , 11 ].
Uncertainty among women diagnosed with malignant illnesses was found to be higher than that among women with a lump in the breast [ 12 ]. Uncertainty among breast cancer patients continues for a long period because of the fear of recurrence [ 13 ] and reduced quality of life [ 11 ]. Similarly, thyroid cancer survivors also show higher levels of fatigue, depression, and anxiety compared to those with no experience of cancer [ 14 , 15 , 16 ].
Social support is a complex and multidimensional concept that is characterized by mutual benefits that include social, psychological, and material support provided by the social support network [ 17 ]. In other words, social support means help provided by social relationships such as family, friends, and significant others, and plays an important role in directly and indirectly reducing uncertainty [ 18 , 19 ]. For cancer survivors, the need for social support is varied and depends largely on the adaptive tasks they face [ 20 ]. Social support is closely related to breast cancer survivor prognosis [ 21 ]; breast cancer survivors’ uncertainty was found to lower their quality of life, but their recognition of social support was found to improve it [ 11 ]. Recognition of social support and uncertainty played a key role in managing and maintaining quality of life. Research has shown that social support differs according to survival stage, as patients who are undergoing treatment receive active support from healthcare professionals and their family, but this support declines notably after the treatment ends [ 14 , 22 , 23 ].
With the number of cancer survivors steadily increasing, there has been an increase in the number of studies published on cancer survivors internationally [ 22 , 24 ]. In Korea in particular, there have been studies on recurrence-prevention behaviors and quality of life [ 25 ], the factors influencing quality of life [ 10 ], fatigue and quality of life [ 26 ], distress and quality of life [ 27 ], and symptoms and quality of life among breast cancer survivors [ 8 ]. Most of these studies focused on breast cancer survivors, but few studies focus on overall quality of life and the related influential factors. Few studies have analyzed the relationships between uncertainty in illness, quality of life, and social support among female breast and thyroid cancer survivors.
This study aimed to identify the relationships among uncertainty in illness, social support, and quality of life in female cancer survivors, and to verify the mediating role of social support, in the relationship between uncertainty in illness and quality of life. Social support may act as a generative mechanism influencing how uncertainty in illness, the predictor variable, affects quality of life, the outcome variable (Fig. 1 ) [ 28 ]. Therefore, this study will provide foundational data for devising practical and helpful intervention strategies to raise the quality of life of cancer survivors.
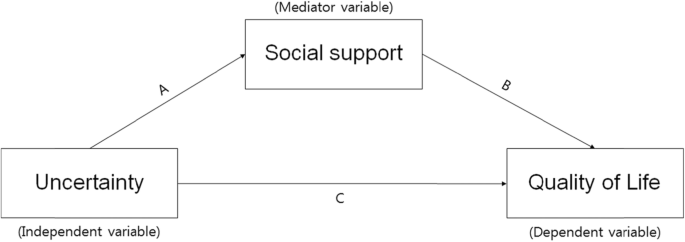
The theoretical research model showing the influence of uncertainty on quality of life and the mediating effect of social support
Participants
Participants were selected using convenience sampling of female cancer patients who were being treated by specialists in breast endocrinology at general hospitals located in J City of Korea. Among the 189 women (138 thyroid and 50 breast cancer patients) who agreed to participate, 156 surveys were collected (response rate: 82.5%). The final sample including 148 participants after excluding eight insincere responses. The data collection period was from April 21 to June 30, 2014. The completion of data collection through the mailed-in copies of surveys occurred on October 15, 2014. Participants were asked to complete the survey, put it in an opaque envelope, and seal it before returning it to the researchers. In cases in which on-site survey completion was difficult, participants were able to complete the survey at home and returned it by mail to the researcher.
The necessary sample size for the multiple regression analysis was confirmed utilizing G*power ver. 3.1.9 with a significance level (α) of .05; power of .80; effect size (f 2 ) of .15 (representing a medium effect size in the multiple regression analysis); and 13 independent variables (age, marital status, religion, level of education, occupation, satisfaction with economic status, smoking, drinking, diagnosis name, clinical stage of cancer, time passed since the end of treatment, uncertainty, and social support). The minimum sample size was determined to be 131. Since a maximum dropout rate of 40% was expected, information was collected from a total of 189 participants who fit the following inclusion criteria: 1) a diagnosis of cancer and no cognitive limitations; 2) the ability to understand and complete the survey in Korean; and 3) an understanding of the purpose of the study and consenting to participate. The exclusion criteria were those suffering from a mental illness, those with difficulties in communication, and those who did not wish to participate in the study.
Uncertainty in illness
Uncertainty occurs when an appropriate subjective interpretation of an illness or event is not formed. This study measured uncertainty using Mishel’s Uncertainty in Illness Scale (MUIS), which is composed of 33 items concerning uncertainty in illness. Mishel [ 19 ] originally developed the scale, and it has been translated into Korean by Lee [ 28 ]. The MUIS is a self-administered survey, with items scored on a 5-point scale from 5 ( strongly agree ) to 1 ( strongly disagree ). Positive items were measured backward, so that total scores ranged from 33 to 165. Higher scores indicated higher rates of uncertainty. The Cronbach’s α for the original 33-item tool was .91–.93; the Cronbach’s α for the tool used in the study of Korean breast cancer patients [ 29 ] was .83. In this study, the Cronbach’s α for the uncertainty scale was .88.
Social support
Social support was measured using Zimet et al.’s [ 30 ] Multidimensional Scale of Perceived Social Support (MSPSS). This 12-item measure is scored on a 7-point, Likert-type scale, and assessed the three dimensions of family, friends, and significant others. Its sub-domains are composed of four items. Overall social support scores are calculated by summing the scores for each item, with higher scores indicating higher levels of social support. At the time of development, the Cronbach’s α reliability was .91; Cronbach’s α for each subscale ranged from .90–.95. In this study, the Cronbach’s α of the social support scale was .95.
Quality of life
Quality of life was measured using a standardized tool that was translated into the Korean and verified validity of the Korean version of the EORTC QLQ-C30, which was developed through a process of international joint study from multiple countries, and it is the most widely used standardized tool to measure the quality of life of cancer patients. This tool is composed of three subdomains and 30 items. It includes two items on overall quality of life and five functional domains (i.e., physical, role, cognitive, emotional, and social functions) that include 15 items; three symptom domains (i.e., fatigue, pain, nausea/vomiting) that include seven items; and one item for each of the symptoms commonly reported by cancer patients (i.e., difficulties in breathing, loss of appetite, sleeping disorders, constipation, diarrhea, and financial hardship) [ 31 ]. The EORTC QLQ-C30 is converted into a score ranging between 0 and 100 points [ 31 ]; higher overall quality of life scores, higher functional domain scores, and lower symptom domain scores indicate higher quality of life. Moreover, overall quality of life can be understood as a measurement of comprehensive quality of life [ 31 ]. This study assess quality of life using the overall quality of life score. At the time of development, Cronbach’s α was .65–.73; the Cronbach’s α for the overall quality of life score in this study was .853.
Ethical considerations
This study was conducted after receiving approval of the research protocol from the Institutional Review Board (Approved number: 2014-L02–01). The purpose and method of the research was explained directly to participants by a trained research assistant. The participants then signed an informed consent form that stated the survey would be used for the purposes of the study only, and that their confidentiality would be safeguarded. The subjects who agreed to participate in the survey received a small amount of goods worth of KRW 3000, but there were no factors that could interfere with the answers in the survey.
Data analysis
The collected data were coded and analyzed using SPSS software (version 24.0; SPSS Inc., Chicago, IL) at .05 significance level. The analysis excluded missing data values. The general characteristics, illness-related characteristics, uncertainty, social support, and quality of life were measured using frequency, percentages, means, and standard deviations. The differences in uncertainty, social support, and quality of life in accordance with general and illness-related characteristics were analyzed using independent t -tests and one-way analysis of variance (ANOVA). Tukey’s post-hoc analysis was used for independent variables of more than three groups to identify which group contained the differences. Pearson’s correlation coefficient was calculated to identify correlations between uncertainty, social support, and quality of life. Multiple regression (stepwise method) was used to test the influence of uncertainty on social support and quality of life. To verify the mediating effects of social support in the relationship between uncertainty and quality of life, simple, and hierarchical multiple regression analyses were conducted as per the method proposed by Baron and Kenny [ 30 ]. The significance of the mediating effects of social support was verified using the Sobel test.
Demographic characteristics of subjects
The general characteristics of the female cancer survivors in this study indicated that their average age was 51.87 ( SD = 11.78) years, with the largest proportion (33.3%) of the population being in their 50s, followed by those in their 40s (30.1%), 60s and over (24.4%), and below 30 (12.2%). Most participants (76.2%) were married; 61.9% practiced a religion, and 66.7% had a high school education or below; 56.2% had jobs; 17.8% had lost their jobs as a result of their cancer diagnosis and treatment, and 73.1% indicated that their satisfaction with their financial status was average. They had an average of 2.26 ( SD = 1.19) children; 94.4% were non-smokers; 64.1% were non-drinkers; 29.1% of the subjects had breast cancer and 70.9% had thyroid cancer; 53.8% of the cancers were early stage, and 46.2% were advanced. The duration after cancer treatment averaged 17.64 ( SD = 31.30) months, with 70.3% reporting a duration of less than a year since they ended their treatment (Table 1 ).
Uncertainty in illness, social support, and quality of life
Average scores of uncertainty in illness, social support, and quality of life are given in Table 2 . The average uncertainty in illness score was 83.06 ( SD = 15.29; range: 44–127 points), and the average quality of life score was 66.90 ( SD = 20.32; range: 0–100 points). Average social support score was 62.62 ( SD = 17.09; range: 12–84 points), with family support being the highest (mean = 21.84, SD = 6.58), followed by support from significant others (mean = 21.28, SD = 5.93) and friends (mean = 19.45, SD = 6.70).
Differences in uncertainty in illness, social support, and quality of life according to general and illness-related characteristics
The results of the analysis of differences in uncertainty in illness, social support, and quality of life according to general and illness-related characteristics are given in Tables 3 and 4 . There were significant differences in uncertainty in illness by educational level ( t = 4.048, p < .001), satisfaction with financial status ( F = 3.760, p = .027), and smoking ( t = 2.195, p = .030). Uncertainty in illness was higher for subjects with less than a high school education, compared to those who had a university degree or higher, when they were dissatisfied with their financial status. Likewise, it was higher for smokers, compared to non-smokers.
Social support had statistically significant differences given satisfaction with financial status ( F = 5.151, p = .007) and duration since cancer treatment completion ( F = 4.292, p = .015). Social support was higher for subjects with average financial status satisfaction, and for subjects for whom it had been less than a year, or between 1 to 5 years, since they completed cancer treatment.
Quality of life significantly differed according to financial status satisfaction ( F = 6.648, p = .002). Participants had higher quality of life when they had high or average financial status satisfaction compared to dissatisfaction.
Correlation between uncertainty in illness, social support, and quality of life
The results of the correlation analyses indicated that uncertainty in illness had a significant negative correlation with social support ( r = −.335, p < .001) and quality of life ( r = −.312, p < .001); social support had a significant positive correlation with quality of life ( r = .321, p < .001). Correlations between the sub-factors of social support and quality of life indicate that there were significant positive correlations between quality of life and support from significant others ( r = .315, p < .001), friends ( r = .284, p = .001), and family ( r = .265, p = .001). Uncertainty and support from significant others ( r = −.326, p = .001), friends ( r = −.294, p = .002), and family ( r = −.244, p = .010) showed significant negative correlations; particularly, the highest correlation was between support from significant others and uncertainty (Table 5 ).
Mediating effect of social support
Four stages of regression analysis were conducted to verify whether social support had mediating effects in the process by which uncertainty in illness influenced quality of life. Prior to verifying the mediating effects of social support, this study examined the multicollinearity between variables. The residual limit was between 0.8–1.0, which is higher than 0.1; and the value of the variance inflation factor was between 1.0–1.2, which was lower than 10, indicating no issues with multicollinearity. Moreover, the Durbin-Watson test, which is the test of independence of residual error, indicated d = 1.903–1.944, which was close to two and met the independence condition, representing no issues with self-correlation.
Using the hierarchy regression, this confirmed the partial mediating effects of social support in the process of uncertainty influencing quality of life (Table 6 , Fig. 2 ). The first regression analysis indicated that the independent variable (uncertainty) had a statistically significant influence on the mediator variable (social support; β = − 0.335, p < .001), and the explanatory power for social support was 10.4%. The second stage regression analysis indicated that the mediator variable (social support) had a significant influence on the dependent variable (quality of life; β = 0.321, p < .001), and the explanatory power for quality of life was 9.7%. The third stage regression analysis indicated that the independent variable (uncertainty) had a significant influence on the dependent variable (quality of life; β = − 0.312, p = .001) with an explanatory power of 8.9%. At the fourth stage, this study aimed to test the influence of the independent variable (uncertainty) on the dependent variable (quality of life) with social support as the mediator variable. The results indicated that uncertainty (β = − 0.241, p = .014) and social support (β = 0.213, p = .030) were significant predictors of quality of life. When social support was set as the mediator variable, uncertainty was found to have a significant influence on quality of life; the unstandardized regression coefficient reduced from − 0.396 to − 0.398, indicating a partial mediation of social support. The explanatory power of these variables in terms of quality of life was 12.1%. This study executed the Sobel test to verify the significance of the mediating effects of social support, confirming that they were significant in the relationship between uncertainty and quality of life.
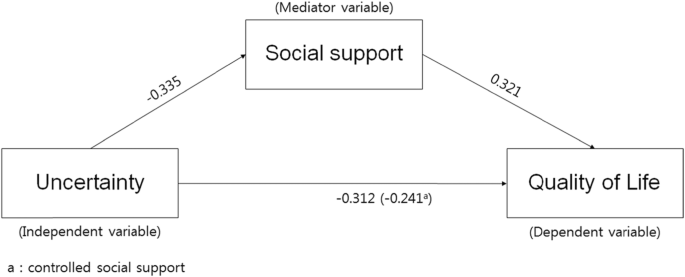
Model showing the influence of uncertainty on quality of life and the mediating effect of social support
Mullen divided the stages of cancer survival into three major classifications [ 32 , 33 ]. First is the acute stage, which marks the period after the cancer diagnosis. Second is the extended stage, in which the active treatment of cancer has ended and the patient is placed under tracking observation or engages in intermittent treatment. During this period, the majority of cancer survivors experience uncertainty toward their cancer treatment and fear recurrence, and they may experience physical and psychological issues. Lastly, the permanent stage marks a period in which the cancer is thought to be fully cured, or the patient is expected to survive long term, with a low risk of recurrence.
The participants in this study averaged a score of 66.90 for quality of life. As it is difficult to draw a direct comparison given the lack of research utilizing this measure, in converting quality of life into a scale of 100 points, this study’s results were similar to those found previously regarding post-hoc management following breast cancer treatment for 200 women [ 8 , 10 ]. However, a study covering regionally based, adult female breast cancer survivors between 6 months and 2 years after anti-cancer treatment completion reported lower scores (e.g., 60.13 points) compared to this study [ 27 ]. Likewise, a study of breast cancer survivors with completed surgeries and assistive treatments, breast cancer survivors whose treatment had ended had scores of 53.4 and 56.66 points, respectively for breast cancer survivors with completed surgeries and assistive treatments [ 25 , 26 ].
On the other hand, a report of 110 adult females with breast cancer or OB/GYN cancers [ 33 ] indicated that quality of life according to cancer survival stage was 58.7, 62.3, and 66.8 points during the acute, extended, and permanent stages, respectively. Quality of life in this study was similar to the level experienced by survivors during the permanent stage. Considering that the average time since treatment was 17.64 months, these results indicate a relatively high quality of life. While these differences cannot be accurately compared and discussed because of the lack of research covering the same variables, the majority of survivors had thyroid cancer (70.9%), and it is known that thyroid cancer has higher rates of survival. Going forward, it is important to develop interventions to improve quality of life by assessing survivors’ specific stages.
There were no significant relationships between quality of life and length of time since completing treatment. Existing research has suggested that quality of life was significantly higher for those surviving more than 5 years after cancer treatment completion [ 8 , 33 ], indicating that quality of life improves as duration of survival increases. The quality of life of these cancer survivors has been reported to improve with the passage of time [ 8 , 33 ]. Therefore, cross-sectional and longitudinal studies are required in the future to identify quality of life by survival stage and changes in quality of life over time.
On the other hand, qualitative studies of Korean female cancer survivors have indicated that the significant others and families of female cancer survivors wanted them to return to their pre-cancer lives to take care of their spouses and children, indicated the demands on female cancer survivors in Korea to fulfill their roles as wives and mothers before fully recovering from cancer [ 33 ]. Thus, customized interventions by survival stage for female cancer survivors are needed along with further research on the relationships between cultural specificity, role conflicts imposed on survivors because they are women, and their quality of life.
The uncertainty toward illness of the participants in this study was similar to existing research in breast cancer patients undergoing chemotherapy averaged 83.08 [ 34 ] and female thyroid cancer patients [ 35 ]. On the other hand, the level of uncertainty faced by cancer patients prior to surgery averaged 81.43 in a study of cancer patients hospitalized for breast, thyroid, and bladder cancer [ 36 ], which was slightly lower than the value found in this study. This appears to be because female cancer survivors in this study were mostly in the extended stage, which comes after the active treatment of their cancer [ 32 , 33 ]. Most cancer survivors face uncertainty toward cancer treatment and fear of recurrence [ 8 , 32 , 33 ]; thus, they experience a diverse range of physical and psychological problems [ 6 , 7 ]. On the other hand, a qualitative study of 25 breast cancer survivors aged over 30 who had undergone surgery and chemotherapy as their primary treatment for breast cancer [ 37 ] indicated that quality of life following treatment for breast cancer survivors saw a coexistence of anxiety and uncertainty about recurrence. A shorter duration of time since treatment led to higher confusion in their own health management efforts and health management in general.
These results indicate that there are limitations to comparing uncertainty results given the lack of domestic studies on cancer survivors; therefore, future studies are needed to fill this gap. Moreover, it is necessary to confirm uncertainty by cancer survival stage and develop interventions to reduce the uncertainty accompanying each stage.
Uncertainty in illness was higher for those with less than a high school education, compared to those with a university education or higher, when they were dissatisfied with their financial status, and for those who were smokers. These results were similar to previous research [ 36 ], which indicated high uncertainty for participants over 60 who had a low monthly income and low level of education. Therefore, it is necessary to consider these socioeconomic factors when developing uncertainty reducing strategies such as customized information delivery and communication.
The social support of female cancer survivors in this study was rather high, at 62.62 out of 84 points; family support was the highest, followed by support from significant others, and finally friends. Social support is known to play an important role in helping individuals reduce their levels of uncertainty [ 37 ]. Particularly, in Korea, family and healthcare professional support have been the most important support resources among all social support types [ 34 ]. The results of this study indicated that family support was the highest, which was in line with the results of existing studies. On the other hand, a qualitative study of 25 breast cancer survivors aged over 30 who had undergone surgery and chemotherapy as their primary breast cancer treatments [ 37 ] indicated that positive support and responses from family, patients with similar illnesses, and those surrounding them helped to strengthen positive self-suggestion, which also helped them to overcome their illnesses. Other studies have reported that patients undergoing treatment receive active support from healthcare professionals and their family, but they receive less support and interest from healthcare professionals, their family, and those surrounding them after the treatment ends [ 22 , 23 , 27 ]. Therefore, it is necessary to take a continuous interest in and facilitate social support for cancer survivors.
Social support was higher for participants with average satisfaction toward their financial status, and for those for whom less than a year, or between 1 and 5 years, had passed since the completion of their cancer treatment, compared to those for whom 5 years or more had passed since treatment. These results were similar to those of studies on cancer patients hospitalized for breast, thyroid, and bladder cancer surgery [ 36 ], which indicated social support differed according to the time that had passed since diagnosis. Moreover, these results are similar to those reporting that breast cancer survivors are required by their spouses or family to fulfill roles they had filled prior to their cancer diagnosis, and this was associated with decreasing support from family [ 38 ]. These results indicate that female cancer survivors require ongoing psychosocial support as well as education and access to information as they live out their lives.
According to Baik and Lim [ 20 ], who studied social support according to different stages of breast and gynecological cancer survival, the social support of patients in the acute stage was comparatively higher, but there were no significant differences in social support across the different stages, which was different from the findings of this study. While there were no significant differences, Baik and Lim [ 20 ] reported that the social support perceived by survivors decreased as they proceeded through the acute to the extended stage. The social support perceived by respondents decreased in the 2 years following the diagnosis but maintained the reduced rate through the permanent stage [ 20 ]. Long-term survivors had a greater need to meet other cancer patients and self-help groups [ 20 ]. Kwon and Yi [ 27 ] asserted that interest and support from family and the society in general are very important in raising breast cancer survivors’ quality of life and survival rates. Moreover, self-help groups were reported to be effective in providing emotional support for long- and short-term cancer survivors [ 39 ], which indicates the need for developing stage-specific social support interventions and various methods of facilitating social support groups. Moreover, further research is required concerning cancer survival stage-dependent social support and quality of life.
The results of this study showed that higher uncertainty in illness among female cancer survivors led to reduced social support and quality of life, while higher social support led to better quality of life. Support from others was found to be the most relevant aspect of the relationship between quality of life and uncertainty. These results were similar to those of studies on early-stage breast cancer patients [ 40 ] and on cancer patients hospitalized for breast, thyroid, and bladder cancer surgery [ 36 ], which indicated that perceived social support was lower as uncertainty increased.
Uncertainty was very influential on female cancer survivors’ quality of life. Higher uncertainty in illness among female cancer survivors led to lower social support and reduce quality of life; higher social support led to improved quality of life. The explanatory power of these variables on quality of life was 12.1%; uncertainty in illness and social support influenced the quality of life of female cancer survivors. Moreover, in the process of uncertainty in illness influencing subjects’ quality of life, social support was confirmed to play a significant, partially mediating, role in the relationship between uncertainty and quality of life. Higher uncertainty toward illness led to lower quality of life, higher social support led to higher quality of life, and social support influenced female cancer survivors’ quality of life by partially mediating its relationship with uncertainty. Social support plays an important role in directly and indirectly reducing uncertainty [ 18 , 19 ]. Social support is closely related to the prognosis of breast cancer survivors [ 21 ]. Uncertainty among breast cancer survivors has been found to lower their quality of life; however, social support has been found to improve quality of life [ 11 ]. Thus, the need for a diverse range of attempts, including developing and applying social support programs, to increase cancer survivors’ quality of life exists. On the other hand, the partially mediating effects of social support indicate that there are other mediating factors in uncertainty in illness’s influence on quality of life. Therefore, it is important for future studies to include other mediating factors in their examinations of what influences quality of life among female cancer survivors.
In Korea, studies on cancer survivors have been conducted since 2010, and the majority of these focused on breast cancer survivors. Particularly, as there has been no overall research into the healthy behaviors of cancer survivors, it is necessary to develop practical guidelines that befit Korea through studies concerning the development and application of health improvement programs based on the study of healthy behaviors, as per the assertion of Kim [ 32 ]. Moreover, attempts are needed to practically apply a diverse range of intervention studies to improve cancer survivors’ quality of life.
Moreover, future studies should include mediator variables other than social support that might influence quality of life. Additionally, both cross-sectional and longitudinal studies are needed to further investigate the quality of life and uncertainty according to the stages of survival.
Our results show that social support partial mediates the relationship between uncertainty and quality of life in female cancer survivors. The results of this study have great implications for improving cancer care, especially in how it relates to quality of life, and they also demonstrate how uncertainty can be decreased. Therefore, it is necessary to develop and apply intervention methods to improve social support thereby improving quality of life among female cancer survivors. A nurse-led social support program may especially contribute to enhancing the quality of life of cancer survivors by providing them with adequate health information and emotional support.
Availability of data and materials
The data used in this study were collected through questionnaires and analyzed by coding the original data. The datasets generated and/or analysed during the current study are not publicly available due [REASON WHY DATA ARE NOT PUBLIC] but are available from the corresponding author on reasonable request.
Abbreviations
Mishel’s Uncertainty in Illness Scale
Multidimensional Scale of Perceived Social Support
European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30
Obstetrics/Gynaecology
Lee JE, Shin DW, Cho BL. The current status of cancer survivorship care and a consideration of appropriate care model in Korea. Korean J Clin Oncol. 2014;10(2):58–62. https://doi.org/10.14216/kjco.14012 .
Article Google Scholar
Yoon HJ, Seok JH. Clinical factors associated with quality of life in patients with thyroid cancer. J Korean Thyroid Assoc. 2014;7(1):62–9. https://doi.org/10.11106/jkta.2014.7.1.62 .
Dow KH, Ferrell BR, Leigh S, Ly J, Gulasekaram P. An evaluation of the quality of life among long-term survivors of breast cancer. Breast Cancer Res Treat. 1996;39(3):261–73. https://doi.org/10.1007/BF01806154 .
Article CAS PubMed Google Scholar
Ferrell BR, Dow KH. Quality of life among long-term cancer survivors. Oncology. 1997;11:565–8.
CAS PubMed Google Scholar
Lee JE, Goo A, Lee KE, Park DJ, Cho B. Management of long-term thyroid cancer survivors in Korea. J Korean Med Assoc. 2016;59(4):287–93. https://doi.org/10.5124/jkma.2016.59.4.287 .
Article CAS Google Scholar
Molassiotis A, Yates P, Li Q, So WK, Pongthavornkamol K, Pittayapan P, et al. Mapping unmet supportive care needs, quality-of-life perceptions and current symptoms in cancer survivors across the Asia-Pacific region: results from the international STEP study. Ann Oncol. 2017;28(10):2552–8. https://doi.org/10.1093/annonc/mdx350 .
Yun YH, Kim YA, Sim JA, Shin AS, Chang YJ, Lee J, et al. Prognostic value of quality of life score in disease-free survivors of surgically-treated lung cancer. BMC Cancer. 2016;16(1):505–14. https://doi.org/10.1186/s12885-016-2504-x .
Article PubMed PubMed Central Google Scholar
Park JH, Jun EY, Kang MY, Joung YS, Kim GS. Symptom experience and quality of life in breast cancer survivors. J Korean Acad Nurs. 2009;39(5):613–21. https://doi.org/10.4040/jkan.2009.39.5.613 .
Article PubMed Google Scholar
Chae YR. Relationships of perceived health status, depression, and quality of life of breast cancer survivors. J Korean Adult Nurs. 2005;17:119–27.
Google Scholar
Kim YS, Tae YS. The influencing factors on quality of life among breast cancer survivors. J Korean Oncol Nurs. 2011;11(3):221–8. https://doi.org/10.5388/jkon.2011.11.3.221 .
Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina breast cancer survivors. Oncol Nurs Forum. 2008;35(5):844–9. https://doi.org/10.1188/08.ONF.844-849 .
Liao MN, Chen MF, Chen SC, Chen PL. Uncertainty and anxiety during the diagnostic period for women with suspected breast cancer. Cancer Nurs. 2008;31(4):274–83. https://doi.org/10.1097/01.NCC.0000305744.64452.fe .
Dirksen S, Erickson J. Well-being in Hispanic and non-Hispanic Caucasian survivors of breast cancer. Oncol Nurs Forum. 2002;29(5):820–6. https://doi.org/10.1188/02.ONF.820-826 .
Husson O, Haak HR, Buffart LM, Nieuwlaat WA, Oranje WA, Mols F, et al. Health-related quality of life and disease specific symptoms in long-term thyroid cancer survivors: a study from the population-based PROFILES registry. Acta Oncol. 2013;52(2):249–58. https://doi.org/10.3109/0284186X.2012.741326 .
Lee JI, Kim SH, Tan AH, Kim HK, Jang HW, Hur KY, et al. Decreased health-related quality of life in disease-free survivors of differentiated thyroid cancer in Korea. Health Qual Life Outcomes. 2010;8(1):101. https://doi.org/10.1186/1477-7525-8-101 .
Yang J, Yi M. Factors influencing quality of life in thyroid cancer patients with thyroidectomy. Asian Oncol Nurs. 2015;15(2):59–66. https://doi.org/10.5388/aon.2015.15.2.59 .
Oh KS. Social support as a prescription theory. J Nurs Query. 2006;15(1):134–54.
Lien CY, Lin HR, Kuo IT, Chen ML. Perceived uncertainty, social support and psychological adjustment in older patients with cancer being treated with surgery. J Clin Nurs. 2009;18(16):2311–9. https://doi.org/10.1111/j.1365-2702.2008.02549.x .
Mishel MH. Uncertainty in illness. Image J Nurs Sch. 1988;20(4):225–32. https://doi.org/10.1111/j.1547-5069.1988.tb00082.x .
Baik OM, Lim J. Social support in Korean breast and gynecological cancer survivors: comparison by the cancer stage at diagnosis and the stage of cancer survivorship. Korean J Family Soc Work. 2011;32(6):5–35.
Nausheen B, Kamal A. Familial social support and depression in breast cancer: an exploratory study on a Pakistani sample. Psychooncology. 2007;16(9):859–62. https://doi.org/10.1002/pon.1136 .
Alfano CM, Rowland JH. Recovery issues in cancer survivorship: a new challenge for supportive care. Cancer J. 2006;12(5):432–43. https://doi.org/10.1097/00130404-200609000-00012 .
Ashing KT, Padilla G, Tejero JS, Kagawa-Singer M. Understanding the breast cancer experience of Asian American women. Psychooncology. 2003;12(1):38–58. https://doi.org/10.1002/pon.632 .
Janz N, Mujahid M, Chung L, Lantz P, Hawley S, Morrow M, et al. Symptom experience and quality of life of women following breast cancer treatment. J Women's Health. 2007;16(9):1348–61. https://doi.org/10.1089/jwh.2006.0255 .
Min HS, Park SY, Lim JS, Park MO, Won HJ, Kim JI. A study on behaviors for preventing recurrence and quality of life in breast cancer survivors. J Korean Acad Nurs. 2008;38(2):187–94. https://doi.org/10.4040/jkan.2008.38.2.187 .
Kim GD. Impact of climacteric symptoms and fatigue on the quality of life in breast cancer survivors: the mediating effect of cognitive dysfunction. Asian Oncol Nurs. 2014;14(2):58–65. https://doi.org/10.5388/aon.2014.14.2.58 .
Kwon EJ, Yi M. Distress and quality of life in breast cancer survivors in Korea. Asian Oncol Nurs. 2012;12(4):289–96. https://doi.org/10.5388/aon.2012.12.4.289 .
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. https://doi.org/10.1037/0022-3514.51.6.1173 .
Lee I. Uncertainty, appraisal and quality of life in patients with breast cancer across treatment phases. J Cheju Halla Collage. 2009;33:94–112.
Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3–4):610–7. https://doi.org/10.1080/00223891.1990.9674095 .
Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A, On behalf of the EORTC Quality of Life Group. EORTC QLQ-C30 scoring manual. 3rd ed. Brussels: European Organization for Research and Treatment of Cancer; 2001. p. 2001.
Kim SH. Understanding cancer survivorship and its new perspectives. J Korean Oncol Nurs. 2010;10(1):19–29.
Lim J, Han I. Comparison of quality of life on the stage of cancer survivorship for breast and gynecological cancer survivors. Korean J Soc Welf. 2008;60(1):5–27. https://doi.org/10.20970/kasw.2008.60.1.001 .
Ahn JY. The influence of symptoms, uncertainty, family support on resilience in patients with breast cancer receiving chemotherapy [master’s thesis]. Seoul: The Seoul National University; 2014.
Lee I, Park CS. Convergent effects of anxiety, depression, uncertainty, and social support on quality of life in women with thyroid cancer. J Korea Convergence Soc. 2017;8(8):163–76. https://doi.org/10.15207/JKCS.2017.8.8.163 .
Park YJ. Uncertainty, anxiety and social support among preoperative patients of cancer: A correlational study [master’s thesis]. Seoul: The Seoul National University; 2015.
Yun M, Song M. A qualitative study on breast cancer survivors’ experiences. Perspect Nurs Sci. 2013;10:41–51.
Ashing-Giwa KT. The contextual model of HRQoL: a paradigm for expanding the HRQoL framework. Qual Life Res. 2005;14(2):297–307. https://doi.org/10.1007/s11136-004-0729-7 .
Adamsen L, Rasmussen J. Sociological perspectives on self-help groups: reflections on conceptualisation and social processes. J Adv Nurs. 2001;35(6):909–17. https://doi.org/10.1046/j.1365-2648.2001.01928.x .
Kim HY, So HS. A structural model for psychosocial adjustment in patients with early breast cancer. J Korean Acad Nurs. 2012;42(1):105–15. https://doi.org/10.4040/jkan.2012.42.1.105 .
Download references
Acknowledgements
We would like to thank Dr. Min, a physician of the Endocrine surgery at Cheju Halla Hospital, for collecting the data. And, we would like to thank the IRB who approved the research and the Editage Company who edited the English.
Conflict of interest
“No conflict of interest has been declared by the author(s).”
The authors did not receive any financial support for this study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
“This research did not received any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.”
Author information
Authors and affiliations.
Department of Nursing, Changwon National University, C.P.O. Box 51140, Changwon, Republic of South Korea
Division of Nursing, Cheju Halla University, Jeju, Republic of South Korea
Changseung Park
You can also search for this author in PubMed Google Scholar
Contributions
IL designed the study, searched the literature, analyzed the data, conducted the interpretation of data, drafted and edited the manuscript, and submitted the manuscript for publishing. CSP collected the data, searched the literature, and critically revised the initial manuscript. And all authors read and approved the final manuscript.
Corresponding author
Correspondence to Insook Lee .
Ethics declarations
Ethics approval and consent to participate.
This study approved by IRB in Cheju Halla Hospital (IRB No. 2014-L02) and informed consent to participate.
Consent for publication
This manuscript has never been published in any other journal, and all authors agree to be published in this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lee, I., Park, C. The mediating effect of social support on uncertainty in illness and quality of life of female cancer survivors: a cross-sectional study. Health Qual Life Outcomes 18 , 143 (2020). https://doi.org/10.1186/s12955-020-01392-2
Download citation
Received : 08 December 2019
Accepted : 05 May 2020
Published : 19 May 2020
DOI : https://doi.org/10.1186/s12955-020-01392-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Health and Quality of Life Outcomes
ISSN: 1477-7525
- Submission enquiries: [email protected]
Advertisement
Challenges of Survivorship for Older Adults Diagnosed with Cancer
- Geriatric Oncology (L Balducci, Section Editor)
- Published: 14 March 2022
- Volume 24 , pages 763–773, ( 2022 )
Cite this article
- Margaret I. Fitch 1 ,
- Irene Nicoll 2 ,
- Lorelei Newton 3 &
- Fay J. Strohschein 4
2686 Accesses
5 Citations
Explore all metrics
Purpose of Review
The purpose of this brief review is to highlight significant recent developments in survivorship research and care of older adults following cancer treatment. The aim is to provide insight into care and support needs of older adults during cancer survivorship as well as directions for future research.
Recent Findings
The numbers of older adult cancer survivors are increasing globally. Increased attention to the interaction between age-related and cancer-related concerns before, during, and after cancer treatment is needed to optimize outcomes and quality of life among older adult survivors. Issues of concern to older survivors, and ones associated with quality of life, include physical and cognitive functioning and emotional well-being. Maintaining activities of daily living, given limitations imposed by cancer treatment and other comorbidities, is of primary importance to older survivors. Evidence concerning the influence of income and rurality, experiences in care coordination and accessing services, and effectiveness of interventions remains scant for older adults during survivorship.
There is a clear need for further research relating to tailored intervention and health care provider knowledge and education. Emerging issues, such as the use of medical assistance in dying, must be considered in this population.
Similar content being viewed by others
Older adults with cancer and their caregivers — current landscape and future directions for clinical care
Sindhuja Kadambi, Kah Poh Loh, … Supriya Mohile

Research Methods: Outcomes and Survivorship Research in Geriatric Oncology

Avoid common mistakes on your manuscript.
Introduction
Older adults constitute one of the fastest-growing subgroups in the cancer population [ 1 ]. Over the next decade, the number of individuals 65 years and older who are diagnosed with cancer is expected to double, accounting for 67% of new cancer cases and reaching levels of 14 million worldwide [ 2 ]. Given advances in screening, treatment, and supportive care which have resulted in improved cancer outcomes, the population of older adult cancer survivors is also expected to escalate [ 3 ].
The aftermath of cancer treatment can have a significant impact on survivors [ 4 , 5 ]. Physical, emotional, and practical changes during and after treatment may carry consequences that have a significant impact on the quality of life of survivors [ 6 ], carrying implications for recovery and maintenance of autonomy and independence. Early evidence illustrates that immediate recovery following cancer treatment and improvements in survival for older adults following cancer is slower than for younger survivors [ 7 ••]. For older adults, who may be already dealing with other comorbid conditions and effects of aging, the added burden of late and long-term effects may be particularly troublesome [ 8 ].
Challenges emerging during survivorship add to the complexity of meeting the needs of older adults after cancer [ 9 , 10 ••]. Evidence is beginning to accumulate regarding the unique, multi-dimensional needs of older adults following cancer [ 11 •], and, with it, an understanding of challenges they may face as cancer survivors [ 12 ]. However, further work is needed to fully understand survivorship experiences for this population, gaps in care delivery, and how those gaps could be mitigated.
This paper highlights significant recent developments in survivorship research and care for older adults following cancer. We define survivorship as the interval from completion of primary cancer treatment until the identification of recurrent or progressive disease [ 13 ]. Our aim is to provide insight into care and support needs of older adults during cancer survivorship as well as directions for future research.
A brief review of literature from the last 3 years reporting on older adult cancer survivors aged 65 years and older was undertaken. Relevant topics were identified through consultation with experts in the field and used for search purposes. Keywords used together with “older adults” and “cancer survivors” were accelerated aging, polypharmacy, late/long-term effects, cognitive changes, neuropathy, comprehensive geriatric assessment, survivorship care plans, depression, ethics, and MAiD. A search of Medline via PubMed using the keywords identified relevant English publications from the past 3 years. All article types were considered (e.g., reviews, perspectives papers, descriptive/intervention studies). Each article was reviewed, significant findings identified, and results grouped into broad topic areas. These broad topics are summarized below, presenting significant developments regarding research and care of older cancer survivors reported over the past 3 years.
Aging and Cancer Survival
Four articles addressed patterns of survival among older adults and the impact of little research that considers age-related concerns on patterns and quality of survival in this group. There have been consistent improvements in cancer survival over the past two decades; however, these improvements are smaller for those aged 75 years and older at diagnosis and there is greater variation in 5-year survival across countries for this age group [ 7 ••]. Cellular and molecular changes that occur in non-cancerous cells with aging contribute to a microenvironment that promotes tumor progression and to treatment responses that may impact outcomes, including survival, but are seldom considered in pre-clinical trials [ 14 •]. In addition, a lack of inclusion of older adults in clinical trials, and consideration of outcomes of importance to older adults, means that treatment decisions for older adults with cancer are often based on evidence acquired from younger adults with fewer comorbidities, less polypharmacy, and different physiology [ 15 ].
Accelerated Aging
Not only does aging impact the experience of cancer, but the disease and treatment can also impact the experience of aging among cancer survivors. There is increasing work documenting patterns of accelerated or accentuated aging among people who have experienced cancer treatment [ 16 , 17 ••, 18 ]. Aging is often understood as the “time-dependent accumulation of cellular damage” [ 14 •]. Accelerated or accentuated aging occurs when cancer and cancer treatments contribute to genotoxic and cytotoxic damage that contributes to anatomic and functional changes that mirror those expected with aging, but at a younger age or to a greater degree than would occur in the absence of cancer [ 17 ••]. We identified seven articles exploring relationships among physiological markers of aging, behavioral or functional changes associated with aging, and the receipt of cancer treatment. The aging phenotype caused by cancer and its treatment has been characterized by adverse physical and cognitive consequences, including fatiguability and poor endurance [ 19 ], persistent cognitive impairment [ 20 ], onset of chronic health conditions [ 16 , 21 ••, 22 ], and decreased survival [ 17 ••, 22 ]. Researchers are exploring physiological mechanisms that may contribute to this accelerated aging phenotype among cancer survivors, including DNA damage [ 17 ••, 22 ], stem cell depletion [ 17 ••], alterations in cerebral blood flow [ 20 ], shortening of telomere length [ 16 ], cellular senescence [ 17 ••, 21 ••], and disruption of pathways that mitigate the damaging effects of inflammation and oxidative stress [ 20 , 21 ••]. These physiological changes may be reflected in clinical measures of functional status, frailty, and cognitive function, including subjective measures, such as self-report measures of activities of daily living, and objective measures, such as gait speed and grip strength [ 17 ••]. These changes may also be reflected in biological measures. The authors of recent reviews present a thorough discussion of the biomarkers associated with aging that may be used to assess and/or predict accelerated aging [ 17 ••] or resilience [ 21 ••].
To increase understanding of cancer treatment on aging, appropriate clinical and biological measures of aging of must be incorporated into clinical trials [ 17 ••]. Resilience, defined as capacity to resist or regain physical, cognitive, or psychological function and well-being after a stressor, diminishes with aging and may be defined by age-related biologic processes [ 21 ••]. If so, then clinical and biological measures of aging may also predict resilience in older survivors, and identifying associated physiological and molecular mechanisms may promote the identification of protective factors and strategies to promote resilience and well-being in survivorship [ 21 ••]. Some strategies to prevent accelerated aging include treatment with pharmaceuticals or nutraceuticals that reduce inflammation, treat cardiovascular risk, or improve cardiac function, as well as behavioral strategies including exercise-based interventions considering the unique needs of survivors [ 16 ].
Issues of Particular Concern Among Older Adult Survivors
Eighteen articles describing physical issues, comorbidities, and polypharmacy for older cancer survivors were identified. Ten were studies of older cancer survivors, five focused on older breast cancer survivors, and others addressed issues with older survivors of hematological, oral-digestive and prostate cancers, and non-Hodgkin’s lymphoma.
Physical Issues
Studies about older adults following cancer treatment have chiefly focused on physical health and function [ 10 ••, 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 ••, 31 , 32 , 33 , 34 , 35 , 36 , 37 ]. The impaired physical function has been studied as a result of treatment [ 25 , 26 , 27 , 28 ] and several studies compared symptom burden with non-cancer controls or younger cancer survivors [ 23 , 26 , 28 , 29 , 30 ••, 31 , 32 , 33 , 35 ]. In a Canadian survey of over 3000 cancer survivors 75 years or older, 80% reported physical concerns [ 11 •]. Specifically impaired physical function, decline in cardiovascular and other health conditions, fatigue, and depression were studied. The effect of cancer treatment on cardiovascular systems, physical balance, mobility, and neuropathy were reported as significant in older cancer survivors [ 10 ••, 25 , 28 ].
While the importance of physical function in older cancer survivors was explored in some studies, cognitive impairment was highlighted in more than half. Cognitive decline was observed as common in older cancer survivors, but findings varied, ranging from 12 to 75% [ 33 ]. One study observed no association between chemotherapy and cognitive function [ 27 ]. In others, older cancer survivors were shown to demonstrate the decline in executive functioning and verbal memory more frequently than younger adults following treatment [ 26 , 33 ]. Regier et al. [ 33 ] found up to 40% of older cancer survivors exhibited cancer-related cognitive impairment (sustained attention, memory, and verbal fluency) 18 months post-diagnosis while survivors who exhibited high psychoneurological symptoms at diagnosis were more likely to experience greater cognitive decline post-treatment [ 25 , 30 ••, 35 ].
Comorbidities and Polypharmacy
It is estimated 25% of older adults with cancer have five or more comorbid conditions [ 10 ••]. In a recent Canadian study, over 70% of adult survivors 75 years and older reported comorbidities, the four most common being cardiovascular/heart disease (45%); arthritis, osteoarthritis, or other rheumatic diseases (40%); diabetes (16%); and mental health (7%) [ 11 •]. Given the prevalence of other diseases and medical conditions, it is interesting that less than half of the articles addressed comorbidities and fewer discussed the importance of polypharmacy and its implications. While older adults comprise less than 15% of the population of the USA, for example, they account for over 30% of both non-prescription and prescription medications [ 30 ••]. Magnusson et al. [ 30 ••] state that polypharmacy is defined as the use of five or more medications but recognize that researchers less often address appropriate versus inappropriate polypharmacy (lacking evidence base, adverse reactions, etc.). On average, older adults with cancer take nearly 10 different medications and many are uncertain about the reasons they need these medications [ 10 ••]. The impacts of adverse drug effects (e.g., falls, cognitive issues) and drug and disease interactions can be severe. In addition, Guerard et al. [ 10 ••] note that a fragmented group of providers is often responsible for the provision of healthcare to older adults which can result in a lack of communication and coordination among the various specialists involved [ 30 ••] and uncertainty on the part of survivors about where they should seek assistance for an issue [ 12 ].
Overall cancer and its treatments are associated with higher levels of symptom burden and greater loss of well-being over time in older adult survivors, as compared to older adults without cancer, suggesting the need for greater surveillance and opportunities for intervention [ 31 ]. In addition, many older adults are at risk for experiencing physical, emotional, and practical concerns following cancer treatment yet are not obtaining desired help [ 12 ]. Coughlin et al. noted that given prevalent age-related issues such as comorbidities, osteoporosis, symptoms, physical functioning, cognitive functioning, nutrition, and physical activity [ 37 ], appropriate surveillance, screening (including pre-screening for at-risk individuals), and interventions both during and post-treatment are critical to improve associated functional/neurological changes and improve the overall quality of life [ 24 , 30 ••, 31 , 32 , 33 ]. Future research is needed about the nature and extent of disability and symptom burden to develop survivorship programs for this distinct patient population [ 29 ] and inform the development of guidelines and policies in conjunction with patients’ preferences and goals [ 10 ••].
Factors Influencing Quality of Life in Older Adult Survivors
A primary direction of research regarding older adult cancer survivors has been identifying factors that influence quality of life. Health-related quality of life (HRQOL) is seen as a primary outcome given that priorities and values for older adults shift as they age [ 38 ] and acknowledge they have few remaining years. However, age alone is insufficient to explain variations in this populations’ HRQOL. Both cancer (e.g., cancer type, treatment modality, recurrence) and non-cancer-related (e.g., education, income, residence) factors contribute [ 38 , 39 , 40 ].
Most studies reviewed included survivors of breast, prostate, lung, and colorectal cancers, making use of existing databases and frequently resulting in sizeable sample sizes (121 [ 41 ] to 271,640 [ 42 •]. Studies involved various time intervals following completion of treatment (1 to > 10 years), definitions of older adults (e.g., 60+, 75+, 70+, 75+, and 80+ years) and combinations of physical, psychological, emotional, social, and demographic variables. Overall, there is agreement that HRQOL is lower in older adult survivors than in general older adult populations [ 42 •, 43 ].
Consistently physical variables have the strongest associations with HRQOL. Although these variables were measured in various ways, (e.g., physical well-being [ 44 •], functional health limitations [ 38 ] disability [ 45 ], mobility [ 46 , 47 ], and physical health status [ 48 ], the capacity to manage activities of daily living and maintain independence were critical for older adult survivors and contributed to HRQOL. Cancer type [ 49 •], the number of comorbidities [ 42 •, 45 ], length of time dealing with side effects, side effect severity [ 43 , 50 , 51 ], duration of chronic illness [ 39 ], and deteriorating health status [ 41 , 45 ] are key variables with negative influence on HRQOL. Experiencing fatigue [ 44 •], frailty [ 53 ••], difficulty performing Activities of Daily Living (ADLs) [ 53 ••], difficulty walking [ 46 ],) and increased risk for falls [ 47 , 48 ] are challenges associated with poor HRQOL outcomes [ 53 ••] in older survivors. In a sample of 3274 older cancer survivors, when asked to identify the main challenge, they experienced in transitioning to survivorship, over 68% identified physical limitations [ 11 •].
Psychosocial variables have not been explored as frequently as physical variables in older cancer survivors. Depression [ 40 , 50 ], body image (appearance) [ 51 , 54 ], reduced optimism [ 55 ], altered sexual intimacy [ 56 ], treatment decision regret [ 57 ], chronic stress (55), lack of emotional support [ 39 ], and post-traumatic growth [ 41 ] are associated with reduced HRQOL. Depression is concerning in this population, reaching levels of 30% in community-dwelling older survivors [ 40 ]. Increased levels of depression are associated with female gender, number of symptoms [ 50 ], living alone [ 40 ], reduced income [ 40 ], and recurrence [ 40 ]. Additionally, social well-being, which is associated with social support and satisfaction with psychosocial need fulfillment [ 58 ], is associated with QOL [ 41 ]. Attending to environmental barriers which hinder engagement in social activities and reintegration in the community is important for older survivors given isolation contributes to reduced QOL [ 58 ].
Two variables beginning to receive attention in survivor populations are income and rurality. A larger proportion of older cancer survivors with low household income have concerns and seek help for physical, emotional, and practical issues than those with higher incomes [ 59 ]. However, similar proportions of low- and high-income older survivors experienced difficulty obtaining help for their concerns. In general, lower levels of subjective socioeconomic status are associated with lower QOL across all domains [ 39 , 41 , 49 •], non-adherence in purchasing medicines and supplies [ 60 ], and foregoing tests, procedures, and care [ 61 ].
Although rurality has been investigated regarding access to screening, diagnostic, and treatment services, few studies have looked at access to services for survivorship care, especially for older adults. Access to services presents different challenges for survivors than for cancer patients; survivors want services close to home rather than traveling for specialist treatment [ 62 ]. Moss et al. [ 42 •] reported QOL is higher for older survivors living in urban settings where access to ancillary services such as social work, physiotherapy, and support groups is easier. The need to leverage the higher social integration in rural communities to enhance emotional support for older adult survivors is recommended.
Interventions for Older Adult Cancer Survivors
Few studies regarding the effectiveness of interventions designed for older adult cancer survivors were identified in our search. Interventions receiving the most attention included incorporating comprehensive geriatric assessment (CGA) and physical exercise.
Comprehensive Geriatric Assessment
Older adults present a wide variation in health and functional status that may be exacerbated by cancer treatment and present various life challenges [ 63 ]. The use of screening and other assessment tools is helpful for identifying patient needs and planning appropriate interventions, particularly for distinct populations such as older adults.
Comprehensive Geriatric Assessment (CGA) is a process of evaluating and improving functional ability, physical health, cognition and mental health, and socio-environmental circumstances of older adults. Assessment results are reviewed by healthcare teams, discussed with patients, and incorporated into care plans. Nishuima et al. [ 64 •], for example, propose an approach to CGA comprised of assessments in 10 impairment domains (cognition, mood, communication, mobility, balance, bowels, bladder, nutrition, daily activities, and social) and a single comorbidity domain. Geriatric assessed impairments were associated with increased hospitalizations and long-term care use in older adults with cancer [ 65 ]. Benefits of CGA include treatment effectiveness and efficacy, prediction of mortality and cancer treatment tolerance, and decision-making to establish the appropriate treatment of cancer [ 66 ••]. CGA also helps identify significant comorbidities and polypharmacy [ 67 ] and patients who might benefit from less invasive and more tolerable evidence-based treatments [ 68 ]. Studies have shown that participants receiving CGA-based intervention report significantly better HRQOL [ 63 ].
While GA is helpful in identifying deficits in older adults with cancer and is considered a critical component in oncology treatment planning, with demonstrated feasibility and effectiveness, it is not widely implemented [ 63 , 65 , 67 , 68 ]. The incorporation of geriatric screening can be taxing to this population particularly if multiple surveys/screening tools related to geriatric domains are used in addition to those related to distress and patient-reported outcomes. In addition, healthcare providers find the incorporation of CGA into daily practice time-consuming [ 63 ]. Successful implementation requires the involvement of the multi-disciplinary team, strong administrative and patient scheduling support, and planning [ 66 ••]. Given the complexities of care for older adults with cancer, the introduction of CGA in post-treatment care, as an aspect of survivorship care planning, for example, could assist in isolating survivors’ critical health issues, identifying appropriate therapies, and enhancing survivorship care coordination.
Physical Activity/Exercise
More than 50% of older cancer survivors are not achieving standards for physical activity (PA) [ 44 •, 54 ]. Given the potential impact of PA on recovery and capacity to perform activities of daily living (ADLs), finding relevant and effective physical programming for older adults with cancer has become a priority. Unfortunately, current guidelines are based on research with younger populations. A recent systematic review of the effectiveness of PA interventions in older survivors identified 14 studies [ 69 ••]. However, interventions varied in duration (1 to 12 months), intensity, settings, and outcome measurements, making it difficult to draw conclusions about specific approaches for older survivors.
Given the choice about what interventions to pursue in one study, older adults selected PA [ 70 ]. Older survivors reported they used PA programs to increase engagement and performance of ADLs and reduce sleep disturbances and fatigue [ 70 , 71 , 72 ]. In addition, interventions help with issues of body image and psychosocial distress [ 44 •, 54 , 72 ]. Barriers included time, transportation, lack of facilities, weather, and pain [ 44 •, 70 , 72 ] while their preferences included structured programs incorporated with cancer care, having supervision, and being able to use equipment aids [ 70 , 72 ].
Older Adult Survivor Perspectives Regarding Experiences with Care
A small but growing body of evidence is emerging which captures survivors’ perspectives about experiences with cancer care delivery and suggestions for improvement. Given the complexity of needs and challenges in addressing concerns, it is important to understand the views of older survivors who have accessed services.
In quantitative investigations, higher access to services and higher self-reported health status were associated with better care experiences [ 73 ]. Variations in care experiences exist by education, gender, and cancer types. Scores indicating patient perceptions of higher care coordination are associated with living rurally at diagnosis, having fewer specialists involved in care, and more frequent visits with a family doctor [ 74 ]. Low scores are reported by women with metastatic disease, those with higher education, and individuals over 80 years of age [ 74 ].
A thematic analysis from Canada described perspectives of older adults regarding challenges experienced during survivorship care and suggestions for improvements. Themes regarding challenges included: “Getting back on my feet,” “Adjusting to life changes,” and “Finding the support I need” [ 11 •], while those regarding suggestions for improvements were, “Offer me support,” “Make access easy for me,” and “Show me you care” [ 36 ]. In this same study, communication, information, and access to a range of services were considered important yet remained gaps in service delivery by 82% of respondents.
During the COVID-19 pandemic, older adult survivors were reported to be among one of the most disadvantaged groups and needed special consideration in terms of support [ 75 ]. One qualitative study reported older survivors [ 76 ] indicated they understood the situation but that they missed interactions with others. Survivors found virtual clinic appointments were helpful, especially in reducing needs for transportation, but they were not as beneficial for social interaction as in-person visits.
Suggestions Regarding Future Research and Care Across Articles
Many articles contained recommendations about screening to identify at-risk individuals and utilizing deeper assessment of needs to build tailored interventions. Incorporating self-report by older survivors for aspects such as physical health, mobility, and emotional distress was emphasized [ 43 , 48 , 50 ] together with a relevant discussion of preferences [ 38 ]. Older survivors are a heterogeneous population with unique and complex needs. The priorities in unmet needs vary [ 12 ] and what will be most effective in meeting those needs differs from other age groups [ 77 ]. Yet health care professionals report a lack of confidence in caring for this population [ 78 ]. Enhancing knowledge and skill for survivorship care of older adults, guided by standards for optimizing care for this population [ 78 , 79 ], needs consideration.
Several areas of interventions used with other populations may have potential relevance for the older adult survivor cohort and could be considered for future program design and implementation. Lay Navigation [ 80 ], nurse coordination models [ 74 ], home telehealth [ 74 , 76 ], use of survivorship care plans [ 81 , 82 ], and active involvement of caregivers/partners in care planning [ 83 , 84 ] could be explored given the interventions were designed with the unique needs of older survivors in mind.
An Emerging Consideration from Clinical Care
An emerging issue regarding the clinical care of older adults with cancer is the marked increase in requests for medical assistance in dying (MAiD) [ 85 ]. The concept of MAiD encompasses the terms assisted suicide and euthanasia [ 86 •] with MAiD legislation originally aimed to ease the burden of suffering of imminent death. Conversation of the right to access MAiD most often centers on individual autonomy and dying with dignity (e.g., Selby et al. [ 87 •]), conceptualized as having control over one’s destiny. It has been strongly associated with an unacceptable situation of being dependent and a burden to the family. Definitions and restrictions of MAiD, guided by healthcare providers’ standards of practice, organizational policies, and professional codes of ethics, vary depending on jurisdiction-specific legislation. MAiD is often framed as a procedure; however, this patient choice also represents an extensive social movement in which a multitude of legal, ethical, regulatory, and clinical factors converge with highly personal values and beliefs involved. No discussion about this issue emerged in the literature regarding older adult cancer survivors, leaving little guidance for negotiating the difficulty of providing ethical options while also countering ageist discourses influencing patient choices.
The majority of people who consider MAiD have a pre-existing cancer diagnosis [ 88 •, 89 , 90 , 91 •]. A recent Canadian survey of oncologists reported 70% encountered a patient request for MAiD [ 92•• ]. Nurses also grapple with requests for medical assistance in dying (MAiD) among older adults with cancer, perceiving it to be a response to suffering, being a burden in survivorship, and not wanting to engage in treatment or transition to palliative care [ 80 ]. Concerns that uncontrolled physical and psychological symptoms may prompt premature requests for MAiD are warranted [ 91 •]. Furthermore, understanding the interplay of depression and demoralization, factors which are often undertreated and unaddressed in older adults, with MAiD requests is essential. The research provides a better understanding of these influences and provides guidance for practice underway [ 93 •].
In support of appropriate access and choice regarding MAiD, current evidence supports that clear and direct discussions with an interdisciplinary approach enhance therapeutic relationships [ 91• , 94 , 95 ]. At the same time, MAiD must remain person-centered to humanize a medicalized activity [ 96 ••]. Such conversations have implications for all patients, and more specifically older adults with cancer. The conversations are apt to occur within a largely unquestioned backdrop of system-level ageism, an often unaccounted for force impacting cancer care [ 36 ]. Healthcare professionals must consider messages they transmit when they commit to having explicit conversations about assistance for dying but not to the assistance required for living with the challenging side effects of cancer and subsequent treatment as patients move in and through survivorship. Evidence-informed guidelines are essential to support the transition through active treatment to survivorship. Clearly, there is need for further research in this area in the context of survivorship.
Existing Guidelines to Inform Intervention
Guidelines established by the National Comprehensive Cancer Network [NCCN] [ 97 ] and the American Society of Clinical Oncology [ 98 ] provide a framework for assessing and managing age-related concerns prior to and during cancer treatment. In addition, priorities to optimize care of older adults with cancer have been identified [ 79 , 99 , 100 ] and recommendations to support quality of life during all phases of the cancer trajectory, including survivorship, have been developed [ 101 ].
The body of evidence for guiding care of older adult cancer survivors is growing and confirms the unique and complex needs of this population. Screening at-risk individuals and connecting them to appropriate resources is important. Tailored assessments and interventions before, during, and after treatment are necessary to optimize survivorship care. However, additional research is required to design truly age appropriate and effective care approaches. By strengthening the evidence base to better inform treatment decision-making, outcomes for older adults with cancer may be improved, both in terms of survival and quality of life in survivorship.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363–85.
Article Google Scholar
Pilleron S, Sarfati D, Janssen-Heijnen M, et al. Global cancer incidence in older adults, 2012 and 2035: a population-based study. Int J Cancer. 2019;144:49–58.
Article CAS Google Scholar
Parry C, Kent EE, Mariotto AB, et al. Cancer survivors: a booming population. Cancer Epidemiol Biomarkers Prev. 2011;20:1996–2005.
Lerro CC, Stein KD, Smith T, Virgo KS. A systematic review of large-scale surveys of cancer survivors conducted in North America, 2000–2011. J Cancer Survivorship. 2012;6:115–45. https://doi.org/10.1007/s11764-012-0214-1 .
Hewitt M, Greenfield S, Stovall E. From cancer patient to cancer survivor: Lost in transition. Institute of Medicine, Washington, DC: The National Academies Press. 2006
Hamrood R, Hamrood H, Merhasin I, Kenan-Boker L. Chronic pain and other symptoms among breast cancer survivors: prevalence predictors and effects on quality of life. Breast Cancer Res Treat. 2018;167(1):157–69. https://doi.org/10.1007/s10549-017-4485-0 ( Epub 2017 Aug 31 ).
Arnold M, Rutherford MJ, Bardot A, Ferlay J, Andersson TML, Myklebust TÅ… Bray F. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995-2014 (ICBP SURVMARK-2): A population-based study. Lancet Oncol. 2019;20(11);1493–1505. https://doi.org/10.1016/S1470-2045(19)30456-5 . Longitudinal, population-based study in which researchers analyzed patient-level data of 3.9 million patients drawn from population-based cancer registries in seven countries. They calculated age-standardized net survival at 1 and 5 years by tumor site, age group, and period of diagnosis.
Corbett T, Bridges J. Multimorbidity in older adults living with and beyond cancer. Current Opinion in Supportive and Palliative Care. 2019;13:220–4. https://doi.org/10.1097/SPC.0000000000000439 .
Article PubMed Google Scholar
Rowland JH, Bellizzi KM. Cancer Survivorship Issues Life after treatment and implications for an aging population. Journal of Clinical Oncology. 2014;32:2662–8. https://doi.org/10.1200/JCO.2014.55.836 .
Article PubMed PubMed Central Google Scholar
Guerard EJ, Nightingale G, Bellizzi K, Burhenn P, Rosko A, Artz AS, et al. Survivorship care for older adults with cancer: U13 Conference Report. J Geriatr Oncol. 2016;(4):305-12. https://doi.org/10.1016/j.jgo.2016.06.005 . This article presents a summary of the Cancer and Aging Research Group (National Institute on Aging and National Cancer Institute) 2015 conference that discussed survivorship care for older adults. Emerging themes included that survivorship must evolve to meet the needs of older adults; older adult survivors require tailored survivorship care and plans; the suitability of the interdisciplinary team to provide older adult survivorship care; and patient advocacy is needed throughout the care continuum.
Fitch MI, Nicoll I, Lockwood G, Strohschein FJ, Newton L. Main challenges in survivorship transitions: perspectives of older adults with cancer. J Geriatr Oncol. 2021;12(4):632–640. https://doi.org/10.1016/j.jgo.2020.09.024 . A secondary analysis of early cancer survivorship for older adults revealing gaps in care and raises concerns about unexamined ageism within the Canadian cancer care system, with the concurrent need for comprehensive geriatric assessments along with multi-modal proactive treatment plans.
Fitch MI, Nicoll I, Lockwood G, Strohschein FJ, Newton L. Cancer survivors 75 years and older: physical, emotional and practical needs. BMJ Support Palliat Care. 2021; Apr 21. https://doi.org/10.1136/bmjspcare-2020-002855 .
Earle CC. Failing to plan is planning to fail: improving the quality of care with survivorship care plans. J Clin Oncol. 2006;24(32):5112–6. https://doi.org/10.1200/JCO.2006.06.5284 .
Fane M, Weeraratna AT. How the ageing microenvironment influences tumour progression. Nat Rev Cancer. 2020;20(2):89–106. https://doi.org/10.1038/s41568-019-0222-9 . A review in which the authors discuss how the ageing microenvironment contributes to tumor progression and responses to cancer therapy, including survival.
Outlaw D, Williams GR. Is the lack of evidence in older adults with cancer compromising safety? Expert Opin Drug Saf. 2020;19(9):1059–61.
Armenian SH, Gibson CJ, Rockne RC, Ness KK. Premature aging in young cancer survivors. J Natl Cancer Inst. 2019; 111(3):226–232.
Guida JL, Ahles TA, Belsky D, Campisi J, Cohen HJ, Degregori J… Hurria, A. Measuring aging and identifying aging phenotypes in cancer survivors. J Natl Cancer Inst 2019;111(12):1245–1254. https://doi.org/10.1093/jnci/djz136 . Provides a summary of the National Cancer Institute’s 2018 interdisciplinary think tank concerning aging-related consequence of cancer and cancer treatment, which addressed conceptual, measurement, and methodological challenges in this field.
Sedrak MS, Hurria A. Cancer in the older adult: implications for therapy and future research. Cancer. 2018;124(6):1108–10. https://doi.org/10.1002/cncr.31236 .
Gresham G, Dy SM, Zipunnikov V, Browner IS, Studenski SA, Simonsick EM, Ferrucci L, Schrack JA. Fatigability and endurance performance in cancer survivors: analyses from the Baltimore Longitudinal Study of Aging. Cancer. 2018;124(6):1279–87.
Carlson BW, Craft MA, Carlson JR, Razaq W, Deardeuff KK, Benbrook DM. Accelerated vascular aging and persistent cognitive impairment in older female breast cancer survivors. Geroscience. 2018;40(3):325–36. https://doi.org/10.1007/s11357-018-0025-z .
Article CAS PubMed PubMed Central Google Scholar
Sedrak MS, Gilmore NJ, Carroll JE, Muss HB, Cohen HJ, Dale W. Measuring biologic resilience in older cancer survivors. J ClinOncol. 2021;39(19):2079–2089. In this review, authors highlight the emerging concept of resilience in older cancer survivors, considering potential biomarkers and interventions that may promote resilience in this population.
Slavin TP, Sun CL, Chavarri-Guerra Y, Sedrak MS, Katheria V, Castillo D, et al. Older breast cancer survivors may harbor hereditary cancer predisposition pathogenic variants and are at risk for clonal hematopoiesis. J Geriatr Oncol. 2020;11(2):316–9. https://doi.org/10.1016/j.jgo.2019.09.004 .
Bevilacqua L, Dulak D, Schofield E, Starr TD, Nelson CJ, Roth AJ. Prevalence and predictors of depression, pain, and fatigue in older- versus younger-adult cancer survivors. Psycho-oncology. 2018;27(3):900–7. https://doi.org/10.1002/pon.4605 .
Blackwood J, Rybicki K, Huang M. Cognitive measures in older cancer survivors: An examination of validity, reliability, and minimal detectable change. J Geriatr Oncol. 2021;1:146–51. https://doi.org/10.1016/j.jgo.2020.06.015 .
La Carpia D, Liperoti R, Guglielmo M, Di Capua B, Devizzi LF, Matteucci P, et al. Cognitive decline in older long-term survivors from Non-Hodgkin Lymphoma: a multicenter cross-sectional study. J Geriatr Oncol. 2020;11(5):790–5. https://doi.org/10.1016/j.jgo.2020.01.007 .
Morin RT, Midlarsky E. Treatment with chemotherapy and cognitive functioning in older adult cancer survivors. Arch Phys Med Rehabil. 2018;99(2):257–63. https://doi.org/10.1016/j.apmr.2017.06.016 .
Fino PC, Horak FB, El-Gohary M, Guidarelli C, Medysky ME, Nagle SJ, Winters-Stone KM. Postural sway, falls, and self-reported neuropathy in aging female cancer survivors. Gait Posture. 2019;69:136–42. https://doi.org/10.1016/j.gaitpost.2019.01.025 .
Götze H, Köhler N, Taubenheim S, Lordick F, Mehnert A. Polypharmacy, limited activity, fatigue and insomnia are the most frequent symptoms and impairments in older hematological cancer survivors (70+): Findings from a register-based study on physical and mental health. J Geriatr Oncol. 2019;10(1):55–9. https://doi.org/10.1016/j.jgo.2018.05.011 .
Magnuson A, Sattar S, Nightingale G, Saracino R, Skonecki E, Trevino KM. A practical guide to geriatric syndromes in older adults with cancer: a focus on falls, cognition, polypharmacy, and depression. Am Soc Clin Oncol Educ Book. 2019n;39:e96–e109. https://doi.org/10.1200/EDBK_237641 . Identifies potential screening tools to identify geriatric syndromes and highlights the significance of falls, cognitive impairment, polypharmacy, and depression in older adults with cancer.
Mandelblatt JS, Zhai W, Ahn J, Small BJ, Ahles TA, Carroll JE, et al. Symptom burden among older breast cancer survivors: the Thinking and Living with Cancer (TLC) study. Cancer. 2020;126(6):1183–92. https://doi.org/10.1002/cncr.32663 .
Meneses K, Benz R, Bail JR, Vo JB, Triebel K, Fazeli P, et al. Speed of processing training in middle-aged and older breast cancer survivors (SOAR): results of a randomized controlled pilot. Breast Cancer Res Treat. 2018;168(1):259–67. https://doi.org/10.1007/s10549-017-4564-2 .
Regier NG, Naik AD, Mulligan EA, Nasreddine ZS, Driver JA, Sada YH, Moye J. Cancer-related cognitive impairment and associated factors in a sample of older male oral-digestive cancer survivors. Psycho-oncology. 2019;28(7):1551–8. https://doi.org/10.1002/pon.5131 .
Shah R, Chou LN, Kuo YF, Raji MA. Long-term opioid therapy in older cancer survivors: a retrospective cohort study. J Am Geriatr Soc. 2019;67(5):945–52. https://doi.org/10.1111/jgs.15945 .
Tometich DB, Small BJ, Carroll JE, Zhai W, Luta G, Zhou X, et al. Thinking and Living with Cancer (TLC) Study. Pretreatment psychoneurological symptoms and their association with longitudinal cognitive function and quality of life in older breast cancer survivors. J Pain Symptom Manage. 2019;57(3):596–606. https://doi.org/10.1016/j.jpainsymman.2018.11.015 .
Fitch MI, Nicoll I, Lockwood G, Newton L, Strohschein FJ. Improving survivorship care: perspectives of cancer survivors 75 years and older. J Geriatr Oncol. 2021;12(3):453–60. https://doi.org/10.1016/j.jgo.2020.09.012 .
Coughlin SS, Paxton RJ, Moore N, Stewart JL, Anglin J. Survivorship issues in older breast cancer survivors. Breast Cancer Res Treat. 2019;174(1):47–53. https://doi.org/10.1007/s10549-018-05078-8 .
Lapinsky E, Man LC, MacKenzie AR. Health-related quality of life in older adults with colorectal cancer. Curr Oncol Rep. 2019;21(9):81. https://doi.org/10.1007/s11912-019-0830-2 ( PMID: 31359163 ).
Doran P, Burden S, Shryane N. Older people living well beyond cancer: the relationship between emotional support and quality of life. J Aging Health. 2019;31(10):1850–71. https://doi.org/10.1177/0898264318799252 .
Doege D, Thong MSY, Koch-Gallenkamp L, Jansen L, Bertram H, Eberle A, et al. Age-specific prevalence and determinants of depression in long-term breast cancer survivors compared to female population controls. Cancer Med. 2020;9(22):8713–21. https://doi.org/10.1002/cam4.3476 .
Yang S-K, Ha Y. Exploring the relationships between posttraumatic growth, wisdom, and quality of life in older cancer survivors. Asian Pac J Cancer Prev. 2019;20(9):2667–72. https://doi.org/10.31557/APJCP.2019.20.9.2667 .
Moss JL, Pinto CN, Mama SK, Rincon M, Kent EE, Yu M, Cronin KA. Rural–urban differences in health-related quality of life: patterns for cancer survivors compared to other older adults. Qual Life Res. 2021;30:1131–1143. https://doi.org/10.1007/s11136-020-02683-3 . This study has a very large sample size and one of the first to explore rural-urban differences among older cancer survivors.
Winters-Stone KM, Medysky ME, Savin MA. Patient-reported and objectively measured physical function in older breast cancer survivors and cancer-free controls. J Geriatr Oncol. 2019;10(2):311–6. https://doi.org/10.1016/j.jgo.2018.10.006 .
Shuk D, Cheung T, Takemura N, Chau PH, Yee A, Ng M, Xu X, Lin CC. Exercise levels and preferences on exercise counselling and programming among older cancer survivors: a mixed-methods study. JGO. 2021;12(8):1173–1180. https://doi.org/10.1016/j.jgo.2021.05.00 . Study provides interesting insight into the preferences of older adult survivors regarding how exercise programs could be designed with their needs in mind.
Diemling GT, Pappada H, Ye M, Nalepa E, Ciaralli S, Phelps E, Burant CJ. Factors affecting perceptions of disability and self-rated health among older adult, long-term cancer survivors. J Aging Health. 2019;31(4):667–84. https://doi.org/10.1177/0898264317745745 .
Brown JC, Narhay MO, Harhay MN. Self-reported major mobility, disability and mortality among cancer survivors. J Geriatr Oncol. 2018; 9(5):459–463. 1016/j.jgo.2018.03.004
Huang MH, Blackwood J, Godoshian M, Pfalzer L. Predictors of falls in older survivors of breast and prostate cancer: a retrospective cohort study of surveillance, epidemiology and end results-Medicare health outcomes survey linkage. J Geriatr Oncol. 2019;10(1):89–97. https://doi.org/10.1016/j.jgo.2018.04.009 .
Sulicka J, Pac A, Puzianowska-Kuźnicka3 M, Zdrojewski T, Chudek J, Tobiasz-Adamczyk B, et al., Health status of older cancer survivors—results of the PolSenior study. J Cancer Survivorship. 2018;12:326–333 https://doi.org/10.1007/s11764-017-0672-6
Ramsey SD, Hall IJ, Smith JL, Ekwueme DU, Fedorenko CR, Kreizenbeck K, et al. A comparison of general, genitourinary, bowel, and sexual quality of life among long term survivors of prostate, bladder, colorectal, and lung cancer. J Geriatr Oncol. 2021;12(2):305–311. https://doi.org/10.1016/j.jgo.2020.07.014 . This study offers insight into an often-overlooked aspect of quality of life in older adults (sexual activity). It includes a sample of various cancer types.
Levkovich I, Cohen, Alon S, Evron E, Pollack S, Fried, et al. Symptom cluster of emotional distress, fatigue and cognitive difficulties among young and older breast cancer survivors: the mediating role f subjective stress. J Geriatr Oncol. 2018;9(5):469–475. 1016/j.jgo.2018.05.002
Davis C, Tami P, Ramsay D, Melanson L, MacLean L, Nersesian S, Ramjeesingh R. Body image in older breast cancer survivors: a systematic review. Psycho-Oncology. 2020;29:823–32. https://doi.org/10.1002/pon.5359 .
Koll TT, Semin JN, Brodsky R, Fisher AL, High R, Beadle JN. Health-related and sociodemographic factors associated with physical frailty among older cancer survivors. J Geriatr Oncol. 2021;12(1):96–101. https://doi.org/10.1016/j.jco.2020.04.015 .
Blackwood J, Karczewski H, Huang MH, Pfalzer L. Katz activities of daily living disability in older cancer survivors by age, stage, and cancer type. J Cancer Surviv. 2020;14(6):769–778. https://doi.org/10.1007/s11764-020-00891-x . This article describes the range of potential impairments in activities of daily living cancer survivors could experience. It is a strong case for screening for ADL impairments as a regular aspect of care for older survivors.
Zhang X, Pennell ML, Bernardo BM, Crane T, Shadyab AH, Paskett ED, et al. Body image, physical activity and psychological health in older female cancer survivors. J Geriatr Oncol. 2021;12(7):1059–67. https://doi.org/10.1016/j.jgo2021.04.007 .
Chow PI, Shaffer LM, Lohman MC, LeBaron VT, Fortuna KL, Ritterband LM. Examining the relationship between changes in personality and depression in older adult cancer survivors. Aging Ment Health. 2019;24(8):1237–45. https://doi.org/10.1080/13607863.2019.1594158 .
Arthur EK, Wordy B, Carpenter KM, Krok-Schoen JL, Quick AM, Jenkins LC, et al. Let’s get it on: addressing sex and intimacy in older cancer survivors. JGO. 2021;12(2):312–5. https://doi.org/10.1016/j.jgo.2020.08.033 .
Karauturi MS, Lei X, Shen Y, Giordano SH, Swanick CW, Smith BD. Long-term decision regret surrounding systemic therapy in older breast cancer survivors: a population-based survey study. J Geriatr Oncol. 2019;10(6):973–9. https://doi.org/10.1016/j.jgo.2019.03.013 .
Loew K, Lynch MF, Lee J. Social support, basic psychological needs, and social well-being among older cancer survivors. Int J Aging Hum Dev. 2021;92:100–14. https://doi.org/10.1177/0091415019887688 .
Fitch MI, Nicoll I, Lockwood G, Loiselle CG, Longo CJ, Newton L, Strohschein FJ. Exploring the relationships between income and emotional/practical concerns and help-seeking by older adult cancer survivors: a secondary analysis. J Geriatr Oncol. 2021. https://doi.org/10.1016/j.jgo.2021.11.007 .
Gu D, Shen C. Cost-related medication nonadherence and cost-reduction strategies among elderly cancer survivors with self-reported symptoms of depression. Popul Health Manag. 2020;23(2):132–9. https://doi.org/10.1089/pop.2019.0035 .
Longo CJ, Fitch MI. Unequal distribution of financial toxicity among people with cancer and its impact on access to care: a rapid review. Current Opinion (ePub 2021) https://doi.org/10.1097/spc.0000000000000561
Fitch MI, Lockwood G, Nicoll I. Physical, emotional, and practical concerns, help-seeking and unmet needs of rural and urban dwelling adult cancer survivors. J Eur Oncol Nurs. 2021;53:101976. https://doi.org/10.1016/j.ejon.2021.101976 .
Fitch MI, Strohschein FJ, Nyrop K. Measuring quality of life in older people with cancer. Curr Opin Support Palliat Care. 2021;15(1):39–47. https://doi.org/10.1097/SPC.0000000000000535 .
Nishijima TF, Shimokawa M, Esaki T, Morita M, Toh Y, Muss HB. A 10-item frailty index based on a Comprehensive Geriatric Assessment (FI-CGA-10) in Older Adults with Cancer: Development and construct validation. Oncologist. 2021;26(10):e1751–e1760. https://doi.org/10.1002/onco.13894 . Study of the creation and testing of a user-friendly frailty index based on comprehensive geriatric assessment with over 500 older adults with various cancer types. Results were determined more quickly and interpreted in a more clinically sensible manner than existing tools.
Williams GR, Dunham L, Chang Y, Deal AM, Pergolotti M, Lund JL, et al. Geriatric assessment predicts hospitalization frequency and long-term care use in older adult cancer survivors. J Oncol Pract. 2019;15(5):e399–409. https://doi.org/10.1200/JOP.18.00368 .
Overcash J, Ford N, Kress E, Ubbing C, Williams N. Comprehensive Geriatric Assessment as a versatile tool to enhance the care of the older person diagnosed with cancer. Geriatrics (Basel). 2019;24;4(2):39. https://doi.org/10.3390/geriatrics4020039 . Examination of how a comprehensive geriatric assessment can be tailored to ambulatory geriatric oncology programs in academic cancer centers and to community oncology practices with varying levels of resources.
Williams GR, Kenzik KM, Parman M, Al-Obaidi M, Francisco L, Rocque GB, et al. Integrating geriatric assessment into routine gastrointestinal (GI) consultation: the Cancer and Aging Resilience Evaluation (CARE). J Geriatr Oncol. 2020;11(2):270–3. https://doi.org/10.1016/j.jgo.2019.04.008 .
Cope DG, Reb A, Schwartz R, Simon J. Older adults with lung cancer: assessment, treatment options, survivorship issues, and palliative care strategies. Clin J Oncol Nurs. 2018;22(6):26–35. https://doi.org/10.1188/18.CJON.S2.26-35 .
Forbes C, Swan F, Greenley SL, Lind M, Johnson MJ. Physical activity and nutrition interventions for older adults with cancer: A systematic review. Journal of Cancer Survivorship. 2020;14:689–711. https://doi.org/10.1007/s11764-020-00883-x / Published online: 24 April 2020. A recent literature review of effectiveness of physical activity interventions for older adult cancer survivors describes various interventions and can inform future designs.
Lyons KD, Newman R, Adachi-Mejia AM, Whipple J, Hegel MT. Content analysis of a participant-directed intervention to optimize activity engagement of older adult cancer survivors. OTJR: Occup Participation Health. 2018;38(1):38–45. https://doi.org/10.1177/1539449217730356
Paulo TRS, Rossi FE, Viezel J, Tosello GT, Seidinger SG, Simões RR, et al. The impact of an exercise program on quality of life in older breast cancer survivors undergoing aromatase inhibitor therapy: a randomized controlled trial. Health Qual Life. 2019;17:17. https://doi.org/10.1186/s12955-019-1090-4 .
Perry CK, Ali WB, Solanki E, Winters-Stone K. Attitudes and beliefs of older female breast cancer survivors and providers about exercise in cancer care. ONF. 2020;47(1):56–69. https://doi.org/10.1188/20.ONF.56-69
Halpern MT, Urato MP, Lines LM, Cohen JB, Arora NK, Kent EE, et al. Healthcare experience among older cancer survivors: analysis of the SEER-CAHPS dataset. J Geriatr Oncol. 2018;9:194–203. https://doi.org/10.1016/j.jgo.2017.11.005 .
Mollica MA, Buckenmaier SS, Halpern MT, McNeel TS, Weaver SJ, Doose M, Kent EE. Perceptions of care coordination among older adult cancer survivors: a SEER-CAHPS study 2020. J Geriatr Oncol. 2021;12:446–52. https://doi.org/10.1016/j.jgo.2020.09.003 .
Galica J, Liu Z, Kain D, Merchant S, Booth C, Koven R, Brundage M, Haase KR. Coping during COVID-19: a mixed methods study of older cancer survivors. Support Care Cancer. 2021;29(6):3389–3398. https://doi.org/10.1007/s00520-020-05929-5 . Erratum in: Support Care Cancer. 2021.
Haase KR, Kain D, Merchant S, Booth C, Koven R, Brundage M, Galica J. Older survivors of cancer in the COVID-19 pandemic: reflections and recommendations for future care. J Geriatr Oncol. 2021;12(3):461–466. https://doi.org/10.1016/j.jgo.2020.11.009 .
Strohschein FJ. Newton L. Fitch MI, Haase K, Puts MTE, Jin R, Loucks A, Kenis C. Optimizing care of older adults with cancer: Canadian perspectives on challenges, solutions, and the need for interprofessional collaboration. Canadian Association of Psychosocial Oncology National Virtual Conference, July 14-16, 2020.
Puts M, Hsu T, Szumacher E, Dawe D, Fitch M, Jones J, Fulop T, Alibhai S, Strohschein F. Never too old to learn new tricks: surveying Canadian health care professionals about learning needs in caring for older adults with cancer. Curr Oncol. 2019;26(2):71–2. https://doi.org/10.3747/co.26.4833 .
Strohschein FJ, Newton L, Puts M, Jin R, Haase, K, Plante A, Loucks A, Kenis C, Fitch MI. Optimizing the care of older Canadians with cancer and their families: a statement articulating the position and contribution of Canadian oncology nurses. Can Oncol Nurs J = Revue canadienne de nursing oncologique. 2021;31(3):352–356.
Pisu M, Rocque GB, Jackson BE, Kenzik KM, Sharma P, Williams CP… Meneses K. Lay navigation across the cancer continuum for older cancer survivors: equally beneficial for Black and White survivors? J Geriatr Oncol. 2019;10(5):779–786. https://doi.org/10.1016/j.jgo.2018.10.013
Krok-Schoen JL, DeSalvo J, Klemanski D, Stephens C, Noonan AM, Brill S, Lustberg MB. Primary care physicians’ perspectives of the survivorship care for older breast cancer survivors: a pilot study. Support Care Cancer. 2020;28(2):645–52. https://doi.org/10.1007/s00520-019-04855-5 .
Krok-Schoen JL, Naughton MJ, Noonan AM, Pisegna J, DeSalvo J, Lustberg MB. Perspectives of survivorship care plans among older breast cancer survivors: a pilot study. Cancer Control. 2020;27(1):1073274820917208. https://doi.org/10.1177/1073274820917208 .
Cohee AA, Bigatti SM, Shields CG, Johns SA, Stump T, Monahan PO, Champion VL. Quality of life in partners of young and old breast cancer survivors. Cancer Nurs. 2018;41(6):491–7. https://doi.org/10.1097/NCC.0000000000000556 .
Kadambi S, Loh KP, Dunne R, Magnuson A, Maggiore R, Zittel J, Mohile S. Older adults with cancer and their caregivers - current landscape and future directions for clinical care. Nat Rev Clin Oncol. 2020;17(12):742–55. https://doi.org/10.1038/s41571-020-0421-z .
Van Den Noortgate N, Van Humbeeck L. Medical assistance in dying and older persons in Belgium: trends, emerging issues and challenges. Age Ageing. 2021;50(1):68–71. https://doi.org/10.1093/ageing/afaa116 .
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum . 2018;53:511–520. https://doi.org/10.1111/nuf.12280 . A Canadian descriptive narrative inquiry examining nurses’ experiences in the first six months of MAiD legalization, highlighting professional impacts of, and the importance of, open and non-judgemental communication with and between patients, families and the multidisciplinary healthcare team.
Selby, D, Bean, S, Isenberg-Grzeda, E, Bioethics, B, & Nolen, A. Medical Assistance in Dying (MAiD): A Descriptive study from a Canadian tertiary care hospital. Am J Hospice Palliat Care. 2020;37(1):58–64. https://doi.org/10.1177/1049909119859844 . A retrospective chart review was conducted to better understand the nature of MAiD requests in a Canadian healthcare institution, finding similarities with requests to other jurisdictions, and indicating that earlier assessments and more careful monitoring would be beneficial for this group at high risk for loss of capacity.
Blanke C, LeBlanc M, Hershman D, Ellis L, Meyskens F. (2017). Characterizing 18 years of the death with dignity act in Oregon. JAMA Oncol 2017;3(10):1403–1406. https://doi.org/10.1001/jamaoncol.2017.0243 . This analysis of publicly available data illuminates how MAiD in the USA is enacted and corroborates how cancer is the prevalent diagnosis of those choosing this option.
Emanuel IJ, Onwuteaka-Philipsen BD, Unwin JW, Cohen J. Attitudes and practices of euthanasia and physician-assisted suicide in the United States, Canada and Europe. JAMA. 2016;316:79–90. Comprehensive review of practices across Europe and North America with extensive data on differing approaches and experiences.
Health Canada. Second Annual Report on Medical Assistance in Dying in Canada: 2020. Ottawa, ON; June 2021. Accessed December 2, 2021 from: https://www.canada.ca/content/dam/hc-sc/documents/services/medical-assistance-dying/annual-report-2020/annual-report-2020-eng.pdf
Selby D, Bean S. Oncologists communicating with patients about assisted dying. Curr Opin Support Palliat Care. 2019;13(1):59–63. https://doi.org/10.1097/SPC.0000000000000411 . A review of recent literature regarding MAiD and communication revealed key themes of perceived barriers and benefits, including the importance of pragmatic and proactive approaches o develop and support best practices
Chandhoke G, Pond G, Levine O, Oczkowski S. Oncologists and medical assistance in dying: where do we stand? Results of a national survey of Canadian oncologists. Curr Oncol (Toronto, Ont.), 2020;27(5):263–269. https://doi.org/10.3747/co.27.6295 . An overview of survey finding to better understand Canadian oncologists’ experiences with MAiD, in which 70% of respondents received MAiD requests, supporting calls for standardized guidelines to safeguard equitable access for oncology patients.
Li M, Shapiro GK, Klein R, et al. Medical Assistance in Dying in patients with advanced cancer and their caregivers: a mixed methods longitudinal study protocol. BMC Palliat Care, 2021;117. https://doi.org/10.1186/s12904-021-00793-4 . This Canadian study is aimed to excavate the prevalence and determinants of depression and demoralization and how these states influence desire for death and MAiD requests, pointing to the importance of appropriate access and further consideration as the legislation for MAiD is broadening.
Jackson ML. Transitional Care: methods and processes for transitioning older adults with cancer in a post-acute setting. Clin J Oncol Nurs. 2018;22(6):37–41. https://doi.org/10.1188/18.CJON.S2.37-41 .
Suva G, Penney T, McPherson CJ. Medical assistance in dying: a scoping review to inform nurses’ practice. J Hospice Palliat Nurs. 2019;21(1):46–53. https://doi.org/10.1097/NJH.0000000000000486 .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. (2020). Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Glob QualNurs Res. 2020;7:2333393620938686 https://doi.org/10.1177/2333393620938686 . The purpose of this qualitative study was to explore ‘good nursing practice’ in the context of MAiD to humanize a somewhat medicalized experience, which includes establishing relationships, planning and supporting the family and underscores the need for best practice guidelines development.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Older adult oncology (Version 1.2021). 2021. Available from: www.nccn.org . Accessed 2 Jan 2022.
Mohile SG, Dale W, Somerfield MR, Schonberg MA, Boyd CM, Burhenn PS, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol. 2018;36:2326–47.
Extermann M, Brain E, Canin B, Cherian MN, Cheung K-L, de Glas N, et al. Priorities for the global advancement of care for older adults with cancer: an update of the International Society of Geriatric Oncology Priorities Initiative. Lancet Oncol. 2021;22(1):e29–36.
Puts M, Strohschein F, Oldenmenger W, Haase K, Newton L, Fitch M, et al. Position statement on oncology and cancer nursing care for older adults with cancer and their caregivers of the International Society of Geriatric Oncology Nursing and Allied Health Interest Group, the Canadian Association of Nurses in Oncology Oncology & Aging Special Interest Group, and the European Oncology Nursing Society. J Geriatr Oncol. 2021;12(7):1000–4.
Scotté F, Bossi P, Carola E, Cudennec T, Dielenseger P, Gomes F, et al. Addressing the quality of life needs of older patients with cancer: a SIOG consensus paper and practical guide. Ann Oncol. 2018;29(8):1718–26.
Download references
Author information
Authors and affiliations.
Bloomberg Faculty of Nursing, University of Toronto, 207 Chisholm Ave, Toronto, ON, M4C 4V9, Canada
Margaret I. Fitch
Health Care Consultant, Toronto, Canada
Irene Nicoll
School of Nursing, STN CSC, University of Victoria, PO Box 1700, Victoria, BC, V8W 2Y2, Canada
Lorelei Newton
Faculty of Nursing, University of Calgary, Calgary, AB, Canada
Fay J. Strohschein
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Margaret I. Fitch .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Geriatric Oncology
Rights and permissions
Reprints and permissions
About this article
Fitch, M.I., Nicoll, I., Newton, L. et al. Challenges of Survivorship for Older Adults Diagnosed with Cancer. Curr Oncol Rep 24 , 763–773 (2022). https://doi.org/10.1007/s11912-022-01255-7
Download citation
Accepted : 05 January 2022
Published : 14 March 2022
Issue Date : June 2022
DOI : https://doi.org/10.1007/s11912-022-01255-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Older adults
- Survivorship
- Quality of life
- Literature review
- Find a journal
- Publish with us
- Track your research
Home > AACR Cancer Disparities Progress Report > Contents > Disparities in Cancer Survivorship
- Disparities in Cancer Survivorship
In this section, you will learn:
- Cancer survivorship encompasses the physical and mental health-related issues, as well as the social and financial challenges, encountered by anyone who has received a cancer diagnosis.
- Those belonging to racial and ethnic minorities and other medically underserved populations experience higher rates of adverse side effects, poorer quality of life, and higher financial toxicity resulting from a cancer diagnosis.
- Pediatric, adolescent, and young adult cancer survivors who belong to medically underserved populations experience increased financial toxicity, adverse side effects, and differences in the types of palliative care services they receive.
- To improve the survivorship experience for racial and ethnic minorities and other underserved populations, patient navigators, patient advocates, and culturally sensitive intervention/navigation programs need to be used.
- Long-term and Late Effects of Cancer Treatment
Health-related Quality of Life
Palliative care, financial toxicity.
- Adherence to Follow-up Care
Impact of COVID-19 on Disparities in Cancer Survivorship
Paving the way for health equity in cancer survivorship.
A cancer survivor is anyone who has been diagnosed with any cancer. Cancer survivorship includes the time from initial diagnosis (often called the acute phase) until end of life (also called the chronic phase). With nearly 17 million cancer survivors in the United States as of 2019, many more people are living through and beyond their cancer. While these numbers are promising, medically underserved populations have higher rates of incidence and mortality for many types of cancers ( 17 ) Miller KD, Ortiz AP, Pinheiro PS, Bandi P, Minihan A, Fuchs HE, et al. Cancer Statistics for the US Hispanic/Latino Population, 2021. CA: A Cancer Journal for Clinicians 2021;71:466-87. [LINK NOT AVAILABLE] ( 642 ) Giaquinto AN, Miller KD, Tossas KY, Winn RA, Jemal A, Siegel RL. Cancer Statistics for African American/Black People 2022. CA: A Cancer Journal for Clinicians 2022. [LINK NOT AVAILABLE] . With the projected increase in cancer survivors who belong to racial and ethnic minorities, disparities across the cancer continuum will potentially widen, because both the numbers of U.S. individuals over the age of 65 and the diversity of the U.S. population are increasing ( 643 ) Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of Cancer Incidence in the United States: Burdens Upon an Aging, Changing Nation. J Clin Oncol 2009;27:2758-65. [LINK NOT AVAILABLE] ( 644 ) Lee Smith J, Hall IJ. Advancing Health Equity in Cancer Survivorship: Opportunities for Public Health. American Journal of Preventive Medicine 2015;49:S477-S82. [LINK NOT AVAILABLE] ( 645 ) Nguyen J, Napalkov P, Richie N, Arndorfer S, Zivkovic M, Surinach A. Impact of US Population Demographic Changes on Projected Incident Cancer Cases from 2019 to 2045 in Three Major Cancer Types. J Clin Oncol 2020;38:e19044. [LINK NOT AVAILABLE] ( 646 ) The Chance That Two People Chosen at Random Are of Different Race or Ethnicity Groups Has Increased since 2010. [updated April 22, 2022, cited .
As more people are living longer and fuller lives after a cancer diagnosis, thanks to improved diagnosis and treatment options, greater attention is needed to understand the survivorship experience. These experiences include the physical, psychosocial, and economic adversities caused by a cancer diagnosis, such as the need for long-term follow-up care and the increased risk of secondary cancers, among others. While all survivors of cancer have unique experiences, it is becoming clear that those belonging to medically underserved populations shoulder a disproportionate burden of the adverse effects of cancer survivorship. Outlining the challenges faced by these groups will help inform cancer care strategies and personalized recommendations for those who are more vulnerable, leading to better quality of life.
Long-Term and Late Effects of Cancer Treatment
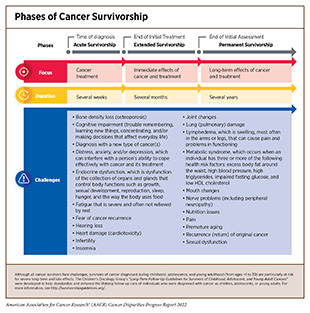
Cancer treatments can impact a patient’s physical and mental health. When a cancer survivor experiences adverse side effects that begin during treatment and continue afterward, these are called long-term side effects; nearly one-third of cancer survivors experience long-term side effects ( 647 ) Wu H-S, Harden JK. Symptom Burden and Quality of Life in Survivorship: A Review of the Literature. Cancer Nursing 2015;38(1):E29-54. [LINK NOT AVAILABLE] . Late-term side effects happen after the conclusion of treatment and can occur for the lifetime of the survivor. Side effects are unique to each individual and are dependent on multiple factors such as cancer type, treatment, physical health, and mental well-being. Recent studies are highlighting the disparities in both long- and late-term effects of cancer treatments in medically underserved populations. As evident from such studies, these groups experience lower rates of fertility preservation ( 648 ) Meernik C, Engel SM, Wardell A, Baggett CD, Gupta P, Rodriguez-Ormaza N, et al. Disparities in Fertility Preservation Use among Adolescent and Young Adult Women with Cancer. J Cancer Surviv 2022. [LINK NOT AVAILABLE] , neurological challenges such as anxiety and post-traumatic stress disorder (PTSD) ( 433 ) Mazor M, Wisnivesky JP, Goel M, Harris YT, Lin JJ. Racial and Ethnic Disparities in Post-Traumatic Stress and Illness Coherence in Breast Cancer Survivors with Comorbid Diabetes. Psycho-Oncology 2021;30:1789-98. [LINK NOT AVAILABLE] ( 469 ) White PM, Itzkowitz SH. Barriers Driving Racial Disparities in Colorectal Cancer Screening in African Americans. Curr Gastroenterol Rep 2020;22:41. [LINK NOT AVAILABLE] , lymphedema ( 650 ) Chang DW, Suami H, Skoracki R. A Prospective Analysis of 100 Consecutive Lymphovenous Bypass Cases for Treatment of Extremity Lymphedema. Plastic and Reconstructive Surgery 2013;133(6):887e-888e. [LINK NOT AVAILABLE] , metabolic disorders ( 651 ) Yoshida Y, Schmaltz CL, Jackson-Thompson J, Simoes EJ. The Effect of Metabolic Risk Factors on Cancer Mortality among Blacks and Whites. Translational Cancer Research 2019:S389-S96. [LINK NOT AVAILABLE] , diabetes ( 652 ) Yao Yuan MT, and Avonne E. Connor. The Effects of Social and Behavioral Determinants of Health on the Relationship between Race and Health Status in U.S. Breast Cancer Survivors. Journal of Women’s Health 2019;28:1632-9. [LINK NOT AVAILABLE] , heart failure ( 653 ) Noyd DH, Yasui Y, Li N, Chow EJ, Bhatia S, Landstrom A, et al. Disparities in Cardiovascular Risk Factors by Race/Ethnicity among Adult Survivors of Childhood Cancer: A Report from the Childhood Cancer Survivorship Study (CCSS). J Clin Oncol 2021;39:10017. [LINK NOT AVAILABLE] , cardiac dysfunction ( 654 ) Yuan Y, Taneja M, Connor AE. The Effects of Social and Behavioral Determinants of Health on the Relationship between Race and Health Status in U.S. Breast Cancer Survivors. Journal of Women’s Health 2018;28:1632-9. [LINK NOT AVAILABLE] ( 655 ) Williams MS, Beech BM, Griffith DM, Jr. Thorpe RJ. The Association between Hypertension and Race/Ethnicity among Breast Cancer Survivors. Journal of Racial and Ethnic Health Disparities 2020;7:1172-7. [LINK NOT AVAILABLE] , recurrence of cancer ( 656 ) Manz CR, Schrag D. Racial Disparities in Colorectal Cancer Recurrence and Mortality: Equitable Care, Inequitable Outcomes? JNCI: Journal of the National Cancer Institute 2021;113:656-7. [LINK NOT AVAILABLE] ( 657 ) Kabat GC, Ginsberg M, Sparano JA, Rohan TE. Risk of Recurrence and Mortality in a Multi-Ethnic Breast Cancer Population. Journal of Racial and Ethnic Health Disparities 2017;4:1181-8. [LINK NOT AVAILABLE] , and development of new, secondary cancers ( 659 ) Lindström L. Racial and Ethnic Disparities in Rates of Invasive Secondary Breast Cancer among Women with Ductal Carcinoma in Situ in Hawai‘i. JAMA Netw Open 2021;4:e2130925. [LINK NOT AVAILABLE] ( 660 ) Scott LC, Yang Q, Dowling NF, Richardson LC. Predicted Heart Age among Cancer Survivors – United States, 2013-2017. MMWR Morb Mortal Wkly Rep 2021;70:1-6. [LINK NOT AVAILABLE] (see sidebar on Phases of Cancer Survivorship ).
Many common cancer treatments damage the cardiovascular system, further exacerbating complications in cancer survivors. Research has shown that cancer survivors have an “excess heart age”—a measure of cardiovascular damage and risk for a heart attack—of eight and a half years in men and six and half years in women compared to those individuals who have never received a cancer diagnosis ( 660 ) Scott LC, Yang Q, Dowling NF, Richardson LC. Predicted Heart Age among Cancer Survivors – United States, 2013-2017. MMWR Morb Mortal Wkly Rep 2021;70:1-6. [LINK NOT AVAILABLE] . Average excess heart age was shown to be higher in cancer patients who are NHB, less educated, and have lower income. Other cardiovascular conditions like thrombosis, which is a result of blood clots in veins and arteries, are more common in patients who are Black, regardless of cancer type (except myeloma) and can lead to pain and swelling as well as stroke and heart attack ( 661 ) Datta T, Brunson A, Mahajan A, Keegan TH, Wun T. Racial Disparities in Cancer-Associated Thrombosis. Blood Adv 2022;6:3167–3177. [LINK NOT AVAILABLE] . Furthermore, several studies have shown disproportionately higher rates of cardiovascular disease in Black cancer patients ( 655 ) Williams MS, Beech BM, Griffith DM, Jr. Thorpe RJ. The Association between Hypertension and Race/Ethnicity among Breast Cancer Survivors. Journal of Racial and Ethnic Health Disparities 2020;7:1172-7. [LINK NOT AVAILABLE] ( 662 ) Ohman RE, Yang EH, Abel ML. Inequity in Cardio-Oncology: Identifying Disparities in Cardiotoxicity and Links to Cardiac and Cancer Outcomes. Journal of the American Heart Association 2021;10:e023852. [LINK NOT AVAILABLE] ( 663 ) Collin LJ, Troeschel AN, Liu Y, Gogineni K, Borger K, Ward KC, et al. A Balancing Act: Racial Disparities in Cardiovascular Disease Mortality among Women Diagnosed with Breast Cancer. Annals of Cancer Epidemiology 2020;4. [LINK NOT AVAILABLE] ( 664 ) Stoltzfus KC, Zhang Y, Sturgeon K, Sinoway LI, Trifiletti DM, Chinchilli VM, et al. Fatal Heart Disease among Cancer Patients. Nature communications 2020;11:2011. [LINK NOT AVAILABLE] , with one study of over 400,000 patients with breast cancer showing mortality related to cardiovascular disease occurring in 13.3 percent of NHB patients compared to only 8.9 percent of NHW patients ( 665 ) Troeschel AN, Liu Y, Collin LJ, Bradshaw PT, Ward KC, Gogineni K, et al. Race Differences in Cardiovascular Disease and Breast Cancer Mortality among US Women Diagnosed with Invasive Breast Cancer. International Journal of Epidemiology 2019;48:1897-905. [LINK NOT AVAILABLE] . Further concerning are data indicating that NHB breast cancer survivors were 15 percent more likely not to adhere to cardiovascular medication schedules after treatment, increasing the likelihood of having a cardiac event ( 666 ) Hershman DL, Accordino MK, Shen S, Buono D, Crew KD, Kalinsky K, et al. Association between Nonadherence to Cardiovascular Risk Factor Medications after Breast Cancer Diagnosis and Incidence of Cardiac Events. Cancer 2020;126:1541-9. [LINK NOT AVAILABLE] .
One challenge faced by cancer survivors is infertility or the inability to conceive a child that can be a consequence of cancer treatments. This can occur in both men and women as a result of surgery on reproductive organs or effects of cancer medications on reproductive cells. In anticipation of impaired reproductive abilities, patients may choose to store reproductive material in a process called fertility preservation prior to cancer treatment. Rates of fertility preservation among patients with cancer is an area of active investigation, but emerging data show that rates vary among men and women, cancer type, treating institution, and age ( 667 ) Lambertini M, Del Mastro L, Pescio MC, Andersen CY, Azim HA, Jr., Peccatori FA, et al. Cancer and Fertility Preservation: International Recommendations from an Expert Meeting. BMC Med 2016;14:1. [LINK NOT AVAILABLE] ( 668 ) Pinelli S, Basile S. Fertility Preservation: Current and Future Perspectives for Oncologic Patients at Risk for Iatrogenic Premature Ovarian Insufficiency. BioMed Research International 2018;2018:6465903. [LINK NOT AVAILABLE] ( 669 ) Patel P, Kohn TP, Cohen J, Shiff B, Kohn J, Ramasamy R. Evaluation of Reported Fertility Preservation Counseling before Chemotherapy Using the Quality Oncology Practice Initiative Survey. JAMA Netw Open 2020;3:e2010806. [LINK NOT AVAILABLE] . Trends show, however, that women cancer survivors who were Black, poor, or lived in rural areas, had decreased rates of fertility preservation ( 648 ) Meernik C, Engel SM, Wardell A, Baggett CD, Gupta P, Rodriguez-Ormaza N, et al. Disparities in Fertility Preservation Use among Adolescent and Young Adult Women with Cancer. J Cancer Surviv 2022. [LINK NOT AVAILABLE] ( 670 ) Voigt P, Persily J, Blakemore JK, Licciardi F, Thakker S, Najari B. Sociodemographic Differences in Utilization of Fertility Services among Reproductive Age Women Diagnosed with Cancer in the USA. J Assist Reprod Genet. 2022;39:963-972. [LINK NOT AVAILABLE] . Currently, cancer-focused organizations have guidelines that discuss fertility preservation and sexual health as an essential part of cancer management, especially in AYA populations ( 671 ) Coccia PF, Pappo AS, Beaupin L, Borges VF, Borinstein SC, Chugh R, et al. Adolescent and Young Adult Oncology, Version 2.2018, Nccn Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw 2018;16:66-97. [LINK NOT AVAILABLE] . Furthermore, as of February 2022, 10 states have mandates, and 12 more have active legislation, requiring insurance coverage of fertility preservation for patients facing infertility due to treatments such as anticancer therapies ( 672 ) Alliance for Fertility Preservation. State Laws & Legislation. [updated March 28, 2022, cited 2022 April 22]. .
Lymphedema is a common long-term side effect among survivors of colorectal, endometrial, and breast cancer that results from damage to the lymphatic system after cancer surgery ( 673 ) Zhang X, McLaughlin EM, Krok-Schoen JL, Naughton M, Bernardo BM, Cheville A, et al. Association of Lower Extremity Lymphedema with Physical Functioning and Activities of Daily Living among Older Survivors of Colorectal, Endometrial, and Ovarian Cancer. JAMA Netw Open 2022;5:e221671. [LINK NOT AVAILABLE] . This damage disrupts normal draining of lymphatic fluid, instead leading to accumulation in the surrounding tissue, resulting in painful swelling most commonly in the arms and legs ( 673 ) Zhang X, McLaughlin EM, Krok-Schoen JL, Naughton M, Bernardo BM, Cheville A, et al. Association of Lower Extremity Lymphedema with Physical Functioning and Activities of Daily Living among Older Survivors of Colorectal, Endometrial, and Ovarian Cancer. JAMA Netw Open 2022;5:e221671. [LINK NOT AVAILABLE] ( 674 ) Hayes SC, Janda M, Cornish B, Battistutta D, Newman B. Lymphedema after Breast Cancer: Incidence, Risk Factors, and Effect on Upper Body Function. J Clin Oncol 2008;26:3536-42. [LINK NOT AVAILABLE] ( 675 ) Armer JM, Ballman KV, McCall L, Ostby PL, Zagar E, Kuerer HM, et al. Factors Associated with Lymphedema in Women with Node-Positive Breast Cancer Treated with Neoadjuvant Chemotherapy and Axillary Dissection. JAMA Surgery 2019;154:800-9. [LINK NOT AVAILABLE] . Black women are 3.85 times and Hispanic women 1.47 times more likely to develop breast cancer-related lymphedemas compared with White women ( 676 ) Kwan ML, Yao S, Lee VS, Roh JM, Zhu Q, Ergas IJ, et al. Race/Ethnicity, Genetic Ancestry, and Breast Cancer-Related Lymphedema in the Pathways Study. Breast Cancer Research and Treatment 2016;159:119-29. [LINK NOT AVAILABLE] ( 677 ) Barrio AV, Montagna G, Sevilimedu V, Gomez EA, Mehrara B, Morrow M. Abstract Gs4-01: Impact of Race and Ethnicity on Incidence and Severity of Breast Cancer Related Lymphedema after Axillary Lymph Node Dissection: Results of a Prospective Screening Study. Cancer Research 2022;82:GS4-01. [LINK NOT AVAILABLE] . Limited access to medical resources including surgery, physical therapy, and medical equipment, coupled with barriers to maintaining a healthy diet and exercise to reduce swelling, increase lymphedema occurrence and severity and reduce quality of life ( 326 ) Rock CL, Thomson CA, Sullivan KR, Howe CL, Kushi LH, Caan BJ, et al. American Cancer Society Nutrition and Physical Activity Guideline for Cancer Survivors. CA: A Cancer Journal for Clinicians;72:230-262. [LINK NOT AVAILABLE] .
Implementation of behavioral strategies that reduce the risk of developing adverse health conditions by promoting risk reduction strategies (e.g., smoking cessation and maintaining a healthy weight) in patients with cancer are important for reducing side effects of cancer treatment. Lifestyle programs to reduce obesity such as the obesity-related behavioral intervention trials (ORBIT) can help combat these risks and are being evaluated in specific vulnerable populations ( 678 ) Porter KJ, Moon KE, LeBaron VT, Zoellner JM. A Novel Behavioral Intervention for Rural Appalachian Cancer Survivors (Wesurvive): Participatory Development and Proof-of-Concept Testing. JMIR Cancer 2021;7:e26010. [LINK NOT AVAILABLE] . Furthermore, activities such as walking have been shown to reduce obesity and improve health outcomes in cancer survivors ( 679 ) Robinson JRM, Beebe-Dimmer JL, Schwartz AG, Ruterbusch JJ, Baird TE, Pandolfi SS, et al. Neighborhood Walkability and Body Mass Index in African American Cancer Survivors: The Detroit Research on Cancer Survivors Study. Cancer 2021;127:4687-93. [LINK NOT AVAILABLE] . For example, one study has shown that exercise benefited the physical well-being of Black breast cancer survivors to a greater degree than White breast cancer survivors ( 680 ) Owusu C, Margevicius S, Nock NL, Austin K, Bennet E, Cerne S, et al. A Randomized Controlled Trial of the Effect of Supervised Exercise on Functional Outcomes in Older African American and Non-Hispanic White Breast Cancer Survivors: Are There Racial Differences in the Effects of Exercise on Functional Outcomes? Cancer 2022. [LINK NOT AVAILABLE] . Unfortunately, neighborhood walkability, (i.e. how much a neighborhood supports walking) is much lower in neighborhoods that are majority Black or have high poverty compared to those that are White and highly affluent, reducing opportunities for exercise among minority and underserved populations. ( 681 ) Conderino SE, Feldman JM, Spoer B, Gourevitch MN, Thorpe LE. Social and Economic Differences in Neighborhood Walkability across 500 U.S. Cities. American Journal of Preventive Medicine 2021;61:394-401. [LINK NOT AVAILABLE] . Because of the importance of the built environment to improving outcomes for patients with cancer, equal access to outdoor spaces is essential to improve health for everyone.

Adverse physical effects are only a part of the impact that a cancer diagnosis can have on cancer survivors. Health-related quality of life (HRQOL) offers a comprehensive view of the impact a disease and its treatment have on a patient’s physical, functional, psychological, social, and financial well-being ( 682 ) Oh H-JS, Menéndez ÁF, Santos VS, Martínez ÁR, Ribeiro FF, Vilanova-Trillo L, et al. Evaluating Health Related Quality of Life in Outpatients Receiving Anti-Cancer Treatment: Results from an Observational, Cross-Sectional Study. Health and Quality of Life Outcomes 2021;19:245. [LINK NOT AVAILABLE] . HRQOL is becoming an important consideration in cancer care, the approval of new drugs, and prediction of long-term survival ( 683 ) Bottomley A, Pe M, Sloan J, Basch E, Bonnetain F, Calvert M, et al. Moving Forward toward Standardizing Analysis of Quality of Life Data in Randomized Cancer Clinical Trials. Clinical Trials 2018;15:624-30. [LINK NOT AVAILABLE] ( 684 ) Mierzynska J, Piccinin C, Pe M, Martinelli F, Gotay C, Coens C, et al. Prognostic Value of Patient-Reported Outcomes from International Randomised Clinical Trials on Cancer: A Systematic Review. Lancet Oncol 2019;20:e685-e98. [LINK NOT AVAILABLE] ( 685 ) Efficace F, Collins GS, Cottone F, Giesinger JM, Sommer K, Anota A, et al. Patient-Reported Outcomes as Independent Prognostic Factors for Survival in Oncology: Systematic Review and Meta-Analysis. Value in Health 2021;24:250-67. [LINK NOT AVAILABLE] . Research has shown that HRQOL is lower for cancer survivors than individuals who have never had a cancer diagnosis or other type of chronic condition. Low HRQOL is exacerbated in cancer survivors who are pediatric (under 1 to 14 years of age) or adolescent and young adult (15-39 years of age) due to a range of factors (see sidebar on Survivorship Disparities in Pediatric, Adolescent, and Young Adult Cancer Patients ). Cancer survivors that belong to medically underserved populations are at an elevated risk of worse HRQOL, which has been shown to increase the likelihood of cancer recurrence and mortality ( 686 ) Sitlinger A, Zafar SY. Health-Related Quality of Life: The Impact on Morbidity and Mortality. Surg Oncol Clin N Am 2018;27:675-84. [LINK NOT AVAILABLE] ( 687 ) Park J, Rodriguez JL, O’Brien KM, Nichols HB, Hodgson ME, Weinberg CR, et al. Health-Related Quality of Life Outcomes among Breast Cancer Survivors. Cancer 2021;127:1114-25. [LINK NOT AVAILABLE] ( 688 ) Eichler M, Singer S, Hentschel L, Richter S, Hohenberger P, Kasper B, et al. The Association of Health-Related Quality of Life and 1-Year-Survival in Sarcoma Patients—Results of a Nationwide Observational Study (Prosa). Br J Can 2022;126:1346–1354. [LINK NOT AVAILABLE] .
Women cancer survivors who identify as lesbian, gay, or bisexual (LGB) report increased depression, anxiety, and PTSD compared to heterosexual women ( 689 ) Schefter A, Thomaier L, Jewett P, Brown K, Stenzel AE, Blaes A, et al. Cross-Sectional Study of Psychosocial Well-Being among Lesbian, Gay, Bisexual, and Heterosexual Gynecologic CancerSurvivors. Cancer Reports 2022;5:e1461. [LINK NOT AVAILABLE] ( 690 ) Megan L. Hutchcraft AAT, Lauren Montemorano, and Joanne G. Patterson. Differences in Health-Related Quality of Life and Health Behaviors among Lesbian, Bisexual, and Heterosexual Women Surviving Cancer from the 2013 to 2018 National Health Interview Survey. LGBT Health 2021;8:68-78. [LINK NOT AVAILABLE] . A similar trend has been observed in gay men with prostate cancer, who reported worse mental health, greater fear of cancer recurrence, and general dissatisfaction with their medical care ( 691 ) Hart TL, Coon DW, Kowalkowski MA, Zhang K, Hersom JI, Goltz HH, et al. Changes in Sexual Roles and Quality of Life for Gay Men after Prostate Cancer: Challenges for Sexual Health Providers. The Journal of Sexual Medicine 2014;11:2308-17. [LINK NOT AVAILABLE] . The disparity widens if the individuals are also Black or Hispanic, who experience poor overall health and physical health, and poor activity, explained by sociodemographic and access-to-care factors, further highlighting the key influence of intersectionality in cancer health disparities ( 692 ) Boehmer U, Jesdale BM, Streed Jr CG, Agénor M. Intersectionality and Cancer Survivorship: Sexual Orientation and Racial/Ethnic Differences in Physical and Mental Health Outcomes among Female and Male Cancer Survivors. Cancer 2022;128:284-91. [LINK NOT AVAILABLE] . Sexual orientation is not a routinely discussed topic between physicians and survivors, which limits the ability to understand the cancer care needs of this population. There is increased interest in implementing standards to collect information on sexual and gender minorities ( 693 ) Griggs J, Maingi S, Blinder V, Denduluri N, Khorana AA, Norton L, et al. American Society of Clinical Oncology Position Statement: Strategies for Reducing Cancer Health Disparities among Sexual and Gender Minority Populations. J Clin Oncol 2017;35:2203-8. [LINK NOT AVAILABLE] . Routine assessment of sexual orientation would establish the need for sensitive and culturally appropriate health care discussions, foster healthy behaviors, and strengthen patient-physician relationships in addition to gathering data to assess cancer outcomes in sexual minorities ( 690 ) Megan L. Hutchcraft AAT, Lauren Montemorano, and Joanne G. Patterson. Differences in Health-Related Quality of Life and Health Behaviors among Lesbian, Bisexual, and Heterosexual Women Surviving Cancer from the 2013 to 2018 National Health Interview Survey. LGBT Health 2021;8:68-78. [LINK NOT AVAILABLE] . Research into the health of SGM populations is necessary to improve outcomes, with nationally funded offices such as the NIH Sexual and Gender Minority Office launched in 2016 ( 694 ) National Institutes of Health – Sexual & Gender Minority Research Office. About SGMRO. [updated April 22, 2022, cited 2022 April 22]. providing resources to more clearly understand these needs.
Studies of breast, prostate, or colorectal cancer survivors who are Black report poorer quality of life, and physical and mental health compared to cancer survivors who are White ( 695 ) Samuel CA, Pinheiro LC, Reeder-Hayes KE, Walker JS, Corbie-Smith G, Fashaw SA, et al. To Be Young, Black, and Living with Breast Cancer: A Systematic Review of Health-Related Quality of Life in Young Black Breast Cancer Survivors. Breast Cancer Research and Treatment 2016;160:1-15. [LINK NOT AVAILABLE] ( 696 ) Pinheiro LC, Wheeler SB, Chen RC, Mayer DK, Lyons JC, Reeve BB. The Effects of Cancer and Racial Disparities in Health-Related Quality of Life among Older Americans: A Case-Control, Population-Based Study. Cancer 2015;121:1312-20. [LINK NOT AVAILABLE] ( 697 ) Claridy MD, Ansa B, Damus F, Alema-Mensah E, Smith SA. Health-Related Quality of Life of African-American Female Breast Cancer Survivors, Survivors of Other Cancers, and Those without Cancer. Quality of Life Research 2018;27:2067-75. [LINK NOT AVAILABLE] ( 698 ) Matthews AK, Tejeda S, Johnson TP, Berbaum ML, Manfredi C. Correlates of Quality of Life among African American and White Cancer Survivors. Cancer Nursing 2012;35:355-64. [LINK NOT AVAILABLE] . Even when sociodemographic and psychosocial factors are accounted for, disparities in survivors’ mental health remain ( 698 ) Matthews AK, Tejeda S, Johnson TP, Berbaum ML, Manfredi C. Correlates of Quality of Life among African American and White Cancer Survivors. Cancer Nursing 2012;35:355-64. [LINK NOT AVAILABLE] . Continued evaluation of quality of life in medically underserved populations and assessment of the contributing factors such as income, education, and stress are important to identify avenues for intervention. For instance, Black cancer survivors report increased social support and spirituality ( 697 ) Claridy MD, Ansa B, Damus F, Alema-Mensah E, Smith SA. Health-Related Quality of Life of African-American Female Breast Cancer Survivors, Survivors of Other Cancers, and Those without Cancer. Quality of Life Research 2018;27:2067-75. [LINK NOT AVAILABLE] as well as communication among family members ( 699 ) Dickey SL, Matthews C, Millender E. An Exploration of Precancer and Post-Cancer Diagnosis and Health Communication among African American Prostate Cancer Survivors and Their Families. American Journal of Men’s Health 2020;14:1557988320927202. [LINK NOT AVAILABLE] compared to those who are White. These data underscore the importance of culturally targeted regimens to improve quality of life for cancer survivors ( 698 ) Matthews AK, Tejeda S, Johnson TP, Berbaum ML, Manfredi C. Correlates of Quality of Life among African American and White Cancer Survivors. Cancer Nursing 2012;35:355-64. [LINK NOT AVAILABLE] ( 699 ) Dickey SL, Matthews C, Millender E. An Exploration of Precancer and Post-Cancer Diagnosis and Health Communication among African American Prostate Cancer Survivors and Their Families. American Journal of Men’s Health 2020;14:1557988320927202. [LINK NOT AVAILABLE] ( 700 ) Bai J, Brubaker A, Meghani SH, Bruner DW, Yeager KA. Spirituality and Quality of Life in Black Patients with Cancer Pain. Journal of Pain and Symptom Management 2018;56:390-8. [LINK NOT AVAILABLE] . To understand the myriad factors that contribute to these disparities, the NCI funded the Detroit Research on Cancer Survivors (ROCS) study which will look at cancer progression, recurrence, mortality, and quality of life of 5,560 African American cancer survivors across three counties surrounding Detroit, Michigan. The study seeks to identify how cancer type, genetics, social, psychological, and racial discrimination influence cancer survivorship in this group through interviews, medical records, and biospecimen collection; the study will also include survivors’ family members, to understand how a cancer diagnosis affects caregivers ( 701 ) National Institutes of Health. Nci Launces Study of African-American Cancer Survivors. [updated February 27, 2017, cited 2022 April 22]. .
Hispanic/Latino cancer survivors experience lower HRQOL compared to other racial and ethnic groups ( 702 ) Samuel CA, Mbah OM, Elkins W, Pinheiro LC, Szymeczek MA, Padilla N, et al. Calidad De Vida: A Systematic Review of Quality of Life in Latino Cancer Survivors in the USA. Quality of Life Research 2020;29:2615-30. [LINK NOT AVAILABLE] ( 703 ) Graves KD, Jensen RE, Cañar J, Perret-Gentil M, Leventhal K-G, Gonzalez F, et al. Through the Lens of Culture: Quality of Life among Latina Breast Cancer Survivors. Breast Cancer Research and Treatment 2012;136:603-13. [LINK NOT AVAILABLE] . Worse survival rates of colorectal, prostate, and breast cancers lead to this population experiencing higher psychosocial burden compared to NHW individuals ( 704 ) McNulty J, Kim S, Thurston T, Kim J, Larkey L. Interventions to Improve Quality of Life, Well Being and Cancer Care in Hispanic/Latino Cancer Survivors: A Systematic Literature Review. Oncology Nursing Forum 2016;43. [LINK NOT AVAILABLE] ( 705 ) Ramirez AG, Gallion KJ, Perez A, Munoz E, Long Parma D, Moreno PI, et al. Improving Quality of Life among Latino Cancer Survivors: Design of a Randomized Trial of Patient Navigation. Contemporary Clinical Trials 2019;76:41-8. [LINK NOT AVAILABLE] . Furthermore, side effects of cancer treatment such as lymphedema may lower the physical and mental quality of life among these patients ( 706 ) Acebedo JC, Haas BK, Hermanns M. Breast Cancer–Related Lymphedema in Hispanic Women: A Phenomenological Study. Journal of Transcultural Nursing 2019;32:41-9. [LINK NOT AVAILABLE] . Finally, food insecurity, a household-level economic and social condition of limited or uncertain access to adequate food is experienced by 26 percent of Hispanic/Latino households and is more prevalent in Hispanics/Latinos as well as other underserved minorities with cancer ( 707 ) Gany F, Leng J, Ramirez J, Phillips S, Aragones A, Roberts N, et al. Health-Related Quality of Life of Food-Insecure Ethnic Minority Patients with Cancer. Journal of oncology practice 2015;11:396-402. [LINK NOT AVAILABLE] . Higher rates of food insecurity experienced by patients and survivors of cancer that are Hispanic/ Latino as well as other underserved groups have been shown to lead to lower HRQOL compared with other races or ethnicities. Other research has shown that persistent food insecurity in cancer patients has led to lower treatment adherence ( 708 ) McDougall JA, Anderson J, Adler Jaffe S, Guest DD, Sussman AL, Meisner ALW, et al. Food Insecurity and Forgone Medical Care among Cancer Survivors. JCO Oncol Pract 2020;16:e922-e32. [LINK NOT AVAILABLE] . It is important for providers to screen for food insecurity in highly vulnerable groups in order to increase adherence to treatment, increase HRQOL, and improve patient outcomes.
Intervention strategies that address HRQOL in Hispanic/Latino populations, such as The National Latino Cancer Research Network and LIVESTRONG cancer navigation services patient navigation program, demonstrate the importance of providing culturally relevant patient navigation to improve quality of life in cancer survivors ( 705 ) Ramirez AG, Gallion KJ, Perez A, Munoz E, Long Parma D, Moreno PI, et al. Improving Quality of Life among Latino Cancer Survivors: Design of a Randomized Trial of Patient Navigation. Contemporary Clinical Trials 2019;76:41-8. [LINK NOT AVAILABLE] . Avanzando Caminos (Leading Pathways): The Hispanic/Latino Cancer Survivorship Study is a 6-year study that aims to recruit 3,000 survivors of breast, colorectal, kidney, lung, prostate, stomach, and cervical cancers to understand the social, cultural, behavioral, psychosocial, biological, and medical influences during cancer survivorship. Studies like these are important in understanding recovery, disease burden, and quality of life after treatment and the unique biological and social burdens experienced by Hispanic/Latino cancer survivors ( 709 ) University of Texas Health. New $9.8 Million Study Is the 1st to Seek Full Understanding of the Latino Cancer Survivorship Journey. [updated May 4, 2021, cited 2022 April 22]. .
American Indian or Alaska Native (AI/AN) groups, which represents highly diverse communities with 560 federally recognized and 100 state tribes in the U.S., experience disparities in cancer survival rates and social and physical quality of life, and have the poorest 5-year survival rate from cancer of any racial group ( 710 ) Bastian TD, Burhansstipanov L. Sharing Wisdom, Sharing Hope: Strategies Used by Native American Cancer Survivors to Restore Quality of Life. JCO Global Oncology 2020:161-6. [LINK NOT AVAILABLE] ( 711 ) Burhansstipanov L, Dignan M, Jones KL, Krebs LU, Marchionda P, Kaur JS. A Comparison of Quality of Life between Native and Non-Native Cancer Survivors. Journal of Cancer Education 2012;27:106-13. [LINK NOT AVAILABLE] ( 712 ) Centers for Disease Control and Prevention. A National Action Plan for Cancer Survivorship: Native American Priorities. [updated April 22, 2022, cited 2022 April 22]. . Due to diversity among AI/AN tribal groups, spirituality characteristics are highly individualistic, and AI/AN cancer survivors have higher spiritual quality of life compared to those who belong to other races and ethnicities ( 711 ) Burhansstipanov L, Dignan M, Jones KL, Krebs LU, Marchionda P, Kaur JS. A Comparison of Quality of Life between Native and Non-Native Cancer Survivors. Journal of Cancer Education 2012;27:106-13. [LINK NOT AVAILABLE] . In one study of AN cancer survivors insight into navigating life after cancer, common themes pointed to the unique challenges survivors faced, such as balancing their responsibility to care for themselves while simultaneously embracing cultural values of selflessness ( 710 ) Bastian TD, Burhansstipanov L. Sharing Wisdom, Sharing Hope: Strategies Used by Native American Cancer Survivors to Restore Quality of Life. JCO Global Oncology 2020:161-6. [LINK NOT AVAILABLE] , which necessitates the study and use of culturally relevant approaches to cancer care and patient navigation such as those utilized by the Native American Cancer Survivors’ Support Network (NACES) ( 712 ) Centers for Disease Control and Prevention. A National Action Plan for Cancer Survivorship: Native American Priorities. [updated April 22, 2022, cited 2022 April 22]. ( 713 ) Burhansstipanov L, Krebs LU, Seals BF, Bradley AA, Kaur JS, Iron P, et al. Native American Breast Cancer Survivors’ Physical Conditions and Quality of Life. Cancer 2010;116:1560-71. [LINK NOT AVAILABLE] ( 714 ) Petereit D, Guadagnolo B, Wong R, Coleman C. Addressing Cancer Disparities among American Indians through Innovative Technologies and Patient Navigation: The Walking Forward Experience. Frontiers in Oncology 2011;1. [LINK NOT AVAILABLE] .
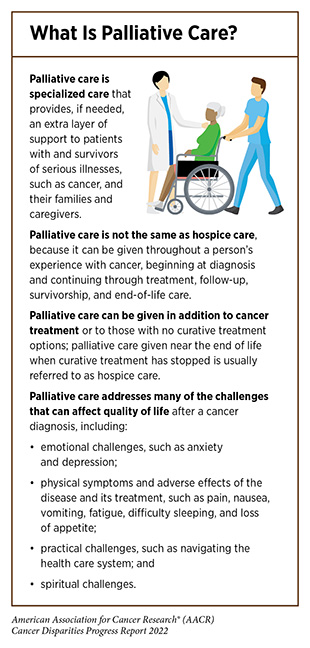
Palliative care is an approach to prevent or treat the symptoms and side effects of any disease, including cancer, by addressing the physical, psychological, financial, social, and spiritual needs that arise from the disease and associated treatments (see sidebar on What Is Palliative Care? ). Palliative care is facilitated by a multidisciplinary team of doctors, nurses, dieticians, pharmacists, therapists, spiritual leaders, and social workers and has been shown to improve quality of life for patients, families, and caregivers ( 715 ) Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, Bhatnaghar S, et al. Redefining Palliative Care—a New Consensus-Based Definition. Journal of Pain and Symptom Management 2020;60:754-64. [LINK NOT AVAILABLE] . Despite the advantages of palliative care, there are disparities ( 716 ) Elk R, Felder TM, Cayir E, Samuel CA. Social Inequalities in Palliative Care for Cancer Patients in the United States: A Structured Review. Seminars in Oncology Nursing 2018;34:303-15. [LINK NOT AVAILABLE] in utilization by racial and ethnic minorities, SGM populations ( 717 ) Haviland K, Burrows Walters C, Newman S. Barriers to Palliative Care in Sexual and Gender Minority Patients with Cancer: A Scoping Review of the Literature. Health & Social Care in the Community 2021;29:305-18. [LINK NOT AVAILABLE] , and those living in geographically remote areas ( 718 ) Bakitas MA, Elk R, Astin M, Ceronsky L, Clifford KN, Dionne-Odom JN, et al. Systematic Review of Palliative Care in the Rural Setting. Cancer Control 2015;22:450-64. [LINK NOT AVAILABLE] ( 719 ) Cancer Network. Challenges of Rural Cancer Care in the United States. [updated September 15, 2015, cited 2022 April 22]. . Unfortunately, most studies examining palliative care in medically underserved populations focus on the end-of-life care and not care during cancer treatment or survivorship. Additional focus needs to be given to identifying the unique needs of cancer patients from medically underserved groups, developing innovative methods to overcome barriers, and implementing policies that provide equitable care ( 720 ) Polite BN, Adams-Campbell LL, Brawley OW, Bickell N, Carethers JM, Flowers CR, et al. Charting the Future of Cancer Health Disparities Research: A Position Statement from the American Association for Cancer Research, the American Cancer Society, the American Society of Clinical Oncology, and the National Cancer Institute. CA: A Cancer Journal for Clinicians 2017;67:353-61. [LINK NOT AVAILABLE] during the chronic phase of cancer survivorship (see sidebar on Phases of Cancer Survivorship ).
End-of-life care is one component of palliative care that places emphasis on improving patient comfort and quality of life through management of pain, psychological burden, and medical events. Unfortunately, there are disparities in access to appropriate end-of-life care services. For instance, over 70 percent of patients with multiple myeloma who are in the final stages of the disease develop bone lesions and related skeletal events, leading to pain. Palliative radiotherapy is an effective treatment to reduce pain. However, based on a recent study, Black patients were 13 percent less likely to receive this treatment compared to NHW patients ( 721 ) Fossum CC, Navarro S, Farias AJ, Ballas LK. Racial Disparities in the Use of Palliative Radiotherapy for Black Patients with Multiple Myeloma in the United States. Leukemia & Lymphoma 2021;62:3235-43. [LINK NOT AVAILABLE] . Management of care during terminal stages of cancer comes with tremendous mental and physical challenges for patients, caregivers, family, and friends. Current guidelines during end-of-life care favor highest quality of life over intense treatment interventions, which can be aggressive, invasive, and expensive ( 722 ) Bickel KE, McNiff K, Buss MK, Kamal A, Lupu D, Abernethy AP, et al. Defining High-Quality Palliative Care in Oncology Practice: An American Society of Clinical Oncology/American Academy of Hospice and Palliative Medicine Guidance Statement. Journal of Oncology Practice 2016;12:e828-e38. [LINK NOT AVAILABLE] ( 723 ) Ferrell BR, Temel JS, Temin S, Alesi ER, Balboni TA, Basch EM, et al. Integration of Palliative Care into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 2017;35:96-112. [LINK NOT AVAILABLE] ( 724 ) Deeb S, Chino FL, Diamond LC, Tao A, Aragones A, Shahrokni A, et al. Disparities in Care Management During Terminal Hospitalization among Adults with Metastatic Cancer from 2010 to 2017. JAMA Netw Open 2021;4:e2125328-e. [LINK NOT AVAILABLE] . Unfortunately, it has been shown that patients from racial and ethnic minorities and those on Medicare or Medicaid that have metastatic cancers and are receiving end of life care are more likely to receive more aggressive, higher cost medical interventions that are not beneficial ( 724 ) Deeb S, Chino FL, Diamond LC, Tao A, Aragones A, Shahrokni A, et al. Disparities in Care Management During Terminal Hospitalization among Adults with Metastatic Cancer from 2010 to 2017. JAMA Netw Open 2021;4:e2125328-e. [LINK NOT AVAILABLE] . More research is needed to understand why patients belonging to these groups are more likely to receive this type of care and to develop prospective interventions that can be implemented in the future.
Financial toxicity refers to the detrimental effects experienced by cancer survivors and their family members caused by the financial strain after a cancer diagnosis. Estimates indicate that out-of-pocket costs for cancer care are higher than for any other chronic illness ( 743 ) Bernard DSM, Farr SL, Fang Z. National Estimates of out-of-Pocket Health Care Expenditure Burdens among Nonelderly Adults with Cancer: 2001 to 2008. J Clin Oncol 2011;29:2821-6. [LINK NOT AVAILABLE] , and at least 50 percent of patients with cancer report financial difficulties irrespective of cancer type or treatment regimen ( 744 ) Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial Hardships Experienced by Cancer Survivors: A Systematic Review. JNCI: Journal of the National Cancer Institute 2016;109. [LINK NOT AVAILABLE] ( 745 ) de Souza JA, Yap BJ, Wroblewski K, Blinder V, Araújo FS, Hlubocky FJ, et al. Measuring Financial Toxicity as a Clinically Relevant Patient-Reported Outcome: The Validation of the Comprehensive Score for Financial Toxicity (Cost). Cancer 2017;123:476-84. [LINK NOT AVAILABLE] . These financial strains lead to financial coping behaviors including taking medications less frequently (e.g. skipping doses, taking less medication than prescribed, or not filling a prescription); taking on debt; reduced follow-up care; and decreased preventative services, all of which increase cancer-related mortality ( 746 ) Bestvina CM, Zullig LL, Rushing C, Chino F, Samsa GP, Altomare I, et al. Patient-Oncologist Cost Communication, Financial Distress, and Medication Adherence. Journal of Oncology Practice 2014;10:162-7. [LINK NOT AVAILABLE] ( 747 ) Doherty M, Gardner D, Finik J. The Financial Coping Strategies of US Cancer Patients and Survivors. Supportive Care in Cancer 2021;29:5753-62. [LINK NOT AVAILABLE] ( 748 ) Gu C, Jewett PI, Yabroff KR, Vogel RI, Parsons HM, Gangnon RE, et al. Forgoing Physician Visits Due to Cost: Regional Clustering among Cancer Survivors by Age, Sex, and Race/Ethnicity. J Cancer Surviv 2022. [LINK NOT AVAILABLE] ( 749 ) Bridgette Thom CB. The Impact of Financial Toxicity on Psychological Well-Being, Coping Self-Efficacy, and Cost-Coping Behaviors in Young Adults with Cancer. Journal of Adolescent and Young Adult Oncology 2019;8:236-42. [LINK NOT AVAILABLE] ( 750 ) Ramsey SD, Bansal A, Fedorenko CR, Blough DK, Overstreet KA, Shankaran V, et al. Financial Insolvency as a Risk Factor for Early Mortality among Patients with Cancer. J Clin Oncol 2016;34:980-6. [LINK NOT AVAILABLE] .
The burden of cancer disproportionately affects those who are poor or are living in poverty (see Cancer Health Disparities Among Other Medically Underserved Populations ). Additionally, chronic diseases such as cancer have consistently high costs of care and unfairly impact populations from low SES pushing them deeper into poverty. To that end, low-income Americans have difficulty paying for cancer care, even when insured. With increasing enrollment of many U.S. workers in high-deductible health insurance plans ( 751 ) Centers for Disease Control and Prevention. High-Deductible Health Plan Enrollment among Adults Aged 18–64 with Employment-Based Insurance Coverage. [updated August 9, 2018, cited 2022 April 22]. , which offer lower up-front costs in exchange for high deductibles (anywhere from $2,500 to $5,000) ( 752 ) Yousuf Zafar S. Financial Toxicity of Cancer Care: It’s Time to Intervene. JNCI: Journal of the National Cancer Institute 2015;108. [LINK NOT AVAILABLE] , even insured patients with cancer may struggle with debt related to treatment and follow up care. In fact, roughly 50% of Americans are not able to afford to pay their deductibles using savings ( 752 ) Yousuf Zafar S. Financial Toxicity of Cancer Care: It’s Time to Intervene. JNCI: Journal of the National Cancer Institute 2015;108. [LINK NOT AVAILABLE] . Unfortunately, the inability to afford treatments or accumulation of debt leads to the increased likelihood of bankruptcy among cancer survivors. Furthermore, finding a new job or returning to a previous job is more difficult after any cancer diagnosis ( 753 ) Meernik C, Sandler DP, Peipins LA, Hodgson ME, Blinder VS, Wheeler SB, et al. Breast Cancer–Related Employment Disruption and Financial Hardship in the Sister Study. JNCI Cancer Spectrum 2021;5. [LINK NOT AVAILABLE] ( 754 ) Hallgren E, Ayers BL, Moore R, Purvis RS, McElfish PA, Maraboyina S, et al. Facilitators and Barriers to Employment for Rural Women Cancer Survivors. J Cancer Surviv. 2022 Feb 10. [LINK NOT AVAILABLE] , further straining survivors financially ( 755 ) Mols F, Tomalin B, Pearce A, Kaambwa B, Koczwara B. Financial Toxicity and Employment Status in Cancer Survivors. A Systematic Literature Review. Supportive Care in Cancer 2020;28:5693-708. [LINK NOT AVAILABLE] . Those who experience financial toxicity are also less likely to enroll in clinical trials ( 756 ) Chino F, Zafar SY. Financial Toxicity and Equitable Access to Clinical Trials. American Society of Clinical Oncology Educational Book 2019:11-8. [LINK NOT AVAILABLE] ( 757 ) Winkfield KM, Phillips JK, Joffe S, Halpern MT, Wollins DS, Moy B. Addressing Financial Barriers to Patient Participation in Clinical Trials: ASCO Policy Statement. J Clin Oncol 2018;36:3331-9. [LINK NOT AVAILABLE] , preventing access to potentially lifesaving treatments and furthering the low participation of medically underserved populations (see Disparities in Cancer Clinical Trial Participation ).
Individuals who belong to medically underserved groups including racial and ethnic minorities, those who live in rural areas, and/or those who are elderly are at a higher risk of experiencing financial toxicity as a result of a cancer diagnosis ( 143 ) Panzone J, Welch C, Pinkhasov R, Jacob JM, Shapiro O, Basnet A, et al. The Influence of Race on Financial Toxicity among Cancer Patients. J Clin Oncol 2021;39:1525. [LINK NOT AVAILABLE] ( 759 ) Jagsi R, Pottow JAE, Griffith KA, Bradley C, Hamilton AS, Graff J, et al. Long-Term Financial Burden of Breast Cancer: Experiences of a Diverse Cohort of Survivors Identified through Population-Based Registries. J Clin Oncol 2014;32:1269-76. [LINK NOT AVAILABLE] ( 760 ) Wheeler SB, Spencer JC, Pinheiro LC, Carey LA, Olshan AF, Reeder-Hayes KE. Financial Impact of Breast Cancer in Black Versus White Women. J Clin Oncol 2018;36:1695-701. [LINK NOT AVAILABLE] ( 761 ) Shah K, Zafar SY, Chino F. Role of Financial Toxicity in Perpetuating Health Disparities. Trends in Cancer 2022;8:266-8. [LINK NOT AVAILABLE] . Compared to 44.5 percent of NHWs, 68 percent of African Americans and 58 percent of Hispanics reported experiencing financial hardships one year after cancer diagnosis ( 762 ) Pisu M, Kenzik KM, Oster RA, Drentea P, Ashing KT, Fouad M, et al. Economic Hardship of Minority and Non-Minority Cancer Survivors 1 Year after Diagnosis: Another Long-Term Effect of Cancer? Cancer 2015;121:1257-64. [LINK NOT AVAILABLE] . In a study that examined the effects of cancer on financial wellness, both Black and Hispanic groups reported being negatively impacted financially twice as often as White individuals ( 759 ) Jagsi R, Pottow JAE, Griffith KA, Bradley C, Hamilton AS, Graff J, et al. Long-Term Financial Burden of Breast Cancer: Experiences of a Diverse Cohort of Survivors Identified through Population-Based Registries. J Clin Oncol 2014;32:1269-76. [LINK NOT AVAILABLE] . This led to increased use of financial coping behaviors like skipping medications ( 747 ) Doherty M, Gardner D, Finik J. The Financial Coping Strategies of US Cancer Patients and Survivors. Supportive Care in Cancer 2021;29:5753-62. [LINK NOT AVAILABLE] . Among rural populations, such as those residing in the Appalachian region of the eastern United States, two thirds of cancer survivors reported financial distress ( 763 ) Vanderpool RC, Chen Q, Johnson MF, Lei F, Stradtman LR, Huang B. Financial Distress among Cancer Survivors in Appalachian Kentucky. Cancer Reports 2020;3:e1221. [LINK NOT AVAILABLE] . Compared to NHWs, elderly Native Hawaiian or Other Pacific Islander were less likely to be able to pay medical bills, more likely to experience psychological distress about paying bills, and more likely to delay or forgo medical care due to cost ( 764 ) Li C, Narcisse M-R, McElfish PA. Medical Financial Hardship Reported by Native Hawaiian and Pacific Islander Cancer Survivors Compared with Non-Hispanic Whites. Cancer 2020;126:2900-14. [LINK NOT AVAILABLE] .
Even after treatment, cancer survivors especially those from racial and ethnic minorities, experience difficulties in obtaining health and life insurance. Compared to NHWs, Black cancer survivors were three to five times more likely to be denied health insurance ( 765 ) Panzone J, Welch C, Morgans A, Bhanvadia SK, Mossanen M, Shenhav-Goldberg R, et al. Association of Race with Cancer-Related Financial Toxicity. JCO Oncology Practice 2022;18:e271-e83. [LINK NOT AVAILABLE] , while Hispanic cancer survivors were twice as likely to be denied health insurance ( 766 ) Lent AB, Garrido CO, Baird EH, Viela R, Harris RB. Racial/Ethnic Disparities in Health and Life Insurance Denial Due to Cancer among Cancer Survivors. International Journal of Environmental Research and Public Health 2022;19:2166. [LINK NOT AVAILABLE] . Lack of, or insufficient, health insurance coverage can further increase mortality among racial and ethnic minorities from side effects of cancer, such as cardiovascular disease, which is increased in NHB cancer survivors ( 767 ) Shi T, Jiang C, Zhu C, Wu F, Fotjhadi I, Zarich S. Insurance Disparity in Cardiovascular Mortality among Non-Elderly Cancer Survivors. Cardio-Oncology 2021;7:11. [LINK NOT AVAILABLE] .
Combating financial toxicity for cancer survivors must occur at multiple levels such as lowering of drug prices, implementation of financial planners, evaluation of high-deductible insurance plans, and practical decision-making about what treatments are necessary such as through the American Board of Internal Medicine’s Choose Wisely campaign. This campaign helps patients choose treatment that has been proven to be effective and avoid unnecessary medical tests, treatments, and procedures. In order to navigate the financial burdens of cancer care, the use of patient navigators and patient advocates, and discussions with the health care team, will be necessary to reduce financial toxicity, which disproportionately affects medically underserved groups.
Adherence to Follow-Up Care
The cancer experience does not end at the completion of the initial treatment plan, as 60 percent of adults diagnosed with cancer are expected to become long-term cancer survivors ( 768 ) DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, et al. Cancer Treatment and Survivorship Statistics, 2014. CA: A Cancer Journal for Clinicians 2014;64:252-71. [LINK NOT AVAILABLE] . Follow-up care for cancer survivors includes developing a survivorship care plan with the health care team, monitoring for signs of cancer recurrence, managing the long- and late-term side effects of treatments, and monitoring overall health. Due to the uniqueness of each individual, their cancer, and their treatment, the needs of each survivor are highly complex and variable, which creates challenges to effective follow-up care.
Following completion of the treatment, continuity of care is an important component of a successful transition to living with and beyond cancer. This includes the coordinated and uninterrupted care of a patient’s physical, mental, and social needs. Fragmentation of care can lead to duplicated services which can increase costs; reduce patient-clinician trust and communication; and decrease a patient’s satisfaction with care and quality of life ( 769 ) Plate S, Emilsson L, Söderberg M, Brandberg Y, Wärnberg F. High Experienced Continuity in Breast Cancer Care Is Associated with High Health Related Quality of Life. BMC Health Services Research 2018;18:127. [LINK NOT AVAILABLE] ( 770 ) Chen Y-Y, Hsieh C-I, Chung K-P. Continuity of Care, Followup Care, and Outcomes among Breast Cancer Survivors. International Journal of Environmental Research and Public Health 2019;16:3050. [LINK NOT AVAILABLE] ( 771 ) Aubin M, Vézina L, Verreault R, Simard S, Hudon É, Desbiens J-F, et al. Continuity of Cancer Care and Collaboration between Family Physicians and Oncologists: Results of a Randomized Clinical Trial. The Annals of Family Medicine 2021;19:117. [LINK NOT AVAILABLE] . As one example, a higher continuity of care benefited Black prostate cancer survivors over two years after the conclusion of treatment and was associated with fewer emergency room visits, lower cost, and lower all-cause mortality compared to White cancer survivors ( 772 ) Chhatre S, Malkowicz SB, Jayadevappa R. Continuity of Care in Acute Survivorship Phase, and Short and Long-Term Outcomes in Prostate Cancer Patients. The Prostate 2021;81:1310-9. [LINK NOT AVAILABLE] . The success of continuity of care immediately following treatment in improving outcomes, especially in medically underserved groups, highlights the importance of incorporating such regimens into the current standard of care.
Follow-up care can be delayed because of lack of insurance and out-of-pocket costs, transportation and language barriers, scheduling challenges, and childcare issues, especially in groups at risk of experiencing difficulties related to these factors such as those in rural communities or immigrants ( 774 ) Milam JE, Meeske K, Slaughter RI, Sherman-Bien S, Ritt-Olson A, Kuperberg A, et al. Cancer-Related Follow-up Care among Hispanic and Non-Hispanic Childhood Cancer Survivors: The Project Forward Study. Cancer 2015;121:605-13. [LINK NOT AVAILABLE] ( 775 ) Rosales M, Ashing K, Napoles A. Quality of Cancer Follow-up Care: A Focus on Latina Breast Cancer Survivors. Journal of Cancer Survivorship 2014;8:364-71. [LINK NOT AVAILABLE] ( 776 ) Jiang C, Yabroff KR, Deng L, Wang Q, Perimbeti S, Shapiro CL, et al. Self-Reported Transportation Barriers to Health Care among US Cancer Survivors. JAMA Oncol 2022;8:775-778. [LINK NOT AVAILABLE] . Notably, breast cancer survivors who were Black reported increased difficulty in accessing follow-up care due to one or more of these factors at a higher rate than survivors who were White ( 777 ) Palmer NRA, Weaver KE, Hauser SP, Lawrence JA, Talton J, Case LD, et al. Disparities in Barriers to Follow-up Care between African American and White Breast Cancer Survivors. Supportive Care in Cancer 2015;23:3201-9. [LINK NOT AVAILABLE] .
Those living in rural areas are less likely to continue follow-up care because of greater distance from large research hospitals, which are usually located in metropolitan areas. This creates barriers for rural residents, such as those living in Appalachia, Mississippi Delta, and Rocky Mountain regions of the United States; for AI/AN communities that live on reservations; or for those in rural communities with limited transportation options. Long travel times compounded by financial strains lead to a reluctance to travel to specialists, opting for local primary care providers who may lack experience and/or access to state-of-the-art facilities and adequate knowledge about frequency of surveillance testing for cancer recurrence ( 778 ) Bober SL, Recklitis CJ, Campbell EG, Park ER, Kutner JS, Najita JS, et al. Caring for Cancer Survivors. Cancer 2009;115:4409-18. [LINK NOT AVAILABLE] . Transfer of care to primary care physicians from oncologists can often create gaps in follow-up care for doctors and patients ( 779 ) Schootman M, Homan S, Weaver KE, Jeffe DB, Yun S. The Health and Welfare of Rural and Urban Cancer Survivors in Missouri. Preventing Chronic Disease 2013;10:E152. [LINK NOT AVAILABLE] ( 780 ) Blanch-Hartigan D, Forsythe LP, Alfano CM, Smith T, Nekhlyudov L, Ganz PA, et al. Provision and Discussion of Survivorship Care Plans among Cancer Survivors: Results of a Nationally Representative Survey of Oncologists and Primary Care Physicians. J Clin Oncol 2014;32:1578-85. [LINK NOT AVAILABLE] . Recommendations to improve transfer of care among patients living in remote areas include the use of telehealth strategies. Although telehealth is highly effective, lack of access to high-speed Internet and computers can limit access to telehealth for medically underserved groups and could exacerbate disparities. Recruitment and retention of oncology providers in rural hospitals through incentives, including loan repayments are also important ways to improve care in rural areas for patients after treatment ( 781 ) ASCO. Asco Announces New Program Designed to Increase Workforce Diversity and Reduce Cancer Care Disparities. Journal of Oncology Practice 2009;5:315-7. [LINK NOT AVAILABLE] .
The COVID-19 pandemic has had a more severe impact on mental and physical health of cancer survivors compared to those without a history of cancer ( 782 ) Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, et al. Clinical Impact of COVID-19 on Patients with Cancer (Ccc19): A Cohort Study. The Lancet 2020;395:1907-18. [LINK NOT AVAILABLE] ( 783 ) Zhao F, Henderson TO, Cipriano TM, Copley BL, Liu M, Burra R, et al. The Impact of Coronavirus Disease 2019 on the Quality of Life and Treatment Disruption of Patients with Breast Cancer in a Multiethnic Cohort. Cancer 2021;127:4072-80. [LINK NOT AVAILABLE] ( 784 ) Ciazynska M, Pabianek M, Szczepaniak K, Ulanska M, Skibinska M, Owczarek W, et al. Quality of Life of Cancer Patients During Coronavirus Disease (COVID-19) Pandemic. Psycho-Oncology 2020;29:1377-9. [LINK NOT AVAILABLE] ( 785 ) Koinig KA, Arnold C, Lehmann J, Giesinger J, Köck S, Willenbacher W, et al. The Cancer Patient’s Perspective of COVID-19-Induced Distress—a Cross-Sectional Study and a Longitudinal Comparison of Hrqol Assessed before and During the Pandemic. Cancer Medicine 2021;10:3928-37. [LINK NOT AVAILABLE] ( 786 ) Katz AJ, Haynes K, Du S, Barron J, Kubik R, Chen RC. Evaluation of Telemedicine Use among US Patients with Newly Diagnosed Cancer by Socioeconomic Status. JAMA Oncol 2022;8:161-3. [LINK NOT AVAILABLE] . The pandemic has increased social isolation, financial stress, and food insecurity, as well as timely access to routine follow-up care. As many of these factors are commonly known mechanisms for disparities in cancer survivorship, COVID-19 has disproportionately affected cancer survivors belonging to racial and ethnic minorities and other underserved populations. Furthermore, Black, Hispanic, and AI/AN individuals have experienced a higher burden of COVID-19 compared to NHW individuals. These compounding factors place racial and ethnic minority survivors at risk of negative outcomes necessitating increased support for these groups through and beyond the pandemic. AACR has outlined many of these challenges in the AACR Report on the Impact of COVID-19 on Cancer Research and Patient Care with a Call to Action to bolster access to health care services, like telehealth, which has been less accessible to minorities but can potentially address health care disparities ( 786 ) Katz AJ, Haynes K, Du S, Barron J, Kubik R, Chen RC. Evaluation of Telemedicine Use among US Patients with Newly Diagnosed Cancer by Socioeconomic Status. JAMA Oncol 2022;8:161-3. [LINK NOT AVAILABLE] ( 787 ) Jewett PI, Vogel RI, Ghebre R, Hui JYC, Parsons HM, Rao A, et al. Telehealth in Cancer Care During COVID-19: Disparities by Age, Race/Ethnicity, and Residential Status. Journal of Cancer Survivorship 2022;16:44-51. [LINK NOT AVAILABLE] .
The disparities in various aspects of cancer survivorship as highlighted in this chapter necessitate a comprehensive multidisciplinary approach to address the deficiencies experienced by underserved groups. This includes researchers, health care systems, professional organizations, insurance groups, and care teams working together to meet the specific needs of the community and the patient.
Community-centered approaches that meet patients where they are, are required if we are to better understand the challenges faced by cancer survivors who belong to racial and ethnic minorities and underserved populations. Patient advocates, such as Sandra Morales and Marlena Murphy , who themselves are often cancer survivors and support those living with and through cancer, are uniquely positioned to bridge a critical gap between survivors and researchers. Patient advocates have immense social capital within their communities because they understand the unique needs and challenges within the community; this can help inform research questions and clinical study designs. Patient advocates can also help disseminate new information gleaned from research studies into the community so that it is readily accessible and favorably received. Organizations such as Turning Point and Guiding Researchers and Advocates to Scientific Partnerships (GRASP) bridge the gap by bringing together all stakeholders including researchers, advocates, and survivors. Utilization of patient advocates is necessary to reduce health disparities, voice community concerns, increase research of underserved groups, increase survival, increase quality of life, and reduce financial strain on survivors.
Patient navigators are individuals dedicated to assisting patients with cancer, survivors, family, and caregivers by facilitating and navigating through the health care system for access to timely and quality care. Utilization of patient navigation has been shown to benefit patients across the cancer care continuum, especially in medically underserved population groups, and to reduce the overall costs associated with cancer ( 788 ) Kline RM, Rocque GB, Rohan EA, Blackley KA, Cantril CA, Pratt-Chapman ML, et al. Patient Navigation in Cancer: The Business Case to Support Clinical Needs. Journal of Oncology Practice 2019;15:585-90. [LINK NOT AVAILABLE] ( 789 ) Dixit N, Rugo H, Burke NJ. Navigating a Path to Equity in Cancer Care: The Role of Patient Navigation. American Society of Clinical Oncology Educational Book 2021:3-10. [LINK NOT AVAILABLE] ( 790 ) The Cancer Center Cessation Initiative Diversity E, and Inclusion Working Group Members. Use of Community Health Workers and Patient Navigators to Improve Cancer Outcomes among Patients Served by Federally Qualified Health Centers: A Systematic Literature Review. Health Equity 2017;1:61-76. [LINK NOT AVAILABLE] . In fact, the first patient navigation program in the U.S. was designed specifically to address racial disparities of breast cancer screening and follow-up in Black women, which led to a 70 percent increase in 5-year survival in this group ( 791 ) Oluwole SF, Ali AO, Adu A, Blane BP, Barlow B, Oropeza R, et al. Impact of a Cancer Screening Program on Breast Cancer Stage at Diagnosis in a Medically Underserved Urban Community. J Am Coll Surg 2003;196:180-8. [LINK NOT AVAILABLE] ( 792 ) Freeman HP. Patient Navigation: A Community Based Strategy to Reduce Cancer Disparities. Journal of Urban Health 2006;83:139-41. [LINK NOT AVAILABLE] . Recognition of the benefits of patient navigators on health outcomes has led to legislative efforts to increase access to patient navigation including the Patient Navigation Outreach and Chronic Disease Prevention Act in 2005 and the Patient Protection and Affordable Care Act in 2010, the latter of which requires each state health insurance exchange to establish a navigator program.
To further increase the use of patient navigators, the American College of Surgeons’ Commission on Cancer (CoC) required all organizations accredited by the CoC to have a patient navigation program by 2015. Despite this requirement, there is high variability in the organization and training of patient navigators in the United States, leading to heterogeneous navigation ( 793 ) Ustjanauskas AE, Bredice M, Nuhaily S, Kath L, Wells KJ. Training in Patient Navigation:A Review of the Research Literature. Health Promotion Practice 2016;17:373-81. [LINK NOT AVAILABLE] ; for instance, navigators can be classified as either health care or non-health care workers leading to confusion surrounding their credentials. Additionally, there is often confusion abou ( 794 ) Pratt-Chapman M, Willis A. Community Cancer Center Administration and Support for Navigation Services. Seminars in Oncology Nursing 2013;29:141-8. [LINK NOT AVAILABLE] t coverage and financial benefits of patient navigator services through Medicare, Medicaid, and private/commercial insurers ( 794 ) Pratt-Chapman M, Willis A. Community Cancer Center Administration and Support for Navigation Services. Seminars in Oncology Nursing 2013;29:141-8. [LINK NOT AVAILABLE] . Broad implementation of patient navigators to assist all patients with cancer will require standardization guidelines and population-specific training, support from government and health care providers, and more universal access through implementation of telehealth (see Sustainably Supporting Patient Navigators and Community Health Workers ).
A key to charting an equitable path forward for cancer survivors who belong to medically underserved populations is the use of community-based tailored solutions that meet the specific needs of every patient and include patient advocates and patient navigators as key partners. Such an approach will help implement strategies that address the specific social, psychological, medical, and physical needs of the patient while tying in cultural norms and perceptions, ultimately increasing quality of life; bolstering adherence to follow-up care; identifying financial concerns; providing equitable health care; and reducing the overall cost of cancer care ( 795 ) Walls M, Chambers R, Begay M, Masten K, Aulandez K, Richards J, et al. Centering the Strengths of American Indian Culture, Families and Communities to Overcome Type 2 Diabetes. Frontiers in Public Health 2022;9:788285. [LINK NOT AVAILABLE] .
- A Message from the AACR
- Executive Summary
- A Snapshot of U.S. Cancer Health Disparities
- The State of Cancer Health Disparities in 2022
- Understanding Cancer Development in the Context of Cancer Health Disparities
- Disparities in the Burden of Preventable Cancer Risk Factors
- Disparities in Cancer Screening for Early Detection
- Disparities in Clinical Research and Cancer Treatment
- Overcoming Cancer Health Disparities Through Diversity in Cancer Training and Workforce
- Overcoming Cancer Health Disparities Through Science-based Public Policy
- AACR Call to Action
- AACR Cancer Disparities Progress Report: Steering Committee
Your donation to the American Association for Cancer Research helps our more than 58,000 members worldwide drive progress against cancer.

- Open access
- Published: 17 January 2024
Breast cancer survivorship needs: a qualitative study
- Rahimeh Khajoei ORCID: orcid.org/0000-0002-3770-6790 1 ,
- Payam Azadeh ORCID: orcid.org/0000-0003-1771-7377 2 ,
- Sima ZohariAnboohi ORCID: orcid.org/0000-0003-3422-9420 3 ,
- Mahnaz Ilkhani ORCID: orcid.org/0000-0002-5454-4041 3 &
- Fatemah Heshmati Nabavi ORCID: orcid.org/0000-0002-9842-966X 4
BMC Cancer volume 24 , Article number: 96 ( 2024 ) Cite this article
787 Accesses
Metrics details
Breast cancer rates and the number of breast cancer survivors have been increasing among women in Iran. Effective responses from healthcare depend on appropriately identifying survivors’ needs. This study investigated the experience and needs of breast cancer survivors in different dimensions.
In this qualitative content analysis, semi-structured in-depth interviews were conducted from April 2023 to July 2023. Data saturation was achieved after interviewing 16 breast cancer survivors (BCSs) and four oncologists using purposive sampling. Survivors were asked to narrate their experiences about their needs during the survivorship. Data were analyzed with an inductive approach in order to extract the themes.
Twenty interviews were conducted. The analysis focused on four central themes: (1) financial toxicity (healthcare costs, unplanned retirement, and insurance coverage of services); (2) family support (emotional support, Physical support); (3) informational needs (management of side effects, management of uncertainty, and balanced diet); and (4) psychological and physical issues (pain, fatigue, hot flashes, and fear of cancer recurrence).
Conclusions
This study provides valuable information for designing survivorship care plans. Identifying the survivorship needs of breast cancer survivors is the first and most important step, leading to optimal healthcare delivery and improving quality of life. It is recommended to check the financial capability of patients and take necessary measures for patients with financial problems. Additionally, support sources should be assessed and appropriate. Psychological interventions should be considered for patients without a support source. Consultation groups can be used to meet the information needs of patients. For patients with physical problems, self-care recommendations may also be useful in addition to doctors’ orders.
Peer Review reports
Introduction
According to the Globocan website, breast cancer is the most common cancer among women. Breast cancer was the most common cancer in Iran in 2020 in both sexes and the fifth cause of death in both sexes; however, it is the leading cause of death in women [ 1 ]. Due to early diagnosis and improvements in treatment methods, the prognosis and survival rate of women with breast cancer have enhanced significantly worldwide [ 2 ]. Breast cancer survivors face many problems and needs in different dimensions: psychological, physical, social, etc. [ 3 ]. These needs and issues during the survivorship period are different during the active phase of cancer treatment [ 4 ]. Physical and psychological symptoms include fatigue, pain, osteoporosis, premature menopause, fear of disease recurrence, sexual problems, and infertility [ 5 , 6 , 7 ]. To deal with these health needs, many patients require medical, psychological, and social care for more than ten years after diagnosis [ 8 , 9 ].
The growing population of survivors, along with their multiple needs, is a challenge for healthcare providers and health policymakers, who need to provide a good standard of care during the survival period and meet the different dimensions of the needs of these patients after treatment [ 3 , 10 ]. Failure to meet these needs is associated with negative consequences such as decreased satisfaction with care, poor adherence to treatment, decreased quality of life, and increased anxiety and depression [ 11 ]. The current trend in modern medicine is changing from a disease-based model to a patient-centered model in which patients are active and their preferences and needs are considered in care [ 12 ]. Therefore, the first step in planning supportive care services for cancer patients is to identify their care needs [ 13 ]. To date, several studies have investigated the needs and experiences of breast cancer survivors and obtained different results. The need for help in dealing with problems such as financial distress [ 14 ], Pain [ 15 ], Memory problems [ 16 ], Fear of disclosure [ 17 ], concerns relating to body image, femininity, altered physical appearance, and self-confidence [ 18 ] are among the needs experienced by breast cancer survivors. In 2023, a systematic study on the needs of breast cancer survivors showed that most of these patients had psychological and informational needs [ 19 ]. In assessing the needs of BCSs, it is essential to consider culture, ethnicity, socioeconomic status, birthplace, and native language. The elements of the survivorship journey may be somewhat similar for all women, yet we cannot assume that their experiences are monolithic, regardless of the context. Ethnic, racial, and cultural diversity may affect survivors’ needs. Iran is a country with unique cultural and religious characteristics and people’s behavior and attitude towards disease are different depending on their culture. As such, conducting research across cultures is necessary. For example, the family holds a valuable position in Iran. Cancer affects physical, mental, social, and economic dimensions of patients and their families. In this situation, preserving and consolidating the family foundation is important and may create different needs for patients. Therefore, considering the differences in the ethnic, cultural, and socioeconomic background of Iran, this study aimed to investigate the needs and experiences of breast cancer survivors in the country.
This qualitative study was conducted using a conventional content analysis approach in order to investigate the experiences and needs of breast cancer survivors. Qualitative research methods seek to discover and understand people’s inner worlds. As experiences form the structure of truth for each person, researchers can discover the meaning of phenomena from their perspective by taking into account people’s experiences [ 20 ]. In conventional content analysis, classes are extracted directly from the data text. This approach is used in studies whose purpose is to describe a phenomenon; this method was used in the present study [ 21 ].
Contributors
The qualitative research participants had deep experience of the phenomenon under study [ 19 ]. The participants in the study were breast cancer survivors (14 participants), patients’ families (two participants), and healthcare professionals (four participants). Women who had completed their treatment courses at a university hospital in Tehran between four and 18 months prior and were visiting the hospital for follow-up care were included in the study using targeted sampling. To achieve the maximum difference in the samples, participants with maximum diversity were included in the study over a period of three months. Participants of different ages, marriages, education levels, income, and ethnicities were included in the study. The sampling was continued until data saturation was achieved. The inclusion criteria were patients between 18 and 60 years of age, literacy, completion of treatment, non-metastatic cancer, and stable clinical conditions. The exclusion criteria were cancer recurrence or metastasis, secondary cancers, and cognitive impairment.
Collecting data
Two separate interview guides for survivors and healthcare professionals were developed by the research team, using expert input on the needs of cancer survivors. These guidelines are based on a literature review of the needs of survivors of breast cancer. In-depth semi-structured interviews were conducted in order to collect the data. After informed consent was obtained, an interview method with open-ended questions focusing on the study objectives was conducted. Each interview was conducted and analyzed. The interviews were scheduled at a convenient time and location for the interviewees. A total of 20 face-to-face and telephone interviews were conducted, lasting 45 min each. The data were collected between April 20 and July 30, 2023. The interviews began with an open-ended question relating to the needs and experiences of breast cancer survivors. Based on the interviewees’ answers, the interview process was directed towards achieving the main goal of the research. Exploratory questions were asked in order to attain a deeper understanding of the phenomena. The interviews continued until complete information saturation was reached. Full saturation occurs when classes and subclasses are completed, and new data do not add anything to these classes; at this point, no new data are obtained from the interviews and only previous information is repeated. Immediately after the end of the interviews, all interviews were recorded verbatim using the recording device and transcribed.
The interview guide questions included the following questions:
What were the most important issues you faced after completing your treatment?
What side effects did you experience and how did you deal with them?
What feelings did you experience during your recovery? Fear, anxiety, depression, despair, anger, fear of cancer returning, loss of self-confidence?
Explain your emotional life.
In addition, according to the participants’ answers, the following questions were addressed:
In what areas did you need more training and information?
What physical problems and complications do you currently face in need of support?
Do you need support in establishing relationships with others and being present in the community and workplace?
Do you feel that you need more support in your emotional and family relationships?
Do you need help from others in performing daily tasks?
Do you have trouble remembering and recalling events?
In addition, interview guide questions for healthcare providers include the following:
From your perspective, what are the most important issues and needs of breast cancer survivors? (in physical, mental, informational, cognitive dimensions, etc.)
Are there any issues that are more problematic for the Iranian recoveries?
The researcher further explored participants’ answers to each question. Furthermore, by restating and returning to the salient points or a summary of the participants’ answers, we confirmed the correctness of the data and increased the credibility of the results. At the end of each session, we asked questions such as “Is there anything else you would like to add?” and “Is there another question I should have asked?” Participants were asked to express any further experience or additional information. In addition, permission was obtained from the participants for future calls or interviews. At the end of each interview, the interviews were listened to several times at the earliest possible time and transcribed verbatim. The moods and characteristics of the participants were recorded along with the interviews. The mood and characteristics of the participants helped code the text of the interviews. That the codes accurately express a person’s understanding of the desired situation. The text of the interviews with pseudonyms was entered into MAXQDA 2020 software for data storage, retrieval, and analysis.
Data analysis
Data analysis was performed using conventional content analysis, based on the steps introduced by Graneheim and Lundman [ 22 ]. The sentences and phrases describing the needs and experiences of survivors were coded. The first and third researchers coded the texts of the interviews separately. The coded text was reviewed by a responsible researcher. Any disagreements were discussed to reach a consensus. Subsequently, the central concept of each class and the main and abstract concepts were defined. Following this, based on a constant comparison of similarities and differences, the codes that indicated a single topic were placed in a class, the subclasses and classes were categorized, and the core codes were formed. In the fifth step, the central concept of each class and the main and abstract concepts were defined.
Data integrity and robustness
To validate the research findings, the criteria of acceptability or validity, transferability, reliability, trust or stability, and ability, based on Lincoln and Guba, were used [ 23 ]. To ensure the validity of the data, in addition to allocating sufficient time for data collection and immersion, semi-structured interviews were conducted; the maximum variety in sampling was observed by interviewing people of different ages, education, income, and use at various stages of the disease. Sampling continued until the data reached saturation and the most appropriate semantic unit was selected. Internal validity of content analysis was condcuted; this was evaluated for its face validity. To validate the content, a panel of experts (research team) supported the generation of concepts or coding topics; these were also reviewed by the participants. For this purpose, the interview text and extracted codes were presented to participants, who commented on their accuracy [ 24 ]. In this study, a research audit, a detailed review of data by an external observer, was used to increase the stability of the research. In addition, the period of data collection (interviews) was carried out as quickly as possible and all participants were asked about the same topic [ 22 ]. To facilitate transferability, the researcher has provided a clear description of the platform, the method of selecting and characterizing the participants, the data collection, and the analysis process so that the reader can judge the applicability of the findings to other situations. In addition, rich and detailed findings with appropriate quotations and authentic documents are presented in order to increase transferability [ 25 ]. To increase the verifiability of the data, all research stages, methodology, and decisions taken in the research stages are explained in clear detail so that they can be followed by other researchers if necessary. In addition, all raw data and recorded notes, documents, and interviews have been retained for future review [ 26 ].
Ethical considerations
This study was approved by the Research Ethics Committee of Shahid Beheshti University of Medical Sciences in Tehran (IR. SBMU. PHARMACY. REC.1402.005). Informed consent was obtained from the research participants, and they were also informed about the confidentiality of their information.
Participants
The medical records of 450 BCSs were reviewed. 56 patients met the inclusion criteria for this study. 28 survivors could not be contacted, 12 declined to participate, and 16 participated in the interviews. Among the survivors, 64% were married and about half were between 30 and 50 years old. 60% had a higher education level and over 85% had an average income. Of the 12 oncologists who were invited to participate in this study, four agreed to participate, with a response rate of 33.3%.
The analysis focused on four central themes: (1) financial toxicity (healthcare costs, unplanned retirement, and insurance coverage of services); (2) family support (emotional support, Physical support); (3) informational needs (management of side effects, management of uncertainty, and balanced diet); and (4) psychological and physical issues (pain, fatigue, hot flashes, and fear of cancer recurrence).
Financial toxicity
The high cost of drugs and treatment, along with reduced work productivity and subsequent loss of income, impose a heavy financial burden on cancer patients, which in turn imposes a unique stress known as financial toxicity [ 27 ]. In this study, most patients mentioned financial problems as their most challenging issue.
Healthcare costs
One source of financial problems is the costs associated with cancer care services (e.g., medications, supplies, copayments, and transportation) [ 28 ]. Patients who report cancer-related financial problems or high healthcare costs are more likely to avoid or delay their medical care or prescribed medications. This may slow their healing process or aggravate the disease [ 29 ]. The participants in this study complained about the high costs of drugs and medical procedures. One participant said:
I had finished chemotherapy three months ago and was told to start radiation. But I couldn’t afford it, so I gave it up.

Coverage of insurance services
Another financial problem for the participants was that insurance did not cover the cost of some treatments. Obtaining health insurance did not fully protect against cancer-related financial problems. One participant said:
I am a worker and I have to work hard to improve my wife’s condition. Thank God, most of my wife’s treatment costs were paid by supplementary insurance. However, now the problem is that my wife has to undergo a mastectomy and she is very upset about the change in her appearance and wants to have breast implants. However, because it is considered a cosmetic procedure, unfortunately, insurance does not accept the payment and we are not able to pay the cost.
Unplanned retirement
One source of financial distress is reduced income due to loss of employment, missing work, or unplanned retirement [ 28 ]. In this study, it was found that some patients were forced to retire and had difficulty with paying the treatment costs. One participant said:
I am a teacher, and I was forced to retire due to illness. My pension is not sufficient to pay for my medicine and treatment. I really don’t know what to do to pay for the treatment.
Family support
Emotional support.
A remarkable finding obtained from the participants’ statements was that emotional support from their family, partner, and children played an important role in reducing their physical and psychological symptoms. Survivors who had a strong source of emotional support experienced fewer physical symptoms and a better mental state; among these patients, psychological symptoms such as stress, anxiety, and depression were far less common. Studies have shown that BCSs face various stresses during the course of the disease and need comprehensive support, including social and family support, to deal with these stressful factors and manage their resulting conditions better [ 30 ]. Family involvement increases their ability to cope [ 31 ]. Some of the participants’ statements support this:
After the radiation treatment, I felt much better because I went to my family in the city. They supported me a lot, making me feel better.
I live alone. Initially, my family supported me, but they left me little by little. Of course, they are right, our problem is ongoing, and I do not like to disturb anyone. I am struggling with several complications. The current problems include severe muscle pain, fatigue, weakness, and lethargy. I feel lonely. I often feel stressed and anxious.
The husband of one of the participants said:
My wife is not experiencing any particular problem at the moment because I am paying attention to her in every way. She is my life partner, and I should be by her side facing difficulties. I will do whatever I can to make her feel better. Thank God; there is no problem now.
Considering that partners play an essential role in providing emotional support, financial management, and decision-making regarding their spouses’ cancer treatment, there is a need to involve them in psychological interventions [ 32 ].
Physical support
Due to the complications of the treatment, the participants needed physical support from the family to fulfill their responsibilities. Patients who lacked physical support from the family had many problems in carrying out daily responsibilities and activities. One participant said:
I separated from my wife and live alone. My hand is swollen and painful, but I have to work with this condition; And I don’t have anyone to help me and this is really hard for me.
Informational needs
Almost all participants stated that they did not receive any information on what to expect. and would have liked to receive more information about management of side effects and balanced diet.
Management of side effects
Information needs were one of the most important needs for the survivors. Most participants said that they had not been given any training program. Many women reported that they had experienced persistent side effects from treatment for which they were poorly prepared. Moreover, they did not receive any related training. This lack of information confused them and exacerbated complications. One participant said:
I was not provided with any training. I was faced with cases where I did not know what to do. For example, because of menopause, I used to get hot flashes and I was very bothered. Later, they said you could use cool liquids like chicory, but I did not know what to do, and I tolerated it.
Management of uncertainty
One of the informational needs for BCSs was ensuring complete recovery. They were confused about being completely healed. Furthermore, they wanted more information about disease prevention for their daughters. One participant said:
My most important question during the recovery period is whether I have fully recovered. Does cancer have a chance of coming back? Is it possible for my daughter to develop cancer in the future?
One of the specialists stated:
Facing an uncertain future and the fear of the disease returning (especially the concern for children) is one of the most important concerns of BCSs. They should know that creating a suitable lifestyle and continuous follow-up can prevent the return of the disease.
Balanced diet
Another need expressed by patients was information about healthy eating or balanced eating (food to eat, food to avoid). One of the participants said:
In this regard, we did not receive sufficient training. I do not know what food is good for me. There is some information on the internet, but it is unreliable. I cannot always ask my doctor these questions. They should teach us about proper nutrition.
Psychological and physical issues
Most participants reported post-mastectomy, chest/arm, musculoskeletal, and lymphatic pain. Chronic pain is one of the most troublesome side effects of breast cancer treatment and affects patients’ quality of life [ 33 ]. Chronic pain causes discomfort and fatigue, reduces appetite and sleep, and interferes with many activities of daily living [ 34 ]. Some of the participants’ statements regarding pain are provided below. One of the specialists stated:
Survivors face long-term complications of treatment, such as myalgia, osteoporosis, and hot flashes due to hormonal treatments, respiratory disorders due to receiving radiotherapy, and paresthesias of limbs due to receiving chemotherapy drugs, and they should have the necessary information and background to face these complications.
Participants stated:
My main problem was that I experienced so much musculoskeletal pain that I could not move. I was admitted to the hospital a couple of times, and a bunch of drugs were injected into me, but it worked temporarily, and the pain recurred.
My left hand is in severe pain due to the removal of the lymph nodes, which makes it difficult for me to do my chores and I need the help of others.
Fatigue was another physical symptom mentioned by most participants. Fatigue is the most common and frequent symptom of BCSs after treatment [ 35 ]. Studies have shown that low physical activity, decreased muscle mass, and impaired physical fitness are potential causes of fatigue in BCSs [ 36 ]. One participant said:
Sometimes I am so tired that I have to take a break several times while doing a normal daily task and continue again.
Hot flashes
Most of the participants stated that they experienced hot flashes due to menopause. Hot flashes are a common problem in breast cancer survivors, affecting their work performance [ 37 ]. One of the participants stated:
I have night sweats and hot flashes due to menopause. It bothers me a lot; it starts with my head and then with the rest of my body. Anyone around me will notice that I am sweating profusely. When I get this condition at night, I wake up, get annoyed, and cannot sleep anymore. I drink cold liquids, and it gets better but not completely.
Fear of cancer recurrence
Fear of cancer recurrence is one of the most commonly reported concerns among cancer survivors [ 38 ]. Most participants experienced FCR; it was the most important source of stress and worry after breast cancer diagnosis and treatment, involving the fear of cancer returning to the breast, metastasizing, or returning as a second cancer. One of the contributors said:
I do not have much stress and anxiety because my doctor told me that my disease has progressed. My only concern is whether my cancer returns?
To the best of our knowledge, this is the first study to examine the needs and experiences of Iranian BCSs. The most important finding of this study was the patients’ experience with financial problems. Most patients had financial problems associated with cancer care services (e.g., therapeutic procedures, supplies, medications, and transportation) and reduced income due to loss of employment, missing work, or unplanned retirement. In Iranian government hospitals, all healthcare services are based on insurance. Patients who use these services in hospitals are required to pay a percentage of the treatment cost. Usually, cosmetic procedures are not included in these insurance programs. However, the increase in inflation and prices has caused most patients to experience financial problems. This finding is consistent with that of a study by Autade and Chauhan, in which all BCSs reported financial problems [ 39 ]. In addition, in a study by Carrera (2018), 28–48% of cancer survivors experienced financial toxicity based on monetary measures and 16–73% experienced financial toxicity based on subjective measures [ 40 ]. In a study by Barthakur et al. (2016), finances relating to treatment were a major concern for survivors and there was a need for information on reducing healthcare costs [ 41 ]. Over 8% reported that providing for the financial needs of their families was a severe problem [ 42 ]. Patients who report cancer-related financial problems or high costs may be more likely to forgo or delay prescription medications or medical care [ 29 ]. The inability to afford household expenses is one of the most commonly reported reasons for delayed medical care among cancer patients [ 43 ]. Financial problems, if not identified, can negatively affect the physical, psychological, and socioeconomic status of survivors and lead to poorer access to health services and consequently poorer health status and health-related quality of life [ 44 ]. Research shows that health professionals recognize patients’ financial concerns but may not be qualified to address them [ 44 ]. Healthcare providers can take several steps to reduce patients’ financial difficulties, including: (1) considering the cost of multiple treatment regimens with similar effects, (2) providing cancer cost estimates to patients, (3) considering treatment benefits, (4) assessing patients for financial toxicity, and (5) educating and assisting patients about insurance benefits and other financial assistance institutions that may be available to them [ 42 ].
Another finding of this study relates to patients’ experience of support resources. Consistent with Iranian culture, in this study family members were a valuable and main source of support for the BCSs. In the study of Lee et al., family members, including adult children and spouses, were the main source of support for all participants [ 45 ].
Upon receiving emotional support from their family, patients felt reassurance, acceptance, and attention. Those who had family support felt less anxious and depressed, and their physical symptoms were much fewer. The effective role of emotional support for patients has been reported in several studies [ 5 , 9 , 46 ]. Wilson et al. reported that support from friends and family is a positive strategy for reducing stress and anxiety and coping with illness [ 47 ]. In a study by Moradi et al. (2013), supportive care needs in women with breast cancer decreased after their husbands were educated about familiarity with breast cancer disease, symptoms and complications of the disease, and treatment. It has been suggested that caregivers use training sessions to reduce the needs of women with cancer [ 48 ]. These results were inconsistent, however, with those of Thewes (2004) and Arora (2007) [ 9 , 49 ]. They both concluded that friends and family members of patients with cancer tend to decrease or withdraw their support after treatment completion. The family’s role in improving patient outcomes cannot be overemphasized.
The study shows that patients who do not have access to a family support source have a greater tendency to use social support networks [ 50 ]. The researchers could create access to social support networks for patients who do not receive family support. Additionally, the role of support groups cannot be ignored. Support groups consisted of people with common experiences. In Iran, there are many support groups for cancer patients. Experiencers with any type of cancer can declare their readiness to participate in these groups by registering on related sites. These groups usually have weekly or monthly meetings. These meetings are held in person or virtually, according to the position of the group members. According to the needs of the members, the content of these meetings can be informative, reminiscent, fun, sports, cooking, or any topic desired by the majority of the members. Chou et al. (2016) showed that support groups help reduce psychological distress and increase the quality of life of patients with breast cancer. It is also possible to educate patients’ families about the needs of those who have recovered. Moghaddam Tabrizi et al. (2018) conducted an interventional study and trained patients’ families in family participation, optimism, coping with cancer, reducing uncertainty, and managing symptoms. The findings indicated a significant improvement in overall cancer coping scores on all subscales, including individual, positive focus, coping, deviation, planning, and interpersonal communication [ 31 ].
The participants also stated that they had unmet information needs in the areas of management of side effects, nutrition, and uncertainty management. Previous studies have also identified informational needs as the most common need for BCSs [ 3 , 5 , 51 ], even for survivors who have been diagnosed and treated for several years. These needs often include information on diet and nutrition, mental health counselling, infertility, and spiritual counselling [ 52 ]. Previous studies have indicated that BCSs often feel unready for the side effects that linger after therapy [ 17 , 18 ]. In a study by Pembroke et al., almost half of the participants reported informational needs associated with side effects of treatment [ 52 ]. In this study, patients met their information needs through the Internet; however, they had doubts regarding the use of this information. The high use of the Internet by patients with cancer suggests that healthcare providers may not be adequately meeting patients’ information needs [ 53 ].
Germino et al. (2013) conducted an intervention study with the aim of determining the impact of uncertainty management intervention on reducing uncertainty, better uncertainty management, fewer breast cancer-specific concerns and more positive psychological outcomes. The intervention consisted of a written CD and a manual with four weekly 20-minute training calls. The findings showed that BCS who received the intervention reported a reduction in uncertainty and significant improvement in behavioral and cognitive coping strategies for managing uncertainty, self-efficacy, and sexual dysfunction [ 54 ].
Physical problems were also reported by most participants. The patients mostly complained of pain, fatigue, and hot flashes. This finding is consistent with the results of the present study [ 9 , 16 , 17 , 39 ]. In the study by Bu et al. (2022), fatigue and pain were reported in 40.7% and 37.2% of the subjects respectively [ 55 ]. Studies have shown that the use of exercise-based interventions plays an effective role in reducing the pain and fatigue of breast cancer survivors [ 56 , 57 ].
Studies have also shown that mobile health education intervention improves cancer-related fatigue among breast cancer survivors [ 58 ]. mHealth interventions involve the adoption of mobile technologies to provide educational information, help users manage their own conditions and behaviors, and deliver healthcare to improve the health of users [ 59 ]. Integrating training to manage fatigue as part of routine care among breast cancer survivors is recommended [ 58 ].
The most important mental disorder experienced by patients was the fear of recurrence. The results of this study are similar to those of a previous study, which showed that the most common unmet need was help with coping with the fear of recurrence [ 60 , 61 , 62 ]. In the study of Brennan et al. (2010), fear of cancer recurrence was reported by 38% of the participants and emerged as the highest-ranked unmet need in all age groups [ 63 ]. In this study, fear of recurrence was identified as a key issue for cancer survivors [ 64 , 65 , 66 , 67 ].
The remarkable findings obtained from the interviews with health care professionals were that they mentioned the long-term complications caused by treatment procedures such as radiotherapy and chemotherapy in breast cancer survivors, including pain, fatigue, and hot flashes. Survivors have also reported these complications. According to healthcare professionals, facing an uncertain future, fear of cancer recurrence, and body image concerns are the most important concerns for breast cancer survivors. These results are consistent with those reported by Wells et al. [ 68 ].
Limitations
This study has several limitations. First, while the BCSs were diverse, all were recruited from a comprehensive cancer center in Tehran, where they were referred to receive survivorship care. They may differ in other centers. Second, we did not use random sampling to obtain a sample of study participants. Instead, we used purposive sampling, a sampling approach commonly used in qualitative research, in order to select participants who were particularly knowledgeable about the phenomenon under study. Third, a qualitative method was used in this study, which does not allow the testing of a specific hypothesis. Fourth, we used literate participants; different results may be obtained from illiterate individuals.
The results of this study can be used to design survival care programs for Iranian BCS. Therefore, patients’ support resources should be reviewed and measured. Appropriate psychological interventions could be used for patients who do not have a source of support. The financial ability of patients should be assessed, and necessary measures should be considered for patients with financial problems. All the patients were provided with an educational program tailored to their needs. Consultation groups could be used to meet the information needs of the patients. In patients with physical problems, self-care recommendations may also be useful in addition to doctors’ orders.
Data availability
The datasets analysed during the current study are not publicly available due to ethical restrictions. but are available from the corresponding author on reasonable request.
Abbreviations
Breast Cancer Survivor
Survivorship care plans
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021;71(3):209–49.
Article Google Scholar
DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, et al. Breast cancer statistics, 2019. Cancer J Clin. 2019;69(6):438–51.
Cheng KKF, Cheng HL, Wong WH, Koh C. A mixed-methods study to explore the supportive care needs of breast cancer survivors. Psychooncology. 2018;27(1):265–71.
Article CAS PubMed Google Scholar
Joshi A, Larkins S, Evans R, Moodley N, Brown A, Sabesan S. Use and impact of breast cancer survivorship care plans: a systematic review. Breast Cancer. 2021;28(6):1292–317.
Article PubMed Google Scholar
Dsouza SM, Vyas N, Narayanan P, Parsekar SS, Gore M, Sharan K. A qualitative study on experiences and needs of breast cancer survivors in Karnataka, India. Clin Epidemiol Global Health. 2018;6(2):69–74.
Fong EJ, Cheah WL. Unmet supportive care needs among breast cancer survivors of community-based support group in Kuching, Sarawak. International journal of breast cancer. 2016;2016.
Hubbeling HG, Rosenberg SM, González-Robledo MC, Cohn JG, Villarreal-Garza C, Partridge AH, et al. Psychosocial needs of young breast cancer survivors in Mexico City, Mexico. PLoS ONE. 2018;13(5):e0197931.
Article PubMed PubMed Central Google Scholar
Lo-Fo‐Wong DN, de Haes HC, Aaronson NK, van Abbema DL, den Boer MD, van Hezewijk M, et al. Risk factors of unmet needs among women with breast cancer in the post‐treatment phase. Psycho‐Oncology. 2020;29(3):539–49.
Thewes B, Butow P, Girgis A, Pendlebury S. The psychosocial needs of breast cancer survivors; a qualitative study of the shared and unique needs of younger versus older survivors. Psychooncology. 2004;13(3):177–89.
Richter-Ehrenstein C, Martinez-Pader J. Impact of breast cancer diagnosis and treatment on work-related life and financial factors. Breast Care. 2021;16(1):72–6.
Mayer DK, Nasso SF, Earp JA. Defining cancer survivors, their needs, and perspectives on survivorship health care in the USA. Lancet Oncol. 2017;18(1):e11–e8.
Chae BJ, Lee J, Lee SK, Shin HJ, Jung SY, Lee JW, et al. Unmet needs and related factors of Korean breast cancer survivors: a multicenter, cross-sectional study. BMC Cancer. 2019;19(1):839.
Rahmani A, Ferguson C, Jabarzadeh F, Mohammadpoorasl A, Moradi N, Pakpour V. Supportive care needs of Iranian cancer patients. Indian J Palliat Care. 2014;20(3):224–8.
Buki LP, Rivera-Ramos ZA, Kanagui-Muñoz M, Heppner PP, Ojeda L, Lehardy EN, et al. I never heard anything about it: knowledge and psychosocial needs of Latina breast cancer survivors with lymphedema. Women’s Health. 2021;17:17455065211002488.
CAS PubMed PubMed Central Google Scholar
Gisiger-Camata S, Adams N, Nolan TS, Meneses K. Multi-level assessment to reach out to rural breast cancer survivors. Women’s Health. 2016;12(6):513–22.
PubMed PubMed Central Google Scholar
Gisiger-Camata S, Adams N, Nolan TS, Meneses K. Multi-level Assessment to Reach out to rural breast Cancer survivors. Womens Health (Lond). 2016;12(6):513–22.
Cappiello M, Cunningham RS, Tish Knobf M, Erdos D. Breast cancer survivors: information and support after treatment. Clin Nurs Res. 2007;16(4):278–93.
Galván N, Buki LP, Garcés DM. Suddenly, a carriage appears: social support needs of Latina breast cancer survivors. J Psychosoc Oncol. 2009;27(3):361–82.
Khajoei R, Ilkhani M, Azadeh P, Anboohi SZ, Nabavi FH. Breast cancer survivors–supportive care needs: systematic review. BMJ Supportive & Palliative Care. 2023;13(2):143–53.
Speziale HS, Streubert HJ, Carpenter DR. Qualitative research in nursing: advancing the humanistic imperative. Lippincott Williams & Wilkins; 2011.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir Program Evaluation. 1986;1986(30):73–84.
Corbin J, Strauss A. Strategies for qualitative data analysis. Basics of Qualitative Research Techniques and Procedures for Developing Grounded Theory. 2008;3(104135):9781452230153.
Google Scholar
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Lietz CA, Langer CL, Furman R. Establishing trustworthiness in qualitative research in social work: implications from a study regarding spirituality. Qualitative Social work. 2006;5(4):441–58.
Lentz R, Benson AB III, Kircher S. Financial toxicity in cancer care: prevalence, causes, consequences, and reduction strategies. J Surg Oncol. 2019;120(1):85–92.
Perry LM, Hoerger M, Seibert K, Gerhart JI, O’Mahony S, Duberstein PR. Financial strain and physical and emotional quality of life in breast cancer. J Pain Symptom Manag. 2019;58(3):454–9.
Kent EE, Forsythe LP, Yabroff KR, Weaver KE, de Moor JS, Rodriguez JL, et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119(20):3710–7.
Hu RY, Wang JY, Chen WL, Zhao J, Shao CH, Wang JW, et al. Stress, coping strategies and expectations among breast cancer survivors in China: a qualitative study. BMC Psychol. 2021;9(1):26.
Moghaddam Tabrizi F, Alizadeh S. Family intervention based on the FOCUS Program effects on Cancer Coping in Iranian breast Cancer patients: a Randomized Control Trial. Asian Pac J Cancer Prev. 2018;19(6):1523–8.
PubMed Google Scholar
Sebri V, Pravettoni G. Tailored psychological interventions to manage body image: an Opinion study on breast Cancer survivors. Int J Environ Res Public Health. 2023;20(4).
Tait RC, Zoberi K, Ferguson M, Levenhagen K, Luebbert RA, Rowland K, et al. Persistent Post-mastectomy Pain: risk factors and current approaches to treatment. J Pain. 2018;19(12):1367–83.
Fitzgerald Jones K, Fu MR, McTernan ML, Ko E, Yazicioglu S, Axelrod D, et al. Lymphatic Pain in breast Cancer survivors. Lymphat Res Biol. 2022;20(5):525–32.
Schmidt ME, Chang-Claude J, Vrieling A, Heinz J, Flesch-Janys D, Steindorf K. Fatigue and quality of life in breast cancer survivors: temporal courses and long-term pattern. J Cancer Surviv. 2012;6(1):11–9.
Neil SE, Klika RJ, Garland SJ, McKenzie DC, Campbell KL. Cardiorespiratory and neuromuscular deconditioning in fatigued and non-fatigued breast cancer survivors. Support Care Cancer. 2013;21(3):873–81.
Harris PF, Remington PL, Trentham-Dietz A, Allen CI, Newcomb PA. Prevalence and treatment of menopausal symptoms among breast cancer survivors. J Pain Symptom Manage. 2002;23(6):501–9.
Thewes B, Lebel S, Seguin Leclair C, Butow P. A qualitative exploration of fear of cancer recurrence (FCR) amongst Australian and Canadian breast cancer survivors. Support Care Cancer. 2016;24(5):2269–76.
Autade YCG. Assess the prevalence for needs of breast cancer survivors’ in the oncology ward at a selected tertiary care hospital. JPRI. 2021;1(33):1–12.
Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin. 2018;68(2):153–65.
Barthakur MS, Sharma MP, Chaturvedi SK, Manjunath SK. Experiences of breast Cancer survivors with Oncology Settings in Urban India: qualitative findings. Indian J Surg Oncol. 2016;7(4):392–6.
Coughlin SS, Ayyala DN, Tingen MS, Cortes JE. Financial distress among breast cancer survivors. Curr Cancer Rep. 2020;2(1):48–53.
Knight TG, Deal AM, Dusetzina SB, Muss HB, Choi SK, Bensen JT et al. Financial toxicity in adults with Cancer: adverse outcomes and noncompliance. J Oncol Pract. 2018:Jop1800120.
Nipp RD, Shui AM, Perez GK, Kirchhoff AC, Peppercorn JM, Moy B, et al. Patterns in Health Care Access and Affordability among Cancer survivors during implementation of the Affordable Care Act. JAMA Oncol. 2018;4(6):791–7.
Lee S, Chen L, Ma GX, Fang CY, Oh Y, Scully L. Challenges and needs of Chinese and Korean American breast Cancer survivors: In-Depth interviews. N Am J Med Sci (Boston). 2013;6(1):1–8.
Shaw MD, Coggin C. Using a Delphi technique to determine the needs of African American breast cancer survivors. Health Promot Pract. 2008;9(1):34–44.
Wilson SE, Andersen MR, Meischke H. Meeting the needs of rural breast cancer survivors: what still needs to be done? J Womens Health Gend Based Med. 2000;9(6):667–77.
Moradi NAF, Rahmani AZV. Effects of husband’s education on meting supportive care needs of breast cancer patients: a clinical trial. Avicenna-J-Nurs-Midwifery-Care. 2013;21(3):40–50.
Arora NK, Finney Rutten LJ, Gustafson DH, Moser R, Hawkins RP. Perceived helpfulness and impact of social support provided by family, friends, and health care providers to women newly diagnosed with breast cancer. Psychooncology. 2007;16(5):474–86.
Namkoong K, Shah DV, Gustafson DH. Offline Social relationships and Online Cancer Communication: effects of Social and Family Support on Online Social Network Building. Health Commun. 2017;32(11):1422–9.
Liao MN, Chen SC, Chen SC, Lin YC, Hsu YH, Hung HC, et al. Changes and predictors of unmet supportive care needs in Taiwanese women with newly diagnosed breast cancer. Oncol Nurs Forum. 2012;39(5):E380–9.
Zebrack B. Information and service needs for young adult cancer survivors. Support Care Cancer. 2009;17(4):349–57.
Winzelberg AJ, Classen C, Alpers GW, Roberts H, Koopman C, Adams RE, et al. Evaluation of an internet support group for women with primary breast cancer. Cancer: Interdisciplinary International Journal of the American Cancer Society. 2003;97(5):1164–73.
Germino BB, Mishel MH, Crandell J, Porter L, Blyler D, Jenerette C, et al. Outcomes of an uncertainty management intervention in younger African American and caucasian breast cancer survivors. Oncol Nurs Forum. 2013;40(1):82–92.
Bu X, Jin C, Fan R, Cheng ASK, Ng PHF, Xia Y, et al. Unmet needs of 1210 Chinese breast cancer survivors and associated factors: a multicentre cross-sectional study. BMC Cancer. 2022;22(1):135.
Galiano-Castillo N, Cantarero‐Villanueva I, Fernández‐Lao C, Ariza‐García A, Díaz‐Rodríguez L, Del‐Moral‐Ávila R, et al. Telehealth system: a randomized controlled trial evaluating the impact of an internet‐based exercise intervention on quality of life, pain, muscle strength, and fatigue in breast cancer survivors. Cancer. 2016;122(20):3166–74.
Lin Y, Wu C, He C, Yan J, Chen Y, Gao L, et al. Effectiveness of three exercise programs and intensive follow-up in improving quality of life, pain, and lymphedema among breast cancer survivors: a randomized, controlled 6-month trial. Support Care Cancer. 2022;31(1):9.
Bandani-Susan B, Montazeri A, Haghighizadeh MH, Araban M. The effect of mobile health educational intervention on body image and fatigue in breast cancer survivors: a randomized controlled trial. Ir J Med Sci. 2022;191(4):1599–605.
Wei Y, Zheng P, Deng H, Wang X, Li X, Fu H. Design features for improving Mobile Health intervention user Engagement: systematic review and thematic analysis. J Med Internet Res. 2020;22(12):e21687.
Hodgkinson K, Butow P, Hunt GE, Pendlebury S, Hobbs KM, Wain G. Breast cancer survivors’ supportive care needs 2–10 years after diagnosis. Support Care Cancer. 2007;15(5):515–23.
Beatty L, Oxlad M, Koczwara B, Wade TD. The psychosocial concerns and needs of women recently diagnosed with breast cancer: a qualitative study of patient, nurse and volunteer perspectives. Health Expect. 2008;11(4):331–42.
Torres E, Dixon C, Richman AR. Understanding the breast Cancer Experience of survivors: a qualitative study of African American Women in Rural Eastern North Carolina. J Cancer Educ. 2016;31(1):198–206.
Brennan ME, Butow P, Spillane AJ, Boyle F. Patient-reported quality of life, unmet needs and care coordination outcomes: moving toward targeted breast cancer survivorship care planning. Asia‐Pacific J Clin Oncol. 2016;12(2):e323–e31.
Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7(3):300–22.
Crist JV, Grunfeld EA. Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psychooncology. 2013;22(5):978–86.
Ellegaard MB, Grau C, Zachariae R, Bonde Jensen A. Fear of cancer recurrence and unmet needs among breast cancer survivors in the first five years. A cross-sectional study. Acta Oncol. 2017;56(2):314–20.
Fang SY, Fetzer SJ, Lee KT, Kuo YL. Fear of recurrence as a predictor of Care needs for long-term breast Cancer survivors. Cancer Nurs. 2018;41(1):69–76.
Wells KJ, Drizin JH, Ustjanauskas AE, Vázquez-Otero C, Pan-Weisz TM, Ung D, et al. The psychosocial needs of underserved breast cancer survivors and perspectives of their clinicians and support providers. Support Care Cancer. 2022;30:105–16.
Download references
Acknowledgements
Not applicable.
Not funded.
Author information
Authors and affiliations.
Student Research Committee, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, IR, Iran
Rahimeh Khajoei
Radiation Oncology Department, School of Medicine, Imam Hossein Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Payam Azadeh
Department of Medical Surgical Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, IR, Iran
Sima ZohariAnboohi & Mahnaz Ilkhani
Nursing and Midwifery Care Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
Fatemah Heshmati Nabavi
You can also search for this author in PubMed Google Scholar
Contributions
R.K. and M.I. conceived and designed the study. R.K. conducted and transcribed interviews, analyzed the data, and wrote the manuscript. M.I., S.Z., P.A. and F.H. assisted in the analysis and interpretation of data, and in the revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mahnaz Ilkhani .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran with code IR.SBMU.PHARMACY.REC.1402.005. Informed consent was obtained from all subjects involved in the study.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Khajoei, R., Azadeh, P., ZohariAnboohi, S. et al. Breast cancer survivorship needs: a qualitative study. BMC Cancer 24 , 96 (2024). https://doi.org/10.1186/s12885-024-11834-5
Download citation
Received : 16 September 2023
Accepted : 03 January 2024
Published : 17 January 2024
DOI : https://doi.org/10.1186/s12885-024-11834-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Survivorship
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
AACR Annual Meeting News: Read the latest session previews and recaps from the official news website.
Select "Patients / Caregivers / Public" or "Researchers / Professionals" to filter your results. To further refine your search, toggle appropriate sections on or off.
Cancer Research Catalyst The Official Blog of the American Association for Cancer Research

Home > Cancer Research Catalyst > Cancer Survivors: In Their Words
Cancer Survivors: In Their Words
This year alone, an estimated 1.8 million people will hear their doctor say they have cancer. The individual impact of each person can be clouded in the vast statistics. In honor of National Cancer Survivor Month, Cancer Today would like to highlight several personal essays we’ve published from cancer survivors at different stages of their treatment.

In this essay , psychiatrist Adam P. Stern’s cerebral processing of his metastatic kidney cancer diagnosis gives rise to piercing questions. When he drops off his 3-year-old son to daycare, he ponders a simple exchange: his son’s request for a routine morning hug before he turns to leave. “Will he remember me, only a little, just enough to mythologize me as a giant who used to carry him up the stairs? As my health declines, will he have to learn to adjust to a dad who used to be like all the other dads but then wasn’t?” he questions.

In another essay from a parent with a young child, Amanda Rose Ferraro describes the abrupt change from healthy to not healthy after being diagnosed with acute myeloid leukemia in May 2017. After a 33-day hospital stay, followed by weeklong chemotherapy treatments, Ferraro’s cancer went into remission, but a recurrence required more chemotherapy and a stem cell transplant. Ferraro describes harrowing guilt over being separated from her 3-year-old son, who at one point wanted nothing to do with her. “Giving up control is hard, but not living up to what I thought a mother should be was harder. I had to put myself first, and it was the hardest thing I had ever done,” she writes.
In January 1995, 37-year-old Melvin Mann was diagnosed with chronic myelogenous leukemia, which would eventually mean he would need to take a chance on a phase I clinical trial that tested an experimental drug called imatinib—a treatment that would go on to receive U.S. Food and Drug Administration approval under the brand name Gleevec. It would also mean trusting a system with a documented history of negligence and abuse of Black people like him: “Many patients, especially some African Americans, are afraid they will be taken advantage of because of past unethical experiments like the infamous Tuskegee syphilis study,” Mann writes, before describing changes that make current trials safer. Mann’s been on imatinib ever since and has enjoyed watching his daughter become a physician and celebrating 35 years of marriage.

In another essay , Carly Flumer addresses the absurdity of hearing doctors reassure her that she had a good cancer after she was diagnosed with stage I papillary thyroid cancer in 2017. “What I did hear repeatedly from various physicians was that I had the ‘good cancer,’ and that ‘if you were to have a cancer, thyroid would be the one to get,’” she writes.
In another piece for Cancer Today , Flumer shares how being diagnosed with cancer just four months after starting a graduate program shaped her education and future career path.
For Liza Bernstein, her breast cancer diagnosis created a paradox as she both acknowledged and denied the disease the opportunity to define who she was. “In the privacy of my own mind, I refused to accept that cancer was part of my identity, even though it was affecting it as surely as erosion transforms the landscape,” she writes . “Out in the world, I’d blurt out, ‘I have cancer,’ because I took questions from acquaintances like ‘How are you, what’s new?’ literally. Answering casual questions with the unvarnished truth wasn’t claiming cancer as my identity. It was an attempt to dismiss the magnitude of it, like saying ‘I have a cold.’” By her third primary breast cancer diagnosis, Bernstein reassesses and moves closer to acceptance as she discovers her role as advocate.

As part of the staff of Cancer Today , a magazine and online resource for cancer patients, survivors and caregivers, we often refer to a succinct tagline to sum up our mission: “Practical knowledge. Real hope.” Part of providing information is also listening closely to cancer survivors’ experiences. As we celebrate National Cancer Survivor Month, we elevate these voices, and all patients and survivors in their journeys.
Cancer Today is a magazine and online resource for cancer patients, survivors, and caregivers published by the American Association for Cancer Research. Subscriptions to the magazine are free to cancer patients, survivors and caregivers who live in the U.S.
- About This Blog
- Blog Policies
- Tips for Contributors

AACR Virtual Annual Meeting I: Results on a Targeted Therapeutic for Lung Cancer Support FDA Approval
Annual Meeting 2022: Understanding and Intercepting Precancer

AACR Annual Meeting 2021: How Do Diet and Ancestry Affect Cancer Development?
Cancel reply
Your email address will not be published. Required fields are marked *
Join the Discussion (max: 750 characters)...
This site uses Akismet to reduce spam. Learn how your comment data is processed .
- Cancer Research Catalyst
- Share Your Story
- National Cancer Survivor Month
DigitalCommons@UNMC
Home > Eppley Institute > Theses & Dissertations
Theses & Dissertations: Cancer Research
Theses/dissertations from 2023 2023.
Development of Combination Therapy Strategies to Treat Cancer Using Dihydroorotate Dehydrogenase Inhibitors , Nicholas Mullen
Overcoming Resistance Mechanisms to CDK4/6 Inhibitor Treatment Using CDK6-Selective PROTAC , Sarah Truong
Theses/Dissertations from 2022 2022
Omics Analysis in Cancer and Development , Emalie J. Clement
Investigating the Role of Splenic Macrophages in Pancreatic Cancer , Daisy V. Gonzalez
Polymeric Chloroquine in Metastatic Pancreatic Cancer Therapy , Rubayat Islam Khan
Evaluating Targets and Therapeutics for the Treatment of Pancreatic Cancer , Shelby M. Knoche
Characterization of 1,1-Diarylethylene FOXM1 Inhibitors Against High-Grade Serous Ovarian Carcinoma Cells , Cassie Liu
Novel Mechanisms of Protein Kinase C α Regulation and Function , Xinyue Li
SOX2 Dosage Governs Tumor Cell Identity and Proliferation , Ethan P. Metz
Post-Transcriptional Control of the Epithelial-to-Mesenchymal Transition (EMT) in Ras-Driven Colorectal Cancers , Chaitra Rao
Use of Machine Learning Algorithms and Highly Multiplexed Immunohistochemistry to Perform In-Depth Characterization of Primary Pancreatic Tumors and Metastatic Sites , Krysten Vance
Characterization of Metastatic Cutaneous Squamous Cell Carcinoma in the Immunosuppressed Patient , Megan E. Wackel
Visceral adipose tissue remodeling in pancreatic ductal adenocarcinoma cachexia: the role of activin A signaling , Pauline Xu
Phos-Tag-Based Screens Identify Novel Therapeutic Targets in Ovarian Cancer and Pancreatic Cancer , Renya Zeng
Theses/Dissertations from 2021 2021
Functional Characterization of Cancer-Associated DNA Polymerase ε Variants , Stephanie R. Barbari
Pancreatic Cancer: Novel Therapy, Research Tools, and Educational Outreach , Ayrianne J. Crawford
Apixaban to Prevent Thrombosis in Adult Patients Treated With Asparaginase , Krishna Gundabolu
Molecular Investigation into the Biologic and Prognostic Elements of Peripheral T-cell Lymphoma with Regulators of Tumor Microenvironment Signaling Explored in Model Systems , Tyler Herek
Utilizing Proteolysis-Targeting Chimeras to Target the Transcriptional Cyclin-Dependent Kinases 9 and 12 , Hannah King
Insights into Cutaneous Squamous Cell Carcinoma Pathogenesis and Metastasis Using a Bedside-to-Bench Approach , Marissa Lobl
Development of a MUC16-Targeted Near-Infrared Antibody Probe for Fluorescence-Guided Surgery of Pancreatic Cancer , Madeline T. Olson
FGFR4 glycosylation and processing in cholangiocarcinoma promote cancer signaling , Andrew J. Phillips
Theses/Dissertations from 2020 2020
Cooperativity of CCNE1 and FOXM1 in High-Grade Serous Ovarian Cancer , Lucy Elge
Characterizing the critical role of metabolic and redox homeostasis in colorectal cancer , Danielle Frodyma
Genomic and Transcriptomic Alterations in Metabolic Regulators and Implications for Anti-tumoral Immune Response , Ryan J. King
Dimers of Isatin Derived Spirocyclic NF-κB Inhibitor Exhibit Potent Anticancer Activity by Inducing UPR Mediated Apoptosis , Smit Kour
From Development to Therapy: A Panoramic Approach to Further Our Understanding of Cancer , Brittany Poelaert
The Cellular Origin and Molecular Drivers of Claudin-Low Mammary Cancer , Patrick D. Raedler
Mitochondrial Metabolism as a Therapeutic Target for Pancreatic Cancer , Simon Shin
Development of Fluorescent Hyaluronic Acid Nanoparticles for Intraoperative Tumor Detection , Nicholas E. Wojtynek
Theses/Dissertations from 2019 2019
The role of E3 ubiquitin ligase FBXO9 in normal and malignant hematopoiesis , R. Willow Hynes-Smith
BRCA1 & CTDP1 BRCT Domainomics in the DNA Damage Response , Kimiko L. Krieger
Targeted Inhibition of Histone Deacetyltransferases for Pancreatic Cancer Therapy , Richard Laschanzky
Human Leukocyte Antigen (HLA) Class I Molecule Components and Amyloid Precursor-Like Protein 2 (APLP2): Roles in Pancreatic Cancer Cell Migration , Bailee Sliker
Theses/Dissertations from 2018 2018
FOXM1 Expression and Contribution to Genomic Instability and Chemoresistance in High-Grade Serous Ovarian Cancer , Carter J. Barger
Overcoming TCF4-Driven BCR Signaling in Diffuse Large B-Cell Lymphoma , Keenan Hartert
Functional Role of Protein Kinase C Alpha in Endometrial Carcinogenesis , Alice Hsu
Functional Signature Ontology-Based Identification and Validation of Novel Therapeutic Targets and Natural Products for the Treatment of Cancer , Beth Neilsen
Elucidating the Roles of Lunatic Fringe in Pancreatic Ductal Adenocarcinoma , Prathamesh Patil
Theses/Dissertations from 2017 2017
Metabolic Reprogramming of Pancreatic Ductal Adenocarcinoma Cells in Response to Chronic Low pH Stress , Jaime Abrego
Understanding the Relationship between TGF-Beta and IGF-1R Signaling in Colorectal Cancer , Katie L. Bailey
The Role of EHD2 in Triple-Negative Breast Cancer Tumorigenesis and Progression , Timothy A. Bielecki
Perturbing anti-apoptotic proteins to develop novel cancer therapies , Jacob Contreras
Role of Ezrin in Colorectal Cancer Cell Survival Regulation , Premila Leiphrakpam
Evaluation of Aminopyrazole Analogs as Cyclin-Dependent Kinase Inhibitors for Colorectal Cancer Therapy , Caroline Robb
Identifying the Role of Janus Kinase 1 in Mammary Gland Development and Breast Cancer , Barbara Swenson
DNMT3A Haploinsufficiency Provokes Hematologic Malignancy of B-Lymphoid, T-Lymphoid, and Myeloid Lineage in Mice , Garland Michael Upchurch
Theses/Dissertations from 2016 2016
EHD1 As a Positive Regulator of Macrophage Colony-Stimulating Factor-1 Receptor , Luke R. Cypher
Inflammation- and Cancer-Associated Neurolymphatic Remodeling and Cachexia in Pancreatic Ductal Adenocarcinoma , Darci M. Fink
Role of CBL-family Ubiquitin Ligases as Critical Negative Regulators of T Cell Activation and Functions , Benjamin Goetz
Exploration into the Functional Impact of MUC1 on the Formation and Regulation of Transcriptional Complexes Containing AP-1 and p53 , Ryan L. Hanson
DNA Polymerase Zeta-Dependent Mutagenesis: Molecular Specificity, Extent of Error-Prone Synthesis, and the Role of dNTP Pools , Olga V. Kochenova
Defining the Role of Phosphorylation and Dephosphorylation in the Regulation of Gap Junction Proteins , Hanjun Li
Molecular Mechanisms Regulating MYC and PGC1β Expression in Colon Cancer , Jamie L. McCall
Pancreatic Cancer Invasion of the Lymphatic Vasculature and Contributions of the Tumor Microenvironment: Roles for E-selectin and CXCR4 , Maria M. Steele
Altered Levels of SOX2, and Its Associated Protein Musashi2, Disrupt Critical Cell Functions in Cancer and Embryonic Stem Cells , Erin L. Wuebben
Theses/Dissertations from 2015 2015
Characterization and target identification of non-toxic IKKβ inhibitors for anticancer therapy , Elizabeth Blowers
Effectors of Ras and KSR1 dependent colon tumorigenesis , Binita Das
Characterization of cancer-associated DNA polymerase delta variants , Tony M. Mertz
A Role for EHD Family Endocytic Regulators in Endothelial Biology , Alexandra E. J. Moffitt
Biochemical pathways regulating mammary epithelial cell homeostasis and differentiation , Chandrani Mukhopadhyay
EPACs: epigenetic regulators that affect cell survival in cancer. , Catherine Murari
Role of the C-terminus of the Catalytic Subunit of Translesion Synthesis Polymerase ζ (Zeta) in UV-induced Mutagensis , Hollie M. Siebler
LGR5 Activates TGFbeta Signaling and Suppresses Metastasis in Colon Cancer , Xiaolin Zhou
LGR5 Activates TGFβ Signaling and Suppresses Metastasis in Colon Cancer , Xiaolin Zhou
Theses/Dissertations from 2014 2014
Genetic dissection of the role of CBL-family ubiquitin ligases and their associated adapters in epidermal growth factor receptor endocytosis , Gulzar Ahmad
Strategies for the identification of chemical probes to study signaling pathways , Jamie Leigh Arnst
Defining the mechanism of signaling through the C-terminus of MUC1 , Roger B. Brown
Targeting telomerase in human pancreatic cancer cells , Katrina Burchett
The identification of KSR1-like molecules in ras-addicted colorectal cancer cells , Drew Gehring
Mechanisms of regulation of AID APOBEC deaminases activity and protection of the genome from promiscuous deamination , Artem Georgievich Lada
Characterization of the DNA-biding properties of human telomeric proteins , Amanda Lakamp-Hawley
Studies on MUC1, p120-catenin, Kaiso: coordinate role of mucins, cell adhesion molecules and cell cycle players in pancreatic cancer , Xiang Liu
Epac interaction with the TGFbeta PKA pathway to regulate cell survival in colon cancer , Meghan Lynn Mendick
Theses/Dissertations from 2013 2013
Deconvolution of the phosphorylation patterns of replication protein A by the DNA damage response to breaks , Kerry D. Brader
Modeling malignant breast cancer occurrence and survival in black and white women , Michael Gleason
The role of dna methyltransferases in myc-induced lymphomagenesis , Ryan A. Hlady
Design and development of inhibitors of CBL (TKB)-protein interactions , Eric A. Kumar
Pancreatic cancer-associated miRNAs : expression, regulation and function , Ashley M. Mohr
Mechanistic studies of mitochondrial outer membrane permeabilization (MOMP) , Xiaming Pang
Novel roles for JAK2/STAT5 signaling in mammary gland development, cancer, and immune dysregulation , Jeffrey Wayne Schmidt
Optimization of therapeutics against lethal pancreatic cancer , Joshua J. Souchek
Theses/Dissertations from 2012 2012
Immune-based novel diagnostic mechanisms for pancreatic cancer , Michael J. Baine
Sox2 associated proteins are essential for cell fate , Jesse Lee Cox
KSR2 regulates cellular proliferation, transformation, and metabolism , Mario R. Fernandez
Discovery of a novel signaling cross-talk between TPX2 and the aurora kinases during mitosis , Jyoti Iyer
Regulation of metabolism by KSR proteins , Paula Jean Klutho
The role of ERK 1/2 signaling in the dna damage-induced G2 , Ryan Kolb
Regulation of the Bcl-2 family network during apoptosis induced by different stimuli , Hernando Lopez
Studies on the role of cullin3 in mitosis , Saili Moghe
Characteristics of amyloid precursor-like protein 2 (APLP2) in pancreatic cancer and Ewing's sarcoma , Haley Louise Capek Peters
Structural and biophysical analysis of a human inosine triphosphate pyrophosphatase polymorphism , Peter David Simone
Functions and regulation of Ron receptor tyrosine kinase in human pancreatic cancer and its therapeutic applications , Yi Zou
Theses/Dissertations from 2011 2011
Coordinate detection of new targets and small molecules for cancer therapy , Kurt Fisher
The role of c-Myc in pancreatic cancer initiation and progression , Wan-Chi Lin
The role of inosine triphosphate pyrophosphatase (ITPA) in maintanence [sic] of genomic stability in human cells , Miriam-Rose Menezes
Molecular insights into major histocompatibility complex class I folding and assembly , Laura Christina Simone
The role of bcl-2 in colon cancer metastatic progression , Wang Wang
A rational peptidomimetic approach towards generation of high affinity BRCT (BRCA1) inhibitors , Ziyan Yuan
D-type cyclins and breast cancer , Quian Zhang
- Eppley Institute Website
- McGoogan Library
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Share full article
Advertisement
Supported by
A Blood Test Shows Promise for Early Colon Cancer Detection
Many patients are reluctant to undergo colonoscopies or conduct at-home fecal tests. Doctors see potential in another screening method.

By Gina Kolata
Early detection of colon cancer can prevent a majority of deaths from this disease, possibly as much as 73 percent of them. But just 50 to 75 percent of middle-aged and older adults who should be screened regularly are being tested .
One reason, doctors say, is that the screening methods put many people off.
There are two options for people of average risk: a colonoscopy every 10 years or a fecal test every one to three years , depending on the type of test.
Or, as Dr. Folasade P. May, a gastroenterologist at UCLA Health puts it, “either you take this horrible laxative and then a doctor puts an instrument up your behind, or you have to manipulate your own poop.”
But something much simpler is on the horizon: a blood test. Gastroenterologists say such tests could become part of the routine blood work that doctors order when, for example, a person comes in for an annual physical exam.
“I think this is going to start taking off,” said Dr. John M. Carethers, a gastroenterologist and the vice chancellor for health sciences at the University of California, San Diego.
About 53,000 Americans are expected to die from colorectal cancer this year. It is the second-most common cause of cancer-related deaths in the United States, and while the death rate in older adults has fallen, it has increased in people under age 55.
Current guidelines recommend screenings starting at age 45. The problem is convincing more people to be screened.
Enter the blood test. It takes advantage of the discovery that colon cancers and large polyps — clumps of cells on the lining of the colon that occasionally turn into cancers — shed fragments of DNA into the blood.
A study published on Wednesday in The New England Journal of Medicine found that a blood test searching for such DNA called Shield and made by the company Guardant Health detected 87 percent of cancers that were at an early and curable stage. The false positive rate was 10 percent.
“This will be big news,” said Dr. May, who consults for Exact Sciences, the maker of the Cologuard fecal test.
But there is a caveat to the blood test: While it detects cancers, it misses most large polyps, finding just 13 percent of them. In contrast, the fecal test detects 43 percent and a colonoscopy finds 94 percent, Dr. Carethers said.
While polyps are usually harmless, a few can turn into cancers, so doctors want to find all of them and remove them to prevent cancers from forming.
Dr. Barbara Jung, the chair of the department of medicine at the University of Washington and president of the American Gastroenterological Association, said that patients should be fully informed before they opt for a blood test. In particular, they need to understand that while this test helps detect cancer early, it does not prevent it because it is not good at finding precancerous polyps.
“We have to have that discussion,” with patients, she said. But, she added, “a lot of this will fall on primary care physicians who are already very pressed for time to get through a litany of screens and counseling.”
Doctors will also need to explain to patients that if the blood test result is abnormal, they will have to schedule a colonoscopy to look for polyps or early-stage cancers and remove them if they are present.
It is also not clear how often people should do the blood test. Guardant suggested every three years but that recommendation is not well established, Dr. Jung said.
Dr. Jung added that she would love to know if the blood test performs well in people too young to qualify for existing screening tests. But that will require additional studies. She worries about rising colon cancer rates in younger people. It would be “very attractive,” she said, if people could get a blood test for colon cancer when they are in their 30s.
“That would be my biggest excitement,” Dr. Jung said.
The big unknown, though, is cost. Guardant has applied to the Food and Drug Administration for approval to market the test. The company sells it now as a “lab-based test,” which does not require F.D.A. approval but is also not covered by health insurance. For those who want to pay out of pocket, the price is $895. But the company will work with Medicare and Medicaid and private insurers to “finalize pricing” if it is approved, said Matt Burns, a Guardant spokesman.
Dr. William Grady, the medical director of the gastrointestinal cancer prevention program at the Fred Hutchinson Cancer Center who is a corresponding author in the trial sponsored by Guardant, said the company might settle on a price that makes it comparable to the price of the other screening methods. The Cologuard fecal test costs $581 to $681 . Colonoscopies, usually needed half as often, typically cost $1,250 to $4,800 , although some hospitals charge more. The average cost of a colonoscopy in the United States is $2,750. The tests are typically covered by insurance.
Dr. May cautioned that patients need to know that these three screening tests are not equivalent. With the blood test, she said, “we are moving from prevention to early detection.”
But, she said, the blood test is pretty easy. When a doctor is ordering routine blood work, all that needs to be done is to add a colorectal colon cancer test.
“That’s phenomenally exciting,” she said.
And its ease of use could outweigh the test’s limitations, said Dr. Carethers, who wrote an editorial in the journal accompanying the study. After all, he said, the goal of screening is to reduce deaths from colon cancer for the population as a whole.
If a blood test means many more people will be screened, the result — fewer deaths from colon cancer — will be beneficial.
“The best screening test is the one that gets completed by the patient,” he wrote.
Gina Kolata reports on diseases and treatments, how treatments are discovered and tested, and how they affect people. More about Gina Kolata
The Fight Against Cancer
Risk calculators can offer a more personalized picture of an individual patient’s breast cancer risk. But experts warn that the results need to be interpreted with the help of a doctor .
Early detection is a powerful weapon in preventing deaths from colon cancer, but many patients are reluctant to undergo colonoscopies or conduct at-home fecal tests. Doctors see potential in another screening method .
The human papillomavirus vaccine provides powerful protection against the leading cause of cervical cancer and against a strong risk factor for anal cancer. Here’s what to know about the shot.
A recent study adds to growing evidence that exercise is an important part of preventing prostate cancer , the second most common and second most fatal cancer in the United States for men.
No single food can prevent cancer on its own, but experts say that there are some that may help you build the best defense .
The F.D.A. has proposed banning the use of formaldehyde in chemical hair straighteners , which have been linked to increased cancer risk, particularly among Black women .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cancer Res Treat
- v.45(3); 2013 Sep
Psychosocial Impact of Cancer Patients on Their Family Members
Sun min lim.
1 Division of Medical Oncology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
Hyeon Chang Kim
2 Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
Soohyeon Lee
A population-based study was conducted in order to examine the characteristics of family members of cancer patients in comparison with the general population and also to evaluate the psychosocial impact of cancer patients on their family members.
Materials and Methods
From the Fourth Korea National Health and Nutrition Examination Surveys (KNHANES IV) (2007-2009) dataset, we identified 460 cancer patients and then selected family members of these patients who were aged 20 years or older (n=565). The control group was sampled from members of families without a cancer patient with matching for sex and age (n=2,260). Serial conditional logistic regression models were used for comparison of characteristics between family members of cancer patients and subjects in the control group.
Family members of cancer patients were less employed (57.9% vs. 63.0%, p<0.001), more functionally limited (20.2% vs. 16.5%, p=0.032), and had lower self-rated health (p=0.023) compared with sex and age-matched control subjects. They also had a significantly higher level of stress (79.7% vs. 76.1%, p=0.008), history of depression (12.9% vs. 10.2%, p=0.035), and current depressive symptoms (5.5% vs. 3.5%, p=0.038). However, higher physical activity was reported in family members of cancer patients (13.6% vs. 9.6%, p=0.003) than in control subjects. The presence of a cancer patient in the family showed an association with current depressive symptoms (odds ratio, 1.62; 95% confidence interval, 1.05 to 2.48; p=0.028), however, the association was no longer significant after adjustment for household income, education level, and employment status (p=0.304).
Family members of cancer patients are more susceptible to depression, probably due to adverse change in socioeconomic status. Use of multidisciplinary approaches for promotion of psychological health and well-being is essential.
Introduction
A continuous increase in cancer incidence and decrease in cancer mortality have resulted in a rising number of people living with cancer. As cancer patients live longer, psychological wellbeing of both cancer patients and their family members is becoming a growing concern. Previous studies have focused on the psychological status of cancer patients, and evaluated sociodemographic variables that make cancer patients more susceptible to depression and increased anxiety [ 1 , 2 ]. With the continuous increase in the number of cancer patients and their family members, knowing which factors contribute to the burden of family members is critical. To date, many studies have been conducted for evaluation of the burden of caregivers in chronic diseases such as stroke and dementia, however, the burden of family members of cancer patients has not been evaluated in depth [ 3 - 5 ]. Meta-analyses have evaluated the burden of caregivers alone, however, socioeconomic status (SES), physical function, perceived health status, psychological factors, health behavior, and health-related quality of life (HRQOL) of the family members in a household have not been investigated [ 6 , 7 ].
In a recent study reported by Palos et al. [ 8 ], who assessed the risk of caring for underserved patients with advanced cancer, sadness and distress were more prevalent among caregivers compared with cancer patients, and approximately 40% of caregivers were found to be at an increased risk for moderate to severe sadness and distress. This finding suggests that more attention is required for family members, and knowing how to support them is imperative.
Economic burden and financial distress are important issues that affect treatment strategy in long-term cancer survivorship. With newly emerging diagnostic and treatment patterns, expenditures on cancer treatment have increased and are expected to show a continuous increase in the future [ 9 ]. All of the factors mentioned above may contribute to greater anxiety, depression, poorer social well-being, and lower HRQOL.
In this study, we compared psychological, socioeconomic, physical function, health behavioral, and HRQOL-related aspects of family members of cancer patients and control subjects. We then performed an evaluation with an emphasis on factors that contribute to psychosocial wellbeing, such as level of stress, history of depression, and current depressive symptoms in all family members of each cancer patient.
1. Research design and participants
The Ministry of Health and Welfare of Korea began conducting the Korea National Health and Nutrition Examination Surveys (KNHANES) in 1998 in order to examine the general health and nutrition status of Koreans. KNHANES IV was conducted from July 2007 to December 2009. The survey used a stratified multistage probability sampling design for the South Korean population [ 10 ]. The uniqueness of this study is that the survey was based on households, and every member of the household was required to complete the survey. KNHANES consisted of four different measures: a health interview, health behavior survey, health examination, and a nutrition survey. In KNHANES IV, 31,705 individuals aged>1 year were invited to participate in the health interview and examination (6,455 in 2007, 12,528 in 2008, and 12,722 in 2009), and 24,871 individuals participated in the survey (4,594 in 2007, 9,744 in 2008, and 10,533 in 2009) at a response rate of 78.4% (71.2% in 2007, 77.8% in 2008, and 82.8% in 2009). Participants who reported a history of cancer (n=460) were considered cancer patients and were excluded from the analysis. Participants under age 19 (n=6,465) were excluded because they were not required to complete questionnaires for HRQOL. We defined 'family members of cancer patients' as individuals who have at least one cancer patient within his/her family. Participants who do not live with cancer patients were considered as candidates for the control group. Because there was a significant age difference between family members of cancer patients (n=565) and non-cancer family members (n=17,351), we sampled the control group with 1:4 individual matching on sex and age. Therefore, the final study population included 565 family members of cancer patients and 2,260 matched control subjects ( Fig. 1 ).

A flow chart showing recruitment of the study population. In Korea National Health and Nutrition Examination Surveys IV, 31,705 individuals aged>1 year were sampled by the health interview. From the initial sample of 31,705 individuals, 6,834 individuals did not complete the survey and participants under 19 (n=6,465) were excluded because they did not complete questionnaires for health-related quality of life; 460 cancer patients were excluded from the study. A total of 565 family members of cancer patients and 17,351 members of the general population were age-, sex-matched to 1 to 4. The final study population included 565 family members of cancer patients and 2,260 matched control subjects.
2. Measurements
Information on demographic and SES, including sex, age, household income, education, and employment was obtained using self-administered questionnaires. Families were divided into four groups according to monthly household income (lowest, lower intermediate, higher intermediate, and highest groups) and education level as four groups (primary [≤6 years of schooling], middle [6-9 years of schooling], high [9-12 years of schooling], and college [≥13 years of schooling]). Employment status was reported as either yes or no. Physical function was categorized according to two groups: limited in anyway and not limited. Participants were asked if they had ever had comorbidities such as hypertension, heart disease, stroke, arthritis, or chronic renal disease. They were also asked to report self-rated health as very good, good, fair, poor, or very poor. For our analyses, self-rated health was regrouped into three categories as very good to good, fair, or poor to very poor.
For evaluation of psychological factors, respondents were asked to report their level of stress, history of depression, and current depressive symptoms. The level of stress was reported as none/small or some/extreme. Respondents reported history of depression and current depressive symptoms as yes or no.
Health related behavioral risk factors were measured using self-reported questionnaires. Smoking status was categorized according to two groups: never smoker/ex-smoker and current smoker. Current alcohol use (average consumption) was measured by obtaining information related to respondents' self-reported alcohol behavior. Specifically, frequency of alcohol consumption was used as the measure of alcohol status: less than once per month, once per month, 2-4 times per month, 2-3 times per week, and more than four times per week. For our analyses, alcohol consumption was coded as yes if respondents reported consuming alcohol≥2 times/wk. Otherwise, alcohol consumption was coded as none [ 11 ]. Physical activity was measured using the frequency of moderate and vigorous physical activity per week. For analyses, recommended physical activity level was coded as yes if participants reported more than two days of moderate activity per week. Otherwise, physical activity level was coded as none for those who reported physical activity less than two days per week.
HIQOL was measured using the EuroQol, which consists of the health-status descriptive system (EQ-5D) and a visual analogue scale (EQ-VAS). The EQ-5D records the level of self-reported problems according to five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) [ 12 , 13 ]. Each of the dimensions is assessed based on a single question with three response levels (no problem, some problems, and extreme problems). Using the combination of these items, a single health index was calculated using the Korea valuation set developed by the Korean Centers for Disease Control and Prevention [ 14 ]. Scores on the EQ-5D index range from -0.171 to 1, where 1 indicates no problem in any of the five dimensions, zero indicates death, and negative values indicate a health status worse than death. Next, respondents described their own health status using a VAS ranging from 0 (worst imaginable health) to 100 (best imaginable health), which is represented as EQ-VAS. Eighty five percent of participants responded to EQ-5D and EQ-VAS.
3. Statistical analysis
Descriptive statistics and χ 2 tests were used for examination of demographic characteristics and differences between the family members of cancer patients and subjects in the control group. The survey year was also included as a controlled variable because the EQ-5D and EQ-VAS scores differed significantly according to survey year (data not shown). Conditional logistic regression analysis was performed, and presence of a cancer survivor, household income, education level, and employment status were dependent variables. All statistical analyses were performed using SAS ver. 9.2 (SAS Institute, Cary, NC) and p<0.05 was considered statistically significant.
1. Characteristics of family members of cancer patients and subjects in the control group
Characteristics of family members of cancer patients and subjects in the control group are shown in Table 1 . We excluded cancer patients from the analysis because our aim was to perform a comparison of the psychosocial status of family members only. The mean age was 51.2±17.6 years. No significant differences in household income and education level were observed between the two groups, although the group of family members of cancer patients had more respondents with lower household income and education level. Employment rates differed significantly among the two groups, with fewer family members of cancer patients currently employed (57.9% vs. 63.0%). Family members of cancer patients reported a significantly higher rate of functional limitation (20.2% vs. 16.5%). Prevalence of comorbidity was similar between the two groups (p for difference=0.091), however, family members of cancer patients were more likely to report their health status as poor to very poor (24.4% vs. 20%). Significantly higher levels of stress (79.7% vs. 76.1%), history of depression (12.9% vs. 10.2%), and current depression (5.5% vs. 3.5%) were reported by family members of cancer patients. Results for health behavioral risk factors, cigarette smoking, and alcohol consumption were similar; however, physical activity was more common in family members of cancer patients than in the control group (13.6% vs. 9.6%). No differences in mean EQ-5D (p for difference=0.361) and EQ-VAS scores (p for difference=0.900) were observed between the two groups.
Psycho-socio-physical status of family members of cancer patients and control subjects (1:4 matched)

Values are presented as mean±SD or total number (%). NA, not applicable. a) Hypertension, heart disease, stroke, arthritis, chronic renal disease, and diabetes.
2. Multivariate analysis of psychosocial distress
Significant difference in psychological and cognition status was observed between family members of cancer patients and the general population. Family members of cancer patients reported a relatively higher level of stress and more past or current depression. We performed univariate and multivariate analyses for determination of which factors would have a greater impact on psychosocial status of family members. In univariate analyses, presence of a cancer patient significantly increased the risk of current depression (odd ratio [OR], 1.62; 95% confidence interval [CI], 1.05 to 2.48). Lower education level (primary school) showed a significant association with history of depression (OR, 1.99; 95% CI, 1.21 to 3.27) and current depression (OR, 3.51; 95% CI, 1.52 to 8.11). Household income and employment status did not show an association with stress, history of depression, and current depressive symptoms ( Table 2 ). However, after adjustment for household income, education level, and employment status, presence of a cancer patient did not show a significant association with stress and depression. In the multivariate adjusted models, only low education showed a significant association with past (OR, 2.11; 95% CI, 1.09 to 4.05) and current (OR, 3.61; 95% CI, 1.19 to 10.89) depressive symptoms ( Table 3 ).
Univariate (unadjusted) analyses of factors influencing psychosocial status of the study population

CI, confidence interval.
Multivariate (adjusted) analyses of factors influencing psychosocial status of the study population

The current study evaluated the psychosocial impact of cancer patients on their family members in a national representative survey. Family members of cancer patients experienced relatively higher levels of stress and depressive symptoms. They were also less employed and more functionally limited. The presence of cancer patients in a family showed an association with current depressive symptoms; however, after adjustment for household income, education level, and employment status, the association was no longer significant. To the best of our knowledge, this is the first study to assess the psychological, socioeconomic, and physical burden of caregivers using family-based questionnaires.
Cancer is a stressful event for both patients and family members [ 14 ]. After the diagnosis of cancer, treatment of cancer and follow-up management are shared among family members. Family members are often expected to deal with cancer-related symptoms and perform clinical tasks. As a result of patients' pre-existing comorbidities, family members of elderly cancer patients face a highly complex set of challenges. In addition, because a large portion of cancer treatment is administered in ambulatory settings, family members are becoming more responsible for providing care [ 15 ].
Previous studies have reported that having a cancer patient in a family can be a distress. In a study reporting on psychosocial status and quality of life of patients and spouses in patients with prostate cancer, spouses had the lowest emotional quality of life of all participants, suggesting that cancer takes an emotional toll on spouses [ 16 ]. Another study examined levels of depression and anxiety in newly diagnosed adult patients and their adult family members. Family members had higher levels of depression and anxiety than cancer patients [ 17 ]. Findings of our study also showed that a diagnosis of cancer impacts on family caregivers from a psychological perspective. Significantly higher levels of stress, history of depression, and current depressive symptoms were observed in family members of cancer patients than in control subjects.
We examined multiple factors representing SES because low SES may be an indication that individuals to live in poorer conditions, have less access to healthcare, and experience greater psychological stress. Our results showed that those with lower household income were more likely to experience depression, although the significance was not met. Low SES is a substantial adverse prognostic factor and a risk factor for all-cause mortality after diagnosis of cancer; therefore, disparities in SES may influence both mental and physical wellbeing and should be considered in evaluation of psychosocial distress associated with cancer [ 18 - 20 ].
With respect to health behavioral risk factors, high occurrence of current smoking among family members of cancer patients draws attention. According to Burke et al. [ 21 ], less than half of smoking cancer patients quit smoking after their cancer diagnosis, and only 62% of smoking cancer patients received smoking cessation counseling from their physicians. Although no study on smoking behavior of family members has been reported, effective promotion of smoking cessation programs is required for secondary cancer prevention. Oncologists and primary care physicians should provide guidance on health promotion interventions to both cancer patients and family members [ 22 ].
The strength of our study is that these data were obtained from a nationwide population and therefore provided representative information on the Korean population. In addition, this is the first large-scaled questionnaire study based on households. Nevertheless, several study limitations should be considered. First, due to the cross-sectional nature of the data, determination of the causal relationship between cancer diagnosis and the identified parameters is difficult. Cancer treatment itself can cause family members to forgo their jobs, leading to lower household income, or it may be that diagnosis of cancer is more likely in populations with low SES [ 23 ]. Therefore, conduct of long-term follow-up studies will be needed for evaluation of the causal relationship between socioeconomic and psychological burdens of family members. Second, the findings of this study were based on self-reported health status, thus, there is a possibility of inaccurate reporting or not answering certain questions. Depression was also assessed using the self-reported questionnaire rather than being diagnosed by a doctor; therefore, it may not provide an accurate indication of the prevalence of clinically relevant depression. In addition, depression may result from other chronic comorbidities, such as stroke and dementia, which should be considered in future studies. Third, we did not differentiate cancer patients who were under active treatment from those who were not. Cancer patients who are under active treatment and those who are not may have different impact on the psychosocial status of their family members; however, we were not able to perform further investigation on this matter. Finally, due to the retrospective nature of this study, we were not able to determine the relationship between caregiver and patient and whether the caregiver was living in the same household or not.
Despite these limitations, the results of the current study suggest that more concern for family members is needed, as cancer may influence the whole family, not just the patient. According to findings of recent studies, caregivers who received intervention reported significantly less burden, less depression, and less distress, compared to those who did not. They also reported more knowledge, better coping, and greater mental well-being [ 24 , 25 ]. Therefore, there is a need for conduct of more effective studies with cancer caregivers or patient-caregiver dyads for implementation of evidence-based interventions in clinical settings. Healthcare professionals should plan risk assessment of caregiver's capacity and assist them in solving practical problems that arise as a result of the cancer diagnosis.
As the number of people living with a history of cancer continues to increase, identification of optimal methods for promoting the psychological health and well-being of both cancer patients and their family members is essential. Family members, who are somewhat invisible to the healthcare team, should be recognized for their mental and physical well-being. Assessment of stress and psychological distress should be followed by guidance and individualized interventions for attenuation of the health consequences.
Conflict of interest relevant to this article was not reported.
University of Notre Dame
Notre Dame News
- Home ›
- News ›
Cancer therapies show promise in combating tuberculosis
Published: March 25, 2024
Author: Brandi Wampler

What could cancer teach us about tuberculosis? That’s a question Meenal Datta has been chasing since she was a graduate student.
Once the body’s immune system is infected with tuberculosis, it forms granulomas — tight clusters of white blood cells — in an attempt to wall off the infection-causing bacteria in the lungs. But more often than not, granulomas do more harm than good.
Charged with analyzing the similarities between granulomas and tumors, Datta discovered that both are structurally and functionally abnormal. In 2015, she and other researchers looked at the vascular structures of granulomas and showed that they are compromised and leaky just like tumor blood vessels, which limits drug delivery and successful treatment in both diseases.
“It was the first time we showed definitively that there was this pathophysiological similarity between these two diseases that present with different causes and symptoms,” said Datta, assistant professor of aerospace and mechanical engineering at the University of Notre Dame. “Cancer doesn’t sound anything like an infectious disease. And yet, here are two different diseases with the same problem of dysfunctional blood vessels.”
Now a study from the same team at the University of Notre Dame, Massachusetts General Hospital and the National Institutes of Health has identified a combination of medications that may improve blood flow within granulomas, benefiting drug delivery. Published in the Proceedings of the National Academy of Sciences , the study leverages decades of cancer research to study tuberculosis-affected lung tissue and improve treatment.
“Much like in tumors, many of the blood vessels in granulomas are compressed or squeezed shut — just like if you stepped on your garden hose,” said Datta, the first author on the study. “In cancer, we know that happens because of the growing tumor mass and the supportive protein scaffolding it puts down, called matrix. We thought maybe the same thing was happening in tuberculosis.”
The study confirmed that a similar phenomenon is occurring in granulomas — too much cell mass and protein scaffolding. This impaired function makes blood flow through blood vessels nearly impossible, crippling the ability to get a medication to the tuberculosis disease site.
Datta and her collaborators used losartan, an affordable drug used to treat high blood pressure. However, it also has the beneficial side effect of reducing the amount of matrix being created inside a granuloma, thus opening the compressed blood vessels and restoring blood flow.
Researchers then combined losartan with bevacizumab, a drug used by cancer patients to stop the overproduction of poorly formed blood vessels. With this two-pronged medicinal approach, Datta and the team were able to make the granuloma blood vessels function and behave more normally.
When the researchers applied the host-directed therapies losartan and bevacizumab along with antibiotics, they showed improved drug delivery and antibiotic concentration within granulomas.
Additionally, Datta’s graduate student Maksym Zarodniuk analyzed genome sequencing data produced by the team, and found that even without antibiotics, there was a reduction in tuberculosis bacteria within the granulomas.
“When we gave just those host-directed therapies, we were getting good treatment benefit even without adding the antibiotics. Those therapies were promoting the body’s inflammatory response to fight against the bacteria, which we did not expect,” Datta said.
For Datta, this study caps off a stretch of tuberculosis research that started when she began her doctoral research at Massachusetts General Hospital and Harvard Medical School in 2011, and has spanned multiple phases of her career. Tuberculosis, although largely controlled in the U.S., is still considered one of the deadliest infectious diseases worldwide.
“The advantage of the host-directed therapies we selected is that these agents or very similar drugs of the same class are already approved by regulatory agencies around the globe, and they are affordable,” Datta said. “We hope that our preclinical results will be found compelling enough to start a clinical trial to benefit tuberculosis patients.”
Today, Datta’s lab at the University of Notre Dame primarily focuses its research on understanding glioblastoma , a rare treatment-resistant brain cancer. Datta said that being an engineer allows her to cross into other areas of research and with a different perspective, making an excellent case for the importance of multidisciplinary research.
“I do believe that really is an advantage of being an engineer. It’s easier for me to sometimes make connections between contexts that seem disparate,” Datta said. “We depend on our life science and clinical colleagues to walk through those details, but engineers are very good at approaching complex problems from a simplified systems approach.”
The study, “Normalizing granuloma vasculature and matrix improves drug delivery and reduces bacterial burden in tuberculosis-infected rabbits,” was funded by the Bill & Melinda Gates Foundation and the National Institutes of Health. Datta is an affiliated member of Notre Dame’s Berthiaume Institute for Precision Health , Eck Institute for Global Health , Harper Cancer Research Institute , Lucy Family Institute for Data and Society , NDnano and Warren Center for Drug Discovery . Datta is an assistant professor in the following doctorate programs: aerospace and mechanical engineering, bioengineering, and materials science and engineering.
Contact: Brandi Wampler, associate director of media relations, 574-631-2632, [email protected]
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
Unlocking mRNA’s cancer-fighting potential
Press contact :.

Previous image Next image
What if training your immune system to attack cancer cells was as easy as training it to fight Covid-19? Many people believe the technology behind some Covid-19 vaccines, messenger RNA, holds great promise for stimulating immune responses to cancer.
But using messenger RNA, or mRNA, to get the immune system to mount a prolonged and aggressive attack on cancer cells — while leaving healthy cells alone — has been a major challenge.
The MIT spinout Strand Therapeutics is attempting to solve that problem with an advanced class of mRNA molecules that are designed to sense what type of cells they encounter in the body and to express therapeutic proteins only once they have entered diseased cells.
“It’s about finding ways to deal with the signal-to-noise ratio, the signal being expression in the target tissue and the noise being expression in the non-target tissue,” Strand CEO Jacob Becraft PhD ’19 explains. “Our technology amplifies the signal to express more proteins for longer while at the same time effectively eliminating the mRNA’s off-target expression.”
Strand is set to begin its first clinical trial in April, which is testing a self-replicating mRNA molecule’s ability to express immune signals directly from a tumor, triggering the immune system to attack and kill the tumor cells directly. It’s also being tested as a possible improvement for existing treatments to a number of solid tumors.
As they work to commercialize its early innovations, Strand’s team is continuing to add capabilities to what it calls its “programmable medicines,” improving mRNA molecules’ ability to sense their environment and generate potent, targeted responses where they’re needed most.
“Self-replicating mRNA was the first thing that we pioneered when we were at MIT and in the first couple years at Strand,” Becraft says. “Now we’ve also moved into approaches like circular mRNAs, which allow each molecule of mRNA to express more of a protein for longer, potentially for weeks at a time. And the bigger our cell-type specific datasets become, the better we are at differentiating cell types, which makes these molecules so targeted we can have a higher level of safety at higher doses and create stronger treatments.”
Making mRNA smarter
Becraft got his first taste of MIT as an undergraduate at the University of Illinois when he secured a summer internship in the lab of MIT Institute Professor Bob Langer.
“That’s where I learned how lab research could be translated into spinout companies,” Becraft recalls.
The experience left enough of an impression on Becraft that he returned to MIT the next fall to earn his PhD, where he worked in the Synthetic Biology Center under professor of bioengineering and electrical engineering and computer science Ron Weiss. During that time, he collaborated with postdoc Tasuku Kitada to create genetic “switches” that could control protein expression in cells.
Becraft and Kitada realized their research could be the foundation of a company around 2017 and started spending time in the Martin Trust Center for MIT Entrepreneurship. They also received support from MIT Sandbox and eventually worked with the Technology Licensing Office to establish Strand’s early intellectual property.
“We started by asking, where is the highest unmet need that also allows us to prove out the thesis of this technology? And where will this approach have therapeutic relevance that is a quantum leap forward from what anyone else is doing?” Becraft says. “The first place we looked was oncology.”
People have been working on cancer immunotherapy, which turns a patient’s immune system against cancer cells, for decades. Scientists in the field have developed drugs that produce some remarkable results in patients with aggressive, late-stage cancers. But most next-generation cancer immunotherapies are based on recombinant (lab-made) proteins that are difficult to deliver to specific targets in the body and don’t remain active for long enough to consistently create a durable response.
More recently, companies like Moderna, whose founders also include MIT alumni , have pioneered the use of mRNAs to create proteins in cells. But to date, those mRNA molecules have not been able to change behavior based on the type of cells they enter, and don’t last for very long in the body.
“If you’re trying to engage the immune system with a tumor cell, the mRNA needs to be expressing from the tumor cell itself, and it needs to be expressing over a long period of time,” Becraft says. “Those challenges are hard to overcome with the first generation of mRNA technologies.”
Strand has developed what it calls the world’s first mRNA programming language that allows the company to specify the tissues its mRNAs express proteins in.
“We built a database that says, ‘Here are all of the different cells that the mRNA could be delivered to, and here are all of their microRNA signatures,’ and then we use computational tools and machine learning to differentiate the cells,” Becraft explains. “For instance, I need to make sure that the messenger RNA turns off when it's in the liver cell, and I need to make sure that it turns on when it's in a tumor cell or a T-cell.”
Strand also uses techniques like mRNA self-replication to create more durable protein expression and immune responses.
“The first versions of mRNA therapeutics, like the Covid-19 vaccines, just recapitulate how our body’s natural mRNAs work,” Becraft explains. “Natural mRNAs last for a few days, maybe less, and they express a single protein. They have no context-dependent actions. That means wherever the mRNA is delivered, it’s only going to express a molecule for a short period of time. That’s perfect for a vaccine, but it’s much more limiting when you want to create a protein that’s actually engaging in a biological process, like activating an immune response against a tumor that could take many days or weeks.”
Technology with broad potential
Strand’s first clinical trial is targeting solid tumors like melanoma and triple-negative breast cancer. The company is also actively developing mRNA therapies that could be used to treat blood cancers.
“We’ll be expanding into new areas as we continue to de-risk the translation of the science and create new technologies,” Becraft says.
Strand plans to partner with large pharmaceutical companies as well as investors to continue developing drugs. Further down the line, the founders believe future versions of its mRNA therapies could be used to treat a broad range of diseases.
“Our thesis is: amplified expression in specific, programmed target cells for long periods of time,” Becraft says. “That approach can be utilized for [immunotherapies like] CAR T-cell therapy, both in oncology and autoimmune conditions. There are also many diseases that require cell-type specific delivery and expression of proteins in treatment, everything from kidney disease to types of liver disease. We can envision our technology being used for all of that.”
Share this news article on:
Related links.
- Strand Therapeutics
- Department of Biological Engineering
Related Topics
- Biological engineering
- Bioengineering and biotechnology
- Drug development
- Tissue engineering
- Synthetic biology
- Innovation and Entrepreneurship (I&E)
Related Articles

Synthetic biology circuits can respond within seconds

MIT launches Center for Multi-Cellular Engineered Living Systems

This RNA-based technique could make gene therapy more effective
Previous item Next item
More MIT News
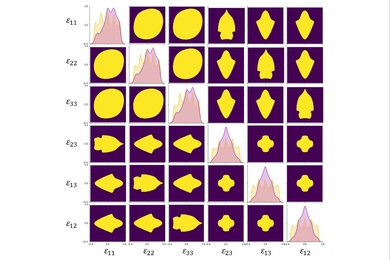
A first-ever complete map for elastic strain engineering
Read full story →

“Life is short, so aim high”

Shining a light on oil fields to make them more sustainable

MIT launches Working Group on Generative AI and the Work of the Future

Atmospheric observations in China show rise in emissions of a potent greenhouse gas

Second round of seed grants awarded to MIT scholars studying the impact and applications of generative AI
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram

IMAGES
COMMENTS
More people are living after a diagnosis of cancer than ever before and now account for around 5% of the US population. The specialty of cancer survivorship has been developing and growing since the mid-1980s, but the term survivor is open to debate by people living with cancer and those caring for them. Regardless of the term used, many ongoing physical, psychological, and social needs affect ...
3.3 Breast Cancer worldwide. Breast cancer is the most common type of cancer in women around the globe. It affects women from low, middle and high-income countries (Rohani, Abedi, Omranipour, & Langius-Eklöf, 2015, 2). Breast cancer prevalence has increased within the last few years in middle- and low-income countries.
Date Thesis Sponsor, Jennifer Ford, Ph.D. April 14, 2022 Date Second Reader, Tracy Dennis, Ph.D. ... The psychosocial outcomes of cancer have been understudied in adolescent and young adult (AYA) cancer survivors, an important group to focus on because of this unique developmental time. Distress is commonly experienced post-treatment due to ...
depth interviews with 20 cancer survivors. Findings indicate cancer patients are motivated to use social media as a therapeutic tool for coping and managing emotions ... gratitude to my thesis advisor, LaKesha Anderson, Ph.D., for her support, guidance, and encouragement throughout this process. She went above-and-beyond on numerous
Cancer patients' rates of insomnia and other sleep disturbances exceed those found in non-cancer populations, with problems reported in about 30% to 87% of cancer patients (J. Savard et al., 2001) compared to 16% to 20% in the general population (Ohayon, 2002). For example, in a prospective study of 823 patients of mixed cancer types
This thesis is dedicated to all childhood cancer survivors. Your strength to endure hardship and continue living life to the fullest inspires me each and every day. This thesis is also ... Cancer survivors may continue to experience "late" or "long-term" effects (Lindell et al.,
Demographic characteristics of subjects. The general characteristics of the female cancer survivors in this study indicated that their average age was 51.87 (SD = 11.78) years, with the largest proportion (33.3%) of the population being in their 50s, followed by those in their 40s (30.1%), 60s and over (24.4%), and below 30 (12.2%).Most participants (76.2%) were married; 61.9% practiced a ...
Background. Breast cancer is the most frequent malignancy affecting women across all ethnic groups in the United States. In 2013, an estimated 232 340 new cases of invasive breast cancer were expected to be diagnosed among women. 1 At the same time, the number of breast cancer survivors is increasing due primarily to advances in biomedical technology leading to an increase in early diagnosis ...
Breast cancer (BC), while highly prevalent globally (highest incidence cancer among women in 159/185 countries) [], has a high survival rateThe average five-year survival rate in Australia for BC from 2013 to 2017 was 91.5%, compared to 69.7% for all cancer types combined [].Cancer survivors are defined as individuals diagnosed with cancer who have completed their initial cancer treatment ...
Breast cancer survivors may need to prepare for ongoing psychosocial challenges in survivorship and proactively seek sup-port to overcome these. Keywords Breast cancer · Survivorship · Qualitative · Meta-review · Systematic review Introduction Breast cancer (BC), while highly prevalent globally (highest incidence cancer among women in 159/ ...
A brief review of literature from the last 3 years reporting on older adult cancer survivors aged 65 years and older was undertaken. Relevant topics were identified through consultation with experts in the field and used for search purposes. Keywords used together with "older adults" and "cancer survivors" were accelerated aging ...
Breast cancer survivors face unique physical and emotional challenges after completing active treatment. This thesis analyzes questionnaires and semi-structured narrative interviews collected from 17 female BCS with the goal of understanding the factors that they deem most significant to their quality of life and identity after completing ...
Cancer treatments can impact a patient's physical and mental health. When a cancer survivor experiences adverse side effects that begin during treatment and continue afterward, these are called long-term side effects; nearly one-third of cancer survivors experience long-term side effects () Wu H-S, Harden JK. Symptom Burden and Quality of Life in Survivorship: A Review of the Literature.
Breast cancer rates and the number of breast cancer survivors have been increasing among women in Iran. Effective responses from healthcare depend on appropriately identifying survivors' needs. This study investigated the experience and needs of breast cancer survivors in different dimensions. In this qualitative content analysis, semi-structured in-depth interviews were conducted from April ...
Cancer Survivors: In Their Words. June 20, 2020 by Marci Landsmann. This year alone, an estimated 1.8 million people will hear their doctor say they have cancer. The individual impact of each person can be clouded in the vast statistics. In honor of National Cancer Survivor Month, Cancer Today would like to highlight several personal essays we ...
Results The result shows that the overall number of cancer survivors is 673 per 100.000 older adults and is higher in Urban areas (874 per 100.000) than in rural areas (535 per 100.000). 43.7% of ...
Introduction. In 2020, there were estimated to be 19.3 million new cancer cases worldwide and almost 10 million cancer-related deaths. Female breast cancer was the most commonly diagnosed cancer, with 2.3 million new cases (11.7%), surpassing lung cancer. 1 Thanks to early diagnosis and improved treatment, the survival rate in patients with breast cancer has improved. 2 Almost 88% of patients ...
among cancer patients and how different psychosocial aspects influence this adaptation. Information regarding the possibilities to predict later well-being is also of great relevance. This thesis has included several diagnoses consid-ered relevant for the aims, namely, gastrointestinal (GI)-, breast-, and ovar-ian cancer and malignant lymphomas.
This study was part of a PhD thesis entitled development and psychometric evaluation of motivation for healing questionnaire in cancer patients that was conducted from November 2019 to November 2020 in the Kashan University of Medical Sciences, Iran. Based on the study objectives, the inductive content analysis method was used.
Theses/Dissertations from 2022. Omics Analysis in Cancer and Development, Emalie J. Clement. Investigating the Role of Splenic Macrophages in Pancreatic Cancer, Daisy V. Gonzalez. Polymeric Chloroquine in Metastatic Pancreatic Cancer Therapy, Rubayat Islam Khan. Evaluating Targets and Therapeutics for the Treatment of Pancreatic Cancer, Shelby ...
Each year in the United States, about 240,000 women and 2,100 men are diagnosed with breast cancer. Although the incidence rate of breast cancer is 4% lower among Black women than White women ...
As news that Catherine, Princess of Wales had announced her cancer diagnosis dominated headlines Friday, I felt a deep and traumatic solidarity, writes Sara Stewart.
The number of breast cancer survivors has increased since 1990 due to advances in biomedical technology that lead to an increase in early diagnosis and treatment. Research on survivorship has focused on the psychological and treatment aspects of the disease. The goal of this study was focused on exploring the lived experiences of breast cancer ...
Early detection is a powerful weapon in preventing deaths from colon cancer, but many patients are reluctant to undergo colonoscopies or conduct at-home fecal tests. Doctors see potential in ...
Early detection is a powerful weapon in preventing deaths from colon cancer, but many patients are reluctant to undergo colonoscopies or conduct at-home fecal tests. Doctors see potential in ...
Many patients are reluctant to undergo colonoscopies or conduct at-home fecal tests. Doctors see potential in another screening method. By Gina Kolata Early detection of colon cancer can prevent a ...
The presence of cancer patients in a family showed an association with current depressive symptoms; however, after adjustment for household income, education level, and employment status, the association was no longer significant. To the best of our knowledge, this is the first study to assess the psychological, socioeconomic, and physical ...
The cancer diagnosis of Catherine, Princess of Wales, is no anomaly, writes oncologist Jalal Baig. He says it is part of a rising global trend in which newly diagnosed cancer patients are getting ...
Researchers then combined losartan with bevacizumab, a drug used by cancer patients to stop the overproduction of poorly formed blood vessels. With this two-pronged medicinal approach, Datta and the team were able to make the granuloma blood vessels function and behave more normally. ... Essays on democracy draw attention to critical threats ...
Scientists in the field have developed drugs that produce some remarkable results in patients with aggressive, late-stage cancers. But most next-generation cancer immunotherapies are based on recombinant (lab-made) proteins that are difficult to deliver to specific targets in the body and don't remain active for long enough to consistently ...