Advertisement

Foodborne Disease Symptoms, Diagnostics, and Predictions Using Artificial Intelligence-Based Learning Approaches: A Systematic Review
- Review article
- Published: 25 August 2023
- Volume 31 , pages 553–578, ( 2024 )
Cite this article

- Yogesh Kumar 1 ,
- Inderpreet Kaur 2 &
- Shakti Mishra ORCID: orcid.org/0000-0002-5961-3114 1
655 Accesses
5 Citations
Explore all metrics
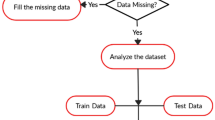
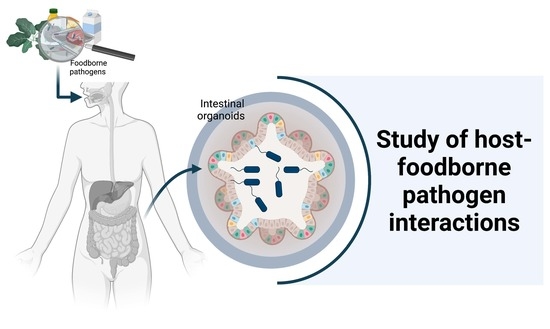
Food-borne diseases have a high worldwide occurrence, substantially impacting public health and the social economy. Most food-borne diseases are contagious or poisonous and are caused by bacteria, viruses or chemicals that enter the body via contaminated food. The most prevalent harmful bacteria ( Salmonella , Escherichia coli , Campylobacter , Clostridium and Listeria ) and viruses (norovirus) may cause acute poisoning or chronic disorders such as cancer. Thus, the detection of pathogenic organisms is crucial for the safety of food. Artificial intelligence has recently been an effective technique for predicting pathogens spreading food-borne diseases. This study compares and contrasts the accuracy of many popular methods for making predictions about the pathogens in food-borne diseases, including decision trees, random forests, k-Nearest Neighbors, stochastic gradient descent and extremely randomized trees, along with an ensemble model incorporating all of these approaches. In addition, principal component analysis and scaling methods were used to normalize and rescale the values of the target variable in order to increase the prediction rate. The performance of classification systems has been examined using precision, accuracy, recall, F1-score and root mean square error (RMSE). The experimental results demonstrate that the suggested new ensemble model beat all other classifiers and achieved the average highest 97.26% accuracy, 0.22 RMSE value, 97.77% recall, 97.66% precision and 98.44% F1-Score. This research investigates the predictability of pathogens in food-borne diseases using ensemble learning techniques.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price excludes VAT (USA) Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
A random forest guided tour.
Heart Disease Prediction using Machine Learning Techniques

A Systematic Review on Supervised and Unsupervised Machine Learning Algorithms for Data Science
Data availability.
Not applicable.
Finger JA, Baroni WS, Maffei DF, Bastos DH, Pinto UM (2019) Overview of foodborne disease outbreaks in Brazil from 2000 to 2018. Foods 8(10):434
Article PubMed PubMed Central Google Scholar
Sharif MK, Javed K, Nasir A (2018) Foodborne illness: threats and control. Foodborne diseases. Academic Press, Cambridge, pp 501–523
Google Scholar
Jung Y, Jang H, Matthews KR (2014) Effect of the food production chain from farm practices to vegetable processing on outbreak incidence. Microb Biotechnol 7(6):517–527
Kaur I, Garg R, Kaur T, Mathur G (2023) Using artificial intelligence to predict clinical requirements in healthcare. J Pharm Negat Results 2023:4177–4180
Vidyadharani G, Vijaya Bhavadharani HK, Sathishnath P, Ramanathan S, Sariga P, Sandhya A, Sugumar S (2022) Present and pioneer methods of early detection of food borne pathogens. J Food Sci Technol 59(6):2087–2107
Article CAS PubMed Google Scholar
Torgerson PR, Devleesschauwer B, Praet N, Speybroeck N, Willingham AL, Kasuga F, de Silva N (2015) World Health Organization estimates of the global and regional disease burden of 11 foodborne parasitic diseases, 2010: a data synthesis. PLoS Med 12(12):e1001920
Vilne B, Meistere I, Grantiņa-Ieviņa L, Ķibilds J (2019) Machine learning approaches for epidemiological investigations of food-borne disease outbreaks. Front Microbiol 10:1722
Kadariya J, Smith TC, Thapaliya D (2014) Staphylococcus aureus and staphylococcal food-borne disease: an ongoing challenge in public health. BioMed Res Int 2014:1–9
Article Google Scholar
Wang H, Cui W, Guo Y, Du Y, Zhou Y (2021) Machine learning prediction of foodborne disease pathogens: algorithm development and validation study. JMIR Med Inform 9(1):e24924
Pandey SK, Bhandari AK (2023) A systematic review of modern approaches in healthcare systems for lung cancer detection and classification. Archiv Comput Methods Eng 30:1–20
Kumar Y, Gupta S (2023) Deep transfer learning approaches to predict glaucoma, cataract, choroidal neovascularization, diabetic macular edema, drusen and healthy eyes: an experimental review. Archiv Comput Methods Eng 30(1):521–541
Heredia N, García S (2018) Animals as sources of food-borne pathogens: a review. Animal nutrition 4(3):250–255
Saravanan A, Kumar PS, Hemavathy RV, Jeevanantham S, Kamalesh R, Sneha S, Yaashikaa PR (2021) Methods of detection of food-borne pathogens: a review. Environ Chem Lett 19:189–207
Article CAS Google Scholar
Chukwu EE, Nwaokorie FO, Coker AO, Avila-Campos MJ, Ogunsola FT (2019) 16S rRNA gene sequencing: a practical approach to confirming the identity of food borne bacteria. IFE J Sci 21(3):13–25
Koul A, Bawa RK, Kumar Y (2023) Artificial intelligence techniques to predict the airway disorders illness: a systematic review. Archiv Comput Methods Eng 30(2):831–864
Hu W, Feng K, Jiang A, Xiu Z, Lao Y, Li Y, Long Y (2020) An in situ-synthesized gene chip for the detection of food-borne pathogens on fresh-cut cantaloupe and lettuce. Front Microbiol 10:3089
Nesakumar N, Lakshmanakumar M, Srinivasan S, Jayalatha Jbb A, Balaguru Rayappan JB (2021) Principles and recent advances in biosensors for pathogens detection. ChemistrySelect 6(37):10063–10091
Zheng S, Yang Q, Yang H, Zhang Y, Guo W, Zhang W (2023) An ultrasensitive and specific ratiometric electrochemical biosensor based on SRCA-CRISPR/Cas12a system for detection of Salmonella in food. Food Control 146:109528
Chenar SS, Deng Z (2021) Hybrid modeling and prediction of oyster norovirus outbreaks. J Water Health 19(2):254–266
Article PubMed Google Scholar
Zhang P, Cui W, Wang H, Du Y, Zhou Y (2021) High-efficiency machine learning method for identifying foodborne disease outbreaks and confounding factors. Foodborne Pathog Dis 18(8):590–598
Article CAS PubMed PubMed Central Google Scholar
Chenar SS, Deng Z (2018) Development of artificial intelligence approach to forecasting oyster norovirus outbreaks along Gulf of Mexico coast. Environ Int 111:212–223
Min HJ, Mina HA, Deering AJ, Bae E (2021) Development of a smartphone-based lateral-flow imaging system using machine-learning classifiers for detection of Salmonella spp. J Microbiol Methods 188:106288
Nguyen M, Long SW, McDermott PF, Olsen RJ, Olson R, Stevens RL, Davis JJ (2018) Using machine learning to predict antimicrobial minimum inhibitory concentrations and associated genomic features for nontyphoidal Salmonella . bioRxiv 2018:380782
Polat H, Topalcengiz Z, Danyluk MD (2020) Prediction of Salmonella presence and absence in agricultural surface waters by artificial intelligence approaches. J Food Saf 40(1):e12733
Amado TM, Bunuan MR, Chicote RF, Espenida SMC, Masangcay HL, Ventura CH, Enriquez LAC (2019) Development of predictive models using machine learning algorithms for food adulterants bacteria detection. 2019 IEEE 11th international conference on humanoid, nanotechnology, information technology, communication and control, environment, and management (HNICEM). IEEE, New York, pp 1–6
Lupolova N, Dallman TJ, Holden NJ, Gally DL (2017) Patchy promiscuity: machine learning applied to predict the host specificity of Salmonella enterica and Escherichia coli . Microb Genom. https://doi.org/10.1099/mgen.0.000135
Hiura S, Koseki S, Koyama K (2021) Prediction of population behavior of Listeria monocytogenes in food using machine learning and a microbial growth and survival database. Sci Rep 11(1):1–11
Njage PMK, Henri C, Leekitcharoenphon P, Mistou MY, Hendriksen RS, Hald T (2019) Machine learning methods as a tool for predicting risk of illness applying next-generation sequencing data. Risk Anal 39(6):1397–1413
Borujeni MS, Ghaderi-Zefrehei M, Ghanegolmohammadi F, Ansari-Mahyari S (2018) A novel LSSVM based algorithm to increase accuracy of bacterial growth modeling. Iran J Biotech 16(2):105
Bandoy DJ, Weimer BC (2020) Biological machine learning combined with campylobacter population genomics reveals virulence gene allelic variants cause disease. Microorganisms 8(4):549
Hill AA, Crotta M, Wall B, Good L, O’Brien SJ, Guitian J (2017) Towards an integrated food safety surveillance system: a simulation study to explore the potential of combining genomic and epidemiological metadata. Royal Soc Open Sci 4(3):160721
Article ADS CAS Google Scholar
Maharana A, Cai K, Hellerstein J, Hswen Y, Munsell M, Staneva V, Nsoesie EO (2019) Detecting reports of unsafe foods in consumer product reviews. JAMIA Open 2(3):330–338
Olm MR, Bhattacharya N, Crits-Christoph A, Firek BA, Baker R, Song YS, Banfield JF (2019) Necrotizing enterocolitis is preceded by increased gut bacterial replication, Klebsiella, and fimbriae-encoding bacteria. Sci Adv 5(12):eaax5727
Article ADS CAS PubMed PubMed Central Google Scholar
Nogales A, Morón RD, García-Tejedor ÁJ (2020) Food safety risk prediction with Deep Learning models using categorical embeddings on European Union data. Preprint at https://arxiv.org/abs/2009.06704
Ahsan MM, Mahmud MA, Saha PK, Gupta KD, Siddique Z (2021) Effect of data scaling methods on machine learning algorithms and model performance. Technologies 9(3):52
Rudra T, Paul P (2021) Heart disease prediction using traditional machine learning.
Kaur I, Sandhu AK, Kumar Y (2022) A hybrid deep transfer learning approach for the detection of vector-borne diseases. 2022 5th international conference on contemporary computing and informatics (IC3I). IEEE, New York, pp 2189–2194
Chapter Google Scholar
Peng T, Chen X, Wan M, Jin L, Wang X, Du X, Yang X (2021) The prediction of hepatitis E through ensemble learning. Int J Environ Res Public Health 18(1):159
Nogales A, Díaz-Morón R, García-Tejedor ÁJ (2022) A comparison of neural and non-neural machine learning models for food safety risk prediction with European Union RASFF data. Food Control 134:108697
Wheeler NE (2019) Tracing outbreaks with machine learning. Nat Rev Microbiol 17(5):269–269
Martínez-García PM, López-Solanilla E, Ramos C, Rodríguez-Palenzuela P (2016) Prediction of bacterial associations with plants using a supervised machine-learning approach. Environ Microbiol 18(12):4847–4861
Bhardwaj P, Bhandari G, Kumar Y, Gupta S (2022) An investigational approach for the prediction of gastric cancer using artificial intelligence techniques: a systematic review. Archiv Comput Methods Eng 29:1–22
Lumogdang CFD, Wata MG, Loyola SJS, Angelia RE, Angelia HLP (2019) Supervised machine learning approach for pork meat freshness identification. Proceedings of the 2019 6th international conference on bioinformatics research and applications. ACM, New York, pp 1–6
Chowdhury NH, Reaz MBI, Haque F, Ahmad S, Ali SHM, Bakar AAA, Bhuiyan MAS (2021) Performance analysis of conventional machine learning algorithms for identification of chronic kidney disease in type 1 diabetes mellitus patients. Diagnostics 11(12):2267
Kader MS, Ahmed F, Akter J (2021) Machine learning techniques to precaution of emerging disease in the poultry industry. 2021 24th international conference on computer and information technology (ICCIT). IEEE, New York, pp 1–6
Rani P, Kumar R, Jain A (2021) Coronary artery disease diagnosis using extra tree-support vector machine: ET-SVMRBF. Int J Comput Appl Technol 66(2):209–218
Ali L, Niamat A, Khan JA, Golilarz NA, Xingzhong X, Noor A, Bukhari SAC (2019) An optimized stacked support vector machines based expert system for the effective prediction of heart failure. IEEE Access 7:54007–54014
Weller DL, Love T, Wiedmann M (2021) Interpretability versus accuracy: a comparison of machine learning models built using different algorithms, performance measures, and features to predict E. coli levels in agricultural water. Front Artif Intell 4:19
Goyal P, Gopala Krishna DN, Jain D, Rathi M (2021) Foodborne disease outbreak prediction using deep learning. Innovations in computational intelligence and computer vision. Springer, Singapore, pp 165–172
Kaur I, Kumar Y, Sandhu AK, Ijaz MF (2023) Predictive modeling of epidemic diseases based on vector-borne diseases using artificial intelligence techniques. Computational intelligence in medical decision making and diagnosis. CRC Press, Boca Raton, pp 81–100
Singh PD, Kaur R, Singh KD, Dhiman G (2021) A novel ensemble-based classifier for detecting the COVID-19 disease for infected patients. Inf Syst Front 23(6):1385–1401
Kaur I, Sandhu AK, Kumar Y (2022) Artificial intelligence techniques for predictive modeling of vector-borne diseases and its pathogens: a systematic review. Archiv Comput Methods Eng 29:1–31
Article MathSciNet Google Scholar
Kaur I, Sandhu AK, Kumar Y (2021) Analyzing and minimizing the effects of Vector-borne diseases using machine and deep learning techniques: a systematic review. 2021 sixth international conference on image information processing (ICIIP), vol 6. IEEE, New York, pp 69–74
Download references
Author information
Authors and affiliations.
Department of CSE, School of Technology, Pandit Deendayal Energy University, Gandhinagar, Gujarat, India
Yogesh Kumar & Shakti Mishra
Department of Computer Applications, Chandigarh Group of Colleges, Landran, Mohali, India
Inderpreet Kaur
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Shakti Mishra .
Ethics declarations
Competing interests.
Non-financial interests and authors have no conflict of interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Kumar, Y., Kaur, I. & Mishra, S. Foodborne Disease Symptoms, Diagnostics, and Predictions Using Artificial Intelligence-Based Learning Approaches: A Systematic Review. Arch Computat Methods Eng 31 , 553–578 (2024). https://doi.org/10.1007/s11831-023-09991-0
Download citation
Received : 26 April 2023
Accepted : 03 August 2023
Published : 25 August 2023
Issue Date : March 2024
DOI : https://doi.org/10.1007/s11831-023-09991-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Food-Borne Disease Prevention and Risk Assessment
Affiliation.
- 1 Ewen Todd Consulting LLC, Okemos, MI 48864, USA.
- PMID: 32708573
- PMCID: PMC7399861
- DOI: 10.3390/ijerph17145129
"Food-borne Disease Prevention and Risk Assessment" is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how food-borne disease is still a global threat to health today and to be able to target strategies to reduce its prevalence [...].
PubMed Disclaimer
Similar articles
- [Endemic, Trend, Research and Direction of Food-borne Parasitic Diseases]. Huang Y, Yu XB. Huang Y, et al. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2015 Dec;33(6):436-42. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2015. PMID: 27089773 Review. Chinese.
- Trends in technology, trade and consumption likely to impact on microbial food safety. Quested TE, Cook PE, Gorris LG, Cole MB. Quested TE, et al. Int J Food Microbiol. 2010 May 30;139 Suppl 1:S29-42. doi: 10.1016/j.ijfoodmicro.2010.01.043. Epub 2010 Feb 10. Int J Food Microbiol. 2010. PMID: 20307911
- Harmonization of international risk assessment protocol. Toyofuku H. Toyofuku H. Mar Pollut Bull. 2006;53(10-12):579-90. doi: 10.1016/j.marpolbul.2006.08.008. Epub 2006 Sep 27. Mar Pollut Bull. 2006. PMID: 17007893 Review.
- [Food-borne infections: do we need further data collection for public health action and research]. Desenclos JC, Vaillant V, De Valk H. Desenclos JC, et al. Rev Epidemiol Sante Publique. 2002 Jan;50(1):67-79. Rev Epidemiol Sante Publique. 2002. PMID: 11938118 French.
- Factors in the emergence of food borne diseases. Altekruse SF, Swerdlow DL, Wells SJ. Altekruse SF, et al. Vet Clin North Am Food Anim Pract. 1998 Mar;14(1):1-15. doi: 10.1016/s0749-0720(15)30275-9. Vet Clin North Am Food Anim Pract. 1998. PMID: 9532663 Review.
- Knowledge, attitudes and practices of fresh Nile perch value chain handlers towards food safety requirements in Uganda. Ssubi JA, Mukisa IM, Muyanja CK. Ssubi JA, et al. Heliyon. 2024 May 20;10(10):e31432. doi: 10.1016/j.heliyon.2024.e31432. eCollection 2024 May 30. Heliyon. 2024. PMID: 38826725 Free PMC article.
- Concurrent emergencies: overlapping Salmonella and COVID-19 concerns in public health strategies and preparedness. Prayoga W. Prayoga W. Front Public Health. 2024 Apr 29;12:1331052. doi: 10.3389/fpubh.2024.1331052. eCollection 2024. Front Public Health. 2024. PMID: 38741915 Free PMC article. No abstract available.
- Vine-Winery Byproducts as Precious Resource of Natural Antimicrobials: In Vitro Antibacterial and Antibiofilm Activity of Grape Pomace Extracts against Foodborne Pathogens. Sateriale D, Forgione G, Di Rosario M, Pagliuca C, Colicchio R, Salvatore P, Paolucci M, Pagliarulo C. Sateriale D, et al. Microorganisms. 2024 Feb 21;12(3):437. doi: 10.3390/microorganisms12030437. Microorganisms. 2024. PMID: 38543488 Free PMC article.
- One Health Perspectives on Food Safety in Minimally Processed Vegetables and Fruits: From Farm to Fork. Santos MI, Grácio M, Silva MC, Pedroso L, Lima A. Santos MI, et al. Microorganisms. 2023 Dec 15;11(12):2990. doi: 10.3390/microorganisms11122990. Microorganisms. 2023. PMID: 38138132 Free PMC article. Review.
- A quantitative prevalence of Escherichia coli O157 in different food samples using real-time qPCR method. Pakbin B, Brück WM, Brück TB, Allahyari S, Ashrafi Tamai I. Pakbin B, et al. Food Sci Nutr. 2022 Sep 15;11(1):228-235. doi: 10.1002/fsn3.3055. eCollection 2023 Jan. Food Sci Nutr. 2022. PMID: 36655112 Free PMC article.
- Scallan E., Hoekstra R.M., Angulo F.J., Tauxe R.V., Widdowson M.-A., Roy S.L., Jones J.L., Griffin P.M. Foodborne illness acquired in the United States—Major pathogens. Emerg. Infect. Dis. 2011;17:7. doi: 10.3201/eid1701.P11101. - DOI - PMC - PubMed
- Kirk M.D., Pires S.M., Black R.E., Caipo M., Crump J.A., Devleesschauwer B., Döpfer D., Fazil A., Fischer-Walker C.L., Hald T., et al. World Health Organization estimates of the global and regional disease burden of 22 foodborne bacterial, protozoal, and viral diseases, 2010: A data synthesis. PLoS Med. 2015;12:e1001921. doi: 10.1371/journal.pmed.1001921. - DOI - PMC - PubMed
- WHO (World Health Organization) WHO Estimates of the Global Burden of Foodborne Diseases: Foodborne Disease Burden Epidemiology Reference Group 2007–2015. [(accessed on 1 June 2020)]; Available online: https://www.who.int/foodsafety/publications/foodborne_disease/fergreport...
- Wen X., Sun S., Li L., He Q., Tsai F.-S. Avian Influenza—Factors Affecting Consumers’ Purchase Intentions toward Poultry Products. Int. J. Environ. Res. Public Health. 2019;16:4139. doi: 10.3390/ijerph16214139. - DOI - PMC - PubMed
- Food and Agriculture Organization (FAO) Avian Influenza and the H5N1 Virus. [(accessed on 1 June 2020)]; Available online: http://www.fao.org/3/a1521e/a1521e01.pdf .
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- PubMed Central

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Journal Menu
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
- arrow_forward_ios Forthcoming issue arrow_forward_ios Current issue
- Vol. 13 (2024)
- Vol. 12 (2023)
- Vol. 11 (2022)
- Vol. 10 (2021)
- Vol. 9 (2020)
- Vol. 8 (2019)
- Vol. 7 (2018)
- Vol. 6 (2017)
- Vol. 5 (2016)
- Vol. 4 (2015)
- Vol. 3 (2014)
- Vol. 2 (2013)
- Vol. 1 (2012)
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
Foodborne Pathogens and Food Safety
- Print Special Issue Flyer
Special Issue Editors
Special issue information.
- Published Papers
A special issue of Foods (ISSN 2304-8158). This special issue belongs to the section " Food Quality and Safety ".
Deadline for manuscript submissions: closed (10 February 2022) | Viewed by 94426

Share This Special Issue

Foodborne pathogens represent a major burden on society as they are the cause of high numbers of illnesses, hospitalizations, and deaths each year. In addition to their detrimental impact on human health, these microorganisms, which include pathogenic bacteria, viruses, fungi, and a range of parasites, also represent a significant economic cost to food companies in the implementation and constant oversight of food hygiene and safety programs, product recalls, and potential litigation if outbreaks occur. Advancing our current knowledge of the food processing chain and its vulnerabilities to the many factors related to foodborne pathogens (e.g., their stress response, survival and persistence in processing environments, acquisition of virulence factors and antimicrobial drug resistance) is paramount to the development of effective strategies for early detection and control of pathogens, thereby improving food safety.
This Special Issue welcomes original research articles contributing to a better understanding of the impact of all aspects of foodborne pathogens on food safety. Papers on the following topics are particularly encouraged:
- Physiology, genetics, biochemistry, and behavior of foodborne pathogens;
- Effects of antimicrobials and packaging systems on foodborne pathogens;
- Predictive microbiology applied to foodborne pathogens in foods;
- Interactions of pathogens in microbial communities and the ecology of foods, food production, and food processing environments;
- Improved or novel methods for the detection, identification and enumeration of foodborne pathogens and microbial toxins;
- Microbiological challenge testing for ensuring the safety of food products;
- Risk assessment and microbial responses to stresses in the food chain.
Dr. Antonio Afonso Lourenco Dr. Catherine Burgess Dr. Timothy Ells Guest Editors
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website . Once you are registered, click here to go to the submission form . Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Foods is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
- foodborne pathogens
- antimicrobial susceptibility
- foodborne illnesses
- food safety
- food contamination
- risk assessment
Published Papers (15 papers)
Jump to: Review
Graphical abstract
Jump to: Research
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Open access
- Published: 28 September 2022
Descriptive study of foodborne disease using disease monitoring data in Zhejiang Province, China, 2016–2020
- Xiaojuan Qi 1 ,
- Xialidan Alifu 2 , 3 ,
- Jiang Chen 1 ,
- Wenliang Luo 3 ,
- Jikai Wang 1 ,
- Yunxian Yu 2 , 3 &
- Ronghua Zhang 1
BMC Public Health volume 22 , Article number: 1831 ( 2022 ) Cite this article
5398 Accesses
10 Citations
Metrics details
This study aimed to identify the epidemiology, seasonality, aetiology and clinical characteristics of sporadic foodborne diseases in Zhejiang province during 2016–2020.
Descriptive statistical methods were used to analyze the data from surveillance network established by the Zhejiang Provincial Center for Disease Control and Prevention. There were 31 designated hospitals in all 11 cities which were selected using probability proportionate to size sampling method.
During the study period, the surveillance system received 75,124 cases with 4826 (6.42%) hospitalizations from 31 hospitals. The most common cause was Norovirus, 6120 cases (42.56%), followed by Salmonella, 3351 cases (23.30%). A significant seasonal trend was observed for the V. parahaemolyticus, with the highest rates over the summer period, peaking in August, 1171 cases (38.75%), a similar trend was also observed with Salmonella and Diarrheagenic E. coli. Norovirus infections showed the highest rate in November (904, 14.77%) and March (660,10.78%), the lowest in August, 215 cases (3.51%). Patients between 19 ~ 40 years were more likely to infected by Norovirus, V. parahaemolyticus and Diarrheagenic E. coli, patients below 1 year were the highest among patients with Salmonella infection, 881 cases (26.3%). The Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection with the highest positive detection rates among the workers were observed. The largest number cases of food categories were from aquatic product infection. The private home was the most common exposure setting.
Our study highlighted the necessity for conducting an active, comprehensive surveillance for pathogens in all age groups, to monitor the changing dynamics in the epidemiology and aetiology of foodborne diseases to guide policies that would reduce related illnesses.
Peer Review reports
Introduction
Foodborne illnesses are usually infectious or virulent and caused by bacteria, viruses, parasites or chemicals that enter the body through contaminated food or water. Although, food science and related technologies are developing rapidly, but still, it remains a challenge to prevent foodborne diseases completely [ 1 ]. An estimated 600 million in the world (almost 1 in 10 people), fall ill after eating contaminated food and 420 000 die every year, resulting in the loss of 33 million healthy life years in terms of Disability Adjusted Life Years (DALYs) according to an estimate based on the 2015 data [ 2 ]. Diarrhoeal diseases account for more than 50% of foodborne diseases, according to the data released by World Health Organization (WHO), foodborne or water-borne diarrhea alone causes about 2.2 million deaths worldwide every year [ 3 ]. As in other countries, foodborne diseases characterized by acute gastrointestinal diseases are the largest food safety problem as well as the most distressing food-related threat to public health in China [ 4 , 5 , 6 ]. In order to reduce the disease burden, China has established a web-based foodborne disease surveillance system since 2011, which has gradually played a role in food safety incidence prevention. The surveillance contents include hygiene indicator bacteria, pathogenic bacteria, viruses, and parasites in many food categories. Moreover, sampling points are no more limited to retail and catering sites, and have been extended to processing, and sales locations.
The studies discussed the characteristics of food contamination by pathogens according to surveillance data and reflects the contamination and distribution trend of foodborne pathogens in different regions. A wide range of representative agents (including pathogenic bacteria, viruses and etc.) are covered to understand their contamination in meat and meat products [ 7 ], milk and dairy products [ 8 ], eggs and egg products [ 9 ], children’s foods [ 10 ] and ready-to-eat foods [ 11 ]. Norovirus, Salmonella spp., Vibrio parahaemolyticus (V. parahaemolyticus), Shigella and Diarrheagenic E. coli have been identified as the most common pathogens responsible for foodborne diseases in China [ 12 , 13 ]. The surveillance data showed that occurrence of V. parahaemolyticus in aquatic products tended to increase over the period from 2015 to 2018 [ 11 , 14 ].
Safe food supplies support national economies, trade and tourism, contribute to food and nutrition security, and underpin sustainable development. As there are a limited number of existing epidemiological studies and reports on the foodborne diseases in Zhejiang province, the need for researches has become important. The aim of this study was to summarize epidemiological characteristics of foodborne disease cases and provide effective interventions to prevent foodborne disease illnesses in Zhejiang province, we analyzed the surveillance data of foodborne disease cases caused by Norovirus, Salmonella spp., Vibrio parahaemolyticus (V. parahaemolyticus), Shigella and Diarrheagenic E. coli in Zhejiang province from 2016 to 2020.
Geographical position, climatic and socio-demographic feature of study site
Zhejiang Province, one of the southeastern coastal provinces of China, is located at 27°02’N to 31°11’N and 118°01’E to 123°10’E [ 15 ], the 11 cities and their subordinate counties are listed in Supplementary Table 1. Zhejiang experience a subtropical humid climate. During summer the weather is hot and humid and the temperature is around 27 to 30 °C (81 to 86 °F). During winter the temperature falls down to a minimum temperature of 2℃ to 8℃ (36 to 46 °F). Rainfall and typhoons are a common phenomenon in summers. Zhejiang province has a permanent population of 65.4 million at the end of 2021, and GDP grew 8.5% year-on-year to 7.35 trillion yuan ($1.16 trillion) in 2021 [ 15 ]. Most of Zhejiang’s wealth derives from light industry and mostly located in rural villages [ 16 ].
Data source
Zhejiang Provincial Center for Disease Control and Prevention (ZJCDC) has collected foodborne disease relevant data through the China National Foodborne Diseases Surveillance Network (NFDSN) since 2012. 31 hospitals were inquired to detect 5 major pathogens and corresponding subtypes, including Salmonella, Norovirus, V. parahaemolyticus, Diarrheagenic E. coli and Shigella for all suspected foodborne disease cases, and reported illnesses through NFDSN since 2016. In this study the cases reported by 31 hospitals in Zhejiang province during the period 2016–2020 were included. Epidemiologists from the health departments first conducted the investigation to ascertain the full extent of the foodborne illness and the information collected for each case includes reporting region, date of occurrence, setting, etiology, food categories, number of illnesses / hospitalizations, and some other details. Unknown etiology refers to those foodborne disease cases where the confirmed etiology has not been identified. Foods was identified as the sources of disease through epidemiologic or laboratory methods and was classified into 13 categories. The food that cannot be determined was classified as “Unknown”. The GIS map data of Zhejiang Province is downloaded by the national basic geographic information center of China ( http://bzdt.ch.mnr.gov.cn/ ).
Statistical analysis
Total positive detection rate and hospitalization rate were calculated for each pathogen and linear trend test was used to test the change of positive detection rate and hospitalization rate annually for each pathogen. Chi-square test was used to compare the demographic characteristics, contaminated food category and food settings among four pathogens, including Salmonella, Norovirus, V. parahaemolyticus, Diarrheagenic E. coli while Shigella was not included due to limited sample sizes. Fisher exact test was used if the conditions were not met for Chi-square test. Post-hoc test was used for pairwise comparisons. Comparison was only programmed within illnesses with single etiology. Open-source software QGIS (Quantum GIS version 3.22.9) was used to map the spatial distribution of cases with positive detection rate caused by five pathogens for the period between 2016 and 2020. All statistical analyses were performed using R 3.6.2 and P -value was considered as significant at < 0.05.
General epidemiological characteristics
During the study period (2016–2020), the surveillance system received 75,124 cases with 4826 (6.42%) hospitalizations from 31 hospitals. As shown in Table 1 , total positive detection rate was 14,381(3.97%). The most common cause was Norovirus, 6120 cases (42.56%), followed by Salmonella, 3351 cases (23.30%), V. parahaemolyticus, 3022 cases (21.01%), Diarrheagenic E. coli,1849 cases (12.86%) and Shigella, 39 cases (0.27%). The positive detection rate increased in Salmonella and E. coli (from 3.37 to 6.59% and from 1.14 to 2.38%, respectively), while the rate for V. parahaemolyticus and Norovirus decreased during 2016–2020 (from 6.29 to 2.39% and from 10.62 to 6.62%, respectively); the rate in Shigella remained low level (Fig. 1 .A). As for hospitalization rate, a significant decrease of Norovirus and Salmonella was observed during the study period as well ( P < 0.001), with the highest in 2016 (from 12.62 to 6.55% and from 8.21 to 6.24%, respectively) (Fig. 1 .B). Among all cases with positive detection, which were being hospitalized, the most common cause was Salmonella (Table 1 ).
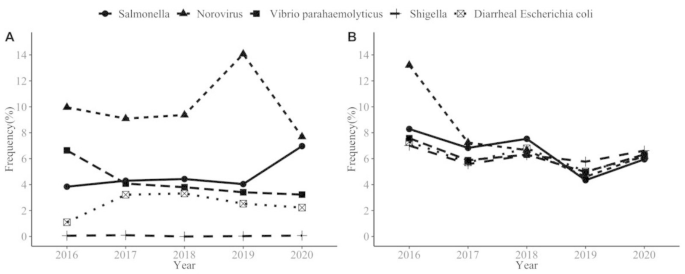
The change of positive detection rate (A) and hospitalization rate (B) of major pathogens during 2016–2020
The regional distribution of cases with positive caused by five pathogens among 11 cities, as shown in Fig. 2 : 2028 cases with 5.34% detection rate in Huzhou city, 1636 (4.89%) cases in Taizhou city, 1073 (4.88%) cases in Lishui city (Fig. 2 ).
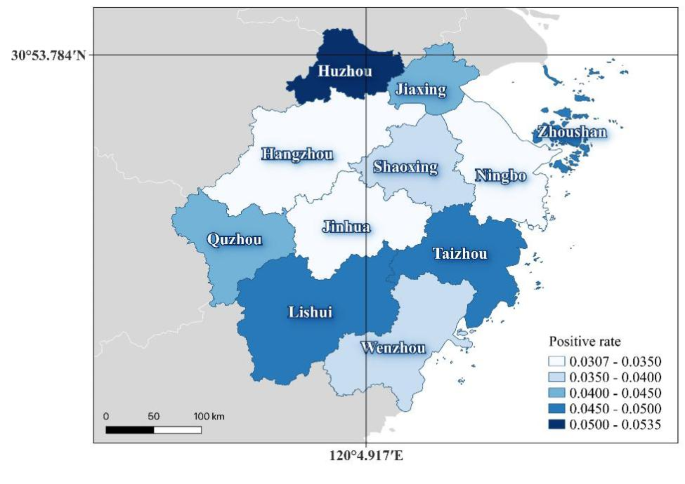
The regional distribution of cases with positive detection rate caused by five pathogens
Characteristics for four pathogens
For this analysis, only the highest contributing pathogens were included (Salmonella, Norovirus, V. parahaemolyticus, and Diarrheagenic E. coli).
Trend and seasonality
A significant seasonal trend was observed for the V. parahaemolyticus, with the highest rates over the summer period, peaking in August, 1171 cases (38.75%). A similar trend was also observed with Salmonella and Diarrheagenic E. coli, with the peak in August, 612 cases (18.26%) and 335 cases (18.12%), respectively. Norovirus infections showed the highest rate in November (904 cases, 14.77%) and March (660 cases,10.78%) and the lowest in August, 215 cases (3.51%) (Fig. 3 ).
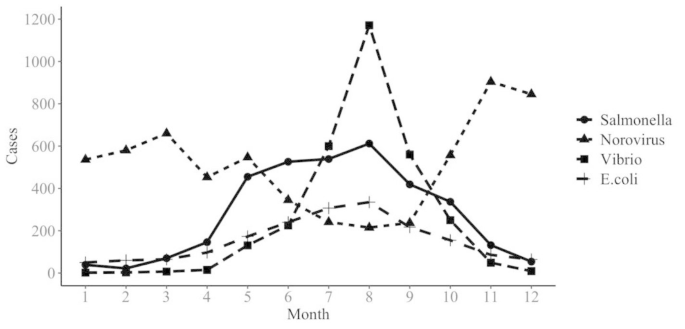
Monthly trends of selected foodborne diseases
Age, gender and occupational differences
A significant difference was observed between different age groups ( P < 0.01), with the majority of reported cases affecting young people aged 19–40 years, as shown in Table 2 . Among Salmonella infections, illnesses below one year old accounted for 26.30%, significantly higher than other three pathogens. V. parahaemolyticus showed much lower proportion for illnesses in population under 18 years old. As for gender distribution, though significantly different among four pathogens, all showed higher proportion in males ( P < 0.05). A significant occupational difference was observed. For Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection with the highest proportion among the workers. Salmonella infections showed the highest proportion in kids living scattered,1180 cases (35.21%) (Table 2 ).
Implicated foods and settings
In this study, four type of foodborne cases were reported due to certain food vehicles, as shown in Fig. 4 . Aquatic products were the most common cause for Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection (17.73%, 39.34% and 15.84%, respectively), followed by cooked meat products (17.04%, 15.57% and 15.73% respectively). The top three food vehicles in Salmonella infection were fruits (16.25%), aquatic products (12.36%) and cereals (12.29%). The places with more cases caused by four pathogens were household settings, followed by restaurants, data shown in Table 3 .
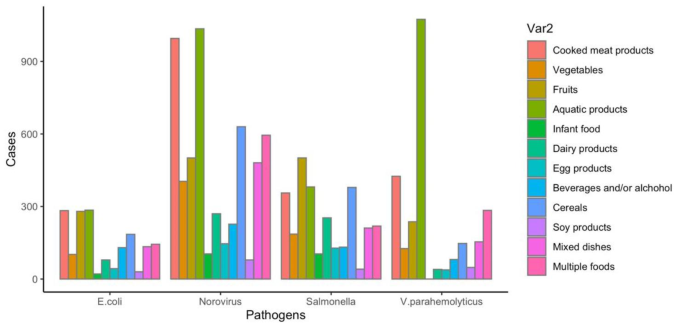
Food categories between foodborne disease cases
Among the Norovirus cases: 52.81% with abdominal cramps, 38.35% with vomiting, 38.28% with nausea; Salmonella caused 49.93% abdominal cramps, 28.20% fever, 19.04% nausea cases; V. parahaemolyticus caused 76.15% abdominal cramps, 46.92% nausea, 37.62% vomiting cases; Diarrheagenic E. coli caused 60.57% abdominal cramps, 25.26% nausea, 19.47% vomiting cases. Watery diarrhea was the most common symptom for four pathogens (Table 4 ).
Foodborne diseases impede socioeconomic development by straining health care systems, and harming national economies, tourism and trade. This study described the epidemiology of foodborne diseases caused by different pathogens in Zhejiang Province during the period 2016–2020. Over the 5 years, 75,124 cases with 4826 (6.42%) hospitalizations caused by Norovirus, Salmonella, V. parahaemolyticus, Diarrheagenic E. coli and Shigella from 31 hospitals were reported. Among 11 cities, 2028 cases in Huzhou city (14.33%), 1933 cases in Wenzhou city (13.66%), 1636 cases in Taizhou city (11.56%). The results were quite different from Sun Liang’s report, in which Wenzhou city accounts for the largest percentage of illnesses [ 17 ].
The number of illnesses caused by Norovirus ranks first among all etiologies, which is consistent with Shanghai, in which Norovirus was the most common pathogen (43.10%) [ 18 ], but quite different from the studies in China’s coastal provinces such as Hainan [ 19 ]. Wang [ 20 ] et al. reviewed 2447 papers in China that reported 1082 foodborne disease cases occurring between 1994 and 2005, in which V. parahaemolyticus caused the most events in littoral provinces, whereas in inland provinces, the largest percentage of cases were caused by Salmonella. Thus, there are regional differences in the distribution of pathogenic bacteria in China. These studies suggests that region-specific policies on foodborne disease control should be established.
Seasonality of foodborne illnesses was observed in this study. A seasonal trend was found for the V. parahaemolyticus, Salmonella and Diarrheagenic E. coli with the highest rates during summer period, peaking in August, this was similar in Enserink’s [ 21 ] and Gong’s [ 18 ] reports. However, the seasonal peak of infection attributed to some foodborne pathogens isn’t in the summer. For instance, Norovirus infections showed the highest rate in November and March and the lowest in summer, which was in line with previous studies [ 18 , 22 , 23 ]. Seasonality related to the temperature, humidity and rainfall, all of which may affect exposure frequency and host immune status. These findings indicated that temperature is an important factor in foodborne illnesses, and investigation of the reasons for the seasonal dominance on foodborne diseases should be the focus of surveillance.
This study showed the distinctive differences between four main pathogens with age groups. In general, the positive detection rate was higher in people aged 19 ~ 30 and 31 ~ 40 years than that in those aged < 18 and 40 + years, which were infected by Norovirus, V. parahaemolyticus and Diarrheagenic E. coli. This was partly consistent with a study in China which found incidence of foodborne diseases in youth group was higher than that in elderly group [ 14 ]. Also, a study in France which found incidence of foodborne diseases in young was higher than that in elders, in which, elders (≥ 60 years) were at least likely to get infected with V. parahaemolyticus, whereas people aged 30 ~ 44 years were the most likely get infected [ 24 ]. Similar results were observed in a Shanghai study [ 25 ]. In contrast to previous studies which found children (< 5 years) and elder people more likely to get infected with Norovirus [ 26 , 27 ], our study found that the highest proportion in Norovirus infections was people aged 19–30 years old. Among Salmonella infections, cases among children aged under 1 year old accounted for 26.30%, significantly higher than other age groups. Similar findings reported in Guangdong Province that children aged < 5 years were the group most affected by Salmonella (73%), of whom the infants under 1 year old were 81.5% [ 28 ]. As for gender distribution, though significantly different among four pathogens, all showed higher proportion in male. The Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection with the highest positive detection rates in the workers were observed. Foodborne illnesses among workers are liable to occur frequently because poor hygienic conditions at workers’ camps and work situations, in the meantime, high summer temperatures impacting the transportation, distribution and storing of foods [ 29 ]. The related knowledge on what is safe should be handed down through families, work sites and credible institutions.
Analysis of exposed foods of foodborne illnesses in this study, the cases caused by Norovirus, V. parahaemolyticus and Diarrheagenic E. coli, the largest number of food categories involved were aquatic product infection (17.73%, 39.34% and 15.84%, respectively). On the contrary, a study showed the analysis of exposed foods of reported cases in Shandong Province, multiple foods (meaning more than two kinds of food) were the most commonly reported classification [ 30 ]. The reason for the different findings may be that Zhejiang is a coastal province with a vast sea area and various aquatic products. Therefore, consumers would be advised to separate raw and cooked foods, cook thoroughly as much as possible and keep food at safe temperatures to reduce the risk of foodborne diseases. However, avoiding all raw seafood should be difficult for those who are in the habit of eating seafood. As for cases infected by Salmonella, fruits, aquatic products and cooked meat products were identified as the most frequent food vehicles in the present study. Conversely, eggs have been reported as the most common classification for Salmonella infection in the US [ 31 ]. The main reason for this difference was cultural differences in eating habits. Yet it’s worth noting that, the reported classification of multiple foods relatively high as well. That means people eat more and more diverse foods, on the other hand, the category of exposed foods in national foodborne disease surveillance system is not specified in enough detail.
Analysis of the settings, according to our analysis, private home was the most common exposure setting, followed by restaurant. However, the average annual case ratios in the Republic of Korea were the highest at restaurant (57%) [ 32 ]. Among cases reported in US, restaurants also the most common settings of preparation [ 31 ]. On the contrary, Wu et al. [ 33 ] from CDC of China found that, foodborne illnesses most frequently occurred in household (32%). Similar results were observed in a EU study [ 34 ]. These findings consistent with present results, this means a large proportion of foodborne diseases caused by foods improperly prepared or mishandled at home. The effective actions can include the following aspects: know the food they use, for example, read labels on food packages, make informed choices, become familiar with common food hazards; furthermore, government should focus on home settings to reduce infections.
In regard to clinical symptoms in general, results showed similar clinical symptoms, such as nausea, abdominal pain and watery diarrhea between patients caused by four pathogens, respectively. The proportion of fever was the highest in Salmonella while lowest in Diarrheagenic E. coli. The proportion of fever in Salmonella infections in our findings was close to that in another research [ 35 ]. As Most foodborne pathogens can cause acute gastroenteritis with gastrointestinal symptoms, it is difficult to distinguish the cases infected by different pathogens by symptoms.
The limitations of this study need to be explained. First, for many reported cases, information on certain aspects, such as food category, settings and etc. were missing or incomplete, so the conclusions might not be representative of unknown classifications. Second, information and detection data were collected from 31 hospitals and several laboratories. Though detection methods were unified and regular trainings were held, there was a chance of bias caused by the different conditions and levels of hospitals and laboratories. Third, inability to conduct an epidemiological investigation due to lack of patient cooperation, there were still some missing information.
Norovirus was the most common enteric pathogen detected in our surveillance during 2016–2020. Since the different epidemiological characteristics of foodborne diseases caused by different pathogens, we suggest that targeted measures be taken according to the characteristics of different etiologies and food vehicles to improve the prevention and control efficiency. The Norovirus, V. parahaemolyticus and Diarrheagenic E. coli infection with the highest positive detection rates over the workers were observed. Foodborne illnesses among workers are liable to occur frequently because hygienic conditions at workers’ camps and work situations are not always at the same standard. The related knowledge on what is safe should be handed down through families, work sites and credible institutions. Most foodborne diseases are preventable, we should further improve the identification rate of the causes of the epidemic, carry out attribution analysis for “precise prevention and control”.
Data availability
The data that support the findings of this study are available from the Foodborne Disease Case Surveillance Reporting System of the China National Center for Food Safety Risk Assessment, and these data are not publicly available.
The data that support the findings of this study are available from the Foodborne Disease Case Surveillance Reporting System ( https://sppt.cfsa.net.cn/goto ), and these data are not publicly available.
Kim JJ, Ryu S, Lee H. Foodborne illness outbreaks in Gyeonggi province, Korea, following seafood consumption potentially caused by Kudoa septempunctata between 2015 and 2016. Osong Public Health Res Perspect. 2018;9:66–72.
Article Google Scholar
World Health Organization. WHO estimates of the global burden of foodborne diseases: foodborne diseases burden epidemiology reference group 2007–2015. https://www.who.int/publications/i/item/9789241565165 . Accessed 3 December 2015.
Food Standards Agency. The FSA food borne disease strategy 2010-15. London: Food Standards Agency; 2011.
Google Scholar
Chung SS, Wong CK. Regulatory and policy control on food safety in China. J Epidemiol Community Health. 2013;67(6):476–7.
Akhtar S, Sarker MR, Hossain A. Microbiological food safety: a dilemma of developing societies. Crit Rev Microbiol. 2014;40(4):348–59.
Article CAS Google Scholar
Wu YN, Liu P, Chen JS. Food safety risk assessment in China: Past, present and future. Food Control. 2018;90:212–21.
Yang S, Yan L, Pei X, Yang D. Study on the contamination status of foodborne pathogens in frozen minced meat products on China market. Chin J Food Hyg. 2020;32:180–3.
Yan L, Li Y, Yang D, et al. Contamination of pathogens in milk powder available in retail markets. Chin J Public Health. 2016;32:602–4.
Li Y, Yang X, Zhang H, et al. Prevalence and antimicrobial susceptibility of Salmonella in the commercial eggs in China. Int J Food Microbiol. 2020;325:108623.
Hu J, Pei X, Li N, Yang D. Survey of microbiological contamination of commercial available infant formula sheep milk powder. Chin J Health Lab Tec 2016;26:1942–1943, 1946.
Kim HW, Hong YJ, Jo JI, et al. Raw ready-to-eat seafood safety: microbiological quality of the various seafood species available in fishery, hyper and online markets. Lett Appl Microbiol. 2017;64(1):27–34.
Li W, Cui Q, Bai L, Fu P, Han H, Liu J, Guo Y. Application of Whole-Genome Sequencing in the National Molecular Tracing Network for Foodborne Disease Surveillance in China. Foodborne Pathog Dis. 2021;18(8):538–46.
Kim SS, Kang DH. Combination treatment of ohmic heating with various essential oil components for inactivation of food-borne pathogens in buffered peptone water and salsa. Food Cont. 2017;80:29–36.
Yan L, Hu J, Pei X, Yang D, Zhang X. Contamination of foodborne pathogens in frozen surimi products sold in China in 2014. J Hyg Res. 2017;46:328–30.
Zhejiang Provincial Bureau of Statistics. http://tjj.zj.gov.cn/ .
Official site of Zhejiang province. China. http://www.ezhejiang.gov.cn/index.html .
Sun L, Chen Ll, Liao NB, Chen J. Analysis of foodborne disease outbreak surveillance data in Zhejiang Province,2006–2017. Chin J Health Lab Tec. 2019;29(15):1874–7.
Gong XH, Wu HY, Li J, Xiao WJ, Zhang X, Chen M, Teng Z, Pan H, Yuan ZA. Epidemiology, aetiology and seasonality of infectious diarrhoea in adult outpatients through active surveillance in Shanghai, China, 2012–2016: a cross-sectional study. BMJ Open. 2018;8(9):e019699.
Wang JX, He J, Wang S, et al. Incidence of foodborne diseases in Hainan province, 2007–2016. Chin J Public Health. 2018;34(9):1288–91.
Wang S, Duan H, Zhang W, Li JW. Analysis of bacterial foodborne disease outbreaks in China between 1994 and 2005. FEMS Immunol Med Microbiol. 2007;51(1):8–13.
Enserink R, van den Wijngaard C, Bruijning-Verhagen P, et al. Gastroenteritis attributable to 16 enteropathogens in children attending day care: significant effects of rotavirus, norovirus, astrovirus, Cryptosporidium and Giardia. Pediatr Infect Dis J. 2015;34(1):5–10.
Karsten C, et al. Incidence and risk factors for community-acquired acute gastroenteritis in north-west Germany in 2004. Eur J Clin Microbiol Infect Dis. 2009;28(8):935–43.
Zhang Z, Lai S, Yu J, et al. Etiology of acute diarrhea in the elderly in China: A six-year observational study. PLoS ONE. 2017;12(3):e0173881.
Arena C, Amoros JP, Vaillant V, et al. Acute diarrhea in adults consulting a general practitioner in France during winter: incidence, clinical characteristics, management and risk factors. BMC Infect Dis. 2014;14:574.
Zhang Y, Zhao Y, Ding K, Wang X, Chen X, Liu Y, Chen Y. Analysis of bacterial pathogens causing acute diarrhea on the basis of sentinel surveillance in Shanghai, China, 2006–2011. Jpn J Infect Dis. 2014;67(4):264–8.
Hossain ME, Islam MM, Miah M, Haque W, Vinjé J, Rahman MZ, Faruque ASG, Khan AI, Ahmed T, Rahman M. Corrigendum to: Viral Etiology of Acute Gastroenteritis Among Forcibly Displaced Myanmar Nationals and Adjacent Host Population in Bangladesh. J Infect Dis. 2022;225(6):1114.
Patel MM, Widdowson MA, Glass RI, Akazawa K, Vinjé J, Parashar UD. Systematic literature review of role of noroviruses in sporadic gastroenteritis. Emerg Infect Dis. 2008;14(8):1224–31.
Liang Z, Ke B, Deng X, Liang J, Ran L, Lu L, He D, Huang Q, Ke C, Li Z, Yu H, Klena JD, Wu S. Serotypes, seasonal trends, and antibiotic resistance of non-typhoidal Salmonella from human patients in Guangdong Province, China, 2009–2012. BMC Infect Dis. 2015;15:53.
Todd ECD. Foodborne disease and food control in the Gulf States. Food Control. 2017;73:341–66.
Wu G, Wang L, Wang Q, et al. Descriptive Study of Foodborne Disease Using Case Monitoring Data in Shandong Province, China, 2016–2017. Iran J Public Health. 2019;48(4):722–9.
PubMed PubMed Central Google Scholar
Dewey-Mattia D, Manikonda K, Hall AJ, Wise ME, Crowe SJ. Surveillance for Foodborne Disease Outbreaks - United States, 2009–2015. MMWR Surveill Summ. 2018;67(10):1–11.
Kim JJ, Ryu S, Lee H. Foodborne Illness Outbreaks in Gyeonggi Province, Korea, Following Seafood Consumption Potentially Caused by Kudoa septempunctata between 2015 and 2016. Osong Public Health Res Perspect. 2018;9(2):66–72.
Wu YN, Liu XM, Chen Q, et al. Surveillance for foodborne disease outbreaks in China, 2003 to 2008. Food Control. 2018;84:382–8.
Schlinkmann KM, Razum O, Werber D. Characteristics of foodborne outbreaks in which use of analytical epidemiological studies contributed to identification of suspected vehicles, European Union, 2007 to 2011. Epidemiol Infect. 2017;145(6):1231–8.
Qi XL, Wang HX, Bu SR, Xu XG, Wu XY, Lin DF. Incidence rates and clinical Symptoms of Salmonella, Vibrio parahaemolyticus, and Shigella infections in China, 1998–2013. J Infect Dev Ctries. 2016;10(2):127–33.
Download references
Acknowledgements
The authors thank the food safety staff of the CDC at all levels of the province for their positive role and responsible handling of foodborne cases and timely submitting accurate reports, which enabled current study to have a large number of data to analyze the epidemiological characteristics of which in our province and put forward targeted intervention measures for further prevention and control.
This research was sponsored by Medical and Health Science and Technology Project of Zhejiang Province (No.2022KY712), Chinese National Natural Science Foundation (81973055), the National Key Research and Development Programme of China (No.2021YFC2701901), Major research and development projects of the Zhejiang Science and Technology Department (2018C03010), Key Laboratory of Intelligent Preventive Medicine of Zhejiang Province (2020E10004), and Leading Innovative and Entrepreneur Team Introduction Program of Zhejiang (2019R01007).

Author information
Authors and affiliations.
Department of Nutrition and Food Safety, Zhejiang Provincial Center for Disease Control and Prevention, 3399 Binsheng Road, Binjiang District, 310051, Hangzhou City, Zhejiang Province, China
Xiaojuan Qi, Jiang Chen, Jikai Wang & Ronghua Zhang
Department of Epidemiology & Health Statistics, School of Public Health, School of Medicine, Zhejiang University, 310058, Hangzhou City, Zhejiang Province, China
Xialidan Alifu & Yunxian Yu
Department of Public Health, Department of Anesthesiology, Second Affiliated Hospital of Zhejiang University School of Medicine, 310003, Hangzhou City, Zhejiang Province, China
Xialidan Alifu, Wenliang Luo & Yunxian Yu
You can also search for this author in PubMed Google Scholar
Contributions
X.J.Q. and X.A. made substantial contributions to the design of the work. X.J.Q. and X.A. drafted the work, Y.X.Y. and R.H.Z. substantively revised it. All authors made substantial contributions to the acquisition, analysis, and interpretation of data. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Yunxian Yu or Ronghua Zhang .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of Zhejiang Provincial Center for Disease Control and Prevention (CDC). The study protocol was performed in accordance with the relevant guidelines. The ethics committee approved the procedure for verbal consent because Zhejiang CDC has the authority of the Zhejiang provincial government to collect and utilize information on foodborne disease cases, which is part of disease surveillance scope in Zhejiang CDC. All participants were informed that they had the right to reject or terminate the study at any time during the interview. Since we have obtained verbal consent, documentation of consent was not required. The information provided by each participant is confidential in Zhejiang CDC. The China’s National Center for Food Safety Risk Assessment (CFSA) is responsible for maintaining and managing the foodborne disease case surveillance system, and our use of the data has been verbally approved by CFSA.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaojuan Qi and Xialidan Alifu contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Qi, X., Alifu, X., Chen, J. et al. Descriptive study of foodborne disease using disease monitoring data in Zhejiang Province, China, 2016–2020. BMC Public Health 22 , 1831 (2022). https://doi.org/10.1186/s12889-022-14226-1
Download citation
Received : 07 May 2022
Revised : 23 August 2022
Accepted : 19 September 2022
Published : 28 September 2022
DOI : https://doi.org/10.1186/s12889-022-14226-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Food safety
- Microbial hazard
- Foodborne pathogen
- Surveillance network
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Burden of Foodborne Illness: Questions and Answers

- Report: Foodborne Illness Acquired in the United States—Major Pathogens
- Report: Foodborne Illness Acquired in the United States—Unspecified Agents
Commentary: How Safe Is Our Food?
What are the main findings?
Foodborne diseases are an important public health burden in the United States.
First, we estimate that 31 of the most important known agents of foodborne disease found in foods consumed in the United States each year cause 9.4 million illnesses, 55,961 hospitalizations, and 1,351 deaths.
Second, not all agents of foodborne disease are known or can be counted as a “known agent of foodborne disease.” These other agents, which we call “unspecified agents,” include:
- Known agents with insufficient data to estimate the agent-specific burden
- Known agents not yet recognized as causing foodborne illness
- Microbes, chemicals, or other substances known to be in food whose ability to cause illness is unproven; and
- Agents not yet described
As a group, we estimate that these unspecified agents in food consumed in the United States, cause an additional 38.4 million gastroenteritis illnesses, 71,878 hospitalizations, and 1,686 deaths each year.
After combining the estimates for the major known pathogens and the unspecified agents, the overall annual estimate of the total burden of disease due to contaminated food consumed in the United States is 47.8 million illnesses, 127,839 hospitalizations, and 3,037 deaths.
What are the leading causes of foodborne deaths, hospitalizations, and illnesses?
- Nontyphoidal Salmonella , Toxoplasma , Listeria , and norovirus caused the most deaths.
- Nontyphoidal Salmonella , norovirus, Campylobacter , and Toxoplasma caused the most hospitalizations.
- Norovirus caused the most illnesses. Although norovirus usually causes a mild illness, norovirus is a leading cause of foodborne deaths because it affects so many people.
Read the Report
Foodborne Illness Acquired in the United States—Unspecified Agents
The paper on unspecified agents says that 38.4 million gastrointestinal illnesses are due to agents not yet described, unrecognized foodborne agents, and noninfectious agents. How does CDC know that these unspecified agents are foodborne? Can’t acute gastroenteritis be caused by conditions or vehicles other than foodborne transmission?
- Gastroenteritis can be caused by agents that are transmitted through food, water, direct contact with animals, or person-to-person contact.
- Based on the data for known pathogens, we estimated the proportion of acute gastroenteritis illnesses that was caused by foodborne transmission.
- We applied that proportion to the number of all gastrointestinal illnesses from unspecified agents to estimate the number of illnesses from unspecified agents that were foodborne.
It is important to note, however, that using this method assumes that the foodborne proportion is the same for illnesses from known agents and from unspecified agents. We believe that this is a reasonable assumption, given the limited information available, but it is certainly possible that the foodborne proportion differs for known and unspecified agents.
How can I get more information about the methods used to create the estimates?
Estimating US foodborne illnesses for 31 known foodborne pathogens
For each pathogen, we gathered data from surveillance systems and corrected for underreporting and under-diagnosis. We then multiplied the adjusted number by the proportion of illnesses that was acquired in the United States (that is, not during international travel) and the proportion transmitted by food to yield an estimated number of illnesses that are domestically acquired and foodborne. Then, we added the estimates for each of the pathogens to arrive at a total, and used an uncertainty model to generate a point estimate and 90% credible interval (upper and lower limits).
Estimating US foodborne illnesses for unspecified agents
Unspecified agents fall into four general categories:
- Agents with insufficient data to estimate agent-specific burden
- Microbes, chemicals, or other substances known to be in food whose pathogenicity is unproven
To estimate foodborne illnesses from unspecified agents, we used symptom-based data from surveys to estimate the total number of AGI and then subtracted the number of illnesses accounted for by known gastroenteritis pathogens. We then multiplied this number by the proportion of domestically acquired illnesses and of illnesses attributable to food, just as we did for the known agents. Finally, again as with the known-pathogens estimate, we used an uncertainty model to generate a point estimate and 90% credible interval (upper and lower limits).
Foodborne illnesses caused by chemicals that cause acute gastroenteritis are included in the estimate of illnesses due to unspecified agents. However, chemicals or unspecified agents that do not cause acute gastroenteritis are not included in the estimates.
Learn more about the methods used >
The paper says that comparing estimates from 1999 with estimates from 2011 would be meaningless because better data sources and methods were used for the new estimates. Were the 1999 estimates wrong? How can you be sure that the new estimates accurately reflect the burden of foodborne illness if they are so different from those in 1999?
The 1999 Mead et al. estimates were based on the best data available and used accepted methodologies of the time, so in 1999 they were the best possible estimates. Those estimates provided important information about the relative frequency of various pathogens and filled a major gap in knowledge that helped in decision making. Public health science is not static. Every year new findings emerge, new methods are developed for research and analysis, new data are added to surveillance systems, and new surveys are conducted. The 2011 estimates are the result of innovations in methodology and improvements in the data made over the past decade, which we believe have resulted in more accurate estimates than their predecessors. We hope future estimates will benefit from additional innovations and improvements.
Learn more about improvements made in the 2011 estimates >
Why is it important to estimate domestically acquired foodborne illnesses?
Because many persons and organizations are involved in food safety in the United States—farmers, product manufacturers, distributors, retailers, restaurant workers, and consumers. We all want the most accurate measure of how well we’re doing in making food safe. Every time someone gets sick from eating food in the United States, we know we have more work to do. Whether we are involved in developing new or improved practices or policies in industry, or in encouraging best consumer practices, specific estimates about domestically acquired foodborne illnesses tell us that improvements are still needed.
Can you tease apart the proportion of the big drop in the estimates that’s due to improved methods from an actual decrease in illness? Put another way, was there any actual decrease in illness? If the answer to the second question is “yes,” to what can the actual reduction in illness be attributed?
Estimates of burden are designed to estimate the overall burden of disease at a point in time. They are not designed or intended to gauge increases or decreases in illnesses. Surveillance systems, such as Foodborne Diseases Active Surveillance Network (FoodNet) , which capture data in a standardized way at regular points in time, are more appropriate for looking at disease trends.
If the new estimates do not really reflect a drop in the number of foodborne illnesses, how can you tell whether or not the government’s policies and programs for preventing these illnesses are working or if changes are needed?
To determine the effects of policies and programs, you need trend data—a way to tell how the incidence of disease has changed over time. The Foodborne Diseases Active Surveillance Network (FoodNet )—provides the best data for watching trends in common foodborne diseases. These data offer insight into whether policies and programs are having the intended effects.
- FoodNet is a surveillance system that collects information from sites in 10 states about diseases that are caused by nine organisms transmitted commonly through food.
- It is designed to identify everyone in the 10 sites who went to a health care provider, had a sample tested in a laboratory, and was diagnosed (laboratory-confirmed) with one of these infections.
- FoodNet gives us important information about which foodborne diseases are becoming less common and which need more concentrated attention.
How does our burden of foodborne illness compare with those of other countries?
Studies estimating the burden of foodborne illness have been done in Canada, England and Wales, and Australia.
- Like our study, the Canadian and Australian studies found that norovirus is responsible for a large portion of foodborne illnesses (31% and 30%, respectively).
- The study in England and Wales found a much lower percentage of norovirus-related illnesses than the US estimates, but when study samples were reexamined with a different technique, the rates were higher.
- Salmonella and Campylobacter were found to be leading causes of foodborne illnesses in the three foreign studies, as in the US study.
- The three foreign studies attributed a large burden of foodborne illness to unspecified agents and estimated a similar proportion of gastrointestinal illness to be transmitted by food.
However, it is important to note that each study used different methods, and therefore their specific estimates are not directly comparable.
If norovirus is the biggest cause of gastroenteritis illness, why isn’t it reportable?
Norovirus and food.
Norovirus is a leading cause of disease from contaminated foods in the United States . Foods that are most commonly involved in foodborne norovirus outbreaks include leafy greens (such as lettuce), fresh fruits, and shellfish (such as oysters). However, any food item that is served raw or handled after being cooked can become contaminated with noroviruses.
Each year, the Council of State and Territorial Epidemiologists, with input from CDC, recommends diseases to include on the list of nationally notifiable conditions (formerly called nationally notifiable diseases).
- Considerations include the frequency, severity, and transmissibility of the disease as well as other considerations, such as whether ill persons are given a specific diagnosis when they receive health care.
- Based on this recommendation, states mandate which diseases must be reported to the state health department.
- Reporting to CDC is voluntary.
- The list changes periodically as new pathogens emerge or incidence of an illness drops over time.
- Norovirus is currently not on the list of nationally notifiable diseases. One of the main reasons is that clinical laboratories do not routinely test for norovirus, so ill persons are usually not specifically diagnosed with norovirus infection.
- Usually, norovirus is specifically diagnosed only in an outbreak situation.
- Beginning in 2009, all norovirus outbreaks have been reportable through outbreak surveillance, including those not transmitted by food; previously only food- and waterborne outbreaks were reported to CDC.
CDC conducts surveillance for norovirus outbreaks through the National Outbreak Reporting System (NORS). Through NORS, states are able to report all outbreaks of gastroenteritis, including those caused by foodborne, waterborne, and person-to-person transmission of norovirus directly to CDC. When states send specimens for testing or sequencing, norovirus outbreaks may also be reported to CDC’s National Calicivirus Laboratory, within the Gastroenteritis and Respiratory Viruses Laboratory Branch. (Calicivirus is the family name for the family of viruses that includes norovirus.)
- Norovirus: Technical Fact Sheet
- Norovirus Illness: Key Facts
- Norovirus: Trends
- Norovirus: Surveillance, Disease Burden, and Disease Reduction Activities
- Norovirus: Facts for Food Handlers
In addition, CDC recently has developed a national surveillance network for norovirus genetic sequences (like DNA “fingerprints”) called CaliciNet, which is modeled after PulseNet, a surveillance network for enteric bacteria. CaliciNet is a national network of public health laboratories that contribute to a database of genetic fingerprints from noroviruses identified in outbreaks. As more states participate, CaliciNet may find links to help identify multistate outbreaks, detect potential norovirus-contaminated food before preparation and serving, and identify the emergence of new norovirus strains.
Other countries have done surveillance for norovirus illnesses; what are the barriers to doing so for the US population?
The UK, the Netherlands, and Australia conducted large community-based studies to estimate the fraction of acute gastroenteritis attributable to norovirus and other pathogens. These studies are very expensive to implement, costing millions of dollars. It would be costly and complex, but could be done here if we devoted the time and money to do it. It is a matter of priorities. In the United States, public health authorities think it is more efficient to focus on improving surveillance, including norovirus in outbreak reporting. However, CDC is engaged in numerous efforts to better assess the burden of norovirus using a variety of methods. When the burden of foodborne disease is estimated again, we will likely use norovirus data from these special studies, outbreaks, or other surveillance gathered here in the United States.
Norovirus can be transmitted through contact with contaminated objects in the environment, so why is it being included in the estimate of foodborne illness?
Although norovirus is, indeed, easily transmitted by touching contaminated objects in the environment as well as by direct person-to-person contact with an infected person, it is also transmitted commonly through food.
- Most often, food is contaminated by infected food handlers.
- Food may also be contaminated if it is grown in or irrigated with water contaminated with norovirus, as has been shown with oysters, lettuce, and raspberries.
- As we did when we estimated the number of foodborne illnesses for each of the other known pathogens, we multiplied the total estimated cases of norovirus-related acute gastroenteritis by the foodborne fraction for the pathogen.
- The foodborne fraction was derived from outbreak surveillance data, risk factor studies, and a literature review.
- This gave us an estimate of the proportion of norovirus infections that were transmitted through food.
What is the government doing to lower the burden of norovirus-related illnesses?
Food handlers are often implicated in outbreaks of norovirus illnesses.
- Many local and state health departments require that food handlers and preparers with gastroenteritis not work until 2 or 3 days after they feel better.
- In addition, strictly enforced rules requiring hand washing after using the bathroom and before handling food items is important in preventing the spread of this virus, even when food handlers do not have symptoms of gastroenteritis.
- Food handlers who were recently sick can often be given different duties in the restaurant so that they do not have to handle food (for example, working the cash register or serving as a host or hostess).
- The presence of kitchen managers trained in appropriate food hygiene practices may also reduce contamination during food preparation.
- The US Environmental Protection Agency has designated several effective disinfectants for killing norovirus. These cleaners should be used in food service, child care, health care, and other settings where transmission of norovirus is likely.
CDC is engaged in additional research to evaluate the specific foods and points in the food distribution systems at which norovirus contamination occurs, as well as the factors that contribute to contamination. These efforts may help identify control points at which interventions can be made to reduce norovirus contamination of food and the associated burden of illness.
There is also ongoing research towards development of a norovirus vaccine. Preliminary evidence shows that this may indeed be an effective strategy, although a great deal of work remains before a vaccine could be available.
The paper on known agents says that more accurate assessment of the foodborne norovirus illness rate is largely responsible for the big drop in the overall number of foodborne illnesses. Can you explain that in plain language?
- In the 1999 estimates, which were based on the best available data which had substantial limitations, the proportion of norovirus-related illnesses that was foodborne was estimated to be 40%.
- In the 2011 estimates, which were based on data from recently reported outbreaks and studies from other developed countries, the proportion of norovirus illnesses that was foodborne was estimated to be 26%.
- We believe that the 2011 estimate (26%) is a more accurate number than 40%. The 2011 estimate would probably have been more accurate in 1999, too, but it was not available then.
- Because norovirus causes millions of illnesses, the drop in the proportion of norovirus-related foodborne illnesses resulted in a sizeable drop in the estimated proportion of foodborne illnesses from all known foodborne pathogens—from 36% in 1999 to 25% in the 2011 study.
- The new, smaller proportion was also used to estimate the foodborne proportion of illnesses from unspecified agents, thus yielding a different overall estimate of foodborne illnesses than in 1999.

The paper says that the estimates help direct food policy. Specifically, what decisions are made based on the burden estimates?
The new estimates identify and rank the most important known pathogens responsible for causing foodborne illness, hospitalizations, and deaths. They provide a foundation for priority setting for interventions, policy development, research and analyses, and advocacy. Regulatory agencies can use these data to conduct risk analyses required in the rulemaking process. Prevention efforts should focus on these pathogens, because these are the pathogens that are causing the biggest problem. Among the 31 known foodborne pathogens:
- Norovirus caused the most illnesses.
From a broad public health perspective, what needs to happen to cause a major decrease in the burden of foodborne illness?
Many actions need to occur for major decreases to be seen:
- Research is needed to understand how foods become contaminated naturally in growing environments or during production, packaging, transporting, and/or preparing processes, so that all involved can take prevention measures at each step in the process.
- Policies need to be in place across the farm-to-fork continuum that support research, prevention, and early identification of and speedy response to problems.
- Everyone needs to adopt practices known to prevent foodborne illness— farms following best practices for safe production of produce or milk or meat, restaurants following practices outlined in the Food Code, and members of the public following the “clean, separate, cook, and chill” guidelines. We all have a role in preventing foodborne illnesses.
This paper gives us more accurate data on the pathogens causing foodborne illness in the United States. Next, we need to better understand what foods are causing these illnesses and where foods are being contaminated. CDC publishes data on the attribution of outbreak-associated illnesses to food commodities in the MMWR. We are currently enhancing this approach by using outbreak data to attribute the burden of illnesses caused by known agents and to food commodities using the new foodborne illness estimates.
Do you know if anyone is working on an estimate of the economic burden of foodborne illness using the figures in the new paper?
Yes, scientists have used the 2011 figures to update estimates of the cost and quality-adjusted and disability-adjusted life years of foodborne illness, including:
- Scallan E, Hoekstra RM, Mahon BE, Jones TF, Griffin PM. An assessment of the human health impact of seven leading foodborne pathogens in the United States using disability adjusted life years. Epidemiol Infect. 2015 Oct;143(13):2795-804. doi: 10.1017/S0950268814003185. Epub 2015 Jan 30.
- Minor T, Lasher A, Klontz K, Brown B, Nardinelli C, Zorn D. The per case and total annual costs of foodborne illness in the United States. Risk Anal. 2015 Jun;35(6):1125-39. doi: 10.1111/risa.12316. Epub 2015 Jan 2.
- Hoffmann S, Batz MB, Morris JG Jr. Annual cost of illness and quality-adjusted life year losses in the United States due to 14 foodborne pathogens. J Food Prot. 2012 Jul;75(7):1292-302. doi: 10.4315/0362-028X.JFP-11-417.
- Scharff R. Economic burden from health losses due to foodborne illness in the United States. J Food Prot. 2012 Jan;75(1):123-31. doi: 10.4315/0362-028X.JFP-11-058.
When will the next estimate of foodborne illness be done? Do you anticipate that further changes in technology and methods will cause the next estimate to change as dramatically as the 2011 estimate?
The burden of foodborne illness will likely be estimated again in about 10 years. New innovations and discoveries are occurring all the time in public health, so it is reasonable to think that methodologies and data sources will have changed by the time we do the next estimates. It is difficult to anticipate how those changes might affect the estimates, but if surveillance systems are maintained or expanded we expect that the accuracy will increase with each new improvement in data or methodology.
Where can I find more information about the seven pathogens that cause 90% of illnesses, hospitalizations, and deaths due to known pathogens?
CDC has information on these pathogens on its website.
- Campylobacter
- E. coli O157
- Clostridium perfringens
- Foodborne Illnesses and Germs
- Foodborne Illness Surveillance Systems
- Foodborne Illness Trends
- Interagency Food Safety Analytics Collaboration
- Enteric Diseases Epidemiology Branch
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can J Infect Dis
- v.14(5); Sep-Oct 2003
Food safety and foodborne disease in 21st century homes
Over the past decade there has been a growing recognition of the involvement of the home in several public health and hygiene issues. Perhaps the best understood of these issues is the role of the home in the transmission and acquisition of foodborne disease. The incidence of foodborne disease is increasing globally. Although foodborne disease data collection systems often miss the mass of home-based outbreaks of sporadic infection, it is now accepted that many cases of foodborne illness occur as a result of improper food handling and preparation by consumers in their own kitchens. Some of the most compelling evidence has come from the international data on Salmonella species and Campylobacter species infections.
By its very nature, the home is a multifunctional setting and this directly impacts upon the need for better food safety in the home. In particular, the growing population of elderly and other immnocompromised individuals living at home who are likely to be more vulnerable to the impact of foodborne disease is an important aspect to consider. In addition, some developed nations are currently undergoing a dramatic shift in healthcare delivery, resulting in millions of patients nursed at home. Other aspects of the home that are unique in terms of food safety are the use of the home as a daycare centre for preschool age children, the presence of domestic animals in the home and the use of the domestic kitchen for small-scale commercial catering operations. At the global level, domestic food safety issues for the 21st century include the continued globalization of the food supply, the impact of international travel and tourism, and the impact of foodborne disease on developing nations.
A number of countries have launched national campaigns to reduce the burden of foodborne disease, including alerting consumers to the need to practice food safety at home. Home hygiene practice and consumer hygiene products are being refined and targeted to areas of risk, including preventing the onward transmission of foodborne illness via the inanimate environment. It has been said that food safety in the home is the last line of defense against foodborne disease, and it is likely that this will remain true for the global population in the foreseeable future.
THE INCIDENCE OF FOODBORNE DISEASE
There are many indicators that point to the fact that the incidence of foodborne disease is increasing globally, and is a substantial cause of morbidity and mortality worldwide. For industrialized countries in general, it has been estimated that up to one-third of the population suffer a foodborne illness each year ( 1 ). In the United States, foodborne diseases cause an estimated 76 million episodes of illness annually ( 2 ). Although the vast majority of cases are mild, a significant number of deaths do occur and the high levels of acute infections and chronic sequelae lead to billions of dollars in medical costs and lost productivity ( 3 ).
It can be assumed that the prevalence of foodborne disease in the developing world is even higher ( 4 ), although it is difficult to obtain the data that would support this assumption. While it has long been considered that most cases of diarrhea in developing countries are waterborne, Kaferstein ( 5 ) has recently stated that it is a grave mistake to ignore the role of contaminated food and that there is an urgent need to integrate food safety, along with water and sanitation programs, as an essential strategy to prevent diarrhea. A recent study of campylobacteriosis in developing countries ( 6 ) gave an insight into the prevalence of Campylobacter species, which is the most commonly isolated bacterial pathogen from children under two years of age suffering from diarrhea. Isolation rates for children under five years of age were estimated to be between 40,000 per 100,000 and 60,000 per 100,000, compared with 300 per 100,000 in developed countries. The study found that the major sources of human infection were food and environmental contamination and a survey of retail poultry sold in Bangkok and Nairobi ( 6 ) found Campylobacter species contamination rates of between 40% and 77%. Coker et al ( 6 ) reported that this disease is projected to remain one of the top ten isolated bacterial pathogens globally in 2020. Campylobacteriosis is considered to be a greater burden in the developing world, partly because Campylobacter species-associated diarrhea and bacteremia occur in HIV/AIDS patients.
THE ROLE OF THE HOME IN FOODBORNE DISEASE
Although foodborne disease data collection systems often miss the mass of home-based outbreaks of sporadic infection, it is now widely accepted that many cases of foodborne illness occur as a result of improper food handling and preparation by consumers in their own kitchens, as shown in a review of studies from both Europe and North America ( 7 ). In addition, a study of Escherichia coli O157 outbreaks in the United States ( 8 ) found that 80% of suspect hamburgers were prepared and eaten at home. In Australia, approximately 90% of Salmonella species infections are generally thought to be associated with nonmanufactured foods and the home ( 9 ). Data available from Canada covering 1996 and 1997 has identified the home as the most common exposure setting for cases of Salmonella species, Campylobacter species and pathogenic E coli infection ( 10 ).
There are a number of factors which are likely to contribute to outbreaks of foodborne illness in the home, including a raw food supply that is frequently contaminated, a lack of awareness among the general public, mistakes in food handling and food preparation at home and the deliberate consumption of raw and undercooked foods of animal origin, often described as 'risky eating behaviour' ( 4 ).
Raw foods, including meat and poultry, raw eggs, fish and shellfish, and fruits and vegetables, should all be considered as potential entry sources of foodborne pathogens into the home. The list of infectious agents that have been introduced into the home via food includes species of Salmonella, Camylobacter, Listeria and E coli O157 ( 11 ).
The human and animal occupants of the home can also serve as sources of foodborne pathogens. Humans and animals can both serve as symptomatic and nonsymptomatic carriers and also as postsymptomatic excreters. Pathogens can be transferred from various sources to inanimate contact surfaces in the home or directly to other foods or human occupants via transient carriage on the hands. Foodborne agents that have been introduced into the home via humans include species of Salmonella, Shigella sonnei, Staphylococcus aureus , rotavirus and hepatitis A virus ( 11 ).
The four most common mistakes in handling and preparing food at home are the inappropriate storage of food (including inadequate refrigeration, the failure to attain a required cooking and/or reheating temperature), any actions that result in cross-contamination, and the presence of an infected food handler. In a study of 101 home-based outbreaks ( 12 ), it was determined that inappropriate food storage and cross-contamination were the most prevalent mistakes, accounting for 50% and 28% of reported causative factors, respectively.
FACTORS THAT IMPACT FOOD SAFETY INSIDE THE 21 st CENTURY HOME
In order to understand the challenges to food safety in the home, it is worthwhile to consider the relevant elements that comprise a typical modern-day home in this early part of the 21 st century. It is also worth noting that in many parts of the world, the home is in fact a multifunctional setting comprising many activities that may have an impact on the need for, and practice of, food safety.
First and foremost, the home is a residence containing occupants of mixed ages and health statuses. In many parts of the world the numbers of immunocompromised individuals living in the community is on the increase and, amongst other things, these people are often at a higher risk for the acquisition of foodborne disease as well as for a more severe disease outcome. In the United States, the population of immunocompromised individuals is estimated at more than 30 million people ( 13 ). In many countries of the developed world, the elderly population is the fastest growing segment of the population, as for example in the United Kingdom, where there are currently nine million senior citizens, most of them living at home ( 14 ). For the developing world, one only has to consider the impact of the AIDS epidemic and the numbers of people living with HIV/AIDS to get some measure of the size of the immunocompromised populations in these areas ( 15 ).
With a dramatic shift in healthcare delivery, the home in the United States is increasingly playing a role as an extension to, or replacement for, traditional in-hospital care. It is estimated that eight million patients are now nursed at home, with 66% of them being over 65 years old ( 16 ). Again, this puts a renewed emphasis on the need for food safety in the home, much as might be expected if these patients were being cared for within the hospital.
Another growing home-based activity that may impact food safety in the home is the presence of young children in home-based daycare. In the United States, 75% of under-five-year-olds are currently enrolled in daycare ( 17 ), representing 13 million preschoolers and six million infants. Much of this child care is home-based, with 25% of all children cared for by relatives and 5% by in-home caregivers. There are many reports of outbreaks of infectious diseases, including diarrhea, in children's day care settings ( 18 ) and the potential for infection to spread within the home via food is inevitably increased in these situations. In addition, small and/or unlicensed home-based daycare settings are less likely to have outbreaks reported and investigated, and may, therefore, miss advice and information about the importance of appropriate food safety practices.
In addition to its human occupants, the home is frequently shelter to a number of pets, ranging from mundane varieties to the exotic, and many zoonoses, including some that can cause foodborne infections, can be acquired from both. Salmonella species and other enteropathogens have long been recognized in association with domestic pets, such as cats and dogs ( 19 ). Household cats and dogs may also serve as reservoirs for species of Campylobacter and, thus, are potential sources of infection (20). Exotic pets may also serve as a source of enteropathogens into the home ( 21 ). More than 50% of homes in the English-speaking world have cats and dogs ( 14 ), with 14 million cats and dogs in the United Kingdom, 60 million in the United States and an estimated 17.8 million household pets in Australia, with three in every five Australian households containing at least one pet ( 22 ). The role of household pets in the acquisition of Salmonella species infections by infants was described by Schutze et al ( 23 ). It was found that infants in this study were probably more likely to have acquired infections by direct contact with inanimate surfaces, such as floors, that had been contaminated by household pets, than by the consumption of contaminated foods.
Finally, when considering the question of food safety in the home, we usually think of food that is prepared and served to the home occupants. However, we should also consider that the home kitchen may also be used for small home-based business operations that prepare food for catered functions outside of the home, as well as for bake sales, school and church picnics, etc. In all of these examples, food prepared at home is served to a wider community. These catering activities are usually unregulated, often take place in kitchens with inadequate facilities and equipment, and are carried out by people who may not have taken a training course in food safety. A study of home-based catering operations in the in the United Kingdom noted that food was stored inappropriately in the home kitchen on 50% of occasions ( 12 ).
GLOBAL IMPACTS ON FOOD SAFETY IN THE HOME
There are also a number of global factors that have an impact on food safety inside the 21 st century home. In particular, the globalization of the food supply impacts homes all over the world.
World meat consumption is expected to double between 1983 and 2020, to 300 million metric tons, and most of this increase will occur in developing countries ( 24 ). The impact on food safety for homes in these countries may be significant, considering that meat processing may not be well regulated, home kitchens may not be equipped for storage and preparation of raw meats and the population may not be familiar with the general food safety guidelines for meat storage and preparation, especially where the consumption of large quantities of meat protein is a new phenomenon. The aforementioned study on campylobacteriosis in the developing world ( 6 ) indicates the potential magnitude of the problem surrounding poultry production.
Import statistics indicate that more than 50% of fresh vegetables in the developed world marketplace are imported from developing countries ( 25 ), prompting food safety experts to quip that consumers only have to travel as far as the local foodmarket and home again to experience 'traveller's diarrhea'.
International travel and tourism to countries with poor standards of food hygiene may also impact the home. Globally, 1.6 billion people travel by air each year ( 26 ). Rapid air travel means that people who have contracted gastroenteric infections may carry these agents back into their homes, with the potential for further spread within the family and the immediate community, both directly by person-to-person contact and indirectly by cross-contamination into the food prepared at home. The potential for this type of transmission is seen in a World Health Organization report ( 27 ) that states that 64% of tourists exiting Thailand in 1995 were suffering from diarrhea.
IMPROVING FOOD SAFETY IN THE 21 st CENTURY HOME
It has been said that there are three major lines of defense against foodborne disease ( 4 ). The first aims at improving the hygienic quality of raw foodstuffs; the second utilizes food processing technologies such as pasteurization and irradiation, and employs hazard analysis and critical control point (HACCP) concepts; and the third line of defense concerns the education of all food handlers, including home-based food handlers. There are a number of national campaigns, for example the Canadian Partnership for Consumer Food Safety Education in Canada ( 28 ), the Partnership for Food Safety Education in the United States ( 29 ), the Food Standards Agency in the United Kingdom ( 30 ), and international campaigns, such as the World Health Organization's Food Safety Program ( 31 , that aim to inform and educate the general public about the need to better understand and practice food safety in the home. These campaigns are comprehensive and address real concerns, but inevitably tend to be web and print media-based and, in this respect, they are a passive form of information transfer and are likely to be taken up only by that segment of the population that is actively searching for information. In many countries, the subject of food safety was traditionally taught as a part of the home economics curriculum in schools, but in recent years the teaching of home economics has largely disappeared from many national education programs and, as a result, food safety is not taught. In addition, changes in family structure, changes in family meal practices and changes in women's roles in the home and workplace have resulted in a breakdown in the transfer of information about safe food practices within the family. With increasing concern in many countries about the levels of foodborne disease and the huge national economic burden associated with these levels, the introduction of mandatory food safety education programs across schools should be considered as a means of actively educating and engaging the population in a basic health issue.
In practical terms, food safety education and information is increasingly incorporating the targeted hygiene approach developed and described by the International Hygiene Forum in their Guidelines for prevention of infection and cross infection in the domestic environment ( 32 ). Targeted hygiene is a risk-based approach to hygiene practice in the home, similar to the HACCP approach so widely used in the commercial food sector. Targeted hygiene assesses the relative need for a hygiene intervention based upon the source of pathogens into the home, the potential routes of transfer of pathogens within the home and the likely risk posed by the transfer of these agents to a family member. Recommendations can then be given for safe and effective hygiene procedures aimed at eliminating pathogens from those surfaces that present a risk, thereby reducing the risk of pathogen transfer to other sites and surfaces.
Foodborne disease will continue to be a matter of major concern around the world in the foreseeable future, despite some important national successes at reducing the levels of certain pathogens in foods resulting from better farm practices, food processing regulations, etc. Therefore, it has to be concluded that the 21 st century home will also continue to remain the last line of defense against foodborne pathogens. Public education is seen as a key factor in improving food safety practices in the home. The benefits of food hygiene education would include not only a reduction in the occurrence of foodborne illness at home, but also a population better prepared to meet the needs of the food industry and food service sectors of local and national economies.

COMMENTS
"Food-borne Disease Prevention and Risk Assessment" is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how food-borne disease is still a global threat to health today and to be able to target strategies to reduce its prevalence. Despite decades of government and industry interventions, food-borne disease remains unexpectedly high in ...
Foodborne diseases can be both acute and chronic, and stem from three sources: biological, chemical, and physical. Bacteria, viruses, and parasites, are the main biological hazards causing acute foodborne diseases. Certain biological toxins can also be considered as causing acute effects, such as most seafood toxins, and these are discussed ...
Food-borne illnesses and diseases are major threats to human health and lives with over 200 foodborne diseases identified . ... This paper reviews the use of culture-based methods, immunological assays, PCR and Next Generation Sequencing-based approaches. ... In addition, more research should be carried out on the development of more effective ...
Introduction. Foodborne diseases (FBD) still cause a substantial public health, economic and social burden worldwide. Recognizing the need to measure the burden and distribution of FBD and encourage evidence-informed policies, in 2015 the World Health Organization (WHO) reported the first estimates of global and regional disease burden due to 31 foodborne hazards [1].
What is a foodborne disease outbreak? A foodborne disease outbreak occurs when two or more people develop a similar illness after ingesting the same contaminated food or drink (WHO, 2008). In some countries, only one case of a rare but severe foodborne disease - like botulism or chemical intoxication - is also considered an outbreak.
Food-borne diseases have a high worldwide occurrence, substantially impacting public health and the social economy. ... predicting disease outbreaks and analyzing the genes of disease pathogens. Foodborne illness research has been enlightened by the effective use of ML in epidemiology; ... The following is the rest of the paper: ...
Versions Notes. "Food-borne Disease Prevention and Risk Assessment" is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how food-borne disease is still a global threat to health today and to be able to target strategies to reduce its prevalence. Despite decades of government and ...
Foodborne diseases pose a significant global health burden. For example, 299 foodborne disease outbreaks occurred in the United States in 2020, causing 5,987 illnesses, 641 hospitalizations, and fourteen deaths (CDC, 2022).In Europe, 3,166 foodborne disease outbreaks occurred during the same period, resulting in 22,010 illnesses, 1,838 hospitalizations, and 48 deaths (EFSA, 2022).
consumption of contaminated food, pathogenic. bacteria, viruses, or p arasites that contaminate food, as well as chemical or natural toxins such as. poisonous mushrooms. It also r eferred to food ...
"Food-borne Disease Prevention and Risk Assessment" is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how ...
Current landscape of national burden of foodborne disease studies. The concept of burden of disease was developed in the 1990s by the Harvard School of Public Health, the World Bank and the WHO to describe death and loss of health due to diseases, injuries and risk factors for all regions of the world [].While burden of disease can be expressed using various indicators, such as incidence ...
Additionally, to ensure food safety and prevent foodborne disease outbreaks, the development of novel methods for the microbiological detection and identification of foodborne pathogens is of great importance and, therefore, welcomed as a topic in this Special Issue, taking both original research papers and reviews into consideration for ...
Abstract. "Food-borne Disease Prevention and Risk Assessment" is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how food-borne ...
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications. ... Foodborne disease caused by ...
Background This study aimed to identify the epidemiology, seasonality, aetiology and clinical characteristics of sporadic foodborne diseases in Zhejiang province during 2016-2020. Methods Descriptive statistical methods were used to analyze the data from surveillance network established by the Zhejiang Provincial Center for Disease Control and Prevention. There were 31 designated hospitals ...
Foodborne Pathogens and Disease is a monthly peer-reviewed international journal that publishes original research articles and short communications on important new information on foodborne pathogens research and diseases caused by foodborne pathogens. Foodborne Pathogens and Disease invites scientists from all countries to submit manuscripts ...
His lectures and papers are arguably some of the most significant illustrations of the foundation of public health prevention philosophy and practice today. ... The CDC established FoodCORE (Foodborne Diseases Centers for Outbreak Response Enhancement), improving foodborne disease outbreak response capacity in ... VA Medicinal Cannabis Research ...
A foodborne disease occurs when a person eats a contaminated food product containing harmful pathogens, which then grow in the intestinal tract and cause illness. Depending on the pathogen, organism, or chemical, foodborne illness symptoms can range from mild to severe and can last from a few hours to several days.
Food Safety Conditions in Home-Kitche ns is defined as adeq uate conditions for stor age and production o f. food and meals, as we ll as adequate conditi ons for water supply a nd sanitary sewage ...
Foodborne diseases are an important public health burden in the United States. First, we estimate that 31 of the most important known agents of foodborne disease found in foods consumed in the United States each year cause 9.4 million illnesses, 55,961 hospitalizations, and 1,351 deaths. Second, not all agents of foodborne disease are known or ...
Foodborne microorganisms substantially impact food safety and contribute considerably to the public health and economic burden of infectious diseases worldwide. In the Special Issue on "Foodborne Pathogens: Infections and Pathogenesis", seven research papers and three reviews were published, between February 2022 and January 2023.
There are a few reports regarding the knowledge, attitude, and practice (KAP) of food handlers about food safety in some subcities of Addis Ababa; 93.7% of food handlers had adequate knowledge of food borne diseases, 52.3% of food handlers had a poor food handling practice in Addis Ababa University students' cafeteria , and 27.4% of food ...
Foodborne infection is a major health issue and its impact on global social and economic development remains unknown ().A paper published in the journal Nature estimates 30% of all infections over the last 60 years were Foodborne ().The Centre for Disease Control in the United States estimates that 76 million people per year are affected by Foodborne illness, with 300,000 requiring hospital ...
At the global level, domestic food safety issues for the 21st century include the continued globalization of the food supply, the impact of international travel and tourism, and the impact of foodborne disease on developing nations. A number of countries have launched national campaigns to reduce the burden of foodborne disease, including ...