

Bipolar Awareness: Understanding and Supporting Individuals with Bipolar Disorder
Amidst the vibrant spectrum of human emotions, bipolar disorder paints a complex and often misunderstood portrait of mental health, challenging society to look beyond the surface and embrace empathy, awareness, and support. This mental health condition, characterized by extreme mood swings ranging from manic highs to depressive lows, affects millions of individuals worldwide, impacting their daily lives, relationships, and overall well-being.
Bipolar disorder, formerly known as manic depression, is a chronic mental health condition that affects approximately 2.8% of the adult population in the United States alone. The disorder is characterized by alternating episodes of mania or hypomania (periods of elevated mood and increased energy) and depression (periods of low mood and decreased energy). These episodes can last for days, weeks, or even months, significantly impacting an individual’s ability to function in their personal and professional lives.
The prevalence of bipolar disorder underscores the critical importance of raising awareness about this condition. By fostering a deeper understanding of bipolar disorder, we can create a more compassionate and supportive environment for those affected by it. Increased awareness can lead to earlier diagnosis, improved access to treatment, and reduced stigma surrounding mental health issues.
National Bipolar Day: A Day to Educate and Advocate
National Bipolar Day, observed annually on March 30th, serves as a powerful platform to educate the public about bipolar disorder and advocate for those affected by it. This day was established to coincide with the birthday of Vincent van Gogh, the renowned Dutch post-impressionist painter who is believed to have suffered from bipolar disorder.
The significance of National Bipolar Day lies in its ability to bring together individuals, organizations, and communities to raise awareness about bipolar disorder. It provides an opportunity to share accurate information, dispel myths, and promote understanding of the challenges faced by those living with the condition.
On National Bipolar Day, various activities and events are organized to engage the public and promote awareness. These may include:
1. Educational seminars and workshops 2. Support group meetings and discussions 3. Art exhibitions showcasing works by individuals with bipolar disorder 4. Social media campaigns using hashtags like #NationalBipolarDay 5. Fundraising events for bipolar disorder research and support programs
These initiatives play a crucial role in promoting understanding and empathy through awareness campaigns. By sharing personal stories, providing factual information, and encouraging open dialogue, National Bipolar Day helps to break down barriers and foster a more inclusive society for individuals with bipolar disorder.
World Bipolar Day 2018: Spreading Awareness Globally
World Bipolar Day, celebrated annually on March 30th, is a global initiative aimed at raising awareness about bipolar disorder on an international scale. The day was initiated by the Asian Network of Bipolar Disorder (ANBD), the International Bipolar Foundation (IBPF), and the International Society for Bipolar Disorders (ISBD) to bring world attention to bipolar disorder and eliminate social stigma.
In 2018, World Bipolar Day focused on the theme “Bipolar Disorder: Know Your Triggers.” This theme emphasized the importance of understanding personal triggers that can lead to manic or depressive episodes, empowering individuals with bipolar disorder to better manage their condition.
Throughout the day, various events and initiatives were undertaken worldwide to spread awareness and educate the public about bipolar disorder. These included:
1. Online webinars featuring mental health professionals and individuals living with bipolar disorder 2. Social media campaigns encouraging people to share their experiences using #WorldBipolarDay 3. Community outreach programs in schools and workplaces 4. Lighting up landmarks in green, the color associated with bipolar awareness
One of the most powerful aspects of World Bipolar Day 2018 was the sharing of personal stories by individuals living with bipolar disorder. These narratives provided invaluable insights into the daily challenges and triumphs of managing the condition, helping to unscramble bipolar disorder for those unfamiliar with its complexities.
For instance, Sarah, a 32-year-old graphic designer, shared her journey of living with bipolar disorder: “Some days, I feel like I can conquer the world, brimming with creative energy and ideas. Other days, it’s a struggle just to get out of bed. Learning to recognize my triggers and developing coping strategies has been crucial in managing my bipolar disorder and leading a fulfilling life.”
World Bipolar Day 2016: Highlighting Advocacy and Support
World Bipolar Day 2016 marked another significant milestone in the ongoing efforts to raise awareness about bipolar disorder. The theme for that year was “More Than A Diagnosis,” emphasizing the importance of seeing individuals with bipolar disorder as whole persons, not just their diagnosis.
The day saw numerous collaborations and partnerships between mental health organizations, healthcare providers, and advocacy groups. These collaborations aimed to provide comprehensive education about bipolar disorder, its symptoms, treatment options, and the importance of early intervention.
Key initiatives during World Bipolar Day 2016 included:
1. Launch of online resources and toolkits for individuals, families, and healthcare providers 2. Partnerships with celebrities and public figures to share their experiences with bipolar disorder 3. Community-based screening programs to promote early detection and intervention 4. Workplace seminars to educate employers about supporting employees with bipolar disorder
A crucial focus of World Bipolar Day 2016 was the importance of reducing stigma and promoting acceptance. Stigma remains one of the biggest barriers to seeking help and receiving proper treatment for bipolar disorder. By encouraging open conversations and challenging misconceptions, the day aimed to create a more supportive environment for individuals living with bipolar disorder.
Bipolar Disorder Day: Recognizing the Challenges and Offering Support
While not an officially recognized day, the concept of a “Bipolar Disorder Day” emphasizes the ongoing need for awareness and support throughout the year. This concept encourages continuous efforts to educate the public about bipolar disorder, its symptoms, diagnosis, and treatment options.
Understanding bipolar disorder is crucial for early detection and effective management. The condition is characterized by distinct episodes of mania or hypomania and depression. Manic episodes may include symptoms such as:
– Increased energy and activity – Decreased need for sleep – Racing thoughts and rapid speech – Impulsive or risky behavior
Depressive episodes, on the other hand, may involve:
– Persistent feelings of sadness or hopelessness – Loss of interest in activities once enjoyed – Changes in appetite and sleep patterns – Difficulty concentrating and making decisions
It’s important to note that bipolar symptoms in men may present differently than in women, highlighting the need for gender-specific awareness and understanding.
Diagnosis of bipolar disorder typically involves a comprehensive evaluation by a mental health professional, including a detailed medical history, physical exam, and psychological assessment. Treatment often includes a combination of medication (such as mood stabilizers and antipsychotics) and psychotherapy (such as cognitive-behavioral therapy or interpersonal therapy).
Support and resources available for individuals with bipolar disorder are crucial for managing the condition effectively. These may include:
1. Support groups (both in-person and online) 2. Educational programs for individuals and families 3. Occupational therapy to help maintain employment 4. Crisis hotlines for immediate support during difficult times
Bipolar bracelets have also gained popularity as a visible symbol of support and awareness, serving as a reminder of the wearer’s journey or as a conversation starter to educate others about the condition.
World Bipolar Day 2022: Looking to the Future
As we look ahead to World Bipolar Day 2022, the focus continues to be on raising awareness, promoting understanding, and improving the lives of individuals with bipolar disorder. The theme for 2022 is expected to build upon previous years’ efforts, emphasizing the importance of holistic care and support for those living with bipolar disorder.
Anticipated activities for World Bipolar Day 2022 include:
1. Virtual conferences and webinars featuring leading researchers and clinicians 2. Global social media campaigns to share information and personal stories 3. Launch of new resources and support tools for individuals and families 4. Collaborative research initiatives to advance understanding and treatment of bipolar disorder
Recent advancements in research, treatment, and support for bipolar disorder offer hope for improved outcomes. These include:
– Development of new medications with fewer side effects – Increased understanding of the genetic factors contributing to bipolar disorder – Innovative psychotherapy approaches tailored for bipolar disorder – Integration of digital health technologies for mood monitoring and early intervention
The role of advocacy and community support remains crucial in improving the lives of individuals with bipolar disorder. Grassroots organizations, online communities, and bipolar quotes shared on social media platforms continue to play a vital role in providing support, sharing information, and reducing stigma.
As we continue to raise awareness about bipolar disorder, it’s important to remember that understanding and support are ongoing processes. The journey towards better mental health care and reduced stigma requires consistent effort and dedication from individuals, communities, and society as a whole.
Bipolar Day , whether observed nationally or globally, serves as a powerful reminder of the importance of mental health awareness. It challenges us to look beyond stereotypes and misconceptions, encouraging empathy and understanding for those living with bipolar disorder.
The ongoing efforts to raise awareness about bipolar disorder are crucial in creating a more inclusive and supportive society. By continuing to educate ourselves and others, we can help reduce the stigma associated with mental health conditions and promote a culture of acceptance and support.
As we move forward, let us remember that every day is an opportunity to learn, understand, and support individuals with bipolar disorder. Whether it’s through sharing information, offering a listening ear, or advocating for better mental health policies, each of us has a role to play in creating a world where individuals with bipolar disorder can thrive.
In the words of Kay Redfield Jamison, a clinical psychologist and author who has written extensively about her own experiences with bipolar disorder, “We all build internal sea walls to keep at bay the sadnesses of life and the often overwhelming forces within our minds. In whatever way we do this—through love, work, family, faith, friends, denial, alcohol, drugs, or medication—we build these walls, stone by stone, over a lifetime.”
Let us continue to build bridges of understanding and support, ensuring that no one faces the challenges of bipolar disorder alone. Through awareness, education, and compassion, we can create a world where the bipolar flag flies high, symbolizing hope, resilience, and unity in the face of mental health challenges.
References:
1. National Institute of Mental Health. (2021). Bipolar Disorder. Retrieved from https://www.nimh.nih.gov/health/topics/bipolar-disorder
2. International Bipolar Foundation. (n.d.). World Bipolar Day. Retrieved from https://ibpf.org/learn/programs/world-bipolar-day/
3. Depression and Bipolar Support Alliance. (n.d.). Bipolar Disorder Statistics. Retrieved from https://www.dbsalliance.org/education/bipolar-disorder/bipolar-disorder-statistics/
4. American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
5. Jamison, K. R. (1995). An Unquiet Mind: A Memoir of Moods and Madness. New York: Vintage Books.
6. World Health Organization. (2019). Mental disorders. Retrieved from https://www.who.int/news-room/fact-sheets/detail/mental-disorders
7. National Alliance on Mental Illness. (n.d.). Bipolar Disorder. Retrieved from https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Bipolar-Disorder
8. Goodwin, F. K., & Jamison, K. R. (2007). Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression (2nd ed.). New York: Oxford University Press.
Similar Posts

Bipolar Fatigue: Understanding and Overcoming the Challenges
Exhaustion creeps in like an unwelcome shadow, draining the vibrant colors from life’s palette—welcome to the world of bipolar fatigue, a relentless adversary that countless individuals battle daily. This pervasive symptom of bipolar disorder can be overwhelming, affecting every aspect of a person’s life. However, understanding its nature and learning effective management strategies can help…

Understanding Postpartum Depression Disability Leave in California
Postpartum depression is a serious mental health condition that affects many new mothers, often requiring time off work to recover and care for their newborn. In California, understanding the intricacies of disability leave for postpartum depression is crucial for both employees and employers. This article delves into the details of postpartum depression disability leave in…

Divorcing a Narcissist: A Comprehensive Guide for Dealing with a Bipolar Narcissist
Shattered mirrors and emotional minefields await those brave souls who dare to untangle the Gordian knot of divorcing a bipolar narcissist. The journey ahead is fraught with challenges, but armed with knowledge and determination, it is possible to navigate this treacherous terrain and emerge stronger on the other side. Divorcing a narcissist is already a…

Newly Coined Synonyms for Depression: Expanding the Vocabulary of Mental Health Awareness
Language plays a crucial role in shaping our perception of mental health, influencing how we understand, discuss, and address various conditions. As our understanding of mental health evolves, so too must the vocabulary we use to describe these complex experiences. This is particularly true when it comes to depression, a condition that affects millions of…

Living with Someone with Bipolar: Understanding, Supporting, and Communicating
Navigating the unpredictable waves of bipolar disorder can be a challenging journey for both the individual affected and their loved ones, but with understanding, support, and effective communication, it’s possible to create a harmonious and loving relationship. The complexities of bipolar disorder often leave partners, family members, and friends feeling overwhelmed and uncertain about how…

Can Anxiety Disorder Cause Death: Understanding the Link between Anxiety and Mortality
Your heart races, your palms sweat, and your mind spirals—but could these familiar symptoms of anxiety be silently shortening your life? Anxiety disorders are more than just fleeting moments of worry or stress; they are persistent, often debilitating conditions that can have far-reaching effects on both mental and physical health. As we delve into the…

- Bipolar Disorder
Manic Depression
Reviewed by Psychology Today Staff
Bipolar disorder, also known as manic depression , is a chronically recurring condition involving moods that swing between the highs of mania and the lows of depression. Depression is by far the most pervasive feature of the illness. The manic phase usually involves a mix of irritability, anger , and depression, with or without euphoria. When euphoria is present, it may manifest as unusual energy and overconfidence, playing out in bouts of overspending or promiscuity, among other behaviors.
The disorder most often starts in young adulthood, but can also occur in children and adolescents. Misdiagnosis is common; the condition is often confused with attention -deficit/hyperactivity disorder, schizophrenia, or borderline personality disorder . Biological factors probably create vulnerability to the disorder within certain individuals, and experiences such as sleep deprivation can kick off manic episodes .
There are two primary types of bipolar disorder: Bipolar I and Bipolar II. A major depressive episode may or may not accompany bipolar I, but does accompany bipolar II. People with bipolar I have had at least one manic episode, which may be very severe and require hospital care. People with bipolar II normally have a major depressive episode that lasts at least two weeks along with hypomania , a mania that is mild to moderate and does not normally require hospital care.
- Signs of Bipolar Disorder
- Causes of Bipolar Disorder
- Treatment for Bipolar Disorder
- Living with Bipolar Disorder

The defining feature of bipolar disorder is mania. It can be the triggering episode of the disorder, followed by a depressive episode, or it can first manifest after years of depressive episodes. The switch between mania and depression can be abrupt, and moods can oscillate rapidly. But while an episode of mania is what distinguishes bipolar disorder from depression, a person may spend far more time in a depressed state than in a manic or hypomanic one.
Hypomania can be deceptive; it is often experienced as a surge in energy that can feel good and even enhance productivity and creativity . As a result, a person experiencing it may deny that anything is wrong. There is great variability in manic symptoms, but features may include increased energy, activity, and restlessness; euphoric mood and extreme optimism ; extreme irritability; racing thoughts, unusually fast speech, or thoughts that jump from one idea to another; distractibility and lack of concentration ; decreased need for sleep; an unrealistic belief in one's abilities and ideas; poor judgment; reckless behavior including spending sprees and dangerous driving, or risky and increased sexual drive; provocative, intrusive, or aggressive behavior; and denial that anything is wrong.
The duration of elevated moods and the frequency with which they alternate with depressive moods can vary enormously from person to person. Frequent fluctuation, known as rapid cycling, is not uncommon and is defined as at least four episodes per year.
Just as there is considerable variability in manic symptoms, there is great variability in the degree and duration of depressive symptoms in bipolar disorder. Features generally include lasting sad, anxious, or empty mood; feelings of hopelessness or pessimism ; feelings of guilt , worthlessness, or helplessness; a loss of interest or pleasure in activities once enjoyed, including sex; decreased energy and feelings of fatigue or of being "slowed down"; difficulty concentrating, remembering, or making decisions; restlessness or irritability; oversleeping or an inability to sleep or stay asleep; change in appetite and/or unintended weight loss or gain; chronic pain or other persistent physical symptoms not accounted for by illness or injury; and thoughts of death or suicide, or suicide attempts.
The symptoms of mania and depression often occur together in "mixed" episodes. Symptoms of a mixed state can include agitation, trouble sleeping , significant change in appetite, psychosis , and suicidal thinking. At these times, a person can feel sad yet highly energized.
About 2.8 percent of American adults have had bipolar disorder in the past year, according to the National Institute of Mental Health, and 4.4 percent experience bipolar disorder at some time in their lives. These rates are similar among men and women. Worldwide, the disorder affects about 45 million people, according to the World Health Organization.
Most people with bipolar disorder develop the condition in their late teens or early twenties, although symptoms can appear in children as young as six years old. The average age of a first episode of mania, hypomania, or depression is 18 years old for bipolar I and mid-20s for bipolar II, according to the DSM-5 .
Symptoms in children and teens are similar to those in adults and include the condition's hallmark mood swings. Children with bipolar disorder undergo extreme changes in mood and behavior, feeling unusually happy and energetic during manic episodes and becoming very sad and less active during depressive episodes. Manic episodes may involve increased energy, distractibility, grandiosity, and inability to sleep while depressive episodes may involve self-harm or suicidal thoughts and gestures, which should be taken seriously.
One key factor: bipolar is episodic while other disorders are pervasive. For example, bipolar symptoms come and go in mood swings, while disorders like ADHD tend to be more consistent if left untreated.
People often struggle with unidentified and untreated bipolar disorder for years. In fact, about two-thirds of people with bipolar disorder are misdiagnosed before bipolar is discovered.
Most of these individuals are misdiagnosed with depression. When thinking about the difference between the two, patients and clinicians can consider family history due to the genetic roots of the disorder, and personal history of unexplained excitability and euphoria or rage , self-harm, and suicidality . Antidepressants can trigger mania in some cases; it’s critical to monitor if a patient feels more agitated, irritable, aggressive, or hyperactive after beginning medication .
In the case of schizophrenia, manic episodes can include or resemble psychosis, while depressive episodes resemble the negative symptoms of schizophrenia. (Such patients may receive a diagnosis of schizoaffective disorder, bipolar type.)

Both genetic and environmental factors can create vulnerability to bipolar disorder. As a result, the causes vary from person to person. While the disorder can run in families, no one has definitively identified specific genes that create a risk for developing the condition. There is some evidence that advanced paternal age at conception can increase the possibility of new genetic mutations that underlie vulnerability. Imaging studies have suggested that there may be differences in the structure and function of certain brain areas, but no differences have been consistently found.
Life events including various types of childhood trauma are thought to play a role in spurring bipolar disorder in those who are already vulnerable to developing the condition. Researchers do know that once bipolar disorder occurs, life events can precipitate its recurrence. Incidents of interpersonal difficulty and abuse are most commonly associated with triggering the disorder.
“Family history is the strongest and most consistent factor for bipolar disorder,” states the DSM-5. The risk is 10 times greater for those who have a relative with bipolar I or bipolar II. Genes that are passed down in a family with bipolar appear to influence how the brain handles mood regulation.
When attempting to explore a bipolar diagnosis, it’s vital to understand the family history of mental health to know whether an individual may be predisposed. For example, it’s worth considering if anyone in the family, particularly one’s closest relatives, has experienced severe mood swings, intensely erratic behavior, or high irritability followed by deep sadness.
Some people with traumatic brain injuries (TBI)—due to a car accident or a sports injury, for example—experience heightened levels of anxiety , depression, and mood swings. Individuals with a TBI are four times more likely to develop a mental illness, according to a Danish study of more than 100,000 people with head injuries. People with a TBI are 28 percent more likely to develop bipolar disorder, 59 percent more likely to develop depression, and 65 percent more likely to develop schizophrenia.
Bipolar disorder has biological roots, but life experiences may trigger or exacerbate it. Many patients cite a specific psychosocial trigger for their first episode of bipolar disorder, such as a breakup, family trauma, substance use, or period of stress. Being aware of these factors is important for both identifying and treating bipolar .

Because bipolar disorder is a recurrent illness, long-term treatment is necessary. Mood stabilizer drugs are typically prescribed to prevent mood swings. Lithium is perhaps the best-known mood stabilizer, but newer drugs such as lamotrigine have been shown to cause fewer side effects while frequently obviating the need for antidepressant medication. Used alone, antidepressants can precipitate mania and may accelerate mood cycling. Getting the full range of symptoms under control may require other drugs as well, either short-term or long-term.
Nutritional approaches have also been found to have therapeutic value. Studies show that omega-3 fatty acids may help lower the number or dosage of medications needed. Omega-3 fatty acids play a role in the functioning of all brain cells and are incorporated into the structure of brain cell membranes.
Work and relationship problems can be both a cause and effect of bipolar episodes, making psychotherapeutic treatment important. Studies show that such treatment reduces the number of mood episodes patients experience. Psychotherapy is also valuable in teaching self-management skills, which help keep one's everyday ups and downs from triggering full-blown episodes.
In addition to medication management, therapy is an important component of treating bipolar disorder. Evidence-based therapies include Cognitive Behavioral Therapy—which helps patients reframe harmful or irrational thoughts to change mood and behavior—as well as Interpersonal Therapy, Family-Focused Therapy, and psychoeducational approaches. Family-Focused therapy may be particularly helpful for children and teens with bipolar disorder.
Therapy helps treat bipolar disorder through many different pathways. Therapy offers psychoeducation to improve medication compliance, skills to cope with the challenges of living with the condition, lifestyle remedies, connection to loved ones for greater support, and immediate help for crises that might trigger a manic or depressive episode. Patients come to treatment with different goals, so a therapist should encourage patients to share those goals and work collaboratively to find the right approach.
People with bipolar disorder typically need medication, but choosing the right drug or drug combination often requires some trial and error. To determine the right treatment, the psychiatrist may start with a low dose and gradually increase it based on the patient’s response and tolerance. They will seek feedback from the patient, and prescribe one medication at a time to find the best fit.
Patients may experience difficult side effects, such as fatigue, weight gain, and nausea. Lifestyle changes can help manage those symptoms —patients can exercise, maintain a healthy diet , keep a regular sleep schedule, and seek social support.
Sharing concerns about medication in therapy is important so that patients and clinicians can determine the best path forward. If one medication has not worked well, there may be other options to explore. If there are concerns around the stigma of psychiatric medication or fears of maintaining one’s sense of self, a therapist can provide clarity and support.

Bipolar disorder can wreak havoc on a person's goals and relationships. But in conjunction with proper medical care, sufferers can learn coping skills and strategies to keep their lives on track. Bipolar disorder, like many mental illnesses, is sometimes a controversial diagnosis. While most sufferers consider the disorder to be a hardship, some appreciate its role in their lives, and others even link it to greater creative output.
While the depression of bipolar disorder is hard to treat, mood swings and recurrences can often be delayed or prevented with a mood stabilizer, on its own or combined with other drugs. Psychotherapy is an important adjunct to pharmacotherapy, especially for dealing with work and relationship problems that typically accompany the disorder. Clinicians are well aware that there is no one-size-fits-all cure: An individual with a first-time manic episode will not be the same as an individual who has lived with bipolar for a decade.
The fear of losing one’s creativity, productivity, and sense of identity can prevent people from seeking help. But neglecting treatment to preserve manic energy often leads to a crash that can threaten every aspect of the person’s well-being.
A therapist can allay these concerns and redefine creativity. The intense rise of manic energy is sometimes confused for creativity rather than disorganized and reckless output; mania can delude the person into believing their skills are greater than they truly are. A therapist can help a patient with bipolar to steadily harness their creative abilities following mood stabilization and develop an organized strategy and timeline to achieve their goals.
Many individuals with bipolar disorder experience hyper-religiosity during mania. Fifteen to 22 percent of those with bipolar mania in the U.S. experience religious delusions, such as thinking that demons are watching them or that they are Christ reborn.
The complex phenomenon of spirituality involves networks of multiple brain regions. Parts of the parietal lobe are associated with feelings of spiritual transcendence, parts of the temporal and frontal cortices are involved in the storage and retrieval of religious beliefs in memory , and still other parts of the frontal lobe and limbic structures are responsible for rational and emotional aspects of religious beliefs. Dopamine levels in those with bipolar disorder may play a role in elevating religious and spiritual experiences.
The experience of bipolar disorder can differ between people. While not discounting the tremendous toll the disorder takes on many lives, some people with bipolar disorder believe the condition confers certain advantages , such as creativity, motivation , and leadership . Famous figures are often cited to illustrate the connection between genius and mental illness, such as Vincent van Gogh, Winston Churchill, and more recently, Kanye West.
One common misconception about bipolar disorder is that mania is always “good” because it’s better than being depressed. But people in a manic episode often do ignorant or foolish things, make mistakes, and hurt other people. Another misunderstanding is that actions during manic periods are fully voluntary, but the person doesn’t have complete control over their faculties.
Another misunderstanding is that treatment ends when a person is stable. Bipolar disorder is chronic, so maintaining stability, incorporating lifestyle changes, and being aware of triggers is an ongoing process.
Do you dance to the beat of your own drum, but fear that others don't hear the music?

Your mental health is unlikely to be diagnosed by #Relatable online.

A Personal Perspective: Societal pressure to be happy all the time sets us up for failure. Here’s how to overcome that trap.

Anxiety often travels with company, and many things masquerade as anxiety.

Inexplicable behavior at work deserves more than outrage. It can be a sign of mental health struggles.

Personal Perspective: The term "behavioral health" was cultivated to reduce the stigma of mental health and psychiatric services. Has it done more harm than good?

The "prodromal" phase, the early rumbles in individuals at high risk of psychosis, may present an opportunity for improved response to interventions.

A Personal Perspective: Let go of preconceived ideas about wellness tools and allow yourself the freedom to find what works for you, no matter how uncommon it seems.

New research is revealing that inherited mental illnesses are promoted by alterations in DNA that were caused by viral infection of our ancestors over a million years ago.

A Personal Perspective: It’s possible to plan a future despite the uncertainties of mental illness.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Bipolar Disorder
- Download PDF
- Order a free hardcopy
Do you have periods of time when you feel unusually “up” (happy and outgoing, or irritable), but other periods when you feel “down” (unusually sad or anxious)? During the “up” periods, do you have increased energy or activity and feel a decreased need for sleep, while during the “down” times you have low energy, hopelessness, and sometimes suicidal thoughts? Do these symptoms of fluctuating mood and energy levels cause you distress or affect your daily functioning? Some people with these symptoms have a lifelong but treatable mental illness called bipolar disorder.
What is bipolar disorder?
Bipolar disorder is a mental illness that can be chronic (persistent or constantly reoccurring) or episodic (occurring occasionally and at irregular intervals). People sometimes refer to bipolar disorder with the older terms “manic-depressive disorder” or “manic depression.”
Everyone experiences normal ups and downs, but with bipolar disorder, the range of mood changes can be extreme. People with the disorder have manic episodes, or unusually elevated moods in which the individual might feel very happy, irritable, or “up,” with a marked increase in activity level. They might also have depressive episodes, in which they feel sad, indifferent, or hopeless, combined with a very low activity level. Some people have hypomanic episodes, which are like manic episodes, but not severe enough to cause marked impairment in social or occupational functioning or require hospitalization.
Most of the time, bipolar disorder symptoms start during late adolescence or early adulthood. Occasionally, children may experience bipolar disorder symptoms. Although symptoms may come and go, bipolar disorder usually requires lifelong treatment and does not go away on its own. Bipolar disorder can be an important factor in suicide, job loss, ability to function, and family discord. However, proper treatment can lead to better functioning and improved quality of life.
What are the symptoms of bipolar disorder?
Symptoms of bipolar disorder can vary. An individual with the disorder may have manic episodes, depressive episodes, or “mixed” episodes. A mixed episode has both manic and depressive symptoms. These mood episodes cause symptoms that last a week or two, or sometimes longer. During an episode, the symptoms last every day for most of the day. Feelings are intense and happen with changes in behavior, energy levels, or activity levels that are noticeable to others. In between episodes, mood usually returns to a healthy baseline. But in many cases, without adequate treatment, episodes occur more frequently as time goes on.
| Feeling very up, high, elated, or extremely irritable or touchy | Feeling very down or sad, or anxious |
| Feeling jumpy or wired, more active than usual | Feeling slowed down or restless |
| Racing thoughts | Trouble concentrating or making decisions |
| Decreased need for sleep | Trouble falling asleep, waking up too early, or sleeping too much |
| Talking fast about a lot of different things (“flight of ideas”) | Talking very slowly, feeling unable to find anything to say, or forgetting a lot |
| Excessive appetite for food, drinking, sex, or other pleasurable activities | Lack of interest in almost all activities |
| Feeling able to do many things at once without getting tired | Unable to do even simple things |
| Feeling unusually important, talented, or powerful | Feeling hopeless or worthless, or thinking about death or suicide |
Some people with bipolar disorder may have milder symptoms than others. For example, hypomanic episodes may make an individual feel very good and productive; they may not feel like anything is wrong. However, family and friends may notice the mood swings and changes in activity levels as unusual behavior, and depressive episodes may follow hypomanic episodes.
Types of Bipolar Disorder
People are diagnosed with three basic types of bipolar disorder that involve clear changes in mood, energy, and activity levels. These moods range from manic episodes to depressive episodes.
- Bipolar I disorder is defined by manic episodes that last at least 7 days (most of the day, nearly every day) or when manic symptoms are so severe that hospital care is needed. Usually, separate depressive episodes occur as well, typically lasting at least 2 weeks. Episodes of mood disturbance with mixed features are also possible. The experience of four or more episodes of mania or depression within a year is termed “rapid cycling.”
- Bipolar II disorder is defined by a pattern of depressive and hypomanic episodes, but the episodes are less severe than the manic episodes in bipolar I disorder.
- Cyclothymic disorder (also called cyclothymia) is defined by recurrent hypomanic and depressive symptoms that are not intense enough or do not last long enough to qualify as hypomanic or depressive episodes.
“Other specified and unspecified bipolar and related disorders” is a diagnosis that refers to bipolar disorder symptoms that do not match the three major types of bipolar disorder outlined above.
What causes bipolar disorder?
The exact cause of bipolar disorder is unknown. However, research suggests that a combination of factors may contribute to the illness.
Bipolar disorder often runs in families, and research suggests this is mostly explained by heredity—people with certain genes are more likely to develop bipolar disorder than others. Many genes are involved, and no one gene can cause the disorder.
But genes are not the only factor. Studies of identical twins have shown that one twin can develop bipolar disorder while the other does not. Though people with a parent or sibling with bipolar disorder are more likely to develop it, most people with a family history of bipolar disorder will not develop it.
Brain Structure and Function
Research shows that the brain structure and function of people with bipolar disorder may differ from those of people who do not have bipolar disorder or other mental disorders. Learning about the nature of these brain changes helps researchers better understand bipolar disorder and, in the future, may help predict which types of treatment will work best for a person with bipolar disorder.
How is bipolar disorder diagnosed?
To diagnose bipolar disorder, a health care provider may complete a physical exam, order medical testing to rule out other illnesses, and refer the person for an evaluation by a mental health professional. Bipolar disorder is diagnosed based on the severity, length, and frequency of an individual’s symptoms and experiences over their lifetime.
Some people have bipolar disorder for years before it’s diagnosed for several reasons. People with bipolar II disorder may seek help only for depressive episodes and hypomanic episodes may go unnoticed. Misdiagnosis may happen because some bipolar disorder symptoms are like those of other illnesses. For example, people with bipolar disorder who also have psychotic symptoms can be misdiagnosed with schizophrenia. Some health conditions, such as thyroid disease, can cause symptoms like those of bipolar disorder. The effects of recreational and illicit drugs can sometimes mimic or worsen mood symptoms.
Conditions That Can Co-Occur With Bipolar Disorder
Many people with bipolar disorder also have other mental disorders or conditions such as anxiety disorders, attention-deficit/hyperactivity disorder (ADHD), misuse of drugs or alcohol, or eating disorders. Sometimes people who have severe manic or depressive episodes also have symptoms of psychosis, such as hallucinations or delusions. The psychotic symptoms tend to match the person’s extreme mood. For example, someone having psychotic symptoms during a depressive episode may falsely believe they are financially ruined, while someone having psychotic symptoms during a manic episode may falsely believe they are famous or have special powers.
Looking at symptoms over the course of the illness and the person’s family history can help determine whether a person has bipolar disorder along with another disorder.
How is bipolar disorder treated?
Treatment helps many people, even those with the most severe forms of bipolar disorder. Mental health professionals treat bipolar disorder with medications, psychotherapy, or a combination of treatments.
Medications
Certain medications can help control the symptoms of bipolar disorder. Some people may need to try several different medications before finding the ones that work best. The most common types of medications that doctors prescribe include mood stabilizers and atypical antipsychotics. Mood stabilizers such as lithium or valproate can help prevent mood episodes or reduce their severity. Lithium also can decrease the risk of suicide. While bipolar depression is often treated with antidepressant medication, a mood stabilizer must be taken as well, as an antidepressant alone can trigger a manic episode or rapid cycling in a person with bipolar disorder. Medications that target sleep or anxiety are sometimes added to mood stabilizers as part of a treatment plan.
Talk with your health care provider to understand the risks and benefits of each medication. Report any concerns about side effects to your health care provider right away. Avoid stopping medication without talking to your health care provider first. Read the latest medication warnings, patient medication guides, and information on newly approved medications on the Food and Drug Administration (FDA) website .
Psychotherapy
Psychotherapy (sometimes called “talk therapy”) is a term for various treatment techniques that aim to help a person identify and change troubling emotions, thoughts, and behaviors. Psychotherapy can offer support, education, skills, and strategies to people with bipolar disorder and their families.
Some types of psychotherapy can be effective treatments for bipolar disorder when used with medications, including interpersonal and social rhythm therapy, which aims to understand and work with an individual’s biological and social rhythms. Cognitive behavioral therapy (CBT) is an important treatment for depression, and CBT adapted for the treatment of insomnia can be especially helpful as a component of the treatment of bipolar depression. Learn more on NIMH’s psychotherapies webpage .
Other Treatments
Some people may find other treatments helpful in managing their bipolar disorder symptoms.
- Electroconvulsive therapy (ECT) is a brain stimulation procedure that can help relieve severe symptoms of bipolar disorder. ECT is usually only considered if an individual’s illness has not improved after other treatments such as medication or psychotherapy, or in cases that require rapid response, such as with suicide risk or catatonia (a state of unresponsiveness).
- Transcranial Magnetic Stimulation (TMS) is a type of brain stimulation that uses magnetic waves, rather than the electrical stimulus of ECT, to relieve depression over a series of treatment sessions. Although not as powerful as ECT, TMS does not require general anesthesia and presents little risk of memory or adverse cognitive effects.
- Light Therapy is the best evidence-based treatment for seasonal affective disorder (SAD), and many people with bipolar disorder experience seasonal worsening of depression in the winter, in some cases to the point of SAD. Light therapy could also be considered for lesser forms of seasonal worsening of bipolar depression.
Complementary Health Approaches
Unlike specific psychotherapy and medication treatments that are scientifically proven to improve bipolar disorder symptoms, complementary health approaches for bipolar disorder, such as natural products, are not based on current knowledge or evidence. For more information, visit the National Center for Complementary and Integrative Health website .
Coping With Bipolar Disorder
Living with bipolar disorder can be challenging, but there are ways to help yourself, as well as your friends and loved ones.
- Get treatment and stick with it. Treatment is the best way to start feeling better.
- Keep medical and therapy appointments and talk with your health care provider about treatment options.
- Take medication as directed.
- Structure activities. Keep a routine for eating, sleeping, and exercising.
- Try regular, vigorous exercise like jogging, swimming, or bicycling, which can help with depression and anxiety, promote better sleep, and is healthy for your heart and brain.
- Keep a life chart to help recognize your mood swings.
- Ask for help when trying to stick with your treatment.
- Be patient. Improvement takes time. Social support helps.
Remember, bipolar disorder is a lifelong illness, but long-term, ongoing treatment can help manage symptoms and enable you to live a healthy life.
Are there clinical trials studying bipolar disorder?
NIMH supports a wide range of research, including clinical trials that look at new ways to prevent, detect, or treat diseases and conditions—including bipolar disorder. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge to help others in the future. Researchers at NIMH and around the country conduct clinical trials with patients and healthy volunteers. Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information, visit the NIMH clinical trials webpage .
Finding Help
Behavioral health treatment services locator.
This online resource, provided by the Substance Abuse and Mental Health Services Administration (SAMHSA), can help you locate mental health treatment facilities and programs. Find a facility in your state by searching SAMHSA’s online Behavioral Health Treatment Services Locator . For additional resources, visit NIMH's Help for Mental Illnesses webpage .
If you or someone you know is in immediate distress or is thinking about hurting themselves, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org. You can also contact the Crisis Text Line ( text HELLO to 741741 ). For medical emergencies, call 911.
Talking to a Health Care Provider About Your Mental Health
Communicating well with a health care provider can improve your care and help you both make good choices about your health. Find tips to help prepare for and get the most out of your visit . For additional resources, including questions to ask a provider, visit the Agency for Healthcare Research and Quality website .
The information in this publication is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
For More Information
MedlinePlus (National Library of Medicine) ( en español )
ClinicalTrials.gov ( en español )
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health NIH Publication No. 22-MH-8088 Revised 2022

Bipolar disorder

Bipolar disorder is a serious mental illness in which common emotions become intensely and often unpredictably magnified. Individuals with bipolar disorder can quickly swing from extremes of happiness, energy, and clarity to sadness, fatigue, and confusion. These shifts can be so devastating that individuals may consider suicide.
All people with bipolar disorder have manic episodes—abnormally elevated or irritable moods that last at least a week and impair functioning. But not all become depressed.
Adapted from the Encyclopedia of Psychology
Resources from APA

Treatment and recovery from serious mental illness
Kim Mueser, PhD, talks about the progress psychology has made in treating serious mental illness

How to live with bipolar disorder
David Miklowitz, PhD, and Terri Cheney talk about diagnosis and treatments of bipolar disorder

Diagnosing and treating bipolar disorders
Patients with bipolar disorder cycle between two or more mood states, such as mania, hypomania, or depression.

Treating bipolar disorder in kids and teens
New research is helping practitioners better understand the symptoms of pediatric bipolar disorder
More resources about bipolar disorder
APA publications
Psychological Assessment of Bipolar Spectrum Disorders
Essay Service Examples Health Bipolar Disorder
Informative Speech about Bipolar Disorder
Bipolar disorder
- Proper editing and formatting
- Free revision, title page, and bibliography
- Flexible prices and money-back guarantee
Biological Factors
- People with bipolar disorder generally have problems with their moods, experiencing extreme highs and lows known as mania or hypomania, respectively.
- An individual with bipolar disorder may also develop problems with perception and thinking such as psychosis.
- They think of things that are not true otherwise known as delusions and hear or see things that are not physically present (hallucinations).
Getting help
Our writers will provide you with an essay sample written from scratch: any topic, any deadline, any instructions.
Cite this paper
Related essay topics.
Get your paper done in as fast as 3 hours, 24/7.
Related articles
Most popular essays
- Bipolar Disorder
- Helping Others
- Mental Illness
The biological model of psychology focuses on treating the underlying physical issues that might...
“No excellent soul is exempt from a mixture of madness.” Aristotle. The link between creativity...
- Human Brain
Approximately 1 in 5 people in the U.S. struggles with a mental illness every year, Hollywood is...
The memoir written by Dr. Kay Jamison, An Unquiet Mind, provides an in-depth look at an...
The research by Caldieraro et al. was designed to study the impact of psychosis on patients with...
The track I chose for this project was track two Psychological Influences of Abnormal Behavior....
- Post Traumatic Stress Disorder
Bipolar disorder is a condition that has several diagnoses. These are, Bipolar Ⅰ, Bipolar Ⅱ,...
Bipolar disorder is a debilitating mental illness that causes extreme fluctuation in mood. One...
- Human Behavior
Bipolar disorder, today, can be defined as a brain disorder that causes changes in a person’s mood...
Join our 150k of happy users
- Get original paper written according to your instructions
- Save time for what matters most
Fair Use Policy
EduBirdie considers academic integrity to be the essential part of the learning process and does not support any violation of the academic standards. Should you have any questions regarding our Fair Use Policy or become aware of any violations, please do not hesitate to contact us via [email protected].
We are here 24/7 to write your paper in as fast as 3 hours.
Provide your email, and we'll send you this sample!
By providing your email, you agree to our Terms & Conditions and Privacy Policy .
Say goodbye to copy-pasting!
Get custom-crafted papers for you.
Enter your email, and we'll promptly send you the full essay. No need to copy piece by piece. It's in your inbox!
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 03 October 2019
Thought and language disturbance in bipolar disorder quantified via process-oriented verbal fluency measures
- Luisa Weiner 1 , 2 ,
- Nadège Doignon-Camus ORCID: orcid.org/0000-0002-0295-2801 1 ,
- Gilles Bertschy 1 , 2 , 3 &
- Anne Giersch ORCID: orcid.org/0000-0002-8577-6021 1
Scientific Reports volume 9 , Article number: 14282 ( 2019 ) Cite this article
27k Accesses
22 Citations
3 Altmetric
Metrics details
- Bipolar disorder
Bipolar disorder (BD) is characterized by speech abnormalities, reflected by symptoms such as pressure of speech in mania and poverty of speech in depression. Here we aimed at investigating speech abnormalities in different episodes of BD, including mixed episodes, via process-oriented measures of verbal fluency performance – i.e., word and error count, semantic and phonological clustering measures, and number of switches–, and their relation to neurocognitive mechanisms and clinical symptoms. 93 patients with BD – i.e., 25 manic, 12 mixed manic, 19 mixed depression, 17 depressed, and 20 euthymic–and 31 healthy controls were administered three verbal fluency tasks – free, letter, semantic–and a clinical and neuropsychological assessment. Compared to depression and euthymia, switching and clustering abnormalities were found in manic and mixed states, mimicking symptoms like flight of ideas. Moreover, the neuropsychological results, as well as the fact that error count did not increase whereas phonological associations did, showed that impaired inhibition abilities and distractibility could not account for the results in patients with manic symptoms. Rather, semantic overactivation in patients with manic symptoms, including mixed depression, may compensate for trait-like deficient semantic retrieval/access found in euthymia.
“For those who are manic, or those who have a history of mania, words move about in all directions possible, in a three-dimensional ‘soup’, making retrieval more fluid, less predictable.” Kay Redfield Jamison (2017, p. 279).
Similar content being viewed by others

Syntactic complexity and diversity of spontaneous speech production in schizophrenia spectrum and major depressive disorders
Altered language network lateralization in euthymic bipolar patients: a pilot study

Natural Language Processing markers in first episode psychosis and people at clinical high-risk
Introduction.
Bipolar disorder (BD) is characterized by acute episodes of mania and depression, mixed episodes wherein depressive and manic symptoms co-occur, and periods of partial or full remission, also called ‘euthymic states’. Language disturbances such as speech pressure or poverty are among the main symptoms of acute episodes in BD 1 , and may prevail during periods of remission 2 . While early studies focused on associational fluency as a measure of creativity and thinking style in mania 3 , 4 , 5 , 6 , 7 , more recent studies have favored the use of verbal fluency tasks (VFT) with more restrained instructions (e.g., starting with a given letter or category) to tackle executive and language impairments mostly in euthymia, i.e., during periods of mood stabilization 8 . Here we investigated language disturbances, by means of both free and restrained VFT across different mood episodes of BD, to determine the contribution of clinical symptoms and executive functioning to word production in BD.
Different kinds of language disturbances have been described during mood episodes of BD. Pressure of speech, with increased rapidity of speech and racing thoughts, is a common symptom of mania, second only to elevated mood 9 . Manic speech has also been characterized as extremely combinatory, shifting quickly from one discourse structure to another, which authors have linked to distractibility and overactivation 10 . Other linguistic features frequently reported during manic episodes include increased verbosity 11 , and clang associations, i.e., associations based on sound rather than on the meaning of words 12 . In contrast, poverty of speech and increased pause times are common in depression, and have been hypothesized to be associated with psychomotor retardation and rumination 11 . In mixed episodes, linguistic features have been understudied, but phenomenological accounts suggest that patients may experience ‘disorganized flight of ideas’ 13 , distractibility and ‘crowded thoughts’ 14 , pressure and poverty of speech 15 . However, few empirical investigations have specifically addressed these thought and language abnormalities, whether in manic, depressed or mixed states. In particular, from a neurocognitive perspective, it is unclear whether manic speech is related to mechanisms such as semantic overactivation and deficient cognitive control.
VFT are widely used neuropsychological methods for studying language disorders 16 . In these tasks, subjects are instructed to generate words according to specified rules based on phonemic or semantic criteria (‘letter’ and ‘semantic’ fluency, respectively), or in the absence of a specified criterion (free word generation). Although traditionally only the total number of words produced within the allotted time period is considered, VFT are multi-faceted 17 , 18 . Indeed, it has been long known that semantically related words occur together as part of a burst of responding in recall protocols 19 . Qualitative process-oriented methods evolved based on findings relative to the dynamics of word retrieval in fluency and semantic memory tasks. Word output requires the integrity of both the storage and organization of concepts in lexico-semantic memory, and the ability to retrieve words from memory, thought to rely on executive functioning 17 . These processes underlie two aspects of word output that are responsible for optimal performance: the ability to produce words within semantic or phonological clusters, and the ability to shift to a new category, i.e., clustering and switching respectively 17 .
According to Troyer et al . 17 , clustering is defined by the production of words within semantic subcategories in the semantic fluency task (e.g., bird subcategory if the category is “animals”), and phonemic subcategories in the letter fluency task (e.g., words that rhyme). The clustering measure of interest is the cluster size, i.e. the number of words within each cluster. In their processing-oriented scoring procedure, Troyer et al . 17 considered task-consistent clustering, i.e., semantic relatedness in semantic fluency and phonemic relatedness in letter fluency. Switching was operationalized as the ability to shift from a subcategory to another. More recent qualitative scoring procedures have integrated ‘task-discrepant’ clustering, consisting of phonemic relatedness in semantic fluency or semantic relatedness in letter fluency 20 . ‘Task-discrepant’ means that when instructed to retrieve words from a given category (e.g. animals), retrieval might include phonologically-related successive words (e.g., cat and bat). Recent scoring procedures have also integrated a measure of cluster ratio (i.e., the number of clusters/number of words), arguing that mean cluster size is an ambiguous measure, as it reflects both the total number of words and the organization of the verbal output 21 . Hence the combined use of the mean cluster size and the cluster ratio is considered a better index of clustering, as it addresses respectively the integrity of lexico-semantic memory as well as retrieval organization throughout the task 22 , 23 .
In BD however, only the total word count has been considered. In a recent meta-analysis of VFT in BD, Raucher-Chéné et al . 8 found that performance in letter and semantic VFT was equally reduced in patients with BD. Most studies were conducted during euthymia (30 out of 39 studies), and only one study 24 included a group of patients in a mixed episode. Importantly, Raucher-Chéné et al . 8 found greater impairment in the semantic (but not letter) VFT in euthymic compared to manic patients. The authors argued that semantic memory dysfunction – i.e., storage and/or functional organization – could explain these results. Moreover, akin to formal thought disorder in schizophrenia, they speculated that the relative “manic advantage” in the semantic VFT was related to an over-activation of the semantic network, which supposedly underlies thought and language disturbances in mania 8 . That is, during manic episodes, the oral production of a given word might lead to faster than usual spreading of activation, hence facilitating the retrieval of more remotely associated words. If such is the case, cluster ratio should be reduced, and switches should be increased in manic and mixed groups compared to controls and euthymic and depressed bipolar groups.
Here we applied a comprehensive process-oriented method in patients with BD in five different mood episodes – i.e., mania, mixed mania, mixed depression, depression, and euthymia. To do so, total word count, but also measures of clustering and switching were calculated in three conditions of VFT – i.e., letter, semantic, and free condition: we calculated semantic and phonological cluster ratios (i.e., number of clusters/number of words), mean cluster sizes, and the raw number of switches. Consistent with earlier studies using associational paradigms 3 , 4 , we expected word production to be decreased in depressed patients and enhanced in patients with manic symptoms. The idiosyncratic combinatory and associational patterns (e.g., clanging) observed in mania 3 , 10 were expected to result in enhanced switches, and, possibly, diminished semantic clustering measures, and increased phonological clustering measures compared to healthy controls, euthymia and depression groups. We were particularly interested in the results of the mixed groups, given that distractibility is also a distinctive feature of mixed states 25 . Since linguistic abnormalities in BD were reported either in free speech or in associational fluency tasks, it was unclear, however, if they would still be observed in restricted conditions of VFT (letter or category). Because subjects have to follow specific retrieval rules, these tasks are considered more effortful 26 . Hence executive impairments and clinical symptoms such as distractibility and/or flight of ideas may result in the production of irrelevant words, i.e., errors. In contrast, if it is overactivation in patients with manic symptoms that subtends the peculiarities of manic speech instead of being the consequence of distractibility and overall executive dysfunction, then more switches should be observed while the production of irrelevant words remains stable in tasks with retrieval rules 27 .
Descriptive statistics
With the exception of working memory, performance in executive tasks was diminished in mania, mixed mania and depression compared to healthy controls. See Table 1 for detailed results on the neuropsychological tasks and the self-report questionnaires assessing clinical symptoms, i.e., racing thoughts and rumination, and the p significance level for the group effect.
Number of words
In the free condition and the letter condition, no significant difference was found in the number of words produced between groups, F(5,118) = 0.45, p = 0.81, η2 = 0.02, and F(5,118) = 0.72, p = 0.60, η2 = 0.04, respectively. In the semantic condition, the number of words produced among groups tended to differ, F(5,118) = 2.14, p = 0.07, η2 = 0.08 (Fig. 1 ). Planned comparisons revealed that the control and the manic groups tended to produce more animal words than the depressed group, F(1,118) = 4.13, p = 0.08, η2 = 0.1, and F(1,118) = 2.85, p = 0.09, η2 = 0.09, respectively. Number of errors did not differ between groups in the letter and semantic conditions, F(5,117) = 1.37, p = 0.25, η2 = 0.06, and F(5,117) = 0.80, p = 0.55, η2 = 0.03, respectively.
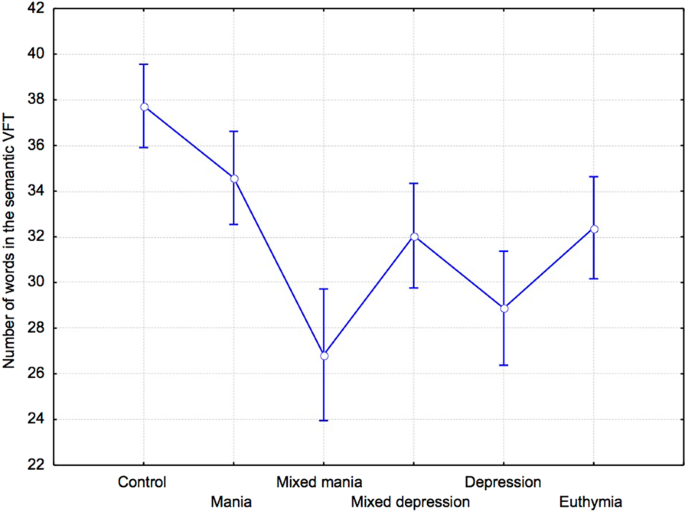
Number of words (mean and standard error) in the semantic VFT.
Cluster analyses
Semantic cluster size.
Average semantic cluster size did not differ between groups in the free, F(5,118) = 1.4, p = 0.23, η2 = 0.06, the semantic, F(5,118) = 1.4, p = 0.23, η2 = 0.06, and the letter conditions, F(5,117) = 1.56, p = 0.17, η2 = 0.06.

Ratio of semantic clusters
The ratio of semantic clusters did not differ between groups in the free, F(5,118) = 1.52, p = 0.19, η2 = 0.06, the letter, F(5,118) = 1.12, p = 0.36, η2 = 0.05, and the semantic conditions, F(5,118) = 0.97 p = 0.44, η2 = 0.42. Nevertheless, in the free condition, planned comparisons revealed that manic groups had significantly smaller cluster ratios than healthy controls, F(1,118) = 4.76, p = 0.03, η2 = 0.09, but not compared to the depressed group, F(1,118) = 0.78, p = 0.77, η2 = 0.02.
Phonological cluster size
Average phonological cluster size did not differ between groups in the free, F(5,118) = 0.94, p = 0.45, η2 = 0.04, and in the letter condition, F(5,117) = 0.35, p = 0.89, η2 = 0.01. In the semantic condition, phonological cluster size tended to differ between groups, F(5,118) = 2.11, p = 0.07, η2 = 0.09 (Fig. 2 ). As expected, planned comparisons revealed that average phonological cluster size in the semantic condition was significantly increased in the manic compared to the control, F(1,118) = 6.2, p = 0.02, η2 = 0.1, and euthymic groups, F(1,118) = 5.29,p = 0.02, η2 = 0.1. Compared to depressed patients, the difference was only tendential, F(1,118) = 3.86, p = 0.07, η2 = 0.09.
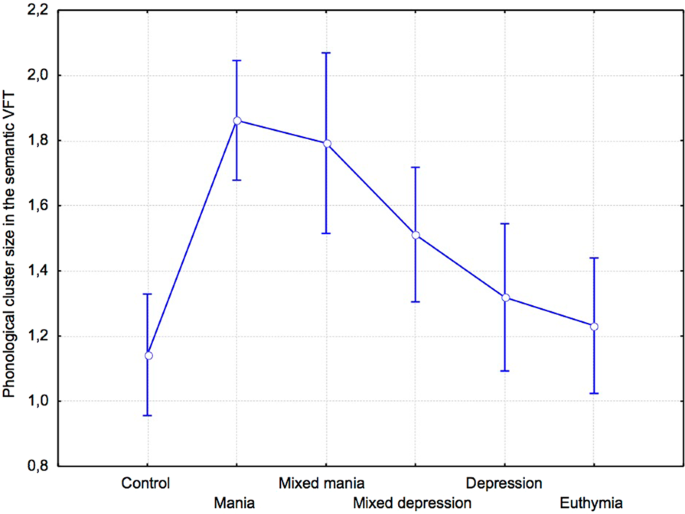
Phonological cluster size (mean and standard error) in the semantic VFT.
Ratio of phonological clusters
The ratio of phonological clusters tended to differ in the free, F(5,118) = 1.91, p = 0.09, η2 = 0.08, and the letter conditions, F(5,117) = 2.3, p = 0.06, η2 = 0.09. In the semantic condition, the ratio of phonological clusters did not differ between groups, F(5,117) = 0.89, p = 0.49, η2 = 0.04.
In the free condition, the number of switches differed significantly between groups, F(5,118) = 3.7, p = 0.004, η2 = 0.14 (Fig. 3A ). Planned comparisons showed that the number of switches was significantly increased in the manic group compared to the control, F(1,118) = 11.42, p < 0.0001, η2 = 0.26, the depressed groups, F(1,118) = 7.64, p < 0.001, η2 = 0.2, and the euthymic group, F(1,118) = 7.35, p < 0.01, η2 = 0.17. Compared to the depression group, switches were increased in the mixed depression group, F(1,118) = 4.65, p = 0.04, η2 = 0.11. In the letter and semantic conditions, there was no significant difference in the number of switches found among groups, F(5,117) = 0.48, p = 0.79, η2 = 0.02, and F(5,117) = 1.77, p = 0.12, η2 = 0.08, respectively (Fig. 3B ). In the semantic condition however, planned comparisons showed that the number of switches was significantly higher in the manic group compared to the depressed and euthymic groups, F(1,117) = 4.37, p = 0.04, η2 = 0.13, and F(1,117) = 4.5, p = 0.04, η2 = 0.13, respectively, but not the control group, F(1,117) = 0.004, p = 0.95, η2 < 0.001.
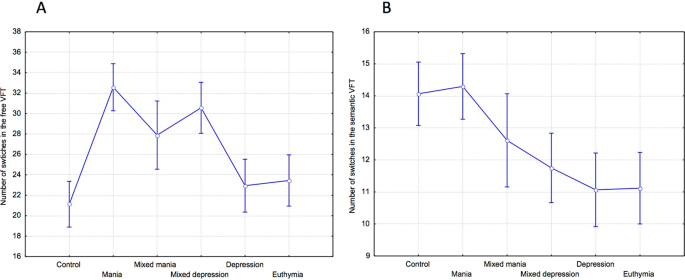
( A ) Number of switches (mean and standard error) in the free and ( B ) the semantic VFT.
Correlation and regression analyses
Correlation analyses were performed within the whole patient group (cf. Table 2 ). Increased working memory, executive functioning, and processing speed scores were related to greater verbal output in all verbal fluency tasks, whereas increased vocabulary score was only involved in semantic and letter fluency performance. Of note, similar patterns of correlations were found when the sample of patients with manic symptoms (n = 53)–i.e., mania, mixed mania and mixed depression–was considered alone (see Table 4 in supplementary information for detailed results). In addition, to investigate the relationship between process-oriented measures and word output in patients, we performed multiple regression analyses on the number of words produced in the three VFT. For the free condition, predictors accounted for 49% of the variance, with significant contributions from (i) semantic cluster size (β = 0.67, p < 0.001), (ii) ratio of semantic clusters (β = 0.62, p < 0.001), and (iii) number of switches (β = 0.37, p < 0.001). For the semantic condition, the predictors accounted for 50% of the variance, with significant effects of (i) semantic cluster size (β = 0.50, p < 0.001) and (ii) number of switches (β = 0.58, p < 0.001). Regarding the letter condition, the predictors accounted for 76% of the variance, with significant contributions from (i) ratio of phonological clusters (β = 0.36, p < 0.001), and (ii) number of switches (β = 0.89, p < 0.001).
Racing thoughts, assessed via the RCTQ, were associated with decreased cluster ratios and fewer words in the letter and semantic conditions. Specifically, ‘thought overexcitability’, i.e., distractibility, was linked to decreased verbal output in these task conditions. Higher brooding rumination scores, assessed via the RRS, were associated with fewer words in the free and the semantic VFT. Phonological and semantic cluster sizes were larger when response times in the Hayling task were longer. In the free VFT, switches decreased when word suppression in the Hayling task was impaired, and they increased with faster processing speed.
Word and error count in VFT could not clearly distinguish between mood episodes in BD. Indeed, only the depression group tended to produce fewer words compared to healthy controls and manic patients in the semantic VFT. These results are consistent with those reported by Raucher-Chéne et al . 8 , suggesting greater impairment in the semantic VFT in subgroups of patients with BD. By contrast, the process-oriented measures proved to better capture the combinatory, tangential, and sound-based speech found in mania 10 . As a matter of fact, in the free condition, manic patients switched more often between semantic subcategories than the healthy and depression groups, and their semantic cluster ratio was also reduced. However, these results were not observed when the tasks had retrieval rules, i.e. letter and semantic conditions. In the semantic condition, switches were increased in the manic group compared only to the depression and euthymic groups, but not the healthy one. Interestingly, we found larger task-discrepant phonological cluster sizes in manic patients compared to controls. Despite this, the error count was similar between groups. In the mixed depression group, the number of switches in the free VFT was also higher than those found in non-mixed depression, suggesting that subthreshold manic symptoms led to discrete structural speech anomalies.
Consistent with a previous study by Fossati et al . 28 in unipolar depression, our results show reduced verbal output and switches in depressed patients, especially in the semantic VFT. Since this result was found in the semantic, but not the letter condition, this could be due either to a deterioration of the semantic system or to aberrant activation/inhibition processes within the semantic network 8 . Our results provide evidence against the storage deficit hypothesis, owing to the calculation of semantic cluster sizes which indexes semantic memory integrity. This index was not significantly different between groups, and vocabulary scores were equivalent between depression and healthy controls. Instead, in the semantic and free conditions, switching was decreased in the euthymic and the depression groups compared to the manic and healthy control groups, suggesting the existence of functional anomalies in the retrieval/access within the semantic system. Since results were similar in depression and euthymic groups, we argue that a trait-like impairment might be compensated for in the presence of manic symptoms 8 , 29 , 30 .
Interestingly, our results are the first to pinpoint switching abilities as affecting semantic fluency performance, and differently so among different types of mood episodes in BD. Like Fossati et al.’s findings 28 , switching was specifically correlated to measures of executive functions and psychomotor speed. Slower processing speed resulted in decreased switches in the semantic task, which might explain the results in depression and euthymia. As a whole, our results in bipolar depression are thus similar to those reported in unipolar depression 28 .
In contrast to depression, switches were increased in mania but also, to a lesser extent, in mixed depression. This was mainly observed in the free condition of VFT: subjects with mixed depression and mania, compared to depressed and euthymic patients, shifted from one discourse unit to the other at a faster rate, mimicking the flight of ideas characteristic of these states 10 . It is noteworthy however that increased switches did not amount to a greater number of words produced in the free VFT, despite the fact that cluster ratios and number of switches predicted the number of word output in all VFT. The stability of word output suggests that switches were increased at the expense of reduced semantic organization, as reflected by reduced cluster ratios in mania. All these results support the hypothesis of an abnormal access/retrieval within the semantic system might be involved in these results.
Indeed, a plausible explanation is that, in mania, there is a semantic overactivation during word retrieval. Clustering performance depends on the spread of semantic activation primed by each word generated 31 . Raucher-Chéné et al . 8 had already put forward the possibility of a faster than usual spread of semantic activation to explain the ‘manic advantage’ in VFT. This hypothesis is consistent with our results in the free task. In addition, the results in VFT with retrieval rules are also supportive of this hypothesis rather than overall inhibition deficits. Deficient inhibition of unrelated words should have led to a greater amount of errors, smaller cluster ratios and increased switches in constrained VFT, but this was not the case in patients with manic symptoms relative to healthy controls. Correlation analyses did not support a straightforward role of inhibition deficits either, as clustering measures increased and switches decreased when inhibition was impaired in the Hayling task 32 (see Supplementary Information).
The contrast between the results found in the free and the constrained VFT is striking, and the difference between these task conditions may be crucial to understand the mechanisms at play. In patients with manic symptoms, the unrestrictive nature of the free VFT may have enhanced diffuse semantic activation and favored the retrieval of more remotely associated words within the semantic network, which were not required to be inhibited in this task 26 . Hence, in the free condition, semantic overactivation was not detrimental to performance since subjects did not have to inhibit words unrelated to the task’s rules. A critical question is the role of distractibility. In the free task, it might have favored conceptual shifts, promoting the production of single words instead of clusters (i.e., reduced cluster ratio and increased switches) in patients with manic symptoms. However, distractibility might be detrimental to performance in tasks with retrieval rules, as suggested by the correlation between elevated racing thoughts, and its distractibility feature in particular (i.e., thought overexcitability), and decreased word output in restricted VFT. Yet again, this did not affect total word output in patients with manic symptoms. This, along with a similar error count, shows that patients with manic symptoms followed the tasks’ rules; that is, distractibility did not lead to irrelevant word production. Instead, the increased phonological cluster sizes in the semantic condition of VFT suggest that they are spontaneously more flexible. More specifically, when they had to produce animal names, manic subjects did so while rhyming and using other sound-based associations, akin to clanging, more than any other group. This is surprising given that phonological clustering is laborious and relies on executive functions 20 , 33 . However, enhanced executive functions in mania seems unlikely to explain our results, as executive performance was generally impaired in our manic group. Unrelated representations might rather be spontaneously activated through semantic spreading and subtend sound-based associations 34 , 35 . As emphasized above, semantic overactivation in mania might compensate for trait-like deficient word access/retrieval based on semantic cues.
It is noteworthy that manic symptoms, brooding rumination and racing thoughts were mainly correlated to decreased word output in patients, and most clinical symptoms were unrelated to switches or clustering measures. This suggests that self-report questionnaires fail to capture what is nonetheless clinically observed in the speech of patients, i.e. clanging and increased combinatory patterns 11 . This might be due to the fact that patients presenting with manic symptoms lack insight, hence underestimate their self-report of symptoms 36 . This makes the process-oriented VFT results all the more useful, as they provide a quantification of this clinical symptom, and improve the phenomenological models and scales aimed at evidencing enhanced spontaneous flexibility potentially involved in racing thoughts 14 . Importantly, clustering and switching abnormalities differentiated patients with manic symptoms, including the mixed depression group with few subthreshold – overlapping or not – hypomanic symptoms, from typical depression, suggesting that very few activation symptoms concurrent with depression might give rise to speech and thought abnormalities similar to those found in mania 25 , 37 .
Finally, we acknowledge the limitations of our study. The main one is the small sample of mixed manic patients. Given the small number of studies which have investigated language and cognition in mixed episodes of BD, results in mixed mania require to be confirmed by future studies. Second, we acknowledge the different lengths of the constrained and free VFT but it seems unlikely to explain the switching and clustering differences found here. Future studies may consider assessing the temporal pattern of process-oriented measures in BD, as it might provide further information regarding the cognitive mechanisms at play. For instance, these might be applied for within-cluster and non-clustered word intervals 20 but also with focus on individual word production over the allotted VFT time, as retrieval during initial intervals (e.g., 15 s) might be associated with semi-automatic word retrieval, whereas later intervals are reflective of effortful word retrieval (e.g. 38 , 39 , 40 , 41 ).
In sum, ours is the first study to capture thought and language abnormalities characteristic of mood episodes of BD, including mixed states, via process-oriented measures of VFT. This suggests that these measures may tackle structural and cognitive abnormalities that are not assessed simply by word or error count. Specifically, our results suggest that the increased combinatory nature of word output is subtended by a faster semantic spread of activation in patients with manic symptoms and might represent a compensatory mechanism for trait-like access/retrieval impairments found in euthymia 30 . Interestingly, these results were found in mania, but also in patients with mixed symptoms; increased switches were greater in mixed depression than non-mixed depression in the free VFT, mimicking the flight of ideas characteristic of mixed states.
Participants
Thirty-one healthy individuals aged 18–64 (M = 38.13, SD = 11.43) and 93 patients aged 18–64 (M = 42.70, SD = 12.83) with BD were recruited. Patients were recruited from inpatient and outpatient clinics at the University Hospital of Strasbourg, and fulfilled criteria for BD according to the DSM-IV-TR 42 . 50.5% patients had BD type 1, and 49.5% BD type 2. Healthy volunteers were recruited from the region by advertisement. They had no current or past personal history of psychiatric or neurological disorders nor did they have any first-degree relatives with psychosis or mood disorders. Patients with BD had no history of neurological disorder, ADHD, borderline personality disorder or substance use disorder within the last 12 months. Two patients were not taking any psychotropic medication at the time of the assessment. Of the remaining 91 patients, 39% were taking lithium, 44.1% were prescribed antiepileptic drugs, 40.9% were taking antipsychotics, 32.3% were on antidepressants, and 18% were taking benzodiazepines (27% of manic patients, 25% mixed manic patients, 20% mixed depression, 14% depressed, and 5% euthymia).
Detailed demographic data are presented in Table 3 . Most patients in the manic and mixed manic groups presented with a hypomanic episode. Subjects provided written informed consent prior to inclusion in the study in accordance with the Declaration of Helsinki. This study was approved by the regional ethics committee of the East of France (CPP EST IV). All methods were performed in accordance with the aforementioned relevant guidelines and regulations.
Materials and procedures
Patients were considered to be in a predominantly depressive or manic/(hypo)manic episode if they fulfilled the DSM-IV-TR criteria for either episode 42 . Comorbidities were assessed by senior psychiatrists using the DSM-IV-TR criteria 42 . Patients had no history of neurological disorder, ADHD, substance use disorder within the last 12 months or borderline personality disorder. Prior to the neuropsychological assessment, mania and depression symptoms were assessed with the Young Mania Rating Scale (YMRS) 43 and the Quick Inventory of Depressive Symptomatology–Clinician-Rated Version (QIDS-C16) 44 . A YMRS score > 5 was considered reflective of hypomania 45 and a QIDS-C16 score > 5 was reflective of depression 43 . A mixed manic/hypomanic state was diagnosed if manic and depressive symptoms were above the cut-off 46 . Mixed depression was diagnosed when scores were above the threshold for depressive symptoms (QIDS-C16 score > 5), and co-occurred with mild hypomanic symptoms (YMRS score > 2 and <6) 47 . Euthymia was defined by scores below the threshold in both the YMRS and the QIDS-C16, reflecting the absence of a significant mood episode. Psychotic features were not part of the affective episodes at the time of testing, as assessed by the YMRS item 8 referring to thought content.
Participants then fulfilled two self-rated questionnaires, the Racing and Crowded Thoughts Questionnaire (RCTQ) 48 assessing three facets of racing thoughts – i.e., ‘thought overactivation’, its ‘burden’, and ‘overexcitability’ features–, and the Ruminative Response Scale State-version (RRS-S) 49 assessing ‘brooding’ and ‘reflection’ rumination. They were also administered a battery of neuropsychological tests, including three VFT.
Neuropsychological assessment
Neuropsychological assessment included measures of processing speed and attention switching – i.e., the Trail Making Test (TMT-A & B) 50 and the digit-symbol subtest of the Wechsler Adult Intelligence Scale—Third Edition (WAIS-III) 51 . Semantic inhibition was assessed via the Hayling test 52 , which requires participants to orally complete a set of 15 sentences, whose last word is missing, with semantically-unrelated ending words. Both response times and errors were recorded. Working memory was assessed via the digit-span task 50 . The Vocabulary Subtest of the WAIS-III assessed subjects’ lexico-semantic abilities and vocabulary size 53 and the French National Adult Reading Test 54 measured their premorbid intellectual functioning 32 .
Verbal fluency tasks
The three conditions of the verbal fluency task were administered in a fixed order, starting with the most unrestrictive condition 55 : the free, the letter and the semantic conditions. In the free fluency trial, participants were asked to produce as many words as possible, with their eyes closed, during 150s 56 . In the letter fluency condition, subjects were asked to produce as many words as possible starting with the letter ‘p’, with the exception of proper nouns, during 120 s. Words starting with a letter other than p and proper nouns were counted as errors 55 . In the semantic VFT, participants had to produce as many animal nouns as possible, during 120 s. Words belonging to different semantic categories were counted as errors 55 .
Scoring procedure: Participants’ oral production was recorded using the Audacity© software. Verbatim output was transcribed by French-speaking psychology undergraduates who were blind to the diagnostic status of the participants.
In addition to total word and error count, semantic and phonological cluster ratios (i.e., number of clusters/number of words), mean cluster sizes, and the raw number of switches were calculated for the three VFT. Two independent raters (graduate-level psychologists) blind to the diagnostic status of participants scored the verbal fluency protocols. Semantic and phonemic relatedness were assessed in the three conditions of the task; this combined procedure allows for the identification of both task-consistent and task-discrepant clustering 20 . Additionally, it allows for the calculation of cluster ratios, i.e., the number of clusters/number of words, and mean cluster size, i.e., total number of words in clusters beginning with the second word divided by the number of clusters produced 21 , 22 . The former indexes output organization whereas the latter indexes the integrity of the lexico-semantic store. Cluster sizes of zero were not considered in the analysis 19 . Semantic clusters were defined as a group of at least two serially produced words related categorically (e.g., fruits), or contextually (e.g., animals that live in the forest). Synonyms and antonyms, but also superordinates, were considered as being related. Phonemic clusters were defined as groupings of at least two serially produced words sharing the first two phonemes (e.g., plot and plight), sharing a syllable (e.g., propensity and pen), rhyming (e.g., daughter and water), differing only by a vowel sound (e.g., pin, pen), as well as homonyms (e.g., sum and some) 17 . Switches were defined by shifts from a cluster to another cluster, but also from a cluster to a word, or from a word to another word 17 , 19 . Intra-class correlations between scoring of the two raters revealed excellent interrater reliability for both semantic and phonemic clustering in the letter (r = 0.86, r = 0.95, respectively), semantic (r = 0.88, r = 0.93, respectively) and free (r = 0.93, r = 0. 95, respectively) conditions.
Statistical analyses
Analyses were undertaken using the Statistica® software. Because data were normally distributed for the whole sample of participants (Kolmogorov-Smirnov test, p > 0.10), for each scoring criterion and condition of the task, we conducted a one-way ANCOVA with group as a between-group variable and the following covariates, given their potential effect on cognitive performance 6 , 57 : (i) number of hospitalizations, (ii) lithium dosage, and (iii) equivalent dosage of antipsychotic drugs. Of note, results were similar when the covariates were not entered in the analyses. Based on our a priori hypotheses, planned comparisons between groups were performed using the false discovery rate (FDR) 58 method of alpha level adjustment for multiple comparisons; statistical significance was set at 0.05 (two-sided tests). Specifically, planned comparisons were conducted between manic patients’ performance compared to depression, euthymia and controls, on the one hand, and depression versus mixed depression, on the other hand. Given the scarce literature on language and cognition in mixed mania, we did not have a priori hypotheses regarding this group and planned comparisons were not performed for this group in particular. Results were similar when subjects taking benzodiazepines at the time of the assessment were removed from the analyses, hence for the sake of simplicity we will present the results averaged over all subjects. Only significant planned comparisons were reported in the results section for greater readability. Correlation analyses, using Pearson’s coefficient, were performed in the whole sample of patients and in patients with manic symptoms alone between the verbal fluency measures, neuropsychological measures, and clinical symptoms. To investigate the relationship between process-oriented measures (clustering and switching) and word output in the three VFT, we conducted multiple regression analyses on the word output within the patient sample. Five predictors – i.e., semantic cluster size, phonological cluster size, ratio of semantic clusters, ratio of phonological clusters, and number of switches –, were simultaneously entered into the model. Statistical significance was set at 0.05.
Data Availability
Data can be made available upon request to authors.
Goodwin, F. K. & Jamison, K. R. Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression . (Oxford University Press, USA 2007).
Harrow, M., Grossman, L. S., Silverstein, M. L., Meltzer, H. Y. & Kettering, R. L. A longitudinal study of thought disorder in manic patients. Arch. Gen. Psychiatry 43 , 781–785 (1986).
Article CAS Google Scholar
KRAEPELIN, E. La folie maniaco-dépressive . (Mollat, 2008).
Giehm, G. Experimentell-psychologische Untersuchungen der Assoziationsgeschwindigkeit bei Geisteskranken. Arch. Für Psychiatr. Nervenkrankh. 100 , 432–438 (1933).
Article Google Scholar
Shaw, E. D., Mann, J. J., Stokes, P. E. & Manevitz, A. Z. Effects of lithium carbonate on associative productivity and idiosyncrasy in bipolar outpatients. Am. J. Psychiatry 143 , 1166–1169 (1986).
Kocsis, J. H. et al . Neuropsychologic Effects of Lithium Discontinuation. J. Clin. Psychopharmacol. 13 , 268 (1993).
Levine, J., Schild, K., Kimhi, R. & Schreiber, G. Word Associative Production in Affective versus Schizophrenic Psychoses. Psychopathology 29 , 7–13 (1996).
Raucher-Chéné, D., Achim, A. M., Kaladjian, A. & Besche-Richard, C. Verbal fluency in bipolar disorders: A systematic review and meta-analysis. J. Affect. Disord. 207 , 359–366 (2017).
Cutting, J. Principles of Psychopathology: Two Worlds - Two Minds - Two Hemispheres . (Oxford University Press, 1997).
Hoffman, R. E., Stopek, S. & Andreasen, N. C. A comparative study of manic vs schizophrenic speech disorganization. Arch. Gen. Psychiatry 43 , 831–838 (1986).
Jamison, K. R. Robert Lowell , Setting the River on Fire: A Study of Genius , Mania , and Character . (Knopf, 2017).
Sass, L. & Pienkos, E. Beyond Words: Linguistic Experience in Melancholia, Mania, and Schizophrenia. Phenomenol. Cogn. Sci. 14 , 475–495 (2015).
Binswanger, L. Sur la fuite des idées . (Editions Jérôme Millon, 2000).
Piguet, C. et al . Phenomenology of racing and crowded thoughts in mood disorders: a theoretical reappraisal. J. Affect. Disord. 121 , 189–198 (2010).
Esmaeelpour, E. & Sasani, F. The Effect of Bipolar Mood Disorder on Sadegh Hedayat’s Letters. J. Psycholinguist. Res. 45 , 367–377 (2016).
Lezak, M. D. Neuropsychological Assessment . (Oxford University Press, 2004).
Troyer, A. K., Moscovitch, M. & Winocur, G. Clustering and switching as two components of verbal fluency: evidence from younger and older healthy adults. Neuropsychology 11 , 138–146 (1997).
Henry, J. D. & Crawford, J. R. A meta-analytic review of verbal fluency performance following focal cortical lesions. Neuropsychology 18 , 284–295 (2004).
Wixted, J. T. & Rohrer, D. Analyzing the dynamics of free recall: An integrative review of the empirical literature. Psychon. Bull. Rev. 1 , 89–106 (1994).
Ledoux, K. et al . Capturing additional information about the organization of entries in the lexicon from verbal fluency productions. J . Clin . Exp . Neuropsychol . 36 (2014).
Helmes, E. & Hall, F. Performance of psychiatric diagnostic groups on measures and strategies of verbal fluency. Appl. Neuropsychol. Adult 23 , 284–294 (2016).
Raskin, S. A., Sliwinski, M. & Borod, J. C. Clustering strategies on tasks of verbal fluency in Parkinson’s disease. Neuropsychologia 30 , 95–99 (1992).
Koren, R., Kofman, O. & Berger, A. Analysis of word clustering in verbal fluency of school-aged children. Arch. Clin. Neuropsychol. Off. J. Natl. Acad. Neuropsychol. 20 , 1087–1104 (2005).
Basso, M. R., Lowery, N., Neel, J., Purdie, R. & Bornstein, R. A. Neuropsychological impairment among manic, depressed, and mixed-episode inpatients with bipolar disorder. Neuropsychology 16 , 84–91 (2002).
Perugi, G. et al . Mixed features in patients with a major depressive episode: the BRIDGE-II-MIX study. J. Clin. Psychiatry 76 , e351–358 (2015).
Phillips, L. H., Bull, R., Adams, E. & Fraser, L. Positive mood and executive function: evidence from stroop and fluency tasks. Emot. Wash. DC 2 , 12–22 (2002).
Google Scholar
Weiner, L. Racing thoughts: Cognitive and Psychopathological Mechanisms. Neuroscience . University of Strasbourg 2017.
Fossati, P., Ergis, A.-M. & Allilaire, J.-F. & others. Qualitative analysis of verbal fluency in depression. Psychiatry Res. 117 , 17–24 (2003).
PubMed Google Scholar
Chang, J. S. et al . Differential pattern of semantic memory organization between bipolar I and II disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 35 , 1053–1058 (2011).
Sung, K., Gordon, B., Vannorsdall, T. D., Ledoux, K. & Schretlen, D. J. Impaired retrieval of semantic information in bipolar disorder: a clustering analysis of category-fluency productions. J. Abnorm. Psychol. 122 , 624–634 (2013).
Collins, A. M. & Loftus, E. F. A Spreading-Activation Theory of Semantic Processing. Psychol. Rev. 82 , 407–428 (1975).
Ross, T. P. et al . The reliability and validity of qualitative scores for the Controlled Oral Word Association. Test. Arch. Clin. Neuropsychol. Off. J. Natl. Acad. Neuropsychol. 22 , 475–488 (2007).
Ho, A. K. et al . Verbal fluency in Huntington’s disease: a longitudinal analysis of phonemic and semantic clustering and switching. Neuropsychologia 40 , 1277–1284 (2002).
Navarrete, E. & Costa, A. Phonological activation of ignored pictures: Further evidence for a cascade model of lexical access. J. Mem. Lang. 53 , 359–377 (2005).
Robinson, G. & Ceslis, A. An unusual presentation of probable dementia: rhyming, associations, and verbal disinhibition. J. Neuropsychol. 8 , 289–294 (2014).
Silva, R. et al . Insight in bipolar mania: evaluation of its heterogeneity and correlation with clinical symptoms. J. Affect. Disord. 199 , 95–98 (2016).
Weiner, L. et al . Racing thoughts revisited: A key dimension of activation in bipolar disorder. J. Affect. Disord. 255 , 69–76 (2019).
Rinaldi, R. & Lefebvre, L. Cued fluency protocol reveals dynamic symptomatic-dependent processes of goal-directed behaviours in schizophrenia. Cognit. Neuropsychiatry 20 , 382–397 (2015).
Krukow, P. et al . What specifically contributes to disturbed non-verbal fluency in patients with bipolar disorder: Ineffective performance initiation, slowed processing or lack of the execution strategy? Psychiatry Res. 271 , 15–22 (2019).
Krukow, P., Harciarek, M., Morylowska-Topolska, J., Karakuła-Juchnowicz, H. & Jonak, K. Ineffective initiation contributes to deficient verbal and non-verbal fluency in patients with schizophrenia. Cognit. Neuropsychiatry 22 , 391–406 (2017).
Crowe, S. F. Decrease in performance on the verbal fluency test as a function of time: evaluation in a young healthy sample. J. Clin. Exp. Neuropsychol. 20 , 391–401 (1998).
Association, A. P. Diagnostic and Statistical Manual of Mental Disorders , 4th Edition , Text Revision . (American Psychiatric Association, 2000).
Young, R. C., Biggs, J. T., Ziegler, V. E. & Meyer, D. A. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry J. Ment. Sci. 133 , 429–435 (1978).
Rush, A. J. et al . The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol. Psychiatry 54 , 573–583 (2003).
Favre, S. et al . Translation and validation of a French version of the Young Mania Rating Scale (YMRS). L’Encephale 29 , 499–505 (2003).
CAS PubMed Google Scholar
Suppes, T. et al . Mixed hypomania in 908 patients with bipolar disorder evaluated prospectively in the Stanley Foundation Bipolar Treatment Network: a sex-specific phenomenon. Arch. Gen. Psychiatry 62 , 1089–1096 (2005).
Miller, S. et al . Mixed Depression in Bipolar Disorder: Prevalence Rate and Clinical Correlates During Naturalistic Follow-Up in the Stanley Bipolar Network. Am. J. Psychiatry 173 , 1015–1023 (2016).
Weiner, L. et al . Measuring racing thoughts in healthy individuals: The Racing and Crowded Thoughts Questionnaire (RCTQ). Compr. Psychiatry 82 , 37–44 (2018).
Treynor, W., Gonzalez, R. & Nolen-Hoeksema, S. Rumination Reconsidered: A Psychometric. Analysis. Cogn. Ther. Res. 27 , 247–259 (2003).
Tombaugh, T. N. Trail Making Test A and B: Normative data stratified by age and education. Arch. Clin. Neuropsychol. 19 , 203–214 (2004).
Wechsler D. Wechsler Adult Intelligence Scale III . San Antonio, Tex, Psychological Corporation; 2017.
Burgess, P. W. & Shallice, T. The Hayling and Brixton Tests. Thames Valley Test Company , Bury St . Edmunds , U . K . (1997) . Available at, http://discovery.ucl.ac.uk/5457/ . (Accessed: 31st October 2017).
Strauss, E., Sherman, E. M. S. & Spreen, O. A Compendium of Neuropsychological Tests: Administration , Norms , and Commentary . (Oxford University Press, 2006).
Mackinnon, A. & Mulligan, R. The estimation of premorbid intelligence levels in French speakers. L’Encephale 31 , 31–43 (2005).
Cardebat, D., Doyon, B., Puel, M., Goulet, P. & Joanette, Y. Formal and semantic lexical evocation in normal subjects. Performance and dynamics of production as a function of sex, age and educational level. Acta Neurol. Belg. 90 , 207–217 (1990).
Béland, R., Lecours, A. R., Giroux, F. & Bois, M. The MT-86 β aphasia battery: A subset of normative data in relation to age and level of school education (Part II). Aphasiology 7 , 359–382 (1993).
Bourne, C. et al . Neuropsychological testing of cognitive impairment in euthymic bipolar disorder: an individual patient data meta-analysis. Acta Psychiatr. Scand. 128 , 149–162 (2013).
Benjamini, Y. & Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B Methodol. 57 , 289–300 (1995).
MathSciNet MATH Google Scholar
Download references
Acknowledgements
This study was conducted as part of the first author’s PhD thesis. An unfinished preliminary version of this manuscript can be found in the thesis document (Weiner, L. Racing thoughts: Cognitive and Psychopathological Mechanisms. Neuroscience. University of Strasbourg, 2017.)
Author information
Authors and affiliations.
INSERM U1114, Strasbourg, France
Luisa Weiner, Nadège Doignon-Camus, Gilles Bertschy & Anne Giersch
Psychiatry Department, University Hospital of Strasbourg, Strasbourg, France
Luisa Weiner & Gilles Bertschy
Translational Medicine Federation, University of Strasbourg, Strasbourg, France
Gilles Bertschy
You can also search for this author in PubMed Google Scholar
Contributions
The protocol was designed by L.W., N.D.C., G.B. and A.G. The first draft of the article was written by L.W. and reviewed by A.G., N.D.C. and G.B. Data were analyzed by L.W. and N.D.C. All authors have given final approval of the version to be published.
Corresponding author
Correspondence to Luisa Weiner .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary results and discussion, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Weiner, L., Doignon-Camus, N., Bertschy, G. et al. Thought and language disturbance in bipolar disorder quantified via process-oriented verbal fluency measures. Sci Rep 9 , 14282 (2019). https://doi.org/10.1038/s41598-019-50818-5
Download citation
Received : 14 February 2019
Accepted : 19 September 2019
Published : 03 October 2019
DOI : https://doi.org/10.1038/s41598-019-50818-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Automated mood disorder symptoms monitoring from multivariate time-series sensory data: getting the full picture beyond a single number.
- Filippo Corponi
- Bryan M. Li
- Antonio Vergari
Translational Psychiatry (2024)
Linguistic characteristics in bipolar disorder versus borderline personality disorder
- Noelia Santos Muriel
- Patricia López Resa
- Esther Moraleda Sepúlveda
Scientific Reports (2023)
Vocal features obtained through automated methods in verbal fluency tasks can aid the identification of mixed episodes in bipolar disorder
- Luisa Weiner
- Andrea Guidi
- Nicola Vanello
Translational Psychiatry (2021)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Gen Intern Med
- v.28(12); 2013 Dec

The Presentation, Recognition and Management of Bipolar Depression in Primary Care
Joseph m. cerimele.
Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, 1959 NE Pacific St, Box 356560, Seattle, WA 98195-6560 USA
Lydia A. Chwastiak
Harborview Medical Center, Seattle, WA USA
Ya-Fen Chan
David a. harrison, jürgen unützer.
Bipolar disorder is a mood disorder characterized by episodes of major depression and mania or hypomania. Most patients experience chronic symptoms of bipolar disorder approximately half of the time, most commonly subsyndromal depressive symptoms or a full depressive episode with concurrent manic symptoms. Consequently, patients with bipolar depression are often misdiagnosed with major depressive disorder. Individual patient characteristics and population screening tools may be helpful in improving recognition of bipolar depression in primary care. Health risk behaviors including tobacco use, sedentary activity level and weight gain are highly prevalent in patients with bipolar disorder, as are the comorbid chronic diseases such as diabetes mellitus and cardiovascular disease. Patients with bipolar illness have about an eight-fold higher risk of suicide and a two-fold increased risk of death from chronic medical illnesses. Recognition of bipolar depression and its associated health risk behaviors and chronic medical problems can lead to the use of appropriate interventions for patients with bipolar disorder, which differ in important ways from the treatments used for major depressive disorder. The above topics are reviewed in detail in this article.
A 38-year-old man presented to the primary care clinic to “have some disability papers filled out”. He reports being unable to work for 6 months because “I am a failure and I don’t have enough energy to get up in the morning”. He reports a long-standing history of sleep problems and now lays awake in bed every day from 4 am until mid-morning. He smokes 15 cigarettes throughout the day “to try to get moving”. He has gained 18 pounds over 6 months and now has a body mass index of 26 and daily low back pain. He endorses problems with concentration, decreased interest in previously pleasurable activities, low energy, and racing thoughts. His girlfriend ended their relationship, reportedly due to his ongoing irritability. He was hospitalized once on a psychiatry ward at the age of 19, “because I smoked a lot of pot, didn’t sleep for 3 weeks and I spent all of my parents’ money on important electronics.” He scores 19 out of 27 on the Patient Health Questionnaire-9.
This article is a narrative review of the diagnosis and treatment of bipolar depression in primary care. We identified articles through search strategies in PubMed, the Cochrane database, and GoogleScholar. We identified additional articles in the references of retrieved studies, and consulted with clinicians in psychiatry and primary care to develop a review that could guide clinicians in recognizing and treating bipolar depression. Much of the literature cited, particularly the studies on prevalence and co-occurring disorders, comes from the United States.
BACKGROUND AND EPIDEMIOLOGY
Bipolar I disorder is a chronic mood disorder characterized by the presence of at least one manic episode and usually recurrent major depressive episodes and often chronic depressive symptoms. 1 , 2 Symptoms of bipolar disorder are shown in Table 1 . Mania is the defining disease state in bipolar I disorder, and consists of a marked departure from baseline behavior and functioning, often accompanied by psychosis and/or a high risk of danger to the patient. 1 Elevated mood can occur in mania, although more commonly irritable or dysphoric mood occur, making associated symptoms such as racing thoughts, grandiosity, distractibility and impulsivity key for diagnosis. Bipolar II disorder is also a chronic disorder usually consisting of recurrent depression and at least one hypomanic episode. The symptoms and impairment of bipolar depression are similar to that of major depressive disorder, including depressed mood, feelings of worthlessness or guilt, psychomotor retardation and suicidal ideation. 3 Patients may also present with a mixed manic-depressive episode, or in a hypomanic state. Depressive symptoms contribute more to functional impairment than manic symptoms over the long-term in bipolar disorder. 4 , 5 Suicidal ideation or recurrent thoughts of death can occur during all phases of bipolar illness. The lifetime prevalence of a suicide attempt is 17 % in bipolar I disorder and 24 % in bipolar II disorder, compared to 12 % in unipolar depression 6 and 0.6 % in the general US population. 7
Symptom Episodes of Bipolar Disorder
| * | |
|---|---|
| Manic Episode | Persistently elevated or irritable mood, often with uncontrollable excitement lasting throughout the day. Generally accompanied by increased energy, overactivity, pressure of speech, and a decreased need for sleep. Loss of social inhibitions may result in reckless and out of character behavior, or engagement in high-risk pleasurable activities. May also be accompanied by delusions, or extreme flight of ideas, making the patient incomprehennsible. |
| Depressive Episode | Depressed mood, reduced energy, decreased energy, diminished capacity for enjoyment, interest and concentration, and guilt or worthlessness are often present. Fatigue often occurs, along with disturbed sleep. Appetite can be diminished or increased. The lowered mood and associated symptoms vary little from day to day. |
| Mixed Affective Episode | Mixture or a rapid alteration of manic and depressive symptoms. |
| Hypomanic Episode | Persistent mild elevation of mood, increased energy and activity, and usually marked feelings of wellbeing and physical and mental efficiency. Increased sociability, talkativeness, over-familiarity, increased sexual energy, and a decreased need for sleep are often present, but not to the extent that they lead to severe disruption of work or result in social rejection. Irritability may also occur. |
* The presence of at least one manic episode is required for the diagnosis of bipolar I disorder. The presence of at least one hypomanic episode and at least one major depressive episode is required for a diagnosis of bipolar II disorder 1
† Adapted with permission from the International Classification of Diseases-10 Version:2010. World Health Organization 2
‡ Symptoms are not due to general medical problem or to the physiologic effects of substances
The National Comorbidity Survey Replication estimated the lifetime prevalence of bipolar disorder in a community sample as 1.0 % for bipolar I disorder, 1.1 % for bipolar II disorder, and 2.4 % for subthreshold bipolar disorder symptoms. 8 The prevalence of bipolar disorder may be higher in primary care clinical samples, though screening instruments used in research to measure bipolar disorder prevalence, such as the Mood Disorder Questionnaire (MDQ), have limitations that are discussed below. Das et al. 9 screened 1,157 random patients from a large, urban, academic primary care clinic and found that 9.8 % (95 % CI 8.0–11.5 %) had a positive MDQ screen for a lifetime history of bipolar disorder. Three studies 10 – 12 using screening measures for bipolar disorder among patients already diagnosed with depression or anxiety showed a prevalence of positive screening measures for bipolar I or II disorder between 3.3 and 23.5 %. Based on a structured interview completed by a family physician, Manning et al. 13 diagnosed 18.5 % of patients with current depression or anxiety with bipolar disorder II, though only 2.8 % with bipolar I disorder.
PRESENTATION AND DIAGNOSIS
In addition to episodes of depression, mania or hypomania, patients with bipolar disorder can experience mood swings and chronic mood symptoms below the level of severity of a mood episode. Judd et al. 14 prospectively followed 146 patients with bipolar I disorder and found that patients experienced mood symptoms 47.3 % (SD 34 %) of weeks over a mean follow-up of 12.8 years, with depressive symptoms occurring three times as often as manic symptoms. Patients in this study had symptoms and impairment consistent with a full manic, hypomanic or major depressive episode 2.3 %, 4.6 % and 8.9 % of the study weeks, respectively. The same group followed 86 patients with bipolar II disorder for a mean of 13.4 years and found that patients experienced symptoms 53.9 % of the follow-up time, with depressive symptoms occurring 39 times as often as hypomanic symptoms. 15 As in bipolar I disorder, subsyndromal depressive symptoms were three times more prevalent than symptoms consistent with a full depressive episode.
Strategies to Improve Recognition in Individuals
Historical, examination and other factors can be helpful in differentiating bipolar disorder from other mood disorders. 16 – 18 In one primary care practice, those with a lifetime history of bipolar disorder were significantly more likely than those without bipolar disorder to have current symptoms of anorexia or overeating, low self-esteem, suicidal ideation, alcohol use, and a history of hallucinations. 12 Mitchell et al. 19 , 20 systematically reviewed the literature and found that the clinical symptoms of hypersomnia, hyperphagia, leaden paralysis, psychomotor retardation, psychotic features, pathological guilt, mood lability and longer speech latency occurred more often in bipolar depression than in unipolar depression (Table 2 ).
Proposed “Probabilistic” Approach to the Diagnosis of Bipolar I Depression in a Person Experiencing a Major Depressive Episode with No Clear Prior Episodes of Mania*
| -Hypersomnia and/or increased daytime napping | -Initial insomnia/reduced sleep |
| -Hyperphagia and/or increased weight | -Reduced appetite and/or weight loss |
| -Other atypical depressive symptoms such as leaden paralysis | |
| -Psychomotor retardation | -Normal or increased activity levels |
| -Psychotic features and/or pathological guilt | -Somatic complaints (e.g. headache) |
| -Lability of mood/co-occurring manic symptoms | |
| -Early onset of first depression (before age 25 | -Later onset of first depression (after age 25) |
| -Multiple prior episodes of depression (five or more episodes) | -Long duration of current episodes (6 months or more) |
| -Positive family history of bipolar disorder | -Negative family history of bipolar disorder |
| Substance use occurs more often in bipolar disorder than unipolar disorder | |
| Post-partum mood episode—many women with bipolar disorder have had a postpartum mood episode | |
| Response to antidepressant medication—may see increased activity, such as onset or worsening of racing thoughts or irritability in patients with bipolar disorder | |
* Adapted with permission from Mitchell et al. 19
Goldberg et al. 21 found that 31.2 % of 1,380 patients with bipolar depression experienced depression episodes without any coexisting manic symptoms. The remaining patients experienced either subsyndromal mania (1–3 manic symptoms, 54 % of patients) during the depressive episode or a mixed manic-depressive episode (14.8 %). Distractibility, racing thoughts and psychomotor agitation were the most commonly occurring manic symptoms. Seventy-one percent of patients with bipolar II disorder and 30 % of patients with bipolar I experienced concurrent manic symptoms during the depressive episode, with male patients and those with illness onset in adolescence being more likely to have concurrent manic symptoms.
Screening and Case Identification Tools
Accurate recognition of bipolar disorder in a patient with current depressive symptoms is important, because treatment of bipolar patients with standard antidepressant medications prior to starting mood stabilizing medications can worsen their clinical outcomes. Patients with bipolar I or II disorder may present with subsyndromal symptoms such as fatigue, concentration problems, irritability, or psychomotor retardation, making a complete history of prior mood symptoms, impairment, treatment and family history vital for accurate diagnosis of bipolar disorder. Patients may also present with symptoms of a co-occurring psychiatric disorder. Among patients with any type of bipolar disorder, approximately 75 %, 42 % and 63 % have a co-occurring anxiety, substance use or impulse control disorder, respectively, 8 making questioning about bipolar disorder important in the assessment of patients with the above disorders. The diagnostic process should include obtaining a comprehensive history (including information from collateral sources and prior clinicians), and completing examinations (mental status, physical and laboratory and possibly neuropsychological testing), which may need to be spread over several clinic appointments. 18 , 22 Patients with bipolar depression should be asked directly about suicidal ideation, and those with positive responses should undergo additional suicide risk assessment. 23 , 24 Clinicians should seek a personal and family history of mania or hypomania, including prior treatments received, and screen for substance use disorders using evidence-based techniques, such as the AUDIT scale for alcohol use. 23 Co-occurring psychiatric disorders should also be assessed and treated. 25
Patients with bipolar disorder may receive specialty mental health care only intermittently, and as many as 10–38 % of patients receive treatment only in the primary care setting. 26 Major depression illness severity can be similar in primary care and psychiatric care settings. 27 Similarly, patients with bipolar disorder seen in primary care and specialty care can have equal degrees of functional impairment and reduced quality of life. 28 , 29
Although screening tools help detect psychiatric disorders among primary care patients, screening alone, without adequate follow-up and treatment, does not improve psychiatric outcomes. 30 The diagnosis of unipolar depression in primary care has been improved by the standardization and use of tools such as the Patient Health Questionnaire-9 (PHQ-9). 31 , 32 Measurement-based care with PHQ-9 has helped demonstrate that patients with depression receiving the same treatment in primary and specialty care settings had comparable treatment outcomes in a large clinical trial. 33 Several screening measures have been developed to identify patients at increased risk for bipolar disorder (see Table 2 ).
Hirschfeld et al. 34 developed the Mood Disorder Questionnaire (MDQ) as a screening instrument for bipolar disorder. In the original validation study, 34 conducted in five psychiatry clinics with a high prevalence of bipolar disorder, a score of 7 or higher on the MDQ had sensitivity of 0.73 and specificity of 0.90 for a diagnosis of bipolar disorder, when compared to the Structured Clinical Interview for DSM-IV (SCID-IV). 34 Subsequent research on the MDQ, however, has suggested that patients with positive MDQ screens were as likely to have borderline personality disorder as bipolar disorder. 35 In another study, most patients who screened positive on the MDQ 36 were found to have posttraumatic stress disorder, eating disorders and substance use disorders (based on a standardized clinical interview, SCID-IV), rather than bipolar disorder. The MDQ is a screening tool rather than a case-finding tool;, the high false positive rate requires that patients who screen positive should undergo further diagnostic assessment 37 (see example follow-up questions in Tables 3 and and4 4 ).
Screening for Bipolar Disorder: MDQ Versus CIDI-3
| • Filled out by patient | • Administered by clinician |
| • Positive screen = ≥ 7/13 yes responses | • Positive screen = Yes on euphoria irritability stem questions |
| • Symptoms occurring at the same time | • Yes on criterion B question |
| • Moderate to severe problem | • Yes on majority of subset questions |
Suggested Follow-up Questions
| . |
| 2. |
| 3. |
| 4. |
| 5. |
| 6. |
| 7. |
| 8. |
| 9. |
The World Health Organization’s Composite International Diagnostic Interview (CIDI) Version 3.0 is a diagnostic tool used to identify psychiatric disorders in the community, and may be a more useful tool for diagnosing bipolar disorder in primary care. 38 The CIDI Bipolar Disorder screening scale is a 3-min clinician-administered screen beginning with two stem questions. (Question 1. “ Some people have periods lasting several days when they feel much more excited and full of energy than usual. Their minds go too fast. They talk a lot. They are very restless or unable to sit still and they sometimes do things that are unusual for them, such as driving too fast or spending too much money. Have you ever had a period like this lasting several days or longer? ” Question 2: “ Have you ever had a period lasting several days or longer when most of the time you were so irritable or grouchy that you either started arguments, shouted at people or hit people? ”) If the answers to the two stem questions are “no”, then the CIDI is considered negative. Patients who answer “yes” to either stem question require a full CIDI assessment. The CIDI scale was concordant with the gold-standard SCID-IV (kappa 0.88 for bipolar I disorder and kappa 0.88 for bipolar II disorder or subthreshold bipolar disorder symptoms) in a national household survey, suggesting that the CIDI could be used as a case-finding measure for bipolar disorder. Clinical guidelines for the evaluation of bipolar disorder, such as the STABLE Toolkit, 23 recommend using the CIDI as the main measure for bipolar disorder case identification. The CIDI could also be used in patients scoring higher than 7 on the MDQ to confirm the likelihood of bipolar disorder diagnosis, given the low positive predictive value of the MDQ.
CO-OCCURRING DISORDERS, HEALTH RISK BEHAVIORS AND SERVICE UTILIZATION
Patients with bipolar disorder experience a 10–20 year reduction in life expectancy compared to the rest of the population, and the majority of this premature mortality is due to chronic medical illnesses. 39 Bipolar disorder is associated with sedentary behavior, obesity and tobacco use, 39 – 43 all of which are associated with an increased risk of cardiovascular disease (CVD). Approximately one-third of patients with bipolar disorder are current smokers, 44 though lifetime smoking prevalence is 44–82.5 %. 45 , 46 Additionally, Simon et al. found that obesity (a body mass index (BMI) greater than 30 kg/ m 2 ) independently increased the risk of a lifetime diagnosis of bipolar disorder, (OR 1.47, 95 % CI 1.12–1.93). 47 Chwastiak et al. found a 39.2 % prevalence of obesity in patients with bipolar disorder. 48 These behaviors contribute to the development of chronic medical disorders such as obesity, type 2 diabetes and coronary heart disease at an earlier age of onset compared to primary care patients without bipolar disorder. 40 , 41
Several United States studies have demonstrated higher prevalence of chronic medical conditions among patients with bipolar disorder compared to the general population. Kilbourne et al. 41 found higher prevalence of diabetes (17.2 % vs. 15.6 %, p = 0.0035), hepatitis C infection (5.9 % vs. 1.1 %, p < 0.001), lower back pain (15.4 % vs. 10.6 %, p < 0.001), chronic obstructive pulmonary disease (COPD) (10.6 % vs. 9.4 %, p = 0.005), among Department of Veterans Affairs (VA) patients with bipolar disorder compared to VA patients without bipolar disorder, even though the patients with bipolar disorder were younger, on average, than patients without bipolar disorder. Higher prevalence of medical conditions among patients with bipolar disorder has also been demonstrated in non-VA samples. 49 , 50 As bipolar disorder progresses, other chronic health conditions develop and accumulate 51 : patients with greater than 21 years of bipolar illness have a significantly higher burden of medical illness compared to patients with 10–20 years (p < 0.001) and 0–9 years of bipolar illness (p < 0.001), independent of patient age. Despite the high burden of general medical problems in this population, patients with bipolar disorder have significantly lower odds of having an identified primary care physician, 52 and are less likely than controls to have at least one primary care visit during a one-year study period (OR 0.63, 95 % CI 0.60–0.67). 53
In a national VA study, Kilbourne et al. 54 compared patients with bipolar disorder seen exclusively in primary care (7.6 % of patients) to those who received specialty mental health treatment. Compared to patients who received specialty care, the patients with bipolar disorder treated exclusively in primary care were more likely to have cardiovascular disease (OR = 1.26, 95 % CI 1.–1-1.58, p < 0.05) or hypertension (OR = 1.31, 95 % CI 1.11–1.53, p < 0.01), but were less likely to receive a mood stabilizing medication for bipolar disorder (OR = 0.18, 95 % CI 0.15–0.21, p < 0.001).
Substance use disorders co-occur in as many as 42 % of outpatients with bipolar disorder, 25 and are present in approximately one-third of patients at the onset of the first mood episode. 55 Health risk behaviors, 56 chronic medical conditions 57 and substance use 58 are associated with decreased level of functioning, increased symptom burden, and lower quality of life among patients with bipolar disorder. 59 Therefore, the recognition and treatment of bipolar disorder and commonly associated health risk behaviors in primary care may lead to reduced psychiatric symptom severity, improved health and improved functioning. 26
TREATMENT PRINCIPLES
Individual interventions.
Table 5 shows the evidence-based pharmacological treatments for bipolar depression and their associated common side effects. It is notable that only two treatments (quetiapine and olanzapine-fluoxetine combination [OFC]) have Food and Drug Administration (FDA) indications for bipolar depression.
Medications with an Evidence Base for the Treatment of Bipolar Depression
| Lithium | 600 mg by mouth at bedtime | Dose to serum level 0.8–1 mEq/L, (usual dose 900–2400 mg / day in divided doses) | Tremor, GI upset, polydipsia, renal impairment, thyroid disease, arrhythmia | No |
| Divalproex sodium, valproic acid | 500 mg by mouth at bedtime | Dose to clinical effect, generally at serum level 50–125mcg/mL (usual dose 1000–2000 mg / day in divided doses) | Nausea, vomiting, weight gain, sedation, hematologic effects, elevated liver enzymes, alopecia, tremor | No |
| Lamotrigine* | 25 mg by mouth daily for 2 weeks, then 50 mg by mouth daily for 2 weeks, then increase daily dose by 25 mg per week | 100–400 mg per day in divided doses | Nausea, non-severe or severe rash (note risk of Stevens-Johnson syndrome is reduced by titrating dose over several weeks) | No |
| Olanzapine-fluoxetine combination | Combination pill – Olanzapine 3–6 mg / fluoxetine 25 mg once daily | Combination pill – Olanzapine 6–12 mg / fluoxetine 25–50 mg once daily | Fluoxetine – restlessness, sleep problems, sexual dysfunction | Yes |
| Separate medications – Olanzapine 2.5-5 mg once daily, fluoxetine 10–20 mg once daily | Separate medications – Olanzapine 5–12.5 mg once daily, fluoxetine 20–50 mg once daily | Olanzapine – weight gain, dyslipidemia, hyperglycemia, sedation, constipation, urinary retention, orthostatic hypotension, prolonged QTc interval | ||
| Quetiapine* | 50 mg by mouth on day 1, 100 mg by mouth on day 2, then increase daily dose by 50–100 mg every 1–2 days | 300–600 mg per day in divided doses | Weight gain, dyslipidemia, hyperglycemia, sedation constipation, urinary retention, orthostatic hypotension, prolonged QTc interval | Yes |
*The doses suggested here exceed the doses FDA-approved for the indication of bipolar depression, but not the doses FDA-approved for other indications. The FDA-approved maximum doses for the indication of bipolar depression are 200 mg per day for lamotrigine and 300 mg per day for quetiapine
Lithium has an FDA indication for the treatment of mania and for maintenance treatment of bipolar disorder, but not for the treatment of bipolar depression. Lithium has been shown to reduce morbidity 60 and suicide risk 61 associated with bipolar disorder. A meta-analysis 62 of long-term lithium treatment in bipolar disorder showed that lithium is effective in reducing the risk of manic relapse, and to a lesser extent, depressive relapse. Quetiapine has shown superiority over lithium in the acute treatment of bipolar depression. 63 Lithium may have a limited role as monotherapy of acute bipolar depression, though lamotrigine added to existing lithium therapy has been effective in treating bipolar depression. 64 Lithium is an important treatment in the long-term management of bipolar disorder. Thiazide diuretics, ACE inhibitors, and non-steroidal anti-inflammatory agents increase serum lithium levels. Treatment with any of these medications requires a reduction in daily lithium dose and close laboratory monitoring.
Anticonvulsant Agents
A meta-analysis showed that divalproex 65 was more effective than placebo in producing a clinical response (risk ratio 2.1, 95 % CI 1.10-4.03) and remission (risk ratio 1.61, 95 % CI 1.02–2.53) in patients with bipolar depression. One meta-analysis of lamotrigine in bipolar depression showed that more people treated with lamotrigine experienced reduced depression symptoms compared to placebo (risk ratio 1.27, 95 % CI 1.09–1.47), and that those patients with more severe depression (measured by the Hamilton Rating Scale for Depression score > 24) had a greater benefit from lamotrigine compared to those with less severe depression. 66 However, a second meta-analysis showed that lamotrigine was not beneficial in the acute treatment of bipolar depression. 67
Antipsychotic Agents
In a meta-analysis of atypical antipsychotics in the treatment of acute bipolar depression, quetiapine (random effects estimate −5.63, 95 % CI −7.05 to −4.21) and olanzapine–fluoxetine in combination (OFC) (random effects estimate −3.10, 95 % CI −5.18 to −1.02) were superior to placebo. A systematic review of randomized, controlled treatment trials showed that OFC and quetiapine monotherapy were the most effective interventions for acute bipolar depression. 64 In newer treatment guidelines, quetiapine monotherapy has become the first-line recommendation for the treatment of bipolar depression. 68 Both olanzapine and quetiapine cause significant weight gain and dyslipidemia in many patients, and these adverse effects associated with atypical antipsychotics should be considered in treatment selection.
Antidepressant Agents
No antidepressant agents (including selective serotonin reuptake inhibitors [SSRIs]) have monotherapy FDA indications for the treatment of bipolar depression, and their use in bipolar disorder remains controversial. A meta-analysis 69 of fifteen studies showed that antidepressant medications lacked efficacy in the acute treatment of bipolar depression. However, a different meta-analysis 70 and subsequent clinical trial 71 suggest that antidepressants may have a role in the maintenance treatment of stabilized patients with bipolar disorder. In a trial without a placebo comparison, 60 patients already receiving a mood stabilizing medication who experienced a depressive episode experienced a significant reduction in depressive symptoms after receiving paroxetine or venlafaxine, although four patients in the venlafaxine group and one in the paroxetine group experienced mania or hypomania. 72 Investigators are continuing to study the role of antidepressant medications in bipolar depression. 73
The STEP-BD study was a large, federally funded multisite comparative effectiveness study of the treatment of bipolar depression. In patients with bipolar disorder treated with a mood stabilizer, there was no effect from adjunctive antidepressant treatment; only 27.3 % of patients randomized to treatment with a mood stabilizer plus placebo and 23.5 % randomized to mood stabilizer plus antidepressant (p = 0.40) recovered from the depressive episode. 74 Treatment-emergent affective switches 74 (e.g. into hypomania or mania), did not differ between treatment groups (10.1 % for the antidepressant group and 10.7 % for the placebo group, p = 0.84), though antidepressant treatment was associated with increased severity of manic symptoms at 3-month follow-up in patients with concurrent manic symptoms at baseline measurement during the depressive episode. 75 A systematic review 76 of anti-depressant associated mood-switching found that 13.8 % of patients with bipolar disorder exposed to antidepressant monotherapy developed elevated mood, hypomania or mania, with tricyclic antidepressants conferring the greatest risk.
There was no increase in suicidal behavior associated with antidepressant treatment of bipolar depression in the STEP-BD study. 77 In a review, McElroy et al. 78 found that patients with unrecognized bipolar disorder who received antidepressant monotherapy, but not antidepressant therapy plus a mood stabilizer, might have increased risk of experiencing suicidal ideation.
Other Treatment Principles
The BALANCE trial 79 showed that compared to valproate monotherapy, lithium monotherapy or in combination with valproate was more likely to prevent mood episode recurrence. Combination treatment (two mood stabilizing medications) may be more beneficial in preventing mood episode recurrence if the patient’s most recent mood episode was treated with combination treatment. 80
Psychosocial interventions such as social rhythm therapy and cognitive behavioral therapy are important components of treatment during depressive episodes or during the maintenance phase. In combination with appropriate pharmacotherapy, they shorten time to recovery of an acute episode, 81 shorten the time needed to achieve premorbid occupational functioning, 82 and lengthen the time until next mood episode. 83 In a randomized controlled trial 84 of stable patients with bipolar I and II disorder who were receiving appropriate pharmacotherapy, twenty one weeks of group psychoeducation was associated with lower incidence of mood episode recurrence, lower total number of mood recurrences per patient, and increased total time until next mood episode compared to a control group.
Population Interventions
Collaborative care models involving a population registry, treat to target guidelines, care managers, supervision by a consulting psychiatrist, brief counseling, patient self-management skills and close patient follow-up are more effective in primary care than usual care. 32 , 85 No randomized controlled trials have developed health services models to test how to improve quality of care and psychiatric outcomes in patients with bipolar disorder seen in primary care. A recent meta-analysis of collaborative care models found only four trials involving patients with bipolar disorder, all of which took place in mental health care settings. 86 However, collaborative care models have improved psychiatric outcomes and slowed the decline in physical health for patients with bipolar disorder treated in psychiatric care settings. 87 – 90 These results suggest that collaborative care for bipolar disorder may be effectively translated into the primary care setting.
Patients with bipolar disorder commonly present to primary care settings. Patients experience distinct depressive, hypomanic and manic episodes, but more commonly patients have subsyndromal depressive symptoms that impair functioning. It is important to ask patients with depression about the presence of current manic symptoms, such as racing thoughts, a history of manic symptoms, hypomania or mania, substance use, family history of bipolar disorder and prior treatments. Validated case identification tools such as the CIDI can be helpful in identifying bipolar disorder in primary care patients. Evidence-based treatments for bipolar depression differ from treatments for unipolar depression. Guidelines are available from the American Psychiatric Association 91 and the STABLE toolkit 23 for additional information on the management of bipolar disorder. Other publications provide resources intended specifically for primary care physicians. 92
Acknowledgements
1. Contributors: Wayne J. Katon MD
2. Funders: National Institute of Mental Health grant 5T32MH020021-15
3. Prior presentations—University of Washington Department of Psychiatry and Behavioral Sciences Grand Rounds on 21 December 2012, and the University of Washington Department of Internal Medicine Chief of Medicine Rounds at Harborview Medical Center on 12 February 2013; both in Seattle, WA
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Verbal fluency in bipolar disorders: A systematic review and meta-analysis
Affiliations.
- 1 Psychiatry Department, University Hospital, Reims, France; Cognition, Health, Socialization Laboratory (C2S EA6291), University of Reims Champagne-Ardenne, Reims, France. Electronic address: [email protected].
- 2 Psychiatry and Neurosciences Department, Faculty of Medicine, Laval University, Canada; Centre de recherche de l'Institut universitaire en santé mentale de Québec, Canada.
- 3 Psychiatry Department, University Hospital, Reims, France; Cognition, Health, Socialization Laboratory (C2S EA6291), University of Reims Champagne-Ardenne, Reims, France.
- 4 Cognition, Health, Socialization Laboratory (C2S EA6291), University of Reims Champagne-Ardenne, Reims, France.
- PMID: 27744224
- DOI: 10.1016/j.jad.2016.09.039
Background: One of the main features of bipolar disorder (BD), besides mood dysregulation, is an alteration of the structure of language. Bipolar patients present changes in semantic contents, impaired verbal associations, abnormal prosody and abnormal speed of language highlighted with various experimental tasks. Verbal fluency tasks are widely used to assess the abilities of bipolar patients to retrieve and produce verbal material from the lexico-semantic memory. Studies using these tasks have however yielded discrepant results. The aim of this study was thus to determine the extent of the verbal fluency impairment in BD patients and to evaluate if the deficits are affected by the type of task or by mood states.
Methods: A systematic literature search was conducted in MEDLINE, EBSCOHost and Google Scholar and relevant data were submitted to a meta-analysis.
Results: Thirty-nine studies were retained providing data for 52 independent groups of BD patients. The overall meta-analysis revealed a moderate verbal fluency impairment in BD compared to healthy controls (effect size d=0.61). Comparisons between mood states showed significant differences only between euthymic and manic patients and only on category fluency performances.
Limitations: This review is limited by the heterogeneity between studies for the characteristics of BD populations. Also, few of the retained studies examined depressive or mixed episodes.
Conclusions: This work confirms that BD patients present with moderate verbal fluency impairments, and underlines the specific effect of mood state on category fluency. This emphasizes the need to distinguish semantic from phonological processes in verbal fluency assessments in BD.
Keywords: Bipolar disorder; Mood state; Verbal fluency.
Copyright © 2016 Elsevier B.V. All rights reserved.
PubMed Disclaimer
Similar articles
- Cognitive deficits in bipolar disorders: Implications for emotion. Lima IMM, Peckham AD, Johnson SL. Lima IMM, et al. Clin Psychol Rev. 2018 Feb;59:126-136. doi: 10.1016/j.cpr.2017.11.006. Epub 2017 Nov 21. Clin Psychol Rev. 2018. PMID: 29195773 Free PMC article. Review.
- Thought and language disturbance in bipolar disorder quantified via process-oriented verbal fluency measures. Weiner L, Doignon-Camus N, Bertschy G, Giersch A. Weiner L, et al. Sci Rep. 2019 Oct 3;9(1):14282. doi: 10.1038/s41598-019-50818-5. Sci Rep. 2019. PMID: 31582814 Free PMC article.
- Neurocognitive endophenotypes (endophenocognitypes) from studies of relatives of bipolar disorder subjects: a systematic review. Balanzá-Martínez V, Rubio C, Selva-Vera G, Martinez-Aran A, Sánchez-Moreno J, Salazar-Fraile J, Vieta E, Tabarés-Seisdedos R. Balanzá-Martínez V, et al. Neurosci Biobehav Rev. 2008 Oct;32(8):1426-38. doi: 10.1016/j.neubiorev.2008.05.019. Epub 2008 May 23. Neurosci Biobehav Rev. 2008. PMID: 18582942 Review.
- Cognitive-linguistic deficits in euthymic elderly patients with bipolar disorder. Radanovic M, Nunes PV, Forlenza OV, Braga Ladeira R, Gattaz WF. Radanovic M, et al. J Affect Disord. 2013 Sep 5;150(2):691-4. doi: 10.1016/j.jad.2013.04.035. Epub 2013 Jun 12. J Affect Disord. 2013. PMID: 23764386
- Executive functioning deficits among adults with Bipolar Disorder (types I and II): A systematic review and meta-analysis. Dickinson T, Becerra R, Coombes J. Dickinson T, et al. J Affect Disord. 2017 Aug 15;218:407-427. doi: 10.1016/j.jad.2017.04.010. Epub 2017 Apr 29. J Affect Disord. 2017. PMID: 28501741 Review.
- The inferior frontal gyrus and familial risk for bipolar disorder. Qin K, Sweeney JA, DelBello MP. Qin K, et al. Psychoradiology. 2022 Dec 6;2(4):171-179. doi: 10.1093/psyrad/kkac022. eCollection 2022 Dec. Psychoradiology. 2022. PMID: 38665274 Free PMC article. Review.
- Linguistic characteristics in bipolar disorder versus borderline personality disorder. Muriel NS, López Resa P, Moraleda Sepúlveda E. Muriel NS, et al. Sci Rep. 2023 Dec 7;13(1):21715. doi: 10.1038/s41598-023-46038-7. Sci Rep. 2023. PMID: 38065986 Free PMC article.
- The relationship between cognitive reserve focused on leisure experiences and cognitive functions in bipolar patients. Sato K, Matsui M, Ono Y, Miyagishi Y, Tsubomoto M, Naito N, Kikuchi M. Sato K, et al. Heliyon. 2023 Nov 1;9(11):e21661. doi: 10.1016/j.heliyon.2023.e21661. eCollection 2023 Nov. Heliyon. 2023. PMID: 38027814 Free PMC article.
- Mindfulness enhances cognitive functioning: a meta-analysis of 111 randomized controlled trials. Zainal NH, Newman MG. Zainal NH, et al. Health Psychol Rev. 2024 Jun;18(2):369-395. doi: 10.1080/17437199.2023.2248222. Epub 2023 Aug 30. Health Psychol Rev. 2024. PMID: 37578065 Review.
- Neurocognitive Deficits in Recently Diagnosed Young Remitted Bipolar I Disorder and At-Risk Subjects: Potential Endophenotypes? Reddy PV, Bojappen N, Reddy RP, Arumugham SS, Muralidharan K. Reddy PV, et al. Indian J Psychol Med. 2023 Jul;45(4):390-396. doi: 10.1177/02537176231165414. Epub 2023 May 11. Indian J Psychol Med. 2023. PMID: 37483584 Free PMC article.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Elsevier Science
Other Literature Sources
- scite Smart Citations
- MedlinePlus Consumer Health Information
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

INFORMATIVE SPEECH

Informative Speech (Mental Illness)
Related Papers
Bipolar Disorders
Michele Raja
World Psychiatry 2012; 11 (suppl. 1): 26-30.
subho chakrabarti
The World Health Organization has stated that clinical utility and cross-cultural applicability will be accorded a very high priority during the process of revising the ICD-10. This brief review highlights the impact of cultural factors on clinical presentations, gender differences, and treatment realities in the area of mood and anxiety disorders, with particular emphasis on research from non-Western settings. Even a cursory examination of these issues reveals significant cross-cultural variations in the clinical and treatment profile of these disorders. The process of revision would greatly benefit by incorporating relevant insights from the growing body of evidence regarding socio-cultural influences on depressive and anxiety disorders. This may eventually help lessen the widespread problems of non-recognition and under-treatment of these disorders, thereby enhancing the global utility of the ICD-11.
World Psychiatry 2012; 11 (suppl. 1): 59-64.
It is debatable whether psychotic and catatonic forms of mood disorders represent distinct categories meriting independent status, or are merely more severe variants of these disorders. Current research evidence indicates that not only are psychotic symptoms quite common in mood disorders, but they are often associated with poorer prognosis, though not invariably so. Catatonia also appears to have a distinct profile, and is more commonly associated with mood disorders than with schizophrenia. Existing classifications have accorded the status of specifiers/subtypes to psychotic and catatonic symptoms of mood disorders. They also link psychotic symptoms with severity of mood episodes, and provide only limited information about the unique characteristics of mood disorders with psychosis or catatonia. Proposals for the DSM- 5 have attempted to remedy some of these deficiencies. The ICD-11 could benefit by introducing some important changes in this area, such as delinking psychosis from severity, providing greater detail about mood-congruent and mood-incongruent psychotic symptoms, and incorporating descriptions of the unique features of psychotic mood disorders. Additionally, catatonic presentations could be designated separately with criteria that are uniformly applicable to mood, schizophrenic and organic disorders.
Neuro endocrinology letters
Jan Prasko , Klára Látalová , Zuzana Sedlackova , Daniela Zmeškalová
Anxiety disorders are common in patients with bipolar disorder and show considerable influence on the course of the disease and response to treatment. We conducted a series of literature searches using key words, such as bipolar disorder and anxiety disorders, as items in indexed fields. The studies were obtained through a MEDLINE search from 1970 to 2012. We also examined additional studies cited in articles from these searches or our previous studies. Several studies have shown poorer outcomes for patients with bipolar and comorbid anxiety disorders. Some studies have indicated worse outcomes in patients with bipolar disorder and associated anxiety disorders. Shorter periods of euthymia, increased suicidal thoughts and an increased number of suicide attempts were observed. Whether the effective treatment of anxiety reduces suicide and the severity of bipolar disorder or improves the response to treatment remains unknown. There are no well-designed intervention studies in bipolar p...
Journal of Affective Disorders
C. Demonfaucon , Hagop Akiskal
Yuna S Chaniago
Hagop Akiskal
Frontiers in Psychiatry
Stefano Pallanti
Depression and Anxiety
Ygor Ferrão
The obsessive–compulsive (OC) spectrum has been discussed in the literature for two decades. Proponents of this concept propose that certain disorders characterized by repetitive thoughts and/or behaviors are related to obsessive–compulsive disorder (OCD), and suggest that such disorders be grouped together in the same category (i.e. grouping, or “chapter”) in DSM. This article addresses this topic and presents options and preliminary recommendations to be considered for DSM-V. The article builds upon and extends prior reviews of this topic that were prepared for and discussed at a DSM-V Research Planning Conference on Obsessive–Compulsive Spectrum Disorders held in 2006. Our preliminary recommendation is that an OC-spectrum grouping of disorders be included in DSM-V. Furthermore, we preliminarily recommend that consideration be given to including this group of disorders within a larger supraordinate category of “Anxiety and Obsessive–Compulsive Spectrum Disorders.” These preliminary recommendations must be evaluated in light of recommendations for, and constraints upon, the overall structure of DSM-V. Depression and Anxiety, 2010. © 2010 Wiley-Liss, Inc.
Bipolar Disorders 2008; 10 (Suppl. 1): 42.
Background and Aim: In India, caregivers play an important role in treatment supervision and decision-making for bipolar affective disorder (BPAD). In recent times there is lot of concern about switch of polarity with use of antidepressants and hence Electroconvulsive therapy (ECT) is quite frequently used for treating BPAD, severe depression. The present study attempted to assess the knowledge and attitude towards ECT of caregivers of BPAD patients at PGIMER, Chandigarh, India. Method: Thirty-five consenting primary caregivers, of BPAD patients who had never received ECT were asked to fill up a selfadministered questionnaire. Results: Majority of the caregivers were male (65.7%), educated & Matric (94.3%) and spouse (57.1%) of the patients. Majority of the caregivers were aware about the nature of ECT treatment, need for consent, but are not aware about the mechanism of action and details of procedure of ECT. More than half of the caregivers also had a positive attitude towards ECT and did not consider it as dangerous, inhuman, cruel, a form of punishment and thought that it shouldn’t be outlawed. Nearly 63% agreed to recommend for family members when required. There was positive correlation between better knowledge and better education level of the caregiver and female caregivers had poorer knowledge. Conclusion: Majority of the caregivers of the BPAD patients were aware about the nature of ECT treatment, need for consent, but are not aware about the mechanism of action and procedure of ECT and have positive attitude towards ECT
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Seetal Dodd
Martin Provencher
Yugashini Paramaswaran
Acta Psychiatrica Scandinavica
Andrea Amerio , C. Liapis
Steven Marwaha , Matthew Broome
Journal of Anxiety Disorders
European Archives of Psychiatry and Clinical Neuroscience
Riccardo Paoli , Marta Serati
… page intentionally left …
Frank Pillmann , Raffaela Blöink
Comprehensive Psychiatry
Juliana Diniz , Roseli Shavitt , Albina Torres
Journal of affective disorders
Maria Travierso
Gustavo Vazquez
Acta Neuropsychiatrica
Roseli Shavitt
Starlin Mythri
Francesca Pellegrini
Progress in Neuro-Psychopharmacology and Biological Psychiatry
Christine Lochner
Marcia Brenner
Current Pharmaceutical Design
Barnaby Nelson
Jasper Eberendu
Annals of Clinical Psychiatry Official Journal of the American Academy of Clinical Psychiatrists
Margaret D Weiss
Raymond Lam
Scott Patten
Depression and …
Erhan Ertekin
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

COMMENTS
Bipolar Disorder Informative Speech Outline. 1202 Words5 Pages. Jasmine Yard SPCH 1500 10/5/14 Topic: Bipolar Disorder General Purpose Statement: To inform. Specific Purposes Statement: To inform my peers of the severity of Bipolar Disorder. Central Idea: To inform my peers of the severity of Bipolar Disorder, including description, the causes ...
A well-structured essay on bipolar disorder should include: 1. Introduction: Provide a brief overview of bipolar disorder and state the essay's main focus or thesis. 2. Background Information: Offer essential context about bipolar disorder, including its definition, types, and prevalence.
Bipolar disorder (formerly called manic-depressive illness or manic depression) is a mental illness that causes unusual shifts in a person's mood, energy, activity levels, and concentration. These shifts can make it difficult to carry out day-to-day tasks. There are three types of bipolar disorder. All three types involve clear changes in ...
Kristen Holmes Ms. Hobbs CMCN 100: Speech Outline 20 April 2016 Having Bipolar Disorder I. Introduction A. Attention Getter- Introduce my sister 1. My sister is 25 years old and has suffered from bipolar disorder since she turned 7 years old. 2. She was not capable of completing high school because of her disorder. 3.
Home > Blog > Informative Speech > Informative Speech Outline Understanding Mental Health: Breaking the Stigma I. Introduction ... anxiety, bipolar disorder, and schizophrenia are just a few examples of common mental health disorders. We'll delve into what each entails." B. Prevalence: "Let's face the facts: these disorders are more common than ...
Bipolar disorder, formerly known as manic depression, is a chronic mental health condition that affects approximately 2.8% of the adult population in the United States alone. ... - Racing thoughts and rapid speech - Impulsive or risky behavior. Depressive episodes, on the other hand, may involve: - Persistent feelings of sadness or ...
Bipolar Disorder: #N# <h2>What Is Bipolar Disorder?</h2>#N# <div class="field field-name-body field-type-text-with-summary field-label-hidden">#N# <div class="field ...
Bipolar I disorder is defined by manic episodes that last at least 7 days (most of the day, nearly every day) or when manic symptoms are so severe that hospital care is needed. Usually, separate depressive episodes occur as well, typically lasting at least 2 weeks. Episodes of mood disturbance with mixed features are also possible.
Bipolar disorder, which used to be called manic depressive illness or manic depression, is a mental disorder characterized by wide mood swings from high (manic) to low (depressed). The expert view of bipolar disorder will continue to evolve, but it is now commonly divided into two subtypes (bipolar I and bipolar II) based on the dividing line ...
Bipolar disorder. Bipolar disorder is a serious mental illness in which common emotions become intensely and often unpredictably magnified. Individuals with bipolar disorder can quickly swing from extremes of happiness, energy, and clarity to sadness, fatigue, and confusion. These shifts can be so devastating that individuals may consider suicide.
reckless or behavior that may have harmful effects. a decreased need or ability to sleep. elevated mood. exaggerated optimism. feeling anxious or jittery. inability to focus. restlessness. Learn ...
Biological Factors. The symptoms of an individual with bipolar disorder include the following. People with bipolar disorder generally have problems with their moods, experiencing extreme highs and lows known as mania or hypomania, respectively. An individual with bipolar disorder may also develop problems with perception and thinking such as ...
Bipolar disorder (BD) is characterized by speech abnormalities, reflected by symptoms such as pressure of speech in mania and poverty of speech in depression. Here we aimed at investigating speech ...
Bipolar Depression is a serious disorder that deals with serious side effects that can result in either being treated easily or dealt with for the rest of the victim's lives. Bipolar Depression associates with a disorder called Bipolar Disorder (known as manic depression) that causes serious shifts in mood, energy, thinking and behavior.
BACKGROUND AND EPIDEMIOLOGY. Bipolar I disorder is a chronic mood disorder characterized by the presence of at least one manic episode and usually recurrent major depressive episodes and often chronic depressive symptoms. 1, 2 Symptoms of bipolar disorder are shown in Table 1.Mania is the defining disease state in bipolar I disorder, and consists of a marked departure from baseline behavior ...
b. The 4 types of bipolar disorder in order from most severe to least starting with Bipolar 1 Disorder - a person has at least 1 manic episode lasting at least a week. He or she has multiple episodes of major depression. Without treatment, the episodes of mania and depression usually repeat over time. The depressive symptoms may outnumber the manic symptoms.
Informative Speech Outline Bipolar Disorder Topic: Bipolar Disorder (Manic-Depressive Behavior) Opening with Impact: Raise your hand if you have heard of the term "bipolar" before? We often associate this term when making a joke or insult in some cases or even when someone is acting erratic, but it is way more complexed. Manic- Depressive Behavior also known as bipolar disorder is ...
Bipolar Disorder.pptx - Bipolar Disorder Informative speech... Pages 13. Total views 19. University of Maryland, University College. PSYC. PSYC MISC. abcmabera. 2/24/2020. 100% (1) View full document. Students also studied. imformative speech- mental illness outline. Georgia Southern University.
Verbal fluency tasks are widely used to assess the abilities of bipolar patients to retrieve and produce verbal material from the lexico-semantic memory. Studies using these tasks have however yielded discrepant results. The aim of this study was thus to determine the extent of the verbal fluency impairment in BD patients and to evaluate if the ...
Anxiety disorders are common in patients with bipolar disorder and show considerable influence on the course of the disease and response to treatment. We conducted a series of literature searches using key words, such as bipolar disorder and anxiety disorders, as items in indexed fields. ... INFORMATIVE SPEECH BY ANGELIANA NATASHA JIMMY GENERAL ...
Bipolar Informative Speech Outline Name: Secoya Hines Topic: Bipolar Disorder Specific Purpose: To inform the audience on the symptoms and treatment options of Bipolar Disorder Central Idea: To inform the audience on the description of Bipolar Disorder, the signs and symptoms, and available treatment options of this mental health disorder INTRODUCTION I. Attention Getter: Talk about my ...
Here is some information on bipolar effective disorder also known as manic depression.
Hatt 1 Rachael Hatt Professor Kilgore Communications 12 April 2024 Informative Speech Outline Understanding the Difference Between Bipolar Disorder and Borderline Personality Disorder. According to the World Health Organization, mental health disorders affect approximately 450 million people worldwide, emphasizing the need for understanding and supporting individuals affected by mental health ...