- Research article
- Open access
- Published: 16 November 2020

Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews
- Pawel Posadzki 1 , 2 ,
- Dawid Pieper ORCID: orcid.org/0000-0002-0715-5182 3 ,
- Ram Bajpai 4 ,
- Hubert Makaruk 5 ,
- Nadja Könsgen 3 ,
- Annika Lena Neuhaus 3 &
- Monika Semwal 6
BMC Public Health volume 20 , Article number: 1724 ( 2020 ) Cite this article
36k Accesses
151 Citations
157 Altmetric
Metrics details
Sedentary lifestyle is a major risk factor for noncommunicable diseases such as cardiovascular diseases, cancer and diabetes. It has been estimated that approximately 3.2 million deaths each year are attributable to insufficient levels of physical activity. We evaluated the available evidence from Cochrane systematic reviews (CSRs) on the effectiveness of exercise/physical activity for various health outcomes.
Overview and meta-analysis. The Cochrane Library was searched from 01.01.2000 to issue 1, 2019. No language restrictions were imposed. Only CSRs of randomised controlled trials (RCTs) were included. Both healthy individuals, those at risk of a disease, and medically compromised patients of any age and gender were eligible. We evaluated any type of exercise or physical activity interventions; against any types of controls; and measuring any type of health-related outcome measures. The AMSTAR-2 tool for assessing the methodological quality of the included studies was utilised.
Hundred and fifty CSRs met the inclusion criteria. There were 54 different conditions. Majority of CSRs were of high methodological quality. Hundred and thirty CSRs employed meta-analytic techniques and 20 did not. Limitations for studies were the most common reasons for downgrading the quality of the evidence. Based on 10 CSRs and 187 RCTs with 27,671 participants, there was a 13% reduction in mortality rates risk ratio (RR) 0.87 [95% confidence intervals (CI) 0.78 to 0.96]; I 2 = 26.6%, [prediction interval (PI) 0.70, 1.07], median effect size (MES) = 0.93 [interquartile range (IQR) 0.81, 1.00]. Data from 15 CSRs and 408 RCTs with 32,984 participants showed a small improvement in quality of life (QOL) standardised mean difference (SMD) 0.18 [95% CI 0.08, 0.28]; I 2 = 74.3%; PI -0.18, 0.53], MES = 0.20 [IQR 0.07, 0.39]. Subgroup analyses by the type of condition showed that the magnitude of effect size was the largest among patients with mental health conditions.
There is a plethora of CSRs evaluating the effectiveness of physical activity/exercise. The evidence suggests that physical activity/exercise reduces mortality rates and improves QOL with minimal or no safety concerns.
Trial registration
Registered in PROSPERO ( CRD42019120295 ) on 10th January 2019.
Peer Review reports
The World Health Organization (WHO) defines physical activity “as any bodily movement produced by skeletal muscles that requires energy expenditure” [ 1 ]. Therefore, physical activity is not only limited to sports but also includes walking, running, swimming, gymnastics, dance, ball games, and martial arts, for example. In the last years, several organizations have published or updated their guidelines on physical activity. For example, the Physical Activity Guidelines for Americans, 2nd edition, provides information and guidance on the types and amounts of physical activity that provide substantial health benefits [ 2 ]. The evidence about the health benefits of regular physical activity is well established and so are the risks of sedentary behaviour [ 2 ]. Exercise is dose dependent, meaning that people who achieve cumulative levels several times higher than the current recommended minimum level have a significant reduction in the risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events [ 3 ]. Benefits of physical activity have been reported for numerous outcomes such as mortality [ 4 , 5 ], cognitive and physical decline [ 5 , 6 , 7 ], glycaemic control [ 8 , 9 ], pain and disability [ 10 , 11 ], muscle and bone strength [ 12 ], depressive symptoms [ 13 ], and functional mobility and well-being [ 14 , 15 ]. Overall benefits of exercise apply to all bodily systems including immunological [ 16 ], musculoskeletal [ 17 ], respiratory [ 18 ], and hormonal [ 19 ]. Specifically for the cardiovascular system, exercise increases fatty acid oxidation, cardiac output, vascular smooth muscle relaxation, endothelial nitric oxide synthase expression and nitric oxide availability, improves plasma lipid profiles [ 15 ] while at the same time reducing resting heart rate and blood pressure, aortic valve calcification, and vascular resistance [ 20 ].
However, the degree of all the above-highlighted benefits vary considerably depending on individual fitness levels, types of populations, age groups and the intensity of different physical activities/exercises [ 21 ]. The majority of guidelines in different countries recommend a goal of 150 min/week of moderate-intensity aerobic physical activity (or equivalent of 75 min of vigorous-intensity) [ 22 ] with differences for cardiovascular disease [ 23 ] or obesity prevention [ 24 ] or age groups [ 25 ].
There is a plethora of systematic reviews published by the Cochrane Library critically evaluating the effectiveness of physical activity/exercise for various health outcomes. Cochrane systematic reviews (CSRs) are known to be a source of high-quality evidence. Thus, it is not only timely but relevant to evaluate the current knowledge, and determine the quality of the evidence-base, and the magnitude of the effect sizes given the negative lifestyle changes and rising physical inactivity-related burden of diseases. This overview will identify the breadth and scope to which CSRs have appraised the evidence for exercise on health outcomes; and this will help in directing future guidelines and identifying current gaps in the literature.
The objectives of this research were to a. answer the following research questions: in children, adolescents and adults (both healthy and medically compromised) what are the effects (and adverse effects) of exercise/physical activity in improving various health outcomes (e.g., pain, function, quality of life) reported in CSRs; b. estimate the magnitude of the effects by pooling the results quantitatively; c. evaluate the strength and quality of the existing evidence; and d. create recommendations for future researchers, patients, and clinicians.
Our overview was registered with PROSPERO (CRD42019120295) on 10th January 2019. The Cochrane Handbook for Systematic Reviews of interventions and Preferred Reporting Items for Overviews of Reviews were adhered to while writing and reporting this overview [ 26 , 27 ].
Search strategy and selection criteria
We followed the practical guidance for conducting overviews of reviews of health care interventions [ 28 ] and searched the Cochrane Database of Systematic Reviews (CDSR), 2019, Issue 1, on the Cochrane Library for relevant papers using the search strategy: (health) and (exercise or activity or physical). The decision to seek CSRs only was based on three main aspects. First, high quality (CSRs are considered to be the ‘gold methodological standard’) [ 29 , 30 , 31 ]. Second, data saturation (enough high-quality evidence to reach meaningful conclusions based on CSRs only). Third, including non-CSRs would have heavily increased the issue of overlapping reviews (also affecting data robustness and credibility of conclusions). One reviewer carried out the searches. The study screening and selection process were performed independently by two reviewers. We imported all identified references into reference manager software EndNote (X8). Any disagreements were resolved by discussion between the authors with third overview author acting as an arbiter, if necessary.
We included CSRs of randomised controlled trials (RCTs) involving both healthy individuals and medically compromised patients of any age and gender. Only CSRs assessing exercise or physical activity as a stand-alone intervention were included. This included interventions that could initially be taught by a professional or involve ongoing supervision (the WHO definition). Complex interventions e.g., assessing both exercise/physical activity and behavioural changes were excluded if the health effects of the interventions could not have been attributed to exercise distinctly.
Any types of controls were admissible. Reviews evaluating any type of health-related outcome measures were deemed eligible. However, we excluded protocols or/and CSRs that have been withdrawn from the Cochrane Library as well as reviews with no included studies.
Data analysis
Three authors (HM, ALN, NK) independently extracted relevant information from all the included studies using a custom-made data collection form. The methodological quality of SRs included was independently evaluated by same reviewers using the AMSTAR-2 tool [ 32 ]. Any disagreements on data extraction or CSR quality were resolved by discussion. The entire dataset was validated by three authors (PP, MS, DP) and any discrepant opinions were settled through discussions.
The results of CSRs are presented in a narrative fashion using descriptive tables. Where feasible, we presented outcome measures across CSRs. Data from the subset of homogeneous outcomes were pooled quantitatively using the approach previously described by Bellou et al. and Posadzki et al. [ 33 , 34 ]. For mortality and quality of life (QOL) outcomes, the number of participants and RCTs involved in the meta-analysis, summary effect sizes [with 95% confidence intervals (CI)] using random-effects model were calculated. For binary outcomes, we considered relative risks (RRs) as surrogate measures of the corresponding odds ratio (OR) or risk ratio/hazard ratio (HR). To stabilise the variance and normalise the distributions, we transformed RRs into their natural logarithms before pooling the data (a variation was allowed, however, it did not change interpretation of results) [ 35 ]. The standard error (SE) of the natural logarithm of RR was derived from the corresponding CIs, which was either provided in the study or calculated with standard formulas [ 36 ]. Binary outcomes reported as risk difference (RD) were also meta-analysed if two more estimates were available. For continuous outcomes, we only meta-analysed estimates that were available as standardised mean difference (SMD), and estimates reported with mean differences (MD) for QOL were presented separately in a supplementary Table 9 . To estimate the overall effect size, each study was weighted by the reciprocal of its variance. Random-effects meta-analysis, using DerSimonian and Laird method [ 37 ] was applied to individual CSR estimates to obtain a pooled summary estimate for RR or SMD. The 95% prediction interval (PI) was also calculated (where ≥3 studies were available), which further accounts for between-study heterogeneity and estimates the uncertainty around the effect that would be anticipated in a new study evaluating that same association. I -squared statistic was used to measure between study heterogeneity; and its various thresholds (small, substantial and considerable) were interpreted considering the size and direction of effects and the p -value from Cochran’s Q test ( p < 0.1 considered as significance) [ 38 ]. Wherever possible, we calculated the median effect size (with interquartile range [IQR]) of each CSR to interpret the direction and magnitude of the effect size. Sub-group analyses are planned for type and intensity of the intervention; age group; gender; type and/or severity of the condition, risk of bias in RCTs, and the overall quality of the evidence (Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria). To assess overlap we calculated the corrected covered area (CCA) [ 39 ]. All statistical analyses were conducted on Stata statistical software version 15.2 (StataCorp LLC, College Station, Texas, USA).
The searches generated 280 potentially relevant CRSs. After removing of duplicates and screening, a total of 150 CSRs met our eligibility criteria [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 , 185 , 186 , 187 , 188 , 189 ] (Fig. 1 ). Reviews were published between September 2002 and December 2018. A total of 130 CSRs employed meta-analytic techniques and 20 did not. The total number of RCTs in the CSRs amounted to 2888; with 485,110 participants (mean = 3234, SD = 13,272). The age ranged from 3 to 87 and gender distribution was inestimable. The main characteristics of included reviews are summarised in supplementary Table 1 . Supplementary Table 2 summarises the effects of physical activity/exercise on health outcomes. Conclusions from CSRs are listed in supplementary Table 3 . Adverse effects are listed in supplementary Table 4 . Supplementary Table 5 presents summary of withdrawals/non-adherence. The methodological quality of CSRs is presented in supplementary Table 6 . Supplementary Table 7 summarises studies assessed at low risk of bias (by the authors of CSRs). GRADE-ings of the review’s main comparison are listed in supplementary Table 8 .
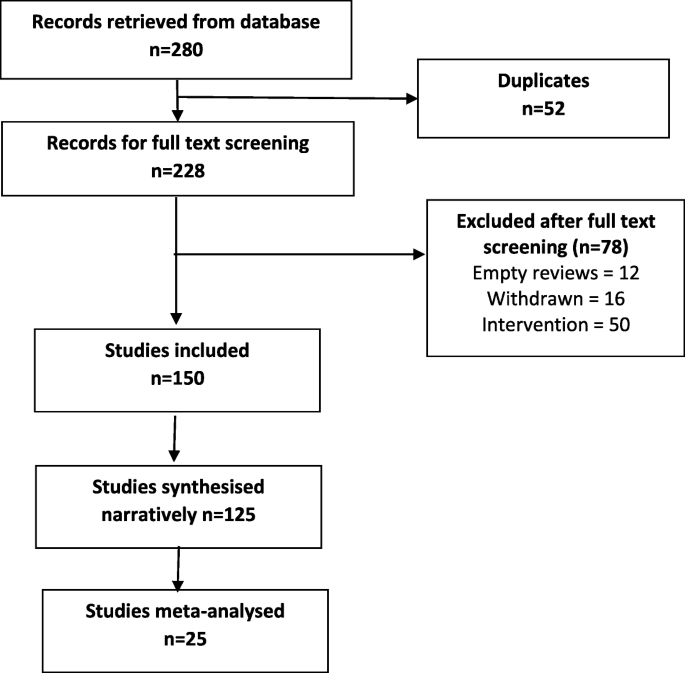
Study selection process
There were 54 separate populations/conditions, considerable range of interventions and comparators, co-interventions, and outcome measures. For detailed description of interventions, please refer to the supplementary tables . Most commonly measured outcomes were - function 112 (75%), QOL 83 (55%), AEs 70 (47%), pain 41 (27%), mortality 28 (19%), strength 30 (20%), costs 47 (31%), disability 14 (9%), and mental health in 35 (23%) CSRs.
There was a 13% reduction in mortality rates risk ratio (RR) 0.87 [95% CI 0.78 to 0.96]; I 2 = 26.6%, [PI 0.70, 1.07], median effect size (MES) = 0.93 [interquartile range (IQR) 0.81, 1.00]; 10 CSRs, 187 RCTs, 27,671 participants) following exercise when compared with various controls (Table 1 ). This reduction was smaller in ‘other groups’ of patients when compared to cardiovascular diseases (CVD) patients - RR 0.97 [95% CI 0.65, 1.45] versus 0.85 [0.76, 0.96] respectively. The effects of exercise were not intensity or frequency dependent. Sessions more than 3 times per week exerted a smaller reduction in mortality as compared with sessions of less than 3 times per week RR 0.87 [95% CI 0.78, 0.98] versus 0.63 [0.39, 1.00]. Subgroup analyses by risk of bias (ROB) in RCTs showed that RCTs at low ROB exerted smaller reductions in mortality when compared to RCTs at an unclear or high ROB, RR 0.90 [95% CI 0.78, 1.02] versus 0.72 [0.42, 1.22] versus 0.86 [0.69, 1.06] respectively. CSRs with moderate quality of evidence (GRADE), showed slightly smaller reductions in mortality when compared with CSRs that relied on very low to low quality evidence RR 0.88 [95% CI 0.79, 0.98] versus 0.70 [0.47, 1.04].
Exercise also showed an improvement in QOL, standardised mean difference (SMD) 0.18 [95% CI 0.08, 0.28]; I 2 = 74.3%; PI -0.18, 0.53], MES = 0.20 [IQR 0.07, 0.39]; 15 CSRs, 408 RCTs, 32,984 participants) when compared with various controls (Table 2 ). These improvements were greater observed for health related QOL when compared to overall QOL SMD 0.30 [95% CI 0.21, 0.39] vs 0.06 [− 0.08, 0.20] respectively. Again, the effects of exercise were duration and frequency dependent. For instance, sessions of more than 90 mins exerted a greater improvement in QOL as compared with sessions up to 90 min SMD 0.24 [95% CI 0.11, 0.37] versus 0.22 [− 0.30, 0.74]. Subgroup analyses by the type of condition showed that the magnitude of effect was the largest among patients with mental health conditions, followed by CVD and cancer. Physical activity exerted negative effects on QOL in patients with respiratory conditions (2 CSRs, 20 RCTs with 601 patients; SMD -0.97 [95% CI -1.43, 0.57]; I 2 = 87.8%; MES = -0.46 [IQR-0.97, 0.05]). Subgroup analyses by risk of bias (ROB) in RCTs showed that RCTs at low or unclear ROB exerted greater improvements in QOL when compared to RCTs at a high ROB SMD 0.21 [95% CI 0.10, 0.31] versus 0.17 [0.03, 0.31]. Analogically, CSRs with moderate to high quality of evidence showed slightly greater improvements in QOL when compared with CSRs that relied on very low to low quality evidence SMD 0.19 [95% CI 0.05, 0.33] versus 0.15 [− 0.02, 0.32]. Please also see supplementary Table 9 more studies reporting QOL outcomes as mean difference (not quantitatively synthesised herein).
Adverse events (AEs) were reported in 100 (66.6%) CSRs; and not reported in 50 (33.3%). The number of AEs ranged from 0 to 84 in the CSRs. The number was inestimable in 83 (55.3%) CSRs. Ten (6.6%) reported no occurrence of AEs. Mild AEs were reported in 28 (18.6%) CSRs, moderate in 9 (6%) and serious/severe in 20 (13.3%). There were 10 deaths and in majority of instances, the causality was not attributed to exercise. For this outcome, we were unable to pool the data as effect sizes were too heterogeneous (Table 3 ).
In 38 CSRs, the total number of trials reporting withdrawals/non-adherence was inestimable. There were different ways of reporting it such as adherence or attrition (high in 23.3% of CSRs) as well as various effect estimates including %, range, total numbers, MD, RD, RR, OR, mean and SD. The overall pooled estimates are reported in Table 3 .
Of all 16 domains of the AMSTAR-2 tool, 1876 (78.1%) scored ‘yes’, 76 (3.1%) ‘partial yes’; 375 (15.6%) ‘no’, and ‘not applicable’ in 25 (1%) CSRs. Ninety-six CSRs (64%) were scored as ‘no’ on reporting sources of funding for the studies followed by 88 (58.6%) failing to explain the selection of study designs for inclusion. One CSR (0.6%) each were judged as ‘no’ for reporting any potential sources of conflict of interest, including any funding for conducting the review as well for performing study selection in duplicate.
In 102 (68%) CSRs, there was predominantly a high risk of bias in RCTs. In 9 (6%) studies, this was reported as a range, e.g., low or unclear or low to high. Two CSRs used different terminology i.e., moderate methodological quality; and the risk of bias was inestimable in one CSR. Sixteen (10.6%) CSRs did not identify any studies (RCTs) at low risk of random sequence generation, 28 (18.6%) allocation concealment, 28 (18.6%) performance bias, 84 (54%) detection bias, 35 (23.3%) attrition bias, 18 (12%) reporting bias, and 29 (19.3%) other bias.
In 114 (76%) CSRs, limitation of studies was the main reason for downgrading the quality of the evidence followed by imprecision in 98 (65.3%) and inconsistency in 68 (45.3%). Publication bias was the least frequent reason for downgrading in 26 (17.3%) CSRs. Ninety-one (60.7%) CSRs reached equivocal conclusions, 49 (32.7%) reviews reached positive conclusions and 10 (6.7%) reached negative conclusions (as judged by the authors of CSRs).
In this systematic review of CSRs, we found a large body of evidence on the beneficial effects of physical activity/exercise on health outcomes in a wide range of heterogeneous populations. Our data shows a 13% reduction in mortality rates among 27,671 participants, and a small improvement in QOL and health-related QOL following various modes of physical activity/exercises. This means that both healthy individuals and medically compromised patients can significantly improve function, physical and mental health; or reduce pain and disability by exercising more [ 190 ]. In line with previous findings [ 191 , 192 , 193 , 194 ], where a dose-specific reduction in mortality has been found, our data shows a greater reduction in mortality in studies with longer follow-up (> 12 months) as compared to those with shorter follow-up (< 12 months). Interestingly, we found a consistent pattern in the findings, the higher the quality of evidence and the lower the risk of bias in primary studies, the smaller reductions in mortality. This pattern is observational in nature and cannot be over-generalised; however this might mean less certainty in the estimates measured. Furthermore, we found that the magnitude of the effect size was the largest among patients with mental health conditions. A possible mechanism of action may involve elevated levels of brain-derived neurotrophic factor or beta-endorphins [ 195 ].
We found the issue of poor reporting or underreporting of adherence/withdrawals in over a quarter of CSRs (25.3%). This is crucial both for improving the accuracy of the estimates at the RCT level as well as maintaining high levels of physical activity and associated health benefits at the population level.
Even the most promising interventions are not entirely risk-free; and some minor AEs such as post-exercise pain and soreness or discomfort related to physical activity/exercise have been reported. These were typically transient; resolved within a few days; and comparable between exercise and various control groups. However worryingly, the issue of poor reporting or underreporting of AEs has been observed in one third of the CSRs. Transparent reporting of AEs is crucial for identifying patients at risk and mitigating any potential negative or unintended consequences of the interventions.
High risk of bias of the RCTs evaluated was evident in more than two thirds of the CSRs. For example, more than half of reviews identified high risk of detection bias as a major source of bias suggesting that lack of blinding is still an issue in trials of behavioural interventions. Other shortcomings included insufficiently described randomisation and allocation concealment methods and often poor outcome reporting. This highlights the methodological challenges in RCTs of exercise and the need to counterbalance those with the underlying aim of strengthening internal and external validity of these trials.
Overall, high risk of bias in the primary trials was the main reason for downgrading the quality of the evidence using the GRADE criteria. Imprecision was frequently an issue, meaning the effective sample size was often small; studies were underpowered to detect the between-group differences. Pooling too heterogeneous results often resulted in inconsistent findings and inability to draw any meaningful conclusions. Indirectness and publication bias were lesser common reasons for downgrading. However, with regards to the latter, the generally accepted minimum number of 10 studies needed for quantitatively estimate the funnel plot asymmetry was not present in 69 (46%) CSRs.
Strengths of this research are the inclusion of large number of ‘gold standard’ systematic reviews, robust screening, data extractions and critical methodological appraisal. Nevertheless, some weaknesses need to be highlighted when interpreting findings of this overview. For instance, some of these CSRs analysed the same primary studies (RCTs) but, arrived at slightly different conclusions. Using, the Pieper et al. [ 39 ] formula, the amount of overlap ranged from 0.01% for AEs to 0.2% for adherence, which indicates slight overlap. All CSRs are vulnerable to publication bias [ 196 ] - hence the conclusions generated by them may be false-positive. Also, exercise was sometimes part of a complex intervention; and the effects of physical activity could not be distinguished from co-interventions. Often there were confounding effects of diet, educational, behavioural or lifestyle interventions; selection, and measurement bias were inevitably inherited in this overview too. Also, including CSRs only might lead to selection bias; and excluding reviews published before 2000 might limit the overall completeness and applicability of the evidence. A future update should consider these limitations, and in particular also including non-CSRs.
Conclusions
Trialists must improve the quality of primary studies. At the same time, strict compliance with the reporting standards should be enforced. Authors of CSRs should better explain eligibility criteria and report sources of funding for the primary studies. There are still insufficient physical activity trends worldwide amongst all age groups; and scalable interventions aimed at increasing physical activity levels should be prioritized [ 197 ]. Hence, policymakers and practitioners need to design and implement comprehensive and coordinated strategies aimed at targeting physical activity programs/interventions, health promotion and disease prevention campaigns at local, regional, national, and international levels [ 198 ].
Availability of data and materials
Data sharing is not applicable to this article as no raw data were analysed during the current study. All information in this article is based on published systematic reviews.
Abbreviations
Adverse events
Cardiovascular diseases
Cochrane Database of Systematic Reviews
Cochrane systematic reviews
Confidence interval
Grading of Recommendations Assessment, Development and Evaluation
Hazard ratio
Interquartile range
Mean difference
Prediction interval
Quality of life
Randomised controlled trials
Relative risk
Risk difference
Risk of bias
Standard error
Standardised mean difference
World Health Organization
https://www.who.int/dietphysicalactivity/pa/en/ . (Accessed 8 June 2020).
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD. The physical activity guidelines for AmericansPhysical activity guidelines for AmericansPhysical activity guidelines for Americans. Jama. 2018;320(19):2020–8.
PubMed Google Scholar
Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, Veerman JL, Delwiche K, Iannarone ML, Moyer ML, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the global burden of disease study 2013. BMJ. 2016;354:i3857.
PubMed PubMed Central Google Scholar
Abell B, Glasziou P, Hoffmann T. The contribution of individual exercise training components to clinical outcomes in randomised controlled trials of cardiac rehabilitation: a systematic review and meta-regression. Sports Med Open. 2017;3(1):19.
Anderson D, Seib C, Rasmussen L. Can physical activity prevent physical and cognitive decline in postmenopausal women? A systematic review of the literature. Maturitas. 2014;79(1):14–33.
Barbaric M, Brooks E, Moore L, Cheifetz O. Effects of physical activity on cancer survival: a systematic review. Physiother Can. 2010;62(1):25–34.
Barlow PA, Otahal P, Schultz MG, Shing CM, Sharman JE. Low exercise blood pressure and risk of cardiovascular events and all-cause mortality: systematic review and meta-analysis. Atherosclerosis. 2014;237(1):13–22.
CAS PubMed Google Scholar
Aljawarneh YM, Wardell DW, Wood GL, Rozmus CL. A systematic review of physical activity and exercise on physiological and biochemical outcomes in children and adolescents with type 1 diabetes. J Nurs Scholarsh. 2019.
Chastin SFM, De Craemer M, De Cocker K, Powell L, Van Cauwenberg J, Dall P, Hamer M, Stamatakis E. How does light-intensity physical activity associate with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br J Sports Med. 2019;53(6):370–6.
Abdulla SY, Southerst D, Cote P, Shearer HM, Sutton D, Randhawa K, Varatharajan S, Wong JJ, Yu H, Marchand AA, et al. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario protocol for traffic injury management (OPTIMa) collaboration. Man Ther. 2015;20(5):646–56.
Alanazi MH, Parent EC, Dennett E. Effect of stabilization exercise on back pain, disability and quality of life in adults with scoliosis: a systematic review. Eur J Phys Rehabil Med. 2018;54(5):647–53.
Adsett JA, Mudge AM, Morris N, Kuys S, Paratz JD. Aquatic exercise training and stable heart failure: a systematic review and meta-analysis. Int J Cardiol. 2015;186:22–8.
Adamson BC, Ensari I, Motl RW. Effect of exercise on depressive symptoms in adults with neurologic disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2015;96(7):1329–38.
Abdin S, Welch RK, Byron-Daniel J, Meyrick J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: a systematic review. Public Health. 2018;160:70–6.
Albalawi H, Coulter E, Ghouri N, Paul L. The effectiveness of structured exercise in the south Asian population with type 2 diabetes: a systematic review. Phys Sportsmed. 2017;45(4):408–17.
Sellami M, Gasmi M, Denham J, Hayes LD, Stratton D, Padulo J, Bragazzi N. Effects of acute and chronic exercise on immunological parameters in the elderly aged: can physical activity counteract the effects of aging? Front Immunol. 2018;9:2187.
Hagen KB, Dagfinrud H, Moe RH, Østerås N, Kjeken I, Grotle M, Smedslund G. Exercise therapy for bone and muscle health: an overview of systematic reviews. BMC Med. 2012;10(1):167.
Burton DA, Stokes K, Hall GM. Physiological effects of exercise. Contin Educ Anaesth Crit Care Pain. 2004;4(6):185–8.
Google Scholar
Kraemer WJ, Ratamess NA. Hormonal responses and adaptations to resistance exercise and training. Sports Med. 2005;35(4):339–61.
Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. 2018;5:135.
CAS PubMed PubMed Central Google Scholar
Vina J, Sanchis-Gomar F, Martinez-Bello V, Gomez-Cabrera MC. Exercise acts as a drug; the pharmacological benefits of exercise. Br J Pharmacol. 2012;167(1):1–12.
Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541–56.
Excellence NIfHaC: Cardiovascular disease prevention public health guideline [PH25] Published date: June 2010. Available at: https://www.nice.org.uk/guidance/ph25/resources/cardiovascular-disease-prevention-pdf-1996238687173 .
Excellence NIfHaC: Obesity prevention clinical guideline [CG43] published date: December 2006 Last updated: March 2015. Available at: https://www.nice.org.uk/guidance/cg43/resources/obesity-prevention-pdf-975445344709 .
Excellence NIfHaC: Physical activity for children and young people public health guideline [PH17] Published date: January 2009. Available at: https://www.nice.org.uk/guidance/ph17/resources/physical-activity-for-children-and-young-people-pdf-1996181580229 .
Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 6 [updated September 2018] edition. Available from www.cochrane-handbook.org : The Cochrane Collaboration, 2011. 2011.
Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich A-B. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. 2018;93:9–24.
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18.
Handoll H, Madhok R. Quality of Cochrane reviews. Another study found that most Cochrane reviews are of a good standard. BMJ. 2002;324(7336):545.
Petticrew M, Wilson P, Wright K, Song F. Quality of Cochrane reviews. Quality of Cochrane reviews is better than that of non-Cochrane reviews. BMJ. 2002;324(7336):545.
Shea B, Moher D, Graham I, Pham B, Tugwell P. A comparison of the quality of Cochrane reviews and systematic reviews published in paper-based journals. Eval Health Prof. 2002;25(1):116–29.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Posadzki PP, Bajpai R, Kyaw BM, Roberts NJ, Brzezinski A, Christopoulos GI, Divakar U, Bajpai S, Soljak M, Dunleavy G, et al. Melatonin and health: an umbrella review of health outcomes and biological mechanisms of action. BMC Med. 2018;16(1):18.
Bellou V, Belbasis L, Tzoulaki I, Evangelou E, Ioannidis JP. Environmental risk factors and Parkinson's disease: an umbrella review of meta-analyses. Parkinsonism Relat Disord. 2016;23:1–9.
Walter SD, Cook RJ. A comparison of several point estimators of the odds ratio in a single 2 x 2 contingency table. Biometrics. 1991;47(3):795–811.
Khan H, Sempos CT. Statistical methods in epidemiology. New York: Oxford University Press; 1989.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
CAS Google Scholar
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019): Cochrane; 2019. Available from www.training.cochrane.org/handbook .
Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Adeniyi FB, Young T. Weight loss interventions for chronic asthma. Cochrane Database Syst Rev. 2012;7.
Al-Khudairy L, Loveman E, Colquitt JL, Mead E, Johnson RE, Fraser H, Olajide J, Murphy M, Velho RM, O'Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev. 2017;6.
Amorim Adegboye AR, Linne YM. Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev. 2013;7.
Anderson L, Nguyen TT, Dall CH, Burgess L, Bridges C, Taylor RS. Exercise-based cardiac rehabilitation in heart transplant recipients. Cochrane Database Syst Rev. 2017;4.
Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;1.
Andriolo RB, El Dib RP, Ramos L, Atallah Á, da Silva EMK. Aerobic exercise training programmes for improving physical and psychosocial health in adults with Down syndrome. Cochrane Database Syst Rev. 2010;5.
Araujo DN, Ribeiro CTD, Maciel ACC, Bruno SS, Fregonezi GAF, Dias FAL. Physical exercise for the treatment of non-ulcerated chronic venous insufficiency. Cochrane Database Syst Rev. 2016;12.
Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC. Home versus center based physical activity programs in older adults. Cochrane Database Syst Rev. 2005;1.
Bartels EM, Juhl CB, Christensen R, Hagen KB, Danneskiold-Samsøe B, Dagfinrud H, Lund H. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2016;3.
Beggs S, Foong YC, Le HCT, Noor D, Wood-Baker R, Walters JAE. Swimming training for asthma in children and adolescents aged 18 years and under. Cochrane Database Syst Rev. 2013;4.
Bergenthal N, Will A, Streckmann F, Wolkewitz KD, Monsef I, Engert A, Elter T, Skoetz N. Aerobic physical exercise for adult patients with haematological malignancies. Cochrane Database Syst Rev. 2014;11.
Bidonde J, Busch AJ, Schachter CL, Overend TJ, Kim SY, Góes SM, Boden C, Foulds HJA. Aerobic exercise training for adults with fibromyalgia. Cochrane Database Syst Rev. 2017;6.
Bidonde J, Busch AJ, van der Spuy I, Tupper S, Kim SY, Boden C. Whole body vibration exercise training for fibromyalgia. Cochrane Database Syst Rev. 2017;9.
Bidonde J, Busch AJ, Webber SC, Schachter CL, Danyliw A, Overend TJ, Richards RS, Rader T. Aquatic exercise training for fibromyalgia. Cochrane Database Syst Rev. 2014;10.
Braam KI, van der Torre P, Takken T, Veening MA, van Dulmen-den Broeder E, Kaspers GJL. Physical exercise training interventions for children and young adults during and after treatment for childhood cancer. Cochrane Database Syst Rev. 2016;3.
Bradt J, Shim M, Goodill SW. Dance/movement therapy for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. 2015;1.
Broderick J, Crumlish N, Waugh A, Vancampfort D. Yoga versus non-standard care for schizophrenia. Cochrane Database Syst Rev. 2017;9.
Broderick J, Knowles A, Chadwick J, Vancampfort D. Yoga versus standard care for schizophrenia. Cochrane Database Syst Rev. 2015;10.
Broderick J, Vancampfort D. Yoga as part of a package of care versus standard care for schizophrenia. Cochrane Database Syst Rev. 2017;9.
Brown J, Ceysens G, Boulvain M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Cochrane Database Syst Rev. 2017;6.
Busch AJ, Barber KA, Overend TJ, Peloso PMJ, Schachter CL. Exercise for treating fibromyalgia syndrome. Cochrane Database Syst Rev. 2007;4.
Busch AJ, Webber SC, Richards RS, Bidonde J, Schachter CL, Schafer LA, Danyliw A, Sawant A, Dal Bello-Haas V, Rader T, et al. Resistance exercise training for fibromyalgia. Cochrane Database Syst Rev. 2013;12.
Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2018;9.
Carson KV, Chandratilleke MG, Picot J, Brinn MP, Esterman AJ, Smith BJ. Physical training for asthma. Cochrane Database Syst Rev. 2013;9.
Carvalho APV, Vital FMR, Soares BGO. Exercise interventions for shoulder dysfunction in patients treated for head and neck cancer. Cochrane Database Syst Rev. 2012;4.
Cavalheri V, Granger C. Preoperative exercise training for patients with non-small cell lung cancer. Cochrane Database Syst Rev. 2017;6.
Cavalheri V, Tahirah F, Nonoyama ML, Jenkins S, Hill K. Exercise training undertaken by people within 12 months of lung resection for non-small cell lung cancer. Cochrane Database Syst Rev. 2013;7.
Ceysens G, Rouiller D, Boulvain M. Exercise for diabetic pregnant women. Cochrane Database Syst Rev. 2006;3.
Choi BKL, Verbeek JH, Tam WWS, Jiang JY. Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev. 2010;1.
Colquitt JL, Loveman E, O'Malley C, Azevedo LB, Mead E, Al-Khudairy L, Ells LJ, Metzendorf MI, Rees K. Diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database Syst Rev. 2016;3.
Connolly B, Salisbury L, O'Neill B, Geneen LJ, Douiri A, Grocott MPW, Hart N, Walsh TS, Blackwood B. Exercise rehabilitation following intensive care unit discharge for recovery from critical illness. Cochrane Database Syst Rev. 2015;6.
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, McMurdo M, Mead GE. Exercise for depression. Cochrane Database Syst Rev. 2013;9.
Corbetta D, Sirtori V, Castellini G, Moja L, Gatti R. Constraint-induced movement therapy for upper extremities in people with stroke. Cochrane Database Syst Rev. 2015;10.
Cramer H, Lauche R, Klose P, Lange S, Langhorst J, Dobos GJ. Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1.
Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11.
Dal Bello-Haas V, Florence JM. Therapeutic exercise for people with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database Syst Rev. 2013;5.
Dale MT, McKeough ZJ, Troosters T, Bye P, Alison JA. Exercise training to improve exercise capacity and quality of life in people with non-malignant dust-related respiratory diseases. Cochrane Database Syst Rev. 2015;11.
Daley A, Stokes-Lampard H, Thomas A, MacArthur C. Exercise for vasomotor menopausal symptoms. Cochrane Database Syst Rev. 2014;11.
de Morton N, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;1.
Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2013;2.
Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. Cochrane Database Syst Rev. 2018;3.
Ekeland E, Heian F, Hagen KB, Abbott JM, Nordheim L. Exercise to improve self-esteem in children and young people. Cochrane Database Syst Rev. 2004;1.
Elbers RG, Verhoef J, van Wegen EEH, Berendse HW, Kwakkel G. Interventions for fatigue in Parkinson's disease. Cochrane Database Syst Rev. 2015;10.
Felbel S, Meerpohl JJ, Monsef I, Engert A, Skoetz N. Yoga in addition to standard care for patients with haematological malignancies. Cochrane Database Syst Rev. 2014;6.
Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S. Exercise programs for people with dementia. Cochrane Database Syst Rev. 2015;4.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1.
Fransen M, McConnell S, Hernandez-Molina G, Reichenbach S. Exercise for osteoarthritis of the hip. Cochrane Database Syst Rev. 2014;4.
Freitas DA, Holloway EA, Bruno SS, Chaves GSS, Fregonezi GAF, Mendonça K. Breathing exercises for adults with asthma. Cochrane Database Syst Rev. 2013;10.
Furmaniak AC, Menig M, Markes MH. Exercise for women receiving adjuvant therapy for breast cancer. Cochrane Database Syst Rev. 2016;9.
Giangregorio LM, MacIntyre NJ, Thabane L, Skidmore CJ, Papaioannou A. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev. 2013;1.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9.
Gorczynski P, Faulkner G. Exercise therapy for schizophrenia. Cochrane Database Syst Rev. 2010;5.
Grande AJ, Keogh J, Hoffmann TC, Beller EM, Del Mar CB. Exercise versus no exercise for the occurrence, severity and duration of acute respiratory infections. Cochrane Database Syst Rev. 2015;6.
Grande AJ, Reid H, Thomas EE, Nunan D, Foster C. Exercise prior to influenza vaccination for limiting influenza incidence and its related complications in adults. Cochrane Database Syst Rev. 2016;8.
Grande AJ, Silva V, Andriolo BNG, Riera R, Parra SA, Peccin MS. Water-based exercise for adults with asthma. Cochrane Database Syst Rev. 2014;7.
Gross A, Kay TM, Paquin JP, Blanchette S, Lalonde P, Christie T, Dupont G, Graham N, Burnie SJ, Gelley G, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2015;1.
Hageman D, Fokkenrood HJP, Gommans LNM, van den Houten MML, Teijink JAW. Supervised exercise therapy versus home-based exercise therapy versus walking advice for intermittent claudication. Cochrane Database Syst Rev. 2018;4.
Han A, Judd M, Welch V, Wu T, Tugwell P, Wells GA. Tai chi for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2004;3.
Han S, Middleton P, Crowther CA. Exercise for pregnant women for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2012;7.
Hartley L, Dyakova M, Holmes J, Clarke A, Lee MS, Ernst E, Rees K. Yoga for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;5.
Hartley L, Flowers N, Lee MS, Ernst E, Rees K. Tai chi for primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;4.
Hartley L, Lee MS, Kwong JSW, Flowers N, Todkill D, Ernst E, Rees K. Qigong for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2015;6.
Hassett L, Moseley AM, Harmer AR. Fitness training for cardiorespiratory conditioning after traumatic brain injury. Cochrane Database Syst Rev. 2017;12.
Hayden J, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005;3.
Hay-Smith EJC, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev. 2011;12.
Heine M, van de Port I, Rietberg MB, van Wegen EEH, Kwakkel G. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev. 2015;9.
Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev. 2011;10.
Hemmingsen B, Gimenez-Perez G, Mauricio D, Roqué i Figuls M, Metzendorf MI, Richter B. Diet, physical activity or both for prevention or delay of type 2 diabetes mellitus and its associated complications in people at increased risk of developing type 2 diabetes mellitus. Cochrane Database Syst Rev. 2017;12.
Herbert RD, de Noronha M, Kamper SJ. Stretching to prevent or reduce muscle soreness after exercise. Cochrane Database Syst Rev. 2011;7.
Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non-specific low-back pain. Cochrane Database Syst Rev. 2004;4.
Holland AE, Hill CJ, Jones AY, McDonald CF. Breathing exercises for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;10.
Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2011;11.
Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011;7.
Hurkmans E, van der Giesen FJ, Vliet Vlieland TPM, Schoones J, Van den Ende E. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst Rev. 2009;4.
Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, Stansfield C, Oliver S. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev. 2018;4.
Jones M, Harvey A, Marston L, O'Connell NE. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013;5.
Katsura M, Kuriyama A, Takeshima T, Fukuhara S, Furukawa TA. Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery. Cochrane Database Syst Rev. 2015;10.
Kendrick D, Kumar A, Carpenter H, Zijlstra GAR, Skelton DA, Cook JR, Stevens Z, Belcher CM, Haworth D, Gawler SJ, et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev. 2014;11.
Kramer MS, McDonald SW. Aerobic exercise for women during pregnancy. Cochrane Database Syst Rev. 2006;3.
Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity for women with breast cancer after adjuvant therapy. Cochrane Database Syst Rev. 2018;1.
Lane R, Harwood A, Watson L, Leng GC. Exercise for intermittent claudication. Cochrane Database Syst Rev. 2017;12.
Larun L, Brurberg KG, Odgaard-Jensen J, Price JR. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev. 2017;4.
Larun L, Nordheim LV, Ekeland E, Hagen KB, Heian F. Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database Syst Rev. 2006;3.
Lauret GJ, Fakhry F, Fokkenrood HJP, Hunink MGM, Teijink JAW, Spronk S. Modes of exercise training for intermittent claudication. Cochrane Database Syst Rev. 2014;7.
Lawrence M, Celestino Junior FT, Matozinho HHS, Govan L, Booth J, Beecher J. Yoga for stroke rehabilitation. Cochrane Database Syst Rev. 2017;12.
Lin CWC, Donkers NAJ, Refshauge KM, Beckenkamp PR, Khera K, Moseley AM. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev. 2012;11.
Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;3.
Long L, Anderson L, Dewhirst AM, He J, Bridges C, Gandhi M, Taylor RS. Exercise-based cardiac rehabilitation for adults with stable angina. Cochrane Database Syst Rev. 2018;2.
Loughney LA, West MA, Kemp GJ, Grocott MPW, Jack S. Exercise interventions for people undergoing multimodal cancer treatment that includes surgery. Cochrane Database Syst Rev. 2018;12.
Macedo LG, Saragiotto BT, Yamato TP, Costa LOP, Menezes Costa LC, Ostelo R, Maher CG. Motor control exercise for acute non-specific low back pain. Cochrane Database Syst Rev. 2016;2.
Macêdo TMF, Freitas DA, Chaves GSS, Holloway EA, Mendonça K. Breathing exercises for children with asthma. Cochrane Database Syst Rev. 2016;4.
Martin A, Booth JN, Laird Y, Sproule J, Reilly JJ, Saunders DH. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database Syst Rev. 2018;3.
McKeough ZJ, Velloso M, Lima VP, Alison JA. Upper limb exercise training for COPD. Cochrane Database Syst Rev. 2016;11.
McNamara RJ, McKeough ZJ, McKenzie DK, Alison JA. Water-based exercise training for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;12.
McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, Mackey J, Courneya K. Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev. 2010;6.
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, Olajide J, Mainardi GM, Corpeleijn E, O'Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6.
Meekums B, Karkou V, Nelson EA. Dance movement therapy for depression. Cochrane Database Syst Rev. 2015;2.
Meher S, Duley L. Exercise or other physical activity for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2006;2.
Mehrholz J, Kugler J, Pohl M. Water-based exercises for improving activities of daily living after stroke. Cochrane Database Syst Rev. 2011;1.
Mehrholz J, Kugler J, Pohl M. Locomotor training for walking after spinal cord injury. Cochrane Database Syst Rev. 2012;11.
Mehrholz J, Thomas S, Elsner B. Treadmill training and body weight support for walking after stroke. Cochrane Database Syst Rev. 2017;8.
Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC, Snyder C. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;8.
Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst Rev. 2012;8.
Montgomery P, Dennis JA. Physical exercise for sleep problems in adults aged 60+. Cochrane Database Syst Rev. 2002;4.
Morris NR, Kermeen FD, Holland AE. Exercise-based rehabilitation programmes for pulmonary hypertension. Cochrane Database Syst Rev. 2017;1.
Muktabhant B, Lawrie TA, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst Rev. 2015;6.
Ngai SPC, Jones AYM, Tam WWS. Tai chi for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2016;6.
Norton C, Cody JD. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. Cochrane Database Syst Rev. 2012;7.
O'Brien K, Nixon S, Glazier R, Tynan AM. Progressive resistive exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2004;4.
O'Brien K, Nixon S, Tynan AM, Glazier R. Aerobic exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2010;8.
Østerås N, Kjeken I, Smedslund G, Moe RH, Slatkowsky-Christensen B, Uhlig T, Hagen KB. Exercise for hand osteoarthritis. Cochrane Database Syst Rev. 2017;1.
Page MJ, Green S, Kramer S, Johnston RV, McBain B, Chau M, Buchbinder R. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014;8.
Page MJ, Green S, McBain B, Surace SJ, Deitch J, Lyttle N, Mrocki MA, Buchbinder R. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev. 2016;6.
Page MJ, O'Connor D, Pitt V, Massy-Westropp N. Exercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;6.
Panebianco M, Sridharan K, Ramaratnam S. Yoga for epilepsy. Cochrane Database Syst Rev. 2017;10.
Perry A, Lee SH, Cotton S, Kennedy C. Therapeutic exercises for affecting post-treatment swallowing in people treated for advanced-stage head and neck cancers. Cochrane Database Syst Rev. 2016;8.
Radtke T, Nevitt SJ, Hebestreit H, Kriemler S. Physical exercise training for cystic fibrosis. Cochrane Database Syst Rev. 2017;11.
Regnaux JP, Lefevre-Colau MM, Trinquart L, Nguyen C, Boutron I, Brosseau L, Ravaud P. High-intensity versus low-intensity physical activity or exercise in people with hip or knee osteoarthritis. Cochrane Database Syst Rev. 2015;10.
Ren J, Xia J. Dance therapy for schizophrenia. Cochrane Database Syst Rev. 2013;10.
Rietberg MB, Brooks D, Uitdehaag BMJ, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;1.
Risom SS, Zwisler AD, Johansen PP, Sibilitz KL, Lindschou J, Gluud C, Taylor RS, Svendsen JH, Berg SK. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst Rev. 2017;2.
Romano M, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Kotwicki T, Maier-Hennes A, Negrini S. Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst Rev. 2012;8.
Ryan JM, Cassidy EE, Noorduyn SG, O'Connell NE. Exercise interventions for cerebral palsy. Cochrane Database Syst Rev. 2017;6.
Saragiotto BT, Maher CG, Yamato TP, Costa LOP, Menezes Costa LC, Ostelo R, Macedo LG. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev. 2016;1.
Saunders DH, Sanderson M, Hayes S, Kilrane M, Greig CA, Brazzelli M, Mead GE. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2016;3.
Schulzke SM, Kaempfen S, Trachsel D, Patole SK. Physical activity programs for promoting bone mineralization and growth in preterm infants. Cochrane Database Syst Rev. 2014;4.
Seron P, Lanas F, Pardo Hernandez H, Bonfill Cosp X. Exercise for people with high cardiovascular risk. Cochrane Database Syst Rev. 2014;8.
Shaw KA, Gennat HC, O'Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006;4.
Shepherd E, Gomersall JC, Tieu J, Han S, Crowther CA, Middleton P. Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2017;11.
Sibilitz KL, Berg SK, Tang LH, Risom SS, Gluud C, Lindschou J, Kober L, Hassager C, Taylor RS, Zwisler AD. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2016;3.
Silva IS, Fregonezi GAF, Dias FAL, Ribeiro CTD, Guerra RO, Ferreira GMH. Inspiratory muscle training for asthma. Cochrane Database Syst Rev. 2013;9.
States RA, Pappas E, Salem Y. Overground physical therapy gait training for chronic stroke patients with mobility deficits. Cochrane Database Syst Rev. 2009;3.
Strike K, Mulder K, Michael R. Exercise for haemophilia. Cochrane Database Syst Rev. 2016;12.
Takken T, Van Brussel M, Engelbert RH, van der Net JJ, Kuis W, Helders P. Exercise therapy in juvenile idiopathic arthritis. Cochrane Database Syst Rev. 2008;2.
Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJS, Dalal H, Lough F, Rees K, Singh SJ, Mordi IR. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014;4.
Thomas D, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2006;3.
Ussher MH, Taylor AH, Faulkner GEJ. Exercise interventions for smoking cessation. Cochrane Database Syst Rev. 2014;8.
Valentín-Gudiol M, Mattern-Baxter K, Girabent-Farrés M, Bagur-Calafat C, Hadders-Algra M, Angulo-Barroso RM. Treadmill interventions in children under six years of age at risk of neuromotor delay. Cochrane Database Syst Rev. 2017;7.
van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma-Zeinstra SMA, van Middelkoop M. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2015;1.
Vloothuis JDM, Mulder M, Veerbeek JM, Konijnenbelt M, Visser-Meily JMA, Ket JCF, Kwakkel G, van Wegen EEH. Caregiver-mediated exercises for improving outcomes after stroke. Cochrane Database Syst Rev. 2016;12.
Voet NBM, van der Kooi EL. Riphagen, II, Lindeman E, van Engelen BGM, Geurts ACH: strength training and aerobic exercise training for muscle disease. Cochrane Database Syst Rev. 2013;7.
White CM, Pritchard J, Turner-Stokes L. Exercise for people with peripheral neuropathy. Cochrane Database Syst Rev. 2004;4.
Wieland LS, Skoetz N, Pilkington K, Vempati R, D'Adamo CR, Berman BM. Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;1.
Williams AD, Bird ML, Hardcastle SGK, Kirschbaum M, Ogden KJ, Walters JAE. Exercise for reducing falls in people living with and beyond cancer. Cochrane Database Syst Rev. 2018;10.
Williams MA, Srikesavan C, Heine PJ, Bruce J, Brosseau L, Hoxey-Thomas N, Lamb SE. Exercise for rheumatoid arthritis of the hand. Cochrane Database Syst Rev. 2018;7.
Yamamoto S, Hotta K, Ota E, Matsunaga A, Mori R. Exercise-based cardiac rehabilitation for people with implantable ventricular assist devices. Cochrane Database Syst Rev. 2018;9.
Yamato TP, Maher CG, Saragiotto BT, Hancock MJ, Ostelo R, Cabral CMN, Menezes Costa LC, Costa LOP. Pilates for low back pain. Cochrane Database Syst Rev. 2015;7.
Yang ZY, Zhong HB, Mao C, Yuan JQ, Huang YF, Wu XY, Gao YM, Tang JL. Yoga for asthma. Cochrane Database Syst Rev. 2016;4.
Young J, Angevaren M, Rusted J, Tabet N. Aerobic exercise to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2015;4.
Zainuldin R, Mackey MG, Alison JA. Optimal intensity and type of leg exercise training for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;11.
Mok A, Khaw K-T, Luben R, Wareham N, Brage S. Physical activity trajectories and mortality: population based cohort study. Bmj. 2019;365:l2323.
Ekelund U, Brown WJ, Steene-Johannessen J, Fagerland MW, Owen N, Powell KE, Bauman AE, Lee IM. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019;53(14):886–94. https://doi.org/10.1136/bjsports-2017-098963 . Epub 2018 Jul 10.
Article PubMed Google Scholar
Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, Bauman A, Lee IM. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–10.
Lear SA, Hu W, Rangarajan S, Gasevic D, Leong D, Iqbal R, Casanova A, Swaminathan S, Anjana RM, Kumar R, et al. The effect of physical activity on mortality and cardiovascular disease in 130000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390(10113):2643–54.
Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–95.
Heyman E, Gamelin FX, Goekint M, Piscitelli F, Roelands B, Leclair E, Di Marzo V, Meeusen R. Intense exercise increases circulating endocannabinoid and BDNF levels in humans--possible implications for reward and depression. Psychoneuroendocrinology. 2012;37(6):844–51.
Horton R. Offline: the gravy train of systematic reviews. Lancet. 2019;394(10211):1790.
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health. 2018;6(10):e1077–86.
Fletcher GF, Landolfo C, Niebauer J, Ozemek C, Arena R, Lavie CJ. Promoting physical activity and exercise: JACC health promotion series. J Am Coll Cardiol. 2018;72(14):1622–39.
Download references
Acknowledgements
Not applicable.
There was no funding source for this study. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Kleijnen Systematic Reviews Ltd., York, UK
Pawel Posadzki
Nanyang Technological University, Singapore, Singapore
Institute for Research in Operative Medicine, Witten/Herdecke University, Witten, Germany
Dawid Pieper, Nadja Könsgen & Annika Lena Neuhaus
School of Medicine, Keele University, Staffordshire, UK
Jozef Pilsudski University of Physical Education in Warsaw, Faculty Physical Education and Health, Biala Podlaska, Poland
Hubert Makaruk
Health Outcomes Division, University of Texas at Austin College of Pharmacy, Austin, USA
Monika Semwal
You can also search for this author in PubMed Google Scholar
Contributions
PP wrote the protocol, ran the searches, validated, analysed and synthesised data, wrote and revised the drafts. HM, NK and ALN screened and extracted data. MS and DP validated and analysed the data. RB ran statistical analyses. All authors contributed to writing and reviewing the manuscript. PP is the guarantor. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Dawid Pieper .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Supplementary Table 1. Main characteristics of included Cochrane systematic reviews evaluating the effects of physical activity/exercise on health outcomes ( n = 150). Supplementary Table 2. Additional information from Cochrane systematic reviews of the effects of physical activity/exercise on health outcomes ( n = 150). Supplementary Table 3. Conclusions from Cochrane systematic reviews “quote”. Supplementary Table 4 . AEs reported in Cochrane systematic reviews. Supplementary Table 5. Summary of withdrawals/non-adherence. Supplementary Table 6. Methodological quality assessment of the included Cochrane reviews with AMSTAR-2. Supplementary Table 7. Number of studies assessed as low risk of bias per domain. Supplementary Table 8. GRADE for the review’s main comparison. Supplementary Table 9. Studies reporting quality of life outcomes as mean difference.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Posadzki, P., Pieper, D., Bajpai, R. et al. Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews. BMC Public Health 20 , 1724 (2020). https://doi.org/10.1186/s12889-020-09855-3
Download citation
Received : 01 April 2020
Accepted : 08 November 2020
Published : 16 November 2020
DOI : https://doi.org/10.1186/s12889-020-09855-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Effectiveness
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 21 June 2024
Effects of different types of exercise intensity on improving health-related physical fitness in children and adolescents: a systematic review
- Xianxian Zhou 1 ,
- Jiayu Li 1 &
- Xiaoping Jiang 1
Scientific Reports volume 14 , Article number: 14301 ( 2024 ) Cite this article
Metrics details
- Health services
- Public health
A substantial body of empirical evidence reveals that physical activity is associated with a wide range of positive physical and mental health outcomes. However, an absence of comprehensive syntheses is observed concerning the varying effects of different exercise intensities on the improvement of physical health among children and adolescents. The aim of this review is to systematically investigate the effects of different exercise intensities on the physical fitness of children and adolescents, to analyses the optimal exercise intensities for improving physical fitness, and to provide a relevant theoretical basis for optimizing school physical education curricula. A systematic search strategy was used in this study in four online databases (PubMed, Scopus, EBSCO and Web of Science). Intervention studies that met the inclusion criteria underwent a thorough screening process, and their methodological quality was assessed utilizing the PEDro scale. The selected literature was systematically analyzed and evaluated through induction, summary, analysis, and evaluation. These findings indicate that high-intensity exercise training exerts significant positive effects on body composition, cardiopulmonary function and muscle fitness in children and adolescents. Therefore, we suggest that schools should focus on high-intensity sports in their physical education curriculum, which can further improve the student's PHYSICAL FITNESS.
Introduction
Overweight and obesity in children and adolescents have become a global public health problem 1 . The prevalence of obesity in children and adolescents has been reported to have increased from 0.7% to 5.6% 2 . The persistence of overweight and obesity into adulthood has the potential to lead to chronic diseases, including type 2 diabetes, cardiometabolic disorders, and a range of psychosocial problems 3 , 4 , 5 , 6 , Numerous studies have shown that physical activity is one of the most important interventions to reduce physical health and psychological problems in adolescents 7 , 8 , 9 . WHO recommends that children and adolescents should engage in an average of 60 min of moderate to high-intensity physical activity (MVPA) per day to obtain health benefits 10 , however, more than 80%of adolescents fail to reach the minimum recommended amount of physical activity 11 . Given that adolescents have difficulty starting and following recommended guidelines for 30–60 min of moderate-intensity training per day 12 , 13 , there is a need to explore and develop engaging alternatives for youth to achieve the many health benefits of regular physical activity. Traditionally, moderate-intensity continuous training (MICT) has been the most common type of exercise recommended to improve body composition and cardiorespiratory fitness (CRF) 14 , 15 . However, in recent years, a growing body of laboratory evidence has shown that high-intensity exercise training is less time-consuming than MICT in improving body composition and other health indicators in obese children and adolescents 16 , 17 , 18 . Whether high-intensity or low-intensity exercise training is more beneficial to the PHYSICAL FITNESS of children and adolescents is still highly debated. Therefore, there is a need to further explore differences in the effectiveness of different exercise intensity interventions in improving PHYSICAL FITNESS in children and adolescents.
PHYSICAL FITNESS is a multidimensional state of being. PHYSICAL FITNESS is the body’s ability to function efficiently and effectively. It is a state of being that consists of at least FIVE HEALTH-RELATED and SIX SKILL-RELATED PHYSICAL FITNESS COMPONENTS, each of which contributes to total quality of life. The five components of health-related PHYSICAL FITNESS are BODY COMPOSITION, CARDIOVASCULAR FITNESS, FLEXIBILITY, MUSCULAR ENDURANCE, AND STRENGTH 19 . A recent narrative and meta-analysis of 20 studies evaluated the efficacy of HIIT for improving HEALTH-RELATED FITNESS (ie, cardiorespiratory fitness, muscular fitness, body composition and flexibility). The results indicated significant improvements in cardiorespiratory fitness and body composition through HIIT, with notable effects observed in these areas 13 . Previous meta-analyses have weakened the interpretation of findings due to small sample sizes. Furthermore, there is less research on exercise interventions to treat PHYSICAL FITNESS in children and adolescents than in adults, particularly in terms of exploring exercise-related variables (intensity and duration).
Therefore, this systematic review aims to systematically summarized the effects of different exercise intensities on health-related fitness in children and adolescents and to analyze which exercise intensity is more conducive to improving health-related fitness in children and adolescents.
This review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines 20 , and the Cochrane Handbook for systematic review 21 . The PRISMA checklist is presented in Additional File 1.
Search strategy
A comprehensive search was done systematically through PubMed, Scopus, EBSCO, and Web of Science up to the 5 of June 2024. Searching terms were based on adapted PICO questions to search through the aforementioned databases to access all the important articles. Free text words and medical subject heading (MeSH) terms were used. (1) children OR childhood OR pre*schooler OR schoolchildren OR preadolescent OR adolescent OR adolescence OR youth;(2) physical*activity OR physical*education OR exercise OR fitness OR sport;(3) strength OR flexibility OR motor OR endurance OR agility OR body composition OR anthropometry OR body mass index OR waist circumference OR overall adiposity OR central adiposity OR overweight OR obesity OR risk factors OR risk score cardiovascular disease OR metabolic syndrome OR blood glucose OR glucose tolerance OR insulin resistance OR insulin sensitivity OR blood lipids OR dyslipidemia OR diabetes OR blood pressure OR hypertension OR inflammatory markers OR bone mineral OR bone mineral content;(4) random OR random*controlled trial OR controlled trial OR trial. (The search strategy used for each database is provided in the supplementary material (table S2). At the same time, the reference lists of included articles and relevant reviews were retrospectively included to supplement the missing literature in the computer search. The systematic search process was conducted by XXZ and JYL. Any disagreement of an included/excluded study was resolved by the author PXJ.
Eligibility criteria of the selected studies
The inclusion criteria for articles were determined using the PICOS (Participants/Interventions/Comparisons/Outcomes/Study Design) principles, as follows. Participants (P): Children and adolescents (individuals in the 10–19 year age group 22 , including samples of overweight/obese children, but excluding samples of children with medical conditions); Interventions (I):interventions in the form of exercise, High-intensity aerobic exercise, Low-intensity aerobic training (LIT), Endurance training (ET), High-intensity interval exercise (HIIE), Moderate-intensity exercise (MIE),HIIT, moderate-intensity continuous (MICT); Comparisons (C): control group performed low to moderate intensity physical activity or no artificially designed physical exercise; Outcomes (O): assessment of at least one of the following indicators (i.e., body composition, cardiorespiratory fitness, muscular fitness, strength, flexibility, motor, endurance, agility, body composition, anthropometry, body mass index, waist circumference, overall adiposity , central adiposity , overweight , obesity ,risk factors , risk score cardiovascular disease, metabolic syndrome, blood glucose, glucose tolerance, insulin resistance, insulin sensitivity, blood lipids, dyslipidemia, diabetes, blood pressure, hypertension, inflammatory markers, bone mineral, bone mineral content); Study Design (S): controlled trial.
Exclusion criteria: (1) studies not related to the topic (non-physical activity, physical activity); (2) non-intervention studies (observational studies, systematic reviews) and studies that did not provide sufficient comparisons to compare; (3) Exclude other age groups other than 3–19 years old. The title, abstract and full text were independently assessed by two authors for eligibility. Finally, randomized controlled trials were limited to articles published in English.
Data extraction
Data extraction from the included studies was independently performed by two authors (XXZ and JYL). For each study, data were extracted for the characteristics of the study population. These include (1) first author’s surname; (2) year of publication; (3) purpose; (4) results; (5) the characteristics, sample size and age of the participants; (6) sampling type; (7) type of research; (8) Characteristics of physical exercise (type, frequency and duration). Any disagreement in data extraction was resolved by the third author PXJ (Table 1 ).
Quality assessment
Papers that met the inclusion criteria were independently assessed by two authors (XXZ and JYL). This review assessed the included literature using the Physiotherapy Evidence Database (PEDro) scale, a credit rating scale developed by the Australian Centre for Evidence-Based Practice. The PEDro scale is a valid measure of the methodological quality of clinical trial 23 . The scale consisted of randomized grouping (2 items), blinding (3 item), data reporting (3 item), data analysis (1 item), and follow-up (1 item), with a total of 10 criteria. Each item was recorded as 1 point when it appeared in the article and 0 points when it was not reflected, for a total score of 0 to 10 points. To avoid subjective opinions, two reviewers assessed the opinions, and the third judged the differences. It classifies papers into three levels: high quality above 8, medium quality 4–7, and low quality below 4 points. Disagreements were solved by a third party (PXJ) (Table 2 ).
Data synthesis and analysis
Due to the heterogeneity of the studies, no meta-analysis was performed. Instead, intervention characteristics for each study were summarized and analyzed and then recorded in a standardized form created by the authors. The effectiveness of the intervention was calculated using the formula: number of effective trials (post-intervention scores significantly higher than pre-intervention or control scores)/total number of trials. Data analysis was performed by the first author XXZ and then validated by the second author JYL.
Literature screening process and results
A preliminary search of the database yielded 10,030 relevant studies. We first imported the documents into the document management software Endnote, and after removing duplicate documents and screening titles and abstracts, we excluded 9990 articles. Of the remaining 40 articles, 30 articles were obtained after screening and checking the full text, and the irrelevant articles were eliminated. The reasons for the exclusion based on the full text were: (1) no intervention studies (3 articles); (2) The age does not meet (3 articles); (3) non-full text (2 articles); (4) non-English articles (2 articles). The PRISMA flowchart is shown in Fig. 1 .

Flow chart of literature retrieval.
The systematic search of relevant literature published as of 5 June 2024 found 30 relevant articles, the earliest of which was published in 1999. The study included 30 related papers from the United States, Canada, Brazil, Denmark, Spain, China, Australia, the United Kingdom, Singapore, France, Portugal, Colombia, and Switzerland.
Study characteristics were summarized in Table 1 , and the final analysis included 6494 children and adolescents with participants ranging in age from 5 to 18 years, with most studies including healthy children and adolescents, but nine studies including overweight or obese children. Study sizes ranged from 10 to 2166. Physical activity interventions mainly included HIIT (8/30; 27%), aerobic training (5/30; 17%), resistance training (2/30; 7%), physical education (1/30; 3%), endurance training (1/30; 3%), acute exercise (1/30; 3%) and other interventions. Outcome measures: body mass index, waist circumference, body fat, cardiorespiratory fitness, and muscle fitness (muscular endurance, muscle strength and muscular flexibility). Quality scores for 30 studies are shown in Table 2 . The studies ranged in their scores from 3 to 10. Only two studies achieved high-quality scores (≥ 8) (Table 2 ). One study scored below 4. Blinding techniques ranged from 0 to 3 in this study, with only one study scoring 3 and four scoring 1; Fifteen studies scored 0.
Effects of different exercise intensity on BODY COMPOSITION in children and adolescents
A total of 11 studies in this study assessed the effects of different exercise intensities on body composition (weight, BMI, body fat, waist circumference, fat-free mass, and other relevant indicators), of which 9 showed that high-intensity exercise interventions had a positive effect on overweight or obese children and adolescents, but 2 had no positive effect.
Weight, BMI and body fat
A total of 8 of the 11 studies assessed changes in body weight, BMI, adiposity, or percentage of body fat measured. Six of the eight studies, reported positive effects of high-intensity exercise interventions on body weight, BMI, or body fat in overweight and obese child adolescents. However, 2 studies showed moderate or no positive effects of high-intensity exercise interventions on BMI, and body fat in overweight or obese children and adolescents.
Tadiotto et al. conducted a 12-week HIIT and MIIT intervention study and found significant reductions in (body mass index) BMI-z, (waist-to-height ratio) WHtR, and LDL-c in HIIT 28 . Benson et al. compared the effects of high-intensity progressive resistance training (PRT) on body composition in obese children and showed that an 8-week PRT intervention resulted in significant improvements in adiposity, percentage body fat, and body mass index 34 . Recent findings have shown that after 12 weeks of HIIT and MICT interventions, there was a significant reduction in BMI and body fat mass in the HIIT group compared to the control group, as well as a significant reduction in visceral adipose tissue (− 53 g vs. − 17 g, p < 0.01), LDL cholesterol was reduced only in the HIIT group, whereas in MICT only the body fat percentage was significantly reduced (− 17.2%, p < 0.05) 31 . In addition, Winn et al. compared the effects of HIIT on adolescents over a 6-month period and showed that after a 6-month school HIIT intervention, BMI was maintained in the HIIT group and significantly increased in the control group, and that HIIT was an effective tool for maintaining BMI 47 .
In a study assessing the effect of different exercise intensities on energy expenditure for spontaneous physical activity in adolescents, Paravidino et al. found that the mean energy expenditure was 82, 286 and 343 kcal in the control, moderate and vigorous exercise groups, respectively ( p < 0.001), and the results suggest that high intensities are more conducive to an increase in energy expenditure, and thus to weight loss 27 . Saidi et al. studied the effect of vigorous exercise on subsequent dietary intake in obese adolescent girls and showed a significant reduction in adiposity in the exercise group compared to the control group ( p < 0.02) 45 .
In the present study, 2 studies reported no significant effects of different intensities of exercise on body composition in overweight or obese children and adolescents. Gomes et al. compared the effects of different aerobic training intensities over a period of 12 on the body composition of obese adolescents, and showed a decrease in body weight, BMI, and body fat in both the intervention and control groups after a 12-week intervention ( p < 0.001), but these results could not be attributed solely to aerobic training intensity due to the multidisciplinary intervention 40 . In another study, Costigan et al. conducted an 8-week study of aerobic training (AEP) and resistance and aerobic programming (RAP) with 68 secondary school students, and the results showed a moderate effect of the BMI intervention for participants in the AEP and RAP groups. It may be related to the small sample size 43 .
Waist circumference
Three randomized controlled trials assessed changes in waist circumference and all found beneficial effects. (Insert literature), a study conducted by Farah et al., showed that after 6 months of high-intensity aerobic training (HIT) and low-intensity aerobic training (LIT), significant beneficial changes in waist circumference were found only in the HIT group 24 . Benson et al. investigated the effects of 8 weeks of high-intensity progressive resistance training (PRT) on body composition in obese children and compared the effects between the experimental and control groups, showing that significant changes in waist circumference were obtained in the intervention group after 8 weeks of PRT training 34 . Costigan et al. conducted an 8-week study of aerobic training (AEP), resistance and aerobic programming (RAP) with 68 secondary school students and showed that participants in the AEP and RAP groups had significant changes in waist circumference ( p = 0.024) 43 .
Fat-free mass
Only 1 study evaluated the effect of different exercise intensities on fat-free mass. Leppanen et al. investigated the effect of physical activity intensity and sedentary behaviours (ST) on body composition in 4 years old children. The results showed that the higher the intensity of moderate-to-vigorous exercise, the lower the percentage of fat (%FM, p = 0.015), the VPA (high intensity) and MVPA (moderate-to-vigorous exercise intensity) the higher the fat-free mass index (FFMI, p = 0.002 and p = 0.011) Time spent on VPA was associated with higher FFMI 38 .
Effects of different exercise intensities on CARDIOPULMONARY FUNCTION (CRF) in children and adolescents
A total of 16 studies investigated the effects of different exercise intensity interventions on cardiorespiratory fitness, and positive effects were found in all studies. In general, cardiorespiratory fitness improved with high-intensity exercise interventions. The included studies assessed vascularity, heart rate, lipids, insulin sensitivity, inflammatory markers, diabetes, and other relevant indicators.
Blood vessels
A total of 4 out of 16 studies investigated the effects of exercise intensity interventions on blood vessels in children and adolescents. Four studies demonstrated that high-intensity training interventions had a positive effect on blood vessels.
Bond et al. investigated the effect of exercise intensity on protecting the vascular system from high-fat diets in adolescents study by intervening with high-intensity interval exercise (HIIE) and moderate-intensity exercise (MIE) in 20 adolescents, and showed that exercise intensity plays an important role in protecting the vascular system from the deleterious effects of HFM, and that in the adolescent population, performing HIIE may be more effective than MIE in Provides better vascular benefits 26 . In a study examining the effects of sprint interval exercise on post-exercise metabolism and blood pressure in adolescents, it was shown that acute sprint interval exercise leads to an increase in short-term oxygen uptake and a decrease in blood pressure in adolescents 37 . Farpour-Lambert et al. investigated the effect of physical activity on systemic blood pressure in adolescent obese children, and after a 3-month intervention, significant changes in systolic and diastolic blood pressure were obtained in the intervention group compared to the control group 51 . Buchan et al. investigated whether a high-intensity training (HIT) intervention could improve the CVD risk profile of adolescents in a time-effective manner, and after a 7-week HIT intervention, a significant reduction in systolic blood pressure was obtained in the intervention group compared to the control group 41 .
Insulin sensitivity
Of the 16 studies, only 2 randomized controlled trials assessed the effect of exercise intensity on insulin sensitivity. Only one study showed that a high-intensity exercise intervention could have a positive effect on insulin sensitivity. In the first randomized controlled trial, the Davis study found that after the intervention, the high-dose aerobic training group had a greater reduction in insulin (AUC), which could be effective in reducing metabolic risk 36 . However, in another randomized trial of 106 overweight and obese adolescents who underwent high-intensity endurance training (ET) and moderate-intensity (ET) for 6 months, the results showed that ET significantly improved cardiorespiratory fitness in obese adolescents, but the effect of exercise intensity on insulin sensitivity and triglycerides remained unclear due to lack of compliance 25 .
Inflammation
A total of 3 out of 16 studies assessed the effect of exercise intensity interventions on inflammation, with only 2 showing a positive effect of high-intensity exercise interventions on the prevention of inflammation. The results of the study by Ramirez-Velez et al. suggest the utility of high-intensity aerobic and resistance training as a means of modulating the levels of certain pro-inflammatory interleukins in adolescent subjects, thereby playing an important role in the prevention of diseases associated with low-grade inflammation, such as cardiovascular disease and type 2 diabetes 30 . A study by Tadiotto et al. found that C-reactive protein (CRP) was significantly reduced in the HIIT group, promoting beneficial changes in obesity and inflammatory processes 28 . However, in a study conducted by Buchan et al. with 89 adolescent students to assess whether the HIIT intervention could improve the cardiovascular disease risk profile of secondary school students in a time-effective manner, after a 7-week intervention, the results showed no significant differences between groups for any of the nine biochemical risk markers for cardiovascular disease, but significantly improved cardiorespiratory fitness 41 .
Two of the 16 studies showed that high-intensity exercise interventions had a positive effect on heart rate. In one study examining the effect of exercise intensity on blood pressure and heart rate in obese adolescents, after a 6-month period of HIT and LIT, beneficial changes in HR and HRV occurred only in the HIT group 24 . In a randomized controlled trial, Ketelhut et al. assessed the effect of implementing school-specific HIIT in a physical education curriculum on various hemodynamics parameters and heart rate variability, and after a 12-week intervention, the results showed that significant changes in heart rate were obtained in the intervention group ( p = 0.010) 52 .
In addition, five other studies have all demonstrated the beneficial effects of high-intensity exercise interventions on cardiorespiratory fitness. Grasten et al. examined the effects of moderate-to-vigorous physical activity and ST with cardiorespiratory fitness in schoolchildren from 2017 to 2020, assessing accelerometer based MVPA by using waist-worn activity monitors and CRFs at four measurement points using the 20-m shuttle run test and ST, which showed a positive correlation between MVPA and CRF, and a negative correlation between ST and CRF 42 . Taber et al. conducted a moderate and vigorous exercise intervention with 1,029 eighth-grade girls and measured cardiorespiratory fitness using the Modified Physical Exercise Capacity Test (MPCT), which showed that vigorous exercise was positively associated with cardiorespiratory fitness 35 . Dias et al. showed that after 12 weeks of HIIT and MICT interventions, the HIIT group had a significant increase in relative peak VO2 compared to MICT, which was very effective in improving cardiorespiratory fitness 32 . Both studies by Gerber et al. and Leppanen et al. showed that higher levels of MVPA were associated with higher CRF scores 39 .
Effects of different exercise intensities on FLEXIBILITY in children and adolescents
Only two studies assessed changes in flexibility and no effects were found. The first study, conducted by Buchan et al., showed that after a 7-week period of high-intensity interval exercise, the intervention group showed an increase in vertical performance, and 10-m sprint speed ( p < = 0.05), while the control group showed a significant decrease in both flexibility and vertical performance 41 . The most recent study, conducted by Juric et al. investigated the effects of a HIIT intervention lasting 12 weeks on balance, coordination, speed, flexibility, strength, and agility in 10- to 15-year-old students, and showed no significant effects. This may be because short-term HIIT interventions of only two 10-min sessions per week do not provide sufficient stimulation for fitness (muscular strength, muscular endurance, power, speed, flexibility, and balance) enhancement 50 .
Effects of different exercise intensities on MUSCLE FITNESS in children and adolescents
Five studies assessed changes in muscle fitness, and four showed that high-intensity exercise interventions had a positive impact on muscle fitness in children and adolescents. Larsen et al. explored whether the musculoskeletal fitness of 8–10 year old schoolchildren is affected by frequent high-intensity physical education classes, and showed that after a 10-month intervention of varying intensities, the intervention group had higher scores for changes in bone mineral content (BMC) and bone mineral density (aBMD) change scores were higher, suggesting that well organized high-intensity physical education sessions can promote the development of musculoskeletal fitness in young children 29 . A study of the effects of different resistance training programs on the development of muscular strength and endurance in children found a significant increase in leg extension muscular endurance with low repetition-heavy loads and high repetition-heavy loads, with high repetition-medium loads being significantly greater than low repetition-heavy loads training, and in the chest press exercise only the high repetition-medium loads exercise group had significantly greater muscular strength and muscular endurance than the control group 33 . Benson et al. found that an 8-week PRT (two sets of high-intensity exercises targeting major muscle groups) intervention resulted in significant increases in upper body strength and lower body strength compared to a control group 34 . Leppanen et al. investigated the effect of physical activity intensity on PHYSICAL FITNESS in children by using the PREFIT PHYSICAL FITNESS test to measure PHYSICAL FITNESS (that is, cardiorespiratory fitness, lower and upper body muscular strength and motor fitness), and the results showed that replacing sedentary, low- or moderate-intensity exercise with 5 min of high-intensity exercise per day promoted an increase in muscle strength 38 .
However, Videira-Silva et al. showed no significant improvement in muscular endurance in participants in the 12-week HIIT group 49 . That's because the study, which only had two 10-min short-term high-intensity interval exercise sessions per week, failed to provide enough stimulation for fitness enhancement. Therefore, long-term, high-intensity training may be necessary to effectively improve muscle fitness in children and adolescents.
This review aimed to summarize the effects of physical activity of different exercise intensities on the PHYSICAL FITNESS of children and adolescents. The analysis included 30 interventional studies from 15 countries. 30 studies were assessed as above average, with good reason to believe that different exercise intensities had different effects on PHYSICAL FITNESS in children and adolescents. Based on strict restrictions on the nature of the intervention included in the studies, the studies included in the study span the years 1999 to 2024 (Table 1 ). It can be guessed that since 1999, researchers have gradually found differences in improving the PHYSICAL FITNESS of adolescents with different exercise intensities. In addition, from the perspective of regions and countries where the literature is published, relevant research is mainly concentrated in developed countries and some developing countries. This may be because, with the increase in material wealth, the PHYSICAL FITNESS of children and adolescents has received a high level of attention. Judging from the number of relevant published literature, there is still a lack of research on the effects of different exercise intensities on the PHYSICAL FITNESS of children and adolescents internationally. Therefore, this study aims to draw the attention of more draw the attention of more researchers from different regions and countries to this topic and encourage the conduction of controlled trials with high-quality evidence to further demonstrate the positive effects of different exercise intensities.
This study shows that high intensity exercise training has significant effects in improving body composition. It was mainly more effective in reducing visceral fat. These results align with a previous review by Batacan et al., which synthesized 65 studies and showed that HIIT can significantly improve waist circumference and body fat percentage in people who are overweight or obese 54 . A meta-analysis of adolescents found that exercise interventions of different intensities were differentially effective in reducing body weight and body mass index, and that high-intensity aerobic exercise and high-intensity aerobic exercise combined with high-intensity resistance training were more effective than low- and moderate-intensity exercise interventions 55 . We suspect that this may be due to the fact that high-intensity exercise leads to excessive post-exercise oxygen consumption and the substrate for this energy oxidation is fat, during high-intensity exercise the body needs to secrete more adrenaline and noradrenaline to control the muscles, and in addition the body has to maintain high metabolic levels for a longer period of time even after exercise. All of these effects lead to an increase in the body's resting metabolic levels, which further stimulates fat burning and leads to weight loss 56 , 57 . It is also interesting to note that Buchan and Kargarfard, when exploring the effects of HIIT on body composition in normal and obese adolescents, did not find any good changes in body composition or waist circumference in the intervention group. Both studies claimed that the lack of effect on body composition was due to the short duration of the training (duration of 7 and 8 weeks) 58 , 59 . Therefore, we suggest that relevant scholars pay more attention to the optimal training time when high-intensity exercise training can effectively improve the body composition of children and adolescents, and provide more effective training programs to reduce the obesity rate of children and adolescents at home and abroad.
This study showed that both high-intensity exercise training and moderate to low-level exercise training can improve cardiorespiratory fitness in children and adolescents, but high-intensity exercise training has a more significant effect on cardiorespiratory function. This finding coincides with previous conclusions 60 , 61 , 62 . A meta-analysis of adolescents aged 11–17 years found that high-intensity exercise training has a significant effect on improving cardiorespiratory fitness in adolescents compared to moderate-intensity exercise 60 , which is consistent with our findings. The mechanism by which this occurs may be due to the fact that high-intensity training increases the oxidative capacity of skeletal muscle more efficiently than conventional training methods. For example, in terms of the molecular adaptive mechanisms of skeletal muscle oxidative capacity, high-intensity exercise activates the activity of AMPK and MAPK exercise-responsive kinases 63 , 64 , while increasing the amount of mRNA for PGC-qα, a transcription factor that regulates the oxidative function of mitochondria. With the activation of the joints leading to increased transcription of mitochondrial substances, this allows the body's aerobic and anaerobic capacity to be enhanced, leading to improved cardiorespiratory fitness 65 . We therefore recommend that schools should incorporate high-intensity program in their physical education curricula so as to improve the cardiorespiratory fitness of children and adolescents and to reduce the probability of children and adolescents suffering from cardiovascular diseases in adulthood.
Muscle fitness is widely recognized as a key fitness component for maintaining overall health and is negatively correlated with obesity 66 .In this review, five studies confirmed the effects of different exercise intensities on muscle fitness function in children and adolescents. A systematic study of school-age children and adolescents suggests that high-intensity physical activity is more beneficial in building muscle 67 . Our findings are supported by Smith et al.'s study, where strenuous physical activity was positively associated with muscle fitness in children and adolescents 68 . In addition, only 1 study in this study showed that high-intensity training was effective in improving muscle flexibility. Muscle flexibility can be expressed as the normal physiological range of joint motion 69 . If adequate flexibility is lacking, daily activities will become difficult. In addition, reduced flexibility can also lead to musculoskeletal injuries 70 . Therefore, maintaining (or increasing) flexibility is essential as it maintains normal joint motion, thereby reducing the risk of injury 71 . A study of adolescents aged 14–17 years found that a 12-week, high-intensity training intervention resulted in adolescents displaying greater flexibility 72 , which is consistent with our findings. Furthermore, in the literature included in this review, only 1 study showed that high-intensity training improves muscle flexibility, but there was insufficient evidence that muscle flexibility is associated with high-intensity training. We speculate that on the one hand, this may be related to limitations in the assessment of muscle flexibility. The currently commonly used methods of assessing muscle flexibility (sitting and stretching) are unable to detect a lack of function due to muscle laxity 73 ; the other side of the coin is that most of the current research on muscle flexibility has focused on the elderly population, with less attention paid to children and adolescents. This is due to the fact that muscle flexibility decreases with age, leading to increased joint stiffness and progressive loss of balance, which increases the risk of falls in older adults 73 . Overall, appropriate levels of flexibility have positive implications for the PHYSICAL FITNESS of children and adolescents, and exploring scientifically sound methods of assessing flexibility and research on flexibility in children and adolescents should receive more attention.
Research limitations and prospects
Although this review discusses the effects of different exercise intensities on the PHYSICAL FITNESS of children and adolescents from four aspects, its limitations should be properly examined. This review provides direction for further research on the effects of different exercise intensities on the PHYSICAL FITNESS of children and adolescents. Although an extensive literature search was conducted, including articles published before 2024, it is possible that some relevant literature may have been overlooked due to variations in keywords used in this study. Additionally, we conducted an extensive literature search in four major databases, but some published non-English foreign studies may have been missed in this review as our search was limited to English-language journal articles.
Despite these limitations, this review systematically collated the literature reports on the different effects of different exercise intensities on the PHYSICAL FITNESS of children and adolescents. Future research could explore higher-quality randomize controlled trials to provide more convincing evidence for optimal exercise intensity to improve the health of children and adolescents. Future research should also focus on the effect of different exercise intensities on muscle flexibility. At the same time, more comprehensive exercise evaluation is needed to support high-intensity exercise training as an effective exercise program to improve the PHYSICAL FITNESS of children and adolescents.
Conclusions
This systematic review demonstrates a positive association between high-intensity exercise training and PHYSICAL FITNESS in children and adolescents. High-intensity exercise training yields notable improvement in body composition (reduced body mass index, waist circumference, and body fat), cardiopulmonary function, and muscle strength in children and adolescents. Furthermore, the high-intensity training group outperforms both the moderate-intensity group and the control group in terms of improving physical fitness. Specifically, participation in HIIT exhibits a more significant effect on improving PHYSICAL FITNESS in children and adolescents. Based on the findings, we recommend that schools optimize their physical education programs by incorporating more high-intensity physical activities, thereby promoting the healthy growth of children and adolescents through effective exercise.
Moreover, the study highlights that the effects of high-intensity physical activity on the PHYSICAL FITNESS of children and adolescents may be influenced by factors such as average age, overweight or obesity of participants. Therefore, further refinement of the study design is necessary, along with additional high-quality research, particularly randomized controlled trials, to ensure the long-term reliability of the results. Additionally, in terms of measurement of related indicators, this study primarily relies on manual measurement and automated equipment, which may introduce measurement errors. Subsequent studies could consider using more advanced instruments to assess relevant indicators of the PHYSICAL FITNESS of children and adolescents.
Data availability
Data is provided within the manuscript or supplementary information files.
Jebeile, H., Kelly, A. S., O’Malley, G. & Baur, L. A. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 10 , 351–365. https://doi.org/10.1016/s2213-8587(22)00047-x (2022).
Article CAS PubMed PubMed Central Google Scholar
Ezzati, M. et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390 , 2627–2642. https://doi.org/10.1016/s0140-6736(17)32129-3 (2017).
Article Google Scholar
Simmonds, M., Llewellyn, A., Owen, C. G. & Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obesity Rev. 17 , 95–107. https://doi.org/10.1111/obr.12334 (2016).
Article CAS Google Scholar
The, N. S., Suchindran, C., North, K. E., Popkin, B. M. & Gordon-Larsen, P. Association of adolescent obesity with risk of severe obesity in adulthood. Jama-J. Am. Med. Associat. 304 , 2042–2047. https://doi.org/10.1001/jama.2010.1635 (2010).
Horesh, A., Tsur, A. M., Bardugo, A. & Twig, G. Adolescent and childhood obesity and excess morbidity and mortality in young adulthood-a systematic review. Curr. Obesity Rep. 10 , 301–310. https://doi.org/10.1007/s13679-021-00439-9 (2021).
Jebeile, H., Cardel, M. I., Kyle, T. K. & Jastreboff, A. M. Addressing psychosocial health in the treatment and care of adolescents with obesity. Obesity 29 , 1413–1422. https://doi.org/10.1002/oby.23194 (2021).
Article PubMed Google Scholar
Weihrauch-Blueher, S., Schwarz, P. & Klusmann, J.-H. Childhood obesity: Increased risk for cardiometabolic disease and cancer in adulthood. Metabolism-Clin. Exp. 92 , 147–152. https://doi.org/10.1016/j.metabol.2018.12.001 (2019).
Li, J., Zhou, X., Huang, Z. & Shao, T. Effect of exercise intervention on depression in children and adolescents: a systematic review and network meta-analysis. Bmc Public Health https://doi.org/10.1186/s12889-023-16824-z (2023).
Article PubMed PubMed Central Google Scholar
Romero-Perez, E. M. et al. Influence of a physical exercise program in the anxiety and depression in children with obesity. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17134655 (2020).
Martin, A. et al. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database Systematic Rev. https://doi.org/10.1002/14651858.CD009728.pub3 (2018).
Cai, Y., Zhu, X. & Wu, X. Overweight, obesity, and screen-time viewing among Chinese school-aged children: National prevalence estimates from the 2016 Physical Activity and Fitness in China-The Youth Study. J. Sport Health Sci. 6 , 404–409. https://doi.org/10.1016/j.jshs.2017.09.002 (2017).
Sedgwick, M. J., Morris, J. G., Nevill, M. E. & Barrett, L. A. Effect of repeated sprints on postprandial endothelial function and triacylglycerol concentrations in adolescent boys. J. Sports Sci. 33 , 806–816. https://doi.org/10.1080/02640414.2014.964749 (2015).
Costigan, S. A., Eather, N., Plotnikoff, R. C., Taaffe, D. R. & Lubans, D. R. High-intensity interval training for improving health-related fitness in adolescents: A systematic review and meta-analysis. Br. J. Sports Med. https://doi.org/10.1136/bjsports-2014-094490 (2015).
Donnelly, J. E. et al. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exercise 41 , 459–471. https://doi.org/10.1249/MSS.0b013e3181949333 (2009).
Reilly, J. J. & Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obesity 35 , 891–898. https://doi.org/10.1038/ijo.2010.222 (2011).
Hopkins, N. D. et al. Relationships between measures of fitness, physical activity, body composition and vascular function in children. Atherosclerosis 204 , 244–249. https://doi.org/10.1016/j.atherosclerosis.2008.09.004 (2009).
Article CAS PubMed Google Scholar
Chuensiri, N., Suksom, D. & Tanaka, H. Effects of high-intensity intermittent training on vascular function in obese preadolescent boys. Childhood Obesity 14 , 41–49. https://doi.org/10.1089/chi.2017.002 (2018).
Weston, K. S., Wisloff, U. & Coombes, J. S. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: A systematic review and meta-analysis. Br. J. Sports Med. 48 , 1227-U1252. https://doi.org/10.1136/bjsports-2013-092576 (2014).
Corbin, C. B., Welk, G. J., Corbin, W. R. & Welk, K. A. Concepts of Physical Fitness: Active Lifestyles for Wellness 14th edn. (William Glass, 2008).
Google Scholar
Hutton, B., Caldwell, D. M., Chaimani, A., Schmid, C. H. & Cameron, C. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Internal Med. 162 (11), 777–784. https://doi.org/10.7326/M14-2385 (2015).
Vrabel, M. Preferred reporting items for systematic reviews and meta-analyses. Oncol. Nursing Forum 42 , 552–554. https://doi.org/10.1188/15.Onf.552-554 (2015).
Adolescent health in the South-East Asia Region , < https://www.who.int/southeastasia/health-topics/adolescent-health > (2022).
de Morton, N. A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 55 , 129–133. https://doi.org/10.1016/s0004-9514(09)70043-1 (2009).
Farah, B. Q., Ritti-Dias, R. M., Balagopal, P., Hill, J. O. & Prado, W. L. Does exercise intensity affect blood pressure and heart rate in obese adolescents? A 6-month multidisciplinary randomized intervention study. Pediatric Obesity 9 , 111–120. https://doi.org/10.1111/j.2047-6310.2012.00145.x (2014).
Hay, J. et al. Physical activity intensity and type 2 diabetes risk in overweight youth: a randomized trial. Int. J. Obesity 40 , 607–614. https://doi.org/10.1038/ijo.2015.241 (2016).
Bond, B. et al. Exercise intensity and the protection from postprandial vascular dysfunction in adolescents. Am. J. Physiol. -Heart Circulatory Physiol. 308 , H1443–H1450. https://doi.org/10.1152/ajpheart.00074.2015 (2015).
Paravidino, V. B., Felix Mediano, M. F., Hoffman, D. J. & Sichieri, R. Effect of exercise intensity on spontaneous physical activity energy expenditure in overweight boys: A crossover study. Plos One https://doi.org/10.1371/journal.pone.0147141 (2016).
Tadiotto, M. C. et al. Effects and individual response of continuous and interval training on adiponectin concentration, cardiometabolic risk factors, and physical fitness in overweight adolescents. Eur. J. Pediatr. 182 , 2881–2889. https://doi.org/10.1007/s00431-023-04974-6 (2023).
Larsen, M. N. et al. Positive effects on bone mineralisation and muscular fitness after 10 months of intense school-based physical training for children aged 8–10 years: The FIT FIRST randomised controlled trial. Br. J. Sports Med. 52 , 254. https://doi.org/10.1136/bjsports-2016-096219 (2018).
Ramirez-Velez, R. et al. Effects of different doses of exercise on inflammation markers among adolescents with overweight/obesity: HEPAFIT study. J. Clin. Endocrinol. Metabolism 107 , E2619–E2627. https://doi.org/10.1210/clinem/dgac021 (2022).
Cao, M., Tang, Y., Li, S. & Zou, Y. Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: A randomized controlled trial. Bmc Pediatr. https://doi.org/10.1186/s12887-021-03079-z (2022).
Dias, K. A. et al. Effect of high-intensity interval training on fitness, fat mass and cardiometabolic biomarkers in children with obesity: A randomised controlled trial. Sports Med. 48 , 733–746. https://doi.org/10.1007/s40279-017-0777-0 (2018).
Faigenbaum, A. D., Westcott, W. L., Loud, R. L. & Long, C. The effects of different resistance training protocols on muscular strength and endurance development in children. Pediatrics 104 , e5–e5. https://doi.org/10.1542/peds.104.1.e5 (1999).
Benson, A. C., Torode, M. E. & Singh, M. A. F. The effect of high-intensity progressive resistance training on adiposity in children: A randomized controlled trial. Int. J. Obesity 32 , 1016–1027. https://doi.org/10.1038/ijo.2008.5 (2008).
Taber, D. R. et al. Participation in vigorous sports, not moderate sports, is positively associated with cardiorespiratory fitness among adolescent girls. J. Phys. Activity Health 11 , 596–603. https://doi.org/10.1123/jpah.2011-0280 (2014).
Davis, C. L. et al. Exercise dose and diabetes risk in overweight and obese children a randomized controlled trial. Jama-J. Am. Med. Associat. 308 , 1103–1112. https://doi.org/10.1001/2012.jama.10762 (2012).
Burns, S. F., Oo, H. H. & Anh Thanh Thuy, T. Effect of sprint interval exercise on postexercise metabolism and blood pressure in adolescents. Int. J. Sport Nutr. Exerc. Metabolism 22 , 47–54. https://doi.org/10.1123/ijsnem.22.1.47 (2012).
Leppanen, M. H. et al. Physical activity intensity, sedentary behavior, body composition and physical fitness in 4-year-old children: Results from the ministop trial. Int. J. Obesity 40 , 1126–1133. https://doi.org/10.1038/ijo.2016.54 (2016).
Leppanen, M. H. et al. Longitudinal physical activity, body composition, and physical fitness in preschoolers. Med. Sci. Sports Exerc. 49 , 2078–2085. https://doi.org/10.1249/mss.0000000000001313 (2017).
Gomes, P. P., Silva, H. J. G. D., Lira, C. T. C. D., Lofrano-Prado, M. C. & Prado, W. L. D. Efeitos de diferentes intensidades de treinamento aeróbio sobre a composição corporal em adolescentes obesos. Revista Brasileira de Cineantropometria Desempenho Humano 15 , 594–603. https://doi.org/10.5007/1980-0037.2013v15n5p594 (2013).
Buchan, D. S. et al. High intensity interval running enhances measures of physical fitness but not metabolic measures of cardiovascular disease risk in healthy adolescents. BMC Public Health 13 , 498–498. https://doi.org/10.1186/1471-2458-13-498 (2013).
Grasten, A., Huhtiniemi, M., Kolunsarka, I. & Jaakkola, T. Developmental associations of accelerometer measured moderate-to-vigorous physical activity and sedentary time with cardiorespiratory fitness in schoolchildren. J. Sci. Med. Sport 25 , 884–889. https://doi.org/10.1016/j.jsams.2022.08.015 (2022).
Costigan, S. A. et al. Preliminary efficacy and feasibility of embedding high intensity interval training into the school day: A pilot randomized controlled trial. Prevent. Med. Rep. 2 , 973–979. https://doi.org/10.1016/j.pmedr.2015.11.001 (2015).
Saidi, O. et al. Acute effect of an intensified exercise program on subsequent sleep, dietary intake, and performance in junior rugby players. Eur. J. Appl. Physiol. 119 , 2075–2082. https://doi.org/10.1007/s00421-019-04196-5 (2019).
Saidi, O., Rochette, E., Bovet, M., Merlin, E. & Duche, P. Acute intense exercise improves sleep and decreases next morning consumption of energy-dense food in adolescent girls with obesity and evening chronotype. Pediatric Obesity https://doi.org/10.1111/ijpo.12613 (2020).
Gerber, M. et al. Moderate-to-vigorous physical activity is associated with cardiorespiratory fitness among primary schoolchildren living in cote D’ivoire, South Africa, and Tanzania. Front. Public Health https://doi.org/10.3389/fpubh.2021.671782 (2021).
Winn, C. O. N. et al. Effect of high-intensity interval training in adolescents with asthma: The exercise for asthma with Commando Joe’s (R) (X4ACJ) trial. J. Sport Health Sci. 10 , 488–498. https://doi.org/10.1016/j.jshs.2019.05.009 (2021).
da Silva, P., Bento, A. F., Paez, L. C., de Mendonca, M. & Raimundo, A. High-intensity interval training in high-school physical education classes: Study protocol for a randomized controlled trial. Contemporary Clin. Trials Commun. 24 , 100867–100867. https://doi.org/10.1016/j.conctc.2021.100867 (2021).
Videira-Silva, A., Sardinha, L. B. B. & Fonseca, H. Atherosclerosis prevention in adolescents with obesity: The role of moderate-vigorous physical activity. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph192315537 (2022).
Juric, P., Dudley, D. A. & Petocz, P. Does incorporating high intensity interval training in physical education classes improve fitness outcomes of students? A cluster randomized controlled trial. Prevent. Med. Rep. 32 , 102127–102127. https://doi.org/10.1016/j.pmedr.2023.102127 (2023).
Farpour-Lambert, N. J. et al. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J. Am. College Cardiol. 54 , 2396–2406. https://doi.org/10.1016/j.jacc.2009.08.030 (2009).
Ketelhut, S., Ketelhut, K., Ketelhut, S. R. & Ketelhut, R. G. Effects of school-based high-intensity interval training on hemodynamic parameters and heart rate variability: A randomized controlled trial. J. Strength Cond. Res. https://doi.org/10.1519/jsc.0000000000004744 (2024).
Migueles, J. H. et al. Effects of an exercise program on cardiometabolic and mental health in children with overweight or obesity a secondary analysis of a randomized clinical trial. Jama Netw. Open https://doi.org/10.1001/jamanetworkopen.2023.24839 (2023).
Batacan, R. B. Jr., Duncan, M. J., Dalbo, V. J., Tucker, P. S. & Fenning, A. S. Effects of high-intensity interval training on cardiometabolic health: A systematic review and meta-analysis of intervention studies. Br. J. Sports Med. https://doi.org/10.1136/bjsports-2015-095841 (2017).
Hao, Z. et al. Which exercise interventions are more helpful in treating primary obesity in young adults? A systematic review and Bayesian network meta-analysis. Archiv. Med. Sci. 19 , 865–883. https://doi.org/10.5114/aoms/153479 (2023).
Borsheim, E. & Bahr, R. Effect of exercise intensity, duration and mode on post-exercise oxygen consumption. Sports medicine (Auckland, NZ) 33 , 1037–1060 (2003).
Sindorf, M. A. G. et al. Excess post-exercise oxygen consumption and substrate oxidation following high-intensity interval training: Effects of recovery manipulation. Int. J. Exerc. Sci. 14 , 1151–1165 (2021).
PubMed PubMed Central Google Scholar
Kargarfard, M. et al. Effects of endurance and high intensity training on ICAM-1 and VCAM-1 levels and arterial pressure in obese and normal weight adolescents. Physician Sportsmedicine 44 , 208–216. https://doi.org/10.1080/00913847.2016.1200442 (2016).
Buchan, D. S. et al. The effects of time and intensity of exercise on novel and established markers of CVD in adolescent youth. Am. J. Hum. Biol. 23 , 517–526. https://doi.org/10.1002/ajhb.21166 (2011).
Martin-Smith, R. et al. High intensity interval training (HIIT) improves cardiorespiratory fitness (CRF) in healthy, overweight and obese adolescents: A systematic review and meta-analysis of controlled studies. Int. J. Environ. Res. Public Health 17 (8), 2955. https://doi.org/10.3390/ijerph17082955 (2020).
Cao, M., Tang, Y., Li, S. & Zou, Y. Effects of high-intensity interval training and moderate-intensity continuous training on cardiometabolic risk factors in overweight and obesity children and adolescents: A meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph182211905 (2021).
Bond, B., Weston, K. L., Williams, C. A. & Barker, A. R. Perspectives on high-intensity interval exercise for health promotion in children and adolescents. Open Access J. Sports Med. 8 , 243–265. https://doi.org/10.2147/oajsm.S127395 (2017).
Little, J. P. et al. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J. Appl. Physiol. 111 , 1554–1560. https://doi.org/10.1152/japplphysiol.00921.2011 (2011).
Gibala, M. J. et al. Brief intense interval exercise activates AMPK and p38 MAPK signaling and increases the expression of PGC-1α in human skeletal muscle. J. Appl. Physiol. 106 , 929–934. https://doi.org/10.1152/japplphysiol.90880.2008 (2009).
Little, J. P., Safdar, A., Bishop, D., Tarnopolsky, M. A. & Gibala, M. J. An acute bout of high-intensity interval training increases the nuclear abundance of PGC-1α and activates mitochondrial biogenesis in human skeletal muscle. Am. J. Physiol. -Regulatory Integrative Comparative Physiol. 300 , R1303–R1310. https://doi.org/10.1152/ajpregu.00538.2010 (2011).
Wearing, S. C., Hennig, E. M., Byrne, N. M., Steele, J. R. & Hills, A. P. The impact of childhood obesity on musculoskeletal form. Obesity Rev.: Off. J. Int. Associat. Study Obesity 7 , 209–218. https://doi.org/10.1111/j.1467-789X.2006.00216.x (2006).
Janssen, I. & LeBlanc, A. G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Activity https://doi.org/10.1186/1479-5868-7-40 (2010).
Smith, J. J. et al. Behavioral correlates of muscular fitness in children and adolescents: A systematic review. Sports Med. 49 , 887–904. https://doi.org/10.1007/s40279-019-01089-7 (2019).
Holland, G. J., Tanaka, K., Shigematsu, R. & Nakagaichi, M. Flexibility and physical functions of older adults: A review. Aging Phys. Activity https://doi.org/10.1123/japa.10.2.169 (2002).
Badley, E. M., Wagstaff, S. & Wood, P. H. Measures of functional ability (disability) in arthritis in relation to impairment of range of joint movement. Ann. Rheumatic Diseases 43 , 563–569. https://doi.org/10.1136/ard.43.4.563 (1984).
D’Onofrio, G., Kirschner, J., Prather, H., Goldman, D. & Rozanski, A. Musculoskeletal exercise: Its role in promoting health and longevity. Progr. Cardiovasc. Diseases 77 , 25–36. https://doi.org/10.1016/j.pcad.2023.02.006 (2023).
Cvetkovic, N. et al. Exercise training in overweight and obese children: Recreational football and high-intensity interval training provide similar benefits to physical fitness. Scandinavian J. Med. Sci. Sports 28 , 18–32. https://doi.org/10.1111/sms.13241 (2018).
Liu, C., Cao, Y., Zhang, Z., Gao, R. & Qu, G. Correlation of fundamental movement skills with health-related fitness elements in children and adolescents: A systematic review. Front. Public Health https://doi.org/10.3389/fpubh.2023.1129258 (2023).
Download references
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
College of Physical Education and Health Sciences, Zhejiang Normal University, Jinhua, 321004, Zhejiang, China
Xianxian Zhou, Jiayu Li & Xiaoping Jiang
You can also search for this author in PubMed Google Scholar
Contributions
X.X.Z. performed the methodological search on the research topic and helped write the draft manuscript. J.Y.L. contributed to the conception and design of the manuscript. X.P.J. critically wrote and revised the manuscript. All authors have read and approved the final version of this paper and agree with the other of its presentation.
Corresponding author
Correspondence to Xiaoping Jiang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhou, X., Li, J. & Jiang, X. Effects of different types of exercise intensity on improving health-related physical fitness in children and adolescents: a systematic review. Sci Rep 14 , 14301 (2024). https://doi.org/10.1038/s41598-024-64830-x
Download citation
Received : 16 January 2024
Accepted : 13 June 2024
Published : 21 June 2024
DOI : https://doi.org/10.1038/s41598-024-64830-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Exercise intensity
- Physical fitness
- Adolescents
- Systematic review
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 11 May 2010
Systematic review of the health benefits of physical activity and fitness in school-aged children and youth
- Ian Janssen 1 , 2 &
- Allana G LeBlanc 1
International Journal of Behavioral Nutrition and Physical Activity volume 7 , Article number: 40 ( 2010 ) Cite this article
364k Accesses
3029 Citations
235 Altmetric
Metrics details
The purpose was to: 1) perform a systematic review of studies examining the relation between physical activity, fitness, and health in school-aged children and youth, and 2) make recommendations based on the findings.
The systematic review was limited to 7 health indicators: high blood cholesterol, high blood pressure, the metabolic syndrome, obesity, low bone density, depression, and injuries. Literature searches were conducted using predefined keywords in 6 key databases. A total of 11,088 potential papers were identified. The abstracts and full-text articles of potentially relevant papers were screened to determine eligibility. Data was abstracted for 113 outcomes from the 86 eligible papers. The evidence was graded for each health outcome using established criteria based on the quantity and quality of studies and strength of effect. The volume, intensity, and type of physical activity were considered.
Physical activity was associated with numerous health benefits. The dose-response relations observed in observational studies indicate that the more physical activity, the greater the health benefit. Results from experimental studies indicate that even modest amounts of physical activity can have health benefits in high-risk youngsters (e.g., obese). To achieve substantive health benefits, the physical activity should be of at least a moderate intensity. Vigorous intensity activities may provide even greater benefit. Aerobic-based activities had the greatest health benefit, other than for bone health, in which case high-impact weight bearing activities were required.
The following recommendations were made: 1) Children and youth 5-17 years of age should accumulate an average of at least 60 minutes per day and up to several hours of at least moderate intensity physical activity. Some of the health benefits can be achieved through an average of 30 minutes per day. [Level 2, Grade A] . 2) More vigorous intensity activities should be incorporated or added when possible, including activities that strengthen muscle and bone [Level 3, Grade B] . 3) Aerobic activities should make up the majority of the physical activity. Muscle and bone strengthening activities should be incorporated on at least 3 days of the week [Level 2, Grade A] .
Canada's first set of physical activity guidelines for children and youth were introduced in 2002 [ 1 , 2 ]. The basic recommendation within these guidelines was that children and youth, independent of their current physical activity level, should increase the time they spend on moderate-to-vigorous intensity physical activity by 30 minutes per day, and over a 5 month period progress to adding an additional 90 minutes of daily physical activity. Recently, a narrative literature review was conduced to provide an update on the evidence related to the biological and psycho-social health benefits of physical activity in school-aged children and youth which has accumulated since the publication of Canada's guidelines [ 3 ]. This narrative review explored whether Canada's physical activity guidelines for children and youth are appropriate, and made recommendations as to how the guidelines could be modified to reflect current knowledge.
Several other narrative reviews have examined the relation between physical activity and health in school aged children, a small sample of which are referenced here [ 4 – 8 ]. Although informative, narrative reviews have severe limitations. First and foremost, it is uncertain as to whether all of the relevant scientific evidence has been examined. The authors of a narrative review may be exclusive with the materials they review, and these materials may have been selected and interpreted in a biased manner. Thus, the reader is faced with uncertainty and doubt when interpreting a narrative review. The reader may be better served when the choices made in the review are explicit, transparent, clearly stated, and reproducible. This can be achieved through a systematic review. Systematic reviews attempt to reduce reviewer bias through the use of objective, reproducible criteria to select relevant publications, to synthesize and critically appraise the findings from these publications, and to employ defined evidence-based criteria when formulating recommendations [ 9 ].
The purpose of this report was to: 1) perform a systematic review of the evidence informing the relation between physical activity and health in school-aged children and youth, defined here as those aged 5-17 years; and 2) make recommendations on the appropriate volume, intensity, and type of physical activity for minimal and optimal health benefits in school-aged children and youth. A previously developed evaluation system was used to set the level of evidence and grade for the recommendations. This report was part of a much larger project around Canada's physical activity guidelines, and comparable systematic reviews for adults [ 10 ] and older adults [ 11 ] have also been published in the journal. Additional details on the scope and purpose of the larger project [ 12 ] and the interpretation of the recommendations from an independent expert panel [ 13 ] can also be found elsewhere in the journal.
Overview of existing physical activity guidelines for children and youth
Before conducting the systematic review, this paper provides a brief overview on existing physical activity guidelines for school-aged children, as well as an explanation of the scientific evidence that informed the guideline development process.
The publication of Canada's physical activity guidelines for children and youth in 2002 represented a joint effort of the Canadian Society for Exercise Physiology and Health Canada. Two sets of guidelines were published, one for children aged 6 to 9 years [ 2 ] and a second for youth aged 10 to14 years [ 1 ]. In addition to the physical activity guides, which highlighted the recommended physical activity levels for these two age groups, a number of other promotional and educational packages were developed, including family booklets [ 14 , 15 ], teacher booklets [ 16 , 17 ], as well as physical activity magazines for children [ 18 ] and youth [ 19 ].
The key recommendations within Canada's child and youth physical activity guides are:
Increase the time currently spent on physical activity by 30 minutes per day, and progress over approximately 5 months to 90 minutes more per day.
Physical activity can be accumulated throughout the day in periods of at least 5 to 10 minutes.
The 90 minute increase in physical activity should include 60 minutes of moderate activity (e.g., brisk walking, skating, bicycle riding) and 30 minutes of vigorous activity (e.g., running, basketball, soccer).
Participate in different types of physical activities - endurance, flexibility, and strength - to achieve the best health results.
Reduce non-active time spent on watching television and videos, playing computer games, and surfing the Internet. Start with 30 minutes less of such activities per day and progress over the course of approximately 5 months to 90 minutes less per day.
Many other countries and organizations have developed physical activity recommendations for school-aged children and youth, as recently summarized [ 3 ]. With few exceptions, these countries and organizations recommend that children and youth participate in at least 60 minutes of moderate-to-vigorous intensity physical activity on a daily basis. One of these recommendations was published in 2005 as part of a systematic review that linked physical activity to several health and behavioural outcomes in school-aged children and youth [ 20 ]. This systematic review was sponsored by the U.S. Centers for Disease Control and Prevention (CDC) and was developed by a multidisciplinary expert panel. The expert panel considered over 850 articles published in 2004 or earlier, identified by computerized database searches and by searching the bibliographies of the panellists' own libraries [ 20 ]. Based on conceptual definitions and inclusion and exclusion criteria developed by the panel, participants systematically evaluated relevant articles (primarily intervention studies) for each of the 14 health and behavioural outcomes considered. On the basis of their reviews, the panel provided a summary of the evidence for strength (strong, >60% of studies reviewed; moderate, 30-59% of studies reviewed; and weak, <30% of studies reviewed) and the direction (positive, null, or negative) of the effects of physical activity on each of the health and behavioural outcomes. The strength of evidence was judged from the statistical significance of the outcomes; it did not include other factors usually considered in systematic review, such as the effect sizes of physical activity and the quality and types of studies.
The expert panel reached the following conclusions: (i) Evidence-based data are strong to conclude that physical activity has beneficial effects on adiposity (within overweight and obese youth), musculoskeletal health and fitness, and several components of cardiovascular health. (ii) Evidence-based data are adequate to conclude that physical activity has beneficial effects on adiposity levels in those with a normal body weight, on blood pressure in normotensive youth, on plasma lipid and lipoproteins levels, on non-traditional cardiovascular risk factors (inflammatory markers, endothelial function and heart rate variability), and on several components of mental health (self-concept, anxiety and depression) [ 20 ]. A summary of evidence concerning the health outcomes examined by the expert panel is shown in Table 1 [Additional file 1 ]. The amount, intensity, and type of physical activity required to achieve the result, when clear, is also shown in the table.
In 2008 a second systematic review of literature examining the relation between physical activity and key fitness and health outcomes within school-aged children and youth was published. This systematic review was part of the "Physical Activity Guidelines for Americans" project that was undertaken by the Unites States Department of Health and Human Services [ 21 ]. Unlike the 2005 CDC sponsored systematic review that focused on intervention studies, the 2008 review considered both observational and experimental studies. The 2008 systematic review concluded that few studies have provided data on the dose-response relation between physical activity and various health and fitness outcomes in children and youth. However, substantial data indicate that health and fitness benefits will occur in most children and youth who participate in 60 or more minutes of moderate-to-vigorous physical activity on a daily basis. For children and youth to gain comprehensive health benefits they need to participate in the following types of physical activity on 3 or more days per week: vigorous aerobic exercise, resistance exercise, and weight-loading activities.
Although informative, the recommendations made within the 2005 and 2008 systematic reviews did not include a level of evidence or grade, which are now becoming a routine part of evidence based reviews. The level of evidence helps inform the reader about the strength of evidence that informed the recommendation. The grade considers the harms and benefits of implementing the intervention, and informs the reader about whether an intervention should be implemented.
Questions addressed in systematic review
The following questions were addressed in this systematic review:
1) How much (volume) physical activity is needed for minimal and optimal health benefits in school-aged children and youth? To address this question careful consideration was given to whether dose-response relations existed between physical activity and fitness with the various health outcomes, and if so, the pattern of these relations (e.g., linear, or curvilinear relations with large improvements in health occurring with limited increases in physical activity at the low end of the physical activity scale, or curvilinear relations with small improvements in health occurring with increases in physical activity at the low end of the physical activity scale).
2) What types of activity are needed to produce health benefits ? Specific consideration was given to what types of activity (aerobic, resistance, etc.) influenced the different health outcomes, and whether more than one type of activity would be needed for overall health and well-being.
3) What is the appropriate physical activity intensity ? Attention was given to the intensity of physical activity measured (observational studies) or prescribed (experimental studies). An underlying assumption was that children and youth would prefer lower intensity activities over higher intensity activities. Therefore, for higher intensity activities to be recommended over lower intensity activities there would need to be either: i) no evidence that low intensity activities were beneficial for health and evidence that higher intensity activities impacted health in a favorable manner, or ii) clear evidence that higher intensity activities impacted the health outcomes to a greater extent than lower intensity activities.
4) Do the effects of physical activity on health in school-aged children and youth vary by sex and/or age ? Results were examined to see if: i) the moderating effects of sex and/or age on the relations between physical activity and health were explored, and if not, iii) whether there were consistent patterns across studies (either statistically or in order of magnitude) that were suggestive of sex or age differences.
Eligibility criteria
This systematic review was limited to key indicators of different health outcomes known to be related to physical activity in school-aged children and youth. Decisions on what health outcomes to include in the systematic review were made by examining what outcomes were studied in previously conducted reviews of this nature [ 20 , 21 ] and in consultation with the Steering Committee for the Canadian Physical Activity Guidelines project. These key indicators consisted of:
High blood cholesterol, high blood pressure, and markers of the metabolic syndrome as a measure of cardiometabolic risk
Overweight/obesity as a measure of adiposity
Low bone density as a measure of skeletal health
Depression as a measure of mental health
Injuries as a negative health outcome of physical activity
We recognized that although cardiorespiratory and musculoskeletal fitness are partially genetic in origin, they are in large measure a reflection of physical activity participation in recent weeks and months [ 22 ]. Therefore, the systematic review also included studies that examined the relation between fitness and health. For our purposes, fitness was assumed to be a proxy measure of physical activity. Any studies evaluating the relationship between physical activity or fitness and one or more of the key health outcomes listed above within school-aged children and youth were eligible for inclusion.
In consultation with the Steering Committee of the Canadian Physical Activity Guidelines and Measurement Project and the authors who were completing the adult and older adult systematic reviews, a decision was made to limit the pediatric systematic review to: 1) studies examining the key health indicators above, and 2) for observational studies, the outcomes must have been measured in a dichotomous (yes or no) manner and presented as prevalences or ratio scores (odds ratio, relative risk, hazard ratio). This decision was made for three reasons: (i) to help ensure that the systematic review would be manageable in size and scope for a single research team to complete in a timely manner, (ii) to eliminate many of the observational studies with small sample sizes, and (iii) to ensure that the health outcomes, at least for the observational studies, were presented in a reasonably consistent pattern from study to study. This helped us to make comparisons between studies and to characterize the magnitude of effect for physical activity.
To further illustrate why the aforementioned limitations were put in place, consider the following. Within children and youth physical activity has been related to over two dozen different health outcomes. For adiposity alone, several adiposity measures have been considered including body weight, BMI, several skinfold and circumference measures, total body fat, and several specific body fat depots. Preliminary literature searches on adiposity - as measured using both continuous (e.g., body weight, BMI, visceral fat, skinfolds) and categorical (overweight/obese vs. normal weight) outcomes to capture the measures indicated above, revealed over 15,000 published papers. The results from these papers were presented in several formats including comparison of group means for continuous adiposity measures according to physical activity level, relations between continuous adiposity and physical activity measures which were presented in a variety of ways (e.g., r values, regression coefficients); comparison of group means for physical activity according to adiposity status; ratio scores (odds ratios, relative risks, hazard ratios) for the prediction of obesity status according to physical activity level; comparison of the prevalence of obesity according to physical activity level; etc. Without employing some criteria to limit the types of measures and outcomes, it would have been virtually impossible to synthesize the results from these studies.
Cross-sectional studies, case-control studies, cohort studies (prospective and retrospective) and intervention studies (including randomized and quasi experimental designs) were eligible for inclusion in the systematic review. Only published, English language studies including human participants were included. To be included studies had to be limited to school-aged children and youth between 5-17 years of age, or present data specifically for a subgroup of participants within this age range.
For the observational studies, there were no limitations placed on the form of physical activity (e.g., questionnaire, activity diary, pedometer, accelerometer) or fitness (cardiorespiratory or musculoskeletal fitness) measurements. For intervention studies, all cardiorespriatory and/or musculoskeletal based interventions were eligible for inclusion. Intervention studies were excluded if they included a dietary (e.g., caloric restriction) or other behavioral risk factor component (e.g., smoking cessation) that may have independently affected the health outcomes and subsequently made it impossible to distinguish the independent effect of the physical activity portion of the intervention.
Search strategy
Literature searches were conducted in MEDLINE (1950-January 2008, OVID Interface), EMBASE (1980-January 2008, OVID Interface), CINAHL (1982-January 2008, OVID Interface), PsycINFO (1967-January 2008, OVID Interface), all Evidence-Based Medicine Reviews (1991-January 2008, OVID Interface), and SPORTDiscus (up to January 2008, EBSCO Interface).
The electronic search strategies were executed by a single researcher (AB) under direction of the primary author (IJ). They were not restricted by publication type or study design; however, they were limited to human participants and English language. The following string of search terms were used for each of the study outcomes to identify physical activity related papers conducted within the age group of interest: ('physical activity' OR 'fitness' OR 'exercise' OR 'energy expenditure') AND ('child' OR 'adolescent' OR 'youth' OR 'juvenile'). The following search terms were added (e.g., AND) for the cholesterol search: ('high cholesterol' OR 'hypercholesterolemia' OR 'hyperlipidemia' OR 'dyslipidemia'). For hypertension the following search terms were added: ('high blood pressure' OR 'hypertension'). For metabolic syndrome the following search terms added: ('metabolic syndrome' OR 'syndrome X' OR 'deadly quartet' OR 'plurimetabolic syndrome' OR 'insulin resistance' OR 'insulin resistant'). For obesity the following search terms were added: ('obese' OR 'obesity' OR 'overweight'). For low bone mineral density the following search terms were added: ('bone density' OR 'bone strength' OR 'bone mass' OR 'bone mineral density'). For depression the following search terms were added: ('depression' OR 'mood disorder'). For injuries the following search terms were added: ('injury' OR 'injuries').
A total of 42 electronic searches were performed (7 health outcomes × 6 search engines) and the information from each search was saved as a text file that included all of the retrieved citations. Using SAS software version 9 (SAS Institute, Carry, NC), the text files were separated back into individual citations and exported into a Microsoft Access database. The database included the following information for each citation: unique identifier for the database, paper title, authors, journal name, volume and issue number, page numbers, and the abstract. See Figure 1 for an illustration of the Microsoft Access database form. Within the Microsoft Access database, duplicate citations - those citations that were identified in more than one of the search engines and/or for more than one of the health outcomes - were identified by a match of the title and were removed using automated procedures.
Copy of electronic abstract review form .
Screening of citations
After duplicate citations were removed from the Access database, the abstract of each citation was reviewed by a single reviewer to determine if it should be included within the systematic review. The full-text articles of all potentially relevant citations were obtained, and saved as Adobe-PDF files that were linked to the Access database. Whenever it was uncertain as to whether a citation was appropriate, the full-text copy was obtained. After the first reviewer screened the database, the citations that were deemed ineligible were reviewed by a second reviewer to determine if any potentially relevant citations were missed, and full-text copies of these citations were also obtained. Copies of all of the full-text articles were then reviewed by the two reviewers for inclusion criteria; if uncertain as whether or not to include an article, the article in question was reviewed again until a final decision was made.
Data abstraction
A single reviewer (AL) abstracted data from all eligible full-text citations using an electronic data abstraction form. Refer to Figure 2 for an illustration of electronic data abstraction form. The data abstraction was completed in a second Microsoft Access Database, which was linked to the first Microsoft Access Database using a unique identifier. The abstracted data included information on the study design, participants, details of the physical activity (or fitness) measures or interventions, and key findings. After data abstraction was completed, the information was checked by a second reviewer (IJ) and corrected when necessary.
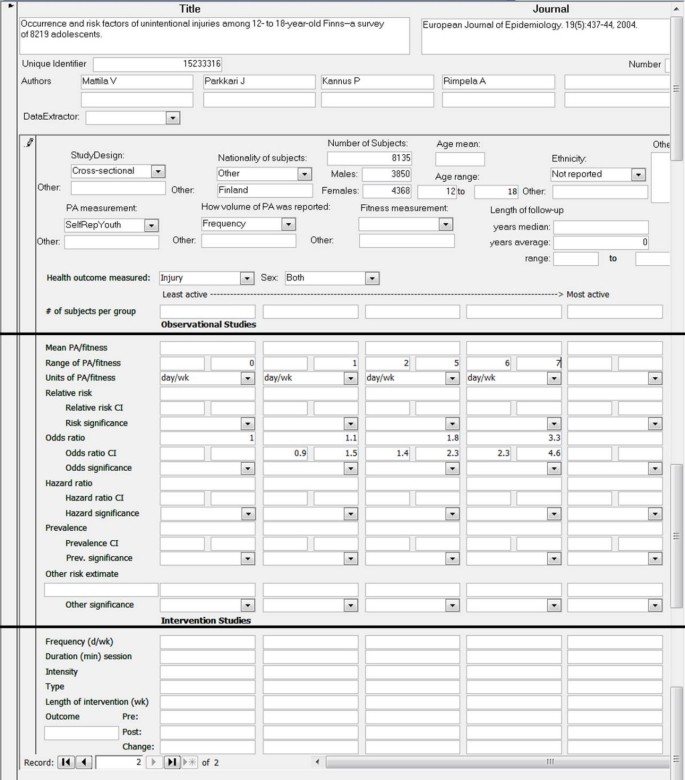
Copy of electronic database abstraction form .
Assigning levels of evidence and formulation of recommendations
The goal was to use a rigorous, evidence-based approach to develop levels of evidence on the relation between physical activity and health in school-aged children that could be used to formulate recommendations for the specific volume, intensity, and type of physical activity needed. At present there is no universally accepted method for formulating evidence-based recommendations. In consultation with the Steering Committee for this project and the authors performing the systematic reviews in adults and older adults, we chose to use the process that was recently employed for the development of Canada's obesity prevention and management guidelines [ 23 ]. Within this system, the level of evidence for a recommendation is based on an objective appraisal of the literature according to a pre-specified scale as reflected by the study designs and quality. As shown in Table 2 [Additional file 2 ], the level of evidence can range from 1 (highest) to 4 (lowest). The grade for a recommendation reflects the level of evidence and several additional features, including: benefits and risks of physical activity participation, magnitude of the effects, cost of the intervention, and value of an intervention to an individual or population. As indicated in Table 3 [Additional file 3 ], the grade for the recommendation may be an A, B, or C. Note that while the level of evidence assigned is not necessarily linked to the corresponding grade, a high grade is less likely in the setting of low-quality of evidence.
Note that the level of evidence in the aforementioned grading system is based in part on the quality of the studies. This grading was particularly relevant for experimental studies wherein the level of evidence would change from Level 1 to Level 2 based on whether or not the randomized controlled trials (RCTs) have important limitations. A single investigator (IJ) assessed the quality of the RCTs included in this systematic review using the validated checklist developed by Downs and Black [ 24 ]. This 27-item checklist assess the quality of reporting (e.g., are the interventions of interest clearly described, have all the adverse events that may be a consequence of the intervention been reported), external validity (e.g., were the subjects representative of the population), internal validity (e.g., was an attempt made to blind those measuring the outcome, were the outcome measures accurate), selection bias (e.g., were the study subjects randomized, was randomization assignment concealed until recruitment was complete), and statistical power.
To evaluate the magnitude of effect of physical activity on the various health outcomes examined, in addition to statistical significance, the following criteria were applied to evaluate the strength of the ratio scores (odds ratio, relative risk, hazard ratio) for the observational studies. For positive associations 1.01-1.50 = weak association, 1.51-3.00 = moderate association, and 3.01 or higher = strong association. For negative associations: 0.71-0.99 = weak association, 0.41-0.70 = moderate association, 0.00-0.40 = strong association [ 25 ]. For the experimental studies, measures of effect were calculated based on Cohen's d, which was calculated as the difference between the pre- and post-treatment mean within a given treatment group divided by the average of the standard deviation of the pre- and post-treatment means [ 26 ]. Cohen's d effect measures ≥ 0.49 were considered to be weak, values ranging from 0.50-0.79 were considered to be moderate, and values ≥ 0.80 were considered to be strong [ 26 ]. Note that several experimental studies did not report the information required to calculate Cohen's d, and for these studies effect measures have not been presented.
When possible (e.g., at least 4 studies) we performed meta-analyses to calculate summary odds ratio and Cohen's d effect size measures for the observational and experimental studies, respectively [ 27 ]. These summary estimates represent a weighted average of the estimates provided in the various studies included in the meta-analysis. These meta-analyses were performed separately for each health outcomes, separately for observational and experimental studies, and separately based on type of physical activity measurement or exercise modality prescribed.
Literature review
The flow of citations through the systematic review process is shown in Figure 3 . For each of the 7 health outcomes, several citations were retrieved in more than one of the 6 search engines. After removing duplicates, a total of 437 citations were identified for cholesterol, 1151 for depression, 2505 for injury, 1181 for bone density, 1677 for blood pressure, 5824 for obesity, and 1677 for the metabolic syndrome. Thus, the grand total was 13174. Many of these 13174 citations were retrieved for 2 or more health outcomes, and after removing these duplicates there was a total of 11,088 unique citations. After the titles and abstracts of these 11,088 citations were reviewed, full-text copies of 454 potentially relevant citations were obtained and reviewed. Of these 454 citations, 86 unique citations passed the eligibility criteria and were included in the systematic review. Several of these 86 citations included results for 2 or more of the 7 relevant health outcomes.
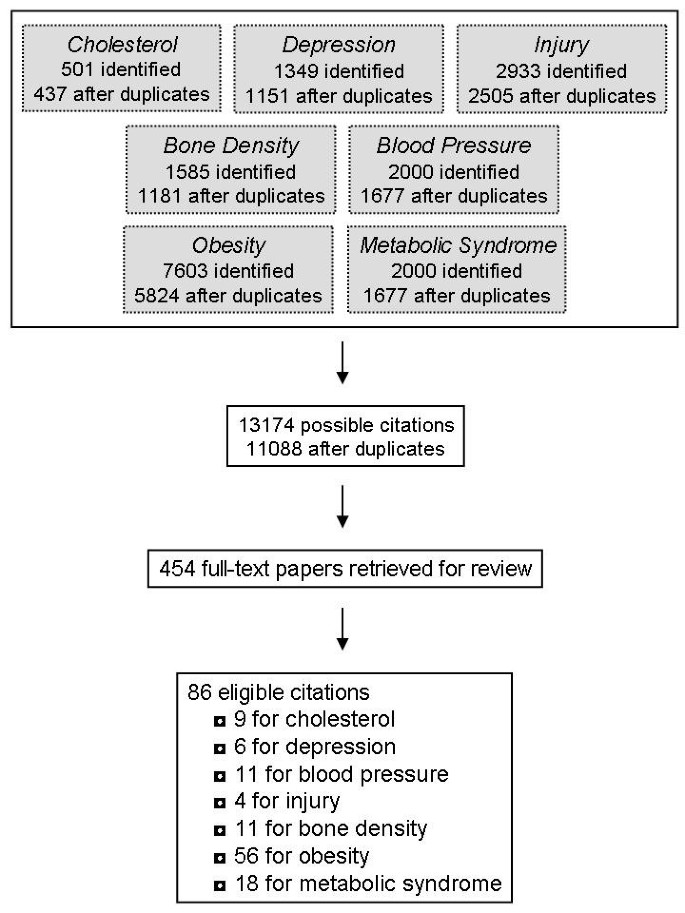
Flow of articles through the systematic review .
Cholesterol and blood lipids
A total of 9 articles examining blood lipids and lipoproteins met the inclusion criteria. Only one of these studies was observational in nature [ 28 ]. This cross-sectional study was conducted on a representative sample (n = 3110) of 12-19 year old American adolescents and measured cardiorespiratory fitness using a submaximal treadmill test. The results indicated that unfit girls, defined as the lowest 20% fit, were 1.89 (95% confidence interval: 1.12-3.17) times more likely to have hypercholesterolemia and 1.03 (0.74-1.43) times more likely to have a low HDL-cholesterol by comparison to moderately and high fit girls. Unfit boys were 3.68 (2.55-5.31) times more likely to have hypercholesterolemia and 1.25 (0.79-1.95) times more likely to have a low HDL-cholesterol by comparison to moderately and high fit boys.
A total of 8 experimental studies (6 RCT, 2 non-randomized) examined the effect of exercise interventions on changes in blood lipids and lipoproteins, as summarized in Table 4 [Additional file 4 ] [ 29 – 36 ]. For the most part, these studies were limited to children and youth with high cholesterol levels [ 30 ] or obesity [ 29 , 32 , 34 , 36 ] at baseline. The sample sizes were quite small and only 2 of these interventions included more than 37 participants [ 32 , 36 ]. The interventions ranged from 6 to 24 weeks in duration and included anywhere from 1 to 4 hours per week (9-34 minutes per day on average) of prescribed exercise. Six of the 8 exercise programs included various forms of moderate-to-vigorous physical activity as explained in the methods sections of the papers.
The results from these intervention studies were mixed. The 5 studies that were based on aerobic exercise alone observed significant improvements in at least one lipid/lipoprotein variable. The summary effects size measures (95% confidence interval) for the aerobic exercise interventions were -3.03 (-3.22, -2.84) for triglycerides and 0.26 (0.03, 0.49) for HDL-cholesterol. The interventions that were based on resistance training [ 33 ] and circuit training [ 34 ] reported small and/or insignificant changes for all of the lipid/lipoprotein variables examined, and the effect sizes within these studies tended to be quite small (eg, <0.5). Not surprisingly, the interventions that produced significant changes were also based on the studies that employed the largest sample sizes. This suggests that many of the studies were underpowered.
Due to the design of these interventions (eg, only one dose of exercise prescribed in a given study), the nature of the dose-response relation between exercise and blood lipids in children and youth remains unclear. Furthermore, the interventions that produced favorable effects on blood lipids did not tend to prescribe higher volumes or intensities of exercise by comparison to the interventions that did not produce significant changes. The favorable interventions were, however, based on 'high risk' participants, implying that low volumes of moderate-to-vigorous exercise may be beneficial for youngsters at the greatest risk.
The effects of age and sex have not been adequately addressed in the existing literature. Thus, conclusions cannot be made on the moderating effects of these demographic characteristics on the relation between physical activity and blood lipids in school-aged children and youth.
High blood pressure
A total of 11 articles examining high blood pressure met the systematic review inclusion criteria. Three of these studies were observational in nature (2 cross-sectional, one prospective cohort) (Table 5) [Additional file 5 ] [ 28 , 37 , 38 ]. Of these 3 studies, one relied on self-reported measures of physical activity [ 37 ] and the remaining two measured cardiorespiratory fitness [ 28 , 38 ]. Within all 3 observational studies the relations between physical activity or fitness with hypertension were weak in magnitude (e.g., odds ratios <1.5), and in one case [ 28 ] was insignificant. Only one study examined more than 2 levels of physical activity or fitness (e.g., compared risk estimates across at least 3 groups), and thus was able to provide some insight into the dose-response relation. Within that study only participants within the least fit quartile were more likely to have hypertension relative to participants in the most fit quartile, a finding that was consistent in boys and girls [ 38 ].
Eight experimental studies, 4 of which were RCTs, examined the influence of exercise interventions on changes in blood pressure (Table 6) [Additional file 6 ] [ 29 , 33 , 34 , 39 – 43 ]. Most of these studies were limited to children and youth with high blood pressure [ 39 – 42 ] or obesity [ 29 , 34 ]. The sample sizes were quite small; only one of these studies included more than 37 participants [ 42 ]. The interventions ranged from 4 to 25 weeks in duration. With one exception [ 43 ], the interventions included between 60 to 180 minutes/week of prescribed exercise. This equates to 9 to 30 minutes/day when averaged over a week.
Despite the small sample sizes, the results from these intervention studies were positive with reports of significant reductions in systolic blood pressure in response to aerobic exercise training, with effect sizes that all tended to be large (>0.80) [ 29 , 39 , 41 – 43 ]. Two of the aerobic based interventions also reported significant reductions (~6% to 11%) in diastolic blood pressure [ 34 , 39 ]. The summary effect size measures for the aerobic exercise interventions were -1.39 (-2.53, -0.24) for systolic blood pressure and -0.39 (-1.72, 0.93) for diastolic blood pressure. Unlike the aerobic-based exercise programs, only two of the four studies that employed other training modalities, such as resistance exercise, reported a significant effect on blood pressure [ 33 , 40 ], with small to modest effect sizes being observed. The summary effect size measures for the non-aerobic exercise interventions were -0.61 (-2.27, 1.05) for systolic blood pressure and -0.51 (-2.18, 1.06) for diastolic blood pressure.
Because the aerobic exercise intervention studies prescribed similar volumes and intensities of exercise, and because they found comparable reductions in blood pressure, the effects of the volume and intensity (moderate vs. vigorous) of exercise on blood pressure remain unclear. Due to limited variations in the age of the participants in these studies, the effects of age on the relation between exercise and blood pressure remains unclear. Most of the studies included both males and females, suggesting that aerobic exercise is effective at controlling blood pressure within box sexes.
Metabolic syndrome
The metabolic syndrome has received considerable research attention in recent years in both adults and youngsters. Sixteen articles examining the metabolic syndrome met the inclusion criteria. The metabolic syndrome components (e.g., abdominal obesity, triglycerides, insulin, HDL-cholesterol, inflammatory markers, etc.) and criteria (e.g., cut-points used to define high-risk values) employed in these studies varied considerably. Eight of the 17 identified studies were observational in nature (7 cross-sectional, 1 prospective), as summarized in Table 7 [Additional file 7 ] [ 28 , 44 – 51 ]. Many of these observational studies examined large and heterogeneous samples of participants, suggesting that the findings are quite generalizable to the general population. Of the 3 cross-sectional studies that employed self-reported measures of physical activity, the reported relations with the metabolic syndrome were either weak or modest in strength, and all were non-significant [ 45 , 48 , 49 ]. The summary odds ratio for the least active group relative to the most active group in these 3 studies was 1.68 (95% confidence interval: 1.22, 2.31). By comparison, the study that used accelerometers to measure physical activity in an objective manner [ 51 ] and the 4 studies that used direct measures of cardiorespiratory fitness [ 28 , 46 , 47 , 50 ] all reported strong and significant relations with the metabolic syndrome. The summary odds ratio for the least fit group relative to the most fit group in the 4 studies that measured fitness was 6.79 (95% confidence interval: 5.11, 9.03). Further examination of these later studies revealed clear dose-response relations; however, the nature (e.g., linear or curvilinear) of the dose-response relation is unclear. In addition, comparison of the risk estimates in males and females suggests that the relation between physical activity and fitness with the metabolic syndrome is stronger in males. The influence of age on these relations remains uncertain.
Eight experimental studies, 5 of which were RCTs, examined the effect of exercise interventions on changes in markers of the metabolic syndrome, primarily in the form of fasting insulin and insulin resistance (Table 8) [Additional file 8 ] [ 32 – 34 , 36 , 52 – 55 ]. All but one of these studies was conducted in an overweight/obese sample [ 33 ]. The number of participants included in these studies was modest, with all but a single study being limited to 52 participants or less [ 36 ]. The exercise interventions ranged from 6 to 40 weeks in duration and included anywhere from 80 to 200 minutes per week (10-30 minutes per average day) of prescribed exercise. About half of the exercise programs were aerobic in nature.
The results from these 8 studies were mixed (Table 8). All of the 4 interventions that focused on aerobic exercise observed significant improvements in at least one of the insulin variables examined. Conversely, only one of the four interventions that employed resistance or circuit training observed any meaningful improvements [ 54 ]. The summary effect size measures (95% confidence interval) for fasting insulin in the aerobic and resistance exercise interventions were -0.60 (-1.71, 0.50) and -0.31 (-0.82, 0.19), respectively. No intervention studies systematically considered the influence of the dose or intensity of exercise, or sex and age effects, on markers of the metabolic syndrome. More research is needed to address these issues.
Overweight and obesity
The relation between physical activity and fitness with obesity in school-aged children and youth has been extensively studied. A total of 31 observational studies (24 cross-sectional, 3 prospective cohort, 2 case-control, 1 mixed) were retrieved that met the appropriate inclusion criteria, as summarized in Table 9 [Additional file 9 ] [ 56 – 86 ]. Overweight and obesity were classified using age- and gender-specific body mass index (BMI) criteria (e.g., BMI z-scores) in the majority of these observational studies. The majority of these studies assessed physical activity or sport participation using self- or parental-reported tools. These studies tended to report weak to modest relationships between physical activity and overweight/obesity, with many risk estimates being non-significant. Of the 25 available data points, the median odds ratio for overweight/obesity in the least active group relative to the most active group was 1.33. It is noteworthy that the studies that assessed moderate-to-vigorous intensity physical activities alone were more consistently and strongly related to obesity than the studies that included low intensity activities within the physical activity measure.
Four studies were identified that employed objective measures of physical activity, including one study that used pedometers [ 73 ] and 3 studies that used accelerometers [ 59 , 67 , 83 ]. These studies tended to report significant relations between physical activity with overweight/obesity that were strong in magnitude. Of the 8 available data points for cross-sectional findings, the median odds ratio was 3.79. An additional 4 studies measured the relation between cardiorespiratory fitness and obesity [ 75 , 76 , 82 ]. All of these studies reported significant relations between physical activity and fitness with overweight/obesity that were modest to strong in magnitude.
Several of the observational studies examining overweight and obesity presented analyses that were stratified by sex [ 56 – 58 , 60 , 64 , 67 , 71 , 73 – 75 , 77 , 79 , 81 ]. Although sex differences were rarely tested for using the appropriate statistical techniques, visual inspection of the risk estimates provided suggests that in 12 of the 14 studies the associations between physical activity and fitness with obesity were stronger in males than in females.
Many of the observational studies presented their results in a manner that permitted the dose-response relations with obesity to be examined [ 57 , 59 , 61 , 62 , 64 , 65 , 69 , 71 , 73 , 74 , 79 , 80 , 82 , 84 ]. From these studies it is apparent that a dose-response relation between physical activity and obesity exists. However, the pattern of this dose-response relation is unclear as some studies observed linear patterns and others observed curvilinear patterns.
In addition to the observational studies discussed above, 24 intervention studies, 17 of which were RCTs, examining changes in obesity measures were included in the systematic review (Table 10) [Additional file 10 ] [ 29 , 32 , 34 – 36 , 39 , 42 , 43 , 52 – 55 , 87 – 98 ]. It is important to note that in many of these studies the primary aim of the intervention was to improve other health measures (e.g., blood lipids, insulin resistance, and bone density) and not obesity measures per se . These studies examined several different measures of total (% fat, BMI, weight) and abdominal (waist circumference, trunk fat, visceral fat) adiposity. The studies ranged in length from 4 weeks to 2 years, with most being 4 to 6 months in duration. The amounts of exercise prescribed typically ranged from 2 to 3.5 hours per week, which averages out to 17 to 30 minutes per day. Half of the studies were limited to overweight and obese participants.
About 50% of the exercise interventions that were aerobic in nature observed significant changes in measures of BMI, total fat, and/or abdominal fat in response to training. Only 3 of the 17 studies that employed other training modalities (resistance training, circuit training, pilates, jumping exercises) observed significant improvements in measures of total fat, abdominal fat, or BMI in response to training. The effect sizes, even for the studies that found significant improvements, tended to be small (<0.50). For the interventions that were based on aerobic exercise, the summary effect size measures were -0.40 (-1.10, 0.31) for % body fat and -0.07 (-0.89, 0.75) for BMI. For the resistance exercise intervention, the summary effect size calculation for % body fat was -0.19 (-1.55, 1.18).
Variations in the effects of age, sex, and exercise dose on changes in obesity measures in response to exercise training have not been systematically addressed in the literature. Thus, no conclusions can be drawn on the potential moderating effects of these variables.
Bone mineral density
Many observational studies have examined the relation between physical activity and continuous measures of bone mineral density such as bone mineral content values in grams, bone density values in g/cm 2 , and cortical bone area measures in cm 2 (see review [ 99 ]). However, no observational studies in the literature search met the systematic review criteria of predicting a low bone mineral density as a dichotomous outcome.
As summarized in Table 11 [Additional file 11 ], a total of 11 experimental studies examining changes in bone mineral density in response to exercise training were retrieved in the systematic review [ 55 , 88 – 94 , 100 – 103 ]. Two of these studies presented identical data on the same group of participants, and were therefore presented as a single study in the table [ 101 , 102 ]. The physical activity programs employed in these interventions typically consisted of moderate-to-high strain anaerobic activities such as impact resistance training, high impact weight bearing, and jumping. These programs were performed anywhere from 3 to 60 minutes in length on at least 2 or 3 days of the week, and lasted from a few months to 2 years in duration.
The results from these studies, although not undisputed, indicate that as little as 10 minutes of moderate-to-high impact activities performed on as little as 2 or 3 days of the week can have a modest effect on bone mineral density when combined with more general weight bearing aerobic activities that are also beneficial for cardiovascular risk factors and obesity prevention (e.g., jogging, play, etc.).
Only 6 studies on depression and related symptoms met the inclusion criteria. Table 12 [Additional file 12 ] outlines the 3 observational studies [ 104 – 106 ]. These were all cross-sectional in design, used self-reported measures of physical activity, and reported small and insignificant [ 104 , 106 ] or modest [ 105 ] relations between physical activity and depression. Interestingly, within the later study the relation between physical activity and depression were more evident at a moderate intensity of physical activity than at a vigorous intensity of physical activity [ 105 ].
The 3 experimental studies that examined changes in depression [ 107 – 109 ], all of which were RCTs based on aerobic exercise, are outlined in Table 13 [Additional file 13 ]. The volume of exercise prescribed in these studies was very modest (60 to 90 minutes per week). All three of these studies observed significant improvements in at least one depressive symptom measure in response to 8 to 12 week exercise programs. The effect sizes were small to modest in these studies, with very broad 95% confidence intervals. One of the studies included both high intensity and moderate intensity exercise programs, and only the high intensity program resulted in significant improvements in depression scores in comparison to the control group, which performed flexibility exercises [ 108 ].
Injuries are a leading cause of disability and mortality in young people. It has been reported that approximately 50% of medically treated injuries within 6 th to 10 th grade Canadian youth occur during physical activity [ 110 ]. Thus, it is not surprising that there is an extensive literature on physical activity and injuries in the pediatric population (see review [ 111 ]). However, most of the published information is limited to groups of participants that have all been injured or groups of participants comprised entirely of athletes (eg, football players, ballet dancers).
Only 3 articles examining injury met the inclusion criteria for this systematic review [ 112 – 114 ]. These studies were all cross-sectional in nature and relied on self- or parental-reported measures of physical activity and sports participation (Table 14) [Additional file 14 ]. These studies examined medically treated injuries; however, limited or no information on the severity of and long-term recovery from these injuries was presented. All 3 of the studies reported higher rates of injury in physically active children and youth compared with inactive children and youth. Furthermore, within all 3 of the papers there was clear evidence of a dose-response relation between physical activity participation and the likelihood of injury. That is, as the physical activity level increased, the likelihood of injury increased in a graded fashion. One study assessed vigorous sports, and within that study the risk estimates for injury within the most active group would be considered high [ 114 ]. Conversely the risk estimates for injury were modest within the 2 studies that measured moderate-to-vigorous intensity activities [ 112 , 113 ]. The quality of the evidence for the injury outcome, which is based on cross-sectional studies, is limited as cross-sectional research only provides a low level of evidence. Follow-up (incidence) studies that also take into consideration the volume of sports participation would provide a more powerful level of evidence.
Quality assessment of RCTs
The RCTs that are listed within the summary tables contained several significant limitations. The study samples were small, and non-representative. Although few of the studies addressed the issue of statistical power, the lack of power was clearly an issue. Specifically, for a number of the health outcomes, the RCTs in which significant findings were observed were also the RCTs with the largest sample sizes. Almost without exception, the RCTs included in the systematic review did not report adverse events for the physical activity interventions (e.g., injuries), provided little or no detail on the drop-outs, and did not perform intent-to-treat analyses. Given the consistency of these limitations across studies, Level 2 was the highest level that could be assigned to any of the recommendations.
Recommendations based on systematic review
Recommendation #1
Children and youth 5-17 years of age should accumulate an average of at least 60 minutes per day and up to several hours of at least moderate intensity physical activity. Some of the health benefits can be achieved through an average of 30 minutes per day. [Level 2, Grade A]
There is strong and consistent evidence based on experimental studies for several health outcomes that participating in as little as 2 or 3 hours of moderate-to-vigorously intense physical activity per week is associated with health benefits. Evidence from observational studies also demonstrates dose-response relations between physical activity and health, with differences in health risk between the least active (or fit) and the second least active (of fit) groups. Thus, it would seem appropriate to set minimal physical activity targets that reflect a low level of physical activity (see Recommendation #1). Furthermore, the current recommendation of 90 minutes more per day (Canadian) or 60 minutes per day (US, UK, Australian) may be quite intimidating, particularly for children and youth who are very inactive. From a behaviour modification perspective, having a target that seems out of reach may actually undermine physical activity participation [ 115 ].
That being said, with the exception of injuries, the dose-response evidence from observational studies for several health outcomes suggests that more physical activity will be better, and that additional health benefits can still be achieved at the higher end of the physical activity spectrum. Therefore, it would also seem appropriate to set higher physical activity targets (60 minutes and up to several hours) that would elicit more pronounced health benefits for those children and youth who are already somewhat active (see Recommendation #1). This approach is consistent with recommendations made by the U.S. National Association for Sports and Physical Education[ 116 ] and the Australia Department of Health and Ageing [ 117 ], both of whom have recommended that children and youth participate in at least 60 minutes, and up to several hours, of moderate to vigorous intensity physical activity every day.
This type of dual message provided in Recommendation #1 will hopefully encourage children and youth who are very inactive to engage in at least a modest amount of physical activity, while at the same time encourage moderately active children and youth to achieve even greater benefits by becoming more active. The minimal and optimal doses of physical activity required for good health in children and youth remain unclear, and more carefully conducted dose-responses studies are warranted in the pediatric age range.
Previous physical activity recommendations and guidelines for school-aged children and youth indicate that a high volume of physical activity needs to be performed everyday. The need for children and youth to engage in physical activity on a daily basis to maintain good health was not supported by the evidence reviewed here. In other words, it is unknown as to whether a child who accumulates 7 hours of activity over the week, with one hour being performed on each day, would have any greater health benefits than a child who accumulates 7 hours of activity over the week, with different amounts of activity being performed each day (including some days with no activity). Thus, the recommendation made in this systematic review calls for an "average" of at least 60 minutes per day instead of at least 60 minutes everyday. Future studies need to address whether a "days per week" recommendation is warranted. In addition, future studies within children and youth should consider whether the daily physical activity needs to be accumulated in bouts of at least a few minutes in duration (eg, 5 or 10 minutes). Most children accumulate the majority of their physical activity in a very sporadic manner (eg, a couple of minutes here and there), and new evidence suggests that this sporadic pattern of activity may not be as beneficial as bouts of activity that last at least 5 minutes in length [ 118 ].
Given the positive effect of physical activity on 6 of the 7 health outcomes examined, including observations from several large and diverse samples, this Recommendation was assigned a Grade A.
Recommendation #2
More vigorous intensity activities should be incorporated or added when possible, including activities that strengthen muscle and bone. [Level 3, Grade B] .
Moderate intensity activity in children and youth has been defined in a variety of ways, depending on the method chosen to measure physical activity. The lower threshold of moderate intensity activity is usually defined as 4 METS (4 × resting metabolic rate), although it is not uncommon for investigators to use 3 METS. In general, the lower threshold of vigorous intensity activity is usually defined as 7 METS (7 × resting metabolic rate) in children.
The majority of observational studies have focused on measuring moderate-to-vigorous intensity physical activity. Furthermore, the relations between overall physical activity (including low intensity activities) and obesity do not appear to be as strong or consistent as the relations between moderate-to-vigorous intensity activity and obesity. In addition, the intervention studies included within this systematic review almost exclusively prescribed physical activity of at least a moderate intensity. Thus, while it is clear that moderate and vigorous intensity activities are associated with many health benefits, the same is not true for low intensity activity. Therefore, Recommendation #1 indicates that the physical activity should be of at least a moderate intensity. More consideration on the impact of low intensity activities on health should be given in future studies.
The next question to address is whether vigorous intensity activities provide benefits above and beyond that of moderate intensity activities. Regrettably, few studies have systematically addressed this question. The available information suggests that vigorous intensity activities provide additional health benefits beyond modest intensity activities. Furthermore, many of the experimental studies that observed significant changes in the health variables examined prescribed exercise that would fall within the vigorous intensity or upper-end of the moderate intensity range. Recommendation #2, therefore, suggests that vigorous intensity activities should be included when possible. This recommendation was assigned a lower level of evidence (Level 3) because of the limited amount of evidence and the inconsistency in the evidence that is available. This recommendation was given a lower grade (Grade C) because of the potential increase in injury risk associated with more vigorous intensity activities and sports. However, the injury data is weak and future studies, particularly intervention studies, should examine and report on injuries associated with physical activity in children.
Recommendation #3
Aerobic activities should make up the majority of the physical activity. Muscle and bone strengthening activities should be incorporated on at least 3 days of the week. [Level 2, Grade A] .
Many of the health outcomes examined, particularly obesity and the cardiometabolic health measures, responded almost exclusively to aerobic exercise interventions. It is also likely that most of the activity that was captured in the observational studies was aerobic in nature. Recommendation #3 therefore suggests that physical activity should focus on aerobic activities. However, bone health was more favorably affected by modest amounts of resistance training and other high-impact activities (jumping) that were performed on at least 2 or 3 days of the week. Thus, this recommendation indicates that a small amount of bone strengthening activities should be incorporated.
Limitations
This systematic review has several limitations, many of which related to practical issues around conducting the study (e.g., budgetary, human resource, and time constraints). First, because we did not include unpublished studies and studies that were published in a language other than English, and because we did not perform an extensive cross-referencing of the references lists from the papers that were retrieved in the electronic databases, several relevant papers may be been excluded. Second, the review was limited to 7 health outcomes and did not include several other outcomes that may be relevant for children and youth such as academic performance, emerging cardiometabolic risk factors (e.g., endothelial function, inflammatory markers), risky and aggressive behaviours (e.g., substance use and abuse, bullying and fighting), and measures of mental health and well-being outside of depression. Third, a large percentage of observational studies in the area were excluded because they did not report their findings in a dichotomous manner. Together, these limitations may have biased the Results and Recommendations that were made. Nonetheless, despite these limitations and the differences in methodology employed, the recommendations made here are remarkably comparable to the recommendations for children and youth that were part of the recently completed "Physical Activity Guidelines for Americans" project [ 21 ]. The reader is referred to the Expert Panel report for a more comprehensive discussion of the limitations of this systematic review [ 13 ].
In summary, the findings of this systematic review confirm that physical activity is associated with numerous health benefits in school-aged children and youth. The dose-response relations between physical activity and health that were observed in several observational studies suggest that the more physical activity, the greater the health benefit. However, the results from several experimental studies suggested that even modest amounts of physical activity can have tremendous health benefits in high-risk youngsters (e.g., obese, high blood pressure). To achieve substantive health benefits, the physical activity should be of at least a moderate intensity, and it should be recognized that vigorous intensity activities may provide an even greater benefit. Aerobic-based activities that stress the cardiovascular and respiratory systems have the greatest health benefit, other than for bone health, in which case high-impact weight bearing activities are required.
Health Canada, Canadian Society for Exercise Physiology: Canada's Physical Activity Guide for Youth. 2002, Ottawa: Minister of Public Works and Government Services Canada
Google Scholar
Health Canada, Canadian Society for Exercise Physiology: Canada's Physical Activity Guideline for Children. 2002, Ottawa: Minister of Public Works and Government Services Canada
Janssen I: Physical activity guidelines for children and youth. Can J Public Health. 2007, 98 (Suppl 2): S109-121.
Twisk JW: Physical activity guidelines for children and adolescents: a critical review. Sports Med. 2001, 31 (8): 617-627. 10.2165/00007256-200131080-00006.
CAS Google Scholar
Tolfrey K, Jones AM, Campbell IG: The effect of aerobic exercise training on the lipid-lipoprotein profile of children and adolescents. Sports Med. 2000, 29 (2): 99-112. 10.2165/00007256-200029020-00003.
Kelley GA, Kelley KS: Exercise and resting blood pressure in children and adolescents: a meta-analysis. Ped Exerc Sci. 2003, 15: 83-97.
Reilly JJ, McDowell ZC: Physical activity interventions in the prevention and treatment of paediatric obesity: systematic review and critical appraisal. Proc Nutr Soc. 2003, 62 (3): 611-619. 10.1079/PNS2003276.
Etnier JL, Nowell PM, Landers DM, Sibley BA: A meta-regression to examine the relationship between aerobic fitness and cognitive performance. Brain Res Brain Res Rev. 2006, 52 (1): 119-130. 10.1016/j.brainresrev.2006.01.002.
Cook DJ, Mulrow CD, Haynes RB: Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med. 1997, 126 (5): 376-380.
Warburton DER, Charlesworth S, Ivey A, Nettlefold L, Bredin SSD: A systematic review of the evidence for Canada's Physical Activity Guidelines for Adults. Int J Behav Nutr Phys Act. 2010, 7: 39.
Paterson DH, Warburton DER: Physical activity and functional limitations in older adults: a systematic review related to Canada's Physical Activity Guidelines. Int J Behav Nutr Phys Act. 2010, 7: 38.
Tremblay MS, Kho ME, Tricco AC, Duggan M: Process description and evaluation of Canadian Physical Activity Guidelines development. Int J Behav Nutr Phys Act. 2010, 7: 42.
Kesaniemi A, Riddoch CJ, Reeder B, Blair SN, Sorensen TIA: Advancing the future of physical activity guidelines in Canada: an independent expert panel interpretation of the evidence. Int J Behav Nutr Phys Act. 2010, 7: 41.
Health Canada, Canadian Society for Exercise Physiology: Family Guide to Physical Activity for Youth 10-14 Years of Age. 2002, Minister of Public Works and Government Services Canada
Health Canada, Canadian Society for Exercise Physiology: Family Guide to Physical Activity for Children 6-9 Years of Age. 2002, Minister of Public Works and Government Services Canada
Health Canada, Canadian Society for Exercise Physiology: Teacher's Guide to Physical Activity for Youth 10-14 Years of Age. 2002, Minister of Public Works and Government Services Canada
Health Canada, Canadian Society for Exercise Physiology: Teacher's Guide to Physical Activity for Children 6-9 Years of Age. 2002, Minister of Public Works and Government Services Canada
Health Canada, Canadian Society for Exercise Physiology: Gotta Move! Magazine for Children 6-9 Years of Age. 2002, Minister of Public Works and Government Services Canada
Health Canada, Canadian Society for Exercise Physiology: Let's Get Active! Magazine for Youth 10-14 Years of Age of Public Works and Government Services Canada. 2002
Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, Hergenroeder AC, Must A, Nixon PA, Pivarnik JM, Rowland T, Trost S, Trudeau F: Evidence based physical activity for school-age youth. J Pediatr. 2005, 146 (6): 732-737. 10.1016/j.jpeds.2005.01.055.
Physical Activity Guidelines Advisory Committee: Physical Activity Guidelines Advisory Committee Report, 2008. 2008, Washington, DC: U.S. Department of Health and Human Services
Baquet G, van Praagh E, Berthoin S: Endurance training and aerobic fitness in young people. Sports Med. 2003, 33 (15): 1127-1143. 10.2165/00007256-200333150-00004.
Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E: 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ. 2007, 176 (8): S1-13.
Downs SH, Black N: The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998, 52: 377-384. 10.1136/jech.52.6.377.
Oleckno WA: Essential Epidemiology: Principles and Applications. 2002, Long Grove, IL: Waveland Press
Cohen J: Statistical power calculations for the behavioral sciences. 1988, Hillsdale: Lawrence Erlbaum Associates, 2
Petitti DB: Meta-Analysis, Decision Analysis, and Cost-Effective Analysis. 1994, New York, NY: Oxford University Press
Carnethon MR, Gulati M, Greenland P: Prevalence and cardiovascular disease correlates of low cardiorespiratory fitness in adolescents and adults. JAMA. 2005, 294 (23): 2981-2988. 10.1001/jama.294.23.2981.
Kahle EB, Zipf WB, Lamb DR, Horswill CA, Ward KM: Association between mild, routine exercise and improved insulin dynamics and glucose control in obese adolescents. Int J Sports Med. 1996, 17 (1): 1-6. 10.1055/s-2007-972799.
Hardin DS, Hebert JD, Bayden T, Dehart M, Mazur L: Treatment of childhood syndrome X. Pediatrics. 1997, 100 (2): E5-10.1542/peds.100.2.e5.
Stergioulas A, Tripolitsioti A, Messinis D, Bouloukos A, Nounopoulos C: The effects of endurance training on selected coronary risk factors in children. Acta Paediatr. 1998, 87 (4): 401-404. 10.1080/08035259850156986.
Ferguson MA, Gutin B, Le NA, Karp W, Litaker M, Humphries M, Okuyama T, Riggs S, Owens S: Effects of exercise training and its cessation on components of the insulin resistance syndrome in obese children. Int J Obes Relat Metab Disord. 1999, 23 (8): 889-895. 10.1038/sj.ijo.0800968.
Lau PWC, CW Y, Lee A, Sung RYT: The physiological and psychological effects of resistance training on Chinese obese adolescents. Journal of Exercise Science and Fitness. 2004, 2 (2): 115-120.
Bell LM, Watts K, Siafarikas A, Thompson A, Ratnam N, Bulsara M, Finn J, O'Driscoll G, Green DJ, Jones TW, Davis EA: Exercise alone reduces insulin resistance in obese children independently of changes in body composition. J Clin Endocrinol Metab. 2007, 92 (11): 4230-4235. 10.1210/jc.2007-0779.
Heyman E, Toutain C, Delamarche P, Berthon P, Briard D, Youssef H, Dekerdanet M, Gratas-Delamarche A: Exercise training and cardiovascular risk factors in type 1 diabetic adolescent girls. Pediatr Exerc Sci. 2007, 19 (4): 408-419.
Meyer AA, Kundt G, Lenschow U, Schuff-Werner P, Kienast W: Improvement of early vascular changes and cardiovascular risk factors in obese children after a six-month exercise program. J Am Coll Cardiol. 2006, 48 (9): 1865-1870. 10.1016/j.jacc.2006.07.035.
Dasgupta K, O'Loughlin J, Chen S, Karp I, Paradis G, Tremblay J, Hamet P, Pilote L: Emergence of sex differences in prevalence of high systolic blood pressure: analysis of a longitudinal adolescent cohort. Circulation. 2006, 114 (24): 2663-2670. 10.1161/CIRCULATIONAHA.106.624536.
Nielsen GA, Andersen LB: The association between high blood pressure, physical fitness, and body mass index in adolescents. Prev Med. 2003, 36 (2): 229-234. 10.1016/S0091-7435(02)00017-8.
Hagberg JM, Goldring D, Ehsani AA, Heath GW, Hernandez A, Schechtman K, Holloszy JO: Effect of exercise training on the blood pressure and hemodynamic features of hypertensive adolescents. Am J Cardiol. 1983, 52 (7): 763-768. 10.1016/0002-9149(83)90412-5.
Hagberg JM, Ehsani AA, Goldring D, Hernandez A, Sinacore DR, Holloszy JO: Effect of weight training on blood pressure and hemodynamics in hypertensive adolescents. J Pediatr. 1984, 104 (1): 147-151. 10.1016/S0022-3476(84)80615-0.
Danforth JS, Allen KD, Fitterling JM, Danforth JA, Farrar D, Brown M, Drabman RS: Exercise as a treatment for hypertension in low-socioeconomic-status black children. J Consult Clin Psychol. 1990, 58 (2): 237-239. 10.1037/0022-006X.58.2.237.
Ewart CK, Young DR, Hagberg JM: Effects of school-based aerobic exercise on blood pressure in adolescent girls at risk for hypertension. Am J Public Health. 1998, 88 (6): 949-951. 10.2105/AJPH.88.6.949.
Jago R, Jonker ML, Missaghian M, Baranowski T: Effect of 4 weeks of Pilates on the body composition of young girls. Prev Med. 2006, 42 (3): 177-180. 10.1016/j.ypmed.2005.11.010.
Yin Z, Davis CL, Moore JB, Treiber FA: Physical activity buffers the effects of chronic stress on adiposity in youth. Ann Behav Med. 2005, 29 (1): 29-36. 10.1207/s15324796abm2901_5.
Ramirez-Lopez G, Gonzalez-Villalpando C, Sanchez-Corona J, Salmeron-Castro J, Gonzalez-Ortiz M, Celis-de la Rosa A, Valles-Sanchez V: Weight, physical activity, and smoking as determinants of insulinemia in adolescents. Arch Med Res. 2001, 32 (3): 208-213. 10.1016/S0188-4409(01)00270-3.
Andersen LB, Hasselstrom H, Gronfeldt V, Hansen SE, Karsten F: The relationship between physical fitness and clustered risk, and tracking of clustered risk from adolescence to young adulthood: eight years follow-up in the Danish Youth and Sport Study. Int J Behav Nutr Phys Act. 2004, 1 (1): 6-10.1186/1479-5868-1-6.
Eiberg A, Hasselstrom H, Gronfeldt V, Froberg K, Cooper A, Andersen LB: Physical fitness as a predictor of cardiovascular disease risk factors in 6- to 7-year-old Danish children: The Copenhagen school-child intervention study. Pediatr Exerc Sci. 2005, 17: 161-170.
Hasselstrom H, Karlsson KM, Hansen SE, Gronfeldt V, Froberg K, Andersen LB: Peripheral bone mineral density and different intensities of physical activity in children 6-8 years old: the Copenhagen School Child Intervention study. Calcif Tissue Int. 2007, 80 (1): 31-38. 10.1007/s00223-006-0137-9.
Kelishadi R, Razaghi EM, Gouya MM, Ardalan G, Gheiratmand R, Delavari A, Motaghian M, Ziaee V, Siadat ZD, Majdzadeh R, Heshmat R, Barekati H, Arabi MS, Heidarzadeh A, Shariatinejad K: Association of physical activity and the metabolic syndrome in children and adolescents: CASPIAN Study. Horm Res. 2007, 67 (1): 46-52. 10.1159/000096121.
Anderssen SA, Cooper AR, Riddoch C, Sardinha LB, Harro M, Brage S, Andersen LB: Low cardiorespiratory fitness is a strong predictor for clustering of cardiovascular disease risk factors in children independent of country, age and sex. Eur J Cardiovasc Prev Rehabil. 2007, 14 (4): 526-531. 10.1097/HJR.0b013e328011efc1.
Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, Anderssen SA: Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study). Lancet. 2006, 368 (9532): 299-304. 10.1016/S0140-6736(06)69075-2.
Carrel AL, Clark RR, Peterson SE, Nemeth BA, Sullivan J, Allen DB: Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: a randomized, controlled study. Arch Pediatr Adolesc Med. 2005, 159 (10): 963-968. 10.1001/archpedi.159.10.963.
Nassis GP, Papantakou K, Skenderi K, Triandafillopoulou M, Kavouras SA, Yannakoulia M, Chrousos GP, Sidossis LS: Aerobic exercise training improves insulin sensitivity without changes in body weight, body fat, adiponectin, and inflammatory markers in overweight and obese girls. Metabolism. 2005, 54 (11): 1472-1479. 10.1016/j.metabol.2005.05.013.
Shaibi GQ, Cruz ML, Ball GD, Weigensberg MJ, Salem GJ, Crespo NC, Goran MI: Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Med Sci Sports Exerc. 2006, 38 (7): 1208-1215. 10.1249/01.mss.0000227304.88406.0f.
Treuth MS, Hunter GR, Figueroa-Colon R, Goran MI: Effects of strength training on intra-abdominal adipose tissue in obese prepubertal girls. Med Sci Sports Exerc. 1998, 30 (12): 1738-1743. 10.1097/00005768-199812000-00013.
Gordon-Larsen P, Adair LS, Popkin BM: Ethnic differences in physical activity and inactivity patterns and overweight status. Obes Res. 2002, 10 (3): 141-149. 10.1038/oby.2002.23.
Eisenmann JC, Bartee RT, Wang MQ: Physical activity, TV viewing, and weight in U.S. youth: 1999 Youth Risk Behavior Survey. Obes Res. 2002, 10 (5): 379-385. 10.1038/oby.2002.52.
Kim J, Must A, Fitzmaurice GM, Gillman MW, Chomitz V, Kramer E, McGowan R, Peterson KE: Relationship of physical fitness to prevalence and incidence of overweight among schoolchildren. Obes Res. 2005, 13 (7): 1246-1254. 10.1038/oby.2005.148.
Dencker M, Thorsson O, Karlsson MK, Linden C, Eiberg S, Wollmer P, Andersen LB: Daily physical activity related to body fat in children aged 8-11 years. J Pediatr. 2006, 149 (1): 38-42. 10.1016/j.jpeds.2006.02.002.
Rosenberg DE, Sallis JF, Conway TL, Cain KL, McKenzie TL: Active transportation to school over 2 years in relation to weight status and physical activity. Obesity (Silver Spring). 2006, 14 (10): 1771-1776. 10.1038/oby.2006.204.
Laxmaiah A, Nagalla B, Vijayaraghavan K, Nair M: Factors affecting prevalence of overweight among 12- to 17-year-old urban adolescents in Hyderabad, India. Obesity (Silver Spring). 2007, 15 (6): 1384-1390. 10.1038/oby.2007.165.
Hernandez B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra-Cabrera S: Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico city. Int J Obes Relat Metab Disord. 1999, 23 (8): 845-854. 10.1038/sj.ijo.0800962.
Tremblay MS, Willms JD: Is the Canadian childhood obesity epidemic related to physical inactivity?. Int J Obes Relat Metab Disord. 2003, 27 (9): 1100-1105. 10.1038/sj.ijo.0802376.
Janssen I, Katzmarzyk PT, Boyce WF, King MA, Pickett W: Overweight and obesity in Canadian adolescents and their associations with dietary habits and physical activity patterns. J Adolesc Health. 2004, 35 (5): 360-367.
Veugelers PJ, Fitzgerald AL: Prevalence of and risk factors for childhood overweight and obesity. CMAJ. 2005, 173 (6): 607-613.
Ha A, Bae S, Urrutia-Rijas X, Singh KP: Eating and physical activity pracitces in risk of overweight and overweight children. Nutrition Research. 2005, 25: 905-915. 10.1016/j.nutres.2005.09.010.
Ness AR, Leary SD, Mattocks C, Blair SN, Reilly JJ, Wells J, Ingle S, Tilling K, Smith GD, Riddoch C: Objectively measured physical activity and fat mass in a large cohort of children. PLoS Med. 2007, 4 (3): e97-10.1371/journal.pmed.0040097.
Li Y, Zhai F, Yang X, Schouten EG, Hu X, He Y, Luan D, Ma G: Determinants of childhood overweight and obesity in China. Br J Nutr. 2007, 97 (1): 210-215. 10.1017/S0007114507280559.
Smith BJ, Phongsavan P, Havea D, Halavatau V, Chey T: Body mass index, physical activity and dietary behaviours among adolescents in the Kingdom of Tonga. Public Health Nutr. 2007, 10 (2): 137-144. 10.1017/S1368980007226060.
Urrutia-Rojas X, Menchaca J: Prevalence of risk for type 2 diabetes in school children. J Sch Health. 2006, 76 (5): 189-194. 10.1111/j.1746-1561.2006.00093.x.
Guerra S, Teixeira-Pinto A, Ribeiro JC, Ascensao A, Magalhaes J, Andersen LB, Duarte JA, Mota J: Relationship between physical activity and obesity in children and adolescents. J Sports Med Phys Fitness. 2006, 46 (1): 79-83.
Ochoa MC, Moreno-Aliaga MJ, Martinez-Gonzalez MA, Martinez JA, Marti A: Predictor factors for childhood obesity in a Spanish case-control study. Nutrition. 2007, 23 (5): 379-384. 10.1016/j.nut.2007.02.004.
Eisenmann JC, Laurson KR, Wickel EE, Gentile D, Walsh D: Utility of pedometer step recommendations for predicting overweight in children. Int J Obes (Lond). 2007, 31 (7): 1179-1182. 10.1038/sj.ijo.0803553.
McMurray RG, Harrell JS, Deng S, Bradley CB, Cox LM, Bangdiwala SI: The influence of physical activity, socioeconomic status, and ethnicity on the weight status of adolescents. Obes Res. 2000, 8 (2): 130-139. 10.1038/oby.2000.14.
Burke V, Beilin LJ, Durkin K, Stritzke WG, Houghton S, Cameron CA: Television, computer use, physical activity, diet and fatness in Australian adolescents. Int J Pediatr Obes. 2006, 1 (4): 248-255. 10.1080/17477160600984975.
Psarra G, Nassis GP, Sidossis LS: Short-term predictors of abdominal obesity in children. Eur J Public Health. 2006, 16 (5): 520-525. 10.1093/eurpub/cki196.
Yang X, Telama R, Viikari J, Raitakari OT: Risk of obesity in relation to physical activity tracking from youth to adulthood. Med Sci Sports Exerc. 2006, 38 (5): 919-925. 10.1249/01.mss.0000218121.19703.f7.
Neutzling MB, Taddei JA, Gigante DP: Risk factors of obesity among Brazilian adolescents: a case-control study. Public Health Nutr. 2003, 6 (8): 743-749. 10.1079/PHN2003490.
O'Loughlin J, Paradis G, Renaud L, Meshefedjian G, Gray-Donald K: Prevalence and correlates of overweight among elementary schoolchildren in multiethnic, low income, inner-city neighbourhoods in Montreal, Canada. Ann Epidemiol. 1998, 8 (7): 422-432. 10.1016/S1047-2797(98)00009-X.
Fiore H, Travis S, Whalen A, Auinger P, Ryan S: Potentially protective factors associated with healthful body mass index in adolescents with obese and nonobese parents: a secondary data analysis of the third national health and nutrition examination survey, 1988-1994. J Am Diet Assoc. 2006, 106 (1): 55-64-64. 10.1016/j.jada.2005.09.046. quiz 76-59
te Velde SJ, De Bourdeaudhuij I, Thorsdottir I, Rasmussen M, Hagstromer M, Klepp KI, Brug J: Patterns in sedentary and exercise behaviors and associations with overweight in 9-14-year-old boys and girls--a cross-sectional study. BMC Public Health. 2007, 7: 16-10.1186/1471-2458-7-16.
Hanley AJ, Harris SB, Gittelsohn J, Wolever TM, Saksvig B, Zinman B: Overweight among children and adolescents in a Native Canadian community: prevalence and associated factors. Am J Clin Nutr. 2000, 71 (3): 693-700.
Stevens J, Murray DM, Baggett CD, Elder JP, Lohman TG, Lytle LA, Pate RR, Pratt CA, Treuth MS, Webber LS, Young DR: Objectively assessed associations between physical activity and body composition in middle-school girls: the Trial of Activity for Adolescent Girls. Am J Epidemiol. 2007, 166 (11): 1298-1305. 10.1093/aje/kwm202.
Kuriyan R, Bhat S, Thomas T, Vaz M, Kurpad AV: Television viewing and sleep are associated with overweight among urban and semi-urban South Indian children. Nutr J. 2007, 6: 25-10.1186/1475-2891-6-25.
Muecke L, Simons-Morton B, Huang IW, Parcel G: Is childhood obesity associated with high-fat foods and low physical activity?. J Sch Health. 1992, 62 (1): 19-23. 10.1111/j.1746-1561.1992.tb01213.x.
Delva J, O'Malley PM, Johnston LD: Health-related behaviors and overweight: a study of Latino adolescents in the United States of America. Rev Panam Salud Publica. 2007, 21 (1): 11-20. 10.1590/S1020-49892007000100002.
Jette M, Barry W, Pearlman L: The effects of an extracurricular physical activity program on obese adolescents. Canadian Journal of Public Health. 1977, 68 (1): 39-42.
Blimkie CJ, Rice S, Webber CE, Martin J, Levy D, Gordon CL: Effects of resistance training on bone mineral content and density in adolescent females. Can J Physiol Pharmacol. 1996, 74 (9): 1025-1033. 10.1139/cjpp-74-9-1025.
Morris FL, Naughton GA, Gibbs JL, Carlson JS, Wark JD: Prospective ten-month exercise intervention in premenarcheal girls: positive effects on bone and lean mass. J Bone Miner Res. 1997, 12 (9): 1453-1462. 10.1359/jbmr.1997.12.9.1453.
McKay HA, Petit MA, Schutz RW, Prior JC, Barr SI, Khan KM: Augmented trochanteric bone mineral density after modified physical education classes: a randomized school-based exercise intervention study in prepubescent and early pubescent children. J Pediatr. 2000, 136 (2): 156-162. 10.1016/S0022-3476(00)70095-3.
Nichols DL, Sanborn CF, Love AM: Resistance training and bone mineral density in adolescent females. J Pediatr. 2001, 139 (4): 494-500. 10.1067/mpd.2001.116698.
MacKelvie KJ, Petit MA, Khan KM, Beck TJ, McKay HA: Bone mass and structure are enhanced following a 2-year randomized controlled trial of exercise in prepubertal boys. Bone. 2004, 34 (4): 755-764. 10.1016/j.bone.2003.12.017.
Linden C, Ahlborg HG, Besjakov J, Gardsell P, Karlsson MK: A school curriculum-based exercise program increases bone mineral accrual and bone size in prepubertal girls: two-year data from the pediatric osteoporosis prevention (POP) study. J Bone Miner Res. 2006, 21 (6): 829-835. 10.1359/jbmr.060304.
MacKelvie KJ, Khan KM, Petit MA, Janssen PA, McKay HA: A school-based exercise intervention elicits substantial bone health benefits: a 2-year randomized controlled trial in girls. Pediatrics. 2003, 112 (6 Pt 1): e447-10.1542/peds.112.6.e447.
Kelly AS, Steinberger J, Olson TP, Dengel DR: In the absence of weight loss, exercise training does not improve adipokines or oxidative stress in overweight children. Metabolism. 2007, 56 (7): 1005-1009. 10.1016/j.metabol.2007.03.009.
Gutin B, Barbeau P, Owens S, Lemmon CR, Bauman M, Allison J, Kang HS, Litaker MS: Effects of exercise intensity on cardiovascular fitness, total body composition, and visceral adiposity of obese adolescents. Am J Clin Nutr. 2002, 75 (5): 818-826.
Owens S, Gutin B, Allison J, Riggs S, Ferguson M, Litaker M, Thompson W: Effect of physical training on total and visceral fat in obese children. Med Sci Sports Exerc. 1999, 31 (1): 143-148. 10.1097/00005768-199901000-00022.
Lazaar N, Aucouturier J, Ratel S, Rance M, Meyer M, Duche P: Effect of physical activity intervention on body composition in young children: influence of body mass index status and gender. Acta Paediatr. 2007, 96 (9): 1315-1320. 10.1111/j.1651-2227.2007.00426.x.
Ondrak KS, Morgan DW: Physical activity, calcium intake and bone health in children and adolescents. Sports Med. 2007, 37 (7): 587-600. 10.2165/00007256-200737070-00003.
Kontulainen SA, Kannus PA, Pasanen ME, Sievanen HT, Heinonen AO, Oja P, Vuori I: Does previous participation in high-impact training result in residual bone gain in growing girls? One year follow-up of a 9-month jumping intervention. Int J Sports Med. 2002, 23 (8): 575-581. 10.1055/s-2002-35543.
Mackelvie KJ, McKay HA, Khan KM, Crocker PR: A school-based exercise intervention augments bone mineral accrual in early pubertal girls. J Pediatr. 2001, 139 (4): 501-508. 10.1067/mpd.2001.118190.
Petit MA, McKay HA, MacKelvie KJ, Heinonen A, Khan KM, Beck TJ: A randomized school-based jumping intervention confers site and maturity-specific benefits on bone structural properties in girls: a hip structural analysis study. J Bone Miner Res. 2002, 17 (3): 363-372. 10.1359/jbmr.2002.17.3.363.
McKay HA, MacLean L, Petit M, MacKelvie-O'Brien K, Janssen P, Beck T, Khan KM: "Bounce at the Bell": a novel program of short bouts of exercise improves proximal femur bone mass in early pubertal children. Br J Sports Med. 2005, 39 (8): 521-526. 10.1136/bjsm.2004.014266.
Brosnahan J, Steffen LM, Lytle L, Patterson J, Boostrom A: The relation between physical activity and mental health among Hispanic and non-Hispanic white adolescents. Arch Pediatr Adolesc Med. 2004, 158 (8): 818-823. 10.1001/archpedi.158.8.818.
Tao FB, Xu ML, Kim SD, Sun Y, Su PY, Huang K: Physical activity might not be the protective factor for health risk behaviours and psychopathological symptoms in adolescents. J Paediatr Child Health. 2007, 43 (11): 762-767. 10.1111/j.1440-1754.2007.01217.x.
Haarasilta LM, Marttunen MJ, Kaprio JA, Aro HM: Correlates of depression in a representative nationwide sample of adolescents (15-19 years) and young adults (20-24 years). Eur J Public Health. 2004, 14 (3): 280-285. 10.1093/eurpub/14.3.280.
Annesi JJ: Correlations of depression and total mood disturbance with physical activity and self-concept in preadolescents enrolled in an after-school exercise program. Psychol Rep. 2005, 96 (3 Pt 2): 891-898.
Norris R, Carroll D, Cochrane R: The effects of physical activity and exercise training on psychological stress and well-being in an adolescent population. J Psychosom Res. 1992, 36 (1): 55-65. 10.1016/0022-3999(92)90114-H.
Goldfield GS, Mallory R, Parker T, Cunningham T, Legg C, Lumb A, Parker K, Prud'homme D, Adamo KB: Effects of modifying physical activity and sedentary behavior on psychosocial adjustment in overweight/obese children. J Pediatr Psychol. 2007, 32 (7): 783-793. 10.1093/jpepsy/jsm017.
Pickett W: Injuries. Young people in Canada: their health and wellbeing. Edited by: Boyce WF. 2004, Ottawa: Health Canada, 101-102.
Collard DC, Verhagen EA, Chin APMJ, van Mechelen W: Acute physical activity and sports injuries in children. Appl Physiol Nutr Metab. 2008, 33 (2): 393-401. 10.1139/H07-182.
Janssen I, Dostaler S, Boyce WF, Pickett W: Influence of multiple risk behaviors on physical activity-related injuries in adolescents. Pediatrics. 2007, 119 (3): e672-680. 10.1542/peds.2006-0339.
Tsuang HCA, Guo YL, Lin YC, Su HJ: School type, stress and sport-related injuries in middle school students in central Taiwan. Safety Science. 2001, 39: 137-144. 10.1016/S0925-7535(00)00057-6.
Mattila V, Parkkari J, Kannus P, Rimpela A: Occurrence and risk factors of unintentional injuries among 12- to 18-year-old Finns--a survey of 8219 adolescents. Eur J Epidemiol. 2004, 19 (5): 437-444. 10.1023/B:EJEP.0000027355.85493.cb.
Brawley LR, Latimer AE: Physical activity guides for Canadians: messaging strategies, realistic expectations for change, and evaluation. Can J Public Health. 2007, 98 (Suppl 2): S170-184.
Corbin CB, Pangrazi RP: Physical Activity for Children: A Statement of Guidelines for Children Aged 5-12. 2004, Reston, VA: National Association for Sport and Physical Education, 2
Department of Health and Aging: National Physical Activity Guidelines for Australians. 1999, Canberra: Commonwealth of Australia
Mark AE, Janssen I: Does physical activity accrued in bouts predict overweight and obesity beyond the total volume of physical activity in youth?. Am J Prev Med. 2009, 36: 416-421. 10.1016/j.amepre.2009.01.027.
Download references
Acknowledgements
Production of this paper has been made possible through a financial contribution from the Public Health Agency of Canada. The views expressed herein do not necessarily represent the views of the Public Health Agency of Canada. The leadership and administrative assistance was provided by the Canadian Society for Exercise Physiology.
Author information
Authors and affiliations.
School of Kinesiology and Health Studies, Queen's University, Kingston, Ontario, Canada
Ian Janssen & Allana G LeBlanc
Department of Community Health and Epidemiology, Queen's University, Kingston, Ontario, Canada
Ian Janssen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ian Janssen .
Additional information
Competing interests.
Production of this paper has been made possible through a financial contribution from the Public Health Agency of Canada. The views expressed herein do not necessarily represent the views of the Public Health Agency of Canada. I Janssen has received honoraria, speaker fees, and consulting fees from several non-profit organizations, including the Public Health Agency of Canada, that have an interest in physical activity and health.
Authors' contributions
IJ designed the methods, assisted with the completion of the systematic review, and drafted the manuscript. AB lead most of the components of the systematic review and helped drafts some of the methodology sections of the paper.
All authors have read and approved the final manuscript.
Electronic supplementary material
12966_2009_346_moesm1_esm.doc.
Additional file 1: Table 1. Association between physical activity and health and behavioural outcomes in children and youth. (DOC 78 KB)
Additional file 2: Table 2. Criteria for assigning a level of evidence to recommendations. (DOC 50 KB)
Additional file 3: table 3. criteria for assigning a grade to recommendations. (doc 50 kb), 12966_2009_346_moesm4_esm.doc.
Additional file 4: Table 4. Experimental studies examining the influence of exercise on changes in traditional blood lipids and lipoproteins in school-aged children and youth. (DOC 158 KB)
12966_2009_346_MOESM5_ESM.DOC
Additional file 5: Table 5. Observational studies examining the relation between physical activity and fitness with hypertension in school-aged children and youth. (DOC 86 KB)
12966_2009_346_MOESM6_ESM.DOC
Additional file 6: Table 6. Experimental studies examining the influence of exercise on changes in blood pressure in school-aged children and youth. (DOC 133 KB)
12966_2009_346_MOESM7_ESM.DOC
Additional file 7: Table 7. Observational studies examining the relation between physical activity and fitness with the metabolic syndrome in school-aged children and youth. (DOC 154 KB)
12966_2009_346_MOESM8_ESM.DOC
Additional file 8: Table 8. Experimental studies examining the influence of exercise on changes in markers of the metabolic syndrome (insulin resistance) in school-aged children and youth. (DOC 125 KB)
12966_2009_346_MOESM9_ESM.DOC
Additional file 9: Table 9. Observational studies examining the relation between physical activity and fitness with obesity in school-aged children and youth. (DOC 458 KB)
12966_2009_346_MOESM10_ESM.DOC
Additional file 10: Table 10. Experimental studies examining the influence of exercise on changes in obesity measures in school-aged children and youth. (DOC 360 KB)
12966_2009_346_MOESM11_ESM.DOC
Additional file 11: Table 11. Experimental studies examining the influence of exercise on changes in bone mineral density in school-aged children and youth. (DOC 190 KB)
12966_2009_346_MOESM12_ESM.DOC
Additional file 12: Table 12. Observational studies examining the relation between physical activity and fitness with depression in school-aged children and youth. (DOC 80 KB)
12966_2009_346_MOESM13_ESM.DOC
Additional file 13: Table 13. Experimental studies examining the influence of exercise on changes in measures of depression in school-aged children and youth. (DOC 91 KB)
12966_2009_346_MOESM14_ESM.DOC
Additional file 14: Table 14. Observational studies examining the relation between physical activity and fitness with injury in school-aged children and youth. (DOC 114 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Janssen, I., LeBlanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 7 , 40 (2010). https://doi.org/10.1186/1479-5868-7-40
Download citation
Received : 20 July 2009
Accepted : 11 May 2010
Published : 11 May 2010
DOI : https://doi.org/10.1186/1479-5868-7-40
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Physical Activity
- Intensity Activity
- Physical Activity Guideline
- Intensity Physical Activity
- Physical Activity Participation

International Journal of Behavioral Nutrition and Physical Activity
ISSN: 1479-5868
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

40 Facts About Elektrostal
Written by Lanette Mayes
Modified & Updated: 01 Jun 2024
Reviewed by Jessica Corbett

Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to captivate you.
This article will provide you with 40 fascinating facts about Elektrostal, giving you a better understanding of why this city is worth exploring. From its origins as an industrial hub to its modern-day charm, we will delve into the various aspects that make Elektrostal a unique and must-visit destination.
So, join us as we uncover the hidden treasures of Elektrostal and discover what makes this city a true gem in the heart of Russia.
Key Takeaways:
- Elektrostal, known as the “Motor City of Russia,” is a vibrant and growing city with a rich industrial history, offering diverse cultural experiences and a strong commitment to environmental sustainability.
- With its convenient location near Moscow, Elektrostal provides a picturesque landscape, vibrant nightlife, and a range of recreational activities, making it an ideal destination for residents and visitors alike.
Known as the “Motor City of Russia.”
Elektrostal, a city located in the Moscow Oblast region of Russia, earned the nickname “Motor City” due to its significant involvement in the automotive industry.
Home to the Elektrostal Metallurgical Plant.
Elektrostal is renowned for its metallurgical plant, which has been producing high-quality steel and alloys since its establishment in 1916.
Boasts a rich industrial heritage.
Elektrostal has a long history of industrial development, contributing to the growth and progress of the region.
Founded in 1916.
The city of Elektrostal was founded in 1916 as a result of the construction of the Elektrostal Metallurgical Plant.
Located approximately 50 kilometers east of Moscow.
Elektrostal is situated in close proximity to the Russian capital, making it easily accessible for both residents and visitors.
Known for its vibrant cultural scene.
Elektrostal is home to several cultural institutions, including museums, theaters, and art galleries that showcase the city’s rich artistic heritage.
A popular destination for nature lovers.
Surrounded by picturesque landscapes and forests, Elektrostal offers ample opportunities for outdoor activities such as hiking, camping, and birdwatching.
Hosts the annual Elektrostal City Day celebrations.
Every year, Elektrostal organizes festive events and activities to celebrate its founding, bringing together residents and visitors in a spirit of unity and joy.
Has a population of approximately 160,000 people.
Elektrostal is home to a diverse and vibrant community of around 160,000 residents, contributing to its dynamic atmosphere.
Boasts excellent education facilities.
The city is known for its well-established educational institutions, providing quality education to students of all ages.
A center for scientific research and innovation.
Elektrostal serves as an important hub for scientific research, particularly in the fields of metallurgy , materials science, and engineering.
Surrounded by picturesque lakes.
The city is blessed with numerous beautiful lakes , offering scenic views and recreational opportunities for locals and visitors alike.
Well-connected transportation system.
Elektrostal benefits from an efficient transportation network, including highways, railways, and public transportation options, ensuring convenient travel within and beyond the city.
Famous for its traditional Russian cuisine.
Food enthusiasts can indulge in authentic Russian dishes at numerous restaurants and cafes scattered throughout Elektrostal.
Home to notable architectural landmarks.
Elektrostal boasts impressive architecture, including the Church of the Transfiguration of the Lord and the Elektrostal Palace of Culture.
Offers a wide range of recreational facilities.
Residents and visitors can enjoy various recreational activities, such as sports complexes, swimming pools, and fitness centers, enhancing the overall quality of life.
Provides a high standard of healthcare.
Elektrostal is equipped with modern medical facilities, ensuring residents have access to quality healthcare services.
Home to the Elektrostal History Museum.
The Elektrostal History Museum showcases the city’s fascinating past through exhibitions and displays.
A hub for sports enthusiasts.
Elektrostal is passionate about sports, with numerous stadiums, arenas, and sports clubs offering opportunities for athletes and spectators.
Celebrates diverse cultural festivals.
Throughout the year, Elektrostal hosts a variety of cultural festivals, celebrating different ethnicities, traditions, and art forms.
Electric power played a significant role in its early development.
Elektrostal owes its name and initial growth to the establishment of electric power stations and the utilization of electricity in the industrial sector.
Boasts a thriving economy.
The city’s strong industrial base, coupled with its strategic location near Moscow, has contributed to Elektrostal’s prosperous economic status.
Houses the Elektrostal Drama Theater.
The Elektrostal Drama Theater is a cultural centerpiece, attracting theater enthusiasts from far and wide.
Popular destination for winter sports.
Elektrostal’s proximity to ski resorts and winter sport facilities makes it a favorite destination for skiing, snowboarding, and other winter activities.
Promotes environmental sustainability.
Elektrostal prioritizes environmental protection and sustainability, implementing initiatives to reduce pollution and preserve natural resources.
Home to renowned educational institutions.
Elektrostal is known for its prestigious schools and universities, offering a wide range of academic programs to students.
Committed to cultural preservation.
The city values its cultural heritage and takes active steps to preserve and promote traditional customs, crafts, and arts.
Hosts an annual International Film Festival.
The Elektrostal International Film Festival attracts filmmakers and cinema enthusiasts from around the world, showcasing a diverse range of films.
Encourages entrepreneurship and innovation.
Elektrostal supports aspiring entrepreneurs and fosters a culture of innovation, providing opportunities for startups and business development .
Offers a range of housing options.
Elektrostal provides diverse housing options, including apartments, houses, and residential complexes, catering to different lifestyles and budgets.
Home to notable sports teams.
Elektrostal is proud of its sports legacy , with several successful sports teams competing at regional and national levels.
Boasts a vibrant nightlife scene.
Residents and visitors can enjoy a lively nightlife in Elektrostal, with numerous bars, clubs, and entertainment venues.
Promotes cultural exchange and international relations.
Elektrostal actively engages in international partnerships, cultural exchanges, and diplomatic collaborations to foster global connections.
Surrounded by beautiful nature reserves.
Nearby nature reserves, such as the Barybino Forest and Luchinskoye Lake, offer opportunities for nature enthusiasts to explore and appreciate the region’s biodiversity.
Commemorates historical events.
The city pays tribute to significant historical events through memorials, monuments, and exhibitions, ensuring the preservation of collective memory.
Promotes sports and youth development.
Elektrostal invests in sports infrastructure and programs to encourage youth participation, health, and physical fitness.
Hosts annual cultural and artistic festivals.
Throughout the year, Elektrostal celebrates its cultural diversity through festivals dedicated to music, dance, art, and theater.
Provides a picturesque landscape for photography enthusiasts.
The city’s scenic beauty, architectural landmarks, and natural surroundings make it a paradise for photographers.
Connects to Moscow via a direct train line.
The convenient train connection between Elektrostal and Moscow makes commuting between the two cities effortless.
A city with a bright future.
Elektrostal continues to grow and develop, aiming to become a model city in terms of infrastructure, sustainability, and quality of life for its residents.
In conclusion, Elektrostal is a fascinating city with a rich history and a vibrant present. From its origins as a center of steel production to its modern-day status as a hub for education and industry, Elektrostal has plenty to offer both residents and visitors. With its beautiful parks, cultural attractions, and proximity to Moscow, there is no shortage of things to see and do in this dynamic city. Whether you’re interested in exploring its historical landmarks, enjoying outdoor activities, or immersing yourself in the local culture, Elektrostal has something for everyone. So, next time you find yourself in the Moscow region, don’t miss the opportunity to discover the hidden gems of Elektrostal.
Q: What is the population of Elektrostal?
A: As of the latest data, the population of Elektrostal is approximately XXXX.
Q: How far is Elektrostal from Moscow?
A: Elektrostal is located approximately XX kilometers away from Moscow.
Q: Are there any famous landmarks in Elektrostal?
A: Yes, Elektrostal is home to several notable landmarks, including XXXX and XXXX.
Q: What industries are prominent in Elektrostal?
A: Elektrostal is known for its steel production industry and is also a center for engineering and manufacturing.
Q: Are there any universities or educational institutions in Elektrostal?
A: Yes, Elektrostal is home to XXXX University and several other educational institutions.
Q: What are some popular outdoor activities in Elektrostal?
A: Elektrostal offers several outdoor activities, such as hiking, cycling, and picnicking in its beautiful parks.
Q: Is Elektrostal well-connected in terms of transportation?
A: Yes, Elektrostal has good transportation links, including trains and buses, making it easily accessible from nearby cities.
Q: Are there any annual events or festivals in Elektrostal?
A: Yes, Elektrostal hosts various events and festivals throughout the year, including XXXX and XXXX.
Elektrostal's fascinating history, vibrant culture, and promising future make it a city worth exploring. For more captivating facts about cities around the world, discover the unique characteristics that define each city . Uncover the hidden gems of Moscow Oblast through our in-depth look at Kolomna. Lastly, dive into the rich industrial heritage of Teesside, a thriving industrial center with its own story to tell.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
Share this Fact:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Glob Adv Health Med
- v.2(4); 2013 Jul
Language: English | Chinese | Spanish
A Systematic Review of the Literature on Health and Wellness Coaching: Defining a Key Behavioral intervention in Healthcare
医疗与健康辅导文献的系统性审查:界定医疗护理领域中的主要行为干预, revisión sistemática de la literatura médica sobre la formación de salud y bienestar: definiendo una intervención conductual clave en la atención sanitaria, ruth q. wolever.
Duke Integrative Medicine, Duke University Health System, Durham, North Carolina and Department of Psychiatry and Behavioral Science, Duke School of Medicine, Durham, NC, United States.
Leigh Ann Simmons
Duke Integrative Medicine, Duke University Health System, Durham, North Carolina and Duke School of Nursing, Durham, United States.
Gary A. Sforzo
Department of Exercise and Sport Sciences, School of Health Science and Human Performance, Ithaca College, Ithaca, NY, United States.
Working Together For Health, Boston, Massachusetts, United States.
Miranda Kaye
Elizabeth m. bechard.
Duke Integrative Medicine, Duke University Health System, Durham, North Carolina, United States.
Mary Elaine Southard
Integrative Health Consulting and Coaching, LLC, Scranton, Pennsylvania, United States.
Mary Kennedy
Institute of Lifestyle Medicine, Department of Physical Medicine and Rehabilitation at Spaulding Rehabilitation Hospital, Boston, Massachusetts, United States.
Justine Vosloo
Duke School of Nursing, Durham, United States.
Primary Objective:
Review the operational definitions of health and wellness coaching as published in the peer-reviewed medical literature.
Background:
As global rates of preventable chronic diseases have reached epidemic proportions, there has been an increased focus on strategies to improve health behaviors and associated outcomes. One such strategy, health and wellness coaching, has been inconsistently defined and shown mixed results.
A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)—guided systematic review of the medical literature on health and wellness coaching allowed for compilation of data on specific features of the coaching interventions and background and training of coaches.
Eight hundred abstracts were initially identified through PubMed, with 284 full-text articles ultimately included. The majority (76%) were empirical articles. The literature operationalized health and wellness coaching as a process that is fully or partially patient-centered (86% of articles), included patient-determined goals (71%), incorporated self-discovery and active learning processes (63%) (vs more passive receipt of advice), encouraged accountability for behaviors (86%), and provided some type of education to patients along with using coaching processes (91%). Additionally, 78% of articles indicated that the coaching occurs in the context of a consistent, ongoing relationship with a human coach who is trained in specific behavior change, communication, and motivational skills.
Conclusions:
Despite disparities in how health and wellness coaching have been operationalized previously, this systematic review observes an emerging consensus in what is referred to as health and wellness coaching; namely, a patient-centered process that is based upon behavior change theory and is delivered by health professionals with diverse backgrounds. The actual coaching process entails goal-setting determined by the patient, encourages self-discovery in addition to content education, and incorporates mechanisms for developing accountability in health behaviors. With a clear definition for health and wellness coaching, robust research can more accurately assess the effectiveness of the approach in bringing about changes in health behaviors, health outcomes and associated costs that are targeted to reduce the global burden of chronic disease.
摘要
主要目标: 审查同行评审的医 疗文献中所发布医疗和健康辅导 的操作性定义。
方法: 在系统性审查和 Meta 分析首选报告项目 (PRIMSA) 指 导下进行的医疗与健康辅导医学 文献的系统性审查,可编辑与辅 导干预指定功能和教练背景和培 训有关的数据。
成效: 通过 PubMed 初步识别 出八百篇摘要,并最终纳入 284 篇全文文章,其中 多数 (76%) 为实证性文章。 文献指实施医 疗和健康辅导为完全或部分以患 者为中心 (86% 的文章)、包含 患者决定的目标 (71%)、合并自 我发现和积极学习流程(63%)(与 较为被动地接受建议相比)、鼓 励对行为负责 (86%)、 并配合 辅导流程向患者提供某种类型的 教育 (91%)。此外,78% 的文章 指出,辅导是在与接受过特定行 为改变、 沟通和激励性技能培 训的教练建立了一贯、持久的关 系的情况下提供 结论:尽管先 前在如何实施医疗与健康辅导方 面存在分歧,但通过本系统性审 查,发现在医疗与健康辅导的定 义方面达成一种共识;即,医疗 与健康辅导是一个由拥有不同背 景的医疗专业人员交付的、以行 为改变理论为基础、以患者为中 心的流程。该实际的辅导流程促 致患者决定目标设定,鼓励除内 容教育以外的自我发现,并且将 多种机制整合在一起,用以发展 健康行为的问责制。有了明确的 医疗与健康辅导定义,人们便可 开展大量研究,更为准确地评估 该等方法在健康行为、健康结果 和相关费用方面所带来变化的有 效性,从而减轻全球的慢性疾病 负担。
Objetivo Principal:
revisar las definiciones operativas de la formación de salud y bienestar según las publicaciones en la literatura médica revisada por pares.
Fundamentación:
Dado que que las tasas mundiales de enfermedades crónicas evitables han alcanzado proporciones epidémicas, se ha hecho cada vez más hincapié en las estrategias para mejorar las conductas sanitarias y los resultados asociados. Una de estas estrategias, la formación de salud y bienestar, se ha definido de forma inconsistente y ha mostrado resultados mixtos.
Métodos:
Una revisión sistemática, guiada por los elementos de información preferidos para las revisiones sistemáticas y el metanálisis (PRIMSA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses), de la literatura médica sobre la formación de salud y bienestar permitió la recopilación de datos sobre las características específicas de las intervenciones de formación, y sobre la procedencia y la formación de los formadores.
Resultados:
se identificaron inicialmente ochocientos resúmenes a través de PubMed y, en última instancia, se incluyeron 284 artículos con texto completo. La mayoría (76 %) eran artículos empíricos. La literatura aportó una definición operativa de la formación de salud y bienestar como un proceso que está total o parcialmente centrado en el paciente (86 % de los artículos), que incluye metas determinadas por los pacientes (71 %), incorpora procesos de aprendizaje activo y descubrimiento personal (63 %) —en comparación con una recepción más pasiva de asesoramiento—, alienta la responsabilidad por las conductas (86 %) e imparte algún tipo de educación a pacientes junto con el uso de procesos de formación (91 %). Además, el 78 % de los artículos indicó que la formación se presenta en el contexto de una relación continua y coherente con un formador humano que está capacitado en aptitudes motivacionales, comunicativas y de cambios conductuales específicos.
Conclusiones:
A pesar de las divergencias en la forma en que la formación de salud y bienestar se ha puesto en marcha con anterioridad, esta revisión sistemática señala un consenso emergente en lo que se refiere a la formación de salud y bienestar, es decir, un proceso centrado en el paciente que se basa en la teoría del cambio conductual y que se administra por parte de profesionales sanitarios con diversas experiencias en el pasado. El proceso real de formación implica el establecimiento de objetivos determinado por el paciente, estimula el descubrimiento personal, además de la formación en contenidos, e incorpora mecanismos para desarrollar la responsabilidad en las conductas de salud. Con una definición clara de la formación de salud y bienestar, la investigación sólida puede evaluar de una forma más precisa la eficacia de la estrategia en la consecución de los cambios en las conductas de salud, los resultados sanitarios y los costos asociados dirigidos a reducir la carga mundial de la enfermedad crónica.
INTRODUCTION
The global prevalence of preventable chronic diseases associated with unhealthy behaviors has reached epidemic proportions and negatively affects healthcare systems and economies worldwide. 1 - 3 Given the strain of chronic illness, public health, disease management, clinical practice, and employee wellness models are evolving to help individuals change their health behaviors to prevent and better manage chronic disease. 4 - 7 One rapidly emerging strategy to help individuals successfully change their health behaviors is health or wellness coaching. Health and wellness coaching has been defined in varying ways over the past decade. In 2003, Palmer et al defined health coaching as
the practice of health education and health promotion within a coaching context, to enhance the well-being of individuals and to facilitate the achievement of their health-related goals. 8
In 2006, Butterworth, Linden, McClay, and Leo defined health coaching as
a service in which providers facilitate participants in changing lifestyle-related behaviors for improved health and quality of life, or establishing and attaining health promoting goals. 9 , 10
More recently, the National Consortium for Credentialing Health and Wellness Coaches (NCCHWC) proposed the following definition of health and wellness coaches, which delineates core elements of the practice of coaching:
Health and wellness coaches are professionals from diverse backgrounds and education who work with individuals and groups in a client-centered process to facilitate and empower the client to achieve self-determined goals related to health and wellness. Successful coaching takes place when coaches apply clearly defined knowledge and skills so that clients mobilize internal strengths and external resources for sustainable change. 11
Although these definitions share some similar components, there is no agreement on what exactly health coaching entails (eg, practices, strategies, delivery methods), what the role of the coach actually is (eg, educator, navigator, facilitator, partner), 9 , 12 and what background and training enable the coach to provide health coaching competently.
As use of the terms health coaching and wellness coaching proliferate without a clear and consistent definition of this intervention, additionally concerning is the increasing rate at which peer-reviewed journals are publishing research results that claim to evaluate “health coaching,” but use widely varying definitions, 12 thereby confusing the value of coaching results. Indeed, numerous studies have used the term health coaching to address chronic disease care in various settings and with mixed results. For example, Wennberg et al found that a targeted care-management program with telephonic health coaching for individuals insured by a large health plan reduced medical costs and hospitalizations. 13 Similarly, studies of health coaching for patients with diabetes, 14 - 17 obesity, 18 , 19 cancer, 20 and risk of 21 or diagnosed cardiovascular disease 22 , 23 demonstrate a positive effect on health behaviors or health outcomes. However, review of the literature reveals other evaluations of coaching that find non-significant benefits for health outcomes. 24 - 27
Likely, one major reason for the variability in findings on the effectiveness of health coaching is that highly disparate interventions are being investigated under the umbrella term of health or wellness coaching . When we consider the interventions carefully, we find a broad range in the following: (1) the techniques used during the coaching process; (2) the theoretical underpinnings of the approach; (3) the frequency and duration of the coaching process; (4) the extent of human contact provided; (5) the degree to which content education is included in the intervention; and (6) the professional background and training of the coaches. At one end of the continuum are well-described and theoretically based interventions delivered through one-on-one relationships that develop over months or years with a highly trained professional who employs well-developed and articulated processes and strategies to help individuals initiate and sustain behavior changes over time. 9 , 17 , 19 , 28 At the other end of the continuum are interventions that require no human contact, 29 - 31 that appear to be purely content education rather than skills-based training, 32 , 33 and/or have no stated theoretical backing. This lack of standardization in both the definition and the operationalization of health coaching makes it difficult, if not impossible, to determine whether health coaching is indeed an effective approach to improving health behaviors and reducing the global burden of chronic disease.
The purpose of the present study was to establish a consensus definition of health and wellness coaching through a systematic review of the related literature. The intention is threefold. First, we intend to answer repeated calls in the literature for evidence-based identification of conceptual and interventional components of health and wellness coaching. 28 , 34 , 35 Second, with a standardized definition, components of this approach can be used as targets to clarify the professional skills needed to appropriately train health and wellness coaches. 12 , 34 , 36 Finally, with a standardized definition, we can more rigorously evaluate both the efficacy and the effectiveness of health and wellness coaching. 12 To these ends, we conducted a comprehensive, systematic review of the peer-reviewed medical literature to determine how health and wellness coaching is operationalized. Using an adapted population, intervention, comparison, outcome (PICO) format, our primary research question was, “How are interventions described as health or wellness coaching defined and operationalized in the peer-reviewed medical literature?” This review will serve as the foundation for future effectiveness research and identification of best practices in health and wellness coaching that may be widely disseminated to mitigate the negative consequences of the global chronic disease epidemic.
We conducted a systematic review of the peer-reviewed literature on health and wellness coaching using the international guidelines established by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). 37 , 38 The PRISMA standards were published in 2009 to update the Quality of Reporting of Meta-Analyses (QUOROM) statement based on conceptual advances in the science of systematic reviews. According to the definitions established by the Cochrane Collaboration, a systematic review addresses “a clearly formulated question that uses systematic and explicit methods to identify, select, and critically appraise relevant research, and to collect and analyze data from the studies that are included in the review.” 39
Research Questions
Our primary aim was to answer the question, “How are interventions that are described as health or wellness coaching defined and operationalized in the peer-reviewed medical literature?” Explicitly, we sought to determine the following.
1. What type of literature has been published on health and wellness coaching? Given this early stage of clarifying the definition of “health and wellness coaching,” we chose to describe all peer-reviewed medical literature rather than only empirical trials. We surmised that articles written by clinicians describing ongoing practices were as useful as randomized controlled trials for understanding key concepts emerging in the field. Once a standardized definition has emerged, review of empirical data will be essential to ascertain the effectiveness of health and wellness coaching and to establish standards for practice guidelines. In answering question 1, we categorized articles as one of four types:
- a research study wherein data were systematically collected;
- a protocol description for an intended (and often funded) study where there is a plan to systematically collect data;
- description of an existing practice or process, labeled as health or wellness coaching, that has already been operationalized and implemented—this category included those practices that had retrospectively culled and reviewed data that were not prospectively and systematically collected; and
- a conceptual piece that describes ideas about health and wellness coaching in research or clinical practice but presented no associated data.
As can be seen in the tables, we separated the results by article type in order to assess potential publication bias. We were concerned that the conceptual elements that did not resemble fully operationalized practices might reflect ideas that had not been tried.
2. What approaches, practices, strategies, and methodologies constitute health coaching as described? After initial full-text review of 66 articles, five investigators (DD, EB, LAS, MES, RQW) developed a consensus on which specific practices were repeatedly mentioned and thus should be quantified to describe the evolving practice of health and wellness coaching. Categorical questions were answered with Yes, No, Partially, Not described, and Not applicable. These included the following:
- 2.1 Was the coaching patient-centered? To determine the answer, we drew from the definition as put forth by the Institute of Medicine. 40 Specifically, was the coaching respectful of and responsive to individual patient preferences, needs and values? Did it appear to ensure that patient values guided all clinical decisions? Was it based on effective communication, shared information, and shared decision-making between clinician and patient? In practice, coding “yes” for 2.1 indicated that the coaching practice was tailored to the individual and allowed some autonomy on the part of the patient.
- 2.2 Were the patients' goals self-determined vs recommended by a provider or the coach? Following along the lines of coaching as a patient-centered process and consistent with several definitions of health and wellness coaching, we evaluated the degree to which articles described a practice wherein patients were able to set their own goals, or whether the goals were predetermined by the intervention, coach, or medical provider(s). If patients were able to set their own goals, this was coded “yes.” If patients had preset goals, this was coded “no.” Interventions that described a procedure where there was a predetermined primary goal (eg, blood pressure control, weight loss) but the patient was able to develop some personal goals that might facilitate the primary goal were coded as “partially.”
- 2.3 Was a self-discovery process used to find solutions vs advice-giving? We assessed each article to evaluate whether or not an active learning process was encouraged for the participant through self-exploration and problem solving vs being advised or instructed by the coach. In practice, if the patient appeared to have any involvement in finding or generating solutions for themselves, we coded “Yes.” This was in contrast to an approach that was strictly content education or simply telling the patient what s/ he needs to do, which was coded as “No.”
- 2.4 Did the coaching process encourage patient accountability in behavior toward the stated goal? Accountability is encouraged when the patient has some way to self-monitor in order to observe their progress (or lack of it) toward their goal. This involves supporting patients in regular data collection on goal-related behaviors and outcomes. The role of the coaching program is to support and/or facilitate this data collection and teach patients how to use it in self-regulation of behaviors.
- 2.5 Was content education provided as part of the defined “coaching” intervention? In some articles, content education was provided in the service of developing patients' abilities to better solve problems for themselves. In others, it was provided in the context of instructing or advising.
- 2.6 What was the typical coaching “dose” (length of a coaching session, the frequency of sessions, and the duration of the coaching process)?
- 2.7 Did the patient develop a relationship with the same coach over time? Some interventions describe an approach where a patient may talk to a different coach depending on when s/he accesses the intervention, while others describe an intervention wherein the patient interacts with the same coach during the entire intervention. We wanted to assess the degree to which patients had a consistent coach, as this may be an important variable when later assessing effectiveness.
3. Who delivers the service that is referred to as “health or wellness coaching?” To better understand the delivery of health and wellness coaching, we asked further background questions regarding the “coach.” Specifically, we asked the following:
- 3.1 Are these individuals professionally trained?
- 3.2 if so, what type of professionals were the coaches? Specifically, were they health professionals or not? If so, what type?
- 3.3. In addition, what type of training have they received, if any, in the specifics of the coaching process and the content of the coaching they are delivering? We synthesized any details provided about their backgrounds, including how many hours of training they received for their coaching roles and the content of that training.
Identification, Screening and Eligibility of the Literature
A professional librarian ran a search on PubMed, which encompassed MEDLINE, life science journals, and online books from the fields of biomedicine and health covering portions of the life sciences, behavioral sciences, chemical sciences, and bioengineering. The librarian used no start date and included all articles with MeSH term “human,” written in English or Spanish, which had been loaded through January 2013. Search index terms included all forms of the words health or wellness and coach . The search included other potential subterms for coach such as educator , mentor , navigator and teacher as well as subterms for “coaching” such as training , feedback , and mentoring . For the full search index list, see Table 1 .
Specific Search Terms
| ((health[tiab] OR wellness[Title/Abstract]) AND (coach[tiab] OR coach/educator[tiab] OR coach/mentor[tiab] OR coach/navigator[tiab] OR coach/teacher[tiab] OR coach'[tiab] OR coach's[tiab] OR coachability[tiab] OR coachable[tiab] OR coachdelivered[tiab] OR coached[tiab] OR coached/trained[tiab] OR coached'[tiab] OR coachee[tiab] OR coaches[tiab] OR coaches/case[tiab] OR coaches/facilitators[tiab] OR coaches/instructors[tiab] OR coaches/trainers[tiab] OR coaches'[tiab] OR coaching[tiab] OR coaching/control[tiab] OR coaching/facilitating[tiab] OR coaching/feedback[tiab] OR coaching/mentoring[tiab] OR coaching/training[tiab] OR coaching'[tiab] OR coaching's[tiab] OR coachwork[tiab])) AND ("humans"[MeSH Terms] AND (English[lang] OR Spanish[lang])) |
Eight hundred abstracts were initially identified through the literature search. An additional 55 articles were added through two separate means. First, articles previously collected by the authors that did not appear in the literature search were contributed for review. Second, three review articles obtained through the PubMed search 28 , 34 , 35 were combed for additional references. To be eligible for inclusion in the review, articles had to be published in a peer-reviewed journal, written in English or Spanish, and discuss coaching in the context of improving patient health and/or wellness. Articles on coaching for the purpose of professional development (eg, supporting a physician or nurse to improve their skills) and coaching in athletics were excluded. One investigator (RQW) reviewed each title and abstract to ensure general relevance. A second researcher (EB) reviewed abstracts for which the first investigator was unclear about its relevance to the current review. As illustrated in Figure 1 , the 800 abstracts were reduced to349 full-text articles for review. Full-text reviews then resulted in an additional 65 exclusions; specific reasons for exclusion are displayed in Figure 1 . As noted above, no exclusions were made based on type of article (eg, research report, protocol description, operating clinical practice, conceptual piece). We also noted when a single study was described by multiple articles (eg, at varying time points or on varying measures) or when a group of investigators or clinicians produced multiple articles on the same approach. Following a series of team discussions, however, we decided to include all such articles for this systematic review (vs one representative paper from a single study or group of investigators or clinicians) so we could report on the “emerging thinking” in both the clinical and research literature. For future reviews that evaluate the quality of the evidence and outcomes, multiple articles on a single study may be counted only once. We are well aware of the potential for descriptive or conceptual pieces (eg, commentaries) to influence the literature—and thus practice—even when they do not include descriptions of operating clinical practices or data. Hence, we also summarize pertinent sections of the literature (such as the descriptions of the actual coaching processes) without these concept articles and assess for potential bias.

PRISMA flow diagram.
From: Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med. 2009;6(6):e1000097. doi:10.1371/journal.pmed.1000097. 37 For more information, visit www.prisma-statement.org .
Pairs of investigators from our team of 10 were assigned full-text articles to independently review and enter pertinent data on a standardized grid. For all full-text articles, the following data were evaluated and abstracted if available:
- type of article (empirical, protocol waiting for data collection, existing practice, conceptual);
- characteristics of the reported coaching process, including techniques used, degree of patient-centeredness, patient role in goal-setting and self-discovery processes, use of accountability strategies to encourage self-monitoring, provision of content education, frequency and duration of the coaching, and use of the same coach or different coaches over time; and
- characteristics of the coaches themselves, including type of professional, background, and breadth and scope of reported training obtained to serve in the coaching role.
A third reviewer resolved any disagreements between the two assigned reviewers on the abstracted data. Third reviews were required for 96 articles, and a fourth review was required for three. Four investigators (DD, MK, GS, and RQW) summarized data by compiling answers to each sub-question above and calculating summary statistics (proportions and ranges) for each question. Five investigators independently confirmed the compilations (MES, JV, EB, LAS, MAK) and together resolved any discrepancies.
1. What Kind of Peer-reviewed Articles Are Describing Health (or Wellness) Coaching?
The bulk of peer-reviewed articles have been empirical trials. For the 284 full-text articles included, 185 (65.1%) were empirical studies wherein data were systematically collected; 31 (10.9%) were protocol descriptions for which data collection was planned but not yet reported; 37 (13.0%) were accounts of existing practices labeled as health or wellness coaching that have reportedly been operationalized and conducted but not formally evaluated; and 31 (10.9%) were concept articles that presented no data.
As seen in Figure 2 , the rapidly increasing slope of peer-reviewed publications is noteworthy. For example, whereas 22 articles were published on health or wellness coaching before 2003, in 2010 through 2012 alone, 152 articles on the topic were published.

Frequency of peer-reviewed articles published on health and wellness coaching across time.
2. What Approaches, Practices, Strategies and Methodologies Constitute Health Coaching as Described?
Depending on the specific feature, between 11% and 23% of the articles did not report adequate details to code the processes used in their coaching interventions. Of those that did, a clear majority of articles operationalized health or wellness coaching as a process that was fully or partially patient-centered (86%), included patient-determined goals (71%), incorporated self-discovery and active learning processes (63%) (vs more passive receipt of advice), encouraged accountability for behaviors (86%), and provided some type of education to patients along with using coaching processes (91%). Details on these components are described below.
2.1 Patient-centeredness. Was the coaching patient-centered, ie, were coaching strategies and processes tailored to the individual's specific needs, concerns, circumstances, or readiness to change, or was the coaching instead applied uniformly without regard to individual differences? Twenty percent of articles did not provide sufficient detail to judge whether the coaching was patient-centered. Of those articles which gave sufficient detail to allow judgment, 61% described a coaching process that was patient-centered and an additional 25% described a coaching process that was partially patient-centered ( Table 2 ). For example, Hendren et al (2010) tested a coaching intervention that appeared to be fully patient-centered, tailored in both intensity and content to patients' assessed barriers to obtaining care. 41 Others used partially patient-centered processes, including some strategies that were individualized in combination with some standardized processes. Aoun et al (2009), for example, used the patient-centered approach of motivational interviewing in combination with standardized guidelines for weight loss and physical activity. 42
Was the Coaching Patient-centered?
| All Articles (n = 228) | Research and Existing Practice Articles (n = 207) | Conceptual Articles (n = 21) | |
|---|---|---|---|
| Yes | 138 (60.5%) | 119 (57.0%) | 19 (90.0%) |
| Partially | 58 (25.4%) | 57 (27.5%) | 1 (5.0%) |
| No | 32 (14.0%) | 31 (15.5%) | 1 (5.0%) |
Fewer than one out of six articles (14%) described a process that was classified as not at all patient-centered as evidenced by every participant receiving the same intervention without any tailoring or interventions that involved non-individualized instruction or prompting. For example, in one wellness program, coaching for weight loss was provided via highly scripted responses to patient statements. 43 In another intervention, the coaching content involved instructions from pharmacists in the correct use of medications without apparent variation according to the individual's situation. 44
2.2 Patient-determined goals. Did patients choose their own change goals as a target of the coaching, or were their goals preset or created by a professional? Twenty-four percent of articles did not provide sufficient detail to judge whether goals were set by the coaching patients themselves or by others. Of those articles that did allow us to judge, 45% described coaching processes in which patients determined their own goals and 26% reported that patients partially determined their coaching goals ( Table 3 ). Examples of interventions with patient-determined goals include Hanks et al's (1995) study of weekly coaching sessions to support patients' capabilities as new mothers. In this intervention, coaches explored and clarified patients' values, provided information as needed, and encouraged design and commitment to achievable goals while constructing a plan sheet. 45 Examples of programs in which patients partially determined their coaching goals include a primary care-based intervention designed to help older adults adhere to medication for hypertension. Although the overall objective was medication adherence, coaches helped participants choose the barriers and habits they wished to change, set their own specific goals around them, and defined action steps to achieve them. 46 Similarly, a program that had the overall intention of improving participants' exercise persistence supported participants in setting individualized exercise plans. 27
Were the Goals of the Coaching Determined by the Patient?
| All Articles (n = 217) | Research and Existing Practice Articles (n = 197) | Conceptual Articles (n = 20) | |
|---|---|---|---|
| Yes | 97 (44.7%) | 84 (42.6%) | 14 (70.0%) |
| Partially | 56 (25.8%) | 52 (26.4%) | 4 (20.0%) |
| No | 64 (29.5%) | 62 (31.5%) | 2 (10.0%) |
Almost 30% of the literature described a coaching process in which goals were set externally without input from the patients. In Elbers et al's (2011) study of personal injury victims, health coaches executed a physician-driven care plan. 47 Likewise, in Allen et al (2008), all patients were given the goal of preparing for their physician visit. While the intervention was patient-centered, the goals themselves were not self-determined. 48
2.3 Use of self-discovery process. Was there a process of discovery, or active learning, included in the coaching process, or was the coaching instead instructional? Thirty-four percent of articles did not provide sufficient detail to judge whether or not self-discovery was involved in the coaching. Of those that did, 42% of the articles reviewed described a self-discovery process, and an additional 21% described a process that was mixed, ie, partly self-discovery and partly instructional or advice-giving ( Table 4 ). Saleh et al's (2010) study of a rural workplace wellness program engaged patients as active learners through goal setting, action planning, self-monitoring, review of results, and conclusions about persisting with the action plan. 49 Another example is Ottaviano et al's (2010) proposed intervention to promote self-efficacy in patients with coronary heart disease. Here the coach continuously helps the patient assess their readiness to make lifestyle changes. 50
Was There a Self-discovery Process Involved?
| All Articles (n = 188) | Research and Existing Practice Articles (n = 172) | Conceptual Articles (n = 16) | |
|---|---|---|---|
| Yes | 79 (42.0%) | 68 (39.5%) | 11 (68.8%) |
| Partially | 40 (21.3%) | 38 (22.1%) | 2 (12.5%) |
| No | 69 (36.7%) | 66 (38.4%) | 3 (18.8%) |
Thirty-seven percent of the articles did not include self-discovery processes as part of the definition of coaching. Examples where study participants did not engage in self-discovery or active learning include Margolius et al's (2012) study of coaching for hypertension control in a low-income sample. 51 In this program, patients were instructed in the importance of blood pressure control and medication adherence without the opportunity to learn about themselves by exploring the relationship of their hypertension to their own overall health, well-being, or key values and drawing conclusions. Similarly, Ovbiosa et al (2012) described a workplace wellness program for weight reduction where participants received instructions on how to increase their physical activity to a preset target, including general educational handouts and calorie-counting books. 43
2.4 Accountability. Coaching that involves patient accountability is coaching in which it is possible for patients to self-monitor in order to observe their progress (or lack of it) toward their goal using some type of data and that encourages reflection on progress. Thirty-one percent of articles did not provide sufficient detail to judge whether the coaching being evaluated encouraged patient accountability. Of those that did, the vast majority of articles (81%) described a coaching process in which accountability of some form was built in, as shown in Table 5 . In these programs, patients actively monitored their efforts, observed results, either reported them or discussed them with their coach, and drew conclusions. Data collection formats ranged from qualitative self-report using coaching preparation forms 17 , 52 to sophisticated web- programs 31 , 52 and innovative mobile apps. 31 For example, in a study reported by Debar et al (2006), adolescent girls' recordings of their diet and exercise goals and achievements were regularly shared with their peer group and their coach. 53 In another study reported by Wennberg et al (2010), participants in a telephone-based care management intervention signed a behavioral contract with their wellness coaches, and had access to a computer program that tracked progress toward goals through the intervention. 54 An additional 5% of articles described coaching in which accountability was partially built in.
Was Accountability for Results Built Into the Coaching Process?
| All Articles (n = 196) | Research and Existing Practice Articles (n = 184) | Conceptual Articles (n = 12) | |
|---|---|---|---|
| Yes | 159 (81.1%) | 150 (81.5%) | 9 (75.0%) |
| Partially | 9 (4.6%) | 8 (4.3%) | 1 (8.3%) |
| No | 28 (14.3%) | 26 (14.1%) | 2 (16.7%) |
Conversely, 14% of articles described a coaching process where there was no opportunity for patients to be accountable to either themselves (eg, through self-monitoring or observation of change against target) or to their coach (eg, through regularly providing information on progress toward goals and getting feedback). Coaching approaches where the coach and patient met once fell into this category since there is no opportunity for support of behavior change over time. For example, Brook et al (2003, 2005) reported on a program in which pharmacists instructed new users of anti-depressant medication about potential side effects in a one-time visit. 44 , 55
2.5 Content education. Content education refers to providing expert information to the patient to facilitate knowledge and understanding of a specific health condition for which behavior change is desirable (eg, disease information, standardized guidelines for clinical markers, consensus recommendations for behavior change, professional opinions on target goals). Eighteen percent (51 of 284) of articles did not provide sufficient information to determine whether or not content education was provided to coaching participants. Of those that did, 91% documented provision of content education. In terms of the type of education provided to participants, 40% of the interventions provided disease-specific information, while 22% more generically defined their content education as lifestyle or health education or specified teaching about nutrition (19%) or physical activity (18%). Only 8% provided the participants with content education on behavior change processes, such as goal setting and the importance of self-monitoring ( Table 6 ).
Frequency (Percentage) of Given Article Types Providing Content Education to Participants
| Was content education provided? | All Articles (n = 233) | Research and Existing Practice Articles (n = 219) | Conceptual Articles (n = 14) |
|---|---|---|---|
| Yes | 212 (91.0%) | 200 (91.3%) | 12 (85.7%) |
| No | 21 (9.0%) | 19 (8.7%) | 2 (14.3%) |
| Disease or condition-based information | 85 (40.1%) | 82 (41.0%) | 3 (25.0%) |
| Behavior change processes | 16 (7.5%) | 16 (8.0%) | 0 (0.0%) |
| Physical activity or exercise | 39 (18.4%) | 37 (18.5%) | 2 (16.7%) |
| Nutrition | 40 (18.9%) | 38 (19.0%) | 2 (16.7%) |
| General lifestyle and health education | 46 (21.7%) | 44 (22.0%) | 2 (16.7%) |
| Communication with care team | 22 (10.4%) | 19 (9.5%) | 3 (25.0%) |
| Smoking and tobacco-related | 11 (5.2%) | 10 (5.0%) | 1 (8.3%) |
| Other | 4 (1.9%) | 4 (2.0%) | 0 (0.0%) |
| No description of content area | 39 (18.4%) | 35 (17.5%) | 4 (33.3%) |
The depth of content and mode of delivery varied substantially. Common delivery modes for content education included provision of written material (eg, notebooks, pamphlets), static and interactive websites, and in-person visits and classes. Many programs used multiple tactics. For example, one disease management program described mailing quarterly newsletters and disease-specific educational pamphlets to participants with diabetes who were also involved in coaching. 56
2.6 Coaching “Dose.” In the majority of articles reviewed, it was not possible to calculate the “dose” of coaching that was being evaluated in terms of length of individual coaching sessions, number of coaching sessions, or duration of the coaching intervention. Overall, 75% (212 of 284) of the peer-reviewed articles did not specify the length of each individual coaching session, 52% (148 of 284) did not specify the total number of coaching sessions used, and 64% (181 of 284) did not specify the duration of the coaching process. Of those that did specify the session length, sessions lasted for an average of 35.8 minutes, ranging from 5 minutes 57 , 58 to 2.5 hours. 59 Of those that specified the number of coaching sessions, the average reported was 10.1 sessions, ranging from 1 to 90, 60 median = 6. For those articles that reported the length and number of coaching sessions (n = 68), the average contact hours with a coach was 6.2, ranging from 15 minutes 61 to 135 hours, 60 median = 3 hours.
A wide range was also observed in the duration of the entire coaching intervention. As depicted in Table 7 , coaching ranged from a single session to 6 years. For interventions that had a consistent coaching schedule, frequency of coaching ranged from biannual sessions to access to a coach twice per week, with the majority reporting weekly sessions. Coaching frequency appeared to be related to length of the intervention, with shorter programs employing more weekly coaching whereas longer interventions were more likely to use monthly coaching.
Frequency (Percentage) of Given Articles Reporting Various Durations of Coaching
| Duration | All Articles (n = 184) | Research and Existing Practice Articles (n = 181) | Conceptual Articles (n = 3) |
|---|---|---|---|
| 1 session to 1 mo | 22 (12.0%) | 22 (12.2%) | 0 (0.0%) |
| 5 wk to 3 mo | 43 (23.4%) | 42 (23.2%) | 1 (33.33%) |
| 3.5 mo to 6 mo | 46 (25.0%) | 45 (24.9%) | 1 (33.33%) |
| 6.5 mo to 9 mo | 9 (4.9%) | 9 (5.0%) | 0 (0.0%) |
| 10 mo to 12.5 mo | 41 (22.3%) | 40 (22.1%) | 1 (33.33%) |
| 15 mo to 2 y | 19 (10.3%) | 19 (10.5%) | 0 (0.0%) |
| 3 y to 6 y | 4 (2.2%) | 4 (2.2%) | 0 (0.0%) |
2.7 Was there a consistent coaching relationship? Just over half of the articles (154 of 284, or 54%) provided adequate information to assess whether the participant had an ongoing relationship with the same coach over time. Of these articles, 60% (92 of 154 articles) overtly stated that participants were matched with the same coach over multiple sessions, and another 18% (28 of 154) implied a consistent relationship. In contrast to the 78% that thus indicated a consistent relationship was formed, only 21% (32 of 154) of the programs clearly did not pair the same coach with the same participant over time. Of those programs that did not rely on a consistent coaching relationship, a third of the programs only offered a single coaching session, precluding development of a relationship, and the rest either used interchangeable coaches or automated contacts that were algorithm driven.
3. Who Delivers the Coaching?
3.1 Are they professionals? In 13% (38 of 284) of the studies, there was not enough information provided to determine the coaches' professional background. Of the remaining articles, 95% (234 of 246) of the studies/practices employed human coaches, while the remaining 5% (12 of 246) employed technology-based coaching only. Of those that employed human coaches, 93% (217 of 234) used professionals while only 7% (17 of 234) used lay individuals.
3.2 What kind of professionals? Of coaches with professional training, coaches were overwhelmingly medical (53%) and allied health (51%) professionals ( Table 8 ). * Nurses comprised the clear majority of these professionals (42%). Mental health providers were the second most common (21%: divided between 11% psychologists [doctorate level] and 10% social workers and other master's-level psychotherapists). Dieticians were the third most common professionals to provide coaching (11%), with health educators/health promotion experts (8%), unspecified health professionals (8%) and exercise physiologists/specialists (6%) also well-represented.
Frequency (Percentage) of Articles With Given Coach Background
| General Category | Specific Background | All Articles (n = 234) | Research and Existing Practice Articles (n = 212) | Conceptual Articles (n = 22) |
|---|---|---|---|---|
| Physicians | 14 (6.0%) | 11 (5.2%) | 3 (13.6%) | |
| Nurses | 98 (41.9%) | 85 (40.1%) | 13 (59.1%) | |
| Pharmacists | 10 (4.3%) | 9 (4.2%) | 1 (4.6%) | |
| Physician assistants | 1 (0.4%) | 0 (0.0%) | 1 (4.6%) | |
| Medical staff | 1 (0.4%) | 1 (0.5%) | 0 (0.0%) | |
| Dieticians or nutritionists | 26 (11.1%) | 25 (11.8%) | 1 (4.6%) | |
| Psychologists (doctorate level) | 25 (10.7%) | 20 (9.4%) | 5 (22.7%) | |
| Social workers, psychotherapists, counselors (master's level) | 23 (9.8%) | 19 (9.0%) | 4 (18.2%) | |
| All mental health providers | 48 (20.5%) | 39 (18.4%) | 9 (40.9%) | |
| Physio- and physical therapists | 10 (4.3%) | 10 (4.7%) | 0 (0.0%) | |
| Medical assistants | 8 (3.4%) | 7 (3.3%) | 1 (4.6%) | |
| Occupational therapists | 3 (1.3%) | 2 (0.9%) | 1 (4.6%) | |
| Exercise physiologists and exercise specialists | 15 (6.4%) | 15 (7.1%) | 0 (0.0%) | |
| Unspecified or other allied health professionals | 10 (4.3%) | 9 (4.2%) | 1 (4.6%) | |
| Unspecified health professionals | 18 (7.7%) | 14 (6.6%) | 4 (18.2%) | |
| Health educators/promotion | 19 (8.1%) | 17 (8.0%) | 2 (9.1%) | |
| Research assistants | 5 (2.1%) | 5 (2.4%) | 0 (0.0%) | |
| Medical or nursing students | 5 (2.1%) | 5 (2.4%) | 0 (0.0%) | |
| Allied health students | 12 (5.1%) | 12 (5.7%) | 0 (0.0%) | |
| Other students | 1 (0.4%) | 1 (0.5%) | 0 (0.0%) | |
| Health/wellness | 15 (6.4%) | 13 (6.1%) | 2 (9.1%) | |
| Life/lifestyle | 2 (0.9%) | 1 (0.5%) | 1 (4.6%) | |
| Personal vitality | 2 (0.9%) | 2 (0.9%) | 0 (0.0%) | |
| Professional coach | 4 (1.7%) | 4 (1.9%) | 0 (0.0%) |
3.3 Training received by the coaches. We considered both intensity of training and content of training given to coaches for the specific coaching under investigation. As can be seen in Tables 9 and and10, 10 , only 22% (59 of 272) of the articles using human coaches provided information on the amount of training obtained by those performing the coaching ( Figure 3a ). Of these, there was a large range in intensity of coaching-specific training, from less than 2 hours to close to 2 years, median between 6 and 40 hours. At the least intensive end, only 1.5 hours of training were provided to content experts in weight loss and consisted of the rationale for health coaching 62 or 2 hours of coaching-specific training were provided to MD, PharmD, or RN student health coaches to support uninsured patients with hyperten-sion. 63 At the most intensive end, a 9-month curriculum was provided to medical assistants to coach patients with chronic health issues, 64 and an estimated 600 hours of training were provided to non-medical professionals to help newly diagnosed cancer patients navigate the healthcare system and their treatment. 41
Frequency (Percentages) of Given Article Type That Describes Amount of Coaches' Training
| Described Coach's Training (n = 57) | No Information Provided (n = 218) | |
|---|---|---|
| Empirical research | 40 (22.3%) | 139 (77.7%) |
| Protocols | 7 (24.1%) | 22 (75.9%) |
| Existing clinical practices | 4 (10.8%) | 33 (89.2%) |
| Conceptual articles | 6 (20.0%) | 24 (80.0%) |
Frequency of Articles Describing the Training Provided to Coaches
| Amount of Training | No. of articles |
|---|---|
| Described | 57 |
| Not sufficiently described | 218 |
| 1-5 h | 4 |
| 6-15 h | 9 |
| 16-23 h | 10 |
| 24-40 h | 9 |
| 41-79 h | 3 |
| 80-120 h | 6 |
| 4-6 wk, full-time | 5 |
| Greater than 6 wk (eg, 1 y experience plus CDE training, 600 h, ICF certification required) | 5 |
| Variable (ie, articles on multiple coaching programs that noted “variable” amounts) | 5 |
| Total | 57 |
Abbreviations: ICF, International Coaching Federation; CDE, Certified Diabetes Educator.

Frequency of articles reporting various amounts of coach training.
In terms of the specific content of the training received by the coaches, only half (50.4% or 143 of 284) of the articles included descriptive information. Of these, three broad types of training could be identified: (1) behavior change skills, (2) health information briefing (content education), and (3) job training.
3.3.1 Behavior change skills include training in specific behavioral theories and skills used to facilitate behavior change. Table 11 presents these data. Sixty-one percent (87 of 143) of articles in which training content was described reported training coaches in behavior change methods (eg, goal setting, action planning, problem solving, navigating obstacles/barriers to goals, finding resources, self-monitoring, and building self-efficacy) based on multiple theories, including the following: Health Beliefs Model, 65 Social Cognitive Theory, 66 , 67 Theory of Planned Behavior, 68 , 69 the Trans theoretical Model, 70 - 72 Self-Determination Theory, 73 - 75 Self-Perception Theory, 76 and Motivational Enhancement. 77 - 79 Sixty-seven percent of articles reported training coaches in communication skills specifically for developing rapport, expressing empathy, and/or providing emotional support. Sixty-three percent of articles reported training coaches in other communication skills that would enhance the change process: these included the use of powerful questions, assertiveness training, negotiation skills, providing feedback, and various types of reflections including those that emphasize possibilities, underline the positive side of an issue, or high-light the gap between where a patient wants to be and where he or she is now. Note that 42% of articles that documented the content of the coaches' training specifically referred to training in “a communication method” called motivational interviewing (MI). 78 - 80 Training in MI typically includes education in five key skill sets that reflect the “four guiding principles” of MI: expressing empathy, developing discrepancy, rolling with resistance, and supporting self-efficacy. The five key skill sets include (1) use of open-ended questions, (2) affirmations, (3) reflections, (4) summaries that highlight both sides of ambivalence, and (5) reinforcement of the patients use of “change talk.” (For a greater understanding, see the article by Simmons and Wolever in this issue. 80 ) Because MI covers both types of communication strategies coded in our study, we also credited articles that explicitly reported MI training with both types of communication training. In addition to the 42% that reported training in MI, training in other motivational approaches was mentioned by 14% of the articles and an additional 4% specifically noted the use of whole-person approaches. Other motivational techniques included additional aspects of Motivation Enhancement Therapy, patient activation, visioning, and exploration of personal values. Finally, 13% reported training coaches in cognitive behavioral skills (CBT) for working with patients' specific health conditions, including reframing, cognitive restructuring, and CBT-based self-management skills.
Frequency (Percentage) of Articles Describing Content of Training to Professionals and Non-professionals Who Delivered the Coaching
| Content of Training (when described) | All literature (n = 143) | When coaches were professionals (n = 116) | When coaches were non-professionals (n = 19) | When unclear or n/A (n = 8) |
|---|---|---|---|---|
| Behavior change (including training in health behavior models and methods) | 87 (60.8%) | 69 (59.5%) | 14 (73.7%) | 4 (50.0%) |
| Communication skills to develop rapport, express empathy, and provide emotional support | 96 (67.1%) | 78 (67.2%) | 12 (63.2%) | 6 (75.0%) |
| Other communication skills (eg, powerful questions, various types of reflection, negotiation skills, assertive-ness, providing feedback) | 90 (62.9%) | 74 (63.8%) | 11 (57.9%) | 5 (62.5%) |
| Motivational interviewing | 60 (42.0%) | 50 (43.1%) | 5 (26.3%) | 5 (62.5%) |
| Other motivational approaches (eg, other aspects of motivation enhancement therapy, patient activation, visioning, values exploration) | 20 (14.0%) | 16 (13.8%) | 3 (15.8%) | 1 (12.5%) |
| Whole person | 6 (4.2%) | 6 (5.2%) | 0 (0.0%) | 0 (0.0%) |
| Cognitive-behavioral skills, including reframing, cognitive restructuring, and self-management | 18 (12.6%) | 16 (13.8%) | 2 (10.5%) | 0 (0.0%) |
| Exercise or physical activity guidelines, information | 12 (8.4%) | 12 (10.3%) | 0 (0.0%) | 0 (0.0%) |
| Nutrition | 13 (9.1%) | 13 (11.2%) | 0 (0.0%) | 0 (0.0%) |
| Disease- or condition-based information | 52 (36.4%) | 39 (33.6%) | 11 (57.9%) | 2 (25.0%) |
| Protocol-specific training | 39 (27.3%) | 32 (27.6%) | 6 (31.6%) | 1 (12.5%) |
| Navigating the health system | 13 (9.1%) | 10 (8.6%) | 3 (15.8%) | 0 (0.0%) |
3.3.2 Health information briefing includes content education regarding healthy lifestyles (eg, physical activity guidelines, nutrition information) and/or information specific to the disease or health condition under investigation (eg, pathophysiology, onset and course of the illness or condition, treatments). Of those articles that described training content, 36% described briefing coaches with disease-or health condition—specific information (eg, regarding diabetes, heart disease risk, etc). Nine percent described providing coaches with information on nutrition, and 8% of articles described providing coaches with information on physical activity/exercise.
3.3.3 Job training includes training related to the coach's job role (eg, training on clinic flow) or study-specific training (eg, review of protocol). Twenty-seven percent of the articles that described the coach training described protocol-specific training, whereas 9% of articles provided coaches with education on navigating the health system.
POTENTIAL SOURCES OF BIAS
While we evaluated our questions of interest using all the obtained medical literature, we also compared the literature on empirical studies and existing, operationalized practices to the literature that was conceptual only to assess potential sources of bias. Several differences emerged that merit mention. First, as can be seen in Tables 2 through through4, 4 , a considerably higher percentage of conceptual articles fully support a definition of coaching as a patient-centric process that uses patient-determined goals and self-discovery processes. Second, compared to research and existing practice articles, a somewhat lower percentage of conceptual articles discusses the inclusion of accountability mechanisms ( Table 5 ) and proposes content education as part of the coaching intervention ( Table 6 ). Third, the conceptual articles, taken together, posit a more intense training trajectory than do the articles on empirical work and existing practices ( Figure 3b ). Finally, the conceptual articles cite greater use of nurses and mental health providers.

Percentage of research and existing practice articles versus conceptual articles reporting various amounts of coach training.
SUMMARY AND DISCUSSION
Early reviews of the effectiveness of health coaching have called for conceptual and operational clarification of health and wellness coaching. 34 Indeed, as the trajectory of peer-reviewed articles on this approach rapidly increases, continued variability in definitions of health coaching precludes the ability to perform rigorous reviews or meta-analyses. This variability also insures continued confusion over the coaching approach and confounds the skills needed by the rapidly growing number of professionals providing health and wellness coaching. To move the field forward, we must first clarify what the intervention is. With an evidence-based, consensus definition, stronger efficacy and effectiveness studies can ensue, and professional training can be improved. Eventually, we will be able to consistently replicate and widely disseminate the intervention while also assessing the cost:benefit ratio of using health coaching to address the myriad behavior changes needed to prevent and manage chronic disease.
Defining Health and Wellness Coaching
Our analysis used a comprehensive, systematic review to evaluate well over 200 peer-reviewed empirical articles and close to 70 expert opinions available in the peer-reviewed medical literature to form the foundation of a definition for health and wellness coaching that can be broadly accepted and adopted for future use. Despite the evident variability in use of the terms health coaching and wellness coaching , our systematic study of the state of academic knowledge on health and wellness coaching reveals areas of consensus emerging in the literature, as well as areas that need clarification for the field to move forward. In sum, the emerging consensus defines the conceptual and interventional components of health and wellness coaching as
a patient-centered approach wherein patients at least partially determine their goals, use self-discovery or active learning processes together with content education to work toward their goals, and self-monitor behaviors to increase accountability, all within the context of an interpersonal relationship with a coach. The coach is a healthcare professional trained in behavior change theory, motivational strategies, and communication techniques, which are used to assist patients to develop intrinsic motivation and obtain skills to create sustainable change for improved health and well-being.
Specifically, 86% of the articles describe health and wellness coaching as a process that is patient-centered. Seventy-one percent describe coaching as an intervention that supports patients' pursuit of self-identified goals (rather than goals prescribed by the provider). Sixty-three percent define coaching as a process in which the patient is an active learner whose own self-discovery process is supported to resolve problems, overcome challenges, and negotiate barriers to goals. Eighty-six percent of articles describe specific mechanisms to support patient accountability for behavior change through various self-monitoring techniques and reporting back to their coach. Seventy-eight percent of articles describe coaching that occurs in the context of a consistent ongoing relationship with a human coach designated to play a defined role.
The definition of health coaching emerging from the peer-reviewed literature is consistent with the evolving science of human motivation and the psycho-social underpinnings of sustainable behavioral change. There is evidence that behavior change and learning occur most reliably when there is a helping relationship that (1) acknowledges the individual, (2) is collaborative, and (3) encourages active learning. (See Dill and Gumpert for review. 81 ) Reaching back to the theoretical roots of Adler, 82 , 83 Jung, 84 , 85 and Rogers, 86 health and wellness coaching conceptualizes patients as lifelong learners whose individual personal values and innate internal resources can be cultivated in the context of a supportive relationship to guide them toward their own desired vision of health. 87 , 88
This systematic review takes the field an important step forward, yet we need to further upgrade the science to better evaluate health and wellness coaching. It is concerning that up to a third of the articles did not describe the actual coaching methods used, making it impossible to fully evaluate or replicate specific processes. Further, only a small minority of articles provided information that allows for calculation of a coaching “dose” (25% reported length of each individual coaching session, 48% reported the number of coaching sessions delivered, 36% reported the duration of the coaching process, and very few reported all three.) Going forward and until there is a well-accepted international standard to determine competency in health and wellness coaching, it is imperative that publications report the theories on which interventions are based and fully describe the processes, techniques, and intensity of the intervention being investigated. To move the field ahead, empirical articles must describe the approaches they are evaluating in a way that allows replication. With a consensus definition of health and wellness coaching in place, we will be able to understand what components of coaching are essential to affect health outcomes and health behavior change in general. For example, it will be of great interest to revisit the issue of whether health coaching will be consistently effective at promoting health change if health coaching is defined, as by this consensus, as patient-centered and incorporating patient-determined goals, self-discovery processes, accountability mechanisms, and content information, in the context of an ongoing helping relationship.
We also will be able to understand what components, at what “dose,” can be adapted in what way, to affect health outcomes and health behavior change for specific patient populations and specific illnesses or conditions. We have statistical capability to evaluate the impact of individual components of heterogeneous interventions. For example, Michie (2009) found strong evidence for the efficacy of the following specific interventions in the behavioral change literature on dietary intake and physical activity: self-monitoring of behavior, prompting intention formation, prompting specific goal setting, providing feedback on performance, and prompting participants to review behavioral goals. 89 Also, Olsen and Nesbitt (2010) found evidence that four specific interventions were the effective components of health coaching programs: (1) goal setting, (2) selected components of motivational interviewing, (3) collaborations with healthcare providers, and (4) program durations of 6 to 12 months. 34 In the near future, we look forward to being able to define best practices in health and wellness coaching applied to specific populations and specific targets for health outcomes and health behavior change.
Who Delivers Health Coaching?
While the specific professional background of health and wellness coaches is diverse, there is an emerging consensus in the literature that coaching be provided by health professionals (currently a diverse range is represented) who, further, have specific training in coaching processes and not only expertise in the knowledge base of their profession. Coaches' training, when described, fell in the general categories of behavior change skills, health information briefing, and job training. However, it is of significant concern that only half of the articles provided descriptions of the content of coaches' training for the specific study, and only 22% of articles reported on the extent of training received by the coaches. As previously stated, if we are to move the field of health coaching forward, empirical articles must describe the approaches they are evaluating in a way that allows replication; this includes concrete descriptions of content and intensity of training provided and/or evidence by replicable standards that coaches had achieved a level of competence relevant for the coaching they delivered. However, if we refer to the emerging consensus definition of what health and wellness coaching is , we can extrapolate coaches' necessary core competencies with the caveat that their effect on health outcomes remains to be determined.
First, coaches must have training in a model of change that is patient-centered , and based on facilitating the patient's personal change process, rather than dictating it. Coaches must also have the interpersonal skills to understand the unique values, motivations, resources, and obstacles that the patient brings to the change process and the ability to express their understanding effectively. Second, and along similar lines, the coach must be able to help patients identify their own goals for change that are personally important and achievable. Third, coaches must be trained in the use of a self-discovery process that facilitates patients working toward their goals through exploration and an active learning process rather than by dictating what should be done. Fourth, coaches must understand how to help patients be accountable to themselves and monitor their progress. Finally, coaches must have the relevant content knowledge to help their patients with the above four processes in the arena of change. Coaches also must have the interpersonal skill to integrate the content information into the patient's change process rather than dictating it. These competencies require not only use of multiple communication skills and empowerment strategies, but also require a consistent stance on the part of the coach to simultaneously hold the patient's agenda, convey that the patient is resourceful and a lifelong learner, and guide them toward sound health decisions without advising, all the while respecting patients as the best experts on what may work best in their individual lives.
It is critical to note that this paradigm is distinct from that of conventional medicine. 87 As well-explicated in Linden, Butterworth, and Prochaska (2010), typical disease management interventions often employ healthcare professionals who do not necessarily value patient empowerment, who may not have exposure to or adequate training in the science of behavioral change, and who may not have the complex interpersonal skills to facilitate behavior change effectively. 90 This leaves those trained in the conventional medical model vulnerable to using approaches that are expert-driven, authoritarian, and advice-giving as opposed to taking stances that are supported by the latest research in behavior change models. 87 , 91 , 92 Thus, we conclude that specific training in these core competencies and credentialing will be necessary if coaches are to deliver health and wellness coaching as described in this consensus definition.
Areas for Further Investigation
Next steps..
The most recent prior review of the effectiveness of health coaching reviewed only 15 articles and concluded that the body of literature as a whole was inconclusive due to theoretical and methodological issues. 34 It will be of great interest to revisit the issue of whether health coaching will be consistently effective at promoting health change now that we have a much larger body of work to review (284 articles), and if health coaching is defined, as by this consensus, as patient-centered, incorporating patient-determined goals, self-discovery processes, accountability, and content information, in the context of an ongoing helping relationship. This unified assessment will be fundamental to establishing the merit of this approach to helping people achieve good health outcomes and change their health behaviors. We also will be able to understand what components of health and wellness coaching, at what “doses,” can be adapted in what way to best promote health outcomes and health behavior change for specific patient populations and specific illnesses or conditions. Several other areas within health and wellness coaching merit more rigorous study, including the role of the coach, individualized vs protocol-driven coaching, and the integration of technology into coaching.
Role of the coach.
One issue for future investigation is the role of the coach and specifically whether one coach can play multiple roles effectively. Of the literature that provided sufficient information to determine the presence of content education for participants, 91% included content education as a key addition to the coaching process. It was not uncommon to see coaching provided as an adjunct to educational modules, as well as to observe education components provided to a primarily coaching intervention. As multiple authors have distinguished between educating and coaching, 28 , 87 , 91 it is undoubtedly important to differentiate the processes. When the health coach is providing information within the context of coaching, plainly defined processes need to be outlined. For example, one component of motivational interviewing, an approach that can be used within the coaching process, 89 emphasizes the importance of obtaining permission to present information. 78 Indeed, asking permission has also been found empirically to benefit the coaching process and serves to empower the patient. 92
A second option identified as a way to provide education in the context of coaching is that of presenting information as tentative and for consideration of possibilities rather than as directive knowledge. 92 This distinction highlights the import of training coaches in skills designed to incorporate educational information so that the process remains patient-centered. Relatedly, there is a stark lack of clarity in the literature regarding the role of health coaches as educators and whether the same person can effectively serve in both roles simultaneously while still ensuring the coaching process is patient-centered. For example, if a healthcare provider is both coaching and educating, a patient may defer to this person's expertise and assume that the education provided is what “should” be done, even if it conflicts with the individual's values, readiness, or desires around the behavior. This raises the need for a clear division of roles with commensurate professional training. Whether the psychological (eg, building self-efficacy) and behavioral (eg, setting goals that are consistent with values) strategies used in health coaching complement or conflict with simultaneous delivery of content information is an intriguing question. It seems that both can be used to the benefit of the patient, however, the best mechanism for delivering these strategies is yet to be determined. Assessing whether, and if so how, the health coach provides content information will be critical to defining health or wellness coaching best practices.
Similarly, in a setting where the provider is serving a dual role as clinician and coach, further investigation into what constitutes the coaching segment of a visit and how that looks different from the clinical care component of the visit will be essential to understanding how such a brief encounter might work. At least 13 articles alluded to the role of the coach as someone to help patients navigate some aspect of the health system. This role presents yet another potential conflict for patient-centered guidance wherein the coach supports, but does not “do for” the patient. Each of these approaches will look different, emphasize different skills, and needs to be carefully considered to ensure that coaches receive the appropriate training to differentiate roles and protect patients. Moreover, there likely will need to be a patient-education component of this approach, where patients learn how coaching is being integrated into a clinical visit, what their “job” or “role” is in this encounter, and how that looks different from when they are receiving information about their health.
Individualized vs protocol-driven coaching
Another area for further investigation is the delicate balance between conducting patient-centric, highly individualized approaches and using more standardized, protocol-based approaches to health and wellness coaching. Of the articles that provided descriptions of the actual coaching processes, a number of them included a more generalized approach with set protocols and prompts that were disease-specific in some cases but not based on the individual needs or values of the participant. Some might argue that such a standardized approach is easier to describe, disseminate, measure, and ultimately compare. However, our review indicates that there are examples of individualized processes that can be standardized with the same effect. For example, although only emerging in the past decade, one brand of integrative health coaching has been well described, standardized within a framework that allows for individual tailoring, 87 , 88 and shown to be effective. 17 , 21 , 93 , 94 Perhaps the best example of standardization of individually tailored processes is seen in motivational interviewing; the MI processes have been well described, standardized within a framework, widely disseminated, and demonstrated to be effective in many settings. 9 , 78 , 79 , 90 , 95 - 97 Moreover, motivational interviewing has the advantage of several psychometrically sound program evaluation measures (eg, Motivational Interviewing Skills Code, 98 Motivational Interviewing Treatment Integrity 99 ) that can be used to ensure intervention integrity and assess intervention outcomes for common threats to validi-ty. 9 While motivational interviewing uses only a subset of skills needed in health or wellness coaching, 80 it serves as an excellent example of how general processes that are used in highly individualized ways can be thoroughly described and well-validated.
Integrating technology into coaching.
Some articles used the term coaching to describe interventions in which there are actually no human providers. Instead, technology (eg, computer programs, algorithm-driven text messages) was used to drive the behavior change process. While there is no doubt that technology provides myriad potential advantages, close to four in five articles posit coaching as a relationship-based approach. We propose that technology has a definite role in supporting individuals in the process of behavior change, particularly in facilitating the process of self-monitoring, the most strongly supported behavior change technique studied at least for eating and physical activity. 89 Many practices described the use of technology including text-based messaging, mobile applications, websites, and even sensor technology (eg, ear buds, wristbands) to facilitate accumulation and tracking of data on behaviors of interest. For example, in the Davis et al study, a TriFit machine was the primary means for tracking data. 100 Despite the important contribution of technology to self-monitoring, three-quarters of the articles stated or implied (78%) that participants were matched with the same coach over multiple sessions whereas a consistent relationship was not developed with a coach about a fifth of the time. Though multiple theorists describe the health and wellness coaching process as building on the critical foundation of a human relationship, further research is needed to determine the degree to which the relationship itself is seminal in facilitating personal learning. The value of human connection to facilitate deep learning is well-described in other evidence bases. 101 In the health and wellness coaching literature, qualitative studies have noted the power of interpersonal support in building courage to try new behaviors, 102 in strengthening a sense of accountability toward the other person (coach), 103 , 104 and in developing a sense of empowerment. 92 Additionally, interpersonal interactions may be necessary for participants to move from cognitive understanding of ambivalence, motivators, and barriers to change to a deeper, “felt sense” understanding more likely to sustain behav-ior. 81 , 101 The potential role of relationship in this emerging approach remains an important area for further exploration.
CONCLUSIONS
This study is not without its limitations. Indeed, for each of the domains for which we abstracted data, there were data missing because the authors did not provide the information in their report. First, we included all studies of health coaching, even when there were multiple reports of the same intervention. This may have inflated certain counts of the various domains of coaching reported. Second, although two to three investigators reviewed each study, there were many instances in which the team made judgment calls regarding a particular domain of the coaching based on limited descriptions in the articles that may or may not have been what was actually implemented. Thus, our review may have mischaracterized some of the coaching interventions in the literature. Third, and relatedly, for several of the review questions for which we abstracted data, anywhere from 11% to 78% of articles did not describe the pertinent domain in sufficient detail to allow us to code them. Finally, our methods included only articles in the PubMed database. Though we expect the vast majority of health and wellness coaching articles to be indexed within PubMed, we are aware that some relevant articles may exist outside this database. Thus, the picture presented here likely does not fully reflect all of the coaching models in the literature. Similarly, health coach training paradigms and programs that are not reflected in PubMed are also not reflected in this systematic review.
Despite these limitations, our systematic review of health and wellness coaching is the first in the literature to characterize this growing field in healthcare. Variation in approaches and practices that have been defined and operationalized as health or wellness coaching makes it difficult to compare approaches and identify those that are most effective for chronic disease prevention and management. Indeed, our findings point to the critical need for future systematic investigations of the effectiveness of various health and wellness coaching approaches in order to identify the best practices in the field, further refine the definition, and iteratively operationalize health or wellness coaching in research and practice. These “best practices” should include both the coach's minimum necessary skills and the coaching processes that facilitate a patient-centric approach to behavioral change. Moreover, future reports of coaching interventions should aim to describe in as much detail as possible the coaching intervention, including a thorough description of the individuals providing coaching with professional background and coaching-specific training, and the breadth and depth of the skills and processes used. These detailed descriptions will enable robust comparison of approaches across disease states and populations, so that a compendium of coaching models that have proven most effective can be generated and disseminated. These efforts will help to ensure that health and wellness coaching is an evidence-based practice that can make a demonstrable difference in the prevention and management of chronic disease in healthcare systems worldwide.
Acknowledgments
We wish to acknowledge the support of Kathy Buarotti in tracking and securing articles and Anita Bhat for her early participation in brainstorming about this review.
Disclosures The authors completed the ICMJE Form for Potential Conflicts of Interest and declared no relevant conflicts.
* Since we could find no consensus among professional organizations about which professions constitute “medical” or “allied health” professions, we chose a common view to classify professionals as indicated on Wikipedia. We thus categorized the professional background of the coaches into six groups: (1) medical professionals (eg, physicians, nurses, pharmacists), (2) allied health professionals (eg, dieticians, psychologists, social workers, physiotherapists, medical assistants, occupational therapists, and exercise physiologists), (3) other health professionals (eg, health educators, medical or allied health students), (4) professional coaches (eg, health, wellness, life), (5) various providers noted in same article but not quantified (eg, used two or more coaches from two or more professional backgrounds), and (6) no information provided. Fourteen articles discussed peer coaching, although 11 of them were excluded because they covered only peer coaching rather than also including coaching provided by professionals.
Contributor Information
Ruth Q. Wolever, Duke Integrative Medicine, Duke University Health System, Durham, North Carolina and Department of Psychiatry and Behavioral Science, Duke School of Medicine, Durham, NC, United States.
Leigh Ann Simmons, Duke Integrative Medicine, Duke University Health System, Durham, North Carolina and Duke School of Nursing, Durham, United States.
Gary A. Sforzo, Department of Exercise and Sport Sciences, School of Health Science and Human Performance, Ithaca College, Ithaca, NY, United States.
Diana Dill, Working Together For Health, Boston, Massachusetts, United States.
Miranda Kaye, Department of Exercise and Sport Sciences, School of Health Science and Human Performance, Ithaca College, Ithaca, NY, United States.
Elizabeth M. Bechard, Duke Integrative Medicine, Duke University Health System, Durham, North Carolina, United States.
Mary Elaine Southard, Integrative Health Consulting and Coaching, LLC, Scranton, Pennsylvania, United States.
Mary Kennedy, Institute of Lifestyle Medicine, Department of Physical Medicine and Rehabilitation at Spaulding Rehabilitation Hospital, Boston, Massachusetts, United States.
Justine Vosloo, Department of Exercise and Sport Sciences, School of Health Science and Human Performance, Ithaca College, Ithaca, NY, United States.
Nancy Yang, Duke School of Nursing, Durham, United States.

- Bahasa Indonesia
- Eastern Europe
- Moscow Oblast
Elektrostal
Elektrostal Localisation : Country Russia , Oblast Moscow Oblast . Available Information : Geographical coordinates , Population, Altitude, Area, Weather and Hotel . Nearby cities and villages : Noginsk , Pavlovsky Posad and Staraya Kupavna .
Information
Find all the information of Elektrostal or click on the section of your choice in the left menu.
- Update data
| Country | |
|---|---|
| Oblast |
Elektrostal Demography
Information on the people and the population of Elektrostal.
| Elektrostal Population | 157,409 inhabitants |
|---|---|
| Elektrostal Population Density | 3,179.3 /km² (8,234.4 /sq mi) |
Elektrostal Geography
Geographic Information regarding City of Elektrostal .
| Elektrostal Geographical coordinates | Latitude: , Longitude: 55° 48′ 0″ North, 38° 27′ 0″ East |
|---|---|
| Elektrostal Area | 4,951 hectares 49.51 km² (19.12 sq mi) |
| Elektrostal Altitude | 164 m (538 ft) |
| Elektrostal Climate | Humid continental climate (Köppen climate classification: Dfb) |
Elektrostal Distance
Distance (in kilometers) between Elektrostal and the biggest cities of Russia.
Elektrostal Map
Locate simply the city of Elektrostal through the card, map and satellite image of the city.
Elektrostal Nearby cities and villages
Elektrostal Weather
Weather forecast for the next coming days and current time of Elektrostal.
Elektrostal Sunrise and sunset
Find below the times of sunrise and sunset calculated 7 days to Elektrostal.
| Day | Sunrise and sunset | Twilight | Nautical twilight | Astronomical twilight |
|---|---|---|---|---|
| 8 June | 02:43 - 11:25 - 20:07 | 01:43 - 21:07 | 01:00 - 01:00 | 01:00 - 01:00 |
| 9 June | 02:42 - 11:25 - 20:08 | 01:42 - 21:08 | 01:00 - 01:00 | 01:00 - 01:00 |
| 10 June | 02:42 - 11:25 - 20:09 | 01:41 - 21:09 | 01:00 - 01:00 | 01:00 - 01:00 |
| 11 June | 02:41 - 11:25 - 20:10 | 01:41 - 21:10 | 01:00 - 01:00 | 01:00 - 01:00 |
| 12 June | 02:41 - 11:26 - 20:11 | 01:40 - 21:11 | 01:00 - 01:00 | 01:00 - 01:00 |
| 13 June | 02:40 - 11:26 - 20:11 | 01:40 - 21:12 | 01:00 - 01:00 | 01:00 - 01:00 |
| 14 June | 02:40 - 11:26 - 20:12 | 01:39 - 21:13 | 01:00 - 01:00 | 01:00 - 01:00 |
Elektrostal Hotel
Our team has selected for you a list of hotel in Elektrostal classified by value for money. Book your hotel room at the best price.
| Located next to Noginskoye Highway in Electrostal, Apelsin Hotel offers comfortable rooms with free Wi-Fi. Free parking is available. The elegant rooms are air conditioned and feature a flat-screen satellite TV and fridge... | from | |
| Located in the green area Yamskiye Woods, 5 km from Elektrostal city centre, this hotel features a sauna and a restaurant. It offers rooms with a kitchen... | from | |
| Ekotel Bogorodsk Hotel is located in a picturesque park near Chernogolovsky Pond. It features an indoor swimming pool and a wellness centre. Free Wi-Fi and private parking are provided... | from | |
| Surrounded by 420,000 m² of parkland and overlooking Kovershi Lake, this hotel outside Moscow offers spa and fitness facilities, and a private beach area with volleyball court and loungers... | from | |
| Surrounded by green parklands, this hotel in the Moscow region features 2 restaurants, a bowling alley with bar, and several spa and fitness facilities. Moscow Ring Road is 17 km away... | from | |
Elektrostal Nearby
Below is a list of activities and point of interest in Elektrostal and its surroundings.
Elektrostal Page
| Direct link | |
|---|---|
| DB-City.com | Elektrostal /5 (2021-10-07 13:22:50) |

- Information /Russian-Federation--Moscow-Oblast--Elektrostal#info
- Demography /Russian-Federation--Moscow-Oblast--Elektrostal#demo
- Geography /Russian-Federation--Moscow-Oblast--Elektrostal#geo
- Distance /Russian-Federation--Moscow-Oblast--Elektrostal#dist1
- Map /Russian-Federation--Moscow-Oblast--Elektrostal#map
- Nearby cities and villages /Russian-Federation--Moscow-Oblast--Elektrostal#dist2
- Weather /Russian-Federation--Moscow-Oblast--Elektrostal#weather
- Sunrise and sunset /Russian-Federation--Moscow-Oblast--Elektrostal#sun
- Hotel /Russian-Federation--Moscow-Oblast--Elektrostal#hotel
- Nearby /Russian-Federation--Moscow-Oblast--Elektrostal#around
- Page /Russian-Federation--Moscow-Oblast--Elektrostal#page
- Terms of Use
- Copyright © 2024 DB-City - All rights reserved
- Change Ad Consent Do not sell my data

COMMENTS
2. Definitions of Physical Activity, Exercise, Training, Sport, and Health. Definitions and terms are based on "Physical activity in the prevention and treatment of disease" (FYSS, www.fyss.se [Swedish] []), World Health Organization (WHO) [] and the US Department of Human Services [].The definition of physical activity in FYSS is: "Physical activity is defined purely physiologically, as ...
Abstract. Purpose of review: The health benefits of physical activity and exercise are clear; virtually everyone can benefit from becoming more physically active. Most international guidelines recommend a goal of 150 min/week of moderate-to-vigorous intensity physical activity. Many agencies have translated these recommendations to indicate ...
Health is a state of complete physical, mental and social well-being and not merely absence of disease [ 1 ]. Fitness is an ability to execute daily functional activities with optimal performance, endurance, and strength to manage minimalist of disease, fatigue, stress and reduced sedentary behavior [ 2 ]. In the modern era with advancement in ...
A review of SRs of Tai Chi studies found fair evidence for increased well-being as a result of participation in Tai Chi but not excellent or good evidence as found for other health outcomes . A review of reviews found that walking programs improved psychological well-being and subjective well-being, although findings varied in effectiveness and ...
changes take place or have already taken place, such as menopause and andropause, which involve. diverse psychological impacts and, frequently, physiological changes. A loss of bone mass, for ...
Level of physical activity. Recommendations regarding the level of PA required for physical health benefits and the prevention of chronic disease, across the lifespan, are well established (U.S. Department of Health and Human Services, Citation 2018).It is recommended that children and adolescents aged 6-17 years engage in PA of moderate to vigorous intensity for a minimum of 60 min per day.
Background Sedentary lifestyle is a major risk factor for noncommunicable diseases such as cardiovascular diseases, cancer and diabetes. It has been estimated that approximately 3.2 million deaths each year are attributable to insufficient levels of physical activity. We evaluated the available evidence from Cochrane systematic reviews (CSRs) on the effectiveness of exercise/physical activity ...
Background: The purpose was to: 1) perform a systematic review of studies examining the relation between physical activity, fitness, and health in school-aged children and youth, and 2) make recommendations based on the findings. Methods: The systematic review was limited to 7 health indicators: high blood cholesterol, high blood pressure, the metabolic syndrome, obesity, low bone density ...
The links between increased participation in Physical Activity (PA) and improvements in health are well established. As this body of evidence has grown, so too has the search for measures of PA with high levels of methodological effectiveness (i.e. validity, reliability and responsiveness to change). The aim of this "review of reviews" was to provide a comprehensive overview of the ...
Muscle fitness is widely recognized as a key fitness component for maintaining overall health and is negatively correlated with obesity 66.In this review, five studies confirmed the effects of ...
1. Our review found that the term "fitness professional" is being used inconsistently to refer to a broad range of occupational roles. For example, these include the related roles of "personal trainer," "fitness instructor," "exercise referral specialist," and many more.
Physical activity reduces cardiovascular risk through lowering of blood pressure, improved glucose tolerance, reduced obesity, improvement in lipid profile, enhanced fibrinolysis, improved endothelial function and enhanced parasympathetic autonomic tone. Conclusion: Physical exercise has many health benefits and the evidence for this continues ...
Find methods information, sources, references or conduct a literature review on PHYSICAL FITNESS Science topics: Medicine Public Health Health Education and Promotion Health Education Physical Fitness
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses reporting guidelines (Liberati et al., 2009). We searched PubMed, Ovid MEDLINE, CINAHL, Bibliography of Native North Americans, and the University of New Mexico's Native Health Databases using keywords and medical subject head-
In 2008 a second systematic review of literature examining the relation between physical activity and key fitness and health outcomes within school-aged children and youth was published. This systematic review was part of the "Physical Activity Guidelines for Americans" project that was undertaken by the Unites States Department of Health and ...
The literature review summary has 4 main sections. This Introduction provides background information about the rationale for focusing on older adults and the process for reviewing the literature and developing the conclusions. The Methods utilized by the Literature Review Team are detailed in the following section.
The purpose was to: 1) perform a systematic review of studies examining the relation between physical activity, fitness, and health in school-aged children and youth, and 2) make recommendations based on the findings. The systematic review was limited to 7 health indicators: high blood cholesterol, high blood pressure, the metabolic syndrome, obesity, low bone density, depression, and injuries.
health services, and more focus is needed on the positive contribution that exercise can exert on life and recovery from mental illness (Mason and Holt, 2012). This literature review will describe evidence-based research that explore the benefits of exercise on mental health. It will integrate evidence connected to the relationship between
A traditional literature review of the academic, policy, and gray literatures was conducted between October 2012 - October 2015. The purpose of this type of review is to analyze a large
40 Facts About Elektrostal. Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to ...
Elektrostal is a city in Moscow Oblast, Russia, located 58 kilometers east of Moscow. Elektrostal has about 158,000 residents. Mapcarta, the open map.
The Moscow oblast is the most highly developed and most populated region in Russia. There was a legend that Moscow was built upon seven hills, just like Rome, was exaggerated, and the truth is that there are a only few small hills in and around the city center. In the southwest corner of the city, there is an upland region, called the ...
The most recent prior review of the effectiveness of health coaching reviewed only 15 articles and concluded that the body of literature as a whole was inconclusive due to theoretical and methodological issues. 34 It will be of great interest to revisit the issue of whether health coaching will be consistently effective at promoting health ...
Elektrostal Geography. Geographic Information regarding City of Elektrostal. Elektrostal Geographical coordinates. Latitude: 55.8, Longitude: 38.45. 55° 48′ 0″ North, 38° 27′ 0″ East. Elektrostal Area. 4,951 hectares. 49.51 km² (19.12 sq mi) Elektrostal Altitude.