Featured Topics
Featured series.
A series of random questions answered by Harvard experts.

Explore the Gazette
Read the latest.

‘Harvard Thinking’: Facing death with dignity

Novel teamwork, promising results for glioblastoma treatment

Study of 4.3M pregnant women clarifies safety of antiseizure meds
Research shows working out gets inflammation-fighting t cells moving.
Ekaterina Pesheva
HMS Communications
Activated by regular exercise, immune cells in muscles found to fend off inflammation, enhance endurance in mice
The connection between exercise and inflammation has captivated the imagination of researchers ever since an early 20th-century study showed a spike of white cells in the blood of Boston marathon runners following the race.
Now, a new Harvard Medical School study published Friday in Science Immunology may offer a molecular explanation behind this century-old observation.
The study, done in mice, suggests that the beneficial effects of exercise may be driven, at least partly, by the immune system. It shows that muscle inflammation caused by exertion mobilizes inflammation-countering T cells, or Tregs, which enhance the muscles’ ability to use energy as fuel and improve overall exercise endurance.
Long known for their role in countering the aberrant inflammation linked to autoimmune diseases, Tregs now also emerge as key players in the body’s immune responses during exercise, the research team said.
“The immune system, and the T cell arm in particular, has a broad impact on tissue health that goes beyond protection against pathogens and controlling cancer. Our study demonstrates that the immune system exerts powerful effects inside the muscle during exercise,” said study senior investigator Diane Mathis , professor of immunology in the Blavatnik Institute at HMS.
Mice are not people, and the findings remain to be replicated in further studies, the researchers cautioned. However, the study is an important step toward detailing the cellular and molecular changes that occur during exercise and confer health benefits.
Understanding the molecular underpinnings of exercise
Protecting from cardiovascular disease, reducing the risk of diabetes, shielding against dementia. The salutary effects of exercise are well established. But exactly how does exercise make us healthy? The question has intrigued researchers for a long time.
The new findings come amid intensifying efforts to understand the molecular underpinnings of exercises. Untangling the immune system’s involvement in this process is but one aspect of these research efforts.
“Our research suggests that with exercise, we have a natural way to boost the body’s immune responses to reduce inflammation.” Diane Mathis, professor of immunology in the Blavatnik Institute
“We’ve known for a long time that physical exertion causes inflammation, but we don’t fully understand the immune processes involved,” said study first author Kent Langston, a postdoctoral researcher in the Mathis lab. “Our study shows, at very high resolution, what T cells do at the site where exercise occurs, in the muscle.”
Most previous research on exercise physiology has focused on the role of various hormones released during exercise and their effects on different organs such as the heart and the lungs. The new study unravels the immunological cascade that unfolds inside the actual site of exertion — the muscle.
T cell heroes and inflammation-fueling villains
Exercise is known to cause temporary damage to the muscles, unleashing a cascade of inflammatory responses. It boosts the expression of genes that regulate muscle structure, metabolism, and the activity of mitochondria, the tiny powerhouses that fuel cell function. Mitochondria play a key role in exercise adaptation by helping cells meet the greater energy demand of exercise.
In the new study, the team analyzed what happens in cells taken from the hind leg muscles of mice that ran on a treadmill once and animals that ran regularly. Then, the researchers compared them with muscle cells obtained from sedentary mice.
The muscle cells of the mice that ran on treadmills, whether once or regularly, showed classic signs of inflammation — greater activity in genes that regulate various metabolic processes and higher levels of chemicals that promote inflammation, including interferon.
Both groups had elevated levels of Treg cells in their muscles. Further analyses showed that in both groups, Tregs lowered exercise-induced inflammation. None of those changes were seen in the muscle cells of sedentary mice.
However, the metabolic and performance benefits of exercise were apparent only in the regular exercisers — the mice that had repeated bouts of running. In that group, Tregs not only subdued exertion-induced inflammation and muscle damage, but also altered muscle metabolism and muscle performance, the experiments showed. This finding aligns with well-established observations in humans that a single bout of exercise does not lead to significant improvements in performance and that regular activity over time is needed to yield benefits.
The hind leg muscles of mice lacking Treg cells (right) showed prominent signs of inflammation after regular exercise, compared with those from mice with intact Tregs (left). The research showed such that this uncontrolled inflammation negatively impacted muscle metabolism and function.
Credit: Kent Langston/Mathis Lab, HMS
Further analyses confirmed that Tregs were, indeed, responsible for the broader benefits seen in regular exercisers. Animals that lacked Tregs had unrestrained muscle inflammation, marked by the rapid accumulation of inflammation-promoting cells in their hind leg muscles. Their muscle cells also had strikingly swollen mitochondria, a sign of metabolic abnormality.
More importantly, animals lacking Tregs did not adapt to increasing demands of exercise over time the way mice with intact Tregs did. They did not derive the same whole-body benefits from exercise and had diminished aerobic fitness.
These animals’ muscles also had excessive amounts of interferon, a known driver of inflammation. Further analyses revealed that interferon acts directly on muscle fibers to alter mitochondrial function and limit energy production. Blocking interferon prevented metabolic abnormalities and improved aerobic fitness in mice lacking Tregs.
“The villain here is interferon,” Langston said. “In the absence of guardian Tregs to counter it, interferon went on to cause uncontrolled damage.”
Interferon is known to promote chronic inflammation, a process that underlies many chronic diseases and age-related conditions and has become a tantalizing target for therapies aimed at reducing inflammation. Tregs have also captured the attention of scientists and industry as treatments for a range of immunologic conditions marked by abnormal inflammation.
The study findings provide a glimpse into the cellular innerworkings behind exercise’s anti-inflammatory effects and underscore its importance in harnessing the body’s own immune defenses, the researchers said.
There are efforts afoot to design interventions targeting Tregs in the context of specific immune-mediated diseases. And while immunologic conditions driven by aberrant inflammation require carefully calibrated therapies, exercise is yet another way to counter inflammation, the researchers said.
“Our research suggests that with exercise, we have a natural way to boost the body’s immune responses to reduce inflammation,” Mathis said. “We’ve only looked in the muscle, but it’s possible that exercise is boosting Treg activity elsewhere in the body as well.”
Co-investigators included Yizhi Sun, Birgitta Ryback, Bruce Spiegelman, Amber Mueller, and Christophe Benoist.
The work was funded by National Institutes of Health grants R01 AR070334, F32 AG072874, and F32 AG069363; and by the JPB Foundation.
Share this article
You might like.
In podcast episode, a chaplain, a bioethicist, and a doctor talk about end-of-life care

Researchers cite ‘academic medicine’ as key factor in success

Using 20 years of data, prenatal exposure to topiramate may not increase children’s risk of autism spectrum disorder
Aspirin cuts liver fat in trial
10 percent reduction seen in small study of disease that affects up to a third of U.S. adults
Parkinson’s warning in skin biopsy
Medical office procedure identifies key biomarker that may lead to more reliable diagnosis of neurodegenerative disorders
So what exactly makes Taylor Swift so great?
Experts weigh in on pop superstar's cultural and financial impact as her tours and albums continue to break records.
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
Scientists chart how exercise affects the body
Press contact :, media download.

*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."

Previous image Next image
Exercise is well-known to help people lose weight and avoid gaining it. However, identifying the cellular mechanisms that underlie this process has proven difficult because so many cells and tissues are involved.
In a new study in mice that expands researchers’ understanding of how exercise and diet affect the body, MIT and Harvard Medical School researchers have mapped out many of the cells, genes, and cellular pathways that are modified by exercise or high-fat diet. The findings could offer potential targets for drugs that could help to enhance or mimic the benefits of exercise, the researchers say.
“It is extremely important to understand the molecular mechanisms that are drivers of the beneficial effects of exercise and the detrimental effects of a high-fat diet, so that we can understand how we can intervene, and develop drugs that mimic the impact of exercise across multiple tissues,” says Manolis Kellis, a professor of computer science in MIT’s Computer Science and Artificial Intelligence Laboratory (CSAIL) and a member of the Broad Institute of MIT and Harvard.
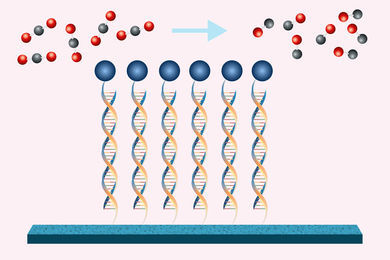
The researchers studied mice with high-fat or normal diets, who were either sedentary or given the opportunity to exercise whenever they wanted. Using single-cell RNA sequencing, the researchers cataloged the responses of 53 types of cells found in skeletal muscle and two types of fatty tissue.
“One of the general points that we found in our study, which is overwhelmingly clear, is how high-fat diets push all of these cells and systems in one way, and exercise seems to be pushing them nearly all in the opposite way,” Kellis says. “It says that exercise can really have a major effect throughout the body.”
Kellis and Laurie Goodyear, a professor of medicine at Harvard Medical School and senior investigator at the Joslin Diabetes Center, are the senior authors of the study, which appears today in the journal Cell Metabolism . Jiekun Yang, a research scientist in MIT CSAIL; Maria Vamvini, an instructor of medicine at the Joslin Diabetes Center; and Pasquale Nigro, an instructor of medicine at the Joslin Diabetes Center, are the lead authors of the paper.
The risks of obesity
Obesity is a growing health problem around the world. In the United States, more than 40 percent of the population is considered obese, and nearly 75 percent is overweight. Being overweight is a risk factor for many diseases, including heart disease, cancer, Alzheimer’s disease, and even infectious diseases such as Covid-19.
“Obesity, along with aging, is a global factor that contributes to every aspect of human health,” Kellis says.
Several years ago, his lab performed a study on the FTO gene region, which has been strongly linked to obesity risk. In that 2015 study, the research team found that genes in this region control a pathway that prompts immature fat cells called progenitor adipocytes to either become fat-burning cells or fat-storing cells.
That finding, which demonstrated a clear genetic component to obesity, motivated Kellis to begin looking at how exercise, a well-known behavioral intervention that can prevent obesity, might act on progenitor adipocytes at the cellular level.
To explore that question, Kellis and his colleagues decided to perform single-cell RNA sequencing of three types of tissue — skeletal muscle, visceral white adipose tissue (found packed around internal organs, where it stores fat), and subcutaneous white adipose tissue (which is found under the skin and primarily burns fat).
These tissues came from mice from four different experimental groups. For three weeks, two groups of mice were fed either a normal diet or a high-fat diet. For the next three weeks, each of those two groups were further divided into a sedentary group and an exercise group, which had continuous access to a treadmill.
By analyzing tissues from those mice, the researchers were able to comprehensively catalog the genes that were activated or suppressed by exercise in 53 different cell types.
The researchers found that in all three tissue types, mesenchymal stem cells (MSCs) appeared to control many of the diet and exercise-induced effects that they observed. MSCs are stem cells that can differentiate into other cell types, including fat cells and fibroblasts. In adipose tissue, the researchers found that a high-fat diet modulated MSCs’ capacity to differentiate into fat-storing cells, while exercise reversed this effect.
In addition to promoting fat storage, the researchers found that a high-fat diet also stimulated MSCs to secrete factors that remodel the extracellular matrix (ECM) — a network of proteins and other molecules that surround and support cells and tissues in the body. This ECM remodeling helps provide structure for enlarged fat-storing cells and also creates a more inflammatory environment.
“As the adipocytes become overloaded with lipids, there’s an extreme amount of stress, and that causes low-grade inflammation, which is systemic and preserved for a long time,” Kellis says. “That is one of the factors that is contributing to many of the adverse effects of obesity.”
Circadian effects
The researchers also found that high-fat diets and exercise had opposing effects on cellular pathways that control circadian rhythms — the 24-hour cycles that govern many functions, from sleep to body temperature, hormone release, and digestion. The study revealed that exercise boosts the expression of genes that regulate these rhythms, while a high-fat diet suppresses them.
“There have been a lot of studies showing that when you eat during the day is extremely important in how you absorb the calories,” Kellis says. “The circadian rhythm connection is a very important one, and shows how obesity and exercise are in fact directly impacting that circadian rhythm in peripheral organs, which could act systemically on distal clocks and regulate stem cell functions and immunity.”
The researchers then compared their results to a database of human genes that have been linked with metabolic traits. They found that two of the circadian rhythm genes they identified in this study, known as DBP and CDKN1A, have genetic variants that have been associated with a higher risk of obesity in humans.
“These results help us see the translational values of these targets, and how we could potentially target specific biological processes in specific cell types,” Yang says.
The researchers are now analyzing samples of small intestine, liver, and brain tissue from the mice in this study, to explore the effects of exercise and high-fat diets on those tissues. They are also conducting work with human volunteers to sample blood and biopsies and study similarities and differences between human and mouse physiology. They hope that their findings will help guide drug developers in designing drugs that might mimic some of the beneficial effects of exercise.
“The message for everyone should be, eat a healthy diet and exercise if possible,” Kellis says. “For those for whom this is not possible, due to low access to healthy foods, or due to disabilities or other factors that prevent exercise, or simply lack of time to have a healthy diet or a healthy lifestyle, what this study says is that we now have a better handle on the pathways, the specific genes, and the specific molecular and cellular processes that we should be manipulating therapeutically.”
The research was funded by the National Institutes of Health and the Novo Nordisk Research Center in Seattle.
Share this news article on:
Press mentions.
Researchers from MIT and Harvard Medical School are investigating how exercise and high-fat diets can alter cells, genes and cellular pathways, reports Abby Patkin for Boston.com . “Their research could eventually help develop drugs that would mimic the effects of exercise and combat obesity,” explains Patkin.
Researchers from MIT and Harvard Medical School have conducted a study to see how exercise and high-fat diets can impact cells, reports WCVB. The researchers “say the data could eventually be used to develop drugs that could help enhance or mimic the benefits of exercise,” writes WCVB.
A new study by researchers from MIT and Harvard Medical School has helped identify the impact of exercise and high-fat diets on cells, reports Darren Botelho for NBC Boston 10 . “Years from now, those researchers say the data could lead to a pill that would help not only with weight loss, but with the overall effect from exercise – a better wellbeing,” explains Botelho.
Boston 25 News
Prof. Manolis Kellis speaks with Boston 25 about his team’s work exploring the underlying mechanisms exploring how exercise influences weight loss, findings that could offer potential targets for drugs that could help to enhance or mimic the benefits of exercise. “Such an intervention would be a complete game changer and the reason for that is that the obesity epidemic has led to the U.S. having a decreased life span compared to all other developed countries,” says Kellis.
Previous item Next item
Related Links
- Manolis Kellis
- MIT Computational Biology Lab
- Computer Science and Artificial Intelligence Laboratory
- Department of Electrical Engineering and Computer Science
- Broad Institute
Related Topics
- Drug discovery
- Electrical Engineering & Computer Science (eecs)
- Computer Science and Artificial Intelligence Laboratory (CSAIL)
- National Institutes of Health (NIH)
Related Articles

A new atlas of cells that carry blood to the brain

Epigenomic map reveals circuitry of 30,000 human disease regions
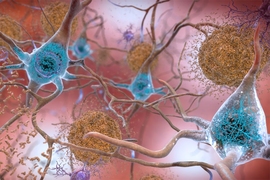
A comprehensive map of how Alzheimer’s affects the brain
A metabolic master switch underlying human obesity
More mit news.

Is it the school, or the students?
Read full story →

Student spotlight: Victory Yinka-Banjo

A delicate dance
Persistent “hiccups” in a far-off galaxy draw astronomers to new black hole behavior

New software enables blind and low-vision users to create interactive, accessible charts
Engineers find a new way to convert carbon dioxide into useful products
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
Women see greater health benefits from regular exercise than men do
Women generally exercise less than men do , but new research suggests they see greater health benefits from it.
A national study found that women who exercised regularly — at least 2½ hours of moderate exercise or 75 minutes of vigorous exercise per week — had a 24% lower risk of dying over the study period compared with women who didn’t exercise. By contrast, men who exercised regularly were 15% less likely to die than men who didn’t exercise.
Men also needed more exercise than women to achieve the same health benefits: Five hours of moderate or vigorous exercise per week reduced their risk of dying by 18% compared with men who didn’t exercise. But just 140 minutes of weekly exercise had the same effect among women.
“Women got the same benefit at lower levels of physical activity,” said a co-author of the study, Dr. Martha Gulati, the director of preventive cardiology at Cedars-Sinai’s Smidt Heart Institute in Los Angeles.

Women who exercised regularly also had a 36% lower risk of dying from a cardiovascular issue such as a heart attack or stroke, the study found, whereas men who exercised regularly had a 14% lower risk.
The findings were published Monday in the Journal of the American College of Cardiology. The researchers analyzed the self-reported exercise habits of more than 412,000 men and women who participated in the National Health Interview Survey from 1997 to 2017.
Roughly one-third of the women regularly engaged in aerobic exercises — ones that elevate the heart rate, such as brisk walking, jumping rope or taking spin classes — compared with 43% of men in the study. Women were also less likely than men to do muscle-strengthening activities, such as lifting weights.
Nevertheless, regular muscle strengthening — roughly one session per week, on average — was associated with a 30% lower risk of women dying from cardiovascular problems and a 19% lower risk of dying overall. Among men, the same weekly exercises lowered the risk of dying from cardiovascular problems by 11% and of death by the same percentage.
Gulati said one major limitation of the study is that it didn't account for how active women were outside workout settings.
“Missing from our data are the things that we do every day — the other physical activity that’s not going to the gym but running after kids, doing gardening, doing household chores,” she said.
Should men and woman have different exercise recommendations?
The Department of Health and Human Services recommends that adults get 150 minutes of moderate physical activity per week, including two days of muscle-strengthening activities.
But Gulati said those guidelines “can be very overwhelming to someone who does zero.” Many of her female patients struggle to find time for exercise, she said.
“Women are busy. Women work. Women usually take the bulk of family responsibilities — whether that’s children, whether that’s elderly parents — and by the time the day finishes, there’s very little time,” Gulati said.
Data from the National Health Interview Survey suggests that women in 2022 were more likely than men to have been advised over the past year by doctors or other health professionals to increase their amounts of physical activity.
"Rather than talking about 150 minutes a week, the way that we should be saying it is: What can you fit in?" Gulati said.
Paul Arciero, a professor of sports, medicine and nutrition at the University of Pittsburgh, said it’s only logical to have separate exercise guidelines for men and women.
“There are clear, sex-based differences in response to exercise,” he said. “We have to move beyond thinking that men and women respond similarly."
What's causing the sex-based difference?
Many studies have shown that exercise doesn't affect men and women in the same way.
Arciero’s research in 2022 found that women had greater reductions in blood pressure when they exercised in the morning, whereas men had greater reductions at night. A 2020 review also found that women’s muscles are more resistant to fatigue from high-intensity exercise.
But scientists have been less certain about how those differences affect people’s long-term health.
The new study shows that “women are basically more efficient in responding to exercise, particularly when it comes to heart health and mortality,” said Arciero, who wasn’t involved in the paper.
Arciero said physiological differences may contribute to the advantage: Women have more capillaries (tiny blood vessels) in a given section of muscle than men do, which could allow more blood and oxygen to flow to the heart during exercise.
Women also have higher levels of the hormone estrogen, which enhances blood flow, said Lynda Ransdell, the chair of the kinesiology department at Boise State University.
Ransdell pointed to a third factor as well: Women tend to be less physically active, so it may take less effort to improve their health relative to their baselines.
“I would call it the principle of diminishing returns,” Ransdell said. “Since women typically start at lower levels of fitness, they can see significant gains with taking up a little less physical activity.”
But scientists have more to learn, she added.
“While I love this study and I think it’s groundbreaking and landmark, I also believe that it’s one piece of a puzzle,” Ransdell said. "I would love to see them do more research with objective measures of physical activity like pedometers or Apple watches.”
Aria Bendix is the breaking health reporter for NBC News Digital.
- Research article
- Open access
- Published: 16 November 2020
Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews
- Pawel Posadzki 1 , 2 ,
- Dawid Pieper ORCID: orcid.org/0000-0002-0715-5182 3 ,
- Ram Bajpai 4 ,
- Hubert Makaruk 5 ,
- Nadja Könsgen 3 ,
- Annika Lena Neuhaus 3 &
- Monika Semwal 6
BMC Public Health volume 20 , Article number: 1724 ( 2020 ) Cite this article
29k Accesses
127 Citations
132 Altmetric
Metrics details
Sedentary lifestyle is a major risk factor for noncommunicable diseases such as cardiovascular diseases, cancer and diabetes. It has been estimated that approximately 3.2 million deaths each year are attributable to insufficient levels of physical activity. We evaluated the available evidence from Cochrane systematic reviews (CSRs) on the effectiveness of exercise/physical activity for various health outcomes.
Overview and meta-analysis. The Cochrane Library was searched from 01.01.2000 to issue 1, 2019. No language restrictions were imposed. Only CSRs of randomised controlled trials (RCTs) were included. Both healthy individuals, those at risk of a disease, and medically compromised patients of any age and gender were eligible. We evaluated any type of exercise or physical activity interventions; against any types of controls; and measuring any type of health-related outcome measures. The AMSTAR-2 tool for assessing the methodological quality of the included studies was utilised.
Hundred and fifty CSRs met the inclusion criteria. There were 54 different conditions. Majority of CSRs were of high methodological quality. Hundred and thirty CSRs employed meta-analytic techniques and 20 did not. Limitations for studies were the most common reasons for downgrading the quality of the evidence. Based on 10 CSRs and 187 RCTs with 27,671 participants, there was a 13% reduction in mortality rates risk ratio (RR) 0.87 [95% confidence intervals (CI) 0.78 to 0.96]; I 2 = 26.6%, [prediction interval (PI) 0.70, 1.07], median effect size (MES) = 0.93 [interquartile range (IQR) 0.81, 1.00]. Data from 15 CSRs and 408 RCTs with 32,984 participants showed a small improvement in quality of life (QOL) standardised mean difference (SMD) 0.18 [95% CI 0.08, 0.28]; I 2 = 74.3%; PI -0.18, 0.53], MES = 0.20 [IQR 0.07, 0.39]. Subgroup analyses by the type of condition showed that the magnitude of effect size was the largest among patients with mental health conditions.
There is a plethora of CSRs evaluating the effectiveness of physical activity/exercise. The evidence suggests that physical activity/exercise reduces mortality rates and improves QOL with minimal or no safety concerns.
Trial registration
Registered in PROSPERO ( CRD42019120295 ) on 10th January 2019.
Peer Review reports
The World Health Organization (WHO) defines physical activity “as any bodily movement produced by skeletal muscles that requires energy expenditure” [ 1 ]. Therefore, physical activity is not only limited to sports but also includes walking, running, swimming, gymnastics, dance, ball games, and martial arts, for example. In the last years, several organizations have published or updated their guidelines on physical activity. For example, the Physical Activity Guidelines for Americans, 2nd edition, provides information and guidance on the types and amounts of physical activity that provide substantial health benefits [ 2 ]. The evidence about the health benefits of regular physical activity is well established and so are the risks of sedentary behaviour [ 2 ]. Exercise is dose dependent, meaning that people who achieve cumulative levels several times higher than the current recommended minimum level have a significant reduction in the risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events [ 3 ]. Benefits of physical activity have been reported for numerous outcomes such as mortality [ 4 , 5 ], cognitive and physical decline [ 5 , 6 , 7 ], glycaemic control [ 8 , 9 ], pain and disability [ 10 , 11 ], muscle and bone strength [ 12 ], depressive symptoms [ 13 ], and functional mobility and well-being [ 14 , 15 ]. Overall benefits of exercise apply to all bodily systems including immunological [ 16 ], musculoskeletal [ 17 ], respiratory [ 18 ], and hormonal [ 19 ]. Specifically for the cardiovascular system, exercise increases fatty acid oxidation, cardiac output, vascular smooth muscle relaxation, endothelial nitric oxide synthase expression and nitric oxide availability, improves plasma lipid profiles [ 15 ] while at the same time reducing resting heart rate and blood pressure, aortic valve calcification, and vascular resistance [ 20 ].
However, the degree of all the above-highlighted benefits vary considerably depending on individual fitness levels, types of populations, age groups and the intensity of different physical activities/exercises [ 21 ]. The majority of guidelines in different countries recommend a goal of 150 min/week of moderate-intensity aerobic physical activity (or equivalent of 75 min of vigorous-intensity) [ 22 ] with differences for cardiovascular disease [ 23 ] or obesity prevention [ 24 ] or age groups [ 25 ].
There is a plethora of systematic reviews published by the Cochrane Library critically evaluating the effectiveness of physical activity/exercise for various health outcomes. Cochrane systematic reviews (CSRs) are known to be a source of high-quality evidence. Thus, it is not only timely but relevant to evaluate the current knowledge, and determine the quality of the evidence-base, and the magnitude of the effect sizes given the negative lifestyle changes and rising physical inactivity-related burden of diseases. This overview will identify the breadth and scope to which CSRs have appraised the evidence for exercise on health outcomes; and this will help in directing future guidelines and identifying current gaps in the literature.
The objectives of this research were to a. answer the following research questions: in children, adolescents and adults (both healthy and medically compromised) what are the effects (and adverse effects) of exercise/physical activity in improving various health outcomes (e.g., pain, function, quality of life) reported in CSRs; b. estimate the magnitude of the effects by pooling the results quantitatively; c. evaluate the strength and quality of the existing evidence; and d. create recommendations for future researchers, patients, and clinicians.
Our overview was registered with PROSPERO (CRD42019120295) on 10th January 2019. The Cochrane Handbook for Systematic Reviews of interventions and Preferred Reporting Items for Overviews of Reviews were adhered to while writing and reporting this overview [ 26 , 27 ].
Search strategy and selection criteria
We followed the practical guidance for conducting overviews of reviews of health care interventions [ 28 ] and searched the Cochrane Database of Systematic Reviews (CDSR), 2019, Issue 1, on the Cochrane Library for relevant papers using the search strategy: (health) and (exercise or activity or physical). The decision to seek CSRs only was based on three main aspects. First, high quality (CSRs are considered to be the ‘gold methodological standard’) [ 29 , 30 , 31 ]. Second, data saturation (enough high-quality evidence to reach meaningful conclusions based on CSRs only). Third, including non-CSRs would have heavily increased the issue of overlapping reviews (also affecting data robustness and credibility of conclusions). One reviewer carried out the searches. The study screening and selection process were performed independently by two reviewers. We imported all identified references into reference manager software EndNote (X8). Any disagreements were resolved by discussion between the authors with third overview author acting as an arbiter, if necessary.
We included CSRs of randomised controlled trials (RCTs) involving both healthy individuals and medically compromised patients of any age and gender. Only CSRs assessing exercise or physical activity as a stand-alone intervention were included. This included interventions that could initially be taught by a professional or involve ongoing supervision (the WHO definition). Complex interventions e.g., assessing both exercise/physical activity and behavioural changes were excluded if the health effects of the interventions could not have been attributed to exercise distinctly.
Any types of controls were admissible. Reviews evaluating any type of health-related outcome measures were deemed eligible. However, we excluded protocols or/and CSRs that have been withdrawn from the Cochrane Library as well as reviews with no included studies.
Data analysis
Three authors (HM, ALN, NK) independently extracted relevant information from all the included studies using a custom-made data collection form. The methodological quality of SRs included was independently evaluated by same reviewers using the AMSTAR-2 tool [ 32 ]. Any disagreements on data extraction or CSR quality were resolved by discussion. The entire dataset was validated by three authors (PP, MS, DP) and any discrepant opinions were settled through discussions.
The results of CSRs are presented in a narrative fashion using descriptive tables. Where feasible, we presented outcome measures across CSRs. Data from the subset of homogeneous outcomes were pooled quantitatively using the approach previously described by Bellou et al. and Posadzki et al. [ 33 , 34 ]. For mortality and quality of life (QOL) outcomes, the number of participants and RCTs involved in the meta-analysis, summary effect sizes [with 95% confidence intervals (CI)] using random-effects model were calculated. For binary outcomes, we considered relative risks (RRs) as surrogate measures of the corresponding odds ratio (OR) or risk ratio/hazard ratio (HR). To stabilise the variance and normalise the distributions, we transformed RRs into their natural logarithms before pooling the data (a variation was allowed, however, it did not change interpretation of results) [ 35 ]. The standard error (SE) of the natural logarithm of RR was derived from the corresponding CIs, which was either provided in the study or calculated with standard formulas [ 36 ]. Binary outcomes reported as risk difference (RD) were also meta-analysed if two more estimates were available. For continuous outcomes, we only meta-analysed estimates that were available as standardised mean difference (SMD), and estimates reported with mean differences (MD) for QOL were presented separately in a supplementary Table 9 . To estimate the overall effect size, each study was weighted by the reciprocal of its variance. Random-effects meta-analysis, using DerSimonian and Laird method [ 37 ] was applied to individual CSR estimates to obtain a pooled summary estimate for RR or SMD. The 95% prediction interval (PI) was also calculated (where ≥3 studies were available), which further accounts for between-study heterogeneity and estimates the uncertainty around the effect that would be anticipated in a new study evaluating that same association. I -squared statistic was used to measure between study heterogeneity; and its various thresholds (small, substantial and considerable) were interpreted considering the size and direction of effects and the p -value from Cochran’s Q test ( p < 0.1 considered as significance) [ 38 ]. Wherever possible, we calculated the median effect size (with interquartile range [IQR]) of each CSR to interpret the direction and magnitude of the effect size. Sub-group analyses are planned for type and intensity of the intervention; age group; gender; type and/or severity of the condition, risk of bias in RCTs, and the overall quality of the evidence (Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria). To assess overlap we calculated the corrected covered area (CCA) [ 39 ]. All statistical analyses were conducted on Stata statistical software version 15.2 (StataCorp LLC, College Station, Texas, USA).
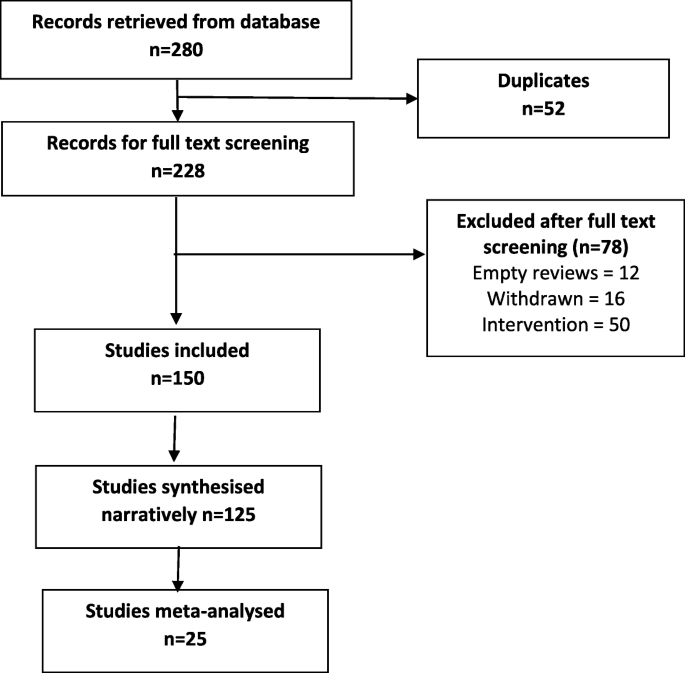
The searches generated 280 potentially relevant CRSs. After removing of duplicates and screening, a total of 150 CSRs met our eligibility criteria [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 , 185 , 186 , 187 , 188 , 189 ] (Fig. 1 ). Reviews were published between September 2002 and December 2018. A total of 130 CSRs employed meta-analytic techniques and 20 did not. The total number of RCTs in the CSRs amounted to 2888; with 485,110 participants (mean = 3234, SD = 13,272). The age ranged from 3 to 87 and gender distribution was inestimable. The main characteristics of included reviews are summarised in supplementary Table 1 . Supplementary Table 2 summarises the effects of physical activity/exercise on health outcomes. Conclusions from CSRs are listed in supplementary Table 3 . Adverse effects are listed in supplementary Table 4 . Supplementary Table 5 presents summary of withdrawals/non-adherence. The methodological quality of CSRs is presented in supplementary Table 6 . Supplementary Table 7 summarises studies assessed at low risk of bias (by the authors of CSRs). GRADE-ings of the review’s main comparison are listed in supplementary Table 8 .
Study selection process
There were 54 separate populations/conditions, considerable range of interventions and comparators, co-interventions, and outcome measures. For detailed description of interventions, please refer to the supplementary tables . Most commonly measured outcomes were - function 112 (75%), QOL 83 (55%), AEs 70 (47%), pain 41 (27%), mortality 28 (19%), strength 30 (20%), costs 47 (31%), disability 14 (9%), and mental health in 35 (23%) CSRs.
There was a 13% reduction in mortality rates risk ratio (RR) 0.87 [95% CI 0.78 to 0.96]; I 2 = 26.6%, [PI 0.70, 1.07], median effect size (MES) = 0.93 [interquartile range (IQR) 0.81, 1.00]; 10 CSRs, 187 RCTs, 27,671 participants) following exercise when compared with various controls (Table 1 ). This reduction was smaller in ‘other groups’ of patients when compared to cardiovascular diseases (CVD) patients - RR 0.97 [95% CI 0.65, 1.45] versus 0.85 [0.76, 0.96] respectively. The effects of exercise were not intensity or frequency dependent. Sessions more than 3 times per week exerted a smaller reduction in mortality as compared with sessions of less than 3 times per week RR 0.87 [95% CI 0.78, 0.98] versus 0.63 [0.39, 1.00]. Subgroup analyses by risk of bias (ROB) in RCTs showed that RCTs at low ROB exerted smaller reductions in mortality when compared to RCTs at an unclear or high ROB, RR 0.90 [95% CI 0.78, 1.02] versus 0.72 [0.42, 1.22] versus 0.86 [0.69, 1.06] respectively. CSRs with moderate quality of evidence (GRADE), showed slightly smaller reductions in mortality when compared with CSRs that relied on very low to low quality evidence RR 0.88 [95% CI 0.79, 0.98] versus 0.70 [0.47, 1.04].
Exercise also showed an improvement in QOL, standardised mean difference (SMD) 0.18 [95% CI 0.08, 0.28]; I 2 = 74.3%; PI -0.18, 0.53], MES = 0.20 [IQR 0.07, 0.39]; 15 CSRs, 408 RCTs, 32,984 participants) when compared with various controls (Table 2 ). These improvements were greater observed for health related QOL when compared to overall QOL SMD 0.30 [95% CI 0.21, 0.39] vs 0.06 [− 0.08, 0.20] respectively. Again, the effects of exercise were duration and frequency dependent. For instance, sessions of more than 90 mins exerted a greater improvement in QOL as compared with sessions up to 90 min SMD 0.24 [95% CI 0.11, 0.37] versus 0.22 [− 0.30, 0.74]. Subgroup analyses by the type of condition showed that the magnitude of effect was the largest among patients with mental health conditions, followed by CVD and cancer. Physical activity exerted negative effects on QOL in patients with respiratory conditions (2 CSRs, 20 RCTs with 601 patients; SMD -0.97 [95% CI -1.43, 0.57]; I 2 = 87.8%; MES = -0.46 [IQR-0.97, 0.05]). Subgroup analyses by risk of bias (ROB) in RCTs showed that RCTs at low or unclear ROB exerted greater improvements in QOL when compared to RCTs at a high ROB SMD 0.21 [95% CI 0.10, 0.31] versus 0.17 [0.03, 0.31]. Analogically, CSRs with moderate to high quality of evidence showed slightly greater improvements in QOL when compared with CSRs that relied on very low to low quality evidence SMD 0.19 [95% CI 0.05, 0.33] versus 0.15 [− 0.02, 0.32]. Please also see supplementary Table 9 more studies reporting QOL outcomes as mean difference (not quantitatively synthesised herein).
Adverse events (AEs) were reported in 100 (66.6%) CSRs; and not reported in 50 (33.3%). The number of AEs ranged from 0 to 84 in the CSRs. The number was inestimable in 83 (55.3%) CSRs. Ten (6.6%) reported no occurrence of AEs. Mild AEs were reported in 28 (18.6%) CSRs, moderate in 9 (6%) and serious/severe in 20 (13.3%). There were 10 deaths and in majority of instances, the causality was not attributed to exercise. For this outcome, we were unable to pool the data as effect sizes were too heterogeneous (Table 3 ).
In 38 CSRs, the total number of trials reporting withdrawals/non-adherence was inestimable. There were different ways of reporting it such as adherence or attrition (high in 23.3% of CSRs) as well as various effect estimates including %, range, total numbers, MD, RD, RR, OR, mean and SD. The overall pooled estimates are reported in Table 3 .
Of all 16 domains of the AMSTAR-2 tool, 1876 (78.1%) scored ‘yes’, 76 (3.1%) ‘partial yes’; 375 (15.6%) ‘no’, and ‘not applicable’ in 25 (1%) CSRs. Ninety-six CSRs (64%) were scored as ‘no’ on reporting sources of funding for the studies followed by 88 (58.6%) failing to explain the selection of study designs for inclusion. One CSR (0.6%) each were judged as ‘no’ for reporting any potential sources of conflict of interest, including any funding for conducting the review as well for performing study selection in duplicate.
In 102 (68%) CSRs, there was predominantly a high risk of bias in RCTs. In 9 (6%) studies, this was reported as a range, e.g., low or unclear or low to high. Two CSRs used different terminology i.e., moderate methodological quality; and the risk of bias was inestimable in one CSR. Sixteen (10.6%) CSRs did not identify any studies (RCTs) at low risk of random sequence generation, 28 (18.6%) allocation concealment, 28 (18.6%) performance bias, 84 (54%) detection bias, 35 (23.3%) attrition bias, 18 (12%) reporting bias, and 29 (19.3%) other bias.
In 114 (76%) CSRs, limitation of studies was the main reason for downgrading the quality of the evidence followed by imprecision in 98 (65.3%) and inconsistency in 68 (45.3%). Publication bias was the least frequent reason for downgrading in 26 (17.3%) CSRs. Ninety-one (60.7%) CSRs reached equivocal conclusions, 49 (32.7%) reviews reached positive conclusions and 10 (6.7%) reached negative conclusions (as judged by the authors of CSRs).
In this systematic review of CSRs, we found a large body of evidence on the beneficial effects of physical activity/exercise on health outcomes in a wide range of heterogeneous populations. Our data shows a 13% reduction in mortality rates among 27,671 participants, and a small improvement in QOL and health-related QOL following various modes of physical activity/exercises. This means that both healthy individuals and medically compromised patients can significantly improve function, physical and mental health; or reduce pain and disability by exercising more [ 190 ]. In line with previous findings [ 191 , 192 , 193 , 194 ], where a dose-specific reduction in mortality has been found, our data shows a greater reduction in mortality in studies with longer follow-up (> 12 months) as compared to those with shorter follow-up (< 12 months). Interestingly, we found a consistent pattern in the findings, the higher the quality of evidence and the lower the risk of bias in primary studies, the smaller reductions in mortality. This pattern is observational in nature and cannot be over-generalised; however this might mean less certainty in the estimates measured. Furthermore, we found that the magnitude of the effect size was the largest among patients with mental health conditions. A possible mechanism of action may involve elevated levels of brain-derived neurotrophic factor or beta-endorphins [ 195 ].
We found the issue of poor reporting or underreporting of adherence/withdrawals in over a quarter of CSRs (25.3%). This is crucial both for improving the accuracy of the estimates at the RCT level as well as maintaining high levels of physical activity and associated health benefits at the population level.
Even the most promising interventions are not entirely risk-free; and some minor AEs such as post-exercise pain and soreness or discomfort related to physical activity/exercise have been reported. These were typically transient; resolved within a few days; and comparable between exercise and various control groups. However worryingly, the issue of poor reporting or underreporting of AEs has been observed in one third of the CSRs. Transparent reporting of AEs is crucial for identifying patients at risk and mitigating any potential negative or unintended consequences of the interventions.
High risk of bias of the RCTs evaluated was evident in more than two thirds of the CSRs. For example, more than half of reviews identified high risk of detection bias as a major source of bias suggesting that lack of blinding is still an issue in trials of behavioural interventions. Other shortcomings included insufficiently described randomisation and allocation concealment methods and often poor outcome reporting. This highlights the methodological challenges in RCTs of exercise and the need to counterbalance those with the underlying aim of strengthening internal and external validity of these trials.
Overall, high risk of bias in the primary trials was the main reason for downgrading the quality of the evidence using the GRADE criteria. Imprecision was frequently an issue, meaning the effective sample size was often small; studies were underpowered to detect the between-group differences. Pooling too heterogeneous results often resulted in inconsistent findings and inability to draw any meaningful conclusions. Indirectness and publication bias were lesser common reasons for downgrading. However, with regards to the latter, the generally accepted minimum number of 10 studies needed for quantitatively estimate the funnel plot asymmetry was not present in 69 (46%) CSRs.
Strengths of this research are the inclusion of large number of ‘gold standard’ systematic reviews, robust screening, data extractions and critical methodological appraisal. Nevertheless, some weaknesses need to be highlighted when interpreting findings of this overview. For instance, some of these CSRs analysed the same primary studies (RCTs) but, arrived at slightly different conclusions. Using, the Pieper et al. [ 39 ] formula, the amount of overlap ranged from 0.01% for AEs to 0.2% for adherence, which indicates slight overlap. All CSRs are vulnerable to publication bias [ 196 ] - hence the conclusions generated by them may be false-positive. Also, exercise was sometimes part of a complex intervention; and the effects of physical activity could not be distinguished from co-interventions. Often there were confounding effects of diet, educational, behavioural or lifestyle interventions; selection, and measurement bias were inevitably inherited in this overview too. Also, including CSRs only might lead to selection bias; and excluding reviews published before 2000 might limit the overall completeness and applicability of the evidence. A future update should consider these limitations, and in particular also including non-CSRs.
Conclusions
Trialists must improve the quality of primary studies. At the same time, strict compliance with the reporting standards should be enforced. Authors of CSRs should better explain eligibility criteria and report sources of funding for the primary studies. There are still insufficient physical activity trends worldwide amongst all age groups; and scalable interventions aimed at increasing physical activity levels should be prioritized [ 197 ]. Hence, policymakers and practitioners need to design and implement comprehensive and coordinated strategies aimed at targeting physical activity programs/interventions, health promotion and disease prevention campaigns at local, regional, national, and international levels [ 198 ].
Availability of data and materials
Data sharing is not applicable to this article as no raw data were analysed during the current study. All information in this article is based on published systematic reviews.
Abbreviations
Adverse events
Cardiovascular diseases
Cochrane Database of Systematic Reviews
Cochrane systematic reviews
Confidence interval
Grading of Recommendations Assessment, Development and Evaluation
Hazard ratio
Interquartile range
Mean difference
Prediction interval
Quality of life
Randomised controlled trials
Relative risk
Risk difference
Risk of bias
Standard error
Standardised mean difference
World Health Organization
https://www.who.int/dietphysicalactivity/pa/en/ . (Accessed 8 June 2020).
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD. The physical activity guidelines for AmericansPhysical activity guidelines for AmericansPhysical activity guidelines for Americans. Jama. 2018;320(19):2020–8.
PubMed Google Scholar
Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, Veerman JL, Delwiche K, Iannarone ML, Moyer ML, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the global burden of disease study 2013. BMJ. 2016;354:i3857.
PubMed PubMed Central Google Scholar
Abell B, Glasziou P, Hoffmann T. The contribution of individual exercise training components to clinical outcomes in randomised controlled trials of cardiac rehabilitation: a systematic review and meta-regression. Sports Med Open. 2017;3(1):19.
Anderson D, Seib C, Rasmussen L. Can physical activity prevent physical and cognitive decline in postmenopausal women? A systematic review of the literature. Maturitas. 2014;79(1):14–33.
Barbaric M, Brooks E, Moore L, Cheifetz O. Effects of physical activity on cancer survival: a systematic review. Physiother Can. 2010;62(1):25–34.
Barlow PA, Otahal P, Schultz MG, Shing CM, Sharman JE. Low exercise blood pressure and risk of cardiovascular events and all-cause mortality: systematic review and meta-analysis. Atherosclerosis. 2014;237(1):13–22.
CAS PubMed Google Scholar
Aljawarneh YM, Wardell DW, Wood GL, Rozmus CL. A systematic review of physical activity and exercise on physiological and biochemical outcomes in children and adolescents with type 1 diabetes. J Nurs Scholarsh. 2019.
Chastin SFM, De Craemer M, De Cocker K, Powell L, Van Cauwenberg J, Dall P, Hamer M, Stamatakis E. How does light-intensity physical activity associate with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br J Sports Med. 2019;53(6):370–6.
Abdulla SY, Southerst D, Cote P, Shearer HM, Sutton D, Randhawa K, Varatharajan S, Wong JJ, Yu H, Marchand AA, et al. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario protocol for traffic injury management (OPTIMa) collaboration. Man Ther. 2015;20(5):646–56.
Alanazi MH, Parent EC, Dennett E. Effect of stabilization exercise on back pain, disability and quality of life in adults with scoliosis: a systematic review. Eur J Phys Rehabil Med. 2018;54(5):647–53.
Adsett JA, Mudge AM, Morris N, Kuys S, Paratz JD. Aquatic exercise training and stable heart failure: a systematic review and meta-analysis. Int J Cardiol. 2015;186:22–8.
Adamson BC, Ensari I, Motl RW. Effect of exercise on depressive symptoms in adults with neurologic disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2015;96(7):1329–38.
Abdin S, Welch RK, Byron-Daniel J, Meyrick J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: a systematic review. Public Health. 2018;160:70–6.
Albalawi H, Coulter E, Ghouri N, Paul L. The effectiveness of structured exercise in the south Asian population with type 2 diabetes: a systematic review. Phys Sportsmed. 2017;45(4):408–17.
Sellami M, Gasmi M, Denham J, Hayes LD, Stratton D, Padulo J, Bragazzi N. Effects of acute and chronic exercise on immunological parameters in the elderly aged: can physical activity counteract the effects of aging? Front Immunol. 2018;9:2187.
Hagen KB, Dagfinrud H, Moe RH, Østerås N, Kjeken I, Grotle M, Smedslund G. Exercise therapy for bone and muscle health: an overview of systematic reviews. BMC Med. 2012;10(1):167.
Burton DA, Stokes K, Hall GM. Physiological effects of exercise. Contin Educ Anaesth Crit Care Pain. 2004;4(6):185–8.
Google Scholar
Kraemer WJ, Ratamess NA. Hormonal responses and adaptations to resistance exercise and training. Sports Med. 2005;35(4):339–61.
Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. 2018;5:135.
CAS PubMed PubMed Central Google Scholar
Vina J, Sanchis-Gomar F, Martinez-Bello V, Gomez-Cabrera MC. Exercise acts as a drug; the pharmacological benefits of exercise. Br J Pharmacol. 2012;167(1):1–12.
Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541–56.
Excellence NIfHaC: Cardiovascular disease prevention public health guideline [PH25] Published date: June 2010. Available at: https://www.nice.org.uk/guidance/ph25/resources/cardiovascular-disease-prevention-pdf-1996238687173 .
Excellence NIfHaC: Obesity prevention clinical guideline [CG43] published date: December 2006 Last updated: March 2015. Available at: https://www.nice.org.uk/guidance/cg43/resources/obesity-prevention-pdf-975445344709 .
Excellence NIfHaC: Physical activity for children and young people public health guideline [PH17] Published date: January 2009. Available at: https://www.nice.org.uk/guidance/ph17/resources/physical-activity-for-children-and-young-people-pdf-1996181580229 .
Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 6 [updated September 2018] edition. Available from www.cochrane-handbook.org : The Cochrane Collaboration, 2011. 2011.
Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich A-B. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. 2018;93:9–24.
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18.
Handoll H, Madhok R. Quality of Cochrane reviews. Another study found that most Cochrane reviews are of a good standard. BMJ. 2002;324(7336):545.
Petticrew M, Wilson P, Wright K, Song F. Quality of Cochrane reviews. Quality of Cochrane reviews is better than that of non-Cochrane reviews. BMJ. 2002;324(7336):545.
Shea B, Moher D, Graham I, Pham B, Tugwell P. A comparison of the quality of Cochrane reviews and systematic reviews published in paper-based journals. Eval Health Prof. 2002;25(1):116–29.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Posadzki PP, Bajpai R, Kyaw BM, Roberts NJ, Brzezinski A, Christopoulos GI, Divakar U, Bajpai S, Soljak M, Dunleavy G, et al. Melatonin and health: an umbrella review of health outcomes and biological mechanisms of action. BMC Med. 2018;16(1):18.
Bellou V, Belbasis L, Tzoulaki I, Evangelou E, Ioannidis JP. Environmental risk factors and Parkinson's disease: an umbrella review of meta-analyses. Parkinsonism Relat Disord. 2016;23:1–9.
Walter SD, Cook RJ. A comparison of several point estimators of the odds ratio in a single 2 x 2 contingency table. Biometrics. 1991;47(3):795–811.
Khan H, Sempos CT. Statistical methods in epidemiology. New York: Oxford University Press; 1989.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
CAS Google Scholar
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019): Cochrane; 2019. Available from www.training.cochrane.org/handbook .
Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Adeniyi FB, Young T. Weight loss interventions for chronic asthma. Cochrane Database Syst Rev. 2012;7.
Al-Khudairy L, Loveman E, Colquitt JL, Mead E, Johnson RE, Fraser H, Olajide J, Murphy M, Velho RM, O'Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev. 2017;6.
Amorim Adegboye AR, Linne YM. Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev. 2013;7.
Anderson L, Nguyen TT, Dall CH, Burgess L, Bridges C, Taylor RS. Exercise-based cardiac rehabilitation in heart transplant recipients. Cochrane Database Syst Rev. 2017;4.
Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;1.
Andriolo RB, El Dib RP, Ramos L, Atallah Á, da Silva EMK. Aerobic exercise training programmes for improving physical and psychosocial health in adults with Down syndrome. Cochrane Database Syst Rev. 2010;5.
Araujo DN, Ribeiro CTD, Maciel ACC, Bruno SS, Fregonezi GAF, Dias FAL. Physical exercise for the treatment of non-ulcerated chronic venous insufficiency. Cochrane Database Syst Rev. 2016;12.
Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC. Home versus center based physical activity programs in older adults. Cochrane Database Syst Rev. 2005;1.
Bartels EM, Juhl CB, Christensen R, Hagen KB, Danneskiold-Samsøe B, Dagfinrud H, Lund H. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2016;3.
Beggs S, Foong YC, Le HCT, Noor D, Wood-Baker R, Walters JAE. Swimming training for asthma in children and adolescents aged 18 years and under. Cochrane Database Syst Rev. 2013;4.
Bergenthal N, Will A, Streckmann F, Wolkewitz KD, Monsef I, Engert A, Elter T, Skoetz N. Aerobic physical exercise for adult patients with haematological malignancies. Cochrane Database Syst Rev. 2014;11.
Bidonde J, Busch AJ, Schachter CL, Overend TJ, Kim SY, Góes SM, Boden C, Foulds HJA. Aerobic exercise training for adults with fibromyalgia. Cochrane Database Syst Rev. 2017;6.
Bidonde J, Busch AJ, van der Spuy I, Tupper S, Kim SY, Boden C. Whole body vibration exercise training for fibromyalgia. Cochrane Database Syst Rev. 2017;9.
Bidonde J, Busch AJ, Webber SC, Schachter CL, Danyliw A, Overend TJ, Richards RS, Rader T. Aquatic exercise training for fibromyalgia. Cochrane Database Syst Rev. 2014;10.
Braam KI, van der Torre P, Takken T, Veening MA, van Dulmen-den Broeder E, Kaspers GJL. Physical exercise training interventions for children and young adults during and after treatment for childhood cancer. Cochrane Database Syst Rev. 2016;3.
Bradt J, Shim M, Goodill SW. Dance/movement therapy for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. 2015;1.
Broderick J, Crumlish N, Waugh A, Vancampfort D. Yoga versus non-standard care for schizophrenia. Cochrane Database Syst Rev. 2017;9.
Broderick J, Knowles A, Chadwick J, Vancampfort D. Yoga versus standard care for schizophrenia. Cochrane Database Syst Rev. 2015;10.
Broderick J, Vancampfort D. Yoga as part of a package of care versus standard care for schizophrenia. Cochrane Database Syst Rev. 2017;9.
Brown J, Ceysens G, Boulvain M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Cochrane Database Syst Rev. 2017;6.
Busch AJ, Barber KA, Overend TJ, Peloso PMJ, Schachter CL. Exercise for treating fibromyalgia syndrome. Cochrane Database Syst Rev. 2007;4.
Busch AJ, Webber SC, Richards RS, Bidonde J, Schachter CL, Schafer LA, Danyliw A, Sawant A, Dal Bello-Haas V, Rader T, et al. Resistance exercise training for fibromyalgia. Cochrane Database Syst Rev. 2013;12.
Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2018;9.
Carson KV, Chandratilleke MG, Picot J, Brinn MP, Esterman AJ, Smith BJ. Physical training for asthma. Cochrane Database Syst Rev. 2013;9.
Carvalho APV, Vital FMR, Soares BGO. Exercise interventions for shoulder dysfunction in patients treated for head and neck cancer. Cochrane Database Syst Rev. 2012;4.
Cavalheri V, Granger C. Preoperative exercise training for patients with non-small cell lung cancer. Cochrane Database Syst Rev. 2017;6.
Cavalheri V, Tahirah F, Nonoyama ML, Jenkins S, Hill K. Exercise training undertaken by people within 12 months of lung resection for non-small cell lung cancer. Cochrane Database Syst Rev. 2013;7.
Ceysens G, Rouiller D, Boulvain M. Exercise for diabetic pregnant women. Cochrane Database Syst Rev. 2006;3.
Choi BKL, Verbeek JH, Tam WWS, Jiang JY. Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev. 2010;1.
Colquitt JL, Loveman E, O'Malley C, Azevedo LB, Mead E, Al-Khudairy L, Ells LJ, Metzendorf MI, Rees K. Diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database Syst Rev. 2016;3.
Connolly B, Salisbury L, O'Neill B, Geneen LJ, Douiri A, Grocott MPW, Hart N, Walsh TS, Blackwood B. Exercise rehabilitation following intensive care unit discharge for recovery from critical illness. Cochrane Database Syst Rev. 2015;6.
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, McMurdo M, Mead GE. Exercise for depression. Cochrane Database Syst Rev. 2013;9.
Corbetta D, Sirtori V, Castellini G, Moja L, Gatti R. Constraint-induced movement therapy for upper extremities in people with stroke. Cochrane Database Syst Rev. 2015;10.
Cramer H, Lauche R, Klose P, Lange S, Langhorst J, Dobos GJ. Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1.
Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11.
Dal Bello-Haas V, Florence JM. Therapeutic exercise for people with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database Syst Rev. 2013;5.
Dale MT, McKeough ZJ, Troosters T, Bye P, Alison JA. Exercise training to improve exercise capacity and quality of life in people with non-malignant dust-related respiratory diseases. Cochrane Database Syst Rev. 2015;11.
Daley A, Stokes-Lampard H, Thomas A, MacArthur C. Exercise for vasomotor menopausal symptoms. Cochrane Database Syst Rev. 2014;11.
de Morton N, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;1.
Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2013;2.
Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. Cochrane Database Syst Rev. 2018;3.
Ekeland E, Heian F, Hagen KB, Abbott JM, Nordheim L. Exercise to improve self-esteem in children and young people. Cochrane Database Syst Rev. 2004;1.
Elbers RG, Verhoef J, van Wegen EEH, Berendse HW, Kwakkel G. Interventions for fatigue in Parkinson's disease. Cochrane Database Syst Rev. 2015;10.
Felbel S, Meerpohl JJ, Monsef I, Engert A, Skoetz N. Yoga in addition to standard care for patients with haematological malignancies. Cochrane Database Syst Rev. 2014;6.
Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S. Exercise programs for people with dementia. Cochrane Database Syst Rev. 2015;4.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1.
Fransen M, McConnell S, Hernandez-Molina G, Reichenbach S. Exercise for osteoarthritis of the hip. Cochrane Database Syst Rev. 2014;4.
Freitas DA, Holloway EA, Bruno SS, Chaves GSS, Fregonezi GAF, Mendonça K. Breathing exercises for adults with asthma. Cochrane Database Syst Rev. 2013;10.
Furmaniak AC, Menig M, Markes MH. Exercise for women receiving adjuvant therapy for breast cancer. Cochrane Database Syst Rev. 2016;9.
Giangregorio LM, MacIntyre NJ, Thabane L, Skidmore CJ, Papaioannou A. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev. 2013;1.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9.
Gorczynski P, Faulkner G. Exercise therapy for schizophrenia. Cochrane Database Syst Rev. 2010;5.
Grande AJ, Keogh J, Hoffmann TC, Beller EM, Del Mar CB. Exercise versus no exercise for the occurrence, severity and duration of acute respiratory infections. Cochrane Database Syst Rev. 2015;6.
Grande AJ, Reid H, Thomas EE, Nunan D, Foster C. Exercise prior to influenza vaccination for limiting influenza incidence and its related complications in adults. Cochrane Database Syst Rev. 2016;8.
Grande AJ, Silva V, Andriolo BNG, Riera R, Parra SA, Peccin MS. Water-based exercise for adults with asthma. Cochrane Database Syst Rev. 2014;7.
Gross A, Kay TM, Paquin JP, Blanchette S, Lalonde P, Christie T, Dupont G, Graham N, Burnie SJ, Gelley G, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2015;1.
Hageman D, Fokkenrood HJP, Gommans LNM, van den Houten MML, Teijink JAW. Supervised exercise therapy versus home-based exercise therapy versus walking advice for intermittent claudication. Cochrane Database Syst Rev. 2018;4.
Han A, Judd M, Welch V, Wu T, Tugwell P, Wells GA. Tai chi for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2004;3.
Han S, Middleton P, Crowther CA. Exercise for pregnant women for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2012;7.
Hartley L, Dyakova M, Holmes J, Clarke A, Lee MS, Ernst E, Rees K. Yoga for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;5.
Hartley L, Flowers N, Lee MS, Ernst E, Rees K. Tai chi for primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;4.
Hartley L, Lee MS, Kwong JSW, Flowers N, Todkill D, Ernst E, Rees K. Qigong for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2015;6.
Hassett L, Moseley AM, Harmer AR. Fitness training for cardiorespiratory conditioning after traumatic brain injury. Cochrane Database Syst Rev. 2017;12.
Hayden J, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005;3.
Hay-Smith EJC, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev. 2011;12.
Heine M, van de Port I, Rietberg MB, van Wegen EEH, Kwakkel G. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev. 2015;9.
Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev. 2011;10.
Hemmingsen B, Gimenez-Perez G, Mauricio D, Roqué i Figuls M, Metzendorf MI, Richter B. Diet, physical activity or both for prevention or delay of type 2 diabetes mellitus and its associated complications in people at increased risk of developing type 2 diabetes mellitus. Cochrane Database Syst Rev. 2017;12.
Herbert RD, de Noronha M, Kamper SJ. Stretching to prevent or reduce muscle soreness after exercise. Cochrane Database Syst Rev. 2011;7.
Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non-specific low-back pain. Cochrane Database Syst Rev. 2004;4.
Holland AE, Hill CJ, Jones AY, McDonald CF. Breathing exercises for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;10.
Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2011;11.
Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011;7.
Hurkmans E, van der Giesen FJ, Vliet Vlieland TPM, Schoones J, Van den Ende E. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst Rev. 2009;4.
Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, Stansfield C, Oliver S. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev. 2018;4.
Jones M, Harvey A, Marston L, O'Connell NE. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013;5.
Katsura M, Kuriyama A, Takeshima T, Fukuhara S, Furukawa TA. Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery. Cochrane Database Syst Rev. 2015;10.
Kendrick D, Kumar A, Carpenter H, Zijlstra GAR, Skelton DA, Cook JR, Stevens Z, Belcher CM, Haworth D, Gawler SJ, et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev. 2014;11.
Kramer MS, McDonald SW. Aerobic exercise for women during pregnancy. Cochrane Database Syst Rev. 2006;3.
Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity for women with breast cancer after adjuvant therapy. Cochrane Database Syst Rev. 2018;1.
Lane R, Harwood A, Watson L, Leng GC. Exercise for intermittent claudication. Cochrane Database Syst Rev. 2017;12.
Larun L, Brurberg KG, Odgaard-Jensen J, Price JR. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev. 2017;4.
Larun L, Nordheim LV, Ekeland E, Hagen KB, Heian F. Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database Syst Rev. 2006;3.
Lauret GJ, Fakhry F, Fokkenrood HJP, Hunink MGM, Teijink JAW, Spronk S. Modes of exercise training for intermittent claudication. Cochrane Database Syst Rev. 2014;7.
Lawrence M, Celestino Junior FT, Matozinho HHS, Govan L, Booth J, Beecher J. Yoga for stroke rehabilitation. Cochrane Database Syst Rev. 2017;12.
Lin CWC, Donkers NAJ, Refshauge KM, Beckenkamp PR, Khera K, Moseley AM. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev. 2012;11.
Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;3.
Long L, Anderson L, Dewhirst AM, He J, Bridges C, Gandhi M, Taylor RS. Exercise-based cardiac rehabilitation for adults with stable angina. Cochrane Database Syst Rev. 2018;2.
Loughney LA, West MA, Kemp GJ, Grocott MPW, Jack S. Exercise interventions for people undergoing multimodal cancer treatment that includes surgery. Cochrane Database Syst Rev. 2018;12.
Macedo LG, Saragiotto BT, Yamato TP, Costa LOP, Menezes Costa LC, Ostelo R, Maher CG. Motor control exercise for acute non-specific low back pain. Cochrane Database Syst Rev. 2016;2.
Macêdo TMF, Freitas DA, Chaves GSS, Holloway EA, Mendonça K. Breathing exercises for children with asthma. Cochrane Database Syst Rev. 2016;4.
Martin A, Booth JN, Laird Y, Sproule J, Reilly JJ, Saunders DH. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database Syst Rev. 2018;3.
McKeough ZJ, Velloso M, Lima VP, Alison JA. Upper limb exercise training for COPD. Cochrane Database Syst Rev. 2016;11.
McNamara RJ, McKeough ZJ, McKenzie DK, Alison JA. Water-based exercise training for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;12.
McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, Mackey J, Courneya K. Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev. 2010;6.
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, Olajide J, Mainardi GM, Corpeleijn E, O'Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6.
Meekums B, Karkou V, Nelson EA. Dance movement therapy for depression. Cochrane Database Syst Rev. 2015;2.
Meher S, Duley L. Exercise or other physical activity for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2006;2.
Mehrholz J, Kugler J, Pohl M. Water-based exercises for improving activities of daily living after stroke. Cochrane Database Syst Rev. 2011;1.
Mehrholz J, Kugler J, Pohl M. Locomotor training for walking after spinal cord injury. Cochrane Database Syst Rev. 2012;11.
Mehrholz J, Thomas S, Elsner B. Treadmill training and body weight support for walking after stroke. Cochrane Database Syst Rev. 2017;8.
Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC, Snyder C. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;8.
Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst Rev. 2012;8.
Montgomery P, Dennis JA. Physical exercise for sleep problems in adults aged 60+. Cochrane Database Syst Rev. 2002;4.
Morris NR, Kermeen FD, Holland AE. Exercise-based rehabilitation programmes for pulmonary hypertension. Cochrane Database Syst Rev. 2017;1.
Muktabhant B, Lawrie TA, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst Rev. 2015;6.
Ngai SPC, Jones AYM, Tam WWS. Tai chi for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2016;6.
Norton C, Cody JD. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. Cochrane Database Syst Rev. 2012;7.
O'Brien K, Nixon S, Glazier R, Tynan AM. Progressive resistive exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2004;4.
O'Brien K, Nixon S, Tynan AM, Glazier R. Aerobic exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2010;8.
Østerås N, Kjeken I, Smedslund G, Moe RH, Slatkowsky-Christensen B, Uhlig T, Hagen KB. Exercise for hand osteoarthritis. Cochrane Database Syst Rev. 2017;1.
Page MJ, Green S, Kramer S, Johnston RV, McBain B, Chau M, Buchbinder R. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014;8.
Page MJ, Green S, McBain B, Surace SJ, Deitch J, Lyttle N, Mrocki MA, Buchbinder R. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev. 2016;6.
Page MJ, O'Connor D, Pitt V, Massy-Westropp N. Exercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;6.
Panebianco M, Sridharan K, Ramaratnam S. Yoga for epilepsy. Cochrane Database Syst Rev. 2017;10.
Perry A, Lee SH, Cotton S, Kennedy C. Therapeutic exercises for affecting post-treatment swallowing in people treated for advanced-stage head and neck cancers. Cochrane Database Syst Rev. 2016;8.
Radtke T, Nevitt SJ, Hebestreit H, Kriemler S. Physical exercise training for cystic fibrosis. Cochrane Database Syst Rev. 2017;11.
Regnaux JP, Lefevre-Colau MM, Trinquart L, Nguyen C, Boutron I, Brosseau L, Ravaud P. High-intensity versus low-intensity physical activity or exercise in people with hip or knee osteoarthritis. Cochrane Database Syst Rev. 2015;10.
Ren J, Xia J. Dance therapy for schizophrenia. Cochrane Database Syst Rev. 2013;10.
Rietberg MB, Brooks D, Uitdehaag BMJ, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;1.
Risom SS, Zwisler AD, Johansen PP, Sibilitz KL, Lindschou J, Gluud C, Taylor RS, Svendsen JH, Berg SK. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst Rev. 2017;2.
Romano M, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Kotwicki T, Maier-Hennes A, Negrini S. Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst Rev. 2012;8.
Ryan JM, Cassidy EE, Noorduyn SG, O'Connell NE. Exercise interventions for cerebral palsy. Cochrane Database Syst Rev. 2017;6.
Saragiotto BT, Maher CG, Yamato TP, Costa LOP, Menezes Costa LC, Ostelo R, Macedo LG. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev. 2016;1.
Saunders DH, Sanderson M, Hayes S, Kilrane M, Greig CA, Brazzelli M, Mead GE. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2016;3.
Schulzke SM, Kaempfen S, Trachsel D, Patole SK. Physical activity programs for promoting bone mineralization and growth in preterm infants. Cochrane Database Syst Rev. 2014;4.
Seron P, Lanas F, Pardo Hernandez H, Bonfill Cosp X. Exercise for people with high cardiovascular risk. Cochrane Database Syst Rev. 2014;8.
Shaw KA, Gennat HC, O'Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006;4.
Shepherd E, Gomersall JC, Tieu J, Han S, Crowther CA, Middleton P. Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2017;11.
Sibilitz KL, Berg SK, Tang LH, Risom SS, Gluud C, Lindschou J, Kober L, Hassager C, Taylor RS, Zwisler AD. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2016;3.
Silva IS, Fregonezi GAF, Dias FAL, Ribeiro CTD, Guerra RO, Ferreira GMH. Inspiratory muscle training for asthma. Cochrane Database Syst Rev. 2013;9.
States RA, Pappas E, Salem Y. Overground physical therapy gait training for chronic stroke patients with mobility deficits. Cochrane Database Syst Rev. 2009;3.
Strike K, Mulder K, Michael R. Exercise for haemophilia. Cochrane Database Syst Rev. 2016;12.
Takken T, Van Brussel M, Engelbert RH, van der Net JJ, Kuis W, Helders P. Exercise therapy in juvenile idiopathic arthritis. Cochrane Database Syst Rev. 2008;2.
Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJS, Dalal H, Lough F, Rees K, Singh SJ, Mordi IR. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014;4.
Thomas D, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2006;3.
Ussher MH, Taylor AH, Faulkner GEJ. Exercise interventions for smoking cessation. Cochrane Database Syst Rev. 2014;8.
Valentín-Gudiol M, Mattern-Baxter K, Girabent-Farrés M, Bagur-Calafat C, Hadders-Algra M, Angulo-Barroso RM. Treadmill interventions in children under six years of age at risk of neuromotor delay. Cochrane Database Syst Rev. 2017;7.
van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma-Zeinstra SMA, van Middelkoop M. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2015;1.
Vloothuis JDM, Mulder M, Veerbeek JM, Konijnenbelt M, Visser-Meily JMA, Ket JCF, Kwakkel G, van Wegen EEH. Caregiver-mediated exercises for improving outcomes after stroke. Cochrane Database Syst Rev. 2016;12.
Voet NBM, van der Kooi EL. Riphagen, II, Lindeman E, van Engelen BGM, Geurts ACH: strength training and aerobic exercise training for muscle disease. Cochrane Database Syst Rev. 2013;7.
White CM, Pritchard J, Turner-Stokes L. Exercise for people with peripheral neuropathy. Cochrane Database Syst Rev. 2004;4.
Wieland LS, Skoetz N, Pilkington K, Vempati R, D'Adamo CR, Berman BM. Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;1.
Williams AD, Bird ML, Hardcastle SGK, Kirschbaum M, Ogden KJ, Walters JAE. Exercise for reducing falls in people living with and beyond cancer. Cochrane Database Syst Rev. 2018;10.
Williams MA, Srikesavan C, Heine PJ, Bruce J, Brosseau L, Hoxey-Thomas N, Lamb SE. Exercise for rheumatoid arthritis of the hand. Cochrane Database Syst Rev. 2018;7.
Yamamoto S, Hotta K, Ota E, Matsunaga A, Mori R. Exercise-based cardiac rehabilitation for people with implantable ventricular assist devices. Cochrane Database Syst Rev. 2018;9.
Yamato TP, Maher CG, Saragiotto BT, Hancock MJ, Ostelo R, Cabral CMN, Menezes Costa LC, Costa LOP. Pilates for low back pain. Cochrane Database Syst Rev. 2015;7.
Yang ZY, Zhong HB, Mao C, Yuan JQ, Huang YF, Wu XY, Gao YM, Tang JL. Yoga for asthma. Cochrane Database Syst Rev. 2016;4.
Young J, Angevaren M, Rusted J, Tabet N. Aerobic exercise to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2015;4.
Zainuldin R, Mackey MG, Alison JA. Optimal intensity and type of leg exercise training for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;11.
Mok A, Khaw K-T, Luben R, Wareham N, Brage S. Physical activity trajectories and mortality: population based cohort study. Bmj. 2019;365:l2323.
Ekelund U, Brown WJ, Steene-Johannessen J, Fagerland MW, Owen N, Powell KE, Bauman AE, Lee IM. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019;53(14):886–94. https://doi.org/10.1136/bjsports-2017-098963 . Epub 2018 Jul 10.
Article PubMed Google Scholar
Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, Bauman A, Lee IM. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–10.
Lear SA, Hu W, Rangarajan S, Gasevic D, Leong D, Iqbal R, Casanova A, Swaminathan S, Anjana RM, Kumar R, et al. The effect of physical activity on mortality and cardiovascular disease in 130000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390(10113):2643–54.
Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–95.
Heyman E, Gamelin FX, Goekint M, Piscitelli F, Roelands B, Leclair E, Di Marzo V, Meeusen R. Intense exercise increases circulating endocannabinoid and BDNF levels in humans--possible implications for reward and depression. Psychoneuroendocrinology. 2012;37(6):844–51.
Horton R. Offline: the gravy train of systematic reviews. Lancet. 2019;394(10211):1790.
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health. 2018;6(10):e1077–86.
Fletcher GF, Landolfo C, Niebauer J, Ozemek C, Arena R, Lavie CJ. Promoting physical activity and exercise: JACC health promotion series. J Am Coll Cardiol. 2018;72(14):1622–39.
Download references
Acknowledgements
Not applicable.
There was no funding source for this study. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Kleijnen Systematic Reviews Ltd., York, UK
Pawel Posadzki
Nanyang Technological University, Singapore, Singapore
Institute for Research in Operative Medicine, Witten/Herdecke University, Witten, Germany
Dawid Pieper, Nadja Könsgen & Annika Lena Neuhaus
School of Medicine, Keele University, Staffordshire, UK
Jozef Pilsudski University of Physical Education in Warsaw, Faculty Physical Education and Health, Biala Podlaska, Poland
Hubert Makaruk
Health Outcomes Division, University of Texas at Austin College of Pharmacy, Austin, USA
Monika Semwal
You can also search for this author in PubMed Google Scholar
Contributions
PP wrote the protocol, ran the searches, validated, analysed and synthesised data, wrote and revised the drafts. HM, NK and ALN screened and extracted data. MS and DP validated and analysed the data. RB ran statistical analyses. All authors contributed to writing and reviewing the manuscript. PP is the guarantor. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Dawid Pieper .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Supplementary Table 1. Main characteristics of included Cochrane systematic reviews evaluating the effects of physical activity/exercise on health outcomes ( n = 150). Supplementary Table 2. Additional information from Cochrane systematic reviews of the effects of physical activity/exercise on health outcomes ( n = 150). Supplementary Table 3. Conclusions from Cochrane systematic reviews “quote”. Supplementary Table 4 . AEs reported in Cochrane systematic reviews. Supplementary Table 5. Summary of withdrawals/non-adherence. Supplementary Table 6. Methodological quality assessment of the included Cochrane reviews with AMSTAR-2. Supplementary Table 7. Number of studies assessed as low risk of bias per domain. Supplementary Table 8. GRADE for the review’s main comparison. Supplementary Table 9. Studies reporting quality of life outcomes as mean difference.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Posadzki, P., Pieper, D., Bajpai, R. et al. Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews. BMC Public Health 20 , 1724 (2020). https://doi.org/10.1186/s12889-020-09855-3
Download citation
Received : 01 April 2020
Accepted : 08 November 2020
Published : 16 November 2020
DOI : https://doi.org/10.1186/s12889-020-09855-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Effectiveness
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
A discovery in the muscles of long COVID patients may explain exercise troubles

For patients with long COVID, exercise can lead to a worsening of symptoms, a condition called post-exertional malaise. New research shows what's going on in their muscles. Erik Isakson/Getty Images/Tetra images RF hide caption
For patients with long COVID, exercise can lead to a worsening of symptoms, a condition called post-exertional malaise. New research shows what's going on in their muscles.
Hit the gym. Get back in shape.
That's what many patients with long COVID are told when they talk of the crushing fatigue that envelops them after even a light bout of physical activity.
These symptoms of exhaustion, or post-exertional malaise as it's called, are a hallmark of long COVID and similar complex illnesses like chronic fatigue syndrome or ME/CFS.
The idea that exercise can help patients has proven difficult to shake — despite evidence suggesting this isn't merely a case of deconditioning that patients can overcome by pushing through the pain.
"I don't think the messaging has been strong enough," says David Putrino , the director of rehabilitation innovation for Mount Sinai Health System. "It is very clear that this is not a typical response to exercise."
Now research published this month in Nature Communications gives new weight to this assessment.
By taking biopsies from long COVID patients before and after exercising, scientists in the Netherlands constructed a startling picture of widespread abnormalities in muscle tissue that may explain this severe reaction to physical activity.
Among the most striking findings were clear signs that the cellular power plants, the mitochondria , are compromised and the tissue starved for energy.
"We saw this immediately and it's very profound," says Braeden Charlton , one of the study's authors at Vrije University in Amsterdam.
The tissue samples from long COVID patients also revealed severe muscle damage, a disturbed immune response, and a buildup of microclots.
"This is a very real disease," says Charlton. "We see this at basically every parameter that we measure."

Goats and Soda
Long covid brain fog may originate in a surprising place, say scientists, exercise tests reveal a cellular energy system gone wrong.
Most people will get delayed onset muscle soreness after a tough workout, but post-exertional malaise is a different animal altogether.
"It's not just soreness," says Charlton. "For a lot of people, it's completely debilitating for days to weeks."
While symptoms vary, the most common tend to be muscle pain, an increase in fatigue, and cognitive problems, usually referred to as "brain fog," that last up to a week after physical exertion.
The study , based at Vrije and Amsterdam UMC health center, compared 25 people with long COVID to healthy controls who'd fully recovered from COVID-19 and had no persistent symptoms. Both groups were asked to work out for about 10-15 minutes on a stationary bike, until gradually reaching their maximum aerobic capacity.
Researchers took multiple blood draws and collected two muscle biopsies from their thighs, a week before they exercised and a day after.
"Their baseline was already impaired and that dropped even lower with the maximal exercise," says Charlton.
As seen in other long COVID studies , the problem wasn't related to how their lungs or heart were functioning. Instead, something was making it hard for the muscle to take up the oxygen in the blood.
Using a technique called respirometry , the Dutch researchers oversupplied oxygen to the muscle tissue and found evidence the mitochondria weren't functioning properly
Further tests revealed more clues
Metabolites in the blood related to energy production were also severely reduced in long COVID patients. And they started producing lactate, a fuel of "last resort" for cells, much sooner during exercise than those who were healthy, yet another sign that their cellular energy system had gone awry.
"The mitochondria are operating at a severely reduced capacity compared to healthy people," says Charlton.
Taken together, the results support the hypothesis that mitochondrial dysfunction plays a role in long COVID symptoms like fatigue and post-exertional malaise, says Dr. David Systrom , a physician at Harvard Medical School and Brigham and Women's Hospital.
"They were able to link symptoms to these organic changes," he says. "I was impressed by that."
In his own research, Systrom has found evidence of abnormal oxygen uptake by the skeletal muscles during peak exercise in both long COVID and ME/CFS patients, which indicates there's a problem with oxygen delivery to the mitochondria.
Meanwhile, the Dutch study suggests there could be "intrinsic dysfunction" of the mitochondria's ability to produce energy, he says.
Systrom says it's possible both could be happening in long COVID patients. "There may be two ends of that spectrum," he says. "That's really something future work will have to look at."

Shots - Health News
Unraveling long covid: here's what scientists who study the illness want to find out, biopsies carry clear signs of muscle damage.
The story doesn't end with mitochondria, either.
The muscle biopsies taken after the exercise test revealed other troubling events.
"They end up having a lot more muscle damage than a healthy person would have," says Charlton. "And because their maximal capacity is now also lower, they have that damage happening at a sooner point ."
A close look at the muscle tissue showed long COVID patients had more atrophy — shrinking of the fibers — than the healthy controls. There were also "immense amounts" of cell death, or "necrosis," which happens when immune cells infiltrate and degrade the tissue, he says.
The data hints at some kind of altered immune response to exercise in post-exertional malaise.
"It's not just the functionality of their muscles, but the way that their immune system is receiving that exercise signal," says Charlton.
The tissue-level analysis of defects in the muscle is "striking" and may help explain the pain, fatigue and weakness that patients experience, says Akiko Iwasaki, a professor of immunobiology at Yale University, who was not involved in the research.
The additional finding that T cells — part of the immune system's arsenal — had infiltrated the muscles of long COVID patients also caught Iwasaki's attention, possibly indicating "an autoimmune response within the muscle cells."
"In the healthy muscle, they find very few, if any T cells," she says.
Microclots portend big problems for blood vessels
The deep dive into muscle tissue also turned up another increasingly familiar character in long COVID pathology — microclots.
The researchers found these were heavily elevated in those with symptoms — a feature that only got worse following exercise.
Researchers in South Africa have zeroed in on these microclots that carry "trapped inflammatory molecules" as an indication of patients' compromised vasculature.
In the Dutch study, there wasn't evidence that microclots were blocking the tiny blood vessels, which was one hypothesis. Instead, they were lodged in the tissue.
The implications of this finding are potentially huge, says Resia Pretorius , a professor of physiological sciences at Stellenbosch University in South Africa, who was not involved in the present study.
"That means the microclots can actually have traveled through the damaged vasculature into the muscle," she says. "What is scary, but possibly very significant, is that this might be happening in other tissues as well."
In this scenario, the microclots could reflect the extent of damage to the lining of the blood vessels, which would also impair the delivery of oxygen to the muscle tissue.
If the vasculature is "totally shot," Pretorius says the "mitochondria will be massively affected," although more work needs to be done before drawing definitive conclusions.
The underlying causes of long COVID remain elusive; however, one leading theory is that an ongoing chronic infection could be driving the downstream consequences.
The researchers probed this hypothesis. They found evidence of viral proteins from SARS-CoV-2 in the muscle tissue, but no difference emerged between the long COVID group and the controls, leading them to conclude these are viral leftovers that don't necessarily figure into post-exertional malaise.

Millions of people have long COVID brain fog — and there's a shortage of answers
Experts warn that exercise can "harm" and other approaches are needed.
The role of exercise in treating post-exertional malaise remains "intensely controversial," says Harvard's Systrom, who has studied exercise in the context of other complex chronic illnesses like ME/CFS.
"Post-exertional malaise is a unique symptom in these disorders and is not a feature of deconditioning," he says. "You cannot simply ask these patients to go to the gym and fix the problem."
Long COVID is itself an umbrella term that encompasses a wide range of symptoms that may have different underlying causes.
Systrom says it's possible a subset of these patients may benefit more than others from gradual exercise, especially after successful medical treatment has been first established.
In their study, Charlton says they looked at other research to verify that what they observed did not stem from physical inactivity. He also notes that the long COVID patients who were enrolled were not bedridden and had an average of 4,000 steps a day.
Putrino at Mount Sinai considers the study a much-needed wake-up call for the broader medical field — clear evidence of a biological basis for the energy crash and onslaught of symptoms that patients with long COVID and similar conditions experience.
"As opposed to what's been sold to patients over the last few decades, that symptoms such as extreme fatigue and exertional malaise are psychological or physical conditioning issues," he says. "Physical exertion does harm to the bodies of people with these illnesses. "
His general guidance is to avoid exercise if you have post-exertional malaise and instead practice "energy conservation."
At his clinic, Putrino prescribes what's called " autonomic rehabilitation " for these patients.
Whereas the aim of exercise is to improve cardiovascular fitness — something he might recommend to patients who're recovering after severe pneumonia — this type of rehabilitation is done at a much lower intensity and duration, and it takes into account post-exertional malaise.
"We need to step out of this erroneous mindset of no pain, no gain," he says.

Why viral reservoirs are a prime suspect for long COVID sleuths
- exercise intolerance
- post-exertional malaise
- chronic fatigue syndrome
- Share full article
Advertisement
Supported by
The Year in Fitness: Shorter Workouts, Greater Clarity, Longer Lives
The most vital exercise science of 2021 provided a reminder that our bodies and minds can flourish, no matter our circumstances.

By Gretchen Reynolds
In a year filled with Covid-related hopes, setbacks, advances and losses, the most vital exercise science of 2021 provided a reminder that for many of us, our bodies and minds can strengthen, endure and flourish, no matter our circumstances. If we move our bodies in the right ways, a growing body of evidence suggests we might live with greater stamina, purpose and cognitive clarity for many years to come. And it may not take much movement.
In fact, some of the year’s biggest fitness news concerned how little exercise we might be able to get away with, while maintaining or even improving our health. A study from January, for instance, showed that just five minutes of intense calisthenics substantially improved college students’ aerobic fitness and leg strength. Another series of studies from the University of Texas found that four seconds — yes, seconds — of ferocious bicycle pedaling, repeated several times, was enough to raise adults’ strength and endurance, whatever their age or health when they started.
Even people whose favorite workout is walking might need less than they think to reach an exercise sweet spot, other new research suggested. As I wrote in July, the familiar goal of 10,000 daily steps, deeply embedded in our activity trackers and collective consciousness, has little scientific validity. It is a myth that grew out of a marketing accident, and a study published this summer further debunked it , finding that people who took between 7,000 and 8,000 steps a day, or a little more than three miles, generally lived longer than those strolling less or accumulating more than 10,000 steps. So keep moving, but there’s no need to fret if your total doesn’t reach a five-figure step count.
Of course, exercise science weighed in on other resonant topics this year, too, including weight. And the news there was not all cheering. Multiple studies this year reinforced an emerging scientific consensus that our bodies compensate for some of the calories we expend during physical activity, by shunting energy away from certain cellular processes or prompting us unconsciously to move and fidget less. A study from July , for example, that examined the metabolisms of almost 2,000 people concluded that we probably compensate, on average, for about a quarter of the calories we burn with exercise. As a result, on days we exercise, we wind up burning far fewer total calories than we might think, making weight loss that much more challenging.
On the other hand, exercise seems essential for weight maintenance, according to other research this year. A new scientific analysis of participants from the TV weight-loss contest “The Biggest Loser” found that those who exercised the most in the years after the program ended were the least likely to have regained all of the pounds they shed during the show.
Exercise also has a disproportionate impact on our odds of enjoying a long, healthy life. According to one of the most inspiring studies this year, overweight people who started working out lowered their risk of premature death by about 30 percent even if they remained overweight, with exercise providing about twice as much benefit as weight loss might.
Exercise enhances our brain power, too, according to other, memorable experiments from this year. They showed physical activity fortifying immune cells that help protect us against dementia; prompting the release of a hormone that improves neuron health and the ability to think (in mice); shoring up the fabric of our brains’ white matter , the stuff that connects and protects our working brain cells; and likely even adding to our creativity. In a nifty study from February , physically active people tended to dream up more-inventive ways to use car tires and umbrellas, a standard test of creativity, than people who seldom moved around much.
Taken together, this year’s exercise neuroscience research makes “a strong case for getting up and moving” if we hope to use our brains with ongoing clarity and in imaginative ways deep into our golden years, as one of the researchers said to me.
Still, the study that stuck with me most this year had less to do with the myriad ways exercise remodels our bodies and brains and more with how it might shape our sense of what matters. In the study, which I wrote about in May , active people reported a stronger sense of purpose in their lives than inactive people.
“A sense of purpose is the feeling you get from having goals and plans that give direction and meaning to life,” the study’s lead researcher told me. “It is about being engaged with life in productive ways.” The study found that exercise amplified people’s purposefulness over time, while simultaneously, a sturdy sense of purpose fortified people’s willingness to exercise. In effect, the more people felt their lives had meaning, the more they wound up moving, and the more they moved, the more meaningful they found their lives.
It’s a result worth remembering as we look ahead with wary optimism. So stay healthy, active and in touch in 2022, everyone. Here’s to a happy new year!
Let Us Help You Pick Your Next Workout
Looking for a new way to get moving we have plenty of options..
To develop a sustainable exercise habit, experts say it helps to tie your workout to something or someone .
Viral online exercise challenges might get you in shape in the short run, but they may not help you build sustainable healthy habits. Here’s what fitness fads get wrong .
Does it really matter how many steps you take each day? The quality of the steps you take might be just as important as the amount .
Is your workout really working for you? Take our quiz to find out .
To help you start moving, we tapped fitness pros for advice on setting realistic goals for exercising and actually enjoying yourself.
You need more than strength to age well — you also need power. Here’s how to measure how much you have and here’s how to increase yours .
Pick the Right Equipment With Wirecutter’s Recommendations
Want to build a home gym? These five things can help you transform your space into a fitness center.
Transform your upper-body workouts with a simple pull-up bar and an adjustable dumbbell set .
Choosing the best running shoes and running gear can be tricky. These tips make the process easier.
A comfortable sports bra can improve your overall workout experience. These are the best on the market .
Few things are more annoying than ill-fitting, hard-to-use headphones. Here are the best ones for the gym and for runners .
- Introduction
- Conclusions
- Article Information
Hazard ratio for obesity was modeled according to mean daily step counts and 25th, 50th, and 75th percentile PRS for body mass index. Shaded regions represent 95% CIs. Model is adjusted for age, sex, mean baseline step counts, cancer status, coronary artery disease status, systolic blood pressure, alcohol use, educational level, and a PRS × mean steps interaction term.
Mean daily steps and polygenic risk score (PRS) for higher body mass index are independently associated with hazard for obesity. Hazard ratios model the difference between the 75th and 25th percentiles for continuous variables. CAD indicate coronary artery disease; and SBP, systolic blood pressure.
Each point estimate is indexed to a hazard ratio for obesity of 1.00 (BMI [calculated as weight in kilograms divided by height in meters squared] ≥30). Error bars represent 95% CIs.
eTable. Cumulative Incidence Estimates of Obesity Based on Polygenic Risk Score for Body Mass Index and Mean Daily Steps at 1, 3, and 5 Years
eFigure 1. CONSORT Diagram
eFigure 2. Risk of Incident Obesity Modeled by Mean Daily Step Count and Polygenic Risk Scores Adjusted for Baseline Body Mass Index
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Brittain EL , Han L , Annis J, et al. Physical Activity and Incident Obesity Across the Spectrum of Genetic Risk for Obesity. JAMA Netw Open. 2024;7(3):e243821. doi:10.1001/jamanetworkopen.2024.3821
Manage citations:
© 2024
- Permissions
Physical Activity and Incident Obesity Across the Spectrum of Genetic Risk for Obesity
- 1 Division of Cardiovascular Medicine, Vanderbilt University Medical Center, Nashville, Tennessee
- 2 Center for Digital Genomic Medicine, Department of Medicine, Vanderbilt University Medical Center, Nashville, Tennessee
- 3 Division of Genetic Medicine, Vanderbilt Genetics Institute, Vanderbilt University Medical Center, Nashville, Tennessee
- 4 Vanderbilt Institute of Clinical and Translational Research, Vanderbilt University Medical Center, Nashville, Tennessee
- 5 Department of Medicine, Vanderbilt University Medical Center, Nashville, Tennessee
- 6 Department of Pharmacology, Vanderbilt University Medical Center, Nashville, Tennessee
- 7 Department of Biomedical Informatics, Vanderbilt University Medical Center, Nashville, Tennessee
- 8 Department of Biomedical Engineering, Vanderbilt University Medical Center, Nashville, Tennessee
- 9 Department of Biostatistics, Vanderbilt University Medical Center, Nashville, Tennessee
- 10 Department of Psychiatry and Behavioral Sciences, Vanderbilt University Medical Center, Nashville, Tennessee
Question Does the degree of physical activity associated with incident obesity vary by genetic risk?
Findings In this cohort study of 3124 adults, individuals at high genetic risk of obesity needed higher daily step counts to reduce the risk of obesity than those at moderate or low genetic risk.
Meaning These findings suggest that individualized physical activity recommendations that incorporate genetic background may reduce obesity risk.
Importance Despite consistent public health recommendations, obesity rates in the US continue to increase. Physical activity recommendations do not account for individual genetic variability, increasing risk of obesity.
Objective To use activity, clinical, and genetic data from the All of Us Research Program (AoURP) to explore the association of genetic risk of higher body mass index (BMI) with the level of physical activity needed to reduce incident obesity.
Design, Setting, and Participants In this US population–based retrospective cohort study, participants were enrolled in the AoURP between May 1, 2018, and July 1, 2022. Enrollees in the AoURP who were of European ancestry, owned a personal activity tracking device, and did not have obesity up to 6 months into activity tracking were included in the analysis.
Exposure Physical activity expressed as daily step counts and a polygenic risk score (PRS) for BMI, calculated as weight in kilograms divided by height in meters squared.
Main Outcome and Measures Incident obesity (BMI ≥30).
Results A total of 3124 participants met inclusion criteria. Among 3051 participants with available data, 2216 (73%) were women, and the median age was 52.7 (IQR, 36.4-62.8) years. The total cohort of 3124 participants walked a median of 8326 (IQR, 6499-10 389) steps/d over a median of 5.4 (IQR, 3.4-7.0) years of personal activity tracking. The incidence of obesity over the study period increased from 13% (101 of 781) to 43% (335 of 781) in the lowest and highest PRS quartiles, respectively ( P = 1.0 × 10 −20 ). The BMI PRS demonstrated an 81% increase in obesity risk ( P = 3.57 × 10 −20 ) while mean step count demonstrated a 43% reduction ( P = 5.30 × 10 −12 ) when comparing the 75th and 25th percentiles, respectively. Individuals with a PRS in the 75th percentile would need to walk a mean of 2280 (95% CI, 1680-3310) more steps per day (11 020 total) than those at the 50th percentile to have a comparable risk of obesity. To have a comparable risk of obesity to individuals at the 25th percentile of PRS, those at the 75th percentile with a baseline BMI of 22 would need to walk an additional 3460 steps/d; with a baseline BMI of 24, an additional 4430 steps/d; with a baseline BMI of 26, an additional 5380 steps/d; and with a baseline BMI of 28, an additional 6350 steps/d.
Conclusions and Relevance In this cohort study, the association between daily step count and obesity risk across genetic background and baseline BMI were quantified. Population-based recommendations may underestimate physical activity needed to prevent obesity among those at high genetic risk.
In 2000, the World Health Organization declared obesity the greatest threat to the health of Westernized nations. 1 In the US, obesity accounts for over 400 000 deaths per year and affects nearly 40% of the adult population. Despite the modifiable nature of obesity through diet, exercise, and pharmacotherapy, rates have continued to increase.
Physical activity recommendations are a crucial component of public health guidelines for maintaining a healthy weight, with increased physical activity being associated with a reduced risk of obesity. 2 - 4 Fitness trackers and wearable devices have provided an objective means to capture physical activity, and their use may be associated with weight loss. 5 Prior work leveraging these devices has suggested that taking around 8000 steps/d substantially mitigates risk of obesity. 3 , 4 However, current recommendations around physical activity do not take into account other contributors such as caloric intake, energy expenditure, or genetic background, likely leading to less effective prevention of obesity for many people. 6
Obesity has a substantial genetic contribution, with heritability estimates ranging from 40% to 70%. 7 , 8 Prior studies 9 - 11 have shown an inverse association between genetic risk and physical activity with obesity, whereby increasing physical activity can help mitigate higher genetic risk for obesity. These results have implications for physical activity recommendations on an individual level. Most of the prior work 9 - 11 focused on a narrow set of obesity-associated variants or genes and relied on self-reported physical activity, and more recent work using wearable devices has been limited to 7 days of physical activity measurements. 12 Longer-term capture in large populations will be required to accurately estimate differences in physical activity needed to prevent incident obesity.
We used longitudinal activity monitoring and genome sequencing data from the All of Us Research Program (AoURP) to quantify the combined association of genetic risk for body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) and physical activity with the risk of incident obesity. Activity monitoring was quantified as daily step counts obtained from fitness tracking devices. Genetic risk was quantified by using a polygenic risk score (PRS) from a large-scale genomewide association study (GWAS) of BMI. 13 We quantified the mean daily step count needed to overcome genetic risk for increased BMI. These findings represent an initial step toward personalized exercise recommendations that integrate genetic information.
Details on the design and execution of the AoURP have been published previously. 14 The present study used AoURP Controlled Tier dataset, version 7 (C2022Q4R9), with data from participants enrolled between May 1, 2018, and July 1, 2022. Participants who provided informed consent could share data from their own activity tracking devices from the time their accounts were first created, which may precede the enrollment date in AoURP. We followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline. In this study, only the authorized authors who completed All of Us Responsible Conduct of Research training accessed the deidentified data from the Researcher Workbench (a secured cloud-based platform). Since the authors were not directly involved with the participants, institutional review board review was exempted in compliance with AoURP policy.
Activity tracking data for this study came from the Bring Your Own Device program that allowed individuals who already owned a tracking device (Fitbit, Inc) to consent to link their activity data with other data in the AoURP. By registering their personal device on the AoURP patient portal, patients could share all activity data collected since the creation of their personal device account. For many participants, this allowed us to examine fitness activity data collected prior to enrollment in the AoURP. Activity data in AoURP are reported as daily step counts. We excluded days with fewer than 10 hours of wear time to enrich our cohort for individuals with consistently high wear time. The initial personal activity device cohort consisted of 12 766 individuals. Consistent with our prior data curation approach, days with less than 10 hours of wear time, less than 100 steps, or greater than 45 000 steps or for which the participant was younger than 18 years were removed. For time-varying analyses, mean daily steps were calculated on a monthly basis for each participant. Months with fewer than 15 valid days of monitoring were removed.
The analytic cohort included only individuals with a BMI of less than 30 at the time activity monitoring began. The primary outcome was incident obesity, defined as a BMI of 30 or greater documented in the medical record at least 6 months after initiation of activity monitoring. The latter stipulation reduced the likelihood that having obesity predated the beginning of monitoring but had not yet been clinically documented. We extracted BMI values and clinical characteristics from longitudinal electronic health records (EHRs) for the consenting participants who were associated with a health care provider organization funded by the AoURP. The EHR data have been standardized using the Observational Medical Outcomes Partnership Common Data Model. 15 In the AoURP, upon consent, participants are asked to complete the Basics survey, in which they may self-report demographic characteristics such as race, ethnicity, and sex at birth.
We filtered the data to include only biallelic, autosomal single-nucleotide variants (SNVs) that had passed AoURP initial quality control. 16 We then removed duplicate-position SNVs and kept only individual genotypes with a genotype quality greater than 20. We further filtered the SNVs based on their Hardy-Weinberg equilibrium P value (>1.0 × 10 −15 ) and missing rate (<5%) across all samples. Next, we divided the samples into 6 groups (Admixed American, African, East Asian, European, Middle Eastern, and South Asian) based on their estimated ancestral populations 16 , 17 and further filtered the SNVs within each population based on minor allele frequency (MAF) (>0.01), missing rate (<0.02), and Hardy-Weinberg equilibrium P value (>1.0 × 10 −6 ). The SNVs were mapped from Genome Reference Consortium Human Build 38 with coordinates to Build 37. Because the existing PRS models have limited transferability across ancestry groups and to ensure appropriate power of the subsequent PRS analysis, we limited our analysis to the populations who had a sample size of greater than 500, resulting in 5964 participants of European ancestry with 5 515 802 common SNVs for analysis.
To generate principal components, we excluded the regions with high linkage disequilibrium, including chr5:44-51.5 megabase (Mb), chr6:25-33.5 Mb, chr8:8-12 Mb, and chr11:45-57 Mb. We then pruned the remaining SNVs using PLINK, version 1.9 (Harvard University), pairwise independence function with 1-kilobase window shifted by 50 base pairs and requiring r 2 < 0.05 between any pair, resulting in 100 983 SNPs for further analysis. 18 Principal component analysis was run using PLINK, version 1.9. The European ancestry linkage disequilibrium reference panel from the 1000 Genomes Project phase 3 was downloaded, and nonambiguous SNPs with MAF greater than 0.01 were kept in the largest European ancestry GWAS summary statistics of BMI. 13 We manually harmonized the strand-flipping SNPs among the SNP information file, GWAS summary statistics files, and the European ancestry PLINK extended map files (.bim).
We used PRS–continuous shrinkage to infer posterior SNP effect sizes under continuous shrinkage priors with a scaling parameter set to 0.01, reflecting the polygenic architecture of BMI. GWAS summary statistics of BMI measured in 681 275 individuals of European ancestry was used to estimate the SNP weights. 19 The scoring command in PLINK, version 1.9, was used to produce the genomewide scores of the AoURP European individuals with their quality-controlled SNP genotype data and these derived SNP weights. 20 Finally, by using the genomewide scores as the dependent variable and the 10 principal components as the independent variable, we performed linear regression, and the obtained residuals were kept for the subsequent analysis. To check the performance of the PRS estimate, we first fit a generalized regression model with obesity status as the dependent variable and the PRS as the independent variable with age, sex, and the top 10 principal components of genetic ancestry as covariates. We then built a subset logistic regression model, which only uses the same set of covariates. By comparing the full model with the subset model, we measured the incremental Nagelkerke R 2 value to quantify how much variance in obesity status was explained by the PRS.
Differences in clinical characteristics across PRS quartiles were assessed using the Wilcoxon rank sum or Kruskal-Wallis test for continuous variables and the Pearson χ 2 test for categorical variables. Cox proportional hazards regression models were used to examine the association among daily step count (considered as a time-varying variable), PRS, and the time to event for obesity, adjusting for age, sex, mean baseline step counts, cancer status, coronary artery disease status, systolic blood pressure, alcohol use, educational level, and interaction term of PRS × mean steps. We presented these results stratified by baseline BMI and provided a model including baseline BMI in eFigure 2 in Supplement 1 as a secondary analysis due to collinearity between BMI and PRS.
Cox proportional hazards regression models were fit on a multiply imputed dataset. Multiple imputation was performed for baseline BMI, alcohol use, educational status, systolic blood pressure, and smoking status using bootstrap and predictive mean matching with the aregImpute function in the Hmisc package of R, version 4.2.2 (R Project for Statistical Computing). Continuous variables were modeled as restricted cubic splines with 3 knots, unless the nonlinear term was not significant, in which case it was modeled as a linear term. Fits and predictions of the Cox proportional hazards regression models were obtained using the rms package in R, version 4.2.2. The Cox proportional hazards regression assumptions were checked using the cox.zph function from the survival package in R, version 4.2.2.
To identify the combinations of PRS and mean daily step counts associated with a hazard ratio (HR) of 1.00, we used a 100-knot spline function to fit the Cox proportional hazards regression ratio model estimations across a range of mean daily step counts for each PRS percentile. We then computed the inverse of the fitted spline function to determine the mean daily step count where the HR equals 1.00 for each PRS percentile. We repeated this process for multiple PRS percentiles to generate a plot of mean daily step counts as a function of PRS percentiles where the HR was 1.00. To estimate the uncertainty around these estimations, we applied a similar spline function to the upper and lower estimated 95% CIs of the Cox proportional hazards regression model to find the 95% CIs for the estimated mean daily step counts at each PRS percentile. Two-sided P < .05 indicated statistical significance.
We identified 3124 participants of European ancestry without obesity at baseline who agreed to link their personal activity data and EHR data and had available genome sequencing. Among those with available data, 2216 of 3051 (73%) were women and 835 of 3051 (27%) were men, and the median age was 52.7 (IQR, 36.4-62.8) years. In terms of race and ethnicity, 2958 participants (95%) were White compared with 141 participants (5%) who were of other race or ethnicity (which may include Asian, Black or African American, Middle Eastern or North African, Native Hawaiian or Other Pacific Islander, multiple races or ethnicities, and unknown race or ethnicity) ( Table ). The analytic sample was restricted to individuals assigned European ancestry based on the All of Us Genomic Research Data Quality Report. 16 A study flowchart detailing the creation of the analytic dataset is provided in eFigure 1 in Supplement 1 . The BMI-based PRS explained 8.3% of the phenotypic variation in obesity (β = 1.76; P = 2 × 10 −16 ). The median follow-up time was 5.4 (IQR, 3.4-7.0) years and participants walked a median of 8326 (IQR, 6499-10 389) steps/d. The incidence of obesity over the study period was 13% (101 of 781 participants) in the lowest PRS quartile and 43% (335 of 781 participants) in the highest PRS quartile ( P = 1.0 × 10 −20 ). We observed a decrease in median daily steps when moving from lowest (8599 [IQR, 6751-10 768]) to highest (8115 [IQR, 6340-10 187]) PRS quartile ( P = .01).
We next modeled obesity risk stratified by PRS percentile with the 50th percentile indexed to an HR for obesity of 1.00 ( Figure 1 ). The association between PRS and incident obesity was direct ( P = .001) and linear (chunk test for nonlinearity was nonsignificant [ P = .07]). The PRS and mean daily step count were both independently associated with obesity risk ( Figure 2 ). The 75th percentile BMI PRS demonstrated an 81% increase in obesity risk (HR, 1.81 [95% CI, 1.59-2.05]; P = 3.57 × 10 −20 ) when compared with the 25th percentile BMI PRS, whereas the 75th percentile median step count demonstrated a 43% reduction in obesity risk (HR, 0.57 [95% CI, 0.49-0.67]; P = 5.30 × 10 −12 ) when compared with the 25th percentile step count. The PRS × mean steps interaction term was not significant (χ 2 = 1.98; P = .37).
Individuals with a PRS at the 75th percentile would need to walk a mean of 2280 (95% CI, 1680-3310) more steps per day (11 020 total) than those at the 50th percentile to reduce the HR for obesity to 1.00 ( Figure 1 ). Conversely, those in the 25th percentile PRS could reach an HR of 1.00 by walking a mean of 3660 (95% CI, 2180-8740) fewer steps than those at the 50th percentile PRS. When assuming a median daily step count of 8740 (cohort median), those in the 75th percentile PRS had an HR for obesity of 1.33 (95% CI, 1.25-1.41), whereas those at the 25th percentile PRS had an obesity HR of 0.74 (95% CI, 0.69-0.79).
The mean daily step count required to achieve an HR for obesity of 1.00 across the full PRS spectrum and stratified by baseline BMI is shown in Figure 3 . To reach an HR of 1.00 for obesity, when stratified by baseline BMI of 22, individuals at the 50th percentile PRS would need to achieve a mean daily step count of 3290 (additional 3460 steps/d); for a baseline BMI of 24, a mean daily step count of 7590 (additional 4430 steps/d); for a baseline BMI of 26, a mean daily step count of 11 890 (additional 5380 steps/d); and for a baseline BMI of 28, a mean daily step count of 16 190 (additional 6350 steps/d).
When adding baseline BMI to the full Cox proportional hazards regression model, daily step count and BMI PRS both remain associated with obesity risk. When comparing individuals at the 75th percentile with those at the 25th percentile, the BMI PRS is associated with a 61% increased risk of obesity (HR, 1.61 [95% CI, 1.45-1.78]). Similarly, when comparing the 75th with the 25th percentiles, daily step count was associated with a 38% lower risk of obesity (HR, 0.62 [95% CI, 0.53-0.72]) (eFigure 2 in Supplement 1 ).
The cumulative incidence of obesity increases over time and with fewer daily steps and higher PRS. The cumulative incidence of obesity would be 2.9% at the 25th percentile, 3.9% at the 50th percentile, and 5.2% at the 75th percentile for PRS in year 1; 10.5% at the 25th percentile, 14.0% at the 50th percentile, and 18.2% at the 75th percentile for PRS in year 3; and 18.5% at the 25th percentile, 24.3% at the 50th percentile, and 30.9% at the 75th percentile for PRS in year 5 ( Figure 4 ). The eTable in Supplement 1 models the expected cumulative incidence of obesity at 1, 3, and 5 years based on PRS and assumed mean daily steps of 7500, 10 000, and 12 500.
We examined the combined association of daily step counts and genetic risk for increased BMI with the incidence of obesity in a large national sample with genome sequencing and long-term activity monitoring data. Lower daily step counts and higher BMI PRS were both independently associated with increased risk of obesity. As the PRS increased, the number of daily steps associated with lower risk of obesity also increased. By combining these data sources, we derived an estimate of the daily step count needed to reduce the risk of obesity based on an individual’s genetic background. Importantly, our findings suggest that genetic risk for obesity is not deterministic but can be overcome by increasing physical activity.
Our findings align with those of prior literature 9 indicating that engaging in physical activity can mitigate genetic obesity risk and highlight the importance of genetic background for individual health and wellness. Using the data from a large population-based sample, Li et al 9 characterized obesity risk by genotyping 12 susceptibility loci and found that higher self-reported physical activity was associated with a 40% reduction in genetic predisposition to obesity. Our study extends these results in 2 important ways. First, we leveraged objectively measured longitudinal activity data from commercial devices to focus on physical activity prior to and leading up to a diagnosis of obesity. Second, we used a more comprehensive genomewide risk assessment in the form of a PRS. Our results indicate that daily step count recommendations to reduce obesity risk may be personalized based on an individual’s genetic background. For instance, individuals with higher genetic risk (ie, 75th percentile PRS) would need to walk a mean of 2280 more steps per day than those at the 50th percentile of genetic risk to have a comparable risk of obesity.
These results suggest that population-based recommendations that do not account for genetic background may not accurately represent the amount of physical activity needed to reduce the risk of obesity. Population-based exercise recommendations may overestimate or underestimate physical activity needs, depending on one’s genetic background. Underestimation of physical activity required to reduce obesity risk has the potential to be particularly detrimental to public health efforts to reduce weight-related morbidity. As such, integration of activity and genetic data could facilitate personalized activity recommendations that account for an individual’s genetic profile. The widespread use of wearable devices and the increasing demand for genetic information from both clinical and direct-to-consumer sources may soon permit testing the value of personalized activity recommendations. Efforts to integrate wearable devices and genomic data into the EHR further support the potential future clinical utility of merging these data sources to personalize lifestyle recommendations. Thus, our findings support the need for a prospective trial investigating the impact of tailoring step counts by genetic risk on chronic disease outcomes.
The most important limitation of this work is the lack of diversity and inclusion only of individuals with European ancestry. These findings will need validation in a more diverse population. Our cohort only included individuals who already owned a fitness tracking device and agreed to link their activity data to the AoURP dataset, which may not be generalizable to other populations. We cannot account for unmeasured confounding, and the potential for reverse causation still exists. We attempted to diminish the latter concern by excluding prevalent obesity and incident cases within the first 6 months of monitoring. Genetic risk was simplified to be specific to increased BMI; however, genetic risk for other cardiometabolic conditions could also inform obesity risk. Nongenetic factors that contribute to obesity risk such as dietary patterns were not available, reducing the explanatory power of the model. It is unlikely that the widespread use of drug classes targeting weight loss affects the generalizability of our results, because such drugs are rarely prescribed for obesity prevention, and our study focused on individuals who were not obese at baseline. Indeed, less than 0.5% of our cohort was exposed to a medication class targeting weight loss (phentermine, orlistat, or glucagonlike peptide-1 receptor agonists) prior to incident obesity or censoring. Finally, some fitness activity tracking devices may not capture nonambulatory activity as well as triaxial accelerometers.
This cohort study used longitudinal activity data from commercial wearable devices, genome sequencing, and clinical data to support the notion that higher daily step counts can mitigate genetic risk for obesity. These results have important clinical and public health implications and may offer a novel strategy for addressing the obesity epidemic by informing activity recommendations that incorporate genetic information.
Accepted for Publication: January 30, 2024.
Published: March 27, 2024. doi:10.1001/jamanetworkopen.2024.3821
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Brittain EL et al. JAMA Network Open .
Corresponding Author: Evan L. Brittain, MD, MSc ( [email protected] ) and Douglas M. Ruderfer, PhD ( [email protected] ), Vanderbilt University Medical Center, 2525 West End Ave, Suite 300A, Nashville, TN 37203.
Author Contributions: Drs Brittain and Ruderfer had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Brittain, Annis, Master, Roden, Ruderfer.
Acquisition, analysis, or interpretation of data: Brittain, Han, Annis, Master, Hughes, Harris, Ruderfer.
Drafting of the manuscript: Brittain, Han, Annis, Master, Ruderfer.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Brittain, Han, Annis, Master.
Obtained funding: Brittain, Harris.
Administrative, technical, or material support: Brittain, Annis, Master, Roden.
Supervision: Brittain, Ruderfer.
Conflict of Interest Disclosures: Dr Brittain reported receiving a gift from Google LLC during the conduct of the study. Dr Ruderfer reported serving on the advisory board of Illumina Inc and Alkermes PLC and receiving grant funding from PTC Therapeutics outside the submitted work. No other disclosures were reported.
Funding/Support: The All of Us Research Program is supported by grants 1 OT2 OD026549, 1 OT2 OD026554, 1 OT2 OD026557, 1 OT2 OD026556, 1 OT2 OD026550, 1 OT2 OD 026552, 1 OT2 OD026553, 1 OT2 OD026548, 1 OT2 OD026551, 1 OT2 OD026555, IAA AOD21037, AOD22003, AOD16037, and AOD21041 (regional medical centers); grant HHSN 263201600085U (federally qualified health centers); grant U2C OD023196 (data and research center); 1 U24 OD023121 (Biobank); U24 OD023176 (participant center); U24 OD023163 (participant technology systems center); grants 3 OT2 OD023205 and 3 OT2 OD023206 (communications and engagement); and grants 1 OT2 OD025277, 3 OT2 OD025315, 1 OT2 OD025337, and 1 OT2 OD025276 (community partners) from the National Institutes of Health (NIH). This study is also supported by grants R01 HL146588 (Dr Brittain), R61 HL158941 (Dr Brittain), and R21 HL172038 (Drs Brittain and Ruderfer) from the NIH.
Role of the Funder/Sponsor: The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: The All of Us Research Program would not be possible without the partnership of its participants.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

- March 26, 2024 | Starry Nights and Snowy Lights: Space Station’s Stunning View of Eastern Canada
- March 26, 2024 | A Simple Way To Run Faster: New Research Reveals That Cranberries Can Boost Athletic Performance
- March 26, 2024 | Epsilon Indi “Starquake” Shatters Astronomical Records and Expectations
- March 26, 2024 | Quasar Conundrum: Brilliant Supermassive Black Hole Defies Expectations
- March 26, 2024 | Soyuz Spacecraft Hatches Open, Expedition 70 Welcomes International Trio Aboard Station
The Magic Number – New Research Sheds Light on How Often You Need To Exercise To Make It Worth It
By Edith Cowan University October 2, 2023

New research indicates that a thrice-weekly, three-second maximum-effort eccentric bicep contraction significantly enhances muscle strength. Though exercising three days a week shows benefits, five days a week brings greater improvements, highlighting the importance of regular short exercises.
A recent study provides insight into the frequency of exercise necessary to reap its benefits.
Interested in the health advantages of exercise but not eager to hit the road or lift weights daily?
New research from Edith Cowan University (ECU) might be able to shed light on how often you need to work out each week to make it worthwhile.
A new study saw participants perform a single three-second, maximum-effort eccentric bicep contraction — similar to slowly lowering a heavy dumbbell, from a bent arm to a straight arm.
Previous ECU research showed this can significantly improve muscle strength when it’s performed daily for five days a week (Monday – Friday), for four weeks.
Participants in the new study were split into two groups, with the first group performing a single three-second contraction two days per week, and the other performing the same exercise on three days per week.
After four weeks, researchers compared the participants’ bicep strength.
Those who performed the exercise two days per week saw no significant changes, however, the three-day group saw small but significant increases in concentric strength (2.5 percent) and eccentric strength (3.9 percent).
Study lead Professor Ken Nosaka said the results helped to further improve our understanding of how our body responds to exercise — and how people can then put that knowledge to good use.
“Our previous work has shown regular, shorter exercise is more beneficial than one or two big training sessions in a week,” Professor Nosaka said. “Now, we have a clearer idea of where the tipping point is where you start to see meaningful benefits from such a minimal exercise. These new results suggest at least three days a week are required, at least for the single three-second eccentric contraction training.”
Three is good… but five is better
While the findings showed three days per week will have an impact, finding the willpower to put in a couple of extra days of exercise per week will produce better results.
The previous study’s participants who performed the exercise five days a week saw greater improvements in strength — more than 10% increases — than the three-day group.
However, Professor Nosaka stressed this didn’t mean exercising every day would improve results even further.
“Muscle adaptations occur when we are resting, so muscles need rest to improve their strength and their muscle mass,” he said. “It should be noted that the exercise was only three seconds, so the rest between exercises in the study was close to 28,800 times more than the exercise time. But muscles do appear to like to be stimulated more frequently, especially for the small volume of muscle strengthening exercise.”
Applying it to real-life
Professor Nosaka said more research was needed to see if the study’s findings apply to other types and volumes of exercise.
“Muscles enjoying frequent stimulation may not necessarily be the case for a greater volume of aerobic exercise to improve cardiovascular function, or muscle strengthening exercise such as working out at a gym,” he said. “However, it may be that exercising once a week for 2 hours is less effective than exercising every day for 20 minutes. If it is not possible to have 20 minutes a day for exercise, even five minutes a day makes a difference for fitness and health. Of course, more studies are needed to confirm this, but our recent studies show the importance of accumulating small amount of exercise as frequently as possible in a week. It is important to note that even a very small amount of exercise can make a difference to our body, if it is performed regularly.”
Reference: “Weekly minimum frequency of one maximal eccentric contraction to increase muscle strength of the elbow flexors” by Riku Yoshida, Kazuki Kasahara, Yuta Murakami, Shigeru Sato, Midori Tanaka, Kazunori Nosaka and Masatoshi Nakamura, 28 July 2023, European Journal of Applied Physiology . DOI: 10.1007/s00421-023-05281-6
More on SciTechDaily


Affecting Millions – Study Finds That Stop-and-Go Traffic May Be Linked to Reduced Birth Weight

Gene Therapy Successfully Restores Cone Function in Colorblind Children

New Research May Explain Severe Virus Attacks on the Lungs, Contribute to Future Treatments for COVID-19
Stunning new species of fish discovered: the rose-veiled fairy wrasse.

Unlocking Climate Secrets: How Ocean Salt Patterns Influence Global Weather
Genome reconstruction opens door to transformation of potato breeding.

New Study: Immune Activation in Depression More Common Than Previously Thought
Progress Continues Toward NASA Artemis I Launch in August
1 comment on "the magic number – new research sheds light on how often you need to exercise to make it worth it".
Wow! Congratulations on completing and publishing the research! Really great work.
It would be interesting to see this experiment over a longer time interval – maybe 6 months. Does the gap between twice vs thrice get larger or is there a plateau effect which causes the gap to get smaller?
Imo, consistency in effort is fundamental to gaining results in exercise and in other aspects of life.
Leave a comment Cancel reply
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.
clock This article was published more than 1 year ago
For a longer life, afternoon exercise may be best, a large study shows
The data collected from more than 90,000 people gives afternoon exercisers the edge for longevity, but morning exercise might burn more fat.

Afternoon exercise may reduce the risks of premature death more than morning or evening workouts, according to a new large-scale study of more 90,000 men and women.
But if morning or evening exercise is your preference, don’t despair. The study also finds that physical activity at any time of day is better for longevity than not exercising.
And other new research indicates that there can be unique benefits to slotting exercise into the morning hours, suggesting that the best time to exercise depends on what we want from a workout.
Why worry about exercise timing?
There is already mounting evidence that the health effects of exercise depend, to some extent, on when we are active. In past research , people at risk for diabetes improved their blood-sugar control more if they worked out in the evening than in the morning, while in other studies , people lost more body fat if they exercised early rather than later in the day.
But most of these studies were small and their results narrow and inconsistent, so it’s been difficult to draw conclusions about when we should exercise.
One of the new studies helpfully steamrolls any concerns about study size, though. Published this month in Nature Communications , the new study marshals data about 92,139 men and women who had joined the UK Biobank, a health study of adults in the United Kingdom, and worn an activity tracker for a week.
Using the trackers’ readouts, the researchers divvied up the volunteers according to how often and when they moved around, checked mortality records for up to seven years after people joined the Biobank, and compared movement patterns and deaths.
The strongest and least-surprising correlation they found was that the men and women who most frequently engaged in moderate or vigorous physical activity (the equivalent of a brisk walk), lived longer than people who rarely worked out, no matter what time of day people got up and moved.
But the researchers also uncovered subtle links between midday exercise and even better odds of a long life.
People who clustered their physical activity between 11 a.m. and 5 p.m. or spread it out throughout the entire day were less likely to die prematurely from heart disease or other causes (except cancer) than people who mainly exercised before 11 a.m. or after 5 p.m.
This afternoon time frame, the researchers point out, neatly coincides with the time of day when, statistically, people are least likely to experience a heart attack.
The benefits of afternoon exercise for longevity were most pronounced for men and the elderly. But, overall, the findings suggest exercise timing “may have the potential to maximize the health benefits of daily [physical activity],” the researchers conclude.
Morning exercise targets body fat
But for many of us, afternoon exercise in the middle of the workday is logistically challenging or temperamentally undesirable.
For those people, a new study featuring healthy mice on tiny treadmills, offers some hope.
The research builds on a separate, ambitious study from last year in which researchers at the Karolinska Institute in Stockholm and other institutions, catalogued almost every molecule that changed in the body tissues of mice, depending on when they ran.
To their surprise, they noticed the changes were especially pronounced in the animals’ fat tissue. “We hadn’t expected fat to be so affected,” said Juleen Zierath, a professor of clinical integrative physiology at the Karolinska Institute and one of the senior authors of the study. She and her co-authors had anticipated that the animals’ muscles and livers, which help fuel exercise, would show the most molecular alterations.
So, for the new study, they decided to focus on fat and how exercise timing changed it. They had male mice run for an hour on tiny treadmills or stand on the same treadmills as a control. Some ran a few hours after they had awaked, equivalent to midmorning for us.
Others ran a few hours into the period when the animals would normally slow and rest.
Some of the animals skipped eating before their workout; others nibbled beforehand on kibble at will.
The researchers drew blood and fat tissue from the animals repeatedly in the hours after they exercised. And they found far more going on in the fat of the animals who ran within a few hours of waking up. Their fat released substantially more fatty acids, the building blocks of fat, into the animals’ bloodstream, ready for use as muscle fuel. And the remaining fat tissue showed larger increases in biochemical markers of heat production and mitochondrial activity than the fat from the evening (in mouse terms) runners, as well as in the activity of certain genes related to fat metabolism.
In effect, a single session of early-day exercise had set up conditions in the animals’ fat tissue that presumably would lead to greater fat burning and fat loss over time than the same exercise in the evening, Zierath said.
How should you decide the best time to exercise?
“This study identified some fascinating effects,” said Jeffrey Horowitz, a professor at the University of Michigan, who studies exercise and metabolism. He was not involved with the new study.
But it also complicates the question of when to work out. Is afternoon exercise preferable if our goal is longevity, while morning exertions are better to narrow our waistline?
In reality, any differences “will be marginal,” Zierath said.
The biggest gains in the longevity study, after all, came from frequent activity, whatever the time of day.
And any increases in fat burning after morning workouts would likely be small, Zierath said.
“We’re talking fine-tuning,” she said. But, over months, years, or a lifetime, “those small changes can be meaningful.”
So, if you’d like to burn a little more fat with each workout and slowly lower your body’s fat stores, there may be advantages to exercising before noon. But if your primary aim is more life, then get up and move around more during the afternoon, if possible.
But most important is to just get up and move.
Do you have a fitness question? Email [email protected] and we may answer your question in a future column.
Sign up for the Well+Being newsletter, your source of expert advice and simple tips to help you live well every day
Read more from Well+Being
Well+Being shares news and advice for living well every day. Sign up for our newsletter to get tips directly in your inbox.
Vitamin B12 for fatigue has no proven benefit unless you have a deficiency that causes anemia.
Flashes, shimmers and blind spots: Here’s what migraine aura looks like.
Sparkling water is a better choice for your teeth than most popular beverages.
You can help your brain form healthy habits and break the bad ones.
Our 7 best tips to build an exercise habit .
- Why a too-tight sports bra may affect your breathing and energy March 13, 2024 Why a too-tight sports bra may affect your breathing and energy March 13, 2024
- Women may get a bigger longevity boost from exercise than men March 6, 2024 Women may get a bigger longevity boost from exercise than men March 6, 2024
- How to start curling March 1, 2024 How to start curling March 1, 2024

Could Regular Exercise Cure Your Insomnia? New Research Says Yes
By Dennis Thompson and Carole Tanzer Miller HealthDay Reporters

WEDNESDAY, March 27, 2024 (HealthDay News) -- Folks who consistently work out two to three times a week are less likely to suffer from insomnia, a new study says.
That sort of long-term commitment to exercise also helps people get the recommended amount of sleep each night, according to findings published March 26 in the journal BMJ Open .
The paper “indicates strongly that consistency in [physical activity] might be an important factor in optimizing sleep duration and reducing the symptoms of insomnia,” concluded the research team led by Icelandic psychologists Erla Bjornsdottir and Elin Helga Thorarinsdottir .
For the study, researchers tracked the exercise habits and sleep quality of nearly 4,400 middle-aged adults from 21 hospitals in nine European countries.
U.S. Cities With the Most Homelessness

Participants were specifically asked how often they exercise to the point that they become out of breath or sweaty.
Researchers found that people who persistently worked out at least a few times a week -- totaling at least one hour of exercise weekly -- were:
42% less likely to find it difficult to fall asleep
22% less likely to suffer any symptoms of insomnia
40% less likely to suffer more than one insomnia symptom
Symptoms of insomnia include taking a long time to go to sleep, waking in the night and feeling excessively sleepy during the day.
People who consistently exercised also were 55% more likely to get the normal, recommended amount of shut-eye, between 6 and 9 hours a night, researchers found.
They were 29% less likely to have short sleep less than 6 hours, and 52% less likely to have long sleep of 9 hours or more, results show.
In addition, folks who became active during the course of the decade-long study were 21% more likely to become normal sleepers than those who remained inactive.
These results jibe with other studies that have linked regular exercise with sound sleep, researchers said in a journal news release.
People who work out not only make their bodies tired enough to get good sleep, but they also are more likely to follow a healthy lifestyle, the researchers noted.
More information
Johns Hopkins Medicine has more on exercising for better sleep .
SOURCE: BMJ , news release, March 26, 2024
Copyright © 2024 HealthDay . All rights reserved.
Join the Conversation
Tags: exercise and fitness , sleep disorders
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

'Very Active' 2024 Hurricane Season
Cecelia Smith-Schoenwalder March 27, 2024

EXPLAINER: The Total Solar Eclipse

Trump’s Checkered Biblical Past
Lauren Camera March 27, 2024

The Baltimore Bridge Collapse, Explained
Elliott Davis Jr. March 26, 2024

In Ala., More GOP Trouble on Abortion
Susan Milligan March 27, 2024

Robert F. Kennedy Jr. Names VP
Susan Milligan March 26, 2024

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.12(5); 2021 Aug
Exercise in Aging: Be Balanced
Joanna gronek.
1 Department of Dance, Poznań University of Physical Education, Poland.
Michał Boraczyński
2 Faculty of Health Sciences, Collegium Medicum, University of Warmia and Mazury, Poland.
Piotr Gronek
Dariusz wieliński.
3 Department of Anthropology and Biometry, Poznań University of Physical Education, Poland.
Jacek Tarnas
4 Department of Physical Education and Lifelong Sports, Poznań University of Physical Education, Poland.
Sławomir Marszałek
5 Department of Physiotherapy, Poznań University of Physical Education, Poland.
6 Department of Physiotherapy, Poznań University of Medical Sciences, Poland.
Yi-Yuan Tang
7 Department of Psychological Sciences, Texas Tech University, USA.
The beneficial effects of exercise are recognized for preventing physical and cognitive decline during the aging process. However, there is still a gap concerning recommended intensity, volume, frequency and mode of exercise especially for older people. The aim of this study was to investigate an appropriate type of physical activity (PA) model for healthy aging. A commentary of the influence of PA and exercise on healthy aging through an online search of the databases Web of Science, PubMed and Google Scholar. Two living groups can be considered as potential references: modern hunter-gatherer small-scale population and master athletes. Greater physical activity is proposed for healthy aging than that recommended by WHO. Additionally, mindfulness meditation techniques during exercise are recommended especially for persons practicing long-duration exercises. Complex and compound exercise and workouts should include challenging exercises adjusted and balanced to provide clients, especially older people, with noticeable changes and progress.
By the year 2030 elderly adults over 65 years of age is estimated to comprise 20% of the population [ 1 ], and by 2050 the number of people 60 years old and over worldwide to be 21.1% or 2 billion [ 2 ]. Because of the increasing aging population in many countries throughout the world, much evidence shows that pharmacological treatment, in some instances, is indispensable during the aging process. However, a non-pharmacological approach can be just as effective if not more given it does not disrupt the normal bodily function of interest and be used in the prevention or management of the disease at hand. Exercise and general physical activity (PA), a prominent non-pharmacological treatment is a promising, low-cost, low-risk and widely available, which is recognized for its reduction impact in cancer, cardiovascular diseases, vascular aging, cardiorespiratory fitness, psycho-motor skills, mood and health-related quality of life (HRQL) [ 3 , 4 , 5 , 6 ]. Moreover, the beneficial effects of habitual exercise and PA on brain structure (cortical and sub-cortical regions), brain function (neural plasticity) [ 7 , 8 ] and consequently on cognition and psychological well-being have been promising elements of in preventing brain deterioration and cognitive decline during the aging process [ 9 , 10 , 11 , 12 , 13 ]. Finally, PA levels are shown to ensure subjective well-being among older adults [ 14 ] which is associated with healthy aging and longevity [ 15 ].
Types of exercise
According to Baar, exercise can broadly be grouped into subclasses: aerobic/endurance and strength/resistance [ 16 ]. An additional subgroup that should be noted is patterned movements. While resistance and endurance exercise significantly influence muscle phenotype, patterned movement exercises are mainly a motor program in the central nervous system and result in relatively small or indistinguishable biochemical changes in myocytes [ 17 ]. Mechanisms underlying muscle adaptation to exercise have been better recognized as a model to explain the concurrent training effect [ 16 ]. The main exercise characteristics are intensity and volume. Their reciprocal relations in the decrease of one variable and simultaneous increase of another variable result in a different adaptation within the myocytes.
The results of resistance and high-resistance training in young, healthy people relate to RNA, protein content [ 18 ], fast-twitch fiber’s cross-sectional area [ 19 , 20 ] and the capacity to generate force [ 21 ]. Complex interventional programs including resistance training are especially important to reverse frailty and sarcopenia and consequently decrease physical disability and early cognitive dysfunction (cognitive frailty) in older persons [ 22 , 23 ]. This type of exercise focuses on the sarcopenic aspects of frailty, because about 70% of frailty is due to sarcopenia [ 24 ] which is defined as low muscle function or strength in the presence of low muscle mass [ 25 , 26 ]. In contrast, increasing the duration and simultaneously decreasing the intensity of exercise results in different adaptations within the myocytes, including decreased glycolytic enzymes [ 27 ], increased oxidative enzymes and slow contractile and regulatory proteins [ 28 , 29 ], increased mitochondrial mass and capillarization [ 30 , 31 ], and a decrease in the fast-fiber area [ 32 ].
All exercise stimulates brain blood flow, but this process depends on the mode (the type of activity) and intensity. During steady-state walking, cycling, running, swimming, etc. total brain blood flow increases in parallel with increasing cardiac output and VO2 consumption, although average arterial pressure remains constant [ 33 ]. Neural adaptation starts at the beginning of the exercise and gradually covers the increase in regional brain blood flow and autonomic nervous system changes. The increased brain blood flow at the beginning of exercise is due to both increased cardiac output as well as to changes in brain metabolism to supply increased neural activation. However, the decisive and most important variable is the intensity of the exercise, since carotid artery blood flow at a higher intensity continues to rise [ 34 ], which is thought to be due to the necessity to maintain thermoregulation during higher-intensity exercise [ 35 ]. Therefore, in theory in comparison to vigorous-intensity training, moderate-intensity training may be enough to result in acute augmentation of blood flow to the brain, thus achieving the equivalent myocyte adaptation that is desired.
WHO and CSEP recommendations for physical activity
Sedentary behavior (SED) is characterized by an energy expenditure less (or equal) than 1.5 metabolic equivalents (MET) [ 36 ] while physical activity (PA) is often classified depends on exercise intensity. Vigorous-intensity PA refers to exercise that is performed at 6.0 or more times the intensity of rest for adults (>6 MET’s, where 1 MET equals to the oxygen cost of sitting quietly, an equivalent of 3.5 mL/kg/min or 1 kcal/kg/hour) while moderate-intensity PA refers to exercise that is performed at 3.0-5.9 times the intensity of rest.
The World Health Organization (WHO) considers both intensity for PA and also the frequency of weekly PA adjusted to age [ 37 ]. Therefore, adults aged 18-64 yrs and for adults > 65 yrs are recommended a minimum seventy-five minutes of vigorous-intensity aerobic PA or at least 150 min of moderate-intensity aerobic activity per week, respectively. These recommendations are important to be considered since sedentary time and total moderate-to-vigorous (MVPA) activities are associated to health risk in adults [ 38 ]. An equivalent combination of MVPA can be suggested, such as 2.5 hours of lawn-mowing t (21 min/day) or 75 min. vigorous biking (11 min/day) fulfills weekly PA energy expenditure recommended by WHO for human health as well.
These examples of recommendations seem low and somewhat conservative, and probably were dictated by the principle primum non-nocere . Unfortunately, approximately 30%-60% of adults aged ≥60 years across the WHO regions fail to meet the recommended PA levels [ 39 ]. Moreover, although reaching current recommended PA levels are sufficient for partially reducing risk factors for cardiovascular disease (CVD), they do not eliminate the additional risk that overweight/obesity poses [ 40 ]. In contrast to the WHO recommendations, some international PA guidelines recommend the incorporation of moderate-intensity PA on all days of the week or add other types of exercise [ 41 ]. However, due to the risk of injury with aging and problems associated with adherence, more vigorous forms of PA are recommended for experienced older adults [ 5 ]. In addition to those by WHO, the Canadian Society for Exercise Physiology (CSEP) recommends the addition of muscle and bone strengthening activities using major muscle groups at least two days per week [ 42 ].
The gap seems especially crucial in context since higher cardiorespiratory fitness is strongly associated with lower rates of age-related decline in gray matter, particularly in the prefrontal, superior parietal, and temporal cortices of cognitively healthy older adults [ 43 , 44 ].
Thus, the starting point in assuming that adequate PA is correlated with the cognitive decline in aging. However, a few interesting questions arise from WHO recommendations. Firstly, concerns to whom should individual recommendations be dedicated to, and should we consider sedentary humans as the “norm”? [ 44 ]. Secondly, what is the ideal model for human PA, especially in the context of healthy aging, should there be a real pattern/model? The argument arises that it is unrealistic to generalize PA by the model since each client requires a personalized approach where the aim is searching for specific exercises that will allow each client to reach the balance in their mind and body.
What model of PA should be a real pattern?
It is widely accepted that the existing human genome was selected in the circumstances of restricted energy intake and increased demand for total energy expenditure (TEE) adjusted for hunter-gatherers Stone Age living in a rough foraging environment. That genetic constitution has stayed relatively unchanged, but nowadays TEE has changed dramatically, including motor activity, body composition with fatter tissue and less skeletal muscle tissue, and energy intake. The change in human TEE/kg/day is estimated to about 65% that of humans from the late Paleolithic Stone Age. Additionally, TEE adjusted per unit body mass of PA for contemporary Westerns is about 38% that of their ancestors [ 45 ].
Two living groups, modern hunter-gatherer small-scale populations and master athletes, seem to be considered as potential references to determine the recommended model for human PA, in the context of healthy aging. The level of hunter-gatherers TEE/kg/day is comparable only to physical fitness enthusiasts exercising the equivalent of running 7.5 mph, 60 min/day. Additionally, hunter-gatherer populations are referenced for their excellent metabolic and cardiovascular health, making them models in public health.
The Hadza hunter-gatherer small-scale population of around 1000 people from a savanna-woodland habitat near Lake Eyasi in northern Tanzania is characterized by moderate and vigorous PA levels, exceeding 100 min×d -1 [ 46 ]. Additionally, this population has an extremely low obesity prevalence (<5%) and a modest mean body-fat content (women: 24-28%, men: 9-18%). Metabolic CVD is not common, but longevity is an analog to that of industrialized populations. However, the Hadza people, significantly differ not only in terms of PA, but also nutrition, gut microbiota, exposure to pathogens, activity budgets and modes of subsistence. Moreover, findings from Western populations do not uniformly match findings from non-Western populations in many other types of investigation [ 47 ]. Thus, some abstinence and awareness are necessary due to certain limitations in accepting this group as a potential reference, even if it arouses highest curiosity. Master athletes with or without sports history exercise four to six days/wk can be the second model group for PA of healthy aging. This group includes athletes over 35-40 years old and are usually referred to as “veteran”, “master”, or “seniors”. This group exercises over the set point, as suggested by Lazarus and Harridge [ 48 ], a given threshold of PA that is needed to age optimally and to maximize the “healthspan”. Exercising at levels of a certain intensity, volume, frequency below the set point will result in aging being contaminated by the pathological and unpredictable effects of inactivity. Exercise over this threshold stimulates maximized athletic performance but is unlikely to have any further beneficial effects on health [ 48 ].
From a gerontological perspective, numerous studies included in a review by Lemez and Baker [ 49 ] reported a longer lifespan for elite athletes compared to age- and sex-matched controls from the general population and other athletes. The previously observed relationship between participation in elite sport and longevity [ 50 , 51 ] can enhance our notion of the benefits of PA at the highest levels of competition in unique athletic cohorts. However, there is still controversy about the recommended intensity, volume, duration and frequency of PA for the elderly. Professional master athletes apply training loads at the highest values, while amateur athletes are recommended by some specialists much lower training loads at light and moderate intensity levels. Prof. Tanaka suggested slow jogging almost at a speed of fast walking to allow comfortable talking, similar to “tiptoe” running [ 52 ]. Furthermore, running is recommended for older people to reduce all-cause mortality, even if they have advanced arthritic changes. However, the distance and intensity should be adjusted to the individual possibilities of the runner [ 53 ].
Physiological and cognitive function
Besides aging and a sedentary lifestyle deterioration in physical function, cardiorespiratory fitness and muscle mass have been established to accelerate physiological decline in later decades of life [ 54 ]. An individualized training programme can minimize this decline, thus preventing older adults (age 65+ years) from crossing functional thresholds of inability [ 55 ]. Vascular function and blood flow regulation form a crucial link between cardiovascular functioning and normal cognitive functions. Moreover, vascular dysfunction appears when blood vessels lose their ability to respond generally due to damage of the endothelial cell layer (caused by advanced glycation end products, inflammation, oxidative stress, etc.) or an increase in the collagen-to-elastin protein ratio within the intimal and medial layers of the vessel wall. Consequently, this disrupts the arterial ability to supply adequate blood flow to the target organs and therefore is at a higher risk of developing into clinical disease [ 56 ].
In continuation, dysfunction in one vascular bed is thought to translate to other vascular beds, resulting in systemic vascular dysfunction that will likely alter blood flow to the brain that in time can affect cognitive impairment [ 44 ]. Measuring relative changes in oxygenated (O2Hb) and deoxygenated (HHb) hemoglobin in the cortex with the fNIRS method in order to compare sedentary reading control (RC), cognitive exercise (CE), physical exercise (PE) and cognitive + physical exercise (CE + PE) demonstrated that combined variant was superior to single exercise for task-efficient cerebral oxygenation and improved oxygen utilization during cortical activation in older individuals [ 57 ].
Moreover, the authors concluded that to maximize cognitive performance, older adults need to undertake more cognitive-demand exercises or more kinds of activity. Unfortunately, the majority of older persons with cognitive dementia were also observed to have vascular dementia with marked leukoariosis (white matter hyperintensities) on CT or MRI [ 58 ]. Thus, monitoring vasculature and blood flow regulation to detect dysfunction in the vascular system has high clinical relevance for both cardiovascular disease and cognitive functions.
However, a positive effect on slow cognitive decline is not univocal, and some authors have observed evidence in systematic reviews for the mostly insufficient effectiveness of single-component PA interventions in preventing cognitive decline [ 59 ]. Although authors indicate several limitations of their studies in which (i) most analyzed trials were small and did not follow participants long term; (ii) the mode, volume, intensity, and frequency of PA interventions varied widely; (iii) numerous trials enrolled sedentary adults, but inactive status was defined or measured unclearly; (iv) trials used numerous different cognitive tests; and (v) many studies measured cognitive outcomes with various instruments and did not correct for multiple comparisons. Nevertheless, it is necessary to analyze the changing situation of the social structure as the total population ages.
Is exercise a real polypill against cognitive decline?
Despite the reservations and skepticism of some authors regarding the positive impact of exercise on healthy aging [ 59 ], practice also has a significant effect on the entire architecture of the human body, including physical, psychological and mental dimension ( Figure 1 ). Verghese et al . [ 6 ] reported on a cohort of 469 subjects over 75 years old in which such leisure activities as reading, playing musical instruments, playing board games and dancing were associated with a reduced risk in dementia. Muscles and nervous tissues are functionally connected, and thus, an exercising person who usually focuses on training muscles also needs to be aware that during exercise, the nervous system is trained as well. The nervous system is characterized by a unique adaptive ability of neuroplasticity, complex molecular and cellular processes that represents the biological basis of the so-called “cerebral reserves”, which can modify itself in response to experience [ 60 ]. Exercise and PA may be considered as enhancers as well as environmental factors promoting neuroplasticity ( Figure 2 ). Nervous tissue allows the creation of new connections in the neuronal network and their reorganization, an adaptation ability and biofeedback to such external stimuli as physical exercise (PE) and cognitive exercise.

Summary of main pathway effect of aerobic exercise.

The main pathway effect of aerobic exercise on the central nervous system.
Numerous studies have demonstrated that, PE stimulates in human adults such structural changes as increased gray matter volume in the frontal and hippocampal regions [ 61 ] as well as reduced damage in the gray matter [ 62 ]. Thus, physically active people are more likely to maintain cognition in older age in than those who are physically inactive. To date, it remains unknown whether these positive adaptations in the nervous system occur only in healthy adults or also concern such pre-AD stages as mild cognitive impairment (MCI) or severe cognitive deficiency (SCD).
Stimulation of neural plasticity and cognitive functions through exercise and inclusion of mindfulness and meditation in physical activity classification
There is “no health without mental health” [ 63 ]. Dual-task conditions, in comparison to single-task ones, are recognized to improve for exercising older people their postural stability [ 64 ], balance and cognition [ 65 ]. Makizako et al. [ 66 ] coined the term “cognicize” to describe the exercises that are conducted in multitask conditions that include physical and cognitive tasks. However, the idea is to focus on meditation or in broader sense mindfulness as a potentially cognitive task during dual-task exercise. Meditation plays a unique role among numerous non-pharmacologic therapies used to maintain or enhance the cognitive function of the body and mind. Studies on mindfulness, awareness, and meditation are fascinating because they bring knowledge closer to mysterious unknown processes that are still being studied to this day [ 67 ].
Although it is not commonly defined or even included in discussions, encyclopedic sources illustrate it as “an intentional and self-regulated focusing of attention that aims to relax and calm the mind and body” [ 68 ]. Encyclopedia Britannica focuses on exercise for self-awareness: “private devotion or mental exercise encompassing various techniques of concentration, contemplation, and abstraction, regarded as conducive to heightened self-awareness, spiritual enlightenment, and physical and mental health.” Oxford Learner's Dictionaries associates it with thinking on/upon something and describes it as, “to think deeply, usually in silence, especially for religious reasons or to make your mind calm”. In a more general description, meditation is the practice of using specific techniques such as mindfulness, focusing the mind on a particular object, thought or activity, and so the aim is to train awareness and attention to achieve a mentally and emotionally transparent, stable state [ 69 , 70 ]. All available definitions of meditation focus on the process of calming thoughts and emotions, which is achieved via a comfortable body position and the slow progress of inaction, including thinking. This non-uniform definition is not the only problem since scientific research on this scope shows at least two limitations.
Firstly, meditation studies show that a selection marker or trait is neither known nor given allowing for including/excluding subjects on the protocol. The only criterion of including/excluding individuals is a subjective and non-verifiable opinion; for instance, experienced meditators are defined as meditating ≥30 minutes per day for at least five days per week over the past five years [ 71 ]. Secondly, authors do not precisely define the meditation process using such sophisticated research methods as morphometric imaging [ 67 ]. Meditation can be classified into three main subclasses depending on body kinesthetics: the sitting position (yoga, zen, Buddhism), the lying position (yoga, vipassana) or in motion (Taijiquan, qigong, whirling dances, circle dances, sustained exercise). The last subclass is crucial in the context of exercising for older people. Meditation can be specified as the disconnection of active consciousness, which may occur in all three mentioned subclasses. In exercise and generally during PA, the third subclass is of particular interest. Recently, Tolahunase et al. [ 72 ] found significant improvements in both the cardinal biomarkers of cellular aging [DNA damage marker 8-hydroxy-2′-deoxyguanosine (8-OH2dG), oxidative stress markers reactive oxygen species (ROS), and total antioxidant capacity (TAC), and telomere attrition markers telomere length and telomerase activity] and the metabotrophic biomarkers influencing cellular aging (cortisol, β -endorphin, IL-6, BDNF, and sirtuin-1) in apparently healthy population after a 12-week yoga- meditation based lifestyle intervention. Furthermore, such mind-body activities that require attention engagement as yoga, tai chi and meditation have been associated with positive changes in brain structure and function, especially in areas related to awareness, attention, executive functions and memory [ 73 , 74 , 75 ]. Long-duration exercise not only concerns the state of the body but also changes in the mental state during a bout [ 76 ]. Progressive fatigue of the peripheral and then central nervous system is universal regardless of whether it is running, swimming, cycling, prolonged climbing or another mode of exercise, so the exploration of even “millimeter” reserves is relevant. That being said, enthusiasm or motivation can be a crucial aspect of exercising by preventing premature fatigue, though as the consequence/reward due to the refusal to cease training.
Overall, mindfulness meditation during training can be helpful during prolonged efforts. Elements that lead to reaching a state of meditation during exercise are known and are as follows: focusing on inhale-exhale breathing rhythm. Nosal mode and oral mode [ 77 ], focusing on cadence (running, biking, hitting) while coordinating bodily movement to the rhythm of the music [ 78 ]. This is especially challenging, for men with more difficulties adjusting the cadence of exercise to a musical rhythm.
Rhythm-based music interventions are considered as useful prevention against dementia [ 79 ], falls [ 80 ], and Parkinson's disease [ 81 ]. and moreover, enhance neuroplasticity of the nervous system [ 82 , 83 ]. Rhythmic auditory stimulation (RAS) has been explained in the process of auditory-motor entertainment [ 84 ] sensorimotor coupling to temporally structured auditory input, and during recruitment of a striato-thalamocortical-system, involving the thalamus, premotor, the basal ganglia, supplementary motor and dorsolateral prefrontal cortex [ 85 ]. Thus, rhythm-based music needs to be recommended for people over 60 years old when exercising.
Visualization techniques from mindfulness meditation may also be recommended for the persons practicing long-duration exercises to shift attention from fatigue and pain to other elements and structures of the body [ 86 ]. Thus, we recommend strict and precise psychological phenomenon (processes) focuses attention both on the top of the body (coronal suture) and at the center of the body (plexus Solaris). These points are recommended since they are generally not painfully “destroyed” or “devastated” during a long-lasting bout and may be easily associated with the imagination.
In summary, an exercise model for physically active people over 60 should be individualized according to health status and include mindfulness meditation during movement and visualization during rhythm-based music long-duration exercise in order to prevent against progressive aging and to slow the decline of cognition functions.
Be balanced
Higher PA can be incorporated with moderate-intensity PA on all days of the week than that recommended by WHO and small hunter-gatherer populations and master athletes can serve as a model group of PA for healthy aging as the next step in rethinking exercise/bout for older adults.
The conventional approach in recent physical activity and fitness clubs is “be balanced” which is understood as psychosomatic harmony, integrity, an optimal mind/psyche level and health-related fitness. Thus, specialists in physical activity and health/fitness coaching must design g individualized exercises and training programs that provide stimulation of motor skills, cognitive functions, interactivity of participants, synergistic impact, external strengthening and evaluation/audit of achieving fitness processes. This issue is of high interest because of the risk of sarcopenia and association of muscle mass with endurance skills since VO 2max is mostly in older people dependent on muscle and bone mass as the working muscles stimulate heart adaptation to exercise as well as the vascular system. We propose for older people a moderate-intensity structured training program composed of endurance and resistance exercises, flexibility, falls prevention programs and coordination stimulation in order to obtain an effective cooperation of muscle-nervous tissues.
Cardiorespiratory fitness should be accompanied by searching to be balanced in the context of cognitive functions and mental states.
Furthermore, older people should regularly involve themselves in mind-body activities that require such attention engagement as yoga and meditation [ 87 ]. Thus, complex lifestyle intervention program should include challenging physical exercises and mindfulness-based practices that adjusted provide older clients with noticeable changes and progress towards the goal of being balanced.
Conflicts of interest
The authors disclose no potential conflicts of interest.
Exercise more effective than medicines to manage mental health, study shows
University of South Australia researchers are calling for exercise to be a mainstay approach for managing depression as a new study shows that physical activity is 1.5 times more effective than counselling or the leading medications.
Published in the British Journal of Sports Medicine , the review is the most comprehensive to date, encompassing 97 reviews, 1039 trials and 128,119 participants. It shows that physical activity is extremely beneficial for improving symptoms of depression, anxiety, and distress.
Specifically, the review showed that exercise interventions that were 12 weeks or shorter were most the effective at reducing mental health symptoms, highlighting the speed at which physical activity can make a change.
The largest benefits were seen among people with depression, pregnant and postpartum women, healthy individuals, and people diagnosed with HIV or kidney disease.
According to the World Health Organization, one in every eight people worldwide (970 million people) live with a mental disorder. Poor mental health costs the world economy approximately $2.5 trillion each year, a cost projected to rise to $6 trillion by 2030. In Australia, an estimated one in five people (aged 16-85) have experienced a mental disorder in the past 12 months.
Lead UniSA researcher, Dr Ben Singh, says physical activity must be prioritised to better manage the growing cases of mental health conditions.
"Physical activity is known to help improve mental health. Yet despite the evidence, it has not been widely adopted as a first-choice treatment," Dr Singh says.
"Our review shows that physical activity interventions can significantly reduce symptoms of depression and anxiety in all clinical populations, with some groups showing even greater signs of improvement.
"Higher intensity exercise had greater improvements for depression and anxiety, while longer durations had smaller effects when compared to short and mid-duration bursts.
"We also found that all types of physical activity and exercise were beneficial, including aerobic exercise such as walking, resistance training, Pilates, and yoga.
"Importantly, the research shows that it doesn't take much for exercise to make a positive change to your mental health."
Senior researcher, UniSA's Prof Carol Maher, says the study is the first to evaluate the effects of all types of physical activity on depression, anxiety, and psychological distress in all adult populations.
"Examining these studies as a whole is an effective way to for clinicians to easily understand the body of evidence that supports physical activity in managing mental health disorders.
"We hope this review will underscore the need for physical activity, including structured exercise interventions, as a mainstay approach for managing depression and anxiety."
- Mental Health Research
- Chronic Illness
- Diseases and Conditions
- Mental Health
- Disorders and Syndromes
- Personalized medicine
- Physical exercise
- Aerobic exercise
- Anaerobic exercise
- Postpartum depression
- Stem cell treatments
- Clinical depression
Story Source:
Materials provided by University of South Australia . Note: Content may be edited for style and length.
Journal Reference :
- Ben Singh, Timothy Olds, Rachel Curtis, Dorothea Dumuid, Rosa Virgara, Amanda Watson, Kimberley Szeto, Edward O'Connor, Ty Ferguson, Emily Eglitis, Aaron Miatke, Catherine EM Simpson, Carol Maher. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews . British Journal of Sports Medicine , 2023; bjsports-2022-106195 DOI: 10.1136/bjsports-2022-106195
Cite This Page :
Explore More
- Could Tardigrade Proteins Slow Aging in Humans?
- Supermassive Black Holes Awakened
- Beethoven's Genes: Low Beat Synchronization
- Common Household Chemicals Threat to Brain?
- Tiniest 'Starquake' Ever Detected
- Amazing Archive of Ancient Human Brains
- Night-Time Light and Stroke Risk
- Toward Secure Quantum Communication Globally
- Artificial Nanofluidic Synapses: Memory
- 49 New Galaxies Discovered in Under Three Hours
Trending Topics
Strange & offbeat.
Articles on Fitness
Displaying 1 - 20 of 230 articles.

Paying people to exercise can be motivating, but the financial rewards don’t have to last forever to work
Marc Mitchell , Western University

Thinking of using an activity tracker to achieve your exercise goals? Here’s where it can help – and where it probably won’t
Corneel Vandelanotte , CQUniversity Australia

How to keep a new year’s resolution: ask yourself why you’re doing it
Abigail Parrish , University of Sheffield and Kimberley Jane Bartholomew , University of East Anglia

Wanting to ‘move on’ is natural – but women’s pandemic experiences can’t be lost to ‘lockdown amnesia’
Holly Thorpe , University of Waikato ; Grace O'Leary , University of Waikato ; Mihi Joy Nemani , University of Waikato , and Nida Ahmad , University of Waikato

Why are my muscles sore after exercise? Hint: it’s nothing to do with lactic acid
Robert Andrew Robergs , Queensland University of Technology and Samuel L. Torrens , Queensland University of Technology

The science behind building healthy habits can help you keep your New Year’s resolution
Scott Lear , Simon Fraser University

Resistance (exercise) is far from futile: The unheralded benefits of weight training
Stuart Phillips , McMaster University

How to jump-start your New Year with cold weather running
Kurt Michael Downes , University of Windsor and Kevin Milne , University of Windsor

How to keep your physical and mental health on track during the holidays

Lifestyle changes can reduce dementia risk by maintaining brain plasticity — but the time to act is now
Saskia Sivananthan , McGill University and Laura Middleton , University of Waterloo

Focusing on functional fitness in your 20s and 30s can help you stay ready for anything — and many exercises can help you achieve it
Sinead Roberts , University of Westminster

Treadmill, exercise bike, rowing machine: what’s the best option for cardio at home?
Lewis Ingram , University of South Australia ; Hunter Bennett , University of South Australia , and Saravana Kumar , University of South Australia

Three rules for adding weight to your backpack that will boost the benefits of exercise
Jen Wilson , Nottingham Trent University and Athalie Redwood-Brown , Nottingham Trent University

What can you do to speed up your metabolism?
Nick Fuller , University of Sydney

Planks and wall sits are best for lowering blood pressure – here are six more reasons they’re such great exercises
Alex Walker , University of East London and Jamie Edwards , University of East London

How your genes may determine whether you can be an endurance athlete
Henry Chung , University of Essex ; Dan Gordon , Anglia Ruskin University , and Justin Roberts , Anglia Ruskin University

How to train your body for hot weather if you are active or work outdoors
Anthony Bain , University of Windsor

Can’t afford a gym membership or fitness class? 3 things to include in a DIY exercise program

Exercise may or may not help you lose weight and keep it off – here’s the evidence for both sides of the debate
Donald M. Lamkin , University of California, Los Angeles

Sleep deprivation benefited our ancestors, yet harms us now — but staying fit may help us cope
Madhura Lotlikar , McGill University
Related Topics
- Coronavirus
- New Year's resolutions
- Physical activity
- Weight loss
Top contributors
Professor of Health Sciences, Simon Fraser University
Reader in Exercise and Health Physiology, University of Hertfordshire
Associate Professor, Cardiorespiratory Exercise Physiology, Anglia Ruskin University
Professor of Nutritional Physiology, Anglia Ruskin University
Senior Lecturer in Sport and Exercise Science, Swansea University
Senior Lecturer in Sport and Exercise, Teesside University
Professor of Physical Activity, Lifestyle, and Population Health, University of Sydney
Senior Lecturer in Physiology, University of Westminster
Director of Sport, Performance and Health, Heriot-Watt University
Clinician Scientist, Canada Research Chair in Injury Prevention and Physical Activity for Health, Sport Medicine Physician, Schulich School of Medicine & Dentistry, Western University
Associate Professor in Neuromuscular Physiology, Liverpool John Moores University
Postdoctoral fellow, Behavioural Medicine Lab, School of Exercise Science, Physical & Health Education, University of Victoria
Lecturer in Biomechanics and Strength and Conditioning, Teesside University
Lecturer in Sport, Health & exercise Science, University of Stirling
Professor in Public Health Data Science, Swansea University
- X (Twitter)
- Unfollow topic Follow topic
The New Science of Exercise

E ver since high school, Dr. Mark Tarnopolsky has blurred the line between jock and nerd. After working out every morning and doing 200 push-ups, he runs three miles to his lab at McMaster University in Ontario. When he was younger, Tarnopolsky dreamed of becoming a gym teacher. But now, in his backup career as a genetic metabolic neurologist, he’s determined to prove that exercise can be used as medicine for even the sickest patients.
“People would always say to me, ‘Exercise? Come on. Scientifically, you can’t come up with a mechanism, so it’s a complete waste of time,'” Tarnopolsky says. “But as time goes on, paper after paper after paper shows that the most effective, potent way that we can improve quality of life and duration of life is exercise.”
Tarnopolsky has published some of those papers himself. In 2011, he and a team studied mice with a terrible genetic disease that caused them to age prematurely. Over the course of five months, half of the mice were sedentary. The other half were coaxed to run three times a week on a miniature treadmill.
By the end of the study, the sedentary mice were barely hanging on. The fur that had yet to fall out had grown coarse and gray, muscles shriveled, hearts weakened, skin thinned–even the mice’s hearing got worse. “They were shivering in the corner, about to die,” Tarnopolsky says.
But the group of mice that exercised, genetically compromised though they were, were nearly indistinguishable from healthy mice. Their coats were sleek and black, they ran around their cages, they could even reproduce. “We almost completely prevented the premature aging in the animals,” Tarnopolsky says.
That’s remarkable news, if you’re a mouse. And though there are obvious differences between rodents and humans, Tarnopolsky has seen something similar happen in his ill patients. “I’ve seen all the hype about gene therapy for people with genetic disease”–Tarnopolsky treats kids with severe genetic diseases like muscular dystrophy–“but it hasn’t delivered in the 25 years I’ve been doing this,” he says. “The most effective therapy available to my patients right now is exercise.”
Looking to get in shape but don’t know where to start? Sign up for TIME’s guide to getting fitter, faster.
Tarnopolsky now thinks he knows why. In studies where blood is drawn immediately after people exercised, researchers have found that many positive changes occur throughout the body during and right after a workout. “Going for a run is going to improve your skin health, your eye health, your gonadal health,” he says. “It’s unbelievable.” If there were a drug that could do for human health everything that exercise can, it would likely be the most valuable pharmaceutical ever developed.
The trouble is only 20% of Americans get the recommended 150 minutes of strength and cardiovascular physical activity per week, more than half of all baby boomers report doing no exercise whatsoever, and 80.2 million Americans over age 6 are entirely inactive.
The consequences of a sedentary life are as well documented as they are dire. People with low levels of physical activity are at higher risk for many different kinds of cancer, heart disease, Alzheimer’s disease and early death by any cause. That’s at the end of life. Long before that, inactivity can worsen arthritis symptoms, increase lower-back pain and lead to depression and anxiety–not to mention cause a sallow complexion.
Despite public-awareness campaigns, the health benefits of exercise have not been effectively communicated to the average American. Humans are notoriously bad at assessing the long-term benefits–and risks–of their lifestyle choices. And vague promises that exercise is “good for you” or even “good for the heart” aren’t powerful enough to motivate most people to do something they think of as a chore. Humans are, however, motivated by rewards. That is why experts like Tarnopolsky are so focused on proving that the scientific benefits of exercise–slower aging, better mood, less chronic pain, stronger vision, the list goes on–are real, measurable and almost immediate.
The U.S. National Institutes of Health (NIH) is on the bandwagon too. Next year the agency will launch a massive new study with the aim of documenting in unprecedented detail exactly what happens inside a body in motion. Its hope: to prove that exercise is medicine.
Before doctors adopted a single-minded focus on treating and curing diseases, their main goal was to keep people healthy. Even back in 400 B.C., doctors knew that diet and exercise were the best ways to do that. “Eating alone will not keep a man well,” Hippocrates famously wrote. “He must also take exercise.” For millennia, doctors were the vanguards of physical education–the original PE teachers.
But in the early 1900s, with the rise of modern surgery and nascent pharmaceuticals, medicine shifted its focus from the prevention of disease to its treatment. Paradoxically, physicians de-emphasized exercise just as the modern Olympics swelled in popularity and colleges began building campus stadiums to accommodate America’s growing love of spectator sports. The authors of a paper published in a 1905 issue of the Journal of the American Medical Association mourned how many people were losing sight of the health benefits of exercise. “The men on the teams are the very ones whom Nature has endowed superabundantly with physical capacity, but on them the physical director bends most of his energies,” they wrote, “while the average student is left to get his physical development by yelling from the bleachers.”
Physical activity was no longer the medicine of the masses but the privilege of elite athletes. When scientists studied exercise, it was to figure out how athletes could improve their peak performance–not how mere mortals could improve their health day to day. This gap persists. At a time when boutique (read: expensive) fitness studios are more popular than ever, fewer people are getting the minimum recommended amount of exercise.
Worse, many U.S. schools have seen gym classes cut from the curriculum; nearly half of high school students don’t have weekly PE class, and only 15% of elementary schools require PE at least three days a week for the school year. The result: the majority of American kids and adolescents have so-called exercise-deficit disorder. Meanwhile, childhood-obesity rates have climbed every year since 1999. “You have whole generations that are soured on exercise,” says Jack Berryman, professor emeritus of medical history at the University of Washington School of Medicine.
Researchers like Tarnopolsky and Marcas Bamman, an exercise physiologist who also wants to be part of the NIH study, are hoping that their work will begin reversing those trends. Next year the NIH will launch its six-year, $170 million study with a group of about 3,000 sedentary people, ranging in age from children to the elderly. They will start an exercise program and then donate blood, fat and muscle before and after they exercise. Scientists will then examine samples for clues to how the body changes with physical activity. A control group that doesn’t exercise will also be tracked for comparison.
As part of the study, researchers will do the same experiment in animals to get tissue samples from places like the brain and the lungs that would be too dangerous to obtain from humans. “It’ll be a tremendously enormous data set,” says Maren Laughlin, program director for integrative metabolism at the NIH, who is also a lead on the new study. In the end, the researchers think they’ll be able to identify every single molecule in the body that’s tweaked or turned on by exercise.
This kind of study–its size, its rigor, its aims–is a first, and experts are hoping it will give doctors the evidence they need to start treating exercise like the miracle drug they’ve long thought it to be. “If you think of exercise as a true form of medicine, which it is, it’s not good enough to just look at a patient and say, ‘You need to do more exercise,'” says Bamman, director of the Center for Exercise Medicine at the University of Alabama at Birmingham. “That’s no better than handing someone a bottle of pills and saying, ‘Here, take a few,'” with no other explanation.
Bamman is betting that with this new data, exercise will one day be prescribed to patients. Instead of leaving the doctor’s office with nothing but a slip of paper with a drug name scrawled on it, patients may also get a detailed exercise plan tailored to make their medication work better. “We think that precision will go a long way in changing behavior,” Bamman says. “We’re at a really important time in the field.”
Think of all the different ways you can sweat and you might be surprised that each falls into one of just two categories. You’re doing aerobic exercise when your breathing speeds up, your blood flows faster and your heart pumps more of it, shooting oxygen out to the tissues in the rest of the body. It’s the most popular kind; about half of Americans meet the recommendations for aerobic physical activity. But only 20% also do the other type, strength training. The phrase may conjure grunting weight lifters and gym dumbbells slick with sweat, but to build muscle and strengthen bones, you really only need to use your body weight as resistance, says Anthony Hackney, an exercise physiologist at the University of North Carolina at Chapel Hill. That’s why things like yoga, tai chi and Pilates–not just pumping iron–are excellent forms of strength training. “People always get the image of the big, muscular guy,” Hackney says. “We try to think of muscle strength and power as a 65-year-old lady picking up a gallon of milk, pouring a glass and feeling comfortable.”
In addition to the heart, muscles, lungs and bones, scientists are finding that another major beneficiary of exercise might be the brain. Recent research links exercise to less depression, better memory and quicker learning. Studies also suggest that exercise is, as of now, the best way to prevent or delay the onset of Alzheimer’s, which is second only to cancer as the disease Americans fear most, according to surveys.
Scientists don’t know exactly why exercise changes the structure and function of the brain for the better, but it’s an area of active research. So far, they’ve found that exercise improves blood flow to the brain, feeding the growth of new blood vessels and even new brain cells, courtesy of the protein BDNF, short for brain-derived neurotrophic factor. BDNF triggers the growth of new neurons and helps repair and protect brain cells from degeneration. “I always tell people that exercise is regenerative medicine–restoring and repairing and basically fixing things that are broken,” Bamman says.
Repairs like this throughout the body may be the reason exercise has been shown to extend life span by as much as five years. A small new study suggests that moderate-intensity exercise may slow down the aging of cells. As humans get older and their cells divide over and over again, their telomeres–the protective caps on the end of chromosomes–get shorter. To see how exercise affects telomeres, researchers took a muscle biopsy and blood samples from 10 healthy people before and after a 45-minute ride on a stationary bicycle. They found that exercise increased levels of a molecule that protects telomeres, ultimately slowing how quickly they shorten over time. Exercise, then, appears to slow aging at the cellular level.
For all its merits, however, exercise is not an effective way to lose weight, research has shown. In a cruel twist, many people actually gain weight after they start exercising, whether from new muscle mass or a fired-up appetite. “Some people say exercise doesn’t do anything,” says researcher John Jakicic of the University of Pittsburgh. “Well, exercise does a lot. It just may not show up on the scale.”
One of the best pieces of news is that so much of what we already do counts as physical activity. “Mowing the grass, raking leaves, washing the car–all that’s exercise,” says Berryman, the exercise historian. “Physical activity includes all movement, not just throwing a ball through a basket.”
What’s more, emerging research suggests that it doesn’t take much movement to get the benefits. “We’ve been interested in the question of, How low can you go?” says Martin Gibala, an exercise physiologist at McMaster University. After all, if it were possible to reap all the health benefits of exercise in a tiny fraction of the time, who wouldn’t be compelled to give it a try?
Gibala wanted to test how efficient and effective a 10-minute workout could be, compared with the standard 50-minutes-at-a-time approach. The micro-workout he devised consists of three exhausting 20-second bouts of all-out, hard-as-you-can exercise, followed by brief recoveries. In a three-month study, he pitted the short workout against the standard one to see which was better.
To his amazement, the workouts resulted in identical improvements in heart function and blood-sugar control, even though one workout was five times longer than the other. “If you’re willing and able to push hard, you can get away with surprisingly little exercise,” Gibala says.
Not everyone can–or wants to–do this kind of excruciating workout, often referred to as high-intensity interval training, or HIIT. Many of us would gladly bounce around in Zumba class for an hour to avoid enduring even a minute of HIIT torture. But considering that a lack of time is the No. 1 reason people say they don’t exercise, a workout far shorter than what’s generally recommended could be a strong motivator. Gibala, for his part, is wondering if the workout can get even shorter. He’s even played around with the idea of a one-minute workout.
Not every type of exercise will work for every person, of course, but a growing body of research indicates that very vigorous exercise–like the interval workouts Gibala is studying–is, in fact, appropriate for people with different chronic conditions, from Type 2 diabetes to heart failure. That’s new thinking, because for decades, people with certain diseases and even pregnant women were advised not to exercise. Now scientists know that far more people can and should exercise. A recent analysis of more than 300 clinical trials discovered that for people recovering from a stroke, for instance, exercise was even more effective at helping them rehabilitate.
Dr. Robert Sallis, a family physician who runs a sports-medicine fellowship at Kaiser Permanente Fontana Medical Center in California, has prescribed exercise to his patients since the early 1990s in hopes of doling out less medication. “It really worked amazingly, particularly in my very sickest patients,” he says. “If I could get them to do it on a regular basis–even just walking, anything that got their heart rate up a bit–I would see dramatic improvements in their chronic disease, not to mention all of these other things like depression, anxiety, mood and energy levels.”
Older people, too, can benefit from strenuous exercise. Until now, all the recommendations for increasing bone density have included low-repetition, high-weight types of training, says Jinger Gottschall, associate professor of kinesiology at Penn State University. “But this just isn’t feasible for a lot of people. You can’t picture your grandma going in and doing that.” Luckily for Grandma, Gottschall’s team found that lifting lighter weights for more reps improves bone density in key parts of the body, making it a good alternative to heavy lifting.
It’s becoming evident that nearly everyone–young, old, pregnant, ill–benefits from exercise. And as scientists learn more about why that is, they’re hoping that those early 20th century missteps–the move away from our being bodies in motion–will be reversed. They’re also hoping that the messaging around exercise gets simpler. “People think now, because of the health-club and fitness movement, that in order to exercise you need to join a fancy club and wear fancy clothes,” says Berryman. In fact, some of the best exercise, research is showing, doesn’t require a gym membership at all.
Back at McMaster University, Tarnopolsky and his team are almost finished doing autopsies on mice from their new study, and even though the scalpel-wielding scientists are blind to which groups the mice were in, they can tell with certainty which animals were allowed to exercise and which were sedentary. “You open up the sedentary mice and there’s fat all over the place,” he says. About half of those mice have tumors. “They just look god-awful.”
As for the mice who hit the wheel every day? “We haven’t found a single tumor,” he says. “I think if people saw, they’d be pretty motivated to exercise.”
More Must-Reads From TIME
- Jane Fonda Champions Climate Action for Every Generation
- Biden’s Campaign Is In Trouble. Will the Turnaround Plan Work?
- Why We're Spending So Much Money Now
- The Financial Influencers Women Actually Want to Listen To
- Breaker Sunny Choi Is Heading to Paris
- Why TV Can’t Stop Making Silly Shows About Lady Journalists
- The Case for Wearing Shoes in the House
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Write to Mandy Oaklander at [email protected]
You May Also Like
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Weight loss caused by common diabetes drug tied to “anti-hunger” molecule in study
A Stanford Medicine study found that metformin, a commonly prescribed diabetes drug associated with moderate weight loss, stimulates production of lac-phe, a molecule abundant after exercise.
March 18, 2024 - By Krista Conger

Jonathan Long co-discovered lac-phe, known as the "anti-hunger" molecule. Courtesy Jonathan Long
An “anti-hunger” molecule produced after vigorous exercise is responsible for the moderate weight loss caused by the diabetes medication metformin, according to a new study in mice and humans. The molecule, lac-phe, was discovered by Stanford Medicine researchers in 2022.
The finding, made jointly by researchers at Stanford Medicine and at Harvard Medical School, further cements the critical role the molecule, called lac-phe, plays in metabolism, exercise and appetite. It may pave the way to a new class of weight loss drugs.
“Until now, the way metformin, which is prescribed to control blood sugar levels, also brings about weight loss has been unclear,” said Jonathan Long , PhD, an assistant professor of pathology. “Now we know that it is acting through the same pathway as vigorous exercise to reduce hunger. Understanding how these pathways are controlled may lead to viable strategies to lower body mass and improve health in millions of people.”
Long, who is supported by the Knight Initiative for Brain Resilience, and Mark Benson, MD, PhD, an assistant professor of medicine at Harvard Medical School, are co-senior authors of the study , which was published on March 18 in Nature Metabolism . Postdoctoral scholar Shuke Xiao , PhD, is the lead author of the study.
Many people with diabetes who are prescribed metformin lose around 2% to 3% of their body weight within the first year of starting the drug. Although this amount of weight loss is modest when compared with the 15% or more often seen by people taking semaglutide drugs such as Ozempic and Wegovy, the discoveries that led to those drugs also grew from observations of relatively minor, but reproducible, weight loss in people taking first-generation versions of the medications.
Post-workout appetite loss
When Long and colleagues at Baylor University discovered lac-phe in 2022, they were on the hunt for small molecules responsible for curtailing hunger after vigorous exercise. What they found was a Frankenbaby of lactate — a byproduct of muscle fatigue — and an amino acid called phenylalanine. They dubbed the hybrid molecule lac-phe and went on to show that it’s not only more abundant after exercise but it also causes people (as well as mice and even racehorses) to feel less hungry immediately after a hard workout.
“There is an intimate connection between lac-phe production and lactate generation,” Long said. “Once we understood this relationship, we started to think about other aspects of lactate metabolism.”
Metformin was an obvious candidate because as it stimulates the breakdown of glucose (thus reducing blood sugar levels) it can trigger the generation of lactate.
The researchers found that obese laboratory mice given metformin had increased levels of lac-phe in their blood. They ate less than their peers and lost about 2 grams of body weight during the nine-day experiment.
The fact that metformin and sprint exercise affect your body weight through the same pathway is both weird and interesting.
Long and his colleagues also analyzed stored blood plasma samples from people with Type 2 diabetes before and 12 weeks after they had begun taking metformin to control their blood sugar. They saw significant increases in the levels of lac-phe in people after metformin compared with their levels before treatment. Finally, 79 participants in a large, multi-ethnic study of atherosclerosis who were also taking metformin had significantly higher levels of lac-phe circulating in their blood than those who were not taking the drug.
“It was nice to confirm our hunch experimentally,” Long said. “The magnitude of effect of metformin on lac-phe production in mice was as great as or greater than what we previously observed with exercise. If you give a mouse metformin at levels comparable to what we prescribe for humans, their lac-phe levels go through the roof and stay high for many hours.”
Further research revealed that lac-phe is made by intestinal epithelial cells in the animals; blocking the ability of mice to make lac-phe erased the appetite suppression and weight loss previously observed.
Finally, a statistical analysis of the people in the atherosclerosis study who lost weight during the several-year study and follow-up period found a meaningful association between metformin use, lac-phe production and weight loss.
“The fact that metformin and sprint exercise affect your body weight through the same pathway is both weird and interesting,” Long said. “And the involvement of the intestinal epithelial cells suggests a layer of gut-to-brain communication that deserves further exploration. Are there other signals involved?”
Long noted that, while semaglutide drugs are injected into the bloodstream, metformin is an oral drug that is already prescribed to millions of people. “These findings suggest there may be a way to optimize oral medications to affect these hunger and energy balance pathways to control body weight, cholesterol and blood pressure. I think what we’re seeing now is just the beginning of new types of weight loss drugs.”
Researchers from Beth Israel Deaconess Medical Center, Harbor-UCLA Medical Center, Cedars-Sinai Medical Center, Baylor College of Medicine, the University of Colorado, the University of Virginia and the Broad Institute contributed to the work.
The study was funded by the National Institutes of Health (grants GM113854, K08HL145095, DK124265, DK136526, HHSN2682015000031, HSN26800004, UM1DK078616 and 1R01HL151855), a Stanford School of Medicine’s Dean’s Fellowship, the American Heart Association, Wu Tsai Human Performance Alliance, Knight Initiative for Brain Resilience and Stanford Diabetes Research Center.

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care

The Serious Side of Kid and Canine Play
Umass amherst kinesiologists expand research into physical activity benefits for youth with a family dog.

With two-thirds of children in the U.S. failing to meet national physical activity guidelines , kinesiologists Katie Potter and Colleen Chase have been looking at the impact of the family dog on the exercise habits of kids.
Could having a canine best friend get kids on their feet and help bring them more in line with the minimum recommendation of 60 minutes of moderate to vigorous physical activity every day?
A preliminary study in 2022, reported in a recent issue of the Journal for the Measurement of Physical Behaviour , tested and validated a new approach for measuring dog-facilitated physical activity among kids.
The study, involving 12 children, found that about 20% of their daily physical activity came from time in close proximity with the family dog. Now a larger study, aimed at including a more diverse population, is underway.
This time, there is an option for participants to complete the weeklong study remotely, allowing families outside of Western Massachusetts to take part.
“There are so many ways we might leverage the human-dog bond to promote physical activity in kids, but first we need to understand how much physical activity dog-owning kids get with their dogs,” says Potter, an assistant professor in the Department of Kinesiology.
Interested families can fill out a screening survey to see if they qualify to participate. The study will include children between 7 and 10 years old, and a dog who has been with the family at least six months.
“Our preliminary study was the first time that this type of research had been done specifically quantifying physical activity with the dog and the kid in proximity together,” says Colleen Chase, lead author of the recent paper and a doctoral student in Potter’s lab. “We’re interested in replicating that study to see whether that 20% value holds at a significant sample size of participants.”
Research has shown that children get more exercise when it is enjoyable, motivational and involves social interaction. “If a child has a dog and is bonded with the dog, that’s going to lead to greater enjoyment of whatever activity they are partaking in. And having a dog is a form of social support,” says Chase, who is leading this research study as part of her doctoral dissertation. “So, we see the way this lines up nicely with what other studies have shown is going to promote kids being more active.”
Chase says if the research continues to show that dogs have a positive impact on the physical activity of children, researchers can look for ways to involve kids who don’t have a family dog. “There’s a financial and time burden associated with pet ownership, and we acknowledge that,” Chase says.
She could envision dog-walking programs in animal shelters or after-school programs involving dog play to expand access to the benefits of hanging out with a dog.
“This is a pretty concerning issue in the United States right now,” Chase says of physical inactivity among kids. “That’s why we’re trying to get creative with methods to address this. It’s a very wholesome line of research. You know, we’re working with kids. We’re working with dogs. But we do have these larger, significant health problems that we are working to address through this research.”
The UMass Behavioral Medicine Lab , directed by Potter, studies ways to help people become more active, with a current focus on children and dogs. Potter is looking for families with kids and one or more dogs to wear ActiGraph accelerometers, with a Bluetooth feature that measures proximity, as they go about their routine life.
Global footer
- ©2024 University of Massachusetts Amherst
- Site policies
- Non-discrimination notice
- Accessibility
- Terms of use

IMAGES
COMMENTS
The new findings come amid intensifying efforts to understand the molecular underpinnings of exercises. Untangling the immune system's involvement in this process is but one aspect of these research efforts. "Our research suggests that with exercise, we have a natural way to boost the body's immune responses to reduce inflammation."
But Raphael Knaier says the existing research is still limited and mostly focuses on young men, so it's hard to generalize. Knaier is an exercise physiologist at the University of Basel.
A new study by researchers from MIT and Harvard Medical School has helped identify the impact of exercise and high-fat diets on cells, reports Darren Botelho for NBC Boston 10.. "Years from now, those researchers say the data could lead to a pill that would help not only with weight loss, but with the overall effect from exercise - a better wellbeing," explains Botelho.
04:18. Regular exercise offers many benefits beyond burning calories — so there are plenty of reasons to keep moving in the new year. "Research shows that exercise affects pretty much every ...
Physical fitness and exercise. Check out the latest articles on physical fitness, weight lifting programs, and new methods for improving exercise performance. Your source for the latest research news
from ScienceDaily. May 16, 2022 — Exercise increases levels of a chemical involved in brain cell growth, which bolsters the release of the 'feel good' hormone dopamine, a new study shows ...
Aug. 9, 2021 — Findings from a new study add to growing evidence that resistance exercise has unique benefits for fat loss. Researchers found that resistance-like exercise regulates fat cell ...
Feb. 19, 2024, 11:01 AM PST. By Aria Bendix. Women generally exercise less than men do, but new research suggests they see greater health benefits from it. A national study found that women who ...
"And males, after a certain number of minutes of exercise per week, almost 110 minutes, they plateau. So, they don't benefit more from the exercise." Dr. Jaber assisted in reviewing this research. He said another interesting finding is that while men plateau after110 minutes of aerobic exercise, women continue to see benefits.
Sedentary lifestyle is a major risk factor for noncommunicable diseases such as cardiovascular diseases, cancer and diabetes. It has been estimated that approximately 3.2 million deaths each year are attributable to insufficient levels of physical activity. We evaluated the available evidence from Cochrane systematic reviews (CSRs) on the effectiveness of exercise/physical activity for various ...
Why long COVID can cause exhaustion, or post-exertional malaise, after exercise : Shots - Health News Long COVID patients can experience severe energy crashes after physical exertion. New research ...
On the other hand, exercise seems essential for weight maintenance, according to other research this year. A new scientific analysis of participants from the TV weight-loss contest "The Biggest ...
To conduct the new study, researchers looked at more than 400,000 U.S. adults who provided survey data on leisure-time activity from 1997 to 2017 and compared that data with death records.
Part of the current scope of research in exercise physiology is represented by 11 papers contributing to the Research Topic "Insights in Exercise Physiology: 2021," from different areas. ... In fact, new research horizons appear in relation to the identification of the mechanisms of exercise-induced damage, both at the gastrointestinal and ...
Importance Despite consistent public health recommendations, obesity rates in the US continue to increase. Physical activity recommendations do not account for individual genetic variability, increasing risk of obesity. Objective To use activity, clinical, and genetic data from the All of Us Research Program (AoURP) to explore the association of genetic risk of higher body mass index (BMI ...
The Magic Number - New Research Sheds Light on How Often You Need To Exercise To Make It Worth It. New research indicates that a thrice-weekly, three-second maximum-effort eccentric bicep contraction significantly enhances muscle strength. Though exercising three days a week shows benefits, five days a week brings greater improvements ...
Running or yoga can help beat depression, research shows - even if exercise is the last thing you feel like. Our new study shows you may be able to walk, run, lift or dance away depression. And ...
A new study collected from more than 90,000 people found afternoon exercisers lived longer, but other research suggests morning exercise might burn more body fat.
Regular exercise has so many health benefits, and treating insomnia could be added to that list, according to a new study.
We know that regular exercise has many health benefits, but new research is showing just what impact that may have on the population. More than 110,000 deaths a year could be prevented if adults ...
New Research Says Yes. WEDNESDAY, March 27, 2024 (HealthDay News) -- Folks who consistently work out two to three times a week are less likely to suffer from insomnia, a new study says. That sort ...
Exercise and PA may be considered as enhancers as well as environmental factors promoting neuroplasticity (Figure 2). Nervous tissue allows the creation of new connections in the neuronal network and their reorganization, an adaptation ability and biofeedback to such external stimuli as physical exercise (PE) and cognitive exercise.
FULL STORY. University of South Australia researchers are calling for exercise to be a mainstay approach for managing depression as a new study shows that physical activity is 1.5 times more ...
Offering financial incentives for exercise may be one way of stimulating, and sustaining, a more active lifestyle. Research suggests that even after rewards stop, exercise gains mostly persist.
In studies where blood is drawn immediately after people exercised, researchers have found that many positive changes occur throughout the body during and right after a workout. "Going for a run ...
An "anti-hunger" molecule produced after vigorous exercise is responsible for the moderate weight loss caused by the diabetes medication metformin, according to a new study in mice and humans. The molecule, lac-phe, was discovered by Stanford Medicine researchers in 2022.
March 27 (UPI) -- Insomniacs looking to get more shut-eye could experience better sleep with consistent exercise, according to new research. The study, published Tuesday in the journal BMJ Open ...
March 27, 2024 Research. Katie Potter (left) and Colleen Chase. With two-thirds of children in the U.S. failing to meet national physical activity guidelines, kinesiologists Katie Potter and Colleen Chase have been looking at the impact of the family dog on the exercise habits of kids.