

‘You have to suffer for your PhD’: poor mental health among doctoral researchers – new research
Lecturer in Social Sciences, University of Westminster
Disclosure statement
Cassie Hazell has received funding from the Office for Students.
University of Westminster provides funding as a member of The Conversation UK.
View all partners
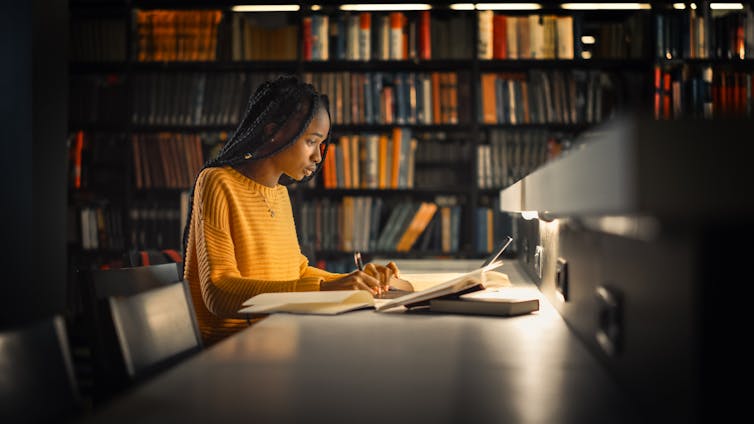
PhD students are the future of research, innovation and teaching at universities and beyond – but this future is at risk. There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.
My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were more likely to meet the criteria for clinical levels of depression and anxiety. They were also more likely to have significantly more severe symptoms than the working-professional control group.
We surveyed 3,352 PhD students, as well as 1,256 working professionals who served as a matched comparison group . We used the questionnaires used by NHS mental health services to assess several mental health symptoms.
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety.
The groups reported an equally high risk of suicide. Between 33% and 35% of both PhD students and working professionals met the criteria for “suicide risk”. The figures for suicide risk might be so high because of the high rates of depression found in our sample.
We also asked PhD students what they thought about their own and their peers’ mental health. More than 40% of PhD students believed that experiencing a mental health problem during your PhD is the norm. A similar number (41%) told us that most of their PhD colleagues had mental health problems.
Just over a third of PhD students had considered ending their studies altogether for mental health reasons.
There is clearly a high prevalence of mental health problems among PhD students, beyond those rates seen in the general public. Our results indicate a problem with the current system of PhD study – or perhaps with academic more widely. Academia notoriously encourages a culture of overwork and under-appreciation.
This mindset is present among PhD students. In our focus groups and surveys for other research , PhD students reported wearing their suffering as a badge of honour and a marker that they are working hard enough rather than too much. One student told us :
“There is a common belief … you have to suffer for the sake of your PhD, if you aren’t anxious or suffering from impostor syndrome, then you aren’t doing it "properly”.
We explored the potential risk factors that could lead to poor mental health among PhD students and the things that could protect their mental health.
Financial insecurity was one risk factor. Not all researchers receive funding to cover their course and personal expenses, and once their PhD is complete, there is no guarantee of a job. The number of people studying for a PhD is increasing without an equivalent increase in postdoctoral positions .
Another risk factor was conflict in their relationship with their academic supervisor . An analogy offered by one of our PhD student collaborators likened the academic supervisor to a “sword” that you can use to defeat the “PhD monster”. If your weapon is ineffective, then it makes tackling the monster a difficult – if not impossible – task. Supervisor difficulties can take many forms. These can include a supervisor being inaccessible, overly critical or lacking expertise.
A lack of interests or relationships outside PhD study, or the presence of stressors in students’ personal lives were also risk factors.
We have also found an association between poor mental health and high levels of perfectionism, impostor syndrome (feeling like you don’t belong or deserve to be studying for your PhD) and the sense of being isolated .
Better conversations
Doctoral research is not all doom and gloom. There are many students who find studying for a PhD to be both enjoyable and fulfilling , and there are many examples of cooperative and nurturing research environments across academia.
Studying for a PhD is an opportunity for researchers to spend several years learning and exploring a topic they are passionate about. It is a training programme intended to equip students with the skills and expertise to further the world’s knowledge. These examples of good practice provide opportunities for us to learn about what works well and disseminate them more widely.
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence, offers balance, and avoids perpetuating unhelpful myths.
Indeed, in our own study, we found that the percentage of PhD students who believed their peers had mental health problems and that poor mental health was the norm, exceeded the rates of students who actually met diagnostic criteria for a common mental health problem . That is, PhD students may be overestimating the already high number of their peers who experienced mental health problems.
We therefore need to be careful about the messages we put out on this topic, as we may inadvertently make the situation worse. If messages are too negative, we may add to the myth that all PhD students experience mental health problems and help maintain the toxicity of academic culture.
- Mental health
- Academic life
- PhD research

Senior Lecturer - Earth System Science

Associate Director, Operational Planning

Sydney Horizon Educators (Identified)

Deputy Social Media Producer

Associate Professor, Occupational Therapy
- Advisory Committees
- CGS Employer Roundtable
- Governance & Financials
- Upcoming Meetings
- Convenings & Special Events
- Partnership and Sponsorship Opportunities
- Press Releases
- Newsletters
- Communications to Policymakers
- Publications
- Data & Infographics
- Dean’s Discussion Board
- For Current & Prospective Graduate Students
- Institutional Membership
- International Membership
- Corresponding Affiliate Membership
- Sustaining Membership Network for Corporate Partners
- Diversity, Equity & Inclusiveness
- Admissions, Enrollment, and Completion
- International Engagement
- Graduate Wellness
- Graduate Professional Development
- Career Pathways
- Microcredentials
- Advocacy Resources
- Master’s Degrees at Work
- Join the Effort
- Graduate Deans
- Faculty and Graduate Education Professionals
- Community Voices
- The National Name Exchange

Graduate Student Mental Health and Well-being
Project summary.
A growing body of evidence indicates that mental health challenges are common among graduate students. Unfortunately, many barriers exist to effective support and care. Beginning in 2019, CGS and The JED Foundation undertook a project to create an evidence base to inform future policies, programs and resources. Below are the results of that project, including the report, “Supporting Graduate Student Mental Health and Well-being: Evidence-Informed Recommendations for the Graduate Community.”

Report and Recommendations
On April 29, 2021, CGS and the JED Foundation released a report, “Supporting Graduate Student Mental Health and Well-being: Evidence-Informed Recommendations for the Graduate Community,” which contextualizes the urgency of this issue and includes results from a CGS member survey, priority areas for future research, and examples of programs aligned with key recommendations. The findings and recommendations summarized in the report are intended to provide a starting point for discussion and action for all campus groups with a vested interest in the quality of graduate education, including presidents and provosts, graduate deans, department chairs, faculty members, graduate students, and funders. Also embedded in the report is a “Statement of Principles and Commitments of Graduate Deans,” which provides institutions a blueprint for action to support the academic success and well-being of all students.
The report and supplemental documents related to it can be viewed and downloaded below.
- Supporting Graduate Student Mental Health and Well-being: Evidence-Informed Recommendations for the Graduate Community (Full Report)
- Executive Summary and Recommendations
- Communications Toolkit
- Call to Action and List of Signatories (last updated January 30th, 2024)
Webinar: Supporting Graduate Student Mental Health and Well-being: Evidence and Recommendations to Catalyze Action
Consultant papers.
CGS and JED commissioned three essays on aspects of graduate student mental health and well-being. Authored by experts in their fields, these explore cultural and organizational issues surrounding graduate student mental health; issues specific to international students, and legal issues.
- “ Unique Challenges and Opportunities for Supporting Mental Health and Promoting the Well-being of International Graduate Students ” by Jenny J. Lee (University of Arizona)
- “ Promoting Graduate Student Wellbeing: Cultural, Organizational, and Environmental Factors in the Academy ” by Julie R. Posselt (University of Southern California)
- “ Balancing Access and Safety for Graduate Students with Mental Health Issues ” by Hannah S. Ross (Middlebury College)
Other Resources
- “ CGS & JED Release Evidence-Informed Recommendations and Resources to Support Graduate Student Mental Health & Well-being ” (Press Release)
- Webinar: “ A Framework on Graduate Student Mental Health: CGS Members Share Ideas and Guidance ” (3.16.2021)
- Hironao Okahana, “Pressing Issue: Mental Wellness of Graduate Students” (4.9.2018)
In Partnership with
Project Funders


Common Graduate Student Challenges
As a graduate student, you may encounter a variety of challenges. Fortunately, there are plenty of resources to support you and help you overcome. Here is an introduction to some common graduate student challenges and the resources available to you.
Struggling with Physical and Mental Health
Nothing works unless you do. Health issues can put a full stop on your progress and affect every part of your life.
There are resources available at UC Davis to help you heal and provide support.
Here are a few to start:
- Mental Health Resources - Counseling, Crisis Management, and Wellness
- Student Health Services
- Student Disability Services
- Student Support Referral for OSSJA Case Management support
Feeling Isolated
Each graduate student is on their own journey. Making connections in graduate school can be intimidating, challenging, and feel like a lot of extra work. It’s normal for students to feel lonely and isolated, but you can take steps to connect with or create a community.
TIPS TO STAY CONNECTED
- Make connections in your program - Many programs have dedicated student groups in-person or virtually. Form a study group with students in your courses. Slack channels or messages can be a low-key way to initiate.
- Find (or create) a graduate student space - If your program doesn’t have a student space, check your UC Davis email. Groups and initiatives are often forwarded. The Graduate Student Association may be able to connect you with student groups. Take a stroll through the Graduate Center at Walker Hall or the Student Community Center . Many of the student clubs on campus are grad student inclusive.
- Attend a colloquium, brown bag, or workshop - Check your email or search UC Davis website and calendar for UC Davis colloquia, brown bags, and graduate student workshops. Sign up for a GradPathways workshop or scroll through the UC Davis events calendar .
- Join a professional organization - Find out what organizations your faculty advisors belong to (this info is often available online if you don’t feel comfortable asking), or search for organizations in your field online. Your program website may point you towards relevant organizations.
- Volunteer in your community - Visit the Internship and Career Center for volunteer ideas .
Managing Personal Life and Relationships
Being a graduate student is no easy feat. Juggling time between work, school, and family requires serious time management and organization skills—not to mention, tons of patience and willpower.
One important thing to remember is that you are more than just a graduate student. Your well-being is greatly affected by maintaining the important relationships in your life.
Here are some tips to help you out during graduate school:
- Engage in Open and Honest Communication and Planning To minimize problems and to enhance your relationship, communicate before and during challenging times. Communication, however, is not simply a matter of exchanging information (although that is an important part of a respectful relationship). Communication about one's feelings is also important. Let them know when you’re overwhelmed. Let them know this week is going to be challenging and you probably won’t be around much. Let them know if you can’t schedule a date this month because you have multiple deadlines to make.
- Plan Ahead It is important to plan ahead and look at your schedule for each quarter. That means knowing when deadlines are coming and being sure that you can finish your work with time to spare.
- Don’t Forget YOU Time: As important as it is to keep up your relationships, don’t forget to have YOU time as well. Because it’s impossible to please and take care of other people if you don’t take care of yourself first.
Food, Housing, and Financial Insecurity
The cost of graduate school adds up fast, and many students don’t have a source for financial support. If you’re struggling to secure basic needs, let your Graduate Program Coordinator know. Your Graduate Program Coordinator’s primary job is connecting you with the right resources.
Here are some of the campus basic needs support resources:
- UC Davis Basic Needs Resource Hub - This is a living document that is updated regularly with the latest information on basic needs resources at UC Davis. Consider bookmarking this for the future.
- Aggie Compass Basic Needs Center - Provides financial, food, housing, and mental wellness support and resources.
- The Pantry - Ensures that no student ever has to miss a meal or go without basic necessities due to Financial reasons.
- Graduate Student Association - Maintains the Graduate Student Pantry and offers other basic needs services to graduate students.
- Student Support Referral for OSSJA Case Management support.
Mentorship Issues
UC Davis Graduate Studies can help you navigate and overcome obstacles to your academic success, including conflicts with your advisors. We offer resources on how to navigate difficult conversations, develop strategies to help you improve communication between you and your advisor or mentor, and to point you to resources outside of your department to navigate these conversations. Visit our Problems and Dispute Resolution Page to learn more.
Imposter Syndrome
Imposter syndrome is the feeling or belief that you've been given something you didn't earn or don't deserve. It affects graduate students of all backgrounds and in different ways. Remember, you are in graduate school to enhance or find your career path, give back to your families and communities, or make important contributions to research and innovation.
For even more tips and strategies on how to counteract feelings that you don’t belong, check out these articles:
- Managing Imposter Syndrome in Graduate School
- Imposter Syndrome Through a First-Gen Perspective
- How to Banish Imposter Syndrome
Too Much to Do!
One of the most challenging aspects of graduate school is finding a way to set priorities, create boundaries, and maintain balance. Most graduate students have multiple roles such as graduate school, additional jobs on or off campus, family and community commitments and self-care.
As a first-year student, your school responsibilities may consist of: taking graduate coursework, working as a TA or GSR, starting research and/or lab rotations, looking for an internship, building relationships with faculty and colleagues, navigating your program requirements, and the minutiae of being an enrolled student.
Graduate school will test your limits, and feeling overwhelmed is expected.
Here are some tips to help you when you feel overwhelmed:
- Talk to your senior colleagues about their own experiences. What worked and what didn’t?
- Find a student support group at UC Davis or online - Check with colleagues and your Graduate Program Coordinator, read through your UC Davis email, search the internet for groups on social media.
- Seek help when you can manage - No one wants to admit they’re overwhelmed, but your advisors and GraduateProgram Coordinator will likely have suggestions you would not have found on your own.
In Conclusion:
Identify and build your support network - There are layers of support available to you, and accessible people who want you to succeed. There’s no need to wait until you’re struggling to meet and interact with your faculty and staff advisors.
Don’t hesitate, communicate. Most issues are fixable, but reaching out early can significantly reduce the level of anxiety and process complications, as well as the risk of long-term impacts.
Accept your limits - Do your best to manage, but be open to admitting when you’re not, take help when it’s offered, and ask for help when you need it.
Take advantage of the campus resources, and ask the experts (your Graduate Coordinator and Graduate Studies SeniorAcademic Advisors) for referrals.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
In CDC survey, 37% of U.S. high school students report regular mental health struggles during COVID-19 pandemic

Many high school students have reported experiencing mental health challenges during the coronavirus outbreak, according to recently published survey findings from the Centers for Disease Control and Prevention (CDC). High school students who are gay, lesbian or bisexual, as well as girls, were especially likely to say their mental health has suffered during the pandemic.
This analysis explores U.S. high school students’ self-reported mental health challenges during the COVID-19 pandemic. It expands on Pew Research Center surveys that have explored U.S. adults’ mental health difficulties during this time. Not all of the survey questions asked specifically about mental health during the pandemic.
This analysis relies on the Center for Disease Control and Prevention’s Adolescent Behaviors and Experiences Survey (ABES), which was conducted from January to June 2021 to assess students’ health-related behaviors and experiences during the COVID-19 pandemic. ABES surveyed high school students in grades 9-12 attending U.S. public and private schools. More information about the survey and its methodology can be found on the CDC’s website.
The results from this one-time survey are not directly comparable to previous CDC surveys on these topics.
Overall, 37% of students at public and private high schools reported that their mental health was not good most or all of the time during the pandemic, according to the CDC’s Adolescent Behaviors and Experiences Survey , which was fielded from January to June 2021. In the survey, “poor mental health” includes stress, anxiety and depression. About three-in-ten high school students (31%) said they experienced poor mental health most or all of the time in the 30 days before the survey. In addition, 44% said that, in the previous 12 months, they felt sad or hopeless almost every day for at least two weeks in a row such that they stopped doing some usual activities. (Not all of the survey questions asked specifically about mental health during the pandemic.)
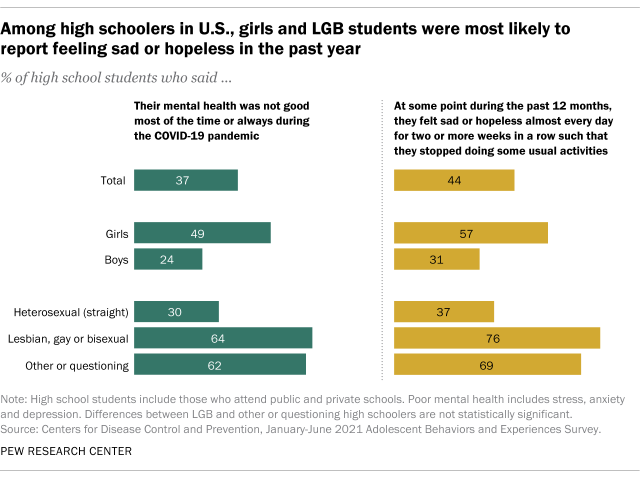
High school students who are gay, lesbian or bisexual reported higher rates of mental health stresses than their heterosexual (straight) peers. The share of LGB high schoolers who said their mental health was not good most of the time or always during the pandemic was more than double that of heterosexual students (64% vs. 30%). More than half of LGB students (55%) said they experienced poor mental health at least most of the time in the 30 days before the survey, while 26% of heterosexual teens said the same. And about three-quarters of LGB high schoolers (76%) said they felt sad or hopeless almost daily for at least two weeks such that they stopped doing some of their usual activities, compared with 37% of heterosexual students.
There were also differences by gender. About half of high school girls (49%) said their mental health was not good most of the time or always during the COVID-19 outbreak – roughly double the share of boys who said this (24%). And roughly four-in-ten girls (42%) reported feeling this way in the 30 days before the survey; 20% of boys said the same. About six-in-ten high school girls (57%) reported that at some point in the 12 months before taking the survey (in the first half of 2021) they felt sad or hopeless almost every day for at least two weeks in a row such that they stopped doing some usual activities, compared with 31% of high school boys who said this.
LGB high schoolers were also more likely than their heterosexual peers to have sought mental health care – including treatment or counseling for alcohol or drug use – via telemedicine during the COVID-19 pandemic. Around one-in-five LGB students (19%) said they received treatment this way at some point during the pandemic, compared with 6% of heterosexual students. Girls were more likely than boys to have received mental health care through telemedicine (10% vs. 7%, respectively).
Pandemic-related disruptions to schooling, socializing and family life have created a situation that the U.S. surgeon general has described as a “ youth mental health crisis ,” with high rates of teens experiencing distress. But public health experts had called attention to teen mental health even before the coronavirus outbreak. For instance, a separate CDC survey conducted in 2015 found that LGB teens were at greater risk of depression than their heterosexual peers. And a Pew Research Center analysis of pre-pandemic data from the National Survey for Drug Use and Health showed teenage girls were more likely than their male peers to report recent experiences with depression , as well as to receive treatment for it.
- Coronavirus (COVID-19)
- Generation Z
- Happiness & Life Satisfaction
- LGBTQ Attitudes & Experiences
- Teens & Youth

How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, mental health and the pandemic: what u.s. surveys have found, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Mental health in medical and biomedical doctoral students during the 2020 COVID-19 pandemic and racial protests
Allison schad.
1 Office of Medical Education, University of North Carolina at Chapel Hill School of Medicine Chapel Hill, United States
Rebekah L Layton
Debra ragland, jeanette gowen cook.
2 Department of Biochemistry and Biophysics, University of North Carolina at Chapel Hill School of Medicine Chapel Hill, United States
Associated Data
Schad A, Layton RL, Ragland D, Cook JG. 2021. Mental health disparities among biomedical trainees during COVID-19 and racial inequity. Open Science Framework. [ CrossRef ]
Underlying data is available on the Open Science Framework at https://doi.org/10.17605/OSF.IO/H9UCX . In accordance with IRB approval, the presentation of data does not include demographic information that could potentially lead to the identification of a student. Furthermore, to protect student anonymity, responses with fewer than ten individuals will not be shared. Accordingly, data sharing is limited to those variables directly relevant to the analyses conducted (e.g., underlying data) and composite categories (e.g., underrepresented vs. well-represented) are shared when applicable rather than granular demographic information to protect the identity of respondents also noted in in the Human Subjects section.
The following dataset was generated:
Concerns about the mental health of students, trainees and staff at universities and medical schools have been growing for many years. Recently, these have been exacerbated by the COVID-19 pandemic and a period of heightened reckoning and protests about systemic racism in the United States in 2020. To better understand the mental health of medical students and biomedical doctoral students at the University of North Carolina at Chapel Hill during this challenging period, we performed a cross-sectional study (n=957) using institutional annual survey data on measures of depression, anxiety, hazardous alcohol use, problems related to substance use, and suicidal ideation. These data were collected in 2019 and 2020, and were analyzed by type of training program, race/ethnicity, gender, sexual orientation, and survey year. Results indicated significant differences for rates of depression, anxiety, and suicidal ideation, with biomedical doctoral students showing greater incidence than medical students, and historically excluded students (e.g., people of color, women, LGBQ+ trainees) showing greater incidence compared to their peers. Of note, mental health remained poor for biomedical doctoral students in 2020 and declined for those belonging to historically excluded populations. The high rates of depression, anxiety, and suicidal ideation reported suggest that training environments need to be improved and support for mental health increased.
Introduction
Graduate and professional programs in the biomedical and health sciences are stressful environments for junior researchers and clinicians. Indeed, the mental health of medical students declines during medical school and is worse than that of the general population by graduation ( Dyrbye et al., 2005 ; Dyrbye et al., 2006 ; Brazeau et al., 2014 ). In fact, poor mental health in medical education is evidenced by a robust, decades-old body of literature, including a systematic review of mental health evidence-based research encompassing nearly 200 relevant studies to date (e.g., Slavin et al., 2014 ; Rotenstein et al., 2016 ; Quek et al., 2019 ).
In comparison, evidence-based research on mental health of doctoral students has only begun to emerge over the past five years. Recent reports indicate elevated rates of anxiety and depression among graduate students in all disciplines ( UC Berkeley Graduate Assembly, 2014 ; Evans et al., 2018 ; Nagy et al., 2019 ; Levecque et al., 2017 ). For example, a multi-campus study of undergraduate and graduate students found that 17.3% scored positive for depression, 9.8% scored positive for anxiety, and 6.3% reported suicidal ideation ( Eisenberg et al., 2013 ). One study found that graduate students in the Faculty of Medicine at the University of Calgary have higher anxiety and depression than undergraduates ( Toews et al., 1993 ), and a survey of graduate students at a university in the United States showed that approximately half of respondents reported emotional or stress-related problems ( Hyun et al., 2006 ). In an international sample of Masters’ and PhD students, 39% of respondents indicated moderate to severe depression, and 41% moderate to severe anxiety scores ( Evans et al., 2018 ). In comparison, the Centers for Disease Control and Prevention (CDC) estimate that approximately 16% of adults in the United States experience anxiety, and approximately 5% depression. Moreover, approximately 1 in 6 Americans will experience depression in their lifetime, and more women than men experience anxiety ( CDC, 2021 ; Terlizzi and Villarroel, 2020 ). However, while these general population incidences can be informative as a benchmark, these rates are not truly comparable to the student population due to multiple potential confounding factors (e.g., age group, socio-economic status, education levels of graduate level students, etc.).
Less is known about the mental health of biomedical doctoral students specifically, as disparate disciplines are often combined when graduate students are included in student mental health studies. Still, these students train in environments which may feature long work hours, pressures to produce, influential and sometimes unsupportive relationships with advisors, as well as financial concerns, uncertainty about future employment, and non-transparent university processes which may all negatively impact doctoral student mental health ( Hazell et al., 2020 ; Mackie and Bates, 2019 ).
Of note, some studies highlight that Asian, Black, Hispanic, and multi-racial undergraduate students score higher for depression than white students ( Eisenberg et al., 2013 ). Many theories have attempted to account for these racial and ethnic disparities, such as the effects of structural racism on symptoms, diagnosis, treatment and access to care ( Kendi, 2019 ) and the use of white populations as the baseline norm ( Legha and Miranda, 2020 ; for review see Conrad, 2022 ). Additionally, studies based on data from the national survey on drug use and health have shown ongoing mental health disparities among people identifying as Black, Indigenous, and people of color (BIPOC), women, and lesbian, gay, bisexual, and queer (LGBQ+) people ( SAMHSA, 2021 ). These populations are also particularly at risk in academia due to structural inequities, barriers, and microaggressions among other challenges (for example, academic cultural barriers and stressors for BIPOC, Halsey et al., 2020 ; barriers for women doctoral students, see Carter et al., 2013 ; LGBQ+ academics experience toxic environments and microaggressions, see Beagan et al., 2021 and Linley and Nguyen, 2015 ) that can impact the mental health of these populations. To acknowledge the systemic barriers faced by historically excluded groups, and to recognize that people of certain backgrounds were intentionally excluded from parts of American society for various political, economic, and social reasons (e.g., Berhe et al., 2021 ; Rollnick, 2015 ) the terms ‘historically excluded by race/ethnicity, gender, or sexual orientation’ will be used to refer to these groups respectively. While the list of historically excluded groups is not comprehensive, we aim to decenter Whiteness by referring to historically excluded (HE) versus non-historically excluded (NHE) groups.
The COVID-19 pandemic has resulted in globally increased symptoms of anxiety, depression, post-traumatic stress disorder and psychological stress, particularly among healthcare workers, those with pre-existing mental health conditions, women, college students, and individuals under 45 ( Xiong et al., 2020 ). Furthermore, it may also have impacted mental health during academic training ( Byrom, 2020 ). Compounding systemic inequities and racial injustice, COVID-19 disproportionally impacted communities of color in the United States ( Li, 2020 ; Webb Hooper et al., 2020 ; CDC, 2020 ). In particular, the highest risk of age-adjusted mortality during COVID was identified for Hawaiian and other Pacific Islander, American Indian or Alaska Native, and Latinx or Hispanic people ( Feldman and Bassett, 2021 ).
While students themselves may be classified as associated with some lower risk groups for direct effects of COVID due to their levels of education, families of students identifying as BIPOC may be disproportionately affected, especially when intersecting with risk factors associated with social class (e.g., Pathak et al., 2021 ; Feldman and Bassett, 2021 ). Hence, students historically excluded because of their race and ethnicity (also termed persons excluded due to ethnicity or race, see Asai, 2020 ) may experience disproportionate impact and heightened concerns about individual, community and family health ( Pathak et al., 2021 ; Feldman and Bassett, 2021 ; Limas, 2021 ; Blake et al., 2021 ). Indeed, a recent longitudinal study on undergraduates at the University of North Carolina at Chapel Hill (UNC-Chapel Hill; same location as the present study) found that the prevalence of anxiety and depression increased among first-year undergraduate students of color, sexual minority students, and women-identifying students during the pandemic ( Fruehwirth et al., 2021 ).
Moreover, the stress caused by the COVID-19 pandemic coincided with heightened responses and protests against the persistent racial injustice found in the United States – notably killings of Black Americans by police and vigilantes. These also took place alongside heightened anti-Asian violence, which may have also affected the mental health of Asian American students within academia.
At UNC-Chapel Hill, a large public university in the United States, the pandemic impacted courses and degrees in different ways. Most biomedical doctoral programs require didactic classes in the first two years only; afterwards students require full-time laboratory access to continue their research for another three to four years, precluding a transition to fully online instruction. Due to health and safety measures, biomedical doctoral student training was severely curtailed at our institution in the spring of 2020, and students returned to labs in June 2020 with strict occupancy limits. In contrast, medical student training is characterized by two years of didactic coursework and frequent test-taking, followed by another two years of sequential clinical experiences in hospitals or other clinical settings. In 2020, medical students could continue their academic progress with online learning options fostered by a switch to remote instruction in place of didactic in-person courses and clinical rotations. Hence, these students were temporarily removed from clinical rotations due to shortages of personal protective equipment; conversely though, graduation dates were not delayed.
Given this background, we sought to examine effects of the concurrent COVID-19 pandemic and heightened community reactions to racial injustice between 2019 and 2020 by exploring the mental health of medical students and biomedical doctoral students at UNC-Chapel Hill. We investigate comparisons between historically excluded (HE) and non-historically excluded (NHE) groups in science, focused on race/ethnicity, gender, and sexual orientation in medical and graduate biomedical students during the intersection of the COVID-19 pandemic and a time of reckoning of persistent racial injustice. Recognizing that an intersectional approach encompasses a multitude of identities ( Cho et al., 2013 ), the facets of identity explored in this study are not intended to be comprehensive, but rather to represent major subpopulations represented in our sample and commonly found in US biomedical graduate and medical education.
The UNC-Chapel Hill School of Medicine annually enrolls approximately 800 medical and 600 biomedical PhD students; part of the student body is representative of diverse identities including trainees from a variety of racial and ethnic groups, genders and LGBQ +identities. For example, a recent report ( UNC School of Medicine Office of Diversity Equity and Inclusion, 2021 ) indicated that the medical student population at UNC-Chapel Hill consisted of 54% women, 58% white, 14% Asian, and 24% underrepresented students (4% not reported); the biomedical graduate student population consisted of 57% white, 15% Asian, and 26% underrepresented students (2% not reported). The present study was reviewed and approved by the Institutional Review Board (#18–0112).
The annual School of Medicine survey used for this study includes self-reported mental health status (examined in this work), as well as assessment of current and desired student-support programs. It is conducted to inform current and future mental health and wellness programming and global satisfaction with services provided ( https://doi.org/10.17605/OSF.IO/H9UCX ). The same School of Medicine survey was administered to medical and biomedical doctoral students approximately one year apart in 2019 and 2020 (n=431, Fall 2020; n=526, Fall 2019). Each survey was open for four weeks between September and October and distributed using the same mechanisms (e.g., same internal listservs) to be as comparable as possible.
In the primary analysis, mental health data was analyzed by type of training program (MD vs. PhD; that is, medical students vs. biomedical doctoral students), year (2019 vs 2020), and historically excluded vs. non-historically excluded (HE vs NHE) populations based on race/ethnicity (HE-RE vs. NHE-RE) and gender (HE-G vs. NHE-G, that is students identifying as women vs. men). A post hoc analysis included the primary variables as well as historically excluded on the basis of sexual orientation (HE-SO vs. NHE-SO, that is LGBQ+ vs. non-LGBQ+ populations).
Demographic data including race/ethnicity were collected. In some cases, partial survey data was recorded (n=957 total responses; n=931 completed the survey; of those, n=740 submitted some or all demographic data). Partial surveys were used, however, only fully completed measures were included in the analysis (a blocked survey design enabled a data cleaning check that ensured participants completed each section/measure they were working on before closing the survey).
We assessed four measures of mental health (depression, anxiety, hazardous alcohol use, and problems related to substance use) using widely utilized and validated questionnaires. For each of these four measures, the values of responses were summed and sorted into categories of increasing severity ranging from 0 (indicating a lack of presentation of symptoms/no problematic substance use) to 3 or 4 (indicating increasing population-normed levels of severity for each variable), and then recoded into no symptoms (0) versus any symptoms (1). Depression scores/categories were calculated using the Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001 ); anxiety scores/categories were calculated using the Generalized Anxiety Disorder Assessment (GAD-7; Spitzer et al., 2006 ); hazardous alcohol use was assessed using the Alcohol Use Disorder Identification Test (AUDIT; World Health Organization, 2001 ); problems with drug use was assessed by the Drug Abuse Screening Test (DAST-10; Skinner, 1982 ; Yudko et al., 2007 ; see Table 1 for details of the categories and how they were created). To assess meaningful categories of symptomatic versus asymptomatic responses, each mental health outcome measure (for depression, anxiety, alcohol use and drug use) was recoded into bivariate (0/1) variables with a value of one (1) indicating symptoms or problems with each category (see Table 1 ).
Each measure of mental health (depression, anxiety, hazardous alcohol use, and problems related to substance use) was examined and coded according to its respective validated scale (PHQ-9, GAD-7, AUDIT, DAST-10). The scores were recoded as interim measures based on symptom severity, from 0 to 4. These were then transferred into a clinically meaningful bivariate category (no symptoms, 0; any symptoms, 1) to facilitate the planned analysis (bivariate logistic regression).
In addition, suicidal ideation was assessed using the following three “Yes” or “No” questions: “Have you ever thought about ending your life?”; “Have you ever thought about ending your life while enrolled?”; “Have you ever thought about ending your life in the last 12 months?”.
Participants
All of the approximately 800 medical students and 600 biomedical doctoral students on campus were invited to participate in the survey each year via student listservs. Respondents included both medical and biomedical doctoral students (Fall 2020 n=431, Fall 2019 n=526, n=957 total respondents). This sample included 622 medical students, 309 biomedical doctoral students, with 26 surveys missing data, for a total of 931 completed surveys. Amongst those 931 respondents, 91 medical students were classified as HE-RE and 531 as NHE-RE; and 57 biomedical doctoral students were classified as HE-RE, with 252 being classified as NHE-RE.
Ages ranged from 18 to 40+, with the majority of students (59%) being ages 21–25 years (59% of medical students, 60% of biomedical doctoral students), followed by 35% being ages 26–30 (34% of medical students, 35% of biomedical doctoral students), and the remainder 5% being ages 31–35 (6% of medical students, 5% of biomedical doctoral students), with <1% each respectively (for both medical students and biomedical doctoral students) for ages 18–20 years and 35–40+years.
Respondents classified as belonging to NHE-RE groups identified as follows: 66% white (67% of medical students, 66% of biomedical doctoral students), 14% Asian (16% of medical students, 9% of biomedical doctoral students), or 2% other (2% of medical students, 3% of biomedical doctoral students). In accordance with National Institutes of Health definitions of ‘underrepresented’ in the biomedical, clinical, behavioral, and social sciences ( National Institutes of Health, 2020 ), respondents were classified as belonging to HE-RE groups if they identified as follows: 7% African American (7% of medical students and biomedical doctoral students), 7% Latinx (4% of medical students, 11% of biomedical doctoral students), 2% Middle Eastern (3% of medical students, 1% of biomedical doctoral students), 1% American Indian/Alaskan Native (1% of medical students and biomedical doctoral students), and <1% Pacific Islander (<1% of medical students and biomedical doctoral students). Historically, Asian Americans have also faced exclusion from American culture, as evidenced by the Chinese Exclusion Act and the internment of Japanese Americans during the Second World War. However, Asian Americans have been well-represented in the sciences and thus are included as NHE-RE for analysis. Additionally, Middle Eastern is not an identity included in the United States Census or NIH definitions as underrepresented; however, this group is included as HE-RE due to the marginalization this population as experienced in the United States, especially in recent years and specifically over the decades following 9/11/2001 (e.g., Crawford et al., 2021 ; Daraiseh, 2012 ; Clay, 2011 ).
The majority of respondents identified as women (67%; 63% of medical students, 75% of biomedical doctoral students), followed by men (32%; 36% of medical students, 24% of biomedical doctoral students), and <1% other (genderqueer, gender nonconforming, gender non-binary, and transgender; equally represented across medical and biomedical doctoral students). Institutionally, the overall medical and biomedical doctoral student populations include more women than men, so these distributions are not unexpected. Women were classified as historically excluded and men as non-historically excluded. Though transgender individuals also experience mental health and substance use disparities ( National Center for Transgender Equality, 2016 ), we were unable to include analyses in this study due the small sample size; future studies focused on the mental health and wellbeing of gender diverse people, including transgender and gender non-conforming individuals are needed.
Respondents were classified as non-historically excluded on the basis of sexual orientation (NHE-SO) if they identified as straight/heterosexual (83%; 85% of medical students, 79% of biomedical doctoral students); or historically excluded on the basis of sexual orientation (HE-SO) if they identified as bisexual (7%; 5% of medical students, 10% biomedical doctoral students), gay/lesbian (5%; 5% of medical students, 4% of biomedical doctoral students), queer (2%; 3% of medical students, 2% of biomedical doctoral students), pansexual (2%; 1% of medical students, 3% of biomedical doctoral students), asexual (1%;<1% of medical students and biomedical doctoral students), or other (1%; <1% of medical students, 2% of biomedical doctoral students).
Analysis plan
A logistic regression was conducted, including significant interaction terms, to examine the effects of each variable on mental health outcomes using a parsimonious model. Full models with main effects and interactions were run for each variable, with stepwise addition of the largest interaction terms to the main effects, until the next largest interaction term added was no longer significant. At that point, the prior model with significant main effects and any significant interactions was retained as the final model for that variable (see Source data 1 ).
As previously described, each mental health outcome variable was split into clinically meaningful bivariate categories for depression, anxiety, problems with drug use and hazardous alcohol use such that the baseline category (none or fewest symptoms, as defined by each scale) was coded as zero (0), and any symptoms, as defined by more or worse symptoms than the baseline category, were coded as one (1). A bivariate logistic regression model was used to assess the impact of our primary factors of interest across the medical and biomedical doctoral student populations to maintain a large sample size and sufficient power to compare historically excluded (HE) and non-historically excluded (NHE) groups pre- and during COVID-19; groups were analyzed via Race/Ethnicity (RE) and Gender (G) for the primary analysis.
Year was coded into a practically meaningful bivariate category, with pre-COVID-19 as zero (2019; 0) and during the COVID-19 pandemic and racial unrest as one (2020; 1). Finally, HE and NHE statuses (based on race/ethnicity, gender, and sexual orientation) were coded into practically meaningful bivariate categories, with endorsement of any historically excluded category being coded as one (1), whereas all others were coded as NHE using the value of zero (0).
The primary analysis included type of program (MD vs. PhD) x Year x Race/Ethnicity x Gender. A post hoc model included all these variables, with the addition of sexual orientation (all three historically excluded social identity groups; HE-RE, HE-G, & HE-SO).
Limitations
Response bias is always a consideration in cross-sectional self-report research. Relatedly, there were no matched controls, hence it is possible that sampling distributions may have differed by chance. Furthermore, it is possible that respondents differed based on how important mental health is to them, potentially skewing the sample; hence we cannot definitively evaluate the respondent sample as representative of the full population. Due to anonymous data collection and optional questions to protect participant identities, we cannot assess granular response rates by demographic characteristics. Future studies could be completed with a controlled sample matched with participant identifiers to know who in the sample is and is not responding, as this could impact findings. Nonetheless, we achieved a response rate commensurate with voluntary survey data, suggesting a typical level of participation. We also had a high percentage of women respondents, who experience higher rates of depression and anxiety compared to men respondents; however, greater response from women is not atypical of our graduate medical and biomedical doctoral student populations, which include more enrolled women than men.
While anonymized data collection was employed as a strategy to increase sample size (e.g., more participants would feel safe responding if they could be anonymous), another limitation introduced as a byproduct of this design was the inability to examine the extent of repeated participants from year to year, which would be ideal to assess and control for in future studies. Nonetheless, using a between-groups design assuming normal variation in participants, there is no reason to believe that the two samples collected should be atypical from their respective populations over the consecutive years sampled. Methodological congruence of data collection was employed to reduce systematic bias in responses from year to year. Hence, results should be interpreted with caution as we cannot assess the percentage of repeated participants from year to year, though we believe the samples to be representative of the populations at each timepoint.
Conversely, we recognize that a large number of participants responding in both samples could be problematic for assumptions of independence for the use of parametric statistics and logistic regression analysis. Because we collected data anonymously to protect respondents’ privacy, we cannot assess to what extent respondents may have participated in both years, hence results should be interpreted with caution. It would be preferable to have identifiable data and be able to use a repeated-measures design to reduce error variance. Yet, to the extent that significant findings were achieved even with the increased error variance inherent in a between-subjects design, these results likely had large enough effect sizes to be identified even given the loss of power from using a between-subjects design rather than the preferred, more sensitive within-subjects design.
Additional limitations included our lack of ability to control for other possible variables of interest such as pandemic-specific factors, years in training, and departmental affiliation or specialty area. Pandemic-specific questions were not asked because we used the same annual survey questions in 2019 and 2020 to maintain comparable responses. Department and specialty information were not asked in order to protect anonymity, to increase comfort with responding, and to maximize response rates. Yet, populations were purposefully defined by reasonably homogenous training experiences into the two major clusters of interest: medical training and biomedical doctoral training. A large portion of the sample did not complete optional demographic questions (such as number of years in training), limiting our ability to include this in the analysis. Future work should consider controlling for as many of these variables as possible.
The logistic regression model identified significant differences on student mental health outcomes for depression and anxiety by year (interactions), as well as by program (biomedical doctoral students scored worse than medical students), and for those historically on the basis of race/ethnicity (HE-RE) and by gender (HE-G) ( Figure 1A ).

Logistic regression tables show main effects and interactions for each of the primary factors (Program, Year, HE-Gender, HE-Race/Ethnicity) across four measures of mental health (Depression, Anxiety, Hazardous Alcohol Use, Problems with Drug Use) and three measures of suicidal ideation (Ever, While Enrolled, In The Last 12 Months); the correlation matrix scatter plots illustrate the relationships between the four mental health measures. All percentages were calculated out of total valid responses; see Figure 2 for percentages. Mental health outcomes were coded into a bivariate 0/1 indicating the absence or presence of the respective symptoms for depression and anxiety (see Measures). For suicidal ideation, response options included ‘Yes’ (indicating suicidal ideations) or ‘No’ (indicating no suicidal ideations) for each of the three categories (see Methods for exact question wording). ( A & B ) Logistic Regression. A significant odds ratio greater than 1 indicates that the target category is more likely than the comparison group to indicate a higher score on that variable, whereas a significant odds ratio of less than 1 indicates that the target category is less likely than the comparison group to indicate a higher score on that variable. Nonsignificant effects suggest odds ratios do not show a difference greater than expected by chance (~1). If the 95% confidence interval includes 1, then the odds ratio does not differ more than expected by chance (e.g., OR = 0.98, CI95%=0.83–1.14 means there is not a significant effect of Year for Suicidal Ideation Ever); if the confidence interval does not include 1, then it differs more than expected by chance. ( C ) Scatterplots of the relationship between variables of interest (Depression, Anxiety, Problems with Drug Use and Hazardous Alcohol Use) displayed include graphical representations in a matrix format.
In the combined population (when medical and biomedical doctoral students are considered together) there was a decrease in depression and anxiety, likely driven by the medical student improvements; see Discussion. In general, HE-RE students exhibited significantly higher rates of depression and anxiety at about 1.5 times the rate of their NHE-RE peers across the combined medical and biomedical doctoral student sample. No differences were evidenced on either drug or alcohol use by year, type of program or historically excluded/non-excluded status.
Overall, across medical and biomedical doctoral students, HE-RE students were approximately twice as likely to say they had thought about ending their life in the last 12months than their NHE-RE peers, and about 1.8 times more likely while enrolled ( Figure 1B ); such high rates are extremely concerning. Due to different patterns emerging for training type and racial/ethnic identity by year, examining effect solely by year obscured these differences, hence interactions were further explored.
Depression and anxiety
Surprisingly, for medical students, there was a significant decrease in depression and anxiety between 2019 and 2020 ( P <.001), whereas doctoral students observed no change between years. However, HE-RE students differed from their NHE-RE peers, being significantly more likely to be depressed ( P <.02) and anxious ( P <.04). Women (HE-G) exhibited higher depression and anxiety scores than men (NHE-G) consistent with known mental health trends; hence these effects are controlled for in the analyses.
Problems with drug use and hazardous alcohol use
No significant differences of note emerged between populations or within populations (e.g., NHE/HE by Program, Race/Ethnicity, Gender) on the primary measures. Reported problems with substance use and hazardous alcohol use were comparatively low in contrast to depression and anxiety, which were more pervasive. Men (NHE-G) exhibited more problems with drug use and hazardous alcohol use than women (HE-G) consistent with known substance use trends; hence these effects are controlled for in the analysis.
Suicidal ideation
Medical students showed trends toward improvement, whereas biomedical doctoral students exhibited no change between 2019 and 2020. As compared with NH-RE peers, there were significant increase in HE-RE student suicidal ideation ‘while enrolled’ ( P =.03), and ‘in the last 12 months’ ( P <.01). There were no significant effects of gender on suicidal ideation ( p s = .58 -.62, not significant).
Medical school versus biomedical doctoral training
Prior to 2020, both medical and biomedical doctoral students suffered from depression (46% of medical students, 65% of biomedical doctoral students) and anxiety (47% of medical students, 67% of biomedical doctoral students) at high rates ( Figure 2A and B ), as defined by no symptoms compared with any symptomatic categories (see Methods for categorical definitions). Doctoral student mental health in 2020 remained very poor (depression: 26% of medical students, 64% of biomedical doctoral students; anxiety: 32% of medical students, 61% of biomedical doctoral students), whereas, surprisingly, the mental health of medical students improved. Suicidal ideation ‘in the last 12 months’ among biomedical doctoral students (compared with medical students) was markedly higher, both before (11% of medical students, 16% of biomedical doctoral students) and during 2020 (6% of medical students, 19% of biomedical doctoral students).

( A ) Percentages of medical (MD) and biomedical doctoral (PhD) students reporting the presence (dark grey) or absence (light grey) of symptoms/problematic use pertaining to depression, anxiety, problems with drug use and hazardous alcohol use. ( B ) Percentages of medical (MD) and biomedical doctoral (PhD) students in 2019 and 2020 reporting having had (dark grey) or not having had (light grey) suicidal thoughts ever, in the last 12 months or while enrolled. ( C ) Percentages of historically excluded and non-historically excluded students based on race and ethnicity (HE-RE vs HE-NRE) reporting the presence (dark grey) or absence (light grey) of symptoms and problematic use pertaining to depression, anxiety, problems with drug use and hazardous alcohol use. HE-RE students showed higher rates of depression in both 2019 (60% of HE-RE, 51% of NHE-RE) and 2020 (48% of HE-RE, 35% of NHE-RE). This pattern was also seen for anxiety (in 2019: 60% of HE-RE, 53% of NHE-RE; in 2020: 51% of HE-RE, 38% of NHE-RE). ( D ) Percentages of historically excluded and non-excluded students based on race and ethnicity (HE-RE vs HE-NRE) reporting, in 2019 and 2020, having had (dark grey) or not having had (light grey) suicidal thoughts ever, in the last 12 months or while enrolled. Historically excluded students exhibit higher rates of suicidal ideation, in particular ‘while enrolled’ and ‘during the last 12 months’ (2019, positive responses for ‘while enrolled’: 23% of HE-RE, 15% of NHE-RE; positive responses for ‘during the last 12 months’: 19% HE-RE, 11% NHE-RE; 2020, positive responses for ‘while enrolled’: 18% of HE-RE, 10% of NHE-RE; positive responses for ‘during the last 12 months’ 17% HE-RE, 12% NHE-RE). All percentages were calculated out of total valid responses. HE-RE students were coded as such if they indicated that they belonged to historically excluded racial or ethnic categories (e.g., African American/Black, Hispanic/Latinx; see Methods for details); NHE-RE included students who did not indicate a marginalized racial/ethnic identity.
We assessed differences between medical and biomedical doctoral students for depression (PHQ-9), anxiety (GAD), problematic drug use (DAST), and hazardous alcohol use (AUDIT) using nominal outcome variables ( Figure 2A and B ). We identified significantly higher rates of depression and anxiety for biomedical doctoral students compared with medical students, as well as higher rates of suicidal ideation ‘while enrolled’ and ‘in the last 12 months’. No significant differences emerged for problems with drug use or hazardous alcohol use by training type, year, or historical exclusion by race/ethnicity; furthermore, problems with drug use rates were comparatively low in contrast to depression and anxiety. Known gender effects were consistent with expectations for both problematic substance use categories (greater use found in prior studies is also reflected in our sample for NHE-G vs. HE-G).
Historically excluded versus non-historically excluded students based on race/ethnicity (HE-RE vs. NHE-RE)
Mental health results for groups historically and non-historically excluded on the basis of race/ethnicity (HE-RE vs. NHE-RE) across a combined pool of biomedical doctoral students and medical students were also compared ( Figure 2C and D ). In both 2019 and 2020, HE-RE students experienced higher rates of depression and anxiety compared to their NHE-RE peers ( Figure 2C and D ). Suicidal ideation was also worse for HE-RE students as compared with their NHE-RE peers, specifically ‘while enrolled’ and ‘in the last 12 months’. In summary, HE-RE outcomes in general were worse for depression and anxiety ( Figure 2C ), as well asthese students experiencing more suicidal ideation ‘while enrolled’ and ‘over the last 12 months’ ( Figure 2D ).
While individuals identifying as Asian are well-represented in the academic workforce, 2020 saw an increase in anti-Asian violence, which led us to conduct additional analyses to compare the mental health of Asian American and HE-RE students in 2019 and 2020. People who identified as of Asian descent generally scored better than other NHE-RE or HE-RE groups, indicating fewer mental health challenges on all four outcome variables and the three suicidal ideation variables. However, conditional odds ratios based on these models indicated some changes by year that may be associated with the negative psychosocial and environmental factors many Asian Americans experienced between 2019–2020. Accounting for the effect of race (3-level: HE-RE Asian, HE-RE Non-Asian, HE-NRE) while controlling for year, type of training and gender, Asian American participants showed greater mean depression scores ( P <.03) and anxiety scores ( P <.04) in 2020 compared with 2019; there was no change in either alcohol use ( P =.07, though marginal) or drug use ( P =.28). There were no significant changes in conditional probabilities for suicidal ideation of Asian American participants during that time.
Associations
A robust positive association was evident between depression and anxiety ( r =.69, P <.001), not surprisingly as these conditions are often comorbid. Both depression ( r =.14) and anxiety ( r =.33) were associated with problems with drug use ( p s <.001). Neither depression ( r =-.01, P =.74) nor anxiety ( r =-.01, P =.77) were associated with hazardous alcohol use. Since this was only correlational in nature, a causal direction cannot be determined; nonetheless, these associations may indicate a connection between problems with drug use either as a precursor to or as an effect of experiencing mental health symptoms.
Post hoc analysis: historically excluded versus non-historically excluded students based on sexual orientation (HE-SO vs. NHE-SO)
To further examine additional aspects of intersectionality, we completed a post hoc analysis including LGBQ+ identities (HE-SO) into a simplified model (controlling for main effects of the four primary variables and identifying any significant two-way interactions). Due to a smaller sample size, this was included as a post hoc analysis.
The HE-SO variable showed significant main effects across main outcome variables, with HE-SO participants more than twice as likely to experience depression (OR = 2.19, P <.0003) and anxiety (OR = 2.66, P <.0001). In addition, there was a significant interaction with ‘Year’ for depression ( P =.03), such that 2020 was significantly worse for HE-SO depression than 2019.
There were also main effects for alcohol use (OR = 2.31, P <.01) and drug use (OR = 2.37, P <.0002), such that HE-SO participants were more at risk for substance use; however, an interaction between gender and sexual orientation ( P =.03) indicated that among HE-SO participants, NHE-G (LGBQ +men) were more likely to report drug use than HE-G participants (LGBQ+ women; conditional OR = .29, P <.003). HE-SO NHE-G participants (LGBQ+ men) compared to NHE-SO HE-G participants (LGBQ+ women) were nearly four times as likely to report drug use (conditional OR = 3.91, P <.0002), whereas HE-SO HE-G participants (LGBQ+ women) were not significantly more likely to report drug use ( P =.19).
HE-SO participants experienced more suicidal ideation (ever, OR = 4.37, P <.001; while enrolled, OR = 3.66, P <.0001; in the last 12 months, OR = 4.77, P <.0001; see Figure 3 for visualization of comparative percentages). In addition, there was a marginal interaction between ‘HE-SO’ and ‘Program’ ( P =.05), such that medical participants were much less likely (OR = .25) than biomedical doctoral students to indicate suicidal ideations while enrolled. Hence, biomedical doctoral HE-SO participants were almost six times more likely to report suicidal ideations than NHE-SO biomedical doctoral participants while enrolled (conditional OR = 5.94, P <.0001) whereas HE-SO medical students where about twice as likely to indicate suicidal ideations while enrolled than NHE-SO medical students (conditional OR = 2.925, P <.02).

Graphical representation displaying the percentages for each of the two primary factors in this figure (Gender and Sexual Orientation) across the four measures of mental health and three measures of suicidal ideation for populations historically excluded on the basis of sexual orientation or gender (HE-SO and HE-G). All percentages were calculated out of total valid responses. Historically excluded versus non-historically excluded students based on sexual orientation (HE-SO vs. NHE-SO) were compared. Members of the HE-SO group were classified as such if they indicated an excluded identity (e.g., Lesbian, Bisexual, Queer – LGBQ+ sexual orientation; see Methods for details); NHE-SO included any students who did not indicate a historically excluded identity. Historically excluded on the basis of gender included women; non-historically excluded students by gender included men (HE-G vs. NHE-G). ( A ) Percentages of LGBQ+ (HE-SO) and non-LGBQ+ (NHE-SO) men and women (NHE-G vs. HE-G) reporting the presence (dark grey) or absence (light grey) of symptoms and problematic use pertaining to depression, anxiety, problems with drug use and hazardous alcohol use. ( B ) Percentages of LGBQ+ (HE-SO) and non-LGBQ+ (NHE-SO) men and women (NHE-G vs. HE-G) reporting having had (dark grey) or not having had (light grey) suicidal thoughts ever, in the last 12 months or while enrolled.
Overall, medical student mental health improved from 2019–2020 on measures of both depression and anxiety, whereas biomedical doctoral students showed no change, their scores remaining concernedly high. HE-RE students were worse off than their NHE-RE peers in measures of depression, anxiety, and suicidal ideation – particularly reporting more suicidal ideation than their counterparts both ‘while enrolled’ and in the ‘last 12 months’. All analyses controlled for gender, for which women (HE-G) generally experienced anxiety and depression more than men (NHE-G), whereas men generally reported higher substance use. Post hoc analyses also indicated that those identifying as HE-SO (LGBQ+ respondents) experienced more anxiety and depression than NHE-SO (non-LGBQ+) respondents, as well as greater suicidal ideation.
Trends in medical students versus biomedical doctoral students
Despite unique challenges between 2019 and 2020, many metrics of medical student mental health improved. In mid-March of 2020, medical students were pulled from clinical settings and from typical coursework due to the pandemic. Usual academic and clinical responsibilities were replaced with a four-week online course named ‘Medical Management of COVID-19’, which focused for instance on wellness, self-care, medical management and personal protective equipment related to COVID-19 ( UNC Health and UNC School of Medicine, 2020 ). It is possible that the pause in traditional medical student training and the new course focused on timely topics mitigated stress-induced mental health erosion. In contrast, biomedical doctoral students did not receive any similar interventions addressing emerging COVID knowledge or mental health coping strategies.
Furthermore, medical students at our institution were able to continue some form of their training remotely, to maintain some social contact and peer support networks through academic training, and to avoid graduation delays. Additionally, while medical students pay for their training, which could contribute to financial stress, these financial demands did not change between 2019 and 2020. This consistency of circumstances, combined with expectations of income post-graduation and a near-guarantee of eventual employment in medicine, could also have mitigated the downward trend in medical student mental health. Furthermore, we also speculate that being in a medical training program with obvious direct impact during a time when medical professionals were publicly celebrated (at least initially) had a positive effect on the mental health of medical students.
Finally, and in contrast to biomedical doctoral programs, medical school accreditation bodies mandate and enforce the presence of more structured mental health and wellness support systems, ensuring that support services for medical students are more easily accessible and freely available (no cost, and/or available funding to cover any out-of-pocket mental health medical expenses). At our institution, both medical and biomedical doctoral students have limited access to facilitated and triaged on-campus resources; however, while the equivalent of 1.5 person working full time is dedicated to support the ~800 medical students (e.g., 533:1 student-counsellor ratio), the ~600 biomedical doctoral trainees only have access to the equivalent of 0.5 full-time employee dedicated to their support (e.g., 1200:1 student-counsellor ratio). The more robust support for medical students, combined with being removed from the acute stressors often encountered in rotations (due to being pulled from clinical duties during the pandemic) may have magnified the ameliorative effect of the cohort-based intervention that medical students received.
In contrast to medical students, biomedical doctoral students exhibited alarmingly high levels of depression and anxiety that dwarfed the rates in the medical student population, which were themselves higher than in the general population. This is similar to previous findings (e.g. Evans et al., 2018 ), even accounting for COVID trends (see Gordon, 2021 ). When considering recent suicidal ideation in particular, the mental health of biomedical doctoral student worsened between 2019 and 2020. This may be linked to changes imposed on biomedical doctoral student training: laboratory research had to be stopped and lab occupancy was then restricted in Spring 2020, which reduced supportive social interactions and peer camaraderie. The loss of progress on dissertation projects (given that graduation times are open-ended) was frustrating and may have exacerbated mental health issues. In addition, the concurrent economic recession may have depressed optimism about job opportunities for biomedical doctoral students, who pursue a much wider range of careers after graduation compared to medical students. The dismissal of science by politicians and the media, popular sentiments against public health policies based on scientific recommendations and public degradation of trust in science and scientists may have all contributed to a worsened experience for biomedical scientists (e.g., Couée, 2020 ; Gross, 2020 ; Kreps and Kriner, 2020 ).
For biomedical doctoral students whose research was not directly related to COVID-19, it may have been harder to find meaning and purpose in their formerly satisfying research on other diseases. Anecdotally, some biomedical doctoral students sought opportunities to volunteer their skills in molecular biology in diagnostic COVID-19 labs, indicating a desire to contribute to the immediate crisis. In contrast, medical students may have found it easier to connect their training with the real-world crisis of COVID-19. Moreover, when labs were shutting down, medical education shifted to COVID-19 prevention topics directly related to the pandemic.
Additionally, medical students will soon become medical doctors in a society where this profession took center stage. On the other hand, the success of the vaccine effort – which received praise but also backlash – may yet improve how basic research scientists are considered in society in the coming years ( Bogel-Burroughs, 2020 ; Kauer, 2020 ; Kolata, 2021 ). Future education and mental health research should delve into the aspects of medical education versus biomedical doctoral training that drive different mental health outcomes during a crisis and in normal times.
Mental health trends for student from historically excluded racial or ethnic groups
Irrespective of medical or doctoral program, mental health metrics for depression, anxiety and suicidal ideation were worse for students from historically excluded groups based on race/ethnicity compared to students from non-historically excluded racial groups, and they worsened between 2019 and 2020. Overall, the incidence of suicidal thoughts for HE-RE students increased proportionately both ‘while enrolled’ and ‘in the last 12 months’ compared with NHE-RE students, and particularly for biomedical doctoral HE-RE students ‘in the last 12 months’. We hypothesize that the COVID-19 pandemic and heightened racial unrest contributed to these differences, although future research is needed to isolate the factors causing the observed effects. This result may be partially explained by the added stressors of systemic racism in academic, medical, and American cultures. Academic culture, in particular, is based on norms that systematically exclude minority groups and create additional mental health challenges for people of color (e.g., persons excluded due to ethnicity or race, see Asai, 2020 ).
Our finding that depression was correlated with both anxiety and problematic drug use was consistent with previous work which demonstrates common comorbidity of depression and anxiety, as well as of substance use disorders with mental illness (e.g., National Institute on Drug Abuse, 2010 ); hence, it is plausible that problematic drug use could represent a contributing factor and/or a coping strategy for depression but this should be interpreted with caution. Furthermore, the lack of association in our sample between hazardous alcohol use and mental illness was surprising given the common associations found between these variables in previous work (e.g., Smith and Randall, 2012 ; McHugh and Weiss, 2019 ).
Mental health trends for students belonging to groups historically excluded because of sexual orientation
Our findings that LGBQ+ students experience worse mental health outcomes align with national studies showing that sexual minorities are approximately twice more likely than heterosexual people to experience mental health conditions such as anxiety, depression, suicide, and substance use ( Medley et al., 2016 ; SAMHSA, 2020 ; SAMHSA, 2021 ). Similar to national trends, gender interacted with sexual orientation to indicate worse effects for LGBQ+ women for depression and anxiety, but worse substance use for LGBQ+ men. While our small sample suggests that these results should be interpreted with caution, the large effect size evident in our analysis was extremely concerning and indicates a crucial need for studies to further examine this population and how it could be better supported. In addition, our inability to evaluate these hypotheses for transgender and gender non-conforming students (due to an insufficient sample size to run a parallel analysis) was a limitation. This should certainly be evaluated in future studies, especially due to transgender people being at increased risk and incidence for mental health problems, as evidenced nationally ( National Center for Transgender Equality, 2016 ).
Conclusions and recommendations
Whereas medical schools have had mental health recommendations in place since 1992 ( AAMC Executive Council, 1992 ; enforced by the Liaison Committee on Medical Education accreditation standards), biomedical doctoral programs have had no such parallel policies regarding mental health provisions nationwide. Our new data suggest a need for swift action to address the very urgent mental health needs of biomedical doctoral students both before and during the COVID-19 pandemic, especially for students who have been traditionally excluded from the academy based on their gender, race/ethnicity, and sexual orientation. Furthermore, the data we present suggests that depression, anxiety, and suicidality for historically excluded medical and biomedical research students have been exacerbated during the ongoing COVID-19 pandemic and climate of heightened visibility of racial inequity. Future studies should explore additional disparities between historically and non-historically excluded students in addition to those highly concerning trends.
It is crucial, now more than ever, to provide mental health support both on campus and remotely to ensure that students have access to the mental health services they need (see Krause and Harris, 2019 ). On-campus mental health resources should reflect the diversity of the student body, including in terms of race/ethnicity and sexual orientation. Meanwhile, mental health resources, communities, and support groups are starting to emerge online (e.g., PhDBalance , TAE Consortium , RVoice ).
While offering more resources is an important step, the increasing national demand for mental health services on university and college campuses may make it difficult to provide comprehensive mental health care to all students who need it ( Seppälä et al., 2020 ). In addition, simply providing services and programs may not be enough due to inequitable access to these resources and systemic issues that negatively impact mental health outcomes. Preventative health measures should therefore be investigated at the graduate level, particularly regarding the learning environment. Prevention, wellness resources, LGBTQ+ Safe Zone, anti-racism and resiliency training as well as assessment of impact are crucial to reduce the acute need for mental health support, including substance use.
Given the higher indicators of distress, the factors driving the mental health crisis, particularly for BIPOC students, those from gender and sexual minorities, and biomedical doctoral students, should be identified. Some potential causes to explore include toxic work environments, systemic racism, sexism, homophobia and unhealthy cultural and academic norms. In addition, the following factors contribute to historical exclusion based on race and ethnicity: bullying and harassment, precarity of work contracts in higher education, science inequities based on barriers and limitations to diversity, inclusion, and accessibility, and a disproportionate effect of the competitive culture in academia on historically excluded groups ( Limas et al., 2022 ; Limas, 2021 ). Researchers must continue to examine how these and other factors may contribute to negative experiences for historically excluded groups particularly, and to extend this research to proposing, implementing and evaluating needed programmatic and policy changes empirically. This should also include evidence-based research focused on the mental health of faculty and staff to better cater to this population’s needs, as well as to recognize and improve the support they provide to students (e.g., Loissel, 2019 ; Loissel, 2020 ).
While individual protective measures can alleviate some negative impacts of operating within a flawed system (e.g., the academic environment), systemic change must occur rather than relying on those most likely to be impacted to create change ( Halsey et al., 2020 ). It is imperative that leaders in higher education use evidence-based quantitative and qualitative research to examine population trends, create visibility for lived experience, and ultimately identify and reduce causes of mental health problems rather than just treating symptoms when they emerge. Academic culture needs to be actively reformed by those in power to model, encourage, and sustain student, faculty and staff wellbeing.
Study limitations and future directions
Limitations related to anonymous data collection include the inability to estimate exact response rates, percentage of repeated versus new respondents, or non-respondents who skipped entering demographic data. In addition, self-reported mental health status may be biased, and independent assessments by a clinician would provide greater accuracy. Importantly, given the observational nature of our data collection, many confounds could also not be accounted for which changed over the course of the year between data collection timepoints. Nonetheless we believe that our work provides a compelling starting point to further examine trends and emergent concerns in the mental health of medical and biomedical doctoral students. Even given the limitations of our dataset, the unexpectedly high rate of suicidal ideation is concerning: among respondents alone, nearly 40 trainees (16 medical students and 21 biomedical doctoral students) reported recent suicidal ideation in 2020.
Many segments of society in the United States have been intentionally excluded from social, economic, and cultural opportunities via law, policy, and cultural expectations in order for dominant groups to retain power and privilege. Some groups have explicitly and implicitly experienced more systemic barriers than others – for example, the legal discrimination against African Americans throughout American history, or the restriction of voting privileges to exclude women and non-white voters. Historically, this has been reinforced by social norms and cultural biases, even in situations when overt racial discrimination has been addressed. We recognize that race is a social construct, and that other social identity groups beyond race and ethnicity ( Rothman et al., 2020 ) may also experience inequitable impacts of COVID-19. For instance, we noted that women and LGBTQ+ students also showed evidence of negative impacts on their mental health in the current study. We have controlled for differences by gender as well as examined effects for sexual orientation (see Salerno et al., 2020 ), but we recognize that these analyses are not comprehensive of all social groups experiencing inequities, and we acknowledge the impact of additional identities that we were not able to study such as, among others, international and undocumented status ( Hunt, 2020 ; Chen et al., 2020 ) and disability ( Goggin and Ellis, 2020 ; Gray et al., 2020 ). In fact, the NIH has recently expanded its definition of underrepresented in science to include women, people with disabilities, first-generation college students and those from disadvantaged backgrounds (including people who have experienced or are experiencing homelessness, foster care participation, recipients of free and reduced lunch, Pell grants, SNAP or WIC, and those who grew up in a low-income or rural areas; National Institutes of Health, 2020 ; National Institutes of Health, 2018 , rescinded and replaced in 2019; National Institutes of Health, 2019 ).
Yet this expanded definition remains flawed as some groups are still excluded from recognition and inclusion as societal norms and practices shift over time. The concept of ‘historically excluded’ should therefore continue to evolve and be re-examined or expanded over time as warranted by newly identified historical trends. For instance, people of Middle Eastern descent have faced heightened discrimination following 9/11/2001. Students identifying as Asian may also face distinct challenges that affect their mental health among rising anti-Asian violence (e.g., Yam, 2021a ; Yam, 2021b ). In fact, our analyses showed that the 2019–2020 year brought additional challenges that impacted mental health in a negative direction for both depression and anxiety in this population, despite overall scores that indicate, on average, better mental health outcomes. This supports the need for examining Asian HE-RE populations separately in future work (and to contrast Asian American with white American experiences) in order to identify distinct experiences, protective factors and challenges. In sum, while not all groups nor all aspects of exclusion were represented in this paper, we aim to amplify the importance of examining multiple layers of identity and historical exclusion: future directions should include examination of the intersectionality of these and other identity groups, as well as systemic barriers that each may encounter differentially.
Furthermore, additional structural factors not accounted for herein (e.g., isolation, financial stressors, policy and law impacts) may have also exacerbated the mental health status of trainees and created systemic inequities for different groups. For instance, while data collection was completed before the 2020 election in the United States, political tensions were building throughout the summer and fall of 2020. Future research should examine the way that political cycles, economic trends and governmental policies impact trainee populations in the United States, and in particular how xenophobic, nationalist, ableist, sexist, and homophobic legislation affect the mental health of students from historically excluded communities.
Acknowledgements
The authors thank the Odum Institute for Research in Social Science at UNC-Chapel Hill for its support, resources and consultations on statistical analyses. We thank Nathan Vanderford for valuable insights on earlier versions of this manuscript. Tables were generated from SAS Output, and figures were created using Numbers and BioRender.
Biographies
Allison Schad is in the Office of Medical Education, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, United States
Rebekah L Layton is in the Office of Graduate Education, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, United States
Debra Ragland is in the Office of Graduate Education, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, United States
Jeanette Gowen Cook is in the Office of Graduate Education and the Department of Biochemistry and Biophysics, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, United States
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
Elsa Loissel, eLife United Kingdom .
Peter Rodgers, eLife United Kingdom .
Funding Information
This paper was supported by the following grant:
- National Institute of General Medical Sciences 1R01GM140282-01 to Rebekah L Layton.
Additional information
No competing interests declared.
Conceptualization, Resources, Data curation, Formal analysis, Funding acquisition, Investigation, Visualization, Methodology, Writing – original draft, Project administration, Writing – review and editing.
Conceptualization, Resources, Data curation, Formal analysis, Supervision, Funding acquisition, Investigation, Visualization, Methodology, Writing – original draft, Project administration, Writing – review and editing.
Validation, Writing – review and editing.
Resources, Funding acquisition, Writing – review and editing.
Human subjects: The study was reviewed and approved as Exempt by the UNC Institutional Review Board (#18-0112). Consent was obtained on the first question of the survey before continuing forward to respond to any additional questions. In accordance with IRB approval, the presentation of data will not include demographic information that could potentially lead to the identification of a student. Furthermore, to protect student anonymity, responses with fewer than ten individuals will not be shared. Accordingly, data sharing is limited to those variables directly relevant to the analyses conducted (e.g., underlying data) and composite categories (e.g., historically excluded by category vs. non-historically excluded by category, such as race/ethnicity, gender, or sexual orientation) are shared when applicable rather than granular demographic information to protect the identity of respondents.
Additional files
Transparent reporting form, source data 1., reporting standard 1., data availability.
- AAMC Executive Council Recommendations regarding health services for medical students. 1992. [August 8, 2022]. https://www.aamc.org/professional-development/affinity-groups/gsa/health-services-recommendations
- Asai D. Excluded. Journal of Microbiology & Biology Education. 2020; 21 :21.1.18. doi: 10.1128/jmbe.v21i1.2071. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beagan BL, Mohamed T, Brooks K, Waterfield B, Weinberg M. Microaggressions experienced by LGBTQ academics in Canada: “just not fitting in… it does take a toll.” International Journal of Qualitative Studies in Education. 2021; 34 :197–212. doi: 10.1080/09518398.2020.1735556. [ CrossRef ] [ Google Scholar ]
- Berhe AA, Barnes RT, Hastings MG, Mattheis A, Schneider B, Williams BM, Marín-Spiotta E. Scientists from historically excluded groups face a hostile obstacle course. Nature Geoscience. 2021; 15 :2–4. doi: 10.1038/s41561-021-00868-0. [ CrossRef ] [ Google Scholar ]
- Blake H, Brown N, Follette C, Morgan J, Yu H. Black, Indigenous, people of color, and international students: experiences and resolutions beyond COVID-19. American Journal of Public Health. 2021; 111 :384–386. doi: 10.2105/AJPH.2020.306118. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bogel-Burroughs N. Antivaccination activists are growing force at virus protests. The New York Times. 2020. [April 5, 2022]. https://www.nytimes.com/2020/05/02/us/anti-vaxxers-coronavirus-protests.html
- Brazeau C, Shanafelt T, Durning SJ, Massie FS, Eacker A, Moutier C, Satele DV, Sloan JA, Dyrbye LN. Distress among matriculating medical students relative to the general population. Academic Medicine. 2014; 89 :1520–1525. doi: 10.1097/ACM.0000000000000482. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Byrom N. COVID-19 and the research community: the challenges of lockdown for early-career researchers. eLife. 2020; 9 :e59634. doi: 10.7554/eLife.59634. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carter S, Blumenstein M, Cook C. Different for women? The challenges of doctoral studies. Teaching in Higher Education. 2013; 18 :339–351. doi: 10.1080/13562517.2012.719159. [ CrossRef ] [ Google Scholar ]
- CDC Health equity considerations & racial & ethnic minority groups. 2020. [April 7, 2022]. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
- CDC Depression. 2021. [April 7, 2022]. https://www.cdc.gov/nchs/fastats/depression.htm
- Chen JH, Li Y, Wu AMS, Tong KK. The overlooked minority: mental health of international students worldwide under the COVID-19 pandemic and beyond. Asian Journal of Psychiatry. 2020; 54 :102333. doi: 10.1016/j.ajp.2020.102333. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cho S, Crenshaw KW, McCall L. Toward a field of intersectionality studies: theory, applications, and praxis. Signs. 2013; 38 :785–810. doi: 10.1086/669608. [ CrossRef ] [ Google Scholar ]
- Clay RA. Muslims in America, post 9/11. American Psychological Association. 2011; 42 :8 [ Google Scholar ]
- Conrad JA. A black and white history of psychiatry in the United States. The Journal of Medical Humanities. 2022; 43 :247–266. doi: 10.1007/s10912-020-09650-6. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Couée I. Restoring public trust in science with the help of the humanities. EMBO Reports. 2020; 21 :e50796. doi: 10.15252/embr.202050796. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crawford NC, Graves L, Katzenstein J. Costs of war: racial profiling and islamophobia. Brown University Watson Institute of International Affairs. 2021. [August 8, 2022]. https://watson.brown.edu/costsofwar/costs/social/rights/profiling
- Daraiseh I. Effects of Arab American discrimination post 9/11 in the contexts of the workplace and education. McNair Scholars Research Journal. 2012; 4 :3 [ Google Scholar ]
- Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clinic Proceedings. 2005; 80 :1613–1622. doi: 10.4065/80.12.1613. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Academic Medicine. 2006; 81 :354–373. doi: 10.1097/00001888-200604000-00009. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eisenberg D, Hunt J, Speer N. Mental health in American colleges and universities: variation across student subgroups and across campuses. The Journal of Nervous and Mental Disease. 2013; 201 :60–67. doi: 10.1097/NMD.0b013e31827ab077. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Evans TM, Bira L, Gastelum JB, Weiss LT, Vanderford NL. Evidence for a mental health crisis in graduate education. Nature Biotechnology. 2018; 36 :282–284. doi: 10.1038/nbt.4089. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Feldman JM, Bassett MT. Variation in COVID-19 mortality in the US by race and ethnicity and educational attainment. JAMA Network Open. 2021; 4 :e2135967. doi: 10.1001/jamanetworkopen.2021.35967. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fruehwirth JC, Biswas S, Perreira KM. The COVID-19 pandemic and mental health of first-year college students: examining the effect of COVID-19 stressors using longitudinal data. PLOS ONE. 2021; 16 :e0247999. doi: 10.1371/journal.pone.0247999. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goggin G, Ellis K. Disability, communication, and life itself in the COVID-19 pandemic. Health Sociology Review. 2020; 29 :168–176. doi: 10.1080/14461242.2020.1784020. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gordon J. One year in: COVID-19 and mental health. National Institutue of Mental Health. 2021. [August 8, 2022]. https://www.nimh.nih.gov/about/director/messages/2021/one-year-in-covid-19-and-mental-health
- Gray DM, Anyane-Yeboa A, Balzora S, Issaka RB, May FP. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nature Reviews. Gastroenterology & Hepatology. 2020; 17 :520–522. doi: 10.1038/s41575-020-0330-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gross M. Communicating science in a crisis. Current Biology. 2020; 30 :R737–R739. doi: 10.1016/j.cub.2020.06.052. [ CrossRef ] [ Google Scholar ]
- Halsey SJ, Strickland LR, Scott-Richardson M, Perrin-Stowe T, Massenburg L. Elevate, don’t assimilate, to revolutionize the experience of scientists who are Black, Indigenous and people of colour. Nature Ecology & Evolution. 2020; 4 :1291–1293. doi: 10.1038/s41559-020-01297-9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hazell CM, Chapman L, Valeix SF, Roberts P, Niven JE, Berry C. Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis. Systematic Reviews. 2020; 9 :1–30. doi: 10.1186/s13643-020-01443-1. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hunt JE. COVID-19 and the research community: being vulnerable. eLife. 2020; 9 :e59285. doi: 10.7554/eLife.59285. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hyun JK, Quinn BC, Madon T, Lustig S. Graduate student mental health: needs assessment and utilization of counseling services. Journal of College Student Development. 2006; 47 :247–266. doi: 10.1353/csd.2006.0030. [ CrossRef ] [ Google Scholar ]
- Kauer H. Fauci wants people to know that one of lead scientists who developed the COVID-19 vaccine is a Black woman. CNN. 2020. [April 7, 2022]. https://www.cnn.com/2020/12/09/us/african-american-scientists-vaccine-development-trnd/index.html
- Kendi IX. How To Be An Antiracist. Random House; 2019. [ Google Scholar ]
- Kolata G. Kati Kariko helped shield the world from the coronavirus. New York Times. 2021. [April 7, 2022]. https://www.nytimes.com/2021/04/08/health/coronavirus-mrna-kariko.html
- Krause LA, Harris SL. Mental health in academia: get online to support wellbeing of graduate students. eLife. 2019; 8 :e53178. doi: 10.7554/eLife.53178. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kreps SE, Kriner DL. Model uncertainty, political contestation, and public trust in science: evidence from the COVID-19 pandemic. Science Advances. 2020; 6 :eabd4563. doi: 10.1126/sciadv.abd4563. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001; 16 :606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Legha RK, Miranda J. An anti-racist approach to achieving mental health equity in clinical care. The Psychiatric Clinics of North America. 2020; 43 :451–469. doi: 10.1016/j.psc.2020.05.002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levecque K, Anseel F, De Beuckelaer A, Van der Heyden J, Gisle L. Work organization and mental health problems in PhD students. Research Policy. 2017; 46 :868–879. doi: 10.1016/j.respol.2017.02.008. [ CrossRef ] [ Google Scholar ]
- Li W. Racial disparities in COVID-19. Harvard University Special Edition Science Policy and Social Justice Blog. 2020. [April 7, 2022]. http://sitn.hms.harvard.edu/flash/2020/racial-disparities-in-covid-19/
- Limas JC. Adaptation to Overexpression of Cyclin E in Epithelial Cells Doctoral Dissertation. University of North Carolina; 2021. [ CrossRef ] [ Google Scholar ]
- Limas JC, Corcoran LC, Baker AN, Cartaya AE, Ayres ZJ. The impact of research culture on mental health & diversity in STEM. Chemistry. 2022; 28 :e202102957. doi: 10.1002/chem.202102957. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Linley JL, Nguyen DJ. LGBTQ experiences in curricular contexts. New Directions for Student Services. 2015; 2015 :41–53. doi: 10.1002/ss.20144. [ CrossRef ] [ Google Scholar ]
- Loissel E. Mental health in academia: a question of support. eLife. 2019; 8 :e52881. doi: 10.7554/eLife.52881. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Loissel E. Mental health in academia: shedding light on those who provide support. eLife. 2020; 9 :e64739. doi: 10.7554/eLife.64739. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mackie SA, Bates GW. Contribution of the doctoral education environment to PhD candidates’ mental health problems: a scoping review. Higher Education Research & Development. 2019; 38 :565–578. doi: 10.1080/07294360.2018.1556620. [ CrossRef ] [ Google Scholar ]
- McHugh RK, Weiss RD. Alcohol use disorder and depressive disorders. Alcohol Research. 2019; 40 :arcr.v40.1.01. doi: 10.35946/arcr.v40.1.01. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Medley G, Lipari RN, Bose J, Cribb DS, Kroutil LS, McHenry G. Sexual orientation and estimates of adult substance use and mental health: Results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review; 2016. https://www.samhsa.gov/data/sites/default/files/NSDUH-SexualOrientation-2015/NSDUH-SexualOrientation-2015/NSDUH-SexualOrientation-2015.htm [ Google Scholar ]
- Nagy GA, Fang CM, Hish AJ, Kelly L, Nicchitta CV, Dzirasa K, Rosenthal MZ. Burnout and mental health problems in biomedical doctoral students. CBE Life Sciences Education. 2019; 18 :ar27. doi: 10.1187/cbe.18-09-0198. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Center for Transgender Equality The report of the 2015 U.S. Transgender Survey. 2016. [April 7, 2022]. https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf
- National Institute on Drug Abuse Comorbidity: addiction and other mental illnesses (NIH Publication Number 10-5771) NIDA Research Report Series. 2010. [April 7, 2022]. https://www.drugabuse.gov/sites/default/files/rrcomorbidity.pdf
- National Institutes of Health RESCINDED - updated notice of NIH’s interest in diversity - notice number: NOT-OD-18-210. 2018. [July 16, 2018]. https://grants.nih.gov/grants/guide/notice-files/NOT-OD-18-210.html
- National Institutes of Health Notice of NIH’s interest in diversity (Notice Number: NOT-OD-20-031) 2019. [November 22, 2019]. https://grants.nih.gov/grants/guide/notice-files/NOT-OD-20-031.html
- National Institutes of Health Populations underrepresented in the extramural scientific workforce. 2020. [April 7, 2020]. https://diversity.nih.gov/about-us/population-underrepresented
- Pathak EB, Menard JM, Garcia RB, Salemi JL. Social Class, Race/Ethnicity, and COVID-19 Mortality among Working Age Adults in the United States. medRxiv. 2021 doi: 10.1101/2021.11.23.21266759. [ PMC free article ] [ PubMed ] [ CrossRef ]
- Quek TT-C, Tam WW-S, Tran BX, Zhang M, Zhang Z, Ho CS-H, Ho RC-M. The global prevalence of anxiety among medical students: a meta-analysis. International Journal of Environmental Research and Public Health. 2019; 16 :E2735. doi: 10.3390/ijerph16152735. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rollnick M. In: Encyclopedia of Science Education. Gunstone R, editor. Dordrecht: Springer; 2015. Access of historically excluded groups to tertiary STEM education; pp. 1–6. [ CrossRef ] [ Google Scholar ]
- Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016; 316 :2214–2236. doi: 10.1001/jama.2016.17324. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rothman S, Gunturu S, Korenis P. The mental health impact of the COVID-19 epidemic on immigrants and racial and ethnic minorities. QJM : Monthly Journal of the Association of Physicians. 2020; 113 :779–782. doi: 10.1093/qjmed/hcaa203. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Salerno JP, Devadas J, Pease M, Nketia B, Fish JN. Sexual and gender minority stress amid the COVID-19 pandemic: implications for LGBTQ young persons’ mental health and well-being. Public Health Reports. 2020; 135 :721–727. doi: 10.1177/0033354920954511. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- SAMHSA . 2019 national survey on drug use and health: lesbian, gay, and bisexual (LGB) adults. SAMHSA; 2020. https://www.samhsa.gov/data/report/2019-nsduh-lesbian-gay-bisexual-lgb-adults [ Google Scholar ]
- SAMHSA . Key substance use and mental health indicators in the United States: results from the 2020 national survey on drug use and health. SAMHSA; 2021. https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.pdf [ Google Scholar ]
- Seppälä EM, Bradley C, Moeller J, Harouni L, Nandamudi D, Brackett MA. Promoting mental health and psychological thriving in university students: a randomized controlled trial of three well-being interventions. Frontiers in Psychiatry. 2020; 11 :590. doi: 10.3389/fpsyt.2020.00590. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Skinner HA. The drug abuse screening test. Addictive Behaviors. 1982; 7 :363–371. doi: 10.1016/0306-4603(82)90005-3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Slavin SJ, Schindler DL, Chibnall JT. Medical student mental health 3.0: improving student wellness through curricular changes. Academic Medicine. 2014; 89 :573–577. doi: 10.1097/ACM.0000000000000166. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith JP, Randall CL. Anxiety and alcohol use disorders: comorbidity and treatment considerations. Alcohol Research. 2012; 34 :414–431. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine. 2006; 166 :1092–1097. doi: 10.1001/archinte.166.10.1092. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Terlizzi EP, Villarroel MA. Symptoms of generalized anxiety disorder among adults: United States. 2020. [April 5, 2022]. https://www.cdc.gov/nchs/products/databriefs/db378.htm [ PubMed ]
- Toews JA, Lockyer JM, Dobson DJ, Brownell AK. Stress among residents, medical students, and graduate science (MSc/PhD) students. Academic Medicine. 1993; 68 :S46–S48. doi: 10.1097/00001888-199310000-00042. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- UC Berkeley Graduate Assembly Graduate student happiness and well-being report. 2014. [April 7, 2022]. http://ga.berkeley.edu/wp-content/uploads/2015/04/wellbeingreport_2014.pdf
- UNC Health and UNC School of Medicine Teaching COVID-19’s real-time lessons. 2020. [April 7, 2022]. https://news.unchealthcare.org/2020/06/teaching-covid-192019s-real-time-lessons/
- UNC School of Medicine Office of Diversity Equity and Inclusion ODEI Annual Report. 2021. [August 8, 2022]. https://www.med.unc.edu/inclusion/about/odei-reports/
- Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020; 323 :2466–2467. doi: 10.1001/jama.2020.8598. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization AUDIT: The alcohol use disorders identification test: guidelines for use in primary health care (no.WHO/MSD/MSB/01.6 a) 2001. [April 7, 2022]. http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6a.pdf
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. Journal of Affective Disorders. 2020; 277 :55–64. doi: 10.1016/j.jad.2020.08.001. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yam K. Anti-Asian hate crimes increased by nearly 150% in 2020, mostly in NY and LA, new report says. NBC News. 2021a. [April 7, 2022]. https://www.nbcnews.com/news/asian-america/anti-asian-hate-crimes-increased-nearly-150-2020-mostly-n-n1260264
- Yam K. Anti-Asian hate incident reports nearly doubled in March, new data says. NBC News. 2021b. [April 7, 2022]. https://www.nbcnews.com/news/asian-america/anti-asian-hate-incident-reports-nearly-doubled-march-new-data-n1266980
- Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the drug abuse screening test. Journal of Substance Abuse Treatment. 2007; 32 :189–198. doi: 10.1016/j.jsat.2006.08.002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- eLife. 2022; 11: e69960.
Decision letter
In the interests of transparency, eLife publishes the most substantive revision requests and the accompanying author responses.
Decision letter after peer review:
Thank you for submitting your article "Mental health disparities among biomedical trainees during COVID-19 and racial inequity" to eLife for consideration as a Feature Article.
Four peer reviewers have reviewed your article, and the evaluation has been overseen by two members of the eLife Features Team (Elsa Loissel and Peter Rodgers). The following individuals involved in reviewing your submission have agreed to reveal their identity: Marcus Lambert and Amanda Haage.
The reviewers and editors have discussed the reviews and we have drafted this decision letter to help you prepare a revised submission.
Please also note that if your manuscript is accepted, we would like to publish some of the relevant code with the article: please let me know if this will be a problem.
In addition, the eLife Features Editor may also contact you separately about some editorial issues that you will need to address.
The article aims to explore the wellbeing of medical students and biomedical PhD students at an R1 institution using self-reported markers of mental health across race/ethnicity. This work was conducted over two years, one of which was marked by the COVID-19 pandemic and a wave of racial and civil unrest. This manuscript is important and timely for a broad biomedical audience, highlighting major concerns around the prevalence of mental health challenges, especially in biomedical PhD and underrepresented students.
However, several points need to be addressed to make the article suitable for publication. In particular, the reviewers were concerned with some aspects of the methodology and the discussion.
Essential revisions:
Comparing medical and PhD students:
1 – Please consider discussing in the introduction (and the discussion) why there may be a difference between medical and biomedical PhD students. In particular, please expand on:
a. The level of institutional support provided by the respective programs: For instance, what are the mental health resources provided to medical and PhD students? Are they the same and are they easily accessible e.g. paid for? facilitated/triaged? on-campus?
b. The awareness of the two populations of their mental health (one might argue that medical students are trained to recognize certain signs and symptoms).
c. The differences that are intrinsic to their training: for example, those familiar with the medical student training process might suggest more acute stressors but more structured support due to LCME requirements.
d. The response to the COVID pandemic from the two different programs: for instance, the curriculum and/or level of support changed for the medical students in 2020, which is highlighted in the discussion. However, this is a big limitation in interpreting the data (comparatively between MD and PhD students). This can be viewed as an intervention that the PhD students did not have.
2 – Following that thought: medical and graduate students have extremely different training paradigms and, in this institution, medical students received an intervention that could have mitigated the effects of the pandemic on their mental health. Therefore, please consider whether directly comparing medical to graduate students is relevant, and if so, how to do so: for example, the bar graphs side by side are fine, but the chi-sq tests may be an unfair comparison. Or at least, please discuss the caveat of the different training paradigms and levels of support provided throughout the 2020 year.
3 – The reason why PhD students have worse PHQ9 outcomes over time comparatively is because the medical students show a decrease from 2019 to 2020. Could you please report whether you have looked at the trends across the medical student years (1 through 4), and justify if not.
Discussing the sample, and how it was coded:
4 – Line 158: Please detail the criteria for sample invitations (e.g. are there any inclusion or exclusion criteria for the study, and if so, are they the same for the 2019 and 2020 surveys?).
5 – Line 158: Please clarify whether the respondents (n=431, Fall 2020; n=526, Fall 2019) are a representative sample that closely matches the characteristics of your population. If not, please address this selection bias in the discussion.
6 – Line 166-167. "Middle Eastern", while an important subcategory, is not a part of the NIH definition of underrepresented groups. If you would like to use the NIH guidelines, please remove this subcategory from the UR coding. Alternatively, please directly justify the coding of "Middle Eastern" as underrepresented. Please see revisions #13 and #14 for further discussion about NIH guidelines.
7 – Please ensure that the in-text reported percentages and N values are easy to understand, as they are quite unclear in the current version. This is particularly the case in the "participants" section of the methods and figure legends, where it is unclear what year each number represents.
Methodological and statistical issues:
8 – The data collected in 2019 and 2020 was combined for data analysis, suggesting that some participants may have participated in both years. Logistic regression requires the observations to be independent of each other: that is, the observations should not come from repeated measurements. This could bias/inflate the results – the larger number of repeated respondents, the higher chance to obtain biased results – and it therefore needs to be carefully justified and addressed. If you can identify repeated respondents, please report how many, and justify why you think you can include them in the analysis: in addition, please consider exploring whether your findings stay the same if you take out those repeated respondents, and/or use a repeated measures design to compare the difference in mental health between 2019 and 2020. If you are not able to identify repeated respondents, please discuss this limitation.
9 – The mental health outcomes are sensitive to recent events and affected by many factors/variables (e.g., variables related to the pandemic, years in the degree, disciplines, etc.): it is possible that the mental health disparities you report might be no longer statistically significant once these covariates are included in the analysis. Please either include these covariates in your logistic regression, or explain in the manuscript why they were not included.
10 – The collected mental health measures could be treated as continuous variables, which could offer better variabilities for statistical modelling. Please clarify why you decided to simplify the scale (0 and 1) to run logistic regression analyses (binary outcome) rather than multiple regressions (continuous outcome). If you are not able to provide the reason, please make sure that both approaches (logistic regression and multiple regression) yield consistent findings.
Additional analyses and discussion points pertaining to intersectionality approaches:
11 – Please consider conducting additional analyses to explore whether they were any differences across gender identity. The N values seem similar to the other populations you have chosen to compare, and this would significantly increase the impact of this study. Otherwise, please justify why this variable was not explored.
12 – If feasible, please adopt an intersectionality approach, in particular by examining how gender AND race/ethnicity impact your findings. Otherwise, please justify why these analyses were not performed, and strengthen your discussion around intersectionality.
13 – While Asians are included as well-represented according to NIH standards, the percentage of Asian-identifying individuals in the sample (at 16% and 9%) clearly demonstrates that they are not. This is discussed at the end, but please also include these comments in the Results section and strengthen the language. In addition, please consider comparing the experiences of Asian and White students, or, if you are concerned with anonymity/statistical power, please consider comparing WR vs. UR where "Asian" is moved from WR to UR, as this would allow the reader to understand if coding "Asian" as WR vs. UR makes a difference (this does not necessarily need to be in the main part of the paper). Alternatively, please justify why these analyses were not performed.
14 – On that note: although discussed at the end, please provide a more nuanced discussion of race and ethnicity, and strengthen your stance. In particular, while it is understandable that you want to use NIH standards, please acknowledge more overtly that race is a social construct (so as to not reinforce the notion that these categories may be biological); and please discuss in more depth how the NIH categories may be lacking and not best represent a marginalized identity in science.
Strengthening certain claims
15 – Please provide evidence for the following statements:
a – Line 40 ("biomedical graduate programs are exposed to unique stressors by the nature of their training"): please consider moving up certain citations (e.g. Hazell et al., 2020 and Mackie and Bates 2019) to support this affirmation. Please also consider replacing the word "unique" as long hours, pressure to produce, and unsupportive mentors may not necessarily support a "uniquely" stressful situation.
b – Line 93 ("Trainees of color, especially people identifying as Black, Indigenous, and people of color (BIPOC), may also be affected by heightened concerns about individual, community, and family health."): While covid disparities are certainly real, and likely at play, please provide supporting evidence for this affirmation.
c – Line 340 ("We also speculate that being in a medical training program with obvious direct impact during a time when medical professionals were publicly celebrated had a positive effect on MD student mental health.") This discussion of MDs being "publicly celebrated" and "heroic" and able to connect their training to the crisis compared to PhD lacks evidence, particularly as we see protests outside of hospitals continue.
d – Line 343 ("Furthermore, medical students were able to continue some form of their training remotely, maintain some social contact and peer support networks through academic training, and avoid graduation delays.") Please provide citations for this statement, and clarify whether this is institution-specific.
e – Line 356 ("Biomedical PhD student training was severely curtailed in the 2020 spring months…"). Please clarify if this refers to specific measures at your institution.
f – Line 410 ("the mental health crisis in graduate biomedical education has only recently received considerable attention from the laboratory research community."): Please provide evidence for this statement.
Author response
Essential revisions: Comparing medical and PhD students: 1 – Please consider discussing in the introduction (and the discussion) why there may be a difference between medical and biomedical PhD students. In particular, please expand on: a. The level of institutional support provided by the respective programs: For instance, what are the mental health resources provided to medical and PhD students? Are they the same and are they easily accessible e.g. paid for? facilitated/triaged? on-campus? b. The awareness of the two populations of their mental health (one might argue that medical students are trained to recognize certain signs and symptoms). c. The differences that are intrinsic to their training: for example, those familiar with the medical student training process might suggest more acute stressors but more structured support due to LCME requirements. d. The response to the COVID pandemic from the two different programs: for instance, the curriculum and/or level of support changed for the medical students in 2020, which is highlighted in the discussion. However, this is a big limitation in interpreting the data (comparatively between MD and PhD students). This can be viewed as an intervention that the PhD students did not have.
We thank the reviewers for this important point and have added the following to the discussion to address these valid critiques:
“In contrast, PhD students continued work at best, or experienced forced absence from the lab, with no specific intervention addressing emerging COVID knowledge or mental health coping strategies.”
“Furthermore, accreditation requirements for MD training provide a more structured support system for medical student mental health and wellness compared with PhD student supports. Given the difference in support offered due to enforced standards, this makes MD support services more easily accessible and freely available (no cost, and/or available funding to cover any out-of-pocket mental health medical expenses). Whereas both MD and PhD have availability of limited initial contact of facilitated and triaged on-campus resources, MDs have access to 1.5 FTE dedicated support for 800 students (e.g., 533:1 student-counselor ratio) whereas PhDs have only.5 FTE dedicated support for 600 students (e.g., 1200:1 student-counselor ratio). The combination of the more robust support for MD students with the removal of exposure to acute stressors often encountered in clinical rotations may have magnified this effect.”
We agree that the nuanced discussion of differences between the two populations is very important, and brings to attention the point that adjustment of the training environment (e.g., MD intervention) can in fact positively impact mental health even amidst difficult times. We have replaced the post hoc chi-squared tests with a more complex logistic regression model that allows for statistical control of differences between the two populations, including marginal means and conditional odds ratios to expresses in terms of differences in each population, while simultaneously controlling for the other variables’ impact.
We agree that analysis by year in program would be important to include in future work; however, in our sample this was a demographic question that was not completed by a sizeable portion of respondents, which would reduce our ability to complete the main analysis if we included it. We also have concerns about including variables with a significant amount of missing data as this would potentially not be representative of the sample or population.
Discussing the sample, and how it was coded: 4 – Line 158: Please detail the criteria for sample invitations (e.g. are there any inclusion or exclusion criteria for the study, and if so, are they the same for the 2019 and 2020 surveys?).
The same listservs were used each year to recruit School of Medicine trainees in Medical Education (MD students) and Graduate Education (biomedical PhDs), as described in Methods. A standard IRB-approved invitation included a brief paragraph explaining the survey, signed by the appropriate administrator (e.g., SOM Wellness Coach). There were no formal inclusion or exclusion criteria in either year other than being enrolled in either the MD or PhD programs, and anyone included on the SOM trainee listservs was invited to respond.
Unfortunately, we can’t directly assess how well our samples were representative of their respective populations, the following has been added in limitations to address this:
“Due to anonymous data collection and optional questions to protect participant identities, we cannot assess granular response rates by demographic characteristics. Future studies could be completed with a controlled sample matched with participant identifiers to know who in the sample is and isn’t responding, as this could impact findings.”
Thank you for pointing out the limitations of NIH definition, here and elsewhere – we have further explained the reasoning for inclusion of Middle Eastern and expanded the discussion of why this category was included. In addition, we adjusted the terminology to better reflect the categories included in our analyses to include identities that have been historically excluded. This category has been retitled accordingly to, “historically excluded (HE)” as reflected in science by race/ethnicity and gender (HE gender discussed elsewhere). Please also see other author responses for a summary; as well as expanded responses about marginalized identity, gender, intersectionality, Asian identity, and an expanded discussion of NIH definition along with limitations thereof.
The following has been added:
“Further, the stress experienced by Asian Americans as scapegoats of the pandemic and targets of anti-Asian violence may also affect the mental health of Asian American students within academia.” (Introduction)
“In the primary analysis, mental health data was analyzed by type of training program (MD vs. PhD), year (2019 vs. 2020), and historically excluded (HE) populations by race/ethnicity (HE-RE vs. NHE-RE) and by gender (HE-G women vs. NHE-G men). A post hoc analysis included the primary variables as wells as historically excluded by sexual orientation (HE-SO LGBQ+ vs. NHE-SO non-LGBQ+).” (Methods)
“in accordance with National Institutes of Health definitions of underrepresented in the biomedical, clinical, behavioral, and social sciences (NIH, 2020). Historically, Asian Americans have also faced exclusion from American culture as evidenced by Japanese Internment and the Chinese Exclusion Act. However, Asian Americans have been well-represented in the sciences and thus are included as NHE-RE for analysis. Additionally, Middle Eastern is not included in the US Census or NIH definitions as underrepresented; however, this identity group is included as HE-RE due to the marginalization especially over the past two decades in the United States following 9/11/2001.” (Methods-Participants)
We have simplified the figures and legends in favor of an expanded unified description in the Methods, as we recognize that the prior version may be confusing. Previously, the chi-squared post hoc analysis relied on specific n and degrees of freedom for each test that impacted interpretation (no longer crucial for the current analyses). Especially given the updated modeling with interaction terms used to replace the previous chi-squared post hoc tests, the exact n per each subgroup is less important and instead the odds ratios and p-values are the primary focus. Accordingly, to reflect this change, Figure 1 has been simplified per the editors and reviewers’ suggestions; Figure 2 and Figure 3 (new Figure 3 added to visualize effects identified in the post hoc analysis) also now include percentages embedded in the figures rather than embedding these details in the legends.
Methodological and statistical issues: 8 – The data collected in 2019 and 2020 was combined for data analysis, suggesting that some participants may have participated in both years. Logistic regression requires the observations to be independent of each other: that is, the observations should not come from repeated measurements. This could bias/inflate the results – the larger number of repeated respondents, the higher chance to obtain biased results – and it therefore needs to be carefully justified and addressed. If you can identify repeated respondents, please report how many, and justify why you think you can include them in the analysis: in addition, please consider exploring whether your findings stay the same if you take out those repeated respondents, and/or use a repeated measures design to compare the difference in mental health between 2019 and 2020. If you are not able to identify repeated respondents, please discuss this limitation.
Due to data being collected anonymously, we cannot confirm if there were any repeated participants across the year timepoints; we recognize that this is a limitation, and have added the following to the discussion to acknowledge this:
“We recognize that if a large number of participants responded in both samples this could be problematic for assumptions of independence for use of parametric statistics and the Logistic Regression analysis used specifically, hence results should be interpreted with caution. Because we collected data anonymously to protect respondents’ privacy, we cannot assess to what extent there may have been respondents who participated in both years. If we did have identifiable data and were able to use a repeated-measures design, this would be preferable to reduce error variance. To the extent that significant findings were achieved even with the increased error variance inherent in a between-subjects design, these results likely had large enough effect sizes to be identified even given the loss of power from using a between-subjects design rather than the more sensitive within-subjects design that would be preferable.”
We did not collect pandemic-specific data as we used the same annual survey questions from the previous year, future evaluations should ask and control for these variables. Limitations for being able to include years in training is discussed elsewhere (see additional author responses to year in training variable). We did not collet specialty or departmental affiliations to protect anonymity, to increase comfort with responding, and to maximize response rates. Furthermore, disciplinary clusters were deemed homogeneous enough to be considered in the two major categories of biomedical PhD training and medical MD training.
“Additional limitations included our lack of ability to control for other possible variables of interest such as pandemic-specific factors, years in training, and departmental affiliation or specialty area. Pandemic-specific questions were not asked because we used the same annual survey questions from the previous year to maintain comparable responses. Department and specialty information were not asked in order to protect anonymity, to increase comfort with responding, and to maximize response rates. Yet, populations were purposefully defined by reasonably homogenous training experiences into the two major clusters of interest: biomedical PhD training and MD training. Optional demographic questions were not completed for number of years in training for a large portion of the sample, limiting our ability to include this in the analysis. Future work should consider controlling for as many of these variables as possible.”
The research question of interest was best captured by a bivariate designation of symptomatic versus asymptomatic (or problematic use versus non-problematic use). Hence, we approached the question from a bivariate logistic regression approach to answer the question accordingly. We felt this was the most appropriate model to answer the research question, and could be best interpreted to determined when respondents were functionally affected by their mental health; hence our decision to define it as such in the statistical modeling. Severity of symptoms at a more granular level, especially relying on self-report approaches rather than clinical diagnoses, posed several limitations that we felt made it a less appropriate approach to the data. Furthermore, for implications and policy purposes, we feel that the defined research question best illustrates the sweeping problem of mental health in graduate biomedical and medical education.
Additional analyses and discussion points pertaining to intersectionality approaches: 11 – Please consider conducting additional analyses to explore whether they were any differences across gender identity. The N values seem similar to the other populations you have chosen to compare, and this would significantly increase the impact of this study. Otherwise, please justify why this variable was not explored.
We agree that including gender as variable would add to the intersectional applicability of our model, and hence have added it as a control variable for all primary analyses.
We also decided that if evaluating the impact of gender were to be added to the model, we would be remiss to not also include sexual orientation status if we had a large enough sample size, as the intersectionality of gender and sexual identity can interact with race/ethnicity, trainee type, and year as well. However, we were also cautious about inadvertently reducing power to evaluate main effects beyond the primary research questions in order to ensure enough power to evaluate the primary intersectional identities (race/ethnicity, gender, and trainee type) by year. Hence, we added a post hoc analysis that accounted for both gender and LGBQ status using an intersectional approach.
We have added sections in the results and discussion describing the revised primary analysis (adding gender using a more sophisticated Logistic Regression model including interaction terms, conditional odds ratios, and marginal means to replace the more simplistic Chi-Squared comparisons previously displayed) as well as the post hoc model which includes LGBQ identity. Along with these substantive changes to the analyses, we have included justification and precedent for including both gender and sexual orientation based on previous studies. Transgender identity could not be included due to the small sample size, but should be included in future work and this limitation is also addressed in the manuscript.
Relatedly, to avoid reductions in power we also ran post hoc tests to further examine the impact of Asian social identities in a more granular way, and have reported the new results accordingly (using the model that also controls for gender).
We have adopted an intersectional approach, with additional citations to justify this in the introduction as well as a deeper dive in the discussion. Thank you for this suggestion, we believe it has strengthened our approach and the applicability of the findings greatly.
Thank you for this suggestion. We agree that a more granular investigation of the impacts on Asian participants is useful, despite having a small sample once dividing HE-RE into 3 classifications; hence have included a supplemental post hoc analysis as mentioned in other author responses which still allows us to address the questions while retaining power for the primary analysis. The following has been added:
“People who identified of Asian descent generally scored better than other NHE or HE groups, indicating fewer mental health challenges on all four outcome variables and the three suicidal ideation variables. However, conditional odds rations based on these models indicated some changes by year that may be associated with the negative psychosocial and environmental factors many Asian Americans experienced between 2019-2020. Accounting for the effect of race (3-level) while controlling for year, MD/PhD, and gender in 2020 compared with 2019, Asian participants showed greater mean depression scores (p<.03) and anxiety scores (p<.04); there was no change in either alcohol use (p=.07, though marginal) or drug use (p=.28). There were no significant changes in conditional probabilities for suicidal ideation of Asian participants during that time. Future directions should include examination of the intersectionality of these and other identity groups, and systemic barriers that each may encounter differentially. Follow-up studies should explore the impact of racism on Asian Americans and contrast Asian American experiences with White American experiences when reporting HE-RE data.”
Thank you for these valuable suggestions, which we have leaned on heavily to reframe much of our discussion and additional analyses. We believe this has strengthened our findings and our ability to interpret implications more broadly. We have: (a) expanded our discussion of intersectionality; (b) added more nuanced analysis controlling for a wider range of identities (including the addition of gender to all of our primary models; c) included a post hoc analysis and discussion of Asian identity as well as sexual orientation); (d) re-envisioned the terminology used to Historically Excluded (HE) in science (HE-RE and HE-G); (e) we have expanded our discussion of limitations to the NIH definitions of WR/UR; and f) we have explicitly noted the social derivation of race.
The following has been added to the discussion (see NIH definition expanded discussion in other author responses):
“We recognize [both that race is a social construct], and that other social identity groups beyond race and ethnicity (Rothman, Gunturu, Korenis, 2020) may also experience inequitable impacts of COVID-19 and similar structural biases may negatively impact mental health for other reasons (Hunt, 2020). (Discussion)
“In fact, the NIH has recently expanded its definition of underrepresented in science to include women, people with disabilities, first generation college students, and those from disadvantaged backgrounds, including people who have experienced or are experiencing homelessness, foster care participation, recipients of free and reduced lunch, Pell grants, SNAP or WIC, and those who grew up in a low-income or rural areas (NIH, 2020; NIH, 2018, rescinded and replaced in 2019; NIH, 2019). This expanded definition is still flawed as some groups are still excluded from recognition and inclusion as societal norms and practices shift over time. For instance, people of middle eastern descent who have faced heightened discrimination, especially following 9/11/2001.” (Discussion)
NIH definition limitations are discussed in a number of other points in the response as well (please see also other author responses regardig Middle Eastern and Asian identities, gender, intersectionality, and NIH definition limitations).
Furthermore, particularly in recent American history, it is noteworthy that over the past 20 years many groups have been systematically marginalized during different periods of time. Future definitions of historically excluded groups may also want to consider the impact of current events with politics and their intersection with discrimination against specific social identities. We must acknowledge that science is not immune from such effects, which can drive out a talented, diverse pool of future scientists in training.
Strengthening certain claims 15 – Please provide evidence for the following statements: a – Line 40 ("biomedical graduate programs are exposed to unique stressors by the nature of their training"): please consider moving up certain citations (e.g. Hazell et al., 2020 and Mackie and Bates 2019) to support this affirmation. Please also consider replacing the word "unique" as long hours, pressure to produce, and unsupportive mentors may not necessarily support a "uniquely" stressful situation. b – Line 93 ("Trainees of color, especially people identifying as Black, Indigenous, and people of color (BIPOC), may also be affected by heightened concerns about individual, community, and family health."): While covid disparities are certainly real, and likely at play, please provide supporting evidence for this affirmation. c – Line 340 ("We also speculate that being in a medical training program with obvious direct impact during a time when medical professionals were publicly celebrated had a positive effect on MD student mental health.") This discussion of MDs being "publicly celebrated" and "heroic" and able to connect their training to the crisis compared to PhD lacks evidence, particularly as we see protests outside of hospitals continue. d – Line 343 ("Furthermore, medical students were able to continue some form of their training remotely, maintain some social contact and peer support networks through academic training, and avoid graduation delays.") Please provide citations for this statement, and clarify whether this is institution-specific. e – Line 356 ("Biomedical PhD student training was severely curtailed in the 2020 spring months…"). Please clarify if this refers to specific measures at your institution. f – Line 410 ("the mental health crisis in graduate biomedical education has only recently received considerable attention from the laboratory research community."): Please provide evidence for this statement.
Unique has been replaced as follows:
“Considering that students in medical school and in biomedical graduate programs are exposed to a multitude of stressors by the nature of their training including long hours, pressure to produce, and unsupportive mentors…”
B – We have reframed the terminology to center on Historically Excluded instead of BIPOC; nonetheless, we have also included an additional reference to support the extension of the COVID-19 impacts to disproportionately impact BIPOC individuals, communities, and family health.
We have also added the following reference, examining HE-RE working class inequities due to COVID-19:
Pathak, E. B., Menard, J. M., Garcia, R. B., and Salemi, J. L. (2021). Social Class, Race/Ethnicity, and COVID-19 Mortality Among Working Age Adults in the United States. medRxiv.
Feldman, J. M., and Bassett, M. T. (2021). Variation in COVID-19 Mortality in the US by Race and Ethnicity and Educational Attainment. JAMA network open, 4(11), e2135967-e2135967.
Limas, J.C. (2021). Adaptation to Overexpression of Cyclin E in Epithelial Cells. (Publication No. 2616907910) [Doctoral dissertation, University of North Carolina at Chapel Hill]. ProQuest Dissertations and Theses Global.
Limas, J. C., Corcoran, L. C., Baker, A. N., Cartaya, A. E., and Ayres, Z. J. (2022). The Impact of Research Culture on Mental Health and Diversity in STEM. Chemistry–A European Journal, e202102957.
“While our students themselves may be classified as associated with some lower risk groups for direct effects COVID due to their levels of education, BIPOC students disproportionately hail from working-class families and identify as first-generation college graduates. Hence, students historically excluded by race and ethnicity (HE-RE; e.g., those identifying as BIPOC) may experience disproportionate impact to their families, in that their families have been most at risk for mortality from COVID during 2020 within each social class (Pathak et al., 2021). Similarly, highest risk of age-adjusted mortality during COVID was identified for Hawaiian and Other Pacific Islander, American Indian or Alaska Native, and Latinx or Hispanic people (Black, Feldman and Bassett, 2021). An illustrative example includes a PhD sharing instances of her own experience as a Mexican-American woman PhD trainee during this time (Limas, 2021).”
C – We acknowledge the very real impact of anti-medical establishment influences as well, and have added the following to address this oversight: “Even so, this was not a ubiquitous experience, as simultaneously continued protests and divisiveness regarding vaccination were also pervasive across the country, which could ameliorate this effect (e.g., Bogel-Burroughs, 2020).”
Bogel-Burroughs, N. (2020). Antivaccination activists are growing force at virus protests. The New York Times. May, 2.
D and E – We have clarified these statements, and qualified them by specifying, “at our institution.”
F – The following has been added to clarify:
“Whereas medical schools have had mental health recommendations in place since 1992 (AAMC, 1992; enforced by Liaison Committee on Medical Education accreditation standards), biomedical PhD programs have had no such parallel policies regarding mental health provisions nationwide. Similarly, while there have been frequent calls for mental health research in higher education and there is already a robust body of literature decades old already in medical education (e.g., Slavin, 2016; a systematic review of medical education mental health evidence-based research included 195 relevant studies, Rotenstein et al., 2016) , evidence-based research on mental health research of PhDs has begun to emerge over the past five years (e.g., Levecque et al., 2017; Evans et al., 2018). Resources have been mobilized to evaluate and respond to the needs of medical students (e.g., 28 studies evaluating interventions, Wasson et al., 2016), which indeed still merit additional attention given high rates of depression, anxiety, and suicidality.”
The following additional references have also been added:
AAMC Executive Council (1992). Recommendations Regarding Health Services for Medical Students. Washington, DC: Association of American Medical Colleges
Available: https://www.aamc.org/professional-development/affinity-groups/gsa/health-services-recommendations
Wasson, L. T., Cusmano, A., Meli, L., Louh, I., Falzon, L., Hampsey, M., … and Davidson, K. W. (2016). Association between learning environment interventions and medical student well-being: a systematic review. Jama, 316(21), 2237-2252.
Student mental health needs, ‘unsustainable’ jobs overwhelm Minnesota school principals

It can be hard to predict what St. Paul Central High School principal Cherise Ayers will encounter when she walks through the doors each day.
“I would describe a day in the life of a principal as everything everywhere all at once,” Ayers said. “I am like the mayor of a small town. There are so many things happening, and Central is actually larger than some small towns.”
Principals like Ayers have an outsized impact on their schools. Research shows effective school leaders have a big impact on student achievement , teacher retention and other outcomes important for kids.
Many, though, are overwhelmed. A newly released University of Minnesota report on Minnesota K-12 school principals found school leaders struggling for traction on instructional leadership and community engagement as they deal with their single greatest challenge, student mental health.
Create a More Connected Minnesota
MPR News is your trusted resource for the news you need. With your support, MPR News brings accessible, courageous journalism and authentic conversation to everyone - free of paywalls and barriers. Your gift makes a difference.
“The principal really, really matters, and they’re overwhelmed,” said Katie Pekel, executive director of educational leadership at the University of Minnesota. “If you’ve got a good principal, you get lower student absenteeism rates and you have better student academic outcomes. So we do need to be concerned about our principals.”
‘More students needing more intense support’
The report from the U’s College of Education and Human Development is based on a statewide survey of thousands of Minnesota principals conducted in November with a strong enough response that the college considers the findings conclusive.
Among those findings, 94 percent agreed that student mental health challenges are a significant barrier to student learning.
For Ayers, social media and technology are major contributors to the anxiety and emotional outbursts she sees students struggling with.
“We can all be everywhere from our living room … you’ve got this device in your hand that takes you everywhere. And you can either experience everyone’s pain and trauma, or you can experience a lot of people’s joy,” Ayers said. “It impacts our students, because they start to internalize all of those things that they’re seeing.”

The effects are not limited to high school students.
Emily Casselius, principal at Goodview Elementary in southeastern Minnesota, said she sees her students struggling with anxiety, depression and friend relationships, making it hard to focus on school work.
“I’m fortunate enough to have a counselor and a school social worker in my building. Both are part time and they’re spread very thin. And we’re just seeing more students needing a more intense level of support than what we can offer within a school day,” Casselius said.
Beyond Goodview’s doors, Casselius said it’s hard to get assistance from providers since there’s a shortage of practitioners.
Mountains of meetings, mandates, demands
Similar to responses recorded in a 2021 survey , principals remain overwhelmed with the amount of work they’re required to do. Many said their job responsibilities far exceed the time they have to fulfill them.
For Cassellius, her job as principal is layered.
“My day is very unpredictable. I come into my day with kind of a plan of these are the things I need to work on, this is going to be maybe time in my office, this is time I’m going to be in a classroom. But then throughout the day, there might be a student with maybe a behavior that needs support, or we have a (substitute) shortage … and maybe I need to sub instead of do the principal tasks that I had planned for the day.”
In addition to last-minute disruptions, Casselius said her goal of instructional leadership is thwarted by a mountain of administrative tasks, district meetings, budget management, timesheet approval and emails.
Over the last 12 months, another mountain of work has been added to the plates of school leaders: dozens of new laws from the Legislature regarding things like reading instruction and non-exclusionary discipline.
“It’s a lot,” Casselius said. “It took a lot of time just to read and digest and truly understand what they were expecting.”
Principals across the state voiced widespread concern that many of the mandates passed in 2023 were not fully funded or supported. Many reported needing more information and guidance to implement the changes as well as time to plan and train staff.
Ben Bakeberg leads Jordan Middle School and also serves in the Minnesota House as a Republican representative from Jordan.
“We passed over 65 mandates on schools last year, and some of them are really good ones. But then if we’re going to do that, we need to make sure that we're very, very explicit in what is expected,” said Bakeberg.
“That’s the biggest thing when I looked at the survey,” he added. “There was all this pent up stuff, especially around discipline, that people wanted to get done because of a political win. And it’s negatively impacting kids right now.”
Many principals reported doing less work now than they were in 2021 on culturally responsive leadership. That’s likely due to a lack of time and a fear about the “potential divisiveness within communities,” Pekel said.
Despite the many concerns raised in the 2023 survey, many school leaders are generally satisfied with their jobs and say they are working slightly less now than in 2021, although they’re still averaging 57 hours per week.
“People that choose to go into education, they do it because they want to love and serve kids. No other reason. People are not going into education to indoctrinate kids … to push their political agenda,” Bakeberg said. “We need to get back to respecting educators.”
Pekel wants to see school systems try a different approach to developing principals, including paid internships and continuing professional development on topics like culturally responsive pedagogy and instructional leadership.
She also wants to see the job itself change to spread the responsibilities that fall squarely on principals.
“The problem with that,” she acknowledged, “is we never want to spend more money on administration.”
- Anoka-Hennepin students to march in defense of diversity programs
- Minnesota child care finances stabilize, but the business remains in flux
- First lady Jill Biden to visit Minnesota on Friday
Monday, April 22
Previous issues, submit a tip.

USG discusses mental health initiatives at final meeting of semester
Nick Kosan, the vice president of internal affairs for the Graduate Student Government (GSG), presents at the USG meeting.
Alena zhang / the daily princetonian..
The Undergraduate Student Government (USG) Senate convened for the final regularly scheduled meeting of the semester on Sunday, April 21, addressing a range of issues from collaboration efforts to mental health initiatives and student group selectivity.
Mental Health Committee Chair Meera Kochhar ’25 presented updates from the committee. She outlined the subcommittees, which focus on various aspects of mental health including therapeutic services, academics and advocacy, diversity, equity, and inclusion (DEI), and mental health space. Kochhar announced an upcoming Mental Health Space event scheduled for Friday, April 26, aimed at providing students with a space for self-care and relaxation.
“The whole purpose of our grand opening is that we want to make sure that students feel like they know that the space exists and like what its purpose is … so we have a variety of activities that students can engage in for self care,” Kochhar said.
As a part of expanded mental health programming, the University previously announced renewed collaboration with the Jed Foundation, a nonprofit focused on emotional health and suicide prevention, at the Council of the Princeton University Community (CPUC) on Monday, March 18. The committee is also gathering student feedback on mental health experiences, particularly related to therapeutic services and financial burdens. One specific issue was the financial burden of copays, and the committee is seeking student voices and data before presenting to the administration.
Additional plans include refreshing mental health training, reviving the Ivy League Mental Health Conference, and organizing reading period wellness events.
Nick Kosan GS, Vice President of Internal Affairs for the Graduate Student Government (GSG), delivered a presentation highlighting potential collaborations between GSG and USG. Emphasizing the need to foster partnerships between the two governing bodies, Kosan outlined priorities including creation of purposeful spaces for professional and social interactions, improved USG-GSG communications, and continued robust wellness programming and resources.
Campus and Community Affairs (CCA) Committee Chair Genevieve Shutt ’26 highlighted recent events organized by the committee, including trips to Six Flags and the Antiquarian Book Fair in New York City. She also presented on Tigers in Town, which this semester contributed to a total of $5,199.32 spent at local businesses in Princeton.
U-Councilor Anuj Krishnan ’27 presented findings from the Student Group Selectivity Working Group, which surveyed club officers on their perspectives and ways to make clubs more accessible. The survey revealed concerns over confusion regarding selectivity processes and a desire for greater transparency. The working group aims to create a more consistent experience in clubs and plans to organize future training to address these issues.
Krishnan said, “This is going to be an opportunity for students to see what we’re doing in order to make clubs accessible, but it is also … a wake up call to club officers [to follow some] best practices.”
USG meetings are open for all students to attend and are held on Sundays from 4 to 5 p.m., typically in Robertson Hall 016. This week’s meeting, the last regularly scheduled Senate meeting of the semester, was held in Robertson Hall 100.
Alena Zhang is a staff News writer for the ‘Prince.’
Please send any corrections to corrections[at]dailyprincetonian.com.
Fast-a-Thon brings Muslim and non-Muslim students together

Today, Daybreak revisits Fast-a-Thon and examines how it brings the University community closer together.
Two Princeton professors testify in election hearings regarding New Jersey county line

The county line system places endorsed candidates in a single column or row, which displays them more prominently on primary ballots, as opposed to the block ballot system, which groups candidates by the office they are seeking. The system is unique to New Jersey.
University’s termination of lease with Nassau Swim Club makes splash of community pushback

Despite pushback from community members, the University’s decision to terminate the lease of the Nassau Swim Club (NSC) on Tuesday will go forward as planned. This decision follows NSC facing financial difficulties for several years. The University refused the appeal put forth by NSC which included detailed financial plans.
Most Popular
The adl gave princeton an f for antisemitism. after the cjl pushed back, they bumped it up to a d., 184 members of the class of 2026 declared economics. we broke down declaration day., protest supporting columbia’s ‘gaza solidarity encampment’ circles cannon green on declaration day, progressives failed a lesson in free speech, genrietta churbanova, john freeman named valedictorian, salutatorian.

‘You have to suffer for your PhD’: Poor mental health among doctoral researchers

PhD students are the future of research, innovation and teaching at universities and beyond – but this future is at risk. There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.
My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were more likely to meet the criteria for clinical levels of depression and anxiety. They were also more likely to have significantly more severe symptoms than the working-professional control group.
We surveyed 3,352 PhD students, as well as 1,256 working professionals who served as a matched comparison group . We used the questionnaires used by NHS mental health services to assess several mental health symptoms.
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety.
The groups reported an equally high risk of suicide. Between 33% and 35% of both PhD students and working professionals met the criteria for “suicide risk”. The figures for suicide risk might be so high because of the high rates of depression found in our sample.
We also asked PhD students what they thought about their own and their peers’ mental health. More than 40% of PhD students believed that experiencing a mental health problem during your PhD is the norm. A similar number (41%) told us that most of their PhD colleagues had mental health problems.
Just over a third of PhD students had considered ending their studies altogether for mental health reasons.

Between 33% and 35% of both PhD students and working professionals met the criteria for “suicide risk”. Source: Philippe Lopez/AFP
There is clearly a high prevalence of mental health problems among PhD students, beyond those rates seen in the general public. Our results indicate a problem with the current system of PhD study – or perhaps with academic more widely. Academia notoriously encourages a culture of overwork and under-appreciation.
This mindset is present among PhD students. In our focus groups and surveys for other research , PhD students reported wearing their suffering as a badge of honour and a marker that they are working hard enough rather than too much. One student told us :
“There is a common belief … you have to suffer for the sake of your PhD, if you aren’t anxious or suffering from impostor syndrome, then you aren’t doing it “properly”.
We explored the potential risk factors that could lead to poor mental health among PhD students and the things that could protect their mental health.
Financial insecurity was one risk factor. Not all researchers receive funding to cover their course and personal expenses, and once their PhD is complete, there is no guarantee of a job. The number of people studying for a PhD is increasing without an equivalent increase in postdoctoral positions .
Another risk factor was conflict in their relationship with their academic supervisor . An analogy offered by one of our PhD student collaborators likened the academic supervisor to a “sword” that you can use to defeat the “PhD monster”. If your weapon is ineffective, then it makes tackling the monster a difficult – if not impossible – task. Supervisor difficulties can take many forms. These can include a supervisor being inaccessible, overly critical or lacking expertise.
A lack of interests or relationships outside PhD study, or the presence of stressors in students’ personal lives were also risk factors.
We have also found an association between poor mental health and high levels of perfectionism, impostor syndrome (feeling like you don’t belong or deserve to be studying for your PhD) and the sense of being isolated .
Better conversations for PhD students
Doctoral research is not all doom and gloom. There are many students who find studying for a PhD to be both enjoyable and fulfilling , and there are many examples of cooperative and nurturing research environments across academia.
Studying for a PhD is an opportunity for researchers to spend several years learning and exploring a topic they are passionate about. It is a training programme intended to equip students with the skills and expertise to further the world’s knowledge. These examples of good practice provide opportunities for us to learn about what works well and disseminate them more widely.
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence, offers balance, and avoids perpetuating unhelpful myths.
Indeed, in our own study, we found that the percentage of PhD students who believed their peers had mental health problems and that poor mental health was the norm, exceeded the rates of students who actually met diagnostic criteria for a common mental health problem . That is, PhD students may be overestimating the already high number of their peers who experienced mental health problems.
Cassie M Hazell , Lecturer in Social Sciences, University of Westminster
This article is republished from The Conversation under a Creative Commons license. Read the original article .
Popular stories
Jobs in tech: 6 countries offering visas to skilled foreign graduates.

The best programming languages to learn in 2024

Super-smart: 10 superheroes with university degrees and doctorates

5 best careers for introverts that lead to both success and fulfilment

This Nigerian PhD student is living his dream at UT Dallas — now he’s helping others go abroad via Twitter

New US Act would give STEM PhD graduates direct pathways to a green card

This PhD student will ride out China's zero-COVID-19 policy
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- CAREER NEWS
- 18 August 2020
Signs of depression and anxiety soar among US graduate students during pandemic
- Chris Woolston 0
Chris Woolston is a freelance writer in Billings, Montana.
You can also search for this author in PubMed Google Scholar
Signs of depression among graduate students in the United States have apparently doubled during the COVID-19 pandemic, according to a survey that drew responses from more than 15,000 graduate and 30,000 undergraduate students at 9 US research universities.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 585 , 147-148 (2020)
doi: https://doi.org/10.1038/d41586-020-02439-6
Related Articles

Londoners see what a scientist looks like up close in 50 photographs
Career News 18 APR 24

Deadly diseases and inflatable suits: how I found my niche in virology research
Spotlight 17 APR 24

How young people benefit from Swiss apprenticeships

The rise of eco-anxiety: scientists wake up to the mental-health toll of climate change
News Feature 10 APR 24

Rwanda 30 years on: understanding the horror of genocide
Editorial 09 APR 24

After the genocide: what scientists are learning from Rwanda
News Feature 05 APR 24

I dive for fish in the longest freshwater lake in the world
Female academics need more support — in China as elsewhere
Correspondence 16 APR 24
2024 Recruitment notice Shenzhen Institute of Synthetic Biology: Shenzhen, China
The wide-ranging expertise drawing from technical, engineering or science professions...
Shenzhen,China
Shenzhen Institute of Synthetic Biology
Recruitment of Global Talent at the Institute of Zoology, Chinese Academy of Sciences (IOZ, CAS)
The Institute of Zoology (IOZ), Chinese Academy of Sciences (CAS), is seeking global talents around the world.
Beijing, China
Institute of Zoology, Chinese Academy of Sciences (IOZ, CAS)
Research Associate - Brain Cancer
Houston, Texas (US)
Baylor College of Medicine (BCM)

Senior Manager, Animal Care
Research associate - genomics.
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Warning Signs and Symptoms
- Mental Health Conditions
- Common with Mental Illness
- Mental Health By the Numbers
- Individuals with Mental Illness
- Family Members and Caregivers
Kids, Teens and Young Adults
- Veterans & Active Duty
- Identity and Cultural Dimensions
- Frontline Professionals
- Mental Health Education
- Support Groups
- NAMI HelpLine
- Publications & Reports
- Podcasts and Webinars
- Video Resource Library
- Justice Library
- Find Your Local NAMI
- Find a NAMIWalks
- Attend the NAMI National Convention
- Fundraise Your Way
- Create a Memorial Fundraiser
- Pledge to Be StigmaFree
- Awareness Events
- Share Your Story
- Partner with Us
- Advocate for Change
- Policy Priorities
- NAMI Advocacy Actions
- Policy Platform
- Crisis Intervention
- State Fact Sheets
- Public Policy Reports
- Your Journey
One of NAMI’s main goals is to ensure that people get help early. Since mental health conditions typically begin during childhood, adolescence or young adulthood, we have compiled essential information and resources intended to help young people get the mental health support they need.
Young Adults
What you need to know about youth suicide, youth and young adult resources, social media and your family, school break resources.

Having a child that is facing mental health symptoms can be incredibly difficult. To make things easier, explore our information, tips and resources for getting your child the treatment, support and accommodations they need.
What to Look For and When to Act
When to worry and how to respond if your child is struggling.
Finding Mental Health Care for Your Child
Finding mental health services for your child can often seem like an immense challenge.
Getting Your Child Mental Health Support and Accommodations in School
Improve your understanding of how to advocate for your child’s needs in school.
What to Do If Your Child Is in Crisis
Learn the warning signs of a mental health crisis and what to do.
How to Talk to Your Child About Their Mental Health
Read our tips on how to start the conversation with your child.
Residential Treatment
Explore whether residential placement is right for your child and what that would entail.

Determining whether certain behavior is normal or a symptom of a mental health condition can be difficult. Learn when to ask for help, how to talk to your friends and family about mental health, and more.
Finding Help
Learn what to do when you need help with your mental health.
How to Talk to My Friends
Read our tips on how to open up to your friends.
How to Talk to My Parents or Guardian
Read our tips on how to start the conversation with your parent or guardian.
Social Media and Mental Health
Explore our suggestions for protecting your mental health while using social media.
Your Mental Health and School
Learn what to do if you need more mental health support in school.

If you are experiencing symptoms that are affecting your everyday life, it is essential to seek help. The following information, resources and tips may be helpful during your journey toward finding the right care and support for you.
Do I Have a Mental Health Condition?
Determine if what you are experiencing might be a symptom of an underlying mental health condit..
How to Seek Help
Learn how to search for a mental health professional.
Understanding Health Insurance
Better your understanding of health insurance and what plan is right for you.
Mental Health in College
Explore our suggestions for managing your mental health while in college.
How to Disclose Your Mental Health Condition
Read our tips on how to disclose to your university, employer and significant other.
Suicidal thoughts are common among teens and young adults. If we can identify and support young people who are experiencing mental health symptoms, including thinking about suicide, we have an opportunity to help prevent tragedy.

Mental health conditions typically begin during childhood, adolescence or young adulthood, here you will find additional information intended to help provide young people, educators, parents and caregivers with the resources they need.
Be a Trusted Adult for Young People in Your Life
Trusted adults can be family members, grandparents, teachers or social workers and this kind of relationship can have a positive impact on physical, mental and social outcomes for children.
Technology is all around our kids — at school, at home, and in their pockets. Keeping our kids safe and well online is top of mind for many of us. We’re also facing tough questions — how much screen time is too much? When is the right time to get a child a phone? Here are some tips to help you and your family navigate social media together!

School breaks offer a much-needed pause from academics and a busy school schedule. Students can take this time to relax and get back into activities they didn’t have time for while they were in school.
Parents of Children 12 and Under During School Breaks
Students and their families take a big hit to their daily schedules when school breaks occur. Every family’s situation is different, but our tips can help make things a little easier.
Parents of Teens During School Breaks
This section provides insight into how you as a parent can communicate with your children effectively and support what they need to maintain their mental health.
Teens (13-18) During School Breaks
Middle school and high school often have more intense academic expectations and school breaks are great opportunities to focus on your mental health and rest up.
Young Adults in College During School Breaks
Young adults attending college will have a different experience during school breaks than high school and younger students.
Thank you to our partners for helping us spread information and resources to our younger audiences. One of our most important goals is to ensure that people get help early and these resources contribute to that goal.
Finding Support Near You
Nami ending the silence.
A presentation for middle and high school students, school staff and parents or guardians.
NAMI In Our Own Voice
A presentation by people with mental health conditions to promote awareness and recovery.
Contact Your Local NAMI
Across the country, thousands of trained volunteers bring peer-led programs and lived experience to your community.
Related Videos

Fighting for Black Mental Health
Depression & Anxiety: Mental Health Advocate Goes Viral

Bullying: Let's Talk About It

How Young Adults Can Seek Help
#NotAlone Conversation – Heading Back To School
Who To Talk To About Mental Health

Navigating College, Protecting Your Mental Health

Making A Mental Health Plan
College Guide

10 Common Warning Signs Of A Mental Health Condition
Helpful Articles & Stories

From Gang Member to Mental Health Advocate
How EMDR Healed My Trauma
Personal Stories
The Blizzard of Depression and the Importance of Compassion
Chronic People Pleasing and My OCD
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264 , text “helpline” to 62640 , or chat online. In a crisis, call or text 988 (24/7).
- Open access
- Published: 15 April 2024
How would you describe a mentally healthy college student based on Chinese culture? A qualitative research from the perspective of college students
- Mingjia Guo 1 ,
- Xiaoming Jia 1 &
- Wenqian Wang 1
BMC Psychology volume 12 , Article number: 207 ( 2024 ) Cite this article
148 Accesses
1 Altmetric
Metrics details
Promoting college students’ mental health remains a significant concern, necessitating a clear understanding of what constitutes good mental health. Variations in the conceptualizations of mental health across cultures, typically derived from academic and authoritative perspectives, have overlooked insights from laypeople. This study aims to investigate the characteristics of mentally healthy college students within Chinese cultural contexts, emphasizing perspectives provided by college students themselves.
Undergraduates with self-reported mental health scores ≥ 7 were randomly selected for in-depth interviews. The sample ( N = 17, 59% female) had a mean age of 20.82 ± 1.33 years and represented diverse regions, backgrounds, and academic fields. Thematic analysis was used in the analysis of the qualitative data, involving initial coding to identify 168 manifestations of mental health among college students, followed by categorizing them into 18 characteristics through focused coding. These characteristics were then organized into five themes via core coding. The Delphi method was utilized to validate the themes with 3 experts, ensuring the trustworthiness of the final findings.
Eighteen characteristics of mentally healthy college students emerged from the interviews, categorized into 5 themes: (1)Value Pursuit (i.e. Having a sense of responsibility and mission and being willing to dedicate oneself to the country at any time.); (2)Life Attitude (i.e. Staying positive and having the ability and quality to cope with hardships.); (3)Interpersonal Ideals (i.e., Showing filial respect to parents appropriately.); (4)Behavior Ability(i.e., Studying diligently and learning well.); and (5)Self-cultivation (i.e., Possessing good qualities advocated by Confucianism, Buddhism, and Taoism coexist harmoniously.). Most of these characteristics directly reflect traditional Chinese culture or culture that has changed with the times. At the same time, some are a reflection of modern Chinese new culture.
Conclusions
On the whole, the characteristics of mentally healthy college students are diverse and with rich connotations, focusing on the individual’s relationship with the country, family, and others, and are good expressions of Chinese cultural features, such as the balance of Yin and Yang, the coexistence of Confucianism, Buddhism, and Taoism, and highlight moral attributes. In essence, these traits hold profound importance in advancing the mental health of Chinese college students.
Peer Review reports
The period of undergraduate study is vital for individual development, physical and mental growth, knowledge reserve, and health literacy development. For undergraduate students, they are in the process of transitioning from late adolescence to early adulthood, navigating various physical, psychological, and social changes [ 1 ]. After entering the university, undergraduates, especially first-year students, are prone to various maladaptation problems due to changes in their living and learning environments [ 2 ]. Notably, a recent nationwide survey of 48,789 undergraduate students from 31 provinces and cities of China showed that 24.17% of undergraduates were at risk of depression, and 49.58% were at risk of anxiety [ 3 ].
Some studies have shown that these psychological problems are related to culture. As a Chinese proverb goes, “Nothing is more important than learning.” Before university, Chinese students focused solely on their studies, with their parents managing all aspects of life [ 4 ]. Consequently, they may lack the ability to independently resolve problems, particularly when confronted with many challenges in university life, often feeling helpless. Furthermore, admission to university is considered an honor to ancestors and a source of pride for parents in Chinese culture [ 5 ]. Attaining good grades and securing an ideal career post-graduation are seen as ways for college students to fulfill their filial duties, like supporting their parents, thus imposing familial and communal pressures.
Cultural influences also play a role in the mental health of college students. Wang et al. (2016) investigated how traditional Chinese philosophies—such as relationship harmony (advocated by Confucianism), dialectical coping (from Taoism), and non-attachment (rooted in Buddhism)—impact college students’ mental health. Their research demonstrated these philosophies’ negative correlation with psychological distress and negative emotions while displaying positive correlations with self-esteem, positive emotions, meaning of life, and happiness [ 6 ]. Another study indicated that Chinese college students scoring higher in Zhongyong thinking exhibit lower anxiety and depressive symptoms, along with higher self-esteem and life satisfaction, versus those with lower scores [ 7 ].
Since culture and mental health are mutually embedded [ 8 ], different cultures may interpret the same things differently. For instance, in Western cultures, pursuing a college education is often viewed as an individual pursuit, whereas in collectivist China, but in China, higher education is commonly sought to elevate social status and offer enhanced financial support to parents, such as securing a comfortable retirement home. In times of conflict, individuals in Chinese society tend to adopt the principle of “taking a step back and yielding vastness and spaciousness to others” [ 9 ], prioritizing long-term harmony over immediate gains by favoring conflict avoidance over confrontation. The values of “harmony is precious” and the practice of “forbearance” are revered in China, whereas in Western societies, it may be considered unhealthy, with individuals opting for direct expression of discontent [ 10 ].
In China, only 8% of the population hold bachelor’s degrees [ 11 ], and college students are seen as the nation’s hope and future [ 12 ], underscoring a heightened focus on their mental health. To enhance the mental health of Chinese college students effectively, it is imperative to grasp the cultural nuances defining mental health across various contexts.
Mental health has always been a focus in the field of psychology. Researchers from diverse backgrounds have extensively investigated mental health within various cultural frameworks. This includes the development of nuanced interpretations and pertinent theories regarding mental health across different cultural settings [ 13 , 14 ]. Moreover, scholars have localized measurement tools through meticulous adaptations [ 1 , 15 , 16 , 17 ] and delved into understanding the impact mechanisms between mental health and its associated determinants [ 18 , 19 ]. In terms of the connotation of mental health, aside from the various approaches of counseling and psychotherapy have their interpretations and definitions of mental health, various organizations and scholars have also put forward different perspectives of mental health from multifaceted viewpoints, clearly demonstrating the impact of culture.
According to the Concise Encyclopaedia Britannica, mental health is defined as “the state of optimal functioning of the individual psyche within the limits of its own and environmental conditions, but not as an absolute state of perfection” [ 20 ]. Meeks and Heit describe mental health as “the ability to perceive and express one’s emotions and state of mind; mental health is the ability to accept reality as it is” [ 21 ]. Meanwhile, Ryan and Deci propose that mental health involves “the ability to feel effective and agile, e.g., to have full self-fulfillment” [ 22 ]. The World Health Organization defines mental health as “a state of well-being in which the individual realizes his or her abilities, can cope with the normal stresses of life, can work productively and fruitfully, and can make a contribution to his or her community” [ 23 ]. These definitions illustrate how Western culture emphasizes individual capabilities, states of being, and overall well-being, focusing on fulfilling potential, fostering self-esteem, and reflecting a culture centered on the individual.
In the Dictionary of Psychology (Chinese version), mental health was defined as “a good state in which the individual’s mental state (e.g., general adaptability, soundness of personality) remains normal or at a good level, and in which harmony is maintained within the self (e.g., self-awareness, self-control, self-experience) and between the self and the environment” [ 24 ]. According to Zhang and Yang, mental health contains objective and subjective components [ 25 ]. An individual’s mental health is mainly expressed by the relationship between the individual and others in a group, so it contains social meaning. Hu suggests that mental health is about “following one’s heart and not exceeding the rules,” which has both its individual (developmental and autonomous) and social (adaptive and normative) aspects [ 26 ]. Yip defines mental health as a direction that suggests self-discipline and obedience to social order to maintain inner balance and external harmony with others [ 27 ]. Specifically, individuals can maintain this balance and harmony across three levels: personal, interpersonal, and moral/ethical. These definitions underscore Chinese scholars’ emphasis on the social aspects of the individual in conjunction with the proper functioning of mental faculties. They highlight Chinese culture’s focus on harmony, interpersonal relationships, societal connections, and moral/ethical considerations.
In summary, concepts and understandings of mental health are closely tied to culture [ 28 ], reflecting that the connotations of mental health defined by different cultural contexts can vary to some extent. Then, how is mental health related to culture? The theory of sociocultural models (TSCM) provides a perspective on the interaction between culture and the individual mind [ 29 ].
The primary thesis of the theory of sociocultural models (TSCM) is that the human mind and culture mutually constitute each other. During continued interactions, individuals internalize the social culture into their psychological realities to regulate their actions and interactions. Conversely, community members will externalize the psychological reality through enactment and instantiation, creating new social cultures through social interactions and co-construction with the existing social culture. The dialectical interactions of these two aspects constitute the mechanism of the sociocultural regulation of human actions and the construction of the sociocultural reality [ 29 ]. Consequently, social culture dictates varying expectations for mental health standards, while the characteristics associated with mental health are also culturally rooted and reflect social culture. Simultaneously, societal depictions of mentally healthy individuals contribute to the evolution of novel cultural norms in a reciprocal manner.
The Chinese culture has a long history of rich mental health concepts deeply rooted in philosophies such as Confucianism, Buddhism, and Taoism. Confucianism seeks to go into the society( Rushi ), i.e., “To ordain conscience for Heaven and Earth, to secure life and fortune for the populace, to carry on lost teachings of ancient sages, to build peace for posterity” (Zhang Zai: Heng Qu Yi Shuo ). When encountering setbacks, Confucianism advocates being adaptable to circumstances and maintaining mental health by being resilient and motivated. Taoism seeks to transcend the world( Chaoshi ) and advocates “letting go.”When encountering difficulties, people maintain mental health by going with the flow and doing what they should do. The philosophy also underscores the importance of balancing Yin and Yang, enabling individuals to perceive challenges holistically by acknowledging both positive and negative aspects. Buddhism seeks to jump out of the material world( Chushi ) and advocate “being free of worried thoughts” when encountering difficulties. As Hui Neng(the Sixth Patriarch of Zen) said in the Tan Jing, “Since everything is naught, where can dust gather?” Individuals can cope better with difficulties if they have a mindset that looks down on gains and losses and that everything is nothingness.
Popular anecdotes and proverbs in Chinese culture also dictate criteria for individuals’ mental health. For instance, the “Three Feet of Space” tale narrates an incident from ancient China where the Guo family faced a boundary dispute with their neighbor during house construction. Upon hearing of this issue, patriarch Guo Pu wisely proposed, “Sending letters a thousand miles just for a wall; why not give him three feet?” This led to the Guo family’s compromise, and finally, both families conceded three feet of space from their walls. This narrative underscores the cultural emphasis on fostering interpersonal harmony through mutual accommodation, viewing discordant relationships as signs of poor mental health.
Contemporary scholars have also endeavored to directly integrate key concepts from Chinese traditional culture into psychological counseling and therapy. Yang and his colleagues(2002) [ 30 ] created Taoist Cognitive Therapy to facilitate cognitive restructuring in psychologically distressed individuals by directly applying the 32 characteristics of the Taoist principle of health, that is: “Benefit without harm, but not disputing; abstinent contentment with little selfishness and desire; under the knowledge and the place, let gentleness overcome rigidity; recover the original simplicity, let it be.” Liu(2023) posits that “unity of universe and human” in Chinese culture is a core idea of mental health [ 31 ]. He pointed out that the psychological phenomenon corresponding to this concept is psychological nothingness. By fusing modern psychotherapy with the concept of “unity of universe and human,” Liu developed the technique of “Moving symptom’s symbol to nothingness” to fulfill the healing role of Chinese culture. These endeavors establish a robust framework for comprehending mental health through the lens of Chinese cultural perspectives.
Over the years, numerous scholars have delved into the attributes of mentally healthy college students. Prominent among these is Wang and Zhang’s widely recognized framework, which outlines eight characteristics drawing from personal experience: understanding and accepting oneself; accepting others and dealing well with them; facing reality squarely and accepting it; loving life and enjoying work; being able to coordinate and control emotions and being in a good state of mind; having a complete and harmonious personality; having normal intelligence; and having age-appropriate mental behavior [ 32 ]. However, this work has predominantly focused on psychological cognition, emotion, and intention, with limited consideration of the cultural context, particularly the influence of Chinese culture on mental health.
Subsequently, scholars such as Zeng and Lei, incorporating social, ethical, and moral perspectives, proposed a culturally nuanced framework emphasizing four main traits in mentally healthy college students: positive and controllable emotions, good moral values, comfortable coping with schoolwork, and healthy social interaction [ 33 ]. While valuable, this perspective primarily mirrors researchers’ subjective experiences and authority-driven viewpoints. It neglects insights from laypeople, omits identification of the aspects of Chinese culture showcasing characteristics of mentally healthy college students, and lacks differentiation between mentally healthy college students and other demographic groups. Consequently, there is a demand for exploring innovative methodologies to scrutinize the attributes of mentally healthy college students, particularly focusing on characteristics within Chinese culture.
Currently, there are various research paradigms for the study of mental health. Jiang (2004) categorized them and concluded that there are two main principles in evaluating mental health: the majority principle and the elite principle [ 34 ]. The majority principle refers to a research paradigm that selects research subjects through large samples and measures whether individuals deviate from the norm through the principle of statistical normal distribution [ 35 ]. An example is applying the Chinese version of Symptom Checklist-90 (SCL-90), one of the most often used self-report symptom inventories to measure the mental health of college students, and individuals scoring exceeding the norm were considered abnormal [ 36 ].
The elite principle refers to a research paradigm that focuses on elite samples, namely a small number of relatively outstanding individuals in the whole population who are at the tip of one side of the normal distribution, and primarily employs qualitative research methods to derive research findings [ 35 ]. For example, Maslow researched some great people in Western history( i.e., self-actualized people) using qualitative research methods such as biographical analysis, depicted 15 characteristics of self-actualized people, that is, “more efficient perception of reality and more comfortable relations with it,” “acceptance (self, others, nature),” “spontaneity; simplicity; naturalness,” “problem centering,” “the quality of detachment; the need for privacy,” “continued freshness of appreciation,” “autonomy; independence of culture and environment; will; active agents,” “the mystic experience: the peak experience,” “gemeinschaftsgefuhl,” “interpersonal relations,” “the democratic character structure,” “discrimination between means and ends, between good and evil,” “philosophical, unhostile sense of humor,” “creativeness,” “resistance to enculturation; the transcendence of any particular culture” [ 37 ].
Maslow’s findings profoundly influenced research on mental health definitions, standards, and interventions. While some researchers have embraced the characteristics of self-actualized people as an ideal standard of mental health [ 38 ], others have leveraged these characteristics by focusing on exceptional psychological qualities rather than normative behavioral performance [ 39 ], and many of these characteristics have been used as ideal indicators of mental health for the promotion of mental health among college students [ 40 ]. Additionally, these characteristics and the conditions that promote or inhibit self-actualization are also applied in methods and paths of healthy human development [ 41 ]. Furthermore, specific characteristics such as a “philosophical, unhostile sense of humor” have been directly applied by researchers to enhance humor quality among college students facing stress and embarrassment, aiming to uphold their mental well-being [ 42 ].
Despite significant value in both theory and practice, Maslow’s study is based on the Western culture and is not aimed at a specific group of college students. Consequently, its direct relevance to enhancing the mental well-being of Chinese college students may be limited, necessitating further investigation into mental health within the framework of Chinese culture. Nonetheless, Maslow’s study of the elite samples of self-actualized people also provides a new research paradigm for mental health research, which has greatly inspired this study.
In the past, most studies on the mental health of college students used quantitative studies based on the majority principle. While some qualitative studies inquiries delved into the characteristics of mentally healthy college students, these studies often focused on specific subgroups like those who experienced being left behind [ 43 ] or childhood trauma [ 44 ]. A gap exists in the mental health characteristics based on the Chinese culture of college students who are the elite samples, i.e., those who exhibit very good mental health. By utilizing the elite principle paradigm, researchers can gain insights into and depict the mental health characteristics of college students within the context of Chinese culture, with the ultimate aim of delineating the mental health characteristics of college students specific to this cultural framework.
This study will apply the elite principle to examine college students with very good mental health. Through a distinctly Chinese cultural lens, this research aims to delineate what mentally healthy college students look like and what characteristics they show. By focusing on college students’ personal experiences and Chinese culture, this study positions college students as knowledge generators, employing a qualitative research approach to uncover the characteristics of mentally healthy college students. The objective is to achieve a new understanding of college students’ mental health based on Chinese culture and provide a theoretical basis for new mental health standards and a reference for promoting, cultivating, and intervening in college students’ mental health.
In this study, mental health refers to the good psychological state of an individual. College students refer to the group of students who are receiving professional higher education. Chinese culture refers to the culture created by the Chinese over thousands of years of development, from ancient times to the present [ 45 ].
The study applied a participatory, exploratory, qualitative design. Qualitative methods are suitable for exploring the meaning of phenomena or life events to the interviewees and their inherent experiences from the subjectivity of the interviewees [ 46 ]. It also emphasizes the participants as a generator of knowledge and the acquisition of significant experiences from the participants [ 47 ]. Thus, it can help researchers to gain a deeper understanding of community members in a specific cultural-historical context. Moreover, qualitative methods hold particular promise for prioritizing participants’ voices, and they contribute to understanding human interaction with the environment in development and helping researchers build and expand new concepts and theories in specific cultural-historical contexts [ 48 ]. This study used semi-structured individual in-depth interviews to explore the characteristics of mentally healthy college students based on Chinese culture. Moreover, the procedure of the study is shown in Fig. 1 .
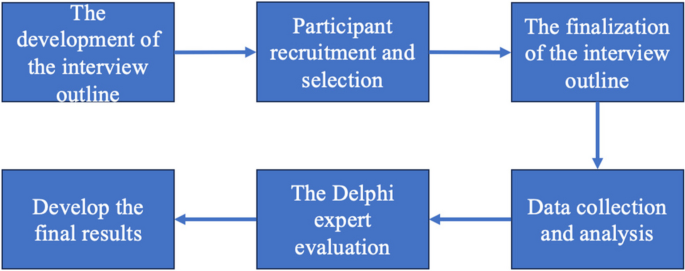
The procedure of the study
The development of the interview outline
The qualitative data for this study was collected through semi-structured interviews. Interviews serve as a tool to help reveal and understand participants’ perspectives and experiences. The interview outline for this study was based on the theory of sociocultural models [ 29 ], focusing on how the interviewed college students understood Chinese culture and which cultures were internalized as characteristics of mentally healthy college students.
The interview outline in the pre-interview includes questions such as “What do you think is mental health? What do you think a ‘mentally healthy’ college student is like? You can use yourself or your classmates as examples.” “What do you think is Chinese culture? What is your understanding of Chinese culture?” “What do you think is related to college students’ mental health in Chinese culture?” (Appendix 1 ).
Participant recruitment and selection
The selection criteria for the participants were: i) undergraduate students enrolled in colleges; ii) having a very good psychological status, with a self-assessment of mental health of 7 or more (out of 10); and iii) self-assessment anxiety/depression scores within the normal range.
The study recruited participants through postings in contact groups and forums among different colleges. Undergraduates who satisfied the selection criteria volunteered to participate in the study. At the time of self-referral, enrolled students rated their mental health with the term “Out of ten, how would you rate your mental health?” as well as filled out self-rated anxiety and depression scales [ 49 , 50 ].
The reasons for considering selection criteria are as follows. Firstly, the research objective is to identify the mental health characteristics of college students with good mental health. Therefore, following the elite principle and referencing Maslow’s self-actualization research paradigm [ 37 ], we have chosen exceptionally mentally healthy college students as elite samples for study. Given that statistical analysis commonly regards the top 27% as the criterion for high-score groups [ 51 , 52 ], a score of 7 out of 10 indicates high mental health levels. Consequently, the study interviewed college students scoring at least 7 points. Secondly, to eliminate individuals with significant biases in the self-assessment of mental health and those potentially experiencing psychological issues, we utilized scores from self-rating scales for depression and anxiety to exclude possible candidates with underlying psychological disorders.
Eventually, 17 college students who met the criteria were selected for interviews in this study. The selection of participants considered factors that might influence college students to develop different understandings of Chinese cultures, such as upbringing, family environment, and educational experiences. The total number of participants was determined based on thematic saturation, i.e., no significant themes emerged with new respondents [ 53 , 54 ]. Finally, 17 undergraduate students volunteered to participate in the formal interviews, and the self-reported mental health score of the interviewees was 8.11(SD = 0.90) (out of 10). Among the participants, seven were male, and ten were female. Their ages ranged from 19 to 23 years old (mean age = 20.82, SD = 1.33 years), five interviewees were from Double World-Class Project Universities in China, and 5 were first-year students, two sophomores, eight juniors, and two seniors. Participants came from different regions of China; 4 grew up in north China, 1 in northwest China, 2 in southwest China, 2 in south China, 1 in east China, and 7 in central China; 1 from an ethnic minority. 65% were from urban areas, and 29% had no siblings. Additional information on parents’ education level and occupation is shown in Table 1 .
After the interviews, participants were thanked for their participation and contribution and were offered 30 RMB (about 4 dollars) for participating.
The finalization of the interview outline
Before the formal interviews, three college students (one male and two female) who met the selection criteria were pre-interviewed, and the interview outline was adjusted based on the pre-interviews. Specifically, the researchers adjusted ambiguous expressions. For example, in the pre-interview, the researchers found that if they asked the interviewees, “What do you think is related to college students’ mental health in Chinese culture?” They answered how Chinese culture affects college students’ mental health rather than the characteristics of mentally healthy college students based on Chinese culture. Therefore, we adjusted the question to “What a ‘mentally healthy’ college student is like based on Chinese culture? You can take yourself or your classmates as an example” to obtain the characteristics of mental health that reflect Chinese culture. A formal interview outline was eventually formed (Appendix 2 ).
Data collection and analysis
The qualitative data was collected through in-depth personal interviews with eligible college students. Each interview lasted between 50- 100 min and was conducted by the researcher (MG), who possessed a doctoral background in psychology, had received training in qualitative research methods, and had three years of experience working in mental health education in universities. All participants signed informed consent forms prior to the interviews. In total, 1252 min of interviews were conducted with 17 participants, which were then manually transcribed by MG, resulting in 289,000 words of interview transcripts.
To accurately ascertain the true meaning expressed by the participants, this study employed manual analysis within the research team to code and analyze the interview transcripts word by word and sentence by sentence. Under the guidance of XJ (a clinical and counseling psychology professor), the research team completed all data analysis work. In addition to MG and WW, the team members included two doctoral students who are also full-time university psychological counselors and two master’s students specializing in mental health education.
The data analysis was conducted using thematic analysis [ 55 ]. The steps are as follows: first, the researcher transcribed each of the digitally recorded interviews, immersed within the data, and repeatedly read through the 289,000-word interview transcripts. Second, researchers identified meaningful texts and created open codes. Each meaningful sentence was marked with a “code number,” totaling 1,889. The study used “F” to represent female interviewees and “M” for male participants. The first number represents the interview orders of interviewees; the second number represents the order of the meaningful statements in the interview. For example, “M5-40” represents the 40th word, sentence, or paragraph spoken by the fifth male interviewee. Third, after contemplating the open codes repeatedly, 168 manifestations of mentally healthy college students were derived through initial coding. These manifestations were then summarized to establish 18 characteristics of psychologically healthy university students via focused coding. Subsequently, these 18 characteristics were further classified through core coding to derive five main themes. Fourth, we checked the themes and adjusted their structure until they met internal homogeneity and external heterogeneity criteria. Fifth, we defined and named the themes; 18 characteristics were obtained and coded into five themes.
The Delphi expert evaluation
Subsequently, three experts were invited to assess the appropriateness of naming, defining, and classifying the identified 18 characteristics and five themes above. These experts are professors in clinical and counseling psychology from institutions such as Beijing University of Chinese Medicine, with in-depth research in Chinese culture and mental health. They have published numerous related monographs and academic papers, such as “When Psychological Counseling Meets Traditional Culture” and “Mind Operations in Meditation.”
The evaluation comprised two rounds. The first round involved a focused group interview where the three experts individually reviewed each theme, characteristic, and original interview data, offering suggestions for revision. They generally approved of the theme divisions and most characteristics, with two main modifications: 1) the integration and categorization of specific characteristics, such as the initial characteristic “Having a pleasant disposition,” which was deemed by experts to contribute to a comfortable interpersonal state and thus was incorporated into “Interpersonal harmony and comfort.” 2) Adjustments to specific nomenclature, such as refining “Showing filial respect to parents” to “Showing filial respect to parents appropriately” to better emphasize the nuance of the characteristic.
The revised results were resent to the three experts for a second round of evaluation, leading to a consensus with no further modifications suggested, thus finalizing the research findings.
The trustworthiness of the data
Trustworthiness was achieved in several ways.
First, to minimize personal biases to the greatest extent possible, the researchers continuously reflect at each stage of the research project, remaining attentive to the influence of their own experiences and biases throughout all research and analysis phases. For instance, MG utilized a reflective journal [ 56 ] to document personal perspectives after each interview, consistently reminding herself to avoid preconceived notions.
Second, the selection of participants considered factors that might influence college students to develop different understandings of Chinese cultures to ensure the diversity of the participants. And, the total number of participants was determined based on thematic saturation [ 53 , 54 ]. In this study, after interviewing the F8(the 14th interviewee), no new significant themes emerged. Then, three more interviews were conducted (F9, F10, M7), and no significant themes emerged with the new respondents.
Third, the research performed investigator triangulation [ 57 ]. Independent researchers completed comparative analyses of individual findings, organized regular research team meetings to compare the analyses, and identified relevant themes. Moreover, XJ frequently reviewed interviews conducted by MG, her reactions to interviews, and the formulation of results. All the researchers discussed the coding and the corresponding original text until a consensus was obtained to bolster the study’s credibility and dependability.
Fourth, external audits are conducted to foster the accuracy or validity of a research study [ 57 ]. The research invited three experts above who have made achievements in Chinese culture and mental health to assess the appropriateness of naming, defining, and classifying the characteristics and themes in order to enhance the reliability of research findings.
College students’ understanding of Chinese culture
The interviewees’ understanding of Chinese culture was focused on the following four main aspects, and the participant’s identifier follows quotations.
Firstly, Chinese culture is undoubtedly distinct from other countries. For example, F1 believes that “Chinese culture is not just some fixed dynasties in history, or language, or what some literati or educators or some people said, it refers to some patterns of behavior or some ideas that distinguish people from other countries” (F1-66) and is unique to China (M3-110).
Secondly, Chinese culture includes both traditional and modern Chinese new cultures (e.g., revolutionary spirit, M2-95, M4-151, M7-85). Moreover, it is argued that Chinese culture is the essence of what has been left behind through history, including all aspects that have been handed down from ancient times to the present (M1-99; M5-128), and that it is a continuous transmission (F2-72, F4-92, F5-170, F7-137; F9-181; M6-132) and a fusion of the old and the new (F7-142). Chinese culture is implicitly formed and constantly influences and permeates everyone or their lives (F3-134; F7-138; M1-102; M3-111).
Thirdly, Chinese culture is a macro concept, encompassing both intangible and physical aspects. Intangible aspects include thoughts, spirits, and qualities (M2-95, M4-151, M5-131). The physical component includes not only literary works such as poetry (as perceived by all respondents) but also Chinese language and writing (Chinese characters, F2-75; oracle bone inscriptions, F9-184; calligraphy, F2-77, F5-170, F8-94), architecture (F3-148; F10-98), costume (F3-141; F10-101), and folkloric performances (drama, F2 -74; shadow puppets, F5-168; martial arts, F7-141), gastronomy (M5-132), art (painting, F8-93; paper-cutting, M1-100, M2-96, F5-169; china, M2-97; F2-75), traditional festivals and customs (M3-107; F3-138; F5-166; F7-140; F0-97. M7-87) and many others.
Fourthly, some important historical and modern figures mainly reflect Chinese culture’s ideological and spiritual aspects. For example, the famous statesman and literary figure Wen Tianxiang of the late Southern Song dynasty, whose poems “Everyone must die; let me but leave a loyal heart shining in the pages of history books” showed the interviewees his righteousness (M4-122), resilient, his moral integrity (F6-77), and his fearlessness in dedicating his life to his country (M2-72). There is also Zhou Enlai’s ambitious pursuit of “Reading for the rise of China” (M4-62), Mao Zedong’s sense of family and country and the importance he attached to learning (M5-43), and Qian Xuesen’s strict demands on himself during his research (M4-126). The interviewees also made many references to literary figures, such as Li Bai, a poet of the Tang dynasty, whom several interviewees mentioned for his free and ease in the face of frustration (M2-92, M6-30), and his ability to show his spontaneous side in life and learn things spontaneously(M5-54). As well as the ambition of Du Fu showed in his poem “When you are standing on the peak, you are on top of the world” (M5-36), and his sense of responsibility (M1-91, F3-56) reflected in his other poem, “To Emperor Yao and Shun, and to make the customs simple again” (M1-91, F3-56). They also talked about Su Shi’s open-mindedness (F8-79; M6-9) and cheerfulness (M5-29) in the face of adversity, who is a famous poet, calligrapher, gourmet, and hydraulic expert in the Northern Song Dynasty; and also the inner peace(M6-15) and indifference (F3-53) of Tao Yuanming (a famous idyllic poet in the Eastern Jin Dynasty) from his poem “I pick fence side asters at will; carefree I see the southern hill,” and so on.
In addition, the spirit of Chinese culture is also reflected in some allusions and some historical events in ancient and modern times, for example, “Mencius’ mother moves her home three times to better her son’s education” (F1-60), “Che Yin makes use of the light of fireflies or the reflected light by the snow to study” and “Kuang Heng dug a small hole on the wall in order to get some light from the neighbor’s house to read books” (F1-61; F8-34). These allusions convey the importance of studying hard even when conditions are limited. Also, the revolutionary spirit of the May Fourth Movement shows that young people are not afraid of sacrifice (M4-29), and the New Democratic and Industrial Revolution embodied the unity of the Chinese people (M7-91).
Characteristics of mentally healthy college students based on Chinese culture
There are eighteen characteristics of mentally healthy college students based on participants’ understanding of Chinese culture as described above, which is coded into five core themes: (1) value pursuit, (2) life attitude, (3) interpersonal ideal, (4) behavior ability, and (5) self-cultivation. It can be seen that the vast majority of the mental health characteristics reflect traditional Chinese culture, which is constantly being passed down and changed, with the remainder reflecting the influence of modern Chinese culture. The five themes and corresponding characteristics are shown in Table 2 . The results are presented below, and the participant’s identifier follows quotations.
Value pursuit
Value pursuit refers to an individual’s understanding and practice of life ideals and beliefs after integrating social consciousness, such as worldview, life view, and values. Participants described that mentally healthy college students based on Chinese culture have strong beliefs and goal pursuits of contributing to the motherland. They exhibit profound loyalty towards their motherland, viewing its service as their sacred duty, and are steadfast in their resolve to contribute through bold exploration, even in the face of daunting challenges or the prospect of personal sacrifice. This theme directly reflects the Chinese Confucian culture of “Self-cultivation is the starting point of several steps moving outward. The next step is managing family affairs, followed by governing the state. The final step is moving to provide peace and sound governance to all under heaven” and “To be the first in the country to worry about the affairs of the state and the last to enjoy oneself.” The following three subthemes were identified regarding students’ value pursuit.
(1) Loving their motherland and identifying with their culture
First and foremost, mentally healthy college students love their country and are firmly convinced that they want to identify with it. Twelve interviewees emphasize that mentally healthy college students should embody love for their country, cultural identification, and a profound sense of belonging and national pride. On the one hand, they are patriotic and loyal to their motherland and have high moral characters. For example, one participant said, “ like the patriotism in Yue Fei (a famous military man, strategist, calligrapher, poet, and national hero in Chinese history, and was the first of the Four generals rebuilding the Song dynasty). His patriotism and loyalty are also what a mentally healthy college student should have ” (#M6-54).
On the other hand, they identify with the country, nation, and culture from the heart and are proud of the motherland. Another participant said, “ Mentally healthy college students should have a real sense of cultural identity. Furthermore, a Chinese should identify with the traditional Chinese culture …… ” (#F3-110).
(2) Having a sense of responsibility and mission and being willing to dedicate oneself to the country at any time
In addition, mentally healthy college students have a firm sense of mission and responsibility to the motherland. Ten interviewees assert that mentally healthy college students should exhibit a sense of national responsibility, ambitious aspirations, and a readiness to devote themselves to their homeland wholeheartedly. Mentally healthy college students should have ambitious ambitions. As M1-75 said: “ ‘To ordain conscience for Heaven and Earth, to secure life and fortune for the populace, to carry on lost teachings of ancient sages, to build peace for posterity’ (Zhang Zai: Heng Qu Yi Shuo), which can also reflect the looks of a mentally healthy college student. ”
The most important thing is to be willing to contribute to their motherland, even at the expense of oneself. Another participant said, “ Mentally healthy college students do not think about personal gains and losses too much but put their country and nation before themselves, ……, ‘Death is not my concern should it benefit the country. How can I pick and choose for my loss or gains?’ (Lin Zexu) …… ” (#M7-22).
(3) Daring to criticize, explore, and innovate
At the same time, mentally healthy college students have the quest and conviction to keep climbing to the top. Sixteen interviewees believe that mentally healthy college students are enterprising, daring to criticize, explore, and innovate to contribute to their country’s development. Mentally healthy college students are active, enterprising, and have goals and plans. One participant said, “ I think mentally healthy college students should have goals and plans for themselves ” (#M6-3). They also have critical thinking and exploratory spirit and will keep innovating. As F7 said, “ If you are a mentally healthy college student, you also need some innovative spirit to break through …… ” (#F7-59). Also, they are willing to explore and contribute to the country’s development, as M4 said: “ Mentally healthy college students should be like Qian Xuesen (also known as Tsien Hsue-she), who has a strong spirit of patriotism. He devoted himself to scientific research, and after countless attempts and explorations, he finally launched the first atomic bomb for China …… ” (#M4-124).
Life Attitude
Life attitude is an individual’s understanding and reaction to things that happen in daily life. Participants highlighted that maintaining a positive, optimistic, dialectical, and open-minded stance towards setbacks and challenges is a key characteristic of mentally healthy college students. This theme directly reflects Chinese culture: “Someday, with my sail piercing the clouds, I will mount the wind, break the waves, and traverse the vast, rolling sea.” and “It is blessed to suffer losses.” The following four subthemes regarding students’ life attitudes were identified.
(1) Loving life and being positive
Mentally healthy college students hold positive attitudes about life. Fourteen interviewees believe that mentally healthy college students exhibit optimistic attitudes toward life. Mentally healthy college students approach life optimistically, viewing it as brimming with hope. As F9 mentioned, “ I think I am mentally healthy because I am quite positive and optimistic about life, and I will face it positively even if there are some bad things ” (#F9-149). Moreover, they love life and experience life from their heart, “ I think mentally healthy college students can live a good life. Particularly, they can still maintain a love for life, have something they want to do, have the energy to fight or to live. ” (#M2-2). They always think life is full of meaning. As F1 said, “ I think some of the cases (of mental ill health) are because they have lost hope in life and do not want to do anything ” (#F1-47).
(2) Staying positive and having the ability and quality to cope with hardships
Mentally healthy college students possess a positive attitude towards suffering and setbacks. All interviewees believe that mentally healthy college students have a positive view and the qualities of coping with suffering when facing life difficulties. They will not shy away from adversity; instead, they proactively address issues, surmount obstacles, and manage them with composure. When facing difficulties or setbacks, mentally healthy college students maintain constructive beliefs. As one participant said: “ ‘Just as heaven keeps moving forward vigorously, a man of virtue should strive continuously to strengthen himself’ (The Change of Book). And ‘When Heaven intends to confer a great responsibility upon a person, it first visits his mind and will with suffering, toils his sinews and bones, subjects his body to hunger, exposes him to poverty and confounds his projects. Through this, his mind is stimulated, his nature strengthened, and his inadequacies repaired’ (Mencius). A mentally healthy college student should be like as described in these statements. ” (#F9-25).
They also exhibit the qualities to cope with hardships, such as striving continuously to strengthen themselves, being indomitable, resilient, enterprising, and so on. “ I think indomitable also reflects the self-control mentioned earlier, that is, they will not give up even after experiencing more difficulties ” (#M4-136).
Furthermore, they can analyze and resolve problems amid adversity and challenges, effectively overcoming them. “ For a long time, when my friends and I encounter setbacks, crises, or challenges, I always use this phrase to encourage myself and others to handle it calmly, ‘to be unchanged in front of the collapse of the mountain Tai, and to face danger without being surprised when it suddenly comes in front of you.’ ” (#M7-6).
(3) Being flexible and dialectical
Mentally healthy college students have a dialectical attitude towards life. Ten interviewees noted that mentally healthy college students demonstrate critical thinking skills by approaching situations objectively, comprehensively, and dialectically. These dialectical concepts, attitudes, and behaviors when facing negative things in life are also characteristics of mentally healthy college students. One participant said, “ Mentally healthy college students should be as objective and comprehensive as possible when dealing with things ” (#F3-118). They do not dwell on the present and have a positive attitude toward the future, “ There are plenty of fish in the sea. Do not miss the whole forest because of a tree. Even if you are sad about a breakup, do not cling to the past, but try to live a new life ” (#M7-12).
Furthermore, they think dialectically and believe that all sufferings have its reward. As F1 said: “ A saying goes that ‘Someday This Pain Will Be Useful to You,’ which means that it is not always bad to suffer Loss; think long term. For example, one may sometimes feel that their interests are being threatened in interpersonal relationships. However, if they are particularly concerned about this, it will make them uncomfortable, while if they are generous or forgiving, their heart will become more open ” (#F1-24).
(4) Being inclusive and broad-minded
Mentally healthy college students have an open-minded attitude toward life. Sixteen interviewees believe mentally healthy college students are tolerant, broad-minded, and open-minded. Both for themselves and others, mentally healthy college students hold tolerant attitudes. A participant said, “ I may lack a little tolerance for others because I am always strict with myself, so I may sometimes be strict with others. So, from this point of view, I think my mental health level needs to be further improved ” (#M2-79). They are broad-minded (“ Be magnanimous, as the saying goes, ‘A prime minister’s mind should be broad enough for poling a boat,’ which is a sign of college students’ mental health, advising people to look at whatever things a little more openly ”, #F6-34).
Moreover, even in the face of life’s misfortunes, they are also very liberal and open-minded, able to accept them openly. As M6 mentioned, “ One should also have positive and healthy perceptions. Su Shi, a famous poet, calligrapher, gourmet, and hydraulic expert in the Northern Song Dynasty, openly accepted the fact that he was deprived of his official position. Instead of being depressed daily, he lived an easy and interesting life, free and relaxed ” (#M6-9).
Interpersonal ideal
Interpersonal ideals refer to the pursuit and aspiration of individuals to achieve the best in interpersonal communication and good relationships. According to these interviewees, the characteristics of mentally healthy college students can be divided into general and specific interpersonal relationships. Regarding general interpersonal relationships, mentally healthy college students are friendly and kind, and their interactions with others are harmonious and comfortable. When navigating specific relationships like those with parents, they are filial but have rational thinking; in terms of friendship and romantic partnerships, they pursue ideal and pure relationships. This theme is a direct reflection of Chinese culture: “benevolence,” “harmony is precious,” “The relations between men of virtue are plain like water,” “filial piety,” and so on. The following four subthemes were identified regarding students’ interpersonal ideals.
1) Being benevolent and kind
Mentally healthy college students are benevolent and kind in their interactions with others. Thirteen interviewees believe mentally healthy college students are kind-hearted, compassionate, sincere, caring, and helping others without discrimination. Mentally healthy college students are benevolent and have compassion for others; as M7 mentioned, “ When I met beggars on the road, …… whether they are pretending or be, I am always willing to give them some money…… ” (#M7-54). They are kind-hearted (“ I think a person should be at least kind-hearted; he may have that kind of empathy inside, have that kind of emotion for either other people or animals, ……, and have a softer heart, which also reflects the mental health of college students ,” #F6-45). They treat people gently and friendly (“ Laozi and Confucius look gentler than others, I feel that this characteristic in them also indicates the mental health of college students ,” #M3-73).
Furthermore, they are helpful and kind to others. As one participant said, “ Imagine this: You’re in a crowd, and a bike tumbles to the ground. Everyone is looking around, unsure of what happened. Now, you’re caught in a bind: Should you lend a hand or stay back to avoid being wrongly accused? Despite the chance of misunderstanding, I feel it’s crucial to step up and help. Ignoring the situation just doesn’t sit right with me—it goes against everything I believe in. ” (#F5-161).
2) Interpersonal harmony and comfort
Mentally healthy college students have a harmonious and comfortable interpersonal state. All interviewees agree that mentally healthy college students exhibit pleasant character and interpersonal adeptness, adhere to fundamental Chinese cultural values, and maintain a more harmonious and comfortable relational environment compared to their peers. Mentally healthy college students experience interpersonal harmony and comfort; one interviewee said, “ A mentally healthy college student has better interpersonal relationships, ……and has a comfortable social state ” (#F1-17). In interpersonal interaction, they prioritize harmony (“ I quite agree with the saying ‘Peace is of paramount importance. Since we are studying together, it is important to take care of each other and try to understand each other ”, #M3-49). Besides, they have good interpersonal interactions (“ ones’ mental health, I think, also shows more in whether they can deal with interpersonal relationships with people around them, …… whatever kind of people may meet, they can deal with the relationship well ”, #F6-9).
Moreover, they appreciate others (“ If other people have gained a certain amount of academic achievement, …… if he is (mentally) healthy, he may be happy for others’ success, achievement ”, #M7-33). Also, they can resolve conflicts or contradictions in interpersonal relationships (“ There is no perfect person; for example, if they cause harm to others, they can recognize their mistakes and apologize timely and honestly ,” #M6-101).
Furthermore, they follow many guidelines to create a harmonious and comfortable interpersonal state. As F3 mentioned, “ I think, when it comes to some unimportant things, it is important not to bother others like that…… one should have the sense of proportion ” (#F3-39).
3) Having a soul mate
Mentally healthy college students seek to have a soul mate in specific friendships or romantic partnerships. Nine interviewees suggest that mentally healthy college students possess the ability and quality to communicate and empathize with others on a deep spiritual level and form corresponding friendships or romantic relationships. Whether in friendship or romantic relationships, mentally healthy college students have the correct attitude toward interaction, as F8 said, “ For example, Zeng Gong and Wang Anshi (both politicians of the Northern Song Dynasty), …… They become good friends for life not based on interests, but on their appreciation of each other, and the same values, which I think mental health of college students should always be ” (#F8-67).
They emphasize the spiritual level of communication more than pursuing each other’s company. They have a more high-quality and pure relationship, in friendship or romantic relationships. As F6 said: “ ‘The friendship of a noble person is as pure as water.’ (Chuang-Tzu). Put simply, relationships should be genuine and straightforward, free from fame-seeking or ulterior motives; Just like the story of Boya and Ziqi, mentally healthy students might find a companion who truly gets them, connecting on a spiritual and empathetic level…… ” (#F6-38). It is the same with romantic relationships, as M6 mentioned, “ When you read the poem of Su Shi, for example, ‘Ten years parted, one living, one dead; Not thinking; Yet never forgetting; A thousand Li from her lonely grave; I have nowhere to tell my grief……’ The affection between him and his wife is so deep that it is enviable ” (#M6-42).
4) Showing filial respect to parents appropriately
Mentally healthy college students have rational conceptions of filial piety towards their parents and appropriate, respectful behavior. Eleven interviewees believe mentally healthy college students are filial and rational in their interactions with their parents. Mentally healthy college students show filial piety to their parents appropriately. On the one hand, they practice filial piety by accompanying their parents, communicating more with them, caring for them, repaying them, and so on. As F5 mentioned, “ ‘Our bodies—to every hair and bit of skin—are received by us from our parents’ (Xiao Jing). Mentally healthy college students are grateful and respectful, often care for their parents, and spend more time with them ” (#F5-109).
On the other hand, they also have rational thinking rather than unprincipled obedience regarding filial piety’s “cognition” aspect. As one participant said, “ Not just any kind of filial piety, that is, you should have your thinking and judgment…… ” (#F3-105). Another participant said, “ Proper filial piety is an aspect of college students’ mental health, not that they are obedient to their parents. When they disagree with parents, they can communicate more with parents and let themselves be understood ” (#M5-102).
Behavior ability
Behavior ability refers to the ability of an individual to behave appropriately. According to these interviewees, mentally healthy college students have a variety of behavioral abilities, such as adapting to different environments, learning well, and regulating their emotions. This theme directly reflects the Chinese culture: “Those who obey heaven survive, and those who defy heaven perish,” “learn without thinking is reckless, think without learning is dangerous,” and “When joy, anger, sorrow, and happiness are not yet expressed as a response to other things, they are in a state of balance. When they are expressed in words and deeds by the rites, harmony is achieved. “The following three subthemes were identified regarding students’ behavior ability.
(1) Adapting to the environment
Mentally healthy college students can adapt to the environment. Seven interviewees believe that mentally healthy college students can adapt to different environments. Adaptability is reflected on the one hand in the interpersonal aspects (“ There is also the adaptation to the university environment. Mentally healthy college students can integrate into groups and clubs, and actively participate in club activities ”, #F2-16). Also, they can adapt to different environments (“ I think social adaptability is quite important…… I went to work part-time this summer, but I feel that I have just been exposed to it ”, #F9-10). Moreover, they also show adaptability to adversity (“ I think mentally healthy college students also can adapt to adversity…… ”, #M5-70).
(2) Studying diligently and learning well
Mentally healthy college students can learn well. Thirteen interviewees suggest that mentally healthy college students exhibit a positive learning attitude, take ownership of their learning, maintain a continuous learning process, and demonstrate good study habits. They learn earnestly and diligently and have good learning attitudes (“ College students with good mental health will keep learning, have the initiative to learn, down-to-earth. Moreover, if they work by fits and starts (Cao Xueqin: The Dream of Red Mansions), there will not be a good result ”, #F5-64).
They also actively take responsibility for learning. As F10 said, “ Responsibility is fundamental. The primary task for students is studying. One should stay in one’s lane ” (#F10-83). Besides, they are good at learning (“ I think Lu Xun, who gave up medicine to pursue literature, …… has a powerful ability to learn ”, #F9-71). In addition, they study diligently and accumulate knowledge. As M2 mentioned, “ Since I have to prepare for the entrance examination, I have to memorize words and take lessons every day. That is, ‘But unless you pile up little steps, you can never journey a thousand li; unless you pile up tiny streams, you can never make a river or a sea.’ (Hsun-Tzu: Encouraging Learning), …… I realized that what I do daily is important ”, #M2-93).
(3) Being emotionally appropriate and can regulate emotions
Mentally healthy college students can regulate and manage their emotions. Nine interviewees posit that mentally healthy students display emotional appropriateness and stability, promptly and effectively managing their emotions. Emotions are often regarded as the signal light of mental health. Thus, mentally healthy college students are emotionally appropriate and relatively stable, “ A mentally healthy college student should be emotionally stable, …… ‘The master was mild, and yet dignified; majestic, and yet not fierce; respectful, and yet easy’ (The Analects). One should have a suitable emotion in which state ” (#F3-78).
Moreover, when encountering adverse events, they have the ability to regulate their emotions. As one participant mentioned, “ A mentally healthy college student can control his emotions and regulate his emotions ” (#F6-1). At the same time, they can adjust themselves in appropriate and healthy ways in time, “ when he meets some bad things, he can just communicate with others, exercise…… instead of drinking or even hurting himself ” (#F8-10).
Self-cultivation
Self-cultivation refers to the inner quality or state an individual constantly improves or achieves through long-term efforts and cultivation. According to the interviewees, mentally healthy college students advocate the continuous improvement of self-cultivation. They try to possess many excellent qualities of Confucianism, Buddhism, and Taoism and perfect them daily by having clear and objective self-knowledge and constantly reflecting on themselves to improve their cultivation. This is a direct reflection of the Chinese culture of “no end to learning” and “Seeing the virtuous and thinking of the wise, seeing the unwise and introspecting”, and so on. The following four subthemes regarding students’ self-cultivation were identified.
(1) Having an objective, positive perception of oneself and can accept one’s mediocrity
The constant improvement of mentally healthy college students’ self-cultivation first requires a clear perception of oneself. Eleven interviewees believe mentally healthy college students have a positive, comprehensive, and clear understanding of themselves. They know their strengths and weaknesses and can accept their mediocre and weak sides, “ For example, an Olympic weightlifter, he can only lift 50 pounds, but he had to go lift 100 pounds…… A mentally healthy person should clearly understand themselves and do according to one’s abilities… ”, #F8-33). They also have a positive view of themselves, “ ‘All things in their being are good for something’ (Li Bai: Invitation to Wine); one should not think too lightly of themselves when disillusioned. They can certainly play their usefulness in life, cannot improperly belittle oneself ” (#F9-35). Furthermore, they can also accept their mediocrity and weakness, “ I think there is also a significant point, which is to accept their mediocrity gradually…… ” (#F1-8).
(2) Being confident and also modest
The constant improvement of mentally healthy college students’ self-cultivation also requires an objective perception of oneself. Thirteen interviewees believe that mentally healthy college students are confident and able to stick to what they believe is correct while also being modest. According to a participant, mentally healthy college students believe in themselves, “ This point of believing in oneself in Qian Xuesen is probably also what a mentally healthy college student should have…… ”, #M4-128). They are assertive and can stand firm on their ideas (“ When faced with two choices, mentally healthy college students listen to others’ opinions and at the same time stick to their ow n,” #F4-77). At the same time, they are also modest (“ A saying goes that, ‘Modesty helps one go forward, whereas conceit makes one lag.’ In my opinion, mentally healthy students may not be so proud of themselves……”, #F5-36). Furthermore, they are not overly confident or modest (“Both confidence and modesty in a mentally healthy college student are appropriate and balanced, that is, I think it is necessary to be confident but also modest……, ” #F7-109).
(3) Focusing on introspection and contemplation to align with the sages
Mentally healthy college students improve themselves through constant introspection. Ten interviewees believe mentally healthy college students focus on introspection and are strict with themselves. They constantly check the gaps to seek progress and expand their horizon. Specifically, mentally healthy college students often reflect on themselves (“ ‘I daily examine myself on three points……’ (The Analects) which I think reflects the mental health of college students, that is, whether you are doing your best in the team…… ”, F2-35). They are also strict with themselves, “ As the sayings go, ‘You cannot expect a better world without cleaning your room first,’ although Du Fu (a famous poet of the Tang Dynasty) is said to be very talented, if one cannot do small things well, like cleaning the house, he can do nothing else well ” (#M5-52).
Moreover, they make constant progress and look to the virtuous, “ ‘When you see a person of virtue and capability, you should think of emulating and equaling the person; when you see a person of low caliber, you should reflect on your weak points’ (The Analects). Mentally healthy people also constantly learn from the strengths of others and reflect on their weaknesses ” (#M2-34).
(4) Possessing good qualities advocated by Confucianism, Buddhism, and Taoism, which coexist harmoniously
The highest level of self-cultivation for mentally healthy college students is to possess many good qualities of Confucianism, Buddhism, and Taoism, which together become the characteristics of mentally healthy college students. Sixteen interviewees suggest that mentally healthy college students exhibit strong moral characteristics and virtues from Confucianism, Buddhism, and Taoism, all coexisting harmoniously. Mentally healthy college students have the excellent qualities of Taoism, such as being calm and bland, indifferent to fame and fortune, and peaceful and happy. As the participants said, “ This sense of ordinariness, which I think may also be a necessity for mental health…… ” (#F7- 34); “ Mentally healthy college students are calm and relaxed, take the rough with the smooth; they have confidence in themselves and take it easy ” (#M7-35).
Moreover, they have the excellent virtues of Confucianism, such as benevolence, righteousness, rites, wisdom, and good faith. As F3 said, “ Mentally healthy college students must be good in these virtues, like ‘loyalty, filial piety, rites, wisdom, good faith, and courage’…… ” (#F3-90). Another participant mentioned, “ After comparing so many fictional characters, it is hard for me to use words to describe him (Qiao Feng), …… very filial and loyal, very righteous, …… doing things very fairly, … … ”, #M6-59).
Besides, they also obtain the main qualities of Buddhism, such as gratitude and kindness (“ ‘Moral character can be built by accumulating goodness’ (Hsun-Tzu: Encouraging Learning). A mentally healthy college student does good deeds, such as attending activities as a volunteer…… ” #F2-30). As F9 said, “ Also, mentally healthy college students often remember others’ kindness and are grateful, and then be nice to others, as the saying goes, ‘You throw a peach to me, I give you a white jade for friendship.’ (The Book of Songs) ”, #F9 -112).
The study identified five themes and 18 characteristics of mentally healthy college students within Chinese culture. These characteristics are deeply rooted in Chinese traditions, highlighting yin-yang balance and moral cultivation. They related closely to college students’ identity, learning stage, and age. Contrasting with characteristics of other cultural backgrounds, they showcase the impact of Chinese culture on college students, validating and expanding the theory of sociocultural models.
Comparison with previous studies
Firstly, compared to existing research on the characteristics of mentally healthy college students, this study presents novel findings and unique insights. Consistent with other related studies rooted in Chinese culture, both this study and previous research accentuate that the characteristics of mentally healthy college students encompass facets such as self-awareness, interpersonal relationships, emotional regulation, and positive learning traits. For instance, Wang (1992) posited that mentally healthy college students exhibit characteristics focusing on self-awareness, interpersonal adeptness, and emotional regulation [ 32 ]. Similarly, Zeng (2021) described the characteristics of mentally healthy college students, highlighting their emotional state, academic performance, and interpersonal skills [ 33 ].
Some characteristics revealed in our study diverge from those proposed in prior research concerning their specific connotations. Taking emotional regulation as an example, the research of Zeng (2021) and Wang (1992) primarily emphasized affirming positive emotions. They depicted mentally healthy college students as “positively emotional and controllable” or “possess the capacity to coordinate and manage emotions effectively, sustaining a positive mood.” In contrast, the characteristic identified in this study of “being emotionally appropriate and can regulate emotions” not only encompasses positive emotions but also includes negative feelings, emphasizing the timely and moderate expression of both. This directly reflects the Confucian concept of “Zhongyong” (doctrine of the mean) in Chinese culture, which advocates for moderation in all things, whether positive or negative. Therefore, it is evident that college students’ mental health is closely intertwined with the concept of moderation. Individuals can achieve mental health in various aspects by expressing emotions moderately, whether positive or negative.
Furthermore, this study has identified characteristics not previously mentioned by Chinese scholars, such as “showing filial respect to parents appropriately.” Filial piety is a unique social behavior within Chinese culture, embodying a comprehensive and intricate ethical framework [ 58 ]. Chinese society dramatically emphasizes family values, where treating parents well and acknowledging their upbringing is paramount. Therefore, if one is not filial, one cannot be said to be mentally healthy. However, with the evolution of societal norms, the essence of filial piety has transformed. Recent research reveals that contemporary society no longer adheres to traditional interpretations of filial piety solely through obedience to parents [ 59 ]. This shift signifies that mentally healthy college students now approach filial piety differently, manifesting altered perspectives, attitudes, and behaviors toward this concept. In ancient China, departing from one’s hometown to pursue education and personal growth was discouraged, as staying by one’s parents’ side was deemed the epitome of filial piety. As Confucius stated, “While the father and mother are living, do not wander afar” ( The Analects ). However, today, individuals are encouraged to venture afar to contribute meaningfully to their country and society [ 60 ]. As a result, modern manifestations of filial piety among mentally healthy college students involve not just reverence, care, and support for their parents but also underscore the significance of preserving autonomy and independence while fulfilling their familial duties.
Secondly, upon comparing our findings with research from other cultural backgrounds, it becomes apparent that our results diverge significantly from those of Western culture but align closely with research outcomes from Africa and Asia.
In the West, the understanding of mental health emphasizes enhancing personal belonging, satisfaction, and well-being, which is very different from Chinese culture, which emphasizes self-sacrifice and self-elimination [ 61 ]. Although this study was conducted in a qualitative study of a group of college students in very good mental health, a research perspective similar to Maslow’s research on self-actualizers, there were significant differences in the specific characteristics of these healthy individuals in different cultures. In particular, this study did not address the characteristics of self-actualizers noted by Maslow, such as “the mystic experience: the peak experience” and “philosophical, unhostile sense of humor,” which emphasize excellent personal features. The characteristics identified from this study emphasize individuals’ relationships with the country and family. Such as “loving their motherland and identifying with their culture,” “having a sense of responsibility and mission and being willing to dedicate oneself to the country at any time,” and “Showing filial respect to parents appropriately.” These characteristics are the direct expression of Chinese culture in terms of devoting oneself to the country and being filial to parents, which were not found in the results of Maslow’s study.
On the other hand, this study aligns more closely with research findings from African and Asian cultural backgrounds. For example, in the view of caregivers in Africa and Asia, mentally healthy individuals are people who contribute to the community and spend an enjoyable time in groups [ 28 ]. Thus, college students with good mental health can meet precise requirements at different levels: the individual and others, the individual and the family, and the individual and the nation, which is more of a relationship-oriented “big self” [ 62 ].
Thirdly, this research’s findings correspond with certain facets of the 24 character strengths and 6 virtues outlined in positive psychology, yet they also reveal disparities in specific aspects.
With the burgeoning of the positive psychology movement, some researchers have suggested that people with good mental health are not articulated merely as the absence of mental illness but as people who possess positive qualities, such as being highly resilient and well-being [ 63 ]. Seligman and colleagues summarized 6 virtues and 24 character strengths contributing to a good life [ 64 ], which have garnered wide attention. A point of convergence is that some positive psychological qualities emphasized by the characteristics identified in this study align with those highlighted in positive psychology. For instance, the characteristic of “being benevolent and kind” identified in this study emphasizes that mentally healthy college students are compassionate and kind. Similarly, one of the 6 virtues in positive psychology is humanity, which also focuses on kindness.
Nonetheless, notable distinctions exist between this study and the character strengths or virtues proposed by positive psychology. Firstly, in terms of the connotation of similar qualities, there are variations between the two. For example, the quality of “modesty” as a traditional Chinese virtue holds different implications than the Western perspective on “humility.” Modesty in Chinese culture carries much richer connotations than in the West, and core characteristics such as being open-minded, down-to-earth, and striving for improvement are unique to Chinese culture [ 65 ]. Additionally, while positive psychology views humility as an important but standalone character strength, this study found that mentally healthy college students are “being confident and also modest,” with modesty and confidence blending and coexisting harmoniously. This aligns with the encouragement of self-esteem, confidence, and self-improvement among the younger generation in China in recent years [ 66 ]. However, Chinese people still highly value modesty as a virtue while simultaneously emphasizing confidence. These seemingly contradictory qualities of confidence and modesty are valued, reflecting the dynamic balance of “yin and yang” in Chinese culture [ 67 ].
More importantly, this study has uncovered additional positive qualities beyond the 24 character strengths, such as “being inclusive and broad-minded”.These qualities carry strong moral attributes; in other words, possessing these moral qualities is essential for mental health. Confucianism emphasizes social morality, self-cultivation, and the development of a gentleman-like sage personality [ 68 ]. Self-cultivation is the basis for the ethical construction of family and society to perfect the ideal personality of governing the state and pacifying the world. The concept of “sageliness within and kingliness without” underscores this philosophy [ 69 ]. The characteristic “being inclusive and broad-minded” implies that mentally healthy college students exhibit tolerant and open-minded attitudes, embracing the principles of “Harmony, but Not Uniformity” and “The sea admits hundreds of rivers for its capacity to hold”(Chinese idioms) when encountering diverse viewpoints or adversity. Therefore, a mentally healthy college student possesses virtues such as tolerance and open-mindedness, showcasing solid moral values. In essence, college students’ mental health is intertwined with their moral attributes. A mentally healthy individual must embody essential moral qualities, which serve as markers of their overall well-being. Acknowledging the significance of moral virtues in defining and nurturing mental health among college students is crucial.
Validation and extension to the theory of sociocultural models
Firstly, this study validates the theory of sociocultural models. On one hand, this study confirms how culture influences individual psychology as proposed in the theory of sociocultural models. In this study, psychological entities represent the characteristics of mentally healthy college students that guide their thoughts, behaviors, and attitudes. According to the findings of this study, Chinese traditional culture plays a significant role in shaping these characteristics. For example, the patriotic sentiments of important historical figures such as Wen Tianxiang and Yue Fei, as well as the thoughts of traditional Chinese culture such as “Death is not my concern should it benefit the country. How can I pick and choose for my loss or gains?” (Lin Zexu: Two poems for family members on the way to the garrison ”) and “To ordain conscience for Heaven and Earth, to secure life and fortune for the populace, to carry on lost teachings of ancient sages, to build peace for posterity’ (Zhang Zai: Heng Qu Yi Shuo ) are internalized in the characteristics of “Having a sense of responsibility and mission and being willing to dedicate oneself to the country at any time.” The country cultivates college students as pillars of talent, and Confucianism teaches “To be the first in the country to worry about the affairs of the state and the last to enjoy oneself.” (Fan Zhongyan: The Yueyang Tower ). Thus, studying is not only for personal development but also for a sense of responsibility and contribution to the country, which arguably demonstrates the mental health characteristics of the specific group of college students with distinct traditional Chinese cultural connotations. Such findings align with the theory of sociocultural models, emphasizing how people internalize societal culture into their psychological entities to regulate their psychological activities.
On the other hand, this study validates how individual psychology externalizes and promotes the generation of new culture as proposed in the theory of sociocultural models. During China’s modernization, people have realized that only by daring to break through the shackles of existing ideas and exploring innovative development opportunities can the country move forward and develop sustainably. Many people have overcome difficulties and carried out the revolution, construction, and innovation in constructing Chinese socialism. Their love for the country and their sense of mission made them always meet the challenges of national reconstruction with high morale and perseverance [ 70 ]. Especially since the reform and opening-up, people’s minds have been fundamentally liberated, and the spring of scientific and technological progress has been ushered in. Their precious spiritual wealth, such as the characteristic of “daring to criticize, explore, and innovate,” has facilitated the development of new cultures like Chinese revolutionary and socialist cultures in modern times. Such findings align with the theory of sociocultural models, highlighting how group members externalize their psychological entities and transform them into new social cultures through social interactions and co-construction with existing social cultures.
Secondly, this study expands the content of the theory of sociocultural models. Due to a lack of specific pathways depicting the interaction between culture and psychology in the theory of sociocultural models, this study found that the significant carriers of interaction between culture and individual psychology are the spiritual world presented by historical and modern figures mentioned by the interviewees, as well as tangible worlds such as Chinese characters, poetry, martial arts, and art. These aspects of Chinese culture are internalized by college students as part of their psychological entities, guiding their words and actions and also shaping their perception of mental health. Conversely, the psychological entities of college students, such as the emergence of new concepts like “daring to criticize, explore, and innovate” in the construction of a new China, are transformed into emerging cultures, such as Chinese socialist culture through the role of figures like Qian Xuesen and stories as carriers.
Strengths, limitations, and future research
This study possesses several strengths. Firstly, it is the first attempt to systematically explore the characteristics of college students’ mental health entirely based on Chinese culture. The 18 identified characteristics directly convey or reflect aspects of Chinese culture, significantly enriching the comprehension of college students’ mental well-being within the context of Chinese culture. Secondly, the study adheres to the elite principle research paradigm by using elite samples as participants. Consequently, the outcomes comprehensively delineate the characteristics of mentally healthy college students possessing an excellent psychological state rooted in Chinese culture. These findings not only provide an ideal model for nurturing mental health among college students but also engender fresh insights into mental well-being, culminating in a novel benchmark for mental health standards. Thirdly, this study delves into the unique characteristics of mentally healthy college students within Chinese culture from the students’ firsthand experiences. In contrast, prior scholars predominantly offered personal opinions on the characteristics of mentally healthy individuals based on their experiences, lacking the direct perspectives of college students.
This study also has some limitations. As a qualitative study, the nature of this research inherently limits the applications of its conclusions. Focused primarily on college students, generalizing the findings to other groups in China (such as civil servants) may be constrained. Moreover, this study exclusively examines Chinese college students without conducting cross-cultural research. The absence of direct comparative studies fails to highlight variations in mentally healthy characteristics across diverse cultures. For instance, the absence of a comparative study between Chinese and students from other cultures (such as American college students) hindered exploration into the distinctive characteristics and differences of mentally healthy college students from varying cultures. Consequently, extrapolating the results of this study to other cultural contexts also has its limitations. Despite some similarities between Chinese culture and certain cultures in Asia and Africa, direct inferences also have significant constraints.
Furthermore, in terms of understanding culture, there is no conclusive definition of what culture is and what Chinese culture is. Scholars have put forward many understandings and definitions of Chinese culture from different perspectives. Understanding and defining Chinese culture are still in the exploratory stage, which challenges this study. The researcher’s understanding and mastery of existing relevant knowledge are somewhat limited regarding the formation of research results and the depth of analysis and discussion.
Future research could consider the following aspects. Firstly, a comparative study of the characteristics of mentally healthy people in different cultural groups can be conducted. Since individualistic/collectivistic cultures influence Americans and Chinese to be more expressive of private selves/collective selves, and religious cultures also influence individual self-esteem [ 71 ] and form religious selves [ 72 ]. Therefore, some comparative studies with students from different cultural backgrounds can be conducted in the future. For example, a comparative study with three groups of college students from the United States, China, and India can be considered to compare whether there are differences in the characteristics of mentally healthy college students from different cultures. Secondly, some quantitative studies can be considered. For example, future research could refine specific characteristics identified in the study, like “being flexible and dialectical,” for more specific operational definitions and develop a scale to measure the mental health of different groups to validate how these characteristics are manifested in university students or other groups so that more further research could be conducted using this new scale, which may help facilitate replication of the findings. Thirdly, based on continuous learning and accumulation of Chinese culture, future research can do in-depth excavation and exploration of the manifestation and nature of these mental health characteristics. For example, future research could select the characteristics reflecting the culture of filial piety or Zhongyong culture and explore how these cultures change and develop into mental health characteristics with the development of science and technology, the change of social structure, and the collision of Chinese and Western cultures, which may also be of great significance.
Practical implications
The Chinese culture has rich treasure resources and cultivated Chinese character traits, characteristics, and lifestyles. The results of this study show that many attitudes, ideas, and behaviors espoused by Chinese culture are manifestations of mental health. In particular, this study found the characteristics of mentally healthy college students based on Chinese culture, which is culturally applicable and more suitable for promoting the mental health of Chinese college students and can provide essential references and bases for mental health education and clinical practice.
On the one hand, this study can provide an overall theoretical framework for developing mental health courses for college students. Mental health courses are the most important and direct form of mental health education for college students in China, and they are also the primary way to improve the psychological quality of college students. The Ministry of Education requires colleges and universities to offer mandatory public courses on mental health for undergraduate students [ 73 ]. However, current mental health courses for Chinese college students rely mainly on Western mental health-related definitions, theories, and techniques for delivery [ 74 , 75 ]. The five themes and 18 characteristics discovered in this study are systematic, providing a comprehensive and systematic theoretical basis for college students’ mental health courses.
In particular, the five themes discovered in this study—values pursuit, life attitude, interpersonal ideals, behavioral ability, and self-cultivation—can be employed as the central pillars for teaching and setting objectives in a college student mental health course rooted in Chinese culture. Furthermore, the 18 identified characteristics can form each lesson’s fundamental content and learning goals, establishing a comprehensive framework. For instance, the characteristics “being confident and also modest” can be one of the key topics under the theme of “self-cultivation.” By comparing Western views of mental health (focused on confidence) with Chinese beliefs (valuing both confidence and modesty) and blending students’ self-awareness with Chinese cultural insights, the course can delve into the importance of confidence and modesty in Chinese culture. Strategies for cultivating these characteristics can be discussed, shedding light on the unique aspects of mental health development among college students within Chinese cultural contexts.
Secondly, this research offers valuable insights for fostering healthy personalities among college students in psychological counseling methods from the perspective of Chinese culture. On the one hand, this study has a guiding significance for setting goals in psychological counseling. Psychological counseling has traditionally emphasized decreasing negative emotions and boosting positive ones. Nevertheless, this study serves as a reminder for counselors to reassess this counseling objective. Throughout the counseling process, counselors should not only focus on diminishing negative emotions but also be wary of potential complications stemming from excessive positive emotions, stressing the importance of a moderate expression of positive and negative emotions.
On the other hand, the discoveries of this study could serve as a wellspring of inspiration for crafting indigenous approaches to psychological counseling. This research reveals that mentally healthy college students possess the characteristic “possessing good qualities advocated by Confucianism, Buddhism, and Taoism coexist harmoniously.” Within Chinese culture, the symbiotic interplay among Confucianism, Buddhism, and Taoism stands out as a cornerstone [ 76 ], where these philosophies coexist compatibly and mutually influence each other in shaping Chinese characters [ 77 ]. Future scholars might devise counseling methodologies rooted in the principle of harmonious coexistence found within Confucianism, Buddhism, and Taoism, potentially empowering individuals to bolster their mental health through these culturally embedded psychological counseling approaches.
This study explores the characteristics of mental health of college students with good psychological states from the perspective of Chinese culture and finds 18 characteristics, based on which five themes are formed: value pursuit, life attitude, interpersonal ideal, behavior ability, and self-cultivation. The 18 characteristics are typical of Chinese culture or its features, focusing on multi-level relationships with others, parents, and the country. They are also typical of Chinese culture with moral attributes, an emphasis on self-cultivation, a balance of Yin and Yang, and the coexistence of Confucianism, Buddhism, and Taoism. These findings help enrich the research on culture and mental health, highlight the Chinese cultural connotations of mental health, and help form an ideal standard of mental health for college students. Findings can serve as a theoretical foundation for improving the mental well-being of Chinese college students, act as a guiding light for enhancing students’ mental health, and be integrated directly into the mental health curriculum as course content. Mental health education activities based on these findings can help promote, maintain, and cultivate college students’ mental health literacy and healthy personalities to fulfill their potential and become the pillars of the nation.
Availability of data and materials
The datasets for this study are not readily available because they consist of interview data, for which confidentiality cannot be safeguarded. Therefore, the data will not be made available. Requests to access the datasets should be directed to XJ, [email protected].
Nooripour R, Ghanbari N, Mozaffari N, Ghahari S, Hosseini SR. The Persian Version of the Difficulties in Emotion Regulation Scale (DERS-18): Psychometric properties and its role in predicting aggression in iranian adolescents. Psychol Stud. 2023;68(2):236–46. https://doi.org/10.1007/s12646-023-00713-x .
Article Google Scholar
Gao F, Xu M, Wang P, Tian Y, Han P. Shyness and adaptation in freshmen: a cross-lagged analysis. J Psychol Sci. 2017;40(2):353–9. https://doi.org/10.16719/j.cnki.1671-6981.20170216 .
Fang Y, Wang L, Chen Z. Report on national mental health development in China (2021–2022). In: Fu X, Zhang K, editors. College Students Mental Health Survey in 2022. Beijing: China Social Sciences Academic Press; 2022.
Google Scholar
Chen M. Analysis of the causes of the phenomenon of college students’ “giant babies” and educational thinking. Lead J Ideol Theor. 2019;11:133–7. https://doi.org/10.16580/j.sxlljydk.2019.11.029 .
Huang Z, Li X. Going to college, is it far enough: a perspective on the expansion of colleges and universities. Fuzhou: Fujian Education Press; 2001.
Wang SY, Wong YJ, Yeh KH. Relationship harmony, dialectical coping, and nonattachment: Chinese indigenous well-being and mental health. Couns Psychol. 2016;44(1):78–108. https://doi.org/10.1177/0011000015616463 .
Yang X, Zhang P, Zhao J, Zhao J, Wang J, Chen Y, et al. Confucian culture still matters: The benefits of Zhongyong thinking (doctrine of the mean) for mental health. J Cross Cult Psychol. 2016;47(8):1097–113. https://doi.org/10.1177/0022022116658 .
Sam DL, Moreira V. Revisiting the mutual embeddedness of culture and mental illness. Online Read Psychol Culture. 2012;10(2):1–20. https://doi.org/10.9707/2307-0919.1078 .
Yu L. Coping with interpersonal stress in Chinese organizations. Master Thesis: National Taiwan University, Faculty of Psychology; 2018. http://tdr.lib.ntu.edu.tw/jspui/handle/123456789/7415
Kim HS, Sherman DK. “Express yourself”: culture and the effect of self-expression on choice. J Pers Soc Psychol. 2007;92(1):1–11. https://doi.org/10.1037/0022-3514.92.1.1 .
Article PubMed Google Scholar
National Bureau of Statistics of China. 2022 China Statistical Yearbook. Beijing, China. 2022. https://www.stats.gov.cn/sj/ndsj/2022/indexch.htm . Accessed 8 Oct. 2023.
Wang L, Luo H. Study on Xi Jinping’s theory of ideological and political education for college students in the new era. The Party Building and Ideological Education in Schools. 2019;03:22–6+68.
Tay AK, Riley A, Islam R, Welton-Mitchell C, Duchesne B, Waters V, et al. The culture, mental health and psychosocial wellbeing of Rohingya refugees: a systematic review. Epidemiol Psychiatr Sci. 2019;28(5):489–94. https://doi.org/10.1017/S2045796019000192 .
Article PubMed PubMed Central Google Scholar
Wang K. The Yin-Yang Definition Model of Mental Health: The Mental Health Definition in Chinese Culture. Front Psychol. 2022;13:832076. https://doi.org/10.3389/fpsyg.2022.832076 .
Nazari N, Shabbir MS, Sevbitov AV, Sadeghi M, Griffiths MD. Psychometric evaluation of the Russian version of the Gaming Disorder Scale for Adolescents. Curr Psychol. 2023;42(16):13754–68. https://doi.org/10.1007/s12144-021-02575-w .
Ghanbari N, Nooripour R, Firoozabadi A, Var TSP, Wisniewski P, Hosseini SR. Psychometric assessment of Persian translation of Yale food addiction scale version 2.0 (YFAS 2.0) in Iranian college students. J Eat Disord. 2022;10(1):158. https://doi.org/10.1186/s40337-022-00689-5 .
Hosseini SR, Tabbassi SS, Mosaferi S, Mousavinezad SH, Nooripour R, Firoozabadi A, Ghanbari N. The Persian version of the Psychotic-Like Experiences Questionnaire for Children (PLEQ-C): Psychometric properties in Iranian school students. Psychol Sch. 2023;60(3):814–29. https://doi.org/10.1002/pits.22797 .
Nooripour R, Hosseinian S, Sobhaninia M, Ghanbari N, Hassanvandi S, Ilanloo H, Kakabraee K. Predicting fear of covid-19 based on spiritual well-being and self-efficacy in Iranian University Students by emphasizing the mediating role of mindfulness. J Prac Clin Psychol. 2022;10(1):1–10. https://doi.org/10.32598/jpcp.10.1.288.6 .
Panter-Brick C, Dajani R, Eggerman M, Hermosilla S, Sancilio A, Ager A. Insecurity, distress and mental health: experimental and randomized controlled trials of a psychosocial intervention for youth affected by the Syrian crisis. J Child Psychol Psychiatry. 2018;59(5):523–41.
Britannica TCE. Beijing. China: Chinese Encyclopedia Publishing House; 1985.
Meeks L, Heit P. Health. In: Charles E, editor. A wellness approach. Columbus,OH: Merrill publishing company; 1991.
Ryan RM, Deci EL. On happiness and human potentials: A review of research on hedonic and eudaimonic well-being. Annu Rev Psychol. 2001;52(1):141–66. https://doi.org/10.1146/annurev.psych.52.1.141 .
Sayers J. The world health report 2001 mental health: new understanding, new hope. Bull World Health Organ. 2001;79(11):1085.
PubMed Central Google Scholar
Lin C, Yang Z, Huang X. The Dictionary of Psychology. Shanghai: Shanghai Education Press; 2003.
Zhang C, Yang G. Psychology. Taipei: Sanmin Bookstore; 1980.
Hu J. “Following one’s heart and not exceeding the rules”-An analysis of the definition and criteria of mental health. Educ Res Exp. 1997;02:45–8.
Yip K. Traditional Confucian concepts of mental health: Its implications to social work practice with Chinese communities. Asia Pacific J Social Work Development. 2003;13(2):65–89. https://doi.org/10.1080/21650993.2003.9755929 .
Keyes CL, Sohail MM, Molokwu NJ, Parnell H, Amanya C, Kaza VGK, et al. How would you describe a mentally healthy person? A cross-cultural qualitative study of caregivers of orphans and separated children. J Happiness Stud. 2021;22:1719–43. https://doi.org/10.1007/s10902-020-00293-x .
Chirkov V. An introduction to the theory of sociocultural models. Asian J Soc Psychol. 2020;23(2):143–62. https://doi.org/10.1111/ajsp.12381 .
Yang D, Zhang Y, Xiao S. Chinese Taoist Cognitive Therapy Introduction. J Chinese Neuropsychosis. 2002;2:152–4.
Liu T. Integrating the core concepts of traditional Chinese culture into modern psychotherapy. Health Research. 2023;43(06):601 605–630 https://doi.org/10.19890/j.cnki.issn1674-6449.2023.06.001 .
Wang D, Zhang B. Mental health and counseling for college students. Beijing, China: Beijing University Press; 1992.
Zeng Y, Lei J. A new theory on the mental health standards of college students in the post-epidemic era. J Shaoyang University (Natural Science Edition). 2021;18(4):103–9.
Jiang G, Liu J, Li S, Duan W. A review on the studies of mental health diathesis. Studies of Psychology and Behavior. 2004;2(4):586–91.
Jiang G. A theoretical analysis of research on mental health standards. Educational Res Experimentation. 1996;03:49–54.
Xin Z, Zhang M, He L. Changes in college students’ mental health: A cross-temporal meta-analysis. Acta Psychologica Sinica. 2012;44(5):664–79. https://doi.org/10.3724/SP.J.1041.2012.00664 .
Maslow AH. Motivation and Personality. 3rd ed. New York: Harper and Row; 1987.
Yip Y. Re-conceptualisation of mental health standards and the research on them. Southeast Academic Research. 2001;06:169–75+168.
Lü Z. The impact of Maslow’s “self-actualisation theory” on university students’ values. The Party Building and Ideological Education in Schools. 1990;1:46–8.
Li L. From Maslow’s “self-actualisation” theory on the shaping of healthy personality of college students. Popular Literature and Art (Academic Edition). 2013;20:254–5.
Bland AM, DeRobertis EM. Maslow’s unacknowledged contributions to developmental psychology. J Humanist Psychol. 2020;60(6):934–58. https://doi.org/10.1177/0022167817739732 .
Chen S, Jie F, Gao S, Sun P, Zheng X. Relationship between self-enhancing humor and life satisfaction A chain mediation model through emotional well-being and social support. J Psychol Sci. 2014;37(2):377–82. https://doi.org/10.16719/j.cnki.1671-6981.2014.02.022 .
Du X. Resilience of college students with rural left-behind experience in China: a qualitative study. China Jqqqqqqqqqq Social Work. 2022;15(2):178–92. https://doi.org/10.1080/17525098.2020.1834968 .
Ding Y. Qualitative research on post-traumatic growth in college students with childhood traumatic experience. The Guide of Science & Education. 2020; (15): 173–174. https://doi.org/10.16400/j.cnki.kjdkx.2020.05.081
Li Z. An experiment on the connotation of excellent Chinese traditional culture. Acad Res. 2013;11:35–9.
Ye H. Qualitative research in western psychology. J Soc Sci. 2009;11:113–8.
Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis (Bian, G. Trans.). Chongqing: Chongqing University Press; 2009.
He W, Zheng J. Qualitative research in psychology: history, current status, and prospect. J Psychol Sci. 2019;4:1017–33. https://doi.org/10.16719/j.cnki.1671-6981.20190435 .
Wang Z, Chi Y. Self-rating anxiety scale (SAS). Shanghai Arch Psychiatry. 1984;2(1):73–4.
Wang Z, Chi Y. Self-rating depression scale (SDS). Shanghai Arch Psychiatry. 1984;2(1):71–2.
Lyu M, Xi J, Luo Y. Daily emotional characteristics in individuals with different resilience levels: Supplementary evidence from experience-sampling method (ESM). Acta Psychol Sin. 2017;49(7):928–40.
Rasmussen A, Verkuilen J, Ho E, Fan Y. Posttraumatic stress disorder among refugees: Measurement invariance of Harvard Trauma Questionnaire scores across global regions and response patterns. Psychol Assess. 2015;27(4):1160.
Given LM. In: 100 questions (and answers) about qualitative research. SAGE publications; 2015.
Birks M, Mills J. Grounded theory. In: A practical guide. Sage; 2015.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Lincoln YS, Guba EG. Naturalistic inquiry. Newberry Park, CA: Sage Publications; 1985.
Book Google Scholar
Creswell JW. Qualitative inquiry and research design: Choosing among five traditions. Thousand Oaks, CA: SAGE Publications; 1998.
Ye G, Yang G. Chinese filial piety: a psychological analysis. Chongqing, China: Chongqing University Press; 2009.
Ge X. Multidimensional psychology of filial piety (xiao): Differences in orientation and changes from ancient to modern times. Acta Psychologica Sinica. 2021;53(3):306–21. https://doi.org/10.3724/SP.J.1041.2021.00306 .
Zheng D, Liao H. An analysis of filial piety culture changes in modern China under the conflict of eastern and western civilizations. Academic Exploration. 2022;1:116–22.
Wang Z, Wang F. The Taiji model of self II: developing self models and self-cultivation theories based on the Chinese cultural traditions of Taoism and Buddhism. Front Psychol. 2020;11:540074. https://doi.org/10.3389/fpsyg.2020.540074 .
Yang Z, Zhang X. The theoretical construct of mental health conceptions of the modern Chinese. J Psychol Sci. 2007;30(3):629–31. https://doi.org/10.16719/j.cnki.1671-6981.2007.03.027 .
Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73(3):539. https://doi.org/10.1037/0022-006X.73.3.539 .
Peterson C, Seligman M. Character strengths and virtues. In: A handbook and classification. New York: Oxford University Press/Washington, DC: American Psychological Association; 2004.
Shi Y, Gregg AP, Sedikides C, Cai H. Lay conceptions of modesty in China: A prototype approach. J Cross Cult Psychol. 2021;52(2):155–77.
Cai H, Kwan VS, Sedikides C. A sociocultural approach to narcissism: The case of modern China. Eur J Pers. 2011;26(5):529–35. https://doi.org/10.1002/per.852 .
Xue Y, Chen J, Xue B. Brief understanding of Tao Te Ching and Yin yang Theory. In: World Journal of Integrated Traditional and Western Medicine. 2014. p. 109–11.
Luo M, Chang J, Chen J. Cross-construction of Confucian culture and Chinese healthy psychology. Psychological Exploration. 2020;40(01):3–8. https://doi.org/CNKI:SUN:XLXT.0.2020-01-001 .
Kou Z. Reflection and modern transformation of Confucian virtue ethics. Soc Sci Guangdong. 2017;5:60–6.
Chu GC. The emergence of the new Chinese culture. In: Tseng W, Wu D, editors. Chinese culture and mental health. Florida, ORL: Academic Press, Inc; 1981. p. 15–27.
Plumwongrot P, Pholphirul P. Participating in religious activities and adolescents’ self-esteem: empirical evidence from buddhist adolescents in Thailand. Int J Adolesc Youth. 2021;26(1):185–200. https://doi.org/10.1080/02673843.2021.1890161 .
Croucher SM. Self-construals, conflict styles, and religious identification in India. Int J Confl Manag. 2013;24(4):421–36. https://doi.org/10.1108/IJCMA-03-2012-0033 .
Ministry of Education of the People’s Republic of China. Notice on Strengthening the Management of Students’ Mental Health: General Office of the Ministry of Education. Beijing, China. 2021. http://www.moe.gov.cn/srcsite/A12/moe_1407/s3020/202107/t20210720_545789.html . Accessed 02 Sept. 2021.
Huang X, Yue T. Bringing psychology to the public: An interview with professor Huang Xiting. J Teach Educ. 2022;9(1):1–9.
Han J. A comparative study of psychological health education between Chinese and American college students. Advances in Psychology. 2022;12(8):2911. https://doi.org/10.12677/AP.2022.128348 .
Huang Y. The integration and co-existence of the three Religions of Confucianism, Buddhism and Taoism and the self-adaptation of Taoism. Journal of Sichuan University (Philosophy and Social Science Edition). 2018;3:197–9.
Lou Y. The character of China. Chengdu, China: Sichuan People’s Publishing House; 2015.
Download references
Acknowledgements
We appreciate Professor Tianjun Liu from Beijing University of Chinese Medicine, Professor Jianjun Zhu, and Professor Ming Li from Beijing Forestry University for their support in assessing the appropriateness of naming, defining, and classifying the 18 characteristics and five themes. We thank our research team and participants who shared their experiences and made this study possible. We thank Dr. Xiaofang Yao at Federation University Australia and Dr. Lixian Tu at Shanghai University of Political Science and Law for their support throughout the English translation.
This study is support by the BIT Research and Innovation Promoting Project (Grant No. 2022YCXY053).
Author information
Authors and affiliations.
School of Humanities and Social Sciences, Beijing Institute of Technology, Beijing, China
Mingjia Guo, Xiaoming Jia & Wenqian Wang
You can also search for this author in PubMed Google Scholar
Contributions
MG conducted the interviews, analyzed the data and wrote the manuscript under the guidance of XJ. XJ formulated this study and contributed to editing of the manuscript and critical revisions. WW assisted with the writing and editing of the final manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Correspondence to Xiaoming Jia .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was provided by the institutional ethics committee (Graduate School of Beijing Institute of Technology).The authors confirm that all methods comply with the current guidelines and regulations which follow the Declaration of Helsinki. All participants received a written participant information leaflet, detailing information including data protection, confidentiality, withdrawal procedures and signposting to relevant organisations. All participants took part in the study with fully informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplemenatary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Guo, M., Jia, X. & Wang, W. How would you describe a mentally healthy college student based on Chinese culture? A qualitative research from the perspective of college students. BMC Psychol 12 , 207 (2024). https://doi.org/10.1186/s40359-024-01689-7
Download citation
Received : 19 August 2023
Accepted : 27 March 2024
Published : 15 April 2024
DOI : https://doi.org/10.1186/s40359-024-01689-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- College students
- Mental health
- Qualitative research
- Mental health promotion
- Chinese culture
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

IMAGES
COMMENTS
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety. The ...
Anxiety and depression among graduate students seems to be on the rise. Systemic change is needed to halt an ongoing crisis. Anxiety and depression in graduate students is worsening.
Mental health issues among graduate students. Even before the COVID-19 pandemic, poor mental health was pervasive among graduate students and in academia 2, 3. In a 2019 global survey of 6,320 PhD students, 36% of respondents reported seeking help for anxiety or depression caused by their studies 4. A synthesis of articles published through ...
A growing body of evidence indicates that mental health challenges are common among graduate students. Unfortunately, many barriers exist to effective support and care. Beginning in 2019, CGS and The JED Foundation undertook a project to create an evidence base to inform future policies, programs and resources.
Graduate students around the world need more support to manage the mental-health issues, such as depression and anxiety, that they are experiencing at worrying rates, according to a report 1 from ...
Even before the COVID-19 pandemic, poor mental health was pervasive among graduate students and in academia 2,3.In a 2019 global survey of 6,320 PhD students, 36% of respondents reported seeking ...
Introduction. Mental health and well-being is an increasingly prominent concern in graduate education [].Sixty-eight percent of university presidents acknowledged that, during the COVID-19 pandemic, student mental health ranked among their most pressing issues [].Doctoral students are an at-risk population with respect to mental health, illustrated by a study of over two thousand Ph.D ...
Despite the increasing concern about graduate student mental health among those in the scientific community (Pain, 2018; "The Mental Health of PhD Researchers," 2019; Puri, 2019), there is a lack of information about how specific aspects of science PhD programs affect students with depression. This is the first study to explicitly ...
The COVID-19 pandemic also, unsurprisingly, worsened the situation, with a more than 10% jump in the number of students with depression and anxiety symptoms. This mental health crisis has been such a big problem that mental health is the major factor behind the high attrition rates in PhD programs. If this issue is left unresolved, the academic ...
There is a mental health crisis in graduate education, and research institutions need to take action to address it. That's the take-home message from a global survey of Ph.D. and master's students published today, which adds to the meager but growing literature on the subject and corroborates anecdotal evidence and discussion about the topic from recent years, including a number of personal ...
Warren Wong/Creative Commons. Approximately one-third of Ph.D. students are at risk of having or developing a common psychiatric disorder like depression, a recent study reports. Although these results come from a small sample—3659 students at universities in Flanders, Belgium, 90% of whom were studying the sciences and social sciences—they ...
It is alarming that graduate students have six times greater risk of experiencing depression and anxiety as compared to the general population. The 2018 study, published by Dr. Theresa M. Evans, a neuroscientist at the University of Texas Health Science Center at San Antonio, surveyed graduate students from different areas of expertise such as ...
Results based on 12 mental health symptoms (GHQ-12) showed that 32% of PhD students are at risk of having or developing a common psychiatric disorder, especially depression. This estimate was significantly higher than those obtained in the comparison groups.
By nearly every metric, student mental health is worsening. During the 2020-2021 school year, more than 60% of college students met the criteria for at least one mental health problem, according to the Healthy Minds Study, which collects data from 373 campuses nationwide (Lipson, S. K., et al., Journal of Affective Disorders, Vol. 306, 2022).In another national survey, almost three quarters ...
Common Graduate Student ChallengesAs a graduate student, you may encounter a variety of challenges. Fortunately, there are plenty of resources to support you and help you overcome. Here is an introduction to some common graduate student challenges and the resources available to you. Struggling with Physical and Mental HealthNothing works unless you do. Health issues can put a full stop on your ...
Mental health problems among graduate students in doctoral degree programs have received increasing attention 1,2,3,4.Ph.D. students (and students completing equivalent degrees, such as the Sc.D ...
A Santa Clara University student holds a sign during a rally demanding better mental health services for students in December 2021 in Santa Clara, Calif. (Dai Sugano/MediaNews Group/The Mercury News via Getty Images) The coronavirus pandemic has been associated with worsening mental health among people in the United States and around the world ...
Overall, 37% of students at public and private high schools reported that their mental health was not good most or all of the time during the pandemic, according to the CDC's Adolescent Behaviors and Experiences Survey, which was fielded from January to June 2021.In the survey, "poor mental health" includes stress, anxiety and depression.
Alla Kholmogorova currently works at the Moscow State University of Psychology and Education (dean of the faculty of Counseling and Clinical Psychology). Alla does research in Health Psychology ...
In comparison, evidence-based research on mental health of doctoral students has only begun to emerge over the past five years. Recent reports indicate elevated rates of anxiety and depression among graduate students in all disciplines (UC Berkeley Graduate Assembly, 2014; Evans et al., 2018; Nagy et al., 2019; Levecque et al., 2017).
A newly released University of Minnesota report on Minnesota K-12 school principals found school leaders struggling to deal with student mental health. It can be hard to predict what St. Paul ...
The Undergraduate Student Government (USG) Senate convened for the final regularly scheduled meeting of the semester on Sunday, April 21, addressing a range of issues from collaboration efforts to mental health initiatives and student group selectivity. Mental Health Committee Chair Meera Kochhar '25 presented updates from the committee.
Suicide rates among people of all ages in the United States have increased over the past two decades, making it a serious public health problem.. Among US college athletes, suicide is now the ...
PhD students are the future of research, innovation and teaching at universities and beyond - but this future is at risk. There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.. My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were ...
The 5th European Conference on Health Promoting Schools Health, Wellbeing and Education: ... As a result of the research and case studies presented and discussions among conference participants, the following recommendations for action have been developed. ... including mental illnesses are threatening the future of many countries' health and ...
US graduate students are experiencing higher levels of mental-health distress amid the COVID-19 pandemic. Credit: Jonathan Knowles/Getty. Signs of depression among graduate students in the United ...
Suicidal thoughts are common among teens and young adults. If we can identify and support young people who are experiencing mental health symptoms, including thinking about suicide, we have an opportunity to help prevent tragedy. ... Youth and Young Adult Resources. Mental health conditions typically begin during childhood, adolescence or young ...
In essence, college students' mental health is intertwined with their moral attributes. A mentally healthy individual must embody essential moral qualities, which serve as markers of their overall well-being. Acknowledging the significance of moral virtues in defining and nurturing mental health among college students is crucial.
«Multidisciplinary aspects of personalized approach to mental health problems» will take place at the Lomonosov Moscow State University, Moscow, Russia, on 27-28 September 2019 During the Congress, it will also take place the Russian-Croatian symposium «Use of biopsychosocial and spiritual model in the diagnosis and therapy of mental disorders»
More than 40 000 students (graduate and postgraduate) and about 7 000 undergraduates study at the university, and over 5 000 specialists do the refresher course here. ... She is the recipient of a Fulbright Scholarship for 2018-2019 on the role of psychology policies and guidelines on mental health access and treatment of sexually and gender ...