- Leadership & Committees
- 2022-2027 Strategic Plan
- Patient Resources
- Sports Medicine Careers
- AOSSM Apparel Store
- Education & Events
- 2024 Annual Meeting
- Featured Programs & Events
- Abstract Submission
- Speaker Resources
- eLearning Zone
- Claiming CME/MOC Credits
- Sports Medicine Fellowships
- Become a Member
- Member Benefits
- Early Career Engagement
- Traveling Fellowship
- AOSSM Hall of Fame
- Awards & Recognitions
- Sports Medicine Update
- Research Agenda
- Grant Opportunities
- Past Grant Recipients
- Member Sponsored Surveys

American Journal of Sports Medicine
- Sports Health: A Multidisciplinary Approach
- Video Journal of Sports Medicine
- Easy Reider Podcast
- Corporate Partners
- Partnership Opportunities
- Support AOSSM
- Member Login

The American Journal of Sports Medicine (AJSM) is the official peer-reviewed scientific journal of the American Orthopaedic Society for Sports Medicine (AOSSM). Founded in 1972, AJSM is an essential forum for independent orthopaedic sports medicine research and education, allowing clinical practitioners the ability to make decisions based on sound scientific information. AJSM is published 14 times a year and contains original articles addressed to orthopaedic surgeons, team physicians, athletic trainers, and physical therapists focusing on the treatment and prevention of athletic injuries.
AJSM has a five-year impact factor of 7.392 and is ranked number two out of 82 orthopaedic publications* and number four out of 88 sports sciences publications*, explore how the AJSM and Bruce Reider, MD, Editor-in-Chief, can expand your knowledge and keep you up-to-date with the latest research through our online content .
View AJSM’s Editorial Board here.
View the Journal
AOSSM is a trusted source among the orthopaedic sports medicine profession for knowledge, skills, and continuing education. Login now to see a complete list of what's next in orthopaedic sports medicine education.
Additional Resources
Explore how the American Journal of Sports Medicine can expand your knowledge and keep you up to date with the latest research through our online content.
Current Concepts/Journal CME
The American Journal of Sports Medicine ’s Current Concepts CME activity tests your knowledge and application of material presented in Current Concept articles. Earn one credit per article towards your Part II MOC CME requirements after completing a short online post-test and evaluation. This activity provides you with researched-based information and application of critical topics in sports medicine with the most updated information for you to reflect, evaluate, and use in your practice.
This is an easy and convenient way to get your Orthopaedic CME credits for articles that you are already reading!
Keep current with AJSM monthly podcasts. The 5-in-5 podcast is an overview of each issue, making this a great start before you dive deep into each issue. After reading an issue, listen to our in-depth podcast to learn more about authors, research and editorial commentary.
Video Abstracts
Each issue features a video abstract that summarizes a feature article.
The AJSM Webinar Series provides an opportunity for authors to discuss their work with readers with ample time set aside for Q&A. Earn up to 1 AMA PRA Category 1 Credit ™ after completing a brief post-test and evaluation.
By clicking "Accept", you agree to the storing of cookies on your device and our use to enhance site navigation, analyze site usage, and assist in our communication efforts. Our cookie policy is available here .
- Open access
- Published: 22 April 2024
Off- to in-season body composition adaptations in elite male and female endurance and power event athletics competitors: an observational study
- Stefan Pettersson 1 , 2 ,
- Anton Kalén 2 , 3 ,
- Mikael Gustafsson 1 ,
- Stefan Grau 1 , 4 &
- Andreas Caspers 1
BMC Sports Science, Medicine and Rehabilitation volume 16 , Article number: 90 ( 2024 ) Cite this article
116 Accesses
1 Altmetric
Metrics details
Monitoring elite athletes’ body composition (BC) is vital for health and optimizing performance in sports emphasizing leanness, such as athletics. This study aims to investigate and compare sex- and event-specific off-to in-season BC changes in endurance and power event athletics competitors.
Elite male and female endurance athletes (> 800 m runners; n = 21) and power event athletes (sprinters, jumpers; n = 32) underwent dual-energy X-ray absorptiometry (DXA) scans for whole and regional lean mass (LM), fat mass (FM), bone mineral content (BMC), and density (BMD) during off-season (September-October) and in-season (April-May). Linear mixed models tested between-group off-season differences in BC, within-group off-season to in-season changes, and between-group differences in change. To assess meaningful or least significant changes (LSC) in BC, DXA precision errors were determined from two consecutive total body scans in a subsample of athletes ( n = 30).
Male athletes ( n = 26) gained significantly ( p < 0.05) more body mass (BM; mean difference 1.5 [95% confidence interval (CI):0.5–2.4] kg), LM (843 [95% CI:-253:1459] g), and trunk LM (756 [-502:1156] g) than female athletes ( n = 27). The proportion of changes in athlete’s BC exceeding the LSC threshold for LM and trunk LM were 70% and 65% in males, and 48% and 26% in females. Significant ( p < 0.05) within-group off-season to in-season increases in LM were found for male endurance and power athletes, and female power athletes. All groups significantly increased BMD ( p < 0.05). Only male and female power athletes had significant in- to-off-season increases in BMC. 80% of all athletes who had a meaningful increase in BMC belonged to the power event group. No significant within- or between group change in FM was observed.
Conclusions
The present study found that male athletes gained more BM, LM and trunk LM than females. Within-group increases in regional and whole-body LM and BMC were predominantly found among power event competitors. Incorporating individual meaningful changes alongside traditional statistics provided additional insights into sex and event-group differences. Future research on elite athletic event groups should include DXA measurements closer to major outdoor-season competitions, coupled with site-specific measures (ultrasound, MRI) for better detection of subtle changes in LM and FM.
Peer Review reports
Introduction
Estimation of whole and regional body composition (BC) may be valuable for improving performance, injury prevention, and assessing health risks in athletes [ 1 ]. Generally, a high power-to weight-ratio, characterized by a greater proportion of lean mass (LM), of which a significant fraction is skeletal muscle, and a lower proportion of fat mass (FM) is considered crucial for locomotion and athletic performance [ 2 ]. On the other hand, an excessive focus on obtaining a low body mass (BM) and FM content has been related to negative outcomes, including decreased bone mineral density (BMD), reduced LM, disordered eating habits and menstrual dysfunction [ 3 ]. Monitoring changes of BC during an athletic season can provide vital information for coaches, athletes, and sport medicine professionals. It facilitates the evaluation of training program effectiveness, and identification of potential health and injury risks in sports emphasizing leanness such as athletics (track and field).
Numerous studies have examined BC in athletics athletes across various events, including middle- to long-distance running (800 m to marathon), sprinting (60–400 m including hurdles), jumping (long jump, triple jump, high jump, pole vault) and throwing (shot put, javelin, discus, hammer) [ 4 , 5 , 6 , 7 , 8 , 9 , 10 ]. Each event category imposes distinct physical demands that necessitate specific anthropometric dimensions and BC for optimal performance. For example, research on middle- to long-distance runners has demonstrated an inverse relationship between regional, total, and relative FM (%FM) and performance, while LM has been positively associated with higher aerobic capacity (e.g., V̇O 2 max) in both male and female runners [ 11 , 12 , 13 , 14 ].
Similarly, sprinters and jumpers, known as power event athletes, typically exhibit a lean physique [ 15 , 16 ]. Cross-sectional studies have demonstrated that the fastest sprinters tend to possess the greatest lower body muscle mass [ 17 , 18 , 19 ]. These findings suggest that during the transition from the off-season to the competitive season, endurance event athletes may benefit from a gradual reduction in total BM by decreasing FM while minimizing changes in LM. Conversely, power event athletes may benefit from increasing LM, particularly in thigh skeletal muscle mass thickness. Studies conducted by Stanforth et al. [ 9 ] and Carbuhn et al. [ 5 ] have reported reductions in FM and %FM, accompanied by increases in LM and BMD over the course of a competitive season in female sprinters and jumpers. However, it is essential to consider the disparities in training methods between sprinters/jumpers (involving sprinting, plyometric exercises, and power lifts) and middle- to long-distance runners (primarily comprising high-volume, low-intensity aerobic exercise). These divergent training approaches likely influence seasonal changes in BC in an event-specific manner [ 20 , 21 ], however event comparisons have not been systematically researched with regards to BC methodology.
Dual-energy X-ray absorptiometry (DXA) has become an increasingly popular method for quantifying whole and regional FM, LM, BMD, and bone mineral content (BMC) in athletes [ 22 ]. While DXA is renowned for its excellent reproducibility, it is important to acknowledge that both biological factors (such as age, sex, body size, prior exercise, and acute food and fluid intake) and technical factors (DXA model, scan mode, and subject positioning on the scanning bed) can contribute to measurement errors [ 22 ]. Although adhering to a meticulous scanning protocol can mitigate some of these issues, understanding the measurement precision of the DXA device is crucial for interpreting meaningful changes when conducting consecutive BC measurements. The International Society for Clinical Densitometry (ISCD) recommends the use of the least significant change (LSC), which is calculated based on the precision error for a specific group. The LSC represents the smallest change in a BC variable that can be considered beyond the margin of error or the inherent variability in the measurement process. The objective of this study was to assess variations in BC changes between sex and event categories, and to determine the proportion of athletes who had BC changes that exceeded the DXA’s LSC.
From a prospective cohort study consisting of 96 participants, which aimed to investigate risk factors and injuries over an eleven-month athletics season [ 23 ], a subsample of 53 elite athletics competitors (26 males (M), 27 females (F)) aged 22.2 ± 2.8 years, were selected for inclusion in this study. The majority of these athletes were part of the Swedish national team and regularly participated in international events. All participants were required to be over 18 years of age, resulting in the exclusion of n = 35 athletes from the initial cohort study. Additionally, one athlete who ceased training due to severe injury for more than three consecutive weeks (10% of the study duration), between the off-season and in-season DXA measurement periods, was excluded from the analysis. Four athletes underwent the off-season DXA measurement, but not the in-season scan and were therefore excluded. Three throwing event athletes were also excluded due to their significantly different training plans, both in terms of frequency and content, compared to the other included event categories (see below). The study was conducted in accordance with the declaration of Helsinki [ 24 ], and all procedures were approved by the Regional Ethical Committee in Gothenburg (dnr. 723–16), Sweden. Additionally, all athletes gave their written informed consent.
DXA measurements
After an overnight fast, the athletes had their BM measured on a digital scale (Seca 764, Hamburg, Germany) to the nearest 0.1 kg while wearing underwear only. Height was measured to the nearest 0.5 cm with a standard wall-mounted stadiometer. Subsequently, BC was assessed using a fan-beam DXA scanner (iDXA GE Medical Systems, Madison, WI, USA) in the standard mode as determined automatically by the DXA software (EnCore, version 16.10) based on BMI. The athletes were positioned in a supine position, centrally aligned with their extremities fitting inside the measuring parameter and their feet and hands placed in custom-made radio-opaque positioning aids [ 22 ]. All scans were inspected for regions of interest misalignments and artefacts by two experienced technicians. The EnCore software automatically calculated whole- and regional FM, LM, BMC, BMD, and BMD Z-score. BMD Z-scores were calculated using the combined NHANES/Lunar database. Fat mass index (FMI) and fat-free mass index (FFMI) were calculated using the following formulas:
The DXA assessments were conducted at two seasonal periods defined in this study: off-season assessments were completed after the outdoor athletic season (September-October), while in-season assessments were conducted at the beginning of the outdoor athletic season (April-May). DXA measurements were conducted during two seasonal periods: off-season assessments occurred after the outdoor athletic season (September-October), while in-season assessments were done at the beginning of the outdoor athletic season (April-May). Time between the off-season and in-season measurements was 5.7 ± 0.7 months. The athletes were classified into one of two event categories: Endurance athletes (M/F = 9/12) competing in running events from 800 m to 10,000 m and Power athletes (M/F = 17/15) including sprinters (M/F = 14/7), long- (F = 1), triple- (M/F = 2/1) and high jumpers (F = 1) and pole-vaulters (M/F = 1/5).
Following the ISCD guidelines [ 25 ], a precision estimation of the DXA equipment was performed on a subsample of the athletes ( n = 30; M/F = 15/15; height 176 ± 6.9, BMI = 21.6 ± 2.0) who underwent duplicate scans with dismounting and repositioning on the scanning bed between measurements. The LSC was calculated following the recommended approach by the ISCD: RMS-SD × 2.77 (95% confidence interval (CI)), see Table 1 .
Training frequencies
Supplementary Fig. 1 provides information on the monthly number of training sessions and training days from October to April. The mean training hours per week (14 ± 3 h) did not significantly differ between event categories or sexes. Throughout the study period, the endurance athletes performed approximately two resistance training sessions per week, while the majority of the power athletes engaged in four strength sessions per week from October to December and two sessions per week from January to April, (as per personal communication with the strength and conditioning coaches).
Statistical analysis
Linear mixed model was fitted for each variable using cluster-robust standard errors. Time (off-season or in-season), sex (male or female), and event type (endurance or power), along with their two- and three-way interactions were included as fixed factors. The model contained a random intercept for each athlete. Difference in estimated marginal means from the models were used to test for between-group off-season differences in BC, within-group off-season to in-season change, and for between-group differences in change.
Based on the LSC calculations (Table 1 ), the off-season to in-season change of each athlete was categorized as meaningful increase, no change or decrease. All statistical analyses were conducted using R software (version 4.1.2). A significance level of p < 0.05 was used to determine statistical significance, and the Benjamini–Hochberg procedure was applied to control for the false discovery rate in all contrasts.
Off-season sex- and event-specific differences in BC
The overall off- and in-season whole and regional BC estimates of the athletes are presented in Table 2 , and off-season sex and event differences (mean [lower: upper, 95% CI]) can be found in Supplementary Table 1 . Male athletes had significantly higher BM, FFMI, BMD, BMD Z-score and total and regional LM and BMC than female athletes (p ≤ 0.042). Males, in comparison to females, also had lower FMI, %FM and total and regional FM ( p ≤ 0.006; Table 2 and Supplementary Table 1 ), except for trunk FM (mean difference − 568; [-1280: 144] g; p = 0.116).
Off-season event comparisons showed that power athletes ( n = 32) had significantly higher BM, FFMI, BMD, BMD Z-score, FMI, and FM, and total- and regional LM and BMC ( p ≤ 0.02) than endurance athletes ( n = 21), while no significant differences between events in % FM and arms FM were observed.
Male power athletes had significantly higher FFMI, FMI, BMC, BMD and BMD Z-score ( p ≤ 0.046) than male endurance athletes, but no significant differences in LM, FM, %FM or BM were observed (mean group BM difference 6.0 [0.6: 11.4] kg; p = 0.051). Female power athletes had, except for total %FM ( p = 0.058) and arms FM ( p = 0.072), significantly higher off-season BMD, BMD Z-score and total- and regional LM, BMC, and FM than the female endurance athletes ( p ≤ 0.041, see Table 2 and Supplementary Table 1 ).
Sex and event-type off- to in-season BC changes
Table 2 presents the within-group differences in total and regional body composition estimates from the off-season to the in-season. Additionally, Fig. 1 illustrates the changes in total body and trunk LM, FM, and BMC from the off- to in-season periods, while Fig. 2 displays the alterations in BC specifically in the extremities (arms and legs). No significant change in absolute or %FM was observed. The male athletes gained 1.1 kg in BM (0.5: 1.8 kg; p = 0.004), a BM change which mainly consisted of LM accretion (mean change 1257 g, [757: 1757] g, p < 0.001) in the trunk and legs (mean change 851 g and 363 g, p = < 0.001 and p = 0.009, respectively). Consequently, mean FFMI increased by 0.4 kg/m 2 ( p < 0.001) and significant increases in BMD, BMD Z-score, total BMC, and legs BMC were also noted ( p ≤ 0.015).
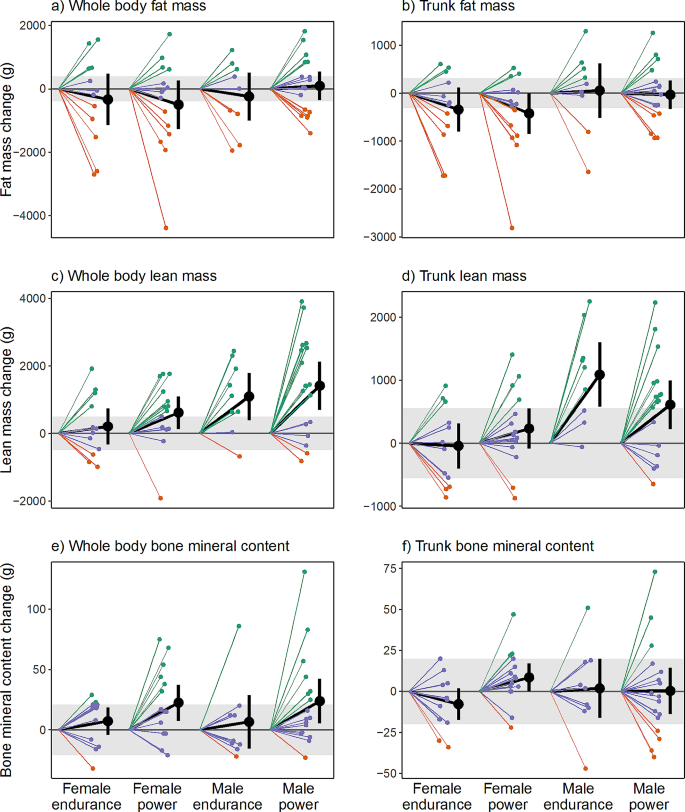
Individual off-season to in-season changes in whole body (a, c, e) and trunk (b, d, f) composition in elite male and female endurance and power athletics event competitors ( n = 53). Grey area represents least significant change (LSC)-95% confidence interval, i.e., precision error of DXA measurement. The green lines represent athletes who experienced off- to in-season changes in LM, FM, and BMC that exceeded the LSC threshold. Red lines indicate athletes who experienced reductions surpassing the LSC threshold, while purple lines represent athletes who neither increased nor reduced beyond the LSC threshold
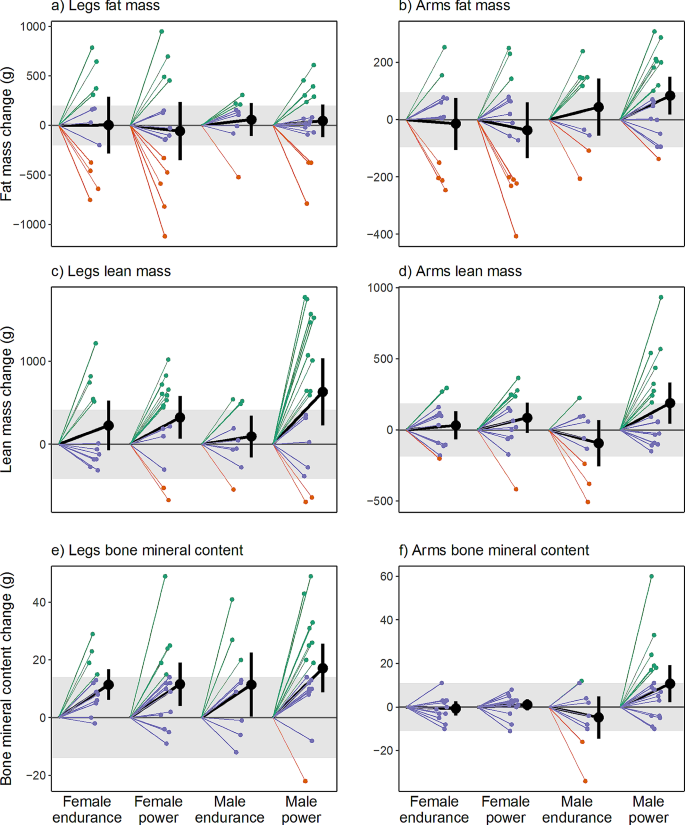
Individual off-season to in-season changes in legs (a, c, e) and arms (b, d, f) composition in elite male and female endurance and power athletics event competitors ( n = 53). Grey area represents least significant change (LSC)-95% confidence interval, i.e., precision error of DXA measurement. The green lines represent athletes who experienced off- to in-season changes in LM, FM, and BMC that exceeded the LSC threshold. Red lines indicate athletes who experienced reductions surpassing the LSC threshold, while purple lines represent athletes who neither increased nor reduced beyond the LSC threshold
Figure 3 illustrates mean changes in total and regional LM and BMC for power and endurance athletes, respectively. The male power athletes significantly increased BM (mean change 1.4 [0.6: 2.3] kg), LM (1416 [703 to 2130] g) and arms, legs, and trunk LM and FFMI ( p ≤ 0.023). BMD, BMD Z-score (Fig. 4 ), total BMC, and legs and arms BMC were also higher in-season than at off-season ( p ≤ 0.023), while no significant change was noted for FM variables except an increase in arms FM ( p = 0.023). In male endurance athletes, increments in LM (1097 [396: 1797] g; p = 0.019), trunk LM (1089 g; p = 0.001) and FFMI (0.3 kg/m 2 ; p = 0.019) were the only significant BC changes noted.
For the female athletes ( n = 27) no significant changes were found for whole or regional FM and LM variables, except legs LM which increased by 275 g from off-season to in-season (79: 475 g, p = 0.030). Furthermore, female athletes BMD, BMD Z-score, total BMC and legs BMC were significantly ( p ≤ 0.030) higher at in-season than off-season.
Female power athletes significantly increased LM (mean change 618 [133: 1103] g, p = 0.041) and FFMI (0.2 kg/m 2 , p = 0.041), total BMC and BMD (22 g and 0.039 g/cm 2 , p = 0.024 and p = 0.001, respectively) and BMD Z-score ( p = 0.008) but also legs LM (324 [67: 581] g; p = 0.041) and legs BMC (12 [4: 19] g; p = 0.024). In the female endurance athlete group, the only significant BC change observed over the course of the season were increased legs BMC (mean change 11 [6: 17] g; p = 0.001) and BMD Z-score (mean change 0.35 [0.15:0.55] p = 0.009).
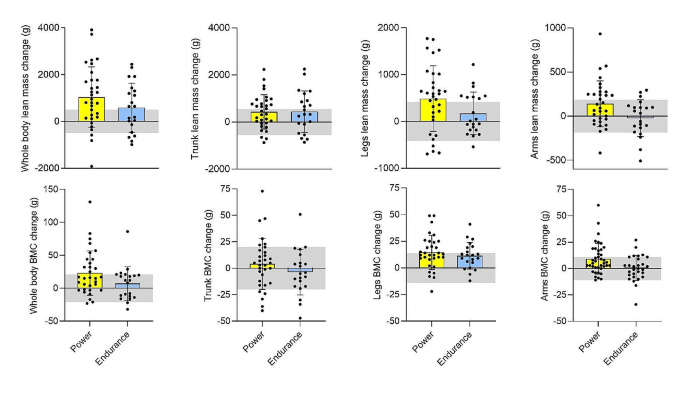
Mean off- to in-season whole and regional lean mass and bone mineral content (BMC) changes in elite male and female power ( n = 32) and endurance ( n = 21) athletics event competitors. Grey area represents least significant change (LSC)-95% confidence interval, i.e., precision error of DXA measurement
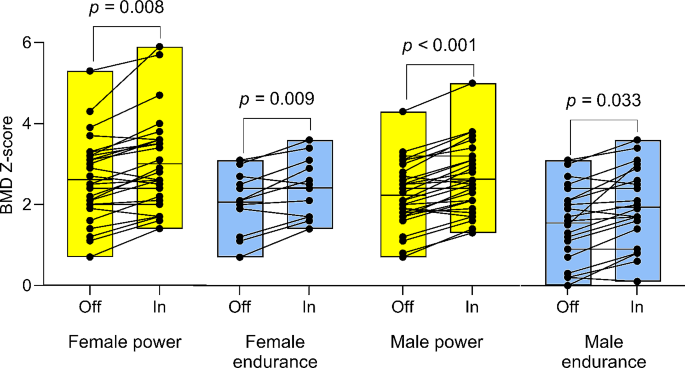
Off-season (Off) to in-season (In) changes in whole-body bone mineral density (BMD) Z-scores among elite female and male competitors in power (F: n = 15, M: n = 17) and endurance (F: n = 12, M: n = 9) athletics events. The box plots depict the mean BMD Z-score and the range of values (min-max distribution). Significant indicators denote within-group off- to in-season changes
Sex and event-type differences in off- to in-season BC changes
The results of the sex and event-type differences in off- to in-season BC changes, including 95% CI and p-values, are presented in Supplementary Table 2 . Male athletes gained significantly more BM (mean difference 1.5 [0.5: 2.4] kg; p = 0.027), LM (mean difference 843 [-253: 1459] g; p = 0.048) and Trunk LM (mean difference 756 [-502: 1156] g; p = 0.007) than female athletes. No other significant differences in BC change were found for sex and event-type.
Meaningful off- to-in-season BC changes
The figures (Figs. 1 , 2 and 3 ) present the number of athletes surpassing the LSC estimates for alterations in whole- and regional LM, BMC, BMD, and FM between the off-season and in-season, while additional statistical inferences are provided in Supplementary Table 3 . Notably, 58% of all athletes (20 power and 11 endurance) experienced a substantial increase (> 496 g) in LM whereas six athletes (11% of the total sample) exhibited a meaningful decrease in LM (> -496 g). In terms of regional LM changes, 51% and 45% respectively demonstrated a significant increase in leg LM (> 417 g) and trunk LM (> 417 g), while five athletes exhibited a decrease in leg LM (see Figs. 1 d and 2 c).
30% of athletes exhibited a verifiable increase, while 40% demonstrated a noteworthy decrease in whole-body FM (LSC = ± 396 g). Among all athletes, 32% ( n = 17) exhibited an increase in leg FM (> 202 g) with a similar relative distribution across sex and event groups (27–35%, Supplementary Table 4 ). One-third of participants ( n = 13) displayed a meaningful decrease in leg FM (Supplementary Table 4 and Fig. 2 a).
All participants had high off-season BMD (1.35 ± 0.11 cm 2 , min-max = 1.14–1.65 cm 2 ) and high BMD Z-score (2.23 ± 1.1, min-max = 0.0–5.3) values; however, 30% ( n = 16) demonstrated a meaningful increase in whole-body BMC (> 21 g), with the majority (81%) comprising power athletes ( n = 13; M/F = 8/5, Fig. 1 e). Three athletes showcased a decrease in whole-body BMC (Figs. 2 e and 3 ) that exceeded the LSC. 38% of all athletes experienced a meaningful increase (> 14 g) in leg BMC, with a larger proportion of the male power athletes (47%; n = 8) compared to the other three groups (33%, respectively).
The study aimed to investigate and compare changes in BC among elite athletics competitors during the transition from off-season to in-season, focusing on sex- and event-related variations. The results highlighted significant increases in BM, total LM, and trunk LM in male athletes compared to females. Significant within-group off-season to in-season increases in regional and whole-body LM, BMC and BMD Z-score were more prominent in power athletes than in endurance athletes. About 60% and 30% of all athletes demonstrated a meaningful increase in LM and BMC, respectively. For BMC, 80% of power athletes had a true increase, distributed equally between sexes. No significant changes were observed in any variable related to FM, except for an increase in arms FM in male power athletes.
Off- to in-season changes in LM
Sex comparisons revealed that male athletes, in contrast to females, exhibited a significant increase in LM and trunk LM from the off-season to the in-season period. The initial lower LM in females during the off-season may induce bias in favor of their increases in both total and trunk LM [ 26 ]. Other factors, such as differences in FFMI during the off-season could also contribute to the observed variation in LM accrual. Although we did not find any significant within- or between-group associations between off-season LM/FFMI and change in LM/FFMI (likely due to small sample sizes), female athletes in power and endurance events exhibited higher off-season FFMI compared to normative sport-specific FFMI values [ 27 ]. In contrast, male athletes had lower off-season muscularity index (FFMI = 19.0 ± 1.5) compared to previously reported values in aged-matched male track and field athletes (FFMI = 22.4 ± 3.7) [ 28 ], suggesting a greater potential for LM increase than in the female athletes. However, it is important to note that skeletal muscle mass only makes up for approximately 30% of total trunk LM [ 29 ]. Still, 68% of the total LM accrual in male athletes consisted of trunk LM, while in females, this proportion was 23%. Previous research on healthy non-athletes [ 30 ] and world-class powerlifters [ 31 ] has indicated that females generally exhibit lower trunk muscle thickness/mass compared to males, implying a lesser potential for significant increases in trunk skeletal mass and thus absolute trunk LM. Sex-differences in trunk LM accrual was also observed regarding meaningful changes, with 25% of all female endurance and power athletes exceeding the LSC, compared to 65% of their male counterparts, respectively.
While no significant between-event-group comparisons were found, there were significant within-group increases in LM observed in all groups, except for female endurance athletes. The off- to in-season increases in LM in the male and female power event group concur with previous findings in male and female NCAA Division 1 jumpers and sprinters [ 5 , 32 ] studied during the same period of the training year as the present study. Correspondingly, Trinschek and colleagues [ 33 ] showed that the percentage of LM in elite male polish endurance runners and sprinters significantly increased between consecutive phases of the annual training cycle. Considering that even modest resistance training frequencies have been shown to be effective in increasing muscle mass and strength [ 34 ] the inclusion of two (for endurance athletes) up to four (for power athletes) resistance training sessions per week during the study period is a plausible explanation as to why almost all athletes (87%) in the present study were able to maintain (28%) or increase (59%) LM above the LSC threshold. However, although the DXA in this study demonstrated commendable short-term precision error values for total LM (0.3%), below the ISCD [ 25 ] recommended limit (LM < 2%), future research should consider combining DXA with site-specific measures (ultrasound, CT, MRI) for improved detection of subtle seasonal changes in LM between different athletic events [ 35 ].
Off- to in-season changes in FM
Contrarily to LM changes, no significant within- or between-group reductions in whole body FM, or %FM, were observed. Off-season %FM ranged from 11.6 to 19.3% (endurance males and female power athletes, respectively) which is similar to some studies [ 9 , 33 ], but higher than other previously published DXA-derived off-season FM values in elite athletics athletes [ 32 ]. Low initial (off-season) FM levels of athletes have previously been suggested as a possible explanation for the lack of change observed during different seasons of training and/or competition [ 36 ]. However, considering that the athletes off-season FM levels in the present cohort are well above the minimum %FM cut-off values proposed by the International Olympic Committee´s Medical Commission [ 3 ] (i.e., < 5 and 12%, males and females respectively), an alternative explanation for the lack of significant off- to in-season change in FM could be the timing of the present study’s BC measurements in relation to the annual training cycle. A systematic review [ 37 ] demonstrated that male and female endurance athletes had a significantly lower percentage of FM during the competition phase compared to the preparation phase, and Mangine et al. [ 32 ] recently reported a ∼ 5% reduction in %FM in collegiate male and female sprint and power athletes between the return from winter break (early January) and the end of the indoor season (early April) but a substantially higher reduction ( ∼ 20%) between April and late May (before the NCAA Championships). Thus, future research on seasonal changes in FM should consider additional BC measurements closer to major outdoor-season competitive events. Nevertheless, the results of the present investigation are still highly relevant since prioritization of BM/FM loss in athletes is generally recommended to take place before, not during, the competitive season [ 3 ]. It is also worth noting that although the present study’s short-term precision error value for total FM (1.3%) was below the recommended limit by the ISCD [ 25 ] (< 3%), it was still considerably high compared to whole body CV’s of LM, BMC and BMD.
Off- to in-season changes in BMC and BMD
Within-group analysis revealed a significant off- to in-season increase in BMD Z-score for all groups. However, only male and female power athletes demonstrated a significant increase in whole-body BMC. Carbuhn et al. [ 5 ] discovered similar off- to in-season mean increases in absolute and relative BMC (26 g and ∼ 0.9% BMC increase, respectively) among collegiate female sprinters and jumpers, as observed in our female power event cohort (22 g and ∼ 0.8% BMC increase, respectively). However, the present LSC-analysis revealed that only 40% of the female sprinters and jumpers experienced a meaningful increase in BMC (≥ 21 g). Furthermore, the majority ( ∼ 80%) of athletes with a meaningful increase in BMC belonged to the power event group, with equal relative distribution between sexes. However, within-group off- to in-season changes in BMD found that both male/female power athletes and female endurance athletes significantly increased BMD (male endurance athletes p = 0.054; BMD Z-score significantly increased in all groups). This finding aligns with previous research [ 38 ] indicating that while the axial loading and weight-bearing nature of middle- to long-distance running can enhance bone turnover and increase BMD, the heavier power event athletes, who impose a greater vertical load on the skeleton, may further augment BMD deposition. Furthermore, all athletes were found to have high whole-body BMD (e.g., a Z-score above − 1.0) [ 39 ]. It is also important to note that three athletes experienced a meaningful decrease in BMC, highlighting the clinical relevance of LSC estimates [ 3 ].
Strength and limitations of the study
The study prioritized a high level of measurement precision by conducting fasted state DXA scans with a standardized positioning protocol [ 22 ]. Another strength of the study was the adherence to recommended guidelines by the ISCD in performing reliability statistics on a subsample of the athletes being studied. Limitations include the small sample size of the participant group, the lack of access to more detailed training diaries, and the absence of data on the athletes’ dietary intake. Training diaries should be developed in close cooperation with the athletes’ coaches to increase compliance, and could be based on e.g., volume and type of training. A 7-day diet-monitoring period during both off- and in-season could have offered insights into implementing periodized energy and macronutrient intakes for changes in BC [ 40 ]. Finally, previous DXA research has illustrated racial differences in body proportion, fat-free mass (FFM) density, and BMD [ 41 ]. Thus, the limited ethnic diversity observed within the current study’s cohort (all Caucasian/White) hinders the ability to generalize these findings to broader populations [ 41 ].
The present study revealed significant sex differences in off-to-in-season changes in total BM, LM, and trunk LM. Significant within-group increases were observed in regional and whole-body LM, BMC, predominantly among power event athletes. Even though all athletes had high off-season BMD, almost all athletes increased BMD over the six-month period. Supplementing traditional statistics with individual meaningful changes in BC also yielded additional insights into the practical relevance of off-to-in-season differences. For example, even though there was a statistically significant difference in BMC in male and female power athletes from off-to-in-season, only 40% in each group showed a meaningful change. Furthermore, it is advisable to include additional DXA measurements closer to major outdoor-season events, coupled with site-specific measures (ultrasound, MRI), to enhance the detection of subtle changes in LM and FM.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
Body composition
Bone mineral content
Bone mineral density
Confidence interval
Coefficients of variation
- Dual-energy X-ray absorptiometry
Fat-free mass index
Fat mass index
International Society for Clinical Densitometry
- Least significant change
Standard deviation
Ackland TR, Lohman TG, Sundgot-Borgen J, Maughan RJ, Meyer NL, Stewart AD et al. Current status of body composition assessment in sport: review and position statement on behalf of the ad hoc research working group on body composition health and performance, under the auspices of the I.O.C. Medical Commission. Sports medicine (Auckland, NZ). 2012;42(3):227–49.
Thomas DT, Erdman KA, Burke LM. Position of the Academy of Nutrition and Dietetics, dietitians of Canada, and the American College of Sports Medicine: Nutrition and athletic performance. J Acad Nutr Diet. 2016;116(3):501–28.
Article PubMed Google Scholar
Sundgot-Borgen J, Meyer NL, Lohman TG, Ackland TR, Maughan RJ, Stewart AD, et al. How to minimise the health risks to athletes who compete in weight-sensitive sports review and position statement on behalf of the Ad Hoc Research Working Group on Body Composition, Health and Performance, under the auspices of the IOC Medical Commission. Br J Sports Med. 2013;47(16):1012–22.
Bennell KL, Malcolm SA, Khan KM, Thomas SA, Reid SJ, Brukner PD, et al. Bone mass and bone turnover in power athletes, endurance athletes, and controls: a 12-month longitudinal study. Bone. 1997;20(5):477–84.
Article CAS PubMed Google Scholar
Carbuhn AF, Fernandez TE, Bragg AF, Green JS, Crouse SF. Sport and training influence bone and body composition in women collegiate athletes. J Strength Conditioning Res. 2010;24(7):1710–7.
Article Google Scholar
Fields JB, Merrigan JJ, White JB, Jones MT. Body composition variables by Sport and Sport-position in Elite Collegiate athletes. J Strength Conditioning Res. 2018;32(11):3153–9.
Hirsch KR, Smith-Ryan AE, Trexler ET, Roelofs EJ. Body composition and Muscle Characteristics of Division I track and field athletes. J Strength Conditioning Res. 2016;30(5):1231–8.
Spenst LF, Martin AD, Drinkwater DT. Muscle mass of competitive male athletes. J Sports Sci. 1993;11(1):3–8.
Stanforth PR, Crim BN, Stanforth D, Stults-Kolehmainen MA. Body composition changes among female NCAA division 1 athletes across the competitive season and over a multiyear time frame. J Strength Conditioning Res. 2014;28(2):300–7.
Vucetić V, Matković BR, Sentija D. Morphological differences of elite Croatian track-and-field athletes. Coll Antropol. 2008;32(3):863–8.
PubMed Google Scholar
Brandon LJ, Boileau RA. The contribution of selected variables to middle and long distance run performance. J Sports Med Phys Fit. 1987;27(2):157–64.
CAS Google Scholar
Brandon LJ, Boileau RA. Influence of metabolic, mechanical and physique variables on middle distance running. J Sports Med Phys Fit. 1992;32(1):1–9.
Hetland ML, Haarbo J, Christiansen C. Regional body composition determined by dual-energy X-ray absorptiometry. Relation to training, sex hormones, and serum lipids in male long-distance runners. Scand J Med Sci Sports. 1998;8(2):102–8.
Yoshiga CC, Higuchi M. Oxygen uptake and ventilation during rowing and running in females and males. Scand J Med Sci Sports. 2003;13(6):359–63.
Malina RM, Harper AB, Avent HH, Campbell DE. Physique of female track and field athletes. Med Sci Sports. 1971;3(1):32–8.
CAS PubMed Google Scholar
Pipes TV. Body composition characteristics of male and female track and field athletes. Res Q. 1977;48(1):244–7.
Kubo K, Ikebukuro T, Yata H, Tomita M, Okada M. Morphological and mechanical properties of muscle and tendon in highly trained sprinters. J Appl Biomech. 2011;27(4):336–44.
Kumagai K, Abe T, Brechue WF, Ryushi T, Takano S, Mizuno M. Sprint performance is related to muscle fascicle length in male 100-m sprinters. Journal of applied physiology (Bethesda, Md: 1985). 2000;88(3):811-6.
Sugisaki N, Kanehisa H, Tauchi K, Okazaki S, Iso S, Okada JJIJS et al. The relationship between 30-m sprint running time and muscle cross-sectional areas of the psoas major and lower limb muscles in male college short and middle distance runners. 2010:1101140066-.
Haugen T, Seiler S, Sandbakk Ø, Tønnessen E. The training and development of Elite Sprint performance: an integration of Scientific and best practice literature. Sports Med - open. 2019;5(1):44.
Article PubMed PubMed Central Google Scholar
Tjelta, LIJIJoSS. Coaching. The training of international level distance runners. 2016;11(1):122– 34.
Nana A, Slater GJ, Stewart AD, Burke LM. Methodology review: using dual-energy X-ray absorptiometry (DXA) for the assessment of body composition in athletes and active people. Int J Sport Nutr Exerc Metab. 2015;25(2):198–215.
Lundberg Zachrisson A, Ivarsson A, Desai, Karlsson J, Grau S. Risk factors for overuse injuries in a cohort of elite Swedish track and field athletes. BMC Sports Sci Med Rehabilitation. 2021;13(1):73.
Association GAotWM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81(3):14–8.
Google Scholar
Hangartner TN, Warner S, Braillon P, Jankowski L, Shepherd J. The Official positions of the International Society for Clinical Densitometry: acquisition of dual-energy X-ray absorptiometry body composition and considerations regarding analysis and repeatability of measures. J Clin Densitometry: Official J Int Soc Clin Densitometry. 2013;16(4):520–36.
Alway SE, Grumbt WH, Gonyea WJ, Stray-Gundersen J. Contrasts in muscle and myofibers of elite male and female bodybuilders. Journal of applied physiology (Bethesda, Md: 1985). 1989;67(1):24–31.
Blue MNM, Hirsch KR, Pihoker AA, Trexler ET, Smith-Ryan AE. Normative fat-free mass index values for a diverse sample of collegiate female athletes. J Sports Sci. 2019;37(15):1741–5.
Currier BS, Harty PS, Zabriskie HA, Stecker RA, Moon JM, Jagim AR, et al. Fat-Free Mass Index in a diverse sample of male Collegiate athletes. J Strength Conditioning Res. 2019;33(6):1474–9.
McCarthy C, Tinsley GM, Bosy-Westphal A, Müller MJ, Shepherd J, Gallagher D, et al. Total and regional appendicular skeletal muscle mass prediction from dual-energy X-ray absorptiometry body composition models. Sci Rep. 2023;13(1):2590.
Article CAS PubMed PubMed Central Google Scholar
Abe T, Kearns CF, Fukunaga T. Sex differences in whole body skeletal muscle mass measured by magnetic resonance imaging and its distribution in young Japanese adults. Br J Sports Med. 2003;37(5):436–40.
Abe T, Bell ZW, Wong V, Spitz RW, Yamada Y, Song JS, et al. Skeletal muscle size distribution in large-sized male and female athletes. Am J Hum Biology: Official J Hum Biology Council. 2021;33(2):e23473.
Mangine GT, Mangine GT, Eggerth A, Gough J, Stratton MT, Feito Y, et al. Endocrine and body composition changes across a competitive season in Collegiate speed-power track and field athletes. J Strength Conditioning Res. 2021;35(8):2067–74.
Trinschek J, Zieliński J, Kusy K. Maximal oxygen uptake adjusted for skeletal muscle Mass in competitive speed-power and endurance male athletes: changes in a one-year training cycle. Int J Environ Res Public Health. 2020;17(17).
Gomes GK, Franco CM, Nunes PRP, Orsatti FL. High-frequency resistance training is not more effective than low-frequency resistance training in increasing muscle Mass and Strength in Well-trained men. J Strength Conditioning Res. 2019;33(Suppl 1):S130–9.
Levine JA, Abboud L, Barry M, Reed JE, Sheedy PF, Jensen MD. Measuring leg muscle and fat mass in humans: comparison of CT and dual-energy X-ray absorptiometry. Journal of applied physiology (Bethesda, Md: 1985). 2000;88(2):452-6.
Koutedakis Y. Seasonal variation in fitness parameters in competitive athletes. Sports Med (Auckland NZ). 1995;19(6):373–92.
Article CAS Google Scholar
Heydenreich J, Kayser B, Schutz Y, Melzer K. Total energy expenditure, Energy Intake, and body composition in Endurance Athletes across the Training Season: a systematic review. Sports Med - open. 2017;3(1):8.
Maïmoun L, Sultan C. Effects of physical activity on bone remodeling. Metab Clin Exp. 2011;60(3):373–88.
Jonvik KL, Torstveit MK, Sundgot-Borgen J, Mathisen TF. Do we need to change the guideline values for determining low bone mineral density in athletes? Journal of applied physiology (Bethesda, Md: 1985). 2022;132(5):1320-2.
Magkos F, Yannakoulia M. Methodology of dietary assessment in athletes: concepts and pitfalls. Curr Opin Clin Nutr Metab Care. 2003;6(5):539–49.
Stults-Kolehmainen MA, Stanforth PR, Bartholomew JB, Lu T, Abolt CJ, Sinha R. DXA estimates of fat in abdominal, trunk and hip regions varies by ethnicity in men. Nutr Diabetes. 2013;3(3):e64.
Download references
Acknowledgements
The authors wish to thank the athletes who volunteered to participate in this study.
Open access funding provided by University of Gothenburg.
Author information
Authors and affiliations.
Center for Health and Performance, Department of Food and Nutrition, and Sport Science, University of Gothenburg, Gothenburg, Sweden
Stefan Pettersson, Mikael Gustafsson, Stefan Grau & Andreas Caspers
Swedish Olympic Committee, Sofiatornet, Olympiastadion, Stockholm, Sweden
Stefan Pettersson & Anton Kalén
Department of Computer Science, Electrical and Space Engineering, Luleå University of Technology, Luleå, Sweden
Anton Kalén
Department of Sports Medicine, University Clinic Tübingen, Tübingen, Germany
Stefan Grau
You can also search for this author in PubMed Google Scholar
Contributions
SP, AC and SG contributed to the original idea, study design and the conception of the work. AC and SP performed measurements and AK performed all statistical analysis except for the DXA’s reliability statistics (MG). SP wrote the main manuscript text. SP, AK, MG, AC and SG revised and edited the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Stefan Pettersson .
Ethics declarations
Ethics approval and consent to participate.
All participants were informed of the potential risks, benefits, and dissemination of the research before providing written informed consent to participate. Furthermore, all participants provided voluntary written informed consent prior to their involvement in the study. During the study process the authors followed the rules of the Helsinki Declaration. Ethics approval was obtained from the Regional Ethical Committee in Gothenburg (dnr. 723–16), Sweden.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pettersson, S., Kalén, A., Gustafsson, M. et al. Off- to in-season body composition adaptations in elite male and female endurance and power event athletics competitors: an observational study. BMC Sports Sci Med Rehabil 16 , 90 (2024). https://doi.org/10.1186/s13102-024-00877-7
Download citation
Received : 07 July 2023
Accepted : 03 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s13102-024-00877-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Track and field
BMC Sports Science, Medicine and Rehabilitation
ISSN: 2052-1847
- General enquiries: [email protected]
Sports Medicine Research

Fair Play rules make ice hockey safer
Fair Play (PDF) is an initiative developed and implemented by Mayo Clinic Sports Medicine Research to reduce the incidence of concussions and make hockey a safer sport.

Research improves all aspects of sports mechanics
Mayo Clinic Sports Medicine Research is using research discoveries to improve strength, power, agility and speed and prevent common injuries such as ACL tears in athletes.

Biomechanics breaks down movement to prevent injury
Mayo Clinic Sports Medicine Research is using biomechanics research to show how pitching and swing mechanics can put an athlete at risk for injury.
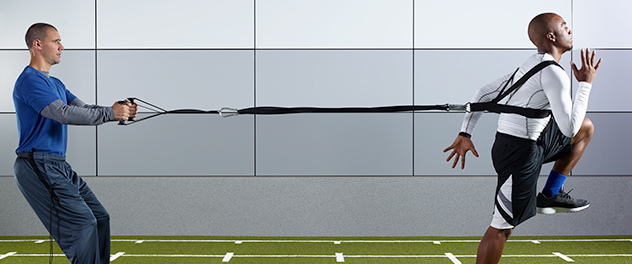
Striving to improve athletic performance
Mayo Clinic Sports Medicine Research: Preventing and treating sports injuries to improve and enhance athletic performance.
Mayo Clinic Sports Medicine Research performs leading-edge research to define the mechanism of injury and utilizes these findings to implement educational programs and therapeutic interventions. This work helps prevent injuries, enhances athletic performance and increases injury prevention during play.
Sports Medicine Research investigates all aspects of sports injury evaluation, treatment and prevention to provide optimal care to those involved in sports- or fitness-related activities. Recent work has addressed neuromuscular interventions to prevent anterior cruciate ligament (ACL) injuries, the use of subsymptom exercise to return athletes who've had concussions to a pre-head-trauma state and the modeling of lower extremity athletic joint injuries.
Research focus areas
Mayo Clinic Sports Medicine Research focuses on the following areas for optimal care and results for athletes:
- Mechanisms that may identify the anatomical and structural causes of injuries
- Screening using algorithms to identify athletes at a high risk of injury
- Intervention and prevention through neuromuscular training protocols
- Treatment strategies (surgical and nonsurgical) to optimize outcomes after injury
Comprehensive care comes from bringing research directly into practice. A complete team of surgeons, physicians, researchers, specialists and therapists work together to return people to physical activity as soon as possible.
- Twitter @mayoclinicsport - Connect Twitter @mayoclinicsport
- Facebook - Connect Facebook
- Instagram #mayoclinicsportsmedicine - Connect Instagram #mayoclinicsportsmedicine
- Contacts - Connect Contacts
Mayo Clinic Sports Medicine
Learn more about clinical services, sports performance training and how to make an appointment.
Focus Areas
Research is focused into specialized areas to diagnose, treat and prevent diseases or conditions that affect athletic performance for the professional and recreational athlete.
Clinical Research Areas
Clinical research areas in ACL, concussion, hip, knee and shoulder apply scientific discoveries to diagnose and treat athletes for the best outcomes.
More about research at Mayo Clinic
- Research Faculty
- Laboratories
- Core Facilities
- Centers & Programs
- Departments & Divisions
- Clinical Trials
- Institutional Review Board
- Postdoctoral Fellowships
- Training Grant Programs
- Publications
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
- Supplements
- Most Read Articles
- Most Cited Articles
- Editorial board
- Authors instructions
- For Reviewers


Original Research Articles
Articles published in Sports Medicine - Open will include a Key Points table. Please provide approximately three short, stand-alone lines/statements summarizing the key findings/implications of the paper. These should be provided after the Abstract under the heading 'Key Points’.
Please note that we advocate the explicit naming of each author in the `Competing Interests’ statement. For example:
`John Smith declares that he has no competing interests’
`Paula Taylor has received research grants from Drug Company A.’
`Mike Schultz has received a speaker honorarium from Drug Company B and own stock in Drug Company C.’
When multiple authors declare no competing interests, this can be stated in one sentence:
`John Smith, Paula Taylor and Mike Schultz declare that they have no competing interests.’
Preparing your manuscript
The title page should:
- present a title that includes, if appropriate, the study design
- if a collaboration group should be listed as an author, please list the Group name as an author. If you would like the names of the individual members of the Group to be searchable through their individual PubMed records, please include this information in the “Acknowledgements” section in accordance with the instructions below
- Large Language Models (LLMs), such as ChatGPT , do not currently satisfy our authorship criteria . Notably an attribution of authorship carries with it accountability for the work, which cannot be effectively applied to LLMs. Use of an LLM should be properly documented in the Methods section (and if a Methods section is not available, in a suitable alternative part) of the manuscript
- indicate the corresponding author
The abstract should not exceed 350 words. Please minimize the use of abbreviations and do not cite references in the abstract. The abstract must include the following separate sections:
- Background : the context and purpose of the study
- Results : the main findings
- Conclusions : a brief summary and potential implications
Three to ten keywords representing the main content of the article.
The Background section should explain the background to the study, its aims, a summary of the existing literature and why this study was necessary.
This should include the findings of the study including, if appropriate, results of statistical analysis which must be included either in the text or as tables and figures.
For research articles this section should discuss the implications of the findings in context of existing research and highlight limitations of the study. For study protocols and methodology manuscripts this section should include a discussion of any practical or operational issues involved in performing the study and any issues not covered in other sections.
Conclusions
This should state clearly the main conclusions and provide an explanation of the importance and relevance of the study to the field.
Methods (can also be placed after Background)
The methods section should include:
- the aim, design and setting of the study
- the characteristics of participants or description of materials
- a clear description of all processes, interventions and comparisons. Generic names should generally be used. When proprietary brands are used in research, include the brand names in parentheses
- the type of statistical analysis used, including a power calculation if appropriate
List of abbreviations
If abbreviations are used in the text they should be defined in the text at first use, and a list of abbreviations should be provided.
Declarations
All manuscripts must contain the following sections under the heading 'Declarations':
Ethics approval and consent to participate
Consent for publication.
- Availability of data and material
Competing interests
Authors' contributions, acknowledgements.
- Authors' information (optional)
Please see below for details on the information to be included in these sections.
If any of the sections are not relevant to your manuscript, please include the heading and write 'Not applicable' for that section.
Manuscripts reporting studies involving human participants, human data or human tissue must:
- include a statement on ethics approval and consent (even where the need for approval was waived)
- include the name of the ethics committee that approved the study and the committee’s reference number if appropriate
Studies involving animals must include a statement on ethics approval.
See our editorial policies for more information.
If your manuscript does not report on or involve the use of any animal or human data or tissue, please state “Not applicable” in this section.
If your manuscript contains any individual person’s data in any form (including individual details, images or videos), consent to publish must be obtained from that person, or in the case of children, their parent or legal guardian. All presentations of case reports must have consent to publish.
You can use your institutional consent form if you prefer. You should not send the form to us on submission, but we may request to see a copy at any stage (including after publication).
See our editorial policies for more information on consent for publication.
If your manuscript does not contain data from any individual person, please state “Not applicable” in this section.
Availability of data and materials
All manuscripts must include an ‘Availability of data and materials’ statement. Data availability statements should include information on where data supporting the results reported in the article can be found including, where applicable, hyperlinks to publicly archived datasets analysed or generated during the study. By data we mean the minimal dataset that would be necessary to interpret, replicate and build upon the findings reported in the article. We recognise it is not always possible to share research data publicly, for instance when individual privacy could be compromised, and in such instances data availability should still be stated in the manuscript along with any conditions for access.
Data availability statements can take one of the following forms (or a combination of more than one if required for multiple datasets):
- The datasets generated and/or analysed during the current study are available in the [NAME] repository, [PERSISTENT WEB LINK TO DATASETS]
- The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
- All data generated or analysed during this study are included in this published article [and its supplementary information files].
- The datasets generated and/or analysed during the current study are not publicly available due [REASON WHY DATA ARE NOT PUBLIC] but are available from the corresponding author on reasonable request.
- Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
- The data that support the findings of this study are available from [third party name] but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of [third party name].
- Not applicable. If your manuscript does not contain any data, please state 'Not applicable' in this section.
More examples of template data availability statements, which include examples of openly available and restricted access datasets, are available here .
SpringerOpen also requires that authors cite any publicly available data on which the conclusions of the paper rely in the manuscript. Data citations should include a persistent identifier (such as a DOI) and should ideally be included in the reference list. Citations of datasets, when they appear in the reference list, should include the minimum information recommended by DataCite and follow journal style. Dataset identifiers including DOIs should be expressed as full URLs. For example:
Hao Z, AghaKouchak A, Nakhjiri N, Farahmand A. Global integrated drought monitoring and prediction system (GIDMaPS) data sets. figshare. 2014. http://dx.doi.org/10.6084/m9.figshare.853801
With the corresponding text in the Availability of data and materials statement:
The datasets generated during and/or analysed during the current study are available in the [NAME] repository, [PERSISTENT WEB LINK TO DATASETS]. [Reference number]
All financial and non-financial competing interests must be declared in this section.
See our editorial policies for a full explanation of competing interests. If you are unsure whether you or any of your co-authors have a competing interest please contact the editorial office.
Please use the authors’ initials to refer to each authors' competing interests in this section.
If you do not have any competing interests, please state "The authors declare that they have no competing interests" in this section.
All sources of funding for the research reported should be declared. The role of the funding body in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript should be declared.
The individual contributions of authors to the manuscript should be specified in this section. Guidance and criteria for authorship can be found in our editorial policies .
Please use initials to refer to each author's contribution in this section, for example: "FC analyzed and interpreted the patient data regarding the hematological disease and the transplant. RH performed the histological examination of the kidney, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript."
Please acknowledge anyone who contributed towards the article who does not meet the criteria for authorship including anyone who provided professional writing services or materials.
Authors should obtain permission to acknowledge from all those mentioned in the Acknowledgements section.
See our editorial policies for a full explanation of acknowledgements and authorship criteria.
If you do not have anyone to acknowledge, please write "Not applicable" in this section.
Group authorship (for manuscripts involving a collaboration group): if you would like the names of the individual members of a collaboration Group to be searchable through their individual PubMed records, please ensure that the title of the collaboration Group is included on the title page and in the submission system and also include collaborating author names as the last paragraph of the “Acknowledgements” section. Please add authors in the format First Name, Middle initial(s) (optional), Last Name. You can add institution or country information for each author if you wish, but this should be consistent across all authors.
Please note that individual names may not be present in the PubMed record at the time a published article is initially included in PubMed as it takes PubMed additional time to code this information.
Authors' information
This section is optional.
You may choose to use this section to include any relevant information about the author(s) that may aid the reader's interpretation of the article, and understand the standpoint of the author(s). This may include details about the authors' qualifications, current positions they hold at institutions or societies, or any other relevant background information. Please refer to authors using their initials. Note this section should not be used to describe any competing interests.
Footnotes should be designated within the text using a superscript number. It is not allowed to use footnotes for references/citations.
Examples of the Vancouver reference style are shown below.
See our editorial policies for author guidance on good citation practice.
Web links and URLs: All web links and URLs, including links to the authors' own websites, should be given a reference number and included in the reference list rather than within the text of the manuscript. They should be provided in full, including both the title of the site and the URL, as well as the date the site was accessed, in the following format: The Mouse Tumor Biology Database. http://tumor.informatics.jax.org/mtbwi/index.do . Accessed 20 May 2013. If an author or group of authors can clearly be associated with a web link, such as for weblogs, then they should be included in the reference.
Example reference style:
Article within a journal
Smith JJ. The world of science. Am J Sci. 1999;36:234-5.
Article within a journal (no page numbers)
Rohrmann S, Overvad K, Bueno-de-Mesquita HB, Jakobsen MU, Egeberg R, Tjønneland A, et al. Meat consumption and mortality - results from the European Prospective Investigation into Cancer and Nutrition. BMC Medicine. 2013;11:63.
Article within a journal by DOI
Slifka MK, Whitton JL. Clinical implications of dysregulated cytokine production. Dig J Mol Med. 2000; doi:10.1007/s801090000086.
Article within a journal supplement
Frumin AM, Nussbaum J, Esposito M. Functional asplenia: demonstration of splenic activity by bone marrow scan. Blood 1979;59 Suppl 1:26-32.
Book chapter, or an article within a book
Wyllie AH, Kerr JFR, Currie AR. Cell death: the significance of apoptosis. In: Bourne GH, Danielli JF, Jeon KW, editors. International review of cytology. London: Academic; 1980. p. 251-306.
OnlineFirst chapter in a series (without a volume designation but with a DOI)
Saito Y, Hyuga H. Rate equation approaches to amplification of enantiomeric excess and chiral symmetry breaking. Top Curr Chem. 2007. doi:10.1007/128_2006_108.
Complete book, authored
Blenkinsopp A, Paxton P. Symptoms in the pharmacy: a guide to the management of common illness. 3rd ed. Oxford: Blackwell Science; 1998.
Online document
Doe J. Title of subordinate document. In: The dictionary of substances and their effects. Royal Society of Chemistry. 1999. http://www.rsc.org/dose/title of subordinate document. Accessed 15 Jan 1999.
Online database
Healthwise Knowledgebase. US Pharmacopeia, Rockville. 1998. http://www.healthwise.org. Accessed 21 Sept 1998.
Supplementary material/private homepage
Doe J. Title of supplementary material. 2000. http://www.privatehomepage.com. Accessed 22 Feb 2000.
University site
Doe, J: Title of preprint. http://www.uni-heidelberg.de/mydata.html (1999). Accessed 25 Dec 1999.
Doe, J: Trivial HTTP, RFC2169. ftp://ftp.isi.edu/in-notes/rfc2169.txt (1999). Accessed 12 Nov 1999.
Organization site
ISSN International Centre: The ISSN register. http://www.issn.org (2006). Accessed 20 Feb 2007.
Dataset with persistent identifier
Zheng L-Y, Guo X-S, He B, Sun L-J, Peng Y, Dong S-S, et al. Genome data from sweet and grain sorghum (Sorghum bicolor). GigaScience Database. 2011. http://dx.doi.org/10.5524/100012 .
General formatting information
Manuscripts must be written in concise English. For help on scientific writing, or preparing your manuscript in English, please see Springer's Author Academy .
Quick points:
- Use double line spacing
- Include line and page numbering
- Use SI units: Please ensure that all special characters used are embedded in the text, otherwise they will be lost during conversion to PDF
- Do not use page breaks in your manuscript
File formats
The following word processor file formats are acceptable for the main manuscript document:
- Microsoft word (DOC, DOCX)
- Rich text format (RTF)
- TeX/LaTeX
Please note: editable files are required for processing in production. If your manuscript contains any non-editable files (such as PDFs) you will be required to re-submit an editable file if your manuscript is accepted.
For more information, see ' Preparing figures ' below.
Additional information for TeX/LaTeX users
You are encouraged to use the Springer Nature LaTeX template when preparing a submission. A PDF of your manuscript files will be compiled during submission using pdfLaTeX and TexLive 2021. All relevant editable source files must be uploaded during the submission process. Failing to submit these source files will cause unnecessary delays in the production process.
Style and language
For editors and reviewers to accurately assess the work presented in your manuscript you need to ensure the English language is of sufficient quality to be understood. If you need help with writing in English you should consider:
- Getting a fast, free online grammar check .
- Visiting the English language tutorial which covers the common mistakes when writing in English.
- Asking a colleague who is proficient in English to review your manuscript for clarity.
- Using a professional language editing service where editors will improve the English to ensure that your meaning is clear and identify problems that require your review. Two such services are provided by our affiliates Nature Research Editing Service and American Journal Experts . SpringerOpen authors are entitled to a 10% discount on their first submission to either of these services. To claim 10% off English editing from Nature Research Editing Service, click here . To claim 10% off American Journal Experts, click here .
Please note that the use of a language editing service is not a requirement for publication in Sports Medicine - Open and does not imply or guarantee that the article will be selected for peer review or accepted. 为便于编辑和评审专家准确评估您稿件中陈述的研究工作,您需要确保文稿英语语言质量足以令人理解。如果您需要英文写作方面的帮助,您可以考虑:
- 获取快速、免费的在线 语法检查 。
- 查看一些有关英语写作中常见语言错误的 教程 。
- 请一位以英语为母语的同事审阅您的稿件是否表意清晰。
- 使用专业语言编辑服务,编辑人员会对英语进行润色,以确保您的意思表达清晰,并提出需要您复核的问题。例如我们的附属机构 Nature Research Editing Service 以及合作伙伴 American Journal Experts 都可以提供此类专业服务。SpringerOpen作者享受首次订单10%优惠,该优惠同时适用于两家公司。您只需点击以下链接即可开始。使用 Nature Research Editing Service的编辑润色10%的优惠服务,请点击 这里 。使用 American Journal Experts的10%优惠服务,请点击 这里 。
请注意,使用语言编辑服务并非在期刊上发表文章的必要条件,这也并不意味或保证文章将被选中进行同行评议或被接受。 エディターと査読者があなたの論文を正しく評価するには、使用されている英語の質が十分であることが必要とされます。英語での論文執筆に際してサポートが必要な場合には、次のオプションがあります:
- 高速なオンライン 文法チェック を無料で受ける。
- 英語で執筆する際のよくある間違いに関する 英語のチュートリアル を参照する。
- 英語を母国語とする同僚に、原稿内の英語が明確であるかをチェックしてもらう。
- プロの英文校正サービスを利用する。校正者が原稿の意味を明確にしたり、問題点を指摘し、英語を向上させます。 Nature Research Editing Service と American Journal Experts の2つは弊社と提携しているサービスです。SpringerOpenのジャーナルの著者は、いずれかのサービスを初めて利用する際に、10%の割引を受けることができます。Nature Research Editing Serviceの10%割引を受けるには、 こちらをクリックしてください 。. American Journal Expertsの10%割引を受けるには、 こちらをクリックしてください 。
英文校正サービスの利用は、このジャーナルに掲載されるための条件ではないこと、また論文審査や受理を保証するものではないことに留意してください。 영어 원고의 경우, 에디터 및 리뷰어들이 귀하의 원고에 실린 결과물을 정확하게 평가할 수 있도록, 그들이 충분히 이해할 수 있을 만한 수준으로 작성되어야 합니다. 만약 영작문과 관련하여 도움을 받기를 원하신다면 다음의 사항들을 고려하여 주십시오:
- 영어 튜토리얼 페이지 에 방문하여 영어로 글을 쓸 때 자주하는 실수들을 확인합니다.
- 귀하의 원고의 표현을 명확히 해줄 영어 원어민 동료를 찾아서 리뷰를 의뢰합니다
- 리뷰에 대비하여, 원고의 의미를 명확하게 해주고 리뷰에서 요구하는 문제점들을 식별해서 영문 수준을 향상시켜주는 전문 영문 교정 서비스를 이용합니다. Nature Research Editing Service 와 American Journal Experts 에서 저희와 협약을 통해 서비스를 제공하고 있습니다. SpringerOpen에서는 위의 두 가지의 서비스를 첫 논문 투고를 위해 사용하시는 경우, 10%의 할인을 제공하고 있습니다. Nature Research Editing Service이용시 10% 할인을 요청하기 위해서는 여기 를 클릭해 주시고, American Journal Experts 이용시 10% 할인을 요청하기 위해서는 여기 를 클릭해 주십시오.
영문 교정 서비스는 게재를 위한 요구사항은 아니며, 해당 서비스의 이용이 피어 리뷰에 논문이 선택되거나 게재가 수락되는 것을 의미하거나 보장하지 않습니다.
Data and materials
For all journals, SpringerOpen strongly encourages all datasets on which the conclusions of the manuscript rely to be either deposited in publicly available repositories (where available and appropriate) or presented in the main paper or additional supporting files, in machine-readable format (such as spread sheets rather than PDFs) whenever possible. Please see the list of recommended repositories in our editorial policies.
For some journals, deposition of the data on which the conclusions of the manuscript rely is an absolute requirement. Please check the Instructions for Authors for the relevant journal and article type for journal specific policies.
For all manuscripts, information about data availability should be detailed in an ‘Availability of data and materials’ section. For more information on the content of this section, please see the Declarations section of the relevant journal’s Instruction for Authors. For more information on SpringerOpen's policies on data availability, please see our editorial policies .
Formatting the 'Availability of data and materials' section of your manuscript
The following format for the 'Availability of data and materials section of your manuscript should be used:
"The dataset(s) supporting the conclusions of this article is(are) available in the [repository name] repository, [unique persistent identifier and hyperlink to dataset(s) in http:// format]."
The following format is required when data are included as additional files:
"The dataset(s) supporting the conclusions of this article is(are) included within the article (and its additional file(s))."
For databases, this section should state the web/ftp address at which the database is available and any restrictions to its use by non-academics.
For software, this section should include:
- Project name: e.g. My bioinformatics project
- Project home page: e.g. http://sourceforge.net/projects/mged
- Archived version: DOI or unique identifier of archived software or code in repository (e.g. enodo)
- Operating system(s): e.g. Platform independent
- Programming language: e.g. Java
- Other requirements: e.g. Java 1.3.1 or higher, Tomcat 4.0 or higher
- License: e.g. GNU GPL, FreeBSD etc.
- Any restrictions to use by non-academics: e.g. licence needed
Information on available repositories for other types of scientific data, including clinical data, can be found in our editorial policies .
What should be cited?
Only articles, clinical trial registration records and abstracts that have been published or are in press, or are available through public e-print/preprint servers, may be cited.
Unpublished abstracts, unpublished data and personal communications should not be included in the reference list, but may be included in the text and referred to as "unpublished observations" or "personal communications" giving the names of the involved researchers. Obtaining permission to quote personal communications and unpublished data from the cited colleagues is the responsibility of the author. Either footnotes or endnotes are permitted. Journal abbreviations follow Index Medicus/MEDLINE.
Any in press articles cited within the references and necessary for the reviewers' assessment of the manuscript should be made available if requested by the editorial office.

Preparing figures
When preparing figures, please follow the formatting instructions below.
- Figure titles (max 15 words) and legends (max 300 words) should be provided in the main manuscript, not in the graphic file.
- Tables should NOT be submitted as figures but should be included in the main manuscript file.
- Multi-panel figures (those with parts a, b, c, d etc.) should be submitted as a single composite file that contains all parts of the figure.
- Figures should be numbered in the order they are first mentioned in the text, and uploaded in this order.
- Figures should be uploaded in the correct orientation.
- Figure keys should be incorporated into the graphic, not into the legend of the figure.
- Each figure should be closely cropped to minimize the amount of white space surrounding the illustration. Cropping figures improves accuracy when placing the figure in combination with other elements when the accepted manuscript is prepared for publication on our site. For more information on individual figure file formats, see our detailed instructions.
- Individual figure files should not exceed 10 MB. If a suitable format is chosen, this file size is adequate for extremely high quality figures.
- Please note that it is the responsibility of the author(s) to obtain permission from the copyright holder to reproduce figures (or tables) that have previously been published elsewhere. In order for all figures to be open access, authors must have permission from the rights holder if they wish to include images that have been published elsewhere in non open access journals. Permission should be indicated in the figure legend, and the original source included in the reference list.
Figure file types
We accept the following file formats for figures:
- EPS (suitable for diagrams and/or images)
- PDF (suitable for diagrams and/or images)
- Microsoft Word (suitable for diagrams and/or images, figures must be a single page)
- PowerPoint (suitable for diagrams and/or images, figures must be a single page)
- TIFF (suitable for images)
- JPEG (suitable for photographic images, less suitable for graphical images)
- PNG (suitable for images)
- BMP (suitable for images)
- CDX (ChemDraw - suitable for molecular structures)
Figure size and resolution
Figures are resized during publication of the final full text and PDF versions to conform to the SpringerOpen standard dimensions, which are detailed below.
Figures on the web:
- width of 600 pixels (standard), 1200 pixels (high resolution).
Figures in the final PDF version:
- width of 85 mm for half page width figure
- width of 170 mm for full page width figure
- maximum height of 225 mm for figure and legend
- image resolution of approximately 300 dpi (dots per inch) at the final size
Figures should be designed such that all information, including text, is legible at these dimensions. All lines should be wider than 0.25 pt when constrained to standard figure widths. All fonts must be embedded.
Figure file compression
Vector figures should if possible be submitted as PDF files, which are usually more compact than EPS files.
- TIFF files should be saved with LZW compression, which is lossless (decreases file size without decreasing quality) in order to minimize upload time.
- JPEG files should be saved at maximum quality.
- Conversion of images between file types (especially lossy formats such as JPEG) should be kept to a minimum to avoid degradation of quality.
If you have any questions or are experiencing a problem with figures, please contact the customer service team at [email protected] .
Preparing tables
When preparing tables, please follow the formatting instructions below.
- Tables should be numbered and cited in the text in sequence using Arabic numerals (i.e. Table 1, Table 2 etc.).
- Tables less than one A4 or Letter page in length can be placed in the appropriate location within the manuscript.
- Tables larger than one A4 or Letter page in length can be placed at the end of the document text file. Please cite and indicate where the table should appear at the relevant location in the text file so that the table can be added in the correct place during production.
- Larger datasets, or tables too wide for A4 or Letter landscape page can be uploaded as additional files. Please see [below] for more information.
- Tabular data provided as additional files can be uploaded as an Excel spreadsheet (.xls ) or comma separated values (.csv). Please use the standard file extensions.
- Table titles (max 15 words) should be included above the table, and legends (max 300 words) should be included underneath the table.
- Tables should not be embedded as figures or spreadsheet files, but should be formatted using ‘Table object’ function in your word processing program.
- Color and shading may not be used. Parts of the table can be highlighted using superscript, numbering, lettering, symbols or bold text, the meaning of which should be explained in a table legend.
- Commas should not be used to indicate numerical values.
If you have any questions or are experiencing a problem with tables, please contact the customer service team at [email protected] .
Preparing additional files
As the length and quantity of data is not restricted for many article types, authors can provide datasets, tables, movies, or other information as additional files.
All Additional files will be published along with the accepted article. Do not include files such as patient consent forms, certificates of language editing, or revised versions of the main manuscript document with tracked changes. Such files, if requested, should be sent by email to the journal’s editorial email address, quoting the manuscript reference number.
Results that would otherwise be indicated as "data not shown" should be included as additional files. Since many web links and URLs rapidly become broken, SpringerOpen requires that supporting data are included as additional files, or deposited in a recognized repository. Please do not link to data on a personal/departmental website. Do not include any individual participant details. The maximum file size for additional files is 20 MB each, and files will be virus-scanned on submission. Each additional file should be cited in sequence within the main body of text.
Submit manuscript
- Editorial Board
- Sign up for article alerts and news from this journal
Annual Journal Metrics
2022 Citation Impact 4.6 - 2-year Impact Factor 5.7 - 5-year Impact Factor 1.705 - SNIP (Source Normalized Impact per Paper) 1.15 - SJR (SCImago Journal Rank)
2023 Speed 15 days submission to first editorial decision for all manuscripts (Median) 216 days submission to accept (Median)
2023 Usage 1,609,820 downloads 4,288 Altmetric mentions
- More about our metrics
- ISSN: 2198-9761 (electronic)
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- New editors
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Strength, power and aerobic capacity of transgender athletes: a cross-sectional study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-7412-1188 Blair Hamilton 1 , 2 ,
- http://orcid.org/0009-0005-9553-3081 Andrew Brown 2 ,
- http://orcid.org/0009-0007-0957-5002 Stephanie Montagner-Moraes 2 ,
- http://orcid.org/0000-0001-9483-3262 Cristina Comeras-Chueca 3 ,
- http://orcid.org/0000-0001-8609-2812 Peter G Bush 2 ,
- http://orcid.org/0000-0002-8526-9169 Fergus M Guppy 4 ,
- http://orcid.org/0000-0001-6210-2449 Yannis P Pitsiladis 5 , 6
- 1 School of Sport and Health Sciences , University of Brighton , Brighton , UK
- 2 School of Applied Sciences University , Brighton , UK
- 3 Health Sciences Faculty , Universidad San Jorge , Zaragoza , Spain
- 4 Heriot-Watt University , Edinburgh , UK
- 5 Department of Movement, Human and Health Sciences , University of Rome ‘Foro Italico’ , Rome , Italy
- 6 Department of Sport, Physical Education and Health , Hong Kong Baptist University , Hong Kong , Hong Kong SAR
- Correspondence to Professor Yannis P Pitsiladis, Department of Sport, Physical Education and Health, Hong Kong Baptist University, Hong Kong, Hong Kong SAR; ypitsiladis{at}hkbu.edu.hk
Objective The primary objective of this cross-sectional study was to compare standard laboratory performance metrics of transgender athletes to cisgender athletes.
Methods 19 cisgender men (CM) (mean±SD, age: 37±9 years), 12 transgender men (TM) (age: 34±7 years), 23 transgender women (TW) (age: 34±10 years) and 21 cisgender women (CW) (age: 30±9 years) underwent a series of standard laboratory performance tests, including body composition, lung function, cardiopulmonary exercise testing, strength and lower body power. Haemoglobin concentration in capillary blood and testosterone and oestradiol in serum were also measured.
Results In this cohort of athletes, TW had similar testosterone concentration (TW 0.7±0.5 nmol/L, CW 0.9±0.4 nmol/), higher oestrogen (TW 742.4±801.9 pmol/L, CW 336.0±266.3 pmol/L, p=0.045), higher absolute handgrip strength (TW 40.7±6.8 kg, CW 34.2±3.7 kg, p=0.01), lower forced expiratory volume in 1 s:forced vital capacity ratio (TW 0.83±0.07, CW 0.88±0.04, p=0.04), lower relative jump height (TW 0.7±0.2 cm/kg; CW 1.0±0.2 cm/kg, p<0.001) and lower relative V̇O 2 max (TW 45.1±13.3 mL/kg/min/, CW 54.1±6.0 mL/kg/min, p<0.001) compared with CW athletes. TM had similar testosterone concentration (TM 20.5±5.8 nmol/L, CM 24.8±12.3 nmol/L), lower absolute hand grip strength (TM 38.8±7.5 kg, CM 45.7±6.9 kg, p = 0.03) and lower absolute V̇O 2 max (TM 3635±644 mL/min, CM 4467±641 mL/min p = 0.002) than CM.
Conclusion While longitudinal transitioning studies of transgender athletes are urgently needed, these results should caution against precautionary bans and sport eligibility exclusions that are not based on sport-specific (or sport-relevant) research.
Data availability statement
Data are available on reasonable request.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bjsports-2023-108029
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
There is currently a lack of laboratory data on strength, power and V̇O 2 max from transgender athlete populations.
WHAT THIS STUDY ADDS
This research compares laboratory measures of strength, power and V̇O 2 max of transgender male and female athletes to their cisgender counterparts.
Transgender women athletes demonstrated lower performance than cisgender women in the metrics of forced expiratory volume in 1 s:forced vital capacity ratio, jump height and relative V̇O 2 max.
Transgender women athletes demonstrated higher absolute handgrip strength than cisgender women, with no difference found relative to fat-free mass or hand size.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE, OR POLICY
This study provides sport governing bodies with laboratory-based performance-related data from transgender athletes.
Longitudinal studies are needed to confirm if these results are a direct result of gender affirmation hormone therapy.
Sports-specific studies are necessary to inform policy-making.
Introduction
Transgender athletes can experience conflict between the gender that they were assigned and their experienced gender. 1 The question of integrating transgender athletes into their affirmed gender categories is becoming more prominent, with sports’ governing bodies using varied approaches, from bans on transgender women in the female category 2 requiring the reduction of testosterone in the female category for some time 3 to self-identification into the athletes chosen category. 4
As part of gender affirmation hormone therapy (GAHT), some transgender women undergo testosterone suppression (target ≤1.8 nmol/L 5 ) coupled with oestrogen supplementation (target 400–600 pmol/L 5 ), while some transgender men undergo testosterone supplementation (National Health Service (NHS, UK) target 15–20 nmol/L, 6 Endocrine Society Target 11–34.7 nmol/L 7 ). Testosterone is known to impact sporting performances, with differences in circulating testosterone concentration between cisgender men (CM) and women proposed to explain most of the laboratory-measured differences in sports performance. 8 9 GAHT of transgender men and women alters the body composition of transgender athletes via testosterone-mediated effects on fat-free mass 8 and oestrogens on subcutaneous fat distribution 9 and maintenance of muscle mass. 10 An often-held assumption against transgender women athletes competing in the female category of sport is that transgender women have benefited from a high testosterone concentration from assigned male-at-birth puberty until the administration of GAHT that cannot be mitigated 11 and that cisgender women competitors are unable to achieve similar benefits naturally. 12 To date, this assumption has yet to be tested and confirmed in transgender athlete cohorts. The low serum testosterone concentrations from an assigned female-at-birth puberty would hypothetically not give transgender men the competitive advantages of higher testosterone concentrations over CM, and this viewpoint is reflected in the current inclusion sports policies for transgender men. 2
Lab-derived data on a cohort of transgender athletes, as requested in article 6.1b of the International Olympic Committee Framework On Fairness, Inclusion And Non-Discrimination based on Gender Identity and Sex Variations, 4 must be generated to better inform a decision-making process. 13 Therefore, the primary aim of this study was to compare cardiorespiratory fitness, strength and body composition of transgender women and men athletes to that of matched cisgender cohorts.
Study design
This cross-sectional study involved a single visit to the laboratory at the School of Applied Sciences, University of Brighton, UK. Each participant arrived at ~9:00 hours. after an overnight fast and departed from testing at ~15:00 hours. The complete study design can be found in the study protocol, available as a preprint. 14
Recruitment
Following ethical approval (ref: 9496), 75 (19 CM, 12 transgender men, 23 transgender women and 21 cisgender women) participants were recruited through social media advertising on Meta Platforms (Facebook and Instagram, Meta Platforms, California, USA) and X (Twitter, California, USA). Following the initial response, all participants were provided with the participant information sheet by email at least 7 days before being invited to travel to the laboratory, with further oral information about the study procedures and written informed consent provided on their visit to the laboratory.
Participants and eligibility criteria
Participants were required to participate in competitive sports or undergo physical training at least three times per week. Following written consent, participants were asked to record their last four training sessions and self-rate their training intensity for each session on a scale of 1–10 (10=maximum intensity). The mean of the four sessions was recorded to represent the athletes’ training intensity. The transgender athletes must have completed ≥1 year of GAHT, voluntarily disclosed during consent and verified during blood test analysis. The full inclusion/exclusion criteria can be found in the study protocol, available as a preprint. 14 Two cisgender women and one transgender man could not provide blood samples and were consequently excluded from all analyses as their endocrine profiles could not be verified. Furthermore, two transgender women and one cisgender woman were excluded from all analyses due to testosterone concentrations exceeding recommended female testosterone concentrations (2.7 nmol/L 15 ).
Laboratory assessments
Blood sampling and analysis.
Prior to venous blood sampling, haemoglobin concentration ((Hb)) was sampled via the third drop of a Unistik 3 Comfort lancet (Owen Mumford, Woodstock, UK) finger prick capillary blood sample analysed immediately using a HemoCue 201+ (HemoCue AB, Ängelholm, Sweden). Capillary blood was used for (Hb) analysis for practical reasons such as ease of use. It is important to note that the HemoCue 201+used in the present study is expected to yield higher (Hb) values than venous blood. 16 After capillary sampling, one 10 mL whole venous blood sample was collected from an antecubital vein into a BD serum tube (Becton, Dickinson and Company, Wokingham, Berkshire, UK) for serum extraction. Once collected, the tubes were left at room temperature (18°C±5°C) for 1 hour and then stored in a fridge (3°C±2°C) for up to 4 hours before being centrifuged (PK 120 centrifuge, ALC, Winchester, Virginia, USA) using a T515 rotor at 1300G for 10 min at 4°C, before storage at −80°C until analysis. Before analysis, the samples were stored between −25°C and −15°C, thawed at room temp until liquid, vortexing to remix samples, centrifuged at 2876G for 8 min to remove any precipitant and then analysed for participant’s testosterone and oestradiol concentrations on an immunoassay analyser (Roche Cobas 8000 e801, Roche Diagnostics, Burgess Hill, UK).
Body composition and bone mass
Participants’ body mass was measured (OMRON Healthcare, Kyoto, Japan) while participants were lightly dressed, representing clothed body mass. Body composition and bone mass were measured by DXA (Horizon W, Hologic, Massachusetts, USA). Each participant underwent a whole-body, a proximal-femur and a lumbar spine scan. The participant was asked to lie on the scan bed, and the first author (BH) performed all participant placement and scanning for the three scans. Due to inbuilt assumptions of body fat percentage for the head and scanning bed area imitations, whole-body less head data are reported for the whole-body scan. Body mass index (BMI), Fat Mass Index (FMI) and Fat-Free Mass Index (FFMI) were calculated by taking the appropriate mass value and dividing it by height (m 2 ).
Lung function
Lung function was measured using a Vitalograph Alpha spirometer (Vitalograph, Kansas, USA) with an antibacterial filter and a nose clip on the bridge of the participant’s nose. Each participant was asked to perform the flow-volume-loop spirometry to test forced vital capacity (FVC), forced expiratory volume in 1 s (FEV 1 ) and peak expiratory flow. The test was repeated until a trend of declining performance occurred. The highest numeric value for each metric obtained during a test with the correct procedure was then recorded. The FEV1:FVC ratio was used to assess the presence of obstructed lung function.
Strength was measured using a handgrip dynamometer (TAKEI 5401, TAKEI Scientific Instruments, Japan). The participants’ hand sizes were also measured around the metacarpophalangeal joints of both hands prior to testing. Each hand was tested three times in sequential order of left-right to allow each hand to rest; the mean scores were taken from the three attempts for each hand.
Lower body power
Lower body power was measured with the countermovement jump on a JUM001 Jump Mat (Probotics, Alabama, USA). During the test, if the participant went beyond 45° of countermovement or the hands came off the hips, the test would be declared void for that attempt. After recording three legitimate attempts, the mean scores were recorded.
Cardiopulmonary exercise testing
Cardiopulmonary exercise testing was performed using a 95T Engage Treadmill ergometer (Life Fitness, Illinois, USA) and a COSMED QUARK (COSMED, Rome, Italy). All V̇O 2 max tests were conducted and analysed by the first author (BH) to avoid interinvestigator variability. 17 The ramp protocol of Badawy and Muaidi treadmill V̇O 2 max testing 18 was used for each V̇O 2 max test, involving gradual increases in speed every 3 min at a 1% incline. One cisgender man and two cisgender women were excluded from the analysis as they did not meet the required respiratory exchange ratio of ≥1.1 to classify the test as maximal (cisgender men (CM), n=18, transgender men (TM), n=11; cisgender women (CW) n=16; transgender women (TW), n=21).
Statistical analysis
Data meeting the assumptions of normality and homogeneity of variance were analysed using a one-way analysis of variance along with Bonferroni post hoc corrections for pairwise comparisons. Data not meeting the parametric assumptions were compared using a Kruskal-Wallis ANOVA with Dwass-Steel-Critchlow-Fligner post hoc test for multiple comparisons, with an alpha level of 0.05 for both types of analysis. Statistical analysis and presentation are consistent with the checklist for statistical assessment of medical papers statement 19 found in online supplemental files 1–3 at Hamilton et al , The Strength, Power and Aerobic Capacity of Transgender Athletes: A Cross-Sectional Study (Internet). OSF; 2023. Available from: osf.io/a684b.
Supplemental material
Equity, diversity and inclusion statement.
The author group consists of early (n=3) and senior researchers (n=3) from different disciplines and universities (n=3). Two authors are members of a marginalised community; the lead early-career author is a transgender woman, and one of the junior authors is a woman from the global south. Our study population included male and female transgender athletes from within the UK participating in competitive sports in comparison with cisgender male and female athletes participating in competitive sports; thus, findings may not be generalisable to global athlete populations.
Participant characteristics
Our investigation encompassed a diverse cohort of athletes, with endurance sports representing 36% of the athlete cohort, team sports representing 26% and power sports representing 38%. No cisgender or transgender athletes were competing at the national or international level. No significant differences were found in age (F (3–66) =1.9, p=0.14), training intensity score (χ 2 (3) =1.2, p=0.76) or length of GAHT between transgender men and transgender women (F (1–32) =0.5, p=0.48, table 1 ).
- View inline
Significant differences were found in height (F (3–66) =21.3, p<0.001), with CM being taller than transgender men (t (66) =3.8, p=0.002, table 1 ). Transgender women were also taller than transgender men (t (66) =3.3, p=0.01) and cisgender women (t (66) =6.5, p<0.001, table 1 ).
Significant differences were found in clothed mass (F (3–66) =10.6, p<0.001), with transgender women found to be heavier than cisgender women (t (66) =5.6, p<0.001, table 1 ).
BMI was also significantly different between the groups in this Study (F (3–66) =3.6, p=0.02). Transgender women athletes demonstrated higher BMI than cisgender women (t (66) =2.9, p=0.03, table 1 ), with no further differences observed.
Blood measures
There was a significant gender effect on testosterone concentration (F (3–66) =80.6, p<0.001). CM (20.5±5.8 nmol/L) exhibited significantly higher total testosterone concentration than transgender women (0.7±0.5 nmol/L, t (66) = 11.1, p<0.001, figure 1A ). Transgender men (24.8±12.3 nmol/L) had elevated total testosterone concentration compared with transgender women (t (66) =11.3) and cisgender women (0.9±0.4 nmol/L, t (66) =10.9, both p<0.001, figure 1A ). There was also a significant gender effect on oestradiol concentration (F (3−66) =7.6, p<0.001), with transgender women (742.4±801.9 pmol/L) showing higher oestradiol concentration than CM (104.3±24.8 pmol/L, t (66) =4.4 p<0.001), cisgender women (336.0±266.3 pmol/L, t (66) =2.7, p=0.045) and transgender men (150.2±59.4 pmol/L, t (66) =3.4, p=0.01, figure 1B ).
- Download figure
- Open in new tab
- Download powerpoint
Blood measures. (A) testosterone; (B) oestradiol; (C) haemoglobin. *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001. CM, cisgender men; CW, cisgender women; TM, transgender men; TW, transgender women.
Transgender women’s total testosterone concentration (0.7±0.5 nmol/L) falls within the recommendations for GAHT of ≤1.8 nmol/L, 5 and oestradiol concentrations (742.4±801.9 pmol/L) exceed the target of 400–600 pmol/L 5 for GAHT. Transgender men’s testosterone concentration (24.8±12.3 nmol/L) exceeds the NHS target of 15–20 nmol/L 6 for GAHT, although not the Endocrine Society target of 11–34.7 nmol/L. 7
Differences were reported in (Hb) concentration (F (3–66) =3.3, p=0.03), although a post hoc Bonferroni analysis showed no differences between the various groups (CM 142.8±12.5 g/L; transgender men, 143.3±19.5 g/L; transgender women, 131.3±14.2 g/L; cisgender women, 133.3±12.7 g/L; figure 1C ).
DXA assessment
There was a significant gender effect on percentage fat mass (F (3–66) =6.6, p<0.001), with CM having a lower percentage fat mass than transgender women (t (66) =−4.4, p<0.001, table 2 ), with no other differences observed. A significant gender effect was also found on absolute fat mass (F (3–66) =6.6, p<0.001), with transgender women having more absolute fat mass than CM (t (66) =3.8, p=0.002, table 2 ) and cisgender women (t (66) =3.9, p=0.002, table 2 ). FMI measures revealed a gender effect (F (3–66) =5.2, p=0.003), with transgender women found to have a higher FMI than CM (t (66) =3.7, p=0.002, table 2 ) and cisgender women (t (66) =2.8, p=0.04, table 2 ). Android to gynoid ratio analysis (F (3–66) =10.7, p<0.001) revealed cisgender women had a lower ratio than transgender men (t (66) =−2.9, p=0.03, table 2 ), and transgender women (t (66) =−4.0, p=0.001, table 2 ).
Body composition, BMD data, handgrip strength, lower anaerobic power and cardiopulmonary exercise testing
Fat-free mass
There was a significant gender effect on absolute fat-free mass (F (3–66) =24.6, p<0.001), with CM having significantly more absolute fat-free mass than transgender men (t (66) =3.5, p=0.01, table 2 ). Cisgender women had less absolute fat-free mass than transgender men (t (66) =−3.5, p=0.01, table 2 ) and transgender women (t (66) =−6.6, p<0.001, table 2 ). No gender-based effects were found when comparing transgender women athletes to cisgender women athletes, or transgender men athletes to CM athletes in the measures of FFMI (F (3–66) =3.7, p=0.02, table 2 ), percentage of fat-free mass (F (3–66) =2.4, p=0.08, table 2 ) or appendicular FFMI (F (3–66) =5.1, p=0.003, table 2 ).
Bone mineral density
No differences in whole-body bone mineral density (BMD) (F (3–66) =4.6, p=0.01), femoral neck BMD (F (3–66) =1.0, p=0.39, table 2 ), total proximal femur BMD (F (3–66) =1.5, p=0.22, table 2 ) or total lumbar spine BMD (F (3–66) =0.4, p=0.78, table 2 ) were found between transgender athletes and cisgender athletes ( table 2 ).
Lung function data for all groups can be found in table 2 . FEV 1 had an effect of gender (F (3–66) =14.7, p<0.001), with CM having greater FEV 1 than transgender men (t (66) = 4.5, p<0.001, figure 2A ). Transgender women also had greater FEV 1 than cisgender women (t (66) =4.2, p<0.001, figure 2A ) and transgender men (t (66) =2.9, p=0.03, figure 2A ). There was a similar effect of gender on FVC (F (3–66) =21.6, p<0.001, figure 2B ), with CM having greater FVC than transgender men (t (66) =5.2, p<0.001, figure 2B ). Transgender women also had greater FVC than cisgender women (t (66) =5.6, p<0.001, figure 2B ) and transgender men (t (66) =4.0, p=0.001, figure 2B ). A significant effect of gender was also seen on the FEV 1 :FVC ratio (F (3–66) =3.3, p=0.03 figure 2C ), with transgender women showing a reduced FEV 1 :FVC ratio compared with cisgender women (t (66) =−2.8, p=0.04, figure 2C ) with no differences observed in transgender or CM. Peak expiratory flow (F (3–66) =5.5, p=0.002) had a minor gender-based effect, with cisgender women having lower peak expiratory flow than transgender women (t (66) −3.0, p=0.02, figure 2D ).
Lung function measures. (A) Forced rxpiratory volume in 1 s (FEV 1 ); (B) forced vital capacity (FVC) (C) modified Tiffeneau-Pinelli Index (FEV 1 :FVC); (D) peak expiratory flow (PEF). *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001. CM, cisgender men; CW, cisgender women; TM, transgender men; TW, transgender women.
Handgrip strength
Handgrip strength data can be found in table 2 . Absolute right handgrip strength was significantly different between the groups (F (3–66) =10.5, p<0.001), with CM having greater absolute right handgrip strength than transgender men (t (66) =2.9, p=0.03, figure 3B ). Transgender women also had greater absolute right handgrip strength than cisgender women (t (66) =3.2, p=0.01, figure 3B ). Absolute left handgrip was significantly different between the groups (F (3–66) =8.6, p<0.001). However, no differences were found between transgender and cisgender athletes ( figure 3A ). There was no effect on the right (F (3–66) =0.8, p=0.53, figure 3F ) or left-hand grip strength (F (3–66) =1.0, p=0.39, figure 3E ) relative to fat-free mass, nor was there any gender effect on the right (F (3–66) =1.6, p=0.20, figure 3D ) or left-hand grip-strength (F (3–66) =2.1, p=0.11) relative to hand size.
Absolute and relative handgrip strength (GS) measures. (A) Absolute strength (right hand); B) Absolute strength (left hand) (C) relative strength to hand size (right hand); (D) relative strength to hand size (left hand); (E) relative strength to fat-free mass (FFM) (right hand); (F) relative strength to fat-free mass (left hand). *p<0.05, ***p<0.001, ****p<0.0001. CM, cisgender men; CW, cisgender women; TM, transgender men; TW, transgender women.
Lower body anaerobic power
Lower body anaerobic power data are shown in table 2 . Gender had a significant effect on absolute countermovement jump height (F (3–66) =7.2, p<0.001), with CM having greater absolute jump height than transgender women (t (66) =4.5, p<0.001, figure 4A ). A significant effect of gender was found in countermovement jump height relative to fat-free mass (F (3–66) =10.1, p<0.001, figure 4B ), with transgender women found to have lower countermovement jump height relative to fat-free mass than both cisgender women (t (66) =−5.3, p<0.001) and transgender men (t (66) =–3.2, p=0.01, figure 4B ).
Absolute and relative anaerobic power measures. (A) Absolute CMJ height; B) Relative CMJ height to fat-free mass (FFM); (C) absolute peak power; (D) relative peak power to FFM; (E) absolute average power; (F) relative average power to FFM. *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001. CM, cisgender men; CMJ, Counter Movement Jump; CW, cisgender women; TM, transgender men; TW, transgender women.
There was a significant difference in absolute peak power (F (3–66) =8.7, p<0.001), with cisgender women having reduced peak power compared with transgender men (t (66) =−3.3, p=0.01) and transgender women (t (66) =−3.6, p=0.004, figure 4C ). Peak power relative to fat-free mass had a more negligible gender effect (F (3–66) =4.2, p=0.01), with no difference in peak power relative to fat-free mass found between transgender and cisgender athletes ( figure 4D ).
There was a significant gender effect of absolute average power (F (3–66) =5.9, p=0.001), with cisgender women having reduced absolute average power compared with transgender men (t (66) =–3.1, p=0.02, figure 4E ). There was no effect of gender on average power relative to fat-free mass (F (3–66) =2.6, p=0.06, figure 4F ).
Cardiopulmonary exercise testing data are shown in table 2 . A significant effect of gender was found on absolute V̇O 2 max (F (3–62) =14.1, p<0.001) with CM having greater absolute V̇O 2 max than transgender men (t (66) =3.8, p=0.002, figure 5A ) and transgender women (t (66) =4.3, p<0.001, figure 5A ). Relative V̇O 2 max to body mass also showed a significant gender effect (F (3–62) =9.8, p<0.001) with transgender women having lower relative V̇O 2 max than CM (t (66) =–5.3, p<0.001, figure 5B ) and cisgender women (t (66) =−3.3, p=0.01, figure 5B ). No significant gender effect was found on the measure of V̇O 2 max relative to fat-free mass (F (3–62) =2.0, p=0.12).
Absolute and relative cardiopulmonary exercise testing measures. (A) Absolute V̇O 2 max; (B) relative V̇O 2 max to body weight; (C) absolute anaerobic threshold (AT); (D) anaerobic threshold (%V̇O 2 max); (E) relative anaerobic threshold relative to body mass; (F) AT relative to at-free mass (FFM). *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001. CM, cisgender men; CW, cisgender women; TM, transgender men; TW, transgender women.
Gender affected the absolute anaerobic threshold (F (3–62) =14.1, p<0.001), with cisgender (3924±628 mL/min) men having a higher absolute anaerobic threshold than transgender men (3089±546 mL/min, t (66) =4.2, p<0.001, figure 5C ), and transgender women (3122±438 mL/min, t (66) =4.8, p<0.001, figure 5C ). No significant gender effect was found on the measure of anaerobic threshold as a percentage of V̇O 2 max (F (3–62) =0.8, p=0.51, figure 5D ). A gender effect was also seen on the anaerobic threshold relative to body mass (F (3–62) =10.7, p<0.001), with transgender women (38.3±6.6 mL/kg/min) showing a lower relative anaerobic threshold than both cisgender women (47.2±6.1 mL/kg/min, t (66) =–3.3, p=0.01, figure 5E ) and CM (52.2±9.5 mL/kg/min, t (66) =−5.4, p<0.001, figure 5E ). CM also showed a higher relative anaerobic threshold than transgender men (42.1±9.9 mL/kg/min, t (66) =3.3, p=0.01, figure 5E ). Anaerobic threshold relative to fat-free mass also had a small gender effect (F (3–62) =3.2, p=0.03), with transgender women (60.8±12.2 mL/kg FFM /min) having a lower anaerobic threshold relative to fat-free mass than CM (71.2±13.3 mL/kg FFM /min, t (66) =−2.8, p=0.045, figure 5F ).
The results presented in this study provide valuable insights into laboratory-based performance-related metrics of gender-diverse athletes participating in competitive sports. Given the primary aim of GAHT, 20 it is noteworthy that although this study is cross-sectional in design, transgender women’s oestradiol was higher than that of cisgender women ( figure 1B ). The presence of outliers affecting transgender women’s oestrogen concentration ( figure 1B ) is evident. This underscores that transgender women in this cohort of athletes exhibit a distinct endocrine profile from CM and share a similar endocrine profile with cisgender women, whom many transgender women aim to integrate into a sporting category. One of the most noticeable disparities between gender groups was in height and mass ( table 1 ), with CM and transgender women being taller and heavier than their cisgender and transgender counterparts ( table 1 ). Body composition measures (fat mass % and fat-free mass %, table 2 ) between transgender women and cisgender women found no difference. However, transgender women are, on average as a cohort taller and heavier.
In this cohort, the average difference in haemoglobin (Hb) between cisgender women and CM athletes was 7% ( figure 1C ), lower than previously described (12% 8 ). Notably, the (Hb) profiles of all the athlete groups were not significantly different, concurring with earlier research 21 and contradicting research in sedentary populations. 22 (Hb) is crucial in O 2 transport 23 and vital for endurance sports performance, 24 with O 2 delivery to the tissues a limiting factor in V̇O 2 max attainment. 25 The lack of differences in (Hb) is consistent with the lack of observed difference in absolute V̇O 2 max between transgender women, transgender men and cisgender women in this cohort. However, as cardiac output, the most crucial variable influencing V̇O 2 max 25 was not assessed in the present study, a more comprehensive mechanistic explanation for the similar maximal aerobic capacity between groups cannot be provided.
No differences in BMD were observed between transgender and cisgender women athletes in this study ( table 2 ), despite prior research hypothesising that transgender women athletes have a significant BMD advantage over cisgender women. 11 The sample size for each gender was n<30 participants and may be insufficient to characterise BMD differences reliably. Exercise has been shown to have a protective effect on BMD in CM 26 and CW, 27 and our results suggest a protective effect of exercise in transgender women, given that there is evidence of low BMD in transgender women with low weekly sports activity. 28 Nevertheless, the results suggest the complexity of bone health in athlete populations and the need for a more comprehensive assessment to understand the long-term impact of GAHT on transgender athletes’ BMD.
The differences observed in body composition in this population ( table 2 ) indirectly show the potential role of androgens in body composition, owing to the role of oestradiol in fat accumulation 29 and transgender women’s oestradiol concentrations ( figure 1B ) and fat mass ( table 2 ) being greater than all other groups. Body composition differences may have implications for sports that prioritise exercise economy, 30 defined as the average V̇O 2 relative to body mass between submaximal intensities, 31 as athletes with a higher fat mass percentage will present with a lower exercise economy owing to the increased O 2 cost of exercise. 32 The android-to-gynoid ratio analysis ( table 2 ) suggests that hormone therapy ( figure 1A,B ) influences differences in fat distribution patterns. However, fat distribution patterns of the present transgender female athlete cohort ( table 2 ) do not reach ratios previously reported in cisgender female populations (0.8). 33 Understanding these variations is essential for evaluating performance in sports where body composition is a determining factor, for example, weightlifting or boxing.
Cisgender women had lower absolute fat-free mass than transgender men and transgender women ( table 2 ). When analysing absolute fat and fat-free mass data ( table 2 ), these results can be affected by sample size and/or athlete diversity limitations. A purposefully designed future study with height-matched and sport-matched cisgender and transgender female athletes is crucial to understanding differences in these parameters, as they are influenced by height disparities ( table 1 ) and variations in sampled sports.
FVC, FEV 1 and FEV 1 :FVC ratio are higher in athletes than in the normal sedentary control individuals, 34 and there is no difference in all three metrics between aerobic athletes and anaerobic athletes. 35 Therefore, the lung function differences observed in figure 2A,B may be attributed to factors such as skeletal size benefiting lung capacity and function, 36 with transgender women’s FVC results ( figure 2B ) suggesting gender-affirming hormone care did not impact changing lung volumes owing to the GAHTs lack of effect on skeletal stature. 11 Transgender women showed a significantly reduced FEV 1 :FVC ratio compared with cisgender women ( figure 2C ). The FEV 1 :FVC ratio has been used as a screening index for identifying obstructive lung conditions globally, 37 as a lower FEV 1 owing to obstruction of air escaping from the lungs will reduce the FEV 1 :FVC ratio. Transgender women’s results ( figure 2C ) suggest obstructed airflow in the lungs 38 when compared with cisgender women. However, this observation of transgender women is unlikely to be pathological (<0.70), 39 as seen in chronic obstructive pulmonary disease.
Nevertheless, this reduced airflow could potentially lead to exercise-induced dyspnoea, resulting in performance limitations 40 in comparison to cisgender women. When comparing both the CM and transgender women athletes’ groups with identical heights (1.8 m, table 1 ), while both groups exhibit similar FVC, transgender women demonstrate a lower FEV 1 , leading to a reduced FEV 1 :FVC ratio compared with CM, although not significant. If there were a significant difference between CM and transgender women, our preliminary hypothesis would have attributed this divergence to testosterone suppression in transgender women. However, comparing transgender women to cisgender women who do not share similar height and or exhibit a comparable FVC, the observed differences become more complex to interpret. The possibility arises that factors beyond hormonal influences, such as varying levels of aerobic training, may contribute to the significant difference found in the FEV 1 :FVC ratio between transgender women and cisgender women. Further longitudinal investigation is required to elucidate if the causation underlying these pulmonary function disparities is indeed testosterone suppression.
Strength results in figure 3 disagree with previous literature in a non-athlete transgender cohort using the same methodology that showed transgender women and CM had significantly different absolute and relative hand grip strength. 41 Our results showed no differences in absolute strength between transgender women and CM and no difference in relative handgrip between any of the groups in this study ( figure 3 ). These results highlight the differences between athlete and sedentary populations. However, the results relative to hand size also concur with the notion that greater handgrip strength is caused by greater hand size, 42 as there were no differences in results between the four groups when normalised for hand size ( figure 3C,D ). Therefore, investigations with more accurate measures of strength are warranted in transgender athletes.
Transgender women presented lower absolute jump height than CM and lower relative jump height, normalised for fat-free mass, than transgender men and cisgender women ( figure 4 ). These results in this study cohort suggest that transgender women lack lower body anaerobic power compared with the other groups. Transgender women’s higher absolute peak power than cisgender women ( figure 4C ), coupled with higher fat mass potentially driven by higher oestradiol concentrations ( figure 1B ), suggest that transgender women had more inertia to overcome during the explosive phase of the countermovement jump, which may lead to decreased performance. However, when normalised for fat-free mass ( figure 4D ), transgender women’s peak power was lower than that of cisgender women, showing that this cohort also lacks peak power relatively, indicating that the higher fat mass may not be the primary contributing factor. Further investigations are warranted to find the causation of this poor lower anaerobic power performance in transgender women.
The lack of differences in anaerobic threshold (%V̇O 2 max, figure 5D ) suggests that the athletes in this study had a similar fitness status, which is an essential underlying finding given that CM showed greater absolute V̇O 2 max than all groups ( figure 5A ), with no differences between transgender women and cisgender women found, and transgender women exhibited lower relative V̇O 2 max compared with both CM and women ( figure 5B ). In this cohort, the finding of no statistical difference in absolute V̇O 2 max between transgender women and cisgender women contrasts the idea that transgender women’s bigger lung size ( table 2 ) is an inherent respiratory function advantage over cisgender women. 11 Both the absolute and relative V̇O 2 max differences between groups contradict one previous study in non-athlete transgender populations that found transgender women had higher absolute V̇O 2 peak and no difference in relative V̇O 2 peak compared with cisgender women. 41 This contradictory finding further highlights population differences between non-athlete and athlete cohorts while also contradicting literature hypothesising that there would be a baseline gap in aerobic capacity between transgender women and cisgender women. 11 The results in this athlete cohort warrant further research to elucidate the mechanisms behind this deviation, as they may be metabolic, as transgender women also exhibited a lower relative anaerobic threshold ( figure 5E ). The findings in table 2 reveal notable disparities in fat mass, fat-free mass, laboratory sports performance measures and hand-grip strength measures between cisgender male and transgender female athletes. These differences underscore the inadequacy of using cisgender male athletes as proxies for transgender women athletes. Therefore, based on these limited findings, we recommend that transgender women athletes be evaluated as their own demographic group, in accordance with the principles outlined in Article 6.1b of the International Olympic Committee Framework on Fairness, Inclusion and Non-Discrimination based on Gender Identity and Sex Variations. 4
Study limitations
The limitations of this study primarily relate to its cross-sectional design, making it challenging to establish causation or examine if the performance of athletes changes as a result of undergoing GAHT. Longitudinal studies are needed to examine how GAHT, and other factors impact athletes’ physiology and performance over time. Additionally, the composition of the study cohort may not fully represent the diversity of athletes in elite sports from worldwide populations. Athletes from various sporting disciplines and performance levels were included, and the athlete training intensity was self-reported. Therefore, the results may suffer from selection and recall bias. 43 The results may not apply to all levels or ages of athletes, specifically as this research did not include any adolescent athletes competing at the national or international level. The athletes participating in the present study represented a variety of different sports, and this would have undoubtedly impacted the results of the study as different sports stress different training and sports modalities. Exercise type, intensity and duration all have an impact on physiological responses and overall laboratory performance metrics. 44 The subgroups of sports that emerged were also too dissimilar to allow meaningful subgroup analysis. The complexity and difficulty of this area of activity means that while this study provides a starting point for understanding the complex physiology in GAHT and athletic performance, this study does not provide evidence that is sufficient to influence policy for either inclusion or exclusion. However, this is the first study to assess laboratory-based measures of performance in transgender athletes, and this opens up interesting avenues for replication and extension into the longitudinal effects of GAHT on athletic performance.
Future research should include more extensive and diverse samples to enhance the generalisability of findings or smaller, more specific cohorts to hone in on a particular sports discipline. However, such studies may be complex due to the low numbers of transgender athletes. The recruitment method of this study also provided a limitation as social media advertising was used rather than recruitment from a clinical provider. Social media recruitment leaves this study open to sample bias as social media advertising, although great for recruiting hard-to-reach participants for observational studies, 44 45 does not represent a clinical population in 86% of comparisons. 44 As the participants were not recruited from a clinic, this also means that the gender-affirming treatment of the transgender athletes was not controlled. For example, different testosterone suppression methods have different efficacies, 46 and future studies should consider differences in the prescribed GAHT to participants. Lastly, the participants were not screened by a clinician before participation, and any medical conditions were self-reported in the physical activity readiness questionnaire (PAR-Q). This method of medical reporting leaves the data open to self-reporting bias, which can mislead descriptive statistics and causal inferences 47 as participants’ cognitive processes, such as social desirability, can alter participants’ responses. 48 Therefore, it is recommended to use a clinic to screen and recruit participants to avoid such bias in a longitudinal study of transgender athlete sports performance.
Conclusions
This research compares transgender male and transgender female athletes to their cisgender counterparts. Compared with cisgender women, transgender women have decreased lung function, increasing their work in breathing. Regardless of fat-free mass distribution, transgender women performed worse on the countermovement jump than cisgender women and CM. Although transgender women have comparable absolute V̇O 2 max values to cisgender women, when normalised for body weight, transgender women’s cardiovascular fitness is lower than CM and women. Therefore, this research shows the potential complexity of transgender athlete physiology and its effects on the laboratory measures of physical performance. A long-term longitudinal study is needed to confirm whether these findings are directly related to gender-affirming hormone therapy owing to the study’s shortcomings, particularly its cross-sectional design and limited sample size, which make confirming the causal effect of gender-affirmative care on sports performance problematic.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and ethical approval for this study has been granted by the School of Applied Sciences Research Ethics Committee of the University of Brighton, Brighton, UK (Ref: 9496). Participants gave informed consent to participate in the study before taking part.
Acknowledgments
We thank Associate Professor Ada Cheung of the Department of Medicine (Austin Health) at the University of Melbourne, Australia for her valuable review of this work prior to publication.
- Arcelus J ,
- Bouman WP , et al
- World Aquatics
- USA Gymnastics
- International Olympic Committee
- National Health Service
- Hembree WC ,
- Cohen-Kettenis PT ,
- Gooren L , et al
- Handelsman DJ ,
- Hirschberg AL ,
- Alvero-Cruz JR ,
- Chilibeck P , et al
- Gharahdaghi N ,
- Phillips BE ,
- Szewczyk NJ , et al
- Hilton EN ,
- Lundberg TR
- Hamilton BR ,
- Barrett J , et al
- Hamilton B ,
- Comeras-Chueca C ,
- Bush P , et al
- Leitman SF , et al
- Popović ZB ,
- Badawy MM ,
- Mansournia MA ,
- Collins GS ,
- Nielsen RO , et al
- Malczewska-Lenczowska J ,
- Sitkowski D ,
- Orysiak J , et al
- Roberts TK ,
- French D , et al
- Schmidt W ,
- Bassett DR ,
- Staines KA ,
- Kelley GA , et al
- Hofmeister M
- Rothman MS ,
- Mareschal J ,
- Karsegard VL , et al
- Losnegard T ,
- Schäfer D ,
- V Mendonca G ,
- Imboden MT ,
- Swartz AM , et al
- Rajaure YS ,
- Budhathoki L , et al
- van der Plaat D ,
- Dharmage S , et al
- Min HK , et al
- Schiöler L ,
- Lindberg A , et al
- Anzueto A , et al
- Alvares LAM ,
- Santos MR ,
- Souza FR , et al
- Alahmari KA ,
- Kakaraparthi VN ,
- Reddy RS , et al
- Tripepi G ,
- Dekker FW , et al
- Topolovec-Vranic J ,
- Natarajan K
- Whitaker C ,
- Stevelink S ,
- Leemaqz S ,
- Ooi O , et al
- Mathiowetz N
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
X @BlairH_PhD
Contributors BH, FMG and YPP designed the study. Material preparation, reporting and critical revision of the work were performed by BH, PGB, FMG and YPP. Data collection was performed by CC-C, AB, SM-M and BH. BH wrote the first draft of the manuscript, and all authors critically revised subsequent versions until all authors could approve the final manuscript. YPP is the guarantor.
Funding The study has been funded by a research grant awarded by the International Olympic Committee, Lausanne, Switzerland.
Competing interests YPP is a member of the IOC Medical and Scientific Commission, which recently published articles and framework documents on the topic. BH and FMG have recently published articles on the topic on behalf of the International Federation of Sports Medicine (FIMS). All authors declare no further conflict of interest or competing interests.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:

Aims and scope
Sports Medicine focuses on definitive and comprehensive review articles that interpret and evaluate the current literature to provide the rationale for and application of research findings in the sports medicine and exercise field. Major topics covered by reviews published in the journal include:
- Sports medicine and sports science, including performance research.
- The medical syndromes associated with sport and exercise.
- The practical role that clinical medicine plays in sport, through injury prevention and treatment.
- The medical use of exercise for rehabilitation and health.
- The application of physiological and biomechanical principles to specific sports.
Sports Medicine also publishes:
- Leading/current opinion articles providing overviews of contentious or emerging issues.
- High-quality original research articles.
Additional digital features (including animated abstracts, video abstracts, slide decks, audio slides, instructional videos, infographics, podcasts and animations) can be published with articles; these are designed to increase the visibility, readership and educational value of the journal’s content. In addition, articles published in Sports Medicine may be accompanied by plain language summaries to assist readers who have some knowledge of, but not in-depth expertise in, the area to understand important medical advances.
All manuscripts are subject to peer review by international experts. Letters to the Editor are welcomed and will be considered for publication.
- Find a journal
- Publish with us
- Track your research
Study debunks longstanding medical myth that a torn ACL can't heal
Personal trainer Danyelle Anderson ruptured the anterior cruciate ligament (ACL) in her right knee during a kickboxing class.
"My whole world came crashing down, pretty much," she said.
She was told by an orthopaedic surgeon that it wasn't possible for her ACL to heal and that a surgical reconstruction was needed.
Reluctant to have an operation, she decided to see if her knee would improve with physiotherapy.
Three months later, a follow-up MRI showed her injury had gone from a grade three complete rupture, where the ligament is torn completely in half, to a less severe grade one tear, where some of the fibres are continuous.
"So basically, my ACL has reattached and is healing," she said.
Ms Anderson's story comes as no surprise to University of Melbourne researcher Associate Professor Stephanie Filbay.
In a study that has garnered worldwide attention, she re-analysed the results of a Swedish trial involving 120 patients, comparing the MRIs of those who had surgery with others who underwent rehabilitation without surgery.
"What we found, surprisingly, was that two years after injury, in those who'd had rehabilitation only, 53 per cent had signs of healing on MRI," Dr Filbay said.
"Even more surprising was that those with signs of healing reported better outcomes than those who'd had ACL surgery."
Evidence of healing was taken to be the presence of continuous ACL fibres where previous MRIs showed a complete disconnect in the rupture zone, as well as the ligament becoming thicker and tauter and taking on a more normal appearance.
The findings have become a hot topic in medical circles, raising questions about whether changes are needed to the way doctors treat ACL injuries.
"Everyone's heard of incidents where someone's on a waitlist for surgery with a torn ACL and they get opened up by the surgeon and then the surgeon says 'well, the ACL is healed'," Dr Filbay said.
"People thought they were extremely rare, and what the research is suggesting is that this occurs more commonly than we thought."
Challenging accepted medical wisdom
Some surgeons have reacted to the study with scepticism, pointing to the small number of young, physically fit adult patients involved in the trial, and the difficulties of assessing healing on an MRI.
The ACL is a rope-like band of tissue that runs through the middle of the knee, connecting the thigh bone to the shin bone and playing a vital role in keeping the joint stable.
For decades, the accepted medical wisdom has been that the ACL can't heal because of poor blood supply inside the knee joint.
"It has been a myth that the ACL never heals, something that's been set in stone," specialist orthopaedic knee surgeon Justin Roe said.
In practice, he said, doctors have observed that ACLs heal in some cases, but not in others.
"And that's the holy grail — predicting who it does heal in and who it doesn't," Dr Roe said.
Surgical reconstruction has been viewed as the gold standard treatment, offering a more predictable outcome.
"We have good surgical techniques that have developed over the years, so we can say with confidence to patients that with a successful ACL reconstruction, they can get back to sport 70 to 80 per cent of the time," Dr Roe said.
Dr Filbay said her research showed that patients treated non-surgically returned to sport at similar rates.
"If you're told by your surgeon or your physio that if you ever want to play sport again, you need surgery, then it really does take away your ability to make an informed decision, because you're going to choose surgery and you're not accurately understanding the pros and cons of each," she said.
"I think the best evidence at the moment shows that rehabilitation on average is just as good a treatment as surgery, but that hasn't translated into current practice in Australia."
Australia has one of the highest per capita rates of ACL surgery in the world.
Around 90 per cent of patients who rupture their ACL undergo an operation, costing around $10,000 a time.
The surgery involves removing the damaged ligament and replacing it with a graft of tissue taken from the patient's hamstring or patellar (kneecap) tendon, or, in some cases, with tissue from a donor.
"If you watch the AFL or the rugby and someone tears their ACL and the commentator says they'll be in for surgery the next day to fix their ACL, that really filters down to society and to the public," Associate Professor Filbay said.
"If they injure their ACL, they think if Sam Kerr is having a reconstruction, that must be the best treatment for me.
"But that's not what the evidence shows."
Every year around 20,000 ACL reconstructions are carried out — and that figure is on the rise, particularly among females and children, with patients as young as nine undergoing surgery.
The finding that the ACL may have a greater ability to heal than previously thought has raised questions about whether all these surgeries are necessary.
"Certainly for a long time, we have known that we've been doing too many," Dr Roe said.
But he said in some cases there was a danger that by not operating, the patient was at risk of doing more damage to their knee.
"What I'm concerned about is the extremism [of] going too far the other way," Dr Roe said.
Orthopaedic knee surgeon Christopher Vertullo said the latest research has shown that around half of ACL patients are no better off having surgery.
"It is concerning that there are too many ACL injuries and too many ACL surgeries," he said.
"There's now lots of studies suggesting that non-surgical management of ACL injuries does very well and [that] for a high proportion of patients, upwards of 50 per cent, they'll do just as well without an operation."
But he said not all patients were open to trying a non-surgical approach.
"There is a mentality that people really want to be fixed and they want it now, and that is hard as a surgeon."
He said Stephanie Filbay's research had contributed to a robust debate on the treatment of ACL injuries, but cautioned that MRIs were not a perfect tool for assessing healing or whether the ACL is intact.
"You certainly see continuous-looking ACLs on MRI and then you examine the person and they've got gross instability," he said.
He said a national ACL injury registry was needed to track patients and collect more data.
"I don't have any doubts that there's healing ability of the ACL," he said.
"A registry will help us then make more informed decisions for our patients and help patients make more informed decisions."
Choosing rehabilitation versus surgery
When sports physiotherapist Clare Walsh did her training 20 years ago, she was taught that the ACL did not heal.
"What we understood was that if somebody had an ACL injury, then they needed surgery," she said.
These days, patients are given the option of surgery with up to a year of rehabilitation or rehabilitation alone.
"Making that decision about surgery isn't urgent, you don't have to make that on day one," she said.
"Surgery may be the most appropriate choice, but if they want to try non-operative management in rehabilitation, then they can give that a go."
A high percentage of the patients Ms Walsh sees choose the non-surgical route, some of them for financial reasons.
"The patients that tend to choose rehabilitation are those that don't have private health cover because it's a very expensive operation," she said.
Patients still have the option of having surgery down the track if their knee proves to be unstable after a period of rehabilitation.
"We have great surgeons and the surgery outcomes are very good for a very high percentage of cases," Ms Walsh said.
That's an option that Dr Filbay pointed out is not available the other way round.
"Once someone undergoes reconstructive surgery, the ACL is removed, and it's replaced by tissue from elsewhere in the body." she said.
"So you'll never have the ability of that natural healing again."
- X (formerly Twitter)
Related Stories
'australia is about to see a tsunami of acl injuries' warns surgeon who fixed ellie carpenter's knee.
Matildas captain Sam Kerr suffers 'devastating' ACL injury six months out from Olympics
Why do more women tear their ACL than men? This physio talked to 13 elite athletes to find out
- Doctors and Medical Professionals
- Medical Procedures
- Medical Research
- Sports injuries
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Athl Train
- v.57(2); 2022 Feb
Athletic Training and Population Health Science
Justin beaupre.
Main Line Health System, Wynnewood, PA
Sam W. Meske
Meghan buckley.
To define and discuss the role of population health as a framework to improve care and clinical decision making in athletic training practice.
Athletic trainers (ATs) are allied health professionals who are uniquely suited to provide preventive and educational health and wellness programs to improve health outcomes across a physically active population. Athletic trainers are often the first contacts for high school athletes seeking health and wellness education, which may allow ATs to be the first intervention or prevention point for reducing or eliminating negative health behaviors and outcomes among their patients.
Conclusions
Integrating a population-health framework into the athletic training setting prepares ATs to address complex health concerns in communities that result from factors that influence determinants of health. The field of athletic training could benefit from a population-health approach to care by broadening consideration of the factors that affect the health of homogeneous populations that are served by ATs.
The Commission for Accreditation of Athletic Training Education implemented new core competency standards in 2020. 1 These revisions include education about public health and the value of population-health tools, such as data-driven research and outcomes, electronic health record utilization, health informatics, and value-based care decisions. 1 Curricular changes to athletic training programs include foundational knowledge in population health, epidemiology, health care delivery systems, and payer systems. 1 Athletic training students will be required to receive educational and clinical experiences that address factors that influence the health of a population, such as behavioral health and substance abuse. Incorporating this knowledge will create a new paradigm that pushes the field of athletic training forward by widening the lens to focus on the external influences that shape health behaviors and create potential health risks for patients.
Athletic trainers (ATs) are well educated in the prevention and management of injuries and regularly collaborate with other health care providers to treat and manage patients with acute and chronic health conditions. However, what if ATs could use data and surveillance methods to predict health risks and potential illnesses in their population and to develop the appropriate interventions earlier? This is the focus of population health. Population health is defined as a cohesive, integrated, and comprehensive approach to health care that considers the distribution of health outcomes within a population, the health determinants that influence the distribution of care, and the policies and interventions that affect and are affected by the determinants. 2 A population-health framework allows health professionals to think critically about how to manage and treat health conditions by focusing specifically on the factors that drive health and disease within groups of people (populations). These factors include biological, social, psychological, geographic, and economic conditions that shape health over the life course. 3 Athletic trainers who adopt a population-health–based approach to injury and illness prevention will be better suited to take leading roles in policy development and assessment and be able to develop and implement large-scale translations to practice initiatives that are informed by public health approaches. 4 Beyond the policy boundaries, ATs have a set of clinical responsibilities and skills that have prepared them to provide high-quality preventive care that can reduce risk and injury to the patients they serve. From a population-health perspective, with its focus on prevention and risk reduction, ATs should consider the characteristics and factors that make a subset of the population more vulnerable.
Athletic trainers are well positioned to provide effective and efficient health care to student-athletes at the secondary school level. 5 They focus on improving the health of their patients under the direction of or in collaboration with physicians and may serve as a liaison to the greater medical community. Because ATs are allied health care professionals with extensive knowledge of disease and illness prevention, they are often capable of working with patients and health professionals to find appropriate solutions to address a wide variety of health-related concerns. 4 As the number of US student-athletes has risen to nearly 8 million, 6 the responsibility of caring for them has increased not only the volume of patients seen by ATs but also the roles that ATs play in health maintenance and care. In 2015, researchers 7 found that nearly 70% of US public schools had access to some athletic training services; however, only 30% of those schools had full-time services. The focus of this paper is on the role high school ATs can play in addressing health determinants that affect the health of their patients. In the high school setting, the AT is often the first contact for care outside of an athlete or patient's primary care physician. Because health behaviors and attitudes are often shaped during these early adolescent years, providing ATs with a population-health framework to recognize and identify the factors that affect health determinants may reduce the risk of worse health outcomes later in the athlete's career.
POPULATION HEALTH
Population-health programs assess the distribution of health outcomes and policies surrounding health determinants. Programs use this evidence to strategize improvements in how determinants of health are affecting large homogeneous groups of individuals throughout a system, which improves health outcomes. Population health seeks to provide a conceptual framework to organize thinking and approaches to the study of wellbeing and variability among populations. 2 In a population-health framework, clinical practice standards shift from care that is individual to care that considers population-level perspectives. This can be achieved by using primary and secondary prevention strategies, improved screening and surveillance, and broadening our focus beyond acute and episodic health care events.
The framework for population health has 4 pillars: chronic care management, quality and safety, health policy, and public health ( Figure ). 2 Athletic trainers are part of an interprofessional health care model that works closely with patients, providers, school officials, and others to improve the health and wellbeing of the population they treat. Although the pillars of population health are all-encompassing for allied health professionals, this does not imply that providers should be responsible for activities in each category. For example, ATs will not often be working in public health settings or actively engaged in policy making at the state or national level. However, it is important that ATs begin to think about the tasks in their daily practice that fit into each of these pillars. In the following paragraphs, ATs' engagement in the pillars of population health are highlighted with examples.

Four pillars of population health.
Chronic Care Management
Care management is a vital role in athletic training practice. Athletic trainers use a variety of health promotion and preventive measures that focus on health behavior modification. Athletic trainers work with patients who have a variety of existing health conditions and help to facilitate and manage both acute and chronic care needs. Because of this relationship, it is imperative that they establish partnerships with a variety of health care providers and resources. Using this care management model, ATs gain information about the patients they serve and are able to share information with those patients by becoming part of a broader community of interprofessional health care teams. For instance, an athlete who was diagnosed with type 1 diabetes and is using an insulin pump will require care coordinated among the AT, primary care provider, and endocrinologist to manage insulin levels that fluctuate due to physical activity. This potentially improves the way in which patients use their health care, both to prevent the misuse of health services and to promote effective and efficient use of health services over the course of their care with ATs.
Quality and Safety
Participating in athletics is associated with an inherent risk of injury. Athletic trainers often use injury surveillance to track and make inferences about the causes and risks of illness and injury among the populations they serve. With the current focus on value-based care models, many ATs collect patient-reported outcomes data to evaluate the quality of interventions and treatments. These tools and practices have advanced the development of evidence-based treatment protocols, as well as the creation and implementation of prevention and screening tools, and informed epidemiologic studies that lead to reductions in the risk of injury or illness.
Health Policy
Health policy in athletic training is likely to occur on the state and national levels. The National Athletic Trainers' Association has developed practice policies and guidelines that keep ATs and athletes safe and protected. Athletic trainers may be part of the policy development process for injury prevention, risk management, behavioral health policy, return-to-play guidelines, and referral guides at the school and district levels. In nearly all 50 states, the athletic training profession is managed by a regulatory body that outlines policies, practice guidelines, and rules and regulations. Athletic trainers have been involved in developing many of these laws and regulations.
Public Health
Public health is a relatively new field for athletic training. The National Athletic Trainers' Association has created a task force to examine the role of ATs in public health and collaborate with the American Public Health Association to bring awareness of public health initiatives to ATs. Collaborating with health departments and community-facing organizations may create opportunities for developing innovative strategies to address the social determinants of health, reducing health disparities and preventing disease transmission. Athletic trainers also regularly engage in injury prevention, health screenings, health education, and injury and disease surveillance within populations. Given ATs' unique skill set and the overlap between the medical and public health models, they are well positioned to lead responses to public health emergencies. For example, the global COVID-19 pandemic has created an opportunity for ATs to begin interpreting and implementing public health policy and data from organizations such as the Centers for Disease Control and Prevention. As a result of the pandemic, ATs are consulting with organizational leadership to implement new policies and procedures that protect the health of the populations they serve.
Characteristics of Population-Health Professionals
An interdisciplinary population-health model suggests that clinicians adopt certain attributes or characteristics that will lead to successful health outcomes. These include taking personalized, patient-centered approaches to health, such as shared decision making about health promotion and case management; calling on interdisciplinary care teams to address complex health needs; gaining knowledge about determinants of health and their effect on population health and individual health outcomes; and using evidence-based care strategies that provide high-quality, value-based, effective care. 2 These attributes of population health align well with ATs' current practices. Athletic trainers use evidence-based treatment guidelines to manage a variety of conditions such as concussions, mental health disorders and addictions, and musculoskeletal injuries.
Translating Population Health Into Athletic Training Practice
Three athletic training competencies can be used to improve health of populations:
- Assess the health status of populations using available data (eg, public health surveillance data, vital statistics, registries, surveys, electronic health records, and health plan claims data).
- Discuss the role of socioeconomic, environmental, cultural, and other population-level determinants of health on the health status and health care of individuals and populations.
- Identify community assets and resources to improve the health of individuals and populations. 8
Population-level data alert us to trends in populations. The field of athletic training should be informed by data that surveil risks and trends to inform assessments, treatments, and health outcomes. Athletic trainers know how to care for individuals and their health needs but may not be attuned to the larger group needs within the populations they serve. Athletic trainers spend numerous hours with patients developing treatment plans, assessing and monitoring their health status, and building relationships that foster trust and engagement. Because population health focuses on homogeneous groups of people and identifying and understanding factors that affect health outcomes in these groups, incorporating these competencies can serve as an additional protective factor for reducing injury, illness, and worse health outcomes. The causes of population health are multilevel (institutions, socioeconomic policies, communities, social relationships, and individual behaviors) and accumulate throughout the life course. 9 This population-health lens of increasingly vigilant surveillance to identify the factors and conditions that put populations at greater risk than others for health disparities, injuries, and risk is critical for the field of athletic training.
Athletic trainers are often in positions where they observe disparities that are caused by health inequity. In a pilot focus group we conducted, ATs discussed health concerns related to poverty, food scarcity, substance abuse, mental health, housing insecurity, crime, and violence. Surveillance and detection of these problems may help ATs develop preventive initiatives that connect patients with the appropriate professionals and resources to prevent worse health outcomes.
CONCLUSIONS
A population-health framework can benefit the field of athletic training by positioning ATs to consider a broader perspective in understanding the factors that affect the health of the populations they serve through interprofessional collaborations and community support. Early detection and prevention of illness and injury has long been the primary role of the AT. The profession can continue to expand on this by shifting toward a population-health framework and recognizing how the distribution of health determinants may place the populations they serve at risk for worse health outcomes. Athletic trainers should take proactive steps to recognize these population-health concerns and implement new preventive health-education opportunities. As ATs become more knowledgeable about population health and begin thinking critically about the conditions affecting the health of their communities and patients, they will be able to implement transformative policies, interventions, and practices that raise the health status of the populations they serve.
- OUR MISSION
- STRATEGIC PLAN
- COLLEGE GOVERNANCE
- WHAT IS OSTEOPATHIC MEDICINE?
- FACTS AND FIGURES
- OUR THREE SITES
- DIVERSITY, INCLUSION AND SAFETY
- CLINICAL OUTREACH
- INTERNATIONAL OPPORTUNITIES
- LEARNING AND ASSESSMENT CENTER
- GRADUATE MEDICAL EDUCATION
- OUR COMMUNITIES
- COMMON GROUND PROFESSIONALISM INITIATIVE
- ACCREDITATION
- CONTACT INFORMATION
- COMPLIMENTS AND CONCERNS
- WHY MSU COLLEGE OF OSTEOPATHIC MEDICINE?
- DUAL DEGREE PROGRAMS
- PA MEDICINE PROGRAM
- GLOBAL HEALTH STUDIES
- PATHWAY PROGRAMS
- ONBOARDING TIMELINE
- FINANCIAL AID AND SCHOLARSHIPS
- SITE SELECTION
- TECHNOLOGY REQUIREMENTS & RECOMMENDATIONS
- PREMATRICULATION CHECKLIST
- DISABILITY SERVICES
- PRECLERKSHIP MEDICAL EDUCATION
- CLERKSHIP MEDICAL EDUCATION
- CLASS-SPECIFIC INFORMATION
- COLLEGE OF OSTEOPATHIC MEDICINE REGISTRAR
- ACADEMIC AND CAREER ADVISING
- STUDENT AFFAIRS
- STUDENT HANDBOOK AND COURSE CATALOG
- MSUCOM MERCHANDISE STORE
- CONVOCATION
- COMMENCEMENT
- GET INVOLVED
- STAY CONNECTED
- MICHIGAN OSTEOPATHIC COLLEGE FOUNDATION
- DEGREE, LICENSURE, AND VERIFICATION
- ANNUAL REPORT
- DEAN&RSQUO;S UPDATE
- COLLEGE NEWS
- SPARTANDO JOURNEYS
- SPARTANDO IN THE NEWS
- SPARTANDO EXPERT TAKE
- COVID-19 INFORMATION
- PATENGE MEDAL OF PUBLIC SERVICE
- IN MEMORIAM
- Faculty/Staff Directory
- Departments
- Research & Scholarly Activity
- Continuing Medical Education
Michigan State University
College of osteopathic medicine, msu omm clinic continues to serve, expand 40 years later.
MSU Health Care Osteopathic Manipulative Medicine comes from humble beginnings, but has grown to accommodate a hefty caseload. What started during the 1980s in the basement of Lansing General Hospital’s professional building eventually expanded to the third floor of the hospital. It later moved to MSU’s Clinical Center before settling at its current location at 4660 S. Hagadorn Road, Suite 500.
“The numbers are daunting,” said Reddog Sina, D.O., assistant professor of Osteopathic Manipulative Medicine at the MSU College of Osteopathic Medicine, who is board-certified in Neuromusculoskeletal Medicine and Osteopathic Manipulative Medicine (NMM/OMM), and sees patients daily at MSU Health Care OMM. These are busy days at the clinic. In 2023 alone, the clinic had 33,550 appointments. Patients range from newborns to centenarians seeking non-surgical treatment for a wide range of arthrodial and neuromuscular conditions including feeding issues, torticollis, neck pain, back pain, joint and muscle pain, headaches and temporomandibular joint dysfunction (commonly referred to as TMJ).
Through it all, MSU Health Care OMM has stayed true to its mission “to maintain a model of osteopathic medical practice, provide leadership in the transformation and promotion of osteopathic principles, and contribute to osteopathic philosophy’s biological, behavioral and clinical science foundation.”
Medical Practice
After being referred by their primary care providers, patients with wide-ranging conditions seek treatment at MSU Health Care OMM. “Our patients are already under the care of a primary care provider, and we are consulted for our expertise in neuromusculoskeletal medicine,” said J’Aimee Lippert, D.O., who is one of the clinic’s physicians, as well as the interim chair and an associate professor for the MSU College of Osteopathic Medicine’s Department of Osteopathic Manipulative Medicine. “We emphasize to patients that maintaining good contact with their primary care provider is important – we value that relationship! When a patient is referred to OMM, it is because of our expertise in the optimal function of the neuromusculoskeletal system.”
Once referred, patients at MSU Health Care OMM receive care that considers more than their signs and symptoms. “Learning OMM teaches trainees to palpate (examine through touch), and osteopathic physicians are the doctors that palpate. Touch is incredibly sensitive, and can be trained to differentiate very different tissue conditions that aren’t obvious by only using observation,” Dr. Sina explained. “We learn to look at our patients through the physical, spiritual and mental approaches to their lives. Our practice helps to integrate those things.”
Educational Outreach
At MSU Health Care OMM, outreach comes in the form of medical education. In addition to undergraduate and D.O. students from MSU, the clinic hosts high school students, visiting undergraduate and medical students and visiting residents. These opportunities demonstrate how osteopathic manipulative medicine works in real patient care. Dr. Lippert noted this experience is especially valuable for students.

“Those students who come to shadow us or do rotations in the clinic really get to see the power – the clinical impact of using our hands. They also have critical opportunities to apply their knowledge in clinical environments during primary care preclerkship courses, throughout clerkship rotations and during extracurricular and cocurricular experiences, such as Student OMM Clinic, Street Medicine and Sports OMT.”
Clinical Research
Doctors at MSU Health Care OMM often publish case studies that contribute to broader research efforts. In a recently published study , for example, Dr. Sina detailed how, in one adult patient experiencing sudden-onset hearing loss from no discernible cause, he used manipulative medicine to open up the patient’s eustachian tube, which connects the ear to the nasopharynx.
In addition to clinical studies, MSU Health Care OMM also produces original projects and quality improvement studies. Of special note is MSU’s Center for Neuromusculoskeletal Clinical Research (CNCR). This lab houses a special treadmill equipped with motion-capture technology to conduct gait research, as well as equipment for concussion research. The CNCR assists researchers in evaluating skeletal motion gait in individuals, which can then be compared to larger populations, such as people with chronic back pain. The lab’s state-of-the-art equipment also makes it a strong candidate for facilitating research partnerships.
Looking Ahead
MSU Health Care OMM is reputed to be the largest OMM clinic in the world. While it carries an impressive caseload, the clinic’s size also measures the fact that the osteopathic neuromusculoskeletal specialty – the doctors who focus on OMM – is among the smallest osteopathic specialties.
“We have the biggest clinic in the country, but as a specialty across the nation, we’re very small,” Dr. Lippert explained. “For many patients, this is all quite novel, and understanding how their body functions can be a new concept.”
Dr. Lippert explained that during an appointment, osteopathic doctors evaluate how a patient’s body moves, identify areas that are moving well and those that are not and connect that information to the patient’s work, hobbies and past experiences. Osteopathic physicians can then use osteopathic manipulative treatment to address areas of concern.
“The very idea that we can use our hands to improve function and mobility, which can help them breathe, circulate, think and perform better, is often a revelation,” said Dr. Lippert. “This message needs to be widely shared. We have a very real opportunity to share what osteopathic medicine contributes to the health of all communities, and we take that obligation and responsibility very seriously.”
The osteopathic medical field is growing. According to the American Osteopathic Association, nearly 149,000 osteopathic physicians were in practice in 2023 , which measured a 30 percent increase since 2018. Today, more than 11 percent of physicians are osteopathic doctors, and 25 percent of all medical students in the U.S. study osteopathic medicine.
Open for enrollment: MSU’s current osteopathic manipulative medicine/treatment (OMM/OMT) clinical studies
- Prospective participants: please contact [email protected]
- Prospective participants: please contact [email protected]
- Prospective participants: please contact [email protected]
- Prospective participants: please contact [email protected]
By E. LaClear
- Outreach and Engagement
- Faculty/Staff

IMAGES
VIDEO
COMMENTS
The American Journal of Sports Medicine, founded in 1972, is the official publication of the American Orthopaedic Society for Sports Medicine.It contains original articles addressed to orthopaedic surgeons specializing in sports medicine, and to team physicians, athletic trainers, and physical therapists focusing on the causes and effects of injury or disease resulting from or affected by ...
The physiological demands of esports are poorly understood and need to be investig... Mitchell Nicholson, Dylan Poulus, Rob Robergs, Vincent Kelly and Craig McNulty. Sports Medicine - Open 2024 10 :44. Original Research Article Published on: 17 April 2024. Full Text.
Lars Donath. Daniel L. Belavy. Systematic Review Open access 14 December 2023 Pages: 711 - 725. 1. 2. …. 78. Next. Sports Medicine bridges the gap between science and practice in the promotion of exercise and health, and in the scientific assessment, study and ...
The American Journal of Sports Medicine (AJSM) is the official peer-reviewed scientific journal of the American Orthopaedic Society for Sports Medicine (AOSSM). Founded in 1972, AJSM is an essential forum for independent orthopaedic sports medicine research and education, allowing clinical practitioners the ability to make decisions based on sound scientific information.
As such, optimising performance, improving the best players' availability, and decreasing the risk of injury have become the main thrusts of sports science and sports medicine when tied to high-performance teams. 5. Sports science research can help lead to evidence-based approaches that will allow athletes and active individuals to exercise ...
British Journal of Sports Medicine (BJSM) is a Plan S compliant Transformative Journal. British Journal of Sports Medicine (BJSM) is a multimedia portal for authoritative original research, systematic reviews, consensus statements and debate in sport and exercise medicine (SEM). We define sport and exercise medicine broadly. BJSM's web, print, video and audio material serves the ...
Medicine & Science in Sports & Exercise (MSSE), ACSM's flagship monthly peer-reviewed journal, is the leading multidisciplinary original research journal for members. Each issue features original investigations, clinical studies and comprehensive reviews on current topics in sports medicine and exercise science.
Clinical Journal of Sport Medicine is an international refereed journal published for clinicians with a primary interest in sports medicine practice. The journal publishes original research and reviews covering diagnostics, therapeutics, and rehabilitation in healthy and physically challenged individuals of all ages and levels of sport and exercise participation.
Sports Medicine also welcomes the submission of high-quality original research in the above fields. As a hybrid journal, Sports Medicine does not charge authors to publish using the traditional subscription-based publishing route, but does offer the option to publish accepted articles open access if authors so wish or if their funders require ...
Research in Sports Medicine is a broad journal that aims to bridge the gap between all professionals in the fields of sports medicine. The journal serves an international audience and is of interest to professionals worldwide. The journal covers major aspects of sports medicine and sports science - prevention, management, and rehabilitation of sports, exercise and physical activity related ...
As injury is an inevitable part of sports participation, more and more attention has been paid to the research of sports medicine. Due to the rapid growth of sports medicine of athletes research, it is a challenge to entirely understand its research status and hotspots. ... From the analysis of Citespace, we found that the annual articles about ...
Sports Medicine. Online first articles. Search within journal. Search. Online first articles Articles not assigned to an issue 50 articles. ... Content type: Original Research Article Open Access; Published: 31 October 2023; This is part of 1 collection: Rugby Health; Exploring the Role of Sprint Biomechanics in Hamstring Strain Injuries: A ...
Together, research shows that organized sports, in clubs or companies, are more important for people's overall physical activity than ever before. Groups that are usually less physically active can be motivated through sport—for example, elderly men in sport supporters' clubs [ 169 ], people in rural areas [ 170 ], migrants [ 171 ], and ...
Sports Medicine - Open focuses on original research and definitive reviews in the field of sport and exercise medicine. The Journal includes medical and scientific research relating to: ... Articles published in Sports Medicine - Open will include a Key Points table. Please provide approximately three short, stand-alone lines/statements ...
The impact of a mid-season FIFA World Cup™ on injury occurrence and patterns in French professional soccer clubs. Emmanuel Orhant et al. Article | Published online: 6 Mar 2024. View all latest articles. Explore the current issue of Research in Sports Medicine, Volume 32, Issue 3, 2024.
Monitoring elite athletes' body composition (BC) is vital for health and optimizing performance in sports emphasizing leanness, such as athletics. This study aims to investigate and compare sex- and event-specific off-to in-season BC changes in endurance and power event athletics competitors. Elite male and female endurance athletes (> 800 m runners; n = 21) and power event athletes ...
Mayo Clinic Sports Medicine Research focuses on the following areas for optimal care and results for athletes: Mechanisms that may identify the anatomical and structural causes of injuries. Screening using algorithms to identify athletes at a high risk of injury. Intervention and prevention through neuromuscular training protocols.
Sports Medicine - Female athletes are four to six times more likely to sustain an anterior cruciate ligament (ACL) injury than male athletes. ... A systematic literature search was conducted across the following scientific databases to identify original research articles published from inception to July 2022 and then updated in May 2023: PubMed ...
Sports medicine also engages amateur sportsmen and strives to promote physical activity and quality of life in the general population. Hence, the field involves all ages from childhood to old age, aiming to preserve and support every person at every age. Sports medicine, which started developing in the 19 th century, is today a medical speciality.
Journal of Sports Science and Medicine. Journal of Sports Science and Medicine (JSSM) is a nonprofit scientific electronic journal, publishing research and case studies, and review article in the fields of sports medicine and exercise sciences. JSSM is an open access journal which means that all content is freely available without charge to the ...
Sports medicine, sports science, dietetics, cultural influences, and even popular media are all included in the topic of "sports nutrition." ... United States has the larger number of articles on sports nutrition, which may be due to the disadvantage of Chinese sports research in writing English articles. The amount of nutrition studies on ...
Articles published in Sports Medicine - Open will include a Key Points table. Please provide approximately three short, stand-alone lines/statements summarizing the key findings/implications of the paper. These should be provided after the Abstract under the heading 'Key Points'. Please note that we advocate the explicit naming of each author ...
Objective The primary objective of this cross-sectional study was to compare standard laboratory performance metrics of transgender athletes to cisgender athletes. Methods 19 cisgender men (CM) (mean±SD, age: 37±9 years), 12 transgender men (TM) (age: 34±7 years), 23 transgender women (TW) (age: 34±10 years) and 21 cisgender women (CW) (age: 30±9 years) underwent a series of standard ...
Sports Medicine focuses on definitive and comprehensive review articles that interpret and evaluate the current literature to provide the rationale for and application of research findings in the sports medicine and exercise field. Major topics covered by reviews published in the journal include: Sports medicine and sports science, including performance research.
Dr Filbay said her research showed that patients treated non-surgically returned to sport at similar rates. ... When sports physiotherapist Clare Walsh did her training 20 years ago, she was ...
The Commission for Accreditation of Athletic Training Education implemented new core competency standards in 2020. 1 These revisions include education about public health and the value of population-health tools, such as data-driven research and outcomes, electronic health record utilization, health informatics, and value-based care decisions. 1 Curricular changes to athletic training programs ...
In addition to clinical studies, MSU Health Care OMM also produces original projects and quality improvement studies. Of special note is MSU's Center for Neuromusculoskeletal Clinical Research (CNCR). This lab houses a special treadmill equipped with motion-capture technology to conduct gait research, as well as equipment for concussion research.