
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.

18.1 Understanding Health, Medicine, and Society
Learning objectives.
- Understand the basic views of the sociological approach to health and medicine.
- List the assumptions of the functionalist, conflict, and symbolic interactionist perspectives on health and medicine.
Health refers to the extent of a person’s physical, mental, and social well-being. This definition, taken from the World Health Organization’s treatment of health, emphasizes that health is a complex concept that involves not just the soundness of a person’s body but also the state of a person’s mind and the quality of the social environment in which she or he lives. The quality of the social environment in turn can affect a person’s physical and mental health, underscoring the importance of social factors for these twin aspects of our overall well-being.
Medicine is the social institution that seeks both to prevent, diagnose, and treat illness and to promote health as just defined. Dissatisfaction with the medical establishment has been growing. Part of this dissatisfaction stems from soaring health-care costs and what many perceive as insensitive stinginess by the health insurance industry, as the 2009 battle over health-care reform illustrated. Some of the dissatisfaction also reflects a growing view that the social and even spiritual realms of human existence play a key role in health and illness. This view has fueled renewed interest in alternative medicine. We return later to these many issues for the social institution of medicine.
The Sociological Approach to Health and Medicine
We usually think of health, illness, and medicine in individual terms. When a person becomes ill, we view the illness as a medical problem with biological causes, and a physician treats the individual accordingly. A sociological approach takes a different view. Unlike physicians, sociologists and other public health scholars do not try to understand why any one person becomes ill. Instead, they typically examine rates of illness to explain why people from certain social backgrounds are more likely than those from others to become sick. Here, as we will see, our social location in society—our social class, race and ethnicity, and gender—makes a critical difference.

A sociological approach emphasizes that our social class, race and ethnicity, and gender, among other aspects of our social backgrounds, influence our levels of health and illness.
U.S. Army Garrison Japan – Arnn students celebrate diversity; weeklong recognition – CC BY-NC-ND 2.0.
The fact that our social backgrounds affect our health may be difficult for many of us to accept. We all know someone, and often someone we love, who has died from a serious illness or currently suffers from one. There is always a “medical” cause of this person’s illness, and physicians do their best to try to cure it and prevent it from recurring. Sometimes they succeed; sometimes they fail. Whether someone suffers a serious illness is often simply a matter of bad luck or bad genes: we can do everything right and still become ill. In saying that our social backgrounds affect our health, sociologists do not deny any of these possibilities. They simply remind us that our social backgrounds also play an important role (Cockerham, 2009).
A sociological approach also emphasizes that a society’s culture shapes its understanding of health and illness and practice of medicine. In particular, culture shapes a society’s perceptions of what it means to be healthy or ill, the reasons to which it attributes illness, and the ways in which it tries to keep its members healthy and to cure those who are sick (Hahn & Inborn, 2009). Knowing about a society’s culture, then, helps us to understand how it perceives health and healing. By the same token, knowing about a society’s health and medicine helps us to understand important aspects of its culture.
An interesting example of culture in this regard is seen in Japan’s aversion to organ transplants, which are much less common in that nation than in other wealthy nations. Japanese families dislike disfiguring the bodies of the dead, even for autopsies, which are also much less common in Japan than other nations. This cultural view often prompts them to refuse permission for organ transplants when a family member dies, and it leads many Japanese to refuse to designate themselves as potential organ donors (Sehata & Kimura, 2009; Shinzo, 2004).
As culture changes over time, it is also true that perceptions of health and medicine may also change. Recall from Chapter 2 “Eye on Society: Doing Sociological Research” that physicians in top medical schools a century ago advised women not to go to college because the stress of higher education would disrupt their menstrual cycles (Ehrenreich & English, 2005). This nonsensical advice reflected the sexism of the times, and we no longer accept it now, but it also shows that what it means to be healthy or ill can change as a society’s culture changes.
A society’s culture matters in these various ways, but so does its social structure, in particular its level of economic development and extent of government involvement in health-care delivery. As we will see, poor societies have much worse health than richer societies. At the same time, richer societies have certain health risks and health problems, such as pollution and liver disease (brought on by high alcohol use), that poor societies avoid. The degree of government involvement in health-care delivery also matters: as we will also see, the United States lags behind many Western European nations in several health indicators, in part because the latter nations provide much more national health care than does the United States. Although illness is often a matter of bad luck or bad genes, the society we live in can nonetheless affect our chances of becoming and staying ill.
Sociological Perspectives on Health and Medicine
The major sociological perspectives on health and medicine all recognize these points but offer different ways of understanding health and medicine that fall into the functional, conflict, and symbolic interactionist approaches. Together they provide us with a more comprehensive understanding of health, medicine, and society than any one approach can do by itself (Cockerham, 2009). Table 18.1 “Theory Snapshot” summarizes what they say.
Table 18.1 Theory Snapshot
| Theoretical perspective | Major assumptions |
|---|---|
| Functionalism | Good health and effective medical care are essential for the smooth functioning of society. Patients must perform the “sick role” in order to be perceived as legitimately ill and to be exempt from their normal obligations. The physician-patient relationship is hierarchical: the physician provides instructions, and the patient needs to follow them. |
| Conflict theory | Social inequality characterizes the quality of health and the quality of health care. People from disadvantaged social backgrounds are more likely to become ill and to receive inadequate health care. Partly to increase their incomes, physicians have tried to control the practice of medicine and to define social problems as medical problems. |
| Symbolic interactionism | Health and illness are : Physical and mental conditions have little or no objective reality but instead are considered healthy or ill conditions only if they are defined as such by a society. Physicians “manage the situation” to display their authority and medical knowledge. |
The Functionalist Approach
As conceived by Talcott Parsons (1951), the functionalist perspective on health and medicine emphasizes that good health and effective medical care are essential for a society’s ability to function. Ill health impairs our ability to perform our roles in society, and if too many people are unhealthy, society’s functioning and stability suffer. This was especially true for premature death, said Parsons, because it prevents individuals from fully carrying out all their social roles and thus represents a “poor return” to society for the various costs of pregnancy, birth, child care, and socialization of the individual who ends up dying early. Poor medical care is likewise dysfunctional for society, as people who are ill face greater difficulty in becoming healthy and people who are healthy are more likely to become ill.
For a person to be considered legitimately sick, said Parsons, several expectations must be met. He referred to these expectations as the sick role . First, sick people should not be perceived as having caused their own health problem. If we eat high-fat food, become obese, and have a heart attack, we evoke less sympathy than if we had practiced good nutrition and maintained a proper weight. If someone is driving drunk and smashes into a tree, there is much less sympathy than if the driver had been sober and skidded off the road in icy weather.
Second, sick people must want to get well. If they do not want to get well or, worse yet, are perceived as faking their illness or malingering after becoming healthier, they are no longer considered legitimately ill by the people who know them or, more generally, by society itself.
Third, sick people are expected to have their illness confirmed by a physician or other health-care professional and to follow the professional’s advice and instructions in order to become well. If a sick person fails to do so, she or he again loses the right to perform the sick role.

Talcott Parsons wrote that for a person to be perceived as legitimately ill, several expectations, called the sick role, must be met. These expectations include the perception that the person did not cause her or his own health problem.
Nathalie Babineau-Griffith – grand-maman’s blanket – CC BY-NC-ND 2.0.
If all of these expectations are met, said Parsons, sick people are treated as sick by their family, their friends, and other people they know, and they become exempt from their normal obligations to all these people. Sometimes they are even told to stay in bed when they want to remain active.
Physicians also have a role to perform, said Parsons. First and foremost, they have to diagnose the person’s illness, decide how to treat it, and help the person become well. To do so, they need the cooperation of the patient, who must answer the physician’s questions accurately and follow the physician’s instructions. Parsons thus viewed the physician-patient relationship as hierarchical: the physician gives the orders (or, more accurately, provides advice and instructions), and the patient follows them.
Parsons was certainly right in emphasizing the importance of individuals’ good health for society’s health, but his perspective has been criticized for several reasons. First, his idea of the sick role applies more to acute (short-term) illness than to chronic (long-term) illness. Although much of his discussion implies a person temporarily enters a sick role and leaves it soon after following adequate medical care, people with chronic illnesses can be locked into a sick role for a very long time or even permanently. Second, Parsons’s discussion ignores the fact, mentioned earlier, that our social location in society in the form of social class, race and ethnicity, and gender affects both the likelihood of becoming ill and the quality of medical care we receive. Third, Parsons wrote approvingly of the hierarchy implicit in the physician-patient relationship. Many experts say today that patients need to reduce this hierarchy by asking more questions of their physicians and by taking a more active role in maintaining their health. To the extent that physicians do not always provide the best medical care, the hierarchy that Parsons favored is at least partly to blame.
The Conflict Approach
The conflict approach emphasizes inequality in the quality of health and of health-care delivery (Conrad, 2009). As noted earlier, the quality of health and health care differ greatly around the world and within the United States. Society’s inequities along social class, race and ethnicity, and gender lines are reproduced in our health and health care. People from disadvantaged social backgrounds are more likely to become ill, and once they do become ill, inadequate health care makes it more difficult for them to become well. As we will see, the evidence of inequities in health and health care is vast and dramatic.
The conflict approach also critiques the degree to which physicians over the decades have tried to control the practice of medicine and to define various social problems as medical ones. Their motivation for doing so has been both good and bad. On the good side, they have believed that they are the most qualified professionals to diagnose problems and treat people who have these problems. On the negative side, they have also recognized that their financial status will improve if they succeed in characterizing social problems as medical problems and in monopolizing the treatment of these problems. Once these problems become “medicalized,” their possible social roots and thus potential solutions are neglected.
Several examples illustrate conflict theory’s criticism. Alternative medicine is becoming increasingly popular (see Chapter 18 “Health and Medicine” , Section 18.4 “Medicine and Health Care in the United States” ), but so has criticism of it by the medical establishment. Physicians may honestly feel that medical alternatives are inadequate, ineffective, or even dangerous, but they also recognize that the use of these alternatives is financially harmful to their own practices. Eating disorders also illustrate conflict theory’s criticism. Many of the women and girls who have eating disorders receive help from a physician, a psychiatrist, a psychologist, or another health-care professional. Although this care is often very helpful, the definition of eating disorders as a medical problem nonetheless provides a good source of income for the professionals who treat it and obscures its cultural roots in society’s standard of beauty for women (Whitehead & Kurz, 2008).
Obstetrical care provides another example. In most of human history, midwives or their equivalent were the people who helped pregnant women deliver their babies. In the 19th century, physicians claimed they were better trained than midwives and won legislation giving them authority to deliver babies. They may have honestly felt that midwives were inadequately trained, but they also fully recognized that obstetrical care would be quite lucrative (Ehrenreich & English, 2005). In a final example, many hyperactive children are now diagnosed with ADHD, or attention deficit/hyperactivity disorder. A generation or more ago, they would have been considered merely as overly active. After Ritalin, a drug that reduces hyperactivity, was developed, their behavior came to be considered a medical problem and the ADHD diagnosis was increasingly applied, and tens of thousands of children went to physicians’ offices and were given Ritalin or similar drugs. The definition of their behavior as a medical problem was very lucrative for physicians and for the company that developed Ritalin, and it also obscured the possible roots of their behavior in inadequate parenting, stultifying schools, or even gender socialization, as most hyperactive kids are boys (Conrad, 2008; Rao & Seaton, 2010).
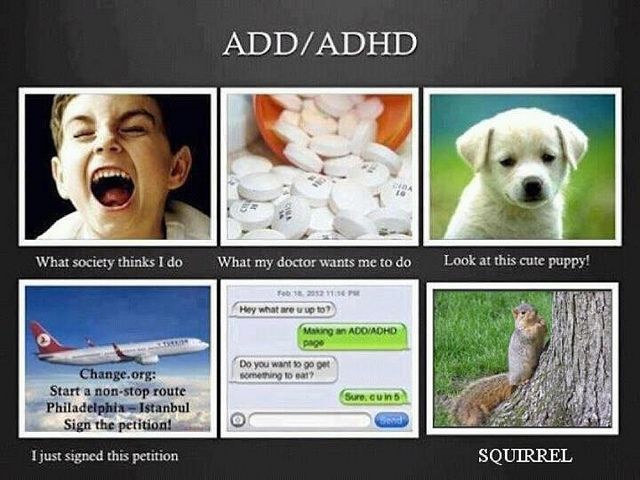
According to conflict theory, physicians have often sought to define various social problems as medical problems. An example is the development of the diagnosis of ADHD, or attention deficit/hyperactivity disorder.
birgerking – What I Really Do… ADD/ADHD – CC BY 2.0.
Critics of the conflict approach say that its assessment of health and medicine is overly harsh and its criticism of physicians’ motivation far too cynical. Scientific medicine has greatly improved the health of people in the industrial world; even in the poorer nations, moreover, health has improved from a century ago, however inadequate it remains today. Although physicians are certainly motivated, as many people are, by economic considerations, their efforts to extend their scope into previously nonmedical areas also stem from honest beliefs that people’s health and lives will improve if these efforts succeed. Certainly there is some truth in this criticism of the conflict approach, but the evidence of inequality in health and medicine and of the negative aspects of the medical establishment’s motivation for extending its reach remains compelling.
The Interactionist Approach
The interactionist approach emphasizes that health and illness are social constructions . This means that various physical and mental conditions have little or no objective reality but instead are considered healthy or ill conditions only if they are defined as such by a society and its members (Buckser, 2009; Lorber & Moore, 2002). The ADHD example just discussed also illustrates interactionist theory’s concerns, as a behavior that was not previously considered an illness came to be defined as one after the development of Ritalin. In another example, in the late 1800s opium use was quite common in the United States, as opium derivatives were included in all sorts of over-the-counter products. Opium use was considered neither a major health nor legal problem. That changed by the end of the century, as prejudice against Chinese Americans led to the banning of the opium dens (similar to today’s bars) they frequented, and calls for the banning of opium led to federal legislation early in the 20th century that banned most opium products except by prescription (Musto, 2002).
In a more current example, an attempt to redefine obesity is now under way in the United States. Obesity is a known health risk, but a “fat pride” movement composed mainly of heavy individuals is arguing that obesity’s health risks are exaggerated and calling attention to society’s discrimination against overweight people. Although such discrimination is certainly unfortunate, critics say the movement is going too far in trying to minimize obesity’s risks (Saulny, 2009).
The symbolic interactionist approach has also provided important studies of the interaction between patients and health-care professionals. Consciously or not, physicians “manage the situation” to display their authority and medical knowledge. Patients usually have to wait a long time for the physician to show up, and the physician is often in a white lab coat; the physician is also often addressed as “Doctor,” while patients are often called by their first name. Physicians typically use complex medical terms to describe a patient’s illness instead of the more simple terms used by laypeople and the patients themselves.
Management of the situation is perhaps especially important during a gynecological exam. When the physician is a man, this situation is fraught with potential embarrassment and uneasiness because a man is examining and touching a woman’s genital area. Under these circumstances, the physician must act in a purely professional manner. He must indicate no personal interest in the woman’s body and must instead treat the exam no differently from any other type of exam. To further “desex” the situation and reduce any potential uneasiness, a female nurse is often present during the exam (Cullum-Swan, 1992).
Critics fault the symbolic interactionist approach for implying that no illnesses have objective reality. Many serious health conditions do exist and put people at risk for their health regardless of what they or their society thinks. Critics also say the approach neglects the effects of social inequality for health and illness. Despite these possible faults, the symbolic interactionist approach reminds us that health and illness do have a subjective as well as an objective reality.
Key Takeaways
- A sociological understanding emphasizes the influence of people’s social backgrounds on the quality of their health and health care. A society’s culture and social structure also affect health and health care.
- The functionalist approach emphasizes that good health and effective health care are essential for a society’s ability to function. The conflict approach emphasizes inequality in the quality of health and in the quality of health care.
- The interactionist approach emphasizes that health and illness are social constructions; physical and mental conditions have little or no objective reality but instead are considered healthy or ill conditions only if they are defined as such by a society and its members.
For Your Review
- Which approach—functionalist, conflict, or symbolic interactionist—do you most favor regarding how you understand health and health care? Explain your answer.
- Think of the last time you visited a physician or another health-care professional. In what ways did this person come across as an authority figure possessing medical knowledge? In formulating your answer, think about the person’s clothing, body position and body language, and other aspects of nonverbal communication.
Buckser, A. (2009). Institutions, agency, and illness in the making of Tourette syndrome. Human Organization, 68 (3), 293–306.
Cockerham, W. C. (2009). Medical sociology (11th ed.). Upper Saddle River, NJ: Prentice Hall.
Conrad, P. (2008). The medicalization of society: On the transformation of human conditions into treatable disorders . Baltimore, MD: Johns Hopkins University Press.
Conrad, P. (Ed.). (2009). Sociology of health and illness: Critical perspectives (8th ed.). New York, NY: Worth.
Cullum-Swan, B. (1992). Behavior in public places: A frame analysis of gynecological exams . Paper presented at the American Sociological Association, Pittsburgh, PA.
Ehrenreich, B., & English, D. (2005). For her own good: Two centuries of the experts’ advice to women (2nd ed.). New York, NY: Anchor Books.
Hahn, R. A., & Inborn, M. (Eds.). (2009). Anthropology and public health: Bridging differences in culture and society (2nd ed.). New York, NY: Oxford University Press.
Lorber, J., & Moore, L. J. (2002). Gender and the social construction of illness (2nd ed.). Lanham, MD: Rowman & Littlefield.
Musto, D. F. (Ed.). (2002). Drugs in America: A documentary history . New York, NY: New York University Press.
Parsons, T. (1951). The social system . New York, NY: Free Press.
Rao, A., & Seaton, M. (2010). The way of boys: Promoting the social and emotional development of young boys . New York, NY: Harper Paperbacks.
Saulny, S. (2009, November 7). Heavier Americans push back on health debate. The New York Times , p. A23.
Sehata, G., & Kimura, T. (2009, February 28). A decade on, organ transplant law falls short. The Daily Yomiuri [Tokyo], p. 3.
Shinzo, K. (2004). Organ transplants and brain-dead donors: A Japanese doctor’s perspective. Mortality, 9 (1), 13–26.
Whitehead, K., & Kurz, T. (2008). Saints, sinners and standards of femininity: Discursive constructions of anorexia nervosa and obesity in women’s magazines. Journal of Gender Studies, 17 , 345–358.
Sociology Copyright © 2016 by University of Minnesota is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Sociology and Health
- First Online: 23 March 2022
Cite this chapter

- Mat Jones 3
1846 Accesses
Illness can seem random; yet, an extensive body of evidence suggests that health and disease are patterned in complex ways suggesting a more systematic and social process of disease causation. The first part of this chapter explores the social patterning of health and illness. Evidence linking social divisions, such as class, gender and ethnicity, with experiences of health and healthcare is examined. Sociology contributes to finding explanations for the persistence of social inequalities in health, as well as strategies to eliminate or reduce them.
Part 2 of the chapter explores the methodological approaches of sociology. Sociologists have looked beyond the assumed altruism of health professionals to examine the individual, group and social impact of professional practice. Sociology relies on both evidence and theory. In addition to a critical examination of evidence such as mortality rates, sociology involves the development and testing of theoretical frameworks and perspectives that seek to explain patterns of health and illness.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Social Determinants of Health

Data, Social Determinants, and Better Decision-making for Health: the 3-D Commission
Further reading.
Annandale, E. (2014). The Sociology of Health and Medicine: A Critical Introduction (2nd ed.). Polity Press.
Google Scholar
Bartley, M. (2016). Health Inequality: An Introduction to Concepts, Theories and Methods . John Wiley & Sons.
Cockerburn, W. C. (2013). Social Causes of Health and Disease (2nd ed.). Polity.
Gabe, J., Kelleher, D., & Williams, G. (Eds.). (2006). Challenging Medicine (2nd ed.). Routledge.
Nettleton, S. (2020). The Sociology of Health and Illness (4th ed.). Polity.
Finally, it is important to remember that sociological research often appears in journals before it is described in books. Relevant journals include the Sociology of Health and Illness, Social Science and Medicine, Health, Health Risk and Society, and Frontiers in Sociology.
Ahmad, W. I. U. (1993). Making Black People Sick: “Race”, Ideology and Health Research. In W. I. U. Ahmad (Ed.), ‘Race’ and Health in Contemporary Britain (pp. 11–13). Open University Press.
Allen, L., Williams, J., Townsend, N., Mikkelsen, B., Roberts, N., Foster, C., & Wickramasinghe, K. (2017). Socioeconomic Status and Non-communicable Disease Behavioural Risk Factors in Low-income and Lower-middle-income Countries: A Systematic Review. The Lancet Global Health, 5 (3), e277–e289.
Article Google Scholar
Allik, M., Brown, D., Dundas, R., & Leyland, A. H. (2019). Differences in Ill Health and in Socioeconomic Inequalities in Health by Ethnic Groups: A Cross-Sectional Study Using 2011 Scottish Census. Ethnicity & Health , 1–19.
Armstrong, D. (1995). The Rise of Surveillance Medicine. Sociology of Health and Illness, 17 (3), 393–404.
Backett-Milburn, K., Wills, W., Gregory, S., & Lawton, J. (2006). Making Sense of Eating, Weight and Risk in the Early Teenage Years: Views and Concerns of Parents in Poorer Socio-economic Circumstances. Social Science and Medicine., 63 (3), 624–635.
Barnett, P., Mackay, E., Matthews, H., Gate, R., Greenwood, H., Ariyo, K., Bhui, K., Halvorsrud, K., Pilling, S., & Smith, S. (2019). Ethnic Variations in Compulsory Detention Under the Mental Health Act: A Systematic Review and Meta-analysis of International Data. The Lancet Psychiatry, 6 (4), 305–317.
Baum, F. (1999). Social Capital: Is It Good for Your Health? Issues for a Public Health Agenda. Journal of Epidemiology and Community Health, 53 , 195–196.
Beck, U. (1992). Risk Society: Towards a New Modernity . Sage.
Ben-Shlomo, Y., & Kuh, D. (2002). A Life Course Approach to Chronic Disease Epidemiology: Conceptual Models, Empirical Challenges and Interdisciplinary Perspectives. International Journal of Epidemiology, 31 , 285–293.
Beresford, P. (2019). Public Participation in Health and Social Care: Exploring the Co-production of Knowledge. Frontiers in Sociology, 3 , 41.
Bor, J., Cohen, G. H., & Galea, S. (2017). Population Health in an Era of Rising Income Inequality: USA, 1980–2015. The Lancet, 389 (10077), 1475–1490.
Bourdieu, P. (1984). Distinction: A Social Critique of the Judgement of Taste . Routledge.
Bury, M. (1982). Chronic Illness as Biographical Disruption. Sociology of Health and Illness, 4 (2), 167–182.
Bury, M. (2001). Illness Narratives: Fact Or Fiction? Sociology of Health & Illness, 23 (3), 263–285.
Cameron, E., & Bernades, J. (1998). Gender and Disadvantage in Health: Men’s Health for a Change. Sociology of Health and Illness, 20 (5), 673–693.
Caraher, M., & Coveney, M. (2004). Public Health Nutrition and Food Policy. Public Health Nutrition, 7 (5), 591–598.
Caroli, E., & Weber-Baghdiguian, L. (2016). Self-Reported Health and Gender: The Role of Social Norms. Social Science & Medicine, 153 , 220–229.
Chan, K. S., Parikh, M. A., Thorpe, R. J., & Gaskin, D. J. (2019). Health Care Disparities in Race-Ethnic Minority Communities and Populations: Does the Availability of Health Care Providers Play a Role? Journal of Racial and Ethnic Health Disparities, 7 , 1–11.
Clapp, J., & Scrinis, G. (2017). Big Food, Nutritionism, and Corporate Power. Globalizations, 14 (4), 578–595.
Crimmins, E. M., Kim, J. K., & Solé-Auró, A. (2011). Gender Differences in Health: Results from SHARE, ELSA and HRS. European Journal of Public Health, 21 (1), 81–91.
Crossley, M. (1998). ‘Sick role’ Or ‘empowerment’: The Ambiguities of Life with an HIV Positive Diagnosis. Sociology of Health and Illness, 20 (4), 507–531.
CSDH [Commission on Social Determinants of Health]. (2008). Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report , Geneva, WHO.
Cummins, S., & Macintyre, S. (2006). Food Environments and Obesity – Neighbourhood Or Nation? International Journal of Epidemiology, 35 , 100–104.
Darmon, N., & Drewnowski, A. (2015). Contribution of Food Prices and Diet Cost to Socioeconomic Disparities in Diet Quality and Health: A Systematic Review and Analysis. Nutrition Reviews, 73 (10), 643–660.
Davey-Smith, G. (Ed.). (2003). Health Inequalities: Lifecourse Approaches . Polity Press.
Davies, C. (1995). Gender and the Professional Predicament in Nursing . Open University Press.
DeVisser, R., & Smith, J. A. (2006). Mister in-Between – A Case Study of, Masculine Identity and Health-Related Behaviour. Journal of Health Psychology, 11 , 685–695.
Diamond, L. M. (2020). Gender Fluidity and Nonbinary Gender Identities Among Children and Adolescents. Child Development Perspectives, 14 (2), 110–115.
Doyal, L. (2001). Sex, Gender and Health: The Need for a New Approach. BMJ, 323 , 1061–1063.
Durkheim, E. (1952). Suicide . Routledge and Kegan Paul.
Ehsan, A., Klaas, H. S., Bastianen, A., & Spini, D. (2019). Social Capital and Health: A Systematic Review of Systematic Reviews. SSM-Population Health, 8 , 100425.
Everingham, C. (2001). Reconstituting Community: Social Justice, Social Order and the Politics of Community. Australian Journal of Social Issues, 36 (2), 105–122.
Fleischhacker, S. E., Evenson, K. R., Rodriguez, D. A., & Ammerman, A. S. (2011). A Systematic Review of Fast Food Access Studies. Obesity Review, 12 (5), e460–e471.
Fleming, P. J., Lee, J. G., & Dworkin, S. L. (2014). “Real Men Don’t”: Constructions of Masculinity and Inadvertent Harm in Public Health Interventions. American Journal of Public Health, 104 (6), 1029–1035.
Foster, P. (1995). Women and the Health Care Industry. An Unhealthy Relationship? Open University Press.
Foucault, M. (1976). The Birth of the Clinic: An Archaeology of Medical Perception . Tavistock.
Foucault, M. (1979a). The History of Sexuality, Vol. 1 . Allen Lane.
Foucault, M. (1979b). Discipline and Punish: The Birth of the Prison . Vintage.
Frank, A. W. (1991). For a Sociology of the Body: An Analytical Review. In M. F. M. Hepworth & B. Turner (Eds.), The Body: Social Process and Cultural Theory . Sage.
Frank, J., Abel, T., Campostrini, S., Cook, S., Lin, V. K., & McQueen, D. V. (2020). The Social Determinants of Health: Time to Re-Think? International Journal of Environmental Research and Public Health, 17 (16), 5856.
Frank, R. (2001). A Reconceptualization of the Role of Biology in Contributing to Race/Ethnic Disparities in Health Outcomes. Population Research and Policy Review, 20 , 441–455.
Freidson, E. (1970). Professional Dominance . Artherton.
Frost, L. (2003). Doing Bodies Differently? Gender, Youth, Appearance and Damage. Journal of Youth Studies, 6 (1), 55–70.
George, J., Mathur, R., Shah, A. D., Pujades-Rodriguez, M., Denaxas, S., Smeeth, L., Timmis, A., & Hemingway, H. (2017). Ethnicity and the First Diagnosis of a Wide Range of Cardiovascular Diseases: Associations in a Linked Electronic Health Record Cohort of 1 Million Patients. PloS One, 12 (6), e0178945.
Gidaris, C. (2019). Surveillance Capitalism, Datafication, and Unwaged Labour: The Rise of Wearable Fitness Devices and Interactive Life Insurance. Surveillance & Society, 17 (1/2), 132–138.
Giddens, A. (1991). Modernity and Self Identity: A Study of Comparative Sociology . Polity Press.
Goffman, E. (1963). Stigma . Penguin.
Gough, B., & Conner, M. T. (2006). Barriers to Healthy Eating Amongst Men: A Qualitative Analysis. Social Science & Medicine, 62 , 387–395.
Green, J., & Dowler, D. A. (2003). Short Cuts to Safety: Risk and ‘rules of thumb’ in Accounts of Food Choice. Health, Risk and Society, 5 (1), 33–52.
Green, M. A., Evans, C. R., & Subramanian, S. V. (2017). Can Intersectionality Theory Enrich Population Health Research? Social Science & Medicine, 178 , 214–216.
Hay, K., McDougal, L., Percival, V., Henry, S., Klugman, J., Wurie, H., Raven, J., Shabalala, F., Fielding-Miller, R., Dey, A., & Dehingia, N. (2019). Disrupting Gender Norms in Health Systems: Making the Case for Change. The Lancet, 393 (10190), 2535–2549.
Higgins, J. A., Carpenter, E., Everett, B. G., Greene, M. Z., Haider, S., & Hendrick, C. E. (2019). Sexual Minority Women and Contraceptive Use: Complex Pathways Between Sexual Orientation and Health Outcomes. American Journal of Public Health, 109 (12), 1680–1686.
IHME [Institute for Health Metrics and Evaluation] (2018). Findings from the Global Burden of Disease Study .
Illich, I. (1977). The Limits to Medicine . Penguin.
Islam, M. M. (2019). Social Determinants of Health and Related Inequalities: Confusion and Implications. Frontiers in Public Health, 7 , 11.
Jecker, N. S. (2018). Age-Related Inequalities in Health and Healthcare: The Life Stages Approach. Developing World Bioethics, 18 (2), 144–155.
Johnson, T. (1993). Expertise and the State. In M. Gane & T. Johnson (Eds.), Foucault’s New Domains . Routledge.
Johnson, T. (1995). Governmentality and the Institutionalisation of Expertise. In T. Johnson, G. Larkin, & M. Saks (Eds.), Professions and the State in Europe . Routledge.
Jones, M. (2004). Anxiety and Containment in the Risk Society: Theorising Young People’s Drugs Policy. International Journal of Drug Policy, 15 , 367–376.
Kawachi, I., Kennedy, B. P., Lochner, K., et al. (1997). Social Capital, Income Inequality, and Mortality. American Journal of Public Health, 87 , 1491–1499.
Knight, R., Shoveller, J. A., Oliffe, J. L., Gilbert, M., Frank, B., & Ogilve, G. (2012). Masculinities, ‘guy talk’ and ‘manning up’: A Discourse Analysis of How Young Men Talk About Sexual Health. Sociology of Health & Illness, 34 (8), 1246–1261.
Kurian, A. K., & Cardarelli, K. M. (2007). Racial and Ethnic Differences in Cardiovascular Disease Risk Factors: A Systematic Review. Ethnicity and Disease, 17 (1), 143.
Lang, T. (2020). Feeding Britain. Our Food Problems and How to Fix Them . Pelican Books.
Leigh, J. A., Alvarez, M., & Rodriguez, C. J. (2016). Ethnic Minorities and Coronary Heart Disease: An Update and Future Directions. Current Atherosclerosis Reports, 18 (2), 9.
Lewington, L., Sebar, B., & Lee, J. (2018). “Becoming the man you always wanted to be”: Exploring the Representation of Health and Masculinity in Men’s Health Magazine. Health Promotion Journal of Australia, 29 (3), 243–250.
Lim, W. Y., Ma, S., Heng, D., Bhalla, V., & Chew, S. K. (2007). Gender, Ethnicity, Health Behaviour & Self-Rated Health in Singapore. BMC Public Health, 7 (1), 184.
Liu, J. (2019). What Does In-Work Poverty Mean for Women: Comparing the Gender Employment Segregation in Belgium and China. Sustainability, 11 (20), 5725.
LSP [Longevity Science Panel]. (2018). Life Expectancy: Is the Socioeconomic Gap Narrowing? Available at https://www.longevitypanel.co.uk/_files/LSP_Report.pdf
Lupton, D. (1995). The Imperative of Health: Public Health and the Regulated Body . Sage.
Book Google Scholar
Lupton, D. (2005). Lay Discourses and Beliefs Related to Food Risks: An Australian Perspective. Sociology of Health and Illness, 27 (4), 448–467.
Lynch, J., Due, P., & Muntaner, C. Davey Smith, G. (2000). Social Capital – Is It a Good Investment Strategy for Public Health? Journal of Epidemiology and Community Health, 54 , 404–408.
Mackenbach, J. (2019). Health Inequalities; Persistence and Change in European Welfare States . Oxford University Press.
Mackenbach, J. D., Nelissen, K. G., Dijkstra, S. C., Poelman, M. P., Daams, J. G., Leijssen, J. B., & Nicolaou, M. (2019). A Systematic Review on Socioeconomic Differences in the Association Between the Food Environment and Dietary Behaviors. Nutrients, 11 (9), 2215.
Marmot, M. (2015). The Health Gap: The Challenge of an Unequal World . Bloomsbury.
Marmot, M., Allen, J., Boyce, T., Goldblatt, P., & Morrison, J. (2020). Health Equity in England: The Marmot Review 10 Years on . Institute of Health Equity.
Marmot, M. G., Stansfeld, S., Patel, C., North, F., Head, J., White, I., Brunner, E., Feeney, A., & Smith, G. D. (1991). Health Inequalities Among British Civil Servants: The Whitehall II Study. The Lancet, 337 (8754), 1387–1393.
Martin, G., & P, Myles L, Minion, J, Willars J, Dixon-Woods, M. (2013). Between Surveillance and Subjectification: Professionals and the Governance of Quality and Patient Safety in English Hospitals. Social Science & Medicine, 99 , 80–88.
McTaggart, L. (1996). What Doctors Don’t Tell You. The Truth About the Dangers of Modern Medicine . Thorsons.
Meeks, K. A., Freitas-Da-Silva, D., Adeyemo, A., Beune, E. J., Modesti, P. A., Stronks, K., Zafarmand, M. H., & Agyemang, C. (2016). Disparities in Type 2 Diabetes Prevalence Among Ethnic Minority Groups Resident in Europe: A Systematic Review and Meta-analysis. Internal and Emergency Medicine, 11 (3), 327–340.
Mills, C. W. (1959/2000). The Sociological Imagination . Oxford University Press.
Monteiro, C. A., Moubarac, J.-C., Cannon, G., Ng, S. W., & Popkin, B. (2013). Ultra-Processed Products Are Becoming Dominant in the Global Food System. Obesity Reviews, 14 (11), 21–28.
Moss, N. E. (2002). Gender Equity and Socioeconomic Inequality: A Framework for the Patterning of Women’s Health. Social Science and Medicine, 54 , 649–661.
Navarro, V. (1979). Medicine Under Capitalism . Croom Helm.
NVSR [National Vital Statistics Reports]. (2019). 68 (13): 1–47. Available at https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_13-508.pdf
Parsons, T. (1951). Illness and the Role of the Physician: A Sociological Perspective. American Journal of Orthopsychiatry, 21 (3), 452.
Parsons, T. (1975, Summer). The Sick Role and the Role of the Physician Reconsidered. Millbank Memorial Fund Quarterly , 257–278.
Patel, N., Ferrer, H. B., Tyrer, F., Wray, P., Farooqi, A., Davies, M. J., & Khunti, K. (2017). Barriers and Facilitators to Healthy Lifestyle Changes in Minority Ethnic Populations in the UK: A Narrative Review. Journal of Racial and Ethnic Health Disparities, 4 (6), 1107–1119.
Pearce, M., Bray, I., & Horswell, M. (2018). Weight Gain in Mid-Childhood and Its Relationship with the Fast Food Environment. Journal of Public Health, 40 (2), 237–244.
Perry-Jenkins, M., & Gerstel, N. (2020). Work and Family in the Second Decade of the 21st Century. Journal of Marriage and Family, 82 (1), 420–453.
Petrovic, D., de Mestral, C., Bochud, M., Bartley, M., Kivimäki, M., Vineis, P., Mackenbach, J., & Stringhini, S. (2018). The Contribution of Health Behaviors to Socioeconomic Inequalities in Health: A Systematic Review. Prev. Med. (Baltim.), 113 , 15–31.
PHE [Public Health England]. (2018). Local Action on Health Inequalities: Understanding and Reducing Ethnic Inequalities in Health . Public Health England. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/730917/local_action_on_health_inequalities.pdf
PHE [Public Health England]. (2020). Disparities in the Risk and Outcomes of COVID-19 . London PHE Publications. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf
Phillimore, J. A., Bradby, H., & Brand, T. (2019). Superdiversity, Population Health and Health Care: Opportunities and Challenges in a Changing World. Public Health , 172 , 93–98.
Porter, S. (1999). Social Theory and Nursing Practice . Macmillan.
Portes, A. (1998). Social Capital: Its Origins and Applications in Modern Sociology. Annual Review of Sociology, 24 , 1–24.
Powell, B. L., Luckett, R., Bekele, A., & Chao, T. E. (2020). Sex Disparities in the Global Burden of Surgical Disease. World Journal of Surgery, 44 , 1–5.
Priest, N., Paradies, Y., Trenerry, B., Truong, M., Karlsen, S., & Kelly, Y. (2013). A Systematic Review of Studies Examining the Relationship Between Reported Racism and Health and Wellbeing for Children and Young People. Social Science & Medicine, 95 , 115–127.
Putnam, R., & D. (1995). Bowling Alone: America’s Declining Social Capital. Journal of Democracy, 6 (1), 65–78.
Radcliffe, E., Lowton, K., & Morgan, M. (2013). Co-construction of Chronic Illness Narratives by Older Stroke Survivors and Their Spouses. Sociology of Health & Illness, 36 (7), 993–1007.
Robertson, S. (2006). ‘Not Living Life in Too Much of an Excess’: Lay Men Understanding Health and Well-Being. Health, 10 , 175–189.
Salway, S., Carter, L., Powell, K., et al. (2014). Race Equality and Health Inequalities: Towards More Integrated Policy and Practice . Race Equality Foundation Better Health Briefing Paper 32. Race Equality Foundation.
Samari, G., Alcalá, H. E., & Sharif, M. Z. (2018). Islamophobia, Health, and Public Health: A Systematic Literature Review. American Journal of Public Health, 108 (6), e1–e9.
Sauer, A. G., Siegel, R. L., Jemal, A., & Fedewa, S. A. (2019). Current Prevalence of Major Cancer Risk Factors and Screening Test Use in the United States: Disparities by Education and Race/Ethnicity. Cancer Epidemiology and Prevention Biomarkers, 28 (4), 629–642.
Schrecker, T. (2019). The Commission on Social Determinants of Health: Ten Years on, a Tale of a Sinking Stone, Or of Promise Yet Unrealised? Critical Public Health, 29 (5), 610–615.
Shakespeare, T. (2013). Disability Rights and Wrongs Revisited . Routledge.
Shaw, A. (2004). Discourses of Risk in Lay Accounts of Microbiological Safety and BSE: A Qualitative Interview Study. Health Risk and Society, 6 (2), 151–171.
Small, M. J., Allen, T. K., & Brown, H. L. (2017). Global Disparities in Maternal Morbidity and Mortality. Seminars in Perinatology, 41 (5), 318–322.
Tai, D. B. G., Shah, A., Doubeni, C. A., Sia, I. G., & Wieland, M. L. (2020). The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clinical Infectious Diseases, 7 , 10.
Thompson, D., Johnson, K. R., Cistrunk, K. M., Vancil-Leap, A., Nyatta, T., Hossfeld, L., Rico Méndez, G., & Jones, C. (2020). Assemblage, Food Justice, and Intersectionality in Rural Mississippi: The Oktibbeha Food Policy Council. Sociological Spectrum, 40 , 1–19.
Townsend, P., & Davidson, N. (1982). Inequalities in Health: The Black Report . Penguin.
UN [United Nations]. (2020). World Population Dashboard . Available at https://www.unfpa.org/data/world-population-dashboard
Vertovec, S. (2007). Super-Diversity and its Implications. Ethnic and Racial Studies, 30 (6), 1024–1054.
Villatoro, A. P., Mays, V. M., Ponce, N. A., & Aneshensel, C. S. (2018). Perceived Need for Mental Health Care: The Intersection of Race, Ethnicity, Gender, and Socioeconomic Status. Society and Mental Health, 8 (1), 1–24.
Walsh, D., Bendel, N., Jones, R., & Hanlon, P. (2010). It’s Not ‘just deprivation’: Why Do Equally Deprived UK Cities Experience Different Health Outcomes? Public Health, 124 (9), 487–495.
Wang, Y. J., Chen, X. P., Chen, W. J., Zhang, Z. L., Zhou, Y. P., & Jia, Z. (2020). Ethnicity and Health Inequalities: An Empirical Study Based on the 2010 China Survey of Social Change (CSSC) in Western China. BMC Public Health, 20 , 1–12.
Wallace, S., Nazroo, J., & Bécares, L. (2016). Cumulative Effect of Racial Discrimination on the Mental Health of Ethnic Minorities in the United Kingdom. American Journal of Public Health, 106 (7), 1294–1300.
Welch, H., Schwartz, L. M., & Woloshin, S. (2011). Overdiagnosed. Making People Sick in the Pursuit of Health . Beacon Press.
WHO. (2017). Gender and Women’s Mental Health . WHO. Available at https://www.who.int/mental_health/prevention/genderwomen/en/
Wilkinson, R. G. (1996). Unhealthy Societies: The Afflictions of Inequality . London: Routledge.
Wilkinson, R. G., & Pickett, K. (2009). The Spirit Level: Why More Equal Societies Almost Always Better . London: Allen Lane.
Williams, D. R., & Mohammed, S. A. (2009). Discrimination and Racial Disparities in Health: Evidence and Needed Research. Journal of Behavioral Medicine, 32 (1), 20–47.
Williams, G. H. (2003). The Determinants of Health: Structure, Context and Agency. Sociology of Health and Illness, 25 , 131–154.
Witz, A. (1992). Professions and Patriarchy . Routledge.
Wong, Y. L. A., & Charles, M. (2020). Gender and Occupational Segregation. Companion to Women’s and Gender Studies , 303–325.
Zimmerman, F. J., & Anderson, N. W. (2019). Trends in Health Equity in the United States by Race/Ethnicity, Sex, and Income, 1993–2017. JAMA Network Open, 2 (6), e196386–e196386.
Zola, I. (1972). Medicine as an Institution of Social Control. Sociological Review, 20 (4), 487–504.
Download references
Author information
Authors and affiliations.
University of the West of England, Bristol, UK
You can also search for this author in PubMed Google Scholar

Corresponding author
Correspondence to Mat Jones .
Editor information
Editors and affiliations.
School of Health, Community & Policy Studies, University of the West of England, Bristol, UK
Jennie Naidoo
London South Bank University, London, UK
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Jones, M. (2022). Sociology and Health. In: Naidoo, J., Wills, J. (eds) Health Studies. Palgrave Macmillan, Singapore. https://doi.org/10.1007/978-981-16-2149-9_7
Download citation
DOI : https://doi.org/10.1007/978-981-16-2149-9_7
Published : 23 March 2022
Publisher Name : Palgrave Macmillan, Singapore
Print ISBN : 978-981-16-2148-2
Online ISBN : 978-981-16-2149-9
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Sociological contributions to race and health: Diversifying the ontological and methodological agenda
AUTHOR CONTRIBUTION
Associated Data
Data sharing not applicable to this article as no datasets were generated or analysed during the current study. This is a review article that reviews current scholarship published in the field of Sociology.
Sociologists have made fundamental contributions to the study of race and health in the United States. They have disrupted biological assumptions of race, uncovered individual and structural factors that drive racial health disparities and explored the effects of racism on health. In recent years, however, with broader shifts towards big data, the work to understand the dynamics between race and health has been increasingly pursued from a quantitative perspective. Often, such analyses isolate intermediary mechanisms to further explain race as a cause of disease. While important, these approaches potentially limit our investigations of underlying assumptions about race and the complexity of this critical social construct. We argue that the resulting dearth of qualitative research on race and health substantially limits the knowledge being produced. After providing an overview of the overwhelming shift towards quantitative methods in the study of race and health, we present three areas of study that would benefit from greater qualitative inquiry as follows: (1) Healthy Immigrant Effect, (2) Maternal Health and (3) End-of-Life Care. We conclude with a call to the discipline to embrace the critical role of qualitative research in exploring the dynamics of race and health in the United States.
INTRODUCTION
From theoretical conceptualisations of race ( Bonilla-Silva, 1999 , 2019 ; Omi & Winant, 1994 ; Ray, 2019 ) to empirical studies exploring mechanisms that drive racial inequality across all facets of social life, sociologists have extensively explored race and racialised experiences in the United States. Quantitatively, scholars have examined the relationship between race and various individual-level outcomes including socioeconomic status, educational attainment ( Telles & Ortiz, 2009 ), employment and housing (for review, see Pager & Shepherd, 2008 ). Sociologists have also analysed neighbourhood effects (for review, see Sampson et al., 2003 ) that lead to concentrated disadvantage (Du Bois, ([1899]1967)), residential segregation, and the creation of the underclass ( Massey & Denton, 1993 ; Wilson, 1987 ), which disproportionately impact people of colour. Qualitatively, scholars have focused on lived experiences, particularly those of people of colour residing in urban settings ( Desmond, 2016 ; Duneier, 2000 ). A robust sociological tradition of urban ethnography, that dates back to the 1940s, has extensively explored neighbourhood contexts and how the increased risk of marginalisation, discrimination and criminalisation directly shapes the social worlds of people of colour living in these spaces ( Goffman, 2014 ). Furthermore, more recently scholars have looked beyond the ‘urban underclass’ and instead have examined the experiences of middle class and elite racial minorities living in urban ( Pattillo, 1999 ), suburban ( Lacy, 2007 ) and rural settings ( Eason, 2017 ). While themes of marginalisation, discrimination and stigma still emerge in this work, this scholarship has also shed much needed light on the multi-dimensional lived experiences, cultural meanings, decision-making and interactional orders surrounding people of colour living in the United States.
In the subfield of medical sociology, US scholars have documented extensive racial disparities in health, often explored from a quantitative demographic tradition. For example, age-adjusted black-white death rate ratios have worsened for blacks for heart disease and cancer over the past several decades, blacks have higher rates of premature mortality than their white counterparts ( Geronimus et al., 2001 ), greater incidence and severity of hypertension ( Kershaw et al., 2011 ), obesity ( Kershaw et al., 2013 ) and Type II diabetes as well ( Bancks et al., 2017 ), and the homicide rate was over seven times higher for Black men than for White men in 2016 ( National Center for Health Statistics, 2018 ). Resonant with several aspects of broader sociological race research, explanations for these racial disparities in health often invoke differences in socioeconomic status, neighbourhood residential conditions and medical care, frequently the consequence of enduring structural inequalities and racism ( Riley, 2017 ; Sewell, 2016 ; Williams & Collins, 2001 ; Yearby, 2018 ).
Despite these strengths, however, the subfield of medical sociology exhibits some key departures from the sociological study of race more broadly. First, as noted by Williams and Sternthal in their contribution to the 2010 special issue of Journal of Health and Social Behavior , ‘for much of the twentieth century, as reflected by publications in the two leading journals in American sociology, the health of the black populations has not been a central focus of the discipline’ ( Williams & Sternthal, 2010 , p. S16). Indeed, their review of American Journal of Sociology and American Sociological Review revealed a total of only 18 publications on racial-ethnic disparities in health by 1989, with fourteen more published from 1990–2008 (six in AJS and 8 in ASR ). In that article, Williams and Sternthal identify a series of important sociological contributions to scholarship on race and health, including, for example: (1) showing that race is largely a social rather than biological category; (2) capitalising on the multidimensionality of socioeconomic status to more fully articulate its relationship to race; (3) developing multilevel constructs of racism; and (4) identifying a multitude of empirical pathways through which segregation can affect health. The authors conclude by calling for quantitative health data to be ‘routinely collected, analysed, and presented simultaneously by race, SES, and gender’ (2010, p. S23). As a whole, this 2010 review characterises flagship medical sociology research on race and health as making critical contributions but also as limited in volume and largely oriented to using quantitative operationalisation and analytic tools in the measurement of racial disparities.
Using the same search terms as Williams and Sternthal (2010 , p. S16), we observe that flagship sociological research on race and health has modestly increased in volume in the intervening decade, but retains the largely quantitative ontological and methodological orientation of earlier work. For the years 2009–2020, out of approximately 385 articles published by American Journal of Sociology , four were captured by our search for the terms ‘race and health’, ‘health inequality and race’, ‘health inequality and ethnicity’ or ‘health disparity’ in abstracts; of those, none were qualitative. For American Sociological Review , eighteen articles addressed these topics, but only three of those used qualitative methods. For Journal of Health and Social Behavior , there was a larger volume of work addressing race, health, and inequality but a similarly small proportion was qualitative (for example, 68 unique articles came up under a search for ‘race and health’, one of which used qualitative methods). In total, only four qualitative JHSB papers were captured with the full set of search terms – a meagre 1.5% of all the articles published over eleven years by American Sociological Association’s lead medical sociology journal. Thus, while flagship publication of research in these areas has certainly increased from the pre-1989 period, and perhaps shown modest gains since 2009, developments have been overwhelmingly in the analysis of large secondary data sets and negligible qualitative approaches. Furthermore, this pattern is not fully explained by assuming that qualitative studies of race and health are simply published in other outlets. A broader search of Dissertation Abstracts International and Sociological Abstracts, using the same search terms and time periods, indicates that the proportion of research on race and health that is qualitative is generally higher than in the flagship journals, yet still quite modest. For example, our search on ‘race and health’ yielded 3741 (English language) doctoral dissertations, of which 419 were qualitative (11.2%). Considering the full set of peer-reviewed scholarly articles and books listed in Sociological Abstracts, the same search yielded 1841 publications, of which 63 (3.4%) were qualitative, a figure more in line with the flagship journals. A search of current NIH grants shows a current portfolio of 35,322 grants on ‘race and health’, but only 6% of those also use qualitative methods. Based on these data, we conclude that methodological foci of US flagship journals may be partially explained by selection biases in the placement of papers but that a broad survey of sociological scholarship suggests that these trends towards quantitative investigations of race and health also hold more generally.
Critically, we are loathe to conflate ‘flagship’ with ‘quality’ in this discussion. We recognise that there is a plethora of excellent qualitative research on race and health published in outlets other than AJS, ASR and JHSB . This type of research is regularly published in respected outlets such as Social Science and Medicine , The Milbank Quarterly and Journal of Health Care for the Poor and Underserved . Indeed, Sociology of Health and Illness has been a leader in this area for many years exploring racialised experiences across different regions and health-care contexts (e.g., see Cain & McCleskey, 2019 ; Gunaratnam 2001 ; Persson & Newman, 2008 ; Smart & Weiner, 2018 ; Younis & Jadhav, 2019 ). However, we believe this ontological and methodological dominance of quantitative approaches to studies of race and health has major implications for sociology more broadly, in the United States and internationally. The assumptions and conceptualisations embedded in the intellectual traditions we see calcifying in sociology around race and health inherently narrow the types of research questions posed, concepts developed, evidence marshalled and conclusions drawn about race and health. This dominance implicitly positions qualitative approaches to these topics as ‘alternative’ or secondary to the main discoveries.
Far from being secondary, we view this type of work as fundamental for moving beyond the treatment of race as an essentialist concept and having a deeper engagement with the ways that race is configured in relational, processual and contextual terms ( Loveman, 1999 ; Morning, 2014 ; Saperstein & Penner, 2012 ). Such understanding entails unpackaging of systems, organisations, variables, racialisation and proxies for race, all of which are embedded in cultural, social, and economic systems and resources which have the potential for multiple types of health influences ( Nazroo et al., 2020 ). Furthermore, stratification systems, including the ways that people explain, rationalise and justify their biases, are reproduced through dynamic interactions ( Bonilla-Silva, 2006 ), which are insufficiently captured in quantitative measures. Qualitative approaches are ideally equipped for the elucidation of such processes and refinement of our assumptions and theories about how race operates. These approaches can help reveal our own biases and points of stagnation as theorists and researchers.
Furthermore, the implications of these patterns are cascading and reifying, mattering for intellectual and professional reasons. To the extent that hiring, funding and career trajectories are tethered to dissemination outlets, and reputations of departments and programmes are built on those indicators of individual researchers’ successes, the type of research that is published in flagship outlets matters. Rather than be relegated to the ‘alternative’ spaces within and around sociology, we believe that qualitative research on race and health should also be central to the modern sociological agenda in order to help the field outgrow outdated essentialist conceptualisations of race and bring health research into alignment with cutting edge race theory and sociological studies of race more broadly. Without research examining assumptions about race categories, racialisation processes, and the ways that racial bias and discrimination become built into our organisations, cultures and emotional economies, our understandings of race and health will be fundamentally limited.
In this article, we examine the implications of this limited qualitative research agenda around race and health in sociology, with careful attention to the types of empirical questions being asked, the methodologies being used, and the potential gains to be had with increased ontological and methodological diversity. Here, we selected three key areas of research that would greatly advance scholarship on race and health through more qualitative inquiry: Healthy Immigrant Effect, Maternal Health and End-of-Life Care. That said, this sort of evaluation is needed in most aspects of research on race and health and could be explored in any area where race is treated as a quantitative variable related to health. We selected these areas as they: (1) represent the full spectrum of the life course; (2) are not entirely centred on clinical interactions, thus providing an opportunity to examine how race is operative upstream of medicine and how those processes are not well understood; and (3) as elaborated below, each of these subfields is faced with prolonged puzzles around the role of race and are thus ripe for qualitative inquiry.
First, we provide a general overview of the current literature in each research area, focusing on empirical studies published in the flagship US sociological journals American Sociological Review, American Journal of Sociology and Journal of Health and Social Behavior . We highlight successes and opportunities lost in each area and propose qualitative research agendas to fill critical gaps in the current scholarship. We must note that the broad, multidisciplinary scope of these topics makes it impossible to fully address all of the studies on each of these areas within a single article, but we do our best to provide comprehensive overviews of the research areas within the United States. We conclude with a discussion of how the dominance of quantitative methodology and ontology in sociology not only hinders intellectual advancements in scholarship on race and health, but also has cascading effects that directly shape institutions and the profession more broadly. We also consider possible reasons for these observed patterns.
HEALTHY IMMIGRANT EFFECT
The Healthy Immigrant Effect, or the Latinx Health Paradox, refers to the fact that foreign-born individuals, particularly Latinx immigrants, tend to perform better on health indicators such as all-cause mortality, infant mortality and self-rated health compared with Whites and their US-born counterparts, despite experiencing lower socioeconomic status and educational attainment ( Markides & Coreil, 1986 ; Scribner, 1996 ). The health assimilation model has been widely accepted to explain this paradox: as Latinx immigrants become more acculturated through prolonged US residence, they lose protective health effects that give them this health advantage. In recent years, however, scholars have increasingly questioned the paradox's efficacy arguing that while Latinx individuals may live longer, they tend to have faster physical decline and poorer quality of life compared with Whites ( Boen & Hummer, 2019 ).
Sociologists have confronted assumptions in the paradox primarily through quantitative methodologies that have been extensively published in the JHSB . Individual-level factors explored include socioeconomic status ( Brown et al., 2016 ), educational attainment ( Crosnoe, 2006 ), gender ( Gorman et al., 2010 ), English language proficiency ( Lebrun, 2012 ), country of origin ( Montazer & Wheaton, 2011 ), arrival year ( Hamilton et al., 2015 ) and length of residence in the United States ( Tegegne, 2018 ). Others have looked to cultural and structural factors, including intergenerational family dynamics ( Schmeer & Tarrence, 2018 ) and the impact of institutions, neighbourhoods and policies on immigrant health ( Dondero et al., 2018 ; Rosenbaum, 2008 ; Viruell-Fuentes et al., 2012 ). One persisting critique of the paradox is that studies have mostly ignored the health status of undocumented individuals. The available scholarship however has found that undocumented individuals are much less likely to access necessary healthcare services ( Torres & Waldinger, 2015 ) and experience an exacerbation of chronic conditions ( Hacker et al., 2011 ).
New empirical research continues to problematise the Healthy Immigrant Effect's depiction of US immigrant health. For example, the relationship between variables like citizenship and English language acquisition, common measures of acculturation and assimilation, and immigrant health do not consistently align with the paradox. Lebrun (2012) found that immigrants who remained in the United States and Canada for longer and acquired greater English proficiency, tended to have better healthcare access, utilisation and experiences with healthcare providers. Tegegne (2018) argued that immigrants who were embedded in diverse networks and acquired greater English language proficiency, reported better health over time and were less likely to be diagnosed with a chronic condition.
While quantitative scholarship on the Healthy Immigrant Effect is robust, qualitative research in the area has been ostensibly absent in the discipline's flagship journals. Sociologists who have utilised qualitative methods have frequently done so to explore the efficacy of the Latina Birth Paradox, which asserts that Latinx immigrant women have better birth outcomes than their White and US-born counterparts ( Fleuriet & Sunil, 2015 ). In their interview study of pregnant Mexican women in Texas, Fleuriet and Sunil (2015) found that while infant birth weight decreased as length of time in the United States increased and Mexican American women reported higher levels of depression and stress, Mexican immigrant women reported higher levels of anxiety directly related to the pregnancy itself. These findings resonate with recent quantitative research that also reveals that foreign-born Latina women do not necessarily have better birth outcomes than White women ( Hoggatt et al., 2012 ) or only in the context of specific birth outcomes and migration histories ( Urquia et al., 2012 ). Collectively, this research points to the ongoing need to reconsider our assumptions of immigrant health. For instance, these inconsistencies may point to the need to embrace a life-course perspective when thinking about immigrant health, recognising that health and immigrant status are fluid and deeply interconnected experiences that cannot be measured simply as single data points in time.
This relative dearth of qualitative explorations of the Healthy Immigrant Effect, which could be attributed to the model's historical roots in epidemiology and assumptions that qualitative measurement of this paradox may be too difficult, leads to persisting gaps in the literature. Variables across studies share the same name yet result in vastly different findings due to their complexity and the great variation across immigrant groups. These inconsistencies beg for greater qualitative inquiry, which is particularly well-equipped for the refinement of our assumptions related to the Healthy Immigrant Effect. One way to target these persisting puzzles would be to incorporate more qualitative inquiry to explore how the paradox relates to undocumented status, racialised experiences, discrimination and other obstacles that emerge in daily life ( Viruell-Fuentes et al., 2012 ). It is important to note that there has been valuable qualitative research on immigrant experiences in health-care encounters, revealing how culture, contexts and social structures directly shape immigrants’ clinical experiences (e.g. Lo, 2010 and Lo & Stacey, 2008 ). We argue that such conceptualisations and approaches should be applied to examine the Healthy Immigrant Effect as well.
Another area of fruitful inquiry is qualitatively exploring the impact of neighbourhood effects on immigrant health. Cagney et al. (2007) found that while foreign-born Latinx have much lower rates of asthma and other respiratory conditions compared to their US-born counterparts, this advantage was contingent on the physical environment. When Latinx immigrants lived in communities with high rates of other immigrants, the respiratory health advantage remained, yet when Latinx immigrants lived in largely non-immigrant communities, their respiratory health deteriorated ( Cagney et al., 2007 ). What are the resources, opportunities and experiences in majority-immigrant communities vs. non-majority-immigrant communities that may lead to such differential health outcomes? How do neighbourhoods reproduce racial inequalities via norms, culture, and various other mechanisms? And how do individuals in a community differentially encounter agency, segregation and discrimination in different structural contexts ( Ray, 2019 ; Wingfield & Chavez, 2020 )? Participant observation, interviews and other qualitative approaches would be able to offer critical insights into these questions.
There is also value in applying qualitative methods to understand how health intersects with race, policing and the implementation of both local and federal immigration policies. Recent qualitative scholarship on policing and incarceration has elucidated the complex, and at times surprising, ways in which race operates in these contexts ( Eason, 2017 ; Western, 2018 ). Negative perceptions, fear of, and past traumatic experiences with providers and law enforcement officials may shape individual decision-making and patient–provider interactions, exacerbating inadequate access to care, leading to undetected, poor health outcomes ( Read & Reynolds, 2012 ) and expectations of poor health and survival in the long-term ( Warner & Swisher, 2015 ). Collectively, these examples of possible qualitative inquiry would help unpack both individual and structural factors that directly shape immigrant health in the United States.
MATERNAL HEALTH
Clinicians and public health scholars have primarily used quantitative methods to explain sustaining racial disparities in pregnancy-related morbidity and mortality in the United States ( Creanga et al., 2012 ). In contrast, within sociology, the relationship between race and maternal health has been less central to the research agenda, which has focused largely on reproductive health, childbearing experiences and maternal and infant outcomes. Much of the scholarship published in top US sociology journals has relied on quantitative methods and have operational-ised maternal health in terms of infant birth weight or pre-term births ( Dooley & Prause, 2005 ) and mothers’ physical and mental health ( Hartnett & Brantley, 2020 ; Williams & Finch, 2019 ). Individual maternal characteristics, like age ( Mirowsky, 2005 ), education ( Kravdal & Rindfuss, 2008 ), socioeconomic status ( Strully et al., 2010 ), employment ( Frech & Damaske, 2012 ) and relationship status ( Meadows et al., 2008 ), and structural factors, such as social networks ( Balbo & Barban, 2014 ; Sandberg, 2006 ), neighbourhood context ( Morenoff, 2003 ) and residential segregation ( Walton, 2009 ), have been targeted as critical factors that shape disparate maternal and infant health outcomes.
In the past decade, quantitative sociologists have accelerated a research agenda exploring how race impacts maternal health ( Colen et al., 2019 ; Reyes et al., 2018 ; Williams et al., 2015 ). Reyes et al. (2018) found that Black women experienced greater emotional distress during pregnancy than their White counterparts. Williams et al. (2015) found that African American women, who had a child when they were adolescents or young adults, reported worse health outcomes later in life compared with White women who had children at similar ages. Furthermore, Colen et al. (2019) found that African American women, whose children experienced acute and chronic discrimination, had faster and poorer declines in health compared to their White counterparts.
In contrast, qualitative scholarship has largely investigated the organisational, sociocultural and political structures that shape women's experiences navigating their reproductive health ( Almeling, 2007 ; Waggoner, 2017 ), pregnancy ( Armstrong, 2003 ; Casper, 1988 ; MacKendrick & Cairns, 2018 ) and childbirth within the United States ( Dillaway & Brubaker, 2006 ; Morris, 2013 ) and abroad ( Storeng et al., 2010 ; Story et al., 2012 ). While this research has provided key insights revealing experiences, mechanisms and consequences of maternal healthcare, race has largely remained on the periphery – particularly in the research that has been featured most prominently in the discipline. For instance, Almeling’s (2007) ASR article exploring the impact of sociocultural notions of gender and family on the markets of egg and sperm donation provides invaluable information on how such market dynamics result in divergent compensation, marketing tactics and interactions with egg versus sperm donors. Yet, there is little discussion of how racial backgrounds of donors and clients inevitably shape the market.
Similarly, in her study on foetal alcohol syndrome, Armstrong (2003) found that while low-income women of colour were generally less likely to drink than White women were, a small group of these women reported high levels of drinking during pregnancy. There, however, is a missed opportunity to unpack the factors that may lead to this pattern of distribution of FAS: although Armstrong (2003) notes structural inequalities that put low-income women of colour at greatest risk, much of her analytical argument focuses on how clinical and policy approaches to FAS lead to the social regulation of all women. Anthropologists, on the other hand, have delved more deeply into the relationship between race and maternal health ( Bridges, 2011 ; Davis, 2019 ; Galvez, 2019 ). Both Bridges (2011) and Gálvez (2019) found that women of colour frequently encountered racialised health-care experiences, often labelled as ‘at’ or ‘high risk’, and were subsequently subject to increased surveillance, interventions and sanctions. And Davis (2019) found that the medical racism of providers and institutions increased negative birth outcomes for African American women across different SES levels.
While maternal health research is extensive, there remain key limitations. In quantitative social scientific scholarship, conceptualisations of maternal health largely rely on infant health outcomes and mothers’ self-reported health status. Research on racial disparities is limited and primarily reveals disparities related to the ‘usual suspects’ (e.g. access to care and SES) without fully exploring broader social contexts and structural inequities. Qualitative sociological scholarship has been more minimal, with little focus on racial dynamics, which is a lost opportunity to unpack current racialised trends in maternal morbidity and mortality. For instance, recent qualitative research published in the JHSB reminds us that patient–provider interactions are directly shaped by provider perceptions ( Fenton, 2019 ; Stevens, 2016 ). Such empirical inquiry is especially necessary in maternal health, where recent publicised cases of maternal (near) deaths point to ineffective interactions with providers.
Despite repeated visits to the hospital after giving birth to her daughter, Dr. Shalon Irving, a 36-year-old African American epidemiologist at the CDC, died three weeks postpartum. Upon waiting over 7 hours for any clinical intervention after first reporting problematic symptoms, Kira Johnson, a 39-year-old African American woman in excellent health, died from the elective c-section of her second child due to haemorrhaging. Serena Williams, a sports icon, nearly lost her life after the birth of her daughter: health-care professionals initially refused to provide her with a CT scan that she requested and failed to adequately acknowledge her pain, even though she had a medical history that placed her at greater risk for maternal morbidity and mortality. These anecdotal cases disrupt the assumptions that racial health disparities largely mirror the racial distribution of poverty within our society, as these women were not short of resources yet struggled to receive necessary care.
Furthermore, pain management research reveals that Black patients are the least likely to have their pain sufficiently treated by health-care providers ( Hausmann et al., 2012 ) and are frequently approached as criminals, especially in the context of opioid medication prescriptions: African American patients are monitored more closely than their White counterparts ( Becker et al., 2001 ; Hausmann et al., 2012 ) and labelled as drug seekers ( Zickmund et al., 2015 ). Patients of colour are also burdened with needing to ‘prove’ their pain and are also subject to racialised assumptions that shape how their concerns are addressed ( Rubin et al., 2018 ). Considering the high morbidity and mortality penalty for Black women, it is crucial that studies similarly examine the relationship between women of colour and providers during their pregnancy and childbirth to discern how discriminatory experiences and inequities contribute to current racial maternal health trends. Qualitative approaches would offer valuable opportunities to explore decision-making processes of both providers and patients and the nature of interactions between providers and patients of colour, which qualitative scholarship has shown frequently reproduces and reinforces broader social inequities ( Shim, 2010 ).
END-OF-LIFE CARE
Vast multidisciplinary literatures spanning sociology, demography, health services and medicine have quantitatively documented socioeconomic and ethnoracial disparities around end-of-life. In a large international review of research on high-income countries, Davies et al. (2019) document robust socioeconomic differences in place of death and type of care received in late life, with blacks at increased risk of adverse events such as having four or more transitions in the last six months of life ( Wang et al., 2019 ), being hospitalised, or treated in the emergency department ( Rizzuto & Aldridge, 2018 ). Similar work has demonstrated that racial differences exist with regard to use of palliative care ( Johnson, 2013 ) and engagement in end-of-life planning ( Orlovic et al., 2019 ). As a backdrop to all of this, persistent disparities in pain assessments and receipt of intensive treatments have been well-documented ( Hoffman et al., 2016 ).
Historically, qualitative sociology has been prominent in the study of end-of-life. In the 1960s, 70s and 80s, substantive studies of death and dying were abundant, supporting, for example, an Annual Review of Sociology piece (1983) and a 1975 special issue of qualitative studies on the topic in Urban Life ( Lofland, 1975 ). Classic qualitative sociological monographs on the topic were generated in this period ( Glaser & Strauss, 1968 ; Sudnow, 1967 ) as well as in more recent decades ( Anspach, 1997 ; Timmermans, 1999 ; Zussman, 1992 ). Today, qualitative research on death, dying and end-of-life remains quite active ( Bandini, 2020 ; Broom & Kirby, 2013 ; Chapple et al., 2015 ; Cortez & Halpin, 2020 ; Exley, 2004 ; MacArtney et al., 2016 ). These works have embraced thick description of the social processes and contexts that surround death and dying, pushing fields beyond quantitative conceptualisations. Unfortunately, however, they have rarely focused on racial, ethnic, or even socioeconomic disparities ( Cain & McCleskey, 2019 ; Livne, 2019 as exceptions).
Furthermore, consistent with broader trends outlined above, there has been a dearth of qualitative research on end-of-life published by flagship American sociology journals in the past twenty years (i.e. American Sociological Review and American Journal of Sociology ). In Journal of Health and Social Behavior , publications in this substantive area have largely used quantitative analyses to examine demographically oriented questions of morbidity, mortality and wellbeing ( Aneshensel et al., 2004 ; Carr, 2003 ; Cornwell & Waite, 2009 ; Turner et al., 2017 ; Umberson, 2017 ). Qualitative exceptions in JHSB are present but rare ( Bloor, 1991 ; Thomeer et al., 2017 ). Several recent monographs written by sociologists have used qualitative methods to study various aspects of ageing, end-of-life, health care and race in this time period ( Abramson, 2015 ; Raudenbush, 2020 ; Rodriquez, 2014 ).
The implications of these methodological biases are considerable, often reifying problematic assumptions underlying quantitative analyses. For example, in a sample of Medicare beneficiaries, Barnato et al. (2009) report that minorities have a greater preference for intensive treatment near end-of-life, including Blacks being more likely to want mechanical ventilation, preferring to die in a hospital, but also being concerned about having too much medical care. By conceptualising the mechanisms for these disparities as a matter of individual preferences, knowledge or attitudes, we miss an opportunity to examine the ways racialised health care, patient–provider interaction, ecologies of care or historical trauma may contribute to black distrust of health care or cultural ideas about end-of-life planning.
Another example is how epidemiologic differences over the life course provide upstream context for end-of-life. We would expect one’s long-term health experience to shape expectations for activities of daily living, thoughts about caregiving and the role of social support. Consider: middle-aged non-Hispanic Blacks start with more chronic diseases and develop multimorbidity at an earlier age than their white counterparts ( Quinones et al., 2019 ), and also fare worse in terms of disability adjusted life years ( McGrath et al., 2019 ). Two late life patients with the same end-stage diagnosis, one white, one black, may have the same diagnostic ICD-10 code in a dataset but have vastly different lived experiences and decision-making processes that are not captured by quantitative measures.
These illness experiences are, in turn, nested in other social structures and environments. Having a caregiver is often touted as a key characteristic of patients who are able to use hospice or to die at home ( National Hospice & Palliative Care Organization, 2019 ). However, authors of quantitative studies have drawn some conflicting conclusions on this matter, for example with Blacks believed to be at increased risk of not having a caregiver because they are less likely to be married ( Carr & Luth, 2019 ) but also possibly more likely to have a caregiver as a result of living in larger households and having stronger social networks ( Orlovic et al., 2019 ). These big data studies are ill-equipped to address the quality and racialised context of these family and caregiving structures, and whether they translate to end-of-life caregiving. Qualitative studies, whether ethnographic, interview, historical or content analyses, are well-positioned to examine the meaning and processes that lead up to these data snapshots.
American systems around death and dying – including hospice – are not race-neutral, but grow out of a specific racialised history and therefore must be studied with intersectional and multilevel lenses of analysis. Questions of what patients have been told, how they have been pressured or supported, whether they have received goal-concordant care and how those narratives are passed through social support systems over time are all part of understanding assessments of quality of care or medical decisions. The role of medical providers must be similarly and seriously assessed. Assumptions and incentives related to the value of hospice itself are deeply embedded in history of medicine and health policy, and those racialised contexts contribute to conceptual frameworks and resulting research agendas. Qualitative approaches are needed to not only clarify assumptions underlying treatment decisions and demographic analyses, but also examine pathways, processes and contexts connecting these domains as end-of-life trajectories unfold.
We began this article with the observation that scholarship on race and health published in sociology's flagship US journals lacks methodological diversity, and this trend is generally consistent with sociological literature broadly. Despite the historical richness of qualitative studies of race in sociology generally, and of qualitative research within the subfield of medical sociology, this pattern has been robust over time and in recent decades it has become more acute. In the past decades, we have instead seen a focus on quantitative approaches and epidemiologic and demographically oriented research questions. In this article, we have explored three substantive cases related to race and health – the healthy immigrant effect, maternal health and end-of-life care – to examine opportunities for qualitative inquiry as well as potential limitations and distortions in our knowledge that may emerge from a penchant for methodological and ontological homogeneity. These alternative research approaches have the potential to not only shed light on context, processes and lived experiences that are essential for understanding race and health, but also help resolve mixed results and paradoxes that are evident in quantitative literatures in these areas.
There are many other cases in the arena of race and health that would similarly benefit from increased qualitative attention, and our selected cases are intended to offer some general observations that may speak to other areas of inquiry. First, our cases speak to the importance of not treating race as a proxy for other characteristics. Rather than seeing race as an individual demographic characteristic, the lived experience of race reveals some of the ways various social institutions and policies become racialised over time. To only seek explanations at the level of the individual or family is a major limitation for our knowledge, inviting continuations of outdated deficit models when we could instead be asking how racism is built and sustained by various social structures. More centrally, our cases illustrate the urgent need for generating valid understandings of context, meaning and processes of race, not only for individuals, but also cultures, institutions, policies and the ways in which these domains interact with one another.
We speculate that race and class confounds, which can be challenging to evaluate qualitatively, may be part of the reason that we see little qualitative work on race and health. This begs the question: Is it better to over- or under-engage race given fear of confounds? Since we know from quantitative data that unexplained race effects exist, it seems not only intellectually myopic but also unethical to avoid the pursuit of explanations of how those racialised effects operate. Erring on the side of attributing disparities to socioeconomic status by default, or avoiding race altogether, has the effect of perpetually relegating race to the far reaches of our inquiry. The risks of this approach, as evidenced with the exemplars we present above, include compromised validity, deracialised assumptions and distorted agendas. Furthermore, per our opening discussion of race and sociology, we observe that urban ethnographers do not shy away from drawing conclusions about how race operates in ethnographic settings – in other words, it is feasible and necessary.
While we have focused on the outcomes of these patterns in research dissemination, we also recognise that there is likely a diversity of upstream causes as well as potential challenges in the implementation of our recommendations. Without more data, much remains unknown about where and how patterns emerge in the publication pipeline. We are not able to assess the types of research submissions received by flagship journal editors in the years we evaluated, who can of course only publish from the pool of submissions they receive. It may be that the sociological workforce lacks the diversity (in training, in experience) to feel compelled to engage these lines of research. (However, we believe this seems implausible given the representation of qualitative dissertations being published in sociology). It may be that there are interested researchers, but the logistical hurdles to conducting time- or resource-intensive qualitative research are obstacles for career, funding, or other related reasons. It may be that authors doing qualitative research on race and health disproportionately submit their articles to non-flagship outlets, or publish them as monographs. Indeed, the data above show that the proportion of qualitative publications on race and health is greater across Sociological Abstracts than in the flagship journals, although that increase is only from zero to three percent. It may be that flagship journals disproportionately lack reviewers or editors with the expertise to review these kinds of submissions, thus affecting their likelihood of being published and reifying methodological biases in journals. Perhaps decision makers are hesitant to publish such work out of other concerns such as reproducing stereotypes, exploiting communities of colour, or facing challenges in ethically recruiting marginalised persons to participate in research. In the end, we lack transparency about the upstream factors preceding the dissemination patterns we observe, but we suspect it is a multifactorial problem.
We have focused on research published in specific flagship sociology journals because we assume these outlets signal key priorities, strengths and results from sociology generally ( ASR and AJS ) and medical sociology specifically ( JHSB ) within the United States. While some of our intellectual neighbours engaged in scholarship on race and health have deep qualitative traditions (e.g. anthropology and science and technology studies (STS)), others either do not use qualitative methods (e.g. demography) or have a more limited tradition in that area (e.g. medicine, health services research). To the extent that quantitative research agendas thrive in sociology to the exclusion of qualitative work, we are concerned that qualitative scholarship on race and health may wither. Even more likely, qualitative scholars of race and health will disperse to areas beyond sociology, publishing in journals that are more ontologically diverse, accepting positions in departments that are more open to these approaches (e.g. African American studies), and cultivating research networks outside of sociology. Indeed, the cases we describe above suggest such changes are already afoot.
In the context of our three cases and the various sorts of qualitative race and health investigations occurring in neighbouring disciplines, we believe sociology has the potential to take a leading role in cultivating a more sophisticated research agenda around health and race. Taking such a role is contingent on the extent to which we are willing to continue to revisit our historical roots, tools, concepts and methods. The point here is not only that quantitative studies can be improved with more accurate measures or models of race, but that we need to fundamentally e-brace these varied forms of knowledge production – an endeavour that requires not only broad intellectual engagement but also collective investment in the research, professional and educational infrastructures that support the diversity inherent in our sociological enterprise.
ACKNOWLEDGEMENTS
We would like to thank the editors and anonymous reviewers for their very thoughtful comments.
DATA AVAILABILITY STATEMENT
- Abramson CM (2015). The end game . Harvard University Press. [ Google Scholar ]
- Almeling R (2007). Selling genes, selling gender: Egg agencies, sperm banks, and the medical market in genetic material . American Sociological Review , 72 ( 3 ), 319–340. [ Google Scholar ]
- Aneshensel CS, Botticello AL, & Yamamoto-Mitani N (2004). When caregiving ends: The course of depressive symptoms after bereavement . Journal of Health and Social Behavior , 45 ( 4 ), 422–440. [ PubMed ] [ Google Scholar ]
- Anspach RR (1997). Deciding who lives: Fateful choices in the intensive-care nursery . University of California Press. [ Google Scholar ]
- Armstrong EM (2003). Conceiving risk, bearing responsibility: Fetal alcohol syndrome and the moral diagnosis of disorder . The Johns Hopkins University Press. [ Google Scholar ]
- Balbo N, & Barban N (2014). Does fertility behavior spread among friends? American Sociological Review , 79 ( 3 ), 412–431. [ Google Scholar ]
- Bancks M, Kershaw K, Carson AP, Gordon-Larsen P, Schreiner P, & Carnethon MR (2017). Association of modifiable risk factors in young adulthood with racial disparity in incident type 2 diabetes during middle adulthood . JAMA: The Journal of the American Medical Association , 318 ( 24 ), 2457. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bandini JI (2020). Negotiating the ‘buffet’ of choice: Advances in technology and end-of-life decision-making in the intensive care unit setting . Sociology of Health and Illness , 42 ( 4 ), 877–891. [ PubMed ] [ Google Scholar ]
- Barnato AE, Anthony DL, Skinner J, Gallagher PM, & Fisher ES (2009). Racial and ethnic differences in preferences for end-of-life treatment . Journal of General Internal Medicine , 24 ( 6 ), 695–701. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Becker WC, Starrels JL, Heo M, Li X, Weiner MG, & Turner BJ (2001). Racial differences in primary care opioid risk reduction strategies . The Annals of Family Medicine , 9 ( 3 ), 219–225. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bloor M (1991). A minor office: The variable and socially constructed character of death certification in a Scottish City . Journal of Health and Social Behavior , 32 ( 3 ), 273–287. [ PubMed ] [ Google Scholar ]
- Boen CE, & Hummer RA (2019). Longer—but harder—Lives? The hispanic health paradox and the social determinants of racial, ethnic, and immigrant—native health disparities from midlife through late life . Journal of Health and Social Behavior , 60 ( 4 ), 434–452. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bonilla-Silva E (1999). The essential social fact of race . American Sociological Review , 64 ( 6 ), 899–906. [ Google Scholar ]
- Bonilla-Silva E (2006). From bi-racial to tri-racial: Towards a new system of racial stratification in the USA . Ethnic and Racial Studies , 27 ( 6 ), 931–950. [ Google Scholar ]
- Bonilla-Silva E (2019). Feeling race: Theorizing the racial economy of emotions . American Sociological Review , 84 ( 1 ), 1–25. [ Google Scholar ]
- Bridges K (2011). Reproducing race: An ethnography of pregnancy as a site of racialization . University of California Press. [ Google Scholar ]
- Broom A, & Kirby E (2013). The end of life and the family: Hospice patients’ views on dying as relational . Sociology of Health and Illness , 35 ( 4 ), 499–513. [ PubMed ] [ Google Scholar ]
- Brown TH, Richardson LJ, Hargrove TW, & Thomas CS (2016). Using multiple-hierarchy stratification and life course approaches to understand health inequalities: The intersecting consequences of race, gender, ses, and age . Journal of Health and Social Behavior , 57 ( 2 ), 200–222. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cagney KA, Browning CR, & Wallace DM (2007). The latino paradox in neighborhood context: The case of asthma and other respiratory conditions . American Journal of Public Health , 97 ( 5 ), 919–925. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cain CL, & McCleskey S (2019). Expanded definitions of the ‘good death’? Race, ethnicity and medical aid in dying . Sociology of Health and Illness , 41 ( 6 ), 1175–1191. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Carr D (2003). A ‘good death’ for whom? Quality of spouse's death and psychological distress among older widowed persons . Journal of Health and Social Behavior , 44 ( 2 ), 215–232. [ PubMed ] [ Google Scholar ]
- Carr D, & Luth EA (2019). Well-being at the end of life . Annual Review of Sociology , 45 ( 21 ), 1–20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Casper MJ (1988). The making of the unborn patient: A social anatomy of fetal surgery . Rutgers University Press. [ Google Scholar ]
- Chapple A, Ziebland S, & Hawton K (2015). Taboo and the different death? Perceptions of those bereaved by suicide or other traumatic death . Sociology of Health and Illness , 37 ( 4 ), 610–625. [ PubMed ] [ Google Scholar ]
- Colen CG, Li Q, Reczek C, & Williams DR (2019). The intergenerational transmission of discrimination: Children’s experiences of unfair treatment and their mothers’ health at midlife . Journal of Health and Social Behavior , 60 ( 4 ), 474–492. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cornwell EY, & Waite LJ (2009). Social disconnectedness, perceived isolation, and health among older adults . Journal of Health and Social Behavior , 50 ( 1 ), 31–48. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cortez D, & Halpin M (2020). Uncertainty and certain death: The role of clinical trials in terminal cancer care . Sociology of Health and Illness , 42 ( Suppl 1 ), 130–144. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce C, & Callaghan WM (2012). Race, ethnicity and nativity differentials in pregnancy-related mortality in the United States: 1993–2006 . Journal of Obstetrics and Gynecology , 120 , 261–268. [ PubMed ] [ Google Scholar ]
- Crosnoe R (2006). Health and the education of children from racial/ethnic minority and immigrant families . Journal of Health and Social Behavior , 47 ( 3 ), 77–93. [ PubMed ] [ Google Scholar ]
- Davies JM, Sleeman KE, Leniz J, Wilson R, Higginson IJ, Verne J, Maddocks M, & Murtagh FEM (2019). Socioeconomic position and use of healthcare in the last year of life: A systematic review and meta-analysis . PLoS Medicine , 16 ( 4 ), e1002782. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Davis D (2019). Reproductive injustice: Racism, pregnancy, and premature birth . New York University Press. [ Google Scholar ]
- Desmond M (2016). Evicted: Poverty and profit in the american city . Crown Publishers. [ Google Scholar ]
- Dillaway H, & Brubaker SJ (2006). Intersectionality and childbirth: How women from different social locations discuss epidural use . Race, Gender & Class , 13 ( 3–4 ), 16–41. [ Google Scholar ]
- Dondero M, Van Hook J, Frisco ML, & Martin MA (2018). Dietary assimilation among mexican children in immigrant households: Code-switching and healthy eating across social institutions . Journal of Health and Social Behavior , 59 ( 4 ), 601–624. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dooley D, & Prause J (2005). Birth weight and mothers’ adverse employment change . Journal of Health and Social Behavior , 46 ( 6 ), 141–155. [ PubMed ] [ Google Scholar ]
- Du Bois WEB (1967). The Philadelphia negro: A social study . Schocken Books. [ Google Scholar ]
- Duneier M (2000). Sidewalk . Farrar, Strauss and Giroux. [ Google Scholar ]
- Eason JM (2017). Big house on the prairie: Rise of the rural ghetto and prison proliferation . The University of Chicago Press. [ Google Scholar ]
- Exley C (2004). Review article: The sociology of dying, death and bereavement . Sociology of Health and Illness , 26 ( 1 ), 110–122. [ PubMed ] [ Google Scholar ]
- Fenton AT (2019). Abandoning medical authority: when medical professionals confront stigmatized adolescent sex and the human papillomavirus (HPV) vaccine . Journal of Health and Social Behavior , 60 ( 2 ), 240–256. [ PubMed ] [ Google Scholar ]
- Fleuriet KJ, & Sunil TS (2015). Reproductive habitus, psychosocial health, and birth weight variation in Mexican immigrant and Mexican American women in south Texas . Social Science and Medicine , 138 , 102–109. [ PubMed ] [ Google Scholar ]
- Frech A, & Damaske S (2012). The relationships between mothers’ work pathways and physical and mental health . Journal of Health and Social Behavior , 53 ( 4 ), 396–412. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gálvez A (2019). Transnational mother blame: Protecting and caring in a globalized context . Medical Anthropology , 38 ( 7 ), 574–587. [ PubMed ] [ Google Scholar ]
- Geronimus AT, Bound J, Waidmann TA, Colen CG, & Steffick D (2001). Inequality in life expectancy, functional status, and active life expectancy across selected black and white populations in the United States . Demography , 38 , 227–251. [ PubMed ] [ Google Scholar ]
- Glaser BG, & Strauss AL (1968). Time for dying . Aldine. [ Google Scholar ]
- Goffman A (2014). On the run: Fugitive life in an American city . University of Chicago Press. [ Google Scholar ]
- Gorman BK, Read JG, & Krueger PM (2010). Gender, acculturation, and health among mexican Americans . Journal of Health and Social Behavior , 51 ( 4 ), 440–457. [ PubMed ] [ Google Scholar ]
- Gunaratnam Y (2001). ‘We mustn’t judge people… but’: Staff dilemmas in dealing with racial harassment amongst hospice service users . Sociology of Health and Illness , 23 ( 1 ), 65–84. [ Google Scholar ]
- Hacker K, Chu J, Leung C, Marra R, Pirie A, Brahimi M, English M, Beckmann J, Acevedo-Garcia D, & Marlin RP (2011). The impact of Immigration and Customs Enforcement on immigrant health: Perceptions of immigrants in Everett, Massachusetts, USA . Social Science and Medicine , 73 , 586–594. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hamilton TG, Palermo T, & Green TL (2015). Health assimilation among hispanic immigrants in the United States: The impact of ignoring arrival-cohort effects . Journal of Health and Social Behavior , 56 ( 4 ), 460–477. [ PubMed ] [ Google Scholar ]
- Hartnett CS, & Brantley M (2020). Racial disparities in emotional well-being during pregnancy . Journal of Health and Social Behavior , 61 ( 2 ), 223–238. [ PubMed ] [ Google Scholar ]
- Hausmann LR, Gao S, Lee ES, & Kwoh CK (2012). Racial disparities in the monitoring of patients on chronic opioid therapy . Pain , 154 , 46–52. [ PubMed ] [ Google Scholar ]
- Hoffman KM, Trawalter S, Axt JR, & Oliver MN (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites . Proceesings of the National Academy of Sciences of the United States of America , 113 ( 16 ), 4296–4301. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hoggatt KJ, Flores M, Solorio R, Wilhelm M, & Ritz B (2012). The “Latina Epidemiologic Paradox” Revisited: The role of birthplace and acculturation in predicting infant low birth weight for latinas in Los Angeles, CA . Journal of Immigrant and Minority Health , 14 , 875–884. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Johnson KS (2013). Racial and ethnic disparities in palliative care . Journal of Palliative Medicine , 16 ( 11 ), 1329–1334. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kershaw KN, Albrecht SS, & Carnethon MR (2013). Racial and ethnic residential segregation, the neighborhood socioeconomic environment, and obesity among blacks and mexican Americans . American Journal of Epidemiology , 177 ( 4 ), 299–309. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kershaw KN, Roux AD, Burgard SA, Lisabeth LD, Mujahid MS, & Schulz AJ (2011). Metropolitan-level racial residential segregation and black-white disparities in hypertension . American Journal of Epidemiology , 174 ( 5 ), 537–545. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kravdal Ø, & Rindfuss RP (2008). Changing relationships between education and fertility: a study of women and men born 1940 to 1964 . American Sociological Review , 73 , 854–873. [ Google Scholar ]
- Lacy K (2007). Blue-chip black: Race, class, and status in the new black middle class . University of California Press. [ Google Scholar ]
- Lebrun LA (2012). Effects of length of stay and language proficiency on health care experiences among Immigrants in Canada and the United States . Social Science and Medicine , 74 , 1062–1072. [ PubMed ] [ Google Scholar ]
- Livne R (2019). Value at the end of life . Harvard University Press. [ Google Scholar ]
- Lo MM (2010). Cultural brokerage: Creating linkages between voices of lifeworld and medicine in cross-cultural clinical settings . Health , 14 ( 5 ), 484–504. [ PubMed ] [ Google Scholar ]
- Lo MM, & Stacey CL (2008). Beyond cultural competency: Bourdieu, patients and clinical encounters . Sociology of Health and Illness , 30 ( 2 ), 741–755. [ PubMed ] [ Google Scholar ]
- Lofland LH (1975). Toward a sociology of death and dying: Editor's introduction . Urban Life , 4 ( 3 ), 243–249. [ Google Scholar ]
- Loveman M (1999). Is “race” essential? American Sociological Review , 64 ( 6 ), 891–898. [ Google Scholar ]
- MacArtney JL, Broom A, Kirby E, Good P, Wootton J, & Adams J (2016). Locating care at the end of life: Burden, vulnerability, and the practical accomplishment of dying . Sociology of Health and Illness , 38 ( 3 ), 479–492. [ PubMed ] [ Google Scholar ]
- MacKendrick N, & Cairns K (2018). The polluted child and maternal responsibility in the US environmental health movement . Signs , 44 ( 2 ), 307–332. [ Google Scholar ]
- Markides KS, & Coreil J (1986). The health of hispanics in the southwestern United States: An epidemiologic paradox . Public Health Records , 101 ( 3 ), 253–265. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Massey DS, & Denton NA (1993). American apartheid: Segregation and the making of the underclass . Harvard University Press. [ Google Scholar ]
- McGrath RP, Snih SA, Markides KS, Faul JD, Vincent BM, Hall OT, & Peterson MD (2019). The burden of health conditions across race and ethnicity for aging Americans . Medicine , 98 ( 46 ), e17964. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meadows SO, McLanahan SS, & Brooks-Gunn J (2008). Stability and change in family structure and maternal health trajectories . American Sociological Review , 73 , 314–334. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mirowsky J (2005). Age at first birth, health, and mortality . Journal of Health and Social Behavior , 46 ( 3 ), 32–50. [ PubMed ] [ Google Scholar ]
- Montazer S, & Wheaton B (2011). The impact of generation and country of origin on the mental health of children of immigrants . Journal of Health and Social Behavior , 52 ( 1 ), 23–42. [ PubMed ] [ Google Scholar ]
- Morenoff JD (2003). Neighborhood mechanisms and the spatial dynamics of birth weight . American Journal of Sociology , 108 ( 5 ), 976–1017. [ PubMed ] [ Google Scholar ]
- Morning A (2014). And you thought we had moved beyond all that: Biological race returns to the social sciences . Ethnic and Racial Studies , 37 ( 1 ), 1676–1685. [ Google Scholar ]
- Morris T (2013). Cut it out: the c-section epidemic in America . New York University Press. [ Google Scholar ]
- National Center for Health Statistics. (2018). Health, United States, 2017: With a special feature on mortality . Hyattsville. [ PubMed ] [ Google Scholar ]
- National Hospice and Palliative Care Organization. (2019). NHPCO facts and figures: Hospice care in America . National Hospice and Palliative Care Organization. [ Google Scholar ]
- Nazroo JY, Bhui KS, & Rhodes J (2020). Where next for understanding race/ethnic inequalities in severe mental illness? Structural, interpersonal and institutional racism . Sociology of Health and Illness , 42 ( 2 ), 262–276. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Omi M, & Winant W (1994). Racial formation in the United States . Routledge. [ Google Scholar ]
- Orlovic M, Smith K, & Mossialos E (2019). Racial and ethnic differences in end-of-life care in the united states: Evidence from the health and retirement study (HRS) . Social Science and Medicine – Population Health , 30 ( 7 ), 100331. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pager D, & Shepherd H (2008). The sociology of discrimination: Racial discrimination in employment, housing, credit, and consumer markets . Annual Review of Sociology , 34 , 181–209. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pattillo M (1999). Black picket fences: Privilege and peril among the black middle class . The University of Chicago Press. [ Google Scholar ]
- Persson A, & Newman C (2008). Making monsters: Heterosexuality, crime and race in recent Western media coverage of HIV . Sociology of Health and Illness , 30 ( 4 ), 632–646. [ PubMed ] [ Google Scholar ]
- Quinones AR, Botoseneanu A, Markwardt S, Nagel CL, Newsom JT, Dorr DA, & Allore HG (2019). Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults . PLoS One , 14 ( 6 ), e0218462. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Raudenbush DT (2020). Health care off the books: poverty, illness, and strategies for survival in urban America . University of California Press. [ Google Scholar ]
- Ray V (2019). A theory of racialized organizations . American Sociological Review , 84 ( 1 ), 26–53. [ Google Scholar ]
- Read JG, & Reynolds MM (2012). Gender differences in immigrant health: The case of Mexican and middle eastern immigrants . Journal of Health and Social Behavior , 53 ( 1 ), 99–123. [ PubMed ] [ Google Scholar ]
- Reyes AM, Hardy M, & Pavalko E (2018). Race differences in linking family formation transitions to women’s mortality . Journal of Health and Social Behavior , 59 ( 2 ), 231–247. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Riley AR (2017). Neighborhood disadvantage, residential segregation, and beyond—lessons for studying structural racism and health . Journal of Racial and Ethnic Health Disparities , 5 ( 2 ), 357–365. 10.1007/s40615-017-0378-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rizzuto J, & Aldridge MD (2018). Racial Disparities in hospice outcomes: A race or hospice-level effect? Journal of the American Geriatric Society , 66 ( 2 ), 407–413. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rodriquez J (2014). Labor of love: Nursing homes and the structures of care work . New York University Press. [ Google Scholar ]
- Rosenbaum E (2008). Racial/ethnic differences in asthma prevalence: The role of housing and neighborhood environments . Journal of Health and Social Behavior , 49 ( 6 ), 131–145. [ PubMed ] [ Google Scholar ]
- Rubin S, Burke N, Van Natta M, Yen I, & Shim JK (2018). Like a fish out of water: Managing chronic pain in the urban safety net . Journal of Health and Social Behavior , 59 ( 4 ), 487–500. [ PubMed ] [ Google Scholar ]
- Sampson RJ, Morenoff JD, & Gannon-Rowley T (2003). Assessing “neighborhood effects”: Social processes and new directions in research . Annual Review of Sociology , 28 , 443–478. [ Google Scholar ]
- Sandberg J (2006). Infant mortality, social networks, and subsequent fertility . American Sociological Review , 71 , 288–309. [ Google Scholar ]
- Saperstein A, & Penner AM (2012). Racial fluidity and inequality in the United State . American Journal of Sociology , 118 ( 3 ), 676–727. [ Google Scholar ]
- Schmeer KK, & Tarrence J (2018). Racial-ethnic disparities in inflammation: Evidence of weathering in childhood? Journal of Health and Social Behavior , 59 ( 3 ), 411–428. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scribner R (1996). Paradox as paradigm—The health outcomes of Mexican Americans . American Journal of Public Health , 86 ( 3 ), 303–305. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sewell AA (2016). The racism-race reification process: A mesolevel political economic framework for understanding racial health disparities . Sociology of Race and Ethnicity , 2 ( 4 ), 402–432. [ Google Scholar ]
- Shim JK (2010). Cultural health capital: A theoretical approach to understanding health care interactions and the dynamics of unequal treatment . Journal of Health and Social Behavior , 51 ( 1 ), 1–15. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smart A, & Weiner K (2018). Racialised prescribing: Enacting race/ethnicity in clinical practice guidelines and in accounts of clinical practice . Sociology of Health and Illness , 40 ( 5 ), 843–858. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stevens LM (2016). Environmental contaminants and reproductive bodies: Provider perspectives on risk, gender, and responsibility . Journal of Health and Social Behavior , 57 ( 4 ), 471–485. [ PubMed ] [ Google Scholar ]
- Storeng KT, Murray SF, Akoum MS, Ouattara F, & Filippi V (2010). Beyond body counts: A qualitative study of lives and loss in Burkina Faso after ‘near-miss’ obstetric complications . Social Science and Medicine , 71 ( 10 ), 1749–1756. [ PubMed ] [ Google Scholar ]
- Story WT, Burgard SA, Lori JR, Taleb F, Ahraf Ali N, & Emdadul Hoque DM (2012). Husbands’ involvement in delivery care utilization in rural Bangladesh: A qualitative study . BMC Pregnancy and Childbirth , 12 ( 28 ), 28–39. 10.1186/1471-2393-12-28 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Strully KW, Rehkopf DH, & Xuan Z (2010). Effects of prenatal poverty on infant health: State earned income tax credits and birth weight . American Sociological Review , 75 ( 4 ), 534–562. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sudnow D (1967). Passing on: The social organization of dying . Prentice Hall. [ Google Scholar ]
- Tegegne MA (2018). Linguistic integration and immigrant health: The longitudinal effects of interethnic social capital . Journal of Health and Social Behavior , 59 ( 2 ), 215–230. [ PubMed ] [ Google Scholar ]
- Telles EE, & Ortiz V (2009). Generations of exclusion: Mexican-americans, assimilation, and race . Russell Sage Foundation. [ Google Scholar ]
- Thomeer MB, Donnelly R, Reczek C, & Umberson D (2017). Planning for future care and the end of life: A qualitative analysis of gay, lesbian, and heterosexual couples . Journal of Health and Social Behavior , 58 ( 4 ), 473–487. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Timmermans S (1999). Sudden death and the myth of CPR . Temple University Press. [ Google Scholar ]
- Torres JM, & Waldinger R (2015). Civic stratification and the exclusion of undocumented immigrants from cross-border health care . Journal of Health and Social Behavior , 56 ( 4 ), 438–459. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Turner RJ, Brown TN, & Hale WB (2017). Race, socioeconomic position, and physical health: A descriptive analysis . Journal of Health and Social Behavior , 58 ( 1 ), 23–36. [ PubMed ] [ Google Scholar ]
- Umberson D (2017). Black deaths matter: Race, relationship loss, and effects on survivors . Journal of Health and Social Behavior , 58 ( 4 ), 405–420. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Urquia ML, O’Campo PJ, & Heaman MI (2012). Revisiting the immigrant paradox in reproductive health: The roles of duration of residence and ethnicity . Social Science and Medicine , 74 , 1610–1621. [ PubMed ] [ Google Scholar ]
- Viruell-Fuentes EA, Miranda PY, & Abdulrahim S (2012). More than culture: Structural racism, intersectionality theory, and immigrant health . Social Science and Medicine , 75 , 2099–2106. [ PubMed ] [ Google Scholar ]
- Waggoner MR (2017). The zero trimester: Pre-pregnancy care and the politics of reproductive risk . University of California Press. [ Google Scholar ]
- Walton E (2009). Residential segregation and birth weight among racial and ethnic minorities in the United States . Journal of Health and Social Behavior , 50 ( 12 ), 427–444. [ PubMed ] [ Google Scholar ]
- Wang S-Y, Hsu SH, Aldridge MD, Cherlin E, & Bradley E (2019). Racial differences in health care transitions and hospice use at the end of life . Journal of Palliative Medicine , 22 ( 6 ), 619–627. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Warner TD, & Swisher RR (2015). Adolescent survival expectations: Variations by race, ethnicity, and nativity . Journal of Health and Social Behavior , 56 ( 4 ), 478–494. [ PubMed ] [ Google Scholar ]
- Western B (2018). Homeward: Life in the year after prison . Russell Sage. [ Google Scholar ]
- Williams DR, & Collins C (2001). Racial residential segregation: A fundamental cause of racial disparities in health . Public Health Reports , 116 , 404–416. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams DR, & Sternthal M (2010). Understanding racial-ethnic disparities in health: Sociological contributions . Journal of Health and Social Behavior , 51 ( S ), S15–S27. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams K, & Finch BK (2019). Adverse childhood experiences, early and nonmarital fertility, and women’s health at midlife . Journal of Health and Social Behavior , 60 ( 3 ), 309–325. [ PubMed ] [ Google Scholar ]
- Williams K, Sassler S, Addo F, & Frech A (2015). First-birth timing, marital history, and women’s health at midlife . Journal of Health and Social Behavior , 56 ( 4 ), 514–533. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wilson WJ (1987). The truly disadvantaged: The inner city, the underclass, and public policy . The University of Chicago Press. [ Google Scholar ]
- Wingfield AH, & Chavez K (2020). Getting in, getting hired, getting sideways looks: Organizationl hierarchy and perceptions of racial discrimination . American Sociological Review , 85 ( 1 ), 31–57. [ Google Scholar ]
- Yearby R (2018). Racial disparities in health status and access to healthcare: The continuation of inequality in the united states due to structural racism . American Journal of Economics and Sociology , 77 ( 3–4 ), 1113–1152. [ Google Scholar ]
- Younis T, & Jadhav S (2019). Islamophobia in the National Health Service: An ethnography of institutional racism in PREVENT’s counter-radicalisation policy . Sociology of Health and Illness , 42 ( 3 ), 610–626. [ PubMed ] [ Google Scholar ]
- Zickmund SL, Burkitt KH, Gao S, Stone RA, Rodriguez KL, Switzer GE, Shea JA, Bayliss NK, Meiksin R, Walsh MB, & Fine MJ (2015). Racial differences in satisfaction with VA health care: A mixed methods pilot study . Journal of Racial and Ethnic Health Disparities , 2 , 317–329. [ PubMed ] [ Google Scholar ]
- Zussman R (1992). Intensive care: Medical ethics and the medical profession . University of Chicago Press. [ Google Scholar ]

COMMENTS
Table 13.1 "Theory Snapshot" summarizes what they say. Good health and effective medical care are essential for the smooth functioning of society. Patients must perform the "sick role" in order to be perceived as legitimately ill and to be exempt from their normal obligations.
This essay has discussed a number of topics within the field of health and social care, where sociological perspectives are relevant. The main perspectives. that constitute sociology have been presented, with the Medical Model and how this impacts on the treatment of patients. Health and social care can be seen.
Understanding health sociologically. Sociology of health and illness has been enlivened with increased understanding of the complex roles, social factors and structures play in individual and societal health and well-being. New insights are simultaneously empirical and conceptual, leading to innovative approaches to analysis, as well as new ...
The social construction of illness is a major research perspective in medical sociology. This article traces the roots of this perspective and presents three overarching constructionist findings. ... Research in the Sociology of Health Care6:1-31. Google Scholar---. 2007. ... Essays on the Social Situation of Mental Patients and Other Inmates ...
fluence of social structures can be examined. Sociological Perspectives of Health & Illness would be welcomed by students across a wide range. courses in sociology and the social sciences. Specifically, students undertaking undergraduate and postgraduate courses in health studies, and health p.
A sociological understanding emphasizes the influence of people's social backgrounds on the quality of their health and health care. A society's culture and social structure also affect health and health care. The functionalist approach emphasizes that good health and effective health care are essential for a society's ability to function.
1. EXPLAINING AND THEORISINGMain pointsSociology is a scientific approa. to understanding people in society.Social structures can often exert more influence ov. our behaviour than we would expect.Sociological perspectives on health emphasise that it is vital to understand the social in order t.
The intellectual roots of 'postmodern health and social care' derive from Jaber F. Gubrium's sociological analysis of the discovery and conceptual elaboration of Alzheimer's disease in the United States and the establishment of boundaries between 'normal' and pathological health and social care, care health and social care are seen ...
Here, hands-on care is conceptualised as 'body work' and in the introduction to this collection Twigg et al. (2011) lay out important theoretical foundations for studying this critical aspect of health and social care, with several papers published under its auspices addressing directly issues raised by Francis.
The February issue of 2018 addressed the role of theory in health inequality research, the relationship between socio-political context and health [], and it also highlighted the recent turn in social epidemiology towards studying the impact of institutional arrangements, social policy and political context on population health [].Moreover, the issue suggested that moving forward from where we ...
in the social world (p. 11).Health consciousness: The degree to which an individual is aware of an. attentive to health (p. 7).Health sociology: Sociological analysis of social structures and behavioral practices that influence both pe. sonal and population health. This perspective focuses on good health as well as ill health and critically ...
After this, its relevance to health will be explained. Sociology has been variously defined since Auguste Comte coined the term in 1838. Simply, sociology is the study of human society and social problems. Sociology is the scientific study of social relations, institutions, and society (Smelser 1994 ) .
1. Sociology—the study of human social life—has addressed many issues concerning people's experiences of health and illness, and the organisation of healthcare services. 2. A key theme in this area is the social patterning of health, ill health and premature death.
The transformation of health and social care: Insights from sociology. ... [email protected] School of Law, Politics and Sociology, University of Sussex, Brighton, UK. Correspondence. Karen Lowton, School of Law, Politics and Sociology, University of Sussex, Brighton BN1 9RH, UK. Email: [email protected] Search for more papers by this author. ...
Sociological Perspectives for health and social care Introduction: This article is based on the sociological perspectives used in health and social care. Sociology is a social science that has arisen from theoretical perspectives in philosophy and political theory. It uses data gathered by different studies to make it more reliable and acceptable.
Timmermans and Berg (2003) highlight the way in which the sociology of health and illness has moved over the years from a view that medical technologies provided healthcare providers with effective tools to coerce others into medically-approved lifestyles (e.g.Conrad's 1979 work considering psychopharmaceuticals) - a view they categorise as ...
Furthermore, consistent with broader trends outlined above, there has been a dearth of qualitative research on end-of-life published by flagship American sociology journals in the past twenty years (i.e. American Sociological Review and American Journal of Sociology). In Journal of Health and Social Behavior, publications in this substantive ...
UNIT 6 - SocIoLogIcaL PErSPEcTIVES for HEaLTH aNd SocIaL carE. learning hours : 30credit value: 5PurPosE of thE unitThis unit emphasises the importance of sociologica. perspectives in the context of health and social care.Sociology can help learners understand the impact of social proces. es upon the health of individuals and social groupings ...
Sociological perception believes that health is a state of complete wellbeing, physical, mental, and emotional. It emphasizes the importance of being more than disease free, and recognises that a healthy body depends upon a healthy environment and a stable mind. This sociological view, points out that society plays a role in sickness and ...
Download. There are 3 main perspectives: • The Structural/Functional Perspective - Relationship between parts of society, i.e. how aspects of society are functional and adaptive. - Macro - all aspects of society contribute to the way society functions as a whole. For example the government pays for school teachers and schools and bin ...