Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

The value of vital sign trends in predicting and monitoring clinical deterioration: A systematic review
Contributed equally to this work with: Idar Johan Brekke, Lars Håland Puntervoll
Roles Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Clinical Research, University of Southern Denmark, Odense, Denmark
Roles Conceptualization, Methodology, Supervision, Writing – review & editing
Affiliations Department of Clinical Research, University of Southern Denmark, Odense, Denmark, Department of Emergency Medicine, Odense University Hospital, Odense, Denmark
Affiliations Department of Emergency Medicine, Hospital of South West Jutland, Esbjerg, Denmark, Department of Regional Health Research, University of Southern Denmark, Odense, Denmark
Affiliations Department of Emergency Medicine, Odense University Hospital, Odense, Denmark, Department of Emergency Medicine, Hospital of South West Jutland, Esbjerg, Denmark, Department of Regional Health Research, University of Southern Denmark, Odense, Denmark
- Idar Johan Brekke,
- Lars Håland Puntervoll,
- Peter Bank Pedersen,
- John Kellett,
- Mikkel Brabrand

- Published: January 15, 2019
- https://doi.org/10.1371/journal.pone.0210875
- Reader Comments
Vital signs, i.e. respiratory rate, oxygen saturation, pulse, blood pressure and temperature, are regarded as an essential part of monitoring hospitalized patients. Changes in vital signs prior to clinical deterioration are well documented and early detection of preventable outcomes is key to timely intervention. Despite their role in clinical practice, how to best monitor and interpret them is still unclear.
To evaluate the ability of vital sign trends to predict clinical deterioration in patients hospitalized with acute illness.
Data Sources
PubMed, Embase, Cochrane Library and CINAHL were searched in December 2017.
Study Selection
Studies examining intermittently monitored vital sign trends in acutely ill adult patients on hospital wards and in emergency departments. Outcomes representing clinical deterioration were of interest.
Data Extraction
Performed separately by two authors using a preformed extraction sheet.
Of 7,366 references screened, only two were eligible for inclusion. Both were retrospective cohort studies without controls. One examined the accuracy of different vital sign trend models using discrete-time survival analysis in 269,999 admissions. One included 44,531 medical admissions examining trend in Vitalpac Early Warning Score weighted vital signs. They stated that vital sign trends increased detection of clinical deterioration. Critical appraisal was performed using evaluation tools. The studies had moderate risk of bias, and a low certainty of evidence. Additionally, four studies examining trends in early warning scores, otherwise eligible for inclusion, were evaluated.
Conclusions
This review illustrates a lack of research in intermittently monitored vital sign trends. The included studies, although heterogeneous and imprecise, indicates an added value of trend analysis. This highlights the need for well-controlled trials to thoroughly assess the research question.
Citation: Brekke IJ, Puntervoll LH, Pedersen PB, Kellett J, Brabrand M (2019) The value of vital sign trends in predicting and monitoring clinical deterioration: A systematic review. PLoS ONE 14(1): e0210875. https://doi.org/10.1371/journal.pone.0210875
Editor: Shane Patman, University of Notre Dame Australia, AUSTRALIA
Received: July 24, 2018; Accepted: January 3, 2019; Published: January 15, 2019
Copyright: © 2019 Brekke et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Protocol for this systematic review is registered in PROSPERO: CRD42017080303 Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017080303 . All other relevant data are within the paper and its Supporting Information files.
Funding: The author received no specific funding for this work.
Competing interests: Dr. John Kellett is a major shareholder, director and chief medical officer of Tapa Healthcare DAC. The authors confirm that this does not alter their adherence to PLOS ONE policies on sharing data and materials.
Introduction
Vital signs, including respiratory rate, oxygen saturation, blood pressure, pulse and temperature, are the simplest, cheapest and probably most important information gathered on hospitalized patients [ 1 ]. However, despite being introduced into clinical practice more than a century ago, surprisingly few attempts have been made to quantify their clinical performance [ 2 ]. In the last few decades, vital signs have become an area of active research [ 1 ] and numerous studies have reported that changes in vital signs occur several hours prior to a serious adverse event [ 3 – 7 ].
Today, vital signs play an important role in emergency departments (ED) and on the wards, to determine patients at risk of deterioration [ 6 – 11 ]. Even though it is accurately predicted by vital sign changes, clinical deterioration often goes unnoticed, or is not detected until it is too late to treat [ 12 – 15 ]. This is mainly caused by inadequate recording of vital signs or as a result of an inappropriate response to abnormal values [ 1 , 14 – 16 ]. Among nurses and doctors there is insufficient knowledge and appreciation of vital sign changes and their implications for patient care [ 17 – 20 ]. The importance of monitoring vital signs in clinical practice is indisputable, but how to best monitor and interpret them and how frequently they should be measured is still unclear [ 21 , 22 ].
This review searched the literature for studies that explicitly tried to determine and quantify the increase or decrease in risk associated with changes of intermittently measured vital signs. We, therefore, confined our search only to those papers that measured vital signs intermittently, and not to those that used continuous monitoring and novel wearable technology
The aim of this systematic review was to evaluate the ability of intermittent vital sign trends to predict clinical deterioration in acutely ill patients in hospital.
Protocol and registration
The protocol for this review was registered in PROSPERO: CRD42017080303. Both the protocol and the article are developed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines ( S1 Appendix ) [ 23 , 24 ].
Eligibility criteria
Inclusion criteria: all studies based on intermittent vital sign trends in acutely ill adult patients on hospital wards and in EDs, including all observational studies and controlled trials assessing prognosis. Trends were defined as the changes between two or more consecutive measurements of vital sign values, with a minimum of 3 hours and a maximum of 24 hours between measurements. Articles in English, Danish, Norwegian or Swedish were included.
Exclusion criteria: case series and case reports, studies on patients with specific conditions or with less than 100 participants, or patients directly admitted to ICU. All studies reporting trends in continuous monitoring were excluded.
Outcomes: in-hospital mortality or mortality up to 30 days after hospital discharge, transfer to ICU, cardiac arrest, calls to a rapid response system, or any other outcome reported that was associated with clinical deterioration.
Information sources
We searched PubMed, Embase, Cochrane Library and CINAHL on October 26th 2017. The databases were searched without time restrictions or filters for language and study design. The search was updated on December 28th 2017, adding the term “trajectory” to the original search ( S2 Appendix ). PROSPERO was searched for relevant ongoing or recently completed systematic reviews, last on December 18th. All studies assessed in full-text were screened for relevant citing articles using Scopus and Web of Science ( S3 Appendix ). Experts in the field were contacted to identify additional relevant studies.
The search strategy was developed through a series of preliminary searches using a broad range of relevant keywords and thesauri, including; vital sign, deterioration and trend ( S2 Appendix ). An information specialist from the Medical Research Library at University of Southern Denmark reviewed the search strategy before the final searches were conducted.
Study selection
Reference handling and duplicate screening was performed using EndNote and Covidence. After removal of duplicates, titles and abstracts were screened independently by two authors (LHP and IJB). Disagreements regarding inclusion were resolved through discussion. In case of continued disagreement, inclusion was decided by a third author.
Eligible studies were read in full length by LHP and IJB and separately assessed against inclusion and exclusion criteria decided by all authors ( S4 Appendix ). Disagreements were discussed with the other authors, and consensus decided inclusion.
Data collection process
Data from included studies were extracted separately by LHP and IJB using a preformed data extraction sheet. Collection included: study characteristics, settings, demographics, intervention details and outcomes.
Risk of bias in individual studies
Critical appraisal was performed in duplicates by the two reviewers. Neither of the authors were blinded. The Quality in Prognosis Studies (QUIPS) tool for prognostic studies [ 25 ] was used to evaluate the included studies. The risk of bias was rated within six domains: study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding and statistical analysis and reporting, assessing the risk of bias as either high, moderate or low.
Risk of bias across studies
The certainty of evidence was evaluated inspired by the Grading of Recommendations Assessment (GRADE) [ 26 ]. GRADE is originally designed to evaluate the certainty of evidence in randomized controlled trials. The approach assesses the strength of the body of evidence within five domains: within-study risk of bias (QUIPS), directness, heterogeneity, precision of effect estimates and risk of publication bias. An overall judgement regarding the certainty of the evidence was awarded for each examined outcome, as high, moderate, low or very low. As our study was observational by nature and did not address effect, evidence was not upgraded based on standard criteria. LHP and IJB evaluated the studies independently. Results were compared and discussed with the other authors.
Study selection and characteristics
The final search yielded 7,366 studies after removal of duplicates. However, 7,340 were deemed irrelevant ( Fig 1 ). Twenty-six were read in full-text and another nine were added through other sources: seven through citation tracking [ 27 – 33 ] and two additional studies recommended by experts [ 34 , 35 ]. Of the thirty-five studies assessed, two were eligible for inclusion. Details of the study selection are presented in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Abbreviation: EWS–early warning score.
https://doi.org/10.1371/journal.pone.0210875.g001
We excluded thirty-three studies assessed in full-text. Twenty-five, as they did not fulfil our eligibility criteria; fourteen did not examine trend, seven focused on trends in clinical scoring systems and three incorporated elements of vital sign trends in multi-parameter risk stratification models, but did not present sufficient data to enable analysis. Five studies examined trends in vital signs or EWS in patients with specific conditions and four studies were excluded due to wrong study design. Reasons for exclusion and details are given in S4 Appendix .
We found two cohort studies eligible for inclusion. One including 269,999 medical and surgical admissions in five hospitals in Illinois, by Churpek et al. [ 36 ] and one including 44,531 medical admissions to a Canadian regional hospital, by Kellett et al. [ 37 ]. Both were retrospective analyses of vital signs collected in electronic medical records that included: respiratory rate, heart rate, systolic and diastolic blood pressure, temperature and oxygen saturation.
Churpek et al. aimed to compare the accuracy of different methods of modelling vital sign trends for detecting clinical deterioration on the wards using discrete-time survival analysis. Six different trend models were tested against the predictive value of current vital signs alone ( Table 1 ). Transfers to intensive care unit (ICU), cardiac arrests and deaths on the ward were analysed as a composite outcome. Vital signs were averaged for each four-hour time block, and the variables at the beginning on each interval used to predict risk of deterioration during that time block.
https://doi.org/10.1371/journal.pone.0210875.t001
Kellett et al. aimed to assess whether changes in vital signs would enable detection of in-hospital mortality. They assigned a weighted Vitalpac Early Warning Score (ViEWS) to each vital sign and averaged the score for each twenty-four hour period of admission. Change in mean score between the first five and the last five days of admission were then compared for survivors and non-survivors. Further study characteristics are given in Table 1 .
Risk of bias within included studies
None of the studies accounted for loss to follow-up and no clear assessment of confounders were stated. Statistical analyses varied substantially and the overall risk of bias was rated as moderate for both studies, S5 Appendix .
As both studies are observational, the certainty of the evidence was regarded as low. With only one article per outcome, inconsistency was not evaluated. We found no serious indirectness in the studies and publication bias was not suspected. Therefore, Churpek et al. received an overall low rating, while Kellett et al. was downgraded to very low, due to serious imprecision. See S5 Appendix for full description.
Results of individual studies
Churpek et al. performed univariate analysis of the different trend models and the current value, followed by bivariate analysis combining the trend models with the current value. Through univariate analysis, they found respiratory rate to be the best predictor of deterioration when using the current value, AUC 0.70 (95% CI 0.70–0.70). Standard deviation of respiratory rate was found to be more accurate than the current value (AUC 0.71 (95% CI 0.71–0.71)). Bivariate analyses increased accuracy for all vital signs compared to the current value alone, but the optimal method varied for the different vital signs. The model including the current respiratory rate and the maximum rate prior to current was the most the accurate predictor (AUC 0.73). When averaging the change in accuracy for all vital signs, vital sign slope resulted in the greatest increase (AUC improvement 0.013), while the change from previous value resulted in an average decrease of model accuracy (AUC -0.002).
Analysing trajectories in ViEWS weighted vital signs for the first five and the last five days of admission, Kellett et al. found that the score for respiratory rate increased the most in non-survivors (0.92 (SD 1.22)–1.46 (SD 1.34)) and decreased the most in survivors (0.24 (SD 0.71)–0.10 (SD 0.49)). Combining respiratory rate with other vital signs was not more accurately associated with in-hospital mortality. Due to large standard deviations, none of the vital sign trends were statistically significant.
The heterogeneity between the two studies was high. Apart from methodology and outcomes, the cohorts differed in several ways: Churpek et al. looked at both medical and surgical ward patients, with an unspecified number of elective surgical patients. Average age was 60 years and in-hospital mortality was 1.0%. Kellett et al. looked at medical admissions, with an average age of 67.5 years and an in-hospital mortality of 4.6%, Table 1 .
The literature search also identified seven studies on trends in EWS. The results of four studies, otherwise eligible for inclusion, were evaluated and summarized in Table 2 . The remaining three studies were based on data from the same cohort as Kellett et al [ 37 ].
https://doi.org/10.1371/journal.pone.0210875.t002
This systematic review looked at trends in intermittently monitored vital signs and identified two studies eligible for inclusion. Both examined intermittent vital sign trends as an independent predictor of clinical deterioration. Although largely heterogeneous, with a low certainty of evidence, they suggested trends to be associated with deterioration.
Churpek et al. found respiratory rate to be the most accurate predictor, both for current value and when adding trend models. The most accurate model varied between the vital signs. Although trend statistically increased model accuracy for all vital signs, the improvements were considered minor. Kellett et al. suggested a correlation between increasing ViEWS weighted vital signs and in-hospital mortality. Similarly to Churpek et al., they found respiratory rate to be best associated with outcome, with the largest increase in score for non-survivors and decrease for survivors. However, due to large standard deviations, their findings were not statistically significant.
In essence, both studies suggest that more precise prognostic information can be obtained from changes in vital signs if they undergo manipulation. Kellett et al suggested that the values should be weighted, and Churpek et al found that the difference from the current and previous value was less valuable than the vital sign slope, vital sign variability, and the most deranged values since admission. Their findings also illustrates the lack of consensus in what constitutes trends, and how to best interpret them.
Considering vital signs central role in daily clinical practice, their results, although only suggestive, should be of interest to clinicians caring for patients on wards or in EDs. A lot of effort is going into developing continuous monitoring on the assumption that the trends it will reveal will be clinically valuable and superior to intermittent monitoring [ 41 ]. Although considering the technology promising, three recent systematic reviews did not find sufficient evidence in to support the implementation of routinely continuous monitoring of vital signs in general wards [ 42 – 44 ]. Results of this systematic review suggest that combining the widespread use of electronic healthcare systems to record intermittently monitored vital signs with trend analysis could improve the prediction of deterioration prior to a serious adverse event and help direct limited resources towards the patients at risk.
As illustrated by this review, there is an apparent lack of high quality evidence regarding trends in intermittently monitored vital signs. The studies included are retrospective analyses of pre-existing cohorts, without control groups, and with complete heterogeneity. Thus, they have a low (or very low) certainty of evidence. Interestingly, both studies found respiratory rate to be best associated with clinical course, a standpoint receiving a growing support [ 1 , 44 , 45 ]. Currently, there is no reliable and convenient way to evaluate respiratory rate, but recent technological advances will soon enable automated monitoring of respiratory rate [ 2 , 44 ], and can prove to be a major advance in monitoring. Ultimately, both trends in vital signs in general and respiratory rate in particular, should be subjected to evaluation through well-controlled prospective multicentre cohort studies.
Several studies examining trajectories of intermittently monitored vital signs were not eligible for inclusion ( S4 Appendix ). These consisted of; risk stratification models with elements of vital sign trends, trends in EWS and in patients with specific conditions, including; cardiac arrest [ 46 ], advanced stage of cancer [ 34 ], acute respiratory condition [ 47 ], repeated emergency team activations [ 48 ] and normotensive ED patients [ 31 ]. Although not subject for inclusion, they are mentioned to give an account of the total number of studies on vital sign trends identified by the review.
Likewise, studies on trends in EWS, otherwise meeting the inclusion criteria, are listed in Table 2 , in order to make the review more informative. They illustrate a potential correlation between trends and clinical deterioration. As observational studies with small sample sizes and low number of events, their findings should be interpreted with caution. They were all evaluated to have a moderate risk of bias and a very low certainty of evidence.
However, there are multiple limitations to such risk stratification models. In a recent article, Baker & Gerdin [ 49 ] discussed the clinical usefulness of the large number of prediction models developed for use in critical care. They emphasised the current focus on trying to optimise the precision of these models, rather than testing the performance of the models to real-world interventions and their impact on outcomes. Similarly, Pedersen et al. [ 10 ] highlighted the need to evaluate the endpoints currently used to validate these predictive models (e.g. ICU-transfer, cardiac arrest and in-hospital mortality). They argued for the importance of developing systems that specifically can identify patients who are salvageable, if provided with optimal treatment and care.
Disappointingly, only two studies were found eligible for inclusion in this review of intermittently monitored vital sign trends. Still, the fact that there is little or no high quality evidence supporting trends in vital signs and the myriads of scoring systems developed to the means of predicting clinical deterioration, should be an essential contribution to evidence based practice.
The search strategy was developed for a high sensitivity, with the aim of identifying all studies examining trend, without filtering for time or language. An information specialist reviewed the search strategy before the final searches were conducted. Only studies examining continuous monitoring were excluded on time criteria, in the abstract screening. Hence, changing the minimum time to 1 hour would not yield any further eligible studies. Reference tracking and outreach to relevant experts did not identify any other eligible studies that were not identified by the original search.
Limitations
This review only descriptively analysed the eligible studies identified and did not quantify data or perform a meta-analysis. Due to the wide applicability of the search terms “vital signs” and “trend”, only a small number of the articles were deemed relevant and assessed in full text. To reflect the clinical ward setting, the protocol for the review narrowed the inclusion criteria to studies analysing trends with a minimum of 3 hours and a maximum of 24 hours between measurements [ 21 , 22 ]. The evidence supporting measurement frequency is limited at best, and as a result, no studies were excluded on this criterion alone during abstract screening. Apart from reference tracking and expert outreach, attempts to pursue grey literature were not made.
The two eligible studies identified suggest that trend analysis of intermittent vital signs would increase the accuracy for detection of clinical deterioration on general wards and in EDs. However, the external validity of these findings is challenging to test–and there is a need to shift the focus towards clinical feasibility. Furthermore, the results of this review show there is no consensus on how to best analyse trends. Given that trend-models are externally validated through well-controlled prospective multicentre cohort studies, authors of this review, consider them promising and welcome as a valuable addition to clinical decision support.
Supporting information
S1 appendix. prisma 2009 checklist..
https://doi.org/10.1371/journal.pone.0210875.s001
S2 Appendix. Search strategy.
https://doi.org/10.1371/journal.pone.0210875.s002
S3 Appendix. Citation tracking.
https://doi.org/10.1371/journal.pone.0210875.s003
S4 Appendix. Full-text screening.
https://doi.org/10.1371/journal.pone.0210875.s004
S5 Appendix. Risk of bias assessment.
https://doi.org/10.1371/journal.pone.0210875.s005
Acknowledgments
We would like to thank the information specialists at the Medical Research Library at University of Southern Denmark for help with the search strategy, Dr. Daanyaal Wasim for his suggestions during revision and the experts that responded to our request for additional literature.
- View Article
- Google Scholar
- 2. Kellett J. The Assessment and Interpretation of Vital Signs. In: DeVita MA, Hillman K, Bellomo R, Odell M, Jones DA, Winters BD, et al., editors. Textbook of Rapid Response Systems: Concept and Implementation. Cham: Springer International Publishing; 2017. p. 63–85.
- PubMed/NCBI
- 30. Mao Y, Chen Y, Hackmann G, Chen M, Lu C, Kollef M, et al., editors. Medical Data Mining for Early Deterioration Warning in General Hospital Wards. 2011 IEEE 11th International Conference on Data Mining Workshops; 2011 11–11 Dec. 2011.
- 41. Cardona-Morrell M, Zimlichman E, Taenzer A. Continuous Monitoring for Early Detection of Deterioration on General Care Units. In: DeVita MA, Hillman K, Bellomo R, Odell M, Jones DA, Winters BD, et al., editors. Textbook of Rapid Response Systems: Concept and Implementation. Cham: Springer International Publishing; 2017. p. 277–87.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 08 March 2023
The quality of vital signs measurements and value preferences in electronic medical records varies by hospital, specialty, and patient demographics
- Niall Jackson 1 ,
- Jessica Woods 2 ,
- Peter Watkinson 3 ,
- Andrew Brent 1 , 3 ,
- Tim E. A. Peto 4 , 5 ,
- A. Sarah Walker 4 , 5 &
- David W. Eyre 5 , 6
Scientific Reports volume 13 , Article number: 3858 ( 2023 ) Cite this article
2514 Accesses
2 Citations
1 Altmetric
Metrics details
- Diagnostic markers
- Epidemiology
We aimed to assess the frequency of value preferences in recording of vital signs in electronic healthcare records (EHRs) and associated patient and hospital factors. We used EHR data from Oxford University Hospitals, UK, between 01-January-2016 and 30-June-2019 and a maximum likelihood estimator to determine the prevalence of value preferences in measurements of systolic and diastolic blood pressure (SBP/DBP), heart rate (HR) (readings ending in zero), respiratory rate (multiples of 2 or 4), and temperature (readings of 36.0 °C). We used multivariable logistic regression to investigate associations between value preferences and patient age, sex, ethnicity, deprivation, comorbidities, calendar time, hour of day, days into admission, hospital, day of week and speciality. In 4,375,654 records from 135,173 patients, there was an excess of temperature readings of 36.0 °C above that expected from the underlying distribution that affected 11.3% (95% CI 10.6–12.1%) of measurements, i.e. these observations were likely inappropriately recorded as 36.0 °C instead of the true value. SBP, DBP and HR were rounded to the nearest 10 in 2.2% (1.4–2.8%) and 2.0% (1.3–5.1%) and 2.4% (1.7–3.1%) of measurements. RR was also more commonly recorded as multiples of 2. BP digit preference and an excess of temperature recordings of 36.0 °C were more common in older and male patients, as length of stay increased, following a previous normal set of vital signs and typically more common in medical vs. surgical specialities. Differences were seen between hospitals, however, digit preference reduced over calendar time. Vital signs may not always be accurately documented, and this may vary by patient groups and hospital settings. Allowances and adjustments may be needed in delivering care to patients and in observational analyses and predictive tools using these factors as outcomes or exposures.
Similar content being viewed by others
Exploring the clinical relevance of vital signs statistical calculations from a new-generation clinical information system

Vital signs in pediatric oncology patients assessed by continuous recording with a wearable device, NCT04134429

Continuous monitoring of physiological data using the patient vital status fusion score in septic critical care patients
Introduction.
Electronic healthcare records (EHR) have been widely adopted across different healthcare settings globally and have become an integral part of health infrastructure: saving time, improving communication and record keeping, and supporting learning 1 . As the scale and breadth of EHR data increases, so does its ability to fulfil secondary functions including quality improvement, product development, and research, contingent on appropriate regulation and transparency 2 . Example applications of EHR data include population-level epidemiological studies 3 , 4 , 5 , machine learning-based diagnostic assistants for clinicians 6 , screening for child maltreatment and family violence 7 , and detecting and tracking infectious disease outbreaks 8 , 9 .
However, conclusions rely on the reliability and accuracy of EHR data, which is not guaranteed 10 , 11 . Indeed, the use of EHR data beyond its original purpose (clinical care and billing) raises specific challenges. Data collection in the clinical environment is imperfect 12 and often incomplete 13 ; it may lack comparability or reproducibility 14 or even simply be wrong 15 , 16 . Additionally, sensor-derived data such vital signs, are also subject to intrinsic measurement errors arising from variation in calibration, accuracy and drift over time. Attempts to quantify or evaluate EHR data quality are limited, and even fewer have investigated causes for variability in quality 17 . Most studies have focused on checking the accuracy of clinical and diagnostic codes rather than numerical observations. In one notable exception, evaluating the quality of vital sign data across multiple hospitals and EHR systems, there was a skew of completeness and correctness in favour of arriving patients and higher fidelity in wholly EHR based systems compared to a combination of paper and EHR 18 .
Digit preference in vital sign measurement is a well-recognized phenomenon, however it is infrequently formally accounted for in healthcare delivery or in studies using EHR data. Additionally, systems to ensure vital signs are attributable, correct, and contemporaneously recorded can be limited. Many hospitals rely on manual transcription of readings into patient records rather than using potentially more accurate automated systems, e.g. because of cost or problems with interoperability of measurement devices and EHR systems. Terminal digit preference for multiples of ten in blood pressure (BP) recordings has been shown to be extremely common 19 , 20 , to introduce systemic bias potentially effecting mortality 21 and to produce inaccurate epidemiological results 22 . This phenomenon has been observed in other vital sign measurements such as respiratory rate 23 , with attempts to rectify inaccuracy through continuous, automated monitoring 24 . Digital preference in vital signs may also impact derived values such as pulse pressure, and platforms that depend on them including early warning systems. However, in addition to standard digit preference, when reviewing data from our hospital group we noted an excess of a specific temperature measurement, 36.0 °C, that appeared unlikely to have arisen from rounding alone, warranting further investigation which we describe here.
We investigated observations of vital signs gathered over 3.5 years from inpatients at a large UK teaching hospital group. We assessed the frequency of recordings with preferences for a specific values (e.g. multiples of ten for BP or temperature readings of 36.0 °C) as a marker of sub-optimal data quality. We extend prior work in this area 19 , 20 , 21 , 22 , 23 by investigating associations between digit preference and patient factors, such as age and sex, and hospital factors, such as the specialty caring for a patient. The associations we describe provide insights into what may drive digit preference and may help healthcare institutions improve the quality of the data they collect and use for patient care.
We conducted a retrospective observational study at Oxford University Hospitals NHS Foundation Trust (OUH) in Oxfordshire, UK. OUH consists of four teaching hospitals with a total of 1000 beds: Hospital A (providing acute care, trauma, and neurosurgery services); Hospital B (elective cancer surgery, transplant, haematology, oncology); Hospital C (district hospital, acute medical services) and Hospital D (elective orthopaedics). OUH acts as a tertiary referral centre for the surrounding region, providing approximately 1 million patient contacts a year and serving a population of around 655,000.
We used individual observations of vital signs conducted at OUH for adult inpatients (≥ 18y) between 01-January-2016 and 30-June-2019. The vital signs observed, with dates and times of collection, included respiratory rate (RR), heart rate (HR), tympanic temperature, systolic and diastolic BP (SBP and DBP) and oxygen saturations. Vital signs were included for all general wards, but those from intensive care units, operating theatre recovery areas, day case units, and OUH’s hospice were not included as these were collected using a separate system or in locations with a different care delivery focus.
Observations were collected by healthcare assistants and registered nurses using a semi-automated vital sign observation system across all 4 hospital sites. HR, SBP, DBP, and oxygen saturations were collected using an observation machine combining an electronic sphygmomanometer and pulse oximeter. RR was manually timed, typically expected to be recorded by counting the number of breaths over 60 s. Temperature was measured with a separate tympanic thermometer. All observations were then manually transcribed into a tablet computer attached to the same stand, this was usually done at the bedside as the tablet computer allowed the patient’s wristband to be scanned to add results to their record. The tablet computer automatically uploaded results into the EHR in real time. Although the tablet computer and observation equipment were co-located on the same mobile stand, there was no automated check that the observations documented had been performed or matched those measured. We do not believe that any of the measurement devices show any intrinsic value preference. All devices produce an error rather than a default reading if measurement is unsuccessful. Supplemental oxygen devices and alertness (alert, responsive to voice, pain or unresponsive, AVPU) were also recorded. However, these non-numerical measurements are not considered further here. Additional data were obtained: hospital-level data (hospital where the observation was made, the specialty managing the patient); and patient data (age, sex, ethnicity, index of multiple deprivation (IMD) score at home address, Charlson comorbidity score).
Statistical analysis
Several approaches have been previously described for identifying and quantifying digit preference 25 . For example, jointly estimating a flexible, but smooth, underlying distribution and modelling rounding from adjacent values to the nearest number showing digit preference, e.g. from 9 or 11 to 10 26 , 27 . Extensions of this approach allow for rounding of groups of adjacent values, e.g. to the nearest 10 28 . However, here we also wanted to account for a phenomenon in temperature recordings which went beyond simple rounding, where a subset of all observations was set to 36.0 °C. We therefore used a simple maximum likelihood-based estimator to jointly estimate the underlying distribution of temperature, HR, SBP, DBP, and respiratory rate measurements, and the proportion of observations affected by digit preference. Oxygen saturation measurements had only limited dynamic range and no clear evidence of digit preference and so were not studied further. For all other vital signs, we assume that a given vital sign follows an underlying distribution, here we fit both normal and gamma distributions. This leads to the following expression for the statistical likelihood of the observed data, given the parameters governing the underlying distribution and any digit preference (i.e. the probability of digit preference and mean/standard deviation or shape/rate):
Pr(observation was subject to digit preference) * Pr(true value is from the interval of the source distribution leading to rounding) + Pr(observation not subject to digit preference) * Pr(true value given the precision values reported at).
In the case of BP and HR recordings, which are initially reported by the measurement device to the nearest whole number, we estimate the extent of rounding to the nearest 10, for example where the BP reading was 120 mmHg, then the likelihood becomes:
Pr(observation rounded) * Pr(observation from the interval [114.5, 124.5)) + Pr(observation not rounded)*Pr(observation from the interval [119.5, 120.5)).
In the case when the HR or BP is not a multiple of ten, then the probability of rounding is set to zero, and only the second term of the likelihood applies. As this term includes the probability that the observation is not rounded it accounts for the fact that rounding leads to depletion in the frequency of observed values relative to the underlying distribution at values that are rounded up/down. The most common way rounding occurs in the RR is by only timing the number of breaths over 15 or 30 s (rather than 60 s), and then multiplying by 4 or 2 respectively to report breaths per minute. We therefore simultaneously estimated the extent of rounding leading to multiples of 4 and 2 for RR. The formula used for the likelihood means that the estimated proportion of observations subject to rounding includes observations where the true value is a multiple of 4 or 2; as such we estimate the total proportion of respiratory rate observations that might have been measured by timing breaths over 15 or 30 s respectively. Similarly, the form of the likelihood for HR and BP rounding means we estimate the total extent of rounding behaviour, including in our calculations the approximately 1 in 10 instances where the true value and the rounded value are the same.
For temperature readings we assume that any true observation can lead to a documented recording of 36.0 °C, as our hypothesis is that an excess of these readings occurs when the temperature is not actually measured but simply documented as 36.0 °C instead, such that the likelihood becomes:
Pr(observation subject to preference for 36.0 °C) + Pr(observation not subject to preference for 36.0 °C) * Pr(observation from the observed interval of the source distribution).
For temperature recordings we make the simplifying assumption that any observation that is not 36.0 °C is not subject to digit preference.
Maximum likelihood estimates were obtained using R, version 4.2 and pnorm, pgamma and optim functions (see Supplement for code). Confidence intervals were estimated by non-parametric bootstrap sampling using 1000 iterations. For computational efficiency only 10,000 observations were included in each iteration. The accuracy of the code was tested through simulation prior to use.
We used multivariable logistic regression to investigate associations between temperature recordings of 36.0 °C and several factors potentially driving value preferences. Analyses were restricted to patients with complete data, and to complete vital sign sets (i.e. all of temperature, HR, RR, SBP, DBP, and oxygen saturations recorded). We used natural cubic splines to account for non-linear relationships for continuous variables (allowing up to five default placed knots, selecting the final number of knots by minimising the Bayesian Information Criterion, BIC). To avoid undue influence of outlying values, continuous variables were truncated at the 1st and 99th percentiles. Pairwise interactions between model main effects were included where this improved model fit based on BIC. We used clustered robust standard errors to account for repeated measurements obtained from the same patient.
To investigate if associations were specific to temperature or applied to vital signs more widely, we also refitted the same model (i.e. with the same spline terms and interactions) with BP digit preference as the outcome, regarding measurements where the SBP and DBP both ended in zero as indicative of possible digit preference. We use this combined measure across both SBP and DBP as it is likely to be most enriched for digit preference. We fitted the same models for HR and RR digit preference regarding readings ending in zero or multiples as two as showing possible digit preference respectively.
We also investigated if the presence of abnormal previous readings affected subsequent digit preference. Temperatures of ≤ 35.5 °C or ≥ 37.5 °C, SBP readings of > 160 or < 90 mmHg, DBP readings of > 100 or < 60 mmHg, HR readings of < 50 or > 120, and RR readings of < 10 and > 24 were arbitrarily considered abnormal. For each observation with a prior observation from the same patient within ≤ 36 h, we selected the most recent prior observation for comparison. A look back period of up to 36 h was allowed to capture vital signs measured just once a day, but at different times. However, where vital signs were measured more frequently only the most recent was considered. We then refitted the regression models above including a term for if the prior vital sign reading (temperature, HR, SBP, DBP, or RR) had been abnormal as a covariate.
Regression analyses were conducted using R, version 4.2.
Ethical approval
Deidentified data were obtained from the Infections in Oxfordshire Research Database which has approvals from the National Research Ethics Service South Central – Oxford C Research Ethics Committee (19/SC/0403), the Health Research Authority and the national Confidentiality Advisory Group (19/CAG/0144), including provision for use of pseudonymised routinely collected data without individual patient consent. Patients who choose to opt out of their data being used in research are not included in the study. The study was carried out in accordance with all relevant guidelines and regulations.
Between 01-January-2016 and 30-June-2019, a total of 5,007,650 sets of vital signs were recorded. Of these, 469,904 (9.4%) did not include temperature, 395,445 (7.9%) were missing SBP and/or DBP, 403,364 (8.1%) missing RR, 353,083 (7.1%) missing HR, and 326,474 (6.5%) missing oxygen saturation recordings. Rates of missing data were similar across different patient groups, but missing data were more common near the start of a hospital admission and outside times of day that vital signs were routinely measured. Missing data were more common at Hospital D (elective orthopaedics) and in some specialties, e.g. obstetrics and gynaecology and cardiology (Table S1 ).
Restricting to complete sets of vital signs left 4,375,654 (87.4%) records in the final dataset from 135,173 patients. The median (IQR) patient age was 61 (42–76) years, 70,515 (52.2%) patients were female, and 100,655 (74.5%) were of white and 27,453 (20.3%) of unstated or unknown ethnicity. The most common specialties recording vital signs were general surgery (882,956, 20.2%), acute and emergency medicine (660,530, 15.1%), and trauma and orthopaedics (597,834, 13.7%).
Prevalence of value preferences in vital signs readings
Compared with the overall distribution of temperature values, there was an excess of temperature readings of 36.0 °C (Fig. 1 ), readings of 36.0 °C accounted for 15.0% (658,124/4,375,654) of all values. The same pattern of excess readings of 36.0 °C was seen across all four hospitals (Fig. S1 ). Assuming true temperature readings followed a normal distribution (Table 1 , Fig. S2 ), then 11.3% (95% CI 10.6–12.1%) of observations were estimated to be inappropriately recorded as 36.0 °C instead of the true value. Similar estimates were obtained assuming an alternative gamma distribution for temperature readings (Table S2 , Fig. S2 ).
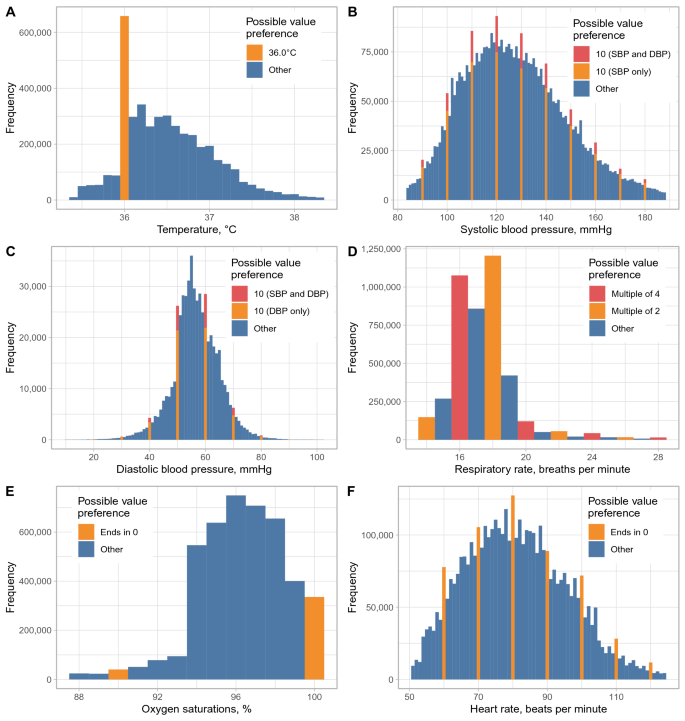
Observed distribution of temperature, systolic blood pressure (SBP), diastolic blood pressure (DBP), respiratory rate, oxygen saturation, and heart rate recordings. Readings showing possible value preferences are shown in orange/red. For SBP and DBP, readings where the SBP and DBP both end in zero are shown in red, readings where only the SBP or DBP respectively end in zero are shown in orange. Values below the 1st percentile or above the 99th percentile are omitted for visualisation purposes.
Approximately 1% of all BP readings would be expected to have both a SBP and DBP ending in zero by chance, however 2.3% (99,209) of readings showed this pattern. Assuming SBP and DBP both followed a normal distribution, 2.2% (95% CI 1.4–2.8%) and 2.0% (1.3–5.1%) of readings respectively were estimated to be rounded to the nearest 10 mmHg. Digit preference also occurred for HR readings, with 12.1% (531,219) ending in zero and 2.4% (1.7–3.1%) of readings estimated to be rounded to the nearest ten. RR readings were also more likely to be multiples of 2 (62.0%, 2,711,524) or 4 (29.1%, 1,273,972) than expected by chance, with digit preference to the nearest multiple of 2 or 4 affecting an estimated 22.5% (22.2–24.8%) and 2.5% (< 0.1–3.5%) of readings respectively. Estimates were similar if SBP, DBP, HR, and RR were assumed to be gamma distributed, with the exception that rounding of RR to the nearest multiple of 4 was found to be less common, < 0.1% (< 0.1–0.1%) (Table S2 ). There was no clear evidence of value preference in oxygen saturation readings (Fig. 1 ).
Value preference associations with patient demographics
Associations with value preferences for each vital sign were investigated using multivariable models (Tables 2 , 3 and Figs. 2 , 3 ). For 41,350 (0.9%) records no deprivation score was documented; these records were excluded. Complete data were available for all other hospital/patient variables. Temperature was independently more likely to be recorded as 36.0 °C with increasing age above 50 years and BP most likely to be recorded with SBP and DBP both ending in zero for those above 80 years (Fig. 2 A). Conversely, RR was less likely to be a multiple of 2 as age increased and HR value preference was greatest in younger and older adults. Male patients were more likely than female patients to have readings with value preferences across all vital signs, with differences by sex increasing for temperature and HR as performance improved overall with passing calendar time (Fig. 2 B). Temperature value preference was slightly less common in patients from less deprived areas (aOR per 10 unit change in deprivation percentile = 0.99 [0.99–0.99, higher percentiles are less deprived]), but with no evidence of a difference in other vital signs. There was no evidence for consistent differences in value preference by ethnicity, however temperatures of 36.0 °C were more commonly recorded in patients of Asian ethnicity (aOR vs. white = 1.08 [1.03–1.13]) and BPs ending in zero were more common in those of unstated or unknown ethnicity (aOR vs. white = 1.13 [1.07–1.19]). Patients with higher Charlson scores were slightly more likely to have recorded temperatures of 36.0 °C (aOR per 5 unit increase = 1.02 [1.02–1.03]), but less likely to have BP ending in zero (aOR per 5 unit increase = 0.93 [0.92–0.94]), with only small changes by Charlson score in HR or RR value preferences.
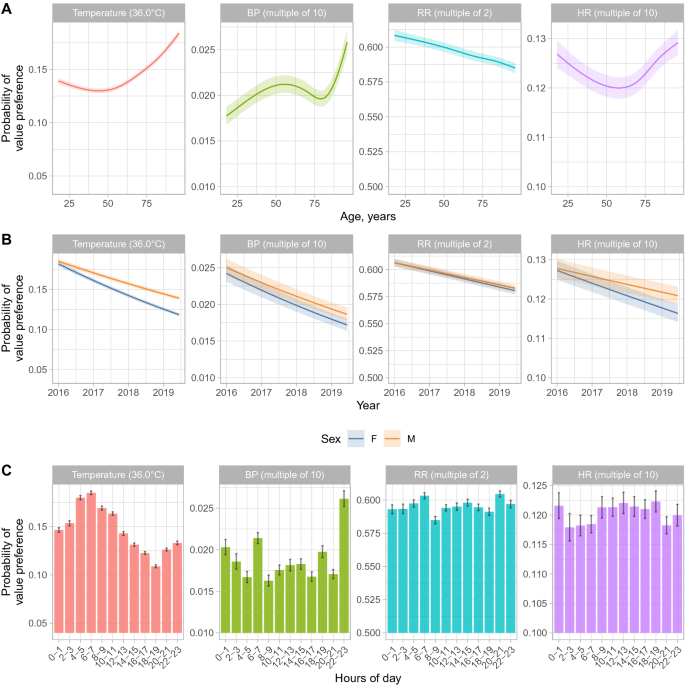
Multivariable associations between age, study year, sex, and time of day and vital sign value preferences. Model predictions from a multivariable model are shown with all other factors set to the reference category or median value as shown in Table 3 and Fig. 3 . The shaded ribbon indicates the 95% confidence interval. BP blood pressure, RR respiratory rate, HR heart rate, M male, F female. The minimum value on each y-axis represents the approximate expected value without any value preference.
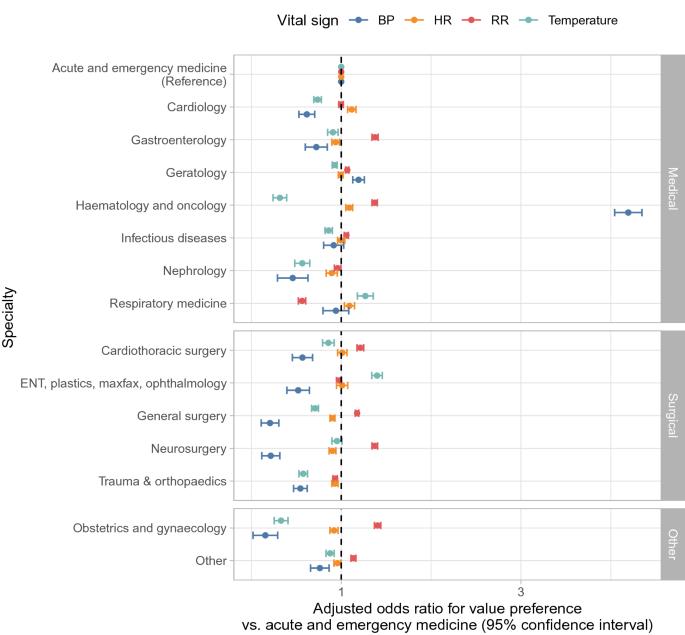
Relationship between specialty and vital sign value preferences. ENT ear, nose and throat, plastics plastic surgery, maxfax maxillofacial surgery, BP blood pressure, RR respiratory rate, HR heart rate. Values plotted are provided in Table S3.
Changes over calendar time, hour of day, and by hospital and time in admission
The frequency of value preferences for all vital signs decreased during the study (Fig. 2 B). Temperatures were most likely to be recorded as 36.0 °C at around 6-8am, i.e. at the first routine set of observations performed per day in most patients, whereas BP was most likely to end in zero during the late evening, and to a lesser extent between 6 and 8am. Relatively little change in HR or RR value preference was seen by time of day (Fig. 2 C). Value preference for all vital signs became slightly more common the greater the prior length of stay (e.g. for temperature, aOR per 7 day increase in prior length of stay = 1.03 [95% CI 1.03–1.03]).
Differences were also seen between hospitals in temperature value preferences. After adjusting for differences in the specialties present and all other factors, compared to hospital A (acute care, trauma, and neurosurgery), value preferences in temperature measurement were more common in hospital C (district hospital) and less common in hospital B (elective cancer surgery, transplant, haematology, oncology) and particularly hospital D (elective orthopaedics) (Table 3 ). RR value preference was also more common in hospital C, as well as D, whereas BP value preference was more common in hospital B. Relatively little difference between hospitals was seen in HR value preference.
Variation by specialty
Value preferences in temperature, BP, and RR readings varied by specialty, whereas differences in HR value preference were more limited (Fig. 3 ). Compared to acute and emergency medicine, value preferences for temperature and BP were less common in most surgical specialties and medical sub-specialties, but RR value preference was more common in several surgical specialties and BP value preferences substantially more common in haematology and oncology. Value preference in temperature readings was least common in haematology and oncology. Both nephrology and trauma and orthopaedics exhibited less value preference across all vital signs than acute and emergency medicine.
Effect of previous abnormal measurements
A total of 4,125,851 sets of observations had a previous measurement from the same patient within ≤ 36 h. Temperature readings of 36.0 °C were less frequent following an abnormal prior temperature measurement, 20,224/354,837 (5.7%), than following a normal prior measurement, 601,092/3,771,014 (16.0%). Given it may take time for temperature to normalise it would not be expected that those with a previously abnormal temperature would have the same proportion of true temperatures of 36.0 °C as the overall hospital population (estimated as 4.0% from the normal distribution fitted above). However even allowing for this, preference for recording a temperature of 36.0 °C was likely more common with a normal prior measurement. Adjusting for the same factors as in the main analysis, a previous abnormal temperature independently reduced the odds of a recording of 36.0 °C (aOR = 0.34, [95% CI 0.34–0.35]). Similarly, 25,091/1,307,048 (1.9%) of BP observations had SBP and DBP both ending in zero after an abnormal SBP or DBP, compared to 69,773/2,818,803 (2.5%) without a prior abnormal reading (aOR = 0.86 [0.84–0.88]). However, the opposite pattern was seen for HR and RR where abnormal previous readings were associated with increased subsequent digit preference (aOR = 1.22 [1.19–1.24] and aOR = 1.12 [1.10–1.14] respectively).
In this analysis of records from a large UK teaching hospital group, we show preference for specific values or digits in vital sign records in EHRs. Our findings have implications for patient management, quality improvement initiatives and for research conducted using EHRs. Three potential mechanisms underlie the value preferences seen. HR and BP measurements exhibit classical digit preference with rounding occurring during human transcription of readings. Value preference in RR most likely occurred during the measurement process, with RR values that are multiples of two arising from recording the number of breaths per minute over 30 s and doubling the measured count. Thirdly, value preferences in temperature readings occurred due to preference for a specific value, 36.0 °C.
A key question is whether temperature value preferences indicate simply convenience rounding on transcribing values or whether they are also a marker for incompletely observed observations. Potentially favouring the latter, we observed differences in the relative frequency of value preferences. We found that around 2% of BP and HR measurements showed evidence of rounding to the nearest 10. In contrast, over 5-times more temperature readings were estimated to affected by value preference: an estimated excess of 11% of all temperature recordings were recorded as 36.0 °C. One alternative explanation to rounding is that these recordings were documented when in fact no temperature was measured, e.g. it was presumed to be normal where the thermometer, which was separate to the rest of the vital sign measuring equipment, was missing or not working, or alternatively where patients appeared well and a normal measurement was assumed as has been hypothesised for respiratory rate measurement too 29 . It is also possible that implausibly low readings, e.g. when thermometers were mis-calibrated, were recorded as 36.0 °C, but this is unlikely to have been common. Although over 20% of RR recordings were estimated to be rounded to the nearest two, this most likely reflects the measurements process described above, rather than digit preference per se. Automated measurements of RR may increase accuracy, depending on the setting and device used, in some instances automated RR measurements have been shown correlated better with outcomes 30 , but not in others 29 .
We found differences between hospital specialties, even after adjustment for other factors. Generally surgical specialities recorded vital signs with greater precision than acute and emergency medicine. However, the prevalence of value preferences also potentially reflects the culture within a speciality, where greater importance may be placed on measured values, e.g. in nephrology, or on specific vital signs, e.g. temperature in neutropenic and other immunosuppressed patients in haematology and oncology or BP in cardiology. We also found marked differences in temperature measurement between the four hospitals in the organisation, even following adjustment for the specialties present. This may reflect systemic factors, e.g. staffing levels and the importance placed on vital signs may vary by setting. In higher acuity settings, reliance on vital signs for treatment escalation could increase vital sign fidelity compared to less acute settings focused on rehabilitation. Although patients are admitted to acute medicine as an emergency, the increased digit preference seen in this specialty may reflect that for many longer staying patients rehabilitation and provision of social care are the dominant issues for much of each admission. We also found that normal prior temperature and BP measurements were more likely to be followed by digital preference in subsequent observations, with previous abnormal measurements being associated with greater accuracy in subsequent observations. However, this effect was not seen consistently with the opposite for HR and RR, where possibly 3 digit heart rates are more likely to be rounded or more rapid respiratory rates more difficult to count precisely.
Older patients and male patients were more likely to have temperature and BP recordings with value preferences, whereas RR value preferences we more common in younger patients. Further work is required to better understand the reasons for this. For example, variation in temperature recording by age may reflect differences in the acuity of patients and associated culture around vital sign measurement, the relative importance placed on curative treatment vs. patient comfort, and physical barriers to temperature measurement including patient agitation. There were no systematic differences by ethnicity across all vital signs.
Changes over time suggest institution-wide improvement is possible, with increased precision of all vital signs seen during the study. The study builds on previous studies of vital sign recording quality 31 , and highlights that institutions may wish to monitor vital sign recording to identify areas of the hospital or patient groups where specific interventions to improve quality may be required.
Multiple variables representing the timing of measurements were investigated. Routine morning temperature measurements, e.g. 6–7am, were most likely to be impacted by digit preference. BP measurements were also more likely to be rounded in morning as well as in late evening. Vital sign precision was greatest around the time of hospital admission with value preferences increasing as length of stay increased, likely reflecting that patients are most unwell when first presenting to hospital and so vital signs are performed and recorded carefully. However, it was also more common to have one or more vital signs missing after short prior lengths of stay, e.g. < 1 day, possibly reflecting different approaches to short stay patients, or rechecking of specific vital signs in some acute settings. There was less temporal variation in digit preference in RR and HR measurements.
Digit preference is a well described phenomenon 19 , 20 . However, particularly for temperature measurement, the question that arises from our findings is; if a vital sign is more difficult to measure for some reason, then why does current culture potentially favour documenting an inaccurate reading instead of leaving it missing, especially within a system where safety is prioritised. There may be explicit or implied pressure to always record a complete set of vital signs but less scrutiny of their accuracy 32 (although ~ 13% of observations in our study were excluded because of missing one or more vital signs), or it may be that recording an observation as unavailable may be more onerous and require entering a justification. There may also be disincentives to recording abnormal values if this requires escalation of care and additional action. Related to this point, value preferences may impact early warning scores, such as NEWS2 33 , e.g. value preferences for temperatures of 36.0 °C may score a point that would not otherwise be scored with temperatures ranging from 36.1 to 38.0 °C.
Limitations of our study include that it is based on a single organisation and data entry system for recording vital signs. Further studies are required to confirm if our findings are replicated more widely. As this was a retrospective study, we were not able to identify the reasons behind missing or potential inaccurate readings; future investigations could consider both practical barriers such as malfunctioning devices and behavioural factors such as perceptions around the importance of vital signs. We did not investigate more granular variation in vital sign recording by hospital ward or individual staff member, the latter as the identity of the healthcare worker recording the vital signs was not available in our data extract. We also did not investigate the downstream consequences of vital sign values (as has been done elsewhere to create early warning systems) or the consequences of value preferences. The latter could be looked at in future work, e.g. considering associations with length of stay or mortality, although care would be required to avoid reverse causation where delays in discharge or a more palliative focus change value preferences.
There are also several technical limitations. Our model for estimating the proportion of vital signs affected by value preference is relatively simple. For BP and HR, we only consider rounding to the nearest 10, which was the most dominant form in our data, but rounding to the nearest 5 or 2 also occurs. However, our main focus here is not the absolute quantification of value preference, but rather to explore the potential drivers of it and to highlight it as an issue. Our estimation framework could be extended to consider multiple types of rounding, e.g. by expanding the likelihood to simultaneously consider rounding to the nearest 2, 5 and 10. We also assume that all underlying temperatures are equally likely to be recorded as 36.0 °C; in reality external signs of a fever, which is often accompanied by other abnormal vital signs, may prompt more accurate recording of the temperature. The underlying distributions chosen result in a good fit for HR and BP, particularly the gamma distribution. For temperature the fit is less good, but a reasonable approximation and a better fitting distribution is unlikely to explain the substantial excess in recordings of 36.0 °C. There are relatively few unique commonly recorded RR values resulting in the fitted continuous distribution being a less good approximation. The logistic regression models fitted include both true values and recordings affected by value preferences as outcomes. Therefore, for temperature where an absolute value preference is common, it is possible that in part the resulting associations are indicative of a normal temperature of 36.0 °C as well as value preferences. For all other vital signs value preferences occur throughout the full range of measurements and so the logistic models are still able to estimate factors associated with a relative increase in value preferences robustly. Finally, inaccuracies not leading to value preferences are not assessed in the current analysis, but also need to be considered when using EHR data, e.g. miscalibration of devices or measurement error arising from failure of tympanic thermometers to accurately record low temperatures.
Our study provides evidence that vital sign measurement displays value preference to a such a degree that it could affect conclusions based on unadjusted vital sign data, in both clinical and research settings. We show that hospital, speciality, admission stage and patient age all have important impacts on the accuracy of vital signs. Changes over time in our hospital suggest improvements in accuracy are possible. Ultimately fully connected systems that automatically measure and/or record vital signs into patient records are likely to address many of the issues identified; however, these are only likely to be implemented if this is prioritised by device manufacturers and healthcare providers. Work with institutions and individuals is required to fully elucidate and understand the mechanisms behind values preferences on a systems, patient and clinician level. Greater consensus on what health information is essential and what level of accuracy is required, across different settings, would help define benchmarks for acceptable performance, which could potentially be monitored automatically. In the meantime, clinicians and researchers need to be aware that vital signs may not always be accurately documented, and to make appropriate allowances and adjustments for this in delivering care to patients and in analyses using these factors as outcomes or exposures.
Data availability
The data analysed are not publicly available as they contain personal data but are available from the Infections in Oxfordshire Research Database ( https://oxfordbrc.nihr.ac.uk/research-themes-overview/antimicrobial-resistance-and-modernising-microbiology/infections-in-oxfordshire-research-database-iord/ ), subject to an application and research proposal meeting on the ethical and governance requirements of the Database. More information is available by emailing [email protected].
Evans, R. S. Electronic health records: Then, now, and in the future. Yearb. Med. Inform. 25 , S48–S61. https://doi.org/10.15265/iys-2016-s006 (2016).
Article Google Scholar
Safran, C. et al. Toward a national framework for the secondary use of health data: An American Medical Informatics Association White Paper. J. Am. Med. Inform. Assoc. 14 , 1–9. https://doi.org/10.1197/jamia.m2273 (2007).
Article PubMed PubMed Central Google Scholar
Casey, J. A., Schwartz, B. S., Stewart, W. F. & Adler, N. E. Using electronic health records for population health research: A review of methods and applications. Annu. Rev. Public Health 37 , 1–21. https://doi.org/10.1146/annurev-publhealth-032315-021353 (2015).
Lin, H. et al. Using big data to improve cardiovascular care and outcomes in China: A protocol for the Chinese Electronic health Records Research in Yinzhou (CHERRY) Study. BMJ Open 8 , e019698. https://doi.org/10.1136/bmjopen-2017-019698 (2018).
Morley, K. I. et al. Defining disease phenotypes using national linked electronic health records: A case study of atrial fibrillation. Plos One 9 , e110900. https://doi.org/10.1371/journal.pone.0110900 (2014).
Article ADS CAS PubMed PubMed Central Google Scholar
Yang, Z. et al. Clinical assistant diagnosis for electronic medical record based on convolutional neural network. Sci. Rep.-UK 8 , 6329. https://doi.org/10.1038/s41598-018-24389-w (2018).
Article ADS CAS Google Scholar
Syed, S. et al. Predictive value of indicators for identifying child maltreatment and intimate partner violence in coded electronic health records: A systematic review and meta-analysis. Arch. Dis. Child. 106 , 44–53. https://doi.org/10.1136/archdischild-2020-319027 (2020).
Article PubMed Google Scholar
Cooper, G. F. et al. A method for detecting and characterizing outbreaks of infectious disease from clinical reports. J. Biomed. Inform. 53 , 15–26. https://doi.org/10.1016/j.jbi.2014.08.011 (2015).
Greene, S. K. et al. Gastrointestinal disease outbreak detection using multiple data streams from electronic medical records. Foodborne Pathog. Dis. 9 , 431–441. https://doi.org/10.1089/fpd.2011.1036 (2012).
Ray, W. A. Improving automated database studies. Epidemiology 22 , 302–304. https://doi.org/10.1097/ede.0b013e31820f31e1 (2011).
Terris, D. D., Litaker, D. G. & Koroukian, S. M. Health state information derived from secondary databases is affected by multiple sources of bias. J. Clin. Epidemiol. 60 , 734–741. https://doi.org/10.1016/j.jclinepi.2006.08.012 (2007).
Verheij, R. A., Curcin, V., Delaney, B. C. & McGilchrist, M. M. Possible sources of bias in primary care electronic health record data use and reuse. J. Med. Internet Res. 20 , e185. https://doi.org/10.2196/jmir.9134 (2018).
Köpcke, F. et al. Evaluation of data completeness in the electronic health record for the purpose of patient recruitment into clinical trials: A retrospective analysis of element presence. BMC Med. Inform. Decis. 13 , 37. https://doi.org/10.1186/1472-6947-13-37 (2013).
Verweij, L. M. et al. Data quality issues impede comparability of hospital treatment delay performance indicators. Neth. Heart J. 23 , 420–427. https://doi.org/10.1007/s12471-015-0708-3 (2015).
Article CAS PubMed PubMed Central Google Scholar
Brennan, L., Watson, M., Klaber, R. & Charles, T. The importance of knowing context of hospital episode statistics when reconfiguring the NHS. BMJ Br. Med. J. 344 , e2432. https://doi.org/10.1136/bmj.e2432 (2012).
Fawcett, N. et al. ‘Caveat emptor’: The cautionary tale of endocarditis and the potential pitfalls of clinical coding data—An electronic health records study. BMC Med. 17 , 169. https://doi.org/10.1186/s12916-019-1390-x (2019).
Hogan, W. R. & Wagner, M. M. Accuracy of data in computer-based patient records. J. Am. Med. Inform. Assoc. 4 , 342–355. https://doi.org/10.1136/jamia.1997.0040342 (1997).
Skyttberg, N., Chen, R., Blomqvist, H. & Koch, S. Exploring vital sign data quality in electronic health records with focus on emergency care warning scores. Appl. Clin. Inform. 08 , 880–892. https://doi.org/10.4338/aci-2017-05-ra-0075 (2017).
Hessel, P. A. Terminal digit preference in blood pressure measurements: Effects on epidemiological associations. Int. J. Epidemiol. 15 , 122–125. https://doi.org/10.1093/ije/15.1.122 (1986).
Article CAS PubMed Google Scholar
Nietert, P. J., Wessell, A. M., Feifer, C. & Ornstein, S. M. Effect of terminal digit preference on blood pressure measurement and treatment in primary care. Am. J. Hypertens. 19 , 147–152. https://doi.org/10.1016/j.amjhyper.2005.08.016 (2006).
Wingfield, D., Freeman, G. K., Bulpitt, C. J., GPHSG. Selective recording in blood pressure readings may increase subsequent mortality. QJM Int. J. Med. 95 , 571–577. https://doi.org/10.1093/qjmed/95.9.571 (2002).
Article CAS Google Scholar
Hense, H. W., Kuulasmaa, K., Zaborskis, A., Kupsc, W. & Tuomilehto, J. Quality assessment of blood pressure measurements in epidemiological surveys. The impact of last digit preference and the proportions of identical duplicate measurements. WHO Monica Project [corrected]. Revue D’épidémiologie Et De Santé Publique 38 , 463–468 (1990).
CAS PubMed Google Scholar
Badawy, J., Nguyen, O. K., Clark, C., Halm, E. A. & Makam, A. N. Is everyone really breathing 20 times a minute? Assessing epidemiology and variation in recorded respiratory rate in hospitalised adults. BMJ Qual. Saf. 26 , 832. https://doi.org/10.1136/bmjqs-2017-006671 (2017).
Granholm, A., Pedersen, N. E., Lippert, A., Petersen, L. F. & Rasmussen, L. S. Respiratory rates measured by a standardised clinical approach, ward staff, and a wireless device. Acta Anaesth. Scand. 60 , 1444–1452. https://doi.org/10.1111/aas.12784 (2016).
Beaman J, Grenier M. Statistical tests and measures for the presence and influence of digit preference. https://www.srs.fs.usda.gov/pubs/17075 . (Accessed 2 December 2022) (1998).
Eilers, P. H. C. & Borgdorff, M. W. Modeling and correction of digit preference in tuberculin surveys. Int. J. Tuberc. Lung Dis. Off. J. Int. Union Against Tuberc. Lung Dis. 8 , 232–239 (2004).
CAS Google Scholar
Camarda, C. G., Eilers, P. H. C. & Gampe, J. Modelling general patterns of digit preference. Stat. Model. 8 , 385–401. https://doi.org/10.1177/1471082x0800800404 (2008).
Article MathSciNet MATH Google Scholar
Camarda, C. G., Eilers, P. H. C. & Gampe, J. Modelling trends in digit preference patterns. J. R. Stat. Soc. Ser. C Appl. Stat. 66 , 893–918. https://doi.org/10.1111/rssc.12205 (2017).
Article MathSciNet Google Scholar
Churpek, M. M., Snyder, A., Twu, N. M. & Edelson, D. P. Accuracy comparisons between manual and automated respiratory rate for detecting clinical deterioration in ward patients. J. Hosp. Med. 13 , 486–487. https://doi.org/10.12788/jhm.2914 (2018).
Kellett, J., Li, M., Rasool, S., Green, G. C. & Seely, A. Comparison of the heart and breathing rate of acutely ill medical patients recorded by nursing staff with those measured over 5min by a piezoelectric belt and ECG monitor at the time of admission to hospital. Resuscitation 82 , 1381–1386. https://doi.org/10.1016/j.resuscitation.2011.07.013 (2011).
Clifton, D. A. et al. ‘Errors’ and omissions in paper-based early warning scores: The association with changes in vital signs—A database analysis. Bmj Open 5 , e007376. https://doi.org/10.1136/bmjopen-2014-007376 (2015).
Reader, T. W. & Gillespie, A. Patient neglect in healthcare institutions: A systematic review and conceptual model. BMC Health Serv. Res. 13 , 156. https://doi.org/10.1186/1472-6963-13-156 (2013).
Kostakis, I. et al. The performance of the National Early Warning Score and National Early Warning Score 2 in hospitalised patients infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Resuscitation 159 , 150–157. https://doi.org/10.1016/j.resuscitation.2020.10.039 (2021).
Download references
Acknowledgements
This work uses data provided by patients and collected by the UK’s National Health Service as part of their care and support. We thank all the people of Oxfordshire who contribute to the Infections in Oxfordshire Research Database. Research Database Team: L Butcher, H Boseley, C Crichton, DW Crook, DW Eyre, O Freeman, J Gearing (community), R Harrington, K Jeffery, M Landray, A Pal, TEA Peto, TP Quan, J Robinson (community), J Sellors, B Shine, AS Walker, D Waller. Patient and Public Panel: G Blower, C Mancey, P McLoughlin, B Nichols.
This work was supported by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Healthcare Associated Infections and Antimicrobial Resistance at Oxford University in partnership with the UK Health Security Agency, and the NIHR Biomedical Research Centre, Oxford. DWE is a Big Data Institute Robertson Fellow. ASW is an NIHR Senior Investigator. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, the Department of Health or the UK Health Security Agency. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Oxford University Hospitals NHS Foundation Trust, Oxford, UK
Niall Jackson & Andrew Brent
N Family Club, London, UK
Jessica Woods
Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, UK
Peter Watkinson & Andrew Brent
Nuffield Department of Medicine, University of Oxford, Oxford, UK
Tim E. A. Peto & A. Sarah Walker
NIHR Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance, University of Oxford, Oxford, UK
Tim E. A. Peto, A. Sarah Walker & David W. Eyre
Big Data Institute, Nuffield Department of Population Health, University of Oxford, Old Road Campus, Oxford, OX3 7LF, UK
David W. Eyre
You can also search for this author in PubMed Google Scholar
Contributions
D.W.E., P.W., A.B., T.E.A.P. and A.S.W. designed the study. D.W.E., N.J. and J.W. analysed the data. D.W.E. and N.J. wrote the manuscript and prepared the figures and tables. All authors reviewed the manuscript.
Corresponding author
Correspondence to David W. Eyre .
Ethics declarations
Competing interests.
DWE declares lecture fees from Gilead outside the submitted work. No other author has a conflict of interest to declare.

Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Jackson, N., Woods, J., Watkinson, P. et al. The quality of vital signs measurements and value preferences in electronic medical records varies by hospital, specialty, and patient demographics. Sci Rep 13 , 3858 (2023). https://doi.org/10.1038/s41598-023-30691-z
Download citation
Received : 02 December 2022
Accepted : 28 February 2023
Published : 08 March 2023
DOI : https://doi.org/10.1038/s41598-023-30691-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Chapter 6: Knowledge Integration
Case Study 1: Adult Client (continued)
1. What infection control measures should the healthcare provider implement? Use correct handwashing techniques before and after your assessment.
2. What method should be used to measure temperature for this adult client? Temperature is best taken using the tympanic or axillary route; because the client is nauseated, the oral route could stimulate the gag reflex.
3. What pulse and blood pressure readings should be taken for this adult client? Orthostatic vital signs (pulse and blood pressure) should be taken because this client is at risk for hypovolemia. The client may be dehydrated as a result of the vomiting and diarrhea and lack of fluid intake. Return to the chapter on blood pressure for more information on hypovolemia and its effects on vital signs.
Next, see and read the vital sign record below. On a piece of paper, write down each of the client’s vital sign readings, and if applicable, the route used and the client’s position.
Vital Sign Measurement Across the Lifespan - 1st Canadian edition Copyright © 2018 by Ryerson University is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Continuous vital signs monitoring with a wireless device on a general ward: a survey to explore nurses’ experiences in a post-implementation period.

1. Introduction
2. materials and methods, 2.1. participants, 2.2. the device and implementation, 2.3. data collection, 2.4. data analysis, 2.5. data presentation, 3.1. theme 1: timely signalling and early action, 3.2. theme 2: time savings and time consumption.
In the day and evening shift, it does give you some gain, but usually only 5–10 min because it almost never happens that all three to six are functioning. In the evening shift, maybe sometimes a little more time gain, because you have more patients there and especially when they all function. On the night shift, the morning round, it certainly saves a lot of time. But also only when they are functioning; otherwise, you still have to calibrate them or manually measure the controls. (Respondent 18)
3.3. Theme 3: Patient Comfort and Satisfaction
3.4. theme 4: preconditions, 3.4.1. device design and technical concerns, 3.4.2. vital signs’ reliability, 3.4.3. internet connectivity, 3.4.4. nurses’ knowledge and training, 3.4.5. logistics, 4. discussion, limitations, 5. conclusions, relevance to clinical practice, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest, appendix a. checklist for reporting of survey studies (cross) [ 31 ].
| Section/Topic | Item | Item Description | Reported on Page # |
|---|---|---|---|
| Title and abstract | 1a | State the word “survey” along with a commonly used term in title or abstract to introduce the study’s design. | #1 |
| 1b | Provide an informative summary in the abstract, covering background, objectives, methods, findings/results, interpretation/discussion, and conclusions. | #1 | |
| Background | 2 | Provide a background about the rationale of study, what has been previously done, and why this survey is needed. | #1–3 |
| Purpose/aim | 3 | Identify specific purposes, aims, goals, or objectives of the study. | #2–3 |
| Study design | 4 | Specify the study design in the methods section with a commonly used term (e.g., cross-sectional or longitudinal). | #3 |
| Data collection methods | 5a | Describe the questionnaire (e.g., number of sections, number of questions, number and names of instruments used). | #4–5 + |
| 5b | Describe all questionnaire instruments that were used in the survey to measure particular concepts. Report target population, reported validity and reliability information, scoring/classification procedure, and reference links (if any). | N/A | |
| 5c | Provide information on pretesting of the questionnaire, if performed (in the article or in an online supplement). Report the method of pretesting, number of times questionnaire was pre-tested, number and demographics of participants used for pretesting, and the level of similarity of demographics between pre-testing participants and sample population. | #4–5 | |
| 5d | Questionnaire if possible, should be fully provided (in the article, or as appendices or as an online supplement). | ||
| Sample characteristics | 6a | Describe the study population (i.e., background, locations, eligibility criteria for participant inclusion in survey, exclusion criteria). | #3 |
| 6b | Describe the sampling techniques used (e.g., single stage or multistage sampling, simple random sampling, stratified sampling, cluster sampling, convenience sampling). Specify the locations of sample participants whenever clustered sampling was applied. | #3 | |
| 6c | Provide information on sample size, along with details of sample size calculation. | #3–4 + N/A | |
| 6d | Describe how representative the sample is of the study population (or target population if possible), particularly for population-based surveys. | N/A | |
| Survey administration | 7a | Provide information on modes of questionnaire administration, including the type and number of contacts, the location where the survey was conducted (e.g., outpatient room or by use of online tools, such as SurveyMonkey). | #4–5 |
| 7b | Provide information of survey’s time frame, such as periods of recruitment, exposure, and follow-up days. | #4–5 | |
| 7c | Provide information on the entry process: | ||
| N/A | |||
| #5 | |||
| Study preparation | 8 | Describe any preparation process before conducting the survey (e.g., interviewers’ training process, advertising the survey). | #4–5 |
| Ethical considerations | 9a | Provide information on ethical approval for the survey if obtained, including informed consent, institutional review board [IRB] approval, Helsinki declaration, and good clinical practice [GCP] declaration (as appropriate). | #3 |
| 9b | Provide information about survey anonymity and confidentiality and describe what mechanisms were used to protect unauthorized access. | #3 | |
| Statistical analysis | 10a | Describe statistical methods and analytical approach. Report the statistical software that was used for data analysis. | #5 |
| 10b | Report any modification of variables used in the analysis, along with reference (if available). | N/A | |
| 10c | Report details about how missing data was handled. Include rate of missing items, missing data mechanism (i.e., missing completely at random [MCAR], missing at random [MAR] or missing not at random [MNAR]) and methods used to deal with missing data (e.g., multiple imputation). | #5 | |
| 10d | State how non-response error was addressed. | N/A | |
| 10e | For longitudinal surveys, state how loss to follow-up was addressed. | N/A | |
| 10f | Indicate whether any methods such as weighting of items or propensity scores have been used to adjust for non-representativeness of the sample. | N/A | |
| 10g | Describe any sensitivity analysis conducted. | N/A | |
| Respondent characteristics | 11a | Report numbers of individuals at each stage of the study. Consider using a flow diagram, if possible. | #5 ( ) |
| 11b | Provide reasons for non-participation at each stage, if possible. | N/A | |
| 11c | Report response rate, present the definition of response rate or the formula used to calculate response rate. | #5 | |
| 11d | Provide information to define how unique visitors are determined. Report number of unique visitors along with relevant proportions (e.g., view proportion, participation proportion, completion proportion). | N/A | |
| Descriptive results | 12 | Provide characteristics of study participants, as well as information on potential confounders and assessed outcomes. | #5–6 |
| Main findings | 13a | Give unadjusted estimates and, if applicable, confounder-adjusted estimates along with 95% confidence intervals and p-values. | N/A |
| 13b | For multivariable analysis, provide information on the model building process, model fit statistics, and model assumptions (as appropriate). | N/A | |
| 13c | Provide details about any sensitivity analysis performed. If there are considerable amount of missing data, report sensitivity analyses comparing the results of complete cases with that of the imputed dataset (if possible). | N/A | |
| Limitations | 14 | Discuss the limitations of the study, considering sources of potential biases and imprecisions, such as non-representativeness of sample, study design, important uncontrolled confounders. | #12 |
| Interpretations | 15 | Give a cautious overall interpretation of results, based on potential biases and imprecisions and suggest areas for future research. | #10–12 |
| Generalizability | 16 | Discuss the external validity of the results. | #12 |
| Role of funding source | 17 | State whether any funding organization has had any roles in the survey’s design, implementation, and analysis. | #13 |
| Conflict of interest | 18 | Declare any potential conflict of interest. | #13 |
| Acknowledgements | 19 | Provide names of organizations/persons that are acknowledged along with their contribution to the research. | #13 |
Appendix B. Working with ViSi Mobile
Appendix c. the survey.
- I see a future in continuously monitoring patients’ vital signs in a general ward independently of the ViSi Mobile device *.
- Explain why you do or do not see a future in continuously monitoring patients’ vital signs.
- If ViSi Mobile is fully functional, I find the device to be of added value *.
- Explain this answer.
- I consider ViSi Mobile to be a user-friendly device *.
- If you find ViSi Mobile a less user-friendly device, explain why.
- If ViSi Mobile is fully functional, the main benefits are (give a maximum of three benefits).
- If ViSi Mobile does not function properly, it is often due to (give a maximum of three answers).
- ViSi Mobile functions for me in …% of cases (please give an estimation between 0% and 100%).
- Give an explanation, if possible.
- Does ViSi Mobile save time compared to MEWS checks (intermittent monitoring) during the day, evening and night shifts per patient? Select the response that applies to you per shift to give a total of three answers. MEWS = Modified Early Warning Score.
- If the answer is no, indicate how much more time you spend on average per patient, per shift, compared to your previous situation.
- ViSi Mobile supplies are kept in an appropriate location on the ward *.
- Indicate what you would like to see change on the ward concerning stock and location.
- On what topics would you like to receive further training?
- How would you like to receive this continuing education?
- What do you consider the main areas of improvement that should be prioritised regarding ViSi Mobile (give a maximum of three answers)?
Appendix D. Figures for Closed Questions 6 and 9
Click here to enlarge figure
Appendix E. Relevance to Clinical Practice
Appendix f. impact statement.
- Nurses are positive towards using remote wireless technology to monitor vital signs continuously because it enables them to detect and react to clinical deterioration in patients early. It also enhances patient safety compared to intermittent monitoring.
- Wireless technology for continuously monitoring vital signs affects nursing care. It consumes time during day shifts and saves time during evening and night shifts.
- Contrary to expectations, nurses do not mention less contact with patients. These findings challenge thinking about if and how wireless technology for continuously monitoring of vital signs optimises fundamental nursing care delivery, which could influence nurse-sensitive outcomes and ‘care left undone’.
- Zhang, W.; Barriball, K.L.; While, A.E. Nurses’ attitudes towards medical devices in healthcare delivery: A systematic review. J. Clin. Nurs. 2014 , 23 , 2725–2739. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cardona-Morrell, M.; Prgomet, M.; Turner, R.M.; Nicholson, M.; Hillman, K. Effectiveness of continuous or intermittent vital signs monitoring in preventing adverse events on general wards: A systematic review and meta-analysis. Int. J. Clin. Pract. 2016 , 70 , 806–824. [ Google Scholar ] [ CrossRef ]
- Prgomet, M.; Cardona-Morrell, M.; Nicholson, M.; Lake, R.; Long, J.; Westbrook, J.; Braithwaite, J.; Hillman, K. Vital signs monitoring on general wards: Clinical staff perceptions of current practices and the planned introduction of continuous monitoring technology. Int. J. Qual. Health Care 2016 , 28 , 515–521. [ Google Scholar ] [ CrossRef ]
- Subbe, C.P.; Duller, B.; Bellomo, R. Effect of an automated notification system for deteriorating ward patients on clinical outcomes. Crit. Care 2017 , 21 , 1–9. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Downey, C.; Randell, R.; Brown, J.; Jayne, D.G. Continuous Versus Intermittent Vital Signs Monitoring Using a Wearable, Wireless Patch in Patients Admitted to Surgical Wards: Pilot Cluster Randomized Controlled Trial. J. Med. Internet Res. 2018 , 20 , e10802. [ Google Scholar ] [ CrossRef ]
- Eddahchouri, Y.; Peelen, R.V.; Koeneman, M.; Touw, H.R.W.; van Goor, H.; Bredie, S.J.H. Effect of continuous wireless vital sign monitoring on unplanned ICU admissions and rapid response team calls: A before-and-after study. Br. J. Anaesth. 2022 , 128 , 857–863. [ Google Scholar ] [ CrossRef ]
- Kitson, A.; Carr, D.; Conroy, T.; Feo, R.; Gronkjaer, M.; Huisman-de Waal, G.; Jackson, D.; Jeffs, L.; Merkley, J.; Muntlin Athlin, A.; et al. Speaking Up for Fundamental Care: The ILC Aalborg Statement. BMJ Open 2019 , 9 , e033077. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Considine, J.; Currey, J. Ensuring a proactive, evidence-based, patient safety approach to patient assessment. J. Clin. Nurs. 2015 , 24 , 300–307. [ Google Scholar ] [ CrossRef ]
- Downey, C.L.; Brown, J.M.; Jayne, D.G.; Randell, R. Patient attitudes towards remote continuous vital signs monitoring on general surgery wards: An interview study. Int. J. Med. Inform. 2018 , 114 , 52–56. [ Google Scholar ] [ CrossRef ]
- Douw, G.; Huisman-de Waal, G.; van Zanten, A.R.H.; van der Hoeven, J.G.; Schoonhoven, L. Surgical ward nurses’ responses to worry: An observational descriptive study. Int. J. Nurs. Stud. 2018 , 85 , 90–95. [ Google Scholar ] [ CrossRef ]
- Weenk, M.; Bredie, S.J.; Koeneman, M.; Hesselink, G.; van Goor, H.; van de Belt, T.H. Continuous Monitoring of Vital Signs in the General Ward Using Wearable Devices: Randomized Controlled Trial. J. Med. Internet Res. 2020 , 22 , e15471. [ Google Scholar ] [ CrossRef ]
- Douw, G. General Discussion. Just Worry, Exploring Triggers Used by Nurses to Identify Surgical Patients at Risk for Clinical Deterioration. Ph.D. Thesis, Radboud Universiteit Nijmegen, Nijmegen, The Netherlands, October 2018. [ Google Scholar ]
- Schoville, R.R.; Titler, M.G. Guiding healthcare technology implementation: A new integrated technology implementation model. Comput. Inform. Nurs. 2015 , 33 , 99–107. [ Google Scholar ] [ CrossRef ]
- Holden, R.J.; Karsh, B.-T. The technology acceptance model: Its past and its future in health care. J. Biomed. Inform. 2010 , 43 , 159–172. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Simon, S.R.; Kaushal, R.; Cleary, P.D.; Jenter, C.A.; Volk, L.A.; Orav, E.J.; Burdick, E.; Poon, E.G.; Bates, D.W. Physicians and electronic health records: A statewide survey. Arch. Intern. Med. 2007 , 167 , 507–512. [ Google Scholar ] [ CrossRef ]
- Downey, C.L.; Chapman, S.; Randell, R.; Brown, J.M.; Jayne, D.G. The impact of continuous versus intermittent vital signs monitoring in hospitals: A systematic review and narrative synthesis. Int. J. Nurs. Stud. 2018 , 84 , 19–27. [ Google Scholar ] [ CrossRef ]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User Acceptance of Computer Technology: A Comparison of Two Theoretical Models. Manag. Sci. 1989 , 35 , 982–1003. [ Google Scholar ] [ CrossRef ]
- Cadmus, E.; Brigley, P.; Pearson, M. Safe patient handling: Is your facility ready for a culture change? Nurs. Manag. 2011 , 42 , 12–15. [ Google Scholar ] [ CrossRef ]
- Stellpflug, C.; Pierson, L.; Roloff, D.; Mosman, E.; Gross, T.; Marsh, S.; Willis, V.; Gabrielson, D. Continuous Physiological Monitoring Improves Patient Outcomes. Am. J. Nurs. 2021 , 121 , 40–46. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jeskey, M.; Card, E.; Nelson, D.; Mercaldo, N.D.; Sanders, N.; Higgins, M.S.; Shi, Y.; Michaels, D.; Miller, A. Nurse adoption of continuous patient monitoring on acute post-surgical units: Managing technology implementation. J. Nurs. Manag. 2011 , 19 , 863–875. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bergmann, J.H.; McGregor, A.H. Body-worn sensor design: What do patients and clinicians want? Ann. Biomed. Eng. 2011 , 39 , 2299–2312. [ Google Scholar ] [ CrossRef ]
- Jeffs, E.; Vollam, S.; Young, J.D.; Horsington, L.; Lynch, B.; Watkinson, P.J. Wearable monitors for patients following discharge from an intensive care unit: Practical lessons learnt from an observational study. J. Adv. Nurs. 2016 , 72 , 1851–1862. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- de Veer, A.J.; Fleuren, M.A.; Bekkema, N.; Francke, A.L. Successful implementation of new technologies in nursing care: A questionnaire survey of nurse-users. BMC Med. Inform. Decis. Mak. 2011 , 11 , 67. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Watkins, T.; Whisman, L.; Booker, P. Nursing assessment of continuous vital sign surveillance to improve patient safety on the medical/surgical unit. J. Clin. Nurs. 2016 , 25 , 278–281. [ Google Scholar ] [ CrossRef ]
- Rouleau, G.; Gagnon, M.P.; Côté, J.; Payne-Gagnon, J.; Hudson, E.; Dubois, C.A. Impact of Information and Communication Technologies on Nursing Care: Results of an Overview of Systematic Reviews. J. Med. Internet Res. 2017 , 19 , e122. [ Google Scholar ] [ CrossRef ]
- Sprogis, S.K.; Currey, J.; Considine, J. Patient acceptability of wearable vital sign monitoring technologies in the acute care setting: A systematic review. J. Clin. Nurs. 2019 , 28 , 2732–2744. [ Google Scholar ] [ CrossRef ]
- Dall’Ora, C.; Griffiths, P.; Hope, J.; Barker, H.; Smith, G.B. What is the nursing time and workload involved in taking and recording patients’ vital signs? A systematic review. J. Clin. Nurs. 2020 , 29 , 2053–2068. [ Google Scholar ] [ CrossRef ]
- Leenen, J.P.L.; Dijkman, E.M.; van Hout, A.; Kalkman, C.J.; Schoonhoven, L.; Patijn, G.A. Nurses’ experiences with continuous vital sign monitoring on the general surgical ward: A qualitative study based on the Behaviour Change Wheel. BMC Nurs. 2022 , 21 , 60. [ Google Scholar ] [ CrossRef ]
- Sotera Wireless. ViSi Mobile System General Information. Available online: https://www.soterawireless.com/faqs (accessed on 27 July 2021).
- World Medical Association. WMA Declaration of Helsinki–Ethical Principles for Medical Research Involving HUMAN subjects ; WMA: Ferney-Voltaire, France, 2018. [ Google Scholar ]
- Sharma, A.; Minh Duc, N.T.; Luu Lam Thang, T.; Nam, N.H.; Ng, S.J.; Abbas, K.S.; Huy, N.T.; Marušić, A.; Paul, C.L.; Kwok, J.; et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J. Gen. Intern. Med. 2021 , 36 , 3179–3187. [ Google Scholar ] [ CrossRef ]
- Leenen, J.P.L.; Leerentveld, C.; van Dijk, J.D.; van Westreenen, H.L.; Schoonhoven, L.; Patijn, G.A. Current Evidence for Continuous Vital Signs Monitoring by Wearable Wireless Devices in Hospitalized Adults: Systematic Review. J. Med. Internet Res. 2020 , 22 , e18636. [ Google Scholar ] [ CrossRef ]
- Weenk, M.; van Goor, H.; Frietman, B.; Engelen, L.J.; van Laarhoven, C.J.; Smit, J.; Bredie, S.J.; van de Belt, T.H. Continuous Monitoring of Vital Signs Using Wearable Devices on the General Ward: Pilot Study. JMIR mHealth uHealth 2017 , 5 , e91. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Schoot, T.S.; Weenk, M.; van de Belt, T.H.; Engelen, L.J.; van Goor, H.; Bredie, S.J. A New Cuffless Device for Measuring Blood Pressure: A Real-Life Validation Study. J. Med. Internet. Res. 2016 , 18 , e85. [ Google Scholar ] [ CrossRef ]
- Haahr-Raunkjaer, C.; Skovbye, M.; Rasmussen, S.M.; Elvekjaer, M.; Sørensen, H.B.D.; Meyhoff, C.S.; Aasvang, E.K. Agreement between standard and continuous wireless vital sign measurements after major abdominal surgery: A clinical comparison study. Physiol. Meas. 2022 , 43 , 115007. [ Google Scholar ] [ CrossRef ]
- Soller, B.; McCombie, D.; Kanter, B. A Blood Pressure Study Demonstrating Equivalence of the ViSi Mobile® System and GE DINAMAP™ CARESCAPE™ V100. 2015. Available online: https://cdn2.hubspot.net/hubfs/5599582/SoteraWireless-April2020/PDF/White-Paper-ViSi-Mobile-and-GE-Dinamap-Carescape-White-Paper-3.pdf?hsCtaTracking=69d7ffd3-0839-4199-87b5-8637d3bf6196%7Ce347d48c-2f99-4db4-ada4-e17a1d32cc1f (accessed on 18 January 2023).
- Nayak, M.S.D.P.; Narayan, K. Strengths and weaknesses of online surveys. IOSR-JHSS 2019 , 24 , 31–38. [ Google Scholar ]
- Williams, M.; Moser, T. The art of coding and thematic exploration in qualitative research. Int. Manag. Rev. 2019 , 15 , 45–55. [ Google Scholar ]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006 , 3 , 77–101. [ Google Scholar ] [ CrossRef ]
- Proot, I.; Van der Lyke, S.; Smits, M. Qualitative research [Kwalitatief onderzoek]. In Evidence-Based Practice for Nurses: Shared Decision-Making [Evidence-Based Practice Voor Verpleegkundigen: Gezamenlijke Geïnformeerde Besluitvorming] , 4th ed.; Munten, G., Verhoef, J., Kuiper, C., Eds.; Boom: Amsterdam, The Netherlands, 2016; pp. 191–208. [ Google Scholar ]
- Zwieten, M.; Willems, D. Valuation of qualitative research [Waardering van kwalitatief onderzoek]. Huisarts Wet. 2004 , 47 , 38–43. [ Google Scholar ] [ CrossRef ]
- Gagnon, M.P.; Desmartis, M.; Labrecque, M.; Car, J.; Pagliari, C.; Pluye, P.; Fremont, P.; Gagnon, J.; Tremblay, N.; Legare, F. Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. J. Med. Syst. 2012 , 36 , 241–277. [ Google Scholar ] [ CrossRef ]
- Schoville, R.; Titler, M.G. Integrated Technology Implementation Model: Examination and Enhancements. Comput. Inform. Nurs. 2020 , 38 , 579–589. [ Google Scholar ] [ CrossRef ]
- Areia, C.; King, E.; Ede, J.; Young, L.; Tarassenko, L.; Watkinson, P.; Vollam, S. Experiences of current vital signs monitoring practices and views of wearable monitoring: A qualitative study in patients and nurses. J. Adv. Nurs. 2021 , 78 , 810–822. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brown, J.; Pope, N.; Bosco, A.M.; Mason, J.; Morgan, A. Issues affecting nurses’ capability to use digital technology at work: An integrative review. J. Clin. Nurs. 2020 , 29 , 2801–2819. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health ; National Academies Press: Washington, DC, USA, 2011. [ Google Scholar ] [ CrossRef ]
- Hamerlijnck, D.; Tummers, M.; Kvaerner, K.; Sampietro-Colom, L.; Siebert, M.; Krahn, M.; Melien, O.; Abrishami, P.; Grutters, J. On the integration of early health technology assessment in the innovation process: Reflections from five stakeholders. Int. J. Technol. Assess. Health Care 2020 , 36 , 481–485. [ Google Scholar ] [ CrossRef ]
- Downey, C.L.; Tahir, W.; Randell, R.; Brown, J.M.; Jayne, D.G. Strengths and limitations of early warning scores: A systematic review and narrative synthesis. Int. J. Nurs. Stud. 2017 , 76 , 106–119. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- van der Weegen, S.; Galle, I. Implementation Toolkit TECHNOLOGY in Healthcare [Implementatie Toolkit Technologie in de zorg]; Vilans: Utrecht, The Netherlands. Available online: https://www.waardigheidentrots.nl/wp-content/uploads/2017/12/Implementatie-toolkit-technologie-definitief.pdf (accessed on 18 January 2023).
- Kooij, L.; Peters, G.M.; Doggen, C.J.M.; van Harten, W.H. Remote continuous monitoring with wireless wearable sensors in clinical practice, nurses perspectives on factors affecting implementation: A qualitative study. BMC Nurs. 2022 , 21 , 53. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- De Leeuw, J.A.; Woltjer, H.; Kool, R.B. Identification of Factors Influencing the Adoption of Health Information Technology by Nurses Who Are Digitally Lagging: In-Depth Interview Study. J. Med. Internet Res. 2020 , 22 , e15630. [ Google Scholar ] [ CrossRef ]
- Khanna, A.K.; Hoppe, P.; Saugel, B. Automated continuous noninvasive ward monitoring: Future directions and challenges. Crit. Care 2019 , 23 , 194. [ Google Scholar ] [ CrossRef ]
- Vears, D.F.; Gillam, L. Inductive content analysis: A guide for beginning qualitative researchers. FoHPE 2022 , 23 , 111–127. Available online: https://search.informit.org/doi/10.3316/informit.455663644555599 (accessed on 18 January 2023). [ CrossRef ]
- Al-rawashdeh, M.; Keikhosrokiani, P.; Belaton, B.; Alawida, M.; Zwiri, A. IoT Adoption and Application for Smart Healthcare: A Systematic Review. Sensors 2022 , 22 , 5377. [ Google Scholar ] [ CrossRef ]
- Dwivedi, Y.K.; Rana, N.P.; Tamilmani, K.; Raman, R. A meta-analysis based modified unified theory of acceptance and use of technology (meta-UTAUT): A review of emerging literature. Curr. Opin. Psychol. 2020 , 36 , 13–18. [ Google Scholar ] [ CrossRef ]
- Dwivedi, Y.K.; Rana, N.P.; Jeyaraj, A.; Clement, M.; Williams, M.D. Re-examining the Unified Theory of Acceptance and Use of Technology (UTAUT): Towards a Revised Theoretical Model. Inf. Syst. Front. 2019 , 21 , 719–734. [ Google Scholar ] [ CrossRef ]
- Banks, J.; McArthur, J.; Gordon, G. Flexible monitoring in the management of patient care processes: A pilot study. Lippincotts Case Manag. 2000 , 5 , 94–103, quiz 104–106. [ Google Scholar ]
- Haddad, L.M.; Annamaraju, P.; Toney-Butler, T.J. Nursing Shortage ; StatPearls: Treasure Island, FL, USA, 2023. [ Google Scholar ]
- Subbe, C.P.; Kruger, M.; Rutherford, P.; Gemmel, L. Validation of a modified Early Warning Score in medical admissions. QJM 2001 , 94 , 521–526. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sotera Wireless. Patient Monitoring System. User Manual ; Sotera Wireless: San Diego, CA, USA, 2016; pp. 1–292. [ Google Scholar ]
| Respondents n = 58 (%) | Non-Respondents n = 53 (%) | |
|---|---|---|
| Gender | ||
| Male (%) | 9 (15.5) | 8 (15.1) |
| Female (%) | 49 (84.5) | 45 (84.9) |
| Education | ||
| Vocational educated nurse (%) | 12 (20.7) | 25 (47.2) |
| Registered nurse (%) | 46 (79.3) | 28 (52.8) |
| Ward | ||
| Abdominal/oncological surgery (%) | 22 (37.9) | 18 (34.0) |
| Internal medicine/rheumatology (%) | 27 (46.6) | 25 (47.2) |
| Gastroenterology (%) | 9 (15.5) | 10 (18.9) |
| Age group | ||
| 21–30 years (%) | 42 (72.4) | 26 (49.1) |
| 31–40 years (%) | 10 (17.2) | 9 (17.0) |
| 41–50 years (%) | 3 (5.2) | 8 (15.1) |
| 51–60 years (%) | 3 (5.2) | 7 (13.2) |
| 61–64 years (%) | 0 (0) | 3 (5.7) |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Becking-Verhaar, F.L.; Verweij, R.P.H.; de Vries, M.; Vermeulen, H.; van Goor, H.; Huisman-de Waal, G.J. Continuous Vital Signs Monitoring with a Wireless Device on a General Ward: A Survey to Explore Nurses’ Experiences in a Post-Implementation Period. Int. J. Environ. Res. Public Health 2023 , 20 , 5794. https://doi.org/10.3390/ijerph20105794
Becking-Verhaar FL, Verweij RPH, de Vries M, Vermeulen H, van Goor H, Huisman-de Waal GJ. Continuous Vital Signs Monitoring with a Wireless Device on a General Ward: A Survey to Explore Nurses’ Experiences in a Post-Implementation Period. International Journal of Environmental Research and Public Health . 2023; 20(10):5794. https://doi.org/10.3390/ijerph20105794
Becking-Verhaar, Femke L., Robin P. H. Verweij, Marjan de Vries, Hester Vermeulen, Harry van Goor, and Getty J. Huisman-de Waal. 2023. "Continuous Vital Signs Monitoring with a Wireless Device on a General Ward: A Survey to Explore Nurses’ Experiences in a Post-Implementation Period" International Journal of Environmental Research and Public Health 20, no. 10: 5794. https://doi.org/10.3390/ijerph20105794
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Case Study: Continuous Monitoring of Patient Vital Signs to Reduce 'Failure-to-Rescue' Events
- PMID: 28103094
- DOI: 10.2345/0899-8205-51.1.41
PubMed Disclaimer
Similar articles
- Adaptive threshold-based alarm strategies for continuous vital signs monitoring. van Rossum MC, Vlaskamp LB, Posthuma LM, Visscher MJ, Breteler MJM, Hermens HJ, Kalkman CJ, Preckel B. van Rossum MC, et al. J Clin Monit Comput. 2022 Apr;36(2):407-417. doi: 10.1007/s10877-021-00666-4. Epub 2021 Feb 11. J Clin Monit Comput. 2022. PMID: 33575922 Free PMC article.
- Beyond 'failure to rescue': the time has come for continuous ward monitoring. Sessler DI, Saugel B. Sessler DI, et al. Br J Anaesth. 2019 Mar;122(3):304-306. doi: 10.1016/j.bja.2018.12.003. Epub 2019 Jan 3. Br J Anaesth. 2019. PMID: 30770047 No abstract available.
- The Afferent Limb of Rapid Response Systems: Continuous Monitoring on General Care Units. Taenzer AH, Spence BC. Taenzer AH, et al. Crit Care Clin. 2018 Apr;34(2):189-198. doi: 10.1016/j.ccc.2017.12.001. Epub 2018 Jan 8. Crit Care Clin. 2018. PMID: 29482899 Review.
- Make vital signs great again - A call for action. Kellett J, Sebat F. Kellett J, et al. Eur J Intern Med. 2017 Nov;45:13-19. doi: 10.1016/j.ejim.2017.09.018. Epub 2017 Sep 20. Eur J Intern Med. 2017. PMID: 28941841 Review.
- Nursing assessment of continuous vital sign surveillance to improve patient safety on the medical/surgical unit. Watkins T, Whisman L, Booker P. Watkins T, et al. J Clin Nurs. 2016 Jan;25(1-2):278-81. doi: 10.1111/jocn.13102. Epub 2015 Nov 4. J Clin Nurs. 2016. PMID: 26531215 Free PMC article.
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Silverchair Information Systems
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
NTI Recorded Session NTI23299
Vital Lessons: A Case-Based Approach to Abnormal Vital Signs
Author(s): Megan Vennero
Activity Message
Get ce message.
Contact Hours 1.00
CERP A 1.00
Expires Nov 15, 2026
Topics: Monitoring
Population: Adult
Role: Staff
Add to Collection
Added to Collection
Activity Summary
Required reading for all learners: Implicit Bias impacts patient outcomes
- Describe an algorithmic approach to assessing abnormal vital signs.
- Articulate a focused differential based in part on specific vital signs.
- Apply knowledge gained in this presentation to interactive clinical case studies.
Continuing Education Disclosure Statement
Learners must attend/view/read the entire activity, read Implicit Bias impacts patient outcomes , and complete the associated evaluation to be awarded the contact hours or CERP. No partial credit will be awarded.
Accreditation
The American Association of Critical-Care Nurses is accredited as a provider of nursing continuing professional development by the American Nurses Credentialing Center's Commission on Accreditation.
Provider approved by the California Board of Registered Nursing, Provider number CEP 1036, for 1.00 contact hours.
Accreditation refers to recognition of continuing education only and does not imply AACN, ANCC, or CBRN approval or endorsement of any commercial products discussed or displayed in conjunction with this educational activity.
Any relevant relationship between an ineligible company and an individual with the ability to influence clinical content will be identified by the Nurse Planner within the activity. Any relevant relationship between an ineligible company and an individual with the ability to influence clinical content has been mitigated.
AACN programming meets the standards for most states that require mandatory continuing education contact hours for license and/or certification renewal. AACN recommends consulting with your state board of nursing or credentialing organization before submitting CE to fulfill continuing education requirements.
Continuing Education Activities are nonrefundable.
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
The Atlas of Shared Learning
Introducing bedside vital signs devices at imperial college healthcare nhs trust.
- Nursing, midwifery and care
Leading change
The Chief Nursing Information Officer (CNIO) at Imperial College Healthcare NHS Trust led the implementation of digitising the National Early Warning Score (NEWS) at the Trust, with support from nursing, midwifery and healthcare assistant colleagues. This has significantly improved patient safety and outcomes, improved staff experience, and streamlined and standardised handovers which has increased time spent caring for patients.
Where to look
NEWS is a tool developed by the Royal College of Physicians which supports practitioners to detect and respond to clinical deterioration in adult patients and is a key element of patient safety and improving patient outcomes.
The tool is based on a simple aggregate scoring system in which a score is allocated to physiological measurements already recorded in routine practice, when patients present to, or are being monitored in, hospital. Six physiological parameters form the basis of the scoring system:
- respiration rate;
- oxygen saturation;
- systolic blood pressure;
- pulse rate;
- level of consciousness or new confusion;
- temperature.
A score is allocated to each parameter as they are measured, with the magnitude of the score reflecting how the parameter varies from normal ranges. The score is then aggregated and guidance given to staff carrying out the assessment as to what actions are needed to support good patient outcomes. NHS England described how this standardised approach can reduce the number of patients whose conditions deteriorate whilst in hospital and potentially save over 1800 lives a year.
Since its initial launch in 2012, NEWS has seen widespread uptake across the NHS. At present around 70% of acute Trusts in England are using NEWS, with other Early Warning Scores in place in other areas.
The senior nursing team at Imperial College Healthcare NHS Trust identified that the existing paper-based approach to documentation of patient’s observations was varied across the Trust and a robust tool to identify deterioration which could contribute to patient safety incidents was not standardized practice – this was unwarranted variation.
What to change
Imperial College Healthcare NHS Trust provides acute and specialist healthcare in north west London. The senior nursing team completed an audit of current practice including patient case note reviews and gathering feedback from the Critical Care Outreach Team (CCOT). The results indicated that the practice of documenting patient information on paper often resulted in a fragmented approach to the recording, visibility and access of information, and ease of escalation of patients at risk of deterioration. There was a risk of transcription errors or incomplete records, paperwork was time consuming, and audits were resource intensive.
To address this unwarranted variation, the ‘Safer Care Project’ was initiated at the Trust with an aim of using digital technology to identify patients at risk of deterioration and provide optimal care to improve their outcomes and experience of care. The nurse leaders took this opportunity to implement a system that would make vital patient information more visible, support staff in decision making, establish and highlight trends and improve clinical judgements on risk and escalation.
How to change
The Chief Nursing Information Officer led an initial pilot to introduce 70 digital bedside vital signs monitors, supported by nurses and midwives providing leadership as local champions supporting decisions on areas for implementation.
Hand held devices were introduced to reduce documentation time with decision support at the bedside. Digital touch screen monitors now capture clinical observations such as blood pressure and temperature and automatically transfer it into the electronic patient record (EPR) by wireless connection. The EPR is supported by a handover page detailing a patient’s latest NEWS score that is automatically calculated, and any escalation instructions automatically on screen.
Face to face training to support staff to understand and use the equipment was rolled out across the Trust.
Following a successful two-month pilot, the digital NEWS system was further rolled out across the Trust, with 200 additional digital bedside vital signs monitors to support staff to implement the system.
Adding value
Better outcomes – Patient assessment is now standardised and information goes directly into the patient record, increasing the accuracy of information. Patient safety has been improved through earlier and consistent referral to CCOT and medical colleagues. The technology provides decision-making support for staff and alerts teams when support is needed. There has been a positive impact on handovers, through streamlining and standardising the process; there is now a real-time digital list of patients for colleagues to review and investigate individual NEWS scores.
Better experience – The NEWS system has been well received by staff, with feedback including: “In the old system it took me at times an hour and a half to take all my patients’ vital signs, but with this system it just takes me 30 minutes.”
Better use of resources – The mean time to take and record vitals has reduced from 2 minutes 35 seconds to 1 minute 12 seconds now that there is a digital solution. This is a 53.5% reduction in the time it takes to document a full set of NEWS observations. By using bedside devices, 600 hours of nursing time has been released from routine documentation and that time can be used in direct patient care. A saving of 30 hours per month of audit time has also been achieved. Together, this is projected as 323,500 hours a year across the Trust.
Challenges and lessons learnt for implementation
It is important to ensure staff are educated, trained and supported correctly from the start and understand the potential benefits. Challenges included ensuring that each time a new patient was admitted, the appropriate electronic link was made through the electronic device and that the previous encounter was not continued. Having sufficient equipment is vital.
Technology was not seen as something new, but rather as something that can support improving patient care. To implement something similar, consider the conditions of change that are needed to affect and improve patient care, better experience for staff and better outcomes for patients. Think about the leadership and what you are trying to achieve; bring staff together and involve them in using technology.
Involve the patient and show them what you are doing with the technology – it’s their clinical information. Graphs are useful, especially to show improvements.
Imperial College Healthcare NHS Trust was selected as a Global Digital Exemplar (GDE), who are internationally recognised NHS providers exceptional care, efficiently, through the use of world-class digital technology and information.
Find out more
For more information contact:
- James Bird, Chief Nursing Information Officer, Imperial College Healthcare NHS Trust, [email protected]
- Diagnostic or screening
- Hospital (acute)
- Urgent and emergency
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Vital sign assessment.
Amit Sapra ; Ahmad Malik ; Priyanka Bhandari .
Affiliations
Last Update: May 1, 2023 .
- Definition/Introduction
Vital signs are an objective measurement of the essential physiological functions of a living organism. They have the name "vital" as their measurement and assessment is the critical first step for any clinical evaluation. The first set of clinical examinations is an evaluation of the vital signs of the patient. Triage of patients in an urgent/prompt care or an emergency department is based on their vital signs as it tells the physician the degree of derangement that is happening from the baseline. Healthcare providers must understand the various physiologic and pathologic processes affecting these sets of measurements and their proper interpretation. If we use a triage method where we select patients without determining their vital signs, it may not give us a reflection of the urgency of the patient's presentation. [1] The degree of vital sign abnormalities may also predict the long-term patient health outcomes, return emergency department visits, and frequency of readmission to hospitals, and utilization of healthcare resources.
Traditionally, the vital signs consist of temperature, pulse rate, blood pressure, and respiratory rate. Even though there are a variety of parameters that may be useful along with the traditional four vital sign parameters, studies have only found pulse oximetry and smoking status to have significance in patient outcomes. [2] Pulse oximetry sometimes helps to clarify the patient's physiological functions, which would sometimes be unclear by checking just the traditional vital signs. The inclusion of smoking status has the premise that the patient will be provided counseling by the provider on quitting smoking. In the past, some health care systems in the United States had used "pain as the fifth vital sign'. This approach is being abandoned due to the unintended opioid crisis that the country is currently facing. [3]
- Issues of Concern
Patient safety is a fundamental concern in any health care organization, and early detection of any clinical deterioration is of paramount importance whether the patient is in the emergency department or on the hospital floor. The early detection of changes in vital signs typically correlates with faster detection of changes in the cardiopulmonary status of the patient as well as up-gradation of the level of service if needed. Vital signs assessment currently uses electronic equipment, but there is evidence that, outside of the intensive care units, respiratory rate assessment through observation, leading to insufficient, subjective, and unreliable results. [4]
In a case-control study conducted by Rothschild and colleagues, early warning criterion among patients on the medical floor, the presence of respiratory rate over 35/min (OR=31.1) was most strongly associated with a life-threatening adverse event. [5] Early warning score (EWS) tools, mostly using vital sign abnormalities, are critical in predicting cardiac arrest and death within 48 hours of measurement, even though the effect on in-hospital health outcomes and utilization of resources remains unknown. [5]
It seems intuitive that the higher the frequency of vital sign measurement, the faster the chances of clinical deterioration are detected. There is variability between institutes within and across nations depending on the acuity of clinical condition, any active intervention carried out, the amount of staff availability, cost issues, organizational practices, and leadership styles. The weighted average score deduced from the vital sign measurements (i.e., an early warning score) is used to determine the timing of the next observation sets. [4] [5]
- Clinical Significance
Temperature
Body temperature is a variable, which is complex as well as nonlinear and is affected by many sources of internal and external variables. The normal body temperature for a healthy adult is approximately 98.6 degrees Fahrenheit/37.0 degrees centigrade. The human body temperature typically ranges from 36.5 to 37.5 degrees centigrade (97.7 to 99.5 degrees Fahrenheit. [6] Body temperature is regulated in the hypothalamus in a narrow thermodynamic range and maintained to optimize the synaptic transmission of biochemical reactions. [7]
Clinical decisions, especially in the pediatric population regarding the investigation and management, are based on the results of temperature measurement alone. Whereas at one end, missing that the patient's fever is severe or detecting a falsely positive fever reading can cause the patient to receive wrongful management. Galileo was the first scientist to uncover the concept of thermometers that began in the 16th century. In the year, 1709 Daniel Fahrenheit developed an alcohol-filled thermometer as well as a mercury-filled thermometer. [8]
Health care providers use the axillary, rectal, oral, and tympanic membrane most commonly to record body temperature, and the devices most commonly used are the electronic and infrared thermometers. They can monitor temperature at different sites, and each site has its range as well as advantages and disadvantages. As clinicians, the understanding of these site-specific differences is crucial. For example, the oral temperature, which is the most commonly used method, is considered very convenient and reliable. Here we place the thermometer under the tongue and close the lips around it. The posterior sublingual pocket is the area that gives the highest reliability. The other commonly used methods are tympanic temperature, where the thermometer where we insert the thermometer into the ear canal, and the axillary temperature where we place the thermometer in the axilla while adducting the arm of the patient. Both these sites are convenient but generally considered less accurate and hence not recommended. [8]
For measuring the rectal temperature, the thermometer is inserted through the anus into the rectum after applying a lubricant. This method is very inconvenient, but since it measures the internal measurement, it is very reliable. It is usually considered the "gold standard" method of recording temperature. Gut temperature, measured with an ingested pill, also gives readings close to the rectal temperature. Besides the site, the time of day is an essential factor leading to variability in the temperature record, secondary to the circadian rhythm. The inability to consider this physiological diurnal variation of temperature can lead to the wrong conclusion that an individual's temperature suggests a disease state when it is a normal temperature at that time of day. There is also a variation of the body temperature in a regularly cycling female, referred to as the "circamensal" rhythm. Understanding of this rhythm is paramount in teaching patients, trying to conceive about the fertile period of the cycle. Besides the change with diurnal variation and menstrual variation, a person's relative physical fitness and age can affect the degree of temperature change during a day. Studies show that younger patients and fitter record larger temperature amplitudes, while older and less fit people record lesser amplitude changes. [9] Some studies have demonstrated a seasonal variation in body temperature; we need more research in this regard to reach a definitive conclusion. [9]
The most common sites of measuring the peripheral pulses are the radial pulse, ulnar pulse, brachial pulse in the upper extremity, and the posterior tibialis or the dorsalis pedis pulse as well as the femoral pulse in the lower extremity. Clinicians measure the carotid pulse in the neck. In day-to-day practice, the radial pulse is the most frequently used site for checking the peripheral pulse, where the pulse is palpated on the radial aspect of the forearm, just proximal to the wrist joint. Parameters for assessment of pulse include its rate, rhythm, volume, amplitude, and rate of increase, besides its symmetry The rate of the pulse is significant to measure for assessing the physiological and pathological processes affecting the body. The normal range used in an adult is between 60 to 100 beats/minute with rates above 100 beats/minute and rates below 60 beats per minute, referred to as tachycardia and bradycardia, respectively. The age-specific heart rate given for the pediatric age range appears in table -2.
Assessing whether the rhythm of the pulse is regular or irregular is essential. The pulse could be regular, irregular, or irregularly irregular. Changes in the rate of the pulse, along with changes in respiration are called sinus arrhythmia. In sinus arrhythmia, the pulse rate becomes faster during inspiration and slows down during expiration. Irregularly irregular pattern is more commonly indicative of processes like atrial flutter or atrial fibrillation. We should also be checking for the radial and the femoral pulse simultaneously. If there is any delay between the pulses, it could indicate conditions like the coarctation of the aorta. Assessing the volume of the pulse is equally essential. A low volume pulse could be indicative of inadequate tissue perfusion; this can be a crucial indicator of indirect prediction of the systolic blood pressure of the patient. If we can palpate the radial pulse, the systolic blood pressure is generally more than 80 mmHg. If we can palpate the femoral pulse, the systolic blood pressure is more than 70 mmHg, and if we can palpate the carotid pulse, the systolic blood pressure is more than 60 mmHg. [10] Checking for symmetry of the pulses is important as asymmetrical pulses could be seen in conditions like aortic dissection, aortic coarctation, Takayasu arteritis, and subclavian steal syndrome. Besides the above-stated parameters, amplitude and rate of increase is also an important consideration. Low amplitude and low rate of increase could be seen in conditions like aortic stenosis, besides weak perfusion states. High amplitude and rapid rise can be indicative of conditions like aortic regurgitation, mitral regurgitation, and hypertrophic cardiomyopathy.
Respiratory Rate
The respiratory rate is the number of breaths per minute. The normal breathing rate is about 12 to 20 breaths per minute in an average adult. In the pediatric age group, it is defined by the particular age group. Parameters important here again include rate, depth of breathing, and pattern of breathing. Rates higher or lower than expected are termed as tachypnea and bradypnea, respectively. Tachypnea is described as a respiratory rate of more than 20 breaths per minute that could occur in physiological conditions like exercise, emotional changes, or pregnancy. Pathological conditions like pain, pneumonia, pulmonary embolism, asthma, foreign body aspiration, anxiety conditions, sepsis, carbon monoxide poisoning, and diabetic ketoacidosis can also present with tachypnea. Bradypnea described as ventilation less than 12 breaths per minute can be seen due to worsening of any underlying respiratory condition leading to respiratory failure or due to usage of central nervous system depressants like alcohol, narcotics, benzodiazepines, or metabolic derangements. Apnea is the complete cessation of airflow to the lungs for a total of 15 seconds. It appears in cardiopulmonary arrests, airway obstructions, the overdose of narcotics, and benzodiazepines.
The depth of breathing is also a crucial parameter. Hyperpnea is described as an increased depth of breathing and is seen during exercise and in anxiety states, lung infections, and congestive heart failure. Hyperventilation, on the other hand, is described as both increased in the rate and depth of breathing and can again be seen in anxiety states like anxiety or due to exercise but is also seen in pathological conditions like diabetic ketoacidosis or lactic acidosis. The term hypoventilation describes the decreased rate and depth of ventilation. This condition results from excessive sedation, metabolic alkalosis, and in instances of obesity hypoventilation syndrome.
The pattern of breathing also gets affected in various conditions and indicates the underlying pathology. Biot respiration is a condition where there are periods of increased rate and depth of breathing, followed by periods of no breathing or apnea. These can vary in length of time. This pattern is suggestive of raised intracranial pressure as in space-occupying lesions of the skull or conditions like meningitis. Cheyne-Stokes respiration is a peculiar pattern of breathing where there is an increase in the depth of ventilation followed by periods of no breathing or apnea. This presentation occurs in conditions of raised intracranial pressure but is also seen with excessive usage of sedatives and worsening congestive heart failure. Kussmaul breathing refers to the increased depth of ventilation, although the rate remains regular. This presentation is in patients with renal failure and diabetic ketoacidosis. Orthopnea refers to difficulty in respiration occurring on lying horizontal but gets better when the patient sits up or stands It is seen characteristically in congestive heart failure. Paradoxical ventilation refers to the inward movement of the abdominal or chest wall during inspiration, and outward movement during expiration, which is seen in cases of diaphragmatic paralysis, muscle fatigue, and trauma to the chest wall.
Blood Pressure
Blood pressure is an essential vital sign to comprehend the hemodynamic condition of the patient. Unfortunately, though, there are a lot of inter-person variabilities when measuring it. Many times, the basic measurement techniques are not followed and lead to erroneous results.
All healthcare providers should be aware of making sure all the essential pre-requisites are met before checking the blood pressure of the patient. The patient should not have taken any caffeinated drink at least one hour before the testing and should not have smoked any nicotine products at least 15 minutes before checking the pressure. They should have emptied their bladder before checking the blood pressure. Full bladder adds 10 mmHg to the pressure readings. It is advisable to have the patient be seated for at least five minutes before checking their blood pressure. This step takes care of or at least minimizes the higher readings that could have occurred secondary to rushing in for the clinic appointment. The providers should not be having a conversation with the patient while checking his blood pressure. Talking or active listening adds 10 mmHg to the pressure readings. The patient’s back and feet should be supported, and their legs should be uncrossed. Unsupported back and feet add 6 mmHg to the pressure readings. Crossed legs add 2 to 4 mmHg to the pressure readings. The arm should be supported at the heart level. Unsupported arm leads to 10 mmHg to the pressure readings. The patient’s blood pressure should get checked in each arm, and in younger patients, it should be tested in an upper and lower extremity to rule out the coarctation of the aorta. Using the correct cuff size is very important. Smaller cuff sizes give falsely high, and larger cuff sizes give a falsely lower blood pressure reading. [11]
- Nursing, Allied Health, and Interprofessional Team Interventions
Variability of Vital Signs in the Geriatric Age Group
Since vital signs are an indication of the changes in physiological processes, they tend to change with age. With age, core body temperature tends to be lower, and the ability of the body to change with different kinds of stressors becomes minimized. Even subtle variation from the core body temperature can be a significant finding as fever in an older patient often indicates a more severe infection and is associated with increased rates of life-threatening consequences. [12]
There can be a decrease in response to changes in the oxygen and carbon dioxide at the molecular level along with anatomical changes resulting due to stiffness of muscles and compliance of the chest wall. Respiratory rate sometimes might be the most neglected of the vital signs reported in hospitalized patients but is more sensitive than other vital signs in picking up a critically ill patient. [13]
The aging blood vessels also lead to higher arterial stiffness, leading to higher systolic blood pressure and increased pulse pressure. There is also the issue of orthostatic hypotension due to decreased autonomic responsiveness. This response becomes exaggerated with the use of polypharmacy and reduced fluid intake. Thus, it is imperative to check orthostatic vitals in this population. Resting heart rate, in contrast, is often observed to increase with age due to deconditioning and autonomic dysregulation. [14]
Limitations of Vital Signs
Accurately measuring vital signs is a clinical skill that needs time and practice to refine. A review of literature is abundant about the inter-observer variability observed and reported secondary to lack of this skill. Clinicians should be wary of this and always re-check the vital signs themselves if there is a profound or unexpected change. Clinics and organizations should continuously strive to check and educate their nursing and ancillary staff to sharpen these skills.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
VItal Sign Tables Table 1: Types of Digital Thermometers for Use by Age 6 Table 2: Normal Heart Rate (beats/minute) as per the Pediatric Advanced Life Support (PALS) Guidelines. Table 3: Normal Respiratory Rate (Beats/Minute) as per the Pediatric Advanced (more...)
Vital Signs Table 5: Acceptable Blood Pressure Dimensions for Various arm sizes. Contributed by Amit Sapra, MD
Vital Signs Table 6: BP targets by different organizations Contributed by Amit Sapra, MD
Vital Signs Table 7: Normal Blood Pressure as per the Pediatric Advanced Life Support (PALS) Guidelines. Contributed by Amit Sapra, MD
Disclosure: Amit Sapra declares no relevant financial relationships with ineligible companies.
Disclosure: Ahmad Malik declares no relevant financial relationships with ineligible companies.
Disclosure: Priyanka Bhandari declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Sapra A, Malik A, Bhandari P. Vital Sign Assessment. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Technology Assessment: Early Sense for Monitoring Vital Signs in Hospitalized Patients [ 2016] Review Technology Assessment: Early Sense for Monitoring Vital Signs in Hospitalized Patients Helfand M, Christensen V, Anderson J. 2016 May
- Assessing sensitivity and specificity of the Manchester Triage System in the evaluation of acute coronary syndrome in adult patients in emergency care: a systematic review protocol. [JBI Database System Rev Implem...] Assessing sensitivity and specificity of the Manchester Triage System in the evaluation of acute coronary syndrome in adult patients in emergency care: a systematic review protocol. Nishi FA, de Motta Maia FO, de Lopes Monteiro da Cruz DA. JBI Database System Rev Implement Rep. 2015 Nov; 13(11):64-73.
- The prevalence and diagnostic utility of systemic inflammatory response syndrome vital signs in a pediatric emergency department. [Acad Emerg Med. 2015] The prevalence and diagnostic utility of systemic inflammatory response syndrome vital signs in a pediatric emergency department. Scott HF, Deakyne SJ, Woods JM, Bajaj L. Acad Emerg Med. 2015 Apr; 22(4):381-9. Epub 2015 Mar 16.
- Measuring vital signs in children with fever at the emergency department: an observational study on adherence to the NICE recommendations in Europe. [Eur J Pediatr. 2020] Measuring vital signs in children with fever at the emergency department: an observational study on adherence to the NICE recommendations in Europe. van de Maat J, Jonkman H, van de Voort E, Mintegi S, Gervaix A, Bressan S, Moll H, Oostenbrink R. Eur J Pediatr. 2020 Jul; 179(7):1097-1106. Epub 2020 Feb 8.
- Review Nursing handover of vital signs at the transition of care from the emergency department to the inpatient ward: An integrative review. [J Clin Nurs. 2019] Review Nursing handover of vital signs at the transition of care from the emergency department to the inpatient ward: An integrative review. Cross R, Considine J, Currey J. J Clin Nurs. 2019 Mar; 28(5-6):1010-1021. Epub 2018 Oct 23.
Recent Activity
- Vital Sign Assessment - StatPearls Vital Sign Assessment - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
In the last few decades, vital signs have become an area of active research and numerous studies have reported that changes in vital signs occur several hours prior to a serious adverse event [3-7]. Today, vital signs play an important role in emergency departments (ED) and on the wards, to determine patients at risk of deterioration [6-11].
Vital signs are regarded as an essential part of patient monitoring as early detection of preventable outcomes is key to timely intervention (Brekke et al., Citation 2019).Vital signs represent the afferent limb of rapid response systems and are thus critical in detecting patient deterioration and facilitating early medical intervention (Difonzo, Citation 2019).
The only change was the addition of surveillance vital sign monitoring for all patients, in order to determine if it would help detect earlier, subtle signs of deterioration. When the unit began this initiative, providers confused the surveillance monitoring with cardiac monitoring, resulting in inappropriate, high-acuity admissions to the unit.
Background Vital signs, i.e. respiratory rate, oxygen saturation, pulse, blood pressure and temperature, are regarded as an essential part of monitoring hospitalized patients. Changes in vital signs prior to clinical deterioration are well documented and early detection of preventable outcomes is key to timely intervention. Despite their role in clinical practice, how to best monitor and ...
1. INTRODUCTION. Failure to monitor patients is associated with adverse outcomes and delayed recognition of deterioration (National Institute for Health and Care Excellence (UK), 2020).In hospitals, routine monitoring practice involves vital signs measurements (oxygen saturation, temperature, blood pressure, heart rate and respiratory rate) and Early Warning Scoring (EWS) systems.
Vital signs are imported into the patient's electronic health record (EHR) every minute. A healthcare professional stores vital signs in the EHR, imported vital signs that are not stored, are deleted after discharge. Transmitting vital signs from patients to the remote viewers and EHRs is only possible with a wireless internet connection.
1 INTRODUCTION. Vital signs' assessment is a critical task performed by nurses as abnormal vital signs are strongly associated with adverse outcomes. 1, 2 It is recognized, for example, that the simultaneous presence of three critically abnormal vital signs is associated with a very high mortality rate. 3 Vital signs assessment is also critical to the success of Early Warning Scoring systems ...
Continuous monitoring of vital signs using a wireless wearable device was implemented in 2018 at a surgical care unit of an academic hospital. This study aimed at gaining insight into nurses' and patients' perspectives regarding the use and innovation of a continuous vital signs monitoring system, three years after its introduction. This qualitative study was performed in a surgical, non ...
In this paper, we present three main themes identified through thematic analysis (Table 3).The first theme, Vital sign data as evidence for escalation, explores how nurses described using vital sign data to inform and defend their decision to escalate.In the second theme, Trustworthiness of vital sign data, the importance of trust in data is discussed, how nurses responded to concern about ...
Background Vital signs, i.e. respiratory rate, oxygen saturation, pulse, blood pressure and temperature, are regarded as an essential part of monitoring hospitalized patients. Changes in vital ...
The first of REVIEW the two patient outcome studies was conducted over a 3-month period in a wing of John Hopkins Hospital, USA, where 40% of sudden deaths were occurring. 24 The study found that ...
The hospital's philoso-phy is that "failure-to-rescue" events (i.e., when a patient dies from a medical complica-tion that was not recognized in a timely manner or treated appropriately) and in-hospital cardiac arrests should never occur. In 2015, 40% of the sudden deaths at Johns Hopkins Hospital occurred on the Zayed 11 East unit.
The study builds on previous studies of vital sign recording quality 31, and highlights that institutions may wish to monitor vital sign recording to identify areas of the hospital or patient ...
Orthostatic vital signs (pulse and blood pressure) should be taken because this client is at risk for hypovolemia. The client may be dehydrated as a result of the vomiting and diarrhea and lack of fluid intake. Return to the chapter on blood pressure for more information on hypovolemia and its effects on vital signs.
Furthermore, an increase in stress levels was observed, as well as in anxiety before their first simulation case. Both study groups (students with and without experience), demonstrated a decrease in the vital signs and levels of stress/anxiety, possibly related to the effects of participating in the case study scenarios as well as the ...
Case Study: Continuous Monitoring of Patient Vital Signs to Reduce 'Failure-to-Rescue' Events Author : Phyllis J. Miller Authors Info & Affiliations Publication : Biomedical Instrumentation & Technology
Nurses' opinions regarding continuous monitoring appear to be positive. However, facilitators and barriers were little studied. This study explored nurses' post-implementation experiences of the facilitators and barriers to continuously monitoring patients' vital signs using a wireless device on general hospital wards.
Case Study: Continuous Monitoring of Patient Vital Signs to Reduce 'Failure-to-Rescue' Events. Case Study: Continuous Monitoring of Patient Vital Signs to Reduce 'Failure-to-Rescue' Events Biomed Instrum Technol. 2017 Jan-Feb;51(1):41-45. doi: 10.2345/0899-8205-51.1.41. ...
A number of studies reported a mean time for taking a vital-sign set, mean time to record vital signs on charts or both. 32, 56, 105, 107, 108, 110, 113, 114, 116, 118 Other studies reported the amount of time that nursing staff spent taking vital signs and/or recording them over a shift, per hour, per patient or over an amount of time (e.g ...
Required reading for all learners: Implicit Bias impacts patient outcomes. This session covers pathophysiology that causes alterations in VS and presents a foundational algorithmic approach to assessing the abnormal vital signs readings of heart rate, blood pressure, respiratory rate and temperature to quickly formulate a focused differential diagnosis.
The only change was the addition of surveillance vital sign monitoring for all patients, in order to determine if it would help detect earlier, subtle signs of deterioration. When the unit began this initiative, providers confused the surveillance monitoring with cardiac monitoring, resulting in inappropriate, high-acuity admissions to the unit.
How to change. The Chief Nursing Information Officer led an initial pilot to introduce 70 digital bedside vital signs monitors, supported by nurses and midwives providing leadership as local champions supporting decisions on areas for implementation. Hand held devices were introduced to reduce documentation time with decision support at the ...
Vital signs are an objective measurement of the essential physiological functions of a living organism. They have the name "vital" as their measurement and assessment is the critical first step for any clinical evaluation. The first set of clinical examinations is an evaluation of the vital signs of the patient. Triage of patients in an urgent/prompt care or an emergency department is based on ...