Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

New Research Sheds Light on Cause of Type 2 Diabetes

St. Petersburg, Fla. – September 12, 2023 – Scientists at Johns Hopkins All Children’s Hospital, along with an international team of researchers, are shedding new light on the causes of Type 2 diabetes. The new research, published in the journal Nature Communications , offers a potential strategy for developing new therapies that could restore dysfunctional pancreatic beta-cells or, perhaps, even prevent Type 2 diabetes from developing.
The new study shows that the beta-cells of Type 2 diabetes patients are deficient in a cell trafficking protein called “phosphatidylinositol transfer protein alpha” (or PITPNA), which can promote the formation of “little packages,” or intracellular granules containing insulin. These structures facilitate processing and maturation of insulin “cargo.” By restoring PITPNA in the Type 2 deficient beta-cells, production of insulin granule is restored and this reverses many of the deficiencies associated with beta-cell failure and Type 2 diabetes.
Researchers say it’s important to understand how specific genes regulate pancreatic beta-cell function, including those that mediate insulin granule production and maturation like PITPNA to provide therapeutic options for people.
Matthew Poy, Ph.D. , an associate professor of Medicine and Biological Chemistry in the Johns Hopkins University School of Medicine and leader of the Johns Hopkins All Children’s team within the Institute for Fundamental Biomedical Research , was lead researcher on the study. He adds that follow-up work is now focused on whether PITPNA can enhance the functionality of stem-cell-derived pancreatic beta-cells. Since stem cell-based therapies are still in their relatively early stages of clinical development, it appears a great deal of the potential of this approach remains untapped. Poy believes that increasing levels of PITPNA in stem cell-derived beta-cells is an approach that could enhance the ability to produce and release mature insulin prior to transplantation in diabetic subjects.
“Our dream is that increasing PITPNA could improve the efficacy and potency of beta-like stem cells,” Poy says. “This is where our research is heading, but we have to discover whether the capacity of these undifferentiated stem cells that can be converted into many different cell types can be optimized — and to what level — to be converted into healthy insulin producing beta-cells. The goal would be to find a cure for type 2 diabetes.”
Read more about this groundbreaking research.
This study was funded through grants from the Johns Hopkins All Children’s Foundation , the National Institute of Health, the Robert A. Welch Foundation, the Helmholtz Gemeinschaft , the European Foundation for the Study of Diabetes, the Swedish Science Council , the NovoNordisk Foundation and the Deutsche Forschungsgemeinschaft . About Johns Hopkins All Children’s Hospital Johns Hopkins All Children’s Hospital in St. Petersburg is a leader in children’s health care, combining a legacy of compassionate care focused solely on children since 1926 with the innovation and experience of one of the world’s leading health care systems. The 259-bed teaching hospital, stands at the forefront of discovery, leading innovative research to cure and prevent childhood diseases while training the next generation of pediatric experts. With a network of Johns Hopkins All Children’s Outpatient Care centers and collaborative care provided by All Children’s Specialty Physicians at regional hospitals, Johns Hopkins All Children’s brings care closer to home. Johns Hopkins All Children’s Hospital consistently keeps the patient and family at the center of care while continuing to expand its mission in treatment, research, education and advocacy. For more information, visit HopkinsAllChildrens.org .

- July 2, 2024 | Scientists Uncover Brain-Boosting Potential of Vitamin B6
- July 2, 2024 | Scientists Crack the Code on Broccoli’s Health Benefits
- July 2, 2024 | Carbon Cataclysm: Scientists Shed New Light on Ancient Apocalypse That Affected the Entire Planet
- July 2, 2024 | Orion Spacecraft to Take a Test Spin in the Vacuum of Space Without Leaving Earth
- July 2, 2024 | Warning From the Deep: Ancient Extinction Holds Clues to Today’s Climate Crisis
Beyond Blood Sugar Control: New Target for Curing Diabetes Unveiled
By Helmholtz Munich March 22, 2024
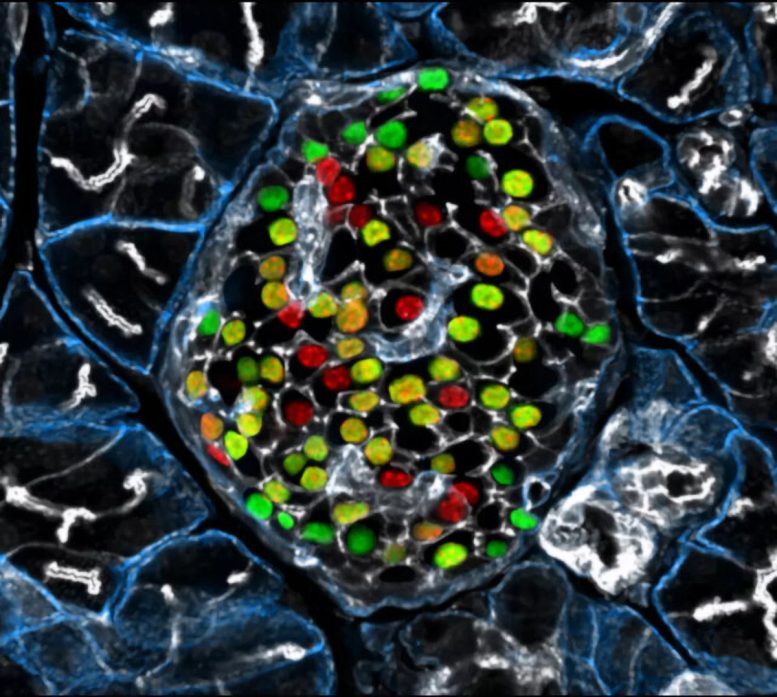
Targeting the inceptor receptor could lead to breakthrough treatments for diabetes by protecting beta cells and improving blood sugar control, with German research institutions leading this promising discovery. Insulin-producing beta cells in the islet of Langerhans. Credit: Helmholtz Munich | Erik Bader
Research focusing on the insulin -inhibitory receptor, known as inceptor, has revealed promising paths for protecting beta cells, providing optimism for therapy that directly addresses diabetes. A groundbreaking study involving mice with obesity caused by diet shows that eliminating inceptor improves glucose management. This finding encourages further investigation into inceptor as a potential therapeutic target for treating type 2 diabetes.
These findings, led by Helmholtz Munich in collaboration with the German Center for Diabetes Research, the Technical University of Munich, and the Ludwig-Maximilians-University Munich, drive advancements in diabetes research.
Targeting Inceptor to Combat Insulin Resistance in Beta Cells
Insulin resistance, often linked to abdominal obesity, presents a significant healthcare dilemma in our era. More importantly, the insulin resistance of beta cells contributes to their dysfunction and the transition from obesity to overt type 2 diabetes. Currently, all pharmacotherapies, including insulin supplementation, focus on managing high blood sugar levels rather than addressing the underlying cause of diabetes: beta cell failure or loss. Therefore, research into beta cell protection and regeneration is crucial and holds promising prospects for addressing the root cause of diabetes, offering potential avenues for causal treatment.
With the recent discovery of inceptor, the research group of beta cell expert Prof. Heiko Lickert has uncovered an interesting molecular target. Upregulated in diabetes, the insulin-inhibitory receptor inceptor may contribute to insulin resistance by acting as a negative regulator of this signaling pathway. Conversely, inhibiting the function of the inceptor could enhance insulin signaling – which in turn is required for overall beta cell function, survival, and compensation upon stress.
In collaboration with Prof. Timo Müller, an expert in molecular pharmacology in obesity and diabetes, the researchers explored the effects of inceptor knock-out in diet-induced obese mice. Their study aimed to determine whether inhibiting inceptor function could also enhance glucose tolerance in diet-induced obesity and insulin resistance, both critical pre-clinical stages in the progression toward diabetes. The results were now published in Nature Metabolism .
Removing Inceptor Improves Blood Sugar Levels in Obese Mice
The researchers delved into the effects of removing inceptor from all body cells in diet-induced obese mice. Interestingly, they found that mice lacking inceptor exhibited improved glucose regulation without experiencing weight loss, which was linked to increased insulin secretion in response to glucose. Next, they investigated the distribution of inceptor in the central nervous system and discovered its widespread presence in neurons. Deleting inceptor from neuronal cells also improved glucose regulation in obese mice. Ultimately, the researchers selectively removed the inceptor from the mice’s beta cells, resulting in enhanced glucose control and a slight increase in beta cell mass.
Research for Inceptor-Blocking Drugs
“Our findings support the idea that enhancing insulin sensitivity through targeting inceptor shows promise as a pharmacological intervention, especially concerning the health and function of beta cells,” says Timo Müller. Unlike intensive early-onset insulin treatments, utilizing inceptor to enhance beta cell function offers promise in alleviating the detrimental effects on blood sugar and metabolism induced by diet-induced obesity. This approach avoids the associated risks of hypoglycemia-associated unawareness and unwanted weight gain typically observed with intensive insulin therapy.
“Since inceptor is expressed on the surface of pancreatic beta cells, it becomes an accessible drug target. Currently, our laboratory is actively researching the potential of several inceptor-blocking drug classes to enhance beta cell health in pre-diabetic and diabetic mice. Looking forward, inceptor emerges as a novel and intriguing molecular target for enhancing beta cell health, not only in prediabetic obese individuals but also in patients diagnosed with type 2 diabetes,” explains Heiko Lickert.
Reference: “Global, neuronal or β cell-specific deletion of inceptor improves glucose homeostasis in male mice with diet-induced obesity” by Gerald Grandl, Gustav Collden, Jin Feng, Sreya Bhattacharya, Felix Klingelhuber, Leopold Schomann, Sara Bilekova, Ansarullah, Weiwei Xu, Fataneh Fathi Far, Monica Tost, Tim Gruber, Aimée Bastidas-Ponce, Qian Zhang, Aaron Novikoff, Arkadiusz Liskiewicz, Daniela Liskiewicz, Cristina Garcia-Caceres, Annette Feuchtinger, Matthias H. Tschöp, Natalie Krahmer, Heiko Lickert and Timo D. Müller, 28 February 2024, Nature Metabolism . DOI: 10.1038/s42255-024-00991-3
More on SciTechDaily

Quantum Breakthrough Reveals Superconductor’s Hidden Nature

Novel Molecules Discovered to Combat Asthma and COVID-Related Lung Diseases

Orbital Engineering, Yale Engineers Change Electron Trajectories

Finding and Erasing Quantum Computing Errors in Real-Time

“Glow-in-the-Dark” Proteins: The Future of Viral Disease Detection?
A black hole – a million times as bright as our sun – offers potential clue to reionization of universe.

Risk Factors for Falls in Older Americans Identified – A Growing Public Health Concern

Common Fireworks Emit Toxic Metals Into the Air – Damage Human Cells and Animal Lungs
1 comment on "beyond blood sugar control: new target for curing diabetes unveiled".
Interesting study and hopefully another tool which will apply to diabetic patients.
Leave a comment Cancel reply
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.
Cornell Chronicle
- Architecture & Design
- Arts & Humanities
- Business, Economics & Entrepreneurship
- Computing & Information Sciences
- Energy, Environment & Sustainability
- Food & Agriculture
- Global Reach
- Health, Nutrition & Medicine
- Law, Government & Public Policy
- Life Sciences & Veterinary Medicine
- Physical Sciences & Engineering
- Social & Behavioral Sciences
- Coronavirus
- News & Events
- Public Engagement
- New York City
- Photos of the Week
- Big Red Sports
- Freedom of Expression
- Student Life
- University Statements
- Around Cornell
- All Stories
- In the News
- Expert Quotes
- Cornellians
Large-scale study reveals new genetic details of diabetes
By wynne parry weill cornell medicine.
In experiments of unprecedented scale, investigators at Weill Cornell Medicine and the National Institutes of Health have revealed new aspects of the complex genetics behind Type 2 diabetes. Through these discoveries, and by providing a template for future studies, this research furthers efforts to better understand and ultimately treat this common metabolic disease.
Previous studies have generally examined the influence of individual genes. In research described Oct. 18 in Cell Metabolism, senior co-author Shuibing Chen , the Kilts Family Professor of Surgery at Weill Cornell Medicine, working alongside senior co-author Dr. Francis Collins , a senior investigator at the Center for Precision Health Research within the National Human Genome Research Institute of the U.S. National Institutes of Health, took a more comprehensive approach. Together, they looked at the contribution of 20 genes in a single effort.
“It’s very difficult to believe all these diabetes-related genes act independently of each other,” Chen said. By using a combination of technologies, the team examined the effects of shutting each down. By comparing the consequences for cell behavior and genetics, she said, “we found some common themes.”
As with other types of diabetes, Type 2 diabetes occurs when sugar levels in the blood are too high. In Type 2 diabetes, this happens in part because specialized cells in the pancreas, known as β-cells, don’t produce enough insulin, a hormone that tells cells to take sugar out of the blood for use as an energy source. Over time, high levels of blood sugar damage tissues and cause other problems, such as heart and kidney disease. According to the United States Centers for Disease Control and Prevention, nearly 9% of adults in the United States have been diagnosed with Type 2 diabetes.
Both genetic and environmental factors, such as obesity and chronic stress, can increase risk for it. Yet evaluating the role of the genetic contributors alone is a massive project. So far, researchers have identified more than 290 locations within the genome where changes to DNA can raise the likelihood of developing the disease. Some of these locations fall within known genes, but most are found in regions that regulate the expression of nearby genes.
For the new research, the team focused on 20 genes clearly identified as contributors. They began their investigation by using the gene editing system CRISPR-Cas9 to shut down these genes, one at a time, within 20 sets of identical stem cells.
These stem cells had the potential to generate any kind of mature cell, but the researchers coaxed them into becoming insulin-producing β-cells. They then examined the effects of losing each gene on five traits related to insulin production and the health of β-cells. They also documented the accompanying changes in gene expression and the accessibility of DNA for expression.
To make sense of the massive amount of data they collected, the team developed their own computational models to analyze it, leading to several discoveries: By comparing the effects of all 20 mutations on β-cells, they identified four additional genes, each representing a newly discovered pathway that contributes to insulin production. They also found that, of the original 20 genes, only one, called HNF4A, contributed to all five traits, apparently by acting as a master controller that regulates the activity of other genes. In one specific example, they explained how a small variation, located in a space between genes, contributes to the risk of diabetes by interfering with HNF4A’s ability to regulate nearby genes.
Ultimately, this study and others like it hold the promise of benefiting patients, Collins said. “We need to understand all the genetic and environmental factors involved so we can do a better job of preventing diabetes, and to develop new ideas about how to effectively treat it.”
Collins and Chen note that their approach may have relevance beyond diabetes, to other common diseases, such as Alzheimer’s, Parkinson’s and Crohn’s disease, that involve many genetic factors.
The work reported in this newsroom story was supported in part by the United States’ National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases and the American Diabetes Association.
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see the profile for Shuibing Chen .
Wynne Parry is a freelance writer for Weill Cornell Medicine.
Media Contact
Krystle lopez.
Get Cornell news delivered right to your inbox.
You might also like

Gallery Heading
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Clinical Research on Type 2 Diabetes: A Promising and Multifaceted Landscape
Type 2 diabetes constitutes an imposing epidemiological, economic, and scientific global challenge. The chronic complications of type 2 diabetes are a major cause of mortality and disability worldwide [ 1 , 2 ]. Clinical research is the main way to gain knowledge about long-term diabetic complications and reduce the burden of diabetes. This allows for designing effective programs for screening and follow-up and fine-targeted therapeutic interventions. However, new research methodologies are needed to obtain more accurate and useful insights into the biological and clinical processes involved in diabetic complication development.
During the last few years, new approaches for clinical research have incorporated digital tools to analyze the complex physiopathological background of type 2 diabetes. In this Special Issue, entitled “ Clinical Research on Type 2 Diabetes and Its Complications ” and published in the Journal of Clinical Medicine ( https://www.mdpi.com/journal/jcm/special_issues/Type_2_Diabetes_Complications ), some valuable digital methodologies were used in different studies focusing on the type 2 diabetes syndrome. Novel machine learning techniques for predicting long-term complications are one of these approaches, as the studies of Huang, Rashid, and Shin et al. depict [ 3 , 4 , 5 ]. The data presented by these authors suggest that machine learning may be more accurate in predicting diabetic microvascular complications than traditional methods. Additionally, digital tools such as artificial intelligence and machine learning can be implemented through an automated and rapid process.
Among the frequent causes of frustration for people with diabetes and the health care providers involved in their management is the delayed detection of diabetic complications. The outlook of clinical research appears promising in the near future owing to the development and implementation of advanced methods for the detection of early alterations in the micro- and macrovascular complications associated with diabetes. Two papers in this Special Issue cover the use of specific biomarkers tracing the progress of diabetic cardiovascular complications [ 6 , 7 ]. In another contribution, Lee et al. revisit the long-term glycemic variability and its relationship with end-stage kidney disease [ 8 ].
Besides the genetic approach, the application of digital techniques, including machine learning and artificial intelligence, and novel biomarkers could be crucial for individualized type 2 diabetes management, which is the backbone of precision medicine.
Two review papers address the complications that are non-traditionally linked to type 2 diabetes, although currently under exhaustive research: bone health and non-alcoholic fatty liver disease [ 9 , 10 ]. The multifaceted nature of type 2 diabetes is clearly visualized owing to the holistic angle used by these approaches.
The efficacy and safety of new type 2 diabetes pharmacological treatment are covered by three original papers [ 11 , 12 , 13 ]. The Yu-Chuan Kang et al. study includes a large population sample and an extended follow-up to evaluate the association between dipeptidyl peptidase-4 inhibitors and diabetic retinopathy [ 13 ]. This could be the first signal for a new safety risk of a pharmacological class of drugs used by millions worldwide.
The COVID-19 pandemic was first reported in China in December 2019 and continues to be a devastating condition for global health and economy. The COVID-19 disease has immediate implications for common chronic metabolic disorders such as type 2 diabetes. Both direct infection and the associated distress due to preventive measures in the general population have worsened the control of type 2 diabetes. Some factors indicate that COVID-19 or other coronavirus-caused diseases can be seasonal or persistent in the future. Type 2 diabetes has a strong negative effect on the prognosis of patients with COVID-19. Three papers in this Special Issue review the implications of this disease in relation to diabetes [ 14 , 15 , 16 ].
Finally, the aim of researchers in this field should be to make all these remarkable advances accessible to those populations experiencing more difficulties due to sociodemographic factors such as cultural deprivation, sex discrimination, or limited income [ 17 , 18 , 19 ].
Acknowledgments
The authors acknowledge the continuous editorial assistance of Nicole Quinn, Always English S.L.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, writing—original draft preparation, writing—review and editing were equally done by F.G.-P. and C.A. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These New Developments Could Make Living With Type 2 Diabetes More Manageable

E xperts often talk about the “burden” of a disease or illness. The word acts as a tidy container for all the unpleasantness people with that condition may experience—from their symptoms, to the cost of their care, to the restrictions imposed on their lifestyle, to the health complications that may arise. For people with Type 2 diabetes , this burden can be high.
Routine management of Type 2 diabetes often involves major changes to one’s diet and physical activity . And for many, especially those taking insulin to manage their blood sugar, the disease can necessitate daily blood-glucose monitoring, a process that entails pricking a finger to draw blood and then dabbing that blood onto a glucose monitor’s test strip. Doing this several times a week—month after month—can present overlapping challenges. According to a 2013 survey in the journal Diabetes Spectrum, people find finger-prick glucose monitoring to be painful, and the results can be confusing or unhelpful.
“Patients don’t want to prick their fingers, and they come in all the time and say, ‘I’m tired of this,’” says Dr. Francisco Pasquel, a diabetes specialist and associate professor of medicine at Emory University School of Medicine in Atlanta.
But relief is on the way. Continuous glucose monitors, or CGMs, are small devices-—often about the size of a quarter-—that use a small under-the-skin needle to continuously monitor blood-glucose levels. This information can be transmitted—in some cases wirelessly and automatically—to a smartphone app or other device. “You can look at glucose levels for a single point in time, but you can also look at trends in values over time,” says Dr. Roy Beck, medical director of the nonprofit Jaeb Center for Health Research in Tampa. Beck’s work has found that continuous glucose monitoring may provide a number of benefits for people with Type 2 diabetes.
These monitors are just one of several new advancements in Type 2 diabetes care and management. From connected technologies to new drug treatments, medical science is making steady and sometimes life-changing progress in the treatment of this condition. Here, experts describe some of the latest and greatest developments.
Continuous glucose monitors
People with Type 1 diabetes typically have to check their blood-sugar levels on a daily basis, or even multiple times each day. Because testing is such a big part of managing that disease, the research on continuous glucose monitors started with these patients. That work has shown that CGMs provide multiple benefits, including reduced hemoglobin A1C (HbA1c) levels, which is an important measure of healthy blood glucose. Continuous glucose monitors are now being studied in people with Type 2 diabetes, and research points to multiple benefits.
For a study published in 2021 in the Journal of the American Medical Association, Beck and his colleagues compared continuous glucose monitoring to standard finger-prick tests among people with Type 2 diabetes who were using insulin. They found that continuous monitoring was associated with a significantly greater drop in HbA1c. They also found that continuous monitoring helped people avoid risky and severe drops in blood sugar (a.k.a. hypoglycemia). “It’s pretty clear that there’s a benefit for people with Type 2 diabetes who are using insulin,” he says.
More than 90% of people with diabetes have Type 2 diabetes, and Beck says that roughly 30% of these people are using insulin. In other words, there are many people with Type 2 diabetes who stand to benefit from continuous glucose monitoring. However, use of these monitors is still mostly confined to people with Type 1 diabetes. “Use is slowly increasing in Type 2 patients, but I think it’s still too low considering this is a non-pharmacological approach”—something many people prefer because it avoids the side effects of medications—“that can help people,” he says.
Even for people with Type 2 diabetes who are not taking insulin, Beck says that continuous glucose monitoring could be helpful. “There’s a need for more studies to prove it, but it makes sense that it would likely have benefits,” he says. For example, monitoring blood sugar in real time could help people make diet or lifestyle changes that reduce their risks for long-term health complications. “Normally, blood glucose following a meal shouldn’t go above 140 [mg/dL],” he says. But based on factors like diet, meal timing, and exercise habits, someone with Type 2 diabetes may experience post-meal blood-sugar spikes that surpass 200 or even 300 mg/dL. These spikes could cause few symptoms or short-term consequences, Beck says, but over time they can contribute to the development of common diabetes-related complications such as kidney failure, heart disease, or diabetic retinopathy (an eye condition that can cause blurry vision or blindness). “The first time people use these continuous monitors, it can be a real eye-opener,” he adds. “I think they could be most helpful for self-management, and Type 2 diabetes is a disease where self-management through diet and exercise can make a huge difference.”
Other experts second this. “Patients using these devices can receive a graph of their glucose values over time, which helps them understand the effects of nutrition on glucose control, or how they could modify their exercise to make improvements,” says Dr. Ilias Spanakis, an associate professor of medicine in the division of endocrinology, diabetes, and nutrition at the University of Maryland School of Medicine.
For patients who are reliant on insulin to manage their blood glucose, combining continuous glucose monitors with insulin pumps—devices that automatically inject insulin as needed—could also lead to major improvements. “Smart algorithms that connect the two can automatically adjust glucose based on glucose values,” Spanakis says. This is already possible, and it’s likely to become much more commonplace, he adds.
For many people with diabetes, continuous glucose monitoring could provide a safer and simpler path forward.
Read More: The Link Between Type 2 Diabetes and Psychiatric Disorders
Bariatric surgery for Type 2 diabetes
Historically, bariatric (weight-loss) surgery has been used primarily to help people manage severe obesity, which the U.S. Centers for Disease Control and Prevention defines as a BMI of 40 or higher. Many people who are severely obese also have diabetes, and research has found that these surgical procedures can help reduce the burden of Type 2 diabetes or even send it into remission.
A 2018 study from researchers at the University of Oklahoma found that Roux-en-Y gastric bypass surgery, a common bariatric procedure, vastly outperformed typical medical management techniques—such as diet changes, doctor’s visits, and prescription drugs—among people with Type 2 diabetes. Surgery led to diabetes remission in roughly 28% of patients, compared with a remission rate of just 4% among the non-surgery group, according to the study results. More research has found that bariatric surgery may effectively send Type 2 diabetes into remission.
“Surgery does not just lead to weight loss, but also to an improvement in glycemic control, which happens even before the weight loss occurs,” says Emory’s Pasquel, who has published work on the benefits of bariatric surgery for people with Type 2 diabetes. Exactly how the surgery does this isn’t well understood, he says. However, bariatric surgery affects appetite, food intake, caloric absorption, and multiple neuroendocrine pathways—all of which could contribute to its beneficial actions for people with Type 2 diabetes.
In the future, Pasquel says these procedures are likely to become more commonplace even for people with Type 2 diabetes who are not severely obese.
More from TIME
New pharmaceutical drugs.
There are a lot of different diabetes drugs on the market, each with its own risks and benefits. But experts say two types are emerging as potential “game changers” when it comes to Type 2 diabetes treatment.
Glucagon-like peptide 1 (GLP-1) is a hormone released in the gut during digestion—one that plays a role in blood-sugar homeostasis. A class of drugs known as GLP-1 receptor agonists can interact with GLP-1 receptors in ways that lower appetite, slow digestion, and provide other benefits for people with Type 2 diabetes. These GLP-1 drugs aren’t new. But Pasquel says the latest versions are different in that they work on two different receptors, not one. “Recent evidence shows that activating both receptors has a remarkable impact on weight loss and glycemic control,” he says. Especially for people with Type 2 diabetes who are at high risk for heart or arterial disease, he says that these new drugs seem to be a big upgrade over previous medications.
A second category of drug has also emerged as a standout in the treatment of Type 2 diabetes. Known as sodium-glucose cotransporter-2 (SGLT-2) inhibitors, these drugs help the kidneys remove sugar from a person’s blood. Not only does this improve blood-sugar control in people with Type 2 diabetes, but it also helps protect them from heart failure and kidney disease—two common and serious complications. Pasquel says these drugs are so effective that they’re now being used in people with heart failure or kidney disease who do not have Type 2 diabetes.
Read More: The Truth About Fasting and Type 2 Diabetes
Emerging ways to think about weight loss
Experts have long understood that weight loss can help people reduce their Type 2 diabetes symptoms and risks . This recognition has led to research on a number of weight-loss diets . More research is needed, but some of the latest studies suggest that fasting plans—in particular, intermittent fasting—may be particularly beneficial for people with Type 2 diabetes.
Intermittent fasting involves cutting out calorie-containing foods and drinks for an extended period of time—anywhere from 12 hours to two days depending on the approach a person chooses. A 2019 research review in the journal Nutrients found that intermittent fasting promotes weight loss, increases insulin sensitivity, and reduces insulin levels in the blood. All of this is helpful for people with Type 2 diabetes. “Essentially, fasting is doing what we prescribe diabetes medications to do, which is to improve insulin sensitivity,” says Benjamin Horne, director of cardiovascular and genetic epidemiology at Intermountain Healthcare in Utah.
It’s not yet clear which form of intermittent fasting is best. But Horne says that time-restricted eating—a type of fasting that involves squeezing all the day’s calories into single six- or eight-hour feeding windows—is leading the pack, largely because patients are able to stick with it.
There are more new advancements in Type 2 diabetes care. The interventions described here—from continuous glucose monitors to novel drugs—are some of the most promising, but they have company. It’s safe to say that, looking ahead, more people with Type 2 diabetes will be able to effectively manage or mitigate their symptoms.
More Must-Reads from TIME
- Welcome to the Noah Lyles Olympics
- Melinda French Gates Is Going It Alone
- What to Do if You Can’t Afford Your Medications
- How to Buy Groceries Without Breaking the Bank
- Sienna Miller Is the Reason to Watch Horizon
- Why So Many Bitcoin Mining Companies Are Pivoting to AI
- The 15 Best Movies to Watch on a Plane
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]

- Weill Cornell Medicine

New Study Reveals Promising Findings to Treat Type 2 Diabetes
A new study published in the Journal of Clinical Investigation has demonstrated that activating a pathway to promote cell division not only expanded the population of insulin-producing cells, but, surprisingly, also enhanced the cells’ function. The findings hold promise for future therapeutics that will improve the lives of individuals with type 2 diabetes—a condition that affects more than half a billion people worldwide.

Dr. Laura Alonso
“That’s reassuring because there is a long-standing belief in the field that proliferation can lead to ‘de-differentiation’ and a loss of cell function,” said study senior author Dr. Laura Alonso , chief of the division of endocrinology, diabetes and metabolism, director of the Weill Center for Metabolic Health , and the E. Hugh Luckey Distinguished Professor in Medicine at Weill Cornell Medicine. “Our result flies in the face of that dogma and suggests if we can find a way to trigger replication of the beta cells in the body, we won’t impair their ability to produce and secrete insulin.”
First author, Rachel Stamateris, also contributed to this work as an MD, PhD student at the University of Massachusetts Medical School and visiting graduate assistant in medicine at Weill Cornell Medicine.
When Beta Cells Fail
In type 2 diabetes, the body’s tissues become resistant to insulin, which means they can’t take in and use blood sugar. At the same time, insulin-producing beta cells in the pancreas fail—diminishing in number and losing their ability to function.
Dr. Alonso and her colleagues reproduced these conditions in a mouse model of diabetes that lacks IRS2, a protein that allows insulin to transmit its signal for cells to absorb blood sugar. These mice displayed insulin resistance, a seminal feature of human type 2 diabetes. “On top of that,” said Dr. Alonso, “the IRS2 protein also turns out to be critical for beta cell function and beta cell number.” So, their pool of beta cells was depleted.
The first order of business to rescue these mice: boost beta cell numbers. But how? She and her team took a closer look at the molecular machinery that controls cell proliferation. The researchers observed that in the IRS-deficient diabetic mice, beta cells failed to elevate production of cyclin D2. This protein, when partnered with a protein called CDK4, drives cell division. Previous studies had shown that mice lacking CDK4 also develop diabetes.
It seemed logical to test if boosting CDK4 activity would help increase beta cell quantity. When Dr. Alonso’s team genetically introduced an active form of CDK4 into the diabetic mice that was more available to attach to cyclin D2, the first thing they noticed was the animals’ blood sugars were restored to normal. Their beta cells were more plentiful than in the untreated, IRS2 mutant mice. But even better: “The beta cells looked amazingly healthy in the treated mice compared with the original diabetic mice, whose beta cells look terrible. Increasing the activity of CDK4 resulted in beta cells packed full of insulin,” said Dr. Alonso, who is also an endocrinologist at NewYork-Presbyterian/Weill Cornell Medical Center.
This supports the concept that beta cell mass can be expanded without compromising function.
While CDK4 is not, itself, a viable therapeutic target because its ability to stimulate proliferation could increase the risk of cancer, Dr. Alonso is confident that probing the molecular pathways that govern beta cell division and function could someday lead to a clinical breakthrough. She pointed to Ozempic, one of the most talked about new treatments for diabetes. “That medication was discovered by a scientist studying toxins in the saliva of the Gila monster,” said Dr. Alonso. “So, it’s clear that understanding how fundamental biology works can lead to real advances in treating or even preventing diabetes.”
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see the profile for Dr. Laura Alonso .
This study was supported by grants K08DK076562, R01DK095140, R01DK124906, and R01DK114686 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Releated Links: Boosting Beta Cells to Treat Type 2 Diabetes
Back to News
- Endocrinology, Diabetes & Metabolism
Talk to us about diabetes
0345 123 2399
customer support
Inhaled insulin and tech for type 2: new research presented from the American Diabetes Association

Every year, over 10,000 scientists meet up at the American Diabetes Association’s Scientific Sessions to share results from major new diabetes research studies. Here are some of the most exciting developments, from inhaled insulin to stem cell transplants.
Vertex’s venture into man-made beta cells
Stem cells can be coaxed to shape-shift into other types of cells in the body, including insulin-making beta cells. Scientists are using them to produce a man-made supply of beta cells that could be transplanted into people with type 1 diabetes , replacing those that the immune system has destroyed.
Biotech company Vertex have been running a clinical trial to test a pioneering stem cell treatment, which they call VX-880. At ADA the team presented the latest promising updates from the first 12 people who’ve received the treatment.
Before the trial, participants had an average HbA1c of 61.7 mmol/mol (7.8%) and were taking around 40 units of insulin per day. They also had dangerous hypo unawareness and a history of severe hypos. And none of them were producing any traces of their own insulin.
After the treatment, participants who had a full dose of VX-880 started to produce insulin again, and saw their blood sugar levels improve significantly. All 12 participants reduced their HbA1c to under 53 mmol/mol (7%), spent more than 70% of time with blood sugar levels in a target range, and had no severe hypos.
After six months, seven participants were no longer injecting any insulin and two reduced the amount of insulin they inject by around 70%. Importantly, all the participants who were followed up after a year were no longer having severe hypos, even with a lower HbA1c.
The trial now has almost 40 participants enrolled and is recruiting globally, helping the team to gather more evidence about the safety and potential of VX-880.
But these exciting findings suggest highlight the potential of growing beta cells from stem cells to transform how type 1 diabetes is treated. This is an area the Type 1 Diabetes Grand Challenge is propelling forward in the UK, to make sure treatments reach people with type 1 sooner.
Inhaled insulin shows promise in type 1 diabetes
Findings from a pivotal trial looking at the use of inhaled insulin in people with type 1 diabetes were announced at the ADA Scientific Sessions.
Everyone with type 1 diabetes needs to take insulin, either by injecting it multiple times everyday, or using an insulin pump. But researchers are searching for easier ways to use insulin, including by inhaling it.
This works like an asthma inhaler. Insulin comes in a powdered form and when you breath it in using an inhaler, it goes into your lungs. And from there, it gets into your blood.
In the INHALE-3 trial, 123 adults with type 1 diabetes were divided into two groups. One group used inhaled insulin (called Afrezza), plus a long-lasting insulin over 17 weeks. While the other group kept their normal insulin regime – taking their quick-acting insulin with injections or pumps.
The researchers found that more participants using inhaled insulin had improved HbA1c levels, compared to standard care.
- 21% of people on inhaled insulin improved their HbA1c by 5 mmol/mol (0.5%) or more. This compared to only 5% of those with standard care.
- For participants who had an HbA1c of 53 mmol/mol (7%) or more at the start of the study, 21% who tried inhaled insulin reduced their HbA1c to below 53 mmol/mol by the end of the study. Whereas no one in the standard care group did.
More than half of the people on the trial said they’d like to continue using inhaled insulin after the study. But the findings also showed that inhaled insulin wasn’t for everyone. 26% of participants in the inhaled insulin group saw their HbA1c increase by 5 mmol/mol (0.5%) or more. This compared to 3% using standard care.
Inhaled insulin has not been approved for use in the UK yet. But these results show its potential to offer people with type 1 diabetes an alternative way of taking insulin.
Technology triumphs for type 2 diabetes
Diabetes technology, like continuous glucose monitoring (CGM) and hybrid closed loop systems , are transforming the lives of people with type 1 diabetes in the UK. But research to understand how they could benefit people with type 2 diabetes has been lacking.
At ADA, a new set of studies illuminated the potential for these technologies to improve blood sugar levels in people living with type 2 diabetes too. This positive impact was seen both in people who were taking insulin, or not.
A world-first study of the Omnipod 5 hybrid closed loop system, involving 305 adults with type 2 diabetes , showed the tech reduced blood sugar levels. Average HbA1c levels went from 72 mmol/mol (8.2%) to 57 mmol/mol (7.4%) over 13 weeks.
We also heard about real-world data from over 6,000 people with type 2 diabetes treating their condition with insulin who had been using CGM. Researchers compared their blood sugar levels before and after using CGM for a year.
Using CGM helped people reduce their HbA1c levels by around 10 mmol/mol (1%). And CGM use led to a 50% reduction in hospitalisations from diabetes or other causes.
Similar positive results were found in people with type 2 diabetes who weren’t using insulin. CGM meant that they spent four more hours a day in target blood sugar range.
The next steps of these studies will be to test the technologies in different groups of people with type 2 diabetes and check if the benefits last for the longer term.
These findings demonstrate how tech could transform how people manage their type 2 diabetes day-to-day and help them live healthier lives. We want to see everyone who could benefit having access to the technology they deserve. And research like this is vital to build the case.
Tackling kidney complications in children with type 1
Medicines called SGLT2 inhibitors are prescribed to manage blood sugar levels in type 2 diabetes. Researchers also found out they can protect kidneys in people with type 2 diabetes, as they help the kidneys to filter extra sugar out of the blood.
A team of researchers in Canada wanted to find out if SGLT2 inhibitors could help children with type 1 as well, and shared their findings at ADA.
The team recruited 98 children and young people with type 1 diabetes to the ATTEMPT study. Half of them were chosen at random to be treated with a low dose of the SGLT2 inhibitor dapaglifozin, while the other half were treated with a harmless placebo. Everyone carried on taking insulin as normal.
Over 16 weeks, the team measured how well the children’s kidneys were working, their HbA1c, and if there were any side effects from the treatment. They found that the children who’d been taking dapaglifozin saw their HbA1c drop by around 5 mmol/mol (0.5).
And, importantly, they saw an improvement in their kidney function. There were also no side effects linked to taking dapaglifozin.
Now we need more research to see how long these benefits could last for, but these early findings are paving the way to new treatments for young people with type 1 diabetes to protect against kidney disease.
Share this Page
© The British Diabetic Association operating as Diabetes UK, a charity registered in England and Wales (no. 215199) and in Scotland (no. SC039136). A company limited by guarantee registered in England and Wales with (no.00339181) and registered office at Wells Lawrence House, 126 Back Church Lane London E1 1FH

Study links gut microbiome changes to increased risk of type 2 diabetes

Brigham, Broad, and Harvard Chan School researchers found that specific species and strains of bacteria were linked to changes in the functioning of the gut microbiome and a person’s risk of type 2 diabetes
For immediate release: June 25, 2024
Boston, MA—The largest and most ethnically and geographically comprehensive investigation to date of the gut microbiome of people with type 2 diabetes (T2D), prediabetes, and healthy glucose status has found that specific viruses and genetic variants within bacteria correspond with changes in gut microbiome function and T2D risk. Results of the study—which represents a collaboration across Brigham and Women’s Hospital (a founding member of the Mass General Brigham healthcare system), the Broad Institute of MIT and Harvard, and Harvard T.H. Chan School of Public Health—are published in Nature Medicine .
“The microbiome is highly variable across different geographic locations and racial and ethnic groups. If you only study a small, homogeneous population, you will probably miss something,” said co-corresponding author Daniel (Dong) Wang , of the Channing Division of Network Medicine at Brigham and Women’s Hospital, Broad, and Harvard Chan School. “Our study is by far the largest and most diverse study of its kind.”
“The gut microbiome’s relationship to complex, chronic, heterogeneous diseases like T2D is quite subtle,” said co-corresponding author Curtis Huttenhower, of Harvard Chan School and Broad. “Much like studies of large human populations have been crucial for understanding human genetic variation, large and diverse populations are necessary—and increasingly feasible—for detailed microbiome variation studies as well.”
T2D affects approximately 537 million people worldwide. In T2D, the body gradually loses its ability to regulate blood sugar effectively. Research over the last decade has linked changes in the gut microbiome—the collection of bacteria, fungi, and viruses that inhabit our intestines—to the development of T2D. However, prior studies of the gut microbiome and its role in T2D have been too small and varied in study design to draw significant conclusions.
This paper analyzed data from the newly established Microbiome and Cardiometabolic Disease Consortium (MicroCardio). The investigation included newly generated data and those originally captured during several other experiments, encompassing a total of 8,117 gut microbiome metagenomes from ethnically and geographically diverse participants. People included in the study had T2D, prediabetes, or no changes in their blood sugar levels and hailed from the U.S., Israel, Sweden, Finland, Denmark, Germany, France, and China. Co-first authors on the paper are Zhendong Mei, of the Channing Division of Network Medicine at Brigham and Women’s Hospital and Broad, as well as Fenglei Wang , of Harvard Chan School and Broad.
“With this large study, we asked two questions. One is, ‘What are the roles of species and strains that make up the gut microbiome in type 2 diabetes?’ The other question is, ‘What are these microbes doing?’” Wang said. “When we analyzed this data, we found a relatively consistent set of microbial species linked to type 2 diabetes across our study populations. Many of those species have never been reported before.”
To understand the role of these microbes in the gut, the team analyzed species’ functional abilities. Different strains of a microbial species can have varied functions, like the ability to make a specific amino acid. The team found that certain strains had functions that may be linked to varied T2D disease risk.
One major functional difference they saw was that a strain of Prevotella copri —a common microbe in the gut that has the capacity to produce large amounts of branched-chain amino acids (BCAAs)—was more commonly seen in diabetes patients’ gut microbiomes. Previous studies have shown that people with chronically high blood levels of BCAAs have a higher risk of obesity and T2D.
The researchers also found evidence suggesting that bacteriophages—viruses that infect bacteria—could be driving some of the changes they detected within certain strains of gut bacteria.
“Our findings related to bacteriophages were very surprising,” Wang said. “This could mean that the virus infects the bacteria and changes its function in a way that increases or decreases type 2 diabetes risk, but more work is needed to understand this connection.”
In another analysis, the team studied a small subset of samples from patients newly diagnosed with T2D to assess microbiomes that are less likely to have been impacted by medication use or long-term high glucose status. Their results were similar to their larger findings, according to Wang.
“We believe that changes in the gut microbiome cause type 2 diabetes,” said Wang. “The changes to the microbiome may happen first, and diabetes develops later, not the other way around—although future prospective or interventional studies are needed to prove this relation firmly.”
“If these microbial features are causal, we can find a way to change the microbiome and reduce type 2 diabetes risk,” he added. “The microbiome is amenable to intervention—meaning you can change your microbiome, for example, with dietary changes, probiotics, or fecal transplants.”
One major limitation of the study is that, for the most part, it looked at patients’ microbiomes at one point in time. It didn’t look at changes to the gut microbiome or disease status over time. Future studies that build on this work include studying this link over an extended period and examining the strain-specific functions to understand better how they lead to T2D.
“A benefit and a challenge of the human microbiome is that it is highly personalized,” said Huttenhower. “The fact that we each have highly distinct microbial communities and microbial genetics means that very large population studies are needed to find consistent patterns. But once we do, individual microbiomes have the potential to be reshaped to help reduce disease risk.”
Other Harvard Chan authors include Amrisha Bhosle , Andrew Ghazi, Yancong Zhang , Yuxi Liu, Eric Rimm , Walter Willett , Frank Hu , Qibin Qi , Meir Stampfer , and Iris Shai .
The study was funded by National Institute of Diabetes and Digestive and Kidney Diseases (R00 DK119412) and Boston Nutrition Obesity Research Center Pilot & Feasibility Program (P30 DK046200; R24 DK110499), National Institute of Nursing Research (R01 NR01999), National Institute on Aging (R01 AG077489; RF1 AG083764), and National Cancer Institute (R35 CA253185). Fenglei Wang is supported by the American Heart Association Postdoctoral Fellowship (Grant 897161).
“Strain-Specific gut microbial signatures in Type 2 Diabetes Revealed by a Cross-Cohort Analysis of 8,117 Metagenomes,” Zhendong Mei, Fenglei Wang, Amrisha Bhosle, Danyue Dong, Raaj Mehta, Andrew Ghazi, Yancong Zhang, Yuxi Liu, Ehud Rinott, Siyuan Ma, Eric B. Rimm, Martha Daviglus, Walter C. Willett, Rob Knight, Frank B. Hu, Qibin Qi, Andrew T. Chan, Robert D. Burk, Meir J. Stampfer, Iris Shai, Robert C. Kaplan, Curtis Huttenhower, Dong D. Wang, Nature Medicine, June 25, 2024, doi: 10.1038/s41591-024-03067-7
Visit the Harvard Chan School website for the latest news , press releases , and multimedia offerings .
Image: iStock/Elif Bayraktar
For more information:
Maya Brownstein [email protected]
Serena Bronda [email protected]
Karen Zusi-Tran [email protected]
Harvard T.H. Chan School of Public Health brings together dedicated experts from many disciplines to educate new generations of global health leaders and produce powerful ideas that improve the lives and health of people everywhere. As a community of leading scientists, educators, and students, we work together to take innovative ideas from the laboratory to people’s lives—not only making scientific breakthroughs, but also working to change individual behaviors, public policies, and health care practices. Each year, more than 400 faculty members at Harvard Chan School teach 1,000-plus full-time students from around the world and train thousands more through online and executive education courses. Founded in 1913 as the Harvard-MIT School of Health Officers, the School is recognized as America’s oldest professional training program in public health.
Brigham and Women’s Hospital is a founding member of Mass General Brigham and a teaching affiliate of Harvard Medical School. With nearly 1,000 inpatient beds, approximately 50,000 inpatient stays, and over 2.6 million outpatient encounters annually, clinicians across the Brigham provide compassionate, high-quality care in virtually every medical and surgical specialty to patients locally, regionally, nationally and around the world. An international leader in basic, clinical, and translational research, Brigham and Women’s Hospital has nearly 5,000 scientists, including physician-investigators, renowned biomedical researchers and faculty supported by nearly $750 million in funding. The Brigham’s medical preeminence and service to the community dates to 1832, with the opening of the Boston Lying In, one of the nation’s first maternity hospitals designed to care for women unable to afford in-home medical care. Its merger with the Free Hospital for Women resulted in the Boston Hospital for Women in 1966. In 1980, the Boston Hospital for Women, the Peter Bent Brigham Hospital and the Robert Breck Brigham Hospital officially merged to become Brigham and Women’s Hospital. With nearly 21,000 employees across the Brigham family – including the Brigham and Women’s Physicians Organization and Brigham and Women’s Faulkner Hospital – that rich history is the foundation for our commitment to providing superb care for some of the most complex cases, pursuing breakthroughs in biomedical research, training the next generation of health care providers, and serving the local and global community.
Broad Institute of MIT and Harvard was launched in 2004 to empower this generation of creative scientists to transform medicine. The Broad Institute seeks to describe the molecular components of life and their connections; discover the molecular basis of major human diseases; develop effective new approaches to diagnostics and therapeutics; and disseminate discoveries, tools, methods and data openly to the entire scientific community. Founded by MIT, Harvard, Harvard-affiliated hospitals, and the visionary Los Angeles philanthropists Eli and Edythe L. Broad, the Broad Institute includes faculty, professional staff and students from throughout the MIT and Harvard biomedical research communities and beyond, with collaborations spanning over a hundred private and public institutions in more than 40 countries worldwide.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
July 1, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
reputable news agency
Few with type 2 diabetes receive guideline-recommended chronic kidney disease screening
by Elana Gotkine
Fewer than one-quarter of patients with type 2 diabetes (T2D) receive recommended chronic kidney disease (CKD) screening, according to a study published online June 26 in JAMA Network Open .
Daniel Edmonston, M.D., from the Duke University School of Medicine in Durham, North Carolina, and colleagues conducted a retrospective cohort study to examine risk factors for nonconcordance with guideline-recommended CKD screening and treatment in patients with T2D. Adults with an outpatient clinician visit linked to T2D diagnosis between Jan 1, 2015, and Dec 31, 2020, were included; concordance with CKD screening guidelines was assessed in 316,234 adults.
The researchers found that 24.9, 56.5, and 18.6% of participants received creatinine and urinary albumin-to-creatinine ratio screening, one screening measurement, and neither measurement, respectively. There was an association observed for Hispanic ethnicity with lack of screening (relative risk, 1.16).
Lower risk of nonconcordance was seen for heart failure , peripheral artery disease, and hypertension. In 4,215 patients with CKD and albuminuria, 78.0, 4.6, and 21.0% received an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, sodium-glucose cotransporter 2 inhibitor, or neither therapy, respectively.
Associations were seen for peripheral artery disease and lower estimated glomerular filtration rate with lack of CKD treatment; however, diuretic or statin prescription and hypertension were associated with treatment.
"These limitations in CKD screening and treatment identify areas of focus for implementation strategies to improve concordance with guideline-recommended screening and therapies for CKD," the authors write.
Several authors disclosed ties to biopharmaceutical companies, including Boehringer Ingelheim and Eli Lilly. The study was funded by the Boehringer Ingelheim & Lilly Diabetes Alliance.
© 2024 HealthDay . All rights reserved.
Explore further
Feedback to editors

Team develops AI model to improve patient response to cancer therapy
3 hours ago

New cancer treatment slows progression of aggressive neuroendocrine tumors, study finds
16 hours ago

Why schizophrenia and apathy go hand in hand
17 hours ago

Study: Women veterans at higher risk for repeat suicide attempts
18 hours ago

Childhood obesity tied to double the risk of dengue hospitalization

Financial incentives found to double smoking cessation rate for people with socioeconomic challenges
19 hours ago

Study discovers connection between between heart and brain in KBG syndrome

Clinical trial could lead to new 'gold standard' test for prostate cancer detection
20 hours ago

Serendipity reveals new method to fight cancer with T cells

The path to Parkinson's disease: All roads lead to the nigrosome
21 hours ago
Related Stories

Greater reduction seen in mortality with bariatric surgery than GLP-1 RAs
Jun 10, 2024

ACE inhibitor, statin no benefit for T1DM, high albumin excretion
Nov 2, 2017

Predicted albumin-creatinine ratio useful for CKD screening
Jul 14, 2020

CVD mortality similar with diuretic, ACE inhibitor, or calcium channel blocker
Dec 4, 2023

Simple automated tool prompts physicians to screen patients with diabetes for kidney disease
Nov 2, 2023

Antihypertensive combos recommended for BTKi-linked hypertension
Feb 19, 2024
Recommended for you

Research shows how insulin-triggering nutrients vary from person to person, with implications for personalized nutrition


Doctors could soon use facial temperature for early diagnosis of metabolic diseases

Study describes how insulinomas, a rare type of pancreatic beta cell tumor, form

Drugs that kill 'zombie' cells may benefit some older women, but not all, study finds
Jul 2, 2024

Scientists turn white fat cells into calorie-burning beige fat
Jul 1, 2024

Largest ever genetic study of age of puberty in girls shows links with weight gain
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
The use of technology in type 2 diabetes and prediabetes: a narrative review
- Open access
- Published: 29 June 2024
Cite this article
You have full access to this open access article

- Alexandros L. Liarakos ORCID: orcid.org/0000-0003-1713-3064 1 , 2 ,
- Jonathan Z. M. Lim ORCID: orcid.org/0000-0003-3682-8910 3 ,
- Lalantha Leelarathna ORCID: orcid.org/0000-0001-9602-1962 3 , 4 , 5 &
- Emma G. Wilmot ORCID: orcid.org/0000-0002-8698-6207 1 , 2
13 Altmetric
The increasing incidence of type 2 diabetes, which represents 90% of diabetes cases globally, is a major public health concern. Improved glucose management reduces the risk of vascular complications and mortality; however, only a small proportion of the type 2 diabetes population have blood glucose levels within the recommended treatment targets. In recent years, diabetes technologies have revolutionised the care of people with type 1 diabetes, and it is becoming increasingly evident that people with type 2 diabetes can also benefit from these advances. In this review, we describe the current knowledge regarding the role of technologies for people living with type 2 diabetes and the evidence supporting their use in clinical practice. We conclude that continuous glucose monitoring systems deliver glycaemic benefits for individuals with type 2 diabetes, whether treated with insulin or non-insulin therapy; further data are required to evaluate the role of these systems in those with prediabetes (defined as impaired glucose tolerance and/or impaired fasting glucose and/or HbA 1c levels between 39 mmol/mol [5.7%] and 47 mmol/mol [6.4%]). The use of insulin pumps seems to be safe and effective in people with type 2 diabetes, especially in those with an HbA 1c significantly above target. Initial results from studies exploring the impact of closed-loop systems in type 2 diabetes are promising. We discuss directions for future research to fully understand the potential benefits of integrating evidence-based technology into care for people living with type 2 diabetes and prediabetes.
Graphical Abstract
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a major public health issue characterised as a worldwide pandemic. A total of 537 million adults live with diabetes globally, with 90% of all cases diagnosed as type 2 diabetes [ 1 ]. This figure is predicted to rise by almost 50% in the next 20 years, which will be associated with increased rates of vascular complications [ 1 ]. Improved glucose management reduces the risk of vascular complications and mortality in people with type 2 diabetes [ 2 , 3 , 4 , 5 ]. However, data suggest that only around 50% of people with type 2 diabetes achieve the recommended HbA 1c target of <53 mmol/mol (7%) [ 6 , 7 ], highlighting the need for better therapeutic options.
Technologies such as continuous glucose monitoring (CGM), insulin pumps and automated insulin delivery (AID) therapies have been shown to improve HbA 1c , reduce hypoglycaemia and diabetes distress, and improve quality of life (QoL) in people with type 1 diabetes [ 8 , 9 , 10 ], and it is becoming increasingly evident that type 2 diabetes populations can also benefit from these advances [ 11 , 12 ].
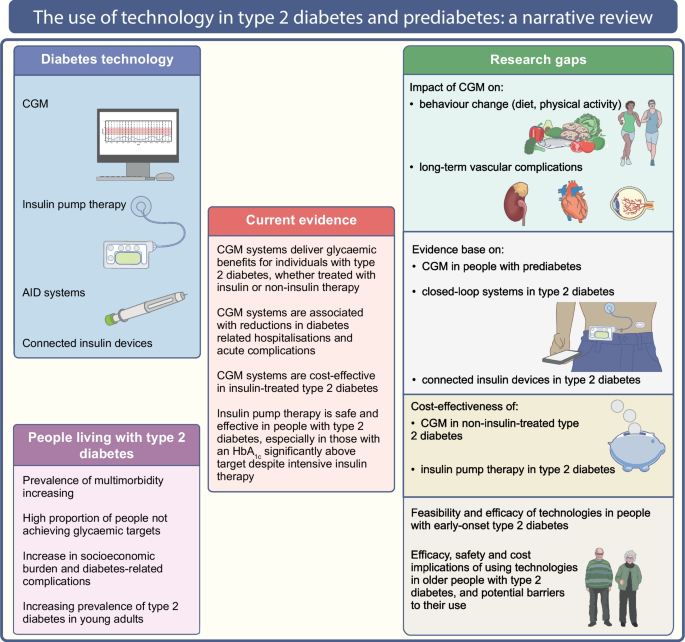
The aim of this review is to describe the current evidence regarding the role of technologies in people with type 2 diabetes, based on randomised trials, observational studies, systematic reviews and meta-analyses. We used the keywords ‘type 2 diabetes’, ‘diabetes technology’, ‘continuous glucose monitoring’, ‘flash glucose monitoring’, ‘intermittently-scanned continuous glucose monitoring’, ‘real-time continuous glucose monitoring’, ‘continuous subcutaneous insulin infusion’, ‘insulin pump’, ‘closed-loop’, ‘automated insulin delivery’, ‘artificial pancreas’, ‘connected insulin devices’, ‘smart insulin pen’ and ‘smart insulin pen caps’ alone and in combination to retrieve available literature from PubMed from inception until January 2024. The current evidence and research gaps in the use of technology in type 2 diabetes and prediabetes (defined as impaired glucose tolerance and/or impaired fasting glucose and/or HbA 1c levels between 39 mmol/mol [5.7%] and 47 mmol/mol [6.4%]) are illustrated in Fig. 1 .

The use of technology in type 2 diabetes and prediabetes. This figure describes the current evidence and research gaps in the use of technology in type 2 diabetes and prediabetes. CGM improves glucose management in insulin- and non-insulin-treated type 2 diabetes, while the role of CGM in prediabetes requires further research. Insulin pumps improve glucose management in individuals with type 2 diabetes, especially in those with high HbA 1c despite intensive insulin therapy. The impact of CGM on behaviour changes and vascular complications, and the evidence base on connected insulin devices and closed-loop systems in type 2 diabetes, require further investigation. This figure is available as a downloadable slide
CGM in type 2 diabetes
Current glucose monitoring technology enables intermittently scanned CGM (isCGM) and real-time CGM (rtCGM). isCGM involves sensors that need to be scanned to provide glucose values, while in rtCGM the sensors display glucose data on a reader or app automatically, without the need for scanning.
A meta-analysis of 26 RCTs (17 rtCGM, nine isCGM), involving 2783 people with type 2 diabetes, showed that, compared with self-monitoring of blood glucose (SMBG), rtCGM and isCGM reduced HbA 1c by 0.19 percentage points (pp) (2 mmol/mol) (95% CI −0.34, −0.04 pp) and 0.31 pp (3 mmol/mol) (95% CI −0.46, −0.17 pp), respectively. Time in range (TIR) increased significantly in isCGM users (three RCTs) and non-significantly in rtCGM users (six RCTs) [ 13 ]. CGM did not significantly impact glucose concentrations, glucose variability, measures of body composition, blood pressure or lipid levels [ 14 , 15 ]. There was no difference in risk of hypoglycaemia between CGM and SMBG [ 14 , 16 , 17 , 18 , 19 ]. Treatment satisfaction improved with CGM use, especially with newer generation systems, compared with SMBG [ 13 , 17 , 20 , 21 ]. A more recent systematic review of CGM in adults with type 2 diabetes, which excluded studies investigating professional CGM and those combining CGM with additional glucose-lowering treatment, identified 12 RCTs (eight rtCGM, four isCGM) involving 1248 people [ 22 ]. Compared with SMBG, CGM (isCGM or rtCGM) resulted in a reduction in HbA 1c (mean difference [MD] −3.43 mmol/mol [−0.31 pp], 95% CI −4.75, −2.11 mmol/mol; p <0.00001). The effect size was comparable between studies including individuals on insulin ± oral therapy (MD −3.27 mmol/mol [−0.30 pp], 95% CI −6.22, −0.31 mmol/mol; p =0.03) and studies including those on oral therapy only (MD −3.22 mmol/mol [−0.29 pp], 95% CI −5.39, −1.05 mmol/mol; p =0.004). Using rtCGM showed a trend towards a larger effect (MD −3.95 mmol/mol [−0.36 pp], 95% CI −5.46, −2.44 mmol/mol; p <0.00001) than using isCGM (MD −1.79 mmol/mol [−0.16 pp], 95% CI −5.28, 1.69 mmol/mol; p =0.31). CGM compared with SMBG was also associated with increased TIR (+6.36%, 95% CI +2.48%, +10.24%; p =0.001) and decreased time below range (TBR) (−0.66 pp, 95% CI −1.21, −0.12 pp; p =0.02). No significant differences in severe hypoglycaemia or macrovascular complications were found between CGM and SMBG. No trials reported data on microvascular complications [ 22 ]. Table 1 summarises the main findings of the key RCTs on CGM use in type 2 diabetes.
CGM use in people with type 2 diabetes on intensive insulin therapies
The DIAMOND RCT [ 15 ] showed that, compared with SMBG, rtCGM resulted in a greater HbA 1c reduction (MD −0.3 pp [–3 mmol/mol]) in a type 2 diabetes population treated with multiple daily insulin injections (MDI). However, the study did not incorporate structured diabetes education to optimise self-management and included people undertaking SMBG at least twice daily at baseline, while the control group were asked to perform SMBG four or more times daily. This may have resulted in underestimation of the impact of rtCGM on plasma glucose levels. In the REPLACE RCT, isCGM resulted in no difference in HbA 1c compared with SMBG. Nevertheless, the hypoglycaemia burden decreased and treatment satisfaction improved in isCGM users. An inclusion criterion of SMBG at least twice daily at baseline was reported and no education on data interpretation was provided [ 17 ], suggesting possible underestimation of the impact of isCGM on HbA 1c . Another RCT of isCGM vs SMBG in a type 2 diabetes population on MDI showed that, although the primary outcome of treatment satisfaction was not met ( p =0.053), users reported more flexibility ( p =0.019) and would recommend isCGM to others ( p =0.023) [ 23 ].
Overall, using CGM in those on intensive insulin therapy is beneficial. Several RCTs and real-world retrospective studies support CGM use, demonstrating improvements in HbA 1c and decreased frequency and severity of hypoglycaemia [ 24 , 25 , 26 , 27 ]. However, to date, no studies have investigated the impact of CGM in people with type 2 diabetes treated with mixed insulin; further research is required to evaluate the potential benefits in this group.
CGM use in people with type 2 diabetes on basal insulin
The MOBILE RCT [ 14 ] found that, compared with SMBG, rtCGM resulted in a greater HbA 1c reduction (MD −4 mmol/mol [–0.4 pp]), improved TIR and decreased time above range (TAR) and TBR in a type 2 diabetes population treated with basal insulin ( p <0.05 for all). The total dose of insulin and body weight did not differ between groups, which raises the possibility that rtCGM use may be directly associated with dietary and activity changes. This is an area that needs to be addressed in future research to gain a more detailed understanding of how CGM may drive glycaemic improvements in this group.
CGM use in people with type 2 diabetes on non-insulin therapy
A pilot RCT of a structured diabetes education programme with episodic rtCGM use in a non-insulin-treated type 2 diabetes population demonstrated no significant HbA 1c improvement compared with SMBG [ 28 ], while an RCT of intermittent short-term use of rtCGM compared with SMBG found a 0.64 pp (6 mmol/mol) HbA 1c reduction ( p =0.014) [ 29 ]. In another RCT [ 30 ], isCGM users showed a higher HbA 1c reduction than SMBG users at 24 weeks (MD –3.2 mmol/mol [−0.29 pp]; p =0.022). The IMMEDIATE RCT explored the glycaemic efficacy of isCGM plus diabetes self-management education compared with education alone in a type 2 diabetes population on at least one non-insulin therapy [ 11 ]. TIR at 4 months was higher in isCGM users ( p =0.009), with little change in medication use (non-insulin glucose-lowering therapies were added for <10% of participants in each arm). This raises the possibility that CGM use may change behaviours, impacting glycaemic outcomes. The effect of CGM use on behaviour change is an area ripe for future research.
A retrospective analysis of 728 people with type 2 diabetes on non-insulin therapies using isCGM found a 1.6 pp (16 mmol/mol) HbA 1c reduction ( p <0.001); a limitation of this analysis was the lack of a control group [ 31 ].
CGM use and acute diabetes-related complications and hospitalisation
The RELIEF [ 32 ] retrospective study evaluated 40,846 people with type 2 diabetes (and 33,165 individuals with type 1 diabetes) in the first 12 months following isCGM initiation. Most within the type 2 diabetes cohort were treated with MDI, while a small proportion were treated with basal insulin or oral agents only. Twelve months following isCGM initiation, hospitalisation for acute diabetes complications decreased by 39% [ 32 ]. Specifically, in the type 2 diabetes population, the annual percentage of hospital admissions decreased for diabetic ketoacidosis (DKA) (from 1.7% to 0.82%), hypoglycaemia (from 0.7% to 0.62%), diabetes-related comas (from 0.23% to 0.16%) and hyperglycaemia (from 0.12% to 0.09%). The 2-year follow-up showed a persistent reduction in acute diabetes-related hospitalisations, from 2.0% before initiating isCGM to 0.75% at 1 year and 0.6% at 2 years follow-up [ 33 ]. Similarly, in a retrospective study carried out in the Netherlands, use of isCGM reduced diabetes-related hospital admissions from 13.7% to 4.7% ( p <0.05) [ 34 ].
The LIBERATES RCT [ 18 ] investigated the effect of isCGM vs SMBG on blood glucose levels in a type 2 diabetes population with acute myocardial infarction, already treated with therapies that may result in hypoglycaemia. Although there was no significant difference in HbA 1c or TIR between groups, isCGM significantly reduced the subsequent risk of hypoglycaemia (Table 1 ).
CGM use in prediabetes
An RCT in individuals with prediabetes showed that isCGM combined with lifestyle coaching improved blood glucose levels and reduced carbohydrate intake and body weight [ 35 ]. A pilot RCT in 13 individuals with prediabetes or type 2 diabetes suggested that rtCGM may facilitate self-monitoring behaviour and increase exercise adherence accompanied by improvements in health-related QoL [ 36 ]. Similarly, a qualitative study in 26 individuals at moderate to high risk of developing type 2 diabetes suggested that using a combination of isCGM and a physical activity monitor may increase self-awareness regarding the impact of lifestyle on short-term health and guide behaviour change [ 37 ]. However, the feedback provided by the devices lacked meaning for several individuals, posing barriers to making changes to diet and physical activity levels. Hence, these findings highlight the need for further research to explore potential modifications required to digital health technologies, including CGM, to sustain engagement and behaviour change in individuals with prediabetes.
In summary, high-quality evidence demonstrates that both isCGM and rtCGM deliver glycaemic benefits for people with type 2 diabetes, whether treated with insulin or non-insulin therapy. The available data suggest that the mechanisms for improvements in blood glucose levels in response to CGM may not be directly reacted to therapeutic change, as one might assume. Further studies are required to provide a detailed understanding of the impact of CGM on dietary intake and physical activity, in addition to exploring the potential benefits of CGM in those with type 2 diabetes treated with mixed insulins.
Continuous subcutaneous insulin infusion in type 2 diabetes
Continuous subcutaneous insulin infusion (CSII), also known as insulin pump therapy, has a clear place in the management of type 1 diabetes [ 38 ]. In contrast, the guidelines for using CSII in type 2 diabetes are less consistent [ 39 , 40 , 41 ].
The OpT2mise RCT, which included 331 individuals with MDI-treated type 2 diabetes, found that, compared with MDI, CSII resulted in a significant 0.7 pp (7 mmol/mol) HbA 1c reduction after 6 months, without increased rates of hypoglycaemia, DKA or hospitalisation [ 42 ]. In another RCT, individuals randomised to the CSII arm achieved a significant 0.9 pp (9 mmol/mol) HbA 1c reduction compared with 0.3 pp (3 mmol/mol) in the MDI arm. After 6 months, the MDI arm crossed over to CSII and at 12 months the individuals continuing CSII had an additional 0.7 pp (7 mmol/mol) reduction in HbA 1c and those switching from MDI to CSII experienced a 0.5 pp (5 mmol/mol) HbA 1c reduction [ 43 ]. Similarly, the VIVID study demonstrated that, compared with MDI, CSII improved HbA 1c without increasing body weight or severe hypoglycaemia [ 44 ].
Real-world data suggest that using CSII in type 2 diabetes can be safe and effective for improving blood glucose levels, particularly in those individuals with higher HbA 1c levels, and is associated with high user satisfaction [ 45 , 46 , 47 ]. In one study, the HbA 1c reduction was sustained for 6 years, indicating the potential long-term benefits of CSII therapy for those with type 2 diabetes [ 46 ].
Initiating CSII in type 2 diabetes has been associated with improved patient-reported outcomes and user satisfaction [ 48 ]. A recent real-world study demonstrated that, compared with MDI, use of a tubeless insulin pump in adults with type 2 diabetes contributed to significant behavioural and psychosocial benefits, including improvements in overall well-being, diabetes distress, hypoglycaemia-related concerns and QoL, as well as greater glycaemic improvement [ 49 ]. User satisfaction and improved glycaemic outcomes have also been shown in studies exploring the use of simplified CSII systems with no need for pump programming or detailed education sessions [ 50 , 51 ].
Overall, CSII is safe and effective in populations with type 2 diabetes, especially in those with an HbA 1c significantly above target despite MDI. CSII may also be associated with decreased healthcare costs as a result of lower rates of diabetes-related complications [ 51 , 52 , 53 , 54 ].
AID systems in type 2 diabetes
AID systems, also known as closed-loop systems, include ‘hybrid’ closed-loop (HCL) therapies, which require carbohydrate counting and user-initiated, pump-delivered meal boluses, and fully closed-loop systems, which eliminate the need for manual mealtime boluses.
An RCT in 136 individuals with type 2 diabetes showed that, compared with subcutaneous insulin therapy, a fully AID system resulted in a significant 24.3 pp TIR increase and 25.9 pp TAR reduction without increasing hypoglycaemia. User satisfaction was also high in the closed-loop group [ 55 ]. Similar results were observed in other RCTs performed in inpatient settings [ 56 , 57 ].
Randomised trials conducted in outpatient settings also suggest glycaemic benefits of fully closed-loop systems [ 58 , 59 , 60 ]. A randomised crossover study in 26 adults with type 2 diabetes compared a fully closed-loop system with standard insulin therapy and a masked glucose sensor (control). The authors demonstrated a significant 15 mmol/mol (1.4 pp) HbA 1c reduction and 35.3 pp TIR increase without elevated hypoglycaemia rates following closed-loop therapy compared with control [ 59 ].
A recent meta-analysis of seven RCTs assessing the efficacy of fully closed-loop systems compared with conventional insulin therapy in 390 people with type 2 diabetes showed that fully closed-loop systems improved TIR (MD +22.40 pp, 95% CI 12.88, 31.91 pp; p <0.01) and reduced TAR (MD −22.67 pp, 95% CI −30.87, −14.46 pp; p <0.01) without a significant difference in hypoglycaemia [ 61 ].
The literature on HCL therapies in type 2 diabetes is limited [ 62 , 63 ]. A feasibility trial in 24 adults with type 2 diabetes managed in an outpatient setting found that HCL was associated with a 14 mmol/mol (1.3 pp) HbA 1c reduction, 21.9 pp TIR increase, 16.9 pp TAR reduction and 0% of time at glucose <3 mmol/l (<54 mg/dl), without a significant change in total daily insulin dose or body weight [ 62 ]. Similarly, a prospective single-arm trial demonstrated a substantial glycaemic improvement (TIR increased by 15 pp) without increased hypoglycaemia in 30 adults with type 2 diabetes using HCL therapy [ 63 ].
In summary, small studies suggest that closed-loop systems could be a potential future therapeutic option in type 2 diabetes. More long-term follow-up studies are required to assess their clinical and cost-effectiveness.
Connected insulin devices in type 2 diabetes
Missed and late insulin injections negatively impact blood glucose levels [ 64 ]. Connected insulin devices, including tracking insulin pens, and smart insulin pens and caps, can record and transfer data about insulin doses and timing to smartphone applications, as well as provide reminders to bolus and facilitate insulin dose calculations [ 65 ]. These features support decision making and inform counselling strategies for the diabetes care team [ 65 , 66 , 67 , 68 ].
In a randomised trial that aimed to assess the efficacy of a smart insulin pen cap for the management of individuals with suboptimally controlled type 2 diabetes (intervention group: feedback and alarm notifications; control group: masked device without alarm notifications), compared with the control group ( n =40), the intervention group ( n =40) experienced a greater HbA 1c reduction (−0.98 pp [–10 mmol/mol] vs −0.72 pp [–7 mmol/mol]; p =0.006) and lower blood glucose levels (8.2 ± 1.9 vs 8.7 ± 2.3 mmol/l [147.0 ± 34 vs 157.6 ± 42 mg/dl]; p <0.01). The device was also associated with high user satisfaction [ 69 ]. In the STYLCONNECT study, people with type 2 diabetes showed a strong interest in using a device that could automate the collection of their insulin data and integrate data from glucose measurement devices [ 70 ]. Another study demonstrated that people with type 2 diabetes preferred connected over non-connected insulin pens because of the capability for automated recording of insulin dose and glucose levels [ 71 ].
Evidence around the use of connected insulin devices in type 2 diabetes is still in an early phase. However, existing literature suggests that these systems may have the potential to improve plasma glucose and user satisfaction, highlighting the importance of further research in this area [ 72 ].
Special groups
Early-onset type 2 diabetes.
Type 2 diabetes in young people is associated with an excess lifetime risk of vascular complications and premature death [ 73 , 74 , 75 , 76 ]. Improving HbA 1c is crucial to reduce long-term diabetes-related complications and mortality rates [ 3 , 4 ]. Despite emerging evidence suggesting the glycaemic benefits of technologies such as CGM in older adults with type 2 diabetes [ 11 , 12 ], research around the use of such systems in young individuals is scarce and limited to small studies [ 77 , 78 ]. Small pilot studies suggest that rtCGM is acceptable and feasible and associated with significant improvements in QoL and glycaemic outcomes in adolescents and young adults with type 2 diabetes [ 77 , 78 ]. To date, there are no studies exploring the impact of CSII or closed-loop systems in young people with type 2 diabetes. Further studies assessing the use of technologies in people with early-onset type 2 diabetes are needed to explore the potential benefit of these therapies in this high-risk cohort.
Pregnancy and type 2 diabetes
Pregnancy complicated by type 2 diabetes is associated with adverse maternal and fetal outcomes [ 79 ]. Maternal hyperglycaemia is a major modifiable risk factor for pregnancy outcomes [ 79 ], and it seems logical that CGM could improve blood glucose levels and optimise the care of pregnant women with pre-existing diabetes. rtCGM reduces the risk of adverse fetal outcomes in women with type 1 diabetes [ 80 ] and may support the management of women with pre-existing diabetes, including the high-risk type 2 diabetes population [ 81 , 82 ]. Non-randomised studies suggest that isCGM can be useful for improving blood glucose levels in pregnant women with type 2 diabetes and is accurate and well-received [ 83 , 84 ]. However, RCT-derived data assessing the efficacy of CGM for maternal glucose management and perinatal outcomes in women with type 2 diabetes are currently lacking, while existing studies involve small numbers of individuals [ 85 , 86 , 87 ]. The ADA clinical practice recommendations for the management of diabetes in pregnancy state that there are insufficient data to support CGM use in all individuals with type 2 diabetes and that the decision to use CGM should be individualised [ 88 ]. NICE guidelines on the management of diabetes in pregnancy indicate that rtCGM should be considered in pregnant women with insulin-treated type 2 diabetes if they have problematic severe hypoglycaemia or unstable blood glucose levels causing concern despite efforts to optimise plasma glucose [ 89 ]. Although the International Consensus on Time in Range defines CGM target ranges for people with diabetes, there are currently no internationally agreed goals for pregnant women with type 2 diabetes [ 88 , 90 ].
Future research should aim to investigate the impact of CGM in pregnant women with type 2 diabetes, assess associations of CGM metrics with pregnancy outcomes and identify the appropriate amount of time spent within defined glucose targets for this population.
End-stage renal disease and type 2 diabetes
The evidence for using technologies in the type 2 diabetes population with end-stage renal disease on dialysis is scarce. Observational studies suggest that CGM is an accurate and efficient method of monitoring interstitial glucose levels in individuals receiving haemodialysis [ 91 , 92 , 93 , 94 , 95 ]. Data suggest that there is increased glucose variability during dialysis days, which could be an additional risk factor for cardiovascular complications [ 96 , 97 ]. CGM can capture glucose variations, guide insulin therapy optimisation and improve glucose levels and hypoglycaemia detection in individuals with insulin-treated type 2 diabetes receiving dialysis [ 98 , 99 , 100 ]. However, these outcomes should be interpreted with caution as most of the existing studies are observational with short-term follow-up, include small numbers of participants and no control group, and provide very limited evidence on peritoneal dialysis. RCTs and studies with longer follow-up are therefore needed.
A post hoc analysis of an RCT in a type 2 diabetes population undergoing inpatient haemodialysis showed that, compared with subcutaneous insulin therapy, a fully closed-loop system was associated with a significant 37.6% increase in the proportion of time when blood glucose was within the target range (5.6–10.0 mmol/l [100–180 mg/dl]), without increasing hypoglycaemia [ 101 ]. Similarly, an RCT in 26 adults with type 2 diabetes requiring dialysis in an outpatient setting showed that a fully AID system significantly increased TIR by 14.6 pp without increased hypoglycaemia compared with standard insulin therapy [ 58 ], suggesting that closed-loop systems could be a novel way to achieve safe and effective glucose management in this vulnerable population.
Older people and type 2 diabetes
The adoption of diabetes technologies in older people remains at an early stage and clinical knowledge is currently modest. Cognitive impairment, multimorbidity and sensory deficits due to increasing age are important challenges in this group [ 102 , 103 ], while the significance of reducing hypoglycaemia is emphasised in international recommendations [ 90 ].
Two RCTs including people with type 2 diabetes on MDI over the age of 60 years found that CGM was associated with a 0.3–0.5 pp (3–5 mmol/mol) HbA 1c reduction compared with SMBG [ 15 , 23 ]. Additional data suggesting that pump therapy may be beneficial in older people with type 2 diabetes on MDI were described in the OpT2mise trial, which included individuals aged up to 75 years [ 42 ]. Another RCT demonstrated that, compared with MDI, a fully closed-loop system resulted in a significant 27.4 pp TIR increase, a 27.7 pp TAR reduction and an unchanged TBR of <1% in 30 people with type 2 diabetes (mean age 69.5 years) requiring nursing support at home. There were no episodes of severe hypoglycaemia or ketoacidosis and both participants and caregivers were highly satisfied with the AID system [ 60 ].
A recent review from the International Geriatric Diabetes Society described the low uptake of diabetes technologies in older adults because of individual and healthcare system-related barriers [ 104 ]. Future studies should aim to explore the efficacy, safety, role, cost implications and potential barriers of using technologies in older people with type 2 diabetes, including those with multimorbidity and cognitive and functional impairment and those living in supervised facilities.
Cost-effectiveness of technologies in type 2 diabetes
The increasing prevalence of type 2 diabetes globally, particularly in younger individuals who will live longer with their disease and have an increased risk of costly diabetes-related complications, is expected to result in several challenges for healthcare systems and clinicians. Increased rates of emergency department use and hospital admissions due to diabetes-related complications are associated with significant healthcare costs [ 105 ]. Hence, using cost-effective technologies, which improve HbA 1c and thereby reduce complications, is imperative.
The cost–benefits of CGM in type 2 diabetes have been described previously [ 106 , 107 ]. A recent retrospective analysis showed that the mean per-patient per-month cost for diabetes-related medical costs in a type 2 diabetes population decreased by US$424 following ≥6 months of rtCGM use. A decrease in hospital admissions was also reported [ 108 ]. Other studies have also demonstrated that CGM use in type 2 diabetes is associated with a reduction in diabetes-related admissions, which would imply cost savings for healthcare systems [ 24 , 33 ]. A base-case analysis showed that long-term isCGM use was cost-effective compared with SMBG in individuals with type 2 diabetes receiving intensive insulin treatment [ 109 ]. Similarly, another analysis demonstrated that rtCGM was likely to be cost-effective compared with SMBG in a type 2 diabetes population receiving insulin therapy, with HbA 1c reduction and QoL benefit from reduced fingerstick testing being the main drivers of the outcomes observed [ 110 ]. Taken together, the available data suggest that CGM is cost-effective, which has led to the inclusion of such systems in guidelines for the management of type 2 diabetes [ 40 , 111 ].
Evidence suggesting the cost-effectiveness of CSII in type 2 diabetes is scarce. Compared with MDI, CSII was associated with a gain in quality-adjusted life-years ranging between 0.17 and 0.43 and a 15–20% reduction in diabetes-related complication costs, which mitigated the higher mean lifetime costs [ 53 , 54 , 112 ]. Sensitivity analyses showed that insulin pump therapy was most cost-effective in individuals with the highest baseline HbA 1c , suggesting that CSII may represent a cost-effective therapeutic alternative for MDI-treated type 2 diabetes populations who have HbA 1c levels above target [ 112 ].
To date, there are no cost-effective analyses of closed-loop systems in type 2 diabetes, and studies comparing the cost-effectiveness of such systems with that of the available glucose-lowering therapies are needed. Lastly, connected insulin devices in this population are potentially cost saving, but further data are required [ 72 ].
People with type 2 diabetes face several challenges in achieving glycaemic targets. Advances in diabetes technologies have provided tools that can facilitate self-management in this high-risk group, especially those on insulin therapy with HbA 1c values above target. Further research will indicate the best place within treatment guidelines of newer technologies such as closed-loop therapies, which have shown very promising results at this initial stage.
Abbreviations
- Automated insulin delivery
- Continuous glucose monitoring
- Continuous subcutaneous insulin infusion
Diabetic ketoacidosis
Hybrid closed-loop
Intermittently scanned continuous glucose monitoring
Mean difference
Multiple daily injections
Percentage points
Quality of life
Real-time continuous glucose monitoring
Self-monitoring of blood glucose
Time above range
Time below range
Time in range
International Diabetes Federation (2021) IDF diabetes atlas, 10th edn. Available from: https://www.diabetesatlas.org . Accessed 14 Jan 2024
UK Prospective Diabetes Study (UKPDS) Group (1998) Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352(9131):854–865. https://doi.org/10.1016/S0140-6736(98)07037-8
Article Google Scholar
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359(15):1577–1589. https://doi.org/10.1056/NEJMoa0806470
Article CAS PubMed Google Scholar
Stratton IM, Adler AI, Neil HA et al (2000) Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321(7258):405–412. https://doi.org/10.1136/bmj.321.7258.405
Article CAS PubMed Central PubMed Google Scholar
Maranta F, Cianfanelli L, Cianflone D (2021) Glycaemic control and vascular complications in diabetes mellitus type 2. Adv Exp Med Biol 1307:129–152. https://doi.org/10.1007/5584_2020_514
NHS Digital (2023) National Diabetes Audit Core Report 1: Care processes and treatment targets 2022-23, underlying data. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/report-1-cp-and-tt-data-release-2022-23/national-diabetes-audit-report-1---care-processes-and-treatment-targets-2022-23-underlying-data . Accessed 15 Jan 2024
Fang M, Wang D, Coresh J, Selvin E (2021) Trends in diabetes treatment and control in U.S. adults, 1999-2018. N Engl J Med 384(23):2219–2228. https://doi.org/10.1056/NEJMsa2032271
Article PubMed Central PubMed Google Scholar
Deshmukh H, Wilmot EG, Gregory R et al (2020) Effect of flash glucose monitoring on glycemic control, hypoglycemia, diabetes-related distress, and resource utilization in the Association of British Clinical Diabetologists (ABCD) nationwide audit. Diabetes Care 43(9):2153–2160. https://doi.org/10.2337/dc20-0738
Jeyam A, Gibb FW, McKnight JA et al (2021) Marked improvements in glycaemic outcomes following insulin pump therapy initiation in people with type 1 diabetes: a nationwide observational study in Scotland. Diabetologia 64(6):1320–1331. https://doi.org/10.1007/s00125-021-05413-7
Crabtree TSJ, Griffin TP, Yap YW et al (2023) Hybrid closed-loop therapy in adults with type 1 diabetes and above-target HbA1c: a real-world observational study. Diabetes Care 46(10):1831–1838. https://doi.org/10.2337/dc23-0635
Aronson R, Brown RE, Chu L et al (2023) IMpact of flash glucose Monitoring in pEople with type 2 Diabetes Inadequately controlled with non-insulin Antihyperglycaemic ThErapy (IMMEDIATE): A randomized controlled trial. Diabetes Obes Metab 25(4):1024–1031. https://doi.org/10.1111/dom.14949
Choe HJ, Rhee EJ, Won JC, Park KS, Lee WY, Cho YM (2022) Effects of patient-driven lifestyle modification using intermittently scanned continuous glucose monitoring in patients with type 2 diabetes: results from the randomized open-label PDF study. Diabetes Care 45(10):2224–2230. https://doi.org/10.2337/dc22-0764
Seidu S, Kunutsor SK, Ajjan RA, Choudhary P (2023) Efficacy and safety of continuous glucose monitoring and intermittently scanned continuous glucose monitoring in patients with type 2 diabetes: a systematic review and meta-analysis of interventional evidence. Diabetes Care 47(1):169–179. https://doi.org/10.2337/dc23-1520
Martens T, Beck RW, Bailey R et al (2021) Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: a randomized clinical trial. JAMA 325(22):2262–2272. https://doi.org/10.1001/jama.2021.7444
Beck RW, Riddlesworth TD, Ruedy K et al (2017) Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med 167(6):365–374. https://doi.org/10.7326/m16-2855
Article PubMed Google Scholar
Ilany J, Bhandari H, Nabriski D, Toledano Y, Konvalina N, Cohen O (2018) Effect of prandial treatment timing adjustment, based on continuous glucose monitoring, in patients with type 2 diabetes uncontrolled with once-daily basal insulin: A randomized, phase IV study. Diabetes, Obes Metab 20(5):1186–1192. https://doi.org/10.1111/dom.13214
Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline JP, Rayman G (2017) Flash glucose-sensing technology as a replacement for blood glucose monitoring for the management of insulin-treated type 2 diabetes: a multicenter, open-label randomized controlled trial. Diabetes Ther 8(1):55–73. https://doi.org/10.1007/s13300-016-0223-6
Ajjan RA, Heller SR, Everett CC et al (2023) Multicenter randomized trial of intermittently scanned continuous glucose monitoring versus self-monitoring of blood glucose in individuals with type 2 diabetes and recent-onset acute myocardial infarction: results of the LIBERATES trial. Diabetes Care 46(2):441–449. https://doi.org/10.2337/dc22-1219
Ajjan RA, Jackson N, Thomson SA (2019) Reduction in HbA1c using professional flash glucose monitoring in insulin-treated type 2 diabetes patients managed in primary and secondary care settings: a pilot, multicentre, randomised controlled trial. Diab Vasc Dis Res 16(4):385–395. https://doi.org/10.1177/1479164119827456
Cox DJ, Banton T, Moncrief M, Conaway M, Diamond A, McCall AL (2020) Minimizing Glucose Excursions (GEM) with continuous glucose monitoring in type 2 diabetes: a randomized clinical trial. J Endocr Soc 4(11):118. https://doi.org/10.1210/jendso/bvaa118
Article CAS Google Scholar
Tang TS, Digby EM, Wright AM et al (2014) Real-time continuous glucose monitoring versus internet-based blood glucose monitoring in adults with type 2 diabetes: a study of treatment satisfaction. Diabetes Res Clin Pract 106(3):481–486. https://doi.org/10.1016/j.diabres.2014.09.050
Jancev M, Vissers T, Visseren FLJ et al (2024) Continuous glucose monitoring in adults with type 2 diabetes: a systematic review and meta-analysis. Diabetologia 67(5):798–810. https://doi.org/10.1007/s00125-024-06107-6
Yaron M, Roitman E, Aharon-Hananel G et al (2019) Effect of flash glucose monitoring technology on glycemic control and treatment satisfaction in patients with type 2 diabetes. Diabetes Care 42(7):1178–1184. https://doi.org/10.2337/dc18-0166
Miller E, Kerr MSD, Roberts GJ, Nabutovsky Y, Wright E (2021) Flash CGM associated with event reduction in nonintensive diabetes therapy. Am J Manag Care 27(11):e372–e377. https://doi.org/10.37765/ajmc.2021.88780
Fokkert M, van Dijk P, Edens M et al (2019) Improved well-being and decreased disease burden after 1-year use of flash glucose monitoring (FLARE-NL4). BMJ Open Diabetes Res Care 7(1):e000809. https://doi.org/10.1136/bmjdrc-2019-000809
Charleer S, Mathieu C, Nobels F et al (2018) Effect of continuous glucose monitoring on glycemic control, acute admissions, and quality of life: a real-world study. J Clin Endocrinol Metab 103(3):1224–1232. https://doi.org/10.1210/jc.2017-02498
Elliott T, Beca S, Beharry R, Tsoukas MA, Zarruk A, Abitbol A (2021) The impact of flash glucose monitoring on glycated hemoglobin in type 2 diabetes managed with basal insulin in Canada: a retrospective real-world chart review study. Diab Vasc Dis Res 18(4):14791641211021374. https://doi.org/10.1177/14791641211021374
Price DA, Deng Q, Kipnes M, Beck SE (2021) Episodic real-time CGM use in adults with type 2 diabetes: results of a pilot randomized controlled trial. Diabetes Ther 12(7):2089–2099. https://doi.org/10.1007/s13300-021-01086-y
Moon SJ, Kim KS, Lee WJ, Lee MY, Vigersky R, Park CY (2023) Efficacy of intermittent short-term use of a real-time continuous glucose monitoring system in non-insulin-treated patients with type 2 diabetes: A randomized controlled trial. Diabetes Obes Metab 25(1):110–120. https://doi.org/10.1111/dom.14852
Wada E, Onoue T, Kobayashi T et al (2020) Flash glucose monitoring helps achieve better glycemic control than conventional self-monitoring of blood glucose in non-insulin-treated type 2 diabetes: a randomized controlled trial. BMJ Open Diabetes Res Care 8(1):e001115. https://doi.org/10.1136/bmjdrc-2019-001115
Wright EE Jr, Kerr MSD, Reyes IJ, Nabutovsky Y, Miller E (2021) Use of flash continuous glucose monitoring is associated with A1C reduction in people with type 2 diabetes treated with basal insulin or noninsulin therapy. Diabetes Spectr 34(2):184–189. https://doi.org/10.2337/ds20-0069
Roussel R, Riveline JP, Vicaut E et al (2021) Important drop in rate of acute diabetes complications in people with type 1 or type 2 diabetes after initiation of flash glucose monitoring in France: the RELIEF study. Diabetes Care 44(6):1368–1376. https://doi.org/10.2337/dc20-1690
Guerci B, Roussel R, Levrat-Guillen F et al (2023) Important decrease in hospitalizations for acute diabetes events following free style libre system initiation in people with type 2 diabetes on basal insulin therapy in France. Diabetes Technol Ther 25(1):20–30. https://doi.org/10.1089/dia.2022.0271
Bergenstal RM, Kerr MSD, Roberts GJ, Souto D, Nabutovsky Y, Hirsch IB (2021) Flash CGM is associated with reduced diabetes events and hospitalizations in insulin-treated type 2 diabetes. J Endocr Soc 5(4):bvab013. https://doi.org/10.1210/jendso/bvab013
Kitazawa M, Takeda Y, Hatta M et al (2023) Lifestyle intervention with smartphone app and is CGM for people at high risk of type 2 diabetes: randomized trial. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgad639
Article PubMed Central Google Scholar
Bailey KJ, Little JP, Jung ME (2016) Self-monitoring using continuous glucose monitors with real-time feedback improves exercise adherence in individuals with impaired blood glucose: a pilot study. Diabetes Technol Ther 18(3):185–193. https://doi.org/10.1089/dia.2015.0285
Whelan ME, Denton F, Bourne CLA et al (2021) A digital lifestyle behaviour change intervention for the prevention of type 2 diabetes: a qualitative study exploring intuitive engagement with real-time glucose and physical activity feedback. BMC Public Health 21(1):130. https://doi.org/10.1186/s12889-020-09740-z
Holt RIG, DeVries JH, Hess-Fischl A et al (2021) The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 64(12):2609–2652. https://doi.org/10.1007/s00125-021-05568-3
National Institute fo Health and Care Excellence (2008) Continuous subcutaneous insulin infusion for the treatment of diabetes mellitus. Technology appraisal guidance [TA151]. Available from: https://www.nice.org.uk/guidance/ta151 . Accessed 16 Jan 2024
American Diabetes Association Professional Practice Committee (2024) 7. Diabetes Technology: Standards of Care in Diabetes-2024. Diabetes Care 47(Suppl 1):S126-s144. https://doi.org/10.2337/dc24-S007
Davies MJ, Aroda VR, Collins BS et al (2022) Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 65(12):1925–1966. https://doi.org/10.1007/s00125-022-05787-2
Reznik Y, Cohen O, Aronson R et al (2014) Insulin pump treatment compared with multiple daily injections for treatment of type 2 diabetes (OpT2mise): a randomised open-label controlled trial. Lancet 384(9950):1265–1272. https://doi.org/10.1016/s0140-6736(14)61037-0
Chlup R, Runzis S, Castaneda J, Lee SW, Nguyen X, Cohen O (2018) Complex assessment of metabolic effectiveness of insulin pump therapy in patients with type 2 diabetes beyond HbA1c reduction. Diabetes Technol Ther 20(2):153–159. https://doi.org/10.1089/dia.2017.0283
Grunberger G, Bhargava A, Ly T et al (2020) Human regular U-500 insulin via continuous subcutaneous insulin infusion versus multiple daily injections in adults with type 2 diabetes: The VIVID study. Diabetes Obes Metab 22(3):434–441. https://doi.org/10.1111/dom.13947
Gentry CK, Cross LB, Gross BN, McFarland MS, Bestermann WH (2011) Retrospective analysis and patient satisfaction assessment of insulin pump therapy in patients with type 2 diabetes. South Med J 104(1):24–28. https://doi.org/10.1097/SMJ.0b013e3181fa7230
Reznik Y, Morera J, Rod A et al (2010) Efficacy of continuous subcutaneous insulin infusion in type 2 diabetes mellitus: a survey on a cohort of 102 patients with prolonged follow-up. Diabetes Technol Ther 12(12):931–936. https://doi.org/10.1089/dia.2010.0110
Stallings DE, Higgins KJ (2023) The use of multiple daily injections versus insulin pump therapy for HgbA1c reduction in patients with insulin-dependent type 2 diabetes. J Am Assoc Nurse Pract 35(10):615–619. https://doi.org/10.1097/jxx.0000000000000890
Frias JP, Bode BW, Bailey TS, Kipnes MS, Brunelle R, Edelman SV (2011) A 16-week open-label, multicenter pilot study assessing insulin pump therapy in patients with type 2 diabetes suboptimally controlled with multiple daily injections. J Diabetes Sci Technol 5(4):887–893. https://doi.org/10.1177/193229681100500410
Polonsky WH, Soriano EC (2023) Psychosocial and glycemic benefits for insulin-using adults with type 2 diabetes after six months of pump therapy: a quasi-experimental approach. J Diabetes Sci Technol 4:19322968231198532. https://doi.org/10.1177/19322968231198533
Mader JK, Lilly LC, Aberer F et al (2018) Improved glycaemic control and treatment satisfaction with a simple wearable 3-day insulin delivery device among people with Type 2 diabetes. Diabet Med 35(10):1448–1456. https://doi.org/10.1111/dme.13708
Ekanayake P, Edelman S (2023) Identifying patients with type 2 diabetes who might benefit from insulin pump therapy: Literature review, clinical opportunities, potential benefits and challenges. Diabetes Obes Metab 25(Suppl 2):3–20. https://doi.org/10.1111/dom.15059
David G, Gill M, Gunnarsson C, Shafiroff J, Edelman S (2014) Switching from multiple daily injections to CSII pump therapy: insulin expenditures in type 2 diabetes. Am J Manag Care 20(11):e490-497
PubMed Google Scholar
Roze S, Duteil E, Smith-Palmer J et al (2016) Cost-effectiveness of continuous subcutaneous insulin infusion in people with type 2 diabetes in the Netherlands. J Med Econ 19(8):742–749. https://doi.org/10.3111/13696998.2016.1167695
Wahlqvist P, Warner J, Morlock R (2018) Cost-effectiveness of simple insulin infusion devices compared to multiple daily injections in uncontrolled type 2 diabetics in the United States based on a simulation model. J Health Econ Outcomes Res 6(1):84–95. https://doi.org/10.36469/9789
Bally L, Thabit H, Hartnell S et al (2018) Closed-loop insulin delivery for glycemic control in noncritical care. N Engl J Med 379(6):547–556. https://doi.org/10.1056/NEJMoa1805233
Thabit H, Hartnell S, Allen JM et al (2017) Closed-loop insulin delivery in inpatients with type 2 diabetes: a randomised, parallel-group trial. Lancet Diabetes Endocrinol 5(2):117–124. https://doi.org/10.1016/s2213-8587(16)30280-7
Boughton CK, Bally L, Martignoni F et al (2019) Fully closed-loop insulin delivery in inpatients receiving nutritional support: a two-centre, open-label, randomised controlled trial. Lancet Diabetes Endocrinol 7(5):368–377. https://doi.org/10.1016/s2213-8587(19)30061-0
Boughton CK, Tripyla A, Hartnell S et al (2021) Fully automated closed-loop glucose control compared with standard insulin therapy in adults with type 2 diabetes requiring dialysis: an open-label, randomized crossover trial. Nat Med 27(8):1471–1476. https://doi.org/10.1038/s41591-021-01453-z
Daly AB, Boughton CK, Nwokolo M et al (2023) Fully automated closed-loop insulin delivery in adults with type 2 diabetes: an open-label, single-center, randomized crossover trial. Nat Med 29(1):203–208. https://doi.org/10.1038/s41591-022-02144-z
Reznik Y, Carvalho M, Fendri S et al (2024) Should people with type 2 diabetes treated by multiple daily insulin injections with home health care support be switched to hybrid closed-loop? The CLOSE AP+ randomized controlled trial. Diabetes Obes Metab 26(2):622–630. https://doi.org/10.1111/dom.15351
Amer BE, Yaqout YE, Abozaid AM, Afifi E, Aboelkhier MM (2024) Does fully closed-loop automated insulin delivery improve glycaemic control in patients with type 2 diabetes? A meta-analysis of randomized controlled trials. Diabet Med 41(1):e15196. https://doi.org/10.1111/dme.15196
Davis GM, Peters AL, Bode BW et al (2023) Safety and efficacy of the omnipod 5 automated insulin delivery system in adults with type 2 diabetes: from injections to hybrid closed-loop therapy. Diabetes Care 46(4):742–750. https://doi.org/10.2337/dc22-1915
Levy CJ, Raghinaru D, Kudva YC et al (2024) Beneficial effects of control-IQ automated insulin delivery in basal-bolus and basal-only insulin users with type 2 diabetes. Clin Diabetes 42(1):116–124. https://doi.org/10.2337/cd23-0025
Randløv J, Poulsen JU (2008) How much do forgotten insulin injections matter to hemoglobin a1c in people with diabetes? A simulation study. J Diabetes Sci Technol 2(2):229–235. https://doi.org/10.1177/193229680800200209
Lingen K, Pikounis T, Bellini N, Isaacs D (2023) Advantages and disadvantages of connected insulin pens in diabetes management. Endocr Connect 12(11):e230108. https://doi.org/10.1530/ec-23-0108
MacLeod J, Im GH, Smith M, Vigersky RA (2024) Shining the spotlight on multiple daily insulin therapy: real-world evidence of the InPen smart insulin pen. Diabetes Technol Ther 26(1):33–39. https://doi.org/10.1089/dia.2023.0365
MacLeod J, Vigersky RA (2023) A review of precision insulin management with smart insulin pens: opening up the digital door to people on insulin injection therapy. J Diabetes Sci Technol 17(2):283–289. https://doi.org/10.1177/19322968221134546
Heinemann L, Jendle J (2023) Language matters: connected pens, smart pens, connected smart pens, or just digital pens? J Diabetes Sci Technol 17(4):875–877. https://doi.org/10.1177/19322968221148508
Galindo RJ, Ramos C, Cardona S et al (2023) Efficacy of a smart insulin pen cap for the management of patients with uncontrolled type 2 diabetes: a randomized cross-over trial. J Diabetes Sci Technol 17(1):201–207. https://doi.org/10.1177/19322968211033837
Naïditch N, Mauchant C, Benabbad I et al (2023) STYLCONNECT study: an assessment of automatic data collection devices by people living with diabetes and using an insulin pen. Diabetes Ther 14(2):303–318. https://doi.org/10.1007/s13300-022-01337-6
Seo J, Heidenreich S, Aldalooj E et al (2023) Patients’ preferences for connected insulin pens: a discrete choice experiment among patients with type 1 and type 2 diabetes. Patient 16(2):127–138. https://doi.org/10.1007/s40271-022-00610-x
Cranston I, Jamdade V, Liao B, Newson RS (2023) Clinical, economic, and patient-reported benefits of connected insulin pen systems: a systematic literature review. Adv Ther 40(5):2015–2037. https://doi.org/10.1007/s12325-023-02478-1
Duncan BB, Schmidt MI (2023) Many years of life lost to young-onset type 2 diabetes. Lancet Diabetes Endocrinol 11(10):709–710. https://doi.org/10.1016/s2213-8587(23)00255-3
Misra S, Ke C, Srinivasan S et al (2023) Current insights and emerging trends in early-onset type 2 diabetes. Lancet Diabetes Endocrinol 11(10):768–782. https://doi.org/10.1016/s2213-8587(23)00225-5
Magliano DJ, Sacre JW, Harding JL, Gregg EW, Zimmet PZ, Shaw JE (2020) Young-onset type 2 diabetes mellitus - implications for morbidity and mortality. Nat Rev Endocrinol 16(6):321–331. https://doi.org/10.1038/s41574-020-0334-z
Emerging Risk Factors Collaboration (2023) Life expectancy associated with different ages at diagnosis of type 2 diabetes in high-income countries: 23 million person-years of observation. Lancet Diabetes Endocrinol 11(10):731–742. https://doi.org/10.1016/s2213-8587(23)00223-1
Chesser H, Srinivasan S, Puckett C, Gitelman SE, Wong JC (2022) Real-time continuous glucose monitoring in adolescents and young adults with type 2 diabetes can improve quality of life. J Diabetes Sci Technol 19322968221139873. https://doi.org/10.1177/19322968221139873
Chang N, Barber ROB, Llovido Alula J, Durazo-Arvizu R, Chao LC (2023) Continuous glucose monitoring versus standard of care in adolescents with type 2 diabetes: a pilot randomized cross-over trial. J Diabetes Sci Technol 17:1419–1420. https://doi.org/10.1177/19322968231178284
Murphy HR, Howgate C, O’Keefe J et al (2021) Characteristics and outcomes of pregnant women with type 1 or type 2 diabetes: a 5-year national population-based cohort study. Lancet Diabetes Endocrinol 9(3):153–164. https://doi.org/10.1016/s2213-8587(20)30406-x
Feig DS, Donovan LE, Corcoy R et al (2017) Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): a multicentre international randomised controlled trial. Lancet 390(10110):2347–2359. https://doi.org/10.1016/s0140-6736(17)32400-5
Sanusi AA, Xue Y, McIlwraith C et al (2024) Association of continuous glucose monitoring metrics with pregnancy outcomes in patients with preexisting diabetes. Diabetes Care 47(1):89–96. https://doi.org/10.2337/dc23-0636
McLean A, Barr E, Tabuai G, Murphy HR, Maple-Brown L (2023) Continuous glucose monitoring metrics in high-risk pregnant women with type 2 diabetes. Diabetes Technol Ther 25(12):836–844. https://doi.org/10.1089/dia.2023.0300
McLean A, Sinha A, Barr E, Maple-Brown L (2023) Feasibility and acceptability of intermittently scanned continuous glucose monitoring for women with type 2 diabetes in pregnancy. J Diabetes Sci Technol 17:256–258. https://doi.org/10.1177/19322968221124956
Scott EM, Bilous RW, Kautzky-Willer A (2018) Accuracy, user acceptability, and safety evaluation for the FreeStyle Libre flash glucose monitoring system when used by pregnant women with diabetes. Diabetes Technol Ther 20(3):180–188. https://doi.org/10.1089/dia.2017.0386
Wilkie G, Melnik V, Brainard L et al (2023) Continuous glucose monitor use in type 2 diabetes mellitus in pregnancy and perinatal outcomes: a systematic review and meta-analysis. Am J Obstet Gynecol MFM 5(7):100969. https://doi.org/10.1016/j.ajogmf.2023.100969
Tumminia A, Milluzzo A, Festa C et al (2021) Efficacy of flash glucose monitoring in pregnant women with poorly controlled pregestational diabetes (FlashMom): a randomized pilot study. Nutr Metab Cardiovasc Dis 31(6):1851–1859. https://doi.org/10.1016/j.numecd.2021.03.013
Rademaker D, van der Wel AWT, van Eekelen R et al (2023) Continuous glucose monitoring metrics and pregnancy outcomes in insulin-treated diabetes: a post-hoc analysis of the GlucoMOMS trial. Diabetes Obes Metab 25(12):3798–3806. https://doi.org/10.1111/dom.15276
American Diabetes Association Professional Practice Committee (2024) 15. Management of diabetes in pregnancy: standards of care in diabetes-2024. Diabetes Care 47(Suppl 1):S282-s294. https://doi.org/10.2337/dc24-S015
National Institute for Health and Care Excellence (2020) Diabetes in pregnancy: management from preconception to the postnatal period. NICE guideline [NG3]. Available from: https://www.nice.org.uk/guidance/ng3 . Accessed 20 Jan 2024
Battelino T, Danne T, Bergenstal RM et al (2019) Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care 42(8):1593–1603. https://doi.org/10.2337/dci19-0028
Villard O, Breton MD, Rao S et al (2022) Accuracy of a factory-calibrated continuous glucose monitor in individuals with diabetes on hemodialysis. Diabetes Care 45(7):1666–1669. https://doi.org/10.2337/dc22-0073
Hissa MRN, Hissa PNG, Guimarães SB, Hissa MN (2021) Use of continuous glucose monitoring system in patients with type 2 mellitus diabetic during hemodialysis treatment. Diabetol Metab Syndr 13(1):104. https://doi.org/10.1186/s13098-021-00722-8
Mambelli E, Cristino S, Mosconi G, Göbl C, Tura A (2021) Flash glucose monitoring to assess glycemic control and variability in hemodialysis patients: the GIOTTO study. Front Med (Lausanne) 8:617891. https://doi.org/10.3389/fmed.2021.617891
Wang F, Wang D, Lu XL, Sun XM, Duan BH (2022) Continuous glucose monitoring in diabetes patients with chronic kidney disease on dialysis: a meta-analysis. Minerva Endocrinol (Torino) 47(3):325–333. https://doi.org/10.23736/s2724-6507.20.03284-8
Avari P, Tang W, Jugnee N et al (2023) The accuracy of continuous glucose sensors in people with diabetes undergoing hemodialysis (ALPHA Study). Diabetes Technol Ther 25(7):447–456. https://doi.org/10.1089/dia.2023.0013
Yusof Khan AHK, Zakaria NF, Zainal Abidin MA, Kamaruddin NA (2021) Prevalence of glycemic variability and factors associated with the glycemic arrays among end-stage kidney disease patients on chronic hemodialysis. Medicine (Baltimore) 100(30):e26729. https://doi.org/10.1097/md.0000000000026729
Colette C, Monnier L (2007) Acute glucose fluctuations and chronic sustained hyperglycemia as risk factors for cardiovascular diseases in patients with type 2 diabetes. Horm Metab Res 39(9):683–686. https://doi.org/10.1055/s-2007-985157
Mirani M, Berra C, Finazzi S et al (2010) Inter-day glycemic variability assessed by continuous glucose monitoring in insulin-treated type 2 diabetes patients on hemodialysis. Diabetes Technol Ther 12(10):749–753. https://doi.org/10.1089/dia.2010.0052
Gallieni M, De Salvo C, Lunati ME et al (2021) Continuous glucose monitoring in patients with type 2 diabetes on hemodialysis. Acta Diabetol 58(8):975–981. https://doi.org/10.1007/s00592-021-01699-6
Jakubowska Z, Malyszko J (2023) Continuous glucose monitoring in people with diabetes and end-stage kidney disease-review of association studies and Evidence-Based discussion. J Nephrol https://doi.org/10.1007/s40620-023-01802-w
Bally L, Gubler P, Thabit H et al (2019) Fully closed-loop insulin delivery improves glucose control of inpatients with type 2 diabetes receiving hemodialysis. Kidney Int 96(3):593–596. https://doi.org/10.1016/j.kint.2019.03.006
Srikanth V, Sinclair AJ, Hill-Briggs F, Moran C, Biessels GJ (2020) Type 2 diabetes and cognitive dysfunction-towards effective management of both comorbidities. Lancet Diabetes Endocrinol 8(6):535–545. https://doi.org/10.1016/s2213-8587(20)30118-2
Espeland MA, Justice JN, Bahnson J et al (2022) Eight-year changes in multimorbidity and frailty in adults with type 2 diabetes mellitus: associations with cognitive and physical function and mortality. J Gerontol A Biol Sci Med Sci 77(8):1691–1698. https://doi.org/10.1093/gerona/glab342
Huang ES, Sinclair A, Conlin PR et al (2023) The growing role of technology in the care of older adults with diabetes. Diabetes Care 46(8):1455–1463. https://doi.org/10.2337/dci23-0021
Stedman M, Lunt M, Davies M et al (2020) Cost of hospital treatment of type 1 diabetes (T1DM) and type 2 diabetes (T2DM) compared to the non-diabetes population: a detailed economic evaluation. BMJ Open 10(5):e033231. https://doi.org/10.1136/bmjopen-2019-033231
Aleppo G, Hirsch IB, Parkin CG et al (2023) Coverage for continuous glucose monitoring for individuals with type 2 diabetes treated with nonintensive therapies: an evidence-based approach to policymaking. Diabetes Technol Ther 25(10):741–751. https://doi.org/10.1089/dia.2023.0268
Fonda SJ, Graham C, Munakata J, Powers JM, Price D, Vigersky RA (2016) The cost-effectiveness of Real-Time Continuous Glucose Monitoring (RT-CGM) in type 2 diabetes. J Diabetes Sci Technol 10(4):898–904. https://doi.org/10.1177/1932296816628547
Norman GJ, Paudel ML, Parkin CG, Bancroft T, Lynch PM (2022) Association between real-time continuous glucose monitor use and diabetes-related medical costs for patients with type 2 diabetes. Diabetes Technol Ther 24(7):520–524. https://doi.org/10.1089/dia.2021.0525
Ajjan R, Bilir SP, Hellmund R, Souto D (2022) Cost-effectiveness analysis of flash glucose monitoring system for people with type 2 diabetes receiving intensive insulin treatment. Diabetes Ther 13(11–12):1933–1945. https://doi.org/10.1007/s13300-022-01325-w
Isitt JJ, Roze S, Sharland H et al (2022) Cost-effectiveness of a real-time continuous glucose monitoring system versus self-monitoring of blood glucose in people with type 2 diabetes on insulin therapy in the UK. Diabetes Ther 13(11–12):1875–1890. https://doi.org/10.1007/s13300-022-01324-x
National Institute for Health and Care Excellence (2022) Type 2 diabetes in adults: management. NICE guideline [NG28]. Available from: https://www.nice.org.uk/guidance/ng28 . Accessed 16 Jan 2024
Roze S, Smith-Palmer J, Delbaere A et al (2019) Cost-effectiveness of continuous subcutaneous insulin infusion versus multiple daily injections in patients with poorly controlled type 2 diabetes in Finland. Diabetes Ther 10(2):563–574. https://doi.org/10.1007/s13300-019-0575-9
Download references
Author information
Authors and affiliations.
Department of Diabetes and Endocrinology, University Hospitals of Derby and Burton NHS Foundation Trust, Royal Derby Hospital, Derby, UK
Alexandros L. Liarakos & Emma G. Wilmot
School of Medicine, Faculty of Medicine and Health Sciences, University of Nottingham, Nottingham, UK
Diabetes, Endocrinology and Metabolism Centre, Manchester University NHS Foundation Trust, Manchester Royal Infirmary, Manchester, UK
Jonathan Z. M. Lim & Lalantha Leelarathna
Department of Diabetes, Imperial College Healthcare NHS Trust, London, UK
Lalantha Leelarathna
Faculty of Medicine, Department of Metabolism, Digestion and Reproduction, Imperial College London, London, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Emma G. Wilmot .
Ethics declarations
This review received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Authors’ relationships and activities
ALL has received support to attend conferences from Eli Lilly and Novo Nordisk and research support from the Association of British Clinical Diabetologists. LL has received research support from Abbott Diabetes Care and Dexcom, participated in advisory groups for Abbott Diabetes Care, Insulet, Dexcom, Medtronic and Roche Diabetes, and received fees for speaking from Sanofi, Insulet, Medtronic and Abbott. EGW has received personal fees from Abbott, AstraZeneca, Dexcom, Eli Lilly, Embecta, Glooko, Insulet, Medtronic, Novo Nordisk, Roche, Sanofi, Sinocare and Ypsomed, research support from the Association of British Clinical Diabetologists, Abbott, Diabetes UK, Embecta, Insulet, Novo Nordisk and Sanofi, and medical writing support from Abbott, Eli Lilly and Embecta, and has participated in consultancy/been an advisory board member for Abbott, Dexcom, Eli Lilly, Embecta, Insulet, Medtronic, Novo Nordisk, Roche and Sanofi. JZML declares that there are no relationships or activities that might bias, or be perceived to bias, this work.
Contribution statement
All authors were responsible for drafting the article and reviewing it critically for important intellectual content. All authors approved the version to be published.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alexandros L. Liarakos and Jonathan Z. M. Lim are joint first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Figure slide (PPTX 238 KB)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Liarakos, A.L., Lim, J.Z.M., Leelarathna, L. et al. The use of technology in type 2 diabetes and prediabetes: a narrative review. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06203-7
Download citation
Received : 05 March 2024
Accepted : 09 May 2024
Published : 29 June 2024
DOI : https://doi.org/10.1007/s00125-024-06203-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Closed loop
- Diabetes technology
- Insulin pump
- Prediabetes
- Type 2 diabetes
- Find a journal
- Publish with us
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Diabetes articles from across Nature Portfolio
Diabetes describes a group of metabolic diseases characterized by high blood sugar levels. Diabetes can be caused by the pancreas not producing insulin (type 1 diabetes) or by insulin resistance (cells do not respond to insulin; type 2 diabetes).

Brain fluid probed by ultrasound using squishy cubes
Soft solids that swell with shifts in pressure, temperature and pH provide a way of detecting such changes in the fluid around the brain. The method could be used to determine other properties of fluids elsewhere in the body.
- Jules J. Magda
Related Subjects
- Diabetes complications
- Diabetes insipidus
- Gestational diabetes
- Type 1 diabetes
- Type 2 diabetes
Latest Research and Reviews

The metabolic consequences of ‘yo-yo’ dieting are markedly influenced by genetic diversity
- Senthil Thillainadesan
- Aaron Lambert
- Samantha L. Hocking
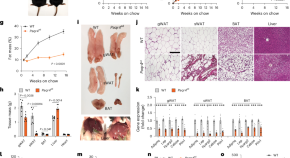
PAQR4 regulates adipocyte function and systemic metabolic health by mediating ceramide levels
PAQR4 regulates cellular ceramide synthesis and accumulation to mediate adipose tissue function, glucose homoeostasis and, thus, systemic metabolic health.
- Qingzhang Zhu
- Shiuhwei Chen
- Philipp E. Scherer

Identification of unique cell type responses in pancreatic islets to stress
Endoplasmic reticulum and inflammatory stress are associated with diabetes. Maestas et al. use single-cell sequencing to profile primary human islets under stress and identified tissue and cell-type responses.
- Marlie M. Maestas
- Matthew Ishahak
- Jeffrey R. Millman
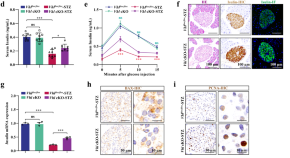
Activation of the osteoblastic HIF-1α pathway partially alleviates the symptoms of STZ-induced type 1 diabetes mellitus via RegIIIγ
- Minglong Qiu
- Leilei Chang
- Changwei Li
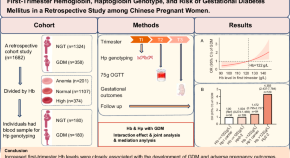
First-trimester hemoglobin, haptoglobin genotype, and risk of gestational diabetes mellitus in a retrospective study among Chinese pregnant women

IFNγ-IL12 axis regulates intercellular crosstalk in metabolic dysfunction-associated steatotic liver disease
Metabolic liver disease is highly prevalent in subjects with obesity and involves inflammation, insulin resistance, and fibrosis, leading to cirrhosis. Here, the authors show the IFNγ-IL12 axis in regulating intercellular crosstalk in the liver and playing a major role in the pathogenesis of metabolic liver disease.
- Randall H. Friedline
- Hye Lim Noh
- Jason K. Kim
News and Comment

Does Ozempic boost fertility? What the science says
Blockbuster weight-loss drugs have been linked to unexplained pregnancies. Research shows it is plausible, but more data are needed.
- Gillian Dohrn

How medical schools can prepare students for new technologies
Patient educators and nurses can demonstrate the real-life use of health technologies.
- Chantal Mathieu
Bile acid receptor protects against diabetic cardiomyopathy
Activation of the bile acid receptor TGR5 inhibits CD36-mediated fatty acid uptake in cardiomyocytes and protects against cardiac lipotoxicity and the development of diabetic cardiomyopathy in mice, according to a new study.
- Irene Fernández-Ruiz
Response to comment on “Credibility of Chat-GPT in the assessment of obesity in type 2 diabetes according to the guidelines”
- Tugba Barlas
- Alev Eroglu Altinova
- Fusun Balos Toruner
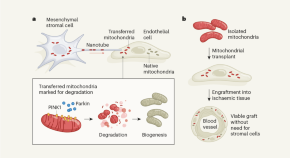
Cells destroy donated mitochondria to build blood vessels
Organelles called mitochondria are transferred to blood-vessel-forming cells by support cells. Unexpectedly, these mitochondria are degraded, kick-starting the production of new ones and boosting vessel formation.
- Chantell S. Evans
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Groundbreaking study shows why drinking from plastic bottles may increase your risk of type 2 diabetes
- BPA is an industrial chemical that scientists have linked to hormone disruption and diabetes risk.
- Plastic water bottles and food containers can leach BPA into what you eat and drink.
- A new study found it can be risky at levels previously considered safe by government agencies.

Scientists have long suspected that industrial chemicals used in plastic water bottles can disrupt human hormones .
But, to date, evidence has been observational, meaning it shows an association between plastics exposure and certain diseases, but can't prove a causal effect.
Now, a groundbreaking new study shows direct evidence that bisphenol A — or, BPA, a chemical used to package food and drink — can reduce sensitivity to insulin, a hormone that helps regulate blood sugar.
An impaired ability to respond to insulin, known as insulin resistance , can mean chronically high blood sugar levels and a much higher risk of type 2 diabetes.
The researchers, who presented their findings at the 2024 Scientific Sessions of the American Diabetes Association , said this study shows the EPA may need to reconsider the safe limits for exposure to BPA in plastic bottles, food containers, and other containers.
Even so-called safe levels of BPA may cause health issues
Researchers from California Polytechnic State University studied 40 healthy adults who were randomly assigned to receive either a placebo or a small dose of BPA daily.
After four days, the participants who were given BPA were less responsive to insulin, while the placebo group did not experience any change.
Related stories
The dose of BPA that participants received, 50 micrograms per kilogram of body weight per day, is an amount currently classified as safe by the EPA .
"These results suggest that maybe the US EPA safe dose should be reconsidered and that healthcare providers could suggest these changes to patients," Todd Hagobian, senior author of the new study and professor at California Polytechnic State University, said in a press release.
The FDA considers BPA to be safe at low levels occurring in food containers, up to 5 mg per kg body weight per day, or 100 times the amount the new study found to be risky. Some researchers argue the FDA guidelines are outdated .
Other regulatory agencies around the world have taken a tougher stance on the chemical — the European Commission proposed to ban BPA in products that come into contact with food or beverages by the end of 2024.
Environmental contaminants can be a major threat to human health
The concern about BPA is part of a broader alarm being raised about our everyday exposure to substances that may be harmful to our health.
Other recent research has found microplastics , particles so tiny they can infiltrate human cells, may potentially wreak havoc with our health. They've been found everywhere, from human lungs to reproductive organs .
Understanding how the substances we encounter every day may affect our health long-term could help us make better decisions about how to reduce the risk of chronic illnesses like type 2 diabetes.
"Given that diabetes is a leading cause of death in the US, it is crucial to understand even the smallest factors that contribute to the disease," Hagobian said in the press release. " We were surprised to see that reducing BPA exposure, such as using stainless steel or glass bottles and BPA-free cans, may lower diabetes risk."
June 24, 2024 — An earlier version of this article misstated the difference between what the EPA considers safe BPA exposure and what the study found to be safe. It is 100 times higher, not 1000.
Watch: Every difference between US and UK Coca-Cola
- Main content

IMAGES
VIDEO
COMMENTS
Semaglutide with affordable, transparent pricing. No membership fee and fast shipping! Don't pay $99/month without any medications. Go to ReflexMD and get your meds now!
Eliminate 3 drinks for better blood sugar control and effectively manage T2D. Lower your blood sugar levels naturally and bid farewell to high blood sugar for good.
The new research, published in the journal Nature Communications, offers a potential strategy for developing new therapies that could restore dysfunctional pancreatic beta-cells or, perhaps, even prevent Type 2 diabetes from developing. The new study shows that the beta-cells of Type 2 diabetes patients are deficient in a cell trafficking ...
June 24, 2021 — Across the world, type 2 diabetes is on the rise. A research group has discovered a new gene that may hold the key to preventing and treating lifestyle related diseases such as ...
This finding encourages further investigation into inceptor as a potential therapeutic target for treating type 2 diabetes. These findings, led by Helmholtz Munich in collaboration with the German Center for Diabetes Research, the Technical University of Munich, and the Ludwig-Maximilians-University Munich, drive advancements in diabetes research.
Your source for the latest research news. Follow: Facebook X/Twitter Subscribe: RSS Feeds. ... 2022 — A novel therapy ameliorates obesity and Type 2 diabetes in mice fed a high-fat diet. The ...
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). ... Latest Research and Reviews. ... and long-term ...
However, type 2 diabetes makes up more than 90% of diagnosed diabetes cases in the United States. 35 Thus, our findings largely reflect risk-factor treatment and control in those with type 2 diabetes.
Methods. In this trial involving participants with type 2 diabetes of less than 10 years' duration who were receiving metformin and had glycated hemoglobin levels of 6.8 to 8.5%, we compared the ...
Large-scale study reveals new genetic details of diabetes. In experiments of unprecedented scale, investigators at Weill Cornell Medicine and the National Institutes of Health have revealed new aspects of the complex genetics behind Type 2 diabetes. Through these discoveries, and by providing a template for future studies, this research ...
New approaches for the treatment of type 2 diabetes aim to induce remission as soon as possible after diagnosis by achieving durable responses to novel medicines designed to target the causes of ...
More than 7,000 clinical trials are currently ongoing involving new drugs for type 2 diabetes mellitus (T2DM). ... Dallas Diabetes Research Center at Medical City, Dallas, TX, USA. Julio Rosenstock.
Despite the successful development of new therapies for the treatment of type 2 diabetes, such as glucagon-like peptide-1 (GLP-1) receptor agonists and sodium-glucose cotransporter-2 inhibitors, the search for novel treatment options that can provide better glycaemic control and at reduce complications is a continuous effort. The present Review aims to present an overview of novel targets and ...
MLA. APA. Chicago. University of Barcelona. "New therapeutic targets to fight type 2 diabetes." ScienceDaily. ScienceDaily, 7 June 2024. <www.sciencedaily.com / releases / 2024 / 06 / 240607121434 ...
Type 2 diabetes accounts for nearly 90% of the approximately 537 million cases of diabetes worldwide. The number affected is increasing rapidly with alarming trends in children and young adults (up to age 40 years). Early detection and proactive management are crucial for prevention and mitigation of microvascular and macrovascular complications and mortality burden. Access to novel therapies ...
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
It also discusses emerging target-based therapies and new potential therapeutic targets that have emerged within the last three years. The aim of our review is to provide a theoretical basis for further advancement in targeted therapies for T2DM. Keywords: type 2 diabetes mellitus, target, mechanism, medicine. 1.
The chronic complications of type 2 diabetes are a major cause of mortality and disability worldwide [ 1, 2 ]. Clinical research is the main way to gain knowledge about long-term diabetic complications and reduce the burden of diabetes. This allows for designing effective programs for screening and follow-up and fine-targeted therapeutic ...
Surgery led to diabetes remission in roughly 28% of patients, compared with a remission rate of just 4% among the non-surgery group, according to the study results. More research has found that ...
Amelioration of Both Central and Peripheral Neuropathy in Mouse Models of Type 1 and Type 2 Diabetes by the Neurogenic Molecule NSI-189. Diabetes, 68(11), 2143-2154. Read more. ADA-funded researcher studying link between ageing and type 2 diabetes. One of the most important risk factors for developing type 2 diabetes is age.
A new study found that tiny biodegradable particles improved insulin sensitivity in the liver cells of humans and in diabetic mice, which could offer a promising new treatment for type 2 diabetes.
A new study published in the Journal of Clinical Investigation has demonstrated that activating a pathway to promote cell division not only expanded the population of insulin-producing cells, but, surprisingly, also enhanced the cells' function. The findings hold promise for future therapeutics that will improve the lives of individuals with type 2 diabetes—a condition that affects more ...
New data focused on advanced technology innovations for managing type 2 diabetes (T2D) highlight the positive impact of automated insulin delivery systems ... the world's largest scientific meeting focused on diabetes research, prevention, and care, will be held in Orlando, FL on June 21-24. More than 11,000 leading physicians, scientists, and ...
Read the latest Research articles in Type 2 diabetes from Nature Reviews Endocrinology ... Evidence indicates an elevated risk of type 2 diabetes mellitus after breast cancer treatment ...
In type 2 diabetes, which affects approximately 537 million people worldwide, a person's body gradually loses its ability to effectively regulate blood sugar. Although prior research has connected changes in the gut microbiome to type 2 diabetes, a diverse large-scale study has been lacking.
But research to understand how they could benefit people with type 2 diabetes has been lacking. At ADA, a new set of studies illuminated the potential for these technologies to improve blood sugar levels in people living with type 2 diabetes too. This positive impact was seen both in people who were taking insulin, or not.
"The changes to the microbiome may happen first, and diabetes develops later, not the other way around—although future prospective or interventional studies are needed to prove this relation firmly." "If these microbial features are causal, we can find a way to change the microbiome and reduce type 2 diabetes risk," he added.
Fewer than one-quarter of patients with type 2 diabetes (T2D) receive recommended chronic kidney disease (CKD) screening, according to a study published online June 26 in JAMA Network Open.
The increasing incidence of type 2 diabetes, which represents 90% of diabetes cases globally, is a major public health concern. Improved glucose management reduces the risk of vascular complications and mortality; however, only a small proportion of the type 2 diabetes population have blood glucose levels within the recommended treatment targets. In recent years, diabetes technologies have ...
Type 1 diabetes; Type 2 diabetes; Latest Research and Reviews. Activation of the osteoblastic HIF-1α pathway partially alleviates the symptoms of STZ-induced type 1 diabetes mellitus via RegIIIγ ...
The demarcation between monogenic and polygenic type 2 diabetes (T2D) is less distinct than previously believed. Notably, recent research has highlighted a new entity, that we suggest calling oligogenic forms of T2D, serving as a genetic link between these two forms. In this opinion article, we have reviewed scientific advances that suggest categorizing genes involved in oligogenic T2D ...
An impaired ability to respond to insulin, known as insulin resistance, can mean chronically high blood sugar levels and a much higher risk of type 2 diabetes. Advertisement